User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Implantable stimulator shows promise for chronic knee pain
NATIONAL HARBOR, MD. – Stimulation of the infrapatellar branch of the saphenous nerve with an implantable electrical device is a potentially effective treatment for chronic, intractable knee pain.
In a small case series consisting of five patients with chronic knee pain, pain intensity scores on the visual analog scale (VAS) dropped from an average of 8 out of 10 before the implant to 1.4 out of 10 when measured 6 months afterward.
Pain relief was also long lasting, with an average score at 2 years still significantly reduced from baseline, at 3 out of 10 on the VAS.
“We have a lot of patients with chronic knee pain, and unfortunately, our hands are tied in terms of what we can do for them,” lead author Kwo Wei David Ho, MD, PhD, Stanford University, California, told Medscape Medical News.
“They can use NSAIDs, physical therapy, some get steroid injections, or genicular nerve blocks, but they don’t work that well. Some have knee replacement surgery, and can still have persistent knee pain after the operation, so here we are using an alternative therapy called peripheral nerve stimulation of the saphenous nerve. This provides a way to relieve pain without nerve destruction or motor dysfunction,” Ho said.
The findings were presented here at the American Academy of Pain Medicine (AAPM) 2020 Annual Meeting.
Patient Controlled
For the study, the investigators surgically implanted five patients with intractable knee pain with the StimRouter™ (Bioness, Inc).
The device takes about 15 to 30 minutes to implant, much like a pacemaker, and reduces pain by delivering gentle electrical stimulation directly to a target peripheral nerve, in this case the saphenous nerve, to interrupt the pain signal, Ho said.
“A thin, threadlike lead, or noodle, is implanted below the skin next to the target peripheral nerve responsible for the pain signal under ultrasound guidance, and then a patch or external pulse transmitter (EPT) is worn on top of the skin. This sends electric stimulation through the skin to the lead,” he explained.
The patient can then control the EPT and adjust stimulation with a wireless handheld programmer.
“Some patients turn it on at night for a couple of hours and then turn it off, some leave it on for the entire night, or the whole day if they prefer. What we’ve been noticing in our series is that after a while, patients are using less and less, and the pain gets better and better, and eventually they stop using it entirely because the pain completely resolves,” Ho said.
Good candidates for this treatment are post-knee replacement patients with residual pain, he added.
Durable Effect
Of the five patients in the case series, four had previous knee arthroplasty.
To determine the chances of a good response to the implant, study participants underwent a diagnostic saphenous nerve block, with the rationale that if the block successfully reduced knee pain by 50% or more in the short term, patients would likely respond well to the implant.
Before the peripheral nerve stimulation implant, the average pain intensity was 7.8 out of 10 on the VAS. After stimulator implantation, the average pain intensity was 1.4 at 6 months (P = .019, in 5 patients). At 1 year, the average pain intensity score was virtually the same, at 1.5 on the VAS, (P = .0032, in 4 patients). At 2 years, the average pain intensity score was 2.75 (P = .12, in 2 patients).
“This study provides preliminary evidence that stimulation at the saphenous nerve may be effective for selected patients with chronic knee pain,” Ho said.
Commenting on the findings for Medscape Medical News, Patrick Tighe, MD, MS, University of Florida, Gainesville, said that chronic knee pain continues to present “numerous diagnostic and therapeutic challenges for many patients.”
“It may be surprising, but there is still so much we don’t know about the innervation of the knee, and we are still learning about different ways to alter the behavior of those nerves,” said Tighe, who was not involved with the current study.
“This work points to some exciting opportunities to help patients suffering from chronic knee pain. We certainly need more research in this area to figure out the optimal approach to applying these findings more widely,” he said.
Ho and Tighe have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
NATIONAL HARBOR, MD. – Stimulation of the infrapatellar branch of the saphenous nerve with an implantable electrical device is a potentially effective treatment for chronic, intractable knee pain.
In a small case series consisting of five patients with chronic knee pain, pain intensity scores on the visual analog scale (VAS) dropped from an average of 8 out of 10 before the implant to 1.4 out of 10 when measured 6 months afterward.
Pain relief was also long lasting, with an average score at 2 years still significantly reduced from baseline, at 3 out of 10 on the VAS.
“We have a lot of patients with chronic knee pain, and unfortunately, our hands are tied in terms of what we can do for them,” lead author Kwo Wei David Ho, MD, PhD, Stanford University, California, told Medscape Medical News.
“They can use NSAIDs, physical therapy, some get steroid injections, or genicular nerve blocks, but they don’t work that well. Some have knee replacement surgery, and can still have persistent knee pain after the operation, so here we are using an alternative therapy called peripheral nerve stimulation of the saphenous nerve. This provides a way to relieve pain without nerve destruction or motor dysfunction,” Ho said.
The findings were presented here at the American Academy of Pain Medicine (AAPM) 2020 Annual Meeting.
Patient Controlled
For the study, the investigators surgically implanted five patients with intractable knee pain with the StimRouter™ (Bioness, Inc).
The device takes about 15 to 30 minutes to implant, much like a pacemaker, and reduces pain by delivering gentle electrical stimulation directly to a target peripheral nerve, in this case the saphenous nerve, to interrupt the pain signal, Ho said.
“A thin, threadlike lead, or noodle, is implanted below the skin next to the target peripheral nerve responsible for the pain signal under ultrasound guidance, and then a patch or external pulse transmitter (EPT) is worn on top of the skin. This sends electric stimulation through the skin to the lead,” he explained.
The patient can then control the EPT and adjust stimulation with a wireless handheld programmer.
“Some patients turn it on at night for a couple of hours and then turn it off, some leave it on for the entire night, or the whole day if they prefer. What we’ve been noticing in our series is that after a while, patients are using less and less, and the pain gets better and better, and eventually they stop using it entirely because the pain completely resolves,” Ho said.
Good candidates for this treatment are post-knee replacement patients with residual pain, he added.
Durable Effect
Of the five patients in the case series, four had previous knee arthroplasty.
To determine the chances of a good response to the implant, study participants underwent a diagnostic saphenous nerve block, with the rationale that if the block successfully reduced knee pain by 50% or more in the short term, patients would likely respond well to the implant.
Before the peripheral nerve stimulation implant, the average pain intensity was 7.8 out of 10 on the VAS. After stimulator implantation, the average pain intensity was 1.4 at 6 months (P = .019, in 5 patients). At 1 year, the average pain intensity score was virtually the same, at 1.5 on the VAS, (P = .0032, in 4 patients). At 2 years, the average pain intensity score was 2.75 (P = .12, in 2 patients).
“This study provides preliminary evidence that stimulation at the saphenous nerve may be effective for selected patients with chronic knee pain,” Ho said.
Commenting on the findings for Medscape Medical News, Patrick Tighe, MD, MS, University of Florida, Gainesville, said that chronic knee pain continues to present “numerous diagnostic and therapeutic challenges for many patients.”
“It may be surprising, but there is still so much we don’t know about the innervation of the knee, and we are still learning about different ways to alter the behavior of those nerves,” said Tighe, who was not involved with the current study.
“This work points to some exciting opportunities to help patients suffering from chronic knee pain. We certainly need more research in this area to figure out the optimal approach to applying these findings more widely,” he said.
Ho and Tighe have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
NATIONAL HARBOR, MD. – Stimulation of the infrapatellar branch of the saphenous nerve with an implantable electrical device is a potentially effective treatment for chronic, intractable knee pain.
In a small case series consisting of five patients with chronic knee pain, pain intensity scores on the visual analog scale (VAS) dropped from an average of 8 out of 10 before the implant to 1.4 out of 10 when measured 6 months afterward.
Pain relief was also long lasting, with an average score at 2 years still significantly reduced from baseline, at 3 out of 10 on the VAS.
“We have a lot of patients with chronic knee pain, and unfortunately, our hands are tied in terms of what we can do for them,” lead author Kwo Wei David Ho, MD, PhD, Stanford University, California, told Medscape Medical News.
“They can use NSAIDs, physical therapy, some get steroid injections, or genicular nerve blocks, but they don’t work that well. Some have knee replacement surgery, and can still have persistent knee pain after the operation, so here we are using an alternative therapy called peripheral nerve stimulation of the saphenous nerve. This provides a way to relieve pain without nerve destruction or motor dysfunction,” Ho said.
The findings were presented here at the American Academy of Pain Medicine (AAPM) 2020 Annual Meeting.
Patient Controlled
For the study, the investigators surgically implanted five patients with intractable knee pain with the StimRouter™ (Bioness, Inc).
The device takes about 15 to 30 minutes to implant, much like a pacemaker, and reduces pain by delivering gentle electrical stimulation directly to a target peripheral nerve, in this case the saphenous nerve, to interrupt the pain signal, Ho said.
“A thin, threadlike lead, or noodle, is implanted below the skin next to the target peripheral nerve responsible for the pain signal under ultrasound guidance, and then a patch or external pulse transmitter (EPT) is worn on top of the skin. This sends electric stimulation through the skin to the lead,” he explained.
The patient can then control the EPT and adjust stimulation with a wireless handheld programmer.
“Some patients turn it on at night for a couple of hours and then turn it off, some leave it on for the entire night, or the whole day if they prefer. What we’ve been noticing in our series is that after a while, patients are using less and less, and the pain gets better and better, and eventually they stop using it entirely because the pain completely resolves,” Ho said.
Good candidates for this treatment are post-knee replacement patients with residual pain, he added.
Durable Effect
Of the five patients in the case series, four had previous knee arthroplasty.
To determine the chances of a good response to the implant, study participants underwent a diagnostic saphenous nerve block, with the rationale that if the block successfully reduced knee pain by 50% or more in the short term, patients would likely respond well to the implant.
Before the peripheral nerve stimulation implant, the average pain intensity was 7.8 out of 10 on the VAS. After stimulator implantation, the average pain intensity was 1.4 at 6 months (P = .019, in 5 patients). At 1 year, the average pain intensity score was virtually the same, at 1.5 on the VAS, (P = .0032, in 4 patients). At 2 years, the average pain intensity score was 2.75 (P = .12, in 2 patients).
“This study provides preliminary evidence that stimulation at the saphenous nerve may be effective for selected patients with chronic knee pain,” Ho said.
Commenting on the findings for Medscape Medical News, Patrick Tighe, MD, MS, University of Florida, Gainesville, said that chronic knee pain continues to present “numerous diagnostic and therapeutic challenges for many patients.”
“It may be surprising, but there is still so much we don’t know about the innervation of the knee, and we are still learning about different ways to alter the behavior of those nerves,” said Tighe, who was not involved with the current study.
“This work points to some exciting opportunities to help patients suffering from chronic knee pain. We certainly need more research in this area to figure out the optimal approach to applying these findings more widely,” he said.
Ho and Tighe have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Telehealth seen as a key tool to help fight COVID-19
Telehealth is increasingly being viewed as a key way to help fight the COVID-19 outbreak in the United States. Recognizing the potential of this technology to slow the spread of the disease, the House of Representatives included a provision in an $8.3 billion emergency response bill it approved today that would temporarily lift restrictions on Medicare telehealth coverage to assist in the efforts to contain the virus.
Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention (CDC), said that hospitals should be prepared to use telehealth as one of their tools in fighting the outbreak, according to a recent news release from the American Hospital Association (AHA).
Congress is responding to that need by including the service in the new coronavirus legislation now headed to the Senate, after the funding bill was approved in a 415-2 vote by the House.
The bill empowers the Secretary of Health and Human Services (HHS) to “waive or modify application of certain Medicare requirements with respect to telehealth services furnished during certain emergency periods.”
While the measure adds telehealth to the waiver authority that the HHS secretary currently has during national emergencies, it’s only for the coronavirus crisis in this case, Krista Drobac, executive director of the Alliance for Connected Care, told Medscape Medical News.
The waiver would apply to originating sites of telehealth visits, she noted. Thus Medicare coverage of telemedicine would be expanded beyond rural areas.
In addition, the waiver would allow coverage of virtual visits conducted on smartphones with audio and video capabilities. A “qualified provider,” as defined by the legislation, would be a practitioner who has an established relationship with the patient or who is in the same practice as the provider who has that relationship.
An advantage of telehealth, proponents say, is that it can enable people who believe they have COVID-19 to be seen at home rather than visit offices or emergency departments (EDs) where they might spread the disease or be in proximity to others who have it.
In an editorial published March 2 in Modern Healthcare, medical directors from Stanford Medicine, MedStar Health, and Intermountain Healthcare also noted that telehealth can give patients 24/7 access to care, allow surveillance of patients at risk while keeping them at home, ensure that treatment in hospitals is reserved for high-need patients, and enable providers to triage and screen more patients than can be handled in brick-and-mortar care settings.
However, telehealth screening would allow physicians only to judge whether a patient’s symptoms might be indicative of COVID-19, the Alliance for Connected Care, a telehealth advocacy group, noted in a letter to Congressional leaders. Patients would still have to be seen in person to be tested for the disease.
The group, which represents technology companies, health insurers, pharmacies, and other healthcare players, has been lobbying Congress to include telehealth in federal funds to combat the outbreak.
The American Telemedicine Association (ATA) also supports this goal, ATA President Joseph Kvedar, MD, told Medscape Medical News. And the authors of the Modern Healthcare editorial also advocated for this legislative solution. Because the fatality rate for COVID-19 is significantly higher for older people than for other age groups, they noted, telehealth should be an economically viable option for all seniors.
The Centers for Medicare and Medicaid Services (CMS) long covered telemedicine only in rural areas and only when initiated in healthcare settings. Recently, however, CMS loosened its approach to some extent. Virtual “check-in visits” can now be initiated from any location, including home, to determine whether a Medicare patient needs to be seen in the office. In addition, CMS allows Medicare Advantage plans to offer telemedicine as a core benefit.
Are healthcare systems prepared?
Some large healthcare systems such as Stanford, MedStar, and Intermountain are already using telehealth to diagnose and treat patients who have traditional influenza. Telehealth providers at Stanford estimate that almost 50% of these patients are being prescribed the antiviral drug Tamiflu.
It’s unclear whether other healthcare systems are this well prepared to offer telehealth on a large scale. But, according to an AHA survey, Kvedar noted, three quarters of AHA members are engaged in some form of telehealth.
Drobac said “it wouldn’t require too much effort” to ramp up a wide-scale telehealth program that could help reduce the impact of the outbreak. “The technology is there,” she noted. “You need a HIPAA-compliant telehealth platform, but there are so many out there.”
Kvedar agreed. To begin with, he said, hospitals might sequester patients who visit the ED with COVID-19 symptoms in a video-equipped “isolation room.” Staff members could then do the patient intake from a different location in the hospital.
He admitted that this approach would be infeasible if a lot of patients arrived in EDs with coronavirus symptoms. However, Kvedar noted, “All the tools are in place to go well beyond that. American Well, Teladoc, and others are all offering ways to get out in front of this. There are plenty of vendors out there, and most people have a connected cell phone that you can do a video call on.”
Hospital leaders would have to decide whether to embrace telehealth, which would mean less use of services in their institutions, he said. “But it would be for the greater good of the public.”
Kvedar recalled that there was some use of telehealth in the New York area after 9/11. Telehealth was also used in the aftermath of Hurricane Katrina in 2005. But the ATA president, who is also vice president of connected health at Partners HealthCare in Boston, noted that the COVID-19 outbreak is the first public health emergency to occur in the era of Skype and smartphones.
If Congress does ultimately authorize CMS to cover telehealth across the board during this emergency, might that lead to a permanent change in Medicare coverage policy? Kvedar wouldn’t venture an opinion. “However, the current CMS leadership has been incredibly telehealth friendly,” he said. “So it’s possible they would [embrace a lifting of restrictions]. As patients get a sense of this modality of care and how convenient it is for them, they’ll start asking for more.”
Meanwhile, he said, the telehealth opportunity goes beyond video visits with doctors to mitigate the outbreak. Telehealth data could also be used to track disease spread, similar to how researchers have studied Google searches to predict the spread of the flu, he noted.
Teladoc, a major telehealth vendor, recently told stock analysts it’s already working with the CDC on disease surveillance, according to a report in FierceHealthcare.
This article first appeared on Medscape.com.
Telehealth is increasingly being viewed as a key way to help fight the COVID-19 outbreak in the United States. Recognizing the potential of this technology to slow the spread of the disease, the House of Representatives included a provision in an $8.3 billion emergency response bill it approved today that would temporarily lift restrictions on Medicare telehealth coverage to assist in the efforts to contain the virus.
Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention (CDC), said that hospitals should be prepared to use telehealth as one of their tools in fighting the outbreak, according to a recent news release from the American Hospital Association (AHA).
Congress is responding to that need by including the service in the new coronavirus legislation now headed to the Senate, after the funding bill was approved in a 415-2 vote by the House.
The bill empowers the Secretary of Health and Human Services (HHS) to “waive or modify application of certain Medicare requirements with respect to telehealth services furnished during certain emergency periods.”
While the measure adds telehealth to the waiver authority that the HHS secretary currently has during national emergencies, it’s only for the coronavirus crisis in this case, Krista Drobac, executive director of the Alliance for Connected Care, told Medscape Medical News.
The waiver would apply to originating sites of telehealth visits, she noted. Thus Medicare coverage of telemedicine would be expanded beyond rural areas.
In addition, the waiver would allow coverage of virtual visits conducted on smartphones with audio and video capabilities. A “qualified provider,” as defined by the legislation, would be a practitioner who has an established relationship with the patient or who is in the same practice as the provider who has that relationship.
An advantage of telehealth, proponents say, is that it can enable people who believe they have COVID-19 to be seen at home rather than visit offices or emergency departments (EDs) where they might spread the disease or be in proximity to others who have it.
In an editorial published March 2 in Modern Healthcare, medical directors from Stanford Medicine, MedStar Health, and Intermountain Healthcare also noted that telehealth can give patients 24/7 access to care, allow surveillance of patients at risk while keeping them at home, ensure that treatment in hospitals is reserved for high-need patients, and enable providers to triage and screen more patients than can be handled in brick-and-mortar care settings.
