User login
The shell game
The shell game is probably the world’s oldest confidence game, going back 2,000-3,000 years. You still see people getting lured into it in cities today.
It’s also played, albeit legally, in physician offices and pharmacies around the country.
You know, the ones piled up in your sample cabinet. Get a month free of Whateveritscalled to try and/or have your copay reduced to $0 or something reasonably low. All, of course, subject to terms and conditions in the small print and that of your insurance carrier. Your mileage may vary.
In my experience these things often don’t work as well as advertised. Sometimes it’s because the patient doesn’t understand how to use them, other times because their pharmacy doesn’t want to have anything to do with the cards, and still other times because their insurance has some exclusion against them.
But they do sometimes work ... until they don’t. Sometimes, out of the blue, they’ll stop. Maybe there was an insurance change, or the pharmacy policy changed, or the manufacturer’s program changed, or the offer expired. I usually don’t know and rarely find out.
So the shell game begins. The patients call multiple pharmacies, trying to find one that may be able to honor the coupons. Then they call my office and ask me to switch the script. So I do. They they go to the pharmacy. Sometimes they can get the script, sometimes not. If not, they move to another pharmacy and call my office to switch it again. Wash, rinse, repeat.
Other times it’s more complicated. They want a new card for each try, so they show up at my office asking for one (usually they can be downloaded online so some try that. Others do both). Like pebbles under a shell, the prescriptions and cards get switched from pharmacy to pharmacy.
This isn’t exclusive to manufacturers’ copay cards. I see the same phenomenon with GoodRx and similar cost-saving programs. People move scripts around to find the best deal. It may be helping them, but it certainly doesn’t help me and my staff as we try to keep up, or the badly overworked pharmacy staff.
I’ve even had some patients take the audacious step of asking me to write a script in the name of their spouses so they can double their supply. Obviously, such requests are refused. I’m not going to play that game.
I understand new drugs are costly, and often outside the reach of many patients today. I know the manufacturers are trying to get their products tried, or even make them more affordable for those who need it.
But, in many cases, this becomes (unintentionally or intentionally; I’m not sure) a shell game. Legal, perhaps, but still equally frustrating for all of us who are trying to keep up with it.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The shell game is probably the world’s oldest confidence game, going back 2,000-3,000 years. You still see people getting lured into it in cities today.
It’s also played, albeit legally, in physician offices and pharmacies around the country.
You know, the ones piled up in your sample cabinet. Get a month free of Whateveritscalled to try and/or have your copay reduced to $0 or something reasonably low. All, of course, subject to terms and conditions in the small print and that of your insurance carrier. Your mileage may vary.
In my experience these things often don’t work as well as advertised. Sometimes it’s because the patient doesn’t understand how to use them, other times because their pharmacy doesn’t want to have anything to do with the cards, and still other times because their insurance has some exclusion against them.
But they do sometimes work ... until they don’t. Sometimes, out of the blue, they’ll stop. Maybe there was an insurance change, or the pharmacy policy changed, or the manufacturer’s program changed, or the offer expired. I usually don’t know and rarely find out.
So the shell game begins. The patients call multiple pharmacies, trying to find one that may be able to honor the coupons. Then they call my office and ask me to switch the script. So I do. They they go to the pharmacy. Sometimes they can get the script, sometimes not. If not, they move to another pharmacy and call my office to switch it again. Wash, rinse, repeat.
Other times it’s more complicated. They want a new card for each try, so they show up at my office asking for one (usually they can be downloaded online so some try that. Others do both). Like pebbles under a shell, the prescriptions and cards get switched from pharmacy to pharmacy.
This isn’t exclusive to manufacturers’ copay cards. I see the same phenomenon with GoodRx and similar cost-saving programs. People move scripts around to find the best deal. It may be helping them, but it certainly doesn’t help me and my staff as we try to keep up, or the badly overworked pharmacy staff.
I’ve even had some patients take the audacious step of asking me to write a script in the name of their spouses so they can double their supply. Obviously, such requests are refused. I’m not going to play that game.
I understand new drugs are costly, and often outside the reach of many patients today. I know the manufacturers are trying to get their products tried, or even make them more affordable for those who need it.
But, in many cases, this becomes (unintentionally or intentionally; I’m not sure) a shell game. Legal, perhaps, but still equally frustrating for all of us who are trying to keep up with it.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The shell game is probably the world’s oldest confidence game, going back 2,000-3,000 years. You still see people getting lured into it in cities today.
It’s also played, albeit legally, in physician offices and pharmacies around the country.
You know, the ones piled up in your sample cabinet. Get a month free of Whateveritscalled to try and/or have your copay reduced to $0 or something reasonably low. All, of course, subject to terms and conditions in the small print and that of your insurance carrier. Your mileage may vary.
In my experience these things often don’t work as well as advertised. Sometimes it’s because the patient doesn’t understand how to use them, other times because their pharmacy doesn’t want to have anything to do with the cards, and still other times because their insurance has some exclusion against them.
But they do sometimes work ... until they don’t. Sometimes, out of the blue, they’ll stop. Maybe there was an insurance change, or the pharmacy policy changed, or the manufacturer’s program changed, or the offer expired. I usually don’t know and rarely find out.
So the shell game begins. The patients call multiple pharmacies, trying to find one that may be able to honor the coupons. Then they call my office and ask me to switch the script. So I do. They they go to the pharmacy. Sometimes they can get the script, sometimes not. If not, they move to another pharmacy and call my office to switch it again. Wash, rinse, repeat.
Other times it’s more complicated. They want a new card for each try, so they show up at my office asking for one (usually they can be downloaded online so some try that. Others do both). Like pebbles under a shell, the prescriptions and cards get switched from pharmacy to pharmacy.
This isn’t exclusive to manufacturers’ copay cards. I see the same phenomenon with GoodRx and similar cost-saving programs. People move scripts around to find the best deal. It may be helping them, but it certainly doesn’t help me and my staff as we try to keep up, or the badly overworked pharmacy staff.
I’ve even had some patients take the audacious step of asking me to write a script in the name of their spouses so they can double their supply. Obviously, such requests are refused. I’m not going to play that game.
I understand new drugs are costly, and often outside the reach of many patients today. I know the manufacturers are trying to get their products tried, or even make them more affordable for those who need it.
But, in many cases, this becomes (unintentionally or intentionally; I’m not sure) a shell game. Legal, perhaps, but still equally frustrating for all of us who are trying to keep up with it.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
PCOS in mothers tied to health problems in children
Children whose mothers have polycystic ovary syndrome (PCOS) have increased rates of hospitalization for various conditions, including asthma, pneumonia, and ear infection, a study of more than 1 million children shows.
The associations were not particularly strong, according to the researchers. But they raise questions about the reasons for the increased risk and whether interventions such as diet, exercise, or medications could lead to healthier outcomes for children whose mothers have PCOS.
“The findings suggest that maternal PCOS may have a negative impact on offspring development, enough to lead to a measurable increase in the risk of childhood hospitalization,” study coauthor Nathalie Auger, MD, associate professor of epidemiology at University of Montreal, and colleagues reported in Human Reproduction.
“They are minor differences, just enough that we can statistically identify them. They’re not something where everyone should be worrying at this point,” Dr. Auger told this news organization.
Still, some of the hospitalizations, such as those related to infection or allergy, could be prevented with earlier ambulatory care, so some degree of greater awareness among parents and clinicians may be warranted, she said.
Thirteen years of follow-up
PCOS – a reproductive disorder characterized by irregular periods, increased male hormones, and metabolic complications – affects some 10% of women. People with the condition are at increased risk for obesity, type 2 diabetes, and cardiovascular disease.
Although prior research has shown that maternal PCOS may be associated with higher body mass index and attention deficit disorder in children, data on long-term childhood health outcomes have been limited, Dr. Auger’s group noted.
To examine illness in children exposed to maternal PCOS, the investigators analyzed hospitalization rates for nearly 1.04 million children in Quebec between 2006 and 2020; 7,160 of the children had mothers with PCOS.
In all, 275,354 children were hospitalized during 13 years of follow-up, including 2,314 whose mothers had PCOS.
Children exposed to PCOS were hospitalized at a rate of 68.9 per 1,000 person-years – roughly 50% more often than the rate of 45.3 per 1,000 person-years for children not exposed to maternal PCOS.
In an analysis that adjusted for maternal characteristics, childhood hospitalization for any reason was 1.32 times more likely for children exposed to maternal PCOS.
Hospitalizations linked to infectious diseases – such as for bronchitis, bronchiolitis, pneumonia, nephritis, otitis media, or meningitis – were 1.31 times more likely among children exposed to PCOS. Allergy-related hospitalizations, such as for allergic asthma and anaphylaxis, were 1.47 times more likely, according to the researchers.
Metabolic hospitalizations were 1.59 times more likely. For gastrointestinal hospitalizations, the hazard ratio was 1.72. For central nervous system hospitalizations, it was 1.74.
The associations were stronger in earlier childhood, and results were similar for boys and girls, the investigators reported.
Hospitalizations for cardiovascular disease, musculoskeletal conditions, or malignancy were not increased.
‘Surprising’ links
“The findings are surprising in that some of the conditions that they showed increased risk for, like asthma and some infections, are not conditions that we think of as being typically associated with PCOS,” said Andrea E. Dunaif, MD, chief of the Hilda and J. Lester Gabrilove Division of Endocrinology, Diabetes, and Bone Disease at Mount Sinai Health System, New York, who was not part of the study team.
Earlier studies of offspring of women with PCOS have suggested that children may be at increased risk for insulin resistance and obesity.
Differences in genetics, intrauterine environments, patterns of health care use by women with PCOS, and behavioral factors, such as diet and how children are raised, are variables that could have contributed to the different hospitalization rates among children exposed to maternal PCOS, Dr. Auger said.
“Everything is interconnected,” she said.
The study was supported by a grant from the Canadian Institutes of Health Research. Dr. Auger has received a career award from Fonds de Recherche du Québec-Santé. Dr. Dunaif has consulted for Novo Nordisk and Fractyl Laboratories (now Fractyl Health).
A version of this article first appeared on Medscape.com.
Children whose mothers have polycystic ovary syndrome (PCOS) have increased rates of hospitalization for various conditions, including asthma, pneumonia, and ear infection, a study of more than 1 million children shows.
The associations were not particularly strong, according to the researchers. But they raise questions about the reasons for the increased risk and whether interventions such as diet, exercise, or medications could lead to healthier outcomes for children whose mothers have PCOS.
“The findings suggest that maternal PCOS may have a negative impact on offspring development, enough to lead to a measurable increase in the risk of childhood hospitalization,” study coauthor Nathalie Auger, MD, associate professor of epidemiology at University of Montreal, and colleagues reported in Human Reproduction.
“They are minor differences, just enough that we can statistically identify them. They’re not something where everyone should be worrying at this point,” Dr. Auger told this news organization.
Still, some of the hospitalizations, such as those related to infection or allergy, could be prevented with earlier ambulatory care, so some degree of greater awareness among parents and clinicians may be warranted, she said.
Thirteen years of follow-up
PCOS – a reproductive disorder characterized by irregular periods, increased male hormones, and metabolic complications – affects some 10% of women. People with the condition are at increased risk for obesity, type 2 diabetes, and cardiovascular disease.
Although prior research has shown that maternal PCOS may be associated with higher body mass index and attention deficit disorder in children, data on long-term childhood health outcomes have been limited, Dr. Auger’s group noted.
To examine illness in children exposed to maternal PCOS, the investigators analyzed hospitalization rates for nearly 1.04 million children in Quebec between 2006 and 2020; 7,160 of the children had mothers with PCOS.
In all, 275,354 children were hospitalized during 13 years of follow-up, including 2,314 whose mothers had PCOS.
Children exposed to PCOS were hospitalized at a rate of 68.9 per 1,000 person-years – roughly 50% more often than the rate of 45.3 per 1,000 person-years for children not exposed to maternal PCOS.
In an analysis that adjusted for maternal characteristics, childhood hospitalization for any reason was 1.32 times more likely for children exposed to maternal PCOS.
Hospitalizations linked to infectious diseases – such as for bronchitis, bronchiolitis, pneumonia, nephritis, otitis media, or meningitis – were 1.31 times more likely among children exposed to PCOS. Allergy-related hospitalizations, such as for allergic asthma and anaphylaxis, were 1.47 times more likely, according to the researchers.
Metabolic hospitalizations were 1.59 times more likely. For gastrointestinal hospitalizations, the hazard ratio was 1.72. For central nervous system hospitalizations, it was 1.74.
The associations were stronger in earlier childhood, and results were similar for boys and girls, the investigators reported.
Hospitalizations for cardiovascular disease, musculoskeletal conditions, or malignancy were not increased.
‘Surprising’ links
“The findings are surprising in that some of the conditions that they showed increased risk for, like asthma and some infections, are not conditions that we think of as being typically associated with PCOS,” said Andrea E. Dunaif, MD, chief of the Hilda and J. Lester Gabrilove Division of Endocrinology, Diabetes, and Bone Disease at Mount Sinai Health System, New York, who was not part of the study team.
Earlier studies of offspring of women with PCOS have suggested that children may be at increased risk for insulin resistance and obesity.
Differences in genetics, intrauterine environments, patterns of health care use by women with PCOS, and behavioral factors, such as diet and how children are raised, are variables that could have contributed to the different hospitalization rates among children exposed to maternal PCOS, Dr. Auger said.
“Everything is interconnected,” she said.
The study was supported by a grant from the Canadian Institutes of Health Research. Dr. Auger has received a career award from Fonds de Recherche du Québec-Santé. Dr. Dunaif has consulted for Novo Nordisk and Fractyl Laboratories (now Fractyl Health).
A version of this article first appeared on Medscape.com.
Children whose mothers have polycystic ovary syndrome (PCOS) have increased rates of hospitalization for various conditions, including asthma, pneumonia, and ear infection, a study of more than 1 million children shows.
The associations were not particularly strong, according to the researchers. But they raise questions about the reasons for the increased risk and whether interventions such as diet, exercise, or medications could lead to healthier outcomes for children whose mothers have PCOS.
“The findings suggest that maternal PCOS may have a negative impact on offspring development, enough to lead to a measurable increase in the risk of childhood hospitalization,” study coauthor Nathalie Auger, MD, associate professor of epidemiology at University of Montreal, and colleagues reported in Human Reproduction.
“They are minor differences, just enough that we can statistically identify them. They’re not something where everyone should be worrying at this point,” Dr. Auger told this news organization.
Still, some of the hospitalizations, such as those related to infection or allergy, could be prevented with earlier ambulatory care, so some degree of greater awareness among parents and clinicians may be warranted, she said.
