User login
Is exercise effective for constipation?
I recently presented a clinical scenario about a patient of mine named Brenda. This 35-year-old woman came to me with symptoms that had been going on for a year already. I asked for readers’ comments about my management of Brenda.
I appreciate the comments I received regarding this case. The most common suggestion was to encourage Brenda to exercise, and a systematic review of randomized clinical trials published in 2019 supports this recommendation. This review included nine studies with a total of 680 participants, and the overall effect of exercise was a twofold improvement in symptoms associated with constipation. Walking was the most common exercise intervention, and along with qigong (which combines body position, breathing, and meditation), these two modes of exercise were effective in improving constipation. However, the one study evaluating resistance training failed to demonstrate a significant effect. Importantly, the reviewers considered the collective research to be at a high risk of bias.
Exercise will probably help Brenda, although some brainstorming might be necessary to help her fit exercise into her busy schedule. Another suggestion focused on her risk for colorectal cancer, and Dr. Cooke and Dr. Boboc both astutely noted that colorectal cancer is increasingly common among adults at early middle age. This stands in contrast to a steady decline in the prevalence of colorectal cancer among U.S. adults at age 65 years or older. Whereas colorectal cancer declined by 3.3% annually among U.S. older adults from 2011 to 2016, there was a reversal of this favorable trend among individuals between 50 and 64 years of age, with rates increasing by 1% annually.
The increase in the incidence of colorectal cancer among adults 50-64 years of age has been outpaced by the increase among adults younger than 50 years, who have experienced a 2.2% increase in the incidence of colorectal cancer annually between 2012 and 2016. Previously, the increase in colorectal cancer among early middle-aged adults was driven by higher rates of rectal cancer, but more recently this trend has included higher rates of proximal and distal colon tumors. In 2020, 12% of new cases of colorectal cancer were expected to be among individuals younger than 50 years.
So how do we act on this context in the case of Brenda? Her history suggests no overt warning signs for cancer. The history did not address a family history of gastrointestinal symptoms or colorectal cancer, which is an important omission.
Although the number of cases of cancer among persons younger than 50 years may be rising, the overall prevalence of colorectal cancer among younger adults is well under 1%. At 35 years of age, it is not necessary to evaluate Brenda for colorectal cancer. However, persistent or worsening symptoms could prompt a referral for colonoscopy at a later time.
Finally, let’s address how to practically manage Brenda’s case, because many options are available. I would begin with recommendations regarding her lifestyle, including regular exercise, adequate sleep, and whatever she can achieve in the FODMAP diet. I would also recommend psyllium as a soluble fiber and expect that these changes would help her constipation. But they might be less effective for abdominal cramping, so I would also recommend peppermint oil at this time.
If Brenda commits to these recommendations, she will very likely improve. If she does not, I will be more concerned regarding anxiety and depression complicating her illness. Treating those disorders can make a big difference.
In addition, if there is an inadequate response to initial therapy, I will initiate linaclotide or lubiprostone. Plecanatide is another reasonable option. At this point, I will also consider referral to a gastroenterologist for a recalcitrant case and will certainly refer if one of these specific treatments fails in Brenda. Conditions such as pelvic floor dysfunction can mimic irritable bowel syndrome with constipation and merit consideration.
However, I really believe that Brenda will feel better. Thanks for all of the insightful and interesting comments. It is easy to see how we are all invested in improving patients’ lives.
Dr. Vega is a clinical professor of family medicine at the University of California, Irvine. He reported disclosures with McNeil Pharmaceuticals. A version of this article first appeared on Medscape.com.
I recently presented a clinical scenario about a patient of mine named Brenda. This 35-year-old woman came to me with symptoms that had been going on for a year already. I asked for readers’ comments about my management of Brenda.
I appreciate the comments I received regarding this case. The most common suggestion was to encourage Brenda to exercise, and a systematic review of randomized clinical trials published in 2019 supports this recommendation. This review included nine studies with a total of 680 participants, and the overall effect of exercise was a twofold improvement in symptoms associated with constipation. Walking was the most common exercise intervention, and along with qigong (which combines body position, breathing, and meditation), these two modes of exercise were effective in improving constipation. However, the one study evaluating resistance training failed to demonstrate a significant effect. Importantly, the reviewers considered the collective research to be at a high risk of bias.
Exercise will probably help Brenda, although some brainstorming might be necessary to help her fit exercise into her busy schedule. Another suggestion focused on her risk for colorectal cancer, and Dr. Cooke and Dr. Boboc both astutely noted that colorectal cancer is increasingly common among adults at early middle age. This stands in contrast to a steady decline in the prevalence of colorectal cancer among U.S. adults at age 65 years or older. Whereas colorectal cancer declined by 3.3% annually among U.S. older adults from 2011 to 2016, there was a reversal of this favorable trend among individuals between 50 and 64 years of age, with rates increasing by 1% annually.
The increase in the incidence of colorectal cancer among adults 50-64 years of age has been outpaced by the increase among adults younger than 50 years, who have experienced a 2.2% increase in the incidence of colorectal cancer annually between 2012 and 2016. Previously, the increase in colorectal cancer among early middle-aged adults was driven by higher rates of rectal cancer, but more recently this trend has included higher rates of proximal and distal colon tumors. In 2020, 12% of new cases of colorectal cancer were expected to be among individuals younger than 50 years.
So how do we act on this context in the case of Brenda? Her history suggests no overt warning signs for cancer. The history did not address a family history of gastrointestinal symptoms or colorectal cancer, which is an important omission.
Although the number of cases of cancer among persons younger than 50 years may be rising, the overall prevalence of colorectal cancer among younger adults is well under 1%. At 35 years of age, it is not necessary to evaluate Brenda for colorectal cancer. However, persistent or worsening symptoms could prompt a referral for colonoscopy at a later time.
Finally, let’s address how to practically manage Brenda’s case, because many options are available. I would begin with recommendations regarding her lifestyle, including regular exercise, adequate sleep, and whatever she can achieve in the FODMAP diet. I would also recommend psyllium as a soluble fiber and expect that these changes would help her constipation. But they might be less effective for abdominal cramping, so I would also recommend peppermint oil at this time.
If Brenda commits to these recommendations, she will very likely improve. If she does not, I will be more concerned regarding anxiety and depression complicating her illness. Treating those disorders can make a big difference.
In addition, if there is an inadequate response to initial therapy, I will initiate linaclotide or lubiprostone. Plecanatide is another reasonable option. At this point, I will also consider referral to a gastroenterologist for a recalcitrant case and will certainly refer if one of these specific treatments fails in Brenda. Conditions such as pelvic floor dysfunction can mimic irritable bowel syndrome with constipation and merit consideration.
However, I really believe that Brenda will feel better. Thanks for all of the insightful and interesting comments. It is easy to see how we are all invested in improving patients’ lives.
Dr. Vega is a clinical professor of family medicine at the University of California, Irvine. He reported disclosures with McNeil Pharmaceuticals. A version of this article first appeared on Medscape.com.
I recently presented a clinical scenario about a patient of mine named Brenda. This 35-year-old woman came to me with symptoms that had been going on for a year already. I asked for readers’ comments about my management of Brenda.
I appreciate the comments I received regarding this case. The most common suggestion was to encourage Brenda to exercise, and a systematic review of randomized clinical trials published in 2019 supports this recommendation. This review included nine studies with a total of 680 participants, and the overall effect of exercise was a twofold improvement in symptoms associated with constipation. Walking was the most common exercise intervention, and along with qigong (which combines body position, breathing, and meditation), these two modes of exercise were effective in improving constipation. However, the one study evaluating resistance training failed to demonstrate a significant effect. Importantly, the reviewers considered the collective research to be at a high risk of bias.
Exercise will probably help Brenda, although some brainstorming might be necessary to help her fit exercise into her busy schedule. Another suggestion focused on her risk for colorectal cancer, and Dr. Cooke and Dr. Boboc both astutely noted that colorectal cancer is increasingly common among adults at early middle age. This stands in contrast to a steady decline in the prevalence of colorectal cancer among U.S. adults at age 65 years or older. Whereas colorectal cancer declined by 3.3% annually among U.S. older adults from 2011 to 2016, there was a reversal of this favorable trend among individuals between 50 and 64 years of age, with rates increasing by 1% annually.
The increase in the incidence of colorectal cancer among adults 50-64 years of age has been outpaced by the increase among adults younger than 50 years, who have experienced a 2.2% increase in the incidence of colorectal cancer annually between 2012 and 2016. Previously, the increase in colorectal cancer among early middle-aged adults was driven by higher rates of rectal cancer, but more recently this trend has included higher rates of proximal and distal colon tumors. In 2020, 12% of new cases of colorectal cancer were expected to be among individuals younger than 50 years.
So how do we act on this context in the case of Brenda? Her history suggests no overt warning signs for cancer. The history did not address a family history of gastrointestinal symptoms or colorectal cancer, which is an important omission.
Although the number of cases of cancer among persons younger than 50 years may be rising, the overall prevalence of colorectal cancer among younger adults is well under 1%. At 35 years of age, it is not necessary to evaluate Brenda for colorectal cancer. However, persistent or worsening symptoms could prompt a referral for colonoscopy at a later time.
Finally, let’s address how to practically manage Brenda’s case, because many options are available. I would begin with recommendations regarding her lifestyle, including regular exercise, adequate sleep, and whatever she can achieve in the FODMAP diet. I would also recommend psyllium as a soluble fiber and expect that these changes would help her constipation. But they might be less effective for abdominal cramping, so I would also recommend peppermint oil at this time.
If Brenda commits to these recommendations, she will very likely improve. If she does not, I will be more concerned regarding anxiety and depression complicating her illness. Treating those disorders can make a big difference.
In addition, if there is an inadequate response to initial therapy, I will initiate linaclotide or lubiprostone. Plecanatide is another reasonable option. At this point, I will also consider referral to a gastroenterologist for a recalcitrant case and will certainly refer if one of these specific treatments fails in Brenda. Conditions such as pelvic floor dysfunction can mimic irritable bowel syndrome with constipation and merit consideration.
However, I really believe that Brenda will feel better. Thanks for all of the insightful and interesting comments. It is easy to see how we are all invested in improving patients’ lives.
Dr. Vega is a clinical professor of family medicine at the University of California, Irvine. He reported disclosures with McNeil Pharmaceuticals. A version of this article first appeared on Medscape.com.
The role of repeat uterine curettage in postmolar gestational trophoblastic neoplasia
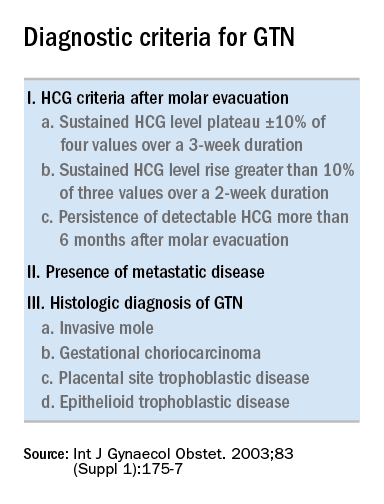
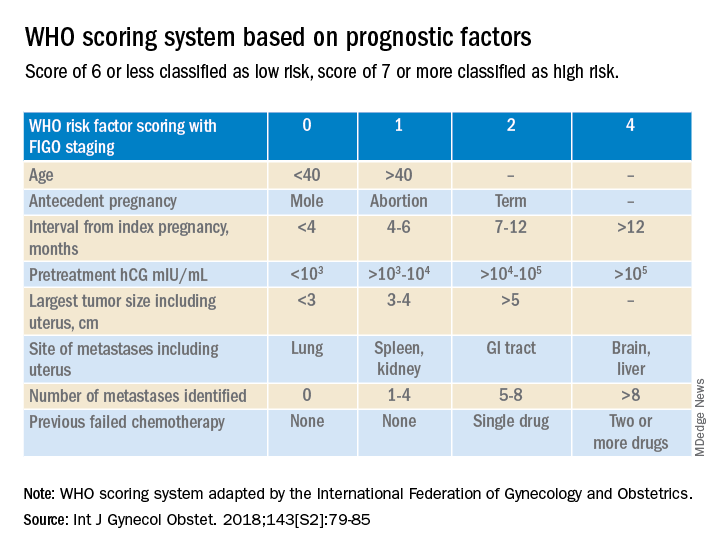
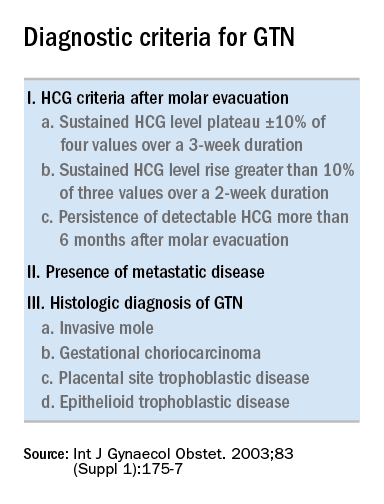
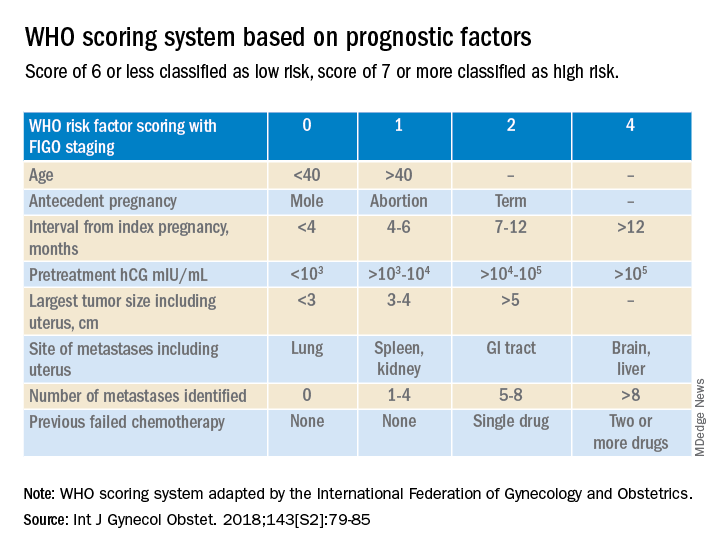
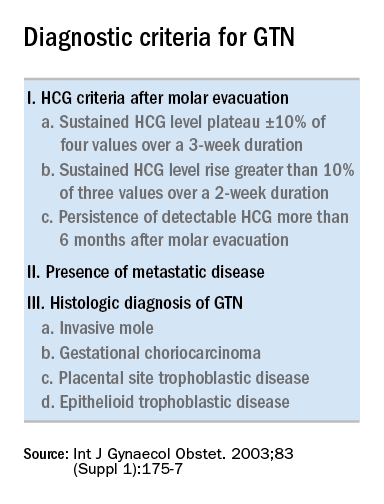
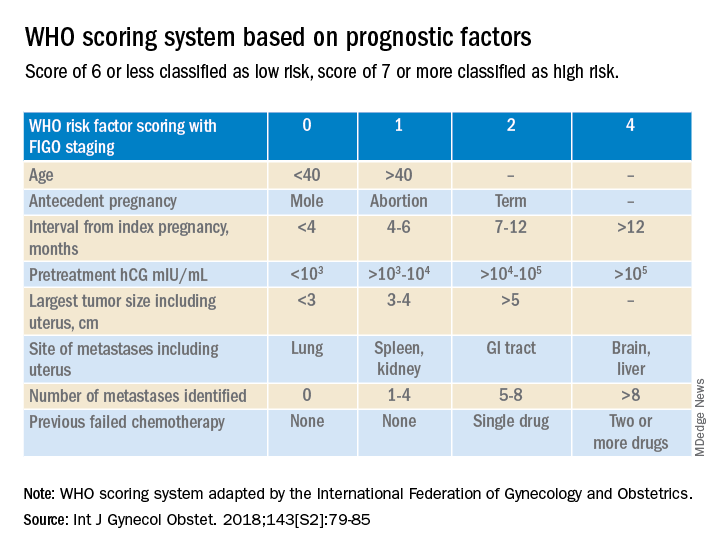
Trophoblastic tissue is responsible for formation of the placenta during pregnancy. Gestational trophoblastic disease (GTD), a group comprising benign (hydatidiform moles) and malignant tumors, occurs when gestational trophoblastic tissue behaves in an abnormal manner. Hydatidiform moles, which are thought to be caused by errors in fertilization, occur in approximately 1 in 1,200 pregnancies in the United States. Gestational trophoblastic neoplasia (GTN) refers to the subgroup of these trophoblastic or placental tumors with malignant behavior and includes postmolar GTN, invasive mole, gestational choriocarcinoma, placental-site trophoblastic tumor (PSTT), and epithelioid trophoblastic tumor. Postmolar GTN arises after evacuation of a molar pregnancy and is most frequently diagnosed by a plateau or increase in human chorionic gonadotropin (hCG).1 The risk of postmolar GTN is much higher after a complete mole (7%-30%) compared with a partial mole (2.5%-7.5%).2 Once postmolar GTN is diagnosed, a World Health Organization score is assigned to determine if patients have low- or high-risk disease.3 The primary treatment for most GTN is chemotherapy. A patient’s WHO score helps determine whether they would benefit from single-agent or multiagent chemotherapy. The standard of care for low-risk disease is single-agent chemotherapy with either methotrexate or actinomycin D.