However, telehealth screening would allow physicians only to judge whether a patient’s symptoms might be indicative of COVID-19, the Alliance for Connected Care, a telehealth advocacy group, noted in a letter to Congressional leaders. Patients would still have to be seen in person to be tested for the disease.
The group, which represents technology companies, health insurers, pharmacies, and other healthcare players, has been lobbying Congress to include telehealth in federal funds to combat the outbreak.
The American Telemedicine Association (ATA) also supports this goal, ATA President Joseph Kvedar, MD, told Medscape Medical News. And the authors of the Modern Healthcare editorial also advocated for this legislative solution. Because the fatality rate for COVID-19 is significantly higher for older people than for other age groups, they noted, telehealth should be an economically viable option for all seniors.
The Centers for Medicare and Medicaid Services (CMS) long covered telemedicine only in rural areas and only when initiated in healthcare settings. Recently, however, CMS loosened its approach to some extent. Virtual “check-in visits” can now be initiated from any location, including home, to determine whether a Medicare patient needs to be seen in the office. In addition, CMS allows Medicare Advantage plans to offer telemedicine as a core benefit.
Are healthcare systems prepared?
Some large healthcare systems such as Stanford, MedStar, and Intermountain are already using telehealth to diagnose and treat patients who have traditional influenza. Telehealth providers at Stanford estimate that almost 50% of these patients are being prescribed the antiviral drug Tamiflu.
It’s unclear whether other healthcare systems are this well prepared to offer telehealth on a large scale. But, according to an AHA survey, Kvedar noted, three quarters of AHA members are engaged in some form of telehealth.
Drobac said “it wouldn’t require too much effort” to ramp up a wide-scale telehealth program that could help reduce the impact of the outbreak. “The technology is there,” she noted. “You need a HIPAA-compliant telehealth platform, but there are so many out there.”
Kvedar agreed. To begin with, he said, hospitals might sequester patients who visit the ED with COVID-19 symptoms in a video-equipped “isolation room.” Staff members could then do the patient intake from a different location in the hospital.
He admitted that this approach would be infeasible if a lot of patients arrived in EDs with coronavirus symptoms. However, Kvedar noted, “All the tools are in place to go well beyond that. American Well, Teladoc, and others are all offering ways to get out in front of this. There are plenty of vendors out there, and most people have a connected cell phone that you can do a video call on.”
Hospital leaders would have to decide whether to embrace telehealth, which would mean less use of services in their institutions, he said. “But it would be for the greater good of the public.”
Kvedar recalled that there was some use of telehealth in the New York area after 9/11. Telehealth was also used in the aftermath of Hurricane Katrina in 2005. But the ATA president, who is also vice president of connected health at Partners HealthCare in Boston, noted that the COVID-19 outbreak is the first public health emergency to occur in the era of Skype and smartphones.
If Congress does ultimately authorize CMS to cover telehealth across the board during this emergency, might that lead to a permanent change in Medicare coverage policy? Kvedar wouldn’t venture an opinion. “However, the current CMS leadership has been incredibly telehealth friendly,” he said. “So it’s possible they would [embrace a lifting of restrictions]. As patients get a sense of this modality of care and how convenient it is for them, they’ll start asking for more.”
Meanwhile, he said, the telehealth opportunity goes beyond video visits with doctors to mitigate the outbreak. Telehealth data could also be used to track disease spread, similar to how researchers have studied Google searches to predict the spread of the flu, he noted.
Teladoc, a major telehealth vendor, recently told stock analysts it’s already working with the CDC on disease surveillance, according to a report in FierceHealthcare.
This article first appeared on Medscape.com.
Telehealth is increasingly being viewed as a key way to help fight the COVID-19 outbreak in the United States. Recognizing the potential of this technology to slow the spread of the disease, the House of Representatives included a provision in an $8.3 billion emergency response bill it approved today that would temporarily lift restrictions on Medicare telehealth coverage to assist in the efforts to contain the virus.
Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention (CDC), said that hospitals should be prepared to use telehealth as one of their tools in fighting the outbreak, according to a recent news release from the American Hospital Association (AHA).
Congress is responding to that need by including the service in the new coronavirus legislation now headed to the Senate, after the funding bill was approved in a 415-2 vote by the House.
The bill empowers the Secretary of Health and Human Services (HHS) to “waive or modify application of certain Medicare requirements with respect to telehealth services furnished during certain emergency periods.”
While the measure adds telehealth to the waiver authority that the HHS secretary currently has during national emergencies, it’s only for the coronavirus crisis in this case, Krista Drobac, executive director of the Alliance for Connected Care, told Medscape Medical News.
The waiver would apply to originating sites of telehealth visits, she noted. Thus Medicare coverage of telemedicine would be expanded beyond rural areas.
In addition, the waiver would allow coverage of virtual visits conducted on smartphones with audio and video capabilities. A “qualified provider,” as defined by the legislation, would be a practitioner who has an established relationship with the patient or who is in the same practice as the provider who has that relationship.
An advantage of telehealth, proponents say, is that it can enable people who believe they have COVID-19 to be seen at home rather than visit offices or emergency departments (EDs) where they might spread the disease or be in proximity to others who have it.
In an editorial published March 2 in Modern Healthcare, medical directors from Stanford Medicine, MedStar Health, and Intermountain Healthcare also noted that telehealth can give patients 24/7 access to care, allow surveillance of patients at risk while keeping them at home, ensure that treatment in hospitals is reserved for high-need patients, and enable providers to triage and screen more patients than can be handled in brick-and-mortar care settings.
However, telehealth screening would allow physicians only to judge whether a patient’s symptoms might be indicative of COVID-19, the Alliance for Connected Care, a telehealth advocacy group, noted in a letter to Congressional leaders. Patients would still have to be seen in person to be tested for the disease.
The group, which represents technology companies, health insurers, pharmacies, and other healthcare players, has been lobbying Congress to include telehealth in federal funds to combat the outbreak.
The American Telemedicine Association (ATA) also supports this goal, ATA President Joseph Kvedar, MD, told Medscape Medical News. And the authors of the Modern Healthcare editorial also advocated for this legislative solution. Because the fatality rate for COVID-19 is significantly higher for older people than for other age groups, they noted, telehealth should be an economically viable option for all seniors.
The Centers for Medicare and Medicaid Services (CMS) long covered telemedicine only in rural areas and only when initiated in healthcare settings. Recently, however, CMS loosened its approach to some extent. Virtual “check-in visits” can now be initiated from any location, including home, to determine whether a Medicare patient needs to be seen in the office. In addition, CMS allows Medicare Advantage plans to offer telemedicine as a core benefit.
Are healthcare systems prepared?
Some large healthcare systems such as Stanford, MedStar, and Intermountain are already using telehealth to diagnose and treat patients who have traditional influenza. Telehealth providers at Stanford estimate that almost 50% of these patients are being prescribed the antiviral drug Tamiflu.
It’s unclear whether other healthcare systems are this well prepared to offer telehealth on a large scale. But, according to an AHA survey, Kvedar noted, three quarters of AHA members are engaged in some form of telehealth.
Drobac said “it wouldn’t require too much effort” to ramp up a wide-scale telehealth program that could help reduce the impact of the outbreak. “The technology is there,” she noted. “You need a HIPAA-compliant telehealth platform, but there are so many out there.”
Kvedar agreed. To begin with, he said, hospitals might sequester patients who visit the ED with COVID-19 symptoms in a video-equipped “isolation room.” Staff members could then do the patient intake from a different location in the hospital.
He admitted that this approach would be infeasible if a lot of patients arrived in EDs with coronavirus symptoms. However, Kvedar noted, “All the tools are in place to go well beyond that. American Well, Teladoc, and others are all offering ways to get out in front of this. There are plenty of vendors out there, and most people have a connected cell phone that you can do a video call on.”
Hospital leaders would have to decide whether to embrace telehealth, which would mean less use of services in their institutions, he said. “But it would be for the greater good of the public.”
Kvedar recalled that there was some use of telehealth in the New York area after 9/11. Telehealth was also used in the aftermath of Hurricane Katrina in 2005. But the ATA president, who is also vice president of connected health at Partners HealthCare in Boston, noted that the COVID-19 outbreak is the first public health emergency to occur in the era of Skype and smartphones.
If Congress does ultimately authorize CMS to cover telehealth across the board during this emergency, might that lead to a permanent change in Medicare coverage policy? Kvedar wouldn’t venture an opinion. “However, the current CMS leadership has been incredibly telehealth friendly,” he said. “So it’s possible they would [embrace a lifting of restrictions]. As patients get a sense of this modality of care and how convenient it is for them, they’ll start asking for more.”
Meanwhile, he said, the telehealth opportunity goes beyond video visits with doctors to mitigate the outbreak. Telehealth data could also be used to track disease spread, similar to how researchers have studied Google searches to predict the spread of the flu, he noted.
Teladoc, a major telehealth vendor, recently told stock analysts it’s already working with the CDC on disease surveillance, according to a report in FierceHealthcare.
This article first appeared on Medscape.com.
SARS epidemiology provides clues to potential treatment for COVID-19
A team of researchers has discovered important commonalities between SARS-CoV-2 and SARS-CoV infection that could lead to a potential targets for antiviral intervention.
Markus Hoffmann, of the Leibniz Institute for Primate Research, Göttingen, Germany, and a team of investigators also found that antibody responses raised against SARS-S during infection or vaccination might offer some level of protection against SARS-CoV-2 infection. Their findings were published in Cell.
In order for coronaviruses to enter a cell, they must first bind their viral spike (S) proteins to cellular receptors and depend on S protein priming by host cell proteases. The study found that the SARS-CoV-2, causal agent for COVID-19, uses the same SARS-CoV receptor, ACE2, for entry and uses the serine protease TMPRSS2 for S protein priming as the original SARS-CoV-1 (SARS). Importantly, the researchers also found that the cellular serine protease TMPRSS2 primes SARS-CoV-2-S for entry and that a serine protease inhibitor blocks SARS-CoV-2 infection of lung cells, providing opportunities for potential therapeutic intervention.
The researchers performed a sequence analysis that showed SARS-CoV-2 clusters with SARS-CoV–related viruses from bats, of which some – but not all – can use ACE2 for host cell entry. Further analysis of the receptor binding motif known to make contact with ACE2 showed that most amino acid residues essential for ACE2 binding by SARS-S were conserved in SARS-2-S but were absent from S proteins of those SARS-related coronaviruses previously found not to use ACE2.
In addition, the researchers found that SARS-CoV-2–infected BHK-21 cells transfected to express ACE2 with high efficiency, but not the parental BHK-21 cells indicating that SARS-CoV-2-S, like the original SARS virus S protein, uses ACE2 for cellular entry.
Using cultured cells, the researchers found that the protease inhibitor, camostat mesylate, inhibited SARS-S and SARS-2-S entry into primary human lung cells, demonstrating that SARS-CoV-2 can use TMPRSS2 for S protein priming and that camostat mesylate can block SARS-CoV-2 infection of lung cells. Camostat mesylate has been used as a therapy for some forms of cancer and other viral infections.
In addition to their research on the protease inhibitor, the researchers also found that sera from convalescent SARS patients cross-neutralized SARS-2-S–driven entry. They found that four sera obtained from three convalescent SARS patients inhibited SARS-S entry into cell lines in a concentration dependent fashion.
“We demonstrate that SARS-CoV-2 uses the SARS55 CoV receptor, ACE2, for entry and the serine protease TMPRSS2 for S protein priming. A TMPRSS2 inhibitor approved for clinical use blocked entry and might constitute a treatment option. Finally, we show that the sera from convalescent SARS patients cross-neutralized SARS-2-S–driven entry,” the authors concluded.
The study was supported by BMBF (RAPID Consortium) and German Research Foundation (DFG). The authors reported that they had no conflicts.
SOURCE: Hoffmann M et al. Cell 2020. doi: 10.1016/j.cell.2020.02.052.
A team of researchers has discovered important commonalities between SARS-CoV-2 and SARS-CoV infection that could lead to a potential targets for antiviral intervention.
Markus Hoffmann, of the Leibniz Institute for Primate Research, Göttingen, Germany, and a team of investigators also found that antibody responses raised against SARS-S during infection or vaccination might offer some level of protection against SARS-CoV-2 infection. Their findings were published in Cell.
In order for coronaviruses to enter a cell, they must first bind their viral spike (S) proteins to cellular receptors and depend on S protein priming by host cell proteases. The study found that the SARS-CoV-2, causal agent for COVID-19, uses the same SARS-CoV receptor, ACE2, for entry and uses the serine protease TMPRSS2 for S protein priming as the original SARS-CoV-1 (SARS). Importantly, the researchers also found that the cellular serine protease TMPRSS2 primes SARS-CoV-2-S for entry and that a serine protease inhibitor blocks SARS-CoV-2 infection of lung cells, providing opportunities for potential therapeutic intervention.
The researchers performed a sequence analysis that showed SARS-CoV-2 clusters with SARS-CoV–related viruses from bats, of which some – but not all – can use ACE2 for host cell entry. Further analysis of the receptor binding motif known to make contact with ACE2 showed that most amino acid residues essential for ACE2 binding by SARS-S were conserved in SARS-2-S but were absent from S proteins of those SARS-related coronaviruses previously found not to use ACE2.
In addition, the researchers found that SARS-CoV-2–infected BHK-21 cells transfected to express ACE2 with high efficiency, but not the parental BHK-21 cells indicating that SARS-CoV-2-S, like the original SARS virus S protein, uses ACE2 for cellular entry.
Using cultured cells, the researchers found that the protease inhibitor, camostat mesylate, inhibited SARS-S and SARS-2-S entry into primary human lung cells, demonstrating that SARS-CoV-2 can use TMPRSS2 for S protein priming and that camostat mesylate can block SARS-CoV-2 infection of lung cells. Camostat mesylate has been used as a therapy for some forms of cancer and other viral infections.
In addition to their research on the protease inhibitor, the researchers also found that sera from convalescent SARS patients cross-neutralized SARS-2-S–driven entry. They found that four sera obtained from three convalescent SARS patients inhibited SARS-S entry into cell lines in a concentration dependent fashion.
“We demonstrate that SARS-CoV-2 uses the SARS55 CoV receptor, ACE2, for entry and the serine protease TMPRSS2 for S protein priming. A TMPRSS2 inhibitor approved for clinical use blocked entry and might constitute a treatment option. Finally, we show that the sera from convalescent SARS patients cross-neutralized SARS-2-S–driven entry,” the authors concluded.
The study was supported by BMBF (RAPID Consortium) and German Research Foundation (DFG). The authors reported that they had no conflicts.
SOURCE: Hoffmann M et al. Cell 2020. doi: 10.1016/j.cell.2020.02.052.
A team of researchers has discovered important commonalities between SARS-CoV-2 and SARS-CoV infection that could lead to a potential targets for antiviral intervention.
Markus Hoffmann, of the Leibniz Institute for Primate Research, Göttingen, Germany, and a team of investigators also found that antibody responses raised against SARS-S during infection or vaccination might offer some level of protection against SARS-CoV-2 infection. Their findings were published in Cell.
In order for coronaviruses to enter a cell, they must first bind their viral spike (S) proteins to cellular receptors and depend on S protein priming by host cell proteases. The study found that the SARS-CoV-2, causal agent for COVID-19, uses the same SARS-CoV receptor, ACE2, for entry and uses the serine protease TMPRSS2 for S protein priming as the original SARS-CoV-1 (SARS). Importantly, the researchers also found that the cellular serine protease TMPRSS2 primes SARS-CoV-2-S for entry and that a serine protease inhibitor blocks SARS-CoV-2 infection of lung cells, providing opportunities for potential therapeutic intervention.
The researchers performed a sequence analysis that showed SARS-CoV-2 clusters with SARS-CoV–related viruses from bats, of which some – but not all – can use ACE2 for host cell entry. Further analysis of the receptor binding motif known to make contact with ACE2 showed that most amino acid residues essential for ACE2 binding by SARS-S were conserved in SARS-2-S but were absent from S proteins of those SARS-related coronaviruses previously found not to use ACE2.
In addition, the researchers found that SARS-CoV-2–infected BHK-21 cells transfected to express ACE2 with high efficiency, but not the parental BHK-21 cells indicating that SARS-CoV-2-S, like the original SARS virus S protein, uses ACE2 for cellular entry.
Using cultured cells, the researchers found that the protease inhibitor, camostat mesylate, inhibited SARS-S and SARS-2-S entry into primary human lung cells, demonstrating that SARS-CoV-2 can use TMPRSS2 for S protein priming and that camostat mesylate can block SARS-CoV-2 infection of lung cells. Camostat mesylate has been used as a therapy for some forms of cancer and other viral infections.
In addition to their research on the protease inhibitor, the researchers also found that sera from convalescent SARS patients cross-neutralized SARS-2-S–driven entry. They found that four sera obtained from three convalescent SARS patients inhibited SARS-S entry into cell lines in a concentration dependent fashion.
“We demonstrate that SARS-CoV-2 uses the SARS55 CoV receptor, ACE2, for entry and the serine protease TMPRSS2 for S protein priming. A TMPRSS2 inhibitor approved for clinical use blocked entry and might constitute a treatment option. Finally, we show that the sera from convalescent SARS patients cross-neutralized SARS-2-S–driven entry,” the authors concluded.
The study was supported by BMBF (RAPID Consortium) and German Research Foundation (DFG). The authors reported that they had no conflicts.
SOURCE: Hoffmann M et al. Cell 2020. doi: 10.1016/j.cell.2020.02.052.
FROM CELL
Infection control protects hospital staff from COVID-19, study shows
Hospital-related infections have been widely reported during the ongoing coronavirus outbreak, with healthcare professionals bearing a disproportionate risk. However, a proactive response in Hong Kong’s public hospital system appears to have bucked this trend and successfully protected both patients and staff from SARS-CoV-2, according to a study published online today in Infection Control & Hospital Epidemiology.
