User login
VIDEO: Hidradenitis suppurativa in pediatrics similar to that in adults
WASHINGTON– Hidradenitis suppurativa (HS) can present early in adolescence, and the approach to treatment in pediatric patients is similar to treatment in adults, “with a few caveats,” A. Yasmine Kirkorian, MD, said in a video interview at an educational session held by George Washington University.
While the literature often states that HS starts in a person’s 20s, it primarily starts in adolescence, sometimes earlier, with a presentation that is similar to that seen in adults and appearing at the same sites, such as the armpits and groin, said Dr. Kirkorian a pediatric dermatologist at Children’s National Health System and George Washington University, Washington.
“As dermatologists, we know this. Kids are getting this disease, but we need to characterize that better in the literature so that we can start to apply the adult style therapeutics in clinical trials ... to children,” she added.
In the interview, Dr. Kirkorian discussed treatment strategies, as well as familial cases of HS and the links between HS and Down syndrome and inflammatory bowel disease in children.
The meeting was sponsored by AbbVie. Dr. Kirkorian had no financial conflicts to disclose.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON– Hidradenitis suppurativa (HS) can present early in adolescence, and the approach to treatment in pediatric patients is similar to treatment in adults, “with a few caveats,” A. Yasmine Kirkorian, MD, said in a video interview at an educational session held by George Washington University.
While the literature often states that HS starts in a person’s 20s, it primarily starts in adolescence, sometimes earlier, with a presentation that is similar to that seen in adults and appearing at the same sites, such as the armpits and groin, said Dr. Kirkorian a pediatric dermatologist at Children’s National Health System and George Washington University, Washington.
“As dermatologists, we know this. Kids are getting this disease, but we need to characterize that better in the literature so that we can start to apply the adult style therapeutics in clinical trials ... to children,” she added.
In the interview, Dr. Kirkorian discussed treatment strategies, as well as familial cases of HS and the links between HS and Down syndrome and inflammatory bowel disease in children.
The meeting was sponsored by AbbVie. Dr. Kirkorian had no financial conflicts to disclose.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON– Hidradenitis suppurativa (HS) can present early in adolescence, and the approach to treatment in pediatric patients is similar to treatment in adults, “with a few caveats,” A. Yasmine Kirkorian, MD, said in a video interview at an educational session held by George Washington University.
While the literature often states that HS starts in a person’s 20s, it primarily starts in adolescence, sometimes earlier, with a presentation that is similar to that seen in adults and appearing at the same sites, such as the armpits and groin, said Dr. Kirkorian a pediatric dermatologist at Children’s National Health System and George Washington University, Washington.
“As dermatologists, we know this. Kids are getting this disease, but we need to characterize that better in the literature so that we can start to apply the adult style therapeutics in clinical trials ... to children,” she added.
In the interview, Dr. Kirkorian discussed treatment strategies, as well as familial cases of HS and the links between HS and Down syndrome and inflammatory bowel disease in children.
The meeting was sponsored by AbbVie. Dr. Kirkorian had no financial conflicts to disclose.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
After the epidemic, Ebola’s destructive power still haunts survivors
VIENNA – The Ebola crisis may be over in Sierra Leone, but the suffering is not.
The last patient from the epidemic was discharged in February 2016, but 78% of survivors now appear to have one or more sequelae of the infection. Some problems are mild, but some are so debilitating that life may never be the same.
Janet Scott, MD, of the University of Liverpool (England), heads a task force studying Ebola’s lingering aftereffects. These fall into four categories, Dr. Scott said at the European Society of Clinical Microbiology and Infectious Diseases annual congress: musculoskeletal pain, headache, eye problems, and psychological disorders.
They add up to an enormous risk of disability – survivors are more than 200 times more likely than controls to express at least moderate disability.
Dr. Scott and her team of researchers are partnering with clinicians and data managers in the Ebola treatment unit in the 34th Regimental Military Hospital (MH34) in Freetown, Sierra Leone. In Sierra Leone alone, she said, there were nearly 9,000 cases and 3,500 deaths from the virus; about 5,000 patients survived. So far, Dr. Scott and her team have collected data on about 500 patients for whom they also provide free health care.
The project has six arms, each headed by an expert: clinical care, data collection, disability, neurology, ophthalmology, and psychiatry.
The team sees patients in a large tent sectioned by a plywood wall*. Wireless Internet access, which she said is “enormously expensive” in Sierra Leone, has been donated by Omline Business Communications*. It’s the team’s lifeline, allowing them to transmit data between Freetown and participating units around the world. Members also Skype regularly, talking with patients and with each other.
All patients who come into the clinic have an initial visit that includes collection of demographics, their Ebola and clinical history (including an exploration of comorbidities), a maternal health screening for women, vital signs and symptom assessment, medication dispensing, and a treatment plan.
Then they visit the specialists, either onsite or through local referral*. These specialist modules include joints, eyes, headache, ears, neurology, cardiac, respiratory, gastrointestinal, renal and urologic, reproductive health for both genders, and psychiatry.
Last year, Dr. Scott published initial data on 44 patients. At ECCMID 2017, she expanded that report to include 203 survivors. They spanned all ages, but about 67% were in their most productive adult years, aged 20-39 years.
Her findings are striking: About 78% report musculoskeletal pain, with many saying they have trouble walking even short distances, climbing stairs, or picking up their children.
Headache was the next most common problem, reported by nearly 40%. About 15% report ocular problems, which include anterior uveitis, cataracts – even in very young children – and retinal lesions. Abdominal and chest pain affect about 10% of the survivors.
Although she didn’t present specific numbers, Dr. Scott also said that many of the survivors experience psychological sequelae, including insomnia, anxiety, and depression. Whether this is related to viral pathology isn’t clear; it could be a not-unexpected response to the trauma of living through the epidemic.
“Many of these people have lost their entire family, and those that are left now shun them,” she said in a live video interview on Facebook. “It’s almost like a post-traumatic stress reaction.”
The other symptoms probably are related to the disease pathology, she observed. “Unfortunately, we don’t have all the clinical details of the acute phase for everyone, but for those for whom we do have details, we are seeing correlation between some of the problems with viral loads at admission, and even episodes of becoming unconscious during the acute illness.”
Patrick Howlett, MD, of the King’s Sierra Leone Partnership, Freetown, leads the neurology study. So far, the researchers have collected data on 19 patients with severe neurological consequences. Of those, 12 (63%) experienced a period of unconsciousness during their acute Ebola episode. In a comparator group of 21 with nonsevere neurologic sequelae, 33% had experienced unconsciousness.
Headache was present in nine (47%) of the patients. Migraine was the most common diagnosis. “We don’t have money for migraine medications, but fortunately, most of our migraine patients seem to be doing well on beta blockers,” Dr. Scott said.
CT scans were performed on 17 patients: three showed cerebral or cerebellar atrophy and two had confirmed stroke.
The brain injuries were severe in two, including a 42-year-old with extensive gliosis in the left middle cerebral artery region and a dilated left ventricle secondary to loss of volume in that hemisphere. A 12-year-old girl showed extensive parietal and temporal lobe atrophy. She is now so disabled that her family can’t care for her at home.
Other neurological problems include peripheral neuropathy, brachial plexus neuropathy, and asymmetric lower limb muscular atrophy.
Paul Steptoe, MD, an ophthalmic registrar from St. Paul’s Eye Unit at the Royal Liverpool Hospital, heads the eye study. He has observed dense cataracts, even in children, and anterior uveitis that has blinded some patients. There is concern about live virus persisting in vitreal fluid, but two eye taps have been negative, Dr. Scott said.
The most exciting recent finding, however, was made possible by the donation of a digital retinal camera, which “enabled us to get dozens of amazing images,” Dr. Scott said. With it, Dr. Steptoe conducted a case-control study of 81 Ebola survivors and 106 community controls. The findings of this study are potentially very, very important, Dr. Scott said.
“The first thing we found out is that retinal scarring is pervasive in our control patients,” she said. “There is just a lot of it out here in the community. But more interesting is that Dr. Steptoe seems to have identified a characteristic retinal lesion seen only in our survivors. It could be evidence of neurotropic aspects of the Ebola virus.”
The lesions occurred in 12 (15%) of the survivors and none of the controls. They are of a striking and consistent shape: straight-edged and sharply angulated. The lesions are only on the surface of the retina and do not penetrate into deeper levels. Nor do they interfere with vision. Dr. Steptoe has proposed that they take their angular shape from the retina’s underlying structures. His paper documenting this finding has been accepted and will be published shortly in the journal Emerging Infectious Diseases.
All of the post-Ebola sequelae add up to general disability for survivors, Dr. Scott said. Soushieta Jagadesh, of the* Liverpool School of Tropical Medicine, is conducting a disability survey. The comparison between 27 survivors and 54 community controls employed the Washington Group extended disability questionnaire. “We noted major limitations 1 year after discharge in mobility, vision, cognition, and affect,” Dr. Scott said.
