User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Aaron Beck: An appreciation
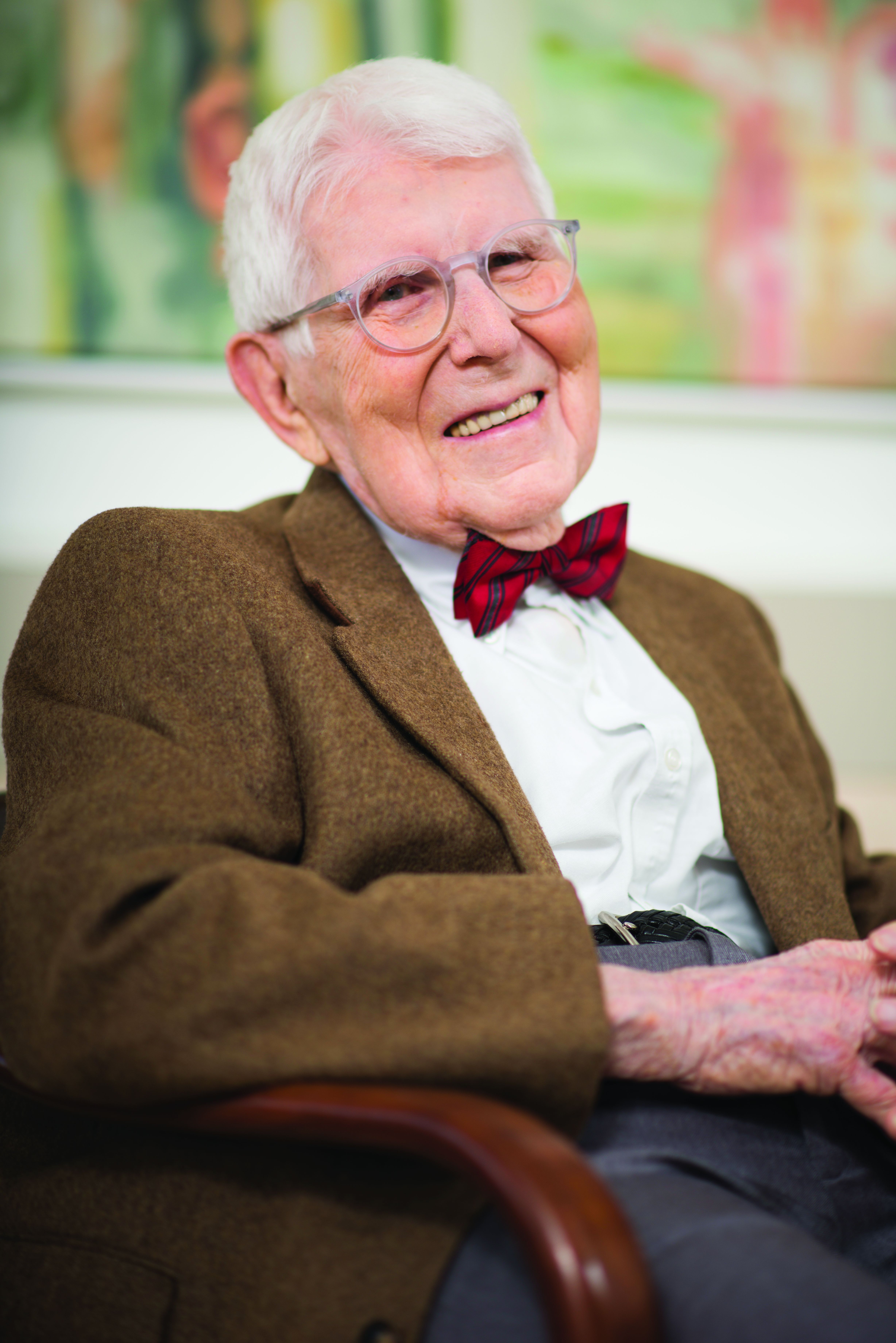
He always dressed the same at conferences: dark suit, white shirt, bright red bow tie.
For all his fame, he was very kind, warmly greeting those who wanted to see him and immediately turning attention toward their research rather than his own. Aaron Beck actually didn’t lecture much; he preferred to roleplay cognitive therapy with an audience member acting as the patient. He would engage in what he called Socratic questioning, or more formally, cognitive restructuring, with warmth and true curiosity:
- What might be another explanation or viewpoint?
- What are the effects of thinking this way?
- Can you think of any evidence that supports the opposite view?
The audience member/patient would benefit not only from thinking about things differently, but also from the captivating interaction with the man, Aaron Temkin Beck, MD, (who went by Tim), youngest child of Jewish immigrants from the Ukraine.
When written up in treatment manuals, cognitive restructuring can seem cold and overly logical, but in person, Dr. Beck made it come to life. This ability to nurture curiosity was a special talent; his friend and fellow cognitive psychologist Donald Meichenbaum, PhD, recalls that even over lunch, he never stopped asking questions, personal and professional, on a wide range of topics.
It is widely accepted that Dr. Beck, who died Nov. 1 at the age of 100 in suburban Philadelphia, was the most important figure in the field of cognitive-behavioral therapy (CBT).
He didn’t invent the field. Behaviorism predated him by generations, founded by figures such as John Watson and B.F. Skinner. Those psychologists set up behaviorism as an alternative to the reigning power of Freudian psychoanalysis, but they ran a distant second.
It wasn’t until Dr. Beck added a new approach, cognitive therapy, to the behavioristic movement that the new mélange, CBT, began to gain traction with clinicians and researchers. Dr. Beck, who had trained in psychiatry, developed his ideas in the 1960s while observing what he believed were limitations in the classic Freudian methods. He recognized that patients had “automatic thoughts,” not just unconscious emotions, when they engaged in Freudian free association, saying whatever came to their minds.
These thoughts often distorted reality, he observed; they were “maladaptive beliefs,” and when they changed, patients’ emotional states improved.
Dr. Beck wasn’t alone. The psychologist Albert Ellis, PhD, in New York, had come to similar conclusions a decade earlier, though with a more coldly logical and challenging style. The prominent British psychologist Hans Eysenck, PhD, had argued strongly that Freudian psychoanalysis was ineffective and that behavioral approaches were better.
Dr. Beck turned the Freudian equation around: Instead of emotion as cause and thought as effect, it was thought which affected emotion, for better or worse. Once you connected behavior as the outcome, you had the essence of CBT: thought, emotion, and behavior – each affecting the other, with thought being the strongest axis of change.
The process wasn’t bloodless. Behaviorists defended their turf against cognitivists, just as much as Freudians rejected both. At one point the behaviorists in the Association for the Advancement of Behavior Therapy tried to expel the advocates of a cognitive approach. Dr. Beck responded by leading the cognitivists in creating a new journal; he emphasized the importance of research being the main mechanism to decide what treatments worked the best.
Putting these ideas out in the 1960s and 1970s, Dr. Beck garnered support from researchers when he manualized the approach. Freudian psychoanalysis was idiosyncratic; it was almost impossible to study empirically, because the therapist would be responding to the unpredictable dreams and memories of patients engaged in free association. Each case was unique.
But CBT was systematic: The same general approach was taken to all patients; the same negative cognitions were found in depression, for instance, like all-or-nothing thinking or overgeneralization. Once manualized, CBT became the standard method of psychotherapy studied with the newly developed method of randomized controlled trials (RCTs).
By the 1980s, RCTs had proven the efficacy of CBT in depression, and the approach took off.
Dr. Beck already had developed a series of rating scales: the Beck Depression Inventory, the Beck Scale for Suicidal Ideation, the Beck Anxiety Inventory, the Beck Hopelessness Scale. Widely used, these scales extended his influence enormously. Copyrighted, they created a new industry of psychological research.
Dr. Beck’s own work was mainly in depression, but his followers extended it everywhere else: anxiety disorders and phobias, eating disorders, substance abuse, bipolar illness, even schizophrenia. Meanwhile, Freudian psychoanalysis fell into a steep decline from which it never recovered.
Some argued that it was abetted by insurance restrictions on psychotherapy, which favored shorter-term CBT; others that its research was biased in its favor because psychotherapy treatments, unlike medications, cannot be blinded; others that its efficacy could not be shown to be specific to its theory, as opposed to the interpersonal relationship between therapist and client.
Still, CBT has transformed psychotherapy and continues to expand its influence. Computer-based CBT has been proven effective, and digital CBT has become a standard approach in many smartphone applications and is central to the claims of multiple new biotechnology companies advocating for digital psychotherapy.
Aaron Beck continued publishing scientific articles to age 98. His last papers reviewed his life’s work. He characteristically gave credit to others, calmly recollected how he traveled away from psychoanalysis, described how his work started and ended in schizophrenia, and noted that the “working relationship with the therapist” remained a key factor for the success of CBT.
That parting comment reminds us that behind all the technology and research stands the kindly man in the dark suit, white shirt, and bright red bow tie, looking at you warmly, asking about your thoughts, and curiously wondering what might be another explanation or viewpoint you hadn’t considered.
Nassir Ghaemi, MD, MPH, is a professor of psychiatry at Tufts Medical Center and a lecturer in psychiatry at Harvard Medical School. He is the author of several general-interest books on psychiatry. A version of this article first appeared on Medscape.com.
He always dressed the same at conferences: dark suit, white shirt, bright red bow tie.
For all his fame, he was very kind, warmly greeting those who wanted to see him and immediately turning attention toward their research rather than his own. Aaron Beck actually didn’t lecture much; he preferred to roleplay cognitive therapy with an audience member acting as the patient. He would engage in what he called Socratic questioning, or more formally, cognitive restructuring, with warmth and true curiosity:
- What might be another explanation or viewpoint?
- What are the effects of thinking this way?
- Can you think of any evidence that supports the opposite view?
The audience member/patient would benefit not only from thinking about things differently, but also from the captivating interaction with the man, Aaron Temkin Beck, MD, (who went by Tim), youngest child of Jewish immigrants from the Ukraine.
When written up in treatment manuals, cognitive restructuring can seem cold and overly logical, but in person, Dr. Beck made it come to life. This ability to nurture curiosity was a special talent; his friend and fellow cognitive psychologist Donald Meichenbaum, PhD, recalls that even over lunch, he never stopped asking questions, personal and professional, on a wide range of topics.
It is widely accepted that Dr. Beck, who died Nov. 1 at the age of 100 in suburban Philadelphia, was the most important figure in the field of cognitive-behavioral therapy (CBT).
He didn’t invent the field. Behaviorism predated him by generations, founded by figures such as John Watson and B.F. Skinner. Those psychologists set up behaviorism as an alternative to the reigning power of Freudian psychoanalysis, but they ran a distant second.
It wasn’t until Dr. Beck added a new approach, cognitive therapy, to the behavioristic movement that the new mélange, CBT, began to gain traction with clinicians and researchers. Dr. Beck, who had trained in psychiatry, developed his ideas in the 1960s while observing what he believed were limitations in the classic Freudian methods. He recognized that patients had “automatic thoughts,” not just unconscious emotions, when they engaged in Freudian free association, saying whatever came to their minds.
These thoughts often distorted reality, he observed; they were “maladaptive beliefs,” and when they changed, patients’ emotional states improved.
Dr. Beck wasn’t alone. The psychologist Albert Ellis, PhD, in New York, had come to similar conclusions a decade earlier, though with a more coldly logical and challenging style. The prominent British psychologist Hans Eysenck, PhD, had argued strongly that Freudian psychoanalysis was ineffective and that behavioral approaches were better.
Dr. Beck turned the Freudian equation around: Instead of emotion as cause and thought as effect, it was thought which affected emotion, for better or worse. Once you connected behavior as the outcome, you had the essence of CBT: thought, emotion, and behavior – each affecting the other, with thought being the strongest axis of change.
The process wasn’t bloodless. Behaviorists defended their turf against cognitivists, just as much as Freudians rejected both. At one point the behaviorists in the Association for the Advancement of Behavior Therapy tried to expel the advocates of a cognitive approach. Dr. Beck responded by leading the cognitivists in creating a new journal; he emphasized the importance of research being the main mechanism to decide what treatments worked the best.
Putting these ideas out in the 1960s and 1970s, Dr. Beck garnered support from researchers when he manualized the approach. Freudian psychoanalysis was idiosyncratic; it was almost impossible to study empirically, because the therapist would be responding to the unpredictable dreams and memories of patients engaged in free association. Each case was unique.
But CBT was systematic: The same general approach was taken to all patients; the same negative cognitions were found in depression, for instance, like all-or-nothing thinking or overgeneralization. Once manualized, CBT became the standard method of psychotherapy studied with the newly developed method of randomized controlled trials (RCTs).
By the 1980s, RCTs had proven the efficacy of CBT in depression, and the approach took off.
Dr. Beck already had developed a series of rating scales: the Beck Depression Inventory, the Beck Scale for Suicidal Ideation, the Beck Anxiety Inventory, the Beck Hopelessness Scale. Widely used, these scales extended his influence enormously. Copyrighted, they created a new industry of psychological research.
Dr. Beck’s own work was mainly in depression, but his followers extended it everywhere else: anxiety disorders and phobias, eating disorders, substance abuse, bipolar illness, even schizophrenia. Meanwhile, Freudian psychoanalysis fell into a steep decline from which it never recovered.
Some argued that it was abetted by insurance restrictions on psychotherapy, which favored shorter-term CBT; others that its research was biased in its favor because psychotherapy treatments, unlike medications, cannot be blinded; others that its efficacy could not be shown to be specific to its theory, as opposed to the interpersonal relationship between therapist and client.
Still, CBT has transformed psychotherapy and continues to expand its influence. Computer-based CBT has been proven effective, and digital CBT has become a standard approach in many smartphone applications and is central to the claims of multiple new biotechnology companies advocating for digital psychotherapy.
Aaron Beck continued publishing scientific articles to age 98. His last papers reviewed his life’s work. He characteristically gave credit to others, calmly recollected how he traveled away from psychoanalysis, described how his work started and ended in schizophrenia, and noted that the “working relationship with the therapist” remained a key factor for the success of CBT.
That parting comment reminds us that behind all the technology and research stands the kindly man in the dark suit, white shirt, and bright red bow tie, looking at you warmly, asking about your thoughts, and curiously wondering what might be another explanation or viewpoint you hadn’t considered.
Nassir Ghaemi, MD, MPH, is a professor of psychiatry at Tufts Medical Center and a lecturer in psychiatry at Harvard Medical School. He is the author of several general-interest books on psychiatry. A version of this article first appeared on Medscape.com.
He always dressed the same at conferences: dark suit, white shirt, bright red bow tie.
For all his fame, he was very kind, warmly greeting those who wanted to see him and immediately turning attention toward their research rather than his own. Aaron Beck actually didn’t lecture much; he preferred to roleplay cognitive therapy with an audience member acting as the patient. He would engage in what he called Socratic questioning, or more formally, cognitive restructuring, with warmth and true curiosity:
- What might be another explanation or viewpoint?
- What are the effects of thinking this way?
- Can you think of any evidence that supports the opposite view?
The audience member/patient would benefit not only from thinking about things differently, but also from the captivating interaction with the man, Aaron Temkin Beck, MD, (who went by Tim), youngest child of Jewish immigrants from the Ukraine.
When written up in treatment manuals, cognitive restructuring can seem cold and overly logical, but in person, Dr. Beck made it come to life. This ability to nurture curiosity was a special talent; his friend and fellow cognitive psychologist Donald Meichenbaum, PhD, recalls that even over lunch, he never stopped asking questions, personal and professional, on a wide range of topics.
It is widely accepted that Dr. Beck, who died Nov. 1 at the age of 100 in suburban Philadelphia, was the most important figure in the field of cognitive-behavioral therapy (CBT).
He didn’t invent the field. Behaviorism predated him by generations, founded by figures such as John Watson and B.F. Skinner. Those psychologists set up behaviorism as an alternative to the reigning power of Freudian psychoanalysis, but they ran a distant second.
It wasn’t until Dr. Beck added a new approach, cognitive therapy, to the behavioristic movement that the new mélange, CBT, began to gain traction with clinicians and researchers. Dr. Beck, who had trained in psychiatry, developed his ideas in the 1960s while observing what he believed were limitations in the classic Freudian methods. He recognized that patients had “automatic thoughts,” not just unconscious emotions, when they engaged in Freudian free association, saying whatever came to their minds.
These thoughts often distorted reality, he observed; they were “maladaptive beliefs,” and when they changed, patients’ emotional states improved.
Dr. Beck wasn’t alone. The psychologist Albert Ellis, PhD, in New York, had come to similar conclusions a decade earlier, though with a more coldly logical and challenging style. The prominent British psychologist Hans Eysenck, PhD, had argued strongly that Freudian psychoanalysis was ineffective and that behavioral approaches were better.
Dr. Beck turned the Freudian equation around: Instead of emotion as cause and thought as effect, it was thought which affected emotion, for better or worse. Once you connected behavior as the outcome, you had the essence of CBT: thought, emotion, and behavior – each affecting the other, with thought being the strongest axis of change.
The process wasn’t bloodless. Behaviorists defended their turf against cognitivists, just as much as Freudians rejected both. At one point the behaviorists in the Association for the Advancement of Behavior Therapy tried to expel the advocates of a cognitive approach. Dr. Beck responded by leading the cognitivists in creating a new journal; he emphasized the importance of research being the main mechanism to decide what treatments worked the best.
Putting these ideas out in the 1960s and 1970s, Dr. Beck garnered support from researchers when he manualized the approach. Freudian psychoanalysis was idiosyncratic; it was almost impossible to study empirically, because the therapist would be responding to the unpredictable dreams and memories of patients engaged in free association. Each case was unique.
But CBT was systematic: The same general approach was taken to all patients; the same negative cognitions were found in depression, for instance, like all-or-nothing thinking or overgeneralization. Once manualized, CBT became the standard method of psychotherapy studied with the newly developed method of randomized controlled trials (RCTs).
By the 1980s, RCTs had proven the efficacy of CBT in depression, and the approach took off.
Dr. Beck already had developed a series of rating scales: the Beck Depression Inventory, the Beck Scale for Suicidal Ideation, the Beck Anxiety Inventory, the Beck Hopelessness Scale. Widely used, these scales extended his influence enormously. Copyrighted, they created a new industry of psychological research.
Dr. Beck’s own work was mainly in depression, but his followers extended it everywhere else: anxiety disorders and phobias, eating disorders, substance abuse, bipolar illness, even schizophrenia. Meanwhile, Freudian psychoanalysis fell into a steep decline from which it never recovered.
Some argued that it was abetted by insurance restrictions on psychotherapy, which favored shorter-term CBT; others that its research was biased in its favor because psychotherapy treatments, unlike medications, cannot be blinded; others that its efficacy could not be shown to be specific to its theory, as opposed to the interpersonal relationship between therapist and client.
Still, CBT has transformed psychotherapy and continues to expand its influence. Computer-based CBT has been proven effective, and digital CBT has become a standard approach in many smartphone applications and is central to the claims of multiple new biotechnology companies advocating for digital psychotherapy.
Aaron Beck continued publishing scientific articles to age 98. His last papers reviewed his life’s work. He characteristically gave credit to others, calmly recollected how he traveled away from psychoanalysis, described how his work started and ended in schizophrenia, and noted that the “working relationship with the therapist” remained a key factor for the success of CBT.
That parting comment reminds us that behind all the technology and research stands the kindly man in the dark suit, white shirt, and bright red bow tie, looking at you warmly, asking about your thoughts, and curiously wondering what might be another explanation or viewpoint you hadn’t considered.
Nassir Ghaemi, MD, MPH, is a professor of psychiatry at Tufts Medical Center and a lecturer in psychiatry at Harvard Medical School. He is the author of several general-interest books on psychiatry. A version of this article first appeared on Medscape.com.
Practicing telepsychiatry: Include backup plans, ground rules
For psychiatrists embarking on a telemedicine consultation, it might be helpful to review a checklist of steps that will reduce the risk of problems when things go wrong, according to an overview of the dangers at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sponsored by Medscape Live.
Ideally, telepsychiatry will function much like an inpatient office visit, but the dynamics differ – as do the things that can go wrong, according to Sanjay Gupta, MD, chief medical officer, BryLin Behavioral Health System, Buffalo, N.Y. “Issues can arise suddenly. You need contingency planning.”
At the outset, psychiatrists should establish the location of the patient. This is necessary at every telemedicine encounter. With a remote device, a patient could be essentially anywhere on Earth. Patients might not even remember to mention that they are vacationing in Australia.
The location of the patient is important in the event of an unexpected crisis. This is not only relevant to an unstable patient at risk of dangerous behavior, such as actively attempting suicide, but to patients who have a seizure or some other emergency that inhibits communication. , and this requires confirming that the patient is where he or she was expected to be.
In addition, there should be a plan for technological failure. As everyone knows, these failures, such as dysfunction of a device, a poor connection, or an Internet outage, can happen at any time. Both the clinician and the patient can derive reassurance from at least one if not two or more plans to reconnect in the event of these failures.
The visit should also begin with questions that will establish the patient has a sense of adequate privacy. This is one of the most common obstacles to an effective telemedicine consultation. Dr. Gupta pointed out that phone or computer cameras do not typically permit the clinician to exclude the presence of another individual sitting even a few feet away from the patient. With spouses and children nearby, there might be a tenuous sense of privacy even if they are unlikely to overhear the telemedicine visit.
One strategy that can be used to assess the patient’s level of comfort is to ask for a description of the patient’s surroundings and any other people at the location. Dr. Gupta also said it is appropriate to establish ground rules about recording of the session, which has its own potential to inhibit the interaction.
Warning that some form of consent to a telemedicine visit is mandatory in most states, Dr. Gupta also cautioned that a formal identification check is appropriate for a first-time visit. The risk of an individual offering a false identification is likely to be low, but it can be eliminated entirely by a protocol that verifies consent and identify before the clinical work begins.
