User login
In some states, voters will get to decide the future of abortion rights
As states grapple with the future of abortion in the United States, Michigan, California, and Vermont could become the first states to let voters decide whether the right to abortion should be written into the state constitution.
In Michigan, a proposed constitutional amendment would override a 90-year-old state law that makes abortion a felony even in cases of rape or incest. The U.S. Supreme Court’s overturning of Roe v. Wade could revive that abortion ban – and has galvanized abortion-rights advocates to secure new protections.
Some of the momentum is coming from activists getting involved for the first time.
“I wanted to do something, but I had no political experience or really any experience in activism,” said Amanda Mazur, who lives in rural northwestern Michigan. “But I thought, ‘Maybe I can volunteer and just offer something tangible to the movement.’”
Michigan organizers like Ms. Mazur submitted more than 750,000 signatures – a record number, they said – to state election officials in hopes of having the amendment appear on the November ballot.
If just over half those signatures are validated, Michigan voters will decide whether to amend the state’s constitution to guarantee broad individual rights to “reproductive freedom” that would cover abortion, contraception, and fertility treatments. It would also prevent the state from regulating abortions later in pregnancy if the patient’s “physical or mental health” is at risk.
The ballot initiative has the backing of medical groups like the American College of Obstetricians and Gynecologists, while conservative groups have called it radical and dangerous, claiming it would “allow late-term abortions for practically any reason.”
In California, the push to expand abortion access starts from a very different vantage point: The right to abortion is protected in state statute. And voters will be asked whether they want to enshrine it in the constitution. Proposition 1, which will be on the ballot in November, would prohibit the state from interfering with Californians’ reproductive health decisions, including those related to abortion or contraception.
“I want to know for sure that that right is protected,” state Sen. Toni Atkins (D-Calif.), the Democratic leader in the Senate and lead author of the amendment, said at a legislative hearing in June. “We are protecting ourselves from future courts and future politicians.”
The amendment is one strategy that several California lawmakers are pursuing to protect abortion access in the state. Gov. Gavin Newsom, a Democrat, has signed legislation to eliminate out-of-pocket expenses for abortion for most Californians and to protect California providers that offer abortion services from lawsuits in other states. The recent state budget deal also includes $200 million for reproductive and abortion care.
Earlier in July, Vermont Gov. Phil Scott, a Republican, announced that Proposal 5 will be on the November ballot. He said in a statement: “In Vermont, we solidified the right to choose in law, and now Vermonters have the opportunity to further protect that right in our constitution.”
For Ms. Mazur, the desire to “do something” started in 2017, when she and her husband gave their daughter, then 2 years old, some happy news: She was going to be a big sister. The family was thrilled.
But then doctors told Ms. Mazur something was wrong.
“I found out halfway through the pregnancy that the baby my husband and I hoped for suffered from a rare and life-limiting genetic condition,” Ms. Mazur said. “We ultimately made the compassionate choice to end the pregnancy for my well-being, and for the well-being of our family, and the life of what we thought would be our child.”
Devastated, Ms. Mazur turned to a national online support group and met people having similar experiences. But many group members said they were having a tough time finding a way to terminate their pregnancies.
“It really broke my heart that you’re going through this already devastating experience but have to travel far away from your home across the country ... [and] advocate for yourself like crazy just to get care that you have decided with your doctor is best for you,” Ms. Mazur said.
At the time, abortion rights in Michigan seemed pretty stable, but Ms. Mazur’s political awakening found an outlet this year.
Reproductive Freedom for All, a petition group backed by the American Civil Liberties Union of Michigan and Planned Parenthood Advocates of Michigan, was gathering signatures for the constitutional amendment to enshrine abortion protections in state law. The effort took on new urgency in May after a draft of the Supreme Court’s decision in Dobbs v. Jackson Women’s Health Organization was leaked and then published.
“Folks realized that this big, scary thing that they did not think would happen might actually happen,” said Jessica Ayoub, a field organizer with the ACLU of Michigan.
Some Michiganders were registering to vote just to be eligible to sign the petition. Jaynie Hoerauf, a 62-year-old attorney in Farwell, drove 40 miles to attend a rally where she knew she could sign it.
“A bunch of us were so ticked off [about Roe being overturned], and we were talking about it. And I was like, ‘I’m just going to go on and find where I can sign the stupid petition,’” Ms. Hoerauf said.
Activists on both sides of the abortion-rights debate expect to spend millions of dollars. They predict that donations will pour in from outside Michigan and that voters in other states will be watching.
“This is just the start of our fight,” Ms. Ayoub said. “We know that it is a long road to November.”
KHN correspondent Rachel Bluth contributed to this report. This story is part of a partnership that includes Michigan Radio, NPR, and KHN. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
As states grapple with the future of abortion in the United States, Michigan, California, and Vermont could become the first states to let voters decide whether the right to abortion should be written into the state constitution.
In Michigan, a proposed constitutional amendment would override a 90-year-old state law that makes abortion a felony even in cases of rape or incest. The U.S. Supreme Court’s overturning of Roe v. Wade could revive that abortion ban – and has galvanized abortion-rights advocates to secure new protections.
Some of the momentum is coming from activists getting involved for the first time.
“I wanted to do something, but I had no political experience or really any experience in activism,” said Amanda Mazur, who lives in rural northwestern Michigan. “But I thought, ‘Maybe I can volunteer and just offer something tangible to the movement.’”
Michigan organizers like Ms. Mazur submitted more than 750,000 signatures – a record number, they said – to state election officials in hopes of having the amendment appear on the November ballot.
If just over half those signatures are validated, Michigan voters will decide whether to amend the state’s constitution to guarantee broad individual rights to “reproductive freedom” that would cover abortion, contraception, and fertility treatments. It would also prevent the state from regulating abortions later in pregnancy if the patient’s “physical or mental health” is at risk.
The ballot initiative has the backing of medical groups like the American College of Obstetricians and Gynecologists, while conservative groups have called it radical and dangerous, claiming it would “allow late-term abortions for practically any reason.”
In California, the push to expand abortion access starts from a very different vantage point: The right to abortion is protected in state statute. And voters will be asked whether they want to enshrine it in the constitution. Proposition 1, which will be on the ballot in November, would prohibit the state from interfering with Californians’ reproductive health decisions, including those related to abortion or contraception.
“I want to know for sure that that right is protected,” state Sen. Toni Atkins (D-Calif.), the Democratic leader in the Senate and lead author of the amendment, said at a legislative hearing in June. “We are protecting ourselves from future courts and future politicians.”
The amendment is one strategy that several California lawmakers are pursuing to protect abortion access in the state. Gov. Gavin Newsom, a Democrat, has signed legislation to eliminate out-of-pocket expenses for abortion for most Californians and to protect California providers that offer abortion services from lawsuits in other states. The recent state budget deal also includes $200 million for reproductive and abortion care.
Earlier in July, Vermont Gov. Phil Scott, a Republican, announced that Proposal 5 will be on the November ballot. He said in a statement: “In Vermont, we solidified the right to choose in law, and now Vermonters have the opportunity to further protect that right in our constitution.”
For Ms. Mazur, the desire to “do something” started in 2017, when she and her husband gave their daughter, then 2 years old, some happy news: She was going to be a big sister. The family was thrilled.
But then doctors told Ms. Mazur something was wrong.
“I found out halfway through the pregnancy that the baby my husband and I hoped for suffered from a rare and life-limiting genetic condition,” Ms. Mazur said. “We ultimately made the compassionate choice to end the pregnancy for my well-being, and for the well-being of our family, and the life of what we thought would be our child.”
Devastated, Ms. Mazur turned to a national online support group and met people having similar experiences. But many group members said they were having a tough time finding a way to terminate their pregnancies.
“It really broke my heart that you’re going through this already devastating experience but have to travel far away from your home across the country ... [and] advocate for yourself like crazy just to get care that you have decided with your doctor is best for you,” Ms. Mazur said.
At the time, abortion rights in Michigan seemed pretty stable, but Ms. Mazur’s political awakening found an outlet this year.
Reproductive Freedom for All, a petition group backed by the American Civil Liberties Union of Michigan and Planned Parenthood Advocates of Michigan, was gathering signatures for the constitutional amendment to enshrine abortion protections in state law. The effort took on new urgency in May after a draft of the Supreme Court’s decision in Dobbs v. Jackson Women’s Health Organization was leaked and then published.
“Folks realized that this big, scary thing that they did not think would happen might actually happen,” said Jessica Ayoub, a field organizer with the ACLU of Michigan.
Some Michiganders were registering to vote just to be eligible to sign the petition. Jaynie Hoerauf, a 62-year-old attorney in Farwell, drove 40 miles to attend a rally where she knew she could sign it.
“A bunch of us were so ticked off [about Roe being overturned], and we were talking about it. And I was like, ‘I’m just going to go on and find where I can sign the stupid petition,’” Ms. Hoerauf said.