The role of a second uterine curettage, after the diagnosis of low-risk postmolar GTN, has been controversial because of the limited data and disparate outcomes reported. In older retrospective series, a second curettage affected treatment or produced remission in only 9%-20% of patients and caused uterine perforation or major hemorrhage in 5%-8% of patients.4,5 Given relatively high rates of major complications compared with surgical cure or decreased chemotherapy cycles needed, only a limited number of patients seemed to benefit from a second procedure. On the other hand, an observational study of 544 patients who underwent second uterine evacuation after a presumed diagnosis of persistent GTD found that up to 60% of patients did not require chemotherapy afterward.6 Those with hCG levels greater than 1,500 IU/L or histologic evidence of GTD were less likely to have a surgical cure after second curettage. The indications for uterine evacuations were varied across these studies and make it nearly impossible to compare their results.
More recently, there have been two prospective trials that have tackled the question of the utility of second uterine evacuation in low-risk, nonmetastatic GTN. The Gynecologic Oncology Group performed a single-arm prospective study in the United States that enrolled patients with postmolar GTN to undergo second curettage as initial treatment of their disease.7 Of 60 eligible patients, 40% had a surgical cure (defined as normalization of hCG followed by at least 6 months of subsequent normal hCG values). Overall, 47% of patients were able to avoid chemotherapy. All surgical cures were seen in patients with WHO scores between 0 and 4. Importantly, three women were diagnosed with PSTT, which tends to be resistant to methotrexate and actinomycin D (treatment for nonmetastatic PSTT is definitive surgery with hysterectomy). The study found that hCG was a poor discriminator for achieving surgical cure. While age appeared to have an association with surgical cure (cure less likely for younger and older ages, younger than 19 and older than 40), patient numbers were too small to make a statistical conclusion. There were no uterine perforations and one patient had a grade 3 hemorrhage (requiring transfusion).
In the second prospective trial, performed in Iran, 62 patients were randomized to either second uterine evacuation or standard treatment after diagnosis of postmolar GTN.8 All patients in the surgical arm received a cervical ripening agent prior to their procedure, had their procedure under ultrasound guidance, and received misoprostol afterward to prevent uterine bleeding. Among those undergoing second uterine evacuation, 50% were cured (no need for chemotherapy). Among those needing chemotherapy after surgery, the mean number of cycles of chemotherapy needed (3.07 vs. 6.69) and the time it took to achieve negative hCG (3.23 vs. 9.19 weeks) were significantly less compared with patients who did not undergo surgery. hCG prior to second uterine evacuation could distinguish response to surgery compared with those needing chemotherapy (hCG of 1,983 IU/L or less was the level determined to best predict response). No complications related to surgery were reported.
Given prospective data available, second uterine evacuation for treatment of nonmetastatic, low-risk postmolar GTN is a reasonable treatment option and one that should be considered and discussed with patients given the potential to avoid chemotherapy or decrease the number of cycles needed. It may be prudent to limit the procedure to patients with an hCG less than 1,500-2,000 IU/L and to those between the ages of 20 and 40. While uterine hemorrhage and perforation have been reported in the literature, more recent data suggest low rates of these complications. Unfortunately, given the rarity of the disease and the historically controversial use of second curettage, little is known about the effects on future fertility that this procedure may have, including the development of uterine synechiae.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Ngan HY et al, FIGO Committee on Gynecologic Oncology. Int J Gynaecol Obstet. 2003 Oct;83 Suppl 1:175-7. Erratum in: Int J Gynaecol Obstet. 2021 Dec;155(3):563.
2. Soper JT. Obstet Gynecol. 2021 Feb.;137(2):355-70.
3. Ngan HY et al. Int J Gynecol Obstet. 2018;143:79-85.
4. Schlaerth JB et al. Am J Obstet Gynecol. 1990 Jun;162(6):1465-70.
5. van Trommel NE et al. Gynecol Oncol. 2005 Oct;99(1):6-13.
6. Pezeshki M et al. Gynecol Oncol. 2004 Dec;95(3):423-9.
7. Osborne RJ et al. Obstet Gynecol. 2016 Sep;128(3):535-42.
8. Ayatollahi H et al. Int J Womens Health. 2017 Sep 21;9:665-71.
Trophoblastic tissue is responsible for formation of the placenta during pregnancy. Gestational trophoblastic disease (GTD), a group comprising benign (hydatidiform moles) and malignant tumors, occurs when gestational trophoblastic tissue behaves in an abnormal manner. Hydatidiform moles, which are thought to be caused by errors in fertilization, occur in approximately 1 in 1,200 pregnancies in the United States. Gestational trophoblastic neoplasia (GTN) refers to the subgroup of these trophoblastic or placental tumors with malignant behavior and includes postmolar GTN, invasive mole, gestational choriocarcinoma, placental-site trophoblastic tumor (PSTT), and epithelioid trophoblastic tumor. Postmolar GTN arises after evacuation of a molar pregnancy and is most frequently diagnosed by a plateau or increase in human chorionic gonadotropin (hCG).1 The risk of postmolar GTN is much higher after a complete mole (7%-30%) compared with a partial mole (2.5%-7.5%).2 Once postmolar GTN is diagnosed, a World Health Organization score is assigned to determine if patients have low- or high-risk disease.3 The primary treatment for most GTN is chemotherapy. A patient’s WHO score helps determine whether they would benefit from single-agent or multiagent chemotherapy. The standard of care for low-risk disease is single-agent chemotherapy with either methotrexate or actinomycin D.
The role of a second uterine curettage, after the diagnosis of low-risk postmolar GTN, has been controversial because of the limited data and disparate outcomes reported. In older retrospective series, a second curettage affected treatment or produced remission in only 9%-20% of patients and caused uterine perforation or major hemorrhage in 5%-8% of patients.4,5 Given relatively high rates of major complications compared with surgical cure or decreased chemotherapy cycles needed, only a limited number of patients seemed to benefit from a second procedure. On the other hand, an observational study of 544 patients who underwent second uterine evacuation after a presumed diagnosis of persistent GTD found that up to 60% of patients did not require chemotherapy afterward.6 Those with hCG levels greater than 1,500 IU/L or histologic evidence of GTD were less likely to have a surgical cure after second curettage. The indications for uterine evacuations were varied across these studies and make it nearly impossible to compare their results.
More recently, there have been two prospective trials that have tackled the question of the utility of second uterine evacuation in low-risk, nonmetastatic GTN. The Gynecologic Oncology Group performed a single-arm prospective study in the United States that enrolled patients with postmolar GTN to undergo second curettage as initial treatment of their disease.7 Of 60 eligible patients, 40% had a surgical cure (defined as normalization of hCG followed by at least 6 months of subsequent normal hCG values). Overall, 47% of patients were able to avoid chemotherapy. All surgical cures were seen in patients with WHO scores between 0 and 4. Importantly, three women were diagnosed with PSTT, which tends to be resistant to methotrexate and actinomycin D (treatment for nonmetastatic PSTT is definitive surgery with hysterectomy). The study found that hCG was a poor discriminator for achieving surgical cure. While age appeared to have an association with surgical cure (cure less likely for younger and older ages, younger than 19 and older than 40), patient numbers were too small to make a statistical conclusion. There were no uterine perforations and one patient had a grade 3 hemorrhage (requiring transfusion).
In the second prospective trial, performed in Iran, 62 patients were randomized to either second uterine evacuation or standard treatment after diagnosis of postmolar GTN.8 All patients in the surgical arm received a cervical ripening agent prior to their procedure, had their procedure under ultrasound guidance, and received misoprostol afterward to prevent uterine bleeding. Among those undergoing second uterine evacuation, 50% were cured (no need for chemotherapy). Among those needing chemotherapy after surgery, the mean number of cycles of chemotherapy needed (3.07 vs. 6.69) and the time it took to achieve negative hCG (3.23 vs. 9.19 weeks) were significantly less compared with patients who did not undergo surgery. hCG prior to second uterine evacuation could distinguish response to surgery compared with those needing chemotherapy (hCG of 1,983 IU/L or less was the level determined to best predict response). No complications related to surgery were reported.
Given prospective data available, second uterine evacuation for treatment of nonmetastatic, low-risk postmolar GTN is a reasonable treatment option and one that should be considered and discussed with patients given the potential to avoid chemotherapy or decrease the number of cycles needed. It may be prudent to limit the procedure to patients with an hCG less than 1,500-2,000 IU/L and to those between the ages of 20 and 40. While uterine hemorrhage and perforation have been reported in the literature, more recent data suggest low rates of these complications. Unfortunately, given the rarity of the disease and the historically controversial use of second curettage, little is known about the effects on future fertility that this procedure may have, including the development of uterine synechiae.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Ngan HY et al, FIGO Committee on Gynecologic Oncology. Int J Gynaecol Obstet. 2003 Oct;83 Suppl 1:175-7. Erratum in: Int J Gynaecol Obstet. 2021 Dec;155(3):563.
2. Soper JT. Obstet Gynecol. 2021 Feb.;137(2):355-70.
3. Ngan HY et al. Int J Gynecol Obstet. 2018;143:79-85.
4. Schlaerth JB et al. Am J Obstet Gynecol. 1990 Jun;162(6):1465-70.
5. van Trommel NE et al. Gynecol Oncol. 2005 Oct;99(1):6-13.
6. Pezeshki M et al. Gynecol Oncol. 2004 Dec;95(3):423-9.
7. Osborne RJ et al. Obstet Gynecol. 2016 Sep;128(3):535-42.
8. Ayatollahi H et al. Int J Womens Health. 2017 Sep 21;9:665-71.
Trophoblastic tissue is responsible for formation of the placenta during pregnancy. Gestational trophoblastic disease (GTD), a group comprising benign (hydatidiform moles) and malignant tumors, occurs when gestational trophoblastic tissue behaves in an abnormal manner. Hydatidiform moles, which are thought to be caused by errors in fertilization, occur in approximately 1 in 1,200 pregnancies in the United States. Gestational trophoblastic neoplasia (GTN) refers to the subgroup of these trophoblastic or placental tumors with malignant behavior and includes postmolar GTN, invasive mole, gestational choriocarcinoma, placental-site trophoblastic tumor (PSTT), and epithelioid trophoblastic tumor. Postmolar GTN arises after evacuation of a molar pregnancy and is most frequently diagnosed by a plateau or increase in human chorionic gonadotropin (hCG).1 The risk of postmolar GTN is much higher after a complete mole (7%-30%) compared with a partial mole (2.5%-7.5%).2 Once postmolar GTN is diagnosed, a World Health Organization score is assigned to determine if patients have low- or high-risk disease.3 The primary treatment for most GTN is chemotherapy. A patient’s WHO score helps determine whether they would benefit from single-agent or multiagent chemotherapy. The standard of care for low-risk disease is single-agent chemotherapy with either methotrexate or actinomycin D.
The role of a second uterine curettage, after the diagnosis of low-risk postmolar GTN, has been controversial because of the limited data and disparate outcomes reported. In older retrospective series, a second curettage affected treatment or produced remission in only 9%-20% of patients and caused uterine perforation or major hemorrhage in 5%-8% of patients.4,5 Given relatively high rates of major complications compared with surgical cure or decreased chemotherapy cycles needed, only a limited number of patients seemed to benefit from a second procedure. On the other hand, an observational study of 544 patients who underwent second uterine evacuation after a presumed diagnosis of persistent GTD found that up to 60% of patients did not require chemotherapy afterward.6 Those with hCG levels greater than 1,500 IU/L or histologic evidence of GTD were less likely to have a surgical cure after second curettage. The indications for uterine evacuations were varied across these studies and make it nearly impossible to compare their results.
More recently, there have been two prospective trials that have tackled the question of the utility of second uterine evacuation in low-risk, nonmetastatic GTN. The Gynecologic Oncology Group performed a single-arm prospective study in the United States that enrolled patients with postmolar GTN to undergo second curettage as initial treatment of their disease.7 Of 60 eligible patients, 40% had a surgical cure (defined as normalization of hCG followed by at least 6 months of subsequent normal hCG values). Overall, 47% of patients were able to avoid chemotherapy. All surgical cures were seen in patients with WHO scores between 0 and 4. Importantly, three women were diagnosed with PSTT, which tends to be resistant to methotrexate and actinomycin D (treatment for nonmetastatic PSTT is definitive surgery with hysterectomy). The study found that hCG was a poor discriminator for achieving surgical cure. While age appeared to have an association with surgical cure (cure less likely for younger and older ages, younger than 19 and older than 40), patient numbers were too small to make a statistical conclusion. There were no uterine perforations and one patient had a grade 3 hemorrhage (requiring transfusion).
In the second prospective trial, performed in Iran, 62 patients were randomized to either second uterine evacuation or standard treatment after diagnosis of postmolar GTN.8 All patients in the surgical arm received a cervical ripening agent prior to their procedure, had their procedure under ultrasound guidance, and received misoprostol afterward to prevent uterine bleeding. Among those undergoing second uterine evacuation, 50% were cured (no need for chemotherapy). Among those needing chemotherapy after surgery, the mean number of cycles of chemotherapy needed (3.07 vs. 6.69) and the time it took to achieve negative hCG (3.23 vs. 9.19 weeks) were significantly less compared with patients who did not undergo surgery. hCG prior to second uterine evacuation could distinguish response to surgery compared with those needing chemotherapy (hCG of 1,983 IU/L or less was the level determined to best predict response). No complications related to surgery were reported.
Given prospective data available, second uterine evacuation for treatment of nonmetastatic, low-risk postmolar GTN is a reasonable treatment option and one that should be considered and discussed with patients given the potential to avoid chemotherapy or decrease the number of cycles needed. It may be prudent to limit the procedure to patients with an hCG less than 1,500-2,000 IU/L and to those between the ages of 20 and 40. While uterine hemorrhage and perforation have been reported in the literature, more recent data suggest low rates of these complications. Unfortunately, given the rarity of the disease and the historically controversial use of second curettage, little is known about the effects on future fertility that this procedure may have, including the development of uterine synechiae.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Ngan HY et al, FIGO Committee on Gynecologic Oncology. Int J Gynaecol Obstet. 2003 Oct;83 Suppl 1:175-7. Erratum in: Int J Gynaecol Obstet. 2021 Dec;155(3):563.