Because of the importance of engaging patients quickly, Dr. Gupta called the first few minutes of a telemedicine visit “crucial.” By initiating the visit with a warm and respectful tone, by relaying a competent and professional appearance, and by establishing an atmosphere that encourages communication, the initial minutes of the call can set a tone that facilitates an effective visit.
Simple and established telehealth etiquette strategies should be employed, according to Dr. Gupta. He suggested paying attention to such issues as lighting, background, and camera position. Descriptions of what constitutes adequate lighting and background are easily obtained on free how-to websites, but the goal is to provide patients with a nondistracting and clear view of the clinician.
During a telemedicine visit, the clinician’s focus should remain on the patient, according to Dr. Gupta. He advised against taking notes or documenting the visit on an electronic health record during the course of the visit. Rather, he advised positioning the camera in a way that the patient feels eye contact is being made.
“It can be helpful to periodically summarize what the patient has said to demonstrate that you are fully engaged,” Dr. Gupta suggested.
Telemedicine is very effective for many but not all patients. Some, such as those with active psychosis, are not suited to this approach, but others are simply uncomfortable with this form of communication. Dr. Gupta suggested that clinicians should be mindful of the advantages and the limitations of telepsychiatry.
Ultimately, Dr. Gupta believes that the substantial expansion of telepsychiatry that took place during the COVID-19 pandemic is likely to persist when the pandemic ends, even if many of the changes that permitted its expansion, such as a relaxation of HIPPA requirements, are withdrawn. However, parity reimbursement for visits offered by telemedicine relative to those that are face-to-face, which greatly facilitated the growth of telepsychiatry, is not guaranteed, so this remains an unanswered question.
“The question is what will happen to the billing codes when we see COVID-19 in the rearview mirror, and the answer is that no one knows,” he said.
Uncertainty about future use
Other experts in this field agreed. James (Jay) H. Shore, MD, MPH, director of telemedicine, Helen and Arthur E. Johnson Depression Center, University of Colorado at Denver, Aurora, has long been an advocate for the value of telepsychiatry for reaching patients with limited psychosocial services. The attention drawn to this practice by the COVID-19 pandemic has been welcome, but he does not know how it will affect the future.
“There is too much uncertainty in the system to make a good prediction of where this may end up,” he said.
It is not just reimbursement that is at risk, according to Peter Yellowlees, MBBS, MD, chief wellness officer at the University of California, Davis. Also a longtime advocate of telepsychiatry, particularly to reach the underserved, Dr. Yellowlees pointed out that the ability to prescribe controlled substances through telemedicine and the ability to consult with patients across state lines might also be in jeopardy if and when rules for telemedicine are revisited after the pandemic.
“Many organizations are lobbying to make the pandemic changes permanent because they greatly support telemedicine delivery,” Dr. Yellowlees said, but agreed about the uncertainty regarding what policy makers will do.
Jayasudha Gude, MD, who is completing her residency in psychiatry at Zucker Hillside Hospital, Northwell Health, New York, recently led a literature review evaluating the needs and viability of telepsychiatry during and after the COVID-19 era (Cureus. 2021 Aug;13:e16974). Based on the benefits she identified in her review, she said, “I would definitely want to advocate for the continued use of telepsychiatry after the pandemic is over.” She hopes that psychiatrists who now have experience in this area will join her.
“I am hopeful that a lot of mental health providers will also be advocating since they have experience, and many will want to continue its use,” she said. Medscape Live and this news organization are owned by the same parent company. Dr. Gupta, Dr. Shore, Dr. Yellowlees, and Dr. Gude reported no potential conflicts of interest.
For psychiatrists embarking on a telemedicine consultation, it might be helpful to review a checklist of steps that will reduce the risk of problems when things go wrong, according to an overview of the dangers at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sponsored by Medscape Live.
Ideally, telepsychiatry will function much like an inpatient office visit, but the dynamics differ – as do the things that can go wrong, according to Sanjay Gupta, MD, chief medical officer, BryLin Behavioral Health System, Buffalo, N.Y. “Issues can arise suddenly. You need contingency planning.”
At the outset, psychiatrists should establish the location of the patient. This is necessary at every telemedicine encounter. With a remote device, a patient could be essentially anywhere on Earth. Patients might not even remember to mention that they are vacationing in Australia.
The location of the patient is important in the event of an unexpected crisis. This is not only relevant to an unstable patient at risk of dangerous behavior, such as actively attempting suicide, but to patients who have a seizure or some other emergency that inhibits communication. , and this requires confirming that the patient is where he or she was expected to be.
In addition, there should be a plan for technological failure. As everyone knows, these failures, such as dysfunction of a device, a poor connection, or an Internet outage, can happen at any time. Both the clinician and the patient can derive reassurance from at least one if not two or more plans to reconnect in the event of these failures.
The visit should also begin with questions that will establish the patient has a sense of adequate privacy. This is one of the most common obstacles to an effective telemedicine consultation. Dr. Gupta pointed out that phone or computer cameras do not typically permit the clinician to exclude the presence of another individual sitting even a few feet away from the patient. With spouses and children nearby, there might be a tenuous sense of privacy even if they are unlikely to overhear the telemedicine visit.
One strategy that can be used to assess the patient’s level of comfort is to ask for a description of the patient’s surroundings and any other people at the location. Dr. Gupta also said it is appropriate to establish ground rules about recording of the session, which has its own potential to inhibit the interaction.
Warning that some form of consent to a telemedicine visit is mandatory in most states, Dr. Gupta also cautioned that a formal identification check is appropriate for a first-time visit. The risk of an individual offering a false identification is likely to be low, but it can be eliminated entirely by a protocol that verifies consent and identify before the clinical work begins.
Because of the importance of engaging patients quickly, Dr. Gupta called the first few minutes of a telemedicine visit “crucial.” By initiating the visit with a warm and respectful tone, by relaying a competent and professional appearance, and by establishing an atmosphere that encourages communication, the initial minutes of the call can set a tone that facilitates an effective visit.
Simple and established telehealth etiquette strategies should be employed, according to Dr. Gupta. He suggested paying attention to such issues as lighting, background, and camera position. Descriptions of what constitutes adequate lighting and background are easily obtained on free how-to websites, but the goal is to provide patients with a nondistracting and clear view of the clinician.
During a telemedicine visit, the clinician’s focus should remain on the patient, according to Dr. Gupta. He advised against taking notes or documenting the visit on an electronic health record during the course of the visit. Rather, he advised positioning the camera in a way that the patient feels eye contact is being made.
“It can be helpful to periodically summarize what the patient has said to demonstrate that you are fully engaged,” Dr. Gupta suggested.
Telemedicine is very effective for many but not all patients. Some, such as those with active psychosis, are not suited to this approach, but others are simply uncomfortable with this form of communication. Dr. Gupta suggested that clinicians should be mindful of the advantages and the limitations of telepsychiatry.
Ultimately, Dr. Gupta believes that the substantial expansion of telepsychiatry that took place during the COVID-19 pandemic is likely to persist when the pandemic ends, even if many of the changes that permitted its expansion, such as a relaxation of HIPPA requirements, are withdrawn. However, parity reimbursement for visits offered by telemedicine relative to those that are face-to-face, which greatly facilitated the growth of telepsychiatry, is not guaranteed, so this remains an unanswered question.
“The question is what will happen to the billing codes when we see COVID-19 in the rearview mirror, and the answer is that no one knows,” he said.
Uncertainty about future use
Other experts in this field agreed. James (Jay) H. Shore, MD, MPH, director of telemedicine, Helen and Arthur E. Johnson Depression Center, University of Colorado at Denver, Aurora, has long been an advocate for the value of telepsychiatry for reaching patients with limited psychosocial services. The attention drawn to this practice by the COVID-19 pandemic has been welcome, but he does not know how it will affect the future.
“There is too much uncertainty in the system to make a good prediction of where this may end up,” he said.
It is not just reimbursement that is at risk, according to Peter Yellowlees, MBBS, MD, chief wellness officer at the University of California, Davis. Also a longtime advocate of telepsychiatry, particularly to reach the underserved, Dr. Yellowlees pointed out that the ability to prescribe controlled substances through telemedicine and the ability to consult with patients across state lines might also be in jeopardy if and when rules for telemedicine are revisited after the pandemic.
“Many organizations are lobbying to make the pandemic changes permanent because they greatly support telemedicine delivery,” Dr. Yellowlees said, but agreed about the uncertainty regarding what policy makers will do.
Jayasudha Gude, MD, who is completing her residency in psychiatry at Zucker Hillside Hospital, Northwell Health, New York, recently led a literature review evaluating the needs and viability of telepsychiatry during and after the COVID-19 era (Cureus. 2021 Aug;13:e16974). Based on the benefits she identified in her review, she said, “I would definitely want to advocate for the continued use of telepsychiatry after the pandemic is over.” She hopes that psychiatrists who now have experience in this area will join her.
“I am hopeful that a lot of mental health providers will also be advocating since they have experience, and many will want to continue its use,” she said. Medscape Live and this news organization are owned by the same parent company. Dr. Gupta, Dr. Shore, Dr. Yellowlees, and Dr. Gude reported no potential conflicts of interest.
For psychiatrists embarking on a telemedicine consultation, it might be helpful to review a checklist of steps that will reduce the risk of problems when things go wrong, according to an overview of the dangers at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sponsored by Medscape Live.
Ideally, telepsychiatry will function much like an inpatient office visit, but the dynamics differ – as do the things that can go wrong, according to Sanjay Gupta, MD, chief medical officer, BryLin Behavioral Health System, Buffalo, N.Y. “Issues can arise suddenly. You need contingency planning.”
At the outset, psychiatrists should establish the location of the patient. This is necessary at every telemedicine encounter. With a remote device, a patient could be essentially anywhere on Earth. Patients might not even remember to mention that they are vacationing in Australia.
The location of the patient is important in the event of an unexpected crisis. This is not only relevant to an unstable patient at risk of dangerous behavior, such as actively attempting suicide, but to patients who have a seizure or some other emergency that inhibits communication. , and this requires confirming that the patient is where he or she was expected to be.
In addition, there should be a plan for technological failure. As everyone knows, these failures, such as dysfunction of a device, a poor connection, or an Internet outage, can happen at any time. Both the clinician and the patient can derive reassurance from at least one if not two or more plans to reconnect in the event of these failures.
The visit should also begin with questions that will establish the patient has a sense of adequate privacy. This is one of the most common obstacles to an effective telemedicine consultation. Dr. Gupta pointed out that phone or computer cameras do not typically permit the clinician to exclude the presence of another individual sitting even a few feet away from the patient. With spouses and children nearby, there might be a tenuous sense of privacy even if they are unlikely to overhear the telemedicine visit.
One strategy that can be used to assess the patient’s level of comfort is to ask for a description of the patient’s surroundings and any other people at the location. Dr. Gupta also said it is appropriate to establish ground rules about recording of the session, which has its own potential to inhibit the interaction.
Warning that some form of consent to a telemedicine visit is mandatory in most states, Dr. Gupta also cautioned that a formal identification check is appropriate for a first-time visit. The risk of an individual offering a false identification is likely to be low, but it can be eliminated entirely by a protocol that verifies consent and identify before the clinical work begins.
Because of the importance of engaging patients quickly, Dr. Gupta called the first few minutes of a telemedicine visit “crucial.” By initiating the visit with a warm and respectful tone, by relaying a competent and professional appearance, and by establishing an atmosphere that encourages communication, the initial minutes of the call can set a tone that facilitates an effective visit.
Simple and established telehealth etiquette strategies should be employed, according to Dr. Gupta. He suggested paying attention to such issues as lighting, background, and camera position. Descriptions of what constitutes adequate lighting and background are easily obtained on free how-to websites, but the goal is to provide patients with a nondistracting and clear view of the clinician.
During a telemedicine visit, the clinician’s focus should remain on the patient, according to Dr. Gupta. He advised against taking notes or documenting the visit on an electronic health record during the course of the visit. Rather, he advised positioning the camera in a way that the patient feels eye contact is being made.
“It can be helpful to periodically summarize what the patient has said to demonstrate that you are fully engaged,” Dr. Gupta suggested.
Telemedicine is very effective for many but not all patients. Some, such as those with active psychosis, are not suited to this approach, but others are simply uncomfortable with this form of communication. Dr. Gupta suggested that clinicians should be mindful of the advantages and the limitations of telepsychiatry.
Ultimately, Dr. Gupta believes that the substantial expansion of telepsychiatry that took place during the COVID-19 pandemic is likely to persist when the pandemic ends, even if many of the changes that permitted its expansion, such as a relaxation of HIPPA requirements, are withdrawn. However, parity reimbursement for visits offered by telemedicine relative to those that are face-to-face, which greatly facilitated the growth of telepsychiatry, is not guaranteed, so this remains an unanswered question.
“The question is what will happen to the billing codes when we see COVID-19 in the rearview mirror, and the answer is that no one knows,” he said.
Uncertainty about future use
Other experts in this field agreed. James (Jay) H. Shore, MD, MPH, director of telemedicine, Helen and Arthur E. Johnson Depression Center, University of Colorado at Denver, Aurora, has long been an advocate for the value of telepsychiatry for reaching patients with limited psychosocial services. The attention drawn to this practice by the COVID-19 pandemic has been welcome, but he does not know how it will affect the future.
“There is too much uncertainty in the system to make a good prediction of where this may end up,” he said.
It is not just reimbursement that is at risk, according to Peter Yellowlees, MBBS, MD, chief wellness officer at the University of California, Davis. Also a longtime advocate of telepsychiatry, particularly to reach the underserved, Dr. Yellowlees pointed out that the ability to prescribe controlled substances through telemedicine and the ability to consult with patients across state lines might also be in jeopardy if and when rules for telemedicine are revisited after the pandemic.
“Many organizations are lobbying to make the pandemic changes permanent because they greatly support telemedicine delivery,” Dr. Yellowlees said, but agreed about the uncertainty regarding what policy makers will do.
Jayasudha Gude, MD, who is completing her residency in psychiatry at Zucker Hillside Hospital, Northwell Health, New York, recently led a literature review evaluating the needs and viability of telepsychiatry during and after the COVID-19 era (Cureus. 2021 Aug;13:e16974). Based on the benefits she identified in her review, she said, “I would definitely want to advocate for the continued use of telepsychiatry after the pandemic is over.” She hopes that psychiatrists who now have experience in this area will join her.
“I am hopeful that a lot of mental health providers will also be advocating since they have experience, and many will want to continue its use,” she said. Medscape Live and this news organization are owned by the same parent company. Dr. Gupta, Dr. Shore, Dr. Yellowlees, and Dr. Gude reported no potential conflicts of interest.
FROM PSYCHOPHARMACOLOGY UPDATE
Newly discovered vascular barrier in the brain may explain IBD-related anxiety, depression
A newly discovered vascular brain barrier that blocks the passage of inflammatory molecules triggered by gut bacteria may be why patients with inflammatory bowel disease (IBD) are at increased risk for certain mental health disorders, including anxiety and depression, early research suggests.
The discovery, which was based on a preclinical model, could lead to new therapeutic targets that could have applications for both gastrointestinal and psychiatric conditions, investigators note.
The research team, which was led by immunologist Maria Rescigno, PhD, and neuroscientist Simona Lodato, PhD, both from Humanitas University, Milan, notes that the barrier resides in the choroid plexus, a region of the brain that is involved in filtering cerebrospinal fluid. The researchers found that the region closes in response to inflammatory molecules produced in reaction to the presence of intestinal bacteria in patients with gut disorders.
Dr. Lodato said in an interview that the brain’s choroid plexus vascular barrier, along with another barrier between the gut and liver, known as the gut vascular barrier, appear to control the movement of molecules along the gut-brain axis.
“We show that in addition to the epithelial barrier in the choroid plexus, there is a functional vascular barrier that only becomes evident in blocking entry of various inflammatory molecules under conditions of systemic inflammation,” Dr. Lodato said.
“This interruption of the gut-brain interaction has developed to protect the brain from inflammation. Why this happens is not yet known, but it is likely to prevent epileptic seizures and imbalanced neuronal activity,” added Dr. Rescigno.
The study was published online October 22 in Science.
The gut a root cause of mental illness?
Nearly 40% of patients with IBD also experience depression and anxiety. It was once thought that these conditions arose because of patients’ difficulties in coping with their disease, said Dr. Rescigno.
“People with these disorders conventionally thought to be caused by an imbalance in the brain may actually find the root cause is located in the intestine. This is the first time these symptoms have been associated with the choroid plexus vascular brain barrier and its closure,” she noted.
Dr. Rescigno added that subtle, rather than overt, inflammation may be all that’s required for closure of the choroid plexus and the subsequent effects on mental health.
In 2015, Dr. Rescigno’s group first described the gut vascular barrier that protects the systemic circulation from gut bacteria or associated bacteria-derived molecules. During intestinal inflammation, such as occurs in IBD, this barrier is compromised and becomes more permeable. This allows microbes to pass across the epithelium of the gut barrier and enter the systemic circulation, including the liver and spleen, explained Dr. Rescigno.
Dr. Rescigno and Dr. Lodato then explored whether this systemic inflammatory condition was connected to the brain along a gut-brain axis and found that it was.
The researchers tested the hypothesis that central nervous system symptoms may be due to vascular changes at the interface between the gut or the brain and elsewhere in the body.
“We set out to test whether opening of the gut vascular barrier would allow gut bacteria to trigger the release of inflammatory molecules that spread to more distant areas, possibly leading to a deficiency of certain nutrients and precipitating mental disorders,” they said.
An experimental preclinical model of the choroid plexus vascular barrier closure led to anxiety-like behavior, as well as short-term memory loss. That this behavior occurred independently of inflammation suggested that it was likely a response to closure itself, they note.
In the noninflammatory state, the epithelium of the choroid plexus filters molecules. Those that are ≤70 kDa are allowed to pass through to the brain. However, the investigators found that during systemic inflammation, this filtration stops, and the blood capillaries of the choroid plexus prevent entry of inflammatory molecules such as cytokines.
Dr. Lodato speculated that when the vascular barrier of the choroid plexus shuts off during the systemic inflammatory state, it responds by bathing the brain in cerebrospinal fluid.
“When the choroid plexus closes, like a door slamming shut, then communication between the brain and the rest of the body is halted. This means that the brain is deprived of certain nutrients and other beneficial molecules that usually enter via the cerebrospinal fluid or enriched of potentially dangerous ones, as drainage could also be affected,” she said.
If confirmed in further studies, these results may open the way to new interventions.
‘A significant leap forward’
Commenting on the findings, David T. Rubin, MD, professor of medicine at the University of Chicago, noted that the study’s results represent “a significant leap forward” and that it highlights “another important cost to uncontrolled gut inflammation that is the potential for worsened mental health disorders.”
Dr. Rubin, whose research involves measuring metabolites of the dietary amino acid tryptophan, including melatonin and serotonin, in patients with IBD, added that the findings offer a possible explanation for the association of both Crohn’s disease and ulcerative colitis with anxiety and depressive disorders.
“There was a belief that the association was in the opposite direction, that the mental health disorder was causing or worsening the gut inflammation, but this has been disavowed,” Dr. Rubin said.
“Most recently, the recognition that the major sources of serotonin and other metabolites of tryptophan that come from the gut microbiome has led to the hypothesis that the inflamed bowel and dysbiotic gut biome may in fact be driving the mental health disorders due to the effect of neurotransmitter imbalance,” he added. Dr. Rubin also suggested that the shutdown of the choroid plexus vascular barrier may contribute to this imbalance but that this needs additional study.
“This further supports my ongoing contention that the gut really is the center of the universe,” said Dr. Rubin.
Also commenting on the findings, Miguel Rigueiro, MD, professor in the department of medicine in the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, Cleveland, said, “There’s an implication that anxiety and depression and other behavioral health disorders may be explained by this mechanism. If that is the case, there may be a way to target medications against the choroid plexus and potentially treat depression or anxiety.”
This prospect was echoed by Dr. Rubin, who said, “The clinical implication is that treatment of gut inflammation may restore a balance to the neurotransmitters and resolve anxiety or depressive disorders.”
To identify new therapeutic targets, investigators will study the regions and circuits of the brain that are more susceptible to this closure of the choroid plexus, said Dr. Lodato.
“If these regions are associated with depression or other psychosocial disorders, then this new understanding around the choroid plexus vascular barrier might eventually have implications for helping treat such disorders,” she noted.
Reflecting a general shift from a brain-centric view of some psychosocial disorders to an intestinal-centric one, Dr. Lodato added, “The brain cannot be considered in isolation. It is part of a much larger body, and we need to think this way.”
Dr. Rescigno, Dr. Lodato, and Dr. Rubin report no relevant financial relationships. Dr. Rigueiro has served on advisory boards and as consultant for AbbVie, Janssen, UCB, Takeda, Pfizer, Miraca Labs, Amgen, Celgene, Seres, Allergan, Genentech, Gilead, Salix, Prometheus, Lilly, TARGET Pharma Solutions, ALFASIGMA, SpA, and Bristol-Meyer Squibb.
A version of this article first appeared on Medscape.com.
A newly discovered vascular brain barrier that blocks the passage of inflammatory molecules triggered by gut bacteria may be why patients with inflammatory bowel disease (IBD) are at increased risk for certain mental health disorders, including anxiety and depression, early research suggests.
The discovery, which was based on a preclinical model, could lead to new therapeutic targets that could have applications for both gastrointestinal and psychiatric conditions, investigators note.
The research team, which was led by immunologist Maria Rescigno, PhD, and neuroscientist Simona Lodato, PhD, both from Humanitas University, Milan, notes that the barrier resides in the choroid plexus, a region of the brain that is involved in filtering cerebrospinal fluid. The researchers found that the region closes in response to inflammatory molecules produced in reaction to the presence of intestinal bacteria in patients with gut disorders.