Activists on both sides of the abortion-rights debate expect to spend millions of dollars. They predict that donations will pour in from outside Michigan and that voters in other states will be watching.
“This is just the start of our fight,” Ms. Ayoub said. “We know that it is a long road to November.”
KHN correspondent Rachel Bluth contributed to this report. This story is part of a partnership that includes Michigan Radio, NPR, and KHN. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
As states grapple with the future of abortion in the United States, Michigan, California, and Vermont could become the first states to let voters decide whether the right to abortion should be written into the state constitution.
In Michigan, a proposed constitutional amendment would override a 90-year-old state law that makes abortion a felony even in cases of rape or incest. The U.S. Supreme Court’s overturning of Roe v. Wade could revive that abortion ban – and has galvanized abortion-rights advocates to secure new protections.
Some of the momentum is coming from activists getting involved for the first time.
“I wanted to do something, but I had no political experience or really any experience in activism,” said Amanda Mazur, who lives in rural northwestern Michigan. “But I thought, ‘Maybe I can volunteer and just offer something tangible to the movement.’”
Michigan organizers like Ms. Mazur submitted more than 750,000 signatures – a record number, they said – to state election officials in hopes of having the amendment appear on the November ballot.
If just over half those signatures are validated, Michigan voters will decide whether to amend the state’s constitution to guarantee broad individual rights to “reproductive freedom” that would cover abortion, contraception, and fertility treatments. It would also prevent the state from regulating abortions later in pregnancy if the patient’s “physical or mental health” is at risk.
The ballot initiative has the backing of medical groups like the American College of Obstetricians and Gynecologists, while conservative groups have called it radical and dangerous, claiming it would “allow late-term abortions for practically any reason.”
In California, the push to expand abortion access starts from a very different vantage point: The right to abortion is protected in state statute. And voters will be asked whether they want to enshrine it in the constitution. Proposition 1, which will be on the ballot in November, would prohibit the state from interfering with Californians’ reproductive health decisions, including those related to abortion or contraception.
“I want to know for sure that that right is protected,” state Sen. Toni Atkins (D-Calif.), the Democratic leader in the Senate and lead author of the amendment, said at a legislative hearing in June. “We are protecting ourselves from future courts and future politicians.”
The amendment is one strategy that several California lawmakers are pursuing to protect abortion access in the state. Gov. Gavin Newsom, a Democrat, has signed legislation to eliminate out-of-pocket expenses for abortion for most Californians and to protect California providers that offer abortion services from lawsuits in other states. The recent state budget deal also includes $200 million for reproductive and abortion care.
Earlier in July, Vermont Gov. Phil Scott, a Republican, announced that Proposal 5 will be on the November ballot. He said in a statement: “In Vermont, we solidified the right to choose in law, and now Vermonters have the opportunity to further protect that right in our constitution.”
For Ms. Mazur, the desire to “do something” started in 2017, when she and her husband gave their daughter, then 2 years old, some happy news: She was going to be a big sister. The family was thrilled.
But then doctors told Ms. Mazur something was wrong.
“I found out halfway through the pregnancy that the baby my husband and I hoped for suffered from a rare and life-limiting genetic condition,” Ms. Mazur said. “We ultimately made the compassionate choice to end the pregnancy for my well-being, and for the well-being of our family, and the life of what we thought would be our child.”
Devastated, Ms. Mazur turned to a national online support group and met people having similar experiences. But many group members said they were having a tough time finding a way to terminate their pregnancies.
“It really broke my heart that you’re going through this already devastating experience but have to travel far away from your home across the country ... [and] advocate for yourself like crazy just to get care that you have decided with your doctor is best for you,” Ms. Mazur said.
At the time, abortion rights in Michigan seemed pretty stable, but Ms. Mazur’s political awakening found an outlet this year.
Reproductive Freedom for All, a petition group backed by the American Civil Liberties Union of Michigan and Planned Parenthood Advocates of Michigan, was gathering signatures for the constitutional amendment to enshrine abortion protections in state law. The effort took on new urgency in May after a draft of the Supreme Court’s decision in Dobbs v. Jackson Women’s Health Organization was leaked and then published.
“Folks realized that this big, scary thing that they did not think would happen might actually happen,” said Jessica Ayoub, a field organizer with the ACLU of Michigan.
Some Michiganders were registering to vote just to be eligible to sign the petition. Jaynie Hoerauf, a 62-year-old attorney in Farwell, drove 40 miles to attend a rally where she knew she could sign it.
“A bunch of us were so ticked off [about Roe being overturned], and we were talking about it. And I was like, ‘I’m just going to go on and find where I can sign the stupid petition,’” Ms. Hoerauf said.
Activists on both sides of the abortion-rights debate expect to spend millions of dollars. They predict that donations will pour in from outside Michigan and that voters in other states will be watching.
“This is just the start of our fight,” Ms. Ayoub said. “We know that it is a long road to November.”
KHN correspondent Rachel Bluth contributed to this report. This story is part of a partnership that includes Michigan Radio, NPR, and KHN. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Focal Palmoplantar Keratoderma and Gingival Keratosis Caused by a KRT16 Mutation
To the Editor:
Focal palmoplantar keratoderma and gingival keratosis (FPGK)(Online Mendelian Inheritance in Man [OMIM] 148730) is a rare autosomal-dominant syndrome featuring focal, pressure-related, painful palmoplantar keratoderma and gingival hyperkeratosis presenting as leukokeratosis. Focal palmoplantar keratoderma and gingival keratosis was first defined by Gorlin1 in 1976. Since then, only a few cases have been reported, but no causative mutations have been identified.2
Focal pressure-related palmoplantar keratoderma (PPK) and oral hyperkeratosis also are seen in pachyonychia congenita (PC)(OMIM 167200, 615726, 615728, 167210), a rare autosomal-dominant disorder of keratinization characterized by PPK and nail dystrophy. Patients with PC often present with plantar pain; more variable features include oral leukokeratosis, follicular hyperkeratosis, pilosebaceous and epidermal inclusion cysts, hoarseness, hyperhidrosis, and natal teeth. Pachyonychia congenita is caused by mutation in keratin genes KRT6A, KRT6B, KRT16, or KRT17.
Focal palmoplantar keratoderma and gingival keratosis as well as PC are distinct from other forms of PPK with gingival involvement such as
Despite the common features of FPGK and PC, they are considered distinct disorders due to absence of nail changes in FPGK and no prior evidence of a common genetic cause. We present a patient with familial FPGK found by whole exome sequencing to be caused by a mutation in KRT16.
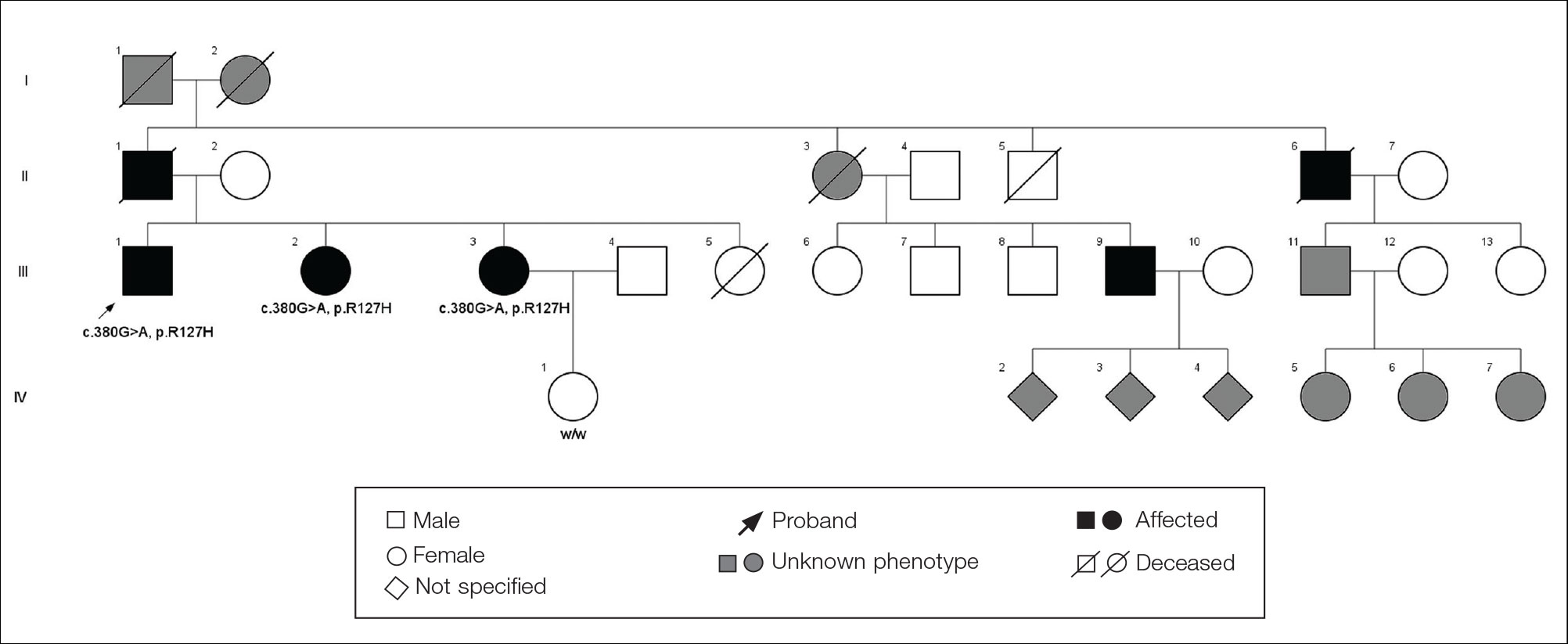
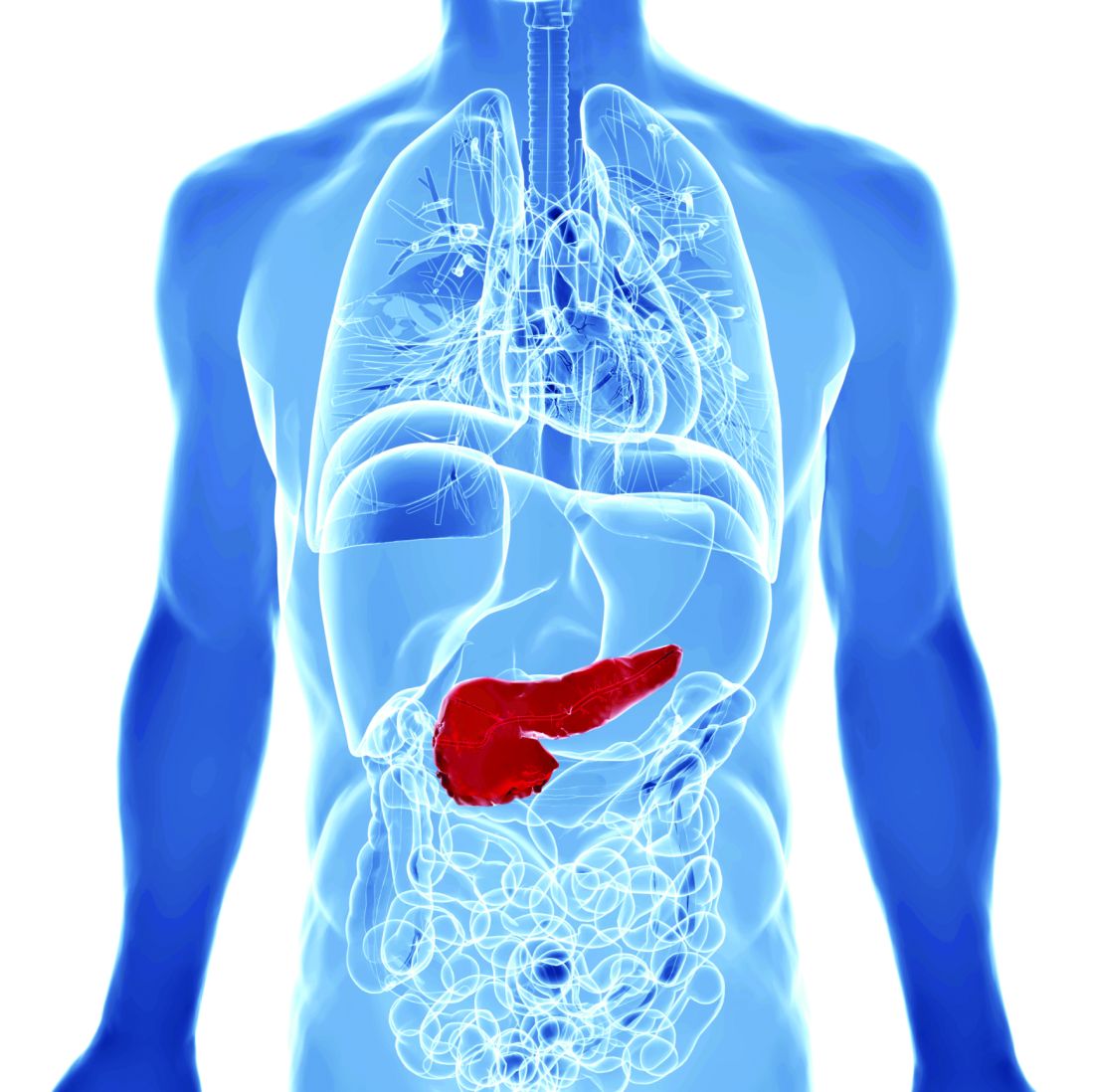
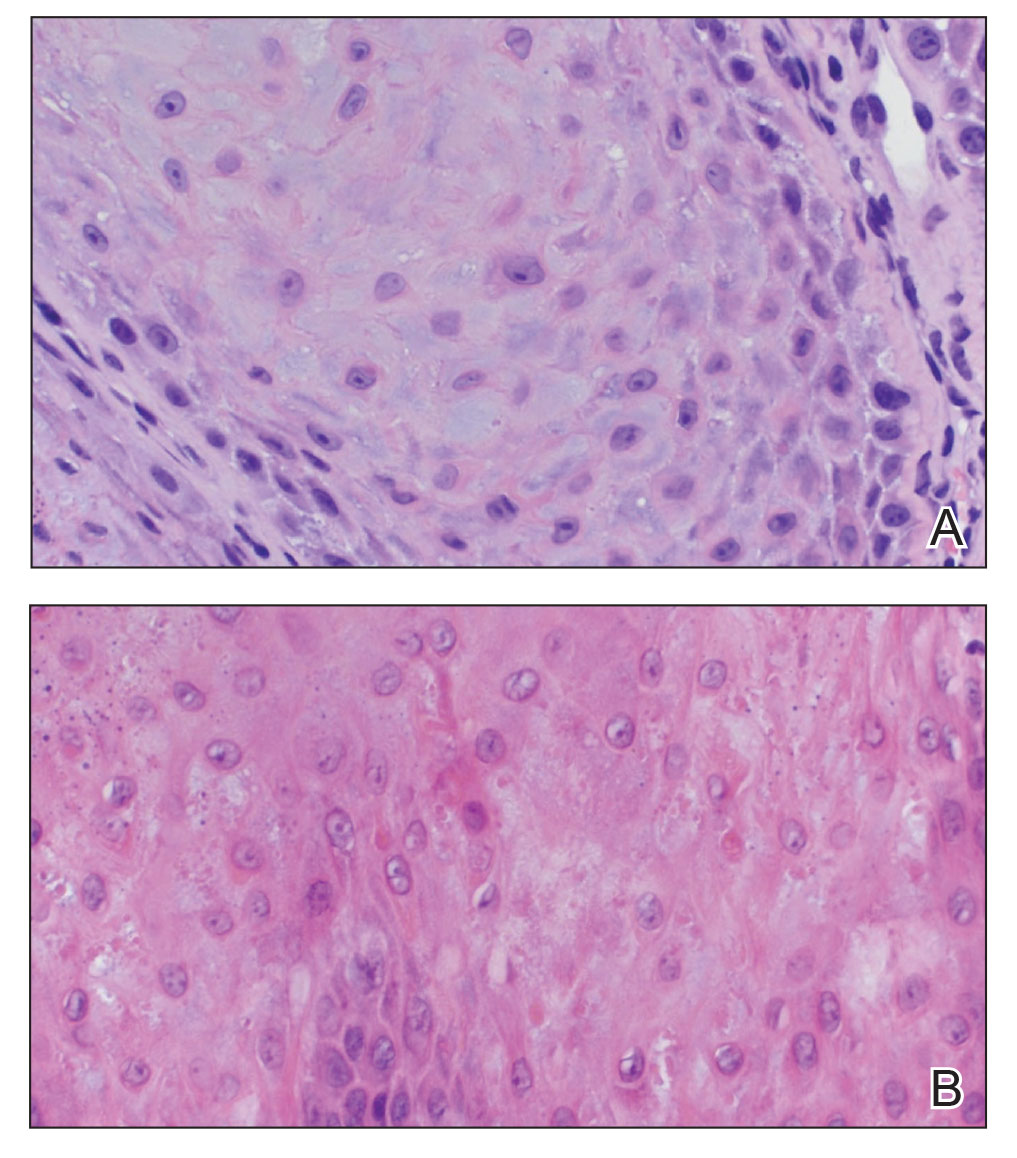
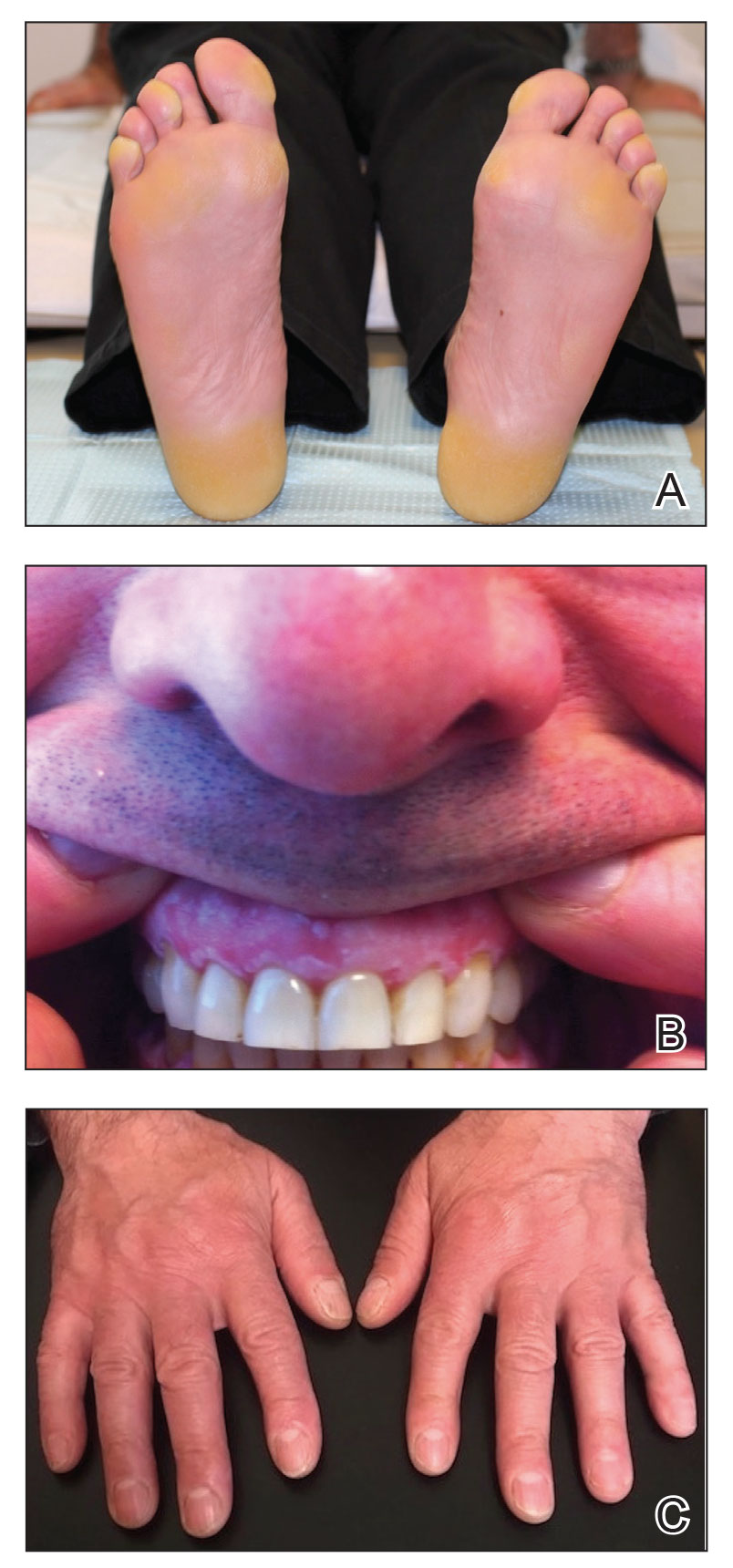
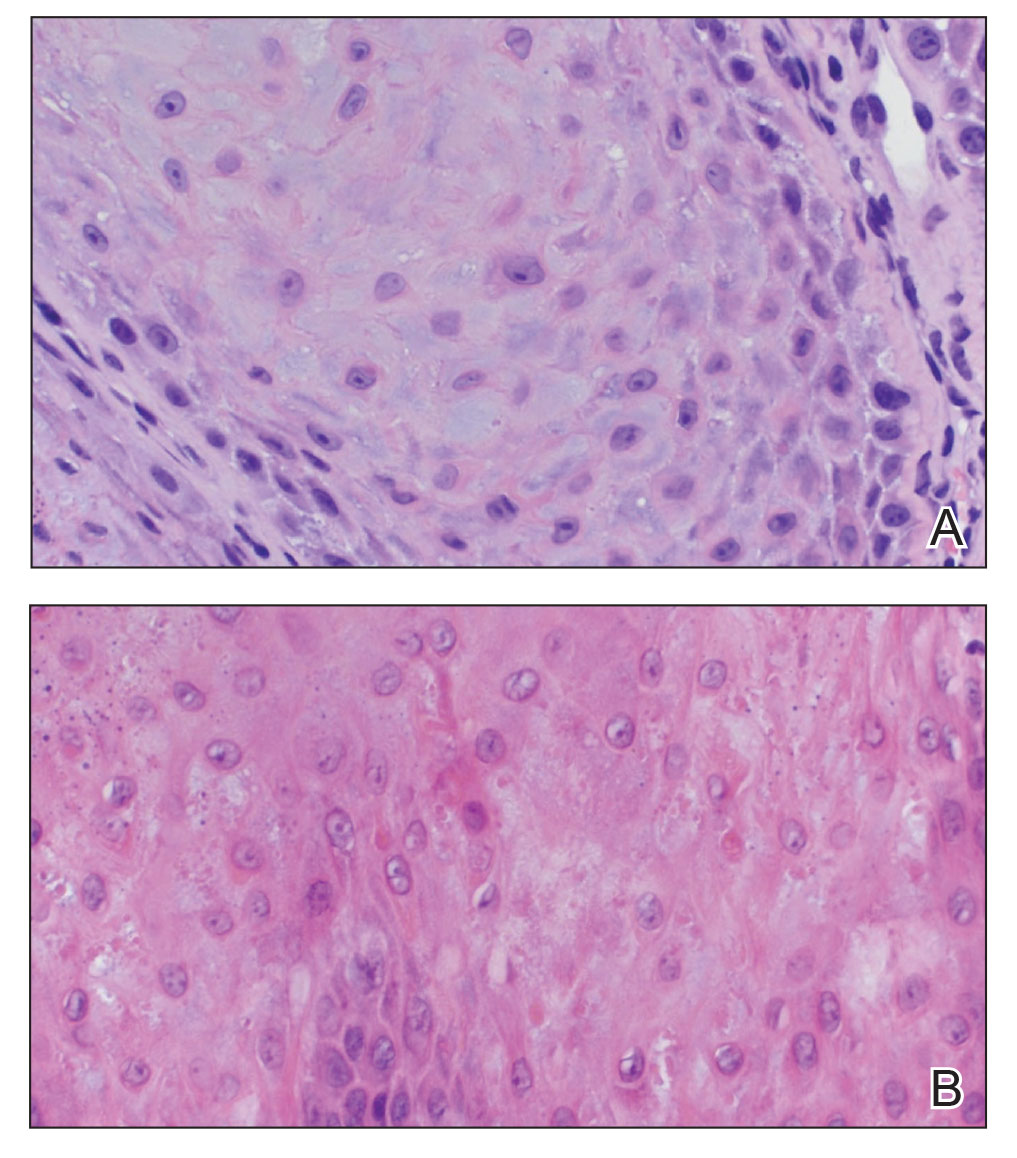
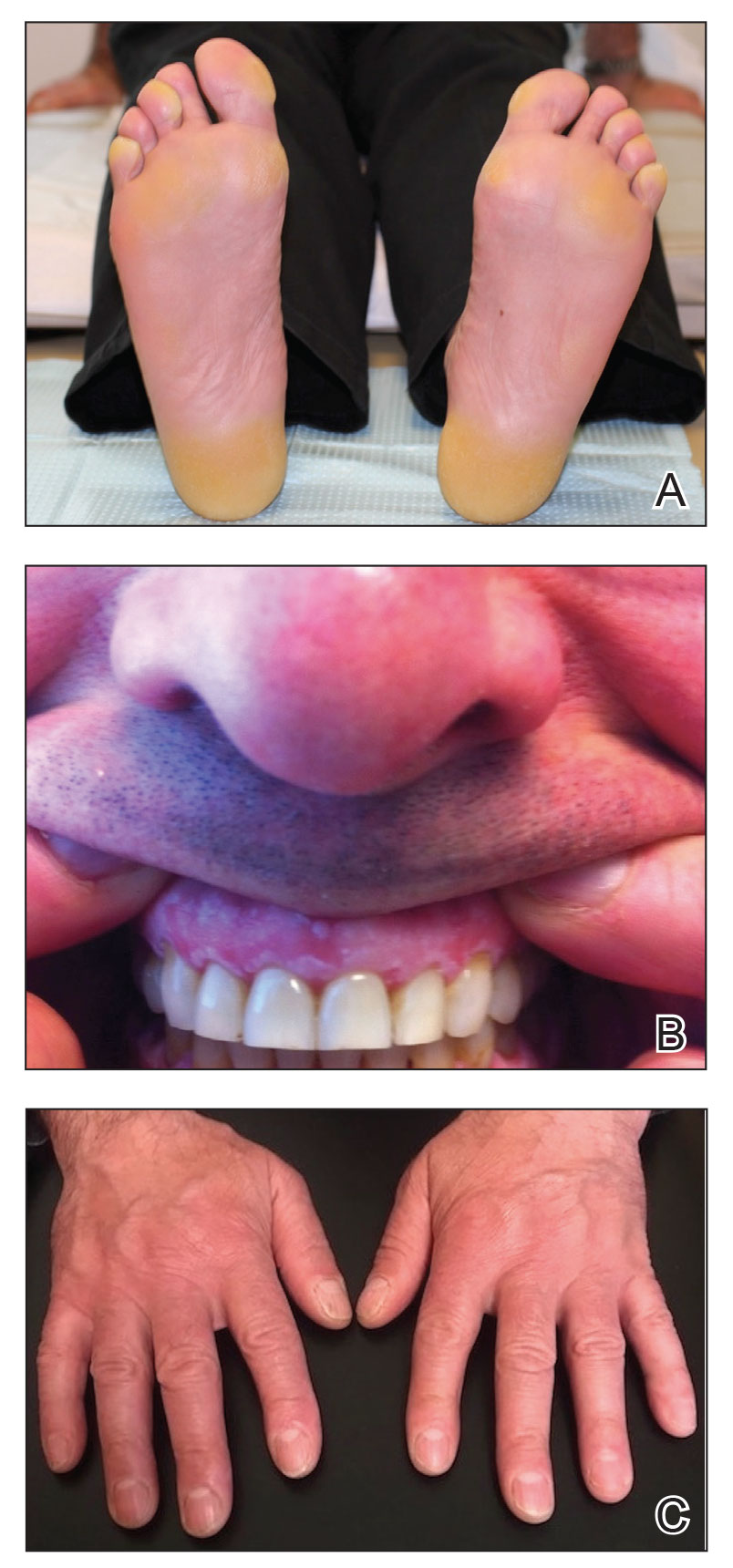
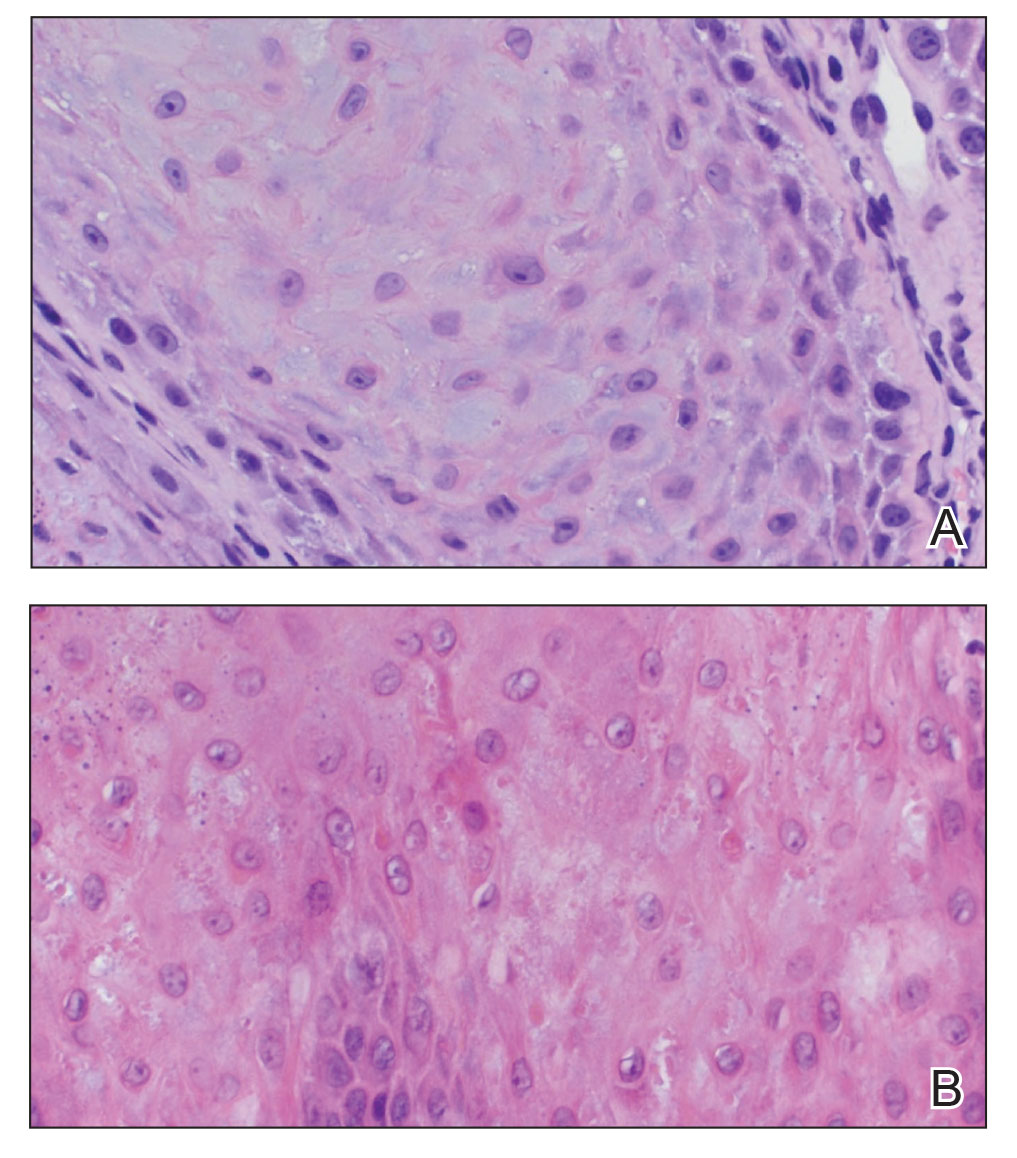
The proband was a 57-year-old man born to unrelated parents (Figure 1). He had no skin problems at birth, and his development was normal. He had painful focal keratoderma since childhood that were most prominent at pressure points on the soles and toes (Figure 2A), in addition to gingival hyperkeratosis and oral leukokeratosis (Figure 2B). He had no associated abnormalities of the skin, hair, or teeth and no nail findings (Figure 2C). He reported that his father and 2 of his 3 sisters were affected with similar symptoms. A punch biopsy of the right fifth toe was consistent with verrucous epidermal hyperplasia with perinuclear keratinization in the spinous layer (Figure 3A). A gingival biopsy showed perinuclear eosinophilic globules and basophilic stranding in the cytoplasm (Figure 3B). His older sister had more severe and painful focal keratoderma of the soles, punctate keratoderma of the palms, gingival hyperkeratosis, and leukokeratosis of the tongue.
Whole exome sequencing of the proband revealed a heterozygous missense mutation in KRT16 (c.380G>A, p.R127H, rs57424749). Sanger sequencing confirmed this mutation and showed that it was heterozygous in both of his affected sisters and absent in his unaffected niece (Figure 1). The patient was treated with topical and systemic retinoids, keratolytics, and mechanical removal to moderate effect, with noted improvement in the appearance and associated pain of the plantar keratoderma.
Phenotypic heterogeneity is common in PC, though PC due to KRT6A mutations demonstrates more severe nail disease with oral lesions, cysts, and follicular hyperkeratosis, while PC caused by KRT16 mutations generally presents with more extensive and painful PPK.4KRT16 mutations affecting p.R127 are frequent causes of PC, and genotype-phenotype correlations have been observed. Individuals with p.R127P mutations exhibit more severe disease with earlier age of onset, more extensive nail involvement and oral leukokeratosis, and greater impact on daily quality of life than in individuals with p.R127C mutations.5 Cases of PC with KRT16 p.R127S and p.R127G mutations also have been observed. The KRT16 c.380G>A, p.R127H mutation we documented has been reported in one kindred with PC who presented with PPK, oral leukokeratosis, toenail thickening, and pilosebaceous and follicular hyperkeratosis.6
Although patients with FPGK lack the thickening of fingernails and/or toenails considered a defining feature of PC, the disorders otherwise are phenotypically similar, suggesting the possibility of common pathogenesis. One linkage study of familial FPGK excluded genetic intervals containing type I and type II keratins but was limited to a single small kindred.2 This study and our data together suggest that, similar to PC, there are multiple genes in which mutations cause FPGK.
Murine Krt16 knockouts show distinct phenotypes depending on the mouse strain in which they are propagated, ranging from perinatal lethality to differences in the severity of oral and PPK lesions.7 These observations provide evidence that additional genetic variants contribute to Krt16 phenotypes in mice and suggest the same could be true for humans.
