User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
New toolkit offers help for climate change anxiety
These strategies include volunteering, building a community, discussing emotions with others, practicing mindfulness, and seeking therapy.
The toolkit, which was developed by nursing experts at the University of British Columbia in Vancouver, also offers reflection questions and a film with diverse voices for people to examine their values, emotions, and behaviors in relation to the environment.
“Many people have a hard time understanding the relationship between climate change and mental health and are experiencing high levels of stress about climate change,” Natania Abebe, MSN/MPH, RN, a registered nurse and graduate student at UBC who developed the toolkit, told this news organization.
“Youth, in particular, appear to have higher levels of consciousness regarding climate change because they’re the ones who are going to inherit the planet,” she said. “A big part of why they have mental health issues is that they feel trapped in sociopolitical structures that they didn’t agree to and didn’t necessarily create.”
The toolkit was published online on April 20.
Empowering agents for change
Ms. Abebe was inspired to create the toolkit after giving guest lectures on climate change and mental health as part of UBC’s Nursing 290 course. Her faculty advisor, Raluca Radu, MSN, a lecturer in the School of Nursing at UBC, developed the course in 2020 to teach students about the broad impacts of climate change on communities.
As the course has grown during the past 2 years, Ms. Abebe wanted to create a coping framework and engaging film for health educators to use with students, as well as for everyday people.
The toolkit includes contributions from three Canadian climate change experts, as well as six students from different backgrounds who have taken the course.
“I wanted to center the voices of youth and empower them to think they can be agents for change,” Ms. Abebe said. “I also wanted to highlight diverse voices and take a collaborative approach because climate change is such a big problem that we have to come together to address it.”
Ms. Abebe and Ms. Radu also noticed an increase in climate anxiety in recent years because of the pandemic, worldwide food and energy shortages, and extreme weather events that hit close to home, such as wildfires and floods in British Columbia.
“With the pandemic, people have been spending more time online and thinking about our world at large,” Ms. Abebe said. “At the same time that they’re thinking about it, climate change events are happening simultaneously – not in the future, but right now.”
Economic, social, and political shifts during the past 2 years have also prompted people to question standard practices and institutions, which has created an opportunity to discuss change, Ms. Radu told this news organization.
“It’s a pivotal time to question our values and highly consumerist society,” she said. “We’re at a point in time where, if we don’t take action, the planetary health will be in an irreversible state, and we won’t be able to turn back time and make changes.”
Our psyches and nature
The toolkit includes three main sections that feature video clips and reflective questions around eco-anxiety, eco-paralysis, and ecological grief.
In the first section, eco-anxiety is defined as a “chronic fear of environmental doom,” which could include anxiousness around the likelihood of a severe weather event because of ongoing news coverage and social media. The reflective questions prompt readers to discuss eco-anxiety in their life, work through their emotions, understand their beliefs and values, and determine how to use them to address climate change anxiety.
The second section defines eco-paralysis as the powerlessness that people may feel when they don’t believe they can do anything meaningful on an individual level to address climate change. Paralysis can look like apathy, complacency, or disengagement. The questions prompt readers to observe how paralysis may show up in their lives, explore the tension between individual versus collective responsibility, and consider ways to address their sense of helplessness about climate change.
In the third section, ecological grief centers around “experienced or anticipated ecological losses,” which could include the loss of species, ecosystems, and landscapes because of short- or long-term environmental change. The questions prompt readers to explore their feelings, beliefs, and values and feel empowered to address their ecological grief over climate change.
The toolkit also includes recommendations for books, journal articles, websites, podcasts, and meditations around mental health and climate change, as well as ways to get involved with others. For instance, health care practitioners can register with PaRx, a program in British Columbia that allows providers to prescribe time in nature to improve a client’s health. The program is being adopted across Canada, and people with a prescription can visit local and national parks, historic sites, and marine conservation areas for free.
“This is about recognizing that there is a connection between our psyches and nature, and by talking about it, we can name what we’re feeling,” Ms. Abebe said. “We can take action not only to handle our emotions, but also to live kinder and more sustainable lifestyles.”
Future work will need to focus on population-level approaches to climate change and mental health as well, including policy and financial support to address environmental changes directly.
“We need to start thinking beyond individualized approaches and focus on how to create supportive and resilient communities to respond to climate change,” Kiffer Card, PhD, executive director of the Mental Health and Climate Change Alliance and an assistant professor of health sciences at Simon Fraser University, Burnaby, B.C., told this news organization.
Dr. Card, who wasn’t involved in developing the toolkit, has researched recent trends around climate change anxiety in Canada and fielded questions from health care practitioners and mental health professionals who are looking for ways to help their patients.
“Communities need to be ready to stand up and respond to acute emergency disasters, and government leaders need to take this seriously,” he said. “Those who are experiencing climate anxiety now are the canaries in the coal mine for the severe weather events and consequences to come.”
The toolkit was developed with funding from the Alma Mater Society of the University of British Columbia, Vancouver. Ms. Abebe, Ms. Radu, and Dr. Card reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
These strategies include volunteering, building a community, discussing emotions with others, practicing mindfulness, and seeking therapy.
The toolkit, which was developed by nursing experts at the University of British Columbia in Vancouver, also offers reflection questions and a film with diverse voices for people to examine their values, emotions, and behaviors in relation to the environment.
“Many people have a hard time understanding the relationship between climate change and mental health and are experiencing high levels of stress about climate change,” Natania Abebe, MSN/MPH, RN, a registered nurse and graduate student at UBC who developed the toolkit, told this news organization.
“Youth, in particular, appear to have higher levels of consciousness regarding climate change because they’re the ones who are going to inherit the planet,” she said. “A big part of why they have mental health issues is that they feel trapped in sociopolitical structures that they didn’t agree to and didn’t necessarily create.”
The toolkit was published online on April 20.
Empowering agents for change
Ms. Abebe was inspired to create the toolkit after giving guest lectures on climate change and mental health as part of UBC’s Nursing 290 course. Her faculty advisor, Raluca Radu, MSN, a lecturer in the School of Nursing at UBC, developed the course in 2020 to teach students about the broad impacts of climate change on communities.
As the course has grown during the past 2 years, Ms. Abebe wanted to create a coping framework and engaging film for health educators to use with students, as well as for everyday people.
The toolkit includes contributions from three Canadian climate change experts, as well as six students from different backgrounds who have taken the course.
“I wanted to center the voices of youth and empower them to think they can be agents for change,” Ms. Abebe said. “I also wanted to highlight diverse voices and take a collaborative approach because climate change is such a big problem that we have to come together to address it.”
Ms. Abebe and Ms. Radu also noticed an increase in climate anxiety in recent years because of the pandemic, worldwide food and energy shortages, and extreme weather events that hit close to home, such as wildfires and floods in British Columbia.
“With the pandemic, people have been spending more time online and thinking about our world at large,” Ms. Abebe said. “At the same time that they’re thinking about it, climate change events are happening simultaneously – not in the future, but right now.”
Economic, social, and political shifts during the past 2 years have also prompted people to question standard practices and institutions, which has created an opportunity to discuss change, Ms. Radu told this news organization.
“It’s a pivotal time to question our values and highly consumerist society,” she said. “We’re at a point in time where, if we don’t take action, the planetary health will be in an irreversible state, and we won’t be able to turn back time and make changes.”
Our psyches and nature
The toolkit includes three main sections that feature video clips and reflective questions around eco-anxiety, eco-paralysis, and ecological grief.
In the first section, eco-anxiety is defined as a “chronic fear of environmental doom,” which could include anxiousness around the likelihood of a severe weather event because of ongoing news coverage and social media. The reflective questions prompt readers to discuss eco-anxiety in their life, work through their emotions, understand their beliefs and values, and determine how to use them to address climate change anxiety.
The second section defines eco-paralysis as the powerlessness that people may feel when they don’t believe they can do anything meaningful on an individual level to address climate change. Paralysis can look like apathy, complacency, or disengagement. The questions prompt readers to observe how paralysis may show up in their lives, explore the tension between individual versus collective responsibility, and consider ways to address their sense of helplessness about climate change.
In the third section, ecological grief centers around “experienced or anticipated ecological losses,” which could include the loss of species, ecosystems, and landscapes because of short- or long-term environmental change. The questions prompt readers to explore their feelings, beliefs, and values and feel empowered to address their ecological grief over climate change.
The toolkit also includes recommendations for books, journal articles, websites, podcasts, and meditations around mental health and climate change, as well as ways to get involved with others. For instance, health care practitioners can register with PaRx, a program in British Columbia that allows providers to prescribe time in nature to improve a client’s health. The program is being adopted across Canada, and people with a prescription can visit local and national parks, historic sites, and marine conservation areas for free.
“This is about recognizing that there is a connection between our psyches and nature, and by talking about it, we can name what we’re feeling,” Ms. Abebe said. “We can take action not only to handle our emotions, but also to live kinder and more sustainable lifestyles.”
Future work will need to focus on population-level approaches to climate change and mental health as well, including policy and financial support to address environmental changes directly.
“We need to start thinking beyond individualized approaches and focus on how to create supportive and resilient communities to respond to climate change,” Kiffer Card, PhD, executive director of the Mental Health and Climate Change Alliance and an assistant professor of health sciences at Simon Fraser University, Burnaby, B.C., told this news organization.
Dr. Card, who wasn’t involved in developing the toolkit, has researched recent trends around climate change anxiety in Canada and fielded questions from health care practitioners and mental health professionals who are looking for ways to help their patients.
“Communities need to be ready to stand up and respond to acute emergency disasters, and government leaders need to take this seriously,” he said. “Those who are experiencing climate anxiety now are the canaries in the coal mine for the severe weather events and consequences to come.”
The toolkit was developed with funding from the Alma Mater Society of the University of British Columbia, Vancouver. Ms. Abebe, Ms. Radu, and Dr. Card reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
These strategies include volunteering, building a community, discussing emotions with others, practicing mindfulness, and seeking therapy.
The toolkit, which was developed by nursing experts at the University of British Columbia in Vancouver, also offers reflection questions and a film with diverse voices for people to examine their values, emotions, and behaviors in relation to the environment.
“Many people have a hard time understanding the relationship between climate change and mental health and are experiencing high levels of stress about climate change,” Natania Abebe, MSN/MPH, RN, a registered nurse and graduate student at UBC who developed the toolkit, told this news organization.
“Youth, in particular, appear to have higher levels of consciousness regarding climate change because they’re the ones who are going to inherit the planet,” she said. “A big part of why they have mental health issues is that they feel trapped in sociopolitical structures that they didn’t agree to and didn’t necessarily create.”
The toolkit was published online on April 20.
Empowering agents for change
Ms. Abebe was inspired to create the toolkit after giving guest lectures on climate change and mental health as part of UBC’s Nursing 290 course. Her faculty advisor, Raluca Radu, MSN, a lecturer in the School of Nursing at UBC, developed the course in 2020 to teach students about the broad impacts of climate change on communities.
As the course has grown during the past 2 years, Ms. Abebe wanted to create a coping framework and engaging film for health educators to use with students, as well as for everyday people.
The toolkit includes contributions from three Canadian climate change experts, as well as six students from different backgrounds who have taken the course.
“I wanted to center the voices of youth and empower them to think they can be agents for change,” Ms. Abebe said. “I also wanted to highlight diverse voices and take a collaborative approach because climate change is such a big problem that we have to come together to address it.”
Ms. Abebe and Ms. Radu also noticed an increase in climate anxiety in recent years because of the pandemic, worldwide food and energy shortages, and extreme weather events that hit close to home, such as wildfires and floods in British Columbia.
“With the pandemic, people have been spending more time online and thinking about our world at large,” Ms. Abebe said. “At the same time that they’re thinking about it, climate change events are happening simultaneously – not in the future, but right now.”
Economic, social, and political shifts during the past 2 years have also prompted people to question standard practices and institutions, which has created an opportunity to discuss change, Ms. Radu told this news organization.
“It’s a pivotal time to question our values and highly consumerist society,” she said. “We’re at a point in time where, if we don’t take action, the planetary health will be in an irreversible state, and we won’t be able to turn back time and make changes.”
Our psyches and nature
The toolkit includes three main sections that feature video clips and reflective questions around eco-anxiety, eco-paralysis, and ecological grief.
In the first section, eco-anxiety is defined as a “chronic fear of environmental doom,” which could include anxiousness around the likelihood of a severe weather event because of ongoing news coverage and social media. The reflective questions prompt readers to discuss eco-anxiety in their life, work through their emotions, understand their beliefs and values, and determine how to use them to address climate change anxiety.
The second section defines eco-paralysis as the powerlessness that people may feel when they don’t believe they can do anything meaningful on an individual level to address climate change. Paralysis can look like apathy, complacency, or disengagement. The questions prompt readers to observe how paralysis may show up in their lives, explore the tension between individual versus collective responsibility, and consider ways to address their sense of helplessness about climate change.
In the third section, ecological grief centers around “experienced or anticipated ecological losses,” which could include the loss of species, ecosystems, and landscapes because of short- or long-term environmental change. The questions prompt readers to explore their feelings, beliefs, and values and feel empowered to address their ecological grief over climate change.
The toolkit also includes recommendations for books, journal articles, websites, podcasts, and meditations around mental health and climate change, as well as ways to get involved with others. For instance, health care practitioners can register with PaRx, a program in British Columbia that allows providers to prescribe time in nature to improve a client’s health. The program is being adopted across Canada, and people with a prescription can visit local and national parks, historic sites, and marine conservation areas for free.
“This is about recognizing that there is a connection between our psyches and nature, and by talking about it, we can name what we’re feeling,” Ms. Abebe said. “We can take action not only to handle our emotions, but also to live kinder and more sustainable lifestyles.”
Future work will need to focus on population-level approaches to climate change and mental health as well, including policy and financial support to address environmental changes directly.
“We need to start thinking beyond individualized approaches and focus on how to create supportive and resilient communities to respond to climate change,” Kiffer Card, PhD, executive director of the Mental Health and Climate Change Alliance and an assistant professor of health sciences at Simon Fraser University, Burnaby, B.C., told this news organization.
Dr. Card, who wasn’t involved in developing the toolkit, has researched recent trends around climate change anxiety in Canada and fielded questions from health care practitioners and mental health professionals who are looking for ways to help their patients.
“Communities need to be ready to stand up and respond to acute emergency disasters, and government leaders need to take this seriously,” he said. “Those who are experiencing climate anxiety now are the canaries in the coal mine for the severe weather events and consequences to come.”
The toolkit was developed with funding from the Alma Mater Society of the University of British Columbia, Vancouver. Ms. Abebe, Ms. Radu, and Dr. Card reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Best antioxidants to prevent age-related dementia identified?
Investigators found that individuals with the highest serum levels of lutein + zeaxanthin and beta-cryptoxanthin at baseline were less likely to have dementia decades later than were their peers with lower levels of these antioxidants.
Lutein and zeaxanthin are found in green leafy vegetables such as kale, spinach, broccoli, and peas. Beta-cryptoxanthin is found in fruits such as oranges, papaya, tangerines, and persimmons.
“Antioxidants may help protect the brain from oxidative stress, which can cause cell damage,” first author May A. Beydoun, PhD, with the National Institute on Aging (NIA), said in a news release.
“This is the first nationally representative study to analyze blood levels of antioxidants in relation to dementia risk,” NIA scientific director Luigi Ferrucci, MD, said in an interview.
“Blood test results may be more representative of the actual antioxidant level than a person’s report of what kind of foods they regularly consume,” Dr. Ferrucci added.
The study was published online in Neurology.
Reduced dementia risk
The researchers tested associations and interactions of serum vitamins A, C and E, and total and individual serum carotenoids and interactions with incident Alzheimer’s disease (AD) and all-cause dementia.
They analyzed data from 7,283 participants in the Third National Health and Nutrition Examination Survey (NHANES III) who were at least 45 years old at baseline and followed for an average of 16-17 years.
They found serum levels of lutein + zeaxanthin were associated with reduced risk of all-cause dementia among people aged 65 and older in models adjusted for lifestyle.
For lutein + zeaxanthin, every standard deviation (SD) increase (roughly 15.4 µmol/liter) was associated with a 7% decrease in risk for dementia (hazard ratio [HR] 0.93; 95% confidence interval [CI], 0.87-0.99, P = .037). This association was attenuated somewhat after adjustment for socioeconomic status.
Serum levels of beta-cryptoxanthin showed a “strong” inverse relationship with all-cause dementia in age- and sex-adjusted models.
For beta-cryptoxanthin, every SD increase (roughly 8.6 µmol/liter) was associated with a 14% reduced risk for dementia in people aged 45 and older (HR, 0.86; 95% CI, 0.80-0.93, P < .001) and 65 and older (HR, 0.86; 95% CI, 0.80-0.93, P = .001).
This relationship remained strong in models adjusted for sociodemographic and socioeconomic factors but attenuated in subsequent models.
No associations were found for lycopene, alpha-carotene, beta-carotene, or vitamins A, C, or E in the fully adjusted models.