2. Soper JT. Obstet Gynecol. 2021 Feb.;137(2):355-70.
3. Ngan HY et al. Int J Gynecol Obstet. 2018;143:79-85.
4. Schlaerth JB et al. Am J Obstet Gynecol. 1990 Jun;162(6):1465-70.
5. van Trommel NE et al. Gynecol Oncol. 2005 Oct;99(1):6-13.
6. Pezeshki M et al. Gynecol Oncol. 2004 Dec;95(3):423-9.
7. Osborne RJ et al. Obstet Gynecol. 2016 Sep;128(3):535-42.
8. Ayatollahi H et al. Int J Womens Health. 2017 Sep 21;9:665-71.
Yes, we should talk politics and religion with patients
From our first days as medical students, we are told that politics and religion are topics to be avoided with patients, but I disagree. Knowing more about our patients allows us to deliver better care.
Politics and religion: New risk factors
The importance of politics and religion in the health of patients was clearly demonstrated during the COVID-19 pandemic. Lives were needlessly lost because of stands taken based on religious beliefs or a political ideology. Families, friends, and the community at large were impacted.
Over my years of practice, I have found that while these are difficult topics to address, they should not be avoided. Studies have shown that open acknowledgement of religious beliefs can affect both clinical outcomes and well-being. Religion and spirituality are as much a part of our patient’s lives as the physical parameters that we measure. To neglect these significant aspects is to miss the very essence of the individual.
I made it a practice to ask patients about their religious beliefs, the extent to which religion shaped their life, and whether they were part of a church community. Knowing this allowed me to separate deep personal belief from stances based on personal freedom, misinformation, conspiracies, and politics.
I found that information about political leanings flowed naturally in discussions with patients as we trusted and respected each other over time. If I approached politics objectively and nonjudgmentally, it generally led to meaningful conversation. This helped me to understand the patient as an individual and informed my diagnosis and treatment plan.
Politics as stress
For example, on more than one occasion, a patient with atrial fibrillation presented with persistent elevated blood pressure and pulse rate despite adherence to the medical regimen that I had prescribed. After a few minutes of discussion, it was clear that excessive attention to political commentary on TV and social media raised their anxiety and anger level, putting them at greater risk for adverse outcomes. I advised that they refocus their leisure activities rather than change or increase medication.
It is disappointing to see how one of the great scientific advances of our lifetime, vaccination science, has been tarnished because of political or religious ideology and to see the extent to which these beliefs influenced COVID-19 vaccination compliance. As health care providers, we must promote information based on the scientific method. If patients challenge us and point out that recommendations based on science seem to change over time, we must explain that science evolves on the basis of new information objectively gathered. We need to find out what information the patient has gotten from the Internet, TV, or conspiracy theories and counter this with scientific facts. If we do not discuss religion and politics with our patients along with other risk factors, we may compromise our ability to give them the best advice and treatment.
Our patients have a right to their own spiritual and political ideology. If it differs dramatically from our own, this should not influence our commitment to care for them. But we have an obligation to challenge unfounded beliefs about medicine and counter with scientific facts. There are times when individual freedoms must be secondary to public health. Ultimately, it is up to the patient to choose, but they should not be given a “free pass” on the basis of religion or politics. If I know something is true and I would do it myself or recommend it for my family, I have an obligation to provide this recommendation to my patients.
Religious preference is included in medical records. It is not appropriate to add political preference, but the patient benefits if a long-term caregiver knows this information.
During the pandemic, for the first time in my 40+ years of practice, some patients questioned my recommendations and placed equal or greater weight on religion, politics, or conspiracy theories. This continues to be a very real struggle.
Knowing and understanding our patients as individuals is critical to providing optimum care and that means tackling these formally taboo topics. If having a potentially uncomfortable conversation with patients allows us to save one life, it is worth it.
Dr. Francis is a cardiologist at Inova Heart and Vascular Institute, McLean, Va. He disclosed no relevant conflict of interest. A version of this article first appeared on Medscape.com.
From our first days as medical students, we are told that politics and religion are topics to be avoided with patients, but I disagree. Knowing more about our patients allows us to deliver better care.
Politics and religion: New risk factors
The importance of politics and religion in the health of patients was clearly demonstrated during the COVID-19 pandemic. Lives were needlessly lost because of stands taken based on religious beliefs or a political ideology. Families, friends, and the community at large were impacted.
Over my years of practice, I have found that while these are difficult topics to address, they should not be avoided. Studies have shown that open acknowledgement of religious beliefs can affect both clinical outcomes and well-being. Religion and spirituality are as much a part of our patient’s lives as the physical parameters that we measure. To neglect these significant aspects is to miss the very essence of the individual.
I made it a practice to ask patients about their religious beliefs, the extent to which religion shaped their life, and whether they were part of a church community. Knowing this allowed me to separate deep personal belief from stances based on personal freedom, misinformation, conspiracies, and politics.
I found that information about political leanings flowed naturally in discussions with patients as we trusted and respected each other over time. If I approached politics objectively and nonjudgmentally, it generally led to meaningful conversation. This helped me to understand the patient as an individual and informed my diagnosis and treatment plan.
Politics as stress
For example, on more than one occasion, a patient with atrial fibrillation presented with persistent elevated blood pressure and pulse rate despite adherence to the medical regimen that I had prescribed. After a few minutes of discussion, it was clear that excessive attention to political commentary on TV and social media raised their anxiety and anger level, putting them at greater risk for adverse outcomes. I advised that they refocus their leisure activities rather than change or increase medication.
It is disappointing to see how one of the great scientific advances of our lifetime, vaccination science, has been tarnished because of political or religious ideology and to see the extent to which these beliefs influenced COVID-19 vaccination compliance. As health care providers, we must promote information based on the scientific method. If patients challenge us and point out that recommendations based on science seem to change over time, we must explain that science evolves on the basis of new information objectively gathered. We need to find out what information the patient has gotten from the Internet, TV, or conspiracy theories and counter this with scientific facts. If we do not discuss religion and politics with our patients along with other risk factors, we may compromise our ability to give them the best advice and treatment.
Our patients have a right to their own spiritual and political ideology. If it differs dramatically from our own, this should not influence our commitment to care for them. But we have an obligation to challenge unfounded beliefs about medicine and counter with scientific facts. There are times when individual freedoms must be secondary to public health. Ultimately, it is up to the patient to choose, but they should not be given a “free pass” on the basis of religion or politics. If I know something is true and I would do it myself or recommend it for my family, I have an obligation to provide this recommendation to my patients.
Religious preference is included in medical records. It is not appropriate to add political preference, but the patient benefits if a long-term caregiver knows this information.
During the pandemic, for the first time in my 40+ years of practice, some patients questioned my recommendations and placed equal or greater weight on religion, politics, or conspiracy theories. This continues to be a very real struggle.
Knowing and understanding our patients as individuals is critical to providing optimum care and that means tackling these formally taboo topics. If having a potentially uncomfortable conversation with patients allows us to save one life, it is worth it.
Dr. Francis is a cardiologist at Inova Heart and Vascular Institute, McLean, Va. He disclosed no relevant conflict of interest. A version of this article first appeared on Medscape.com.
From our first days as medical students, we are told that politics and religion are topics to be avoided with patients, but I disagree. Knowing more about our patients allows us to deliver better care.
Politics and religion: New risk factors
The importance of politics and religion in the health of patients was clearly demonstrated during the COVID-19 pandemic. Lives were needlessly lost because of stands taken based on religious beliefs or a political ideology. Families, friends, and the community at large were impacted.
Over my years of practice, I have found that while these are difficult topics to address, they should not be avoided. Studies have shown that open acknowledgement of religious beliefs can affect both clinical outcomes and well-being. Religion and spirituality are as much a part of our patient’s lives as the physical parameters that we measure. To neglect these significant aspects is to miss the very essence of the individual.
I made it a practice to ask patients about their religious beliefs, the extent to which religion shaped their life, and whether they were part of a church community. Knowing this allowed me to separate deep personal belief from stances based on personal freedom, misinformation, conspiracies, and politics.
I found that information about political leanings flowed naturally in discussions with patients as we trusted and respected each other over time. If I approached politics objectively and nonjudgmentally, it generally led to meaningful conversation. This helped me to understand the patient as an individual and informed my diagnosis and treatment plan.
Politics as stress
For example, on more than one occasion, a patient with atrial fibrillation presented with persistent elevated blood pressure and pulse rate despite adherence to the medical regimen that I had prescribed. After a few minutes of discussion, it was clear that excessive attention to political commentary on TV and social media raised their anxiety and anger level, putting them at greater risk for adverse outcomes. I advised that they refocus their leisure activities rather than change or increase medication.
It is disappointing to see how one of the great scientific advances of our lifetime, vaccination science, has been tarnished because of political or religious ideology and to see the extent to which these beliefs influenced COVID-19 vaccination compliance. As health care providers, we must promote information based on the scientific method. If patients challenge us and point out that recommendations based on science seem to change over time, we must explain that science evolves on the basis of new information objectively gathered. We need to find out what information the patient has gotten from the Internet, TV, or conspiracy theories and counter this with scientific facts. If we do not discuss religion and politics with our patients along with other risk factors, we may compromise our ability to give them the best advice and treatment.
Our patients have a right to their own spiritual and political ideology. If it differs dramatically from our own, this should not influence our commitment to care for them. But we have an obligation to challenge unfounded beliefs about medicine and counter with scientific facts. There are times when individual freedoms must be secondary to public health. Ultimately, it is up to the patient to choose, but they should not be given a “free pass” on the basis of religion or politics. If I know something is true and I would do it myself or recommend it for my family, I have an obligation to provide this recommendation to my patients.
Religious preference is included in medical records. It is not appropriate to add political preference, but the patient benefits if a long-term caregiver knows this information.
During the pandemic, for the first time in my 40+ years of practice, some patients questioned my recommendations and placed equal or greater weight on religion, politics, or conspiracy theories. This continues to be a very real struggle.
Knowing and understanding our patients as individuals is critical to providing optimum care and that means tackling these formally taboo topics. If having a potentially uncomfortable conversation with patients allows us to save one life, it is worth it.
Dr. Francis is a cardiologist at Inova Heart and Vascular Institute, McLean, Va. He disclosed no relevant conflict of interest. A version of this article first appeared on Medscape.com.
No such thing as an easy fix
Recently an article crossed my screen that drinking 4 cups of tea per day lowered the risk of type 2 diabetes by 17%. As these thing always seem to, it ended with a variant of “further research is needed.”
Encouraging? Sure. Definite? Nope.
I’ve seen plenty of articles suggesting coffee and/or tea have health benefits, though specifically on what varies, from lifespan to lowering the risk of a chronic medical condition (in this case, type 2 diabetes).
There are always numerous variables that aren’t clear. What kind of tea? Decaf or regular? Hot or iced? When you say cup, what do you mean? A lot of people, including me, probably consider anything smaller that a Starbucks grande to be for wimps.
While I can’t think of any off the top of my head, there’s probably a reasonable chance that, if I looked, I could find something that says coffee or tea are bad for you in some way, too.
Not that I’m planning on changing my already caffeinated drinking habits, which is probably the crux of these things for most of us. In a given day I have 1-2 cups of coffee and 3-4 bottles of diet green tea. Maybe 1-2 Diet Cokes in there some days. In winter more hot black tea. I’m probably a poster child for methylyxanthine toxicity.
I have no idea if all that coffee and tea are doing anything besides keeping me awake and alert for my patients. If they are, I certainly hope they’re lowering my risk of something bad.
Articles like this always get attention, and are often picked up by the general media. People love to think something so simple as drinking more tea or coffee would make a big difference in their lives. So it gets forwarded, people never read past the first paragraph or two, and don’t make it to the “further research is needed” line.
If an article ever came out refuting it, it probably wouldn’t get nearly as much press (who wants to read bad news?) and would be quickly forgotten outside of medical circles.
But the reality is that people are really looking for shortcuts. Unless you live under a rock, it’s pretty clear to both medical and lay people that such things as exercise and a healthy diet can help avoid multiple chronic health conditions. This doesn’t mean most of us, myself included, will do such faithfully. It just takes less time and effort to drink more tea than it does to go to the gym, so we want to believe.
That’s just human nature.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Recently an article crossed my screen that drinking 4 cups of tea per day lowered the risk of type 2 diabetes by 17%. As these thing always seem to, it ended with a variant of “further research is needed.”
Encouraging? Sure. Definite? Nope.
I’ve seen plenty of articles suggesting coffee and/or tea have health benefits, though specifically on what varies, from lifespan to lowering the risk of a chronic medical condition (in this case, type 2 diabetes).
There are always numerous variables that aren’t clear. What kind of tea? Decaf or regular? Hot or iced? When you say cup, what do you mean? A lot of people, including me, probably consider anything smaller that a Starbucks grande to be for wimps.
While I can’t think of any off the top of my head, there’s probably a reasonable chance that, if I looked, I could find something that says coffee or tea are bad for you in some way, too.
Not that I’m planning on changing my already caffeinated drinking habits, which is probably the crux of these things for most of us. In a given day I have 1-2 cups of coffee and 3-4 bottles of diet green tea. Maybe 1-2 Diet Cokes in there some days. In winter more hot black tea. I’m probably a poster child for methylyxanthine toxicity.
I have no idea if all that coffee and tea are doing anything besides keeping me awake and alert for my patients. If they are, I certainly hope they’re lowering my risk of something bad.
Articles like this always get attention, and are often picked up by the general media. People love to think something so simple as drinking more tea or coffee would make a big difference in their lives. So it gets forwarded, people never read past the first paragraph or two, and don’t make it to the “further research is needed” line.
If an article ever came out refuting it, it probably wouldn’t get nearly as much press (who wants to read bad news?) and would be quickly forgotten outside of medical circles.
But the reality is that people are really looking for shortcuts. Unless you live under a rock, it’s pretty clear to both medical and lay people that such things as exercise and a healthy diet can help avoid multiple chronic health conditions. This doesn’t mean most of us, myself included, will do such faithfully. It just takes less time and effort to drink more tea than it does to go to the gym, so we want to believe.
That’s just human nature.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Recently an article crossed my screen that drinking 4 cups of tea per day lowered the risk of type 2 diabetes by 17%. As these thing always seem to, it ended with a variant of “further research is needed.”
Encouraging? Sure. Definite? Nope.
I’ve seen plenty of articles suggesting coffee and/or tea have health benefits, though specifically on what varies, from lifespan to lowering the risk of a chronic medical condition (in this case, type 2 diabetes).
There are always numerous variables that aren’t clear. What kind of tea? Decaf or regular? Hot or iced? When you say cup, what do you mean? A lot of people, including me, probably consider anything smaller that a Starbucks grande to be for wimps.
While I can’t think of any off the top of my head, there’s probably a reasonable chance that, if I looked, I could find something that says coffee or tea are bad for you in some way, too.
Not that I’m planning on changing my already caffeinated drinking habits, which is probably the crux of these things for most of us. In a given day I have 1-2 cups of coffee and 3-4 bottles of diet green tea. Maybe 1-2 Diet Cokes in there some days. In winter more hot black tea. I’m probably a poster child for methylyxanthine toxicity.
I have no idea if all that coffee and tea are doing anything besides keeping me awake and alert for my patients. If they are, I certainly hope they’re lowering my risk of something bad.
Articles like this always get attention, and are often picked up by the general media. People love to think something so simple as drinking more tea or coffee would make a big difference in their lives. So it gets forwarded, people never read past the first paragraph or two, and don’t make it to the “further research is needed” line.
If an article ever came out refuting it, it probably wouldn’t get nearly as much press (who wants to read bad news?) and would be quickly forgotten outside of medical circles.
