User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Bad sleep cuts years off life, but exercise can save us
Experts recommend that most adults get 7-9 hours of sleep a night.
Plenty of research points to sleep and physical activity as crucial factors affecting life expectancy. Regular exercise can lengthen life, while too little or too much sleep may cut it short.
But evidence is growing that exercise may counteract the negative effects of poor sleep. A 2022 study found that being physically active for at least 25 minutes a day can erase the risk of early death associated with too much sleep or trouble falling asleep. And a 2021 study found that lower levels of physical activity may exacerbate the impact of poor sleep on early death, heart disease, and cancer.
The latest such study, published in the European Journal of Preventive Cardiology, suggests that higher volumes of exercise can virtually eliminate the risk of early death associated with sleeping too little or too long.
This study is unique, the researchers say, because it used accelerometers (motion-tracking sensors) to quantify sleep and physical activity. Other studies asked participants to report their own data, opening the door to false reports and mistakes.
Some 92,000 participants in the United Kingdom (mean age, 62 years; 56% women) wore the activity trackers for a week to measure how much they moved and slept. In the following 7 years, 3,080 participants died, mostly from cardiovascular disease or cancer.
As one might expect, the participants who were least likely to die also exercised the most and slept the “normal” amount (6-8 hours a night, as defined by the study).
Compared with that group, those who exercised the least and slept less than 6 hours were 2.5 times more likely to die during those 7 years (P < .001). Less active persons who got the recommended sleep were 79% more likely to die (P < .001). The risk was slightly higher than that for those who logged more than 8 hours a night.
But those risks disappeared for short- or long-sleeping participants who logged at least 150 minutes a week of moderate to vigorous activity.
“Exercise fights inflammatory and metabolic dysregulations and abnormal sympathetic nervous system activity,” said study author Jihui Zhang, PhD, of the Affiliated Brain Hospital of Guangzhou (China). Those problems are associated with cardiovascular diseases and other potentially fatal conditions.
More objective data – with tech
A study’s findings are only as good as the data it relies on. That’s why obtaining objective data not influenced by individual perception is key.
“Self-report questionnaires are prone to misperception, or recall or response bias,” Dr. Zhang explains.
Take sleep, for example. Research reveals that several factors can affect how we judge our sleep. When people have to sleep at irregular times, they often underestimate how many hours they sleep but overestimate how long they nap, found a study in the Journal of Clinical Sleep Medicine.
Another study showed that when people are under a lot of stress, they’ll report more sleep problems than they actually have, as revealed by an Actiheart monitor.
With exercise, participants often report doing more exercise, and doing it at a higher intensity, than objective measurements show they did. At the same time, self-reports typically don’t account for much of the unplanned, low-effort movement people do throughout the day.
Staying active when you’re tired
The study raises a practical question: If you don’t get the proper amount of sleep, how are you supposed to find the time, energy, and motivation to exercise?
The solution is to use one to fix the other.
Exercise and sleep have “a robust directional relationship,” Dr. Zhang said. Exercise improves sleep, while better sleep makes it easier to stick with an exercise program.
Ideally, that program will include a mix of cardio and resistance exercise, said Mitch Duncan, PhD, a professor of public health at the University of Newcastle, Australia.
As Dr. Duncan and his co-authors showed in a recent study, “the largest benefits to health occur when people do a combination of both aerobic and muscle-strengthening activity,” Dr. Duncan said.
“In terms of benefits to sleep, there doesn’t seem to be consistent evidence that favors either as being most effective.”
The timing or intensity of exercise doesn’t seem to matter much, either.
“But there is evidence that a greater duration contributes to larger improvements in sleep,” Dr. Duncan said.
In other words, longer workouts are generally better, but they don’t necessarily have to be super-intense.
The strongest evidence of all, however, shows that recent and regular exercise offer the biggest benefits at bedtime.
Today’s workout will improve tonight’s sleep. And the better you sleep tonight, the more likely you are to stick with the program.
A version of this article first appeared on WebMD.com.
Experts recommend that most adults get 7-9 hours of sleep a night.
Plenty of research points to sleep and physical activity as crucial factors affecting life expectancy. Regular exercise can lengthen life, while too little or too much sleep may cut it short.
But evidence is growing that exercise may counteract the negative effects of poor sleep. A 2022 study found that being physically active for at least 25 minutes a day can erase the risk of early death associated with too much sleep or trouble falling asleep. And a 2021 study found that lower levels of physical activity may exacerbate the impact of poor sleep on early death, heart disease, and cancer.
The latest such study, published in the European Journal of Preventive Cardiology, suggests that higher volumes of exercise can virtually eliminate the risk of early death associated with sleeping too little or too long.
This study is unique, the researchers say, because it used accelerometers (motion-tracking sensors) to quantify sleep and physical activity. Other studies asked participants to report their own data, opening the door to false reports and mistakes.
Some 92,000 participants in the United Kingdom (mean age, 62 years; 56% women) wore the activity trackers for a week to measure how much they moved and slept. In the following 7 years, 3,080 participants died, mostly from cardiovascular disease or cancer.
As one might expect, the participants who were least likely to die also exercised the most and slept the “normal” amount (6-8 hours a night, as defined by the study).
Compared with that group, those who exercised the least and slept less than 6 hours were 2.5 times more likely to die during those 7 years (P < .001). Less active persons who got the recommended sleep were 79% more likely to die (P < .001). The risk was slightly higher than that for those who logged more than 8 hours a night.
But those risks disappeared for short- or long-sleeping participants who logged at least 150 minutes a week of moderate to vigorous activity.
“Exercise fights inflammatory and metabolic dysregulations and abnormal sympathetic nervous system activity,” said study author Jihui Zhang, PhD, of the Affiliated Brain Hospital of Guangzhou (China). Those problems are associated with cardiovascular diseases and other potentially fatal conditions.
More objective data – with tech
A study’s findings are only as good as the data it relies on. That’s why obtaining objective data not influenced by individual perception is key.
“Self-report questionnaires are prone to misperception, or recall or response bias,” Dr. Zhang explains.
Take sleep, for example. Research reveals that several factors can affect how we judge our sleep. When people have to sleep at irregular times, they often underestimate how many hours they sleep but overestimate how long they nap, found a study in the Journal of Clinical Sleep Medicine.
Another study showed that when people are under a lot of stress, they’ll report more sleep problems than they actually have, as revealed by an Actiheart monitor.
With exercise, participants often report doing more exercise, and doing it at a higher intensity, than objective measurements show they did. At the same time, self-reports typically don’t account for much of the unplanned, low-effort movement people do throughout the day.
Staying active when you’re tired
The study raises a practical question: If you don’t get the proper amount of sleep, how are you supposed to find the time, energy, and motivation to exercise?
The solution is to use one to fix the other.
Exercise and sleep have “a robust directional relationship,” Dr. Zhang said. Exercise improves sleep, while better sleep makes it easier to stick with an exercise program.
Ideally, that program will include a mix of cardio and resistance exercise, said Mitch Duncan, PhD, a professor of public health at the University of Newcastle, Australia.
As Dr. Duncan and his co-authors showed in a recent study, “the largest benefits to health occur when people do a combination of both aerobic and muscle-strengthening activity,” Dr. Duncan said.
“In terms of benefits to sleep, there doesn’t seem to be consistent evidence that favors either as being most effective.”
The timing or intensity of exercise doesn’t seem to matter much, either.
“But there is evidence that a greater duration contributes to larger improvements in sleep,” Dr. Duncan said.
In other words, longer workouts are generally better, but they don’t necessarily have to be super-intense.
The strongest evidence of all, however, shows that recent and regular exercise offer the biggest benefits at bedtime.
Today’s workout will improve tonight’s sleep. And the better you sleep tonight, the more likely you are to stick with the program.
A version of this article first appeared on WebMD.com.
Experts recommend that most adults get 7-9 hours of sleep a night.
Plenty of research points to sleep and physical activity as crucial factors affecting life expectancy. Regular exercise can lengthen life, while too little or too much sleep may cut it short.
But evidence is growing that exercise may counteract the negative effects of poor sleep. A 2022 study found that being physically active for at least 25 minutes a day can erase the risk of early death associated with too much sleep or trouble falling asleep. And a 2021 study found that lower levels of physical activity may exacerbate the impact of poor sleep on early death, heart disease, and cancer.
The latest such study, published in the European Journal of Preventive Cardiology, suggests that higher volumes of exercise can virtually eliminate the risk of early death associated with sleeping too little or too long.
This study is unique, the researchers say, because it used accelerometers (motion-tracking sensors) to quantify sleep and physical activity. Other studies asked participants to report their own data, opening the door to false reports and mistakes.
Some 92,000 participants in the United Kingdom (mean age, 62 years; 56% women) wore the activity trackers for a week to measure how much they moved and slept. In the following 7 years, 3,080 participants died, mostly from cardiovascular disease or cancer.
As one might expect, the participants who were least likely to die also exercised the most and slept the “normal” amount (6-8 hours a night, as defined by the study).
Compared with that group, those who exercised the least and slept less than 6 hours were 2.5 times more likely to die during those 7 years (P < .001). Less active persons who got the recommended sleep were 79% more likely to die (P < .001). The risk was slightly higher than that for those who logged more than 8 hours a night.
But those risks disappeared for short- or long-sleeping participants who logged at least 150 minutes a week of moderate to vigorous activity.
“Exercise fights inflammatory and metabolic dysregulations and abnormal sympathetic nervous system activity,” said study author Jihui Zhang, PhD, of the Affiliated Brain Hospital of Guangzhou (China). Those problems are associated with cardiovascular diseases and other potentially fatal conditions.
More objective data – with tech
A study’s findings are only as good as the data it relies on. That’s why obtaining objective data not influenced by individual perception is key.
“Self-report questionnaires are prone to misperception, or recall or response bias,” Dr. Zhang explains.
Take sleep, for example. Research reveals that several factors can affect how we judge our sleep. When people have to sleep at irregular times, they often underestimate how many hours they sleep but overestimate how long they nap, found a study in the Journal of Clinical Sleep Medicine.
Another study showed that when people are under a lot of stress, they’ll report more sleep problems than they actually have, as revealed by an Actiheart monitor.
With exercise, participants often report doing more exercise, and doing it at a higher intensity, than objective measurements show they did. At the same time, self-reports typically don’t account for much of the unplanned, low-effort movement people do throughout the day.
Staying active when you’re tired
The study raises a practical question: If you don’t get the proper amount of sleep, how are you supposed to find the time, energy, and motivation to exercise?
The solution is to use one to fix the other.
Exercise and sleep have “a robust directional relationship,” Dr. Zhang said. Exercise improves sleep, while better sleep makes it easier to stick with an exercise program.
Ideally, that program will include a mix of cardio and resistance exercise, said Mitch Duncan, PhD, a professor of public health at the University of Newcastle, Australia.
As Dr. Duncan and his co-authors showed in a recent study, “the largest benefits to health occur when people do a combination of both aerobic and muscle-strengthening activity,” Dr. Duncan said.
“In terms of benefits to sleep, there doesn’t seem to be consistent evidence that favors either as being most effective.”
The timing or intensity of exercise doesn’t seem to matter much, either.
“But there is evidence that a greater duration contributes to larger improvements in sleep,” Dr. Duncan said.
In other words, longer workouts are generally better, but they don’t necessarily have to be super-intense.
The strongest evidence of all, however, shows that recent and regular exercise offer the biggest benefits at bedtime.
Today’s workout will improve tonight’s sleep. And the better you sleep tonight, the more likely you are to stick with the program.
A version of this article first appeared on WebMD.com.
FROM EUROPEAN JOURNAL OF PREVENTIVE CARDIOLOGY
Single-dose psilocybin promising for resistant depression
PARIS –
Known as COMP360, the synthetic agent, a proprietary, purified form of psilocybin, improved symptoms related to mood and anhedonia while leaving aspects such as appetite and weight changes unaffected, reported investigators led by Guy M. Goodwin, PhD, emeritus professor of psychiatry, University of Oxford, England, and chief medical officer, COMPASS Pathways.
The study was presented at the European Psychiatric Association (EPA) 2023 Congress.
100 million affected
Affecting up to 100 million people globally, TRD is “not an official diagnosis,” although it is often defined as the failure to elicit a response with at least two antidepressant treatments, said Dr. Goodwin.
Compared to their counterparts with non-TRD, those with TRD experience higher relapse rates, higher rates of suicidal behavior, and more residual symptoms even when they do respond to treatment.
Previous results from the study known as P-TRD indicated that a single 25-mg dose of COMP360 significantly reduced depression scores for up to 12 weeks when given along with psychological support, although a later analysis suggested the effect subsequently dropped off.
The vast majority of the patients in the trial were naive to psychedelics, and so, Dr. Goodwin explained, they undergo a preparation phase during which they receive psychoeducation and have at least two visits with a therapist, who then stays with them during administration of the drug to offer support if they experience psychological distress.
Following the psilocybin session, participants go through a process known as integration, which involves two sessions with a therapist within 2 weeks.
“That, in our view, is essentially about safety, and about identifying problems that have arisen as a result of taking the drug,” said Dr. Goodwin.
The phase 2b trial examined changes in specific depression symptoms after psilocybin treatment in 233 patients with TRD. Participants were a mean age of 39.8 years and 59% were women. They were randomized to receive one of three doses of the drug: a 1-mg dose (n = 79), a 10-mg dose (n = 75), or a 25-mg dose (n = 79).
The primary outcome was changes in individual items on the Montgomery-Åsberg Depression Rating Scale (MADRS) and 16-item Quick Inventory of Depressive Symptomatology–Self Report (QIDS-SR-16) scale.
While the effect on overall depression scores is important, said Dr. Goodwin, many of the items included in the depression assessment scales are “uninformative.”
Reduction in ‘core’ symptoms
Participants were assessed by a blinded rater at baseline, day 1, day 2, and at 1, 2, 3, 6, 9, and 12 weeks after administration of COMP360. The primary endpoint was a reduction in individual items on MADRS and scores from baseline to 3 weeks. Individual items on the QIDS-SR-16 were rated by participants at the same time points.
Investigators found the largest mean changes from baseline were on reported and apparent sadness, lassitude, inability to feel, and concentration difficulties, with “very nice and clear dose-related differences,” Dr. Goodwin said.
The results indicate that the significant benefit with the largest dose at 3 weeks versus baseline was confined to items such as inability to feel and reported and apparent sadness on the MADRS and feeling sad and general interest on the QIDS-SR-16 (Table 1).
The results suggest the effect of COMP360 is “on the core symptoms of depression,” said Dr. Goodwin.
Results were similar for individual items on the QIDS-SR-16, with the greatest changes in items including feeling sad, general interest, energy level, falling asleep, view of myself, concentration/decision-making, and feeling down.
Other scale items, such as decreased appetite, feel restless, and weight changes, showed negligible changes in response to COMP360 therapy and were described by Dr. Goodwin as “inconsequential.”
“Essentially, these items are contributing nothing but noise to the signal,” he said.
He added the results of the study need to be replicated and that plans for phase 3 trials are underway. These studies, he said, are designed to convince the Food and Drug Administration that “this is not just a recreational drug, it’s a medicine.”
Enthusiasm running ahead of the data
Commenting on the findings, Bertha K. Madras, PhD, professor of psychobiology, department of psychiatry, Harvard Medical School, Boston, who was not involved in the study, said “hallucinogens are an intriguing class of drugs and I support ongoing high-quality research in this area.”
However, she told this news organization that the “breathtaking endorsement of this drug is far ahead of scientific data.”
She cited concerns such as the “narrow demographics” of participants, their previous experience with and expectations of hallucinogens, the “potential for symptom fluidity of enrollees,” such as depression evolving into psychosis, and the “undefined role” of the therapist during a hallucinogenic session.
“Finally, I am concerned that enthusiasm for therapeutic potential has been, and will continue to be, preempted and directed towards legalization and widespread access for vulnerable populations,” Dr. Madras said.
This, she said, “is occurring at breakneck speed in the U.S., with scant resistance or skepticism from the investigators engaged in therapeutic assessment.”
The study was funded by COMPASS Pathways. Dr. Goodwin has reported relationships with COMPASS Pathways, Buckley Psytech, Boehringer Ingelheim, Clerkenwell Health, EVA Pharma, Lundbeck, Janssen Global Services, Novartis, Ocean Neurosciences, P1vital, Sage Therapeutics, Servier, Takeda, and WebMD.
A version of this article first appeared on Medscape.com.
PARIS –
Known as COMP360, the synthetic agent, a proprietary, purified form of psilocybin, improved symptoms related to mood and anhedonia while leaving aspects such as appetite and weight changes unaffected, reported investigators led by Guy M. Goodwin, PhD, emeritus professor of psychiatry, University of Oxford, England, and chief medical officer, COMPASS Pathways.
The study was presented at the European Psychiatric Association (EPA) 2023 Congress.
100 million affected
Affecting up to 100 million people globally, TRD is “not an official diagnosis,” although it is often defined as the failure to elicit a response with at least two antidepressant treatments, said Dr. Goodwin.
Compared to their counterparts with non-TRD, those with TRD experience higher relapse rates, higher rates of suicidal behavior, and more residual symptoms even when they do respond to treatment.
Previous results from the study known as P-TRD indicated that a single 25-mg dose of COMP360 significantly reduced depression scores for up to 12 weeks when given along with psychological support, although a later analysis suggested the effect subsequently dropped off.
The vast majority of the patients in the trial were naive to psychedelics, and so, Dr. Goodwin explained, they undergo a preparation phase during which they receive psychoeducation and have at least two visits with a therapist, who then stays with them during administration of the drug to offer support if they experience psychological distress.
Following the psilocybin session, participants go through a process known as integration, which involves two sessions with a therapist within 2 weeks.
“That, in our view, is essentially about safety, and about identifying problems that have arisen as a result of taking the drug,” said Dr. Goodwin.
The phase 2b trial examined changes in specific depression symptoms after psilocybin treatment in 233 patients with TRD. Participants were a mean age of 39.8 years and 59% were women. They were randomized to receive one of three doses of the drug: a 1-mg dose (n = 79), a 10-mg dose (n = 75), or a 25-mg dose (n = 79).
The primary outcome was changes in individual items on the Montgomery-Åsberg Depression Rating Scale (MADRS) and 16-item Quick Inventory of Depressive Symptomatology–Self Report (QIDS-SR-16) scale.
While the effect on overall depression scores is important, said Dr. Goodwin, many of the items included in the depression assessment scales are “uninformative.”
Reduction in ‘core’ symptoms
Participants were assessed by a blinded rater at baseline, day 1, day 2, and at 1, 2, 3, 6, 9, and 12 weeks after administration of COMP360. The primary endpoint was a reduction in individual items on MADRS and scores from baseline to 3 weeks. Individual items on the QIDS-SR-16 were rated by participants at the same time points.