We propose that some cases of FPGK are due to mutations in KRT16 and thus share a genetic pathogenesis with PC, underscoring the utility of whole exome sequencing in providing genetic diagnoses for disorders that are genetically and clinically heterogeneous. Further biologic investigation of phenotypes caused by KRT16 mutation may reveal respective contributions of additional genetic variation and environmental effects to the variable clinical presentations.
- Gorlin RJ. Focal palmoplantar and marginal gingival hyperkeratosis—a syndrome. Birth Defects Orig Artic Ser. 1976;12:239-242.
- Kolde G, Hennies HC, Bethke G, et al. Focal palmoplantar and gingival keratosis: a distinct palmoplantar ectodermal dysplasia with epidermolytic alterations but lack of mutations in known keratins. J Am Acad Dermatol. 2005;52(3 pt 1):403-409.
- Duchatelet S, Hovnanian A. Olmsted syndrome: clinical, molecular and therapeutic aspects. Orphanet J Rare Dis. 2015;10:33.
- Spaunhurst KM, Hogendorf AM, Smith FJ, et al. Pachyonychia congenita patients with mutations in KRT6A have more extensive disease compared with patients who have mutations in KRT16. Br J Dermatol. 2012;166:875-878.
- Fu T, Leachman SA, Wilson NJ, et al. Genotype-phenotype correlations among pachyonychia congenita patients with K16 mutations. J Invest Dermatol. 2011;131:1025-1028.
- Wilson NJ, O’Toole EA, Milstone LM, et al. The molecular genetic analysis of the expanding pachyonychia congenita case collection. Br J Dermatol. 2014;171:343-355.
- Zieman A, Coulombe PA. The keratin 16 null phenotype is modestly impacted by genetic strain background in mice. Exp Dermatol. 2018;27:672-674.
To the Editor:
Focal palmoplantar keratoderma and gingival keratosis (FPGK)(Online Mendelian Inheritance in Man [OMIM] 148730) is a rare autosomal-dominant syndrome featuring focal, pressure-related, painful palmoplantar keratoderma and gingival hyperkeratosis presenting as leukokeratosis. Focal palmoplantar keratoderma and gingival keratosis was first defined by Gorlin1 in 1976. Since then, only a few cases have been reported, but no causative mutations have been identified.2
Focal pressure-related palmoplantar keratoderma (PPK) and oral hyperkeratosis also are seen in pachyonychia congenita (PC)(OMIM 167200, 615726, 615728, 167210), a rare autosomal-dominant disorder of keratinization characterized by PPK and nail dystrophy. Patients with PC often present with plantar pain; more variable features include oral leukokeratosis, follicular hyperkeratosis, pilosebaceous and epidermal inclusion cysts, hoarseness, hyperhidrosis, and natal teeth. Pachyonychia congenita is caused by mutation in keratin genes KRT6A, KRT6B, KRT16, or KRT17.
Focal palmoplantar keratoderma and gingival keratosis as well as PC are distinct from other forms of PPK with gingival involvement such as
Despite the common features of FPGK and PC, they are considered distinct disorders due to absence of nail changes in FPGK and no prior evidence of a common genetic cause. We present a patient with familial FPGK found by whole exome sequencing to be caused by a mutation in KRT16.
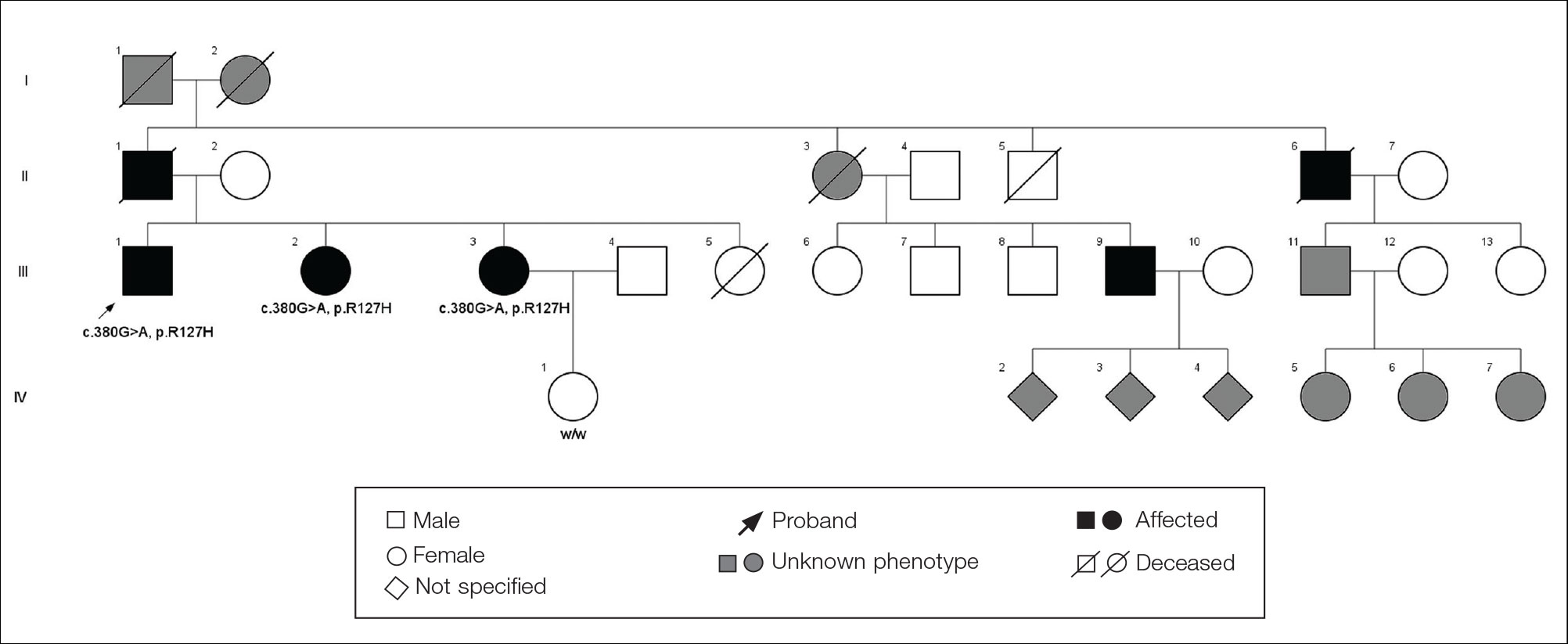
The proband was a 57-year-old man born to unrelated parents (Figure 1). He had no skin problems at birth, and his development was normal. He had painful focal keratoderma since childhood that were most prominent at pressure points on the soles and toes (Figure 2A), in addition to gingival hyperkeratosis and oral leukokeratosis (Figure 2B). He had no associated abnormalities of the skin, hair, or teeth and no nail findings (Figure 2C). He reported that his father and 2 of his 3 sisters were affected with similar symptoms. A punch biopsy of the right fifth toe was consistent with verrucous epidermal hyperplasia with perinuclear keratinization in the spinous layer (Figure 3A). A gingival biopsy showed perinuclear eosinophilic globules and basophilic stranding in the cytoplasm (Figure 3B). His older sister had more severe and painful focal keratoderma of the soles, punctate keratoderma of the palms, gingival hyperkeratosis, and leukokeratosis of the tongue.
Whole exome sequencing of the proband revealed a heterozygous missense mutation in KRT16 (c.380G>A, p.R127H, rs57424749). Sanger sequencing confirmed this mutation and showed that it was heterozygous in both of his affected sisters and absent in his unaffected niece (Figure 1). The patient was treated with topical and systemic retinoids, keratolytics, and mechanical removal to moderate effect, with noted improvement in the appearance and associated pain of the plantar keratoderma.
Phenotypic heterogeneity is common in PC, though PC due to KRT6A mutations demonstrates more severe nail disease with oral lesions, cysts, and follicular hyperkeratosis, while PC caused by KRT16 mutations generally presents with more extensive and painful PPK.4KRT16 mutations affecting p.R127 are frequent causes of PC, and genotype-phenotype correlations have been observed. Individuals with p.R127P mutations exhibit more severe disease with earlier age of onset, more extensive nail involvement and oral leukokeratosis, and greater impact on daily quality of life than in individuals with p.R127C mutations.5 Cases of PC with KRT16 p.R127S and p.R127G mutations also have been observed. The KRT16 c.380G>A, p.R127H mutation we documented has been reported in one kindred with PC who presented with PPK, oral leukokeratosis, toenail thickening, and pilosebaceous and follicular hyperkeratosis.6
Although patients with FPGK lack the thickening of fingernails and/or toenails considered a defining feature of PC, the disorders otherwise are phenotypically similar, suggesting the possibility of common pathogenesis. One linkage study of familial FPGK excluded genetic intervals containing type I and type II keratins but was limited to a single small kindred.2 This study and our data together suggest that, similar to PC, there are multiple genes in which mutations cause FPGK.
Murine Krt16 knockouts show distinct phenotypes depending on the mouse strain in which they are propagated, ranging from perinatal lethality to differences in the severity of oral and PPK lesions.7 These observations provide evidence that additional genetic variants contribute to Krt16 phenotypes in mice and suggest the same could be true for humans.
We propose that some cases of FPGK are due to mutations in KRT16 and thus share a genetic pathogenesis with PC, underscoring the utility of whole exome sequencing in providing genetic diagnoses for disorders that are genetically and clinically heterogeneous. Further biologic investigation of phenotypes caused by KRT16 mutation may reveal respective contributions of additional genetic variation and environmental effects to the variable clinical presentations.
To the Editor:
Focal palmoplantar keratoderma and gingival keratosis (FPGK)(Online Mendelian Inheritance in Man [OMIM] 148730) is a rare autosomal-dominant syndrome featuring focal, pressure-related, painful palmoplantar keratoderma and gingival hyperkeratosis presenting as leukokeratosis. Focal palmoplantar keratoderma and gingival keratosis was first defined by Gorlin1 in 1976. Since then, only a few cases have been reported, but no causative mutations have been identified.2
Focal pressure-related palmoplantar keratoderma (PPK) and oral hyperkeratosis also are seen in pachyonychia congenita (PC)(OMIM 167200, 615726, 615728, 167210), a rare autosomal-dominant disorder of keratinization characterized by PPK and nail dystrophy. Patients with PC often present with plantar pain; more variable features include oral leukokeratosis, follicular hyperkeratosis, pilosebaceous and epidermal inclusion cysts, hoarseness, hyperhidrosis, and natal teeth. Pachyonychia congenita is caused by mutation in keratin genes KRT6A, KRT6B, KRT16, or KRT17.
Focal palmoplantar keratoderma and gingival keratosis as well as PC are distinct from other forms of PPK with gingival involvement such as
Despite the common features of FPGK and PC, they are considered distinct disorders due to absence of nail changes in FPGK and no prior evidence of a common genetic cause. We present a patient with familial FPGK found by whole exome sequencing to be caused by a mutation in KRT16.
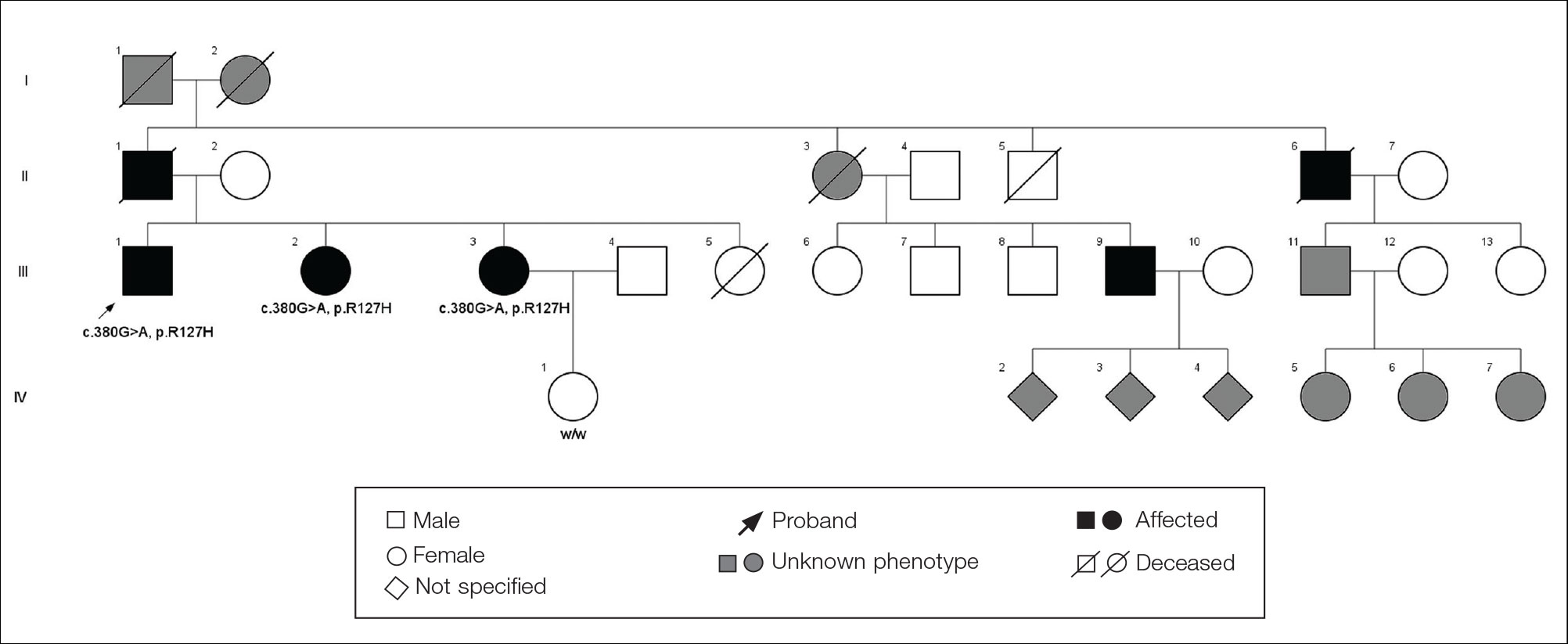
The proband was a 57-year-old man born to unrelated parents (Figure 1). He had no skin problems at birth, and his development was normal. He had painful focal keratoderma since childhood that were most prominent at pressure points on the soles and toes (Figure 2A), in addition to gingival hyperkeratosis and oral leukokeratosis (Figure 2B). He had no associated abnormalities of the skin, hair, or teeth and no nail findings (Figure 2C). He reported that his father and 2 of his 3 sisters were affected with similar symptoms. A punch biopsy of the right fifth toe was consistent with verrucous epidermal hyperplasia with perinuclear keratinization in the spinous layer (Figure 3A). A gingival biopsy showed perinuclear eosinophilic globules and basophilic stranding in the cytoplasm (Figure 3B). His older sister had more severe and painful focal keratoderma of the soles, punctate keratoderma of the palms, gingival hyperkeratosis, and leukokeratosis of the tongue.
Whole exome sequencing of the proband revealed a heterozygous missense mutation in KRT16 (c.380G>A, p.R127H, rs57424749). Sanger sequencing confirmed this mutation and showed that it was heterozygous in both of his affected sisters and absent in his unaffected niece (Figure 1). The patient was treated with topical and systemic retinoids, keratolytics, and mechanical removal to moderate effect, with noted improvement in the appearance and associated pain of the plantar keratoderma.
Phenotypic heterogeneity is common in PC, though PC due to KRT6A mutations demonstrates more severe nail disease with oral lesions, cysts, and follicular hyperkeratosis, while PC caused by KRT16 mutations generally presents with more extensive and painful PPK.4KRT16 mutations affecting p.R127 are frequent causes of PC, and genotype-phenotype correlations have been observed. Individuals with p.R127P mutations exhibit more severe disease with earlier age of onset, more extensive nail involvement and oral leukokeratosis, and greater impact on daily quality of life than in individuals with p.R127C mutations.5 Cases of PC with KRT16 p.R127S and p.R127G mutations also have been observed. The KRT16 c.380G>A, p.R127H mutation we documented has been reported in one kindred with PC who presented with PPK, oral leukokeratosis, toenail thickening, and pilosebaceous and follicular hyperkeratosis.6
Although patients with FPGK lack the thickening of fingernails and/or toenails considered a defining feature of PC, the disorders otherwise are phenotypically similar, suggesting the possibility of common pathogenesis. One linkage study of familial FPGK excluded genetic intervals containing type I and type II keratins but was limited to a single small kindred.2 This study and our data together suggest that, similar to PC, there are multiple genes in which mutations cause FPGK.
Murine Krt16 knockouts show distinct phenotypes depending on the mouse strain in which they are propagated, ranging from perinatal lethality to differences in the severity of oral and PPK lesions.7 These observations provide evidence that additional genetic variants contribute to Krt16 phenotypes in mice and suggest the same could be true for humans.
We propose that some cases of FPGK are due to mutations in KRT16 and thus share a genetic pathogenesis with PC, underscoring the utility of whole exome sequencing in providing genetic diagnoses for disorders that are genetically and clinically heterogeneous. Further biologic investigation of phenotypes caused by KRT16 mutation may reveal respective contributions of additional genetic variation and environmental effects to the variable clinical presentations.
- Gorlin RJ. Focal palmoplantar and marginal gingival hyperkeratosis—a syndrome. Birth Defects Orig Artic Ser. 1976;12:239-242.
- Kolde G, Hennies HC, Bethke G, et al. Focal palmoplantar and gingival keratosis: a distinct palmoplantar ectodermal dysplasia with epidermolytic alterations but lack of mutations in known keratins. J Am Acad Dermatol. 2005;52(3 pt 1):403-409.
- Duchatelet S, Hovnanian A. Olmsted syndrome: clinical, molecular and therapeutic aspects. Orphanet J Rare Dis. 2015;10:33.
- Spaunhurst KM, Hogendorf AM, Smith FJ, et al. Pachyonychia congenita patients with mutations in KRT6A have more extensive disease compared with patients who have mutations in KRT16. Br J Dermatol. 2012;166:875-878.
- Fu T, Leachman SA, Wilson NJ, et al. Genotype-phenotype correlations among pachyonychia congenita patients with K16 mutations. J Invest Dermatol. 2011;131:1025-1028.
- Wilson NJ, O’Toole EA, Milstone LM, et al. The molecular genetic analysis of the expanding pachyonychia congenita case collection. Br J Dermatol. 2014;171:343-355.
- Zieman A, Coulombe PA. The keratin 16 null phenotype is modestly impacted by genetic strain background in mice. Exp Dermatol. 2018;27:672-674.
- Gorlin RJ. Focal palmoplantar and marginal gingival hyperkeratosis—a syndrome. Birth Defects Orig Artic Ser. 1976;12:239-242.
- Kolde G, Hennies HC, Bethke G, et al. Focal palmoplantar and gingival keratosis: a distinct palmoplantar ectodermal dysplasia with epidermolytic alterations but lack of mutations in known keratins. J Am Acad Dermatol. 2005;52(3 pt 1):403-409.
- Duchatelet S, Hovnanian A. Olmsted syndrome: clinical, molecular and therapeutic aspects. Orphanet J Rare Dis. 2015;10:33.
- Spaunhurst KM, Hogendorf AM, Smith FJ, et al. Pachyonychia congenita patients with mutations in KRT6A have more extensive disease compared with patients who have mutations in KRT16. Br J Dermatol. 2012;166:875-878.
- Fu T, Leachman SA, Wilson NJ, et al. Genotype-phenotype correlations among pachyonychia congenita patients with K16 mutations. J Invest Dermatol. 2011;131:1025-1028.
- Wilson NJ, O’Toole EA, Milstone LM, et al. The molecular genetic analysis of the expanding pachyonychia congenita case collection. Br J Dermatol. 2014;171:343-355.
- Zieman A, Coulombe PA. The keratin 16 null phenotype is modestly impacted by genetic strain background in mice. Exp Dermatol. 2018;27:672-674.
Practice Points
- Focal palmoplantar keratoderma and gingival keratosis (FPGK) is a rare autosomal-dominant syndrome featuring focal, pressure-related, painful palmoplantar keratoderma (PPK) and gingival hyperkeratosis presenting as leukokeratosis.
- Focal pressure-related PPK and oral hyperkeratosis also are seen in pachyonychia congenita (PC), which is caused by mutations in keratin genes and is distinguished from FPGK by characteristic nail changes.
- A shared causative gene suggests that FPGK should be considered part of the PC spectrum.
Statins linked to lower diabetes risk after acute pancreatitis
Use of cholesterol-lowering statins was linked to a lower risk of developing a subtype of diabetes that occurs after acute pancreatitis, according to a new report.
The benefits of statins depended on the consistency of usage, with regular users having a lower risk of developing postpancreatitis diabetes than irregular users. The results were similar with low, moderate, and high statin doses, as well as in cases of both mild and severe acute pancreatitis.
“About 15% of patients with acute pancreatitis will develop diabetes mellitus in the next 5 years, and although we can monitor for it, we can’t do anything to prevent it,” Nikhil Thiruvengadam, MD, the lead study author and a gastroenterologist at Loma Linda (Calif.) University, told this news organization.
“This could push you as a clinician to prescribe [a statin if you have a reason to] because it could provide two benefits instead of just one,” he said.
The study was published online in Clinical Gastroenterology and Hepatology.
Steady use mattered, not dose
Patients with acute pancreatitis face at least a twofold increased risk of developing postpancreatitis diabetes, the study authors write. Although previous studies have shown that statins can lower the incidence and severity of acute pancreatitis, they haven’t been studied for the prevention of postpancreatitis diabetes.
In a collaborative study with several other universities, Dr. Thiruvengadam and colleagues examined commercial insurance claims from the Optum Clinformatics database to assess the impact of statins on 118,479 patients without preexisting diabetes admitted for a first episode of acute pancreatitis between 2008 and 2020.
They compared patients who consistently used statins with irregular users and nonusers. Regular statin usage was defined as patients who had statin prescriptions filled for at least 80% of the year prior to their acute pancreatitis diagnosis. The analysis included 9,048 patients (7.6%) who used statins regularly, 27,272 (23%) who used statins irregularly, and 82,159 (69.3%) nonusers.