But the reality is that people are really looking for shortcuts. Unless you live under a rock, it’s pretty clear to both medical and lay people that such things as exercise and a healthy diet can help avoid multiple chronic health conditions. This doesn’t mean most of us, myself included, will do such faithfully. It just takes less time and effort to drink more tea than it does to go to the gym, so we want to believe.
That’s just human nature.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
How to make the best of your worst reviews
I have a love-hate relationship with patient reviews and satisfaction scores. I love good reviews and hate bad ones. Actually, I skim good reviews and then dwell for days on the negative ones, trying to rack my brain as to what I did wrong. Like everyone else, I have off days when I’m tired or distracted or just overwhelmed. Though I try to bring my A game to every patient visit, realistically, I know that I don’t always achieve this. But, for me, the difference in my best visits and good-enough visits is the difference between a 4-star and 5-star review. What’s up with those 1-star reviews?
Many, many years ago, when patient satisfaction scores were in their infancy, our clinic rewarded any physician who got a 100% satisfaction score. On the surface that makes perfect sense – of course, our patients should be satisfied 100% of the time, right? When I asked one of the winners of this competition how he did it (I never scored 100%), he told me, “I just do whatever the patient wants me to do.” Yikes, I thought at the time. That may be the recipe for an A+ for patient satisfaction but not for quality or outcomes.
Sometimes, I know that they are going to be unhappy, such as when I decline to refill their drug of abuse. Other times, I have to exercise my best medical judgment and hope that my explanation does not alienate the patient. After all, when I say “no” to a patient request, it is with their overall health and well-being in mind. But I would be lying if I said that I have matured to the point that I’m not bothered by a negative review or a patient choosing to take their care elsewhere.
Most of us seek and welcome feedback. Over time, I’ve learned to do this during the visit by asking “Am I giving you too much information?” or “What do you think of the plan?” or “What’s most important to you?” There are times when I conclude the visit and know that the patient is not satisfied but remain unable to ferret out where I let them down – even, on occasion, when I ask them directly. Ideally, any feedback we get from our patients, positive or negative, would be specific and actionable. It rarely is.
There is no doubt we have entered the era of consumer medicine. Everything from the physical appearance of our clinics to the response time to electronic messages is fair game in how patients judge us. As we all know, patients assume competence – they are not usually impressed by your training or quality outcomes because they already believe you are clinically competent (or arguably they’d never set foot in your office). Instead of judging us how we often judge ourselves, patients form opinions about us by how we enter the room, whether we sit or stand, how long they wait in the exam room before we come in, or whether they like the nurse with whom we work. So many subtle things – many of which are outside of our control.
I often struggle with staying on time. When I am invariably walking into the room late, I make a point of thanking patients for their patience. When I’m very late, I offer a more detailed, HIPAA-compliant explanation. What I wish my patients saw was that I am often accommodating a patient who arrives late for their appointment or who wants me to address every concern they’ve had for the past 5 years. While I aspire to not allow the patient’s perception of the visit to unduly influence how I handle the visit, it inevitably does. I do want to have patients who are happy with their experience.
One of my friends is enviously pragmatic in her view on patient experience. “I’m not their friend and they don’t have to like me.” She emphasizes the clinical care she is providing and does not allow patients who are upset with some aspect of the care to weigh heavy on her. It may be that specialists are more likely to enjoy the luxury of putting aside how patients feel about them personally. In primary care, the patient-physician relationship is so central to what we do that ignoring your “likability” has the potential to threaten your professional viability.
I conclude this blog much like I started it. My desire is to allow the negative reviews, particularly if they have nothing actionable in them, to roll off my back and to keep my focus on the clinical care that I am providing. In actuality, I care deeply about how my patients experience their visit with me and will likely continue to take my reviews to heart.
Dr. Frank is a family physician in Neenah, Wisc. She disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
I have a love-hate relationship with patient reviews and satisfaction scores. I love good reviews and hate bad ones. Actually, I skim good reviews and then dwell for days on the negative ones, trying to rack my brain as to what I did wrong. Like everyone else, I have off days when I’m tired or distracted or just overwhelmed. Though I try to bring my A game to every patient visit, realistically, I know that I don’t always achieve this. But, for me, the difference in my best visits and good-enough visits is the difference between a 4-star and 5-star review. What’s up with those 1-star reviews?
Many, many years ago, when patient satisfaction scores were in their infancy, our clinic rewarded any physician who got a 100% satisfaction score. On the surface that makes perfect sense – of course, our patients should be satisfied 100% of the time, right? When I asked one of the winners of this competition how he did it (I never scored 100%), he told me, “I just do whatever the patient wants me to do.” Yikes, I thought at the time. That may be the recipe for an A+ for patient satisfaction but not for quality or outcomes.
Sometimes, I know that they are going to be unhappy, such as when I decline to refill their drug of abuse. Other times, I have to exercise my best medical judgment and hope that my explanation does not alienate the patient. After all, when I say “no” to a patient request, it is with their overall health and well-being in mind. But I would be lying if I said that I have matured to the point that I’m not bothered by a negative review or a patient choosing to take their care elsewhere.
Most of us seek and welcome feedback. Over time, I’ve learned to do this during the visit by asking “Am I giving you too much information?” or “What do you think of the plan?” or “What’s most important to you?” There are times when I conclude the visit and know that the patient is not satisfied but remain unable to ferret out where I let them down – even, on occasion, when I ask them directly. Ideally, any feedback we get from our patients, positive or negative, would be specific and actionable. It rarely is.
There is no doubt we have entered the era of consumer medicine. Everything from the physical appearance of our clinics to the response time to electronic messages is fair game in how patients judge us. As we all know, patients assume competence – they are not usually impressed by your training or quality outcomes because they already believe you are clinically competent (or arguably they’d never set foot in your office). Instead of judging us how we often judge ourselves, patients form opinions about us by how we enter the room, whether we sit or stand, how long they wait in the exam room before we come in, or whether they like the nurse with whom we work. So many subtle things – many of which are outside of our control.
I often struggle with staying on time. When I am invariably walking into the room late, I make a point of thanking patients for their patience. When I’m very late, I offer a more detailed, HIPAA-compliant explanation. What I wish my patients saw was that I am often accommodating a patient who arrives late for their appointment or who wants me to address every concern they’ve had for the past 5 years. While I aspire to not allow the patient’s perception of the visit to unduly influence how I handle the visit, it inevitably does. I do want to have patients who are happy with their experience.
One of my friends is enviously pragmatic in her view on patient experience. “I’m not their friend and they don’t have to like me.” She emphasizes the clinical care she is providing and does not allow patients who are upset with some aspect of the care to weigh heavy on her. It may be that specialists are more likely to enjoy the luxury of putting aside how patients feel about them personally. In primary care, the patient-physician relationship is so central to what we do that ignoring your “likability” has the potential to threaten your professional viability.
I conclude this blog much like I started it. My desire is to allow the negative reviews, particularly if they have nothing actionable in them, to roll off my back and to keep my focus on the clinical care that I am providing. In actuality, I care deeply about how my patients experience their visit with me and will likely continue to take my reviews to heart.
Dr. Frank is a family physician in Neenah, Wisc. She disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
I have a love-hate relationship with patient reviews and satisfaction scores. I love good reviews and hate bad ones. Actually, I skim good reviews and then dwell for days on the negative ones, trying to rack my brain as to what I did wrong. Like everyone else, I have off days when I’m tired or distracted or just overwhelmed. Though I try to bring my A game to every patient visit, realistically, I know that I don’t always achieve this. But, for me, the difference in my best visits and good-enough visits is the difference between a 4-star and 5-star review. What’s up with those 1-star reviews?
Many, many years ago, when patient satisfaction scores were in their infancy, our clinic rewarded any physician who got a 100% satisfaction score. On the surface that makes perfect sense – of course, our patients should be satisfied 100% of the time, right? When I asked one of the winners of this competition how he did it (I never scored 100%), he told me, “I just do whatever the patient wants me to do.” Yikes, I thought at the time. That may be the recipe for an A+ for patient satisfaction but not for quality or outcomes.
Sometimes, I know that they are going to be unhappy, such as when I decline to refill their drug of abuse. Other times, I have to exercise my best medical judgment and hope that my explanation does not alienate the patient. After all, when I say “no” to a patient request, it is with their overall health and well-being in mind. But I would be lying if I said that I have matured to the point that I’m not bothered by a negative review or a patient choosing to take their care elsewhere.
Most of us seek and welcome feedback. Over time, I’ve learned to do this during the visit by asking “Am I giving you too much information?” or “What do you think of the plan?” or “What’s most important to you?” There are times when I conclude the visit and know that the patient is not satisfied but remain unable to ferret out where I let them down – even, on occasion, when I ask them directly. Ideally, any feedback we get from our patients, positive or negative, would be specific and actionable. It rarely is.
There is no doubt we have entered the era of consumer medicine. Everything from the physical appearance of our clinics to the response time to electronic messages is fair game in how patients judge us. As we all know, patients assume competence – they are not usually impressed by your training or quality outcomes because they already believe you are clinically competent (or arguably they’d never set foot in your office). Instead of judging us how we often judge ourselves, patients form opinions about us by how we enter the room, whether we sit or stand, how long they wait in the exam room before we come in, or whether they like the nurse with whom we work. So many subtle things – many of which are outside of our control.
I often struggle with staying on time. When I am invariably walking into the room late, I make a point of thanking patients for their patience. When I’m very late, I offer a more detailed, HIPAA-compliant explanation. What I wish my patients saw was that I am often accommodating a patient who arrives late for their appointment or who wants me to address every concern they’ve had for the past 5 years. While I aspire to not allow the patient’s perception of the visit to unduly influence how I handle the visit, it inevitably does. I do want to have patients who are happy with their experience.
One of my friends is enviously pragmatic in her view on patient experience. “I’m not their friend and they don’t have to like me.” She emphasizes the clinical care she is providing and does not allow patients who are upset with some aspect of the care to weigh heavy on her. It may be that specialists are more likely to enjoy the luxury of putting aside how patients feel about them personally. In primary care, the patient-physician relationship is so central to what we do that ignoring your “likability” has the potential to threaten your professional viability.
I conclude this blog much like I started it. My desire is to allow the negative reviews, particularly if they have nothing actionable in them, to roll off my back and to keep my focus on the clinical care that I am providing. In actuality, I care deeply about how my patients experience their visit with me and will likely continue to take my reviews to heart.
Dr. Frank is a family physician in Neenah, Wisc. She disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Is corporate telepsychiatry the solution to access to care problems?
When Sue W’s mother died in 2018, she struggled terribly. She was already seeing a psychotherapist and was taking duloxetine, prescribed by her primary care physician. But her grief was profound, and her depression became paralyzing. She needed to see a psychiatrist, and there were many available in or near her hometown, a Connecticut suburb of New York City, but neither Sue, her therapist, nor her primary care doctor could find a psychiatrist who participated with her insurance. Finally, she was given the name of a psychiatrist in Manhattan who practiced online, and she made an appointment on the Skypiatrist (a telepsychiatry group founded in 2016) website.
“I hesitated about it at first,” Sue said. “The doctor was nice, and I liked the convenience. Appointments were 15 minutes long, although the first session was longer. He focused on the medications, which was okay because I already have a therapist. And it was really easy. I made appointments on their website and I saw the doctor through the same site, and I really liked that I could send him messages.” The psychiatrist was responsive when Sue had trouble coming off duloxetine, and he gave her instructions for a slower taper. The treatment was affordable and accessible, and she got better.
When you also consider that many private-practice psychiatrists do not participate with insurance panels, online companies that do accept insurance may add value, convenience, and access.
Cerebral, the largest online psychiatric service in the country, began seeing patients in January 2020, offering medications and psychotherapy. They participate with a number of commercial insurers, and this varies by state, but not with Medicaid or Medicare. Patients pay a monthly fee, and an initial 30-minute medication evaluation session is conducted, often with a nurse practitioner. They advertise wait times of less than 7 days.
Another company, Done, offers treatment specifically for ADHD. They don’t accept insurance for appointments; patients must submit their own claims for reimbursement. Their pricing structure involves a fee of $199 for the first month, then $79 a month thereafter, which does not include medications. Hims – another online company – targets men with a variety of health issues, including mental health problems.
Some of these internet companies have been in the news recently for concerns related to quality of care and prescribing practices. A The Wall Street Journal article of March 26, 2022, quoted clinicians who had previously worked for Cerebral and Done who left because they felt pressured to see patients quickly and to prescribe stimulants. Not all of the prescribers were unhappy, however. Yina Cruz-Harris, a nurse practitioner at Done who has a doctorate in nursing practice, said that she manages 2,300 patients with ADHD for Done. Virtually all are on stimulants. She renews each patient’s monthly prescription from her New Jersey home, based mostly on online forms filled out by the patients. She’s fast, doing two renewals per minute, and Done pays her almost $10 per patient, working out to around $20,000 in monthly earnings.
In May, the Department of Justice began looking into Cerebral’s practices around controlled substances and more recently, Cerebral has been in the news for complaints from patients that they have been unable to reach their prescribers when problems arise. Some pharmacy chains have refused to fill prescriptions for controlled medications from online telehealth providers, and some online providers, including Cerebral, are no longer prescribing controlled substances. A front-page The Wall Street Journal article on Aug. 19, 2022, told the story of a man with a history of addiction who was prescribed stimulants after a brief appointment with a prescriber at Done. Family and friends in his sober house believe that the stimulants triggered a relapse, and he died of an opioid overdose.
During the early days of the pandemic, nonemergency psychiatric care was shut down and we all became virtual psychiatrists. Many of us saw new patients and prescribed controlled medications to people we had never met in real life.
“John Brown,” MD, PhD, spoke with me on the condition that I don’t use his real name or the name of the practice he left. He was hired by a traditional group practice with a multidisciplinary staff and several offices in his state. Most of the clinicians worked part time and were contractual employees, and Dr. Brown was hired to develop a specialty service. He soon learned that the practice – which participates with a number of insurance plans – was not financially stable, and it was acquired by an investment firm with no medical experience.
“They wanted everyone to work 40-hour weeks and see 14 patients a day, including 3-4 new patients, and suddenly everyone was overextended and exhausted. Overnight, most of the therapists left, and they hired nurse practitioners to replace many of the psychiatrists. People weren’t getting good care.” While this was not a telepsychiatry startup, it was a corporate takeover of a traditional practice that was unable to remain financially solvent while participating with insurance panels.
Like Sue W, Elizabeth K struggled to get treatment for ADHD even before the pandemic.
“I work multiple part-time jobs, don’t own a car, and don’t have insurance. Before telehealth became available, it was difficult and discouraging for me to maintain consistent treatment. It took me months to get initial appointments with a doctor and I live in one of the largest cities in the country.” She was pleased with the care she received by Done.
“I was pleasantly surprised by the authenticity and thoroughness of my first telehealth provider,” Elizabeth noted. “She remembered and considered more about me, my medical history, and details of my personal life than nearly every psychiatric doctor I’ve ever seen. They informed me of the long-term effects of medications and the importance of routine cardiovascular check-ups. Also, they wouldn’t prescribe more than 5 mg of Adderall (even though I had been prescribed 30-90 mg a day for most of my life) until I completed a medical check-up with blood pressure and blood test results.”
Corporate telepsychiatry may fill an important void and provide care to many people who have been unable to access traditional treatment. Something, however, has to account for the fact that care is more affordable through startups than through traditional psychiatric practices. Startups have expensive technological and infrastructure costs and added layers of administration. This translates to either higher volumes with shorter appointments, less compensation for prescribers, or both. How this will affect the future of psychiatric care remains to be seen.