Investigators found the largest mean changes from baseline were on reported and apparent sadness, lassitude, inability to feel, and concentration difficulties, with “very nice and clear dose-related differences,” Dr. Goodwin said.
The results indicate that the significant benefit with the largest dose at 3 weeks versus baseline was confined to items such as inability to feel and reported and apparent sadness on the MADRS and feeling sad and general interest on the QIDS-SR-16 (Table 1).
The results suggest the effect of COMP360 is “on the core symptoms of depression,” said Dr. Goodwin.
Results were similar for individual items on the QIDS-SR-16, with the greatest changes in items including feeling sad, general interest, energy level, falling asleep, view of myself, concentration/decision-making, and feeling down.
Other scale items, such as decreased appetite, feel restless, and weight changes, showed negligible changes in response to COMP360 therapy and were described by Dr. Goodwin as “inconsequential.”
“Essentially, these items are contributing nothing but noise to the signal,” he said.
He added the results of the study need to be replicated and that plans for phase 3 trials are underway. These studies, he said, are designed to convince the Food and Drug Administration that “this is not just a recreational drug, it’s a medicine.”
Enthusiasm running ahead of the data
Commenting on the findings, Bertha K. Madras, PhD, professor of psychobiology, department of psychiatry, Harvard Medical School, Boston, who was not involved in the study, said “hallucinogens are an intriguing class of drugs and I support ongoing high-quality research in this area.”
However, she told this news organization that the “breathtaking endorsement of this drug is far ahead of scientific data.”
She cited concerns such as the “narrow demographics” of participants, their previous experience with and expectations of hallucinogens, the “potential for symptom fluidity of enrollees,” such as depression evolving into psychosis, and the “undefined role” of the therapist during a hallucinogenic session.
“Finally, I am concerned that enthusiasm for therapeutic potential has been, and will continue to be, preempted and directed towards legalization and widespread access for vulnerable populations,” Dr. Madras said.
This, she said, “is occurring at breakneck speed in the U.S., with scant resistance or skepticism from the investigators engaged in therapeutic assessment.”
The study was funded by COMPASS Pathways. Dr. Goodwin has reported relationships with COMPASS Pathways, Buckley Psytech, Boehringer Ingelheim, Clerkenwell Health, EVA Pharma, Lundbeck, Janssen Global Services, Novartis, Ocean Neurosciences, P1vital, Sage Therapeutics, Servier, Takeda, and WebMD.
A version of this article first appeared on Medscape.com.
PARIS –
Known as COMP360, the synthetic agent, a proprietary, purified form of psilocybin, improved symptoms related to mood and anhedonia while leaving aspects such as appetite and weight changes unaffected, reported investigators led by Guy M. Goodwin, PhD, emeritus professor of psychiatry, University of Oxford, England, and chief medical officer, COMPASS Pathways.
The study was presented at the European Psychiatric Association (EPA) 2023 Congress.
100 million affected
Affecting up to 100 million people globally, TRD is “not an official diagnosis,” although it is often defined as the failure to elicit a response with at least two antidepressant treatments, said Dr. Goodwin.
Compared to their counterparts with non-TRD, those with TRD experience higher relapse rates, higher rates of suicidal behavior, and more residual symptoms even when they do respond to treatment.
Previous results from the study known as P-TRD indicated that a single 25-mg dose of COMP360 significantly reduced depression scores for up to 12 weeks when given along with psychological support, although a later analysis suggested the effect subsequently dropped off.
The vast majority of the patients in the trial were naive to psychedelics, and so, Dr. Goodwin explained, they undergo a preparation phase during which they receive psychoeducation and have at least two visits with a therapist, who then stays with them during administration of the drug to offer support if they experience psychological distress.
Following the psilocybin session, participants go through a process known as integration, which involves two sessions with a therapist within 2 weeks.
“That, in our view, is essentially about safety, and about identifying problems that have arisen as a result of taking the drug,” said Dr. Goodwin.
The phase 2b trial examined changes in specific depression symptoms after psilocybin treatment in 233 patients with TRD. Participants were a mean age of 39.8 years and 59% were women. They were randomized to receive one of three doses of the drug: a 1-mg dose (n = 79), a 10-mg dose (n = 75), or a 25-mg dose (n = 79).
The primary outcome was changes in individual items on the Montgomery-Åsberg Depression Rating Scale (MADRS) and 16-item Quick Inventory of Depressive Symptomatology–Self Report (QIDS-SR-16) scale.
While the effect on overall depression scores is important, said Dr. Goodwin, many of the items included in the depression assessment scales are “uninformative.”
Reduction in ‘core’ symptoms
Participants were assessed by a blinded rater at baseline, day 1, day 2, and at 1, 2, 3, 6, 9, and 12 weeks after administration of COMP360. The primary endpoint was a reduction in individual items on MADRS and scores from baseline to 3 weeks. Individual items on the QIDS-SR-16 were rated by participants at the same time points.
Investigators found the largest mean changes from baseline were on reported and apparent sadness, lassitude, inability to feel, and concentration difficulties, with “very nice and clear dose-related differences,” Dr. Goodwin said.
The results indicate that the significant benefit with the largest dose at 3 weeks versus baseline was confined to items such as inability to feel and reported and apparent sadness on the MADRS and feeling sad and general interest on the QIDS-SR-16 (Table 1).
The results suggest the effect of COMP360 is “on the core symptoms of depression,” said Dr. Goodwin.
Results were similar for individual items on the QIDS-SR-16, with the greatest changes in items including feeling sad, general interest, energy level, falling asleep, view of myself, concentration/decision-making, and feeling down.
Other scale items, such as decreased appetite, feel restless, and weight changes, showed negligible changes in response to COMP360 therapy and were described by Dr. Goodwin as “inconsequential.”
“Essentially, these items are contributing nothing but noise to the signal,” he said.
He added the results of the study need to be replicated and that plans for phase 3 trials are underway. These studies, he said, are designed to convince the Food and Drug Administration that “this is not just a recreational drug, it’s a medicine.”
Enthusiasm running ahead of the data
Commenting on the findings, Bertha K. Madras, PhD, professor of psychobiology, department of psychiatry, Harvard Medical School, Boston, who was not involved in the study, said “hallucinogens are an intriguing class of drugs and I support ongoing high-quality research in this area.”
However, she told this news organization that the “breathtaking endorsement of this drug is far ahead of scientific data.”
She cited concerns such as the “narrow demographics” of participants, their previous experience with and expectations of hallucinogens, the “potential for symptom fluidity of enrollees,” such as depression evolving into psychosis, and the “undefined role” of the therapist during a hallucinogenic session.
“Finally, I am concerned that enthusiasm for therapeutic potential has been, and will continue to be, preempted and directed towards legalization and widespread access for vulnerable populations,” Dr. Madras said.
This, she said, “is occurring at breakneck speed in the U.S., with scant resistance or skepticism from the investigators engaged in therapeutic assessment.”
The study was funded by COMPASS Pathways. Dr. Goodwin has reported relationships with COMPASS Pathways, Buckley Psytech, Boehringer Ingelheim, Clerkenwell Health, EVA Pharma, Lundbeck, Janssen Global Services, Novartis, Ocean Neurosciences, P1vital, Sage Therapeutics, Servier, Takeda, and WebMD.
A version of this article first appeared on Medscape.com.
AT EPA 2023
Seven ‘simple’ cardiovascular health measures linked to reduced dementia risk in women
according to results of a study that was released early, ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology.
Epidemiologist Pamela M. Rist, ScD, assistant professor of medicine at Harvard Medical School and associate epidemiologist at Brigham and Women’s Hospital, both in Boston, and colleagues, used data from 13,720 women whose mean age was 54 when they enrolled in the Harvard-based Women’s Health Study between 1992 and 1995. Subjects in that study were followed up in 2004.
Putting ‘Life’s Simple 7’ to the test
Dr. Rist and colleagues used the Harvard data to discern how well closely women conformed, during the initial study period and at 10-year follow up, to what the American Heart Association describes as “Life’s Simple 7,” a list of behavioral and biometric measures that indicate and predict cardiovascular health. The measures include four modifiable behaviors – not smoking, healthy weight, a healthy diet, and being physically active – along with three biometric measures of blood pressure, cholesterol, and blood sugar (AHA has since added a sleep component).
Researchers assigned women one point for each desirable habit or measure on the list, with subjects’ average Simple 7 score at baseline 4.3, and 4.2 at 10 years’ follow-up.
The investigators then looked at Medicare data for the study subjects from 2011 to 2018 – approximately 20 years after their enrollment in the Women’s Health Study – seeking dementia diagnoses. Some 13% of the study cohort (n = 1,771) had gone on to develop dementia.
Each point on the Simple 7 score at baseline corresponded with a 6% reduction in later dementia risk, Dr. Rist and her colleagues found after adjusting for variables including age and education (odds ratio per one unit change in score, 0.94; 95% CI, 0.90-0.98). This effect was similar for Simple 7 scores measured at 10 years of follow-up (OR, 0.95; 95% CI, 0.91-1.00).
“It can be empowering for people to know that by taking steps such as exercising for a half an hour a day or keeping their blood pressure under control, they can reduce their risk of dementia,” Dr. Rist said in a statement on the findings.
‘A simple take-home message’
Reached for comment, Andrew E. Budson, MD, chief of cognitive-behavioral neurology at the VA Boston Healthcare System, praised Dr. Rist and colleagues’ study as one that “builds on existing knowledge to provide a simple take-home message that empowers women to take control of their dementia risk.”
Each of the seven known risk factors – being active, eating better, maintaining a healthy weight, not smoking, maintaining a healthy blood pressure, controlling cholesterol, and having low blood sugar – “was associated with a 6% reduced risk of dementia,” Dr. Budson continued. “So, women who work to address all seven risk factors can reduce their risk of developing dementia by 42%: a huge amount. Moreover, although this study only looked at women, I am confident that if men follow this same advice they will also be able to reduce their risk of dementia, although we don’t know if the size of the effect will be the same.”
Dr. Rist and colleagues’ study was supported by the National Institutes of Health. None of the study authors reported conflicts of interest. Dr. Budson has reported receiving past compensation as a speaker for Eli Lilly.
according to results of a study that was released early, ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology.
Epidemiologist Pamela M. Rist, ScD, assistant professor of medicine at Harvard Medical School and associate epidemiologist at Brigham and Women’s Hospital, both in Boston, and colleagues, used data from 13,720 women whose mean age was 54 when they enrolled in the Harvard-based Women’s Health Study between 1992 and 1995. Subjects in that study were followed up in 2004.
Putting ‘Life’s Simple 7’ to the test
Dr. Rist and colleagues used the Harvard data to discern how well closely women conformed, during the initial study period and at 10-year follow up, to what the American Heart Association describes as “Life’s Simple 7,” a list of behavioral and biometric measures that indicate and predict cardiovascular health. The measures include four modifiable behaviors – not smoking, healthy weight, a healthy diet, and being physically active – along with three biometric measures of blood pressure, cholesterol, and blood sugar (AHA has since added a sleep component).
Researchers assigned women one point for each desirable habit or measure on the list, with subjects’ average Simple 7 score at baseline 4.3, and 4.2 at 10 years’ follow-up.
The investigators then looked at Medicare data for the study subjects from 2011 to 2018 – approximately 20 years after their enrollment in the Women’s Health Study – seeking dementia diagnoses. Some 13% of the study cohort (n = 1,771) had gone on to develop dementia.
Each point on the Simple 7 score at baseline corresponded with a 6% reduction in later dementia risk, Dr. Rist and her colleagues found after adjusting for variables including age and education (odds ratio per one unit change in score, 0.94; 95% CI, 0.90-0.98). This effect was similar for Simple 7 scores measured at 10 years of follow-up (OR, 0.95; 95% CI, 0.91-1.00).
“It can be empowering for people to know that by taking steps such as exercising for a half an hour a day or keeping their blood pressure under control, they can reduce their risk of dementia,” Dr. Rist said in a statement on the findings.
‘A simple take-home message’
Reached for comment, Andrew E. Budson, MD, chief of cognitive-behavioral neurology at the VA Boston Healthcare System, praised Dr. Rist and colleagues’ study as one that “builds on existing knowledge to provide a simple take-home message that empowers women to take control of their dementia risk.”
Each of the seven known risk factors – being active, eating better, maintaining a healthy weight, not smoking, maintaining a healthy blood pressure, controlling cholesterol, and having low blood sugar – “was associated with a 6% reduced risk of dementia,” Dr. Budson continued. “So, women who work to address all seven risk factors can reduce their risk of developing dementia by 42%: a huge amount. Moreover, although this study only looked at women, I am confident that if men follow this same advice they will also be able to reduce their risk of dementia, although we don’t know if the size of the effect will be the same.”
Dr. Rist and colleagues’ study was supported by the National Institutes of Health. None of the study authors reported conflicts of interest. Dr. Budson has reported receiving past compensation as a speaker for Eli Lilly.
according to results of a study that was released early, ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology.
Epidemiologist Pamela M. Rist, ScD, assistant professor of medicine at Harvard Medical School and associate epidemiologist at Brigham and Women’s Hospital, both in Boston, and colleagues, used data from 13,720 women whose mean age was 54 when they enrolled in the Harvard-based Women’s Health Study between 1992 and 1995. Subjects in that study were followed up in 2004.
Putting ‘Life’s Simple 7’ to the test
Dr. Rist and colleagues used the Harvard data to discern how well closely women conformed, during the initial study period and at 10-year follow up, to what the American Heart Association describes as “Life’s Simple 7,” a list of behavioral and biometric measures that indicate and predict cardiovascular health. The measures include four modifiable behaviors – not smoking, healthy weight, a healthy diet, and being physically active – along with three biometric measures of blood pressure, cholesterol, and blood sugar (AHA has since added a sleep component).
Researchers assigned women one point for each desirable habit or measure on the list, with subjects’ average Simple 7 score at baseline 4.3, and 4.2 at 10 years’ follow-up.
The investigators then looked at Medicare data for the study subjects from 2011 to 2018 – approximately 20 years after their enrollment in the Women’s Health Study – seeking dementia diagnoses. Some 13% of the study cohort (n = 1,771) had gone on to develop dementia.
Each point on the Simple 7 score at baseline corresponded with a 6% reduction in later dementia risk, Dr. Rist and her colleagues found after adjusting for variables including age and education (odds ratio per one unit change in score, 0.94; 95% CI, 0.90-0.98). This effect was similar for Simple 7 scores measured at 10 years of follow-up (OR, 0.95; 95% CI, 0.91-1.00).
“It can be empowering for people to know that by taking steps such as exercising for a half an hour a day or keeping their blood pressure under control, they can reduce their risk of dementia,” Dr. Rist said in a statement on the findings.
‘A simple take-home message’
Reached for comment, Andrew E. Budson, MD, chief of cognitive-behavioral neurology at the VA Boston Healthcare System, praised Dr. Rist and colleagues’ study as one that “builds on existing knowledge to provide a simple take-home message that empowers women to take control of their dementia risk.”
Each of the seven known risk factors – being active, eating better, maintaining a healthy weight, not smoking, maintaining a healthy blood pressure, controlling cholesterol, and having low blood sugar – “was associated with a 6% reduced risk of dementia,” Dr. Budson continued. “So, women who work to address all seven risk factors can reduce their risk of developing dementia by 42%: a huge amount. Moreover, although this study only looked at women, I am confident that if men follow this same advice they will also be able to reduce their risk of dementia, although we don’t know if the size of the effect will be the same.”
Dr. Rist and colleagues’ study was supported by the National Institutes of Health. None of the study authors reported conflicts of interest. Dr. Budson has reported receiving past compensation as a speaker for Eli Lilly.
FROM AAN 2023
Family violence after COVID: Understanding coercive relationships
Despite the ability of some couples to pull together and manage through the COVID-19 pandemic, other couples and families failed to thrive. Increasing divorce rates have been noted nationwide with many disagreements being specifically about COVID.1
A review of over 1 million tweets, between April 12 and July 16, 2020, found an increase in calls to hotlines and increased reports of a variety of types of family violence. There were also more inquiries about social services for family violence, an increased presence from social movements, and more domestic violence-related news.2
The literature addressing family violence uses a variety of terms, so here are some definitions.
Domestic violence is defined as a pattern of behaviors used to gain or maintain power and control. Broadly speaking, domestic violence includes elder abuse, sibling abuse, child abuse, intimate partner abuse, parent abuse, and can also include people who don’t necessarily live together but who have an intimate relationship. Domestic violence centers use the Power and Control Wheel (see graphic) developed by the Domestic Abuse Intervention Project in Duluth, Minn., to describe how domestic violence occurs.
Intimate partner violence is more specific, referring to violence that happens between people in an ongoing or former intimate or romantic relationship, and is a subcategory of domestic violence.
