User login
FDA approves first targeted treatment for rare DMD mutation
, the agency has announced.
This particular mutation of the DMD gene “is amenable to exon 45 skipping,” the FDA noted in a press release. The agency added that this is its first approval of a targeted treatment for patients with the mutation.
“Developing drugs designed for patients with specific mutations is a critical part of personalized medicine,” Eric Bastings, MD, deputy director of the Office of Neuroscience at the FDA’s Center for Drug Evaluation and Research, said in a statement.
The approval was based on results from a 43-person randomized controlled trial. Patients who received casimersen had a greater increase in production of the muscle-fiber protein dystrophin compared with their counterparts who received placebo.
Approved – with cautions
The FDA noted that DMD prevalence worldwide is about 1 in 3,600 boys – although it can also affect girls in rare cases. Symptoms of the disorder are commonly first observed around age 3 years but worsen steadily over time. DMD gene mutations lead to a decrease in dystrophin.
As reported by Medscape Medical News in August, the FDA approved viltolarsen (Viltepso, NS Pharma) for the treatment of DMD in patients with a confirmed mutation amenable to exon 53 skipping, following approval of golodirsen injection (Vyondys 53, Sarepta Therapeutics) for the same indication in December 2019.
The DMD gene mutation that is amenable to exon 45 skipping is present in about 8% of patients with DMD.
The trial that carried weight with the FDA included 43 male participants with DMD aged 7-20 years. All were confirmed to have the exon 45-skipping gene mutation and all were randomly assigned 2:1 to received IV casimersen 30 mg/kg or matching placebo.
Results showed that, between baseline and 48 weeks post treatment, the casimersen group showed a significantly higher increase in levels of dystrophin protein than in the placebo group.
Upper respiratory tract infections, fever, joint and throat pain, headache, and cough were the most common adverse events experienced by the active-treatment group.
Although the clinical studies assessing casimersen did not show any reports of kidney toxicity, the adverse event was observed in some nonclinical studies. Therefore, clinicians should monitor kidney function in any patient receiving this treatment, the FDA recommended.
Overall, “the FDA has concluded that the data submitted by the applicant demonstrated an increase in dystrophin production that is reasonably likely to predict clinical benefit” in this patient population, the agency said in its press release.
However, it noted that definitive clinical benefits such as improved motor function were not “established.”
“In making this decision, the FDA considered the potential risks associated with the drug, the life-threatening and debilitating nature of the disease, and the lack of [other] available therapy,” the agency said.
It added that the manufacturer is currently conducting a multicenter study focused on the safety and efficacy of the drug in ambulatory patients with DMD.
The FDA approved casimersen using its Accelerated Approval pathway, granted Fast Track and Priority Review designations to its applications, and gave the treatment Orphan Drug designation.
A version of this article first appeared on Medscape.com.
, the agency has announced.
This particular mutation of the DMD gene “is amenable to exon 45 skipping,” the FDA noted in a press release. The agency added that this is its first approval of a targeted treatment for patients with the mutation.
“Developing drugs designed for patients with specific mutations is a critical part of personalized medicine,” Eric Bastings, MD, deputy director of the Office of Neuroscience at the FDA’s Center for Drug Evaluation and Research, said in a statement.
The approval was based on results from a 43-person randomized controlled trial. Patients who received casimersen had a greater increase in production of the muscle-fiber protein dystrophin compared with their counterparts who received placebo.
Approved – with cautions
The FDA noted that DMD prevalence worldwide is about 1 in 3,600 boys – although it can also affect girls in rare cases. Symptoms of the disorder are commonly first observed around age 3 years but worsen steadily over time. DMD gene mutations lead to a decrease in dystrophin.
As reported by Medscape Medical News in August, the FDA approved viltolarsen (Viltepso, NS Pharma) for the treatment of DMD in patients with a confirmed mutation amenable to exon 53 skipping, following approval of golodirsen injection (Vyondys 53, Sarepta Therapeutics) for the same indication in December 2019.
The DMD gene mutation that is amenable to exon 45 skipping is present in about 8% of patients with DMD.
The trial that carried weight with the FDA included 43 male participants with DMD aged 7-20 years. All were confirmed to have the exon 45-skipping gene mutation and all were randomly assigned 2:1 to received IV casimersen 30 mg/kg or matching placebo.
Results showed that, between baseline and 48 weeks post treatment, the casimersen group showed a significantly higher increase in levels of dystrophin protein than in the placebo group.
Upper respiratory tract infections, fever, joint and throat pain, headache, and cough were the most common adverse events experienced by the active-treatment group.
Although the clinical studies assessing casimersen did not show any reports of kidney toxicity, the adverse event was observed in some nonclinical studies. Therefore, clinicians should monitor kidney function in any patient receiving this treatment, the FDA recommended.
Overall, “the FDA has concluded that the data submitted by the applicant demonstrated an increase in dystrophin production that is reasonably likely to predict clinical benefit” in this patient population, the agency said in its press release.
However, it noted that definitive clinical benefits such as improved motor function were not “established.”
“In making this decision, the FDA considered the potential risks associated with the drug, the life-threatening and debilitating nature of the disease, and the lack of [other] available therapy,” the agency said.
It added that the manufacturer is currently conducting a multicenter study focused on the safety and efficacy of the drug in ambulatory patients with DMD.
The FDA approved casimersen using its Accelerated Approval pathway, granted Fast Track and Priority Review designations to its applications, and gave the treatment Orphan Drug designation.
A version of this article first appeared on Medscape.com.
, the agency has announced.
This particular mutation of the DMD gene “is amenable to exon 45 skipping,” the FDA noted in a press release. The agency added that this is its first approval of a targeted treatment for patients with the mutation.
“Developing drugs designed for patients with specific mutations is a critical part of personalized medicine,” Eric Bastings, MD, deputy director of the Office of Neuroscience at the FDA’s Center for Drug Evaluation and Research, said in a statement.
The approval was based on results from a 43-person randomized controlled trial. Patients who received casimersen had a greater increase in production of the muscle-fiber protein dystrophin compared with their counterparts who received placebo.
Approved – with cautions
The FDA noted that DMD prevalence worldwide is about 1 in 3,600 boys – although it can also affect girls in rare cases. Symptoms of the disorder are commonly first observed around age 3 years but worsen steadily over time. DMD gene mutations lead to a decrease in dystrophin.
As reported by Medscape Medical News in August, the FDA approved viltolarsen (Viltepso, NS Pharma) for the treatment of DMD in patients with a confirmed mutation amenable to exon 53 skipping, following approval of golodirsen injection (Vyondys 53, Sarepta Therapeutics) for the same indication in December 2019.
The DMD gene mutation that is amenable to exon 45 skipping is present in about 8% of patients with DMD.
The trial that carried weight with the FDA included 43 male participants with DMD aged 7-20 years. All were confirmed to have the exon 45-skipping gene mutation and all were randomly assigned 2:1 to received IV casimersen 30 mg/kg or matching placebo.
Results showed that, between baseline and 48 weeks post treatment, the casimersen group showed a significantly higher increase in levels of dystrophin protein than in the placebo group.
Upper respiratory tract infections, fever, joint and throat pain, headache, and cough were the most common adverse events experienced by the active-treatment group.
Although the clinical studies assessing casimersen did not show any reports of kidney toxicity, the adverse event was observed in some nonclinical studies. Therefore, clinicians should monitor kidney function in any patient receiving this treatment, the FDA recommended.
Overall, “the FDA has concluded that the data submitted by the applicant demonstrated an increase in dystrophin production that is reasonably likely to predict clinical benefit” in this patient population, the agency said in its press release.
However, it noted that definitive clinical benefits such as improved motor function were not “established.”
“In making this decision, the FDA considered the potential risks associated with the drug, the life-threatening and debilitating nature of the disease, and the lack of [other] available therapy,” the agency said.
It added that the manufacturer is currently conducting a multicenter study focused on the safety and efficacy of the drug in ambulatory patients with DMD.
The FDA approved casimersen using its Accelerated Approval pathway, granted Fast Track and Priority Review designations to its applications, and gave the treatment Orphan Drug designation.
A version of this article first appeared on Medscape.com.
Repeated ketamine infusions linked to rapid relief of PTSD
Repeated intravenous infusions of ketamine provide rapid relief for patients with posttraumatic stress disorder, new research suggests.
In what investigators are calling the first randomized controlled trial of repeated ketamine administration for chronic PTSD, 30 patients received six infusions of ketamine or midazolam (used as a psychoactive placebo) over 2 consecutive weeks.
Between baseline and week 2, those receiving ketamine showed significantly greater improvement than those receiving midazolam. Total scores on the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) for the first group were almost 12 points lower than the latter group at week 2, meeting the study’s primary outcome measure.
In addition, 67% vs. 20% of the patients, respectively, were considered to be treatment responders; time to loss of response for those in the ketamine group was 28 days.
Although the overall findings were as expected, “what was surprising was how robust the results were,” lead author Adriana Feder, MD, associate professor of psychiatry, Icahn School of Medicine, Mount Sinai, New York, told this news organization.
It was also a bit surprising that, in a study of just 30 participants, “we were able to show such a clear difference” between the two treatment groups, said Dr. Feder, who is also a coinventor on issued patents for the use of ketamine as therapy for PTSD, and codirector of the Ehrenkranz Lab for the Study of Human Resilience at Mount Sinai.
The findings were published online Jan. 5 in the American Journal of Psychiatry.
Unmet need
Ketamine is a glutamate N-methyl-D-aspartate (NMDA) receptor antagonist that was first approved by the U.S. Food and Drug Administration for anesthetic use in 1970. It has also been shown to be effective for treatment-resistant depression.
PTSD has a lifetime prevalence of about 6% in the United States. “While trauma-focused psychotherapies have the most empirical support, they are limited by significant rates of nonresponse, partial response, and treatment dropout,” the investigators write. Also, there are “few available pharmacotherapies for PTSD, and their efficacy is insufficient,” they add.
“There’s a real need for new treatment interventions that are effective for PTSD and also work rapidly, because it can take weeks to months for currently available treatments to work for PTSD,” Dr. Feder said.
The researchers previously conducted a “proof-of-concept” randomized controlled trial of single infusions of ketamine for chronic PTSD. Results published in 2014 in JAMA Psychiatry showed significant reduction in PTSD symptoms 24 hours after infusion.
For the current study, the investigative team wanted to assess whether ketamine was viable as a longer-term treatment.
“We were encouraged by our initial promising findings” of the earlier trial, Dr. Feder said. “We wanted to do the second study to see if ketamine really works for PTSD, to see if we could replicate the rapid improvement and also examine whether a course of six infusions over 2 weeks could maintain the improvement.”
Thirty patients (aged 18-70; mean age, 39 years) with chronic PTSD from civilian or military trauma were enrolled (mean PTSD duration, 15 years).
The most cited primary trauma was sexual assault or molestation (n = 13), followed by physical assault or abuse (n = 8), witnessing a violent assault or death (n = 4), witnessing the 9/11 attacks (n = 3), and combat exposure (n = 2).
During the 2-week treatment phase, half of the patients were randomly assigned to receive six infusions of ketamine hydrochloride at a dose of 0.5 mg/kg (86.7% women; mean CAPS-5 score, 42), while the other half received six infusions of midazolam at a dose of 0.045 mg/kg (66.7% women; mean CAPS-5 score, 40).
In addition to the primary outcome measure of 2-week changes on the CAPS-5, secondary outcomes included score changes on the Montgomery-Åsberg Depression Rating Scale (MADRS) and the Impact of Event Scale-Revised (IES-R).
Treatment response was defined as a 30% or more improvement in symptoms on the CAPS-5. A number of measures were also used to assess potential treatment-related adverse events (AEs).
Safe, effective
Results showed significantly lower total CAPS-5 scores for the ketamine group vs. the midazolam group at week 1 (score difference, 8.8 points; P = .03) and at week 2 (score difference, 11.88 points; P = .004).
Those receiving ketamine also showed improvements in three of the four PTSD symptom clusters on the CAPS-5: avoidance (P < .0001), negative mood and cognitions (P = .02), and intrusions (P = .03). The fourth symptom cluster – arousal and reactivity – did not show a significant improvement.
In addition, the ketamine group showed significantly greater improvement scores on the MADRS at both week 1 and week 2.
Treatment response at 2 weeks was achieved by 10 members of the ketamine group and by three members of the midazolam group (P = .03).
Secondary analyses showed rapid improvement in the treatment responders within the ketamine group, with a mean change of 26 points on the total IES-R score between baseline and 24 hours after their first infusion, and a mean change of 13.4 points on the MADRS total past-24-hour score, a 53% improvement on average.
“A response at 2 weeks is very rapid but they got better sometimes within the first day,” Dr. Feder noted.
There were no serious AEs reported. Although some dissociative symptoms occurred during ketamine infusions, with the highest levels reported at the end of the infusion, these symptoms had resolved by the next assessment, conducted 2 hours after infusion.
The most frequently reported AE in the ketamine group, compared with midazolam, after the start of infusions was blurred vision (53% vs. 0%), followed by dizziness (33% vs. 13%), fatigue (33% vs. 87%), headache (27% vs. 13%), and nausea or vomiting (20% vs. 7%).
‘Large-magnitude improvement’
The overall findings show that, in this patient population, “repeated intravenous ketamine infusions administered over 2 weeks were associated with a large-magnitude, clinically significant improvement in PTSD symptoms,” the investigators write.
The results “were very satisfying,” added Dr. Feder. “It was heartening also to hear what some of the participants would say. Some told us about how their symptoms and feelings had changed during the course of treatment with ketamine, where they felt stronger and better able to cope with their trauma and memories.”
She noted, however, that this was not a study designed to specifically assess ketamine in treatment-resistant PTSD. “Some patients had had multiple treatments before that hadn’t worked, while others had not received treatment before. Efficacy for treatment-resistant PTSD is an important question for future research,” Dr. Feder said.
Other areas worth future exploration include treatment efficacy in patients with different types of trauma and whether outcomes can last longer in patients receiving ketamine plus psychotherapy treatment, she noted.
“I don’t want to ignore the fact that currently available treatments work for a number of people with chronic PTSD. But because there are many more for whom [the treatments] don’t work, or they’re insufficiently helped by those treatments, this is certainly one potentially very promising approach that can be added” to a clinician’s toolbox, Dr. Feder said.
Speaks to clinical utility
Commenting for this news organization, Gerard Sanacora, MD, PhD, professor of psychiatry at Yale University, New Haven, Connecticut, called this a “very solid and well-designed” study.
“It definitely builds on what’s been found in the past, but it’s a critical piece of information speaking to the clinical utility of this treatment for PTSD,” said Dr. Sanacora, who is also director of the Yale Depression Research Program and was not involved with the current research.
He agreed with the investigators that PTSD has long been a condition that is difficult to treat.
“It’s an area that has a great unmet need for treatment options. Beyond that, as ketamine is becoming more widely used, there’s increasing demand for off-label uses. This [study] actually provides some evidence that there may be efficacy there,” Dr. Sanacora said.
Although he cautioned that this was a small study, and thus further research with a larger patient population will be needed, it provides a compelling foundation to build upon.
“This study provides clear evidence to support a larger study to really give a definitive statement on the efficacy and safety of its use for PTSD. I don’t think this is the study that provides that definitive evidence, but it is a very strong indication, and it very strongly supports the initiation of a large study to address that,” said Dr. Sanacora.
He noted that, although he’s used the term “cautious optimism” for studies in the past, he has “real optimism” that ketamine will be effective for PTSD based on the results of this current study.
“We still need some more data to really convince us of that before we can say with any clear statement that it is effective and safe, but I’m very optimistic,” Dr. Sanacora concluded.
The study was funded by the Brain and Behavior Research Foundation, Mount Sinai Innovation Partners and the Mount Sinai i3 Accelerator, Gerald and Glenda Greenwald, and the Ehrenkranz Laboratory for Human Resilience. Dr. Feder is a coinventor on issued patents for the use of ketamine as therapy for PTSD. A list of all disclosures for the other study authors are listed in the original article.
A version of this article first appeared on Medscape.com.
Repeated intravenous infusions of ketamine provide rapid relief for patients with posttraumatic stress disorder, new research suggests.
In what investigators are calling the first randomized controlled trial of repeated ketamine administration for chronic PTSD, 30 patients received six infusions of ketamine or midazolam (used as a psychoactive placebo) over 2 consecutive weeks.
Between baseline and week 2, those receiving ketamine showed significantly greater improvement than those receiving midazolam. Total scores on the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) for the first group were almost 12 points lower than the latter group at week 2, meeting the study’s primary outcome measure.
In addition, 67% vs. 20% of the patients, respectively, were considered to be treatment responders; time to loss of response for those in the ketamine group was 28 days.
Although the overall findings were as expected, “what was surprising was how robust the results were,” lead author Adriana Feder, MD, associate professor of psychiatry, Icahn School of Medicine, Mount Sinai, New York, told this news organization.
It was also a bit surprising that, in a study of just 30 participants, “we were able to show such a clear difference” between the two treatment groups, said Dr. Feder, who is also a coinventor on issued patents for the use of ketamine as therapy for PTSD, and codirector of the Ehrenkranz Lab for the Study of Human Resilience at Mount Sinai.
The findings were published online Jan. 5 in the American Journal of Psychiatry.
Unmet need
Ketamine is a glutamate N-methyl-D-aspartate (NMDA) receptor antagonist that was first approved by the U.S. Food and Drug Administration for anesthetic use in 1970. It has also been shown to be effective for treatment-resistant depression.
PTSD has a lifetime prevalence of about 6% in the United States. “While trauma-focused psychotherapies have the most empirical support, they are limited by significant rates of nonresponse, partial response, and treatment dropout,” the investigators write. Also, there are “few available pharmacotherapies for PTSD, and their efficacy is insufficient,” they add.
“There’s a real need for new treatment interventions that are effective for PTSD and also work rapidly, because it can take weeks to months for currently available treatments to work for PTSD,” Dr. Feder said.
The researchers previously conducted a “proof-of-concept” randomized controlled trial of single infusions of ketamine for chronic PTSD. Results published in 2014 in JAMA Psychiatry showed significant reduction in PTSD symptoms 24 hours after infusion.
For the current study, the investigative team wanted to assess whether ketamine was viable as a longer-term treatment.
“We were encouraged by our initial promising findings” of the earlier trial, Dr. Feder said. “We wanted to do the second study to see if ketamine really works for PTSD, to see if we could replicate the rapid improvement and also examine whether a course of six infusions over 2 weeks could maintain the improvement.”
Thirty patients (aged 18-70; mean age, 39 years) with chronic PTSD from civilian or military trauma were enrolled (mean PTSD duration, 15 years).
The most cited primary trauma was sexual assault or molestation (n = 13), followed by physical assault or abuse (n = 8), witnessing a violent assault or death (n = 4), witnessing the 9/11 attacks (n = 3), and combat exposure (n = 2).
During the 2-week treatment phase, half of the patients were randomly assigned to receive six infusions of ketamine hydrochloride at a dose of 0.5 mg/kg (86.7% women; mean CAPS-5 score, 42), while the other half received six infusions of midazolam at a dose of 0.045 mg/kg (66.7% women; mean CAPS-5 score, 40).
In addition to the primary outcome measure of 2-week changes on the CAPS-5, secondary outcomes included score changes on the Montgomery-Åsberg Depression Rating Scale (MADRS) and the Impact of Event Scale-Revised (IES-R).
Treatment response was defined as a 30% or more improvement in symptoms on the CAPS-5. A number of measures were also used to assess potential treatment-related adverse events (AEs).
Safe, effective
Results showed significantly lower total CAPS-5 scores for the ketamine group vs. the midazolam group at week 1 (score difference, 8.8 points; P = .03) and at week 2 (score difference, 11.88 points; P = .004).
Those receiving ketamine also showed improvements in three of the four PTSD symptom clusters on the CAPS-5: avoidance (P < .0001), negative mood and cognitions (P = .02), and intrusions (P = .03). The fourth symptom cluster – arousal and reactivity – did not show a significant improvement.
In addition, the ketamine group showed significantly greater improvement scores on the MADRS at both week 1 and week 2.
Treatment response at 2 weeks was achieved by 10 members of the ketamine group and by three members of the midazolam group (P = .03).
Secondary analyses showed rapid improvement in the treatment responders within the ketamine group, with a mean change of 26 points on the total IES-R score between baseline and 24 hours after their first infusion, and a mean change of 13.4 points on the MADRS total past-24-hour score, a 53% improvement on average.
“A response at 2 weeks is very rapid but they got better sometimes within the first day,” Dr. Feder noted.
There were no serious AEs reported. Although some dissociative symptoms occurred during ketamine infusions, with the highest levels reported at the end of the infusion, these symptoms had resolved by the next assessment, conducted 2 hours after infusion.
The most frequently reported AE in the ketamine group, compared with midazolam, after the start of infusions was blurred vision (53% vs. 0%), followed by dizziness (33% vs. 13%), fatigue (33% vs. 87%), headache (27% vs. 13%), and nausea or vomiting (20% vs. 7%).
‘Large-magnitude improvement’
The overall findings show that, in this patient population, “repeated intravenous ketamine infusions administered over 2 weeks were associated with a large-magnitude, clinically significant improvement in PTSD symptoms,” the investigators write.
The results “were very satisfying,” added Dr. Feder. “It was heartening also to hear what some of the participants would say. Some told us about how their symptoms and feelings had changed during the course of treatment with ketamine, where they felt stronger and better able to cope with their trauma and memories.”
She noted, however, that this was not a study designed to specifically assess ketamine in treatment-resistant PTSD. “Some patients had had multiple treatments before that hadn’t worked, while others had not received treatment before. Efficacy for treatment-resistant PTSD is an important question for future research,” Dr. Feder said.
Other areas worth future exploration include treatment efficacy in patients with different types of trauma and whether outcomes can last longer in patients receiving ketamine plus psychotherapy treatment, she noted.
“I don’t want to ignore the fact that currently available treatments work for a number of people with chronic PTSD. But because there are many more for whom [the treatments] don’t work, or they’re insufficiently helped by those treatments, this is certainly one potentially very promising approach that can be added” to a clinician’s toolbox, Dr. Feder said.
