User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Benzodiazepines, hypnotics don’t increase Alzheimer’s pathology
LOS ANGELES – Benzodiazepines and hypnotics, including the so-called “Z drugs,” don’t significantly increase the pathological features typical of Alzheimer’s disease but long-term users may experience some neuronal loss in the nucleus basalis, Chris Fox, MD, reported at the Alzheimer’s Association International Conference.
The nucleus basalis is rich in cholinergic neurons and associated with arousing stimuli, including positive and aversive appetite, sustained attention, and the interplay of reality and visual perception.
“Neuronal loss in the nucleus basalis offers mechanisms for the impact of benzodiazepine and anticholinergic drug use on the aging brain and highlights important areas for future research,” said Dr. Fox, professor of clinical psychiatry at the University of East Anglia, Norwich, England.
“The risk [for taking a Z drug] in the United Kingdom is high, with about 7.5 million older adults using potentially inappropriately prescribed anticholinergic and/or Z-drug medications. Despite well-documented cognitive impairment associated with these medicines, hypnotics are still used for long durations and exceed the recommended limits,” Dr. Fox said. “There’s no association with better cognition, quality of life, or improved behavior when they are given to people with dementia. In fact, we’ve seen a 60% increased risk of hip fractures – an increase from a 3% to a 15% yearly risk.”
Dr. Fox and colleagues studied the brains of 337 subjects who were included in the U.K. Medical Research Council’s Cognitive Function and Ageing Studies (CFAS). The study was intended to explore the incidence of dementia in the United Kingdom, examine incidence variation among regions, and explore factors increasing dementia risk and rate of progression.
The first study, which began in 1989 and lasted until 2015, followed subjects older than 65 years for up to 12 years. Each subject was regularly interviewed and underwent cognitive testing about every 1.5 years. Benzodiazepine use was considered an especially important aspect, because the medications are frequently used in the elderly and seem linked to injuries and cognitive status at last follow-up.
In CFAS, 21% of subjects reported at least one incidence of anticholinergic use, and 12% reported recurrent use. Another 17% reported any hypnotic use, and 11% reported recurrent use. The main indications were as an antidepressant (13%), for urological issues (4%), as antiparkinsonism drugs (1%), as antipsychotics (3%), and as antihistamines (3%). Overall, 18% reported concurrent use of benzodiazepines and hypnotics. At time of death, 46% had a diagnosis of dementia.
“Those reporting benzodiazepine use were more likely to be women and to have depression or sleep problems,” Dr. Fox noted, although he didn’t give specific hazard ratios. After adjustment for numerous factors, including age, sex, stroke, hypertension, depression, anxiety, asthma, Parkinson’s disease, duration of sleep problems, education, and smoking, he found no statistically increased risk of amyloid brain plaques or tau tangles, the pathologic hallmarks of Alzheimer’s disease.
Anticholinergic use was associated with a significant 60% reduction in cortical atrophy (odds ratio, 0.40) and recurrent use with a 61% reduction in amyloid angiopathy (OR, 0.39).
However, both medication classes were associated with greater neuronal loss in the nucleus basalis. Recurrent use of anticholinergic drugs increased neuronal loss by 300% (OR, 4.12), while any use nearly tripled it (OR, 2.87). Recurrent use of benzodiazepines was associated with increased neuronal loss in the region (OR, 3.76) as well. However, these associations did not reach statistical significance. But there was a statistically significant association with any use of benzodiazepines and neuronal loss in the nucleus basalis (OR, 6.84).
“We did find greater neuronal loss in the nucleus basalis associated with benzodiazepine and anticholinergic drugs use,” Dr. Fox said. “The nucleus basalis is rich in neurons that stimulate the cholinergic system of the neocortex. Neuronal loss in this region is thought to occur in the early stages of Alzheimer’s. Other studies have suggested that volume loss in the basal forebrain cholinergic site leads to widespread cortical atrophy in patients with mild cognitive impairment. We did not observe the widespread cortical atrophy, however.
“Given that the strongest associations were observed for benzodiazepines and neuronal loss in the nucleus basalis, it may be that the drugs were prescribed to treat the symptoms of ‘cholinergic deficiency syndrome,’ Our findings suggest that the symptoms of dementia lead to an increase of benzodiazepines as opposed to the medications actually causing Alzheimer’s disease,” he said.
Dr. Fox reported no financial disclosures.
SOURCE: Fox C et al. AAIC 2019, Abstract 34017.
LOS ANGELES – Benzodiazepines and hypnotics, including the so-called “Z drugs,” don’t significantly increase the pathological features typical of Alzheimer’s disease but long-term users may experience some neuronal loss in the nucleus basalis, Chris Fox, MD, reported at the Alzheimer’s Association International Conference.
The nucleus basalis is rich in cholinergic neurons and associated with arousing stimuli, including positive and aversive appetite, sustained attention, and the interplay of reality and visual perception.
“Neuronal loss in the nucleus basalis offers mechanisms for the impact of benzodiazepine and anticholinergic drug use on the aging brain and highlights important areas for future research,” said Dr. Fox, professor of clinical psychiatry at the University of East Anglia, Norwich, England.
“The risk [for taking a Z drug] in the United Kingdom is high, with about 7.5 million older adults using potentially inappropriately prescribed anticholinergic and/or Z-drug medications. Despite well-documented cognitive impairment associated with these medicines, hypnotics are still used for long durations and exceed the recommended limits,” Dr. Fox said. “There’s no association with better cognition, quality of life, or improved behavior when they are given to people with dementia. In fact, we’ve seen a 60% increased risk of hip fractures – an increase from a 3% to a 15% yearly risk.”
Dr. Fox and colleagues studied the brains of 337 subjects who were included in the U.K. Medical Research Council’s Cognitive Function and Ageing Studies (CFAS). The study was intended to explore the incidence of dementia in the United Kingdom, examine incidence variation among regions, and explore factors increasing dementia risk and rate of progression.
The first study, which began in 1989 and lasted until 2015, followed subjects older than 65 years for up to 12 years. Each subject was regularly interviewed and underwent cognitive testing about every 1.5 years. Benzodiazepine use was considered an especially important aspect, because the medications are frequently used in the elderly and seem linked to injuries and cognitive status at last follow-up.
In CFAS, 21% of subjects reported at least one incidence of anticholinergic use, and 12% reported recurrent use. Another 17% reported any hypnotic use, and 11% reported recurrent use. The main indications were as an antidepressant (13%), for urological issues (4%), as antiparkinsonism drugs (1%), as antipsychotics (3%), and as antihistamines (3%). Overall, 18% reported concurrent use of benzodiazepines and hypnotics. At time of death, 46% had a diagnosis of dementia.
“Those reporting benzodiazepine use were more likely to be women and to have depression or sleep problems,” Dr. Fox noted, although he didn’t give specific hazard ratios. After adjustment for numerous factors, including age, sex, stroke, hypertension, depression, anxiety, asthma, Parkinson’s disease, duration of sleep problems, education, and smoking, he found no statistically increased risk of amyloid brain plaques or tau tangles, the pathologic hallmarks of Alzheimer’s disease.
Anticholinergic use was associated with a significant 60% reduction in cortical atrophy (odds ratio, 0.40) and recurrent use with a 61% reduction in amyloid angiopathy (OR, 0.39).
However, both medication classes were associated with greater neuronal loss in the nucleus basalis. Recurrent use of anticholinergic drugs increased neuronal loss by 300% (OR, 4.12), while any use nearly tripled it (OR, 2.87). Recurrent use of benzodiazepines was associated with increased neuronal loss in the region (OR, 3.76) as well. However, these associations did not reach statistical significance. But there was a statistically significant association with any use of benzodiazepines and neuronal loss in the nucleus basalis (OR, 6.84).
“We did find greater neuronal loss in the nucleus basalis associated with benzodiazepine and anticholinergic drugs use,” Dr. Fox said. “The nucleus basalis is rich in neurons that stimulate the cholinergic system of the neocortex. Neuronal loss in this region is thought to occur in the early stages of Alzheimer’s. Other studies have suggested that volume loss in the basal forebrain cholinergic site leads to widespread cortical atrophy in patients with mild cognitive impairment. We did not observe the widespread cortical atrophy, however.
“Given that the strongest associations were observed for benzodiazepines and neuronal loss in the nucleus basalis, it may be that the drugs were prescribed to treat the symptoms of ‘cholinergic deficiency syndrome,’ Our findings suggest that the symptoms of dementia lead to an increase of benzodiazepines as opposed to the medications actually causing Alzheimer’s disease,” he said.
Dr. Fox reported no financial disclosures.
SOURCE: Fox C et al. AAIC 2019, Abstract 34017.
LOS ANGELES – Benzodiazepines and hypnotics, including the so-called “Z drugs,” don’t significantly increase the pathological features typical of Alzheimer’s disease but long-term users may experience some neuronal loss in the nucleus basalis, Chris Fox, MD, reported at the Alzheimer’s Association International Conference.
The nucleus basalis is rich in cholinergic neurons and associated with arousing stimuli, including positive and aversive appetite, sustained attention, and the interplay of reality and visual perception.
“Neuronal loss in the nucleus basalis offers mechanisms for the impact of benzodiazepine and anticholinergic drug use on the aging brain and highlights important areas for future research,” said Dr. Fox, professor of clinical psychiatry at the University of East Anglia, Norwich, England.
“The risk [for taking a Z drug] in the United Kingdom is high, with about 7.5 million older adults using potentially inappropriately prescribed anticholinergic and/or Z-drug medications. Despite well-documented cognitive impairment associated with these medicines, hypnotics are still used for long durations and exceed the recommended limits,” Dr. Fox said. “There’s no association with better cognition, quality of life, or improved behavior when they are given to people with dementia. In fact, we’ve seen a 60% increased risk of hip fractures – an increase from a 3% to a 15% yearly risk.”
Dr. Fox and colleagues studied the brains of 337 subjects who were included in the U.K. Medical Research Council’s Cognitive Function and Ageing Studies (CFAS). The study was intended to explore the incidence of dementia in the United Kingdom, examine incidence variation among regions, and explore factors increasing dementia risk and rate of progression.
The first study, which began in 1989 and lasted until 2015, followed subjects older than 65 years for up to 12 years. Each subject was regularly interviewed and underwent cognitive testing about every 1.5 years. Benzodiazepine use was considered an especially important aspect, because the medications are frequently used in the elderly and seem linked to injuries and cognitive status at last follow-up.
In CFAS, 21% of subjects reported at least one incidence of anticholinergic use, and 12% reported recurrent use. Another 17% reported any hypnotic use, and 11% reported recurrent use. The main indications were as an antidepressant (13%), for urological issues (4%), as antiparkinsonism drugs (1%), as antipsychotics (3%), and as antihistamines (3%). Overall, 18% reported concurrent use of benzodiazepines and hypnotics. At time of death, 46% had a diagnosis of dementia.
“Those reporting benzodiazepine use were more likely to be women and to have depression or sleep problems,” Dr. Fox noted, although he didn’t give specific hazard ratios. After adjustment for numerous factors, including age, sex, stroke, hypertension, depression, anxiety, asthma, Parkinson’s disease, duration of sleep problems, education, and smoking, he found no statistically increased risk of amyloid brain plaques or tau tangles, the pathologic hallmarks of Alzheimer’s disease.
Anticholinergic use was associated with a significant 60% reduction in cortical atrophy (odds ratio, 0.40) and recurrent use with a 61% reduction in amyloid angiopathy (OR, 0.39).
However, both medication classes were associated with greater neuronal loss in the nucleus basalis. Recurrent use of anticholinergic drugs increased neuronal loss by 300% (OR, 4.12), while any use nearly tripled it (OR, 2.87). Recurrent use of benzodiazepines was associated with increased neuronal loss in the region (OR, 3.76) as well. However, these associations did not reach statistical significance. But there was a statistically significant association with any use of benzodiazepines and neuronal loss in the nucleus basalis (OR, 6.84).
“We did find greater neuronal loss in the nucleus basalis associated with benzodiazepine and anticholinergic drugs use,” Dr. Fox said. “The nucleus basalis is rich in neurons that stimulate the cholinergic system of the neocortex. Neuronal loss in this region is thought to occur in the early stages of Alzheimer’s. Other studies have suggested that volume loss in the basal forebrain cholinergic site leads to widespread cortical atrophy in patients with mild cognitive impairment. We did not observe the widespread cortical atrophy, however.
“Given that the strongest associations were observed for benzodiazepines and neuronal loss in the nucleus basalis, it may be that the drugs were prescribed to treat the symptoms of ‘cholinergic deficiency syndrome,’ Our findings suggest that the symptoms of dementia lead to an increase of benzodiazepines as opposed to the medications actually causing Alzheimer’s disease,” he said.
Dr. Fox reported no financial disclosures.
SOURCE: Fox C et al. AAIC 2019, Abstract 34017.
REPORTING FROM AAIC 2019
Researchers examine potential causes of dementia in CTE
, according to a cross-sectional study published online Aug. 5 in JAMA Neurology.
The study of older, deceased former American football players with CTE showed that more years of play were associated with more severe white matter rarefaction and greater burden of neurofibrillary tau tangles in the dorsolateral frontal cortex, wrote Michael L. Alosco, PhD, assistant professor of neurology at Boston University’s CTE Center, and colleagues.