Coercive control is the use of power for control and compliance. It is a dynamic and systematic process described in the top left corner of the Power and Control Wheel. Overt control occurs with the implication that “if you don’t follow the rules, I’ll kill you.” More subtle control is when obedience is forced through monopolizing resources, dictating preferred choices, microregulating a partner’s behavior, and deprivation of supports needed to exercise independent judgment.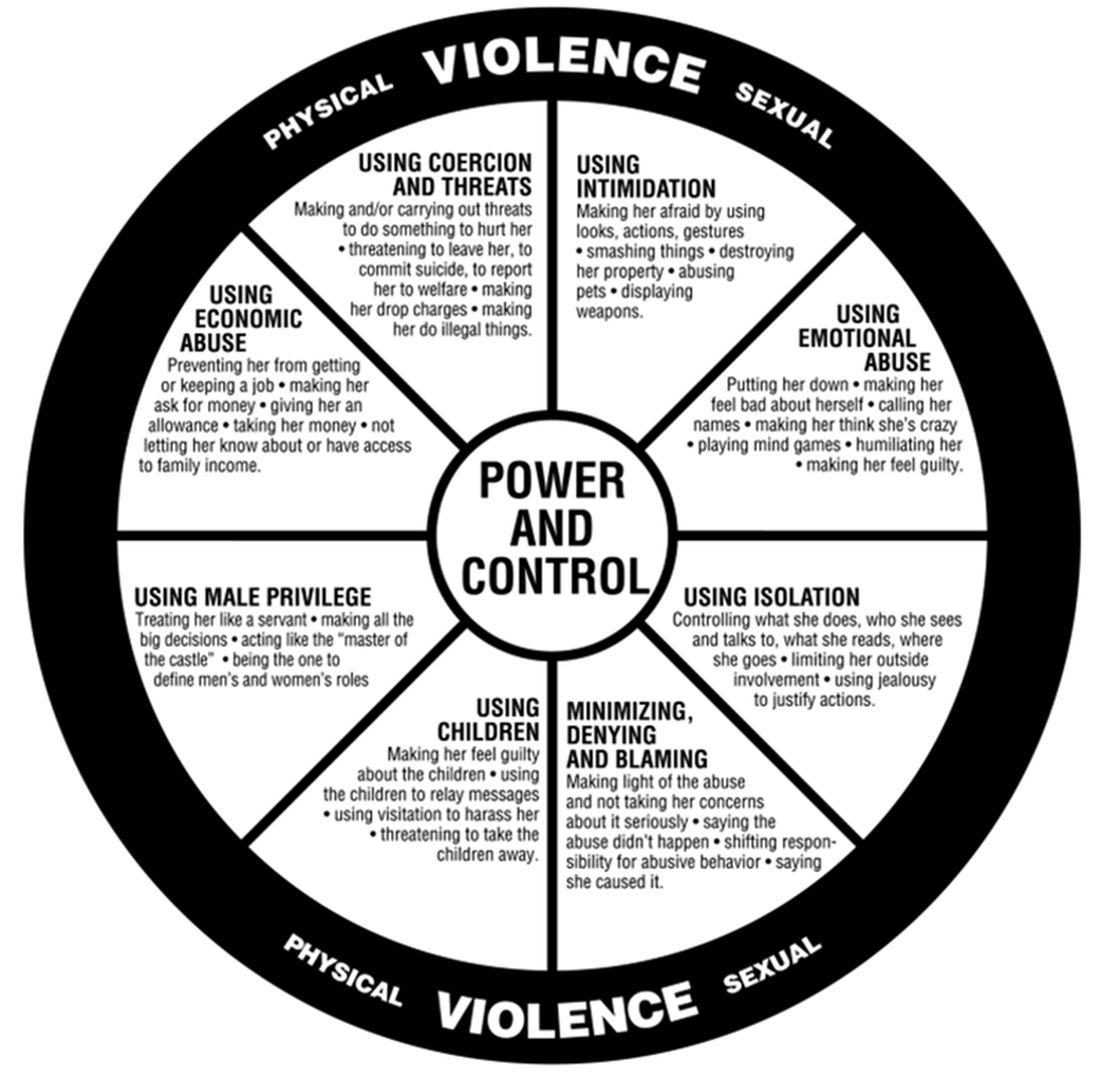
All interpersonal relationships have elements of persuasion and influence; however, the goal of coercive relationships is to maintain power and control. It is a dynamic of the relationship. Coercive control emphasizes the systematic, organized, multifaceted, and patterned nature of this interpersonal dynamic and can be considered to originate in the patriarchal dynamic where men control women.
Most professionals who work in this interdisciplinary area now refer to domestic violence as coercive control. Victimizers target women whom they sense they can control to get their own needs met. They are disinclined to invest in relationships with women who stress their own points of view, who do not readily accept blame when there is a disagreement, and who offer nurturing only when it is reciprocated.
In my office, if I think there are elements of coercion in a relationship, I bring out the Power and Control Wheel and the patient and I go over it. Good education is our responsibility. However, we all have met women who decide to stay in unhealthy relationships.
Assessing people who stay in coercive relationships
Fear
The most important first step is to assess safety. Are they afraid of increased violence if they challenge their partner? Restraining orders or other legal deterrents may not offer solace, as many women are clear that their spouse will come after them, if not tomorrow, then next week, or even next month. They are sure that they will not be safe.
In these cases, I go over safety steps with them so that if they decide to go, they will be prepared. I bring out the “safety box,” which includes the following action steps:
- Memorize important phone numbers of people to call in an emergency.
- If your children are old enough, teach them important phone numbers, including when to dial 911.
- If you can, open your own bank account.
- Stay in touch with friends. Get to know your neighbors. Don’t cut yourself off from people, even if you feel like you want to be alone.
- Rehearse your escape plan until you know it by heart.
- Leave a set of car keys, extra money, a change of clothes and copies of important documents with a trusted friend or relative: your own and your children’s birth certificates, children’s school and medical records, bank books, welfare identification, passport/green card, immigration papers, social security card, lease agreements or mortgage payment books, insurance papers, important addresses, and telephone numbers.
- Keep information about domestic violence in a safe place, where your abuser won’t find it, but where you can get it when you need to review it.
Some women may acknowledge that the risk of physical violence is not the determining factor in their decision to stay and have difficulty explaining why they choose to stay. I suggest that we then consider the following frames that have their origin in the study of the impact of trauma.
Shame
From this lens, abusive events are humiliating experiences, now represented as shame experiences. Humiliation and shame hide hostile feelings that the patient is not able to acknowledge.
“In shame, the self is the failure and others may reject or be critical of this exposed, flawed self.”3 Women will therefore remain attached to an abuser to avoid the exposure of their defective self.
Action steps: Empathic engagement and acknowledgment of shame and humiliation are key. For someone to overcome shame, they must face their sense of their defective self and have strategies to manage these feelings. The development of such strategies is the next step.
Trauma repetition and trauma bonding
Women subjected to domestic violence often respond with incapacitating traumatic syndromes. The concept of “trauma repetition” is suggested as a cause of vulnerability to repeated abuse, and “trauma bonding” is the term for the intense and tenacious bond that can form between abusers and victims.4
Trauma bonding implies that a sense of safety and closeness and secure attachment can only be reached through highly abusive engagement; anything else is experienced as “superficial, cold, or irrelevant.”5 Trauma bonding may have its origins in emotional neglect, according to self reports of 116 women.6Action steps: The literature on trauma is growing and many patients will benefit from good curated sources. Having a good list of books and website on hand is important. Discussion and exploration of the impact of trauma will be needed, and can be provided by someone who is available on a consistent and frequent basis. This work may be time consuming and difficult.
Some asides
1. Some psychiatrists proffer the explanation that these women who stay must be masochistic. The misogynistic concept of masochism still haunts the halls of psychiatry. It is usually offered as a way to dismiss these women’s concerns.
2. One of the obstacles to recognizing chronic mistreatment in relationships is that most abusive men simply “do not seem like abusers.” They have many good qualities, including times of kindness, warmth, and humor, especially in the initial period of a relationship. An abuser’s friends may think the world of him. He may have a successful work life and have no problems with drugs or alcohol. He may simply not fit anyone’s image of a cruel or intimidating person. So, when a woman feels her relationship spinning out of control, it may not occur to her that her partner is an abuser. Even if she does consider her partner to be overly controlling, others may question her perception.
3. Neutrality in family courts is systemic sexism/misogyny. When it comes to domestic violence, family courts tend to split the difference. Stephanie Brandt, MD, notes that The assumption that it is violence alone that matters has formed the basis of much clinical and legal confusion.7 As an analyst, she has gone against the grain of a favored neutrality and become active in the courts, noting the secondary victimization that occurs when a woman enters the legal system.
In summary, psychiatrists must reclaim our expertise in systemic dynamics and point out the role of systemic misogyny. Justices and other court officials need to be educated. Ideally, justice should be based on the equality of men and women in a society free of systemic misogyny. Unfortunately our society has not yet reached this position. In the meanwhile, we must think systemically about interpersonal dynamics. This is our lane. This should not be controversial.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alisonheru@gmail.com. Dr. Heru would like to thank Dr. Stephanie Brandt for discussing this topic with her and supporting this work.
References
1. Ellyatt H. Arguing with your partner over Covid? You’re not alone, with the pandemic straining many relationships. 2022 Jan 21. https://www.cnbc.com/2022/01/21/covid-has-put-pressures-and-strains-on-relationships.html
2. Xue J et al. J Med Internet Res. 2020 Nov 6;22(11):e24361. doi: 10.2196/24361.
3. Dorahy MJ. J Trauma Dissociation. 2017 May-Jun;18(3):383-96. doi: 10.1080/15299732.2017.1295422.
4. Dutton DG and Painter SL. Victimology. 1981 Jan;6(1):139-55.
5. Sachs A. J Trauma Dissociation. 2017 May-Jun;18(3):319-39. doi: 10.1080/15299732.2017.1295400.
6. Krüger C and Fletcher L. J Trauma Dissociation. 2017 May-Jun;18(3):356-72. doi: 10.1080/15299732.2017.1295420.
7. Brandt S and Rudden M. Int J Appl Psychoanal Studies. 2020 Sept;17(3):215-31. doi: 10.1002/aps.1671.
Despite the ability of some couples to pull together and manage through the COVID-19 pandemic, other couples and families failed to thrive. Increasing divorce rates have been noted nationwide with many disagreements being specifically about COVID.1
A review of over 1 million tweets, between April 12 and July 16, 2020, found an increase in calls to hotlines and increased reports of a variety of types of family violence. There were also more inquiries about social services for family violence, an increased presence from social movements, and more domestic violence-related news.2
The literature addressing family violence uses a variety of terms, so here are some definitions.
Domestic violence is defined as a pattern of behaviors used to gain or maintain power and control. Broadly speaking, domestic violence includes elder abuse, sibling abuse, child abuse, intimate partner abuse, parent abuse, and can also include people who don’t necessarily live together but who have an intimate relationship. Domestic violence centers use the Power and Control Wheel (see graphic) developed by the Domestic Abuse Intervention Project in Duluth, Minn., to describe how domestic violence occurs.
Intimate partner violence is more specific, referring to violence that happens between people in an ongoing or former intimate or romantic relationship, and is a subcategory of domestic violence.
Coercive control is the use of power for control and compliance. It is a dynamic and systematic process described in the top left corner of the Power and Control Wheel. Overt control occurs with the implication that “if you don’t follow the rules, I’ll kill you.” More subtle control is when obedience is forced through monopolizing resources, dictating preferred choices, microregulating a partner’s behavior, and deprivation of supports needed to exercise independent judgment.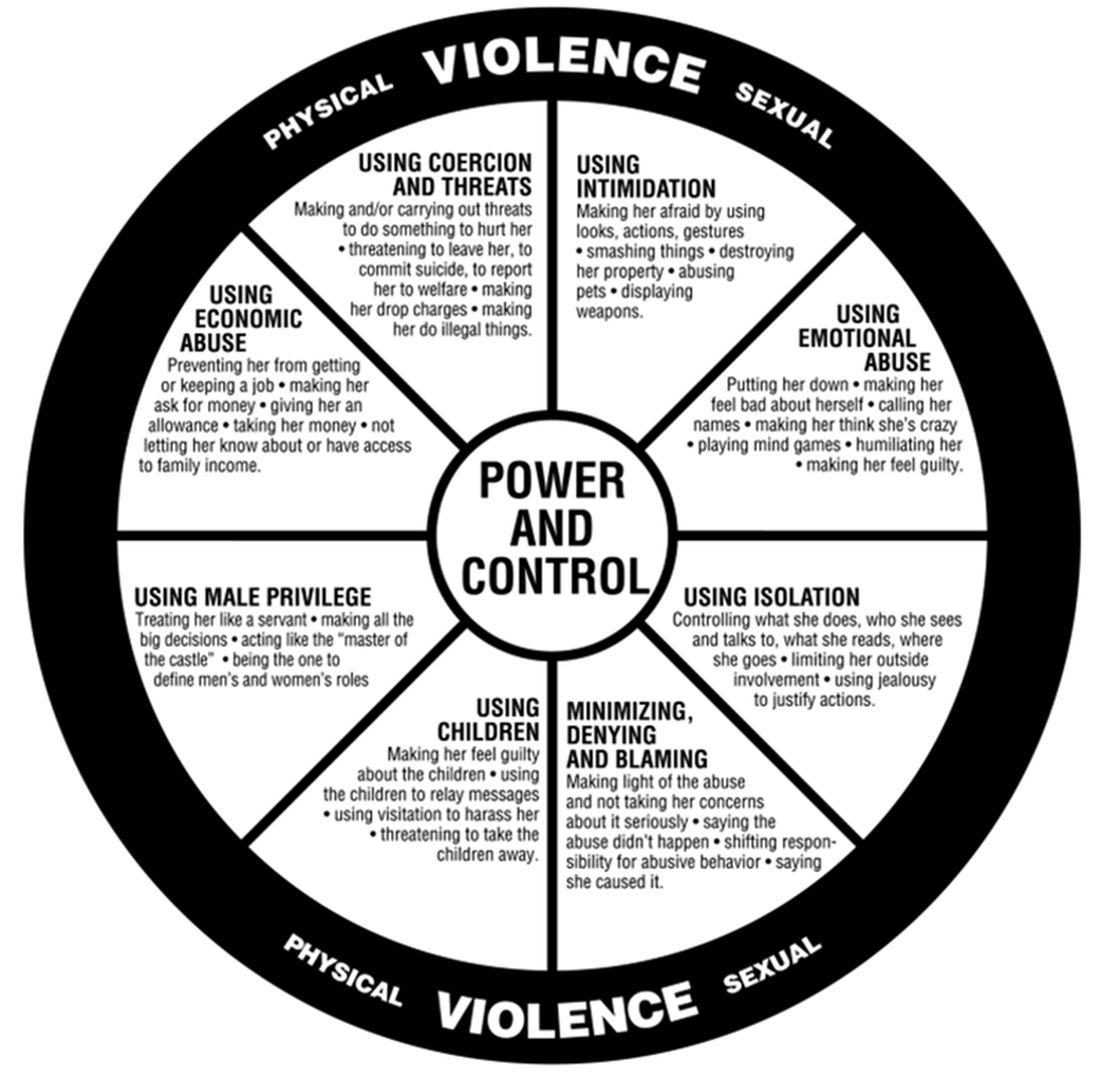
All interpersonal relationships have elements of persuasion and influence; however, the goal of coercive relationships is to maintain power and control. It is a dynamic of the relationship. Coercive control emphasizes the systematic, organized, multifaceted, and patterned nature of this interpersonal dynamic and can be considered to originate in the patriarchal dynamic where men control women.
Most professionals who work in this interdisciplinary area now refer to domestic violence as coercive control. Victimizers target women whom they sense they can control to get their own needs met. They are disinclined to invest in relationships with women who stress their own points of view, who do not readily accept blame when there is a disagreement, and who offer nurturing only when it is reciprocated.
In my office, if I think there are elements of coercion in a relationship, I bring out the Power and Control Wheel and the patient and I go over it. Good education is our responsibility. However, we all have met women who decide to stay in unhealthy relationships.
Assessing people who stay in coercive relationships
Fear
The most important first step is to assess safety. Are they afraid of increased violence if they challenge their partner? Restraining orders or other legal deterrents may not offer solace, as many women are clear that their spouse will come after them, if not tomorrow, then next week, or even next month. They are sure that they will not be safe.
In these cases, I go over safety steps with them so that if they decide to go, they will be prepared. I bring out the “safety box,” which includes the following action steps:
- Memorize important phone numbers of people to call in an emergency.
- If your children are old enough, teach them important phone numbers, including when to dial 911.
- If you can, open your own bank account.
- Stay in touch with friends. Get to know your neighbors. Don’t cut yourself off from people, even if you feel like you want to be alone.
- Rehearse your escape plan until you know it by heart.
- Leave a set of car keys, extra money, a change of clothes and copies of important documents with a trusted friend or relative: your own and your children’s birth certificates, children’s school and medical records, bank books, welfare identification, passport/green card, immigration papers, social security card, lease agreements or mortgage payment books, insurance papers, important addresses, and telephone numbers.
- Keep information about domestic violence in a safe place, where your abuser won’t find it, but where you can get it when you need to review it.
Some women may acknowledge that the risk of physical violence is not the determining factor in their decision to stay and have difficulty explaining why they choose to stay. I suggest that we then consider the following frames that have their origin in the study of the impact of trauma.
Shame
From this lens, abusive events are humiliating experiences, now represented as shame experiences. Humiliation and shame hide hostile feelings that the patient is not able to acknowledge.
“In shame, the self is the failure and others may reject or be critical of this exposed, flawed self.”3 Women will therefore remain attached to an abuser to avoid the exposure of their defective self.
Action steps: Empathic engagement and acknowledgment of shame and humiliation are key. For someone to overcome shame, they must face their sense of their defective self and have strategies to manage these feelings. The development of such strategies is the next step.
Trauma repetition and trauma bonding
Women subjected to domestic violence often respond with incapacitating traumatic syndromes. The concept of “trauma repetition” is suggested as a cause of vulnerability to repeated abuse, and “trauma bonding” is the term for the intense and tenacious bond that can form between abusers and victims.4
Trauma bonding implies that a sense of safety and closeness and secure attachment can only be reached through highly abusive engagement; anything else is experienced as “superficial, cold, or irrelevant.”5 Trauma bonding may have its origins in emotional neglect, according to self reports of 116 women.6Action steps: The literature on trauma is growing and many patients will benefit from good curated sources. Having a good list of books and website on hand is important. Discussion and exploration of the impact of trauma will be needed, and can be provided by someone who is available on a consistent and frequent basis. This work may be time consuming and difficult.
Some asides
1. Some psychiatrists proffer the explanation that these women who stay must be masochistic. The misogynistic concept of masochism still haunts the halls of psychiatry. It is usually offered as a way to dismiss these women’s concerns.
2. One of the obstacles to recognizing chronic mistreatment in relationships is that most abusive men simply “do not seem like abusers.” They have many good qualities, including times of kindness, warmth, and humor, especially in the initial period of a relationship. An abuser’s friends may think the world of him. He may have a successful work life and have no problems with drugs or alcohol. He may simply not fit anyone’s image of a cruel or intimidating person. So, when a woman feels her relationship spinning out of control, it may not occur to her that her partner is an abuser. Even if she does consider her partner to be overly controlling, others may question her perception.
3. Neutrality in family courts is systemic sexism/misogyny. When it comes to domestic violence, family courts tend to split the difference. Stephanie Brandt, MD, notes that The assumption that it is violence alone that matters has formed the basis of much clinical and legal confusion.7 As an analyst, she has gone against the grain of a favored neutrality and become active in the courts, noting the secondary victimization that occurs when a woman enters the legal system.
In summary, psychiatrists must reclaim our expertise in systemic dynamics and point out the role of systemic misogyny. Justices and other court officials need to be educated. Ideally, justice should be based on the equality of men and women in a society free of systemic misogyny. Unfortunately our society has not yet reached this position. In the meanwhile, we must think systemically about interpersonal dynamics. This is our lane. This should not be controversial.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alisonheru@gmail.com. Dr. Heru would like to thank Dr. Stephanie Brandt for discussing this topic with her and supporting this work.
References
1. Ellyatt H. Arguing with your partner over Covid? You’re not alone, with the pandemic straining many relationships. 2022 Jan 21. https://www.cnbc.com/2022/01/21/covid-has-put-pressures-and-strains-on-relationships.html
2. Xue J et al. J Med Internet Res. 2020 Nov 6;22(11):e24361. doi: 10.2196/24361.
3. Dorahy MJ. J Trauma Dissociation. 2017 May-Jun;18(3):383-96. doi: 10.1080/15299732.2017.1295422.
4. Dutton DG and Painter SL. Victimology. 1981 Jan;6(1):139-55.
5. Sachs A. J Trauma Dissociation. 2017 May-Jun;18(3):319-39. doi: 10.1080/15299732.2017.1295400.
6. Krüger C and Fletcher L. J Trauma Dissociation. 2017 May-Jun;18(3):356-72. doi: 10.1080/15299732.2017.1295420.
7. Brandt S and Rudden M. Int J Appl Psychoanal Studies. 2020 Sept;17(3):215-31. doi: 10.1002/aps.1671.
Despite the ability of some couples to pull together and manage through the COVID-19 pandemic, other couples and families failed to thrive. Increasing divorce rates have been noted nationwide with many disagreements being specifically about COVID.1
A review of over 1 million tweets, between April 12 and July 16, 2020, found an increase in calls to hotlines and increased reports of a variety of types of family violence. There were also more inquiries about social services for family violence, an increased presence from social movements, and more domestic violence-related news.2
The literature addressing family violence uses a variety of terms, so here are some definitions.