During the first 42 days of the outbreak, the 43 hospitals in the network tested 1275 suspected cases and treated 42 patients with confirmed COVID-19, the disease caused by SARS-CoV-2 infection. Yet, there were no nosocomial infections or infections among healthcare personnel, report Vincent C.C. Cheng, MD, FRCPath, the hospital’s infection control officer, and colleagues.
Cheng and colleagues note that 11 out of 413 healthcare workers who treat patients with confirmed infections had unprotected exposure and were in quarantine for 14 days, but none became ill.
In comparison, they note, the 2003 SARS outbreak saw almost 60% of nosocomial cases occurring in healthcare workers.
Proactive bundle
The Hong Kong success story may be due to a stepped-up proactive bundle of measures that included enhanced laboratory surveillance, early airborne infection isolation, and rapid-turnaround molecular diagnostics. Other strategies included staff forums and one-on-one discussions about infection control, employee training in protective equipment use, hand-hygiene compliance enforcement, and contact tracing for workers with unprotected exposure.
In addition, surgical masks were provided for all healthcare workers, patients, and visitors to clinical areas, a practice previously associated with reduced in-hospital transmission during influenza outbreaks, the authors note.
Hospitals also mandated use of personal protective equipment (PPE) for aerosol-generating procedures (AGPs), such as endotracheal intubation, open suctioning, and high-flow oxygen use, as AGPs had been linked to nosocomial transmission to healthcare workers during the 2003 SARS outbreak.
The infection control measures, which were part of a preparedness plan developed after the SARS outbreak, were initiated on December 31, when the first reports of a cluster of infections came from Wuhan, China.
As the outbreak evolved, the Hong Kong hospitals quickly widened the epidemiologic criteria for screening, from initially including only those who had been to a wet market in Wuhan within 14 days of symptom onset, to eventually including anyone who had been to Hubei province, been in a medical facility in mainland China, or in contact with a known case.
All suspected cases were sent to an airborne-infection isolation room (AIIR) or a ward with at least a meter of space between patients.
“Appropriate hospital infection control measures could prevent nosocomial transmission of SARS-CoV-2,” the authors write. “Vigilance in hand hygiene practice, wearing of surgical mask in the hospital, and appropriate use of PPE in patient care, especially [when] performing AGPs, are the key infection control measures to prevent nosocomial transmission of SARS-CoV-2 even before the availability of effective antiviral agents and vaccine.”
Asked for his perspective on the report, Aaron E. Glatt, MD, chairman of the department of medicine and chief of infectious diseases at Mount Sinai South Nassau in Oceanside, New York, said that apart from the widespread issuing of surgical masks to workers, patients, and visitors, the measures taken in Hong Kong are not different from standard infection-control practices in American hospitals. Glatt, who is also a hospital epidemiologist, said it was unclear how much impact the masks would have.
“Although the infection control was impressive, I don’t see any evidence of a difference in care,” he told Medscape Medical News.
Could zero infection transmission be achieved in the more far-flung and variable settings of hospitals across the United States? “The ability to get zero transmission is only possible if people adhere to the strictest infection-control guidelines,” Glatt said. “That is clearly the goal, and it will take time to see if our existing strict guidelines are sufficient to maintain zero or close to zero contamination and transmission rates in our hospitals.”
Rather than looking to change US practices, he stressed adherence to widely established tenets of care. “It’s critically important to keep paying close attention to the basics, to the simple blocking and tackling, and to identify which patients are at risk, and therefore, when workers need protective equipment,” he said.
“Follow the recommended standards,” continued Glatt, who is also a spokesperson for the Infectious Diseases Society of America and did not participate in this study.
In a finding from an ancillary pilot experiment, the Hong Kong researchers found exhaled air from a patient with a moderate coronavirus load showed no evidence of the virus, whether the patient was breathing normally or heavily, speaking, or coughing. And spot tests around the room detected the virus in just one location.
“We may not be able to make a definite conclusion based on the analysis of a single patient,” the authors write. “However, it may help to reassure our staff that the exhaled air may be rapidly diluted inside the AIIR with 12 air changes per hour, or probably the SARS-CoV-2 may not be predominantly transmitted by [the] airborne route.”
However, a recent Singapore study showed widespread environmental contamination by SARS-CoV-2 through respiratory droplets and fecal shedding, underlining the need for strict adherence to environmental and hand hygiene. Post-cleaning samples tested negative, suggesting that standard decontamination practices are effective.
This work was partly supported by the Consultancy Service for Enhancing Laboratory Surveillance of Emerging Infectious Diseases of the Department of Health, Hong Kong Special Administrative Region; and the Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases, Ministry of Education of China. The authors and Glatt have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Hospital-related infections have been widely reported during the ongoing coronavirus outbreak, with healthcare professionals bearing a disproportionate risk. However, a proactive response in Hong Kong’s public hospital system appears to have bucked this trend and successfully protected both patients and staff from SARS-CoV-2, according to a study published online today in Infection Control & Hospital Epidemiology.
During the first 42 days of the outbreak, the 43 hospitals in the network tested 1275 suspected cases and treated 42 patients with confirmed COVID-19, the disease caused by SARS-CoV-2 infection. Yet, there were no nosocomial infections or infections among healthcare personnel, report Vincent C.C. Cheng, MD, FRCPath, the hospital’s infection control officer, and colleagues.
Cheng and colleagues note that 11 out of 413 healthcare workers who treat patients with confirmed infections had unprotected exposure and were in quarantine for 14 days, but none became ill.
In comparison, they note, the 2003 SARS outbreak saw almost 60% of nosocomial cases occurring in healthcare workers.
Proactive bundle
The Hong Kong success story may be due to a stepped-up proactive bundle of measures that included enhanced laboratory surveillance, early airborne infection isolation, and rapid-turnaround molecular diagnostics. Other strategies included staff forums and one-on-one discussions about infection control, employee training in protective equipment use, hand-hygiene compliance enforcement, and contact tracing for workers with unprotected exposure.
In addition, surgical masks were provided for all healthcare workers, patients, and visitors to clinical areas, a practice previously associated with reduced in-hospital transmission during influenza outbreaks, the authors note.
Hospitals also mandated use of personal protective equipment (PPE) for aerosol-generating procedures (AGPs), such as endotracheal intubation, open suctioning, and high-flow oxygen use, as AGPs had been linked to nosocomial transmission to healthcare workers during the 2003 SARS outbreak.
The infection control measures, which were part of a preparedness plan developed after the SARS outbreak, were initiated on December 31, when the first reports of a cluster of infections came from Wuhan, China.
As the outbreak evolved, the Hong Kong hospitals quickly widened the epidemiologic criteria for screening, from initially including only those who had been to a wet market in Wuhan within 14 days of symptom onset, to eventually including anyone who had been to Hubei province, been in a medical facility in mainland China, or in contact with a known case.
All suspected cases were sent to an airborne-infection isolation room (AIIR) or a ward with at least a meter of space between patients.
“Appropriate hospital infection control measures could prevent nosocomial transmission of SARS-CoV-2,” the authors write. “Vigilance in hand hygiene practice, wearing of surgical mask in the hospital, and appropriate use of PPE in patient care, especially [when] performing AGPs, are the key infection control measures to prevent nosocomial transmission of SARS-CoV-2 even before the availability of effective antiviral agents and vaccine.”
Asked for his perspective on the report, Aaron E. Glatt, MD, chairman of the department of medicine and chief of infectious diseases at Mount Sinai South Nassau in Oceanside, New York, said that apart from the widespread issuing of surgical masks to workers, patients, and visitors, the measures taken in Hong Kong are not different from standard infection-control practices in American hospitals. Glatt, who is also a hospital epidemiologist, said it was unclear how much impact the masks would have.
“Although the infection control was impressive, I don’t see any evidence of a difference in care,” he told Medscape Medical News.
Could zero infection transmission be achieved in the more far-flung and variable settings of hospitals across the United States? “The ability to get zero transmission is only possible if people adhere to the strictest infection-control guidelines,” Glatt said. “That is clearly the goal, and it will take time to see if our existing strict guidelines are sufficient to maintain zero or close to zero contamination and transmission rates in our hospitals.”
Rather than looking to change US practices, he stressed adherence to widely established tenets of care. “It’s critically important to keep paying close attention to the basics, to the simple blocking and tackling, and to identify which patients are at risk, and therefore, when workers need protective equipment,” he said.
“Follow the recommended standards,” continued Glatt, who is also a spokesperson for the Infectious Diseases Society of America and did not participate in this study.
In a finding from an ancillary pilot experiment, the Hong Kong researchers found exhaled air from a patient with a moderate coronavirus load showed no evidence of the virus, whether the patient was breathing normally or heavily, speaking, or coughing. And spot tests around the room detected the virus in just one location.
“We may not be able to make a definite conclusion based on the analysis of a single patient,” the authors write. “However, it may help to reassure our staff that the exhaled air may be rapidly diluted inside the AIIR with 12 air changes per hour, or probably the SARS-CoV-2 may not be predominantly transmitted by [the] airborne route.”
However, a recent Singapore study showed widespread environmental contamination by SARS-CoV-2 through respiratory droplets and fecal shedding, underlining the need for strict adherence to environmental and hand hygiene. Post-cleaning samples tested negative, suggesting that standard decontamination practices are effective.
This work was partly supported by the Consultancy Service for Enhancing Laboratory Surveillance of Emerging Infectious Diseases of the Department of Health, Hong Kong Special Administrative Region; and the Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases, Ministry of Education of China. The authors and Glatt have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Hospital-related infections have been widely reported during the ongoing coronavirus outbreak, with healthcare professionals bearing a disproportionate risk. However, a proactive response in Hong Kong’s public hospital system appears to have bucked this trend and successfully protected both patients and staff from SARS-CoV-2, according to a study published online today in Infection Control & Hospital Epidemiology.
During the first 42 days of the outbreak, the 43 hospitals in the network tested 1275 suspected cases and treated 42 patients with confirmed COVID-19, the disease caused by SARS-CoV-2 infection. Yet, there were no nosocomial infections or infections among healthcare personnel, report Vincent C.C. Cheng, MD, FRCPath, the hospital’s infection control officer, and colleagues.
Cheng and colleagues note that 11 out of 413 healthcare workers who treat patients with confirmed infections had unprotected exposure and were in quarantine for 14 days, but none became ill.
In comparison, they note, the 2003 SARS outbreak saw almost 60% of nosocomial cases occurring in healthcare workers.
Proactive bundle
The Hong Kong success story may be due to a stepped-up proactive bundle of measures that included enhanced laboratory surveillance, early airborne infection isolation, and rapid-turnaround molecular diagnostics. Other strategies included staff forums and one-on-one discussions about infection control, employee training in protective equipment use, hand-hygiene compliance enforcement, and contact tracing for workers with unprotected exposure.
In addition, surgical masks were provided for all healthcare workers, patients, and visitors to clinical areas, a practice previously associated with reduced in-hospital transmission during influenza outbreaks, the authors note.
Hospitals also mandated use of personal protective equipment (PPE) for aerosol-generating procedures (AGPs), such as endotracheal intubation, open suctioning, and high-flow oxygen use, as AGPs had been linked to nosocomial transmission to healthcare workers during the 2003 SARS outbreak.
The infection control measures, which were part of a preparedness plan developed after the SARS outbreak, were initiated on December 31, when the first reports of a cluster of infections came from Wuhan, China.
As the outbreak evolved, the Hong Kong hospitals quickly widened the epidemiologic criteria for screening, from initially including only those who had been to a wet market in Wuhan within 14 days of symptom onset, to eventually including anyone who had been to Hubei province, been in a medical facility in mainland China, or in contact with a known case.
All suspected cases were sent to an airborne-infection isolation room (AIIR) or a ward with at least a meter of space between patients.
“Appropriate hospital infection control measures could prevent nosocomial transmission of SARS-CoV-2,” the authors write. “Vigilance in hand hygiene practice, wearing of surgical mask in the hospital, and appropriate use of PPE in patient care, especially [when] performing AGPs, are the key infection control measures to prevent nosocomial transmission of SARS-CoV-2 even before the availability of effective antiviral agents and vaccine.”
Asked for his perspective on the report, Aaron E. Glatt, MD, chairman of the department of medicine and chief of infectious diseases at Mount Sinai South Nassau in Oceanside, New York, said that apart from the widespread issuing of surgical masks to workers, patients, and visitors, the measures taken in Hong Kong are not different from standard infection-control practices in American hospitals. Glatt, who is also a hospital epidemiologist, said it was unclear how much impact the masks would have.
“Although the infection control was impressive, I don’t see any evidence of a difference in care,” he told Medscape Medical News.
Could zero infection transmission be achieved in the more far-flung and variable settings of hospitals across the United States? “The ability to get zero transmission is only possible if people adhere to the strictest infection-control guidelines,” Glatt said. “That is clearly the goal, and it will take time to see if our existing strict guidelines are sufficient to maintain zero or close to zero contamination and transmission rates in our hospitals.”
Rather than looking to change US practices, he stressed adherence to widely established tenets of care. “It’s critically important to keep paying close attention to the basics, to the simple blocking and tackling, and to identify which patients are at risk, and therefore, when workers need protective equipment,” he said.
“Follow the recommended standards,” continued Glatt, who is also a spokesperson for the Infectious Diseases Society of America and did not participate in this study.
In a finding from an ancillary pilot experiment, the Hong Kong researchers found exhaled air from a patient with a moderate coronavirus load showed no evidence of the virus, whether the patient was breathing normally or heavily, speaking, or coughing. And spot tests around the room detected the virus in just one location.
“We may not be able to make a definite conclusion based on the analysis of a single patient,” the authors write. “However, it may help to reassure our staff that the exhaled air may be rapidly diluted inside the AIIR with 12 air changes per hour, or probably the SARS-CoV-2 may not be predominantly transmitted by [the] airborne route.”
However, a recent Singapore study showed widespread environmental contamination by SARS-CoV-2 through respiratory droplets and fecal shedding, underlining the need for strict adherence to environmental and hand hygiene. Post-cleaning samples tested negative, suggesting that standard decontamination practices are effective.
This work was partly supported by the Consultancy Service for Enhancing Laboratory Surveillance of Emerging Infectious Diseases of the Department of Health, Hong Kong Special Administrative Region; and the Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases, Ministry of Education of China. The authors and Glatt have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Survey: 2020 will see more attacks on ACA
When physicians gaze into their crystal balls to predict what’s coming in 2020, they see continued efforts to defund the Affordable Care Act – meaning the ACA will still be around to be defunded – but they don’t see a lot of support for universal health care, according to health care market research company InCrowd.
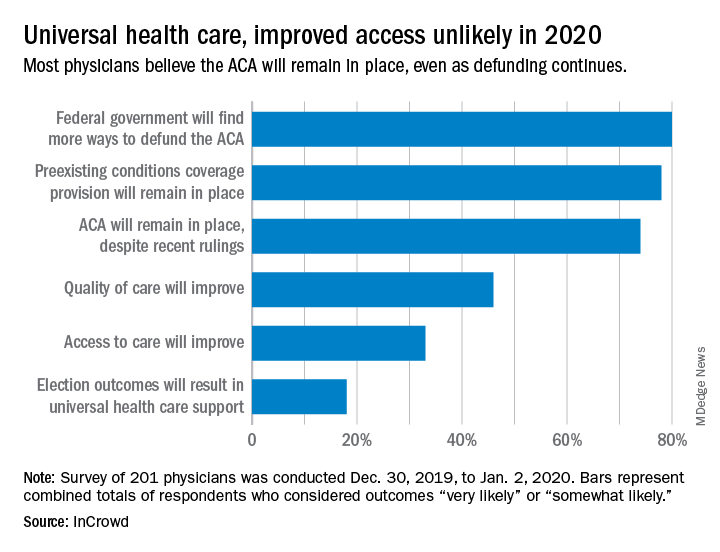
Expectations for universal health care came in at 18% of the 100 generalists and 101 specialists who responded to InCrowd’s fifth annual health care predictions survey, which left 82% who thought that “election outcomes will result in universal healthcare support” was somewhat or very unlikely in 2020.
One respondent, a specialist from California, commented that “the global data on universal healthcare for all shows that it results in overall improved population health. Unfortunately, we are so polarized in the US against universal healthcare driven by bias from health insurance companies and decision makers that are quick to ignore scientific data.”
This was the first time InCrowd asked physicians about universal health care, but ACA-related predictions have been included before, and all three scenarios presented were deemed to be increasingly likely, compared with 2019.
Respondents thought that federal government defunding was more likely to occur in 2020 (80%) than in 2019 (73%), but increased majorities also said that preexisting conditions coverage would continue (78% in 2020 vs. 70% in 2019) and that the ACA would remain in place (74% in 2020 vs. 60% in 2019), InCrowd reported after the survey, which was conducted from Dec. 30, 2019, to Jan. 2, 2020.
A respondent who thought the ACA will be eliminated said, “I have as many uninsured today as before the ACA. They are just different. Mainly younger patients who spend less in a year on healthcare than one month’s premium.” Another suggested that eliminateing it “will limit access to care and overload [emergency departments]. More people will die.”
Cost was addressed in a separate survey question that asked how physicians could help to reduce health care spending in 2020.
The leading answer, given by 37% of respondents, was for physicians to “inform themselves of costs and adapt cost-saving prescription practices.” Next came “limit use of expensive tests and scans” with 21%, followed by “prescribe generics when possible” at 20%, which was a substantial drop from the 38% it garnered in 2019, InCrowd noted.
“Participation in [shared savings] programs and risk-based incentive programs and pay-for-performance programs” would provide “better stewardship of resources,” a primary care physician from Michigan wrote.
When the survey turned to pharmaceutical industry predictions for 2020, cost was the major issue.
