User login
Pfizer recalls BP drugs because of potential carcinogen
Pfizer is voluntarily recalling some antihypertensive medications because of unacceptable levels of a potential carcinogen, the company announced.
The affected products are quinapril HCI/hydrochlorothiazide (Accuretic) tablets that Pfizer distributes, and two authorized generics, quinapril plus hydrochlorothiazide and quinapril HCI/hydrochlorothiazide, distributed by Greenstone. The drugs have been withdrawn because of the presence of nitrosamine, N-nitroso-quinapril.
“Although long-term ingestion of N-nitroso-quinapril may be associated with a potential increased cancer risk in humans, there is no immediate risk to patients taking this medication,” Pfizer said in a news release.
The tablets are indicated for the treatment of hypertension. Patients currently taking the products are asked to consult with their doctor about alternative treatment options.
To date, there have been no reports of adverse events related to the recall, the company said.
In all, Pfizer is recalling six lots of Accuretic tablets (two at 10 mg/12.5 mg, three at 20 mg/12.5 mg, and one at 20 mg/25 mg), one lot of quinapril plus hydrochlorothiazide 20-mg/25-mg tablets, and four lots of quinapril HCl/ hydrochlorothiazide tablets (three at 20 mg/12.5 mg and one at 20 mg/25 mg)
The recalled tablets were sold in 90-count bottles distributed in the United States and Puerto Rico between November 2019 and March 2022. Product codes and lot numbers of the recalled medications are listed on the Pfizer website.
Patients who are taking this product should consult with their health care provider or pharmacy to determine if they have the affected product. Those with the affected tablets should contact claims management firm Sedgwick by phone at 888-843-0247 Monday through Friday from 8 a.m. to 5 p.m. ET for instructions on how to return their product and obtain reimbursement.
Health care providers with medical questions regarding the recall can contact Pfizer by telephone at 800-438-1985, option 3, Monday through Friday 8 a.m. to 9 p.m. ET.
Providers should report adverse reactions or quality problems they experience using these tablets to Pfizer either by telephone at 800-438-1985, option 1, by regular mail or by fax, or to the Food and Drug Administration’s MedWatch program.
A version of this article first appeared on Medscape.com.
Pfizer is voluntarily recalling some antihypertensive medications because of unacceptable levels of a potential carcinogen, the company announced.
The affected products are quinapril HCI/hydrochlorothiazide (Accuretic) tablets that Pfizer distributes, and two authorized generics, quinapril plus hydrochlorothiazide and quinapril HCI/hydrochlorothiazide, distributed by Greenstone. The drugs have been withdrawn because of the presence of nitrosamine, N-nitroso-quinapril.
“Although long-term ingestion of N-nitroso-quinapril may be associated with a potential increased cancer risk in humans, there is no immediate risk to patients taking this medication,” Pfizer said in a news release.
The tablets are indicated for the treatment of hypertension. Patients currently taking the products are asked to consult with their doctor about alternative treatment options.
To date, there have been no reports of adverse events related to the recall, the company said.
In all, Pfizer is recalling six lots of Accuretic tablets (two at 10 mg/12.5 mg, three at 20 mg/12.5 mg, and one at 20 mg/25 mg), one lot of quinapril plus hydrochlorothiazide 20-mg/25-mg tablets, and four lots of quinapril HCl/ hydrochlorothiazide tablets (three at 20 mg/12.5 mg and one at 20 mg/25 mg)
The recalled tablets were sold in 90-count bottles distributed in the United States and Puerto Rico between November 2019 and March 2022. Product codes and lot numbers of the recalled medications are listed on the Pfizer website.
Patients who are taking this product should consult with their health care provider or pharmacy to determine if they have the affected product. Those with the affected tablets should contact claims management firm Sedgwick by phone at 888-843-0247 Monday through Friday from 8 a.m. to 5 p.m. ET for instructions on how to return their product and obtain reimbursement.
Health care providers with medical questions regarding the recall can contact Pfizer by telephone at 800-438-1985, option 3, Monday through Friday 8 a.m. to 9 p.m. ET.
Providers should report adverse reactions or quality problems they experience using these tablets to Pfizer either by telephone at 800-438-1985, option 1, by regular mail or by fax, or to the Food and Drug Administration’s MedWatch program.
A version of this article first appeared on Medscape.com.
Pfizer is voluntarily recalling some antihypertensive medications because of unacceptable levels of a potential carcinogen, the company announced.
The affected products are quinapril HCI/hydrochlorothiazide (Accuretic) tablets that Pfizer distributes, and two authorized generics, quinapril plus hydrochlorothiazide and quinapril HCI/hydrochlorothiazide, distributed by Greenstone. The drugs have been withdrawn because of the presence of nitrosamine, N-nitroso-quinapril.
“Although long-term ingestion of N-nitroso-quinapril may be associated with a potential increased cancer risk in humans, there is no immediate risk to patients taking this medication,” Pfizer said in a news release.
The tablets are indicated for the treatment of hypertension. Patients currently taking the products are asked to consult with their doctor about alternative treatment options.
To date, there have been no reports of adverse events related to the recall, the company said.
In all, Pfizer is recalling six lots of Accuretic tablets (two at 10 mg/12.5 mg, three at 20 mg/12.5 mg, and one at 20 mg/25 mg), one lot of quinapril plus hydrochlorothiazide 20-mg/25-mg tablets, and four lots of quinapril HCl/ hydrochlorothiazide tablets (three at 20 mg/12.5 mg and one at 20 mg/25 mg)
The recalled tablets were sold in 90-count bottles distributed in the United States and Puerto Rico between November 2019 and March 2022. Product codes and lot numbers of the recalled medications are listed on the Pfizer website.
Patients who are taking this product should consult with their health care provider or pharmacy to determine if they have the affected product. Those with the affected tablets should contact claims management firm Sedgwick by phone at 888-843-0247 Monday through Friday from 8 a.m. to 5 p.m. ET for instructions on how to return their product and obtain reimbursement.
Health care providers with medical questions regarding the recall can contact Pfizer by telephone at 800-438-1985, option 3, Monday through Friday 8 a.m. to 9 p.m. ET.
Providers should report adverse reactions or quality problems they experience using these tablets to Pfizer either by telephone at 800-438-1985, option 1, by regular mail or by fax, or to the Food and Drug Administration’s MedWatch program.
A version of this article first appeared on Medscape.com.
Complex surgery 10 times more likely with some ovarian tumors
according to a report at the Society of Gynecologic Oncology annual meeting.
Investigators found that women with those features, compared with those without them, are 10 times more likely to have a high-complexity surgery and almost 27 times more likely to have something other than a complete (RD0) resection.
The findings speak to a common dilemma in advanced ovarian cancer, whether women should have surgery or chemotherapy first. Part of the decision hinges on the likelihood of surgical success, explained lead investigator Diogo Torres, MD, a gynecologic oncologist at Ochsner Health in New Orleans.
He and his team concluded that “preoperative CT imaging combined with tumor molecular subtyping can identify a subset of women for whom successful primary surgery is unlikely. Preoperative tumor sampling may be useful in advanced [ovarian cancer] to better triage these cases to alternative approaches.”
For years “we’ve been trying to figure out” how best to make the call between primary debulking and neoadjuvant chemotherapy, said Pamela T. Soliman, MD, MPH,a gynecologic oncologist at the University of Texas MD Anderson Cancer Center, Houston, who discussed the abstract at the meeting.
Imaging alone or CA-125 are often used to make the decision, but they’re unreliable. Diagnostic laparoscopy is accurate, but it isn’t used much, she said.
What’s unique about Dr. Torres’s approach is that, by including tumor subtype, it incorporates tumor biology. It makes sense because his team previously found that women with mesenchymal (MES) tumors are more likely than those with other subtypes to have upper abdominal and miliary disease.
The approach needs validation in a larger study, but “I really commend” the team “for incorporating biology into the decision-making because it is clearly a step in the right direction,” Dr. Soliman said.
The study included 129 women who underwent primary debulking surgery for stage 3c or 4 high-grade serous ovarian cancer; 46x women (36%) had MES tumors according to RNA profiling of surgical specimens.
Preoperative CTs were reviewed to assess diaphragmatic disease; gastrohepatic/portahepatis lesions; root of superior mesenteric artery involvement; presence of moderate to severe ascites; intrahepatic lesions, and diffuse peritoneal thickening greater than 4 mm.
Fifty-nine women (46%) were classified as “CT high,” meaning that they had two or more of those findings. Women with no more than one were categorized as “CT low.”
Patients with MES tumors and CT-high disease had the lowest rates of complete resections, 8% versus 46% for the entire cohort and 72% for non-MES, CT-low women. MES, CT-high women were also the most likely to have high-complexity surgery (81% versus 35% in the non-MES, CT-low group).
Adjusting for age, stage, and American Society of Anesthesiologists score, the odds of high-complexity surgery were 9.53 times higher and the odds of something less than a complete resection were 26.73 times greater in MES, CT-high patients, compared with non-MES, CT-low women.
“Further studies are needed to evaluate and validate this model using preoperative biopsy specimens” instead of surgical specimens, the investigators said.
No funding was reported for the work. Dr. Torres didn’t have any disclosures. Dr. Soliman is an adviser for Eisai and Amgen, a consultant for Medscape, and receives research funding from Novartis and Incyte.
according to a report at the Society of Gynecologic Oncology annual meeting.
Investigators found that women with those features, compared with those without them, are 10 times more likely to have a high-complexity surgery and almost 27 times more likely to have something other than a complete (RD0) resection.
The findings speak to a common dilemma in advanced ovarian cancer, whether women should have surgery or chemotherapy first. Part of the decision hinges on the likelihood of surgical success, explained lead investigator Diogo Torres, MD, a gynecologic oncologist at Ochsner Health in New Orleans.
He and his team concluded that “preoperative CT imaging combined with tumor molecular subtyping can identify a subset of women for whom successful primary surgery is unlikely. Preoperative tumor sampling may be useful in advanced [ovarian cancer] to better triage these cases to alternative approaches.”
For years “we’ve been trying to figure out” how best to make the call between primary debulking and neoadjuvant chemotherapy, said Pamela T. Soliman, MD, MPH,a gynecologic oncologist at the University of Texas MD Anderson Cancer Center, Houston, who discussed the abstract at the meeting.
Imaging alone or CA-125 are often used to make the decision, but they’re unreliable. Diagnostic laparoscopy is accurate, but it isn’t used much, she said.
What’s unique about Dr. Torres’s approach is that, by including tumor subtype, it incorporates tumor biology. It makes sense because his team previously found that women with mesenchymal (MES) tumors are more likely than those with other subtypes to have upper abdominal and miliary disease.
The approach needs validation in a larger study, but “I really commend” the team “for incorporating biology into the decision-making because it is clearly a step in the right direction,” Dr. Soliman said.
The study included 129 women who underwent primary debulking surgery for stage 3c or 4 high-grade serous ovarian cancer; 46x women (36%) had MES tumors according to RNA profiling of surgical specimens.
Preoperative CTs were reviewed to assess diaphragmatic disease; gastrohepatic/portahepatis lesions; root of superior mesenteric artery involvement; presence of moderate to severe ascites; intrahepatic lesions, and diffuse peritoneal thickening greater than 4 mm.
Fifty-nine women (46%) were classified as “CT high,” meaning that they had two or more of those findings. Women with no more than one were categorized as “CT low.”
Patients with MES tumors and CT-high disease had the lowest rates of complete resections, 8% versus 46% for the entire cohort and 72% for non-MES, CT-low women. MES, CT-high women were also the most likely to have high-complexity surgery (81% versus 35% in the non-MES, CT-low group).
Adjusting for age, stage, and American Society of Anesthesiologists score, the odds of high-complexity surgery were 9.53 times higher and the odds of something less than a complete resection were 26.73 times greater in MES, CT-high patients, compared with non-MES, CT-low women.
“Further studies are needed to evaluate and validate this model using preoperative biopsy specimens” instead of surgical specimens, the investigators said.
No funding was reported for the work. Dr. Torres didn’t have any disclosures. Dr. Soliman is an adviser for Eisai and Amgen, a consultant for Medscape, and receives research funding from Novartis and Incyte.
according to a report at the Society of Gynecologic Oncology annual meeting.
Investigators found that women with those features, compared with those without them, are 10 times more likely to have a high-complexity surgery and almost 27 times more likely to have something other than a complete (RD0) resection.
The findings speak to a common dilemma in advanced ovarian cancer, whether women should have surgery or chemotherapy first. Part of the decision hinges on the likelihood of surgical success, explained lead investigator Diogo Torres, MD, a gynecologic oncologist at Ochsner Health in New Orleans.
He and his team concluded that “preoperative CT imaging combined with tumor molecular subtyping can identify a subset of women for whom successful primary surgery is unlikely. Preoperative tumor sampling may be useful in advanced [ovarian cancer] to better triage these cases to alternative approaches.”
For years “we’ve been trying to figure out” how best to make the call between primary debulking and neoadjuvant chemotherapy, said Pamela T. Soliman, MD, MPH,a gynecologic oncologist at the University of Texas MD Anderson Cancer Center, Houston, who discussed the abstract at the meeting.
Imaging alone or CA-125 are often used to make the decision, but they’re unreliable. Diagnostic laparoscopy is accurate, but it isn’t used much, she said.
What’s unique about Dr. Torres’s approach is that, by including tumor subtype, it incorporates tumor biology. It makes sense because his team previously found that women with mesenchymal (MES) tumors are more likely than those with other subtypes to have upper abdominal and miliary disease.
The approach needs validation in a larger study, but “I really commend” the team “for incorporating biology into the decision-making because it is clearly a step in the right direction,” Dr. Soliman said.
The study included 129 women who underwent primary debulking surgery for stage 3c or 4 high-grade serous ovarian cancer; 46x women (36%) had MES tumors according to RNA profiling of surgical specimens.
Preoperative CTs were reviewed to assess diaphragmatic disease; gastrohepatic/portahepatis lesions; root of superior mesenteric artery involvement; presence of moderate to severe ascites; intrahepatic lesions, and diffuse peritoneal thickening greater than 4 mm.
Fifty-nine women (46%) were classified as “CT high,” meaning that they had two or more of those findings. Women with no more than one were categorized as “CT low.”
Patients with MES tumors and CT-high disease had the lowest rates of complete resections, 8% versus 46% for the entire cohort and 72% for non-MES, CT-low women. MES, CT-high women were also the most likely to have high-complexity surgery (81% versus 35% in the non-MES, CT-low group).
Adjusting for age, stage, and American Society of Anesthesiologists score, the odds of high-complexity surgery were 9.53 times higher and the odds of something less than a complete resection were 26.73 times greater in MES, CT-high patients, compared with non-MES, CT-low women.
“Further studies are needed to evaluate and validate this model using preoperative biopsy specimens” instead of surgical specimens, the investigators said.
No funding was reported for the work. Dr. Torres didn’t have any disclosures. Dr. Soliman is an adviser for Eisai and Amgen, a consultant for Medscape, and receives research funding from Novartis and Incyte.
FROM SGO 2022
As a nurse faces prison for a deadly error, her colleagues worry: Could I be next?
Four years ago, inside the most prestigious hospital in Tennessee, nurse RaDonda Vaught withdrew a vial from an electronic medication cabinet, administered the drug to a patient, and somehow overlooked signs of a terrible and deadly mistake.
The patient was supposed to get Versed, a sedative intended to calm her before being scanned in a large, MRI-like machine. But Ms. Vaught accidentally grabbed vecuronium, a powerful paralyzer, which stopped the patient’s breathing and left her brain-dead before the error was discovered.
Ms. Vaught, 38, admitted her mistake at a Tennessee Board of Nursing hearing last year, saying she became “complacent” in her job and “distracted” by a trainee while operating the computerized medication cabinet. She did not shirk responsibility for the error, but she said the blame was not hers alone.
“I know the reason this patient is no longer here is because of me,” Ms. Vaught said, starting to cry. “There won’t ever be a day that goes by that I don’t think about what I did.”
If Ms. Vaught’s story followed the path of most medical errors, it would have been over hours later, when the Board of Nursing revoked her RN license and almost certainly ended her nursing career. But Ms. Vaught’s case is different: This week she goes on trial in Nashville on criminal charges of reckless homicide and felony abuse of an impaired adult for the killing of Charlene Murphey, a 75-year-old patient who died at Vanderbilt University Medical Center on Dec. 27, 2017.
Prosecutors do not allege in their court filings that Ms. Vaught intended to hurt Ms. Murphey or was impaired by any substance when she made the mistake, so Fatal errors are generally handled by licensing boards and civil courts. And experts say prosecutions like Ms. Vaught’s loom large for a profession terrified of the criminalization of such mistakes — especially because her case hinges on an automated system for dispensing drugs that many nurses use every day.
