User login
Flattening the curve: Viral graphic shows COVID-19 containment needs
Editor’s note: Find the latest COVID-19 news and guidance in Medscape’s Coronavirus Resource Center.
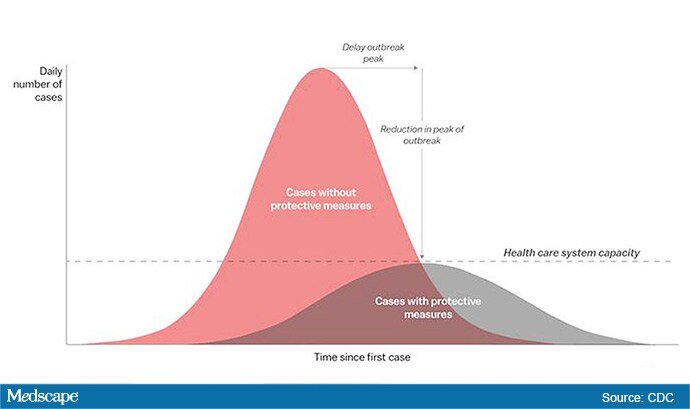
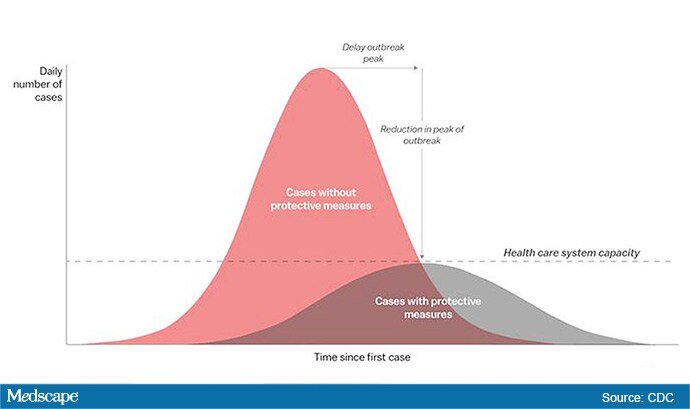
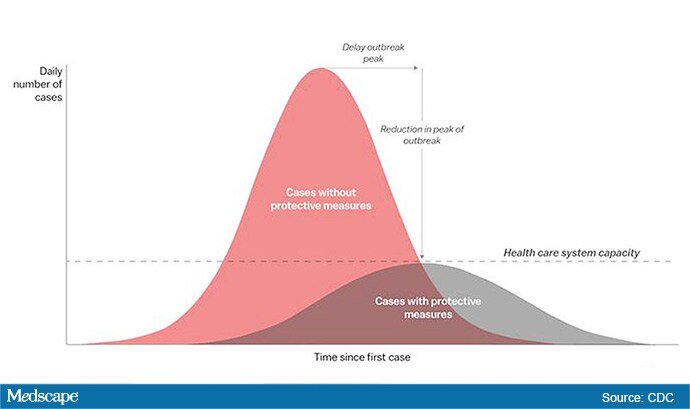
The “Flattening the Curve” graphic, which has, to not use the term lightly, gone viral on social media, visually explains the best currently available strategy to stop the COVID-19 spread, experts told Medscape Medical News.
The height of the curve is the number of potential cases in the United States; along the horizontal X axis, or the breadth, is the amount of time. The line across the middle represents the point at which too many cases in too short a time overwhelm the healthcare system.
Jeanne Marrazzo, MD, MPH, director of the Division of Infectious Diseases at the University of Alabama at Birmingham’s School of Medicine explained.
“Not only are you spreading out the new cases but the rate at which people recover,” she told Medscape Medical News. “You have time to get people out of the hospital so you can get new people in and clear out those beds.”
The strategy, with its own Twitter hashtag, #Flattenthecurve, “is about all we have,” without a vaccine, Marrazzo said.
Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, said avoiding spikes in cases could mean fewer deaths.
“If you look at the curves of outbreaks, you know, they go big peaks, and then they come down. What we need to do is flatten that down,” Fauci said March 10 in a White House briefing. “You do that by trying to interfere with the natural flow of the outbreak.”
Wuhan, China, at the epicenter of the pandemic, “had an explosive curve” and quickly got overwhelmed without early containment measures, Marrazzo noted. “If you look at Italy right now, it’s clearly in the same situation.”
The Race Is On to Interrupt the Spread
The race is on in the US to interrupt the transmission of the virus and slow the spread, meaning containment measures have increasingly higher and wider stakes.
Closing down Broadway shows and some theme parks and massive sporting events; the escalating numbers of people working from home; and businesses cutting hours or closing all demonstrate the level of US confidence that “social distancing” will work, Marrazzo said.
“We’re clearly ready to disrupt the economy and social infrastructure,” she said.
That appears to have made a difference in Wuhan, Marrazzo said, as the new infections are coming down.
The question, she said, is “we’re not China – so are Americans really going to take to this? Americans greatly value their liberty and there’s some skepticism about public health and its directives. People have never seen a pandemic like this before.”
Dena Grayson, MD, PhD, a Florida-based expert in Ebola and other pandemic threats, told Medscape Medical News that EvergreenHealth in Kirkland, Washington, is a good example of what it means when a virus overwhelms healthcare operations.
The New York Times reported that supplies were so strained at the facility that staff were using sanitary napkins to pad protective helmets.
As of March 11, 65 people who had come into the hospital have tested positive for the virus, and 15 of them had died.
Grayson points out that the COVID-19 cases come on top of a severe flu season and the usual cases hospitals see, so the bar on the graphic is even lower than it usually would be.
“We have a relatively limited capacity with ICU beds to begin with,” she said.
So far, closures, postponements, and cancellations are woefully inadequate, Grayson said.
“We can’t stop this virus. We can hope to contain it and slow down the rate of infection,” she said.
“We need to right now shut down all the schools, preschools, and universities,” Grayson said. “We need to look at shutting down public transportation. We need people to stay home – and not for a day but for a couple of weeks.”
The graphic was developed by visual-data journalist Rosamund Pearce, based on a graphic that had appeared in a Centers for Disease Control and Prevention (CDC) article titled “Community Mitigation Guidelines to Prevent Pandemic Influenza,” the Times reports.
Marrazzo and Grayson have disclosed no relevant financial relationships.
This story first appeared on Medscape.com .
Editor’s note: Find the latest COVID-19 news and guidance in Medscape’s Coronavirus Resource Center.
The “Flattening the Curve” graphic, which has, to not use the term lightly, gone viral on social media, visually explains the best currently available strategy to stop the COVID-19 spread, experts told Medscape Medical News.
The height of the curve is the number of potential cases in the United States; along the horizontal X axis, or the breadth, is the amount of time. The line across the middle represents the point at which too many cases in too short a time overwhelm the healthcare system.
Jeanne Marrazzo, MD, MPH, director of the Division of Infectious Diseases at the University of Alabama at Birmingham’s School of Medicine explained.
“Not only are you spreading out the new cases but the rate at which people recover,” she told Medscape Medical News. “You have time to get people out of the hospital so you can get new people in and clear out those beds.”
The strategy, with its own Twitter hashtag, #Flattenthecurve, “is about all we have,” without a vaccine, Marrazzo said.
Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, said avoiding spikes in cases could mean fewer deaths.
“If you look at the curves of outbreaks, you know, they go big peaks, and then they come down. What we need to do is flatten that down,” Fauci said March 10 in a White House briefing. “You do that by trying to interfere with the natural flow of the outbreak.”
Wuhan, China, at the epicenter of the pandemic, “had an explosive curve” and quickly got overwhelmed without early containment measures, Marrazzo noted. “If you look at Italy right now, it’s clearly in the same situation.”
The Race Is On to Interrupt the Spread
The race is on in the US to interrupt the transmission of the virus and slow the spread, meaning containment measures have increasingly higher and wider stakes.
Closing down Broadway shows and some theme parks and massive sporting events; the escalating numbers of people working from home; and businesses cutting hours or closing all demonstrate the level of US confidence that “social distancing” will work, Marrazzo said.
“We’re clearly ready to disrupt the economy and social infrastructure,” she said.
That appears to have made a difference in Wuhan, Marrazzo said, as the new infections are coming down.
The question, she said, is “we’re not China – so are Americans really going to take to this? Americans greatly value their liberty and there’s some skepticism about public health and its directives. People have never seen a pandemic like this before.”
Dena Grayson, MD, PhD, a Florida-based expert in Ebola and other pandemic threats, told Medscape Medical News that EvergreenHealth in Kirkland, Washington, is a good example of what it means when a virus overwhelms healthcare operations.
The New York Times reported that supplies were so strained at the facility that staff were using sanitary napkins to pad protective helmets.
As of March 11, 65 people who had come into the hospital have tested positive for the virus, and 15 of them had died.
Grayson points out that the COVID-19 cases come on top of a severe flu season and the usual cases hospitals see, so the bar on the graphic is even lower than it usually would be.
“We have a relatively limited capacity with ICU beds to begin with,” she said.
So far, closures, postponements, and cancellations are woefully inadequate, Grayson said.
“We can’t stop this virus. We can hope to contain it and slow down the rate of infection,” she said.
“We need to right now shut down all the schools, preschools, and universities,” Grayson said. “We need to look at shutting down public transportation. We need people to stay home – and not for a day but for a couple of weeks.”
The graphic was developed by visual-data journalist Rosamund Pearce, based on a graphic that had appeared in a Centers for Disease Control and Prevention (CDC) article titled “Community Mitigation Guidelines to Prevent Pandemic Influenza,” the Times reports.
Marrazzo and Grayson have disclosed no relevant financial relationships.
This story first appeared on Medscape.com .
Editor’s note: Find the latest COVID-19 news and guidance in Medscape’s Coronavirus Resource Center.
The “Flattening the Curve” graphic, which has, to not use the term lightly, gone viral on social media, visually explains the best currently available strategy to stop the COVID-19 spread, experts told Medscape Medical News.
The height of the curve is the number of potential cases in the United States; along the horizontal X axis, or the breadth, is the amount of time. The line across the middle represents the point at which too many cases in too short a time overwhelm the healthcare system.
Jeanne Marrazzo, MD, MPH, director of the Division of Infectious Diseases at the University of Alabama at Birmingham’s School of Medicine explained.
“Not only are you spreading out the new cases but the rate at which people recover,” she told Medscape Medical News. “You have time to get people out of the hospital so you can get new people in and clear out those beds.”
The strategy, with its own Twitter hashtag, #Flattenthecurve, “is about all we have,” without a vaccine, Marrazzo said.
Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, said avoiding spikes in cases could mean fewer deaths.
“If you look at the curves of outbreaks, you know, they go big peaks, and then they come down. What we need to do is flatten that down,” Fauci said March 10 in a White House briefing. “You do that by trying to interfere with the natural flow of the outbreak.”
Wuhan, China, at the epicenter of the pandemic, “had an explosive curve” and quickly got overwhelmed without early containment measures, Marrazzo noted. “If you look at Italy right now, it’s clearly in the same situation.”
The Race Is On to Interrupt the Spread
The race is on in the US to interrupt the transmission of the virus and slow the spread, meaning containment measures have increasingly higher and wider stakes.
Closing down Broadway shows and some theme parks and massive sporting events; the escalating numbers of people working from home; and businesses cutting hours or closing all demonstrate the level of US confidence that “social distancing” will work, Marrazzo said.
“We’re clearly ready to disrupt the economy and social infrastructure,” she said.