Domestic violence is defined as a pattern of behaviors used to gain or maintain power and control. Broadly speaking, domestic violence includes elder abuse, sibling abuse, child abuse, intimate partner abuse, parent abuse, and can also include people who don’t necessarily live together but who have an intimate relationship. Domestic violence centers use the Power and Control Wheel (see graphic) developed by the Domestic Abuse Intervention Project in Duluth, Minn., to describe how domestic violence occurs.
Intimate partner violence is more specific, referring to violence that happens between people in an ongoing or former intimate or romantic relationship, and is a subcategory of domestic violence.
Coercive control is the use of power for control and compliance. It is a dynamic and systematic process described in the top left corner of the Power and Control Wheel. Overt control occurs with the implication that “if you don’t follow the rules, I’ll kill you.” More subtle control is when obedience is forced through monopolizing resources, dictating preferred choices, microregulating a partner’s behavior, and deprivation of supports needed to exercise independent judgment.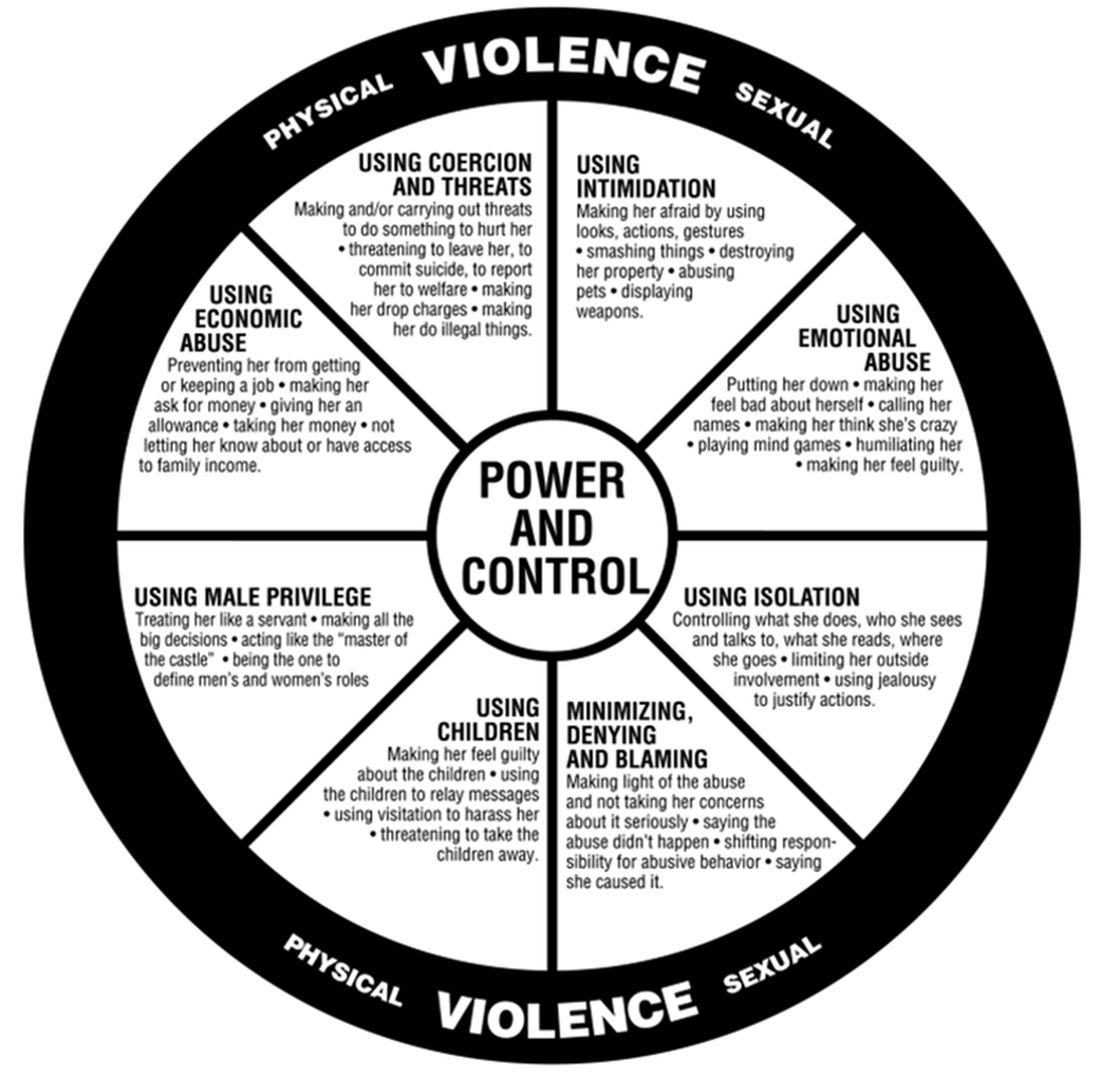
All interpersonal relationships have elements of persuasion and influence; however, the goal of coercive relationships is to maintain power and control. It is a dynamic of the relationship. Coercive control emphasizes the systematic, organized, multifaceted, and patterned nature of this interpersonal dynamic and can be considered to originate in the patriarchal dynamic where men control women.
Most professionals who work in this interdisciplinary area now refer to domestic violence as coercive control. Victimizers target women whom they sense they can control to get their own needs met. They are disinclined to invest in relationships with women who stress their own points of view, who do not readily accept blame when there is a disagreement, and who offer nurturing only when it is reciprocated.
In my office, if I think there are elements of coercion in a relationship, I bring out the Power and Control Wheel and the patient and I go over it. Good education is our responsibility. However, we all have met women who decide to stay in unhealthy relationships.
Assessing people who stay in coercive relationships
Fear
The most important first step is to assess safety. Are they afraid of increased violence if they challenge their partner? Restraining orders or other legal deterrents may not offer solace, as many women are clear that their spouse will come after them, if not tomorrow, then next week, or even next month. They are sure that they will not be safe.
In these cases, I go over safety steps with them so that if they decide to go, they will be prepared. I bring out the “safety box,” which includes the following action steps:
- Memorize important phone numbers of people to call in an emergency.
- If your children are old enough, teach them important phone numbers, including when to dial 911.
- If you can, open your own bank account.
- Stay in touch with friends. Get to know your neighbors. Don’t cut yourself off from people, even if you feel like you want to be alone.
- Rehearse your escape plan until you know it by heart.
- Leave a set of car keys, extra money, a change of clothes and copies of important documents with a trusted friend or relative: your own and your children’s birth certificates, children’s school and medical records, bank books, welfare identification, passport/green card, immigration papers, social security card, lease agreements or mortgage payment books, insurance papers, important addresses, and telephone numbers.
- Keep information about domestic violence in a safe place, where your abuser won’t find it, but where you can get it when you need to review it.
Some women may acknowledge that the risk of physical violence is not the determining factor in their decision to stay and have difficulty explaining why they choose to stay. I suggest that we then consider the following frames that have their origin in the study of the impact of trauma.
Shame
From this lens, abusive events are humiliating experiences, now represented as shame experiences. Humiliation and shame hide hostile feelings that the patient is not able to acknowledge.
“In shame, the self is the failure and others may reject or be critical of this exposed, flawed self.”3 Women will therefore remain attached to an abuser to avoid the exposure of their defective self.
Action steps: Empathic engagement and acknowledgment of shame and humiliation are key. For someone to overcome shame, they must face their sense of their defective self and have strategies to manage these feelings. The development of such strategies is the next step.
Trauma repetition and trauma bonding
Women subjected to domestic violence often respond with incapacitating traumatic syndromes. The concept of “trauma repetition” is suggested as a cause of vulnerability to repeated abuse, and “trauma bonding” is the term for the intense and tenacious bond that can form between abusers and victims.4
Trauma bonding implies that a sense of safety and closeness and secure attachment can only be reached through highly abusive engagement; anything else is experienced as “superficial, cold, or irrelevant.”5 Trauma bonding may have its origins in emotional neglect, according to self reports of 116 women.6Action steps: The literature on trauma is growing and many patients will benefit from good curated sources. Having a good list of books and website on hand is important. Discussion and exploration of the impact of trauma will be needed, and can be provided by someone who is available on a consistent and frequent basis. This work may be time consuming and difficult.
Some asides
1. Some psychiatrists proffer the explanation that these women who stay must be masochistic. The misogynistic concept of masochism still haunts the halls of psychiatry. It is usually offered as a way to dismiss these women’s concerns.
2. One of the obstacles to recognizing chronic mistreatment in relationships is that most abusive men simply “do not seem like abusers.” They have many good qualities, including times of kindness, warmth, and humor, especially in the initial period of a relationship. An abuser’s friends may think the world of him. He may have a successful work life and have no problems with drugs or alcohol. He may simply not fit anyone’s image of a cruel or intimidating person. So, when a woman feels her relationship spinning out of control, it may not occur to her that her partner is an abuser. Even if she does consider her partner to be overly controlling, others may question her perception.
3. Neutrality in family courts is systemic sexism/misogyny. When it comes to domestic violence, family courts tend to split the difference. Stephanie Brandt, MD, notes that The assumption that it is violence alone that matters has formed the basis of much clinical and legal confusion.7 As an analyst, she has gone against the grain of a favored neutrality and become active in the courts, noting the secondary victimization that occurs when a woman enters the legal system.
In summary, psychiatrists must reclaim our expertise in systemic dynamics and point out the role of systemic misogyny. Justices and other court officials need to be educated. Ideally, justice should be based on the equality of men and women in a society free of systemic misogyny. Unfortunately our society has not yet reached this position. In the meanwhile, we must think systemically about interpersonal dynamics. This is our lane. This should not be controversial.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alisonheru@gmail.com. Dr. Heru would like to thank Dr. Stephanie Brandt for discussing this topic with her and supporting this work.
References
1. Ellyatt H. Arguing with your partner over Covid? You’re not alone, with the pandemic straining many relationships. 2022 Jan 21. https://www.cnbc.com/2022/01/21/covid-has-put-pressures-and-strains-on-relationships.html
2. Xue J et al. J Med Internet Res. 2020 Nov 6;22(11):e24361. doi: 10.2196/24361.
3. Dorahy MJ. J Trauma Dissociation. 2017 May-Jun;18(3):383-96. doi: 10.1080/15299732.2017.1295422.
4. Dutton DG and Painter SL. Victimology. 1981 Jan;6(1):139-55.
5. Sachs A. J Trauma Dissociation. 2017 May-Jun;18(3):319-39. doi: 10.1080/15299732.2017.1295400.
6. Krüger C and Fletcher L. J Trauma Dissociation. 2017 May-Jun;18(3):356-72. doi: 10.1080/15299732.2017.1295420.
7. Brandt S and Rudden M. Int J Appl Psychoanal Studies. 2020 Sept;17(3):215-31. doi: 10.1002/aps.1671.
New Medicare rule streamlines prior authorization in Medicare Advantage plans
A new federal rule seeks to reduce Medicare Advantage insurance plans’ prior authorization burdens on physicians while also ensuring that enrollees have the same access to necessary care that they would receive under traditional fee-for-service Medicare.
The prior authorization changes, announced this week, are part of the Centers for Medicare & Medicaid Services’ 2024 update of policy changes for Medicare Advantage and Part D pharmacy plans
Medicare Advantage plans’ business practices have raised significant concerns in recent years. More than 28 million Americans were enrolled in a Medicare Advantage plan in 2022, which is nearly half of all Medicare enrollees, according to the Kaiser Family Foundation.
Medicare pays a fixed amount per enrollee per year to these privately run managed care plans, in contrast to traditional fee-for-service Medicare. Medicare Advantage plans have been criticized for aggressive marketing, for overbilling the federal government for care, and for using prior authorization to inappropriately deny needed care to patients.
About 13% of prior authorization requests that are denied by Medicare Advantage plans actually met Medicare coverage rules and should have been approved, the Office of the Inspector General at the U.S. Department of Health & Human Services reported in 2022.
The newly finalized rule now requires Medicare Advantage plans to do the following.
- Ensure that a prior authorization approval, once granted, remains valid for as long as medically necessary to avoid disruptions in care.
- Conduct an annual review of utilization management policies.
- Ensure that coverage denials based on medical necessity be reviewed by health care professionals with relevant expertise before a denial can be issued.
Physician groups welcomed the changes. In a statement, the American Medical Association said that an initial reading of the rule suggested CMS had “taken important steps toward right-sizing the prior authorization process.”
The Medical Group Management Association praised CMS in a statement for having limited “dangerous disruptions and delays to necessary patient care” resulting from the cumbersome processes of prior approval. With the new rules, CMS will provide greater consistency across Advantage plans as well as traditional Medicare, said Anders Gilberg, MGMA’s senior vice president of government affairs, in a statement.
Peer consideration
The final rule did disappoint physician groups in one key way. CMS rebuffed requests to have CMS require Advantage plans to use reviewers of the same specialty as treating physicians in handling disputes about prior authorization. CMS said it expects plans to exercise judgment in finding reviewers with “sufficient expertise to make an informed and supportable decision.”
“In some instances, we expect that plans will use a physician or other health care professional of the same specialty or subspecialty as the treating physician,” CMS said. “In other instances, we expect that plans will utilize a reviewer with specialized training, certification, or clinical experience in the applicable field of medicine.”
Medicare Advantage marketing ‘sowing confusion’
With this final rule, CMS also sought to protect consumers from “potentially misleading marketing practices” used in promoting Medicare Advantage and Part D prescription drug plans.
The agency said it had received complaints about people who have received official-looking promotional materials for Medicare that directed them not to government sources of information but to Medicare Advantage and Part D plans or their agents and brokers.
Ads now must mention a specific plan name, and they cannot use the Medicare name, CMS logo, Medicare card, or other government information in a misleading way, CMS said.
“CMS can see no value or purpose in a non-governmental entity’s use of the Medicare logo or HHS logo except for the express purpose of sowing confusion and misrepresenting itself as the government,” the agency said.
A version of this article first appeared on Medscape.com.
A new federal rule seeks to reduce Medicare Advantage insurance plans’ prior authorization burdens on physicians while also ensuring that enrollees have the same access to necessary care that they would receive under traditional fee-for-service Medicare.
The prior authorization changes, announced this week, are part of the Centers for Medicare & Medicaid Services’ 2024 update of policy changes for Medicare Advantage and Part D pharmacy plans
Medicare Advantage plans’ business practices have raised significant concerns in recent years. More than 28 million Americans were enrolled in a Medicare Advantage plan in 2022, which is nearly half of all Medicare enrollees, according to the Kaiser Family Foundation.
Medicare pays a fixed amount per enrollee per year to these privately run managed care plans, in contrast to traditional fee-for-service Medicare. Medicare Advantage plans have been criticized for aggressive marketing, for overbilling the federal government for care, and for using prior authorization to inappropriately deny needed care to patients.
About 13% of prior authorization requests that are denied by Medicare Advantage plans actually met Medicare coverage rules and should have been approved, the Office of the Inspector General at the U.S. Department of Health & Human Services reported in 2022.
The newly finalized rule now requires Medicare Advantage plans to do the following.
- Ensure that a prior authorization approval, once granted, remains valid for as long as medically necessary to avoid disruptions in care.
- Conduct an annual review of utilization management policies.
- Ensure that coverage denials based on medical necessity be reviewed by health care professionals with relevant expertise before a denial can be issued.
Physician groups welcomed the changes. In a statement, the American Medical Association said that an initial reading of the rule suggested CMS had “taken important steps toward right-sizing the prior authorization process.”
The Medical Group Management Association praised CMS in a statement for having limited “dangerous disruptions and delays to necessary patient care” resulting from the cumbersome processes of prior approval. With the new rules, CMS will provide greater consistency across Advantage plans as well as traditional Medicare, said Anders Gilberg, MGMA’s senior vice president of government affairs, in a statement.
Peer consideration
The final rule did disappoint physician groups in one key way. CMS rebuffed requests to have CMS require Advantage plans to use reviewers of the same specialty as treating physicians in handling disputes about prior authorization. CMS said it expects plans to exercise judgment in finding reviewers with “sufficient expertise to make an informed and supportable decision.”
“In some instances, we expect that plans will use a physician or other health care professional of the same specialty or subspecialty as the treating physician,” CMS said. “In other instances, we expect that plans will utilize a reviewer with specialized training, certification, or clinical experience in the applicable field of medicine.”
Medicare Advantage marketing ‘sowing confusion’
With this final rule, CMS also sought to protect consumers from “potentially misleading marketing practices” used in promoting Medicare Advantage and Part D prescription drug plans.
The agency said it had received complaints about people who have received official-looking promotional materials for Medicare that directed them not to government sources of information but to Medicare Advantage and Part D plans or their agents and brokers.
Ads now must mention a specific plan name, and they cannot use the Medicare name, CMS logo, Medicare card, or other government information in a misleading way, CMS said.
“CMS can see no value or purpose in a non-governmental entity’s use of the Medicare logo or HHS logo except for the express purpose of sowing confusion and misrepresenting itself as the government,” the agency said.
A version of this article first appeared on Medscape.com.
A new federal rule seeks to reduce Medicare Advantage insurance plans’ prior authorization burdens on physicians while also ensuring that enrollees have the same access to necessary care that they would receive under traditional fee-for-service Medicare.
The prior authorization changes, announced this week, are part of the Centers for Medicare & Medicaid Services’ 2024 update of policy changes for Medicare Advantage and Part D pharmacy plans
Medicare Advantage plans’ business practices have raised significant concerns in recent years. More than 28 million Americans were enrolled in a Medicare Advantage plan in 2022, which is nearly half of all Medicare enrollees, according to the Kaiser Family Foundation.
Medicare pays a fixed amount per enrollee per year to these privately run managed care plans, in contrast to traditional fee-for-service Medicare. Medicare Advantage plans have been criticized for aggressive marketing, for overbilling the federal government for care, and for using prior authorization to inappropriately deny needed care to patients.
About 13% of prior authorization requests that are denied by Medicare Advantage plans actually met Medicare coverage rules and should have been approved, the Office of the Inspector General at the U.S. Department of Health & Human Services reported in 2022.
The newly finalized rule now requires Medicare Advantage plans to do the following.