Speaks to clinical utility
Commenting for this news organization, Gerard Sanacora, MD, PhD, professor of psychiatry at Yale University, New Haven, Connecticut, called this a “very solid and well-designed” study.
“It definitely builds on what’s been found in the past, but it’s a critical piece of information speaking to the clinical utility of this treatment for PTSD,” said Dr. Sanacora, who is also director of the Yale Depression Research Program and was not involved with the current research.
He agreed with the investigators that PTSD has long been a condition that is difficult to treat.
“It’s an area that has a great unmet need for treatment options. Beyond that, as ketamine is becoming more widely used, there’s increasing demand for off-label uses. This [study] actually provides some evidence that there may be efficacy there,” Dr. Sanacora said.
Although he cautioned that this was a small study, and thus further research with a larger patient population will be needed, it provides a compelling foundation to build upon.
“This study provides clear evidence to support a larger study to really give a definitive statement on the efficacy and safety of its use for PTSD. I don’t think this is the study that provides that definitive evidence, but it is a very strong indication, and it very strongly supports the initiation of a large study to address that,” said Dr. Sanacora.
He noted that, although he’s used the term “cautious optimism” for studies in the past, he has “real optimism” that ketamine will be effective for PTSD based on the results of this current study.
“We still need some more data to really convince us of that before we can say with any clear statement that it is effective and safe, but I’m very optimistic,” Dr. Sanacora concluded.
The study was funded by the Brain and Behavior Research Foundation, Mount Sinai Innovation Partners and the Mount Sinai i3 Accelerator, Gerald and Glenda Greenwald, and the Ehrenkranz Laboratory for Human Resilience. Dr. Feder is a coinventor on issued patents for the use of ketamine as therapy for PTSD. A list of all disclosures for the other study authors are listed in the original article.
A version of this article first appeared on Medscape.com.
Repeated intravenous infusions of ketamine provide rapid relief for patients with posttraumatic stress disorder, new research suggests.
In what investigators are calling the first randomized controlled trial of repeated ketamine administration for chronic PTSD, 30 patients received six infusions of ketamine or midazolam (used as a psychoactive placebo) over 2 consecutive weeks.
Between baseline and week 2, those receiving ketamine showed significantly greater improvement than those receiving midazolam. Total scores on the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) for the first group were almost 12 points lower than the latter group at week 2, meeting the study’s primary outcome measure.
In addition, 67% vs. 20% of the patients, respectively, were considered to be treatment responders; time to loss of response for those in the ketamine group was 28 days.
Although the overall findings were as expected, “what was surprising was how robust the results were,” lead author Adriana Feder, MD, associate professor of psychiatry, Icahn School of Medicine, Mount Sinai, New York, told this news organization.
It was also a bit surprising that, in a study of just 30 participants, “we were able to show such a clear difference” between the two treatment groups, said Dr. Feder, who is also a coinventor on issued patents for the use of ketamine as therapy for PTSD, and codirector of the Ehrenkranz Lab for the Study of Human Resilience at Mount Sinai.
The findings were published online Jan. 5 in the American Journal of Psychiatry.
Unmet need
Ketamine is a glutamate N-methyl-D-aspartate (NMDA) receptor antagonist that was first approved by the U.S. Food and Drug Administration for anesthetic use in 1970. It has also been shown to be effective for treatment-resistant depression.
PTSD has a lifetime prevalence of about 6% in the United States. “While trauma-focused psychotherapies have the most empirical support, they are limited by significant rates of nonresponse, partial response, and treatment dropout,” the investigators write. Also, there are “few available pharmacotherapies for PTSD, and their efficacy is insufficient,” they add.
“There’s a real need for new treatment interventions that are effective for PTSD and also work rapidly, because it can take weeks to months for currently available treatments to work for PTSD,” Dr. Feder said.
The researchers previously conducted a “proof-of-concept” randomized controlled trial of single infusions of ketamine for chronic PTSD. Results published in 2014 in JAMA Psychiatry showed significant reduction in PTSD symptoms 24 hours after infusion.
For the current study, the investigative team wanted to assess whether ketamine was viable as a longer-term treatment.
“We were encouraged by our initial promising findings” of the earlier trial, Dr. Feder said. “We wanted to do the second study to see if ketamine really works for PTSD, to see if we could replicate the rapid improvement and also examine whether a course of six infusions over 2 weeks could maintain the improvement.”
Thirty patients (aged 18-70; mean age, 39 years) with chronic PTSD from civilian or military trauma were enrolled (mean PTSD duration, 15 years).
The most cited primary trauma was sexual assault or molestation (n = 13), followed by physical assault or abuse (n = 8), witnessing a violent assault or death (n = 4), witnessing the 9/11 attacks (n = 3), and combat exposure (n = 2).
During the 2-week treatment phase, half of the patients were randomly assigned to receive six infusions of ketamine hydrochloride at a dose of 0.5 mg/kg (86.7% women; mean CAPS-5 score, 42), while the other half received six infusions of midazolam at a dose of 0.045 mg/kg (66.7% women; mean CAPS-5 score, 40).
In addition to the primary outcome measure of 2-week changes on the CAPS-5, secondary outcomes included score changes on the Montgomery-Åsberg Depression Rating Scale (MADRS) and the Impact of Event Scale-Revised (IES-R).
Treatment response was defined as a 30% or more improvement in symptoms on the CAPS-5. A number of measures were also used to assess potential treatment-related adverse events (AEs).
Safe, effective
Results showed significantly lower total CAPS-5 scores for the ketamine group vs. the midazolam group at week 1 (score difference, 8.8 points; P = .03) and at week 2 (score difference, 11.88 points; P = .004).
Those receiving ketamine also showed improvements in three of the four PTSD symptom clusters on the CAPS-5: avoidance (P < .0001), negative mood and cognitions (P = .02), and intrusions (P = .03). The fourth symptom cluster – arousal and reactivity – did not show a significant improvement.
In addition, the ketamine group showed significantly greater improvement scores on the MADRS at both week 1 and week 2.
Treatment response at 2 weeks was achieved by 10 members of the ketamine group and by three members of the midazolam group (P = .03).
Secondary analyses showed rapid improvement in the treatment responders within the ketamine group, with a mean change of 26 points on the total IES-R score between baseline and 24 hours after their first infusion, and a mean change of 13.4 points on the MADRS total past-24-hour score, a 53% improvement on average.
“A response at 2 weeks is very rapid but they got better sometimes within the first day,” Dr. Feder noted.
There were no serious AEs reported. Although some dissociative symptoms occurred during ketamine infusions, with the highest levels reported at the end of the infusion, these symptoms had resolved by the next assessment, conducted 2 hours after infusion.
The most frequently reported AE in the ketamine group, compared with midazolam, after the start of infusions was blurred vision (53% vs. 0%), followed by dizziness (33% vs. 13%), fatigue (33% vs. 87%), headache (27% vs. 13%), and nausea or vomiting (20% vs. 7%).
‘Large-magnitude improvement’
The overall findings show that, in this patient population, “repeated intravenous ketamine infusions administered over 2 weeks were associated with a large-magnitude, clinically significant improvement in PTSD symptoms,” the investigators write.
The results “were very satisfying,” added Dr. Feder. “It was heartening also to hear what some of the participants would say. Some told us about how their symptoms and feelings had changed during the course of treatment with ketamine, where they felt stronger and better able to cope with their trauma and memories.”
She noted, however, that this was not a study designed to specifically assess ketamine in treatment-resistant PTSD. “Some patients had had multiple treatments before that hadn’t worked, while others had not received treatment before. Efficacy for treatment-resistant PTSD is an important question for future research,” Dr. Feder said.
Other areas worth future exploration include treatment efficacy in patients with different types of trauma and whether outcomes can last longer in patients receiving ketamine plus psychotherapy treatment, she noted.
“I don’t want to ignore the fact that currently available treatments work for a number of people with chronic PTSD. But because there are many more for whom [the treatments] don’t work, or they’re insufficiently helped by those treatments, this is certainly one potentially very promising approach that can be added” to a clinician’s toolbox, Dr. Feder said.
Speaks to clinical utility
Commenting for this news organization, Gerard Sanacora, MD, PhD, professor of psychiatry at Yale University, New Haven, Connecticut, called this a “very solid and well-designed” study.
“It definitely builds on what’s been found in the past, but it’s a critical piece of information speaking to the clinical utility of this treatment for PTSD,” said Dr. Sanacora, who is also director of the Yale Depression Research Program and was not involved with the current research.
He agreed with the investigators that PTSD has long been a condition that is difficult to treat.
“It’s an area that has a great unmet need for treatment options. Beyond that, as ketamine is becoming more widely used, there’s increasing demand for off-label uses. This [study] actually provides some evidence that there may be efficacy there,” Dr. Sanacora said.
Although he cautioned that this was a small study, and thus further research with a larger patient population will be needed, it provides a compelling foundation to build upon.
“This study provides clear evidence to support a larger study to really give a definitive statement on the efficacy and safety of its use for PTSD. I don’t think this is the study that provides that definitive evidence, but it is a very strong indication, and it very strongly supports the initiation of a large study to address that,” said Dr. Sanacora.
He noted that, although he’s used the term “cautious optimism” for studies in the past, he has “real optimism” that ketamine will be effective for PTSD based on the results of this current study.
“We still need some more data to really convince us of that before we can say with any clear statement that it is effective and safe, but I’m very optimistic,” Dr. Sanacora concluded.
The study was funded by the Brain and Behavior Research Foundation, Mount Sinai Innovation Partners and the Mount Sinai i3 Accelerator, Gerald and Glenda Greenwald, and the Ehrenkranz Laboratory for Human Resilience. Dr. Feder is a coinventor on issued patents for the use of ketamine as therapy for PTSD. A list of all disclosures for the other study authors are listed in the original article.
A version of this article first appeared on Medscape.com.
Microvascular injury of brain, olfactory bulb seen in COVID-19
new research suggests.
Postmortem MRI brain scans of 13 patients who died from COVID-19 showed abnormalities in 10 of the participants. Of these, nine showed punctate hyperintensities, “which represented areas of microvascular injury and fibrinogen leakage,” the investigators reported. Immunostaining also showed a thinning of the basal lamina in five of these patients.
Further analyses showed punctate hypointensities linked to congested blood vessels in 10 patients. These areas were “interpreted as microhemorrhages,” the researchers noted.
There was no evidence of viral infection, including SARS-CoV-2.
“These findings may inform the interpretation of changes observed on [MRI] of punctate hyperintensities and linear hypointensities in patients with COVID-19,” wrote Myoung-Hwa Lee, PhD, a research fellow at the National Institute of Neurological Disorders and Stroke, and colleagues. The findings were published online Dec. 30 in a “correspondence” piece in the New England Journal of Medicine.
Interpret with caution
The investigators examined brains from a convenience sample of 19 patients (mean age, 50 years), all of whom died from COVID-19 between March and July 2020.
An 11.7-tesla scanner was used to obtain magnetic resonance microscopy images for 13 of the patients. In order to scan the olfactory bulb, the scanner was set at a resolution of 25 mcm; for the brain, it was set at 100 mcm.
Chromogenic immunostaining was used to assess brain abnormalities found in 10 of the patients. Multiplex fluorescence imaging was also used for some of the patients.
For 18 study participants, a histopathological brain examination was performed. In the patients who also had medical histories available to the researchers, five had mild respiratory syndrome, four had acute respiratory distress syndrome, two had pulmonary embolism, one had delirium, and three had unknown symptoms.
The punctate hyperintensities found on magnetic resonance microscopy were also found on histopathological exam. Collagen IV immunostaining showed a thinning in the basal lamina of endothelial cells in these areas.
In addition to congested blood vessels, punctate hypointensities were linked to areas of fibrinogen leakage – but also to “relatively intact vasculature,” the investigators reported.
“There was minimal perivascular inflammation in the specimens examined, but there was no vascular occlusion,” they added.
SARS-CoV-2 was also not found in any of the participants. “It is possible that the virus was cleared by the time of death or that viral copy numbers were below the level of detection by our assays,” the researchers noted.
In 13 of the patients, hypertrophic astrocytes, macrophage infiltrates, and perivascular-activated microglia were found. Eight patients showed CD3+ and CD8+ T cells in spaces and lumens next to endothelial cells.
Finally, five patients showed activated microglia next to neurons. This is “suggestive of neuronophagia in the olfactory bulb, substantial nigra, dorsal motor nucleus of the vagal nerve, and the pre-Bötzinger complex in the medulla, which is involved in the generation of spontaneous rhythmic breathing,” wrote the investigators.
In summary, vascular pathology was found in 10 cases, perivascular infiltrates were present in 13 cases, acute ischemic hypoxic neurons were present in 6 cases, and changes suggestive of neuronophagia were present in 5 cases.
The researchers noted that, although the study findings may be helpful when interpreting brain changes on MRI scan in this patient population, availability of clinical information for the participants was limited.
Therefore, “no conclusions can be drawn in relation to neurologic features of COVID-19,” they wrote.
The study was funded by NINDS. Dr. Lee and all but one of the other investigators reported no relevant financial relationships; the remaining investigator reported having received grants from NINDS during the conduct of this study.
A version of this article first appeared on Medscape.com.
new research suggests.
Postmortem MRI brain scans of 13 patients who died from COVID-19 showed abnormalities in 10 of the participants. Of these, nine showed punctate hyperintensities, “which represented areas of microvascular injury and fibrinogen leakage,” the investigators reported. Immunostaining also showed a thinning of the basal lamina in five of these patients.
Further analyses showed punctate hypointensities linked to congested blood vessels in 10 patients. These areas were “interpreted as microhemorrhages,” the researchers noted.
There was no evidence of viral infection, including SARS-CoV-2.
“These findings may inform the interpretation of changes observed on [MRI] of punctate hyperintensities and linear hypointensities in patients with COVID-19,” wrote Myoung-Hwa Lee, PhD, a research fellow at the National Institute of Neurological Disorders and Stroke, and colleagues. The findings were published online Dec. 30 in a “correspondence” piece in the New England Journal of Medicine.
Interpret with caution
The investigators examined brains from a convenience sample of 19 patients (mean age, 50 years), all of whom died from COVID-19 between March and July 2020.
An 11.7-tesla scanner was used to obtain magnetic resonance microscopy images for 13 of the patients. In order to scan the olfactory bulb, the scanner was set at a resolution of 25 mcm; for the brain, it was set at 100 mcm.
Chromogenic immunostaining was used to assess brain abnormalities found in 10 of the patients. Multiplex fluorescence imaging was also used for some of the patients.
For 18 study participants, a histopathological brain examination was performed. In the patients who also had medical histories available to the researchers, five had mild respiratory syndrome, four had acute respiratory distress syndrome, two had pulmonary embolism, one had delirium, and three had unknown symptoms.
The punctate hyperintensities found on magnetic resonance microscopy were also found on histopathological exam. Collagen IV immunostaining showed a thinning in the basal lamina of endothelial cells in these areas.
In addition to congested blood vessels, punctate hypointensities were linked to areas of fibrinogen leakage – but also to “relatively intact vasculature,” the investigators reported.
“There was minimal perivascular inflammation in the specimens examined, but there was no vascular occlusion,” they added.
SARS-CoV-2 was also not found in any of the participants. “It is possible that the virus was cleared by the time of death or that viral copy numbers were below the level of detection by our assays,” the researchers noted.
In 13 of the patients, hypertrophic astrocytes, macrophage infiltrates, and perivascular-activated microglia were found. Eight patients showed CD3+ and CD8+ T cells in spaces and lumens next to endothelial cells.
Finally, five patients showed activated microglia next to neurons. This is “suggestive of neuronophagia in the olfactory bulb, substantial nigra, dorsal motor nucleus of the vagal nerve, and the pre-Bötzinger complex in the medulla, which is involved in the generation of spontaneous rhythmic breathing,” wrote the investigators.
In summary, vascular pathology was found in 10 cases, perivascular infiltrates were present in 13 cases, acute ischemic hypoxic neurons were present in 6 cases, and changes suggestive of neuronophagia were present in 5 cases.
The researchers noted that, although the study findings may be helpful when interpreting brain changes on MRI scan in this patient population, availability of clinical information for the participants was limited.
Therefore, “no conclusions can be drawn in relation to neurologic features of COVID-19,” they wrote.
The study was funded by NINDS. Dr. Lee and all but one of the other investigators reported no relevant financial relationships; the remaining investigator reported having received grants from NINDS during the conduct of this study.
A version of this article first appeared on Medscape.com.
new research suggests.
Postmortem MRI brain scans of 13 patients who died from COVID-19 showed abnormalities in 10 of the participants. Of these, nine showed punctate hyperintensities, “which represented areas of microvascular injury and fibrinogen leakage,” the investigators reported. Immunostaining also showed a thinning of the basal lamina in five of these patients.
Further analyses showed punctate hypointensities linked to congested blood vessels in 10 patients. These areas were “interpreted as microhemorrhages,” the researchers noted.
There was no evidence of viral infection, including SARS-CoV-2.
“These findings may inform the interpretation of changes observed on [MRI] of punctate hyperintensities and linear hypointensities in patients with COVID-19,” wrote Myoung-Hwa Lee, PhD, a research fellow at the National Institute of Neurological Disorders and Stroke, and colleagues. The findings were published online Dec. 30 in a “correspondence” piece in the New England Journal of Medicine.
Interpret with caution
The investigators examined brains from a convenience sample of 19 patients (mean age, 50 years), all of whom died from COVID-19 between March and July 2020.
An 11.7-tesla scanner was used to obtain magnetic resonance microscopy images for 13 of the patients. In order to scan the olfactory bulb, the scanner was set at a resolution of 25 mcm; for the brain, it was set at 100 mcm.
Chromogenic immunostaining was used to assess brain abnormalities found in 10 of the patients. Multiplex fluorescence imaging was also used for some of the patients.
For 18 study participants, a histopathological brain examination was performed. In the patients who also had medical histories available to the researchers, five had mild respiratory syndrome, four had acute respiratory distress syndrome, two had pulmonary embolism, one had delirium, and three had unknown symptoms.
The punctate hyperintensities found on magnetic resonance microscopy were also found on histopathological exam. Collagen IV immunostaining showed a thinning in the basal lamina of endothelial cells in these areas.
In addition to congested blood vessels, punctate hypointensities were linked to areas of fibrinogen leakage – but also to “relatively intact vasculature,” the investigators reported.
“There was minimal perivascular inflammation in the specimens examined, but there was no vascular occlusion,” they added.
SARS-CoV-2 was also not found in any of the participants. “It is possible that the virus was cleared by the time of death or that viral copy numbers were below the level of detection by our assays,” the researchers noted.
In 13 of the patients, hypertrophic astrocytes, macrophage infiltrates, and perivascular-activated microglia were found. Eight patients showed CD3+ and CD8+ T cells in spaces and lumens next to endothelial cells.
Finally, five patients showed activated microglia next to neurons. This is “suggestive of neuronophagia in the olfactory bulb, substantial nigra, dorsal motor nucleus of the vagal nerve, and the pre-Bötzinger complex in the medulla, which is involved in the generation of spontaneous rhythmic breathing,” wrote the investigators.
In summary, vascular pathology was found in 10 cases, perivascular infiltrates were present in 13 cases, acute ischemic hypoxic neurons were present in 6 cases, and changes suggestive of neuronophagia were present in 5 cases.
The researchers noted that, although the study findings may be helpful when interpreting brain changes on MRI scan in this patient population, availability of clinical information for the participants was limited.
Therefore, “no conclusions can be drawn in relation to neurologic features of COVID-19,” they wrote.
The study was funded by NINDS. Dr. Lee and all but one of the other investigators reported no relevant financial relationships; the remaining investigator reported having received grants from NINDS during the conduct of this study.
A version of this article first appeared on Medscape.com.
‘She’s not a real doctor, she’s a psych doctor’
During a particularly hectic day, Janeni Nayagan, MD, a first-year resident in the department of psychiatry and behavioral health at Cooper University Hospital, Camden, N.J., was taken aback – but not surprised – by a patient’s comment.
In the middle of an emergent situation, she overheard a patient say that Dr. Nayagan wasn’t a “real doctor, she’s a psych doctor.”
“When it happened, I wasn’t particularly angry. It was something I knew I would hear eventually because I’d heard of others experiencing it,” Dr. Nayagan said in an interview. “Psychiatry is one of the fields of medicine that is often questioned in terms of legitimacy, and I knew that when I applied for psych residency,” she said.
Nevertheless, she wrote a post about the incident on Twitter, and she discovered she was far from alone. She posted her original tweet at the start of a night shift and was surprised by the number of responses when she opened her account the next day.
So far, Dr. Nayagan’s initial tweet has garnered 86 replies, 960 likes, and 35 retweets. Some clinicians reported similar experiences from both patients and colleagues, and others offered advice on how to handle such slights.
“There were a lot from people within mental health, but I also received responses from pathologists, radiologists, and others. I didn’t realize how much this experience pervaded through medicine, where a certain specialty would be told: You’re not a real doctor. So it was nice having that support,” Dr. Nayagan said.
Dr. Nayagan noted that psychiatrists encounter “specialty bias” to a greater extent than other medical professionals, and it can be a deterrent for medical students when considering psychiatry as a career path.
“It is something that has been around for a while, but it’s surprising that it’s still prevalent in 2020,” Dr. Nayagan said.
‘Busting the myth’
This type of bias is real, agreed Kaz Nelson, MD, associate professor of psychiatry and behavioral sciences and vice chair for education at the University of Minnesota, Minneapolis, and former director of the psychiatry residency program at the school for 8 years.
She said there is “discrimination” toward psychiatrists, but noted that the problem is improving.
“I think we’re better now than 2 years or 5 years or 10 years ago, so we’re heading in the right direction. But ,” Dr. Nelson said in an interview.
“Psychiatrists have the same robust biomedical training as all specialties. They completed medical school and have this additional specialty and in some cases subspecialty training that is comprehensive of biology, psychology, and social components. We call that using a biopsychosocial model,” she said.
However, she noted that, when talking with students about the field of psychiatry, there’s an awareness “that perhaps we aren’t wearing a white coat” or a stethoscope around the neck.