The hazard ratios for these issues are enormous: Overall, compared with controls, survivors were 23 times more likely to have some level of disability. They were 94 times more likely to have walking limitations and 65 times more likely to have problems with stairs. Survivors were over 200 times more likely to have moderate disability than were their unaffected neighbors.
If funding for the project is renewed – and Dr. Scott admitted this is an “if,” not a “when” – caring for and studying these survivors will continue. Just in this one city, she said, the need is huge.
According to data from the U.S. Centers for Disease Control and Prevention, more than 17,000 patients in Sierra Leone, Liberia, and Guinea survived the 2014 Ebola outbreak.
If the assessments of Freetown survivors hold true across this population, thousands of survivors face life-limiting sequelae of the disease.
“We still have patients walk in every day with musculoskeletal pain, headaches, and ocular issues,” Dr. Scott said. “At the beginning of the epidemic, we were just focusing on containing it and reducing transmission. Now, we are faced with the long-term consequences.”
The Wellcome Trust supported the study. The authors have been awarded a grant from the Enhancing Research Activity in Epidemic Situations (ERAES) program, funded by the Wellcome Trust to support further research into the sequelae of Ebola virus disease.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
msullivan@frontlinemedcom.com
On Twitter @Alz_gal
*This story was updated May 2, 2017.
VIENNA – The Ebola crisis may be over in Sierra Leone, but the suffering is not.
The last patient from the epidemic was discharged in February 2016, but 78% of survivors now appear to have one or more sequelae of the infection. Some problems are mild, but some are so debilitating that life may never be the same.
Janet Scott, MD, of the University of Liverpool (England), heads a task force studying Ebola’s lingering aftereffects. These fall into four categories, Dr. Scott said at the European Society of Clinical Microbiology and Infectious Diseases annual congress: musculoskeletal pain, headache, eye problems, and psychological disorders.
They add up to an enormous risk of disability – survivors are more than 200 times more likely than controls to express at least moderate disability.
Dr. Scott and her team of researchers are partnering with clinicians and data managers in the Ebola treatment unit in the 34th Regimental Military Hospital (MH34) in Freetown, Sierra Leone. In Sierra Leone alone, she said, there were nearly 9,000 cases and 3,500 deaths from the virus; about 5,000 patients survived. So far, Dr. Scott and her team have collected data on about 500 patients for whom they also provide free health care.
The project has six arms, each headed by an expert: clinical care, data collection, disability, neurology, ophthalmology, and psychiatry.
The team sees patients in a large tent sectioned by a plywood wall*. Wireless Internet access, which she said is “enormously expensive” in Sierra Leone, has been donated by Omline Business Communications*. It’s the team’s lifeline, allowing them to transmit data between Freetown and participating units around the world. Members also Skype regularly, talking with patients and with each other.
All patients who come into the clinic have an initial visit that includes collection of demographics, their Ebola and clinical history (including an exploration of comorbidities), a maternal health screening for women, vital signs and symptom assessment, medication dispensing, and a treatment plan.
Then they visit the specialists, either onsite or through local referral*. These specialist modules include joints, eyes, headache, ears, neurology, cardiac, respiratory, gastrointestinal, renal and urologic, reproductive health for both genders, and psychiatry.
Last year, Dr. Scott published initial data on 44 patients. At ECCMID 2017, she expanded that report to include 203 survivors. They spanned all ages, but about 67% were in their most productive adult years, aged 20-39 years.
Her findings are striking: About 78% report musculoskeletal pain, with many saying they have trouble walking even short distances, climbing stairs, or picking up their children.
Headache was the next most common problem, reported by nearly 40%. About 15% report ocular problems, which include anterior uveitis, cataracts – even in very young children – and retinal lesions. Abdominal and chest pain affect about 10% of the survivors.
Although she didn’t present specific numbers, Dr. Scott also said that many of the survivors experience psychological sequelae, including insomnia, anxiety, and depression. Whether this is related to viral pathology isn’t clear; it could be a not-unexpected response to the trauma of living through the epidemic.
“Many of these people have lost their entire family, and those that are left now shun them,” she said in a live video interview on Facebook. “It’s almost like a post-traumatic stress reaction.”
The other symptoms probably are related to the disease pathology, she observed. “Unfortunately, we don’t have all the clinical details of the acute phase for everyone, but for those for whom we do have details, we are seeing correlation between some of the problems with viral loads at admission, and even episodes of becoming unconscious during the acute illness.”
Patrick Howlett, MD, of the King’s Sierra Leone Partnership, Freetown, leads the neurology study. So far, the researchers have collected data on 19 patients with severe neurological consequences. Of those, 12 (63%) experienced a period of unconsciousness during their acute Ebola episode. In a comparator group of 21 with nonsevere neurologic sequelae, 33% had experienced unconsciousness.
Headache was present in nine (47%) of the patients. Migraine was the most common diagnosis. “We don’t have money for migraine medications, but fortunately, most of our migraine patients seem to be doing well on beta blockers,” Dr. Scott said.
CT scans were performed on 17 patients: three showed cerebral or cerebellar atrophy and two had confirmed stroke.
The brain injuries were severe in two, including a 42-year-old with extensive gliosis in the left middle cerebral artery region and a dilated left ventricle secondary to loss of volume in that hemisphere. A 12-year-old girl showed extensive parietal and temporal lobe atrophy. She is now so disabled that her family can’t care for her at home.
Other neurological problems include peripheral neuropathy, brachial plexus neuropathy, and asymmetric lower limb muscular atrophy.
Paul Steptoe, MD, an ophthalmic registrar from St. Paul’s Eye Unit at the Royal Liverpool Hospital, heads the eye study. He has observed dense cataracts, even in children, and anterior uveitis that has blinded some patients. There is concern about live virus persisting in vitreal fluid, but two eye taps have been negative, Dr. Scott said.
The most exciting recent finding, however, was made possible by the donation of a digital retinal camera, which “enabled us to get dozens of amazing images,” Dr. Scott said. With it, Dr. Steptoe conducted a case-control study of 81 Ebola survivors and 106 community controls. The findings of this study are potentially very, very important, Dr. Scott said.
“The first thing we found out is that retinal scarring is pervasive in our control patients,” she said. “There is just a lot of it out here in the community. But more interesting is that Dr. Steptoe seems to have identified a characteristic retinal lesion seen only in our survivors. It could be evidence of neurotropic aspects of the Ebola virus.”
The lesions occurred in 12 (15%) of the survivors and none of the controls. They are of a striking and consistent shape: straight-edged and sharply angulated. The lesions are only on the surface of the retina and do not penetrate into deeper levels. Nor do they interfere with vision. Dr. Steptoe has proposed that they take their angular shape from the retina’s underlying structures. His paper documenting this finding has been accepted and will be published shortly in the journal Emerging Infectious Diseases.
All of the post-Ebola sequelae add up to general disability for survivors, Dr. Scott said. Soushieta Jagadesh, of the* Liverpool School of Tropical Medicine, is conducting a disability survey. The comparison between 27 survivors and 54 community controls employed the Washington Group extended disability questionnaire. “We noted major limitations 1 year after discharge in mobility, vision, cognition, and affect,” Dr. Scott said.
The hazard ratios for these issues are enormous: Overall, compared with controls, survivors were 23 times more likely to have some level of disability. They were 94 times more likely to have walking limitations and 65 times more likely to have problems with stairs. Survivors were over 200 times more likely to have moderate disability than were their unaffected neighbors.
If funding for the project is renewed – and Dr. Scott admitted this is an “if,” not a “when” – caring for and studying these survivors will continue. Just in this one city, she said, the need is huge.
According to data from the U.S. Centers for Disease Control and Prevention, more than 17,000 patients in Sierra Leone, Liberia, and Guinea survived the 2014 Ebola outbreak.
If the assessments of Freetown survivors hold true across this population, thousands of survivors face life-limiting sequelae of the disease.
“We still have patients walk in every day with musculoskeletal pain, headaches, and ocular issues,” Dr. Scott said. “At the beginning of the epidemic, we were just focusing on containing it and reducing transmission. Now, we are faced with the long-term consequences.”
The Wellcome Trust supported the study. The authors have been awarded a grant from the Enhancing Research Activity in Epidemic Situations (ERAES) program, funded by the Wellcome Trust to support further research into the sequelae of Ebola virus disease.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
msullivan@frontlinemedcom.com
On Twitter @Alz_gal
*This story was updated May 2, 2017.
VIENNA – The Ebola crisis may be over in Sierra Leone, but the suffering is not.