An analysis of donated brains
Repetitive head impacts are associated with CTE. The clinical presentation of CTE includes cognitive, behavioral, and mood changes that can progress to dementia. The contributions of pathologic changes in phosphorylated tau, white matter degeneration, and cerebrovascular disease to dementia in the context of CTE are poorly understood. Dr. Alosco and colleagues examined arteriosclerosis, infarcts, microinfarcts, microbleeds, and white matter rarefaction in donated brains to illuminate these contributions.
The researchers examined data from the Understanding Neurologic Injury and Traumatic Encephalopathy (UNITE) Study and Veterans Affairs–Boston University–Concussion Legacy Foundation brain bank. The population included deceased men who had played football and had received a neuropathologic diagnosis of CTE. Eligible participants had a history of repetitive head impacts. Brains that had been donated after a prolonged time postmortem and those with poor tissue quality were excluded.
Neuropathologists blinded to clinical data analyzed patients’ CTE stage and severity of neurofibrillary tangle burden in the dorsolateral frontal cortex as semiquantitative scales of phosphorylated tau severity. Neurofibrillary tangle burden was dichotomized as none or mild versus moderate or severe. The neuropathologists also rated white matter rarefaction and arteriolosclerosis severity using a scale of 0 points (i.e., none) to 3 points (i.e., severe changes). The investigators obtained clinical data through online surveys and retrospective telephone interviews with informants. They adjudicated consensus diagnoses of dementia based on modified criteria from DSM-IV.
White matter rarefaction was common
Dr. Alosco and colleagues included 180 individuals in their analysis, excluding those aged younger than 40 years because of low pathologic burden and minimal presence of dementia. Mean age at death was nearly 68 years. Fifty patients had no or mild neurofibrillary tangle burden, and 130 had moderate to severe burden. Thirty-five patients had CTE at stage I or II, and 145 had CTE at stage III or IV. In all, 120 patients were determined to have had dementia. About 47% of the sample had moderate to severe white matter rarefaction, and about 47% had arteriolosclerosis. Infarcts, microinfarcts, and microbleeds were uncommon.
When the investigators created a simultaneous equations regression model and controlled for age and race, they found that more years of play was associated with more severe white matter rarefaction, greater phosphorylated tau accumulation, and high CTE stage. Furthermore, white matter rarefaction and dorsolateral frontal cortex neurofibrillary tangles were associated with dementia. The association of years of play with dementia was mediated by white matter rarefaction and neurofibrillary tangle burden. Arteriolosclerosis was not associated with years of play, but arteriolosclerosis was independently associated with dementia.
The odds ratio for dementia was 1.69 among participants with more severe white matter rarefaction and 1.81 among patients with arteriolosclerosis. After the researchers controlled for age and race, the odds ratio of dementia was 2.65 among participants with a high neurofibrillary tangle burden, compared with participants with a low burden.
“Studies that include direct cardiovascular disease and repetitive head impacts metrics and refined measures of white matter integrity are needed to improve understanding of the pathogenesis of white matter rarefaction and cerebral small vessel changes in CTE,” Dr. Alosco and colleagues wrote.
The study was funded by grants from the National Institute on Aging, National Institute of Neurological Disorders and Stroke, the Department of Veterans Affairs, the Nick and Lynn Buoniconti Foundation, and the National Center for Advancing Translational Sciences. Some of the authors reported financial ties to the pharmaceutical industry and serving on professional sports committees.
SOURCE: Alosco ML et al. JAMA Neurol. 2019 Aug 5. doi: 10.1001/jamaneurol.2019.2244.
The study by Alosco et al. provides new insights into the pathogenesis of dementia in deceased former football players with chronic traumatic encephalopathy (CTE), Julie A. Schneider, MD, professor of neuropathology at Rush University, Chicago, wrote in an accompanying editorial (JAMA Neurol. 2019 Aug 5. doi: 10.1001/jamaneurol.2019.1089).
Significant and widespread white matter injury is an established result of head trauma resulting from acceleration-deceleration injuries. In addition, studies of single and repetitive traumatic brain injury have shown disruption of axons and white matter. The findings of Alosco et al. “underscore the importance of studying the risk factors and mechanisms for the white matter rarefaction, in addition to the tauopathy, in individuals who have played U.S. football and have CTE,” Dr. Schneider wrote.
The comprehensive neuropathologic examinations, advanced statistical techniques, and multiple sensitivity analyses that the investigators performed are among the study’s strengths. An important limitation, however, is selection bias. “The frequency of pathologic characteristics in this group should not be generalized to estimate the prevalence of neuropathologic conditions in living individuals who have played or are playing U.S. football,” Dr. Schneider wrote. “Moreover, individuals who played football who were selected for autopsy and found to have CTE may differ in other important ways from those who did not undergo autopsy or did not have CTE.” Recall bias could alter associations between years of play and dementia diagnosis, and the study’s semiquantitative assessments could result in decreased power to observe relevant associations, she said.
“In spite of these limitations, the authors should be applauded for elegant work and compelling support for multiple pathologic pathways to dementia in football players with CTE,” Dr. Schneider concluded.
Dr. Schneider is with the Rush Alzheimer’s Disease Center at Rush University, Chicago. She has been an expert consultant for the National Football League and the National Hockey League.
The study by Alosco et al. provides new insights into the pathogenesis of dementia in deceased former football players with chronic traumatic encephalopathy (CTE), Julie A. Schneider, MD, professor of neuropathology at Rush University, Chicago, wrote in an accompanying editorial (JAMA Neurol. 2019 Aug 5. doi: 10.1001/jamaneurol.2019.1089).
Significant and widespread white matter injury is an established result of head trauma resulting from acceleration-deceleration injuries. In addition, studies of single and repetitive traumatic brain injury have shown disruption of axons and white matter. The findings of Alosco et al. “underscore the importance of studying the risk factors and mechanisms for the white matter rarefaction, in addition to the tauopathy, in individuals who have played U.S. football and have CTE,” Dr. Schneider wrote.
The comprehensive neuropathologic examinations, advanced statistical techniques, and multiple sensitivity analyses that the investigators performed are among the study’s strengths. An important limitation, however, is selection bias. “The frequency of pathologic characteristics in this group should not be generalized to estimate the prevalence of neuropathologic conditions in living individuals who have played or are playing U.S. football,” Dr. Schneider wrote. “Moreover, individuals who played football who were selected for autopsy and found to have CTE may differ in other important ways from those who did not undergo autopsy or did not have CTE.” Recall bias could alter associations between years of play and dementia diagnosis, and the study’s semiquantitative assessments could result in decreased power to observe relevant associations, she said.
“In spite of these limitations, the authors should be applauded for elegant work and compelling support for multiple pathologic pathways to dementia in football players with CTE,” Dr. Schneider concluded.
Dr. Schneider is with the Rush Alzheimer’s Disease Center at Rush University, Chicago. She has been an expert consultant for the National Football League and the National Hockey League.
The study by Alosco et al. provides new insights into the pathogenesis of dementia in deceased former football players with chronic traumatic encephalopathy (CTE), Julie A. Schneider, MD, professor of neuropathology at Rush University, Chicago, wrote in an accompanying editorial (JAMA Neurol. 2019 Aug 5. doi: 10.1001/jamaneurol.2019.1089).
Significant and widespread white matter injury is an established result of head trauma resulting from acceleration-deceleration injuries. In addition, studies of single and repetitive traumatic brain injury have shown disruption of axons and white matter. The findings of Alosco et al. “underscore the importance of studying the risk factors and mechanisms for the white matter rarefaction, in addition to the tauopathy, in individuals who have played U.S. football and have CTE,” Dr. Schneider wrote.
The comprehensive neuropathologic examinations, advanced statistical techniques, and multiple sensitivity analyses that the investigators performed are among the study’s strengths. An important limitation, however, is selection bias. “The frequency of pathologic characteristics in this group should not be generalized to estimate the prevalence of neuropathologic conditions in living individuals who have played or are playing U.S. football,” Dr. Schneider wrote. “Moreover, individuals who played football who were selected for autopsy and found to have CTE may differ in other important ways from those who did not undergo autopsy or did not have CTE.” Recall bias could alter associations between years of play and dementia diagnosis, and the study’s semiquantitative assessments could result in decreased power to observe relevant associations, she said.
“In spite of these limitations, the authors should be applauded for elegant work and compelling support for multiple pathologic pathways to dementia in football players with CTE,” Dr. Schneider concluded.
Dr. Schneider is with the Rush Alzheimer’s Disease Center at Rush University, Chicago. She has been an expert consultant for the National Football League and the National Hockey League.
, according to a cross-sectional study published online Aug. 5 in JAMA Neurology.
The study of older, deceased former American football players with CTE showed that more years of play were associated with more severe white matter rarefaction and greater burden of neurofibrillary tau tangles in the dorsolateral frontal cortex, wrote Michael L. Alosco, PhD, assistant professor of neurology at Boston University’s CTE Center, and colleagues.
An analysis of donated brains
Repetitive head impacts are associated with CTE. The clinical presentation of CTE includes cognitive, behavioral, and mood changes that can progress to dementia. The contributions of pathologic changes in phosphorylated tau, white matter degeneration, and cerebrovascular disease to dementia in the context of CTE are poorly understood. Dr. Alosco and colleagues examined arteriosclerosis, infarcts, microinfarcts, microbleeds, and white matter rarefaction in donated brains to illuminate these contributions.
The researchers examined data from the Understanding Neurologic Injury and Traumatic Encephalopathy (UNITE) Study and Veterans Affairs–Boston University–Concussion Legacy Foundation brain bank. The population included deceased men who had played football and had received a neuropathologic diagnosis of CTE. Eligible participants had a history of repetitive head impacts. Brains that had been donated after a prolonged time postmortem and those with poor tissue quality were excluded.
Neuropathologists blinded to clinical data analyzed patients’ CTE stage and severity of neurofibrillary tangle burden in the dorsolateral frontal cortex as semiquantitative scales of phosphorylated tau severity. Neurofibrillary tangle burden was dichotomized as none or mild versus moderate or severe. The neuropathologists also rated white matter rarefaction and arteriolosclerosis severity using a scale of 0 points (i.e., none) to 3 points (i.e., severe changes). The investigators obtained clinical data through online surveys and retrospective telephone interviews with informants. They adjudicated consensus diagnoses of dementia based on modified criteria from DSM-IV.
White matter rarefaction was common
Dr. Alosco and colleagues included 180 individuals in their analysis, excluding those aged younger than 40 years because of low pathologic burden and minimal presence of dementia. Mean age at death was nearly 68 years. Fifty patients had no or mild neurofibrillary tangle burden, and 130 had moderate to severe burden. Thirty-five patients had CTE at stage I or II, and 145 had CTE at stage III or IV. In all, 120 patients were determined to have had dementia. About 47% of the sample had moderate to severe white matter rarefaction, and about 47% had arteriolosclerosis. Infarcts, microinfarcts, and microbleeds were uncommon.
When the investigators created a simultaneous equations regression model and controlled for age and race, they found that more years of play was associated with more severe white matter rarefaction, greater phosphorylated tau accumulation, and high CTE stage. Furthermore, white matter rarefaction and dorsolateral frontal cortex neurofibrillary tangles were associated with dementia. The association of years of play with dementia was mediated by white matter rarefaction and neurofibrillary tangle burden. Arteriolosclerosis was not associated with years of play, but arteriolosclerosis was independently associated with dementia.
The odds ratio for dementia was 1.69 among participants with more severe white matter rarefaction and 1.81 among patients with arteriolosclerosis. After the researchers controlled for age and race, the odds ratio of dementia was 2.65 among participants with a high neurofibrillary tangle burden, compared with participants with a low burden.
“Studies that include direct cardiovascular disease and repetitive head impacts metrics and refined measures of white matter integrity are needed to improve understanding of the pathogenesis of white matter rarefaction and cerebral small vessel changes in CTE,” Dr. Alosco and colleagues wrote.
The study was funded by grants from the National Institute on Aging, National Institute of Neurological Disorders and Stroke, the Department of Veterans Affairs, the Nick and Lynn Buoniconti Foundation, and the National Center for Advancing Translational Sciences. Some of the authors reported financial ties to the pharmaceutical industry and serving on professional sports committees.
SOURCE: Alosco ML et al. JAMA Neurol. 2019 Aug 5. doi: 10.1001/jamaneurol.2019.2244.
, according to a cross-sectional study published online Aug. 5 in JAMA Neurology.
The study of older, deceased former American football players with CTE showed that more years of play were associated with more severe white matter rarefaction and greater burden of neurofibrillary tau tangles in the dorsolateral frontal cortex, wrote Michael L. Alosco, PhD, assistant professor of neurology at Boston University’s CTE Center, and colleagues.
An analysis of donated brains
Repetitive head impacts are associated with CTE. The clinical presentation of CTE includes cognitive, behavioral, and mood changes that can progress to dementia. The contributions of pathologic changes in phosphorylated tau, white matter degeneration, and cerebrovascular disease to dementia in the context of CTE are poorly understood. Dr. Alosco and colleagues examined arteriosclerosis, infarcts, microinfarcts, microbleeds, and white matter rarefaction in donated brains to illuminate these contributions.