“That gets translated as, You are giving up medicine – you got this medical training, and you’re not using it. And I have to bust that myth and convey that it really is a privilege to be able to integrate these aspects of knowledge and expertise. It’s in no way giving up medicine – we’re practicing medicine every single day,” said Dr. Nelson.
Remnants of stigma remain
Tristan Gorrindo, MD, deputy medical director and chief of the division of education at the American Psychiatric Association, noted “remnants of stigma” still occur.
“In my mind, it’s really a misunderstanding of the relationship between mental health and physical health,” Dr. Gorrindo said in an interview.
“There’s still this notion that holds over from an old belief that the mind and the body are separate. However, the contemporary thinking in most of modern medicine is that mental illness and physical illness are really one and the same, and they influence each other in a very dynamic way all the time,” he said.
“Psychiatrists stand in both worlds. They’re really the bridge to both the psychiatric and physical aspects,” he added.
Dr. Gorrindo agreed with Dr. Nelson that this understanding has become more prevalent during past few decades.
“Within society, it’s become much more acceptable for people to talk about their mental illness and seek treatment. In a way, shedding daylight on this issue has allowed psychiatry to step forward and demonstrate its value,” he said.
“I think over time we’re going to see that stigma or specialty bias become an anachronism that will fall by the wayside as we see psychiatry more broadly integrated and accepted within the entire house of medicine,” said Dr. Gorrindo.
Taking a toll
Although some responders on Twitter advised Dr. Nayagan and other psychiatrists to “educate with a smile” when faced with specialty discrimination, Dr. Nelson noted that it’s important to recognize that experiencing “microaggressions” takes a toll.
“Anytime you’re given a signal that you aren’t really a physician or you’re not doing a real job, whether it’s based on race, gender, ethnicity, or being a psychiatrist, there is a cost. I’d say, know what you’re doing and hold your head up high, but recognize that there’s a cost for which you may need community and support from colleagues,” she said.
“Together, our culture is changing, and the future is bright. But it’s a little bit of an oversimplification to say, ‘Just brush it off.’ We must recognize that there’s a burden that comes from those forms of exclusion,” Dr. Nelson concluded.
A version of this article first appeared on Medscape.com.
During a particularly hectic day, Janeni Nayagan, MD, a first-year resident in the department of psychiatry and behavioral health at Cooper University Hospital, Camden, N.J., was taken aback – but not surprised – by a patient’s comment.
In the middle of an emergent situation, she overheard a patient say that Dr. Nayagan wasn’t a “real doctor, she’s a psych doctor.”
“When it happened, I wasn’t particularly angry. It was something I knew I would hear eventually because I’d heard of others experiencing it,” Dr. Nayagan said in an interview. “Psychiatry is one of the fields of medicine that is often questioned in terms of legitimacy, and I knew that when I applied for psych residency,” she said.
Nevertheless, she wrote a post about the incident on Twitter, and she discovered she was far from alone. She posted her original tweet at the start of a night shift and was surprised by the number of responses when she opened her account the next day.
So far, Dr. Nayagan’s initial tweet has garnered 86 replies, 960 likes, and 35 retweets. Some clinicians reported similar experiences from both patients and colleagues, and others offered advice on how to handle such slights.
“There were a lot from people within mental health, but I also received responses from pathologists, radiologists, and others. I didn’t realize how much this experience pervaded through medicine, where a certain specialty would be told: You’re not a real doctor. So it was nice having that support,” Dr. Nayagan said.
Dr. Nayagan noted that psychiatrists encounter “specialty bias” to a greater extent than other medical professionals, and it can be a deterrent for medical students when considering psychiatry as a career path.
“It is something that has been around for a while, but it’s surprising that it’s still prevalent in 2020,” Dr. Nayagan said.
‘Busting the myth’
This type of bias is real, agreed Kaz Nelson, MD, associate professor of psychiatry and behavioral sciences and vice chair for education at the University of Minnesota, Minneapolis, and former director of the psychiatry residency program at the school for 8 years.
She said there is “discrimination” toward psychiatrists, but noted that the problem is improving.
“I think we’re better now than 2 years or 5 years or 10 years ago, so we’re heading in the right direction. But ,” Dr. Nelson said in an interview.
“Psychiatrists have the same robust biomedical training as all specialties. They completed medical school and have this additional specialty and in some cases subspecialty training that is comprehensive of biology, psychology, and social components. We call that using a biopsychosocial model,” she said.
However, she noted that, when talking with students about the field of psychiatry, there’s an awareness “that perhaps we aren’t wearing a white coat” or a stethoscope around the neck.
“That gets translated as, You are giving up medicine – you got this medical training, and you’re not using it. And I have to bust that myth and convey that it really is a privilege to be able to integrate these aspects of knowledge and expertise. It’s in no way giving up medicine – we’re practicing medicine every single day,” said Dr. Nelson.
Remnants of stigma remain
Tristan Gorrindo, MD, deputy medical director and chief of the division of education at the American Psychiatric Association, noted “remnants of stigma” still occur.
“In my mind, it’s really a misunderstanding of the relationship between mental health and physical health,” Dr. Gorrindo said in an interview.
“There’s still this notion that holds over from an old belief that the mind and the body are separate. However, the contemporary thinking in most of modern medicine is that mental illness and physical illness are really one and the same, and they influence each other in a very dynamic way all the time,” he said.
“Psychiatrists stand in both worlds. They’re really the bridge to both the psychiatric and physical aspects,” he added.
Dr. Gorrindo agreed with Dr. Nelson that this understanding has become more prevalent during past few decades.
“Within society, it’s become much more acceptable for people to talk about their mental illness and seek treatment. In a way, shedding daylight on this issue has allowed psychiatry to step forward and demonstrate its value,” he said.
“I think over time we’re going to see that stigma or specialty bias become an anachronism that will fall by the wayside as we see psychiatry more broadly integrated and accepted within the entire house of medicine,” said Dr. Gorrindo.
Taking a toll
Although some responders on Twitter advised Dr. Nayagan and other psychiatrists to “educate with a smile” when faced with specialty discrimination, Dr. Nelson noted that it’s important to recognize that experiencing “microaggressions” takes a toll.
“Anytime you’re given a signal that you aren’t really a physician or you’re not doing a real job, whether it’s based on race, gender, ethnicity, or being a psychiatrist, there is a cost. I’d say, know what you’re doing and hold your head up high, but recognize that there’s a cost for which you may need community and support from colleagues,” she said.
“Together, our culture is changing, and the future is bright. But it’s a little bit of an oversimplification to say, ‘Just brush it off.’ We must recognize that there’s a burden that comes from those forms of exclusion,” Dr. Nelson concluded.
A version of this article first appeared on Medscape.com.
During a particularly hectic day, Janeni Nayagan, MD, a first-year resident in the department of psychiatry and behavioral health at Cooper University Hospital, Camden, N.J., was taken aback – but not surprised – by a patient’s comment.
In the middle of an emergent situation, she overheard a patient say that Dr. Nayagan wasn’t a “real doctor, she’s a psych doctor.”
“When it happened, I wasn’t particularly angry. It was something I knew I would hear eventually because I’d heard of others experiencing it,” Dr. Nayagan said in an interview. “Psychiatry is one of the fields of medicine that is often questioned in terms of legitimacy, and I knew that when I applied for psych residency,” she said.
Nevertheless, she wrote a post about the incident on Twitter, and she discovered she was far from alone. She posted her original tweet at the start of a night shift and was surprised by the number of responses when she opened her account the next day.
So far, Dr. Nayagan’s initial tweet has garnered 86 replies, 960 likes, and 35 retweets. Some clinicians reported similar experiences from both patients and colleagues, and others offered advice on how to handle such slights.
“There were a lot from people within mental health, but I also received responses from pathologists, radiologists, and others. I didn’t realize how much this experience pervaded through medicine, where a certain specialty would be told: You’re not a real doctor. So it was nice having that support,” Dr. Nayagan said.
Dr. Nayagan noted that psychiatrists encounter “specialty bias” to a greater extent than other medical professionals, and it can be a deterrent for medical students when considering psychiatry as a career path.
“It is something that has been around for a while, but it’s surprising that it’s still prevalent in 2020,” Dr. Nayagan said.
‘Busting the myth’
This type of bias is real, agreed Kaz Nelson, MD, associate professor of psychiatry and behavioral sciences and vice chair for education at the University of Minnesota, Minneapolis, and former director of the psychiatry residency program at the school for 8 years.
She said there is “discrimination” toward psychiatrists, but noted that the problem is improving.
“I think we’re better now than 2 years or 5 years or 10 years ago, so we’re heading in the right direction. But ,” Dr. Nelson said in an interview.
“Psychiatrists have the same robust biomedical training as all specialties. They completed medical school and have this additional specialty and in some cases subspecialty training that is comprehensive of biology, psychology, and social components. We call that using a biopsychosocial model,” she said.
However, she noted that, when talking with students about the field of psychiatry, there’s an awareness “that perhaps we aren’t wearing a white coat” or a stethoscope around the neck.
“That gets translated as, You are giving up medicine – you got this medical training, and you’re not using it. And I have to bust that myth and convey that it really is a privilege to be able to integrate these aspects of knowledge and expertise. It’s in no way giving up medicine – we’re practicing medicine every single day,” said Dr. Nelson.
Remnants of stigma remain
Tristan Gorrindo, MD, deputy medical director and chief of the division of education at the American Psychiatric Association, noted “remnants of stigma” still occur.
“In my mind, it’s really a misunderstanding of the relationship between mental health and physical health,” Dr. Gorrindo said in an interview.
“There’s still this notion that holds over from an old belief that the mind and the body are separate. However, the contemporary thinking in most of modern medicine is that mental illness and physical illness are really one and the same, and they influence each other in a very dynamic way all the time,” he said.
“Psychiatrists stand in both worlds. They’re really the bridge to both the psychiatric and physical aspects,” he added.
Dr. Gorrindo agreed with Dr. Nelson that this understanding has become more prevalent during past few decades.
“Within society, it’s become much more acceptable for people to talk about their mental illness and seek treatment. In a way, shedding daylight on this issue has allowed psychiatry to step forward and demonstrate its value,” he said.
“I think over time we’re going to see that stigma or specialty bias become an anachronism that will fall by the wayside as we see psychiatry more broadly integrated and accepted within the entire house of medicine,” said Dr. Gorrindo.
Taking a toll
Although some responders on Twitter advised Dr. Nayagan and other psychiatrists to “educate with a smile” when faced with specialty discrimination, Dr. Nelson noted that it’s important to recognize that experiencing “microaggressions” takes a toll.
“Anytime you’re given a signal that you aren’t really a physician or you’re not doing a real job, whether it’s based on race, gender, ethnicity, or being a psychiatrist, there is a cost. I’d say, know what you’re doing and hold your head up high, but recognize that there’s a cost for which you may need community and support from colleagues,” she said.
“Together, our culture is changing, and the future is bright. But it’s a little bit of an oversimplification to say, ‘Just brush it off.’ We must recognize that there’s a burden that comes from those forms of exclusion,” Dr. Nelson concluded.
A version of this article first appeared on Medscape.com.
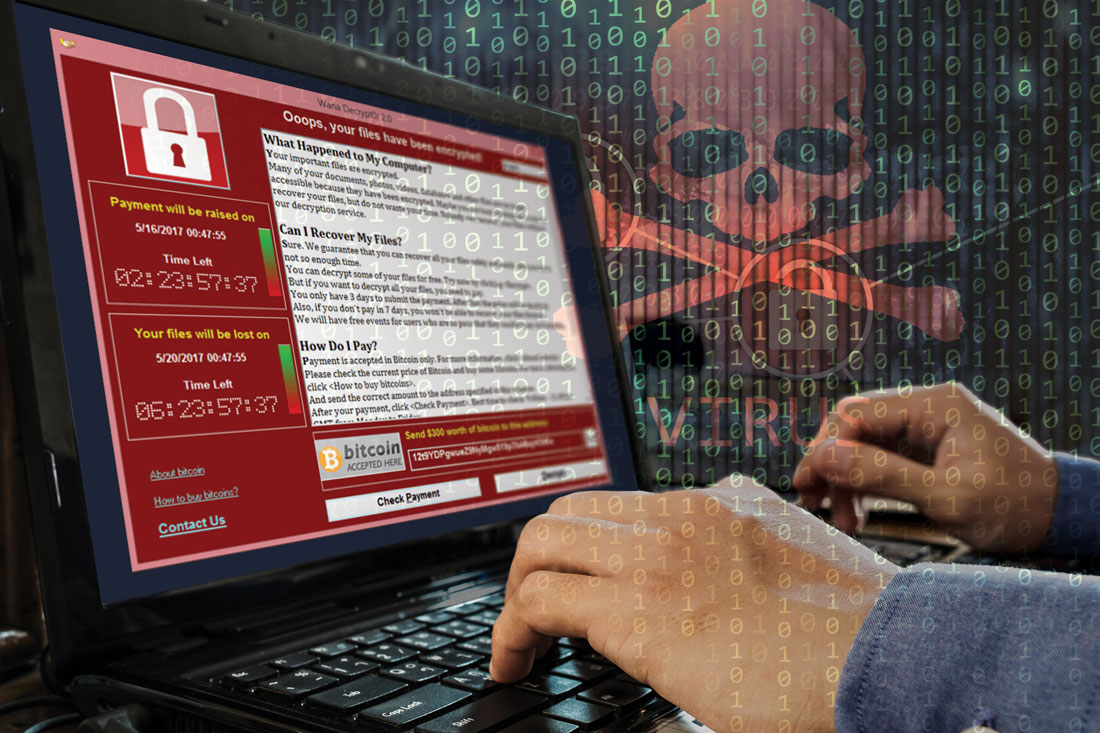
FBI warns of ‘imminent’ cyberattacks on U.S. hospitals
Amid recent reports of hackers targeting and blackmailing health care systems and even patients, the Federal Bureau of Investigation and other agencies have issued warning of “imminent” cyberattacks on more U.S. hospitals.
A new report released by the Cybersecurity and Infrastructure Security Agency, part of the Department of Homeland Security, noted that the FBI and the Department of Health & Human Services have “credible information of an increased and imminent cybercrime threat to U.S. hospitals and health care providers.”
The agencies are urging “timely and reasonable precautions” to protect health care networks from these threats.
As reported, hackers accessed patient records at Vastaamo, Finland’s largest private psychotherapy system, and emailed some patients last month demanding €200 in bitcoin or else personal health data would be released online.
In June, the University of California, San Francisco, experienced an information technology (IT) “security incident” that led to the payout of $1.14 million to individuals responsible for a malware attack in exchange for the return of data.
In addition, last week, Sky Lakes Medical Center in Klamath Falls, Ore., released a statement in which it said there had been a ransomware attack on its computer systems. Although “there is no evidence that patient information has been compromised,” some of its systems are still down.
“We’re open for business, it’s just not business as usual,” Tom Hottman, public information officer at Sky Lakes, said in an interview.
Paul S. Appelbaum, MD, Dollard Professor of Psychiatry, Medicine, and Law at Columbia University, New York, said in an interview, “People have known for a long time that there are nefarious actors out there.” He said all health care systems should be prepared to deal with these problems.
“In the face of a warning from the FBI, I’d say that’s even more important now,” Dr. Appelbaum added.
‘Malicious cyber actors’
In the new CISA report, the agency noted that it, the FBI, and the HHS have been assessing “malicious cyber actors” targeting health care systems with malware loaders such as TrickBot and BazarLoader, which often lead to data theft, ransomware attacks, and service disruptions.
“The cybercriminal enterprise behind TrickBot, which is likely also the creator of BazarLoader malware, has continued to develop new functionality and tools, increasing the ease, speed, and profitability of victimization,” the report authors wrote.
Phishing campaigns often contain attachments with malware or links to malicious websites. “Loaders start the infection chain by distributing the payload,” the report noted. A backdoor mechanism is then installed on the victim’s device.
In addition to TrickBot and BazarLoader (or BazarBackdoor), the report discussed other malicious tools, including Ryuk and Conti, which are types of ransomware that can infect systems for hackers’ financial gain.
“These issues will be particularly challenging for organizations within the COVID-19 pandemic; therefore, administrators will need to balance this risk when determining their cybersecurity investments,” the agencies wrote.
Dr. Appelbaum said his organization is taking the warning seriously.
“When the report first came out, I received emails from every system that I’m affiliated with warning about it and encouraging me as a member of the medical staff to take the usual prudent precautions,” such as not opening attachments or links from unknown sources, he said.
“The FBI warning has what seems like very reasonable advice, which is that every system should automatically back up their data off site in a separate system that’s differently accessible,” he added.
After a ransomware attack, the most recently entered information may not be backed up and could get lost, but “that’s a lot easier to deal with then losing access to all of your medical records,” said Dr. Appelbaum.
Ipsit Vahia, MD, medical director at the Institute for Technology and Psychiatry at McLean Hospital, Belmont, Mass., noted that, in answer to the FBI warning, he has heard that many centers, including his own, are warning their clinicians not to open any email attachments at this time.
Recent attacks
UCSF issued a statement noting that malware detected in early June led to the encryption of “a limited number of servers” in its medical school, making them temporarily inaccessible.
“We do not currently believe patient medical records were exposed,” the university said in the statement.
It added that because the encrypted data were necessary for “some of the academic work” conducted at UCSF, they agreed to pay a portion of the ransom demand – about $1.14 million. The hackers then provided a tool that unlocked the encrypted data.
“We continue to cooperate with law enforcement and we appreciate everyone’s understanding that we are limited in what we can share while we continue our investigation,” the statement reads. UCSF declined a request for further comment.
At Sky Lakes Medical Center, computer systems are still down after its ransomware attack, including use of electronic medical records, but the Oregon-based health care system is still seeing patients.
They are “being interviewed old school,” with the admitting process being conducted on paper, “but patient care goes on,” said Mr. Hottman.
In addition to a teaching hospital, Sky Lakes comprises specialty and primary care clinics, including a cancer treatment center. All remain open to patients at this time.
Diagnostic imaging is also continuing, but “getting the image to a place it can be read” has become more complicated, said Mr. Hottman.
“We have some work-arounds in process, and a plan is being assembled that we think will be in place as early as this weekend so that we can get those images read starting next week,” he said.
In addition, “scheduling is a little clunky,” he reported. However, “we have an awesome staff with a good attitude, so there’s still a whole lot we can do.”
He also noted that his institution has reconfirmed that, as of Nov. 4, no patient data had been compromised.
‘Especially chilling’
Targeting hospitals through cyberattacks isn’t new. In 2017, the WannaCry virus affected more than 200,000 computers in 150 countries, including the operating system of the U.K. National Health Service. The cyberattack locked clinicians out of NHS patient records and other digital tools for 3 days.
Dr. Appelbaum noted that, as hospital systems become more dependent on the Internet and on electronic communications, they become more vulnerable to data breaches.
“I think it’s clear that there have been concerted efforts lately to undertake attacks on health care IT systems to either hold them hostage, as in a ransomware attack, or to download files and use that information for profit,” he said.
Still, Dr. Vahia noted that contacting patients directly, which occurred in the Finland data breach and blackmail scheme, is something new. It is “especially chilling” that individual psychiatric patients were targeted.
It’s difficult to overstate how big a deal this is, and we should be treating it with the appropriate level of urgency,” he said in an interview.
“It shows how badly things can go wrong when security is compromised; and it should make us take a step back and survey the world of digital health to gain recognition of how much risk there might be that we haven’t really understood before,” Dr. Vahia said.
Clinical tips
Asked whether he had any tips to share with clinicians, Mr. Hottman noted that the best time to have a plan is before something dire happens.
“I would make [the possibility of cyberattacks] part of the emergency preparedness program. What if you don’t have access to computers? What do you do?” It’s important to answer those questions prior to systems going down, he said.
Mr. Hottman reported that after a mechanical failure last year put their computer systems offline for a day, “we started putting all critical information on paper and in a binder,” including phone numbers for the state police.
Dr. Vahia noted that another important step for clinicians “is to just pause and take stock of how digitally dependent” health care is becoming. He also warned that precautions should be taken regarding wearables and apps, as well as for electronic medical records. He noted the importance of strong passwords and two-step verification processes.
Even with the risks, digital technology has had a major impact on health care efficiency. “It’s not perfect, the work is ongoing, and there are big questions that need to be addressed, but in the end, the ability of technology when used right and securely” leads to better patient care, he said.
John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, agreed that digital health care is and will remain very important; but at the same time, security issues need proper attention.
“When you look back at medical hacks that have happened, there’s often a human error behind it. It’s rare for someone to break encryption. I think we have pretty darn good security, but we need to realize that sometimes errors will happen,” he said in an interview.
As an example, Dr. Torous, who is also chair of the American Psychiatric Association’s Health and Technology Committee, cited phishing emails, which depend on a user clicking a link that can cause a virus to be downloaded into their network.
“You can be cautious, but it takes just one person to download an attachment with a virus in it” to cause disruptions, Dr. Torous said.
Telehealth implications
After its data breach, Vastaamo posted on its website a notice that video is never recorded during the centers’ telehealth sessions, and so patients need not worry that any videos could be leaked online.
Asked whether video is commonly recorded during telehealth sessions in the United States, Dr. Vahia said that he was not aware of sessions being recorded, especially because the amount of the data would be too great to store indefinitely.
Dr. Appelbaum agreed and said that, to his knowledge, no clinicians at Columbia University are recording telehealth sessions. He said that it would represent a privacy threat, and he noted that most health care providers “don’t have the time to go back and watch videos of their interactions with patients.”
In the case of recordings for research purposes, he emphasized that it would be important to get consent and then store the health information offline.
As for other telehealth security risks, Dr. Vahia noted that it is possible that if a computer or device is compromised, an individual could hack into a camera and observe the session. In addition to microphones, “these pose some especially high vulnerabilities,” he said. “Clinicians need to pay attention as to whether the cameras they’re using for telecare are on or if they’re covered when not in use. And they should pay attention to security settings on smartphones and ensure microphones are not turned on as the default.”
