User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Emergency Contraception Recommended for Teens on Isotretinoin
TORONTO —
That was one of the main messages from Andrea L. Zaenglein, MD, professor of dermatology and pediatrics, Penn State University, Hershey, who discussed hormonal therapies for pediatric acne at the annual meeting of the Society for Pediatric Dermatology.
Many doctors are reluctant to prescribe EC, which refers to contraceptive methods used to prevent unintended pregnancy after unprotected sexual intercourse or contraceptive failure, whether that’s from discomfort with EC or lack of training, Dr. Zaenglein said in an interview.
Isotretinoin, a retinoid marketed as Accutane and other brand names, is an effective treatment for acne but carries serious teratogenicity risks; the iPLEDGE Risk Evaluation and Mitigation Strategy is designed to manage this risk and minimize fetal exposure. Yet from 2011 to 2017, 210-310 pregnancies per year were reported to the Food and Drug Administration, according to a 2019 study.
There is a knowledge gap regarding EC among dermatologists who prescribe isotretinoin, which “is perpetuated by the iPLEDGE program because it is inadequate in guiding clinicians or educating patients about the use of EC,” Dr. Zaenglein and colleagues wrote in a recently published viewpoint on EC prescribing in patients on isotretinoin.
Types of EC include oral levonorgestrel (plan B), available over the counter; oral ulipristal acetate (ella), which requires a prescription; and the copper/hormonal intrauterine device.
Not all teens taking isotretinoin can be trusted to be sexually abstinent. Dr. Zaenglein cited research showing 39% of female high school students have had sexual relations. “In my opinion, these patients should have emergency contraception prescribed to them as a backup,” she said.
Dr. Zaenglein believes there’s a fair amount of “misunderstanding” about EC, with many people thinking it’s an abortion pill. “It’s a totally different medicine. This is contraception; if you’re pregnant, it’s not going to affect your fetus.”
Outgoing SPD President Sheilagh Maguiness, MD, professor of dermatology and pediatrics, University of Minnesota, Minneapolis, agreed that Dr. Zaenglein raised an important issue. “She has identified a practice gap and a knowledge gap that we need to address,” she said in an interview.
When discussing contraception with female patients taking isotretinoin, assume they’re sexually active or could be, Dr. Zaenglein told meeting attendees. Be explicit about the risks to the fetus and consider their past compliance.
Complex Disorder
During her presentation, Dr. Zaenglein described acne as a “very complex, multifactorial inflammatory disorder” of the skin. It involves four steps: Increased sebum production, hyperkeratinization, Cutibacterium acnes, and inflammation. External factors such as diet, genes, and the environment play a role.
“But at the heart of all of it is androgens; if you didn’t have androgens, you wouldn’t have acne.” That’s why some acne treatments block androgen receptors.
Clinicians are increasingly using one such therapy, spironolactone, to treat acne in female adolescents. Dr. Zaenglein referred to a Mayo Clinic study of 80 patients (mean age, 19 years), who had moderate to severe acne treated with a mean dose of 100 mg/day, that found 80% had improvement with a favorable side effect profile. This included nearly 23% who had a complete response (90% or more) and 36% who had a partial response (more than 50%); 20% had no response.
However, response rates are higher in adults, said Dr. Zaenglein, noting that spironolactone works “much better” in adult women.
Side effects of spironolactone can include menstrual disturbances, breast enlargement and tenderness, and premenstrual syndrome–like symptoms.
Dermatologists should also consider combined oral contraceptives (COCs) in their adolescent patients with acne. These have an estrogen component as well as a progestin component.
They have proven effectiveness for acne in adolescents, yet a US survey of 170 dermatology residents found only 60% felt comfortable prescribing them to healthy adolescents. The survey also found only 62% of respondents felt adequately trained on the efficacy of COCs, and 42% felt adequately trained on their safety.
Contraindications for COCs include thrombosis, migraine with aura, lupus, seizures, and hypertension. Complex valvular heart disease and liver tumors also need to be ruled out, said Dr. Zaenglein. One of the “newer concerns” with COCs is depression. “There’s biological plausibility because, obviously, hormones impact the brain.”
Preventing Drug Interactions
Before prescribing hormonal therapy, clinicians should carry out an acne assessment, aimed in part at preventing drug interactions. “The one we mostly have to watch out for is rifampin,” an antibiotic that could interact with COCs, said Dr. Zaenglein.
The herbal supplement St John’s Wort can reduce the efficacy of COCs. “You also want to make sure that they’re not on any medicines that will increase potassium, such as ACE inhibitors,” said Dr. Zaenglein. But tetracyclines, ampicillin, or metronidazole are usually “all okay” when combined with COCs.
It’s important to get baseline blood pressure levels and to check these along with weight on a regular basis, she added.
Always Consider PCOS
Before starting hormonal therapy, she advises dermatologists to “always consider” polycystic ovary syndrome (PCOS), a condition that’s “probably much underdiagnosed.” Acne is common in adolescents with PCOS. She suggests using a PCOS checklist, a reminder to ask about irregular periods, hirsutism, signs of insulin resistance such as increased body mass index, a history of premature adrenarche, and a family history of PCOS, said Dr. Zaenglein, noting that a person with a sibling who has PCOS has about a 40% chance of developing the condition.
“We play an important role in getting kids diagnosed at an early age so that we can make interventions because the impact of the metabolic syndrome can have lifelong effects on their cardiovascular system, as well as infertility.”
Dr. Zaenglein is a member of the American Academy of Dermatology (AAD) Acne Guidelines work group, the immediate past president of the American Acne and Rosacea Society, a member of the AAD iPLEDGE work group, co–editor in chief of Pediatric Dermatology, an advisory board member of Ortho Dermatologics, and a consultant for Church & Dwight. Dr. Maguiness had no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TORONTO —
That was one of the main messages from Andrea L. Zaenglein, MD, professor of dermatology and pediatrics, Penn State University, Hershey, who discussed hormonal therapies for pediatric acne at the annual meeting of the Society for Pediatric Dermatology.
Many doctors are reluctant to prescribe EC, which refers to contraceptive methods used to prevent unintended pregnancy after unprotected sexual intercourse or contraceptive failure, whether that’s from discomfort with EC or lack of training, Dr. Zaenglein said in an interview.
Isotretinoin, a retinoid marketed as Accutane and other brand names, is an effective treatment for acne but carries serious teratogenicity risks; the iPLEDGE Risk Evaluation and Mitigation Strategy is designed to manage this risk and minimize fetal exposure. Yet from 2011 to 2017, 210-310 pregnancies per year were reported to the Food and Drug Administration, according to a 2019 study.
There is a knowledge gap regarding EC among dermatologists who prescribe isotretinoin, which “is perpetuated by the iPLEDGE program because it is inadequate in guiding clinicians or educating patients about the use of EC,” Dr. Zaenglein and colleagues wrote in a recently published viewpoint on EC prescribing in patients on isotretinoin.
Types of EC include oral levonorgestrel (plan B), available over the counter; oral ulipristal acetate (ella), which requires a prescription; and the copper/hormonal intrauterine device.
Not all teens taking isotretinoin can be trusted to be sexually abstinent. Dr. Zaenglein cited research showing 39% of female high school students have had sexual relations. “In my opinion, these patients should have emergency contraception prescribed to them as a backup,” she said.
Dr. Zaenglein believes there’s a fair amount of “misunderstanding” about EC, with many people thinking it’s an abortion pill. “It’s a totally different medicine. This is contraception; if you’re pregnant, it’s not going to affect your fetus.”
Outgoing SPD President Sheilagh Maguiness, MD, professor of dermatology and pediatrics, University of Minnesota, Minneapolis, agreed that Dr. Zaenglein raised an important issue. “She has identified a practice gap and a knowledge gap that we need to address,” she said in an interview.
When discussing contraception with female patients taking isotretinoin, assume they’re sexually active or could be, Dr. Zaenglein told meeting attendees. Be explicit about the risks to the fetus and consider their past compliance.
Complex Disorder
During her presentation, Dr. Zaenglein described acne as a “very complex, multifactorial inflammatory disorder” of the skin. It involves four steps: Increased sebum production, hyperkeratinization, Cutibacterium acnes, and inflammation. External factors such as diet, genes, and the environment play a role.
“But at the heart of all of it is androgens; if you didn’t have androgens, you wouldn’t have acne.” That’s why some acne treatments block androgen receptors.
Clinicians are increasingly using one such therapy, spironolactone, to treat acne in female adolescents. Dr. Zaenglein referred to a Mayo Clinic study of 80 patients (mean age, 19 years), who had moderate to severe acne treated with a mean dose of 100 mg/day, that found 80% had improvement with a favorable side effect profile. This included nearly 23% who had a complete response (90% or more) and 36% who had a partial response (more than 50%); 20% had no response.
However, response rates are higher in adults, said Dr. Zaenglein, noting that spironolactone works “much better” in adult women.
Side effects of spironolactone can include menstrual disturbances, breast enlargement and tenderness, and premenstrual syndrome–like symptoms.
Dermatologists should also consider combined oral contraceptives (COCs) in their adolescent patients with acne. These have an estrogen component as well as a progestin component.
They have proven effectiveness for acne in adolescents, yet a US survey of 170 dermatology residents found only 60% felt comfortable prescribing them to healthy adolescents. The survey also found only 62% of respondents felt adequately trained on the efficacy of COCs, and 42% felt adequately trained on their safety.
Contraindications for COCs include thrombosis, migraine with aura, lupus, seizures, and hypertension. Complex valvular heart disease and liver tumors also need to be ruled out, said Dr. Zaenglein. One of the “newer concerns” with COCs is depression. “There’s biological plausibility because, obviously, hormones impact the brain.”
Preventing Drug Interactions
Before prescribing hormonal therapy, clinicians should carry out an acne assessment, aimed in part at preventing drug interactions. “The one we mostly have to watch out for is rifampin,” an antibiotic that could interact with COCs, said Dr. Zaenglein.
The herbal supplement St John’s Wort can reduce the efficacy of COCs. “You also want to make sure that they’re not on any medicines that will increase potassium, such as ACE inhibitors,” said Dr. Zaenglein. But tetracyclines, ampicillin, or metronidazole are usually “all okay” when combined with COCs.
It’s important to get baseline blood pressure levels and to check these along with weight on a regular basis, she added.
Always Consider PCOS
Before starting hormonal therapy, she advises dermatologists to “always consider” polycystic ovary syndrome (PCOS), a condition that’s “probably much underdiagnosed.” Acne is common in adolescents with PCOS. She suggests using a PCOS checklist, a reminder to ask about irregular periods, hirsutism, signs of insulin resistance such as increased body mass index, a history of premature adrenarche, and a family history of PCOS, said Dr. Zaenglein, noting that a person with a sibling who has PCOS has about a 40% chance of developing the condition.
“We play an important role in getting kids diagnosed at an early age so that we can make interventions because the impact of the metabolic syndrome can have lifelong effects on their cardiovascular system, as well as infertility.”
Dr. Zaenglein is a member of the American Academy of Dermatology (AAD) Acne Guidelines work group, the immediate past president of the American Acne and Rosacea Society, a member of the AAD iPLEDGE work group, co–editor in chief of Pediatric Dermatology, an advisory board member of Ortho Dermatologics, and a consultant for Church & Dwight. Dr. Maguiness had no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TORONTO —
That was one of the main messages from Andrea L. Zaenglein, MD, professor of dermatology and pediatrics, Penn State University, Hershey, who discussed hormonal therapies for pediatric acne at the annual meeting of the Society for Pediatric Dermatology.
Many doctors are reluctant to prescribe EC, which refers to contraceptive methods used to prevent unintended pregnancy after unprotected sexual intercourse or contraceptive failure, whether that’s from discomfort with EC or lack of training, Dr. Zaenglein said in an interview.
Isotretinoin, a retinoid marketed as Accutane and other brand names, is an effective treatment for acne but carries serious teratogenicity risks; the iPLEDGE Risk Evaluation and Mitigation Strategy is designed to manage this risk and minimize fetal exposure. Yet from 2011 to 2017, 210-310 pregnancies per year were reported to the Food and Drug Administration, according to a 2019 study.
There is a knowledge gap regarding EC among dermatologists who prescribe isotretinoin, which “is perpetuated by the iPLEDGE program because it is inadequate in guiding clinicians or educating patients about the use of EC,” Dr. Zaenglein and colleagues wrote in a recently published viewpoint on EC prescribing in patients on isotretinoin.
Types of EC include oral levonorgestrel (plan B), available over the counter; oral ulipristal acetate (ella), which requires a prescription; and the copper/hormonal intrauterine device.
Not all teens taking isotretinoin can be trusted to be sexually abstinent. Dr. Zaenglein cited research showing 39% of female high school students have had sexual relations. “In my opinion, these patients should have emergency contraception prescribed to them as a backup,” she said.
Dr. Zaenglein believes there’s a fair amount of “misunderstanding” about EC, with many people thinking it’s an abortion pill. “It’s a totally different medicine. This is contraception; if you’re pregnant, it’s not going to affect your fetus.”
Outgoing SPD President Sheilagh Maguiness, MD, professor of dermatology and pediatrics, University of Minnesota, Minneapolis, agreed that Dr. Zaenglein raised an important issue. “She has identified a practice gap and a knowledge gap that we need to address,” she said in an interview.
When discussing contraception with female patients taking isotretinoin, assume they’re sexually active or could be, Dr. Zaenglein told meeting attendees. Be explicit about the risks to the fetus and consider their past compliance.
Complex Disorder
During her presentation, Dr. Zaenglein described acne as a “very complex, multifactorial inflammatory disorder” of the skin. It involves four steps: Increased sebum production, hyperkeratinization, Cutibacterium acnes, and inflammation. External factors such as diet, genes, and the environment play a role.
“But at the heart of all of it is androgens; if you didn’t have androgens, you wouldn’t have acne.” That’s why some acne treatments block androgen receptors.
Clinicians are increasingly using one such therapy, spironolactone, to treat acne in female adolescents. Dr. Zaenglein referred to a Mayo Clinic study of 80 patients (mean age, 19 years), who had moderate to severe acne treated with a mean dose of 100 mg/day, that found 80% had improvement with a favorable side effect profile. This included nearly 23% who had a complete response (90% or more) and 36% who had a partial response (more than 50%); 20% had no response.
However, response rates are higher in adults, said Dr. Zaenglein, noting that spironolactone works “much better” in adult women.
Side effects of spironolactone can include menstrual disturbances, breast enlargement and tenderness, and premenstrual syndrome–like symptoms.
Dermatologists should also consider combined oral contraceptives (COCs) in their adolescent patients with acne. These have an estrogen component as well as a progestin component.
They have proven effectiveness for acne in adolescents, yet a US survey of 170 dermatology residents found only 60% felt comfortable prescribing them to healthy adolescents. The survey also found only 62% of respondents felt adequately trained on the efficacy of COCs, and 42% felt adequately trained on their safety.
Contraindications for COCs include thrombosis, migraine with aura, lupus, seizures, and hypertension. Complex valvular heart disease and liver tumors also need to be ruled out, said Dr. Zaenglein. One of the “newer concerns” with COCs is depression. “There’s biological plausibility because, obviously, hormones impact the brain.”
Preventing Drug Interactions
Before prescribing hormonal therapy, clinicians should carry out an acne assessment, aimed in part at preventing drug interactions. “The one we mostly have to watch out for is rifampin,” an antibiotic that could interact with COCs, said Dr. Zaenglein.
The herbal supplement St John’s Wort can reduce the efficacy of COCs. “You also want to make sure that they’re not on any medicines that will increase potassium, such as ACE inhibitors,” said Dr. Zaenglein. But tetracyclines, ampicillin, or metronidazole are usually “all okay” when combined with COCs.
It’s important to get baseline blood pressure levels and to check these along with weight on a regular basis, she added.
Always Consider PCOS
Before starting hormonal therapy, she advises dermatologists to “always consider” polycystic ovary syndrome (PCOS), a condition that’s “probably much underdiagnosed.” Acne is common in adolescents with PCOS. She suggests using a PCOS checklist, a reminder to ask about irregular periods, hirsutism, signs of insulin resistance such as increased body mass index, a history of premature adrenarche, and a family history of PCOS, said Dr. Zaenglein, noting that a person with a sibling who has PCOS has about a 40% chance of developing the condition.
“We play an important role in getting kids diagnosed at an early age so that we can make interventions because the impact of the metabolic syndrome can have lifelong effects on their cardiovascular system, as well as infertility.”
Dr. Zaenglein is a member of the American Academy of Dermatology (AAD) Acne Guidelines work group, the immediate past president of the American Acne and Rosacea Society, a member of the AAD iPLEDGE work group, co–editor in chief of Pediatric Dermatology, an advisory board member of Ortho Dermatologics, and a consultant for Church & Dwight. Dr. Maguiness had no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM SPD 2024
Several Skin Conditions More Likely in Children With Obesity
TORONTO — results of new research show.
The retrospective cohort study found markedly higher rates of skin infections, atopic dermatitis (AD), and acanthosis nigricans among children with overweight, compared with children with average weight.
“Many conditions associated with obesity are strong predictors of cardiovascular mortality as these children age, so doctors can play a key role in advocating for weight loss strategies in this population,” lead study author Samantha Epstein, third-year medical student at Case Western Reserve University, Cleveland, Ohio, said in an interview. The findings were presented at the annual meeting of the Society for Pediatric Dermatology.
Previous research has linked obesity, a chronic inflammatory condition, to psoriasis, AD, hidradenitis suppurativa (HS), acne vulgaris, infections, and rosacea in adults. However, there’s scant research exploring the connection between obesity and cutaneous conditions in children.
According to the Cleveland Clinic, childhood obesity is defined as a body mass index, which is weight in kg divided by the square of height in m2, at or above the 95th percentile for age and sex in children aged 2 years or older.
For the study, Ms. Epstein and coauthor Sonal D. Shah, MD, associate professor, Department of Dermatology, Case Western Reserve University, and a board-certified pediatric dermatologist accessed a large national research database and used diagnostic codes to identify over 1 million children (mean age, 8.5 years). Most (about 44%) were White; about one-quarter were Black. The groups were propensity matched, so there were about equal numbers of youngsters with and without obesity and of boys and girls.
They collected data on AD, HS, rosacea, psoriasis, and acanthosis nigricans (a thickened purplish discoloration typically found in body folds around the armpits, groin, and neck). They also gathered information on comorbidities.
Acanthosis nigricans, which is linked to metabolic syndrome, type 2 diabetes, and insulin resistance , was more prevalent among children with obesity (20,885 cases in the with-obesity group and 336 in the without-obesity group, for a relative risk [RR] of 62.16 and an odds ratio [OR] of 64.38).
Skin and subcutaneous tissue infections were also more common among those with obesity (14,795 cases) vs 4720 cases among those without obesity (RR, 3.14; OR, 3.2). As for AD, there were 11,892 cases in the with-obesity group and 2983 in the without-obesity group (RR, 3.99; OR, 4.06). There were 1166 cases of psoriasis among those with obesity and 408 among those without obesity (RR, 2.86; OR, 2.88).
HS (587 cases in the with-obesity group and 70 in the without-obesity group; RR, 8.39; OR, 8.39) and rosacea (351 in the with-obesity group and 138 in the without-obesity group; RR, 2.54; OR, 2.55) were the least common skin conditions.
Higher Comorbidity Rates
Compared with their average-weight counterparts, the children with obesity had higher rates of comorbidities, including type 2 diabetes. Ms. Epstein noted that children with diabetes and obesity had increased risks for every skin condition except for infections of the skin and subcutaneous tissue when compared with children without obesity.
Such infections were the most common skin conditions among children without obesity. “This was expected just due to the fact that children are outside, they’re playing in the grass and the dirt, and they get infected,” said Ms. Epstein. Still, these infections were three times more common in youngsters with obesity.
Although acanthosis nigricans is “highly correlated” with type 2 diabetes, “not as many children as we would expect in this population have developed type 2 diabetes,” said Ms. Epstein. This might make some sense, though, because these children are still quite young. “When dermatologists recognize this skin condition, they can advocate for weight loss management to try to prevent it.”
Other conditions seen more often in the overweight children with overweight included: hypertension, hyperlipidemia, obstructive sleep apnea, polycystic ovarian syndrome, attention-deficit/hyperactivity disorder, major depressive disorder, depressive episodes, and anxiety (all P < .001).
Commenting on the results, Sonia Havele, MD, a pediatrician and dermatology resident at Children’s Mercy Hospital, Kansas City, Missouri, said in an interview that the study reflects trends that she and her colleagues see in clinic: There are more common skin conditions in their patients with obesity.
She agreed that it offers an opening for education. “The results of this study highlight the opportunity we have as pediatric dermatologists to provide additional counseling on obesity and offer referrals to our colleagues in endocrinology, gastroenterology, and nutrition if needed.”
No conflicts of interest were reported.
TORONTO — results of new research show.
The retrospective cohort study found markedly higher rates of skin infections, atopic dermatitis (AD), and acanthosis nigricans among children with overweight, compared with children with average weight.
“Many conditions associated with obesity are strong predictors of cardiovascular mortality as these children age, so doctors can play a key role in advocating for weight loss strategies in this population,” lead study author Samantha Epstein, third-year medical student at Case Western Reserve University, Cleveland, Ohio, said in an interview. The findings were presented at the annual meeting of the Society for Pediatric Dermatology.
Previous research has linked obesity, a chronic inflammatory condition, to psoriasis, AD, hidradenitis suppurativa (HS), acne vulgaris, infections, and rosacea in adults. However, there’s scant research exploring the connection between obesity and cutaneous conditions in children.
According to the Cleveland Clinic, childhood obesity is defined as a body mass index, which is weight in kg divided by the square of height in m2, at or above the 95th percentile for age and sex in children aged 2 years or older.
For the study, Ms. Epstein and coauthor Sonal D. Shah, MD, associate professor, Department of Dermatology, Case Western Reserve University, and a board-certified pediatric dermatologist accessed a large national research database and used diagnostic codes to identify over 1 million children (mean age, 8.5 years). Most (about 44%) were White; about one-quarter were Black. The groups were propensity matched, so there were about equal numbers of youngsters with and without obesity and of boys and girls.
They collected data on AD, HS, rosacea, psoriasis, and acanthosis nigricans (a thickened purplish discoloration typically found in body folds around the armpits, groin, and neck). They also gathered information on comorbidities.
Acanthosis nigricans, which is linked to metabolic syndrome, type 2 diabetes, and insulin resistance , was more prevalent among children with obesity (20,885 cases in the with-obesity group and 336 in the without-obesity group, for a relative risk [RR] of 62.16 and an odds ratio [OR] of 64.38).
Skin and subcutaneous tissue infections were also more common among those with obesity (14,795 cases) vs 4720 cases among those without obesity (RR, 3.14; OR, 3.2). As for AD, there were 11,892 cases in the with-obesity group and 2983 in the without-obesity group (RR, 3.99; OR, 4.06). There were 1166 cases of psoriasis among those with obesity and 408 among those without obesity (RR, 2.86; OR, 2.88).
HS (587 cases in the with-obesity group and 70 in the without-obesity group; RR, 8.39; OR, 8.39) and rosacea (351 in the with-obesity group and 138 in the without-obesity group; RR, 2.54; OR, 2.55) were the least common skin conditions.
Higher Comorbidity Rates
Compared with their average-weight counterparts, the children with obesity had higher rates of comorbidities, including type 2 diabetes. Ms. Epstein noted that children with diabetes and obesity had increased risks for every skin condition except for infections of the skin and subcutaneous tissue when compared with children without obesity.
Such infections were the most common skin conditions among children without obesity. “This was expected just due to the fact that children are outside, they’re playing in the grass and the dirt, and they get infected,” said Ms. Epstein. Still, these infections were three times more common in youngsters with obesity.
Although acanthosis nigricans is “highly correlated” with type 2 diabetes, “not as many children as we would expect in this population have developed type 2 diabetes,” said Ms. Epstein. This might make some sense, though, because these children are still quite young. “When dermatologists recognize this skin condition, they can advocate for weight loss management to try to prevent it.”
Other conditions seen more often in the overweight children with overweight included: hypertension, hyperlipidemia, obstructive sleep apnea, polycystic ovarian syndrome, attention-deficit/hyperactivity disorder, major depressive disorder, depressive episodes, and anxiety (all P < .001).
Commenting on the results, Sonia Havele, MD, a pediatrician and dermatology resident at Children’s Mercy Hospital, Kansas City, Missouri, said in an interview that the study reflects trends that she and her colleagues see in clinic: There are more common skin conditions in their patients with obesity.
She agreed that it offers an opening for education. “The results of this study highlight the opportunity we have as pediatric dermatologists to provide additional counseling on obesity and offer referrals to our colleagues in endocrinology, gastroenterology, and nutrition if needed.”
No conflicts of interest were reported.
TORONTO — results of new research show.
The retrospective cohort study found markedly higher rates of skin infections, atopic dermatitis (AD), and acanthosis nigricans among children with overweight, compared with children with average weight.
