User login
Exercise tied to 50% reduction in mortality after stroke
, with a greater than 50% reduction in risk.
Lead study author Raed A. Joundi, MD, DPhil, of the University of Calgary (Alta.), said he expected results to show exercise was beneficial, but was surprised by the magnitude of the association between physical activity and lower mortality risk.
The impact of physical activity also differed significantly by age; those younger than 75 had a 79% reduction in mortality risk, compared with 32% in those age 75 and older.
“This is even after adjusting for factors such heart disease, respiratory conditions, smoking, and other functional limitations,” said Dr. Joundi.
The study was published online Aug. 11 in the journal Neurology.
For this analysis, the researchers used data on a cohort of people across Canada (excluding the province of Quebec) over 3-9 years. The 895 patients with prior stroke averaged 72 years of age, while the 97,805 in the control group had an average age of 63.
Weekly physical activity averages were evaluated using the self-reporting Canadian Community Health Survey, which was linked with administrative databases to evaluate the association of physical activity with long-term risk for mortality among stroke survivors, compared with controls.
Physical activity was measured in metabolic equivalents (METs); meeting minimum physical activity guidelines was defined as 10 MET-hours/week.
During the study period, more stroke patients than controls died (24.7% vs. 5.7%). However, those who met the physical activity guideline recommendations of 10 MET-hours/week had a lower mortality, both in the stroke survivor group (14.6% vs. 33.2%; adjusted hazard ratio, 0.46; 95% confidence interval, 0.29-0.73) and among control participants (3.6% vs. 7.9%; aHR 0.69; 95% CI, 0.62-0.76).
The largest absolute and relative reduction in mortality was among stroke respondents younger than 75 (10.5% vs. 29%; aHR, 0.21; 95% CI, 0.10-0.43), the researchers note.
There was a significant interaction with age for the stroke patients but not the control group.
“The greatest reduction in mortality was seen between 0 and 10 METs per week … so the main point is that something is better than nothing,” said Dr. Joundi.
Exercise guidelines for the future
Although current guidelines recommend physical activity in stroke survivors, investigators noted that these are largely based on studies in the general population. Therefore, the aim of this research was to get a better understanding of the role of physical activity in the health of stroke survivors in the community, which could ultimately be used to design improved public health campaigns and physical activity interventions.
Given that this is a large study of stroke survivors in the community, Dr. Joundi hopes the results will influence future activity guidelines for those who have suffered a stroke.
“We found a log-linear relationship between physical activity and mortality such that 10 MET-hours/week was associated with large reductions in mortality with most benefit achieved by 20 MET-hours/week,” the authors concluded. “These thresholds could be considered for use in future guidelines for stroke.”
Clinical trials are underway to provide evidence for the implementation of exercise programs after stroke, they add, and offering physical activity programs to stroke survivors in the community “is an increasing priority in the U.S., Canada, and Europe.”
“People are at higher risk of death early on after a stroke but also months and years later, so if we can identify a relatively low-cost and easy intervention like physical activity to improve health and reduce the risk of death for stroke survivors it would be important,” Dr. Joundi said.
Key barriers
Paul George, MD, PhD, a stroke and vascular neurologist at Stanford (Calif.) University, said findings such as these further strengthen the argument that physical exercise is important after stroke.
“Because the study looked specifically at stroke patients, it can provide further guidance on physical activity recommendations that we provide to our patients following stroke,” said Dr. George, who was not associated with the study.
Going forward, he said, more research is needed to identify specifically what is preventing stroke patients from exercising more. What is required, he said, is “future research to determine the key barriers to physical activity following stroke and methods to reduce these will also be important to increasing physical activity in stroke survivors.”
Dr. Joundi said determining how to tailor exercise recommendations to meet the wide range of capabilities of stroke survivors will be another key factor.
“Stroke survivors may have some disabilities, so we need to be able to engage them at an [exercise] level that’s possible for them,” he said.
The study did not include stroke survivors living in long-term care homes.
The study had no targeted funding. Coauthor Eric E. Smith, MD, MPH, reports royalties from UpToDate, and consulting fees from Alnylam, Biogen, and Javelin. Dr. Joundi and the other coauthors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, with a greater than 50% reduction in risk.
Lead study author Raed A. Joundi, MD, DPhil, of the University of Calgary (Alta.), said he expected results to show exercise was beneficial, but was surprised by the magnitude of the association between physical activity and lower mortality risk.
The impact of physical activity also differed significantly by age; those younger than 75 had a 79% reduction in mortality risk, compared with 32% in those age 75 and older.
“This is even after adjusting for factors such heart disease, respiratory conditions, smoking, and other functional limitations,” said Dr. Joundi.
The study was published online Aug. 11 in the journal Neurology.
For this analysis, the researchers used data on a cohort of people across Canada (excluding the province of Quebec) over 3-9 years. The 895 patients with prior stroke averaged 72 years of age, while the 97,805 in the control group had an average age of 63.
Weekly physical activity averages were evaluated using the self-reporting Canadian Community Health Survey, which was linked with administrative databases to evaluate the association of physical activity with long-term risk for mortality among stroke survivors, compared with controls.
Physical activity was measured in metabolic equivalents (METs); meeting minimum physical activity guidelines was defined as 10 MET-hours/week.
During the study period, more stroke patients than controls died (24.7% vs. 5.7%). However, those who met the physical activity guideline recommendations of 10 MET-hours/week had a lower mortality, both in the stroke survivor group (14.6% vs. 33.2%; adjusted hazard ratio, 0.46; 95% confidence interval, 0.29-0.73) and among control participants (3.6% vs. 7.9%; aHR 0.69; 95% CI, 0.62-0.76).
The largest absolute and relative reduction in mortality was among stroke respondents younger than 75 (10.5% vs. 29%; aHR, 0.21; 95% CI, 0.10-0.43), the researchers note.
There was a significant interaction with age for the stroke patients but not the control group.
“The greatest reduction in mortality was seen between 0 and 10 METs per week … so the main point is that something is better than nothing,” said Dr. Joundi.
Exercise guidelines for the future
Although current guidelines recommend physical activity in stroke survivors, investigators noted that these are largely based on studies in the general population. Therefore, the aim of this research was to get a better understanding of the role of physical activity in the health of stroke survivors in the community, which could ultimately be used to design improved public health campaigns and physical activity interventions.
Given that this is a large study of stroke survivors in the community, Dr. Joundi hopes the results will influence future activity guidelines for those who have suffered a stroke.
“We found a log-linear relationship between physical activity and mortality such that 10 MET-hours/week was associated with large reductions in mortality with most benefit achieved by 20 MET-hours/week,” the authors concluded. “These thresholds could be considered for use in future guidelines for stroke.”
Clinical trials are underway to provide evidence for the implementation of exercise programs after stroke, they add, and offering physical activity programs to stroke survivors in the community “is an increasing priority in the U.S., Canada, and Europe.”
“People are at higher risk of death early on after a stroke but also months and years later, so if we can identify a relatively low-cost and easy intervention like physical activity to improve health and reduce the risk of death for stroke survivors it would be important,” Dr. Joundi said.
