User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Empagliflozin gets HFrEF approval from FDA
The U.S. Food and Drug Administration approved empagliflozin (Jardiance) as a treatment for adults with heart failure with reduced ejection fraction (HFrEF) regardless of whether patients have diabetes on Aug. 18, making it the second agent from the sodium-glucose transporter 2 inhibitor class to received this indication.
Empagliflozin first received FDA marketing approval in 2014 for improving glycemic control in patients with type 2 diabetes, and in 2016 the agency added a second indication of reducing cardiovascular death in patients with type 2 diabetes and cardiovascular disease. The newly granted indication for patients with HFrEF without regard to glycemic status was for reducing the risk for cardiovascular death and hospitalization for heart failure, according to a statement from Boehringer Ingelheim and Lilly, the two companies that together market empagliflozin.
The statement also said that the approval allowed for empagliflozin treatment in patients with HFrEF and an estimated glomerular filtration rate (eGFR) as low as 20 mL/min per 1.73 m2, in contrast to its indication for improving glycemic control in patients with type 2 diabetes that limits use to patients with an eGFR of at least 30 mL per 1.73 m2.
EMPEROR-Reduced results drive approval
The FDA based its decision on results from the EMPEROR-Reduced study, first reported in August 2020, that showed treatment of patients with HFrEF with empagliflozin on top of standard therapy for a median of 16 months cut the incidence of cardiovascular death or hospitalization for worsening heart failure by 25% relative to placebo, and by an absolute 5.3%, compared with placebo-treated patients.
Patients enrolled in EMPEROR-Reduced had chronic heart failure in New York Heart Association functional class II-IV and with a left ventricular ejection fraction of 40% or less, the standard ejection fraction criterion for defining HFrEF. Half the enrolled patients had diabetes, and analysis showed no heterogeneity in the primary outcome response based on diabetes status at enrollment.
Empagliflozin joins dapagliflozin for treating HFrEF
Dapagliflozin (Farxiga) was the first agent from the SGLT2 inhibitor class to receive an FDA indication, in 2020, for treating patients with HFrEF regardless of their diabetes status, a decision based on results from the DAPA-HF trial. Results from DAPA-HF showed that treatment with dapagliflozin in patients with HFrEF for a median of 18 months led to a 26% relative reduction in the incidence of cardiovascular death or worsening heart failure and a 4.9% absolute reduction, compared with placebo when added to standard treatment. DAPA-HF enrolled patients using similar criteria to EMPEROR-Reduced, and 42% of enrolled patients had diabetes with no heterogeneity in the primary outcome related to baseline diabetes status.
Subsequent to the report of results from the EMPEROR-Reduced trial nearly a year ago, heart failure experts declared that treatment with an agent from the SGLT2 inhibitor class had become a “new pillar of foundational therapy for HFrEF,” and they urged rapid initiation of an SGLT2 inhibitor (along with other appropriate medications) at the time of initial diagnosis of HFrEF.
The U.S. Food and Drug Administration approved empagliflozin (Jardiance) as a treatment for adults with heart failure with reduced ejection fraction (HFrEF) regardless of whether patients have diabetes on Aug. 18, making it the second agent from the sodium-glucose transporter 2 inhibitor class to received this indication.
Empagliflozin first received FDA marketing approval in 2014 for improving glycemic control in patients with type 2 diabetes, and in 2016 the agency added a second indication of reducing cardiovascular death in patients with type 2 diabetes and cardiovascular disease. The newly granted indication for patients with HFrEF without regard to glycemic status was for reducing the risk for cardiovascular death and hospitalization for heart failure, according to a statement from Boehringer Ingelheim and Lilly, the two companies that together market empagliflozin.
The statement also said that the approval allowed for empagliflozin treatment in patients with HFrEF and an estimated glomerular filtration rate (eGFR) as low as 20 mL/min per 1.73 m2, in contrast to its indication for improving glycemic control in patients with type 2 diabetes that limits use to patients with an eGFR of at least 30 mL per 1.73 m2.
EMPEROR-Reduced results drive approval
The FDA based its decision on results from the EMPEROR-Reduced study, first reported in August 2020, that showed treatment of patients with HFrEF with empagliflozin on top of standard therapy for a median of 16 months cut the incidence of cardiovascular death or hospitalization for worsening heart failure by 25% relative to placebo, and by an absolute 5.3%, compared with placebo-treated patients.
Patients enrolled in EMPEROR-Reduced had chronic heart failure in New York Heart Association functional class II-IV and with a left ventricular ejection fraction of 40% or less, the standard ejection fraction criterion for defining HFrEF. Half the enrolled patients had diabetes, and analysis showed no heterogeneity in the primary outcome response based on diabetes status at enrollment.
Empagliflozin joins dapagliflozin for treating HFrEF
Dapagliflozin (Farxiga) was the first agent from the SGLT2 inhibitor class to receive an FDA indication, in 2020, for treating patients with HFrEF regardless of their diabetes status, a decision based on results from the DAPA-HF trial. Results from DAPA-HF showed that treatment with dapagliflozin in patients with HFrEF for a median of 18 months led to a 26% relative reduction in the incidence of cardiovascular death or worsening heart failure and a 4.9% absolute reduction, compared with placebo when added to standard treatment. DAPA-HF enrolled patients using similar criteria to EMPEROR-Reduced, and 42% of enrolled patients had diabetes with no heterogeneity in the primary outcome related to baseline diabetes status.
Subsequent to the report of results from the EMPEROR-Reduced trial nearly a year ago, heart failure experts declared that treatment with an agent from the SGLT2 inhibitor class had become a “new pillar of foundational therapy for HFrEF,” and they urged rapid initiation of an SGLT2 inhibitor (along with other appropriate medications) at the time of initial diagnosis of HFrEF.
The U.S. Food and Drug Administration approved empagliflozin (Jardiance) as a treatment for adults with heart failure with reduced ejection fraction (HFrEF) regardless of whether patients have diabetes on Aug. 18, making it the second agent from the sodium-glucose transporter 2 inhibitor class to received this indication.
Empagliflozin first received FDA marketing approval in 2014 for improving glycemic control in patients with type 2 diabetes, and in 2016 the agency added a second indication of reducing cardiovascular death in patients with type 2 diabetes and cardiovascular disease. The newly granted indication for patients with HFrEF without regard to glycemic status was for reducing the risk for cardiovascular death and hospitalization for heart failure, according to a statement from Boehringer Ingelheim and Lilly, the two companies that together market empagliflozin.
The statement also said that the approval allowed for empagliflozin treatment in patients with HFrEF and an estimated glomerular filtration rate (eGFR) as low as 20 mL/min per 1.73 m2, in contrast to its indication for improving glycemic control in patients with type 2 diabetes that limits use to patients with an eGFR of at least 30 mL per 1.73 m2.
EMPEROR-Reduced results drive approval
The FDA based its decision on results from the EMPEROR-Reduced study, first reported in August 2020, that showed treatment of patients with HFrEF with empagliflozin on top of standard therapy for a median of 16 months cut the incidence of cardiovascular death or hospitalization for worsening heart failure by 25% relative to placebo, and by an absolute 5.3%, compared with placebo-treated patients.
Patients enrolled in EMPEROR-Reduced had chronic heart failure in New York Heart Association functional class II-IV and with a left ventricular ejection fraction of 40% or less, the standard ejection fraction criterion for defining HFrEF. Half the enrolled patients had diabetes, and analysis showed no heterogeneity in the primary outcome response based on diabetes status at enrollment.
Empagliflozin joins dapagliflozin for treating HFrEF
Dapagliflozin (Farxiga) was the first agent from the SGLT2 inhibitor class to receive an FDA indication, in 2020, for treating patients with HFrEF regardless of their diabetes status, a decision based on results from the DAPA-HF trial. Results from DAPA-HF showed that treatment with dapagliflozin in patients with HFrEF for a median of 18 months led to a 26% relative reduction in the incidence of cardiovascular death or worsening heart failure and a 4.9% absolute reduction, compared with placebo when added to standard treatment. DAPA-HF enrolled patients using similar criteria to EMPEROR-Reduced, and 42% of enrolled patients had diabetes with no heterogeneity in the primary outcome related to baseline diabetes status.
Subsequent to the report of results from the EMPEROR-Reduced trial nearly a year ago, heart failure experts declared that treatment with an agent from the SGLT2 inhibitor class had become a “new pillar of foundational therapy for HFrEF,” and they urged rapid initiation of an SGLT2 inhibitor (along with other appropriate medications) at the time of initial diagnosis of HFrEF.
Pandemic derails small success in lowering diabetes-related amputations
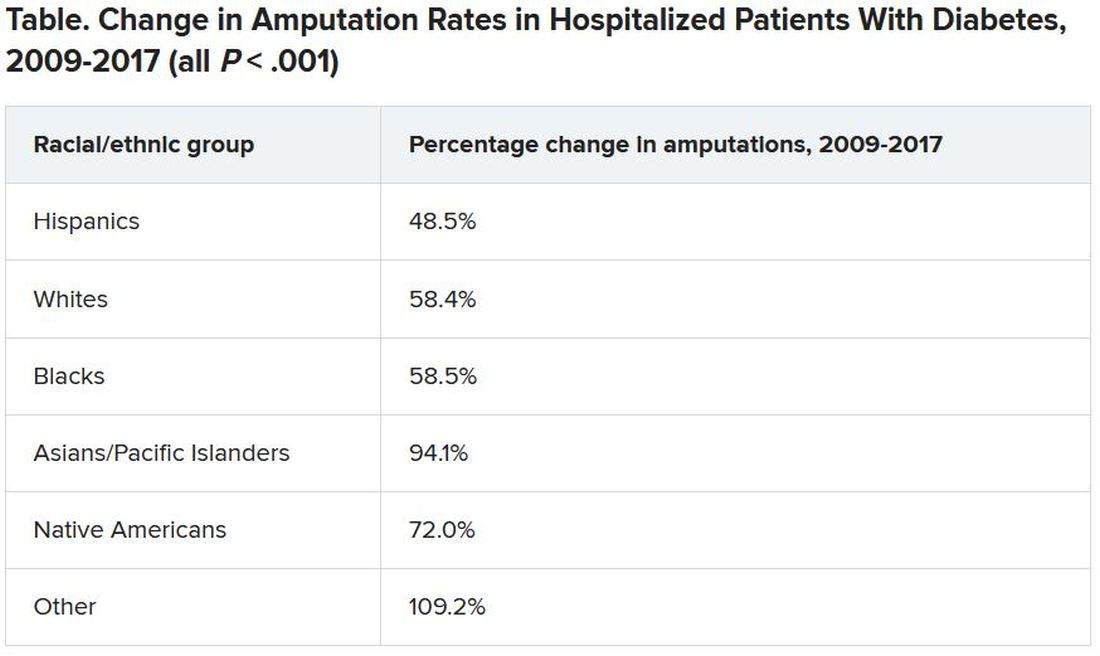
Rates of minor diabetes-related lower extremity amputations (LEAs) in hospitalized patients increased between 2009 and 2017 in all racial and ethnic groups, in both rural and urban areas, and in all geographic regions across the United States, a new retrospective, observational study indicates.
In contrast, major lower extremity amputation rates held steady during the study period with a few exceptions.
There was also a decline in major-to-minor amputation ratios, especially among Native Americans – a sign that diabetes was being better managed and foot ulcers were being caught earlier, preventing the need for a major amputation above the foot or below or above the knee.
Minor LEAs include the loss of a toe, toes, or a foot.
“While I know an amputation is devastating either way, having a minor amputation is better than having a major amputation, and trends [at least to 2017] show that comprehensive foot examinations are paying off,” lead author Marvellous Akinlotan, PhD, MPH, a research associate at the Southwest Rural Health Research Center in Bryan, Texas, said in an interview.
Asked to comment, Marcia Ory, PhD, MPH, director of the Center for Population Health & Aging, Texas A&M School of Public Health, College Station, who was not involved in the study, said: “It points to some successes, but it also points to the need for continued education and preventive care to reduce all types of amputations.”
The study was published online in Diabetes Care.
Amputations increased during COVID-19
However, the study was conducted prior to the COVID-19 pandemic, and amputation rates appear to have significantly worsened during the past 18 months.
In a summary of recent evidence collated by the Amputee Coalition, the authors point out that not only does COVID-19 itself put patients at higher risk for limb loss because severe infection increases the risk of blood clots, but patients with diabetes appear to have been far more likely to undergo any level of amputation during the pandemic than before it began.
In a study of patients with diabetes attending a foot and ankle surgery service in Ohio, the risk of having any level of amputation was 10.8 times higher during compared with before the pandemic. And of patients undergoing any amputation, the odds for receiving a major amputation was 3.1 times higher than before the pandemic.
Telehealth and web-based options for diabetes care and education could help improve health outcomes, particularly during lockdowns.
“Having a diabetes-related amputation is life-changing – it brings disability and functional limitations to the individual – and within the health care system, it reflects the failure of secondary prevention efforts, which ideally should slow the progression of diabetic complications,” noted Dr. Akinlotan.
Race and geography affect risk of amputation
In their study, Dr. Akinlotan and colleagues used data from the National Inpatient Sample to identify trends in LEAs among patients primarily hospitalized for diabetes in the United States between 2009 and 2017.
“The primary outcome variable was documentation of either minor or major LEA during a diabetes-related admission,” they explain.
Minor LEAs increased significantly across all ethnic groups.
Although major amputation rates remained steady, “we did find that some groups remained at risk for having a major amputation,” Dr. Akinlotan noted.