“What’s interesting about this year’s data is that we’re seeing less emphasis on the importance of bringing innovative, new therapies to market faster … versus expanding affordability, which was nearly a unanimous top priority for respondents,” Daniel S. Fitzgerald, InCrowd’s CEO and president, said in a separate statement.
When physicians gaze into their crystal balls to predict what’s coming in 2020, they see continued efforts to defund the Affordable Care Act – meaning the ACA will still be around to be defunded – but they don’t see a lot of support for universal health care, according to health care market research company InCrowd.
Expectations for universal health care came in at 18% of the 100 generalists and 101 specialists who responded to InCrowd’s fifth annual health care predictions survey, which left 82% who thought that “election outcomes will result in universal healthcare support” was somewhat or very unlikely in 2020.
One respondent, a specialist from California, commented that “the global data on universal healthcare for all shows that it results in overall improved population health. Unfortunately, we are so polarized in the US against universal healthcare driven by bias from health insurance companies and decision makers that are quick to ignore scientific data.”
This was the first time InCrowd asked physicians about universal health care, but ACA-related predictions have been included before, and all three scenarios presented were deemed to be increasingly likely, compared with 2019.
Respondents thought that federal government defunding was more likely to occur in 2020 (80%) than in 2019 (73%), but increased majorities also said that preexisting conditions coverage would continue (78% in 2020 vs. 70% in 2019) and that the ACA would remain in place (74% in 2020 vs. 60% in 2019), InCrowd reported after the survey, which was conducted from Dec. 30, 2019, to Jan. 2, 2020.
A respondent who thought the ACA will be eliminated said, “I have as many uninsured today as before the ACA. They are just different. Mainly younger patients who spend less in a year on healthcare than one month’s premium.” Another suggested that eliminateing it “will limit access to care and overload [emergency departments]. More people will die.”
Cost was addressed in a separate survey question that asked how physicians could help to reduce health care spending in 2020.
The leading answer, given by 37% of respondents, was for physicians to “inform themselves of costs and adapt cost-saving prescription practices.” Next came “limit use of expensive tests and scans” with 21%, followed by “prescribe generics when possible” at 20%, which was a substantial drop from the 38% it garnered in 2019, InCrowd noted.
“Participation in [shared savings] programs and risk-based incentive programs and pay-for-performance programs” would provide “better stewardship of resources,” a primary care physician from Michigan wrote.
When the survey turned to pharmaceutical industry predictions for 2020, cost was the major issue.
“What’s interesting about this year’s data is that we’re seeing less emphasis on the importance of bringing innovative, new therapies to market faster … versus expanding affordability, which was nearly a unanimous top priority for respondents,” Daniel S. Fitzgerald, InCrowd’s CEO and president, said in a separate statement.
When physicians gaze into their crystal balls to predict what’s coming in 2020, they see continued efforts to defund the Affordable Care Act – meaning the ACA will still be around to be defunded – but they don’t see a lot of support for universal health care, according to health care market research company InCrowd.
Expectations for universal health care came in at 18% of the 100 generalists and 101 specialists who responded to InCrowd’s fifth annual health care predictions survey, which left 82% who thought that “election outcomes will result in universal healthcare support” was somewhat or very unlikely in 2020.
One respondent, a specialist from California, commented that “the global data on universal healthcare for all shows that it results in overall improved population health. Unfortunately, we are so polarized in the US against universal healthcare driven by bias from health insurance companies and decision makers that are quick to ignore scientific data.”
This was the first time InCrowd asked physicians about universal health care, but ACA-related predictions have been included before, and all three scenarios presented were deemed to be increasingly likely, compared with 2019.
Respondents thought that federal government defunding was more likely to occur in 2020 (80%) than in 2019 (73%), but increased majorities also said that preexisting conditions coverage would continue (78% in 2020 vs. 70% in 2019) and that the ACA would remain in place (74% in 2020 vs. 60% in 2019), InCrowd reported after the survey, which was conducted from Dec. 30, 2019, to Jan. 2, 2020.
A respondent who thought the ACA will be eliminated said, “I have as many uninsured today as before the ACA. They are just different. Mainly younger patients who spend less in a year on healthcare than one month’s premium.” Another suggested that eliminateing it “will limit access to care and overload [emergency departments]. More people will die.”
Cost was addressed in a separate survey question that asked how physicians could help to reduce health care spending in 2020.
The leading answer, given by 37% of respondents, was for physicians to “inform themselves of costs and adapt cost-saving prescription practices.” Next came “limit use of expensive tests and scans” with 21%, followed by “prescribe generics when possible” at 20%, which was a substantial drop from the 38% it garnered in 2019, InCrowd noted.
“Participation in [shared savings] programs and risk-based incentive programs and pay-for-performance programs” would provide “better stewardship of resources,” a primary care physician from Michigan wrote.
When the survey turned to pharmaceutical industry predictions for 2020, cost was the major issue.
“What’s interesting about this year’s data is that we’re seeing less emphasis on the importance of bringing innovative, new therapies to market faster … versus expanding affordability, which was nearly a unanimous top priority for respondents,” Daniel S. Fitzgerald, InCrowd’s CEO and president, said in a separate statement.
AFib patients do best on a DOAC started 7-10 days post stroke
LOS ANGELES – When a patient with atrial fibrillation (AFib) has a cardioembolic stroke, the best blood thinner to start may be a direct-acting oral anticoagulant (DOAC), possibly beginning 7-10 days after the index stroke, according to an analysis of 90-day, observational outcomes data from nearly 1,300 patients.
The analysis also suggested that the use of “bridging” anticoagulant treatment by injection before a patient with atrial fibrillation (AFib) starts a daily oral anticoagulant regimen following a cardioembolic stroke is not a good idea. Patients who received bridging anticoagulation had a nearly threefold higher rate of symptomatic intracranial hemorrhage than did patients who did not, and their bridging treatment failed to protect them from recurrent ischemic events, Shadi Yaghi, MD, said at the International Stroke Conference, sponsored by the American Heart Association. The bridging regimens delivered either heparin or low-molecular-weight heparin.
Based on the findings, “it seems reasonable to avoid bridging unless absolutely necessary, to initiate a DOAC unless it’s contraindicated, and to start the DOAC on day 7-10 following the stroke in most patients,” said Dr. Yaghi, a vascular neurologist and director of stroke research at NYU Langone Health in New York.
“It’s been hard to develop a broad guideline on when to start oral anticoagulation” after a cardioembolic stroke in AFib patients. The best time “depends on a lot of variables and how the patient responded to acute treatment,” commented Alexis Simpkins, MD, a vascular and stroke neurologist at the University of Florida in Gainesville. “You want to start treatment before the patient has another stroke, but not so soon that the treatment causes symptomatic hemorrhagic transformation.”
Dr. Yaghi’s suggestion, based on his findings, to start treatment for most patients with a DOAC 7-10 days after their index stroke “shows consistency” with the prevailing guideline recommendation from the AHA/American Stroke Association to start oral anticoagulation in this patient population 4-14 days after the index stroke (Stroke. 2018 March;49[3]:e46-e99), she noted.
A recent article reviewed the uncertainty about the best time to start oral anticoagulation in AFib patients after a cardioembolic stroke and the subtle differences that distinguish various international medical groups that, like the ASA, have made recommendations (Lancet Neurol. 2019 Jan 1;18[1]:117-26). According to this review, a major limitation of these various recommendations has been the lack of actual evidence collected from AFib patients who began receiving a DOAC shortly after a cardioembolic stroke, although the article added that several studies in progress are collecting these data.
The study reported by Dr. Yaghi pooled data collected from 2,084 recent AFib patients with a cardioembolic stroke treated at any of eight comprehensive U.S. stroke centers. They excluded patients who died from causes unrelated to the primary endpoint, those who did not receive an anticoagulant or had incomplete data, and patients lost to follow-up, leaving 1,289 evaluable patients. During their 90-day follow-up, 10% of the patients had an ischemic event, a symptomatic intracranial hemorrhage, or an extracranial hemorrhage.
The study’s primary analysis showed no statistically significant difference in the incidence of recurrent ischemic events, symptomatic intracranial hemorrhage, or both based on when oral anticoagulant treatment began: 0-3 days, 4-14 days, or more than 14 days after the index stroke.
The investigators then subdivided patients into the subgroup that started treatment with a DOAC and the subgroup that started treatment with warfarin and also further subdivided the 4-14 day time window for starting treatment. Results of this analysis showed that patients who received a DOAC and began this treatment 7-10 days after their stroke had a 50% cut in their 90-day events compared with other patients, a difference that fell just short of statistical significance at P = .07. All the other combinations of oral anticoagulant and time of treatment initiation analyzed showed neutral effects that never came near statistical significance.
Secondary data analyses also showed that both patients with a history of a stroke prior to their index stroke and patients with ipsilateral atherosclerosis came close to having a statistically significant increased rate of a subsequent ischemic event during 90-day follow-up. Furthermore, women, patients with a history of hyperlipidemia, and patients who developed hemorrhagic transformation of their index stroke all had significantly increased rates of developing a symptomatic intracranial hemorrhage during 90-day follow-up. When the endpoint was limited to recurrent ischemic events only, patients who received a DOAC were 50% less likely to have an event than were patients treated with warfarin, a statistically significant difference.
Although starting a DOAC 7-10 days after the index stroke seems reasonable based on this analysis, the question needs a prospective, randomized study to create an appropriate evidence base, Dr. Yaghi said.
Dr. Yaghi disclosed a financial relationship with Medtronic. Dr. Simpkins had no disclosures.
SOURCE: Yaghi S et al. Stroke. 2020 Feb;51(suppl 1):A119.
LOS ANGELES – When a patient with atrial fibrillation (AFib) has a cardioembolic stroke, the best blood thinner to start may be a direct-acting oral anticoagulant (DOAC), possibly beginning 7-10 days after the index stroke, according to an analysis of 90-day, observational outcomes data from nearly 1,300 patients.
The analysis also suggested that the use of “bridging” anticoagulant treatment by injection before a patient with atrial fibrillation (AFib) starts a daily oral anticoagulant regimen following a cardioembolic stroke is not a good idea. Patients who received bridging anticoagulation had a nearly threefold higher rate of symptomatic intracranial hemorrhage than did patients who did not, and their bridging treatment failed to protect them from recurrent ischemic events, Shadi Yaghi, MD, said at the International Stroke Conference, sponsored by the American Heart Association. The bridging regimens delivered either heparin or low-molecular-weight heparin.
Based on the findings, “it seems reasonable to avoid bridging unless absolutely necessary, to initiate a DOAC unless it’s contraindicated, and to start the DOAC on day 7-10 following the stroke in most patients,” said Dr. Yaghi, a vascular neurologist and director of stroke research at NYU Langone Health in New York.
“It’s been hard to develop a broad guideline on when to start oral anticoagulation” after a cardioembolic stroke in AFib patients. The best time “depends on a lot of variables and how the patient responded to acute treatment,” commented Alexis Simpkins, MD, a vascular and stroke neurologist at the University of Florida in Gainesville. “You want to start treatment before the patient has another stroke, but not so soon that the treatment causes symptomatic hemorrhagic transformation.”
Dr. Yaghi’s suggestion, based on his findings, to start treatment for most patients with a DOAC 7-10 days after their index stroke “shows consistency” with the prevailing guideline recommendation from the AHA/American Stroke Association to start oral anticoagulation in this patient population 4-14 days after the index stroke (Stroke. 2018 March;49[3]:e46-e99), she noted.
A recent article reviewed the uncertainty about the best time to start oral anticoagulation in AFib patients after a cardioembolic stroke and the subtle differences that distinguish various international medical groups that, like the ASA, have made recommendations (Lancet Neurol. 2019 Jan 1;18[1]:117-26). According to this review, a major limitation of these various recommendations has been the lack of actual evidence collected from AFib patients who began receiving a DOAC shortly after a cardioembolic stroke, although the article added that several studies in progress are collecting these data.
The study reported by Dr. Yaghi pooled data collected from 2,084 recent AFib patients with a cardioembolic stroke treated at any of eight comprehensive U.S. stroke centers. They excluded patients who died from causes unrelated to the primary endpoint, those who did not receive an anticoagulant or had incomplete data, and patients lost to follow-up, leaving 1,289 evaluable patients. During their 90-day follow-up, 10% of the patients had an ischemic event, a symptomatic intracranial hemorrhage, or an extracranial hemorrhage.
The study’s primary analysis showed no statistically significant difference in the incidence of recurrent ischemic events, symptomatic intracranial hemorrhage, or both based on when oral anticoagulant treatment began: 0-3 days, 4-14 days, or more than 14 days after the index stroke.
The investigators then subdivided patients into the subgroup that started treatment with a DOAC and the subgroup that started treatment with warfarin and also further subdivided the 4-14 day time window for starting treatment. Results of this analysis showed that patients who received a DOAC and began this treatment 7-10 days after their stroke had a 50% cut in their 90-day events compared with other patients, a difference that fell just short of statistical significance at P = .07. All the other combinations of oral anticoagulant and time of treatment initiation analyzed showed neutral effects that never came near statistical significance.
Secondary data analyses also showed that both patients with a history of a stroke prior to their index stroke and patients with ipsilateral atherosclerosis came close to having a statistically significant increased rate of a subsequent ischemic event during 90-day follow-up. Furthermore, women, patients with a history of hyperlipidemia, and patients who developed hemorrhagic transformation of their index stroke all had significantly increased rates of developing a symptomatic intracranial hemorrhage during 90-day follow-up. When the endpoint was limited to recurrent ischemic events only, patients who received a DOAC were 50% less likely to have an event than were patients treated with warfarin, a statistically significant difference.
Although starting a DOAC 7-10 days after the index stroke seems reasonable based on this analysis, the question needs a prospective, randomized study to create an appropriate evidence base, Dr. Yaghi said.
Dr. Yaghi disclosed a financial relationship with Medtronic. Dr. Simpkins had no disclosures.
SOURCE: Yaghi S et al. Stroke. 2020 Feb;51(suppl 1):A119.
LOS ANGELES – When a patient with atrial fibrillation (AFib) has a cardioembolic stroke, the best blood thinner to start may be a direct-acting oral anticoagulant (DOAC), possibly beginning 7-10 days after the index stroke, according to an analysis of 90-day, observational outcomes data from nearly 1,300 patients.
The analysis also suggested that the use of “bridging” anticoagulant treatment by injection before a patient with atrial fibrillation (AFib) starts a daily oral anticoagulant regimen following a cardioembolic stroke is not a good idea. Patients who received bridging anticoagulation had a nearly threefold higher rate of symptomatic intracranial hemorrhage than did patients who did not, and their bridging treatment failed to protect them from recurrent ischemic events, Shadi Yaghi, MD, said at the International Stroke Conference, sponsored by the American Heart Association. The bridging regimens delivered either heparin or low-molecular-weight heparin.
Based on the findings, “it seems reasonable to avoid bridging unless absolutely necessary, to initiate a DOAC unless it’s contraindicated, and to start the DOAC on day 7-10 following the stroke in most patients,” said Dr. Yaghi, a vascular neurologist and director of stroke research at NYU Langone Health in New York.
“It’s been hard to develop a broad guideline on when to start oral anticoagulation” after a cardioembolic stroke in AFib patients. The best time “depends on a lot of variables and how the patient responded to acute treatment,” commented Alexis Simpkins, MD, a vascular and stroke neurologist at the University of Florida in Gainesville. “You want to start treatment before the patient has another stroke, but not so soon that the treatment causes symptomatic hemorrhagic transformation.”
Dr. Yaghi’s suggestion, based on his findings, to start treatment for most patients with a DOAC 7-10 days after their index stroke “shows consistency” with the prevailing guideline recommendation from the AHA/American Stroke Association to start oral anticoagulation in this patient population 4-14 days after the index stroke (Stroke. 2018 March;49[3]:e46-e99), she noted.
A recent article reviewed the uncertainty about the best time to start oral anticoagulation in AFib patients after a cardioembolic stroke and the subtle differences that distinguish various international medical groups that, like the ASA, have made recommendations (Lancet Neurol. 2019 Jan 1;18[1]:117-26). According to this review, a major limitation of these various recommendations has been the lack of actual evidence collected from AFib patients who began receiving a DOAC shortly after a cardioembolic stroke, although the article added that several studies in progress are collecting these data.
The study reported by Dr. Yaghi pooled data collected from 2,084 recent AFib patients with a cardioembolic stroke treated at any of eight comprehensive U.S. stroke centers. They excluded patients who died from causes unrelated to the primary endpoint, those who did not receive an anticoagulant or had incomplete data, and patients lost to follow-up, leaving 1,289 evaluable patients. During their 90-day follow-up, 10% of the patients had an ischemic event, a symptomatic intracranial hemorrhage, or an extracranial hemorrhage.
The study’s primary analysis showed no statistically significant difference in the incidence of recurrent ischemic events, symptomatic intracranial hemorrhage, or both based on when oral anticoagulant treatment began: 0-3 days, 4-14 days, or more than 14 days after the index stroke.
The investigators then subdivided patients into the subgroup that started treatment with a DOAC and the subgroup that started treatment with warfarin and also further subdivided the 4-14 day time window for starting treatment. Results of this analysis showed that patients who received a DOAC and began this treatment 7-10 days after their stroke had a 50% cut in their 90-day events compared with other patients, a difference that fell just short of statistical significance at P = .07. All the other combinations of oral anticoagulant and time of treatment initiation analyzed showed neutral effects that never came near statistical significance.
Secondary data analyses also showed that both patients with a history of a stroke prior to their index stroke and patients with ipsilateral atherosclerosis came close to having a statistically significant increased rate of a subsequent ischemic event during 90-day follow-up. Furthermore, women, patients with a history of hyperlipidemia, and patients who developed hemorrhagic transformation of their index stroke all had significantly increased rates of developing a symptomatic intracranial hemorrhage during 90-day follow-up. When the endpoint was limited to recurrent ischemic events only, patients who received a DOAC were 50% less likely to have an event than were patients treated with warfarin, a statistically significant difference.