The Nashville district attorney’s office declined to discuss Ms. Vaught’s trial. Ms. Vaught’s lawyer, Peter Strianse, did not respond to requests for comment. Vanderbilt University Medical Center has repeatedly declined to comment on Ms. Vaught’s trial or its procedures.
Ms. Vaught’s trial will be followed by nurses nationwide, many of whom worry a conviction may set a precedent even as the coronavirus pandemic leaves countless nurses exhausted, demoralized, and likely more prone to error.
Janie Harvey Garner, a St. Louis registered nurse and founder of Show Me Your Stethoscope, a nursing group with more than 600,000 members on Facebook, said the group has closely watched Ms. Vaught’s case for years out of concern for her fate — and their own.
Ms. Garner said most nurses know all too well the pressures that contribute to such an error: long hours, crowded hospitals, imperfect protocols, and the inevitable creep of complacency in a job with daily life-or-death stakes.
Ms. Garner said she once switched powerful medications just as Ms. Vaught did and caught her mistake only in a last-minute triple-check.
“In response to a story like this one, there are two kinds of nurses,” Ms. Garner said. “You have the nurses who assume they would never make a mistake like that, and usually it’s because they don’t realize they could. And the second kind are the ones who know this could happen, any day, no matter how careful they are. This could be me. I could be RaDonda.”
As the trial begins, the Nashville DA’s prosecutors will argue that Ms. Vaught’s error was anything but a common mistake any nurse could make. Prosecutors will say she ignored a cascade of warnings that led to the deadly error.
The case hinges on the nurse’s use of an electronic medication cabinet, a computerized device that dispenses a range of drugs. According to documents filed in the case, Ms. Vaught initially tried to withdraw Versed from a cabinet by typing “VE” into its search function without realizing she should have been looking for its generic name, midazolam. When the cabinet did not produce Versed, Ms. Vaught triggered an “override” that unlocked a much larger swath of medications, then searched for “VE” again. This time, the cabinet offered vecuronium.
Ms. Vaught then overlooked or bypassed at least five warnings or pop-ups saying she was withdrawing a paralyzing medication, documents state. She also did not recognize that Versed is a liquid but vecuronium is a powder that must be mixed into liquid, documents state.
Finally, just before injecting the vecuronium, Ms. Vaught stuck a syringe into the vial, which would have required her to “look directly” at a bottle cap that read “Warning: Paralyzing Agent,” the DA’s documents state.
The DA’s office points to this override as central to Ms. Vaught’s reckless homicide charge. Ms. Vaught acknowledges she performed an override on the cabinet. But she and others say overrides are a normal operating procedure used daily at hospitals.
While testifying before the nursing board last year, foreshadowing her defense in the upcoming trial, Ms. Vaught said at the time of Ms. Murphey’s death that Vanderbilt was instructing nurses to use overrides to overcome cabinet delays and constant technical problems caused by an ongoing overhaul of the hospital’s electronic health records system.
Ms. Murphey’s care alone required at least 20 cabinet overrides in just three days, Ms. Vaught said.
“Overriding was something we did as part of our practice every day,” Ms. Vaught said. “You couldn’t get a bag of fluids for a patient without using an override function.”
Overrides are common outside of Vanderbilt too, according to experts following Ms. Vaught’s case.
Michael Cohen, president emeritus of the Institute for Safe Medication Practices, and Lorie Brown, past president of the American Association of Nurse Attorneys, each said it is common for nurses to use an override to obtain medication in a hospital.
Mr. Cohen and Ms. Brown stressed that even with an override it should not have been so easy to access vecuronium.
“This is a medication that you should never, ever, be able to override to,” Ms. Brown said. “It’s probably the most dangerous medication out there.”
Mr. Cohen said that in response to Ms. Vaught’s case, manufacturers of medication cabinets modified the devices’ software to require up to five letters to be typed when searching for drugs during an override, but not all hospitals have implemented this safeguard. Two years after Ms. Vaught’s error, Mr. Cohen’s organization documented a “strikingly similar” incident in which another nurse swapped Versed with another drug, verapamil, while using an override and searching with just the first few letters. That incident did not result in a patient’s death or criminal prosecution, Mr. Cohen said.
Maureen Shawn Kennedy, the editor-in-chief emerita of the American Journal of Nursing, wrote in 2019 that Ms. Vaught’s case was “every nurse’s nightmare.”
In the pandemic, she said, this is truer than ever.
“We know that the more patients a nurse has, the more room there is for errors,” Ms. Kennedy said. “We know that when nurses work longer shifts, there is more room for errors. So I think nurses get very concerned because they know this could be them.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Four years ago, inside the most prestigious hospital in Tennessee, nurse RaDonda Vaught withdrew a vial from an electronic medication cabinet, administered the drug to a patient, and somehow overlooked signs of a terrible and deadly mistake.
The patient was supposed to get Versed, a sedative intended to calm her before being scanned in a large, MRI-like machine. But Ms. Vaught accidentally grabbed vecuronium, a powerful paralyzer, which stopped the patient’s breathing and left her brain-dead before the error was discovered.
Ms. Vaught, 38, admitted her mistake at a Tennessee Board of Nursing hearing last year, saying she became “complacent” in her job and “distracted” by a trainee while operating the computerized medication cabinet. She did not shirk responsibility for the error, but she said the blame was not hers alone.
“I know the reason this patient is no longer here is because of me,” Ms. Vaught said, starting to cry. “There won’t ever be a day that goes by that I don’t think about what I did.”
If Ms. Vaught’s story followed the path of most medical errors, it would have been over hours later, when the Board of Nursing revoked her RN license and almost certainly ended her nursing career. But Ms. Vaught’s case is different: This week she goes on trial in Nashville on criminal charges of reckless homicide and felony abuse of an impaired adult for the killing of Charlene Murphey, a 75-year-old patient who died at Vanderbilt University Medical Center on Dec. 27, 2017.
Prosecutors do not allege in their court filings that Ms. Vaught intended to hurt Ms. Murphey or was impaired by any substance when she made the mistake, so Fatal errors are generally handled by licensing boards and civil courts. And experts say prosecutions like Ms. Vaught’s loom large for a profession terrified of the criminalization of such mistakes — especially because her case hinges on an automated system for dispensing drugs that many nurses use every day.
The Nashville district attorney’s office declined to discuss Ms. Vaught’s trial. Ms. Vaught’s lawyer, Peter Strianse, did not respond to requests for comment. Vanderbilt University Medical Center has repeatedly declined to comment on Ms. Vaught’s trial or its procedures.
Ms. Vaught’s trial will be followed by nurses nationwide, many of whom worry a conviction may set a precedent even as the coronavirus pandemic leaves countless nurses exhausted, demoralized, and likely more prone to error.
Janie Harvey Garner, a St. Louis registered nurse and founder of Show Me Your Stethoscope, a nursing group with more than 600,000 members on Facebook, said the group has closely watched Ms. Vaught’s case for years out of concern for her fate — and their own.
Ms. Garner said most nurses know all too well the pressures that contribute to such an error: long hours, crowded hospitals, imperfect protocols, and the inevitable creep of complacency in a job with daily life-or-death stakes.
Ms. Garner said she once switched powerful medications just as Ms. Vaught did and caught her mistake only in a last-minute triple-check.
“In response to a story like this one, there are two kinds of nurses,” Ms. Garner said. “You have the nurses who assume they would never make a mistake like that, and usually it’s because they don’t realize they could. And the second kind are the ones who know this could happen, any day, no matter how careful they are. This could be me. I could be RaDonda.”
As the trial begins, the Nashville DA’s prosecutors will argue that Ms. Vaught’s error was anything but a common mistake any nurse could make. Prosecutors will say she ignored a cascade of warnings that led to the deadly error.
The case hinges on the nurse’s use of an electronic medication cabinet, a computerized device that dispenses a range of drugs. According to documents filed in the case, Ms. Vaught initially tried to withdraw Versed from a cabinet by typing “VE” into its search function without realizing she should have been looking for its generic name, midazolam. When the cabinet did not produce Versed, Ms. Vaught triggered an “override” that unlocked a much larger swath of medications, then searched for “VE” again. This time, the cabinet offered vecuronium.
Ms. Vaught then overlooked or bypassed at least five warnings or pop-ups saying she was withdrawing a paralyzing medication, documents state. She also did not recognize that Versed is a liquid but vecuronium is a powder that must be mixed into liquid, documents state.
Finally, just before injecting the vecuronium, Ms. Vaught stuck a syringe into the vial, which would have required her to “look directly” at a bottle cap that read “Warning: Paralyzing Agent,” the DA’s documents state.
The DA’s office points to this override as central to Ms. Vaught’s reckless homicide charge. Ms. Vaught acknowledges she performed an override on the cabinet. But she and others say overrides are a normal operating procedure used daily at hospitals.
While testifying before the nursing board last year, foreshadowing her defense in the upcoming trial, Ms. Vaught said at the time of Ms. Murphey’s death that Vanderbilt was instructing nurses to use overrides to overcome cabinet delays and constant technical problems caused by an ongoing overhaul of the hospital’s electronic health records system.
Ms. Murphey’s care alone required at least 20 cabinet overrides in just three days, Ms. Vaught said.
“Overriding was something we did as part of our practice every day,” Ms. Vaught said. “You couldn’t get a bag of fluids for a patient without using an override function.”
Overrides are common outside of Vanderbilt too, according to experts following Ms. Vaught’s case.
Michael Cohen, president emeritus of the Institute for Safe Medication Practices, and Lorie Brown, past president of the American Association of Nurse Attorneys, each said it is common for nurses to use an override to obtain medication in a hospital.
Mr. Cohen and Ms. Brown stressed that even with an override it should not have been so easy to access vecuronium.
“This is a medication that you should never, ever, be able to override to,” Ms. Brown said. “It’s probably the most dangerous medication out there.”
Mr. Cohen said that in response to Ms. Vaught’s case, manufacturers of medication cabinets modified the devices’ software to require up to five letters to be typed when searching for drugs during an override, but not all hospitals have implemented this safeguard. Two years after Ms. Vaught’s error, Mr. Cohen’s organization documented a “strikingly similar” incident in which another nurse swapped Versed with another drug, verapamil, while using an override and searching with just the first few letters. That incident did not result in a patient’s death or criminal prosecution, Mr. Cohen said.
Maureen Shawn Kennedy, the editor-in-chief emerita of the American Journal of Nursing, wrote in 2019 that Ms. Vaught’s case was “every nurse’s nightmare.”
In the pandemic, she said, this is truer than ever.
“We know that the more patients a nurse has, the more room there is for errors,” Ms. Kennedy said. “We know that when nurses work longer shifts, there is more room for errors. So I think nurses get very concerned because they know this could be them.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Four years ago, inside the most prestigious hospital in Tennessee, nurse RaDonda Vaught withdrew a vial from an electronic medication cabinet, administered the drug to a patient, and somehow overlooked signs of a terrible and deadly mistake.
The patient was supposed to get Versed, a sedative intended to calm her before being scanned in a large, MRI-like machine. But Ms. Vaught accidentally grabbed vecuronium, a powerful paralyzer, which stopped the patient’s breathing and left her brain-dead before the error was discovered.
Ms. Vaught, 38, admitted her mistake at a Tennessee Board of Nursing hearing last year, saying she became “complacent” in her job and “distracted” by a trainee while operating the computerized medication cabinet. She did not shirk responsibility for the error, but she said the blame was not hers alone.
“I know the reason this patient is no longer here is because of me,” Ms. Vaught said, starting to cry. “There won’t ever be a day that goes by that I don’t think about what I did.”
If Ms. Vaught’s story followed the path of most medical errors, it would have been over hours later, when the Board of Nursing revoked her RN license and almost certainly ended her nursing career. But Ms. Vaught’s case is different: This week she goes on trial in Nashville on criminal charges of reckless homicide and felony abuse of an impaired adult for the killing of Charlene Murphey, a 75-year-old patient who died at Vanderbilt University Medical Center on Dec. 27, 2017.
Prosecutors do not allege in their court filings that Ms. Vaught intended to hurt Ms. Murphey or was impaired by any substance when she made the mistake, so Fatal errors are generally handled by licensing boards and civil courts. And experts say prosecutions like Ms. Vaught’s loom large for a profession terrified of the criminalization of such mistakes — especially because her case hinges on an automated system for dispensing drugs that many nurses use every day.
The Nashville district attorney’s office declined to discuss Ms. Vaught’s trial. Ms. Vaught’s lawyer, Peter Strianse, did not respond to requests for comment. Vanderbilt University Medical Center has repeatedly declined to comment on Ms. Vaught’s trial or its procedures.
Ms. Vaught’s trial will be followed by nurses nationwide, many of whom worry a conviction may set a precedent even as the coronavirus pandemic leaves countless nurses exhausted, demoralized, and likely more prone to error.
Janie Harvey Garner, a St. Louis registered nurse and founder of Show Me Your Stethoscope, a nursing group with more than 600,000 members on Facebook, said the group has closely watched Ms. Vaught’s case for years out of concern for her fate — and their own.
Ms. Garner said most nurses know all too well the pressures that contribute to such an error: long hours, crowded hospitals, imperfect protocols, and the inevitable creep of complacency in a job with daily life-or-death stakes.
Ms. Garner said she once switched powerful medications just as Ms. Vaught did and caught her mistake only in a last-minute triple-check.
“In response to a story like this one, there are two kinds of nurses,” Ms. Garner said. “You have the nurses who assume they would never make a mistake like that, and usually it’s because they don’t realize they could. And the second kind are the ones who know this could happen, any day, no matter how careful they are. This could be me. I could be RaDonda.”
As the trial begins, the Nashville DA’s prosecutors will argue that Ms. Vaught’s error was anything but a common mistake any nurse could make. Prosecutors will say she ignored a cascade of warnings that led to the deadly error.
The case hinges on the nurse’s use of an electronic medication cabinet, a computerized device that dispenses a range of drugs. According to documents filed in the case, Ms. Vaught initially tried to withdraw Versed from a cabinet by typing “VE” into its search function without realizing she should have been looking for its generic name, midazolam. When the cabinet did not produce Versed, Ms. Vaught triggered an “override” that unlocked a much larger swath of medications, then searched for “VE” again. This time, the cabinet offered vecuronium.
Ms. Vaught then overlooked or bypassed at least five warnings or pop-ups saying she was withdrawing a paralyzing medication, documents state. She also did not recognize that Versed is a liquid but vecuronium is a powder that must be mixed into liquid, documents state.
Finally, just before injecting the vecuronium, Ms. Vaught stuck a syringe into the vial, which would have required her to “look directly” at a bottle cap that read “Warning: Paralyzing Agent,” the DA’s documents state.
The DA’s office points to this override as central to Ms. Vaught’s reckless homicide charge. Ms. Vaught acknowledges she performed an override on the cabinet. But she and others say overrides are a normal operating procedure used daily at hospitals.
While testifying before the nursing board last year, foreshadowing her defense in the upcoming trial, Ms. Vaught said at the time of Ms. Murphey’s death that Vanderbilt was instructing nurses to use overrides to overcome cabinet delays and constant technical problems caused by an ongoing overhaul of the hospital’s electronic health records system.
Ms. Murphey’s care alone required at least 20 cabinet overrides in just three days, Ms. Vaught said.
“Overriding was something we did as part of our practice every day,” Ms. Vaught said. “You couldn’t get a bag of fluids for a patient without using an override function.”
Overrides are common outside of Vanderbilt too, according to experts following Ms. Vaught’s case.
Michael Cohen, president emeritus of the Institute for Safe Medication Practices, and Lorie Brown, past president of the American Association of Nurse Attorneys, each said it is common for nurses to use an override to obtain medication in a hospital.
Mr. Cohen and Ms. Brown stressed that even with an override it should not have been so easy to access vecuronium.
“This is a medication that you should never, ever, be able to override to,” Ms. Brown said. “It’s probably the most dangerous medication out there.”
Mr. Cohen said that in response to Ms. Vaught’s case, manufacturers of medication cabinets modified the devices’ software to require up to five letters to be typed when searching for drugs during an override, but not all hospitals have implemented this safeguard. Two years after Ms. Vaught’s error, Mr. Cohen’s organization documented a “strikingly similar” incident in which another nurse swapped Versed with another drug, verapamil, while using an override and searching with just the first few letters. That incident did not result in a patient’s death or criminal prosecution, Mr. Cohen said.
Maureen Shawn Kennedy, the editor-in-chief emerita of the American Journal of Nursing, wrote in 2019 that Ms. Vaught’s case was “every nurse’s nightmare.”
In the pandemic, she said, this is truer than ever.