Thirteen years of follow-up
PCOS – a reproductive disorder characterized by irregular periods, increased male hormones, and metabolic complications – affects some 10% of women. People with the condition are at increased risk for obesity, type 2 diabetes, and cardiovascular disease.
Although prior research has shown that maternal PCOS may be associated with higher body mass index and attention deficit disorder in children, data on long-term childhood health outcomes have been limited, Dr. Auger’s group noted.
To examine illness in children exposed to maternal PCOS, the investigators analyzed hospitalization rates for nearly 1.04 million children in Quebec between 2006 and 2020; 7,160 of the children had mothers with PCOS.
In all, 275,354 children were hospitalized during 13 years of follow-up, including 2,314 whose mothers had PCOS.
Children exposed to PCOS were hospitalized at a rate of 68.9 per 1,000 person-years – roughly 50% more often than the rate of 45.3 per 1,000 person-years for children not exposed to maternal PCOS.
In an analysis that adjusted for maternal characteristics, childhood hospitalization for any reason was 1.32 times more likely for children exposed to maternal PCOS.
Hospitalizations linked to infectious diseases – such as for bronchitis, bronchiolitis, pneumonia, nephritis, otitis media, or meningitis – were 1.31 times more likely among children exposed to PCOS. Allergy-related hospitalizations, such as for allergic asthma and anaphylaxis, were 1.47 times more likely, according to the researchers.
Metabolic hospitalizations were 1.59 times more likely. For gastrointestinal hospitalizations, the hazard ratio was 1.72. For central nervous system hospitalizations, it was 1.74.
The associations were stronger in earlier childhood, and results were similar for boys and girls, the investigators reported.
Hospitalizations for cardiovascular disease, musculoskeletal conditions, or malignancy were not increased.
‘Surprising’ links
“The findings are surprising in that some of the conditions that they showed increased risk for, like asthma and some infections, are not conditions that we think of as being typically associated with PCOS,” said Andrea E. Dunaif, MD, chief of the Hilda and J. Lester Gabrilove Division of Endocrinology, Diabetes, and Bone Disease at Mount Sinai Health System, New York, who was not part of the study team.
Earlier studies of offspring of women with PCOS have suggested that children may be at increased risk for insulin resistance and obesity.
Differences in genetics, intrauterine environments, patterns of health care use by women with PCOS, and behavioral factors, such as diet and how children are raised, are variables that could have contributed to the different hospitalization rates among children exposed to maternal PCOS, Dr. Auger said.
“Everything is interconnected,” she said.
The study was supported by a grant from the Canadian Institutes of Health Research. Dr. Auger has received a career award from Fonds de Recherche du Québec-Santé. Dr. Dunaif has consulted for Novo Nordisk and Fractyl Laboratories (now Fractyl Health).
A version of this article first appeared on Medscape.com.
FROM HUMAN REPRODUCTION
Our role in preventing postpartum depression
Tragic, embarrassing, criminal ... Choose your own adjective. The maternal mortality rate in this country is the worst of any developed nation in the world. And the numbers are getting worse with an increase of 14% over the previous year. One-third of these deaths occur weeks or months after the delivery.
In a recent issue of Harvard Public Health, researchers at the T.H. Chan School of Public Health discuss some of the possible remedies for what they describe as a crisis. While some of the solutions they list will require major restructuring of how we deliver health care to mothers, others could take advantage of our current systems by employing a slight shift in emphasis. And here is where those of us on the frontline of care delivery can make a difference.
The researchers point out that “More than 90% of maternal deaths could be prevented if women had access to quality care.” They also observe that most mothers have a single postpartum check with the ob.gyn. facility that delivered the baby and then are often left to navigate the health system because transfer to their primary care and/or mental health professional is haphazard or lacking in follow-up.
As I read through the article it struck me that as pediatricians we could and should be playing a larger role in this critical postpartum period when so many women seem to be falling through the cracks in our health care nonsystem. This is not a great “Ah-ha” moment for which I deserve any credit. In 2010 the American Academy of Pediatrics recommended that mothers be screened for depression at the 1-, 2-, and 4-month visits using either a validated 10-question screening instrument or a more direct 2-question tool (Pediatrics 2010;126[5]:1032-9). However, a periodic survey of AAP members 3 years later revealed that less than a third of the respondents were screening regularly for postpartum depression. In 2019 the academy reemphasized the important role that pediatric primary care givers can play in the detection and early management of the condition.
The reasons for the disappointing response include the list of usual suspects of inadequate training, workload demands, reimbursement, liability concerns, and the difficulty in finding and establishing effective referral networks. Unfortunately, these factors continue to exist, and many cases have multiplied in the wake of the pandemic.
In some states, educational outreach, funding, and changes in the reimbursement structure have resulted in improved outcomes. Not all of us are fortunate enough to live in a state that has made postpartum depression detection and management a priority. However, simply making it our own professional priority can save lives, ease suffering, and improve postpartum outcomes. Here I am talking about first caring and then inquiring about a mother’s mental health. Asking how much sleep she is getting. And then spending the time to give personalized advice on feeding and sleep schedules. Even, if this means ignoring half of the topics on the recommended health maintenance. It doesn’t take but a few minutes to convince yourself that the baby is healthy, and you know that 90% of them are.
However, a new mother who is sleep deprived and already has one foot on the spiral staircase down into postpartum depression represents an emergency. And, you should have the skills to turn it around. But, you have to care about the problem and make it your own priority – high enough on the list to make a follow-up appointment or call in a week instead of waiting a month or 2 until the next visit.
Unfortunately, even with your best efforts there are some families who need services beyond the scope of your practice. Making the necessary referrals can be frustrating and time consuming but not dropping ball until it lands in the appropriate place may save a life.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Tragic, embarrassing, criminal ... Choose your own adjective. The maternal mortality rate in this country is the worst of any developed nation in the world. And the numbers are getting worse with an increase of 14% over the previous year. One-third of these deaths occur weeks or months after the delivery.
In a recent issue of Harvard Public Health, researchers at the T.H. Chan School of Public Health discuss some of the possible remedies for what they describe as a crisis. While some of the solutions they list will require major restructuring of how we deliver health care to mothers, others could take advantage of our current systems by employing a slight shift in emphasis. And here is where those of us on the frontline of care delivery can make a difference.
The researchers point out that “More than 90% of maternal deaths could be prevented if women had access to quality care.” They also observe that most mothers have a single postpartum check with the ob.gyn. facility that delivered the baby and then are often left to navigate the health system because transfer to their primary care and/or mental health professional is haphazard or lacking in follow-up.
As I read through the article it struck me that as pediatricians we could and should be playing a larger role in this critical postpartum period when so many women seem to be falling through the cracks in our health care nonsystem. This is not a great “Ah-ha” moment for which I deserve any credit. In 2010 the American Academy of Pediatrics recommended that mothers be screened for depression at the 1-, 2-, and 4-month visits using either a validated 10-question screening instrument or a more direct 2-question tool (Pediatrics 2010;126[5]:1032-9). However, a periodic survey of AAP members 3 years later revealed that less than a third of the respondents were screening regularly for postpartum depression. In 2019 the academy reemphasized the important role that pediatric primary care givers can play in the detection and early management of the condition.
The reasons for the disappointing response include the list of usual suspects of inadequate training, workload demands, reimbursement, liability concerns, and the difficulty in finding and establishing effective referral networks. Unfortunately, these factors continue to exist, and many cases have multiplied in the wake of the pandemic.
In some states, educational outreach, funding, and changes in the reimbursement structure have resulted in improved outcomes. Not all of us are fortunate enough to live in a state that has made postpartum depression detection and management a priority. However, simply making it our own professional priority can save lives, ease suffering, and improve postpartum outcomes. Here I am talking about first caring and then inquiring about a mother’s mental health. Asking how much sleep she is getting. And then spending the time to give personalized advice on feeding and sleep schedules. Even, if this means ignoring half of the topics on the recommended health maintenance. It doesn’t take but a few minutes to convince yourself that the baby is healthy, and you know that 90% of them are.
However, a new mother who is sleep deprived and already has one foot on the spiral staircase down into postpartum depression represents an emergency. And, you should have the skills to turn it around. But, you have to care about the problem and make it your own priority – high enough on the list to make a follow-up appointment or call in a week instead of waiting a month or 2 until the next visit.
Unfortunately, even with your best efforts there are some families who need services beyond the scope of your practice. Making the necessary referrals can be frustrating and time consuming but not dropping ball until it lands in the appropriate place may save a life.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Tragic, embarrassing, criminal ... Choose your own adjective. The maternal mortality rate in this country is the worst of any developed nation in the world. And the numbers are getting worse with an increase of 14% over the previous year. One-third of these deaths occur weeks or months after the delivery.
In a recent issue of Harvard Public Health, researchers at the T.H. Chan School of Public Health discuss some of the possible remedies for what they describe as a crisis. While some of the solutions they list will require major restructuring of how we deliver health care to mothers, others could take advantage of our current systems by employing a slight shift in emphasis. And here is where those of us on the frontline of care delivery can make a difference.
The researchers point out that “More than 90% of maternal deaths could be prevented if women had access to quality care.” They also observe that most mothers have a single postpartum check with the ob.gyn. facility that delivered the baby and then are often left to navigate the health system because transfer to their primary care and/or mental health professional is haphazard or lacking in follow-up.
As I read through the article it struck me that as pediatricians we could and should be playing a larger role in this critical postpartum period when so many women seem to be falling through the cracks in our health care nonsystem. This is not a great “Ah-ha” moment for which I deserve any credit. In 2010 the American Academy of Pediatrics recommended that mothers be screened for depression at the 1-, 2-, and 4-month visits using either a validated 10-question screening instrument or a more direct 2-question tool (Pediatrics 2010;126[5]:1032-9). However, a periodic survey of AAP members 3 years later revealed that less than a third of the respondents were screening regularly for postpartum depression. In 2019 the academy reemphasized the important role that pediatric primary care givers can play in the detection and early management of the condition.
The reasons for the disappointing response include the list of usual suspects of inadequate training, workload demands, reimbursement, liability concerns, and the difficulty in finding and establishing effective referral networks. Unfortunately, these factors continue to exist, and many cases have multiplied in the wake of the pandemic.
In some states, educational outreach, funding, and changes in the reimbursement structure have resulted in improved outcomes. Not all of us are fortunate enough to live in a state that has made postpartum depression detection and management a priority. However, simply making it our own professional priority can save lives, ease suffering, and improve postpartum outcomes. Here I am talking about first caring and then inquiring about a mother’s mental health. Asking how much sleep she is getting. And then spending the time to give personalized advice on feeding and sleep schedules. Even, if this means ignoring half of the topics on the recommended health maintenance. It doesn’t take but a few minutes to convince yourself that the baby is healthy, and you know that 90% of them are.
However, a new mother who is sleep deprived and already has one foot on the spiral staircase down into postpartum depression represents an emergency. And, you should have the skills to turn it around. But, you have to care about the problem and make it your own priority – high enough on the list to make a follow-up appointment or call in a week instead of waiting a month or 2 until the next visit.
Unfortunately, even with your best efforts there are some families who need services beyond the scope of your practice. Making the necessary referrals can be frustrating and time consuming but not dropping ball until it lands in the appropriate place may save a life.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Strictures in Crohn’s: Balloon dilation avoids later surgery
Endoscopic balloon dilation (EBD) is an effective treatment option for strictures of the small bowel in patients with Crohn’s disease, based on a nationwide Danish cohort study.
Approximately three out of four patients who underwent an EBD were spared subsequent small bowel surgery. Similar outcomes were seen across primary and postsurgical strictures, reported lead author Mads Damsgaard Wewer, BSc, of the University of Copenhagen, and colleagues.
“Retrospective studies investigating EBD are available with variable follow-up periods; however, a nationwide study to demonstrate more precise durability of EBD in unselected patients is lacking,” the investigators wrote in European Journal of Gastroenterology & Hepatology. Their aim was to understand the use of EBD and the need for redilation and surgery. This retrospective study used a cohort of adult patients with Crohn’s disease who had strictures of the small bowel during a 19-year period.
The population comprised 9,737 patients with incident Crohn’s disease, among whom 90 (1%) underwent EBD during a median 8.2-year follow-up period. Of these 90 patients, 49 had primary strictures, while the remaining 41 had postsurgical strictures.
In the primary stricture group, 59% of patients had one EBD procedure and did not require subsequent small bowel surgery, 14% of patients required redilation but no further surgery, and 27% of patients required small bowel surgery after dilation. In this same group, the 1-, 3-, and 5-year cumulative incidence rates of EBD failure were 19%, 21%, and 25%, respectively. Of note, just 8% of patients with primary stricture who were treated with EBD ultimately required enterotomy, compared with 16% of patients with primary stricture who underwent small bowel resection without first attempting EBD.
In the postsurgical stricture group, 49% of patients underwent one EBD procedure without need for another small bowel surgery, 27% needed redilation but avoided surgery, and 24% required surgery after dilation. One-, three-, and five-year cumulative incidence rates of EBD failure in this group trended slightly higher than the primary stricture group over time, at 19%, 25%, and 29%, respectively.
The researchers noted that 25% of patients required small bowel surgery after EBD, which falls below rates of 29% to 33% reported by recent studies. They explained that this edge may be “partly explained by the careful selection of patients (with few and short strictures) receiving EBD,” as well as exclusion of patients with strictures outside the small intestine. They concluded that, “... small bowel-related EBD is an effective treatment option, and one that could be offered to more patients with Crohn’s disease in the future.”
‘Reassuring study’
David H. Bruining, MD, associate professor of medicine and section head of the inflammatory bowel disease interest group at Mayo Clinic, Rochester, Minn., called it a “reassuring study that confirms previous data regarding the efficacy of endoscopic balloon dilation of Crohn’s disease strictures.”
Dr. Bruining suggested in an interview that the findings, while drawn from Denmark, can be applied to a U.S. population; he also noted the “impressive” size of the study, as well the duration of follow-up, which extended up to 19 years.
EBD is “gaining more traction,” Dr. Bruining said, “as far as the belief among both referring physicians, and gastroenterologists, that it is effective, and it is safe. I think that body of literature is growing, and it’s more widely established at this point.”
Dr. Bruining noted that EBD should be reserved for patients who have short strictures no longer than 4-5 mm “without associated internal penetrating disease.”
In the future, such patients may have even more treatment options, Dr. Bruining predicted. New antifibrotic medications are “on the horizon,” which could one day be used with or without EBD to address fibrotic strictures in Crohn’s disease. Dr. Bruining is a part of the Stenosis Therapy and Anti-Fibrotic Research (STAR) Consortium, a group that aims to develop this emerging approach. He and his colleagues recently published a review of research into antifibrotic therapy to date.