Dr. Appelbaum said the HIPAA requires that telehealth sessions be conducted on secure systems, so clinicians need to ascertain whether the system they’re using complies with that rule.
“Particularly people who are not part of larger systems and would not usually take on that responsibility, maybe they’re in private practice or a small group, they really need to check on the security level and on HIPAA compliance and not just assume that it is adequately secure,” he said.
Dr. Appelbaum, who is also a past president of the APA and director of the Center for Law, Ethics, and Psychiatry at Columbia University, noted that the major risk for hospitals after a cyberattack is probably not liability to individual patients.
“It’s much more likely that they would face fines from HIPAA if it’s found that they failed to live up to HIPAA requirements,” he said.
A version of this article originally appeared on Medscape.com.
Amid recent reports of hackers targeting and blackmailing health care systems and even patients, the Federal Bureau of Investigation and other agencies have issued warning of “imminent” cyberattacks on more U.S. hospitals.
A new report released by the Cybersecurity and Infrastructure Security Agency, part of the Department of Homeland Security, noted that the FBI and the Department of Health & Human Services have “credible information of an increased and imminent cybercrime threat to U.S. hospitals and health care providers.”
The agencies are urging “timely and reasonable precautions” to protect health care networks from these threats.
As reported, hackers accessed patient records at Vastaamo, Finland’s largest private psychotherapy system, and emailed some patients last month demanding €200 in bitcoin or else personal health data would be released online.
In June, the University of California, San Francisco, experienced an information technology (IT) “security incident” that led to the payout of $1.14 million to individuals responsible for a malware attack in exchange for the return of data.
In addition, last week, Sky Lakes Medical Center in Klamath Falls, Ore., released a statement in which it said there had been a ransomware attack on its computer systems. Although “there is no evidence that patient information has been compromised,” some of its systems are still down.
“We’re open for business, it’s just not business as usual,” Tom Hottman, public information officer at Sky Lakes, said in an interview.
Paul S. Appelbaum, MD, Dollard Professor of Psychiatry, Medicine, and Law at Columbia University, New York, said in an interview, “People have known for a long time that there are nefarious actors out there.” He said all health care systems should be prepared to deal with these problems.
“In the face of a warning from the FBI, I’d say that’s even more important now,” Dr. Appelbaum added.
‘Malicious cyber actors’
In the new CISA report, the agency noted that it, the FBI, and the HHS have been assessing “malicious cyber actors” targeting health care systems with malware loaders such as TrickBot and BazarLoader, which often lead to data theft, ransomware attacks, and service disruptions.
“The cybercriminal enterprise behind TrickBot, which is likely also the creator of BazarLoader malware, has continued to develop new functionality and tools, increasing the ease, speed, and profitability of victimization,” the report authors wrote.
Phishing campaigns often contain attachments with malware or links to malicious websites. “Loaders start the infection chain by distributing the payload,” the report noted. A backdoor mechanism is then installed on the victim’s device.
In addition to TrickBot and BazarLoader (or BazarBackdoor), the report discussed other malicious tools, including Ryuk and Conti, which are types of ransomware that can infect systems for hackers’ financial gain.
“These issues will be particularly challenging for organizations within the COVID-19 pandemic; therefore, administrators will need to balance this risk when determining their cybersecurity investments,” the agencies wrote.
Dr. Appelbaum said his organization is taking the warning seriously.
“When the report first came out, I received emails from every system that I’m affiliated with warning about it and encouraging me as a member of the medical staff to take the usual prudent precautions,” such as not opening attachments or links from unknown sources, he said.
“The FBI warning has what seems like very reasonable advice, which is that every system should automatically back up their data off site in a separate system that’s differently accessible,” he added.
After a ransomware attack, the most recently entered information may not be backed up and could get lost, but “that’s a lot easier to deal with then losing access to all of your medical records,” said Dr. Appelbaum.
Ipsit Vahia, MD, medical director at the Institute for Technology and Psychiatry at McLean Hospital, Belmont, Mass., noted that, in answer to the FBI warning, he has heard that many centers, including his own, are warning their clinicians not to open any email attachments at this time.
Recent attacks
UCSF issued a statement noting that malware detected in early June led to the encryption of “a limited number of servers” in its medical school, making them temporarily inaccessible.
“We do not currently believe patient medical records were exposed,” the university said in the statement.
It added that because the encrypted data were necessary for “some of the academic work” conducted at UCSF, they agreed to pay a portion of the ransom demand – about $1.14 million. The hackers then provided a tool that unlocked the encrypted data.
“We continue to cooperate with law enforcement and we appreciate everyone’s understanding that we are limited in what we can share while we continue our investigation,” the statement reads. UCSF declined a request for further comment.
At Sky Lakes Medical Center, computer systems are still down after its ransomware attack, including use of electronic medical records, but the Oregon-based health care system is still seeing patients.
They are “being interviewed old school,” with the admitting process being conducted on paper, “but patient care goes on,” said Mr. Hottman.
In addition to a teaching hospital, Sky Lakes comprises specialty and primary care clinics, including a cancer treatment center. All remain open to patients at this time.
Diagnostic imaging is also continuing, but “getting the image to a place it can be read” has become more complicated, said Mr. Hottman.
“We have some work-arounds in process, and a plan is being assembled that we think will be in place as early as this weekend so that we can get those images read starting next week,” he said.
In addition, “scheduling is a little clunky,” he reported. However, “we have an awesome staff with a good attitude, so there’s still a whole lot we can do.”
He also noted that his institution has reconfirmed that, as of Nov. 4, no patient data had been compromised.
‘Especially chilling’
Targeting hospitals through cyberattacks isn’t new. In 2017, the WannaCry virus affected more than 200,000 computers in 150 countries, including the operating system of the U.K. National Health Service. The cyberattack locked clinicians out of NHS patient records and other digital tools for 3 days.
Dr. Appelbaum noted that, as hospital systems become more dependent on the Internet and on electronic communications, they become more vulnerable to data breaches.
“I think it’s clear that there have been concerted efforts lately to undertake attacks on health care IT systems to either hold them hostage, as in a ransomware attack, or to download files and use that information for profit,” he said.
Still, Dr. Vahia noted that contacting patients directly, which occurred in the Finland data breach and blackmail scheme, is something new. It is “especially chilling” that individual psychiatric patients were targeted.
It’s difficult to overstate how big a deal this is, and we should be treating it with the appropriate level of urgency,” he said in an interview.
“It shows how badly things can go wrong when security is compromised; and it should make us take a step back and survey the world of digital health to gain recognition of how much risk there might be that we haven’t really understood before,” Dr. Vahia said.
Clinical tips
Asked whether he had any tips to share with clinicians, Mr. Hottman noted that the best time to have a plan is before something dire happens.
“I would make [the possibility of cyberattacks] part of the emergency preparedness program. What if you don’t have access to computers? What do you do?” It’s important to answer those questions prior to systems going down, he said.
Mr. Hottman reported that after a mechanical failure last year put their computer systems offline for a day, “we started putting all critical information on paper and in a binder,” including phone numbers for the state police.
Dr. Vahia noted that another important step for clinicians “is to just pause and take stock of how digitally dependent” health care is becoming. He also warned that precautions should be taken regarding wearables and apps, as well as for electronic medical records. He noted the importance of strong passwords and two-step verification processes.
Even with the risks, digital technology has had a major impact on health care efficiency. “It’s not perfect, the work is ongoing, and there are big questions that need to be addressed, but in the end, the ability of technology when used right and securely” leads to better patient care, he said.
John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, agreed that digital health care is and will remain very important; but at the same time, security issues need proper attention.
“When you look back at medical hacks that have happened, there’s often a human error behind it. It’s rare for someone to break encryption. I think we have pretty darn good security, but we need to realize that sometimes errors will happen,” he said in an interview.
As an example, Dr. Torous, who is also chair of the American Psychiatric Association’s Health and Technology Committee, cited phishing emails, which depend on a user clicking a link that can cause a virus to be downloaded into their network.
“You can be cautious, but it takes just one person to download an attachment with a virus in it” to cause disruptions, Dr. Torous said.
Telehealth implications
After its data breach, Vastaamo posted on its website a notice that video is never recorded during the centers’ telehealth sessions, and so patients need not worry that any videos could be leaked online.
Asked whether video is commonly recorded during telehealth sessions in the United States, Dr. Vahia said that he was not aware of sessions being recorded, especially because the amount of the data would be too great to store indefinitely.
Dr. Appelbaum agreed and said that, to his knowledge, no clinicians at Columbia University are recording telehealth sessions. He said that it would represent a privacy threat, and he noted that most health care providers “don’t have the time to go back and watch videos of their interactions with patients.”
In the case of recordings for research purposes, he emphasized that it would be important to get consent and then store the health information offline.
As for other telehealth security risks, Dr. Vahia noted that it is possible that if a computer or device is compromised, an individual could hack into a camera and observe the session. In addition to microphones, “these pose some especially high vulnerabilities,” he said. “Clinicians need to pay attention as to whether the cameras they’re using for telecare are on or if they’re covered when not in use. And they should pay attention to security settings on smartphones and ensure microphones are not turned on as the default.”
Dr. Appelbaum said the HIPAA requires that telehealth sessions be conducted on secure systems, so clinicians need to ascertain whether the system they’re using complies with that rule.
“Particularly people who are not part of larger systems and would not usually take on that responsibility, maybe they’re in private practice or a small group, they really need to check on the security level and on HIPAA compliance and not just assume that it is adequately secure,” he said.
Dr. Appelbaum, who is also a past president of the APA and director of the Center for Law, Ethics, and Psychiatry at Columbia University, noted that the major risk for hospitals after a cyberattack is probably not liability to individual patients.
“It’s much more likely that they would face fines from HIPAA if it’s found that they failed to live up to HIPAA requirements,” he said.
A version of this article originally appeared on Medscape.com.
Amid recent reports of hackers targeting and blackmailing health care systems and even patients, the Federal Bureau of Investigation and other agencies have issued warning of “imminent” cyberattacks on more U.S. hospitals.
A new report released by the Cybersecurity and Infrastructure Security Agency, part of the Department of Homeland Security, noted that the FBI and the Department of Health & Human Services have “credible information of an increased and imminent cybercrime threat to U.S. hospitals and health care providers.”
The agencies are urging “timely and reasonable precautions” to protect health care networks from these threats.
As reported, hackers accessed patient records at Vastaamo, Finland’s largest private psychotherapy system, and emailed some patients last month demanding €200 in bitcoin or else personal health data would be released online.
In June, the University of California, San Francisco, experienced an information technology (IT) “security incident” that led to the payout of $1.14 million to individuals responsible for a malware attack in exchange for the return of data.
In addition, last week, Sky Lakes Medical Center in Klamath Falls, Ore., released a statement in which it said there had been a ransomware attack on its computer systems. Although “there is no evidence that patient information has been compromised,” some of its systems are still down.
“We’re open for business, it’s just not business as usual,” Tom Hottman, public information officer at Sky Lakes, said in an interview.
Paul S. Appelbaum, MD, Dollard Professor of Psychiatry, Medicine, and Law at Columbia University, New York, said in an interview, “People have known for a long time that there are nefarious actors out there.” He said all health care systems should be prepared to deal with these problems.
“In the face of a warning from the FBI, I’d say that’s even more important now,” Dr. Appelbaum added.
‘Malicious cyber actors’
In the new CISA report, the agency noted that it, the FBI, and the HHS have been assessing “malicious cyber actors” targeting health care systems with malware loaders such as TrickBot and BazarLoader, which often lead to data theft, ransomware attacks, and service disruptions.
“The cybercriminal enterprise behind TrickBot, which is likely also the creator of BazarLoader malware, has continued to develop new functionality and tools, increasing the ease, speed, and profitability of victimization,” the report authors wrote.
Phishing campaigns often contain attachments with malware or links to malicious websites. “Loaders start the infection chain by distributing the payload,” the report noted. A backdoor mechanism is then installed on the victim’s device.
In addition to TrickBot and BazarLoader (or BazarBackdoor), the report discussed other malicious tools, including Ryuk and Conti, which are types of ransomware that can infect systems for hackers’ financial gain.
“These issues will be particularly challenging for organizations within the COVID-19 pandemic; therefore, administrators will need to balance this risk when determining their cybersecurity investments,” the agencies wrote.
Dr. Appelbaum said his organization is taking the warning seriously.
“When the report first came out, I received emails from every system that I’m affiliated with warning about it and encouraging me as a member of the medical staff to take the usual prudent precautions,” such as not opening attachments or links from unknown sources, he said.
“The FBI warning has what seems like very reasonable advice, which is that every system should automatically back up their data off site in a separate system that’s differently accessible,” he added.
After a ransomware attack, the most recently entered information may not be backed up and could get lost, but “that’s a lot easier to deal with then losing access to all of your medical records,” said Dr. Appelbaum.
Ipsit Vahia, MD, medical director at the Institute for Technology and Psychiatry at McLean Hospital, Belmont, Mass., noted that, in answer to the FBI warning, he has heard that many centers, including his own, are warning their clinicians not to open any email attachments at this time.
Recent attacks
UCSF issued a statement noting that malware detected in early June led to the encryption of “a limited number of servers” in its medical school, making them temporarily inaccessible.
“We do not currently believe patient medical records were exposed,” the university said in the statement.
It added that because the encrypted data were necessary for “some of the academic work” conducted at UCSF, they agreed to pay a portion of the ransom demand – about $1.14 million. The hackers then provided a tool that unlocked the encrypted data.
“We continue to cooperate with law enforcement and we appreciate everyone’s understanding that we are limited in what we can share while we continue our investigation,” the statement reads. UCSF declined a request for further comment.
At Sky Lakes Medical Center, computer systems are still down after its ransomware attack, including use of electronic medical records, but the Oregon-based health care system is still seeing patients.
They are “being interviewed old school,” with the admitting process being conducted on paper, “but patient care goes on,” said Mr. Hottman.
In addition to a teaching hospital, Sky Lakes comprises specialty and primary care clinics, including a cancer treatment center. All remain open to patients at this time.
Diagnostic imaging is also continuing, but “getting the image to a place it can be read” has become more complicated, said Mr. Hottman.
“We have some work-arounds in process, and a plan is being assembled that we think will be in place as early as this weekend so that we can get those images read starting next week,” he said.
In addition, “scheduling is a little clunky,” he reported. However, “we have an awesome staff with a good attitude, so there’s still a whole lot we can do.”
He also noted that his institution has reconfirmed that, as of Nov. 4, no patient data had been compromised.
‘Especially chilling’
Targeting hospitals through cyberattacks isn’t new. In 2017, the WannaCry virus affected more than 200,000 computers in 150 countries, including the operating system of the U.K. National Health Service. The cyberattack locked clinicians out of NHS patient records and other digital tools for 3 days.
Dr. Appelbaum noted that, as hospital systems become more dependent on the Internet and on electronic communications, they become more vulnerable to data breaches.
“I think it’s clear that there have been concerted efforts lately to undertake attacks on health care IT systems to either hold them hostage, as in a ransomware attack, or to download files and use that information for profit,” he said.
Still, Dr. Vahia noted that contacting patients directly, which occurred in the Finland data breach and blackmail scheme, is something new. It is “especially chilling” that individual psychiatric patients were targeted.
It’s difficult to overstate how big a deal this is, and we should be treating it with the appropriate level of urgency,” he said in an interview.
“It shows how badly things can go wrong when security is compromised; and it should make us take a step back and survey the world of digital health to gain recognition of how much risk there might be that we haven’t really understood before,” Dr. Vahia said.
Clinical tips
Asked whether he had any tips to share with clinicians, Mr. Hottman noted that the best time to have a plan is before something dire happens.
“I would make [the possibility of cyberattacks] part of the emergency preparedness program. What if you don’t have access to computers? What do you do?” It’s important to answer those questions prior to systems going down, he said.
Mr. Hottman reported that after a mechanical failure last year put their computer systems offline for a day, “we started putting all critical information on paper and in a binder,” including phone numbers for the state police.
Dr. Vahia noted that another important step for clinicians “is to just pause and take stock of how digitally dependent” health care is becoming. He also warned that precautions should be taken regarding wearables and apps, as well as for electronic medical records. He noted the importance of strong passwords and two-step verification processes.
Even with the risks, digital technology has had a major impact on health care efficiency. “It’s not perfect, the work is ongoing, and there are big questions that need to be addressed, but in the end, the ability of technology when used right and securely” leads to better patient care, he said.
John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, agreed that digital health care is and will remain very important; but at the same time, security issues need proper attention.
“When you look back at medical hacks that have happened, there’s often a human error behind it. It’s rare for someone to break encryption. I think we have pretty darn good security, but we need to realize that sometimes errors will happen,” he said in an interview.
As an example, Dr. Torous, who is also chair of the American Psychiatric Association’s Health and Technology Committee, cited phishing emails, which depend on a user clicking a link that can cause a virus to be downloaded into their network.
“You can be cautious, but it takes just one person to download an attachment with a virus in it” to cause disruptions, Dr. Torous said.
Telehealth implications
After its data breach, Vastaamo posted on its website a notice that video is never recorded during the centers’ telehealth sessions, and so patients need not worry that any videos could be leaked online.
Asked whether video is commonly recorded during telehealth sessions in the United States, Dr. Vahia said that he was not aware of sessions being recorded, especially because the amount of the data would be too great to store indefinitely.
Dr. Appelbaum agreed and said that, to his knowledge, no clinicians at Columbia University are recording telehealth sessions. He said that it would represent a privacy threat, and he noted that most health care providers “don’t have the time to go back and watch videos of their interactions with patients.”
In the case of recordings for research purposes, he emphasized that it would be important to get consent and then store the health information offline.
As for other telehealth security risks, Dr. Vahia noted that it is possible that if a computer or device is compromised, an individual could hack into a camera and observe the session. In addition to microphones, “these pose some especially high vulnerabilities,” he said. “Clinicians need to pay attention as to whether the cameras they’re using for telecare are on or if they’re covered when not in use. And they should pay attention to security settings on smartphones and ensure microphones are not turned on as the default.”
Dr. Appelbaum said the HIPAA requires that telehealth sessions be conducted on secure systems, so clinicians need to ascertain whether the system they’re using complies with that rule.
“Particularly people who are not part of larger systems and would not usually take on that responsibility, maybe they’re in private practice or a small group, they really need to check on the security level and on HIPAA compliance and not just assume that it is adequately secure,” he said.
Dr. Appelbaum, who is also a past president of the APA and director of the Center for Law, Ethics, and Psychiatry at Columbia University, noted that the major risk for hospitals after a cyberattack is probably not liability to individual patients.
“It’s much more likely that they would face fines from HIPAA if it’s found that they failed to live up to HIPAA requirements,” he said.
A version of this article originally appeared on Medscape.com.
Security breach in Finland leads to psychiatric patient blackmail
Hackers have accessed patient records at Finland’s largest private psychotherapy system, emailing some patients to pay up or face having their private medical records released online.
Vastaamo treats about 40,000 patients and runs 25 centers across the country. Hackers emailed some of the centers’ patients asking for a blackmail payment of 200 euro in bitcoin, The Guardian reports.
Agencies such as the country’s National Bureau of Investigation are urging victims not to comply with the blackmailers’ demand and instead requesting that patients report these incidents to authorities and turn over incriminating emails. However, some data from patient records have already been released online.
“We deeply regret what happened and on behalf of our [patients] who have been compromised, we apologize for the shortcoming in data security, the consequences and human cost of which have been extremely heavy,” the center said in a statement. They added that the investigation into the situation is ongoing.
‘Sobering reminder’
In a comment, John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, Massachusetts, said this is “a sobering reminder that any digital data is subject to hacking.”
Torous is also chair of the American Psychiatric Association’s Health and Technology Committee.
“This is not the first time psychotherapy notes have been targeted and it actually happened, on a smaller scale, in the US in 2017,” he said.
In April of that year, confidential patient record information from a mental health center in Maine, including evaluations, session notes, and names of sex-abuse victims, was listed on the dark web.
Also in April, computer hackers released the WannaCry virus into the operating system of the United Kingdom’s National Health Service, which subsequently locked clinicians out of patient records and other digital tools for 3 days.
In addition, in 2016 hackers took Hollywood Presbyterian Medical Center in Los Angeles offline for more than a week after demanding a ransom of $3.6 million.
Criminal investigation
For Vastaamo, three of its employees were approached by the blackmailer via email at the end of September, the company reports. These incidents were immediately disclosed and the Central Criminal Police launched a criminal investigation.
In addition, several agencies were contacted, including the Finnish Cyber Security Center, the Data Protection Commission, and a cyber security company.
Investigators believe the breach, which led to the customer database theft, occurred back in November 2018. In addition, security “deficiencies” remained until March 2019.
“We do not know that the database was stolen after November 2018, but it is possible that individual data [have been] viewed or copied,” Vastaamo said in a press release. No additional “vulnerabilities were identified after March 2019.”
The center’s CEO, Ville Tapio, who did not disclose any of these incidents to the parent company and its board of directors, was subsequently fired.
Once the police investigation began, Vastaamo said it was not granted permission by the authorities to communicate the occurrence to its patients. However, after the blackmailer released some patient information online early on Oct. 21, permission to inform patients was granted.
The company noted that the blackmailer has started emailing victims, informing of the data breach, and demanding ransom. So far, the emails have not contained harmful digital content or “malware,” but authorities warn that any attachments should not be opened. The police have requested that such emails be kept so they can be used as evidence.
In a Q&A section on its website, Vastaamo noted that videos are never recorded during its centers’ telehealth sessions and patients should not be concerned about the possibility of leaked videos.
In addition, the cybercrime has not interrupted Vastaamo’s operations.
“The authorities and the response office will do their utmost to find out what happened, to prevent the dissemination of information, and to bring the perpetrators to justice,” the center said.
“The most important task ... is to support customers in the midst of an exceptionally serious and difficult situation,” it added.
“Worst-case scenario”
In a comment, Ipsit Vahia, MD, medical director at the Institute for Technology and Psychiatry at McLean Hospital, Belmont, Mass., said Vastaamo’s data breach “represents the worst-case scenario for digital health.”
He added that more information is needed about the specifics of the case, including exactly what happened, how the system was hacked, and what information was compromised.