“We know that the more patients a nurse has, the more room there is for errors,” Ms. Kennedy said. “We know that when nurses work longer shifts, there is more room for errors. So I think nurses get very concerned because they know this could be them.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Are ‘antibiotic diets’ good practice?
Antibiotics are among the most commonly prescribed medications in both outpatient and hospital settings. Global efforts at curbing antibiotic-resistant strains have prompted clinicians to pursue better stewardship, whereby they limit their prescribing of such medications to those who truly need them.
Yet there’s another possible means of addressing antibiotic resistance – using dietary interventions to reduce the gastrointestinal complaints that so often accompany the use of antibiotics: vomiting, nausea, diarrhea, bloating/indigestion, abdominal pain, and loss of appetite. Far from being a mere nuisance, these complications can have major ramifications.
“Often [these side effects] will result in people stopping an antibiotic they need or taking a second- or third-generation one, which potentially causes even more problems with resistance,” explained Daniel J. Merenstein, MD, a professor of family medicine at Georgetown University, Washington, who has conducted multiple trials on antibiotic stewardship and probiotics.
And it’s not just clinicians who would like to find a way around these common complaints. On lifestyle blogs such as Livestrong and Goop, medical news websites, and via academic institutions, patients can learn how the right probiotic supplement or certain fermented or high-fiber foods, for example, might spare them the upset stomach that often accompanies a course of antibiotics.
Yet according to experts in the field, there are notable questions to be answered about whether there’s evidence to support this approach.
The cost of GI discomfort
Pinpointing the exact manner by which antibiotics upend GI tracts is a complex task, according to Gail Cresci, PhD, RD, a microbiome researcher in the department of pediatric gastroenterology, hepatology, and nutrition and director of nutrition research at the Cleveland Clinic.
“A lot of different mechanisms can go awry,” Dr. Cresci said. “But normally, the good microbes are there to help keep the balance, so when that balance is gone, the pathogens can take over and lead to this disruption.”
According to Lynne V. McFarland, PhD, a recently retired infectious disease epidemiologist who now serves as a private consultant, such complications can have substantial ramifications for patients and health care systems.
“If you’re an inpatient and develop antibiotic-associated diarrhea, it usually increases the length of stay from 8 to 20 days. It also increases the cost of care. And small children who have this can get severely dehydrated, which can become life threatening.”
Proponents of probiotics
Several of the researchers who were interviewed believe there’s convincing evidence supporting probiotics for the treatment of common antibiotic-related GI complaints. In many instances, they were involved in the studies themselves.
During Dr. McFarland’s 4-decade career in probiotics research, she has participated in early animal studies with strains such as Saccharomyces boulardii and was involved in meta-analyses of their role in Clostridioides difficile infection and associated diarrhea and even as a potential GI intervention for COVID-19 patients (Antibiotics (Basel). 2021 Apr 9;10(4):408).
In mouse model studies from 2013 and 2018, Dr. Cresci and colleagues showed that the probiotic strains Lactobacillus GG and Faecalibacterium prausnitzii reduced the structural gut changes that lead to antibiotic-associated diarrhea and minimized the risk of C. difficile infection.
In a 2021 randomized controlled trial led by Merenstein, healthy participants were given a trial of amoxicillin/clavulanate (days 1-7) in conjunction with either yogurt containing the probiotic Bifidobacterium animalis subsp lactis BB-12 or control yogurt (days 1-14). After assessing feces samples over a 30-day period, they found that those who received the probiotic yogurt had a significantly smaller decrease in short-chain fatty acid levels and a more stable taxonomic microbiota profile than control persons.
Dr. Merenstein said that, on the basis of results such as these and others, he’s comfortable being relatively definitive about the value of probiotics.
“I believe it’s close to standard of care that if you’re prescribing antibiotics, especially for more than 7 days, you really need to put people on probiotics that have been studied, simply because the evidence is robust enough now,” he said.
Even for proponents, there are caveats
However, all the researchers recommending the use of probiotics did so with caveats. First and foremost, they advise clinicians that the term “probiotics” is an imprecise catchall and is essentially meaningless.
“A lot of products label themselves as probiotic. It’s a great marketing scheme, but many of the products out there aren’t really probiotics; they’re not proven with randomized control trials and don’t have the scientific background,” said Dr. McFarland. “We’ve found that the efficacy is extremely strain specific and disease specific. A strain may work for one disease and not work for another.”
In 2018, Dr. McFarland coauthored an evidence-based practical guide to help clinicians and patients identify the specific strain that works in certain indications. Dr. Cresci recommends that clinicians consult websites such as Probiotics.org or the National Institutes of Health’s database to find the strains that have been proven to work in well-designed clinical trials.
There was also agreement that, to date, the most robust data support probiotics for the treatment of antibiotic-associated diarrhea.
Although the optimal timing of probiotics is a subject of debate, most proponents agreed that the general rule is “the sooner the better.”
Dr. McFarland recommended incorporating probiotics within 24 hours of starting an antibiotic “because the damage done to your GI tract microbiome is pretty quick, and the probiotics work best if they’re established before major disruption occurs.” She added that patients should continue taking probiotics for 2-8 weeks after stopping antibiotics.
“It takes a long time for your normal flora to get restored,” she said. “It’s best to cover your bases.”
For others, the evidence is not definitive
Opinions on the value of probiotics to combat antibiotic-related GI side effects are divergent, though.
“I would not recommend the routine use of probiotics, and certainly not in the prevention of C. difficile or antibiotic-related diarrhea,” said David A. Johnson, MD, professor of medicine and chief of gastroenterology at Eastern Virginia Medical School, Norfolk. “I think the evidence does not support that, and I stand strongly on that recommendation.”
Dr. Johnson cited the 2020 guidelines from the American Gastroenterological Association, which offer only a conditional recommendation for the use of specific probiotics and only in preventing antibiotic-associated C. difficile infection.
Geoffrey A. Preidis, MD, PhD, an assistant professor of pediatrics in the section of gastroenterology, hepatology, and nutrition at Baylor College of Medicine, Houston, served as a coauthor of the AGA’s guidelines. He noted that after reviewing 39 published trials of approximately 10,000 patients given probiotics while receiving antibiotics, the authors “did find some evidence that specific probiotics might decrease the risk of C. difficile diarrhea, but the quality of that evidence was low.”
Dr. Preidis attributed this to the lack of well-designed multicenter trials that can isolate the effects of certain strains and determine their benefit in this application.
“The majority of published trials have not reported safety data as rigorously as these data are reported in pharmaceutical trials, so the risk of side effects could be higher than we think,” said Dr. Preidis. “As living microbes, probiotics can move from the intestines into the bloodstream, causing sepsis. Contamination in the manufacturing process has been reported. There might be other long-term effects that we are not yet aware of.”
When asked to characterize the available data on probiotics, Dr. Johnson replied, “I’d generally label it, ‘caveat emptor.’ ”
Dr. McFarland agreed that the field would benefit from better-designed studies and called out meta-analyses that pool outcomes with various strains for particular criticism.
“When researchers do that, it’s no longer valid and shouldn’t have been published, in my opinion,” she told this news organization.
‘Antibiotic diets’ as a possible approach
A compromise between the two sides may be the so-called antibiotic diet. The theory behind such diets is that foods and beverages with biome-boosting properties may be a risk-free intervention that patients can adopt to alleviate antibiotic-related side effects.
“You want your diet to include more soluble fibers to help support the good bacteria, particularly when you’re taking antibiotics,” said Dr. Cresci. “You can get this through eating fresh fruits and vegetables, whole grains, and foods that have more prebiotic, like potatoes. You can also eat fermented food, such as kefir, kombucha, kimchi, and yogurt, so you’re adding more beneficial bacteria into your intestinal tract.”
There is ample published evidence that such foods can boost microbiome diversity and decrease inflammation, including a July 2021 study in Cell. However, the protection this may confer while taking antibiotics isn’t known. Establishing a clear role for the efficacy of such interventions is made additionally difficult by the well-established limitations of conducting dietary clinical trials.
Dr. Merenstein said that there is no compelling evidence that antibiotic-related complications can be offset by changing what goes onto our dinner plates. He joked: “We can’t say, ‘Here’s amoxicillin for your ear infection, now make sure you increase your fermented food, fiber, and water.’ ”
Dr. Johnson said he’s intrigued by studies of prebiotics – fibers that boost beneficial bacteria in the GI system.
“I would love to have more findings about prebiotic identification; that is, things we could do in a healthy way to keep the gut balanced while it’s subject to a change with antibiotics,” he said. “We’re just not there yet.”
Dr. Johnson added that he generally recommends that patients taking antibiotics eat “a bland diet, avoiding things that may have been provocative in the past.”
If patients are already enjoying foods with microbiome-boosting reputations, Dr. Johnson sees “very little downside to continuing that [while on antibiotics].” However, he noted that the period in which you’re taking antibiotics isn’t ideal for trying new foods, given the lack of experience with how the gut bacteria will react.
There are data about foods to avoid while taking antibiotics, which generally fall in line with common dietary knowledge. Many patients may know not to drink grapefruit juice with certain medications, but it’s worth a reminder. Certain antibiotics may also require delaying or avoiding dairy products, although this does not apply to yogurt.
A fiber-deficient diet can aggravate microbiota collapse following antibiotics. In a 2020 study, researchers showed that people on a high-fat diet who were using antibiotics were 8.6 times more likely to have preinflammatory bowel disease than those eating low-fat foods and who had no recent history of antibiotic use. Mouse model data from the same study indicated that poor diet and antibiotics may have worked in conjunction to reduce oxygen in the gut.
Dr. McFarland noted that building a healthy microbiome is a lifelong pursuit and that several factors (for example, environmental or genetic) are out of individuals’ hands. The general public might want a quick fix – ironically, one of the main drivers behind their requesting and receiving antibiotics when they’re not indicated – but it’s likely not available to them.
“You can’t eat one salad and suddenly have a healthy gut, unfortunately.”
A version of this article first appeared on Medscape.com.
Antibiotics are among the most commonly prescribed medications in both outpatient and hospital settings. Global efforts at curbing antibiotic-resistant strains have prompted clinicians to pursue better stewardship, whereby they limit their prescribing of such medications to those who truly need them.
Yet there’s another possible means of addressing antibiotic resistance – using dietary interventions to reduce the gastrointestinal complaints that so often accompany the use of antibiotics: vomiting, nausea, diarrhea, bloating/indigestion, abdominal pain, and loss of appetite. Far from being a mere nuisance, these complications can have major ramifications.
“Often [these side effects] will result in people stopping an antibiotic they need or taking a second- or third-generation one, which potentially causes even more problems with resistance,” explained Daniel J. Merenstein, MD, a professor of family medicine at Georgetown University, Washington, who has conducted multiple trials on antibiotic stewardship and probiotics.
And it’s not just clinicians who would like to find a way around these common complaints. On lifestyle blogs such as Livestrong and Goop, medical news websites, and via academic institutions, patients can learn how the right probiotic supplement or certain fermented or high-fiber foods, for example, might spare them the upset stomach that often accompanies a course of antibiotics.
Yet according to experts in the field, there are notable questions to be answered about whether there’s evidence to support this approach.
The cost of GI discomfort
Pinpointing the exact manner by which antibiotics upend GI tracts is a complex task, according to Gail Cresci, PhD, RD, a microbiome researcher in the department of pediatric gastroenterology, hepatology, and nutrition and director of nutrition research at the Cleveland Clinic.
“A lot of different mechanisms can go awry,” Dr. Cresci said. “But normally, the good microbes are there to help keep the balance, so when that balance is gone, the pathogens can take over and lead to this disruption.”
According to Lynne V. McFarland, PhD, a recently retired infectious disease epidemiologist who now serves as a private consultant, such complications can have substantial ramifications for patients and health care systems.
“If you’re an inpatient and develop antibiotic-associated diarrhea, it usually increases the length of stay from 8 to 20 days. It also increases the cost of care. And small children who have this can get severely dehydrated, which can become life threatening.”
Proponents of probiotics
Several of the researchers who were interviewed believe there’s convincing evidence supporting probiotics for the treatment of common antibiotic-related GI complaints. In many instances, they were involved in the studies themselves.
During Dr. McFarland’s 4-decade career in probiotics research, she has participated in early animal studies with strains such as Saccharomyces boulardii and was involved in meta-analyses of their role in Clostridioides difficile infection and associated diarrhea and even as a potential GI intervention for COVID-19 patients (Antibiotics (Basel). 2021 Apr 9;10(4):408).
In mouse model studies from 2013 and 2018, Dr. Cresci and colleagues showed that the probiotic strains Lactobacillus GG and Faecalibacterium prausnitzii reduced the structural gut changes that lead to antibiotic-associated diarrhea and minimized the risk of C. difficile infection.
In a 2021 randomized controlled trial led by Merenstein, healthy participants were given a trial of amoxicillin/clavulanate (days 1-7) in conjunction with either yogurt containing the probiotic Bifidobacterium animalis subsp lactis BB-12 or control yogurt (days 1-14). After assessing feces samples over a 30-day period, they found that those who received the probiotic yogurt had a significantly smaller decrease in short-chain fatty acid levels and a more stable taxonomic microbiota profile than control persons.
Dr. Merenstein said that, on the basis of results such as these and others, he’s comfortable being relatively definitive about the value of probiotics.
“I believe it’s close to standard of care that if you’re prescribing antibiotics, especially for more than 7 days, you really need to put people on probiotics that have been studied, simply because the evidence is robust enough now,” he said.
Even for proponents, there are caveats
However, all the researchers recommending the use of probiotics did so with caveats. First and foremost, they advise clinicians that the term “probiotics” is an imprecise catchall and is essentially meaningless.
“A lot of products label themselves as probiotic. It’s a great marketing scheme, but many of the products out there aren’t really probiotics; they’re not proven with randomized control trials and don’t have the scientific background,” said Dr. McFarland. “We’ve found that the efficacy is extremely strain specific and disease specific. A strain may work for one disease and not work for another.”
In 2018, Dr. McFarland coauthored an evidence-based practical guide to help clinicians and patients identify the specific strain that works in certain indications. Dr. Cresci recommends that clinicians consult websites such as Probiotics.org or the National Institutes of Health’s database to find the strains that have been proven to work in well-designed clinical trials.
There was also agreement that, to date, the most robust data support probiotics for the treatment of antibiotic-associated diarrhea.
Although the optimal timing of probiotics is a subject of debate, most proponents agreed that the general rule is “the sooner the better.”
Dr. McFarland recommended incorporating probiotics within 24 hours of starting an antibiotic “because the damage done to your GI tract microbiome is pretty quick, and the probiotics work best if they’re established before major disruption occurs.” She added that patients should continue taking probiotics for 2-8 weeks after stopping antibiotics.
“It takes a long time for your normal flora to get restored,” she said. “It’s best to cover your bases.”
For others, the evidence is not definitive
Opinions on the value of probiotics to combat antibiotic-related GI side effects are divergent, though.
“I would not recommend the routine use of probiotics, and certainly not in the prevention of C. difficile or antibiotic-related diarrhea,” said David A. Johnson, MD, professor of medicine and chief of gastroenterology at Eastern Virginia Medical School, Norfolk. “I think the evidence does not support that, and I stand strongly on that recommendation.”
Dr. Johnson cited the 2020 guidelines from the American Gastroenterological Association, which offer only a conditional recommendation for the use of specific probiotics and only in preventing antibiotic-associated C. difficile infection.
Geoffrey A. Preidis, MD, PhD, an assistant professor of pediatrics in the section of gastroenterology, hepatology, and nutrition at Baylor College of Medicine, Houston, served as a coauthor of the AGA’s guidelines. He noted that after reviewing 39 published trials of approximately 10,000 patients given probiotics while receiving antibiotics, the authors “did find some evidence that specific probiotics might decrease the risk of C. difficile diarrhea, but the quality of that evidence was low.”
Dr. Preidis attributed this to the lack of well-designed multicenter trials that can isolate the effects of certain strains and determine their benefit in this application.
“The majority of published trials have not reported safety data as rigorously as these data are reported in pharmaceutical trials, so the risk of side effects could be higher than we think,” said Dr. Preidis. “As living microbes, probiotics can move from the intestines into the bloodstream, causing sepsis. Contamination in the manufacturing process has been reported. There might be other long-term effects that we are not yet aware of.”
When asked to characterize the available data on probiotics, Dr. Johnson replied, “I’d generally label it, ‘caveat emptor.’ ”
Dr. McFarland agreed that the field would benefit from better-designed studies and called out meta-analyses that pool outcomes with various strains for particular criticism.
“When researchers do that, it’s no longer valid and shouldn’t have been published, in my opinion,” she told this news organization.