Dr. Lodato said in an interview that the brain’s choroid plexus vascular barrier, along with another barrier between the gut and liver, known as the gut vascular barrier, appear to control the movement of molecules along the gut-brain axis.
“We show that in addition to the epithelial barrier in the choroid plexus, there is a functional vascular barrier that only becomes evident in blocking entry of various inflammatory molecules under conditions of systemic inflammation,” Dr. Lodato said.
“This interruption of the gut-brain interaction has developed to protect the brain from inflammation. Why this happens is not yet known, but it is likely to prevent epileptic seizures and imbalanced neuronal activity,” added Dr. Rescigno.
The study was published online October 22 in Science.
The gut a root cause of mental illness?
Nearly 40% of patients with IBD also experience depression and anxiety. It was once thought that these conditions arose because of patients’ difficulties in coping with their disease, said Dr. Rescigno.
“People with these disorders conventionally thought to be caused by an imbalance in the brain may actually find the root cause is located in the intestine. This is the first time these symptoms have been associated with the choroid plexus vascular brain barrier and its closure,” she noted.
Dr. Rescigno added that subtle, rather than overt, inflammation may be all that’s required for closure of the choroid plexus and the subsequent effects on mental health.
In 2015, Dr. Rescigno’s group first described the gut vascular barrier that protects the systemic circulation from gut bacteria or associated bacteria-derived molecules. During intestinal inflammation, such as occurs in IBD, this barrier is compromised and becomes more permeable. This allows microbes to pass across the epithelium of the gut barrier and enter the systemic circulation, including the liver and spleen, explained Dr. Rescigno.
Dr. Rescigno and Dr. Lodato then explored whether this systemic inflammatory condition was connected to the brain along a gut-brain axis and found that it was.
The researchers tested the hypothesis that central nervous system symptoms may be due to vascular changes at the interface between the gut or the brain and elsewhere in the body.
“We set out to test whether opening of the gut vascular barrier would allow gut bacteria to trigger the release of inflammatory molecules that spread to more distant areas, possibly leading to a deficiency of certain nutrients and precipitating mental disorders,” they said.
An experimental preclinical model of the choroid plexus vascular barrier closure led to anxiety-like behavior, as well as short-term memory loss. That this behavior occurred independently of inflammation suggested that it was likely a response to closure itself, they note.
In the noninflammatory state, the epithelium of the choroid plexus filters molecules. Those that are ≤70 kDa are allowed to pass through to the brain. However, the investigators found that during systemic inflammation, this filtration stops, and the blood capillaries of the choroid plexus prevent entry of inflammatory molecules such as cytokines.
Dr. Lodato speculated that when the vascular barrier of the choroid plexus shuts off during the systemic inflammatory state, it responds by bathing the brain in cerebrospinal fluid.
“When the choroid plexus closes, like a door slamming shut, then communication between the brain and the rest of the body is halted. This means that the brain is deprived of certain nutrients and other beneficial molecules that usually enter via the cerebrospinal fluid or enriched of potentially dangerous ones, as drainage could also be affected,” she said.
If confirmed in further studies, these results may open the way to new interventions.
‘A significant leap forward’
Commenting on the findings, David T. Rubin, MD, professor of medicine at the University of Chicago, noted that the study’s results represent “a significant leap forward” and that it highlights “another important cost to uncontrolled gut inflammation that is the potential for worsened mental health disorders.”
Dr. Rubin, whose research involves measuring metabolites of the dietary amino acid tryptophan, including melatonin and serotonin, in patients with IBD, added that the findings offer a possible explanation for the association of both Crohn’s disease and ulcerative colitis with anxiety and depressive disorders.
“There was a belief that the association was in the opposite direction, that the mental health disorder was causing or worsening the gut inflammation, but this has been disavowed,” Dr. Rubin said.
“Most recently, the recognition that the major sources of serotonin and other metabolites of tryptophan that come from the gut microbiome has led to the hypothesis that the inflamed bowel and dysbiotic gut biome may in fact be driving the mental health disorders due to the effect of neurotransmitter imbalance,” he added. Dr. Rubin also suggested that the shutdown of the choroid plexus vascular barrier may contribute to this imbalance but that this needs additional study.
“This further supports my ongoing contention that the gut really is the center of the universe,” said Dr. Rubin.
Also commenting on the findings, Miguel Rigueiro, MD, professor in the department of medicine in the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, Cleveland, said, “There’s an implication that anxiety and depression and other behavioral health disorders may be explained by this mechanism. If that is the case, there may be a way to target medications against the choroid plexus and potentially treat depression or anxiety.”
This prospect was echoed by Dr. Rubin, who said, “The clinical implication is that treatment of gut inflammation may restore a balance to the neurotransmitters and resolve anxiety or depressive disorders.”
To identify new therapeutic targets, investigators will study the regions and circuits of the brain that are more susceptible to this closure of the choroid plexus, said Dr. Lodato.
“If these regions are associated with depression or other psychosocial disorders, then this new understanding around the choroid plexus vascular barrier might eventually have implications for helping treat such disorders,” she noted.
Reflecting a general shift from a brain-centric view of some psychosocial disorders to an intestinal-centric one, Dr. Lodato added, “The brain cannot be considered in isolation. It is part of a much larger body, and we need to think this way.”
Dr. Rescigno, Dr. Lodato, and Dr. Rubin report no relevant financial relationships. Dr. Rigueiro has served on advisory boards and as consultant for AbbVie, Janssen, UCB, Takeda, Pfizer, Miraca Labs, Amgen, Celgene, Seres, Allergan, Genentech, Gilead, Salix, Prometheus, Lilly, TARGET Pharma Solutions, ALFASIGMA, SpA, and Bristol-Meyer Squibb.
A version of this article first appeared on Medscape.com.
A newly discovered vascular brain barrier that blocks the passage of inflammatory molecules triggered by gut bacteria may be why patients with inflammatory bowel disease (IBD) are at increased risk for certain mental health disorders, including anxiety and depression, early research suggests.
The discovery, which was based on a preclinical model, could lead to new therapeutic targets that could have applications for both gastrointestinal and psychiatric conditions, investigators note.
The research team, which was led by immunologist Maria Rescigno, PhD, and neuroscientist Simona Lodato, PhD, both from Humanitas University, Milan, notes that the barrier resides in the choroid plexus, a region of the brain that is involved in filtering cerebrospinal fluid. The researchers found that the region closes in response to inflammatory molecules produced in reaction to the presence of intestinal bacteria in patients with gut disorders.
Dr. Lodato said in an interview that the brain’s choroid plexus vascular barrier, along with another barrier between the gut and liver, known as the gut vascular barrier, appear to control the movement of molecules along the gut-brain axis.
“We show that in addition to the epithelial barrier in the choroid plexus, there is a functional vascular barrier that only becomes evident in blocking entry of various inflammatory molecules under conditions of systemic inflammation,” Dr. Lodato said.
“This interruption of the gut-brain interaction has developed to protect the brain from inflammation. Why this happens is not yet known, but it is likely to prevent epileptic seizures and imbalanced neuronal activity,” added Dr. Rescigno.
The study was published online October 22 in Science.
The gut a root cause of mental illness?
Nearly 40% of patients with IBD also experience depression and anxiety. It was once thought that these conditions arose because of patients’ difficulties in coping with their disease, said Dr. Rescigno.
“People with these disorders conventionally thought to be caused by an imbalance in the brain may actually find the root cause is located in the intestine. This is the first time these symptoms have been associated with the choroid plexus vascular brain barrier and its closure,” she noted.
Dr. Rescigno added that subtle, rather than overt, inflammation may be all that’s required for closure of the choroid plexus and the subsequent effects on mental health.
In 2015, Dr. Rescigno’s group first described the gut vascular barrier that protects the systemic circulation from gut bacteria or associated bacteria-derived molecules. During intestinal inflammation, such as occurs in IBD, this barrier is compromised and becomes more permeable. This allows microbes to pass across the epithelium of the gut barrier and enter the systemic circulation, including the liver and spleen, explained Dr. Rescigno.
Dr. Rescigno and Dr. Lodato then explored whether this systemic inflammatory condition was connected to the brain along a gut-brain axis and found that it was.
The researchers tested the hypothesis that central nervous system symptoms may be due to vascular changes at the interface between the gut or the brain and elsewhere in the body.
“We set out to test whether opening of the gut vascular barrier would allow gut bacteria to trigger the release of inflammatory molecules that spread to more distant areas, possibly leading to a deficiency of certain nutrients and precipitating mental disorders,” they said.
An experimental preclinical model of the choroid plexus vascular barrier closure led to anxiety-like behavior, as well as short-term memory loss. That this behavior occurred independently of inflammation suggested that it was likely a response to closure itself, they note.
In the noninflammatory state, the epithelium of the choroid plexus filters molecules. Those that are ≤70 kDa are allowed to pass through to the brain. However, the investigators found that during systemic inflammation, this filtration stops, and the blood capillaries of the choroid plexus prevent entry of inflammatory molecules such as cytokines.
Dr. Lodato speculated that when the vascular barrier of the choroid plexus shuts off during the systemic inflammatory state, it responds by bathing the brain in cerebrospinal fluid.
“When the choroid plexus closes, like a door slamming shut, then communication between the brain and the rest of the body is halted. This means that the brain is deprived of certain nutrients and other beneficial molecules that usually enter via the cerebrospinal fluid or enriched of potentially dangerous ones, as drainage could also be affected,” she said.
If confirmed in further studies, these results may open the way to new interventions.
‘A significant leap forward’
Commenting on the findings, David T. Rubin, MD, professor of medicine at the University of Chicago, noted that the study’s results represent “a significant leap forward” and that it highlights “another important cost to uncontrolled gut inflammation that is the potential for worsened mental health disorders.”
Dr. Rubin, whose research involves measuring metabolites of the dietary amino acid tryptophan, including melatonin and serotonin, in patients with IBD, added that the findings offer a possible explanation for the association of both Crohn’s disease and ulcerative colitis with anxiety and depressive disorders.
“There was a belief that the association was in the opposite direction, that the mental health disorder was causing or worsening the gut inflammation, but this has been disavowed,” Dr. Rubin said.
“Most recently, the recognition that the major sources of serotonin and other metabolites of tryptophan that come from the gut microbiome has led to the hypothesis that the inflamed bowel and dysbiotic gut biome may in fact be driving the mental health disorders due to the effect of neurotransmitter imbalance,” he added. Dr. Rubin also suggested that the shutdown of the choroid plexus vascular barrier may contribute to this imbalance but that this needs additional study.
“This further supports my ongoing contention that the gut really is the center of the universe,” said Dr. Rubin.
Also commenting on the findings, Miguel Rigueiro, MD, professor in the department of medicine in the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, Cleveland, said, “There’s an implication that anxiety and depression and other behavioral health disorders may be explained by this mechanism. If that is the case, there may be a way to target medications against the choroid plexus and potentially treat depression or anxiety.”
This prospect was echoed by Dr. Rubin, who said, “The clinical implication is that treatment of gut inflammation may restore a balance to the neurotransmitters and resolve anxiety or depressive disorders.”
To identify new therapeutic targets, investigators will study the regions and circuits of the brain that are more susceptible to this closure of the choroid plexus, said Dr. Lodato.
“If these regions are associated with depression or other psychosocial disorders, then this new understanding around the choroid plexus vascular barrier might eventually have implications for helping treat such disorders,” she noted.
Reflecting a general shift from a brain-centric view of some psychosocial disorders to an intestinal-centric one, Dr. Lodato added, “The brain cannot be considered in isolation. It is part of a much larger body, and we need to think this way.”
Dr. Rescigno, Dr. Lodato, and Dr. Rubin report no relevant financial relationships. Dr. Rigueiro has served on advisory boards and as consultant for AbbVie, Janssen, UCB, Takeda, Pfizer, Miraca Labs, Amgen, Celgene, Seres, Allergan, Genentech, Gilead, Salix, Prometheus, Lilly, TARGET Pharma Solutions, ALFASIGMA, SpA, and Bristol-Meyer Squibb.
A version of this article first appeared on Medscape.com.
FROM SCIENCE
COVID vaccines’ protection dropped sharply over 6 months: Study
, a study of almost 800,000 veterans found.
The study, published in the journal Science ., says the three vaccines offered about the same protection against the virus in March, when the Delta variant was first detected in the United States, but that changed 6 months later.
The Moderna two-dose vaccine went from being 89% effective in March to 58% effective in September, according to a story about the study in theLos Angeles Times.
Meanwhile, the Pfizer/BioNTech vaccine went from being 87% effective to 45% effective over the same time period.
The Johnson & Johnson vaccine showed the biggest drop -- from 86% effectiveness to 13% over those 6 months.
“In summary, although vaccination remains protective against SARS-CoV-2 infection, protection waned as the Delta variant emerged in the U.S., and this decline did not differ by age,” the study said.
The three vaccines also lost effectiveness in the ability to protect against death in veterans 65 and over after only 3 months, the Los Angeles Times reported.
Compared to unvaccinated veterans in that age group, veterans who got the Moderna vaccine and had a breakthrough case were 76% less likely to die of COVID-19 by July.
The protection was 70% for Pfizer/BioNTech vaccine recipients and 52% for J&J vaccine recipients for the same age group, compared to unvaccinated veterans, according to the newspaper.
For veterans under 65, the protectiveness against a fatal case of COVID was 84% for Pfizer/BioNTech recipients, 82% for Moderna recipients, and 73% for J&J recipients, compared to unvaccinated veterans in that age group.
The study confirms the need for booster vaccines and protective measures such as vaccine passports, vaccine mandates, masking, hand-washing, and social distancing, the researchers said.
Of the veterans studied, about 500,000 were vaccinated and 300,000 were not. Researchers noted that the study population had 6 times as many men as women. About 48% of the study group was 65 or older, 29% was 50-64, while 24% was under 50.
Researchers from the Public Health Institute in Oakland, the Veterans Affairs Medical Center in San Francisco, and the University of Texas Health Science Center conducted the study.
A version of this article first appeared on WebMD.com.
, a study of almost 800,000 veterans found.
The study, published in the journal Science ., says the three vaccines offered about the same protection against the virus in March, when the Delta variant was first detected in the United States, but that changed 6 months later.
The Moderna two-dose vaccine went from being 89% effective in March to 58% effective in September, according to a story about the study in theLos Angeles Times.
Meanwhile, the Pfizer/BioNTech vaccine went from being 87% effective to 45% effective over the same time period.
The Johnson & Johnson vaccine showed the biggest drop -- from 86% effectiveness to 13% over those 6 months.
“In summary, although vaccination remains protective against SARS-CoV-2 infection, protection waned as the Delta variant emerged in the U.S., and this decline did not differ by age,” the study said.
The three vaccines also lost effectiveness in the ability to protect against death in veterans 65 and over after only 3 months, the Los Angeles Times reported.
Compared to unvaccinated veterans in that age group, veterans who got the Moderna vaccine and had a breakthrough case were 76% less likely to die of COVID-19 by July.
The protection was 70% for Pfizer/BioNTech vaccine recipients and 52% for J&J vaccine recipients for the same age group, compared to unvaccinated veterans, according to the newspaper.
For veterans under 65, the protectiveness against a fatal case of COVID was 84% for Pfizer/BioNTech recipients, 82% for Moderna recipients, and 73% for J&J recipients, compared to unvaccinated veterans in that age group.
The study confirms the need for booster vaccines and protective measures such as vaccine passports, vaccine mandates, masking, hand-washing, and social distancing, the researchers said.
Of the veterans studied, about 500,000 were vaccinated and 300,000 were not. Researchers noted that the study population had 6 times as many men as women. About 48% of the study group was 65 or older, 29% was 50-64, while 24% was under 50.
Researchers from the Public Health Institute in Oakland, the Veterans Affairs Medical Center in San Francisco, and the University of Texas Health Science Center conducted the study.
A version of this article first appeared on WebMD.com.
, a study of almost 800,000 veterans found.
The study, published in the journal Science ., says the three vaccines offered about the same protection against the virus in March, when the Delta variant was first detected in the United States, but that changed 6 months later.
The Moderna two-dose vaccine went from being 89% effective in March to 58% effective in September, according to a story about the study in theLos Angeles Times.
Meanwhile, the Pfizer/BioNTech vaccine went from being 87% effective to 45% effective over the same time period.
The Johnson & Johnson vaccine showed the biggest drop -- from 86% effectiveness to 13% over those 6 months.
“In summary, although vaccination remains protective against SARS-CoV-2 infection, protection waned as the Delta variant emerged in the U.S., and this decline did not differ by age,” the study said.
The three vaccines also lost effectiveness in the ability to protect against death in veterans 65 and over after only 3 months, the Los Angeles Times reported.
Compared to unvaccinated veterans in that age group, veterans who got the Moderna vaccine and had a breakthrough case were 76% less likely to die of COVID-19 by July.
The protection was 70% for Pfizer/BioNTech vaccine recipients and 52% for J&J vaccine recipients for the same age group, compared to unvaccinated veterans, according to the newspaper.
For veterans under 65, the protectiveness against a fatal case of COVID was 84% for Pfizer/BioNTech recipients, 82% for Moderna recipients, and 73% for J&J recipients, compared to unvaccinated veterans in that age group.
The study confirms the need for booster vaccines and protective measures such as vaccine passports, vaccine mandates, masking, hand-washing, and social distancing, the researchers said.
Of the veterans studied, about 500,000 were vaccinated and 300,000 were not. Researchers noted that the study population had 6 times as many men as women. About 48% of the study group was 65 or older, 29% was 50-64, while 24% was under 50.
Researchers from the Public Health Institute in Oakland, the Veterans Affairs Medical Center in San Francisco, and the University of Texas Health Science Center conducted the study.
A version of this article first appeared on WebMD.com.
FROM SCIENCE
Detransitioners received poor evaluation when transitioning
Over half of people who believed they were transgender, transitioned to the opposite sex, but then regretted it and transitioned back – known as detransitioners – felt they did not receive adequate evaluation from a doctor or mental health professional before starting transition, new research indicates.
In what is thought to be the first study to ask whether detransitioners informed their original clinicians of their regret at transitioning, only 24 of the 100 surveyed said they had done so.
This strongly suggests that records on detransition may understate the real numbers, said Lisa Littman, MD, MPH, president of The Institute for Comprehensive Gender Dysphoria Research (ICGDR), who is the sole author of the study, published in Archives of Sexual Behavior.
She stressed that the findings illustrate the complexity surrounding gender dysphoria. “We need to recognize that there are many different types of experiences around gender dysphoria, transition, and detransition,” she told this news organization.
She said there is some resistance among certain health care professionals, and in society in general, to the idea that transitioning is not always successful.
‘We need to understand why this is happening’
“Detransition exists and we need to understand why this is happening,” Dr. Littman emphasized.
She observed that some supporters of “rapid transition” do not want to accept that transitioning helps some individuals but harms others.
“In the end, our goals should be providing the right treatment for the right patient, and without a thorough evaluation, clinicians are at serious risk of giving patients the wrong treatment,” she urged.
She noted that, despite some individuals feeling better after transition, these people still felt inclined to detransition because of discrimination and pressure.
“Individuals should not be pressured to detransition, nor should they be pressured to transition. Both types of pressure were reported by respondents.”
The recently recognized shift from mostly natal males to natal females seeking to transition was borne out by her study data, with the proportion of natal girls who detransitioned at 69%.
‘Shedding light’ on often ignored population
Asked to comment on the study, Laura Edwards-Leeper, PhD, a clinical psychologist from Beaverton, Ore., who specializes in gender-diverse and transgender children, welcomed Dr. Littman’s study.
It is, said Dr. Edwards-Leeper, a “critical preliminary step toward shedding light on this often-ignored and dismissed population of individuals who deserve support, compassion, and sometimes medical intervention from health care providers.”
She added that multiple online reports attest to detransitioners feeling they had not received adequate evaluation prior to medically transitioning, as well as many who expressed feeling too ashamed or angry to return to their same clinicians to detransition.
“Littman’s study provides quantitative support for both of these reported experiences, further emphasizing the importance of the field taking a closer look at the processes currently in place for those experiencing gender dysphoria,” said Dr. Edwards-Leeper.
And Miroslav L. Djordjevic, MD, PhD, professor of surgery/urology, University of Belgrade (Serbia), who is a specialist in urogenital reconstructive surgery and has performed over 2,000 gender-reassignment surgeries in transgender individuals, has recently seen many cases of regret after such surgeries, with requests for reversal operations.
“Despite the fact that medical detransition is relatively safe and without severe consequences, surgical detransition presents one of the most difficult issues in transgender medicine,” Dr. Djordjevic told this news organization.
Commending Dr. Littman on her study, he drew attention to some of the bioethical questions that arise relating to those who detransition.
“I ask what happened in the period before medical transitioning? Was there proper psychological care during medical transitioning? Who confirmed their desire for detransition – the same professionals who did the transition?” or someone else, he continued. “And who accepted these individuals for gender-affirming surgery and what were the criteria for this decision?”
Substantial study of reasons for both transitioning and detransitioning
In her article, Dr. Littman describes a 100-strong population of individuals (66 Americans, 9 British, 9 Canadian, 4 Australians, and 12 from “other” nations), ranging in age from 18 years to over 60 years with a mean age of 29.2 years, who had experienced gender dysphoria, chosen to undergo medical and/or surgical transition, and then detransitioned by discontinuing medications, having reversal surgery, or both.
Participants completed a 115-question survey providing data including age at first experience of gender dysphoria, when participants first sought transitioning care and from whom, and whether they felt pressured to do so. Friendship group dynamics were also explored.
Various narratives of participants’ transitioning-detransitioning experiences were gathered and grouped, for example, those related to discrimination pressures, experiences of trauma or mental health conditions prior to transition, and reports of internalized homophobia.