Dr. Miller, is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
When Sue W’s mother died in 2018, she struggled terribly. She was already seeing a psychotherapist and was taking duloxetine, prescribed by her primary care physician. But her grief was profound, and her depression became paralyzing. She needed to see a psychiatrist, and there were many available in or near her hometown, a Connecticut suburb of New York City, but neither Sue, her therapist, nor her primary care doctor could find a psychiatrist who participated with her insurance. Finally, she was given the name of a psychiatrist in Manhattan who practiced online, and she made an appointment on the Skypiatrist (a telepsychiatry group founded in 2016) website.
“I hesitated about it at first,” Sue said. “The doctor was nice, and I liked the convenience. Appointments were 15 minutes long, although the first session was longer. He focused on the medications, which was okay because I already have a therapist. And it was really easy. I made appointments on their website and I saw the doctor through the same site, and I really liked that I could send him messages.” The psychiatrist was responsive when Sue had trouble coming off duloxetine, and he gave her instructions for a slower taper. The treatment was affordable and accessible, and she got better.
When you also consider that many private-practice psychiatrists do not participate with insurance panels, online companies that do accept insurance may add value, convenience, and access.
Cerebral, the largest online psychiatric service in the country, began seeing patients in January 2020, offering medications and psychotherapy. They participate with a number of commercial insurers, and this varies by state, but not with Medicaid or Medicare. Patients pay a monthly fee, and an initial 30-minute medication evaluation session is conducted, often with a nurse practitioner. They advertise wait times of less than 7 days.
Another company, Done, offers treatment specifically for ADHD. They don’t accept insurance for appointments; patients must submit their own claims for reimbursement. Their pricing structure involves a fee of $199 for the first month, then $79 a month thereafter, which does not include medications. Hims – another online company – targets men with a variety of health issues, including mental health problems.
Some of these internet companies have been in the news recently for concerns related to quality of care and prescribing practices. A The Wall Street Journal article of March 26, 2022, quoted clinicians who had previously worked for Cerebral and Done who left because they felt pressured to see patients quickly and to prescribe stimulants. Not all of the prescribers were unhappy, however. Yina Cruz-Harris, a nurse practitioner at Done who has a doctorate in nursing practice, said that she manages 2,300 patients with ADHD for Done. Virtually all are on stimulants. She renews each patient’s monthly prescription from her New Jersey home, based mostly on online forms filled out by the patients. She’s fast, doing two renewals per minute, and Done pays her almost $10 per patient, working out to around $20,000 in monthly earnings.
In May, the Department of Justice began looking into Cerebral’s practices around controlled substances and more recently, Cerebral has been in the news for complaints from patients that they have been unable to reach their prescribers when problems arise. Some pharmacy chains have refused to fill prescriptions for controlled medications from online telehealth providers, and some online providers, including Cerebral, are no longer prescribing controlled substances. A front-page The Wall Street Journal article on Aug. 19, 2022, told the story of a man with a history of addiction who was prescribed stimulants after a brief appointment with a prescriber at Done. Family and friends in his sober house believe that the stimulants triggered a relapse, and he died of an opioid overdose.
During the early days of the pandemic, nonemergency psychiatric care was shut down and we all became virtual psychiatrists. Many of us saw new patients and prescribed controlled medications to people we had never met in real life.
“John Brown,” MD, PhD, spoke with me on the condition that I don’t use his real name or the name of the practice he left. He was hired by a traditional group practice with a multidisciplinary staff and several offices in his state. Most of the clinicians worked part time and were contractual employees, and Dr. Brown was hired to develop a specialty service. He soon learned that the practice – which participates with a number of insurance plans – was not financially stable, and it was acquired by an investment firm with no medical experience.
“They wanted everyone to work 40-hour weeks and see 14 patients a day, including 3-4 new patients, and suddenly everyone was overextended and exhausted. Overnight, most of the therapists left, and they hired nurse practitioners to replace many of the psychiatrists. People weren’t getting good care.” While this was not a telepsychiatry startup, it was a corporate takeover of a traditional practice that was unable to remain financially solvent while participating with insurance panels.
Like Sue W, Elizabeth K struggled to get treatment for ADHD even before the pandemic.
“I work multiple part-time jobs, don’t own a car, and don’t have insurance. Before telehealth became available, it was difficult and discouraging for me to maintain consistent treatment. It took me months to get initial appointments with a doctor and I live in one of the largest cities in the country.” She was pleased with the care she received by Done.
“I was pleasantly surprised by the authenticity and thoroughness of my first telehealth provider,” Elizabeth noted. “She remembered and considered more about me, my medical history, and details of my personal life than nearly every psychiatric doctor I’ve ever seen. They informed me of the long-term effects of medications and the importance of routine cardiovascular check-ups. Also, they wouldn’t prescribe more than 5 mg of Adderall (even though I had been prescribed 30-90 mg a day for most of my life) until I completed a medical check-up with blood pressure and blood test results.”
Corporate telepsychiatry may fill an important void and provide care to many people who have been unable to access traditional treatment. Something, however, has to account for the fact that care is more affordable through startups than through traditional psychiatric practices. Startups have expensive technological and infrastructure costs and added layers of administration. This translates to either higher volumes with shorter appointments, less compensation for prescribers, or both. How this will affect the future of psychiatric care remains to be seen.
Dr. Miller, is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
When Sue W’s mother died in 2018, she struggled terribly. She was already seeing a psychotherapist and was taking duloxetine, prescribed by her primary care physician. But her grief was profound, and her depression became paralyzing. She needed to see a psychiatrist, and there were many available in or near her hometown, a Connecticut suburb of New York City, but neither Sue, her therapist, nor her primary care doctor could find a psychiatrist who participated with her insurance. Finally, she was given the name of a psychiatrist in Manhattan who practiced online, and she made an appointment on the Skypiatrist (a telepsychiatry group founded in 2016) website.
“I hesitated about it at first,” Sue said. “The doctor was nice, and I liked the convenience. Appointments were 15 minutes long, although the first session was longer. He focused on the medications, which was okay because I already have a therapist. And it was really easy. I made appointments on their website and I saw the doctor through the same site, and I really liked that I could send him messages.” The psychiatrist was responsive when Sue had trouble coming off duloxetine, and he gave her instructions for a slower taper. The treatment was affordable and accessible, and she got better.
When you also consider that many private-practice psychiatrists do not participate with insurance panels, online companies that do accept insurance may add value, convenience, and access.
Cerebral, the largest online psychiatric service in the country, began seeing patients in January 2020, offering medications and psychotherapy. They participate with a number of commercial insurers, and this varies by state, but not with Medicaid or Medicare. Patients pay a monthly fee, and an initial 30-minute medication evaluation session is conducted, often with a nurse practitioner. They advertise wait times of less than 7 days.
Another company, Done, offers treatment specifically for ADHD. They don’t accept insurance for appointments; patients must submit their own claims for reimbursement. Their pricing structure involves a fee of $199 for the first month, then $79 a month thereafter, which does not include medications. Hims – another online company – targets men with a variety of health issues, including mental health problems.
Some of these internet companies have been in the news recently for concerns related to quality of care and prescribing practices. A The Wall Street Journal article of March 26, 2022, quoted clinicians who had previously worked for Cerebral and Done who left because they felt pressured to see patients quickly and to prescribe stimulants. Not all of the prescribers were unhappy, however. Yina Cruz-Harris, a nurse practitioner at Done who has a doctorate in nursing practice, said that she manages 2,300 patients with ADHD for Done. Virtually all are on stimulants. She renews each patient’s monthly prescription from her New Jersey home, based mostly on online forms filled out by the patients. She’s fast, doing two renewals per minute, and Done pays her almost $10 per patient, working out to around $20,000 in monthly earnings.
In May, the Department of Justice began looking into Cerebral’s practices around controlled substances and more recently, Cerebral has been in the news for complaints from patients that they have been unable to reach their prescribers when problems arise. Some pharmacy chains have refused to fill prescriptions for controlled medications from online telehealth providers, and some online providers, including Cerebral, are no longer prescribing controlled substances. A front-page The Wall Street Journal article on Aug. 19, 2022, told the story of a man with a history of addiction who was prescribed stimulants after a brief appointment with a prescriber at Done. Family and friends in his sober house believe that the stimulants triggered a relapse, and he died of an opioid overdose.
During the early days of the pandemic, nonemergency psychiatric care was shut down and we all became virtual psychiatrists. Many of us saw new patients and prescribed controlled medications to people we had never met in real life.
“John Brown,” MD, PhD, spoke with me on the condition that I don’t use his real name or the name of the practice he left. He was hired by a traditional group practice with a multidisciplinary staff and several offices in his state. Most of the clinicians worked part time and were contractual employees, and Dr. Brown was hired to develop a specialty service. He soon learned that the practice – which participates with a number of insurance plans – was not financially stable, and it was acquired by an investment firm with no medical experience.
“They wanted everyone to work 40-hour weeks and see 14 patients a day, including 3-4 new patients, and suddenly everyone was overextended and exhausted. Overnight, most of the therapists left, and they hired nurse practitioners to replace many of the psychiatrists. People weren’t getting good care.” While this was not a telepsychiatry startup, it was a corporate takeover of a traditional practice that was unable to remain financially solvent while participating with insurance panels.
Like Sue W, Elizabeth K struggled to get treatment for ADHD even before the pandemic.
“I work multiple part-time jobs, don’t own a car, and don’t have insurance. Before telehealth became available, it was difficult and discouraging for me to maintain consistent treatment. It took me months to get initial appointments with a doctor and I live in one of the largest cities in the country.” She was pleased with the care she received by Done.
“I was pleasantly surprised by the authenticity and thoroughness of my first telehealth provider,” Elizabeth noted. “She remembered and considered more about me, my medical history, and details of my personal life than nearly every psychiatric doctor I’ve ever seen. They informed me of the long-term effects of medications and the importance of routine cardiovascular check-ups. Also, they wouldn’t prescribe more than 5 mg of Adderall (even though I had been prescribed 30-90 mg a day for most of my life) until I completed a medical check-up with blood pressure and blood test results.”
Corporate telepsychiatry may fill an important void and provide care to many people who have been unable to access traditional treatment. Something, however, has to account for the fact that care is more affordable through startups than through traditional psychiatric practices. Startups have expensive technological and infrastructure costs and added layers of administration. This translates to either higher volumes with shorter appointments, less compensation for prescribers, or both. How this will affect the future of psychiatric care remains to be seen.
Dr. Miller, is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
A 10-year-old with a red bump on her lower lip
The patient’s history and examination are consistent with a diagnosis of pyogenic granuloma. Specifically, the history of rapid growth, friable nature, associated bleeding, and hemorrhagic crusting point to pyogenic granuloma as the most likely diagnosis.
Pyogenic granuloma is an acquired benign vascular growth of the skin or mucous membranes.1 It most frequently occurs in children and young adults and most commonly affects the skin of the head, trunk, and extremities.2 Common mucosal sites include the gingiva, lips, and tongue.2 The etiology of pyogenic granuloma is unknown, though it is thought to be a process akin to the overgrowth of granulation tissue.3,4 Expression of angiogenic factors and subsequent vascular hyperplasia are also implicated as key players in the pathogenesis of pyogenic granuloma.1,4 In addition, several associated factors and inciting triggers have been proposed including trauma, infections, and hormonal fluctuations.3-5 However, the majority of patients do not report predisposing factors or a history of prior trauma at the site.3,6
Clinically, pyogenic granuloma usually presents as a painless, erythematous, dome-shaped friable papule or nodule that easily bleeds and may ulcerate. It typically undergoes a period of growth over weeks to months followed by stabilization. Occasionally, pyogenic granulomas will spontaneously involute, though most do not.7 Pyogenic granuloma may occur within an existing capillary malformation, such as a port wine stain, spontaneously or as a sequela of laser treatment.8,9 Diagnosis of pyogenic granuloma can typically be made clinically on the basis of history and exam. Dermoscopic evaluation of pyogenic granuloma will reveal a homogeneous papule with a surrounding white-brown collarette, and potentially white intersecting lines.10 Histopathologic evaluation may be necessary to differentiate lesions from conditions that may mimic pyogenic granuloma.
What’s on the differential?
The differential diagnosis for pyogenic granuloma consists of Spitz nevus, cherry hemangioma, amelanotic melanoma, and glomus tumor.
Spitz nevus
Spitz nevus (spindle and epithelial cell nevus) is a benign melanocytic lesion that classically appears as a sharply circumscribed, smooth, dome-shaped, pink-red, or brown papule or plaque. There is typically a history of rapid growth over several months followed by stabilization. It usually presents in childhood or adolescence and is most commonly located on the face and extremities. While there are similarities in the appearance of Spitz nevi and pyogenic granuloma, Spitz nevi are not usually friable nor associated with bleeding as in our patient. Furthermore, on dermoscopy, Spitz nevus typically exhibits a starburst pattern with regularly distributed dotted vessels, or a peripheral globular pattern with reticular depigmentation. The definitive diagnosis of Spitz nevi relies on histopathologic evaluation, which is critical for discriminating Spitz nevi from melanoma.
Cherry hemangioma
Cherry angiomas are the most common type of acquired benign vascular proliferation. They present as small, bright red or violaceous macules or papules. However, they typically appear in early to midadulthood and increase in number with age. The age of our patient and solitary presentation of the lesion make this diagnosis unlikely. In addition, cherry angiomas are not usually associated with bleeding. It is important to note that, depending on the age of the patient, pyogenic granuloma may also be confused with infantile hemangioma. Infantile hemangiomas may become bright red papules, nodules, or plaques that appear in early infancy. They characteristically involute, which does not typically happen with pyogenic granuloma.
Amelanotic melanoma
Amelanotic melanoma is an uncommon variant of melanoma with little to no pigmentation. It may appear as a skin-colored to light-brown, pink, or red macule, papule, or nodule. The lesion may be asymmetric with irregular and well-defined borders. The variable and uncharacteristic appearance of this melanoma variant makes it diagnostically challenging and it is often confused with benign lesions including pyogenic granuloma. Dermoscopy can help distinguish amelanotic melanoma from other benign conditions, and will reveal areas of pink to white, polymorphous vessels and crystalline structures. However, ultimately biopsy and histopathological evaluation is necessary for accurate diagnosis.
Glomus tumor
Glomus tumors are rare, benign neoplasms originating from cells of the glomus body that presents as a red-purple, vascular papule or nodule. They are usually found in areas rich in glomus bodies, such as the subungual regions, fingertips, palms, wrists, and forearms. Glomus tumors are typically associated with tenderness, paroxysmal pain, and cold sensitivity. They do not bleed or ulcerate. While pyogenic granuloma may be confused for glomus tumor when present on the fingers or extremities, the location of the lesion in our patient is not consistent with a diagnosis of glomus tumor.
Management and disease course
Management with procedural or topical interventions is usually pursued for pyogenic granuloma because of frequent bleeding and ulceration of lesions. The most common approach is simple excision by a scoop or shave technique, with or without curettage and most commonly with electrocautery of the base. Other options include full-thickness excision, destruction with laser therapy, cryotherapy, or topical treatments (for example, timolol).11 Lesion recurrence can occur with both surgical and nonsurgical management.11 Regardless of management technique, it is useful to obtain histopathologic evaluation of tissue for accurate diagnosis.
Our patient underwent surgical destruction of her lower-lip lesion with shave excision followed by electrocautery. The surgical specimen was sent for pathology, which confirmed the diagnosis of pyogenic granuloma. The patient experienced no complications from the procedure and did not have recurrence of the lesion.
Ms. Sui is a research associate in the department of dermatology, division of pediatric and adolescent dermatology, University of California, San Diego, and Rady Children’s Hospital, San Diego. Dr. Eichenfield is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego, and Rady Children’s Hospital, San Diego. Neither Ms. Sui nor Dr. Eichenfield have any relevant financial disclosures.