The researchers examined data from the Understanding Neurologic Injury and Traumatic Encephalopathy (UNITE) Study and Veterans Affairs–Boston University–Concussion Legacy Foundation brain bank. The population included deceased men who had played football and had received a neuropathologic diagnosis of CTE. Eligible participants had a history of repetitive head impacts. Brains that had been donated after a prolonged time postmortem and those with poor tissue quality were excluded.
Neuropathologists blinded to clinical data analyzed patients’ CTE stage and severity of neurofibrillary tangle burden in the dorsolateral frontal cortex as semiquantitative scales of phosphorylated tau severity. Neurofibrillary tangle burden was dichotomized as none or mild versus moderate or severe. The neuropathologists also rated white matter rarefaction and arteriolosclerosis severity using a scale of 0 points (i.e., none) to 3 points (i.e., severe changes). The investigators obtained clinical data through online surveys and retrospective telephone interviews with informants. They adjudicated consensus diagnoses of dementia based on modified criteria from DSM-IV.
White matter rarefaction was common
Dr. Alosco and colleagues included 180 individuals in their analysis, excluding those aged younger than 40 years because of low pathologic burden and minimal presence of dementia. Mean age at death was nearly 68 years. Fifty patients had no or mild neurofibrillary tangle burden, and 130 had moderate to severe burden. Thirty-five patients had CTE at stage I or II, and 145 had CTE at stage III or IV. In all, 120 patients were determined to have had dementia. About 47% of the sample had moderate to severe white matter rarefaction, and about 47% had arteriolosclerosis. Infarcts, microinfarcts, and microbleeds were uncommon.
When the investigators created a simultaneous equations regression model and controlled for age and race, they found that more years of play was associated with more severe white matter rarefaction, greater phosphorylated tau accumulation, and high CTE stage. Furthermore, white matter rarefaction and dorsolateral frontal cortex neurofibrillary tangles were associated with dementia. The association of years of play with dementia was mediated by white matter rarefaction and neurofibrillary tangle burden. Arteriolosclerosis was not associated with years of play, but arteriolosclerosis was independently associated with dementia.
The odds ratio for dementia was 1.69 among participants with more severe white matter rarefaction and 1.81 among patients with arteriolosclerosis. After the researchers controlled for age and race, the odds ratio of dementia was 2.65 among participants with a high neurofibrillary tangle burden, compared with participants with a low burden.
“Studies that include direct cardiovascular disease and repetitive head impacts metrics and refined measures of white matter integrity are needed to improve understanding of the pathogenesis of white matter rarefaction and cerebral small vessel changes in CTE,” Dr. Alosco and colleagues wrote.
The study was funded by grants from the National Institute on Aging, National Institute of Neurological Disorders and Stroke, the Department of Veterans Affairs, the Nick and Lynn Buoniconti Foundation, and the National Center for Advancing Translational Sciences. Some of the authors reported financial ties to the pharmaceutical industry and serving on professional sports committees.
SOURCE: Alosco ML et al. JAMA Neurol. 2019 Aug 5. doi: 10.1001/jamaneurol.2019.2244.
FROM JAMA NEUROLOGY
The states of health care: Ranking the best and worst
and the last frontier is also last in the nation in health care.
In the 2019 edition of its annual ranking of state health care systems, personal finance website WalletHub named Minnesota the best less than a week after U.S. News & World Report called the Mayo Clinic the top hospital in the country.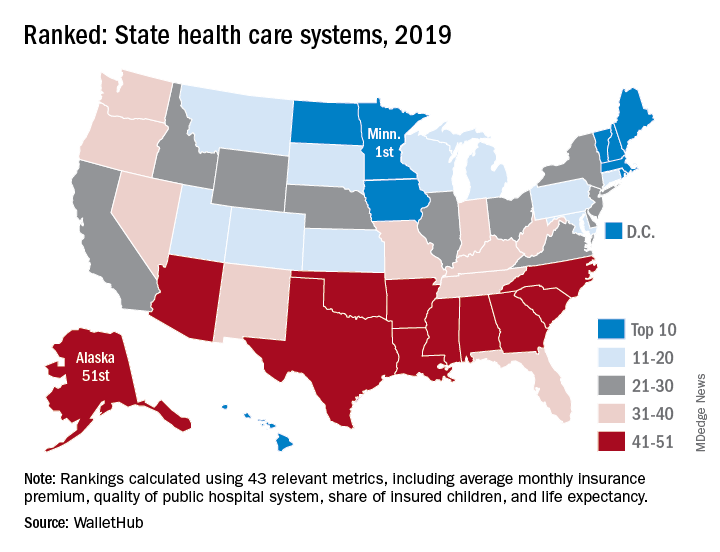
The WalletHub ranking, which included Washington, D.C., also put Alaska’s health care system at No. 51. Just one step above in the 50th spot was North Carolina, with Mississippi (49), South Carolina (48), and Arkansas (47) occupying the rest of the bottom five. Louisiana, which jumped from 51st in 2018 to 44th this year, was the only state to move out of the bottom five, WalletHub reported.
Joining Minnesota in the top five were Massachusetts (2), Rhode Island (3), D.C. (4), and Vermont (5), which was the home of last year’s best health care. North Dakota, which moved up 12 spots this year all the way to 9th, had the second-largest climb of any state: Montana catapulted 15 spots this year to finish 17th overall, WalletHub said.
For 2019, the company compared the states and D.C. using 43 measures of cost, accessibility, and outcome. The cost dimension’s six metrics included cost of a medical visit and share of adults with no doctor visits because of cost. The accessibility dimension consisted of 23 metrics, including hospital beds per capita, geriatricians per population aged 65 years and older, and Medicaid acceptance rate among physicians. The outcomes dimension included 14 metrics, among them share of patients readmitted to hospitals and share of nonimmunized children.
Minnesota was the only state to finish in the top 10 of all three dimensions. D.C. was ranked first in cost and Maine was the leader in access – as each was last year – and Massachusetts was ranked first in outcomes, the WalletHub data show.
The lowest-ranked states for each category in 2019 were the same as in 2018: Alaska (cost), Texas (access), and Mississippi (outcomes), according to the WalletHub analysis, which was based on data from 21 sources, including the Bureau of Labor Statistics, the Centers for Medicare & Medicaid Services, and the Kaiser Family Foundation.
and the last frontier is also last in the nation in health care.
In the 2019 edition of its annual ranking of state health care systems, personal finance website WalletHub named Minnesota the best less than a week after U.S. News & World Report called the Mayo Clinic the top hospital in the country.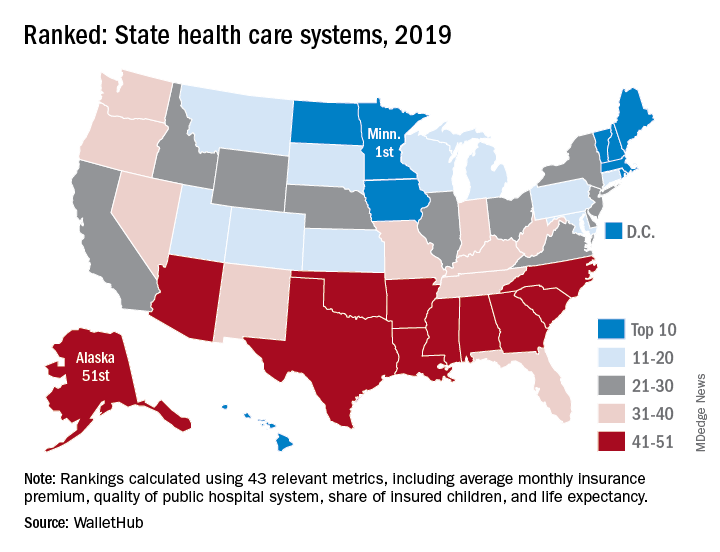
The WalletHub ranking, which included Washington, D.C., also put Alaska’s health care system at No. 51. Just one step above in the 50th spot was North Carolina, with Mississippi (49), South Carolina (48), and Arkansas (47) occupying the rest of the bottom five. Louisiana, which jumped from 51st in 2018 to 44th this year, was the only state to move out of the bottom five, WalletHub reported.
Joining Minnesota in the top five were Massachusetts (2), Rhode Island (3), D.C. (4), and Vermont (5), which was the home of last year’s best health care. North Dakota, which moved up 12 spots this year all the way to 9th, had the second-largest climb of any state: Montana catapulted 15 spots this year to finish 17th overall, WalletHub said.
For 2019, the company compared the states and D.C. using 43 measures of cost, accessibility, and outcome. The cost dimension’s six metrics included cost of a medical visit and share of adults with no doctor visits because of cost. The accessibility dimension consisted of 23 metrics, including hospital beds per capita, geriatricians per population aged 65 years and older, and Medicaid acceptance rate among physicians. The outcomes dimension included 14 metrics, among them share of patients readmitted to hospitals and share of nonimmunized children.
Minnesota was the only state to finish in the top 10 of all three dimensions. D.C. was ranked first in cost and Maine was the leader in access – as each was last year – and Massachusetts was ranked first in outcomes, the WalletHub data show.
The lowest-ranked states for each category in 2019 were the same as in 2018: Alaska (cost), Texas (access), and Mississippi (outcomes), according to the WalletHub analysis, which was based on data from 21 sources, including the Bureau of Labor Statistics, the Centers for Medicare & Medicaid Services, and the Kaiser Family Foundation.
and the last frontier is also last in the nation in health care.
In the 2019 edition of its annual ranking of state health care systems, personal finance website WalletHub named Minnesota the best less than a week after U.S. News & World Report called the Mayo Clinic the top hospital in the country.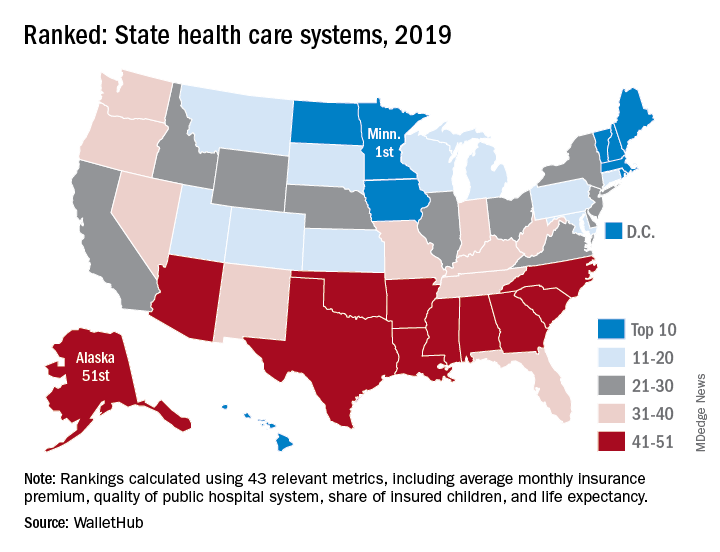
The WalletHub ranking, which included Washington, D.C., also put Alaska’s health care system at No. 51. Just one step above in the 50th spot was North Carolina, with Mississippi (49), South Carolina (48), and Arkansas (47) occupying the rest of the bottom five. Louisiana, which jumped from 51st in 2018 to 44th this year, was the only state to move out of the bottom five, WalletHub reported.
Joining Minnesota in the top five were Massachusetts (2), Rhode Island (3), D.C. (4), and Vermont (5), which was the home of last year’s best health care. North Dakota, which moved up 12 spots this year all the way to 9th, had the second-largest climb of any state: Montana catapulted 15 spots this year to finish 17th overall, WalletHub said.
For 2019, the company compared the states and D.C. using 43 measures of cost, accessibility, and outcome. The cost dimension’s six metrics included cost of a medical visit and share of adults with no doctor visits because of cost. The accessibility dimension consisted of 23 metrics, including hospital beds per capita, geriatricians per population aged 65 years and older, and Medicaid acceptance rate among physicians. The outcomes dimension included 14 metrics, among them share of patients readmitted to hospitals and share of nonimmunized children.
Minnesota was the only state to finish in the top 10 of all three dimensions. D.C. was ranked first in cost and Maine was the leader in access – as each was last year – and Massachusetts was ranked first in outcomes, the WalletHub data show.
The lowest-ranked states for each category in 2019 were the same as in 2018: Alaska (cost), Texas (access), and Mississippi (outcomes), according to the WalletHub analysis, which was based on data from 21 sources, including the Bureau of Labor Statistics, the Centers for Medicare & Medicaid Services, and the Kaiser Family Foundation.
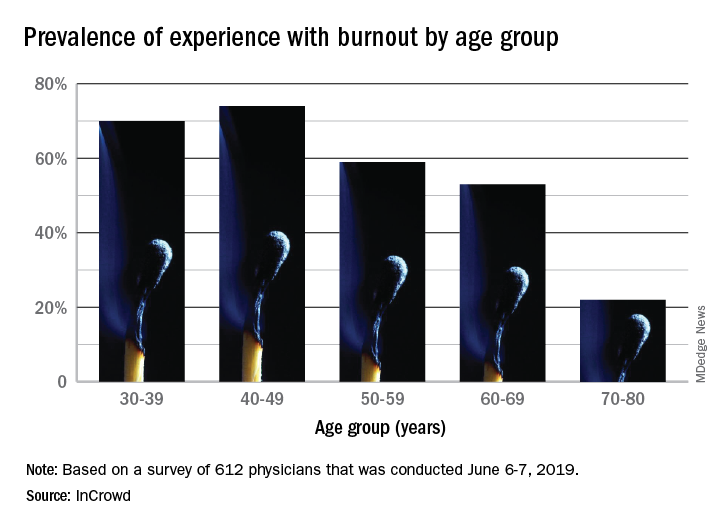
Burnout gets personal for 68% of physicians
by real-time market insights technology firm InCrowd.