Key barriers
Paul George, MD, PhD, a stroke and vascular neurologist at Stanford (Calif.) University, said findings such as these further strengthen the argument that physical exercise is important after stroke.
“Because the study looked specifically at stroke patients, it can provide further guidance on physical activity recommendations that we provide to our patients following stroke,” said Dr. George, who was not associated with the study.
Going forward, he said, more research is needed to identify specifically what is preventing stroke patients from exercising more. What is required, he said, is “future research to determine the key barriers to physical activity following stroke and methods to reduce these will also be important to increasing physical activity in stroke survivors.”
Dr. Joundi said determining how to tailor exercise recommendations to meet the wide range of capabilities of stroke survivors will be another key factor.
“Stroke survivors may have some disabilities, so we need to be able to engage them at an [exercise] level that’s possible for them,” he said.
The study did not include stroke survivors living in long-term care homes.
The study had no targeted funding. Coauthor Eric E. Smith, MD, MPH, reports royalties from UpToDate, and consulting fees from Alnylam, Biogen, and Javelin. Dr. Joundi and the other coauthors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, with a greater than 50% reduction in risk.
Lead study author Raed A. Joundi, MD, DPhil, of the University of Calgary (Alta.), said he expected results to show exercise was beneficial, but was surprised by the magnitude of the association between physical activity and lower mortality risk.
The impact of physical activity also differed significantly by age; those younger than 75 had a 79% reduction in mortality risk, compared with 32% in those age 75 and older.
“This is even after adjusting for factors such heart disease, respiratory conditions, smoking, and other functional limitations,” said Dr. Joundi.
The study was published online Aug. 11 in the journal Neurology.
For this analysis, the researchers used data on a cohort of people across Canada (excluding the province of Quebec) over 3-9 years. The 895 patients with prior stroke averaged 72 years of age, while the 97,805 in the control group had an average age of 63.
Weekly physical activity averages were evaluated using the self-reporting Canadian Community Health Survey, which was linked with administrative databases to evaluate the association of physical activity with long-term risk for mortality among stroke survivors, compared with controls.
Physical activity was measured in metabolic equivalents (METs); meeting minimum physical activity guidelines was defined as 10 MET-hours/week.
During the study period, more stroke patients than controls died (24.7% vs. 5.7%). However, those who met the physical activity guideline recommendations of 10 MET-hours/week had a lower mortality, both in the stroke survivor group (14.6% vs. 33.2%; adjusted hazard ratio, 0.46; 95% confidence interval, 0.29-0.73) and among control participants (3.6% vs. 7.9%; aHR 0.69; 95% CI, 0.62-0.76).
The largest absolute and relative reduction in mortality was among stroke respondents younger than 75 (10.5% vs. 29%; aHR, 0.21; 95% CI, 0.10-0.43), the researchers note.
There was a significant interaction with age for the stroke patients but not the control group.
“The greatest reduction in mortality was seen between 0 and 10 METs per week … so the main point is that something is better than nothing,” said Dr. Joundi.
Exercise guidelines for the future
Although current guidelines recommend physical activity in stroke survivors, investigators noted that these are largely based on studies in the general population. Therefore, the aim of this research was to get a better understanding of the role of physical activity in the health of stroke survivors in the community, which could ultimately be used to design improved public health campaigns and physical activity interventions.
Given that this is a large study of stroke survivors in the community, Dr. Joundi hopes the results will influence future activity guidelines for those who have suffered a stroke.
“We found a log-linear relationship between physical activity and mortality such that 10 MET-hours/week was associated with large reductions in mortality with most benefit achieved by 20 MET-hours/week,” the authors concluded. “These thresholds could be considered for use in future guidelines for stroke.”
Clinical trials are underway to provide evidence for the implementation of exercise programs after stroke, they add, and offering physical activity programs to stroke survivors in the community “is an increasing priority in the U.S., Canada, and Europe.”
“People are at higher risk of death early on after a stroke but also months and years later, so if we can identify a relatively low-cost and easy intervention like physical activity to improve health and reduce the risk of death for stroke survivors it would be important,” Dr. Joundi said.
Key barriers
Paul George, MD, PhD, a stroke and vascular neurologist at Stanford (Calif.) University, said findings such as these further strengthen the argument that physical exercise is important after stroke.
“Because the study looked specifically at stroke patients, it can provide further guidance on physical activity recommendations that we provide to our patients following stroke,” said Dr. George, who was not associated with the study.
Going forward, he said, more research is needed to identify specifically what is preventing stroke patients from exercising more. What is required, he said, is “future research to determine the key barriers to physical activity following stroke and methods to reduce these will also be important to increasing physical activity in stroke survivors.”
Dr. Joundi said determining how to tailor exercise recommendations to meet the wide range of capabilities of stroke survivors will be another key factor.
“Stroke survivors may have some disabilities, so we need to be able to engage them at an [exercise] level that’s possible for them,” he said.
The study did not include stroke survivors living in long-term care homes.
The study had no targeted funding. Coauthor Eric E. Smith, MD, MPH, reports royalties from UpToDate, and consulting fees from Alnylam, Biogen, and Javelin. Dr. Joundi and the other coauthors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Is this a psychiatric emergency? How to screen, assess, and triage safety concerns from the primary care office
Case vignette: Laura is a 14-year-old biological girl who presents to your office for a routine well-child visit. She is doing well medically but notes that over the past 3 months she has been having increasing thoughts of suicide and has self-harmed via cutting on her wrists with a blade removed from a shaving razor. You contemplate what the most salient questions are in order to determine the best disposition for your patient.
The case vignette above may sound like one that you have heard before, and if not, you undoubtedly will encounter such a situation moving forward. The rate of suicidal ideation amongst youth ages 10-24 has increased by 57.4% between 2007 and 2018.1 Furthermore, suicide is the second leading cause of death in those aged 10 through young adulthood.2 According to the Centers for Disease Control and Prevention’s 2019 High School Youth Risk Behavior Survey, 18.8% of high school students seriously considered attempting suicide, 15.7% made a plan about how they would attempt suicide, and 8.9% actually attempted suicide, with 2.5% having a suicide attempt that resulted in an injury, poisoning, or overdose that had to be treated by a doctor or nurse during the 12 months before the survey.3 Children often present first to their primary care provider, and they may be the first individual who the child shares their suicidal or self-harm thoughts with. It may be useful to have a standardized approach, while using your own clinical judgment, to determine best next steps. Given the significant recent surge in children presenting to the emergency department for psychiatric needs and that environment having its own limitations (for example, long wait times, nontherapeutic space, etc.), a simple screen and brief assessment may lead to being able to maintain a patient safely outside of the hospital.
Screen all appropriate patients for suicide
There are, at minimum, three validated screening tools that can be used as to determine what the best next step should be. They include the Ask Suicide-Screening Questions (ASQ) developed by the National Institute of Mental Health, the Columbia-Suicide Severity Rating Scale (C-SSRS), and the PHQ-9 (modified for adolescents). We can highlight one of the screening tools here as noted below, but the choice of screener may be based on facility and/or clinician preference.