References
1. Lin RL and Janniger CK. Cutis. 2004 Oct;74(4):229-33.
2. Harris MN et al. J Am Acad Dermatol. 2000 Jun;42(6):1012-6.
3. Pagliai KA and Cohen BA. Pediatr Dermatol. 2004 Jan-Feb;21(1):10-3.
4. Kamal R et al. J Oral Maxillofac Pathol. 2012 Jan;16(1):79-82.
5. Requena L and Sangueza OP. J Am Acad Dermatol. 1997 Dec;37(6):887-919.
6. Patrice SJ et al. Pediatr Dermatol. 1991 Dec;8(4):267-76.
7. Luba MC et al. Am Fam Physician. 2003 Feb 15;67(4):729-38.
8. Swerlick RA and Cooper PH. J Am Acad Dermatol. 1983 May;8(5):627-30.
9. Sheehan DJ and Lesher JL Jr. Cutis. 2004 Mar;73(3):175-80.
10. Zaballos P et al. Br J Dermatol. 2006 Jun;154(6):1108-11.
11. Lee J et al. J Plast Reconstr Aesthet Surg. 2011 Sep;64(9):1216-20. .
The patient’s history and examination are consistent with a diagnosis of pyogenic granuloma. Specifically, the history of rapid growth, friable nature, associated bleeding, and hemorrhagic crusting point to pyogenic granuloma as the most likely diagnosis.
Pyogenic granuloma is an acquired benign vascular growth of the skin or mucous membranes.1 It most frequently occurs in children and young adults and most commonly affects the skin of the head, trunk, and extremities.2 Common mucosal sites include the gingiva, lips, and tongue.2 The etiology of pyogenic granuloma is unknown, though it is thought to be a process akin to the overgrowth of granulation tissue.3,4 Expression of angiogenic factors and subsequent vascular hyperplasia are also implicated as key players in the pathogenesis of pyogenic granuloma.1,4 In addition, several associated factors and inciting triggers have been proposed including trauma, infections, and hormonal fluctuations.3-5 However, the majority of patients do not report predisposing factors or a history of prior trauma at the site.3,6
Clinically, pyogenic granuloma usually presents as a painless, erythematous, dome-shaped friable papule or nodule that easily bleeds and may ulcerate. It typically undergoes a period of growth over weeks to months followed by stabilization. Occasionally, pyogenic granulomas will spontaneously involute, though most do not.7 Pyogenic granuloma may occur within an existing capillary malformation, such as a port wine stain, spontaneously or as a sequela of laser treatment.8,9 Diagnosis of pyogenic granuloma can typically be made clinically on the basis of history and exam. Dermoscopic evaluation of pyogenic granuloma will reveal a homogeneous papule with a surrounding white-brown collarette, and potentially white intersecting lines.10 Histopathologic evaluation may be necessary to differentiate lesions from conditions that may mimic pyogenic granuloma.
What’s on the differential?
The differential diagnosis for pyogenic granuloma consists of Spitz nevus, cherry hemangioma, amelanotic melanoma, and glomus tumor.
Spitz nevus
Spitz nevus (spindle and epithelial cell nevus) is a benign melanocytic lesion that classically appears as a sharply circumscribed, smooth, dome-shaped, pink-red, or brown papule or plaque. There is typically a history of rapid growth over several months followed by stabilization. It usually presents in childhood or adolescence and is most commonly located on the face and extremities. While there are similarities in the appearance of Spitz nevi and pyogenic granuloma, Spitz nevi are not usually friable nor associated with bleeding as in our patient. Furthermore, on dermoscopy, Spitz nevus typically exhibits a starburst pattern with regularly distributed dotted vessels, or a peripheral globular pattern with reticular depigmentation. The definitive diagnosis of Spitz nevi relies on histopathologic evaluation, which is critical for discriminating Spitz nevi from melanoma.
Cherry hemangioma
Cherry angiomas are the most common type of acquired benign vascular proliferation. They present as small, bright red or violaceous macules or papules. However, they typically appear in early to midadulthood and increase in number with age. The age of our patient and solitary presentation of the lesion make this diagnosis unlikely. In addition, cherry angiomas are not usually associated with bleeding. It is important to note that, depending on the age of the patient, pyogenic granuloma may also be confused with infantile hemangioma. Infantile hemangiomas may become bright red papules, nodules, or plaques that appear in early infancy. They characteristically involute, which does not typically happen with pyogenic granuloma.
Amelanotic melanoma
Amelanotic melanoma is an uncommon variant of melanoma with little to no pigmentation. It may appear as a skin-colored to light-brown, pink, or red macule, papule, or nodule. The lesion may be asymmetric with irregular and well-defined borders. The variable and uncharacteristic appearance of this melanoma variant makes it diagnostically challenging and it is often confused with benign lesions including pyogenic granuloma. Dermoscopy can help distinguish amelanotic melanoma from other benign conditions, and will reveal areas of pink to white, polymorphous vessels and crystalline structures. However, ultimately biopsy and histopathological evaluation is necessary for accurate diagnosis.
Glomus tumor
Glomus tumors are rare, benign neoplasms originating from cells of the glomus body that presents as a red-purple, vascular papule or nodule. They are usually found in areas rich in glomus bodies, such as the subungual regions, fingertips, palms, wrists, and forearms. Glomus tumors are typically associated with tenderness, paroxysmal pain, and cold sensitivity. They do not bleed or ulcerate. While pyogenic granuloma may be confused for glomus tumor when present on the fingers or extremities, the location of the lesion in our patient is not consistent with a diagnosis of glomus tumor.
Management and disease course
Management with procedural or topical interventions is usually pursued for pyogenic granuloma because of frequent bleeding and ulceration of lesions. The most common approach is simple excision by a scoop or shave technique, with or without curettage and most commonly with electrocautery of the base. Other options include full-thickness excision, destruction with laser therapy, cryotherapy, or topical treatments (for example, timolol).11 Lesion recurrence can occur with both surgical and nonsurgical management.11 Regardless of management technique, it is useful to obtain histopathologic evaluation of tissue for accurate diagnosis.
Our patient underwent surgical destruction of her lower-lip lesion with shave excision followed by electrocautery. The surgical specimen was sent for pathology, which confirmed the diagnosis of pyogenic granuloma. The patient experienced no complications from the procedure and did not have recurrence of the lesion.
Ms. Sui is a research associate in the department of dermatology, division of pediatric and adolescent dermatology, University of California, San Diego, and Rady Children’s Hospital, San Diego. Dr. Eichenfield is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego, and Rady Children’s Hospital, San Diego. Neither Ms. Sui nor Dr. Eichenfield have any relevant financial disclosures.
References
1. Lin RL and Janniger CK. Cutis. 2004 Oct;74(4):229-33.
2. Harris MN et al. J Am Acad Dermatol. 2000 Jun;42(6):1012-6.
3. Pagliai KA and Cohen BA. Pediatr Dermatol. 2004 Jan-Feb;21(1):10-3.
4. Kamal R et al. J Oral Maxillofac Pathol. 2012 Jan;16(1):79-82.
5. Requena L and Sangueza OP. J Am Acad Dermatol. 1997 Dec;37(6):887-919.
6. Patrice SJ et al. Pediatr Dermatol. 1991 Dec;8(4):267-76.
7. Luba MC et al. Am Fam Physician. 2003 Feb 15;67(4):729-38.
8. Swerlick RA and Cooper PH. J Am Acad Dermatol. 1983 May;8(5):627-30.
9. Sheehan DJ and Lesher JL Jr. Cutis. 2004 Mar;73(3):175-80.
10. Zaballos P et al. Br J Dermatol. 2006 Jun;154(6):1108-11.
11. Lee J et al. J Plast Reconstr Aesthet Surg. 2011 Sep;64(9):1216-20. .
The patient’s history and examination are consistent with a diagnosis of pyogenic granuloma. Specifically, the history of rapid growth, friable nature, associated bleeding, and hemorrhagic crusting point to pyogenic granuloma as the most likely diagnosis.
Pyogenic granuloma is an acquired benign vascular growth of the skin or mucous membranes.1 It most frequently occurs in children and young adults and most commonly affects the skin of the head, trunk, and extremities.2 Common mucosal sites include the gingiva, lips, and tongue.2 The etiology of pyogenic granuloma is unknown, though it is thought to be a process akin to the overgrowth of granulation tissue.3,4 Expression of angiogenic factors and subsequent vascular hyperplasia are also implicated as key players in the pathogenesis of pyogenic granuloma.1,4 In addition, several associated factors and inciting triggers have been proposed including trauma, infections, and hormonal fluctuations.3-5 However, the majority of patients do not report predisposing factors or a history of prior trauma at the site.3,6
Clinically, pyogenic granuloma usually presents as a painless, erythematous, dome-shaped friable papule or nodule that easily bleeds and may ulcerate. It typically undergoes a period of growth over weeks to months followed by stabilization. Occasionally, pyogenic granulomas will spontaneously involute, though most do not.7 Pyogenic granuloma may occur within an existing capillary malformation, such as a port wine stain, spontaneously or as a sequela of laser treatment.8,9 Diagnosis of pyogenic granuloma can typically be made clinically on the basis of history and exam. Dermoscopic evaluation of pyogenic granuloma will reveal a homogeneous papule with a surrounding white-brown collarette, and potentially white intersecting lines.10 Histopathologic evaluation may be necessary to differentiate lesions from conditions that may mimic pyogenic granuloma.
What’s on the differential?
The differential diagnosis for pyogenic granuloma consists of Spitz nevus, cherry hemangioma, amelanotic melanoma, and glomus tumor.
Spitz nevus
Spitz nevus (spindle and epithelial cell nevus) is a benign melanocytic lesion that classically appears as a sharply circumscribed, smooth, dome-shaped, pink-red, or brown papule or plaque. There is typically a history of rapid growth over several months followed by stabilization. It usually presents in childhood or adolescence and is most commonly located on the face and extremities. While there are similarities in the appearance of Spitz nevi and pyogenic granuloma, Spitz nevi are not usually friable nor associated with bleeding as in our patient. Furthermore, on dermoscopy, Spitz nevus typically exhibits a starburst pattern with regularly distributed dotted vessels, or a peripheral globular pattern with reticular depigmentation. The definitive diagnosis of Spitz nevi relies on histopathologic evaluation, which is critical for discriminating Spitz nevi from melanoma.
Cherry hemangioma
Cherry angiomas are the most common type of acquired benign vascular proliferation. They present as small, bright red or violaceous macules or papules. However, they typically appear in early to midadulthood and increase in number with age. The age of our patient and solitary presentation of the lesion make this diagnosis unlikely. In addition, cherry angiomas are not usually associated with bleeding. It is important to note that, depending on the age of the patient, pyogenic granuloma may also be confused with infantile hemangioma. Infantile hemangiomas may become bright red papules, nodules, or plaques that appear in early infancy. They characteristically involute, which does not typically happen with pyogenic granuloma.
Amelanotic melanoma
Amelanotic melanoma is an uncommon variant of melanoma with little to no pigmentation. It may appear as a skin-colored to light-brown, pink, or red macule, papule, or nodule. The lesion may be asymmetric with irregular and well-defined borders. The variable and uncharacteristic appearance of this melanoma variant makes it diagnostically challenging and it is often confused with benign lesions including pyogenic granuloma. Dermoscopy can help distinguish amelanotic melanoma from other benign conditions, and will reveal areas of pink to white, polymorphous vessels and crystalline structures. However, ultimately biopsy and histopathological evaluation is necessary for accurate diagnosis.
Glomus tumor
Glomus tumors are rare, benign neoplasms originating from cells of the glomus body that presents as a red-purple, vascular papule or nodule. They are usually found in areas rich in glomus bodies, such as the subungual regions, fingertips, palms, wrists, and forearms. Glomus tumors are typically associated with tenderness, paroxysmal pain, and cold sensitivity. They do not bleed or ulcerate. While pyogenic granuloma may be confused for glomus tumor when present on the fingers or extremities, the location of the lesion in our patient is not consistent with a diagnosis of glomus tumor.
Management and disease course
Management with procedural or topical interventions is usually pursued for pyogenic granuloma because of frequent bleeding and ulceration of lesions. The most common approach is simple excision by a scoop or shave technique, with or without curettage and most commonly with electrocautery of the base. Other options include full-thickness excision, destruction with laser therapy, cryotherapy, or topical treatments (for example, timolol).11 Lesion recurrence can occur with both surgical and nonsurgical management.11 Regardless of management technique, it is useful to obtain histopathologic evaluation of tissue for accurate diagnosis.
Our patient underwent surgical destruction of her lower-lip lesion with shave excision followed by electrocautery. The surgical specimen was sent for pathology, which confirmed the diagnosis of pyogenic granuloma. The patient experienced no complications from the procedure and did not have recurrence of the lesion.
Ms. Sui is a research associate in the department of dermatology, division of pediatric and adolescent dermatology, University of California, San Diego, and Rady Children’s Hospital, San Diego. Dr. Eichenfield is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego, and Rady Children’s Hospital, San Diego. Neither Ms. Sui nor Dr. Eichenfield have any relevant financial disclosures.
References
1. Lin RL and Janniger CK. Cutis. 2004 Oct;74(4):229-33.
2. Harris MN et al. J Am Acad Dermatol. 2000 Jun;42(6):1012-6.
3. Pagliai KA and Cohen BA. Pediatr Dermatol. 2004 Jan-Feb;21(1):10-3.
4. Kamal R et al. J Oral Maxillofac Pathol. 2012 Jan;16(1):79-82.
5. Requena L and Sangueza OP. J Am Acad Dermatol. 1997 Dec;37(6):887-919.
6. Patrice SJ et al. Pediatr Dermatol. 1991 Dec;8(4):267-76.
7. Luba MC et al. Am Fam Physician. 2003 Feb 15;67(4):729-38.
8. Swerlick RA and Cooper PH. J Am Acad Dermatol. 1983 May;8(5):627-30.
9. Sheehan DJ and Lesher JL Jr. Cutis. 2004 Mar;73(3):175-80.
10. Zaballos P et al. Br J Dermatol. 2006 Jun;154(6):1108-11.
11. Lee J et al. J Plast Reconstr Aesthet Surg. 2011 Sep;64(9):1216-20. .
Dignity
Queen Elizabeth is everywhere. She was even on the last slide of a presentation on COVID, monkeypox, and influenza vaccines given by our physician in charge of quality. This was odd. The presenter wasn’t English. The Queen had nothing to do with vaccines. Nor apparently would she have said even if she did have an opinion about them. But there we were, an audience of physicians and staff pausing for a moment of remembrance of her.
I’m not a Monarchist – except perhaps for the Kennedys. I grew up in New England. I don’t have an opinion on whether or not the British Crown should endure. But I do marvel at the astounding effect Queen Elizabeth’s passing had on so many around the world. Her personal qualities, particularly her steadiness and humane sympathy, might explain why so many are sad hearing the news. But also I think there was something in her role that we all wished for: Not the owning of palaces and sceptres, but rather, the respect that was given to her.
She was a stateswoman of “unmatched dignity,” the White House wrote. That was true, but it seems being the Queen might have been the last job on earth where such dignity is still possible. Certainly in politics, education, and even health care, there doesn’t seem to be much left lately.
The same day of that presentation I walked into the room of a patient 22 minutes late, she held her arm forth tapping her watch to indicate the time and my tardiness. Unnecessary, if not impertinent. Covering for one of my female physician colleagues, I read an email from a patient which began, “Dear Julie, With all due respect …” Another patient submitted a photo for us to review that was clearly taken from her car while waiting at a stop light. Hardly the consideration a clinical encounter should be given.
Much has been lost for patients. too. There are patients trying to make appointments lately who are told: “There are none. Call back later.” . There is no dignified way to remove exam paper stuck to your backside before introducing yourself to the doctor. Maybe that last slide of Her Majesty was in fact for us to have a moment of silence for what we’ve all lost.