That appears to have made a difference in Wuhan, Marrazzo said, as the new infections are coming down.
The question, she said, is “we’re not China – so are Americans really going to take to this? Americans greatly value their liberty and there’s some skepticism about public health and its directives. People have never seen a pandemic like this before.”
Dena Grayson, MD, PhD, a Florida-based expert in Ebola and other pandemic threats, told Medscape Medical News that EvergreenHealth in Kirkland, Washington, is a good example of what it means when a virus overwhelms healthcare operations.
The New York Times reported that supplies were so strained at the facility that staff were using sanitary napkins to pad protective helmets.
As of March 11, 65 people who had come into the hospital have tested positive for the virus, and 15 of them had died.
Grayson points out that the COVID-19 cases come on top of a severe flu season and the usual cases hospitals see, so the bar on the graphic is even lower than it usually would be.
“We have a relatively limited capacity with ICU beds to begin with,” she said.
So far, closures, postponements, and cancellations are woefully inadequate, Grayson said.
“We can’t stop this virus. We can hope to contain it and slow down the rate of infection,” she said.
“We need to right now shut down all the schools, preschools, and universities,” Grayson said. “We need to look at shutting down public transportation. We need people to stay home – and not for a day but for a couple of weeks.”
The graphic was developed by visual-data journalist Rosamund Pearce, based on a graphic that had appeared in a Centers for Disease Control and Prevention (CDC) article titled “Community Mitigation Guidelines to Prevent Pandemic Influenza,” the Times reports.
Marrazzo and Grayson have disclosed no relevant financial relationships.
This story first appeared on Medscape.com .
Bad behavior by medical trainees target of new proposal
Some instances of unprofessional behavior by medical trainees are universally deemed egregious and worthy of discipline — for example, looking up a friend’s medical data after HIPAA training.
Conversely, some professionalism lapses may be widely thought of as a teaching and consoling moment, such as the human error involved in forgetting a scheduled repositioning of a patient.
But between the extremes is a vast gray area. To deal with those cases appropriately, Jason Wasserman, PhD, and colleagues propose a new framework by which to judge each infraction.
The framework draws from “just culture” concepts used to evaluate medical errors, Wasserman, associate professor of biomedical science at Oakland University William Beaumont School of Medicine in Rochester, Michigan, told Medscape Medical News. Such an approach takes into account the environment in which the error was made, the knowledge and intent of the person making the error, and the severity and consequences of the infraction so that trainees and institutions can learn from mistakes.
“Trainees by definition are not going to fully get it,” he explained. “By definition they’re not going to fully achieve professional expectations. So how can we respond to the things we need to respond to, but do it in a way that’s educational?”
Wasserman and coauthors’ framework for remediation, which they published February 20 in The New England Journal of Medicine, takes into account several questions: Was the expectation clear? Were there factors beyond the trainees› control? What were the trainees› intentions and did they understand the consequences? Did the person genuinely believe the action was inconsequential?
An example requiring discipline, the authors say, would be using a crib sheet during an exam. In that case the intent is clear, there is no defensible belief that the action is inconsequential, and there is a clear understanding the action is wrong.
But a response of “affirm, support, and advise” is more appropriate, for example, when a student’s alarm doesn’t go off after a power outage and they miss a mandatory meeting.
Wasserman points out that this framework won’t cover all situations.
“This is not an algorithm for answering your questions about what to do,” he said. “It’s an architecture for clarifying the discussion about that. It can really tease out all the threads that need to be considered to best respond to and correct the professionalism lapse, but do it in a way that is developmentally appropriate.”
A Core Competency
For two decades, professionalism has been considered a core competency of medical education. In 1999, the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties formalized it as such. In 2013, the Association of American Medical Colleges formally required related professionalism competencies.
However, identifying lapses has operated largely on an “I-know-it-when-I-see-it” basis, leading to widely varying remediation practices judged by a small number of faculty members or administrators.
The ideas outlined by Wasserman and colleagues are “a terrific application of the ‘just-culture’ framework,” according to Nicole Treadway, MD, a first-year primary care resident at Emory School of Medicine in Atlanta, Georgia.
At Emory, discussions of professionalism start from day 1 of medical school and the subject is revisited throughout training in small groups, Treadway told Medscape Medical News.
But, she said, as the authors point out, definitions of unprofessionalism are not always clear and the examples the authors put forward help put lapses in context.
The framework also allows for looking at mistakes in light of the stress trainees encounter and the greater chance of making a professionalism error in those situations, she noted.
In her own work, she says, because she is juggling both inpatient and outpatient care, she is finding it is easy to get behind on correspondence or communicating lab results or having follow-up conversations.
Those delays could be seen as lapses in professionalism, but under this framework, there may be system solutions or training opportunities to consider.
“We do need this organizational architecture, and I think it could serve us well in really helping us identify and appropriately respond to what we see regarding professionalism,” she said.
Framework Helps Standardize Thinking
She said having a universal framework also helps because while standards of professionalism are easier to monitor in a single medical school, when students scatter to other hospitals for clinical training, those hospitals may have different professionalism standards.
Wasserman agrees, saying, “This could be easily adopted in any environment where people deal with professionalism lapses. I don’t even think it’s necessarily relegated to trainees. It’s a great way to think about any kind of lapses, just as hospitals think about medical errors.”
He said the next step is presenting the framework at various medical schools for feedback and research to see whether the framework improves processes.
Potential criticism, he said, might come from those who say such a construct avoids punishing students who make errors.
“There will always be people who say we’re pandering to medical students whenever we worry about the learning environment,” he said. “There are old-school purists who say when people screw up you should punish them.”
But he adds healthcare broadly has moved past that thinking.
“People recognized 20 years ago or more from the standpoint of improving healthcare systems and safety that is a bad strategy. You’ll never get error-free humans working in your system, and what you have to do is consider how the system is functioning and think about ways to optimize the system so people can be their best within it.”
Wasserman and Treadway have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Some instances of unprofessional behavior by medical trainees are universally deemed egregious and worthy of discipline — for example, looking up a friend’s medical data after HIPAA training.
Conversely, some professionalism lapses may be widely thought of as a teaching and consoling moment, such as the human error involved in forgetting a scheduled repositioning of a patient.
But between the extremes is a vast gray area. To deal with those cases appropriately, Jason Wasserman, PhD, and colleagues propose a new framework by which to judge each infraction.
The framework draws from “just culture” concepts used to evaluate medical errors, Wasserman, associate professor of biomedical science at Oakland University William Beaumont School of Medicine in Rochester, Michigan, told Medscape Medical News. Such an approach takes into account the environment in which the error was made, the knowledge and intent of the person making the error, and the severity and consequences of the infraction so that trainees and institutions can learn from mistakes.
“Trainees by definition are not going to fully get it,” he explained. “By definition they’re not going to fully achieve professional expectations. So how can we respond to the things we need to respond to, but do it in a way that’s educational?”
Wasserman and coauthors’ framework for remediation, which they published February 20 in The New England Journal of Medicine, takes into account several questions: Was the expectation clear? Were there factors beyond the trainees› control? What were the trainees› intentions and did they understand the consequences? Did the person genuinely believe the action was inconsequential?
An example requiring discipline, the authors say, would be using a crib sheet during an exam. In that case the intent is clear, there is no defensible belief that the action is inconsequential, and there is a clear understanding the action is wrong.
But a response of “affirm, support, and advise” is more appropriate, for example, when a student’s alarm doesn’t go off after a power outage and they miss a mandatory meeting.
Wasserman points out that this framework won’t cover all situations.
“This is not an algorithm for answering your questions about what to do,” he said. “It’s an architecture for clarifying the discussion about that. It can really tease out all the threads that need to be considered to best respond to and correct the professionalism lapse, but do it in a way that is developmentally appropriate.”
A Core Competency
For two decades, professionalism has been considered a core competency of medical education. In 1999, the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties formalized it as such. In 2013, the Association of American Medical Colleges formally required related professionalism competencies.
However, identifying lapses has operated largely on an “I-know-it-when-I-see-it” basis, leading to widely varying remediation practices judged by a small number of faculty members or administrators.
The ideas outlined by Wasserman and colleagues are “a terrific application of the ‘just-culture’ framework,” according to Nicole Treadway, MD, a first-year primary care resident at Emory School of Medicine in Atlanta, Georgia.
At Emory, discussions of professionalism start from day 1 of medical school and the subject is revisited throughout training in small groups, Treadway told Medscape Medical News.
But, she said, as the authors point out, definitions of unprofessionalism are not always clear and the examples the authors put forward help put lapses in context.
The framework also allows for looking at mistakes in light of the stress trainees encounter and the greater chance of making a professionalism error in those situations, she noted.
In her own work, she says, because she is juggling both inpatient and outpatient care, she is finding it is easy to get behind on correspondence or communicating lab results or having follow-up conversations.
Those delays could be seen as lapses in professionalism, but under this framework, there may be system solutions or training opportunities to consider.
“We do need this organizational architecture, and I think it could serve us well in really helping us identify and appropriately respond to what we see regarding professionalism,” she said.
Framework Helps Standardize Thinking
She said having a universal framework also helps because while standards of professionalism are easier to monitor in a single medical school, when students scatter to other hospitals for clinical training, those hospitals may have different professionalism standards.
Wasserman agrees, saying, “This could be easily adopted in any environment where people deal with professionalism lapses. I don’t even think it’s necessarily relegated to trainees. It’s a great way to think about any kind of lapses, just as hospitals think about medical errors.”
He said the next step is presenting the framework at various medical schools for feedback and research to see whether the framework improves processes.
Potential criticism, he said, might come from those who say such a construct avoids punishing students who make errors.
“There will always be people who say we’re pandering to medical students whenever we worry about the learning environment,” he said. “There are old-school purists who say when people screw up you should punish them.”
But he adds healthcare broadly has moved past that thinking.
“People recognized 20 years ago or more from the standpoint of improving healthcare systems and safety that is a bad strategy. You’ll never get error-free humans working in your system, and what you have to do is consider how the system is functioning and think about ways to optimize the system so people can be their best within it.”
Wasserman and Treadway have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Some instances of unprofessional behavior by medical trainees are universally deemed egregious and worthy of discipline — for example, looking up a friend’s medical data after HIPAA training.
Conversely, some professionalism lapses may be widely thought of as a teaching and consoling moment, such as the human error involved in forgetting a scheduled repositioning of a patient.
But between the extremes is a vast gray area. To deal with those cases appropriately, Jason Wasserman, PhD, and colleagues propose a new framework by which to judge each infraction.
The framework draws from “just culture” concepts used to evaluate medical errors, Wasserman, associate professor of biomedical science at Oakland University William Beaumont School of Medicine in Rochester, Michigan, told Medscape Medical News. Such an approach takes into account the environment in which the error was made, the knowledge and intent of the person making the error, and the severity and consequences of the infraction so that trainees and institutions can learn from mistakes.
“Trainees by definition are not going to fully get it,” he explained. “By definition they’re not going to fully achieve professional expectations. So how can we respond to the things we need to respond to, but do it in a way that’s educational?”
Wasserman and coauthors’ framework for remediation, which they published February 20 in The New England Journal of Medicine, takes into account several questions: Was the expectation clear? Were there factors beyond the trainees› control? What were the trainees› intentions and did they understand the consequences? Did the person genuinely believe the action was inconsequential?