‘Antibiotic diets’ as a possible approach
A compromise between the two sides may be the so-called antibiotic diet. The theory behind such diets is that foods and beverages with biome-boosting properties may be a risk-free intervention that patients can adopt to alleviate antibiotic-related side effects.
“You want your diet to include more soluble fibers to help support the good bacteria, particularly when you’re taking antibiotics,” said Dr. Cresci. “You can get this through eating fresh fruits and vegetables, whole grains, and foods that have more prebiotic, like potatoes. You can also eat fermented food, such as kefir, kombucha, kimchi, and yogurt, so you’re adding more beneficial bacteria into your intestinal tract.”
There is ample published evidence that such foods can boost microbiome diversity and decrease inflammation, including a July 2021 study in Cell. However, the protection this may confer while taking antibiotics isn’t known. Establishing a clear role for the efficacy of such interventions is made additionally difficult by the well-established limitations of conducting dietary clinical trials.
Dr. Merenstein said that there is no compelling evidence that antibiotic-related complications can be offset by changing what goes onto our dinner plates. He joked: “We can’t say, ‘Here’s amoxicillin for your ear infection, now make sure you increase your fermented food, fiber, and water.’ ”
Dr. Johnson said he’s intrigued by studies of prebiotics – fibers that boost beneficial bacteria in the GI system.
“I would love to have more findings about prebiotic identification; that is, things we could do in a healthy way to keep the gut balanced while it’s subject to a change with antibiotics,” he said. “We’re just not there yet.”
Dr. Johnson added that he generally recommends that patients taking antibiotics eat “a bland diet, avoiding things that may have been provocative in the past.”
If patients are already enjoying foods with microbiome-boosting reputations, Dr. Johnson sees “very little downside to continuing that [while on antibiotics].” However, he noted that the period in which you’re taking antibiotics isn’t ideal for trying new foods, given the lack of experience with how the gut bacteria will react.
There are data about foods to avoid while taking antibiotics, which generally fall in line with common dietary knowledge. Many patients may know not to drink grapefruit juice with certain medications, but it’s worth a reminder. Certain antibiotics may also require delaying or avoiding dairy products, although this does not apply to yogurt.
A fiber-deficient diet can aggravate microbiota collapse following antibiotics. In a 2020 study, researchers showed that people on a high-fat diet who were using antibiotics were 8.6 times more likely to have preinflammatory bowel disease than those eating low-fat foods and who had no recent history of antibiotic use. Mouse model data from the same study indicated that poor diet and antibiotics may have worked in conjunction to reduce oxygen in the gut.
Dr. McFarland noted that building a healthy microbiome is a lifelong pursuit and that several factors (for example, environmental or genetic) are out of individuals’ hands. The general public might want a quick fix – ironically, one of the main drivers behind their requesting and receiving antibiotics when they’re not indicated – but it’s likely not available to them.
“You can’t eat one salad and suddenly have a healthy gut, unfortunately.”
A version of this article first appeared on Medscape.com.
Antibiotics are among the most commonly prescribed medications in both outpatient and hospital settings. Global efforts at curbing antibiotic-resistant strains have prompted clinicians to pursue better stewardship, whereby they limit their prescribing of such medications to those who truly need them.
Yet there’s another possible means of addressing antibiotic resistance – using dietary interventions to reduce the gastrointestinal complaints that so often accompany the use of antibiotics: vomiting, nausea, diarrhea, bloating/indigestion, abdominal pain, and loss of appetite. Far from being a mere nuisance, these complications can have major ramifications.
“Often [these side effects] will result in people stopping an antibiotic they need or taking a second- or third-generation one, which potentially causes even more problems with resistance,” explained Daniel J. Merenstein, MD, a professor of family medicine at Georgetown University, Washington, who has conducted multiple trials on antibiotic stewardship and probiotics.
And it’s not just clinicians who would like to find a way around these common complaints. On lifestyle blogs such as Livestrong and Goop, medical news websites, and via academic institutions, patients can learn how the right probiotic supplement or certain fermented or high-fiber foods, for example, might spare them the upset stomach that often accompanies a course of antibiotics.
Yet according to experts in the field, there are notable questions to be answered about whether there’s evidence to support this approach.
The cost of GI discomfort
Pinpointing the exact manner by which antibiotics upend GI tracts is a complex task, according to Gail Cresci, PhD, RD, a microbiome researcher in the department of pediatric gastroenterology, hepatology, and nutrition and director of nutrition research at the Cleveland Clinic.
“A lot of different mechanisms can go awry,” Dr. Cresci said. “But normally, the good microbes are there to help keep the balance, so when that balance is gone, the pathogens can take over and lead to this disruption.”
According to Lynne V. McFarland, PhD, a recently retired infectious disease epidemiologist who now serves as a private consultant, such complications can have substantial ramifications for patients and health care systems.
“If you’re an inpatient and develop antibiotic-associated diarrhea, it usually increases the length of stay from 8 to 20 days. It also increases the cost of care. And small children who have this can get severely dehydrated, which can become life threatening.”
Proponents of probiotics
Several of the researchers who were interviewed believe there’s convincing evidence supporting probiotics for the treatment of common antibiotic-related GI complaints. In many instances, they were involved in the studies themselves.
During Dr. McFarland’s 4-decade career in probiotics research, she has participated in early animal studies with strains such as Saccharomyces boulardii and was involved in meta-analyses of their role in Clostridioides difficile infection and associated diarrhea and even as a potential GI intervention for COVID-19 patients (Antibiotics (Basel). 2021 Apr 9;10(4):408).
In mouse model studies from 2013 and 2018, Dr. Cresci and colleagues showed that the probiotic strains Lactobacillus GG and Faecalibacterium prausnitzii reduced the structural gut changes that lead to antibiotic-associated diarrhea and minimized the risk of C. difficile infection.
In a 2021 randomized controlled trial led by Merenstein, healthy participants were given a trial of amoxicillin/clavulanate (days 1-7) in conjunction with either yogurt containing the probiotic Bifidobacterium animalis subsp lactis BB-12 or control yogurt (days 1-14). After assessing feces samples over a 30-day period, they found that those who received the probiotic yogurt had a significantly smaller decrease in short-chain fatty acid levels and a more stable taxonomic microbiota profile than control persons.
Dr. Merenstein said that, on the basis of results such as these and others, he’s comfortable being relatively definitive about the value of probiotics.
“I believe it’s close to standard of care that if you’re prescribing antibiotics, especially for more than 7 days, you really need to put people on probiotics that have been studied, simply because the evidence is robust enough now,” he said.
Even for proponents, there are caveats
However, all the researchers recommending the use of probiotics did so with caveats. First and foremost, they advise clinicians that the term “probiotics” is an imprecise catchall and is essentially meaningless.
“A lot of products label themselves as probiotic. It’s a great marketing scheme, but many of the products out there aren’t really probiotics; they’re not proven with randomized control trials and don’t have the scientific background,” said Dr. McFarland. “We’ve found that the efficacy is extremely strain specific and disease specific. A strain may work for one disease and not work for another.”
In 2018, Dr. McFarland coauthored an evidence-based practical guide to help clinicians and patients identify the specific strain that works in certain indications. Dr. Cresci recommends that clinicians consult websites such as Probiotics.org or the National Institutes of Health’s database to find the strains that have been proven to work in well-designed clinical trials.
There was also agreement that, to date, the most robust data support probiotics for the treatment of antibiotic-associated diarrhea.
Although the optimal timing of probiotics is a subject of debate, most proponents agreed that the general rule is “the sooner the better.”
Dr. McFarland recommended incorporating probiotics within 24 hours of starting an antibiotic “because the damage done to your GI tract microbiome is pretty quick, and the probiotics work best if they’re established before major disruption occurs.” She added that patients should continue taking probiotics for 2-8 weeks after stopping antibiotics.
“It takes a long time for your normal flora to get restored,” she said. “It’s best to cover your bases.”
For others, the evidence is not definitive
Opinions on the value of probiotics to combat antibiotic-related GI side effects are divergent, though.
“I would not recommend the routine use of probiotics, and certainly not in the prevention of C. difficile or antibiotic-related diarrhea,” said David A. Johnson, MD, professor of medicine and chief of gastroenterology at Eastern Virginia Medical School, Norfolk. “I think the evidence does not support that, and I stand strongly on that recommendation.”
Dr. Johnson cited the 2020 guidelines from the American Gastroenterological Association, which offer only a conditional recommendation for the use of specific probiotics and only in preventing antibiotic-associated C. difficile infection.
Geoffrey A. Preidis, MD, PhD, an assistant professor of pediatrics in the section of gastroenterology, hepatology, and nutrition at Baylor College of Medicine, Houston, served as a coauthor of the AGA’s guidelines. He noted that after reviewing 39 published trials of approximately 10,000 patients given probiotics while receiving antibiotics, the authors “did find some evidence that specific probiotics might decrease the risk of C. difficile diarrhea, but the quality of that evidence was low.”
Dr. Preidis attributed this to the lack of well-designed multicenter trials that can isolate the effects of certain strains and determine their benefit in this application.
“The majority of published trials have not reported safety data as rigorously as these data are reported in pharmaceutical trials, so the risk of side effects could be higher than we think,” said Dr. Preidis. “As living microbes, probiotics can move from the intestines into the bloodstream, causing sepsis. Contamination in the manufacturing process has been reported. There might be other long-term effects that we are not yet aware of.”
When asked to characterize the available data on probiotics, Dr. Johnson replied, “I’d generally label it, ‘caveat emptor.’ ”
Dr. McFarland agreed that the field would benefit from better-designed studies and called out meta-analyses that pool outcomes with various strains for particular criticism.
“When researchers do that, it’s no longer valid and shouldn’t have been published, in my opinion,” she told this news organization.
‘Antibiotic diets’ as a possible approach
A compromise between the two sides may be the so-called antibiotic diet. The theory behind such diets is that foods and beverages with biome-boosting properties may be a risk-free intervention that patients can adopt to alleviate antibiotic-related side effects.
“You want your diet to include more soluble fibers to help support the good bacteria, particularly when you’re taking antibiotics,” said Dr. Cresci. “You can get this through eating fresh fruits and vegetables, whole grains, and foods that have more prebiotic, like potatoes. You can also eat fermented food, such as kefir, kombucha, kimchi, and yogurt, so you’re adding more beneficial bacteria into your intestinal tract.”
There is ample published evidence that such foods can boost microbiome diversity and decrease inflammation, including a July 2021 study in Cell. However, the protection this may confer while taking antibiotics isn’t known. Establishing a clear role for the efficacy of such interventions is made additionally difficult by the well-established limitations of conducting dietary clinical trials.
Dr. Merenstein said that there is no compelling evidence that antibiotic-related complications can be offset by changing what goes onto our dinner plates. He joked: “We can’t say, ‘Here’s amoxicillin for your ear infection, now make sure you increase your fermented food, fiber, and water.’ ”
Dr. Johnson said he’s intrigued by studies of prebiotics – fibers that boost beneficial bacteria in the GI system.
“I would love to have more findings about prebiotic identification; that is, things we could do in a healthy way to keep the gut balanced while it’s subject to a change with antibiotics,” he said. “We’re just not there yet.”
Dr. Johnson added that he generally recommends that patients taking antibiotics eat “a bland diet, avoiding things that may have been provocative in the past.”
If patients are already enjoying foods with microbiome-boosting reputations, Dr. Johnson sees “very little downside to continuing that [while on antibiotics].” However, he noted that the period in which you’re taking antibiotics isn’t ideal for trying new foods, given the lack of experience with how the gut bacteria will react.
There are data about foods to avoid while taking antibiotics, which generally fall in line with common dietary knowledge. Many patients may know not to drink grapefruit juice with certain medications, but it’s worth a reminder. Certain antibiotics may also require delaying or avoiding dairy products, although this does not apply to yogurt.
A fiber-deficient diet can aggravate microbiota collapse following antibiotics. In a 2020 study, researchers showed that people on a high-fat diet who were using antibiotics were 8.6 times more likely to have preinflammatory bowel disease than those eating low-fat foods and who had no recent history of antibiotic use. Mouse model data from the same study indicated that poor diet and antibiotics may have worked in conjunction to reduce oxygen in the gut.
Dr. McFarland noted that building a healthy microbiome is a lifelong pursuit and that several factors (for example, environmental or genetic) are out of individuals’ hands. The general public might want a quick fix – ironically, one of the main drivers behind their requesting and receiving antibiotics when they’re not indicated – but it’s likely not available to them.
“You can’t eat one salad and suddenly have a healthy gut, unfortunately.”
A version of this article first appeared on Medscape.com.
Executive-function deficits a new treatment target for PTSD?
DENVER –
“To our knowledge, this study is the first to show that executive-function deficits maintain PTSD symptoms following trauma exposure,” investigators noted in research presented at the Anxiety and Depression Association of America (ADAA) Anxiety & Depression conference.
The results are important in “developing precision medicine–based approaches for alleviating [posttraumatic stress] symptoms, and improving well-established PTSD treatments for those with relative deficits in executive function,” study investigator Joseph R. Bardeen, PhD, associate professor at Auburn (Ala.) University, told meeting attendees.
The findings were published in the Journal of Anxiety Disorders.
Cognitive impairment
In earlier research, deficits in EF were associated with an increased vulnerability for PTSD symptoms. However, less is known about the role of these deficits, which can impair higher-level cognitive ability, in sustaining PTSD symptoms.
To investigate, the authors conducted a longitudinal study that included 98 participants aged 18-65 years who had been identified via phone screening as experiencing clinically significant PTSD symptoms.
Participants completed self-report measures for PTSD symptoms, as well as measures for EF deficits at baseline and 6-month (n = 92) and 12-month (n = 91) follow-up sessions.
A path analysis showed a significant relationship between baseline PTSD symptoms and EF deficits at 6 months (P < .001). Baseline PTSD symptoms were associated with 12-month PTSD symptoms (P < .04).
EF deficits at 6 months were also associated with 12-month PTSD symptoms (P = .02).
Importantly, no associations were observed between baseline or 6-month PTSD symptoms and EF deficits at 12 months. However, EF deficits at 6 months drove the relationship between PTSD symptoms at baseline and at 1 year (indirect effect = .061).
“What this suggests is that executive-function deficits are a mechanism that maintains patients’ symptoms over the course of 1 year,” Dr. Bardeen said.
“And you don’t see the reverse,” he added. “You don’t see that PTSD symptoms at [6 months] mediate the relationship between [baseline] and 6 month executive-function deficits.”
Surprising finding
The findings suggest deficits in executive functioning have a stronger role in maintaining PTSD symptoms than these symptoms have in maintaining EF deficits, Dr. Bardeen told this news organization.
“I had originally hypothesized a bidirectional relationship in which PTSD symptoms influenced future executive-function deficits and executive-function deficits influenced future PTSD symptoms,” he said.
“So, it was a surprise that, when accounting for both variables in the same model, executive-function deficits predicted future PTSD symptoms, but PTSD symptoms did not significantly predict future EF deficits,” he added.
Dr. Bardeen noted this suggests that EF deficits “may be a particularly important maintenance factor.”
In addition, he recommended the use of neuropsychological assessments prior to treatment to identify individuals with EF deficits and distinguish those deficits from PTSD symptoms.
“There is certainly overlap between executive-function deficits and PTSD symptoms,” Dr. Bardeen said. “For example, several of the symptoms of PTSD, such as concentration difficulties, may be indicators of executive-function deficits.”
He noted assessments such as the Delis Kaplan Executive Function System, and Clinician Administered PTSD Scale for DSM-5, when used as part of a larger assessment battery, can help differentiate between the EF deficits and PTSD.
“This would take several hours to administer, but in cases in which serious cognitive impairment is suspected, a comprehensive assessment is the way to go,” Dr. Bardeen said.
The standard approaches of prolonged exposure therapy and cognitive processing therapy can be effective in patients without EF deficits, while some modifications may benefit those with these deficits, he added.
“For example, it’s important to provide a more directive and structured environment in which the practitioner repeats key points frequently, uses concrete language, simplifies worksheets, and provides written summaries and reminder cards,” he said.
Further findings
In additional research presented at the meeting, Elsa Mattson, a PhD student from Case Western Reserve University, Cleveland, and colleagues reported findings further distinguishing the role of EF in PTSD.
In that study of 149 patients with chronic PTSD, those with low performing working memory, but not high working memory, had higher pre- as well as posttreatment PTSD symptom severity and depressive symptoms.
“Clinicians should consider that impairments in executive function may play a role in reduced treatment response, potentially impairing a client’s ability to learn new information in treatment,” the investigators wrote.
“Understanding how executive function processes change over the course of treatment, particularly in relation to processing the trauma memories, is an important next step,” they added.