“Many conditions associated with obesity are strong predictors of cardiovascular mortality as these children age, so doctors can play a key role in advocating for weight loss strategies in this population,” lead study author Samantha Epstein, third-year medical student at Case Western Reserve University, Cleveland, Ohio, said in an interview. The findings were presented at the annual meeting of the Society for Pediatric Dermatology.
Previous research has linked obesity, a chronic inflammatory condition, to psoriasis, AD, hidradenitis suppurativa (HS), acne vulgaris, infections, and rosacea in adults. However, there’s scant research exploring the connection between obesity and cutaneous conditions in children.
According to the Cleveland Clinic, childhood obesity is defined as a body mass index, which is weight in kg divided by the square of height in m2, at or above the 95th percentile for age and sex in children aged 2 years or older.
For the study, Ms. Epstein and coauthor Sonal D. Shah, MD, associate professor, Department of Dermatology, Case Western Reserve University, and a board-certified pediatric dermatologist accessed a large national research database and used diagnostic codes to identify over 1 million children (mean age, 8.5 years). Most (about 44%) were White; about one-quarter were Black. The groups were propensity matched, so there were about equal numbers of youngsters with and without obesity and of boys and girls.
They collected data on AD, HS, rosacea, psoriasis, and acanthosis nigricans (a thickened purplish discoloration typically found in body folds around the armpits, groin, and neck). They also gathered information on comorbidities.
Acanthosis nigricans, which is linked to metabolic syndrome, type 2 diabetes, and insulin resistance , was more prevalent among children with obesity (20,885 cases in the with-obesity group and 336 in the without-obesity group, for a relative risk [RR] of 62.16 and an odds ratio [OR] of 64.38).
Skin and subcutaneous tissue infections were also more common among those with obesity (14,795 cases) vs 4720 cases among those without obesity (RR, 3.14; OR, 3.2). As for AD, there were 11,892 cases in the with-obesity group and 2983 in the without-obesity group (RR, 3.99; OR, 4.06). There were 1166 cases of psoriasis among those with obesity and 408 among those without obesity (RR, 2.86; OR, 2.88).
HS (587 cases in the with-obesity group and 70 in the without-obesity group; RR, 8.39; OR, 8.39) and rosacea (351 in the with-obesity group and 138 in the without-obesity group; RR, 2.54; OR, 2.55) were the least common skin conditions.
Higher Comorbidity Rates
Compared with their average-weight counterparts, the children with obesity had higher rates of comorbidities, including type 2 diabetes. Ms. Epstein noted that children with diabetes and obesity had increased risks for every skin condition except for infections of the skin and subcutaneous tissue when compared with children without obesity.
Such infections were the most common skin conditions among children without obesity. “This was expected just due to the fact that children are outside, they’re playing in the grass and the dirt, and they get infected,” said Ms. Epstein. Still, these infections were three times more common in youngsters with obesity.
Although acanthosis nigricans is “highly correlated” with type 2 diabetes, “not as many children as we would expect in this population have developed type 2 diabetes,” said Ms. Epstein. This might make some sense, though, because these children are still quite young. “When dermatologists recognize this skin condition, they can advocate for weight loss management to try to prevent it.”
Other conditions seen more often in the overweight children with overweight included: hypertension, hyperlipidemia, obstructive sleep apnea, polycystic ovarian syndrome, attention-deficit/hyperactivity disorder, major depressive disorder, depressive episodes, and anxiety (all P < .001).
Commenting on the results, Sonia Havele, MD, a pediatrician and dermatology resident at Children’s Mercy Hospital, Kansas City, Missouri, said in an interview that the study reflects trends that she and her colleagues see in clinic: There are more common skin conditions in their patients with obesity.
She agreed that it offers an opening for education. “The results of this study highlight the opportunity we have as pediatric dermatologists to provide additional counseling on obesity and offer referrals to our colleagues in endocrinology, gastroenterology, and nutrition if needed.”
No conflicts of interest were reported.
FROM SPD 2024
Topical Ruxolitinib: Analysis Finds Repigmentation Rates in Adolescents with Vitiligo
data showed.
“We consider repigmenting vitiligo a two-step process, where the overactive immune system needs to be calmed down and then the melanocytes need to repopulate to the white areas,” one of the study investigators, David Rosmarin, MD, chair of the Department of Dermatology at Indiana University School of Medicine, Indianapolis, said in an interview in advance of the annual meeting of the Society for Pediatric Dermatology, where the study results were presented during a poster session. “In younger patients, it may be that the melanocytes are more rapidly repigmenting the patches, which is why we see this effect.”
Ruxolitinib, 1.5% cream (Opzelura) is a Janus kinase inhibitor approved for the treatment of nonsegmental vitiligo in patients 12 years of age and older. Dr. Rosmarin and colleagues sought to evaluate differences in rates of complete or near-complete repigmentation and repigmentation by body region between adolescents 12-17 years of age and adults 18 years of age and older who applied ruxolitinib cream twice daily. The researchers evaluated patients who were initially randomized to ruxolitinib cream, 1.5% in the pivotal TRuE-V1 and TRuE-V2 studies and applied it for up to 104 weeks. Complete facial improvement was defined as 100% improvement on the Facial Vitiligo Area Scoring Index (F-VASI 100) from baseline, and near-total improvement was categorized as a ≥ 75% or ≥ 90% improvement from baseline on the Total body VASI (T-VASI). Responses for each of six body regions, excluding the face, were assessed by the proportion of patients who achieved at least a 50% improvement from baseline on the T-VASI.
Compared with adults, a greater proportion of adolescents achieved F-VASI 100 at week 24 (5.7% [3/53] vs 2.9% [10/341], respectively), but there were no differences between the two groups at week 52 (8.0% [4/50] vs 8.0% [24/300]). Response rates were greater among adolescents vs adults for T-VASI 75 at weeks 24 (13.2% [7/53] vs 5.6% [19/341]) and 52 (22.0% [11/50] vs 20.3% [61/300]), as well as T-VASI 90 at weeks 24 (3.8% [2/53] vs 0.3% [1/341]) and 52 (12.0% [6/50] vs 4.0% [12/300]).
The researchers observed that VASI 50 responses by body region were generally similar between adolescents and adults, but a greater proportion of adolescents achieved a VASI 50 in lower extremities (67.3% [33/49] vs 51.8% [118/228]) and feet (37.5% [12/32] vs 27.9% [51/183]) at week 52.
“Adolescents repigmented more rapidly than adults, so that at 24 weeks, more teens had complete facial repigmentation and T-VASI 75 and T-VASI 90 results,” Dr. Rosmarin said. “With continued use of ruxolitinib cream, both more adults and adolescents achieved greater repigmentation.” He acknowledged certain limitations of the study, including the fact that it was only vehicle controlled up through 24 weeks and that, after week 52, there were fewer patients who completed the long-term extension.
“The take-home message is that ruxolitinib cream can effectively and safely help many patients repigment, including adolescents,” he said.
The study was funded by topical ruxolitinib manufacturer Incyte. Dr. Rosmarin disclosed that he has consulted, spoken for, or conducted trials for AbbVie, Abcuro, Almirall, AltruBio, Amgen, Arena, Astria, Boehringer Ingelheim, Bristol Meyers Squibb, Celgene, Concert, CSL Behring, Dermavant Sciences, Dermira, Galderma, Incyte, Janssen, Kyowa Kirin, Lilly, Merck, Nektar, Novartis, Pfizer, RAPT, Regeneron, Recludix Pharma, Revolo Biotherapeutics, Sanofi, Sun Pharmaceuticals, UCB, Viela Bio, and Zura.
A version of this article first appeared on Medscape.com.
data showed.
“We consider repigmenting vitiligo a two-step process, where the overactive immune system needs to be calmed down and then the melanocytes need to repopulate to the white areas,” one of the study investigators, David Rosmarin, MD, chair of the Department of Dermatology at Indiana University School of Medicine, Indianapolis, said in an interview in advance of the annual meeting of the Society for Pediatric Dermatology, where the study results were presented during a poster session. “In younger patients, it may be that the melanocytes are more rapidly repigmenting the patches, which is why we see this effect.”
Ruxolitinib, 1.5% cream (Opzelura) is a Janus kinase inhibitor approved for the treatment of nonsegmental vitiligo in patients 12 years of age and older. Dr. Rosmarin and colleagues sought to evaluate differences in rates of complete or near-complete repigmentation and repigmentation by body region between adolescents 12-17 years of age and adults 18 years of age and older who applied ruxolitinib cream twice daily. The researchers evaluated patients who were initially randomized to ruxolitinib cream, 1.5% in the pivotal TRuE-V1 and TRuE-V2 studies and applied it for up to 104 weeks. Complete facial improvement was defined as 100% improvement on the Facial Vitiligo Area Scoring Index (F-VASI 100) from baseline, and near-total improvement was categorized as a ≥ 75% or ≥ 90% improvement from baseline on the Total body VASI (T-VASI). Responses for each of six body regions, excluding the face, were assessed by the proportion of patients who achieved at least a 50% improvement from baseline on the T-VASI.
Compared with adults, a greater proportion of adolescents achieved F-VASI 100 at week 24 (5.7% [3/53] vs 2.9% [10/341], respectively), but there were no differences between the two groups at week 52 (8.0% [4/50] vs 8.0% [24/300]). Response rates were greater among adolescents vs adults for T-VASI 75 at weeks 24 (13.2% [7/53] vs 5.6% [19/341]) and 52 (22.0% [11/50] vs 20.3% [61/300]), as well as T-VASI 90 at weeks 24 (3.8% [2/53] vs 0.3% [1/341]) and 52 (12.0% [6/50] vs 4.0% [12/300]).
The researchers observed that VASI 50 responses by body region were generally similar between adolescents and adults, but a greater proportion of adolescents achieved a VASI 50 in lower extremities (67.3% [33/49] vs 51.8% [118/228]) and feet (37.5% [12/32] vs 27.9% [51/183]) at week 52.
“Adolescents repigmented more rapidly than adults, so that at 24 weeks, more teens had complete facial repigmentation and T-VASI 75 and T-VASI 90 results,” Dr. Rosmarin said. “With continued use of ruxolitinib cream, both more adults and adolescents achieved greater repigmentation.” He acknowledged certain limitations of the study, including the fact that it was only vehicle controlled up through 24 weeks and that, after week 52, there were fewer patients who completed the long-term extension.
“The take-home message is that ruxolitinib cream can effectively and safely help many patients repigment, including adolescents,” he said.
The study was funded by topical ruxolitinib manufacturer Incyte. Dr. Rosmarin disclosed that he has consulted, spoken for, or conducted trials for AbbVie, Abcuro, Almirall, AltruBio, Amgen, Arena, Astria, Boehringer Ingelheim, Bristol Meyers Squibb, Celgene, Concert, CSL Behring, Dermavant Sciences, Dermira, Galderma, Incyte, Janssen, Kyowa Kirin, Lilly, Merck, Nektar, Novartis, Pfizer, RAPT, Regeneron, Recludix Pharma, Revolo Biotherapeutics, Sanofi, Sun Pharmaceuticals, UCB, Viela Bio, and Zura.
A version of this article first appeared on Medscape.com.
data showed.
“We consider repigmenting vitiligo a two-step process, where the overactive immune system needs to be calmed down and then the melanocytes need to repopulate to the white areas,” one of the study investigators, David Rosmarin, MD, chair of the Department of Dermatology at Indiana University School of Medicine, Indianapolis, said in an interview in advance of the annual meeting of the Society for Pediatric Dermatology, where the study results were presented during a poster session. “In younger patients, it may be that the melanocytes are more rapidly repigmenting the patches, which is why we see this effect.”
Ruxolitinib, 1.5% cream (Opzelura) is a Janus kinase inhibitor approved for the treatment of nonsegmental vitiligo in patients 12 years of age and older. Dr. Rosmarin and colleagues sought to evaluate differences in rates of complete or near-complete repigmentation and repigmentation by body region between adolescents 12-17 years of age and adults 18 years of age and older who applied ruxolitinib cream twice daily. The researchers evaluated patients who were initially randomized to ruxolitinib cream, 1.5% in the pivotal TRuE-V1 and TRuE-V2 studies and applied it for up to 104 weeks. Complete facial improvement was defined as 100% improvement on the Facial Vitiligo Area Scoring Index (F-VASI 100) from baseline, and near-total improvement was categorized as a ≥ 75% or ≥ 90% improvement from baseline on the Total body VASI (T-VASI). Responses for each of six body regions, excluding the face, were assessed by the proportion of patients who achieved at least a 50% improvement from baseline on the T-VASI.
Compared with adults, a greater proportion of adolescents achieved F-VASI 100 at week 24 (5.7% [3/53] vs 2.9% [10/341], respectively), but there were no differences between the two groups at week 52 (8.0% [4/50] vs 8.0% [24/300]). Response rates were greater among adolescents vs adults for T-VASI 75 at weeks 24 (13.2% [7/53] vs 5.6% [19/341]) and 52 (22.0% [11/50] vs 20.3% [61/300]), as well as T-VASI 90 at weeks 24 (3.8% [2/53] vs 0.3% [1/341]) and 52 (12.0% [6/50] vs 4.0% [12/300]).
The researchers observed that VASI 50 responses by body region were generally similar between adolescents and adults, but a greater proportion of adolescents achieved a VASI 50 in lower extremities (67.3% [33/49] vs 51.8% [118/228]) and feet (37.5% [12/32] vs 27.9% [51/183]) at week 52.
“Adolescents repigmented more rapidly than adults, so that at 24 weeks, more teens had complete facial repigmentation and T-VASI 75 and T-VASI 90 results,” Dr. Rosmarin said. “With continued use of ruxolitinib cream, both more adults and adolescents achieved greater repigmentation.” He acknowledged certain limitations of the study, including the fact that it was only vehicle controlled up through 24 weeks and that, after week 52, there were fewer patients who completed the long-term extension.
“The take-home message is that ruxolitinib cream can effectively and safely help many patients repigment, including adolescents,” he said.
The study was funded by topical ruxolitinib manufacturer Incyte. Dr. Rosmarin disclosed that he has consulted, spoken for, or conducted trials for AbbVie, Abcuro, Almirall, AltruBio, Amgen, Arena, Astria, Boehringer Ingelheim, Bristol Meyers Squibb, Celgene, Concert, CSL Behring, Dermavant Sciences, Dermira, Galderma, Incyte, Janssen, Kyowa Kirin, Lilly, Merck, Nektar, Novartis, Pfizer, RAPT, Regeneron, Recludix Pharma, Revolo Biotherapeutics, Sanofi, Sun Pharmaceuticals, UCB, Viela Bio, and Zura.
A version of this article first appeared on Medscape.com.
FROM SPD 2024
Mysteries Persist About Tissue Resident Memory T Cells in Psoriasis
SEATTLE — In fact, flare-ups often recur at the same site, a phenomenon that might be driven by these resident memory cells, according to Liv Eidsmo, MD, PhD.
This has led to their use as biomarkers in clinical trials for new therapies, but TRM T cells have a complex biology that is far from fully understood, Dr. Eidsmo said at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis. “With time, we’re understanding that the regulation of the functionality is more complicated than we thought, so following these cells as a positive outcome of a clinical trial is a little bit premature,” said Dr. Eidsmo, who is a consultant dermatologist at the University of Copenhagen, Copenhagen, Denmark.
Treatment strategies focus on inhibition of interleukin (IL)-23, which is an activator of TRM T cells and probably keeps them alive, according to Dr. Eidsmo. “The hope is that these cells can be silenced by IL-23 inhibition, which is a great idea, and it probably works. It’s just a matter of what is the readout of long-term remission, because the big challenge in the clinical world is when do we stop these expensive biological treatments? When can we feel secure that patients are in deep remission?” she asked.
TRM cells are also far from the only immune cells involved in psoriasis. Others include keratinocytes, Langerhans cells, and fibroblasts. Dr. Eidsmo referenced a recent spatial analysis that used single-cell and spatial RNA sequencing to identify the localization of specific cell populations and inflammatory pathways within psoriasis lesions and epidermal compartments as well as also suggested crosstalk links between cell types. Epigenetic changes in stem cells may also maintain a lower threshold for tissue inflammation.
Dr. Eidsmo advised caution in eliminating TRM T cells, which play a key role in protecting against melanoma and other cancers, especially later in life. “We don’t want to get rid of them. We want to have the right balance.”
She noted a study in her own lab that mapped TRM T cells in healthy epidermis and found that they could be renewed from both circulating precursors and cells within the epidermis. “So getting rid of the mature TRM T cells will most likely just lead to a new generation of the same subset.”
Other data show that there are a wide range of subsets of TRM T cells, and she recommended focusing on the functionality of TRM T cells rather than sheer numbers. “This is something we’re working on now: Can we change the functionality [of TRM T cells], rather than eradicate them and hope for the best in the next generation? Can we change the functionality of the T cells we already have in the skin?”
There is also epigenetic data in TRM T cells, keratinocytes, stem cells, and other cells thus suggesting complexity and plasticity in the system that remains poorly understood.
Taken together, the research is at too early of a stage to be clinically useful, said Dr. Eidsmo. “We need to go back to the drawing board and just realize what we need to measure, and with the new techniques coming out, maybe spatial [measurement] at a high resolution, we can find biomarkers that better dictate the future of this. Be a little bit wary when you read the outcomes from the clinical trials that are ongoing, because right now, it’s a bit of a race between different biologics. These cells are used as a readout of efficacy of the treatments, and we’re not quite there yet.”
During the Q&A session after the presentation, one audience member asked about the heterogeneity of cells found within the skin of patients with psoriasis and pointed out that many proinflammatory cells likely play a role in tumor control. Dr. Eidsmo responded that her group’s analysis of a large database of patients with metastatic melanoma found that a factor that is important to the development of TRM T cells was strongly correlated to survival in patients with metastatic melanoma receiving immune checkpoint blockade. “So we really don’t want to eradicate them,” she said.
Also during the Q&A, Iain McInnes, MD, PhD, commented about the need to understand the previous events that drove the creation of memory T cells. “For me, the question is about the hierarchy, the primacy of what really drives the memory. In the infectious world, we’re trained to think [that memory responses] are T cell driven memory, but I wonder whether you have an idea of whether the T cell is responding to other memories, particularly in the stroma. Because certainly in the arthropathies, we have really good evidence now of epigenetic change in the synovial stroma and subsets,” said Dr. McInnes, who is director of the Institute of Infection, Immunity, and Inflammation at the University of Glasgow, Glasgow, Scotland.
Dr. Eidsmo responded that she believes responses are different among different individuals. “We know too little about how these two systems interact with one another. I think the TRM T cells are very good at amplifying the stroma to recruit cells in. I think we need to think of two-step therapies. You need to normalize this [stromal] environment. How you can do that, I don’t know.”
Dr. McInnes agreed. “As a myeloid doctor, I strongly believe that perpetuators are innate and the adaptive is following on. But how do we test that? That’s really hard,” he said.
Dr. Eidsmo did not list any disclosures. Dr. McInnes has financial relationships with AbbVie, AstraZeneca, Bristol-Myers Squibb, Boehringer, Compugen, Cabaletta, Causeway, Dextera, Eli Lilly, Celgene, MoonLake, Pfizer, Novartis, Janssen, Roche, Versus Arthritis, MRC, and UCB.
SEATTLE — In fact, flare-ups often recur at the same site, a phenomenon that might be driven by these resident memory cells, according to Liv Eidsmo, MD, PhD.
This has led to their use as biomarkers in clinical trials for new therapies, but TRM T cells have a complex biology that is far from fully understood, Dr. Eidsmo said at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis. “With time, we’re understanding that the regulation of the functionality is more complicated than we thought, so following these cells as a positive outcome of a clinical trial is a little bit premature,” said Dr. Eidsmo, who is a consultant dermatologist at the University of Copenhagen, Copenhagen, Denmark.
Treatment strategies focus on inhibition of interleukin (IL)-23, which is an activator of TRM T cells and probably keeps them alive, according to Dr. Eidsmo. “The hope is that these cells can be silenced by IL-23 inhibition, which is a great idea, and it probably works. It’s just a matter of what is the readout of long-term remission, because the big challenge in the clinical world is when do we stop these expensive biological treatments? When can we feel secure that patients are in deep remission?” she asked.
TRM cells are also far from the only immune cells involved in psoriasis. Others include keratinocytes, Langerhans cells, and fibroblasts. Dr. Eidsmo referenced a recent spatial analysis that used single-cell and spatial RNA sequencing to identify the localization of specific cell populations and inflammatory pathways within psoriasis lesions and epidermal compartments as well as also suggested crosstalk links between cell types. Epigenetic changes in stem cells may also maintain a lower threshold for tissue inflammation.
Dr. Eidsmo advised caution in eliminating TRM T cells, which play a key role in protecting against melanoma and other cancers, especially later in life. “We don’t want to get rid of them. We want to have the right balance.”
She noted a study in her own lab that mapped TRM T cells in healthy epidermis and found that they could be renewed from both circulating precursors and cells within the epidermis. “So getting rid of the mature TRM T cells will most likely just lead to a new generation of the same subset.”
Other data show that there are a wide range of subsets of TRM T cells, and she recommended focusing on the functionality of TRM T cells rather than sheer numbers. “This is something we’re working on now: Can we change the functionality [of TRM T cells], rather than eradicate them and hope for the best in the next generation? Can we change the functionality of the T cells we already have in the skin?”
There is also epigenetic data in TRM T cells, keratinocytes, stem cells, and other cells thus suggesting complexity and plasticity in the system that remains poorly understood.
Taken together, the research is at too early of a stage to be clinically useful, said Dr. Eidsmo. “We need to go back to the drawing board and just realize what we need to measure, and with the new techniques coming out, maybe spatial [measurement] at a high resolution, we can find biomarkers that better dictate the future of this. Be a little bit wary when you read the outcomes from the clinical trials that are ongoing, because right now, it’s a bit of a race between different biologics. These cells are used as a readout of efficacy of the treatments, and we’re not quite there yet.”
During the Q&A session after the presentation, one audience member asked about the heterogeneity of cells found within the skin of patients with psoriasis and pointed out that many proinflammatory cells likely play a role in tumor control. Dr. Eidsmo responded that her group’s analysis of a large database of patients with metastatic melanoma found that a factor that is important to the development of TRM T cells was strongly correlated to survival in patients with metastatic melanoma receiving immune checkpoint blockade. “So we really don’t want to eradicate them,” she said.
Also during the Q&A, Iain McInnes, MD, PhD, commented about the need to understand the previous events that drove the creation of memory T cells. “For me, the question is about the hierarchy, the primacy of what really drives the memory. In the infectious world, we’re trained to think [that memory responses] are T cell driven memory, but I wonder whether you have an idea of whether the T cell is responding to other memories, particularly in the stroma. Because certainly in the arthropathies, we have really good evidence now of epigenetic change in the synovial stroma and subsets,” said Dr. McInnes, who is director of the Institute of Infection, Immunity, and Inflammation at the University of Glasgow, Glasgow, Scotland.
Dr. Eidsmo responded that she believes responses are different among different individuals. “We know too little about how these two systems interact with one another. I think the TRM T cells are very good at amplifying the stroma to recruit cells in. I think we need to think of two-step therapies. You need to normalize this [stromal] environment. How you can do that, I don’t know.”
Dr. McInnes agreed. “As a myeloid doctor, I strongly believe that perpetuators are innate and the adaptive is following on. But how do we test that? That’s really hard,” he said.
Dr. Eidsmo did not list any disclosures. Dr. McInnes has financial relationships with AbbVie, AstraZeneca, Bristol-Myers Squibb, Boehringer, Compugen, Cabaletta, Causeway, Dextera, Eli Lilly, Celgene, MoonLake, Pfizer, Novartis, Janssen, Roche, Versus Arthritis, MRC, and UCB.
SEATTLE — In fact, flare-ups often recur at the same site, a phenomenon that might be driven by these resident memory cells, according to Liv Eidsmo, MD, PhD.
This has led to their use as biomarkers in clinical trials for new therapies, but TRM T cells have a complex biology that is far from fully understood, Dr. Eidsmo said at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis. “With time, we’re understanding that the regulation of the functionality is more complicated than we thought, so following these cells as a positive outcome of a clinical trial is a little bit premature,” said Dr. Eidsmo, who is a consultant dermatologist at the University of Copenhagen, Copenhagen, Denmark.
Treatment strategies focus on inhibition of interleukin (IL)-23, which is an activator of TRM T cells and probably keeps them alive, according to Dr. Eidsmo. “The hope is that these cells can be silenced by IL-23 inhibition, which is a great idea, and it probably works. It’s just a matter of what is the readout of long-term remission, because the big challenge in the clinical world is when do we stop these expensive biological treatments? When can we feel secure that patients are in deep remission?” she asked.