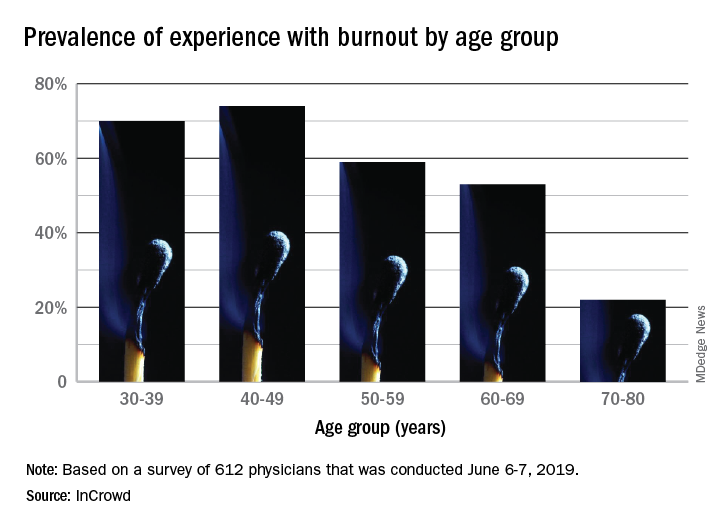
The overall prevalence of personal burnout experience was 68% among respondents, and another 28% said that they had not felt burned out but knew other physicians who had, InCrowd reported Aug. 6.
Specialty appeared to play a part given that 79% of primary care physicians reported experiencing burnout versus 57% of specialists. In response to an open-ended question about ability to manage burnout, the most common answer (23%) was that specialty played a large role, with “no role/all specialties affected equally” next at 13%. Equal proportions of respondents, however, said that specialists (24%) and primary care physicians (24%) were the group most affected, InCrowd said.
There was also a disconnect regarding age. When answering another open-ended question about the effects of age, 23% of those surveyed said that older physicians are more affected, compared with 9% who put the greater burden on younger physicians. The self-reporting of burnout, however, showed that younger physicians were much more likely to experience its effects than their older counterparts: 70% of those aged 30-39 years and 74% of those 40-49 versus 22% of those aged 70-80, InCrowd reported.
InCrowd noted that its results fall within the range of other recent surveys involving burnout in physicians that have shown levels that were lower, at 44% (MedScape, 2019) or 43.9% (American Academy of Family Physicians, 2019), and those that were higher, at 77.8% (The Physicians Foundation/Merritt Hawkins, 2018).
“The alarming persistence of physician burnout over the years and across multiple studies unfortunately demonstrates that we have not yet turned the tide on this problematic issue,” Diane Hayes, PhD, president of InCrowd, said in a statement accompanying the survey results. “Since we last looked at this in 2016, there really haven’t been any notable improvements. The healthcare industry would benefit from refining and expanding current initiatives to assure adequate staffing levels needed to deliver the quality care patients deserve.”
The survey was conducted June 6-7, 2019, and involved responses from 612 physicians (51% primary care providers, 49% specialists).
by real-time market insights technology firm InCrowd.
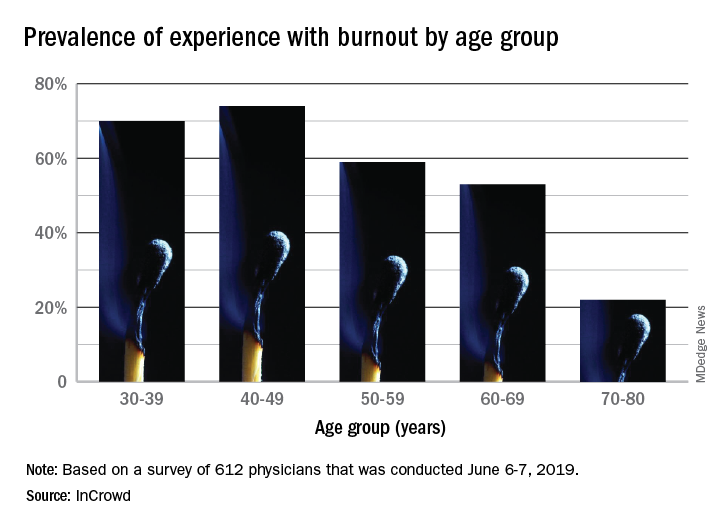
The overall prevalence of personal burnout experience was 68% among respondents, and another 28% said that they had not felt burned out but knew other physicians who had, InCrowd reported Aug. 6.
Specialty appeared to play a part given that 79% of primary care physicians reported experiencing burnout versus 57% of specialists. In response to an open-ended question about ability to manage burnout, the most common answer (23%) was that specialty played a large role, with “no role/all specialties affected equally” next at 13%. Equal proportions of respondents, however, said that specialists (24%) and primary care physicians (24%) were the group most affected, InCrowd said.
There was also a disconnect regarding age. When answering another open-ended question about the effects of age, 23% of those surveyed said that older physicians are more affected, compared with 9% who put the greater burden on younger physicians. The self-reporting of burnout, however, showed that younger physicians were much more likely to experience its effects than their older counterparts: 70% of those aged 30-39 years and 74% of those 40-49 versus 22% of those aged 70-80, InCrowd reported.
InCrowd noted that its results fall within the range of other recent surveys involving burnout in physicians that have shown levels that were lower, at 44% (MedScape, 2019) or 43.9% (American Academy of Family Physicians, 2019), and those that were higher, at 77.8% (The Physicians Foundation/Merritt Hawkins, 2018).
“The alarming persistence of physician burnout over the years and across multiple studies unfortunately demonstrates that we have not yet turned the tide on this problematic issue,” Diane Hayes, PhD, president of InCrowd, said in a statement accompanying the survey results. “Since we last looked at this in 2016, there really haven’t been any notable improvements. The healthcare industry would benefit from refining and expanding current initiatives to assure adequate staffing levels needed to deliver the quality care patients deserve.”
The survey was conducted June 6-7, 2019, and involved responses from 612 physicians (51% primary care providers, 49% specialists).
by real-time market insights technology firm InCrowd.
The overall prevalence of personal burnout experience was 68% among respondents, and another 28% said that they had not felt burned out but knew other physicians who had, InCrowd reported Aug. 6.
Specialty appeared to play a part given that 79% of primary care physicians reported experiencing burnout versus 57% of specialists. In response to an open-ended question about ability to manage burnout, the most common answer (23%) was that specialty played a large role, with “no role/all specialties affected equally” next at 13%. Equal proportions of respondents, however, said that specialists (24%) and primary care physicians (24%) were the group most affected, InCrowd said.
There was also a disconnect regarding age. When answering another open-ended question about the effects of age, 23% of those surveyed said that older physicians are more affected, compared with 9% who put the greater burden on younger physicians. The self-reporting of burnout, however, showed that younger physicians were much more likely to experience its effects than their older counterparts: 70% of those aged 30-39 years and 74% of those 40-49 versus 22% of those aged 70-80, InCrowd reported.
InCrowd noted that its results fall within the range of other recent surveys involving burnout in physicians that have shown levels that were lower, at 44% (MedScape, 2019) or 43.9% (American Academy of Family Physicians, 2019), and those that were higher, at 77.8% (The Physicians Foundation/Merritt Hawkins, 2018).
“The alarming persistence of physician burnout over the years and across multiple studies unfortunately demonstrates that we have not yet turned the tide on this problematic issue,” Diane Hayes, PhD, president of InCrowd, said in a statement accompanying the survey results. “Since we last looked at this in 2016, there really haven’t been any notable improvements. The healthcare industry would benefit from refining and expanding current initiatives to assure adequate staffing levels needed to deliver the quality care patients deserve.”
The survey was conducted June 6-7, 2019, and involved responses from 612 physicians (51% primary care providers, 49% specialists).
Efficacy of erenumab is sustained over more than 4 years of treatment
PHILADELPHIA – “Erenumab was well tolerated and safe, with no safety signals detected over this period,” said Messoud Ashina, MD, PhD, professor of neurology at the University of Copenhagen. Dr. Ashina presented the interim data from a 5-year, open-label extension study of erenumab at the annual meeting of the American Headache Society.
Erenumab is a monoclonal antibody that targets and blocks the calcitonin gene-related peptide (CGRP) receptor. In May 2018, the Food and Drug Administration approved erenumab for the preventive treatment of migraine in adults. The treatment, marketed as Aimovig, is administered once monthly by self-injection.
During the open-label study, patients initially received 70 mg of erenumab monthly. After approximately 2 years, patients switched to 140 mg of erenumab monthly. The researchers’ interim efficacy analysis included all patients on 140 mg of erenumab with data about monthly migraine days after more than 4 years of treatment. The safety analysis included all patients who enrolled in the open-label treatment period and received at least one dose of erenumab.
Of 250 patients who increased the erenumab dose from 70 mg to 140 mg, a total of 221 (88%) completed the open-label treatment period or remained on 140 mg after more than 4 years. Patients’ average number of monthly migraine days at study baseline was 8.7, and the average change from baseline to the most recent month in the interim analysis was –5.8.
During the most recent month of assessment, 77% of patients had at least a 50% reduction in monthly migraine days from baseline, 56% had at least a 75% reduction, and 33% had a 100% reduction.
Mean change from baseline in acute migraine‐specific medication treatment days was –4.6, from a baseline of 6.1.
Among the 383 patients who entered the open-label treatment period and received at least one dose of erenumab (mean age, 41.3; 79% female), the median erenumab exposure was 58.5 months. The exposure‐adjusted incidence of adverse events per 100 patient‐years was 124.9, and the three most frequent adverse events (per 100 patient-years) were nasopharyngitis (10.9), upper respiratory tract infection (6.8), and influenza (4.7). The exposure‐adjusted incidence rate per 100 patient‐years for constipation was 1.3 (9/383) for 70-mg erenumab and 2.6 (15/250) for 140-mg erenumab.
“The exposure‐adjusted incidence rate per 100 patient‐years of serious adverse events was 3.8, similar to the rate observed for erenumab and placebo during the placebo‐controlled periods of studies,” the researchers said.
The study was sponsored by Amgen, and several study authors are employees of Amgen or Novartis, the companies that market erenumab. Dr. Ashina is a consultant for Amgen, Novartis, and other companies.
SOURCE: Ashina M et al. AHS 2019, Abstract IOR10.
PHILADELPHIA – “Erenumab was well tolerated and safe, with no safety signals detected over this period,” said Messoud Ashina, MD, PhD, professor of neurology at the University of Copenhagen. Dr. Ashina presented the interim data from a 5-year, open-label extension study of erenumab at the annual meeting of the American Headache Society.
Erenumab is a monoclonal antibody that targets and blocks the calcitonin gene-related peptide (CGRP) receptor. In May 2018, the Food and Drug Administration approved erenumab for the preventive treatment of migraine in adults. The treatment, marketed as Aimovig, is administered once monthly by self-injection.
During the open-label study, patients initially received 70 mg of erenumab monthly. After approximately 2 years, patients switched to 140 mg of erenumab monthly. The researchers’ interim efficacy analysis included all patients on 140 mg of erenumab with data about monthly migraine days after more than 4 years of treatment. The safety analysis included all patients who enrolled in the open-label treatment period and received at least one dose of erenumab.
Of 250 patients who increased the erenumab dose from 70 mg to 140 mg, a total of 221 (88%) completed the open-label treatment period or remained on 140 mg after more than 4 years. Patients’ average number of monthly migraine days at study baseline was 8.7, and the average change from baseline to the most recent month in the interim analysis was –5.8.
During the most recent month of assessment, 77% of patients had at least a 50% reduction in monthly migraine days from baseline, 56% had at least a 75% reduction, and 33% had a 100% reduction.
Mean change from baseline in acute migraine‐specific medication treatment days was –4.6, from a baseline of 6.1.
Among the 383 patients who entered the open-label treatment period and received at least one dose of erenumab (mean age, 41.3; 79% female), the median erenumab exposure was 58.5 months. The exposure‐adjusted incidence of adverse events per 100 patient‐years was 124.9, and the three most frequent adverse events (per 100 patient-years) were nasopharyngitis (10.9), upper respiratory tract infection (6.8), and influenza (4.7). The exposure‐adjusted incidence rate per 100 patient‐years for constipation was 1.3 (9/383) for 70-mg erenumab and 2.6 (15/250) for 140-mg erenumab.
“The exposure‐adjusted incidence rate per 100 patient‐years of serious adverse events was 3.8, similar to the rate observed for erenumab and placebo during the placebo‐controlled periods of studies,” the researchers said.
The study was sponsored by Amgen, and several study authors are employees of Amgen or Novartis, the companies that market erenumab. Dr. Ashina is a consultant for Amgen, Novartis, and other companies.
SOURCE: Ashina M et al. AHS 2019, Abstract IOR10.