Although starting a DOAC 7-10 days after the index stroke seems reasonable based on this analysis, the question needs a prospective, randomized study to create an appropriate evidence base, Dr. Yaghi said.
Dr. Yaghi disclosed a financial relationship with Medtronic. Dr. Simpkins had no disclosures.
SOURCE: Yaghi S et al. Stroke. 2020 Feb;51(suppl 1):A119.
REPORTING FROM ISC 2020
DAPT may benefit symptomatic carotid endarterectomy patients
LOS ANGELES –
The only patients who benefited from postsurgical treatment with dual antiplatelet therapy (DAPT) were those who were symptomatic (had a stroke or transient ischemic attack) prior to their carotid endarterectomy surgery, a minority of the more than 17,000 matched U.S. patients who underwent carotid endarterectomy during 2003-2018 and were part of this analysis, Nathan Belkin, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
Among patients with symptoms prior to their carotid endarterectomy, DAPT at the time of hospital discharge was associated with a 2-year follow-up rate of stroke, transient ischemic attack (TIA), or death of about 8%, compared with a rate of about 11% among similar patients discharged on aspirin only, a statistically significant difference. In contrast, among patients who were asymptomatic prior to their carotid endarterectomy, discharge treatment with aspirin only was associated with a 2-year event rate similar to the rate among patients discharged on DAPT.
Based in part on this finding, Dr. Belkin and associates at the University of Pennsylvania, Philadelphia, now start symptomatic patients scheduled for carotid endarterectomy on DAPT with aspirin plus clopidogrel (Plavix) about 2 weeks before surgery, and then continue the combined regimen long term after surgery. A prospective, randomized study is needed to fully resolve the optimal use of DAPT in patients with significant carotid artery disease scheduled for carotid endarterectomy, but until then, “we’re individualizing DAPT” to patients at high risk because of a prior stroke or TIA who also have no evidence of an elevated bleeding risk, said Dr. Belkin, a vascular surgeon.
“We hypothesize that patients with systemic carotid disease have a systemic disease process and more activated platelets,” which suggests a potential benefit from DAPT, he explained. But the data that Dr. Belkin reported also indicated that recent U.S. use of DAPT in patients undergoing carotid endarterectomy has moved beyond this subgroup. The U.S. national data set that Dr. Belkin used for the analysis, the Vascular Quality Initiative registry maintained by the Society for Vascular Surgery, included 87,074 patients who underwent carotid endarterectomy during 2003-2018. During the entire 16-year period, 30% of patients overall received a prescription for DAPT at hospital discharge, but this level went steadily up during those years. In 2003, the rate of DAPT prescriptions at discharge was below 10% of patients but then rose incrementally over the following years and by 2018 had increased to about 44% despite a prevalence of symptomatic carotid disease closer to about a third of patients.
“It’s surprising that so many patients received DAPT for carotid disease” in recent years, commented Mai N. Nguyen-Huynh, MD, a vascular neurologist with Kaiser Permanente Northern California in Oakland. “It’s been thought that DAPT, and especially clopidogrel, was more beneficial for patients with intracranial atherosclerotic disease, but not so much for patients with carotid disease,” she said in an interview. “We don’t always see systemic atherosclerotic disease in patients with carotid artery disease. It’s not standard practice to look for systemic atherosclerotic disease in patients with carotid disease,” unless something in the patient’s presentation suggests wider vascular-disease progression.
The primary analysis that Dr. Belkin and associates ran removed about 16% of the patients who underwent carotid endarterectomy from the database: those who received no antiplatelet drug, those who received only clopidogrel, and those who went home from surgery on an anticoagulant. Among the remaining 72,122 patients, 35% received DAPT at discharge and 65% received aspirin only. The patients averaged 70 years old, 61% were men, 37% had a history of stroke or TIA, and their overall 2-year incidence of stroke, TIA, or death was 7.3%. To adjust for many baseline differences between the patients discharged on DAPT and those who got only aspirin, the researchers used propensity-score sorting to identify 17,398 matched patients from the two treatment subgroups, 24% of the total population. Comparison of these DAPT and aspirin-only subgroups showed no difference in the overall, 2-year rate of stroke, TIA, or death.
However, when the analysis divided the patients into asymptomatic and symptomatic subgroups, those discharged on DAPT showed a statistically significant lower rate of stroke, TIA, or death during 2 years of follow-up. The same symptomatic subgroup also showed a statistically significant lower rate of total mortality during 5 years of follow-up when treated with DAPT compared with aspirin only, again an absolute, between-group difference of about 3 percentage points that was statistically significant, a difference not seen in the asymptomatic patients. The type of treatment that symptomatic patients received had no relationship to their 2-year incidence of stroke or TIA.
To confirm these findings, Dr. Belkin and coworkers ran a multivariate logistic regression analysis on the data collected from all 72,122 patients who underwent carotid endarterectomy and subsequently received either DAPT or aspirin only. The only statistically significant association between treatment and outcome was among the symptomatic patients who received DAPT, who had a significant reduction in their 5-year mortality, compared with symptomatic patients who received only aspirin at hospital discharge.
Ideally, a comparison of DAPT and aspirin-only treatment should also assess the incidence and severity of bleeding events associated with these treatments, but bleeding data were not available in the database, Dr. Belkin said.
Dr. Belkin and Dr. Nguyen-Huynh had no relevant disclosures.
SOURCE: Belkin N et al. Stroke. 2020 Feb;51(suppl 1): Abstract 67.
LOS ANGELES –
The only patients who benefited from postsurgical treatment with dual antiplatelet therapy (DAPT) were those who were symptomatic (had a stroke or transient ischemic attack) prior to their carotid endarterectomy surgery, a minority of the more than 17,000 matched U.S. patients who underwent carotid endarterectomy during 2003-2018 and were part of this analysis, Nathan Belkin, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
Among patients with symptoms prior to their carotid endarterectomy, DAPT at the time of hospital discharge was associated with a 2-year follow-up rate of stroke, transient ischemic attack (TIA), or death of about 8%, compared with a rate of about 11% among similar patients discharged on aspirin only, a statistically significant difference. In contrast, among patients who were asymptomatic prior to their carotid endarterectomy, discharge treatment with aspirin only was associated with a 2-year event rate similar to the rate among patients discharged on DAPT.
Based in part on this finding, Dr. Belkin and associates at the University of Pennsylvania, Philadelphia, now start symptomatic patients scheduled for carotid endarterectomy on DAPT with aspirin plus clopidogrel (Plavix) about 2 weeks before surgery, and then continue the combined regimen long term after surgery. A prospective, randomized study is needed to fully resolve the optimal use of DAPT in patients with significant carotid artery disease scheduled for carotid endarterectomy, but until then, “we’re individualizing DAPT” to patients at high risk because of a prior stroke or TIA who also have no evidence of an elevated bleeding risk, said Dr. Belkin, a vascular surgeon.
“We hypothesize that patients with systemic carotid disease have a systemic disease process and more activated platelets,” which suggests a potential benefit from DAPT, he explained. But the data that Dr. Belkin reported also indicated that recent U.S. use of DAPT in patients undergoing carotid endarterectomy has moved beyond this subgroup. The U.S. national data set that Dr. Belkin used for the analysis, the Vascular Quality Initiative registry maintained by the Society for Vascular Surgery, included 87,074 patients who underwent carotid endarterectomy during 2003-2018. During the entire 16-year period, 30% of patients overall received a prescription for DAPT at hospital discharge, but this level went steadily up during those years. In 2003, the rate of DAPT prescriptions at discharge was below 10% of patients but then rose incrementally over the following years and by 2018 had increased to about 44% despite a prevalence of symptomatic carotid disease closer to about a third of patients.
“It’s surprising that so many patients received DAPT for carotid disease” in recent years, commented Mai N. Nguyen-Huynh, MD, a vascular neurologist with Kaiser Permanente Northern California in Oakland. “It’s been thought that DAPT, and especially clopidogrel, was more beneficial for patients with intracranial atherosclerotic disease, but not so much for patients with carotid disease,” she said in an interview. “We don’t always see systemic atherosclerotic disease in patients with carotid artery disease. It’s not standard practice to look for systemic atherosclerotic disease in patients with carotid disease,” unless something in the patient’s presentation suggests wider vascular-disease progression.
The primary analysis that Dr. Belkin and associates ran removed about 16% of the patients who underwent carotid endarterectomy from the database: those who received no antiplatelet drug, those who received only clopidogrel, and those who went home from surgery on an anticoagulant. Among the remaining 72,122 patients, 35% received DAPT at discharge and 65% received aspirin only. The patients averaged 70 years old, 61% were men, 37% had a history of stroke or TIA, and their overall 2-year incidence of stroke, TIA, or death was 7.3%. To adjust for many baseline differences between the patients discharged on DAPT and those who got only aspirin, the researchers used propensity-score sorting to identify 17,398 matched patients from the two treatment subgroups, 24% of the total population. Comparison of these DAPT and aspirin-only subgroups showed no difference in the overall, 2-year rate of stroke, TIA, or death.
However, when the analysis divided the patients into asymptomatic and symptomatic subgroups, those discharged on DAPT showed a statistically significant lower rate of stroke, TIA, or death during 2 years of follow-up. The same symptomatic subgroup also showed a statistically significant lower rate of total mortality during 5 years of follow-up when treated with DAPT compared with aspirin only, again an absolute, between-group difference of about 3 percentage points that was statistically significant, a difference not seen in the asymptomatic patients. The type of treatment that symptomatic patients received had no relationship to their 2-year incidence of stroke or TIA.
To confirm these findings, Dr. Belkin and coworkers ran a multivariate logistic regression analysis on the data collected from all 72,122 patients who underwent carotid endarterectomy and subsequently received either DAPT or aspirin only. The only statistically significant association between treatment and outcome was among the symptomatic patients who received DAPT, who had a significant reduction in their 5-year mortality, compared with symptomatic patients who received only aspirin at hospital discharge.
Ideally, a comparison of DAPT and aspirin-only treatment should also assess the incidence and severity of bleeding events associated with these treatments, but bleeding data were not available in the database, Dr. Belkin said.
Dr. Belkin and Dr. Nguyen-Huynh had no relevant disclosures.
SOURCE: Belkin N et al. Stroke. 2020 Feb;51(suppl 1): Abstract 67.
LOS ANGELES –
The only patients who benefited from postsurgical treatment with dual antiplatelet therapy (DAPT) were those who were symptomatic (had a stroke or transient ischemic attack) prior to their carotid endarterectomy surgery, a minority of the more than 17,000 matched U.S. patients who underwent carotid endarterectomy during 2003-2018 and were part of this analysis, Nathan Belkin, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
Among patients with symptoms prior to their carotid endarterectomy, DAPT at the time of hospital discharge was associated with a 2-year follow-up rate of stroke, transient ischemic attack (TIA), or death of about 8%, compared with a rate of about 11% among similar patients discharged on aspirin only, a statistically significant difference. In contrast, among patients who were asymptomatic prior to their carotid endarterectomy, discharge treatment with aspirin only was associated with a 2-year event rate similar to the rate among patients discharged on DAPT.
Based in part on this finding, Dr. Belkin and associates at the University of Pennsylvania, Philadelphia, now start symptomatic patients scheduled for carotid endarterectomy on DAPT with aspirin plus clopidogrel (Plavix) about 2 weeks before surgery, and then continue the combined regimen long term after surgery. A prospective, randomized study is needed to fully resolve the optimal use of DAPT in patients with significant carotid artery disease scheduled for carotid endarterectomy, but until then, “we’re individualizing DAPT” to patients at high risk because of a prior stroke or TIA who also have no evidence of an elevated bleeding risk, said Dr. Belkin, a vascular surgeon.
“We hypothesize that patients with systemic carotid disease have a systemic disease process and more activated platelets,” which suggests a potential benefit from DAPT, he explained. But the data that Dr. Belkin reported also indicated that recent U.S. use of DAPT in patients undergoing carotid endarterectomy has moved beyond this subgroup. The U.S. national data set that Dr. Belkin used for the analysis, the Vascular Quality Initiative registry maintained by the Society for Vascular Surgery, included 87,074 patients who underwent carotid endarterectomy during 2003-2018. During the entire 16-year period, 30% of patients overall received a prescription for DAPT at hospital discharge, but this level went steadily up during those years. In 2003, the rate of DAPT prescriptions at discharge was below 10% of patients but then rose incrementally over the following years and by 2018 had increased to about 44% despite a prevalence of symptomatic carotid disease closer to about a third of patients.
“It’s surprising that so many patients received DAPT for carotid disease” in recent years, commented Mai N. Nguyen-Huynh, MD, a vascular neurologist with Kaiser Permanente Northern California in Oakland. “It’s been thought that DAPT, and especially clopidogrel, was more beneficial for patients with intracranial atherosclerotic disease, but not so much for patients with carotid disease,” she said in an interview. “We don’t always see systemic atherosclerotic disease in patients with carotid artery disease. It’s not standard practice to look for systemic atherosclerotic disease in patients with carotid disease,” unless something in the patient’s presentation suggests wider vascular-disease progression.
The primary analysis that Dr. Belkin and associates ran removed about 16% of the patients who underwent carotid endarterectomy from the database: those who received no antiplatelet drug, those who received only clopidogrel, and those who went home from surgery on an anticoagulant. Among the remaining 72,122 patients, 35% received DAPT at discharge and 65% received aspirin only. The patients averaged 70 years old, 61% were men, 37% had a history of stroke or TIA, and their overall 2-year incidence of stroke, TIA, or death was 7.3%. To adjust for many baseline differences between the patients discharged on DAPT and those who got only aspirin, the researchers used propensity-score sorting to identify 17,398 matched patients from the two treatment subgroups, 24% of the total population. Comparison of these DAPT and aspirin-only subgroups showed no difference in the overall, 2-year rate of stroke, TIA, or death.
However, when the analysis divided the patients into asymptomatic and symptomatic subgroups, those discharged on DAPT showed a statistically significant lower rate of stroke, TIA, or death during 2 years of follow-up. The same symptomatic subgroup also showed a statistically significant lower rate of total mortality during 5 years of follow-up when treated with DAPT compared with aspirin only, again an absolute, between-group difference of about 3 percentage points that was statistically significant, a difference not seen in the asymptomatic patients. The type of treatment that symptomatic patients received had no relationship to their 2-year incidence of stroke or TIA.
To confirm these findings, Dr. Belkin and coworkers ran a multivariate logistic regression analysis on the data collected from all 72,122 patients who underwent carotid endarterectomy and subsequently received either DAPT or aspirin only. The only statistically significant association between treatment and outcome was among the symptomatic patients who received DAPT, who had a significant reduction in their 5-year mortality, compared with symptomatic patients who received only aspirin at hospital discharge.
Ideally, a comparison of DAPT and aspirin-only treatment should also assess the incidence and severity of bleeding events associated with these treatments, but bleeding data were not available in the database, Dr. Belkin said.
Dr. Belkin and Dr. Nguyen-Huynh had no relevant disclosures.
SOURCE: Belkin N et al. Stroke. 2020 Feb;51(suppl 1): Abstract 67.
REPORTING FROM ISC 2020
FDA moves to expand coronavirus testing capacity; CDC clarifies testing criteria
The White House Coronavirus Task Force appeared at a press briefing March 2 to provide updates about testing strategies and public health coordination to address the current outbreak of the coronavirus COVID-19. Speaking at the briefing, led by Vice President Mike Pence, Centers for Disease Control and Prevention (CDC) director Robert Redfield, MD, said, “Working with our public health partners we continue to be able to identify new community cases and use our public health efforts to aggressively confirm, isolate, and do contact tracking.” Calling state, local, tribal, and territorial public health departments “the backbone of the public health system in our country,” Dr. Redfield noted that he expected many more confirmed COVID-19 cases to emerge.
At least some of the expected increase in confirmed cases of COVID-19 will occur because of expanded testing capacity, noted several of the task force members. On Feb. 29, the Food and Drug Administration issued a the virus that is causing the current outbreak of COVID-19.
Highly qualified laboratories, including both those run by public agencies and private labs, are now authorized to begin using their own validated test for the virus as long as they submit an Emergency Use Authorization (EUA) to the Food and Drug Administration within 15 days of notifying the agency of validation.
“To effectively respond to the COVID-19 outbreak, rapid detection of cases and contacts, appropriate clinical management and infection control, and implementation of community mitigation efforts are critical. This can best be achieved with wide availability of testing capabilities in health care settings, reference and commercial laboratories, and at the point of care,” the agency wrote in a press announcement of the expedited test expansion.
On Feb. 4, the Secretary of the Department of Health & Human Services declared a coronavirus public health emergency. The FDA was then authorized to allow individual laboratories with validated coronavirus tests to begin testing samples immediately. The goal is a more rapid and expanded testing capacity in the United States.
“The global emergence of COVID-19 is concerning, and we appreciate the efforts of the FDA to help bring more testing capability to the U.S.,” Nancy Messonnier, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases (NCIRD), said in the press release.
The new guidance that permits the immediate use of clinical tests after individual development and validation, said the FDA, only applies to labs already certified to perform high complexity testing under Clinical Laboratory Improvement Amendments. Many governmental, academic, and private laboratories fall into this category, however.
“Under this policy, we expect certain laboratories who develop validated tests for coronavirus would begin using them right away prior to FDA review,” said Jeffrey Shuren, MD, JD, director of the FDA’s Center for Devices and Radiological Health. “We believe this action will support laboratories across the country working on this urgent public health situation,” he added in the press release.
“By the end of this week, close to a million tests will be available,” FDA Commissioner Stephen M. Hahn, MD, said during the March 2 briefing.*
Updated criteria
The CDC is maintaining updated criteria for the virus testing on its website. Testing criteria are based both on clinical features and epidemiologic risk.