- Ensure that a prior authorization approval, once granted, remains valid for as long as medically necessary to avoid disruptions in care.
- Conduct an annual review of utilization management policies.
- Ensure that coverage denials based on medical necessity be reviewed by health care professionals with relevant expertise before a denial can be issued.
Physician groups welcomed the changes. In a statement, the American Medical Association said that an initial reading of the rule suggested CMS had “taken important steps toward right-sizing the prior authorization process.”
The Medical Group Management Association praised CMS in a statement for having limited “dangerous disruptions and delays to necessary patient care” resulting from the cumbersome processes of prior approval. With the new rules, CMS will provide greater consistency across Advantage plans as well as traditional Medicare, said Anders Gilberg, MGMA’s senior vice president of government affairs, in a statement.
Peer consideration
The final rule did disappoint physician groups in one key way. CMS rebuffed requests to have CMS require Advantage plans to use reviewers of the same specialty as treating physicians in handling disputes about prior authorization. CMS said it expects plans to exercise judgment in finding reviewers with “sufficient expertise to make an informed and supportable decision.”
“In some instances, we expect that plans will use a physician or other health care professional of the same specialty or subspecialty as the treating physician,” CMS said. “In other instances, we expect that plans will utilize a reviewer with specialized training, certification, or clinical experience in the applicable field of medicine.”
Medicare Advantage marketing ‘sowing confusion’
With this final rule, CMS also sought to protect consumers from “potentially misleading marketing practices” used in promoting Medicare Advantage and Part D prescription drug plans.
The agency said it had received complaints about people who have received official-looking promotional materials for Medicare that directed them not to government sources of information but to Medicare Advantage and Part D plans or their agents and brokers.
Ads now must mention a specific plan name, and they cannot use the Medicare name, CMS logo, Medicare card, or other government information in a misleading way, CMS said.
“CMS can see no value or purpose in a non-governmental entity’s use of the Medicare logo or HHS logo except for the express purpose of sowing confusion and misrepresenting itself as the government,” the agency said.
A version of this article first appeared on Medscape.com.
Glutathione a potential biomarker for postpartum suicide
Approximately 10,000 suicide deaths are recorded in Brazil every year. The suicide risk is highest among patients with depressive disorders, particularly women (> 18% vs. 11% for men).
There are countless people who work to prevent suicide, and the challenges they face are many. But now, on the horizon, there are new tools that could prove invaluable to their efforts – tools such as biomarkers. In a study recently published in the journal Frontiers in Psychiatry, researchers from the Catholic University of Pelotas (UCPel), Brazil, reported an association of glutathione (GSH) with the degree of suicide risk in women at 18 months postpartum. Specifically, they found that reduced serum GSH levels were significantly lower for those with moderate to high suicide risk than for those without suicide risk. Their findings suggest that GSH may be a potential biomarker or etiologic factor among women at risk for suicide, with therapeutic implications.
This was a case-control study nested within a cohort study. From this cohort, 45 women were selected at 18 months postpartum. Thirty of them had mood disorders, such as major depression and bipolar disorder. The other 15 participants, none of whom had a mood disorder, made up the control group.
Depression and the risk for suicide were assessed using the Mini International Neuropsychiatric Interview Plus (MINI-Plus 5.0.0 Brazilian version), module A and module C, respectively. Blood samples were collected to evaluate serum levels of the following oxidative stress biomarkers: reactive oxygen species, superoxide dismutase, and GSH.
The prevalence of suicide risk observed in the women at 18 months postpartum was 24.4%. The prevalence of suicide risk in the mood disorder group was 36.7%.
In addition, the statistical analysis found that women with moderate to high suicide risk had cerebral redox imbalance, resulting in a decrease in blood GSH levels.
The study team was led by neuroscientist Adriano Martimbianco de Assis, PhD, the coordinator of UCPel’s postgraduate program in health and behavior. He said that the correlation identified between GSH serum levels and suicide risk gives rise to two possible applications: using GSH as a biomarker for suicide risk and using GSH therapeutically.
Regarding the former application, Dr. Martimbianco de Assis explained that additional studies are needed to take a step forward. “Although we believe that most of the GSH came from the brain – given that it’s the brain’s main antioxidant – as we analyze blood samples, we’re not yet able to rule out the possibility that it came from other organs,” he said in an interview. So, confirming that hypothesis will require studies that involve imaging brain tissue. According to Dr. Martimbianco de Assis, once there is confirmation, it will be possible to move to using the antioxidant as a biomarker for suicide risk.
He also shared his views about the second application: using GSH therapeutically. “We already know that there are very simple alternatives that can influence GSH levels, [and they] mostly have to do with exercise and [improving the quality of] the food one eats. But there are also drugs: for example, N-acetyl cysteine, which is a precursor of GSH.” Adopting strategies to increase the levels of this antioxidant in the body should reverse the imbalance identified in the study and, as a result, may lead to lowering the risk for suicide. But, he reiterated, “getting to a place where GSH [can be used] in clinical practice hinges on getting that confirmation that it did, in fact, come from the brain. Recall that our study found lower levels of GSH in women at risk for suicide.”
Even though the study evaluated postpartum women, it’s possible that the results can be extrapolated to other populations, said Dr. Martimbianco de Assis. This is because when the data were collected, 18 months had already passed since giving birth. The participants’ physiological condition at that point was more similar to the one prior to becoming pregnant.
The UCPel researchers continue to follow the cohort. “We intend to continue monitoring GSH levels at other times. Forty-eight months have now passed since the women gave birth, and the idea is to continue studying [the patients involved in the study],” said Dr. Martimbianco de Assis, adding that the team also intends to analyze brain tissue from in vitro studies using cell cultures.
This article was translated from the Medscape Portuguese Edition and a version appeared on Medscape.com.
Approximately 10,000 suicide deaths are recorded in Brazil every year. The suicide risk is highest among patients with depressive disorders, particularly women (> 18% vs. 11% for men).
There are countless people who work to prevent suicide, and the challenges they face are many. But now, on the horizon, there are new tools that could prove invaluable to their efforts – tools such as biomarkers. In a study recently published in the journal Frontiers in Psychiatry, researchers from the Catholic University of Pelotas (UCPel), Brazil, reported an association of glutathione (GSH) with the degree of suicide risk in women at 18 months postpartum. Specifically, they found that reduced serum GSH levels were significantly lower for those with moderate to high suicide risk than for those without suicide risk. Their findings suggest that GSH may be a potential biomarker or etiologic factor among women at risk for suicide, with therapeutic implications.
This was a case-control study nested within a cohort study. From this cohort, 45 women were selected at 18 months postpartum. Thirty of them had mood disorders, such as major depression and bipolar disorder. The other 15 participants, none of whom had a mood disorder, made up the control group.
Depression and the risk for suicide were assessed using the Mini International Neuropsychiatric Interview Plus (MINI-Plus 5.0.0 Brazilian version), module A and module C, respectively. Blood samples were collected to evaluate serum levels of the following oxidative stress biomarkers: reactive oxygen species, superoxide dismutase, and GSH.
The prevalence of suicide risk observed in the women at 18 months postpartum was 24.4%. The prevalence of suicide risk in the mood disorder group was 36.7%.
In addition, the statistical analysis found that women with moderate to high suicide risk had cerebral redox imbalance, resulting in a decrease in blood GSH levels.
The study team was led by neuroscientist Adriano Martimbianco de Assis, PhD, the coordinator of UCPel’s postgraduate program in health and behavior. He said that the correlation identified between GSH serum levels and suicide risk gives rise to two possible applications: using GSH as a biomarker for suicide risk and using GSH therapeutically.
Regarding the former application, Dr. Martimbianco de Assis explained that additional studies are needed to take a step forward. “Although we believe that most of the GSH came from the brain – given that it’s the brain’s main antioxidant – as we analyze blood samples, we’re not yet able to rule out the possibility that it came from other organs,” he said in an interview. So, confirming that hypothesis will require studies that involve imaging brain tissue. According to Dr. Martimbianco de Assis, once there is confirmation, it will be possible to move to using the antioxidant as a biomarker for suicide risk.
He also shared his views about the second application: using GSH therapeutically. “We already know that there are very simple alternatives that can influence GSH levels, [and they] mostly have to do with exercise and [improving the quality of] the food one eats. But there are also drugs: for example, N-acetyl cysteine, which is a precursor of GSH.” Adopting strategies to increase the levels of this antioxidant in the body should reverse the imbalance identified in the study and, as a result, may lead to lowering the risk for suicide. But, he reiterated, “getting to a place where GSH [can be used] in clinical practice hinges on getting that confirmation that it did, in fact, come from the brain. Recall that our study found lower levels of GSH in women at risk for suicide.”
Even though the study evaluated postpartum women, it’s possible that the results can be extrapolated to other populations, said Dr. Martimbianco de Assis. This is because when the data were collected, 18 months had already passed since giving birth. The participants’ physiological condition at that point was more similar to the one prior to becoming pregnant.
The UCPel researchers continue to follow the cohort. “We intend to continue monitoring GSH levels at other times. Forty-eight months have now passed since the women gave birth, and the idea is to continue studying [the patients involved in the study],” said Dr. Martimbianco de Assis, adding that the team also intends to analyze brain tissue from in vitro studies using cell cultures.
This article was translated from the Medscape Portuguese Edition and a version appeared on Medscape.com.
Approximately 10,000 suicide deaths are recorded in Brazil every year. The suicide risk is highest among patients with depressive disorders, particularly women (> 18% vs. 11% for men).
There are countless people who work to prevent suicide, and the challenges they face are many. But now, on the horizon, there are new tools that could prove invaluable to their efforts – tools such as biomarkers. In a study recently published in the journal Frontiers in Psychiatry, researchers from the Catholic University of Pelotas (UCPel), Brazil, reported an association of glutathione (GSH) with the degree of suicide risk in women at 18 months postpartum. Specifically, they found that reduced serum GSH levels were significantly lower for those with moderate to high suicide risk than for those without suicide risk. Their findings suggest that GSH may be a potential biomarker or etiologic factor among women at risk for suicide, with therapeutic implications.
This was a case-control study nested within a cohort study. From this cohort, 45 women were selected at 18 months postpartum. Thirty of them had mood disorders, such as major depression and bipolar disorder. The other 15 participants, none of whom had a mood disorder, made up the control group.
Depression and the risk for suicide were assessed using the Mini International Neuropsychiatric Interview Plus (MINI-Plus 5.0.0 Brazilian version), module A and module C, respectively. Blood samples were collected to evaluate serum levels of the following oxidative stress biomarkers: reactive oxygen species, superoxide dismutase, and GSH.
The prevalence of suicide risk observed in the women at 18 months postpartum was 24.4%. The prevalence of suicide risk in the mood disorder group was 36.7%.
In addition, the statistical analysis found that women with moderate to high suicide risk had cerebral redox imbalance, resulting in a decrease in blood GSH levels.
The study team was led by neuroscientist Adriano Martimbianco de Assis, PhD, the coordinator of UCPel’s postgraduate program in health and behavior. He said that the correlation identified between GSH serum levels and suicide risk gives rise to two possible applications: using GSH as a biomarker for suicide risk and using GSH therapeutically.
Regarding the former application, Dr. Martimbianco de Assis explained that additional studies are needed to take a step forward. “Although we believe that most of the GSH came from the brain – given that it’s the brain’s main antioxidant – as we analyze blood samples, we’re not yet able to rule out the possibility that it came from other organs,” he said in an interview. So, confirming that hypothesis will require studies that involve imaging brain tissue. According to Dr. Martimbianco de Assis, once there is confirmation, it will be possible to move to using the antioxidant as a biomarker for suicide risk.
He also shared his views about the second application: using GSH therapeutically. “We already know that there are very simple alternatives that can influence GSH levels, [and they] mostly have to do with exercise and [improving the quality of] the food one eats. But there are also drugs: for example, N-acetyl cysteine, which is a precursor of GSH.” Adopting strategies to increase the levels of this antioxidant in the body should reverse the imbalance identified in the study and, as a result, may lead to lowering the risk for suicide. But, he reiterated, “getting to a place where GSH [can be used] in clinical practice hinges on getting that confirmation that it did, in fact, come from the brain. Recall that our study found lower levels of GSH in women at risk for suicide.”
Even though the study evaluated postpartum women, it’s possible that the results can be extrapolated to other populations, said Dr. Martimbianco de Assis. This is because when the data were collected, 18 months had already passed since giving birth. The participants’ physiological condition at that point was more similar to the one prior to becoming pregnant.
The UCPel researchers continue to follow the cohort. “We intend to continue monitoring GSH levels at other times. Forty-eight months have now passed since the women gave birth, and the idea is to continue studying [the patients involved in the study],” said Dr. Martimbianco de Assis, adding that the team also intends to analyze brain tissue from in vitro studies using cell cultures.
This article was translated from the Medscape Portuguese Edition and a version appeared on Medscape.com.
New insight into the growing problem of gaming disorder
A team of international researchers led by Orsolya Király, PhD, of the Institute of Psychology, Eötvös Loránd University, Budapest, reviewed the characteristics and etiology of GD. They concluded that its genesis arises from the interaction of environmental factors, game-specific factors and individual factors, including personality traits, comorbid psychopathology, and genetic predisposition.
“The development of GD is a complex process and we identified three major factors involved,” study coauthor Mark Griffiths, PhD, distinguished professor of behavioral addiction and director of the international gaming research unit, psychology department, Nottingham (England) Trent University, said in an interview. Because of this complexity, “prevention and intervention in GD require multiprofessional action.”
The review was published in Comprehensive Psychiatry.
In a second paper, published online in Frontiers in Psychiatry, Chinese investigators reviewing randomized controlled trials (RCTs) presented “compelling evidence” to support four effective interventions for GD: group counseling, acceptance and cognitive restructuring intervention program (ACRIP), short-term cognitive-behavioral therapy (CBT), and craving behavioral intervention (CBI).
A third paper, published online in the Journal of Behavioral Addictions, in which researchers analyzed close to 50 studies of GD, found that the concept of “recovery” is rarely mentioned in GD research. Lead author Belle Gavriel-Fried, PhD, senior professor, Bob Shapell School of Social Work, Tel Aviv University, said in an interview that recovery is a “holistic concept that taps into many aspects of life.”
Understanding the “differences in the impact and availability” of negative and positive human resources and their effect on recovery “can help clinicians to customize treatment,” she said.
Complex interplay
GD is garnering increasing attention in the clinical community, especially since 2019, when the World Health Organization included it in the ICD-11.
“Although for most individuals, gaming is a recreational activity or even a passion, a small group of gamers experiences negative symptoms which impact their mental and physical health and cause functional impairment,” wrote Dr. Király and colleagues.
Dr. Griffiths explained that his team wanted to provide an “up-to-date primer – a ‘one-stop shop’ – on all things etiologic concerning gaming disorder for academics and practitioners” as well as others, such as health policy makers, teachers, and individuals in the gaming industry.
The researchers identified three factors that increase the risk of developing GD, the first being gaming-related factors, which make video games “addictive in a way that vulnerable individuals may develop GD.”
For example, GD is more prevalent among online versus offline game players, possibly because online multiplayer games “provide safe environments in which players can fulfill their social needs while remaining invisible and anonymous.”
Game genre also matters, with massively multiplayer online role-playing games, first-person/third-person shooter games, real-time strategy games, and multiplayer online battle arena games most implicated in problematic gaming. Moreover, the “monetization techniques” of certain games also increase their addictive potential.
The researchers point to individual factors that increase the risk of developing GD, including male sex and younger age, personality traits like impulsivity and sensation-seeking, and comorbidities including ADHD, anxiety, and depression.
Poor self-esteem and lack of social competencies make gaming “an easy and efficient way to compensate for these deficiencies, which in turn, heightens the risk for developing GD,” they add. Neurobiological processes and genetic predisposition also play a role.
Lastly, the authors mentioned environmental factors, including family and peer-group issues, problems at work or school, and cultural factors.
“The take-home messages are that problematic gaming has had a long history of empirical research; that the psychiatric community now views GD as a legitimate mental health issue; and that the reasons for GD are complex, with many different factors involved in the acquisition, development, and maintenance of GD,” said Dr. Griffiths.
Beneficial behavioral therapies
Yuzhou Chen and colleagues, Southwest University, Chongqing, China, conducted a systematic review of RCTs investigating interventions for treating GD. Despite the “large number of intervention approaches developed over the past decade, as yet, there are no authoritative guidelines for what makes an effective GD intervention,” they wrote.
Few studies have focused specifically on GD but instead have focused on a combination of internet addiction and GD. But the interventions used to treat internet addiction may not apply to GD. And few studies have utilized an RCT design. The researchers therefore set out to review studies that specifically used an RCT design to investigate interventions for GD.
They searched six databases to identify RCTs that tested GD interventions from the inception of each database until the end of 2021. To be included, participants had to be diagnosed with GD and receive either a “complete and systematic intervention” or be in a comparator control group receiving no intervention or placebo.
Seven studies met the inclusion criteria (n = 332 participants). The studies tested five interventions:
- Group counseling with three different themes (interpersonal interaction, acceptance and commitment, cognition and behavior)
- CBI, which addresses cravings
- Transcranial direct current stimulation (tDCS)
- ACRIP with the main objectives of reducing GD symptoms and improving psychological well-being
- Short-term CBT, which addresses maladaptive cognitions
The mean duration of the interventions ranged from 3 to 15 weeks.
The primary outcome was GD severity, with secondary outcomes including depression, anxiety, cognition, game time, self-esteem, self-compassion, shyness, impulsivity, and psychological well-being.
Group counseling, CBI, ACRIP, and short-term CBT interventions had “a significant effect on decreasing the severity of GD,” while tDCS had “no significant effect.”
Behavioral therapy “exerts its effect on the behavioral mechanism of GD; for example, by reducing the association between game-related stimuli and the game player’s response to them,” the authors suggested.
Behavioral therapy “exerts its effect on the behavioral mechanism of GD; for example, by reducing the association between game-related stimuli and the game-player’s response to them,” the authors suggested.
Recovery vs. pathology
Recovery “traditionally represents the transition from trauma and illness to health,” Dr. Gavriel-Fried and colleagues noted.
Two paradigms of recovery are “deficit based” and “strength based.” The first assesses recovery in terms of abstinence, sobriety, and symptom reduction; and the second focuses on “growth, rather than a reduction in pathology.”
But although recovery is “embedded within mental health addiction policies and practice,” the concept has received “scant attention” in GD research.
The researchers therefore aimed to “map and summarize the state of the art on recovery from GD,” defining “recovery” as the “ability to handle conflicting feelings and emotions without external mediation.”
They conducted a scoping review of all literature regarding GD or internet GD published before February 2022 (47 studies, 2,924 participants with GD; mean age range, 13-26 years).
Most studies (n = 32) consisted of exclusively male subjects. Only 10 included both sexes, and female participants were in the minority.