An example requiring discipline, the authors say, would be using a crib sheet during an exam. In that case the intent is clear, there is no defensible belief that the action is inconsequential, and there is a clear understanding the action is wrong.
But a response of “affirm, support, and advise” is more appropriate, for example, when a student’s alarm doesn’t go off after a power outage and they miss a mandatory meeting.
Wasserman points out that this framework won’t cover all situations.
“This is not an algorithm for answering your questions about what to do,” he said. “It’s an architecture for clarifying the discussion about that. It can really tease out all the threads that need to be considered to best respond to and correct the professionalism lapse, but do it in a way that is developmentally appropriate.”
A Core Competency
For two decades, professionalism has been considered a core competency of medical education. In 1999, the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties formalized it as such. In 2013, the Association of American Medical Colleges formally required related professionalism competencies.
However, identifying lapses has operated largely on an “I-know-it-when-I-see-it” basis, leading to widely varying remediation practices judged by a small number of faculty members or administrators.
The ideas outlined by Wasserman and colleagues are “a terrific application of the ‘just-culture’ framework,” according to Nicole Treadway, MD, a first-year primary care resident at Emory School of Medicine in Atlanta, Georgia.
At Emory, discussions of professionalism start from day 1 of medical school and the subject is revisited throughout training in small groups, Treadway told Medscape Medical News.
But, she said, as the authors point out, definitions of unprofessionalism are not always clear and the examples the authors put forward help put lapses in context.
The framework also allows for looking at mistakes in light of the stress trainees encounter and the greater chance of making a professionalism error in those situations, she noted.
In her own work, she says, because she is juggling both inpatient and outpatient care, she is finding it is easy to get behind on correspondence or communicating lab results or having follow-up conversations.
Those delays could be seen as lapses in professionalism, but under this framework, there may be system solutions or training opportunities to consider.
“We do need this organizational architecture, and I think it could serve us well in really helping us identify and appropriately respond to what we see regarding professionalism,” she said.
Framework Helps Standardize Thinking
She said having a universal framework also helps because while standards of professionalism are easier to monitor in a single medical school, when students scatter to other hospitals for clinical training, those hospitals may have different professionalism standards.
Wasserman agrees, saying, “This could be easily adopted in any environment where people deal with professionalism lapses. I don’t even think it’s necessarily relegated to trainees. It’s a great way to think about any kind of lapses, just as hospitals think about medical errors.”
He said the next step is presenting the framework at various medical schools for feedback and research to see whether the framework improves processes.
Potential criticism, he said, might come from those who say such a construct avoids punishing students who make errors.
“There will always be people who say we’re pandering to medical students whenever we worry about the learning environment,” he said. “There are old-school purists who say when people screw up you should punish them.”
But he adds healthcare broadly has moved past that thinking.
“People recognized 20 years ago or more from the standpoint of improving healthcare systems and safety that is a bad strategy. You’ll never get error-free humans working in your system, and what you have to do is consider how the system is functioning and think about ways to optimize the system so people can be their best within it.”
Wasserman and Treadway have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Obesity expert: Time to embrace growing array of options
MAUI, HAWAII – Specialists who study obesity and embrace the increasing number of treatment options are poised to lead the way in stemming the disease, which Andres Acosta, MD, PhD, calls the “epidemic of the century.”
“Gastroenterologists are in the first line of treatment for obesity management,” said Acosta, who runs the precision medicine for obesity lab at the Mayo Clinic in Rochester, Minn.
“Patients with obesity are already in our clinics,” he said in an interview. And too many physicians “are ignoring the problem.”
The vast majority of people with acid reflux have obesity, as do those with nonalcoholic fatty liver disease, he explained. “By targeting those two areas, we’ll be targeting more than 50% of our patients.” Recurring polyps and colon cancer are also often associated with obesity, he said.
Because of their skill as endoscopists, internists, and nutrition experts, gastroenterologists are uniquely positioned to care for obesity, said Acosta, who is first author of a white paper – Practice Guide on Obesity and Weight Management, Education and Resources – developed by the American Gastroenterological Association with input from nine medical societies.
More treatment choices
Physicians heard an update on options available in the continuum of obesity care from Christopher Thompson, MD, director of endoscopy at Brigham and Women’s Hospital in Boston, at the Gastroenterology Updates IBD Liver Disease Conference 2020. He discussed the potential weight-loss range and safety profile of each.
Some medications result in a body-weight loss of 5%, whereas gastric bypass surgeries can result in a loss of up to 40%, he said in an interview. And weight loss is typically 10% with intragastric balloon, 15%-20% with aspiration therapies and with endoscopic suturing techniques, and 25%-30% with sleeve gastrectomy.
“It’s nice to be able to offer all of those to patients,” he said, adding that he wants to get the message across to hesitant physicians that obesity management “is not as difficult as they think.”
Physicians can be reluctant to address obesity because of the social stigma associated with excess weight and a discomfort in talking about it.
But “there are ways to open that conversation, and it needs to start happening more,” said Thompson, who pointed out that obesity is the underlying cause of many other illnesses, including diabetes and heart diseases.
And new strategies are in the offing, he explained. His team at Brigham is currently involved in clinical trials to test whether the diversion of food and bile to the lower part of the bowel will generate a metabolic signal that affects insulin resistance and weight, he reported.
They are also testing whether gastric procedures can be combined with small bowel procedures to achieve the weight loss seen with bariatric surgery.
As treatment options for obesity increase, precision medicine will help maximize their potential, said Acosta.
Precision medicine will amp up treatments
Acosta outlined the four categories that patients who are obese generally fall into: those with a “hungry brain,” who think they need to eat more than they do; those with a “hungry gut,” whose gut is not sending the proper signal to the brain that it is full; those with “emotional hunger”; and those with abnormal metabolism.
“For each of those, there are genetic circumstances, metabolism, a hormonal profile, as well as pathophysiologic aspects of obesity, that make these groups unique,” he said.
Deciding which patients should get which treatment is the next frontier, he explained. “For example, if you give an intragastric balloon to all comers, patients will lose about 12% of their body weight. But if you separate responders from nonresponders and you select the right intervention, you can achieve an 18% loss of body weight in the right responders.”
At Mayo, they are working on a blood test to break down phenotypes and identify who will respond best to which treatment, he reported. That could lead to a much more efficient use of scarce resources.
“At the same time, I hope that more insurance companies will cover more obesity treatments,” said Acosta.
This article first appeared on Medscape.com.
MAUI, HAWAII – Specialists who study obesity and embrace the increasing number of treatment options are poised to lead the way in stemming the disease, which Andres Acosta, MD, PhD, calls the “epidemic of the century.”
“Gastroenterologists are in the first line of treatment for obesity management,” said Acosta, who runs the precision medicine for obesity lab at the Mayo Clinic in Rochester, Minn.
“Patients with obesity are already in our clinics,” he said in an interview. And too many physicians “are ignoring the problem.”
The vast majority of people with acid reflux have obesity, as do those with nonalcoholic fatty liver disease, he explained. “By targeting those two areas, we’ll be targeting more than 50% of our patients.” Recurring polyps and colon cancer are also often associated with obesity, he said.
Because of their skill as endoscopists, internists, and nutrition experts, gastroenterologists are uniquely positioned to care for obesity, said Acosta, who is first author of a white paper – Practice Guide on Obesity and Weight Management, Education and Resources – developed by the American Gastroenterological Association with input from nine medical societies.
More treatment choices
Physicians heard an update on options available in the continuum of obesity care from Christopher Thompson, MD, director of endoscopy at Brigham and Women’s Hospital in Boston, at the Gastroenterology Updates IBD Liver Disease Conference 2020. He discussed the potential weight-loss range and safety profile of each.
Some medications result in a body-weight loss of 5%, whereas gastric bypass surgeries can result in a loss of up to 40%, he said in an interview. And weight loss is typically 10% with intragastric balloon, 15%-20% with aspiration therapies and with endoscopic suturing techniques, and 25%-30% with sleeve gastrectomy.
“It’s nice to be able to offer all of those to patients,” he said, adding that he wants to get the message across to hesitant physicians that obesity management “is not as difficult as they think.”
Physicians can be reluctant to address obesity because of the social stigma associated with excess weight and a discomfort in talking about it.
But “there are ways to open that conversation, and it needs to start happening more,” said Thompson, who pointed out that obesity is the underlying cause of many other illnesses, including diabetes and heart diseases.
And new strategies are in the offing, he explained. His team at Brigham is currently involved in clinical trials to test whether the diversion of food and bile to the lower part of the bowel will generate a metabolic signal that affects insulin resistance and weight, he reported.
They are also testing whether gastric procedures can be combined with small bowel procedures to achieve the weight loss seen with bariatric surgery.
As treatment options for obesity increase, precision medicine will help maximize their potential, said Acosta.
Precision medicine will amp up treatments
Acosta outlined the four categories that patients who are obese generally fall into: those with a “hungry brain,” who think they need to eat more than they do; those with a “hungry gut,” whose gut is not sending the proper signal to the brain that it is full; those with “emotional hunger”; and those with abnormal metabolism.
“For each of those, there are genetic circumstances, metabolism, a hormonal profile, as well as pathophysiologic aspects of obesity, that make these groups unique,” he said.
Deciding which patients should get which treatment is the next frontier, he explained. “For example, if you give an intragastric balloon to all comers, patients will lose about 12% of their body weight. But if you separate responders from nonresponders and you select the right intervention, you can achieve an 18% loss of body weight in the right responders.”
At Mayo, they are working on a blood test to break down phenotypes and identify who will respond best to which treatment, he reported. That could lead to a much more efficient use of scarce resources.
“At the same time, I hope that more insurance companies will cover more obesity treatments,” said Acosta.
This article first appeared on Medscape.com.
MAUI, HAWAII – Specialists who study obesity and embrace the increasing number of treatment options are poised to lead the way in stemming the disease, which Andres Acosta, MD, PhD, calls the “epidemic of the century.”
“Gastroenterologists are in the first line of treatment for obesity management,” said Acosta, who runs the precision medicine for obesity lab at the Mayo Clinic in Rochester, Minn.
“Patients with obesity are already in our clinics,” he said in an interview. And too many physicians “are ignoring the problem.”
The vast majority of people with acid reflux have obesity, as do those with nonalcoholic fatty liver disease, he explained. “By targeting those two areas, we’ll be targeting more than 50% of our patients.” Recurring polyps and colon cancer are also often associated with obesity, he said.
Because of their skill as endoscopists, internists, and nutrition experts, gastroenterologists are uniquely positioned to care for obesity, said Acosta, who is first author of a white paper – Practice Guide on Obesity and Weight Management, Education and Resources – developed by the American Gastroenterological Association with input from nine medical societies.
More treatment choices
Physicians heard an update on options available in the continuum of obesity care from Christopher Thompson, MD, director of endoscopy at Brigham and Women’s Hospital in Boston, at the Gastroenterology Updates IBD Liver Disease Conference 2020. He discussed the potential weight-loss range and safety profile of each.
Some medications result in a body-weight loss of 5%, whereas gastric bypass surgeries can result in a loss of up to 40%, he said in an interview. And weight loss is typically 10% with intragastric balloon, 15%-20% with aspiration therapies and with endoscopic suturing techniques, and 25%-30% with sleeve gastrectomy.
“It’s nice to be able to offer all of those to patients,” he said, adding that he wants to get the message across to hesitant physicians that obesity management “is not as difficult as they think.”