PHILADELPHIA – “Erenumab was well tolerated and safe, with no safety signals detected over this period,” said Messoud Ashina, MD, PhD, professor of neurology at the University of Copenhagen. Dr. Ashina presented the interim data from a 5-year, open-label extension study of erenumab at the annual meeting of the American Headache Society.
Erenumab is a monoclonal antibody that targets and blocks the calcitonin gene-related peptide (CGRP) receptor. In May 2018, the Food and Drug Administration approved erenumab for the preventive treatment of migraine in adults. The treatment, marketed as Aimovig, is administered once monthly by self-injection.
During the open-label study, patients initially received 70 mg of erenumab monthly. After approximately 2 years, patients switched to 140 mg of erenumab monthly. The researchers’ interim efficacy analysis included all patients on 140 mg of erenumab with data about monthly migraine days after more than 4 years of treatment. The safety analysis included all patients who enrolled in the open-label treatment period and received at least one dose of erenumab.
Of 250 patients who increased the erenumab dose from 70 mg to 140 mg, a total of 221 (88%) completed the open-label treatment period or remained on 140 mg after more than 4 years. Patients’ average number of monthly migraine days at study baseline was 8.7, and the average change from baseline to the most recent month in the interim analysis was –5.8.
During the most recent month of assessment, 77% of patients had at least a 50% reduction in monthly migraine days from baseline, 56% had at least a 75% reduction, and 33% had a 100% reduction.
Mean change from baseline in acute migraine‐specific medication treatment days was –4.6, from a baseline of 6.1.
Among the 383 patients who entered the open-label treatment period and received at least one dose of erenumab (mean age, 41.3; 79% female), the median erenumab exposure was 58.5 months. The exposure‐adjusted incidence of adverse events per 100 patient‐years was 124.9, and the three most frequent adverse events (per 100 patient-years) were nasopharyngitis (10.9), upper respiratory tract infection (6.8), and influenza (4.7). The exposure‐adjusted incidence rate per 100 patient‐years for constipation was 1.3 (9/383) for 70-mg erenumab and 2.6 (15/250) for 140-mg erenumab.
“The exposure‐adjusted incidence rate per 100 patient‐years of serious adverse events was 3.8, similar to the rate observed for erenumab and placebo during the placebo‐controlled periods of studies,” the researchers said.
The study was sponsored by Amgen, and several study authors are employees of Amgen or Novartis, the companies that market erenumab. Dr. Ashina is a consultant for Amgen, Novartis, and other companies.
SOURCE: Ashina M et al. AHS 2019, Abstract IOR10.
REPORTING FROM AHS 2019
Professional coaching keeps doctors in the game
Physicians who receive professional coaching are less emotionally exhausted and less vulnerable to burnout, according to the results of a pilot study.
“This intervention adds to the growing literature of evidence-based approaches to promote physician well-being and should be considered a complementary strategy to be deployed in combination with other organizational approaches to improve system-level drivers of work-related stressors,” wrote Liselotte N. Dyrbye, MD, of the Mayo Clinic in Rochester, Minn., and coauthors in JAMA Internal Medicine.
Dr. Dyrbye and colleagues conducted a randomized pilot study of 88 Mayo Clinic physicians in the departments of medicine, family medicine, and pediatrics. Half (n = 44) received 3.5 hours of sessions facilitated by a professional coach. The other half (n = 44) served as controls. Participants’ well-being – in regard to burnout, quality of life, resilience, job satisfaction, engagement, and meaning at work – was surveyed at baseline and the study’s completion.
Physicians in the coaching group participated in a 1-hour initial telephone session, designed to establish a relationship between the physician and coach, as well as to assess needs, set goals, identify values, and create an action plan. During follow-up sessions, coaches would check in, help plan and set goals, and suggest strategies/changes to incorporate into daily life. Physicians were permitted to ask for support on any issue, but also were expected to see as many patients as their colleagues outside of the study.
After 6 months, physicians in the coaching group saw a significant decrease in emotional exhaustion by a mean of 5.2 points, compared with an increase of 1.5 points in the control group. At 5 months, absolute rates of high emotional exhaustion decreased by 19.5% in the coaching group and increased by 9.8% in the control group and absolute rates of overall burnout decreased by 17.1% in the coaching group and increased by 4.9% in the control group. Quality of life and resilience scores also improved, though there were no notable differences between groups in measures of job satisfaction, engagement, and meaning at work.
The authors noted their study’s limitations, which included a modest sample size and a volunteer group of participants.
In addition, the lower percentage of men in the study – 48 of 88 participants were women – may be a result of factors that deserve further investigation. Finally, burnout rates among volunteers were higher than those among other physicians, suggesting that “the study appealed to those in greatest need of the intervention.”
The study was funded by the Mayo Clinic department of medicine’s Program on Physician Well-Being and the Physician Foundation. Two of the authors – Dr. Dyrbye and Tait D. Shanafelt, MD, of Stanford (Calif.) University – reported being the coinventors of, and receiving royalties for, the Physician Well-Being Index, Medical Student Well-Being Index, Nurse Well-Being Index, and the Well-Being Index.
SOURCE: Dyrbye LN et al. JAMA Intern Med. 2019 Aug 5. doi: 10.1001/jamainternmed.2019.2425.
Physicians who receive professional coaching are less emotionally exhausted and less vulnerable to burnout, according to the results of a pilot study.
“This intervention adds to the growing literature of evidence-based approaches to promote physician well-being and should be considered a complementary strategy to be deployed in combination with other organizational approaches to improve system-level drivers of work-related stressors,” wrote Liselotte N. Dyrbye, MD, of the Mayo Clinic in Rochester, Minn., and coauthors in JAMA Internal Medicine.
Dr. Dyrbye and colleagues conducted a randomized pilot study of 88 Mayo Clinic physicians in the departments of medicine, family medicine, and pediatrics. Half (n = 44) received 3.5 hours of sessions facilitated by a professional coach. The other half (n = 44) served as controls. Participants’ well-being – in regard to burnout, quality of life, resilience, job satisfaction, engagement, and meaning at work – was surveyed at baseline and the study’s completion.
Physicians in the coaching group participated in a 1-hour initial telephone session, designed to establish a relationship between the physician and coach, as well as to assess needs, set goals, identify values, and create an action plan. During follow-up sessions, coaches would check in, help plan and set goals, and suggest strategies/changes to incorporate into daily life. Physicians were permitted to ask for support on any issue, but also were expected to see as many patients as their colleagues outside of the study.
After 6 months, physicians in the coaching group saw a significant decrease in emotional exhaustion by a mean of 5.2 points, compared with an increase of 1.5 points in the control group. At 5 months, absolute rates of high emotional exhaustion decreased by 19.5% in the coaching group and increased by 9.8% in the control group and absolute rates of overall burnout decreased by 17.1% in the coaching group and increased by 4.9% in the control group. Quality of life and resilience scores also improved, though there were no notable differences between groups in measures of job satisfaction, engagement, and meaning at work.
The authors noted their study’s limitations, which included a modest sample size and a volunteer group of participants.
In addition, the lower percentage of men in the study – 48 of 88 participants were women – may be a result of factors that deserve further investigation. Finally, burnout rates among volunteers were higher than those among other physicians, suggesting that “the study appealed to those in greatest need of the intervention.”
The study was funded by the Mayo Clinic department of medicine’s Program on Physician Well-Being and the Physician Foundation. Two of the authors – Dr. Dyrbye and Tait D. Shanafelt, MD, of Stanford (Calif.) University – reported being the coinventors of, and receiving royalties for, the Physician Well-Being Index, Medical Student Well-Being Index, Nurse Well-Being Index, and the Well-Being Index.
SOURCE: Dyrbye LN et al. JAMA Intern Med. 2019 Aug 5. doi: 10.1001/jamainternmed.2019.2425.
Physicians who receive professional coaching are less emotionally exhausted and less vulnerable to burnout, according to the results of a pilot study.
“This intervention adds to the growing literature of evidence-based approaches to promote physician well-being and should be considered a complementary strategy to be deployed in combination with other organizational approaches to improve system-level drivers of work-related stressors,” wrote Liselotte N. Dyrbye, MD, of the Mayo Clinic in Rochester, Minn., and coauthors in JAMA Internal Medicine.
Dr. Dyrbye and colleagues conducted a randomized pilot study of 88 Mayo Clinic physicians in the departments of medicine, family medicine, and pediatrics. Half (n = 44) received 3.5 hours of sessions facilitated by a professional coach. The other half (n = 44) served as controls. Participants’ well-being – in regard to burnout, quality of life, resilience, job satisfaction, engagement, and meaning at work – was surveyed at baseline and the study’s completion.
Physicians in the coaching group participated in a 1-hour initial telephone session, designed to establish a relationship between the physician and coach, as well as to assess needs, set goals, identify values, and create an action plan. During follow-up sessions, coaches would check in, help plan and set goals, and suggest strategies/changes to incorporate into daily life. Physicians were permitted to ask for support on any issue, but also were expected to see as many patients as their colleagues outside of the study.
After 6 months, physicians in the coaching group saw a significant decrease in emotional exhaustion by a mean of 5.2 points, compared with an increase of 1.5 points in the control group. At 5 months, absolute rates of high emotional exhaustion decreased by 19.5% in the coaching group and increased by 9.8% in the control group and absolute rates of overall burnout decreased by 17.1% in the coaching group and increased by 4.9% in the control group. Quality of life and resilience scores also improved, though there were no notable differences between groups in measures of job satisfaction, engagement, and meaning at work.
The authors noted their study’s limitations, which included a modest sample size and a volunteer group of participants.
In addition, the lower percentage of men in the study – 48 of 88 participants were women – may be a result of factors that deserve further investigation. Finally, burnout rates among volunteers were higher than those among other physicians, suggesting that “the study appealed to those in greatest need of the intervention.”
The study was funded by the Mayo Clinic department of medicine’s Program on Physician Well-Being and the Physician Foundation. Two of the authors – Dr. Dyrbye and Tait D. Shanafelt, MD, of Stanford (Calif.) University – reported being the coinventors of, and receiving royalties for, the Physician Well-Being Index, Medical Student Well-Being Index, Nurse Well-Being Index, and the Well-Being Index.
SOURCE: Dyrbye LN et al. JAMA Intern Med. 2019 Aug 5. doi: 10.1001/jamainternmed.2019.2425.
FROM JAMA INTERNAL MEDICINE
Antiepileptic drug outcomes have remained flat for 3 decades
BANGKOK – Since founding the Epilepsy Unit at Glasgow’s Western Infirmary 37 years ago, Martin J. Brodie, MD, has seen many changes in the field, including the introduction of more than a dozen new antiepileptic drugs (AEDs) in the past 2 decades.
And based upon this vast clinical experience coupled with his leadership of landmark studies, he has a message for his physician colleagues and their epilepsy patients. And it’s not pretty.
“Has the probability of achieving seizure freedom increased significantly in the last 3 decades? Regrettably, the answer is no,” he declared at the International Epilepsy Congress.
“Over all these years, in terms of seizure freedom there has been no real difference in outcome. There’s really quite a long way to go before we can say that we are doing all that well for people,” he said at the congress sponsored by the International League Against Epilepsy.
In the year 2000, he and his coinvestigators published a prospective, longitudinal, observational cohort study of 470 newly diagnosed patients with epilepsy treated at the Western Infirmary during 1982-1997, all with a minimum of 2 years’ follow-up. Sixty-one percent achieved complete freedom from seizures for at least 1 year on monotherapy, and another 3% did so on polytherapy, for a total rate of 64% (N Engl J Med. 2000 Feb 3;342[5]:314-19).
But these were patients who by and large were treated with older AEDs such as carbamazepine, which has since fallen by the wayside because of toxicities. Scottish neurologists now generally turn to lamotrigine (Lamictal), levetiracetam (Spritam), and other, newer AEDs. So Dr. Brodie and his coworkers recently published a follow-up study, this one featuring 30 years of longitudinal follow-up of 1,795 patients newly treated for epilepsy with AEDs, new and old, during 1982-2012. The investigators demonstrated that the seizure-free survival curves over time were virtually superimposable. In the larger, more recent study, remission was achieved in 55% of patients with AED monotherapy and in another 9% with polytherapy, for a total rate of 64%, identical to the rate in the 2000 study, and as was the case in the earlier study, 36% of patients remained uncontrolled (JAMA Neurol. 2018 Mar 1;75[3]:279-86).
“Overall, the way this population behaves, there’s no difference in efficacy and no difference in tolerability whether you’re using old drugs used properly or new drugs used properly,” said Dr. Brodie, professor of neurology at the University of Glasgow (Scotland).
It’s noteworthy that Sir William R. Gowers, the Londoner who has been called the greatest neurologist of all time, reported a 70% seizure-free rate in 1881, while Dr. Brodie and workers achieved a 64% rate in their 30-year study. “It’s interesting that the numbers are so bad, really, I suppose,” Dr. Brodie commented.
How about outcomes in pediatric epilepsy?
Dr. Brodie and coworkers recently published a 30-year prospective cohort study of 332 adolescent epilepsy patients newly diagnosed and treated at the Western Infirmary during 1982-2012. At the end of the study, 67% were seizure-free for at least the past year, a feat accomplished via monotherapy in 83% of cases. The seizure-free rate was 72% in those with generalized epilepsy, significantly better than the 60% figure in those with focal epilepsy. The efficacy rate was 74% with newer AED monotherapy and similar at 77% with monotherapy older drugs. Adverse event rates ranged from a low of 12% with lamotrigine to 56% with topiramate (Topamax), according to the findings published in Epilepsia (2019 Jun;60[6]:1083-90).