With a median follow-up of 3.5 years, the 5-year cumulative incidence of postpancreatitis diabetes was 7.5% among regular statin users and 12.7% among nonusers. Regular statin users had a 42% lower risk of developing postpancreatitis diabetes, compared with nonusers. Irregular statin users had a 15% lower risk of postpancreatitis diabetes.
In addition, the 5-year cumulative incidence of insulin-dependent postpancreatitis diabetes was 2.4% among regular statin users and 6.6% among nonusers. Regular statin users had a 52% lower risk of developing insulin-dependent diabetes as compared with nonusers.
Daily dosage didn’t demonstrate a linear dose-response relationship. That means high-dose statins may not be more effective in preventing diabetes as compared with lower doses, the study authors write.
Statin usage was effective across additional analyses, including sex, etiologies of pancreatitis, and in both mild and severe acute pancreatitis. According to the study authors, this suggests that a broad population of these patients may benefit from statins.
“We were pleasantly surprised by the variety of findings,” Dr. Thiruvengadam said. “We’re seeing strong signals, especially with consistency of usage.”
Ongoing studies
The results may seem paradoxical, the study authors write, given an epidemiologic association with a slight increase in new-onset diabetes with statin initiation. But, as other researchers have reported, postpancreatitis diabetes and type 2 diabetes have different clinical features and underlying pathophysiology. For example, patients with postpancreatitis diabetes have much higher rates of requiring insulin, hospitalization, and all-cause mortality, the study authors write.
In fact, postpancreatitis diabetes is thought to be driven by chronic low-grade inflammation attributable to interleukin-6 and tumor necrosis factor–alpha. Statins have been shown to reduce tumor necrosis factor–alpha secretion and the production of C-reactive protein in response to circulating interleukin-6 in hepatocytes, they write.
The results should inform long-term prospective studies of acute pancreatitis, the study authors write, as well as randomized controlled trials of statins.
In the meantime, gastroenterologists and primary care physicians who see outpatients after hospitalization for acute pancreatitis may consider using statins, particularly in those who may have another possible indication for statin therapy, such as mild hyperlipidemia.
“There appears to be a low-dose benefit, which is another reason why providers may consider using statins, though it’s not for everyone with pancreatitis,” Dr. Thiruvengadam said. “This could be an exploratory pathway and suggested for use in the right setting.”
The Type 1 Diabetes in Acute Pancreatitis Consortium, sponsored by the National Institute of Diabetes and Digestive and Kidney Diseases, is conducting an observational cohort study at more than a dozen locations across the country to investigate the incidence, etiology, and pathophysiology of diabetes after acute pancreatitis.
“Diabetes is surprisingly common after even a single attack of acute pancreatitis,” Chris Forsmark, MD, professor of medicine and chief of the division of gastroenterology, hepatology, and nutrition at the University of Florida, Gainesville, told this news organization.
Dr. Forsmark, who wasn’t involved with this study, is a member of T1DAPC and one of the principal investigators in Florida.
“The reduction of risk by 42% is quite substantial,” he said. “Like all such studies, there is risk of bias and confounding in determining the actual risk. Nonetheless, the results provide a strong reason for confirmation in other datasets and for further study.”
The study didn’t report funding support. Dr. Thiruvengadam and Dr. Forsmark report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Use of cholesterol-lowering statins was linked to a lower risk of developing a subtype of diabetes that occurs after acute pancreatitis, according to a new report.
The benefits of statins depended on the consistency of usage, with regular users having a lower risk of developing postpancreatitis diabetes than irregular users. The results were similar with low, moderate, and high statin doses, as well as in cases of both mild and severe acute pancreatitis.
“About 15% of patients with acute pancreatitis will develop diabetes mellitus in the next 5 years, and although we can monitor for it, we can’t do anything to prevent it,” Nikhil Thiruvengadam, MD, the lead study author and a gastroenterologist at Loma Linda (Calif.) University, told this news organization.
“This could push you as a clinician to prescribe [a statin if you have a reason to] because it could provide two benefits instead of just one,” he said.
The study was published online in Clinical Gastroenterology and Hepatology.
Steady use mattered, not dose
Patients with acute pancreatitis face at least a twofold increased risk of developing postpancreatitis diabetes, the study authors write. Although previous studies have shown that statins can lower the incidence and severity of acute pancreatitis, they haven’t been studied for the prevention of postpancreatitis diabetes.
In a collaborative study with several other universities, Dr. Thiruvengadam and colleagues examined commercial insurance claims from the Optum Clinformatics database to assess the impact of statins on 118,479 patients without preexisting diabetes admitted for a first episode of acute pancreatitis between 2008 and 2020.
They compared patients who consistently used statins with irregular users and nonusers. Regular statin usage was defined as patients who had statin prescriptions filled for at least 80% of the year prior to their acute pancreatitis diagnosis. The analysis included 9,048 patients (7.6%) who used statins regularly, 27,272 (23%) who used statins irregularly, and 82,159 (69.3%) nonusers.
With a median follow-up of 3.5 years, the 5-year cumulative incidence of postpancreatitis diabetes was 7.5% among regular statin users and 12.7% among nonusers. Regular statin users had a 42% lower risk of developing postpancreatitis diabetes, compared with nonusers. Irregular statin users had a 15% lower risk of postpancreatitis diabetes.
In addition, the 5-year cumulative incidence of insulin-dependent postpancreatitis diabetes was 2.4% among regular statin users and 6.6% among nonusers. Regular statin users had a 52% lower risk of developing insulin-dependent diabetes as compared with nonusers.
Daily dosage didn’t demonstrate a linear dose-response relationship. That means high-dose statins may not be more effective in preventing diabetes as compared with lower doses, the study authors write.
Statin usage was effective across additional analyses, including sex, etiologies of pancreatitis, and in both mild and severe acute pancreatitis. According to the study authors, this suggests that a broad population of these patients may benefit from statins.
“We were pleasantly surprised by the variety of findings,” Dr. Thiruvengadam said. “We’re seeing strong signals, especially with consistency of usage.”
Ongoing studies
The results may seem paradoxical, the study authors write, given an epidemiologic association with a slight increase in new-onset diabetes with statin initiation. But, as other researchers have reported, postpancreatitis diabetes and type 2 diabetes have different clinical features and underlying pathophysiology. For example, patients with postpancreatitis diabetes have much higher rates of requiring insulin, hospitalization, and all-cause mortality, the study authors write.
In fact, postpancreatitis diabetes is thought to be driven by chronic low-grade inflammation attributable to interleukin-6 and tumor necrosis factor–alpha. Statins have been shown to reduce tumor necrosis factor–alpha secretion and the production of C-reactive protein in response to circulating interleukin-6 in hepatocytes, they write.
The results should inform long-term prospective studies of acute pancreatitis, the study authors write, as well as randomized controlled trials of statins.
In the meantime, gastroenterologists and primary care physicians who see outpatients after hospitalization for acute pancreatitis may consider using statins, particularly in those who may have another possible indication for statin therapy, such as mild hyperlipidemia.
“There appears to be a low-dose benefit, which is another reason why providers may consider using statins, though it’s not for everyone with pancreatitis,” Dr. Thiruvengadam said. “This could be an exploratory pathway and suggested for use in the right setting.”
The Type 1 Diabetes in Acute Pancreatitis Consortium, sponsored by the National Institute of Diabetes and Digestive and Kidney Diseases, is conducting an observational cohort study at more than a dozen locations across the country to investigate the incidence, etiology, and pathophysiology of diabetes after acute pancreatitis.
“Diabetes is surprisingly common after even a single attack of acute pancreatitis,” Chris Forsmark, MD, professor of medicine and chief of the division of gastroenterology, hepatology, and nutrition at the University of Florida, Gainesville, told this news organization.
Dr. Forsmark, who wasn’t involved with this study, is a member of T1DAPC and one of the principal investigators in Florida.
“The reduction of risk by 42% is quite substantial,” he said. “Like all such studies, there is risk of bias and confounding in determining the actual risk. Nonetheless, the results provide a strong reason for confirmation in other datasets and for further study.”
The study didn’t report funding support. Dr. Thiruvengadam and Dr. Forsmark report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Use of cholesterol-lowering statins was linked to a lower risk of developing a subtype of diabetes that occurs after acute pancreatitis, according to a new report.
The benefits of statins depended on the consistency of usage, with regular users having a lower risk of developing postpancreatitis diabetes than irregular users. The results were similar with low, moderate, and high statin doses, as well as in cases of both mild and severe acute pancreatitis.
“About 15% of patients with acute pancreatitis will develop diabetes mellitus in the next 5 years, and although we can monitor for it, we can’t do anything to prevent it,” Nikhil Thiruvengadam, MD, the lead study author and a gastroenterologist at Loma Linda (Calif.) University, told this news organization.
“This could push you as a clinician to prescribe [a statin if you have a reason to] because it could provide two benefits instead of just one,” he said.
The study was published online in Clinical Gastroenterology and Hepatology.
Steady use mattered, not dose
Patients with acute pancreatitis face at least a twofold increased risk of developing postpancreatitis diabetes, the study authors write. Although previous studies have shown that statins can lower the incidence and severity of acute pancreatitis, they haven’t been studied for the prevention of postpancreatitis diabetes.
In a collaborative study with several other universities, Dr. Thiruvengadam and colleagues examined commercial insurance claims from the Optum Clinformatics database to assess the impact of statins on 118,479 patients without preexisting diabetes admitted for a first episode of acute pancreatitis between 2008 and 2020.
They compared patients who consistently used statins with irregular users and nonusers. Regular statin usage was defined as patients who had statin prescriptions filled for at least 80% of the year prior to their acute pancreatitis diagnosis. The analysis included 9,048 patients (7.6%) who used statins regularly, 27,272 (23%) who used statins irregularly, and 82,159 (69.3%) nonusers.
With a median follow-up of 3.5 years, the 5-year cumulative incidence of postpancreatitis diabetes was 7.5% among regular statin users and 12.7% among nonusers. Regular statin users had a 42% lower risk of developing postpancreatitis diabetes, compared with nonusers. Irregular statin users had a 15% lower risk of postpancreatitis diabetes.
In addition, the 5-year cumulative incidence of insulin-dependent postpancreatitis diabetes was 2.4% among regular statin users and 6.6% among nonusers. Regular statin users had a 52% lower risk of developing insulin-dependent diabetes as compared with nonusers.
Daily dosage didn’t demonstrate a linear dose-response relationship. That means high-dose statins may not be more effective in preventing diabetes as compared with lower doses, the study authors write.
Statin usage was effective across additional analyses, including sex, etiologies of pancreatitis, and in both mild and severe acute pancreatitis. According to the study authors, this suggests that a broad population of these patients may benefit from statins.
“We were pleasantly surprised by the variety of findings,” Dr. Thiruvengadam said. “We’re seeing strong signals, especially with consistency of usage.”
Ongoing studies
The results may seem paradoxical, the study authors write, given an epidemiologic association with a slight increase in new-onset diabetes with statin initiation. But, as other researchers have reported, postpancreatitis diabetes and type 2 diabetes have different clinical features and underlying pathophysiology. For example, patients with postpancreatitis diabetes have much higher rates of requiring insulin, hospitalization, and all-cause mortality, the study authors write.
In fact, postpancreatitis diabetes is thought to be driven by chronic low-grade inflammation attributable to interleukin-6 and tumor necrosis factor–alpha. Statins have been shown to reduce tumor necrosis factor–alpha secretion and the production of C-reactive protein in response to circulating interleukin-6 in hepatocytes, they write.
The results should inform long-term prospective studies of acute pancreatitis, the study authors write, as well as randomized controlled trials of statins.
In the meantime, gastroenterologists and primary care physicians who see outpatients after hospitalization for acute pancreatitis may consider using statins, particularly in those who may have another possible indication for statin therapy, such as mild hyperlipidemia.
“There appears to be a low-dose benefit, which is another reason why providers may consider using statins, though it’s not for everyone with pancreatitis,” Dr. Thiruvengadam said. “This could be an exploratory pathway and suggested for use in the right setting.”
The Type 1 Diabetes in Acute Pancreatitis Consortium, sponsored by the National Institute of Diabetes and Digestive and Kidney Diseases, is conducting an observational cohort study at more than a dozen locations across the country to investigate the incidence, etiology, and pathophysiology of diabetes after acute pancreatitis.
“Diabetes is surprisingly common after even a single attack of acute pancreatitis,” Chris Forsmark, MD, professor of medicine and chief of the division of gastroenterology, hepatology, and nutrition at the University of Florida, Gainesville, told this news organization.
Dr. Forsmark, who wasn’t involved with this study, is a member of T1DAPC and one of the principal investigators in Florida.
“The reduction of risk by 42% is quite substantial,” he said. “Like all such studies, there is risk of bias and confounding in determining the actual risk. Nonetheless, the results provide a strong reason for confirmation in other datasets and for further study.”
The study didn’t report funding support. Dr. Thiruvengadam and Dr. Forsmark report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
COVID-19 infection late in pregnancy linked to sevenfold risk of preterm birth
Pregnant women who get infected with SARS-CoV-2 in their third trimester are almost three times as likely to have a preterm birth, while infection after 34 weeks’ gestation raises this risk sevenfold, based on the largest matched population-based cohort study published to date.
These findings support previous studies, underscoring the need for pregnant women and their families to take preventive measures against infection, lead author Noga Fallach, MA, of the Kahn-Sagol-Maccabi Research and Innovation Center, Tel Aviv, and colleagues reported.
Past research has suggested that COVID-19 may cause low birth weights and preterm birth in pregnant women, but those studies didn’t report outcomes for each trimester, the investigators wrote in PLoS ONE, noting that “timing of viral infection during fetal development may affect birth and other health outcomes.”
To address this knowledge gap, the investigators looked back at data from 2,703 pregnant women in Israel who tested positive for SARS-CoV-2 from Feb. 21, 2020, to July 2, 2021. Pregnancy outcomes in these women were compared with outcomes in an equal number of uninfected pregnant women. Vaccination status was not reported.
Comparing the two groups showed that catching COVID-19 in the third trimester was linked with nearly triple the risk of preterm birth (odds ratio, 2.76; 95% confidence interval, 1.63-4.67), and more than quadruple the risk if COVID-19 symptoms were present (OR, 4.28; 95% CI, 1.94-9.41). Women who tested positive for SARS-CoV-2 after 34 weeks’ gestation were seven times more likely than uninfected women to deliver early (OR, 7.10; 95% CI, 2.44-20.61).
Pregnant women who caught COVID-19 in the first two trimesters were not significantly more likely to have a preterm birth. Infection was not associated with abnormally low birth rates, or pregnancy loss, in any trimester.
Tal Patalon, MD, coauthor and head of the Kahn-Sagol-Maccabi Research and Innovation Center, focused on these more optimistic findings in an interview.
“The results are encouraging, and reassuring that COVID-19 infection during pregnancy is not associated with any type of pregnancy loss,” Dr. Patalon said.
She also pointed out that the women in the study were infected with SARS-CoV-2 variants that are no longer common.
“It should be remembered that the research group tested the COVID-19 pre-Delta variants, and does not refer to the dominant variant today, which is Omicron,” Dr. Patalon said.
Still, the investigators concluded that the “results underline the importance of preventive measures taken against SARS-CoV-2 infection among pregnant women and their families.”
Sonja A. Rasmussen, MD, of the University of Florida, Gainesville, said that the issue with out-of-date variants in published research has been one of the “real challenges” in studying the ever-evolving COVID-19 pandemic; however, it’s not a good enough reason to dismiss this study.
“I think at this point, we need to assume that it applies to Omicron too,” Dr. Rasmussen said, noting that other respiratory viruses, like influenza, have also been shown to increase the risk of preterm birth when contracted in late pregnancy.
While the present findings highlight the risk of infection in the third trimester, Dr. Rasmussen advised women in all stages of pregnancy to protect themselves against COVID-19, based on the knowledge that illness in a mother can affect normal growth and development in a fetus, even if it doesn’t lead to preterm birth.
“A mom getting sick during pregnancy is not good for the baby,” Dr. Rasmussen said. “The baby’s really dependent on the mom. So you want that baby to have good nutrition throughout the pregnancy. It’s just as important earlier on as later. And you want that baby to get good oxygenation no matter what time [in the pregnancy]. I know that people want a little bit of a break [from preventive measures]. But I would emphasize that if you’re pregnant, we do all sorts of things during pregnancy to make sure that our babies are safe and healthy, and I would continue that for the whole pregnancy.”
Specifically, Dr. Rasmussen advised social distancing, use of an N95 mask, and vaccination. Getting vaccinated during pregnancy helps newborns fight off infection until 6 months of age, she added, when they become eligible for vaccination themselves. This added benefit was recently reported in a study published in the New England Journal of Medicine , for which Dr. Rasmussen cowrote an editorial .
“Vaccines have been approved for 6 months and older,” Dr. Rasmussen said. “But what do you do in those first 6 months of life? That’s a high-risk time for kids.”
Despite these risks, convincing pregnant women to get vaccinated remains a key challenge for health care providers, according to Dr. Rasmussen, even with an abundance of safety data. “Early on [in the pandemic], we said we didn’t know a lot about risks. We knew that other vaccines were safe during pregnancy, but we didn’t have a lot of information about a COVID-19 vaccine. But now we have a lot of data on safety during pregnancy, and these vaccines appear to be completely safe, based on the information we have. There have been many, many pregnant women vaccinated in the United States and in other countries.”
For reluctant expecting mothers, Dr. Rasmussen offered some words of advice: “I know that you worry about anything you do when you’re pregnant. But this is something that you can do to help your baby – now, to make a preterm birth less likely, and later, after the baby is born.
“The most important thing is for the pregnant person to hear this [vaccine recommendation] from their doctor,” she added. “If they’re going to listen to anybody, they’re going to listen to their physician. That’s what the data have shown for a long time.”
The investigators and Dr. Rasmussen disclosed no conflicts of interest.
Pregnant women who get infected with SARS-CoV-2 in their third trimester are almost three times as likely to have a preterm birth, while infection after 34 weeks’ gestation raises this risk sevenfold, based on the largest matched population-based cohort study published to date.
These findings support previous studies, underscoring the need for pregnant women and their families to take preventive measures against infection, lead author Noga Fallach, MA, of the Kahn-Sagol-Maccabi Research and Innovation Center, Tel Aviv, and colleagues reported.
Past research has suggested that COVID-19 may cause low birth weights and preterm birth in pregnant women, but those studies didn’t report outcomes for each trimester, the investigators wrote in PLoS ONE, noting that “timing of viral infection during fetal development may affect birth and other health outcomes.”
To address this knowledge gap, the investigators looked back at data from 2,703 pregnant women in Israel who tested positive for SARS-CoV-2 from Feb. 21, 2020, to July 2, 2021. Pregnancy outcomes in these women were compared with outcomes in an equal number of uninfected pregnant women. Vaccination status was not reported.
Comparing the two groups showed that catching COVID-19 in the third trimester was linked with nearly triple the risk of preterm birth (odds ratio, 2.76; 95% confidence interval, 1.63-4.67), and more than quadruple the risk if COVID-19 symptoms were present (OR, 4.28; 95% CI, 1.94-9.41). Women who tested positive for SARS-CoV-2 after 34 weeks’ gestation were seven times more likely than uninfected women to deliver early (OR, 7.10; 95% CI, 2.44-20.61).
Pregnant women who caught COVID-19 in the first two trimesters were not significantly more likely to have a preterm birth. Infection was not associated with abnormally low birth rates, or pregnancy loss, in any trimester.
Tal Patalon, MD, coauthor and head of the Kahn-Sagol-Maccabi Research and Innovation Center, focused on these more optimistic findings in an interview.
“The results are encouraging, and reassuring that COVID-19 infection during pregnancy is not associated with any type of pregnancy loss,” Dr. Patalon said.
She also pointed out that the women in the study were infected with SARS-CoV-2 variants that are no longer common.
“It should be remembered that the research group tested the COVID-19 pre-Delta variants, and does not refer to the dominant variant today, which is Omicron,” Dr. Patalon said.
Still, the investigators concluded that the “results underline the importance of preventive measures taken against SARS-CoV-2 infection among pregnant women and their families.”
Sonja A. Rasmussen, MD, of the University of Florida, Gainesville, said that the issue with out-of-date variants in published research has been one of the “real challenges” in studying the ever-evolving COVID-19 pandemic; however, it’s not a good enough reason to dismiss this study.
“I think at this point, we need to assume that it applies to Omicron too,” Dr. Rasmussen said, noting that other respiratory viruses, like influenza, have also been shown to increase the risk of preterm birth when contracted in late pregnancy.
While the present findings highlight the risk of infection in the third trimester, Dr. Rasmussen advised women in all stages of pregnancy to protect themselves against COVID-19, based on the knowledge that illness in a mother can affect normal growth and development in a fetus, even if it doesn’t lead to preterm birth.
“A mom getting sick during pregnancy is not good for the baby,” Dr. Rasmussen said. “The baby’s really dependent on the mom. So you want that baby to have good nutrition throughout the pregnancy. It’s just as important earlier on as later. And you want that baby to get good oxygenation no matter what time [in the pregnancy]. I know that people want a little bit of a break [from preventive measures]. But I would emphasize that if you’re pregnant, we do all sorts of things during pregnancy to make sure that our babies are safe and healthy, and I would continue that for the whole pregnancy.”
Specifically, Dr. Rasmussen advised social distancing, use of an N95 mask, and vaccination. Getting vaccinated during pregnancy helps newborns fight off infection until 6 months of age, she added, when they become eligible for vaccination themselves. This added benefit was recently reported in a study published in the New England Journal of Medicine , for which Dr. Rasmussen cowrote an editorial .
“Vaccines have been approved for 6 months and older,” Dr. Rasmussen said. “But what do you do in those first 6 months of life? That’s a high-risk time for kids.”