Most studies (n = 42) did not address the concept of recovery, although all studies did report significant improvements in gaming-related pathology. Typical terminology used to describe changes in participants’ GD were “reduction” and/or “decrease” in symptom severity.
Although 18 studies mentioned the word “recovery,” only 5 actually discussed issues related to the notion of recovery, and only 5 used the term “abstinence.”
In addition, only 13 studies examined positive components of life in patients with GD, such as increased psychological well-being, life satisfaction, quality of life, improved emotional state, relational skills, and executive control, as well as improved self-care, hygiene, sleep, and interest in school studies.
“As a person and researcher who believes that words shape the way we perceive things, I think we should use the word ‘recovery’ rather than ‘pathology’ much more in research, therapy, and policy,” said Dr. Gavriel-Fried.
She noted that, because GD is a “relatively new behavioral addictive disorder, theories are still being developed and definitions of the symptoms are still being fine-tuned.”
“The field as a whole will benefit from future theoretical work that will lead to practical solutions for treating GD and ways to identify the risk factors,” Dr. Gavriel-Fried said.
Filling a research gap
In a comment, David Greenfield, MD, founder and medical director of the Connecticut-based Center for Internet and Technology Addiction, noted that 3 decades ago, there was almost no research into this area.
“The fact that we have these reviews and studies is good because all of the research adds to the science providing more data about an area we still don’t know that much about, where research is still in its infancy,” said Dr. Greenfield, who was not involved with the present study.
“Although we have definitions, there’s no complete agreement about the definitions of GD, and we do not yet have a unified approach,” continued Dr. Greenfield, who wrote the books Overcoming Internet Addiction for Dummies and Virtual Addiction.
He suggested that “recovery” is rarely used as a concept in GD research perhaps because there’s a “bifurcation in the field of addiction medicine in which behavioral addictions are not seen as equivalent to substance addictions,” and, particularly with GD, the principles of “recovery” have not yet matured.
“Recovery means meaningful life away from the screen, not just abstinence from the screen,” said Dr. Greenfield.
The study by Mr. Chen and colleagues was supported by grants from the National Social Science Foundation of China, the Chongqing Research Program of Basic Research and Frontier Technology, and the Fundamental Research Funds for the Central Universities. Dr. Griffiths has reported receiving research funding from Norsk Tipping (the gambling operator owned by the Norwegian government). The study by Dr. Király and colleagues received support from the Hungarian National Research Development and Innovation Office and the Janos Bolyai Research Scholarship Academy of Sciences to individual investigators. The study by Dr. Gavriel-Fried and colleagues received support from the Hungarian National Research Development and Innovation Office and the Janos Bolyai Research Scholarship Academy of Sciences to individual investigators. Dr. Gavriel-Fried has reported receiving grants from the Israel National Insurance Institute and the Committee for Independent Studies of the Israel Lottery. Dr. Greenfield reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A team of international researchers led by Orsolya Király, PhD, of the Institute of Psychology, Eötvös Loránd University, Budapest, reviewed the characteristics and etiology of GD. They concluded that its genesis arises from the interaction of environmental factors, game-specific factors and individual factors, including personality traits, comorbid psychopathology, and genetic predisposition.
“The development of GD is a complex process and we identified three major factors involved,” study coauthor Mark Griffiths, PhD, distinguished professor of behavioral addiction and director of the international gaming research unit, psychology department, Nottingham (England) Trent University, said in an interview. Because of this complexity, “prevention and intervention in GD require multiprofessional action.”
The review was published in Comprehensive Psychiatry.
In a second paper, published online in Frontiers in Psychiatry, Chinese investigators reviewing randomized controlled trials (RCTs) presented “compelling evidence” to support four effective interventions for GD: group counseling, acceptance and cognitive restructuring intervention program (ACRIP), short-term cognitive-behavioral therapy (CBT), and craving behavioral intervention (CBI).
A third paper, published online in the Journal of Behavioral Addictions, in which researchers analyzed close to 50 studies of GD, found that the concept of “recovery” is rarely mentioned in GD research. Lead author Belle Gavriel-Fried, PhD, senior professor, Bob Shapell School of Social Work, Tel Aviv University, said in an interview that recovery is a “holistic concept that taps into many aspects of life.”
Understanding the “differences in the impact and availability” of negative and positive human resources and their effect on recovery “can help clinicians to customize treatment,” she said.
Complex interplay
GD is garnering increasing attention in the clinical community, especially since 2019, when the World Health Organization included it in the ICD-11.
“Although for most individuals, gaming is a recreational activity or even a passion, a small group of gamers experiences negative symptoms which impact their mental and physical health and cause functional impairment,” wrote Dr. Király and colleagues.
Dr. Griffiths explained that his team wanted to provide an “up-to-date primer – a ‘one-stop shop’ – on all things etiologic concerning gaming disorder for academics and practitioners” as well as others, such as health policy makers, teachers, and individuals in the gaming industry.
The researchers identified three factors that increase the risk of developing GD, the first being gaming-related factors, which make video games “addictive in a way that vulnerable individuals may develop GD.”
For example, GD is more prevalent among online versus offline game players, possibly because online multiplayer games “provide safe environments in which players can fulfill their social needs while remaining invisible and anonymous.”
Game genre also matters, with massively multiplayer online role-playing games, first-person/third-person shooter games, real-time strategy games, and multiplayer online battle arena games most implicated in problematic gaming. Moreover, the “monetization techniques” of certain games also increase their addictive potential.
The researchers point to individual factors that increase the risk of developing GD, including male sex and younger age, personality traits like impulsivity and sensation-seeking, and comorbidities including ADHD, anxiety, and depression.
Poor self-esteem and lack of social competencies make gaming “an easy and efficient way to compensate for these deficiencies, which in turn, heightens the risk for developing GD,” they add. Neurobiological processes and genetic predisposition also play a role.
Lastly, the authors mentioned environmental factors, including family and peer-group issues, problems at work or school, and cultural factors.
“The take-home messages are that problematic gaming has had a long history of empirical research; that the psychiatric community now views GD as a legitimate mental health issue; and that the reasons for GD are complex, with many different factors involved in the acquisition, development, and maintenance of GD,” said Dr. Griffiths.
Beneficial behavioral therapies
Yuzhou Chen and colleagues, Southwest University, Chongqing, China, conducted a systematic review of RCTs investigating interventions for treating GD. Despite the “large number of intervention approaches developed over the past decade, as yet, there are no authoritative guidelines for what makes an effective GD intervention,” they wrote.
Few studies have focused specifically on GD but instead have focused on a combination of internet addiction and GD. But the interventions used to treat internet addiction may not apply to GD. And few studies have utilized an RCT design. The researchers therefore set out to review studies that specifically used an RCT design to investigate interventions for GD.
They searched six databases to identify RCTs that tested GD interventions from the inception of each database until the end of 2021. To be included, participants had to be diagnosed with GD and receive either a “complete and systematic intervention” or be in a comparator control group receiving no intervention or placebo.
Seven studies met the inclusion criteria (n = 332 participants). The studies tested five interventions:
- Group counseling with three different themes (interpersonal interaction, acceptance and commitment, cognition and behavior)
- CBI, which addresses cravings
- Transcranial direct current stimulation (tDCS)
- ACRIP with the main objectives of reducing GD symptoms and improving psychological well-being
- Short-term CBT, which addresses maladaptive cognitions
The mean duration of the interventions ranged from 3 to 15 weeks.
The primary outcome was GD severity, with secondary outcomes including depression, anxiety, cognition, game time, self-esteem, self-compassion, shyness, impulsivity, and psychological well-being.
Group counseling, CBI, ACRIP, and short-term CBT interventions had “a significant effect on decreasing the severity of GD,” while tDCS had “no significant effect.”
Behavioral therapy “exerts its effect on the behavioral mechanism of GD; for example, by reducing the association between game-related stimuli and the game player’s response to them,” the authors suggested.
Behavioral therapy “exerts its effect on the behavioral mechanism of GD; for example, by reducing the association between game-related stimuli and the game-player’s response to them,” the authors suggested.
Recovery vs. pathology
Recovery “traditionally represents the transition from trauma and illness to health,” Dr. Gavriel-Fried and colleagues noted.
Two paradigms of recovery are “deficit based” and “strength based.” The first assesses recovery in terms of abstinence, sobriety, and symptom reduction; and the second focuses on “growth, rather than a reduction in pathology.”
But although recovery is “embedded within mental health addiction policies and practice,” the concept has received “scant attention” in GD research.
The researchers therefore aimed to “map and summarize the state of the art on recovery from GD,” defining “recovery” as the “ability to handle conflicting feelings and emotions without external mediation.”
They conducted a scoping review of all literature regarding GD or internet GD published before February 2022 (47 studies, 2,924 participants with GD; mean age range, 13-26 years).
Most studies (n = 32) consisted of exclusively male subjects. Only 10 included both sexes, and female participants were in the minority.
Most studies (n = 42) did not address the concept of recovery, although all studies did report significant improvements in gaming-related pathology. Typical terminology used to describe changes in participants’ GD were “reduction” and/or “decrease” in symptom severity.
Although 18 studies mentioned the word “recovery,” only 5 actually discussed issues related to the notion of recovery, and only 5 used the term “abstinence.”
In addition, only 13 studies examined positive components of life in patients with GD, such as increased psychological well-being, life satisfaction, quality of life, improved emotional state, relational skills, and executive control, as well as improved self-care, hygiene, sleep, and interest in school studies.
“As a person and researcher who believes that words shape the way we perceive things, I think we should use the word ‘recovery’ rather than ‘pathology’ much more in research, therapy, and policy,” said Dr. Gavriel-Fried.
She noted that, because GD is a “relatively new behavioral addictive disorder, theories are still being developed and definitions of the symptoms are still being fine-tuned.”
“The field as a whole will benefit from future theoretical work that will lead to practical solutions for treating GD and ways to identify the risk factors,” Dr. Gavriel-Fried said.
Filling a research gap
In a comment, David Greenfield, MD, founder and medical director of the Connecticut-based Center for Internet and Technology Addiction, noted that 3 decades ago, there was almost no research into this area.
“The fact that we have these reviews and studies is good because all of the research adds to the science providing more data about an area we still don’t know that much about, where research is still in its infancy,” said Dr. Greenfield, who was not involved with the present study.
“Although we have definitions, there’s no complete agreement about the definitions of GD, and we do not yet have a unified approach,” continued Dr. Greenfield, who wrote the books Overcoming Internet Addiction for Dummies and Virtual Addiction.
He suggested that “recovery” is rarely used as a concept in GD research perhaps because there’s a “bifurcation in the field of addiction medicine in which behavioral addictions are not seen as equivalent to substance addictions,” and, particularly with GD, the principles of “recovery” have not yet matured.
“Recovery means meaningful life away from the screen, not just abstinence from the screen,” said Dr. Greenfield.
The study by Mr. Chen and colleagues was supported by grants from the National Social Science Foundation of China, the Chongqing Research Program of Basic Research and Frontier Technology, and the Fundamental Research Funds for the Central Universities. Dr. Griffiths has reported receiving research funding from Norsk Tipping (the gambling operator owned by the Norwegian government). The study by Dr. Király and colleagues received support from the Hungarian National Research Development and Innovation Office and the Janos Bolyai Research Scholarship Academy of Sciences to individual investigators. The study by Dr. Gavriel-Fried and colleagues received support from the Hungarian National Research Development and Innovation Office and the Janos Bolyai Research Scholarship Academy of Sciences to individual investigators. Dr. Gavriel-Fried has reported receiving grants from the Israel National Insurance Institute and the Committee for Independent Studies of the Israel Lottery. Dr. Greenfield reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A team of international researchers led by Orsolya Király, PhD, of the Institute of Psychology, Eötvös Loránd University, Budapest, reviewed the characteristics and etiology of GD. They concluded that its genesis arises from the interaction of environmental factors, game-specific factors and individual factors, including personality traits, comorbid psychopathology, and genetic predisposition.
“The development of GD is a complex process and we identified three major factors involved,” study coauthor Mark Griffiths, PhD, distinguished professor of behavioral addiction and director of the international gaming research unit, psychology department, Nottingham (England) Trent University, said in an interview. Because of this complexity, “prevention and intervention in GD require multiprofessional action.”
The review was published in Comprehensive Psychiatry.
In a second paper, published online in Frontiers in Psychiatry, Chinese investigators reviewing randomized controlled trials (RCTs) presented “compelling evidence” to support four effective interventions for GD: group counseling, acceptance and cognitive restructuring intervention program (ACRIP), short-term cognitive-behavioral therapy (CBT), and craving behavioral intervention (CBI).
A third paper, published online in the Journal of Behavioral Addictions, in which researchers analyzed close to 50 studies of GD, found that the concept of “recovery” is rarely mentioned in GD research. Lead author Belle Gavriel-Fried, PhD, senior professor, Bob Shapell School of Social Work, Tel Aviv University, said in an interview that recovery is a “holistic concept that taps into many aspects of life.”
Understanding the “differences in the impact and availability” of negative and positive human resources and their effect on recovery “can help clinicians to customize treatment,” she said.
Complex interplay
GD is garnering increasing attention in the clinical community, especially since 2019, when the World Health Organization included it in the ICD-11.
“Although for most individuals, gaming is a recreational activity or even a passion, a small group of gamers experiences negative symptoms which impact their mental and physical health and cause functional impairment,” wrote Dr. Király and colleagues.
Dr. Griffiths explained that his team wanted to provide an “up-to-date primer – a ‘one-stop shop’ – on all things etiologic concerning gaming disorder for academics and practitioners” as well as others, such as health policy makers, teachers, and individuals in the gaming industry.
The researchers identified three factors that increase the risk of developing GD, the first being gaming-related factors, which make video games “addictive in a way that vulnerable individuals may develop GD.”
For example, GD is more prevalent among online versus offline game players, possibly because online multiplayer games “provide safe environments in which players can fulfill their social needs while remaining invisible and anonymous.”
Game genre also matters, with massively multiplayer online role-playing games, first-person/third-person shooter games, real-time strategy games, and multiplayer online battle arena games most implicated in problematic gaming. Moreover, the “monetization techniques” of certain games also increase their addictive potential.
The researchers point to individual factors that increase the risk of developing GD, including male sex and younger age, personality traits like impulsivity and sensation-seeking, and comorbidities including ADHD, anxiety, and depression.
Poor self-esteem and lack of social competencies make gaming “an easy and efficient way to compensate for these deficiencies, which in turn, heightens the risk for developing GD,” they add. Neurobiological processes and genetic predisposition also play a role.
Lastly, the authors mentioned environmental factors, including family and peer-group issues, problems at work or school, and cultural factors.
“The take-home messages are that problematic gaming has had a long history of empirical research; that the psychiatric community now views GD as a legitimate mental health issue; and that the reasons for GD are complex, with many different factors involved in the acquisition, development, and maintenance of GD,” said Dr. Griffiths.
Beneficial behavioral therapies
Yuzhou Chen and colleagues, Southwest University, Chongqing, China, conducted a systematic review of RCTs investigating interventions for treating GD. Despite the “large number of intervention approaches developed over the past decade, as yet, there are no authoritative guidelines for what makes an effective GD intervention,” they wrote.
Few studies have focused specifically on GD but instead have focused on a combination of internet addiction and GD. But the interventions used to treat internet addiction may not apply to GD. And few studies have utilized an RCT design. The researchers therefore set out to review studies that specifically used an RCT design to investigate interventions for GD.
They searched six databases to identify RCTs that tested GD interventions from the inception of each database until the end of 2021. To be included, participants had to be diagnosed with GD and receive either a “complete and systematic intervention” or be in a comparator control group receiving no intervention or placebo.
Seven studies met the inclusion criteria (n = 332 participants). The studies tested five interventions:
- Group counseling with three different themes (interpersonal interaction, acceptance and commitment, cognition and behavior)
- CBI, which addresses cravings
- Transcranial direct current stimulation (tDCS)
- ACRIP with the main objectives of reducing GD symptoms and improving psychological well-being
- Short-term CBT, which addresses maladaptive cognitions
The mean duration of the interventions ranged from 3 to 15 weeks.
The primary outcome was GD severity, with secondary outcomes including depression, anxiety, cognition, game time, self-esteem, self-compassion, shyness, impulsivity, and psychological well-being.
Group counseling, CBI, ACRIP, and short-term CBT interventions had “a significant effect on decreasing the severity of GD,” while tDCS had “no significant effect.”
Behavioral therapy “exerts its effect on the behavioral mechanism of GD; for example, by reducing the association between game-related stimuli and the game player’s response to them,” the authors suggested.
Behavioral therapy “exerts its effect on the behavioral mechanism of GD; for example, by reducing the association between game-related stimuli and the game-player’s response to them,” the authors suggested.
Recovery vs. pathology
Recovery “traditionally represents the transition from trauma and illness to health,” Dr. Gavriel-Fried and colleagues noted.
Two paradigms of recovery are “deficit based” and “strength based.” The first assesses recovery in terms of abstinence, sobriety, and symptom reduction; and the second focuses on “growth, rather than a reduction in pathology.”
But although recovery is “embedded within mental health addiction policies and practice,” the concept has received “scant attention” in GD research.
The researchers therefore aimed to “map and summarize the state of the art on recovery from GD,” defining “recovery” as the “ability to handle conflicting feelings and emotions without external mediation.”
They conducted a scoping review of all literature regarding GD or internet GD published before February 2022 (47 studies, 2,924 participants with GD; mean age range, 13-26 years).
Most studies (n = 32) consisted of exclusively male subjects. Only 10 included both sexes, and female participants were in the minority.
Most studies (n = 42) did not address the concept of recovery, although all studies did report significant improvements in gaming-related pathology. Typical terminology used to describe changes in participants’ GD were “reduction” and/or “decrease” in symptom severity.
Although 18 studies mentioned the word “recovery,” only 5 actually discussed issues related to the notion of recovery, and only 5 used the term “abstinence.”
In addition, only 13 studies examined positive components of life in patients with GD, such as increased psychological well-being, life satisfaction, quality of life, improved emotional state, relational skills, and executive control, as well as improved self-care, hygiene, sleep, and interest in school studies.
“As a person and researcher who believes that words shape the way we perceive things, I think we should use the word ‘recovery’ rather than ‘pathology’ much more in research, therapy, and policy,” said Dr. Gavriel-Fried.
She noted that, because GD is a “relatively new behavioral addictive disorder, theories are still being developed and definitions of the symptoms are still being fine-tuned.”
“The field as a whole will benefit from future theoretical work that will lead to practical solutions for treating GD and ways to identify the risk factors,” Dr. Gavriel-Fried said.
Filling a research gap
In a comment, David Greenfield, MD, founder and medical director of the Connecticut-based Center for Internet and Technology Addiction, noted that 3 decades ago, there was almost no research into this area.
“The fact that we have these reviews and studies is good because all of the research adds to the science providing more data about an area we still don’t know that much about, where research is still in its infancy,” said Dr. Greenfield, who was not involved with the present study.