Walter Bagehot (pronounce it “Baj-et” if you tell this story to your Harlan wine friends) was a political writer and editor of The Economist in the 1860s. He famously said that the secret to the English government was having two kinds of institutions, the dignified and the efficient. The efficient, Parliament, was responsible for all the work. The dignified, the Crown, gives significance and holds everyone’s respect. If medicine ever once was both dignified and efficient, we aren’t lately. We push to reduce backlogs, offer same-time virtual care, work to reduce costs. We’ve driven medicine to the efficient and left little of the dignity it seems.
The Queen will be remembered for her lifelong dedication to the laborious service of others. Even though each of us in medicine pledges the same, we also mourn this week the loss of dignity that once came with it.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Queen Elizabeth is everywhere. She was even on the last slide of a presentation on COVID, monkeypox, and influenza vaccines given by our physician in charge of quality. This was odd. The presenter wasn’t English. The Queen had nothing to do with vaccines. Nor apparently would she have said even if she did have an opinion about them. But there we were, an audience of physicians and staff pausing for a moment of remembrance of her.
I’m not a Monarchist – except perhaps for the Kennedys. I grew up in New England. I don’t have an opinion on whether or not the British Crown should endure. But I do marvel at the astounding effect Queen Elizabeth’s passing had on so many around the world. Her personal qualities, particularly her steadiness and humane sympathy, might explain why so many are sad hearing the news. But also I think there was something in her role that we all wished for: Not the owning of palaces and sceptres, but rather, the respect that was given to her.
She was a stateswoman of “unmatched dignity,” the White House wrote. That was true, but it seems being the Queen might have been the last job on earth where such dignity is still possible. Certainly in politics, education, and even health care, there doesn’t seem to be much left lately.
The same day of that presentation I walked into the room of a patient 22 minutes late, she held her arm forth tapping her watch to indicate the time and my tardiness. Unnecessary, if not impertinent. Covering for one of my female physician colleagues, I read an email from a patient which began, “Dear Julie, With all due respect …” Another patient submitted a photo for us to review that was clearly taken from her car while waiting at a stop light. Hardly the consideration a clinical encounter should be given.
Much has been lost for patients. too. There are patients trying to make appointments lately who are told: “There are none. Call back later.” . There is no dignified way to remove exam paper stuck to your backside before introducing yourself to the doctor. Maybe that last slide of Her Majesty was in fact for us to have a moment of silence for what we’ve all lost.
Walter Bagehot (pronounce it “Baj-et” if you tell this story to your Harlan wine friends) was a political writer and editor of The Economist in the 1860s. He famously said that the secret to the English government was having two kinds of institutions, the dignified and the efficient. The efficient, Parliament, was responsible for all the work. The dignified, the Crown, gives significance and holds everyone’s respect. If medicine ever once was both dignified and efficient, we aren’t lately. We push to reduce backlogs, offer same-time virtual care, work to reduce costs. We’ve driven medicine to the efficient and left little of the dignity it seems.
The Queen will be remembered for her lifelong dedication to the laborious service of others. Even though each of us in medicine pledges the same, we also mourn this week the loss of dignity that once came with it.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Queen Elizabeth is everywhere. She was even on the last slide of a presentation on COVID, monkeypox, and influenza vaccines given by our physician in charge of quality. This was odd. The presenter wasn’t English. The Queen had nothing to do with vaccines. Nor apparently would she have said even if she did have an opinion about them. But there we were, an audience of physicians and staff pausing for a moment of remembrance of her.
I’m not a Monarchist – except perhaps for the Kennedys. I grew up in New England. I don’t have an opinion on whether or not the British Crown should endure. But I do marvel at the astounding effect Queen Elizabeth’s passing had on so many around the world. Her personal qualities, particularly her steadiness and humane sympathy, might explain why so many are sad hearing the news. But also I think there was something in her role that we all wished for: Not the owning of palaces and sceptres, but rather, the respect that was given to her.
She was a stateswoman of “unmatched dignity,” the White House wrote. That was true, but it seems being the Queen might have been the last job on earth where such dignity is still possible. Certainly in politics, education, and even health care, there doesn’t seem to be much left lately.
The same day of that presentation I walked into the room of a patient 22 minutes late, she held her arm forth tapping her watch to indicate the time and my tardiness. Unnecessary, if not impertinent. Covering for one of my female physician colleagues, I read an email from a patient which began, “Dear Julie, With all due respect …” Another patient submitted a photo for us to review that was clearly taken from her car while waiting at a stop light. Hardly the consideration a clinical encounter should be given.
Much has been lost for patients. too. There are patients trying to make appointments lately who are told: “There are none. Call back later.” . There is no dignified way to remove exam paper stuck to your backside before introducing yourself to the doctor. Maybe that last slide of Her Majesty was in fact for us to have a moment of silence for what we’ve all lost.
Walter Bagehot (pronounce it “Baj-et” if you tell this story to your Harlan wine friends) was a political writer and editor of The Economist in the 1860s. He famously said that the secret to the English government was having two kinds of institutions, the dignified and the efficient. The efficient, Parliament, was responsible for all the work. The dignified, the Crown, gives significance and holds everyone’s respect. If medicine ever once was both dignified and efficient, we aren’t lately. We push to reduce backlogs, offer same-time virtual care, work to reduce costs. We’ve driven medicine to the efficient and left little of the dignity it seems.
The Queen will be remembered for her lifelong dedication to the laborious service of others. Even though each of us in medicine pledges the same, we also mourn this week the loss of dignity that once came with it.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Me, my spouse, and COVID
Managing family conflict and cohesion
I watched you in the garage, with your wipes and your mask, your gloves and bottles of sprays and potions. I admired your fealty to CNN’s Dr. Sanjay Gupta as he demonstrated the proper technique for disinfecting groceries. I watched sterile protocol being broken and quietly closed the garage door.
I listened to your descriptions of the agility of the virus with each exhalation of breath, and how far the virus could travel with a tailwind and in cold dry air. I listen as closely and with the same intention as I listen to my yoga teacher’s explication of the benefits of attention to the breath.
Relatives and friends came prepared to be entertained outdoors. Even masked, you eschewed the world. Your version of science clashes with my laissez-faire attitude. We blow up as a couple. Then we settle down and learn how to cope with the stress, as a team, together.
The COVID factor
In the first few months of any stressor, family and couple functioning must reorganize to manage well.
During lockdown, social scientists accessed an eager public ready to participate in their studies. With nowhere to go, many people, especially women, completed online COVID surveys. Community-based tools such as the Centers for Disease Control and Prevention’s Social Vulnerability Index identified populations of high social vulnerability (as caused by external stresses on human health, such as unemployment, overcrowding, presence of an individual with caregiving needs, and low educational attainment). It is assumed that such populations will experience more stress and have more difficulty coping and adjusting.
In a study by a team at the University of Miami, social vulnerability was associated with more disrupted family functioning, except when households with children (n = 2,666) were compared to households without children (n = 1,456).1 What allowed these families with children to enjoy better functioning?
Looking more closely at the Miami study, what can we find? It is a large survey study (n = 4,122), disseminated through professional networks and social media via purchased Facebook and Instagram ads. Data were logged in REDCap, and participants had the option of taking the survey in English or Spanish. Most participants were female (93.5%), 55.7% responded in English, and 44.3% in Spanish. There were few differences between the women who had and did not have children, in terms of their age, employment status, and education level. The number of children in the household did not affect the results.
This study used a new tool called the COVID-19 Household Environment Scale. This tool has 25 items measuring individual and household characteristics, and associated COVID-19 stressors. This tool also includes two family functioning measures: conflict and cohesion, asking the respondent to reflect on the change in “conflict” or “togetherness,” as it relates to household experiences and activities, compared with the period before social distancing.
The surprising finding was that even though households with children reported more conflict than before the start of the pandemic, they also reported more cohesion. This syncs with my experience. My niece and nephew found that having their teenage children at home brought them closer as a family, cut down on some of the extracurricular activities they did not support, and generally “slowed the world down.”
However, in a study in Germany, survey respondents (n = 1,042) noted that having children up to 17 years old was associated with decreases in satisfaction with family life, although this was not related to changes in family demands. The study assessed changes over 6 months and underscores the fact that perceptions of family demands and family well-being are independent of each other.2
These findings also resonate with prior research that measured burden and reward in couples. High burden is not associated with low reward; these two constructs are independent of each other.3
What about couples?
It is no surprise that poor relationships begat poor coping. In an online Belgian survey of 1,491 cohabiting couples during the shutdown, both men and women felt significantly more stress than before, because they felt restricted in their relationship.4
However, only women reported significantly more stress during the lockdown than before, because of relationship conflicts, such as feeling neglected by their partner. These feelings had predated lockdown.
In another lockdown online survey of 782 U.S. adults (89.8% White, 84.5% female), cohabitating intimate partners reported that there were higher thoughts of separation if the participants were younger, or if there was higher verbal aggression, higher relationship invalidation, and lower relationship satisfaction. Higher relationship satisfaction was reported when there was lower money stress, higher sexual fulfillment, lower relationship invalidation, and higher perceived fairness of relationship power. High relationship satisfaction was also reported where there were no children in the home.5
It should be noted that none of these relationship variables was measured in the Miami study discussed above, and this study did not measure perceived conflict or perceived cohesion, so we know less about these aspects of the family unit.
What about teens?
The COVID-19 lockdown had a positive effect on the dynamics in some families, according to a naturalistic study of adolescents (n = 155) who completed surveys at two time periods (initial and 8 weeks).6
These adolescents reported a reduction in perceived psychological control by their mothers, and no change in autonomy support. The changes did not vary according to gender or the mother’s employment situation. The decrease in psychological control was greater with higher initial levels of satisfaction with the mother, and lower levels of the teens disobeying their parents.
What about hospital settings?
The worst of the COVID experience was in the hospital. The pain was displayed on the faces of the staff as they labored to figure out how to care for the dying patients who had no contact with their families. Hospitals, out of fear of contamination and viral dissemination, excluded visitors. In those early days of uncertainty, the stress among staff, patients, and family members was high.
In response to family members feeling disconnected from the health care team and the psychological and moral distress of the staff, Nadine J. Kaslow and colleagues revised policies and procedures at Emory University, Atlanta, facilities to reprioritize patient- and family-centered care.7
The guiding principles focus on providing safe yet compassionate and ethical care, balancing community health and the mitigation of viral transmission, while appreciating family members as essential partners in care; fostering communication between patients and their families; and promoting interactions and decision-making among health care providers, patients, and families.
COVID continues to intrude in many of our lives. Many people are mourning family members and friends who died after contracting the disease. Many people choose to ignore their risk and live their lives as before. Many people, like my spouse and me, continue to debate the merits of venturing into public spaces. Personally, COVID has given me time to read many more books than I could ever have imagined and allowed my spouse to explore the delicate nuances of cooking.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alisonheru@gmail.com.
References
1. Chavez JV et al. Assessing the impact of COVID-19 social distancing and social vulnerability on family functioning in an international sample of households with and without children. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 233-48. doi: 10.1037/cfp0000166.
2. Rudolph CW, Zacher H. Family demands and satisfaction with family life during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 249-59. doi: 10.1037/cfp0000170.
3. Heru AM et al. Family functioning in the caregivers of patients with dementia. Int J Geriatr Psychiatry. 2004 Jun;19(6):533-7. doi: 10.1002/gps.1119.
4. Schokkenbroek JM et al. Partners in lockdown: Relationship stress in men and women during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 149-57. doi: 10.1037/cfp0000172.
5. Eubanks Fleming CJ, Franzese AT. Should I stay or should I go? Evaluating intimate relationship outcomes during the 2020 pandemic shutdown. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 158-67. doi: 10.1037/cfp0000169.
6. Bacikova-Sleskova M,et al. Did perceived parenting in adolescence change as a result of the COVID-19 lockdown? A natural experiment. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 271-80. doi: 10.1037/cfp0000167.
7. Kaslow NJ et al. A roadmap for patient- and family-centered care during the pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 223-32. doi: 10.1037/cfp0000176.
Managing family conflict and cohesion
Managing family conflict and cohesion
I watched you in the garage, with your wipes and your mask, your gloves and bottles of sprays and potions. I admired your fealty to CNN’s Dr. Sanjay Gupta as he demonstrated the proper technique for disinfecting groceries. I watched sterile protocol being broken and quietly closed the garage door.
I listened to your descriptions of the agility of the virus with each exhalation of breath, and how far the virus could travel with a tailwind and in cold dry air. I listen as closely and with the same intention as I listen to my yoga teacher’s explication of the benefits of attention to the breath.
Relatives and friends came prepared to be entertained outdoors. Even masked, you eschewed the world. Your version of science clashes with my laissez-faire attitude. We blow up as a couple. Then we settle down and learn how to cope with the stress, as a team, together.
The COVID factor
In the first few months of any stressor, family and couple functioning must reorganize to manage well.
During lockdown, social scientists accessed an eager public ready to participate in their studies. With nowhere to go, many people, especially women, completed online COVID surveys. Community-based tools such as the Centers for Disease Control and Prevention’s Social Vulnerability Index identified populations of high social vulnerability (as caused by external stresses on human health, such as unemployment, overcrowding, presence of an individual with caregiving needs, and low educational attainment). It is assumed that such populations will experience more stress and have more difficulty coping and adjusting.
In a study by a team at the University of Miami, social vulnerability was associated with more disrupted family functioning, except when households with children (n = 2,666) were compared to households without children (n = 1,456).1 What allowed these families with children to enjoy better functioning?
Looking more closely at the Miami study, what can we find? It is a large survey study (n = 4,122), disseminated through professional networks and social media via purchased Facebook and Instagram ads. Data were logged in REDCap, and participants had the option of taking the survey in English or Spanish. Most participants were female (93.5%), 55.7% responded in English, and 44.3% in Spanish. There were few differences between the women who had and did not have children, in terms of their age, employment status, and education level. The number of children in the household did not affect the results.
This study used a new tool called the COVID-19 Household Environment Scale. This tool has 25 items measuring individual and household characteristics, and associated COVID-19 stressors. This tool also includes two family functioning measures: conflict and cohesion, asking the respondent to reflect on the change in “conflict” or “togetherness,” as it relates to household experiences and activities, compared with the period before social distancing.
The surprising finding was that even though households with children reported more conflict than before the start of the pandemic, they also reported more cohesion. This syncs with my experience. My niece and nephew found that having their teenage children at home brought them closer as a family, cut down on some of the extracurricular activities they did not support, and generally “slowed the world down.”
However, in a study in Germany, survey respondents (n = 1,042) noted that having children up to 17 years old was associated with decreases in satisfaction with family life, although this was not related to changes in family demands. The study assessed changes over 6 months and underscores the fact that perceptions of family demands and family well-being are independent of each other.2
These findings also resonate with prior research that measured burden and reward in couples. High burden is not associated with low reward; these two constructs are independent of each other.3
What about couples?
It is no surprise that poor relationships begat poor coping. In an online Belgian survey of 1,491 cohabiting couples during the shutdown, both men and women felt significantly more stress than before, because they felt restricted in their relationship.4
However, only women reported significantly more stress during the lockdown than before, because of relationship conflicts, such as feeling neglected by their partner. These feelings had predated lockdown.
In another lockdown online survey of 782 U.S. adults (89.8% White, 84.5% female), cohabitating intimate partners reported that there were higher thoughts of separation if the participants were younger, or if there was higher verbal aggression, higher relationship invalidation, and lower relationship satisfaction. Higher relationship satisfaction was reported when there was lower money stress, higher sexual fulfillment, lower relationship invalidation, and higher perceived fairness of relationship power. High relationship satisfaction was also reported where there were no children in the home.5
It should be noted that none of these relationship variables was measured in the Miami study discussed above, and this study did not measure perceived conflict or perceived cohesion, so we know less about these aspects of the family unit.