TRM cells are also far from the only immune cells involved in psoriasis. Others include keratinocytes, Langerhans cells, and fibroblasts. Dr. Eidsmo referenced a recent spatial analysis that used single-cell and spatial RNA sequencing to identify the localization of specific cell populations and inflammatory pathways within psoriasis lesions and epidermal compartments as well as also suggested crosstalk links between cell types. Epigenetic changes in stem cells may also maintain a lower threshold for tissue inflammation.
Dr. Eidsmo advised caution in eliminating TRM T cells, which play a key role in protecting against melanoma and other cancers, especially later in life. “We don’t want to get rid of them. We want to have the right balance.”
She noted a study in her own lab that mapped TRM T cells in healthy epidermis and found that they could be renewed from both circulating precursors and cells within the epidermis. “So getting rid of the mature TRM T cells will most likely just lead to a new generation of the same subset.”
Other data show that there are a wide range of subsets of TRM T cells, and she recommended focusing on the functionality of TRM T cells rather than sheer numbers. “This is something we’re working on now: Can we change the functionality [of TRM T cells], rather than eradicate them and hope for the best in the next generation? Can we change the functionality of the T cells we already have in the skin?”
There is also epigenetic data in TRM T cells, keratinocytes, stem cells, and other cells thus suggesting complexity and plasticity in the system that remains poorly understood.
Taken together, the research is at too early of a stage to be clinically useful, said Dr. Eidsmo. “We need to go back to the drawing board and just realize what we need to measure, and with the new techniques coming out, maybe spatial [measurement] at a high resolution, we can find biomarkers that better dictate the future of this. Be a little bit wary when you read the outcomes from the clinical trials that are ongoing, because right now, it’s a bit of a race between different biologics. These cells are used as a readout of efficacy of the treatments, and we’re not quite there yet.”
During the Q&A session after the presentation, one audience member asked about the heterogeneity of cells found within the skin of patients with psoriasis and pointed out that many proinflammatory cells likely play a role in tumor control. Dr. Eidsmo responded that her group’s analysis of a large database of patients with metastatic melanoma found that a factor that is important to the development of TRM T cells was strongly correlated to survival in patients with metastatic melanoma receiving immune checkpoint blockade. “So we really don’t want to eradicate them,” she said.
Also during the Q&A, Iain McInnes, MD, PhD, commented about the need to understand the previous events that drove the creation of memory T cells. “For me, the question is about the hierarchy, the primacy of what really drives the memory. In the infectious world, we’re trained to think [that memory responses] are T cell driven memory, but I wonder whether you have an idea of whether the T cell is responding to other memories, particularly in the stroma. Because certainly in the arthropathies, we have really good evidence now of epigenetic change in the synovial stroma and subsets,” said Dr. McInnes, who is director of the Institute of Infection, Immunity, and Inflammation at the University of Glasgow, Glasgow, Scotland.
Dr. Eidsmo responded that she believes responses are different among different individuals. “We know too little about how these two systems interact with one another. I think the TRM T cells are very good at amplifying the stroma to recruit cells in. I think we need to think of two-step therapies. You need to normalize this [stromal] environment. How you can do that, I don’t know.”
Dr. McInnes agreed. “As a myeloid doctor, I strongly believe that perpetuators are innate and the adaptive is following on. But how do we test that? That’s really hard,” he said.
Dr. Eidsmo did not list any disclosures. Dr. McInnes has financial relationships with AbbVie, AstraZeneca, Bristol-Myers Squibb, Boehringer, Compugen, Cabaletta, Causeway, Dextera, Eli Lilly, Celgene, MoonLake, Pfizer, Novartis, Janssen, Roche, Versus Arthritis, MRC, and UCB.
FROM GRAPPA 2024
Cyclosporine for Recalcitrant Bullous Pemphigoid Induced by Nivolumab Therapy for Malignant Melanoma
To the Editor:
Immune checkpoint inhibitors have revolutionized the treatment of advanced-stage melanoma, with remarkably improved progression-free survival.1 Anti–programmed death receptor 1 (anti–PD-1) therapies, such as nivolumab and pembrolizumab, are a class of checkpoint inhibitors that have been approved by the US Food and Drug Administration for unresectable metastatic melanoma. Anti–PD-1 agents block the interaction of programmed death-ligand 1 (PD-L1) found on tumor cells with the PD-1 receptor on T cells, facilitating a positive immune response.2
Although these therapies have demonstrated notable antitumor efficacy, they also give rise to numerous immune-related adverse events (irAEs). As many as 70% of patients treated with PD-1/PD-L1 inhibitors experience some type of organ system irAE, of which 30% to 40% are cutaneous.3-6 Dermatologic adverse events are the most common irAEs, specifically spongiotic dermatitis, lichenoid dermatitis, pruritus, and vitiligo.7 Bullous pemphigoid (BP), an autoimmune bullous skin disorder caused by autoantibodies to basement membrane zone antigens, is a rare but potentially serious cutaneous irAE.8 Systemic corticosteroids commonly are used to treat immune checkpoint inhibitor–induced BP; other options include tetracyclines for maintenance therapy and rituximab for corticosteroid-refractory BP associated with anti-PD-1.9 We present a case of recalcitrant BP secondary to nivolumab therapy in a patient with metastatic melanoma who had near-complete resolution of BP following 2 months of cyclosporine.
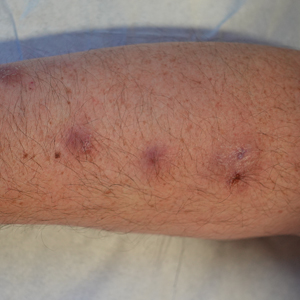
A 41-year-old man presented with a generalized papular skin eruption of 1 month’s duration. He had a history of stage IIIC malignant melanoma of the lower right leg with positive sentinel lymph node biopsy. The largest lymph node deposit was 0.03 mm without extracapsular extension. Whole-body positron emission tomography–computed tomography showed no evidence of distant disease. The patient was treated with wide local excision with clear surgical margins plus 12 cycles of nivolumab, which was discontinued due to colitis. Four months after the final cycle of nivolumab, the patient developed widespread erythematous papules with hemorrhagic yellow crusting and no mucosal involvement. He was referred to dermatology by his primary oncologist for further evaluation.
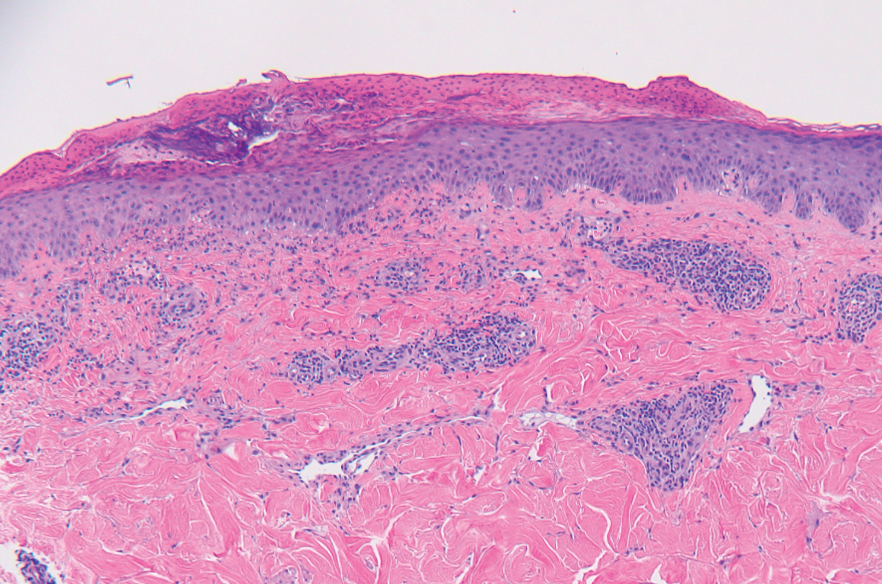
A punch biopsy from the abdomen showed parakeratosis with leukocytoclasis and a superficial dermal infiltrate of neutrophils and eosinophils (Figure 1). Direct immunofluorescence revealed linear basement membrane deposits of IgG and C3, consistent with subepidermal blistering disease. Indirect immunofluorescence demonstrated trace IgG and IgG4 antibodies localized to the epidermal roof of salt-split skin and was negative for IgA antibodies. An enzyme-linked immunoassay was positive for BP antigen 2 (BP180) antibodies (98.4 U/mL [positive, ≥9 U/mL]) and negative for BP antigen 1 (BP230) antibodies (4.3 U/mL [positive, ≥9 U/mL]). Overall, these findings were consistent with a diagnosis of BP.
The patient was treated with prednisone 60 mg daily with initial response; however, there was disease recurrence with tapering. Doxycycline 100 mg twice daily and nicotinamide 500 mg twice daily were added as steroid-sparing agents, as prednisone was discontinued due to mood changes. Three months after the prednisone taper, the patient continued to develop new blisters. He completed treatment with doxycycline and nicotinamide. Rituximab 375 mg weekly was then initiated for 4 weeks.
At 2-week follow-up after completing the rituximab course, the patient reported worsening symptoms and presented with new bullae on the abdomen and upper extremities (Figure 2). Because of the recent history of mood changes while taking prednisone, a trial of cyclosporine 100 mg twice daily (1.37 mg/kg/d) was initiated, with notable improvement within 2 weeks of treatment. After 2 months of cyclosporine, approximately 90% of the rash had resolved with a few tense bullae remaining on the left frontal scalp but no new flares (Figure 3). One month after treatment ended, the patient remained clear of lesions without relapse.
Programmed death receptor 1 inhibitors have shown dramatic efficacy for a growing number of solid and hematologic malignancies, especially malignant melanoma. However, their use is accompanied by nonspecific activation of the immune system, resulting in a variety of adverse events, many manifesting on the skin. Several cases of BP in patients treated with PD-1/PD-L1 inhibitors have been reported.9 Cutaneous irAEs usually manifest within 3 weeks of initiation of PD-1 inhibitor therapy; however, the onset of BP typically occurs later at approximately 21 weeks.4,9 Our patient developed cutaneous manifestations 4 months after cessation of nivolumab.


Bullous pemphigoid classically manifests with pruritus and tense bullae. Notably, our patient’s clinical presentation included a widespread eruption of papules without bullae, which was similar to a review by Tsiogka et al,9 which reported that one-third of patients first present with a nonspecific cutaneous eruption. Bullous pemphigoid induced by anti–PD-1 may manifest differently than traditional BP, illuminating the importance of a thorough diagnostic workup.
Although the pathogenesis of immune checkpoint inhibitor–induced BP has not been fully elucidated, it is hypothesized to be caused by increased T cell cytotoxic activity leading to tumor lysis and release of numerous autoantigens. These autoantigens cause priming of abnormal T cells that can lead to further tissue damage in peripheral tissue and to generation of aberrant B cells and subsequent autoantibodies such as BP180 in germinal centers.4,10,11
Cyclosporine is a calcineurin inhibitor that reduces synthesis of IL-2, resulting in reduced cell activation.12 Therefore, cyclosporine may alleviate BP in patients who are being treated, or were previously treated, with an immune checkpoint inhibitor by suppressing T cell–mediated immune reaction and may be a rapid alternative for patients who cannot tolerate systemic steroids.
Treatment options for mild to moderate cases of BP include topical corticosteroids and antihistamines, while severe cases may require high-dose systemic corticosteroids. In recalcitrant cases, rituximab infusion with or without intravenous immunoglobulin often is utilized.8,13 The use of cyclosporine for various bullous disorders, including pemphigus vulgaris and epidermolysis bullosa acquisita, has been described.14 In recent years there has been a shift away from the use of cyclosporine for these conditions following the introduction of rituximab, a monoclonal antibody directed against the CD20 antigen on B lymphocytes. We utilized cyclosporine in our patient after he experienced worsening symptoms 1 month after completing treatment with rituximab.
Improvement from rituximab therapy may be delayed because it can take months to deplete CD20+ B lymphocytes from circulation, which may necessitate additional immunosuppressants or re-treatment with rituximab.15,16 In these instances, cyclosporine may be beneficial as a low-cost alternative in patients who are unable to tolerate systemic steroids, with a relatively good safety profile. The dosage of cyclosporine prescribed to the patient was chosen based on Joint American Academy of Dermatology–National Psoriasis Foundation management guidelines for psoriasis with systemic nonbiologic therapies, which recommends an initial dosage of 1 to 3 mg/kg/d in 2 divided doses.17
As immunotherapy for treating various cancers gains popularity, the frequency of dermatologic irAEs will increase. Therefore, dermatologists must be aware of the array of cutaneous manifestations, such as BP, and potential treatment options. When first-line and second-line therapies are contraindicated or do not provide notable improvement, cyclosporine may be an effective alternative for immune checkpoint inhibitor–induced BP.
- Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med. 2015;373:23-34. doi:10.1056/NEJMoa1504030
- Alsaab HO, Sau S, Alzhrani R, et al. PD-1 and PD-L1 checkpoint signaling inhibition for cancer immunotherapy: mechanism, combinations, and clinical outcome. Front Pharmacol. 2017;8:561. doi:10.3389/fphar.2017.00561
- Puzanov I, Diab A, Abdallah K, et al; . Managing toxicities associated with immune checkpoint inhibitors: consensus recommendations from the Society for Immunotherapy of Cancer (SITC) Toxicity Management Working Group. J Immunother Cancer. 2017;5:95. doi:10.1186/s40425-017-0300-z
- Geisler AN, Phillips GS, Barrios DM, et al. Immune checkpoint inhibitor-related dermatologic adverse events. J Am Acad Dermatol. 2020;83:1255-1268. doi:10.1016/j.jaad.2020.03.132
- Villadolid J, Amin A. Immune checkpoint inhibitors in clinical practice: update on management of immune-related toxicities. Transl Lung Cancer Res. 2015;4:560-575. doi:10.3978/j.issn.2218-6751.2015.06.06
- Kumar V, Chaudhary N, Garg M, et al. Current diagnosis and management of immune related adverse events (irAEs) induced by immune checkpoint inhibitor therapy. Front Pharmacol. 2017;8:49. doi:10.3389/fphar.2017.00049
- Belum VR, Benhuri B, Postow MA, et al. Characterisation and management of dermatologic adverse events to agents targeting the PD-1 receptor. Eur J Cancer. 2016;60:12-25. doi:10.1016/j.ejca.2016.02.010
- Schauer F, Rafei-Shamsabadi D, Mai S, et al. Hemidesmosomal reactivity and treatment recommendations in immune checkpoint inhibitor-induced bullous pemphigoid—a retrospective, monocentric study. Front Immunol. 2022;13:953546. doi:10.3389/fimmu.2022.953546
- Tsiogka A, Bauer JW, Patsatsi A. Bullous pemphigoid associated with anti-programmed cell death protein 1 and anti-programmed cell death ligand 1 therapy: a review of the literature. Acta Derm Venereol. 2021;101:adv00377. doi:10.2340/00015555-3740
- Lopez AT, Khanna T, Antonov N, et al. A review of bullous pemphigoid associated with PD-1 and PD-L1 inhibitors. Int J Dermatol. 2018;57:664-669. doi:10.1111/ijd.13984
- Yang H, Yao Z, Zhou X, et al. Immune-related adverse events of checkpoint inhibitors: insights into immunological dysregulation. Clin Immunol. 2020;213:108377. doi:10.1016/j.clim.2020.108377
- Russell G, Graveley R, Seid J, et al. Mechanisms of action of cyclosporine and effects on connective tissues. Semin Arthritis Rheum. 1992;21(6 suppl 3):16-22. doi:10.1016/0049-0172(92)90009-3
- Ahmed AR, Shetty S, Kaveri S, et al. Treatment of recalcitrant bullous pemphigoid (BP) with a novel protocol: a retrospective study with a 6-year follow-up. J Am Acad Dermatol. 2016;74:700-708.e3. doi:10.1016/j.jaad.2015.11.030
- Amor KT, Ryan C, Menter A. The use of cyclosporine in dermatology: part I. J Am Acad Dermatol. 2010;63:925-946. doi:10.1016/j.jaad.2010.02.063
- Schmidt E, Hunzelmann N, Zillikens D, et al. Rituximab in refractory autoimmune bullous diseases. Clin Exp Dermatol. 2006;31:503-508. doi:10.1111/j.1365-2230.2006.02151.x
- Kasperkiewicz M, Shimanovich I, Ludwig RJ, et al. Rituximab for treatment-refractory pemphigus and pemphigoid: a case series of 17 patients. J Am Acad Dermatol. 2011;65:552-558.
- Menter A, Gelfand JM, Connor C, et al. Joint American Academy of Dermatology–National Psoriasis Foundation guidelines of care for the management of psoriasis with systemic nonbiologic therapies. J Am Acad Dermatol. 2020;82:1445-1486. doi:10.1016/j.jaad.2020.02.044
To the Editor:
Immune checkpoint inhibitors have revolutionized the treatment of advanced-stage melanoma, with remarkably improved progression-free survival.1 Anti–programmed death receptor 1 (anti–PD-1) therapies, such as nivolumab and pembrolizumab, are a class of checkpoint inhibitors that have been approved by the US Food and Drug Administration for unresectable metastatic melanoma. Anti–PD-1 agents block the interaction of programmed death-ligand 1 (PD-L1) found on tumor cells with the PD-1 receptor on T cells, facilitating a positive immune response.2
Although these therapies have demonstrated notable antitumor efficacy, they also give rise to numerous immune-related adverse events (irAEs). As many as 70% of patients treated with PD-1/PD-L1 inhibitors experience some type of organ system irAE, of which 30% to 40% are cutaneous.3-6 Dermatologic adverse events are the most common irAEs, specifically spongiotic dermatitis, lichenoid dermatitis, pruritus, and vitiligo.7 Bullous pemphigoid (BP), an autoimmune bullous skin disorder caused by autoantibodies to basement membrane zone antigens, is a rare but potentially serious cutaneous irAE.8 Systemic corticosteroids commonly are used to treat immune checkpoint inhibitor–induced BP; other options include tetracyclines for maintenance therapy and rituximab for corticosteroid-refractory BP associated with anti-PD-1.9 We present a case of recalcitrant BP secondary to nivolumab therapy in a patient with metastatic melanoma who had near-complete resolution of BP following 2 months of cyclosporine.
A 41-year-old man presented with a generalized papular skin eruption of 1 month’s duration. He had a history of stage IIIC malignant melanoma of the lower right leg with positive sentinel lymph node biopsy. The largest lymph node deposit was 0.03 mm without extracapsular extension. Whole-body positron emission tomography–computed tomography showed no evidence of distant disease. The patient was treated with wide local excision with clear surgical margins plus 12 cycles of nivolumab, which was discontinued due to colitis. Four months after the final cycle of nivolumab, the patient developed widespread erythematous papules with hemorrhagic yellow crusting and no mucosal involvement. He was referred to dermatology by his primary oncologist for further evaluation.
A punch biopsy from the abdomen showed parakeratosis with leukocytoclasis and a superficial dermal infiltrate of neutrophils and eosinophils (Figure 1). Direct immunofluorescence revealed linear basement membrane deposits of IgG and C3, consistent with subepidermal blistering disease. Indirect immunofluorescence demonstrated trace IgG and IgG4 antibodies localized to the epidermal roof of salt-split skin and was negative for IgA antibodies. An enzyme-linked immunoassay was positive for BP antigen 2 (BP180) antibodies (98.4 U/mL [positive, ≥9 U/mL]) and negative for BP antigen 1 (BP230) antibodies (4.3 U/mL [positive, ≥9 U/mL]). Overall, these findings were consistent with a diagnosis of BP.
The patient was treated with prednisone 60 mg daily with initial response; however, there was disease recurrence with tapering. Doxycycline 100 mg twice daily and nicotinamide 500 mg twice daily were added as steroid-sparing agents, as prednisone was discontinued due to mood changes. Three months after the prednisone taper, the patient continued to develop new blisters. He completed treatment with doxycycline and nicotinamide. Rituximab 375 mg weekly was then initiated for 4 weeks.
At 2-week follow-up after completing the rituximab course, the patient reported worsening symptoms and presented with new bullae on the abdomen and upper extremities (Figure 2). Because of the recent history of mood changes while taking prednisone, a trial of cyclosporine 100 mg twice daily (1.37 mg/kg/d) was initiated, with notable improvement within 2 weeks of treatment. After 2 months of cyclosporine, approximately 90% of the rash had resolved with a few tense bullae remaining on the left frontal scalp but no new flares (Figure 3). One month after treatment ended, the patient remained clear of lesions without relapse.
Programmed death receptor 1 inhibitors have shown dramatic efficacy for a growing number of solid and hematologic malignancies, especially malignant melanoma. However, their use is accompanied by nonspecific activation of the immune system, resulting in a variety of adverse events, many manifesting on the skin. Several cases of BP in patients treated with PD-1/PD-L1 inhibitors have been reported.9 Cutaneous irAEs usually manifest within 3 weeks of initiation of PD-1 inhibitor therapy; however, the onset of BP typically occurs later at approximately 21 weeks.4,9 Our patient developed cutaneous manifestations 4 months after cessation of nivolumab.
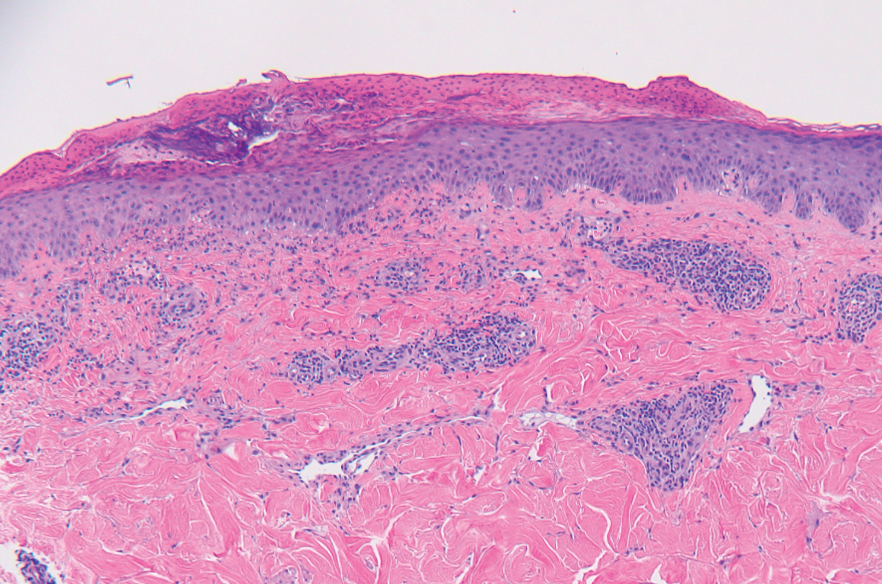


Bullous pemphigoid classically manifests with pruritus and tense bullae. Notably, our patient’s clinical presentation included a widespread eruption of papules without bullae, which was similar to a review by Tsiogka et al,9 which reported that one-third of patients first present with a nonspecific cutaneous eruption. Bullous pemphigoid induced by anti–PD-1 may manifest differently than traditional BP, illuminating the importance of a thorough diagnostic workup.
Although the pathogenesis of immune checkpoint inhibitor–induced BP has not been fully elucidated, it is hypothesized to be caused by increased T cell cytotoxic activity leading to tumor lysis and release of numerous autoantigens. These autoantigens cause priming of abnormal T cells that can lead to further tissue damage in peripheral tissue and to generation of aberrant B cells and subsequent autoantibodies such as BP180 in germinal centers.4,10,11
Cyclosporine is a calcineurin inhibitor that reduces synthesis of IL-2, resulting in reduced cell activation.12 Therefore, cyclosporine may alleviate BP in patients who are being treated, or were previously treated, with an immune checkpoint inhibitor by suppressing T cell–mediated immune reaction and may be a rapid alternative for patients who cannot tolerate systemic steroids.
Treatment options for mild to moderate cases of BP include topical corticosteroids and antihistamines, while severe cases may require high-dose systemic corticosteroids. In recalcitrant cases, rituximab infusion with or without intravenous immunoglobulin often is utilized.8,13 The use of cyclosporine for various bullous disorders, including pemphigus vulgaris and epidermolysis bullosa acquisita, has been described.14 In recent years there has been a shift away from the use of cyclosporine for these conditions following the introduction of rituximab, a monoclonal antibody directed against the CD20 antigen on B lymphocytes. We utilized cyclosporine in our patient after he experienced worsening symptoms 1 month after completing treatment with rituximab.
Improvement from rituximab therapy may be delayed because it can take months to deplete CD20+ B lymphocytes from circulation, which may necessitate additional immunosuppressants or re-treatment with rituximab.15,16 In these instances, cyclosporine may be beneficial as a low-cost alternative in patients who are unable to tolerate systemic steroids, with a relatively good safety profile. The dosage of cyclosporine prescribed to the patient was chosen based on Joint American Academy of Dermatology–National Psoriasis Foundation management guidelines for psoriasis with systemic nonbiologic therapies, which recommends an initial dosage of 1 to 3 mg/kg/d in 2 divided doses.17
As immunotherapy for treating various cancers gains popularity, the frequency of dermatologic irAEs will increase. Therefore, dermatologists must be aware of the array of cutaneous manifestations, such as BP, and potential treatment options. When first-line and second-line therapies are contraindicated or do not provide notable improvement, cyclosporine may be an effective alternative for immune checkpoint inhibitor–induced BP.