Despite these risks, convincing pregnant women to get vaccinated remains a key challenge for health care providers, according to Dr. Rasmussen, even with an abundance of safety data. “Early on [in the pandemic], we said we didn’t know a lot about risks. We knew that other vaccines were safe during pregnancy, but we didn’t have a lot of information about a COVID-19 vaccine. But now we have a lot of data on safety during pregnancy, and these vaccines appear to be completely safe, based on the information we have. There have been many, many pregnant women vaccinated in the United States and in other countries.”
For reluctant expecting mothers, Dr. Rasmussen offered some words of advice: “I know that you worry about anything you do when you’re pregnant. But this is something that you can do to help your baby – now, to make a preterm birth less likely, and later, after the baby is born.
“The most important thing is for the pregnant person to hear this [vaccine recommendation] from their doctor,” she added. “If they’re going to listen to anybody, they’re going to listen to their physician. That’s what the data have shown for a long time.”
The investigators and Dr. Rasmussen disclosed no conflicts of interest.
Pregnant women who get infected with SARS-CoV-2 in their third trimester are almost three times as likely to have a preterm birth, while infection after 34 weeks’ gestation raises this risk sevenfold, based on the largest matched population-based cohort study published to date.
These findings support previous studies, underscoring the need for pregnant women and their families to take preventive measures against infection, lead author Noga Fallach, MA, of the Kahn-Sagol-Maccabi Research and Innovation Center, Tel Aviv, and colleagues reported.
Past research has suggested that COVID-19 may cause low birth weights and preterm birth in pregnant women, but those studies didn’t report outcomes for each trimester, the investigators wrote in PLoS ONE, noting that “timing of viral infection during fetal development may affect birth and other health outcomes.”
To address this knowledge gap, the investigators looked back at data from 2,703 pregnant women in Israel who tested positive for SARS-CoV-2 from Feb. 21, 2020, to July 2, 2021. Pregnancy outcomes in these women were compared with outcomes in an equal number of uninfected pregnant women. Vaccination status was not reported.
Comparing the two groups showed that catching COVID-19 in the third trimester was linked with nearly triple the risk of preterm birth (odds ratio, 2.76; 95% confidence interval, 1.63-4.67), and more than quadruple the risk if COVID-19 symptoms were present (OR, 4.28; 95% CI, 1.94-9.41). Women who tested positive for SARS-CoV-2 after 34 weeks’ gestation were seven times more likely than uninfected women to deliver early (OR, 7.10; 95% CI, 2.44-20.61).
Pregnant women who caught COVID-19 in the first two trimesters were not significantly more likely to have a preterm birth. Infection was not associated with abnormally low birth rates, or pregnancy loss, in any trimester.
Tal Patalon, MD, coauthor and head of the Kahn-Sagol-Maccabi Research and Innovation Center, focused on these more optimistic findings in an interview.
“The results are encouraging, and reassuring that COVID-19 infection during pregnancy is not associated with any type of pregnancy loss,” Dr. Patalon said.
She also pointed out that the women in the study were infected with SARS-CoV-2 variants that are no longer common.
“It should be remembered that the research group tested the COVID-19 pre-Delta variants, and does not refer to the dominant variant today, which is Omicron,” Dr. Patalon said.
Still, the investigators concluded that the “results underline the importance of preventive measures taken against SARS-CoV-2 infection among pregnant women and their families.”
Sonja A. Rasmussen, MD, of the University of Florida, Gainesville, said that the issue with out-of-date variants in published research has been one of the “real challenges” in studying the ever-evolving COVID-19 pandemic; however, it’s not a good enough reason to dismiss this study.
“I think at this point, we need to assume that it applies to Omicron too,” Dr. Rasmussen said, noting that other respiratory viruses, like influenza, have also been shown to increase the risk of preterm birth when contracted in late pregnancy.
While the present findings highlight the risk of infection in the third trimester, Dr. Rasmussen advised women in all stages of pregnancy to protect themselves against COVID-19, based on the knowledge that illness in a mother can affect normal growth and development in a fetus, even if it doesn’t lead to preterm birth.
“A mom getting sick during pregnancy is not good for the baby,” Dr. Rasmussen said. “The baby’s really dependent on the mom. So you want that baby to have good nutrition throughout the pregnancy. It’s just as important earlier on as later. And you want that baby to get good oxygenation no matter what time [in the pregnancy]. I know that people want a little bit of a break [from preventive measures]. But I would emphasize that if you’re pregnant, we do all sorts of things during pregnancy to make sure that our babies are safe and healthy, and I would continue that for the whole pregnancy.”
Specifically, Dr. Rasmussen advised social distancing, use of an N95 mask, and vaccination. Getting vaccinated during pregnancy helps newborns fight off infection until 6 months of age, she added, when they become eligible for vaccination themselves. This added benefit was recently reported in a study published in the New England Journal of Medicine , for which Dr. Rasmussen cowrote an editorial .
“Vaccines have been approved for 6 months and older,” Dr. Rasmussen said. “But what do you do in those first 6 months of life? That’s a high-risk time for kids.”
Despite these risks, convincing pregnant women to get vaccinated remains a key challenge for health care providers, according to Dr. Rasmussen, even with an abundance of safety data. “Early on [in the pandemic], we said we didn’t know a lot about risks. We knew that other vaccines were safe during pregnancy, but we didn’t have a lot of information about a COVID-19 vaccine. But now we have a lot of data on safety during pregnancy, and these vaccines appear to be completely safe, based on the information we have. There have been many, many pregnant women vaccinated in the United States and in other countries.”
For reluctant expecting mothers, Dr. Rasmussen offered some words of advice: “I know that you worry about anything you do when you’re pregnant. But this is something that you can do to help your baby – now, to make a preterm birth less likely, and later, after the baby is born.
“The most important thing is for the pregnant person to hear this [vaccine recommendation] from their doctor,” she added. “If they’re going to listen to anybody, they’re going to listen to their physician. That’s what the data have shown for a long time.”
The investigators and Dr. Rasmussen disclosed no conflicts of interest.
FROM PLOS ONE
Safest, most effective medications for spine-related pain in older adults?
, a new comprehensive literature review suggests.
Investigators assessed the evidence for medications used for this indication in older adults by reviewing 138 double-blind, placebo-controlled trials.
Among their key findings and recommendations: Acetaminophen has a favorable safety profile for spine-related pain but nonsteroidal anti-inflammatory drugs (NSAIDs) have greater efficacy.
However, NSAIDs should be used in lower doses in the short term, with gastrointestinal precaution, the researchers note.
Corticosteroids have the least evidence for treating nonspecific back pain, they add.
“Most older people experience neck or low back pain at some point, bothersome enough to see their doctor,” coinvestigator Michael Perloff, MD, PhD, department of neurology, Boston University, said in a news release.
“Our findings provide a helpful medication guide for physicians to use for spine pain in an older population that can have a complex medical history,” Dr. Perloff added.
The results were published online in Drugs and Aging.
Recommendations, warnings
With the graying of the U.S. population, spine-related pain is increasingly common, the investigators note.
Medications play an important role in pain management, but their use has limitations in the elderly, owing to reduced liver and renal function, comorbid medical problems, and polypharmacy.
Other key findings from the literature review include that, although the nerve pain medications gabapentin and pregabalin may cause dizziness or difficulty walking, they also have some demonstrated benefit for neck and back nerve pain, such as sciatica, in older adults.
These agents should be used in lower doses with smaller dose adjustments, the researchers note.
They caution that the muscle relaxants carisoprodol, chlorzoxazone, cyclobenzaprine, metaxalone, methocarbamol, and orphenadrine should be avoided in older adults because of their association with risk for sedation and falls.
‘Rational therapeutic choices’
Three other muscle relaxants – tizanidine, baclofen, and dantrolene – may be helpful for neck and back pain. The most evidence favors tizanidine and baclofen. These should be used in reduced doses. Tizanidine should be avoided in patients with liver disease, and for patients with kidney disease, the dosing of baclofen should be reduced, the investigators write.
Other findings include the following:
- Older tricyclic antidepressants should typically be avoided in this population because of their side effects, but nortriptyline and desipramine may be better tolerated for neck and back nerve pain at lower doses.
- Newer antidepressants, particularly the selective serotonin-norepinephrine reuptake inhibitor duloxetine, have a better safety profile and good efficacy for spine-related nerve pain.
- Traditional opioids are typically avoided in the treatment of spine-related pain in older adults, owing to their associated risks.
However, low-dose opioid therapy may be helpful for severe refractory pain, with close monitoring of patients, the researchers note.
Weaker opioids, such as tramadol, may be better tolerated by older patients. They work well when combined with acetaminophen, but they carry the risk for sedation, upset stomach, and constipation.
“Medications used at the correct dose, for the correct diagnosis, adjusting for preexisting medical problems can result in better use of treatments for spine pain,” coinvestigator Jonathan Fu, MD, also with the department of neurology, Boston University, said in the release.
“Rational therapeutic choices should be targeted to spine pain diagnosis, such as NSAIDs and acetaminophen for arthritic and myofascial-based complaints, gabapentinoids or duloxetine for neuropathic and radicular symptoms, antispastic agents for myofascial-based pain, and combination therapy for mixed etiologies,” the investigators write.
They also emphasize that medications should be coupled with physical therapy and exercise programs, as well as treatment of the underlying degenerative disease process and medical illness, while keeping in mind the need for possible interventions and/or corrective surgery.
The research had no specific funding. The investigators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, a new comprehensive literature review suggests.
Investigators assessed the evidence for medications used for this indication in older adults by reviewing 138 double-blind, placebo-controlled trials.
Among their key findings and recommendations: Acetaminophen has a favorable safety profile for spine-related pain but nonsteroidal anti-inflammatory drugs (NSAIDs) have greater efficacy.
However, NSAIDs should be used in lower doses in the short term, with gastrointestinal precaution, the researchers note.
Corticosteroids have the least evidence for treating nonspecific back pain, they add.
“Most older people experience neck or low back pain at some point, bothersome enough to see their doctor,” coinvestigator Michael Perloff, MD, PhD, department of neurology, Boston University, said in a news release.
“Our findings provide a helpful medication guide for physicians to use for spine pain in an older population that can have a complex medical history,” Dr. Perloff added.
The results were published online in Drugs and Aging.
Recommendations, warnings
With the graying of the U.S. population, spine-related pain is increasingly common, the investigators note.
Medications play an important role in pain management, but their use has limitations in the elderly, owing to reduced liver and renal function, comorbid medical problems, and polypharmacy.
Other key findings from the literature review include that, although the nerve pain medications gabapentin and pregabalin may cause dizziness or difficulty walking, they also have some demonstrated benefit for neck and back nerve pain, such as sciatica, in older adults.
These agents should be used in lower doses with smaller dose adjustments, the researchers note.
They caution that the muscle relaxants carisoprodol, chlorzoxazone, cyclobenzaprine, metaxalone, methocarbamol, and orphenadrine should be avoided in older adults because of their association with risk for sedation and falls.
‘Rational therapeutic choices’
Three other muscle relaxants – tizanidine, baclofen, and dantrolene – may be helpful for neck and back pain. The most evidence favors tizanidine and baclofen. These should be used in reduced doses. Tizanidine should be avoided in patients with liver disease, and for patients with kidney disease, the dosing of baclofen should be reduced, the investigators write.
Other findings include the following:
- Older tricyclic antidepressants should typically be avoided in this population because of their side effects, but nortriptyline and desipramine may be better tolerated for neck and back nerve pain at lower doses.
- Newer antidepressants, particularly the selective serotonin-norepinephrine reuptake inhibitor duloxetine, have a better safety profile and good efficacy for spine-related nerve pain.
- Traditional opioids are typically avoided in the treatment of spine-related pain in older adults, owing to their associated risks.
However, low-dose opioid therapy may be helpful for severe refractory pain, with close monitoring of patients, the researchers note.
Weaker opioids, such as tramadol, may be better tolerated by older patients. They work well when combined with acetaminophen, but they carry the risk for sedation, upset stomach, and constipation.
“Medications used at the correct dose, for the correct diagnosis, adjusting for preexisting medical problems can result in better use of treatments for spine pain,” coinvestigator Jonathan Fu, MD, also with the department of neurology, Boston University, said in the release.
“Rational therapeutic choices should be targeted to spine pain diagnosis, such as NSAIDs and acetaminophen for arthritic and myofascial-based complaints, gabapentinoids or duloxetine for neuropathic and radicular symptoms, antispastic agents for myofascial-based pain, and combination therapy for mixed etiologies,” the investigators write.
They also emphasize that medications should be coupled with physical therapy and exercise programs, as well as treatment of the underlying degenerative disease process and medical illness, while keeping in mind the need for possible interventions and/or corrective surgery.
The research had no specific funding. The investigators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, a new comprehensive literature review suggests.
Investigators assessed the evidence for medications used for this indication in older adults by reviewing 138 double-blind, placebo-controlled trials.
Among their key findings and recommendations: Acetaminophen has a favorable safety profile for spine-related pain but nonsteroidal anti-inflammatory drugs (NSAIDs) have greater efficacy.
However, NSAIDs should be used in lower doses in the short term, with gastrointestinal precaution, the researchers note.
Corticosteroids have the least evidence for treating nonspecific back pain, they add.
“Most older people experience neck or low back pain at some point, bothersome enough to see their doctor,” coinvestigator Michael Perloff, MD, PhD, department of neurology, Boston University, said in a news release.
“Our findings provide a helpful medication guide for physicians to use for spine pain in an older population that can have a complex medical history,” Dr. Perloff added.
The results were published online in Drugs and Aging.
Recommendations, warnings
With the graying of the U.S. population, spine-related pain is increasingly common, the investigators note.
Medications play an important role in pain management, but their use has limitations in the elderly, owing to reduced liver and renal function, comorbid medical problems, and polypharmacy.
Other key findings from the literature review include that, although the nerve pain medications gabapentin and pregabalin may cause dizziness or difficulty walking, they also have some demonstrated benefit for neck and back nerve pain, such as sciatica, in older adults.
These agents should be used in lower doses with smaller dose adjustments, the researchers note.
They caution that the muscle relaxants carisoprodol, chlorzoxazone, cyclobenzaprine, metaxalone, methocarbamol, and orphenadrine should be avoided in older adults because of their association with risk for sedation and falls.
‘Rational therapeutic choices’
Three other muscle relaxants – tizanidine, baclofen, and dantrolene – may be helpful for neck and back pain. The most evidence favors tizanidine and baclofen. These should be used in reduced doses. Tizanidine should be avoided in patients with liver disease, and for patients with kidney disease, the dosing of baclofen should be reduced, the investigators write.
Other findings include the following:
- Older tricyclic antidepressants should typically be avoided in this population because of their side effects, but nortriptyline and desipramine may be better tolerated for neck and back nerve pain at lower doses.
- Newer antidepressants, particularly the selective serotonin-norepinephrine reuptake inhibitor duloxetine, have a better safety profile and good efficacy for spine-related nerve pain.
- Traditional opioids are typically avoided in the treatment of spine-related pain in older adults, owing to their associated risks.
However, low-dose opioid therapy may be helpful for severe refractory pain, with close monitoring of patients, the researchers note.
Weaker opioids, such as tramadol, may be better tolerated by older patients. They work well when combined with acetaminophen, but they carry the risk for sedation, upset stomach, and constipation.
“Medications used at the correct dose, for the correct diagnosis, adjusting for preexisting medical problems can result in better use of treatments for spine pain,” coinvestigator Jonathan Fu, MD, also with the department of neurology, Boston University, said in the release.
“Rational therapeutic choices should be targeted to spine pain diagnosis, such as NSAIDs and acetaminophen for arthritic and myofascial-based complaints, gabapentinoids or duloxetine for neuropathic and radicular symptoms, antispastic agents for myofascial-based pain, and combination therapy for mixed etiologies,” the investigators write.
They also emphasize that medications should be coupled with physical therapy and exercise programs, as well as treatment of the underlying degenerative disease process and medical illness, while keeping in mind the need for possible interventions and/or corrective surgery.
The research had no specific funding. The investigators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM DRUGS AND AGING
An avocado a day doesn’t shrink belly fat, but helps with cholesterol
according to the findings of a new study.
But it did improve diet quality and led to modest lowering of total cholesterol.
More than 1,000 adults with overweight or obesity and a large waist – at least 35 inches in women and 40 inches in men – took part in this U.S. study, called the Habitual Diet and Avocado Trial (HAT).
The people in the study were divided into two groups: usual diet plus one large avocado every day and usual diet with two avocados at most per month (control group).
Those in the avocado-a-day group were given a regular supply of fresh avocados along with written instructions for how to ripen and prepare them.
They had MRI scans to measure belly fat and fat around other organs at the beginning of the study and after 6 months.
After 6 months, the people who ate an avocado a day did not have less fat around their middles – the main trial outcome – compared with people in the control group.
But at 6 months, those in the avocado-a-day group had:
- No weight gain. People’s weight remained stable in both groups.
- Improved diet quality by 8 points on a 100-point scale
- A 2.9-mg/dL decrease in total cholesterol
- A 2.5-mg/dL decrease in LDL cholesterol
The study was done by researchers at Penn State University; Tufts University; Loma Linda University; and the University of California, Los Angeles, with coordinating support from Wake Forest University.
It was published in the Journal of the American Heart Association.
“While the avocados did not affect belly fat or weight gain, the study still provides evidence that avocados can be a beneficial addition to a well-balanced diet,” Penny M. Kris-Etherton, PhD, one of the researchers and a professor of nutritional sciences at Penn State University, University Park, said in a news release.
“Incorporating an avocado per day in this study did not cause weight gain and also caused a slight decrease in LDL cholesterol, which are all important findings for better health,” she said.
Similarly, study researcher Joan Sabaté, MD, a professor at Loma Linda (Calif.) University, said: “While one avocado a day did not lead to clinically significant improvements in abdominal fat and other cardiometabolic risk factors, consuming one avocado a day did not result in body weight gain.”
“This is positive,” he said, “because eating extra calories from avocados doesn’t impact body weight or abdominal fat, and it slightly decreases total and LDL cholesterol.”
Kristina S. Petersen, PhD, another of the researchers and an assistant professor of nutritional sciences at Texas Tech University, Lubbock, pointed out that people are generally poor at adhering to the Dietary Guidelines for Americans.
This study suggests that an avocado a day can improve diet quality, she noted, which “ is important because we know a higher diet quality is associated with lower risk of several diseases, including heart disease, type 2 diabetes, and some cancers.”
But the researchers also stressed that it is important to consider the diet as a whole.
“Consistent with prior observations, a change in dietary patterns rather than a single food or nutrient may be necessary to achieve clinically significant improvements” in belly fat and other risk factors for heart attack, stroke, and diabetes, they wrote.
HAT was funded by the Hass Avocado Board, which also supplied the avocados.
A version of this article first appeared on WebMD.com.
according to the findings of a new study.
But it did improve diet quality and led to modest lowering of total cholesterol.
More than 1,000 adults with overweight or obesity and a large waist – at least 35 inches in women and 40 inches in men – took part in this U.S. study, called the Habitual Diet and Avocado Trial (HAT).
The people in the study were divided into two groups: usual diet plus one large avocado every day and usual diet with two avocados at most per month (control group).
Those in the avocado-a-day group were given a regular supply of fresh avocados along with written instructions for how to ripen and prepare them.
They had MRI scans to measure belly fat and fat around other organs at the beginning of the study and after 6 months.
After 6 months, the people who ate an avocado a day did not have less fat around their middles – the main trial outcome – compared with people in the control group.
But at 6 months, those in the avocado-a-day group had:
- No weight gain. People’s weight remained stable in both groups.
- Improved diet quality by 8 points on a 100-point scale
- A 2.9-mg/dL decrease in total cholesterol
- A 2.5-mg/dL decrease in LDL cholesterol
The study was done by researchers at Penn State University; Tufts University; Loma Linda University; and the University of California, Los Angeles, with coordinating support from Wake Forest University.
It was published in the Journal of the American Heart Association.
“While the avocados did not affect belly fat or weight gain, the study still provides evidence that avocados can be a beneficial addition to a well-balanced diet,” Penny M. Kris-Etherton, PhD, one of the researchers and a professor of nutritional sciences at Penn State University, University Park, said in a news release.
“Incorporating an avocado per day in this study did not cause weight gain and also caused a slight decrease in LDL cholesterol, which are all important findings for better health,” she said.
Similarly, study researcher Joan Sabaté, MD, a professor at Loma Linda (Calif.) University, said: “While one avocado a day did not lead to clinically significant improvements in abdominal fat and other cardiometabolic risk factors, consuming one avocado a day did not result in body weight gain.”
“This is positive,” he said, “because eating extra calories from avocados doesn’t impact body weight or abdominal fat, and it slightly decreases total and LDL cholesterol.”
Kristina S. Petersen, PhD, another of the researchers and an assistant professor of nutritional sciences at Texas Tech University, Lubbock, pointed out that people are generally poor at adhering to the Dietary Guidelines for Americans.
This study suggests that an avocado a day can improve diet quality, she noted, which “ is important because we know a higher diet quality is associated with lower risk of several diseases, including heart disease, type 2 diabetes, and some cancers.”
But the researchers also stressed that it is important to consider the diet as a whole.
“Consistent with prior observations, a change in dietary patterns rather than a single food or nutrient may be necessary to achieve clinically significant improvements” in belly fat and other risk factors for heart attack, stroke, and diabetes, they wrote.
HAT was funded by the Hass Avocado Board, which also supplied the avocados.
A version of this article first appeared on WebMD.com.
according to the findings of a new study.
But it did improve diet quality and led to modest lowering of total cholesterol.
More than 1,000 adults with overweight or obesity and a large waist – at least 35 inches in women and 40 inches in men – took part in this U.S. study, called the Habitual Diet and Avocado Trial (HAT).
The people in the study were divided into two groups: usual diet plus one large avocado every day and usual diet with two avocados at most per month (control group).