Still, “it raises fundamental questions that healthcare systems, clinicians, and patients everywhere should be asking about what measures are in place to protect electronic medical records and other personal digital information,” said Dr. Vahia.
“This incident also serves as another reminder that the issue of data security and privacy is foundational to digital mental health. Ultimately, without a commitment from all stakeholders to maintaining the strictest levels of security, as well as transparency around how data are handled there will be little to no trust from clinicians or patients,” he said. All of that could prevent digital healthcare from achieving its full potential, he added.
In addition, Dr. Vahia noted that the rapid uptick of telemedicine because of the pandemic has accelerated the use of other forms of digital information in mental healthcare.
“This unfortunate incident should serve as a wake-up call and bring the issue of data protection back firmly into the spotlight,” said Dr. Vahia.
Now that telehealth has become a larger part of clinical practice, said Torous, it’s important for clinicians to be vigilant regarding security procedures.
“Telehealth and digital data are here to stay, and with them new benefits as well as risks. We can continue to work to minimize the risks and protect privacy while ensuring the benefits to patients expand,” he added.
This article first appeared on Medscape.com.
Hackers have accessed patient records at Finland’s largest private psychotherapy system, emailing some patients to pay up or face having their private medical records released online.
Vastaamo treats about 40,000 patients and runs 25 centers across the country. Hackers emailed some of the centers’ patients asking for a blackmail payment of 200 euro in bitcoin, The Guardian reports.
Agencies such as the country’s National Bureau of Investigation are urging victims not to comply with the blackmailers’ demand and instead requesting that patients report these incidents to authorities and turn over incriminating emails. However, some data from patient records have already been released online.
“We deeply regret what happened and on behalf of our [patients] who have been compromised, we apologize for the shortcoming in data security, the consequences and human cost of which have been extremely heavy,” the center said in a statement. They added that the investigation into the situation is ongoing.
‘Sobering reminder’
In a comment, John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, Massachusetts, said this is “a sobering reminder that any digital data is subject to hacking.”
Torous is also chair of the American Psychiatric Association’s Health and Technology Committee.
“This is not the first time psychotherapy notes have been targeted and it actually happened, on a smaller scale, in the US in 2017,” he said.
In April of that year, confidential patient record information from a mental health center in Maine, including evaluations, session notes, and names of sex-abuse victims, was listed on the dark web.
Also in April, computer hackers released the WannaCry virus into the operating system of the United Kingdom’s National Health Service, which subsequently locked clinicians out of patient records and other digital tools for 3 days.
In addition, in 2016 hackers took Hollywood Presbyterian Medical Center in Los Angeles offline for more than a week after demanding a ransom of $3.6 million.
Criminal investigation
For Vastaamo, three of its employees were approached by the blackmailer via email at the end of September, the company reports. These incidents were immediately disclosed and the Central Criminal Police launched a criminal investigation.
In addition, several agencies were contacted, including the Finnish Cyber Security Center, the Data Protection Commission, and a cyber security company.
Investigators believe the breach, which led to the customer database theft, occurred back in November 2018. In addition, security “deficiencies” remained until March 2019.
“We do not know that the database was stolen after November 2018, but it is possible that individual data [have been] viewed or copied,” Vastaamo said in a press release. No additional “vulnerabilities were identified after March 2019.”
The center’s CEO, Ville Tapio, who did not disclose any of these incidents to the parent company and its board of directors, was subsequently fired.
Once the police investigation began, Vastaamo said it was not granted permission by the authorities to communicate the occurrence to its patients. However, after the blackmailer released some patient information online early on Oct. 21, permission to inform patients was granted.
The company noted that the blackmailer has started emailing victims, informing of the data breach, and demanding ransom. So far, the emails have not contained harmful digital content or “malware,” but authorities warn that any attachments should not be opened. The police have requested that such emails be kept so they can be used as evidence.
In a Q&A section on its website, Vastaamo noted that videos are never recorded during its centers’ telehealth sessions and patients should not be concerned about the possibility of leaked videos.
In addition, the cybercrime has not interrupted Vastaamo’s operations.
“The authorities and the response office will do their utmost to find out what happened, to prevent the dissemination of information, and to bring the perpetrators to justice,” the center said.
“The most important task ... is to support customers in the midst of an exceptionally serious and difficult situation,” it added.
“Worst-case scenario”
In a comment, Ipsit Vahia, MD, medical director at the Institute for Technology and Psychiatry at McLean Hospital, Belmont, Mass., said Vastaamo’s data breach “represents the worst-case scenario for digital health.”
He added that more information is needed about the specifics of the case, including exactly what happened, how the system was hacked, and what information was compromised.
Still, “it raises fundamental questions that healthcare systems, clinicians, and patients everywhere should be asking about what measures are in place to protect electronic medical records and other personal digital information,” said Dr. Vahia.
“This incident also serves as another reminder that the issue of data security and privacy is foundational to digital mental health. Ultimately, without a commitment from all stakeholders to maintaining the strictest levels of security, as well as transparency around how data are handled there will be little to no trust from clinicians or patients,” he said. All of that could prevent digital healthcare from achieving its full potential, he added.
In addition, Dr. Vahia noted that the rapid uptick of telemedicine because of the pandemic has accelerated the use of other forms of digital information in mental healthcare.
“This unfortunate incident should serve as a wake-up call and bring the issue of data protection back firmly into the spotlight,” said Dr. Vahia.
Now that telehealth has become a larger part of clinical practice, said Torous, it’s important for clinicians to be vigilant regarding security procedures.
“Telehealth and digital data are here to stay, and with them new benefits as well as risks. We can continue to work to minimize the risks and protect privacy while ensuring the benefits to patients expand,” he added.
This article first appeared on Medscape.com.
Hackers have accessed patient records at Finland’s largest private psychotherapy system, emailing some patients to pay up or face having their private medical records released online.
Vastaamo treats about 40,000 patients and runs 25 centers across the country. Hackers emailed some of the centers’ patients asking for a blackmail payment of 200 euro in bitcoin, The Guardian reports.
Agencies such as the country’s National Bureau of Investigation are urging victims not to comply with the blackmailers’ demand and instead requesting that patients report these incidents to authorities and turn over incriminating emails. However, some data from patient records have already been released online.
“We deeply regret what happened and on behalf of our [patients] who have been compromised, we apologize for the shortcoming in data security, the consequences and human cost of which have been extremely heavy,” the center said in a statement. They added that the investigation into the situation is ongoing.
‘Sobering reminder’
In a comment, John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, Massachusetts, said this is “a sobering reminder that any digital data is subject to hacking.”
Torous is also chair of the American Psychiatric Association’s Health and Technology Committee.
“This is not the first time psychotherapy notes have been targeted and it actually happened, on a smaller scale, in the US in 2017,” he said.
In April of that year, confidential patient record information from a mental health center in Maine, including evaluations, session notes, and names of sex-abuse victims, was listed on the dark web.
Also in April, computer hackers released the WannaCry virus into the operating system of the United Kingdom’s National Health Service, which subsequently locked clinicians out of patient records and other digital tools for 3 days.
In addition, in 2016 hackers took Hollywood Presbyterian Medical Center in Los Angeles offline for more than a week after demanding a ransom of $3.6 million.
Criminal investigation
For Vastaamo, three of its employees were approached by the blackmailer via email at the end of September, the company reports. These incidents were immediately disclosed and the Central Criminal Police launched a criminal investigation.
In addition, several agencies were contacted, including the Finnish Cyber Security Center, the Data Protection Commission, and a cyber security company.
Investigators believe the breach, which led to the customer database theft, occurred back in November 2018. In addition, security “deficiencies” remained until March 2019.
“We do not know that the database was stolen after November 2018, but it is possible that individual data [have been] viewed or copied,” Vastaamo said in a press release. No additional “vulnerabilities were identified after March 2019.”
The center’s CEO, Ville Tapio, who did not disclose any of these incidents to the parent company and its board of directors, was subsequently fired.
Once the police investigation began, Vastaamo said it was not granted permission by the authorities to communicate the occurrence to its patients. However, after the blackmailer released some patient information online early on Oct. 21, permission to inform patients was granted.
The company noted that the blackmailer has started emailing victims, informing of the data breach, and demanding ransom. So far, the emails have not contained harmful digital content or “malware,” but authorities warn that any attachments should not be opened. The police have requested that such emails be kept so they can be used as evidence.
In a Q&A section on its website, Vastaamo noted that videos are never recorded during its centers’ telehealth sessions and patients should not be concerned about the possibility of leaked videos.
In addition, the cybercrime has not interrupted Vastaamo’s operations.
“The authorities and the response office will do their utmost to find out what happened, to prevent the dissemination of information, and to bring the perpetrators to justice,” the center said.
“The most important task ... is to support customers in the midst of an exceptionally serious and difficult situation,” it added.
“Worst-case scenario”
In a comment, Ipsit Vahia, MD, medical director at the Institute for Technology and Psychiatry at McLean Hospital, Belmont, Mass., said Vastaamo’s data breach “represents the worst-case scenario for digital health.”
He added that more information is needed about the specifics of the case, including exactly what happened, how the system was hacked, and what information was compromised.
Still, “it raises fundamental questions that healthcare systems, clinicians, and patients everywhere should be asking about what measures are in place to protect electronic medical records and other personal digital information,” said Dr. Vahia.
“This incident also serves as another reminder that the issue of data security and privacy is foundational to digital mental health. Ultimately, without a commitment from all stakeholders to maintaining the strictest levels of security, as well as transparency around how data are handled there will be little to no trust from clinicians or patients,” he said. All of that could prevent digital healthcare from achieving its full potential, he added.
In addition, Dr. Vahia noted that the rapid uptick of telemedicine because of the pandemic has accelerated the use of other forms of digital information in mental healthcare.
“This unfortunate incident should serve as a wake-up call and bring the issue of data protection back firmly into the spotlight,” said Dr. Vahia.
Now that telehealth has become a larger part of clinical practice, said Torous, it’s important for clinicians to be vigilant regarding security procedures.
“Telehealth and digital data are here to stay, and with them new benefits as well as risks. We can continue to work to minimize the risks and protect privacy while ensuring the benefits to patients expand,” he added.
This article first appeared on Medscape.com.
Is patient suicide in psychiatry a medical error?
When Rodney Vivian, MD, a psychiatrist in Cincinnati, was sued for medical malpractice after a psychiatric inpatient died by suicide, he recalls being naive about the process and how difficult it would be. “I was thinking that truth and common sense would prevail. How stupid I was,” he said.
Although Dr. Vivian, who was at the time the medical director of a hospital psychiatric unit in Ohio, was found not liable in two appeals, the legal process dragged on for 6 years, creating an emotional roller coaster of sadness, fear, vulnerability, and anxiety.
“The lawsuit took a big chunk out of me, and there was a sense of unfairness. It was incredibly humiliating and destructive; and it did not make me a better person or psychiatrist,” Dr. Vivian said.
Dr. Vivian is just one of the many psychiatrists who have had their world turned upside down after a patient suicide. When such events occur, grief-stricken families often point the finger at the treating psychiatrist. Although lawsuits are rare in psychiatry, patient suicide can lead to a myriad of emotional, legal, and career consequences.
Tyler Black, MD, child and adolescent psychiatrist and assistant clinical professor at the University of British Columbia, Vancouver, likens patient suicide to “a nuclear bomb” but emphasizes the importance of not classifying such events as a medical error or assigning blame.
“Starting with the assumption that suicide is always avoidable is not evidence based,” Dr. Black said.
Although patient suicide can occur across medicine, the odds are alarmingly high in psychiatry.
“There’s at least a 50-50 chance that a psychiatrist is going to face the suicide of a patient,” said Eric Plakun, MD, medical director/CEO at the Austen Riggs Center, Stockbridge, Mass. a hospital-based facility that offers a continuum of psychiatric treatment. Quoting forensic psychiatrist Robert Simon, Dr. Plakun said: “There are two kinds of psychiatrists – those who have had a patient die by suicide, and those who will.”
Research from 2015 shows that, among specialists, psychiatrists are among the least likely to be sued. A 2007/2008 Physician Survey from the American Medical Association showed that 22.2% of psychiatrists had been sued for malpractice; the probability that they would face a claim each year was only 2.6%. However, failure to prevent suicide is one of the top reasons for lawsuits.
One report from 2008 suggests that 20%-68% of psychiatrists will lose a patient to suicide. A report cowritten by Dr. Plakun in 2005 notes that about one in six psychiatric interns and one in three psychiatric residents will experience a patient suicide some time during their training. The authors added that 50% of all psychiatrists will have a patient die by suicide during their career. That risk stays at about 50% for future patients even after a clinician experiences the death of a previous patient.
Although mental health professionals prevail in up to 80% of suicide-related malpractice cases, such events are still emotionally devastating for everyone involved.
When a patient dies by suicide, it is a huge event, he noted. “It fuels a lot of fear and a lot of guilt, worry, and sadness.”
Paul S. Appelbaum, MD, past president of the American Psychiatric Association and Dollard Professor of Psychiatry, Medicine, and Law at Columbia University, New York, noted that patient suicide will happen.
The problem with many administrators who talk about a target of “zero suicide” is that when suicide does occur, it can lead to the erroneous conclusion that someone is to blame, said Dr. Appelbaum, who is also director of the Center for Law, Ethics, and Psychiatry at Columbia University. “That’s not necessarily true and contributes to finger-pointing.”
Stopping the blame game
Dr. Black’s first experience as a psychiatry resident was arriving at the hospital and finding the body of a patient who had died by suicide by hanging. Although he did not know the patient, Dr. Black said he had a strong emotional response that was coupled with an intense and sometimes confusing reaction by the hospital administration, including what he called “nonsensical banning” of pencils on the ward.
Dr. Black is now the medical director of emergency psychiatry at BC Children’s Hospital in Vancouver and specializes in suicidology and emergency/crisis youth mental health care. He said during a recent live chat on Twitter that he does not predict suicide but instead “assesses risk,” meaning he examines potential risk factors in his patients.
“If systems and administrators (and consulting doctors) could recognize this, the ‘blame game’ would severely decrease. From the advocacy end, we have to stop seeing suicide as a ‘medical error,’ ” Dr. Black tweeted.
“There’s a strong administrative push, especially in the face of suicide, to dive into the [occurrence] as if it must be that an error was made,” he said in an interview.
To help counteract any potential finger-pointing, Dr. Black created a free-to-download patient risk assessment document called the Assessment of Suicide and Risk Inventory (ASARI) for use at every patient visit.
“ASARI was designed to walk an assessor through their thinking process such that they can put all of their thoughts down on one piece of paper. It makes it a better communication document, and it’s definitely better medicolegal documentation,” he said.
Dr. Appelbaum noted that, although having documentation is beneficial, “I don’t think that you necessarily need to separate actions that are ‘protective’ from actions that are intended to help a patient.”
However, he pointed out that, if a psychiatrist conforms to or exceeds the standard of care, including conducting appropriate suicide risk assessments, developing an appropriate treatment plan, and keeping comprehensive documentation, these measures “should provide an effective defense to claims of malpractice or negligence.”
‘Horrendous event’
Dr. Vivian said that, during his 40-year career in psychiatry, there have been about 12 “office patients” who died by suicide. However, nothing prepared him for the fallout from a lawsuit.
In 2010, a patient who had overdosed was transferred to the psychiatric unit of Mercy Health–Clermont (Ohio) Hospital, where Dr. Vivian was the admitting physician. Although the hospital staff was ordered to check on her every 15 minutes, her husband found her unconscious from a hanging attempt when he came to visit the next evening. After she was transferred to the ICU, she was taken off life support and died a few days later.
“It was a horrendous event,” Dr. Vivian said.
The family sued the hospital, and the matter was settled out of court without Dr. Vivian’s knowledge. The family also filed a separate lawsuit against Dr. Vivian, which went to trial 3 years later.
“My insurance company’s claims person was very supportive and wanted me to not settle. She agreed that I didn’t do anything wrong and that I needed to face this,” he added.
In the first trial, a jury found Dr. Vivian not liable. Six months later, the plaintiff’s attorney filed an appeal. A year after the first trial, the court of appeals also came back with a new ruling in his favor and, in a subsequent appeal, the Ohio Supreme Court also ruled in his favor.
Dr. Vivian noted that there really are no winners in these situations. “Even though the jury ruled in my favor, there was never a sense of ‘success.’ I could never feel good about what happened.” He was told the insurance company spent more than $300,000 on his defense.
Although he no longer performs psychiatric inpatient admissions, Dr. Vivian continues to work in private practice and provides psychiatric consultation to patients at a local medical center.
“I consider my work as a blessing in my life, and I continue to learn from my patients,” he said.
‘Will I be sued?’
Dr. Appelbaum noted there is a difference between a malpractice claim that may be filed and a “payout” to plaintiffs because of a negotiated resolution of a case or an award that is made at trial.
Malpractice insurers may raise the rates of a physician who has been found at fault in one or more legal actions in which financial settlements have been paid out, he said.
The issue in any malpractice case is whether the psychiatrist met the standard of care, which is traditionally defined as “skill and learning that is ordinarily possessed and exercised by members of that profession in good standing.”
“No physician is expected to be the guarantor of a good outcome of a case. Sometimes things go wrong. Merely because there’s a bad outcome, merely because a suicide has occurred, doesn’t mean that the psychiatrist was negligent,” Dr. Appelbaum said.
He believes all large centers should have a “clear-cut plan” in place to assist clinicians in the event of a patient suicide. Such plans should help in dealing with stress from losing a patient and should provide guidance about how to handle any potential lawsuit.
For those worried that a patient’s suicide will shadow them through their career, Dr. Appelbaum said that it can happen, especially in cases involving a financial settlement against the clinician.
Such cases must be reported to the national practitioner data bank, where they can be accessed by any licensing body in any state when physicians apply for a medical license.
In addition, Dr. Appelbaum pointed out that licensure, medical staff, and malpractice applications typically require disclosure of a history of successful or unsuccessful claims filed against a physician. Although that may be limited to the past 10 years, the requirement can go on indefinitely.
Beware how you share
Dr. Plakun noted that there is a sense of isolation for a clinician in cases of patient suicide and that physicians often turn inward. He added that, although it is important to talk with others, in institutions, this is best done in a “peer-review, protected space” – and perhaps with a lawyer present.
However, Dr. Appelbaum warned that sharing information, even in this type of setting, may not offer legal protection. Talking to others in order to get some emotional support is permitted once the statute of limitations for filing a claim has lapsed or if a claim has been closed.
Discussing a case of patient suicide with peers prior to that can have serious legal implications, he added. Colleagues can be called to testify in any resulting legal case and disclose what was said during such conversations.
“The typical advice that a risk manager, a claims manager, or an attorney would give to a clinician is, don’t talk to other people about it other than the lawyer or claims manager who’s dealing with the case,” he noted.
That said, there are three general exceptions to this rule. These include attorney-client privilege, any matters discussed with the physician’s own therapist, and, “depending on the state, there are varying protections for what’s considered ‘peer review.’ ”
For instance, when hospitals implement a formal review process after an event, what is said during discovery may be protected. However, not all states have such protection. That’s why it is important to understand what the law is in your particular state, said Dr. Appelbaum.
Support for psychiatrists
Kaz J. Nelson, MD, psychiatrist and associate professor at the University of Minnesota, Minneapolis, also works with high-risk populations, including those with acute suicidality and self-injury.
During a recent chat on patient suicide, Dr. Nelson tweeted: “Sadly in our field, suicide is not an IF but a WHEN. Don’t keep the inevitable shame and sadness to yourself.”
Dr. Nelson agreed with Dr. Black that it’s important to look into these occurrences as a quality improvement measure, but not as a way to assign blame. Preparing for potential patient loss “and having very solid, very supportive, very inclusive ‘postvention’ procedures” is critical, she noted. “When you don’t have these policies and procedures in place and have them very transparent, it creates a culture of silence around the issue.”
Dr. Plakun reiterated the importance of not staying silent. “We can’t simply surrender to the idea of not talking about patient suicide. We have to find a way to speak.”
A version of this story originally appeared on Medscape.com.
When Rodney Vivian, MD, a psychiatrist in Cincinnati, was sued for medical malpractice after a psychiatric inpatient died by suicide, he recalls being naive about the process and how difficult it would be. “I was thinking that truth and common sense would prevail. How stupid I was,” he said.
Although Dr. Vivian, who was at the time the medical director of a hospital psychiatric unit in Ohio, was found not liable in two appeals, the legal process dragged on for 6 years, creating an emotional roller coaster of sadness, fear, vulnerability, and anxiety.
“The lawsuit took a big chunk out of me, and there was a sense of unfairness. It was incredibly humiliating and destructive; and it did not make me a better person or psychiatrist,” Dr. Vivian said.
Dr. Vivian is just one of the many psychiatrists who have had their world turned upside down after a patient suicide. When such events occur, grief-stricken families often point the finger at the treating psychiatrist. Although lawsuits are rare in psychiatry, patient suicide can lead to a myriad of emotional, legal, and career consequences.
Tyler Black, MD, child and adolescent psychiatrist and assistant clinical professor at the University of British Columbia, Vancouver, likens patient suicide to “a nuclear bomb” but emphasizes the importance of not classifying such events as a medical error or assigning blame.
“Starting with the assumption that suicide is always avoidable is not evidence based,” Dr. Black said.
Although patient suicide can occur across medicine, the odds are alarmingly high in psychiatry.
“There’s at least a 50-50 chance that a psychiatrist is going to face the suicide of a patient,” said Eric Plakun, MD, medical director/CEO at the Austen Riggs Center, Stockbridge, Mass. a hospital-based facility that offers a continuum of psychiatric treatment. Quoting forensic psychiatrist Robert Simon, Dr. Plakun said: “There are two kinds of psychiatrists – those who have had a patient die by suicide, and those who will.”
Research from 2015 shows that, among specialists, psychiatrists are among the least likely to be sued. A 2007/2008 Physician Survey from the American Medical Association showed that 22.2% of psychiatrists had been sued for malpractice; the probability that they would face a claim each year was only 2.6%. However, failure to prevent suicide is one of the top reasons for lawsuits.