White populations, people in the Midwest, and rural areas saw notable increases in major LEAs, as did “... Blacks, Hispanics, [and] those living in the South,” she said.
Patients need to be encouraged to monitor and control their blood glucose, to offset modifiable risk factors, and to seek regular medical attention to prevent an insidious diabetic complication from developing further, she said.
“It’s important for patients to know that continuing care is necessary,” Dr. Akinlotan stressed. “Diabetes is chronic and complex, but it can be managed, so that’s the good news.”
Dr. Ory agrees: “Effective management will require an all-in approach, with doctors and patients working together.
“Given the limited time in doctor-patient encounters, physicians can benefit patients by referring them to evidence-based, self-management education programs, which are proliferating around in the county,” she added.
The authors and Dr. Ory have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Rates of minor diabetes-related lower extremity amputations (LEAs) in hospitalized patients increased between 2009 and 2017 in all racial and ethnic groups, in both rural and urban areas, and in all geographic regions across the United States, a new retrospective, observational study indicates.
In contrast, major lower extremity amputation rates held steady during the study period with a few exceptions.
There was also a decline in major-to-minor amputation ratios, especially among Native Americans – a sign that diabetes was being better managed and foot ulcers were being caught earlier, preventing the need for a major amputation above the foot or below or above the knee.
Minor LEAs include the loss of a toe, toes, or a foot.
“While I know an amputation is devastating either way, having a minor amputation is better than having a major amputation, and trends [at least to 2017] show that comprehensive foot examinations are paying off,” lead author Marvellous Akinlotan, PhD, MPH, a research associate at the Southwest Rural Health Research Center in Bryan, Texas, said in an interview.
Asked to comment, Marcia Ory, PhD, MPH, director of the Center for Population Health & Aging, Texas A&M School of Public Health, College Station, who was not involved in the study, said: “It points to some successes, but it also points to the need for continued education and preventive care to reduce all types of amputations.”
The study was published online in Diabetes Care.
Amputations increased during COVID-19
However, the study was conducted prior to the COVID-19 pandemic, and amputation rates appear to have significantly worsened during the past 18 months.
In a summary of recent evidence collated by the Amputee Coalition, the authors point out that not only does COVID-19 itself put patients at higher risk for limb loss because severe infection increases the risk of blood clots, but patients with diabetes appear to have been far more likely to undergo any level of amputation during the pandemic than before it began.
In a study of patients with diabetes attending a foot and ankle surgery service in Ohio, the risk of having any level of amputation was 10.8 times higher during compared with before the pandemic. And of patients undergoing any amputation, the odds for receiving a major amputation was 3.1 times higher than before the pandemic.
Telehealth and web-based options for diabetes care and education could help improve health outcomes, particularly during lockdowns.
“Having a diabetes-related amputation is life-changing – it brings disability and functional limitations to the individual – and within the health care system, it reflects the failure of secondary prevention efforts, which ideally should slow the progression of diabetic complications,” noted Dr. Akinlotan.
Race and geography affect risk of amputation
In their study, Dr. Akinlotan and colleagues used data from the National Inpatient Sample to identify trends in LEAs among patients primarily hospitalized for diabetes in the United States between 2009 and 2017.
“The primary outcome variable was documentation of either minor or major LEA during a diabetes-related admission,” they explain.
Minor LEAs increased significantly across all ethnic groups.
Although major amputation rates remained steady, “we did find that some groups remained at risk for having a major amputation,” Dr. Akinlotan noted.
White populations, people in the Midwest, and rural areas saw notable increases in major LEAs, as did “... Blacks, Hispanics, [and] those living in the South,” she said.
Patients need to be encouraged to monitor and control their blood glucose, to offset modifiable risk factors, and to seek regular medical attention to prevent an insidious diabetic complication from developing further, she said.
“It’s important for patients to know that continuing care is necessary,” Dr. Akinlotan stressed. “Diabetes is chronic and complex, but it can be managed, so that’s the good news.”
Dr. Ory agrees: “Effective management will require an all-in approach, with doctors and patients working together.
“Given the limited time in doctor-patient encounters, physicians can benefit patients by referring them to evidence-based, self-management education programs, which are proliferating around in the county,” she added.
The authors and Dr. Ory have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Rates of minor diabetes-related lower extremity amputations (LEAs) in hospitalized patients increased between 2009 and 2017 in all racial and ethnic groups, in both rural and urban areas, and in all geographic regions across the United States, a new retrospective, observational study indicates.
In contrast, major lower extremity amputation rates held steady during the study period with a few exceptions.
There was also a decline in major-to-minor amputation ratios, especially among Native Americans – a sign that diabetes was being better managed and foot ulcers were being caught earlier, preventing the need for a major amputation above the foot or below or above the knee.
Minor LEAs include the loss of a toe, toes, or a foot.
“While I know an amputation is devastating either way, having a minor amputation is better than having a major amputation, and trends [at least to 2017] show that comprehensive foot examinations are paying off,” lead author Marvellous Akinlotan, PhD, MPH, a research associate at the Southwest Rural Health Research Center in Bryan, Texas, said in an interview.
Asked to comment, Marcia Ory, PhD, MPH, director of the Center for Population Health & Aging, Texas A&M School of Public Health, College Station, who was not involved in the study, said: “It points to some successes, but it also points to the need for continued education and preventive care to reduce all types of amputations.”
The study was published online in Diabetes Care.
Amputations increased during COVID-19
However, the study was conducted prior to the COVID-19 pandemic, and amputation rates appear to have significantly worsened during the past 18 months.
In a summary of recent evidence collated by the Amputee Coalition, the authors point out that not only does COVID-19 itself put patients at higher risk for limb loss because severe infection increases the risk of blood clots, but patients with diabetes appear to have been far more likely to undergo any level of amputation during the pandemic than before it began.
In a study of patients with diabetes attending a foot and ankle surgery service in Ohio, the risk of having any level of amputation was 10.8 times higher during compared with before the pandemic. And of patients undergoing any amputation, the odds for receiving a major amputation was 3.1 times higher than before the pandemic.
Telehealth and web-based options for diabetes care and education could help improve health outcomes, particularly during lockdowns.
“Having a diabetes-related amputation is life-changing – it brings disability and functional limitations to the individual – and within the health care system, it reflects the failure of secondary prevention efforts, which ideally should slow the progression of diabetic complications,” noted Dr. Akinlotan.
Race and geography affect risk of amputation
In their study, Dr. Akinlotan and colleagues used data from the National Inpatient Sample to identify trends in LEAs among patients primarily hospitalized for diabetes in the United States between 2009 and 2017.
“The primary outcome variable was documentation of either minor or major LEA during a diabetes-related admission,” they explain.
Minor LEAs increased significantly across all ethnic groups.
Although major amputation rates remained steady, “we did find that some groups remained at risk for having a major amputation,” Dr. Akinlotan noted.
White populations, people in the Midwest, and rural areas saw notable increases in major LEAs, as did “... Blacks, Hispanics, [and] those living in the South,” she said.
Patients need to be encouraged to monitor and control their blood glucose, to offset modifiable risk factors, and to seek regular medical attention to prevent an insidious diabetic complication from developing further, she said.
“It’s important for patients to know that continuing care is necessary,” Dr. Akinlotan stressed. “Diabetes is chronic and complex, but it can be managed, so that’s the good news.”
Dr. Ory agrees: “Effective management will require an all-in approach, with doctors and patients working together.
“Given the limited time in doctor-patient encounters, physicians can benefit patients by referring them to evidence-based, self-management education programs, which are proliferating around in the county,” she added.
The authors and Dr. Ory have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ED docs are cleaning up the messes of medical tourism
It was a typical, busy evening shift in the emergency department (ED) when Steve Carroll, DO, an emergency medicine physician in the Philadelphia area, noticed an odd listing on the tracking board. In the waiting room, there was someone whose chief complaint was that she needed to have surgical drains pulled.
According to the woman’s chart, she’d undergone liposuction in Miami a week before. The surgeon had effectively relinquished all follow-up care to the woman’s local ED.
Dr. Carroll searched the name of her surgeon and found that his site “specifically advertised medical tourism,” Dr. Carroll said. The site lured patients with the idea of recovering by the beach and that a local nurse would come to their room every day.
But when Dr. Carroll told the patient that her surgeon should be the one who removes the drains, she became concerned. She didn’t know that her surgeon wasn’t providing the standard of care, he said. Somewhat appalled that a board-certified plastic surgeon would place the burden of follow-up care on an ED doctor hundreds of miles away, Dr. Carroll posted the case to Twitter and several Facebook groups.
“Yes I could refuse to take [the drains] out but that’s not patient-centered care,” Dr. Carroll wrote in a Twitter thread. “It’s unfairly shifting routine outpatient surgical followup (and liability) onto me and extra cost to [the patient].” Comments from ED physicians and sympathetic surgeons across the country flowed in. Dr. Carroll quickly realized his situation was part of a much larger problem than he’d thought.
Dr. Carroll’s patient told him that the Miami surgery cost less than undergoing the surgery locally; that’s why she’d made the trip. She’s not alone. Traveling to get the lowest price for a plastic surgery procedure has been a rising phenomenon since the early 2000s, according to the American Society of Plastic Surgeons (ASPS). Many countries are actively fostering their medical tourism industries, as are states such as Florida.
People have long traveled to get the best medical care. But “medical tourism is completely different,” said Alan Matarasso, MD, FACS, a Manhattan-based plastic surgeon and member of the ASPS Executive Committee. “People [are] traveling to get a simultaneous vacation or lower cost,” he said.
Choosing facilities on the basis of these criteria comes with myriad problems, and the quality of medical care may be lower. It’s difficult to verify the credentials of the surgeons, anesthesiologists, and facilities involved. Medical records can be in a different language, and traveling immediately after surgery increases the risk for pulmonary embolism and death, not to mention the added complications of traveling and being a surgical patient during the COVID-19 pandemic, he said.
Typically, surgeons are protective of their patients. But Murtaza Akhter, MD, an emergency medicine physician based in Miami, says it’s the opposite with the medical tourism surgeons whose patients regularly end up in his ED. “There’s almost no ownership,” he said. “Every time, [the patients] say, ‘My doctor isn’t responding,’ or they said go to the ER.” And that’s before they’ve even made it out of Miami.
The most common cosmetic surgery complications Dr. Akhter sees occur in patients who’ve undergone so-called Brazilian butt lifts. They show up in his ED face down, suffering from severe blood loss. He has them undergo a transfusion and maybe some imaging, but if they need a higher degree of care, they have to be transferred. “There’s a reason it’s cheaper,” he said.
Medical tourism mishaps are such a regular occurrence in Miami that no one flinches when the patients show up in the ED, Dr. Akhter said. He had begun to think he was overreacting to the problem until he saw Dr. Carroll’s Twitter thread.
“Since it’s daily, I just thought maybe I had gone crazy and that it’s considered normal for plastic surgeons to do this. Thanks for making me feel sane again,” Dr. Akhter tweeted in a reply to Dr. Carroll.
There are no reliable data as to of how often or where such surgeries are occurring or of patients’ outcomes. But Nicholas Genes, MD, an ED physician in Manhattan, says he sees far more postsurgical patients who traveled for their procedures than ones who underwent surgery locally. He can’t say for certain whether that’s because procedures performed by doctors in New York City have fewer complications or the physicians just handle postprocedure problems themselves.
In a 2021 systematic review of aesthetic breast surgeries performed through medical tourism, researchers found that of 171 patients who traveled for surgery, 88 (51%) had a total of 106 complications that required returning to the operating room and undergoing general anesthesia. They also found that 39% of breast augmentation implant surgeries required either a unilateral or bilateral explantation procedure after patients returned home.
The rate of complications was higher than the study authors had expected. “These are totally elective procedures,” Dr. Matarasso said. “They should be optimized.” And high rates of complications come with hefty price tags.
The cost of managing these complications, which falls to the home healthcare system or the patient themselves, can range from $5,500 (determined on the basis of data from a 2019 study in the United Kingdom) to as much as $123,000, researchers in New York City calculated, if the patient develops a complicated mycobacterium infection.
“In your effort to get a good deal or around the system, you could still end up with a lot of extensive medical bills if something goes wrong,” Dr. Genes said.
The liability dilemma
Many of the ED physicians Dr. Carroll heard from said that they wouldn’t have treated the woman who needed to have drains removed. Unlike the Brazilian-butt-lifts-gone-wrong in Miami or the complications Dr. Genes sees in New York City, Dr. Carroll’s patient wasn’t in a state of emergency. Most ED physicians said they would have sent her on her way to find a surgeon.
“In general, we shouldn’t be doing things we aren’t trained to do. It’s sort of a slippery slope,” Dr. Genes said. He’s comfortable with removing stitches, but for surgical drains and plastic apparatuses, “I don’t feel particularly well trained. I’d have to consult a colleague in general surgery,” he said. When he does get one of these patients, he works the phones to find a plastic surgeon who will see the patient, something he says their original plastic surgeon should have done.
“Sitting there with the patient, I felt a little bad for her,” Dr. Carroll said. “I knew if I didn’t do it, it would be weeks while she bounced around to urgent care, primary care, and finally found a surgeon.” But by removing the drains, he did shift some of the liability to himself. “If she developed a wound infection, then I’m on the hook for [that],” he said. “If I send her away, I have less liability but didn’t quite do the right thing for the patient.”
In replies to Dr. Carroll’s thread, some doctors debated whether these types of cases, particularly those in which surgeons forgo follow-up care, could be considered medical abandonment. Legal experts say that’s not exactly the case, at least it would not be the case with Dr. Carroll’s patient.