Individuals with less severe clinical features – those who have either fever or signs and symptoms of lower respiratory disease such as cough or shortness of breath, but who don’t require hospitalization – should be tested if they have high epidemiologic risk. “High risk” is defined by the CDC as any individual, including health care workers, who has had close contact with a person with confirmed COVID-19 within the past 2 weeks. For health care workers, testing can be considered even if they have relatively mild respiratory symptoms or have had contact with a person who is suspected, but not yet confirmed, to have coronavirus.
In its testing guidance, the CDC recognizes that defining close contact is difficult. General guidelines are that individuals are considered to have been in close contact with a person who has COVID-19 if they were within about six feet of the person for a prolonged period, or cared for or have spent a prolonged amount of time in the same room or house as a person with confirmed COVID-19.
Individuals who have both fever and signs or symptoms of lower respiratory illness who require hospitalization should be tested if they have a history of travel from any affected geographic area within 14 days of the onset of their symptoms. The CDC now defines “affected geographic area” as any country or region that has at least a CDC Level 2 Travel Health Notice for COVID-19, so that the testing criteria themselves don’t need to be updated when new geographic areas are included in these alerts. As of March 3, China, Iran, Italy, Japan, and South Korea all have Level 2 or 3 travel alerts.
The CDC now recommends that any patient who has severe acute lower respiratory illness that requires hospitalization and doesn’t have an alternative diagnosis should be tested, even without any identified source of exposure.
“Despite seeing these new cases, the risk to the American people is low,” said the CDC’s Dr. Redfield. In response to a question from the press about how fast the coronavirus will spread across the United States, Dr. Redfield said, “From the beginning we’ve anticipated seeing community cases pop up.” He added that as these cases arise, testing and public health strategies will focus on unearthing linkages and contacts to learn how the virus is spreading. “We’ll use the public health strategies that we can to limit that transmission,” he said.
*An earlier version of this article misattributed this quote.
The White House Coronavirus Task Force appeared at a press briefing March 2 to provide updates about testing strategies and public health coordination to address the current outbreak of the coronavirus COVID-19. Speaking at the briefing, led by Vice President Mike Pence, Centers for Disease Control and Prevention (CDC) director Robert Redfield, MD, said, “Working with our public health partners we continue to be able to identify new community cases and use our public health efforts to aggressively confirm, isolate, and do contact tracking.” Calling state, local, tribal, and territorial public health departments “the backbone of the public health system in our country,” Dr. Redfield noted that he expected many more confirmed COVID-19 cases to emerge.
At least some of the expected increase in confirmed cases of COVID-19 will occur because of expanded testing capacity, noted several of the task force members. On Feb. 29, the Food and Drug Administration issued a the virus that is causing the current outbreak of COVID-19.
Highly qualified laboratories, including both those run by public agencies and private labs, are now authorized to begin using their own validated test for the virus as long as they submit an Emergency Use Authorization (EUA) to the Food and Drug Administration within 15 days of notifying the agency of validation.
“To effectively respond to the COVID-19 outbreak, rapid detection of cases and contacts, appropriate clinical management and infection control, and implementation of community mitigation efforts are critical. This can best be achieved with wide availability of testing capabilities in health care settings, reference and commercial laboratories, and at the point of care,” the agency wrote in a press announcement of the expedited test expansion.
On Feb. 4, the Secretary of the Department of Health & Human Services declared a coronavirus public health emergency. The FDA was then authorized to allow individual laboratories with validated coronavirus tests to begin testing samples immediately. The goal is a more rapid and expanded testing capacity in the United States.
“The global emergence of COVID-19 is concerning, and we appreciate the efforts of the FDA to help bring more testing capability to the U.S.,” Nancy Messonnier, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases (NCIRD), said in the press release.
The new guidance that permits the immediate use of clinical tests after individual development and validation, said the FDA, only applies to labs already certified to perform high complexity testing under Clinical Laboratory Improvement Amendments. Many governmental, academic, and private laboratories fall into this category, however.
“Under this policy, we expect certain laboratories who develop validated tests for coronavirus would begin using them right away prior to FDA review,” said Jeffrey Shuren, MD, JD, director of the FDA’s Center for Devices and Radiological Health. “We believe this action will support laboratories across the country working on this urgent public health situation,” he added in the press release.
“By the end of this week, close to a million tests will be available,” FDA Commissioner Stephen M. Hahn, MD, said during the March 2 briefing.*
Updated criteria
The CDC is maintaining updated criteria for the virus testing on its website. Testing criteria are based both on clinical features and epidemiologic risk.
Individuals with less severe clinical features – those who have either fever or signs and symptoms of lower respiratory disease such as cough or shortness of breath, but who don’t require hospitalization – should be tested if they have high epidemiologic risk. “High risk” is defined by the CDC as any individual, including health care workers, who has had close contact with a person with confirmed COVID-19 within the past 2 weeks. For health care workers, testing can be considered even if they have relatively mild respiratory symptoms or have had contact with a person who is suspected, but not yet confirmed, to have coronavirus.
In its testing guidance, the CDC recognizes that defining close contact is difficult. General guidelines are that individuals are considered to have been in close contact with a person who has COVID-19 if they were within about six feet of the person for a prolonged period, or cared for or have spent a prolonged amount of time in the same room or house as a person with confirmed COVID-19.
Individuals who have both fever and signs or symptoms of lower respiratory illness who require hospitalization should be tested if they have a history of travel from any affected geographic area within 14 days of the onset of their symptoms. The CDC now defines “affected geographic area” as any country or region that has at least a CDC Level 2 Travel Health Notice for COVID-19, so that the testing criteria themselves don’t need to be updated when new geographic areas are included in these alerts. As of March 3, China, Iran, Italy, Japan, and South Korea all have Level 2 or 3 travel alerts.
The CDC now recommends that any patient who has severe acute lower respiratory illness that requires hospitalization and doesn’t have an alternative diagnosis should be tested, even without any identified source of exposure.
“Despite seeing these new cases, the risk to the American people is low,” said the CDC’s Dr. Redfield. In response to a question from the press about how fast the coronavirus will spread across the United States, Dr. Redfield said, “From the beginning we’ve anticipated seeing community cases pop up.” He added that as these cases arise, testing and public health strategies will focus on unearthing linkages and contacts to learn how the virus is spreading. “We’ll use the public health strategies that we can to limit that transmission,” he said.
*An earlier version of this article misattributed this quote.
The White House Coronavirus Task Force appeared at a press briefing March 2 to provide updates about testing strategies and public health coordination to address the current outbreak of the coronavirus COVID-19. Speaking at the briefing, led by Vice President Mike Pence, Centers for Disease Control and Prevention (CDC) director Robert Redfield, MD, said, “Working with our public health partners we continue to be able to identify new community cases and use our public health efforts to aggressively confirm, isolate, and do contact tracking.” Calling state, local, tribal, and territorial public health departments “the backbone of the public health system in our country,” Dr. Redfield noted that he expected many more confirmed COVID-19 cases to emerge.
At least some of the expected increase in confirmed cases of COVID-19 will occur because of expanded testing capacity, noted several of the task force members. On Feb. 29, the Food and Drug Administration issued a the virus that is causing the current outbreak of COVID-19.
Highly qualified laboratories, including both those run by public agencies and private labs, are now authorized to begin using their own validated test for the virus as long as they submit an Emergency Use Authorization (EUA) to the Food and Drug Administration within 15 days of notifying the agency of validation.
“To effectively respond to the COVID-19 outbreak, rapid detection of cases and contacts, appropriate clinical management and infection control, and implementation of community mitigation efforts are critical. This can best be achieved with wide availability of testing capabilities in health care settings, reference and commercial laboratories, and at the point of care,” the agency wrote in a press announcement of the expedited test expansion.
On Feb. 4, the Secretary of the Department of Health & Human Services declared a coronavirus public health emergency. The FDA was then authorized to allow individual laboratories with validated coronavirus tests to begin testing samples immediately. The goal is a more rapid and expanded testing capacity in the United States.
“The global emergence of COVID-19 is concerning, and we appreciate the efforts of the FDA to help bring more testing capability to the U.S.,” Nancy Messonnier, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases (NCIRD), said in the press release.
The new guidance that permits the immediate use of clinical tests after individual development and validation, said the FDA, only applies to labs already certified to perform high complexity testing under Clinical Laboratory Improvement Amendments. Many governmental, academic, and private laboratories fall into this category, however.
“Under this policy, we expect certain laboratories who develop validated tests for coronavirus would begin using them right away prior to FDA review,” said Jeffrey Shuren, MD, JD, director of the FDA’s Center for Devices and Radiological Health. “We believe this action will support laboratories across the country working on this urgent public health situation,” he added in the press release.
“By the end of this week, close to a million tests will be available,” FDA Commissioner Stephen M. Hahn, MD, said during the March 2 briefing.*
Updated criteria
The CDC is maintaining updated criteria for the virus testing on its website. Testing criteria are based both on clinical features and epidemiologic risk.
Individuals with less severe clinical features – those who have either fever or signs and symptoms of lower respiratory disease such as cough or shortness of breath, but who don’t require hospitalization – should be tested if they have high epidemiologic risk. “High risk” is defined by the CDC as any individual, including health care workers, who has had close contact with a person with confirmed COVID-19 within the past 2 weeks. For health care workers, testing can be considered even if they have relatively mild respiratory symptoms or have had contact with a person who is suspected, but not yet confirmed, to have coronavirus.
In its testing guidance, the CDC recognizes that defining close contact is difficult. General guidelines are that individuals are considered to have been in close contact with a person who has COVID-19 if they were within about six feet of the person for a prolonged period, or cared for or have spent a prolonged amount of time in the same room or house as a person with confirmed COVID-19.
Individuals who have both fever and signs or symptoms of lower respiratory illness who require hospitalization should be tested if they have a history of travel from any affected geographic area within 14 days of the onset of their symptoms. The CDC now defines “affected geographic area” as any country or region that has at least a CDC Level 2 Travel Health Notice for COVID-19, so that the testing criteria themselves don’t need to be updated when new geographic areas are included in these alerts. As of March 3, China, Iran, Italy, Japan, and South Korea all have Level 2 or 3 travel alerts.
The CDC now recommends that any patient who has severe acute lower respiratory illness that requires hospitalization and doesn’t have an alternative diagnosis should be tested, even without any identified source of exposure.
“Despite seeing these new cases, the risk to the American people is low,” said the CDC’s Dr. Redfield. In response to a question from the press about how fast the coronavirus will spread across the United States, Dr. Redfield said, “From the beginning we’ve anticipated seeing community cases pop up.” He added that as these cases arise, testing and public health strategies will focus on unearthing linkages and contacts to learn how the virus is spreading. “We’ll use the public health strategies that we can to limit that transmission,” he said.
*An earlier version of this article misattributed this quote.
FROM A PRESS BRIEFING BY THE WHITE HOUSE CORONAVIRUS TASK FORCE
Varied nightly bedtime, sleep duration linked to CVD risk
People who frequently alter the amount of sleep and time they go to bed each night are twofold more likely to develop cardiovascular disease, independent of traditional CVD risk factors, new research suggests.
Prior studies have focused on shift workers because night shift work will influence circadian rhythm and increase CVD risk. But it is increasingly recognized that circadian disruption may occur outside of shift work and accumulate over time, particularly given modern lifestyle factors such as increased use of mobile devices and television at night, said study coauthor Tianyi Huang, ScD, MSc, of Brigham and Women’s Hospital and Harvard Medical School in Boston, Massachusetts.
“Even if they tend to go to sleep at certain times, by following that lifestyle or behavior, it can interfere with their planned sleep timing,” he said.
“One thing that surprised me in this sample is that about one third of participants have irregular sleep patterns that can put them at increased risk of cardiovascular disease. So I think the prevalence is higher than expected,” Huang added.
As reported today in the Journal of the American College of Cardiology, the investigators used data from 7-day wrist actigraphy, 1 night of at-home polysomnography, and sleep questionnaires to assess sleep duration and sleep-onset timing among 1,992 Multi-Ethnic Study of Atherosclerosis () participants, aged 45 to 84 years, who were free of CVD and prospectively followed for a me MESA dian of 4.9 years.
A total of 786 patients (39.5%) had sleep duration standard deviation (SD) > 90 minutes and 510 (25.6%) had sleep-onset timing SD > 90 minutes.
During follow-up, there were 111 incident CVD events, including myocardial infarction, coronary heart disease death, stroke, and other coronary events.
Compared with people who had less than 1 hour of variation in sleep duration, the risk for incident CVD was 9% higher for people whose sleep duration varied 61 to 90 minutes (hazard ratio [HR], 1.09; 95% confidence interval [CI], 0.62 - 1.92), even after controlling for a variety of cardiovascular and sleep-related risk factors such as body mass index, systolic blood pressure, smoking status, total cholesterol, average sleep duration, insomnia symptoms, and sleep apnea.
Moreover, the adjusted CVD risk was substantially increased with 91 to 120 minutes of variation (HR, 1.59; 95% CI, 0.91 - 2.76) and more than 120 minutes of variation in sleep duration (HR, 2.14; 95% CI, 1.24 - 3.68).
Every 1-hour increase in sleep duration SD was associated with 36% higher CVD risk (95% CI; 1.07 - 1.73).
Compared with people with no more than a half hour of variation in nightly bedtimes, the adjusted hazard ratios for CVD were 1.16 (95% CI, 0.64 - 2.13), 1.52 (95% CI, 0.81 - 2.88), and 2.11 (95% CI, 1.13 - 3.91) when bedtimes varied by 31 to 60 minutes, 61 to 90 minutes, and more than 90 minutes.
For every 1-hour increase in sleep-onset timing SD, the risk of CVD was 18% higher (95% CI; 1.06 - 1.31).
“The results are similar for the regularity of sleep timing and the regularity of sleep duration, which means that both can contribute to circadian disruption and then lead to development of cardiovascular disease,” Huang said.
This is an important article and signals how sleep is an important marker and possibly a mediator of cardiovascular risk, said Harlan Krumholz, MD, of Yale School of Medicine in New Haven, Connecticut, who was not involved with the study.
“What I like about this is it’s a nice longitudinal, epidemiologic study with not just self-report, but sensor-detected sleep, that has been correlated with well-curated and adjudicated outcomes to give us a strong sense of this association,” he told theheart.org/Medscape Cardiology. “And also, that it goes beyond just the duration — they combine the duration and timing in order to give a fuller picture of sleep.”
Nevertheless, Krumholz said researchers are only at the beginning of being able to quantify the various dimensions of sleep and the degree to which sleep is a reflection of underlying physiologic issues, or whether patients are having erratic sleep patterns that are having a toxic effect on their overall health.
Questions also remain about the mechanism behind the association, whether the increased risk is universal or more harmful for some people, and the best way to measure factors during sleep that can most comprehensively and precisely predict risk.
“As we get more information flowing in from sensors, I think we will begin to develop more sophisticated approaches toward understanding risk, and it will be accompanied by other studies that will help us understand whether, again, this is a reflection of other processes that we should be paying attention to or whether it is a cause of disease and risk,” Krumholz said.
Subgroup analyses suggested positive associations between irregular sleep and CVD in African Americans, Hispanics, and Chinese Americans but not in whites. This could be because sleep irregularity, both timing and duration, was substantially higher in minorities, especially African Americans, but may also be as a result of chance because the study sample is relatively small, Huang explained.
The authors note that the overall findings are biologically plausible because of their previous work linking sleep irregularity with metabolic risk factors that predispose to atherosclerosis, such as obesity, diabetes, and hypertension. Participants with irregular sleep tended to have worse baseline cardiometabolic profiles, but this only explained a small portion of the associations between sleep irregularity and CVD, they note.
Other possible explanations include circadian clock genes, such as clock, per2 and bmal1, which have been shown experimentally to control a broad range of cardiovascular functions, from blood pressure and endothelial functions to vascular thrombosis and cardiac remodeling.
Irregular sleep may also influence the rhythms of the autonomic nervous system, and behavioral rhythms with regard to timing and/or amount of eating or exercise.
Further research is needed to understand the mechanisms driving the associations, the impact of sleep irregularity on individual CVD outcomes, and to determine whether a 7-day SD of more than 90 minutes for either sleep duration or sleep-onset timing can be used clinically as a threshold target for promoting cardiometabolically healthy sleep, Huang said.
“When providers communicate with their patients regarding strategies for CVD prevention, usually they focus on healthy diet and physical activity; and even when they talk about sleep, they talk about whether they have good sleep quality or sufficient sleep,” he said. “But one thing they should provide is advice regarding sleep regularity and [they should] recommend their patients follow a regular sleep pattern for the purpose of cardiovascular prevention.”
In a related editorial, Olaf Oldenburg, MD, Luderus-Kliniken Münster, Clemenshospital, Münster, Germany, and Jens Spiesshoefer, MD, Institute of Life Sciences, Scuola Superiore Sant’Anna, Pisa, Italy, write that the observed independent association between sleep irregularity and CVD “is a particularly striking finding given that impaired circadian rhythm is likely to be much more prevalent than the extreme example of shift work.”
They call on researchers to utilize big data to facilitate understanding of the association and say it is essential to test whether experimental data support the hypothesis that altered circadian rhythms would translate into unfavorable changes in 24-hour sympathovagal and neurohormonal balance, and ultimately CVD.
The present study “will, and should, stimulate much needed additional research on the association between sleep and CVD that may offer novel approaches to help improve the prognosis and daily symptom burden of patients with CVD, and might make sleep itself a therapeutic target in CVD,” the editorialists conclude.
This research was supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI), and by grants from the National Center for Advancing Translational Sciences. The MESA Sleep Study was supported by an NHLBI grant. Huang was supported by a career development grant from the National Institutes of Health.