The first study was supported by a grant from the National Institute of Mental Health. The investigators have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
DENVER –
“To our knowledge, this study is the first to show that executive-function deficits maintain PTSD symptoms following trauma exposure,” investigators noted in research presented at the Anxiety and Depression Association of America (ADAA) Anxiety & Depression conference.
The results are important in “developing precision medicine–based approaches for alleviating [posttraumatic stress] symptoms, and improving well-established PTSD treatments for those with relative deficits in executive function,” study investigator Joseph R. Bardeen, PhD, associate professor at Auburn (Ala.) University, told meeting attendees.
The findings were published in the Journal of Anxiety Disorders.
Cognitive impairment
In earlier research, deficits in EF were associated with an increased vulnerability for PTSD symptoms. However, less is known about the role of these deficits, which can impair higher-level cognitive ability, in sustaining PTSD symptoms.
To investigate, the authors conducted a longitudinal study that included 98 participants aged 18-65 years who had been identified via phone screening as experiencing clinically significant PTSD symptoms.
Participants completed self-report measures for PTSD symptoms, as well as measures for EF deficits at baseline and 6-month (n = 92) and 12-month (n = 91) follow-up sessions.
A path analysis showed a significant relationship between baseline PTSD symptoms and EF deficits at 6 months (P < .001). Baseline PTSD symptoms were associated with 12-month PTSD symptoms (P < .04).
EF deficits at 6 months were also associated with 12-month PTSD symptoms (P = .02).
Importantly, no associations were observed between baseline or 6-month PTSD symptoms and EF deficits at 12 months. However, EF deficits at 6 months drove the relationship between PTSD symptoms at baseline and at 1 year (indirect effect = .061).
“What this suggests is that executive-function deficits are a mechanism that maintains patients’ symptoms over the course of 1 year,” Dr. Bardeen said.
“And you don’t see the reverse,” he added. “You don’t see that PTSD symptoms at [6 months] mediate the relationship between [baseline] and 6 month executive-function deficits.”
Surprising finding
The findings suggest deficits in executive functioning have a stronger role in maintaining PTSD symptoms than these symptoms have in maintaining EF deficits, Dr. Bardeen told this news organization.
“I had originally hypothesized a bidirectional relationship in which PTSD symptoms influenced future executive-function deficits and executive-function deficits influenced future PTSD symptoms,” he said.
“So, it was a surprise that, when accounting for both variables in the same model, executive-function deficits predicted future PTSD symptoms, but PTSD symptoms did not significantly predict future EF deficits,” he added.
Dr. Bardeen noted this suggests that EF deficits “may be a particularly important maintenance factor.”
In addition, he recommended the use of neuropsychological assessments prior to treatment to identify individuals with EF deficits and distinguish those deficits from PTSD symptoms.
“There is certainly overlap between executive-function deficits and PTSD symptoms,” Dr. Bardeen said. “For example, several of the symptoms of PTSD, such as concentration difficulties, may be indicators of executive-function deficits.”
He noted assessments such as the Delis Kaplan Executive Function System, and Clinician Administered PTSD Scale for DSM-5, when used as part of a larger assessment battery, can help differentiate between the EF deficits and PTSD.
“This would take several hours to administer, but in cases in which serious cognitive impairment is suspected, a comprehensive assessment is the way to go,” Dr. Bardeen said.
The standard approaches of prolonged exposure therapy and cognitive processing therapy can be effective in patients without EF deficits, while some modifications may benefit those with these deficits, he added.
“For example, it’s important to provide a more directive and structured environment in which the practitioner repeats key points frequently, uses concrete language, simplifies worksheets, and provides written summaries and reminder cards,” he said.
Further findings
In additional research presented at the meeting, Elsa Mattson, a PhD student from Case Western Reserve University, Cleveland, and colleagues reported findings further distinguishing the role of EF in PTSD.
In that study of 149 patients with chronic PTSD, those with low performing working memory, but not high working memory, had higher pre- as well as posttreatment PTSD symptom severity and depressive symptoms.
“Clinicians should consider that impairments in executive function may play a role in reduced treatment response, potentially impairing a client’s ability to learn new information in treatment,” the investigators wrote.
“Understanding how executive function processes change over the course of treatment, particularly in relation to processing the trauma memories, is an important next step,” they added.
The first study was supported by a grant from the National Institute of Mental Health. The investigators have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
DENVER –
“To our knowledge, this study is the first to show that executive-function deficits maintain PTSD symptoms following trauma exposure,” investigators noted in research presented at the Anxiety and Depression Association of America (ADAA) Anxiety & Depression conference.
The results are important in “developing precision medicine–based approaches for alleviating [posttraumatic stress] symptoms, and improving well-established PTSD treatments for those with relative deficits in executive function,” study investigator Joseph R. Bardeen, PhD, associate professor at Auburn (Ala.) University, told meeting attendees.
The findings were published in the Journal of Anxiety Disorders.
Cognitive impairment
In earlier research, deficits in EF were associated with an increased vulnerability for PTSD symptoms. However, less is known about the role of these deficits, which can impair higher-level cognitive ability, in sustaining PTSD symptoms.
To investigate, the authors conducted a longitudinal study that included 98 participants aged 18-65 years who had been identified via phone screening as experiencing clinically significant PTSD symptoms.
Participants completed self-report measures for PTSD symptoms, as well as measures for EF deficits at baseline and 6-month (n = 92) and 12-month (n = 91) follow-up sessions.
A path analysis showed a significant relationship between baseline PTSD symptoms and EF deficits at 6 months (P < .001). Baseline PTSD symptoms were associated with 12-month PTSD symptoms (P < .04).
EF deficits at 6 months were also associated with 12-month PTSD symptoms (P = .02).
Importantly, no associations were observed between baseline or 6-month PTSD symptoms and EF deficits at 12 months. However, EF deficits at 6 months drove the relationship between PTSD symptoms at baseline and at 1 year (indirect effect = .061).
“What this suggests is that executive-function deficits are a mechanism that maintains patients’ symptoms over the course of 1 year,” Dr. Bardeen said.
“And you don’t see the reverse,” he added. “You don’t see that PTSD symptoms at [6 months] mediate the relationship between [baseline] and 6 month executive-function deficits.”
Surprising finding
The findings suggest deficits in executive functioning have a stronger role in maintaining PTSD symptoms than these symptoms have in maintaining EF deficits, Dr. Bardeen told this news organization.
“I had originally hypothesized a bidirectional relationship in which PTSD symptoms influenced future executive-function deficits and executive-function deficits influenced future PTSD symptoms,” he said.
“So, it was a surprise that, when accounting for both variables in the same model, executive-function deficits predicted future PTSD symptoms, but PTSD symptoms did not significantly predict future EF deficits,” he added.
Dr. Bardeen noted this suggests that EF deficits “may be a particularly important maintenance factor.”
In addition, he recommended the use of neuropsychological assessments prior to treatment to identify individuals with EF deficits and distinguish those deficits from PTSD symptoms.
“There is certainly overlap between executive-function deficits and PTSD symptoms,” Dr. Bardeen said. “For example, several of the symptoms of PTSD, such as concentration difficulties, may be indicators of executive-function deficits.”
He noted assessments such as the Delis Kaplan Executive Function System, and Clinician Administered PTSD Scale for DSM-5, when used as part of a larger assessment battery, can help differentiate between the EF deficits and PTSD.
“This would take several hours to administer, but in cases in which serious cognitive impairment is suspected, a comprehensive assessment is the way to go,” Dr. Bardeen said.
The standard approaches of prolonged exposure therapy and cognitive processing therapy can be effective in patients without EF deficits, while some modifications may benefit those with these deficits, he added.
“For example, it’s important to provide a more directive and structured environment in which the practitioner repeats key points frequently, uses concrete language, simplifies worksheets, and provides written summaries and reminder cards,” he said.
Further findings
In additional research presented at the meeting, Elsa Mattson, a PhD student from Case Western Reserve University, Cleveland, and colleagues reported findings further distinguishing the role of EF in PTSD.
In that study of 149 patients with chronic PTSD, those with low performing working memory, but not high working memory, had higher pre- as well as posttreatment PTSD symptom severity and depressive symptoms.
“Clinicians should consider that impairments in executive function may play a role in reduced treatment response, potentially impairing a client’s ability to learn new information in treatment,” the investigators wrote.
“Understanding how executive function processes change over the course of treatment, particularly in relation to processing the trauma memories, is an important next step,” they added.
The first study was supported by a grant from the National Institute of Mental Health. The investigators have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
REPORTING FROM ADAA 2022
Jury is out on universal screening for eating disorders
Eating disorders (binge eating disorder, bulimia nervosa, and anorexia nervosa) can cause “serious harms to physical and psychosocial health and take a tremendous toll on individuals and families,” task force member Lori Pbert, PhD, told this news organization.
“Screening for eating disorders has the potential to improve health by leading to early detection and effective treatment,” said Dr. Pbert, with the department of population and quantitative health sciences, University of Massachusetts, Worcester.
However, a “deep dive” into the available literature failed to turn up adequate evidence to recommend for or against routine screening for eating disorders for children and adolescents aged 10 years and older and for adults who have no signs or symptoms of an eating disorder or concerns about their eating and who have not previously been diagnosed with an eating disorder, Dr. Pbert said.
The task force, therefore, issued an “I” statement (insufficient evidence), meaning it cannot at this time recommend for or against screening for eating disorders.
An “I” statement is “fundamentally a call for more research,” Dr. Pbert noted.
Adolescents and adults who have signs and symptoms of an eating disorder – which include rapid weight loss; weight gain or pronounced deviation from growth trajectory; pubertal delay; bradycardia; oligomenorrhea; and amenorrhea – are not included in this recommendation.
The USPSTF recommendation statement and accompanying evidence report were published online March 15 in JAMA.
Clinical judgment key
In the absence of evidence, clinicians should use their judgment when determining whether or not to screen an individual patient for an eating disorder, Dr. Pbert advised.
One thing to consider is whether the patient is in a group at higher risk for eating disorders, such as athletes, females, young adults aged 18-29, and transgender individuals.
Another is whether the patient reports engaging in unhealthy weight control behaviors, such as fasting or skipping meals, Dr. Pbert said.
Importantly, any patient who has signs or symptoms of an eating disorder or is expressing concerns about their eating should be assessed and referred for appropriate care, Dr. Pbert said.
“The good news is that eating disorders can be treated,” she said.
Several organizations currently recommend screening in the context of monitoring changes in weight and other vital signs or signs and symptoms to determine whether a patient might have an eating disorder.
Dr. Pbert said it’s important to recognize that the USPSTF statement “doesn’t really conflict” with the recommendations of other organizations. “We all agree that patients who present with signs or symptoms of an eating disorder should be assessed further.”
Evidence gaps
The authors of an invited commentary in JAMA) say the task force has identified several “notable deficiencies” in the available data on screening for eating disorders.
“Directing attention to rigorous research to close this evidence gap will be important to find optimal approaches to identify patients with these complex disorders and improve their health outcomes,” write Evelyn Attia, MD, with Weill Cornell Medicine in New York, and Angela Guarda, MD, with Johns Hopkins University, Baltimore.
This “I” statement, they say, “highlights the need to prioritize research aimed at closing the evidence gap identified by USPSTF in a timely manner and underscores the need for new studies that address screening for eating disorders, treatment trials that enroll screen-detected populations from primary care settings, and screening in specific populations.
“Research on screening in primary care also should be paired with development and assessment of early brief intervention strategies for those individuals who screen positive, especially adolescents,” Dr. Attia and Dr. Guarda say.
Members of the USPSTF have disclosed no relevant financial relationships. Dr. Attia has received research support from the National Institute of Mental Health and the Hilda & Preston David Foundation; royalties from UpToDate; and has served as a clinical advisor to Equip Health. Dr. Guarda has received support from the Stephen and Jean Robinson Fund and research funding from the Klarman Family Foundation.
A version of this article first appeared on Medscape.com.
Eating disorders (binge eating disorder, bulimia nervosa, and anorexia nervosa) can cause “serious harms to physical and psychosocial health and take a tremendous toll on individuals and families,” task force member Lori Pbert, PhD, told this news organization.
“Screening for eating disorders has the potential to improve health by leading to early detection and effective treatment,” said Dr. Pbert, with the department of population and quantitative health sciences, University of Massachusetts, Worcester.
However, a “deep dive” into the available literature failed to turn up adequate evidence to recommend for or against routine screening for eating disorders for children and adolescents aged 10 years and older and for adults who have no signs or symptoms of an eating disorder or concerns about their eating and who have not previously been diagnosed with an eating disorder, Dr. Pbert said.
The task force, therefore, issued an “I” statement (insufficient evidence), meaning it cannot at this time recommend for or against screening for eating disorders.
An “I” statement is “fundamentally a call for more research,” Dr. Pbert noted.
Adolescents and adults who have signs and symptoms of an eating disorder – which include rapid weight loss; weight gain or pronounced deviation from growth trajectory; pubertal delay; bradycardia; oligomenorrhea; and amenorrhea – are not included in this recommendation.
The USPSTF recommendation statement and accompanying evidence report were published online March 15 in JAMA.
Clinical judgment key
In the absence of evidence, clinicians should use their judgment when determining whether or not to screen an individual patient for an eating disorder, Dr. Pbert advised.
One thing to consider is whether the patient is in a group at higher risk for eating disorders, such as athletes, females, young adults aged 18-29, and transgender individuals.
Another is whether the patient reports engaging in unhealthy weight control behaviors, such as fasting or skipping meals, Dr. Pbert said.
Importantly, any patient who has signs or symptoms of an eating disorder or is expressing concerns about their eating should be assessed and referred for appropriate care, Dr. Pbert said.
“The good news is that eating disorders can be treated,” she said.
Several organizations currently recommend screening in the context of monitoring changes in weight and other vital signs or signs and symptoms to determine whether a patient might have an eating disorder.
Dr. Pbert said it’s important to recognize that the USPSTF statement “doesn’t really conflict” with the recommendations of other organizations. “We all agree that patients who present with signs or symptoms of an eating disorder should be assessed further.”
Evidence gaps
The authors of an invited commentary in JAMA) say the task force has identified several “notable deficiencies” in the available data on screening for eating disorders.
“Directing attention to rigorous research to close this evidence gap will be important to find optimal approaches to identify patients with these complex disorders and improve their health outcomes,” write Evelyn Attia, MD, with Weill Cornell Medicine in New York, and Angela Guarda, MD, with Johns Hopkins University, Baltimore.
This “I” statement, they say, “highlights the need to prioritize research aimed at closing the evidence gap identified by USPSTF in a timely manner and underscores the need for new studies that address screening for eating disorders, treatment trials that enroll screen-detected populations from primary care settings, and screening in specific populations.
“Research on screening in primary care also should be paired with development and assessment of early brief intervention strategies for those individuals who screen positive, especially adolescents,” Dr. Attia and Dr. Guarda say.
Members of the USPSTF have disclosed no relevant financial relationships. Dr. Attia has received research support from the National Institute of Mental Health and the Hilda & Preston David Foundation; royalties from UpToDate; and has served as a clinical advisor to Equip Health. Dr. Guarda has received support from the Stephen and Jean Robinson Fund and research funding from the Klarman Family Foundation.
A version of this article first appeared on Medscape.com.
Eating disorders (binge eating disorder, bulimia nervosa, and anorexia nervosa) can cause “serious harms to physical and psychosocial health and take a tremendous toll on individuals and families,” task force member Lori Pbert, PhD, told this news organization.
“Screening for eating disorders has the potential to improve health by leading to early detection and effective treatment,” said Dr. Pbert, with the department of population and quantitative health sciences, University of Massachusetts, Worcester.
However, a “deep dive” into the available literature failed to turn up adequate evidence to recommend for or against routine screening for eating disorders for children and adolescents aged 10 years and older and for adults who have no signs or symptoms of an eating disorder or concerns about their eating and who have not previously been diagnosed with an eating disorder, Dr. Pbert said.
The task force, therefore, issued an “I” statement (insufficient evidence), meaning it cannot at this time recommend for or against screening for eating disorders.
An “I” statement is “fundamentally a call for more research,” Dr. Pbert noted.
Adolescents and adults who have signs and symptoms of an eating disorder – which include rapid weight loss; weight gain or pronounced deviation from growth trajectory; pubertal delay; bradycardia; oligomenorrhea; and amenorrhea – are not included in this recommendation.
The USPSTF recommendation statement and accompanying evidence report were published online March 15 in JAMA.
Clinical judgment key
In the absence of evidence, clinicians should use their judgment when determining whether or not to screen an individual patient for an eating disorder, Dr. Pbert advised.
One thing to consider is whether the patient is in a group at higher risk for eating disorders, such as athletes, females, young adults aged 18-29, and transgender individuals.