“I don’t think they’ve abandoned the patient; I think they’ve abandoned care,” said Michael Flynn, JD, professor of personal injury law at Nova Southeastern University, in Fort Lauderdale–Davie, Fla. “And that abandonment of follow-up care, if it falls below the standard of what medical professionals should do, then it’s malpractice.”
“The doctor didn’t just walk away and become unreachable,” said Bernard Black, JD, a medical malpractice attorney and law professor at Northwestern University, in Evanston, Ill. Technically, the surgeon referred the patient to the ED. Mr. Black agreed that it sounds more like a question of malpractice, “but without real damages, there’s no claim.”
Even if not illegal, sending these patients to the ED is still highly unethical, Dr. Carroll said. The authors of a 2014 article in Aesthetic Plastic Surgery concur: “It is the duty and ethical responsibility of plastic surgeons to prevent unnecessary complications following tourism medicine by adequately counseling patients, defining perioperative treatment protocols, and reporting complications to regional and specialty-specific governing bodies,” they write.
Sometimes patients need to travel, Dr. Matarasso said. Recently, three out-of-state patients came to him for procedures. Two stayed in Manhattan until their follow-up care was finished; he arranged care elsewhere for the third. It’s the operating surgeon’s job to connect patients with someone who can provide follow-up care when they go home, Dr. Matarasso said. If a surgeon doesn’t have a connection in a patient’s home city, the ASPS has a referral service to help, he said.
“My frustration was never with the patient,” Dr. Carroll said. “No one should feel bad about coming to an ED for literally anything, and I mean that. My frustration is with the surgeon who didn’t go the one extra step to arrange her follow-up.”
A version of this article first appeared on Medscape.com.
It was a typical, busy evening shift in the emergency department (ED) when Steve Carroll, DO, an emergency medicine physician in the Philadelphia area, noticed an odd listing on the tracking board. In the waiting room, there was someone whose chief complaint was that she needed to have surgical drains pulled.
According to the woman’s chart, she’d undergone liposuction in Miami a week before. The surgeon had effectively relinquished all follow-up care to the woman’s local ED.
Dr. Carroll searched the name of her surgeon and found that his site “specifically advertised medical tourism,” Dr. Carroll said. The site lured patients with the idea of recovering by the beach and that a local nurse would come to their room every day.
But when Dr. Carroll told the patient that her surgeon should be the one who removes the drains, she became concerned. She didn’t know that her surgeon wasn’t providing the standard of care, he said. Somewhat appalled that a board-certified plastic surgeon would place the burden of follow-up care on an ED doctor hundreds of miles away, Dr. Carroll posted the case to Twitter and several Facebook groups.
“Yes I could refuse to take [the drains] out but that’s not patient-centered care,” Dr. Carroll wrote in a Twitter thread. “It’s unfairly shifting routine outpatient surgical followup (and liability) onto me and extra cost to [the patient].” Comments from ED physicians and sympathetic surgeons across the country flowed in. Dr. Carroll quickly realized his situation was part of a much larger problem than he’d thought.
Dr. Carroll’s patient told him that the Miami surgery cost less than undergoing the surgery locally; that’s why she’d made the trip. She’s not alone. Traveling to get the lowest price for a plastic surgery procedure has been a rising phenomenon since the early 2000s, according to the American Society of Plastic Surgeons (ASPS). Many countries are actively fostering their medical tourism industries, as are states such as Florida.
People have long traveled to get the best medical care. But “medical tourism is completely different,” said Alan Matarasso, MD, FACS, a Manhattan-based plastic surgeon and member of the ASPS Executive Committee. “People [are] traveling to get a simultaneous vacation or lower cost,” he said.
Choosing facilities on the basis of these criteria comes with myriad problems, and the quality of medical care may be lower. It’s difficult to verify the credentials of the surgeons, anesthesiologists, and facilities involved. Medical records can be in a different language, and traveling immediately after surgery increases the risk for pulmonary embolism and death, not to mention the added complications of traveling and being a surgical patient during the COVID-19 pandemic, he said.
Typically, surgeons are protective of their patients. But Murtaza Akhter, MD, an emergency medicine physician based in Miami, says it’s the opposite with the medical tourism surgeons whose patients regularly end up in his ED. “There’s almost no ownership,” he said. “Every time, [the patients] say, ‘My doctor isn’t responding,’ or they said go to the ER.” And that’s before they’ve even made it out of Miami.
The most common cosmetic surgery complications Dr. Akhter sees occur in patients who’ve undergone so-called Brazilian butt lifts. They show up in his ED face down, suffering from severe blood loss. He has them undergo a transfusion and maybe some imaging, but if they need a higher degree of care, they have to be transferred. “There’s a reason it’s cheaper,” he said.
Medical tourism mishaps are such a regular occurrence in Miami that no one flinches when the patients show up in the ED, Dr. Akhter said. He had begun to think he was overreacting to the problem until he saw Dr. Carroll’s Twitter thread.
“Since it’s daily, I just thought maybe I had gone crazy and that it’s considered normal for plastic surgeons to do this. Thanks for making me feel sane again,” Dr. Akhter tweeted in a reply to Dr. Carroll.
There are no reliable data as to of how often or where such surgeries are occurring or of patients’ outcomes. But Nicholas Genes, MD, an ED physician in Manhattan, says he sees far more postsurgical patients who traveled for their procedures than ones who underwent surgery locally. He can’t say for certain whether that’s because procedures performed by doctors in New York City have fewer complications or the physicians just handle postprocedure problems themselves.
In a 2021 systematic review of aesthetic breast surgeries performed through medical tourism, researchers found that of 171 patients who traveled for surgery, 88 (51%) had a total of 106 complications that required returning to the operating room and undergoing general anesthesia. They also found that 39% of breast augmentation implant surgeries required either a unilateral or bilateral explantation procedure after patients returned home.
The rate of complications was higher than the study authors had expected. “These are totally elective procedures,” Dr. Matarasso said. “They should be optimized.” And high rates of complications come with hefty price tags.
The cost of managing these complications, which falls to the home healthcare system or the patient themselves, can range from $5,500 (determined on the basis of data from a 2019 study in the United Kingdom) to as much as $123,000, researchers in New York City calculated, if the patient develops a complicated mycobacterium infection.
“In your effort to get a good deal or around the system, you could still end up with a lot of extensive medical bills if something goes wrong,” Dr. Genes said.
The liability dilemma
Many of the ED physicians Dr. Carroll heard from said that they wouldn’t have treated the woman who needed to have drains removed. Unlike the Brazilian-butt-lifts-gone-wrong in Miami or the complications Dr. Genes sees in New York City, Dr. Carroll’s patient wasn’t in a state of emergency. Most ED physicians said they would have sent her on her way to find a surgeon.
“In general, we shouldn’t be doing things we aren’t trained to do. It’s sort of a slippery slope,” Dr. Genes said. He’s comfortable with removing stitches, but for surgical drains and plastic apparatuses, “I don’t feel particularly well trained. I’d have to consult a colleague in general surgery,” he said. When he does get one of these patients, he works the phones to find a plastic surgeon who will see the patient, something he says their original plastic surgeon should have done.
“Sitting there with the patient, I felt a little bad for her,” Dr. Carroll said. “I knew if I didn’t do it, it would be weeks while she bounced around to urgent care, primary care, and finally found a surgeon.” But by removing the drains, he did shift some of the liability to himself. “If she developed a wound infection, then I’m on the hook for [that],” he said. “If I send her away, I have less liability but didn’t quite do the right thing for the patient.”
In replies to Dr. Carroll’s thread, some doctors debated whether these types of cases, particularly those in which surgeons forgo follow-up care, could be considered medical abandonment. Legal experts say that’s not exactly the case, at least it would not be the case with Dr. Carroll’s patient.
“I don’t think they’ve abandoned the patient; I think they’ve abandoned care,” said Michael Flynn, JD, professor of personal injury law at Nova Southeastern University, in Fort Lauderdale–Davie, Fla. “And that abandonment of follow-up care, if it falls below the standard of what medical professionals should do, then it’s malpractice.”
“The doctor didn’t just walk away and become unreachable,” said Bernard Black, JD, a medical malpractice attorney and law professor at Northwestern University, in Evanston, Ill. Technically, the surgeon referred the patient to the ED. Mr. Black agreed that it sounds more like a question of malpractice, “but without real damages, there’s no claim.”
Even if not illegal, sending these patients to the ED is still highly unethical, Dr. Carroll said. The authors of a 2014 article in Aesthetic Plastic Surgery concur: “It is the duty and ethical responsibility of plastic surgeons to prevent unnecessary complications following tourism medicine by adequately counseling patients, defining perioperative treatment protocols, and reporting complications to regional and specialty-specific governing bodies,” they write.
Sometimes patients need to travel, Dr. Matarasso said. Recently, three out-of-state patients came to him for procedures. Two stayed in Manhattan until their follow-up care was finished; he arranged care elsewhere for the third. It’s the operating surgeon’s job to connect patients with someone who can provide follow-up care when they go home, Dr. Matarasso said. If a surgeon doesn’t have a connection in a patient’s home city, the ASPS has a referral service to help, he said.
“My frustration was never with the patient,” Dr. Carroll said. “No one should feel bad about coming to an ED for literally anything, and I mean that. My frustration is with the surgeon who didn’t go the one extra step to arrange her follow-up.”
A version of this article first appeared on Medscape.com.
It was a typical, busy evening shift in the emergency department (ED) when Steve Carroll, DO, an emergency medicine physician in the Philadelphia area, noticed an odd listing on the tracking board. In the waiting room, there was someone whose chief complaint was that she needed to have surgical drains pulled.
According to the woman’s chart, she’d undergone liposuction in Miami a week before. The surgeon had effectively relinquished all follow-up care to the woman’s local ED.
Dr. Carroll searched the name of her surgeon and found that his site “specifically advertised medical tourism,” Dr. Carroll said. The site lured patients with the idea of recovering by the beach and that a local nurse would come to their room every day.
But when Dr. Carroll told the patient that her surgeon should be the one who removes the drains, she became concerned. She didn’t know that her surgeon wasn’t providing the standard of care, he said. Somewhat appalled that a board-certified plastic surgeon would place the burden of follow-up care on an ED doctor hundreds of miles away, Dr. Carroll posted the case to Twitter and several Facebook groups.
“Yes I could refuse to take [the drains] out but that’s not patient-centered care,” Dr. Carroll wrote in a Twitter thread. “It’s unfairly shifting routine outpatient surgical followup (and liability) onto me and extra cost to [the patient].” Comments from ED physicians and sympathetic surgeons across the country flowed in. Dr. Carroll quickly realized his situation was part of a much larger problem than he’d thought.
Dr. Carroll’s patient told him that the Miami surgery cost less than undergoing the surgery locally; that’s why she’d made the trip. She’s not alone. Traveling to get the lowest price for a plastic surgery procedure has been a rising phenomenon since the early 2000s, according to the American Society of Plastic Surgeons (ASPS). Many countries are actively fostering their medical tourism industries, as are states such as Florida.
People have long traveled to get the best medical care. But “medical tourism is completely different,” said Alan Matarasso, MD, FACS, a Manhattan-based plastic surgeon and member of the ASPS Executive Committee. “People [are] traveling to get a simultaneous vacation or lower cost,” he said.
Choosing facilities on the basis of these criteria comes with myriad problems, and the quality of medical care may be lower. It’s difficult to verify the credentials of the surgeons, anesthesiologists, and facilities involved. Medical records can be in a different language, and traveling immediately after surgery increases the risk for pulmonary embolism and death, not to mention the added complications of traveling and being a surgical patient during the COVID-19 pandemic, he said.
Typically, surgeons are protective of their patients. But Murtaza Akhter, MD, an emergency medicine physician based in Miami, says it’s the opposite with the medical tourism surgeons whose patients regularly end up in his ED. “There’s almost no ownership,” he said. “Every time, [the patients] say, ‘My doctor isn’t responding,’ or they said go to the ER.” And that’s before they’ve even made it out of Miami.
The most common cosmetic surgery complications Dr. Akhter sees occur in patients who’ve undergone so-called Brazilian butt lifts. They show up in his ED face down, suffering from severe blood loss. He has them undergo a transfusion and maybe some imaging, but if they need a higher degree of care, they have to be transferred. “There’s a reason it’s cheaper,” he said.
Medical tourism mishaps are such a regular occurrence in Miami that no one flinches when the patients show up in the ED, Dr. Akhter said. He had begun to think he was overreacting to the problem until he saw Dr. Carroll’s Twitter thread.
“Since it’s daily, I just thought maybe I had gone crazy and that it’s considered normal for plastic surgeons to do this. Thanks for making me feel sane again,” Dr. Akhter tweeted in a reply to Dr. Carroll.
There are no reliable data as to of how often or where such surgeries are occurring or of patients’ outcomes. But Nicholas Genes, MD, an ED physician in Manhattan, says he sees far more postsurgical patients who traveled for their procedures than ones who underwent surgery locally. He can’t say for certain whether that’s because procedures performed by doctors in New York City have fewer complications or the physicians just handle postprocedure problems themselves.
In a 2021 systematic review of aesthetic breast surgeries performed through medical tourism, researchers found that of 171 patients who traveled for surgery, 88 (51%) had a total of 106 complications that required returning to the operating room and undergoing general anesthesia. They also found that 39% of breast augmentation implant surgeries required either a unilateral or bilateral explantation procedure after patients returned home.