Antagonistic interactions were observed for vitamin A and alpha-carotene, vitamin A and beta-carotene, vitamin E and lycopene, and lycopene and beta-carotene, suggesting putative protective effects of one antioxidant at lower levels of the other, the researchers noted.
“This analysis of an observational study found that the most important carotenoids in potentially protecting the brain may be lutein + zeaxanthin and beta-cryptoxanthin. However, randomized controlled trials are needed to prove causality,” said Dr. Ferrucci.
“Experts do not yet know the daily level of antioxidant intake to promote healthy aging of the brain. More research is needed to establish the necessary level of antioxidant intake – through the diet and/or supplements – to promote brain health and healthy aging,” he added.
An important step forward
In an accompanying editorial, Babak Hooshmand, MD, PhD, and Miia Kivipelto, MD, PhD, with Karolinska Institute, Stockholm, noted that while nutrition and dietary components are “potential targets” for dementia risk reduction, observational studies to date have reported “inconsistent findings.”
This study is “an important step towards exploring the complex relationship between antioxidants and dementia because it accounts for factors that could possibly influence the associations and considers interactions between different components,” they wrote.
The findings are “challenging,” they added, because they may lead to the hypothesis that inhibition of oxidative damage by antioxidants might have beneficial effects on preventing dementia.
However, clinical trials of antioxidant supplementation have been mainly “disappointing” and a recent Cochrane review found a lack of evidence for supplement use to preserve cognitive function or prevent dementia, Dr. Hooshmand and Dr. Kivipelto noted.
They added that the study contributes to the belief that antioxidants don’t act independently of each other or other factors, including socioeconomic status and lifestyle, in the mediation of dementia risk.
“A careful examination of the evidence is required to learn how antioxidants influence the complex pathology of dementia, because it appears to be more to it than meets the eye,”they concluded.
The research was supported in part by the Intramural Research Program of the National Institutes of Health and the National Institute on Aging. Dr. Beydoun, Dr. Ferrucci, and Dr. Hooshmand report no relevant disclosures. Dr. Kivipelto has supported advisory boards for Combinostics, Roche, and Biogen.
A version of this article first appeared on Medscape.com.
Investigators found that individuals with the highest serum levels of lutein + zeaxanthin and beta-cryptoxanthin at baseline were less likely to have dementia decades later than were their peers with lower levels of these antioxidants.
Lutein and zeaxanthin are found in green leafy vegetables such as kale, spinach, broccoli, and peas. Beta-cryptoxanthin is found in fruits such as oranges, papaya, tangerines, and persimmons.
“Antioxidants may help protect the brain from oxidative stress, which can cause cell damage,” first author May A. Beydoun, PhD, with the National Institute on Aging (NIA), said in a news release.
“This is the first nationally representative study to analyze blood levels of antioxidants in relation to dementia risk,” NIA scientific director Luigi Ferrucci, MD, said in an interview.
“Blood test results may be more representative of the actual antioxidant level than a person’s report of what kind of foods they regularly consume,” Dr. Ferrucci added.
The study was published online in Neurology.
Reduced dementia risk
The researchers tested associations and interactions of serum vitamins A, C and E, and total and individual serum carotenoids and interactions with incident Alzheimer’s disease (AD) and all-cause dementia.
They analyzed data from 7,283 participants in the Third National Health and Nutrition Examination Survey (NHANES III) who were at least 45 years old at baseline and followed for an average of 16-17 years.
They found serum levels of lutein + zeaxanthin were associated with reduced risk of all-cause dementia among people aged 65 and older in models adjusted for lifestyle.
For lutein + zeaxanthin, every standard deviation (SD) increase (roughly 15.4 µmol/liter) was associated with a 7% decrease in risk for dementia (hazard ratio [HR] 0.93; 95% confidence interval [CI], 0.87-0.99, P = .037). This association was attenuated somewhat after adjustment for socioeconomic status.
Serum levels of beta-cryptoxanthin showed a “strong” inverse relationship with all-cause dementia in age- and sex-adjusted models.
For beta-cryptoxanthin, every SD increase (roughly 8.6 µmol/liter) was associated with a 14% reduced risk for dementia in people aged 45 and older (HR, 0.86; 95% CI, 0.80-0.93, P < .001) and 65 and older (HR, 0.86; 95% CI, 0.80-0.93, P = .001).
This relationship remained strong in models adjusted for sociodemographic and socioeconomic factors but attenuated in subsequent models.
No associations were found for lycopene, alpha-carotene, beta-carotene, or vitamins A, C, or E in the fully adjusted models.
Antagonistic interactions were observed for vitamin A and alpha-carotene, vitamin A and beta-carotene, vitamin E and lycopene, and lycopene and beta-carotene, suggesting putative protective effects of one antioxidant at lower levels of the other, the researchers noted.
“This analysis of an observational study found that the most important carotenoids in potentially protecting the brain may be lutein + zeaxanthin and beta-cryptoxanthin. However, randomized controlled trials are needed to prove causality,” said Dr. Ferrucci.
“Experts do not yet know the daily level of antioxidant intake to promote healthy aging of the brain. More research is needed to establish the necessary level of antioxidant intake – through the diet and/or supplements – to promote brain health and healthy aging,” he added.
An important step forward
In an accompanying editorial, Babak Hooshmand, MD, PhD, and Miia Kivipelto, MD, PhD, with Karolinska Institute, Stockholm, noted that while nutrition and dietary components are “potential targets” for dementia risk reduction, observational studies to date have reported “inconsistent findings.”
This study is “an important step towards exploring the complex relationship between antioxidants and dementia because it accounts for factors that could possibly influence the associations and considers interactions between different components,” they wrote.
The findings are “challenging,” they added, because they may lead to the hypothesis that inhibition of oxidative damage by antioxidants might have beneficial effects on preventing dementia.
However, clinical trials of antioxidant supplementation have been mainly “disappointing” and a recent Cochrane review found a lack of evidence for supplement use to preserve cognitive function or prevent dementia, Dr. Hooshmand and Dr. Kivipelto noted.
They added that the study contributes to the belief that antioxidants don’t act independently of each other or other factors, including socioeconomic status and lifestyle, in the mediation of dementia risk.
“A careful examination of the evidence is required to learn how antioxidants influence the complex pathology of dementia, because it appears to be more to it than meets the eye,”they concluded.
The research was supported in part by the Intramural Research Program of the National Institutes of Health and the National Institute on Aging. Dr. Beydoun, Dr. Ferrucci, and Dr. Hooshmand report no relevant disclosures. Dr. Kivipelto has supported advisory boards for Combinostics, Roche, and Biogen.
A version of this article first appeared on Medscape.com.
Investigators found that individuals with the highest serum levels of lutein + zeaxanthin and beta-cryptoxanthin at baseline were less likely to have dementia decades later than were their peers with lower levels of these antioxidants.
Lutein and zeaxanthin are found in green leafy vegetables such as kale, spinach, broccoli, and peas. Beta-cryptoxanthin is found in fruits such as oranges, papaya, tangerines, and persimmons.
“Antioxidants may help protect the brain from oxidative stress, which can cause cell damage,” first author May A. Beydoun, PhD, with the National Institute on Aging (NIA), said in a news release.
“This is the first nationally representative study to analyze blood levels of antioxidants in relation to dementia risk,” NIA scientific director Luigi Ferrucci, MD, said in an interview.
“Blood test results may be more representative of the actual antioxidant level than a person’s report of what kind of foods they regularly consume,” Dr. Ferrucci added.
The study was published online in Neurology.
Reduced dementia risk
The researchers tested associations and interactions of serum vitamins A, C and E, and total and individual serum carotenoids and interactions with incident Alzheimer’s disease (AD) and all-cause dementia.
They analyzed data from 7,283 participants in the Third National Health and Nutrition Examination Survey (NHANES III) who were at least 45 years old at baseline and followed for an average of 16-17 years.
They found serum levels of lutein + zeaxanthin were associated with reduced risk of all-cause dementia among people aged 65 and older in models adjusted for lifestyle.
For lutein + zeaxanthin, every standard deviation (SD) increase (roughly 15.4 µmol/liter) was associated with a 7% decrease in risk for dementia (hazard ratio [HR] 0.93; 95% confidence interval [CI], 0.87-0.99, P = .037). This association was attenuated somewhat after adjustment for socioeconomic status.
Serum levels of beta-cryptoxanthin showed a “strong” inverse relationship with all-cause dementia in age- and sex-adjusted models.
For beta-cryptoxanthin, every SD increase (roughly 8.6 µmol/liter) was associated with a 14% reduced risk for dementia in people aged 45 and older (HR, 0.86; 95% CI, 0.80-0.93, P < .001) and 65 and older (HR, 0.86; 95% CI, 0.80-0.93, P = .001).
This relationship remained strong in models adjusted for sociodemographic and socioeconomic factors but attenuated in subsequent models.
No associations were found for lycopene, alpha-carotene, beta-carotene, or vitamins A, C, or E in the fully adjusted models.
Antagonistic interactions were observed for vitamin A and alpha-carotene, vitamin A and beta-carotene, vitamin E and lycopene, and lycopene and beta-carotene, suggesting putative protective effects of one antioxidant at lower levels of the other, the researchers noted.
“This analysis of an observational study found that the most important carotenoids in potentially protecting the brain may be lutein + zeaxanthin and beta-cryptoxanthin. However, randomized controlled trials are needed to prove causality,” said Dr. Ferrucci.
“Experts do not yet know the daily level of antioxidant intake to promote healthy aging of the brain. More research is needed to establish the necessary level of antioxidant intake – through the diet and/or supplements – to promote brain health and healthy aging,” he added.
An important step forward
In an accompanying editorial, Babak Hooshmand, MD, PhD, and Miia Kivipelto, MD, PhD, with Karolinska Institute, Stockholm, noted that while nutrition and dietary components are “potential targets” for dementia risk reduction, observational studies to date have reported “inconsistent findings.”
This study is “an important step towards exploring the complex relationship between antioxidants and dementia because it accounts for factors that could possibly influence the associations and considers interactions between different components,” they wrote.
The findings are “challenging,” they added, because they may lead to the hypothesis that inhibition of oxidative damage by antioxidants might have beneficial effects on preventing dementia.
However, clinical trials of antioxidant supplementation have been mainly “disappointing” and a recent Cochrane review found a lack of evidence for supplement use to preserve cognitive function or prevent dementia, Dr. Hooshmand and Dr. Kivipelto noted.
They added that the study contributes to the belief that antioxidants don’t act independently of each other or other factors, including socioeconomic status and lifestyle, in the mediation of dementia risk.
“A careful examination of the evidence is required to learn how antioxidants influence the complex pathology of dementia, because it appears to be more to it than meets the eye,”they concluded.
The research was supported in part by the Intramural Research Program of the National Institutes of Health and the National Institute on Aging. Dr. Beydoun, Dr. Ferrucci, and Dr. Hooshmand report no relevant disclosures. Dr. Kivipelto has supported advisory boards for Combinostics, Roche, and Biogen.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
Vagus nerve stimulation: A little-known option for depression
Standard therapies for depression are antidepressants and psychotherapy. In particularly severe cases, electroconvulsive therapy (ECT) or vagus nerve stimulation (VNS) may also be indicated. VNS is an approved, effective, well-tolerated, long-term therapy for chronic and therapy-resistant depression, wrote Christine Reif-Leonhardt, MD, and associates from the University Hospital Frankfurt am Main (Germany), in a recent journal article. The cost of VNS is covered by health insurance funds in Germany.
Available since 1994
As the authors reported, invasive VNS was approved in the European Union in 1994 and in the United States in 1997 for the treatment of children with medicinal therapy–refractory epilepsy. Because positive and lasting effects on mood could be seen in adults after around 3 months of VNS, irrespective of the effectiveness of anticonvulsive medication, “a genuinely antidepressant effect of VNS [was] postulated,” and therefore it was further developed as an antidepressant therapy.
A VNS system first received a CE certification in 2001 in the European Union for the treatment of patients with chronic or relapsing depression who had therapy-resistant depression or who were intolerant of the current depression therapy. In 2005, VNS was approved in the United States for the treatment of patients aged 18 years or older with therapy-resistant major depression for which at least four antidepressant therapies had not helped sufficiently.
Few sham-controlled studies
According to Dr. Reif-Leonhardt and colleagues, there have been multiple studies and case series on VNS in patients with therapy-resistant depression in the past 20 years. Many of the studies highlighted the additional benefits of VNS as an adjuvant procedure, but they were observational studies. Sham-controlled studies are in short supply because of methodologic difficulties and ethical problems.
The largest long-term study is a registry study in which 494 patients with therapy-resistant depression received the combination of the usual antidepressant therapy and VNS. The study lasted 5 years; 301 patients served as a control group and received the usual therapy. The cumulative response to the therapy (68% vs. 41%) and the remission rate (43% vs. 26%) were significantly greater in the group that received VNS, according to the authors. Patients who underwent at least one ECT series of at least seven sessions responded particularly well to VNS. The combined therapy was also more effective in ECT nonresponders than the usual therapy alone.
To date, only one sham-controlled study of VNS treatment for therapy-resistant depression has been conducted. In it, VNS was not significantly superior to a sham stimulation over an observation period of 10 weeks. However, observational studies have provided evidence that the antidepressant effect of VNS only develops after at least 12 months of treatment. According to Dr. Reif-Leonhardt and colleagues, the data indicate that differences in response rate and therapy effect can only be observed in the longer term after 3-12 months and that as the therapy duration increases, so do the effects of VNS. From this, it can be assumed “that the VNS mechanism of action can be attributed to neuroplastic and adaptive phenomena.”
The typical, common side effects of surgery are pain and paresthesia. Through irritation of the nerve, approximately every third patient experiences postoperative hoarseness and a voice change. Serious side effects and complications, such as temporary swallowing disorders, are rare. By reducing the stimulation intensity or lowering the stimulation frequency or impulse width, the side effects associated with stimulation can be alleviated or even eliminated. A second small surgical intervention may become necessary to replace broken cables or the battery (life span, 3-8 years).
Criteria for VNS therapy
When should VNS be considered? The authors specified the following criteria:
- An insufficient response to at least two antidepressants from different substance classes (ideally including one tricyclic) at a sufficient dosage and duration, as well as to two augmentation agents (such as lithium and quetiapine) in combination with guideline psychotherapy
- Intolerable side effects from pharmacotherapy or contraindications to medicinal therapy
- For patients who respond to ECT, the occurrence of relapses or residual symptoms after cessation of (maintenance) ECT, intolerable ECT side effects, or the need for maintenance ECT
- Repeated or long hospital treatments because of depression
This article is a translation of an article from Univadis Germany and first appeared on Medscape.com.
Standard therapies for depression are antidepressants and psychotherapy. In particularly severe cases, electroconvulsive therapy (ECT) or vagus nerve stimulation (VNS) may also be indicated. VNS is an approved, effective, well-tolerated, long-term therapy for chronic and therapy-resistant depression, wrote Christine Reif-Leonhardt, MD, and associates from the University Hospital Frankfurt am Main (Germany), in a recent journal article. The cost of VNS is covered by health insurance funds in Germany.
Available since 1994
As the authors reported, invasive VNS was approved in the European Union in 1994 and in the United States in 1997 for the treatment of children with medicinal therapy–refractory epilepsy. Because positive and lasting effects on mood could be seen in adults after around 3 months of VNS, irrespective of the effectiveness of anticonvulsive medication, “a genuinely antidepressant effect of VNS [was] postulated,” and therefore it was further developed as an antidepressant therapy.
A VNS system first received a CE certification in 2001 in the European Union for the treatment of patients with chronic or relapsing depression who had therapy-resistant depression or who were intolerant of the current depression therapy. In 2005, VNS was approved in the United States for the treatment of patients aged 18 years or older with therapy-resistant major depression for which at least four antidepressant therapies had not helped sufficiently.
Few sham-controlled studies
According to Dr. Reif-Leonhardt and colleagues, there have been multiple studies and case series on VNS in patients with therapy-resistant depression in the past 20 years. Many of the studies highlighted the additional benefits of VNS as an adjuvant procedure, but they were observational studies. Sham-controlled studies are in short supply because of methodologic difficulties and ethical problems.
The largest long-term study is a registry study in which 494 patients with therapy-resistant depression received the combination of the usual antidepressant therapy and VNS. The study lasted 5 years; 301 patients served as a control group and received the usual therapy. The cumulative response to the therapy (68% vs. 41%) and the remission rate (43% vs. 26%) were significantly greater in the group that received VNS, according to the authors. Patients who underwent at least one ECT series of at least seven sessions responded particularly well to VNS. The combined therapy was also more effective in ECT nonresponders than the usual therapy alone.
To date, only one sham-controlled study of VNS treatment for therapy-resistant depression has been conducted. In it, VNS was not significantly superior to a sham stimulation over an observation period of 10 weeks. However, observational studies have provided evidence that the antidepressant effect of VNS only develops after at least 12 months of treatment. According to Dr. Reif-Leonhardt and colleagues, the data indicate that differences in response rate and therapy effect can only be observed in the longer term after 3-12 months and that as the therapy duration increases, so do the effects of VNS. From this, it can be assumed “that the VNS mechanism of action can be attributed to neuroplastic and adaptive phenomena.”