One report from 2008 suggests that 20%-68% of psychiatrists will lose a patient to suicide. A report cowritten by Dr. Plakun in 2005 notes that about one in six psychiatric interns and one in three psychiatric residents will experience a patient suicide some time during their training. The authors added that 50% of all psychiatrists will have a patient die by suicide during their career. That risk stays at about 50% for future patients even after a clinician experiences the death of a previous patient.
Although mental health professionals prevail in up to 80% of suicide-related malpractice cases, such events are still emotionally devastating for everyone involved.
When a patient dies by suicide, it is a huge event, he noted. “It fuels a lot of fear and a lot of guilt, worry, and sadness.”
Paul S. Appelbaum, MD, past president of the American Psychiatric Association and Dollard Professor of Psychiatry, Medicine, and Law at Columbia University, New York, noted that patient suicide will happen.
The problem with many administrators who talk about a target of “zero suicide” is that when suicide does occur, it can lead to the erroneous conclusion that someone is to blame, said Dr. Appelbaum, who is also director of the Center for Law, Ethics, and Psychiatry at Columbia University. “That’s not necessarily true and contributes to finger-pointing.”
Stopping the blame game
Dr. Black’s first experience as a psychiatry resident was arriving at the hospital and finding the body of a patient who had died by suicide by hanging. Although he did not know the patient, Dr. Black said he had a strong emotional response that was coupled with an intense and sometimes confusing reaction by the hospital administration, including what he called “nonsensical banning” of pencils on the ward.
Dr. Black is now the medical director of emergency psychiatry at BC Children’s Hospital in Vancouver and specializes in suicidology and emergency/crisis youth mental health care. He said during a recent live chat on Twitter that he does not predict suicide but instead “assesses risk,” meaning he examines potential risk factors in his patients.
“If systems and administrators (and consulting doctors) could recognize this, the ‘blame game’ would severely decrease. From the advocacy end, we have to stop seeing suicide as a ‘medical error,’ ” Dr. Black tweeted.
“There’s a strong administrative push, especially in the face of suicide, to dive into the [occurrence] as if it must be that an error was made,” he said in an interview.
To help counteract any potential finger-pointing, Dr. Black created a free-to-download patient risk assessment document called the Assessment of Suicide and Risk Inventory (ASARI) for use at every patient visit.
“ASARI was designed to walk an assessor through their thinking process such that they can put all of their thoughts down on one piece of paper. It makes it a better communication document, and it’s definitely better medicolegal documentation,” he said.
Dr. Appelbaum noted that, although having documentation is beneficial, “I don’t think that you necessarily need to separate actions that are ‘protective’ from actions that are intended to help a patient.”
However, he pointed out that, if a psychiatrist conforms to or exceeds the standard of care, including conducting appropriate suicide risk assessments, developing an appropriate treatment plan, and keeping comprehensive documentation, these measures “should provide an effective defense to claims of malpractice or negligence.”
‘Horrendous event’
Dr. Vivian said that, during his 40-year career in psychiatry, there have been about 12 “office patients” who died by suicide. However, nothing prepared him for the fallout from a lawsuit.
In 2010, a patient who had overdosed was transferred to the psychiatric unit of Mercy Health–Clermont (Ohio) Hospital, where Dr. Vivian was the admitting physician. Although the hospital staff was ordered to check on her every 15 minutes, her husband found her unconscious from a hanging attempt when he came to visit the next evening. After she was transferred to the ICU, she was taken off life support and died a few days later.
“It was a horrendous event,” Dr. Vivian said.
The family sued the hospital, and the matter was settled out of court without Dr. Vivian’s knowledge. The family also filed a separate lawsuit against Dr. Vivian, which went to trial 3 years later.
“My insurance company’s claims person was very supportive and wanted me to not settle. She agreed that I didn’t do anything wrong and that I needed to face this,” he added.
In the first trial, a jury found Dr. Vivian not liable. Six months later, the plaintiff’s attorney filed an appeal. A year after the first trial, the court of appeals also came back with a new ruling in his favor and, in a subsequent appeal, the Ohio Supreme Court also ruled in his favor.
Dr. Vivian noted that there really are no winners in these situations. “Even though the jury ruled in my favor, there was never a sense of ‘success.’ I could never feel good about what happened.” He was told the insurance company spent more than $300,000 on his defense.
Although he no longer performs psychiatric inpatient admissions, Dr. Vivian continues to work in private practice and provides psychiatric consultation to patients at a local medical center.
“I consider my work as a blessing in my life, and I continue to learn from my patients,” he said.
‘Will I be sued?’
Dr. Appelbaum noted there is a difference between a malpractice claim that may be filed and a “payout” to plaintiffs because of a negotiated resolution of a case or an award that is made at trial.
Malpractice insurers may raise the rates of a physician who has been found at fault in one or more legal actions in which financial settlements have been paid out, he said.
The issue in any malpractice case is whether the psychiatrist met the standard of care, which is traditionally defined as “skill and learning that is ordinarily possessed and exercised by members of that profession in good standing.”
“No physician is expected to be the guarantor of a good outcome of a case. Sometimes things go wrong. Merely because there’s a bad outcome, merely because a suicide has occurred, doesn’t mean that the psychiatrist was negligent,” Dr. Appelbaum said.
He believes all large centers should have a “clear-cut plan” in place to assist clinicians in the event of a patient suicide. Such plans should help in dealing with stress from losing a patient and should provide guidance about how to handle any potential lawsuit.
For those worried that a patient’s suicide will shadow them through their career, Dr. Appelbaum said that it can happen, especially in cases involving a financial settlement against the clinician.
Such cases must be reported to the national practitioner data bank, where they can be accessed by any licensing body in any state when physicians apply for a medical license.
In addition, Dr. Appelbaum pointed out that licensure, medical staff, and malpractice applications typically require disclosure of a history of successful or unsuccessful claims filed against a physician. Although that may be limited to the past 10 years, the requirement can go on indefinitely.
Beware how you share
Dr. Plakun noted that there is a sense of isolation for a clinician in cases of patient suicide and that physicians often turn inward. He added that, although it is important to talk with others, in institutions, this is best done in a “peer-review, protected space” – and perhaps with a lawyer present.
However, Dr. Appelbaum warned that sharing information, even in this type of setting, may not offer legal protection. Talking to others in order to get some emotional support is permitted once the statute of limitations for filing a claim has lapsed or if a claim has been closed.
Discussing a case of patient suicide with peers prior to that can have serious legal implications, he added. Colleagues can be called to testify in any resulting legal case and disclose what was said during such conversations.
“The typical advice that a risk manager, a claims manager, or an attorney would give to a clinician is, don’t talk to other people about it other than the lawyer or claims manager who’s dealing with the case,” he noted.
That said, there are three general exceptions to this rule. These include attorney-client privilege, any matters discussed with the physician’s own therapist, and, “depending on the state, there are varying protections for what’s considered ‘peer review.’ ”
For instance, when hospitals implement a formal review process after an event, what is said during discovery may be protected. However, not all states have such protection. That’s why it is important to understand what the law is in your particular state, said Dr. Appelbaum.
Support for psychiatrists
Kaz J. Nelson, MD, psychiatrist and associate professor at the University of Minnesota, Minneapolis, also works with high-risk populations, including those with acute suicidality and self-injury.
During a recent chat on patient suicide, Dr. Nelson tweeted: “Sadly in our field, suicide is not an IF but a WHEN. Don’t keep the inevitable shame and sadness to yourself.”
Dr. Nelson agreed with Dr. Black that it’s important to look into these occurrences as a quality improvement measure, but not as a way to assign blame. Preparing for potential patient loss “and having very solid, very supportive, very inclusive ‘postvention’ procedures” is critical, she noted. “When you don’t have these policies and procedures in place and have them very transparent, it creates a culture of silence around the issue.”
Dr. Plakun reiterated the importance of not staying silent. “We can’t simply surrender to the idea of not talking about patient suicide. We have to find a way to speak.”
A version of this story originally appeared on Medscape.com.
When Rodney Vivian, MD, a psychiatrist in Cincinnati, was sued for medical malpractice after a psychiatric inpatient died by suicide, he recalls being naive about the process and how difficult it would be. “I was thinking that truth and common sense would prevail. How stupid I was,” he said.
Although Dr. Vivian, who was at the time the medical director of a hospital psychiatric unit in Ohio, was found not liable in two appeals, the legal process dragged on for 6 years, creating an emotional roller coaster of sadness, fear, vulnerability, and anxiety.
“The lawsuit took a big chunk out of me, and there was a sense of unfairness. It was incredibly humiliating and destructive; and it did not make me a better person or psychiatrist,” Dr. Vivian said.
Dr. Vivian is just one of the many psychiatrists who have had their world turned upside down after a patient suicide. When such events occur, grief-stricken families often point the finger at the treating psychiatrist. Although lawsuits are rare in psychiatry, patient suicide can lead to a myriad of emotional, legal, and career consequences.
Tyler Black, MD, child and adolescent psychiatrist and assistant clinical professor at the University of British Columbia, Vancouver, likens patient suicide to “a nuclear bomb” but emphasizes the importance of not classifying such events as a medical error or assigning blame.
“Starting with the assumption that suicide is always avoidable is not evidence based,” Dr. Black said.
Although patient suicide can occur across medicine, the odds are alarmingly high in psychiatry.
“There’s at least a 50-50 chance that a psychiatrist is going to face the suicide of a patient,” said Eric Plakun, MD, medical director/CEO at the Austen Riggs Center, Stockbridge, Mass. a hospital-based facility that offers a continuum of psychiatric treatment. Quoting forensic psychiatrist Robert Simon, Dr. Plakun said: “There are two kinds of psychiatrists – those who have had a patient die by suicide, and those who will.”
Research from 2015 shows that, among specialists, psychiatrists are among the least likely to be sued. A 2007/2008 Physician Survey from the American Medical Association showed that 22.2% of psychiatrists had been sued for malpractice; the probability that they would face a claim each year was only 2.6%. However, failure to prevent suicide is one of the top reasons for lawsuits.
One report from 2008 suggests that 20%-68% of psychiatrists will lose a patient to suicide. A report cowritten by Dr. Plakun in 2005 notes that about one in six psychiatric interns and one in three psychiatric residents will experience a patient suicide some time during their training. The authors added that 50% of all psychiatrists will have a patient die by suicide during their career. That risk stays at about 50% for future patients even after a clinician experiences the death of a previous patient.
Although mental health professionals prevail in up to 80% of suicide-related malpractice cases, such events are still emotionally devastating for everyone involved.
When a patient dies by suicide, it is a huge event, he noted. “It fuels a lot of fear and a lot of guilt, worry, and sadness.”
Paul S. Appelbaum, MD, past president of the American Psychiatric Association and Dollard Professor of Psychiatry, Medicine, and Law at Columbia University, New York, noted that patient suicide will happen.
The problem with many administrators who talk about a target of “zero suicide” is that when suicide does occur, it can lead to the erroneous conclusion that someone is to blame, said Dr. Appelbaum, who is also director of the Center for Law, Ethics, and Psychiatry at Columbia University. “That’s not necessarily true and contributes to finger-pointing.”
Stopping the blame game
Dr. Black’s first experience as a psychiatry resident was arriving at the hospital and finding the body of a patient who had died by suicide by hanging. Although he did not know the patient, Dr. Black said he had a strong emotional response that was coupled with an intense and sometimes confusing reaction by the hospital administration, including what he called “nonsensical banning” of pencils on the ward.
Dr. Black is now the medical director of emergency psychiatry at BC Children’s Hospital in Vancouver and specializes in suicidology and emergency/crisis youth mental health care. He said during a recent live chat on Twitter that he does not predict suicide but instead “assesses risk,” meaning he examines potential risk factors in his patients.
“If systems and administrators (and consulting doctors) could recognize this, the ‘blame game’ would severely decrease. From the advocacy end, we have to stop seeing suicide as a ‘medical error,’ ” Dr. Black tweeted.
“There’s a strong administrative push, especially in the face of suicide, to dive into the [occurrence] as if it must be that an error was made,” he said in an interview.
To help counteract any potential finger-pointing, Dr. Black created a free-to-download patient risk assessment document called the Assessment of Suicide and Risk Inventory (ASARI) for use at every patient visit.
“ASARI was designed to walk an assessor through their thinking process such that they can put all of their thoughts down on one piece of paper. It makes it a better communication document, and it’s definitely better medicolegal documentation,” he said.
Dr. Appelbaum noted that, although having documentation is beneficial, “I don’t think that you necessarily need to separate actions that are ‘protective’ from actions that are intended to help a patient.”
However, he pointed out that, if a psychiatrist conforms to or exceeds the standard of care, including conducting appropriate suicide risk assessments, developing an appropriate treatment plan, and keeping comprehensive documentation, these measures “should provide an effective defense to claims of malpractice or negligence.”
‘Horrendous event’
Dr. Vivian said that, during his 40-year career in psychiatry, there have been about 12 “office patients” who died by suicide. However, nothing prepared him for the fallout from a lawsuit.
In 2010, a patient who had overdosed was transferred to the psychiatric unit of Mercy Health–Clermont (Ohio) Hospital, where Dr. Vivian was the admitting physician. Although the hospital staff was ordered to check on her every 15 minutes, her husband found her unconscious from a hanging attempt when he came to visit the next evening. After she was transferred to the ICU, she was taken off life support and died a few days later.
“It was a horrendous event,” Dr. Vivian said.
The family sued the hospital, and the matter was settled out of court without Dr. Vivian’s knowledge. The family also filed a separate lawsuit against Dr. Vivian, which went to trial 3 years later.
“My insurance company’s claims person was very supportive and wanted me to not settle. She agreed that I didn’t do anything wrong and that I needed to face this,” he added.
In the first trial, a jury found Dr. Vivian not liable. Six months later, the plaintiff’s attorney filed an appeal. A year after the first trial, the court of appeals also came back with a new ruling in his favor and, in a subsequent appeal, the Ohio Supreme Court also ruled in his favor.
Dr. Vivian noted that there really are no winners in these situations. “Even though the jury ruled in my favor, there was never a sense of ‘success.’ I could never feel good about what happened.” He was told the insurance company spent more than $300,000 on his defense.
Although he no longer performs psychiatric inpatient admissions, Dr. Vivian continues to work in private practice and provides psychiatric consultation to patients at a local medical center.
“I consider my work as a blessing in my life, and I continue to learn from my patients,” he said.
‘Will I be sued?’
Dr. Appelbaum noted there is a difference between a malpractice claim that may be filed and a “payout” to plaintiffs because of a negotiated resolution of a case or an award that is made at trial.
Malpractice insurers may raise the rates of a physician who has been found at fault in one or more legal actions in which financial settlements have been paid out, he said.
The issue in any malpractice case is whether the psychiatrist met the standard of care, which is traditionally defined as “skill and learning that is ordinarily possessed and exercised by members of that profession in good standing.”
“No physician is expected to be the guarantor of a good outcome of a case. Sometimes things go wrong. Merely because there’s a bad outcome, merely because a suicide has occurred, doesn’t mean that the psychiatrist was negligent,” Dr. Appelbaum said.
He believes all large centers should have a “clear-cut plan” in place to assist clinicians in the event of a patient suicide. Such plans should help in dealing with stress from losing a patient and should provide guidance about how to handle any potential lawsuit.
For those worried that a patient’s suicide will shadow them through their career, Dr. Appelbaum said that it can happen, especially in cases involving a financial settlement against the clinician.
Such cases must be reported to the national practitioner data bank, where they can be accessed by any licensing body in any state when physicians apply for a medical license.
In addition, Dr. Appelbaum pointed out that licensure, medical staff, and malpractice applications typically require disclosure of a history of successful or unsuccessful claims filed against a physician. Although that may be limited to the past 10 years, the requirement can go on indefinitely.
Beware how you share
Dr. Plakun noted that there is a sense of isolation for a clinician in cases of patient suicide and that physicians often turn inward. He added that, although it is important to talk with others, in institutions, this is best done in a “peer-review, protected space” – and perhaps with a lawyer present.
However, Dr. Appelbaum warned that sharing information, even in this type of setting, may not offer legal protection. Talking to others in order to get some emotional support is permitted once the statute of limitations for filing a claim has lapsed or if a claim has been closed.
Discussing a case of patient suicide with peers prior to that can have serious legal implications, he added. Colleagues can be called to testify in any resulting legal case and disclose what was said during such conversations.
“The typical advice that a risk manager, a claims manager, or an attorney would give to a clinician is, don’t talk to other people about it other than the lawyer or claims manager who’s dealing with the case,” he noted.
That said, there are three general exceptions to this rule. These include attorney-client privilege, any matters discussed with the physician’s own therapist, and, “depending on the state, there are varying protections for what’s considered ‘peer review.’ ”
For instance, when hospitals implement a formal review process after an event, what is said during discovery may be protected. However, not all states have such protection. That’s why it is important to understand what the law is in your particular state, said Dr. Appelbaum.
Support for psychiatrists
Kaz J. Nelson, MD, psychiatrist and associate professor at the University of Minnesota, Minneapolis, also works with high-risk populations, including those with acute suicidality and self-injury.
During a recent chat on patient suicide, Dr. Nelson tweeted: “Sadly in our field, suicide is not an IF but a WHEN. Don’t keep the inevitable shame and sadness to yourself.”
Dr. Nelson agreed with Dr. Black that it’s important to look into these occurrences as a quality improvement measure, but not as a way to assign blame. Preparing for potential patient loss “and having very solid, very supportive, very inclusive ‘postvention’ procedures” is critical, she noted. “When you don’t have these policies and procedures in place and have them very transparent, it creates a culture of silence around the issue.”
Dr. Plakun reiterated the importance of not staying silent. “We can’t simply surrender to the idea of not talking about patient suicide. We have to find a way to speak.”
A version of this story originally appeared on Medscape.com.
Substance use tied to increased COVID-19 risk
Substance use disorders (SUD), particularly opioid addiction and smoking, are tied to an increased risk for COVID-19 and serious adverse outcomes including hospitalization and death, new research suggests.
A study funded by the National Institutes of Health assessed electronic health records of more than 73 million patients in the United States. Although only 10.3% of the participants had an SUD, “they represented 15.6% of the COVID-19 cases,” the investigators reported.
In addition, those with a recent diagnosis of SUD were eight times more likely to develop COVID-19 versus those without such a diagnosis. For specific SUDs, the greatest risk was for those with an opioid addiction followed by those who were addicted to cigarettes.
coinvestigator Nora Volkow, MD, director of the National Institute on Drug Abuse, said in a press release.
It may also be harder for individuals with addiction to access health care services for a variety of reasons, including low socioeconomic status or stigma, she said in an interview.
Dr. Volkow said she has encountered patients with medical emergencies who refuse to seek treatment at the emergency department because of previous experiences where they have been mistreated and encountered discrimination, and “that’s really very tragic.”
The findings were published online Sept. 14 in Molecular Psychiatry.
Is nicotine protective?
Dr. Volkow, her fellow senior author Rong Xu, PhD, Case Western Reserve University, Cleveland, and their team conducted the study because data released before the pandemic showed a significant increase in opioid overdose in 2019. “We were in an opioid crisis where we again saw an increase in mortality associated with overdose – and then COVID comes along. So the question was how are people who are already struggling faring? And if they were getting infected [with the coronavirus], what happened to them?”
Patients with SUDs have multiple medical comorbidities that are known risk factors for COVID-19, Dr. Volkow noted.
However, the only specific SUD that has been previously studied in this context is tobacco use disorder, she said. A report from Chinese investigators released early in the pandemic showed that smokers were more likely to be infected by coronavirus and more likely to die from COVID-19.
Interestingly, a cross-sectional study published in April suggested that smoking may be protective against COVID, and Dr. Volkow noted that a clinical study currently being conducted in France is assessing whether wearing a nicotine patch has the potential to prevent the virus.
“That’s very different from looking at a chronic smoker,” she pointed out. “It’s a potential that nicotine as a chemical [could be] a preventive measure as opposed to saying smoking will prevent you from getting COVID.”
Patients with SUDs, said Dr. Volkow, “are likely to be at greater risk because of the effects of drugs in the metabolic system and the interfering with oxygenation in the pulmonary vessels.”
The retrospective case-control study included EHR data from 73.1 million patients. In the study population, 54% were women, 55% were White, 10% Black, 2% Asian, 1% Hispanic/Latino, and the others were classified as other or unknown.
EHRs were collected through June 15 at 360 hospitals in all 50 states and were deidentified to ensure privacy. SUDs included alcohol, tobacco, cannabis, opioid, and cocaine.
Racial disparities
Results showed that about 7.5 million participants had a previous SUD diagnosis; of these, 722,370 had been diagnosed within the past year.
Tobacco use disorder was the most common diagnosis (n = 6,414,580), followed by alcohol (1,264,990), cannabis (490,420), opioid (471,520), and cocaine (222,680).
In addition, 12,030 (60% women) were diagnosed with COVID-19 and 1,880 had both COVID-19 and an SUD.
Adjusted analyses revealed that those who had a recent diagnosis of SUD were at a significantly greater increased risk for COVID-19 than individuals without an SUD (adjusted odds ratio, 8.7; 95% confidence interval, 8.4-9.0; P < 10–30).
This increased risk was greatest in participants with opioid use disorder (aOR, 10.2; 95% CI, 9.1-11.5; P < 10–30), followed by those with tobacco use disorder (aOR, 8.2; 95% CI, 7.9 - 8.5; P < 10–30).
Alcohol, cocaine, and cannabis had aORs of 7.7, 6.5, and 5.3, respectively. The aOR for lifetime SUD and COVID-19 was 1.5.
Among all patients with COVID-19, hospitalization rates were significantly greater in those with an SUD (43.8%) versus those without (30.1%), as were death rates at 9.6% versus 6.6%, respectively.
Race was a significant risk factor. Black patients with a recent SUD diagnosis were twice as likely as White patients to develop COVID-19 (aOR, 2.2; P < 10–30), and those specifically with opioid use disorder were four times more likely to develop the disease (aOR, 4.2 P < 10–25).
Black patients with both COVID-19 and lifetime SUD also had greater hospitalization and death rates versus their White peers (50.7% vs. 35.2% and 13% vs. 8.6%, respectively).
“This surprised me,” Dr. Volkow noted. “You can see the emergence of the racial disparities even under these conditions of really negative outcomes.”
Vulnerable populations
Cancer; obesity; HIV; diabetes; cardiovascular disease; and chronic kidney, liver, and lung diseases, which are all risk factors for COVID-19, were more prevalent in the group of patients with a recent SUD diagnosis versus those without.
In addition, asthma, type 2 diabetes, hypertension, obesity, and chronic kidney disease were more prevalent in the Black patents with a recent SUD than in the White patients.
Overall, the findings “identify individuals with SUD as a vulnerable population, especially African Americans with SUDs, who are at significantly increased risk for COVID-19 and its adverse outcomes,” the investigators wrote.
The results also highlight “the need to screen and treat individuals with SUD as part of the strategy to control the pandemic while ensuring no disparities in access to healthcare support,” they added.
Dr. Volkow noted that “marginalization” often occurs for individuals with addiction, making it more difficult for them to access health care services.
“It is incumbent upon clinicians to meet the unique challenges of caring for this vulnerable population, just as they would any other high-risk group,” she said.
“Patients should not just be treated for COVID, but should also be provided with treatment for their substance use disorder,” Dr. Volkow added.
‘Pretty convincing’
Andrew J. Saxon, MD, professor in the department of psychiatry and behavioral sciences at the University of Washington, Seattle, called the findings interesting.
“I found it pretty convincing that people who have substance use disorders are probably at higher risk for getting COVID-19 infection and more complications once they are infected,” he said.
Dr. Saxon, who was not involved with the research, is also director of the Center of Excellence in Substance Addiction Treatment and Education and is a member of the American Psychiatric Association’s Council on Addiction Psychiatry.
He noted that an important point from the study was not just about a patient having an SUD being at increased risk for COVID-19 “and a more severe disease trajectory.” Other factors associated with having an SUD, such as increased comorbidities, also likely play a part.
Dr. Saxon agreed that the ongoing opioid epidemic combined with the pandemic led to a “perfect storm” of problems.
“We were making slow but some progress getting more people the medications they need [to treat opioid use disorder], but the pandemic coming along disrupted those efforts. A lot of health care entities had to shut down for a while, seeing patients only remotely,” which led to barriers as many clinicians needed to learn how to proceed using telehealth options, said Dr. Saxon.
Universal screening?
Asked whether physicians should screen all patients for SUDs, Dr. Saxon said it’s a complicated question.
“Screening for tobacco and alcohol has a really good evidence base and practices should be doing that. The stigma is there but it’s a lot less than with illegal substances,” he said.
Screening for illegal substances or misuse of prescription substances may not be a good idea in health care settings “when it’s something they can’t do anything about. If you’re going to screen, you would have to have either referral processes in place or treatment available in your facility,” Dr. Saxon said.
Opioid use disorder is “especially amenable to treatment in a primary care or health care setting with prescribers,” he noted.
However, stimulant or cannabis use disorders “require fairly intensive behavioral interventions that are not easy to deliver in many health care settings. And we don›t have the workforce trained up to provide those treatments as widely as they should be,” said Dr. Saxon.
“Unless there’s some way to treat the issue, what’s the point of screening for it? That just creates frustration for patients and clinicians, as well,” he said. “It’s something we’re moving toward but we’re not quite there yet.”
The report authors and Dr. Saxon have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Substance use disorders (SUD), particularly opioid addiction and smoking, are tied to an increased risk for COVID-19 and serious adverse outcomes including hospitalization and death, new research suggests.
A study funded by the National Institutes of Health assessed electronic health records of more than 73 million patients in the United States. Although only 10.3% of the participants had an SUD, “they represented 15.6% of the COVID-19 cases,” the investigators reported.
In addition, those with a recent diagnosis of SUD were eight times more likely to develop COVID-19 versus those without such a diagnosis. For specific SUDs, the greatest risk was for those with an opioid addiction followed by those who were addicted to cigarettes.
coinvestigator Nora Volkow, MD, director of the National Institute on Drug Abuse, said in a press release.
It may also be harder for individuals with addiction to access health care services for a variety of reasons, including low socioeconomic status or stigma, she said in an interview.
Dr. Volkow said she has encountered patients with medical emergencies who refuse to seek treatment at the emergency department because of previous experiences where they have been mistreated and encountered discrimination, and “that’s really very tragic.”
The findings were published online Sept. 14 in Molecular Psychiatry.
Is nicotine protective?
Dr. Volkow, her fellow senior author Rong Xu, PhD, Case Western Reserve University, Cleveland, and their team conducted the study because data released before the pandemic showed a significant increase in opioid overdose in 2019. “We were in an opioid crisis where we again saw an increase in mortality associated with overdose – and then COVID comes along. So the question was how are people who are already struggling faring? And if they were getting infected [with the coronavirus], what happened to them?”
Patients with SUDs have multiple medical comorbidities that are known risk factors for COVID-19, Dr. Volkow noted.
However, the only specific SUD that has been previously studied in this context is tobacco use disorder, she said. A report from Chinese investigators released early in the pandemic showed that smokers were more likely to be infected by coronavirus and more likely to die from COVID-19.
Interestingly, a cross-sectional study published in April suggested that smoking may be protective against COVID, and Dr. Volkow noted that a clinical study currently being conducted in France is assessing whether wearing a nicotine patch has the potential to prevent the virus.
“That’s very different from looking at a chronic smoker,” she pointed out. “It’s a potential that nicotine as a chemical [could be] a preventive measure as opposed to saying smoking will prevent you from getting COVID.”
Patients with SUDs, said Dr. Volkow, “are likely to be at greater risk because of the effects of drugs in the metabolic system and the interfering with oxygenation in the pulmonary vessels.”
The retrospective case-control study included EHR data from 73.1 million patients. In the study population, 54% were women, 55% were White, 10% Black, 2% Asian, 1% Hispanic/Latino, and the others were classified as other or unknown.
EHRs were collected through June 15 at 360 hospitals in all 50 states and were deidentified to ensure privacy. SUDs included alcohol, tobacco, cannabis, opioid, and cocaine.
Racial disparities
Results showed that about 7.5 million participants had a previous SUD diagnosis; of these, 722,370 had been diagnosed within the past year.
Tobacco use disorder was the most common diagnosis (n = 6,414,580), followed by alcohol (1,264,990), cannabis (490,420), opioid (471,520), and cocaine (222,680).
In addition, 12,030 (60% women) were diagnosed with COVID-19 and 1,880 had both COVID-19 and an SUD.
Adjusted analyses revealed that those who had a recent diagnosis of SUD were at a significantly greater increased risk for COVID-19 than individuals without an SUD (adjusted odds ratio, 8.7; 95% confidence interval, 8.4-9.0; P < 10–30).
This increased risk was greatest in participants with opioid use disorder (aOR, 10.2; 95% CI, 9.1-11.5; P < 10–30), followed by those with tobacco use disorder (aOR, 8.2; 95% CI, 7.9 - 8.5; P < 10–30).
Alcohol, cocaine, and cannabis had aORs of 7.7, 6.5, and 5.3, respectively. The aOR for lifetime SUD and COVID-19 was 1.5.
Among all patients with COVID-19, hospitalization rates were significantly greater in those with an SUD (43.8%) versus those without (30.1%), as were death rates at 9.6% versus 6.6%, respectively.
Race was a significant risk factor. Black patients with a recent SUD diagnosis were twice as likely as White patients to develop COVID-19 (aOR, 2.2; P < 10–30), and those specifically with opioid use disorder were four times more likely to develop the disease (aOR, 4.2 P < 10–25).
Black patients with both COVID-19 and lifetime SUD also had greater hospitalization and death rates versus their White peers (50.7% vs. 35.2% and 13% vs. 8.6%, respectively).
“This surprised me,” Dr. Volkow noted. “You can see the emergence of the racial disparities even under these conditions of really negative outcomes.”
Vulnerable populations
Cancer; obesity; HIV; diabetes; cardiovascular disease; and chronic kidney, liver, and lung diseases, which are all risk factors for COVID-19, were more prevalent in the group of patients with a recent SUD diagnosis versus those without.
In addition, asthma, type 2 diabetes, hypertension, obesity, and chronic kidney disease were more prevalent in the Black patents with a recent SUD than in the White patients.
Overall, the findings “identify individuals with SUD as a vulnerable population, especially African Americans with SUDs, who are at significantly increased risk for COVID-19 and its adverse outcomes,” the investigators wrote.
The results also highlight “the need to screen and treat individuals with SUD as part of the strategy to control the pandemic while ensuring no disparities in access to healthcare support,” they added.
Dr. Volkow noted that “marginalization” often occurs for individuals with addiction, making it more difficult for them to access health care services.
“It is incumbent upon clinicians to meet the unique challenges of caring for this vulnerable population, just as they would any other high-risk group,” she said.
“Patients should not just be treated for COVID, but should also be provided with treatment for their substance use disorder,” Dr. Volkow added.
‘Pretty convincing’
Andrew J. Saxon, MD, professor in the department of psychiatry and behavioral sciences at the University of Washington, Seattle, called the findings interesting.
“I found it pretty convincing that people who have substance use disorders are probably at higher risk for getting COVID-19 infection and more complications once they are infected,” he said.
Dr. Saxon, who was not involved with the research, is also director of the Center of Excellence in Substance Addiction Treatment and Education and is a member of the American Psychiatric Association’s Council on Addiction Psychiatry.
He noted that an important point from the study was not just about a patient having an SUD being at increased risk for COVID-19 “and a more severe disease trajectory.” Other factors associated with having an SUD, such as increased comorbidities, also likely play a part.
Dr. Saxon agreed that the ongoing opioid epidemic combined with the pandemic led to a “perfect storm” of problems.
“We were making slow but some progress getting more people the medications they need [to treat opioid use disorder], but the pandemic coming along disrupted those efforts. A lot of health care entities had to shut down for a while, seeing patients only remotely,” which led to barriers as many clinicians needed to learn how to proceed using telehealth options, said Dr. Saxon.
Universal screening?
Asked whether physicians should screen all patients for SUDs, Dr. Saxon said it’s a complicated question.
“Screening for tobacco and alcohol has a really good evidence base and practices should be doing that. The stigma is there but it’s a lot less than with illegal substances,” he said.
Screening for illegal substances or misuse of prescription substances may not be a good idea in health care settings “when it’s something they can’t do anything about. If you’re going to screen, you would have to have either referral processes in place or treatment available in your facility,” Dr. Saxon said.
Opioid use disorder is “especially amenable to treatment in a primary care or health care setting with prescribers,” he noted.
However, stimulant or cannabis use disorders “require fairly intensive behavioral interventions that are not easy to deliver in many health care settings. And we don›t have the workforce trained up to provide those treatments as widely as they should be,” said Dr. Saxon.
“Unless there’s some way to treat the issue, what’s the point of screening for it? That just creates frustration for patients and clinicians, as well,” he said. “It’s something we’re moving toward but we’re not quite there yet.”
The report authors and Dr. Saxon have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Substance use disorders (SUD), particularly opioid addiction and smoking, are tied to an increased risk for COVID-19 and serious adverse outcomes including hospitalization and death, new research suggests.
A study funded by the National Institutes of Health assessed electronic health records of more than 73 million patients in the United States. Although only 10.3% of the participants had an SUD, “they represented 15.6% of the COVID-19 cases,” the investigators reported.
In addition, those with a recent diagnosis of SUD were eight times more likely to develop COVID-19 versus those without such a diagnosis. For specific SUDs, the greatest risk was for those with an opioid addiction followed by those who were addicted to cigarettes.
coinvestigator Nora Volkow, MD, director of the National Institute on Drug Abuse, said in a press release.
It may also be harder for individuals with addiction to access health care services for a variety of reasons, including low socioeconomic status or stigma, she said in an interview.
Dr. Volkow said she has encountered patients with medical emergencies who refuse to seek treatment at the emergency department because of previous experiences where they have been mistreated and encountered discrimination, and “that’s really very tragic.”
The findings were published online Sept. 14 in Molecular Psychiatry.
Is nicotine protective?
Dr. Volkow, her fellow senior author Rong Xu, PhD, Case Western Reserve University, Cleveland, and their team conducted the study because data released before the pandemic showed a significant increase in opioid overdose in 2019. “We were in an opioid crisis where we again saw an increase in mortality associated with overdose – and then COVID comes along. So the question was how are people who are already struggling faring? And if they were getting infected [with the coronavirus], what happened to them?”
Patients with SUDs have multiple medical comorbidities that are known risk factors for COVID-19, Dr. Volkow noted.
However, the only specific SUD that has been previously studied in this context is tobacco use disorder, she said. A report from Chinese investigators released early in the pandemic showed that smokers were more likely to be infected by coronavirus and more likely to die from COVID-19.
Interestingly, a cross-sectional study published in April suggested that smoking may be protective against COVID, and Dr. Volkow noted that a clinical study currently being conducted in France is assessing whether wearing a nicotine patch has the potential to prevent the virus.
“That’s very different from looking at a chronic smoker,” she pointed out. “It’s a potential that nicotine as a chemical [could be] a preventive measure as opposed to saying smoking will prevent you from getting COVID.”
Patients with SUDs, said Dr. Volkow, “are likely to be at greater risk because of the effects of drugs in the metabolic system and the interfering with oxygenation in the pulmonary vessels.”
The retrospective case-control study included EHR data from 73.1 million patients. In the study population, 54% were women, 55% were White, 10% Black, 2% Asian, 1% Hispanic/Latino, and the others were classified as other or unknown.
EHRs were collected through June 15 at 360 hospitals in all 50 states and were deidentified to ensure privacy. SUDs included alcohol, tobacco, cannabis, opioid, and cocaine.
Racial disparities
Results showed that about 7.5 million participants had a previous SUD diagnosis; of these, 722,370 had been diagnosed within the past year.
Tobacco use disorder was the most common diagnosis (n = 6,414,580), followed by alcohol (1,264,990), cannabis (490,420), opioid (471,520), and cocaine (222,680).
In addition, 12,030 (60% women) were diagnosed with COVID-19 and 1,880 had both COVID-19 and an SUD.
Adjusted analyses revealed that those who had a recent diagnosis of SUD were at a significantly greater increased risk for COVID-19 than individuals without an SUD (adjusted odds ratio, 8.7; 95% confidence interval, 8.4-9.0; P < 10–30).
This increased risk was greatest in participants with opioid use disorder (aOR, 10.2; 95% CI, 9.1-11.5; P < 10–30), followed by those with tobacco use disorder (aOR, 8.2; 95% CI, 7.9 - 8.5; P < 10–30).
Alcohol, cocaine, and cannabis had aORs of 7.7, 6.5, and 5.3, respectively. The aOR for lifetime SUD and COVID-19 was 1.5.
Among all patients with COVID-19, hospitalization rates were significantly greater in those with an SUD (43.8%) versus those without (30.1%), as were death rates at 9.6% versus 6.6%, respectively.
Race was a significant risk factor. Black patients with a recent SUD diagnosis were twice as likely as White patients to develop COVID-19 (aOR, 2.2; P < 10–30), and those specifically with opioid use disorder were four times more likely to develop the disease (aOR, 4.2 P < 10–25).
Black patients with both COVID-19 and lifetime SUD also had greater hospitalization and death rates versus their White peers (50.7% vs. 35.2% and 13% vs. 8.6%, respectively).
“This surprised me,” Dr. Volkow noted. “You can see the emergence of the racial disparities even under these conditions of really negative outcomes.”
Vulnerable populations
Cancer; obesity; HIV; diabetes; cardiovascular disease; and chronic kidney, liver, and lung diseases, which are all risk factors for COVID-19, were more prevalent in the group of patients with a recent SUD diagnosis versus those without.
In addition, asthma, type 2 diabetes, hypertension, obesity, and chronic kidney disease were more prevalent in the Black patents with a recent SUD than in the White patients.
Overall, the findings “identify individuals with SUD as a vulnerable population, especially African Americans with SUDs, who are at significantly increased risk for COVID-19 and its adverse outcomes,” the investigators wrote.
The results also highlight “the need to screen and treat individuals with SUD as part of the strategy to control the pandemic while ensuring no disparities in access to healthcare support,” they added.
Dr. Volkow noted that “marginalization” often occurs for individuals with addiction, making it more difficult for them to access health care services.
“It is incumbent upon clinicians to meet the unique challenges of caring for this vulnerable population, just as they would any other high-risk group,” she said.
“Patients should not just be treated for COVID, but should also be provided with treatment for their substance use disorder,” Dr. Volkow added.
‘Pretty convincing’
Andrew J. Saxon, MD, professor in the department of psychiatry and behavioral sciences at the University of Washington, Seattle, called the findings interesting.
“I found it pretty convincing that people who have substance use disorders are probably at higher risk for getting COVID-19 infection and more complications once they are infected,” he said.
Dr. Saxon, who was not involved with the research, is also director of the Center of Excellence in Substance Addiction Treatment and Education and is a member of the American Psychiatric Association’s Council on Addiction Psychiatry.
He noted that an important point from the study was not just about a patient having an SUD being at increased risk for COVID-19 “and a more severe disease trajectory.” Other factors associated with having an SUD, such as increased comorbidities, also likely play a part.
Dr. Saxon agreed that the ongoing opioid epidemic combined with the pandemic led to a “perfect storm” of problems.
“We were making slow but some progress getting more people the medications they need [to treat opioid use disorder], but the pandemic coming along disrupted those efforts. A lot of health care entities had to shut down for a while, seeing patients only remotely,” which led to barriers as many clinicians needed to learn how to proceed using telehealth options, said Dr. Saxon.
Universal screening?
Asked whether physicians should screen all patients for SUDs, Dr. Saxon said it’s a complicated question.
“Screening for tobacco and alcohol has a really good evidence base and practices should be doing that. The stigma is there but it’s a lot less than with illegal substances,” he said.
Screening for illegal substances or misuse of prescription substances may not be a good idea in health care settings “when it’s something they can’t do anything about. If you’re going to screen, you would have to have either referral processes in place or treatment available in your facility,” Dr. Saxon said.
Opioid use disorder is “especially amenable to treatment in a primary care or health care setting with prescribers,” he noted.
However, stimulant or cannabis use disorders “require fairly intensive behavioral interventions that are not easy to deliver in many health care settings. And we don›t have the workforce trained up to provide those treatments as widely as they should be,” said Dr. Saxon.
“Unless there’s some way to treat the issue, what’s the point of screening for it? That just creates frustration for patients and clinicians, as well,” he said. “It’s something we’re moving toward but we’re not quite there yet.”
The report authors and Dr. Saxon have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
TNF inhibitors linked to inflammatory CNS events
, new research suggests
The nested case-control study included more than 200 participants with diseases such as rheumatoid arthritis, psoriasis, and Crohn’s disease. Results showed that exposure to TNF inhibitors was significantly associated with increased risk for demyelinating CNS events, such as multiple sclerosis, and nondemyelinating events, such as meningitis and encephalitis.
Interestingly, disease-specific secondary analyses showed that the strongest association for inflammatory events was in patients with rheumatoid arthritis.
Lead author Amy Kunchok, MD, of Mayo Clinic, Rochester, Minn., noted that “these are highly effective therapies for patients” and that these CNS events are likely uncommon.
“Our study has observed an association, but this does not imply causality. Therefore, we are not cautioning against using these therapies in appropriate patients,” Dr. Kunchok said in an interview.
“Rather, we recommend that clinicians assessing patients with both inflammatory demyelinating and nondemyelinating CNS events consider a detailed evaluation of the medication history, particularly in patients with coexistent autoimmune diseases who may have a current or past history of biological therapies,” she said.
The findings were published in JAMA Neurology.
Poorly understood
TNF inhibitors “are common therapies for certain autoimmune diseases,” the investigators noted.
Previously, a link between exposure to these inhibitors and inflammatory CNS events “has been postulated but is poorly understood,” they wrote.
In the current study, they examined records for 106 patients who were treated at Mayo clinics in Minnesota, Arizona, or Florida from January 2003 through February 2019. All participants had been diagnosed with an autoimmune disease that the Food and Drug Administration has listed as an indication for TNF inhibitor use. This included rheumatoid arthritis (n = 48), ankylosing spondylitis (n = 4), psoriasis and psoriatic arthritis (n = 21), Crohn’s disease (n = 27), and ulcerative colitis (n = 6). Their records also showed diagnostic codes for the inflammatory demyelinating CNS events of relapsing-remitting or primary progressive MS, clinically isolated syndrome, radiologically isolated syndrome, neuromyelitis optica spectrum disorder, and transverse myelitis or for the inflammatory nondemyelinating CNS events of meningitis, meningoencephalitis, encephalitis, neurosarcoidosis, and CNS vasculitis. The investigators also included 106 age-, sex-, and autoimmune disease–matched participants 1:1 to act as the control group.
In the total study population, 64% were women and the median age at disease onset was 52 years. In addition, 60% of the patient group and 40% of the control group were exposed to TNF inhibitors.
Novel finding?
Results showed that TNF inhibitor exposure was significantly linked to increased risk for developing any inflammatory CNS event (adjusted odds ratio, 3.01; 95% CI, 1.55-5.82; P = .001). When the outcomes were stratified by class of inflammatory event, these results were similar. The aOR was 3.09 (95% CI, 1.19-8.04; P = .02) for inflammatory demyelinating CNS events and was 2.97 (95% CI, 1.15-7.65; P = .02) for inflammatory nondemyelinating events.
Dr. Kunchok noted that the association between the inhibitors and nondemyelinating events was “a novel finding from this study.”
In secondary analyses, patients with rheumatoid arthritis and exposure to TNF inhibitors had the strongest association with any inflammatory CNS event (aOR, 4.82; 95% CI, 1.62-14.36; P = .005).
A pooled cohort comprising only the participants with the other autoimmune diseases did not show a significant association between exposure to TNF inhibitors and development of CNS events (P = .09).
“Because of the lack of power, further stratification by individual autoimmune diseases was not analyzed,” the investigators reported.
Although the overall findings showed that exposure to TNF inhibitors was linked to increased risk for inflammatory events, whether this association “represents de novo or exacerbated inflammatory pathways requires further research,” the authors wrote.