Dr. Edwards-Leeper observed that the study offers a more extensive assessment of reasons for detransitioning than any other prior research in the field, which has been sparse.
A survey published in April found that detransitioners report significant unmet medical and psychological needs, and a lack of compassion and help from medical and mental health practitioners.
But another 2021 study concluded most detransitioners only reverted to their birth sex because of societal or family pressure, discrimination, or shift to a nonbinary identity.
“However, [Dr.] Littman’s study found that only a small percentage actually detransitioned for that reason [23%], whereas the majority detransitioned because of a change in how the individual understood being a male or female, resulting in becoming comfortable in their assigned gender [60%],” noted Dr. Edwards-Leeper.
Reasons for detransitioning
Asked to expand upon the motives for detransition identified in her study, Dr. Littman told this news organization: “We found remarkable breadth in the reasons given for detransitioning.”
“I believe that we were able to capture the diversity of experiences around detransition because we reached out to communities that were strongly ‘protransition’ – like the World Professional Association for Transgender Health – and communities where individuals might be more skeptical about transition being universally beneficial, like detransition forums,” she said.
Speaking to the complexity of the experiences, 87% selected more than one reason for detransitioning.
The most common reason (60%) was becoming more comfortable identifying with their birth sex, followed by having concerns about potential medical complications from transitioning (49.0%).
Regarding those who became more comfortable with their natal sex, Dr. Littman noted that the finding adds “further support that gender dysphoria is not always permanent.”
She added that, “because most gender-dysphoric youth who are allowed to go through puberty grow up to be lesbian, gay, or bisexual (LGB) nontransgender adults, intervening too soon with medical treatments risks derailing their development as LGB individuals.”
Internalized homophobia or difficulty accepting themselves as lesbian, gay, or bisexual was reported by 23% of participants as a reason for transition and subsequent detransition.
“For these people, transitioning could be interpreted as an attempt to escape the reality of being same-sex attracted and detransitioning was part of accepting themselves as homosexual or bisexual,” explained Dr. Littman.
“Exploring their distress and discomfort around sexual orientation issues may have been more helpful to them than medical and surgical transition or at least an important part of exploration,” she added in the article.
Societal pressure, friends, and social media also play a role
The latest first-hand reports also support prior work by Dr. Littman when she first identified the concept she termed rapid-onset gender dysphoria (ROGD) to describe a sudden transgender identification, usually in the early teenage years, and with no prior indication of any gender questioning.
ROGD, Dr. Littman believes, is strongly related to psychosocial factors, such as trauma, mental health problems, or social influence contributing to the development of gender dysphoria.
The current study found that 58% of respondents expressed the belief that the cause of their gender dysphoria was something specific, such as trauma, abuse, or a mental health condition, with respondents suggesting that transitioning prevented, or delayed, them from addressing their underlying mental health conditions.
One participant is quoted as saying: “I was deeply uncomfortable with my secondary sex characteristics, which I now understand was a result of childhood trauma and associating my secondary sex characteristics with those events.”
Reflecting on their previous identification as transgender, more than a third of respondents reported that someone else told them their feelings meant they were transgender, and they believed them.
“This speaks to the effect social influence can have on people’s interpretation of their own feelings and their development of a transgender identity,” Dr. Littman remarked.
“Participants also listed several social media sources that encouraged them to believe that transitioning would help them,” she added.
Several friendship group dynamics suggestive of social influence were reported by a subset of respondents, including the fact that their friendship groups mocked people who were not transgender and their popularity increased when they announced they were going to transition.
Pendulum has swung too far the other way
Natal females, who in recent years have made up most referrals, were younger than natal males when they sought transition and decided to detransition; and they stayed “transitioned” for a shorter period than natal males. They were also more likely to have experienced a trauma less than 1 year before the onset of gender dysphoria and were more likely to have felt pressured to transition.
“Because the females in the study transitioned more recently than the males, they may have experienced a culture where there is more of a ‘push’ to transition,” Dr. Littman pointed out.
She added that, “20 years ago, gender-dysphoric patients were most likely to be underdiagnosed and undertreated. Now, the pendulum has swung the other way and patients are, in my opinion, more likely to be overdiagnosed and overtreated. I think we need to aim for somewhere between these two extremes and prioritize people getting the right treatment for the right reason for their distress.”
Dr. Djordjevic added that, with colleagues from Belgrade and the Netherlands, he has published accounts of the experiences of seven individuals who showed regret after gender-affirming surgery.
All of them were born male, “and we confirmed the very poor evaluation and transition process they underwent. We conclude that clinicians should be aware that not everyone with gender identity disorders need or want all elements of hormonal or surgical therapy,” he told this news organization.
Dr. Edwards-Leeper said that more long-term longitudinal studies are needed that follow individuals who undergo transition under different models of care.
“My prediction is that those who first engage in supportive, gender exploratory therapy, followed by comprehensive assessment, will have the best outcomes, perhaps even if they ultimately detransition, as these individuals will know that they did not jump into irreversible interventions too quickly and had time to make the best decision for themselves at the time,” she concluded.
A version of this article first appeared on Medscape.com.
Over half of people who believed they were transgender, transitioned to the opposite sex, but then regretted it and transitioned back – known as detransitioners – felt they did not receive adequate evaluation from a doctor or mental health professional before starting transition, new research indicates.
In what is thought to be the first study to ask whether detransitioners informed their original clinicians of their regret at transitioning, only 24 of the 100 surveyed said they had done so.
This strongly suggests that records on detransition may understate the real numbers, said Lisa Littman, MD, MPH, president of The Institute for Comprehensive Gender Dysphoria Research (ICGDR), who is the sole author of the study, published in Archives of Sexual Behavior.
She stressed that the findings illustrate the complexity surrounding gender dysphoria. “We need to recognize that there are many different types of experiences around gender dysphoria, transition, and detransition,” she told this news organization.
She said there is some resistance among certain health care professionals, and in society in general, to the idea that transitioning is not always successful.
‘We need to understand why this is happening’
“Detransition exists and we need to understand why this is happening,” Dr. Littman emphasized.
She observed that some supporters of “rapid transition” do not want to accept that transitioning helps some individuals but harms others.
“In the end, our goals should be providing the right treatment for the right patient, and without a thorough evaluation, clinicians are at serious risk of giving patients the wrong treatment,” she urged.
She noted that, despite some individuals feeling better after transition, these people still felt inclined to detransition because of discrimination and pressure.
“Individuals should not be pressured to detransition, nor should they be pressured to transition. Both types of pressure were reported by respondents.”
The recently recognized shift from mostly natal males to natal females seeking to transition was borne out by her study data, with the proportion of natal girls who detransitioned at 69%.
‘Shedding light’ on often ignored population
Asked to comment on the study, Laura Edwards-Leeper, PhD, a clinical psychologist from Beaverton, Ore., who specializes in gender-diverse and transgender children, welcomed Dr. Littman’s study.
It is, said Dr. Edwards-Leeper, a “critical preliminary step toward shedding light on this often-ignored and dismissed population of individuals who deserve support, compassion, and sometimes medical intervention from health care providers.”
She added that multiple online reports attest to detransitioners feeling they had not received adequate evaluation prior to medically transitioning, as well as many who expressed feeling too ashamed or angry to return to their same clinicians to detransition.
“Littman’s study provides quantitative support for both of these reported experiences, further emphasizing the importance of the field taking a closer look at the processes currently in place for those experiencing gender dysphoria,” said Dr. Edwards-Leeper.
And Miroslav L. Djordjevic, MD, PhD, professor of surgery/urology, University of Belgrade (Serbia), who is a specialist in urogenital reconstructive surgery and has performed over 2,000 gender-reassignment surgeries in transgender individuals, has recently seen many cases of regret after such surgeries, with requests for reversal operations.
“Despite the fact that medical detransition is relatively safe and without severe consequences, surgical detransition presents one of the most difficult issues in transgender medicine,” Dr. Djordjevic told this news organization.
Commending Dr. Littman on her study, he drew attention to some of the bioethical questions that arise relating to those who detransition.
“I ask what happened in the period before medical transitioning? Was there proper psychological care during medical transitioning? Who confirmed their desire for detransition – the same professionals who did the transition?” or someone else, he continued. “And who accepted these individuals for gender-affirming surgery and what were the criteria for this decision?”
Substantial study of reasons for both transitioning and detransitioning
In her article, Dr. Littman describes a 100-strong population of individuals (66 Americans, 9 British, 9 Canadian, 4 Australians, and 12 from “other” nations), ranging in age from 18 years to over 60 years with a mean age of 29.2 years, who had experienced gender dysphoria, chosen to undergo medical and/or surgical transition, and then detransitioned by discontinuing medications, having reversal surgery, or both.
Participants completed a 115-question survey providing data including age at first experience of gender dysphoria, when participants first sought transitioning care and from whom, and whether they felt pressured to do so. Friendship group dynamics were also explored.
Various narratives of participants’ transitioning-detransitioning experiences were gathered and grouped, for example, those related to discrimination pressures, experiences of trauma or mental health conditions prior to transition, and reports of internalized homophobia.
Dr. Edwards-Leeper observed that the study offers a more extensive assessment of reasons for detransitioning than any other prior research in the field, which has been sparse.
A survey published in April found that detransitioners report significant unmet medical and psychological needs, and a lack of compassion and help from medical and mental health practitioners.
But another 2021 study concluded most detransitioners only reverted to their birth sex because of societal or family pressure, discrimination, or shift to a nonbinary identity.
“However, [Dr.] Littman’s study found that only a small percentage actually detransitioned for that reason [23%], whereas the majority detransitioned because of a change in how the individual understood being a male or female, resulting in becoming comfortable in their assigned gender [60%],” noted Dr. Edwards-Leeper.
Reasons for detransitioning
Asked to expand upon the motives for detransition identified in her study, Dr. Littman told this news organization: “We found remarkable breadth in the reasons given for detransitioning.”
“I believe that we were able to capture the diversity of experiences around detransition because we reached out to communities that were strongly ‘protransition’ – like the World Professional Association for Transgender Health – and communities where individuals might be more skeptical about transition being universally beneficial, like detransition forums,” she said.
Speaking to the complexity of the experiences, 87% selected more than one reason for detransitioning.
The most common reason (60%) was becoming more comfortable identifying with their birth sex, followed by having concerns about potential medical complications from transitioning (49.0%).
Regarding those who became more comfortable with their natal sex, Dr. Littman noted that the finding adds “further support that gender dysphoria is not always permanent.”
She added that, “because most gender-dysphoric youth who are allowed to go through puberty grow up to be lesbian, gay, or bisexual (LGB) nontransgender adults, intervening too soon with medical treatments risks derailing their development as LGB individuals.”
Internalized homophobia or difficulty accepting themselves as lesbian, gay, or bisexual was reported by 23% of participants as a reason for transition and subsequent detransition.
“For these people, transitioning could be interpreted as an attempt to escape the reality of being same-sex attracted and detransitioning was part of accepting themselves as homosexual or bisexual,” explained Dr. Littman.
“Exploring their distress and discomfort around sexual orientation issues may have been more helpful to them than medical and surgical transition or at least an important part of exploration,” she added in the article.
Societal pressure, friends, and social media also play a role
The latest first-hand reports also support prior work by Dr. Littman when she first identified the concept she termed rapid-onset gender dysphoria (ROGD) to describe a sudden transgender identification, usually in the early teenage years, and with no prior indication of any gender questioning.
ROGD, Dr. Littman believes, is strongly related to psychosocial factors, such as trauma, mental health problems, or social influence contributing to the development of gender dysphoria.
The current study found that 58% of respondents expressed the belief that the cause of their gender dysphoria was something specific, such as trauma, abuse, or a mental health condition, with respondents suggesting that transitioning prevented, or delayed, them from addressing their underlying mental health conditions.
One participant is quoted as saying: “I was deeply uncomfortable with my secondary sex characteristics, which I now understand was a result of childhood trauma and associating my secondary sex characteristics with those events.”
Reflecting on their previous identification as transgender, more than a third of respondents reported that someone else told them their feelings meant they were transgender, and they believed them.
“This speaks to the effect social influence can have on people’s interpretation of their own feelings and their development of a transgender identity,” Dr. Littman remarked.
“Participants also listed several social media sources that encouraged them to believe that transitioning would help them,” she added.
Several friendship group dynamics suggestive of social influence were reported by a subset of respondents, including the fact that their friendship groups mocked people who were not transgender and their popularity increased when they announced they were going to transition.
Pendulum has swung too far the other way
Natal females, who in recent years have made up most referrals, were younger than natal males when they sought transition and decided to detransition; and they stayed “transitioned” for a shorter period than natal males. They were also more likely to have experienced a trauma less than 1 year before the onset of gender dysphoria and were more likely to have felt pressured to transition.
“Because the females in the study transitioned more recently than the males, they may have experienced a culture where there is more of a ‘push’ to transition,” Dr. Littman pointed out.
She added that, “20 years ago, gender-dysphoric patients were most likely to be underdiagnosed and undertreated. Now, the pendulum has swung the other way and patients are, in my opinion, more likely to be overdiagnosed and overtreated. I think we need to aim for somewhere between these two extremes and prioritize people getting the right treatment for the right reason for their distress.”
Dr. Djordjevic added that, with colleagues from Belgrade and the Netherlands, he has published accounts of the experiences of seven individuals who showed regret after gender-affirming surgery.
All of them were born male, “and we confirmed the very poor evaluation and transition process they underwent. We conclude that clinicians should be aware that not everyone with gender identity disorders need or want all elements of hormonal or surgical therapy,” he told this news organization.
Dr. Edwards-Leeper said that more long-term longitudinal studies are needed that follow individuals who undergo transition under different models of care.
“My prediction is that those who first engage in supportive, gender exploratory therapy, followed by comprehensive assessment, will have the best outcomes, perhaps even if they ultimately detransition, as these individuals will know that they did not jump into irreversible interventions too quickly and had time to make the best decision for themselves at the time,” she concluded.
A version of this article first appeared on Medscape.com.
Over half of people who believed they were transgender, transitioned to the opposite sex, but then regretted it and transitioned back – known as detransitioners – felt they did not receive adequate evaluation from a doctor or mental health professional before starting transition, new research indicates.
In what is thought to be the first study to ask whether detransitioners informed their original clinicians of their regret at transitioning, only 24 of the 100 surveyed said they had done so.
This strongly suggests that records on detransition may understate the real numbers, said Lisa Littman, MD, MPH, president of The Institute for Comprehensive Gender Dysphoria Research (ICGDR), who is the sole author of the study, published in Archives of Sexual Behavior.
She stressed that the findings illustrate the complexity surrounding gender dysphoria. “We need to recognize that there are many different types of experiences around gender dysphoria, transition, and detransition,” she told this news organization.
She said there is some resistance among certain health care professionals, and in society in general, to the idea that transitioning is not always successful.
‘We need to understand why this is happening’
“Detransition exists and we need to understand why this is happening,” Dr. Littman emphasized.
She observed that some supporters of “rapid transition” do not want to accept that transitioning helps some individuals but harms others.
“In the end, our goals should be providing the right treatment for the right patient, and without a thorough evaluation, clinicians are at serious risk of giving patients the wrong treatment,” she urged.
She noted that, despite some individuals feeling better after transition, these people still felt inclined to detransition because of discrimination and pressure.
“Individuals should not be pressured to detransition, nor should they be pressured to transition. Both types of pressure were reported by respondents.”
The recently recognized shift from mostly natal males to natal females seeking to transition was borne out by her study data, with the proportion of natal girls who detransitioned at 69%.
‘Shedding light’ on often ignored population
Asked to comment on the study, Laura Edwards-Leeper, PhD, a clinical psychologist from Beaverton, Ore., who specializes in gender-diverse and transgender children, welcomed Dr. Littman’s study.
It is, said Dr. Edwards-Leeper, a “critical preliminary step toward shedding light on this often-ignored and dismissed population of individuals who deserve support, compassion, and sometimes medical intervention from health care providers.”
She added that multiple online reports attest to detransitioners feeling they had not received adequate evaluation prior to medically transitioning, as well as many who expressed feeling too ashamed or angry to return to their same clinicians to detransition.
“Littman’s study provides quantitative support for both of these reported experiences, further emphasizing the importance of the field taking a closer look at the processes currently in place for those experiencing gender dysphoria,” said Dr. Edwards-Leeper.
And Miroslav L. Djordjevic, MD, PhD, professor of surgery/urology, University of Belgrade (Serbia), who is a specialist in urogenital reconstructive surgery and has performed over 2,000 gender-reassignment surgeries in transgender individuals, has recently seen many cases of regret after such surgeries, with requests for reversal operations.
“Despite the fact that medical detransition is relatively safe and without severe consequences, surgical detransition presents one of the most difficult issues in transgender medicine,” Dr. Djordjevic told this news organization.
Commending Dr. Littman on her study, he drew attention to some of the bioethical questions that arise relating to those who detransition.
“I ask what happened in the period before medical transitioning? Was there proper psychological care during medical transitioning? Who confirmed their desire for detransition – the same professionals who did the transition?” or someone else, he continued. “And who accepted these individuals for gender-affirming surgery and what were the criteria for this decision?”
Substantial study of reasons for both transitioning and detransitioning
In her article, Dr. Littman describes a 100-strong population of individuals (66 Americans, 9 British, 9 Canadian, 4 Australians, and 12 from “other” nations), ranging in age from 18 years to over 60 years with a mean age of 29.2 years, who had experienced gender dysphoria, chosen to undergo medical and/or surgical transition, and then detransitioned by discontinuing medications, having reversal surgery, or both.
Participants completed a 115-question survey providing data including age at first experience of gender dysphoria, when participants first sought transitioning care and from whom, and whether they felt pressured to do so. Friendship group dynamics were also explored.
Various narratives of participants’ transitioning-detransitioning experiences were gathered and grouped, for example, those related to discrimination pressures, experiences of trauma or mental health conditions prior to transition, and reports of internalized homophobia.
Dr. Edwards-Leeper observed that the study offers a more extensive assessment of reasons for detransitioning than any other prior research in the field, which has been sparse.
A survey published in April found that detransitioners report significant unmet medical and psychological needs, and a lack of compassion and help from medical and mental health practitioners.
But another 2021 study concluded most detransitioners only reverted to their birth sex because of societal or family pressure, discrimination, or shift to a nonbinary identity.
“However, [Dr.] Littman’s study found that only a small percentage actually detransitioned for that reason [23%], whereas the majority detransitioned because of a change in how the individual understood being a male or female, resulting in becoming comfortable in their assigned gender [60%],” noted Dr. Edwards-Leeper.
Reasons for detransitioning
Asked to expand upon the motives for detransition identified in her study, Dr. Littman told this news organization: “We found remarkable breadth in the reasons given for detransitioning.”
“I believe that we were able to capture the diversity of experiences around detransition because we reached out to communities that were strongly ‘protransition’ – like the World Professional Association for Transgender Health – and communities where individuals might be more skeptical about transition being universally beneficial, like detransition forums,” she said.
Speaking to the complexity of the experiences, 87% selected more than one reason for detransitioning.
The most common reason (60%) was becoming more comfortable identifying with their birth sex, followed by having concerns about potential medical complications from transitioning (49.0%).
Regarding those who became more comfortable with their natal sex, Dr. Littman noted that the finding adds “further support that gender dysphoria is not always permanent.”
She added that, “because most gender-dysphoric youth who are allowed to go through puberty grow up to be lesbian, gay, or bisexual (LGB) nontransgender adults, intervening too soon with medical treatments risks derailing their development as LGB individuals.”
Internalized homophobia or difficulty accepting themselves as lesbian, gay, or bisexual was reported by 23% of participants as a reason for transition and subsequent detransition.
“For these people, transitioning could be interpreted as an attempt to escape the reality of being same-sex attracted and detransitioning was part of accepting themselves as homosexual or bisexual,” explained Dr. Littman.
“Exploring their distress and discomfort around sexual orientation issues may have been more helpful to them than medical and surgical transition or at least an important part of exploration,” she added in the article.
Societal pressure, friends, and social media also play a role
The latest first-hand reports also support prior work by Dr. Littman when she first identified the concept she termed rapid-onset gender dysphoria (ROGD) to describe a sudden transgender identification, usually in the early teenage years, and with no prior indication of any gender questioning.
ROGD, Dr. Littman believes, is strongly related to psychosocial factors, such as trauma, mental health problems, or social influence contributing to the development of gender dysphoria.
The current study found that 58% of respondents expressed the belief that the cause of their gender dysphoria was something specific, such as trauma, abuse, or a mental health condition, with respondents suggesting that transitioning prevented, or delayed, them from addressing their underlying mental health conditions.
One participant is quoted as saying: “I was deeply uncomfortable with my secondary sex characteristics, which I now understand was a result of childhood trauma and associating my secondary sex characteristics with those events.”
Reflecting on their previous identification as transgender, more than a third of respondents reported that someone else told them their feelings meant they were transgender, and they believed them.
“This speaks to the effect social influence can have on people’s interpretation of their own feelings and their development of a transgender identity,” Dr. Littman remarked.
“Participants also listed several social media sources that encouraged them to believe that transitioning would help them,” she added.
Several friendship group dynamics suggestive of social influence were reported by a subset of respondents, including the fact that their friendship groups mocked people who were not transgender and their popularity increased when they announced they were going to transition.
Pendulum has swung too far the other way
Natal females, who in recent years have made up most referrals, were younger than natal males when they sought transition and decided to detransition; and they stayed “transitioned” for a shorter period than natal males. They were also more likely to have experienced a trauma less than 1 year before the onset of gender dysphoria and were more likely to have felt pressured to transition.
“Because the females in the study transitioned more recently than the males, they may have experienced a culture where there is more of a ‘push’ to transition,” Dr. Littman pointed out.