The typical, common side effects of surgery are pain and paresthesia. Through irritation of the nerve, approximately every third patient experiences postoperative hoarseness and a voice change. Serious side effects and complications, such as temporary swallowing disorders, are rare. By reducing the stimulation intensity or lowering the stimulation frequency or impulse width, the side effects associated with stimulation can be alleviated or even eliminated. A second small surgical intervention may become necessary to replace broken cables or the battery (life span, 3-8 years).
Criteria for VNS therapy
When should VNS be considered? The authors specified the following criteria:
- An insufficient response to at least two antidepressants from different substance classes (ideally including one tricyclic) at a sufficient dosage and duration, as well as to two augmentation agents (such as lithium and quetiapine) in combination with guideline psychotherapy
- Intolerable side effects from pharmacotherapy or contraindications to medicinal therapy
- For patients who respond to ECT, the occurrence of relapses or residual symptoms after cessation of (maintenance) ECT, intolerable ECT side effects, or the need for maintenance ECT
- Repeated or long hospital treatments because of depression
This article is a translation of an article from Univadis Germany and first appeared on Medscape.com.
Standard therapies for depression are antidepressants and psychotherapy. In particularly severe cases, electroconvulsive therapy (ECT) or vagus nerve stimulation (VNS) may also be indicated. VNS is an approved, effective, well-tolerated, long-term therapy for chronic and therapy-resistant depression, wrote Christine Reif-Leonhardt, MD, and associates from the University Hospital Frankfurt am Main (Germany), in a recent journal article. The cost of VNS is covered by health insurance funds in Germany.
Available since 1994
As the authors reported, invasive VNS was approved in the European Union in 1994 and in the United States in 1997 for the treatment of children with medicinal therapy–refractory epilepsy. Because positive and lasting effects on mood could be seen in adults after around 3 months of VNS, irrespective of the effectiveness of anticonvulsive medication, “a genuinely antidepressant effect of VNS [was] postulated,” and therefore it was further developed as an antidepressant therapy.
A VNS system first received a CE certification in 2001 in the European Union for the treatment of patients with chronic or relapsing depression who had therapy-resistant depression or who were intolerant of the current depression therapy. In 2005, VNS was approved in the United States for the treatment of patients aged 18 years or older with therapy-resistant major depression for which at least four antidepressant therapies had not helped sufficiently.
Few sham-controlled studies
According to Dr. Reif-Leonhardt and colleagues, there have been multiple studies and case series on VNS in patients with therapy-resistant depression in the past 20 years. Many of the studies highlighted the additional benefits of VNS as an adjuvant procedure, but they were observational studies. Sham-controlled studies are in short supply because of methodologic difficulties and ethical problems.
The largest long-term study is a registry study in which 494 patients with therapy-resistant depression received the combination of the usual antidepressant therapy and VNS. The study lasted 5 years; 301 patients served as a control group and received the usual therapy. The cumulative response to the therapy (68% vs. 41%) and the remission rate (43% vs. 26%) were significantly greater in the group that received VNS, according to the authors. Patients who underwent at least one ECT series of at least seven sessions responded particularly well to VNS. The combined therapy was also more effective in ECT nonresponders than the usual therapy alone.
To date, only one sham-controlled study of VNS treatment for therapy-resistant depression has been conducted. In it, VNS was not significantly superior to a sham stimulation over an observation period of 10 weeks. However, observational studies have provided evidence that the antidepressant effect of VNS only develops after at least 12 months of treatment. According to Dr. Reif-Leonhardt and colleagues, the data indicate that differences in response rate and therapy effect can only be observed in the longer term after 3-12 months and that as the therapy duration increases, so do the effects of VNS. From this, it can be assumed “that the VNS mechanism of action can be attributed to neuroplastic and adaptive phenomena.”
The typical, common side effects of surgery are pain and paresthesia. Through irritation of the nerve, approximately every third patient experiences postoperative hoarseness and a voice change. Serious side effects and complications, such as temporary swallowing disorders, are rare. By reducing the stimulation intensity or lowering the stimulation frequency or impulse width, the side effects associated with stimulation can be alleviated or even eliminated. A second small surgical intervention may become necessary to replace broken cables or the battery (life span, 3-8 years).
Criteria for VNS therapy
When should VNS be considered? The authors specified the following criteria:
- An insufficient response to at least two antidepressants from different substance classes (ideally including one tricyclic) at a sufficient dosage and duration, as well as to two augmentation agents (such as lithium and quetiapine) in combination with guideline psychotherapy
- Intolerable side effects from pharmacotherapy or contraindications to medicinal therapy
- For patients who respond to ECT, the occurrence of relapses or residual symptoms after cessation of (maintenance) ECT, intolerable ECT side effects, or the need for maintenance ECT
- Repeated or long hospital treatments because of depression
This article is a translation of an article from Univadis Germany and first appeared on Medscape.com.
FROM DER NERVENARZT
Residential green space linked to better cognitive function
Exposure to green space may boost cognitive function, new research suggests.
This association may be explained by a reduction in depression, researchers note. Scores for overall cognition and psychomotor speed/attention among women with high green-space exposure were equivalent to those of women an average of 1.2 years younger, they add.
“Despite the fact that the women in our study were relatively younger than those in previous studies, we were still able to detect protective associations between green space and cognition,” lead author Marcia Pescador Jimenez, PhD, assistant professor of epidemiology, Boston University School of Public Health, told this news organization.
“This may signal the public health importance of green space and the important clinical implications at the population level,” she said.
The findings were published online in JAMA Network Open.
Better psychomotor speed, attention
Recent studies on the benefits of green space have shown a link between higher exposure and reduced risks for schizophrenia and ischemic stroke. Other studies have explored the link between green space and dementia and Alzheimer’s disease.
Cognitive function in middle age is associated with subsequent dementia, so Dr. Jimenez said she and her colleagues wanted to analyze the effect of residential green space on cognitive function in middle-aged women.
The study included 13,594 women (median age, 61.2 years) who are participants in the ongoing Nurses’ Health Study II, one of the largest studies to examine risk factors for chronic illness in women.
To calculate the amount of green space, researchers used the Normalized Difference Vegetation Index (NDVI), a satellite-based indicator of green vegetation around a residential address. The data were based on each participant’s 2013 residence.
After adjusting for age at assessment, race, and childhood, adulthood, and neighborhood socioeconomic status, green space was associated with higher scores on the global CogState composite (mean difference per interquartile range in green space, 0.05; 95% confidence interval, .02-.07) and psychomotor speed and attention (mean difference in score, 0.05 standard units; 95% CI, .02-.08) scales.
There was no association between green-space exposure and learning and working memory. Investigators also found no differences based on urbanicity, suggesting the benefits were similar for urban versus rural settings.
Specific to cognitive domains
“We were surprised to see that while our study found that higher levels of residential green space were associated with higher scores on processing speed and attention and on overall cognition, we also found that higher levels of residential green space were not associated with learning/working memory battery scores,” Dr. Jimenez said.
“This is actually in-line with previous research suggesting differing associations between green space and cognition based on the cognitive domain examined,” she added.
About 98% of participants were White, limiting the generalizability of the findings, the researchers note. There was also no information on proximity to or size of green space, or how much time individuals spent in the green space and what kinds of activities they engaged in.
Dr. Jimenez said projects examining the amount of time of green-space exposure are underway.
In addition, the researchers found lower rates of depression might contribute to the cognitive benefits associated with green-space exposure, explaining 3.95% (95% CI, .35%-7.55%) of the association between green space and psychomotor speed/attention and 6.3% (95% CI, .77%-11.81%) of the association between green space and overall cognition.
Reduced air pollution and increased physical activity, which are other factors often thought to contribute to the cognitive benefits of green space, were not significant in this study.
‘Interesting and novel’
Commenting on the findings, Payam Dadvand, MD, PhD, associate research professor, Barcelona Institute for Global Health, called the finding that depression may mediate green-space benefits “quite interesting and novel.”
“The results of this study, given its large sample size and its geographical coverage, adds to an emerging body of evidence on the beneficial association of exposure to green space on aging, and in particular, cognitive aging in older adults,” said Dr. Dadvand, who was not involved with the research.
The study was funded by the National Institutes of Health. Dr. Jimenez and Dr. Dadvand have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Exposure to green space may boost cognitive function, new research suggests.
This association may be explained by a reduction in depression, researchers note. Scores for overall cognition and psychomotor speed/attention among women with high green-space exposure were equivalent to those of women an average of 1.2 years younger, they add.
“Despite the fact that the women in our study were relatively younger than those in previous studies, we were still able to detect protective associations between green space and cognition,” lead author Marcia Pescador Jimenez, PhD, assistant professor of epidemiology, Boston University School of Public Health, told this news organization.
“This may signal the public health importance of green space and the important clinical implications at the population level,” she said.
The findings were published online in JAMA Network Open.
Better psychomotor speed, attention
Recent studies on the benefits of green space have shown a link between higher exposure and reduced risks for schizophrenia and ischemic stroke. Other studies have explored the link between green space and dementia and Alzheimer’s disease.
Cognitive function in middle age is associated with subsequent dementia, so Dr. Jimenez said she and her colleagues wanted to analyze the effect of residential green space on cognitive function in middle-aged women.
The study included 13,594 women (median age, 61.2 years) who are participants in the ongoing Nurses’ Health Study II, one of the largest studies to examine risk factors for chronic illness in women.
To calculate the amount of green space, researchers used the Normalized Difference Vegetation Index (NDVI), a satellite-based indicator of green vegetation around a residential address. The data were based on each participant’s 2013 residence.
After adjusting for age at assessment, race, and childhood, adulthood, and neighborhood socioeconomic status, green space was associated with higher scores on the global CogState composite (mean difference per interquartile range in green space, 0.05; 95% confidence interval, .02-.07) and psychomotor speed and attention (mean difference in score, 0.05 standard units; 95% CI, .02-.08) scales.
There was no association between green-space exposure and learning and working memory. Investigators also found no differences based on urbanicity, suggesting the benefits were similar for urban versus rural settings.
Specific to cognitive domains
“We were surprised to see that while our study found that higher levels of residential green space were associated with higher scores on processing speed and attention and on overall cognition, we also found that higher levels of residential green space were not associated with learning/working memory battery scores,” Dr. Jimenez said.
“This is actually in-line with previous research suggesting differing associations between green space and cognition based on the cognitive domain examined,” she added.
About 98% of participants were White, limiting the generalizability of the findings, the researchers note. There was also no information on proximity to or size of green space, or how much time individuals spent in the green space and what kinds of activities they engaged in.
Dr. Jimenez said projects examining the amount of time of green-space exposure are underway.
In addition, the researchers found lower rates of depression might contribute to the cognitive benefits associated with green-space exposure, explaining 3.95% (95% CI, .35%-7.55%) of the association between green space and psychomotor speed/attention and 6.3% (95% CI, .77%-11.81%) of the association between green space and overall cognition.
Reduced air pollution and increased physical activity, which are other factors often thought to contribute to the cognitive benefits of green space, were not significant in this study.
‘Interesting and novel’
Commenting on the findings, Payam Dadvand, MD, PhD, associate research professor, Barcelona Institute for Global Health, called the finding that depression may mediate green-space benefits “quite interesting and novel.”
“The results of this study, given its large sample size and its geographical coverage, adds to an emerging body of evidence on the beneficial association of exposure to green space on aging, and in particular, cognitive aging in older adults,” said Dr. Dadvand, who was not involved with the research.
The study was funded by the National Institutes of Health. Dr. Jimenez and Dr. Dadvand have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Exposure to green space may boost cognitive function, new research suggests.
This association may be explained by a reduction in depression, researchers note. Scores for overall cognition and psychomotor speed/attention among women with high green-space exposure were equivalent to those of women an average of 1.2 years younger, they add.
“Despite the fact that the women in our study were relatively younger than those in previous studies, we were still able to detect protective associations between green space and cognition,” lead author Marcia Pescador Jimenez, PhD, assistant professor of epidemiology, Boston University School of Public Health, told this news organization.
“This may signal the public health importance of green space and the important clinical implications at the population level,” she said.
The findings were published online in JAMA Network Open.
Better psychomotor speed, attention
Recent studies on the benefits of green space have shown a link between higher exposure and reduced risks for schizophrenia and ischemic stroke. Other studies have explored the link between green space and dementia and Alzheimer’s disease.
Cognitive function in middle age is associated with subsequent dementia, so Dr. Jimenez said she and her colleagues wanted to analyze the effect of residential green space on cognitive function in middle-aged women.
The study included 13,594 women (median age, 61.2 years) who are participants in the ongoing Nurses’ Health Study II, one of the largest studies to examine risk factors for chronic illness in women.
To calculate the amount of green space, researchers used the Normalized Difference Vegetation Index (NDVI), a satellite-based indicator of green vegetation around a residential address. The data were based on each participant’s 2013 residence.
After adjusting for age at assessment, race, and childhood, adulthood, and neighborhood socioeconomic status, green space was associated with higher scores on the global CogState composite (mean difference per interquartile range in green space, 0.05; 95% confidence interval, .02-.07) and psychomotor speed and attention (mean difference in score, 0.05 standard units; 95% CI, .02-.08) scales.
There was no association between green-space exposure and learning and working memory. Investigators also found no differences based on urbanicity, suggesting the benefits were similar for urban versus rural settings.
Specific to cognitive domains
“We were surprised to see that while our study found that higher levels of residential green space were associated with higher scores on processing speed and attention and on overall cognition, we also found that higher levels of residential green space were not associated with learning/working memory battery scores,” Dr. Jimenez said.
“This is actually in-line with previous research suggesting differing associations between green space and cognition based on the cognitive domain examined,” she added.
About 98% of participants were White, limiting the generalizability of the findings, the researchers note. There was also no information on proximity to or size of green space, or how much time individuals spent in the green space and what kinds of activities they engaged in.
Dr. Jimenez said projects examining the amount of time of green-space exposure are underway.
In addition, the researchers found lower rates of depression might contribute to the cognitive benefits associated with green-space exposure, explaining 3.95% (95% CI, .35%-7.55%) of the association between green space and psychomotor speed/attention and 6.3% (95% CI, .77%-11.81%) of the association between green space and overall cognition.
Reduced air pollution and increased physical activity, which are other factors often thought to contribute to the cognitive benefits of green space, were not significant in this study.
‘Interesting and novel’
Commenting on the findings, Payam Dadvand, MD, PhD, associate research professor, Barcelona Institute for Global Health, called the finding that depression may mediate green-space benefits “quite interesting and novel.”
“The results of this study, given its large sample size and its geographical coverage, adds to an emerging body of evidence on the beneficial association of exposure to green space on aging, and in particular, cognitive aging in older adults,” said Dr. Dadvand, who was not involved with the research.
The study was funded by the National Institutes of Health. Dr. Jimenez and Dr. Dadvand have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Adherence to ADHD meds may lower unemployment risk
Investigators analyzed data for almost 13,000 working-age adults with ADHD and found ADHD medication use during the previous 2 years was associated with a 10% lower risk for long-term unemployment in the following year.
In addition, among the female participants, longer treatment duration was associated with a lower risk for subsequent long-term unemployment. In both genders, within-individual comparisons showed long-term unemployment was lower during periods of ADHD medication treatment, compared with nontreatment periods.
“This evidence should be considered together with the existing knowledge of risks and benefits of ADHD medications when developing treatment plans for working-aged adults,” lead author Lin Li, MSc, a doctoral candidate at the School of Medical Science, Örebro University, Sweden, told this news organization.
“However, the effect size is relatively small in magnitude, indicating that other treatment programs, such as psychotherapy, are also needed to help individuals with ADHD in work-related settings,” Ms. Li said.
The findings were published online in JAMA Network Open.
Evidence gap
Adults with ADHD “have occupational impairments, such as poor work performance, less job stability, financial problems, and increased risk for unemployment,” the investigators write.
However, “less is known about the extent to which pharmacological treatment of ADHD is associated with reductions in unemployment rates,” they add.
“People with ADHD have been reported to have problems in work-related performance,” Ms. Li noted. “ADHD medications could reduce ADHD symptoms and also help with academic achievement, but there is limited evidence on the association between ADHD medication and occupational outcomes.”
To address this gap in evidence, the researchers turned to several major Swedish registries to identify 25,358 individuals with ADHD born between 1958 and 1978 who were aged 30 to 55 years during the study period of Jan. 1, 2008, through Dec. 31, 2013).
Of these, 12,875 (41.5% women; mean age, 37.9 years) were included in the analysis. Most participants (81.19%) had more than 9 years of education.
The registers provided information not only about diagnosis, but also about prescription medications these individuals took for ADHD, including methylphenidate, amphetamine, dexamphetamine, lisdexamfetamine, and atomoxetine.
