User login
Late to the game: Parenting after 40
As they rolled me down the hallway to the OR, ceiling lights rhythmically passing above, I zoned out into a 1,000-mile stare. How did I get here? I started humming “Swing Low, Sweet Chariot,” praying for a miracle to happen. I thought back to my birth plan, meticulously crafted, a one-pager so that the no-nonsense labor and delivery nurses wouldn›t think me completely off my rocker. No C-section unless medically necessary. Those words laughed back at me – cackling, even. I’d planned out the whole birthing process and here we were, my team almost jogging me to the OR. I lay still, utterly gobsmacked and partially anesthetized.
If I squint my eyes and hallucinate just a bit, that is sort of what motherhood has been like.
It’s about knowing all the things that could go wrong and meeting the unplanned head-on. Motherhood has indeed been a whirlwind – so many physical, psychological, and emotional transformations. And to top it off, the added effort of giving birth in a pandemic. As an over-40 physician, you’d think I would have been better prepared.
I was, but in a sense, I was not. The knowledge, the wisdom, the experience of my medical training surrounded me, but even I panicked at times in the beginning: Am I feeding her correctly? Am I making enough food for her? Am I doing the best that I can for her? What more could I be doing for her?
Over time, I’ve learned to lighten up. Some. In those teachable moments with my daughter Gia, I’ve learned to not sugarcoat reality but encourage the hopeful. If Gia falls on the ground? “You’re okay, sweetie. Now get back up.” If Gia has a tantrum and starts hitting herself? “Honey, our hands are for hugs, not hurting ourselves. Let’s go play.” Eighty percent of motherhood right now is redirection and the other 20% is patience.
I remember this one time I was rushing out the door for work. After getting in the car with my keys, I realized I forgot my coffee back in the house. I left the car, went back in the house to grab the blessed joe, went back to the car, and couldn’t get in because it was locked. I panicked at that moment, went back inside the house, and found Gia playing with my extra key fob. My own daughter locked me out of my car. Of course, it wasn’t her fault. Deep breath and I offered her another kiss while simultaneously taking the key fob from her.
Before Gia could walk, she could climb the stairs in our home. Her father and I sometimes refer to her as “Lil Bamm-Bamm” because she is so strong. One day, Daddy was supposed to be watching her while Mommy was folding laundry upstairs. She was not allowed on the stairs, but what should I hear? Literally, the pitter-patter of little feet, running down the upstairs hallway. Her father had drifted off watching yet another episode of something Star Wars–related. My strong little girl made it up the stairs all by herself and Dad received a strong word. The Force was with me that day.
I would say that I feel like having a child ages you, but what does that really mean when you’re already old? I’ve become acutely aware of my lack of endurance, stamina, and bodily strength. My knees will creak when taking her upstairs to bed, an osseous dirge of a lullaby. Date nights become unintentionally less and less frequent. Friday night dress-up becomes Friday night dress-down. I’ve replaced stiletto heels with comfy sweats.
Once we put Gia down for the night, we are usually exhausted from the day, and the couch and TV are welcome respites. We exhale. As over-40 parents, we knew that having children late in life would bring its challenges. But I’d like to think that we are meeting them the best way that we can. Often I encourage my body to meet Gia at her eye level, see what she sees, play with her on her own terms, and match her energy. She absolutely loves it when I do this. I’m out of breath and my knees are sore by the end of our play session, but I wouldn’t have it any other way.
We are learning from each other. She has a bright and assertive personality, and I am protective of that innocence. Her innocence is without fear. I often wonder what she is thinking when I see her facial expressions. A side-eye, a fleeting giggle. Is she secretly contemplating the chronicity of the cosmos, or is it just gas? I look at her in stolen moments and still can’t believe that I grew a human inside me, and said human was extracted from me and is now walking around my house commanding her bidding. So surreal. The unromanticized, scientific ingredients that are at play from conception to delivery are nothing short of miraculous. And the miracles of parenting over 40 are present every day.
Dr. Tolliver is a family medicine physician at The Ohio State University Wexner Medical Center in Columbus. A version of this article first appeared on Medscape.com.
As they rolled me down the hallway to the OR, ceiling lights rhythmically passing above, I zoned out into a 1,000-mile stare. How did I get here? I started humming “Swing Low, Sweet Chariot,” praying for a miracle to happen. I thought back to my birth plan, meticulously crafted, a one-pager so that the no-nonsense labor and delivery nurses wouldn›t think me completely off my rocker. No C-section unless medically necessary. Those words laughed back at me – cackling, even. I’d planned out the whole birthing process and here we were, my team almost jogging me to the OR. I lay still, utterly gobsmacked and partially anesthetized.
If I squint my eyes and hallucinate just a bit, that is sort of what motherhood has been like.
It’s about knowing all the things that could go wrong and meeting the unplanned head-on. Motherhood has indeed been a whirlwind – so many physical, psychological, and emotional transformations. And to top it off, the added effort of giving birth in a pandemic. As an over-40 physician, you’d think I would have been better prepared.
I was, but in a sense, I was not. The knowledge, the wisdom, the experience of my medical training surrounded me, but even I panicked at times in the beginning: Am I feeding her correctly? Am I making enough food for her? Am I doing the best that I can for her? What more could I be doing for her?
Over time, I’ve learned to lighten up. Some. In those teachable moments with my daughter Gia, I’ve learned to not sugarcoat reality but encourage the hopeful. If Gia falls on the ground? “You’re okay, sweetie. Now get back up.” If Gia has a tantrum and starts hitting herself? “Honey, our hands are for hugs, not hurting ourselves. Let’s go play.” Eighty percent of motherhood right now is redirection and the other 20% is patience.
I remember this one time I was rushing out the door for work. After getting in the car with my keys, I realized I forgot my coffee back in the house. I left the car, went back in the house to grab the blessed joe, went back to the car, and couldn’t get in because it was locked. I panicked at that moment, went back inside the house, and found Gia playing with my extra key fob. My own daughter locked me out of my car. Of course, it wasn’t her fault. Deep breath and I offered her another kiss while simultaneously taking the key fob from her.
Before Gia could walk, she could climb the stairs in our home. Her father and I sometimes refer to her as “Lil Bamm-Bamm” because she is so strong. One day, Daddy was supposed to be watching her while Mommy was folding laundry upstairs. She was not allowed on the stairs, but what should I hear? Literally, the pitter-patter of little feet, running down the upstairs hallway. Her father had drifted off watching yet another episode of something Star Wars–related. My strong little girl made it up the stairs all by herself and Dad received a strong word. The Force was with me that day.
I would say that I feel like having a child ages you, but what does that really mean when you’re already old? I’ve become acutely aware of my lack of endurance, stamina, and bodily strength. My knees will creak when taking her upstairs to bed, an osseous dirge of a lullaby. Date nights become unintentionally less and less frequent. Friday night dress-up becomes Friday night dress-down. I’ve replaced stiletto heels with comfy sweats.
Once we put Gia down for the night, we are usually exhausted from the day, and the couch and TV are welcome respites. We exhale. As over-40 parents, we knew that having children late in life would bring its challenges. But I’d like to think that we are meeting them the best way that we can. Often I encourage my body to meet Gia at her eye level, see what she sees, play with her on her own terms, and match her energy. She absolutely loves it when I do this. I’m out of breath and my knees are sore by the end of our play session, but I wouldn’t have it any other way.
We are learning from each other. She has a bright and assertive personality, and I am protective of that innocence. Her innocence is without fear. I often wonder what she is thinking when I see her facial expressions. A side-eye, a fleeting giggle. Is she secretly contemplating the chronicity of the cosmos, or is it just gas? I look at her in stolen moments and still can’t believe that I grew a human inside me, and said human was extracted from me and is now walking around my house commanding her bidding. So surreal. The unromanticized, scientific ingredients that are at play from conception to delivery are nothing short of miraculous. And the miracles of parenting over 40 are present every day.
Dr. Tolliver is a family medicine physician at The Ohio State University Wexner Medical Center in Columbus. A version of this article first appeared on Medscape.com.
As they rolled me down the hallway to the OR, ceiling lights rhythmically passing above, I zoned out into a 1,000-mile stare. How did I get here? I started humming “Swing Low, Sweet Chariot,” praying for a miracle to happen. I thought back to my birth plan, meticulously crafted, a one-pager so that the no-nonsense labor and delivery nurses wouldn›t think me completely off my rocker. No C-section unless medically necessary. Those words laughed back at me – cackling, even. I’d planned out the whole birthing process and here we were, my team almost jogging me to the OR. I lay still, utterly gobsmacked and partially anesthetized.
If I squint my eyes and hallucinate just a bit, that is sort of what motherhood has been like.
It’s about knowing all the things that could go wrong and meeting the unplanned head-on. Motherhood has indeed been a whirlwind – so many physical, psychological, and emotional transformations. And to top it off, the added effort of giving birth in a pandemic. As an over-40 physician, you’d think I would have been better prepared.
I was, but in a sense, I was not. The knowledge, the wisdom, the experience of my medical training surrounded me, but even I panicked at times in the beginning: Am I feeding her correctly? Am I making enough food for her? Am I doing the best that I can for her? What more could I be doing for her?
Over time, I’ve learned to lighten up. Some. In those teachable moments with my daughter Gia, I’ve learned to not sugarcoat reality but encourage the hopeful. If Gia falls on the ground? “You’re okay, sweetie. Now get back up.” If Gia has a tantrum and starts hitting herself? “Honey, our hands are for hugs, not hurting ourselves. Let’s go play.” Eighty percent of motherhood right now is redirection and the other 20% is patience.
I remember this one time I was rushing out the door for work. After getting in the car with my keys, I realized I forgot my coffee back in the house. I left the car, went back in the house to grab the blessed joe, went back to the car, and couldn’t get in because it was locked. I panicked at that moment, went back inside the house, and found Gia playing with my extra key fob. My own daughter locked me out of my car. Of course, it wasn’t her fault. Deep breath and I offered her another kiss while simultaneously taking the key fob from her.
Before Gia could walk, she could climb the stairs in our home. Her father and I sometimes refer to her as “Lil Bamm-Bamm” because she is so strong. One day, Daddy was supposed to be watching her while Mommy was folding laundry upstairs. She was not allowed on the stairs, but what should I hear? Literally, the pitter-patter of little feet, running down the upstairs hallway. Her father had drifted off watching yet another episode of something Star Wars–related. My strong little girl made it up the stairs all by herself and Dad received a strong word. The Force was with me that day.
I would say that I feel like having a child ages you, but what does that really mean when you’re already old? I’ve become acutely aware of my lack of endurance, stamina, and bodily strength. My knees will creak when taking her upstairs to bed, an osseous dirge of a lullaby. Date nights become unintentionally less and less frequent. Friday night dress-up becomes Friday night dress-down. I’ve replaced stiletto heels with comfy sweats.
Once we put Gia down for the night, we are usually exhausted from the day, and the couch and TV are welcome respites. We exhale. As over-40 parents, we knew that having children late in life would bring its challenges. But I’d like to think that we are meeting them the best way that we can. Often I encourage my body to meet Gia at her eye level, see what she sees, play with her on her own terms, and match her energy. She absolutely loves it when I do this. I’m out of breath and my knees are sore by the end of our play session, but I wouldn’t have it any other way.
We are learning from each other. She has a bright and assertive personality, and I am protective of that innocence. Her innocence is without fear. I often wonder what she is thinking when I see her facial expressions. A side-eye, a fleeting giggle. Is she secretly contemplating the chronicity of the cosmos, or is it just gas? I look at her in stolen moments and still can’t believe that I grew a human inside me, and said human was extracted from me and is now walking around my house commanding her bidding. So surreal. The unromanticized, scientific ingredients that are at play from conception to delivery are nothing short of miraculous. And the miracles of parenting over 40 are present every day.
Dr. Tolliver is a family medicine physician at The Ohio State University Wexner Medical Center in Columbus. A version of this article first appeared on Medscape.com.
Histologic remission predicts relapse-free survival in UC
Histologic remission using the Nancy Histologic Index (NHI) was superior to endoscopic mucosal healing in predicting relapse-free survival in ulcerative colitis (UC), based on data from 74 patients.
A growing body of evidence suggests that UC patients in both histologic and endoscopic remission experience longer relapse-free survival and improved outcomes, but data on specific histologic assessments are limited, wrote Hunter Wang, MBBS, of Canberra Hospital, Australia, and colleagues. The NHI is a validated score drawing interest as an option for predicting survival, they said.
In a retrospective cohort study published Feb. 28 in the Journal of Clinical Gastroenterology, the researchers identified 74 adults aged 18 years and older with UC who were treated at a single center between 2009 and 2017. All patients were in clinical and endoscopic remission without concurrent corticosteroid use. Mucosal healing was defined as Mayo endoscopic subscore (MES) of 1 or less, and clinical remission was defined as partial Mayo score (MSp) less than 2. The median age of the participants was 41 years, and the median disease duration was 8 years at the time of surveillance colonoscopy.
Over a median follow-up of 42 months, patients with an MES of 0 and histologic remission had significantly longer relapse-free survival compared to those with MES 1 and NHI 2 to 4, respectively.
Thirty-three patients relapsed during the study period. Clinical relapse rates were similar for patients with MES 0 and MES 1 (40% and 52%, respectively), but only 29% of patients in histologic remission at baseline relapsed vs. 64% of those with histologic activity at baseline (P = 0.0064).
Risk factors for earlier relapse on univariate analysis included MES 1 and NHI 2 to 4. Only histologic activity predicted future relapse in a multivariate analysis (hazard ratio, 4.36, P = 0.002).
The study findings reflect data from previous research supporting the prognostic value of histologic remission using NHI, the researchers noted in their discussion. Barriers to adoption of histologic indices include “their multiplicity, complexity, lack of validation, and inconsistent incorporation in randomized controlled trials,” which create challenges in interpreting and comparing research outcomes, they wrote.
The study findings were limited by several factors, including the retrospective design, collection of clinical and endoscopic variables from electronic medical records without objective measures of relapse, lack of standardization of colonic biopsies, and lack of power to detect differences in dysplasia and colectomy, the researchers noted.
The results suggest that histologic remission using the NHI serves as an effective predictor of longer relapse-free survival in UC patients with clinical and endoscopic remission, they said.
“Further prospective trials are needed to clarify whether histologic remission as a therapeutic endpoint in addition to endoscopic remission will alter disease course and patient outcomes,” while helping guide treatment management decisions for patients and clinicians, the researchers concluded.
Not the ultimate endpoint?
“There is ongoing interest in whether histological findings (biopsies) of the mucosa are a clinically important and reachable treatment goal in ulcerative colitis,” David T. Rubin, MD, of the University of Chicago, who was not involved in the study, said in an interview.
Questions about this approach remain, such as how findings should be incorporated into clinical care and whether histology offers advantages over patient-reported symptoms, endoscopic findings, or other surrogates of inflammation like calprotectin, a protein related to histology detected in stool, Dr. Rubin explained.
“A number of retrospective studies have demonstrated the clinical importance of achieving histological remission, but the details of how to get there are not yet clearly defined. In this study, using one of the established indices of histological activity, the Nancy Histological Index, those patients who achieved histological remission had better clinical outcomes (stable remission) than symptoms alone or endoscopy alone.”
According to Dr. Rubin, clinicians can inform patients that histological remission supports that the therapy is working and they have a very good likelihood of staying in remission over the next year.
“Importantly, this is not the same as saying we should treat to get to this endpoint,” Dr. Rubin emphasized. “If a patient is in clinical remission with normalized labs and endoscopy (or calprotectin) that show healing, we do not yet recommend adjusting therapy for histological endpoints. This was edified in the consensus paper called STRIDE 2, published in Gastroenterology in 2021.”
As for additional research, the ongoing prospective randomized VERDICT trial is exploring different endpoints of treatment, “one of which is the combination of symptoms, endoscopy, and histology to assess whether this is better than symptoms or endoscopy alone,” said Dr. Rubin. “We also need more work to understand the timing of this finding, the number of biopsies that may be required to get an adequate assessment of the bowel, how pathologists should read and interpret our findings, when we should relook if we adjust therapy, and whether some therapies are more or less likely to achieve this endpoint,” he said.
The study received no outside funding. Neither the researchers nor Dr. Rubin reported any financial disclosures.
Histologic remission using the Nancy Histologic Index (NHI) was superior to endoscopic mucosal healing in predicting relapse-free survival in ulcerative colitis (UC), based on data from 74 patients.
A growing body of evidence suggests that UC patients in both histologic and endoscopic remission experience longer relapse-free survival and improved outcomes, but data on specific histologic assessments are limited, wrote Hunter Wang, MBBS, of Canberra Hospital, Australia, and colleagues. The NHI is a validated score drawing interest as an option for predicting survival, they said.
In a retrospective cohort study published Feb. 28 in the Journal of Clinical Gastroenterology, the researchers identified 74 adults aged 18 years and older with UC who were treated at a single center between 2009 and 2017. All patients were in clinical and endoscopic remission without concurrent corticosteroid use. Mucosal healing was defined as Mayo endoscopic subscore (MES) of 1 or less, and clinical remission was defined as partial Mayo score (MSp) less than 2. The median age of the participants was 41 years, and the median disease duration was 8 years at the time of surveillance colonoscopy.
Over a median follow-up of 42 months, patients with an MES of 0 and histologic remission had significantly longer relapse-free survival compared to those with MES 1 and NHI 2 to 4, respectively.
Thirty-three patients relapsed during the study period. Clinical relapse rates were similar for patients with MES 0 and MES 1 (40% and 52%, respectively), but only 29% of patients in histologic remission at baseline relapsed vs. 64% of those with histologic activity at baseline (P = 0.0064).
Risk factors for earlier relapse on univariate analysis included MES 1 and NHI 2 to 4. Only histologic activity predicted future relapse in a multivariate analysis (hazard ratio, 4.36, P = 0.002).
The study findings reflect data from previous research supporting the prognostic value of histologic remission using NHI, the researchers noted in their discussion. Barriers to adoption of histologic indices include “their multiplicity, complexity, lack of validation, and inconsistent incorporation in randomized controlled trials,” which create challenges in interpreting and comparing research outcomes, they wrote.
The study findings were limited by several factors, including the retrospective design, collection of clinical and endoscopic variables from electronic medical records without objective measures of relapse, lack of standardization of colonic biopsies, and lack of power to detect differences in dysplasia and colectomy, the researchers noted.
The results suggest that histologic remission using the NHI serves as an effective predictor of longer relapse-free survival in UC patients with clinical and endoscopic remission, they said.
“Further prospective trials are needed to clarify whether histologic remission as a therapeutic endpoint in addition to endoscopic remission will alter disease course and patient outcomes,” while helping guide treatment management decisions for patients and clinicians, the researchers concluded.
Not the ultimate endpoint?
“There is ongoing interest in whether histological findings (biopsies) of the mucosa are a clinically important and reachable treatment goal in ulcerative colitis,” David T. Rubin, MD, of the University of Chicago, who was not involved in the study, said in an interview.
Questions about this approach remain, such as how findings should be incorporated into clinical care and whether histology offers advantages over patient-reported symptoms, endoscopic findings, or other surrogates of inflammation like calprotectin, a protein related to histology detected in stool, Dr. Rubin explained.
“A number of retrospective studies have demonstrated the clinical importance of achieving histological remission, but the details of how to get there are not yet clearly defined. In this study, using one of the established indices of histological activity, the Nancy Histological Index, those patients who achieved histological remission had better clinical outcomes (stable remission) than symptoms alone or endoscopy alone.”
According to Dr. Rubin, clinicians can inform patients that histological remission supports that the therapy is working and they have a very good likelihood of staying in remission over the next year.
“Importantly, this is not the same as saying we should treat to get to this endpoint,” Dr. Rubin emphasized. “If a patient is in clinical remission with normalized labs and endoscopy (or calprotectin) that show healing, we do not yet recommend adjusting therapy for histological endpoints. This was edified in the consensus paper called STRIDE 2, published in Gastroenterology in 2021.”
As for additional research, the ongoing prospective randomized VERDICT trial is exploring different endpoints of treatment, “one of which is the combination of symptoms, endoscopy, and histology to assess whether this is better than symptoms or endoscopy alone,” said Dr. Rubin. “We also need more work to understand the timing of this finding, the number of biopsies that may be required to get an adequate assessment of the bowel, how pathologists should read and interpret our findings, when we should relook if we adjust therapy, and whether some therapies are more or less likely to achieve this endpoint,” he said.
The study received no outside funding. Neither the researchers nor Dr. Rubin reported any financial disclosures.
Histologic remission using the Nancy Histologic Index (NHI) was superior to endoscopic mucosal healing in predicting relapse-free survival in ulcerative colitis (UC), based on data from 74 patients.
A growing body of evidence suggests that UC patients in both histologic and endoscopic remission experience longer relapse-free survival and improved outcomes, but data on specific histologic assessments are limited, wrote Hunter Wang, MBBS, of Canberra Hospital, Australia, and colleagues. The NHI is a validated score drawing interest as an option for predicting survival, they said.
In a retrospective cohort study published Feb. 28 in the Journal of Clinical Gastroenterology, the researchers identified 74 adults aged 18 years and older with UC who were treated at a single center between 2009 and 2017. All patients were in clinical and endoscopic remission without concurrent corticosteroid use. Mucosal healing was defined as Mayo endoscopic subscore (MES) of 1 or less, and clinical remission was defined as partial Mayo score (MSp) less than 2. The median age of the participants was 41 years, and the median disease duration was 8 years at the time of surveillance colonoscopy.
Over a median follow-up of 42 months, patients with an MES of 0 and histologic remission had significantly longer relapse-free survival compared to those with MES 1 and NHI 2 to 4, respectively.
Thirty-three patients relapsed during the study period. Clinical relapse rates were similar for patients with MES 0 and MES 1 (40% and 52%, respectively), but only 29% of patients in histologic remission at baseline relapsed vs. 64% of those with histologic activity at baseline (P = 0.0064).
Risk factors for earlier relapse on univariate analysis included MES 1 and NHI 2 to 4. Only histologic activity predicted future relapse in a multivariate analysis (hazard ratio, 4.36, P = 0.002).
The study findings reflect data from previous research supporting the prognostic value of histologic remission using NHI, the researchers noted in their discussion. Barriers to adoption of histologic indices include “their multiplicity, complexity, lack of validation, and inconsistent incorporation in randomized controlled trials,” which create challenges in interpreting and comparing research outcomes, they wrote.
The study findings were limited by several factors, including the retrospective design, collection of clinical and endoscopic variables from electronic medical records without objective measures of relapse, lack of standardization of colonic biopsies, and lack of power to detect differences in dysplasia and colectomy, the researchers noted.
The results suggest that histologic remission using the NHI serves as an effective predictor of longer relapse-free survival in UC patients with clinical and endoscopic remission, they said.
“Further prospective trials are needed to clarify whether histologic remission as a therapeutic endpoint in addition to endoscopic remission will alter disease course and patient outcomes,” while helping guide treatment management decisions for patients and clinicians, the researchers concluded.
Not the ultimate endpoint?
“There is ongoing interest in whether histological findings (biopsies) of the mucosa are a clinically important and reachable treatment goal in ulcerative colitis,” David T. Rubin, MD, of the University of Chicago, who was not involved in the study, said in an interview.
Questions about this approach remain, such as how findings should be incorporated into clinical care and whether histology offers advantages over patient-reported symptoms, endoscopic findings, or other surrogates of inflammation like calprotectin, a protein related to histology detected in stool, Dr. Rubin explained.
“A number of retrospective studies have demonstrated the clinical importance of achieving histological remission, but the details of how to get there are not yet clearly defined. In this study, using one of the established indices of histological activity, the Nancy Histological Index, those patients who achieved histological remission had better clinical outcomes (stable remission) than symptoms alone or endoscopy alone.”
According to Dr. Rubin, clinicians can inform patients that histological remission supports that the therapy is working and they have a very good likelihood of staying in remission over the next year.
“Importantly, this is not the same as saying we should treat to get to this endpoint,” Dr. Rubin emphasized. “If a patient is in clinical remission with normalized labs and endoscopy (or calprotectin) that show healing, we do not yet recommend adjusting therapy for histological endpoints. This was edified in the consensus paper called STRIDE 2, published in Gastroenterology in 2021.”
As for additional research, the ongoing prospective randomized VERDICT trial is exploring different endpoints of treatment, “one of which is the combination of symptoms, endoscopy, and histology to assess whether this is better than symptoms or endoscopy alone,” said Dr. Rubin. “We also need more work to understand the timing of this finding, the number of biopsies that may be required to get an adequate assessment of the bowel, how pathologists should read and interpret our findings, when we should relook if we adjust therapy, and whether some therapies are more or less likely to achieve this endpoint,” he said.
The study received no outside funding. Neither the researchers nor Dr. Rubin reported any financial disclosures.
FROM THE JOURNAL OF CLINICAL GASTROENTEROLOGY
Monitor children’s thyroids after iodine exposure for imaging, FDA says
The Food and Drug Administration has recommended thyroid monitoring for newborns and children through 3 years of age within 3 weeks of receiving injections of iodine-containing contrast media as part of imaging procedures.
A recent FDA review showed that “underactive thyroid or a temporary decrease in thyroid hormone levels were uncommon,” according to an updated Drug Safety Communication issued on March 30, 2022.
However, early monitoring will help identify and treat any thyroid abnormalities as a result of the injections to help prevent potential complications in the future, according to the FDA, as babies and children do not generally show visible signs of thyroid problems and may not do so after an iodinated contrast media (ICM) injection.
ICM have been approved and used for decades to enhance images on x-rays or computed tomography (CT) scans, according to the communication.
The new FDA warning and recommendation for monitoring applies to the prescribing information for the entire class of ICM products. The new communication is an update to the 2015 Drug Safety Communication that advised medical professionals of the potential for underactive thyroid in response to ICM injections in newborns and young children. The update reflects new studies since that time.
The recent research showed that most reported cases of adverse effects were transient subclinical hypothyroidism and did not require treatment, according to the FDA. “The reported rate ranged from 1 percent to 15 percent and tended to be higher in neonates, particularly preterm neonates,” they said. Others at increased risk are those with underlying medical conditions, especially those with cardiac conditions who often require higher doses of contrast during invasive procedures.
In the recent studies, the time from ICM exposure to a diagnosis of thyroid dysfunction ranged from 8.5 to 138 days, but most occurred within 3 weeks, according to the update.
Patients and clinicians can report any adverse events from ICM or other medications to the FDA via FDA MedWatch program.
For more information, read the complete Drug Safety Communication.
The Food and Drug Administration has recommended thyroid monitoring for newborns and children through 3 years of age within 3 weeks of receiving injections of iodine-containing contrast media as part of imaging procedures.
A recent FDA review showed that “underactive thyroid or a temporary decrease in thyroid hormone levels were uncommon,” according to an updated Drug Safety Communication issued on March 30, 2022.
However, early monitoring will help identify and treat any thyroid abnormalities as a result of the injections to help prevent potential complications in the future, according to the FDA, as babies and children do not generally show visible signs of thyroid problems and may not do so after an iodinated contrast media (ICM) injection.
ICM have been approved and used for decades to enhance images on x-rays or computed tomography (CT) scans, according to the communication.
The new FDA warning and recommendation for monitoring applies to the prescribing information for the entire class of ICM products. The new communication is an update to the 2015 Drug Safety Communication that advised medical professionals of the potential for underactive thyroid in response to ICM injections in newborns and young children. The update reflects new studies since that time.
The recent research showed that most reported cases of adverse effects were transient subclinical hypothyroidism and did not require treatment, according to the FDA. “The reported rate ranged from 1 percent to 15 percent and tended to be higher in neonates, particularly preterm neonates,” they said. Others at increased risk are those with underlying medical conditions, especially those with cardiac conditions who often require higher doses of contrast during invasive procedures.
In the recent studies, the time from ICM exposure to a diagnosis of thyroid dysfunction ranged from 8.5 to 138 days, but most occurred within 3 weeks, according to the update.
Patients and clinicians can report any adverse events from ICM or other medications to the FDA via FDA MedWatch program.
For more information, read the complete Drug Safety Communication.
The Food and Drug Administration has recommended thyroid monitoring for newborns and children through 3 years of age within 3 weeks of receiving injections of iodine-containing contrast media as part of imaging procedures.
A recent FDA review showed that “underactive thyroid or a temporary decrease in thyroid hormone levels were uncommon,” according to an updated Drug Safety Communication issued on March 30, 2022.
However, early monitoring will help identify and treat any thyroid abnormalities as a result of the injections to help prevent potential complications in the future, according to the FDA, as babies and children do not generally show visible signs of thyroid problems and may not do so after an iodinated contrast media (ICM) injection.
ICM have been approved and used for decades to enhance images on x-rays or computed tomography (CT) scans, according to the communication.
The new FDA warning and recommendation for monitoring applies to the prescribing information for the entire class of ICM products. The new communication is an update to the 2015 Drug Safety Communication that advised medical professionals of the potential for underactive thyroid in response to ICM injections in newborns and young children. The update reflects new studies since that time.
The recent research showed that most reported cases of adverse effects were transient subclinical hypothyroidism and did not require treatment, according to the FDA. “The reported rate ranged from 1 percent to 15 percent and tended to be higher in neonates, particularly preterm neonates,” they said. Others at increased risk are those with underlying medical conditions, especially those with cardiac conditions who often require higher doses of contrast during invasive procedures.
In the recent studies, the time from ICM exposure to a diagnosis of thyroid dysfunction ranged from 8.5 to 138 days, but most occurred within 3 weeks, according to the update.
Patients and clinicians can report any adverse events from ICM or other medications to the FDA via FDA MedWatch program.
For more information, read the complete Drug Safety Communication.
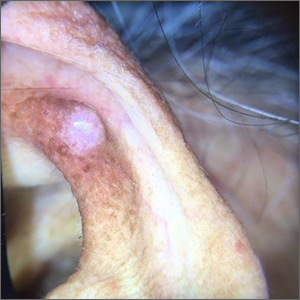
Melanoma increasing, but is this overdiagnosis?
Melanoma has been increasing in incidence in the United States over the last few decades, but is this a true increase? Or is this a case of overdiagnosis, fueled by screening?
A new study argues the case for overdiagnosis.
commented lead author lead author Adewole Adamson, MD, an assistant professor of internal medicine, division of dermatology, at the University of Texas at Austin.
He posted this conclusion on Twitter after the study was published in JAMA Dermatology.
“The discrepancies in incidence and mortality trends found in this cohort study suggest considerable overdiagnosis of melanoma occurring among White patients in the U.S.,” the authors concluded.
They estimated that an estimated 59% of White women and 60% of White men with melanoma were overdiagnosed in 2014.
These results are similar to those from a recent study from Australia, which used a different method of assessing overdiagnosis. Those findings estimated that 54%-58% of melanoma cases represented overdiagnosis in Australia, Dr. Adamson noted.
“Our estimates shed light on the HUGE scope of this problem in the United States that we need to address,” Dr. Adamson commented on Twitter. “Calls for screening for melanoma in the general public will only push these numbers higher, and make patients out of healthy people.”
“Screening the general population for melanoma has never been shown to save lives and likely is responsible for the increase in melanoma overdiagnosis,” Dr. Adamson said in an interview. “Screening average- and/or low-risk patients is of low value and the harms may outweigh the theoretical benefits.”
Screening programs should be directed to those who may derive the most benefit. “Screening should be limited to high-risk patients such as older White men, patients with a lot of atypical nevi, heavy sun exposure, fair skin, and red hair,” he said. “Just like for other cancers, such as breast, prostate, and colorectal, there should be clear guidelines as to which populations to screen, as well as when to start and when to stop screening.”
Overdiagnosis is defined as the diagnosis of cancer that would never have caused any symptoms or problems in a patient’s lifetime. But therein lies the problem, explained Dr. Adamson. “Because we do not know which early, screen-detected skin cancers would be destined to progress, we are obligated to treat all of them.” There is evidence to suggest that melanoma in situ is not an obligate precursor lesion to invasive melanoma, similar to the situation in which not all ductal carcinoma in situ leads to invasive breast cancer. “It is possible that less aggressive management strategies could be the subject of future studies,” he said.
Patients out of healthy people
For their study, Dr. Adamson and colleagues compared rates of melanoma among White and Black patients. Melanoma is much less common among Black individuals, and they are also less likely to be screened. Additionally, screening rates among Black patients have remained more or less the same over the last decades, whereas screening has increased in White patients.
The team used trends in mortality as a result of melanoma in Black patients as a marker for improvements in medical care. From this, they estimated the expected mortality trends in White patients if medical care had not improved. This served as a marker for the change in true cancer occurrence. Overdiagnosis was calculated as the difference between observed incidence and estimated true cancer occurrence.
The incidence of melanoma rose dramatically among White patients from 1975 to 2014, increasing about fourfold in White women (incidence rate ratio, 4.01) and sixfold in White men (IRR, 5.97).
At the same time, there was much smaller increase (of less than 25%) in the incidence of melanoma in both Black women and Black men.
In that time period, melanoma-related mortality decreased approximately 25% in Black women and men; it remained stable in White women, but increased almost 50% in White men.
Had medical care not improved, estimated mortality would have increased 60% in White women and more than doubled in White men, the authors assert.
Guidelines needed
“Recognizing and addressing overdiagnosis is important,” said Anthony J. Olszanski, MD, RPh, associate professor, department of hematology/oncology at Fox Chase Cancer Center, Philadelphia, who was approached for comment on the paper.
That said, Dr. Olszanski noted that this particular study has important limitations. “It is, by nature, a retrospective study using data from the [Surveillance, Epidemiology, and End Results] database registry, limited to patients only in the U.S., and uses a control group of Black patients to estimate overdiagnosis in White patients. These important factors can certainly influence their findings. However, the paper also notes that White men have realized a true increase in diagnosis, backed by a notable increase in mortality.”
The findings should and do raise a number of provocative questions, Dr. Olszanski emphasized. “Should we curtail public screening? Should we mandate revised guidelines for biopsies or pathologic diagnosis?
“As a medical oncologist,” he continued, “I treat patients who clearly do not have benign disease and so it is easy for me to be biased toward aggressive screening. However, it is my opinion that we should develop guidelines aimed at lessening this apparent overdiagnosis.”
These guidelines should be based on prospective studies and would better define which lesions are most suspect and should be biopsied, which are rational for ongoing surveillance, and what pathologic features are most consistent with melanoma, he noted. “We also need to continue to educate the public, as all too often I see the patient who ignored a lesion that was changing over time. A changing lesion requires medical attention. Importantly, we likewise need to improve our commitment in educating the public about the risks of excessive ultraviolet radiation exposure and how to avoid it, as prevention continues to be a most prudent course.”
Screening catches disease early
Another expert approached for comment emphasized that identifying melanomas early on may prevent the need for aggressive therapy. “Many primary melanomas in the U.S. are diagnosed now at an early stage and are cured with surgery, and that hardly constitutes overdiagnosis,” said Jeffrey S. Weber, MD, PhD, deputy director of the Perlmutter Cancer Center and codirector of the melanoma research program, New York University Langone Health.
“In addition, the death rate from melanoma is likely decreased due to the advent of more effective therapies for metastatic disease, and the increasing use of adjuvant immune and targeted therapies that are highly effective at preventing relapse and undoubtedly at prolonging survival, but they have been approved only since 2017-2018,” he added.
This study was supported in part by the Robert Wood Johnson Foundation. Dr. Adamson and Dr. Olszanski disclosed no relevant financial relationships. Dr. Weber disclosed relationships with numerous pharmaceutical companies and holds equity in CytoMx, Biond, Neximmune, and Immunimax.
A version of this article first appeared on Medscape.com.
Melanoma has been increasing in incidence in the United States over the last few decades, but is this a true increase? Or is this a case of overdiagnosis, fueled by screening?
A new study argues the case for overdiagnosis.
commented lead author lead author Adewole Adamson, MD, an assistant professor of internal medicine, division of dermatology, at the University of Texas at Austin.
He posted this conclusion on Twitter after the study was published in JAMA Dermatology.
“The discrepancies in incidence and mortality trends found in this cohort study suggest considerable overdiagnosis of melanoma occurring among White patients in the U.S.,” the authors concluded.
They estimated that an estimated 59% of White women and 60% of White men with melanoma were overdiagnosed in 2014.
These results are similar to those from a recent study from Australia, which used a different method of assessing overdiagnosis. Those findings estimated that 54%-58% of melanoma cases represented overdiagnosis in Australia, Dr. Adamson noted.
“Our estimates shed light on the HUGE scope of this problem in the United States that we need to address,” Dr. Adamson commented on Twitter. “Calls for screening for melanoma in the general public will only push these numbers higher, and make patients out of healthy people.”
“Screening the general population for melanoma has never been shown to save lives and likely is responsible for the increase in melanoma overdiagnosis,” Dr. Adamson said in an interview. “Screening average- and/or low-risk patients is of low value and the harms may outweigh the theoretical benefits.”
Screening programs should be directed to those who may derive the most benefit. “Screening should be limited to high-risk patients such as older White men, patients with a lot of atypical nevi, heavy sun exposure, fair skin, and red hair,” he said. “Just like for other cancers, such as breast, prostate, and colorectal, there should be clear guidelines as to which populations to screen, as well as when to start and when to stop screening.”
Overdiagnosis is defined as the diagnosis of cancer that would never have caused any symptoms or problems in a patient’s lifetime. But therein lies the problem, explained Dr. Adamson. “Because we do not know which early, screen-detected skin cancers would be destined to progress, we are obligated to treat all of them.” There is evidence to suggest that melanoma in situ is not an obligate precursor lesion to invasive melanoma, similar to the situation in which not all ductal carcinoma in situ leads to invasive breast cancer. “It is possible that less aggressive management strategies could be the subject of future studies,” he said.
Patients out of healthy people
For their study, Dr. Adamson and colleagues compared rates of melanoma among White and Black patients. Melanoma is much less common among Black individuals, and they are also less likely to be screened. Additionally, screening rates among Black patients have remained more or less the same over the last decades, whereas screening has increased in White patients.
The team used trends in mortality as a result of melanoma in Black patients as a marker for improvements in medical care. From this, they estimated the expected mortality trends in White patients if medical care had not improved. This served as a marker for the change in true cancer occurrence. Overdiagnosis was calculated as the difference between observed incidence and estimated true cancer occurrence.
The incidence of melanoma rose dramatically among White patients from 1975 to 2014, increasing about fourfold in White women (incidence rate ratio, 4.01) and sixfold in White men (IRR, 5.97).
At the same time, there was much smaller increase (of less than 25%) in the incidence of melanoma in both Black women and Black men.
In that time period, melanoma-related mortality decreased approximately 25% in Black women and men; it remained stable in White women, but increased almost 50% in White men.
Had medical care not improved, estimated mortality would have increased 60% in White women and more than doubled in White men, the authors assert.
Guidelines needed
“Recognizing and addressing overdiagnosis is important,” said Anthony J. Olszanski, MD, RPh, associate professor, department of hematology/oncology at Fox Chase Cancer Center, Philadelphia, who was approached for comment on the paper.
That said, Dr. Olszanski noted that this particular study has important limitations. “It is, by nature, a retrospective study using data from the [Surveillance, Epidemiology, and End Results] database registry, limited to patients only in the U.S., and uses a control group of Black patients to estimate overdiagnosis in White patients. These important factors can certainly influence their findings. However, the paper also notes that White men have realized a true increase in diagnosis, backed by a notable increase in mortality.”
The findings should and do raise a number of provocative questions, Dr. Olszanski emphasized. “Should we curtail public screening? Should we mandate revised guidelines for biopsies or pathologic diagnosis?
“As a medical oncologist,” he continued, “I treat patients who clearly do not have benign disease and so it is easy for me to be biased toward aggressive screening. However, it is my opinion that we should develop guidelines aimed at lessening this apparent overdiagnosis.”
These guidelines should be based on prospective studies and would better define which lesions are most suspect and should be biopsied, which are rational for ongoing surveillance, and what pathologic features are most consistent with melanoma, he noted. “We also need to continue to educate the public, as all too often I see the patient who ignored a lesion that was changing over time. A changing lesion requires medical attention. Importantly, we likewise need to improve our commitment in educating the public about the risks of excessive ultraviolet radiation exposure and how to avoid it, as prevention continues to be a most prudent course.”
Screening catches disease early
Another expert approached for comment emphasized that identifying melanomas early on may prevent the need for aggressive therapy. “Many primary melanomas in the U.S. are diagnosed now at an early stage and are cured with surgery, and that hardly constitutes overdiagnosis,” said Jeffrey S. Weber, MD, PhD, deputy director of the Perlmutter Cancer Center and codirector of the melanoma research program, New York University Langone Health.
“In addition, the death rate from melanoma is likely decreased due to the advent of more effective therapies for metastatic disease, and the increasing use of adjuvant immune and targeted therapies that are highly effective at preventing relapse and undoubtedly at prolonging survival, but they have been approved only since 2017-2018,” he added.
This study was supported in part by the Robert Wood Johnson Foundation. Dr. Adamson and Dr. Olszanski disclosed no relevant financial relationships. Dr. Weber disclosed relationships with numerous pharmaceutical companies and holds equity in CytoMx, Biond, Neximmune, and Immunimax.
A version of this article first appeared on Medscape.com.
Melanoma has been increasing in incidence in the United States over the last few decades, but is this a true increase? Or is this a case of overdiagnosis, fueled by screening?
A new study argues the case for overdiagnosis.
commented lead author lead author Adewole Adamson, MD, an assistant professor of internal medicine, division of dermatology, at the University of Texas at Austin.
He posted this conclusion on Twitter after the study was published in JAMA Dermatology.
“The discrepancies in incidence and mortality trends found in this cohort study suggest considerable overdiagnosis of melanoma occurring among White patients in the U.S.,” the authors concluded.
They estimated that an estimated 59% of White women and 60% of White men with melanoma were overdiagnosed in 2014.
These results are similar to those from a recent study from Australia, which used a different method of assessing overdiagnosis. Those findings estimated that 54%-58% of melanoma cases represented overdiagnosis in Australia, Dr. Adamson noted.
“Our estimates shed light on the HUGE scope of this problem in the United States that we need to address,” Dr. Adamson commented on Twitter. “Calls for screening for melanoma in the general public will only push these numbers higher, and make patients out of healthy people.”
“Screening the general population for melanoma has never been shown to save lives and likely is responsible for the increase in melanoma overdiagnosis,” Dr. Adamson said in an interview. “Screening average- and/or low-risk patients is of low value and the harms may outweigh the theoretical benefits.”
Screening programs should be directed to those who may derive the most benefit. “Screening should be limited to high-risk patients such as older White men, patients with a lot of atypical nevi, heavy sun exposure, fair skin, and red hair,” he said. “Just like for other cancers, such as breast, prostate, and colorectal, there should be clear guidelines as to which populations to screen, as well as when to start and when to stop screening.”
Overdiagnosis is defined as the diagnosis of cancer that would never have caused any symptoms or problems in a patient’s lifetime. But therein lies the problem, explained Dr. Adamson. “Because we do not know which early, screen-detected skin cancers would be destined to progress, we are obligated to treat all of them.” There is evidence to suggest that melanoma in situ is not an obligate precursor lesion to invasive melanoma, similar to the situation in which not all ductal carcinoma in situ leads to invasive breast cancer. “It is possible that less aggressive management strategies could be the subject of future studies,” he said.
Patients out of healthy people
For their study, Dr. Adamson and colleagues compared rates of melanoma among White and Black patients. Melanoma is much less common among Black individuals, and they are also less likely to be screened. Additionally, screening rates among Black patients have remained more or less the same over the last decades, whereas screening has increased in White patients.
The team used trends in mortality as a result of melanoma in Black patients as a marker for improvements in medical care. From this, they estimated the expected mortality trends in White patients if medical care had not improved. This served as a marker for the change in true cancer occurrence. Overdiagnosis was calculated as the difference between observed incidence and estimated true cancer occurrence.
The incidence of melanoma rose dramatically among White patients from 1975 to 2014, increasing about fourfold in White women (incidence rate ratio, 4.01) and sixfold in White men (IRR, 5.97).
At the same time, there was much smaller increase (of less than 25%) in the incidence of melanoma in both Black women and Black men.
In that time period, melanoma-related mortality decreased approximately 25% in Black women and men; it remained stable in White women, but increased almost 50% in White men.
Had medical care not improved, estimated mortality would have increased 60% in White women and more than doubled in White men, the authors assert.
Guidelines needed
“Recognizing and addressing overdiagnosis is important,” said Anthony J. Olszanski, MD, RPh, associate professor, department of hematology/oncology at Fox Chase Cancer Center, Philadelphia, who was approached for comment on the paper.
That said, Dr. Olszanski noted that this particular study has important limitations. “It is, by nature, a retrospective study using data from the [Surveillance, Epidemiology, and End Results] database registry, limited to patients only in the U.S., and uses a control group of Black patients to estimate overdiagnosis in White patients. These important factors can certainly influence their findings. However, the paper also notes that White men have realized a true increase in diagnosis, backed by a notable increase in mortality.”
The findings should and do raise a number of provocative questions, Dr. Olszanski emphasized. “Should we curtail public screening? Should we mandate revised guidelines for biopsies or pathologic diagnosis?
“As a medical oncologist,” he continued, “I treat patients who clearly do not have benign disease and so it is easy for me to be biased toward aggressive screening. However, it is my opinion that we should develop guidelines aimed at lessening this apparent overdiagnosis.”
These guidelines should be based on prospective studies and would better define which lesions are most suspect and should be biopsied, which are rational for ongoing surveillance, and what pathologic features are most consistent with melanoma, he noted. “We also need to continue to educate the public, as all too often I see the patient who ignored a lesion that was changing over time. A changing lesion requires medical attention. Importantly, we likewise need to improve our commitment in educating the public about the risks of excessive ultraviolet radiation exposure and how to avoid it, as prevention continues to be a most prudent course.”
Screening catches disease early
Another expert approached for comment emphasized that identifying melanomas early on may prevent the need for aggressive therapy. “Many primary melanomas in the U.S. are diagnosed now at an early stage and are cured with surgery, and that hardly constitutes overdiagnosis,” said Jeffrey S. Weber, MD, PhD, deputy director of the Perlmutter Cancer Center and codirector of the melanoma research program, New York University Langone Health.
“In addition, the death rate from melanoma is likely decreased due to the advent of more effective therapies for metastatic disease, and the increasing use of adjuvant immune and targeted therapies that are highly effective at preventing relapse and undoubtedly at prolonging survival, but they have been approved only since 2017-2018,” he added.
This study was supported in part by the Robert Wood Johnson Foundation. Dr. Adamson and Dr. Olszanski disclosed no relevant financial relationships. Dr. Weber disclosed relationships with numerous pharmaceutical companies and holds equity in CytoMx, Biond, Neximmune, and Immunimax.
A version of this article first appeared on Medscape.com.
FROM JAMA DERMATOLOGY
Progressive muscle relaxation outperforms mindfulness in reducing grief severity
DENVER –
“Both progressive muscle relaxation and mindfulness training were shown to improve grief severity, yearning, depression symptoms, and stress, [but] the results from this study suggest that progressive muscle relaxation is most effective, compared to a wait-list control condition for improving grief,” study investigator Lindsey Knowles, PhD, senior fellow, MS Center of Excellence, Veterans Affairs Puget Sound Health Care System, and University of Washington, Seattle, told this news organization.
“With replication, progressive muscle relaxation could be a standalone intervention for nondisordered grief or a component of treatment for disordered grief,” Dr. Knowles said.
The findings were presented as part of the Anxiety and Depression Association of America Anxiety & Depression conference.
Disordered grief
Approximately 10% of individuals grappling with loss “get stuck” in their grief and develop disordered grief, which is distinguished by repetitive thought processes of yearning and grief rumination, the investigators noted.
The researchers hypothesized that mindfulness training, which has been shown to reduce maladaptive repetitive thought, could be an effective intervention to prevent disordered grief.
To investigate, they enrolled 94 widows and widowers (mean age, 67.5 years) who were experiencing bereavement-related grief and were between 6 months and 4 years post loss.
The researchers compared a 6-week mindfulness intervention (n = 37) with a 6-week progressive muscle relaxation intervention (n = 35), Dr. Knowles said, because there has been speculation that benefits from mindfulness training may be related more to the relaxation response than to the actual mindfulness component.
Both study groups received the intervention in similar settings with matched instructors.
The mindfulness intervention sessions included 10-25 minutes of meditation and mindfulness practices. It also included instructions for home practice.
Participants in the progressive muscle relaxation group were trained to tense and relax the body’s various muscle groups with an end goal of learning to relax four key muscle groups without initial tensing.
A third group of patients were placed on a wait list with no intervention (n = 22).
Measures taken throughout the study interventions and at 1 month postintervention showed reductions in the study’s two primary outcomes of grief severity and yearning for both interventions versus baseline (P = < .003).
However, only the progressive muscle relaxation group had a significantly greater reduction in grief severity vs the wait-list control group (P = .020).
The muscle relaxation group also showed lower grief severity at 1month follow-up versus the wait-list group (P = .049) – with a value at that time falling below an established cutoff for complicated grief, based on the Revised Inventory of Complicated Grief.
All three treatment groups showed a drop in the third primary outcome of grief rumination (P < .001).
Secondary outcomes of depression and stress were reduced in both active study groups versus the wait-list group (P = .028). Sleep quality also improved in both active intervention groups.
Simple technique
Dr. Knowles said the study’s findings were unexpected.
“We had hypothesized that mindfulness training would outperform progressive muscle relaxation and wait-list for improving grief outcomes,” she said.
Mindfulness experts underscore that a state of global relaxation is considered integral to the benefits of mindfulness, which could explain the benefits of progressive muscle relaxation, Dr. Knowles noted.
Importantly, progressive muscle relaxation has a key advantage: It is quickly and easily learned, which may partially explain the study’s findings, she added.
“Progressive muscle relaxation is a relatively simple technique, so it is also likely that participants were able to master [the technique] over the 6-week intervention,” Dr. Knowles said. “On the other hand, the mindfulness intervention was an introduction to mindfulness, and mastery was not expected or likely over the 6-week intervention.”
Either way, the results shed important light on a potentially beneficial grief intervention.
“Although mindfulness training and progressive muscle relaxation practices may both be perceived as relaxing, mastering progressive muscle relaxation may in fact enable people to maintain better focus in the present moment and generalize nonreactive awareness to both positively and negatively balanced phenomena,” Dr. Knowles said.
However, “more research is necessary to clarify how progressive muscle relaxation improves grief outcomes in widows and widowers.”
CNS benefits?
Zoe Donaldson, PhD, assistant professor in behavioral neuroscience, department of psychology and neuroscience, University of Colorado, Boulder, said the study is important for ongoing efforts in finding effective therapies for grief.
“We often struggle to try to help those experiencing the pain of loss and this study suggests a discrete set of exercises that may help,” said Dr. Donaldson, who was not involved with the research.
She also described the study results as surprising, and speculated that a combination of factors could explain the findings.
“First, mindfulness is hard to achieve, so the moderate beneficial effects might increase with more substantial mindfulness training. Secondly, it is not clear why progressive muscle relaxation had an effect, but the focus and attention to detail may engage the central nervous system in a beneficial way that we don’t fully understand,” Dr. Donaldson said.
Importantly, it’s key to remember that grief is an individual condition when investigating therapies, Dr. Donaldson noted.
“We likely need to develop multiple interventions to help those who are grieving. Incorporating loss can take many forms,” she said.
The investigators and Dr. Donaldson reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
DENVER –
“Both progressive muscle relaxation and mindfulness training were shown to improve grief severity, yearning, depression symptoms, and stress, [but] the results from this study suggest that progressive muscle relaxation is most effective, compared to a wait-list control condition for improving grief,” study investigator Lindsey Knowles, PhD, senior fellow, MS Center of Excellence, Veterans Affairs Puget Sound Health Care System, and University of Washington, Seattle, told this news organization.
“With replication, progressive muscle relaxation could be a standalone intervention for nondisordered grief or a component of treatment for disordered grief,” Dr. Knowles said.
The findings were presented as part of the Anxiety and Depression Association of America Anxiety & Depression conference.
Disordered grief
Approximately 10% of individuals grappling with loss “get stuck” in their grief and develop disordered grief, which is distinguished by repetitive thought processes of yearning and grief rumination, the investigators noted.
The researchers hypothesized that mindfulness training, which has been shown to reduce maladaptive repetitive thought, could be an effective intervention to prevent disordered grief.
To investigate, they enrolled 94 widows and widowers (mean age, 67.5 years) who were experiencing bereavement-related grief and were between 6 months and 4 years post loss.
The researchers compared a 6-week mindfulness intervention (n = 37) with a 6-week progressive muscle relaxation intervention (n = 35), Dr. Knowles said, because there has been speculation that benefits from mindfulness training may be related more to the relaxation response than to the actual mindfulness component.
Both study groups received the intervention in similar settings with matched instructors.
The mindfulness intervention sessions included 10-25 minutes of meditation and mindfulness practices. It also included instructions for home practice.
Participants in the progressive muscle relaxation group were trained to tense and relax the body’s various muscle groups with an end goal of learning to relax four key muscle groups without initial tensing.
A third group of patients were placed on a wait list with no intervention (n = 22).
Measures taken throughout the study interventions and at 1 month postintervention showed reductions in the study’s two primary outcomes of grief severity and yearning for both interventions versus baseline (P = < .003).
However, only the progressive muscle relaxation group had a significantly greater reduction in grief severity vs the wait-list control group (P = .020).
The muscle relaxation group also showed lower grief severity at 1month follow-up versus the wait-list group (P = .049) – with a value at that time falling below an established cutoff for complicated grief, based on the Revised Inventory of Complicated Grief.
All three treatment groups showed a drop in the third primary outcome of grief rumination (P < .001).
Secondary outcomes of depression and stress were reduced in both active study groups versus the wait-list group (P = .028). Sleep quality also improved in both active intervention groups.
Simple technique
Dr. Knowles said the study’s findings were unexpected.
“We had hypothesized that mindfulness training would outperform progressive muscle relaxation and wait-list for improving grief outcomes,” she said.
Mindfulness experts underscore that a state of global relaxation is considered integral to the benefits of mindfulness, which could explain the benefits of progressive muscle relaxation, Dr. Knowles noted.
Importantly, progressive muscle relaxation has a key advantage: It is quickly and easily learned, which may partially explain the study’s findings, she added.
“Progressive muscle relaxation is a relatively simple technique, so it is also likely that participants were able to master [the technique] over the 6-week intervention,” Dr. Knowles said. “On the other hand, the mindfulness intervention was an introduction to mindfulness, and mastery was not expected or likely over the 6-week intervention.”
Either way, the results shed important light on a potentially beneficial grief intervention.
“Although mindfulness training and progressive muscle relaxation practices may both be perceived as relaxing, mastering progressive muscle relaxation may in fact enable people to maintain better focus in the present moment and generalize nonreactive awareness to both positively and negatively balanced phenomena,” Dr. Knowles said.
However, “more research is necessary to clarify how progressive muscle relaxation improves grief outcomes in widows and widowers.”
CNS benefits?
Zoe Donaldson, PhD, assistant professor in behavioral neuroscience, department of psychology and neuroscience, University of Colorado, Boulder, said the study is important for ongoing efforts in finding effective therapies for grief.
“We often struggle to try to help those experiencing the pain of loss and this study suggests a discrete set of exercises that may help,” said Dr. Donaldson, who was not involved with the research.
She also described the study results as surprising, and speculated that a combination of factors could explain the findings.
“First, mindfulness is hard to achieve, so the moderate beneficial effects might increase with more substantial mindfulness training. Secondly, it is not clear why progressive muscle relaxation had an effect, but the focus and attention to detail may engage the central nervous system in a beneficial way that we don’t fully understand,” Dr. Donaldson said.
Importantly, it’s key to remember that grief is an individual condition when investigating therapies, Dr. Donaldson noted.
“We likely need to develop multiple interventions to help those who are grieving. Incorporating loss can take many forms,” she said.
The investigators and Dr. Donaldson reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
DENVER –
“Both progressive muscle relaxation and mindfulness training were shown to improve grief severity, yearning, depression symptoms, and stress, [but] the results from this study suggest that progressive muscle relaxation is most effective, compared to a wait-list control condition for improving grief,” study investigator Lindsey Knowles, PhD, senior fellow, MS Center of Excellence, Veterans Affairs Puget Sound Health Care System, and University of Washington, Seattle, told this news organization.
“With replication, progressive muscle relaxation could be a standalone intervention for nondisordered grief or a component of treatment for disordered grief,” Dr. Knowles said.
The findings were presented as part of the Anxiety and Depression Association of America Anxiety & Depression conference.
Disordered grief
Approximately 10% of individuals grappling with loss “get stuck” in their grief and develop disordered grief, which is distinguished by repetitive thought processes of yearning and grief rumination, the investigators noted.
The researchers hypothesized that mindfulness training, which has been shown to reduce maladaptive repetitive thought, could be an effective intervention to prevent disordered grief.
To investigate, they enrolled 94 widows and widowers (mean age, 67.5 years) who were experiencing bereavement-related grief and were between 6 months and 4 years post loss.
The researchers compared a 6-week mindfulness intervention (n = 37) with a 6-week progressive muscle relaxation intervention (n = 35), Dr. Knowles said, because there has been speculation that benefits from mindfulness training may be related more to the relaxation response than to the actual mindfulness component.
Both study groups received the intervention in similar settings with matched instructors.
The mindfulness intervention sessions included 10-25 minutes of meditation and mindfulness practices. It also included instructions for home practice.
Participants in the progressive muscle relaxation group were trained to tense and relax the body’s various muscle groups with an end goal of learning to relax four key muscle groups without initial tensing.
A third group of patients were placed on a wait list with no intervention (n = 22).
Measures taken throughout the study interventions and at 1 month postintervention showed reductions in the study’s two primary outcomes of grief severity and yearning for both interventions versus baseline (P = < .003).
However, only the progressive muscle relaxation group had a significantly greater reduction in grief severity vs the wait-list control group (P = .020).
The muscle relaxation group also showed lower grief severity at 1month follow-up versus the wait-list group (P = .049) – with a value at that time falling below an established cutoff for complicated grief, based on the Revised Inventory of Complicated Grief.
All three treatment groups showed a drop in the third primary outcome of grief rumination (P < .001).
Secondary outcomes of depression and stress were reduced in both active study groups versus the wait-list group (P = .028). Sleep quality also improved in both active intervention groups.
Simple technique
Dr. Knowles said the study’s findings were unexpected.
“We had hypothesized that mindfulness training would outperform progressive muscle relaxation and wait-list for improving grief outcomes,” she said.
Mindfulness experts underscore that a state of global relaxation is considered integral to the benefits of mindfulness, which could explain the benefits of progressive muscle relaxation, Dr. Knowles noted.
Importantly, progressive muscle relaxation has a key advantage: It is quickly and easily learned, which may partially explain the study’s findings, she added.
“Progressive muscle relaxation is a relatively simple technique, so it is also likely that participants were able to master [the technique] over the 6-week intervention,” Dr. Knowles said. “On the other hand, the mindfulness intervention was an introduction to mindfulness, and mastery was not expected or likely over the 6-week intervention.”
Either way, the results shed important light on a potentially beneficial grief intervention.
“Although mindfulness training and progressive muscle relaxation practices may both be perceived as relaxing, mastering progressive muscle relaxation may in fact enable people to maintain better focus in the present moment and generalize nonreactive awareness to both positively and negatively balanced phenomena,” Dr. Knowles said.
However, “more research is necessary to clarify how progressive muscle relaxation improves grief outcomes in widows and widowers.”
CNS benefits?
Zoe Donaldson, PhD, assistant professor in behavioral neuroscience, department of psychology and neuroscience, University of Colorado, Boulder, said the study is important for ongoing efforts in finding effective therapies for grief.
“We often struggle to try to help those experiencing the pain of loss and this study suggests a discrete set of exercises that may help,” said Dr. Donaldson, who was not involved with the research.
She also described the study results as surprising, and speculated that a combination of factors could explain the findings.
“First, mindfulness is hard to achieve, so the moderate beneficial effects might increase with more substantial mindfulness training. Secondly, it is not clear why progressive muscle relaxation had an effect, but the focus and attention to detail may engage the central nervous system in a beneficial way that we don’t fully understand,” Dr. Donaldson said.
Importantly, it’s key to remember that grief is an individual condition when investigating therapies, Dr. Donaldson noted.
“We likely need to develop multiple interventions to help those who are grieving. Incorporating loss can take many forms,” she said.
The investigators and Dr. Donaldson reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ADAA 2022
Ear growth
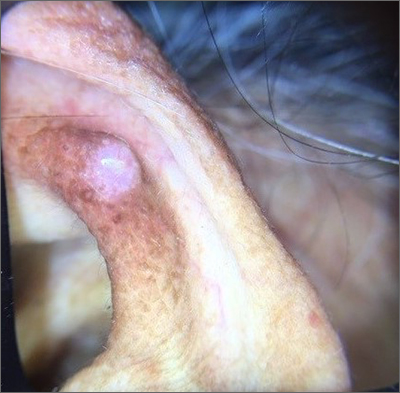
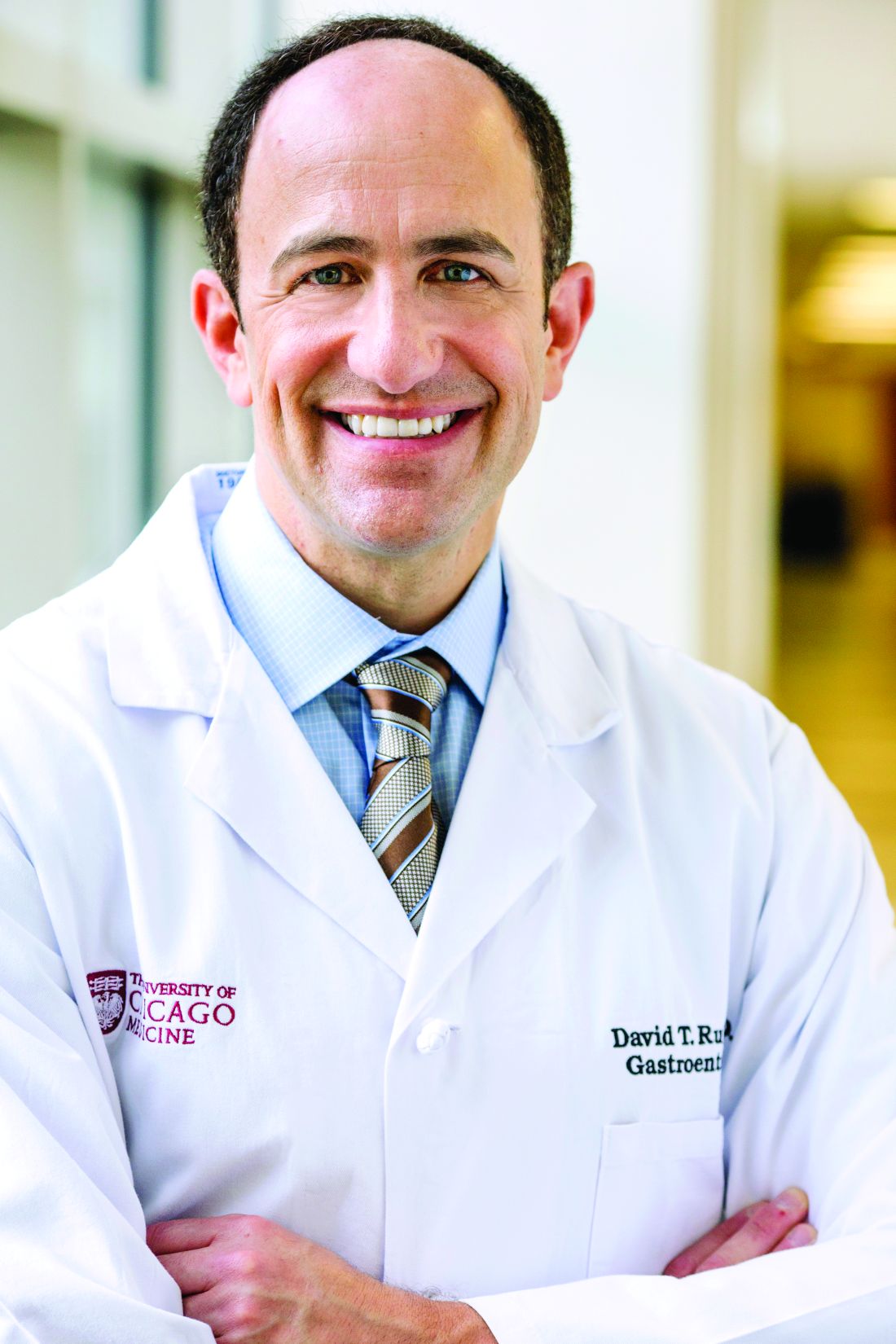
A shave biopsy of the lesion was performed and it confirmed the diagnosis of chondrodermatitis nodularis helicis (CNH).
CNH is an inflammatory process that most commonly occurs on the helix of the ear but can also occur on the antihelix and, rarely, on other areas of the ear. It generally manifests as a firm nodule with surrounding erythema that may be painful only when pressure is applied. Patients may describe bleeding, ulceration, and exudate. They will usually report discomfort from sleeping on the affected side.
The pathogenesis of CNH is poorly understood but is thought to be related to vasculitis and inflammation from prolonged pressure to the affected ear during sleep or from devices that are worn in or around the ear (eg, hearing aids, headphones). Other factors such as actinic damage or ear trauma have also been described. Histopathologic studies have identified arteriolar narrowing with ischemic changes and necrosis of cartilage causing localized inflammation.1
The differential diagnosis for this lesion includes nonmelanoma skin cancer, as well as tophaceous gout and seborrheic keratosis.
There are multiple conservative treatment options. One option is to relieve pressure by sleeping on the unaffected side or using commercially available pillows with a cutout or window where the affected ear can rest. Pharmacologic treatments include topical nitroglycerin1 and intralesional collagen or corticosteroid injections. If previous treatments are unsuccessful, consider surgical excision of the affected tissue and curettage of the underlying abnormal cartilage. Recurrence is possible with both conservative and surgical treatment.
This patient was counseled on the benign nature of her biopsy findings and treatment options were discussed. She elected to proceed with pressure-relieving measures when sleeping and planned to follow up if there was no improvement.
Image courtesy of Marion Cook, MD, First Choice Community Healthcare, Albuquerque, New Mexico. Text courtesy of Spenser Squire, MD, and Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
1. Nielsen LJ, Olsen CH, Lock-Anderson J. Therapeutic options of chondrodermatitis nodularis helicis. Plast Surg Int. 2016;2016:4340168. doi: 10.1155/2016/4340168
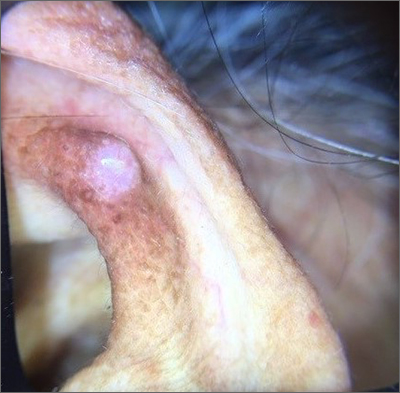
A shave biopsy of the lesion was performed and it confirmed the diagnosis of chondrodermatitis nodularis helicis (CNH).
CNH is an inflammatory process that most commonly occurs on the helix of the ear but can also occur on the antihelix and, rarely, on other areas of the ear. It generally manifests as a firm nodule with surrounding erythema that may be painful only when pressure is applied. Patients may describe bleeding, ulceration, and exudate. They will usually report discomfort from sleeping on the affected side.
The pathogenesis of CNH is poorly understood but is thought to be related to vasculitis and inflammation from prolonged pressure to the affected ear during sleep or from devices that are worn in or around the ear (eg, hearing aids, headphones). Other factors such as actinic damage or ear trauma have also been described. Histopathologic studies have identified arteriolar narrowing with ischemic changes and necrosis of cartilage causing localized inflammation.1
The differential diagnosis for this lesion includes nonmelanoma skin cancer, as well as tophaceous gout and seborrheic keratosis.
There are multiple conservative treatment options. One option is to relieve pressure by sleeping on the unaffected side or using commercially available pillows with a cutout or window where the affected ear can rest. Pharmacologic treatments include topical nitroglycerin1 and intralesional collagen or corticosteroid injections. If previous treatments are unsuccessful, consider surgical excision of the affected tissue and curettage of the underlying abnormal cartilage. Recurrence is possible with both conservative and surgical treatment.
This patient was counseled on the benign nature of her biopsy findings and treatment options were discussed. She elected to proceed with pressure-relieving measures when sleeping and planned to follow up if there was no improvement.
Image courtesy of Marion Cook, MD, First Choice Community Healthcare, Albuquerque, New Mexico. Text courtesy of Spenser Squire, MD, and Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
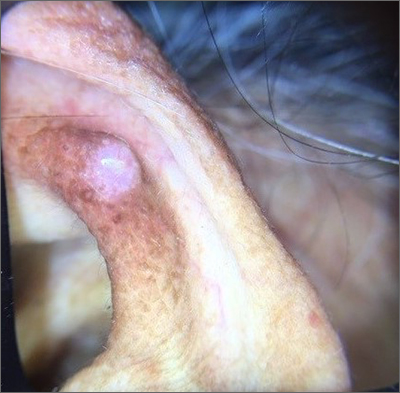
A shave biopsy of the lesion was performed and it confirmed the diagnosis of chondrodermatitis nodularis helicis (CNH).
CNH is an inflammatory process that most commonly occurs on the helix of the ear but can also occur on the antihelix and, rarely, on other areas of the ear. It generally manifests as a firm nodule with surrounding erythema that may be painful only when pressure is applied. Patients may describe bleeding, ulceration, and exudate. They will usually report discomfort from sleeping on the affected side.
The pathogenesis of CNH is poorly understood but is thought to be related to vasculitis and inflammation from prolonged pressure to the affected ear during sleep or from devices that are worn in or around the ear (eg, hearing aids, headphones). Other factors such as actinic damage or ear trauma have also been described. Histopathologic studies have identified arteriolar narrowing with ischemic changes and necrosis of cartilage causing localized inflammation.1
The differential diagnosis for this lesion includes nonmelanoma skin cancer, as well as tophaceous gout and seborrheic keratosis.
There are multiple conservative treatment options. One option is to relieve pressure by sleeping on the unaffected side or using commercially available pillows with a cutout or window where the affected ear can rest. Pharmacologic treatments include topical nitroglycerin1 and intralesional collagen or corticosteroid injections. If previous treatments are unsuccessful, consider surgical excision of the affected tissue and curettage of the underlying abnormal cartilage. Recurrence is possible with both conservative and surgical treatment.
This patient was counseled on the benign nature of her biopsy findings and treatment options were discussed. She elected to proceed with pressure-relieving measures when sleeping and planned to follow up if there was no improvement.
Image courtesy of Marion Cook, MD, First Choice Community Healthcare, Albuquerque, New Mexico. Text courtesy of Spenser Squire, MD, and Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
1. Nielsen LJ, Olsen CH, Lock-Anderson J. Therapeutic options of chondrodermatitis nodularis helicis. Plast Surg Int. 2016;2016:4340168. doi: 10.1155/2016/4340168
1. Nielsen LJ, Olsen CH, Lock-Anderson J. Therapeutic options of chondrodermatitis nodularis helicis. Plast Surg Int. 2016;2016:4340168. doi: 10.1155/2016/4340168
Meet a fierce advocate for women’s health: Jen Gunter, MD
Jen Gunter, MD, refuses to stay silent when she sees misleading claims about women’s health products.
In fact, the world’s most famous – and outspoken – ob.gyn. (as described by The Guardian), is on a social media mission to speak up whenever she sees companies or governments “prey on women’s health and vaginal shame.”
With nearly 400,000 followers, Dr. Gunter never shies away from a controversy.
Recently, she railed against vitamin and supplement maker Olly’s vaginal probiotic, taking the company to task for its product premise and objectionable ad copy.
This news organization caught up with the San Francisco–based doctor and author of two books, “The Vagina Bible” and “The Menopause Manifesto.” The following interview has been lightly edited for length and clarity.
Question: So these Olly capsules purport to be “Probiotics for Your Panty Hamster.” What was your reaction to this?
Answer: Seeing the word “panty hamsters” is so egregious. I’m so used to baseline vaginal opportunism, but this was just absolutely egregious and I had to call it out.
Question: What are vaginal probiotics anyway?
Answer: These are one of these big wellness scams where companies try to sell you on somehow hacking your microbiome by taking them. They’re not inexpensive, either, and can range in price from $30 to $150 per month, depending on how bespoke they are. And yet the data isn’t good. There is little to no evidence of the value of these probiotics except to shareholders.
Question: What’s one claim made in the Olly probiotic packaging that bothers you the most?
Answer: The product claims to balance the vaginal pH. To say that is a gross misunderstanding of the vaginal ecosystem. If that tagline is what you’re leading with, what else don’t you know?
Also, if these things worked, we’d recommend them. Vaginitis is complex and often misdiagnosed, and it’s easy for a company to be predatory and swoop in and say they have a product for you.
If I think your product for the vagina is awful and you have not studied it in at least one quality clinical trial (never mind company-funded or not), and your marketing displays a stunning ignorance about vaginal health, don’t approach me about your product. Really.
Question: When there’s a pop culture reference to, say, menstruation, you’re quick to weigh in.
Answer: I saw these viral messages from a boy mom (that’s what she called herself) where she wrote about being disgusted that there were mentions of periods in Turning Red, the animated movie.
Everything is here because of menstruation. If you didn’t menstruate, you wouldn’t have a kid, we wouldn’t have the person who had the intelligence to build the computer you’re spreading this message on. Menstruation is a vital part of human reproduction, and it’s far more complex than people think. For that reason alone, people should know about it.
Question: Do you ever get worried about being so “out there” on social media?
Answer: I have my stalkers I suppose, but the trolls don’t bother me. I don’t care if some whatever art dealer in New York thinks I have mental illness for promoting masks. That’s the best you’ve got? Honestly, this doesn’t even register with me. It’s like throwing a grain of sand at a car.
Question: You also got into an exchange with Dr. Leana Wen, CNN’s medical analyst, about mask wearing.
Answer: She obviously has a different opinion than I do. I think one of the biggest issues in the pandemic is the change in messaging and this idea that somehow people aren’t living their normal lives right now. I was sad to see her promote that concept.
This weekend I went out for lunch, I went furniture shopping, I went to the movies, I took a hike. My family and I wear masks everywhere. I fail to understand how wearing a mask means you’re not living a normal life when it’s clearly linked with the reduced spread of the virus.
Almost everything in medicine is about risk reduction. You can do things to lower your risk of heart disease. It’s not 100% guaranteed, but wouldn’t we want a lower risk of bad things? I’m going to keep wearing a mask forever!
Question: Do you wish more doctors were more vocal like you?
Answer: I wish more doctors would have conversations about health outside of the office in ways they’re comfortable with. Like, you’re at the hairdresser and you share information, or you share information with 15 of your Facebook friends. If you’re a doctor and post an article about COVID-19 and how it impacts the heart, your 15 friends are more likely to read that article than if your friend who’s a lawyer puts that up.
As doctors, I believe we can often influence people in big and small ways.
A version of this article first appeared on WebMD.com.
Jen Gunter, MD, refuses to stay silent when she sees misleading claims about women’s health products.
In fact, the world’s most famous – and outspoken – ob.gyn. (as described by The Guardian), is on a social media mission to speak up whenever she sees companies or governments “prey on women’s health and vaginal shame.”
With nearly 400,000 followers, Dr. Gunter never shies away from a controversy.
Recently, she railed against vitamin and supplement maker Olly’s vaginal probiotic, taking the company to task for its product premise and objectionable ad copy.
This news organization caught up with the San Francisco–based doctor and author of two books, “The Vagina Bible” and “The Menopause Manifesto.” The following interview has been lightly edited for length and clarity.
Question: So these Olly capsules purport to be “Probiotics for Your Panty Hamster.” What was your reaction to this?
Answer: Seeing the word “panty hamsters” is so egregious. I’m so used to baseline vaginal opportunism, but this was just absolutely egregious and I had to call it out.
Question: What are vaginal probiotics anyway?
Answer: These are one of these big wellness scams where companies try to sell you on somehow hacking your microbiome by taking them. They’re not inexpensive, either, and can range in price from $30 to $150 per month, depending on how bespoke they are. And yet the data isn’t good. There is little to no evidence of the value of these probiotics except to shareholders.
Question: What’s one claim made in the Olly probiotic packaging that bothers you the most?
Answer: The product claims to balance the vaginal pH. To say that is a gross misunderstanding of the vaginal ecosystem. If that tagline is what you’re leading with, what else don’t you know?
Also, if these things worked, we’d recommend them. Vaginitis is complex and often misdiagnosed, and it’s easy for a company to be predatory and swoop in and say they have a product for you.
If I think your product for the vagina is awful and you have not studied it in at least one quality clinical trial (never mind company-funded or not), and your marketing displays a stunning ignorance about vaginal health, don’t approach me about your product. Really.
Question: When there’s a pop culture reference to, say, menstruation, you’re quick to weigh in.
Answer: I saw these viral messages from a boy mom (that’s what she called herself) where she wrote about being disgusted that there were mentions of periods in Turning Red, the animated movie.
Everything is here because of menstruation. If you didn’t menstruate, you wouldn’t have a kid, we wouldn’t have the person who had the intelligence to build the computer you’re spreading this message on. Menstruation is a vital part of human reproduction, and it’s far more complex than people think. For that reason alone, people should know about it.
Question: Do you ever get worried about being so “out there” on social media?
Answer: I have my stalkers I suppose, but the trolls don’t bother me. I don’t care if some whatever art dealer in New York thinks I have mental illness for promoting masks. That’s the best you’ve got? Honestly, this doesn’t even register with me. It’s like throwing a grain of sand at a car.
Question: You also got into an exchange with Dr. Leana Wen, CNN’s medical analyst, about mask wearing.
Answer: She obviously has a different opinion than I do. I think one of the biggest issues in the pandemic is the change in messaging and this idea that somehow people aren’t living their normal lives right now. I was sad to see her promote that concept.
This weekend I went out for lunch, I went furniture shopping, I went to the movies, I took a hike. My family and I wear masks everywhere. I fail to understand how wearing a mask means you’re not living a normal life when it’s clearly linked with the reduced spread of the virus.
Almost everything in medicine is about risk reduction. You can do things to lower your risk of heart disease. It’s not 100% guaranteed, but wouldn’t we want a lower risk of bad things? I’m going to keep wearing a mask forever!
Question: Do you wish more doctors were more vocal like you?
Answer: I wish more doctors would have conversations about health outside of the office in ways they’re comfortable with. Like, you’re at the hairdresser and you share information, or you share information with 15 of your Facebook friends. If you’re a doctor and post an article about COVID-19 and how it impacts the heart, your 15 friends are more likely to read that article than if your friend who’s a lawyer puts that up.
As doctors, I believe we can often influence people in big and small ways.
A version of this article first appeared on WebMD.com.
Jen Gunter, MD, refuses to stay silent when she sees misleading claims about women’s health products.
In fact, the world’s most famous – and outspoken – ob.gyn. (as described by The Guardian), is on a social media mission to speak up whenever she sees companies or governments “prey on women’s health and vaginal shame.”
With nearly 400,000 followers, Dr. Gunter never shies away from a controversy.
Recently, she railed against vitamin and supplement maker Olly’s vaginal probiotic, taking the company to task for its product premise and objectionable ad copy.
This news organization caught up with the San Francisco–based doctor and author of two books, “The Vagina Bible” and “The Menopause Manifesto.” The following interview has been lightly edited for length and clarity.
Question: So these Olly capsules purport to be “Probiotics for Your Panty Hamster.” What was your reaction to this?
Answer: Seeing the word “panty hamsters” is so egregious. I’m so used to baseline vaginal opportunism, but this was just absolutely egregious and I had to call it out.
Question: What are vaginal probiotics anyway?
Answer: These are one of these big wellness scams where companies try to sell you on somehow hacking your microbiome by taking them. They’re not inexpensive, either, and can range in price from $30 to $150 per month, depending on how bespoke they are. And yet the data isn’t good. There is little to no evidence of the value of these probiotics except to shareholders.
Question: What’s one claim made in the Olly probiotic packaging that bothers you the most?
Answer: The product claims to balance the vaginal pH. To say that is a gross misunderstanding of the vaginal ecosystem. If that tagline is what you’re leading with, what else don’t you know?
Also, if these things worked, we’d recommend them. Vaginitis is complex and often misdiagnosed, and it’s easy for a company to be predatory and swoop in and say they have a product for you.
If I think your product for the vagina is awful and you have not studied it in at least one quality clinical trial (never mind company-funded or not), and your marketing displays a stunning ignorance about vaginal health, don’t approach me about your product. Really.
Question: When there’s a pop culture reference to, say, menstruation, you’re quick to weigh in.
Answer: I saw these viral messages from a boy mom (that’s what she called herself) where she wrote about being disgusted that there were mentions of periods in Turning Red, the animated movie.
Everything is here because of menstruation. If you didn’t menstruate, you wouldn’t have a kid, we wouldn’t have the person who had the intelligence to build the computer you’re spreading this message on. Menstruation is a vital part of human reproduction, and it’s far more complex than people think. For that reason alone, people should know about it.
Question: Do you ever get worried about being so “out there” on social media?
Answer: I have my stalkers I suppose, but the trolls don’t bother me. I don’t care if some whatever art dealer in New York thinks I have mental illness for promoting masks. That’s the best you’ve got? Honestly, this doesn’t even register with me. It’s like throwing a grain of sand at a car.
Question: You also got into an exchange with Dr. Leana Wen, CNN’s medical analyst, about mask wearing.
Answer: She obviously has a different opinion than I do. I think one of the biggest issues in the pandemic is the change in messaging and this idea that somehow people aren’t living their normal lives right now. I was sad to see her promote that concept.
This weekend I went out for lunch, I went furniture shopping, I went to the movies, I took a hike. My family and I wear masks everywhere. I fail to understand how wearing a mask means you’re not living a normal life when it’s clearly linked with the reduced spread of the virus.
Almost everything in medicine is about risk reduction. You can do things to lower your risk of heart disease. It’s not 100% guaranteed, but wouldn’t we want a lower risk of bad things? I’m going to keep wearing a mask forever!
Question: Do you wish more doctors were more vocal like you?
Answer: I wish more doctors would have conversations about health outside of the office in ways they’re comfortable with. Like, you’re at the hairdresser and you share information, or you share information with 15 of your Facebook friends. If you’re a doctor and post an article about COVID-19 and how it impacts the heart, your 15 friends are more likely to read that article than if your friend who’s a lawyer puts that up.
As doctors, I believe we can often influence people in big and small ways.
A version of this article first appeared on WebMD.com.
Medications for opioid addiction vastly underutilized
Based on data from the National Survey on Drug Use and Health (NSDUH), investigators found only one in four individuals with OUD receive drug treatment.
In addition, receipt of medication for OUD (MOUD) was lowest among women, the uninsured, non-Hispanic Black or Hispanic people, people with low incomes, and those over age 50. Teens with OUD had the lowest rate of medication use among all demographic groups – zero.
The study is the first to estimate past-year MOUD use in a nationally representative community sample of individuals who may have needed OUD treatment.
“The overdose crisis in the U.S. is continuing unabated, unfortunately, and medication access is an important tool to target and reduce overdose deaths,” lead author Pia Mauro, PhD, assistant professor of epidemiology at Columbia University’s Mailman School of Public Health, New York, told this news organization. “Putting numbers to the distribution of people who are getting medication is important, because it shows that what we’re doing is not enough.”
The study was published online March 23 in JAMA Network Open.
Overdose deaths at an all-time high
U.S. drug overdose deaths are at a record high, with 100,306 American deaths between April 2020 and April 2021, a nearly 30% increase from the previous year. Nearly three-quarters of those deaths involved opioids.
There are currently three Food and Drug Administration–approved medications to treat OUD: methadone, buprenorphine, or naltrexone, all of which are highly effective. Buprenorphine is the only one approved for use in adolescents, and only in those 16 and older.
Before 2019, information about MOUD treatment use was not collected in the NSDUH, an annual survey conducted by the Substance Abuse and Mental Health Services Administration (SAMHSA).
Drawing on responses to the newly added MOUD-use question, Dr. Mauro and colleagues identified participants who may have needed MOUD in the previous year, including those who reported having a heroin or opioid use disorder, receiving medication for their disorder, or undergoing a non-medication OUD treatment, including cognitive behavioral therapy and self-help.
Only 27.8% of those eligible for OUD treatment received MOUD in the past year; 57.0% received no treatment; and 15.3% received non-MOUD services.
Individuals aged 18-25 were most likely to receive MOUD, with just 13.2% of those over age 50 and no one under age 18 receiving medication.
“This study points to extremely low medication use for people who may need it, and given the continued increase in drug-related overdose deaths, the majority of which involve opioids, the necessity to increase access to medication is more important than ever,” Dr. Mauro said.
MOUD use was significantly lower in non-Hispanic Black people, (adjusted relative risk ratio, 0.82; 95% confidence interval, 0.27-2.46), Hispanic people (aRRR, 0.57; 95% CI, 0.14-2.28), and in Asian, Native American or Alaska Native, Native Hawaiian, Pacific Islander, or multiracial people (aRRR, 0.28; 95% CI, 0.08-0.92) compared to White people.
Medication use was less likely in women than men (aRRR, 0.52; 95% CI, 0.29-0.95) and more likely in people who had both prescription opioid and heroin use disorder, compared with those who misused just one of the substances (aRRR, 5.07; 95% CI, 1.50-17.12).
MOUD was more common among people with public insurance than those with private or no insurance, but the overall use remained very low regardless of insurance status.
“Public insurance has consistently been positively associated with MOUD access, so our study builds on this showing the importance of public insurance to increase medication access,” Dr. Mauro said. “But even among those with public insurance, only 35% got medication. That’s only one in three.”
About 85% of participants who may have needed treatment for OUD had at least one contact with a health care provider in the past year, and more than half had contact with the criminal legal system. Only about one-third of these individuals received MOUD, which Dr. Mauro lamented as a lost opportunity for treatment.
Persistent barriers to treatment
The findings highlight persistent barriers to medication-based therapy for OUD, said Alan Leshner, PhD, chief executive officer emeritus of the American Association for the Advancement of Science and a former director of the National Institute on Drug Abuse.
“These kinds of data are critical to increase our understanding of the nature of the opioid epidemic and what to do about it,” Dr. Leshner said. “It’s particularly important to understand who does, and doesn’t, have access to lifesaving medications, but also where to focus efforts at working on the problem.”
In 2019, Dr. Leshner coauthored a report on the underutilization of medication to treat OUD. As previously reported by this news organization, that report argued that stigma, burdensome regulations, unfounded concerns about diversion of MOUDs, lack of insurance coverage, and inadequate professional training for health care providers, law enforcement, and criminal justice officials all acted as barriers that separate people with a medical disorder from desperately needed – and effective – treatment.
“The barriers are the same and have not been vigorously addressed,” Dr. Leshner said. However, recent moves by government leaders may signal a positive trend toward expanded treatment, he added.
Earlier this month, Dr. Leshner chaired a workshop on ways to improve access to methadone, one of the approved medications to treat OUD. Officials from SAMHSA, the Drug Enforcement Administration, and the FDA participated, as did Rahul Gupta, MD, director of the Office of National Drug Control Policy and the nation’s top drug policy official.
“I am optimistic that there may be a new commitment to working on this epidemic using a health-centered approach that takes into account the array of social issues that surround the problem, as well as the criminal justice issues,” Dr. Leshner said.
The study was funded by the National Institute on Drug Abuse grant. Dr. Mauro and Dr. Leshner reported no conflicts. Full disclosures are reported in the original article.
A version of this article first appeared on Medscape.com.
Based on data from the National Survey on Drug Use and Health (NSDUH), investigators found only one in four individuals with OUD receive drug treatment.
In addition, receipt of medication for OUD (MOUD) was lowest among women, the uninsured, non-Hispanic Black or Hispanic people, people with low incomes, and those over age 50. Teens with OUD had the lowest rate of medication use among all demographic groups – zero.
The study is the first to estimate past-year MOUD use in a nationally representative community sample of individuals who may have needed OUD treatment.
“The overdose crisis in the U.S. is continuing unabated, unfortunately, and medication access is an important tool to target and reduce overdose deaths,” lead author Pia Mauro, PhD, assistant professor of epidemiology at Columbia University’s Mailman School of Public Health, New York, told this news organization. “Putting numbers to the distribution of people who are getting medication is important, because it shows that what we’re doing is not enough.”
The study was published online March 23 in JAMA Network Open.
Overdose deaths at an all-time high
U.S. drug overdose deaths are at a record high, with 100,306 American deaths between April 2020 and April 2021, a nearly 30% increase from the previous year. Nearly three-quarters of those deaths involved opioids.
There are currently three Food and Drug Administration–approved medications to treat OUD: methadone, buprenorphine, or naltrexone, all of which are highly effective. Buprenorphine is the only one approved for use in adolescents, and only in those 16 and older.
Before 2019, information about MOUD treatment use was not collected in the NSDUH, an annual survey conducted by the Substance Abuse and Mental Health Services Administration (SAMHSA).
Drawing on responses to the newly added MOUD-use question, Dr. Mauro and colleagues identified participants who may have needed MOUD in the previous year, including those who reported having a heroin or opioid use disorder, receiving medication for their disorder, or undergoing a non-medication OUD treatment, including cognitive behavioral therapy and self-help.
Only 27.8% of those eligible for OUD treatment received MOUD in the past year; 57.0% received no treatment; and 15.3% received non-MOUD services.
Individuals aged 18-25 were most likely to receive MOUD, with just 13.2% of those over age 50 and no one under age 18 receiving medication.
“This study points to extremely low medication use for people who may need it, and given the continued increase in drug-related overdose deaths, the majority of which involve opioids, the necessity to increase access to medication is more important than ever,” Dr. Mauro said.
MOUD use was significantly lower in non-Hispanic Black people, (adjusted relative risk ratio, 0.82; 95% confidence interval, 0.27-2.46), Hispanic people (aRRR, 0.57; 95% CI, 0.14-2.28), and in Asian, Native American or Alaska Native, Native Hawaiian, Pacific Islander, or multiracial people (aRRR, 0.28; 95% CI, 0.08-0.92) compared to White people.
Medication use was less likely in women than men (aRRR, 0.52; 95% CI, 0.29-0.95) and more likely in people who had both prescription opioid and heroin use disorder, compared with those who misused just one of the substances (aRRR, 5.07; 95% CI, 1.50-17.12).
MOUD was more common among people with public insurance than those with private or no insurance, but the overall use remained very low regardless of insurance status.
“Public insurance has consistently been positively associated with MOUD access, so our study builds on this showing the importance of public insurance to increase medication access,” Dr. Mauro said. “But even among those with public insurance, only 35% got medication. That’s only one in three.”
About 85% of participants who may have needed treatment for OUD had at least one contact with a health care provider in the past year, and more than half had contact with the criminal legal system. Only about one-third of these individuals received MOUD, which Dr. Mauro lamented as a lost opportunity for treatment.
Persistent barriers to treatment
The findings highlight persistent barriers to medication-based therapy for OUD, said Alan Leshner, PhD, chief executive officer emeritus of the American Association for the Advancement of Science and a former director of the National Institute on Drug Abuse.
“These kinds of data are critical to increase our understanding of the nature of the opioid epidemic and what to do about it,” Dr. Leshner said. “It’s particularly important to understand who does, and doesn’t, have access to lifesaving medications, but also where to focus efforts at working on the problem.”
In 2019, Dr. Leshner coauthored a report on the underutilization of medication to treat OUD. As previously reported by this news organization, that report argued that stigma, burdensome regulations, unfounded concerns about diversion of MOUDs, lack of insurance coverage, and inadequate professional training for health care providers, law enforcement, and criminal justice officials all acted as barriers that separate people with a medical disorder from desperately needed – and effective – treatment.
“The barriers are the same and have not been vigorously addressed,” Dr. Leshner said. However, recent moves by government leaders may signal a positive trend toward expanded treatment, he added.
Earlier this month, Dr. Leshner chaired a workshop on ways to improve access to methadone, one of the approved medications to treat OUD. Officials from SAMHSA, the Drug Enforcement Administration, and the FDA participated, as did Rahul Gupta, MD, director of the Office of National Drug Control Policy and the nation’s top drug policy official.
“I am optimistic that there may be a new commitment to working on this epidemic using a health-centered approach that takes into account the array of social issues that surround the problem, as well as the criminal justice issues,” Dr. Leshner said.
The study was funded by the National Institute on Drug Abuse grant. Dr. Mauro and Dr. Leshner reported no conflicts. Full disclosures are reported in the original article.
A version of this article first appeared on Medscape.com.
Based on data from the National Survey on Drug Use and Health (NSDUH), investigators found only one in four individuals with OUD receive drug treatment.
In addition, receipt of medication for OUD (MOUD) was lowest among women, the uninsured, non-Hispanic Black or Hispanic people, people with low incomes, and those over age 50. Teens with OUD had the lowest rate of medication use among all demographic groups – zero.
The study is the first to estimate past-year MOUD use in a nationally representative community sample of individuals who may have needed OUD treatment.
“The overdose crisis in the U.S. is continuing unabated, unfortunately, and medication access is an important tool to target and reduce overdose deaths,” lead author Pia Mauro, PhD, assistant professor of epidemiology at Columbia University’s Mailman School of Public Health, New York, told this news organization. “Putting numbers to the distribution of people who are getting medication is important, because it shows that what we’re doing is not enough.”
The study was published online March 23 in JAMA Network Open.
Overdose deaths at an all-time high
U.S. drug overdose deaths are at a record high, with 100,306 American deaths between April 2020 and April 2021, a nearly 30% increase from the previous year. Nearly three-quarters of those deaths involved opioids.
There are currently three Food and Drug Administration–approved medications to treat OUD: methadone, buprenorphine, or naltrexone, all of which are highly effective. Buprenorphine is the only one approved for use in adolescents, and only in those 16 and older.
Before 2019, information about MOUD treatment use was not collected in the NSDUH, an annual survey conducted by the Substance Abuse and Mental Health Services Administration (SAMHSA).
Drawing on responses to the newly added MOUD-use question, Dr. Mauro and colleagues identified participants who may have needed MOUD in the previous year, including those who reported having a heroin or opioid use disorder, receiving medication for their disorder, or undergoing a non-medication OUD treatment, including cognitive behavioral therapy and self-help.
Only 27.8% of those eligible for OUD treatment received MOUD in the past year; 57.0% received no treatment; and 15.3% received non-MOUD services.
Individuals aged 18-25 were most likely to receive MOUD, with just 13.2% of those over age 50 and no one under age 18 receiving medication.
“This study points to extremely low medication use for people who may need it, and given the continued increase in drug-related overdose deaths, the majority of which involve opioids, the necessity to increase access to medication is more important than ever,” Dr. Mauro said.
MOUD use was significantly lower in non-Hispanic Black people, (adjusted relative risk ratio, 0.82; 95% confidence interval, 0.27-2.46), Hispanic people (aRRR, 0.57; 95% CI, 0.14-2.28), and in Asian, Native American or Alaska Native, Native Hawaiian, Pacific Islander, or multiracial people (aRRR, 0.28; 95% CI, 0.08-0.92) compared to White people.
Medication use was less likely in women than men (aRRR, 0.52; 95% CI, 0.29-0.95) and more likely in people who had both prescription opioid and heroin use disorder, compared with those who misused just one of the substances (aRRR, 5.07; 95% CI, 1.50-17.12).
MOUD was more common among people with public insurance than those with private or no insurance, but the overall use remained very low regardless of insurance status.
“Public insurance has consistently been positively associated with MOUD access, so our study builds on this showing the importance of public insurance to increase medication access,” Dr. Mauro said. “But even among those with public insurance, only 35% got medication. That’s only one in three.”
About 85% of participants who may have needed treatment for OUD had at least one contact with a health care provider in the past year, and more than half had contact with the criminal legal system. Only about one-third of these individuals received MOUD, which Dr. Mauro lamented as a lost opportunity for treatment.
Persistent barriers to treatment
The findings highlight persistent barriers to medication-based therapy for OUD, said Alan Leshner, PhD, chief executive officer emeritus of the American Association for the Advancement of Science and a former director of the National Institute on Drug Abuse.
“These kinds of data are critical to increase our understanding of the nature of the opioid epidemic and what to do about it,” Dr. Leshner said. “It’s particularly important to understand who does, and doesn’t, have access to lifesaving medications, but also where to focus efforts at working on the problem.”
In 2019, Dr. Leshner coauthored a report on the underutilization of medication to treat OUD. As previously reported by this news organization, that report argued that stigma, burdensome regulations, unfounded concerns about diversion of MOUDs, lack of insurance coverage, and inadequate professional training for health care providers, law enforcement, and criminal justice officials all acted as barriers that separate people with a medical disorder from desperately needed – and effective – treatment.
“The barriers are the same and have not been vigorously addressed,” Dr. Leshner said. However, recent moves by government leaders may signal a positive trend toward expanded treatment, he added.
Earlier this month, Dr. Leshner chaired a workshop on ways to improve access to methadone, one of the approved medications to treat OUD. Officials from SAMHSA, the Drug Enforcement Administration, and the FDA participated, as did Rahul Gupta, MD, director of the Office of National Drug Control Policy and the nation’s top drug policy official.
“I am optimistic that there may be a new commitment to working on this epidemic using a health-centered approach that takes into account the array of social issues that surround the problem, as well as the criminal justice issues,” Dr. Leshner said.
The study was funded by the National Institute on Drug Abuse grant. Dr. Mauro and Dr. Leshner reported no conflicts. Full disclosures are reported in the original article.
A version of this article first appeared on Medscape.com.
Calcium scores predict sudden-death risk in preclinical CAD
The risk for sudden cardiac death (SCD) climbs steadily in tandem with coronary artery calcium (CAC) burden, independent of more conventional risk factors, in primary-prevention patients considered low- to intermediate-risk, researchers say.
The findings, based on a large cohort study, strengthen the case for initial CAC imaging as a gatekeeper to further testing in such patients who have mostly subclinical atherosclerotic cardiovascular disease (ASCVD), they conclude.
The CAC scan is “evolving into a primary-prevention screening test, not only for initiating statin therapy, but now as a screening modality for risk stratifying someone for sudden cardiac arrest,” Alexander C. Razavi, MD, MPH, PhD, Johns Hopkins University School of Medicine, Baltimore, told this news organization.
“Our data reinforce this and give some quantitative measures of when we should start to consider that.”
A CAC score of 100 to 399 in this “primarily asymptomatic,” predominantly White and male cohort elevated the risk for SCD over an average of 10.6 years by a factor of 2.8, compared with a score of 0. The risk went up four times with CAC scores of 400-999, and almost five times with scores above 1,000.
The risk association was independent of age and sex but also diabetes, smoking, hypertension, dyslipidemia, and family history of heart disease.
That and other findings, Dr. Razavi said, suggest CAC scores in low- to intermediate-risk patients like those studied may sharpen SCD risk-stratification beyond what is possible using traditional risk factors.
Dr. Razavi is lead author on the study’s March 21 publication in JACC Cardiovascular Imaging, and is slated to present the results April 2 during the American College of Cardiology (ACC) 2022 Scientific Session, to be held virtually and in-person in Washington, D.C.
The study’s 66,636 primary-prevention patients, part of the Coronary Artery Calcium Consortium observational cohort, were without known coronary disease at enrollment, from 1991-2010, at four major American centers. They had been referred to CAC imaging because of the presence of at least one ASCVD risk factor, such as dyslipidemia, family history of premature heart disease, hypertension, or diabetes, the researchers note.
They observed 211 SCD events, for a rate of about 0.3%, over a median of 10.6 years. The adjusted stepwise higher risk (SHR) for an SCD event went up continuously with CAC scores (P for trend < .001). The SHR values, compared with a CAC score of 0, were:
- 1.3 (95% CI, 0.7-2.4) for a CAC score score of 1 to 99
- 2.8 (95% CI, 1.6-5.0) for a CAC score of 100 to 399
- 4.0 (95% CI, 2.2-7.3) for a CAC score of 400 to 999
- 4.9 (95% CI, 2.6-9.9) for a CAC score above 1,000
The magnitude of the CAC score’s association with SCD risk in the study was “surprising,” Dr. Razavi said. The CAC score, starting at about 100, seems “more strongly associated with a sudden cardiac arrest” than more familiar SCD risk predictors, such as prolonged heart-rate-corrected QT interval or QRS duration.
Dr. Razavi reported no conflicts. Disclosures for the other authors are in the report.
A version of this article first appeared on Medscape.com.
The risk for sudden cardiac death (SCD) climbs steadily in tandem with coronary artery calcium (CAC) burden, independent of more conventional risk factors, in primary-prevention patients considered low- to intermediate-risk, researchers say.
The findings, based on a large cohort study, strengthen the case for initial CAC imaging as a gatekeeper to further testing in such patients who have mostly subclinical atherosclerotic cardiovascular disease (ASCVD), they conclude.
The CAC scan is “evolving into a primary-prevention screening test, not only for initiating statin therapy, but now as a screening modality for risk stratifying someone for sudden cardiac arrest,” Alexander C. Razavi, MD, MPH, PhD, Johns Hopkins University School of Medicine, Baltimore, told this news organization.
“Our data reinforce this and give some quantitative measures of when we should start to consider that.”
A CAC score of 100 to 399 in this “primarily asymptomatic,” predominantly White and male cohort elevated the risk for SCD over an average of 10.6 years by a factor of 2.8, compared with a score of 0. The risk went up four times with CAC scores of 400-999, and almost five times with scores above 1,000.
The risk association was independent of age and sex but also diabetes, smoking, hypertension, dyslipidemia, and family history of heart disease.
That and other findings, Dr. Razavi said, suggest CAC scores in low- to intermediate-risk patients like those studied may sharpen SCD risk-stratification beyond what is possible using traditional risk factors.
Dr. Razavi is lead author on the study’s March 21 publication in JACC Cardiovascular Imaging, and is slated to present the results April 2 during the American College of Cardiology (ACC) 2022 Scientific Session, to be held virtually and in-person in Washington, D.C.
The study’s 66,636 primary-prevention patients, part of the Coronary Artery Calcium Consortium observational cohort, were without known coronary disease at enrollment, from 1991-2010, at four major American centers. They had been referred to CAC imaging because of the presence of at least one ASCVD risk factor, such as dyslipidemia, family history of premature heart disease, hypertension, or diabetes, the researchers note.
They observed 211 SCD events, for a rate of about 0.3%, over a median of 10.6 years. The adjusted stepwise higher risk (SHR) for an SCD event went up continuously with CAC scores (P for trend < .001). The SHR values, compared with a CAC score of 0, were:
- 1.3 (95% CI, 0.7-2.4) for a CAC score score of 1 to 99
- 2.8 (95% CI, 1.6-5.0) for a CAC score of 100 to 399
- 4.0 (95% CI, 2.2-7.3) for a CAC score of 400 to 999
- 4.9 (95% CI, 2.6-9.9) for a CAC score above 1,000
The magnitude of the CAC score’s association with SCD risk in the study was “surprising,” Dr. Razavi said. The CAC score, starting at about 100, seems “more strongly associated with a sudden cardiac arrest” than more familiar SCD risk predictors, such as prolonged heart-rate-corrected QT interval or QRS duration.
Dr. Razavi reported no conflicts. Disclosures for the other authors are in the report.
A version of this article first appeared on Medscape.com.
The risk for sudden cardiac death (SCD) climbs steadily in tandem with coronary artery calcium (CAC) burden, independent of more conventional risk factors, in primary-prevention patients considered low- to intermediate-risk, researchers say.
The findings, based on a large cohort study, strengthen the case for initial CAC imaging as a gatekeeper to further testing in such patients who have mostly subclinical atherosclerotic cardiovascular disease (ASCVD), they conclude.
The CAC scan is “evolving into a primary-prevention screening test, not only for initiating statin therapy, but now as a screening modality for risk stratifying someone for sudden cardiac arrest,” Alexander C. Razavi, MD, MPH, PhD, Johns Hopkins University School of Medicine, Baltimore, told this news organization.
“Our data reinforce this and give some quantitative measures of when we should start to consider that.”
A CAC score of 100 to 399 in this “primarily asymptomatic,” predominantly White and male cohort elevated the risk for SCD over an average of 10.6 years by a factor of 2.8, compared with a score of 0. The risk went up four times with CAC scores of 400-999, and almost five times with scores above 1,000.
The risk association was independent of age and sex but also diabetes, smoking, hypertension, dyslipidemia, and family history of heart disease.
That and other findings, Dr. Razavi said, suggest CAC scores in low- to intermediate-risk patients like those studied may sharpen SCD risk-stratification beyond what is possible using traditional risk factors.
Dr. Razavi is lead author on the study’s March 21 publication in JACC Cardiovascular Imaging, and is slated to present the results April 2 during the American College of Cardiology (ACC) 2022 Scientific Session, to be held virtually and in-person in Washington, D.C.
The study’s 66,636 primary-prevention patients, part of the Coronary Artery Calcium Consortium observational cohort, were without known coronary disease at enrollment, from 1991-2010, at four major American centers. They had been referred to CAC imaging because of the presence of at least one ASCVD risk factor, such as dyslipidemia, family history of premature heart disease, hypertension, or diabetes, the researchers note.
They observed 211 SCD events, for a rate of about 0.3%, over a median of 10.6 years. The adjusted stepwise higher risk (SHR) for an SCD event went up continuously with CAC scores (P for trend < .001). The SHR values, compared with a CAC score of 0, were:
- 1.3 (95% CI, 0.7-2.4) for a CAC score score of 1 to 99
- 2.8 (95% CI, 1.6-5.0) for a CAC score of 100 to 399
- 4.0 (95% CI, 2.2-7.3) for a CAC score of 400 to 999
- 4.9 (95% CI, 2.6-9.9) for a CAC score above 1,000
The magnitude of the CAC score’s association with SCD risk in the study was “surprising,” Dr. Razavi said. The CAC score, starting at about 100, seems “more strongly associated with a sudden cardiac arrest” than more familiar SCD risk predictors, such as prolonged heart-rate-corrected QT interval or QRS duration.
Dr. Razavi reported no conflicts. Disclosures for the other authors are in the report.
A version of this article first appeared on Medscape.com.
Cancer Data Trends 2022: Cancer in Women
Zullig LL, Goldstein KM, Sims KJ, et al. Cancer among women treated in the Veterans Affairs Healthcare System. J Womens Health (Larchmt). 2019;28(2):268-275. doi:10.1089/jwh.2018.6936
Kondo K, Low A, Everson T, et al. Prevalence of and interventions to reduce health disparities in vulnerable veteran populations: a map of the evidence. VA Evidence-based Synthesis Program (ESP) project #05-225. Published May 2017. Accessed December 22, 2021. https://www.hsrd.research.va.gov/publications/esp/DisparitiesInterventions-REPORT.pdf
Aggarwal A, Liu ML, Krasnow SH. Breast cancer in male veteran population: an analysis from VA cancer registry. J Community Support Oncol. 2014;12(8):293-297. doi:10.12788/jcso.0066
Department of Defense Breast Cancer Research Program. The breast cancer landscape. Published October 2020. Accessed December 23, 2021. https://cdmrp.army.mil/bcrp/pdfs/Breast%20Cancer%20Landscape2020.pdf
Zhu K, Devesa SS, Wu H, et al. Cancer incidence in the US military population: comparison with rates from the SEER program. Cancer Epidemiol Biomarkers Prev. 2009;18(6):1740-1745. doi:10.1158/1055-9965.EPI-09-0041
Kennedy K. “The enemy is lurking in our bodies”— Women veterans say toxic exposure caused breast cancer. The War Horse. Published October 14, 2021. Accessed December 29, 2021. https://thewarhorse.org/military-women-face-higher-breast-cancer-rates-from-exposure
US Department of Veteran Affairs, National Center for Health Promotion and Disease Prevention. Get recommended screening tests and immunizations for women. Updated November 24, 2021. Accessed December 29, 2021. https://www.prevention.va.gov/Healthy_Living/Get_Recommended_Screening_Tests_and_Immunizations_for_Women.asp
Zullig LL, Goldstein KM, Sims KJ, et al. Cancer among women treated in the Veterans Affairs Healthcare System. J Womens Health (Larchmt). 2019;28(2):268-275. doi:10.1089/jwh.2018.6936
Kondo K, Low A, Everson T, et al. Prevalence of and interventions to reduce health disparities in vulnerable veteran populations: a map of the evidence. VA Evidence-based Synthesis Program (ESP) project #05-225. Published May 2017. Accessed December 22, 2021. https://www.hsrd.research.va.gov/publications/esp/DisparitiesInterventions-REPORT.pdf
Aggarwal A, Liu ML, Krasnow SH. Breast cancer in male veteran population: an analysis from VA cancer registry. J Community Support Oncol. 2014;12(8):293-297. doi:10.12788/jcso.0066
Department of Defense Breast Cancer Research Program. The breast cancer landscape. Published October 2020. Accessed December 23, 2021. https://cdmrp.army.mil/bcrp/pdfs/Breast%20Cancer%20Landscape2020.pdf
Zhu K, Devesa SS, Wu H, et al. Cancer incidence in the US military population: comparison with rates from the SEER program. Cancer Epidemiol Biomarkers Prev. 2009;18(6):1740-1745. doi:10.1158/1055-9965.EPI-09-0041
Kennedy K. “The enemy is lurking in our bodies”— Women veterans say toxic exposure caused breast cancer. The War Horse. Published October 14, 2021. Accessed December 29, 2021. https://thewarhorse.org/military-women-face-higher-breast-cancer-rates-from-exposure
US Department of Veteran Affairs, National Center for Health Promotion and Disease Prevention. Get recommended screening tests and immunizations for women. Updated November 24, 2021. Accessed December 29, 2021. https://www.prevention.va.gov/Healthy_Living/Get_Recommended_Screening_Tests_and_Immunizations_for_Women.asp
Zullig LL, Goldstein KM, Sims KJ, et al. Cancer among women treated in the Veterans Affairs Healthcare System. J Womens Health (Larchmt). 2019;28(2):268-275. doi:10.1089/jwh.2018.6936
Kondo K, Low A, Everson T, et al. Prevalence of and interventions to reduce health disparities in vulnerable veteran populations: a map of the evidence. VA Evidence-based Synthesis Program (ESP) project #05-225. Published May 2017. Accessed December 22, 2021. https://www.hsrd.research.va.gov/publications/esp/DisparitiesInterventions-REPORT.pdf
Aggarwal A, Liu ML, Krasnow SH. Breast cancer in male veteran population: an analysis from VA cancer registry. J Community Support Oncol. 2014;12(8):293-297. doi:10.12788/jcso.0066
Department of Defense Breast Cancer Research Program. The breast cancer landscape. Published October 2020. Accessed December 23, 2021. https://cdmrp.army.mil/bcrp/pdfs/Breast%20Cancer%20Landscape2020.pdf
Zhu K, Devesa SS, Wu H, et al. Cancer incidence in the US military population: comparison with rates from the SEER program. Cancer Epidemiol Biomarkers Prev. 2009;18(6):1740-1745. doi:10.1158/1055-9965.EPI-09-0041
Kennedy K. “The enemy is lurking in our bodies”— Women veterans say toxic exposure caused breast cancer. The War Horse. Published October 14, 2021. Accessed December 29, 2021. https://thewarhorse.org/military-women-face-higher-breast-cancer-rates-from-exposure
US Department of Veteran Affairs, National Center for Health Promotion and Disease Prevention. Get recommended screening tests and immunizations for women. Updated November 24, 2021. Accessed December 29, 2021. https://www.prevention.va.gov/Healthy_Living/Get_Recommended_Screening_Tests_and_Immunizations_for_Women.asp