To the Editor:
Immune checkpoint inhibitors have revolutionized the treatment of advanced-stage melanoma, with remarkably improved progression-free survival.1 Anti–programmed death receptor 1 (anti–PD-1) therapies, such as nivolumab and pembrolizumab, are a class of checkpoint inhibitors that have been approved by the US Food and Drug Administration for unresectable metastatic melanoma. Anti–PD-1 agents block the interaction of programmed death-ligand 1 (PD-L1) found on tumor cells with the PD-1 receptor on T cells, facilitating a positive immune response.2
Although these therapies have demonstrated notable antitumor efficacy, they also give rise to numerous immune-related adverse events (irAEs). As many as 70% of patients treated with PD-1/PD-L1 inhibitors experience some type of organ system irAE, of which 30% to 40% are cutaneous.3-6 Dermatologic adverse events are the most common irAEs, specifically spongiotic dermatitis, lichenoid dermatitis, pruritus, and vitiligo.7 Bullous pemphigoid (BP), an autoimmune bullous skin disorder caused by autoantibodies to basement membrane zone antigens, is a rare but potentially serious cutaneous irAE.8 Systemic corticosteroids commonly are used to treat immune checkpoint inhibitor–induced BP; other options include tetracyclines for maintenance therapy and rituximab for corticosteroid-refractory BP associated with anti-PD-1.9 We present a case of recalcitrant BP secondary to nivolumab therapy in a patient with metastatic melanoma who had near-complete resolution of BP following 2 months of cyclosporine.
A 41-year-old man presented with a generalized papular skin eruption of 1 month’s duration. He had a history of stage IIIC malignant melanoma of the lower right leg with positive sentinel lymph node biopsy. The largest lymph node deposit was 0.03 mm without extracapsular extension. Whole-body positron emission tomography–computed tomography showed no evidence of distant disease. The patient was treated with wide local excision with clear surgical margins plus 12 cycles of nivolumab, which was discontinued due to colitis. Four months after the final cycle of nivolumab, the patient developed widespread erythematous papules with hemorrhagic yellow crusting and no mucosal involvement. He was referred to dermatology by his primary oncologist for further evaluation.
A punch biopsy from the abdomen showed parakeratosis with leukocytoclasis and a superficial dermal infiltrate of neutrophils and eosinophils (Figure 1). Direct immunofluorescence revealed linear basement membrane deposits of IgG and C3, consistent with subepidermal blistering disease. Indirect immunofluorescence demonstrated trace IgG and IgG4 antibodies localized to the epidermal roof of salt-split skin and was negative for IgA antibodies. An enzyme-linked immunoassay was positive for BP antigen 2 (BP180) antibodies (98.4 U/mL [positive, ≥9 U/mL]) and negative for BP antigen 1 (BP230) antibodies (4.3 U/mL [positive, ≥9 U/mL]). Overall, these findings were consistent with a diagnosis of BP.
The patient was treated with prednisone 60 mg daily with initial response; however, there was disease recurrence with tapering. Doxycycline 100 mg twice daily and nicotinamide 500 mg twice daily were added as steroid-sparing agents, as prednisone was discontinued due to mood changes. Three months after the prednisone taper, the patient continued to develop new blisters. He completed treatment with doxycycline and nicotinamide. Rituximab 375 mg weekly was then initiated for 4 weeks.
At 2-week follow-up after completing the rituximab course, the patient reported worsening symptoms and presented with new bullae on the abdomen and upper extremities (Figure 2). Because of the recent history of mood changes while taking prednisone, a trial of cyclosporine 100 mg twice daily (1.37 mg/kg/d) was initiated, with notable improvement within 2 weeks of treatment. After 2 months of cyclosporine, approximately 90% of the rash had resolved with a few tense bullae remaining on the left frontal scalp but no new flares (Figure 3). One month after treatment ended, the patient remained clear of lesions without relapse.
Programmed death receptor 1 inhibitors have shown dramatic efficacy for a growing number of solid and hematologic malignancies, especially malignant melanoma. However, their use is accompanied by nonspecific activation of the immune system, resulting in a variety of adverse events, many manifesting on the skin. Several cases of BP in patients treated with PD-1/PD-L1 inhibitors have been reported.9 Cutaneous irAEs usually manifest within 3 weeks of initiation of PD-1 inhibitor therapy; however, the onset of BP typically occurs later at approximately 21 weeks.4,9 Our patient developed cutaneous manifestations 4 months after cessation of nivolumab.
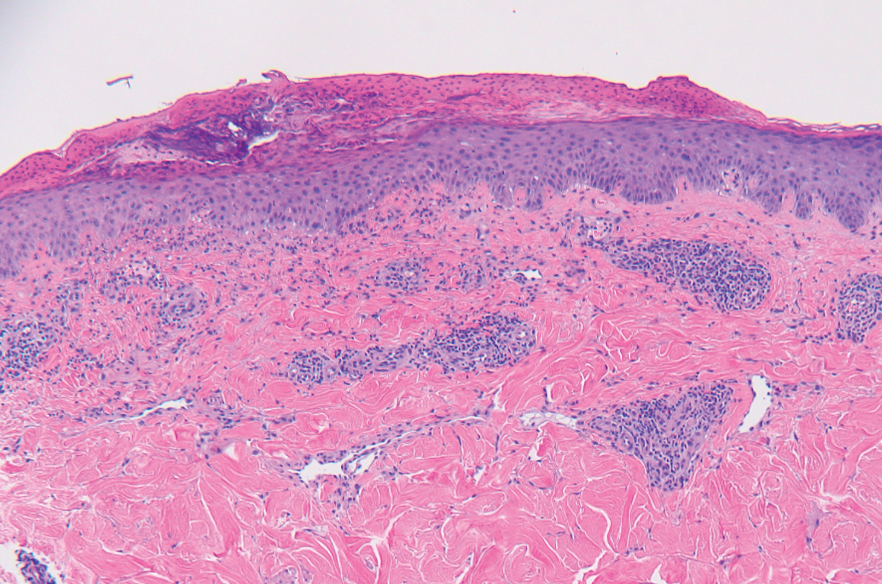


Bullous pemphigoid classically manifests with pruritus and tense bullae. Notably, our patient’s clinical presentation included a widespread eruption of papules without bullae, which was similar to a review by Tsiogka et al,9 which reported that one-third of patients first present with a nonspecific cutaneous eruption. Bullous pemphigoid induced by anti–PD-1 may manifest differently than traditional BP, illuminating the importance of a thorough diagnostic workup.
Although the pathogenesis of immune checkpoint inhibitor–induced BP has not been fully elucidated, it is hypothesized to be caused by increased T cell cytotoxic activity leading to tumor lysis and release of numerous autoantigens. These autoantigens cause priming of abnormal T cells that can lead to further tissue damage in peripheral tissue and to generation of aberrant B cells and subsequent autoantibodies such as BP180 in germinal centers.4,10,11
Cyclosporine is a calcineurin inhibitor that reduces synthesis of IL-2, resulting in reduced cell activation.12 Therefore, cyclosporine may alleviate BP in patients who are being treated, or were previously treated, with an immune checkpoint inhibitor by suppressing T cell–mediated immune reaction and may be a rapid alternative for patients who cannot tolerate systemic steroids.
Treatment options for mild to moderate cases of BP include topical corticosteroids and antihistamines, while severe cases may require high-dose systemic corticosteroids. In recalcitrant cases, rituximab infusion with or without intravenous immunoglobulin often is utilized.8,13 The use of cyclosporine for various bullous disorders, including pemphigus vulgaris and epidermolysis bullosa acquisita, has been described.14 In recent years there has been a shift away from the use of cyclosporine for these conditions following the introduction of rituximab, a monoclonal antibody directed against the CD20 antigen on B lymphocytes. We utilized cyclosporine in our patient after he experienced worsening symptoms 1 month after completing treatment with rituximab.
Improvement from rituximab therapy may be delayed because it can take months to deplete CD20+ B lymphocytes from circulation, which may necessitate additional immunosuppressants or re-treatment with rituximab.15,16 In these instances, cyclosporine may be beneficial as a low-cost alternative in patients who are unable to tolerate systemic steroids, with a relatively good safety profile. The dosage of cyclosporine prescribed to the patient was chosen based on Joint American Academy of Dermatology–National Psoriasis Foundation management guidelines for psoriasis with systemic nonbiologic therapies, which recommends an initial dosage of 1 to 3 mg/kg/d in 2 divided doses.17
As immunotherapy for treating various cancers gains popularity, the frequency of dermatologic irAEs will increase. Therefore, dermatologists must be aware of the array of cutaneous manifestations, such as BP, and potential treatment options. When first-line and second-line therapies are contraindicated or do not provide notable improvement, cyclosporine may be an effective alternative for immune checkpoint inhibitor–induced BP.
- Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med. 2015;373:23-34. doi:10.1056/NEJMoa1504030
- Alsaab HO, Sau S, Alzhrani R, et al. PD-1 and PD-L1 checkpoint signaling inhibition for cancer immunotherapy: mechanism, combinations, and clinical outcome. Front Pharmacol. 2017;8:561. doi:10.3389/fphar.2017.00561
- Puzanov I, Diab A, Abdallah K, et al; . Managing toxicities associated with immune checkpoint inhibitors: consensus recommendations from the Society for Immunotherapy of Cancer (SITC) Toxicity Management Working Group. J Immunother Cancer. 2017;5:95. doi:10.1186/s40425-017-0300-z
- Geisler AN, Phillips GS, Barrios DM, et al. Immune checkpoint inhibitor-related dermatologic adverse events. J Am Acad Dermatol. 2020;83:1255-1268. doi:10.1016/j.jaad.2020.03.132
- Villadolid J, Amin A. Immune checkpoint inhibitors in clinical practice: update on management of immune-related toxicities. Transl Lung Cancer Res. 2015;4:560-575. doi:10.3978/j.issn.2218-6751.2015.06.06
- Kumar V, Chaudhary N, Garg M, et al. Current diagnosis and management of immune related adverse events (irAEs) induced by immune checkpoint inhibitor therapy. Front Pharmacol. 2017;8:49. doi:10.3389/fphar.2017.00049
- Belum VR, Benhuri B, Postow MA, et al. Characterisation and management of dermatologic adverse events to agents targeting the PD-1 receptor. Eur J Cancer. 2016;60:12-25. doi:10.1016/j.ejca.2016.02.010
- Schauer F, Rafei-Shamsabadi D, Mai S, et al. Hemidesmosomal reactivity and treatment recommendations in immune checkpoint inhibitor-induced bullous pemphigoid—a retrospective, monocentric study. Front Immunol. 2022;13:953546. doi:10.3389/fimmu.2022.953546
- Tsiogka A, Bauer JW, Patsatsi A. Bullous pemphigoid associated with anti-programmed cell death protein 1 and anti-programmed cell death ligand 1 therapy: a review of the literature. Acta Derm Venereol. 2021;101:adv00377. doi:10.2340/00015555-3740
- Lopez AT, Khanna T, Antonov N, et al. A review of bullous pemphigoid associated with PD-1 and PD-L1 inhibitors. Int J Dermatol. 2018;57:664-669. doi:10.1111/ijd.13984
- Yang H, Yao Z, Zhou X, et al. Immune-related adverse events of checkpoint inhibitors: insights into immunological dysregulation. Clin Immunol. 2020;213:108377. doi:10.1016/j.clim.2020.108377
- Russell G, Graveley R, Seid J, et al. Mechanisms of action of cyclosporine and effects on connective tissues. Semin Arthritis Rheum. 1992;21(6 suppl 3):16-22. doi:10.1016/0049-0172(92)90009-3
- Ahmed AR, Shetty S, Kaveri S, et al. Treatment of recalcitrant bullous pemphigoid (BP) with a novel protocol: a retrospective study with a 6-year follow-up. J Am Acad Dermatol. 2016;74:700-708.e3. doi:10.1016/j.jaad.2015.11.030
- Amor KT, Ryan C, Menter A. The use of cyclosporine in dermatology: part I. J Am Acad Dermatol. 2010;63:925-946. doi:10.1016/j.jaad.2010.02.063
- Schmidt E, Hunzelmann N, Zillikens D, et al. Rituximab in refractory autoimmune bullous diseases. Clin Exp Dermatol. 2006;31:503-508. doi:10.1111/j.1365-2230.2006.02151.x
- Kasperkiewicz M, Shimanovich I, Ludwig RJ, et al. Rituximab for treatment-refractory pemphigus and pemphigoid: a case series of 17 patients. J Am Acad Dermatol. 2011;65:552-558.
- Menter A, Gelfand JM, Connor C, et al. Joint American Academy of Dermatology–National Psoriasis Foundation guidelines of care for the management of psoriasis with systemic nonbiologic therapies. J Am Acad Dermatol. 2020;82:1445-1486. doi:10.1016/j.jaad.2020.02.044
- Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med. 2015;373:23-34. doi:10.1056/NEJMoa1504030
- Alsaab HO, Sau S, Alzhrani R, et al. PD-1 and PD-L1 checkpoint signaling inhibition for cancer immunotherapy: mechanism, combinations, and clinical outcome. Front Pharmacol. 2017;8:561. doi:10.3389/fphar.2017.00561
- Puzanov I, Diab A, Abdallah K, et al; . Managing toxicities associated with immune checkpoint inhibitors: consensus recommendations from the Society for Immunotherapy of Cancer (SITC) Toxicity Management Working Group. J Immunother Cancer. 2017;5:95. doi:10.1186/s40425-017-0300-z
- Geisler AN, Phillips GS, Barrios DM, et al. Immune checkpoint inhibitor-related dermatologic adverse events. J Am Acad Dermatol. 2020;83:1255-1268. doi:10.1016/j.jaad.2020.03.132
- Villadolid J, Amin A. Immune checkpoint inhibitors in clinical practice: update on management of immune-related toxicities. Transl Lung Cancer Res. 2015;4:560-575. doi:10.3978/j.issn.2218-6751.2015.06.06
- Kumar V, Chaudhary N, Garg M, et al. Current diagnosis and management of immune related adverse events (irAEs) induced by immune checkpoint inhibitor therapy. Front Pharmacol. 2017;8:49. doi:10.3389/fphar.2017.00049
- Belum VR, Benhuri B, Postow MA, et al. Characterisation and management of dermatologic adverse events to agents targeting the PD-1 receptor. Eur J Cancer. 2016;60:12-25. doi:10.1016/j.ejca.2016.02.010
- Schauer F, Rafei-Shamsabadi D, Mai S, et al. Hemidesmosomal reactivity and treatment recommendations in immune checkpoint inhibitor-induced bullous pemphigoid—a retrospective, monocentric study. Front Immunol. 2022;13:953546. doi:10.3389/fimmu.2022.953546
- Tsiogka A, Bauer JW, Patsatsi A. Bullous pemphigoid associated with anti-programmed cell death protein 1 and anti-programmed cell death ligand 1 therapy: a review of the literature. Acta Derm Venereol. 2021;101:adv00377. doi:10.2340/00015555-3740
- Lopez AT, Khanna T, Antonov N, et al. A review of bullous pemphigoid associated with PD-1 and PD-L1 inhibitors. Int J Dermatol. 2018;57:664-669. doi:10.1111/ijd.13984
- Yang H, Yao Z, Zhou X, et al. Immune-related adverse events of checkpoint inhibitors: insights into immunological dysregulation. Clin Immunol. 2020;213:108377. doi:10.1016/j.clim.2020.108377
- Russell G, Graveley R, Seid J, et al. Mechanisms of action of cyclosporine and effects on connective tissues. Semin Arthritis Rheum. 1992;21(6 suppl 3):16-22. doi:10.1016/0049-0172(92)90009-3
- Ahmed AR, Shetty S, Kaveri S, et al. Treatment of recalcitrant bullous pemphigoid (BP) with a novel protocol: a retrospective study with a 6-year follow-up. J Am Acad Dermatol. 2016;74:700-708.e3. doi:10.1016/j.jaad.2015.11.030
- Amor KT, Ryan C, Menter A. The use of cyclosporine in dermatology: part I. J Am Acad Dermatol. 2010;63:925-946. doi:10.1016/j.jaad.2010.02.063
- Schmidt E, Hunzelmann N, Zillikens D, et al. Rituximab in refractory autoimmune bullous diseases. Clin Exp Dermatol. 2006;31:503-508. doi:10.1111/j.1365-2230.2006.02151.x
- Kasperkiewicz M, Shimanovich I, Ludwig RJ, et al. Rituximab for treatment-refractory pemphigus and pemphigoid: a case series of 17 patients. J Am Acad Dermatol. 2011;65:552-558.
- Menter A, Gelfand JM, Connor C, et al. Joint American Academy of Dermatology–National Psoriasis Foundation guidelines of care for the management of psoriasis with systemic nonbiologic therapies. J Am Acad Dermatol. 2020;82:1445-1486. doi:10.1016/j.jaad.2020.02.044
Practice Points
- Bullous pemphigoid is a rare dermatologic immune-related adverse event that can occur secondary to anti–programmed death receptor 1 therapy.
- For cases of immune checkpoint inhibitor–induced bullous pemphigoid that are recalcitrant to corticosteroids and rituximab, cyclosporine might be an effective alternative.
Study Finds Varying Skin Cancer Rates Based on Sexual Orientation
Addressing dynamics of each SM subgroup will require increasingly tailored prevention, screening, and research efforts, the study authors said.
“We identified specific subgroups within the sexual minority community who are at higher risk for skin cancer, specifically White gay males and Hispanic and non-Hispanic Black SM men and women — particularly individuals who identify as bisexual,” senior author Matthew Mansh, MD, said in an interview. He is an assistant professor of dermatology at the University of California, San Francisco. The study was published online in JAMA Dermatology.
Using data of adults in the US general population from the Behavioral Risk Factor Surveillance System from January 2014 to December 2021, investigators included more than 1.5 million respondents. The proportions of SM women and men (who self-identified as bisexual, lesbian, gay, “something else,” or other) were 2.6% and 2.0%, respectively.
Lifetime skin cancer prevalence was higher among SM men than among heterosexual men (7.4% vs 6.8%; adjusted odds ratio [aOR], 1.16). In analyses stratified by racial and ethnic group, AORs for non-Hispanic Black and Hispanic SM men vs their heterosexual counterparts were 2.18 and 3.81, respectively. The corresponding figures for non-Hispanic Black and Hispanic SM women were 2.33 and 2.46, respectively.
When investigators combined all minority respondents along gender lines, lifetime skin cancer prevalence was higher in bisexual men (aOR, 3.94), bisexual women (aOR, 1.51), and women identifying as something else or other (aOR, 2.70) than in their heterosexual peers.
“I wasn’t expecting that Hispanic or non-Hispanic Black SMs would be at higher risk for skin cancer,” Dr. Mansh said. Even if these groups have more behavioral risk factors for UV radiation (UVR) exposure, he explained, UVR exposure is less strongly linked with skin cancer in darker skin than in lighter skin. Reasons for the counterintuitive finding could include different screening habits among SM people of different racial and ethnic groups, he said, and analyzing such factors will require further research.
Although some effect sizes were modest, the authors wrote, their findings may have important implications for population-based research and public health efforts aimed at early skin cancer detection and prevention. Presently, the United States lacks established guidelines for skin cancer screening. In a 2023 statement published in JAMA, the US Preventive Services Task Force said that there is insufficient evidence to determine the benefit-harm balance of skin cancer screening in asymptomatic people.
“So there has been a lot of recent talk and a need to identify which subset groups of patients might be higher risk for skin cancer and might benefit from more screening,” Dr. Mansh said in an interview. “Understanding more about the high-risk demographic and clinical features that predispose someone to skin cancer helps identify these high-risk populations that could be used to develop better screening guidelines.”
Identifying groups at a higher risk for skin cancer also allows experts to design more targeted counseling or public health interventions focused on these groups, Dr. Mansh added. Absent screening guidelines, experts emphasize changing modifiable risk factors such as UVR exposure, smoking, and alcohol use. “And we know that the message that might change behaviors in a cisgender heterosexual man might be different than in a gay White male or a Hispanic bisexual male.”
A 2017 review showed that interventions to reduce behaviors involving UVR exposure, such as indoor tanning, among young cisgender women focused largely on aging and appearance-based concerns. A 2019 study showed that messages focused on avoiding skin cancer may help motivate SM men to reduce tanning behaviors.
Furthermore, said Dr. Mansh, all electronic health record products available in the United States must provide data fields for sexual orientation. “I don’t believe many dermatologists, depending on the setting, collect that information routinely. Integrating sexual orientation and/or gender identity data into patient intake forms so that it can be integrated into the electronic health record is probably very helpful, not only for your clinical practice but also for future research studies.”
Asked to comment on the results, Rebecca I. Hartman, MD, MPH, who was not involved with the study, said that its impact on clinical practice will be challenging to ascertain. She is chief of dermatology with the VA Boston Healthcare System, assistant professor of dermatology at Harvard Medical School, and director of melanoma epidemiology at Brigham and Women’s Hospital, all in Boston, Massachusetts.
“The study found significant adjusted odds ratios,” Dr. Hartman explained, “but for some of the different populations, the overall lifetime rate of skin cancer is still quite low.” For example, 1.0% for SM non-Hispanic Black men or a difference of 2.1% vs 1.8% in SM Hispanic women. “Thus, I am not sure specific screening recommendations are warranted, although some populations, such as Hispanic sexual minority males, seemed to have a much higher risk (3.8-fold on adjusted analysis) that warrants further investigation.”
For now, she advised assessing patients’ risks for skin cancer based on well-established risk factors such as sun exposure/indoor tanning, skin phototype, immunosuppression, and age.
Dr. Mansh reported no relevant conflicts or funding sources for the study. Dr. Hartman reported no relevant conflicts.
A version of this article appeared on Medscape.com.
Addressing dynamics of each SM subgroup will require increasingly tailored prevention, screening, and research efforts, the study authors said.
“We identified specific subgroups within the sexual minority community who are at higher risk for skin cancer, specifically White gay males and Hispanic and non-Hispanic Black SM men and women — particularly individuals who identify as bisexual,” senior author Matthew Mansh, MD, said in an interview. He is an assistant professor of dermatology at the University of California, San Francisco. The study was published online in JAMA Dermatology.
Using data of adults in the US general population from the Behavioral Risk Factor Surveillance System from January 2014 to December 2021, investigators included more than 1.5 million respondents. The proportions of SM women and men (who self-identified as bisexual, lesbian, gay, “something else,” or other) were 2.6% and 2.0%, respectively.
Lifetime skin cancer prevalence was higher among SM men than among heterosexual men (7.4% vs 6.8%; adjusted odds ratio [aOR], 1.16). In analyses stratified by racial and ethnic group, AORs for non-Hispanic Black and Hispanic SM men vs their heterosexual counterparts were 2.18 and 3.81, respectively. The corresponding figures for non-Hispanic Black and Hispanic SM women were 2.33 and 2.46, respectively.
When investigators combined all minority respondents along gender lines, lifetime skin cancer prevalence was higher in bisexual men (aOR, 3.94), bisexual women (aOR, 1.51), and women identifying as something else or other (aOR, 2.70) than in their heterosexual peers.
“I wasn’t expecting that Hispanic or non-Hispanic Black SMs would be at higher risk for skin cancer,” Dr. Mansh said. Even if these groups have more behavioral risk factors for UV radiation (UVR) exposure, he explained, UVR exposure is less strongly linked with skin cancer in darker skin than in lighter skin. Reasons for the counterintuitive finding could include different screening habits among SM people of different racial and ethnic groups, he said, and analyzing such factors will require further research.
Although some effect sizes were modest, the authors wrote, their findings may have important implications for population-based research and public health efforts aimed at early skin cancer detection and prevention. Presently, the United States lacks established guidelines for skin cancer screening. In a 2023 statement published in JAMA, the US Preventive Services Task Force said that there is insufficient evidence to determine the benefit-harm balance of skin cancer screening in asymptomatic people.
“So there has been a lot of recent talk and a need to identify which subset groups of patients might be higher risk for skin cancer and might benefit from more screening,” Dr. Mansh said in an interview. “Understanding more about the high-risk demographic and clinical features that predispose someone to skin cancer helps identify these high-risk populations that could be used to develop better screening guidelines.”
Identifying groups at a higher risk for skin cancer also allows experts to design more targeted counseling or public health interventions focused on these groups, Dr. Mansh added. Absent screening guidelines, experts emphasize changing modifiable risk factors such as UVR exposure, smoking, and alcohol use. “And we know that the message that might change behaviors in a cisgender heterosexual man might be different than in a gay White male or a Hispanic bisexual male.”
A 2017 review showed that interventions to reduce behaviors involving UVR exposure, such as indoor tanning, among young cisgender women focused largely on aging and appearance-based concerns. A 2019 study showed that messages focused on avoiding skin cancer may help motivate SM men to reduce tanning behaviors.