Physicians can be reluctant to address obesity because of the social stigma associated with excess weight and a discomfort in talking about it.
But “there are ways to open that conversation, and it needs to start happening more,” said Thompson, who pointed out that obesity is the underlying cause of many other illnesses, including diabetes and heart diseases.
And new strategies are in the offing, he explained. His team at Brigham is currently involved in clinical trials to test whether the diversion of food and bile to the lower part of the bowel will generate a metabolic signal that affects insulin resistance and weight, he reported.
They are also testing whether gastric procedures can be combined with small bowel procedures to achieve the weight loss seen with bariatric surgery.
As treatment options for obesity increase, precision medicine will help maximize their potential, said Acosta.
Precision medicine will amp up treatments
Acosta outlined the four categories that patients who are obese generally fall into: those with a “hungry brain,” who think they need to eat more than they do; those with a “hungry gut,” whose gut is not sending the proper signal to the brain that it is full; those with “emotional hunger”; and those with abnormal metabolism.
“For each of those, there are genetic circumstances, metabolism, a hormonal profile, as well as pathophysiologic aspects of obesity, that make these groups unique,” he said.
Deciding which patients should get which treatment is the next frontier, he explained. “For example, if you give an intragastric balloon to all comers, patients will lose about 12% of their body weight. But if you separate responders from nonresponders and you select the right intervention, you can achieve an 18% loss of body weight in the right responders.”
At Mayo, they are working on a blood test to break down phenotypes and identify who will respond best to which treatment, he reported. That could lead to a much more efficient use of scarce resources.
“At the same time, I hope that more insurance companies will cover more obesity treatments,” said Acosta.
This article first appeared on Medscape.com.
EXPERT ANALYSIS FROM GUILD 2020
Older adults with IBD often undertreated
MAUI, HAWAII – said Christina Ha, MD, from the Inflammatory Bowel Disease Center at Cedars-Sinai in Los Angeles.
Clinicians sometimes fall back on steroids because they are typically inexpensive and because there are fears that the new anti-TNF biologics can cause adverse events in older patients, Ha said at the Gastroenterology Updates, IBD, Liver Disease Conference.
“There are not a lot of safety data for the age group, which is not well represented in clinical trials,” she explained. “We can’t necessarily extrapolate data from a study of people with an average age in the 40s to someone in their 70s.”
But, she emphasized, steroid use for more than 3 months is potentially inappropriate.
“If we have a patient on steroids, we should be saying which steroid-sparing strategy will be incorporated into their regimen when we start them on their course of steroids,” she explained.
Ha said she gets asked frequently whether the man-made steroid budesonide, which is readily available, should be considered an acceptable alternative to prednisone.
“Steroids are not maintenance therapies,” she pointed out. “One could argue that maybe someone who has symptomatic mild Crohn’s disease could be kept on low doses of budesonide. But I would argue whether it is really the budesonide that’s helping them or some other disease process related to polypharmacy.”
There are no long-term safety or efficacy data for budesonide in patients with ulcerative colitis or Crohn’s disease, she added.
Special considerations
Older patients with IBD have a decreased ability to handle disease activity; they have more comorbidities and a susceptibility to falls, said Ha. Early control of the disease is therefore essential.
Sarcopenia, an inherent part of aging when muscle mass decreases over time, is central to physiologic changes, which have implications for older adults with IBD, she said.
“We’re learning that sarcopenia is also prevalent in our patients with moderate to severe inflammatory bowel disease,” she explained. “Sarcopenia is associated with increased risk of infections, hospitalizations, and postoperative complications.”
Other changes occur in the intestines as patients age, Ha reported. “Recent studies have shown that there are changes in the intestinal barrier in terms of the junctions within the mucosal lining that increase intestinal permeability, which may help explain why some patients respond to treatments and others don’t.”
Physical therapy underused
Other treatment options, such as physical therapy, have also been underused in older patients with IBD. For example, there’s often considerable pushback against doing a physical therapy assessment on a hospitalized older patient, said Ha.
Medicare covers up to 80% of those services, but referral wording is key. “They’re not going to cover it for a primary diagnosis of ulcerative colitis or Crohn’s,” she explained. However, “they will cover it for a primary diagnosis of deconditioning with a secondary diagnoses of steroid exposure, anemia, Crohn’s disease, or ulcerative colitis.”
Physical therapy can improve muscle function, decrease muscle pain, potentially decrease analgesics, improve bone mass, and decrease joint pain, stress, fatigue, and debility. Fatigue is prevalent in patients with IBD, Ha explained.
Another underused resource is psychosocial assessment, she added. Although depression is not part of the aging process, it is common in those with chronic conditions.
Visits with licensed psychiatrists and clinical psychologists are covered under Medicare Part B, Ha pointed out, as are psychiatric evaluation and testing and individual and group therapy.
Older patients with IBD are often not receiving the care they need, said Uma Mahadevan, MD, a gastroenterologist at UCSF Health in San Francisco.
The need for awareness of polypharmacy, which Ha also discussed, is a concern in all older patients, but especially those with IBD, Mahadevan said in an interview. Clinicians need to be aware of the cascading effect of pharmacy, in which one drug’s adverse effect leads to the prescription of another drug, with different adverse effects.
Ha gave the example of a patient with IBD who started to have diarrhea as an adverse effect of a medication. A clinician might then prescribe a medication for Clostridium difficile, but that might lead to nausea, leading to the prescription of an antinausea medicine.
A multidisciplinary team is needed to perform medication reconciliation, Ha noted.
Correcting anemia important for IBD
Anemia is also underidentified and undertreated in older patients with IBD, Ha said.
“Across the board with inflammatory bowel disease, we don’t do a great job of being aggressive and correcting anemia. That has implications for fatigue and implications with functional status and circulating volume,” she said.
In older patients, it might be that the decline in hemoglobin over time is more important to outcomes than the number itself, she said. “A hemoglobin of 8 g/dL is one thing, but if it was at 12 g/dL 6 months ago, that’s a different story.”
“For older patients, anemia is associated with a high incidence of cardiovascular disease, cognitive impairment, increased risks of falls and fractures, longer hospitalizations (and thus increased costs of care), increased frailty and dementia, and increased risk of mortality,” Ha said. But, she pointed out, Medicare benefits do cover intravenous iron formulations.
This article originally appeared on Medscape.com.
MAUI, HAWAII – said Christina Ha, MD, from the Inflammatory Bowel Disease Center at Cedars-Sinai in Los Angeles.
Clinicians sometimes fall back on steroids because they are typically inexpensive and because there are fears that the new anti-TNF biologics can cause adverse events in older patients, Ha said at the Gastroenterology Updates, IBD, Liver Disease Conference.
“There are not a lot of safety data for the age group, which is not well represented in clinical trials,” she explained. “We can’t necessarily extrapolate data from a study of people with an average age in the 40s to someone in their 70s.”
But, she emphasized, steroid use for more than 3 months is potentially inappropriate.
“If we have a patient on steroids, we should be saying which steroid-sparing strategy will be incorporated into their regimen when we start them on their course of steroids,” she explained.
Ha said she gets asked frequently whether the man-made steroid budesonide, which is readily available, should be considered an acceptable alternative to prednisone.
“Steroids are not maintenance therapies,” she pointed out. “One could argue that maybe someone who has symptomatic mild Crohn’s disease could be kept on low doses of budesonide. But I would argue whether it is really the budesonide that’s helping them or some other disease process related to polypharmacy.”
There are no long-term safety or efficacy data for budesonide in patients with ulcerative colitis or Crohn’s disease, she added.
Special considerations
Older patients with IBD have a decreased ability to handle disease activity; they have more comorbidities and a susceptibility to falls, said Ha. Early control of the disease is therefore essential.
Sarcopenia, an inherent part of aging when muscle mass decreases over time, is central to physiologic changes, which have implications for older adults with IBD, she said.
“We’re learning that sarcopenia is also prevalent in our patients with moderate to severe inflammatory bowel disease,” she explained. “Sarcopenia is associated with increased risk of infections, hospitalizations, and postoperative complications.”
Other changes occur in the intestines as patients age, Ha reported. “Recent studies have shown that there are changes in the intestinal barrier in terms of the junctions within the mucosal lining that increase intestinal permeability, which may help explain why some patients respond to treatments and others don’t.”
Physical therapy underused
Other treatment options, such as physical therapy, have also been underused in older patients with IBD. For example, there’s often considerable pushback against doing a physical therapy assessment on a hospitalized older patient, said Ha.
Medicare covers up to 80% of those services, but referral wording is key. “They’re not going to cover it for a primary diagnosis of ulcerative colitis or Crohn’s,” she explained. However, “they will cover it for a primary diagnosis of deconditioning with a secondary diagnoses of steroid exposure, anemia, Crohn’s disease, or ulcerative colitis.”
Physical therapy can improve muscle function, decrease muscle pain, potentially decrease analgesics, improve bone mass, and decrease joint pain, stress, fatigue, and debility. Fatigue is prevalent in patients with IBD, Ha explained.
Another underused resource is psychosocial assessment, she added. Although depression is not part of the aging process, it is common in those with chronic conditions.
Visits with licensed psychiatrists and clinical psychologists are covered under Medicare Part B, Ha pointed out, as are psychiatric evaluation and testing and individual and group therapy.
Older patients with IBD are often not receiving the care they need, said Uma Mahadevan, MD, a gastroenterologist at UCSF Health in San Francisco.
The need for awareness of polypharmacy, which Ha also discussed, is a concern in all older patients, but especially those with IBD, Mahadevan said in an interview. Clinicians need to be aware of the cascading effect of pharmacy, in which one drug’s adverse effect leads to the prescription of another drug, with different adverse effects.
Ha gave the example of a patient with IBD who started to have diarrhea as an adverse effect of a medication. A clinician might then prescribe a medication for Clostridium difficile, but that might lead to nausea, leading to the prescription of an antinausea medicine.
A multidisciplinary team is needed to perform medication reconciliation, Ha noted.
Correcting anemia important for IBD
Anemia is also underidentified and undertreated in older patients with IBD, Ha said.
“Across the board with inflammatory bowel disease, we don’t do a great job of being aggressive and correcting anemia. That has implications for fatigue and implications with functional status and circulating volume,” she said.
In older patients, it might be that the decline in hemoglobin over time is more important to outcomes than the number itself, she said. “A hemoglobin of 8 g/dL is one thing, but if it was at 12 g/dL 6 months ago, that’s a different story.”
“For older patients, anemia is associated with a high incidence of cardiovascular disease, cognitive impairment, increased risks of falls and fractures, longer hospitalizations (and thus increased costs of care), increased frailty and dementia, and increased risk of mortality,” Ha said. But, she pointed out, Medicare benefits do cover intravenous iron formulations.
This article originally appeared on Medscape.com.
MAUI, HAWAII – said Christina Ha, MD, from the Inflammatory Bowel Disease Center at Cedars-Sinai in Los Angeles.
Clinicians sometimes fall back on steroids because they are typically inexpensive and because there are fears that the new anti-TNF biologics can cause adverse events in older patients, Ha said at the Gastroenterology Updates, IBD, Liver Disease Conference.
“There are not a lot of safety data for the age group, which is not well represented in clinical trials,” she explained. “We can’t necessarily extrapolate data from a study of people with an average age in the 40s to someone in their 70s.”
But, she emphasized, steroid use for more than 3 months is potentially inappropriate.
“If we have a patient on steroids, we should be saying which steroid-sparing strategy will be incorporated into their regimen when we start them on their course of steroids,” she explained.