The last patient from the epidemic was discharged in February 2016, but 78% of survivors now appear to have one or more sequelae of the infection. Some problems are mild, but some are so debilitating that life may never be the same.
Janet Scott, MD, of the University of Liverpool (England), heads a task force studying Ebola’s lingering aftereffects. These fall into four categories, Dr. Scott said at the European Society of Clinical Microbiology and Infectious Diseases annual congress: musculoskeletal pain, headache, eye problems, and psychological disorders.
They add up to an enormous risk of disability – survivors are more than 200 times more likely than controls to express at least moderate disability.
Dr. Scott and her team of researchers are partnering with clinicians and data managers in the Ebola treatment unit in the 34th Regimental Military Hospital (MH34) in Freetown, Sierra Leone. In Sierra Leone alone, she said, there were nearly 9,000 cases and 3,500 deaths from the virus; about 5,000 patients survived. So far, Dr. Scott and her team have collected data on about 500 patients for whom they also provide free health care.
The project has six arms, each headed by an expert: clinical care, data collection, disability, neurology, ophthalmology, and psychiatry.
The team sees patients in a large tent sectioned by a plywood wall*. Wireless Internet access, which she said is “enormously expensive” in Sierra Leone, has been donated by Omline Business Communications*. It’s the team’s lifeline, allowing them to transmit data between Freetown and participating units around the world. Members also Skype regularly, talking with patients and with each other.
All patients who come into the clinic have an initial visit that includes collection of demographics, their Ebola and clinical history (including an exploration of comorbidities), a maternal health screening for women, vital signs and symptom assessment, medication dispensing, and a treatment plan.
Then they visit the specialists, either onsite or through local referral*. These specialist modules include joints, eyes, headache, ears, neurology, cardiac, respiratory, gastrointestinal, renal and urologic, reproductive health for both genders, and psychiatry.
Last year, Dr. Scott published initial data on 44 patients. At ECCMID 2017, she expanded that report to include 203 survivors. They spanned all ages, but about 67% were in their most productive adult years, aged 20-39 years.
Her findings are striking: About 78% report musculoskeletal pain, with many saying they have trouble walking even short distances, climbing stairs, or picking up their children.
Headache was the next most common problem, reported by nearly 40%. About 15% report ocular problems, which include anterior uveitis, cataracts – even in very young children – and retinal lesions. Abdominal and chest pain affect about 10% of the survivors.
Although she didn’t present specific numbers, Dr. Scott also said that many of the survivors experience psychological sequelae, including insomnia, anxiety, and depression. Whether this is related to viral pathology isn’t clear; it could be a not-unexpected response to the trauma of living through the epidemic.
“Many of these people have lost their entire family, and those that are left now shun them,” she said in a live video interview on Facebook. “It’s almost like a post-traumatic stress reaction.”
The other symptoms probably are related to the disease pathology, she observed. “Unfortunately, we don’t have all the clinical details of the acute phase for everyone, but for those for whom we do have details, we are seeing correlation between some of the problems with viral loads at admission, and even episodes of becoming unconscious during the acute illness.”
Patrick Howlett, MD, of the King’s Sierra Leone Partnership, Freetown, leads the neurology study. So far, the researchers have collected data on 19 patients with severe neurological consequences. Of those, 12 (63%) experienced a period of unconsciousness during their acute Ebola episode. In a comparator group of 21 with nonsevere neurologic sequelae, 33% had experienced unconsciousness.
Headache was present in nine (47%) of the patients. Migraine was the most common diagnosis. “We don’t have money for migraine medications, but fortunately, most of our migraine patients seem to be doing well on beta blockers,” Dr. Scott said.
CT scans were performed on 17 patients: three showed cerebral or cerebellar atrophy and two had confirmed stroke.
The brain injuries were severe in two, including a 42-year-old with extensive gliosis in the left middle cerebral artery region and a dilated left ventricle secondary to loss of volume in that hemisphere. A 12-year-old girl showed extensive parietal and temporal lobe atrophy. She is now so disabled that her family can’t care for her at home.
Other neurological problems include peripheral neuropathy, brachial plexus neuropathy, and asymmetric lower limb muscular atrophy.
Paul Steptoe, MD, an ophthalmic registrar from St. Paul’s Eye Unit at the Royal Liverpool Hospital, heads the eye study. He has observed dense cataracts, even in children, and anterior uveitis that has blinded some patients. There is concern about live virus persisting in vitreal fluid, but two eye taps have been negative, Dr. Scott said.
The most exciting recent finding, however, was made possible by the donation of a digital retinal camera, which “enabled us to get dozens of amazing images,” Dr. Scott said. With it, Dr. Steptoe conducted a case-control study of 81 Ebola survivors and 106 community controls. The findings of this study are potentially very, very important, Dr. Scott said.
“The first thing we found out is that retinal scarring is pervasive in our control patients,” she said. “There is just a lot of it out here in the community. But more interesting is that Dr. Steptoe seems to have identified a characteristic retinal lesion seen only in our survivors. It could be evidence of neurotropic aspects of the Ebola virus.”
The lesions occurred in 12 (15%) of the survivors and none of the controls. They are of a striking and consistent shape: straight-edged and sharply angulated. The lesions are only on the surface of the retina and do not penetrate into deeper levels. Nor do they interfere with vision. Dr. Steptoe has proposed that they take their angular shape from the retina’s underlying structures. His paper documenting this finding has been accepted and will be published shortly in the journal Emerging Infectious Diseases.
All of the post-Ebola sequelae add up to general disability for survivors, Dr. Scott said. Soushieta Jagadesh, of the* Liverpool School of Tropical Medicine, is conducting a disability survey. The comparison between 27 survivors and 54 community controls employed the Washington Group extended disability questionnaire. “We noted major limitations 1 year after discharge in mobility, vision, cognition, and affect,” Dr. Scott said.
The hazard ratios for these issues are enormous: Overall, compared with controls, survivors were 23 times more likely to have some level of disability. They were 94 times more likely to have walking limitations and 65 times more likely to have problems with stairs. Survivors were over 200 times more likely to have moderate disability than were their unaffected neighbors.
If funding for the project is renewed – and Dr. Scott admitted this is an “if,” not a “when” – caring for and studying these survivors will continue. Just in this one city, she said, the need is huge.
According to data from the U.S. Centers for Disease Control and Prevention, more than 17,000 patients in Sierra Leone, Liberia, and Guinea survived the 2014 Ebola outbreak.
If the assessments of Freetown survivors hold true across this population, thousands of survivors face life-limiting sequelae of the disease.
“We still have patients walk in every day with musculoskeletal pain, headaches, and ocular issues,” Dr. Scott said. “At the beginning of the epidemic, we were just focusing on containing it and reducing transmission. Now, we are faced with the long-term consequences.”
The Wellcome Trust supported the study. The authors have been awarded a grant from the Enhancing Research Activity in Epidemic Situations (ERAES) program, funded by the Wellcome Trust to support further research into the sequelae of Ebola virus disease.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
msullivan@frontlinemedcom.com
On Twitter @Alz_gal
*This story was updated May 2, 2017.
AT ECCMID 2017
VIDEO: Study confirms uneven access to liver cancer treatment at VA hospitals
Only 25% of Veterans Affairs (VA) patients with potentially curable (Barcelona Clinic Liver Cancer stage 0/A) hepatocellular carcinoma received resection, transplantation, or ablative therapy, according to the results of a national retrospective cohort study published in the June issue of Gastroenterology (doi: 10.1053/j.gastro.2017.02.040).
Furthermore, 13% of the fittest (ECOG performance status 1-2) patients received no active treatment for their hepatocellular carcinoma, Marina Serper, MD, of Corporal Michael J. Crescenz VA Medical Center, Philadelphia, and Tamar H. Taddei, MD, of VA New York Harbor Health Care System, Brooklyn, New York, wrote with their associates in Gastroenterology.
Source: American Gastroenterological Association
“Delivery of curative therapies conferred the highest survival benefit, and notable geographic and specialist variation was observed in the delivery of active treatment,” they added. “Future studies should further evaluate modifiable health system and provider-specific barriers to delivering high quality, multidisciplinary care in hepatocellular carcinoma [in order] to optimize patient outcomes.”
Hepatocellular carcinoma ranks second worldwide and fifth in the United States as a cause of cancer mortality. Gastroenterologists, hepatologists, medical oncologists, or surgeons may take primary responsibility for treatment in community settings, but little is known about how provider and health system factors affect outcomes or the likelihood of receiving active treatments, such as liver transplantation, resection, ablative or transarterial therapy, sorafenib, systemic chemotherapy, or radiation. Accordingly, the researchers reviewed medical records and demographic data from all 3,988 U.S. patients diagnosed with hepatocellular carcinoma between 2008 and 2010 who received care at 128 Veterans Affairs centers. Patients were followed through the end of 2014. Data were from the Veterans Outcomes and Costs Associated with Liver Disease (VOCAL) cohort study (Gastroenterology. 2017 Mar 7. doi: 10.1053/j.gastro.2017.02.040).