Administrative records provided data about yearly accumulated unemployment days, with long-term unemployment defined as having at least 90 days of unemployment in a calendar year.
Covariates included age at baseline, sex, country of birth, highest educational level, crime records, and psychiatric comorbidities.
Most patients (69.34%) had at least one psychiatric comorbidity, with depressive, anxiety, and substance use disorders being the most common (in 40.28%, 35.27%, and 28.77%, respectively).
Symptom reduction
The mean length of medication use was 49 days (range, 0-366 days) per year. Of participants in whom these data were available, 31.29% of women and 31.03% of men never used ADHD medications. Among participants treated with ADHD medication (68.71%), only 3.23% of the women and 3.46% of the men had persistent use during the follow-up period.
Among women and men in whom these data were available, (38.85% of the total sample), 35.70% and 41.08%, respectively, were recorded as having one or more long-term unemployment stretches across the study period. In addition, 0.15% and 0.4%, respectively, had long-term unemployment during each of those years.
Use of ADHD medications during the previous 2 years was associated with a 10% lower risk for long-term unemployment in the following year (adjusted relative risk, 0.90; 95% confidence interval, 0.87-0.95).
The researchers also found an association between use of ADHD medications and long-term unemployment among women (RR, 0.82; 95% CI, 0.76-0.89) but not among men (RR, 0.96; 95% CI, 0.91-1.01).
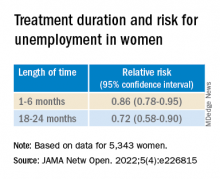
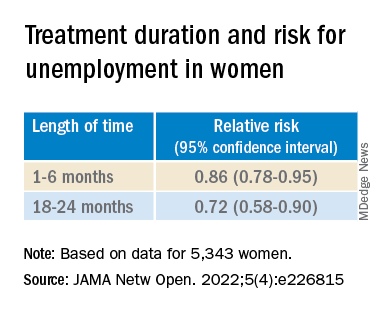
Among women in particular, longer treatment duration was associated with a lower risk of subsequent long-term unemployment (P < .001 for trend).
Within-individual comparisons showed the long-term unemployment rate was lower during periods when individuals were being treated with ADHD medication vs. periods of nontreatment (RR, 0.89; 95% CI, 0.85-0.94).
“Among 12,875 working-aged adults with ADHD in Sweden, we found the use of ADHD medication is associated with a lower risk of long-term unemployment, especially for women,” Ms. Li said.
“The hypothesis of this study is that ADHD medications are effective in reducing ADHD symptoms, which may in turn help to improve work performance among individuals with ADHD,” she added.
However, Ms. Li cautioned, “the information on ADHD symptoms is not available in Swedish National Registers, so more research is needed to test the hypothesis.”
The investigators also suggest that future research “should further explore the effectiveness of stimulant and nonstimulant ADHD medications” and replicate their findings in other settings.
Findings ‘make sense’
Commenting on the study, Ari Tuckman PsyD, expert spokesman for Children and Adults with Attention-Deficit/Hyperactivity Disorder, said, there is “a lot to like about this study, specifically the large sample size and within-individual comparisons that the Scandinavians’ databases allow.”
“We know that ADHD can impact both finding and keeping a job, so it absolutely makes sense that medication use would reduce duration of unemployment,” said Dr. Tuckman, who is in private practice in West Chester, Pa., and was not involved with the research.
However, “I would venture that the results would have been more robust if the authors had been able to only look at those on optimized medication regimens, which is far too few,” he added. “This lack of optimization would have been even more true 10 years ago, which is when the data was from.”
The study was supported by a grant from the Swedish Council for Health, Working Life, and Welfare, an award from the Swedish Research Council, and a grant from Shire International GmbH, a member of the Takeda group of companies. Ms. Li and Dr. Tuckman have disclosed no relevant financial relationships. The other authors’ disclosures are listed in the original paper.
A version of this article first appeared on Medscape.com.
Investigators analyzed data for almost 13,000 working-age adults with ADHD and found ADHD medication use during the previous 2 years was associated with a 10% lower risk for long-term unemployment in the following year.
In addition, among the female participants, longer treatment duration was associated with a lower risk for subsequent long-term unemployment. In both genders, within-individual comparisons showed long-term unemployment was lower during periods of ADHD medication treatment, compared with nontreatment periods.
“This evidence should be considered together with the existing knowledge of risks and benefits of ADHD medications when developing treatment plans for working-aged adults,” lead author Lin Li, MSc, a doctoral candidate at the School of Medical Science, Örebro University, Sweden, told this news organization.
“However, the effect size is relatively small in magnitude, indicating that other treatment programs, such as psychotherapy, are also needed to help individuals with ADHD in work-related settings,” Ms. Li said.
The findings were published online in JAMA Network Open.
Evidence gap
Adults with ADHD “have occupational impairments, such as poor work performance, less job stability, financial problems, and increased risk for unemployment,” the investigators write.
However, “less is known about the extent to which pharmacological treatment of ADHD is associated with reductions in unemployment rates,” they add.
“People with ADHD have been reported to have problems in work-related performance,” Ms. Li noted. “ADHD medications could reduce ADHD symptoms and also help with academic achievement, but there is limited evidence on the association between ADHD medication and occupational outcomes.”
To address this gap in evidence, the researchers turned to several major Swedish registries to identify 25,358 individuals with ADHD born between 1958 and 1978 who were aged 30 to 55 years during the study period of Jan. 1, 2008, through Dec. 31, 2013).
Of these, 12,875 (41.5% women; mean age, 37.9 years) were included in the analysis. Most participants (81.19%) had more than 9 years of education.
The registers provided information not only about diagnosis, but also about prescription medications these individuals took for ADHD, including methylphenidate, amphetamine, dexamphetamine, lisdexamfetamine, and atomoxetine.
Administrative records provided data about yearly accumulated unemployment days, with long-term unemployment defined as having at least 90 days of unemployment in a calendar year.
Covariates included age at baseline, sex, country of birth, highest educational level, crime records, and psychiatric comorbidities.
Most patients (69.34%) had at least one psychiatric comorbidity, with depressive, anxiety, and substance use disorders being the most common (in 40.28%, 35.27%, and 28.77%, respectively).
Symptom reduction
The mean length of medication use was 49 days (range, 0-366 days) per year. Of participants in whom these data were available, 31.29% of women and 31.03% of men never used ADHD medications. Among participants treated with ADHD medication (68.71%), only 3.23% of the women and 3.46% of the men had persistent use during the follow-up period.
Among women and men in whom these data were available, (38.85% of the total sample), 35.70% and 41.08%, respectively, were recorded as having one or more long-term unemployment stretches across the study period. In addition, 0.15% and 0.4%, respectively, had long-term unemployment during each of those years.
Use of ADHD medications during the previous 2 years was associated with a 10% lower risk for long-term unemployment in the following year (adjusted relative risk, 0.90; 95% confidence interval, 0.87-0.95).
The researchers also found an association between use of ADHD medications and long-term unemployment among women (RR, 0.82; 95% CI, 0.76-0.89) but not among men (RR, 0.96; 95% CI, 0.91-1.01).
Among women in particular, longer treatment duration was associated with a lower risk of subsequent long-term unemployment (P < .001 for trend).
Within-individual comparisons showed the long-term unemployment rate was lower during periods when individuals were being treated with ADHD medication vs. periods of nontreatment (RR, 0.89; 95% CI, 0.85-0.94).
“Among 12,875 working-aged adults with ADHD in Sweden, we found the use of ADHD medication is associated with a lower risk of long-term unemployment, especially for women,” Ms. Li said.
“The hypothesis of this study is that ADHD medications are effective in reducing ADHD symptoms, which may in turn help to improve work performance among individuals with ADHD,” she added.
However, Ms. Li cautioned, “the information on ADHD symptoms is not available in Swedish National Registers, so more research is needed to test the hypothesis.”
The investigators also suggest that future research “should further explore the effectiveness of stimulant and nonstimulant ADHD medications” and replicate their findings in other settings.
Findings ‘make sense’
Commenting on the study, Ari Tuckman PsyD, expert spokesman for Children and Adults with Attention-Deficit/Hyperactivity Disorder, said, there is “a lot to like about this study, specifically the large sample size and within-individual comparisons that the Scandinavians’ databases allow.”
“We know that ADHD can impact both finding and keeping a job, so it absolutely makes sense that medication use would reduce duration of unemployment,” said Dr. Tuckman, who is in private practice in West Chester, Pa., and was not involved with the research.
However, “I would venture that the results would have been more robust if the authors had been able to only look at those on optimized medication regimens, which is far too few,” he added. “This lack of optimization would have been even more true 10 years ago, which is when the data was from.”
The study was supported by a grant from the Swedish Council for Health, Working Life, and Welfare, an award from the Swedish Research Council, and a grant from Shire International GmbH, a member of the Takeda group of companies. Ms. Li and Dr. Tuckman have disclosed no relevant financial relationships. The other authors’ disclosures are listed in the original paper.
A version of this article first appeared on Medscape.com.
Investigators analyzed data for almost 13,000 working-age adults with ADHD and found ADHD medication use during the previous 2 years was associated with a 10% lower risk for long-term unemployment in the following year.
In addition, among the female participants, longer treatment duration was associated with a lower risk for subsequent long-term unemployment. In both genders, within-individual comparisons showed long-term unemployment was lower during periods of ADHD medication treatment, compared with nontreatment periods.
“This evidence should be considered together with the existing knowledge of risks and benefits of ADHD medications when developing treatment plans for working-aged adults,” lead author Lin Li, MSc, a doctoral candidate at the School of Medical Science, Örebro University, Sweden, told this news organization.
“However, the effect size is relatively small in magnitude, indicating that other treatment programs, such as psychotherapy, are also needed to help individuals with ADHD in work-related settings,” Ms. Li said.
The findings were published online in JAMA Network Open.
Evidence gap
Adults with ADHD “have occupational impairments, such as poor work performance, less job stability, financial problems, and increased risk for unemployment,” the investigators write.
However, “less is known about the extent to which pharmacological treatment of ADHD is associated with reductions in unemployment rates,” they add.
“People with ADHD have been reported to have problems in work-related performance,” Ms. Li noted. “ADHD medications could reduce ADHD symptoms and also help with academic achievement, but there is limited evidence on the association between ADHD medication and occupational outcomes.”
To address this gap in evidence, the researchers turned to several major Swedish registries to identify 25,358 individuals with ADHD born between 1958 and 1978 who were aged 30 to 55 years during the study period of Jan. 1, 2008, through Dec. 31, 2013).
Of these, 12,875 (41.5% women; mean age, 37.9 years) were included in the analysis. Most participants (81.19%) had more than 9 years of education.
The registers provided information not only about diagnosis, but also about prescription medications these individuals took for ADHD, including methylphenidate, amphetamine, dexamphetamine, lisdexamfetamine, and atomoxetine.
Administrative records provided data about yearly accumulated unemployment days, with long-term unemployment defined as having at least 90 days of unemployment in a calendar year.
Covariates included age at baseline, sex, country of birth, highest educational level, crime records, and psychiatric comorbidities.
Most patients (69.34%) had at least one psychiatric comorbidity, with depressive, anxiety, and substance use disorders being the most common (in 40.28%, 35.27%, and 28.77%, respectively).
Symptom reduction
The mean length of medication use was 49 days (range, 0-366 days) per year. Of participants in whom these data were available, 31.29% of women and 31.03% of men never used ADHD medications. Among participants treated with ADHD medication (68.71%), only 3.23% of the women and 3.46% of the men had persistent use during the follow-up period.
Among women and men in whom these data were available, (38.85% of the total sample), 35.70% and 41.08%, respectively, were recorded as having one or more long-term unemployment stretches across the study period. In addition, 0.15% and 0.4%, respectively, had long-term unemployment during each of those years.
Use of ADHD medications during the previous 2 years was associated with a 10% lower risk for long-term unemployment in the following year (adjusted relative risk, 0.90; 95% confidence interval, 0.87-0.95).
The researchers also found an association between use of ADHD medications and long-term unemployment among women (RR, 0.82; 95% CI, 0.76-0.89) but not among men (RR, 0.96; 95% CI, 0.91-1.01).
Among women in particular, longer treatment duration was associated with a lower risk of subsequent long-term unemployment (P < .001 for trend).
Within-individual comparisons showed the long-term unemployment rate was lower during periods when individuals were being treated with ADHD medication vs. periods of nontreatment (RR, 0.89; 95% CI, 0.85-0.94).
“Among 12,875 working-aged adults with ADHD in Sweden, we found the use of ADHD medication is associated with a lower risk of long-term unemployment, especially for women,” Ms. Li said.
“The hypothesis of this study is that ADHD medications are effective in reducing ADHD symptoms, which may in turn help to improve work performance among individuals with ADHD,” she added.
However, Ms. Li cautioned, “the information on ADHD symptoms is not available in Swedish National Registers, so more research is needed to test the hypothesis.”
The investigators also suggest that future research “should further explore the effectiveness of stimulant and nonstimulant ADHD medications” and replicate their findings in other settings.
Findings ‘make sense’
Commenting on the study, Ari Tuckman PsyD, expert spokesman for Children and Adults with Attention-Deficit/Hyperactivity Disorder, said, there is “a lot to like about this study, specifically the large sample size and within-individual comparisons that the Scandinavians’ databases allow.”
“We know that ADHD can impact both finding and keeping a job, so it absolutely makes sense that medication use would reduce duration of unemployment,” said Dr. Tuckman, who is in private practice in West Chester, Pa., and was not involved with the research.
However, “I would venture that the results would have been more robust if the authors had been able to only look at those on optimized medication regimens, which is far too few,” he added. “This lack of optimization would have been even more true 10 years ago, which is when the data was from.”
The study was supported by a grant from the Swedish Council for Health, Working Life, and Welfare, an award from the Swedish Research Council, and a grant from Shire International GmbH, a member of the Takeda group of companies. Ms. Li and Dr. Tuckman have disclosed no relevant financial relationships. The other authors’ disclosures are listed in the original paper.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Multistate opioid crackdown nets indictment against seven physicians
In coordination with federal and state law enforcement, the DOJ charged the defendants for their involvement in the illegal distribution of opioids. At the time that they were charged with the alleged offenses, 12 of the defendants were medical professionals.
The 12 persons in eight federal districts across the country distributed more than 115 million controlled substances, including buprenorphine, clonazepam, dextroamphetamine-amphetamine, hydrocodone, morphine sulfate, oxycodone, oxymorphone, and Suboxone, per the DOJ.
“Doctors and health care professionals are entrusted with prescribing medicine responsibly and in the best interests of their patients. Today’s takedown targets medical providers across the country whose greed drove them to abandon this responsibility in favor of criminal profits,” said Anne Milgram, administrator of the Drug Enforcement Administration.
Medical professionals, others across six states charged
One former nurse, one business manager, and one individual who practiced medicine without a medical credential are among those listed in the indictment. These include the following:
- Eskender Getachew, MD, a Columbus, Ohio, sleep medicine specialist, was charged with unlawful distribution of controlled substances outside the use of professional practice and not for a legitimate medical practice.
- Charles Kistler, DO, an Upper Arlington, Ohio, family practice physician, was charged with unlawful distribution of controlled substances for unlawful prescribing at Midtown Family Practice Clinic in Columbus.
- Yogeshwar Gil, MBBS, a Manchester, Tenn., family medicine doctor and owner of a medical practice, was charged with conspiracy to unlawfully distribute controlled substances and maintaining a drug-involved premises. Dr. Gil was charged in connection with an alleged scheme to distribute opioids and Suboxone outside the usual course of professional practice and without a legitimate medical purpose.
- Contessa Holley, RN, a Pulaski, Tenn., former nurse and clinical director, was charged with wire fraud, aggravated identity theft, and possession of a controlled substance with intent to distribute. She’s alleged to be connected with a scheme to unlawfully obtain opioids by filling fraudulent prescriptions in the names of current and former patients who were in hospice. The indictment alleged that Ms. Holley used the patients’ hospice benefits to cover the opioids’ costs while keeping the drugs for her own use and for further distribution.
- Francene Aretha Gayle, MD, an Orlando, Fla., physician, was charged with conspiracy to unlawfully distribute controlled substances, conspiracy to commit health care fraud, health care fraud, and several substantive counts of illegally issuing opioid prescriptions. Dr. Gayle was charged along with Schara Monique Davis, a Huntsville, Ala.–based business manager. Per the indictment, Dr. Gayle and Ms. Davis operated three medical clinics in Alabama, where Dr. Gayle was the sole physician. The medical clinics billed health insurers for millions of dollars in patient visits that Dr. Gayle had supposedly conducted but during which she was allegedly absent from the clinics; other staff members conducted the visits instead. It’s alleged that Dr. Gayle presigned prescriptions for opioids that were given to patients.