Ha said she gets asked frequently whether the man-made steroid budesonide, which is readily available, should be considered an acceptable alternative to prednisone.
“Steroids are not maintenance therapies,” she pointed out. “One could argue that maybe someone who has symptomatic mild Crohn’s disease could be kept on low doses of budesonide. But I would argue whether it is really the budesonide that’s helping them or some other disease process related to polypharmacy.”
There are no long-term safety or efficacy data for budesonide in patients with ulcerative colitis or Crohn’s disease, she added.
Special considerations
Older patients with IBD have a decreased ability to handle disease activity; they have more comorbidities and a susceptibility to falls, said Ha. Early control of the disease is therefore essential.
Sarcopenia, an inherent part of aging when muscle mass decreases over time, is central to physiologic changes, which have implications for older adults with IBD, she said.
“We’re learning that sarcopenia is also prevalent in our patients with moderate to severe inflammatory bowel disease,” she explained. “Sarcopenia is associated with increased risk of infections, hospitalizations, and postoperative complications.”
Other changes occur in the intestines as patients age, Ha reported. “Recent studies have shown that there are changes in the intestinal barrier in terms of the junctions within the mucosal lining that increase intestinal permeability, which may help explain why some patients respond to treatments and others don’t.”
Physical therapy underused
Other treatment options, such as physical therapy, have also been underused in older patients with IBD. For example, there’s often considerable pushback against doing a physical therapy assessment on a hospitalized older patient, said Ha.
Medicare covers up to 80% of those services, but referral wording is key. “They’re not going to cover it for a primary diagnosis of ulcerative colitis or Crohn’s,” she explained. However, “they will cover it for a primary diagnosis of deconditioning with a secondary diagnoses of steroid exposure, anemia, Crohn’s disease, or ulcerative colitis.”
Physical therapy can improve muscle function, decrease muscle pain, potentially decrease analgesics, improve bone mass, and decrease joint pain, stress, fatigue, and debility. Fatigue is prevalent in patients with IBD, Ha explained.
Another underused resource is psychosocial assessment, she added. Although depression is not part of the aging process, it is common in those with chronic conditions.
Visits with licensed psychiatrists and clinical psychologists are covered under Medicare Part B, Ha pointed out, as are psychiatric evaluation and testing and individual and group therapy.
Older patients with IBD are often not receiving the care they need, said Uma Mahadevan, MD, a gastroenterologist at UCSF Health in San Francisco.
The need for awareness of polypharmacy, which Ha also discussed, is a concern in all older patients, but especially those with IBD, Mahadevan said in an interview. Clinicians need to be aware of the cascading effect of pharmacy, in which one drug’s adverse effect leads to the prescription of another drug, with different adverse effects.
Ha gave the example of a patient with IBD who started to have diarrhea as an adverse effect of a medication. A clinician might then prescribe a medication for Clostridium difficile, but that might lead to nausea, leading to the prescription of an antinausea medicine.
A multidisciplinary team is needed to perform medication reconciliation, Ha noted.
Correcting anemia important for IBD
Anemia is also underidentified and undertreated in older patients with IBD, Ha said.
“Across the board with inflammatory bowel disease, we don’t do a great job of being aggressive and correcting anemia. That has implications for fatigue and implications with functional status and circulating volume,” she said.
In older patients, it might be that the decline in hemoglobin over time is more important to outcomes than the number itself, she said. “A hemoglobin of 8 g/dL is one thing, but if it was at 12 g/dL 6 months ago, that’s a different story.”
“For older patients, anemia is associated with a high incidence of cardiovascular disease, cognitive impairment, increased risks of falls and fractures, longer hospitalizations (and thus increased costs of care), increased frailty and dementia, and increased risk of mortality,” Ha said. But, she pointed out, Medicare benefits do cover intravenous iron formulations.
This article originally appeared on Medscape.com.
EXPERT ANALYSIS FROM GUILD 2020
Rising number of young people dying after heavy drinking
MAUI, HAWAII – Alcohol use and deaths related to alcohol-use disorders are increasing, and young adults might be the group to watch, said Norah Terrault, MD, MPH, professor at the Keck School of Medicine of USC in Los Angeles.
“A lot of young people are drinking large amounts and they don’t know they’re at risk. They may not drink much during the week but then drink 30 drinks on the weekend,” Dr. Terrault told Medscape Medical News.
The largest relative increase in deaths from alcoholic cirrhosis – 10.5% from 2009 to 2016 – was in the 25- to 34-year age group, she reported here at the Gastroenterology Updates IBD Liver Disease Conference 2020.
This highlights the importance of asking for details about alcohol use during primary care visits; not only how much, but also what time of day, for instance, she explained.
Dr. Terrault’s team at Keck is part of the ACCELERATE-AH consortium, a group of 12 transplant centers looking at patterns of alcohol use before and after liver transplantation.
In their retrospective study of 147 consecutive transplant patients from 2006 to 2018, they found that young age, a history of multiple rehab attempts, and overt encephalopathy at time of transplantation were predictors of alcohol use after the procedure.
Corticosteroids remain the only proven therapy for alcoholic hepatitis. “We have not seen a new therapy in this arena in decades,” said Dr. Terrault. “We really have nothing to offer these patients, yet it’s an incredibly common presentation with a high mortality.”
More treatment options
The good news is that some phase 2 data look promising for new therapies, she reported.
“Some of them are targeting injury and regeneration primarily. Others are looking at the anti-inflammatory and antifibrotic effects. Some are also looking at how gut permeability and the microbiome are influencing outcomes,” she explained.
Transplantation has become very important for patients who do not respond to current therapy, and selection criteria have evolved over the years to take this into account, she pointed out.
In the early 1980s, alcoholic hepatitis was considered an inappropriate indication for liver transplantation. In the early 2000s, the guidance moved to setting 6 months of alcohol abstinence as a criterion for transplantation. The 6-month rule effectively eliminated patients with severe alcoholic hepatitis, who, by the time they needed a new liver, would not have 6 months to live.
Recently, guidelines have added the option of transplantation for patients with alcoholic hepatitis. The option was always there for people who developed alcohol cirrhosis or liver cancer, but now alcoholic hepatitis is recognized as a potential indication for transplantation, Dr. Terrault explained.
Today, transplant centers are moving away from the 6-month rule for two main reasons, she said. One is that few data support the 6-month time period as the duration that makes a difference.
“There is nothing magical about 6 months vs. 3 months or 12 months,” she said, adding that studies have shown that other factors might be better indicators, such as family support and whether the person is employed.
Second, recent studies have shown that rates of 3-year survival are similar in people who did not abstain at all before the procedure and those who undergo transplantation for other reasons.
The ACCELERATE-AH consortium also found that 70% of patients with severe alcoholic hepatitis remained abstinent up to 3 years after transplantation.
Anytime we give an organ to anyone on the list, someone else may die without one. Every year, 20% of patients on the list die without a transplant.
The selection process remains complicated and controversial, Dr. Terrault acknowledged.
“Anytime we give an organ to anyone on the list, someone else may die without one. Every year, 20% of patients on the list die without a transplant,” she said.
And there is concern that because patients with severe alcoholic hepatitis present with severe illness, they get moved to the top of the wait list. The rationale for that, she explained, is that it is done that way in other acute situations.
“We transplant individuals who have an acetaminophen overdose, for example. That’s common in many programs,” she said.
“My issue is that some patients with acute alcoholic hepatitis that have a very high severity score, but some of them, just with abstinence, will get better,” said Guadalupe Garcia-Tsao, MD, professor of medicine at Yale University in New Haven, Conn.
There are cases in which acute alcoholic hepatitis will resolve with abstinence, “and patients can return to an entirely compensated state of cirrhosis, in which they are entirely asymptomatic and they can live,” she told Medscape Medical News.
But it’s hard to know without a control group which patients would have that kind of success with just abstinence, she acknowledged.
Terrault said she agreed, and added that “our tools are not that good,” so determining which patients can be “pulled back from the brink” without transplantation is a challenge.
“There’s still a lot to learn about how we do this, and how we do it well,” she said.
Alcoholic hepatitis as an indication for liver transplantation is rare – less than 1% – but growing.
“This is a potential therapy for your patient who is sick in the ICU with a high severity of disease who has failed steroids. We should call out to see if there’s a transplant program that might be willing to evaluate them,” she said.
This article first appeared on Medscape.com.
MAUI, HAWAII – Alcohol use and deaths related to alcohol-use disorders are increasing, and young adults might be the group to watch, said Norah Terrault, MD, MPH, professor at the Keck School of Medicine of USC in Los Angeles.
“A lot of young people are drinking large amounts and they don’t know they’re at risk. They may not drink much during the week but then drink 30 drinks on the weekend,” Dr. Terrault told Medscape Medical News.
The largest relative increase in deaths from alcoholic cirrhosis – 10.5% from 2009 to 2016 – was in the 25- to 34-year age group, she reported here at the Gastroenterology Updates IBD Liver Disease Conference 2020.
This highlights the importance of asking for details about alcohol use during primary care visits; not only how much, but also what time of day, for instance, she explained.
Dr. Terrault’s team at Keck is part of the ACCELERATE-AH consortium, a group of 12 transplant centers looking at patterns of alcohol use before and after liver transplantation.
In their retrospective study of 147 consecutive transplant patients from 2006 to 2018, they found that young age, a history of multiple rehab attempts, and overt encephalopathy at time of transplantation were predictors of alcohol use after the procedure.
Corticosteroids remain the only proven therapy for alcoholic hepatitis. “We have not seen a new therapy in this arena in decades,” said Dr. Terrault. “We really have nothing to offer these patients, yet it’s an incredibly common presentation with a high mortality.”
More treatment options
The good news is that some phase 2 data look promising for new therapies, she reported.
“Some of them are targeting injury and regeneration primarily. Others are looking at the anti-inflammatory and antifibrotic effects. Some are also looking at how gut permeability and the microbiome are influencing outcomes,” she explained.
Transplantation has become very important for patients who do not respond to current therapy, and selection criteria have evolved over the years to take this into account, she pointed out.
In the early 1980s, alcoholic hepatitis was considered an inappropriate indication for liver transplantation. In the early 2000s, the guidance moved to setting 6 months of alcohol abstinence as a criterion for transplantation. The 6-month rule effectively eliminated patients with severe alcoholic hepatitis, who, by the time they needed a new liver, would not have 6 months to live.
Recently, guidelines have added the option of transplantation for patients with alcoholic hepatitis. The option was always there for people who developed alcohol cirrhosis or liver cancer, but now alcoholic hepatitis is recognized as a potential indication for transplantation, Dr. Terrault explained.
Today, transplant centers are moving away from the 6-month rule for two main reasons, she said. One is that few data support the 6-month time period as the duration that makes a difference.
“There is nothing magical about 6 months vs. 3 months or 12 months,” she said, adding that studies have shown that other factors might be better indicators, such as family support and whether the person is employed.
Second, recent studies have shown that rates of 3-year survival are similar in people who did not abstain at all before the procedure and those who undergo transplantation for other reasons.
The ACCELERATE-AH consortium also found that 70% of patients with severe alcoholic hepatitis remained abstinent up to 3 years after transplantation.
Anytime we give an organ to anyone on the list, someone else may die without one. Every year, 20% of patients on the list die without a transplant.
The selection process remains complicated and controversial, Dr. Terrault acknowledged.