“Although we have definitions, there’s no complete agreement about the definitions of GD, and we do not yet have a unified approach,” continued Dr. Greenfield, who wrote the books Overcoming Internet Addiction for Dummies and Virtual Addiction.
He suggested that “recovery” is rarely used as a concept in GD research perhaps because there’s a “bifurcation in the field of addiction medicine in which behavioral addictions are not seen as equivalent to substance addictions,” and, particularly with GD, the principles of “recovery” have not yet matured.
“Recovery means meaningful life away from the screen, not just abstinence from the screen,” said Dr. Greenfield.
The study by Mr. Chen and colleagues was supported by grants from the National Social Science Foundation of China, the Chongqing Research Program of Basic Research and Frontier Technology, and the Fundamental Research Funds for the Central Universities. Dr. Griffiths has reported receiving research funding from Norsk Tipping (the gambling operator owned by the Norwegian government). The study by Dr. Király and colleagues received support from the Hungarian National Research Development and Innovation Office and the Janos Bolyai Research Scholarship Academy of Sciences to individual investigators. The study by Dr. Gavriel-Fried and colleagues received support from the Hungarian National Research Development and Innovation Office and the Janos Bolyai Research Scholarship Academy of Sciences to individual investigators. Dr. Gavriel-Fried has reported receiving grants from the Israel National Insurance Institute and the Committee for Independent Studies of the Israel Lottery. Dr. Greenfield reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New guidelines for cannabis in chronic pain management released
New clinical practice guidelines for cannabis in chronic pain management have been released.
Developed by a group of Canadian researchers, clinicians, and patients, the guidelines note that cannabinoid-based medicines (CBM) may help clinicians offer an effective, less addictive, alternative to opioids in patients with chronic noncancer pain and comorbid conditions.
“We don’t recommend using CBM first line for anything pretty much because there are other alternatives that may be more effective and also offer fewer side effects,” lead guideline author Alan Bell, MD, assistant professor of family and community medicine at the University of Toronto, told this news organization.
“But I would strongly argue that I would use cannabis-based medicine over opioids every time. Why would you use a high potency-high toxicity agent when there’s a low potency-low toxicity alternative?” he said.
The guidelines were published online in the journal Cannabis and Cannabinoid Research.
Examining the evidence
A consistent criticism of CBM has been the lack of quality research supporting its therapeutic utility. To develop the current recommendations, the task force reviewed 47 pain management studies enrolling more than 11,000 patients. Almost half of the studies (n = 22) were randomized controlled trials (RCTs) and 12 of the 19 included systematic reviews focused solely on RCTs.
Overall, 38 of the 47 included studies demonstrated that CBM provided at least moderate benefits for chronic pain, resulting in a “strong” recommendation – mostly as an adjunct or replacement treatment in individuals living with chronic pain.
Overall, the guidelines place a high value on improving chronic pain and functionality, and addressing co-occurring conditions such as insomnia, anxiety and depression, mobility, and inflammation. They also provide practical dosing and formulation tips to support the use of CBM in the clinical setting.
When it comes to chronic pain, CBM is not a panacea. However, prior research suggests cannabinoids and opioids share several pharmacologic properties, including independent but possibly related mechanisms for antinociception, making them an intriguing combination.
In the current guidelines, all of the four studies specifically addressing combined opioids and vaporized cannabis flower demonstrated further pain reduction, reinforcing the conclusion that the benefits of CBM for improving pain control in patients taking opioids outweigh the risk of nonserious adverse events (AEs), such as dry mouth, dizziness, increased appetite, sedation, and concentration difficulties.
The recommendations also highlighted evidence demonstrating that a majority of participants were able to reduce use of routine pain medications with concomitant CBM/opioid administration, while simultaneously offering secondary benefits such as improved sleep, anxiety, and mood, as well as prevention of opioid tolerance and dose escalation.
Importantly, the guidelines offer an evidence-based algorithm with a clear framework for tapering patients off opioids, especially those who are on > 50 mg MED, which places them with a twofold greater risk for fatal overdose.
An effective alternative
Commenting on the new guidelines, Mark Wallace, MD, who has extensive experience researching and treating pain patients with medical cannabis, said the genesis of his interest in medical cannabis mirrors the guidelines’ focus.
“What got me interested in medical cannabis was trying to get patients off of opioids,” said Dr. Wallace, professor of anesthesiology and chief of the division of pain medicine in the department of anesthesiology at the University of California, San Diego. Dr. Wallace, who was not involved in the guidelines’ development study, said that he’s “titrated hundreds of patients off of opioids using cannabis.”
Dr. Wallace said he found the guidelines’ dosing recommendations helpful.
“If you stay within the 1- to 5-mg dosing range, the risks are so incredibly low, you’re not going to harm the patient.”
While there are patients who abuse cannabis and CBMs, Dr. Wallace noted that he has seen only one patient in the past 20 years who was overusing the medical cannabis. He added that his patient population does not use medical cannabis to get high and, in fact, wants to avoid doses that produce that effect at all costs.
Also commenting on the guidelines, Christopher Gilligan, MD, MBA, associate chief medical officer and a pain medicine physician at Brigham and Women’s Hospital in Boston, who was not involved in the guidelines’ development, points to the risks.
“When we have an opportunity to use cannabinoids in place of opioids for our patients, I think that that’s a positive thing ... and a wise choice in terms of risk benefit,” Dr. Gilligan said.
On the other hand, he cautioned that “freely prescribing” cannabinoids for chronic pain in patients who aren’t on opioids is not good practice.
“We have to take seriously the potential adverse effects of [cannabis], including marijuana use disorder, interference with learning, memory impairment, and psychotic breakthroughs,” said Dr. Gilligan.
Given the current climate, it would appear that CBM is a long way from being endorsed by the Food and Drug Administration, but for clinicians interested in trying CBM for chronic pain patients, the guidelines may offer a roadmap for initiation and an alternative to prescribing opioids.
Dr. Bell, Dr. Gilligan, and Dr. Wallace report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New clinical practice guidelines for cannabis in chronic pain management have been released.
Developed by a group of Canadian researchers, clinicians, and patients, the guidelines note that cannabinoid-based medicines (CBM) may help clinicians offer an effective, less addictive, alternative to opioids in patients with chronic noncancer pain and comorbid conditions.
“We don’t recommend using CBM first line for anything pretty much because there are other alternatives that may be more effective and also offer fewer side effects,” lead guideline author Alan Bell, MD, assistant professor of family and community medicine at the University of Toronto, told this news organization.
“But I would strongly argue that I would use cannabis-based medicine over opioids every time. Why would you use a high potency-high toxicity agent when there’s a low potency-low toxicity alternative?” he said.
The guidelines were published online in the journal Cannabis and Cannabinoid Research.
Examining the evidence
A consistent criticism of CBM has been the lack of quality research supporting its therapeutic utility. To develop the current recommendations, the task force reviewed 47 pain management studies enrolling more than 11,000 patients. Almost half of the studies (n = 22) were randomized controlled trials (RCTs) and 12 of the 19 included systematic reviews focused solely on RCTs.
Overall, 38 of the 47 included studies demonstrated that CBM provided at least moderate benefits for chronic pain, resulting in a “strong” recommendation – mostly as an adjunct or replacement treatment in individuals living with chronic pain.
Overall, the guidelines place a high value on improving chronic pain and functionality, and addressing co-occurring conditions such as insomnia, anxiety and depression, mobility, and inflammation. They also provide practical dosing and formulation tips to support the use of CBM in the clinical setting.
When it comes to chronic pain, CBM is not a panacea. However, prior research suggests cannabinoids and opioids share several pharmacologic properties, including independent but possibly related mechanisms for antinociception, making them an intriguing combination.
In the current guidelines, all of the four studies specifically addressing combined opioids and vaporized cannabis flower demonstrated further pain reduction, reinforcing the conclusion that the benefits of CBM for improving pain control in patients taking opioids outweigh the risk of nonserious adverse events (AEs), such as dry mouth, dizziness, increased appetite, sedation, and concentration difficulties.
The recommendations also highlighted evidence demonstrating that a majority of participants were able to reduce use of routine pain medications with concomitant CBM/opioid administration, while simultaneously offering secondary benefits such as improved sleep, anxiety, and mood, as well as prevention of opioid tolerance and dose escalation.
Importantly, the guidelines offer an evidence-based algorithm with a clear framework for tapering patients off opioids, especially those who are on > 50 mg MED, which places them with a twofold greater risk for fatal overdose.
An effective alternative
Commenting on the new guidelines, Mark Wallace, MD, who has extensive experience researching and treating pain patients with medical cannabis, said the genesis of his interest in medical cannabis mirrors the guidelines’ focus.
“What got me interested in medical cannabis was trying to get patients off of opioids,” said Dr. Wallace, professor of anesthesiology and chief of the division of pain medicine in the department of anesthesiology at the University of California, San Diego. Dr. Wallace, who was not involved in the guidelines’ development study, said that he’s “titrated hundreds of patients off of opioids using cannabis.”
Dr. Wallace said he found the guidelines’ dosing recommendations helpful.
“If you stay within the 1- to 5-mg dosing range, the risks are so incredibly low, you’re not going to harm the patient.”
While there are patients who abuse cannabis and CBMs, Dr. Wallace noted that he has seen only one patient in the past 20 years who was overusing the medical cannabis. He added that his patient population does not use medical cannabis to get high and, in fact, wants to avoid doses that produce that effect at all costs.
Also commenting on the guidelines, Christopher Gilligan, MD, MBA, associate chief medical officer and a pain medicine physician at Brigham and Women’s Hospital in Boston, who was not involved in the guidelines’ development, points to the risks.
“When we have an opportunity to use cannabinoids in place of opioids for our patients, I think that that’s a positive thing ... and a wise choice in terms of risk benefit,” Dr. Gilligan said.
On the other hand, he cautioned that “freely prescribing” cannabinoids for chronic pain in patients who aren’t on opioids is not good practice.
“We have to take seriously the potential adverse effects of [cannabis], including marijuana use disorder, interference with learning, memory impairment, and psychotic breakthroughs,” said Dr. Gilligan.
Given the current climate, it would appear that CBM is a long way from being endorsed by the Food and Drug Administration, but for clinicians interested in trying CBM for chronic pain patients, the guidelines may offer a roadmap for initiation and an alternative to prescribing opioids.
Dr. Bell, Dr. Gilligan, and Dr. Wallace report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New clinical practice guidelines for cannabis in chronic pain management have been released.
Developed by a group of Canadian researchers, clinicians, and patients, the guidelines note that cannabinoid-based medicines (CBM) may help clinicians offer an effective, less addictive, alternative to opioids in patients with chronic noncancer pain and comorbid conditions.
“We don’t recommend using CBM first line for anything pretty much because there are other alternatives that may be more effective and also offer fewer side effects,” lead guideline author Alan Bell, MD, assistant professor of family and community medicine at the University of Toronto, told this news organization.
“But I would strongly argue that I would use cannabis-based medicine over opioids every time. Why would you use a high potency-high toxicity agent when there’s a low potency-low toxicity alternative?” he said.
The guidelines were published online in the journal Cannabis and Cannabinoid Research.
Examining the evidence
A consistent criticism of CBM has been the lack of quality research supporting its therapeutic utility. To develop the current recommendations, the task force reviewed 47 pain management studies enrolling more than 11,000 patients. Almost half of the studies (n = 22) were randomized controlled trials (RCTs) and 12 of the 19 included systematic reviews focused solely on RCTs.
Overall, 38 of the 47 included studies demonstrated that CBM provided at least moderate benefits for chronic pain, resulting in a “strong” recommendation – mostly as an adjunct or replacement treatment in individuals living with chronic pain.
Overall, the guidelines place a high value on improving chronic pain and functionality, and addressing co-occurring conditions such as insomnia, anxiety and depression, mobility, and inflammation. They also provide practical dosing and formulation tips to support the use of CBM in the clinical setting.
When it comes to chronic pain, CBM is not a panacea. However, prior research suggests cannabinoids and opioids share several pharmacologic properties, including independent but possibly related mechanisms for antinociception, making them an intriguing combination.
In the current guidelines, all of the four studies specifically addressing combined opioids and vaporized cannabis flower demonstrated further pain reduction, reinforcing the conclusion that the benefits of CBM for improving pain control in patients taking opioids outweigh the risk of nonserious adverse events (AEs), such as dry mouth, dizziness, increased appetite, sedation, and concentration difficulties.
The recommendations also highlighted evidence demonstrating that a majority of participants were able to reduce use of routine pain medications with concomitant CBM/opioid administration, while simultaneously offering secondary benefits such as improved sleep, anxiety, and mood, as well as prevention of opioid tolerance and dose escalation.
Importantly, the guidelines offer an evidence-based algorithm with a clear framework for tapering patients off opioids, especially those who are on > 50 mg MED, which places them with a twofold greater risk for fatal overdose.
An effective alternative
Commenting on the new guidelines, Mark Wallace, MD, who has extensive experience researching and treating pain patients with medical cannabis, said the genesis of his interest in medical cannabis mirrors the guidelines’ focus.
“What got me interested in medical cannabis was trying to get patients off of opioids,” said Dr. Wallace, professor of anesthesiology and chief of the division of pain medicine in the department of anesthesiology at the University of California, San Diego. Dr. Wallace, who was not involved in the guidelines’ development study, said that he’s “titrated hundreds of patients off of opioids using cannabis.”
Dr. Wallace said he found the guidelines’ dosing recommendations helpful.
“If you stay within the 1- to 5-mg dosing range, the risks are so incredibly low, you’re not going to harm the patient.”
While there are patients who abuse cannabis and CBMs, Dr. Wallace noted that he has seen only one patient in the past 20 years who was overusing the medical cannabis. He added that his patient population does not use medical cannabis to get high and, in fact, wants to avoid doses that produce that effect at all costs.
Also commenting on the guidelines, Christopher Gilligan, MD, MBA, associate chief medical officer and a pain medicine physician at Brigham and Women’s Hospital in Boston, who was not involved in the guidelines’ development, points to the risks.
“When we have an opportunity to use cannabinoids in place of opioids for our patients, I think that that’s a positive thing ... and a wise choice in terms of risk benefit,” Dr. Gilligan said.
On the other hand, he cautioned that “freely prescribing” cannabinoids for chronic pain in patients who aren’t on opioids is not good practice.
“We have to take seriously the potential adverse effects of [cannabis], including marijuana use disorder, interference with learning, memory impairment, and psychotic breakthroughs,” said Dr. Gilligan.
Given the current climate, it would appear that CBM is a long way from being endorsed by the Food and Drug Administration, but for clinicians interested in trying CBM for chronic pain patients, the guidelines may offer a roadmap for initiation and an alternative to prescribing opioids.
Dr. Bell, Dr. Gilligan, and Dr. Wallace report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CANNABIS AND CANNABINOID RESEARCH
Four PTSD blood biomarkers identified
“More accurate means of predicting or screening for PTSD could help to overcome the disorder by identifying individuals at high risk of developing PTSD and providing them with early intervention or prevention strategies,” said study investigator Stacy-Ann Miller, MS.
She also noted that the biomarkers could be used to monitor treatment for PTSD, identify subtypes of PTSD, and lead to a new understanding of the mechanisms underlying PTSD.
The findings were presented at Discover BMB, the annual meeting of the American Society for Biochemistry and Molecular Biology.
Toward better clinical assessment
The findings originated from research conducted by the Department of Defense–initiated PTSD Systems Biology Consortium. The consortium’s goals include developing a reproducible panel of blood-based biomarkers with high sensitivity and specificity for PTSD diagnosis and is made up of about 45 researchers, led by Marti Jett, PhD, Charles Marmar, MD, and Francis J. Doyle III, PhD.
The researchers analyzed blood samples from 1,000 active-duty Army personnel from the 101st Airborne at Fort Campbell, Ky. Participants were assessed before and after deployment to Afghanistan in February 2014 and are referred to as the Fort Campbell Cohort (FCC). Participants’ age ranged from 25 to 30 and approximately 6% were female.
Investigators collected blood samples from the service members and looked for four biomarkers: glycolytic ratio, arginine, serotonin, and glutamate. The team then divided the participants into four groups – those with PTSD (PTSD Checklist score above 30), those who were subthreshold for PTSD (PTSD Checklist score 15-30), those who had high resilience, and those who had low levels of resilience.
The resilience groups were determined based on answers to the Generalized Anxiety Disorder Questionnaire, Patient Health Questionnaire, Pittsburgh Sleep Quality Index, Intensive Combat Exposure (DRRI-D), the number of deployments, whether they had moderate or severe traumatic brain injury, and scores on the Alcohol Use Disorders Identification Test.
Those who scored in the high range at current or prior time points or who were PTSD/subthreshold at prior time points were placed in the low resilience group.
Ms. Miller noted that those in the PTSD group had more severe symptoms than those in the PTSD subthreshold group based on the longitudinal clinical assessment at 3-6 months, 5 years, and longer post deployment. The low resilience group had a much higher rate of PTSD post deployment than the high resilience group.
Investigators found participants with PTSD or subthreshold PTSD had significantly higher glycolic ratios and lower arginine than those with high resilience. They also found that those with PTSD had significantly lower serotonin and higher glutamate levels versus those with high resilience. These associations were independent of factors such as sex, age, body mass index, smoking, and caffeine consumption.
Ms. Miller said that the study results require further validation by the consortium’s labs and third-party labs.
“We are also interested in determining the most appropriate time to screen soldiers for PTSD, as it has been noted that the time period where we see the most psychological issues is around 2-3 months post return from deployment and when the soldier is preparing for their next assignment, perhaps a next deployment,” she said.
She added that previous studies have identified several promising biomarkers of PTSD. “However, like much of the research data, the study sample was comprised mainly of combat-exposed males. With more women serving on the front lines, the military faces new challenges in how combat affects females in the military,” including sex-specific biomarkers that will improve clinical assessment for female soldiers.
Eventually, the team would also like to be able to apply their research to the civilian population experiencing PTSD.
“Our research is anticipated to be useful in helping the medical provider select appropriate therapeutic interventions,” Ms. Miller said.
A version of this article first appeared on Medscape.com.
“More accurate means of predicting or screening for PTSD could help to overcome the disorder by identifying individuals at high risk of developing PTSD and providing them with early intervention or prevention strategies,” said study investigator Stacy-Ann Miller, MS.
She also noted that the biomarkers could be used to monitor treatment for PTSD, identify subtypes of PTSD, and lead to a new understanding of the mechanisms underlying PTSD.
The findings were presented at Discover BMB, the annual meeting of the American Society for Biochemistry and Molecular Biology.
Toward better clinical assessment
The findings originated from research conducted by the Department of Defense–initiated PTSD Systems Biology Consortium. The consortium’s goals include developing a reproducible panel of blood-based biomarkers with high sensitivity and specificity for PTSD diagnosis and is made up of about 45 researchers, led by Marti Jett, PhD, Charles Marmar, MD, and Francis J. Doyle III, PhD.