Krumholz and Oldenburg have disclosed no relevant financial relationships. Spiesshoefer is supported by grants from the Else-Kröner-Fresenius Stiftung, the Innovative Medical Research program at the University of Münster, and Deutsche Herzstiftung; and by young investigator research support from Scuola Superiore Sant’Anna Pisa. He also has received travel grants and lecture honoraria from Boehringer Ingelheim and Chiesi.
Source: J Am Coll Cardiol. 2020 Mar 2. doi: 10.1016/j.jacc.2019.12.054.
This article first appeared on Medscape.com.
People who frequently alter the amount of sleep and time they go to bed each night are twofold more likely to develop cardiovascular disease, independent of traditional CVD risk factors, new research suggests.
Prior studies have focused on shift workers because night shift work will influence circadian rhythm and increase CVD risk. But it is increasingly recognized that circadian disruption may occur outside of shift work and accumulate over time, particularly given modern lifestyle factors such as increased use of mobile devices and television at night, said study coauthor Tianyi Huang, ScD, MSc, of Brigham and Women’s Hospital and Harvard Medical School in Boston, Massachusetts.
“Even if they tend to go to sleep at certain times, by following that lifestyle or behavior, it can interfere with their planned sleep timing,” he said.
“One thing that surprised me in this sample is that about one third of participants have irregular sleep patterns that can put them at increased risk of cardiovascular disease. So I think the prevalence is higher than expected,” Huang added.
As reported today in the Journal of the American College of Cardiology, the investigators used data from 7-day wrist actigraphy, 1 night of at-home polysomnography, and sleep questionnaires to assess sleep duration and sleep-onset timing among 1,992 Multi-Ethnic Study of Atherosclerosis () participants, aged 45 to 84 years, who were free of CVD and prospectively followed for a me MESA dian of 4.9 years.
A total of 786 patients (39.5%) had sleep duration standard deviation (SD) > 90 minutes and 510 (25.6%) had sleep-onset timing SD > 90 minutes.
During follow-up, there were 111 incident CVD events, including myocardial infarction, coronary heart disease death, stroke, and other coronary events.
Compared with people who had less than 1 hour of variation in sleep duration, the risk for incident CVD was 9% higher for people whose sleep duration varied 61 to 90 minutes (hazard ratio [HR], 1.09; 95% confidence interval [CI], 0.62 - 1.92), even after controlling for a variety of cardiovascular and sleep-related risk factors such as body mass index, systolic blood pressure, smoking status, total cholesterol, average sleep duration, insomnia symptoms, and sleep apnea.
Moreover, the adjusted CVD risk was substantially increased with 91 to 120 minutes of variation (HR, 1.59; 95% CI, 0.91 - 2.76) and more than 120 minutes of variation in sleep duration (HR, 2.14; 95% CI, 1.24 - 3.68).
Every 1-hour increase in sleep duration SD was associated with 36% higher CVD risk (95% CI; 1.07 - 1.73).
Compared with people with no more than a half hour of variation in nightly bedtimes, the adjusted hazard ratios for CVD were 1.16 (95% CI, 0.64 - 2.13), 1.52 (95% CI, 0.81 - 2.88), and 2.11 (95% CI, 1.13 - 3.91) when bedtimes varied by 31 to 60 minutes, 61 to 90 minutes, and more than 90 minutes.
For every 1-hour increase in sleep-onset timing SD, the risk of CVD was 18% higher (95% CI; 1.06 - 1.31).
“The results are similar for the regularity of sleep timing and the regularity of sleep duration, which means that both can contribute to circadian disruption and then lead to development of cardiovascular disease,” Huang said.
This is an important article and signals how sleep is an important marker and possibly a mediator of cardiovascular risk, said Harlan Krumholz, MD, of Yale School of Medicine in New Haven, Connecticut, who was not involved with the study.
“What I like about this is it’s a nice longitudinal, epidemiologic study with not just self-report, but sensor-detected sleep, that has been correlated with well-curated and adjudicated outcomes to give us a strong sense of this association,” he told theheart.org/Medscape Cardiology. “And also, that it goes beyond just the duration — they combine the duration and timing in order to give a fuller picture of sleep.”
Nevertheless, Krumholz said researchers are only at the beginning of being able to quantify the various dimensions of sleep and the degree to which sleep is a reflection of underlying physiologic issues, or whether patients are having erratic sleep patterns that are having a toxic effect on their overall health.
Questions also remain about the mechanism behind the association, whether the increased risk is universal or more harmful for some people, and the best way to measure factors during sleep that can most comprehensively and precisely predict risk.
“As we get more information flowing in from sensors, I think we will begin to develop more sophisticated approaches toward understanding risk, and it will be accompanied by other studies that will help us understand whether, again, this is a reflection of other processes that we should be paying attention to or whether it is a cause of disease and risk,” Krumholz said.
Subgroup analyses suggested positive associations between irregular sleep and CVD in African Americans, Hispanics, and Chinese Americans but not in whites. This could be because sleep irregularity, both timing and duration, was substantially higher in minorities, especially African Americans, but may also be as a result of chance because the study sample is relatively small, Huang explained.
The authors note that the overall findings are biologically plausible because of their previous work linking sleep irregularity with metabolic risk factors that predispose to atherosclerosis, such as obesity, diabetes, and hypertension. Participants with irregular sleep tended to have worse baseline cardiometabolic profiles, but this only explained a small portion of the associations between sleep irregularity and CVD, they note.
Other possible explanations include circadian clock genes, such as clock, per2 and bmal1, which have been shown experimentally to control a broad range of cardiovascular functions, from blood pressure and endothelial functions to vascular thrombosis and cardiac remodeling.
Irregular sleep may also influence the rhythms of the autonomic nervous system, and behavioral rhythms with regard to timing and/or amount of eating or exercise.
Further research is needed to understand the mechanisms driving the associations, the impact of sleep irregularity on individual CVD outcomes, and to determine whether a 7-day SD of more than 90 minutes for either sleep duration or sleep-onset timing can be used clinically as a threshold target for promoting cardiometabolically healthy sleep, Huang said.
“When providers communicate with their patients regarding strategies for CVD prevention, usually they focus on healthy diet and physical activity; and even when they talk about sleep, they talk about whether they have good sleep quality or sufficient sleep,” he said. “But one thing they should provide is advice regarding sleep regularity and [they should] recommend their patients follow a regular sleep pattern for the purpose of cardiovascular prevention.”
In a related editorial, Olaf Oldenburg, MD, Luderus-Kliniken Münster, Clemenshospital, Münster, Germany, and Jens Spiesshoefer, MD, Institute of Life Sciences, Scuola Superiore Sant’Anna, Pisa, Italy, write that the observed independent association between sleep irregularity and CVD “is a particularly striking finding given that impaired circadian rhythm is likely to be much more prevalent than the extreme example of shift work.”
They call on researchers to utilize big data to facilitate understanding of the association and say it is essential to test whether experimental data support the hypothesis that altered circadian rhythms would translate into unfavorable changes in 24-hour sympathovagal and neurohormonal balance, and ultimately CVD.
The present study “will, and should, stimulate much needed additional research on the association between sleep and CVD that may offer novel approaches to help improve the prognosis and daily symptom burden of patients with CVD, and might make sleep itself a therapeutic target in CVD,” the editorialists conclude.
This research was supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI), and by grants from the National Center for Advancing Translational Sciences. The MESA Sleep Study was supported by an NHLBI grant. Huang was supported by a career development grant from the National Institutes of Health.
Krumholz and Oldenburg have disclosed no relevant financial relationships. Spiesshoefer is supported by grants from the Else-Kröner-Fresenius Stiftung, the Innovative Medical Research program at the University of Münster, and Deutsche Herzstiftung; and by young investigator research support from Scuola Superiore Sant’Anna Pisa. He also has received travel grants and lecture honoraria from Boehringer Ingelheim and Chiesi.
Source: J Am Coll Cardiol. 2020 Mar 2. doi: 10.1016/j.jacc.2019.12.054.
This article first appeared on Medscape.com.
People who frequently alter the amount of sleep and time they go to bed each night are twofold more likely to develop cardiovascular disease, independent of traditional CVD risk factors, new research suggests.
Prior studies have focused on shift workers because night shift work will influence circadian rhythm and increase CVD risk. But it is increasingly recognized that circadian disruption may occur outside of shift work and accumulate over time, particularly given modern lifestyle factors such as increased use of mobile devices and television at night, said study coauthor Tianyi Huang, ScD, MSc, of Brigham and Women’s Hospital and Harvard Medical School in Boston, Massachusetts.
“Even if they tend to go to sleep at certain times, by following that lifestyle or behavior, it can interfere with their planned sleep timing,” he said.
“One thing that surprised me in this sample is that about one third of participants have irregular sleep patterns that can put them at increased risk of cardiovascular disease. So I think the prevalence is higher than expected,” Huang added.
As reported today in the Journal of the American College of Cardiology, the investigators used data from 7-day wrist actigraphy, 1 night of at-home polysomnography, and sleep questionnaires to assess sleep duration and sleep-onset timing among 1,992 Multi-Ethnic Study of Atherosclerosis () participants, aged 45 to 84 years, who were free of CVD and prospectively followed for a me MESA dian of 4.9 years.
A total of 786 patients (39.5%) had sleep duration standard deviation (SD) > 90 minutes and 510 (25.6%) had sleep-onset timing SD > 90 minutes.
During follow-up, there were 111 incident CVD events, including myocardial infarction, coronary heart disease death, stroke, and other coronary events.
Compared with people who had less than 1 hour of variation in sleep duration, the risk for incident CVD was 9% higher for people whose sleep duration varied 61 to 90 minutes (hazard ratio [HR], 1.09; 95% confidence interval [CI], 0.62 - 1.92), even after controlling for a variety of cardiovascular and sleep-related risk factors such as body mass index, systolic blood pressure, smoking status, total cholesterol, average sleep duration, insomnia symptoms, and sleep apnea.
Moreover, the adjusted CVD risk was substantially increased with 91 to 120 minutes of variation (HR, 1.59; 95% CI, 0.91 - 2.76) and more than 120 minutes of variation in sleep duration (HR, 2.14; 95% CI, 1.24 - 3.68).
Every 1-hour increase in sleep duration SD was associated with 36% higher CVD risk (95% CI; 1.07 - 1.73).
Compared with people with no more than a half hour of variation in nightly bedtimes, the adjusted hazard ratios for CVD were 1.16 (95% CI, 0.64 - 2.13), 1.52 (95% CI, 0.81 - 2.88), and 2.11 (95% CI, 1.13 - 3.91) when bedtimes varied by 31 to 60 minutes, 61 to 90 minutes, and more than 90 minutes.
For every 1-hour increase in sleep-onset timing SD, the risk of CVD was 18% higher (95% CI; 1.06 - 1.31).
“The results are similar for the regularity of sleep timing and the regularity of sleep duration, which means that both can contribute to circadian disruption and then lead to development of cardiovascular disease,” Huang said.
This is an important article and signals how sleep is an important marker and possibly a mediator of cardiovascular risk, said Harlan Krumholz, MD, of Yale School of Medicine in New Haven, Connecticut, who was not involved with the study.
“What I like about this is it’s a nice longitudinal, epidemiologic study with not just self-report, but sensor-detected sleep, that has been correlated with well-curated and adjudicated outcomes to give us a strong sense of this association,” he told theheart.org/Medscape Cardiology. “And also, that it goes beyond just the duration — they combine the duration and timing in order to give a fuller picture of sleep.”
Nevertheless, Krumholz said researchers are only at the beginning of being able to quantify the various dimensions of sleep and the degree to which sleep is a reflection of underlying physiologic issues, or whether patients are having erratic sleep patterns that are having a toxic effect on their overall health.
Questions also remain about the mechanism behind the association, whether the increased risk is universal or more harmful for some people, and the best way to measure factors during sleep that can most comprehensively and precisely predict risk.
“As we get more information flowing in from sensors, I think we will begin to develop more sophisticated approaches toward understanding risk, and it will be accompanied by other studies that will help us understand whether, again, this is a reflection of other processes that we should be paying attention to or whether it is a cause of disease and risk,” Krumholz said.
Subgroup analyses suggested positive associations between irregular sleep and CVD in African Americans, Hispanics, and Chinese Americans but not in whites. This could be because sleep irregularity, both timing and duration, was substantially higher in minorities, especially African Americans, but may also be as a result of chance because the study sample is relatively small, Huang explained.
The authors note that the overall findings are biologically plausible because of their previous work linking sleep irregularity with metabolic risk factors that predispose to atherosclerosis, such as obesity, diabetes, and hypertension. Participants with irregular sleep tended to have worse baseline cardiometabolic profiles, but this only explained a small portion of the associations between sleep irregularity and CVD, they note.
Other possible explanations include circadian clock genes, such as clock, per2 and bmal1, which have been shown experimentally to control a broad range of cardiovascular functions, from blood pressure and endothelial functions to vascular thrombosis and cardiac remodeling.
Irregular sleep may also influence the rhythms of the autonomic nervous system, and behavioral rhythms with regard to timing and/or amount of eating or exercise.
Further research is needed to understand the mechanisms driving the associations, the impact of sleep irregularity on individual CVD outcomes, and to determine whether a 7-day SD of more than 90 minutes for either sleep duration or sleep-onset timing can be used clinically as a threshold target for promoting cardiometabolically healthy sleep, Huang said.
“When providers communicate with their patients regarding strategies for CVD prevention, usually they focus on healthy diet and physical activity; and even when they talk about sleep, they talk about whether they have good sleep quality or sufficient sleep,” he said. “But one thing they should provide is advice regarding sleep regularity and [they should] recommend their patients follow a regular sleep pattern for the purpose of cardiovascular prevention.”
In a related editorial, Olaf Oldenburg, MD, Luderus-Kliniken Münster, Clemenshospital, Münster, Germany, and Jens Spiesshoefer, MD, Institute of Life Sciences, Scuola Superiore Sant’Anna, Pisa, Italy, write that the observed independent association between sleep irregularity and CVD “is a particularly striking finding given that impaired circadian rhythm is likely to be much more prevalent than the extreme example of shift work.”
They call on researchers to utilize big data to facilitate understanding of the association and say it is essential to test whether experimental data support the hypothesis that altered circadian rhythms would translate into unfavorable changes in 24-hour sympathovagal and neurohormonal balance, and ultimately CVD.
The present study “will, and should, stimulate much needed additional research on the association between sleep and CVD that may offer novel approaches to help improve the prognosis and daily symptom burden of patients with CVD, and might make sleep itself a therapeutic target in CVD,” the editorialists conclude.
This research was supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI), and by grants from the National Center for Advancing Translational Sciences. The MESA Sleep Study was supported by an NHLBI grant. Huang was supported by a career development grant from the National Institutes of Health.
Krumholz and Oldenburg have disclosed no relevant financial relationships. Spiesshoefer is supported by grants from the Else-Kröner-Fresenius Stiftung, the Innovative Medical Research program at the University of Münster, and Deutsche Herzstiftung; and by young investigator research support from Scuola Superiore Sant’Anna Pisa. He also has received travel grants and lecture honoraria from Boehringer Ingelheim and Chiesi.
Source: J Am Coll Cardiol. 2020 Mar 2. doi: 10.1016/j.jacc.2019.12.054.
This article first appeared on Medscape.com.
Transradial access gains converts among U.S. interventional neurologists
LOS ANGELES –
“It’s growing dramatically in U.S. practice. It may be hype, but there is big excitement. We are still in an assessment mode, but the adoption rate has been high,” Raul G. Nogueira, MD, said in an interview during the International Stroke Conference sponsored by the American Heart Association. “The big advantage [of transradial catheterization entry] is elimination of groin complications, some of which can be pretty bad. Is it safe for the brain? It’s probably okay, but that needs more study,” said Dr. Nogueira, professor of neurology at Emory University and director of the Neurovascular Service at the Grady Marcus Stroke and Neuroscience Center in Atlanta.
His uncertainty stems from the more difficult route taken to advance a catheter from the wrist into brain vessels, a maneuver that requires significant manipulation of the catheter tip, unlike the path from the right radial artery into the heart’s arteries, a “straight shot,” he explained. To reach the brain’s vasculature, the tip must execute a spin “that may scrape small emboli from the arch or arteries, so we need to look at this a little more carefully.” Ideally in a prospective, randomized study, he said. “We need to see whether the burden of [magnetic resonance] lesions is any higher when you go through the radial [artery].”
Some of the first-reported, large-scale U.S. experiences using a radial-artery approach for various neurovascular procedures, including a few thrombectomy cases, came in a series of 1,272 patients treated at any of four U.S. centers during July 2018 to June 2019, a period when the neurovascular staffs at all four centers transitioned from primarily using femoral-artery access to using radial access as their default mode. During the 12-month transition period, overall use of radial access at all four centers rose from roughly a quarter of all neurovascular interventions during July to September 2018 to closer to 80% by April to June 2019, Eyad Almallouhi, MD, reported at the conference.
During the entire 12 months, the operators ran up a 94% rate of successfully completed procedures using radial access, a rate that rose from about 88% during the first quarter to roughly 95% success during the fourth quarter tracked, said Dr. Almallouhi, a neurologist at the Medical University of South Carolina in Charleston. The rate of crossover from what began as a transradial procedure but switched to transfemoral was just under 6% overall, with a nearly 14% crossover rate during the first quarter that then dropped to around 5% for the rest of the transition year. Crossovers for interventional procedures throughout the study year occurred at a 12% rate, while crossovers for diagnostic procedures occurred at a 5% clip throughout the entire year.
None of the transradial patients had a major access-site complication, and minor complications occurred in less than 2% of the patients, including 11 with a forearm hematoma, 6 with forearm pain, and 5 with oozing at their access site. The absence of any major access-site complications among the transradial-access patients in this series contrasts with a recent report of a 1.7% rate of major complications secondary to femoral-artery access for mechanical thrombectomy in a combined analysis of data from seven published studies that included 660 thrombectomy procedures (Am J Neuroradiol. 2019 Feb. doi: 10.3174/ajnr.A6423). The other three centers that participated in the study Dr. Almallouhi presented were the University of Miami, Thomas Jefferson University in Philadelphia, and the University of Pittsburgh.