The rate of complications was higher than the study authors had expected. “These are totally elective procedures,” Dr. Matarasso said. “They should be optimized.” And high rates of complications come with hefty price tags.
The cost of managing these complications, which falls to the home healthcare system or the patient themselves, can range from $5,500 (determined on the basis of data from a 2019 study in the United Kingdom) to as much as $123,000, researchers in New York City calculated, if the patient develops a complicated mycobacterium infection.
“In your effort to get a good deal or around the system, you could still end up with a lot of extensive medical bills if something goes wrong,” Dr. Genes said.
The liability dilemma
Many of the ED physicians Dr. Carroll heard from said that they wouldn’t have treated the woman who needed to have drains removed. Unlike the Brazilian-butt-lifts-gone-wrong in Miami or the complications Dr. Genes sees in New York City, Dr. Carroll’s patient wasn’t in a state of emergency. Most ED physicians said they would have sent her on her way to find a surgeon.
“In general, we shouldn’t be doing things we aren’t trained to do. It’s sort of a slippery slope,” Dr. Genes said. He’s comfortable with removing stitches, but for surgical drains and plastic apparatuses, “I don’t feel particularly well trained. I’d have to consult a colleague in general surgery,” he said. When he does get one of these patients, he works the phones to find a plastic surgeon who will see the patient, something he says their original plastic surgeon should have done.
“Sitting there with the patient, I felt a little bad for her,” Dr. Carroll said. “I knew if I didn’t do it, it would be weeks while she bounced around to urgent care, primary care, and finally found a surgeon.” But by removing the drains, he did shift some of the liability to himself. “If she developed a wound infection, then I’m on the hook for [that],” he said. “If I send her away, I have less liability but didn’t quite do the right thing for the patient.”
In replies to Dr. Carroll’s thread, some doctors debated whether these types of cases, particularly those in which surgeons forgo follow-up care, could be considered medical abandonment. Legal experts say that’s not exactly the case, at least it would not be the case with Dr. Carroll’s patient.
“I don’t think they’ve abandoned the patient; I think they’ve abandoned care,” said Michael Flynn, JD, professor of personal injury law at Nova Southeastern University, in Fort Lauderdale–Davie, Fla. “And that abandonment of follow-up care, if it falls below the standard of what medical professionals should do, then it’s malpractice.”
“The doctor didn’t just walk away and become unreachable,” said Bernard Black, JD, a medical malpractice attorney and law professor at Northwestern University, in Evanston, Ill. Technically, the surgeon referred the patient to the ED. Mr. Black agreed that it sounds more like a question of malpractice, “but without real damages, there’s no claim.”
Even if not illegal, sending these patients to the ED is still highly unethical, Dr. Carroll said. The authors of a 2014 article in Aesthetic Plastic Surgery concur: “It is the duty and ethical responsibility of plastic surgeons to prevent unnecessary complications following tourism medicine by adequately counseling patients, defining perioperative treatment protocols, and reporting complications to regional and specialty-specific governing bodies,” they write.
Sometimes patients need to travel, Dr. Matarasso said. Recently, three out-of-state patients came to him for procedures. Two stayed in Manhattan until their follow-up care was finished; he arranged care elsewhere for the third. It’s the operating surgeon’s job to connect patients with someone who can provide follow-up care when they go home, Dr. Matarasso said. If a surgeon doesn’t have a connection in a patient’s home city, the ASPS has a referral service to help, he said.
“My frustration was never with the patient,” Dr. Carroll said. “No one should feel bad about coming to an ED for literally anything, and I mean that. My frustration is with the surgeon who didn’t go the one extra step to arrange her follow-up.”
A version of this article first appeared on Medscape.com.
Medicinal liquor and edited mosquitoes
Drink to your health?
Whether you drink or not, most of us can agree that liquor is not the first thing that comes to mind when looking to make health improvements. But researchers have found a small exception in something traditional.
We’ve added buckwheat to pancakes, bread, and other baked goodies we made during the height of quarantine, but it’s also used to create a traditional liquor in some East Asian countries, where it is used medicinally.
Investigators have found that extracts in the Tartary buckwheat used to make the liquor induce autophagy, a process cells go through to remove proteins that are damaged or not needed anymore – sort of like a cellular spring cleaning.
To test this, the researchers treated liver and skin cells with Tartary buckwheat extract and looked to see how the cells responded with fluorescent markers. The results were clear.
“Treating cells with the extract stimulated the formation of autophagosomes, specialized cellular structures that carry out autophagy, and altered the location of proteins involved in regulating autophagy,” said senior author Takeshi Noda of Osaka (Japan) University.
Looking deeper, the researchers found that quercetin, a component of the buckwheat extract, had the same autophagic effect. And both the buckwheat and the quercetin gave the green light for liver cells to induce aggrephagy, the process of cleaning up protein aggregates.
Those protein aggregates in liver cells are closely linked to alcoholic liver disease, suggesting that quercetin could be a game changer in its treatment. In other words, liquor could help fix the problem that liquor started. Go figure.
From hospital bills to X-rated
Ralph Puglisi was an accounting manager for the University Medical Service Association (UMSA), a nonprofit that supports the massive University of South Florida health system. The association took in over $300 million in revenue in the 2019-2020 fiscal year, which is a rather large sum of money, but we’ll glide over the ethics of a “nonprofit” making a few hundred million for now.
Mr. Puglisi was in very close proximity to the money, generated from patient care, and he pled guilty to stealing it using UMSA credit cards. Now, that wouldn’t be LOTME worthy on its own, but what elevates this above garden-variety embezzlement is how the intrepid Mr. Puglisi chose to spend the millions he stole from the university health system: Adult entertainment.
And before you ask, he didn’t spend $11.5 million on something most people so inclined can find for free with judicious Google searches. What Mr. Puglisi actually did was invest in a website providing adult content through individual user profiles, one of which is believed to belong to his stepson’s fiancée, which brings a whole new level of sleaze to this enterprise. Over the course of 2 years, he visited her profile 2,800 times, an amount some might view as excessive.
While the vast majority of the embezzled money went to the adult website, Mr. Puglisi also used thousands of UMSA dollars to pay for travel, household improvements, rent, the works. Almost $44,000 was spent at a resort sometimes known as the happiest place on earth.
Then there’s Mr. Puglisi’s wife. Oh yes, this guy is married. He poured over $600,000 into a company he and his wife owned, which is a lot, but how much do you think went to the woman he married? Probably quite a bit. Go ahead, try to think of a number. It’s not like it was his money.
Did you guess $100 went into his wife’s PayPal account? No? Clearly you don’t understand the criminal mind. His stepson’s fiancée got millions, and his wife got a hundred. Now there are some priorities.
Step 1: Sit at desk. Step 2: Get in shape
Being a physician is not really a desk job, but doctors must spend a fair share of their time sitting, yes? Dealing with recalcitrant EHRs or talking on the phone to insurers or PBMs? If you are one of these physicians, or if you have patients who spend a lot of time sitting at their desks and might need to get a bit of exercise, then we’ve got a multitasking tip for you.
It came to us via one of our favorite websites, Sad and Useless. It’s the site that declares itself “the most depressive humor site on the Internet” and they’re offering up the “12 Best Exercises To Do At Your Desk.” It may not sound like much, but we think that the gang at Dunder-Mifflin would approve. And besides, who couldn’t stand to burn a few calories without having to leave the chair?
We won’t spoil your fun by going through all 12 – each one comes with step-by-step instructions and a helpful illustration or GIF – but here are just a few:
- Bending over backwards: “Agree to do something you don’t want to do. Spend twice as long as expected doing that thing. Hate yourself.”
- Fake laughter: “Hear a joke that isn’t even remotely funny. Open your mouth and make laughing sounds.”
- Bang your head: Feel the “pointlessness of your job overwhelm you” and then “bring your head forcefully down to your desk.”
Now, we here at LOTME are, of course [Bang!], highly skilled, professional wordsmithing humorists [Bang!], so when we tell you that this is a great workout [Bang!] … that this is a great workout [Bang!] … it’s great … uggh.
Wooooo. Feel the burn.
One order of mosquitoes, extra Crispr
What would it be like to have a barbecue in your backyard on a humid summer night and not get eaten alive by mosquitoes? If you’re like us, you probably thought you’d never see that day.
Mosquitoes cause itchy bites, but, more importantly, they can carry dengue, malaria, yellow fever, and Zika virus. New research shows that protection from these diseases may be possible with use of the Crispr-Cas9 gene-editing tool, which could make humans invisible to mosquitoes by taking away their light-sensing abilities and, thus, their ability to find us.
“The better we understand how they sense the human, the better we can control the mosquito in an eco-friendly manner,” Yinpeng Zhan, a postdoctoral researcher at the University of California, Santa Barbara, and the study’s lead author, told the New York Times.
After studying the mosquitoes and figuring out their hunting patterns, the researchers found that mosquitoes are attracted to dark spots more than white spots and used this to their advantage. After knocking out two of the proteins that mosquitoes need for vision – via Crispr – the little suckers could not distinguish the difference between the white and dark spots.
We’re sure mosquitoes don’t mean any harm – they’re just trying to survive and reproduce like any other species – but thanks to this new tool, gone might be the days of having to douse yourself in bug spray that smells like a mix of chemicals and melon.
Drink to your health?
Whether you drink or not, most of us can agree that liquor is not the first thing that comes to mind when looking to make health improvements. But researchers have found a small exception in something traditional.
We’ve added buckwheat to pancakes, bread, and other baked goodies we made during the height of quarantine, but it’s also used to create a traditional liquor in some East Asian countries, where it is used medicinally.
Investigators have found that extracts in the Tartary buckwheat used to make the liquor induce autophagy, a process cells go through to remove proteins that are damaged or not needed anymore – sort of like a cellular spring cleaning.
To test this, the researchers treated liver and skin cells with Tartary buckwheat extract and looked to see how the cells responded with fluorescent markers. The results were clear.
“Treating cells with the extract stimulated the formation of autophagosomes, specialized cellular structures that carry out autophagy, and altered the location of proteins involved in regulating autophagy,” said senior author Takeshi Noda of Osaka (Japan) University.
Looking deeper, the researchers found that quercetin, a component of the buckwheat extract, had the same autophagic effect. And both the buckwheat and the quercetin gave the green light for liver cells to induce aggrephagy, the process of cleaning up protein aggregates.
Those protein aggregates in liver cells are closely linked to alcoholic liver disease, suggesting that quercetin could be a game changer in its treatment. In other words, liquor could help fix the problem that liquor started. Go figure.
From hospital bills to X-rated
Ralph Puglisi was an accounting manager for the University Medical Service Association (UMSA), a nonprofit that supports the massive University of South Florida health system. The association took in over $300 million in revenue in the 2019-2020 fiscal year, which is a rather large sum of money, but we’ll glide over the ethics of a “nonprofit” making a few hundred million for now.
Mr. Puglisi was in very close proximity to the money, generated from patient care, and he pled guilty to stealing it using UMSA credit cards. Now, that wouldn’t be LOTME worthy on its own, but what elevates this above garden-variety embezzlement is how the intrepid Mr. Puglisi chose to spend the millions he stole from the university health system: Adult entertainment.
And before you ask, he didn’t spend $11.5 million on something most people so inclined can find for free with judicious Google searches. What Mr. Puglisi actually did was invest in a website providing adult content through individual user profiles, one of which is believed to belong to his stepson’s fiancée, which brings a whole new level of sleaze to this enterprise. Over the course of 2 years, he visited her profile 2,800 times, an amount some might view as excessive.
While the vast majority of the embezzled money went to the adult website, Mr. Puglisi also used thousands of UMSA dollars to pay for travel, household improvements, rent, the works. Almost $44,000 was spent at a resort sometimes known as the happiest place on earth.
Then there’s Mr. Puglisi’s wife. Oh yes, this guy is married. He poured over $600,000 into a company he and his wife owned, which is a lot, but how much do you think went to the woman he married? Probably quite a bit. Go ahead, try to think of a number. It’s not like it was his money.
Did you guess $100 went into his wife’s PayPal account? No? Clearly you don’t understand the criminal mind. His stepson’s fiancée got millions, and his wife got a hundred. Now there are some priorities.
Step 1: Sit at desk. Step 2: Get in shape
Being a physician is not really a desk job, but doctors must spend a fair share of their time sitting, yes? Dealing with recalcitrant EHRs or talking on the phone to insurers or PBMs? If you are one of these physicians, or if you have patients who spend a lot of time sitting at their desks and might need to get a bit of exercise, then we’ve got a multitasking tip for you.
It came to us via one of our favorite websites, Sad and Useless. It’s the site that declares itself “the most depressive humor site on the Internet” and they’re offering up the “12 Best Exercises To Do At Your Desk.” It may not sound like much, but we think that the gang at Dunder-Mifflin would approve. And besides, who couldn’t stand to burn a few calories without having to leave the chair?
We won’t spoil your fun by going through all 12 – each one comes with step-by-step instructions and a helpful illustration or GIF – but here are just a few:
- Bending over backwards: “Agree to do something you don’t want to do. Spend twice as long as expected doing that thing. Hate yourself.”
- Fake laughter: “Hear a joke that isn’t even remotely funny. Open your mouth and make laughing sounds.”
- Bang your head: Feel the “pointlessness of your job overwhelm you” and then “bring your head forcefully down to your desk.”
Now, we here at LOTME are, of course [Bang!], highly skilled, professional wordsmithing humorists [Bang!], so when we tell you that this is a great workout [Bang!] … that this is a great workout [Bang!] … it’s great … uggh.
Wooooo. Feel the burn.
One order of mosquitoes, extra Crispr
What would it be like to have a barbecue in your backyard on a humid summer night and not get eaten alive by mosquitoes? If you’re like us, you probably thought you’d never see that day.
Mosquitoes cause itchy bites, but, more importantly, they can carry dengue, malaria, yellow fever, and Zika virus. New research shows that protection from these diseases may be possible with use of the Crispr-Cas9 gene-editing tool, which could make humans invisible to mosquitoes by taking away their light-sensing abilities and, thus, their ability to find us.
“The better we understand how they sense the human, the better we can control the mosquito in an eco-friendly manner,” Yinpeng Zhan, a postdoctoral researcher at the University of California, Santa Barbara, and the study’s lead author, told the New York Times.
After studying the mosquitoes and figuring out their hunting patterns, the researchers found that mosquitoes are attracted to dark spots more than white spots and used this to their advantage. After knocking out two of the proteins that mosquitoes need for vision – via Crispr – the little suckers could not distinguish the difference between the white and dark spots.
We’re sure mosquitoes don’t mean any harm – they’re just trying to survive and reproduce like any other species – but thanks to this new tool, gone might be the days of having to douse yourself in bug spray that smells like a mix of chemicals and melon.
Drink to your health?
Whether you drink or not, most of us can agree that liquor is not the first thing that comes to mind when looking to make health improvements. But researchers have found a small exception in something traditional.
We’ve added buckwheat to pancakes, bread, and other baked goodies we made during the height of quarantine, but it’s also used to create a traditional liquor in some East Asian countries, where it is used medicinally.
Investigators have found that extracts in the Tartary buckwheat used to make the liquor induce autophagy, a process cells go through to remove proteins that are damaged or not needed anymore – sort of like a cellular spring cleaning.
To test this, the researchers treated liver and skin cells with Tartary buckwheat extract and looked to see how the cells responded with fluorescent markers. The results were clear.
“Treating cells with the extract stimulated the formation of autophagosomes, specialized cellular structures that carry out autophagy, and altered the location of proteins involved in regulating autophagy,” said senior author Takeshi Noda of Osaka (Japan) University.
Looking deeper, the researchers found that quercetin, a component of the buckwheat extract, had the same autophagic effect. And both the buckwheat and the quercetin gave the green light for liver cells to induce aggrephagy, the process of cleaning up protein aggregates.
Those protein aggregates in liver cells are closely linked to alcoholic liver disease, suggesting that quercetin could be a game changer in its treatment. In other words, liquor could help fix the problem that liquor started. Go figure.
From hospital bills to X-rated
Ralph Puglisi was an accounting manager for the University Medical Service Association (UMSA), a nonprofit that supports the massive University of South Florida health system. The association took in over $300 million in revenue in the 2019-2020 fiscal year, which is a rather large sum of money, but we’ll glide over the ethics of a “nonprofit” making a few hundred million for now.
Mr. Puglisi was in very close proximity to the money, generated from patient care, and he pled guilty to stealing it using UMSA credit cards. Now, that wouldn’t be LOTME worthy on its own, but what elevates this above garden-variety embezzlement is how the intrepid Mr. Puglisi chose to spend the millions he stole from the university health system: Adult entertainment.
And before you ask, he didn’t spend $11.5 million on something most people so inclined can find for free with judicious Google searches. What Mr. Puglisi actually did was invest in a website providing adult content through individual user profiles, one of which is believed to belong to his stepson’s fiancée, which brings a whole new level of sleaze to this enterprise. Over the course of 2 years, he visited her profile 2,800 times, an amount some might view as excessive.
While the vast majority of the embezzled money went to the adult website, Mr. Puglisi also used thousands of UMSA dollars to pay for travel, household improvements, rent, the works. Almost $44,000 was spent at a resort sometimes known as the happiest place on earth.
Then there’s Mr. Puglisi’s wife. Oh yes, this guy is married. He poured over $600,000 into a company he and his wife owned, which is a lot, but how much do you think went to the woman he married? Probably quite a bit. Go ahead, try to think of a number. It’s not like it was his money.
Did you guess $100 went into his wife’s PayPal account? No? Clearly you don’t understand the criminal mind. His stepson’s fiancée got millions, and his wife got a hundred. Now there are some priorities.
Step 1: Sit at desk. Step 2: Get in shape
Being a physician is not really a desk job, but doctors must spend a fair share of their time sitting, yes? Dealing with recalcitrant EHRs or talking on the phone to insurers or PBMs? If you are one of these physicians, or if you have patients who spend a lot of time sitting at their desks and might need to get a bit of exercise, then we’ve got a multitasking tip for you.
It came to us via one of our favorite websites, Sad and Useless. It’s the site that declares itself “the most depressive humor site on the Internet” and they’re offering up the “12 Best Exercises To Do At Your Desk.” It may not sound like much, but we think that the gang at Dunder-Mifflin would approve. And besides, who couldn’t stand to burn a few calories without having to leave the chair?
We won’t spoil your fun by going through all 12 – each one comes with step-by-step instructions and a helpful illustration or GIF – but here are just a few:
- Bending over backwards: “Agree to do something you don’t want to do. Spend twice as long as expected doing that thing. Hate yourself.”
- Fake laughter: “Hear a joke that isn’t even remotely funny. Open your mouth and make laughing sounds.”
- Bang your head: Feel the “pointlessness of your job overwhelm you” and then “bring your head forcefully down to your desk.”
Now, we here at LOTME are, of course [Bang!], highly skilled, professional wordsmithing humorists [Bang!], so when we tell you that this is a great workout [Bang!] … that this is a great workout [Bang!] … it’s great … uggh.
Wooooo. Feel the burn.
One order of mosquitoes, extra Crispr
What would it be like to have a barbecue in your backyard on a humid summer night and not get eaten alive by mosquitoes? If you’re like us, you probably thought you’d never see that day.
Mosquitoes cause itchy bites, but, more importantly, they can carry dengue, malaria, yellow fever, and Zika virus. New research shows that protection from these diseases may be possible with use of the Crispr-Cas9 gene-editing tool, which could make humans invisible to mosquitoes by taking away their light-sensing abilities and, thus, their ability to find us.
“The better we understand how they sense the human, the better we can control the mosquito in an eco-friendly manner,” Yinpeng Zhan, a postdoctoral researcher at the University of California, Santa Barbara, and the study’s lead author, told the New York Times.
After studying the mosquitoes and figuring out their hunting patterns, the researchers found that mosquitoes are attracted to dark spots more than white spots and used this to their advantage. After knocking out two of the proteins that mosquitoes need for vision – via Crispr – the little suckers could not distinguish the difference between the white and dark spots.
We’re sure mosquitoes don’t mean any harm – they’re just trying to survive and reproduce like any other species – but thanks to this new tool, gone might be the days of having to douse yourself in bug spray that smells like a mix of chemicals and melon.
COVID-19 booster shots to start in September: Officials
at a press briefing August 18.
Those who received the Pfizer-BioNTech and Moderna vaccines would be eligible to get a booster shot 8 months after they received the second dose of those vaccines, officials said. Information on boosters for those who got the one-dose Johnson & Johnson vaccine will be forthcoming.
“We anticipate a booster will [also] likely be needed,” said U.S. Surgeon General Vivek Murthy, MD. The J&J vaccine was not available in the U.S. until March, he said, and ‘’we expect more data on J&J in the coming weeks, so that plan is coming.”
The plan for boosters for the two mRNA vaccines is pending the FDA’s conducting of an independent review and authorizing the third dose of the Moderna and Pfizer-BioNTech vaccines, as well as an advisory committee of the CDC making the recommendation.
“We know that even highly effective vaccines become less effective over time,” Dr. Murthy said. “Having reviewed the most current data, it is now our clinical judgment that the time to lay out a plan for the COVID-19 boosters is now.”
Research released Aug. 18 shows waning effectiveness of the two mRNA vaccines.
At the briefing, Dr. Murthy and others continually reassured listeners that while effectiveness against infection declines, the vaccines continue to protect against severe infections, hospitalizations, and death.
“If you are fully vaccinated, you still have a high degree of protection against the worst outcomes,” Dr. Murthy said.
Data driving the plan
CDC Director Rochelle Walensky, MD, cited three research studies published Aug. 18 in the CDC’s Morbidity and Mortality Weekly Report that helped to drive the decision to recommend boosters.
Analysis of nursing home COVID-19 data from the CDC’s National Healthcare Safety Network showed a significant decline in the effectiveness of the full mRNA vaccine against lab-confirmed COVID-19 infection, from 74.7% before the Delta variant (March 1-May 9, 2021) to 53% when the Delta variant became predominant in the United States. The analysis during the Delta dominant period included 85,000 weekly reports from nearly 15,000 facilities.
Another study looked at more than 10 million New York adults who had been fully vaccinated with either the Moderna, Pfizer, or J&J vaccine by July 25. During the period from May 3 to July 25, overall, the age-adjusted vaccine effectiveness against infection decreased from 91.7% to 79.8%.
Vaccine effectiveness against hospitalization remains high, another study found. An analysis of 1,129 patients who had gotten two doses of an mRNA vaccine showed vaccine effectiveness against hospitalization after 24 weeks. It was 86% at weeks 2-12 and 84% at weeks 13-24.
Immunologic facts
Immunologic information also points to the need for a booster, said Anthony Fauci, MD, the chief medical advisor to the president and director of the National Institute of Allergy and Infectious Diseases.
“Antibody levels decline over time,” he said, “and higher antibody levels are associated with higher efficacy of the vaccine. Higher levels of antibody may be needed to protect against Delta.”
A booster increased antibody levels by ‘’at least tenfold and possibly more,” he said. And higher levels of antibody may be required to protect against Delta. Taken together, he said, the data support the use of a booster to increase the overall level of protection.
Booster details
“We will make sure it is convenient and easy to get the booster shot,” said Jeff Zients, the White House COVID-19 response coordinator. As with the previous immunization, he said, the booster will be free, and no one will be asked about immigration status.
The plan for booster shots is an attempt to stay ahead of the virus, officials stressed
Big picture
Not everyone agrees with the booster dose idea. At a World Health Organization briefing Aug. 18, WHO’s Chief Scientist Soumya Swaminathan, MD, an Indian pediatrician, said that the right thing to do right now ‘’is to wait for the science to tell us when boosters, which groups of people, and which vaccines need boosters.”
Like others, she also broached the ‘’moral and ethical argument of giving people third doses, when they’re already well protected and while the rest of the world is waiting for their primary immunization.”
Dr. Swaminathan does see a role for boosters to protect immunocompromised people but noted that ‘’that’s a small number of people.” Widespread boosters ‘’will only lead to more variants, to more escape variants, and perhaps we’re heading into more dire situations.”
A version of this article first appeared on WebMD.com.
at a press briefing August 18.
Those who received the Pfizer-BioNTech and Moderna vaccines would be eligible to get a booster shot 8 months after they received the second dose of those vaccines, officials said. Information on boosters for those who got the one-dose Johnson & Johnson vaccine will be forthcoming.
“We anticipate a booster will [also] likely be needed,” said U.S. Surgeon General Vivek Murthy, MD. The J&J vaccine was not available in the U.S. until March, he said, and ‘’we expect more data on J&J in the coming weeks, so that plan is coming.”
The plan for boosters for the two mRNA vaccines is pending the FDA’s conducting of an independent review and authorizing the third dose of the Moderna and Pfizer-BioNTech vaccines, as well as an advisory committee of the CDC making the recommendation.
“We know that even highly effective vaccines become less effective over time,” Dr. Murthy said. “Having reviewed the most current data, it is now our clinical judgment that the time to lay out a plan for the COVID-19 boosters is now.”
Research released Aug. 18 shows waning effectiveness of the two mRNA vaccines.
At the briefing, Dr. Murthy and others continually reassured listeners that while effectiveness against infection declines, the vaccines continue to protect against severe infections, hospitalizations, and death.
“If you are fully vaccinated, you still have a high degree of protection against the worst outcomes,” Dr. Murthy said.
Data driving the plan
CDC Director Rochelle Walensky, MD, cited three research studies published Aug. 18 in the CDC’s Morbidity and Mortality Weekly Report that helped to drive the decision to recommend boosters.
Analysis of nursing home COVID-19 data from the CDC’s National Healthcare Safety Network showed a significant decline in the effectiveness of the full mRNA vaccine against lab-confirmed COVID-19 infection, from 74.7% before the Delta variant (March 1-May 9, 2021) to 53% when the Delta variant became predominant in the United States. The analysis during the Delta dominant period included 85,000 weekly reports from nearly 15,000 facilities.
Another study looked at more than 10 million New York adults who had been fully vaccinated with either the Moderna, Pfizer, or J&J vaccine by July 25. During the period from May 3 to July 25, overall, the age-adjusted vaccine effectiveness against infection decreased from 91.7% to 79.8%.
Vaccine effectiveness against hospitalization remains high, another study found. An analysis of 1,129 patients who had gotten two doses of an mRNA vaccine showed vaccine effectiveness against hospitalization after 24 weeks. It was 86% at weeks 2-12 and 84% at weeks 13-24.
Immunologic facts
Immunologic information also points to the need for a booster, said Anthony Fauci, MD, the chief medical advisor to the president and director of the National Institute of Allergy and Infectious Diseases.
“Antibody levels decline over time,” he said, “and higher antibody levels are associated with higher efficacy of the vaccine. Higher levels of antibody may be needed to protect against Delta.”
A booster increased antibody levels by ‘’at least tenfold and possibly more,” he said. And higher levels of antibody may be required to protect against Delta. Taken together, he said, the data support the use of a booster to increase the overall level of protection.