The Ask Suicide-Screening Questions
The ASQ, developed by the National Institute of Mental Health, include the following four binary questions plus a fifth acuity question, as follows:
1. In the past few weeks, have you wished you were dead?
2. In the past few weeks, have you felt that you or your family would be better off if you were dead?
3. In the past week, have you been having thoughts about killing yourself?
4. Have you ever tried to kill yourself?
a. If yes, how?
b. When?
The following acuity question is to be asked if any of the above are answered “yes”:
5. Are you having thoughts of killing yourself right now?
a. If yes, please describe.
Assess the level of risk
Once you have screened a patient, you need to assess the level of risk to help determine the level of care required. Returning to our original case vignette, does the patient warrant outpatient management, crisis evaluation, or an emergency psychiatric evaluation? You may have already decided that the patient needs an emergency mental health evaluation from a local crisis clinician evaluation and/or the emergency department. However, you may also find that the screen did not elicit imminent concern, but it does warrant a brief assessment to further elucidate the level of risk and proper disposition. One such instrument that may be helpful is the Brief Suicide Safety Assessment (BSSA) – also developed by the NIMH as a tool linked to the ASQ. There are clear and specific instructions in the BSSA with suggestions on how to ask questions. Important components to the BSSA include:
- A focus on a more thorough clinical history – including frequency of suicidal ideation, suicide plan, past behavior, associated symptoms, and social support/stressors
- Collateral information (e.g., further details from those who know the patient such as family/friends).
- Safety planning.
- Determining disposition.
The BSSA may suggest that a crisis/psychiatric evaluation is warranted or suggest that a safety plan with a mental health referral will likely be sufficient.
Triage and safety planning
A safety plan should be created if you determine that a patient can be safely maintained as an outpatient based on your screening, assessment, and triaging. Traditional safety plans come in many different forms and can be found online (Example of a Safety Plan Template). However, most safety plans include some version of the following:
- Increased supervision: 24/7 supervision with doors open/unlocked.
- Reduced access: medications (prescription and OTC) locked away; sharps and firearms secured.
- Adaptive coping strategies (e.g., relaxation techniques such as drawing or listening to music).
- Reliable persons for support (e.g., parent, therapist, school counselor).
- Outpatient mental health provider follow-up and/or referral.
- Provision of local crisis and national hotline contact information.
- Use of a safety plan phone app completed with patient.
Envision a safety plan as a living document that evolves, grows, and changes with your patient/family – one that can be easily reviewed/updated at each visit.
Returning to our case vignette
Laura returns to your office for a follow-up after a 10-day stay at a hospital-diversion program or inpatient psychiatric unit. The decision is made to use the primary care NIMH ASQ/BSSA algorithm, and you determine the patient to not be at imminent risk following the screen and assessment. Laura is triaged as appropriate for outpatient care, you collaborate to update the safety plan, regular follow-ups are scheduled, and a mental health referral has been placed. Thus, there are tools to assist with screening, assessing, and triaging pediatric patients with suicidal ideation that provide the patient with appropriate care and treatment and may help alleviate the need to have a patient present to the emergency department.
Dr. Abdul-Karim is a child psychiatrist at the University of Vermont University Children’s Hospital in Burlington.
Additional resources
The American Academy of Child and Adolescent Psychiatry has developed information that can be provided to families about suicide safety precautions that can be taken at home, which can be found here: Facts for Families. Suicide Safety: Precautions at Home.
Screening tools listed above can be found here:
ASQ Toolkit.
C-SSRS.
PHQ-9 Modified for Adolescents (PHQ-A).
References
1. Curtin SC. National Center for Health Statistics. “State Suicide Rates Among Adolescents and Young Adults Aged 10-24: United States, 2000-2018” National Vital Statistics Reports..
2. Centers for Disease Control and Prevention, National Center for Health Statistics. “Underlying Cause of Death 2018-2019” CDC WONDER Online Database. Accessed 2021 Jul 31, 6:57:39 p.m.
3. Centers for Disease Control and Prevention. 1991-2019 High School Youth Risk Behavior Survey Data.
Case vignette: Laura is a 14-year-old biological girl who presents to your office for a routine well-child visit. She is doing well medically but notes that over the past 3 months she has been having increasing thoughts of suicide and has self-harmed via cutting on her wrists with a blade removed from a shaving razor. You contemplate what the most salient questions are in order to determine the best disposition for your patient.
The case vignette above may sound like one that you have heard before, and if not, you undoubtedly will encounter such a situation moving forward. The rate of suicidal ideation amongst youth ages 10-24 has increased by 57.4% between 2007 and 2018.1 Furthermore, suicide is the second leading cause of death in those aged 10 through young adulthood.2 According to the Centers for Disease Control and Prevention’s 2019 High School Youth Risk Behavior Survey, 18.8% of high school students seriously considered attempting suicide, 15.7% made a plan about how they would attempt suicide, and 8.9% actually attempted suicide, with 2.5% having a suicide attempt that resulted in an injury, poisoning, or overdose that had to be treated by a doctor or nurse during the 12 months before the survey.3 Children often present first to their primary care provider, and they may be the first individual who the child shares their suicidal or self-harm thoughts with. It may be useful to have a standardized approach, while using your own clinical judgment, to determine best next steps. Given the significant recent surge in children presenting to the emergency department for psychiatric needs and that environment having its own limitations (for example, long wait times, nontherapeutic space, etc.), a simple screen and brief assessment may lead to being able to maintain a patient safely outside of the hospital.
Screen all appropriate patients for suicide
There are, at minimum, three validated screening tools that can be used as to determine what the best next step should be. They include the Ask Suicide-Screening Questions (ASQ) developed by the National Institute of Mental Health, the Columbia-Suicide Severity Rating Scale (C-SSRS), and the PHQ-9 (modified for adolescents). We can highlight one of the screening tools here as noted below, but the choice of screener may be based on facility and/or clinician preference.
The Ask Suicide-Screening Questions
The ASQ, developed by the National Institute of Mental Health, include the following four binary questions plus a fifth acuity question, as follows:
1. In the past few weeks, have you wished you were dead?
2. In the past few weeks, have you felt that you or your family would be better off if you were dead?
3. In the past week, have you been having thoughts about killing yourself?
4. Have you ever tried to kill yourself?
a. If yes, how?
b. When?
The following acuity question is to be asked if any of the above are answered “yes”:
5. Are you having thoughts of killing yourself right now?
a. If yes, please describe.
Assess the level of risk
Once you have screened a patient, you need to assess the level of risk to help determine the level of care required. Returning to our original case vignette, does the patient warrant outpatient management, crisis evaluation, or an emergency psychiatric evaluation? You may have already decided that the patient needs an emergency mental health evaluation from a local crisis clinician evaluation and/or the emergency department. However, you may also find that the screen did not elicit imminent concern, but it does warrant a brief assessment to further elucidate the level of risk and proper disposition. One such instrument that may be helpful is the Brief Suicide Safety Assessment (BSSA) – also developed by the NIMH as a tool linked to the ASQ. There are clear and specific instructions in the BSSA with suggestions on how to ask questions. Important components to the BSSA include:
- A focus on a more thorough clinical history – including frequency of suicidal ideation, suicide plan, past behavior, associated symptoms, and social support/stressors
- Collateral information (e.g., further details from those who know the patient such as family/friends).