Limiting factors
“This is an important study that really adds something to the literature,” noted Joseph Carmichael, MD, chief medical officer and chief of colon and rectal surgery at the University of California, Irvine. “The cohort is a little unusual in this area in that it encompasses a whole country. Yet this is exactly what makes the data stand apart from previous studies, since the patient population was unselected. That’s how you get a true incidence of the intervention.”
Beyond the generally favorable outcomes associated with EBD, Dr. Carmichael highlighted similar rates of success across both primary and postsurgical strictures. “Some of the previous data suggest postsurgical strictures don’t do as well with endoscopic dilation, and this [study] seems to go against that,” he said. “Which really deserves a closer look.”
Reflecting on the researchers’ call for more frequent use of EBD in patients with Crohn’s disease, Dr. Carmichael speculated that several factors may be limiting current utilization in Europe and the U.S. For one, there may not be enough interventional gastroenterologists. Also, the procedure “generally requires a high-volume provider who’s got surgical backup because these [procedures] have a 2% to 4% incidence of technical failure – including perforation or bleeding. These risks may deter patients from undergoing the procedure.
“Patients with Crohn’s disease can be pretty remarkable in their ability to endure obstruction,” he added. “If someone’s feeling their symptoms aren’t altering their quality of life, they may choose not to proceed with it.”
With all candidate patients, Dr. Carmichael recommended discussing the risks of EBD compared with the risks of declining the intervention, such as complete bowel obstruction, bowel perforation, or fistula. “That’s a question that needs to be included with every conversation when we discuss procedures,” he explained.
The researchers report that, among others, they have relationships with Janssen-Cilag, AbbVie A/S, and Celgene. Dr. Bruining and Dr. Carmichael reports no relevant conflicts of interest.
This article was updated 7/29/22.
Endoscopic balloon dilation (EBD) is an effective treatment option for strictures of the small bowel in patients with Crohn’s disease, based on a nationwide Danish cohort study.
Approximately three out of four patients who underwent an EBD were spared subsequent small bowel surgery. Similar outcomes were seen across primary and postsurgical strictures, reported lead author Mads Damsgaard Wewer, BSc, of the University of Copenhagen, and colleagues.
“Retrospective studies investigating EBD are available with variable follow-up periods; however, a nationwide study to demonstrate more precise durability of EBD in unselected patients is lacking,” the investigators wrote in European Journal of Gastroenterology & Hepatology. Their aim was to understand the use of EBD and the need for redilation and surgery. This retrospective study used a cohort of adult patients with Crohn’s disease who had strictures of the small bowel during a 19-year period.
The population comprised 9,737 patients with incident Crohn’s disease, among whom 90 (1%) underwent EBD during a median 8.2-year follow-up period. Of these 90 patients, 49 had primary strictures, while the remaining 41 had postsurgical strictures.
In the primary stricture group, 59% of patients had one EBD procedure and did not require subsequent small bowel surgery, 14% of patients required redilation but no further surgery, and 27% of patients required small bowel surgery after dilation. In this same group, the 1-, 3-, and 5-year cumulative incidence rates of EBD failure were 19%, 21%, and 25%, respectively. Of note, just 8% of patients with primary stricture who were treated with EBD ultimately required enterotomy, compared with 16% of patients with primary stricture who underwent small bowel resection without first attempting EBD.
In the postsurgical stricture group, 49% of patients underwent one EBD procedure without need for another small bowel surgery, 27% needed redilation but avoided surgery, and 24% required surgery after dilation. One-, three-, and five-year cumulative incidence rates of EBD failure in this group trended slightly higher than the primary stricture group over time, at 19%, 25%, and 29%, respectively.
The researchers noted that 25% of patients required small bowel surgery after EBD, which falls below rates of 29% to 33% reported by recent studies. They explained that this edge may be “partly explained by the careful selection of patients (with few and short strictures) receiving EBD,” as well as exclusion of patients with strictures outside the small intestine. They concluded that, “... small bowel-related EBD is an effective treatment option, and one that could be offered to more patients with Crohn’s disease in the future.”
‘Reassuring study’
David H. Bruining, MD, associate professor of medicine and section head of the inflammatory bowel disease interest group at Mayo Clinic, Rochester, Minn., called it a “reassuring study that confirms previous data regarding the efficacy of endoscopic balloon dilation of Crohn’s disease strictures.”
Dr. Bruining suggested in an interview that the findings, while drawn from Denmark, can be applied to a U.S. population; he also noted the “impressive” size of the study, as well the duration of follow-up, which extended up to 19 years.
EBD is “gaining more traction,” Dr. Bruining said, “as far as the belief among both referring physicians, and gastroenterologists, that it is effective, and it is safe. I think that body of literature is growing, and it’s more widely established at this point.”
Dr. Bruining noted that EBD should be reserved for patients who have short strictures no longer than 4-5 mm “without associated internal penetrating disease.”
In the future, such patients may have even more treatment options, Dr. Bruining predicted. New antifibrotic medications are “on the horizon,” which could one day be used with or without EBD to address fibrotic strictures in Crohn’s disease. Dr. Bruining is a part of the Stenosis Therapy and Anti-Fibrotic Research (STAR) Consortium, a group that aims to develop this emerging approach. He and his colleagues recently published a review of research into antifibrotic therapy to date.
Limiting factors
“This is an important study that really adds something to the literature,” noted Joseph Carmichael, MD, chief medical officer and chief of colon and rectal surgery at the University of California, Irvine. “The cohort is a little unusual in this area in that it encompasses a whole country. Yet this is exactly what makes the data stand apart from previous studies, since the patient population was unselected. That’s how you get a true incidence of the intervention.”
Beyond the generally favorable outcomes associated with EBD, Dr. Carmichael highlighted similar rates of success across both primary and postsurgical strictures. “Some of the previous data suggest postsurgical strictures don’t do as well with endoscopic dilation, and this [study] seems to go against that,” he said. “Which really deserves a closer look.”
Reflecting on the researchers’ call for more frequent use of EBD in patients with Crohn’s disease, Dr. Carmichael speculated that several factors may be limiting current utilization in Europe and the U.S. For one, there may not be enough interventional gastroenterologists. Also, the procedure “generally requires a high-volume provider who’s got surgical backup because these [procedures] have a 2% to 4% incidence of technical failure – including perforation or bleeding. These risks may deter patients from undergoing the procedure.
“Patients with Crohn’s disease can be pretty remarkable in their ability to endure obstruction,” he added. “If someone’s feeling their symptoms aren’t altering their quality of life, they may choose not to proceed with it.”
With all candidate patients, Dr. Carmichael recommended discussing the risks of EBD compared with the risks of declining the intervention, such as complete bowel obstruction, bowel perforation, or fistula. “That’s a question that needs to be included with every conversation when we discuss procedures,” he explained.
The researchers report that, among others, they have relationships with Janssen-Cilag, AbbVie A/S, and Celgene. Dr. Bruining and Dr. Carmichael reports no relevant conflicts of interest.
This article was updated 7/29/22.
Endoscopic balloon dilation (EBD) is an effective treatment option for strictures of the small bowel in patients with Crohn’s disease, based on a nationwide Danish cohort study.
Approximately three out of four patients who underwent an EBD were spared subsequent small bowel surgery. Similar outcomes were seen across primary and postsurgical strictures, reported lead author Mads Damsgaard Wewer, BSc, of the University of Copenhagen, and colleagues.
“Retrospective studies investigating EBD are available with variable follow-up periods; however, a nationwide study to demonstrate more precise durability of EBD in unselected patients is lacking,” the investigators wrote in European Journal of Gastroenterology & Hepatology. Their aim was to understand the use of EBD and the need for redilation and surgery. This retrospective study used a cohort of adult patients with Crohn’s disease who had strictures of the small bowel during a 19-year period.
The population comprised 9,737 patients with incident Crohn’s disease, among whom 90 (1%) underwent EBD during a median 8.2-year follow-up period. Of these 90 patients, 49 had primary strictures, while the remaining 41 had postsurgical strictures.
In the primary stricture group, 59% of patients had one EBD procedure and did not require subsequent small bowel surgery, 14% of patients required redilation but no further surgery, and 27% of patients required small bowel surgery after dilation. In this same group, the 1-, 3-, and 5-year cumulative incidence rates of EBD failure were 19%, 21%, and 25%, respectively. Of note, just 8% of patients with primary stricture who were treated with EBD ultimately required enterotomy, compared with 16% of patients with primary stricture who underwent small bowel resection without first attempting EBD.
In the postsurgical stricture group, 49% of patients underwent one EBD procedure without need for another small bowel surgery, 27% needed redilation but avoided surgery, and 24% required surgery after dilation. One-, three-, and five-year cumulative incidence rates of EBD failure in this group trended slightly higher than the primary stricture group over time, at 19%, 25%, and 29%, respectively.
The researchers noted that 25% of patients required small bowel surgery after EBD, which falls below rates of 29% to 33% reported by recent studies. They explained that this edge may be “partly explained by the careful selection of patients (with few and short strictures) receiving EBD,” as well as exclusion of patients with strictures outside the small intestine. They concluded that, “... small bowel-related EBD is an effective treatment option, and one that could be offered to more patients with Crohn’s disease in the future.”
‘Reassuring study’
David H. Bruining, MD, associate professor of medicine and section head of the inflammatory bowel disease interest group at Mayo Clinic, Rochester, Minn., called it a “reassuring study that confirms previous data regarding the efficacy of endoscopic balloon dilation of Crohn’s disease strictures.”
Dr. Bruining suggested in an interview that the findings, while drawn from Denmark, can be applied to a U.S. population; he also noted the “impressive” size of the study, as well the duration of follow-up, which extended up to 19 years.
EBD is “gaining more traction,” Dr. Bruining said, “as far as the belief among both referring physicians, and gastroenterologists, that it is effective, and it is safe. I think that body of literature is growing, and it’s more widely established at this point.”
Dr. Bruining noted that EBD should be reserved for patients who have short strictures no longer than 4-5 mm “without associated internal penetrating disease.”
In the future, such patients may have even more treatment options, Dr. Bruining predicted. New antifibrotic medications are “on the horizon,” which could one day be used with or without EBD to address fibrotic strictures in Crohn’s disease. Dr. Bruining is a part of the Stenosis Therapy and Anti-Fibrotic Research (STAR) Consortium, a group that aims to develop this emerging approach. He and his colleagues recently published a review of research into antifibrotic therapy to date.
Limiting factors
“This is an important study that really adds something to the literature,” noted Joseph Carmichael, MD, chief medical officer and chief of colon and rectal surgery at the University of California, Irvine. “The cohort is a little unusual in this area in that it encompasses a whole country. Yet this is exactly what makes the data stand apart from previous studies, since the patient population was unselected. That’s how you get a true incidence of the intervention.”
Beyond the generally favorable outcomes associated with EBD, Dr. Carmichael highlighted similar rates of success across both primary and postsurgical strictures. “Some of the previous data suggest postsurgical strictures don’t do as well with endoscopic dilation, and this [study] seems to go against that,” he said. “Which really deserves a closer look.”
Reflecting on the researchers’ call for more frequent use of EBD in patients with Crohn’s disease, Dr. Carmichael speculated that several factors may be limiting current utilization in Europe and the U.S. For one, there may not be enough interventional gastroenterologists. Also, the procedure “generally requires a high-volume provider who’s got surgical backup because these [procedures] have a 2% to 4% incidence of technical failure – including perforation or bleeding. These risks may deter patients from undergoing the procedure.
“Patients with Crohn’s disease can be pretty remarkable in their ability to endure obstruction,” he added. “If someone’s feeling their symptoms aren’t altering their quality of life, they may choose not to proceed with it.”
With all candidate patients, Dr. Carmichael recommended discussing the risks of EBD compared with the risks of declining the intervention, such as complete bowel obstruction, bowel perforation, or fistula. “That’s a question that needs to be included with every conversation when we discuss procedures,” he explained.
The researchers report that, among others, they have relationships with Janssen-Cilag, AbbVie A/S, and Celgene. Dr. Bruining and Dr. Carmichael reports no relevant conflicts of interest.
This article was updated 7/29/22.
FROM EUROPEAN JOURNAL OF GASTROENTEROLOGY & HEPATOLOGY
Does choice of biologic affect outcomes in perianal Crohn’s disease?
Choice of biologic therapy in the first line and later may impact long-term outcomes in patients with perianal Crohn’s disease (pCD), according to a retrospective study.
John Gubatan, MD, of Stanford (Calif.) University, and colleagues reported that, compared with no biologic therapy, first-line treatment with an anti–tumor necrosis factor (TNF) agent or ustekinumab significantly reduced risk of perianal abscess recurrence at 5 years, whereas vedolizumab offered no such benefit. After failure of the initial anti-TNF, switching to another anti-TNF agent is the most effective option.
“Although pCD is recognized to be an aggressive phenotype, data on whether escalating to a biologic at the time of perianal disease diagnosis may alter the natural history and long-term clinical outcomes of pCD is limited,” the researchers wrote in Journal of Clinical Gastroenterology. “This is the first study to explore how the type of biologic therapy at the time of perianal disease diagnosis and change in biologic therapy after first anti-TNF failure are associated with rates of long-term clinical outcomes.”
The study included 311 patients with pCD treated at Stanford University from 1998 to 2020. At the time of diagnosis, 168 of these patients started a biologic, most often an anti-TNF agent (n = 138), followed distantly by ustekinumab (n = 16) or vedolizumab (n = 14). Efficacy of these first-line biologics was compared with no biologic therapy in terms of five clinical outcomes at 5 years: surgical intervention, colectomy, permanent diversion, fistula closure, and perianal abscess recurrence.
Although both reduced risk of perianal abscess recurrence, it was still higher with anti-TNF therapy (hazard ratio, 0.48; 95% confidence interval, 0.32-0.74) than with ustekinumab (HR, 0.20; 95% CI, 0.07-0.56). Ustekinumab also increased the rate of perianal fistula closure by more than threefold (HR, 3.58; 95% CI, 1.04-12.35).
Vedolizumab, on the other hand, offered no significant benefit across any of the five outcomes.
None of the biologics had an impact on rates of surgical intervention, colectomy, or permanent diversion.
Further analyses explored the long-term effects of second-line biologic choice after initial failure with anti-TNF therapy. Switching to another anti-TNF agent was more effective than switching to ustekinumab at reducing risks of colectomy (HR, 0.20; 95% CI, 0.04-0.90) and permanent diversion (HR, 0.16; 95% CI, 0.03-0.94); switching to ustekinumab was more effective than switching to vedolizumab for perianal fistula closure (HR, 0.22; 95% CI, 0.05-0.96).
Switching to another anti-TNF biologic or ustekinumab may be associated with better 5-year outcomes, compared with switching to vedolizumab in patients with pCD, according to Dr. Gubatan. Other guidelines or data that might steer this sequencing decision are scant. However, the findings should be validated with prospective data, ideally from head-to-head trials.
Jordan E. Axelrad, MD, of NYU Langone Health, New York, said the present study is noteworthy for addressing a “very-difficult-to-treat condition that has limited data as well as very limited long-term outcome data for our currently available interventions.”
Dr. Axelrad appreciated how the study focused on the distribution of clinical manifestations of pCD, including ulcers (10%), fissures (23.2%), abscesses (76.1%), and fistulas (84.2%). According to Dr. Axelrad, the efficacy data provide really important insights for clinicians who choose biologic therapies. He noted that, in the absence of head-to-head clinical trials, “it’s absolutely important that we use these results to help us guide therapy” for patients with pCD.
While the biologics included in the study were efficacious to varying degrees, Dr. Axelrad pointed out that no choice was associated with a reduced risk of surgical intervention. “That really underscored for me how complex this patient population is,” he said. “Despite good medical therapies … we’re still not necessarily making a huge dent in the risk of surgical intervention requirements for this complex patient group.”
Dr. Gubatan disclosed support from a Chan Zuckerberg Biohub Physician Scientist Scholar Award, a National Institutes of Health NIDDK LRP Award, and a Doris Duke Physician Scientist Fellowship Award; his colleagues reported no conflicts of interest. Dr. Axelrad reports relationships with Janssen, AbbVie, Pfizer, and others.
Choice of biologic therapy in the first line and later may impact long-term outcomes in patients with perianal Crohn’s disease (pCD), according to a retrospective study.
John Gubatan, MD, of Stanford (Calif.) University, and colleagues reported that, compared with no biologic therapy, first-line treatment with an anti–tumor necrosis factor (TNF) agent or ustekinumab significantly reduced risk of perianal abscess recurrence at 5 years, whereas vedolizumab offered no such benefit. After failure of the initial anti-TNF, switching to another anti-TNF agent is the most effective option.
“Although pCD is recognized to be an aggressive phenotype, data on whether escalating to a biologic at the time of perianal disease diagnosis may alter the natural history and long-term clinical outcomes of pCD is limited,” the researchers wrote in Journal of Clinical Gastroenterology. “This is the first study to explore how the type of biologic therapy at the time of perianal disease diagnosis and change in biologic therapy after first anti-TNF failure are associated with rates of long-term clinical outcomes.”
The study included 311 patients with pCD treated at Stanford University from 1998 to 2020. At the time of diagnosis, 168 of these patients started a biologic, most often an anti-TNF agent (n = 138), followed distantly by ustekinumab (n = 16) or vedolizumab (n = 14). Efficacy of these first-line biologics was compared with no biologic therapy in terms of five clinical outcomes at 5 years: surgical intervention, colectomy, permanent diversion, fistula closure, and perianal abscess recurrence.
Although both reduced risk of perianal abscess recurrence, it was still higher with anti-TNF therapy (hazard ratio, 0.48; 95% confidence interval, 0.32-0.74) than with ustekinumab (HR, 0.20; 95% CI, 0.07-0.56). Ustekinumab also increased the rate of perianal fistula closure by more than threefold (HR, 3.58; 95% CI, 1.04-12.35).
Vedolizumab, on the other hand, offered no significant benefit across any of the five outcomes.
None of the biologics had an impact on rates of surgical intervention, colectomy, or permanent diversion.
Further analyses explored the long-term effects of second-line biologic choice after initial failure with anti-TNF therapy. Switching to another anti-TNF agent was more effective than switching to ustekinumab at reducing risks of colectomy (HR, 0.20; 95% CI, 0.04-0.90) and permanent diversion (HR, 0.16; 95% CI, 0.03-0.94); switching to ustekinumab was more effective than switching to vedolizumab for perianal fistula closure (HR, 0.22; 95% CI, 0.05-0.96).
Switching to another anti-TNF biologic or ustekinumab may be associated with better 5-year outcomes, compared with switching to vedolizumab in patients with pCD, according to Dr. Gubatan. Other guidelines or data that might steer this sequencing decision are scant. However, the findings should be validated with prospective data, ideally from head-to-head trials.
Jordan E. Axelrad, MD, of NYU Langone Health, New York, said the present study is noteworthy for addressing a “very-difficult-to-treat condition that has limited data as well as very limited long-term outcome data for our currently available interventions.”
Dr. Axelrad appreciated how the study focused on the distribution of clinical manifestations of pCD, including ulcers (10%), fissures (23.2%), abscesses (76.1%), and fistulas (84.2%). According to Dr. Axelrad, the efficacy data provide really important insights for clinicians who choose biologic therapies. He noted that, in the absence of head-to-head clinical trials, “it’s absolutely important that we use these results to help us guide therapy” for patients with pCD.
While the biologics included in the study were efficacious to varying degrees, Dr. Axelrad pointed out that no choice was associated with a reduced risk of surgical intervention. “That really underscored for me how complex this patient population is,” he said. “Despite good medical therapies … we’re still not necessarily making a huge dent in the risk of surgical intervention requirements for this complex patient group.”
Dr. Gubatan disclosed support from a Chan Zuckerberg Biohub Physician Scientist Scholar Award, a National Institutes of Health NIDDK LRP Award, and a Doris Duke Physician Scientist Fellowship Award; his colleagues reported no conflicts of interest. Dr. Axelrad reports relationships with Janssen, AbbVie, Pfizer, and others.
Choice of biologic therapy in the first line and later may impact long-term outcomes in patients with perianal Crohn’s disease (pCD), according to a retrospective study.
John Gubatan, MD, of Stanford (Calif.) University, and colleagues reported that, compared with no biologic therapy, first-line treatment with an anti–tumor necrosis factor (TNF) agent or ustekinumab significantly reduced risk of perianal abscess recurrence at 5 years, whereas vedolizumab offered no such benefit. After failure of the initial anti-TNF, switching to another anti-TNF agent is the most effective option.
“Although pCD is recognized to be an aggressive phenotype, data on whether escalating to a biologic at the time of perianal disease diagnosis may alter the natural history and long-term clinical outcomes of pCD is limited,” the researchers wrote in Journal of Clinical Gastroenterology. “This is the first study to explore how the type of biologic therapy at the time of perianal disease diagnosis and change in biologic therapy after first anti-TNF failure are associated with rates of long-term clinical outcomes.”
The study included 311 patients with pCD treated at Stanford University from 1998 to 2020. At the time of diagnosis, 168 of these patients started a biologic, most often an anti-TNF agent (n = 138), followed distantly by ustekinumab (n = 16) or vedolizumab (n = 14). Efficacy of these first-line biologics was compared with no biologic therapy in terms of five clinical outcomes at 5 years: surgical intervention, colectomy, permanent diversion, fistula closure, and perianal abscess recurrence.
Although both reduced risk of perianal abscess recurrence, it was still higher with anti-TNF therapy (hazard ratio, 0.48; 95% confidence interval, 0.32-0.74) than with ustekinumab (HR, 0.20; 95% CI, 0.07-0.56). Ustekinumab also increased the rate of perianal fistula closure by more than threefold (HR, 3.58; 95% CI, 1.04-12.35).
Vedolizumab, on the other hand, offered no significant benefit across any of the five outcomes.
None of the biologics had an impact on rates of surgical intervention, colectomy, or permanent diversion.
Further analyses explored the long-term effects of second-line biologic choice after initial failure with anti-TNF therapy. Switching to another anti-TNF agent was more effective than switching to ustekinumab at reducing risks of colectomy (HR, 0.20; 95% CI, 0.04-0.90) and permanent diversion (HR, 0.16; 95% CI, 0.03-0.94); switching to ustekinumab was more effective than switching to vedolizumab for perianal fistula closure (HR, 0.22; 95% CI, 0.05-0.96).
Switching to another anti-TNF biologic or ustekinumab may be associated with better 5-year outcomes, compared with switching to vedolizumab in patients with pCD, according to Dr. Gubatan. Other guidelines or data that might steer this sequencing decision are scant. However, the findings should be validated with prospective data, ideally from head-to-head trials.
Jordan E. Axelrad, MD, of NYU Langone Health, New York, said the present study is noteworthy for addressing a “very-difficult-to-treat condition that has limited data as well as very limited long-term outcome data for our currently available interventions.”
Dr. Axelrad appreciated how the study focused on the distribution of clinical manifestations of pCD, including ulcers (10%), fissures (23.2%), abscesses (76.1%), and fistulas (84.2%). According to Dr. Axelrad, the efficacy data provide really important insights for clinicians who choose biologic therapies. He noted that, in the absence of head-to-head clinical trials, “it’s absolutely important that we use these results to help us guide therapy” for patients with pCD.
While the biologics included in the study were efficacious to varying degrees, Dr. Axelrad pointed out that no choice was associated with a reduced risk of surgical intervention. “That really underscored for me how complex this patient population is,” he said. “Despite good medical therapies … we’re still not necessarily making a huge dent in the risk of surgical intervention requirements for this complex patient group.”
Dr. Gubatan disclosed support from a Chan Zuckerberg Biohub Physician Scientist Scholar Award, a National Institutes of Health NIDDK LRP Award, and a Doris Duke Physician Scientist Fellowship Award; his colleagues reported no conflicts of interest. Dr. Axelrad reports relationships with Janssen, AbbVie, Pfizer, and others.
FROM JOURNAL OF CLINICAL GASTROENTEROLOGY
Pre-endoscopy COVID-19 testing may not be needed
Pre-endoscopy viral testing may not be necessary to prevent coronavirus transmission from patients to endoscopy staff members, according to a new study published in Gut.
Instead, using personal protective equipment (PPE) and ensuring up-to-date COVID-19 vaccination among the medical team was found to be enough to substantially reduce the risk of spreading SARS-CoV-2, wrote Alexander Hann, Dr.med., gastroenterologist at University Hospital W
“We suggest that pre-selection of patients using respective questionnaires, vaccination, and particularly PPE appears to be sufficient for the prevention of SARS-CoV-2 transmission in GI endoscopy,” they wrote.
Dr. Hann and colleagues analyzed 15,750 endoscopies performed by 29 staff members during the period between May 2020 and December 2021. The researchers looked at three test approaches: No testing (4,543 patients), rapid antigen testing (682 patients), and real-time PCR testing (10,465 patients). In addition, 60 endoscopies were performed in patients with known COVID-19. Overall, no staff members became infected with SARS-CoV-2 during the study period. In all three scenarios, staff used PPE, and the vaccination rate of the team was 97%.
University Hospital W
All patients were interviewed before admission for COVID-19 symptoms, close contact with infected people, and recent travel to high-risk countries. Moreover, some endoscopies were performed even if a patient had positive markers for COVID-19.
The clinical team wore recommended PPE, including a high-filter FFP2 mask, one pair of gloves, protective eyewear, and disposable gowns. For patients with known COVID-19, staff wore two pairs of gloves, a disposable hairnet, and a water-resistant disposable gown. In addition, endoscopies were performed in negative pressure intervention rooms.
Among the 29 staff members involved, 16 physicians and 13 assistants worked in the endoscopy unit for at least 2 days per week for at least 6 months. The hospital’s internal policy required medical staff to undergo PCR testing if a rapid antigen test was positive or symptoms developed. Staff were vaccinated with two doses of the Pfizer-BioNTech vaccine in January and February 2021. A single booster dose of the Pfizer or Moderna vaccine was administered in November and December 2021.
The clinical team was not tested routinely, so asymptomatic infections may have existed. Moreover, the relatively low COVID-19 incidence in the local area might have influenced the risk of transmission. “However, even at the end of 2021, when the incidence was increasing, we did not see any higher risk of transmission,” the researchers explained.
“An important limitation of our study relates to the new variant Omicron that was dominant in our local area after the analyzed time frame.” Additional studies may be needed to understand the risk of transmission with the latest Omicron variants, and given the additional costs and implications on routine activity, current testing guidelines may need to be reconsidered.
“Although our data were not part of a randomized prospective study, we were able to demonstrate on a fairly high number of patients that PPE measures in addition to a short interview for assessment of a patient’s individual risks appear to be highly effective to control transmission of SARS-CoV-2 during an endoscopy. ... Pre-procedural RT-PCR testing or RA testing did not show any additional benefit,” Dr. Hann and colleagues concluded.
The authors reported no conflicts of interest.
Pre-endoscopy viral testing may not be necessary to prevent coronavirus transmission from patients to endoscopy staff members, according to a new study published in Gut.
Instead, using personal protective equipment (PPE) and ensuring up-to-date COVID-19 vaccination among the medical team was found to be enough to substantially reduce the risk of spreading SARS-CoV-2, wrote Alexander Hann, Dr.med., gastroenterologist at University Hospital W
“We suggest that pre-selection of patients using respective questionnaires, vaccination, and particularly PPE appears to be sufficient for the prevention of SARS-CoV-2 transmission in GI endoscopy,” they wrote.
Dr. Hann and colleagues analyzed 15,750 endoscopies performed by 29 staff members during the period between May 2020 and December 2021. The researchers looked at three test approaches: No testing (4,543 patients), rapid antigen testing (682 patients), and real-time PCR testing (10,465 patients). In addition, 60 endoscopies were performed in patients with known COVID-19. Overall, no staff members became infected with SARS-CoV-2 during the study period. In all three scenarios, staff used PPE, and the vaccination rate of the team was 97%.
University Hospital W
All patients were interviewed before admission for COVID-19 symptoms, close contact with infected people, and recent travel to high-risk countries. Moreover, some endoscopies were performed even if a patient had positive markers for COVID-19.
The clinical team wore recommended PPE, including a high-filter FFP2 mask, one pair of gloves, protective eyewear, and disposable gowns. For patients with known COVID-19, staff wore two pairs of gloves, a disposable hairnet, and a water-resistant disposable gown. In addition, endoscopies were performed in negative pressure intervention rooms.
Among the 29 staff members involved, 16 physicians and 13 assistants worked in the endoscopy unit for at least 2 days per week for at least 6 months. The hospital’s internal policy required medical staff to undergo PCR testing if a rapid antigen test was positive or symptoms developed. Staff were vaccinated with two doses of the Pfizer-BioNTech vaccine in January and February 2021. A single booster dose of the Pfizer or Moderna vaccine was administered in November and December 2021.
The clinical team was not tested routinely, so asymptomatic infections may have existed. Moreover, the relatively low COVID-19 incidence in the local area might have influenced the risk of transmission. “However, even at the end of 2021, when the incidence was increasing, we did not see any higher risk of transmission,” the researchers explained.
“An important limitation of our study relates to the new variant Omicron that was dominant in our local area after the analyzed time frame.” Additional studies may be needed to understand the risk of transmission with the latest Omicron variants, and given the additional costs and implications on routine activity, current testing guidelines may need to be reconsidered.
“Although our data were not part of a randomized prospective study, we were able to demonstrate on a fairly high number of patients that PPE measures in addition to a short interview for assessment of a patient’s individual risks appear to be highly effective to control transmission of SARS-CoV-2 during an endoscopy. ... Pre-procedural RT-PCR testing or RA testing did not show any additional benefit,” Dr. Hann and colleagues concluded.
The authors reported no conflicts of interest.
Pre-endoscopy viral testing may not be necessary to prevent coronavirus transmission from patients to endoscopy staff members, according to a new study published in Gut.
Instead, using personal protective equipment (PPE) and ensuring up-to-date COVID-19 vaccination among the medical team was found to be enough to substantially reduce the risk of spreading SARS-CoV-2, wrote Alexander Hann, Dr.med., gastroenterologist at University Hospital W
“We suggest that pre-selection of patients using respective questionnaires, vaccination, and particularly PPE appears to be sufficient for the prevention of SARS-CoV-2 transmission in GI endoscopy,” they wrote.
Dr. Hann and colleagues analyzed 15,750 endoscopies performed by 29 staff members during the period between May 2020 and December 2021. The researchers looked at three test approaches: No testing (4,543 patients), rapid antigen testing (682 patients), and real-time PCR testing (10,465 patients). In addition, 60 endoscopies were performed in patients with known COVID-19. Overall, no staff members became infected with SARS-CoV-2 during the study period. In all three scenarios, staff used PPE, and the vaccination rate of the team was 97%.
University Hospital W
All patients were interviewed before admission for COVID-19 symptoms, close contact with infected people, and recent travel to high-risk countries. Moreover, some endoscopies were performed even if a patient had positive markers for COVID-19.
The clinical team wore recommended PPE, including a high-filter FFP2 mask, one pair of gloves, protective eyewear, and disposable gowns. For patients with known COVID-19, staff wore two pairs of gloves, a disposable hairnet, and a water-resistant disposable gown. In addition, endoscopies were performed in negative pressure intervention rooms.
Among the 29 staff members involved, 16 physicians and 13 assistants worked in the endoscopy unit for at least 2 days per week for at least 6 months. The hospital’s internal policy required medical staff to undergo PCR testing if a rapid antigen test was positive or symptoms developed. Staff were vaccinated with two doses of the Pfizer-BioNTech vaccine in January and February 2021. A single booster dose of the Pfizer or Moderna vaccine was administered in November and December 2021.
The clinical team was not tested routinely, so asymptomatic infections may have existed. Moreover, the relatively low COVID-19 incidence in the local area might have influenced the risk of transmission. “However, even at the end of 2021, when the incidence was increasing, we did not see any higher risk of transmission,” the researchers explained.
“An important limitation of our study relates to the new variant Omicron that was dominant in our local area after the analyzed time frame.” Additional studies may be needed to understand the risk of transmission with the latest Omicron variants, and given the additional costs and implications on routine activity, current testing guidelines may need to be reconsidered.
“Although our data were not part of a randomized prospective study, we were able to demonstrate on a fairly high number of patients that PPE measures in addition to a short interview for assessment of a patient’s individual risks appear to be highly effective to control transmission of SARS-CoV-2 during an endoscopy. ... Pre-procedural RT-PCR testing or RA testing did not show any additional benefit,” Dr. Hann and colleagues concluded.
The authors reported no conflicts of interest.
FROM GUT
Steroids no cure for obstructive sleep apnea in children
Children with obstructive sleep apnea syndrome (OSAS) who undergo treatment with intranasal corticosteroids (INCS) did not experience significant improvement in polysomnographic, neurobehavioral, and other symptoms at 3 and 12 months of treatment. At 12 months of INCS treatment, there was a statistically significant but not clinically relevant reduction in the obstructive apnea hypopnea index (OHAI).
“Previous studies were done in children with OSA with an obstructive apnea hypopnea index of less than 5, so they had very mild OSA,” Ignacio Tapia, MD, associate professor of pediatrics, University of Pennsylvania, Philadelphia, said in an interview.
“But then people started using the INCS for a whole range of OSA, so this is why we wanted to do the trial, to make sure that these drugs were being used correctly,” he added.
“The main message from this paper is that I think INCS may still have a role to play in OSA to treat some of the symptoms, like snoring, and in our study, quality of life indices also improved, ,” Dr. Tapia emphasized.
The study was published online in the journal Chest.
3 months of INCS
A total of 134 children between 5 and 12 years of age were randomly assigned to receive INCS for 3 months or placebo. Children in the original INCS arm were then reassigned to receive 9 more months of the same treatment or placebo. Symptoms as well as polysomnographic and neurobehavioral findings were measured at baseline, at 3 months, and again at 12 months.
“The primary outcome was OAHI change at 3 months, available for 122 children,” the authors explained. The OSAS was defined as an OAHI of between two and three events per hour. The median age of the children at baseline was 7.9 years, and the median OAHI baseline score was 5.8/hr (95% confidence interval, 3.6-9.7/hr). The total daily dose of the INCS used was 110 mcg.
At 3 months, the mean change in the OAHI from baseline was –1.73/hr (95% CI, –3.91 to 1.92/hr), while at 12 months, the mean change in the same index was –1.21 (–4.22 to 1.71/hr). These changes were not significantly different from OAHI changes observed among control participants. “OSAS symptoms and neurobehavioral results were not different [either] between the INCS and placebo groups at 3 and12 months,” the authors added.
However, among those children who received INCS treatment for the entire 12 months, the OAHI decreased significantly from 7.2/hr (95% CI, 3.62-9.88/hr) at baseline to 3.71/hr (95% CI, 1.56-6.4/hr; P = .039), although the OAHI did not normalize, the authors noted. Asked to clarify whether this change was not significant, Dr. Tapia said that it did meet statistical significance, but clinically, it meant that the children still needed some form of treatment, because they still had OSA in the range needing treatment.
The placebo group had more asthma exacerbations, upper respiratory tract infections, and exacerbations of OSAS symptoms, compared with children in the INCS group. It is possible that INCS provided a certain degree of protection from asthma exacerbation, the authors suggested.
However, recent guidelines from the American Academy of Pediatrics suggest that clinicians may prescribe these agents for children with mild OSAS in whom adenotonsillectomy is contraindicated; for those with mild postoperative OSAS, adenotonsillectomy remains the treatment of choice for childhood OSA. “The low level of enthusiasm for INCS in these guidelines is based on results from studies of INCS treatment of OSAS that had been limited by small sample size, lack of placebo control, limited duration, and variability in baseline data,” the authors wrote.
“The results of the current larger and more rigorous study of children with a wider range of OSAS also do not support the currently liberal use of INCS for the treatment of OSAS,” they wrote.
Complex issue
In a comment, Rakesh Bhattacharjee, MD, associate professor of pediatrics, University of California, San Diego, noted that he does prescribe INCS for children with mild OSA but not for all children. “We based our decisions on polysomnography, which we use to categorize OSA as mild, moderate, or severe.
“But we certainly do offer this treatment for children with mild sleep apnea as a way to avoid surgical treatment,” Dr. Bhattacharjee added. He also uses INCS for residual sleep apnea that some children experience following adenotonsillectomy. As the current study suggests, many people are treating sleep apnea empirically without confirming the severity of the disorder by a sleep study.
“If a sleep study is not done, we don’t know how severe it is, so this would advocate for the utility of a sleep study so that you can quantify the severity of symptoms and target your therapy to children who might be appropriate for INCS therapy,” Dr. Bhattacharjee said.
On the other hand, surgery is not always relevant even if a child has enlarged adenoids and tonsils, as, for example, a child with obesity. In these children, physicians need to think about other treatments, such as continuous positive airways pressure. “CPAP is not perfect,” Dr. Bhattacharjee observed. “And as pediatricians, we need to do a lot of work to improve the use of CPAP, but, that said, there are children for whom INCS and surgery might be a waste of time, and this is where CPAP might be an alternative.”
Dr. Bhattacharjee previously was the lead author of a large study of children who underwent treatment with CPAP. While findings suggested that adherence to treatment is lower in children than it is for adults, the authors also showed that numerous actionable factors could used to improve adherence to CPAP among children who might otherwise benefit from it.
The authors disclosed no relevant financial relationships. Dr. Bhattacharjee has served as a scientific adviser for Jazz Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Children with obstructive sleep apnea syndrome (OSAS) who undergo treatment with intranasal corticosteroids (INCS) did not experience significant improvement in polysomnographic, neurobehavioral, and other symptoms at 3 and 12 months of treatment. At 12 months of INCS treatment, there was a statistically significant but not clinically relevant reduction in the obstructive apnea hypopnea index (OHAI).
“Previous studies were done in children with OSA with an obstructive apnea hypopnea index of less than 5, so they had very mild OSA,” Ignacio Tapia, MD, associate professor of pediatrics, University of Pennsylvania, Philadelphia, said in an interview.
“But then people started using the INCS for a whole range of OSA, so this is why we wanted to do the trial, to make sure that these drugs were being used correctly,” he added.
“The main message from this paper is that I think INCS may still have a role to play in OSA to treat some of the symptoms, like snoring, and in our study, quality of life indices also improved, ,” Dr. Tapia emphasized.
The study was published online in the journal Chest.
3 months of INCS
A total of 134 children between 5 and 12 years of age were randomly assigned to receive INCS for 3 months or placebo. Children in the original INCS arm were then reassigned to receive 9 more months of the same treatment or placebo. Symptoms as well as polysomnographic and neurobehavioral findings were measured at baseline, at 3 months, and again at 12 months.
“The primary outcome was OAHI change at 3 months, available for 122 children,” the authors explained. The OSAS was defined as an OAHI of between two and three events per hour. The median age of the children at baseline was 7.9 years, and the median OAHI baseline score was 5.8/hr (95% confidence interval, 3.6-9.7/hr). The total daily dose of the INCS used was 110 mcg.
At 3 months, the mean change in the OAHI from baseline was –1.73/hr (95% CI, –3.91 to 1.92/hr), while at 12 months, the mean change in the same index was –1.21 (–4.22 to 1.71/hr). These changes were not significantly different from OAHI changes observed among control participants. “OSAS symptoms and neurobehavioral results were not different [either] between the INCS and placebo groups at 3 and12 months,” the authors added.
However, among those children who received INCS treatment for the entire 12 months, the OAHI decreased significantly from 7.2/hr (95% CI, 3.62-9.88/hr) at baseline to 3.71/hr (95% CI, 1.56-6.4/hr; P = .039), although the OAHI did not normalize, the authors noted. Asked to clarify whether this change was not significant, Dr. Tapia said that it did meet statistical significance, but clinically, it meant that the children still needed some form of treatment, because they still had OSA in the range needing treatment.
The placebo group had more asthma exacerbations, upper respiratory tract infections, and exacerbations of OSAS symptoms, compared with children in the INCS group. It is possible that INCS provided a certain degree of protection from asthma exacerbation, the authors suggested.
However, recent guidelines from the American Academy of Pediatrics suggest that clinicians may prescribe these agents for children with mild OSAS in whom adenotonsillectomy is contraindicated; for those with mild postoperative OSAS, adenotonsillectomy remains the treatment of choice for childhood OSA. “The low level of enthusiasm for INCS in these guidelines is based on results from studies of INCS treatment of OSAS that had been limited by small sample size, lack of placebo control, limited duration, and variability in baseline data,” the authors wrote.
“The results of the current larger and more rigorous study of children with a wider range of OSAS also do not support the currently liberal use of INCS for the treatment of OSAS,” they wrote.
Complex issue
In a comment, Rakesh Bhattacharjee, MD, associate professor of pediatrics, University of California, San Diego, noted that he does prescribe INCS for children with mild OSA but not for all children. “We based our decisions on polysomnography, which we use to categorize OSA as mild, moderate, or severe.
“But we certainly do offer this treatment for children with mild sleep apnea as a way to avoid surgical treatment,” Dr. Bhattacharjee added. He also uses INCS for residual sleep apnea that some children experience following adenotonsillectomy. As the current study suggests, many people are treating sleep apnea empirically without confirming the severity of the disorder by a sleep study.
“If a sleep study is not done, we don’t know how severe it is, so this would advocate for the utility of a sleep study so that you can quantify the severity of symptoms and target your therapy to children who might be appropriate for INCS therapy,” Dr. Bhattacharjee said.
On the other hand, surgery is not always relevant even if a child has enlarged adenoids and tonsils, as, for example, a child with obesity. In these children, physicians need to think about other treatments, such as continuous positive airways pressure. “CPAP is not perfect,” Dr. Bhattacharjee observed. “And as pediatricians, we need to do a lot of work to improve the use of CPAP, but, that said, there are children for whom INCS and surgery might be a waste of time, and this is where CPAP might be an alternative.”
Dr. Bhattacharjee previously was the lead author of a large study of children who underwent treatment with CPAP. While findings suggested that adherence to treatment is lower in children than it is for adults, the authors also showed that numerous actionable factors could used to improve adherence to CPAP among children who might otherwise benefit from it.
The authors disclosed no relevant financial relationships. Dr. Bhattacharjee has served as a scientific adviser for Jazz Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Children with obstructive sleep apnea syndrome (OSAS) who undergo treatment with intranasal corticosteroids (INCS) did not experience significant improvement in polysomnographic, neurobehavioral, and other symptoms at 3 and 12 months of treatment. At 12 months of INCS treatment, there was a statistically significant but not clinically relevant reduction in the obstructive apnea hypopnea index (OHAI).
“Previous studies were done in children with OSA with an obstructive apnea hypopnea index of less than 5, so they had very mild OSA,” Ignacio Tapia, MD, associate professor of pediatrics, University of Pennsylvania, Philadelphia, said in an interview.
“But then people started using the INCS for a whole range of OSA, so this is why we wanted to do the trial, to make sure that these drugs were being used correctly,” he added.
“The main message from this paper is that I think INCS may still have a role to play in OSA to treat some of the symptoms, like snoring, and in our study, quality of life indices also improved, ,” Dr. Tapia emphasized.
The study was published online in the journal Chest.
3 months of INCS
A total of 134 children between 5 and 12 years of age were randomly assigned to receive INCS for 3 months or placebo. Children in the original INCS arm were then reassigned to receive 9 more months of the same treatment or placebo. Symptoms as well as polysomnographic and neurobehavioral findings were measured at baseline, at 3 months, and again at 12 months.
“The primary outcome was OAHI change at 3 months, available for 122 children,” the authors explained. The OSAS was defined as an OAHI of between two and three events per hour. The median age of the children at baseline was 7.9 years, and the median OAHI baseline score was 5.8/hr (95% confidence interval, 3.6-9.7/hr). The total daily dose of the INCS used was 110 mcg.
At 3 months, the mean change in the OAHI from baseline was –1.73/hr (95% CI, –3.91 to 1.92/hr), while at 12 months, the mean change in the same index was –1.21 (–4.22 to 1.71/hr). These changes were not significantly different from OAHI changes observed among control participants. “OSAS symptoms and neurobehavioral results were not different [either] between the INCS and placebo groups at 3 and12 months,” the authors added.
However, among those children who received INCS treatment for the entire 12 months, the OAHI decreased significantly from 7.2/hr (95% CI, 3.62-9.88/hr) at baseline to 3.71/hr (95% CI, 1.56-6.4/hr; P = .039), although the OAHI did not normalize, the authors noted. Asked to clarify whether this change was not significant, Dr. Tapia said that it did meet statistical significance, but clinically, it meant that the children still needed some form of treatment, because they still had OSA in the range needing treatment.
The placebo group had more asthma exacerbations, upper respiratory tract infections, and exacerbations of OSAS symptoms, compared with children in the INCS group. It is possible that INCS provided a certain degree of protection from asthma exacerbation, the authors suggested.
However, recent guidelines from the American Academy of Pediatrics suggest that clinicians may prescribe these agents for children with mild OSAS in whom adenotonsillectomy is contraindicated; for those with mild postoperative OSAS, adenotonsillectomy remains the treatment of choice for childhood OSA. “The low level of enthusiasm for INCS in these guidelines is based on results from studies of INCS treatment of OSAS that had been limited by small sample size, lack of placebo control, limited duration, and variability in baseline data,” the authors wrote.
“The results of the current larger and more rigorous study of children with a wider range of OSAS also do not support the currently liberal use of INCS for the treatment of OSAS,” they wrote.
Complex issue
In a comment, Rakesh Bhattacharjee, MD, associate professor of pediatrics, University of California, San Diego, noted that he does prescribe INCS for children with mild OSA but not for all children. “We based our decisions on polysomnography, which we use to categorize OSA as mild, moderate, or severe.
“But we certainly do offer this treatment for children with mild sleep apnea as a way to avoid surgical treatment,” Dr. Bhattacharjee added. He also uses INCS for residual sleep apnea that some children experience following adenotonsillectomy. As the current study suggests, many people are treating sleep apnea empirically without confirming the severity of the disorder by a sleep study.
“If a sleep study is not done, we don’t know how severe it is, so this would advocate for the utility of a sleep study so that you can quantify the severity of symptoms and target your therapy to children who might be appropriate for INCS therapy,” Dr. Bhattacharjee said.
On the other hand, surgery is not always relevant even if a child has enlarged adenoids and tonsils, as, for example, a child with obesity. In these children, physicians need to think about other treatments, such as continuous positive airways pressure. “CPAP is not perfect,” Dr. Bhattacharjee observed. “And as pediatricians, we need to do a lot of work to improve the use of CPAP, but, that said, there are children for whom INCS and surgery might be a waste of time, and this is where CPAP might be an alternative.”
Dr. Bhattacharjee previously was the lead author of a large study of children who underwent treatment with CPAP. While findings suggested that adherence to treatment is lower in children than it is for adults, the authors also showed that numerous actionable factors could used to improve adherence to CPAP among children who might otherwise benefit from it.
The authors disclosed no relevant financial relationships. Dr. Bhattacharjee has served as a scientific adviser for Jazz Pharmaceuticals.
A version of this article first appeared on Medscape.com.
FROM CHEST
Global data provide new insight into problem gambling
Across the globe few individuals at risk for gambling problems seek help for the issue, new research shows.
In the first study to examine global prevalence of help-seeking for problem gambling, the systematic review showed that
“Our findings suggest a considerable need for help among those experiencing problems related to their gambling,” Rimke Bijker, PhD, of the University of Auckland (New Zealand) and colleagues wrote.
The findings were published online in Addiction.
A public health concern
An increase in online gambling and stress and isolation during the COVID-19 pandemic led to experts sounding the alarm about gambling disorders. But despite its emergence as a public health concern, systematic investigation of help-seeking for problem gambling has been lacking, the investigators noted.
In their review, they included 24 studies conducted between 2010 and 2020 and involving a total of 188,234 individuals. More than 70% of the studies were conducted in Australia and New Zealand and 25% were conducted in the United States and Canada.
The overall prevalence of help-seeking for problem gambling among adults worldwide was 0.23% (95% confidence interval, 0.16-0.33).
Prevalence estimates were significantly higher in studies assessing lifetime help-seeking (0.50%; 95% CI, 0.35-0.71), compared with studies that examined current help-seeking (0.14%; 95% CI, 0.1-0.2, P < .001).
There were no significant differences in prevalence by gambling participation, region, type of help-seeking (professional only or mixed options), or year of data collection.
Gambling severity was measured by the Problem Gambling Severity Index as low risk, as moderate risk, or as problem gambling. Help-seeking was highest in the problem gambling and the moderate-risk groups, compared with the low-risk group (20.63%, 3.73%, and 0.27%, respectively; P < .001).
“A public health approach to gambling problems should be grounded in robust evidence on what people currently do to minimize and reduce their gambling harm and this should be inclusive of professional and nonprofessional support and self-help,” the investigators wrote.
Around 40% of individuals with problem gambling recover with or without professional oversight, they added.
Historically, gambling interventions have focused on those with more severe gambling problems. To truly address the issue, gambling reduction efforts should consider individuals with problems across the full continuum of risk, including those experiencing less severe problem gambling, the researchers wrote.
They added that those with more severe gambling issues “are likely to have comorbidities and may require more intensive interventions, guided by professionals,” such as general practitioners, psychiatrists, or psychologists.
Those with a less severe form “may prefer non-professional options and self-help strategies, which highlights the importance of information on such sources of help being promoted and easily accessible,” the investigators wrote.
No funding source for the study was reported. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Across the globe few individuals at risk for gambling problems seek help for the issue, new research shows.
In the first study to examine global prevalence of help-seeking for problem gambling, the systematic review showed that
“Our findings suggest a considerable need for help among those experiencing problems related to their gambling,” Rimke Bijker, PhD, of the University of Auckland (New Zealand) and colleagues wrote.
The findings were published online in Addiction.
A public health concern
An increase in online gambling and stress and isolation during the COVID-19 pandemic led to experts sounding the alarm about gambling disorders. But despite its emergence as a public health concern, systematic investigation of help-seeking for problem gambling has been lacking, the investigators noted.
In their review, they included 24 studies conducted between 2010 and 2020 and involving a total of 188,234 individuals. More than 70% of the studies were conducted in Australia and New Zealand and 25% were conducted in the United States and Canada.
The overall prevalence of help-seeking for problem gambling among adults worldwide was 0.23% (95% confidence interval, 0.16-0.33).
Prevalence estimates were significantly higher in studies assessing lifetime help-seeking (0.50%; 95% CI, 0.35-0.71), compared with studies that examined current help-seeking (0.14%; 95% CI, 0.1-0.2, P < .001).
There were no significant differences in prevalence by gambling participation, region, type of help-seeking (professional only or mixed options), or year of data collection.
Gambling severity was measured by the Problem Gambling Severity Index as low risk, as moderate risk, or as problem gambling. Help-seeking was highest in the problem gambling and the moderate-risk groups, compared with the low-risk group (20.63%, 3.73%, and 0.27%, respectively; P < .001).
“A public health approach to gambling problems should be grounded in robust evidence on what people currently do to minimize and reduce their gambling harm and this should be inclusive of professional and nonprofessional support and self-help,” the investigators wrote.
Around 40% of individuals with problem gambling recover with or without professional oversight, they added.
Historically, gambling interventions have focused on those with more severe gambling problems. To truly address the issue, gambling reduction efforts should consider individuals with problems across the full continuum of risk, including those experiencing less severe problem gambling, the researchers wrote.
They added that those with more severe gambling issues “are likely to have comorbidities and may require more intensive interventions, guided by professionals,” such as general practitioners, psychiatrists, or psychologists.
Those with a less severe form “may prefer non-professional options and self-help strategies, which highlights the importance of information on such sources of help being promoted and easily accessible,” the investigators wrote.
No funding source for the study was reported. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Across the globe few individuals at risk for gambling problems seek help for the issue, new research shows.
In the first study to examine global prevalence of help-seeking for problem gambling, the systematic review showed that
“Our findings suggest a considerable need for help among those experiencing problems related to their gambling,” Rimke Bijker, PhD, of the University of Auckland (New Zealand) and colleagues wrote.
The findings were published online in Addiction.
A public health concern
An increase in online gambling and stress and isolation during the COVID-19 pandemic led to experts sounding the alarm about gambling disorders. But despite its emergence as a public health concern, systematic investigation of help-seeking for problem gambling has been lacking, the investigators noted.
In their review, they included 24 studies conducted between 2010 and 2020 and involving a total of 188,234 individuals. More than 70% of the studies were conducted in Australia and New Zealand and 25% were conducted in the United States and Canada.
The overall prevalence of help-seeking for problem gambling among adults worldwide was 0.23% (95% confidence interval, 0.16-0.33).
Prevalence estimates were significantly higher in studies assessing lifetime help-seeking (0.50%; 95% CI, 0.35-0.71), compared with studies that examined current help-seeking (0.14%; 95% CI, 0.1-0.2, P < .001).
There were no significant differences in prevalence by gambling participation, region, type of help-seeking (professional only or mixed options), or year of data collection.
Gambling severity was measured by the Problem Gambling Severity Index as low risk, as moderate risk, or as problem gambling. Help-seeking was highest in the problem gambling and the moderate-risk groups, compared with the low-risk group (20.63%, 3.73%, and 0.27%, respectively; P < .001).
“A public health approach to gambling problems should be grounded in robust evidence on what people currently do to minimize and reduce their gambling harm and this should be inclusive of professional and nonprofessional support and self-help,” the investigators wrote.
Around 40% of individuals with problem gambling recover with or without professional oversight, they added.
Historically, gambling interventions have focused on those with more severe gambling problems. To truly address the issue, gambling reduction efforts should consider individuals with problems across the full continuum of risk, including those experiencing less severe problem gambling, the researchers wrote.
They added that those with more severe gambling issues “are likely to have comorbidities and may require more intensive interventions, guided by professionals,” such as general practitioners, psychiatrists, or psychologists.
Those with a less severe form “may prefer non-professional options and self-help strategies, which highlights the importance of information on such sources of help being promoted and easily accessible,” the investigators wrote.
No funding source for the study was reported. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ADDICTION
Electroacupuncture promising for depression-related insomnia
In a study of more than 200 adults with depression and comorbid insomnia, change from baseline to week 8 on the Pittsburgh Sleep Quality Index (PSQI) was 3 points greater in the group receiving EA versus a group receiving sham acupuncture (SA) plus standard care, and 5 points greater vs a control group receiving standard care only. The improvements were sustained during a 24-week postintervention follow-up.
The EA group also showed significant improvement in depression, insomnia, self-rated anxiety, and total sleep time – all of which were not found in the SA or control groups.
“Based on the results of our trial, we recommend patients with depression and insomnia seek the treatment of EA as an alternative and complementary therapy for better results,” study investigator Shifen Xu, PhD, Shanghai (China) Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, told this news organization.
The findings were published online in JAMA Network Open.
Bidirectional relationship
“Sleep disturbance is the prominent symptom in patients with depression,” the investigators noted.
Depression and sleep issues have a bidirectional relationship, in that “poor sleep quality contributes to the development of depression, and having depression makes a person more likely to develop sleep issues,” they wrote.
Patients with co-occurring depression and sleep disorders are more difficult to treat and have a greater risk for relapse and recurrence of depression, they added.
Acupuncture may be an “effective drug-free approach to help treat mental illness and sleep disorders,” the researchers noted. A previous study suggested acupuncture may improve sleep efficacy and prolong total sleep in patients with primary insomnia.
“EA is the combination of traditional Chinese acupuncture with electric-impulse stimulation, and it can enhance the therapeutic effect of the acupoints throughout the needle retention time,” Dr. Xu said.
A previous pilot study of EA for depression-related insomnia showed significant improvements in sleep quality after EA treatment, but the sample size was small.
The current researchers, therefore, undertook the present study – with a larger sample size and comparison with SA and standard care. They divided 270 adults (mean age, 50.3 years; 71.9% women) at three tertiary hospitals in Shanghai into three groups, each consisting of 90 participants.
The EA plus standard care group and the SA plus standard care group received 30-minute treatments three times per week for 8 weeks. The control group received standard care only.
All participants had DSM-5–diagnosed depression; baseline PSQI scores greater than 7, with higher scores indicating worse sleep quality and a greater number or sleep disorders; and Hamilton Depression Rating Scales (HDRS-17) scores of 20-35, with higher scores indicating higher depression levels.
Patients with secondary depressive disorders caused by other conditions, medication, or psychotic disorders were excluded, as were patients with a history of alcohol abuse or drug dependence or those who had received acupuncture within the previous year.
Of the patients who completed the 8-week intervention, 83 were in the EA group, 81 in the SA group, and 83 in the control group. Almost all participants (91.5%) completed all outcome measurements by the end of the 24-week follow-up period (also known as week 32).
Calm mind, balanced mood
At the 8-week posttreatment assessment, which was the primary endpoint, the EA group had a mean reduction from baseline of 6.2 points (95% confidence interval, −6.9 to −5.6) in PSQI score.
There was a significant difference in PSQI score between the EA versus the SA group (−3.6 points; 95% CI, −4.4 to −2.8; P < .001) and vs the control group (−5.1 points; 95% CI, −6.0 to −4.2; P < .001).
The efficacy of EA in treating insomnia was sustained during the postintervention follow-up period when the EA group had a significantly greater reduction in PSQI score, compared with the SA group (−4.7; 95% CI, −5.4 to −3.9; P < .001) and the control group (−5.0; 95% CI, −5.8 to −4.1; P < .001).
Patients receiving EA also experienced significant (all P values < .001) improvement from baseline on secondary outcomes, including:
- Scores on the HDRS (−10.7; 95% CI, −11.8 to −9.7)
- Scores on the Insomnia Severity Index, (−7.6; 95% CI,−8.5 to −6.7)
- Scores on the Self-rated Anxiety Scale (−2.9; 95% CI, −4.1 to −1.7)
- Total sleep time, as recorded by sleep actigraphy (29.1 minutes; 95% CI, 21.5-36.7)
In addition, the EA group showed significant improvement in depression scores compared with the SA and control groups at both 8 and 32 weeks (all P values < .001).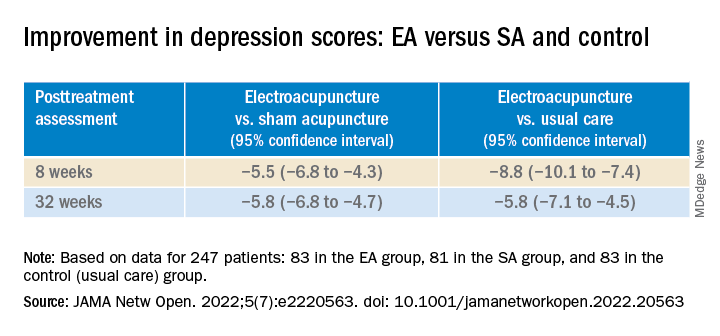
Participants in the EA group also had a 4.2% (95% CI, 2.6% - 5.8%) higher sleep efficiency score at week 8, compared with those in the SA group (P < .001).
In addition, they had lower scores on the Insomnia Severity Index and the Self-rated Anxiety Scale, and longer total sleep time, compared with the control group at week 8.
None of the participants reported any serious adverse events.
“Our findings constitute subjective and objective evidence of the efficacy and safety of EA with standard care in treating comorbid depression and insomnia compared with SA with standard care or standard care alone,” the investigators wrote.
“The acupoints we used in this trial mainly act on calming mind, relieving negative mood, and balancing the yin-yang,” Dr. Xu added.
Viable adjunctive treatment
Commenting on the study, Albert Yeung, MD, ScD, associate director of the Mass General Depression and Clinical Research Program and associate professor of psychiatry, Harvard Medical School, Boston, said that, with the evidence from this study, “acupuncture and/or electroacupuncture could be a viable adjunctive treatment for depressed patients who suffer from insomnia.”
Dr. Yeung, who was not involved with the study, is the coauthor of an accompanying editorial.
“More well-designed studies are warranted to provide evidence for integrating holistic treatment in medicine,” he said.
The study was funded by grants from the National Natural Science Foundation of China, and Shanghai Municipal Health. The investigators and Dr. Yeung reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a study of more than 200 adults with depression and comorbid insomnia, change from baseline to week 8 on the Pittsburgh Sleep Quality Index (PSQI) was 3 points greater in the group receiving EA versus a group receiving sham acupuncture (SA) plus standard care, and 5 points greater vs a control group receiving standard care only. The improvements were sustained during a 24-week postintervention follow-up.
The EA group also showed significant improvement in depression, insomnia, self-rated anxiety, and total sleep time – all of which were not found in the SA or control groups.
“Based on the results of our trial, we recommend patients with depression and insomnia seek the treatment of EA as an alternative and complementary therapy for better results,” study investigator Shifen Xu, PhD, Shanghai (China) Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, told this news organization.
The findings were published online in JAMA Network Open.
Bidirectional relationship
“Sleep disturbance is the prominent symptom in patients with depression,” the investigators noted.
Depression and sleep issues have a bidirectional relationship, in that “poor sleep quality contributes to the development of depression, and having depression makes a person more likely to develop sleep issues,” they wrote.
Patients with co-occurring depression and sleep disorders are more difficult to treat and have a greater risk for relapse and recurrence of depression, they added.
Acupuncture may be an “effective drug-free approach to help treat mental illness and sleep disorders,” the researchers noted. A previous study suggested acupuncture may improve sleep efficacy and prolong total sleep in patients with primary insomnia.
“EA is the combination of traditional Chinese acupuncture with electric-impulse stimulation, and it can enhance the therapeutic effect of the acupoints throughout the needle retention time,” Dr. Xu said.
A previous pilot study of EA for depression-related insomnia showed significant improvements in sleep quality after EA treatment, but the sample size was small.
The current researchers, therefore, undertook the present study – with a larger sample size and comparison with SA and standard care. They divided 270 adults (mean age, 50.3 years; 71.9% women) at three tertiary hospitals in Shanghai into three groups, each consisting of 90 participants.
The EA plus standard care group and the SA plus standard care group received 30-minute treatments three times per week for 8 weeks. The control group received standard care only.
All participants had DSM-5–diagnosed depression; baseline PSQI scores greater than 7, with higher scores indicating worse sleep quality and a greater number or sleep disorders; and Hamilton Depression Rating Scales (HDRS-17) scores of 20-35, with higher scores indicating higher depression levels.
Patients with secondary depressive disorders caused by other conditions, medication, or psychotic disorders were excluded, as were patients with a history of alcohol abuse or drug dependence or those who had received acupuncture within the previous year.
Of the patients who completed the 8-week intervention, 83 were in the EA group, 81 in the SA group, and 83 in the control group. Almost all participants (91.5%) completed all outcome measurements by the end of the 24-week follow-up period (also known as week 32).
Calm mind, balanced mood
At the 8-week posttreatment assessment, which was the primary endpoint, the EA group had a mean reduction from baseline of 6.2 points (95% confidence interval, −6.9 to −5.6) in PSQI score.
There was a significant difference in PSQI score between the EA versus the SA group (−3.6 points; 95% CI, −4.4 to −2.8; P < .001) and vs the control group (−5.1 points; 95% CI, −6.0 to −4.2; P < .001).
The efficacy of EA in treating insomnia was sustained during the postintervention follow-up period when the EA group had a significantly greater reduction in PSQI score, compared with the SA group (−4.7; 95% CI, −5.4 to −3.9; P < .001) and the control group (−5.0; 95% CI, −5.8 to −4.1; P < .001).
Patients receiving EA also experienced significant (all P values < .001) improvement from baseline on secondary outcomes, including:
- Scores on the HDRS (−10.7; 95% CI, −11.8 to −9.7)
- Scores on the Insomnia Severity Index, (−7.6; 95% CI,−8.5 to −6.7)
- Scores on the Self-rated Anxiety Scale (−2.9; 95% CI, −4.1 to −1.7)
- Total sleep time, as recorded by sleep actigraphy (29.1 minutes; 95% CI, 21.5-36.7)
In addition, the EA group showed significant improvement in depression scores compared with the SA and control groups at both 8 and 32 weeks (all P values < .001).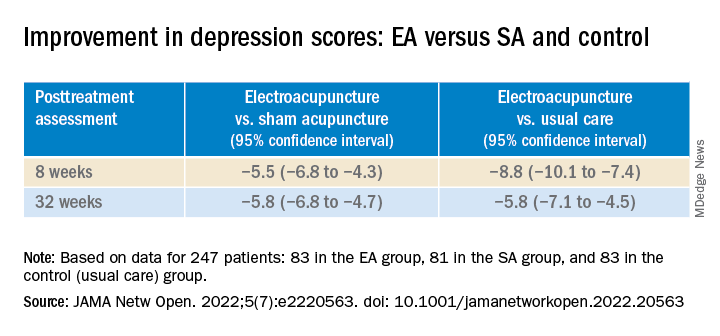
Participants in the EA group also had a 4.2% (95% CI, 2.6% - 5.8%) higher sleep efficiency score at week 8, compared with those in the SA group (P < .001).
In addition, they had lower scores on the Insomnia Severity Index and the Self-rated Anxiety Scale, and longer total sleep time, compared with the control group at week 8.
None of the participants reported any serious adverse events.
“Our findings constitute subjective and objective evidence of the efficacy and safety of EA with standard care in treating comorbid depression and insomnia compared with SA with standard care or standard care alone,” the investigators wrote.
“The acupoints we used in this trial mainly act on calming mind, relieving negative mood, and balancing the yin-yang,” Dr. Xu added.
Viable adjunctive treatment
Commenting on the study, Albert Yeung, MD, ScD, associate director of the Mass General Depression and Clinical Research Program and associate professor of psychiatry, Harvard Medical School, Boston, said that, with the evidence from this study, “acupuncture and/or electroacupuncture could be a viable adjunctive treatment for depressed patients who suffer from insomnia.”
Dr. Yeung, who was not involved with the study, is the coauthor of an accompanying editorial.
“More well-designed studies are warranted to provide evidence for integrating holistic treatment in medicine,” he said.
The study was funded by grants from the National Natural Science Foundation of China, and Shanghai Municipal Health. The investigators and Dr. Yeung reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a study of more than 200 adults with depression and comorbid insomnia, change from baseline to week 8 on the Pittsburgh Sleep Quality Index (PSQI) was 3 points greater in the group receiving EA versus a group receiving sham acupuncture (SA) plus standard care, and 5 points greater vs a control group receiving standard care only. The improvements were sustained during a 24-week postintervention follow-up.
The EA group also showed significant improvement in depression, insomnia, self-rated anxiety, and total sleep time – all of which were not found in the SA or control groups.
“Based on the results of our trial, we recommend patients with depression and insomnia seek the treatment of EA as an alternative and complementary therapy for better results,” study investigator Shifen Xu, PhD, Shanghai (China) Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, told this news organization.
The findings were published online in JAMA Network Open.
Bidirectional relationship
“Sleep disturbance is the prominent symptom in patients with depression,” the investigators noted.
Depression and sleep issues have a bidirectional relationship, in that “poor sleep quality contributes to the development of depression, and having depression makes a person more likely to develop sleep issues,” they wrote.
Patients with co-occurring depression and sleep disorders are more difficult to treat and have a greater risk for relapse and recurrence of depression, they added.
Acupuncture may be an “effective drug-free approach to help treat mental illness and sleep disorders,” the researchers noted. A previous study suggested acupuncture may improve sleep efficacy and prolong total sleep in patients with primary insomnia.
“EA is the combination of traditional Chinese acupuncture with electric-impulse stimulation, and it can enhance the therapeutic effect of the acupoints throughout the needle retention time,” Dr. Xu said.
A previous pilot study of EA for depression-related insomnia showed significant improvements in sleep quality after EA treatment, but the sample size was small.
The current researchers, therefore, undertook the present study – with a larger sample size and comparison with SA and standard care. They divided 270 adults (mean age, 50.3 years; 71.9% women) at three tertiary hospitals in Shanghai into three groups, each consisting of 90 participants.
The EA plus standard care group and the SA plus standard care group received 30-minute treatments three times per week for 8 weeks. The control group received standard care only.
All participants had DSM-5–diagnosed depression; baseline PSQI scores greater than 7, with higher scores indicating worse sleep quality and a greater number or sleep disorders; and Hamilton Depression Rating Scales (HDRS-17) scores of 20-35, with higher scores indicating higher depression levels.
Patients with secondary depressive disorders caused by other conditions, medication, or psychotic disorders were excluded, as were patients with a history of alcohol abuse or drug dependence or those who had received acupuncture within the previous year.
Of the patients who completed the 8-week intervention, 83 were in the EA group, 81 in the SA group, and 83 in the control group. Almost all participants (91.5%) completed all outcome measurements by the end of the 24-week follow-up period (also known as week 32).
Calm mind, balanced mood
At the 8-week posttreatment assessment, which was the primary endpoint, the EA group had a mean reduction from baseline of 6.2 points (95% confidence interval, −6.9 to −5.6) in PSQI score.
There was a significant difference in PSQI score between the EA versus the SA group (−3.6 points; 95% CI, −4.4 to −2.8; P < .001) and vs the control group (−5.1 points; 95% CI, −6.0 to −4.2; P < .001).
The efficacy of EA in treating insomnia was sustained during the postintervention follow-up period when the EA group had a significantly greater reduction in PSQI score, compared with the SA group (−4.7; 95% CI, −5.4 to −3.9; P < .001) and the control group (−5.0; 95% CI, −5.8 to −4.1; P < .001).
Patients receiving EA also experienced significant (all P values < .001) improvement from baseline on secondary outcomes, including:
- Scores on the HDRS (−10.7; 95% CI, −11.8 to −9.7)
- Scores on the Insomnia Severity Index, (−7.6; 95% CI,−8.5 to −6.7)
- Scores on the Self-rated Anxiety Scale (−2.9; 95% CI, −4.1 to −1.7)
- Total sleep time, as recorded by sleep actigraphy (29.1 minutes; 95% CI, 21.5-36.7)
In addition, the EA group showed significant improvement in depression scores compared with the SA and control groups at both 8 and 32 weeks (all P values < .001).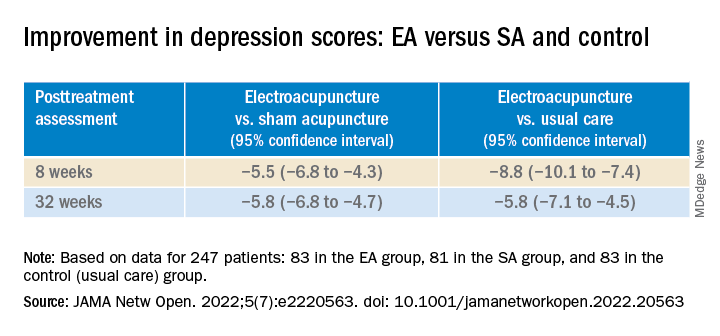
Participants in the EA group also had a 4.2% (95% CI, 2.6% - 5.8%) higher sleep efficiency score at week 8, compared with those in the SA group (P < .001).
In addition, they had lower scores on the Insomnia Severity Index and the Self-rated Anxiety Scale, and longer total sleep time, compared with the control group at week 8.
None of the participants reported any serious adverse events.
“Our findings constitute subjective and objective evidence of the efficacy and safety of EA with standard care in treating comorbid depression and insomnia compared with SA with standard care or standard care alone,” the investigators wrote.
“The acupoints we used in this trial mainly act on calming mind, relieving negative mood, and balancing the yin-yang,” Dr. Xu added.
Viable adjunctive treatment
Commenting on the study, Albert Yeung, MD, ScD, associate director of the Mass General Depression and Clinical Research Program and associate professor of psychiatry, Harvard Medical School, Boston, said that, with the evidence from this study, “acupuncture and/or electroacupuncture could be a viable adjunctive treatment for depressed patients who suffer from insomnia.”
Dr. Yeung, who was not involved with the study, is the coauthor of an accompanying editorial.
“More well-designed studies are warranted to provide evidence for integrating holistic treatment in medicine,” he said.
The study was funded by grants from the National Natural Science Foundation of China, and Shanghai Municipal Health. The investigators and Dr. Yeung reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Children and COVID: Does latest rise in new cases point toward stabilization?
New COVID-19 cases rose for the second time in 3 weeks, as the effort to vaccinate the youngest children continued to slow after just 3 full weeks.