The researchers analyzed blood samples from 1,000 active-duty Army personnel from the 101st Airborne at Fort Campbell, Ky. Participants were assessed before and after deployment to Afghanistan in February 2014 and are referred to as the Fort Campbell Cohort (FCC). Participants’ age ranged from 25 to 30 and approximately 6% were female.
Investigators collected blood samples from the service members and looked for four biomarkers: glycolytic ratio, arginine, serotonin, and glutamate. The team then divided the participants into four groups – those with PTSD (PTSD Checklist score above 30), those who were subthreshold for PTSD (PTSD Checklist score 15-30), those who had high resilience, and those who had low levels of resilience.
The resilience groups were determined based on answers to the Generalized Anxiety Disorder Questionnaire, Patient Health Questionnaire, Pittsburgh Sleep Quality Index, Intensive Combat Exposure (DRRI-D), the number of deployments, whether they had moderate or severe traumatic brain injury, and scores on the Alcohol Use Disorders Identification Test.
Those who scored in the high range at current or prior time points or who were PTSD/subthreshold at prior time points were placed in the low resilience group.
Ms. Miller noted that those in the PTSD group had more severe symptoms than those in the PTSD subthreshold group based on the longitudinal clinical assessment at 3-6 months, 5 years, and longer post deployment. The low resilience group had a much higher rate of PTSD post deployment than the high resilience group.
Investigators found participants with PTSD or subthreshold PTSD had significantly higher glycolic ratios and lower arginine than those with high resilience. They also found that those with PTSD had significantly lower serotonin and higher glutamate levels versus those with high resilience. These associations were independent of factors such as sex, age, body mass index, smoking, and caffeine consumption.
Ms. Miller said that the study results require further validation by the consortium’s labs and third-party labs.
“We are also interested in determining the most appropriate time to screen soldiers for PTSD, as it has been noted that the time period where we see the most psychological issues is around 2-3 months post return from deployment and when the soldier is preparing for their next assignment, perhaps a next deployment,” she said.
She added that previous studies have identified several promising biomarkers of PTSD. “However, like much of the research data, the study sample was comprised mainly of combat-exposed males. With more women serving on the front lines, the military faces new challenges in how combat affects females in the military,” including sex-specific biomarkers that will improve clinical assessment for female soldiers.
Eventually, the team would also like to be able to apply their research to the civilian population experiencing PTSD.
“Our research is anticipated to be useful in helping the medical provider select appropriate therapeutic interventions,” Ms. Miller said.
A version of this article first appeared on Medscape.com.
“More accurate means of predicting or screening for PTSD could help to overcome the disorder by identifying individuals at high risk of developing PTSD and providing them with early intervention or prevention strategies,” said study investigator Stacy-Ann Miller, MS.
She also noted that the biomarkers could be used to monitor treatment for PTSD, identify subtypes of PTSD, and lead to a new understanding of the mechanisms underlying PTSD.
The findings were presented at Discover BMB, the annual meeting of the American Society for Biochemistry and Molecular Biology.
Toward better clinical assessment
The findings originated from research conducted by the Department of Defense–initiated PTSD Systems Biology Consortium. The consortium’s goals include developing a reproducible panel of blood-based biomarkers with high sensitivity and specificity for PTSD diagnosis and is made up of about 45 researchers, led by Marti Jett, PhD, Charles Marmar, MD, and Francis J. Doyle III, PhD.
The researchers analyzed blood samples from 1,000 active-duty Army personnel from the 101st Airborne at Fort Campbell, Ky. Participants were assessed before and after deployment to Afghanistan in February 2014 and are referred to as the Fort Campbell Cohort (FCC). Participants’ age ranged from 25 to 30 and approximately 6% were female.
Investigators collected blood samples from the service members and looked for four biomarkers: glycolytic ratio, arginine, serotonin, and glutamate. The team then divided the participants into four groups – those with PTSD (PTSD Checklist score above 30), those who were subthreshold for PTSD (PTSD Checklist score 15-30), those who had high resilience, and those who had low levels of resilience.
The resilience groups were determined based on answers to the Generalized Anxiety Disorder Questionnaire, Patient Health Questionnaire, Pittsburgh Sleep Quality Index, Intensive Combat Exposure (DRRI-D), the number of deployments, whether they had moderate or severe traumatic brain injury, and scores on the Alcohol Use Disorders Identification Test.
Those who scored in the high range at current or prior time points or who were PTSD/subthreshold at prior time points were placed in the low resilience group.
Ms. Miller noted that those in the PTSD group had more severe symptoms than those in the PTSD subthreshold group based on the longitudinal clinical assessment at 3-6 months, 5 years, and longer post deployment. The low resilience group had a much higher rate of PTSD post deployment than the high resilience group.
Investigators found participants with PTSD or subthreshold PTSD had significantly higher glycolic ratios and lower arginine than those with high resilience. They also found that those with PTSD had significantly lower serotonin and higher glutamate levels versus those with high resilience. These associations were independent of factors such as sex, age, body mass index, smoking, and caffeine consumption.
Ms. Miller said that the study results require further validation by the consortium’s labs and third-party labs.
“We are also interested in determining the most appropriate time to screen soldiers for PTSD, as it has been noted that the time period where we see the most psychological issues is around 2-3 months post return from deployment and when the soldier is preparing for their next assignment, perhaps a next deployment,” she said.
She added that previous studies have identified several promising biomarkers of PTSD. “However, like much of the research data, the study sample was comprised mainly of combat-exposed males. With more women serving on the front lines, the military faces new challenges in how combat affects females in the military,” including sex-specific biomarkers that will improve clinical assessment for female soldiers.
Eventually, the team would also like to be able to apply their research to the civilian population experiencing PTSD.
“Our research is anticipated to be useful in helping the medical provider select appropriate therapeutic interventions,” Ms. Miller said.
A version of this article first appeared on Medscape.com.
FROM DISCOVER BMB
Lack of food for thought: Starve a bacterium, feed an infection
A whole new, tiny level of hangry
Ever been so hungry that everything just got on your nerves? Maybe you feel a little snappy right now? Like you’ll just lash out unless you get something to eat? Been there. And so have bacteria.
New research shows that some bacteria go into a full-on Hulk smash if they’re not getting the nutrients they need by releasing toxins into the body. Sounds like a bacterial temper tantrum.
Even though two cells may be genetically identical, they don’t always behave the same in a bacterial community. Some do their job and stay in line, but some evil twins rage out and make people sick by releasing toxins into the environment, Adam Rosenthal, PhD, of the University of North Carolina and his colleagues discovered.
To figure out why some cells were all business as usual while others were not, the investigators looked at Clostridium perfringens, a bacterium found in the intestines of humans and other vertebrates. When the C. perfringens cells were fed a little acetate to munch on, the hangry cells calmed down faster than a kid with a bag of fruit snacks, reducing toxin levels. Some cells even disappeared, falling in line with their model-citizen counterparts.
So what does this really mean? More research, duh. Now that we know nutrients play a role in toxicity, it may open the door to finding a way to fight against antibiotic resistance in humans and reduce antibiotic use in the food industry.
So think to yourself. Are you bothered for no reason? Getting a little testy with your friends and coworkers? Maybe you just haven’t eaten in a while. You’re literally not alone. Even a single-cell organism can behave based on its hunger levels.
Now go have a snack. Your bacteria are getting restless.
The very hangry iguana?
Imagine yourself on a warm, sunny tropical beach. You are enjoying a piece of cake as you take in the slow beat of the waves lapping against the shore. Life is as good as it could be.
Then you feel a presence nearby. Hostility. Hunger. A set of feral, covetous eyes in the nearby jungle. A reptilian beast stalks you, and its all-encompassing sweet tooth desires your cake.
Wait, hold on, what?
As an unfortunate 3-year-old on vacation in Costa Rica found out, there’s at least one iguana in the world out there with a taste for sugar (better than a taste for blood, we suppose).
While out on the beach, the lizard darted out of nowhere, bit the girl on the back of the hand, and stole her cake. Still not the worst party guest ever. The child was taken to a local clinic, where the wound was cleaned and a 5-day antibiotic treatment (lizards carry salmonella) was provided. Things seemed fine, and the girl returned home without incident.
But of course, that’s not the end of the story. Five months later, the girl’s parents noticed a red bump at the wound site. Over the next 3 months, the surrounding skin grew red and painful. A trip to the hospital in California revealed that she had a ganglion cyst and a discharge of pus. Turns out our cake-obsessed lizard friend did give the little girl a gift: the first known human case of Mycobacterium marinum infection following an iguana bite on record.
M. marinum, which causes a disease similar to tuberculosis, typically infects fish but can infect humans if skin wounds are exposed to contaminated water. It’s also resistant to most antibiotics, which is why the first round didn’t clear up the infection. A second round of more-potent antibiotics seems to be working well.
So, to sum up, this poor child got bitten by a lizard, had her cake stolen, and contracted a rare illness in exchange. For a 3-year-old, that’s gotta be in the top-10 worst days ever. Unless, of course, we’re actually living in the Marvel universe (sorry, multiverse at this point). Then we’re totally going to see the emergence of the new superhero Iguana Girl in 15 years or so. Keep your eyes open.
No allergies? Let them give up cake
Allergy season is already here – starting earlier every year, it seems – and many people are not happy about it. So unhappy, actually, that there’s a list of things they would be willing to give up for a year to get rid of their of allergies, according to a survey conducted by OnePoll on behalf of Flonase.
Nearly 40% of 2,000 respondents with allergies would go a year without eating cake or chocolate or playing video games in exchange for allergy-free status, the survey results show. Almost as many would forgo coffee (38%) or pizza (37%) for a year, while 36% would stay off social media and 31% would take a pay cut or give up their smartphones, the Independent reported.
More than half of the allergic Americans – 54%, to be exact – who were polled this past winter – Feb. 24 to March 1, to be exact – consider allergy symptoms to be the most frustrating part of the spring. Annoying things that were less frustrating to the group included mosquitoes (41%), filing tax returns (38%), and daylight savings time (37%).
The Trump arraignment circus, of course, occurred too late to make the list, as did the big “We’re going back to the office! No wait, we’re closing the office forever!” email extravaganza and emotional roller coaster. That second one, however, did not get nearly as much media coverage.
A whole new, tiny level of hangry
Ever been so hungry that everything just got on your nerves? Maybe you feel a little snappy right now? Like you’ll just lash out unless you get something to eat? Been there. And so have bacteria.
New research shows that some bacteria go into a full-on Hulk smash if they’re not getting the nutrients they need by releasing toxins into the body. Sounds like a bacterial temper tantrum.
Even though two cells may be genetically identical, they don’t always behave the same in a bacterial community. Some do their job and stay in line, but some evil twins rage out and make people sick by releasing toxins into the environment, Adam Rosenthal, PhD, of the University of North Carolina and his colleagues discovered.
To figure out why some cells were all business as usual while others were not, the investigators looked at Clostridium perfringens, a bacterium found in the intestines of humans and other vertebrates. When the C. perfringens cells were fed a little acetate to munch on, the hangry cells calmed down faster than a kid with a bag of fruit snacks, reducing toxin levels. Some cells even disappeared, falling in line with their model-citizen counterparts.
So what does this really mean? More research, duh. Now that we know nutrients play a role in toxicity, it may open the door to finding a way to fight against antibiotic resistance in humans and reduce antibiotic use in the food industry.
So think to yourself. Are you bothered for no reason? Getting a little testy with your friends and coworkers? Maybe you just haven’t eaten in a while. You’re literally not alone. Even a single-cell organism can behave based on its hunger levels.
Now go have a snack. Your bacteria are getting restless.
The very hangry iguana?
Imagine yourself on a warm, sunny tropical beach. You are enjoying a piece of cake as you take in the slow beat of the waves lapping against the shore. Life is as good as it could be.
Then you feel a presence nearby. Hostility. Hunger. A set of feral, covetous eyes in the nearby jungle. A reptilian beast stalks you, and its all-encompassing sweet tooth desires your cake.
Wait, hold on, what?
As an unfortunate 3-year-old on vacation in Costa Rica found out, there’s at least one iguana in the world out there with a taste for sugar (better than a taste for blood, we suppose).
While out on the beach, the lizard darted out of nowhere, bit the girl on the back of the hand, and stole her cake. Still not the worst party guest ever. The child was taken to a local clinic, where the wound was cleaned and a 5-day antibiotic treatment (lizards carry salmonella) was provided. Things seemed fine, and the girl returned home without incident.
But of course, that’s not the end of the story. Five months later, the girl’s parents noticed a red bump at the wound site. Over the next 3 months, the surrounding skin grew red and painful. A trip to the hospital in California revealed that she had a ganglion cyst and a discharge of pus. Turns out our cake-obsessed lizard friend did give the little girl a gift: the first known human case of Mycobacterium marinum infection following an iguana bite on record.
M. marinum, which causes a disease similar to tuberculosis, typically infects fish but can infect humans if skin wounds are exposed to contaminated water. It’s also resistant to most antibiotics, which is why the first round didn’t clear up the infection. A second round of more-potent antibiotics seems to be working well.
So, to sum up, this poor child got bitten by a lizard, had her cake stolen, and contracted a rare illness in exchange. For a 3-year-old, that’s gotta be in the top-10 worst days ever. Unless, of course, we’re actually living in the Marvel universe (sorry, multiverse at this point). Then we’re totally going to see the emergence of the new superhero Iguana Girl in 15 years or so. Keep your eyes open.
No allergies? Let them give up cake
Allergy season is already here – starting earlier every year, it seems – and many people are not happy about it. So unhappy, actually, that there’s a list of things they would be willing to give up for a year to get rid of their of allergies, according to a survey conducted by OnePoll on behalf of Flonase.
Nearly 40% of 2,000 respondents with allergies would go a year without eating cake or chocolate or playing video games in exchange for allergy-free status, the survey results show. Almost as many would forgo coffee (38%) or pizza (37%) for a year, while 36% would stay off social media and 31% would take a pay cut or give up their smartphones, the Independent reported.
More than half of the allergic Americans – 54%, to be exact – who were polled this past winter – Feb. 24 to March 1, to be exact – consider allergy symptoms to be the most frustrating part of the spring. Annoying things that were less frustrating to the group included mosquitoes (41%), filing tax returns (38%), and daylight savings time (37%).
The Trump arraignment circus, of course, occurred too late to make the list, as did the big “We’re going back to the office! No wait, we’re closing the office forever!” email extravaganza and emotional roller coaster. That second one, however, did not get nearly as much media coverage.
A whole new, tiny level of hangry
Ever been so hungry that everything just got on your nerves? Maybe you feel a little snappy right now? Like you’ll just lash out unless you get something to eat? Been there. And so have bacteria.
New research shows that some bacteria go into a full-on Hulk smash if they’re not getting the nutrients they need by releasing toxins into the body. Sounds like a bacterial temper tantrum.
Even though two cells may be genetically identical, they don’t always behave the same in a bacterial community. Some do their job and stay in line, but some evil twins rage out and make people sick by releasing toxins into the environment, Adam Rosenthal, PhD, of the University of North Carolina and his colleagues discovered.
To figure out why some cells were all business as usual while others were not, the investigators looked at Clostridium perfringens, a bacterium found in the intestines of humans and other vertebrates. When the C. perfringens cells were fed a little acetate to munch on, the hangry cells calmed down faster than a kid with a bag of fruit snacks, reducing toxin levels. Some cells even disappeared, falling in line with their model-citizen counterparts.
So what does this really mean? More research, duh. Now that we know nutrients play a role in toxicity, it may open the door to finding a way to fight against antibiotic resistance in humans and reduce antibiotic use in the food industry.
So think to yourself. Are you bothered for no reason? Getting a little testy with your friends and coworkers? Maybe you just haven’t eaten in a while. You’re literally not alone. Even a single-cell organism can behave based on its hunger levels.
Now go have a snack. Your bacteria are getting restless.
The very hangry iguana?
Imagine yourself on a warm, sunny tropical beach. You are enjoying a piece of cake as you take in the slow beat of the waves lapping against the shore. Life is as good as it could be.
Then you feel a presence nearby. Hostility. Hunger. A set of feral, covetous eyes in the nearby jungle. A reptilian beast stalks you, and its all-encompassing sweet tooth desires your cake.
Wait, hold on, what?
As an unfortunate 3-year-old on vacation in Costa Rica found out, there’s at least one iguana in the world out there with a taste for sugar (better than a taste for blood, we suppose).
While out on the beach, the lizard darted out of nowhere, bit the girl on the back of the hand, and stole her cake. Still not the worst party guest ever. The child was taken to a local clinic, where the wound was cleaned and a 5-day antibiotic treatment (lizards carry salmonella) was provided. Things seemed fine, and the girl returned home without incident.
But of course, that’s not the end of the story. Five months later, the girl’s parents noticed a red bump at the wound site. Over the next 3 months, the surrounding skin grew red and painful. A trip to the hospital in California revealed that she had a ganglion cyst and a discharge of pus. Turns out our cake-obsessed lizard friend did give the little girl a gift: the first known human case of Mycobacterium marinum infection following an iguana bite on record.
M. marinum, which causes a disease similar to tuberculosis, typically infects fish but can infect humans if skin wounds are exposed to contaminated water. It’s also resistant to most antibiotics, which is why the first round didn’t clear up the infection. A second round of more-potent antibiotics seems to be working well.
So, to sum up, this poor child got bitten by a lizard, had her cake stolen, and contracted a rare illness in exchange. For a 3-year-old, that’s gotta be in the top-10 worst days ever. Unless, of course, we’re actually living in the Marvel universe (sorry, multiverse at this point). Then we’re totally going to see the emergence of the new superhero Iguana Girl in 15 years or so. Keep your eyes open.
No allergies? Let them give up cake
Allergy season is already here – starting earlier every year, it seems – and many people are not happy about it. So unhappy, actually, that there’s a list of things they would be willing to give up for a year to get rid of their of allergies, according to a survey conducted by OnePoll on behalf of Flonase.
Nearly 40% of 2,000 respondents with allergies would go a year without eating cake or chocolate or playing video games in exchange for allergy-free status, the survey results show. Almost as many would forgo coffee (38%) or pizza (37%) for a year, while 36% would stay off social media and 31% would take a pay cut or give up their smartphones, the Independent reported.
More than half of the allergic Americans – 54%, to be exact – who were polled this past winter – Feb. 24 to March 1, to be exact – consider allergy symptoms to be the most frustrating part of the spring. Annoying things that were less frustrating to the group included mosquitoes (41%), filing tax returns (38%), and daylight savings time (37%).
The Trump arraignment circus, of course, occurred too late to make the list, as did the big “We’re going back to the office! No wait, we’re closing the office forever!” email extravaganza and emotional roller coaster. That second one, however, did not get nearly as much media coverage.