- Robert Taffet, MD, a Haddonfield, N.J., orthopedic surgeon and owner of a medical practice in Sicklerville, N.J., was charged with conspiracy to unlawfully distribute controlled substances. The indictment alleges that he falsified patient files to state that he interacted with patients when he didn’t and that he issued prescriptions for opioids and other controlled substances without assessing the patients in person or by telemedicine. It’s alleged that Dr. Taffett issued prescriptions for more than 179,000 pills that were dispensed by New Jersey pharmacies between April 2020 and December 2021.
- Hau La, MD, a Brentwood, Tenn., family medicine physician and the operator of Absolute Medical Care in Smyrna, Tenn., was charged with sixteen counts of unlawful distribution of a controlled substance. The physician is alleged to have unlawfully prescribed opioids to eight patients outside the usual course of practice and without a legitimate medical purpose.
- Frederick De Mesa, of War, W.Va., practiced as a physician and used a DEA registration number that allowed him to prescribe controlled substances. Mr. De Mesa prescribed these substances without a medical license and didn’t have an active DEA registration number, according to the indictment.
- Loey Kousa, a former internist from Paintsville, Ky., was charged with unlawful distribution of controlled substances, healthcare fraud, and making false statements in connection with the delivery of health care services. The indictment alleges that the former physician issued prescriptions for opioids outside the usual course of professional practice and without a legitimate medical purpose in his capacity as owner and operator of East KY Clinic in Paintsville. He is alleged to have issued the unlawful prescriptions for patients whose treatments were covered by taxpayer-funded programs such as Medicare and Medicaid; he also billed these programs for medically unnecessary procedures for these patients.
Also included in the indictment were Jay Sadrinia, DMD, a Villa Hills, Ky., dentist, who was charged with four counts of illegal distribution of oxycodone and morphine sulfate and one count of illegal distribution of morphine sulfate that resulted in death or serious bodily injury; and Casey Kelleher, an owner-operator of Neighborhood Pharmacy in Boynton Beach, Fla., who allegedly sold large amounts of oxycodone and hydromorphone on the black market.
The Centers for Medicare & Medicaid Services’ Center for Program Integrity has taken six administrative actions against health care providers for their alleged involvement in these offenses, per the DOJ’s announcement.
“Patient care and safety are top priorities for us, and CMS has taken administrative action against six providers to protect critical resources entrusted to Medicare while also safeguarding people with Medicare,” said CMS Administrator Chiquita Brooks-LaSure.
“These actions to combat fraud, waste, and abuse in our federal programs would not be possible without the close and successful partnership of the Centers for Medicare & Medicaid Services, the Department of Justice, and the U.S. Department of Health and Human Services Office of Inspector General,” she added.
A version of this article first appeared on Medscape.com.
In coordination with federal and state law enforcement, the DOJ charged the defendants for their involvement in the illegal distribution of opioids. At the time that they were charged with the alleged offenses, 12 of the defendants were medical professionals.
The 12 persons in eight federal districts across the country distributed more than 115 million controlled substances, including buprenorphine, clonazepam, dextroamphetamine-amphetamine, hydrocodone, morphine sulfate, oxycodone, oxymorphone, and Suboxone, per the DOJ.
“Doctors and health care professionals are entrusted with prescribing medicine responsibly and in the best interests of their patients. Today’s takedown targets medical providers across the country whose greed drove them to abandon this responsibility in favor of criminal profits,” said Anne Milgram, administrator of the Drug Enforcement Administration.
Medical professionals, others across six states charged
One former nurse, one business manager, and one individual who practiced medicine without a medical credential are among those listed in the indictment. These include the following:
- Eskender Getachew, MD, a Columbus, Ohio, sleep medicine specialist, was charged with unlawful distribution of controlled substances outside the use of professional practice and not for a legitimate medical practice.
- Charles Kistler, DO, an Upper Arlington, Ohio, family practice physician, was charged with unlawful distribution of controlled substances for unlawful prescribing at Midtown Family Practice Clinic in Columbus.
- Yogeshwar Gil, MBBS, a Manchester, Tenn., family medicine doctor and owner of a medical practice, was charged with conspiracy to unlawfully distribute controlled substances and maintaining a drug-involved premises. Dr. Gil was charged in connection with an alleged scheme to distribute opioids and Suboxone outside the usual course of professional practice and without a legitimate medical purpose.
- Contessa Holley, RN, a Pulaski, Tenn., former nurse and clinical director, was charged with wire fraud, aggravated identity theft, and possession of a controlled substance with intent to distribute. She’s alleged to be connected with a scheme to unlawfully obtain opioids by filling fraudulent prescriptions in the names of current and former patients who were in hospice. The indictment alleged that Ms. Holley used the patients’ hospice benefits to cover the opioids’ costs while keeping the drugs for her own use and for further distribution.
- Francene Aretha Gayle, MD, an Orlando, Fla., physician, was charged with conspiracy to unlawfully distribute controlled substances, conspiracy to commit health care fraud, health care fraud, and several substantive counts of illegally issuing opioid prescriptions. Dr. Gayle was charged along with Schara Monique Davis, a Huntsville, Ala.–based business manager. Per the indictment, Dr. Gayle and Ms. Davis operated three medical clinics in Alabama, where Dr. Gayle was the sole physician. The medical clinics billed health insurers for millions of dollars in patient visits that Dr. Gayle had supposedly conducted but during which she was allegedly absent from the clinics; other staff members conducted the visits instead. It’s alleged that Dr. Gayle presigned prescriptions for opioids that were given to patients.
- Robert Taffet, MD, a Haddonfield, N.J., orthopedic surgeon and owner of a medical practice in Sicklerville, N.J., was charged with conspiracy to unlawfully distribute controlled substances. The indictment alleges that he falsified patient files to state that he interacted with patients when he didn’t and that he issued prescriptions for opioids and other controlled substances without assessing the patients in person or by telemedicine. It’s alleged that Dr. Taffett issued prescriptions for more than 179,000 pills that were dispensed by New Jersey pharmacies between April 2020 and December 2021.
- Hau La, MD, a Brentwood, Tenn., family medicine physician and the operator of Absolute Medical Care in Smyrna, Tenn., was charged with sixteen counts of unlawful distribution of a controlled substance. The physician is alleged to have unlawfully prescribed opioids to eight patients outside the usual course of practice and without a legitimate medical purpose.
- Frederick De Mesa, of War, W.Va., practiced as a physician and used a DEA registration number that allowed him to prescribe controlled substances. Mr. De Mesa prescribed these substances without a medical license and didn’t have an active DEA registration number, according to the indictment.
- Loey Kousa, a former internist from Paintsville, Ky., was charged with unlawful distribution of controlled substances, healthcare fraud, and making false statements in connection with the delivery of health care services. The indictment alleges that the former physician issued prescriptions for opioids outside the usual course of professional practice and without a legitimate medical purpose in his capacity as owner and operator of East KY Clinic in Paintsville. He is alleged to have issued the unlawful prescriptions for patients whose treatments were covered by taxpayer-funded programs such as Medicare and Medicaid; he also billed these programs for medically unnecessary procedures for these patients.
Also included in the indictment were Jay Sadrinia, DMD, a Villa Hills, Ky., dentist, who was charged with four counts of illegal distribution of oxycodone and morphine sulfate and one count of illegal distribution of morphine sulfate that resulted in death or serious bodily injury; and Casey Kelleher, an owner-operator of Neighborhood Pharmacy in Boynton Beach, Fla., who allegedly sold large amounts of oxycodone and hydromorphone on the black market.
The Centers for Medicare & Medicaid Services’ Center for Program Integrity has taken six administrative actions against health care providers for their alleged involvement in these offenses, per the DOJ’s announcement.
“Patient care and safety are top priorities for us, and CMS has taken administrative action against six providers to protect critical resources entrusted to Medicare while also safeguarding people with Medicare,” said CMS Administrator Chiquita Brooks-LaSure.
“These actions to combat fraud, waste, and abuse in our federal programs would not be possible without the close and successful partnership of the Centers for Medicare & Medicaid Services, the Department of Justice, and the U.S. Department of Health and Human Services Office of Inspector General,” she added.
A version of this article first appeared on Medscape.com.
In coordination with federal and state law enforcement, the DOJ charged the defendants for their involvement in the illegal distribution of opioids. At the time that they were charged with the alleged offenses, 12 of the defendants were medical professionals.
The 12 persons in eight federal districts across the country distributed more than 115 million controlled substances, including buprenorphine, clonazepam, dextroamphetamine-amphetamine, hydrocodone, morphine sulfate, oxycodone, oxymorphone, and Suboxone, per the DOJ.
“Doctors and health care professionals are entrusted with prescribing medicine responsibly and in the best interests of their patients. Today’s takedown targets medical providers across the country whose greed drove them to abandon this responsibility in favor of criminal profits,” said Anne Milgram, administrator of the Drug Enforcement Administration.
Medical professionals, others across six states charged
One former nurse, one business manager, and one individual who practiced medicine without a medical credential are among those listed in the indictment. These include the following:
- Eskender Getachew, MD, a Columbus, Ohio, sleep medicine specialist, was charged with unlawful distribution of controlled substances outside the use of professional practice and not for a legitimate medical practice.
- Charles Kistler, DO, an Upper Arlington, Ohio, family practice physician, was charged with unlawful distribution of controlled substances for unlawful prescribing at Midtown Family Practice Clinic in Columbus.
- Yogeshwar Gil, MBBS, a Manchester, Tenn., family medicine doctor and owner of a medical practice, was charged with conspiracy to unlawfully distribute controlled substances and maintaining a drug-involved premises. Dr. Gil was charged in connection with an alleged scheme to distribute opioids and Suboxone outside the usual course of professional practice and without a legitimate medical purpose.
- Contessa Holley, RN, a Pulaski, Tenn., former nurse and clinical director, was charged with wire fraud, aggravated identity theft, and possession of a controlled substance with intent to distribute. She’s alleged to be connected with a scheme to unlawfully obtain opioids by filling fraudulent prescriptions in the names of current and former patients who were in hospice. The indictment alleged that Ms. Holley used the patients’ hospice benefits to cover the opioids’ costs while keeping the drugs for her own use and for further distribution.
- Francene Aretha Gayle, MD, an Orlando, Fla., physician, was charged with conspiracy to unlawfully distribute controlled substances, conspiracy to commit health care fraud, health care fraud, and several substantive counts of illegally issuing opioid prescriptions. Dr. Gayle was charged along with Schara Monique Davis, a Huntsville, Ala.–based business manager. Per the indictment, Dr. Gayle and Ms. Davis operated three medical clinics in Alabama, where Dr. Gayle was the sole physician. The medical clinics billed health insurers for millions of dollars in patient visits that Dr. Gayle had supposedly conducted but during which she was allegedly absent from the clinics; other staff members conducted the visits instead. It’s alleged that Dr. Gayle presigned prescriptions for opioids that were given to patients.
- Robert Taffet, MD, a Haddonfield, N.J., orthopedic surgeon and owner of a medical practice in Sicklerville, N.J., was charged with conspiracy to unlawfully distribute controlled substances. The indictment alleges that he falsified patient files to state that he interacted with patients when he didn’t and that he issued prescriptions for opioids and other controlled substances without assessing the patients in person or by telemedicine. It’s alleged that Dr. Taffett issued prescriptions for more than 179,000 pills that were dispensed by New Jersey pharmacies between April 2020 and December 2021.
- Hau La, MD, a Brentwood, Tenn., family medicine physician and the operator of Absolute Medical Care in Smyrna, Tenn., was charged with sixteen counts of unlawful distribution of a controlled substance. The physician is alleged to have unlawfully prescribed opioids to eight patients outside the usual course of practice and without a legitimate medical purpose.
- Frederick De Mesa, of War, W.Va., practiced as a physician and used a DEA registration number that allowed him to prescribe controlled substances. Mr. De Mesa prescribed these substances without a medical license and didn’t have an active DEA registration number, according to the indictment.
- Loey Kousa, a former internist from Paintsville, Ky., was charged with unlawful distribution of controlled substances, healthcare fraud, and making false statements in connection with the delivery of health care services. The indictment alleges that the former physician issued prescriptions for opioids outside the usual course of professional practice and without a legitimate medical purpose in his capacity as owner and operator of East KY Clinic in Paintsville. He is alleged to have issued the unlawful prescriptions for patients whose treatments were covered by taxpayer-funded programs such as Medicare and Medicaid; he also billed these programs for medically unnecessary procedures for these patients.
Also included in the indictment were Jay Sadrinia, DMD, a Villa Hills, Ky., dentist, who was charged with four counts of illegal distribution of oxycodone and morphine sulfate and one count of illegal distribution of morphine sulfate that resulted in death or serious bodily injury; and Casey Kelleher, an owner-operator of Neighborhood Pharmacy in Boynton Beach, Fla., who allegedly sold large amounts of oxycodone and hydromorphone on the black market.
The Centers for Medicare & Medicaid Services’ Center for Program Integrity has taken six administrative actions against health care providers for their alleged involvement in these offenses, per the DOJ’s announcement.
“Patient care and safety are top priorities for us, and CMS has taken administrative action against six providers to protect critical resources entrusted to Medicare while also safeguarding people with Medicare,” said CMS Administrator Chiquita Brooks-LaSure.
“These actions to combat fraud, waste, and abuse in our federal programs would not be possible without the close and successful partnership of the Centers for Medicare & Medicaid Services, the Department of Justice, and the U.S. Department of Health and Human Services Office of Inspector General,” she added.
A version of this article first appeared on Medscape.com.
Study provides new analysis of isotretinoin and risk for adverse neuropsychiatric outcomes
The use of , in a large retrospective cohort study published in the British Journal of Dermatology.
Although severe neuropsychiatric effects associated with isotretinoin therapy in patients with acne have been reported, “the evidence base ... is mixed and inconclusive,” and many studies are small, Seena Fazel, MBChB, MD, of the department of psychiatry, Oxford University, England, and co-authors write in the study.
The study results suggest that isotretinoin is conferring protection against adverse neuropsychiatric outcomes, particularly when compared with using oral antibiotics to treat acne, Dr. Fazel, professor of forensic psychiatry at Oxford University and the study’s senior author, said in an interview.
In the study, the investigators reviewed electronic health records (2013-2019) from a primarily United States–based dataset (TriNetX) of patients with acne aged 12-27 who had been followed for up to 1 year after their prescriptions had been dispensed.
There were four arms: those prescribed isotretinoin (30,866), oral antibiotics (44,748), topical anti-acne treatments (108,367), and those who had not been prescribed any acne treatment (78,666). The primary outcomes were diagnoses of a neuropsychiatric disorder (psychotic, mood, anxiety, personality, behavioral, and sleep disorders; and non-fatal self-harm) within one year of being prescribed treatment.
After using propensity score matching to adjust for confounders at baseline, the investigators determined that the odds ratio for any incident neuropsychiatric outcomes among patients with acne treated with isotretinoin was 0.80 (95% confidence interval, 0.74-0.87), compared with patients on oral antibiotics; 0.94 (95% CI, 0.87-1.02), compared with patients on topical anti-acne medications; and 1.06 (95% CI, 0.97-1.16), compared with those without a prescription for anti-acne medicines.
Side effects of isotretinoin – such as headache, dry mouth, and fatigue – were higher among those on isotretinoin than in the other three groups.
The authors concluded that isotretinoin was not independently linked to excess adverse neuropsychiatric outcomes at a population level. “We observed a consistent association between increasing acne severity as indicated by anti-acne treatment options and incidence of adverse neuropsychiatric outcomes, but the findings showed that isotretinoin exposure did not add to the risk of neuropsychiatric adverse outcomes over and above what was associated with oral antibiotics,” they write.
Isotretinoin treatment “appeared to mitigate the excess neuropsychiatric risk associated with recalcitrant moderate-to-severe acne,” they add.
The dermatology community has been interested in the impact isotretinoin has on mental health, and “I think clinically, they see that people get better on isotretinoin and their mental health improves,” Dr. Fazel told this news organization.
Asked to comment on the study results, John Barbieri, MD, MBA, director of the Advanced Acne Therapeutics Clinic, Brigham and Women’s Hospital, Boston, commended the investigators for the design of the trial.
“One of the strengths of this study is that they use a technique called propensity-score matching, where you try to make the groups of patients similar with respect to their other characteristics to minimize the risks of confounding and bias in the study, which I think is a real strength,” he told this news organization. “The other thing that they do, which I think is a strength, is to think about the impact of acne severity on these outcomes, because we know acne itself is associated with depression and risk for suicide and other neuropsychiatric outcomes.”
Including a cohort of patients who had acne and received oral antibiotics for comparison “is a nice way to address the potential for confounding by severity and confounding by indication,” Dr. Barbieri said. “Those who get antibiotics usually have more severe acne. They may not have it as severely as those who get isotretinoin, but it is a nice approach to account for background levels of depression and neuropsychiatric outcomes in patients with acne. I think that is a real strength of the study. This is one of the best studies to have looked at this question.”
However, although the study found that isotretinoin decreased the excess psychiatric risk associated with refractory moderate-to-severe acne, it does not rule out the possibility that individuals may experience an adverse psychiatric outcome while on isotretinoin, Dr. Barbieri said.