- Safety planning.
- Determining disposition.
The BSSA may suggest that a crisis/psychiatric evaluation is warranted or suggest that a safety plan with a mental health referral will likely be sufficient.
Triage and safety planning
A safety plan should be created if you determine that a patient can be safely maintained as an outpatient based on your screening, assessment, and triaging. Traditional safety plans come in many different forms and can be found online (Example of a Safety Plan Template). However, most safety plans include some version of the following:
- Increased supervision: 24/7 supervision with doors open/unlocked.
- Reduced access: medications (prescription and OTC) locked away; sharps and firearms secured.
- Adaptive coping strategies (e.g., relaxation techniques such as drawing or listening to music).
- Reliable persons for support (e.g., parent, therapist, school counselor).
- Outpatient mental health provider follow-up and/or referral.
- Provision of local crisis and national hotline contact information.
- Use of a safety plan phone app completed with patient.
Envision a safety plan as a living document that evolves, grows, and changes with your patient/family – one that can be easily reviewed/updated at each visit.
Returning to our case vignette
Laura returns to your office for a follow-up after a 10-day stay at a hospital-diversion program or inpatient psychiatric unit. The decision is made to use the primary care NIMH ASQ/BSSA algorithm, and you determine the patient to not be at imminent risk following the screen and assessment. Laura is triaged as appropriate for outpatient care, you collaborate to update the safety plan, regular follow-ups are scheduled, and a mental health referral has been placed. Thus, there are tools to assist with screening, assessing, and triaging pediatric patients with suicidal ideation that provide the patient with appropriate care and treatment and may help alleviate the need to have a patient present to the emergency department.
Dr. Abdul-Karim is a child psychiatrist at the University of Vermont University Children’s Hospital in Burlington.
Additional resources
The American Academy of Child and Adolescent Psychiatry has developed information that can be provided to families about suicide safety precautions that can be taken at home, which can be found here: Facts for Families. Suicide Safety: Precautions at Home.
Screening tools listed above can be found here:
ASQ Toolkit.
C-SSRS.
PHQ-9 Modified for Adolescents (PHQ-A).
References
1. Curtin SC. National Center for Health Statistics. “State Suicide Rates Among Adolescents and Young Adults Aged 10-24: United States, 2000-2018” National Vital Statistics Reports..
2. Centers for Disease Control and Prevention, National Center for Health Statistics. “Underlying Cause of Death 2018-2019” CDC WONDER Online Database. Accessed 2021 Jul 31, 6:57:39 p.m.
3. Centers for Disease Control and Prevention. 1991-2019 High School Youth Risk Behavior Survey Data.
Case vignette: Laura is a 14-year-old biological girl who presents to your office for a routine well-child visit. She is doing well medically but notes that over the past 3 months she has been having increasing thoughts of suicide and has self-harmed via cutting on her wrists with a blade removed from a shaving razor. You contemplate what the most salient questions are in order to determine the best disposition for your patient.
The case vignette above may sound like one that you have heard before, and if not, you undoubtedly will encounter such a situation moving forward. The rate of suicidal ideation amongst youth ages 10-24 has increased by 57.4% between 2007 and 2018.1 Furthermore, suicide is the second leading cause of death in those aged 10 through young adulthood.2 According to the Centers for Disease Control and Prevention’s 2019 High School Youth Risk Behavior Survey, 18.8% of high school students seriously considered attempting suicide, 15.7% made a plan about how they would attempt suicide, and 8.9% actually attempted suicide, with 2.5% having a suicide attempt that resulted in an injury, poisoning, or overdose that had to be treated by a doctor or nurse during the 12 months before the survey.3 Children often present first to their primary care provider, and they may be the first individual who the child shares their suicidal or self-harm thoughts with. It may be useful to have a standardized approach, while using your own clinical judgment, to determine best next steps. Given the significant recent surge in children presenting to the emergency department for psychiatric needs and that environment having its own limitations (for example, long wait times, nontherapeutic space, etc.), a simple screen and brief assessment may lead to being able to maintain a patient safely outside of the hospital.
Screen all appropriate patients for suicide
There are, at minimum, three validated screening tools that can be used as to determine what the best next step should be. They include the Ask Suicide-Screening Questions (ASQ) developed by the National Institute of Mental Health, the Columbia-Suicide Severity Rating Scale (C-SSRS), and the PHQ-9 (modified for adolescents). We can highlight one of the screening tools here as noted below, but the choice of screener may be based on facility and/or clinician preference.
The Ask Suicide-Screening Questions
The ASQ, developed by the National Institute of Mental Health, include the following four binary questions plus a fifth acuity question, as follows:
1. In the past few weeks, have you wished you were dead?
2. In the past few weeks, have you felt that you or your family would be better off if you were dead?
3. In the past week, have you been having thoughts about killing yourself?
4. Have you ever tried to kill yourself?
a. If yes, how?
b. When?
The following acuity question is to be asked if any of the above are answered “yes”:
5. Are you having thoughts of killing yourself right now?
a. If yes, please describe.
Assess the level of risk
Once you have screened a patient, you need to assess the level of risk to help determine the level of care required. Returning to our original case vignette, does the patient warrant outpatient management, crisis evaluation, or an emergency psychiatric evaluation? You may have already decided that the patient needs an emergency mental health evaluation from a local crisis clinician evaluation and/or the emergency department. However, you may also find that the screen did not elicit imminent concern, but it does warrant a brief assessment to further elucidate the level of risk and proper disposition. One such instrument that may be helpful is the Brief Suicide Safety Assessment (BSSA) – also developed by the NIMH as a tool linked to the ASQ. There are clear and specific instructions in the BSSA with suggestions on how to ask questions. Important components to the BSSA include:
- A focus on a more thorough clinical history – including frequency of suicidal ideation, suicide plan, past behavior, associated symptoms, and social support/stressors
- Collateral information (e.g., further details from those who know the patient such as family/friends).
- Safety planning.
- Determining disposition.
The BSSA may suggest that a crisis/psychiatric evaluation is warranted or suggest that a safety plan with a mental health referral will likely be sufficient.
Triage and safety planning
A safety plan should be created if you determine that a patient can be safely maintained as an outpatient based on your screening, assessment, and triaging. Traditional safety plans come in many different forms and can be found online (Example of a Safety Plan Template). However, most safety plans include some version of the following:
- Increased supervision: 24/7 supervision with doors open/unlocked.
- Reduced access: medications (prescription and OTC) locked away; sharps and firearms secured.
- Adaptive coping strategies (e.g., relaxation techniques such as drawing or listening to music).
- Reliable persons for support (e.g., parent, therapist, school counselor).
- Outpatient mental health provider follow-up and/or referral.
- Provision of local crisis and national hotline contact information.
- Use of a safety plan phone app completed with patient.
Envision a safety plan as a living document that evolves, grows, and changes with your patient/family – one that can be easily reviewed/updated at each visit.