Furthermore, said Dr. Mansh, all electronic health record products available in the United States must provide data fields for sexual orientation. “I don’t believe many dermatologists, depending on the setting, collect that information routinely. Integrating sexual orientation and/or gender identity data into patient intake forms so that it can be integrated into the electronic health record is probably very helpful, not only for your clinical practice but also for future research studies.”
Asked to comment on the results, Rebecca I. Hartman, MD, MPH, who was not involved with the study, said that its impact on clinical practice will be challenging to ascertain. She is chief of dermatology with the VA Boston Healthcare System, assistant professor of dermatology at Harvard Medical School, and director of melanoma epidemiology at Brigham and Women’s Hospital, all in Boston, Massachusetts.
“The study found significant adjusted odds ratios,” Dr. Hartman explained, “but for some of the different populations, the overall lifetime rate of skin cancer is still quite low.” For example, 1.0% for SM non-Hispanic Black men or a difference of 2.1% vs 1.8% in SM Hispanic women. “Thus, I am not sure specific screening recommendations are warranted, although some populations, such as Hispanic sexual minority males, seemed to have a much higher risk (3.8-fold on adjusted analysis) that warrants further investigation.”
For now, she advised assessing patients’ risks for skin cancer based on well-established risk factors such as sun exposure/indoor tanning, skin phototype, immunosuppression, and age.
Dr. Mansh reported no relevant conflicts or funding sources for the study. Dr. Hartman reported no relevant conflicts.
A version of this article appeared on Medscape.com.
Addressing dynamics of each SM subgroup will require increasingly tailored prevention, screening, and research efforts, the study authors said.
“We identified specific subgroups within the sexual minority community who are at higher risk for skin cancer, specifically White gay males and Hispanic and non-Hispanic Black SM men and women — particularly individuals who identify as bisexual,” senior author Matthew Mansh, MD, said in an interview. He is an assistant professor of dermatology at the University of California, San Francisco. The study was published online in JAMA Dermatology.
Using data of adults in the US general population from the Behavioral Risk Factor Surveillance System from January 2014 to December 2021, investigators included more than 1.5 million respondents. The proportions of SM women and men (who self-identified as bisexual, lesbian, gay, “something else,” or other) were 2.6% and 2.0%, respectively.
Lifetime skin cancer prevalence was higher among SM men than among heterosexual men (7.4% vs 6.8%; adjusted odds ratio [aOR], 1.16). In analyses stratified by racial and ethnic group, AORs for non-Hispanic Black and Hispanic SM men vs their heterosexual counterparts were 2.18 and 3.81, respectively. The corresponding figures for non-Hispanic Black and Hispanic SM women were 2.33 and 2.46, respectively.
When investigators combined all minority respondents along gender lines, lifetime skin cancer prevalence was higher in bisexual men (aOR, 3.94), bisexual women (aOR, 1.51), and women identifying as something else or other (aOR, 2.70) than in their heterosexual peers.
“I wasn’t expecting that Hispanic or non-Hispanic Black SMs would be at higher risk for skin cancer,” Dr. Mansh said. Even if these groups have more behavioral risk factors for UV radiation (UVR) exposure, he explained, UVR exposure is less strongly linked with skin cancer in darker skin than in lighter skin. Reasons for the counterintuitive finding could include different screening habits among SM people of different racial and ethnic groups, he said, and analyzing such factors will require further research.
Although some effect sizes were modest, the authors wrote, their findings may have important implications for population-based research and public health efforts aimed at early skin cancer detection and prevention. Presently, the United States lacks established guidelines for skin cancer screening. In a 2023 statement published in JAMA, the US Preventive Services Task Force said that there is insufficient evidence to determine the benefit-harm balance of skin cancer screening in asymptomatic people.
“So there has been a lot of recent talk and a need to identify which subset groups of patients might be higher risk for skin cancer and might benefit from more screening,” Dr. Mansh said in an interview. “Understanding more about the high-risk demographic and clinical features that predispose someone to skin cancer helps identify these high-risk populations that could be used to develop better screening guidelines.”
Identifying groups at a higher risk for skin cancer also allows experts to design more targeted counseling or public health interventions focused on these groups, Dr. Mansh added. Absent screening guidelines, experts emphasize changing modifiable risk factors such as UVR exposure, smoking, and alcohol use. “And we know that the message that might change behaviors in a cisgender heterosexual man might be different than in a gay White male or a Hispanic bisexual male.”
A 2017 review showed that interventions to reduce behaviors involving UVR exposure, such as indoor tanning, among young cisgender women focused largely on aging and appearance-based concerns. A 2019 study showed that messages focused on avoiding skin cancer may help motivate SM men to reduce tanning behaviors.
Furthermore, said Dr. Mansh, all electronic health record products available in the United States must provide data fields for sexual orientation. “I don’t believe many dermatologists, depending on the setting, collect that information routinely. Integrating sexual orientation and/or gender identity data into patient intake forms so that it can be integrated into the electronic health record is probably very helpful, not only for your clinical practice but also for future research studies.”
Asked to comment on the results, Rebecca I. Hartman, MD, MPH, who was not involved with the study, said that its impact on clinical practice will be challenging to ascertain. She is chief of dermatology with the VA Boston Healthcare System, assistant professor of dermatology at Harvard Medical School, and director of melanoma epidemiology at Brigham and Women’s Hospital, all in Boston, Massachusetts.
“The study found significant adjusted odds ratios,” Dr. Hartman explained, “but for some of the different populations, the overall lifetime rate of skin cancer is still quite low.” For example, 1.0% for SM non-Hispanic Black men or a difference of 2.1% vs 1.8% in SM Hispanic women. “Thus, I am not sure specific screening recommendations are warranted, although some populations, such as Hispanic sexual minority males, seemed to have a much higher risk (3.8-fold on adjusted analysis) that warrants further investigation.”
For now, she advised assessing patients’ risks for skin cancer based on well-established risk factors such as sun exposure/indoor tanning, skin phototype, immunosuppression, and age.
Dr. Mansh reported no relevant conflicts or funding sources for the study. Dr. Hartman reported no relevant conflicts.
A version of this article appeared on Medscape.com.
FROM JAMA DERMATOLOGY
Infection Co-occurring With Lupus Raises Flare Risk
TOPLINE:
Intercurrent infections are associated with an increased risk for systemic lupus erythematosus (SLE) flares within 3 months, with major infections associated with a 7.4 times higher risk for major flares.
METHODOLOGY:
- The researchers prospectively examined the association between intercurrent infections and subsequent SLE flares in 203 patients (median age, 40 years; 91% women) with SLE from the Amsterdam SLE cohort study.
- SLE flares were defined as an increase in disease activity combined with an intensification of immunosuppressive therapy. They were categorized into minor and major flares according to the severity and required treatment.
- Major infections were defined as those requiring hospital admission or intravenous antibiotic therapy, while minor infections did not require hospital admission.
- The risk interval for the occurrence of a disease flare was defined as 3 months from the index date of an infection.
- Patients were followed for a median duration of 6 years.
TAKEAWAY:
- The incidence of major and minor infections was 5.3 (95% CI, 4.1-6.9) and 63.9 per 100 patient-years (95% CI, 59.3-69.0), respectively.
- Intercurrent infections were associated with a 1.9 times higher risk for SLE flares within 3 months (95% CI, 1.3-2.9).
- Intercurrent infections were significantly associated with minor SLE flares (hazard ratio, 1.9; 95% CI, 1.2-3.0) but not with major flares.
- Major infections were linked to a 7.4 times higher risk for major SLE flares within 3 months (95% CI, 2.2-24.6).
IN PRACTICE:
“This finding stresses the importance of awareness and strict monitoring of disease activity in patients with SLE suffering a major infection and prompt adequate treatment in case of the development of a disease flare,” the authors wrote.
SOURCE:
The study was led by Fatma el Hadiyen, Amsterdam Rheumatology and Immunology Center, Amsterdam University Medical Center in the Netherlands. It was published online on July 1, 2024, in Lupus Science & Medicine.
LIMITATIONS:
The reliance on patient recall for minor infections may have introduced recall bias. The small number of patients with identified causative organisms limited the generalizability of the findings. The Bootsma criteria were used for defining SLE flares, which may not align with more recent international standards.
DISCLOSURES:
No specific funding source was reported. One author reported receiving personal fees from various pharmaceutical companies outside the submitted work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
Intercurrent infections are associated with an increased risk for systemic lupus erythematosus (SLE) flares within 3 months, with major infections associated with a 7.4 times higher risk for major flares.
METHODOLOGY:
- The researchers prospectively examined the association between intercurrent infections and subsequent SLE flares in 203 patients (median age, 40 years; 91% women) with SLE from the Amsterdam SLE cohort study.
- SLE flares were defined as an increase in disease activity combined with an intensification of immunosuppressive therapy. They were categorized into minor and major flares according to the severity and required treatment.
- Major infections were defined as those requiring hospital admission or intravenous antibiotic therapy, while minor infections did not require hospital admission.
- The risk interval for the occurrence of a disease flare was defined as 3 months from the index date of an infection.
- Patients were followed for a median duration of 6 years.
TAKEAWAY:
- The incidence of major and minor infections was 5.3 (95% CI, 4.1-6.9) and 63.9 per 100 patient-years (95% CI, 59.3-69.0), respectively.
- Intercurrent infections were associated with a 1.9 times higher risk for SLE flares within 3 months (95% CI, 1.3-2.9).
- Intercurrent infections were significantly associated with minor SLE flares (hazard ratio, 1.9; 95% CI, 1.2-3.0) but not with major flares.
- Major infections were linked to a 7.4 times higher risk for major SLE flares within 3 months (95% CI, 2.2-24.6).
IN PRACTICE:
“This finding stresses the importance of awareness and strict monitoring of disease activity in patients with SLE suffering a major infection and prompt adequate treatment in case of the development of a disease flare,” the authors wrote.
SOURCE:
The study was led by Fatma el Hadiyen, Amsterdam Rheumatology and Immunology Center, Amsterdam University Medical Center in the Netherlands. It was published online on July 1, 2024, in Lupus Science & Medicine.
LIMITATIONS:
The reliance on patient recall for minor infections may have introduced recall bias. The small number of patients with identified causative organisms limited the generalizability of the findings. The Bootsma criteria were used for defining SLE flares, which may not align with more recent international standards.
DISCLOSURES:
No specific funding source was reported. One author reported receiving personal fees from various pharmaceutical companies outside the submitted work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
Intercurrent infections are associated with an increased risk for systemic lupus erythematosus (SLE) flares within 3 months, with major infections associated with a 7.4 times higher risk for major flares.
METHODOLOGY:
- The researchers prospectively examined the association between intercurrent infections and subsequent SLE flares in 203 patients (median age, 40 years; 91% women) with SLE from the Amsterdam SLE cohort study.
- SLE flares were defined as an increase in disease activity combined with an intensification of immunosuppressive therapy. They were categorized into minor and major flares according to the severity and required treatment.
- Major infections were defined as those requiring hospital admission or intravenous antibiotic therapy, while minor infections did not require hospital admission.
- The risk interval for the occurrence of a disease flare was defined as 3 months from the index date of an infection.
- Patients were followed for a median duration of 6 years.
TAKEAWAY:
- The incidence of major and minor infections was 5.3 (95% CI, 4.1-6.9) and 63.9 per 100 patient-years (95% CI, 59.3-69.0), respectively.
- Intercurrent infections were associated with a 1.9 times higher risk for SLE flares within 3 months (95% CI, 1.3-2.9).
- Intercurrent infections were significantly associated with minor SLE flares (hazard ratio, 1.9; 95% CI, 1.2-3.0) but not with major flares.
- Major infections were linked to a 7.4 times higher risk for major SLE flares within 3 months (95% CI, 2.2-24.6).
IN PRACTICE:
“This finding stresses the importance of awareness and strict monitoring of disease activity in patients with SLE suffering a major infection and prompt adequate treatment in case of the development of a disease flare,” the authors wrote.
SOURCE:
The study was led by Fatma el Hadiyen, Amsterdam Rheumatology and Immunology Center, Amsterdam University Medical Center in the Netherlands. It was published online on July 1, 2024, in Lupus Science & Medicine.
LIMITATIONS:
The reliance on patient recall for minor infections may have introduced recall bias. The small number of patients with identified causative organisms limited the generalizability of the findings. The Bootsma criteria were used for defining SLE flares, which may not align with more recent international standards.
DISCLOSURES:
No specific funding source was reported. One author reported receiving personal fees from various pharmaceutical companies outside the submitted work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Generalized Fixed Drug Eruptions Require Urgent Care: A Case Series
Recognizing cutaneous drug eruptions is important for treatment and prevention of recurrence. Fixed drug eruptions (FDEs) typically are harmless but can have major negative cosmetic consequences for patients. In its more severe forms, patients are at risk for widespread epithelial necrosis with accompanying complications. We report 1 patient with generalized FDE and 2 with generalized bullous FDE. We also discuss the recognition and treatment of the condition. Two patients previously had been diagnosed with systemic lupus erythematosus (SLE).
Case Series
Patient 1—A 60-year-old woman presented to dermatology with a rash on the trunk and groin folds of 4 days’ duration. She had a history of SLE and cutaneous lupus treated with hydroxychloroquine 200 mg twice daily and topical corticosteroids. She had started sulfamethoxazole-trimethoprim for a urinary tract infection with a rash appearing 1 day later. She reported burning skin pain with progression to blisters that “sloughed” off. She denied any known history of allergy to sulfa drugs. Prior to evaluation by dermatology, she visited an urgent care facility and was prescribed hydroxyzine and intramuscular corticosteroids. At presentation to dermatology 3 days after taking sulfamethoxazole-trimethoprim, she had annular flaccid bullae and superficial erosions with dusky borders on the right posterior thigh, right side of the chest, left inframammary fold, and right inguinal fold (Figure 1). She had no ocular, oral, or vaginal erosions. A diagnosis of generalized bullous FDE was favored over erythema multiforme or Stevens-Johnson syndrome (SJS)/toxic epidermal necrolysis (TEN). Shave biopsies from lesions on the right posterior thigh and right inguinal fold demonstrated interface dermatitis with epidermal necrosis, pigment incontinence, and numerous eosinophils. Direct immunofluorescence of the perilesional skin was negative for immunoprotein deposition. These findings were consistent with the clinical impression of generalized bullous FDE. Prior to receiving the histopathology report, the patient was initiated on a regimen of cyclosporine 5 mg/kg/d in the setting of normal renal function and followed until the eruption resolved completely. Cyclosporine was tapered at 2 weeks and discontinued at 3 weeks.

Patient 2—A 32-year-old woman presented for follow-up management of discoid lupus erythematosus. She had a history of systemic and cutaneous lupus, juvenile rheumatoid arthritis, and mixed connective tissue disease managed with prednisone, hydroxychloroquine, azathioprine, and belimumab. Physical examination revealed scarring alopecia with dyspigmentation and active inflammation consistent with uncontrolled cutaneous lupus. However, she also had oval-shaped hyperpigmented patches over the left breast, clavicle, and anterior chest consistent with a generalized FDE (Figure 2). The patient did not recall a history of similar lesions and could not identify a possible trigger. She was counseled on possible culprits and advised to avoid unnecessary medications. She had an unremarkable clinical course; therefore, no further intervention was necessary.

Patient 3—A 33-year-old man presented to the emergency department with a painful rash on the chest and back of 2 days’ duration that began 1 hour after taking naproxen (dosage unknown) for back pain. He had no notable medical history. The patient stated that the rash had slowly worsened and started to develop blisters. He visited an urgent care facility 1 day prior to the current presentation and was started on a 5-day course of prednisone 40 mg daily; the first 2 doses did not help. He denied any mucosal involvement apart from a tender lesion on the penis. He reported a history of an allergic reaction to penicillin. Physical examination revealed extensive dusky violaceous annular plaques with erythematous borders across the anterior and posterior trunk (Figure 3). Multiple flaccid bullae developed within these plaques, involving 15% of the body surface area. He was diagnosed with generalized bullous FDE based on the clinical history and histopathology. He was admitted to the burn intensive care unit and treated with cyclosporine 3 mg/kg/d with subsequent resolution of the eruption.
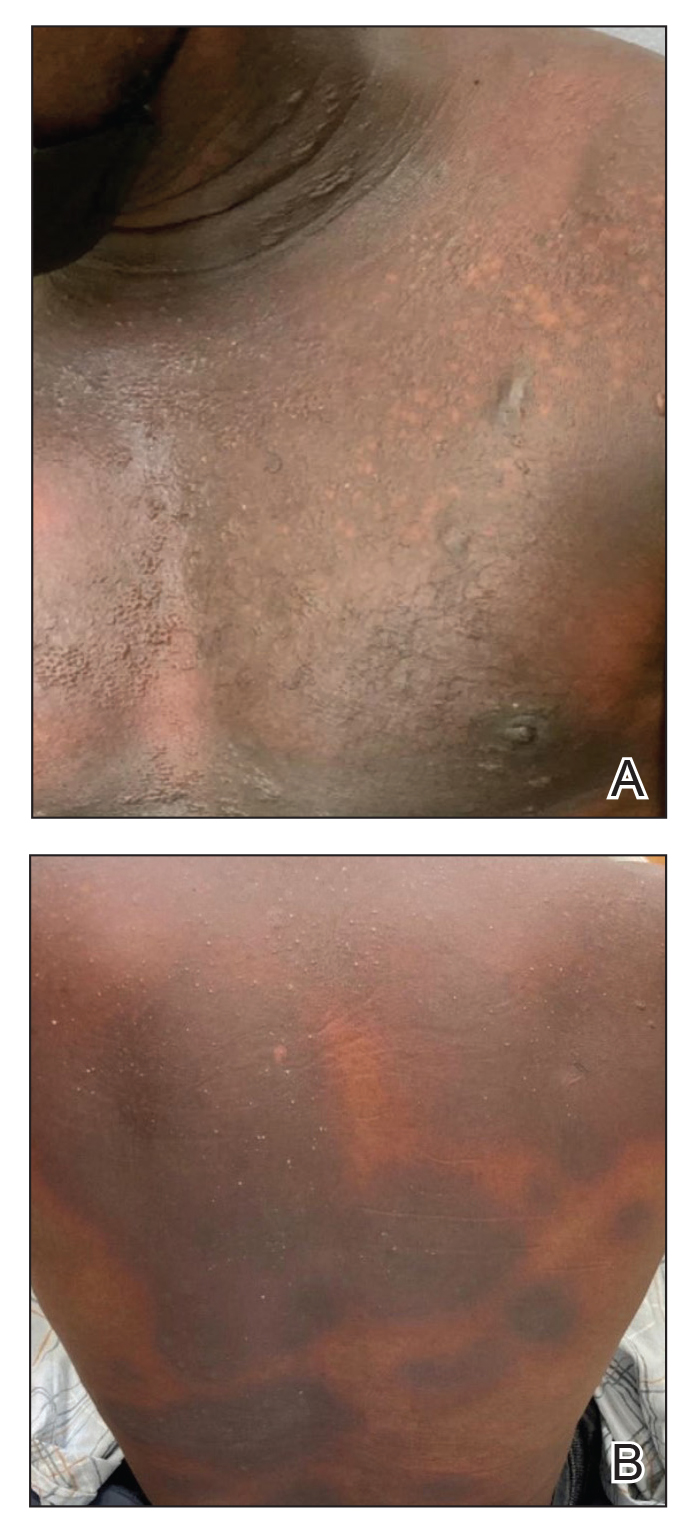
Comment
Presentation of FDEs—A fixed drug eruption manifests with 1 or more well-demarcated, red or violaceous, annular patches that resolve with postinflammatory hyperpigmentation; it occasionally may manifest with bullae. Initial eruptions may occur up to 2 weeks following medication exposure, but recurrent eruptions usually happen within minutes to hours later. They often are in the same location as prior lesions. A fixed drug eruption can be solitary, scattered, or generalized; a generalized FDE typically demonstrates multiple bilateral lesions that may itch, burn, or cause no symptoms. Patients can experience an FDE at any age, though the median age is reported as 35 to 60 years of age.1 A fixed drug eruption usually occurs after ingestion of oral medications, though there have been a few reports with iodinated contrast.2 Well-known culprits include antibiotics (eg, sulfamethoxazole-trimethoprim, tetracyclines, penicillins/cephalosporins, quinolones, dapsone), nonsteroidal anti-inflammatory drugs, acetaminophen (eg, paracetamol), barbiturates, antimalarials, and anticonvulsants. It also can occur with vaccines or with certain foods (fixed food eruption).3,4 Clinicians may try an oral drug challenge to identify the cause of an FDE, but in patients with a history of a generalized FDE, the risk for developing an increasingly severe reaction with repeated exposure to the medication is too high.5
Histopathology—Patch testing at the site of prior eruption with suspected drug culprits may be useful.6 Histopathology of FDE typically demonstrates vacuolar changes at the dermoepidermal junction with a lichenoid lymphocytic infiltrate. Early lesions often show a predominance of eosinophils. Subepidermal clefting is a feature of the bullous variant. In an active lesion, there are large numbers of CD8+ T lymphocytes expressing natural killer cell–associated molecules.7 The pathologic mechanism is not well understood, though it has been hypothesized that memory CD8+ cells are maintained in specific regions of the epidermis by IL-15 produced in the microenvironment and are activated upon rechallenge.7Considerations in Generalized Bullous FDE—Generalized FDE is defined in the literature as an FDE with involvement of 3 of 6 body areas: head, neck, trunk, upper limbs, lower limbs, and genital area. It may cover more or less than 10% of the body surface area.8-10 Although an isolated FDE frequently is asymptomatic and may not be cause for alarm, recurring drug eruptions increase the risk for development of generalized bullous FDE. Generalized bullous FDE is a rare subset. It is frequently misdiagnosed, and data on its incidence are uncertain.11 Of note, several pathologies causing bullous lesions may be in the differential diagnosis, including bullous pemphigoid; pemphigus vulgaris; bullous SLE; or bullae from cutaneous lupus, staphylococcal scalded skin syndrome, erythema multiforme, or SJS/TEN.12 When matched for body surface area involvement with SJS/TEN, generalized bullous FDE shares nearly identical mortality rates10; therefore, these patients should be treated with the same level of urgency and admitted to a critical care or burn unit, as they are at serious risk for infection and other complications.13
Clinical history and presentation along with histopathologic findings help to narrow down the differential diagnosis. Clinically, generalized bullous FDE does not affect the surrounding skin and manifests sooner after drug exposure (1–24 hours) with less mucosal involvement than SJS/TEN.9 Additionally, SJS/TEN patients frequently have generalized malaise and/or fever, while generalized bullous FDE patients do not. Finally, patients with generalized bullous FDE may report a history of a cutaneous eruption similar in morphology or in the same location.
Histopathologically, generalized bullous FDE may be similar to FDE with the addition of a subepidermal blister. Generalized bullous FDE patients have greater eosinophil infiltration and dermal melanophages than patients with SJS/TEN.9 Cellular infiltrates in generalized bullous FDE include more dermal CD41 cells, such as Foxp31 regulatory T cells; fewer intraepidermal CD561 cells; and fewer intraepidermal cells with granulysin.9 Occasionally, generalized bullous FDE causes full-thickness necrosis. In those cases, generalized bullous FDE cannot reliably be distinguished from other conditions with epidermal necrolysis on histopathology.13
FDE Diagnostics—A cytotoxin produced by
Management—Avoidance of the inciting drug often is sufficient for patients with an FDE, as demonstrated in patient 2 in our case series. Clinicians also should counsel patients on avoidance of potential cross-reacting drugs. Symptomatic treatment for itch or pain is appropriate and may include antihistamines or topical steroids. Nonsteroidal anti-inflammatory drugs may exacerbate or be causative of FDE. For generalized bullous FDE, cyclosporine is favored in the literature15,16 and was used to successfully treat both patients 1 and 3 in our case series. A short course of systemic corticosteroids or intravenous immunoglobulin also may be considered. Mild cases of generalized bullous FDE may be treated with close outpatient follow-up (patient 1), while severe cases require inpatient or even critical care monitoring with aggressive medical management to prevent the progression of skin desquamation (patient 3). Patients with severe oral lesions may require inpatient support for fluid maintenance.
Lupus History—Two patients in our case series had a history of lupus. Lupus itself can cause primary bullous lesions. Similar to FDE, bullous SLE can involve sun-exposed and nonexposed areas of the skin as well as the mucous membranes with a predilection for the lower vermilion lip.17 In bullous SLE, tense subepidermal blisters with a neutrophil-rich infiltrate form due to circulating antibodies to type VII collagen. These blisters have an erythematous or urticated base, most commonly on the face, upper trunk, and proximal extremities.18 In both SLE with skin manifestations and lupus limited to the skin, bullae may form due to extensive vacuolar degeneration. Similar to TEN, they can form rapidly in a widespread distribution.17 However, there is limited mucosal involvement, no clear drug association, and a better prognosis. Bullae caused by lupus will frequently demonstrate deposition of immunoproteins IgG, IgM, IgA, and complement component 3 at the basement membrane zone in perilesional skin on direct immunofluorescence. However, negative direct immunofluorescence does not rule out lupus.12 At the same time, patients with lupus frequently have comorbidities requiring multiple medications; the need for these medications may predispose patients to higher rates of cutaneous drug eruptions.19 To our knowledge, there is no known association between FDE and lupus.