She added that, “20 years ago, gender-dysphoric patients were most likely to be underdiagnosed and undertreated. Now, the pendulum has swung the other way and patients are, in my opinion, more likely to be overdiagnosed and overtreated. I think we need to aim for somewhere between these two extremes and prioritize people getting the right treatment for the right reason for their distress.”
Dr. Djordjevic added that, with colleagues from Belgrade and the Netherlands, he has published accounts of the experiences of seven individuals who showed regret after gender-affirming surgery.
All of them were born male, “and we confirmed the very poor evaluation and transition process they underwent. We conclude that clinicians should be aware that not everyone with gender identity disorders need or want all elements of hormonal or surgical therapy,” he told this news organization.
Dr. Edwards-Leeper said that more long-term longitudinal studies are needed that follow individuals who undergo transition under different models of care.
“My prediction is that those who first engage in supportive, gender exploratory therapy, followed by comprehensive assessment, will have the best outcomes, perhaps even if they ultimately detransition, as these individuals will know that they did not jump into irreversible interventions too quickly and had time to make the best decision for themselves at the time,” she concluded.
A version of this article first appeared on Medscape.com.
Universal depression screening in schools doubles odds for teen treatment
Universal screening for adolescent depression in schools, compared with the usual process of targeting students for referral after observing behaviors, resulted in significantly higher odds of identifying major depressive disorder (MDD) and of starting treatment for it, a study of more than 12,000 students suggests. Findings were published online in JAMA Network Open.
Deepa L. Sekhar, MD, MSc, with the department of pediatrics at Pennsylvania State College of Medicine in Hershey, Pa., and colleagues conducted a randomized clinical trial comparing the two screening methods from November 2018 to November 2020.
The trial included students in grades 9 through 12 enrolled at any of the 14 participating Pennsylvania public high schools. Researchers compared the two groups using mixed-effects logistic regression.
They found that adolescents in the universal screening intervention group had 5.92 times higher odds (95% confidence interval [CI], 5.07-6.93) of being identified with MDD symptoms, 3.30 times higher odds (95% CI, 2.49-4.38) of the Student Assistance Program (SAP) confirming follow-up needs, and 2.07 times higher odds (95% CI, 1.39-3.10) of starting MDD treatment.
The study comprised 12,909 students, with an average age of 16 years. Of those students, 2,687 (20.8%) were Hispanic; 2,891 (22.4%) were non-Hispanic Black, 5,842 (45.3%) were non-Hispanic White; and 1,489 (11.5%) were multiracial or of other race or ethnicity.
In the universal screening intervention (n = 6,473) all students completed the Patient Health Questionnaire–9 (PHQ-9). Students who screened positive proceeded to the Student Assistance Program. Students could receive a targeted referral to SAP if they had concerning behavior beyond the PHQ-9.
In the targeted screening group (n = 6,436), students with behaviors prompting concern for MDD were referred to the Student Assistance Program (SAP), mandated in all Pennsylvania schools. The SAP determined follow-up.
The U.S. Preventive Services Task Force (USPSTF) endorsed primary care screening in 2009 and again in 2016 for all adolescents 12-18 years old.
However, the study authors wrote, most U.S. adolescents (more than 60%) don’t have routine access to preventive health care, which limits primary care offices’ ability to properly address the growing numbers.
“[S]creening is inconsistent, with inequalities by race and ethnicity and region, and potential worsening with the COVID-19 pandemic,” they noted.
Depression rates see sharp increase
Meanwhile, the prevalence of adolescents reporting MDD symptoms has “nearly doubled in the last decade, increasing from 8.3% in 2008 to 14.4% in 2018.”
The American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and Children’s Hospital Association recently declared a national emergency in children’s mental health, citing COVID-19’s toll on top of existing challenges.
This study provides further evidence that universal screening is the better approach to identify and treat adolescent depression to save lives, Andres Pumariega, MD, a child and adolescent psychiatrist at University of Florida in Gainesville, told this news organization.
“If you catch these kids early, you can prevent suicide attempts and suicide. You can also prevent complicating costs of care,” he said.
He noted the universal screening removes the potential for bias.
“Relying purely on referral and clinical identification means a lot of kids in minority groups will not be identified and will not be treated accurately. Many clinicians have a problem identifying depression in diverse kids,” he said.
Pushback for universal screening likely
However, he said he has been part of such efforts to implement such programs in Mexico and the United States and said in the Unites States, the political climate will guarantee pushback from having schools more involved in health care and prevention. Recent controversy around COVID-19 vaccines for children illustrates the potential backlash, he said.
Parents often fight such programs as attempts to “label” their children, he said.
“If I have cancer, I sure want to be labeled. A label is used to get them help. We need to find ways to educate parents and support them in facing these issues,” he added.
One concern he has with this intervention is having the SAPs, composed largely of nonclinicians, be the triage point “instead of doing that objectively through objective criteria and by clinicians,” he said. “If we are to have a comprehensive health system where we can serve all kids and manage costs, schools need to be a major part of it.”
School settings offer the chance to see more children, collaborate with teachers and counselors, and integrate results with educational outcomes, he added.
In the study by Sekhar and colleagues, 7 of the 14 schools were classified as urban, with a median size of 370 students.
Researchers noted that the benefit of the universal screening is likely understated because of COVID-19–related school closures during the study period. The closures meant screening wasn’t completed for 7% of students.
The authors concluded that universal screening finds teens living with depression who otherwise would not be found. They said such a program likely works best in schools with strong SAP.
“Adolescents’ consistent contact with schools has been used to support physical health screenings that affect academic success,” the authors wrote. “Major depressive disorder similarly affects academic success, suggesting school-based screening may be especially beneficial.”
In the past 3 years, Dr. Sekhar reported receiving funding from Pfizer through the American Academy of Pediatrics, the Penn State Clinical and Translational Science Awards Program, and a Eugene Washington Patient-Centered Outcomes Research Institute Engagement Award. Full disclosures for coauthors are available in the journal article.
This work was supported in part by the Patient-Centered Outcomes Research Institute. The use of REDCap (Research Electronic Data Capture) in this project was supported by the National Institutes of Health.
Universal screening for adolescent depression in schools, compared with the usual process of targeting students for referral after observing behaviors, resulted in significantly higher odds of identifying major depressive disorder (MDD) and of starting treatment for it, a study of more than 12,000 students suggests. Findings were published online in JAMA Network Open.
Deepa L. Sekhar, MD, MSc, with the department of pediatrics at Pennsylvania State College of Medicine in Hershey, Pa., and colleagues conducted a randomized clinical trial comparing the two screening methods from November 2018 to November 2020.
The trial included students in grades 9 through 12 enrolled at any of the 14 participating Pennsylvania public high schools. Researchers compared the two groups using mixed-effects logistic regression.
They found that adolescents in the universal screening intervention group had 5.92 times higher odds (95% confidence interval [CI], 5.07-6.93) of being identified with MDD symptoms, 3.30 times higher odds (95% CI, 2.49-4.38) of the Student Assistance Program (SAP) confirming follow-up needs, and 2.07 times higher odds (95% CI, 1.39-3.10) of starting MDD treatment.
The study comprised 12,909 students, with an average age of 16 years. Of those students, 2,687 (20.8%) were Hispanic; 2,891 (22.4%) were non-Hispanic Black, 5,842 (45.3%) were non-Hispanic White; and 1,489 (11.5%) were multiracial or of other race or ethnicity.
In the universal screening intervention (n = 6,473) all students completed the Patient Health Questionnaire–9 (PHQ-9). Students who screened positive proceeded to the Student Assistance Program. Students could receive a targeted referral to SAP if they had concerning behavior beyond the PHQ-9.
In the targeted screening group (n = 6,436), students with behaviors prompting concern for MDD were referred to the Student Assistance Program (SAP), mandated in all Pennsylvania schools. The SAP determined follow-up.
The U.S. Preventive Services Task Force (USPSTF) endorsed primary care screening in 2009 and again in 2016 for all adolescents 12-18 years old.
However, the study authors wrote, most U.S. adolescents (more than 60%) don’t have routine access to preventive health care, which limits primary care offices’ ability to properly address the growing numbers.
“[S]creening is inconsistent, with inequalities by race and ethnicity and region, and potential worsening with the COVID-19 pandemic,” they noted.
Depression rates see sharp increase
Meanwhile, the prevalence of adolescents reporting MDD symptoms has “nearly doubled in the last decade, increasing from 8.3% in 2008 to 14.4% in 2018.”
The American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and Children’s Hospital Association recently declared a national emergency in children’s mental health, citing COVID-19’s toll on top of existing challenges.
This study provides further evidence that universal screening is the better approach to identify and treat adolescent depression to save lives, Andres Pumariega, MD, a child and adolescent psychiatrist at University of Florida in Gainesville, told this news organization.
“If you catch these kids early, you can prevent suicide attempts and suicide. You can also prevent complicating costs of care,” he said.
He noted the universal screening removes the potential for bias.
“Relying purely on referral and clinical identification means a lot of kids in minority groups will not be identified and will not be treated accurately. Many clinicians have a problem identifying depression in diverse kids,” he said.
Pushback for universal screening likely
However, he said he has been part of such efforts to implement such programs in Mexico and the United States and said in the Unites States, the political climate will guarantee pushback from having schools more involved in health care and prevention. Recent controversy around COVID-19 vaccines for children illustrates the potential backlash, he said.
Parents often fight such programs as attempts to “label” their children, he said.
“If I have cancer, I sure want to be labeled. A label is used to get them help. We need to find ways to educate parents and support them in facing these issues,” he added.
One concern he has with this intervention is having the SAPs, composed largely of nonclinicians, be the triage point “instead of doing that objectively through objective criteria and by clinicians,” he said. “If we are to have a comprehensive health system where we can serve all kids and manage costs, schools need to be a major part of it.”
School settings offer the chance to see more children, collaborate with teachers and counselors, and integrate results with educational outcomes, he added.
In the study by Sekhar and colleagues, 7 of the 14 schools were classified as urban, with a median size of 370 students.
Researchers noted that the benefit of the universal screening is likely understated because of COVID-19–related school closures during the study period. The closures meant screening wasn’t completed for 7% of students.
The authors concluded that universal screening finds teens living with depression who otherwise would not be found. They said such a program likely works best in schools with strong SAP.
“Adolescents’ consistent contact with schools has been used to support physical health screenings that affect academic success,” the authors wrote. “Major depressive disorder similarly affects academic success, suggesting school-based screening may be especially beneficial.”
In the past 3 years, Dr. Sekhar reported receiving funding from Pfizer through the American Academy of Pediatrics, the Penn State Clinical and Translational Science Awards Program, and a Eugene Washington Patient-Centered Outcomes Research Institute Engagement Award. Full disclosures for coauthors are available in the journal article.
This work was supported in part by the Patient-Centered Outcomes Research Institute. The use of REDCap (Research Electronic Data Capture) in this project was supported by the National Institutes of Health.
Universal screening for adolescent depression in schools, compared with the usual process of targeting students for referral after observing behaviors, resulted in significantly higher odds of identifying major depressive disorder (MDD) and of starting treatment for it, a study of more than 12,000 students suggests. Findings were published online in JAMA Network Open.
Deepa L. Sekhar, MD, MSc, with the department of pediatrics at Pennsylvania State College of Medicine in Hershey, Pa., and colleagues conducted a randomized clinical trial comparing the two screening methods from November 2018 to November 2020.
The trial included students in grades 9 through 12 enrolled at any of the 14 participating Pennsylvania public high schools. Researchers compared the two groups using mixed-effects logistic regression.
They found that adolescents in the universal screening intervention group had 5.92 times higher odds (95% confidence interval [CI], 5.07-6.93) of being identified with MDD symptoms, 3.30 times higher odds (95% CI, 2.49-4.38) of the Student Assistance Program (SAP) confirming follow-up needs, and 2.07 times higher odds (95% CI, 1.39-3.10) of starting MDD treatment.
The study comprised 12,909 students, with an average age of 16 years. Of those students, 2,687 (20.8%) were Hispanic; 2,891 (22.4%) were non-Hispanic Black, 5,842 (45.3%) were non-Hispanic White; and 1,489 (11.5%) were multiracial or of other race or ethnicity.
In the universal screening intervention (n = 6,473) all students completed the Patient Health Questionnaire–9 (PHQ-9). Students who screened positive proceeded to the Student Assistance Program. Students could receive a targeted referral to SAP if they had concerning behavior beyond the PHQ-9.
In the targeted screening group (n = 6,436), students with behaviors prompting concern for MDD were referred to the Student Assistance Program (SAP), mandated in all Pennsylvania schools. The SAP determined follow-up.
The U.S. Preventive Services Task Force (USPSTF) endorsed primary care screening in 2009 and again in 2016 for all adolescents 12-18 years old.
However, the study authors wrote, most U.S. adolescents (more than 60%) don’t have routine access to preventive health care, which limits primary care offices’ ability to properly address the growing numbers.
“[S]creening is inconsistent, with inequalities by race and ethnicity and region, and potential worsening with the COVID-19 pandemic,” they noted.
Depression rates see sharp increase
Meanwhile, the prevalence of adolescents reporting MDD symptoms has “nearly doubled in the last decade, increasing from 8.3% in 2008 to 14.4% in 2018.”
The American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and Children’s Hospital Association recently declared a national emergency in children’s mental health, citing COVID-19’s toll on top of existing challenges.
This study provides further evidence that universal screening is the better approach to identify and treat adolescent depression to save lives, Andres Pumariega, MD, a child and adolescent psychiatrist at University of Florida in Gainesville, told this news organization.
“If you catch these kids early, you can prevent suicide attempts and suicide. You can also prevent complicating costs of care,” he said.
He noted the universal screening removes the potential for bias.
“Relying purely on referral and clinical identification means a lot of kids in minority groups will not be identified and will not be treated accurately. Many clinicians have a problem identifying depression in diverse kids,” he said.
Pushback for universal screening likely
However, he said he has been part of such efforts to implement such programs in Mexico and the United States and said in the Unites States, the political climate will guarantee pushback from having schools more involved in health care and prevention. Recent controversy around COVID-19 vaccines for children illustrates the potential backlash, he said.
Parents often fight such programs as attempts to “label” their children, he said.
“If I have cancer, I sure want to be labeled. A label is used to get them help. We need to find ways to educate parents and support them in facing these issues,” he added.
One concern he has with this intervention is having the SAPs, composed largely of nonclinicians, be the triage point “instead of doing that objectively through objective criteria and by clinicians,” he said. “If we are to have a comprehensive health system where we can serve all kids and manage costs, schools need to be a major part of it.”
School settings offer the chance to see more children, collaborate with teachers and counselors, and integrate results with educational outcomes, he added.
In the study by Sekhar and colleagues, 7 of the 14 schools were classified as urban, with a median size of 370 students.
Researchers noted that the benefit of the universal screening is likely understated because of COVID-19–related school closures during the study period. The closures meant screening wasn’t completed for 7% of students.
The authors concluded that universal screening finds teens living with depression who otherwise would not be found. They said such a program likely works best in schools with strong SAP.
“Adolescents’ consistent contact with schools has been used to support physical health screenings that affect academic success,” the authors wrote. “Major depressive disorder similarly affects academic success, suggesting school-based screening may be especially beneficial.”
In the past 3 years, Dr. Sekhar reported receiving funding from Pfizer through the American Academy of Pediatrics, the Penn State Clinical and Translational Science Awards Program, and a Eugene Washington Patient-Centered Outcomes Research Institute Engagement Award. Full disclosures for coauthors are available in the journal article.
This work was supported in part by the Patient-Centered Outcomes Research Institute. The use of REDCap (Research Electronic Data Capture) in this project was supported by the National Institutes of Health.
JAMA NETWORK OPEN
COVID-19 has brought more complex, longer office visits
Evidence of this came from the latest Primary Care Collaborative (PCC) survey, which found that primary care clinicians are seeing more complex patients requiring longer appointments in the wake of COVID-19.
The PCC with the Larry A. Green Center regularly surveys primary care clinicians. This round of questions came August 14-17 and included 1,263 respondents from 49 states, the District of Columbia, and two territories.
More than 7 in 10 (71%) respondents said their patients are more complex and nearly the same percentage said appointments are taking more time.
Ann Greiner, president and CEO of the PCC, said in an interview that 55% of respondents reported that clinicians are struggling to keep up with pent-up demand after patients have delayed or canceled care. Sixty-five percent in the survey said they had seen a rise in children’s mental health issues, and 58% said they were unsure how to help their patients with long COVID.
In addition, primary care clinicians are having repeated conversations with patients on why they should get a vaccine and which one.
“I think that’s adding to the complexity. There is a lot going on here with patient trust,” Ms. Greiner said.
‘We’re going to be playing catch-up’
Jacqueline Fincher, MD, an internist in Thompson, Ga., said in an interview that appointments have gotten longer and more complex in the wake of the pandemic – “no question.”
The immediate past president of the American College of Physicians is seeing patients with chronic disease that has gone untreated for sometimes a year or more, she said.
“Their blood pressure was not under good control, they were under more stress, their sugars were up and weren’t being followed as closely for conditions such as congestive heart failure,” she said.
Dr. Fincher, who works in a rural practice 40 miles from Augusta, Ga., with her physician husband and two other physicians, said patients are ready to come back in, “but I don’t have enough slots for them.”
She said she prioritizes what to help patients with first and schedules the next tier for the next appointment, but added, “honestly, over the next 2 years we’re going to be playing catch-up.”
At the same time, the CDC has estimated that 45% of U.S. adults are at increased risk for complications from COVID-19 because of cardiovascular disease, diabetes, respiratory disease, hypertension, or cancer. Rates ranged from 19.8% for people 18-29 years old to 80.7% for people over 80 years of age.
Long COVID could overwhelm existing health care capacity
Primary care physicians are also having to diagnose sometimes “invisible” symptoms after people have recovered from acute COVID-19 infection. Diagnosing takes intent listening to patients who describe symptoms that tests can’t confirm.
As this news organization has previously reported, half of COVID-19 survivors report postacute sequelae of COVID-19 (PASC) lasting longer than 6 months.
“These long-term PASC effects occur on a scale that could overwhelm existing health care capacity, particularly in low- and middle-income countries,” the authors wrote.
Anxiety, depression ‘have gone off the charts’
Danielle Loeb, MD, MPH, associate professor of internal medicine at the University of Colorado in Denver, who studies complexity in primary care, said in the wake of COVID-19, more patients have developed “new, serious anxiety.”
“That got extremely exacerbated during the pandemic. Anxiety and depression have gone off the charts,” said Dr. Loeb, who prefers the pronoun “they.”
Dr. Loeb cares for a large number of transgender patients. As offices reopen, some patients are having trouble reintegrating into the workplace and resuming social contacts. The primary care doctor says appointments can get longer because of the need to complete tasks, such as filling out forms for Family Medical Leave Act for those not yet ready to return to work.
COVID-19–related fears are keeping many patients from coming into the office, Dr. Loeb said, either from fear of exposure or because they have mental health issues that keep them from feeling safe leaving the house.
“That really affects my ability to care for them,” they said.
Loss of employment in the pandemic or fear of job loss and subsequent changing of insurance has complicated primary care in terms of treatment and administrative tasks, according to Dr. Loeb.
To help treat patients with acute mental health issues and manage other patients, Dr. Loeb’s practice has brought in a social worker and a therapist.
Team-based care is key in the survival of primary care practices, though providing that is difficult in the smaller clinics because of the critical mass of patients needed to make it viable, they said.
“It’s the only answer. It’s the only way you don’t drown,” Dr. Loeb added. “I’m not drowning, and I credit that to my clinic having the help to support the mental health piece of things.”
Rethinking workflow
Tricia McGinnis, MPP, MPH, executive vice president of the nonprofit Center for Health Care Strategies (CHCS) says complexity has forced rethinking workflow.
“A lot of the trends we’re seeing in primary care were there pre-COVID, but COVID has exacerbated those trends,” she said in an interview.
“The good news ... is that it was already becoming clear that primary care needed to provide basic mental health services and integrate with behavioral health. It had also become clear that effective primary care needed to address social issues that keep patients from accessing health care,” she said.
Expanding care teams, as Dr. Loeb mentioned, is a key strategy, according to Ms. McGinnis. Potential teams would include the clinical staff, but also social workers and community health workers – people who come from the community primary care is serving who can help build trust with patients and connect the patient to the primary care team.
“There’s a lot that needs to happen that the clinician doesn’t need to do,” she said.
Telehealth can be a big factor in coordinating the team, Ms. McGinnis added.
“It’s thinking less about who’s doing the work, but more about the work that needs to be done to keep people healthy. Then let’s think about the type of workers best suited to perform those tasks,” she said.
As for reimbursing more complex care, population-based, up-front capitated payments linked to high-quality care and better outcomes will need to replace fee-for-service models, according to Ms. McGinnis.
That will provide reliable incomes for primary care offices, but also flexibility in how each patient with different levels of complexity is managed, she said.
Ms. Greiner, Dr. Fincher, Dr. Loeb, and Ms. McGinnis have no relevant financial relationships.
Evidence of this came from the latest Primary Care Collaborative (PCC) survey, which found that primary care clinicians are seeing more complex patients requiring longer appointments in the wake of COVID-19.
The PCC with the Larry A. Green Center regularly surveys primary care clinicians. This round of questions came August 14-17 and included 1,263 respondents from 49 states, the District of Columbia, and two territories.
More than 7 in 10 (71%) respondents said their patients are more complex and nearly the same percentage said appointments are taking more time.
Ann Greiner, president and CEO of the PCC, said in an interview that 55% of respondents reported that clinicians are struggling to keep up with pent-up demand after patients have delayed or canceled care. Sixty-five percent in the survey said they had seen a rise in children’s mental health issues, and 58% said they were unsure how to help their patients with long COVID.
In addition, primary care clinicians are having repeated conversations with patients on why they should get a vaccine and which one.