Returning to our case vignette
Laura returns to your office for a follow-up after a 10-day stay at a hospital-diversion program or inpatient psychiatric unit. The decision is made to use the primary care NIMH ASQ/BSSA algorithm, and you determine the patient to not be at imminent risk following the screen and assessment. Laura is triaged as appropriate for outpatient care, you collaborate to update the safety plan, regular follow-ups are scheduled, and a mental health referral has been placed. Thus, there are tools to assist with screening, assessing, and triaging pediatric patients with suicidal ideation that provide the patient with appropriate care and treatment and may help alleviate the need to have a patient present to the emergency department.
Dr. Abdul-Karim is a child psychiatrist at the University of Vermont University Children’s Hospital in Burlington.
Additional resources
The American Academy of Child and Adolescent Psychiatry has developed information that can be provided to families about suicide safety precautions that can be taken at home, which can be found here: Facts for Families. Suicide Safety: Precautions at Home.
Screening tools listed above can be found here:
ASQ Toolkit.
C-SSRS.
PHQ-9 Modified for Adolescents (PHQ-A).
References
1. Curtin SC. National Center for Health Statistics. “State Suicide Rates Among Adolescents and Young Adults Aged 10-24: United States, 2000-2018” National Vital Statistics Reports..
2. Centers for Disease Control and Prevention, National Center for Health Statistics. “Underlying Cause of Death 2018-2019” CDC WONDER Online Database. Accessed 2021 Jul 31, 6:57:39 p.m.
3. Centers for Disease Control and Prevention. 1991-2019 High School Youth Risk Behavior Survey Data.
One center’s experience delivering monochorionic twins
Between 2005 and 2021, mode of delivery of diamniotic twins at this practice did not significantly differ by chorionicity, researchers affiliated with Maternal Fetal Medicine Associates and the department of obstetrics, gynecology, and reproductive science at Icahn School of Medicine at Mount Sinai, New York reported in Obstetrics & Gynecology.
The study supports a recommendation from the American College of Obstetricians and Gynecologists that vaginal delivery “is a reasonable option in well selected diamniotic twin pregnancies, irrespective of chorionicity, and should be considered, provided that an experienced obstetrician is available,” said Iris Krishna, MD, assistant professor of maternal-fetal medicine at Emory University, Atlanta.
The experience at this practice, however, may not apply to many practices in the United States, said Dr. Krishna, who was not involved in the study.
Of 1,121 diamniotic twin pregnancies included in the analysis, 202 (18%) were monochorionic. The cesarean delivery rate was not significantly different between groups: 61% for monochorionic and 63% for dichorionic pregnancies.
Among women with planned vaginal delivery (101 monochorionic pregnancies and 422 dichorionic pregnancies), the cesarean delivery rate likewise did not significantly differ by chorionicity. Twenty-two percent of the monochorionic pregnancies and 21% of the dichorionic pregnancies in this subgroup had a cesarean delivery.
Among patients with a vaginal delivery of twin A, chorionicity was not associated with mode of delivery for twin B. Combined vaginal-cesarean deliveries occurred less than 1% of the time, and breech extraction of twin B occurred approximately 75% of the time, regardless of chorionicity.
The researchers also compared neonatal outcomes for monochorionic-diamniotic twin pregnancies at or after 34 weeks of gestation, based on the intended mode of delivery (95 women with planned vaginal delivery and 68 with planned cesarean delivery). Neonatal outcomes generally were similar, although the incidence of mechanical ventilation was less common in cases with planned vaginal delivery (7% vs. 21%).
“Our data affirm that an attempt at a vaginal birth for twin pregnancies, without contraindications to vaginal delivery and regardless of chorionicity, is reasonable and achievable,” wrote study author Henry N. Lesser, MD, with the department of obstetrics and gynecology at Sinai Hospital in Baltimore, and colleagues.
The patients with planned cesarean delivery had a contraindication to vaginal delivery or otherwise chose to have a cesarean delivery. The researchers excluded from their analysis pregnancies with intrauterine fetal demise of either twin before labor or planned cesarean delivery.
The study’s reliance on data from a single practice decreases its external validity, the researchers noted. Induction of labor at this center typically occurs at 37 weeks’ gestation for monochorionic twins and at 38 weeks for dichorionic twins, and “senior personnel experienced in intrauterine twin manipulation are always present at delivery,” the study authors said.
The study describes “the experience of a single site with skilled obstetricians following a standardized approach to management of diamniotic twin deliveries,” Dr. Krishna said. “Findings may not be generalizable to many U.S. practices as obstetrics and gynecology residents often lack training in breech extraction or internal podalic version of the second twin. This underscores the importance of a concerted effort by skilled senior physicians to train junior physicians in vaginal delivery of the second twin to improve overall outcomes amongst women with diamniotic twin gestations.”
Michael F. Greene, MD, professor emeritus of obstetrics, gynecology, and reproductive biology at Massachusetts General Hospital, Boston, agreed that the findings are not generalizable to the national population. Approximately 10% of the patients in the study had prepregnancy obesity, whereas doctors practicing in other areas likely encounter higher rates, Dr. Greene said in an interview.
He also wondered about other data points that could be of interest but were not reported, such as the racial or ethnic distribution of the patients, rates of birth defects, the use of instruments to aid delivery, and neonatal outcomes for the dichorionic twins.
Monochorionic pregnancies entail a risk of twin-twin transfusion syndrome and other complications, including an increased likelihood of birth defects.
Dr. Greene is an associate editor with the New England Journal of Medicine, which in 2013 published results from the Twin Birth Study, an international trial where women with dichorionic or monochorionic twins were randomly assigned to planned vaginal delivery or planned cesarean delivery. Outcomes did not significantly differ between groups. In the trial, the rate of cesarean delivery in the group with planned vaginal delivery was 43.8%, and Dr. Greene discussed the implications of the study in an accompanying editorial.
Since then, the obstetrics and gynecology community “has been focusing in recent years on trying to avoid the first cesarean section” when it is safe to do so, Dr. Greene said. “That has become almost a bumper sticker in modern obstetrics.”
And patients should know that it is an option, Dr. Krishna added.
“Women with monochorionic-diamniotic twins should be counseled that with an experienced obstetrician that an attempt at vaginal delivery is not associated with adverse neonatal outcomes when compared with planned cesarean delivery,” Dr. Krishna said.
A study coauthor disclosed serving on the speakers bureau for Natera and Hologic. Dr. Krishna is a member of the editorial advisory board for Ob.Gyn. News.
Between 2005 and 2021, mode of delivery of diamniotic twins at this practice did not significantly differ by chorionicity, researchers affiliated with Maternal Fetal Medicine Associates and the department of obstetrics, gynecology, and reproductive science at Icahn School of Medicine at Mount Sinai, New York reported in Obstetrics & Gynecology.
The study supports a recommendation from the American College of Obstetricians and Gynecologists that vaginal delivery “is a reasonable option in well selected diamniotic twin pregnancies, irrespective of chorionicity, and should be considered, provided that an experienced obstetrician is available,” said Iris Krishna, MD, assistant professor of maternal-fetal medicine at Emory University, Atlanta.
The experience at this practice, however, may not apply to many practices in the United States, said Dr. Krishna, who was not involved in the study.
Of 1,121 diamniotic twin pregnancies included in the analysis, 202 (18%) were monochorionic. The cesarean delivery rate was not significantly different between groups: 61% for monochorionic and 63% for dichorionic pregnancies.
Among women with planned vaginal delivery (101 monochorionic pregnancies and 422 dichorionic pregnancies), the cesarean delivery rate likewise did not significantly differ by chorionicity. Twenty-two percent of the monochorionic pregnancies and 21% of the dichorionic pregnancies in this subgroup had a cesarean delivery.
Among patients with a vaginal delivery of twin A, chorionicity was not associated with mode of delivery for twin B. Combined vaginal-cesarean deliveries occurred less than 1% of the time, and breech extraction of twin B occurred approximately 75% of the time, regardless of chorionicity.
The researchers also compared neonatal outcomes for monochorionic-diamniotic twin pregnancies at or after 34 weeks of gestation, based on the intended mode of delivery (95 women with planned vaginal delivery and 68 with planned cesarean delivery). Neonatal outcomes generally were similar, although the incidence of mechanical ventilation was less common in cases with planned vaginal delivery (7% vs. 21%).
“Our data affirm that an attempt at a vaginal birth for twin pregnancies, without contraindications to vaginal delivery and regardless of chorionicity, is reasonable and achievable,” wrote study author Henry N. Lesser, MD, with the department of obstetrics and gynecology at Sinai Hospital in Baltimore, and colleagues.
The patients with planned cesarean delivery had a contraindication to vaginal delivery or otherwise chose to have a cesarean delivery. The researchers excluded from their analysis pregnancies with intrauterine fetal demise of either twin before labor or planned cesarean delivery.
The study’s reliance on data from a single practice decreases its external validity, the researchers noted. Induction of labor at this center typically occurs at 37 weeks’ gestation for monochorionic twins and at 38 weeks for dichorionic twins, and “senior personnel experienced in intrauterine twin manipulation are always present at delivery,” the study authors said.
The study describes “the experience of a single site with skilled obstetricians following a standardized approach to management of diamniotic twin deliveries,” Dr. Krishna said. “Findings may not be generalizable to many U.S. practices as obstetrics and gynecology residents often lack training in breech extraction or internal podalic version of the second twin. This underscores the importance of a concerted effort by skilled senior physicians to train junior physicians in vaginal delivery of the second twin to improve overall outcomes amongst women with diamniotic twin gestations.”
Michael F. Greene, MD, professor emeritus of obstetrics, gynecology, and reproductive biology at Massachusetts General Hospital, Boston, agreed that the findings are not generalizable to the national population. Approximately 10% of the patients in the study had prepregnancy obesity, whereas doctors practicing in other areas likely encounter higher rates, Dr. Greene said in an interview.
He also wondered about other data points that could be of interest but were not reported, such as the racial or ethnic distribution of the patients, rates of birth defects, the use of instruments to aid delivery, and neonatal outcomes for the dichorionic twins.
Monochorionic pregnancies entail a risk of twin-twin transfusion syndrome and other complications, including an increased likelihood of birth defects.
Dr. Greene is an associate editor with the New England Journal of Medicine, which in 2013 published results from the Twin Birth Study, an international trial where women with dichorionic or monochorionic twins were randomly assigned to planned vaginal delivery or planned cesarean delivery. Outcomes did not significantly differ between groups. In the trial, the rate of cesarean delivery in the group with planned vaginal delivery was 43.8%, and Dr. Greene discussed the implications of the study in an accompanying editorial.
Since then, the obstetrics and gynecology community “has been focusing in recent years on trying to avoid the first cesarean section” when it is safe to do so, Dr. Greene said. “That has become almost a bumper sticker in modern obstetrics.”
And patients should know that it is an option, Dr. Krishna added.
“Women with monochorionic-diamniotic twins should be counseled that with an experienced obstetrician that an attempt at vaginal delivery is not associated with adverse neonatal outcomes when compared with planned cesarean delivery,” Dr. Krishna said.
A study coauthor disclosed serving on the speakers bureau for Natera and Hologic. Dr. Krishna is a member of the editorial advisory board for Ob.Gyn. News.
Between 2005 and 2021, mode of delivery of diamniotic twins at this practice did not significantly differ by chorionicity, researchers affiliated with Maternal Fetal Medicine Associates and the department of obstetrics, gynecology, and reproductive science at Icahn School of Medicine at Mount Sinai, New York reported in Obstetrics & Gynecology.
The study supports a recommendation from the American College of Obstetricians and Gynecologists that vaginal delivery “is a reasonable option in well selected diamniotic twin pregnancies, irrespective of chorionicity, and should be considered, provided that an experienced obstetrician is available,” said Iris Krishna, MD, assistant professor of maternal-fetal medicine at Emory University, Atlanta.
The experience at this practice, however, may not apply to many practices in the United States, said Dr. Krishna, who was not involved in the study.
Of 1,121 diamniotic twin pregnancies included in the analysis, 202 (18%) were monochorionic. The cesarean delivery rate was not significantly different between groups: 61% for monochorionic and 63% for dichorionic pregnancies.
Among women with planned vaginal delivery (101 monochorionic pregnancies and 422 dichorionic pregnancies), the cesarean delivery rate likewise did not significantly differ by chorionicity. Twenty-two percent of the monochorionic pregnancies and 21% of the dichorionic pregnancies in this subgroup had a cesarean delivery.
Among patients with a vaginal delivery of twin A, chorionicity was not associated with mode of delivery for twin B. Combined vaginal-cesarean deliveries occurred less than 1% of the time, and breech extraction of twin B occurred approximately 75% of the time, regardless of chorionicity.
The researchers also compared neonatal outcomes for monochorionic-diamniotic twin pregnancies at or after 34 weeks of gestation, based on the intended mode of delivery (95 women with planned vaginal delivery and 68 with planned cesarean delivery). Neonatal outcomes generally were similar, although the incidence of mechanical ventilation was less common in cases with planned vaginal delivery (7% vs. 21%).
“Our data affirm that an attempt at a vaginal birth for twin pregnancies, without contraindications to vaginal delivery and regardless of chorionicity, is reasonable and achievable,” wrote study author Henry N. Lesser, MD, with the department of obstetrics and gynecology at Sinai Hospital in Baltimore, and colleagues.
The patients with planned cesarean delivery had a contraindication to vaginal delivery or otherwise chose to have a cesarean delivery. The researchers excluded from their analysis pregnancies with intrauterine fetal demise of either twin before labor or planned cesarean delivery.
The study’s reliance on data from a single practice decreases its external validity, the researchers noted. Induction of labor at this center typically occurs at 37 weeks’ gestation for monochorionic twins and at 38 weeks for dichorionic twins, and “senior personnel experienced in intrauterine twin manipulation are always present at delivery,” the study authors said.
The study describes “the experience of a single site with skilled obstetricians following a standardized approach to management of diamniotic twin deliveries,” Dr. Krishna said. “Findings may not be generalizable to many U.S. practices as obstetrics and gynecology residents often lack training in breech extraction or internal podalic version of the second twin. This underscores the importance of a concerted effort by skilled senior physicians to train junior physicians in vaginal delivery of the second twin to improve overall outcomes amongst women with diamniotic twin gestations.”