Roughly similar outcomes have been reported from Norway in a study of 600 children with epilepsy, median age 7 years, with a median follow-up of 5.8 years that is considerably shorter than that in the Glasgow pediatric study. Overall, 59% of the Norwegian children remained seizure free for at least 1 year, 30% developed drug-resistant epilepsy, and 11% followed an intermediate remitting/relapsing course (Pediatrics. 2018 Jun. doi: 10.1542/peds.2017-4016).
Why the decades of flat pharmacologic outcomes?
The consistently suboptimal seizure-free outcomes obtained over the past 30 years shouldn’t really be surprising, according to Dr. Brodie.
“Although we think we have lots of mechanisms of action and lots of differences between the drugs, they’re arguably all antiseizure drugs and not antiepilepsy drugs. We don’t treat the whale; we treat the spout. We don’t treat what we cannot see; we treat what we can see, which is the seizures, but we’re not influencing the long-term outcome,” the neurologist explained.
The compelling case for early epilepsy surgery
Epilepsy surgery remains underutilized, according to Dr. Brodie and other experts.
The International League Against Epilepsy defines drug-resistant epilepsy as failure to achieve sustained seizure freedom after adequate trials of two tolerated and appropriately chosen and used AED schedules. Dr. Brodie’s work was influential in creating that definition because his data demonstrated the sharply diminishing returns of additional drug trials.
“When do we consider epilepsy surgery? Arguably, the earlier, the better. After two drugs have failed appropriately, I don’t think anybody in this room would argue about that, although people in some of the other rooms might,” he said at the congress.
Influential in his thinking on this score were the impressive results of an early study, the first-ever randomized trial of surgery for epilepsy. In 80 patients with a 21-year history of drug-refractory temporal lobe epilepsy who were randomized to surgery or 1 year of AED therapy, at 1 year of follow-up blinded epileptologists rated 58% of surgically treated patients as free from seizures that impair awareness of self and surroundings, compared with just 8% in the AED group (N Engl J Med. 2001 Aug 2;345[5]:311-8).
“That’s a big outcome, and I’m very keen to ensure that my data continue to drive the push for early surgery,” according to the neurologist.
A Cochrane review of 177 studies totaling more than 16,000 patients concluded that 65% of epilepsy patients had good outcomes following surgery. Prognostic factors associated with better surgical outcomes included complete surgical resection of the epileptogenic focus, the presence of mesial temporal sclerosis, concordance of MRI and EEG findings, and an absence of cortical dysplasia (Cochrane Database Syst Rev. 2019;6:CD010541. doi: 10.1002/14651858.CD010541.pub3).
In addition, a systematic review and meta-analysis by Canadian investigators found that 72% of adults with lesional epilepsy identified by MRI or histopathology were seizure-free after surgery, compared with 36% of those with nonlesional epilepsy. The disparity in outcomes was similar in pediatric epilepsy patients, with seizure freedom after surgery in 74% of those with lesional disease versus 45% with nonlesional epilepsy (Epilepsy Res. 2010 May;89[2-3]:310-8).
Whither are neurostimulatory device therapies headed?
Dr. Brodie was quick to admit that as a pharmacologic researcher, device modalities including vagus nerve stimulation, responsive neurostimulation, and deep brain stimulation are outside his area of expertise. But he’s been following developments in the field with interest.
“These device therapies have shown efficacy in short-term randomized trials, but very few patients attain long-term seizure freedom. I think these are largely palliative techniques. I gave up on these techniques a long time ago because I felt it was a very costly way of reducing seizures by a relatively small margin, and really we need to go a little bit further than that. But I know there’s a lot of work going on at the moment,” he said.
Dr. Brodie reported serving on the scientific advisory boards of more than a half dozen pharmaceutical companies.
BANGKOK – Since founding the Epilepsy Unit at Glasgow’s Western Infirmary 37 years ago, Martin J. Brodie, MD, has seen many changes in the field, including the introduction of more than a dozen new antiepileptic drugs (AEDs) in the past 2 decades.
And based upon this vast clinical experience coupled with his leadership of landmark studies, he has a message for his physician colleagues and their epilepsy patients. And it’s not pretty.
“Has the probability of achieving seizure freedom increased significantly in the last 3 decades? Regrettably, the answer is no,” he declared at the International Epilepsy Congress.
“Over all these years, in terms of seizure freedom there has been no real difference in outcome. There’s really quite a long way to go before we can say that we are doing all that well for people,” he said at the congress sponsored by the International League Against Epilepsy.
In the year 2000, he and his coinvestigators published a prospective, longitudinal, observational cohort study of 470 newly diagnosed patients with epilepsy treated at the Western Infirmary during 1982-1997, all with a minimum of 2 years’ follow-up. Sixty-one percent achieved complete freedom from seizures for at least 1 year on monotherapy, and another 3% did so on polytherapy, for a total rate of 64% (N Engl J Med. 2000 Feb 3;342[5]:314-19).
But these were patients who by and large were treated with older AEDs such as carbamazepine, which has since fallen by the wayside because of toxicities. Scottish neurologists now generally turn to lamotrigine (Lamictal), levetiracetam (Spritam), and other, newer AEDs. So Dr. Brodie and his coworkers recently published a follow-up study, this one featuring 30 years of longitudinal follow-up of 1,795 patients newly treated for epilepsy with AEDs, new and old, during 1982-2012. The investigators demonstrated that the seizure-free survival curves over time were virtually superimposable. In the larger, more recent study, remission was achieved in 55% of patients with AED monotherapy and in another 9% with polytherapy, for a total rate of 64%, identical to the rate in the 2000 study, and as was the case in the earlier study, 36% of patients remained uncontrolled (JAMA Neurol. 2018 Mar 1;75[3]:279-86).
“Overall, the way this population behaves, there’s no difference in efficacy and no difference in tolerability whether you’re using old drugs used properly or new drugs used properly,” said Dr. Brodie, professor of neurology at the University of Glasgow (Scotland).
It’s noteworthy that Sir William R. Gowers, the Londoner who has been called the greatest neurologist of all time, reported a 70% seizure-free rate in 1881, while Dr. Brodie and workers achieved a 64% rate in their 30-year study. “It’s interesting that the numbers are so bad, really, I suppose,” Dr. Brodie commented.
How about outcomes in pediatric epilepsy?
Dr. Brodie and coworkers recently published a 30-year prospective cohort study of 332 adolescent epilepsy patients newly diagnosed and treated at the Western Infirmary during 1982-2012. At the end of the study, 67% were seizure-free for at least the past year, a feat accomplished via monotherapy in 83% of cases. The seizure-free rate was 72% in those with generalized epilepsy, significantly better than the 60% figure in those with focal epilepsy. The efficacy rate was 74% with newer AED monotherapy and similar at 77% with monotherapy older drugs. Adverse event rates ranged from a low of 12% with lamotrigine to 56% with topiramate (Topamax), according to the findings published in Epilepsia (2019 Jun;60[6]:1083-90).
Roughly similar outcomes have been reported from Norway in a study of 600 children with epilepsy, median age 7 years, with a median follow-up of 5.8 years that is considerably shorter than that in the Glasgow pediatric study. Overall, 59% of the Norwegian children remained seizure free for at least 1 year, 30% developed drug-resistant epilepsy, and 11% followed an intermediate remitting/relapsing course (Pediatrics. 2018 Jun. doi: 10.1542/peds.2017-4016).
Why the decades of flat pharmacologic outcomes?
The consistently suboptimal seizure-free outcomes obtained over the past 30 years shouldn’t really be surprising, according to Dr. Brodie.
“Although we think we have lots of mechanisms of action and lots of differences between the drugs, they’re arguably all antiseizure drugs and not antiepilepsy drugs. We don’t treat the whale; we treat the spout. We don’t treat what we cannot see; we treat what we can see, which is the seizures, but we’re not influencing the long-term outcome,” the neurologist explained.
The compelling case for early epilepsy surgery
Epilepsy surgery remains underutilized, according to Dr. Brodie and other experts.
The International League Against Epilepsy defines drug-resistant epilepsy as failure to achieve sustained seizure freedom after adequate trials of two tolerated and appropriately chosen and used AED schedules. Dr. Brodie’s work was influential in creating that definition because his data demonstrated the sharply diminishing returns of additional drug trials.
“When do we consider epilepsy surgery? Arguably, the earlier, the better. After two drugs have failed appropriately, I don’t think anybody in this room would argue about that, although people in some of the other rooms might,” he said at the congress.
Influential in his thinking on this score were the impressive results of an early study, the first-ever randomized trial of surgery for epilepsy. In 80 patients with a 21-year history of drug-refractory temporal lobe epilepsy who were randomized to surgery or 1 year of AED therapy, at 1 year of follow-up blinded epileptologists rated 58% of surgically treated patients as free from seizures that impair awareness of self and surroundings, compared with just 8% in the AED group (N Engl J Med. 2001 Aug 2;345[5]:311-8).
“That’s a big outcome, and I’m very keen to ensure that my data continue to drive the push for early surgery,” according to the neurologist.
A Cochrane review of 177 studies totaling more than 16,000 patients concluded that 65% of epilepsy patients had good outcomes following surgery. Prognostic factors associated with better surgical outcomes included complete surgical resection of the epileptogenic focus, the presence of mesial temporal sclerosis, concordance of MRI and EEG findings, and an absence of cortical dysplasia (Cochrane Database Syst Rev. 2019;6:CD010541. doi: 10.1002/14651858.CD010541.pub3).
In addition, a systematic review and meta-analysis by Canadian investigators found that 72% of adults with lesional epilepsy identified by MRI or histopathology were seizure-free after surgery, compared with 36% of those with nonlesional epilepsy. The disparity in outcomes was similar in pediatric epilepsy patients, with seizure freedom after surgery in 74% of those with lesional disease versus 45% with nonlesional epilepsy (Epilepsy Res. 2010 May;89[2-3]:310-8).
Whither are neurostimulatory device therapies headed?
Dr. Brodie was quick to admit that as a pharmacologic researcher, device modalities including vagus nerve stimulation, responsive neurostimulation, and deep brain stimulation are outside his area of expertise. But he’s been following developments in the field with interest.
“These device therapies have shown efficacy in short-term randomized trials, but very few patients attain long-term seizure freedom. I think these are largely palliative techniques. I gave up on these techniques a long time ago because I felt it was a very costly way of reducing seizures by a relatively small margin, and really we need to go a little bit further than that. But I know there’s a lot of work going on at the moment,” he said.
Dr. Brodie reported serving on the scientific advisory boards of more than a half dozen pharmaceutical companies.
BANGKOK – Since founding the Epilepsy Unit at Glasgow’s Western Infirmary 37 years ago, Martin J. Brodie, MD, has seen many changes in the field, including the introduction of more than a dozen new antiepileptic drugs (AEDs) in the past 2 decades.
And based upon this vast clinical experience coupled with his leadership of landmark studies, he has a message for his physician colleagues and their epilepsy patients. And it’s not pretty.
“Has the probability of achieving seizure freedom increased significantly in the last 3 decades? Regrettably, the answer is no,” he declared at the International Epilepsy Congress.
“Over all these years, in terms of seizure freedom there has been no real difference in outcome. There’s really quite a long way to go before we can say that we are doing all that well for people,” he said at the congress sponsored by the International League Against Epilepsy.
In the year 2000, he and his coinvestigators published a prospective, longitudinal, observational cohort study of 470 newly diagnosed patients with epilepsy treated at the Western Infirmary during 1982-1997, all with a minimum of 2 years’ follow-up. Sixty-one percent achieved complete freedom from seizures for at least 1 year on monotherapy, and another 3% did so on polytherapy, for a total rate of 64% (N Engl J Med. 2000 Feb 3;342[5]:314-19).
But these were patients who by and large were treated with older AEDs such as carbamazepine, which has since fallen by the wayside because of toxicities. Scottish neurologists now generally turn to lamotrigine (Lamictal), levetiracetam (Spritam), and other, newer AEDs. So Dr. Brodie and his coworkers recently published a follow-up study, this one featuring 30 years of longitudinal follow-up of 1,795 patients newly treated for epilepsy with AEDs, new and old, during 1982-2012. The investigators demonstrated that the seizure-free survival curves over time were virtually superimposable. In the larger, more recent study, remission was achieved in 55% of patients with AED monotherapy and in another 9% with polytherapy, for a total rate of 64%, identical to the rate in the 2000 study, and as was the case in the earlier study, 36% of patients remained uncontrolled (JAMA Neurol. 2018 Mar 1;75[3]:279-86).
“Overall, the way this population behaves, there’s no difference in efficacy and no difference in tolerability whether you’re using old drugs used properly or new drugs used properly,” said Dr. Brodie, professor of neurology at the University of Glasgow (Scotland).
It’s noteworthy that Sir William R. Gowers, the Londoner who has been called the greatest neurologist of all time, reported a 70% seizure-free rate in 1881, while Dr. Brodie and workers achieved a 64% rate in their 30-year study. “It’s interesting that the numbers are so bad, really, I suppose,” Dr. Brodie commented.