Those in the avocado-a-day group were given a regular supply of fresh avocados along with written instructions for how to ripen and prepare them.
They had MRI scans to measure belly fat and fat around other organs at the beginning of the study and after 6 months.
After 6 months, the people who ate an avocado a day did not have less fat around their middles – the main trial outcome – compared with people in the control group.
But at 6 months, those in the avocado-a-day group had:
- No weight gain. People’s weight remained stable in both groups.
- Improved diet quality by 8 points on a 100-point scale
- A 2.9-mg/dL decrease in total cholesterol
- A 2.5-mg/dL decrease in LDL cholesterol
The study was done by researchers at Penn State University; Tufts University; Loma Linda University; and the University of California, Los Angeles, with coordinating support from Wake Forest University.
It was published in the Journal of the American Heart Association.
“While the avocados did not affect belly fat or weight gain, the study still provides evidence that avocados can be a beneficial addition to a well-balanced diet,” Penny M. Kris-Etherton, PhD, one of the researchers and a professor of nutritional sciences at Penn State University, University Park, said in a news release.
“Incorporating an avocado per day in this study did not cause weight gain and also caused a slight decrease in LDL cholesterol, which are all important findings for better health,” she said.
Similarly, study researcher Joan Sabaté, MD, a professor at Loma Linda (Calif.) University, said: “While one avocado a day did not lead to clinically significant improvements in abdominal fat and other cardiometabolic risk factors, consuming one avocado a day did not result in body weight gain.”
“This is positive,” he said, “because eating extra calories from avocados doesn’t impact body weight or abdominal fat, and it slightly decreases total and LDL cholesterol.”
Kristina S. Petersen, PhD, another of the researchers and an assistant professor of nutritional sciences at Texas Tech University, Lubbock, pointed out that people are generally poor at adhering to the Dietary Guidelines for Americans.
This study suggests that an avocado a day can improve diet quality, she noted, which “ is important because we know a higher diet quality is associated with lower risk of several diseases, including heart disease, type 2 diabetes, and some cancers.”
But the researchers also stressed that it is important to consider the diet as a whole.
“Consistent with prior observations, a change in dietary patterns rather than a single food or nutrient may be necessary to achieve clinically significant improvements” in belly fat and other risk factors for heart attack, stroke, and diabetes, they wrote.
HAT was funded by the Hass Avocado Board, which also supplied the avocados.
A version of this article first appeared on WebMD.com.
When and for whom is telehealth OCD treatment appropriate?
It is no secret that the COVID-19 pandemic resulted in widespread disruptions in health care services. While providers and resources were limited and many patients were apprehensive to present to health care settings out of concern of disease contraction, telehealth services did offer some relief.
Compared to other specialty care services, mental health care providers were well equipped to handle the expansion of telehealth services, as extensive treatment literature provides strong support for the use of psychotherapeutic interventions over telehealth mediums.1 This holds true in the context of obsessive-compulsive disorder (OCD), where an impressive literature supports the use of telehealth delivery for the gold-standard psychotherapeutic, exposure and response prevention (ERP).2,3,4
Through ERP, patients work with a clinician to systematically expose themselves to anxiety-providing triggers while actively resisting compulsive behaviors to learn the distress does go away with time and/or the distress is within their ability to cope. This intervention is conceptually similar to repeatedly watching a scary film, by which continued exposure results in less pronounced emotional reaction with subsequent viewings.
Fortunately for patients and providers, the expansion of telehealth ERP across different treatment settings has had many unintended benefits, including increased access to care, lower no-show rates due to the ease of attending appointments, and the ability to offer higher levels of care, including intensive outpatient programs, over telehealth mediums. Anecdotally, our clinic has been able to increase patient reach by providing telehealth ERP to those who historically would not have been able to access care due to geography. Even for those living within driving distance to our clinic, the ease of joining a video visit for a 45-minute appointment far outweighs driving into the clinic, in many circumstances. With these benefits, the delivery of ERP over telehealth appears likely to stay, although OCD providers delivering ERP will need to consider when and for whom this medium may not be appropriate.
To this end, we recently conducted a study examining ERP providers perceptions of telehealth and in-person ERP, patient characteristics best suited for telehealth services, and provider ability to identify and address factors that adversely impact the course of treatment (e.g., substance use, limited symptom insight, distractions during ERP, etc.).5 Providers reported lower feasibility ratings for telehealth compared to in-person ERP for younger patients (aged under 13 years), and patients with more severe OCD presentations. Providers also reported more difficulty identifying and addressing ERP interfering factors over telehealth relative to in-person. The findings from our research do not necessarily speak to the effectiveness of telehealth ERP, which has repeatedly been documented in treatment literature, but rather our findings highlight that ERP providers endorse reservations about the feasibility of ERP for certain OCD patient profiles, and that telehealth ERP may not be appropriate for all patients with OCD.
Mental health care providers, including those delivering ERP, should consider when telehealth is and is not appropriate. Importantly, telehealth offers a limited field of view compared to in-person, and providers can only observe what is captured by the camera. In the context of telehealth ERP, patients may engage in subtle avoidant behaviors that are more difficult to observe, which may prevent them from experiencing necessary anxiety during exposure practice. Many providers may have firsthand experience with this, or patients who appear distracted over telehealth mediums because of environmental factors that can be controlled for during in-person services.
As telehealth treatment options appear increasingly likely to stay, ERP providers and intervention researchers should continue identifying patient characteristics that are more and less appropriate for telehealth settings in order to maximize treatment outcomes. Providers should share concerns with patients when delivering telehealth ERP and work to address interfering factors impacting the course of treatment. In circumstances where this is not possible, such as when the patients age or symptom severity prevents effective telehealth ERP, or when treatment progress stalls, providers should speak with patients to determine if it would be beneficial to transition to in-person services.
Both in-person and telehealth ERP are fundamentally the same, however it does appear that subtle differences across these modalities may have differential impacts on treatment outcomes for certain OCD patient presentations. , however appropriate caution should be exhibited, and providers should use clinical judgment when offering telehealth services.
Dr. Wiese is a clinical psychologist in the department of psychiatry and behavioral sciences at Baylor College of Medicine, Houston, Texas. He is primarily focused on conducting research on OCD and related disorders and providing empirically supported treatments to individuals diagnosed with these conditions.
References
1. Fernandez E et al. Live psychotherapy by video versus in‐person: A meta‐analysis of efficacy and its relationship to types and targets of treatment. Clin Psychol Psychother. 2021 Nov;28(6):1535-49. doi: 10.1002/cpp.2594.
2. Storch EA et al. Preliminary investigation of web-camera delivered cognitive-behavioral therapy for youth with obsessive-compulsive disorder. Psychiatry Res. 2011 Oct 30;189(3):407-12. doi: 10.1016/j.psychres.2011.05.047.
3. Fletcher TL et al. A pilot open trial of video telehealth-delivered exposure and response prevention for obsessive-compulsive disorder in rural Veterans. Mil Psychol. 2021 Oct 28;34(1):83-90. doi: 10.1080/08995605.2021.1970983.
4. Wootton BM. Remote cognitive–behavior therapy for obsessive–compulsive symptoms: a meta-analysis. Clin Psychol Rev. 2016 Feb;43:103-13. doi: 10.1016/j.cpr.2015.10.001.
5. Wiese AD et al. Provider perceptions of telehealth and in-person exposure and response prevention for obsessive–compulsive disorder. Psychiatry Res. 2022 Jul;313:114610. doi: 10.1016/j.psychres.2022.114610.
It is no secret that the COVID-19 pandemic resulted in widespread disruptions in health care services. While providers and resources were limited and many patients were apprehensive to present to health care settings out of concern of disease contraction, telehealth services did offer some relief.
Compared to other specialty care services, mental health care providers were well equipped to handle the expansion of telehealth services, as extensive treatment literature provides strong support for the use of psychotherapeutic interventions over telehealth mediums.1 This holds true in the context of obsessive-compulsive disorder (OCD), where an impressive literature supports the use of telehealth delivery for the gold-standard psychotherapeutic, exposure and response prevention (ERP).2,3,4
Through ERP, patients work with a clinician to systematically expose themselves to anxiety-providing triggers while actively resisting compulsive behaviors to learn the distress does go away with time and/or the distress is within their ability to cope. This intervention is conceptually similar to repeatedly watching a scary film, by which continued exposure results in less pronounced emotional reaction with subsequent viewings.
Fortunately for patients and providers, the expansion of telehealth ERP across different treatment settings has had many unintended benefits, including increased access to care, lower no-show rates due to the ease of attending appointments, and the ability to offer higher levels of care, including intensive outpatient programs, over telehealth mediums. Anecdotally, our clinic has been able to increase patient reach by providing telehealth ERP to those who historically would not have been able to access care due to geography. Even for those living within driving distance to our clinic, the ease of joining a video visit for a 45-minute appointment far outweighs driving into the clinic, in many circumstances. With these benefits, the delivery of ERP over telehealth appears likely to stay, although OCD providers delivering ERP will need to consider when and for whom this medium may not be appropriate.
To this end, we recently conducted a study examining ERP providers perceptions of telehealth and in-person ERP, patient characteristics best suited for telehealth services, and provider ability to identify and address factors that adversely impact the course of treatment (e.g., substance use, limited symptom insight, distractions during ERP, etc.).5 Providers reported lower feasibility ratings for telehealth compared to in-person ERP for younger patients (aged under 13 years), and patients with more severe OCD presentations. Providers also reported more difficulty identifying and addressing ERP interfering factors over telehealth relative to in-person. The findings from our research do not necessarily speak to the effectiveness of telehealth ERP, which has repeatedly been documented in treatment literature, but rather our findings highlight that ERP providers endorse reservations about the feasibility of ERP for certain OCD patient profiles, and that telehealth ERP may not be appropriate for all patients with OCD.
Mental health care providers, including those delivering ERP, should consider when telehealth is and is not appropriate. Importantly, telehealth offers a limited field of view compared to in-person, and providers can only observe what is captured by the camera. In the context of telehealth ERP, patients may engage in subtle avoidant behaviors that are more difficult to observe, which may prevent them from experiencing necessary anxiety during exposure practice. Many providers may have firsthand experience with this, or patients who appear distracted over telehealth mediums because of environmental factors that can be controlled for during in-person services.
As telehealth treatment options appear increasingly likely to stay, ERP providers and intervention researchers should continue identifying patient characteristics that are more and less appropriate for telehealth settings in order to maximize treatment outcomes. Providers should share concerns with patients when delivering telehealth ERP and work to address interfering factors impacting the course of treatment. In circumstances where this is not possible, such as when the patients age or symptom severity prevents effective telehealth ERP, or when treatment progress stalls, providers should speak with patients to determine if it would be beneficial to transition to in-person services.
Both in-person and telehealth ERP are fundamentally the same, however it does appear that subtle differences across these modalities may have differential impacts on treatment outcomes for certain OCD patient presentations. , however appropriate caution should be exhibited, and providers should use clinical judgment when offering telehealth services.
Dr. Wiese is a clinical psychologist in the department of psychiatry and behavioral sciences at Baylor College of Medicine, Houston, Texas. He is primarily focused on conducting research on OCD and related disorders and providing empirically supported treatments to individuals diagnosed with these conditions.
References
1. Fernandez E et al. Live psychotherapy by video versus in‐person: A meta‐analysis of efficacy and its relationship to types and targets of treatment. Clin Psychol Psychother. 2021 Nov;28(6):1535-49. doi: 10.1002/cpp.2594.
2. Storch EA et al. Preliminary investigation of web-camera delivered cognitive-behavioral therapy for youth with obsessive-compulsive disorder. Psychiatry Res. 2011 Oct 30;189(3):407-12. doi: 10.1016/j.psychres.2011.05.047.
3. Fletcher TL et al. A pilot open trial of video telehealth-delivered exposure and response prevention for obsessive-compulsive disorder in rural Veterans. Mil Psychol. 2021 Oct 28;34(1):83-90. doi: 10.1080/08995605.2021.1970983.
4. Wootton BM. Remote cognitive–behavior therapy for obsessive–compulsive symptoms: a meta-analysis. Clin Psychol Rev. 2016 Feb;43:103-13. doi: 10.1016/j.cpr.2015.10.001.
5. Wiese AD et al. Provider perceptions of telehealth and in-person exposure and response prevention for obsessive–compulsive disorder. Psychiatry Res. 2022 Jul;313:114610. doi: 10.1016/j.psychres.2022.114610.
It is no secret that the COVID-19 pandemic resulted in widespread disruptions in health care services. While providers and resources were limited and many patients were apprehensive to present to health care settings out of concern of disease contraction, telehealth services did offer some relief.
Compared to other specialty care services, mental health care providers were well equipped to handle the expansion of telehealth services, as extensive treatment literature provides strong support for the use of psychotherapeutic interventions over telehealth mediums.1 This holds true in the context of obsessive-compulsive disorder (OCD), where an impressive literature supports the use of telehealth delivery for the gold-standard psychotherapeutic, exposure and response prevention (ERP).2,3,4
Through ERP, patients work with a clinician to systematically expose themselves to anxiety-providing triggers while actively resisting compulsive behaviors to learn the distress does go away with time and/or the distress is within their ability to cope. This intervention is conceptually similar to repeatedly watching a scary film, by which continued exposure results in less pronounced emotional reaction with subsequent viewings.
Fortunately for patients and providers, the expansion of telehealth ERP across different treatment settings has had many unintended benefits, including increased access to care, lower no-show rates due to the ease of attending appointments, and the ability to offer higher levels of care, including intensive outpatient programs, over telehealth mediums. Anecdotally, our clinic has been able to increase patient reach by providing telehealth ERP to those who historically would not have been able to access care due to geography. Even for those living within driving distance to our clinic, the ease of joining a video visit for a 45-minute appointment far outweighs driving into the clinic, in many circumstances. With these benefits, the delivery of ERP over telehealth appears likely to stay, although OCD providers delivering ERP will need to consider when and for whom this medium may not be appropriate.
To this end, we recently conducted a study examining ERP providers perceptions of telehealth and in-person ERP, patient characteristics best suited for telehealth services, and provider ability to identify and address factors that adversely impact the course of treatment (e.g., substance use, limited symptom insight, distractions during ERP, etc.).5 Providers reported lower feasibility ratings for telehealth compared to in-person ERP for younger patients (aged under 13 years), and patients with more severe OCD presentations. Providers also reported more difficulty identifying and addressing ERP interfering factors over telehealth relative to in-person. The findings from our research do not necessarily speak to the effectiveness of telehealth ERP, which has repeatedly been documented in treatment literature, but rather our findings highlight that ERP providers endorse reservations about the feasibility of ERP for certain OCD patient profiles, and that telehealth ERP may not be appropriate for all patients with OCD.
Mental health care providers, including those delivering ERP, should consider when telehealth is and is not appropriate. Importantly, telehealth offers a limited field of view compared to in-person, and providers can only observe what is captured by the camera. In the context of telehealth ERP, patients may engage in subtle avoidant behaviors that are more difficult to observe, which may prevent them from experiencing necessary anxiety during exposure practice. Many providers may have firsthand experience with this, or patients who appear distracted over telehealth mediums because of environmental factors that can be controlled for during in-person services.
As telehealth treatment options appear increasingly likely to stay, ERP providers and intervention researchers should continue identifying patient characteristics that are more and less appropriate for telehealth settings in order to maximize treatment outcomes. Providers should share concerns with patients when delivering telehealth ERP and work to address interfering factors impacting the course of treatment. In circumstances where this is not possible, such as when the patients age or symptom severity prevents effective telehealth ERP, or when treatment progress stalls, providers should speak with patients to determine if it would be beneficial to transition to in-person services.
Both in-person and telehealth ERP are fundamentally the same, however it does appear that subtle differences across these modalities may have differential impacts on treatment outcomes for certain OCD patient presentations. , however appropriate caution should be exhibited, and providers should use clinical judgment when offering telehealth services.
Dr. Wiese is a clinical psychologist in the department of psychiatry and behavioral sciences at Baylor College of Medicine, Houston, Texas. He is primarily focused on conducting research on OCD and related disorders and providing empirically supported treatments to individuals diagnosed with these conditions.
References
1. Fernandez E et al. Live psychotherapy by video versus in‐person: A meta‐analysis of efficacy and its relationship to types and targets of treatment. Clin Psychol Psychother. 2021 Nov;28(6):1535-49. doi: 10.1002/cpp.2594.
2. Storch EA et al. Preliminary investigation of web-camera delivered cognitive-behavioral therapy for youth with obsessive-compulsive disorder. Psychiatry Res. 2011 Oct 30;189(3):407-12. doi: 10.1016/j.psychres.2011.05.047.
3. Fletcher TL et al. A pilot open trial of video telehealth-delivered exposure and response prevention for obsessive-compulsive disorder in rural Veterans. Mil Psychol. 2021 Oct 28;34(1):83-90. doi: 10.1080/08995605.2021.1970983.
4. Wootton BM. Remote cognitive–behavior therapy for obsessive–compulsive symptoms: a meta-analysis. Clin Psychol Rev. 2016 Feb;43:103-13. doi: 10.1016/j.cpr.2015.10.001.
5. Wiese AD et al. Provider perceptions of telehealth and in-person exposure and response prevention for obsessive–compulsive disorder. Psychiatry Res. 2022 Jul;313:114610. doi: 10.1016/j.psychres.2022.114610.
Pediatric obesity treatment options: Beyond lifestyle modification
Pediatric obesity is a serious problem, not only in the United States but worldwide. Unfortunately, the ongoing COVID-19 pandemic has worsened the epidemic of childhood obesity. Solutions for treating the millions of children and adolescents with obesity are desperately needed because prevention efforts over the past several decades have not been sufficient in slowing the steady rise in obesity prevalence.
Lifestyle modification, including dietary changes, increases in activity, and behavioral modification, are the cornerstone of any obesity treatment, but they alone are not powerful enough to treat obesity by itself in the vast majority of children and adolescents. This is because obesity is not a lifestyle choice; rather, it is a disease, and a disease that has a tremendous amount of biology driving individuals toward weight gain and the propensity toward weight regain if weight is lost.
Fortunately, the tools to treat the underlying biology driving obesity are becoming safer, more effective, and more widely used every year. The two most effective biology-based treatments for pediatric obesity are antiobesity medications and bariatric surgery. These two treatments, when accompanied by lifestyle modification, have the potential to reduce not only body weight but also treat many other risk factors, such as prediabetes, diabetes, high blood pressure, poor cholesterol, liver disease, and sleep apnea, as well as others.
Rise in antiobesity medications
Antiobesity medications are developing at a rapid pace. Seven medications have been approved by the Food and Drug Administration for adults, and three medications (phentermine, orlistat, and liraglutide) are now approved for children and adolescents.
The number of antiobesity medications for use in children and adolescents is expected to expand to five, with semaglutide and phentermine-topiramate (Qsymia) both completing trials in adolescents in 2022. Each of these medications works by treating the biology that drives weight gain, whether it is decreasing impulsivity, reducing hunger and appetite hormone pathways, or improving energy regulation pathways. Weight loss at 1 year for currently FDA-approved medications in adolescents ranges from 3% to 6% on average, depending on the medications. The newer medications already FDA approved in adults that will soon, hopefully, be available in pediatrics result in 10%-16% weight loss on average.
A common parent and patient question regarding antiobesity medications is: “If I start an antiobesity medication, how long will I need to be on it?” The simple answer is: “Probably for the rest of your life.”
This can be a shock to hear, but obesity treatment is very similar to that of hypertension or diabetes. Using high blood pressure as an example: If a patient has high blood pressure (for example, 160/90 mm Hg), they will be prescribed a medication to treat it. Once blood pressure comes down to near-normal levels (for example, 120/80 mm Hg), a dose will be maintained, not removed, because that is the biological mediator keeping the blood pressure low. Removal of the medication would result in blood pressure going back to homeostasis (160/90 mm Hg in our example) in a short period of time).
The same can be said for obesity. For example, if a 16-year-old girl is prescribed liraglutide, a glucagonlike peptide–1 receptor agonist, and loses 10% of her body weight at 1 year, that is great success. Why would we remove the medication that is treating the underlying biology causing successful weight loss?
In short, we would not want to do that. Even if our example patient only maintained that 10% initial weight loss, that would be very successful, just like someone maintaining their low blood pressure. As medications begin to develop at a rapid pace and become more available to pediatric patients, the messaging and conversation around anti-obesity medications must continue to focus on obesity being a biological disease and not a behavior for treatment to be effective and not stigmatized.
Bariatric surgery most effective treatment for pediatric obesity
Currently, the most effective treatment for pediatric obesity is bariatric surgery. The two most commonly used surgical procedures today are the sleeve gastrectomy and gastric bypass. Sleeve gastrectomy works by removing 75%-85% of the stomach and creating a new stomach, called a “sleeve.” Gastric bypass works by separating the stomach into two parts and connecting one part of the new stomach into the intestine.
Both surgeries are very effective at treating obesity in adolescents, with an average weight loss of 30%-35%. Surgery is not just a restrictive means of controlling body weight; it also changes key hormones for appetite and satiety that signal the brain. In fact, many of the same biological signals that are changed by surgery are the same signals being targeted by antiobesity medications. Long-term outcome of bariatric surgery in adolescents, provided by Teen-LABS, show it to be safe and maybe even more effective than in adults for treating diabetes and hypertension, with similar weight loss.
Does treatment outweigh the potential risks?
Although obesity surgery and antiobesity medications are more successful at treating obesity in children and adolescents than lifestyle medications, they do have some risks. Surgery, depending on the type of surgery, can cause nutritional deficiencies, reduce body mineral density, and is a life-changing medical procedure. Antiobesity medications, depending on the type, can cause nausea and vomiting and increase heart rate – and because they are relatively new, we do not fully understand the long-term impact of continued use past 1 year.