After diagnosis, most (54%) patients only underwent transarterial palliative therapy, and 24% received no cancer treatment, the researchers reported. Being treated at an academically affiliated VA hospital nearly doubled the odds of receiving active therapy (odds ratio, 1.97; 95% confidence interval, 1.6 to 2.4; P less than .001), even after the researchers controlled for race, Charlson-Deyo comorbidity, and presenting Barcelona Clinic Liver Cancer stage. Evaluation by multiple specialists also significantly increased the odds of active treatment (OR, 1.60; 95% CI, 1.15 to 2.21; P = .005), but review by a multidisciplinary tumor board did not (OR, 1.19; P = .1).
Receipt of active therapy also varied significantly by region. Compared with patients in the Northeastern United States, those in the mid-South were significantly less likely to receive active therapy (HR, 0.62; 95% CI, 0.44-0.85). Patients in the Southeast, Central, and Western United States also were less likely to receive active treatment than were those in the Northeast, but 95% CIs for these hazard ratios were nonsignificant. Virtual tumor boards could help overcome diagnostic and treatment delays, but costs, care coordination, patient factors, and compensation issues are major barriers against implementation, the investigators noted.
Overall survival was associated with active treatment of hepatocellular carcinoma, including liver transplantation (hazard ratio, 0.22; 95% CI, 0.16-0.31), liver resection (HR, 0.38; 95% CI, 0.28-0.52), ablative therapy (HR, 0.63; 95% CI, 0.52-0.76), and transarterial therapy (HR, 0.83; 95% CI, 0.74-0.92). Reduced mortality was associated with seeing a hepatologist (HR, 0.7), medical oncologist (HR, 0.82), or surgeon (HR, 0.79) within 30 days of diagnosis (P less than .001 for each). Undergoing review by a multidisciplinary tumor board was associated with significantly reduced mortality (HR, 0.83; P less than .001), said the researchers.
“Findings from the VOCAL cohort of predominantly older males with significant medical comorbidities are important in light of the aging U.S. population and a nearly 70% expected increase in cancer among older adults,” they wrote. Together, the results indicate that access to multidisciplinary and expert care “is critical for optimizing treatment choices and for maximizing survival, but that such access is non-uniform,” they noted. “Detailed national VA clinical and administrative data are a unique resource that may be tapped to facilitate development of a parsimonious set of evidence-based, patient-centered, liver cancer–specific quality measures,” they emphasized. Quality measures based on timeliness, receipt of appropriate care, survival, or patient-reported outcomes “could be applicable both within and outside the VA system.”
The study was funded by unrestricted grants from Bayer Healthcare Pharmaceuticals and the VA HIV, Hepatitis and Public Health Pathogens Programs. The investigators had no conflicts.
The treatment of hepatocellular carcinoma (HCC) can be challenging because of the presence of underlying chronic liver disease and cirrhosis in the majority of patients. The study by Dr. Serper and colleagues evaluated the care of patients diagnosed with HCC in the Veterans Affairs (VA) system between 2008 and 2010. There are important aspects of this study worth highlighting.
First, 36% of patients presented with early-stage HCC and clearly had a better overall survival. This highlights the need for surveillance of patients with cirrhosis not only in the VA but also in other health systems. Second, only a minority of patients with early-stage HCC received curative interventions. In order to improve outcomes, patients with early stage disease should receive appropriate curative interventions. Third, gastroenterologists saw a large number of patients with HCC in the VA system, but, unfortunately, this led to less receipt of active therapy and a trend for a worse all-cause mortality, compared with hepatologists and other specialties. It is critical that gastroenterologists refer patients to specialties more adept at treating HCC in order to achieve better outcomes.
Lastly, only 34% of patients with HCC were managed via a multidisciplinary tumor conference. Importantly, these patients had an increased probability of receipt of active treatment and a 17% reduction in all-cause mortality. Our group has shown that a multidisciplinary approach to treating HCC improves overall survival. It is critical that medical centers develop a multidisciplinary treatment approach to HCC.
Jorge A. Marrero, MD, MS, AGAF, is professor of medicine and medical director for liver transplantation at UT Southwestern Medical Center Dallas. He has no conflicts of interest to report regarding this manuscript or commentary.
The treatment of hepatocellular carcinoma (HCC) can be challenging because of the presence of underlying chronic liver disease and cirrhosis in the majority of patients. The study by Dr. Serper and colleagues evaluated the care of patients diagnosed with HCC in the Veterans Affairs (VA) system between 2008 and 2010. There are important aspects of this study worth highlighting.
First, 36% of patients presented with early-stage HCC and clearly had a better overall survival. This highlights the need for surveillance of patients with cirrhosis not only in the VA but also in other health systems. Second, only a minority of patients with early-stage HCC received curative interventions. In order to improve outcomes, patients with early stage disease should receive appropriate curative interventions. Third, gastroenterologists saw a large number of patients with HCC in the VA system, but, unfortunately, this led to less receipt of active therapy and a trend for a worse all-cause mortality, compared with hepatologists and other specialties. It is critical that gastroenterologists refer patients to specialties more adept at treating HCC in order to achieve better outcomes.
Lastly, only 34% of patients with HCC were managed via a multidisciplinary tumor conference. Importantly, these patients had an increased probability of receipt of active treatment and a 17% reduction in all-cause mortality. Our group has shown that a multidisciplinary approach to treating HCC improves overall survival. It is critical that medical centers develop a multidisciplinary treatment approach to HCC.
Jorge A. Marrero, MD, MS, AGAF, is professor of medicine and medical director for liver transplantation at UT Southwestern Medical Center Dallas. He has no conflicts of interest to report regarding this manuscript or commentary.
The treatment of hepatocellular carcinoma (HCC) can be challenging because of the presence of underlying chronic liver disease and cirrhosis in the majority of patients. The study by Dr. Serper and colleagues evaluated the care of patients diagnosed with HCC in the Veterans Affairs (VA) system between 2008 and 2010. There are important aspects of this study worth highlighting.
First, 36% of patients presented with early-stage HCC and clearly had a better overall survival. This highlights the need for surveillance of patients with cirrhosis not only in the VA but also in other health systems. Second, only a minority of patients with early-stage HCC received curative interventions. In order to improve outcomes, patients with early stage disease should receive appropriate curative interventions. Third, gastroenterologists saw a large number of patients with HCC in the VA system, but, unfortunately, this led to less receipt of active therapy and a trend for a worse all-cause mortality, compared with hepatologists and other specialties. It is critical that gastroenterologists refer patients to specialties more adept at treating HCC in order to achieve better outcomes.
Lastly, only 34% of patients with HCC were managed via a multidisciplinary tumor conference. Importantly, these patients had an increased probability of receipt of active treatment and a 17% reduction in all-cause mortality. Our group has shown that a multidisciplinary approach to treating HCC improves overall survival. It is critical that medical centers develop a multidisciplinary treatment approach to HCC.
Jorge A. Marrero, MD, MS, AGAF, is professor of medicine and medical director for liver transplantation at UT Southwestern Medical Center Dallas. He has no conflicts of interest to report regarding this manuscript or commentary.
Only 25% of Veterans Affairs (VA) patients with potentially curable (Barcelona Clinic Liver Cancer stage 0/A) hepatocellular carcinoma received resection, transplantation, or ablative therapy, according to the results of a national retrospective cohort study published in the June issue of Gastroenterology (doi: 10.1053/j.gastro.2017.02.040).
Furthermore, 13% of the fittest (ECOG performance status 1-2) patients received no active treatment for their hepatocellular carcinoma, Marina Serper, MD, of Corporal Michael J. Crescenz VA Medical Center, Philadelphia, and Tamar H. Taddei, MD, of VA New York Harbor Health Care System, Brooklyn, New York, wrote with their associates in Gastroenterology.
Source: American Gastroenterological Association
“Delivery of curative therapies conferred the highest survival benefit, and notable geographic and specialist variation was observed in the delivery of active treatment,” they added. “Future studies should further evaluate modifiable health system and provider-specific barriers to delivering high quality, multidisciplinary care in hepatocellular carcinoma [in order] to optimize patient outcomes.”
Hepatocellular carcinoma ranks second worldwide and fifth in the United States as a cause of cancer mortality. Gastroenterologists, hepatologists, medical oncologists, or surgeons may take primary responsibility for treatment in community settings, but little is known about how provider and health system factors affect outcomes or the likelihood of receiving active treatments, such as liver transplantation, resection, ablative or transarterial therapy, sorafenib, systemic chemotherapy, or radiation. Accordingly, the researchers reviewed medical records and demographic data from all 3,988 U.S. patients diagnosed with hepatocellular carcinoma between 2008 and 2010 who received care at 128 Veterans Affairs centers. Patients were followed through the end of 2014. Data were from the Veterans Outcomes and Costs Associated with Liver Disease (VOCAL) cohort study (Gastroenterology. 2017 Mar 7. doi: 10.1053/j.gastro.2017.02.040).