Michael F. Greene, MD, professor emeritus of obstetrics, gynecology, and reproductive biology at Massachusetts General Hospital, Boston, agreed that the findings are not generalizable to the national population. Approximately 10% of the patients in the study had prepregnancy obesity, whereas doctors practicing in other areas likely encounter higher rates, Dr. Greene said in an interview.
He also wondered about other data points that could be of interest but were not reported, such as the racial or ethnic distribution of the patients, rates of birth defects, the use of instruments to aid delivery, and neonatal outcomes for the dichorionic twins.
Monochorionic pregnancies entail a risk of twin-twin transfusion syndrome and other complications, including an increased likelihood of birth defects.
Dr. Greene is an associate editor with the New England Journal of Medicine, which in 2013 published results from the Twin Birth Study, an international trial where women with dichorionic or monochorionic twins were randomly assigned to planned vaginal delivery or planned cesarean delivery. Outcomes did not significantly differ between groups. In the trial, the rate of cesarean delivery in the group with planned vaginal delivery was 43.8%, and Dr. Greene discussed the implications of the study in an accompanying editorial.
Since then, the obstetrics and gynecology community “has been focusing in recent years on trying to avoid the first cesarean section” when it is safe to do so, Dr. Greene said. “That has become almost a bumper sticker in modern obstetrics.”
And patients should know that it is an option, Dr. Krishna added.
“Women with monochorionic-diamniotic twins should be counseled that with an experienced obstetrician that an attempt at vaginal delivery is not associated with adverse neonatal outcomes when compared with planned cesarean delivery,” Dr. Krishna said.
A study coauthor disclosed serving on the speakers bureau for Natera and Hologic. Dr. Krishna is a member of the editorial advisory board for Ob.Gyn. News.
FROM OBSTETRICS & GYNECOLOGY
Can a blood-based test predict TNFi nonresponse in RA?
A blood test that uses a patient’s unique genetic signature has shown some ability to predict nonresponse to tumor necrosis factor inhibitors as treatment for rheumatoid arthritis, an observational clinical study has found, but the test’s predictive accuracy was well below 100%.
The test is the blood-based molecular signature response classifier (MSRC) that uses RNA sequencing data based on 23 different biomarkers: 19 RNA transcripts and 4 clinical features. The clinical features are body mass index, gender, patient global assessment, and anticyclic citrullinated protein (anti-CCP) status.
The NETWORK-004 study, published in Rheumatology and Therapy, was able to stratify patients who were likely to respond inadequately to TNFi therapy and could provide patient-specific information to guide therapy choice in RA patients regardless of whether they’ve already been on TNFi therapy. The study evaluated the MSRC test in 504 patients, 391 of whom were treatment naive.
Avoiding ‘fail first’ approach
The idea behind the test is to circumvent the “fail first” approach in finding the right therapy for RA in an individual patient. While the test costs $4,995, Alif Saleh, chief executive officer of Scipher Medicine, which markets the test under the name PrismRA, said in a press release that it has the potential to reduce costs by $19,000 or more per patient per year by avoiding treatments that don’t work. A previous study, which Scipher funded, reported that the test resulted in savings of $7,379 in per-patient costs of ineffective therapy. The same study reported a 25% decrease in costs for ineffective treatments for Medicare-eligible patients.
The price of RA drugs, particularly anti-TNF agents, is hefty and rising. GoodRx has reported that the price of RA drugs increased 92% from 2014 to 2019, and the prices for anti-TNF agents such as etanercept and adalimumab more than doubled in that period. Adalimumab can cost upwards of $84,000 per year while etanercept has a list price of around $72,000 a year. The pharmacy benefit manager WellDyne started covering the test MSRC in February.
Nehad Soloman, MD, a rheumatologist and internist at Midwestern University Arizona College of Osteopathic Medicine in Glendale and a compensated NETWORK-004 investigator, said the MSRC test would be indicated for confirmed RA patients for whom rheumatologists are considering biologic agents, particularly TNFi drugs. “You wouldn’t do it on an RA patient who’s been on several different medications because it doesn’t serve a purpose at that point,” he said.
The potential cost savings may not be the only reason to use the test, Dr. Soloman said. “You don’t want to be dabbling with the wrong drug if there’s another path you can try and save society some money as well as the time and energy it takes to monitor the patients – as well as the patient’s pain,” he said.
How the MSRC test works
The MSRC test detects a signal that’s associated with a high or very high likelihood of inadequate response to TNFi therapies and indicates that the patient is unlikely to achieve low disease activity or remission with TNFi therapies. Response is defined as achieving ACR50 – meaning 50% improvement in American College of Rheumatology response criteria – at 6 months.
Test results are reported on a continuous 1-25 scale, explained Slava Akmaev, PhD, chief technology officer and head of therapeutics at Scipher. “The higher the score, the more likely the patient will have an inadequate response to TNFi therapies and be unable to reach low disease activity; the lower the score, the less likely the patient will have an inadequate response to TNFi therapies,” he said. However, Dr. Akmaev noted that a low score does not ensure a positive response to TNFi therapies.
The MSRC test differs from the multibiomarker disease activity blood test (MBDA; marketed as Vectra by Myriad Genetics) in the number of biomarkers it measures: 19 RNA transcripts vs. 12 serum protein biomarkers in MBDA. The MBDA test is also intended to provide a quantitative, objective measurement of RA disease activity rather than to predict nonresponse to TNFi or other biologics. A number of studies have validated the MBDA test for predicting disease control in RA patients, but not necessarily response to TNFi therapy.
The “high” category threshold of the MSRC test corresponds to an approximate 90% chance of inadequate response to TNFi therapy, or a 10% chance of responding. The “very high” category threshold corresponds to an approximate 95% chance of inadequate response to TNFi therapy, Dr. Akmaev said.
NETWORK-004 used area under the curve (AUC) to measure the accuracy of the MSRC test. An AUC of 1 represents 100% accuracy. Overall, the MSRC had an AUC of 0.64, or 64% accuracy of predicting patients unlikely to respond to TNFi therapy and to achieve ACR50 at 6 months, with an odds ratio of 4.1 (95% confidence interval, 2.0-8.3; P = .0001).
The predictive accuracy went up to 74% with ORs of 3.4-8.8 for additional endpoints at 3 and 6 months (P < .01). Among patients who had already been on TNFi therapy, the predictive accuracy was 83% and associated with ORs of 3.3-26.6 based on ACR, 28-joint Disease Activity Score using C-reactive protein (DAS28-CRP), and Clinical Disease Activity Index (CDAI) metrics.
The investigators also performed an in-cohort cross-validation of the MSRC using baseline blood samples of 245 treatment-naive patients from the CERTAIN study, which yielded a 66% predictive accuracy for the ACR50 outcome at 6 months. Using the 19 RNA transcripts from the test, but not the clinical factors, the predictive accuracy was 62.5%. Using ACR70, CDAI, and DAS28 as measures for 6-month response, the cross-validation analysis of all 23 MSRC features yielded predictive accuracy of 64%-67%.
The study found significant differences in model scores between patients who did and did not have the molecular signal of nonresponse, and the proportion of patients who achieved low disease activity or remission at 6 months based on CDAI and DAS28-CRP measures was greater among those who lacked a molecular signature of nonresponse.