However, an important question to ask is: “Do the risks of obesity surgery and antiobesity medications outweigh the risk of having lifelong obesity?” The answer to me and many of my colleagues is: “Yes!” Although there are risks associated with the two best treatments for pediatric obesity, those risks under proper supervision of a medical professional far outweigh the risks of not properly treating obesity and allowing it to persist and get worse over many years to come. Obesity is a disease deeply rooted in biology, and we must use biology-based treatments to tackle this problem in children and adolescents, who deserve the best care and treatments possible.
Dr. Ryder is assistant professor of pediatrics and associate director of research, Center for Pediatric Obesity Medicine, at the University of Minnesota, Minneapolis. She reported receiving donations for clinical trials from Boehringer Ingelheim. A version of this article first appeared on Medscape.com.
Pediatric obesity is a serious problem, not only in the United States but worldwide. Unfortunately, the ongoing COVID-19 pandemic has worsened the epidemic of childhood obesity. Solutions for treating the millions of children and adolescents with obesity are desperately needed because prevention efforts over the past several decades have not been sufficient in slowing the steady rise in obesity prevalence.
Lifestyle modification, including dietary changes, increases in activity, and behavioral modification, are the cornerstone of any obesity treatment, but they alone are not powerful enough to treat obesity by itself in the vast majority of children and adolescents. This is because obesity is not a lifestyle choice; rather, it is a disease, and a disease that has a tremendous amount of biology driving individuals toward weight gain and the propensity toward weight regain if weight is lost.
Fortunately, the tools to treat the underlying biology driving obesity are becoming safer, more effective, and more widely used every year. The two most effective biology-based treatments for pediatric obesity are antiobesity medications and bariatric surgery. These two treatments, when accompanied by lifestyle modification, have the potential to reduce not only body weight but also treat many other risk factors, such as prediabetes, diabetes, high blood pressure, poor cholesterol, liver disease, and sleep apnea, as well as others.
Rise in antiobesity medications
Antiobesity medications are developing at a rapid pace. Seven medications have been approved by the Food and Drug Administration for adults, and three medications (phentermine, orlistat, and liraglutide) are now approved for children and adolescents.
The number of antiobesity medications for use in children and adolescents is expected to expand to five, with semaglutide and phentermine-topiramate (Qsymia) both completing trials in adolescents in 2022. Each of these medications works by treating the biology that drives weight gain, whether it is decreasing impulsivity, reducing hunger and appetite hormone pathways, or improving energy regulation pathways. Weight loss at 1 year for currently FDA-approved medications in adolescents ranges from 3% to 6% on average, depending on the medications. The newer medications already FDA approved in adults that will soon, hopefully, be available in pediatrics result in 10%-16% weight loss on average.
A common parent and patient question regarding antiobesity medications is: “If I start an antiobesity medication, how long will I need to be on it?” The simple answer is: “Probably for the rest of your life.”
This can be a shock to hear, but obesity treatment is very similar to that of hypertension or diabetes. Using high blood pressure as an example: If a patient has high blood pressure (for example, 160/90 mm Hg), they will be prescribed a medication to treat it. Once blood pressure comes down to near-normal levels (for example, 120/80 mm Hg), a dose will be maintained, not removed, because that is the biological mediator keeping the blood pressure low. Removal of the medication would result in blood pressure going back to homeostasis (160/90 mm Hg in our example) in a short period of time).
The same can be said for obesity. For example, if a 16-year-old girl is prescribed liraglutide, a glucagonlike peptide–1 receptor agonist, and loses 10% of her body weight at 1 year, that is great success. Why would we remove the medication that is treating the underlying biology causing successful weight loss?
In short, we would not want to do that. Even if our example patient only maintained that 10% initial weight loss, that would be very successful, just like someone maintaining their low blood pressure. As medications begin to develop at a rapid pace and become more available to pediatric patients, the messaging and conversation around anti-obesity medications must continue to focus on obesity being a biological disease and not a behavior for treatment to be effective and not stigmatized.
Bariatric surgery most effective treatment for pediatric obesity
Currently, the most effective treatment for pediatric obesity is bariatric surgery. The two most commonly used surgical procedures today are the sleeve gastrectomy and gastric bypass. Sleeve gastrectomy works by removing 75%-85% of the stomach and creating a new stomach, called a “sleeve.” Gastric bypass works by separating the stomach into two parts and connecting one part of the new stomach into the intestine.
Both surgeries are very effective at treating obesity in adolescents, with an average weight loss of 30%-35%. Surgery is not just a restrictive means of controlling body weight; it also changes key hormones for appetite and satiety that signal the brain. In fact, many of the same biological signals that are changed by surgery are the same signals being targeted by antiobesity medications. Long-term outcome of bariatric surgery in adolescents, provided by Teen-LABS, show it to be safe and maybe even more effective than in adults for treating diabetes and hypertension, with similar weight loss.
Does treatment outweigh the potential risks?
Although obesity surgery and antiobesity medications are more successful at treating obesity in children and adolescents than lifestyle medications, they do have some risks. Surgery, depending on the type of surgery, can cause nutritional deficiencies, reduce body mineral density, and is a life-changing medical procedure. Antiobesity medications, depending on the type, can cause nausea and vomiting and increase heart rate – and because they are relatively new, we do not fully understand the long-term impact of continued use past 1 year.
However, an important question to ask is: “Do the risks of obesity surgery and antiobesity medications outweigh the risk of having lifelong obesity?” The answer to me and many of my colleagues is: “Yes!” Although there are risks associated with the two best treatments for pediatric obesity, those risks under proper supervision of a medical professional far outweigh the risks of not properly treating obesity and allowing it to persist and get worse over many years to come. Obesity is a disease deeply rooted in biology, and we must use biology-based treatments to tackle this problem in children and adolescents, who deserve the best care and treatments possible.
Dr. Ryder is assistant professor of pediatrics and associate director of research, Center for Pediatric Obesity Medicine, at the University of Minnesota, Minneapolis. She reported receiving donations for clinical trials from Boehringer Ingelheim. A version of this article first appeared on Medscape.com.
Pediatric obesity is a serious problem, not only in the United States but worldwide. Unfortunately, the ongoing COVID-19 pandemic has worsened the epidemic of childhood obesity. Solutions for treating the millions of children and adolescents with obesity are desperately needed because prevention efforts over the past several decades have not been sufficient in slowing the steady rise in obesity prevalence.
Lifestyle modification, including dietary changes, increases in activity, and behavioral modification, are the cornerstone of any obesity treatment, but they alone are not powerful enough to treat obesity by itself in the vast majority of children and adolescents. This is because obesity is not a lifestyle choice; rather, it is a disease, and a disease that has a tremendous amount of biology driving individuals toward weight gain and the propensity toward weight regain if weight is lost.
Fortunately, the tools to treat the underlying biology driving obesity are becoming safer, more effective, and more widely used every year. The two most effective biology-based treatments for pediatric obesity are antiobesity medications and bariatric surgery. These two treatments, when accompanied by lifestyle modification, have the potential to reduce not only body weight but also treat many other risk factors, such as prediabetes, diabetes, high blood pressure, poor cholesterol, liver disease, and sleep apnea, as well as others.
Rise in antiobesity medications
Antiobesity medications are developing at a rapid pace. Seven medications have been approved by the Food and Drug Administration for adults, and three medications (phentermine, orlistat, and liraglutide) are now approved for children and adolescents.
The number of antiobesity medications for use in children and adolescents is expected to expand to five, with semaglutide and phentermine-topiramate (Qsymia) both completing trials in adolescents in 2022. Each of these medications works by treating the biology that drives weight gain, whether it is decreasing impulsivity, reducing hunger and appetite hormone pathways, or improving energy regulation pathways. Weight loss at 1 year for currently FDA-approved medications in adolescents ranges from 3% to 6% on average, depending on the medications. The newer medications already FDA approved in adults that will soon, hopefully, be available in pediatrics result in 10%-16% weight loss on average.
A common parent and patient question regarding antiobesity medications is: “If I start an antiobesity medication, how long will I need to be on it?” The simple answer is: “Probably for the rest of your life.”
This can be a shock to hear, but obesity treatment is very similar to that of hypertension or diabetes. Using high blood pressure as an example: If a patient has high blood pressure (for example, 160/90 mm Hg), they will be prescribed a medication to treat it. Once blood pressure comes down to near-normal levels (for example, 120/80 mm Hg), a dose will be maintained, not removed, because that is the biological mediator keeping the blood pressure low. Removal of the medication would result in blood pressure going back to homeostasis (160/90 mm Hg in our example) in a short period of time).
The same can be said for obesity. For example, if a 16-year-old girl is prescribed liraglutide, a glucagonlike peptide–1 receptor agonist, and loses 10% of her body weight at 1 year, that is great success. Why would we remove the medication that is treating the underlying biology causing successful weight loss?
In short, we would not want to do that. Even if our example patient only maintained that 10% initial weight loss, that would be very successful, just like someone maintaining their low blood pressure. As medications begin to develop at a rapid pace and become more available to pediatric patients, the messaging and conversation around anti-obesity medications must continue to focus on obesity being a biological disease and not a behavior for treatment to be effective and not stigmatized.
Bariatric surgery most effective treatment for pediatric obesity
Currently, the most effective treatment for pediatric obesity is bariatric surgery. The two most commonly used surgical procedures today are the sleeve gastrectomy and gastric bypass. Sleeve gastrectomy works by removing 75%-85% of the stomach and creating a new stomach, called a “sleeve.” Gastric bypass works by separating the stomach into two parts and connecting one part of the new stomach into the intestine.
Both surgeries are very effective at treating obesity in adolescents, with an average weight loss of 30%-35%. Surgery is not just a restrictive means of controlling body weight; it also changes key hormones for appetite and satiety that signal the brain. In fact, many of the same biological signals that are changed by surgery are the same signals being targeted by antiobesity medications. Long-term outcome of bariatric surgery in adolescents, provided by Teen-LABS, show it to be safe and maybe even more effective than in adults for treating diabetes and hypertension, with similar weight loss.
Does treatment outweigh the potential risks?
Although obesity surgery and antiobesity medications are more successful at treating obesity in children and adolescents than lifestyle medications, they do have some risks. Surgery, depending on the type of surgery, can cause nutritional deficiencies, reduce body mineral density, and is a life-changing medical procedure. Antiobesity medications, depending on the type, can cause nausea and vomiting and increase heart rate – and because they are relatively new, we do not fully understand the long-term impact of continued use past 1 year.
However, an important question to ask is: “Do the risks of obesity surgery and antiobesity medications outweigh the risk of having lifelong obesity?” The answer to me and many of my colleagues is: “Yes!” Although there are risks associated with the two best treatments for pediatric obesity, those risks under proper supervision of a medical professional far outweigh the risks of not properly treating obesity and allowing it to persist and get worse over many years to come. Obesity is a disease deeply rooted in biology, and we must use biology-based treatments to tackle this problem in children and adolescents, who deserve the best care and treatments possible.
Dr. Ryder is assistant professor of pediatrics and associate director of research, Center for Pediatric Obesity Medicine, at the University of Minnesota, Minneapolis. She reported receiving donations for clinical trials from Boehringer Ingelheim. A version of this article first appeared on Medscape.com.
Meet Argireline, the neurotoxinlike cosmeceutical
Acetyl hexapeptide-8 (or -3), better known by its brand name, Argireline (Lubrizol; Wickliffe, Ohio), is a synthetic peptide gaining popularity in cosmeceutical products for its antiaging benefits. Argireline was developed by the company Lipotec in 2001. Media, beauty bloggers, and product claims have likened this product to a “Botox [or other neurotoxin] alternative,” or “Botox mimicker.”
Mechanism of action
Understanding how Argireline works requires a brief refresher on the mechanism of action of botulinum neurotoxin (BoNT). BoNT relaxes facial muscles and smooths expression lines by inhibiting acetylcholine release at the neuromuscular junction.1 More specifically, the various serotypes of BoNT are single-chain polypeptides that target members of the SNARE complex: SNAP-25, syntaxin, and Vamp. The proteins within the SNARE complex are involved in the docking and fusion of presynaptic vesicles to the presynaptic membrane, necessary steps for acetylcholine release into the neuromuscular junction and muscle contraction. By blocking the action of the SNARE complex proteins, BoNT inhibits release of acetylcholine in the neuromuscular junction and prevents muscle contraction.
Argireline is a synthetic peptide with the sequence Ac-EEMQRR-NH2.2 It is patterned after the N-terminal domain of SNAP-25, one of the members of the SNARE complex targeted by BoNT, and functions to interfere with the assembly of the SNARE complex. In this manner, Argireline would theoretically inhibit fusion of presynaptic vesicles and release of acetylcholine into the neuromuscular junction, thus impeding muscle movement. For this reason, it has been likened to topical Botox. Unlike Botox and other neurotoxins, Argireline was developed for topical application rather than injection.
Preclinical studies
In vitro work done 20 years ago demonstrated that Argireline can prevent assembly of the SNARE complex and inhibit neurotransmitter release with a potency similar to that of BoNT A (Botox).2
In 2013, Wang et al. evaluated the histologic effects of Argireline in aged mouse skin induced by D-galactose. For 6 weeks, Argireline was applied twice daily, and histological changes were assessed using hematoxylin and eosin (H&E) and picrosirius–polarization (PSP) stains. The researchers found elevated levels of type I collagen (P < .01) and reduced type III collagen (P < .05) with the Argireline treatment. These results demonstrated that Argireline could histologically enhance collagen in a manner consistent with skin rejuvenation.3
Clinical studies
In 2002, Blanes et al. assessed the antiwrinkle activity of Argireline by measuring skin topography from silicone implants in the lateral periorbital region of an oil/water (O/W) emulsion containing 10% of the acetyl-hexapeptide in 10 healthy women volunteers. The hexapeptide emulsion was applied twice daily in one lateral periorbital area, and the emulsion vehicle alone was applied twice daily on the contralateral side. Over 30 days of treatment, wrinkle depth was found to have decreased by 30%. The investigators also found that Argireline significantly hindered neurotransmitter release in vitro as robustly as BoNT A, though with notably lower efficacy. No toxicity or irritation was associated with this treatment.2 However, it should be noted that this small study conducted 2 decades ago evaluated only silicone implants with confocal microscopy to evaluate wrinkle depth. There was no subjective clinical assessment of dynamic facial wrinkles. As such, their study is an insufficient basis for drawing conclusions that Argireline is a BoNT mimic. Botox and other types of BoNT affect dynamic facial wrinkles mostly (i.e., wrinkles created by moving muscles of facial expression). This study primarily considers static wrinkles on periorbital skin. While static wrinkles may result from longstanding dynamic wrinkles, BoNT mainly targets dynamic wrinkles, again not comparing apples to apples.
At the same time that Wang et al. conducted their experiment on the skin of aged mice as noted above, they performed a multicenter clinical trial in 60 human subjects who received a randomized treatment of Argireline or placebo in a ratio of 3:1 to assess its safety and efficacy. For 4 weeks, the test product or placebo was applied to periorbital wrinkles twice daily. The researchers found the total antiwrinkle efficacy in the Argireline group to be 48.9% based on the subjective evaluation, compared with 0% in the placebo group. The objective evaluation indicated that all parameters of roughness were diminished in the Argireline group (P < .01), with no reduction observed in the placebo group (P < .05).4 There was a little more to appreciate from this study compared with the one reported by Blanes et al., insofar as subjective evaluations and objective evaluations with silica replicas were done. However, this study was not blinded, so the 48.9% wrinkle reduction in the Argireline group vs. 0% in the control group seems suspicious. Additionally, there was a greater focus on static rather than dynamic wrinkles.
In 2017, Raikou et al. conducted a prospective, randomized controlled study to assess the effects of acetyl hexapeptide-3 (Argireline) and tripeptide-10 citrulline in 24 healthy female volunteers (aged 30-60 years) and determine if there was any synergistic action between the peptides. Subjects were randomized to receive a combination of the peptides, tripeptide-10 citrulline only, acetyl hexapeptide-3 only, or neither peptide for 60 days. The researchers found a significant reduction in transepidermal water loss (TEWL) in the Argireline group, compared with the placebo group.5 The result of this study makes me question if the decrease in depth of the wrinkles measured in the former studies is really just a measure of increased skin hydration from the Argireline, rather than a neurotoxic effect of Argireline.
Formulation and penetration: Can Argireline get through your skin?
One of the fundamental questions regarding Argireline is whether it can penetrate through the stratum corneum and find its target – the facial muscles – where it is intended to function. Argireline is a charged, hydrophilic, and large–molecular weight peptide, and each of these factors impairs penetration through the stratum corneum. Therefore, studies assessing penetration are particularly important.
In 2015, Kraeling et al. conducted an in vitro evaluation of the skin penetration of acetyl hexapeptide-8 in hairless guinea pig and human cadaver skin. An oil-in-water (O/W) emulsion containing 10% acetyl hexapeptide-8 was applied (2 mg/cm2) and penetration was quantified in skin layers via hydrophilic interaction liquid chromatography with tandem mass spectrometry. Most of the acetyl hexapeptide-8 was found to have been washed from human cadaver, as well as guinea pig, skin. Less than 1% of the peptide penetrated the guinea pig or human skin. Of this small amount that penetrated the skin, most stayed in the stratum corneum of guinea pigs (0.54%) and human cadavers (0.22%). The levels of acetyl hexapeptide-8 declined further with each layer of tape stripping removal. Epidermal levels of the peptide in tested skin were similar at 0.01%, and none of the peptide was found in the dermis.6 These results indicate negligible penetration by this highly touted peptide ingredient.
Some studies have shown that altering the formulation of acetyl hexapeptide-8 can enhance penetration. Hoppel et al. demonstrated that formulations of the peptide, especially in a water-oil-water (W/O/W emulsion [as compared with O/W and W/O emulsions] can increase penetration into the stratum corneum in porcine skin.7 Notably, this is still very superficial relative to the dermis and muscles. Irrespective of formulation, studies have shown that Argireline barely penetrates the stratum corneum, let alone the dermis. Therefore, I would give pause to attributing any clinical impact or benefit of Argireline to its neurotoxinlike effects measured in vitro.
Conclusion
Despite the growing popularity of this ingredient in cosmeceuticals and the praise it gets in media for acting as a topical neurotoxin, there are no rigorous clinical trials or data demonstrating its efficacy in suppressing dynamic facial wrinkles like BoNT does. Most importantly, without penetration into the stratum corneum and deeper layers of the skin, it seems unlikely that Argireline’s clinical benefit derives from a neurotoxiclike mechanism of action. It seems more likely that the Argireline-containing product enhances hydration or imparts some other quality to the skin surface. While there is certainly great appeal for a neurotoxinlike product without injections, I do not believe this ingredient will replace injections of BoNT in the foreseeable future, or at least until scientists can figure out how to enable these products to penetrate into the deeper layers of the skin.
Dr. Goldman is a dermatologist in private practice in Miami and specializes in cosmetic and general dermatology. She practices at Baumann Cosmetic & Research Institute and is also opening a general dermatology practice. Dr. Goldman has no relevant disclosures. Write to her at dermnews@mdedge.com or message her on Instagram @DrChloeGoldman.
References
1. Reddy BY et al. Exp Dermatol. 2012 Aug;21(8):569-75.
2. Blanes-Mira C et al. Int J Cosmet Sci. 2002 Oct;24(5):303-10.
3. Wang Y et al. J Cosmet Laser Ther. 2013 Aug;15(4):237-41.
4. Wang Y et al. J Cosmet Laser Ther. 2013;14(2):147-53.
5. Raikou V et al. J Cosmet Dermatol. 2017 Jun;16(2):271-8.
6. Kraeling ME et al. Cutan Ocul Toxicol. 2015 Mar;34(1):46-52.
7. Hoppel M et al. Eur J Pharm Sci. 2015 Feb 20;68:27-35.
Acetyl hexapeptide-8 (or -3), better known by its brand name, Argireline (Lubrizol; Wickliffe, Ohio), is a synthetic peptide gaining popularity in cosmeceutical products for its antiaging benefits. Argireline was developed by the company Lipotec in 2001. Media, beauty bloggers, and product claims have likened this product to a “Botox [or other neurotoxin] alternative,” or “Botox mimicker.”
Mechanism of action
Understanding how Argireline works requires a brief refresher on the mechanism of action of botulinum neurotoxin (BoNT). BoNT relaxes facial muscles and smooths expression lines by inhibiting acetylcholine release at the neuromuscular junction.1 More specifically, the various serotypes of BoNT are single-chain polypeptides that target members of the SNARE complex: SNAP-25, syntaxin, and Vamp. The proteins within the SNARE complex are involved in the docking and fusion of presynaptic vesicles to the presynaptic membrane, necessary steps for acetylcholine release into the neuromuscular junction and muscle contraction. By blocking the action of the SNARE complex proteins, BoNT inhibits release of acetylcholine in the neuromuscular junction and prevents muscle contraction.
Argireline is a synthetic peptide with the sequence Ac-EEMQRR-NH2.2 It is patterned after the N-terminal domain of SNAP-25, one of the members of the SNARE complex targeted by BoNT, and functions to interfere with the assembly of the SNARE complex. In this manner, Argireline would theoretically inhibit fusion of presynaptic vesicles and release of acetylcholine into the neuromuscular junction, thus impeding muscle movement. For this reason, it has been likened to topical Botox. Unlike Botox and other neurotoxins, Argireline was developed for topical application rather than injection.