Booster details
“We will make sure it is convenient and easy to get the booster shot,” said Jeff Zients, the White House COVID-19 response coordinator. As with the previous immunization, he said, the booster will be free, and no one will be asked about immigration status.
The plan for booster shots is an attempt to stay ahead of the virus, officials stressed
Big picture
Not everyone agrees with the booster dose idea. At a World Health Organization briefing Aug. 18, WHO’s Chief Scientist Soumya Swaminathan, MD, an Indian pediatrician, said that the right thing to do right now ‘’is to wait for the science to tell us when boosters, which groups of people, and which vaccines need boosters.”
Like others, she also broached the ‘’moral and ethical argument of giving people third doses, when they’re already well protected and while the rest of the world is waiting for their primary immunization.”
Dr. Swaminathan does see a role for boosters to protect immunocompromised people but noted that ‘’that’s a small number of people.” Widespread boosters ‘’will only lead to more variants, to more escape variants, and perhaps we’re heading into more dire situations.”
A version of this article first appeared on WebMD.com.
at a press briefing August 18.
Those who received the Pfizer-BioNTech and Moderna vaccines would be eligible to get a booster shot 8 months after they received the second dose of those vaccines, officials said. Information on boosters for those who got the one-dose Johnson & Johnson vaccine will be forthcoming.
“We anticipate a booster will [also] likely be needed,” said U.S. Surgeon General Vivek Murthy, MD. The J&J vaccine was not available in the U.S. until March, he said, and ‘’we expect more data on J&J in the coming weeks, so that plan is coming.”
The plan for boosters for the two mRNA vaccines is pending the FDA’s conducting of an independent review and authorizing the third dose of the Moderna and Pfizer-BioNTech vaccines, as well as an advisory committee of the CDC making the recommendation.
“We know that even highly effective vaccines become less effective over time,” Dr. Murthy said. “Having reviewed the most current data, it is now our clinical judgment that the time to lay out a plan for the COVID-19 boosters is now.”
Research released Aug. 18 shows waning effectiveness of the two mRNA vaccines.
At the briefing, Dr. Murthy and others continually reassured listeners that while effectiveness against infection declines, the vaccines continue to protect against severe infections, hospitalizations, and death.
“If you are fully vaccinated, you still have a high degree of protection against the worst outcomes,” Dr. Murthy said.
Data driving the plan
CDC Director Rochelle Walensky, MD, cited three research studies published Aug. 18 in the CDC’s Morbidity and Mortality Weekly Report that helped to drive the decision to recommend boosters.
Analysis of nursing home COVID-19 data from the CDC’s National Healthcare Safety Network showed a significant decline in the effectiveness of the full mRNA vaccine against lab-confirmed COVID-19 infection, from 74.7% before the Delta variant (March 1-May 9, 2021) to 53% when the Delta variant became predominant in the United States. The analysis during the Delta dominant period included 85,000 weekly reports from nearly 15,000 facilities.
Another study looked at more than 10 million New York adults who had been fully vaccinated with either the Moderna, Pfizer, or J&J vaccine by July 25. During the period from May 3 to July 25, overall, the age-adjusted vaccine effectiveness against infection decreased from 91.7% to 79.8%.
Vaccine effectiveness against hospitalization remains high, another study found. An analysis of 1,129 patients who had gotten two doses of an mRNA vaccine showed vaccine effectiveness against hospitalization after 24 weeks. It was 86% at weeks 2-12 and 84% at weeks 13-24.
Immunologic facts
Immunologic information also points to the need for a booster, said Anthony Fauci, MD, the chief medical advisor to the president and director of the National Institute of Allergy and Infectious Diseases.
“Antibody levels decline over time,” he said, “and higher antibody levels are associated with higher efficacy of the vaccine. Higher levels of antibody may be needed to protect against Delta.”
A booster increased antibody levels by ‘’at least tenfold and possibly more,” he said. And higher levels of antibody may be required to protect against Delta. Taken together, he said, the data support the use of a booster to increase the overall level of protection.
Booster details
“We will make sure it is convenient and easy to get the booster shot,” said Jeff Zients, the White House COVID-19 response coordinator. As with the previous immunization, he said, the booster will be free, and no one will be asked about immigration status.
The plan for booster shots is an attempt to stay ahead of the virus, officials stressed
Big picture
Not everyone agrees with the booster dose idea. At a World Health Organization briefing Aug. 18, WHO’s Chief Scientist Soumya Swaminathan, MD, an Indian pediatrician, said that the right thing to do right now ‘’is to wait for the science to tell us when boosters, which groups of people, and which vaccines need boosters.”
Like others, she also broached the ‘’moral and ethical argument of giving people third doses, when they’re already well protected and while the rest of the world is waiting for their primary immunization.”
Dr. Swaminathan does see a role for boosters to protect immunocompromised people but noted that ‘’that’s a small number of people.” Widespread boosters ‘’will only lead to more variants, to more escape variants, and perhaps we’re heading into more dire situations.”
A version of this article first appeared on WebMD.com.
Latest data show increase in breakthrough COVID-19 cases
Breakthrough cases accounted for about one in five newly diagnosed cases in six of the states, according to the New York Times. Hospitalizations and deaths among vaccinated people may be higher than previously thought as well.
“Remember when the early vaccine studies came out, it was like nobody gets hospitalized, nobody dies,” Robert Wachter, MD, chairman of the department of medicine at the University of California, San Francisco, said in an interview. “That clearly is not true.”
The New York Times analyzed data in seven states – California, Colorado, Massachusetts, Oregon, Utah, Vermont, and Virginia – that are tracking the most detailed information. The trends in these states may not reflect the numbers throughout the country, the newspaper reported.
Even still, the numbers back up the idea that vaccinated people may need booster shots this fall to support their earlier vaccine doses. Federal health officials are scheduled to approve the extra shots in coming weeks, potentially in September. The first people to receive booster shots will likely be health care workers and nursing home residents who took the first vaccines in December and January.
“If the chances of a breakthrough infection have gone up considerably, and I think the evidence is clear that they have, and the level of protection against severe illness is no longer as robust as it was, I think the case for boosters goes up pretty quickly,” Dr. Wachter said.
Previous analyses of breakthrough cases included data from June and earlier, the newspaper reported. But since July, COVID-19 cases have soared again because of the Delta variant, and the most recent numbers show an uptick among vaccinated people. In Los Angeles County, for instance, fully vaccinated people account for 20% of new COVID-19 cases, which is up from 11% in May, 5% in April, and 2% in March, according to a late July report from the Los Angeles County Department of Public Health.
What’s more, breakthrough infections in the seven states accounted for 12%-24% of COVID-19 hospitalizations in those states. About 8,000 breakthrough hospitalizations have been reported to the CDC. Still, the overall numbers remain low – in California, for instance, about 1,615 people have been hospitalized with breakthrough infections, which accounts for 0.007% of the state’s 22 million vaccinated people, the Times reported.
The breakthrough infections appear to be more severe among vaccinated people who are older or have weakened immune systems. About 74% of breakthrough cases are among adults 65 or older, the CDC reported.
The increase may shift how vaccinated people see their risks for infection and interact with loved ones. Public health officials have suggested that people follow some COVID-19 safety protocols again, such as wearing masks in public indoor spaces regardless of vaccination status.
As the Delta variant continues to circulate this fall, public health researchers will be researching more about breakthrough cases among vaccinated people, including whether they have prolonged symptoms and how easily they may pass the virus to others.
“I think some of us have been challenged by the numbers of clusters that we’ve seen,” Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, told this news organization.
“I think that really needs to be examined more,” he said.
A version of this article first appeared on WebMD.com.
Breakthrough cases accounted for about one in five newly diagnosed cases in six of the states, according to the New York Times. Hospitalizations and deaths among vaccinated people may be higher than previously thought as well.
“Remember when the early vaccine studies came out, it was like nobody gets hospitalized, nobody dies,” Robert Wachter, MD, chairman of the department of medicine at the University of California, San Francisco, said in an interview. “That clearly is not true.”
The New York Times analyzed data in seven states – California, Colorado, Massachusetts, Oregon, Utah, Vermont, and Virginia – that are tracking the most detailed information. The trends in these states may not reflect the numbers throughout the country, the newspaper reported.
Even still, the numbers back up the idea that vaccinated people may need booster shots this fall to support their earlier vaccine doses. Federal health officials are scheduled to approve the extra shots in coming weeks, potentially in September. The first people to receive booster shots will likely be health care workers and nursing home residents who took the first vaccines in December and January.
“If the chances of a breakthrough infection have gone up considerably, and I think the evidence is clear that they have, and the level of protection against severe illness is no longer as robust as it was, I think the case for boosters goes up pretty quickly,” Dr. Wachter said.
Previous analyses of breakthrough cases included data from June and earlier, the newspaper reported. But since July, COVID-19 cases have soared again because of the Delta variant, and the most recent numbers show an uptick among vaccinated people. In Los Angeles County, for instance, fully vaccinated people account for 20% of new COVID-19 cases, which is up from 11% in May, 5% in April, and 2% in March, according to a late July report from the Los Angeles County Department of Public Health.
What’s more, breakthrough infections in the seven states accounted for 12%-24% of COVID-19 hospitalizations in those states. About 8,000 breakthrough hospitalizations have been reported to the CDC. Still, the overall numbers remain low – in California, for instance, about 1,615 people have been hospitalized with breakthrough infections, which accounts for 0.007% of the state’s 22 million vaccinated people, the Times reported.
The breakthrough infections appear to be more severe among vaccinated people who are older or have weakened immune systems. About 74% of breakthrough cases are among adults 65 or older, the CDC reported.
The increase may shift how vaccinated people see their risks for infection and interact with loved ones. Public health officials have suggested that people follow some COVID-19 safety protocols again, such as wearing masks in public indoor spaces regardless of vaccination status.
As the Delta variant continues to circulate this fall, public health researchers will be researching more about breakthrough cases among vaccinated people, including whether they have prolonged symptoms and how easily they may pass the virus to others.
“I think some of us have been challenged by the numbers of clusters that we’ve seen,” Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, told this news organization.
“I think that really needs to be examined more,” he said.
A version of this article first appeared on WebMD.com.
Breakthrough cases accounted for about one in five newly diagnosed cases in six of the states, according to the New York Times. Hospitalizations and deaths among vaccinated people may be higher than previously thought as well.
“Remember when the early vaccine studies came out, it was like nobody gets hospitalized, nobody dies,” Robert Wachter, MD, chairman of the department of medicine at the University of California, San Francisco, said in an interview. “That clearly is not true.”
The New York Times analyzed data in seven states – California, Colorado, Massachusetts, Oregon, Utah, Vermont, and Virginia – that are tracking the most detailed information. The trends in these states may not reflect the numbers throughout the country, the newspaper reported.
Even still, the numbers back up the idea that vaccinated people may need booster shots this fall to support their earlier vaccine doses. Federal health officials are scheduled to approve the extra shots in coming weeks, potentially in September. The first people to receive booster shots will likely be health care workers and nursing home residents who took the first vaccines in December and January.
“If the chances of a breakthrough infection have gone up considerably, and I think the evidence is clear that they have, and the level of protection against severe illness is no longer as robust as it was, I think the case for boosters goes up pretty quickly,” Dr. Wachter said.
Previous analyses of breakthrough cases included data from June and earlier, the newspaper reported. But since July, COVID-19 cases have soared again because of the Delta variant, and the most recent numbers show an uptick among vaccinated people. In Los Angeles County, for instance, fully vaccinated people account for 20% of new COVID-19 cases, which is up from 11% in May, 5% in April, and 2% in March, according to a late July report from the Los Angeles County Department of Public Health.
What’s more, breakthrough infections in the seven states accounted for 12%-24% of COVID-19 hospitalizations in those states. About 8,000 breakthrough hospitalizations have been reported to the CDC. Still, the overall numbers remain low – in California, for instance, about 1,615 people have been hospitalized with breakthrough infections, which accounts for 0.007% of the state’s 22 million vaccinated people, the Times reported.
The breakthrough infections appear to be more severe among vaccinated people who are older or have weakened immune systems. About 74% of breakthrough cases are among adults 65 or older, the CDC reported.
The increase may shift how vaccinated people see their risks for infection and interact with loved ones. Public health officials have suggested that people follow some COVID-19 safety protocols again, such as wearing masks in public indoor spaces regardless of vaccination status.
As the Delta variant continues to circulate this fall, public health researchers will be researching more about breakthrough cases among vaccinated people, including whether they have prolonged symptoms and how easily they may pass the virus to others.
“I think some of us have been challenged by the numbers of clusters that we’ve seen,” Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, told this news organization.
“I think that really needs to be examined more,” he said.
A version of this article first appeared on WebMD.com.
FDA approves Abbott’s Amplatzer Amulet for AFib
The Food and Drug Administration has approved the Amplatzer Amulet left atrial appendage occluder (Abbott) to treat people with nonvalvular atrial fibrillation who are at increased risk for stroke and systemic embolism.
The Amulet and its competitor, Boston Scientific’s Watchman, are minimally invasive devices used to close off the left atrial appendage (LAA), an area where blood clots tend to form in people with atrial fibrillation.
Amulet uses dual-seal technology to completely and immediately seal the LAA, the company says, whereas the other minimally invasive solution uses a single component to seal the LAA that requires blood-thinning drugs to heal and additional patient monitoring. The Amulet also has the widest range of occluder sizes on the market and is recapturable and repositionable to ensure optimal placement.