“While I think on a population level, we absolutely can feel reassured by these data, I do think there are individual patients who have idiosyncratic, unpredictable reactions to isotretinoin where they have mood changes, whether it be irritability, depression, or other mood changes,” he cautioned. “Given the association of acne itself with mental health comorbidities, it is important to screen for comorbidities such as depression in all patients with acne.”
The study was funded by the Wellcome Trust, which provided Dr. Fazel and the first author with financial support for the study. One author is an employee of TriNetX; the other authors had no relevant disclosures. Dr. Barbieri reported no financial disclosures. He is cochair of the AAD’s Acne Guidelines Workgroup and associate editor at JAMA Dermatology.
A version of this article first appeared on Medscape.com.
The use of , in a large retrospective cohort study published in the British Journal of Dermatology.
Although severe neuropsychiatric effects associated with isotretinoin therapy in patients with acne have been reported, “the evidence base ... is mixed and inconclusive,” and many studies are small, Seena Fazel, MBChB, MD, of the department of psychiatry, Oxford University, England, and co-authors write in the study.
The study results suggest that isotretinoin is conferring protection against adverse neuropsychiatric outcomes, particularly when compared with using oral antibiotics to treat acne, Dr. Fazel, professor of forensic psychiatry at Oxford University and the study’s senior author, said in an interview.
In the study, the investigators reviewed electronic health records (2013-2019) from a primarily United States–based dataset (TriNetX) of patients with acne aged 12-27 who had been followed for up to 1 year after their prescriptions had been dispensed.
There were four arms: those prescribed isotretinoin (30,866), oral antibiotics (44,748), topical anti-acne treatments (108,367), and those who had not been prescribed any acne treatment (78,666). The primary outcomes were diagnoses of a neuropsychiatric disorder (psychotic, mood, anxiety, personality, behavioral, and sleep disorders; and non-fatal self-harm) within one year of being prescribed treatment.
After using propensity score matching to adjust for confounders at baseline, the investigators determined that the odds ratio for any incident neuropsychiatric outcomes among patients with acne treated with isotretinoin was 0.80 (95% confidence interval, 0.74-0.87), compared with patients on oral antibiotics; 0.94 (95% CI, 0.87-1.02), compared with patients on topical anti-acne medications; and 1.06 (95% CI, 0.97-1.16), compared with those without a prescription for anti-acne medicines.
Side effects of isotretinoin – such as headache, dry mouth, and fatigue – were higher among those on isotretinoin than in the other three groups.
The authors concluded that isotretinoin was not independently linked to excess adverse neuropsychiatric outcomes at a population level. “We observed a consistent association between increasing acne severity as indicated by anti-acne treatment options and incidence of adverse neuropsychiatric outcomes, but the findings showed that isotretinoin exposure did not add to the risk of neuropsychiatric adverse outcomes over and above what was associated with oral antibiotics,” they write.
Isotretinoin treatment “appeared to mitigate the excess neuropsychiatric risk associated with recalcitrant moderate-to-severe acne,” they add.
The dermatology community has been interested in the impact isotretinoin has on mental health, and “I think clinically, they see that people get better on isotretinoin and their mental health improves,” Dr. Fazel told this news organization.
Asked to comment on the study results, John Barbieri, MD, MBA, director of the Advanced Acne Therapeutics Clinic, Brigham and Women’s Hospital, Boston, commended the investigators for the design of the trial.
“One of the strengths of this study is that they use a technique called propensity-score matching, where you try to make the groups of patients similar with respect to their other characteristics to minimize the risks of confounding and bias in the study, which I think is a real strength,” he told this news organization. “The other thing that they do, which I think is a strength, is to think about the impact of acne severity on these outcomes, because we know acne itself is associated with depression and risk for suicide and other neuropsychiatric outcomes.”
Including a cohort of patients who had acne and received oral antibiotics for comparison “is a nice way to address the potential for confounding by severity and confounding by indication,” Dr. Barbieri said. “Those who get antibiotics usually have more severe acne. They may not have it as severely as those who get isotretinoin, but it is a nice approach to account for background levels of depression and neuropsychiatric outcomes in patients with acne. I think that is a real strength of the study. This is one of the best studies to have looked at this question.”
However, although the study found that isotretinoin decreased the excess psychiatric risk associated with refractory moderate-to-severe acne, it does not rule out the possibility that individuals may experience an adverse psychiatric outcome while on isotretinoin, Dr. Barbieri said.
“While I think on a population level, we absolutely can feel reassured by these data, I do think there are individual patients who have idiosyncratic, unpredictable reactions to isotretinoin where they have mood changes, whether it be irritability, depression, or other mood changes,” he cautioned. “Given the association of acne itself with mental health comorbidities, it is important to screen for comorbidities such as depression in all patients with acne.”
The study was funded by the Wellcome Trust, which provided Dr. Fazel and the first author with financial support for the study. One author is an employee of TriNetX; the other authors had no relevant disclosures. Dr. Barbieri reported no financial disclosures. He is cochair of the AAD’s Acne Guidelines Workgroup and associate editor at JAMA Dermatology.
A version of this article first appeared on Medscape.com.
The use of , in a large retrospective cohort study published in the British Journal of Dermatology.
Although severe neuropsychiatric effects associated with isotretinoin therapy in patients with acne have been reported, “the evidence base ... is mixed and inconclusive,” and many studies are small, Seena Fazel, MBChB, MD, of the department of psychiatry, Oxford University, England, and co-authors write in the study.
The study results suggest that isotretinoin is conferring protection against adverse neuropsychiatric outcomes, particularly when compared with using oral antibiotics to treat acne, Dr. Fazel, professor of forensic psychiatry at Oxford University and the study’s senior author, said in an interview.
In the study, the investigators reviewed electronic health records (2013-2019) from a primarily United States–based dataset (TriNetX) of patients with acne aged 12-27 who had been followed for up to 1 year after their prescriptions had been dispensed.
There were four arms: those prescribed isotretinoin (30,866), oral antibiotics (44,748), topical anti-acne treatments (108,367), and those who had not been prescribed any acne treatment (78,666). The primary outcomes were diagnoses of a neuropsychiatric disorder (psychotic, mood, anxiety, personality, behavioral, and sleep disorders; and non-fatal self-harm) within one year of being prescribed treatment.
After using propensity score matching to adjust for confounders at baseline, the investigators determined that the odds ratio for any incident neuropsychiatric outcomes among patients with acne treated with isotretinoin was 0.80 (95% confidence interval, 0.74-0.87), compared with patients on oral antibiotics; 0.94 (95% CI, 0.87-1.02), compared with patients on topical anti-acne medications; and 1.06 (95% CI, 0.97-1.16), compared with those without a prescription for anti-acne medicines.
Side effects of isotretinoin – such as headache, dry mouth, and fatigue – were higher among those on isotretinoin than in the other three groups.
The authors concluded that isotretinoin was not independently linked to excess adverse neuropsychiatric outcomes at a population level. “We observed a consistent association between increasing acne severity as indicated by anti-acne treatment options and incidence of adverse neuropsychiatric outcomes, but the findings showed that isotretinoin exposure did not add to the risk of neuropsychiatric adverse outcomes over and above what was associated with oral antibiotics,” they write.
Isotretinoin treatment “appeared to mitigate the excess neuropsychiatric risk associated with recalcitrant moderate-to-severe acne,” they add.
The dermatology community has been interested in the impact isotretinoin has on mental health, and “I think clinically, they see that people get better on isotretinoin and their mental health improves,” Dr. Fazel told this news organization.
Asked to comment on the study results, John Barbieri, MD, MBA, director of the Advanced Acne Therapeutics Clinic, Brigham and Women’s Hospital, Boston, commended the investigators for the design of the trial.
“One of the strengths of this study is that they use a technique called propensity-score matching, where you try to make the groups of patients similar with respect to their other characteristics to minimize the risks of confounding and bias in the study, which I think is a real strength,” he told this news organization. “The other thing that they do, which I think is a strength, is to think about the impact of acne severity on these outcomes, because we know acne itself is associated with depression and risk for suicide and other neuropsychiatric outcomes.”
Including a cohort of patients who had acne and received oral antibiotics for comparison “is a nice way to address the potential for confounding by severity and confounding by indication,” Dr. Barbieri said. “Those who get antibiotics usually have more severe acne. They may not have it as severely as those who get isotretinoin, but it is a nice approach to account for background levels of depression and neuropsychiatric outcomes in patients with acne. I think that is a real strength of the study. This is one of the best studies to have looked at this question.”
However, although the study found that isotretinoin decreased the excess psychiatric risk associated with refractory moderate-to-severe acne, it does not rule out the possibility that individuals may experience an adverse psychiatric outcome while on isotretinoin, Dr. Barbieri said.
“While I think on a population level, we absolutely can feel reassured by these data, I do think there are individual patients who have idiosyncratic, unpredictable reactions to isotretinoin where they have mood changes, whether it be irritability, depression, or other mood changes,” he cautioned. “Given the association of acne itself with mental health comorbidities, it is important to screen for comorbidities such as depression in all patients with acne.”
The study was funded by the Wellcome Trust, which provided Dr. Fazel and the first author with financial support for the study. One author is an employee of TriNetX; the other authors had no relevant disclosures. Dr. Barbieri reported no financial disclosures. He is cochair of the AAD’s Acne Guidelines Workgroup and associate editor at JAMA Dermatology.
A version of this article first appeared on Medscape.com.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
FDA clears diagnostic test for early Alzheimer’s
The Lumipulse G β-Amyloid Ratio 1-42/1-40 (Fujirebio Diagnostics) test detects amyloid plaques associated with AD in adults age 55 or older who are under investigation for AD and other causes of cognitive decline.
“The availability of an in vitro diagnostic test that can potentially eliminate the need for time-consuming and expensive [positron emission tomography (PET)] scans is great news for individuals and families concerned with the possibility of an Alzheimer’s disease diagnosis,” Jeff Shuren, MD, JD, director of the FDA’s Center for Devices and Radiological Health, said in a statement.
“With the Lumipulse test, there is a new option that can typically be completed the same day and can give doctors the same information regarding brain amyloid status, without the radiation risk, to help determine if a patient’s cognitive impairment is due to Alzheimer’s disease,” he added.
In its statement, the FDA notes that there is an “unmet need for a reliable and safe test that can accurately identify patients with amyloid plaques consistent with Alzheimer’s disease.”
The agency goes on to state that this new test may eliminate the need to use PET brain scans, a “potentially costly and cumbersome option” to visualize amyloid plaques for the diagnosis of AD.
The Lumipulse test measures the ratio of β-amyloid 1-42 and β-amyloid 1-40 concentrations in human cerebral spinal fluid (CSF). A positive Lumipulse G β-amyloid Ratio (1-42/1-40) test result is consistent with the presence of amyloid plaques, similar to that revealed in a PET scan. A negative result is consistent with a negative amyloid PET scan result.
However, the FDA notes that the test is not a stand-alone assay and should be used in conjunction with other clinical evaluations and additional tests to determine treatment options.
The FDA reports that it evaluated the safety and efficacy of the test in a clinical study of 292 CSF samples from the Alzheimer’s Disease Neuroimaging Initiative sample bank.
The samples were tested by the Lumipulse G β-amyloid Ratio (1-42/1-40) and compared with amyloid PET scan results. In this clinical study, 97% of individuals with Lumipulse G β-amyloid Ratio (1-42/1-40) positive results had the presence of amyloid plaques by PET scan and 84% of individuals with negative results had a negative amyloid PET scan.
The risks associated with the Lumipulse G β-amyloid Ratio (1-42/1-40) test are mainly the possibility of false-positive and false-negative test results.
False-positive results, in conjunction with other clinical information, could lead to an inappropriate diagnosis of, and unnecessary treatment for AD.
False-negative test results could result in additional unnecessary diagnostic tests and potential delay in effective treatment for AD.
The FDA reviewed the device through the De Novo premarket review pathway, a regulatory pathway for low- to moderate-risk devices of a new type.
The agency says this action “creates a new regulatory classification, which means that subsequent devices of the same type with the same intended use may go through FDA’s 510(k) premarket process, whereby devices can obtain marketing authorization by demonstrating substantial equivalence to a predicate device.”
The Lumipulse G β-amyloid Ratio (1-42/1-40) was granted Breakthrough Device designation, a process designed to expedite the development and review of devices that may provide for more effective treatment or diagnosis of life-threatening or irreversibly debilitating diseases or conditions.
A version of this article first appeared on Medscape.com.
The Lumipulse G β-Amyloid Ratio 1-42/1-40 (Fujirebio Diagnostics) test detects amyloid plaques associated with AD in adults age 55 or older who are under investigation for AD and other causes of cognitive decline.
“The availability of an in vitro diagnostic test that can potentially eliminate the need for time-consuming and expensive [positron emission tomography (PET)] scans is great news for individuals and families concerned with the possibility of an Alzheimer’s disease diagnosis,” Jeff Shuren, MD, JD, director of the FDA’s Center for Devices and Radiological Health, said in a statement.
“With the Lumipulse test, there is a new option that can typically be completed the same day and can give doctors the same information regarding brain amyloid status, without the radiation risk, to help determine if a patient’s cognitive impairment is due to Alzheimer’s disease,” he added.
In its statement, the FDA notes that there is an “unmet need for a reliable and safe test that can accurately identify patients with amyloid plaques consistent with Alzheimer’s disease.”
The agency goes on to state that this new test may eliminate the need to use PET brain scans, a “potentially costly and cumbersome option” to visualize amyloid plaques for the diagnosis of AD.
The Lumipulse test measures the ratio of β-amyloid 1-42 and β-amyloid 1-40 concentrations in human cerebral spinal fluid (CSF). A positive Lumipulse G β-amyloid Ratio (1-42/1-40) test result is consistent with the presence of amyloid plaques, similar to that revealed in a PET scan. A negative result is consistent with a negative amyloid PET scan result.
However, the FDA notes that the test is not a stand-alone assay and should be used in conjunction with other clinical evaluations and additional tests to determine treatment options.
The FDA reports that it evaluated the safety and efficacy of the test in a clinical study of 292 CSF samples from the Alzheimer’s Disease Neuroimaging Initiative sample bank.
The samples were tested by the Lumipulse G β-amyloid Ratio (1-42/1-40) and compared with amyloid PET scan results. In this clinical study, 97% of individuals with Lumipulse G β-amyloid Ratio (1-42/1-40) positive results had the presence of amyloid plaques by PET scan and 84% of individuals with negative results had a negative amyloid PET scan.
The risks associated with the Lumipulse G β-amyloid Ratio (1-42/1-40) test are mainly the possibility of false-positive and false-negative test results.
False-positive results, in conjunction with other clinical information, could lead to an inappropriate diagnosis of, and unnecessary treatment for AD.
False-negative test results could result in additional unnecessary diagnostic tests and potential delay in effective treatment for AD.
The FDA reviewed the device through the De Novo premarket review pathway, a regulatory pathway for low- to moderate-risk devices of a new type.
The agency says this action “creates a new regulatory classification, which means that subsequent devices of the same type with the same intended use may go through FDA’s 510(k) premarket process, whereby devices can obtain marketing authorization by demonstrating substantial equivalence to a predicate device.”
The Lumipulse G β-amyloid Ratio (1-42/1-40) was granted Breakthrough Device designation, a process designed to expedite the development and review of devices that may provide for more effective treatment or diagnosis of life-threatening or irreversibly debilitating diseases or conditions.
A version of this article first appeared on Medscape.com.
The Lumipulse G β-Amyloid Ratio 1-42/1-40 (Fujirebio Diagnostics) test detects amyloid plaques associated with AD in adults age 55 or older who are under investigation for AD and other causes of cognitive decline.
“The availability of an in vitro diagnostic test that can potentially eliminate the need for time-consuming and expensive [positron emission tomography (PET)] scans is great news for individuals and families concerned with the possibility of an Alzheimer’s disease diagnosis,” Jeff Shuren, MD, JD, director of the FDA’s Center for Devices and Radiological Health, said in a statement.
“With the Lumipulse test, there is a new option that can typically be completed the same day and can give doctors the same information regarding brain amyloid status, without the radiation risk, to help determine if a patient’s cognitive impairment is due to Alzheimer’s disease,” he added.
In its statement, the FDA notes that there is an “unmet need for a reliable and safe test that can accurately identify patients with amyloid plaques consistent with Alzheimer’s disease.”
The agency goes on to state that this new test may eliminate the need to use PET brain scans, a “potentially costly and cumbersome option” to visualize amyloid plaques for the diagnosis of AD.
The Lumipulse test measures the ratio of β-amyloid 1-42 and β-amyloid 1-40 concentrations in human cerebral spinal fluid (CSF). A positive Lumipulse G β-amyloid Ratio (1-42/1-40) test result is consistent with the presence of amyloid plaques, similar to that revealed in a PET scan. A negative result is consistent with a negative amyloid PET scan result.