“Anytime we give an organ to anyone on the list, someone else may die without one. Every year, 20% of patients on the list die without a transplant,” she said.
And there is concern that because patients with severe alcoholic hepatitis present with severe illness, they get moved to the top of the wait list. The rationale for that, she explained, is that it is done that way in other acute situations.
“We transplant individuals who have an acetaminophen overdose, for example. That’s common in many programs,” she said.
“My issue is that some patients with acute alcoholic hepatitis that have a very high severity score, but some of them, just with abstinence, will get better,” said Guadalupe Garcia-Tsao, MD, professor of medicine at Yale University in New Haven, Conn.
There are cases in which acute alcoholic hepatitis will resolve with abstinence, “and patients can return to an entirely compensated state of cirrhosis, in which they are entirely asymptomatic and they can live,” she told Medscape Medical News.
But it’s hard to know without a control group which patients would have that kind of success with just abstinence, she acknowledged.
Terrault said she agreed, and added that “our tools are not that good,” so determining which patients can be “pulled back from the brink” without transplantation is a challenge.
“There’s still a lot to learn about how we do this, and how we do it well,” she said.
Alcoholic hepatitis as an indication for liver transplantation is rare – less than 1% – but growing.
“This is a potential therapy for your patient who is sick in the ICU with a high severity of disease who has failed steroids. We should call out to see if there’s a transplant program that might be willing to evaluate them,” she said.
This article first appeared on Medscape.com.
MAUI, HAWAII – Alcohol use and deaths related to alcohol-use disorders are increasing, and young adults might be the group to watch, said Norah Terrault, MD, MPH, professor at the Keck School of Medicine of USC in Los Angeles.
“A lot of young people are drinking large amounts and they don’t know they’re at risk. They may not drink much during the week but then drink 30 drinks on the weekend,” Dr. Terrault told Medscape Medical News.
The largest relative increase in deaths from alcoholic cirrhosis – 10.5% from 2009 to 2016 – was in the 25- to 34-year age group, she reported here at the Gastroenterology Updates IBD Liver Disease Conference 2020.
This highlights the importance of asking for details about alcohol use during primary care visits; not only how much, but also what time of day, for instance, she explained.
Dr. Terrault’s team at Keck is part of the ACCELERATE-AH consortium, a group of 12 transplant centers looking at patterns of alcohol use before and after liver transplantation.
In their retrospective study of 147 consecutive transplant patients from 2006 to 2018, they found that young age, a history of multiple rehab attempts, and overt encephalopathy at time of transplantation were predictors of alcohol use after the procedure.
Corticosteroids remain the only proven therapy for alcoholic hepatitis. “We have not seen a new therapy in this arena in decades,” said Dr. Terrault. “We really have nothing to offer these patients, yet it’s an incredibly common presentation with a high mortality.”
More treatment options
The good news is that some phase 2 data look promising for new therapies, she reported.
“Some of them are targeting injury and regeneration primarily. Others are looking at the anti-inflammatory and antifibrotic effects. Some are also looking at how gut permeability and the microbiome are influencing outcomes,” she explained.
Transplantation has become very important for patients who do not respond to current therapy, and selection criteria have evolved over the years to take this into account, she pointed out.
In the early 1980s, alcoholic hepatitis was considered an inappropriate indication for liver transplantation. In the early 2000s, the guidance moved to setting 6 months of alcohol abstinence as a criterion for transplantation. The 6-month rule effectively eliminated patients with severe alcoholic hepatitis, who, by the time they needed a new liver, would not have 6 months to live.
Recently, guidelines have added the option of transplantation for patients with alcoholic hepatitis. The option was always there for people who developed alcohol cirrhosis or liver cancer, but now alcoholic hepatitis is recognized as a potential indication for transplantation, Dr. Terrault explained.
Today, transplant centers are moving away from the 6-month rule for two main reasons, she said. One is that few data support the 6-month time period as the duration that makes a difference.
“There is nothing magical about 6 months vs. 3 months or 12 months,” she said, adding that studies have shown that other factors might be better indicators, such as family support and whether the person is employed.
Second, recent studies have shown that rates of 3-year survival are similar in people who did not abstain at all before the procedure and those who undergo transplantation for other reasons.
The ACCELERATE-AH consortium also found that 70% of patients with severe alcoholic hepatitis remained abstinent up to 3 years after transplantation.
Anytime we give an organ to anyone on the list, someone else may die without one. Every year, 20% of patients on the list die without a transplant.
The selection process remains complicated and controversial, Dr. Terrault acknowledged.
“Anytime we give an organ to anyone on the list, someone else may die without one. Every year, 20% of patients on the list die without a transplant,” she said.
And there is concern that because patients with severe alcoholic hepatitis present with severe illness, they get moved to the top of the wait list. The rationale for that, she explained, is that it is done that way in other acute situations.
“We transplant individuals who have an acetaminophen overdose, for example. That’s common in many programs,” she said.
“My issue is that some patients with acute alcoholic hepatitis that have a very high severity score, but some of them, just with abstinence, will get better,” said Guadalupe Garcia-Tsao, MD, professor of medicine at Yale University in New Haven, Conn.
There are cases in which acute alcoholic hepatitis will resolve with abstinence, “and patients can return to an entirely compensated state of cirrhosis, in which they are entirely asymptomatic and they can live,” she told Medscape Medical News.
But it’s hard to know without a control group which patients would have that kind of success with just abstinence, she acknowledged.
Terrault said she agreed, and added that “our tools are not that good,” so determining which patients can be “pulled back from the brink” without transplantation is a challenge.
“There’s still a lot to learn about how we do this, and how we do it well,” she said.
Alcoholic hepatitis as an indication for liver transplantation is rare – less than 1% – but growing.
“This is a potential therapy for your patient who is sick in the ICU with a high severity of disease who has failed steroids. We should call out to see if there’s a transplant program that might be willing to evaluate them,” she said.
This article first appeared on Medscape.com.
EXPERT ANALYSIS FROM GUILD 2020
Osteoporosis, fracture risk higher in patients with IBD
MAUI, HAWAII –
In the general population, those who develop osteoporosis are typically women who are thin and postmenopausal, and family history, smoking status, and alcohol use usually play a role, Long said at the Gastroenterology Updates, IBD, Liver Disease Conference.
But in the population with IBD, the risk for osteoporosis is similar in women and men, age plays a large role, and corticosteroid use seems to be a driving factor in the development of the disease, she explained.
A previous study that looked at fractures in patients with IBD showed that the risk “is 40% greater than in the general population,” Long reported. In patients younger than 40 years, the risk for fracture was 37% higher than in the general population, and this rate increased with age.
Preventing fractures
Fractures to the hip and spine are linked to significant morbidity, including hospitalization, major surgery, and even death, Long noted. But they are one of the preventable downstream effects of IBD, and patients need to understand that there’s something they can do about their elevated risk.
Patients should be educated on the importance of weight-bearing exercise and quitting smoking, she said.
“We need to think of preventive measures for anyone on more than 5 mg of prednisone a day for a time period of about 3 months,” she added. “Unfortunately, most of our patients meet this criterion.”
Patients with IBD should undergo dual-energy x-ray absorptiometry (DXA) to calculate bone density and establish the need for calcium and vitamin D supplementation.
“One of the things I’m starting to do in my practice is check vitamin D levels annually on my patients. I do this in the springtime and try to optimize their levels,” Long said.
Higher risk for herpes zoster
The risk for infection is also elevated in patients with IBD, including the risk for herpes zoster, which is already high, affecting one in three people in the general population.
In fact, the risk for herpes zoster in patients with IBD in their 20s is similar to the risk for people in their 50s in the general population. This is “something we need to be addressing in all of our patients,” said Long.
Physicians should emphasize the need for zoster vaccination in patients at least 50 years of age, and potentially younger patients on certain therapies, she added.
But because the Shingrix shingles vaccine (GlaxoSmithKline) is so much more powerful than the previous live vaccine, some have wondered whether it could stimulate an immune response, causing the IBD to flare after vaccination, she said.
However, a recent study of IBD patients followed for 207 days after shingles vaccination showed that only one of the 67 study participants (1.5%) experienced a flare. But fever is fairly common after the shot.
“I counsel my patients that they may feel pretty wiped out for 24 hours; they may have myalgias,” Long reported. “If you have someone who has to travel for work, you want them to time this vaccination so they can have a day of rest afterward. It’s the real deal.”
Screening for TB
Screening to rule out latent tuberculosis (TB) is also important in IBD.
“We should be looking at whether they’ve had close contact with active TB or people from endemic areas,” said Long. “The reason we really care about this is that the risk of serious infection is doubled with anti-TNF therapy.”
The treatment of latent TB prior to the initiation of an anti-TNF “reduces the incidence of active TB by over 80%. This is why it’s imperative to screen prior to initiation, and then periodically based on risk factors,” she explained.
“It’s profound how much maintenance is required for patients with IBD,” said Christopher Stanke, MD, from the Oregon Medical Group in Eugene.
He said he is particularly struck by the collective risks for younger patients with IBD.
“Young people look to us as their only doctor. They don’t even see their primary care physicians very often. We have to take over a lot of this stuff,” he told Medscape Medical News.
And osteoporosis doesn’t often get the attention it needs in gastroenterologists’ offices, he acknowledged.
“I often check it on people as they get close to 50 or 60,” said Stanke, who added that Long’s presentation is a good reminder that younger patients, especially those who have been on steroids for a while, need more attention.
This article first appeared on Medscape.com.
MAUI, HAWAII –
In the general population, those who develop osteoporosis are typically women who are thin and postmenopausal, and family history, smoking status, and alcohol use usually play a role, Long said at the Gastroenterology Updates, IBD, Liver Disease Conference.
But in the population with IBD, the risk for osteoporosis is similar in women and men, age plays a large role, and corticosteroid use seems to be a driving factor in the development of the disease, she explained.
A previous study that looked at fractures in patients with IBD showed that the risk “is 40% greater than in the general population,” Long reported. In patients younger than 40 years, the risk for fracture was 37% higher than in the general population, and this rate increased with age.
Preventing fractures
Fractures to the hip and spine are linked to significant morbidity, including hospitalization, major surgery, and even death, Long noted. But they are one of the preventable downstream effects of IBD, and patients need to understand that there’s something they can do about their elevated risk.
Patients should be educated on the importance of weight-bearing exercise and quitting smoking, she said.
“We need to think of preventive measures for anyone on more than 5 mg of prednisone a day for a time period of about 3 months,” she added. “Unfortunately, most of our patients meet this criterion.”
Patients with IBD should undergo dual-energy x-ray absorptiometry (DXA) to calculate bone density and establish the need for calcium and vitamin D supplementation.
“One of the things I’m starting to do in my practice is check vitamin D levels annually on my patients. I do this in the springtime and try to optimize their levels,” Long said.
Higher risk for herpes zoster
The risk for infection is also elevated in patients with IBD, including the risk for herpes zoster, which is already high, affecting one in three people in the general population.
In fact, the risk for herpes zoster in patients with IBD in their 20s is similar to the risk for people in their 50s in the general population. This is “something we need to be addressing in all of our patients,” said Long.
Physicians should emphasize the need for zoster vaccination in patients at least 50 years of age, and potentially younger patients on certain therapies, she added.
But because the Shingrix shingles vaccine (GlaxoSmithKline) is so much more powerful than the previous live vaccine, some have wondered whether it could stimulate an immune response, causing the IBD to flare after vaccination, she said.
However, a recent study of IBD patients followed for 207 days after shingles vaccination showed that only one of the 67 study participants (1.5%) experienced a flare. But fever is fairly common after the shot.
“I counsel my patients that they may feel pretty wiped out for 24 hours; they may have myalgias,” Long reported. “If you have someone who has to travel for work, you want them to time this vaccination so they can have a day of rest afterward. It’s the real deal.”
Screening for TB
Screening to rule out latent tuberculosis (TB) is also important in IBD.
“We should be looking at whether they’ve had close contact with active TB or people from endemic areas,” said Long. “The reason we really care about this is that the risk of serious infection is doubled with anti-TNF therapy.”
The treatment of latent TB prior to the initiation of an anti-TNF “reduces the incidence of active TB by over 80%. This is why it’s imperative to screen prior to initiation, and then periodically based on risk factors,” she explained.
“It’s profound how much maintenance is required for patients with IBD,” said Christopher Stanke, MD, from the Oregon Medical Group in Eugene.
He said he is particularly struck by the collective risks for younger patients with IBD.
“Young people look to us as their only doctor. They don’t even see their primary care physicians very often. We have to take over a lot of this stuff,” he told Medscape Medical News.
And osteoporosis doesn’t often get the attention it needs in gastroenterologists’ offices, he acknowledged.
“I often check it on people as they get close to 50 or 60,” said Stanke, who added that Long’s presentation is a good reminder that younger patients, especially those who have been on steroids for a while, need more attention.
This article first appeared on Medscape.com.
MAUI, HAWAII –
In the general population, those who develop osteoporosis are typically women who are thin and postmenopausal, and family history, smoking status, and alcohol use usually play a role, Long said at the Gastroenterology Updates, IBD, Liver Disease Conference.
But in the population with IBD, the risk for osteoporosis is similar in women and men, age plays a large role, and corticosteroid use seems to be a driving factor in the development of the disease, she explained.
A previous study that looked at fractures in patients with IBD showed that the risk “is 40% greater than in the general population,” Long reported. In patients younger than 40 years, the risk for fracture was 37% higher than in the general population, and this rate increased with age.
Preventing fractures
Fractures to the hip and spine are linked to significant morbidity, including hospitalization, major surgery, and even death, Long noted. But they are one of the preventable downstream effects of IBD, and patients need to understand that there’s something they can do about their elevated risk.
Patients should be educated on the importance of weight-bearing exercise and quitting smoking, she said.
“We need to think of preventive measures for anyone on more than 5 mg of prednisone a day for a time period of about 3 months,” she added. “Unfortunately, most of our patients meet this criterion.”
Patients with IBD should undergo dual-energy x-ray absorptiometry (DXA) to calculate bone density and establish the need for calcium and vitamin D supplementation.
“One of the things I’m starting to do in my practice is check vitamin D levels annually on my patients. I do this in the springtime and try to optimize their levels,” Long said.
Higher risk for herpes zoster
The risk for infection is also elevated in patients with IBD, including the risk for herpes zoster, which is already high, affecting one in three people in the general population.
In fact, the risk for herpes zoster in patients with IBD in their 20s is similar to the risk for people in their 50s in the general population. This is “something we need to be addressing in all of our patients,” said Long.
Physicians should emphasize the need for zoster vaccination in patients at least 50 years of age, and potentially younger patients on certain therapies, she added.
But because the Shingrix shingles vaccine (GlaxoSmithKline) is so much more powerful than the previous live vaccine, some have wondered whether it could stimulate an immune response, causing the IBD to flare after vaccination, she said.
However, a recent study of IBD patients followed for 207 days after shingles vaccination showed that only one of the 67 study participants (1.5%) experienced a flare. But fever is fairly common after the shot.
“I counsel my patients that they may feel pretty wiped out for 24 hours; they may have myalgias,” Long reported. “If you have someone who has to travel for work, you want them to time this vaccination so they can have a day of rest afterward. It’s the real deal.”
Screening for TB
Screening to rule out latent tuberculosis (TB) is also important in IBD.
“We should be looking at whether they’ve had close contact with active TB or people from endemic areas,” said Long. “The reason we really care about this is that the risk of serious infection is doubled with anti-TNF therapy.”
The treatment of latent TB prior to the initiation of an anti-TNF “reduces the incidence of active TB by over 80%. This is why it’s imperative to screen prior to initiation, and then periodically based on risk factors,” she explained.
“It’s profound how much maintenance is required for patients with IBD,” said Christopher Stanke, MD, from the Oregon Medical Group in Eugene.
He said he is particularly struck by the collective risks for younger patients with IBD.
“Young people look to us as their only doctor. They don’t even see their primary care physicians very often. We have to take over a lot of this stuff,” he told Medscape Medical News.
And osteoporosis doesn’t often get the attention it needs in gastroenterologists’ offices, he acknowledged.
“I often check it on people as they get close to 50 or 60,” said Stanke, who added that Long’s presentation is a good reminder that younger patients, especially those who have been on steroids for a while, need more attention.
This article first appeared on Medscape.com.
REPORTING FROM GUILD 2020
‘Momentous’ USMLE change: New pass/fail format stuns medicine
News that the United States Medical Licensing Examination (USMLE) program will change its Step 1 scoring from a 3-digit number to pass/fail starting Jan. 1, 2022, has set off a flurry of shocked responses from students and physicians.
J. Bryan Carmody, MD, MPH, an assistant professor at Eastern Virginia Medical School in Norfolk, said in an interview that he was “stunned” when he heard the news on Wednesday and said the switch presents “the single biggest opportunity for medical school education reform since the Flexner Report,” which in 1910 established standards for modern medical education.
Numbers will continue for some tests
The USMLE cosponsors – the Federation of State Medical Boards (FSMB) and the National Board of Medical Examiners (NBME) – said that the Step 2 Clinical Knowledge (CK) exam and Step 3 will continue to be scored numerically. Step 2 Clinical Skills (CS) will continue its pass/fail system.
The change was made after Step 1 had been roundly criticized as playing too big a role in the process of becoming a physician and for causing students to study for the test instead of engaging fully in their medical education.
Ramie Fathy, a third-year medical student at the University of Pennsylvania, Philadelphia, currently studying for Step 1, said in an interview that it would have been nice personally to have the pass/fail choice, but he predicts both good and unintended consequences in the change.
The positive news, Mr. Fathy said, is that less emphasis will be put on the Step 1 test, which includes memorizing basic science details that may or not be relevant depending on later specialty choice.
“It’s not necessarily measuring what the test makers intended, which was whether or not a student can understand and apply basic science concepts to the practice of medicine,” he said.
“The current system encourages students to get as high a score as possible, which – after a certain point – translates to memorizing many little details that become increasingly less practically relevant,” Mr. Fathy said.
Pressure may move elsewhere?
However, Mr. Fathy worries that, without a scoring system to help decide who stands out in Step 1, residency program directors will depend more on the reputation of candidates’ medical school and the clout of the person writing a letter of recommendation – factors that are often influenced by family resources and social standing. That could wedge a further economic divide into the path to becoming a physician.
Mr. Fathy said he and fellow students are watching for information on what the passing bar will be and what happens with Step 2 Clinical Knowledge exam. USMLE has promised more information as soon as it is available.
“The question is whether that test will replace Step 1 as the standardized metric of student competency,” Mr. Fathy said, which would put more pressure on students further down the medical path.
Will Step 2 anxiety increase?
Dr. Carmody agreed that there is the danger that students now will spend their time studying for Step 2 CK at the expense of other parts of their education.
Meaningful reform will depend on the pass/fail move being coupled with other reforms, most importantly application caps, said Dr. Carmody, who teaches preclinical medical students and works with the residency program.
He has been blogging about Step 1 pass/fail for the past year.
Currently students can apply for as many residencies as they can pay for and Carmody said the number of applications per student has been rising over the past decade.
“That puts program directors under an impossible burden,” he said. “With our Step 1-based system, there’s significant inequality in the number of interviews people get. Programs end up overinviting the same group of people who look good on paper.”
People outside that group respond by sending more applications than they need to just to get a few interviews, Dr. Carmody added.
With caps, students would have an incentive to apply to only those programs in which they had a sincere interest, he said. Program directors also would then be better able to evaluate each application.
Switching Step 1 to pass/fail may have some effect on medical school burnout, Dr. Carmody said.
“It’s one thing to work hard when you’re on call and your patients depend on it,” he said. “But I would have a hard time staying up late every night studying something that I know in my heart is not going to help my patients, but I have to do it because I have to do better than the person who’s studying in the apartment next to me.”
Test has strayed from original purpose
Joseph Safdieh, MD, an assistant dean for clinical curriculum and director of the medical student neurology clerkship for the Weill Cornell Medicine, New York, sees the move as positive overall.
“We should not be using any single metric to define or describe our students’ overall profile,” he said in an interview.
“This has been a very significant anxiety point for our medical students for quite a number of years,” Dr. Safdieh said. “They were frustrated that their entire 4 years of medical school seemingly came down to one number.”
The test was created originally as one of three parts of licensure, he pointed out.
“Over the past 10 or 15 years, the exam has morphed to become a litmus test for very specific residency programs,” he said.
However, Dr. Safdieh has concerns that Step 2 will cultivate the same anxiety and may get too big a spotlight without the Step 1 metric, “although one could argue that test does more accurately reflect clinical material,” he said.
He also worries that students who have selected a specialty by the time they take Step 2 may find late in the game that they are less competitive in their field than they thought they were and may have to make a last-minute switch.
Dr. Safdieh said he thinks Step 2 will be next to go the pass/fail route. In reading between the lines of the announcement, he believes the test cosponsors didn’t make both pass/fail at once because it would have been “a nuclear bomb to the system.”
He credited the cosponsors with making what he called a “bold and momentous decision to initiate radical change in the overall transition between undergraduate and graduate medical education.”
Dr. Safdieh added that few in medicine were expecting Wednesday’s announcement.
“I think many of us were expecting them to go to quartile grading, not to go this far,” he said.
Dr. Safdieh suggested that, among those who may see downstream effects from the pass/fail move are offshore schools, such as those in the Caribbean. “Those schools rely on Step 1 to demonstrate that their students are meeting the rigor,” he said. But he hopes that this will lead to more holistic review.
“We’re hoping that this will force change in the system so that residency directors will look at more than just test-taking ability. They’ll look at publications and scholarship, community service and advocacy and performance in medical school,” Dr. Safdieh said.
Alison J. Whelan, MD, chief medical education officer of the Association of American Medical Colleges said in a statement, “The transition from medical school to residency training is a matter of great concern throughout academic medicine.
“The decision by the NBME and FSMB to change USMLE Step 1 score reporting to pass/fail was very carefully considered to balance student learning and student well-being,” she said. “The medical education community must now work together to identify and implement additional changes to improve the overall UME-GME [undergraduate and graduate medical education] transition system for all stakeholders and the AAMC is committed to helping lead this work.”
Dr. Fathy, Dr. Carmody, and Dr. Safdieh have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
News that the United States Medical Licensing Examination (USMLE) program will change its Step 1 scoring from a 3-digit number to pass/fail starting Jan. 1, 2022, has set off a flurry of shocked responses from students and physicians.
J. Bryan Carmody, MD, MPH, an assistant professor at Eastern Virginia Medical School in Norfolk, said in an interview that he was “stunned” when he heard the news on Wednesday and said the switch presents “the single biggest opportunity for medical school education reform since the Flexner Report,” which in 1910 established standards for modern medical education.