Of the 1,272 total procedures studied, 83% were diagnostic procedures, which had an overall 95% success rate, and 17% were interventional procedures, which had a success rate of 89%. The interventional transradial procedures included 62 primary coilings of aneurysms, 44 stent-assisted aneurysm coilings, 40 patients who underwent a flow diversion, 21 balloon-assisted aneurysm coilings, and 24 patients who underwent stroke thrombectomy.
The size of the devices commonly used for thrombectomy are often too large to allow for radial-artery access, noted Dr. Nogueira. For urgent interventions like thrombectomy “we use balloon-guided catheters that are large-bore and don’t fit well in the radial,” he said, although thrombectomy via the radial artery without a balloon-guided catheter is possible for clots located in the basilar artery. Last year, researchers in Germany reported using a balloon-guided catheter to perform mechanical thrombectomy via the radial artery (Interv Neuroradiol. 2019 Oct 1;25[5]:508-10). But it’s a different story for elective, diagnostic procedures. “I have moved most of these to transradial,” Dr. Nogueira said. He and his coauthors summarized the case for transradial access for cerebral angiography in a recent review; in addition to enhanced safety they cited other advantages including improved patient satisfaction and reduced cost because of a shorter length of stay (Interv Cardiol Clin. 2020 Jan;9[1]:75-86).
Despite his enthusiasm and the enthusiasm of other neurointerventionalists for the transradial approach, other stroke neurologists have been more cautious and slower to shift away from the femoral approach. “Our experience has been that for most cases it’s a bit more challenging to access the cervical vessels from the radial artery than from the traditional femoral approach. For arches with complex anatomy, however, the transradial approach can be of benefit in some cases, depending on the angles that need to be traversed,” commented Jeremy Payne, MD, director of the Banner Center for Neurovascular Medicine and medical director of the Banner—University Medical Center Phoenix Comprehensive Stroke Program. Dr. Payne highlighted that, while he is not an interventionalist himself, he and his interventional staff have regularly discussed the transradial option.
“In the cardiology literature the radial approach has been very successful, with better overall safety than the traditional femoral approach. Largely this seems to do with the anatomy of the aortic arch. It’s simply a more direct approach to the coronaries via the right radial artery; getting the wire into the correct vessel is significantly more difficult the more acute the angle it has to traverse,” such as when the target is an intracerebral vessel, Dr. Payne said in an interview.
“Our experience in the past 6 months has been about 25% transradial for some of our procedures, mainly diagnostic angiograms. We don’t find any difference in safety, however, as our transfemoral procedures are already very safe. One of the benefits of a transradial approach has been that a closure device may not be needed, with fewer vascular complications at the access site, such as fistula formation. We use ultrasound for access, and have not seen a difference in those approaches at all so far. One might argue that using ultrasound to establish access would slow us down, but so far our fastest case start-to-recanalization time in an acute stroke this year was 6 minutes, so speed does not appear to be a limiting issue. Another concern overall for transradial access is the potential limitation in the tools we may be able to deploy, given the smaller size of the vessel. It is reassuring [in the report from Dr. Almallouhi] that a variety of cases were successfully completed via this approach. However, fewer than 2% of their cases [24 patients] were apparently emergent, acute strokes, lending no specific support to that context. I do not expect that to change based on this paper,” Dr. Payne concluded.
“It is not clear to me that transradial neurointervention will change much. We have excellent safety data for the femoral approach, a proven track record of efficacy, and for most patients it seems to afford a somewhat wider range of tools that can be deployed, with simpler anatomy for accessing the cervical vessels in most arches. It is reassuring that the results reported by Dr. Almallouhi did not suggest negative outcomes, and as such I suspect the transradial approach at least gives us an additional option in a minority of patients. We have seen in the past 5-10 years an explosion of tools for the endovascular treatment of stroke; transradial access represents another potential strategy that appears so far to be safe,” Dr. Payne said.
Drs. Nogueira, Almallouhi, and Payne had no relevant disclosures.
SOURCE: Almallouhi E et al. Stroke. 2020 Feb;51(suppl 1):A64.
LOS ANGELES –
“It’s growing dramatically in U.S. practice. It may be hype, but there is big excitement. We are still in an assessment mode, but the adoption rate has been high,” Raul G. Nogueira, MD, said in an interview during the International Stroke Conference sponsored by the American Heart Association. “The big advantage [of transradial catheterization entry] is elimination of groin complications, some of which can be pretty bad. Is it safe for the brain? It’s probably okay, but that needs more study,” said Dr. Nogueira, professor of neurology at Emory University and director of the Neurovascular Service at the Grady Marcus Stroke and Neuroscience Center in Atlanta.
His uncertainty stems from the more difficult route taken to advance a catheter from the wrist into brain vessels, a maneuver that requires significant manipulation of the catheter tip, unlike the path from the right radial artery into the heart’s arteries, a “straight shot,” he explained. To reach the brain’s vasculature, the tip must execute a spin “that may scrape small emboli from the arch or arteries, so we need to look at this a little more carefully.” Ideally in a prospective, randomized study, he said. “We need to see whether the burden of [magnetic resonance] lesions is any higher when you go through the radial [artery].”
Some of the first-reported, large-scale U.S. experiences using a radial-artery approach for various neurovascular procedures, including a few thrombectomy cases, came in a series of 1,272 patients treated at any of four U.S. centers during July 2018 to June 2019, a period when the neurovascular staffs at all four centers transitioned from primarily using femoral-artery access to using radial access as their default mode. During the 12-month transition period, overall use of radial access at all four centers rose from roughly a quarter of all neurovascular interventions during July to September 2018 to closer to 80% by April to June 2019, Eyad Almallouhi, MD, reported at the conference.
During the entire 12 months, the operators ran up a 94% rate of successfully completed procedures using radial access, a rate that rose from about 88% during the first quarter to roughly 95% success during the fourth quarter tracked, said Dr. Almallouhi, a neurologist at the Medical University of South Carolina in Charleston. The rate of crossover from what began as a transradial procedure but switched to transfemoral was just under 6% overall, with a nearly 14% crossover rate during the first quarter that then dropped to around 5% for the rest of the transition year. Crossovers for interventional procedures throughout the study year occurred at a 12% rate, while crossovers for diagnostic procedures occurred at a 5% clip throughout the entire year.
None of the transradial patients had a major access-site complication, and minor complications occurred in less than 2% of the patients, including 11 with a forearm hematoma, 6 with forearm pain, and 5 with oozing at their access site. The absence of any major access-site complications among the transradial-access patients in this series contrasts with a recent report of a 1.7% rate of major complications secondary to femoral-artery access for mechanical thrombectomy in a combined analysis of data from seven published studies that included 660 thrombectomy procedures (Am J Neuroradiol. 2019 Feb. doi: 10.3174/ajnr.A6423). The other three centers that participated in the study Dr. Almallouhi presented were the University of Miami, Thomas Jefferson University in Philadelphia, and the University of Pittsburgh.
Of the 1,272 total procedures studied, 83% were diagnostic procedures, which had an overall 95% success rate, and 17% were interventional procedures, which had a success rate of 89%. The interventional transradial procedures included 62 primary coilings of aneurysms, 44 stent-assisted aneurysm coilings, 40 patients who underwent a flow diversion, 21 balloon-assisted aneurysm coilings, and 24 patients who underwent stroke thrombectomy.
The size of the devices commonly used for thrombectomy are often too large to allow for radial-artery access, noted Dr. Nogueira. For urgent interventions like thrombectomy “we use balloon-guided catheters that are large-bore and don’t fit well in the radial,” he said, although thrombectomy via the radial artery without a balloon-guided catheter is possible for clots located in the basilar artery. Last year, researchers in Germany reported using a balloon-guided catheter to perform mechanical thrombectomy via the radial artery (Interv Neuroradiol. 2019 Oct 1;25[5]:508-10). But it’s a different story for elective, diagnostic procedures. “I have moved most of these to transradial,” Dr. Nogueira said. He and his coauthors summarized the case for transradial access for cerebral angiography in a recent review; in addition to enhanced safety they cited other advantages including improved patient satisfaction and reduced cost because of a shorter length of stay (Interv Cardiol Clin. 2020 Jan;9[1]:75-86).
Despite his enthusiasm and the enthusiasm of other neurointerventionalists for the transradial approach, other stroke neurologists have been more cautious and slower to shift away from the femoral approach. “Our experience has been that for most cases it’s a bit more challenging to access the cervical vessels from the radial artery than from the traditional femoral approach. For arches with complex anatomy, however, the transradial approach can be of benefit in some cases, depending on the angles that need to be traversed,” commented Jeremy Payne, MD, director of the Banner Center for Neurovascular Medicine and medical director of the Banner—University Medical Center Phoenix Comprehensive Stroke Program. Dr. Payne highlighted that, while he is not an interventionalist himself, he and his interventional staff have regularly discussed the transradial option.
“In the cardiology literature the radial approach has been very successful, with better overall safety than the traditional femoral approach. Largely this seems to do with the anatomy of the aortic arch. It’s simply a more direct approach to the coronaries via the right radial artery; getting the wire into the correct vessel is significantly more difficult the more acute the angle it has to traverse,” such as when the target is an intracerebral vessel, Dr. Payne said in an interview.
“Our experience in the past 6 months has been about 25% transradial for some of our procedures, mainly diagnostic angiograms. We don’t find any difference in safety, however, as our transfemoral procedures are already very safe. One of the benefits of a transradial approach has been that a closure device may not be needed, with fewer vascular complications at the access site, such as fistula formation. We use ultrasound for access, and have not seen a difference in those approaches at all so far. One might argue that using ultrasound to establish access would slow us down, but so far our fastest case start-to-recanalization time in an acute stroke this year was 6 minutes, so speed does not appear to be a limiting issue. Another concern overall for transradial access is the potential limitation in the tools we may be able to deploy, given the smaller size of the vessel. It is reassuring [in the report from Dr. Almallouhi] that a variety of cases were successfully completed via this approach. However, fewer than 2% of their cases [24 patients] were apparently emergent, acute strokes, lending no specific support to that context. I do not expect that to change based on this paper,” Dr. Payne concluded.
“It is not clear to me that transradial neurointervention will change much. We have excellent safety data for the femoral approach, a proven track record of efficacy, and for most patients it seems to afford a somewhat wider range of tools that can be deployed, with simpler anatomy for accessing the cervical vessels in most arches. It is reassuring that the results reported by Dr. Almallouhi did not suggest negative outcomes, and as such I suspect the transradial approach at least gives us an additional option in a minority of patients. We have seen in the past 5-10 years an explosion of tools for the endovascular treatment of stroke; transradial access represents another potential strategy that appears so far to be safe,” Dr. Payne said.
Drs. Nogueira, Almallouhi, and Payne had no relevant disclosures.
SOURCE: Almallouhi E et al. Stroke. 2020 Feb;51(suppl 1):A64.
LOS ANGELES –
“It’s growing dramatically in U.S. practice. It may be hype, but there is big excitement. We are still in an assessment mode, but the adoption rate has been high,” Raul G. Nogueira, MD, said in an interview during the International Stroke Conference sponsored by the American Heart Association. “The big advantage [of transradial catheterization entry] is elimination of groin complications, some of which can be pretty bad. Is it safe for the brain? It’s probably okay, but that needs more study,” said Dr. Nogueira, professor of neurology at Emory University and director of the Neurovascular Service at the Grady Marcus Stroke and Neuroscience Center in Atlanta.
His uncertainty stems from the more difficult route taken to advance a catheter from the wrist into brain vessels, a maneuver that requires significant manipulation of the catheter tip, unlike the path from the right radial artery into the heart’s arteries, a “straight shot,” he explained. To reach the brain’s vasculature, the tip must execute a spin “that may scrape small emboli from the arch or arteries, so we need to look at this a little more carefully.” Ideally in a prospective, randomized study, he said. “We need to see whether the burden of [magnetic resonance] lesions is any higher when you go through the radial [artery].”
Some of the first-reported, large-scale U.S. experiences using a radial-artery approach for various neurovascular procedures, including a few thrombectomy cases, came in a series of 1,272 patients treated at any of four U.S. centers during July 2018 to June 2019, a period when the neurovascular staffs at all four centers transitioned from primarily using femoral-artery access to using radial access as their default mode. During the 12-month transition period, overall use of radial access at all four centers rose from roughly a quarter of all neurovascular interventions during July to September 2018 to closer to 80% by April to June 2019, Eyad Almallouhi, MD, reported at the conference.
During the entire 12 months, the operators ran up a 94% rate of successfully completed procedures using radial access, a rate that rose from about 88% during the first quarter to roughly 95% success during the fourth quarter tracked, said Dr. Almallouhi, a neurologist at the Medical University of South Carolina in Charleston. The rate of crossover from what began as a transradial procedure but switched to transfemoral was just under 6% overall, with a nearly 14% crossover rate during the first quarter that then dropped to around 5% for the rest of the transition year. Crossovers for interventional procedures throughout the study year occurred at a 12% rate, while crossovers for diagnostic procedures occurred at a 5% clip throughout the entire year.
None of the transradial patients had a major access-site complication, and minor complications occurred in less than 2% of the patients, including 11 with a forearm hematoma, 6 with forearm pain, and 5 with oozing at their access site. The absence of any major access-site complications among the transradial-access patients in this series contrasts with a recent report of a 1.7% rate of major complications secondary to femoral-artery access for mechanical thrombectomy in a combined analysis of data from seven published studies that included 660 thrombectomy procedures (Am J Neuroradiol. 2019 Feb. doi: 10.3174/ajnr.A6423). The other three centers that participated in the study Dr. Almallouhi presented were the University of Miami, Thomas Jefferson University in Philadelphia, and the University of Pittsburgh.
Of the 1,272 total procedures studied, 83% were diagnostic procedures, which had an overall 95% success rate, and 17% were interventional procedures, which had a success rate of 89%. The interventional transradial procedures included 62 primary coilings of aneurysms, 44 stent-assisted aneurysm coilings, 40 patients who underwent a flow diversion, 21 balloon-assisted aneurysm coilings, and 24 patients who underwent stroke thrombectomy.
The size of the devices commonly used for thrombectomy are often too large to allow for radial-artery access, noted Dr. Nogueira. For urgent interventions like thrombectomy “we use balloon-guided catheters that are large-bore and don’t fit well in the radial,” he said, although thrombectomy via the radial artery without a balloon-guided catheter is possible for clots located in the basilar artery. Last year, researchers in Germany reported using a balloon-guided catheter to perform mechanical thrombectomy via the radial artery (Interv Neuroradiol. 2019 Oct 1;25[5]:508-10). But it’s a different story for elective, diagnostic procedures. “I have moved most of these to transradial,” Dr. Nogueira said. He and his coauthors summarized the case for transradial access for cerebral angiography in a recent review; in addition to enhanced safety they cited other advantages including improved patient satisfaction and reduced cost because of a shorter length of stay (Interv Cardiol Clin. 2020 Jan;9[1]:75-86).
Despite his enthusiasm and the enthusiasm of other neurointerventionalists for the transradial approach, other stroke neurologists have been more cautious and slower to shift away from the femoral approach. “Our experience has been that for most cases it’s a bit more challenging to access the cervical vessels from the radial artery than from the traditional femoral approach. For arches with complex anatomy, however, the transradial approach can be of benefit in some cases, depending on the angles that need to be traversed,” commented Jeremy Payne, MD, director of the Banner Center for Neurovascular Medicine and medical director of the Banner—University Medical Center Phoenix Comprehensive Stroke Program. Dr. Payne highlighted that, while he is not an interventionalist himself, he and his interventional staff have regularly discussed the transradial option.
“In the cardiology literature the radial approach has been very successful, with better overall safety than the traditional femoral approach. Largely this seems to do with the anatomy of the aortic arch. It’s simply a more direct approach to the coronaries via the right radial artery; getting the wire into the correct vessel is significantly more difficult the more acute the angle it has to traverse,” such as when the target is an intracerebral vessel, Dr. Payne said in an interview.
“Our experience in the past 6 months has been about 25% transradial for some of our procedures, mainly diagnostic angiograms. We don’t find any difference in safety, however, as our transfemoral procedures are already very safe. One of the benefits of a transradial approach has been that a closure device may not be needed, with fewer vascular complications at the access site, such as fistula formation. We use ultrasound for access, and have not seen a difference in those approaches at all so far. One might argue that using ultrasound to establish access would slow us down, but so far our fastest case start-to-recanalization time in an acute stroke this year was 6 minutes, so speed does not appear to be a limiting issue. Another concern overall for transradial access is the potential limitation in the tools we may be able to deploy, given the smaller size of the vessel. It is reassuring [in the report from Dr. Almallouhi] that a variety of cases were successfully completed via this approach. However, fewer than 2% of their cases [24 patients] were apparently emergent, acute strokes, lending no specific support to that context. I do not expect that to change based on this paper,” Dr. Payne concluded.
“It is not clear to me that transradial neurointervention will change much. We have excellent safety data for the femoral approach, a proven track record of efficacy, and for most patients it seems to afford a somewhat wider range of tools that can be deployed, with simpler anatomy for accessing the cervical vessels in most arches. It is reassuring that the results reported by Dr. Almallouhi did not suggest negative outcomes, and as such I suspect the transradial approach at least gives us an additional option in a minority of patients. We have seen in the past 5-10 years an explosion of tools for the endovascular treatment of stroke; transradial access represents another potential strategy that appears so far to be safe,” Dr. Payne said.
Drs. Nogueira, Almallouhi, and Payne had no relevant disclosures.
SOURCE: Almallouhi E et al. Stroke. 2020 Feb;51(suppl 1):A64.
REPORTING FROM ISC 2020