How about outcomes in pediatric epilepsy?
Dr. Brodie and coworkers recently published a 30-year prospective cohort study of 332 adolescent epilepsy patients newly diagnosed and treated at the Western Infirmary during 1982-2012. At the end of the study, 67% were seizure-free for at least the past year, a feat accomplished via monotherapy in 83% of cases. The seizure-free rate was 72% in those with generalized epilepsy, significantly better than the 60% figure in those with focal epilepsy. The efficacy rate was 74% with newer AED monotherapy and similar at 77% with monotherapy older drugs. Adverse event rates ranged from a low of 12% with lamotrigine to 56% with topiramate (Topamax), according to the findings published in Epilepsia (2019 Jun;60[6]:1083-90).
Roughly similar outcomes have been reported from Norway in a study of 600 children with epilepsy, median age 7 years, with a median follow-up of 5.8 years that is considerably shorter than that in the Glasgow pediatric study. Overall, 59% of the Norwegian children remained seizure free for at least 1 year, 30% developed drug-resistant epilepsy, and 11% followed an intermediate remitting/relapsing course (Pediatrics. 2018 Jun. doi: 10.1542/peds.2017-4016).
Why the decades of flat pharmacologic outcomes?
The consistently suboptimal seizure-free outcomes obtained over the past 30 years shouldn’t really be surprising, according to Dr. Brodie.
“Although we think we have lots of mechanisms of action and lots of differences between the drugs, they’re arguably all antiseizure drugs and not antiepilepsy drugs. We don’t treat the whale; we treat the spout. We don’t treat what we cannot see; we treat what we can see, which is the seizures, but we’re not influencing the long-term outcome,” the neurologist explained.
The compelling case for early epilepsy surgery
Epilepsy surgery remains underutilized, according to Dr. Brodie and other experts.
The International League Against Epilepsy defines drug-resistant epilepsy as failure to achieve sustained seizure freedom after adequate trials of two tolerated and appropriately chosen and used AED schedules. Dr. Brodie’s work was influential in creating that definition because his data demonstrated the sharply diminishing returns of additional drug trials.
“When do we consider epilepsy surgery? Arguably, the earlier, the better. After two drugs have failed appropriately, I don’t think anybody in this room would argue about that, although people in some of the other rooms might,” he said at the congress.
Influential in his thinking on this score were the impressive results of an early study, the first-ever randomized trial of surgery for epilepsy. In 80 patients with a 21-year history of drug-refractory temporal lobe epilepsy who were randomized to surgery or 1 year of AED therapy, at 1 year of follow-up blinded epileptologists rated 58% of surgically treated patients as free from seizures that impair awareness of self and surroundings, compared with just 8% in the AED group (N Engl J Med. 2001 Aug 2;345[5]:311-8).
“That’s a big outcome, and I’m very keen to ensure that my data continue to drive the push for early surgery,” according to the neurologist.
A Cochrane review of 177 studies totaling more than 16,000 patients concluded that 65% of epilepsy patients had good outcomes following surgery. Prognostic factors associated with better surgical outcomes included complete surgical resection of the epileptogenic focus, the presence of mesial temporal sclerosis, concordance of MRI and EEG findings, and an absence of cortical dysplasia (Cochrane Database Syst Rev. 2019;6:CD010541. doi: 10.1002/14651858.CD010541.pub3).
In addition, a systematic review and meta-analysis by Canadian investigators found that 72% of adults with lesional epilepsy identified by MRI or histopathology were seizure-free after surgery, compared with 36% of those with nonlesional epilepsy. The disparity in outcomes was similar in pediatric epilepsy patients, with seizure freedom after surgery in 74% of those with lesional disease versus 45% with nonlesional epilepsy (Epilepsy Res. 2010 May;89[2-3]:310-8).
Whither are neurostimulatory device therapies headed?
Dr. Brodie was quick to admit that as a pharmacologic researcher, device modalities including vagus nerve stimulation, responsive neurostimulation, and deep brain stimulation are outside his area of expertise. But he’s been following developments in the field with interest.
“These device therapies have shown efficacy in short-term randomized trials, but very few patients attain long-term seizure freedom. I think these are largely palliative techniques. I gave up on these techniques a long time ago because I felt it was a very costly way of reducing seizures by a relatively small margin, and really we need to go a little bit further than that. But I know there’s a lot of work going on at the moment,” he said.
Dr. Brodie reported serving on the scientific advisory boards of more than a half dozen pharmaceutical companies.
EXPERT ANALYSIS FROM IEC 2019
Seeing former patients’ graves at the cemetery gives perspective
Around once a month I go to the cemetery to visit my Dad. Although this was difficult 6 years ago when I started, it’s become easier thanks to that great healer, time.
His grave is a short distance from the parking spot, so I have to walk past a number of others to get there. As a result you see these change over time.
A few times in the last several years I’ve noticed a new grave marker that, to my surprise, has the name of one of my (former) patients on it. Granted, a lot of my practice is the above-75 crowd, and they wouldn’t be coming to me if they didn’t have health issues.
But still, it jolts me a bit when it happens. I may not have thought about them for a while, but suddenly I see the marker and realize why that person hadn’t been in recently. I can usually picture them, too, and remember something they may have said that concerned me or just made me laugh.
Obviously, regardless of age we all end up there, and I certainly don’t consider this a personal medical failing on my part. It’s the nature of life on Earth, no matter how good a job we do as physicians.
But it still surprises me. If it was a patient I have fond memories of, I’ll often stop and say a few words to them, too. To date no one has answered, but I suspect there’s something therapeutic for me in doing so. The cemetery is generally peaceful, and certainly not a place where I feel rushed.
Besides getting to talk to my Dad, the occasional patient visit there is a reminder of the limits of being a physician, and of our own lives. If nothing else it helps keep a perspective on those things, such as family and health, that are truly important.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Around once a month I go to the cemetery to visit my Dad. Although this was difficult 6 years ago when I started, it’s become easier thanks to that great healer, time.
His grave is a short distance from the parking spot, so I have to walk past a number of others to get there. As a result you see these change over time.
A few times in the last several years I’ve noticed a new grave marker that, to my surprise, has the name of one of my (former) patients on it. Granted, a lot of my practice is the above-75 crowd, and they wouldn’t be coming to me if they didn’t have health issues.
But still, it jolts me a bit when it happens. I may not have thought about them for a while, but suddenly I see the marker and realize why that person hadn’t been in recently. I can usually picture them, too, and remember something they may have said that concerned me or just made me laugh.
Obviously, regardless of age we all end up there, and I certainly don’t consider this a personal medical failing on my part. It’s the nature of life on Earth, no matter how good a job we do as physicians.
But it still surprises me. If it was a patient I have fond memories of, I’ll often stop and say a few words to them, too. To date no one has answered, but I suspect there’s something therapeutic for me in doing so. The cemetery is generally peaceful, and certainly not a place where I feel rushed.
Besides getting to talk to my Dad, the occasional patient visit there is a reminder of the limits of being a physician, and of our own lives. If nothing else it helps keep a perspective on those things, such as family and health, that are truly important.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Around once a month I go to the cemetery to visit my Dad. Although this was difficult 6 years ago when I started, it’s become easier thanks to that great healer, time.
His grave is a short distance from the parking spot, so I have to walk past a number of others to get there. As a result you see these change over time.
A few times in the last several years I’ve noticed a new grave marker that, to my surprise, has the name of one of my (former) patients on it. Granted, a lot of my practice is the above-75 crowd, and they wouldn’t be coming to me if they didn’t have health issues.
But still, it jolts me a bit when it happens. I may not have thought about them for a while, but suddenly I see the marker and realize why that person hadn’t been in recently. I can usually picture them, too, and remember something they may have said that concerned me or just made me laugh.
Obviously, regardless of age we all end up there, and I certainly don’t consider this a personal medical failing on my part. It’s the nature of life on Earth, no matter how good a job we do as physicians.
But it still surprises me. If it was a patient I have fond memories of, I’ll often stop and say a few words to them, too. To date no one has answered, but I suspect there’s something therapeutic for me in doing so. The cemetery is generally peaceful, and certainly not a place where I feel rushed.
Besides getting to talk to my Dad, the occasional patient visit there is a reminder of the limits of being a physician, and of our own lives. If nothing else it helps keep a perspective on those things, such as family and health, that are truly important.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Poll: Medicare-for-all sees slight drop in support
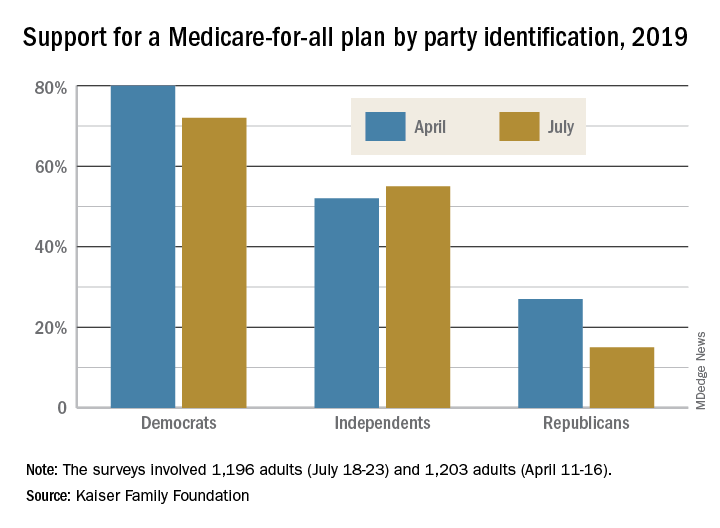
The two polls showed that Americans’ overall favorability for a national Medicare-for-all plan declined from 56% in April to 51% in July. That drop came from Democratic respondents, whose support went from 80% to 72%, and from Republicans, whose support declined from 27% to 15%. Overall favorability increased from 52% to 55% among independents, Kaiser reported in its latest Health Tracking Poll.
“The small dip in Medicare-for-all support may reflect recent debate over the role of private insurance, including employer-sponsored coverage, which would largely disappear under the leading Medicare-for-all plans but would continue under a public option,” Kaiser said in a statement accompanying the report.
When given a choice, 55% of Democrats and Democratic-leaning Independents (Republicans were not asked) would rather build on the existing Affordable Care Act, compared with 39% who want to replace it with Medicare-for-all, the Kaiser investigators said.
Support is currently greater for a public option that would give all residents the ability to choose a government-sponsored insurance plan. Almost two-thirds of those surveyed said that they favor such a proposal, with support at 85% for Democrats, 68% for independents, and 36% for Republicans, the report’s authors said.
The two polls were conducted among 1,196 adults during July 18-23, 2019, and 1,203 adults during April 11-16, 2019. The margin of sampling error for both polls was plus or minus 3 percentage points.
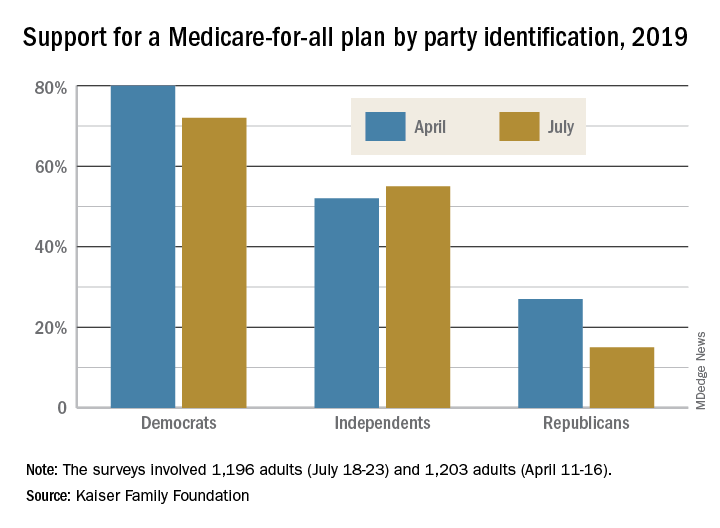
The two polls showed that Americans’ overall favorability for a national Medicare-for-all plan declined from 56% in April to 51% in July. That drop came from Democratic respondents, whose support went from 80% to 72%, and from Republicans, whose support declined from 27% to 15%. Overall favorability increased from 52% to 55% among independents, Kaiser reported in its latest Health Tracking Poll.
“The small dip in Medicare-for-all support may reflect recent debate over the role of private insurance, including employer-sponsored coverage, which would largely disappear under the leading Medicare-for-all plans but would continue under a public option,” Kaiser said in a statement accompanying the report.
When given a choice, 55% of Democrats and Democratic-leaning Independents (Republicans were not asked) would rather build on the existing Affordable Care Act, compared with 39% who want to replace it with Medicare-for-all, the Kaiser investigators said.
Support is currently greater for a public option that would give all residents the ability to choose a government-sponsored insurance plan. Almost two-thirds of those surveyed said that they favor such a proposal, with support at 85% for Democrats, 68% for independents, and 36% for Republicans, the report’s authors said.
The two polls were conducted among 1,196 adults during July 18-23, 2019, and 1,203 adults during April 11-16, 2019. The margin of sampling error for both polls was plus or minus 3 percentage points.