Nationally, over 75,000 children under age 5 years received their first dose of COVID-19 vaccine during the week of July 7-13. That number is down from the previous week – 118,000 from June 30 to July 6 – which, in turn, was lower than the 206,000 doses administered through the first 10 days after approval, based on data from the Centers for Disease Control and Prevention. That all adds up to just under 400,000 vaccinated children, or 2% of the eligible population under age 5, as of July 13.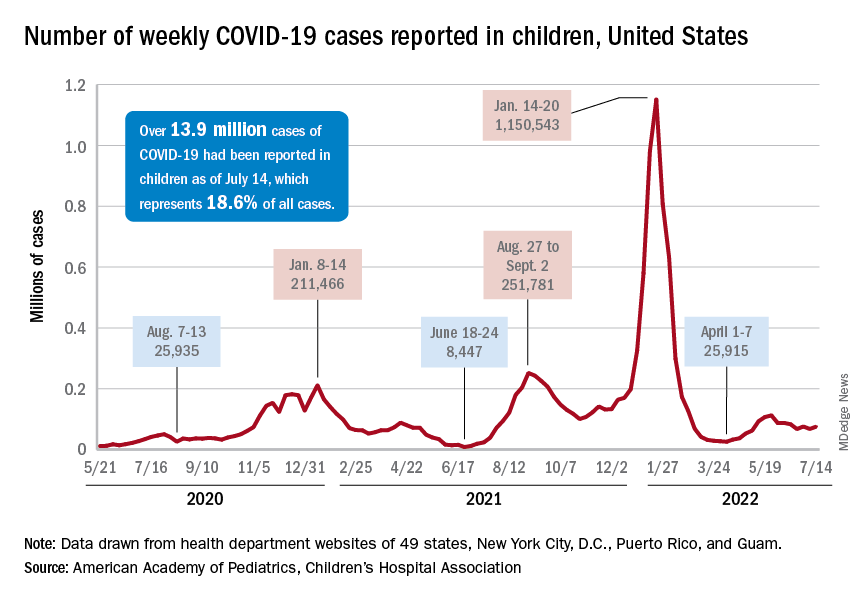
State-level data, meanwhile, show considerable variation, the American Academy of Pediatrics noted in its weekly analysis of the CDC vaccine data. Vermont has already vaccinated 10.0% of children under age 5 years, and Massachusetts is at 9.5%, while Mississippi (0.3%), Alabama (0.5%), and Louisiana (0.8%) are still below 1%, the AAP said.
New cases show signs of steadying
The national count was up by 11.1% for the week of July 8-14, rising to 75,000 new cases, compared with 68,000 the previous week, but the recent trend seems to be leaning toward steadiness. The overall number has been between 67,000 and 76,000 over the past 4 weeks, alternating between rising and falling in that time span, according to data gathered by the AAP and the Children’s Hospital Association from state and territorial health departments.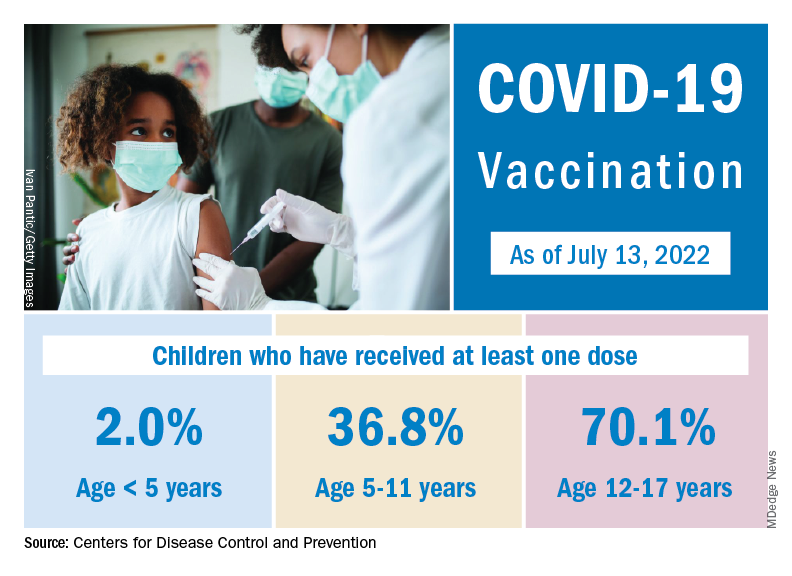
the two groups said, also noting that several states have stopped updating their online dashboards over the past year, making the current total artificially low in comparison.
Taken with that grain of salt, the cumulative number of child cases since the start of the pandemic is just over 13.9 million, which represents 18.6% of all cases in the United States. That proportion has been declining in recent weeks and was as high as 19.0% as late as mid-May. “While COVID-19 cases are likely increasingly underreported for all age groups, this decline indicates that children are disproportionately undercounted in reported COVID-19 cases,” the AAP and CHA said.
New COVID-19 cases rose for the second time in 3 weeks, as the effort to vaccinate the youngest children continued to slow after just 3 full weeks.
Nationally, over 75,000 children under age 5 years received their first dose of COVID-19 vaccine during the week of July 7-13. That number is down from the previous week – 118,000 from June 30 to July 6 – which, in turn, was lower than the 206,000 doses administered through the first 10 days after approval, based on data from the Centers for Disease Control and Prevention. That all adds up to just under 400,000 vaccinated children, or 2% of the eligible population under age 5, as of July 13.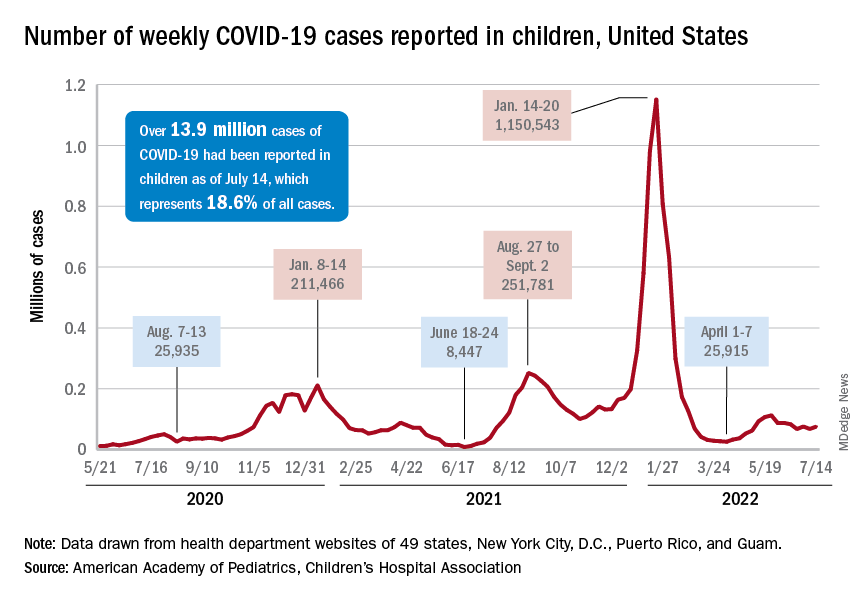
State-level data, meanwhile, show considerable variation, the American Academy of Pediatrics noted in its weekly analysis of the CDC vaccine data. Vermont has already vaccinated 10.0% of children under age 5 years, and Massachusetts is at 9.5%, while Mississippi (0.3%), Alabama (0.5%), and Louisiana (0.8%) are still below 1%, the AAP said.
New cases show signs of steadying
The national count was up by 11.1% for the week of July 8-14, rising to 75,000 new cases, compared with 68,000 the previous week, but the recent trend seems to be leaning toward steadiness. The overall number has been between 67,000 and 76,000 over the past 4 weeks, alternating between rising and falling in that time span, according to data gathered by the AAP and the Children’s Hospital Association from state and territorial health departments.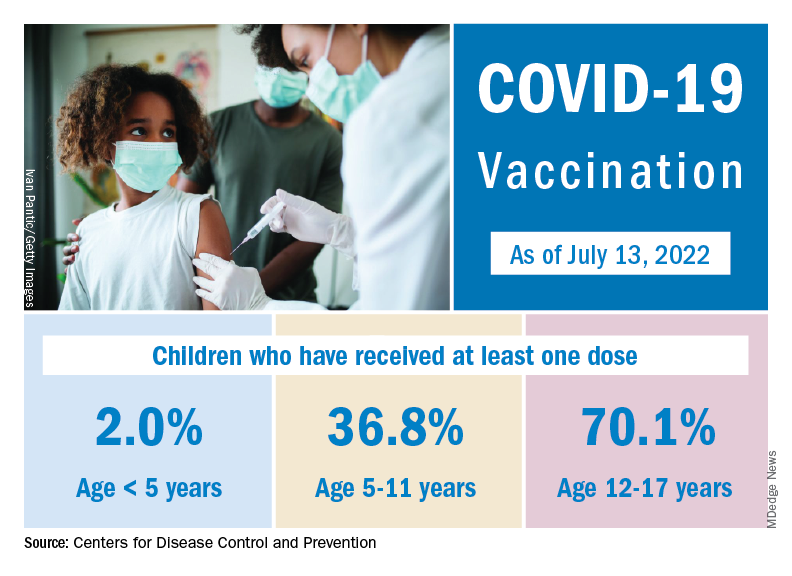
the two groups said, also noting that several states have stopped updating their online dashboards over the past year, making the current total artificially low in comparison.
Taken with that grain of salt, the cumulative number of child cases since the start of the pandemic is just over 13.9 million, which represents 18.6% of all cases in the United States. That proportion has been declining in recent weeks and was as high as 19.0% as late as mid-May. “While COVID-19 cases are likely increasingly underreported for all age groups, this decline indicates that children are disproportionately undercounted in reported COVID-19 cases,” the AAP and CHA said.
New COVID-19 cases rose for the second time in 3 weeks, as the effort to vaccinate the youngest children continued to slow after just 3 full weeks.
Nationally, over 75,000 children under age 5 years received their first dose of COVID-19 vaccine during the week of July 7-13. That number is down from the previous week – 118,000 from June 30 to July 6 – which, in turn, was lower than the 206,000 doses administered through the first 10 days after approval, based on data from the Centers for Disease Control and Prevention. That all adds up to just under 400,000 vaccinated children, or 2% of the eligible population under age 5, as of July 13.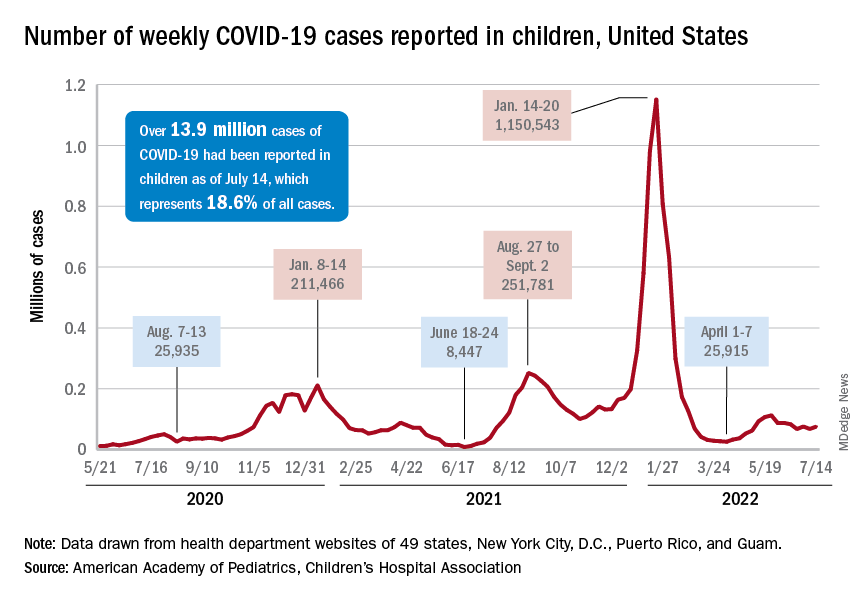
State-level data, meanwhile, show considerable variation, the American Academy of Pediatrics noted in its weekly analysis of the CDC vaccine data. Vermont has already vaccinated 10.0% of children under age 5 years, and Massachusetts is at 9.5%, while Mississippi (0.3%), Alabama (0.5%), and Louisiana (0.8%) are still below 1%, the AAP said.
New cases show signs of steadying
The national count was up by 11.1% for the week of July 8-14, rising to 75,000 new cases, compared with 68,000 the previous week, but the recent trend seems to be leaning toward steadiness. The overall number has been between 67,000 and 76,000 over the past 4 weeks, alternating between rising and falling in that time span, according to data gathered by the AAP and the Children’s Hospital Association from state and territorial health departments.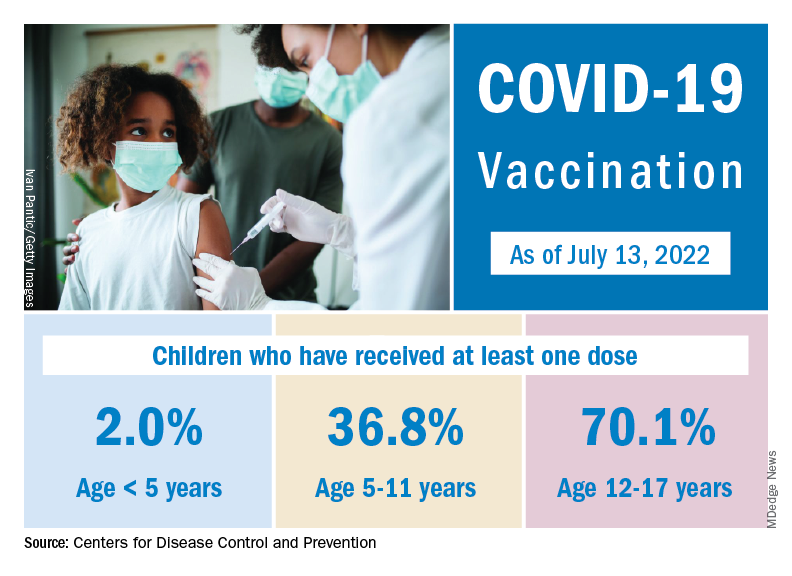
the two groups said, also noting that several states have stopped updating their online dashboards over the past year, making the current total artificially low in comparison.
Taken with that grain of salt, the cumulative number of child cases since the start of the pandemic is just over 13.9 million, which represents 18.6% of all cases in the United States. That proportion has been declining in recent weeks and was as high as 19.0% as late as mid-May. “While COVID-19 cases are likely increasingly underreported for all age groups, this decline indicates that children are disproportionately undercounted in reported COVID-19 cases,” the AAP and CHA said.