After diagnosis, most (54%) patients only underwent transarterial palliative therapy, and 24% received no cancer treatment, the researchers reported. Being treated at an academically affiliated VA hospital nearly doubled the odds of receiving active therapy (odds ratio, 1.97; 95% confidence interval, 1.6 to 2.4; P less than .001), even after the researchers controlled for race, Charlson-Deyo comorbidity, and presenting Barcelona Clinic Liver Cancer stage. Evaluation by multiple specialists also significantly increased the odds of active treatment (OR, 1.60; 95% CI, 1.15 to 2.21; P = .005), but review by a multidisciplinary tumor board did not (OR, 1.19; P = .1).
Receipt of active therapy also varied significantly by region. Compared with patients in the Northeastern United States, those in the mid-South were significantly less likely to receive active therapy (HR, 0.62; 95% CI, 0.44-0.85). Patients in the Southeast, Central, and Western United States also were less likely to receive active treatment than were those in the Northeast, but 95% CIs for these hazard ratios were nonsignificant. Virtual tumor boards could help overcome diagnostic and treatment delays, but costs, care coordination, patient factors, and compensation issues are major barriers against implementation, the investigators noted.
Overall survival was associated with active treatment of hepatocellular carcinoma, including liver transplantation (hazard ratio, 0.22; 95% CI, 0.16-0.31), liver resection (HR, 0.38; 95% CI, 0.28-0.52), ablative therapy (HR, 0.63; 95% CI, 0.52-0.76), and transarterial therapy (HR, 0.83; 95% CI, 0.74-0.92). Reduced mortality was associated with seeing a hepatologist (HR, 0.7), medical oncologist (HR, 0.82), or surgeon (HR, 0.79) within 30 days of diagnosis (P less than .001 for each). Undergoing review by a multidisciplinary tumor board was associated with significantly reduced mortality (HR, 0.83; P less than .001), said the researchers.
“Findings from the VOCAL cohort of predominantly older males with significant medical comorbidities are important in light of the aging U.S. population and a nearly 70% expected increase in cancer among older adults,” they wrote. Together, the results indicate that access to multidisciplinary and expert care “is critical for optimizing treatment choices and for maximizing survival, but that such access is non-uniform,” they noted. “Detailed national VA clinical and administrative data are a unique resource that may be tapped to facilitate development of a parsimonious set of evidence-based, patient-centered, liver cancer–specific quality measures,” they emphasized. Quality measures based on timeliness, receipt of appropriate care, survival, or patient-reported outcomes “could be applicable both within and outside the VA system.”
The study was funded by unrestricted grants from Bayer Healthcare Pharmaceuticals and the VA HIV, Hepatitis and Public Health Pathogens Programs. The investigators had no conflicts.
Only 25% of Veterans Affairs (VA) patients with potentially curable (Barcelona Clinic Liver Cancer stage 0/A) hepatocellular carcinoma received resection, transplantation, or ablative therapy, according to the results of a national retrospective cohort study published in the June issue of Gastroenterology (doi: 10.1053/j.gastro.2017.02.040).
Furthermore, 13% of the fittest (ECOG performance status 1-2) patients received no active treatment for their hepatocellular carcinoma, Marina Serper, MD, of Corporal Michael J. Crescenz VA Medical Center, Philadelphia, and Tamar H. Taddei, MD, of VA New York Harbor Health Care System, Brooklyn, New York, wrote with their associates in Gastroenterology.
Source: American Gastroenterological Association
“Delivery of curative therapies conferred the highest survival benefit, and notable geographic and specialist variation was observed in the delivery of active treatment,” they added. “Future studies should further evaluate modifiable health system and provider-specific barriers to delivering high quality, multidisciplinary care in hepatocellular carcinoma [in order] to optimize patient outcomes.”
Hepatocellular carcinoma ranks second worldwide and fifth in the United States as a cause of cancer mortality. Gastroenterologists, hepatologists, medical oncologists, or surgeons may take primary responsibility for treatment in community settings, but little is known about how provider and health system factors affect outcomes or the likelihood of receiving active treatments, such as liver transplantation, resection, ablative or transarterial therapy, sorafenib, systemic chemotherapy, or radiation. Accordingly, the researchers reviewed medical records and demographic data from all 3,988 U.S. patients diagnosed with hepatocellular carcinoma between 2008 and 2010 who received care at 128 Veterans Affairs centers. Patients were followed through the end of 2014. Data were from the Veterans Outcomes and Costs Associated with Liver Disease (VOCAL) cohort study (Gastroenterology. 2017 Mar 7. doi: 10.1053/j.gastro.2017.02.040).
After diagnosis, most (54%) patients only underwent transarterial palliative therapy, and 24% received no cancer treatment, the researchers reported. Being treated at an academically affiliated VA hospital nearly doubled the odds of receiving active therapy (odds ratio, 1.97; 95% confidence interval, 1.6 to 2.4; P less than .001), even after the researchers controlled for race, Charlson-Deyo comorbidity, and presenting Barcelona Clinic Liver Cancer stage. Evaluation by multiple specialists also significantly increased the odds of active treatment (OR, 1.60; 95% CI, 1.15 to 2.21; P = .005), but review by a multidisciplinary tumor board did not (OR, 1.19; P = .1).
Receipt of active therapy also varied significantly by region. Compared with patients in the Northeastern United States, those in the mid-South were significantly less likely to receive active therapy (HR, 0.62; 95% CI, 0.44-0.85). Patients in the Southeast, Central, and Western United States also were less likely to receive active treatment than were those in the Northeast, but 95% CIs for these hazard ratios were nonsignificant. Virtual tumor boards could help overcome diagnostic and treatment delays, but costs, care coordination, patient factors, and compensation issues are major barriers against implementation, the investigators noted.
Overall survival was associated with active treatment of hepatocellular carcinoma, including liver transplantation (hazard ratio, 0.22; 95% CI, 0.16-0.31), liver resection (HR, 0.38; 95% CI, 0.28-0.52), ablative therapy (HR, 0.63; 95% CI, 0.52-0.76), and transarterial therapy (HR, 0.83; 95% CI, 0.74-0.92). Reduced mortality was associated with seeing a hepatologist (HR, 0.7), medical oncologist (HR, 0.82), or surgeon (HR, 0.79) within 30 days of diagnosis (P less than .001 for each). Undergoing review by a multidisciplinary tumor board was associated with significantly reduced mortality (HR, 0.83; P less than .001), said the researchers.
“Findings from the VOCAL cohort of predominantly older males with significant medical comorbidities are important in light of the aging U.S. population and a nearly 70% expected increase in cancer among older adults,” they wrote. Together, the results indicate that access to multidisciplinary and expert care “is critical for optimizing treatment choices and for maximizing survival, but that such access is non-uniform,” they noted. “Detailed national VA clinical and administrative data are a unique resource that may be tapped to facilitate development of a parsimonious set of evidence-based, patient-centered, liver cancer–specific quality measures,” they emphasized. Quality measures based on timeliness, receipt of appropriate care, survival, or patient-reported outcomes “could be applicable both within and outside the VA system.”
The study was funded by unrestricted grants from Bayer Healthcare Pharmaceuticals and the VA HIV, Hepatitis and Public Health Pathogens Programs. The investigators had no conflicts.
FROM GASTROENTEROLOGY
Key clinical point: Undertreatment of hepatocellular carcinoma was common within the Veterans Affairs system, and varied by geographic region.
Major finding: Only 25% of Barcelona Clinic Liver Cancer stage 0/A patients received potentially curative therapies. Those in the mid-South were significantly less likely to receive active treatment than were those in the Northeast (HR, 0.62; 95% CI, 0.44-0.85). In an adjusted model, treatment at an academically affiliated VA hospital nearly doubled the odds of receiving active therapy (odds ratio, 1.97; P less than .001).
Data source: A national, retrospective cohort study of all 3,988 patients who were diagnosed with hepatocellular carcinoma between 2008 and 2010 and received care through Veterans Affairs.
Disclosures: The study was funded by unrestricted grants from Bayer Healthcare Pharmaceuticals and the VA HIV, Hepatitis and Public Health Pathogens Programs. The investigators had no conflicts.
VIDEO: Geeks brave rain to March for Science
WASHINGTON – Peaceful protesters in hundreds of cities around the globe gathered on Earth Day, April 22, to voice their support for evidence-based policies and funding for scientific research at the March for Science.