However, the FDA notes that the test is not a stand-alone assay and should be used in conjunction with other clinical evaluations and additional tests to determine treatment options.
The FDA reports that it evaluated the safety and efficacy of the test in a clinical study of 292 CSF samples from the Alzheimer’s Disease Neuroimaging Initiative sample bank.
The samples were tested by the Lumipulse G β-amyloid Ratio (1-42/1-40) and compared with amyloid PET scan results. In this clinical study, 97% of individuals with Lumipulse G β-amyloid Ratio (1-42/1-40) positive results had the presence of amyloid plaques by PET scan and 84% of individuals with negative results had a negative amyloid PET scan.
The risks associated with the Lumipulse G β-amyloid Ratio (1-42/1-40) test are mainly the possibility of false-positive and false-negative test results.
False-positive results, in conjunction with other clinical information, could lead to an inappropriate diagnosis of, and unnecessary treatment for AD.
False-negative test results could result in additional unnecessary diagnostic tests and potential delay in effective treatment for AD.
The FDA reviewed the device through the De Novo premarket review pathway, a regulatory pathway for low- to moderate-risk devices of a new type.
The agency says this action “creates a new regulatory classification, which means that subsequent devices of the same type with the same intended use may go through FDA’s 510(k) premarket process, whereby devices can obtain marketing authorization by demonstrating substantial equivalence to a predicate device.”
The Lumipulse G β-amyloid Ratio (1-42/1-40) was granted Breakthrough Device designation, a process designed to expedite the development and review of devices that may provide for more effective treatment or diagnosis of life-threatening or irreversibly debilitating diseases or conditions.
A version of this article first appeared on Medscape.com.
Mood instability in childhood as a precursor to bipolar disorder
Mood instability, or sudden, unpredictable, and frequent shifts in emotional states, characterizes many types of psychiatric disorder, including attention-deficit/hyperactivity disorder (ADHD), personality disorders, depression, and posttraumatic stress disorder. To say that individuals with bipolar disorder (BD) have mood instability sounds like a tautology. Nonetheless, mood instability has particular relevance to BD: Many patients have irregular or labile moods even when they are between major episodes of mania and depression.1
Children of parents with BD who have high levels of mood instability are at particularly high risk for developing BD (types I or II) in late adolescence or early adulthood.2 The following case provides an illustration:
Patrick, age 14, entered treatment with diagnoses of ADHD and other specified bipolar disorder. His mother felt that his behavior resembled that of his father, who had been treated for manic episodes. During the COVID-19 pandemic, Patrick had become increasingly difficult at home, with significant oppositionality, impulsive behavior, and difficulty following through on school assignments or household tasks. His mother’s most significant complaints concerned Patrick’s sudden outbursts of anger and abrupt verbal abuse when she asked him to stop playing video games. When interrupted, he cursed loudly and sometimes turned violent; he had broken a window and a door at home and had on one occasion physically attacked his younger brother. Patrick agreed that he became angry at times, but felt that others provoked him. When queried about depression, he described anxiety and worry. He was unable to describe a particular trigger for his anxiety except for being interrupted in online games with his friends, which made him “feel like a total loser.”
His mother reported that Patrick had multiple 1- to 2-day intervals in which he became “really silly, laughing at nothing,” talking rapidly, jumping from one topic to another, and becoming annoyed when others didn’t share his enthusiasm. In these activated intervals, he slept little and seemed to be full of energy; his mother would hear him talking loudly into his phone throughout the night. During one such interval he had become verbally aggressive with a peer, which had ruined their friendship. Both Patrick and his mother reported that they had been fighting constantly and, in her words, “our house has become a war zone.”
In our recent article in the Journal of the American Academy of Child and Adolescent Psychiatry,3 my coauthors and I examined the association between parents’ ratings of mood instability and clinicians’ longitudinal ratings of symptoms and functioning among youth (ages 9-17 years) who were at high risk for BD. The participants met DSM-5 diagnostic criteria for major depressive disorder or other specified BD, defined as recurrent and brief periods of elevation and activation that did not meet syndromal mania or hypomania criteria. All participants had at least one first- or second-degree family member with a history of BD I or II. Following a period of evaluation, participants were randomly assigned to one of two 4-month psychological therapies: Family-focused therapy (12 sessions of psychoeducation, communication training, and problem-solving skills training) or enhanced usual care (6 sessions of family and individual psychoeducation and support). They also received pharmacological management from study-affiliated psychiatrists when warranted.
We measured mood instability at intake and every 4-6 months over an average of 2 years (range 0-255 weeks). We used a brief parent questionnaire – the Children’s Affective Lability Scale4 – which enables measurement of lability on the dimensions of elevation or activation (e.g., bursts of silliness or hilarity, excessive familiarity with others), irritability (e.g., temper outbursts), or anxious-depression (e.g., sudden bouts of crying).
Over the 1- to 4-year period of follow-up, mood instability was associated with poor prognosis indicators in high-risk youth: Being younger, having younger ages at first symptom onset, being diagnosed with other specified BD (vs. major depression), and having more complex patterns of comorbid disorders. Mood instability tracked closely with levels of mania, depression, and global functioning over the follow-up. There was a temporal pathway between a diagnosis of other specified bipolar disorder at intake and higher levels of mood instability at follow-up, which in turn predicted higher levels of parent/child conflict. High levels of mood lability may lead to isolation from peers and tension within family relationships, which may fuel further children’s expressions of frustration, rage, depression, or impulsive behavior.
Youth with higher levels of mood instability required more complex medication regimens over 1 year than did those with lower instability. There was an overall reduction in mood instability as children aged (or spent more time in treatment). Over the 1- to 4-year follow-up, family-focused therapy was associated with longer intervals prior to new mood episodes than was enhanced usual care, but reductions in mood instability were independent of the type of psychosocial treatment assigned to children.
The participants in this study could not be followed long enough to determine whether levels of mood instability were associated with the later development of syndromal BD. Other studies, however, have documented this relationship. Large-scale longitudinal studies of high-risk children find that measures of mood lability – along with early onset manic symptoms, depression, anxiety, and a family history of mania or hypomania – can be combined to calculate the risk that any individual child will develop BD I or II over the next 5-8 years.2,5
Clinicians should include measurement of the severity and psychosocial determinants of persistent mood shifts in youth under their care, particularly those with a family history of BD. Mood instability is associated with more severe symptom trajectories, more social isolation, and greater distress and conflict within the family. It may require a greater intensity of both pharmacological and psychosocial treatments to treat existing symptoms and functional impairments, and to prevent further mood deterioration.
Dr. Miklowitz is Distinguished Professor of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles, Semel Institute for Neuroscience and Human Behavior. He is the author of “The Bipolar Disorder Survival Guide, 3rd Ed.” (New York: Guilford Press, 2019) and “Bipolar Disorder: A Family-Focused Treatment Approach, 2nd Ed” (New York: Guilford Press, 2010). He has no conflicts of interest to disclose. Contact Dr. Miklowitz at dmiklowitz@mednet.ucla.edu.
References
1. Bonsall MB, et al. Nonlinear time-series approaches in characterizing mood stability and mood instability in bipolar disorder. Proc Biol Sci. Mar 7 2012;279(1730):916-24. doi: 10.1098/rspb.2011.1246.
2. Hafeman DM, et al. Toward the definition of a bipolar prodrome: Dimensional predictors of bipolar spectrum disorders in at-risk youths. Am J Psychiatry. 2016;173(7):695-704. doi: 10.1176/appi.ajp.2015.15040414.
3. Miklowitz DJ, et al. Mood instability in youth at high risk for bipolar disorder. J Am Acad Child Adol Psychiatry. 2022 Mar 17;S0890-8567(22)00118-6. doi: 10.1016/j.jaac.2022.03.009.
4. Gerson AC, et al. The Children’s Affective Lability Scale: a psychometric evaluation of reliability. Psychiatry Res. Dec 20 1996;65(3):189-98. doi: 10.1016/s0165-1781(96)02851-x.
5. Birmaher B, et al. A risk calculator to predict the individual risk of conversion from subthreshold bipolar symptoms to bipolar disorder I or II in youth. J Am Acad Child Adol Psychiatry. 2018;57(10):755-63. doi: 10.1016/j.jaac.2018.05.023.
Mood instability, or sudden, unpredictable, and frequent shifts in emotional states, characterizes many types of psychiatric disorder, including attention-deficit/hyperactivity disorder (ADHD), personality disorders, depression, and posttraumatic stress disorder. To say that individuals with bipolar disorder (BD) have mood instability sounds like a tautology. Nonetheless, mood instability has particular relevance to BD: Many patients have irregular or labile moods even when they are between major episodes of mania and depression.1
Children of parents with BD who have high levels of mood instability are at particularly high risk for developing BD (types I or II) in late adolescence or early adulthood.2 The following case provides an illustration:
Patrick, age 14, entered treatment with diagnoses of ADHD and other specified bipolar disorder. His mother felt that his behavior resembled that of his father, who had been treated for manic episodes. During the COVID-19 pandemic, Patrick had become increasingly difficult at home, with significant oppositionality, impulsive behavior, and difficulty following through on school assignments or household tasks. His mother’s most significant complaints concerned Patrick’s sudden outbursts of anger and abrupt verbal abuse when she asked him to stop playing video games. When interrupted, he cursed loudly and sometimes turned violent; he had broken a window and a door at home and had on one occasion physically attacked his younger brother. Patrick agreed that he became angry at times, but felt that others provoked him. When queried about depression, he described anxiety and worry. He was unable to describe a particular trigger for his anxiety except for being interrupted in online games with his friends, which made him “feel like a total loser.”
His mother reported that Patrick had multiple 1- to 2-day intervals in which he became “really silly, laughing at nothing,” talking rapidly, jumping from one topic to another, and becoming annoyed when others didn’t share his enthusiasm. In these activated intervals, he slept little and seemed to be full of energy; his mother would hear him talking loudly into his phone throughout the night. During one such interval he had become verbally aggressive with a peer, which had ruined their friendship. Both Patrick and his mother reported that they had been fighting constantly and, in her words, “our house has become a war zone.”
In our recent article in the Journal of the American Academy of Child and Adolescent Psychiatry,3 my coauthors and I examined the association between parents’ ratings of mood instability and clinicians’ longitudinal ratings of symptoms and functioning among youth (ages 9-17 years) who were at high risk for BD. The participants met DSM-5 diagnostic criteria for major depressive disorder or other specified BD, defined as recurrent and brief periods of elevation and activation that did not meet syndromal mania or hypomania criteria. All participants had at least one first- or second-degree family member with a history of BD I or II. Following a period of evaluation, participants were randomly assigned to one of two 4-month psychological therapies: Family-focused therapy (12 sessions of psychoeducation, communication training, and problem-solving skills training) or enhanced usual care (6 sessions of family and individual psychoeducation and support). They also received pharmacological management from study-affiliated psychiatrists when warranted.
We measured mood instability at intake and every 4-6 months over an average of 2 years (range 0-255 weeks). We used a brief parent questionnaire – the Children’s Affective Lability Scale4 – which enables measurement of lability on the dimensions of elevation or activation (e.g., bursts of silliness or hilarity, excessive familiarity with others), irritability (e.g., temper outbursts), or anxious-depression (e.g., sudden bouts of crying).
Over the 1- to 4-year period of follow-up, mood instability was associated with poor prognosis indicators in high-risk youth: Being younger, having younger ages at first symptom onset, being diagnosed with other specified BD (vs. major depression), and having more complex patterns of comorbid disorders. Mood instability tracked closely with levels of mania, depression, and global functioning over the follow-up. There was a temporal pathway between a diagnosis of other specified bipolar disorder at intake and higher levels of mood instability at follow-up, which in turn predicted higher levels of parent/child conflict. High levels of mood lability may lead to isolation from peers and tension within family relationships, which may fuel further children’s expressions of frustration, rage, depression, or impulsive behavior.
Youth with higher levels of mood instability required more complex medication regimens over 1 year than did those with lower instability. There was an overall reduction in mood instability as children aged (or spent more time in treatment). Over the 1- to 4-year follow-up, family-focused therapy was associated with longer intervals prior to new mood episodes than was enhanced usual care, but reductions in mood instability were independent of the type of psychosocial treatment assigned to children.
The participants in this study could not be followed long enough to determine whether levels of mood instability were associated with the later development of syndromal BD. Other studies, however, have documented this relationship. Large-scale longitudinal studies of high-risk children find that measures of mood lability – along with early onset manic symptoms, depression, anxiety, and a family history of mania or hypomania – can be combined to calculate the risk that any individual child will develop BD I or II over the next 5-8 years.2,5
Clinicians should include measurement of the severity and psychosocial determinants of persistent mood shifts in youth under their care, particularly those with a family history of BD. Mood instability is associated with more severe symptom trajectories, more social isolation, and greater distress and conflict within the family. It may require a greater intensity of both pharmacological and psychosocial treatments to treat existing symptoms and functional impairments, and to prevent further mood deterioration.
Dr. Miklowitz is Distinguished Professor of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles, Semel Institute for Neuroscience and Human Behavior. He is the author of “The Bipolar Disorder Survival Guide, 3rd Ed.” (New York: Guilford Press, 2019) and “Bipolar Disorder: A Family-Focused Treatment Approach, 2nd Ed” (New York: Guilford Press, 2010). He has no conflicts of interest to disclose. Contact Dr. Miklowitz at dmiklowitz@mednet.ucla.edu.
References
1. Bonsall MB, et al. Nonlinear time-series approaches in characterizing mood stability and mood instability in bipolar disorder. Proc Biol Sci. Mar 7 2012;279(1730):916-24. doi: 10.1098/rspb.2011.1246.
2. Hafeman DM, et al. Toward the definition of a bipolar prodrome: Dimensional predictors of bipolar spectrum disorders in at-risk youths. Am J Psychiatry. 2016;173(7):695-704. doi: 10.1176/appi.ajp.2015.15040414.
3. Miklowitz DJ, et al. Mood instability in youth at high risk for bipolar disorder. J Am Acad Child Adol Psychiatry. 2022 Mar 17;S0890-8567(22)00118-6. doi: 10.1016/j.jaac.2022.03.009.
4. Gerson AC, et al. The Children’s Affective Lability Scale: a psychometric evaluation of reliability. Psychiatry Res. Dec 20 1996;65(3):189-98. doi: 10.1016/s0165-1781(96)02851-x.
5. Birmaher B, et al. A risk calculator to predict the individual risk of conversion from subthreshold bipolar symptoms to bipolar disorder I or II in youth. J Am Acad Child Adol Psychiatry. 2018;57(10):755-63. doi: 10.1016/j.jaac.2018.05.023.
Mood instability, or sudden, unpredictable, and frequent shifts in emotional states, characterizes many types of psychiatric disorder, including attention-deficit/hyperactivity disorder (ADHD), personality disorders, depression, and posttraumatic stress disorder. To say that individuals with bipolar disorder (BD) have mood instability sounds like a tautology. Nonetheless, mood instability has particular relevance to BD: Many patients have irregular or labile moods even when they are between major episodes of mania and depression.1
Children of parents with BD who have high levels of mood instability are at particularly high risk for developing BD (types I or II) in late adolescence or early adulthood.2 The following case provides an illustration:
Patrick, age 14, entered treatment with diagnoses of ADHD and other specified bipolar disorder. His mother felt that his behavior resembled that of his father, who had been treated for manic episodes. During the COVID-19 pandemic, Patrick had become increasingly difficult at home, with significant oppositionality, impulsive behavior, and difficulty following through on school assignments or household tasks. His mother’s most significant complaints concerned Patrick’s sudden outbursts of anger and abrupt verbal abuse when she asked him to stop playing video games. When interrupted, he cursed loudly and sometimes turned violent; he had broken a window and a door at home and had on one occasion physically attacked his younger brother. Patrick agreed that he became angry at times, but felt that others provoked him. When queried about depression, he described anxiety and worry. He was unable to describe a particular trigger for his anxiety except for being interrupted in online games with his friends, which made him “feel like a total loser.”
His mother reported that Patrick had multiple 1- to 2-day intervals in which he became “really silly, laughing at nothing,” talking rapidly, jumping from one topic to another, and becoming annoyed when others didn’t share his enthusiasm. In these activated intervals, he slept little and seemed to be full of energy; his mother would hear him talking loudly into his phone throughout the night. During one such interval he had become verbally aggressive with a peer, which had ruined their friendship. Both Patrick and his mother reported that they had been fighting constantly and, in her words, “our house has become a war zone.”
In our recent article in the Journal of the American Academy of Child and Adolescent Psychiatry,3 my coauthors and I examined the association between parents’ ratings of mood instability and clinicians’ longitudinal ratings of symptoms and functioning among youth (ages 9-17 years) who were at high risk for BD. The participants met DSM-5 diagnostic criteria for major depressive disorder or other specified BD, defined as recurrent and brief periods of elevation and activation that did not meet syndromal mania or hypomania criteria. All participants had at least one first- or second-degree family member with a history of BD I or II. Following a period of evaluation, participants were randomly assigned to one of two 4-month psychological therapies: Family-focused therapy (12 sessions of psychoeducation, communication training, and problem-solving skills training) or enhanced usual care (6 sessions of family and individual psychoeducation and support). They also received pharmacological management from study-affiliated psychiatrists when warranted.