“I think that’s adding to the complexity. There is a lot going on here with patient trust,” Ms. Greiner said.
‘We’re going to be playing catch-up’
Jacqueline Fincher, MD, an internist in Thompson, Ga., said in an interview that appointments have gotten longer and more complex in the wake of the pandemic – “no question.”
The immediate past president of the American College of Physicians is seeing patients with chronic disease that has gone untreated for sometimes a year or more, she said.
“Their blood pressure was not under good control, they were under more stress, their sugars were up and weren’t being followed as closely for conditions such as congestive heart failure,” she said.
Dr. Fincher, who works in a rural practice 40 miles from Augusta, Ga., with her physician husband and two other physicians, said patients are ready to come back in, “but I don’t have enough slots for them.”
She said she prioritizes what to help patients with first and schedules the next tier for the next appointment, but added, “honestly, over the next 2 years we’re going to be playing catch-up.”
At the same time, the CDC has estimated that 45% of U.S. adults are at increased risk for complications from COVID-19 because of cardiovascular disease, diabetes, respiratory disease, hypertension, or cancer. Rates ranged from 19.8% for people 18-29 years old to 80.7% for people over 80 years of age.
Long COVID could overwhelm existing health care capacity
Primary care physicians are also having to diagnose sometimes “invisible” symptoms after people have recovered from acute COVID-19 infection. Diagnosing takes intent listening to patients who describe symptoms that tests can’t confirm.
As this news organization has previously reported, half of COVID-19 survivors report postacute sequelae of COVID-19 (PASC) lasting longer than 6 months.
“These long-term PASC effects occur on a scale that could overwhelm existing health care capacity, particularly in low- and middle-income countries,” the authors wrote.
Anxiety, depression ‘have gone off the charts’
Danielle Loeb, MD, MPH, associate professor of internal medicine at the University of Colorado in Denver, who studies complexity in primary care, said in the wake of COVID-19, more patients have developed “new, serious anxiety.”
“That got extremely exacerbated during the pandemic. Anxiety and depression have gone off the charts,” said Dr. Loeb, who prefers the pronoun “they.”
Dr. Loeb cares for a large number of transgender patients. As offices reopen, some patients are having trouble reintegrating into the workplace and resuming social contacts. The primary care doctor says appointments can get longer because of the need to complete tasks, such as filling out forms for Family Medical Leave Act for those not yet ready to return to work.
COVID-19–related fears are keeping many patients from coming into the office, Dr. Loeb said, either from fear of exposure or because they have mental health issues that keep them from feeling safe leaving the house.
“That really affects my ability to care for them,” they said.
Loss of employment in the pandemic or fear of job loss and subsequent changing of insurance has complicated primary care in terms of treatment and administrative tasks, according to Dr. Loeb.
To help treat patients with acute mental health issues and manage other patients, Dr. Loeb’s practice has brought in a social worker and a therapist.
Team-based care is key in the survival of primary care practices, though providing that is difficult in the smaller clinics because of the critical mass of patients needed to make it viable, they said.
“It’s the only answer. It’s the only way you don’t drown,” Dr. Loeb added. “I’m not drowning, and I credit that to my clinic having the help to support the mental health piece of things.”
Rethinking workflow
Tricia McGinnis, MPP, MPH, executive vice president of the nonprofit Center for Health Care Strategies (CHCS) says complexity has forced rethinking workflow.
“A lot of the trends we’re seeing in primary care were there pre-COVID, but COVID has exacerbated those trends,” she said in an interview.
“The good news ... is that it was already becoming clear that primary care needed to provide basic mental health services and integrate with behavioral health. It had also become clear that effective primary care needed to address social issues that keep patients from accessing health care,” she said.
Expanding care teams, as Dr. Loeb mentioned, is a key strategy, according to Ms. McGinnis. Potential teams would include the clinical staff, but also social workers and community health workers – people who come from the community primary care is serving who can help build trust with patients and connect the patient to the primary care team.
“There’s a lot that needs to happen that the clinician doesn’t need to do,” she said.
Telehealth can be a big factor in coordinating the team, Ms. McGinnis added.
“It’s thinking less about who’s doing the work, but more about the work that needs to be done to keep people healthy. Then let’s think about the type of workers best suited to perform those tasks,” she said.
As for reimbursing more complex care, population-based, up-front capitated payments linked to high-quality care and better outcomes will need to replace fee-for-service models, according to Ms. McGinnis.
That will provide reliable incomes for primary care offices, but also flexibility in how each patient with different levels of complexity is managed, she said.
Ms. Greiner, Dr. Fincher, Dr. Loeb, and Ms. McGinnis have no relevant financial relationships.
Evidence of this came from the latest Primary Care Collaborative (PCC) survey, which found that primary care clinicians are seeing more complex patients requiring longer appointments in the wake of COVID-19.
The PCC with the Larry A. Green Center regularly surveys primary care clinicians. This round of questions came August 14-17 and included 1,263 respondents from 49 states, the District of Columbia, and two territories.
More than 7 in 10 (71%) respondents said their patients are more complex and nearly the same percentage said appointments are taking more time.
Ann Greiner, president and CEO of the PCC, said in an interview that 55% of respondents reported that clinicians are struggling to keep up with pent-up demand after patients have delayed or canceled care. Sixty-five percent in the survey said they had seen a rise in children’s mental health issues, and 58% said they were unsure how to help their patients with long COVID.
In addition, primary care clinicians are having repeated conversations with patients on why they should get a vaccine and which one.
“I think that’s adding to the complexity. There is a lot going on here with patient trust,” Ms. Greiner said.
‘We’re going to be playing catch-up’
Jacqueline Fincher, MD, an internist in Thompson, Ga., said in an interview that appointments have gotten longer and more complex in the wake of the pandemic – “no question.”
The immediate past president of the American College of Physicians is seeing patients with chronic disease that has gone untreated for sometimes a year or more, she said.
“Their blood pressure was not under good control, they were under more stress, their sugars were up and weren’t being followed as closely for conditions such as congestive heart failure,” she said.
Dr. Fincher, who works in a rural practice 40 miles from Augusta, Ga., with her physician husband and two other physicians, said patients are ready to come back in, “but I don’t have enough slots for them.”
She said she prioritizes what to help patients with first and schedules the next tier for the next appointment, but added, “honestly, over the next 2 years we’re going to be playing catch-up.”
At the same time, the CDC has estimated that 45% of U.S. adults are at increased risk for complications from COVID-19 because of cardiovascular disease, diabetes, respiratory disease, hypertension, or cancer. Rates ranged from 19.8% for people 18-29 years old to 80.7% for people over 80 years of age.
Long COVID could overwhelm existing health care capacity
Primary care physicians are also having to diagnose sometimes “invisible” symptoms after people have recovered from acute COVID-19 infection. Diagnosing takes intent listening to patients who describe symptoms that tests can’t confirm.
As this news organization has previously reported, half of COVID-19 survivors report postacute sequelae of COVID-19 (PASC) lasting longer than 6 months.
“These long-term PASC effects occur on a scale that could overwhelm existing health care capacity, particularly in low- and middle-income countries,” the authors wrote.
Anxiety, depression ‘have gone off the charts’
Danielle Loeb, MD, MPH, associate professor of internal medicine at the University of Colorado in Denver, who studies complexity in primary care, said in the wake of COVID-19, more patients have developed “new, serious anxiety.”
“That got extremely exacerbated during the pandemic. Anxiety and depression have gone off the charts,” said Dr. Loeb, who prefers the pronoun “they.”
Dr. Loeb cares for a large number of transgender patients. As offices reopen, some patients are having trouble reintegrating into the workplace and resuming social contacts. The primary care doctor says appointments can get longer because of the need to complete tasks, such as filling out forms for Family Medical Leave Act for those not yet ready to return to work.
COVID-19–related fears are keeping many patients from coming into the office, Dr. Loeb said, either from fear of exposure or because they have mental health issues that keep them from feeling safe leaving the house.
“That really affects my ability to care for them,” they said.
Loss of employment in the pandemic or fear of job loss and subsequent changing of insurance has complicated primary care in terms of treatment and administrative tasks, according to Dr. Loeb.
To help treat patients with acute mental health issues and manage other patients, Dr. Loeb’s practice has brought in a social worker and a therapist.
Team-based care is key in the survival of primary care practices, though providing that is difficult in the smaller clinics because of the critical mass of patients needed to make it viable, they said.
“It’s the only answer. It’s the only way you don’t drown,” Dr. Loeb added. “I’m not drowning, and I credit that to my clinic having the help to support the mental health piece of things.”
Rethinking workflow
Tricia McGinnis, MPP, MPH, executive vice president of the nonprofit Center for Health Care Strategies (CHCS) says complexity has forced rethinking workflow.
“A lot of the trends we’re seeing in primary care were there pre-COVID, but COVID has exacerbated those trends,” she said in an interview.
“The good news ... is that it was already becoming clear that primary care needed to provide basic mental health services and integrate with behavioral health. It had also become clear that effective primary care needed to address social issues that keep patients from accessing health care,” she said.
Expanding care teams, as Dr. Loeb mentioned, is a key strategy, according to Ms. McGinnis. Potential teams would include the clinical staff, but also social workers and community health workers – people who come from the community primary care is serving who can help build trust with patients and connect the patient to the primary care team.
“There’s a lot that needs to happen that the clinician doesn’t need to do,” she said.
Telehealth can be a big factor in coordinating the team, Ms. McGinnis added.
“It’s thinking less about who’s doing the work, but more about the work that needs to be done to keep people healthy. Then let’s think about the type of workers best suited to perform those tasks,” she said.
As for reimbursing more complex care, population-based, up-front capitated payments linked to high-quality care and better outcomes will need to replace fee-for-service models, according to Ms. McGinnis.
That will provide reliable incomes for primary care offices, but also flexibility in how each patient with different levels of complexity is managed, she said.
Ms. Greiner, Dr. Fincher, Dr. Loeb, and Ms. McGinnis have no relevant financial relationships.
Alopecia tied to a threefold increased risk for dementia
Alopecia areata (AA) has been linked to a significantly increased risk for dementia, new research shows.
After controlling for an array of potential confounders, investigators found a threefold higher risk of developing any form of dementia and a fourfold higher risk of developing Alzheimer’s disease (AD) in those with AA versus the controls.
“AA shares a similar inflammatory signature with dementia and has great psychological impacts that lead to poor social engagement,” lead author Cheng-Yuan Li, MD, MSc, of the department of dermatology, Taipei (Taiwan) Veterans General Hospital.
“Poor social engagement and shared inflammatory cytokines might both be important links between AA and dementia,” said Dr. Li, who is also affiliated with the School of Medicine and the Institute of Brain Science at National Yang Ming Chiao Tung University, Taipei.
The study was published online Oct. 26, 2021, in the Journal of Clinical Psychiatry (doi: 10.4088/JCP.21m13931).
Significant psychological impact
Patients with AA often experience anxiety and depression, possibly caused by the negative emotional and psychological impact of the hair loss and partial or even complete baldness associated with the disease, the authors noted.
However, AA is also associated with an array of other atopic and autoimmune diseases, including psoriasis and systemic lupus erythematosus (SLE).
Epidemiologic research has suggested a link between dementia and autoimmune diseases such as psoriasis and SLE, with some evidence suggesting that autoimmune and inflammatory mechanisms may “play a role” in the development of AD.
Dementia in general and AD in particular, “have been shown to include an inflammatory component” that may share some of the same mediators seen in AA (eg, IL-1 beta, IL-6, and tumor necrosis factor–alpha).
Moreover, “the great negative psychosocial impact of AA might result in poor social engagement, a typical risk factor for dementia,” said Dr. Li. The investigators sought to investigate whether patients with AA actually do have a higher dementia risk than individuals without AA.
The researchers used data from the Taiwan National Health Insurance Research Database, comparing 2,534 patients with AA against 25,340 controls matched for age, sex, residence, income, dementia-related comorbidities, systemic steroid use, and annual outpatient visits. Participants were enrolled between 1998 and 2011 and followed to the end of 2013.
The mean age of the cohort was 53.9 years, and a little over half (57.6%) were female. The most common comorbidity was hypertension (32.3%), followed by dyslipidemia (27%) and diabetes (15.4%).
Dual intervention
After adjusting for potential confounders, those with AA were more likely to develop dementia, AD, and unspecified dementia, compared with controls. They also had a numerically higher risk for vascular dementia, compared with controls, but it was not statistically significant.
When participants were stratified by age, investigators found a significant association between AA and higher risk for any dementia as well as unspecified dementia in individuals of all ages and an increased risk for AD in patients with dementia age at onset of 65 years and older.
The mean age of dementia diagnosis was considerably younger in patients with AA versus controls (73.4 vs. 78.9 years, P = .002). The risk for any dementia and unspecified dementia was higher in patients of both sexes, but the risk for AD was higher only in male patients.
Sensitivity analyses that excluded the first year or first 3 years of observation yielded similar and consistent findings.
“Intervention targeting poor social engagement and inflammatory cytokines may be beneficial to AA-associated dementia,” said Dr. Li.
“Physicians should be more aware of this possible association, help reduce disease discrimination among the public, and encourage more social engagement for AA patients,” he said.
“Further studies are needed to elucidate the underlying pathophysiology between AA and dementia risk,” he added.
No cause and effect
Commenting on the study, Heather M. Snyder, PhD, vice president of medical and scientific affairs, Alzheimer’s Association, said, “We continue to learn about and better understand factors that may increase or decrease a person’s risk of dementia.”
“While we know the immune system plays a role in Alzheimer’s and other dementia, we are still investigating links between, and impact of, autoimmune diseases – like alopecia areata, rheumatoid arthritis, and others – on our overall health and our brains, [which] may eventually give us important information on risk reduction strategies as well,” said Dr. Snyder, who was not involved in the research.
She cautioned that although the study did show a correlation between AA and dementia risk, this does not equate to a demonstration of cause and effect.
At present, “the message for clinicians is that when a patient comes to your office with complaints about their memory, they should, No. 1, be taken seriously; and, No. 2, receive a thorough evaluation that takes into account the many factors that may lead to cognitive decline,” Dr. Snyder said.
The study was supported by a grant from Taipei Veterans General Hospital and the Ministry of Science and Technology, Taiwan. Dr. Li, coauthors, and Dr. Snyder disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Alopecia areata (AA) has been linked to a significantly increased risk for dementia, new research shows.
After controlling for an array of potential confounders, investigators found a threefold higher risk of developing any form of dementia and a fourfold higher risk of developing Alzheimer’s disease (AD) in those with AA versus the controls.
“AA shares a similar inflammatory signature with dementia and has great psychological impacts that lead to poor social engagement,” lead author Cheng-Yuan Li, MD, MSc, of the department of dermatology, Taipei (Taiwan) Veterans General Hospital.
“Poor social engagement and shared inflammatory cytokines might both be important links between AA and dementia,” said Dr. Li, who is also affiliated with the School of Medicine and the Institute of Brain Science at National Yang Ming Chiao Tung University, Taipei.
The study was published online Oct. 26, 2021, in the Journal of Clinical Psychiatry (doi: 10.4088/JCP.21m13931).
Significant psychological impact
Patients with AA often experience anxiety and depression, possibly caused by the negative emotional and psychological impact of the hair loss and partial or even complete baldness associated with the disease, the authors noted.
However, AA is also associated with an array of other atopic and autoimmune diseases, including psoriasis and systemic lupus erythematosus (SLE).
Epidemiologic research has suggested a link between dementia and autoimmune diseases such as psoriasis and SLE, with some evidence suggesting that autoimmune and inflammatory mechanisms may “play a role” in the development of AD.
Dementia in general and AD in particular, “have been shown to include an inflammatory component” that may share some of the same mediators seen in AA (eg, IL-1 beta, IL-6, and tumor necrosis factor–alpha).
Moreover, “the great negative psychosocial impact of AA might result in poor social engagement, a typical risk factor for dementia,” said Dr. Li. The investigators sought to investigate whether patients with AA actually do have a higher dementia risk than individuals without AA.
The researchers used data from the Taiwan National Health Insurance Research Database, comparing 2,534 patients with AA against 25,340 controls matched for age, sex, residence, income, dementia-related comorbidities, systemic steroid use, and annual outpatient visits. Participants were enrolled between 1998 and 2011 and followed to the end of 2013.
The mean age of the cohort was 53.9 years, and a little over half (57.6%) were female. The most common comorbidity was hypertension (32.3%), followed by dyslipidemia (27%) and diabetes (15.4%).
Dual intervention
After adjusting for potential confounders, those with AA were more likely to develop dementia, AD, and unspecified dementia, compared with controls. They also had a numerically higher risk for vascular dementia, compared with controls, but it was not statistically significant.
When participants were stratified by age, investigators found a significant association between AA and higher risk for any dementia as well as unspecified dementia in individuals of all ages and an increased risk for AD in patients with dementia age at onset of 65 years and older.
The mean age of dementia diagnosis was considerably younger in patients with AA versus controls (73.4 vs. 78.9 years, P = .002). The risk for any dementia and unspecified dementia was higher in patients of both sexes, but the risk for AD was higher only in male patients.
Sensitivity analyses that excluded the first year or first 3 years of observation yielded similar and consistent findings.
“Intervention targeting poor social engagement and inflammatory cytokines may be beneficial to AA-associated dementia,” said Dr. Li.
“Physicians should be more aware of this possible association, help reduce disease discrimination among the public, and encourage more social engagement for AA patients,” he said.
“Further studies are needed to elucidate the underlying pathophysiology between AA and dementia risk,” he added.
No cause and effect
Commenting on the study, Heather M. Snyder, PhD, vice president of medical and scientific affairs, Alzheimer’s Association, said, “We continue to learn about and better understand factors that may increase or decrease a person’s risk of dementia.”
“While we know the immune system plays a role in Alzheimer’s and other dementia, we are still investigating links between, and impact of, autoimmune diseases – like alopecia areata, rheumatoid arthritis, and others – on our overall health and our brains, [which] may eventually give us important information on risk reduction strategies as well,” said Dr. Snyder, who was not involved in the research.
She cautioned that although the study did show a correlation between AA and dementia risk, this does not equate to a demonstration of cause and effect.
At present, “the message for clinicians is that when a patient comes to your office with complaints about their memory, they should, No. 1, be taken seriously; and, No. 2, receive a thorough evaluation that takes into account the many factors that may lead to cognitive decline,” Dr. Snyder said.
The study was supported by a grant from Taipei Veterans General Hospital and the Ministry of Science and Technology, Taiwan. Dr. Li, coauthors, and Dr. Snyder disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Alopecia areata (AA) has been linked to a significantly increased risk for dementia, new research shows.
After controlling for an array of potential confounders, investigators found a threefold higher risk of developing any form of dementia and a fourfold higher risk of developing Alzheimer’s disease (AD) in those with AA versus the controls.
“AA shares a similar inflammatory signature with dementia and has great psychological impacts that lead to poor social engagement,” lead author Cheng-Yuan Li, MD, MSc, of the department of dermatology, Taipei (Taiwan) Veterans General Hospital.
“Poor social engagement and shared inflammatory cytokines might both be important links between AA and dementia,” said Dr. Li, who is also affiliated with the School of Medicine and the Institute of Brain Science at National Yang Ming Chiao Tung University, Taipei.
The study was published online Oct. 26, 2021, in the Journal of Clinical Psychiatry (doi: 10.4088/JCP.21m13931).
Significant psychological impact
Patients with AA often experience anxiety and depression, possibly caused by the negative emotional and psychological impact of the hair loss and partial or even complete baldness associated with the disease, the authors noted.
However, AA is also associated with an array of other atopic and autoimmune diseases, including psoriasis and systemic lupus erythematosus (SLE).
Epidemiologic research has suggested a link between dementia and autoimmune diseases such as psoriasis and SLE, with some evidence suggesting that autoimmune and inflammatory mechanisms may “play a role” in the development of AD.
Dementia in general and AD in particular, “have been shown to include an inflammatory component” that may share some of the same mediators seen in AA (eg, IL-1 beta, IL-6, and tumor necrosis factor–alpha).
Moreover, “the great negative psychosocial impact of AA might result in poor social engagement, a typical risk factor for dementia,” said Dr. Li. The investigators sought to investigate whether patients with AA actually do have a higher dementia risk than individuals without AA.
The researchers used data from the Taiwan National Health Insurance Research Database, comparing 2,534 patients with AA against 25,340 controls matched for age, sex, residence, income, dementia-related comorbidities, systemic steroid use, and annual outpatient visits. Participants were enrolled between 1998 and 2011 and followed to the end of 2013.
The mean age of the cohort was 53.9 years, and a little over half (57.6%) were female. The most common comorbidity was hypertension (32.3%), followed by dyslipidemia (27%) and diabetes (15.4%).
Dual intervention
After adjusting for potential confounders, those with AA were more likely to develop dementia, AD, and unspecified dementia, compared with controls. They also had a numerically higher risk for vascular dementia, compared with controls, but it was not statistically significant.
When participants were stratified by age, investigators found a significant association between AA and higher risk for any dementia as well as unspecified dementia in individuals of all ages and an increased risk for AD in patients with dementia age at onset of 65 years and older.
The mean age of dementia diagnosis was considerably younger in patients with AA versus controls (73.4 vs. 78.9 years, P = .002). The risk for any dementia and unspecified dementia was higher in patients of both sexes, but the risk for AD was higher only in male patients.
Sensitivity analyses that excluded the first year or first 3 years of observation yielded similar and consistent findings.
“Intervention targeting poor social engagement and inflammatory cytokines may be beneficial to AA-associated dementia,” said Dr. Li.
“Physicians should be more aware of this possible association, help reduce disease discrimination among the public, and encourage more social engagement for AA patients,” he said.
“Further studies are needed to elucidate the underlying pathophysiology between AA and dementia risk,” he added.