In Washington, thousands of participants gathered on the rainy National Mall for teach-ins and speeches, then marched from the Washington Monument to Capitol Hill. A key concern for marchers here was cuts in science agency funding in the Trump administration’s budget proposal for fiscal year 2018.
Organizers now are calling on supporters to participate in a week of action to continue to demonstrate widespread support for their positions.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
dfulton@frontlinemedcom.com
On Twitter @denisefulton
WASHINGTON – Peaceful protesters in hundreds of cities around the globe gathered on Earth Day, April 22, to voice their support for evidence-based policies and funding for scientific research at the March for Science.
In Washington, thousands of participants gathered on the rainy National Mall for teach-ins and speeches, then marched from the Washington Monument to Capitol Hill. A key concern for marchers here was cuts in science agency funding in the Trump administration’s budget proposal for fiscal year 2018.
Organizers now are calling on supporters to participate in a week of action to continue to demonstrate widespread support for their positions.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
dfulton@frontlinemedcom.com
On Twitter @denisefulton
WASHINGTON – Peaceful protesters in hundreds of cities around the globe gathered on Earth Day, April 22, to voice their support for evidence-based policies and funding for scientific research at the March for Science.
In Washington, thousands of participants gathered on the rainy National Mall for teach-ins and speeches, then marched from the Washington Monument to Capitol Hill. A key concern for marchers here was cuts in science agency funding in the Trump administration’s budget proposal for fiscal year 2018.
Organizers now are calling on supporters to participate in a week of action to continue to demonstrate widespread support for their positions.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
dfulton@frontlinemedcom.com
On Twitter @denisefulton
VIDEO: Surgery succeeds with select hidradenitis suppurativa patients
WASHINGTON – Medication has its limits for some patients with more severe hidradenitis suppurativa, and these patients can often benefit from surgical treatment, Chris Sayed, MD, said at an educational session held by George Washington University.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Especially if patients have relatively limited areas of sinus, being able to do some local procedures [is] what will get the patient a lot better,” Dr. Sayed of the department of dermatology at the University of North Carolina, Chapel Hill, said in a video interview. “Whereas the medicines would never have made that sinus go away.”
The meeting was supported by AbbVie. Dr. Sayed disclosed financial relationships with the company.
WASHINGTON – Medication has its limits for some patients with more severe hidradenitis suppurativa, and these patients can often benefit from surgical treatment, Chris Sayed, MD, said at an educational session held by George Washington University.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Especially if patients have relatively limited areas of sinus, being able to do some local procedures [is] what will get the patient a lot better,” Dr. Sayed of the department of dermatology at the University of North Carolina, Chapel Hill, said in a video interview. “Whereas the medicines would never have made that sinus go away.”
The meeting was supported by AbbVie. Dr. Sayed disclosed financial relationships with the company.
WASHINGTON – Medication has its limits for some patients with more severe hidradenitis suppurativa, and these patients can often benefit from surgical treatment, Chris Sayed, MD, said at an educational session held by George Washington University.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Especially if patients have relatively limited areas of sinus, being able to do some local procedures [is] what will get the patient a lot better,” Dr. Sayed of the department of dermatology at the University of North Carolina, Chapel Hill, said in a video interview. “Whereas the medicines would never have made that sinus go away.”
The meeting was supported by AbbVie. Dr. Sayed disclosed financial relationships with the company.
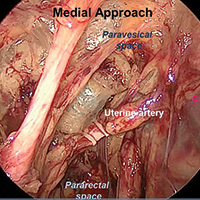
Approaches to isolating the uterine artery at its origin from the internal iliac artery

Visit the Society of Gynecologic Surgeons online: sgsonline.org
More videos from SGS:
- Advanced techniques in cystectomy for mature cystic teratomas
- Novel classification of labial anatomy and evaluation in the treatment of labial agglutination
- Strategies for prophylactic oophoropexy
- Tips and tricks for open laparoscopy
- Complete colpectomy & colpocleisis: Model for simulation
- Natural orifice sacral colpopexy
- Alternative options for visualizing ureteral patency during intraoperative cystoscopy
- Use of suprapubic Carter-Thomason needle to assist in cystoscopic excision of an intravesical foreign object
- Uterine artery ligation: Advanced techniques and considerations for the difficult laparoscopic hysterectomy
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist

Visit the Society of Gynecologic Surgeons online: sgsonline.org
More videos from SGS:
- Advanced techniques in cystectomy for mature cystic teratomas
- Novel classification of labial anatomy and evaluation in the treatment of labial agglutination
- Strategies for prophylactic oophoropexy
- Tips and tricks for open laparoscopy
- Complete colpectomy & colpocleisis: Model for simulation
- Natural orifice sacral colpopexy
- Alternative options for visualizing ureteral patency during intraoperative cystoscopy
- Use of suprapubic Carter-Thomason needle to assist in cystoscopic excision of an intravesical foreign object
- Uterine artery ligation: Advanced techniques and considerations for the difficult laparoscopic hysterectomy
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist

Visit the Society of Gynecologic Surgeons online: sgsonline.org
More videos from SGS:
- Advanced techniques in cystectomy for mature cystic teratomas
- Novel classification of labial anatomy and evaluation in the treatment of labial agglutination
- Strategies for prophylactic oophoropexy
- Tips and tricks for open laparoscopy
- Complete colpectomy & colpocleisis: Model for simulation
- Natural orifice sacral colpopexy
- Alternative options for visualizing ureteral patency during intraoperative cystoscopy
- Use of suprapubic Carter-Thomason needle to assist in cystoscopic excision of an intravesical foreign object
- Uterine artery ligation: Advanced techniques and considerations for the difficult laparoscopic hysterectomy
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist
This video is brought to you by
Reflectance Confocal Microscopy Videomosaic of Melanoma In Situ
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Medial Patellofemoral Ligament Repair
Video, Part 1. Femoral Attachment
1. Ultrasound is used to identify femoral and patellar attachments of medial patellofemoral ligament (MPFL).
2. MPFL is followed from patella to its attachment near adductor tubercle.
3. In-plane ultrasound guidance is used to place needle anterior and distal to tubercle.
4. Percutaneous incision is made down to needle tip. Spear is placed at needle tip for anatomical placement of socket.
5. Socket is drilled.
6. 3.0-mm suture anchor (BioComposite Knotless SutureTak; Arthrex) is placed.
7. Leading edge of torn MPFL is identified.
8. Suture passer (Labral FastPass Scorpion; Arthrex) is used to pass sutures through leading edge of torn MPFL to create horizontal mattress.
9. Sutures are tied.
10. Repair is complete.
Video, Part 2. Patellar Attachment
1. Ultrasound is used to scan patella to identify ideal or exact location of tear. In-plane ultrasound guidance is used to place spinal needle at desired socket location.
2. After spinal needle is positioned, in-line percutaneous incision is made, and needle is palpated at patella.
3. Spear is then placed at spinal needle tip for anatomical positioning of socket.
4. Socket is drilled.
5. 3.0-mm suture anchor (BioComposite Knotless SutureTak; Arthrex) is placed in socket.
6. Leading edge of torn medial patellofemoral ligament (MPFL) is identified.
7. Suture passer (Labral Past Pass Scorpion; Arthrex) is used to pass suture from anchor in horizontal mattress fashion through leading edge of torn MPFL.
8. Wire with loop (FiberSnare; Arthrex) is used as part of knotless technology to pull suture back through anchor to create knotless fixation.
9. Suture is pulled for appropriate tensioning of tissue.
10. Ultrasound is used to visualize construct to confirm that MPFL tissue abuts anchor and that repair is complete.
Video, Part 1. Femoral Attachment
1. Ultrasound is used to identify femoral and patellar attachments of medial patellofemoral ligament (MPFL).
2. MPFL is followed from patella to its attachment near adductor tubercle.
3. In-plane ultrasound guidance is used to place needle anterior and distal to tubercle.
4. Percutaneous incision is made down to needle tip. Spear is placed at needle tip for anatomical placement of socket.
5. Socket is drilled.
6. 3.0-mm suture anchor (BioComposite Knotless SutureTak; Arthrex) is placed.
7. Leading edge of torn MPFL is identified.
8. Suture passer (Labral FastPass Scorpion; Arthrex) is used to pass sutures through leading edge of torn MPFL to create horizontal mattress.
9. Sutures are tied.
10. Repair is complete.
Video, Part 2. Patellar Attachment
1. Ultrasound is used to scan patella to identify ideal or exact location of tear. In-plane ultrasound guidance is used to place spinal needle at desired socket location.
2. After spinal needle is positioned, in-line percutaneous incision is made, and needle is palpated at patella.
3. Spear is then placed at spinal needle tip for anatomical positioning of socket.
4. Socket is drilled.
5. 3.0-mm suture anchor (BioComposite Knotless SutureTak; Arthrex) is placed in socket.