Another is whether the patient reports engaging in unhealthy weight control behaviors, such as fasting or skipping meals, Dr. Pbert said.
Importantly, any patient who has signs or symptoms of an eating disorder or is expressing concerns about their eating should be assessed and referred for appropriate care, Dr. Pbert said.
“The good news is that eating disorders can be treated,” she said.
Several organizations currently recommend screening in the context of monitoring changes in weight and other vital signs or signs and symptoms to determine whether a patient might have an eating disorder.
Dr. Pbert said it’s important to recognize that the USPSTF statement “doesn’t really conflict” with the recommendations of other organizations. “We all agree that patients who present with signs or symptoms of an eating disorder should be assessed further.”
Evidence gaps
The authors of an invited commentary in JAMA) say the task force has identified several “notable deficiencies” in the available data on screening for eating disorders.
“Directing attention to rigorous research to close this evidence gap will be important to find optimal approaches to identify patients with these complex disorders and improve their health outcomes,” write Evelyn Attia, MD, with Weill Cornell Medicine in New York, and Angela Guarda, MD, with Johns Hopkins University, Baltimore.
This “I” statement, they say, “highlights the need to prioritize research aimed at closing the evidence gap identified by USPSTF in a timely manner and underscores the need for new studies that address screening for eating disorders, treatment trials that enroll screen-detected populations from primary care settings, and screening in specific populations.
“Research on screening in primary care also should be paired with development and assessment of early brief intervention strategies for those individuals who screen positive, especially adolescents,” Dr. Attia and Dr. Guarda say.
Members of the USPSTF have disclosed no relevant financial relationships. Dr. Attia has received research support from the National Institute of Mental Health and the Hilda & Preston David Foundation; royalties from UpToDate; and has served as a clinical advisor to Equip Health. Dr. Guarda has received support from the Stephen and Jean Robinson Fund and research funding from the Klarman Family Foundation.
A version of this article first appeared on Medscape.com.
ACC looks to build inclusive, bully-free cardiology workplaces
The American College of Cardiology has issued a new health policy statement directed at eliminating the bias, discrimination, bullying, and harassment that hamstrings the delivery of quality cardiovascular care.
“We pay a lot of attention, of course, to our patients and patient care issues but our ability to care optimally for patients is limited if the workforce is handicapped in any way,” said Pamela S. Douglas, MD, of Duke University, Durham, N.C., who cochaired the writing committee.
The document is the second in the ACC’s diversity inclusion initiative, following the 2019 report on equal compensation and opportunity in cardiology, but the foundation for the work actually started 5 years ago, she told this news organization.
“Unfortunately, COVID and other world events have created a climate in the United States where people don’t treat each other terribly well,” Dr. Douglas said. “It’s divisive and confrontational often, when it should be collaborative. So this document, at this time, was serendipitous but wonderful timing.”
The 2022 ACC Health Policy Statement on Building Respect, Civility, and Inclusion in the Cardiovascular Workforce was published online March 17 in the Journal of the American College of Cardiology.
The 63-page document provides 12 principles for building a better workplace, starting with the belief that civil behavior and respect are inherent in its core values of teamwork, collaboration, and professionalism.
The ACC calls on all organizations and individuals involved in providing cardiovascular care, education, or research to recognize the “ubiquity” of uncivil behavior and the continuum of bias, discrimination, bullying, and harassment (BDBH) that characterize it.
Some of the recommendations they offer to eliminate these behaviors include:
- Creating institutional policies and resources to ensure hiring decisions, evaluations, and departmental/program/center reviews are objective.
- Including assessments of personal behaviors related to respect and civility in performance reviews.
- Establishing confidential, fair, and transparent mechanisms for reporting and investigating individuals and/or departments suspected of BDBH.
- Adopting longitudinal metrics and accurate data collection to track progress and inform future policy and interventions.
- Encouraging independent evaluation of institutional culture and efforts to reduce BDBH.
- Celebrating those who promote and achieve excellence in reducing BDBH.
Patients behaving badly
What’s new, especially since the COVID-19 pandemic, is the number of patients who themselves engage in disrespectful and uncivil behavior, observed Dr. Douglas.
“As physicians, it was the patient’s always right. So you work to do backflips to accommodate the patient,” she said. “But when the patient says: I don’t want to be treated by anybody that comes from outside the United States, that’s not our society anymore. And that has to be addressed and dealt with.”
The policy statement features a suite of online tools and resources including 15 case examples and 30 sample policies from institutions that have been anonymized and some provide an action framework for addressing this type of patient behavior, Dr. Douglas said. An individual, for example, can ask the patient why they made the remark, explaining that the provider is qualified and someone they’d like to have care for their own family. If it was a trainee on the receiving end, it’s fair for them to go back to their supervisor, mentor, or training director.
“They should back you up and explain to the patient that it’s not who we are at this hospital and that they’re happy to provide care, but they are part of the hospital and need to obey the rules and environment in this hospital,” she said.
Writing committee cochair Michael J. Mack, MD, of Baylor Scott & White Health, Plano, Tex., told tthis news organization that “one of the concepts that I hadn’t heard before that resonated with me was the term ‘upstander’ – that you can’t just be a bystander and watch this happen and do nothing. If you’re witness to this in the workplace, if it’s gender bias or racial bias, you need to get involved and reach out to that individual and see what you can do to help and be a reporter of it.”
But it’s all too costly
Financial constraints are often cited as a reason not to focus on bias, discrimination, bullying, and harassment in the workplace or to shelve initiatives, but it’s a false argument, say Dr. Mack and Dr. Douglas.
“One of the case examples is a cardiology practice that is suffering a decline in finances, and the board makes the recommendation that the efforts at diversity and civil workplaces need to be the first to go,” Dr. Mack explained. “And the point that’s being made in this is you can’t afford not to do it because it ends up being more costly to the business in the long run.”
Part of that cost is associated with losing valuable employees that were contributing but left because there wasn’t a culture of respectfulness and positivity in their workplace. While that’s always been a risk, it’s become a particularly compelling issue because of the workforce shortages present 3 years on in the pandemic, he said.
“There’s a new reexamination to be sure that we have a positive work environment that people want to come to work at every day,” he said. “I run our Research Institute, and normally we have a 5% vacancy rate, and our unfilled-position rate is 25% right now.”
Health care is delivered as a team today, but if a member feels disrespected, or worse – harassed, bullied, or discriminated against – they’re not going to contribute at the top of their game, Dr. Douglas said.
“It’s very well documented that bad behavior exists and that it has negative consequences for patient care for institutions, who are at great risk legally and regulatory wise,” she said. “And the document makes that clear that that risk is increasing.”
Dr. Douglas pointed out that the Joint Commission now requires good behavior in institutions that it accredits and that the Accreditation Council for Graduate Medical Education requires education around professionalism and evidence that their trainees are treated as professionals.
Funding agencies like the National Institutes of Health have also jumped into this space, recently establishing a hotline to report harassment, discrimination, and bullying perpetrated by an NIH-funded investigator, and giving institutions 30 days to investigate.
“In the last 2 years they have defunded, taken away the grants of 75 investigators, compared to zero in the 5 years before that,” Dr. Douglas said. “So I think, even though the bad behavior may be escalating, the consequences are escalating too.”
The new “2022 ACC Health Policy Statement on Building Respect, Civility, and Inclusion in the Cardiovascular Workplace” will be discussed in a session at the ACC 2022 Scientific Sessions on April 2 at 4:15 p.m. ET.
A version of this article first appeared on Medscape.com.
The American College of Cardiology has issued a new health policy statement directed at eliminating the bias, discrimination, bullying, and harassment that hamstrings the delivery of quality cardiovascular care.
“We pay a lot of attention, of course, to our patients and patient care issues but our ability to care optimally for patients is limited if the workforce is handicapped in any way,” said Pamela S. Douglas, MD, of Duke University, Durham, N.C., who cochaired the writing committee.
The document is the second in the ACC’s diversity inclusion initiative, following the 2019 report on equal compensation and opportunity in cardiology, but the foundation for the work actually started 5 years ago, she told this news organization.
“Unfortunately, COVID and other world events have created a climate in the United States where people don’t treat each other terribly well,” Dr. Douglas said. “It’s divisive and confrontational often, when it should be collaborative. So this document, at this time, was serendipitous but wonderful timing.”
The 2022 ACC Health Policy Statement on Building Respect, Civility, and Inclusion in the Cardiovascular Workforce was published online March 17 in the Journal of the American College of Cardiology.
The 63-page document provides 12 principles for building a better workplace, starting with the belief that civil behavior and respect are inherent in its core values of teamwork, collaboration, and professionalism.
The ACC calls on all organizations and individuals involved in providing cardiovascular care, education, or research to recognize the “ubiquity” of uncivil behavior and the continuum of bias, discrimination, bullying, and harassment (BDBH) that characterize it.
Some of the recommendations they offer to eliminate these behaviors include:
- Creating institutional policies and resources to ensure hiring decisions, evaluations, and departmental/program/center reviews are objective.
- Including assessments of personal behaviors related to respect and civility in performance reviews.
- Establishing confidential, fair, and transparent mechanisms for reporting and investigating individuals and/or departments suspected of BDBH.
- Adopting longitudinal metrics and accurate data collection to track progress and inform future policy and interventions.
- Encouraging independent evaluation of institutional culture and efforts to reduce BDBH.
- Celebrating those who promote and achieve excellence in reducing BDBH.
Patients behaving badly
What’s new, especially since the COVID-19 pandemic, is the number of patients who themselves engage in disrespectful and uncivil behavior, observed Dr. Douglas.
“As physicians, it was the patient’s always right. So you work to do backflips to accommodate the patient,” she said. “But when the patient says: I don’t want to be treated by anybody that comes from outside the United States, that’s not our society anymore. And that has to be addressed and dealt with.”
The policy statement features a suite of online tools and resources including 15 case examples and 30 sample policies from institutions that have been anonymized and some provide an action framework for addressing this type of patient behavior, Dr. Douglas said. An individual, for example, can ask the patient why they made the remark, explaining that the provider is qualified and someone they’d like to have care for their own family. If it was a trainee on the receiving end, it’s fair for them to go back to their supervisor, mentor, or training director.
“They should back you up and explain to the patient that it’s not who we are at this hospital and that they’re happy to provide care, but they are part of the hospital and need to obey the rules and environment in this hospital,” she said.
Writing committee cochair Michael J. Mack, MD, of Baylor Scott & White Health, Plano, Tex., told tthis news organization that “one of the concepts that I hadn’t heard before that resonated with me was the term ‘upstander’ – that you can’t just be a bystander and watch this happen and do nothing. If you’re witness to this in the workplace, if it’s gender bias or racial bias, you need to get involved and reach out to that individual and see what you can do to help and be a reporter of it.”
But it’s all too costly
Financial constraints are often cited as a reason not to focus on bias, discrimination, bullying, and harassment in the workplace or to shelve initiatives, but it’s a false argument, say Dr. Mack and Dr. Douglas.
“One of the case examples is a cardiology practice that is suffering a decline in finances, and the board makes the recommendation that the efforts at diversity and civil workplaces need to be the first to go,” Dr. Mack explained. “And the point that’s being made in this is you can’t afford not to do it because it ends up being more costly to the business in the long run.”
Part of that cost is associated with losing valuable employees that were contributing but left because there wasn’t a culture of respectfulness and positivity in their workplace. While that’s always been a risk, it’s become a particularly compelling issue because of the workforce shortages present 3 years on in the pandemic, he said.
“There’s a new reexamination to be sure that we have a positive work environment that people want to come to work at every day,” he said. “I run our Research Institute, and normally we have a 5% vacancy rate, and our unfilled-position rate is 25% right now.”
Health care is delivered as a team today, but if a member feels disrespected, or worse – harassed, bullied, or discriminated against – they’re not going to contribute at the top of their game, Dr. Douglas said.
“It’s very well documented that bad behavior exists and that it has negative consequences for patient care for institutions, who are at great risk legally and regulatory wise,” she said. “And the document makes that clear that that risk is increasing.”
Dr. Douglas pointed out that the Joint Commission now requires good behavior in institutions that it accredits and that the Accreditation Council for Graduate Medical Education requires education around professionalism and evidence that their trainees are treated as professionals.
Funding agencies like the National Institutes of Health have also jumped into this space, recently establishing a hotline to report harassment, discrimination, and bullying perpetrated by an NIH-funded investigator, and giving institutions 30 days to investigate.
“In the last 2 years they have defunded, taken away the grants of 75 investigators, compared to zero in the 5 years before that,” Dr. Douglas said. “So I think, even though the bad behavior may be escalating, the consequences are escalating too.”
The new “2022 ACC Health Policy Statement on Building Respect, Civility, and Inclusion in the Cardiovascular Workplace” will be discussed in a session at the ACC 2022 Scientific Sessions on April 2 at 4:15 p.m. ET.
A version of this article first appeared on Medscape.com.
The American College of Cardiology has issued a new health policy statement directed at eliminating the bias, discrimination, bullying, and harassment that hamstrings the delivery of quality cardiovascular care.
“We pay a lot of attention, of course, to our patients and patient care issues but our ability to care optimally for patients is limited if the workforce is handicapped in any way,” said Pamela S. Douglas, MD, of Duke University, Durham, N.C., who cochaired the writing committee.
The document is the second in the ACC’s diversity inclusion initiative, following the 2019 report on equal compensation and opportunity in cardiology, but the foundation for the work actually started 5 years ago, she told this news organization.
“Unfortunately, COVID and other world events have created a climate in the United States where people don’t treat each other terribly well,” Dr. Douglas said. “It’s divisive and confrontational often, when it should be collaborative. So this document, at this time, was serendipitous but wonderful timing.”
The 2022 ACC Health Policy Statement on Building Respect, Civility, and Inclusion in the Cardiovascular Workforce was published online March 17 in the Journal of the American College of Cardiology.
The 63-page document provides 12 principles for building a better workplace, starting with the belief that civil behavior and respect are inherent in its core values of teamwork, collaboration, and professionalism.
The ACC calls on all organizations and individuals involved in providing cardiovascular care, education, or research to recognize the “ubiquity” of uncivil behavior and the continuum of bias, discrimination, bullying, and harassment (BDBH) that characterize it.
Some of the recommendations they offer to eliminate these behaviors include:
- Creating institutional policies and resources to ensure hiring decisions, evaluations, and departmental/program/center reviews are objective.
- Including assessments of personal behaviors related to respect and civility in performance reviews.
- Establishing confidential, fair, and transparent mechanisms for reporting and investigating individuals and/or departments suspected of BDBH.
- Adopting longitudinal metrics and accurate data collection to track progress and inform future policy and interventions.
- Encouraging independent evaluation of institutional culture and efforts to reduce BDBH.
- Celebrating those who promote and achieve excellence in reducing BDBH.
Patients behaving badly
What’s new, especially since the COVID-19 pandemic, is the number of patients who themselves engage in disrespectful and uncivil behavior, observed Dr. Douglas.
“As physicians, it was the patient’s always right. So you work to do backflips to accommodate the patient,” she said. “But when the patient says: I don’t want to be treated by anybody that comes from outside the United States, that’s not our society anymore. And that has to be addressed and dealt with.”
The policy statement features a suite of online tools and resources including 15 case examples and 30 sample policies from institutions that have been anonymized and some provide an action framework for addressing this type of patient behavior, Dr. Douglas said. An individual, for example, can ask the patient why they made the remark, explaining that the provider is qualified and someone they’d like to have care for their own family. If it was a trainee on the receiving end, it’s fair for them to go back to their supervisor, mentor, or training director.
“They should back you up and explain to the patient that it’s not who we are at this hospital and that they’re happy to provide care, but they are part of the hospital and need to obey the rules and environment in this hospital,” she said.
Writing committee cochair Michael J. Mack, MD, of Baylor Scott & White Health, Plano, Tex., told tthis news organization that “one of the concepts that I hadn’t heard before that resonated with me was the term ‘upstander’ – that you can’t just be a bystander and watch this happen and do nothing. If you’re witness to this in the workplace, if it’s gender bias or racial bias, you need to get involved and reach out to that individual and see what you can do to help and be a reporter of it.”
But it’s all too costly
Financial constraints are often cited as a reason not to focus on bias, discrimination, bullying, and harassment in the workplace or to shelve initiatives, but it’s a false argument, say Dr. Mack and Dr. Douglas.
“One of the case examples is a cardiology practice that is suffering a decline in finances, and the board makes the recommendation that the efforts at diversity and civil workplaces need to be the first to go,” Dr. Mack explained. “And the point that’s being made in this is you can’t afford not to do it because it ends up being more costly to the business in the long run.”
Part of that cost is associated with losing valuable employees that were contributing but left because there wasn’t a culture of respectfulness and positivity in their workplace. While that’s always been a risk, it’s become a particularly compelling issue because of the workforce shortages present 3 years on in the pandemic, he said.