Conclusion
Patients with acute eruptions following the initiation of a new prescription or over-the-counter medication require urgent evaluation. Generalized bullous FDE requires timely diagnosis and intervention. Patients with lupus have an increased risk for cutaneous drug eruptions due to polypharmacy. Further investigation is necessary to determine if there is a pathophysiologic mechanism responsible for the development of FDE in lupus patients.
- Anderson HJ, Lee JB. A review of fixed drug eruption with a special focus on generalized bullous fixed drug eruption. Medicina (Kaunas). 2021;57:925.
- Gavin M, Sharp L, Walker K, et al. Contrast-induced generalized bullous fixed drug eruption resembling Stevens-Johnson syndrome. Proc (Bayl Univ Med Cent). 2019;32:601-602.
- Kabir S, Feit EJ, Heilman ER. Generalized fixed drug eruption following Pfizer-BioNtech COVID-19 vaccination. Clin Case Rep. 2022;10:E6684.
- Choi S, Kim SH, Hwang JH, et al. Rapidly progressing generalized bullous fixed drug eruption after the first dose of COVID-19 messenger RNA vaccination. J Dermatol. 2023;50:1190-1193.
- Mahboob A, Haroon TS. Drugs causing fixed eruptions: a study of 450 cases. Int J Dermatol. 1998;37:833-838.
- Shiohara T. Fixed drug eruption: pathogenesis and diagnostic tests. Curr Opin Allergy Clin Immunol. 2009;9:316-321.
- Mizukawa Y, Yamazaki Y, Shiohara T. In vivo dynamics of intraepidermal CD8+ T cells and CD4+ T cells during the evolution of fixed drug eruption. Br J Dermatol. 2008;158:1230-1238.
- Lee CH, Chen YC, Cho YT, et al. Fixed-drug eruption: a retrospective study in a single referral center in northern Taiwan. Dermatologica Sinica. 2012;30:11-15.
- Cho YT, Lin JW, Chen YC, et al. Generalized bullous fixed drug eruption is distinct from Stevens-Johnson syndrome/toxic epidermal necrolysis by immunohistopathological features. J Am Acad Dermatol. 2014;70:539-548.
- Lipowicz S, Sekula P, Ingen-Housz-Oro S, et al. Prognosis of generalized bullous fixed drug eruption: comparison with Stevens-Johnson syndrome and toxic epidermal necrolysis. Br J Dermatol. 2013;168:726-732.
- Patel S, John AM, Handler MZ, et al. Fixed drug eruptions: an update, emphasizing the potentially lethal generalized bullous fixed drug eruption. Am J Clin Dermatol. 2020;21:393-399.
- Ranario JS, Smith JL. Bullous lesions in a patient with systemic lupus erythematosus. J Clin Aesthet Dermatol. 2014;7:44-49.
- Perron E, Viarnaud A, Marciano L, et al. Clinical and histological features of fixed drug eruption: a single-centre series of 73 cases with comparison between bullous and non-bullous forms. Eur J Dermatol. 2021;31:372-380.
- Chen CB, Kuo KL, Wang CW, et al. Detecting lesional granulysin levels for rapid diagnosis of cytotoxic T lymphocyte-mediated bullous skin disorders. J Allergy Clin Immunol Pract. 2021;9:1327-1337.e3.
- Beniwal R, Gupta LK, Khare AK, et al. Cyclosporine in generalized bullous-fixed drug eruption. Indian J Dermatol. 2018;63:432-433.
- Vargas Mora P, García S, Valenzuela F, et al. Generalized bullous fixed drug eruption successfully treated with cyclosporine. Dermatol Ther. 2020;33:E13492.
- Montagnon CM, Tolkachjov SN, Murrell DF, et al. Subepithelial autoimmune blistering dermatoses: clinical features and diagnosis. J Am Acad Dermatol. 2021;85:1-14.
- Sebaratnam DF, Murrell DF. Bullous systemic lupus erythematosus. Dermatol Clin. 2011;29:649-653.
- Zonzits E, Aberer W, Tappeiner G. Drug eruptions from mesna. After cyclophosphamide treatment of patients with systemic lupus erythematosus and dermatomyositis. Arch Dermatol. 1992;128:80-82.
Recognizing cutaneous drug eruptions is important for treatment and prevention of recurrence. Fixed drug eruptions (FDEs) typically are harmless but can have major negative cosmetic consequences for patients. In its more severe forms, patients are at risk for widespread epithelial necrosis with accompanying complications. We report 1 patient with generalized FDE and 2 with generalized bullous FDE. We also discuss the recognition and treatment of the condition. Two patients previously had been diagnosed with systemic lupus erythematosus (SLE).
Case Series
Patient 1—A 60-year-old woman presented to dermatology with a rash on the trunk and groin folds of 4 days’ duration. She had a history of SLE and cutaneous lupus treated with hydroxychloroquine 200 mg twice daily and topical corticosteroids. She had started sulfamethoxazole-trimethoprim for a urinary tract infection with a rash appearing 1 day later. She reported burning skin pain with progression to blisters that “sloughed” off. She denied any known history of allergy to sulfa drugs. Prior to evaluation by dermatology, she visited an urgent care facility and was prescribed hydroxyzine and intramuscular corticosteroids. At presentation to dermatology 3 days after taking sulfamethoxazole-trimethoprim, she had annular flaccid bullae and superficial erosions with dusky borders on the right posterior thigh, right side of the chest, left inframammary fold, and right inguinal fold (Figure 1). She had no ocular, oral, or vaginal erosions. A diagnosis of generalized bullous FDE was favored over erythema multiforme or Stevens-Johnson syndrome (SJS)/toxic epidermal necrolysis (TEN). Shave biopsies from lesions on the right posterior thigh and right inguinal fold demonstrated interface dermatitis with epidermal necrosis, pigment incontinence, and numerous eosinophils. Direct immunofluorescence of the perilesional skin was negative for immunoprotein deposition. These findings were consistent with the clinical impression of generalized bullous FDE. Prior to receiving the histopathology report, the patient was initiated on a regimen of cyclosporine 5 mg/kg/d in the setting of normal renal function and followed until the eruption resolved completely. Cyclosporine was tapered at 2 weeks and discontinued at 3 weeks.

Patient 2—A 32-year-old woman presented for follow-up management of discoid lupus erythematosus. She had a history of systemic and cutaneous lupus, juvenile rheumatoid arthritis, and mixed connective tissue disease managed with prednisone, hydroxychloroquine, azathioprine, and belimumab. Physical examination revealed scarring alopecia with dyspigmentation and active inflammation consistent with uncontrolled cutaneous lupus. However, she also had oval-shaped hyperpigmented patches over the left breast, clavicle, and anterior chest consistent with a generalized FDE (Figure 2). The patient did not recall a history of similar lesions and could not identify a possible trigger. She was counseled on possible culprits and advised to avoid unnecessary medications. She had an unremarkable clinical course; therefore, no further intervention was necessary.

Patient 3—A 33-year-old man presented to the emergency department with a painful rash on the chest and back of 2 days’ duration that began 1 hour after taking naproxen (dosage unknown) for back pain. He had no notable medical history. The patient stated that the rash had slowly worsened and started to develop blisters. He visited an urgent care facility 1 day prior to the current presentation and was started on a 5-day course of prednisone 40 mg daily; the first 2 doses did not help. He denied any mucosal involvement apart from a tender lesion on the penis. He reported a history of an allergic reaction to penicillin. Physical examination revealed extensive dusky violaceous annular plaques with erythematous borders across the anterior and posterior trunk (Figure 3). Multiple flaccid bullae developed within these plaques, involving 15% of the body surface area. He was diagnosed with generalized bullous FDE based on the clinical history and histopathology. He was admitted to the burn intensive care unit and treated with cyclosporine 3 mg/kg/d with subsequent resolution of the eruption.
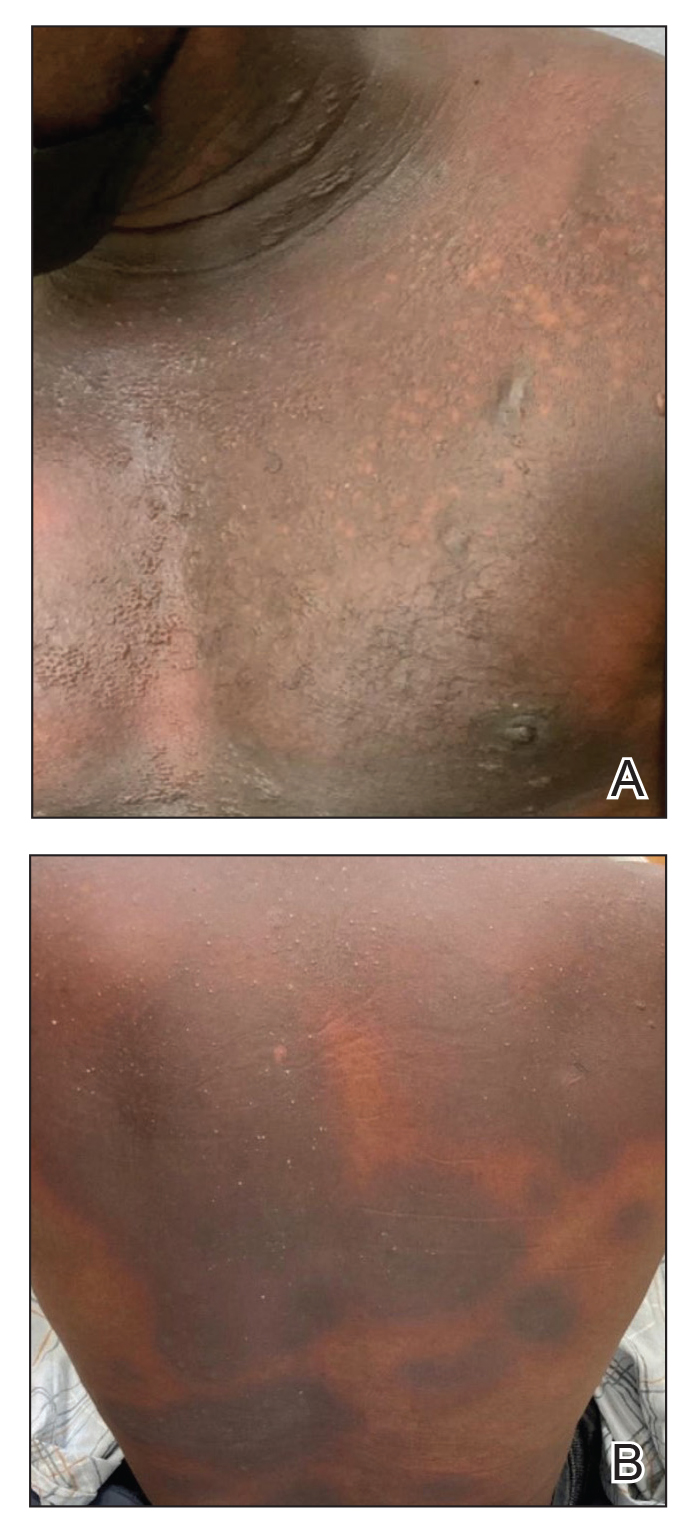
Comment
Presentation of FDEs—A fixed drug eruption manifests with 1 or more well-demarcated, red or violaceous, annular patches that resolve with postinflammatory hyperpigmentation; it occasionally may manifest with bullae. Initial eruptions may occur up to 2 weeks following medication exposure, but recurrent eruptions usually happen within minutes to hours later. They often are in the same location as prior lesions. A fixed drug eruption can be solitary, scattered, or generalized; a generalized FDE typically demonstrates multiple bilateral lesions that may itch, burn, or cause no symptoms. Patients can experience an FDE at any age, though the median age is reported as 35 to 60 years of age.1 A fixed drug eruption usually occurs after ingestion of oral medications, though there have been a few reports with iodinated contrast.2 Well-known culprits include antibiotics (eg, sulfamethoxazole-trimethoprim, tetracyclines, penicillins/cephalosporins, quinolones, dapsone), nonsteroidal anti-inflammatory drugs, acetaminophen (eg, paracetamol), barbiturates, antimalarials, and anticonvulsants. It also can occur with vaccines or with certain foods (fixed food eruption).3,4 Clinicians may try an oral drug challenge to identify the cause of an FDE, but in patients with a history of a generalized FDE, the risk for developing an increasingly severe reaction with repeated exposure to the medication is too high.5
Histopathology—Patch testing at the site of prior eruption with suspected drug culprits may be useful.6 Histopathology of FDE typically demonstrates vacuolar changes at the dermoepidermal junction with a lichenoid lymphocytic infiltrate. Early lesions often show a predominance of eosinophils. Subepidermal clefting is a feature of the bullous variant. In an active lesion, there are large numbers of CD8+ T lymphocytes expressing natural killer cell–associated molecules.7 The pathologic mechanism is not well understood, though it has been hypothesized that memory CD8+ cells are maintained in specific regions of the epidermis by IL-15 produced in the microenvironment and are activated upon rechallenge.7Considerations in Generalized Bullous FDE—Generalized FDE is defined in the literature as an FDE with involvement of 3 of 6 body areas: head, neck, trunk, upper limbs, lower limbs, and genital area. It may cover more or less than 10% of the body surface area.8-10 Although an isolated FDE frequently is asymptomatic and may not be cause for alarm, recurring drug eruptions increase the risk for development of generalized bullous FDE. Generalized bullous FDE is a rare subset. It is frequently misdiagnosed, and data on its incidence are uncertain.11 Of note, several pathologies causing bullous lesions may be in the differential diagnosis, including bullous pemphigoid; pemphigus vulgaris; bullous SLE; or bullae from cutaneous lupus, staphylococcal scalded skin syndrome, erythema multiforme, or SJS/TEN.12 When matched for body surface area involvement with SJS/TEN, generalized bullous FDE shares nearly identical mortality rates10; therefore, these patients should be treated with the same level of urgency and admitted to a critical care or burn unit, as they are at serious risk for infection and other complications.13
Clinical history and presentation along with histopathologic findings help to narrow down the differential diagnosis. Clinically, generalized bullous FDE does not affect the surrounding skin and manifests sooner after drug exposure (1–24 hours) with less mucosal involvement than SJS/TEN.9 Additionally, SJS/TEN patients frequently have generalized malaise and/or fever, while generalized bullous FDE patients do not. Finally, patients with generalized bullous FDE may report a history of a cutaneous eruption similar in morphology or in the same location.
Histopathologically, generalized bullous FDE may be similar to FDE with the addition of a subepidermal blister. Generalized bullous FDE patients have greater eosinophil infiltration and dermal melanophages than patients with SJS/TEN.9 Cellular infiltrates in generalized bullous FDE include more dermal CD41 cells, such as Foxp31 regulatory T cells; fewer intraepidermal CD561 cells; and fewer intraepidermal cells with granulysin.9 Occasionally, generalized bullous FDE causes full-thickness necrosis. In those cases, generalized bullous FDE cannot reliably be distinguished from other conditions with epidermal necrolysis on histopathology.13
FDE Diagnostics—A cytotoxin produced by
Management—Avoidance of the inciting drug often is sufficient for patients with an FDE, as demonstrated in patient 2 in our case series. Clinicians also should counsel patients on avoidance of potential cross-reacting drugs. Symptomatic treatment for itch or pain is appropriate and may include antihistamines or topical steroids. Nonsteroidal anti-inflammatory drugs may exacerbate or be causative of FDE. For generalized bullous FDE, cyclosporine is favored in the literature15,16 and was used to successfully treat both patients 1 and 3 in our case series. A short course of systemic corticosteroids or intravenous immunoglobulin also may be considered. Mild cases of generalized bullous FDE may be treated with close outpatient follow-up (patient 1), while severe cases require inpatient or even critical care monitoring with aggressive medical management to prevent the progression of skin desquamation (patient 3). Patients with severe oral lesions may require inpatient support for fluid maintenance.
Lupus History—Two patients in our case series had a history of lupus. Lupus itself can cause primary bullous lesions. Similar to FDE, bullous SLE can involve sun-exposed and nonexposed areas of the skin as well as the mucous membranes with a predilection for the lower vermilion lip.17 In bullous SLE, tense subepidermal blisters with a neutrophil-rich infiltrate form due to circulating antibodies to type VII collagen. These blisters have an erythematous or urticated base, most commonly on the face, upper trunk, and proximal extremities.18 In both SLE with skin manifestations and lupus limited to the skin, bullae may form due to extensive vacuolar degeneration. Similar to TEN, they can form rapidly in a widespread distribution.17 However, there is limited mucosal involvement, no clear drug association, and a better prognosis. Bullae caused by lupus will frequently demonstrate deposition of immunoproteins IgG, IgM, IgA, and complement component 3 at the basement membrane zone in perilesional skin on direct immunofluorescence. However, negative direct immunofluorescence does not rule out lupus.12 At the same time, patients with lupus frequently have comorbidities requiring multiple medications; the need for these medications may predispose patients to higher rates of cutaneous drug eruptions.19 To our knowledge, there is no known association between FDE and lupus.
Conclusion
Patients with acute eruptions following the initiation of a new prescription or over-the-counter medication require urgent evaluation. Generalized bullous FDE requires timely diagnosis and intervention. Patients with lupus have an increased risk for cutaneous drug eruptions due to polypharmacy. Further investigation is necessary to determine if there is a pathophysiologic mechanism responsible for the development of FDE in lupus patients.
Recognizing cutaneous drug eruptions is important for treatment and prevention of recurrence. Fixed drug eruptions (FDEs) typically are harmless but can have major negative cosmetic consequences for patients. In its more severe forms, patients are at risk for widespread epithelial necrosis with accompanying complications. We report 1 patient with generalized FDE and 2 with generalized bullous FDE. We also discuss the recognition and treatment of the condition. Two patients previously had been diagnosed with systemic lupus erythematosus (SLE).
Case Series
Patient 1—A 60-year-old woman presented to dermatology with a rash on the trunk and groin folds of 4 days’ duration. She had a history of SLE and cutaneous lupus treated with hydroxychloroquine 200 mg twice daily and topical corticosteroids. She had started sulfamethoxazole-trimethoprim for a urinary tract infection with a rash appearing 1 day later. She reported burning skin pain with progression to blisters that “sloughed” off. She denied any known history of allergy to sulfa drugs. Prior to evaluation by dermatology, she visited an urgent care facility and was prescribed hydroxyzine and intramuscular corticosteroids. At presentation to dermatology 3 days after taking sulfamethoxazole-trimethoprim, she had annular flaccid bullae and superficial erosions with dusky borders on the right posterior thigh, right side of the chest, left inframammary fold, and right inguinal fold (Figure 1). She had no ocular, oral, or vaginal erosions. A diagnosis of generalized bullous FDE was favored over erythema multiforme or Stevens-Johnson syndrome (SJS)/toxic epidermal necrolysis (TEN). Shave biopsies from lesions on the right posterior thigh and right inguinal fold demonstrated interface dermatitis with epidermal necrosis, pigment incontinence, and numerous eosinophils. Direct immunofluorescence of the perilesional skin was negative for immunoprotein deposition. These findings were consistent with the clinical impression of generalized bullous FDE. Prior to receiving the histopathology report, the patient was initiated on a regimen of cyclosporine 5 mg/kg/d in the setting of normal renal function and followed until the eruption resolved completely. Cyclosporine was tapered at 2 weeks and discontinued at 3 weeks.

Patient 2—A 32-year-old woman presented for follow-up management of discoid lupus erythematosus. She had a history of systemic and cutaneous lupus, juvenile rheumatoid arthritis, and mixed connective tissue disease managed with prednisone, hydroxychloroquine, azathioprine, and belimumab. Physical examination revealed scarring alopecia with dyspigmentation and active inflammation consistent with uncontrolled cutaneous lupus. However, she also had oval-shaped hyperpigmented patches over the left breast, clavicle, and anterior chest consistent with a generalized FDE (Figure 2). The patient did not recall a history of similar lesions and could not identify a possible trigger. She was counseled on possible culprits and advised to avoid unnecessary medications. She had an unremarkable clinical course; therefore, no further intervention was necessary.

Patient 3—A 33-year-old man presented to the emergency department with a painful rash on the chest and back of 2 days’ duration that began 1 hour after taking naproxen (dosage unknown) for back pain. He had no notable medical history. The patient stated that the rash had slowly worsened and started to develop blisters. He visited an urgent care facility 1 day prior to the current presentation and was started on a 5-day course of prednisone 40 mg daily; the first 2 doses did not help. He denied any mucosal involvement apart from a tender lesion on the penis. He reported a history of an allergic reaction to penicillin. Physical examination revealed extensive dusky violaceous annular plaques with erythematous borders across the anterior and posterior trunk (Figure 3). Multiple flaccid bullae developed within these plaques, involving 15% of the body surface area. He was diagnosed with generalized bullous FDE based on the clinical history and histopathology. He was admitted to the burn intensive care unit and treated with cyclosporine 3 mg/kg/d with subsequent resolution of the eruption.
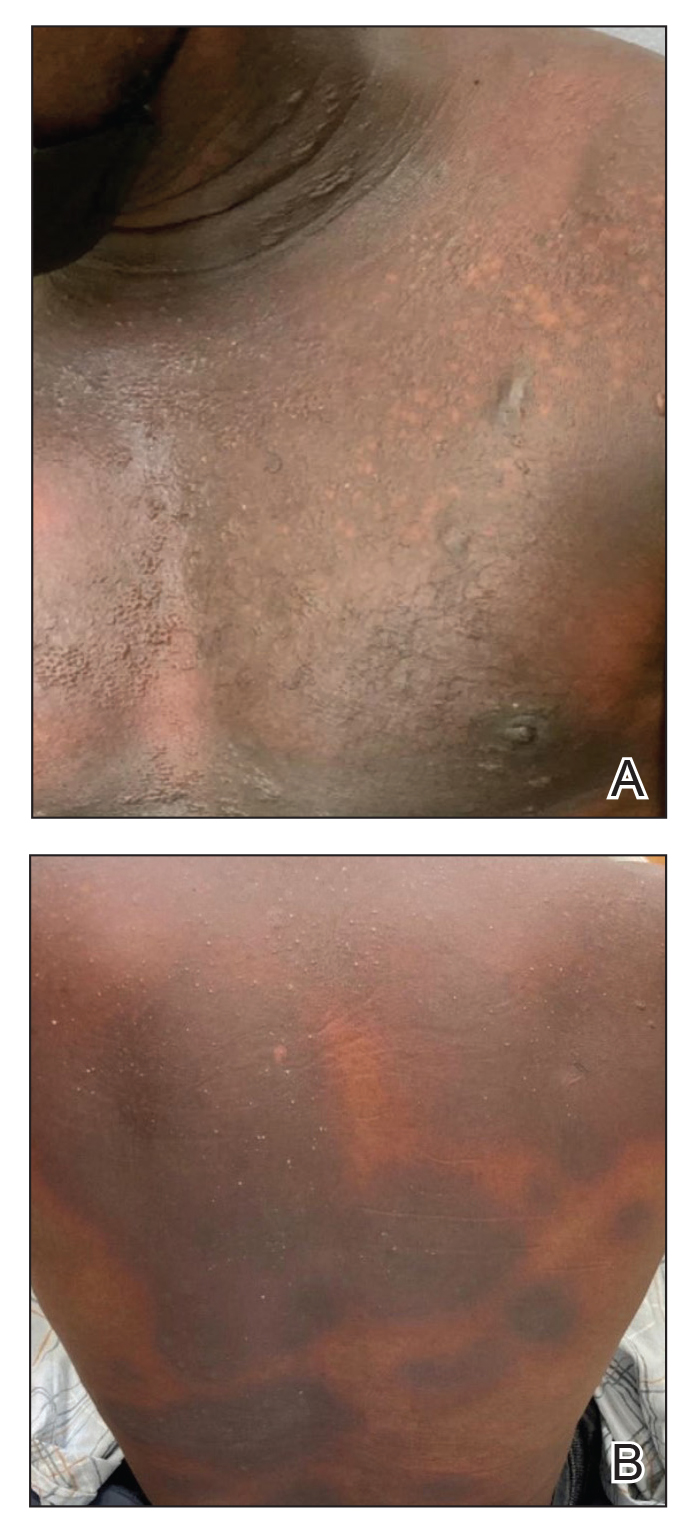
Comment
Presentation of FDEs—A fixed drug eruption manifests with 1 or more well-demarcated, red or violaceous, annular patches that resolve with postinflammatory hyperpigmentation; it occasionally may manifest with bullae. Initial eruptions may occur up to 2 weeks following medication exposure, but recurrent eruptions usually happen within minutes to hours later. They often are in the same location as prior lesions. A fixed drug eruption can be solitary, scattered, or generalized; a generalized FDE typically demonstrates multiple bilateral lesions that may itch, burn, or cause no symptoms. Patients can experience an FDE at any age, though the median age is reported as 35 to 60 years of age.1 A fixed drug eruption usually occurs after ingestion of oral medications, though there have been a few reports with iodinated contrast.2 Well-known culprits include antibiotics (eg, sulfamethoxazole-trimethoprim, tetracyclines, penicillins/cephalosporins, quinolones, dapsone), nonsteroidal anti-inflammatory drugs, acetaminophen (eg, paracetamol), barbiturates, antimalarials, and anticonvulsants. It also can occur with vaccines or with certain foods (fixed food eruption).3,4 Clinicians may try an oral drug challenge to identify the cause of an FDE, but in patients with a history of a generalized FDE, the risk for developing an increasingly severe reaction with repeated exposure to the medication is too high.5
Histopathology—Patch testing at the site of prior eruption with suspected drug culprits may be useful.6 Histopathology of FDE typically demonstrates vacuolar changes at the dermoepidermal junction with a lichenoid lymphocytic infiltrate. Early lesions often show a predominance of eosinophils. Subepidermal clefting is a feature of the bullous variant. In an active lesion, there are large numbers of CD8+ T lymphocytes expressing natural killer cell–associated molecules.7 The pathologic mechanism is not well understood, though it has been hypothesized that memory CD8+ cells are maintained in specific regions of the epidermis by IL-15 produced in the microenvironment and are activated upon rechallenge.7Considerations in Generalized Bullous FDE—Generalized FDE is defined in the literature as an FDE with involvement of 3 of 6 body areas: head, neck, trunk, upper limbs, lower limbs, and genital area. It may cover more or less than 10% of the body surface area.8-10 Although an isolated FDE frequently is asymptomatic and may not be cause for alarm, recurring drug eruptions increase the risk for development of generalized bullous FDE. Generalized bullous FDE is a rare subset. It is frequently misdiagnosed, and data on its incidence are uncertain.11 Of note, several pathologies causing bullous lesions may be in the differential diagnosis, including bullous pemphigoid; pemphigus vulgaris; bullous SLE; or bullae from cutaneous lupus, staphylococcal scalded skin syndrome, erythema multiforme, or SJS/TEN.12 When matched for body surface area involvement with SJS/TEN, generalized bullous FDE shares nearly identical mortality rates10; therefore, these patients should be treated with the same level of urgency and admitted to a critical care or burn unit, as they are at serious risk for infection and other complications.13
Clinical history and presentation along with histopathologic findings help to narrow down the differential diagnosis. Clinically, generalized bullous FDE does not affect the surrounding skin and manifests sooner after drug exposure (1–24 hours) with less mucosal involvement than SJS/TEN.9 Additionally, SJS/TEN patients frequently have generalized malaise and/or fever, while generalized bullous FDE patients do not. Finally, patients with generalized bullous FDE may report a history of a cutaneous eruption similar in morphology or in the same location.