What about teens?
The COVID-19 lockdown had a positive effect on the dynamics in some families, according to a naturalistic study of adolescents (n = 155) who completed surveys at two time periods (initial and 8 weeks).6
These adolescents reported a reduction in perceived psychological control by their mothers, and no change in autonomy support. The changes did not vary according to gender or the mother’s employment situation. The decrease in psychological control was greater with higher initial levels of satisfaction with the mother, and lower levels of the teens disobeying their parents.
What about hospital settings?
The worst of the COVID experience was in the hospital. The pain was displayed on the faces of the staff as they labored to figure out how to care for the dying patients who had no contact with their families. Hospitals, out of fear of contamination and viral dissemination, excluded visitors. In those early days of uncertainty, the stress among staff, patients, and family members was high.
In response to family members feeling disconnected from the health care team and the psychological and moral distress of the staff, Nadine J. Kaslow and colleagues revised policies and procedures at Emory University, Atlanta, facilities to reprioritize patient- and family-centered care.7
The guiding principles focus on providing safe yet compassionate and ethical care, balancing community health and the mitigation of viral transmission, while appreciating family members as essential partners in care; fostering communication between patients and their families; and promoting interactions and decision-making among health care providers, patients, and families.
COVID continues to intrude in many of our lives. Many people are mourning family members and friends who died after contracting the disease. Many people choose to ignore their risk and live their lives as before. Many people, like my spouse and me, continue to debate the merits of venturing into public spaces. Personally, COVID has given me time to read many more books than I could ever have imagined and allowed my spouse to explore the delicate nuances of cooking.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alisonheru@gmail.com.
References
1. Chavez JV et al. Assessing the impact of COVID-19 social distancing and social vulnerability on family functioning in an international sample of households with and without children. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 233-48. doi: 10.1037/cfp0000166.
2. Rudolph CW, Zacher H. Family demands and satisfaction with family life during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 249-59. doi: 10.1037/cfp0000170.
3. Heru AM et al. Family functioning in the caregivers of patients with dementia. Int J Geriatr Psychiatry. 2004 Jun;19(6):533-7. doi: 10.1002/gps.1119.
4. Schokkenbroek JM et al. Partners in lockdown: Relationship stress in men and women during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 149-57. doi: 10.1037/cfp0000172.
5. Eubanks Fleming CJ, Franzese AT. Should I stay or should I go? Evaluating intimate relationship outcomes during the 2020 pandemic shutdown. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 158-67. doi: 10.1037/cfp0000169.
6. Bacikova-Sleskova M,et al. Did perceived parenting in adolescence change as a result of the COVID-19 lockdown? A natural experiment. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 271-80. doi: 10.1037/cfp0000167.
7. Kaslow NJ et al. A roadmap for patient- and family-centered care during the pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 223-32. doi: 10.1037/cfp0000176.
I watched you in the garage, with your wipes and your mask, your gloves and bottles of sprays and potions. I admired your fealty to CNN’s Dr. Sanjay Gupta as he demonstrated the proper technique for disinfecting groceries. I watched sterile protocol being broken and quietly closed the garage door.
I listened to your descriptions of the agility of the virus with each exhalation of breath, and how far the virus could travel with a tailwind and in cold dry air. I listen as closely and with the same intention as I listen to my yoga teacher’s explication of the benefits of attention to the breath.
Relatives and friends came prepared to be entertained outdoors. Even masked, you eschewed the world. Your version of science clashes with my laissez-faire attitude. We blow up as a couple. Then we settle down and learn how to cope with the stress, as a team, together.
The COVID factor
In the first few months of any stressor, family and couple functioning must reorganize to manage well.
During lockdown, social scientists accessed an eager public ready to participate in their studies. With nowhere to go, many people, especially women, completed online COVID surveys. Community-based tools such as the Centers for Disease Control and Prevention’s Social Vulnerability Index identified populations of high social vulnerability (as caused by external stresses on human health, such as unemployment, overcrowding, presence of an individual with caregiving needs, and low educational attainment). It is assumed that such populations will experience more stress and have more difficulty coping and adjusting.
In a study by a team at the University of Miami, social vulnerability was associated with more disrupted family functioning, except when households with children (n = 2,666) were compared to households without children (n = 1,456).1 What allowed these families with children to enjoy better functioning?
Looking more closely at the Miami study, what can we find? It is a large survey study (n = 4,122), disseminated through professional networks and social media via purchased Facebook and Instagram ads. Data were logged in REDCap, and participants had the option of taking the survey in English or Spanish. Most participants were female (93.5%), 55.7% responded in English, and 44.3% in Spanish. There were few differences between the women who had and did not have children, in terms of their age, employment status, and education level. The number of children in the household did not affect the results.
This study used a new tool called the COVID-19 Household Environment Scale. This tool has 25 items measuring individual and household characteristics, and associated COVID-19 stressors. This tool also includes two family functioning measures: conflict and cohesion, asking the respondent to reflect on the change in “conflict” or “togetherness,” as it relates to household experiences and activities, compared with the period before social distancing.
The surprising finding was that even though households with children reported more conflict than before the start of the pandemic, they also reported more cohesion. This syncs with my experience. My niece and nephew found that having their teenage children at home brought them closer as a family, cut down on some of the extracurricular activities they did not support, and generally “slowed the world down.”
However, in a study in Germany, survey respondents (n = 1,042) noted that having children up to 17 years old was associated with decreases in satisfaction with family life, although this was not related to changes in family demands. The study assessed changes over 6 months and underscores the fact that perceptions of family demands and family well-being are independent of each other.2
These findings also resonate with prior research that measured burden and reward in couples. High burden is not associated with low reward; these two constructs are independent of each other.3
What about couples?
It is no surprise that poor relationships begat poor coping. In an online Belgian survey of 1,491 cohabiting couples during the shutdown, both men and women felt significantly more stress than before, because they felt restricted in their relationship.4
However, only women reported significantly more stress during the lockdown than before, because of relationship conflicts, such as feeling neglected by their partner. These feelings had predated lockdown.
In another lockdown online survey of 782 U.S. adults (89.8% White, 84.5% female), cohabitating intimate partners reported that there were higher thoughts of separation if the participants were younger, or if there was higher verbal aggression, higher relationship invalidation, and lower relationship satisfaction. Higher relationship satisfaction was reported when there was lower money stress, higher sexual fulfillment, lower relationship invalidation, and higher perceived fairness of relationship power. High relationship satisfaction was also reported where there were no children in the home.5
It should be noted that none of these relationship variables was measured in the Miami study discussed above, and this study did not measure perceived conflict or perceived cohesion, so we know less about these aspects of the family unit.
What about teens?
The COVID-19 lockdown had a positive effect on the dynamics in some families, according to a naturalistic study of adolescents (n = 155) who completed surveys at two time periods (initial and 8 weeks).6
These adolescents reported a reduction in perceived psychological control by their mothers, and no change in autonomy support. The changes did not vary according to gender or the mother’s employment situation. The decrease in psychological control was greater with higher initial levels of satisfaction with the mother, and lower levels of the teens disobeying their parents.
What about hospital settings?
The worst of the COVID experience was in the hospital. The pain was displayed on the faces of the staff as they labored to figure out how to care for the dying patients who had no contact with their families. Hospitals, out of fear of contamination and viral dissemination, excluded visitors. In those early days of uncertainty, the stress among staff, patients, and family members was high.
In response to family members feeling disconnected from the health care team and the psychological and moral distress of the staff, Nadine J. Kaslow and colleagues revised policies and procedures at Emory University, Atlanta, facilities to reprioritize patient- and family-centered care.7
The guiding principles focus on providing safe yet compassionate and ethical care, balancing community health and the mitigation of viral transmission, while appreciating family members as essential partners in care; fostering communication between patients and their families; and promoting interactions and decision-making among health care providers, patients, and families.
COVID continues to intrude in many of our lives. Many people are mourning family members and friends who died after contracting the disease. Many people choose to ignore their risk and live their lives as before. Many people, like my spouse and me, continue to debate the merits of venturing into public spaces. Personally, COVID has given me time to read many more books than I could ever have imagined and allowed my spouse to explore the delicate nuances of cooking.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alisonheru@gmail.com.
References
1. Chavez JV et al. Assessing the impact of COVID-19 social distancing and social vulnerability on family functioning in an international sample of households with and without children. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 233-48. doi: 10.1037/cfp0000166.
2. Rudolph CW, Zacher H. Family demands and satisfaction with family life during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 249-59. doi: 10.1037/cfp0000170.
3. Heru AM et al. Family functioning in the caregivers of patients with dementia. Int J Geriatr Psychiatry. 2004 Jun;19(6):533-7. doi: 10.1002/gps.1119.
4. Schokkenbroek JM et al. Partners in lockdown: Relationship stress in men and women during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 149-57. doi: 10.1037/cfp0000172.
5. Eubanks Fleming CJ, Franzese AT. Should I stay or should I go? Evaluating intimate relationship outcomes during the 2020 pandemic shutdown. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 158-67. doi: 10.1037/cfp0000169.
6. Bacikova-Sleskova M,et al. Did perceived parenting in adolescence change as a result of the COVID-19 lockdown? A natural experiment. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 271-80. doi: 10.1037/cfp0000167.
7. Kaslow NJ et al. A roadmap for patient- and family-centered care during the pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 223-32. doi: 10.1037/cfp0000176.
A White male presented with a 1-month history of recurrent, widespread, painful sores
Coinfection of staphylococci and streptococci can make it more challenging to treat. Lesions typically begin as a vesicle that enlarges and forms an ulcer with a hemorrhagic crust. Even with treatment, the depth of the lesions may result in scarring. Shins and dorsal feet are nearly always involved. Systemic involvement is rare.
Open wounds, bites, or dermatoses are risk factors for the development of ecthyma. Additionally, poor hygiene and malnutrition play a major role in inoculation and severity of the disease. Poor hygiene may serve as the initiating factor for infection, but malnutrition permits further development because of the body’s inability to mount a sufficient immune response. Intravenous drug users and patients with HIV tend to be affected.
When diagnosing ecthyma, it is important to correlate clinical signs with a bacterial culture. This condition can be difficult to treat because of both coinfection and growing antibiotic resistance in staphylococcal and streptococcal species. Specifically, S. aureus has been found to be resistant to beta-lactam antibiotics for many years, with methicillin-resistant S. aureus (MRSA) being first detected in 1961. While a variety of antibiotics are indicated, the prescription should be tailored to cover the cultured organism.
Topical antibiotics are sufficient for more superficial lesions. Both topical and oral antibiotics may be recommended for ecthyma as the infection can spread more deeply into the skin, eventually causing a cellulitis. Treatment protocol for oral agents varies based on which drug is indicated. This patient was seen in the emergency room. His white blood cell count was elevated at 9 × 109/L. He was started empirically on amoxicillin/clavulanate (Augmentin) and ciprofloxacin. Bacterial cultures grew out Streptococcus pyogenes.
The case and photos were submitted by Lucas Shapiro, BS, Nova Southeastern University College of Osteopathic Medicine, Fort Lauderdale, Fla., and Susannah Berke, MD, Three Rivers Dermatology, Coraopolis, Pa. Dr. Bilu Martin edited the column. Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
1. Kwak Y et al. Infect Chemother. 2017 Dec;49(4):301-25.
2. Pereira LB. An Bras Dermatol. 2014 Mar-Apr;89(2):293-9.
3. Wasserzug O et al. Clin Infect Dis. 2009 May 1;48(9):1213-9.
Coinfection of staphylococci and streptococci can make it more challenging to treat. Lesions typically begin as a vesicle that enlarges and forms an ulcer with a hemorrhagic crust. Even with treatment, the depth of the lesions may result in scarring. Shins and dorsal feet are nearly always involved. Systemic involvement is rare.
Open wounds, bites, or dermatoses are risk factors for the development of ecthyma. Additionally, poor hygiene and malnutrition play a major role in inoculation and severity of the disease. Poor hygiene may serve as the initiating factor for infection, but malnutrition permits further development because of the body’s inability to mount a sufficient immune response. Intravenous drug users and patients with HIV tend to be affected.
When diagnosing ecthyma, it is important to correlate clinical signs with a bacterial culture. This condition can be difficult to treat because of both coinfection and growing antibiotic resistance in staphylococcal and streptococcal species. Specifically, S. aureus has been found to be resistant to beta-lactam antibiotics for many years, with methicillin-resistant S. aureus (MRSA) being first detected in 1961. While a variety of antibiotics are indicated, the prescription should be tailored to cover the cultured organism.
Topical antibiotics are sufficient for more superficial lesions. Both topical and oral antibiotics may be recommended for ecthyma as the infection can spread more deeply into the skin, eventually causing a cellulitis. Treatment protocol for oral agents varies based on which drug is indicated. This patient was seen in the emergency room. His white blood cell count was elevated at 9 × 109/L. He was started empirically on amoxicillin/clavulanate (Augmentin) and ciprofloxacin. Bacterial cultures grew out Streptococcus pyogenes.
The case and photos were submitted by Lucas Shapiro, BS, Nova Southeastern University College of Osteopathic Medicine, Fort Lauderdale, Fla., and Susannah Berke, MD, Three Rivers Dermatology, Coraopolis, Pa. Dr. Bilu Martin edited the column. Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
1. Kwak Y et al. Infect Chemother. 2017 Dec;49(4):301-25.
2. Pereira LB. An Bras Dermatol. 2014 Mar-Apr;89(2):293-9.
3. Wasserzug O et al. Clin Infect Dis. 2009 May 1;48(9):1213-9.
Coinfection of staphylococci and streptococci can make it more challenging to treat. Lesions typically begin as a vesicle that enlarges and forms an ulcer with a hemorrhagic crust. Even with treatment, the depth of the lesions may result in scarring. Shins and dorsal feet are nearly always involved. Systemic involvement is rare.
Open wounds, bites, or dermatoses are risk factors for the development of ecthyma. Additionally, poor hygiene and malnutrition play a major role in inoculation and severity of the disease. Poor hygiene may serve as the initiating factor for infection, but malnutrition permits further development because of the body’s inability to mount a sufficient immune response. Intravenous drug users and patients with HIV tend to be affected.
When diagnosing ecthyma, it is important to correlate clinical signs with a bacterial culture. This condition can be difficult to treat because of both coinfection and growing antibiotic resistance in staphylococcal and streptococcal species. Specifically, S. aureus has been found to be resistant to beta-lactam antibiotics for many years, with methicillin-resistant S. aureus (MRSA) being first detected in 1961. While a variety of antibiotics are indicated, the prescription should be tailored to cover the cultured organism.
Topical antibiotics are sufficient for more superficial lesions. Both topical and oral antibiotics may be recommended for ecthyma as the infection can spread more deeply into the skin, eventually causing a cellulitis. Treatment protocol for oral agents varies based on which drug is indicated. This patient was seen in the emergency room. His white blood cell count was elevated at 9 × 109/L. He was started empirically on amoxicillin/clavulanate (Augmentin) and ciprofloxacin. Bacterial cultures grew out Streptococcus pyogenes.
The case and photos were submitted by Lucas Shapiro, BS, Nova Southeastern University College of Osteopathic Medicine, Fort Lauderdale, Fla., and Susannah Berke, MD, Three Rivers Dermatology, Coraopolis, Pa. Dr. Bilu Martin edited the column. Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
1. Kwak Y et al. Infect Chemother. 2017 Dec;49(4):301-25.
2. Pereira LB. An Bras Dermatol. 2014 Mar-Apr;89(2):293-9.
3. Wasserzug O et al. Clin Infect Dis. 2009 May 1;48(9):1213-9.
