“There’s a new reexamination to be sure that we have a positive work environment that people want to come to work at every day,” he said. “I run our Research Institute, and normally we have a 5% vacancy rate, and our unfilled-position rate is 25% right now.”
Health care is delivered as a team today, but if a member feels disrespected, or worse – harassed, bullied, or discriminated against – they’re not going to contribute at the top of their game, Dr. Douglas said.
“It’s very well documented that bad behavior exists and that it has negative consequences for patient care for institutions, who are at great risk legally and regulatory wise,” she said. “And the document makes that clear that that risk is increasing.”
Dr. Douglas pointed out that the Joint Commission now requires good behavior in institutions that it accredits and that the Accreditation Council for Graduate Medical Education requires education around professionalism and evidence that their trainees are treated as professionals.
Funding agencies like the National Institutes of Health have also jumped into this space, recently establishing a hotline to report harassment, discrimination, and bullying perpetrated by an NIH-funded investigator, and giving institutions 30 days to investigate.
“In the last 2 years they have defunded, taken away the grants of 75 investigators, compared to zero in the 5 years before that,” Dr. Douglas said. “So I think, even though the bad behavior may be escalating, the consequences are escalating too.”
The new “2022 ACC Health Policy Statement on Building Respect, Civility, and Inclusion in the Cardiovascular Workplace” will be discussed in a session at the ACC 2022 Scientific Sessions on April 2 at 4:15 p.m. ET.
A version of this article first appeared on Medscape.com.
FROM JACC
Children and COVID: CDC gives perspective on hospitalizations
New COVID-19 cases in children fell by 23% as the latest weekly count dropped to its lowest level since July of 2021, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
, when the early stages of the Delta surge led to 23,551 cases, the AAP and CHA said in their weekly COVID report.
The two organizations put the total number of cases at nearly 12.8 million from the start of the pandemic to March 17, with children representing 19.0% of cases among all ages. The Centers for Disease Control and Prevention puts the cumulative number of COVID-19 cases at almost 12.0 million as of March 21, or 17.5% of the nationwide total.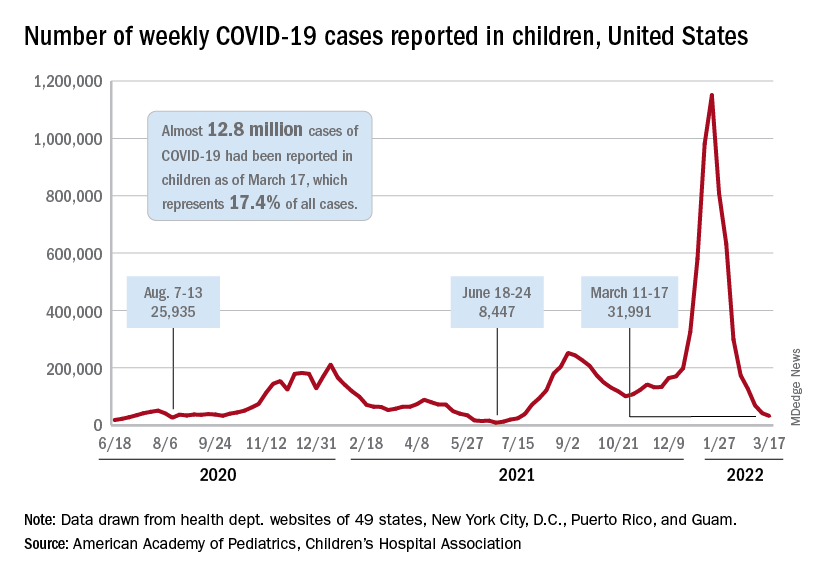
COVID-related hospitalizations also continue to fall, and two new studies from the CDC put children’s experiences during the Omicron surge and the larger pandemic into perspective.
One study showed that hospitalization rates for children aged 4 years and younger during the Omicron surge were five times higher than at the peak of the Delta surge, with the highest rates occurring in infants under 6 months of age. That report was based on the CDC’s COVID-19–Associated Hospitalization Surveillance Network (COVID-NET), which covers 99 counties across 14 states (MMWR. 2022 March 18;71[11]:429-36).
The second study compared child hospitalizations during 1 year of the COVID pandemic (Oct. 1, 2020, to Sept. 30, 2021) with three influenza seasons (2017-2018 through 2019-2020). The pre-Omicron hospitalization rate for those under age 18 years, 48.2 per 100,000 children, was higher than any of the three flu seasons: 33.5 per 100,000 in 2017-2018, 33.8 in 2018-2019, and 41.7 for 2019-2020, the investigators said in a medRxiv preprint.
Most of the increased COVID burden fell on adolescents aged 12-17, they said. The COVID hospitalization rate for that age group was 59.9 per 100,000, versus 12.2-14.1 for influenza, while children aged 5-11 had a COVID-related rate of 25.0 and flu-related rates of 24.3-31.7, and those aged 0-4 had rates of 66.8 for COVID and 70.9-91.5 for the flu, Miranda J. Delahoy of the CDC’s COVID-19 Response Team and associates reported.
New COVID-19 cases in children fell by 23% as the latest weekly count dropped to its lowest level since July of 2021, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
, when the early stages of the Delta surge led to 23,551 cases, the AAP and CHA said in their weekly COVID report.
The two organizations put the total number of cases at nearly 12.8 million from the start of the pandemic to March 17, with children representing 19.0% of cases among all ages. The Centers for Disease Control and Prevention puts the cumulative number of COVID-19 cases at almost 12.0 million as of March 21, or 17.5% of the nationwide total.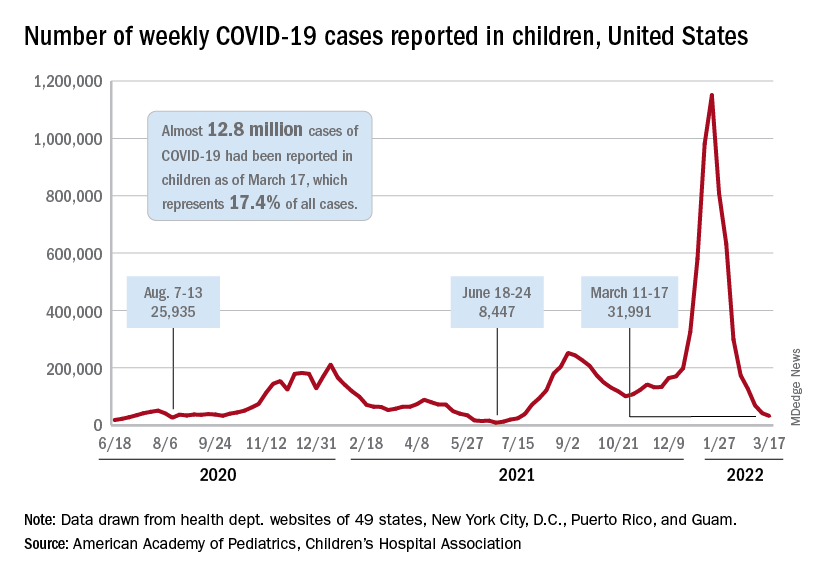
COVID-related hospitalizations also continue to fall, and two new studies from the CDC put children’s experiences during the Omicron surge and the larger pandemic into perspective.
One study showed that hospitalization rates for children aged 4 years and younger during the Omicron surge were five times higher than at the peak of the Delta surge, with the highest rates occurring in infants under 6 months of age. That report was based on the CDC’s COVID-19–Associated Hospitalization Surveillance Network (COVID-NET), which covers 99 counties across 14 states (MMWR. 2022 March 18;71[11]:429-36).
The second study compared child hospitalizations during 1 year of the COVID pandemic (Oct. 1, 2020, to Sept. 30, 2021) with three influenza seasons (2017-2018 through 2019-2020). The pre-Omicron hospitalization rate for those under age 18 years, 48.2 per 100,000 children, was higher than any of the three flu seasons: 33.5 per 100,000 in 2017-2018, 33.8 in 2018-2019, and 41.7 for 2019-2020, the investigators said in a medRxiv preprint.
Most of the increased COVID burden fell on adolescents aged 12-17, they said. The COVID hospitalization rate for that age group was 59.9 per 100,000, versus 12.2-14.1 for influenza, while children aged 5-11 had a COVID-related rate of 25.0 and flu-related rates of 24.3-31.7, and those aged 0-4 had rates of 66.8 for COVID and 70.9-91.5 for the flu, Miranda J. Delahoy of the CDC’s COVID-19 Response Team and associates reported.
New COVID-19 cases in children fell by 23% as the latest weekly count dropped to its lowest level since July of 2021, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
, when the early stages of the Delta surge led to 23,551 cases, the AAP and CHA said in their weekly COVID report.
The two organizations put the total number of cases at nearly 12.8 million from the start of the pandemic to March 17, with children representing 19.0% of cases among all ages. The Centers for Disease Control and Prevention puts the cumulative number of COVID-19 cases at almost 12.0 million as of March 21, or 17.5% of the nationwide total.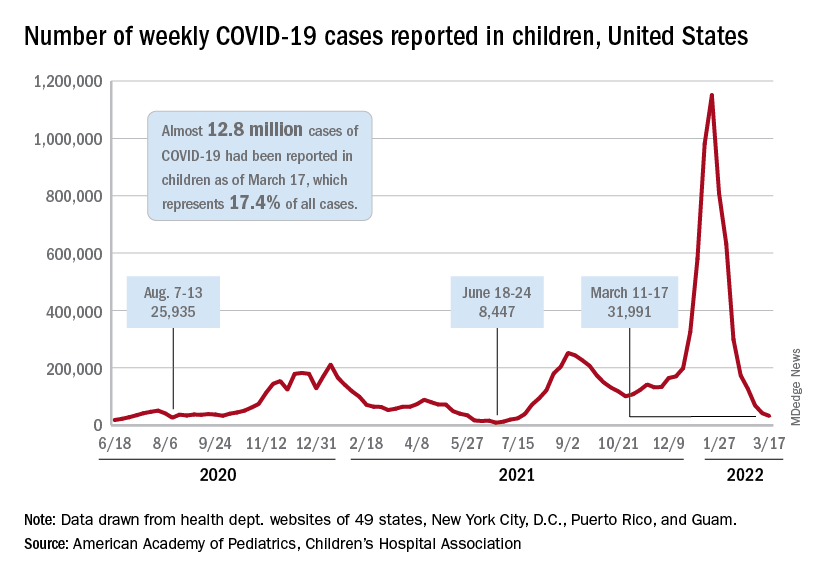
COVID-related hospitalizations also continue to fall, and two new studies from the CDC put children’s experiences during the Omicron surge and the larger pandemic into perspective.
One study showed that hospitalization rates for children aged 4 years and younger during the Omicron surge were five times higher than at the peak of the Delta surge, with the highest rates occurring in infants under 6 months of age. That report was based on the CDC’s COVID-19–Associated Hospitalization Surveillance Network (COVID-NET), which covers 99 counties across 14 states (MMWR. 2022 March 18;71[11]:429-36).
The second study compared child hospitalizations during 1 year of the COVID pandemic (Oct. 1, 2020, to Sept. 30, 2021) with three influenza seasons (2017-2018 through 2019-2020). The pre-Omicron hospitalization rate for those under age 18 years, 48.2 per 100,000 children, was higher than any of the three flu seasons: 33.5 per 100,000 in 2017-2018, 33.8 in 2018-2019, and 41.7 for 2019-2020, the investigators said in a medRxiv preprint.
Most of the increased COVID burden fell on adolescents aged 12-17, they said. The COVID hospitalization rate for that age group was 59.9 per 100,000, versus 12.2-14.1 for influenza, while children aged 5-11 had a COVID-related rate of 25.0 and flu-related rates of 24.3-31.7, and those aged 0-4 had rates of 66.8 for COVID and 70.9-91.5 for the flu, Miranda J. Delahoy of the CDC’s COVID-19 Response Team and associates reported.
Racial disparities seen in pediatric postoperative mortality rates
Among Black and White children, higher socioeconomic status (SES) was associated with lower pediatric postoperative mortality, according to a cohort study published in JAMA Network Open. However, this association was not equitable when comparing Black and White children.
The results showed that postoperative mortality rates were significantly higher in Black children in the highest income category, compared with White children in the same category.
“[We] assessed whether increasing family SES is associated with lower pediatric postoperative mortality and, if so, whether this association is equitable among Black and White children,” Brittany L. Willer, MD, of Nationwide Children’s Hospital in Columbus, Ohio, and colleagues wrote.
The researchers retrospectively analyzed data from 51 pediatric tertiary care hospitals apart of the Children’s Hospital Association Pediatric Health Information System. The cohort included children younger than 18 years who underwent inpatient surgical procedures between January 2004 and December 2020.
The exposures of interest were race and parental income quartile; the primary endpoint was risk-adjusted in-hospital mortality rates by race and parental income quartile.
Results
The study cohort included 1,378,111 participants, including 248,464 (18.0%) Black and 1,129,647 (82.0%) White children, respectively.
The overall mortality rate was 1.2%, and rates decreased as income quartile increased (1.4% in quartile 1 [lowest income]; 1.3% in quartile 2; 1.0% in quartile 3; and 0.9% in quartile 4 [highest income]; P < .001).
Among participants in the three lowest income quartiles, Black children had 33% greater odds of postoperative death versus White children (adjusted odds ratio, 1.33; 95% confidence interval, 1.27-1.39; P < .001). This difference persisted in children in the highest income quartile (aOR, 1.39; 95% CI, 1.25-1.54; P < .001).
In addition, postoperative mortality rates in Black children in the highest income quartile (1.30%; 95% CI, 1.19%-1.42%) were similar to those of White children in the lowest income quartile (1.20%; 95% CI, 1.16%-1.25%).
“These findings suggest that increasing family SES did not provide equitable advantage to Black, compared with White children, and interventions that target socioeconomic inequities alone may not fully address persistent racial disparities in pediatric postoperative mortality,” wrote Dr. Willer and colleagues. “A multifaceted approach that includes dismantling of socioeconomic barriers, equitable availability of comprehensive pediatric surgical care, and personalized care for children of all races is needed.”
The researchers acknowledged that a potential limitation of the study was the use of zip code–level median household income as a proxy for family SES.
A perspective
In an interview, Timothy Joos, MD, a Seattle internist and pediatrician in private practice, said “there is a fair dose of racism and classism inside all of us – recognizing and coming to terms with it are steps toward improving equity issues.
“As providers, we have to remind ourselves to give our most prompt and thorough care to the patients with the most acute and severe illnesses,” Dr. Joos said. “As organizations, we have to pursue feedback from all our clients, but with special outreach to those that are used to not having their voices heard.”
No funding sources were reported. The authors reported no relevant disclosures. Dr. Joos is a member of the Pediatric News editorial advisory board but had no other disclosures.
Among Black and White children, higher socioeconomic status (SES) was associated with lower pediatric postoperative mortality, according to a cohort study published in JAMA Network Open. However, this association was not equitable when comparing Black and White children.
The results showed that postoperative mortality rates were significantly higher in Black children in the highest income category, compared with White children in the same category.
“[We] assessed whether increasing family SES is associated with lower pediatric postoperative mortality and, if so, whether this association is equitable among Black and White children,” Brittany L. Willer, MD, of Nationwide Children’s Hospital in Columbus, Ohio, and colleagues wrote.
The researchers retrospectively analyzed data from 51 pediatric tertiary care hospitals apart of the Children’s Hospital Association Pediatric Health Information System. The cohort included children younger than 18 years who underwent inpatient surgical procedures between January 2004 and December 2020.
The exposures of interest were race and parental income quartile; the primary endpoint was risk-adjusted in-hospital mortality rates by race and parental income quartile.
Results
The study cohort included 1,378,111 participants, including 248,464 (18.0%) Black and 1,129,647 (82.0%) White children, respectively.
The overall mortality rate was 1.2%, and rates decreased as income quartile increased (1.4% in quartile 1 [lowest income]; 1.3% in quartile 2; 1.0% in quartile 3; and 0.9% in quartile 4 [highest income]; P < .001).
Among participants in the three lowest income quartiles, Black children had 33% greater odds of postoperative death versus White children (adjusted odds ratio, 1.33; 95% confidence interval, 1.27-1.39; P < .001). This difference persisted in children in the highest income quartile (aOR, 1.39; 95% CI, 1.25-1.54; P < .001).
In addition, postoperative mortality rates in Black children in the highest income quartile (1.30%; 95% CI, 1.19%-1.42%) were similar to those of White children in the lowest income quartile (1.20%; 95% CI, 1.16%-1.25%).