Histopathologically, generalized bullous FDE may be similar to FDE with the addition of a subepidermal blister. Generalized bullous FDE patients have greater eosinophil infiltration and dermal melanophages than patients with SJS/TEN.9 Cellular infiltrates in generalized bullous FDE include more dermal CD41 cells, such as Foxp31 regulatory T cells; fewer intraepidermal CD561 cells; and fewer intraepidermal cells with granulysin.9 Occasionally, generalized bullous FDE causes full-thickness necrosis. In those cases, generalized bullous FDE cannot reliably be distinguished from other conditions with epidermal necrolysis on histopathology.13
FDE Diagnostics—A cytotoxin produced by
Management—Avoidance of the inciting drug often is sufficient for patients with an FDE, as demonstrated in patient 2 in our case series. Clinicians also should counsel patients on avoidance of potential cross-reacting drugs. Symptomatic treatment for itch or pain is appropriate and may include antihistamines or topical steroids. Nonsteroidal anti-inflammatory drugs may exacerbate or be causative of FDE. For generalized bullous FDE, cyclosporine is favored in the literature15,16 and was used to successfully treat both patients 1 and 3 in our case series. A short course of systemic corticosteroids or intravenous immunoglobulin also may be considered. Mild cases of generalized bullous FDE may be treated with close outpatient follow-up (patient 1), while severe cases require inpatient or even critical care monitoring with aggressive medical management to prevent the progression of skin desquamation (patient 3). Patients with severe oral lesions may require inpatient support for fluid maintenance.
Lupus History—Two patients in our case series had a history of lupus. Lupus itself can cause primary bullous lesions. Similar to FDE, bullous SLE can involve sun-exposed and nonexposed areas of the skin as well as the mucous membranes with a predilection for the lower vermilion lip.17 In bullous SLE, tense subepidermal blisters with a neutrophil-rich infiltrate form due to circulating antibodies to type VII collagen. These blisters have an erythematous or urticated base, most commonly on the face, upper trunk, and proximal extremities.18 In both SLE with skin manifestations and lupus limited to the skin, bullae may form due to extensive vacuolar degeneration. Similar to TEN, they can form rapidly in a widespread distribution.17 However, there is limited mucosal involvement, no clear drug association, and a better prognosis. Bullae caused by lupus will frequently demonstrate deposition of immunoproteins IgG, IgM, IgA, and complement component 3 at the basement membrane zone in perilesional skin on direct immunofluorescence. However, negative direct immunofluorescence does not rule out lupus.12 At the same time, patients with lupus frequently have comorbidities requiring multiple medications; the need for these medications may predispose patients to higher rates of cutaneous drug eruptions.19 To our knowledge, there is no known association between FDE and lupus.
Conclusion
Patients with acute eruptions following the initiation of a new prescription or over-the-counter medication require urgent evaluation. Generalized bullous FDE requires timely diagnosis and intervention. Patients with lupus have an increased risk for cutaneous drug eruptions due to polypharmacy. Further investigation is necessary to determine if there is a pathophysiologic mechanism responsible for the development of FDE in lupus patients.
- Anderson HJ, Lee JB. A review of fixed drug eruption with a special focus on generalized bullous fixed drug eruption. Medicina (Kaunas). 2021;57:925.
- Gavin M, Sharp L, Walker K, et al. Contrast-induced generalized bullous fixed drug eruption resembling Stevens-Johnson syndrome. Proc (Bayl Univ Med Cent). 2019;32:601-602.
- Kabir S, Feit EJ, Heilman ER. Generalized fixed drug eruption following Pfizer-BioNtech COVID-19 vaccination. Clin Case Rep. 2022;10:E6684.
- Choi S, Kim SH, Hwang JH, et al. Rapidly progressing generalized bullous fixed drug eruption after the first dose of COVID-19 messenger RNA vaccination. J Dermatol. 2023;50:1190-1193.
- Mahboob A, Haroon TS. Drugs causing fixed eruptions: a study of 450 cases. Int J Dermatol. 1998;37:833-838.
- Shiohara T. Fixed drug eruption: pathogenesis and diagnostic tests. Curr Opin Allergy Clin Immunol. 2009;9:316-321.
- Mizukawa Y, Yamazaki Y, Shiohara T. In vivo dynamics of intraepidermal CD8+ T cells and CD4+ T cells during the evolution of fixed drug eruption. Br J Dermatol. 2008;158:1230-1238.
- Lee CH, Chen YC, Cho YT, et al. Fixed-drug eruption: a retrospective study in a single referral center in northern Taiwan. Dermatologica Sinica. 2012;30:11-15.
- Cho YT, Lin JW, Chen YC, et al. Generalized bullous fixed drug eruption is distinct from Stevens-Johnson syndrome/toxic epidermal necrolysis by immunohistopathological features. J Am Acad Dermatol. 2014;70:539-548.
- Lipowicz S, Sekula P, Ingen-Housz-Oro S, et al. Prognosis of generalized bullous fixed drug eruption: comparison with Stevens-Johnson syndrome and toxic epidermal necrolysis. Br J Dermatol. 2013;168:726-732.
- Patel S, John AM, Handler MZ, et al. Fixed drug eruptions: an update, emphasizing the potentially lethal generalized bullous fixed drug eruption. Am J Clin Dermatol. 2020;21:393-399.
- Ranario JS, Smith JL. Bullous lesions in a patient with systemic lupus erythematosus. J Clin Aesthet Dermatol. 2014;7:44-49.
- Perron E, Viarnaud A, Marciano L, et al. Clinical and histological features of fixed drug eruption: a single-centre series of 73 cases with comparison between bullous and non-bullous forms. Eur J Dermatol. 2021;31:372-380.
- Chen CB, Kuo KL, Wang CW, et al. Detecting lesional granulysin levels for rapid diagnosis of cytotoxic T lymphocyte-mediated bullous skin disorders. J Allergy Clin Immunol Pract. 2021;9:1327-1337.e3.
- Beniwal R, Gupta LK, Khare AK, et al. Cyclosporine in generalized bullous-fixed drug eruption. Indian J Dermatol. 2018;63:432-433.
- Vargas Mora P, García S, Valenzuela F, et al. Generalized bullous fixed drug eruption successfully treated with cyclosporine. Dermatol Ther. 2020;33:E13492.
- Montagnon CM, Tolkachjov SN, Murrell DF, et al. Subepithelial autoimmune blistering dermatoses: clinical features and diagnosis. J Am Acad Dermatol. 2021;85:1-14.
- Sebaratnam DF, Murrell DF. Bullous systemic lupus erythematosus. Dermatol Clin. 2011;29:649-653.
- Zonzits E, Aberer W, Tappeiner G. Drug eruptions from mesna. After cyclophosphamide treatment of patients with systemic lupus erythematosus and dermatomyositis. Arch Dermatol. 1992;128:80-82.
- Anderson HJ, Lee JB. A review of fixed drug eruption with a special focus on generalized bullous fixed drug eruption. Medicina (Kaunas). 2021;57:925.
- Gavin M, Sharp L, Walker K, et al. Contrast-induced generalized bullous fixed drug eruption resembling Stevens-Johnson syndrome. Proc (Bayl Univ Med Cent). 2019;32:601-602.
- Kabir S, Feit EJ, Heilman ER. Generalized fixed drug eruption following Pfizer-BioNtech COVID-19 vaccination. Clin Case Rep. 2022;10:E6684.
- Choi S, Kim SH, Hwang JH, et al. Rapidly progressing generalized bullous fixed drug eruption after the first dose of COVID-19 messenger RNA vaccination. J Dermatol. 2023;50:1190-1193.
- Mahboob A, Haroon TS. Drugs causing fixed eruptions: a study of 450 cases. Int J Dermatol. 1998;37:833-838.
- Shiohara T. Fixed drug eruption: pathogenesis and diagnostic tests. Curr Opin Allergy Clin Immunol. 2009;9:316-321.
- Mizukawa Y, Yamazaki Y, Shiohara T. In vivo dynamics of intraepidermal CD8+ T cells and CD4+ T cells during the evolution of fixed drug eruption. Br J Dermatol. 2008;158:1230-1238.
- Lee CH, Chen YC, Cho YT, et al. Fixed-drug eruption: a retrospective study in a single referral center in northern Taiwan. Dermatologica Sinica. 2012;30:11-15.
- Cho YT, Lin JW, Chen YC, et al. Generalized bullous fixed drug eruption is distinct from Stevens-Johnson syndrome/toxic epidermal necrolysis by immunohistopathological features. J Am Acad Dermatol. 2014;70:539-548.
- Lipowicz S, Sekula P, Ingen-Housz-Oro S, et al. Prognosis of generalized bullous fixed drug eruption: comparison with Stevens-Johnson syndrome and toxic epidermal necrolysis. Br J Dermatol. 2013;168:726-732.
- Patel S, John AM, Handler MZ, et al. Fixed drug eruptions: an update, emphasizing the potentially lethal generalized bullous fixed drug eruption. Am J Clin Dermatol. 2020;21:393-399.
- Ranario JS, Smith JL. Bullous lesions in a patient with systemic lupus erythematosus. J Clin Aesthet Dermatol. 2014;7:44-49.
- Perron E, Viarnaud A, Marciano L, et al. Clinical and histological features of fixed drug eruption: a single-centre series of 73 cases with comparison between bullous and non-bullous forms. Eur J Dermatol. 2021;31:372-380.
- Chen CB, Kuo KL, Wang CW, et al. Detecting lesional granulysin levels for rapid diagnosis of cytotoxic T lymphocyte-mediated bullous skin disorders. J Allergy Clin Immunol Pract. 2021;9:1327-1337.e3.
- Beniwal R, Gupta LK, Khare AK, et al. Cyclosporine in generalized bullous-fixed drug eruption. Indian J Dermatol. 2018;63:432-433.
- Vargas Mora P, García S, Valenzuela F, et al. Generalized bullous fixed drug eruption successfully treated with cyclosporine. Dermatol Ther. 2020;33:E13492.
- Montagnon CM, Tolkachjov SN, Murrell DF, et al. Subepithelial autoimmune blistering dermatoses: clinical features and diagnosis. J Am Acad Dermatol. 2021;85:1-14.
- Sebaratnam DF, Murrell DF. Bullous systemic lupus erythematosus. Dermatol Clin. 2011;29:649-653.
- Zonzits E, Aberer W, Tappeiner G. Drug eruptions from mesna. After cyclophosphamide treatment of patients with systemic lupus erythematosus and dermatomyositis. Arch Dermatol. 1992;128:80-82.
Practice Points
- Although localized fixed drug eruption (FDE) is a relatively benign diagnosis, generalized bullous FDE requires urgent management and may necessitate intensive burn care.
- Patients with lupus are at increased risk for drug eruptions due to polypharmacy, and there is a wide differential for bullous eruptions in these patients.
Mycobacterium interjectum Infection in an Immunocompetent Host Following Contact With Aquarium Fish
To the Editor:
A 48-year-old man presented with nodular lesions in a sporotrichoid pattern on the right hand and forearm of 3 months’ duration (Figure). There were no lymphadeno-pathies, and he had no notable medical history. He denied fever and other systemic symptoms. The patient recently had manipulated a warm water fish aquarium. Although he did not recall a clear injury, inadvertent mild trauma was a possibility. He denied other contact or trauma in relation to animals or vegetables.
Histopathology from a punch biopsy of the forearm revealed a granulomatous infiltrate with necrosis at the deep dermis level at the interface with the subcutaneous cellular tissue that was composed of mainly epithelioid cells with a few multinucleated giant cells. No acid-fast bacilli or fungi were observed with special stains.
A polymerase chain reaction assay for atypical mycobacteria was positive for Mycobacterium interjectum. The culture of the skin biopsy was negative for fungi and mycobacteria after long incubation (6 weeks) on 2 occasions, and an antibiogram was not available. Complementary tests including hemogram, HIV serology, and chest and upper extremity radiographs did not reveal any abnormalities.
The patient was treated with rifampicin 600 mg/d, clarithromycin 500 mg every 12 hours, and co-trimoxazole 160/800 mg every 12 hours for 9 months with some resolution but persistence of some residual scarring lesions. There was no recurrence at 6-month follow-up.
Mycobacterium interjectum is a rare, slow-growing, scotochromogenic mycobacteria. Case reports usually refer to lymphadenitis in healthy children and pulmonary infections in immunocompromised or immunocompetent adults.1,2 A case of M interjectum with cutaneous involvement was reported by Fukuoka et al,3 with ulcerated nodules and abscesses on the leg identified in an immunocompromised patient. Our patient did not present with any cause of immunosuppression or clear injury predisposing him to infection. This microorganism has been detected in water, soil,3 and aquarium fish,4 the latter being the most likely source of infection in our patient. Given its slow growth rate and the need for a specific polymerase chain reaction assay, which is not widely available, M interjectum infection may be underdiagnosed.
No standard antibiotic regimen has been established, but M interjectum has proven to be a multidrug-resistant bacterium with frequent therapy failures. Treatment options have ranged from standard tuberculostatic therapy to combination therapy with medications such as amikacin, levofloxacin, rifampicin, and co-trimoxazole.1 Because an antibiogram was not available for our patient, empiric treatment with rifampicin, clarithromycin, and co-trimoxazole was prescribed for 9 months, with satisfactory response and tolerance. These drugs were selected because of their susceptibility profile in the literature.1,5
- Sotello D, Hata DJ, Reza M, et al. Disseminated Mycobacterium interjectum infection with bacteremia, hepatic and pulmonary involvement associated with a long-term catheter infection. Case Rep Infect Dis. 2017;2017:1-5.
- Dholakia YN. Mycobacterium interjectum isolated from an immunocompetent host with lung infection. Int J Mycobacteriol. 2017;6:401-403.
- Fukuoka M, Matsumura Y, Kore-eda S, et al. Cutaneous infection due to Mycobacterium interjectum in an immunosuppressed patient with microscopic polyangiitis. Br J Dermatol. 2008;159:1382-1384.
- Zanoni RG, Florio D, Fioravanti ML, et al. Occurrence of Mycobacterium spp. in ornamental fish in Italy. J Fish Dis. 2008;31:433-441.
- Emler S, Rochat T, Rohner P, et al. Chronic destructive lung disease associated with a novel mycobacterium. Am J Respir Crit Care Med. 1994;150:261-265.
To the Editor:
A 48-year-old man presented with nodular lesions in a sporotrichoid pattern on the right hand and forearm of 3 months’ duration (Figure). There were no lymphadeno-pathies, and he had no notable medical history. He denied fever and other systemic symptoms. The patient recently had manipulated a warm water fish aquarium. Although he did not recall a clear injury, inadvertent mild trauma was a possibility. He denied other contact or trauma in relation to animals or vegetables.
Histopathology from a punch biopsy of the forearm revealed a granulomatous infiltrate with necrosis at the deep dermis level at the interface with the subcutaneous cellular tissue that was composed of mainly epithelioid cells with a few multinucleated giant cells. No acid-fast bacilli or fungi were observed with special stains.
A polymerase chain reaction assay for atypical mycobacteria was positive for Mycobacterium interjectum. The culture of the skin biopsy was negative for fungi and mycobacteria after long incubation (6 weeks) on 2 occasions, and an antibiogram was not available. Complementary tests including hemogram, HIV serology, and chest and upper extremity radiographs did not reveal any abnormalities.
The patient was treated with rifampicin 600 mg/d, clarithromycin 500 mg every 12 hours, and co-trimoxazole 160/800 mg every 12 hours for 9 months with some resolution but persistence of some residual scarring lesions. There was no recurrence at 6-month follow-up.
Mycobacterium interjectum is a rare, slow-growing, scotochromogenic mycobacteria. Case reports usually refer to lymphadenitis in healthy children and pulmonary infections in immunocompromised or immunocompetent adults.1,2 A case of M interjectum with cutaneous involvement was reported by Fukuoka et al,3 with ulcerated nodules and abscesses on the leg identified in an immunocompromised patient. Our patient did not present with any cause of immunosuppression or clear injury predisposing him to infection. This microorganism has been detected in water, soil,3 and aquarium fish,4 the latter being the most likely source of infection in our patient. Given its slow growth rate and the need for a specific polymerase chain reaction assay, which is not widely available, M interjectum infection may be underdiagnosed.
No standard antibiotic regimen has been established, but M interjectum has proven to be a multidrug-resistant bacterium with frequent therapy failures. Treatment options have ranged from standard tuberculostatic therapy to combination therapy with medications such as amikacin, levofloxacin, rifampicin, and co-trimoxazole.1 Because an antibiogram was not available for our patient, empiric treatment with rifampicin, clarithromycin, and co-trimoxazole was prescribed for 9 months, with satisfactory response and tolerance. These drugs were selected because of their susceptibility profile in the literature.1,5
To the Editor:
A 48-year-old man presented with nodular lesions in a sporotrichoid pattern on the right hand and forearm of 3 months’ duration (Figure). There were no lymphadeno-pathies, and he had no notable medical history. He denied fever and other systemic symptoms. The patient recently had manipulated a warm water fish aquarium. Although he did not recall a clear injury, inadvertent mild trauma was a possibility. He denied other contact or trauma in relation to animals or vegetables.
Histopathology from a punch biopsy of the forearm revealed a granulomatous infiltrate with necrosis at the deep dermis level at the interface with the subcutaneous cellular tissue that was composed of mainly epithelioid cells with a few multinucleated giant cells. No acid-fast bacilli or fungi were observed with special stains.
A polymerase chain reaction assay for atypical mycobacteria was positive for Mycobacterium interjectum. The culture of the skin biopsy was negative for fungi and mycobacteria after long incubation (6 weeks) on 2 occasions, and an antibiogram was not available. Complementary tests including hemogram, HIV serology, and chest and upper extremity radiographs did not reveal any abnormalities.
The patient was treated with rifampicin 600 mg/d, clarithromycin 500 mg every 12 hours, and co-trimoxazole 160/800 mg every 12 hours for 9 months with some resolution but persistence of some residual scarring lesions. There was no recurrence at 6-month follow-up.
Mycobacterium interjectum is a rare, slow-growing, scotochromogenic mycobacteria. Case reports usually refer to lymphadenitis in healthy children and pulmonary infections in immunocompromised or immunocompetent adults.1,2 A case of M interjectum with cutaneous involvement was reported by Fukuoka et al,3 with ulcerated nodules and abscesses on the leg identified in an immunocompromised patient. Our patient did not present with any cause of immunosuppression or clear injury predisposing him to infection. This microorganism has been detected in water, soil,3 and aquarium fish,4 the latter being the most likely source of infection in our patient. Given its slow growth rate and the need for a specific polymerase chain reaction assay, which is not widely available, M interjectum infection may be underdiagnosed.
No standard antibiotic regimen has been established, but M interjectum has proven to be a multidrug-resistant bacterium with frequent therapy failures. Treatment options have ranged from standard tuberculostatic therapy to combination therapy with medications such as amikacin, levofloxacin, rifampicin, and co-trimoxazole.1 Because an antibiogram was not available for our patient, empiric treatment with rifampicin, clarithromycin, and co-trimoxazole was prescribed for 9 months, with satisfactory response and tolerance. These drugs were selected because of their susceptibility profile in the literature.1,5
- Sotello D, Hata DJ, Reza M, et al. Disseminated Mycobacterium interjectum infection with bacteremia, hepatic and pulmonary involvement associated with a long-term catheter infection. Case Rep Infect Dis. 2017;2017:1-5.
- Dholakia YN. Mycobacterium interjectum isolated from an immunocompetent host with lung infection. Int J Mycobacteriol. 2017;6:401-403.
- Fukuoka M, Matsumura Y, Kore-eda S, et al. Cutaneous infection due to Mycobacterium interjectum in an immunosuppressed patient with microscopic polyangiitis. Br J Dermatol. 2008;159:1382-1384.
- Zanoni RG, Florio D, Fioravanti ML, et al. Occurrence of Mycobacterium spp. in ornamental fish in Italy. J Fish Dis. 2008;31:433-441.
- Emler S, Rochat T, Rohner P, et al. Chronic destructive lung disease associated with a novel mycobacterium. Am J Respir Crit Care Med. 1994;150:261-265.
- Sotello D, Hata DJ, Reza M, et al. Disseminated Mycobacterium interjectum infection with bacteremia, hepatic and pulmonary involvement associated with a long-term catheter infection. Case Rep Infect Dis. 2017;2017:1-5.
- Dholakia YN. Mycobacterium interjectum isolated from an immunocompetent host with lung infection. Int J Mycobacteriol. 2017;6:401-403.
- Fukuoka M, Matsumura Y, Kore-eda S, et al. Cutaneous infection due to Mycobacterium interjectum in an immunosuppressed patient with microscopic polyangiitis. Br J Dermatol. 2008;159:1382-1384.
- Zanoni RG, Florio D, Fioravanti ML, et al. Occurrence of Mycobacterium spp. in ornamental fish in Italy. J Fish Dis. 2008;31:433-441.
- Emler S, Rochat T, Rohner P, et al. Chronic destructive lung disease associated with a novel mycobacterium. Am J Respir Crit Care Med. 1994;150:261-265.
Practice Points
- Mycobacterium interjectum can cause cutaneous nodules in a sporotrichoid or lymphocutaneous pattern and may affect immunocompromised and immunocompetent patients.
- This mycobacteria has been detected in water, soil, and aquarium fish. The latter could be a source of infection and should be taken into account in the anamnesis.
- There is no established therapeutic regimen for M interjectum infection. Combination therapy with rifampicin, clarithromycin, and co-trimoxazole could be an option, though it must always be adapted to an antibiogram if results are available.
Dermatoporosis in Older Adults: A Condition That Requires Holistic, Creative Management
WASHINGTON — and conveys the skin’s vulnerability to serious medical complications, said Adam Friedman, MD, at the ElderDerm conference on dermatology in the older patient.