No cause and effect
Commenting on the study, Heather M. Snyder, PhD, vice president of medical and scientific affairs, Alzheimer’s Association, said, “We continue to learn about and better understand factors that may increase or decrease a person’s risk of dementia.”
“While we know the immune system plays a role in Alzheimer’s and other dementia, we are still investigating links between, and impact of, autoimmune diseases – like alopecia areata, rheumatoid arthritis, and others – on our overall health and our brains, [which] may eventually give us important information on risk reduction strategies as well,” said Dr. Snyder, who was not involved in the research.
She cautioned that although the study did show a correlation between AA and dementia risk, this does not equate to a demonstration of cause and effect.
At present, “the message for clinicians is that when a patient comes to your office with complaints about their memory, they should, No. 1, be taken seriously; and, No. 2, receive a thorough evaluation that takes into account the many factors that may lead to cognitive decline,” Dr. Snyder said.
The study was supported by a grant from Taipei Veterans General Hospital and the Ministry of Science and Technology, Taiwan. Dr. Li, coauthors, and Dr. Snyder disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
City or country life? Genetic risk for mental illness may decide
Individuals with a genetic predisposition to schizophrenia, bipolar disorder (BD), autism spectrum disorder (ASD), or anorexia nervosa (AN) are significantly more likely to move from a rural to an urban setting, whereas those at high genetic risk for attention-deficit/hyperactivity disorder were more likely to do the opposite.
The findings held even in those at high genetic risk who had never been diagnosed with a psychiatric disorder, highlighting a genetic factor that previous research linking urban living to mental illness has not explored.
“It’s not as simple as saying that urban environment is responsible for schizophrenia and everyone should move out of urban environments and they will be safe,” study investigator Evangelos Vassos, MD, PhD, senior clinical research fellow at King’s College London, and a consulting psychiatrist, said in an interview. “If you are genetically predisposed to schizophrenia, you will still be predisposed to schizophrenia even if you move.”
The study was published online in JAMA Psychiatry.
Genetic influence
The study results don’t rule out environmental influence, but offer evidence that the migration pattern researchers have tracked for years may have a multifactorial explanation.
“Our research shows that, at some level, an individual’s genes select their environment and that the relationship between environmental and genetic influences on mental health is interrelated,” Jessye Maxwell, MSc, lead author and a PhD candidate in psychiatry at King’s College, said in a statement. “This overlap needs to be considered when developing models to predict the risk of people developing mental health conditions in the future.”
For the study, the investigators calculated polygenic risk scores (PRS) of different psychiatric illnesses for 385,793 U.K. Biobank participants aged 37-73. PRS analyzes genetic information across a person’s entire genome, rather than by individual genes.
They used address history and U.K. census records from 1931 to 2011 to map population density over time.
PRS analyses showed significant associations with higher population density throughout adulthood, reaching highest significance between age 45 and 55 years for schizophrenia (88 people/km2; 95% confidence interval, 65-98 people/km2), BD (44 people/km2; 95%CI, 34-54 people/km2), AN (36 people/km2; 95%CI, 22-50 people/km2), and ASD (35 people/km2; 95%CI, 25-45 people/km2).
When they compared those who were born and stayed in rural or suburban areas to their counterparts who moved from those areas to cities, they found the odds of moving to urban areas ranged from 5% among people at high genetic risk for schizophrenia to 13% of those with a high risk for BD. Only people at high risk for ADHD were more likely to move to rural areas.
However, the study is not without its limitations. Only people of European descent were included, family medical history was unavailable for some participants, and only about 50,000 people had a lifetime diagnosis of mental illness, which is not representative of the general population.
‘Convincing evidence’
Still, the research adds another piece of the puzzle scientists seek to solve about where people live and mental illness risk, said Jordan DeVylder, PhD, associate professor of social work at Fordham University, New York, who commented on the study for this news organization.
Dr. DeVylder, who has also published research on the topic but was not part of the current study, noted that urban living has long been thought to be among the most consistent environmental risk factors for psychosis. However, he noted, “this association can also be explained by genetic selection, in which the same genes that predispose one to schizophrenia also predispose one to choose urban living.”
“This study presents the most convincing evidence to date that genetics have a major role in this association, at least in the countries where this association between urban living and psychosis exists,” he said.
The study was funded by National Institute for Health Research, Biomedical Research Centre at South London and Maudsley National Health Service Foundation Trust and King’s College London. The authors and Dr. DeVylder have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Individuals with a genetic predisposition to schizophrenia, bipolar disorder (BD), autism spectrum disorder (ASD), or anorexia nervosa (AN) are significantly more likely to move from a rural to an urban setting, whereas those at high genetic risk for attention-deficit/hyperactivity disorder were more likely to do the opposite.
The findings held even in those at high genetic risk who had never been diagnosed with a psychiatric disorder, highlighting a genetic factor that previous research linking urban living to mental illness has not explored.
“It’s not as simple as saying that urban environment is responsible for schizophrenia and everyone should move out of urban environments and they will be safe,” study investigator Evangelos Vassos, MD, PhD, senior clinical research fellow at King’s College London, and a consulting psychiatrist, said in an interview. “If you are genetically predisposed to schizophrenia, you will still be predisposed to schizophrenia even if you move.”
The study was published online in JAMA Psychiatry.
Genetic influence
The study results don’t rule out environmental influence, but offer evidence that the migration pattern researchers have tracked for years may have a multifactorial explanation.
“Our research shows that, at some level, an individual’s genes select their environment and that the relationship between environmental and genetic influences on mental health is interrelated,” Jessye Maxwell, MSc, lead author and a PhD candidate in psychiatry at King’s College, said in a statement. “This overlap needs to be considered when developing models to predict the risk of people developing mental health conditions in the future.”
For the study, the investigators calculated polygenic risk scores (PRS) of different psychiatric illnesses for 385,793 U.K. Biobank participants aged 37-73. PRS analyzes genetic information across a person’s entire genome, rather than by individual genes.
They used address history and U.K. census records from 1931 to 2011 to map population density over time.
PRS analyses showed significant associations with higher population density throughout adulthood, reaching highest significance between age 45 and 55 years for schizophrenia (88 people/km2; 95% confidence interval, 65-98 people/km2), BD (44 people/km2; 95%CI, 34-54 people/km2), AN (36 people/km2; 95%CI, 22-50 people/km2), and ASD (35 people/km2; 95%CI, 25-45 people/km2).
When they compared those who were born and stayed in rural or suburban areas to their counterparts who moved from those areas to cities, they found the odds of moving to urban areas ranged from 5% among people at high genetic risk for schizophrenia to 13% of those with a high risk for BD. Only people at high risk for ADHD were more likely to move to rural areas.
However, the study is not without its limitations. Only people of European descent were included, family medical history was unavailable for some participants, and only about 50,000 people had a lifetime diagnosis of mental illness, which is not representative of the general population.
‘Convincing evidence’
Still, the research adds another piece of the puzzle scientists seek to solve about where people live and mental illness risk, said Jordan DeVylder, PhD, associate professor of social work at Fordham University, New York, who commented on the study for this news organization.
Dr. DeVylder, who has also published research on the topic but was not part of the current study, noted that urban living has long been thought to be among the most consistent environmental risk factors for psychosis. However, he noted, “this association can also be explained by genetic selection, in which the same genes that predispose one to schizophrenia also predispose one to choose urban living.”
“This study presents the most convincing evidence to date that genetics have a major role in this association, at least in the countries where this association between urban living and psychosis exists,” he said.
The study was funded by National Institute for Health Research, Biomedical Research Centre at South London and Maudsley National Health Service Foundation Trust and King’s College London. The authors and Dr. DeVylder have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Individuals with a genetic predisposition to schizophrenia, bipolar disorder (BD), autism spectrum disorder (ASD), or anorexia nervosa (AN) are significantly more likely to move from a rural to an urban setting, whereas those at high genetic risk for attention-deficit/hyperactivity disorder were more likely to do the opposite.
The findings held even in those at high genetic risk who had never been diagnosed with a psychiatric disorder, highlighting a genetic factor that previous research linking urban living to mental illness has not explored.
“It’s not as simple as saying that urban environment is responsible for schizophrenia and everyone should move out of urban environments and they will be safe,” study investigator Evangelos Vassos, MD, PhD, senior clinical research fellow at King’s College London, and a consulting psychiatrist, said in an interview. “If you are genetically predisposed to schizophrenia, you will still be predisposed to schizophrenia even if you move.”
The study was published online in JAMA Psychiatry.
Genetic influence
The study results don’t rule out environmental influence, but offer evidence that the migration pattern researchers have tracked for years may have a multifactorial explanation.
“Our research shows that, at some level, an individual’s genes select their environment and that the relationship between environmental and genetic influences on mental health is interrelated,” Jessye Maxwell, MSc, lead author and a PhD candidate in psychiatry at King’s College, said in a statement. “This overlap needs to be considered when developing models to predict the risk of people developing mental health conditions in the future.”
For the study, the investigators calculated polygenic risk scores (PRS) of different psychiatric illnesses for 385,793 U.K. Biobank participants aged 37-73. PRS analyzes genetic information across a person’s entire genome, rather than by individual genes.
They used address history and U.K. census records from 1931 to 2011 to map population density over time.
PRS analyses showed significant associations with higher population density throughout adulthood, reaching highest significance between age 45 and 55 years for schizophrenia (88 people/km2; 95% confidence interval, 65-98 people/km2), BD (44 people/km2; 95%CI, 34-54 people/km2), AN (36 people/km2; 95%CI, 22-50 people/km2), and ASD (35 people/km2; 95%CI, 25-45 people/km2).
When they compared those who were born and stayed in rural or suburban areas to their counterparts who moved from those areas to cities, they found the odds of moving to urban areas ranged from 5% among people at high genetic risk for schizophrenia to 13% of those with a high risk for BD. Only people at high risk for ADHD were more likely to move to rural areas.
However, the study is not without its limitations. Only people of European descent were included, family medical history was unavailable for some participants, and only about 50,000 people had a lifetime diagnosis of mental illness, which is not representative of the general population.
‘Convincing evidence’
Still, the research adds another piece of the puzzle scientists seek to solve about where people live and mental illness risk, said Jordan DeVylder, PhD, associate professor of social work at Fordham University, New York, who commented on the study for this news organization.
Dr. DeVylder, who has also published research on the topic but was not part of the current study, noted that urban living has long been thought to be among the most consistent environmental risk factors for psychosis. However, he noted, “this association can also be explained by genetic selection, in which the same genes that predispose one to schizophrenia also predispose one to choose urban living.”
“This study presents the most convincing evidence to date that genetics have a major role in this association, at least in the countries where this association between urban living and psychosis exists,” he said.
The study was funded by National Institute for Health Research, Biomedical Research Centre at South London and Maudsley National Health Service Foundation Trust and King’s College London. The authors and Dr. DeVylder have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Resident doctor who attempted suicide three times fights for change
In early 2020, Justin Bullock, MD, MPH, did what few, if any, resident physicians have done: He published an honest account in the New England Journal of Medicine of a would-be suicide attempt during medical training.
In the article, Dr. Bullock matter-of-factly laid out how, in 2019, intern-year night shifts contributed to a depressive episode. For Dr. Bullock, who has a bipolar disorder, sleep dysregulation can be deadly. He had a plan for completing suicide, and this wouldn’t have been his first attempt. Thanks to his history and openness about his condition, Dr. Bullock had an experienced care team that helped him get to a psychiatric hospital before anything happened. While there for around 5 days, he wrote the bulk of the NEJM article.
The article took Dr. Bullock’s impact nationwide. On Twitter and in interviews, Dr. Bullock is an unapologetic advocate for accommodations for people in medicine with mental illness. “One of the things that inspired me to speak out early on is that I feel I stand in a place of so much privilege,” Dr. Bullock told this news organization. “I often feel this sense of ... ‘you have to speak up, Justin; no one else can.’ ”
Dr. Bullock’s activism is especially noteworthy, given that he is still establishing his career. In August, while an internal medicine resident at the University of California, San Francisco, he received a lifetime teaching award from UCSF because he had received three prior teaching awards; a recognition like this is considered rare someone so early in their career. Now in his final year of residency, he actively researches medical education, advocates for mental health support, and is working to become a leading voice on related issues.
“It seems to be working,” his older sister, Jacquis Mahoney, RN, said during a visit to the UCSF campus. Instead of any awkwardness, everyone is thrilled to learn that she is Justin’s sister. “There’s a lot of pride and excitement.”
Suicide attempts during medical training
Now 28, Dr. Bullock grew up in Detroit, with his mom and two older sisters. His father was incarcerated for much of Dr. Bullock’s childhood, in part because of his own bipolar disorder not being well controlled, Dr. Bullock said.
When he was younger, Dr. Bullock was the peacekeeper in the house between his two sisters, said Ms. Mahoney: “Justin was always very delicate and kind.”
He played soccer and ran track but also loved math and science. While outwardly accumulating an impressive resume, Dr. Bullock was internally struggling. In high school, he made what he now calls an “immature” attempt at suicide after coming out as gay to his family. While Dr. Bullock said he doesn’t necessarily dwell on the discrimination he has faced as a gay, Black man, his awareness of how others perceive and treat him because of his identity increases the background stress present in his daily life.
After high school, Dr. Bullock went to MIT in Boston, where he continued running and studied chemical-biological engineering. During college, Dr. Bullock thought he was going to have to withdraw from MIT because of his depression. Thankfully, he received counseling from student services and advice from a track coach who sat him down and talked about pragmatic solutions, like medication. “That was life-changing,” said Dr. Bullock.
When trying to decide between engineering and medicine, Dr. Bullock realized he preferred contemplating medical problems to engineering ones. So he applied to medical school. Dr. Bullock eventually ended up at UCSF, where he was selected to participate in the Program in Medical Education for the Urban Underserved, a 5-year track at the college for students committed to working with underserved communities.
By the time Dr. Bullock got to medical school, he was feeling good. In consultation with his psychiatrist, he thought it worthwhile to take a break from his medications. At that time, his diagnosis was major depressive disorder and he had only had one serious depressive episode, which didn’t necessarily indicate that he would need medication long-term, he said.
Dr. Bullock loved everything about medical school. “One day when I was in my first year of med school, I called my mom and said: ‘It’s like science summer camp but every day!’” he recalled.
Despite his enthusiasm, though, he began feeling something troubling. Recognizing the symptoms of early depression, Dr. Bullock restarted his medication. But this time, the same SSRI only made things worse. He went from sleeping 8 hours to 90 minutes a night. He felt angry. One day, he went on a furious 22-mile run. Plus, within the first 6 months of moving to San Francisco, Dr. Bullock was stopped by the police three different times while riding his bike. He attributes this to his race, which has only further added to his stress. In September 2015, during his second year of medical school, Dr. Bullock attempted suicide again. This time, he was intubated in the ED and rushed to the ICU.
He was given a new diagnosis: bipolar disorder. He changed medications and lived for a time with Ms. Mahoney and his other sister, who moved from Chicago to California to be with him. “My family has helped me a lot,” he said.
Dr. Bullock was initially not sure whether he would be able to return to school after his attempted suicide. Overall, UCSF was extremely supportive, he said. That came as a relief. Medical school was a grounding force in his life, not a destabilizing one: “If I had been pushed out, it would have been really harmful to me.”
Then Dr. Bullock started residency. The sleep disruption that comes with the night shift – the resident rite of passage – triggered another episode. At first, Dr. Bullock was overly productive; his mind was active and alert after staying up all night. He worked on new research during the day instead of sleeping.
Sleep disturbance is a hallmark symptom of bipolar disorder. “Justin should never be on a 24-hour call,” said Lisa Meeks, PhD, associate professor of psychiatry and family medicine at the University of Colorado at Denver, Aurora, and a leading scholar on disability advocacy for medical trainees. When he started residency, Dr. Bullock was open with his program director about his diagnosis and sought accommodations to go to therapy each week. But he didn’t try to get out of night shifts or 24-hour calls, despite his care team urging him to do so. “I have this sense of wanting to tough it out,” he said. He also felt guilty making his peers take on his share of those challenging shifts.
In December 2019, Dr. Bullock was voluntarily hospitalized for a few days and started writing the article that would later appear in NEJM. In January, a friend and UCSF medical student completed suicide. In March, the same month his NEJM article came out, Dr. Bullock attempted suicide again. This time, he quickly recognized that he was making a mistake and called an ambulance. “For me, as far as suicide attempts go, it’s the most positive one.”
Advocating for changes in medical training
Throughout his medical training, Dr. Bullock was always open about his struggles with his peers and with the administration. He shared his suicidal thoughts at a Mental Illness Among Us event during medical school. His story resonated with peers who were surprised that Dr. Bullock, who was thriving academically, could be struggling emotionally.
During residency, he led small group discussions and gave lectures at the medical school, including a talk about his attempts to create institutional change at UCSF, such as his public fight against the college’s Fitness for Duty (FFD) assessment process. That discussion earned him an Outstanding Lecturer award. Because it was the third award he had received from the medical school, Dr. Bullock also automatically earned a lifetime teaching award. When he told his mom, a teacher herself, about the award, she joked: “Are you old enough for ‘lifetime’ anything?”
Dr. Bullock has also spoken out and actively fought against the processes within the medical community that prevent people from coming forward until it is too late. Physicians and trainees often fear that if they seek mental health treatment, they will have to disclose that treatment to a potential employer or licensing board and then be barred from practicing medicine. Because he has been open about his mental health for so long, Dr. Bullock feels that he is in a position to push back against these norms. For example, in June he coauthored another article, this time for the Journal of Hospital Medicine, describing the traumatizing FFD assessment that followed his March 2020 suicide attempt.
In that article, Dr. Bullock wrote how no mental health professional served on the UCSF Physician Well Being Committee – comprising physicians and lawyers who evaluate physician impairment or potential physician impairment – that evaluated him. Dr. Bullock was referred to an outside psychiatrist. He also describes how he was forced to release all of his psychiatric records and undergo extensive drug testing, despite having no history of substance abuse. To return to work, he had to sign a contract, agreeing to be monitored and to attend a specific kind of therapy.
While steps like these can, in the right circumstances, protect both the public and doctors-in-training in important ways, they can also “be very punitive and isolating for someone going through a mental health crisis,” said Dr. Meeks. There were also no Black physicians or lawyers on the committee evaluating Dr. Bullock. “That was really egregious, when you look back.” Dr. Meeks is a coauthor on Dr. Bullock’s JHM article and a mentor and previous student disability officer at UCSF.
Dr. Bullock raised objections to UCSF administrators about how he felt that the committee was discriminating against him because of his mental illness despite assurances from the director of his program that there have never been any performance or professionalism concerns with him. He said the administrators told him he was the first person to question the FFD process. This isn’t surprising, given that all the power in such situations usually lies with the hospital and the administrators, whereas the resident or physician is worried about losing their job and their license, said Dr. Meeks.
Dr. Bullock contends that he’s in a unique position to speak out, considering his stellar academic and work records, openness about his mental illness before a crisis, access to quality mental health care, and extensive personal network among the UCSF administration. “I know that I hold power within my institution; I spoke out because I could,” Dr. Bullock said. In addition to writing an article about his experience, Dr. Bullock shared his story with a task force appointed by the medical staff president to review the Physician Well-Being Committee and the overall FFD process. Even before Dr. Bullock shared his story with the public, the task force had already been appointed as a result of the increased concern about physician mental health during the ongoing COVID-19 pandemic, Michelle Guy, MD, clinical professor of medicine at UCSF, told this news organization.
Elizabeth Fernandez, a UCSF senior public information representative, declined to comment on Dr. Bullock’s specific experience as reported in the JHM. “As with every hospital accredited by the Joint Commission, UCSF Medical Center has a Physician Well Being Committee that provides resources for physicians who may need help with chemical dependency or mental illness,” Ms. Fernandez said.
“Our goal through this program is always, first, to provide the compassion and assistance our physicians need to address the issues they face and continue to pursue their careers. This program is entirely voluntary and is bound by federal and state laws and regulations to protect the confidentiality of its participants, while ensuring that – first and foremost – no one is harmed by the situation, including the participant.”
Overcoming stigma to change the system
All of the attention – from national media outlets such as Vox to struggling peers and others – is fulfilling, Dr. Bullock said. But it can also be overwhelming. “I have definitely been praised as ‘Black excellence,’ and that definitely has added to the pressure to keep going ... to keep pushing at times,” he said.
Ms. Mahoney added: “He’s willing to sacrifice himself in order to make a difference. He would be a sacrificial lamb” for the Black community, the gay community, or any minority community.
Despite these concerns and his past suicide attempts, colleagues feel that Dr. Bullock is in a strong place to make decisions. “I trust Justin to put the boundaries up when they are needed and to engage in a way that feels comfortable for him,” said Ms. Meeks. “He is someone who has incredible self-awareness.”
Dr. Bullock’s history isn’t just something he overcame: It’s something that makes him a better, more empathetic doctor, said Ms. Mahoney. He knows what it’s like to be hospitalized, to deal with the frustration of insurance, to navigate the complexity of the health care system as a patient, or to be facing a deep internal darkness. He “can genuinely hold that person’s hand and say: ‘I know what you’re going through and we’re going to work through this day by day,’ ” she said. “That is something he can bring that no other physician can bring.”
In his advocacy on Twitter, in lectures, and in conversations with UCSF administrators, Dr. Bullock is pushing for board licensing questions to be reformed so physicians are no longer penalized for seeking mental health treatment. He would also like residency programs to make it easier and less stigmatizing for trainees to receive accommodations for a disability or mental illness.
“They say one person can’t change a system,” said Dr. Meeks, “but I do think Justin is calling an awful lot of attention to the system and I do think there will be changes because of his advocacy.”
A version of this article first appeared on Medscape.com.