“As the world’s population continues to age, we’re seeing a surge in atrial fibrillation cases, and with that comes increased risk of stroke. The approval of Abbott’s Amulet device provides physicians with a treatment option that reduces the risk of stroke and eliminates the need for blood-thinning medication immediately after the procedure, which is incredibly valuable given the bleeding risks associated with these medicines,” Dhanunjaya Lakkireddy, MD, Kansas City Heart Rhythm Institute at HCA Midwest Health, Overland Park, Kan., and principal investigator for the study that led to FDA approval, said in a news release from Abbott.
The FDA approval is supported by findings from the global Amulet IDE trial, a head-to-head comparison of the Amulet and Watchman devices in 1,878 participants with nonvalvular atrial fibrillation. The results will be presented virtually on Aug. 30 at the 2021 annual congress of the European Society of Cardiology.
The Amplatzer Amulet received CE Mark designation in 2013 and is approved for use in more than 80 countries, including in Australia, Canada, and European countries.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved the Amplatzer Amulet left atrial appendage occluder (Abbott) to treat people with nonvalvular atrial fibrillation who are at increased risk for stroke and systemic embolism.
The Amulet and its competitor, Boston Scientific’s Watchman, are minimally invasive devices used to close off the left atrial appendage (LAA), an area where blood clots tend to form in people with atrial fibrillation.
Amulet uses dual-seal technology to completely and immediately seal the LAA, the company says, whereas the other minimally invasive solution uses a single component to seal the LAA that requires blood-thinning drugs to heal and additional patient monitoring. The Amulet also has the widest range of occluder sizes on the market and is recapturable and repositionable to ensure optimal placement.
“As the world’s population continues to age, we’re seeing a surge in atrial fibrillation cases, and with that comes increased risk of stroke. The approval of Abbott’s Amulet device provides physicians with a treatment option that reduces the risk of stroke and eliminates the need for blood-thinning medication immediately after the procedure, which is incredibly valuable given the bleeding risks associated with these medicines,” Dhanunjaya Lakkireddy, MD, Kansas City Heart Rhythm Institute at HCA Midwest Health, Overland Park, Kan., and principal investigator for the study that led to FDA approval, said in a news release from Abbott.
The FDA approval is supported by findings from the global Amulet IDE trial, a head-to-head comparison of the Amulet and Watchman devices in 1,878 participants with nonvalvular atrial fibrillation. The results will be presented virtually on Aug. 30 at the 2021 annual congress of the European Society of Cardiology.
The Amplatzer Amulet received CE Mark designation in 2013 and is approved for use in more than 80 countries, including in Australia, Canada, and European countries.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved the Amplatzer Amulet left atrial appendage occluder (Abbott) to treat people with nonvalvular atrial fibrillation who are at increased risk for stroke and systemic embolism.
The Amulet and its competitor, Boston Scientific’s Watchman, are minimally invasive devices used to close off the left atrial appendage (LAA), an area where blood clots tend to form in people with atrial fibrillation.
Amulet uses dual-seal technology to completely and immediately seal the LAA, the company says, whereas the other minimally invasive solution uses a single component to seal the LAA that requires blood-thinning drugs to heal and additional patient monitoring. The Amulet also has the widest range of occluder sizes on the market and is recapturable and repositionable to ensure optimal placement.
“As the world’s population continues to age, we’re seeing a surge in atrial fibrillation cases, and with that comes increased risk of stroke. The approval of Abbott’s Amulet device provides physicians with a treatment option that reduces the risk of stroke and eliminates the need for blood-thinning medication immediately after the procedure, which is incredibly valuable given the bleeding risks associated with these medicines,” Dhanunjaya Lakkireddy, MD, Kansas City Heart Rhythm Institute at HCA Midwest Health, Overland Park, Kan., and principal investigator for the study that led to FDA approval, said in a news release from Abbott.
The FDA approval is supported by findings from the global Amulet IDE trial, a head-to-head comparison of the Amulet and Watchman devices in 1,878 participants with nonvalvular atrial fibrillation. The results will be presented virtually on Aug. 30 at the 2021 annual congress of the European Society of Cardiology.
The Amplatzer Amulet received CE Mark designation in 2013 and is approved for use in more than 80 countries, including in Australia, Canada, and European countries.
A version of this article first appeared on Medscape.com.
Children and COVID: New cases rise to winter levels
Weekly cases of COVID-19 in children topped 100,000 for the first time since early February, according to the American Academy of Pediatrics and the Children’s Hospital Association.
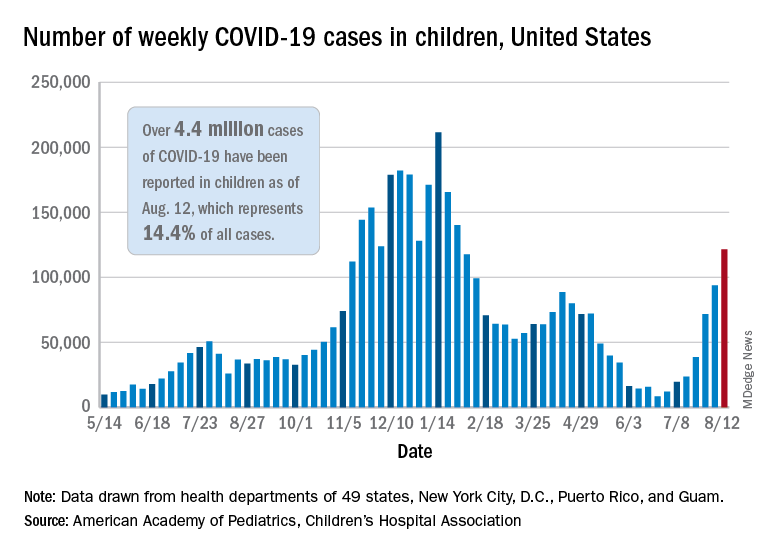
the AAP and CHA said in their weekly COVD-19 report. The recent surge in child COVID has also brought a record high in hospitalizations and shortages of pediatric ICU beds in some areas.
The 121,000 new cases represent an increase of almost 1,400% since June 18-24, when the weekly tally was just 8,447 and at its lowest point in over a year, the AAP/CHA data show.
On the vaccination front in the last week (Aug. 10-16), vaccine initiation for 12- to 17-year-olds was fairly robust but still down slightly, compared with the previous week. Just over 402,000 children aged 12-15 years received a first vaccination, which was down slightly from 411,000 the week before but still higher than any of the 6 weeks from June 22 to Aug. 2, based on data from the Centers for Disease Control and Prevention. Vaccinations were down by a similar margin for 15- to-17-year-olds.
Over 10.9 million children aged 12-17 have had at least one dose of COVID-19 vaccine administered, of whom 8.1 million are fully vaccinated. Among those aged 12-15 years, 44.5% have gotten at least one dose and 31.8% are fully vaccinated, with corresponding figures of 53.9% and 42.5% for 16- and 17-year-olds, according to the CDC’s COVID Data Tracker.
The number of COVID-19 cases reported in children since the start of the pandemic is up to 4.4 million, which makes up 14.4% of all cases in the United States, the AAP and CHA said. Other cumulative figures through Aug. 12 include almost 18,000 hospitalizations – reported by 23 states and New York City – and 378 deaths – reported by 43 states, New York City, Puerto Rico, and Guam.
In the latest edition of their ongoing report, compiled using state data since the summer of 2020, the two groups noted that, “in the summer of 2021, some states have revised cases counts previously reported, begun reporting less frequently, or dropped metrics previously reported.” Among those states are Nebraska, which shut down its online COVID dashboard in late June, and Alabama, which stopped reporting cumulative cases and deaths after July 29.
Weekly cases of COVID-19 in children topped 100,000 for the first time since early February, according to the American Academy of Pediatrics and the Children’s Hospital Association.
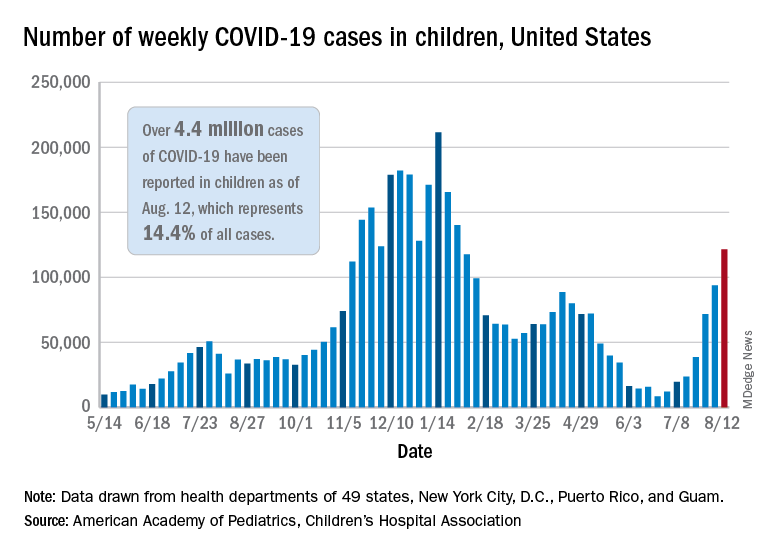
the AAP and CHA said in their weekly COVD-19 report. The recent surge in child COVID has also brought a record high in hospitalizations and shortages of pediatric ICU beds in some areas.
The 121,000 new cases represent an increase of almost 1,400% since June 18-24, when the weekly tally was just 8,447 and at its lowest point in over a year, the AAP/CHA data show.
On the vaccination front in the last week (Aug. 10-16), vaccine initiation for 12- to 17-year-olds was fairly robust but still down slightly, compared with the previous week. Just over 402,000 children aged 12-15 years received a first vaccination, which was down slightly from 411,000 the week before but still higher than any of the 6 weeks from June 22 to Aug. 2, based on data from the Centers for Disease Control and Prevention. Vaccinations were down by a similar margin for 15- to-17-year-olds.
Over 10.9 million children aged 12-17 have had at least one dose of COVID-19 vaccine administered, of whom 8.1 million are fully vaccinated. Among those aged 12-15 years, 44.5% have gotten at least one dose and 31.8% are fully vaccinated, with corresponding figures of 53.9% and 42.5% for 16- and 17-year-olds, according to the CDC’s COVID Data Tracker.
The number of COVID-19 cases reported in children since the start of the pandemic is up to 4.4 million, which makes up 14.4% of all cases in the United States, the AAP and CHA said. Other cumulative figures through Aug. 12 include almost 18,000 hospitalizations – reported by 23 states and New York City – and 378 deaths – reported by 43 states, New York City, Puerto Rico, and Guam.
In the latest edition of their ongoing report, compiled using state data since the summer of 2020, the two groups noted that, “in the summer of 2021, some states have revised cases counts previously reported, begun reporting less frequently, or dropped metrics previously reported.” Among those states are Nebraska, which shut down its online COVID dashboard in late June, and Alabama, which stopped reporting cumulative cases and deaths after July 29.
Weekly cases of COVID-19 in children topped 100,000 for the first time since early February, according to the American Academy of Pediatrics and the Children’s Hospital Association.
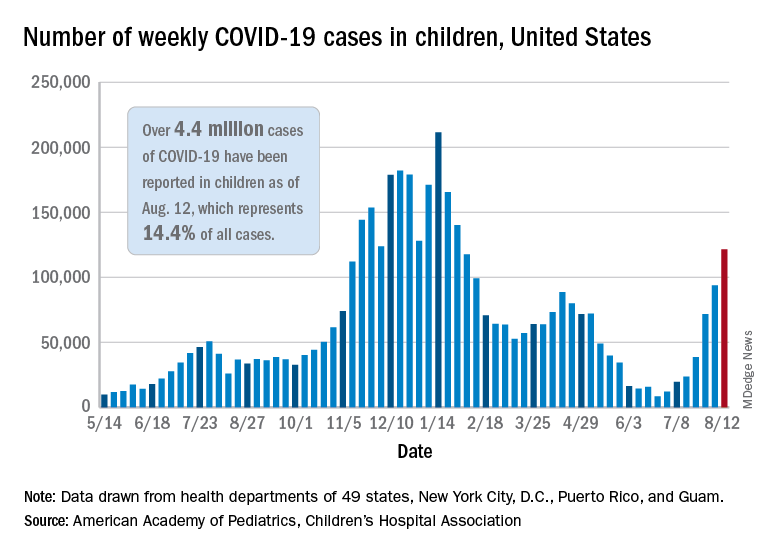
the AAP and CHA said in their weekly COVD-19 report. The recent surge in child COVID has also brought a record high in hospitalizations and shortages of pediatric ICU beds in some areas.
The 121,000 new cases represent an increase of almost 1,400% since June 18-24, when the weekly tally was just 8,447 and at its lowest point in over a year, the AAP/CHA data show.
On the vaccination front in the last week (Aug. 10-16), vaccine initiation for 12- to 17-year-olds was fairly robust but still down slightly, compared with the previous week. Just over 402,000 children aged 12-15 years received a first vaccination, which was down slightly from 411,000 the week before but still higher than any of the 6 weeks from June 22 to Aug. 2, based on data from the Centers for Disease Control and Prevention. Vaccinations were down by a similar margin for 15- to-17-year-olds.
Over 10.9 million children aged 12-17 have had at least one dose of COVID-19 vaccine administered, of whom 8.1 million are fully vaccinated. Among those aged 12-15 years, 44.5% have gotten at least one dose and 31.8% are fully vaccinated, with corresponding figures of 53.9% and 42.5% for 16- and 17-year-olds, according to the CDC’s COVID Data Tracker.