6. Leading edge of torn medial patellofemoral ligament (MPFL) is identified.
7. Suture passer (Labral Past Pass Scorpion; Arthrex) is used to pass suture from anchor in horizontal mattress fashion through leading edge of torn MPFL.
8. Wire with loop (FiberSnare; Arthrex) is used as part of knotless technology to pull suture back through anchor to create knotless fixation.
9. Suture is pulled for appropriate tensioning of tissue.
10. Ultrasound is used to visualize construct to confirm that MPFL tissue abuts anchor and that repair is complete.
Video, Part 1. Femoral Attachment
1. Ultrasound is used to identify femoral and patellar attachments of medial patellofemoral ligament (MPFL).
2. MPFL is followed from patella to its attachment near adductor tubercle.
3. In-plane ultrasound guidance is used to place needle anterior and distal to tubercle.
4. Percutaneous incision is made down to needle tip. Spear is placed at needle tip for anatomical placement of socket.
5. Socket is drilled.
6. 3.0-mm suture anchor (BioComposite Knotless SutureTak; Arthrex) is placed.
7. Leading edge of torn MPFL is identified.
8. Suture passer (Labral FastPass Scorpion; Arthrex) is used to pass sutures through leading edge of torn MPFL to create horizontal mattress.
9. Sutures are tied.
10. Repair is complete.
Video, Part 2. Patellar Attachment
1. Ultrasound is used to scan patella to identify ideal or exact location of tear. In-plane ultrasound guidance is used to place spinal needle at desired socket location.
2. After spinal needle is positioned, in-line percutaneous incision is made, and needle is palpated at patella.
3. Spear is then placed at spinal needle tip for anatomical positioning of socket.
4. Socket is drilled.
5. 3.0-mm suture anchor (BioComposite Knotless SutureTak; Arthrex) is placed in socket.
6. Leading edge of torn medial patellofemoral ligament (MPFL) is identified.
7. Suture passer (Labral Past Pass Scorpion; Arthrex) is used to pass suture from anchor in horizontal mattress fashion through leading edge of torn MPFL.
8. Wire with loop (FiberSnare; Arthrex) is used as part of knotless technology to pull suture back through anchor to create knotless fixation.
9. Suture is pulled for appropriate tensioning of tissue.
10. Ultrasound is used to visualize construct to confirm that MPFL tissue abuts anchor and that repair is complete.
VIDEO: GI innovators dive into the Shark Tank
BOSTON – The innovators who presented their novel technologies to a “shark tank” panel during the 2017 AGA Tech Summit sponsored by the AGA Center for GI Innovation and Technology proved that innovation is alive and well in the field of gastroenterology.
“Shark Tank this year was fabulous,” Dr. Michael L. Kochman, MD, AGAF, executive committee chair of the AGA Center for GI Innovation and Technology, said in a video interview. “It was great to see some really novel ideas and some great, innovative applications.”
Presenters received feedback on their proposals from representatives of the physician, medtech, and regulatory communities and were uniformly positive about the experience, citing the value of such information to decide whether or how to move their projects forward.
“Diving into meet with the “sharks” was “a great opportunity,” says Susan Hutfless, PhD., an epidemiologist at Johns Hopkins University School of Medicine, Baltimore. “I’m still swimming, still alive ... I would do it again.”
BOSTON – The innovators who presented their novel technologies to a “shark tank” panel during the 2017 AGA Tech Summit sponsored by the AGA Center for GI Innovation and Technology proved that innovation is alive and well in the field of gastroenterology.
“Shark Tank this year was fabulous,” Dr. Michael L. Kochman, MD, AGAF, executive committee chair of the AGA Center for GI Innovation and Technology, said in a video interview. “It was great to see some really novel ideas and some great, innovative applications.”
Presenters received feedback on their proposals from representatives of the physician, medtech, and regulatory communities and were uniformly positive about the experience, citing the value of such information to decide whether or how to move their projects forward.
“Diving into meet with the “sharks” was “a great opportunity,” says Susan Hutfless, PhD., an epidemiologist at Johns Hopkins University School of Medicine, Baltimore. “I’m still swimming, still alive ... I would do it again.”
BOSTON – The innovators who presented their novel technologies to a “shark tank” panel during the 2017 AGA Tech Summit sponsored by the AGA Center for GI Innovation and Technology proved that innovation is alive and well in the field of gastroenterology.
“Shark Tank this year was fabulous,” Dr. Michael L. Kochman, MD, AGAF, executive committee chair of the AGA Center for GI Innovation and Technology, said in a video interview. “It was great to see some really novel ideas and some great, innovative applications.”
Presenters received feedback on their proposals from representatives of the physician, medtech, and regulatory communities and were uniformly positive about the experience, citing the value of such information to decide whether or how to move their projects forward.
“Diving into meet with the “sharks” was “a great opportunity,” says Susan Hutfless, PhD., an epidemiologist at Johns Hopkins University School of Medicine, Baltimore. “I’m still swimming, still alive ... I would do it again.”
FROM THE AGA 2017 TECH SUMMIT
VIDEO: Awardee's work targets mucosal stem cells in Crohn’s, ulcerative colitis
BOSTON – A series of important technological advances in cloning stem cells of the gastrointestinal tract is rewriting the basic concepts surrounding these cells and has the potential to advance understanding of GI conditions such as Barrett’s esophagus and Crohn’s disease, according to the winner of the 2016 AGA-Medtronic Research and Development Pilot Award in Technology.
The award is sponsored by Medtronic and administered through the AGA Research Foundation. “Medtronic is pleased to partner with the AGA Research Foundation in supporting research to improve patient outcomes,” said Vafa Jamali, president of Early Technologies’ business with Medtronic. “We are dedicated to support patient-friendly innovations enabling the early detection and treatment of chronic GI diseases and cancers.”
“The enabling technology we developed is the means of cloning and propagating single mucosal stem cells from discrete regions of the gastrointestinal tract in their most immature form. What we have shown is that these stem cells from normal individuals are essentially immortal, are genetically stable, and, critically, are rigorously regiospecific,” Dr. Xian of the Institute of Molecular Medicine for the Prevention of Human Diseases, University of Texas Health Science Center, Houston, said in an interview.
“This regiospecificity – duodenum stem cells always yield duodenum epithelia, ascending colon stem cells produce ascending colon epithelia – has important implications for both regenerative medicine and drug discovery,” she added.
With regard to the dominant stem cell technologies in use today, including induced pluripotent stem cells and organoid cultures of the gastrointestinal tract, Dr. Xian’s technology represents a paradigm shift.
Dr. Xian’s system generates pure “ground state” stem cells that differentiate in 3-D culture to an epithelium indistinguishable from textbook images of in situ epithelia, at rates 250 times faster than intestinal organoid systems.
This system is being applied in major investigations into Barrett’s esophagus and inflammatory bowel disease in collaboration with investigators at multiple centers in the United States and Singapore.
For Barrett’s, Dr. Xian has developed patient-matched stem cells from endoscopic biopsies of esophageal, Barrett’s, and gastric cardia to show that each arises from distinct lineages, and that the Barrett’s stem cells accumulate genetic alterations not found in those of the matched normal epithelia. These stem cells have been adapted to a drug-screening platform to identify leads that specifically eliminate Barrett’s with an eye on preemptive therapies.
Her work on mucosal stem cells in patients with Crohn’s and ulcerative colitis is revealing a coexistence of normal and pathogenic stem cells in these patients that may alter concepts of both the etiology and treatment of these conditions.
Dr. Xian suggests that treatment of Crohn’s may become analogous to treatment of cancer – emphasizing preservation of healthy cells while eliminating diseased cells – and move therapy from the current effort to induce a quiescent inflammatory state to one in which the goal is cure.
“These findings appear to indicate that some of the chronic inflammatory conditions so prevalent in gastroenterology, as well as the cancers arising from them, may have as their basis profound alterations in mucosal stem cell biology,” she added.
Though it’s still early days with this technology, its single-cell resolution naturally melds with other emerging genomic and genome editing technologies into a powerful means of dissecting the molecular basis of disease and realizing the potential of autologous regenerative medicine, according to Dr. Xian.
Following Dr. Xian’s presentation, Michael L. Kochman, MD, who is executive committee chair of the AGA Center for GI Innovation and Technology, announced the winner of the 2017 AGA-Medtronic Research and Development Pilot Award in Technology. The award was presented to Bani Chander Roland, MD, of Lenox Hill Hospital & Northwell Health System, New York. Her research will involve assessment of the ileocecal valve.
“She has several aims in this proposal to really understand better the causes of ileosphincter dysfunction using a novel method of measuring ileocecal junction pressures,” reported Dr. Kochman. He explained that other parts of the proposal included ileocecal evaluation with wireless capsule endoscopy as well as an evaluation of flora across the GI tract.