“These findings suggest that increasing family SES did not provide equitable advantage to Black, compared with White children, and interventions that target socioeconomic inequities alone may not fully address persistent racial disparities in pediatric postoperative mortality,” wrote Dr. Willer and colleagues. “A multifaceted approach that includes dismantling of socioeconomic barriers, equitable availability of comprehensive pediatric surgical care, and personalized care for children of all races is needed.”
The researchers acknowledged that a potential limitation of the study was the use of zip code–level median household income as a proxy for family SES.
A perspective
In an interview, Timothy Joos, MD, a Seattle internist and pediatrician in private practice, said “there is a fair dose of racism and classism inside all of us – recognizing and coming to terms with it are steps toward improving equity issues.
“As providers, we have to remind ourselves to give our most prompt and thorough care to the patients with the most acute and severe illnesses,” Dr. Joos said. “As organizations, we have to pursue feedback from all our clients, but with special outreach to those that are used to not having their voices heard.”
No funding sources were reported. The authors reported no relevant disclosures. Dr. Joos is a member of the Pediatric News editorial advisory board but had no other disclosures.
Among Black and White children, higher socioeconomic status (SES) was associated with lower pediatric postoperative mortality, according to a cohort study published in JAMA Network Open. However, this association was not equitable when comparing Black and White children.
The results showed that postoperative mortality rates were significantly higher in Black children in the highest income category, compared with White children in the same category.
“[We] assessed whether increasing family SES is associated with lower pediatric postoperative mortality and, if so, whether this association is equitable among Black and White children,” Brittany L. Willer, MD, of Nationwide Children’s Hospital in Columbus, Ohio, and colleagues wrote.
The researchers retrospectively analyzed data from 51 pediatric tertiary care hospitals apart of the Children’s Hospital Association Pediatric Health Information System. The cohort included children younger than 18 years who underwent inpatient surgical procedures between January 2004 and December 2020.
The exposures of interest were race and parental income quartile; the primary endpoint was risk-adjusted in-hospital mortality rates by race and parental income quartile.
Results
The study cohort included 1,378,111 participants, including 248,464 (18.0%) Black and 1,129,647 (82.0%) White children, respectively.
The overall mortality rate was 1.2%, and rates decreased as income quartile increased (1.4% in quartile 1 [lowest income]; 1.3% in quartile 2; 1.0% in quartile 3; and 0.9% in quartile 4 [highest income]; P < .001).
Among participants in the three lowest income quartiles, Black children had 33% greater odds of postoperative death versus White children (adjusted odds ratio, 1.33; 95% confidence interval, 1.27-1.39; P < .001). This difference persisted in children in the highest income quartile (aOR, 1.39; 95% CI, 1.25-1.54; P < .001).
In addition, postoperative mortality rates in Black children in the highest income quartile (1.30%; 95% CI, 1.19%-1.42%) were similar to those of White children in the lowest income quartile (1.20%; 95% CI, 1.16%-1.25%).
“These findings suggest that increasing family SES did not provide equitable advantage to Black, compared with White children, and interventions that target socioeconomic inequities alone may not fully address persistent racial disparities in pediatric postoperative mortality,” wrote Dr. Willer and colleagues. “A multifaceted approach that includes dismantling of socioeconomic barriers, equitable availability of comprehensive pediatric surgical care, and personalized care for children of all races is needed.”
The researchers acknowledged that a potential limitation of the study was the use of zip code–level median household income as a proxy for family SES.
A perspective
In an interview, Timothy Joos, MD, a Seattle internist and pediatrician in private practice, said “there is a fair dose of racism and classism inside all of us – recognizing and coming to terms with it are steps toward improving equity issues.
“As providers, we have to remind ourselves to give our most prompt and thorough care to the patients with the most acute and severe illnesses,” Dr. Joos said. “As organizations, we have to pursue feedback from all our clients, but with special outreach to those that are used to not having their voices heard.”
No funding sources were reported. The authors reported no relevant disclosures. Dr. Joos is a member of the Pediatric News editorial advisory board but had no other disclosures.
FROM JAMA NETWORK OPEN
Knowns and unknowns about SSRI use during pregnancy in 2022
The last 15-20 years have brought enormous attention to the relevant clinical issues regarding prescribing antidepressants during pregnancy. Concern about the effects of fetal exposure to selective serotonin reuptake inhibitors (SSRIs) is appropriate given the consistent data that approximately 7% of women use antidepressants during pregnancy, and that risk for relapse of depression during pregnancy in women who have stopped antidepressants during pregnancy is very high.
We have learned so much from studies of relevant questions regarding SSRI exposure. Concerns about increased risk for organ malformation have been set aside. An extraordinary number of studies across a broad range of patients around the globe looked at the issue of risk for organ malformation following in utero SSRI exposure – even looking specifically at risk for cardiac malformations, which had been an earlier concern in the literature – with the evidence supporting absence of increased risk. Also clarified has been, first, the absence of risk of complications such as persistent pulmonary hypertension of the newborn (PPHN) and, second, a delineation of the prevalence and clinical implications of transient neonatal symptoms such as jitteriness and tachypnea in offspring of women who used antidepressants during pregnancy – so-called “poor neonatal adaptation syndrome.”
However, for so many clinicians and for patients, the missing piece in the risk-benefit equation has been the issue of long-term neurodevelopmental sequelae in children whose mothers used antidepressants during pregnancy. While the accumulated data have shown sparse evidence linking SSRI exposure with autism or attention-deficit/hyperactivity disorder (ADHD), the evidence has been mixed regarding neurobehavioral sequelae associated with fetal exposure using developmental outcomes such as language ability, cognition, academic performance, language, math, and other cognitive outcomes. As far back as the 1990s, colleagues in Canada failed to show a difference in neurobehavioral outcomes in 5- to 7-year-old children whose mothers used SSRIs or older tricyclic antidepressants during pregnancy compared to nonexposed women (N Engl J Med. 1997 Jan 23;336[4]:258-62). Even early on, it was noted that one of the strongest predictors of neurodevelopmental outcome was untreated maternal psychiatric illness.
Since those early studies and over the last decade, there have been numerous small studies with conflicting data regarding a whole host of neurodevelopmental outcomes with inconsistent methodologies, different assessments, and failure to control for the presence or absence of maternal psychiatric illness during pregnancy – one of the most critical predictors of neurodevelopmental outcome and one we are beginning to appreciate plays a very significant role.
Most recently, the authors of a very large population-based retrospective cohort study in Denmark linked population-based registries with obstetrical data and examined language and math performance among 575,369 public schoolchildren whose mothers used or didn’t use antidepressants during pregnancy (JAMA. 2021 Nov 2;326[17]:1725-35). These investigators found a decrease in mean test scores for language (53.4 vs. 56.6) and math (52.1 vs. 57.4) in children whose mothers received antidepressant prescriptions during pregnancy compared with children who did not have that exposure. However, when they adjusted for maternal psychiatric illness and other relevant confounders, the finding went to null for language (adjusted difference, –0.1; 95% confidence interval, –0.6 to 0.3), but did not for math (adjusted difference, −2.2; 95% CI, −2.7 to −1.6). The results ultimately showed a modest finding for exposure and a small decrement in mathematical performance. The takeaway is that antidepressant use may be a proxy for neurodevelopmental deficit but is unlikely to be the etiology or direct cause of that deficit.
With that said, patients and their doctors can be reassured with respect to how much we have learned about SSRIs during pregnancy across the last decade. Yet there are appropriate concerns about long-term neurodevelopmental sequelae in this patient population. I think that what we can say in 2022 is that there is a growing appreciation for the effect of maternal psychiatric illness on long-term outcomes in children and the effect of maternal psychiatric illness on risk for postpartum depression, which we know influences long-term neurodevelopmental outcomes in children. Perhaps more than in years past, there is now also an appreciation of the effect of a dysregulated stress axis on the intrauterine fetal neuronal programming, which is perhaps the newest frontier, and which may hold the answers with respect to how to weigh the effect of maternal psychiatric illness on decisions about psychotropic use during pregnancy. But for today, there is an appreciation that exposure to maternal psychopathology is not a benign exposure.
Although some of the data remain incomplete, in 2022, patients will continue to make individual decisions based on the available data, factoring in the effect of maternal adversity in a more deliberate way and with a refined lens through with which to see their options with respect to using or not using SSRIs during pregnancy.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at obnews@mdedge.com.
The last 15-20 years have brought enormous attention to the relevant clinical issues regarding prescribing antidepressants during pregnancy. Concern about the effects of fetal exposure to selective serotonin reuptake inhibitors (SSRIs) is appropriate given the consistent data that approximately 7% of women use antidepressants during pregnancy, and that risk for relapse of depression during pregnancy in women who have stopped antidepressants during pregnancy is very high.
We have learned so much from studies of relevant questions regarding SSRI exposure. Concerns about increased risk for organ malformation have been set aside. An extraordinary number of studies across a broad range of patients around the globe looked at the issue of risk for organ malformation following in utero SSRI exposure – even looking specifically at risk for cardiac malformations, which had been an earlier concern in the literature – with the evidence supporting absence of increased risk. Also clarified has been, first, the absence of risk of complications such as persistent pulmonary hypertension of the newborn (PPHN) and, second, a delineation of the prevalence and clinical implications of transient neonatal symptoms such as jitteriness and tachypnea in offspring of women who used antidepressants during pregnancy – so-called “poor neonatal adaptation syndrome.”
However, for so many clinicians and for patients, the missing piece in the risk-benefit equation has been the issue of long-term neurodevelopmental sequelae in children whose mothers used antidepressants during pregnancy. While the accumulated data have shown sparse evidence linking SSRI exposure with autism or attention-deficit/hyperactivity disorder (ADHD), the evidence has been mixed regarding neurobehavioral sequelae associated with fetal exposure using developmental outcomes such as language ability, cognition, academic performance, language, math, and other cognitive outcomes. As far back as the 1990s, colleagues in Canada failed to show a difference in neurobehavioral outcomes in 5- to 7-year-old children whose mothers used SSRIs or older tricyclic antidepressants during pregnancy compared to nonexposed women (N Engl J Med. 1997 Jan 23;336[4]:258-62). Even early on, it was noted that one of the strongest predictors of neurodevelopmental outcome was untreated maternal psychiatric illness.
Since those early studies and over the last decade, there have been numerous small studies with conflicting data regarding a whole host of neurodevelopmental outcomes with inconsistent methodologies, different assessments, and failure to control for the presence or absence of maternal psychiatric illness during pregnancy – one of the most critical predictors of neurodevelopmental outcome and one we are beginning to appreciate plays a very significant role.
Most recently, the authors of a very large population-based retrospective cohort study in Denmark linked population-based registries with obstetrical data and examined language and math performance among 575,369 public schoolchildren whose mothers used or didn’t use antidepressants during pregnancy (JAMA. 2021 Nov 2;326[17]:1725-35). These investigators found a decrease in mean test scores for language (53.4 vs. 56.6) and math (52.1 vs. 57.4) in children whose mothers received antidepressant prescriptions during pregnancy compared with children who did not have that exposure. However, when they adjusted for maternal psychiatric illness and other relevant confounders, the finding went to null for language (adjusted difference, –0.1; 95% confidence interval, –0.6 to 0.3), but did not for math (adjusted difference, −2.2; 95% CI, −2.7 to −1.6). The results ultimately showed a modest finding for exposure and a small decrement in mathematical performance. The takeaway is that antidepressant use may be a proxy for neurodevelopmental deficit but is unlikely to be the etiology or direct cause of that deficit.
With that said, patients and their doctors can be reassured with respect to how much we have learned about SSRIs during pregnancy across the last decade. Yet there are appropriate concerns about long-term neurodevelopmental sequelae in this patient population. I think that what we can say in 2022 is that there is a growing appreciation for the effect of maternal psychiatric illness on long-term outcomes in children and the effect of maternal psychiatric illness on risk for postpartum depression, which we know influences long-term neurodevelopmental outcomes in children. Perhaps more than in years past, there is now also an appreciation of the effect of a dysregulated stress axis on the intrauterine fetal neuronal programming, which is perhaps the newest frontier, and which may hold the answers with respect to how to weigh the effect of maternal psychiatric illness on decisions about psychotropic use during pregnancy. But for today, there is an appreciation that exposure to maternal psychopathology is not a benign exposure.
Although some of the data remain incomplete, in 2022, patients will continue to make individual decisions based on the available data, factoring in the effect of maternal adversity in a more deliberate way and with a refined lens through with which to see their options with respect to using or not using SSRIs during pregnancy.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at obnews@mdedge.com.
The last 15-20 years have brought enormous attention to the relevant clinical issues regarding prescribing antidepressants during pregnancy. Concern about the effects of fetal exposure to selective serotonin reuptake inhibitors (SSRIs) is appropriate given the consistent data that approximately 7% of women use antidepressants during pregnancy, and that risk for relapse of depression during pregnancy in women who have stopped antidepressants during pregnancy is very high.
We have learned so much from studies of relevant questions regarding SSRI exposure. Concerns about increased risk for organ malformation have been set aside. An extraordinary number of studies across a broad range of patients around the globe looked at the issue of risk for organ malformation following in utero SSRI exposure – even looking specifically at risk for cardiac malformations, which had been an earlier concern in the literature – with the evidence supporting absence of increased risk. Also clarified has been, first, the absence of risk of complications such as persistent pulmonary hypertension of the newborn (PPHN) and, second, a delineation of the prevalence and clinical implications of transient neonatal symptoms such as jitteriness and tachypnea in offspring of women who used antidepressants during pregnancy – so-called “poor neonatal adaptation syndrome.”
However, for so many clinicians and for patients, the missing piece in the risk-benefit equation has been the issue of long-term neurodevelopmental sequelae in children whose mothers used antidepressants during pregnancy. While the accumulated data have shown sparse evidence linking SSRI exposure with autism or attention-deficit/hyperactivity disorder (ADHD), the evidence has been mixed regarding neurobehavioral sequelae associated with fetal exposure using developmental outcomes such as language ability, cognition, academic performance, language, math, and other cognitive outcomes. As far back as the 1990s, colleagues in Canada failed to show a difference in neurobehavioral outcomes in 5- to 7-year-old children whose mothers used SSRIs or older tricyclic antidepressants during pregnancy compared to nonexposed women (N Engl J Med. 1997 Jan 23;336[4]:258-62). Even early on, it was noted that one of the strongest predictors of neurodevelopmental outcome was untreated maternal psychiatric illness.
Since those early studies and over the last decade, there have been numerous small studies with conflicting data regarding a whole host of neurodevelopmental outcomes with inconsistent methodologies, different assessments, and failure to control for the presence or absence of maternal psychiatric illness during pregnancy – one of the most critical predictors of neurodevelopmental outcome and one we are beginning to appreciate plays a very significant role.
Most recently, the authors of a very large population-based retrospective cohort study in Denmark linked population-based registries with obstetrical data and examined language and math performance among 575,369 public schoolchildren whose mothers used or didn’t use antidepressants during pregnancy (JAMA. 2021 Nov 2;326[17]:1725-35). These investigators found a decrease in mean test scores for language (53.4 vs. 56.6) and math (52.1 vs. 57.4) in children whose mothers received antidepressant prescriptions during pregnancy compared with children who did not have that exposure. However, when they adjusted for maternal psychiatric illness and other relevant confounders, the finding went to null for language (adjusted difference, –0.1; 95% confidence interval, –0.6 to 0.3), but did not for math (adjusted difference, −2.2; 95% CI, −2.7 to −1.6). The results ultimately showed a modest finding for exposure and a small decrement in mathematical performance. The takeaway is that antidepressant use may be a proxy for neurodevelopmental deficit but is unlikely to be the etiology or direct cause of that deficit.
With that said, patients and their doctors can be reassured with respect to how much we have learned about SSRIs during pregnancy across the last decade. Yet there are appropriate concerns about long-term neurodevelopmental sequelae in this patient population. I think that what we can say in 2022 is that there is a growing appreciation for the effect of maternal psychiatric illness on long-term outcomes in children and the effect of maternal psychiatric illness on risk for postpartum depression, which we know influences long-term neurodevelopmental outcomes in children. Perhaps more than in years past, there is now also an appreciation of the effect of a dysregulated stress axis on the intrauterine fetal neuronal programming, which is perhaps the newest frontier, and which may hold the answers with respect to how to weigh the effect of maternal psychiatric illness on decisions about psychotropic use during pregnancy. But for today, there is an appreciation that exposure to maternal psychopathology is not a benign exposure.
Although some of the data remain incomplete, in 2022, patients will continue to make individual decisions based on the available data, factoring in the effect of maternal adversity in a more deliberate way and with a refined lens through with which to see their options with respect to using or not using SSRIs during pregnancy.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at obnews@mdedge.com.