The number of COVID-19 cases reported in children since the start of the pandemic is up to 4.4 million, which makes up 14.4% of all cases in the United States, the AAP and CHA said. Other cumulative figures through Aug. 12 include almost 18,000 hospitalizations – reported by 23 states and New York City – and 378 deaths – reported by 43 states, New York City, Puerto Rico, and Guam.
In the latest edition of their ongoing report, compiled using state data since the summer of 2020, the two groups noted that, “in the summer of 2021, some states have revised cases counts previously reported, begun reporting less frequently, or dropped metrics previously reported.” Among those states are Nebraska, which shut down its online COVID dashboard in late June, and Alabama, which stopped reporting cumulative cases and deaths after July 29.
FDA approves rapid-acting insulin, Lyumjev, for pump use
The Food and Drug Administration has expanded the label for Eli Lilly’s ultra–rapid-acting insulin lispro-aabc injection 100 units/mL (Lyumjev) for use in insulin pumps.
Lyumjev (insulin lispro-aabc injection 100 and 200 units/mL) was initially approved in June 2020 to improve glycemic control in adults with type 1 or type 2 diabetes. That formulation is administered by injection from a pen or syringe. Now, the 100 units/mL formulation can also be delivered via continuous subcutaneous insulin infusion with an insulin pump.
Lyumjev will compete with Novo Nordisk’s fast-acting insulin aspart injection 100 units/mL (Fiasp). Fiasp had a head start: it was approved for use in adults in the United States in September 2017. It was approved for use in insulin pumps in October 2019 and for use in children with diabetes in January 2020.
The new approval for Lyumjev was based on data from a phase 3 trial, PRONTO-Pump-2. That trial, which included 432 participants with type 1 diabetes, confirmed the drug’s safety and efficacy when used in pumps.
The study met the primary endpoint of noninferiority in reduction of hemoglobin A1c from baseline to week 16, compared with insulin lispro (Humalog 100 units/mL). It was superior in both 1-hour and 2-hour postprandial glucose reduction when delivered 0-2 minutes before meals, according to a Lilly statement.
Patients who cannot afford the drug can go to www.insulinaffordability.com for assistance. Those with commercial insurance can also visit www.Lyumjev.com to access the Lyumjev Savings Card.
Lyumjev is available in several global markets, including Japan and the European Union, where it is also approved for use in insulin pumps.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has expanded the label for Eli Lilly’s ultra–rapid-acting insulin lispro-aabc injection 100 units/mL (Lyumjev) for use in insulin pumps.
Lyumjev (insulin lispro-aabc injection 100 and 200 units/mL) was initially approved in June 2020 to improve glycemic control in adults with type 1 or type 2 diabetes. That formulation is administered by injection from a pen or syringe. Now, the 100 units/mL formulation can also be delivered via continuous subcutaneous insulin infusion with an insulin pump.
Lyumjev will compete with Novo Nordisk’s fast-acting insulin aspart injection 100 units/mL (Fiasp). Fiasp had a head start: it was approved for use in adults in the United States in September 2017. It was approved for use in insulin pumps in October 2019 and for use in children with diabetes in January 2020.
The new approval for Lyumjev was based on data from a phase 3 trial, PRONTO-Pump-2. That trial, which included 432 participants with type 1 diabetes, confirmed the drug’s safety and efficacy when used in pumps.
The study met the primary endpoint of noninferiority in reduction of hemoglobin A1c from baseline to week 16, compared with insulin lispro (Humalog 100 units/mL). It was superior in both 1-hour and 2-hour postprandial glucose reduction when delivered 0-2 minutes before meals, according to a Lilly statement.
Patients who cannot afford the drug can go to www.insulinaffordability.com for assistance. Those with commercial insurance can also visit www.Lyumjev.com to access the Lyumjev Savings Card.
Lyumjev is available in several global markets, including Japan and the European Union, where it is also approved for use in insulin pumps.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has expanded the label for Eli Lilly’s ultra–rapid-acting insulin lispro-aabc injection 100 units/mL (Lyumjev) for use in insulin pumps.
Lyumjev (insulin lispro-aabc injection 100 and 200 units/mL) was initially approved in June 2020 to improve glycemic control in adults with type 1 or type 2 diabetes. That formulation is administered by injection from a pen or syringe. Now, the 100 units/mL formulation can also be delivered via continuous subcutaneous insulin infusion with an insulin pump.
Lyumjev will compete with Novo Nordisk’s fast-acting insulin aspart injection 100 units/mL (Fiasp). Fiasp had a head start: it was approved for use in adults in the United States in September 2017. It was approved for use in insulin pumps in October 2019 and for use in children with diabetes in January 2020.
The new approval for Lyumjev was based on data from a phase 3 trial, PRONTO-Pump-2. That trial, which included 432 participants with type 1 diabetes, confirmed the drug’s safety and efficacy when used in pumps.
The study met the primary endpoint of noninferiority in reduction of hemoglobin A1c from baseline to week 16, compared with insulin lispro (Humalog 100 units/mL). It was superior in both 1-hour and 2-hour postprandial glucose reduction when delivered 0-2 minutes before meals, according to a Lilly statement.
Patients who cannot afford the drug can go to www.insulinaffordability.com for assistance. Those with commercial insurance can also visit www.Lyumjev.com to access the Lyumjev Savings Card.
Lyumjev is available in several global markets, including Japan and the European Union, where it is also approved for use in insulin pumps.
A version of this article first appeared on Medscape.com.
U.S. reports record COVID-19 hospitalizations of children
The number of children hospitalized with COVID-19 in the U.S. hit a record high on Aug. 14, with more than 1,900 in hospitals.
Hospitals across the South are running out of beds as the contagious Delta variant spreads, mostly among unvaccinated people. Children make up about 2.4% of the country’s COVID-19 hospitalizations, and those under 12 are particularly vulnerable since they’re not eligible to receive a vaccine.
“This is not last year’s COVID,” Sally Goza, MD, former president of the American Academy of Pediatrics, told CNN on Aug. 14.
“This one is worse, and our children are the ones that are going to be affected by it the most,” she said.
The number of newly hospitalized COVID-19 patients for ages 18-49 also hit record highs during the week of Aug. 9. A fifth of the nation’s hospitalizations are in Florida, where the number of COVID-19 patients hit a record high of 16,100 on Aug. 14. More than 90% of the state’s intensive care unit beds are filled.
More than 90% of the ICU beds in Texas are full as well. On Aug. 13, there were no pediatric ICU beds available in Dallas or the 19 surrounding counties, which means that young patients would be transported father away for care – even Oklahoma City.
“That means if your child’s in a car wreck, if your child has a congenital heart defect or something and needs an ICU bed, or more likely, if they have COVID and need an ICU bed, we don’t have one,” Clay Jenkins, a Dallas County judge, said on Aug. 13.
“Your child will wait for another child to die,” he said.
As children return to classes, educators are talking about the possibility of vaccine mandates. The National Education Association announced its support of mandatory vaccination for its members.
“Our students under 12 can’t get vaccinated,” Becky Pringle, president of the association, told CNN.
“It’s our responsibility to keep them safe,” she said. “Keeping them safe means that everyone who can be vaccinated should be vaccinated.”
The U.S. now has an average of about 129,000 new COVID-19 cases per day, Reuters reported, which has doubled in about 2 weeks. The number of hospitalized patients is at a 6-month high, and about 600 people are dying each day.
Arkansas, Florida, Louisiana, Mississippi, and Oregon have reported record numbers of COVID-19 hospitalizations.
In addition, eight states make up half of all the COVID-19 hospitalizations in the U.S. but only 24% of the nation’s population – Alabama, Arkansas, Florida, Georgia, Louisiana, Mississippi, Nevada, and Texas. These states have vaccination rates lower than the national average, and their COVID-19 patients account for at least 15% of their overall hospitalizations.
To address the surge in hospitalizations, Oregon Gov. Kate Brown has ordered the deployment of up to 1,500 Oregon National Guard members to help health care workers.
“I know this is not the summer many of us envisioned,” Gov. Brown said Aug. 13. “The harsh and frustrating reality is that the Delta variant has changed everything. Delta is highly contagious, and we must take action now.”
A version of this article first appeared on WebMD.com.
The number of children hospitalized with COVID-19 in the U.S. hit a record high on Aug. 14, with more than 1,900 in hospitals.
Hospitals across the South are running out of beds as the contagious Delta variant spreads, mostly among unvaccinated people. Children make up about 2.4% of the country’s COVID-19 hospitalizations, and those under 12 are particularly vulnerable since they’re not eligible to receive a vaccine.
“This is not last year’s COVID,” Sally Goza, MD, former president of the American Academy of Pediatrics, told CNN on Aug. 14.
“This one is worse, and our children are the ones that are going to be affected by it the most,” she said.
The number of newly hospitalized COVID-19 patients for ages 18-49 also hit record highs during the week of Aug. 9. A fifth of the nation’s hospitalizations are in Florida, where the number of COVID-19 patients hit a record high of 16,100 on Aug. 14. More than 90% of the state’s intensive care unit beds are filled.
More than 90% of the ICU beds in Texas are full as well. On Aug. 13, there were no pediatric ICU beds available in Dallas or the 19 surrounding counties, which means that young patients would be transported father away for care – even Oklahoma City.
“That means if your child’s in a car wreck, if your child has a congenital heart defect or something and needs an ICU bed, or more likely, if they have COVID and need an ICU bed, we don’t have one,” Clay Jenkins, a Dallas County judge, said on Aug. 13.
“Your child will wait for another child to die,” he said.
As children return to classes, educators are talking about the possibility of vaccine mandates. The National Education Association announced its support of mandatory vaccination for its members.
“Our students under 12 can’t get vaccinated,” Becky Pringle, president of the association, told CNN.
“It’s our responsibility to keep them safe,” she said. “Keeping them safe means that everyone who can be vaccinated should be vaccinated.”
The U.S. now has an average of about 129,000 new COVID-19 cases per day, Reuters reported, which has doubled in about 2 weeks. The number of hospitalized patients is at a 6-month high, and about 600 people are dying each day.
Arkansas, Florida, Louisiana, Mississippi, and Oregon have reported record numbers of COVID-19 hospitalizations.
In addition, eight states make up half of all the COVID-19 hospitalizations in the U.S. but only 24% of the nation’s population – Alabama, Arkansas, Florida, Georgia, Louisiana, Mississippi, Nevada, and Texas. These states have vaccination rates lower than the national average, and their COVID-19 patients account for at least 15% of their overall hospitalizations.
To address the surge in hospitalizations, Oregon Gov. Kate Brown has ordered the deployment of up to 1,500 Oregon National Guard members to help health care workers.
“I know this is not the summer many of us envisioned,” Gov. Brown said Aug. 13. “The harsh and frustrating reality is that the Delta variant has changed everything. Delta is highly contagious, and we must take action now.”
A version of this article first appeared on WebMD.com.
The number of children hospitalized with COVID-19 in the U.S. hit a record high on Aug. 14, with more than 1,900 in hospitals.
Hospitals across the South are running out of beds as the contagious Delta variant spreads, mostly among unvaccinated people. Children make up about 2.4% of the country’s COVID-19 hospitalizations, and those under 12 are particularly vulnerable since they’re not eligible to receive a vaccine.
“This is not last year’s COVID,” Sally Goza, MD, former president of the American Academy of Pediatrics, told CNN on Aug. 14.
“This one is worse, and our children are the ones that are going to be affected by it the most,” she said.
The number of newly hospitalized COVID-19 patients for ages 18-49 also hit record highs during the week of Aug. 9. A fifth of the nation’s hospitalizations are in Florida, where the number of COVID-19 patients hit a record high of 16,100 on Aug. 14. More than 90% of the state’s intensive care unit beds are filled.
More than 90% of the ICU beds in Texas are full as well. On Aug. 13, there were no pediatric ICU beds available in Dallas or the 19 surrounding counties, which means that young patients would be transported father away for care – even Oklahoma City.
“That means if your child’s in a car wreck, if your child has a congenital heart defect or something and needs an ICU bed, or more likely, if they have COVID and need an ICU bed, we don’t have one,” Clay Jenkins, a Dallas County judge, said on Aug. 13.
“Your child will wait for another child to die,” he said.
As children return to classes, educators are talking about the possibility of vaccine mandates. The National Education Association announced its support of mandatory vaccination for its members.
“Our students under 12 can’t get vaccinated,” Becky Pringle, president of the association, told CNN.
“It’s our responsibility to keep them safe,” she said. “Keeping them safe means that everyone who can be vaccinated should be vaccinated.”
The U.S. now has an average of about 129,000 new COVID-19 cases per day, Reuters reported, which has doubled in about 2 weeks. The number of hospitalized patients is at a 6-month high, and about 600 people are dying each day.
Arkansas, Florida, Louisiana, Mississippi, and Oregon have reported record numbers of COVID-19 hospitalizations.
In addition, eight states make up half of all the COVID-19 hospitalizations in the U.S. but only 24% of the nation’s population – Alabama, Arkansas, Florida, Georgia, Louisiana, Mississippi, Nevada, and Texas. These states have vaccination rates lower than the national average, and their COVID-19 patients account for at least 15% of their overall hospitalizations.
To address the surge in hospitalizations, Oregon Gov. Kate Brown has ordered the deployment of up to 1,500 Oregon National Guard members to help health care workers.
“I know this is not the summer many of us envisioned,” Gov. Brown said Aug. 13. “The harsh and frustrating reality is that the Delta variant has changed everything. Delta is highly contagious, and we must take action now.”
A version of this article first appeared on WebMD.com.