In early 2020, Justin Bullock, MD, MPH, did what few, if any, resident physicians have done: He published an honest account in the New England Journal of Medicine of a would-be suicide attempt during medical training.
In the article, Dr. Bullock matter-of-factly laid out how, in 2019, intern-year night shifts contributed to a depressive episode. For Dr. Bullock, who has a bipolar disorder, sleep dysregulation can be deadly. He had a plan for completing suicide, and this wouldn’t have been his first attempt. Thanks to his history and openness about his condition, Dr. Bullock had an experienced care team that helped him get to a psychiatric hospital before anything happened. While there for around 5 days, he wrote the bulk of the NEJM article.
The article took Dr. Bullock’s impact nationwide. On Twitter and in interviews, Dr. Bullock is an unapologetic advocate for accommodations for people in medicine with mental illness. “One of the things that inspired me to speak out early on is that I feel I stand in a place of so much privilege,” Dr. Bullock told this news organization. “I often feel this sense of ... ‘you have to speak up, Justin; no one else can.’ ”
Dr. Bullock’s activism is especially noteworthy, given that he is still establishing his career. In August, while an internal medicine resident at the University of California, San Francisco, he received a lifetime teaching award from UCSF because he had received three prior teaching awards; a recognition like this is considered rare someone so early in their career. Now in his final year of residency, he actively researches medical education, advocates for mental health support, and is working to become a leading voice on related issues.
“It seems to be working,” his older sister, Jacquis Mahoney, RN, said during a visit to the UCSF campus. Instead of any awkwardness, everyone is thrilled to learn that she is Justin’s sister. “There’s a lot of pride and excitement.”
Suicide attempts during medical training
Now 28, Dr. Bullock grew up in Detroit, with his mom and two older sisters. His father was incarcerated for much of Dr. Bullock’s childhood, in part because of his own bipolar disorder not being well controlled, Dr. Bullock said.
When he was younger, Dr. Bullock was the peacekeeper in the house between his two sisters, said Ms. Mahoney: “Justin was always very delicate and kind.”
He played soccer and ran track but also loved math and science. While outwardly accumulating an impressive resume, Dr. Bullock was internally struggling. In high school, he made what he now calls an “immature” attempt at suicide after coming out as gay to his family. While Dr. Bullock said he doesn’t necessarily dwell on the discrimination he has faced as a gay, Black man, his awareness of how others perceive and treat him because of his identity increases the background stress present in his daily life.
After high school, Dr. Bullock went to MIT in Boston, where he continued running and studied chemical-biological engineering. During college, Dr. Bullock thought he was going to have to withdraw from MIT because of his depression. Thankfully, he received counseling from student services and advice from a track coach who sat him down and talked about pragmatic solutions, like medication. “That was life-changing,” said Dr. Bullock.
When trying to decide between engineering and medicine, Dr. Bullock realized he preferred contemplating medical problems to engineering ones. So he applied to medical school. Dr. Bullock eventually ended up at UCSF, where he was selected to participate in the Program in Medical Education for the Urban Underserved, a 5-year track at the college for students committed to working with underserved communities.
By the time Dr. Bullock got to medical school, he was feeling good. In consultation with his psychiatrist, he thought it worthwhile to take a break from his medications. At that time, his diagnosis was major depressive disorder and he had only had one serious depressive episode, which didn’t necessarily indicate that he would need medication long-term, he said.
Dr. Bullock loved everything about medical school. “One day when I was in my first year of med school, I called my mom and said: ‘It’s like science summer camp but every day!’” he recalled.
Despite his enthusiasm, though, he began feeling something troubling. Recognizing the symptoms of early depression, Dr. Bullock restarted his medication. But this time, the same SSRI only made things worse. He went from sleeping 8 hours to 90 minutes a night. He felt angry. One day, he went on a furious 22-mile run. Plus, within the first 6 months of moving to San Francisco, Dr. Bullock was stopped by the police three different times while riding his bike. He attributes this to his race, which has only further added to his stress. In September 2015, during his second year of medical school, Dr. Bullock attempted suicide again. This time, he was intubated in the ED and rushed to the ICU.
He was given a new diagnosis: bipolar disorder. He changed medications and lived for a time with Ms. Mahoney and his other sister, who moved from Chicago to California to be with him. “My family has helped me a lot,” he said.
Dr. Bullock was initially not sure whether he would be able to return to school after his attempted suicide. Overall, UCSF was extremely supportive, he said. That came as a relief. Medical school was a grounding force in his life, not a destabilizing one: “If I had been pushed out, it would have been really harmful to me.”
Then Dr. Bullock started residency. The sleep disruption that comes with the night shift – the resident rite of passage – triggered another episode. At first, Dr. Bullock was overly productive; his mind was active and alert after staying up all night. He worked on new research during the day instead of sleeping.
Sleep disturbance is a hallmark symptom of bipolar disorder. “Justin should never be on a 24-hour call,” said Lisa Meeks, PhD, associate professor of psychiatry and family medicine at the University of Colorado at Denver, Aurora, and a leading scholar on disability advocacy for medical trainees. When he started residency, Dr. Bullock was open with his program director about his diagnosis and sought accommodations to go to therapy each week. But he didn’t try to get out of night shifts or 24-hour calls, despite his care team urging him to do so. “I have this sense of wanting to tough it out,” he said. He also felt guilty making his peers take on his share of those challenging shifts.
In December 2019, Dr. Bullock was voluntarily hospitalized for a few days and started writing the article that would later appear in NEJM. In January, a friend and UCSF medical student completed suicide. In March, the same month his NEJM article came out, Dr. Bullock attempted suicide again. This time, he quickly recognized that he was making a mistake and called an ambulance. “For me, as far as suicide attempts go, it’s the most positive one.”
Advocating for changes in medical training
Throughout his medical training, Dr. Bullock was always open about his struggles with his peers and with the administration. He shared his suicidal thoughts at a Mental Illness Among Us event during medical school. His story resonated with peers who were surprised that Dr. Bullock, who was thriving academically, could be struggling emotionally.
During residency, he led small group discussions and gave lectures at the medical school, including a talk about his attempts to create institutional change at UCSF, such as his public fight against the college’s Fitness for Duty (FFD) assessment process. That discussion earned him an Outstanding Lecturer award. Because it was the third award he had received from the medical school, Dr. Bullock also automatically earned a lifetime teaching award. When he told his mom, a teacher herself, about the award, she joked: “Are you old enough for ‘lifetime’ anything?”
Dr. Bullock has also spoken out and actively fought against the processes within the medical community that prevent people from coming forward until it is too late. Physicians and trainees often fear that if they seek mental health treatment, they will have to disclose that treatment to a potential employer or licensing board and then be barred from practicing medicine. Because he has been open about his mental health for so long, Dr. Bullock feels that he is in a position to push back against these norms. For example, in June he coauthored another article, this time for the Journal of Hospital Medicine, describing the traumatizing FFD assessment that followed his March 2020 suicide attempt.
In that article, Dr. Bullock wrote how no mental health professional served on the UCSF Physician Well Being Committee – comprising physicians and lawyers who evaluate physician impairment or potential physician impairment – that evaluated him. Dr. Bullock was referred to an outside psychiatrist. He also describes how he was forced to release all of his psychiatric records and undergo extensive drug testing, despite having no history of substance abuse. To return to work, he had to sign a contract, agreeing to be monitored and to attend a specific kind of therapy.
While steps like these can, in the right circumstances, protect both the public and doctors-in-training in important ways, they can also “be very punitive and isolating for someone going through a mental health crisis,” said Dr. Meeks. There were also no Black physicians or lawyers on the committee evaluating Dr. Bullock. “That was really egregious, when you look back.” Dr. Meeks is a coauthor on Dr. Bullock’s JHM article and a mentor and previous student disability officer at UCSF.
Dr. Bullock raised objections to UCSF administrators about how he felt that the committee was discriminating against him because of his mental illness despite assurances from the director of his program that there have never been any performance or professionalism concerns with him. He said the administrators told him he was the first person to question the FFD process. This isn’t surprising, given that all the power in such situations usually lies with the hospital and the administrators, whereas the resident or physician is worried about losing their job and their license, said Dr. Meeks.
Dr. Bullock contends that he’s in a unique position to speak out, considering his stellar academic and work records, openness about his mental illness before a crisis, access to quality mental health care, and extensive personal network among the UCSF administration. “I know that I hold power within my institution; I spoke out because I could,” Dr. Bullock said. In addition to writing an article about his experience, Dr. Bullock shared his story with a task force appointed by the medical staff president to review the Physician Well-Being Committee and the overall FFD process. Even before Dr. Bullock shared his story with the public, the task force had already been appointed as a result of the increased concern about physician mental health during the ongoing COVID-19 pandemic, Michelle Guy, MD, clinical professor of medicine at UCSF, told this news organization.
Elizabeth Fernandez, a UCSF senior public information representative, declined to comment on Dr. Bullock’s specific experience as reported in the JHM. “As with every hospital accredited by the Joint Commission, UCSF Medical Center has a Physician Well Being Committee that provides resources for physicians who may need help with chemical dependency or mental illness,” Ms. Fernandez said.
“Our goal through this program is always, first, to provide the compassion and assistance our physicians need to address the issues they face and continue to pursue their careers. This program is entirely voluntary and is bound by federal and state laws and regulations to protect the confidentiality of its participants, while ensuring that – first and foremost – no one is harmed by the situation, including the participant.”
Overcoming stigma to change the system
All of the attention – from national media outlets such as Vox to struggling peers and others – is fulfilling, Dr. Bullock said. But it can also be overwhelming. “I have definitely been praised as ‘Black excellence,’ and that definitely has added to the pressure to keep going ... to keep pushing at times,” he said.
Ms. Mahoney added: “He’s willing to sacrifice himself in order to make a difference. He would be a sacrificial lamb” for the Black community, the gay community, or any minority community.
Despite these concerns and his past suicide attempts, colleagues feel that Dr. Bullock is in a strong place to make decisions. “I trust Justin to put the boundaries up when they are needed and to engage in a way that feels comfortable for him,” said Ms. Meeks. “He is someone who has incredible self-awareness.”
Dr. Bullock’s history isn’t just something he overcame: It’s something that makes him a better, more empathetic doctor, said Ms. Mahoney. He knows what it’s like to be hospitalized, to deal with the frustration of insurance, to navigate the complexity of the health care system as a patient, or to be facing a deep internal darkness. He “can genuinely hold that person’s hand and say: ‘I know what you’re going through and we’re going to work through this day by day,’ ” she said. “That is something he can bring that no other physician can bring.”
In his advocacy on Twitter, in lectures, and in conversations with UCSF administrators, Dr. Bullock is pushing for board licensing questions to be reformed so physicians are no longer penalized for seeking mental health treatment. He would also like residency programs to make it easier and less stigmatizing for trainees to receive accommodations for a disability or mental illness.
“They say one person can’t change a system,” said Dr. Meeks, “but I do think Justin is calling an awful lot of attention to the system and I do think there will be changes because of his advocacy.”
A version of this article first appeared on Medscape.com.
In early 2020, Justin Bullock, MD, MPH, did what few, if any, resident physicians have done: He published an honest account in the New England Journal of Medicine of a would-be suicide attempt during medical training.
In the article, Dr. Bullock matter-of-factly laid out how, in 2019, intern-year night shifts contributed to a depressive episode. For Dr. Bullock, who has a bipolar disorder, sleep dysregulation can be deadly. He had a plan for completing suicide, and this wouldn’t have been his first attempt. Thanks to his history and openness about his condition, Dr. Bullock had an experienced care team that helped him get to a psychiatric hospital before anything happened. While there for around 5 days, he wrote the bulk of the NEJM article.
The article took Dr. Bullock’s impact nationwide. On Twitter and in interviews, Dr. Bullock is an unapologetic advocate for accommodations for people in medicine with mental illness. “One of the things that inspired me to speak out early on is that I feel I stand in a place of so much privilege,” Dr. Bullock told this news organization. “I often feel this sense of ... ‘you have to speak up, Justin; no one else can.’ ”
Dr. Bullock’s activism is especially noteworthy, given that he is still establishing his career. In August, while an internal medicine resident at the University of California, San Francisco, he received a lifetime teaching award from UCSF because he had received three prior teaching awards; a recognition like this is considered rare someone so early in their career. Now in his final year of residency, he actively researches medical education, advocates for mental health support, and is working to become a leading voice on related issues.
“It seems to be working,” his older sister, Jacquis Mahoney, RN, said during a visit to the UCSF campus. Instead of any awkwardness, everyone is thrilled to learn that she is Justin’s sister. “There’s a lot of pride and excitement.”
Suicide attempts during medical training
Now 28, Dr. Bullock grew up in Detroit, with his mom and two older sisters. His father was incarcerated for much of Dr. Bullock’s childhood, in part because of his own bipolar disorder not being well controlled, Dr. Bullock said.
When he was younger, Dr. Bullock was the peacekeeper in the house between his two sisters, said Ms. Mahoney: “Justin was always very delicate and kind.”
He played soccer and ran track but also loved math and science. While outwardly accumulating an impressive resume, Dr. Bullock was internally struggling. In high school, he made what he now calls an “immature” attempt at suicide after coming out as gay to his family. While Dr. Bullock said he doesn’t necessarily dwell on the discrimination he has faced as a gay, Black man, his awareness of how others perceive and treat him because of his identity increases the background stress present in his daily life.
After high school, Dr. Bullock went to MIT in Boston, where he continued running and studied chemical-biological engineering. During college, Dr. Bullock thought he was going to have to withdraw from MIT because of his depression. Thankfully, he received counseling from student services and advice from a track coach who sat him down and talked about pragmatic solutions, like medication. “That was life-changing,” said Dr. Bullock.
When trying to decide between engineering and medicine, Dr. Bullock realized he preferred contemplating medical problems to engineering ones. So he applied to medical school. Dr. Bullock eventually ended up at UCSF, where he was selected to participate in the Program in Medical Education for the Urban Underserved, a 5-year track at the college for students committed to working with underserved communities.
By the time Dr. Bullock got to medical school, he was feeling good. In consultation with his psychiatrist, he thought it worthwhile to take a break from his medications. At that time, his diagnosis was major depressive disorder and he had only had one serious depressive episode, which didn’t necessarily indicate that he would need medication long-term, he said.
Dr. Bullock loved everything about medical school. “One day when I was in my first year of med school, I called my mom and said: ‘It’s like science summer camp but every day!’” he recalled.
Despite his enthusiasm, though, he began feeling something troubling. Recognizing the symptoms of early depression, Dr. Bullock restarted his medication. But this time, the same SSRI only made things worse. He went from sleeping 8 hours to 90 minutes a night. He felt angry. One day, he went on a furious 22-mile run. Plus, within the first 6 months of moving to San Francisco, Dr. Bullock was stopped by the police three different times while riding his bike. He attributes this to his race, which has only further added to his stress. In September 2015, during his second year of medical school, Dr. Bullock attempted suicide again. This time, he was intubated in the ED and rushed to the ICU.
He was given a new diagnosis: bipolar disorder. He changed medications and lived for a time with Ms. Mahoney and his other sister, who moved from Chicago to California to be with him. “My family has helped me a lot,” he said.
Dr. Bullock was initially not sure whether he would be able to return to school after his attempted suicide. Overall, UCSF was extremely supportive, he said. That came as a relief. Medical school was a grounding force in his life, not a destabilizing one: “If I had been pushed out, it would have been really harmful to me.”
Then Dr. Bullock started residency. The sleep disruption that comes with the night shift – the resident rite of passage – triggered another episode. At first, Dr. Bullock was overly productive; his mind was active and alert after staying up all night. He worked on new research during the day instead of sleeping.
Sleep disturbance is a hallmark symptom of bipolar disorder. “Justin should never be on a 24-hour call,” said Lisa Meeks, PhD, associate professor of psychiatry and family medicine at the University of Colorado at Denver, Aurora, and a leading scholar on disability advocacy for medical trainees. When he started residency, Dr. Bullock was open with his program director about his diagnosis and sought accommodations to go to therapy each week. But he didn’t try to get out of night shifts or 24-hour calls, despite his care team urging him to do so. “I have this sense of wanting to tough it out,” he said. He also felt guilty making his peers take on his share of those challenging shifts.
In December 2019, Dr. Bullock was voluntarily hospitalized for a few days and started writing the article that would later appear in NEJM. In January, a friend and UCSF medical student completed suicide. In March, the same month his NEJM article came out, Dr. Bullock attempted suicide again. This time, he quickly recognized that he was making a mistake and called an ambulance. “For me, as far as suicide attempts go, it’s the most positive one.”
Advocating for changes in medical training
Throughout his medical training, Dr. Bullock was always open about his struggles with his peers and with the administration. He shared his suicidal thoughts at a Mental Illness Among Us event during medical school. His story resonated with peers who were surprised that Dr. Bullock, who was thriving academically, could be struggling emotionally.
During residency, he led small group discussions and gave lectures at the medical school, including a talk about his attempts to create institutional change at UCSF, such as his public fight against the college’s Fitness for Duty (FFD) assessment process. That discussion earned him an Outstanding Lecturer award. Because it was the third award he had received from the medical school, Dr. Bullock also automatically earned a lifetime teaching award. When he told his mom, a teacher herself, about the award, she joked: “Are you old enough for ‘lifetime’ anything?”
Dr. Bullock has also spoken out and actively fought against the processes within the medical community that prevent people from coming forward until it is too late. Physicians and trainees often fear that if they seek mental health treatment, they will have to disclose that treatment to a potential employer or licensing board and then be barred from practicing medicine. Because he has been open about his mental health for so long, Dr. Bullock feels that he is in a position to push back against these norms. For example, in June he coauthored another article, this time for the Journal of Hospital Medicine, describing the traumatizing FFD assessment that followed his March 2020 suicide attempt.
In that article, Dr. Bullock wrote how no mental health professional served on the UCSF Physician Well Being Committee – comprising physicians and lawyers who evaluate physician impairment or potential physician impairment – that evaluated him. Dr. Bullock was referred to an outside psychiatrist. He also describes how he was forced to release all of his psychiatric records and undergo extensive drug testing, despite having no history of substance abuse. To return to work, he had to sign a contract, agreeing to be monitored and to attend a specific kind of therapy.
While steps like these can, in the right circumstances, protect both the public and doctors-in-training in important ways, they can also “be very punitive and isolating for someone going through a mental health crisis,” said Dr. Meeks. There were also no Black physicians or lawyers on the committee evaluating Dr. Bullock. “That was really egregious, when you look back.” Dr. Meeks is a coauthor on Dr. Bullock’s JHM article and a mentor and previous student disability officer at UCSF.
Dr. Bullock raised objections to UCSF administrators about how he felt that the committee was discriminating against him because of his mental illness despite assurances from the director of his program that there have never been any performance or professionalism concerns with him. He said the administrators told him he was the first person to question the FFD process. This isn’t surprising, given that all the power in such situations usually lies with the hospital and the administrators, whereas the resident or physician is worried about losing their job and their license, said Dr. Meeks.
Dr. Bullock contends that he’s in a unique position to speak out, considering his stellar academic and work records, openness about his mental illness before a crisis, access to quality mental health care, and extensive personal network among the UCSF administration. “I know that I hold power within my institution; I spoke out because I could,” Dr. Bullock said. In addition to writing an article about his experience, Dr. Bullock shared his story with a task force appointed by the medical staff president to review the Physician Well-Being Committee and the overall FFD process. Even before Dr. Bullock shared his story with the public, the task force had already been appointed as a result of the increased concern about physician mental health during the ongoing COVID-19 pandemic, Michelle Guy, MD, clinical professor of medicine at UCSF, told this news organization.
Elizabeth Fernandez, a UCSF senior public information representative, declined to comment on Dr. Bullock’s specific experience as reported in the JHM. “As with every hospital accredited by the Joint Commission, UCSF Medical Center has a Physician Well Being Committee that provides resources for physicians who may need help with chemical dependency or mental illness,” Ms. Fernandez said.
“Our goal through this program is always, first, to provide the compassion and assistance our physicians need to address the issues they face and continue to pursue their careers. This program is entirely voluntary and is bound by federal and state laws and regulations to protect the confidentiality of its participants, while ensuring that – first and foremost – no one is harmed by the situation, including the participant.”
Overcoming stigma to change the system
All of the attention – from national media outlets such as Vox to struggling peers and others – is fulfilling, Dr. Bullock said. But it can also be overwhelming. “I have definitely been praised as ‘Black excellence,’ and that definitely has added to the pressure to keep going ... to keep pushing at times,” he said.
Ms. Mahoney added: “He’s willing to sacrifice himself in order to make a difference. He would be a sacrificial lamb” for the Black community, the gay community, or any minority community.
Despite these concerns and his past suicide attempts, colleagues feel that Dr. Bullock is in a strong place to make decisions. “I trust Justin to put the boundaries up when they are needed and to engage in a way that feels comfortable for him,” said Ms. Meeks. “He is someone who has incredible self-awareness.”
Dr. Bullock’s history isn’t just something he overcame: It’s something that makes him a better, more empathetic doctor, said Ms. Mahoney. He knows what it’s like to be hospitalized, to deal with the frustration of insurance, to navigate the complexity of the health care system as a patient, or to be facing a deep internal darkness. He “can genuinely hold that person’s hand and say: ‘I know what you’re going through and we’re going to work through this day by day,’ ” she said. “That is something he can bring that no other physician can bring.”
In his advocacy on Twitter, in lectures, and in conversations with UCSF administrators, Dr. Bullock is pushing for board licensing questions to be reformed so physicians are no longer penalized for seeking mental health treatment. He would also like residency programs to make it easier and less stigmatizing for trainees to receive accommodations for a disability or mental illness.
“They say one person can’t change a system,” said Dr. Meeks, “but I do think Justin is calling an awful lot of attention to the system and I do think there will be changes because of his advocacy.”
A version of this article first appeared on Medscape.com.