Key features of dermatoporosis include atrophic skin, solar purpura, white pseudoscars, easily acquired skin lacerations and tears, bruises, and delayed healing. “We’re going to see more of this, and it will more and more be a chief complaint of patients,” said Dr. Friedman, professor and chair of dermatology at George Washington University (GWU) in Washington, and co-chair of the meeting. GWU hosted the conference, describing it as a first-of-its-kind meeting dedicated to improving dermatologic care for older adults.
Dermatoporosis was described in the literature in 2007 by dermatologists at the University of Geneva in Switzerland. “It is not only a cosmetic problem,” Dr. Friedman said. “This is a medical problem ... which can absolutely lead to comorbidities [such as deep dissecting hematomas] that are a huge strain on the healthcare system.”
Dermatologists can meet the moment with holistic, creative combination treatment and counseling approaches aimed at improving the mechanical strength of skin and preventing potential complications in older patients, Dr. Friedman said at the meeting.
He described the case of a 76-year-old woman who presented with dermatoporosis on her arms involving pronounced skin atrophy, solar purpura, and a small covered laceration. “This was a patient who was both devastated by the appearance” and impacted by the pain and burden of dressing frequent wounds, said Dr. Friedman, who is also the director of the Residency Program, of Translational Research, and of Supportive Oncodermatology, all within the Department of Dermatology at GWU.
With 11 months of topical treatment that included daily application of calcipotriene 0.05% ointment and nightly application of tazarotene 0.045% lotion and oral supplementation with 1000-mg vitamin C twice daily and 1000-mg citrus bioflavonoid complex daily, as well as no changes to the medications she took for various comorbidities, the solar purpura improved significantly and “we made a huge difference in the integrity of her skin,” he said.
Dr. Friedman also described this case in a recently published article in the Journal of Drugs in Dermatology titled “What’s Old Is New: An Emerging Focus on Dermatoporosis”.
Likely Pathophysiology
Advancing age and chronic ultraviolet (UV) radiation exposure are the chief drivers of dermatoporosis. In addition to UVA and UVB light, other secondary drivers include genetic susceptibility, topical and systematic corticosteroid use, and anticoagulant treatment.
Its pathogenesis is not well described in the literature but is easy to envision, Dr. Friedman said. For one, both advancing age and exposure to UV light lead to a reduction in hygroscopic glycosaminoglycans, including hyaluronate (HA), and the impact of this diminishment is believed to go “beyond [the loss of] buoyancy,” he noted. Researchers have “been showing these are not just water-loving molecules, they also have some biologic properties” relating to keratinocyte production and epidermal turnover that appear to be intricately linked to the pathogenesis of dermatoporosis.
HAs have been shown to interact with the cell surface receptor CD44 to stimulate keratinocyte proliferation, and low levels of CD44 have been reported in skin with dermatoporosis compared with a younger control population. (A newly characterized organelle, the hyaluronosome, serves as an HA factory and contains CD44 and heparin-binding epidermal growth factor, Dr. Friedman noted. Inadequate functioning may be involved in skin atrophy.)
Advancing age also brings an increase in matrix metalloproteinases (MMPs)–1, –2, and –3, which are “the demolition workers of the skin,” and downregulation of a tissue inhibitor of MMPs, he said.
Adding insult to injury, dermis-penetrating UVA also activates MMPs, “obliterating collagen and elastin.” UVB generates DNA photoproducts, including oxidative stress and damaging skin cell DNA. “That UV light induces breakdown [of the skin] through different mechanisms and inhibits buildup is a simple concept I think our patients can understand,” Dr. Friedman said.
Multifaceted Treatment
For an older adult, “there is never a wrong time to start sun-protective measures” to prevent or try to halt the progression of dermatoporosis, Dr. Friedman said, noting that “UV radiation is an immunosuppressant, so there are many good reasons to start” if the adult is not already taking measures on a regular basis.
Potential treatments for the syndrome of dermatoporosis are backed by few clinical studies, but dermatologists are skilled at translating the use of products from one disease state to another based on understandings of pathophysiology and mechanistic pathways, Dr. Friedman commented in an interview after the meeting.
For instance, “from decades of research, we know what retinoids will do to the skin,” he said in the interview. “We know they will turn on collagen-1 and -3 genes in the skin, and that they will increase the production of glycosaminoglycans ... By understanding the biology, we can translate this to dermatoporosis.” These changes were demonstrated, for instance, in a small study of topical retinol in older adults.
Studies of topical alpha hydroxy acid (AHA), moreover, have demonstrated epidermal thickening and firmness, and “some studies show they can limit steroid-induced atrophy,” Dr. Friedman said at the meeting. “And things like lactic acid and urea are super accessible.”
Topical dehydroepiandrosterone is backed by even less data than retinoids or AHAs are, “but it’s still something to consider” as part of a multimechanistic approach to dermatoporosis, Dr. Friedman shared, noting that a small study demonstrated beneficial effects on epidermal atrophy in aging skin.
The use of vitamin D analogues such as calcipotriene, which is approved for the treatment of psoriasis, may also be promising. “One concept is that [vitamin D analogues] increase calcium concentrations in the epidermis, and calcium is so central to keratinocyte differentiation” and epidermal function that calcipotriene in combination with topical steroid therapy has been shown to limit skin atrophy, he noted.
Nutritionally, low protein intake is a known problem in the older population and is associated with increased skin fragility and poorer healing. From a prevention and treatment standpoint, therefore, patients can be counseled to be attentive to their diets, Dr. Friedman said. Experts have recommended a higher protein intake for older adults than for younger adults; in 2013, an international group recommended a protein intake of 1-1.5 g/kg/d for healthy older adults and more for those with acute or chronic illness.
“Patients love talking about diet and skin disease ... and they love over-the-counter nutraceuticals as well because they want something natural,” Dr. Friedman said. “I like using bioflavonoids in combination with vitamin C, which can be effective especially for solar purpura.”
A 6-week randomized, placebo-controlled, double-blind trial involving 67 patients with purpura associated with aging found a 50% reduction in purpura lesions among those took a particular citrus bioflavonoid blend twice daily. “I thought this was a pretty well-done study,” he said, noting that patient self-assessment and investigator global assessment were utilized.
Skin Injury and Wound Prevention
In addition to recommending gentle skin cleansers and daily moisturizing, dermatologists should talk to their older patients with dermatoporosis about their home environments. “What is it like? Is there furniture with sharp edges?” Dr. Friedman advised. If so, could they use sleeves or protectors on their arms or legs “to protect against injury?”
In a later meeting session about lower-extremity wounds on geriatric patients, Michael Stempel, DPM, assistant professor of medicine and surgery and chief of podiatry at GWU, said that he was happy to hear the term dermatoporosis being used because like diabetes, it’s a risk factor for developing lower-extremity wounds and poor wound healing.
He shared the case of an older woman with dermatoporosis who “tripped and skinned her knee against a step and then self-treated it for over a month by pouring hydrogen peroxide over it and letting air get to it.” The wound developed into “full-thickness tissue loss,” said Dr. Stempel, also medical director of the Wound Healing and Limb Preservation Center at GWU Hospital.
Misperceptions are common among older patients about how a simple wound should be managed; for instance, the adage “just let it get air” is not uncommon. This makes anticipatory guidance about basic wound care — such as the importance of a moist and occlusive environment and the safe use of hydrogen peroxide — especially important for patients with dermatoporosis, Dr. Friedman commented after the meeting.
Dermatoporosis is quantifiable, Dr. Friedman said during the meeting, with a scoring system having been developed by the researchers in Switzerland who originally coined the term. Its use in practice is unnecessary, but its existence is “nice to share with patients who feel bothered because oftentimes, patients feel it’s been dismissed by other providers,” he said. “Telling your patients there’s an actual name for their problem, and that there are ways to quantify and measure changes over time, is validating.”
Its recognition as a medical condition, Dr. Friedman added, also enables the dermatologist to bring it up and counsel appropriately — without a patient feeling shame — when it is identified in the context of a skin excision, treatment of a primary inflammatory skin disease, or management of another dermatologic problem.
Dr. Friedman disclosed that he is a consultant/advisory board member for L’Oréal, La Roche-Posay, Galderma, and other companies; a speaker for Regeneron/Sanofi, Incyte, BMD, and Janssen; and has grants from Pfizer, Lilly, Incyte, and other companies. Dr. Stempel reported no disclosures.
A version of this article first appeared on Medscape.com.
WASHINGTON — and conveys the skin’s vulnerability to serious medical complications, said Adam Friedman, MD, at the ElderDerm conference on dermatology in the older patient.
Key features of dermatoporosis include atrophic skin, solar purpura, white pseudoscars, easily acquired skin lacerations and tears, bruises, and delayed healing. “We’re going to see more of this, and it will more and more be a chief complaint of patients,” said Dr. Friedman, professor and chair of dermatology at George Washington University (GWU) in Washington, and co-chair of the meeting. GWU hosted the conference, describing it as a first-of-its-kind meeting dedicated to improving dermatologic care for older adults.
Dermatoporosis was described in the literature in 2007 by dermatologists at the University of Geneva in Switzerland. “It is not only a cosmetic problem,” Dr. Friedman said. “This is a medical problem ... which can absolutely lead to comorbidities [such as deep dissecting hematomas] that are a huge strain on the healthcare system.”
Dermatologists can meet the moment with holistic, creative combination treatment and counseling approaches aimed at improving the mechanical strength of skin and preventing potential complications in older patients, Dr. Friedman said at the meeting.
He described the case of a 76-year-old woman who presented with dermatoporosis on her arms involving pronounced skin atrophy, solar purpura, and a small covered laceration. “This was a patient who was both devastated by the appearance” and impacted by the pain and burden of dressing frequent wounds, said Dr. Friedman, who is also the director of the Residency Program, of Translational Research, and of Supportive Oncodermatology, all within the Department of Dermatology at GWU.
With 11 months of topical treatment that included daily application of calcipotriene 0.05% ointment and nightly application of tazarotene 0.045% lotion and oral supplementation with 1000-mg vitamin C twice daily and 1000-mg citrus bioflavonoid complex daily, as well as no changes to the medications she took for various comorbidities, the solar purpura improved significantly and “we made a huge difference in the integrity of her skin,” he said.
Dr. Friedman also described this case in a recently published article in the Journal of Drugs in Dermatology titled “What’s Old Is New: An Emerging Focus on Dermatoporosis”.
Likely Pathophysiology
Advancing age and chronic ultraviolet (UV) radiation exposure are the chief drivers of dermatoporosis. In addition to UVA and UVB light, other secondary drivers include genetic susceptibility, topical and systematic corticosteroid use, and anticoagulant treatment.
Its pathogenesis is not well described in the literature but is easy to envision, Dr. Friedman said. For one, both advancing age and exposure to UV light lead to a reduction in hygroscopic glycosaminoglycans, including hyaluronate (HA), and the impact of this diminishment is believed to go “beyond [the loss of] buoyancy,” he noted. Researchers have “been showing these are not just water-loving molecules, they also have some biologic properties” relating to keratinocyte production and epidermal turnover that appear to be intricately linked to the pathogenesis of dermatoporosis.
HAs have been shown to interact with the cell surface receptor CD44 to stimulate keratinocyte proliferation, and low levels of CD44 have been reported in skin with dermatoporosis compared with a younger control population. (A newly characterized organelle, the hyaluronosome, serves as an HA factory and contains CD44 and heparin-binding epidermal growth factor, Dr. Friedman noted. Inadequate functioning may be involved in skin atrophy.)
Advancing age also brings an increase in matrix metalloproteinases (MMPs)–1, –2, and –3, which are “the demolition workers of the skin,” and downregulation of a tissue inhibitor of MMPs, he said.
Adding insult to injury, dermis-penetrating UVA also activates MMPs, “obliterating collagen and elastin.” UVB generates DNA photoproducts, including oxidative stress and damaging skin cell DNA. “That UV light induces breakdown [of the skin] through different mechanisms and inhibits buildup is a simple concept I think our patients can understand,” Dr. Friedman said.
Multifaceted Treatment
For an older adult, “there is never a wrong time to start sun-protective measures” to prevent or try to halt the progression of dermatoporosis, Dr. Friedman said, noting that “UV radiation is an immunosuppressant, so there are many good reasons to start” if the adult is not already taking measures on a regular basis.
Potential treatments for the syndrome of dermatoporosis are backed by few clinical studies, but dermatologists are skilled at translating the use of products from one disease state to another based on understandings of pathophysiology and mechanistic pathways, Dr. Friedman commented in an interview after the meeting.
For instance, “from decades of research, we know what retinoids will do to the skin,” he said in the interview. “We know they will turn on collagen-1 and -3 genes in the skin, and that they will increase the production of glycosaminoglycans ... By understanding the biology, we can translate this to dermatoporosis.” These changes were demonstrated, for instance, in a small study of topical retinol in older adults.
Studies of topical alpha hydroxy acid (AHA), moreover, have demonstrated epidermal thickening and firmness, and “some studies show they can limit steroid-induced atrophy,” Dr. Friedman said at the meeting. “And things like lactic acid and urea are super accessible.”
Topical dehydroepiandrosterone is backed by even less data than retinoids or AHAs are, “but it’s still something to consider” as part of a multimechanistic approach to dermatoporosis, Dr. Friedman shared, noting that a small study demonstrated beneficial effects on epidermal atrophy in aging skin.
The use of vitamin D analogues such as calcipotriene, which is approved for the treatment of psoriasis, may also be promising. “One concept is that [vitamin D analogues] increase calcium concentrations in the epidermis, and calcium is so central to keratinocyte differentiation” and epidermal function that calcipotriene in combination with topical steroid therapy has been shown to limit skin atrophy, he noted.
Nutritionally, low protein intake is a known problem in the older population and is associated with increased skin fragility and poorer healing. From a prevention and treatment standpoint, therefore, patients can be counseled to be attentive to their diets, Dr. Friedman said. Experts have recommended a higher protein intake for older adults than for younger adults; in 2013, an international group recommended a protein intake of 1-1.5 g/kg/d for healthy older adults and more for those with acute or chronic illness.
“Patients love talking about diet and skin disease ... and they love over-the-counter nutraceuticals as well because they want something natural,” Dr. Friedman said. “I like using bioflavonoids in combination with vitamin C, which can be effective especially for solar purpura.”
A 6-week randomized, placebo-controlled, double-blind trial involving 67 patients with purpura associated with aging found a 50% reduction in purpura lesions among those took a particular citrus bioflavonoid blend twice daily. “I thought this was a pretty well-done study,” he said, noting that patient self-assessment and investigator global assessment were utilized.
Skin Injury and Wound Prevention
In addition to recommending gentle skin cleansers and daily moisturizing, dermatologists should talk to their older patients with dermatoporosis about their home environments. “What is it like? Is there furniture with sharp edges?” Dr. Friedman advised. If so, could they use sleeves or protectors on their arms or legs “to protect against injury?”
In a later meeting session about lower-extremity wounds on geriatric patients, Michael Stempel, DPM, assistant professor of medicine and surgery and chief of podiatry at GWU, said that he was happy to hear the term dermatoporosis being used because like diabetes, it’s a risk factor for developing lower-extremity wounds and poor wound healing.
He shared the case of an older woman with dermatoporosis who “tripped and skinned her knee against a step and then self-treated it for over a month by pouring hydrogen peroxide over it and letting air get to it.” The wound developed into “full-thickness tissue loss,” said Dr. Stempel, also medical director of the Wound Healing and Limb Preservation Center at GWU Hospital.
Misperceptions are common among older patients about how a simple wound should be managed; for instance, the adage “just let it get air” is not uncommon. This makes anticipatory guidance about basic wound care — such as the importance of a moist and occlusive environment and the safe use of hydrogen peroxide — especially important for patients with dermatoporosis, Dr. Friedman commented after the meeting.
Dermatoporosis is quantifiable, Dr. Friedman said during the meeting, with a scoring system having been developed by the researchers in Switzerland who originally coined the term. Its use in practice is unnecessary, but its existence is “nice to share with patients who feel bothered because oftentimes, patients feel it’s been dismissed by other providers,” he said. “Telling your patients there’s an actual name for their problem, and that there are ways to quantify and measure changes over time, is validating.”
Its recognition as a medical condition, Dr. Friedman added, also enables the dermatologist to bring it up and counsel appropriately — without a patient feeling shame — when it is identified in the context of a skin excision, treatment of a primary inflammatory skin disease, or management of another dermatologic problem.
Dr. Friedman disclosed that he is a consultant/advisory board member for L’Oréal, La Roche-Posay, Galderma, and other companies; a speaker for Regeneron/Sanofi, Incyte, BMD, and Janssen; and has grants from Pfizer, Lilly, Incyte, and other companies. Dr. Stempel reported no disclosures.
A version of this article first appeared on Medscape.com.
WASHINGTON — and conveys the skin’s vulnerability to serious medical complications, said Adam Friedman, MD, at the ElderDerm conference on dermatology in the older patient.
Key features of dermatoporosis include atrophic skin, solar purpura, white pseudoscars, easily acquired skin lacerations and tears, bruises, and delayed healing. “We’re going to see more of this, and it will more and more be a chief complaint of patients,” said Dr. Friedman, professor and chair of dermatology at George Washington University (GWU) in Washington, and co-chair of the meeting. GWU hosted the conference, describing it as a first-of-its-kind meeting dedicated to improving dermatologic care for older adults.
Dermatoporosis was described in the literature in 2007 by dermatologists at the University of Geneva in Switzerland. “It is not only a cosmetic problem,” Dr. Friedman said. “This is a medical problem ... which can absolutely lead to comorbidities [such as deep dissecting hematomas] that are a huge strain on the healthcare system.”
Dermatologists can meet the moment with holistic, creative combination treatment and counseling approaches aimed at improving the mechanical strength of skin and preventing potential complications in older patients, Dr. Friedman said at the meeting.
He described the case of a 76-year-old woman who presented with dermatoporosis on her arms involving pronounced skin atrophy, solar purpura, and a small covered laceration. “This was a patient who was both devastated by the appearance” and impacted by the pain and burden of dressing frequent wounds, said Dr. Friedman, who is also the director of the Residency Program, of Translational Research, and of Supportive Oncodermatology, all within the Department of Dermatology at GWU.
With 11 months of topical treatment that included daily application of calcipotriene 0.05% ointment and nightly application of tazarotene 0.045% lotion and oral supplementation with 1000-mg vitamin C twice daily and 1000-mg citrus bioflavonoid complex daily, as well as no changes to the medications she took for various comorbidities, the solar purpura improved significantly and “we made a huge difference in the integrity of her skin,” he said.
Dr. Friedman also described this case in a recently published article in the Journal of Drugs in Dermatology titled “What’s Old Is New: An Emerging Focus on Dermatoporosis”.
Likely Pathophysiology
Advancing age and chronic ultraviolet (UV) radiation exposure are the chief drivers of dermatoporosis. In addition to UVA and UVB light, other secondary drivers include genetic susceptibility, topical and systematic corticosteroid use, and anticoagulant treatment.
Its pathogenesis is not well described in the literature but is easy to envision, Dr. Friedman said. For one, both advancing age and exposure to UV light lead to a reduction in hygroscopic glycosaminoglycans, including hyaluronate (HA), and the impact of this diminishment is believed to go “beyond [the loss of] buoyancy,” he noted. Researchers have “been showing these are not just water-loving molecules, they also have some biologic properties” relating to keratinocyte production and epidermal turnover that appear to be intricately linked to the pathogenesis of dermatoporosis.
HAs have been shown to interact with the cell surface receptor CD44 to stimulate keratinocyte proliferation, and low levels of CD44 have been reported in skin with dermatoporosis compared with a younger control population. (A newly characterized organelle, the hyaluronosome, serves as an HA factory and contains CD44 and heparin-binding epidermal growth factor, Dr. Friedman noted. Inadequate functioning may be involved in skin atrophy.)
Advancing age also brings an increase in matrix metalloproteinases (MMPs)–1, –2, and –3, which are “the demolition workers of the skin,” and downregulation of a tissue inhibitor of MMPs, he said.
Adding insult to injury, dermis-penetrating UVA also activates MMPs, “obliterating collagen and elastin.” UVB generates DNA photoproducts, including oxidative stress and damaging skin cell DNA. “That UV light induces breakdown [of the skin] through different mechanisms and inhibits buildup is a simple concept I think our patients can understand,” Dr. Friedman said.
Multifaceted Treatment
For an older adult, “there is never a wrong time to start sun-protective measures” to prevent or try to halt the progression of dermatoporosis, Dr. Friedman said, noting that “UV radiation is an immunosuppressant, so there are many good reasons to start” if the adult is not already taking measures on a regular basis.
Potential treatments for the syndrome of dermatoporosis are backed by few clinical studies, but dermatologists are skilled at translating the use of products from one disease state to another based on understandings of pathophysiology and mechanistic pathways, Dr. Friedman commented in an interview after the meeting.
For instance, “from decades of research, we know what retinoids will do to the skin,” he said in the interview. “We know they will turn on collagen-1 and -3 genes in the skin, and that they will increase the production of glycosaminoglycans ... By understanding the biology, we can translate this to dermatoporosis.” These changes were demonstrated, for instance, in a small study of topical retinol in older adults.
Studies of topical alpha hydroxy acid (AHA), moreover, have demonstrated epidermal thickening and firmness, and “some studies show they can limit steroid-induced atrophy,” Dr. Friedman said at the meeting. “And things like lactic acid and urea are super accessible.”
Topical dehydroepiandrosterone is backed by even less data than retinoids or AHAs are, “but it’s still something to consider” as part of a multimechanistic approach to dermatoporosis, Dr. Friedman shared, noting that a small study demonstrated beneficial effects on epidermal atrophy in aging skin.
The use of vitamin D analogues such as calcipotriene, which is approved for the treatment of psoriasis, may also be promising. “One concept is that [vitamin D analogues] increase calcium concentrations in the epidermis, and calcium is so central to keratinocyte differentiation” and epidermal function that calcipotriene in combination with topical steroid therapy has been shown to limit skin atrophy, he noted.
Nutritionally, low protein intake is a known problem in the older population and is associated with increased skin fragility and poorer healing. From a prevention and treatment standpoint, therefore, patients can be counseled to be attentive to their diets, Dr. Friedman said. Experts have recommended a higher protein intake for older adults than for younger adults; in 2013, an international group recommended a protein intake of 1-1.5 g/kg/d for healthy older adults and more for those with acute or chronic illness.
“Patients love talking about diet and skin disease ... and they love over-the-counter nutraceuticals as well because they want something natural,” Dr. Friedman said. “I like using bioflavonoids in combination with vitamin C, which can be effective especially for solar purpura.”
A 6-week randomized, placebo-controlled, double-blind trial involving 67 patients with purpura associated with aging found a 50% reduction in purpura lesions among those took a particular citrus bioflavonoid blend twice daily. “I thought this was a pretty well-done study,” he said, noting that patient self-assessment and investigator global assessment were utilized.
Skin Injury and Wound Prevention
In addition to recommending gentle skin cleansers and daily moisturizing, dermatologists should talk to their older patients with dermatoporosis about their home environments. “What is it like? Is there furniture with sharp edges?” Dr. Friedman advised. If so, could they use sleeves or protectors on their arms or legs “to protect against injury?”
In a later meeting session about lower-extremity wounds on geriatric patients, Michael Stempel, DPM, assistant professor of medicine and surgery and chief of podiatry at GWU, said that he was happy to hear the term dermatoporosis being used because like diabetes, it’s a risk factor for developing lower-extremity wounds and poor wound healing.
He shared the case of an older woman with dermatoporosis who “tripped and skinned her knee against a step and then self-treated it for over a month by pouring hydrogen peroxide over it and letting air get to it.” The wound developed into “full-thickness tissue loss,” said Dr. Stempel, also medical director of the Wound Healing and Limb Preservation Center at GWU Hospital.
Misperceptions are common among older patients about how a simple wound should be managed; for instance, the adage “just let it get air” is not uncommon. This makes anticipatory guidance about basic wound care — such as the importance of a moist and occlusive environment and the safe use of hydrogen peroxide — especially important for patients with dermatoporosis, Dr. Friedman commented after the meeting.
Dermatoporosis is quantifiable, Dr. Friedman said during the meeting, with a scoring system having been developed by the researchers in Switzerland who originally coined the term. Its use in practice is unnecessary, but its existence is “nice to share with patients who feel bothered because oftentimes, patients feel it’s been dismissed by other providers,” he said. “Telling your patients there’s an actual name for their problem, and that there are ways to quantify and measure changes over time, is validating.”
Its recognition as a medical condition, Dr. Friedman added, also enables the dermatologist to bring it up and counsel appropriately — without a patient feeling shame — when it is identified in the context of a skin excision, treatment of a primary inflammatory skin disease, or management of another dermatologic problem.
Dr. Friedman disclosed that he is a consultant/advisory board member for L’Oréal, La Roche-Posay, Galderma, and other companies; a speaker for Regeneron/Sanofi, Incyte, BMD, and Janssen; and has grants from Pfizer, Lilly, Incyte, and other companies. Dr. Stempel reported no disclosures.
A version of this article first appeared on Medscape.com.
FROM ELDERDERM 2024