A new award to foster innovation in GI medtech is also planned. In partnership with Boston Scientific, the AGA has established the AGA-Boston Scientific Technology and Innovation Pilot Award. This $30,000 research grant will support investigators at any career stage who are developing and testing new medical devices and technologies with applications in gastroenterology and hepatology. The details of the award will be available on the AGA’s website in May. Applications for the award will be accepted beginning in the fall.
BOSTON – A series of important technological advances in cloning stem cells of the gastrointestinal tract is rewriting the basic concepts surrounding these cells and has the potential to advance understanding of GI conditions such as Barrett’s esophagus and Crohn’s disease, according to the winner of the 2016 AGA-Medtronic Research and Development Pilot Award in Technology.
The award is sponsored by Medtronic and administered through the AGA Research Foundation. “Medtronic is pleased to partner with the AGA Research Foundation in supporting research to improve patient outcomes,” said Vafa Jamali, president of Early Technologies’ business with Medtronic. “We are dedicated to support patient-friendly innovations enabling the early detection and treatment of chronic GI diseases and cancers.”
“The enabling technology we developed is the means of cloning and propagating single mucosal stem cells from discrete regions of the gastrointestinal tract in their most immature form. What we have shown is that these stem cells from normal individuals are essentially immortal, are genetically stable, and, critically, are rigorously regiospecific,” Dr. Xian of the Institute of Molecular Medicine for the Prevention of Human Diseases, University of Texas Health Science Center, Houston, said in an interview.
“This regiospecificity – duodenum stem cells always yield duodenum epithelia, ascending colon stem cells produce ascending colon epithelia – has important implications for both regenerative medicine and drug discovery,” she added.
With regard to the dominant stem cell technologies in use today, including induced pluripotent stem cells and organoid cultures of the gastrointestinal tract, Dr. Xian’s technology represents a paradigm shift.
Dr. Xian’s system generates pure “ground state” stem cells that differentiate in 3-D culture to an epithelium indistinguishable from textbook images of in situ epithelia, at rates 250 times faster than intestinal organoid systems.
This system is being applied in major investigations into Barrett’s esophagus and inflammatory bowel disease in collaboration with investigators at multiple centers in the United States and Singapore.
For Barrett’s, Dr. Xian has developed patient-matched stem cells from endoscopic biopsies of esophageal, Barrett’s, and gastric cardia to show that each arises from distinct lineages, and that the Barrett’s stem cells accumulate genetic alterations not found in those of the matched normal epithelia. These stem cells have been adapted to a drug-screening platform to identify leads that specifically eliminate Barrett’s with an eye on preemptive therapies.
Her work on mucosal stem cells in patients with Crohn’s and ulcerative colitis is revealing a coexistence of normal and pathogenic stem cells in these patients that may alter concepts of both the etiology and treatment of these conditions.
Dr. Xian suggests that treatment of Crohn’s may become analogous to treatment of cancer – emphasizing preservation of healthy cells while eliminating diseased cells – and move therapy from the current effort to induce a quiescent inflammatory state to one in which the goal is cure.
“These findings appear to indicate that some of the chronic inflammatory conditions so prevalent in gastroenterology, as well as the cancers arising from them, may have as their basis profound alterations in mucosal stem cell biology,” she added.
Though it’s still early days with this technology, its single-cell resolution naturally melds with other emerging genomic and genome editing technologies into a powerful means of dissecting the molecular basis of disease and realizing the potential of autologous regenerative medicine, according to Dr. Xian.
Following Dr. Xian’s presentation, Michael L. Kochman, MD, who is executive committee chair of the AGA Center for GI Innovation and Technology, announced the winner of the 2017 AGA-Medtronic Research and Development Pilot Award in Technology. The award was presented to Bani Chander Roland, MD, of Lenox Hill Hospital & Northwell Health System, New York. Her research will involve assessment of the ileocecal valve.
“She has several aims in this proposal to really understand better the causes of ileosphincter dysfunction using a novel method of measuring ileocecal junction pressures,” reported Dr. Kochman. He explained that other parts of the proposal included ileocecal evaluation with wireless capsule endoscopy as well as an evaluation of flora across the GI tract.
A new award to foster innovation in GI medtech is also planned. In partnership with Boston Scientific, the AGA has established the AGA-Boston Scientific Technology and Innovation Pilot Award. This $30,000 research grant will support investigators at any career stage who are developing and testing new medical devices and technologies with applications in gastroenterology and hepatology. The details of the award will be available on the AGA’s website in May. Applications for the award will be accepted beginning in the fall.
BOSTON – A series of important technological advances in cloning stem cells of the gastrointestinal tract is rewriting the basic concepts surrounding these cells and has the potential to advance understanding of GI conditions such as Barrett’s esophagus and Crohn’s disease, according to the winner of the 2016 AGA-Medtronic Research and Development Pilot Award in Technology.
The award is sponsored by Medtronic and administered through the AGA Research Foundation. “Medtronic is pleased to partner with the AGA Research Foundation in supporting research to improve patient outcomes,” said Vafa Jamali, president of Early Technologies’ business with Medtronic. “We are dedicated to support patient-friendly innovations enabling the early detection and treatment of chronic GI diseases and cancers.”
“The enabling technology we developed is the means of cloning and propagating single mucosal stem cells from discrete regions of the gastrointestinal tract in their most immature form. What we have shown is that these stem cells from normal individuals are essentially immortal, are genetically stable, and, critically, are rigorously regiospecific,” Dr. Xian of the Institute of Molecular Medicine for the Prevention of Human Diseases, University of Texas Health Science Center, Houston, said in an interview.
“This regiospecificity – duodenum stem cells always yield duodenum epithelia, ascending colon stem cells produce ascending colon epithelia – has important implications for both regenerative medicine and drug discovery,” she added.
With regard to the dominant stem cell technologies in use today, including induced pluripotent stem cells and organoid cultures of the gastrointestinal tract, Dr. Xian’s technology represents a paradigm shift.
Dr. Xian’s system generates pure “ground state” stem cells that differentiate in 3-D culture to an epithelium indistinguishable from textbook images of in situ epithelia, at rates 250 times faster than intestinal organoid systems.
This system is being applied in major investigations into Barrett’s esophagus and inflammatory bowel disease in collaboration with investigators at multiple centers in the United States and Singapore.
For Barrett’s, Dr. Xian has developed patient-matched stem cells from endoscopic biopsies of esophageal, Barrett’s, and gastric cardia to show that each arises from distinct lineages, and that the Barrett’s stem cells accumulate genetic alterations not found in those of the matched normal epithelia. These stem cells have been adapted to a drug-screening platform to identify leads that specifically eliminate Barrett’s with an eye on preemptive therapies.
Her work on mucosal stem cells in patients with Crohn’s and ulcerative colitis is revealing a coexistence of normal and pathogenic stem cells in these patients that may alter concepts of both the etiology and treatment of these conditions.
Dr. Xian suggests that treatment of Crohn’s may become analogous to treatment of cancer – emphasizing preservation of healthy cells while eliminating diseased cells – and move therapy from the current effort to induce a quiescent inflammatory state to one in which the goal is cure.
“These findings appear to indicate that some of the chronic inflammatory conditions so prevalent in gastroenterology, as well as the cancers arising from them, may have as their basis profound alterations in mucosal stem cell biology,” she added.
Though it’s still early days with this technology, its single-cell resolution naturally melds with other emerging genomic and genome editing technologies into a powerful means of dissecting the molecular basis of disease and realizing the potential of autologous regenerative medicine, according to Dr. Xian.
Following Dr. Xian’s presentation, Michael L. Kochman, MD, who is executive committee chair of the AGA Center for GI Innovation and Technology, announced the winner of the 2017 AGA-Medtronic Research and Development Pilot Award in Technology. The award was presented to Bani Chander Roland, MD, of Lenox Hill Hospital & Northwell Health System, New York. Her research will involve assessment of the ileocecal valve.
“She has several aims in this proposal to really understand better the causes of ileosphincter dysfunction using a novel method of measuring ileocecal junction pressures,” reported Dr. Kochman. He explained that other parts of the proposal included ileocecal evaluation with wireless capsule endoscopy as well as an evaluation of flora across the GI tract.
A new award to foster innovation in GI medtech is also planned. In partnership with Boston Scientific, the AGA has established the AGA-Boston Scientific Technology and Innovation Pilot Award. This $30,000 research grant will support investigators at any career stage who are developing and testing new medical devices and technologies with applications in gastroenterology and hepatology. The details of the award will be available on the AGA’s website in May. Applications for the award will be accepted beginning in the fall.
FROM THE AGA 2017 TECH SUMMIT