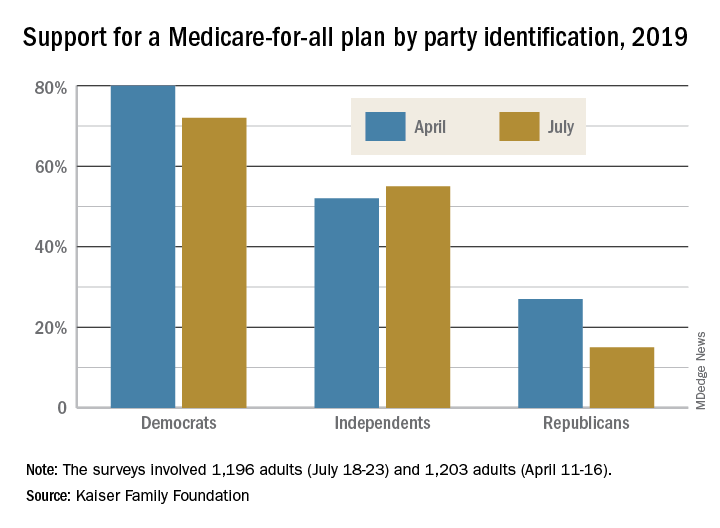
The two polls showed that Americans’ overall favorability for a national Medicare-for-all plan declined from 56% in April to 51% in July. That drop came from Democratic respondents, whose support went from 80% to 72%, and from Republicans, whose support declined from 27% to 15%. Overall favorability increased from 52% to 55% among independents, Kaiser reported in its latest Health Tracking Poll.
“The small dip in Medicare-for-all support may reflect recent debate over the role of private insurance, including employer-sponsored coverage, which would largely disappear under the leading Medicare-for-all plans but would continue under a public option,” Kaiser said in a statement accompanying the report.
When given a choice, 55% of Democrats and Democratic-leaning Independents (Republicans were not asked) would rather build on the existing Affordable Care Act, compared with 39% who want to replace it with Medicare-for-all, the Kaiser investigators said.
Support is currently greater for a public option that would give all residents the ability to choose a government-sponsored insurance plan. Almost two-thirds of those surveyed said that they favor such a proposal, with support at 85% for Democrats, 68% for independents, and 36% for Republicans, the report’s authors said.
The two polls were conducted among 1,196 adults during July 18-23, 2019, and 1,203 adults during April 11-16, 2019. The margin of sampling error for both polls was plus or minus 3 percentage points.
Posttraumatic headache may be associated with reduced pain thresholds
PHILADELPHIA – , according to results of a pilot study presented at the annual meeting of the American Headache Society. The findings suggest that patients with posttraumatic headache have abnormal, multimodal sensory processing, said Amaal J. Starling, MD, a neurologist at Mayo Clinic in Phoenix.
Mild traumatic brain injury (TBI) is a growing public health problem. Headache is the most common symptom after mild TBI, and often the most debilitating symptom for these patients. No Food and Drug Administration–approved treatments are available for patients with posttraumatic headache, and about three-quarters of these patients report that current treatments bring them no relief.
Identifying novel targets and developing new treatment options will require a deeper understanding of the pathophysiology of posttraumatic headache, said Dr. Starling. She and her colleagues conducted a pilot study to characterize allodynia, cutaneous heat pain thresholds, photophobia, and light-induced pain thresholds objectively in patients with posttraumatic headache, compared with healthy controls.
Participants were exposed to a bright-light stressor
The researchers enrolled 20 patients between ages 18 years and 65 years with posttraumatic headache attributed to mild TBI in their study. They matched these patients by age with 20 healthy controls. Dr. Starling and colleagues evaluated all participants prospectively using the Allodynia Symptom Checklist (ASC-12), Photosensitivity Assessment Questionnaire (PAQ), State-Trait Anxiety Inventory (STAI), and Beck Depression Inventory (BDI).
The investigators performed quantitative sensory testing to measure each participant’s cutaneous forearm heat pain threshold. Using a progressive light stimulation device, they quantified each participant’s light-induced pain threshold. Finally, Dr. Starling and colleagues obtained participants’ cutaneous heat pain thresholds immediately after, 10 minutes after, and 40 minutes after exposing them to a bright-light stressor.
The researchers found no significant differences between groups in age, gender, or race. The population’s average age was 41 years. Approximately 70% of the sample was female. Among participants with posttraumatic headache, the average time since the onset of posttraumatic headache was 46 months. The average number of headache days per month in that group was 17.2, which represented “a significantly high headache burden,” said Dr. Starling. Approximately 80% of patients with posttraumatic headache had headaches with a migraine phenotype.
Patients’ pain thresholds were lower
STAI and BDI scores were significantly higher among patients with posttraumatic headache, compared with controls. Mean PAQ score was 0.62 among patients and 0.24 among controls, representing significantly greater photophobia symptom severity among patients, said Dr. Starling.
Light-induced pain thresholds were significantly lower in patients with posttraumatic headache (median, 90.5 lux), compared with healthy controls (median, 863.5 lux), independent of depression and anxiety. Allodynia symptom severity was significantly higher in patients with posttraumatic headache (mean ASC-12 score, 5.7), compared with controls (mean ASC-12 score, 0.98).
In addition, the mean baseline cutaneous heat pain threshold was 40.8° C in patients with posttraumatic headache and 44.4° C in healthy controls. When participants were subjected to the bright-light stressor, the immediate change in heat pain threshold was significant in patients with posttraumatic headache (−1.9° C), compared with healthy controls. The difference between groups was not significant at 10 and 40 minutes after exposure to the stressor, however. The light intensity inducing moderate pain was 688 lux in patients with posttraumatic headache, compared with 6,000 lux in healthy controls.
“Our next steps are going to be replicating this [study] in a larger population, as well as determining whether any type of intervention would change these different types of sensory sensitivities and thresholds,” said Dr. Starling. She and her colleagues will use this human research model to examine whether posttraumatic headache differs from other headache disorders such as migraine and to examine potential differences between acute and persistent posttraumatic headache.
The study was funded through an intramural Mayo Clinic early career research award.
SOURCE: Starling AJ et al. AHS 2019. Abstract OR14.
PHILADELPHIA – , according to results of a pilot study presented at the annual meeting of the American Headache Society. The findings suggest that patients with posttraumatic headache have abnormal, multimodal sensory processing, said Amaal J. Starling, MD, a neurologist at Mayo Clinic in Phoenix.
Mild traumatic brain injury (TBI) is a growing public health problem. Headache is the most common symptom after mild TBI, and often the most debilitating symptom for these patients. No Food and Drug Administration–approved treatments are available for patients with posttraumatic headache, and about three-quarters of these patients report that current treatments bring them no relief.
Identifying novel targets and developing new treatment options will require a deeper understanding of the pathophysiology of posttraumatic headache, said Dr. Starling. She and her colleagues conducted a pilot study to characterize allodynia, cutaneous heat pain thresholds, photophobia, and light-induced pain thresholds objectively in patients with posttraumatic headache, compared with healthy controls.
Participants were exposed to a bright-light stressor
The researchers enrolled 20 patients between ages 18 years and 65 years with posttraumatic headache attributed to mild TBI in their study. They matched these patients by age with 20 healthy controls. Dr. Starling and colleagues evaluated all participants prospectively using the Allodynia Symptom Checklist (ASC-12), Photosensitivity Assessment Questionnaire (PAQ), State-Trait Anxiety Inventory (STAI), and Beck Depression Inventory (BDI).
The investigators performed quantitative sensory testing to measure each participant’s cutaneous forearm heat pain threshold. Using a progressive light stimulation device, they quantified each participant’s light-induced pain threshold. Finally, Dr. Starling and colleagues obtained participants’ cutaneous heat pain thresholds immediately after, 10 minutes after, and 40 minutes after exposing them to a bright-light stressor.
The researchers found no significant differences between groups in age, gender, or race. The population’s average age was 41 years. Approximately 70% of the sample was female. Among participants with posttraumatic headache, the average time since the onset of posttraumatic headache was 46 months. The average number of headache days per month in that group was 17.2, which represented “a significantly high headache burden,” said Dr. Starling. Approximately 80% of patients with posttraumatic headache had headaches with a migraine phenotype.
Patients’ pain thresholds were lower
STAI and BDI scores were significantly higher among patients with posttraumatic headache, compared with controls. Mean PAQ score was 0.62 among patients and 0.24 among controls, representing significantly greater photophobia symptom severity among patients, said Dr. Starling.
Light-induced pain thresholds were significantly lower in patients with posttraumatic headache (median, 90.5 lux), compared with healthy controls (median, 863.5 lux), independent of depression and anxiety. Allodynia symptom severity was significantly higher in patients with posttraumatic headache (mean ASC-12 score, 5.7), compared with controls (mean ASC-12 score, 0.98).
In addition, the mean baseline cutaneous heat pain threshold was 40.8° C in patients with posttraumatic headache and 44.4° C in healthy controls. When participants were subjected to the bright-light stressor, the immediate change in heat pain threshold was significant in patients with posttraumatic headache (−1.9° C), compared with healthy controls. The difference between groups was not significant at 10 and 40 minutes after exposure to the stressor, however. The light intensity inducing moderate pain was 688 lux in patients with posttraumatic headache, compared with 6,000 lux in healthy controls.
“Our next steps are going to be replicating this [study] in a larger population, as well as determining whether any type of intervention would change these different types of sensory sensitivities and thresholds,” said Dr. Starling. She and her colleagues will use this human research model to examine whether posttraumatic headache differs from other headache disorders such as migraine and to examine potential differences between acute and persistent posttraumatic headache.
The study was funded through an intramural Mayo Clinic early career research award.
SOURCE: Starling AJ et al. AHS 2019. Abstract OR14.
PHILADELPHIA – , according to results of a pilot study presented at the annual meeting of the American Headache Society. The findings suggest that patients with posttraumatic headache have abnormal, multimodal sensory processing, said Amaal J. Starling, MD, a neurologist at Mayo Clinic in Phoenix.
Mild traumatic brain injury (TBI) is a growing public health problem. Headache is the most common symptom after mild TBI, and often the most debilitating symptom for these patients. No Food and Drug Administration–approved treatments are available for patients with posttraumatic headache, and about three-quarters of these patients report that current treatments bring them no relief.
Identifying novel targets and developing new treatment options will require a deeper understanding of the pathophysiology of posttraumatic headache, said Dr. Starling. She and her colleagues conducted a pilot study to characterize allodynia, cutaneous heat pain thresholds, photophobia, and light-induced pain thresholds objectively in patients with posttraumatic headache, compared with healthy controls.
Participants were exposed to a bright-light stressor
The researchers enrolled 20 patients between ages 18 years and 65 years with posttraumatic headache attributed to mild TBI in their study. They matched these patients by age with 20 healthy controls. Dr. Starling and colleagues evaluated all participants prospectively using the Allodynia Symptom Checklist (ASC-12), Photosensitivity Assessment Questionnaire (PAQ), State-Trait Anxiety Inventory (STAI), and Beck Depression Inventory (BDI).
The investigators performed quantitative sensory testing to measure each participant’s cutaneous forearm heat pain threshold. Using a progressive light stimulation device, they quantified each participant’s light-induced pain threshold. Finally, Dr. Starling and colleagues obtained participants’ cutaneous heat pain thresholds immediately after, 10 minutes after, and 40 minutes after exposing them to a bright-light stressor.
The researchers found no significant differences between groups in age, gender, or race. The population’s average age was 41 years. Approximately 70% of the sample was female. Among participants with posttraumatic headache, the average time since the onset of posttraumatic headache was 46 months. The average number of headache days per month in that group was 17.2, which represented “a significantly high headache burden,” said Dr. Starling. Approximately 80% of patients with posttraumatic headache had headaches with a migraine phenotype.
Patients’ pain thresholds were lower
STAI and BDI scores were significantly higher among patients with posttraumatic headache, compared with controls. Mean PAQ score was 0.62 among patients and 0.24 among controls, representing significantly greater photophobia symptom severity among patients, said Dr. Starling.
Light-induced pain thresholds were significantly lower in patients with posttraumatic headache (median, 90.5 lux), compared with healthy controls (median, 863.5 lux), independent of depression and anxiety. Allodynia symptom severity was significantly higher in patients with posttraumatic headache (mean ASC-12 score, 5.7), compared with controls (mean ASC-12 score, 0.98).
In addition, the mean baseline cutaneous heat pain threshold was 40.8° C in patients with posttraumatic headache and 44.4° C in healthy controls. When participants were subjected to the bright-light stressor, the immediate change in heat pain threshold was significant in patients with posttraumatic headache (−1.9° C), compared with healthy controls. The difference between groups was not significant at 10 and 40 minutes after exposure to the stressor, however. The light intensity inducing moderate pain was 688 lux in patients with posttraumatic headache, compared with 6,000 lux in healthy controls.
“Our next steps are going to be replicating this [study] in a larger population, as well as determining whether any type of intervention would change these different types of sensory sensitivities and thresholds,” said Dr. Starling. She and her colleagues will use this human research model to examine whether posttraumatic headache differs from other headache disorders such as migraine and to examine potential differences between acute and persistent posttraumatic headache.
The study was funded through an intramural Mayo Clinic early career research award.
SOURCE: Starling AJ et al. AHS 2019. Abstract OR14.
REPORTING FROM AHS 2019