We measured mood instability at intake and every 4-6 months over an average of 2 years (range 0-255 weeks). We used a brief parent questionnaire – the Children’s Affective Lability Scale4 – which enables measurement of lability on the dimensions of elevation or activation (e.g., bursts of silliness or hilarity, excessive familiarity with others), irritability (e.g., temper outbursts), or anxious-depression (e.g., sudden bouts of crying).
Over the 1- to 4-year period of follow-up, mood instability was associated with poor prognosis indicators in high-risk youth: Being younger, having younger ages at first symptom onset, being diagnosed with other specified BD (vs. major depression), and having more complex patterns of comorbid disorders. Mood instability tracked closely with levels of mania, depression, and global functioning over the follow-up. There was a temporal pathway between a diagnosis of other specified bipolar disorder at intake and higher levels of mood instability at follow-up, which in turn predicted higher levels of parent/child conflict. High levels of mood lability may lead to isolation from peers and tension within family relationships, which may fuel further children’s expressions of frustration, rage, depression, or impulsive behavior.
Youth with higher levels of mood instability required more complex medication regimens over 1 year than did those with lower instability. There was an overall reduction in mood instability as children aged (or spent more time in treatment). Over the 1- to 4-year follow-up, family-focused therapy was associated with longer intervals prior to new mood episodes than was enhanced usual care, but reductions in mood instability were independent of the type of psychosocial treatment assigned to children.
The participants in this study could not be followed long enough to determine whether levels of mood instability were associated with the later development of syndromal BD. Other studies, however, have documented this relationship. Large-scale longitudinal studies of high-risk children find that measures of mood lability – along with early onset manic symptoms, depression, anxiety, and a family history of mania or hypomania – can be combined to calculate the risk that any individual child will develop BD I or II over the next 5-8 years.2,5
Clinicians should include measurement of the severity and psychosocial determinants of persistent mood shifts in youth under their care, particularly those with a family history of BD. Mood instability is associated with more severe symptom trajectories, more social isolation, and greater distress and conflict within the family. It may require a greater intensity of both pharmacological and psychosocial treatments to treat existing symptoms and functional impairments, and to prevent further mood deterioration.
Dr. Miklowitz is Distinguished Professor of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles, Semel Institute for Neuroscience and Human Behavior. He is the author of “The Bipolar Disorder Survival Guide, 3rd Ed.” (New York: Guilford Press, 2019) and “Bipolar Disorder: A Family-Focused Treatment Approach, 2nd Ed” (New York: Guilford Press, 2010). He has no conflicts of interest to disclose. Contact Dr. Miklowitz at dmiklowitz@mednet.ucla.edu.
References
1. Bonsall MB, et al. Nonlinear time-series approaches in characterizing mood stability and mood instability in bipolar disorder. Proc Biol Sci. Mar 7 2012;279(1730):916-24. doi: 10.1098/rspb.2011.1246.
2. Hafeman DM, et al. Toward the definition of a bipolar prodrome: Dimensional predictors of bipolar spectrum disorders in at-risk youths. Am J Psychiatry. 2016;173(7):695-704. doi: 10.1176/appi.ajp.2015.15040414.
3. Miklowitz DJ, et al. Mood instability in youth at high risk for bipolar disorder. J Am Acad Child Adol Psychiatry. 2022 Mar 17;S0890-8567(22)00118-6. doi: 10.1016/j.jaac.2022.03.009.
4. Gerson AC, et al. The Children’s Affective Lability Scale: a psychometric evaluation of reliability. Psychiatry Res. Dec 20 1996;65(3):189-98. doi: 10.1016/s0165-1781(96)02851-x.
5. Birmaher B, et al. A risk calculator to predict the individual risk of conversion from subthreshold bipolar symptoms to bipolar disorder I or II in youth. J Am Acad Child Adol Psychiatry. 2018;57(10):755-63. doi: 10.1016/j.jaac.2018.05.023.
Fecal transfer could be the transplant of youth
Fecal matter may be in the fountain of youth
Yes, you read that headline correctly. New research by scientists at Quadram Institute and the University of East Anglia, both in Norwich, England, supports the claim that transferring fecal microbes might actually have some positive effects on reversing the aging process in the eyes, brain, and gut.
How do they know? Mice, of course. In the study, scientists took the gut microbes from older mice and transferred them into the younger mince. The young mice displayed inflamed signs of aging in their guts, brains, and eyes, which, we all know, decline in function as we age. What happens is a chronic inflammation of cells as we get older that can be found in the brain or gut that leads to a degenerative state over time.
When the older mice received the gut microbes from younger mice, the investigators saw the reverse: Gut, brain, and eye functionality improved. In a way, minimizing the inflammation.
There’s tons of research out there that suggests gut health is the key to a healthy life, but this study points directly to an improvement in brain and vision functionality as a result of the transfer.
Now, we’re not insinuating you get a poo transfer as you reach old age. And the shift to human studies on microbiota replacement therapy is still in the works. But this definitely is a topic to watch and could be a game changer in the age-old quest to bottle youth or at least improve quality of life as we age.
For now, the scientists did find some connections between the beneficial bacteria in the transplants and the human diet that could have similar effects, like changes in the metabolism of certain fats and vitamin that could have effects on the inflammatory cells in the eye and brain.
The more you know!
It’s not lying, it’s preemptive truth
Lying is bad. Bold statement, we know, but a true one. After all, God spent an entire commandment telling people not to do the whole bearing false witness thing, and God is generally known for not joking around. He’s a pretty serious dude.
In case you’ve been wandering around the desert for a while and haven’t had wifi, we have a bit of a misinformation problem these days. People lie all the time about a lot of things, and a lot of people believe the lies. According to new research, however, there are also a lot of people who recognize the lies but accept them anyway because they believe that the lies will become true in the future.
Imagine the following scenario: A friend gets a job he’s not qualified for because he listed a skill he doesn’t have. That’s bad, right? And the people the researchers interviewed agreed, at least initially. But when informed that our friend is planning on obtaining the skill in summer classes in the near future, the study participants became far more willing to excuse the initial lie.
A friend jumping the gun on training he doesn’t have yet is fairly innocuous as far as lying goes, but as the researchers found, this willingness to forgive lies because they could become true extends far further. For example, millions of people do not vote illegally in U.S. elections, nor do White people get approved for mortgages at rates 300% higher than minorities, but when asked to imagine scenarios in which those statements could be true, study participants were less likely to condemn the lie and prevent it from spreading further, especially if their political viewpoints aligned with the respective falsehood.
It seems, then, that while we may aspire to not tell lies, we take after another guy with magic powers who spent too much time in the desert: “What I told you was true, from a certain point of view.”
It tastes like feng shui, but it’s not
You know about biomes. You’ve read about various microbiomes. Allow us to introduce you to the envirome,
The envirome “includes all the natural and man-made elements of our environment throughout the lifespan, notably the built environment,” said Robert Schneider, dean of the College of Integrative Medicine at Maharishi International University. Located in – you guessed it – Fairfield, Iowa, and home of the Fighting Transcendentalists. MAHARISHI RULES!
[Editor’s note: You made that up, right? Well, it really is in Iowa, but they don’t seem to have an athletic program.]
In an effort to maximize the envirome’s potential to improve quality of life, Dr. Schneider and his associates systematically integrated the principles of Maharishi Vastu architecture (MVA) into a comprehensive building system. MVA is “a holistic wellness architectural system that aligns buildings with nature’s intelligence, creating balanced, orderly, and integrated living environments with the goal of improving occupants’ lives,” the university explained in a written statement.
Since “modern medicine now recognizes the powerful effects of the ‘envirome’ on health,” Dr. Schneider said in that statement, the researchers reviewed 40 years’ worth of published studies on MVA’s benefits – an analysis that appears in Global Advances in Health and Medicine.
As far as our homes are concerned, here are some of the things MVA says we should be doing:
- The headboard of a bed should be oriented to the east or south when you sleep. This will improve mental health.
- While sitting at a desk or work area, a person should face east or north to improve brain coherence.
- The main entrance of a house should face east because morning light is superior to afternoon light.
And you were worried about feng shui. Well, forget feng shui. Feng shui is for amateurs. MVA is the way to go. MVA is the GOAT. MAHARISHI RULES!
Fecal matter may be in the fountain of youth
Yes, you read that headline correctly. New research by scientists at Quadram Institute and the University of East Anglia, both in Norwich, England, supports the claim that transferring fecal microbes might actually have some positive effects on reversing the aging process in the eyes, brain, and gut.
How do they know? Mice, of course. In the study, scientists took the gut microbes from older mice and transferred them into the younger mince. The young mice displayed inflamed signs of aging in their guts, brains, and eyes, which, we all know, decline in function as we age. What happens is a chronic inflammation of cells as we get older that can be found in the brain or gut that leads to a degenerative state over time.
When the older mice received the gut microbes from younger mice, the investigators saw the reverse: Gut, brain, and eye functionality improved. In a way, minimizing the inflammation.
There’s tons of research out there that suggests gut health is the key to a healthy life, but this study points directly to an improvement in brain and vision functionality as a result of the transfer.
Now, we’re not insinuating you get a poo transfer as you reach old age. And the shift to human studies on microbiota replacement therapy is still in the works. But this definitely is a topic to watch and could be a game changer in the age-old quest to bottle youth or at least improve quality of life as we age.
For now, the scientists did find some connections between the beneficial bacteria in the transplants and the human diet that could have similar effects, like changes in the metabolism of certain fats and vitamin that could have effects on the inflammatory cells in the eye and brain.
The more you know!
It’s not lying, it’s preemptive truth
Lying is bad. Bold statement, we know, but a true one. After all, God spent an entire commandment telling people not to do the whole bearing false witness thing, and God is generally known for not joking around. He’s a pretty serious dude.
In case you’ve been wandering around the desert for a while and haven’t had wifi, we have a bit of a misinformation problem these days. People lie all the time about a lot of things, and a lot of people believe the lies. According to new research, however, there are also a lot of people who recognize the lies but accept them anyway because they believe that the lies will become true in the future.
Imagine the following scenario: A friend gets a job he’s not qualified for because he listed a skill he doesn’t have. That’s bad, right? And the people the researchers interviewed agreed, at least initially. But when informed that our friend is planning on obtaining the skill in summer classes in the near future, the study participants became far more willing to excuse the initial lie.
A friend jumping the gun on training he doesn’t have yet is fairly innocuous as far as lying goes, but as the researchers found, this willingness to forgive lies because they could become true extends far further. For example, millions of people do not vote illegally in U.S. elections, nor do White people get approved for mortgages at rates 300% higher than minorities, but when asked to imagine scenarios in which those statements could be true, study participants were less likely to condemn the lie and prevent it from spreading further, especially if their political viewpoints aligned with the respective falsehood.
It seems, then, that while we may aspire to not tell lies, we take after another guy with magic powers who spent too much time in the desert: “What I told you was true, from a certain point of view.”
It tastes like feng shui, but it’s not
You know about biomes. You’ve read about various microbiomes. Allow us to introduce you to the envirome,
The envirome “includes all the natural and man-made elements of our environment throughout the lifespan, notably the built environment,” said Robert Schneider, dean of the College of Integrative Medicine at Maharishi International University. Located in – you guessed it – Fairfield, Iowa, and home of the Fighting Transcendentalists. MAHARISHI RULES!
[Editor’s note: You made that up, right? Well, it really is in Iowa, but they don’t seem to have an athletic program.]
In an effort to maximize the envirome’s potential to improve quality of life, Dr. Schneider and his associates systematically integrated the principles of Maharishi Vastu architecture (MVA) into a comprehensive building system. MVA is “a holistic wellness architectural system that aligns buildings with nature’s intelligence, creating balanced, orderly, and integrated living environments with the goal of improving occupants’ lives,” the university explained in a written statement.
Since “modern medicine now recognizes the powerful effects of the ‘envirome’ on health,” Dr. Schneider said in that statement, the researchers reviewed 40 years’ worth of published studies on MVA’s benefits – an analysis that appears in Global Advances in Health and Medicine.
As far as our homes are concerned, here are some of the things MVA says we should be doing:
- The headboard of a bed should be oriented to the east or south when you sleep. This will improve mental health.
- While sitting at a desk or work area, a person should face east or north to improve brain coherence.
- The main entrance of a house should face east because morning light is superior to afternoon light.
And you were worried about feng shui. Well, forget feng shui. Feng shui is for amateurs. MVA is the way to go. MVA is the GOAT. MAHARISHI RULES!
Fecal matter may be in the fountain of youth
Yes, you read that headline correctly. New research by scientists at Quadram Institute and the University of East Anglia, both in Norwich, England, supports the claim that transferring fecal microbes might actually have some positive effects on reversing the aging process in the eyes, brain, and gut.
How do they know? Mice, of course. In the study, scientists took the gut microbes from older mice and transferred them into the younger mince. The young mice displayed inflamed signs of aging in their guts, brains, and eyes, which, we all know, decline in function as we age. What happens is a chronic inflammation of cells as we get older that can be found in the brain or gut that leads to a degenerative state over time.
When the older mice received the gut microbes from younger mice, the investigators saw the reverse: Gut, brain, and eye functionality improved. In a way, minimizing the inflammation.
There’s tons of research out there that suggests gut health is the key to a healthy life, but this study points directly to an improvement in brain and vision functionality as a result of the transfer.
Now, we’re not insinuating you get a poo transfer as you reach old age. And the shift to human studies on microbiota replacement therapy is still in the works. But this definitely is a topic to watch and could be a game changer in the age-old quest to bottle youth or at least improve quality of life as we age.
For now, the scientists did find some connections between the beneficial bacteria in the transplants and the human diet that could have similar effects, like changes in the metabolism of certain fats and vitamin that could have effects on the inflammatory cells in the eye and brain.
The more you know!
It’s not lying, it’s preemptive truth
Lying is bad. Bold statement, we know, but a true one. After all, God spent an entire commandment telling people not to do the whole bearing false witness thing, and God is generally known for not joking around. He’s a pretty serious dude.
In case you’ve been wandering around the desert for a while and haven’t had wifi, we have a bit of a misinformation problem these days. People lie all the time about a lot of things, and a lot of people believe the lies. According to new research, however, there are also a lot of people who recognize the lies but accept them anyway because they believe that the lies will become true in the future.
Imagine the following scenario: A friend gets a job he’s not qualified for because he listed a skill he doesn’t have. That’s bad, right? And the people the researchers interviewed agreed, at least initially. But when informed that our friend is planning on obtaining the skill in summer classes in the near future, the study participants became far more willing to excuse the initial lie.
A friend jumping the gun on training he doesn’t have yet is fairly innocuous as far as lying goes, but as the researchers found, this willingness to forgive lies because they could become true extends far further. For example, millions of people do not vote illegally in U.S. elections, nor do White people get approved for mortgages at rates 300% higher than minorities, but when asked to imagine scenarios in which those statements could be true, study participants were less likely to condemn the lie and prevent it from spreading further, especially if their political viewpoints aligned with the respective falsehood.
It seems, then, that while we may aspire to not tell lies, we take after another guy with magic powers who spent too much time in the desert: “What I told you was true, from a certain point of view.”
It tastes like feng shui, but it’s not
You know about biomes. You’ve read about various microbiomes. Allow us to introduce you to the envirome,
The envirome “includes all the natural and man-made elements of our environment throughout the lifespan, notably the built environment,” said Robert Schneider, dean of the College of Integrative Medicine at Maharishi International University. Located in – you guessed it – Fairfield, Iowa, and home of the Fighting Transcendentalists. MAHARISHI RULES!
[Editor’s note: You made that up, right? Well, it really is in Iowa, but they don’t seem to have an athletic program.]
In an effort to maximize the envirome’s potential to improve quality of life, Dr. Schneider and his associates systematically integrated the principles of Maharishi Vastu architecture (MVA) into a comprehensive building system. MVA is “a holistic wellness architectural system that aligns buildings with nature’s intelligence, creating balanced, orderly, and integrated living environments with the goal of improving occupants’ lives,” the university explained in a written statement.
Since “modern medicine now recognizes the powerful effects of the ‘envirome’ on health,” Dr. Schneider said in that statement, the researchers reviewed 40 years’ worth of published studies on MVA’s benefits – an analysis that appears in Global Advances in Health and Medicine.
As far as our homes are concerned, here are some of the things MVA says we should be doing:
- The headboard of a bed should be oriented to the east or south when you sleep. This will improve mental health.
- While sitting at a desk or work area, a person should face east or north to improve brain coherence.
- The main entrance of a house should face east because morning light is superior to afternoon light.
And you were worried about feng shui. Well, forget feng shui. Feng shui is for amateurs. MVA is the way to go. MVA is the GOAT. MAHARISHI RULES!