Preclinical studies
In vitro work done 20 years ago demonstrated that Argireline can prevent assembly of the SNARE complex and inhibit neurotransmitter release with a potency similar to that of BoNT A (Botox).2
In 2013, Wang et al. evaluated the histologic effects of Argireline in aged mouse skin induced by D-galactose. For 6 weeks, Argireline was applied twice daily, and histological changes were assessed using hematoxylin and eosin (H&E) and picrosirius–polarization (PSP) stains. The researchers found elevated levels of type I collagen (P < .01) and reduced type III collagen (P < .05) with the Argireline treatment. These results demonstrated that Argireline could histologically enhance collagen in a manner consistent with skin rejuvenation.3
Clinical studies
In 2002, Blanes et al. assessed the antiwrinkle activity of Argireline by measuring skin topography from silicone implants in the lateral periorbital region of an oil/water (O/W) emulsion containing 10% of the acetyl-hexapeptide in 10 healthy women volunteers. The hexapeptide emulsion was applied twice daily in one lateral periorbital area, and the emulsion vehicle alone was applied twice daily on the contralateral side. Over 30 days of treatment, wrinkle depth was found to have decreased by 30%. The investigators also found that Argireline significantly hindered neurotransmitter release in vitro as robustly as BoNT A, though with notably lower efficacy. No toxicity or irritation was associated with this treatment.2 However, it should be noted that this small study conducted 2 decades ago evaluated only silicone implants with confocal microscopy to evaluate wrinkle depth. There was no subjective clinical assessment of dynamic facial wrinkles. As such, their study is an insufficient basis for drawing conclusions that Argireline is a BoNT mimic. Botox and other types of BoNT affect dynamic facial wrinkles mostly (i.e., wrinkles created by moving muscles of facial expression). This study primarily considers static wrinkles on periorbital skin. While static wrinkles may result from longstanding dynamic wrinkles, BoNT mainly targets dynamic wrinkles, again not comparing apples to apples.
At the same time that Wang et al. conducted their experiment on the skin of aged mice as noted above, they performed a multicenter clinical trial in 60 human subjects who received a randomized treatment of Argireline or placebo in a ratio of 3:1 to assess its safety and efficacy. For 4 weeks, the test product or placebo was applied to periorbital wrinkles twice daily. The researchers found the total antiwrinkle efficacy in the Argireline group to be 48.9% based on the subjective evaluation, compared with 0% in the placebo group. The objective evaluation indicated that all parameters of roughness were diminished in the Argireline group (P < .01), with no reduction observed in the placebo group (P < .05).4 There was a little more to appreciate from this study compared with the one reported by Blanes et al., insofar as subjective evaluations and objective evaluations with silica replicas were done. However, this study was not blinded, so the 48.9% wrinkle reduction in the Argireline group vs. 0% in the control group seems suspicious. Additionally, there was a greater focus on static rather than dynamic wrinkles.
In 2017, Raikou et al. conducted a prospective, randomized controlled study to assess the effects of acetyl hexapeptide-3 (Argireline) and tripeptide-10 citrulline in 24 healthy female volunteers (aged 30-60 years) and determine if there was any synergistic action between the peptides. Subjects were randomized to receive a combination of the peptides, tripeptide-10 citrulline only, acetyl hexapeptide-3 only, or neither peptide for 60 days. The researchers found a significant reduction in transepidermal water loss (TEWL) in the Argireline group, compared with the placebo group.5 The result of this study makes me question if the decrease in depth of the wrinkles measured in the former studies is really just a measure of increased skin hydration from the Argireline, rather than a neurotoxic effect of Argireline.
Formulation and penetration: Can Argireline get through your skin?
One of the fundamental questions regarding Argireline is whether it can penetrate through the stratum corneum and find its target – the facial muscles – where it is intended to function. Argireline is a charged, hydrophilic, and large–molecular weight peptide, and each of these factors impairs penetration through the stratum corneum. Therefore, studies assessing penetration are particularly important.
In 2015, Kraeling et al. conducted an in vitro evaluation of the skin penetration of acetyl hexapeptide-8 in hairless guinea pig and human cadaver skin. An oil-in-water (O/W) emulsion containing 10% acetyl hexapeptide-8 was applied (2 mg/cm2) and penetration was quantified in skin layers via hydrophilic interaction liquid chromatography with tandem mass spectrometry. Most of the acetyl hexapeptide-8 was found to have been washed from human cadaver, as well as guinea pig, skin. Less than 1% of the peptide penetrated the guinea pig or human skin. Of this small amount that penetrated the skin, most stayed in the stratum corneum of guinea pigs (0.54%) and human cadavers (0.22%). The levels of acetyl hexapeptide-8 declined further with each layer of tape stripping removal. Epidermal levels of the peptide in tested skin were similar at 0.01%, and none of the peptide was found in the dermis.6 These results indicate negligible penetration by this highly touted peptide ingredient.
Some studies have shown that altering the formulation of acetyl hexapeptide-8 can enhance penetration. Hoppel et al. demonstrated that formulations of the peptide, especially in a water-oil-water (W/O/W emulsion [as compared with O/W and W/O emulsions] can increase penetration into the stratum corneum in porcine skin.7 Notably, this is still very superficial relative to the dermis and muscles. Irrespective of formulation, studies have shown that Argireline barely penetrates the stratum corneum, let alone the dermis. Therefore, I would give pause to attributing any clinical impact or benefit of Argireline to its neurotoxinlike effects measured in vitro.
Conclusion
Despite the growing popularity of this ingredient in cosmeceuticals and the praise it gets in media for acting as a topical neurotoxin, there are no rigorous clinical trials or data demonstrating its efficacy in suppressing dynamic facial wrinkles like BoNT does. Most importantly, without penetration into the stratum corneum and deeper layers of the skin, it seems unlikely that Argireline’s clinical benefit derives from a neurotoxiclike mechanism of action. It seems more likely that the Argireline-containing product enhances hydration or imparts some other quality to the skin surface. While there is certainly great appeal for a neurotoxinlike product without injections, I do not believe this ingredient will replace injections of BoNT in the foreseeable future, or at least until scientists can figure out how to enable these products to penetrate into the deeper layers of the skin.
Dr. Goldman is a dermatologist in private practice in Miami and specializes in cosmetic and general dermatology. She practices at Baumann Cosmetic & Research Institute and is also opening a general dermatology practice. Dr. Goldman has no relevant disclosures. Write to her at dermnews@mdedge.com or message her on Instagram @DrChloeGoldman.
References
1. Reddy BY et al. Exp Dermatol. 2012 Aug;21(8):569-75.
2. Blanes-Mira C et al. Int J Cosmet Sci. 2002 Oct;24(5):303-10.
3. Wang Y et al. J Cosmet Laser Ther. 2013 Aug;15(4):237-41.
4. Wang Y et al. J Cosmet Laser Ther. 2013;14(2):147-53.
5. Raikou V et al. J Cosmet Dermatol. 2017 Jun;16(2):271-8.
6. Kraeling ME et al. Cutan Ocul Toxicol. 2015 Mar;34(1):46-52.
7. Hoppel M et al. Eur J Pharm Sci. 2015 Feb 20;68:27-35.
Acetyl hexapeptide-8 (or -3), better known by its brand name, Argireline (Lubrizol; Wickliffe, Ohio), is a synthetic peptide gaining popularity in cosmeceutical products for its antiaging benefits. Argireline was developed by the company Lipotec in 2001. Media, beauty bloggers, and product claims have likened this product to a “Botox [or other neurotoxin] alternative,” or “Botox mimicker.”
Mechanism of action
Understanding how Argireline works requires a brief refresher on the mechanism of action of botulinum neurotoxin (BoNT). BoNT relaxes facial muscles and smooths expression lines by inhibiting acetylcholine release at the neuromuscular junction.1 More specifically, the various serotypes of BoNT are single-chain polypeptides that target members of the SNARE complex: SNAP-25, syntaxin, and Vamp. The proteins within the SNARE complex are involved in the docking and fusion of presynaptic vesicles to the presynaptic membrane, necessary steps for acetylcholine release into the neuromuscular junction and muscle contraction. By blocking the action of the SNARE complex proteins, BoNT inhibits release of acetylcholine in the neuromuscular junction and prevents muscle contraction.
Argireline is a synthetic peptide with the sequence Ac-EEMQRR-NH2.2 It is patterned after the N-terminal domain of SNAP-25, one of the members of the SNARE complex targeted by BoNT, and functions to interfere with the assembly of the SNARE complex. In this manner, Argireline would theoretically inhibit fusion of presynaptic vesicles and release of acetylcholine into the neuromuscular junction, thus impeding muscle movement. For this reason, it has been likened to topical Botox. Unlike Botox and other neurotoxins, Argireline was developed for topical application rather than injection.
Preclinical studies
In vitro work done 20 years ago demonstrated that Argireline can prevent assembly of the SNARE complex and inhibit neurotransmitter release with a potency similar to that of BoNT A (Botox).2
In 2013, Wang et al. evaluated the histologic effects of Argireline in aged mouse skin induced by D-galactose. For 6 weeks, Argireline was applied twice daily, and histological changes were assessed using hematoxylin and eosin (H&E) and picrosirius–polarization (PSP) stains. The researchers found elevated levels of type I collagen (P < .01) and reduced type III collagen (P < .05) with the Argireline treatment. These results demonstrated that Argireline could histologically enhance collagen in a manner consistent with skin rejuvenation.3
Clinical studies
In 2002, Blanes et al. assessed the antiwrinkle activity of Argireline by measuring skin topography from silicone implants in the lateral periorbital region of an oil/water (O/W) emulsion containing 10% of the acetyl-hexapeptide in 10 healthy women volunteers. The hexapeptide emulsion was applied twice daily in one lateral periorbital area, and the emulsion vehicle alone was applied twice daily on the contralateral side. Over 30 days of treatment, wrinkle depth was found to have decreased by 30%. The investigators also found that Argireline significantly hindered neurotransmitter release in vitro as robustly as BoNT A, though with notably lower efficacy. No toxicity or irritation was associated with this treatment.2 However, it should be noted that this small study conducted 2 decades ago evaluated only silicone implants with confocal microscopy to evaluate wrinkle depth. There was no subjective clinical assessment of dynamic facial wrinkles. As such, their study is an insufficient basis for drawing conclusions that Argireline is a BoNT mimic. Botox and other types of BoNT affect dynamic facial wrinkles mostly (i.e., wrinkles created by moving muscles of facial expression). This study primarily considers static wrinkles on periorbital skin. While static wrinkles may result from longstanding dynamic wrinkles, BoNT mainly targets dynamic wrinkles, again not comparing apples to apples.
At the same time that Wang et al. conducted their experiment on the skin of aged mice as noted above, they performed a multicenter clinical trial in 60 human subjects who received a randomized treatment of Argireline or placebo in a ratio of 3:1 to assess its safety and efficacy. For 4 weeks, the test product or placebo was applied to periorbital wrinkles twice daily. The researchers found the total antiwrinkle efficacy in the Argireline group to be 48.9% based on the subjective evaluation, compared with 0% in the placebo group. The objective evaluation indicated that all parameters of roughness were diminished in the Argireline group (P < .01), with no reduction observed in the placebo group (P < .05).4 There was a little more to appreciate from this study compared with the one reported by Blanes et al., insofar as subjective evaluations and objective evaluations with silica replicas were done. However, this study was not blinded, so the 48.9% wrinkle reduction in the Argireline group vs. 0% in the control group seems suspicious. Additionally, there was a greater focus on static rather than dynamic wrinkles.
In 2017, Raikou et al. conducted a prospective, randomized controlled study to assess the effects of acetyl hexapeptide-3 (Argireline) and tripeptide-10 citrulline in 24 healthy female volunteers (aged 30-60 years) and determine if there was any synergistic action between the peptides. Subjects were randomized to receive a combination of the peptides, tripeptide-10 citrulline only, acetyl hexapeptide-3 only, or neither peptide for 60 days. The researchers found a significant reduction in transepidermal water loss (TEWL) in the Argireline group, compared with the placebo group.5 The result of this study makes me question if the decrease in depth of the wrinkles measured in the former studies is really just a measure of increased skin hydration from the Argireline, rather than a neurotoxic effect of Argireline.
Formulation and penetration: Can Argireline get through your skin?
One of the fundamental questions regarding Argireline is whether it can penetrate through the stratum corneum and find its target – the facial muscles – where it is intended to function. Argireline is a charged, hydrophilic, and large–molecular weight peptide, and each of these factors impairs penetration through the stratum corneum. Therefore, studies assessing penetration are particularly important.
In 2015, Kraeling et al. conducted an in vitro evaluation of the skin penetration of acetyl hexapeptide-8 in hairless guinea pig and human cadaver skin. An oil-in-water (O/W) emulsion containing 10% acetyl hexapeptide-8 was applied (2 mg/cm2) and penetration was quantified in skin layers via hydrophilic interaction liquid chromatography with tandem mass spectrometry. Most of the acetyl hexapeptide-8 was found to have been washed from human cadaver, as well as guinea pig, skin. Less than 1% of the peptide penetrated the guinea pig or human skin. Of this small amount that penetrated the skin, most stayed in the stratum corneum of guinea pigs (0.54%) and human cadavers (0.22%). The levels of acetyl hexapeptide-8 declined further with each layer of tape stripping removal. Epidermal levels of the peptide in tested skin were similar at 0.01%, and none of the peptide was found in the dermis.6 These results indicate negligible penetration by this highly touted peptide ingredient.
Some studies have shown that altering the formulation of acetyl hexapeptide-8 can enhance penetration. Hoppel et al. demonstrated that formulations of the peptide, especially in a water-oil-water (W/O/W emulsion [as compared with O/W and W/O emulsions] can increase penetration into the stratum corneum in porcine skin.7 Notably, this is still very superficial relative to the dermis and muscles. Irrespective of formulation, studies have shown that Argireline barely penetrates the stratum corneum, let alone the dermis. Therefore, I would give pause to attributing any clinical impact or benefit of Argireline to its neurotoxinlike effects measured in vitro.
Conclusion
Despite the growing popularity of this ingredient in cosmeceuticals and the praise it gets in media for acting as a topical neurotoxin, there are no rigorous clinical trials or data demonstrating its efficacy in suppressing dynamic facial wrinkles like BoNT does. Most importantly, without penetration into the stratum corneum and deeper layers of the skin, it seems unlikely that Argireline’s clinical benefit derives from a neurotoxiclike mechanism of action. It seems more likely that the Argireline-containing product enhances hydration or imparts some other quality to the skin surface. While there is certainly great appeal for a neurotoxinlike product without injections, I do not believe this ingredient will replace injections of BoNT in the foreseeable future, or at least until scientists can figure out how to enable these products to penetrate into the deeper layers of the skin.
Dr. Goldman is a dermatologist in private practice in Miami and specializes in cosmetic and general dermatology. She practices at Baumann Cosmetic & Research Institute and is also opening a general dermatology practice. Dr. Goldman has no relevant disclosures. Write to her at dermnews@mdedge.com or message her on Instagram @DrChloeGoldman.
References
1. Reddy BY et al. Exp Dermatol. 2012 Aug;21(8):569-75.
2. Blanes-Mira C et al. Int J Cosmet Sci. 2002 Oct;24(5):303-10.
3. Wang Y et al. J Cosmet Laser Ther. 2013 Aug;15(4):237-41.
4. Wang Y et al. J Cosmet Laser Ther. 2013;14(2):147-53.
5. Raikou V et al. J Cosmet Dermatol. 2017 Jun;16(2):271-8.
6. Kraeling ME et al. Cutan Ocul Toxicol. 2015 Mar;34(1):46-52.
7. Hoppel M et al. Eur J Pharm Sci. 2015 Feb 20;68:27-35.
No increase in overdose deaths with take-home methadone
new research shows.
Overdose deaths both with and without methadone rose sharply in March 2020, when the policy was announced. Of note, methadone-related deaths decreased in the following months, whereas deaths not involving methadone continued to increase.
“Coupled with research demonstrating improved patient satisfaction, treatment access, and engagement from these policies, these findings can inform decisions about permanently expanding take-home methadone,” the investigators wrote.
The study was published online in JAMA Psychiatry.
An essential tool
Before the pandemic, patients seeking methadone treatment for OUD in the United States had to visit a federally certified opioid treatment clinic every day to receive the medication.
In response to the pandemic, the Substance Abuse and Mental Health Services Administration instituted a new policy that allowed states to request exceptions to provide take-home methadone for up to 4 weeks for stable patients and up to 2 weeks for those who were less stable.
To determine the effect of this policy change on overdose death rates, researchers analyzed data on overdose deaths from January 2019 to August 2021.
Overall, the percentage of deaths involving methadone decreased from 4.5% in 2019 to 3.2% in 2021.
The investigators found a sharp increase in all overdose deaths in March 2020. Deaths that did not involve methadone increased by an average of 78.12 more each month before March 2020, increased by an average of 1,078.27 during March 2020, and then continued to increase by an average of 69.07 more each month after March 2020.
Overdose deaths involving methadone increased by a similar amount in March 2020, stabilized, and then decreased 0.05% per month.
Researchers attributed the increase in methadone-related deaths in March 2020 with the rise in overall drug overdose deaths driven by illicitly made fentanyl in the early months of the COVID-19 pandemic.
A study published in JAMA Network Open in March 2022 showed that methadone and other medications to treat OUD are widely underutilized.
That research cited concern over misuse as a key reason for clinicians’ reluctance to prescribe the drugs. The researchers of the current study hope that these new findings lay some of these fears to rest.
“Treatment is an essential tool to stop the addiction and overdose crises, but it is vastly underused,” Nora Volkow, MD, coinvestigator, and director of the National Institute on Drug Abuse, said in a press release. “This evidence adds significant weight to the argument that effective treatment for substance use disorders should be offered in an accessible and practical way that works for people who need it.”
The study was funded by the Centers for Disease Control and Prevention and the National Institutes of Health. The authors reported no relevant disclosures related to the study.
A version of this article first appeared on Medscape.com.
new research shows.
Overdose deaths both with and without methadone rose sharply in March 2020, when the policy was announced. Of note, methadone-related deaths decreased in the following months, whereas deaths not involving methadone continued to increase.
“Coupled with research demonstrating improved patient satisfaction, treatment access, and engagement from these policies, these findings can inform decisions about permanently expanding take-home methadone,” the investigators wrote.
The study was published online in JAMA Psychiatry.
An essential tool
Before the pandemic, patients seeking methadone treatment for OUD in the United States had to visit a federally certified opioid treatment clinic every day to receive the medication.
In response to the pandemic, the Substance Abuse and Mental Health Services Administration instituted a new policy that allowed states to request exceptions to provide take-home methadone for up to 4 weeks for stable patients and up to 2 weeks for those who were less stable.
To determine the effect of this policy change on overdose death rates, researchers analyzed data on overdose deaths from January 2019 to August 2021.
Overall, the percentage of deaths involving methadone decreased from 4.5% in 2019 to 3.2% in 2021.
The investigators found a sharp increase in all overdose deaths in March 2020. Deaths that did not involve methadone increased by an average of 78.12 more each month before March 2020, increased by an average of 1,078.27 during March 2020, and then continued to increase by an average of 69.07 more each month after March 2020.
Overdose deaths involving methadone increased by a similar amount in March 2020, stabilized, and then decreased 0.05% per month.
Researchers attributed the increase in methadone-related deaths in March 2020 with the rise in overall drug overdose deaths driven by illicitly made fentanyl in the early months of the COVID-19 pandemic.
A study published in JAMA Network Open in March 2022 showed that methadone and other medications to treat OUD are widely underutilized.
That research cited concern over misuse as a key reason for clinicians’ reluctance to prescribe the drugs. The researchers of the current study hope that these new findings lay some of these fears to rest.
“Treatment is an essential tool to stop the addiction and overdose crises, but it is vastly underused,” Nora Volkow, MD, coinvestigator, and director of the National Institute on Drug Abuse, said in a press release. “This evidence adds significant weight to the argument that effective treatment for substance use disorders should be offered in an accessible and practical way that works for people who need it.”
The study was funded by the Centers for Disease Control and Prevention and the National Institutes of Health. The authors reported no relevant disclosures related to the study.
A version of this article first appeared on Medscape.com.
new research shows.
Overdose deaths both with and without methadone rose sharply in March 2020, when the policy was announced. Of note, methadone-related deaths decreased in the following months, whereas deaths not involving methadone continued to increase.
“Coupled with research demonstrating improved patient satisfaction, treatment access, and engagement from these policies, these findings can inform decisions about permanently expanding take-home methadone,” the investigators wrote.
The study was published online in JAMA Psychiatry.
An essential tool
Before the pandemic, patients seeking methadone treatment for OUD in the United States had to visit a federally certified opioid treatment clinic every day to receive the medication.
In response to the pandemic, the Substance Abuse and Mental Health Services Administration instituted a new policy that allowed states to request exceptions to provide take-home methadone for up to 4 weeks for stable patients and up to 2 weeks for those who were less stable.
To determine the effect of this policy change on overdose death rates, researchers analyzed data on overdose deaths from January 2019 to August 2021.
Overall, the percentage of deaths involving methadone decreased from 4.5% in 2019 to 3.2% in 2021.
The investigators found a sharp increase in all overdose deaths in March 2020. Deaths that did not involve methadone increased by an average of 78.12 more each month before March 2020, increased by an average of 1,078.27 during March 2020, and then continued to increase by an average of 69.07 more each month after March 2020.
Overdose deaths involving methadone increased by a similar amount in March 2020, stabilized, and then decreased 0.05% per month.
Researchers attributed the increase in methadone-related deaths in March 2020 with the rise in overall drug overdose deaths driven by illicitly made fentanyl in the early months of the COVID-19 pandemic.
A study published in JAMA Network Open in March 2022 showed that methadone and other medications to treat OUD are widely underutilized.
That research cited concern over misuse as a key reason for clinicians’ reluctance to prescribe the drugs. The researchers of the current study hope that these new findings lay some of these fears to rest.
“Treatment is an essential tool to stop the addiction and overdose crises, but it is vastly underused,” Nora Volkow, MD, coinvestigator, and director of the National Institute on Drug Abuse, said in a press release. “This evidence adds significant weight to the argument that effective treatment for substance use disorders should be offered in an accessible and practical way that works for people who need it.”
The study was funded by the Centers for Disease Control and Prevention and the National Institutes of Health. The authors reported no relevant disclosures related to the study.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY