User login
Inadequate ultrasound quality negatively influences HCC surveillance test performance
Key clinical point: Hampered ultrasound visualization in patients with cirrhosis receiving hepatocellular carcinoma (HCC) surveillance is associated with worse test performance, negatively affecting both sensitivity and specificity of surveillance.
Major finding: Patients with cirrhosis and HCC having severely impaired ultrasound visualization before HCC diagnosis showed increased odds of false-negative results (adjusted odds ratio [aOR] 7.94; 95% CI 1.23-51.16), whereas those with only cirrhosis having moderately impaired visualization showed increased odds of false-positive results (aOR 1.60; 95% CI 1.13-2.27).
Study details: This was a retrospective cohort study involving 2,238 patients with cirrhosis, with (n = 186) or without (n = 2,052) HCC, who underwent at least one abdominal ultrasound examination.
Disclosures: The study was supported by the United States National Institute of Health. A Singal and D Fetzer declared serving as consultants or advisory board members of or having research agreements with various organizations.
Source: Chong N et al. Association between ultrasound quality and test performance for HCC surveillance in patients with cirrhosis: a retrospective cohort study. Aliment Pharmacol Ther. 2022;55(6):683-690 (Feb 15). Doi: 10.1111/apt.16779
Key clinical point: Hampered ultrasound visualization in patients with cirrhosis receiving hepatocellular carcinoma (HCC) surveillance is associated with worse test performance, negatively affecting both sensitivity and specificity of surveillance.
Major finding: Patients with cirrhosis and HCC having severely impaired ultrasound visualization before HCC diagnosis showed increased odds of false-negative results (adjusted odds ratio [aOR] 7.94; 95% CI 1.23-51.16), whereas those with only cirrhosis having moderately impaired visualization showed increased odds of false-positive results (aOR 1.60; 95% CI 1.13-2.27).
Study details: This was a retrospective cohort study involving 2,238 patients with cirrhosis, with (n = 186) or without (n = 2,052) HCC, who underwent at least one abdominal ultrasound examination.
Disclosures: The study was supported by the United States National Institute of Health. A Singal and D Fetzer declared serving as consultants or advisory board members of or having research agreements with various organizations.
Source: Chong N et al. Association between ultrasound quality and test performance for HCC surveillance in patients with cirrhosis: a retrospective cohort study. Aliment Pharmacol Ther. 2022;55(6):683-690 (Feb 15). Doi: 10.1111/apt.16779
Key clinical point: Hampered ultrasound visualization in patients with cirrhosis receiving hepatocellular carcinoma (HCC) surveillance is associated with worse test performance, negatively affecting both sensitivity and specificity of surveillance.
Major finding: Patients with cirrhosis and HCC having severely impaired ultrasound visualization before HCC diagnosis showed increased odds of false-negative results (adjusted odds ratio [aOR] 7.94; 95% CI 1.23-51.16), whereas those with only cirrhosis having moderately impaired visualization showed increased odds of false-positive results (aOR 1.60; 95% CI 1.13-2.27).
Study details: This was a retrospective cohort study involving 2,238 patients with cirrhosis, with (n = 186) or without (n = 2,052) HCC, who underwent at least one abdominal ultrasound examination.
Disclosures: The study was supported by the United States National Institute of Health. A Singal and D Fetzer declared serving as consultants or advisory board members of or having research agreements with various organizations.
Source: Chong N et al. Association between ultrasound quality and test performance for HCC surveillance in patients with cirrhosis: a retrospective cohort study. Aliment Pharmacol Ther. 2022;55(6):683-690 (Feb 15). Doi: 10.1111/apt.16779
MRE-based shear strain mapping may preoperatively predict microvascular invasion in HCC
Key clinical point: Magnetic resonance elastography (MRE)-based shear strain mapping may serve as a noninvasive biomarker enabling the characterization of the tumor-liver interface and preoperative prediction of microvascular invasion (MVI) in patients with hepatocellular carcinoma (HCC).
Major finding: The positive MVI vs. negative MVI group displayed a significantly higher octahedral shear strain (OSS) percentage of low-shear-strain length (pLSL) at three evaluation frequencies (60 Hz: 75% vs. 40%, 40 Hz: 85% vs. 40%, and 30 Hz: 70% vs. 20%; all P < .01). The peritumor OSS-pLSL area under the receiver operating characteristic curve (0.73-0.90) for MVI prediction was good/excellent at all frequencies.
Study details: The data are derived from a retrospective study of 59 patients with HCC, all of whom underwent the conventional 60 Hz MRE examination; of these, 29 patients also underwent 40 and 30 Hz MRE examinations.
Disclosures: The study was funded by the National Natural Science Foundation of China, among others. The authors declared no conflict of interests.
Source: Li M et al. MR elastography-based shear strain mapping for assessment of microvascular invasion in hepatocellular carcinoma. Eur Radiol. 2022 (Feb 11). Doi: 10.1007/s00330-022-08578-w
Key clinical point: Magnetic resonance elastography (MRE)-based shear strain mapping may serve as a noninvasive biomarker enabling the characterization of the tumor-liver interface and preoperative prediction of microvascular invasion (MVI) in patients with hepatocellular carcinoma (HCC).
Major finding: The positive MVI vs. negative MVI group displayed a significantly higher octahedral shear strain (OSS) percentage of low-shear-strain length (pLSL) at three evaluation frequencies (60 Hz: 75% vs. 40%, 40 Hz: 85% vs. 40%, and 30 Hz: 70% vs. 20%; all P < .01). The peritumor OSS-pLSL area under the receiver operating characteristic curve (0.73-0.90) for MVI prediction was good/excellent at all frequencies.
Study details: The data are derived from a retrospective study of 59 patients with HCC, all of whom underwent the conventional 60 Hz MRE examination; of these, 29 patients also underwent 40 and 30 Hz MRE examinations.
Disclosures: The study was funded by the National Natural Science Foundation of China, among others. The authors declared no conflict of interests.
Source: Li M et al. MR elastography-based shear strain mapping for assessment of microvascular invasion in hepatocellular carcinoma. Eur Radiol. 2022 (Feb 11). Doi: 10.1007/s00330-022-08578-w
Key clinical point: Magnetic resonance elastography (MRE)-based shear strain mapping may serve as a noninvasive biomarker enabling the characterization of the tumor-liver interface and preoperative prediction of microvascular invasion (MVI) in patients with hepatocellular carcinoma (HCC).
Major finding: The positive MVI vs. negative MVI group displayed a significantly higher octahedral shear strain (OSS) percentage of low-shear-strain length (pLSL) at three evaluation frequencies (60 Hz: 75% vs. 40%, 40 Hz: 85% vs. 40%, and 30 Hz: 70% vs. 20%; all P < .01). The peritumor OSS-pLSL area under the receiver operating characteristic curve (0.73-0.90) for MVI prediction was good/excellent at all frequencies.
Study details: The data are derived from a retrospective study of 59 patients with HCC, all of whom underwent the conventional 60 Hz MRE examination; of these, 29 patients also underwent 40 and 30 Hz MRE examinations.
Disclosures: The study was funded by the National Natural Science Foundation of China, among others. The authors declared no conflict of interests.
Source: Li M et al. MR elastography-based shear strain mapping for assessment of microvascular invasion in hepatocellular carcinoma. Eur Radiol. 2022 (Feb 11). Doi: 10.1007/s00330-022-08578-w
Ramucirumab-mediated survival benefit in advanced HCC unperturbed by baseline prognostic covariates
Key clinical point: Patients with advanced hepatocellular carcinoma (aHCC) and alpha-fetoprotein (AFP) levels ≥400 ng/mL experience a consistent survival benefit with ramucirumab therapy irrespective of baseline prognostic covariates.
Major finding: Ramucirumab vs. placebo improved overall survival in patients with viral (hazard ratio [HR] 0.76; 95% CI 0.60-0.97) and nonviral (HR 0.56; 95% CI 0.49-0.79) etiologies and in those with above-median AFP levels (≥4,081.5 ng/mL; HR 0.71; 95% CI 0.54-0.95).
Study details: Findings are from a post hoc meta-analysis of the phase 3 REACH and REACH-2 trials involving 542 patients with aHCC and AFP levels ≥400 ng/mL who were randomly assigned to receive ramucirumab (n = 316) or placebo (n = 226).
Disclosures: The study was sponsored by Eli Lilly and Company. JM Llovet, A Singal, A Villanueva, R Finn, M Kudo, P Galle, M Ikeda, and A Zhu reported receiving grants, personal/advisory board/consulting fees, or honoraria from various sources, including Eli Lilly. The other authors are employees or shareholders of Eli Lilly.
Source: Llovet JM et al. Prognostic and predictive factors in patients with advanced HCC and elevated alpha-fetoprotein treated with ramucirumab in two randomized phase III trial. Clin Cancer Res. 2022 (Mar 4). Doi: 10.1158/1078-0432.CCR-21-4000
Key clinical point: Patients with advanced hepatocellular carcinoma (aHCC) and alpha-fetoprotein (AFP) levels ≥400 ng/mL experience a consistent survival benefit with ramucirumab therapy irrespective of baseline prognostic covariates.
Major finding: Ramucirumab vs. placebo improved overall survival in patients with viral (hazard ratio [HR] 0.76; 95% CI 0.60-0.97) and nonviral (HR 0.56; 95% CI 0.49-0.79) etiologies and in those with above-median AFP levels (≥4,081.5 ng/mL; HR 0.71; 95% CI 0.54-0.95).
Study details: Findings are from a post hoc meta-analysis of the phase 3 REACH and REACH-2 trials involving 542 patients with aHCC and AFP levels ≥400 ng/mL who were randomly assigned to receive ramucirumab (n = 316) or placebo (n = 226).
Disclosures: The study was sponsored by Eli Lilly and Company. JM Llovet, A Singal, A Villanueva, R Finn, M Kudo, P Galle, M Ikeda, and A Zhu reported receiving grants, personal/advisory board/consulting fees, or honoraria from various sources, including Eli Lilly. The other authors are employees or shareholders of Eli Lilly.
Source: Llovet JM et al. Prognostic and predictive factors in patients with advanced HCC and elevated alpha-fetoprotein treated with ramucirumab in two randomized phase III trial. Clin Cancer Res. 2022 (Mar 4). Doi: 10.1158/1078-0432.CCR-21-4000
Key clinical point: Patients with advanced hepatocellular carcinoma (aHCC) and alpha-fetoprotein (AFP) levels ≥400 ng/mL experience a consistent survival benefit with ramucirumab therapy irrespective of baseline prognostic covariates.
Major finding: Ramucirumab vs. placebo improved overall survival in patients with viral (hazard ratio [HR] 0.76; 95% CI 0.60-0.97) and nonviral (HR 0.56; 95% CI 0.49-0.79) etiologies and in those with above-median AFP levels (≥4,081.5 ng/mL; HR 0.71; 95% CI 0.54-0.95).
Study details: Findings are from a post hoc meta-analysis of the phase 3 REACH and REACH-2 trials involving 542 patients with aHCC and AFP levels ≥400 ng/mL who were randomly assigned to receive ramucirumab (n = 316) or placebo (n = 226).
Disclosures: The study was sponsored by Eli Lilly and Company. JM Llovet, A Singal, A Villanueva, R Finn, M Kudo, P Galle, M Ikeda, and A Zhu reported receiving grants, personal/advisory board/consulting fees, or honoraria from various sources, including Eli Lilly. The other authors are employees or shareholders of Eli Lilly.
Source: Llovet JM et al. Prognostic and predictive factors in patients with advanced HCC and elevated alpha-fetoprotein treated with ramucirumab in two randomized phase III trial. Clin Cancer Res. 2022 (Mar 4). Doi: 10.1158/1078-0432.CCR-21-4000
Meta-analysis underscores the need for improved HCC surveillance in NAFLD without cirrhosis
Key clinical point: Compared with patients with hepatocellular carcinoma (HCC) due to other causes, a higher proportion of those with nonalcoholic fatty liver disease (NAFLD)-related HCC do not have cirrhosis and lack an indication for HCC surveillance, thus calling for surveillance strategies for patients with NAFLD without cirrhosis but at high risk for HCC.
Major finding: The proportion of patients without cirrhosis was higher among those with NAFLD-related HCC vs. HCC due to other causes (38.5% vs. 14.6%; P < .0001). Before cancer diagnosis, only 32.8% of patients with NAFLD-related HCC underwent HCC surveillance relative to 55.7% of those with HCC due to other causes (odds ratio 0.36; P < .0001).
Study details: This was a meta-analysis of 61 studies including 94,636 patients with HCC related to either NAFLD (n = 15,377) or other causes (n = 79,259).
Disclosures: No funding was received for the study. Some authors declared having stock options from, serving as paid/unpaid consultants or advisory board members for, and receiving royalties or research grants from various organizations.
Source: Tan DJH et al. Clinical characteristics, surveillance, treatment allocation, and outcomes of non-alcoholic fatty liver disease-related hepatocellular carcinoma: a systematic review and meta-analysis. Lancet Oncol. 2022 (Mar 4). Doi: 10.1016/S1470-2045(22)00078-X
Key clinical point: Compared with patients with hepatocellular carcinoma (HCC) due to other causes, a higher proportion of those with nonalcoholic fatty liver disease (NAFLD)-related HCC do not have cirrhosis and lack an indication for HCC surveillance, thus calling for surveillance strategies for patients with NAFLD without cirrhosis but at high risk for HCC.
Major finding: The proportion of patients without cirrhosis was higher among those with NAFLD-related HCC vs. HCC due to other causes (38.5% vs. 14.6%; P < .0001). Before cancer diagnosis, only 32.8% of patients with NAFLD-related HCC underwent HCC surveillance relative to 55.7% of those with HCC due to other causes (odds ratio 0.36; P < .0001).
Study details: This was a meta-analysis of 61 studies including 94,636 patients with HCC related to either NAFLD (n = 15,377) or other causes (n = 79,259).
Disclosures: No funding was received for the study. Some authors declared having stock options from, serving as paid/unpaid consultants or advisory board members for, and receiving royalties or research grants from various organizations.
Source: Tan DJH et al. Clinical characteristics, surveillance, treatment allocation, and outcomes of non-alcoholic fatty liver disease-related hepatocellular carcinoma: a systematic review and meta-analysis. Lancet Oncol. 2022 (Mar 4). Doi: 10.1016/S1470-2045(22)00078-X
Key clinical point: Compared with patients with hepatocellular carcinoma (HCC) due to other causes, a higher proportion of those with nonalcoholic fatty liver disease (NAFLD)-related HCC do not have cirrhosis and lack an indication for HCC surveillance, thus calling for surveillance strategies for patients with NAFLD without cirrhosis but at high risk for HCC.
Major finding: The proportion of patients without cirrhosis was higher among those with NAFLD-related HCC vs. HCC due to other causes (38.5% vs. 14.6%; P < .0001). Before cancer diagnosis, only 32.8% of patients with NAFLD-related HCC underwent HCC surveillance relative to 55.7% of those with HCC due to other causes (odds ratio 0.36; P < .0001).
Study details: This was a meta-analysis of 61 studies including 94,636 patients with HCC related to either NAFLD (n = 15,377) or other causes (n = 79,259).
Disclosures: No funding was received for the study. Some authors declared having stock options from, serving as paid/unpaid consultants or advisory board members for, and receiving royalties or research grants from various organizations.
Source: Tan DJH et al. Clinical characteristics, surveillance, treatment allocation, and outcomes of non-alcoholic fatty liver disease-related hepatocellular carcinoma: a systematic review and meta-analysis. Lancet Oncol. 2022 (Mar 4). Doi: 10.1016/S1470-2045(22)00078-X
Inpatient Dermatology Consultations for Suspected Skin Cancer: A Retrospective Review
To the Editor:
Dermatologists sometimes are consulted in the inpatient setting to rule out possible skin cancer. This scenario provides an opportunity to facilitate the diagnosis and treatment of cutaneous malignancy, often in patients who might not have sought regular outpatient dermatology care. Few studies have described the outcomes of inpatient biopsies to identify skin cancer.1,2
Seeking to better understand the nature of these patient encounters, we reviewed all consultations at a medical center for which the referring physician suspected skin cancer rather than only those lesions that were biopsied by the dermatologist. We also collected data about subsequent treatment to better understand the outcomes of these patient encounters.
We conducted a retrospective review of inpatient dermatology referrals at an academic-affiliated tertiary medical center. We identified all patients who were provided with an inpatient dermatology consultation for suspected skin cancer or what was identified as a “skin lesion” between July 1, 2013, and July 1, 2019. We collected information on each patient’s sex, age at time of consultation, and race, as well as the specialty of the referring provider, lesion location, maximum diameter of the lesion, whether a biopsy was performed, where the biopsy was performed (inpatient or outpatient setting), clinical diagnosis, histopathologic diagnosis, and subsequent treatment.
The institutional review board at Eastern Virginia Medical School (Norfolk, Virginia) approved this study, and all protocol conformed to the ethical guidelines of the Declaration of Helsinki.
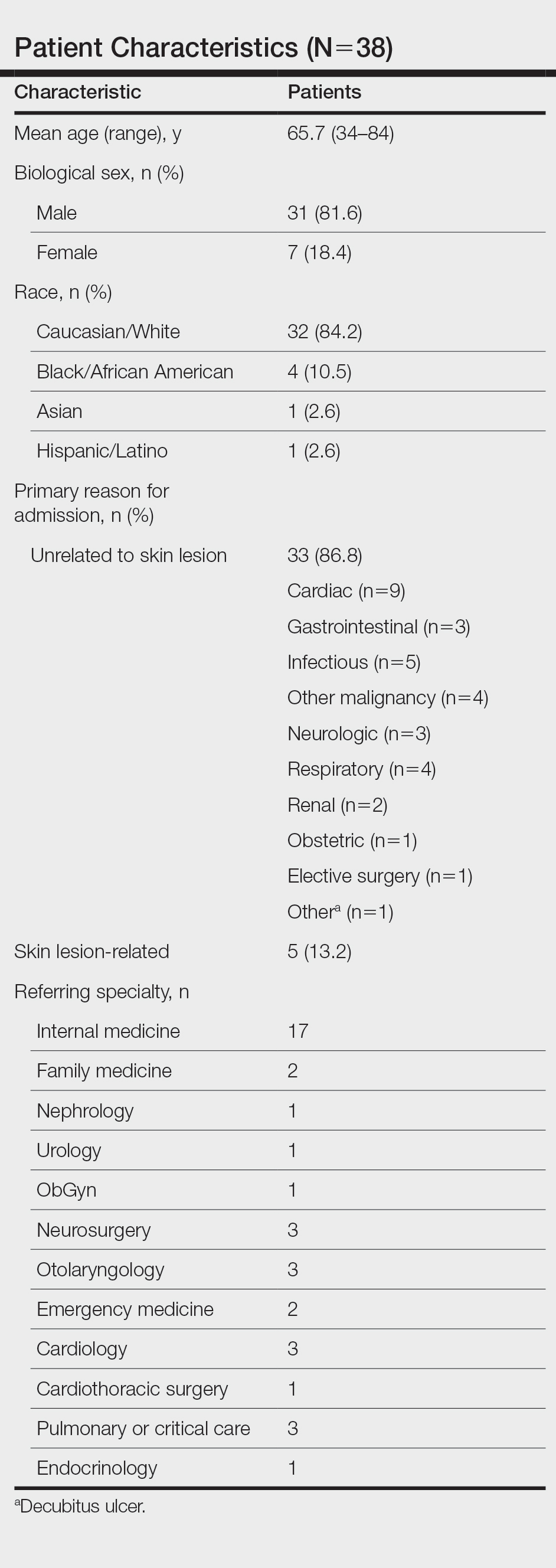
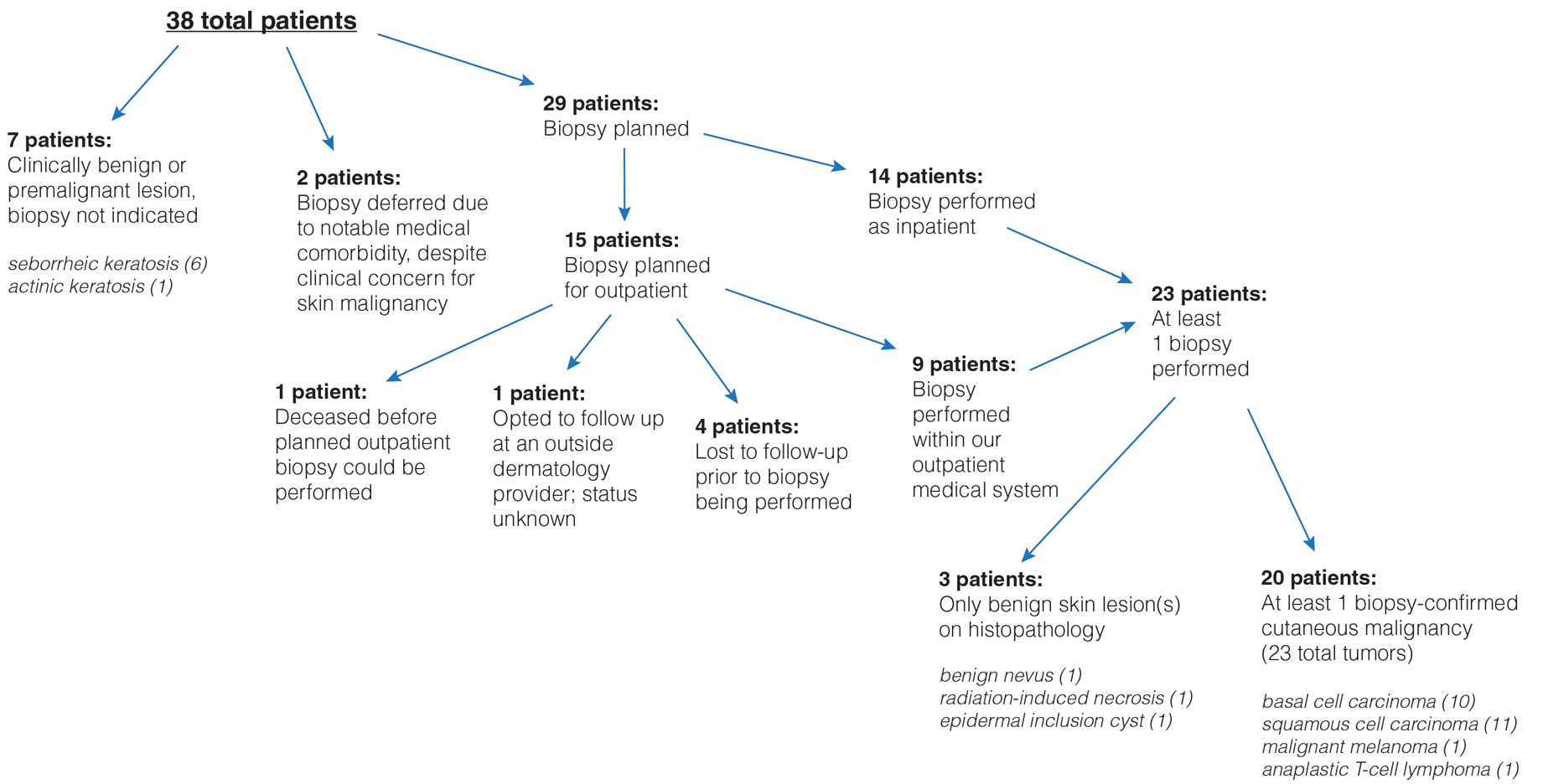
Thirty-eight patients met the inclusion criteria. Their characteristics are listed in the Table. Consultations for possible skin cancer accounted for 4% (38/950) of all inpatient dermatology consultations over the study period. Outcomes of the referrals are shown in the Figure. Consultations were received from 12 different physician specialties.
In the 38 patients, 47 lesions were identified; most (66% [31/47]) were on the head and neck. Twenty of 38 patients were found to have at least 1 biopsy-confirmed cutaneous malignancy (23 total tumors). Of those 23 identified malignancies, 10 were basal cell carcinoma, 11 squamous cell carcinoma, 1 malignant melanoma, and 1 anaplastic T-cell lymphoma. Of note, 17 of 23 (74%) identified cutaneous malignancies were 2.0 cm in diameter at biopsy or larger. Subsequently performed treatments for these patients included wide local excision (n=3), Mohs micrographic surgery (n=5), radiation therapy (n=3), topical fluorouracil (n=1), electrodesiccation and curettage (n=4), and chemotherapy or immunotherapy (n=2). Two patients who were diagnosed with skin cancer died of unrelated causes before treatment was completed.
In 10 of 38 patients, only nonmalignant entities were diagnosed, including seborrheic keratosis (n=6), benign melanocytic nevus (n=1), epidermal inclusion cyst (n=1), actinic keratosis (n=1), and radiation-induced necrosis (n=1). Of the 8 remaining patients, 4 were ultimately lost to follow-up before planned outpatient biopsy could be completed; 1 opted to follow up for biopsy at an unaffiliated outpatient dermatology provider. For 2 patients, the decision was made to forgo biopsy despite clinical suspicion of skin cancer because of overall poor health status, and 1 additional patient died before a planned outpatient biopsy could be performed.
In summary, approximately half of the inpatient dermatology consultations for suspected cutaneous malignancy resulted in a diagnosis of skin cancer. The patients in this population were admitted for a range of diagnoses, most unrelated to their cutaneous malignancy, suggesting that the inpatient setting offers the opportunity for physicians in a variety of specialties to help identify skin cancer that might otherwise be unaddressed and then facilitate management, whether ultimately in an inpatient or outpatient setting.
In many of these cases, it might be most appropriate to arrange subsequent outpatient dermatology follow-up after hospitalization, rather than making an inpatient consultation, as these situations usually are nonurgent and not directly related to hospitalization. However, in cases in which the lesion is directly related to admission, the lesion is advanced, there is concern for metastatic disease, or extenuating circumstances make outpatient follow-up difficult, inpatient dermatology consultation may be reasonable. There sometimes can be compelling reasons to expedite diagnosis and treatment as an inpatient.
In hospitalized, medically complex patients, in whom a new cutaneous malignancy is identified, dermatologists should discuss the situation thoughtfully with the patient, the patient’s family (when appropriate), and other physicians on the treatment team to determine the most appropriate course of action. In some cases, the most appropriate course might be to delay biopsy or treatment until the outpatient setting or to even defer further action completely when the prognosis is very limited. Consulting dermatologists must be mindful of patients’ overall medical situation in planning care for a cutaneous malignancy in these inpatient situations.
This study also highlights the surprising number of large-diameter, high-risk tumors identified in these scenarios. Limitations of this study include a relatively small sample size from a single facility that might not be representative of other practice settings and locations. Future multicenter studies could further explore the impact of inpatient dermatologic consultation on the diagnosis and management of skin cancer.
- Bauer J, Maroon M. Dermatology inpatient consultations: a retrospective study. J Am Acad Dermatol. 2010;62:518-519. doi:10.1016/j.jaad.2009.06.030
- Tsai S, Scott JF, Keller JJ, et al. Cutaneous malignancies identified in an inpatient dermatology consultation service. Br J Dermatol. 2017;177:E116-E118. doi:10.1111/bjd.15401
To the Editor:
Dermatologists sometimes are consulted in the inpatient setting to rule out possible skin cancer. This scenario provides an opportunity to facilitate the diagnosis and treatment of cutaneous malignancy, often in patients who might not have sought regular outpatient dermatology care. Few studies have described the outcomes of inpatient biopsies to identify skin cancer.1,2
Seeking to better understand the nature of these patient encounters, we reviewed all consultations at a medical center for which the referring physician suspected skin cancer rather than only those lesions that were biopsied by the dermatologist. We also collected data about subsequent treatment to better understand the outcomes of these patient encounters.
We conducted a retrospective review of inpatient dermatology referrals at an academic-affiliated tertiary medical center. We identified all patients who were provided with an inpatient dermatology consultation for suspected skin cancer or what was identified as a “skin lesion” between July 1, 2013, and July 1, 2019. We collected information on each patient’s sex, age at time of consultation, and race, as well as the specialty of the referring provider, lesion location, maximum diameter of the lesion, whether a biopsy was performed, where the biopsy was performed (inpatient or outpatient setting), clinical diagnosis, histopathologic diagnosis, and subsequent treatment.
The institutional review board at Eastern Virginia Medical School (Norfolk, Virginia) approved this study, and all protocol conformed to the ethical guidelines of the Declaration of Helsinki.
Thirty-eight patients met the inclusion criteria. Their characteristics are listed in the Table. Consultations for possible skin cancer accounted for 4% (38/950) of all inpatient dermatology consultations over the study period. Outcomes of the referrals are shown in the Figure. Consultations were received from 12 different physician specialties.
In the 38 patients, 47 lesions were identified; most (66% [31/47]) were on the head and neck. Twenty of 38 patients were found to have at least 1 biopsy-confirmed cutaneous malignancy (23 total tumors). Of those 23 identified malignancies, 10 were basal cell carcinoma, 11 squamous cell carcinoma, 1 malignant melanoma, and 1 anaplastic T-cell lymphoma. Of note, 17 of 23 (74%) identified cutaneous malignancies were 2.0 cm in diameter at biopsy or larger. Subsequently performed treatments for these patients included wide local excision (n=3), Mohs micrographic surgery (n=5), radiation therapy (n=3), topical fluorouracil (n=1), electrodesiccation and curettage (n=4), and chemotherapy or immunotherapy (n=2). Two patients who were diagnosed with skin cancer died of unrelated causes before treatment was completed.
In 10 of 38 patients, only nonmalignant entities were diagnosed, including seborrheic keratosis (n=6), benign melanocytic nevus (n=1), epidermal inclusion cyst (n=1), actinic keratosis (n=1), and radiation-induced necrosis (n=1). Of the 8 remaining patients, 4 were ultimately lost to follow-up before planned outpatient biopsy could be completed; 1 opted to follow up for biopsy at an unaffiliated outpatient dermatology provider. For 2 patients, the decision was made to forgo biopsy despite clinical suspicion of skin cancer because of overall poor health status, and 1 additional patient died before a planned outpatient biopsy could be performed.
In summary, approximately half of the inpatient dermatology consultations for suspected cutaneous malignancy resulted in a diagnosis of skin cancer. The patients in this population were admitted for a range of diagnoses, most unrelated to their cutaneous malignancy, suggesting that the inpatient setting offers the opportunity for physicians in a variety of specialties to help identify skin cancer that might otherwise be unaddressed and then facilitate management, whether ultimately in an inpatient or outpatient setting.
In many of these cases, it might be most appropriate to arrange subsequent outpatient dermatology follow-up after hospitalization, rather than making an inpatient consultation, as these situations usually are nonurgent and not directly related to hospitalization. However, in cases in which the lesion is directly related to admission, the lesion is advanced, there is concern for metastatic disease, or extenuating circumstances make outpatient follow-up difficult, inpatient dermatology consultation may be reasonable. There sometimes can be compelling reasons to expedite diagnosis and treatment as an inpatient.
In hospitalized, medically complex patients, in whom a new cutaneous malignancy is identified, dermatologists should discuss the situation thoughtfully with the patient, the patient’s family (when appropriate), and other physicians on the treatment team to determine the most appropriate course of action. In some cases, the most appropriate course might be to delay biopsy or treatment until the outpatient setting or to even defer further action completely when the prognosis is very limited. Consulting dermatologists must be mindful of patients’ overall medical situation in planning care for a cutaneous malignancy in these inpatient situations.
This study also highlights the surprising number of large-diameter, high-risk tumors identified in these scenarios. Limitations of this study include a relatively small sample size from a single facility that might not be representative of other practice settings and locations. Future multicenter studies could further explore the impact of inpatient dermatologic consultation on the diagnosis and management of skin cancer.
To the Editor:
Dermatologists sometimes are consulted in the inpatient setting to rule out possible skin cancer. This scenario provides an opportunity to facilitate the diagnosis and treatment of cutaneous malignancy, often in patients who might not have sought regular outpatient dermatology care. Few studies have described the outcomes of inpatient biopsies to identify skin cancer.1,2
Seeking to better understand the nature of these patient encounters, we reviewed all consultations at a medical center for which the referring physician suspected skin cancer rather than only those lesions that were biopsied by the dermatologist. We also collected data about subsequent treatment to better understand the outcomes of these patient encounters.
We conducted a retrospective review of inpatient dermatology referrals at an academic-affiliated tertiary medical center. We identified all patients who were provided with an inpatient dermatology consultation for suspected skin cancer or what was identified as a “skin lesion” between July 1, 2013, and July 1, 2019. We collected information on each patient’s sex, age at time of consultation, and race, as well as the specialty of the referring provider, lesion location, maximum diameter of the lesion, whether a biopsy was performed, where the biopsy was performed (inpatient or outpatient setting), clinical diagnosis, histopathologic diagnosis, and subsequent treatment.
The institutional review board at Eastern Virginia Medical School (Norfolk, Virginia) approved this study, and all protocol conformed to the ethical guidelines of the Declaration of Helsinki.
Thirty-eight patients met the inclusion criteria. Their characteristics are listed in the Table. Consultations for possible skin cancer accounted for 4% (38/950) of all inpatient dermatology consultations over the study period. Outcomes of the referrals are shown in the Figure. Consultations were received from 12 different physician specialties.
In the 38 patients, 47 lesions were identified; most (66% [31/47]) were on the head and neck. Twenty of 38 patients were found to have at least 1 biopsy-confirmed cutaneous malignancy (23 total tumors). Of those 23 identified malignancies, 10 were basal cell carcinoma, 11 squamous cell carcinoma, 1 malignant melanoma, and 1 anaplastic T-cell lymphoma. Of note, 17 of 23 (74%) identified cutaneous malignancies were 2.0 cm in diameter at biopsy or larger. Subsequently performed treatments for these patients included wide local excision (n=3), Mohs micrographic surgery (n=5), radiation therapy (n=3), topical fluorouracil (n=1), electrodesiccation and curettage (n=4), and chemotherapy or immunotherapy (n=2). Two patients who were diagnosed with skin cancer died of unrelated causes before treatment was completed.
In 10 of 38 patients, only nonmalignant entities were diagnosed, including seborrheic keratosis (n=6), benign melanocytic nevus (n=1), epidermal inclusion cyst (n=1), actinic keratosis (n=1), and radiation-induced necrosis (n=1). Of the 8 remaining patients, 4 were ultimately lost to follow-up before planned outpatient biopsy could be completed; 1 opted to follow up for biopsy at an unaffiliated outpatient dermatology provider. For 2 patients, the decision was made to forgo biopsy despite clinical suspicion of skin cancer because of overall poor health status, and 1 additional patient died before a planned outpatient biopsy could be performed.
In summary, approximately half of the inpatient dermatology consultations for suspected cutaneous malignancy resulted in a diagnosis of skin cancer. The patients in this population were admitted for a range of diagnoses, most unrelated to their cutaneous malignancy, suggesting that the inpatient setting offers the opportunity for physicians in a variety of specialties to help identify skin cancer that might otherwise be unaddressed and then facilitate management, whether ultimately in an inpatient or outpatient setting.
In many of these cases, it might be most appropriate to arrange subsequent outpatient dermatology follow-up after hospitalization, rather than making an inpatient consultation, as these situations usually are nonurgent and not directly related to hospitalization. However, in cases in which the lesion is directly related to admission, the lesion is advanced, there is concern for metastatic disease, or extenuating circumstances make outpatient follow-up difficult, inpatient dermatology consultation may be reasonable. There sometimes can be compelling reasons to expedite diagnosis and treatment as an inpatient.
In hospitalized, medically complex patients, in whom a new cutaneous malignancy is identified, dermatologists should discuss the situation thoughtfully with the patient, the patient’s family (when appropriate), and other physicians on the treatment team to determine the most appropriate course of action. In some cases, the most appropriate course might be to delay biopsy or treatment until the outpatient setting or to even defer further action completely when the prognosis is very limited. Consulting dermatologists must be mindful of patients’ overall medical situation in planning care for a cutaneous malignancy in these inpatient situations.
This study also highlights the surprising number of large-diameter, high-risk tumors identified in these scenarios. Limitations of this study include a relatively small sample size from a single facility that might not be representative of other practice settings and locations. Future multicenter studies could further explore the impact of inpatient dermatologic consultation on the diagnosis and management of skin cancer.
- Bauer J, Maroon M. Dermatology inpatient consultations: a retrospective study. J Am Acad Dermatol. 2010;62:518-519. doi:10.1016/j.jaad.2009.06.030
- Tsai S, Scott JF, Keller JJ, et al. Cutaneous malignancies identified in an inpatient dermatology consultation service. Br J Dermatol. 2017;177:E116-E118. doi:10.1111/bjd.15401
- Bauer J, Maroon M. Dermatology inpatient consultations: a retrospective study. J Am Acad Dermatol. 2010;62:518-519. doi:10.1016/j.jaad.2009.06.030
- Tsai S, Scott JF, Keller JJ, et al. Cutaneous malignancies identified in an inpatient dermatology consultation service. Br J Dermatol. 2017;177:E116-E118. doi:10.1111/bjd.15401
Practice Points
- Dermatologists who perform inpatient consultations should be prepared to be consulted for cutaneous malignancies.
- Relatively large skin tumors may be identified, often incidentally, in the inpatient population.
- Careful consideration should be involved when deciding how to diagnose and manage cutaneous malignancies identified in the inpatient setting, taking the overall medical and social context into account.
LEN-TACE sequential therapy tops LEN monotherapy in unresectable HCC responsive to initial LEN treatment
Key clinical point: Lenvatinib (LEN)-transcatheter arterial chemoembolization (LEN-TACE) sequential therapy may be more clinically beneficial than LEN monotherapy in patients with unresectable hepatocellular carcinoma (HCC) responsive to initial LEN treatment without exerting any additional adverse effects.
Major finding: The LEN-TACE vs. LEN monotherapy group showed a significantly higher median overall survival (31.2 months vs. 13.9 months; P = .002) and progression-free survival (12.2 months vs. 7.1 months; P = .037). The LEN-TACE group had an acceptable safety profile, with only liver dysfunction being significantly higher (P = .04).
Study details: Findings are from a retrospective, multicenter cohort study on patients with intermediate- or advanced-stage unresectable HCC who responded to initial LEN treatment. Among these, 63 patients receiving LEN-TACE sequential therapy were propensity-score matched to those receiving LEN monotherapy.
Disclosures: The authors declared no source of funding or conflict of interests.
Source: Kuroda H et al. Objective response by mRECIST to initial lenvatinib therapy is an independent factor contributing to deep response in hepatocellular carcinoma treated with lenvatinib-transcatheter arterial chemoembolization sequential therapy. Liver Cancer. 2022 (Feb 15). Doi: 10.1159/000522424
Key clinical point: Lenvatinib (LEN)-transcatheter arterial chemoembolization (LEN-TACE) sequential therapy may be more clinically beneficial than LEN monotherapy in patients with unresectable hepatocellular carcinoma (HCC) responsive to initial LEN treatment without exerting any additional adverse effects.
Major finding: The LEN-TACE vs. LEN monotherapy group showed a significantly higher median overall survival (31.2 months vs. 13.9 months; P = .002) and progression-free survival (12.2 months vs. 7.1 months; P = .037). The LEN-TACE group had an acceptable safety profile, with only liver dysfunction being significantly higher (P = .04).
Study details: Findings are from a retrospective, multicenter cohort study on patients with intermediate- or advanced-stage unresectable HCC who responded to initial LEN treatment. Among these, 63 patients receiving LEN-TACE sequential therapy were propensity-score matched to those receiving LEN monotherapy.
Disclosures: The authors declared no source of funding or conflict of interests.
Source: Kuroda H et al. Objective response by mRECIST to initial lenvatinib therapy is an independent factor contributing to deep response in hepatocellular carcinoma treated with lenvatinib-transcatheter arterial chemoembolization sequential therapy. Liver Cancer. 2022 (Feb 15). Doi: 10.1159/000522424
Key clinical point: Lenvatinib (LEN)-transcatheter arterial chemoembolization (LEN-TACE) sequential therapy may be more clinically beneficial than LEN monotherapy in patients with unresectable hepatocellular carcinoma (HCC) responsive to initial LEN treatment without exerting any additional adverse effects.
Major finding: The LEN-TACE vs. LEN monotherapy group showed a significantly higher median overall survival (31.2 months vs. 13.9 months; P = .002) and progression-free survival (12.2 months vs. 7.1 months; P = .037). The LEN-TACE group had an acceptable safety profile, with only liver dysfunction being significantly higher (P = .04).
Study details: Findings are from a retrospective, multicenter cohort study on patients with intermediate- or advanced-stage unresectable HCC who responded to initial LEN treatment. Among these, 63 patients receiving LEN-TACE sequential therapy were propensity-score matched to those receiving LEN monotherapy.
Disclosures: The authors declared no source of funding or conflict of interests.
Source: Kuroda H et al. Objective response by mRECIST to initial lenvatinib therapy is an independent factor contributing to deep response in hepatocellular carcinoma treated with lenvatinib-transcatheter arterial chemoembolization sequential therapy. Liver Cancer. 2022 (Feb 15). Doi: 10.1159/000522424
Final phase 2 results testify to the clinical advantage of TACE plus sorafenib in unresectable HCC
Key clinical point: Although treatment with transarterial chemoembolization (TACE) plus sorafenib does not significantly increase overall survival (OS) in patients with unresectable hepatocellular carcinoma (HCC) relative to TACE alone, it does offer a clinically meaningful OS prolongation.
Major finding: Patients receiving TACE plus sorafenib vs. TACE monotherapy showed a median OS of 36.2 months vs. 30.8 months (hazard ratio 0.861; P = .40). Despite being nonsignificant, the benefit (ΔOS 5.4 months) was clinically meaningful.
Study details: The data represent the final results of the multicenter, prospective phase 2 TACTICS trial including 156 patients aged >20 years with unresectable HCC having a life expectancy of ≥12 weeks who were randomly assigned to TACE plus sorafenib (n = 80) or TACE alone (n = 76).
Disclosures: The study was sponsored by Bayer Yakuhin Ltd., Japan. Some authors reported serving as speakers/advisory consultants for and receiving grants, personal fees, and consulting/advisory fees from various sources including Bayer. M Kudo is the Editor-in-Chief of Liver Cancer, and some others are its editorial board members.
Source: Kudo M et al. Final results of TACTICS: A randomized, prospective trial comparing transarterial chemoembolization plus sorafenib to transarterial chemoembolization alone in patients with unresectable hepatocellular carcinoma. Liver Cancer. 2022 (Feb 10). Doi: 10.1159/000522547
Key clinical point: Although treatment with transarterial chemoembolization (TACE) plus sorafenib does not significantly increase overall survival (OS) in patients with unresectable hepatocellular carcinoma (HCC) relative to TACE alone, it does offer a clinically meaningful OS prolongation.
Major finding: Patients receiving TACE plus sorafenib vs. TACE monotherapy showed a median OS of 36.2 months vs. 30.8 months (hazard ratio 0.861; P = .40). Despite being nonsignificant, the benefit (ΔOS 5.4 months) was clinically meaningful.
Study details: The data represent the final results of the multicenter, prospective phase 2 TACTICS trial including 156 patients aged >20 years with unresectable HCC having a life expectancy of ≥12 weeks who were randomly assigned to TACE plus sorafenib (n = 80) or TACE alone (n = 76).
Disclosures: The study was sponsored by Bayer Yakuhin Ltd., Japan. Some authors reported serving as speakers/advisory consultants for and receiving grants, personal fees, and consulting/advisory fees from various sources including Bayer. M Kudo is the Editor-in-Chief of Liver Cancer, and some others are its editorial board members.
Source: Kudo M et al. Final results of TACTICS: A randomized, prospective trial comparing transarterial chemoembolization plus sorafenib to transarterial chemoembolization alone in patients with unresectable hepatocellular carcinoma. Liver Cancer. 2022 (Feb 10). Doi: 10.1159/000522547
Key clinical point: Although treatment with transarterial chemoembolization (TACE) plus sorafenib does not significantly increase overall survival (OS) in patients with unresectable hepatocellular carcinoma (HCC) relative to TACE alone, it does offer a clinically meaningful OS prolongation.
Major finding: Patients receiving TACE plus sorafenib vs. TACE monotherapy showed a median OS of 36.2 months vs. 30.8 months (hazard ratio 0.861; P = .40). Despite being nonsignificant, the benefit (ΔOS 5.4 months) was clinically meaningful.
Study details: The data represent the final results of the multicenter, prospective phase 2 TACTICS trial including 156 patients aged >20 years with unresectable HCC having a life expectancy of ≥12 weeks who were randomly assigned to TACE plus sorafenib (n = 80) or TACE alone (n = 76).
Disclosures: The study was sponsored by Bayer Yakuhin Ltd., Japan. Some authors reported serving as speakers/advisory consultants for and receiving grants, personal fees, and consulting/advisory fees from various sources including Bayer. M Kudo is the Editor-in-Chief of Liver Cancer, and some others are its editorial board members.
Source: Kudo M et al. Final results of TACTICS: A randomized, prospective trial comparing transarterial chemoembolization plus sorafenib to transarterial chemoembolization alone in patients with unresectable hepatocellular carcinoma. Liver Cancer. 2022 (Feb 10). Doi: 10.1159/000522547
Overall survival after curative resection for HBV-related HCC is better with tenofovir vs. entecavir
Key clinical point: Patients receiving tenofovir disoproxil fumarate (TDF) vs. entecavir (ETV) after curative liver resection for hepatitis B virus (HBV)-related hepatocellular carcinoma (HCC) showed significantly better overall survival and protection of liver function but no significant difference in the cumulative incidences of HCC recurrence.
Major finding: Although patients receiving TDF vs. ETV showed no significant difference in recurrence-free survival after propensity-score matching (hazard ratio [HR] 0.91; P = .45), they had significantly better overall survival (HR 0.37; P = .002) and liver function (P = .001).
Study details: This retrospective, single-center study reviewed data on 1,173 adult patients with HBV-related HCC who had undergone liver resection and were initially treated with either TDF or ETV for chronic HBV infection.
Disclosures: The study was funded by Sun Yat-sen University Cancer Center physician-scientist funding and National Science and Technology Major Project of China. The authors reported having no conflict of interests.
Source: Wang XH et al. Tenofovir vs. entecavir on prognosis of hepatitis B virus-related hepatocellular carcinoma after curative resection. J Gastroenterol. 2022;57:185-198 (Feb 13). Doi: 10.1007/s00535-022-01855-x
Key clinical point: Patients receiving tenofovir disoproxil fumarate (TDF) vs. entecavir (ETV) after curative liver resection for hepatitis B virus (HBV)-related hepatocellular carcinoma (HCC) showed significantly better overall survival and protection of liver function but no significant difference in the cumulative incidences of HCC recurrence.
Major finding: Although patients receiving TDF vs. ETV showed no significant difference in recurrence-free survival after propensity-score matching (hazard ratio [HR] 0.91; P = .45), they had significantly better overall survival (HR 0.37; P = .002) and liver function (P = .001).
Study details: This retrospective, single-center study reviewed data on 1,173 adult patients with HBV-related HCC who had undergone liver resection and were initially treated with either TDF or ETV for chronic HBV infection.
Disclosures: The study was funded by Sun Yat-sen University Cancer Center physician-scientist funding and National Science and Technology Major Project of China. The authors reported having no conflict of interests.
Source: Wang XH et al. Tenofovir vs. entecavir on prognosis of hepatitis B virus-related hepatocellular carcinoma after curative resection. J Gastroenterol. 2022;57:185-198 (Feb 13). Doi: 10.1007/s00535-022-01855-x
Key clinical point: Patients receiving tenofovir disoproxil fumarate (TDF) vs. entecavir (ETV) after curative liver resection for hepatitis B virus (HBV)-related hepatocellular carcinoma (HCC) showed significantly better overall survival and protection of liver function but no significant difference in the cumulative incidences of HCC recurrence.
Major finding: Although patients receiving TDF vs. ETV showed no significant difference in recurrence-free survival after propensity-score matching (hazard ratio [HR] 0.91; P = .45), they had significantly better overall survival (HR 0.37; P = .002) and liver function (P = .001).
Study details: This retrospective, single-center study reviewed data on 1,173 adult patients with HBV-related HCC who had undergone liver resection and were initially treated with either TDF or ETV for chronic HBV infection.
Disclosures: The study was funded by Sun Yat-sen University Cancer Center physician-scientist funding and National Science and Technology Major Project of China. The authors reported having no conflict of interests.
Source: Wang XH et al. Tenofovir vs. entecavir on prognosis of hepatitis B virus-related hepatocellular carcinoma after curative resection. J Gastroenterol. 2022;57:185-198 (Feb 13). Doi: 10.1007/s00535-022-01855-x
New test for Lp(a) allows more accurate LDL-cholesterol results
A new study has drawn attention to inaccurate measurement of LDL-cholesterol levels in some patients with current assays, which could lead to incorrect therapeutic approaches.
The patient groups most affected are those with high levels of the lipoprotein Lp(a), in whom LDL-cholesterol levels are being overestimated in current laboratory tests, the authors say.
“Current laboratory assays all have the limitation that they cannot measure or report LDL cholesterol accurately. They are actually measuring the combination of LDL and Lp(a),” senior study author Sotirios Tsimikas, MD, University of California, San Diego, explained to this news organization.
“While this may not matter much in individuals with normal Lp(a) levels, in those with elevated Lp(a), the Lp(a) cholesterol may constitute a substantial proportion of the reported LDL cholesterol, and the actual LDL-cholesterol levels could be much lower that the value the lab is telling us,” he said.
Dr. Tsimikas gave the example of a patient with an LDL-cholesterol lab measurement of 75 mg/dL. “If that patient has an Lp(a) level of zero, then they do actually have an LDL level of 75. But as the Lp(a) increases, then the proportion of the result accounted for by LDL cholesterol decreases. So, if a patient with a measured LDL cholesterol of 75 has an Lp(a)-cholesterol level of 20, then their actual LDL level is 55.”
Dr. Tsimikas said it is important to know levels of both lipoproteins individually, so the correct therapeutic approach is used in situations where the Lp(a) cholesterol might be elevated.
“By understanding the actual values of LDL cholesterol and Lp(a) cholesterol, this will allow us to personalize the use of cholesterol-lowering medications and decide where to focus treatment. In the patient with a high level of Lp(a), their residual risk could be coming from Lp(a) cholesterol and less so from LDL cholesterol,” he added. “As we develop drugs to lower Lp(a), this patient might be better off on one of these rather than increasing efforts to lower LDL cholesterol, which might already be at goal.”
The study was published in the March 22 issue of the Journal of the American College of Cardiology.
Dr. Tsimikas noted that Lp(a) is now accepted as a genetic, independent, causal risk factor for cardiovascular disease, but current LDL-lowering drugs do not have much effect on Lp(a).
“Lp(a) can be lowered a little with niacin and PCSK9 inhibitors, but both have a quite a weak effect, and statins increase Lp(a). However, there are now multiple RNA-based therapeutics specifically targeting Lp(a) in clinical development,” he said.
At present, Lp(a) cholesterol has to be mathematically estimated, most commonly with the Dahlén formula, because of the lack of a validated, quantitative method to measure Lp(a) cholesterol, Dr. Tsimikas says.
For the current study, the researchers used a novel, quantitative, sensitive method to directly measure Lp(a) cholesterol, then applied this method to data from a recent study with the one of the new Lp(a)-lowering drugs in development – pelacarsen – which was conducted in patients with elevated Lp(a) levels.
Results showed that direct Lp(a)-cholesterol assessment, and subtracting this value from the laboratory LDL-cholesterol value, provides a more accurate reflection of the baseline and change in LDL cholesterol, the authors report. In the current study, corrected LDL cholesterol was 13 to 16 mg/dL lower than laboratory-reported LDL cholesterol.
Using the corrected LDL-cholesterol results, the study showed that pelacarsen significantly decreases Lp(a) cholesterol, with neutral to modest effects on LDL.
The study also suggests that the current method of calculating Lp(a) cholesterol, and then deriving a corrected LDL cholesterol – the Dahlén formula – is not accurate.
“The Dahlén formula relies on the assumption that Lp(a) cholesterol is universally a fixed 30% of Lp(a) mass, but this usually isn’t the case. The Dahlén formula needs to be discontinued. It can be highly inaccurate,” Dr. Tsimikas said.
Important implications
In an accompanying editorial, Guillaume Paré, MD, Michael Chong, PhD student, and Pedrum Mohammadi-Shemirani, BSc, all of McMaster University, Hamilton, Ont., say the current findings have three important clinical implications.
“First, they provide further proof that in individuals with elevated Lp(a), the contribution of Lp(a)-cholesterol to LDL-cholesterol is non-negligible using standard assays, with 13-16 mg/dL lower LDL-cholesterol post-correction.”
Secondly, the editorialists point out that these new findings confirm that the effect of Lp(a) inhibitors is likely to be mostly confined to Lp(a), “as would be expected.”
Finally, “and perhaps more importantly, the authors highlight the need to improve clinical reporting of lipid fractions to properly treat LDL-cholesterol and Lp(a) in high-risk patients,” they note.
“The report paves the way for future studies investigating the clinical utility of these additional measurements to initiate and monitor lipid-lowering therapy,” they conclude.
The clinical trial was funded by Ionis Pharmaceuticals, and the direct Lp(a)-cholesterol measurements were funded by Novartis through a research grant to the University of California, San Diego. Dr. Tsimikas is an employee of Ionis Pharmaceuticals and of the University of California, San Diego, and he is a cofounder of Covicept Therapeutics. He is also a coinventor and receives royalties from patents owned by UCSD on oxidation-specific antibodies and on biomarkers related to oxidized lipoproteins, as well as a cofounder and has equity interest in Oxitope and Kleanthi Diagnostics.
A version of this article first appeared on Medscape.com.
A new study has drawn attention to inaccurate measurement of LDL-cholesterol levels in some patients with current assays, which could lead to incorrect therapeutic approaches.
The patient groups most affected are those with high levels of the lipoprotein Lp(a), in whom LDL-cholesterol levels are being overestimated in current laboratory tests, the authors say.
“Current laboratory assays all have the limitation that they cannot measure or report LDL cholesterol accurately. They are actually measuring the combination of LDL and Lp(a),” senior study author Sotirios Tsimikas, MD, University of California, San Diego, explained to this news organization.
“While this may not matter much in individuals with normal Lp(a) levels, in those with elevated Lp(a), the Lp(a) cholesterol may constitute a substantial proportion of the reported LDL cholesterol, and the actual LDL-cholesterol levels could be much lower that the value the lab is telling us,” he said.
Dr. Tsimikas gave the example of a patient with an LDL-cholesterol lab measurement of 75 mg/dL. “If that patient has an Lp(a) level of zero, then they do actually have an LDL level of 75. But as the Lp(a) increases, then the proportion of the result accounted for by LDL cholesterol decreases. So, if a patient with a measured LDL cholesterol of 75 has an Lp(a)-cholesterol level of 20, then their actual LDL level is 55.”
Dr. Tsimikas said it is important to know levels of both lipoproteins individually, so the correct therapeutic approach is used in situations where the Lp(a) cholesterol might be elevated.
“By understanding the actual values of LDL cholesterol and Lp(a) cholesterol, this will allow us to personalize the use of cholesterol-lowering medications and decide where to focus treatment. In the patient with a high level of Lp(a), their residual risk could be coming from Lp(a) cholesterol and less so from LDL cholesterol,” he added. “As we develop drugs to lower Lp(a), this patient might be better off on one of these rather than increasing efforts to lower LDL cholesterol, which might already be at goal.”
The study was published in the March 22 issue of the Journal of the American College of Cardiology.
Dr. Tsimikas noted that Lp(a) is now accepted as a genetic, independent, causal risk factor for cardiovascular disease, but current LDL-lowering drugs do not have much effect on Lp(a).
“Lp(a) can be lowered a little with niacin and PCSK9 inhibitors, but both have a quite a weak effect, and statins increase Lp(a). However, there are now multiple RNA-based therapeutics specifically targeting Lp(a) in clinical development,” he said.
At present, Lp(a) cholesterol has to be mathematically estimated, most commonly with the Dahlén formula, because of the lack of a validated, quantitative method to measure Lp(a) cholesterol, Dr. Tsimikas says.
For the current study, the researchers used a novel, quantitative, sensitive method to directly measure Lp(a) cholesterol, then applied this method to data from a recent study with the one of the new Lp(a)-lowering drugs in development – pelacarsen – which was conducted in patients with elevated Lp(a) levels.
Results showed that direct Lp(a)-cholesterol assessment, and subtracting this value from the laboratory LDL-cholesterol value, provides a more accurate reflection of the baseline and change in LDL cholesterol, the authors report. In the current study, corrected LDL cholesterol was 13 to 16 mg/dL lower than laboratory-reported LDL cholesterol.
Using the corrected LDL-cholesterol results, the study showed that pelacarsen significantly decreases Lp(a) cholesterol, with neutral to modest effects on LDL.
The study also suggests that the current method of calculating Lp(a) cholesterol, and then deriving a corrected LDL cholesterol – the Dahlén formula – is not accurate.
“The Dahlén formula relies on the assumption that Lp(a) cholesterol is universally a fixed 30% of Lp(a) mass, but this usually isn’t the case. The Dahlén formula needs to be discontinued. It can be highly inaccurate,” Dr. Tsimikas said.
Important implications
In an accompanying editorial, Guillaume Paré, MD, Michael Chong, PhD student, and Pedrum Mohammadi-Shemirani, BSc, all of McMaster University, Hamilton, Ont., say the current findings have three important clinical implications.
“First, they provide further proof that in individuals with elevated Lp(a), the contribution of Lp(a)-cholesterol to LDL-cholesterol is non-negligible using standard assays, with 13-16 mg/dL lower LDL-cholesterol post-correction.”
Secondly, the editorialists point out that these new findings confirm that the effect of Lp(a) inhibitors is likely to be mostly confined to Lp(a), “as would be expected.”
Finally, “and perhaps more importantly, the authors highlight the need to improve clinical reporting of lipid fractions to properly treat LDL-cholesterol and Lp(a) in high-risk patients,” they note.
“The report paves the way for future studies investigating the clinical utility of these additional measurements to initiate and monitor lipid-lowering therapy,” they conclude.
The clinical trial was funded by Ionis Pharmaceuticals, and the direct Lp(a)-cholesterol measurements were funded by Novartis through a research grant to the University of California, San Diego. Dr. Tsimikas is an employee of Ionis Pharmaceuticals and of the University of California, San Diego, and he is a cofounder of Covicept Therapeutics. He is also a coinventor and receives royalties from patents owned by UCSD on oxidation-specific antibodies and on biomarkers related to oxidized lipoproteins, as well as a cofounder and has equity interest in Oxitope and Kleanthi Diagnostics.
A version of this article first appeared on Medscape.com.
A new study has drawn attention to inaccurate measurement of LDL-cholesterol levels in some patients with current assays, which could lead to incorrect therapeutic approaches.
The patient groups most affected are those with high levels of the lipoprotein Lp(a), in whom LDL-cholesterol levels are being overestimated in current laboratory tests, the authors say.
“Current laboratory assays all have the limitation that they cannot measure or report LDL cholesterol accurately. They are actually measuring the combination of LDL and Lp(a),” senior study author Sotirios Tsimikas, MD, University of California, San Diego, explained to this news organization.
“While this may not matter much in individuals with normal Lp(a) levels, in those with elevated Lp(a), the Lp(a) cholesterol may constitute a substantial proportion of the reported LDL cholesterol, and the actual LDL-cholesterol levels could be much lower that the value the lab is telling us,” he said.
Dr. Tsimikas gave the example of a patient with an LDL-cholesterol lab measurement of 75 mg/dL. “If that patient has an Lp(a) level of zero, then they do actually have an LDL level of 75. But as the Lp(a) increases, then the proportion of the result accounted for by LDL cholesterol decreases. So, if a patient with a measured LDL cholesterol of 75 has an Lp(a)-cholesterol level of 20, then their actual LDL level is 55.”
Dr. Tsimikas said it is important to know levels of both lipoproteins individually, so the correct therapeutic approach is used in situations where the Lp(a) cholesterol might be elevated.
“By understanding the actual values of LDL cholesterol and Lp(a) cholesterol, this will allow us to personalize the use of cholesterol-lowering medications and decide where to focus treatment. In the patient with a high level of Lp(a), their residual risk could be coming from Lp(a) cholesterol and less so from LDL cholesterol,” he added. “As we develop drugs to lower Lp(a), this patient might be better off on one of these rather than increasing efforts to lower LDL cholesterol, which might already be at goal.”
The study was published in the March 22 issue of the Journal of the American College of Cardiology.
Dr. Tsimikas noted that Lp(a) is now accepted as a genetic, independent, causal risk factor for cardiovascular disease, but current LDL-lowering drugs do not have much effect on Lp(a).
“Lp(a) can be lowered a little with niacin and PCSK9 inhibitors, but both have a quite a weak effect, and statins increase Lp(a). However, there are now multiple RNA-based therapeutics specifically targeting Lp(a) in clinical development,” he said.
At present, Lp(a) cholesterol has to be mathematically estimated, most commonly with the Dahlén formula, because of the lack of a validated, quantitative method to measure Lp(a) cholesterol, Dr. Tsimikas says.
For the current study, the researchers used a novel, quantitative, sensitive method to directly measure Lp(a) cholesterol, then applied this method to data from a recent study with the one of the new Lp(a)-lowering drugs in development – pelacarsen – which was conducted in patients with elevated Lp(a) levels.
Results showed that direct Lp(a)-cholesterol assessment, and subtracting this value from the laboratory LDL-cholesterol value, provides a more accurate reflection of the baseline and change in LDL cholesterol, the authors report. In the current study, corrected LDL cholesterol was 13 to 16 mg/dL lower than laboratory-reported LDL cholesterol.
Using the corrected LDL-cholesterol results, the study showed that pelacarsen significantly decreases Lp(a) cholesterol, with neutral to modest effects on LDL.
The study also suggests that the current method of calculating Lp(a) cholesterol, and then deriving a corrected LDL cholesterol – the Dahlén formula – is not accurate.
“The Dahlén formula relies on the assumption that Lp(a) cholesterol is universally a fixed 30% of Lp(a) mass, but this usually isn’t the case. The Dahlén formula needs to be discontinued. It can be highly inaccurate,” Dr. Tsimikas said.
Important implications
In an accompanying editorial, Guillaume Paré, MD, Michael Chong, PhD student, and Pedrum Mohammadi-Shemirani, BSc, all of McMaster University, Hamilton, Ont., say the current findings have three important clinical implications.
“First, they provide further proof that in individuals with elevated Lp(a), the contribution of Lp(a)-cholesterol to LDL-cholesterol is non-negligible using standard assays, with 13-16 mg/dL lower LDL-cholesterol post-correction.”
Secondly, the editorialists point out that these new findings confirm that the effect of Lp(a) inhibitors is likely to be mostly confined to Lp(a), “as would be expected.”
Finally, “and perhaps more importantly, the authors highlight the need to improve clinical reporting of lipid fractions to properly treat LDL-cholesterol and Lp(a) in high-risk patients,” they note.
“The report paves the way for future studies investigating the clinical utility of these additional measurements to initiate and monitor lipid-lowering therapy,” they conclude.
The clinical trial was funded by Ionis Pharmaceuticals, and the direct Lp(a)-cholesterol measurements were funded by Novartis through a research grant to the University of California, San Diego. Dr. Tsimikas is an employee of Ionis Pharmaceuticals and of the University of California, San Diego, and he is a cofounder of Covicept Therapeutics. He is also a coinventor and receives royalties from patents owned by UCSD on oxidation-specific antibodies and on biomarkers related to oxidized lipoproteins, as well as a cofounder and has equity interest in Oxitope and Kleanthi Diagnostics.
A version of this article first appeared on Medscape.com.
HCC risk differs among various liver cirrhosis etiologies
Key clinical point: The risk for hepatocellular carcinoma (HCC) varies with underlying etiologies, with active hepatitis C virus (HCV) cirrhosis posing the highest and alcoholic or nonalcoholic fatty liver disease (NAFLD) cirrhosis posing the lowest risk of developing HCC.
Major finding: Patients with active HCV (3.36%) showed the highest annual HCC incidence rate, followed by those with cured HCV (1.71%), alcoholic liver disease (1.32%), and NAFLD cirrhosis (1.24%). Patients with active HCV vs. NAFLD were at a 2.1-fold higher risk for HCC (adjusted hazard ratio 2.16; 95% CI, 1.16-4.04).
Study details: This multicenter, prospective cohort study analyzed data from two multiethnic cohorts enrolling a total of 2,733 patients with cirrhosis.
Disclosures: The study received financial support from the National Cancer Institute; Cancer Prevention & Research Institute of Texas grant; and Center for Gastrointestinal Development, Infection, and Injury. No conflicts of interest were reported.
Source: Kanwal F et al. Risk factors for hepatocellular cancer in contemporary cohorts of patients with cirrhosis. Hepatology. 2022 (Mar 1). Doi: 10.1002/hep.32434
Key clinical point: The risk for hepatocellular carcinoma (HCC) varies with underlying etiologies, with active hepatitis C virus (HCV) cirrhosis posing the highest and alcoholic or nonalcoholic fatty liver disease (NAFLD) cirrhosis posing the lowest risk of developing HCC.
Major finding: Patients with active HCV (3.36%) showed the highest annual HCC incidence rate, followed by those with cured HCV (1.71%), alcoholic liver disease (1.32%), and NAFLD cirrhosis (1.24%). Patients with active HCV vs. NAFLD were at a 2.1-fold higher risk for HCC (adjusted hazard ratio 2.16; 95% CI, 1.16-4.04).
Study details: This multicenter, prospective cohort study analyzed data from two multiethnic cohorts enrolling a total of 2,733 patients with cirrhosis.
Disclosures: The study received financial support from the National Cancer Institute; Cancer Prevention & Research Institute of Texas grant; and Center for Gastrointestinal Development, Infection, and Injury. No conflicts of interest were reported.
Source: Kanwal F et al. Risk factors for hepatocellular cancer in contemporary cohorts of patients with cirrhosis. Hepatology. 2022 (Mar 1). Doi: 10.1002/hep.32434
Key clinical point: The risk for hepatocellular carcinoma (HCC) varies with underlying etiologies, with active hepatitis C virus (HCV) cirrhosis posing the highest and alcoholic or nonalcoholic fatty liver disease (NAFLD) cirrhosis posing the lowest risk of developing HCC.
Major finding: Patients with active HCV (3.36%) showed the highest annual HCC incidence rate, followed by those with cured HCV (1.71%), alcoholic liver disease (1.32%), and NAFLD cirrhosis (1.24%). Patients with active HCV vs. NAFLD were at a 2.1-fold higher risk for HCC (adjusted hazard ratio 2.16; 95% CI, 1.16-4.04).
Study details: This multicenter, prospective cohort study analyzed data from two multiethnic cohorts enrolling a total of 2,733 patients with cirrhosis.
Disclosures: The study received financial support from the National Cancer Institute; Cancer Prevention & Research Institute of Texas grant; and Center for Gastrointestinal Development, Infection, and Injury. No conflicts of interest were reported.
Source: Kanwal F et al. Risk factors for hepatocellular cancer in contemporary cohorts of patients with cirrhosis. Hepatology. 2022 (Mar 1). Doi: 10.1002/hep.32434