Dr. Kunchok added that more research, especially population-based studies, is also needed to examine the incidence of these inflammatory CNS events in patients exposed to TNF-alpha inhibitors.
Adds to the literature
In an accompanying editorial, Jeffrey M. Gelfand, MD, department of neurology at the University of California, San Francisco, and Jinoos Yazdany, MD, Zuckerberg San Francisco General Hospital at UCSF, noted that although the study adds to the literature, the magnitude of the risk found “remains unclear.”
“Randomized clinical trials are not suited to the study of rare adverse events,” Dr. Gelfand and Dr. Yazdany wrote. They agree with Dr. Kunchok that “next steps should include population-based observational studies that control for disease severity.”
Still, the current study provides additional evidence of rare adverse events in patients receiving TNF inhibitors, they noted. So how should prescribers proceed?
“As with all treatments, the risk-benefit ratio for the individual patient’s situation must be weighed and appropriate counseling must be given to facilitate shared decision-making discussions,” wrote the editorialists.
“Given what is known about the risk of harm, avoiding TNF inhibitors is advisable in patients with known MS,” they wrote.
In addition, neurologic consultation can be helpful for clarifying diagnoses and providing advice on monitoring strategies for TNF inhibitor treatment in those with possible MS or other demyelinating conditions, noted the editorialists.
“In patients who develop new concerning neurological symptoms while receiving TNF inhibitor treatment, timely evaluation is indicated, including consideration of neuroinflammatory, infectious, and neurological diagnoses that may be unrelated to treatment,” they added.
“Broader awareness of risks that studies such as this one by Kunchok et al provide can ... encourage timelier recognition of potential TNF inhibitor–associated neuroinflammatory events and may improve outcomes for patients,” Dr. Gelfand and Dr. Yazdany concluded.
The study was funded by a grant from the National Center for Advancing Translational Sciences. Dr. Kunchok reports having received research funding from Biogen outside this study. A full list of disclosures for the other study authors is in the original article. Dr. Gelfand reports having received g rants for a clinical trial from Genentech and consulting fees from Biogen, Alexion, Theranica, Impel Neuropharma, Advanced Clinical, Biohaven, and Satsuma. Dr. Yazdany reports having received grants from Pfizer and consulting fees from AstraZeneca and Eli Lilly outside the submitted work.
A version of this article originally appeared on Medscape.com.
, new research suggests
The nested case-control study included more than 200 participants with diseases such as rheumatoid arthritis, psoriasis, and Crohn’s disease. Results showed that exposure to TNF inhibitors was significantly associated with increased risk for demyelinating CNS events, such as multiple sclerosis, and nondemyelinating events, such as meningitis and encephalitis.
Interestingly, disease-specific secondary analyses showed that the strongest association for inflammatory events was in patients with rheumatoid arthritis.
Lead author Amy Kunchok, MD, of Mayo Clinic, Rochester, Minn., noted that “these are highly effective therapies for patients” and that these CNS events are likely uncommon.
“Our study has observed an association, but this does not imply causality. Therefore, we are not cautioning against using these therapies in appropriate patients,” Dr. Kunchok said in an interview.
“Rather, we recommend that clinicians assessing patients with both inflammatory demyelinating and nondemyelinating CNS events consider a detailed evaluation of the medication history, particularly in patients with coexistent autoimmune diseases who may have a current or past history of biological therapies,” she said.
The findings were published in JAMA Neurology.
Poorly understood
TNF inhibitors “are common therapies for certain autoimmune diseases,” the investigators noted.
Previously, a link between exposure to these inhibitors and inflammatory CNS events “has been postulated but is poorly understood,” they wrote.
In the current study, they examined records for 106 patients who were treated at Mayo clinics in Minnesota, Arizona, or Florida from January 2003 through February 2019. All participants had been diagnosed with an autoimmune disease that the Food and Drug Administration has listed as an indication for TNF inhibitor use. This included rheumatoid arthritis (n = 48), ankylosing spondylitis (n = 4), psoriasis and psoriatic arthritis (n = 21), Crohn’s disease (n = 27), and ulcerative colitis (n = 6). Their records also showed diagnostic codes for the inflammatory demyelinating CNS events of relapsing-remitting or primary progressive MS, clinically isolated syndrome, radiologically isolated syndrome, neuromyelitis optica spectrum disorder, and transverse myelitis or for the inflammatory nondemyelinating CNS events of meningitis, meningoencephalitis, encephalitis, neurosarcoidosis, and CNS vasculitis. The investigators also included 106 age-, sex-, and autoimmune disease–matched participants 1:1 to act as the control group.
In the total study population, 64% were women and the median age at disease onset was 52 years. In addition, 60% of the patient group and 40% of the control group were exposed to TNF inhibitors.
Novel finding?
Results showed that TNF inhibitor exposure was significantly linked to increased risk for developing any inflammatory CNS event (adjusted odds ratio, 3.01; 95% CI, 1.55-5.82; P = .001). When the outcomes were stratified by class of inflammatory event, these results were similar. The aOR was 3.09 (95% CI, 1.19-8.04; P = .02) for inflammatory demyelinating CNS events and was 2.97 (95% CI, 1.15-7.65; P = .02) for inflammatory nondemyelinating events.
Dr. Kunchok noted that the association between the inhibitors and nondemyelinating events was “a novel finding from this study.”
In secondary analyses, patients with rheumatoid arthritis and exposure to TNF inhibitors had the strongest association with any inflammatory CNS event (aOR, 4.82; 95% CI, 1.62-14.36; P = .005).
A pooled cohort comprising only the participants with the other autoimmune diseases did not show a significant association between exposure to TNF inhibitors and development of CNS events (P = .09).
“Because of the lack of power, further stratification by individual autoimmune diseases was not analyzed,” the investigators reported.
Although the overall findings showed that exposure to TNF inhibitors was linked to increased risk for inflammatory events, whether this association “represents de novo or exacerbated inflammatory pathways requires further research,” the authors wrote.
Dr. Kunchok added that more research, especially population-based studies, is also needed to examine the incidence of these inflammatory CNS events in patients exposed to TNF-alpha inhibitors.
Adds to the literature
In an accompanying editorial, Jeffrey M. Gelfand, MD, department of neurology at the University of California, San Francisco, and Jinoos Yazdany, MD, Zuckerberg San Francisco General Hospital at UCSF, noted that although the study adds to the literature, the magnitude of the risk found “remains unclear.”
“Randomized clinical trials are not suited to the study of rare adverse events,” Dr. Gelfand and Dr. Yazdany wrote. They agree with Dr. Kunchok that “next steps should include population-based observational studies that control for disease severity.”
Still, the current study provides additional evidence of rare adverse events in patients receiving TNF inhibitors, they noted. So how should prescribers proceed?
“As with all treatments, the risk-benefit ratio for the individual patient’s situation must be weighed and appropriate counseling must be given to facilitate shared decision-making discussions,” wrote the editorialists.
“Given what is known about the risk of harm, avoiding TNF inhibitors is advisable in patients with known MS,” they wrote.
In addition, neurologic consultation can be helpful for clarifying diagnoses and providing advice on monitoring strategies for TNF inhibitor treatment in those with possible MS or other demyelinating conditions, noted the editorialists.
“In patients who develop new concerning neurological symptoms while receiving TNF inhibitor treatment, timely evaluation is indicated, including consideration of neuroinflammatory, infectious, and neurological diagnoses that may be unrelated to treatment,” they added.
“Broader awareness of risks that studies such as this one by Kunchok et al provide can ... encourage timelier recognition of potential TNF inhibitor–associated neuroinflammatory events and may improve outcomes for patients,” Dr. Gelfand and Dr. Yazdany concluded.
The study was funded by a grant from the National Center for Advancing Translational Sciences. Dr. Kunchok reports having received research funding from Biogen outside this study. A full list of disclosures for the other study authors is in the original article. Dr. Gelfand reports having received g rants for a clinical trial from Genentech and consulting fees from Biogen, Alexion, Theranica, Impel Neuropharma, Advanced Clinical, Biohaven, and Satsuma. Dr. Yazdany reports having received grants from Pfizer and consulting fees from AstraZeneca and Eli Lilly outside the submitted work.
A version of this article originally appeared on Medscape.com.
, new research suggests
The nested case-control study included more than 200 participants with diseases such as rheumatoid arthritis, psoriasis, and Crohn’s disease. Results showed that exposure to TNF inhibitors was significantly associated with increased risk for demyelinating CNS events, such as multiple sclerosis, and nondemyelinating events, such as meningitis and encephalitis.
Interestingly, disease-specific secondary analyses showed that the strongest association for inflammatory events was in patients with rheumatoid arthritis.
Lead author Amy Kunchok, MD, of Mayo Clinic, Rochester, Minn., noted that “these are highly effective therapies for patients” and that these CNS events are likely uncommon.
“Our study has observed an association, but this does not imply causality. Therefore, we are not cautioning against using these therapies in appropriate patients,” Dr. Kunchok said in an interview.
“Rather, we recommend that clinicians assessing patients with both inflammatory demyelinating and nondemyelinating CNS events consider a detailed evaluation of the medication history, particularly in patients with coexistent autoimmune diseases who may have a current or past history of biological therapies,” she said.
The findings were published in JAMA Neurology.
Poorly understood
TNF inhibitors “are common therapies for certain autoimmune diseases,” the investigators noted.
Previously, a link between exposure to these inhibitors and inflammatory CNS events “has been postulated but is poorly understood,” they wrote.
In the current study, they examined records for 106 patients who were treated at Mayo clinics in Minnesota, Arizona, or Florida from January 2003 through February 2019. All participants had been diagnosed with an autoimmune disease that the Food and Drug Administration has listed as an indication for TNF inhibitor use. This included rheumatoid arthritis (n = 48), ankylosing spondylitis (n = 4), psoriasis and psoriatic arthritis (n = 21), Crohn’s disease (n = 27), and ulcerative colitis (n = 6). Their records also showed diagnostic codes for the inflammatory demyelinating CNS events of relapsing-remitting or primary progressive MS, clinically isolated syndrome, radiologically isolated syndrome, neuromyelitis optica spectrum disorder, and transverse myelitis or for the inflammatory nondemyelinating CNS events of meningitis, meningoencephalitis, encephalitis, neurosarcoidosis, and CNS vasculitis. The investigators also included 106 age-, sex-, and autoimmune disease–matched participants 1:1 to act as the control group.
In the total study population, 64% were women and the median age at disease onset was 52 years. In addition, 60% of the patient group and 40% of the control group were exposed to TNF inhibitors.
Novel finding?
Results showed that TNF inhibitor exposure was significantly linked to increased risk for developing any inflammatory CNS event (adjusted odds ratio, 3.01; 95% CI, 1.55-5.82; P = .001). When the outcomes were stratified by class of inflammatory event, these results were similar. The aOR was 3.09 (95% CI, 1.19-8.04; P = .02) for inflammatory demyelinating CNS events and was 2.97 (95% CI, 1.15-7.65; P = .02) for inflammatory nondemyelinating events.
Dr. Kunchok noted that the association between the inhibitors and nondemyelinating events was “a novel finding from this study.”
In secondary analyses, patients with rheumatoid arthritis and exposure to TNF inhibitors had the strongest association with any inflammatory CNS event (aOR, 4.82; 95% CI, 1.62-14.36; P = .005).
A pooled cohort comprising only the participants with the other autoimmune diseases did not show a significant association between exposure to TNF inhibitors and development of CNS events (P = .09).
“Because of the lack of power, further stratification by individual autoimmune diseases was not analyzed,” the investigators reported.
Although the overall findings showed that exposure to TNF inhibitors was linked to increased risk for inflammatory events, whether this association “represents de novo or exacerbated inflammatory pathways requires further research,” the authors wrote.
Dr. Kunchok added that more research, especially population-based studies, is also needed to examine the incidence of these inflammatory CNS events in patients exposed to TNF-alpha inhibitors.
Adds to the literature
In an accompanying editorial, Jeffrey M. Gelfand, MD, department of neurology at the University of California, San Francisco, and Jinoos Yazdany, MD, Zuckerberg San Francisco General Hospital at UCSF, noted that although the study adds to the literature, the magnitude of the risk found “remains unclear.”
“Randomized clinical trials are not suited to the study of rare adverse events,” Dr. Gelfand and Dr. Yazdany wrote. They agree with Dr. Kunchok that “next steps should include population-based observational studies that control for disease severity.”
Still, the current study provides additional evidence of rare adverse events in patients receiving TNF inhibitors, they noted. So how should prescribers proceed?
“As with all treatments, the risk-benefit ratio for the individual patient’s situation must be weighed and appropriate counseling must be given to facilitate shared decision-making discussions,” wrote the editorialists.
“Given what is known about the risk of harm, avoiding TNF inhibitors is advisable in patients with known MS,” they wrote.
In addition, neurologic consultation can be helpful for clarifying diagnoses and providing advice on monitoring strategies for TNF inhibitor treatment in those with possible MS or other demyelinating conditions, noted the editorialists.
“In patients who develop new concerning neurological symptoms while receiving TNF inhibitor treatment, timely evaluation is indicated, including consideration of neuroinflammatory, infectious, and neurological diagnoses that may be unrelated to treatment,” they added.
“Broader awareness of risks that studies such as this one by Kunchok et al provide can ... encourage timelier recognition of potential TNF inhibitor–associated neuroinflammatory events and may improve outcomes for patients,” Dr. Gelfand and Dr. Yazdany concluded.
The study was funded by a grant from the National Center for Advancing Translational Sciences. Dr. Kunchok reports having received research funding from Biogen outside this study. A full list of disclosures for the other study authors is in the original article. Dr. Gelfand reports having received g rants for a clinical trial from Genentech and consulting fees from Biogen, Alexion, Theranica, Impel Neuropharma, Advanced Clinical, Biohaven, and Satsuma. Dr. Yazdany reports having received grants from Pfizer and consulting fees from AstraZeneca and Eli Lilly outside the submitted work.
A version of this article originally appeared on Medscape.com.
FDA approves ofatumumab (Kesimpta) for relapsing forms of MS
including relapsing-remitting MS, active secondary progressive MS, and clinically isolated syndrome, Novartis announced in a press release. This is the first FDA approval of a self-administered, targeted B-cell therapy for these conditions, and is delivered via an autoinjector pen.
“This approval is wonderful news for patients with relapsing multiple sclerosis,” Stephen Hauser, MD, director of the Weill Institute for Neurosciences at the University of California, San Francisco, said in the press release. “Through its favorable safety profile and well-tolerated monthly injection regimen, patients can self-administer the treatment at home, avoiding visits to the infusion center,” he noted.
Dr. Hauser is cochair of the steering committee for the phase 3 ASCLEPIOS I and II studies that were part of the basis for the FDA’s approval.
Bruce Bebo, PhD, executive vice president of research at the National MS Society, said because response to disease-modifying treatments varies among individuals with MS, it’s important to have a range of treatment options available with differing mechanisms of action. “We are pleased to have an additional option approved for the treatment of relapsing forms of MS,” he said.
Twin studies
Formerly known as OMB157, ofatumumab is a precisely-dosed anti-CD20 monoclonal antibody administered subcutaneously via once-monthly injection. However, Novartis noted that initial doses are given at weeks 0, 1, and 2 – with the first injection occurring with a health care professional present.
The drug “is thought to work by binding to a distinct epitope on the CD20 molecule inducing potent B-cell lysis and depletion,” the manufacturer noted.
As previously reported, results for the ACLEPIOS I and II studies were presented at the 2019 Congress of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS), with additional results presented at the 2020 Virtual Annual Meeting of the Consortium of Multiple Sclerosis Centers. In addition, the findings were published in the New England Journal of Medicine.
The twin, identically designed phase 3 studies assessed the safety and efficacy of the drug at a monthly subcutaneous dose of 20 mg versus once daily teriflunomide 14-mg oral tablets. Together, the studies included 1,882 adult patients at more than 350 sites in 37 countries.
Results showed that the study drug reduced the annualized relapse rate (ARR) by 51% in the first study and by 59% in the second versus teriflunomide (P < .001 in both studies), meeting the primary endpoint. Both studies also showed significant reductions of gadolinium-enhancing (Gd+) T1 lesions (by 98% and 94%, respectively) and new or enlarging T2 lesions (by 82% and 85%).
The most commonly observed treatment-related adverse events for ofatumumab were upper respiratory tract infection, headache, and injection-related reactions.
Although the FDA first approved ofatumumab in 2009 for treating chronic lymphocytic leukemia (CLL), it was administered as a high-dose intravenous infusion by a healthcare provider. “This is a different dosing regimen and route of administration than was previously approved for the CLL indication,” the company noted.
The drug is expected to be available in the United States in September.
A version of this article originally appeared on Medscape.com.
including relapsing-remitting MS, active secondary progressive MS, and clinically isolated syndrome, Novartis announced in a press release. This is the first FDA approval of a self-administered, targeted B-cell therapy for these conditions, and is delivered via an autoinjector pen.
“This approval is wonderful news for patients with relapsing multiple sclerosis,” Stephen Hauser, MD, director of the Weill Institute for Neurosciences at the University of California, San Francisco, said in the press release. “Through its favorable safety profile and well-tolerated monthly injection regimen, patients can self-administer the treatment at home, avoiding visits to the infusion center,” he noted.
Dr. Hauser is cochair of the steering committee for the phase 3 ASCLEPIOS I and II studies that were part of the basis for the FDA’s approval.
Bruce Bebo, PhD, executive vice president of research at the National MS Society, said because response to disease-modifying treatments varies among individuals with MS, it’s important to have a range of treatment options available with differing mechanisms of action. “We are pleased to have an additional option approved for the treatment of relapsing forms of MS,” he said.
Twin studies
Formerly known as OMB157, ofatumumab is a precisely-dosed anti-CD20 monoclonal antibody administered subcutaneously via once-monthly injection. However, Novartis noted that initial doses are given at weeks 0, 1, and 2 – with the first injection occurring with a health care professional present.
The drug “is thought to work by binding to a distinct epitope on the CD20 molecule inducing potent B-cell lysis and depletion,” the manufacturer noted.
As previously reported, results for the ACLEPIOS I and II studies were presented at the 2019 Congress of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS), with additional results presented at the 2020 Virtual Annual Meeting of the Consortium of Multiple Sclerosis Centers. In addition, the findings were published in the New England Journal of Medicine.
The twin, identically designed phase 3 studies assessed the safety and efficacy of the drug at a monthly subcutaneous dose of 20 mg versus once daily teriflunomide 14-mg oral tablets. Together, the studies included 1,882 adult patients at more than 350 sites in 37 countries.
Results showed that the study drug reduced the annualized relapse rate (ARR) by 51% in the first study and by 59% in the second versus teriflunomide (P < .001 in both studies), meeting the primary endpoint. Both studies also showed significant reductions of gadolinium-enhancing (Gd+) T1 lesions (by 98% and 94%, respectively) and new or enlarging T2 lesions (by 82% and 85%).
The most commonly observed treatment-related adverse events for ofatumumab were upper respiratory tract infection, headache, and injection-related reactions.
Although the FDA first approved ofatumumab in 2009 for treating chronic lymphocytic leukemia (CLL), it was administered as a high-dose intravenous infusion by a healthcare provider. “This is a different dosing regimen and route of administration than was previously approved for the CLL indication,” the company noted.
The drug is expected to be available in the United States in September.
A version of this article originally appeared on Medscape.com.
including relapsing-remitting MS, active secondary progressive MS, and clinically isolated syndrome, Novartis announced in a press release. This is the first FDA approval of a self-administered, targeted B-cell therapy for these conditions, and is delivered via an autoinjector pen.
“This approval is wonderful news for patients with relapsing multiple sclerosis,” Stephen Hauser, MD, director of the Weill Institute for Neurosciences at the University of California, San Francisco, said in the press release. “Through its favorable safety profile and well-tolerated monthly injection regimen, patients can self-administer the treatment at home, avoiding visits to the infusion center,” he noted.
Dr. Hauser is cochair of the steering committee for the phase 3 ASCLEPIOS I and II studies that were part of the basis for the FDA’s approval.
Bruce Bebo, PhD, executive vice president of research at the National MS Society, said because response to disease-modifying treatments varies among individuals with MS, it’s important to have a range of treatment options available with differing mechanisms of action. “We are pleased to have an additional option approved for the treatment of relapsing forms of MS,” he said.
Twin studies
Formerly known as OMB157, ofatumumab is a precisely-dosed anti-CD20 monoclonal antibody administered subcutaneously via once-monthly injection. However, Novartis noted that initial doses are given at weeks 0, 1, and 2 – with the first injection occurring with a health care professional present.
The drug “is thought to work by binding to a distinct epitope on the CD20 molecule inducing potent B-cell lysis and depletion,” the manufacturer noted.
As previously reported, results for the ACLEPIOS I and II studies were presented at the 2019 Congress of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS), with additional results presented at the 2020 Virtual Annual Meeting of the Consortium of Multiple Sclerosis Centers. In addition, the findings were published in the New England Journal of Medicine.
The twin, identically designed phase 3 studies assessed the safety and efficacy of the drug at a monthly subcutaneous dose of 20 mg versus once daily teriflunomide 14-mg oral tablets. Together, the studies included 1,882 adult patients at more than 350 sites in 37 countries.
Results showed that the study drug reduced the annualized relapse rate (ARR) by 51% in the first study and by 59% in the second versus teriflunomide (P < .001 in both studies), meeting the primary endpoint. Both studies also showed significant reductions of gadolinium-enhancing (Gd+) T1 lesions (by 98% and 94%, respectively) and new or enlarging T2 lesions (by 82% and 85%).
The most commonly observed treatment-related adverse events for ofatumumab were upper respiratory tract infection, headache, and injection-related reactions.
Although the FDA first approved ofatumumab in 2009 for treating chronic lymphocytic leukemia (CLL), it was administered as a high-dose intravenous infusion by a healthcare provider. “This is a different dosing regimen and route of administration than was previously approved for the CLL indication,” the company noted.
The drug is expected to be available in the United States in September.
A version of this article originally appeared on Medscape.com.