Numbers will continue for some tests
The USMLE cosponsors – the Federation of State Medical Boards (FSMB) and the National Board of Medical Examiners (NBME) – said that the Step 2 Clinical Knowledge (CK) exam and Step 3 will continue to be scored numerically. Step 2 Clinical Skills (CS) will continue its pass/fail system.
The change was made after Step 1 had been roundly criticized as playing too big a role in the process of becoming a physician and for causing students to study for the test instead of engaging fully in their medical education.
Ramie Fathy, a third-year medical student at the University of Pennsylvania, Philadelphia, currently studying for Step 1, said in an interview that it would have been nice personally to have the pass/fail choice, but he predicts both good and unintended consequences in the change.
The positive news, Mr. Fathy said, is that less emphasis will be put on the Step 1 test, which includes memorizing basic science details that may or not be relevant depending on later specialty choice.
“It’s not necessarily measuring what the test makers intended, which was whether or not a student can understand and apply basic science concepts to the practice of medicine,” he said.
“The current system encourages students to get as high a score as possible, which – after a certain point – translates to memorizing many little details that become increasingly less practically relevant,” Mr. Fathy said.
Pressure may move elsewhere?
However, Mr. Fathy worries that, without a scoring system to help decide who stands out in Step 1, residency program directors will depend more on the reputation of candidates’ medical school and the clout of the person writing a letter of recommendation – factors that are often influenced by family resources and social standing. That could wedge a further economic divide into the path to becoming a physician.
Mr. Fathy said he and fellow students are watching for information on what the passing bar will be and what happens with Step 2 Clinical Knowledge exam. USMLE has promised more information as soon as it is available.
“The question is whether that test will replace Step 1 as the standardized metric of student competency,” Mr. Fathy said, which would put more pressure on students further down the medical path.
Will Step 2 anxiety increase?
Dr. Carmody agreed that there is the danger that students now will spend their time studying for Step 2 CK at the expense of other parts of their education.
Meaningful reform will depend on the pass/fail move being coupled with other reforms, most importantly application caps, said Dr. Carmody, who teaches preclinical medical students and works with the residency program.
He has been blogging about Step 1 pass/fail for the past year.
Currently students can apply for as many residencies as they can pay for and Carmody said the number of applications per student has been rising over the past decade.
“That puts program directors under an impossible burden,” he said. “With our Step 1-based system, there’s significant inequality in the number of interviews people get. Programs end up overinviting the same group of people who look good on paper.”
People outside that group respond by sending more applications than they need to just to get a few interviews, Dr. Carmody added.
With caps, students would have an incentive to apply to only those programs in which they had a sincere interest, he said. Program directors also would then be better able to evaluate each application.
Switching Step 1 to pass/fail may have some effect on medical school burnout, Dr. Carmody said.
“It’s one thing to work hard when you’re on call and your patients depend on it,” he said. “But I would have a hard time staying up late every night studying something that I know in my heart is not going to help my patients, but I have to do it because I have to do better than the person who’s studying in the apartment next to me.”
Test has strayed from original purpose
Joseph Safdieh, MD, an assistant dean for clinical curriculum and director of the medical student neurology clerkship for the Weill Cornell Medicine, New York, sees the move as positive overall.
“We should not be using any single metric to define or describe our students’ overall profile,” he said in an interview.
“This has been a very significant anxiety point for our medical students for quite a number of years,” Dr. Safdieh said. “They were frustrated that their entire 4 years of medical school seemingly came down to one number.”
The test was created originally as one of three parts of licensure, he pointed out.
“Over the past 10 or 15 years, the exam has morphed to become a litmus test for very specific residency programs,” he said.
However, Dr. Safdieh has concerns that Step 2 will cultivate the same anxiety and may get too big a spotlight without the Step 1 metric, “although one could argue that test does more accurately reflect clinical material,” he said.
He also worries that students who have selected a specialty by the time they take Step 2 may find late in the game that they are less competitive in their field than they thought they were and may have to make a last-minute switch.
Dr. Safdieh said he thinks Step 2 will be next to go the pass/fail route. In reading between the lines of the announcement, he believes the test cosponsors didn’t make both pass/fail at once because it would have been “a nuclear bomb to the system.”
He credited the cosponsors with making what he called a “bold and momentous decision to initiate radical change in the overall transition between undergraduate and graduate medical education.”
Dr. Safdieh added that few in medicine were expecting Wednesday’s announcement.
“I think many of us were expecting them to go to quartile grading, not to go this far,” he said.
Dr. Safdieh suggested that, among those who may see downstream effects from the pass/fail move are offshore schools, such as those in the Caribbean. “Those schools rely on Step 1 to demonstrate that their students are meeting the rigor,” he said. But he hopes that this will lead to more holistic review.
“We’re hoping that this will force change in the system so that residency directors will look at more than just test-taking ability. They’ll look at publications and scholarship, community service and advocacy and performance in medical school,” Dr. Safdieh said.
Alison J. Whelan, MD, chief medical education officer of the Association of American Medical Colleges said in a statement, “The transition from medical school to residency training is a matter of great concern throughout academic medicine.
“The decision by the NBME and FSMB to change USMLE Step 1 score reporting to pass/fail was very carefully considered to balance student learning and student well-being,” she said. “The medical education community must now work together to identify and implement additional changes to improve the overall UME-GME [undergraduate and graduate medical education] transition system for all stakeholders and the AAMC is committed to helping lead this work.”
Dr. Fathy, Dr. Carmody, and Dr. Safdieh have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
News that the United States Medical Licensing Examination (USMLE) program will change its Step 1 scoring from a 3-digit number to pass/fail starting Jan. 1, 2022, has set off a flurry of shocked responses from students and physicians.
J. Bryan Carmody, MD, MPH, an assistant professor at Eastern Virginia Medical School in Norfolk, said in an interview that he was “stunned” when he heard the news on Wednesday and said the switch presents “the single biggest opportunity for medical school education reform since the Flexner Report,” which in 1910 established standards for modern medical education.
Numbers will continue for some tests
The USMLE cosponsors – the Federation of State Medical Boards (FSMB) and the National Board of Medical Examiners (NBME) – said that the Step 2 Clinical Knowledge (CK) exam and Step 3 will continue to be scored numerically. Step 2 Clinical Skills (CS) will continue its pass/fail system.
The change was made after Step 1 had been roundly criticized as playing too big a role in the process of becoming a physician and for causing students to study for the test instead of engaging fully in their medical education.
Ramie Fathy, a third-year medical student at the University of Pennsylvania, Philadelphia, currently studying for Step 1, said in an interview that it would have been nice personally to have the pass/fail choice, but he predicts both good and unintended consequences in the change.
The positive news, Mr. Fathy said, is that less emphasis will be put on the Step 1 test, which includes memorizing basic science details that may or not be relevant depending on later specialty choice.
“It’s not necessarily measuring what the test makers intended, which was whether or not a student can understand and apply basic science concepts to the practice of medicine,” he said.
“The current system encourages students to get as high a score as possible, which – after a certain point – translates to memorizing many little details that become increasingly less practically relevant,” Mr. Fathy said.
Pressure may move elsewhere?
However, Mr. Fathy worries that, without a scoring system to help decide who stands out in Step 1, residency program directors will depend more on the reputation of candidates’ medical school and the clout of the person writing a letter of recommendation – factors that are often influenced by family resources and social standing. That could wedge a further economic divide into the path to becoming a physician.
Mr. Fathy said he and fellow students are watching for information on what the passing bar will be and what happens with Step 2 Clinical Knowledge exam. USMLE has promised more information as soon as it is available.
“The question is whether that test will replace Step 1 as the standardized metric of student competency,” Mr. Fathy said, which would put more pressure on students further down the medical path.
Will Step 2 anxiety increase?
Dr. Carmody agreed that there is the danger that students now will spend their time studying for Step 2 CK at the expense of other parts of their education.
Meaningful reform will depend on the pass/fail move being coupled with other reforms, most importantly application caps, said Dr. Carmody, who teaches preclinical medical students and works with the residency program.
He has been blogging about Step 1 pass/fail for the past year.
Currently students can apply for as many residencies as they can pay for and Carmody said the number of applications per student has been rising over the past decade.
“That puts program directors under an impossible burden,” he said. “With our Step 1-based system, there’s significant inequality in the number of interviews people get. Programs end up overinviting the same group of people who look good on paper.”
People outside that group respond by sending more applications than they need to just to get a few interviews, Dr. Carmody added.
With caps, students would have an incentive to apply to only those programs in which they had a sincere interest, he said. Program directors also would then be better able to evaluate each application.
Switching Step 1 to pass/fail may have some effect on medical school burnout, Dr. Carmody said.
“It’s one thing to work hard when you’re on call and your patients depend on it,” he said. “But I would have a hard time staying up late every night studying something that I know in my heart is not going to help my patients, but I have to do it because I have to do better than the person who’s studying in the apartment next to me.”
Test has strayed from original purpose
Joseph Safdieh, MD, an assistant dean for clinical curriculum and director of the medical student neurology clerkship for the Weill Cornell Medicine, New York, sees the move as positive overall.
“We should not be using any single metric to define or describe our students’ overall profile,” he said in an interview.
“This has been a very significant anxiety point for our medical students for quite a number of years,” Dr. Safdieh said. “They were frustrated that their entire 4 years of medical school seemingly came down to one number.”
The test was created originally as one of three parts of licensure, he pointed out.
“Over the past 10 or 15 years, the exam has morphed to become a litmus test for very specific residency programs,” he said.
However, Dr. Safdieh has concerns that Step 2 will cultivate the same anxiety and may get too big a spotlight without the Step 1 metric, “although one could argue that test does more accurately reflect clinical material,” he said.
He also worries that students who have selected a specialty by the time they take Step 2 may find late in the game that they are less competitive in their field than they thought they were and may have to make a last-minute switch.
Dr. Safdieh said he thinks Step 2 will be next to go the pass/fail route. In reading between the lines of the announcement, he believes the test cosponsors didn’t make both pass/fail at once because it would have been “a nuclear bomb to the system.”
He credited the cosponsors with making what he called a “bold and momentous decision to initiate radical change in the overall transition between undergraduate and graduate medical education.”
Dr. Safdieh added that few in medicine were expecting Wednesday’s announcement.
“I think many of us were expecting them to go to quartile grading, not to go this far,” he said.
Dr. Safdieh suggested that, among those who may see downstream effects from the pass/fail move are offshore schools, such as those in the Caribbean. “Those schools rely on Step 1 to demonstrate that their students are meeting the rigor,” he said. But he hopes that this will lead to more holistic review.
“We’re hoping that this will force change in the system so that residency directors will look at more than just test-taking ability. They’ll look at publications and scholarship, community service and advocacy and performance in medical school,” Dr. Safdieh said.
Alison J. Whelan, MD, chief medical education officer of the Association of American Medical Colleges said in a statement, “The transition from medical school to residency training is a matter of great concern throughout academic medicine.
“The decision by the NBME and FSMB to change USMLE Step 1 score reporting to pass/fail was very carefully considered to balance student learning and student well-being,” she said. “The medical education community must now work together to identify and implement additional changes to improve the overall UME-GME [undergraduate and graduate medical education] transition system for all stakeholders and the AAMC is committed to helping lead this work.”
Dr. Fathy, Dr. Carmody, and Dr. Safdieh have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.