“Those who lack this signature can proceed with TNFi therapy and possibly achieve an increased response rate relative to the unstratified population,” wrote lead study author Stanley B. Cohen, MD, and colleagues.
Daniel E. Furst, MD, emeritus professor at the University of California, Los Angeles, described the design of the NETWORK-004 study as “excellent,” but said that it didn’t overcome potential issues with the MSRC test itself. “The results unfortunately are great for group data but not for individuals, with a predictive area under the curve of 60% to 80%, it really is not that useful,” he said. “Let’s say you’re a patient who’s not doing well, and I do a test and it’s positive; that still means that 20% of the time you will respond.”
He also noted that he coauthored a paper that used decreases in DAS28 to predict nonresponse to certolizumab pegol plus methotrexate with 95% probability in the first 12 weeks of treatment. “That’s closer to what we need,” Dr. Furst said.
However, the MSRC test is a promising sign of where testing for predicting RA therapy is headed, he said. “We are steadily working toward genetic signatures that really are predictive on an individual basis,” Dr. Furst said. “It’s coming; it’s just not here yet.”
Dr. Furst had no relevant financial relationships to disclose. Dr. Soloman is a paid investigator and consultant to Scipher Medicine.
A blood test that uses a patient’s unique genetic signature has shown some ability to predict nonresponse to tumor necrosis factor inhibitors as treatment for rheumatoid arthritis, an observational clinical study has found, but the test’s predictive accuracy was well below 100%.
The test is the blood-based molecular signature response classifier (MSRC) that uses RNA sequencing data based on 23 different biomarkers: 19 RNA transcripts and 4 clinical features. The clinical features are body mass index, gender, patient global assessment, and anticyclic citrullinated protein (anti-CCP) status.
The NETWORK-004 study, published in Rheumatology and Therapy, was able to stratify patients who were likely to respond inadequately to TNFi therapy and could provide patient-specific information to guide therapy choice in RA patients regardless of whether they’ve already been on TNFi therapy. The study evaluated the MSRC test in 504 patients, 391 of whom were treatment naive.
Avoiding ‘fail first’ approach
The idea behind the test is to circumvent the “fail first” approach in finding the right therapy for RA in an individual patient. While the test costs $4,995, Alif Saleh, chief executive officer of Scipher Medicine, which markets the test under the name PrismRA, said in a press release that it has the potential to reduce costs by $19,000 or more per patient per year by avoiding treatments that don’t work. A previous study, which Scipher funded, reported that the test resulted in savings of $7,379 in per-patient costs of ineffective therapy. The same study reported a 25% decrease in costs for ineffective treatments for Medicare-eligible patients.
The price of RA drugs, particularly anti-TNF agents, is hefty and rising. GoodRx has reported that the price of RA drugs increased 92% from 2014 to 2019, and the prices for anti-TNF agents such as etanercept and adalimumab more than doubled in that period. Adalimumab can cost upwards of $84,000 per year while etanercept has a list price of around $72,000 a year. The pharmacy benefit manager WellDyne started covering the test MSRC in February.
Nehad Soloman, MD, a rheumatologist and internist at Midwestern University Arizona College of Osteopathic Medicine in Glendale and a compensated NETWORK-004 investigator, said the MSRC test would be indicated for confirmed RA patients for whom rheumatologists are considering biologic agents, particularly TNFi drugs. “You wouldn’t do it on an RA patient who’s been on several different medications because it doesn’t serve a purpose at that point,” he said.
The potential cost savings may not be the only reason to use the test, Dr. Soloman said. “You don’t want to be dabbling with the wrong drug if there’s another path you can try and save society some money as well as the time and energy it takes to monitor the patients – as well as the patient’s pain,” he said.
How the MSRC test works
The MSRC test detects a signal that’s associated with a high or very high likelihood of inadequate response to TNFi therapies and indicates that the patient is unlikely to achieve low disease activity or remission with TNFi therapies. Response is defined as achieving ACR50 – meaning 50% improvement in American College of Rheumatology response criteria – at 6 months.
Test results are reported on a continuous 1-25 scale, explained Slava Akmaev, PhD, chief technology officer and head of therapeutics at Scipher. “The higher the score, the more likely the patient will have an inadequate response to TNFi therapies and be unable to reach low disease activity; the lower the score, the less likely the patient will have an inadequate response to TNFi therapies,” he said. However, Dr. Akmaev noted that a low score does not ensure a positive response to TNFi therapies.
The MSRC test differs from the multibiomarker disease activity blood test (MBDA; marketed as Vectra by Myriad Genetics) in the number of biomarkers it measures: 19 RNA transcripts vs. 12 serum protein biomarkers in MBDA. The MBDA test is also intended to provide a quantitative, objective measurement of RA disease activity rather than to predict nonresponse to TNFi or other biologics. A number of studies have validated the MBDA test for predicting disease control in RA patients, but not necessarily response to TNFi therapy.
The “high” category threshold of the MSRC test corresponds to an approximate 90% chance of inadequate response to TNFi therapy, or a 10% chance of responding. The “very high” category threshold corresponds to an approximate 95% chance of inadequate response to TNFi therapy, Dr. Akmaev said.
NETWORK-004 used area under the curve (AUC) to measure the accuracy of the MSRC test. An AUC of 1 represents 100% accuracy. Overall, the MSRC had an AUC of 0.64, or 64% accuracy of predicting patients unlikely to respond to TNFi therapy and to achieve ACR50 at 6 months, with an odds ratio of 4.1 (95% confidence interval, 2.0-8.3; P = .0001).
The predictive accuracy went up to 74% with ORs of 3.4-8.8 for additional endpoints at 3 and 6 months (P < .01). Among patients who had already been on TNFi therapy, the predictive accuracy was 83% and associated with ORs of 3.3-26.6 based on ACR, 28-joint Disease Activity Score using C-reactive protein (DAS28-CRP), and Clinical Disease Activity Index (CDAI) metrics.
The investigators also performed an in-cohort cross-validation of the MSRC using baseline blood samples of 245 treatment-naive patients from the CERTAIN study, which yielded a 66% predictive accuracy for the ACR50 outcome at 6 months. Using the 19 RNA transcripts from the test, but not the clinical factors, the predictive accuracy was 62.5%. Using ACR70, CDAI, and DAS28 as measures for 6-month response, the cross-validation analysis of all 23 MSRC features yielded predictive accuracy of 64%-67%.
The study found significant differences in model scores between patients who did and did not have the molecular signal of nonresponse, and the proportion of patients who achieved low disease activity or remission at 6 months based on CDAI and DAS28-CRP measures was greater among those who lacked a molecular signature of nonresponse.
“Those who lack this signature can proceed with TNFi therapy and possibly achieve an increased response rate relative to the unstratified population,” wrote lead study author Stanley B. Cohen, MD, and colleagues.
Daniel E. Furst, MD, emeritus professor at the University of California, Los Angeles, described the design of the NETWORK-004 study as “excellent,” but said that it didn’t overcome potential issues with the MSRC test itself. “The results unfortunately are great for group data but not for individuals, with a predictive area under the curve of 60% to 80%, it really is not that useful,” he said. “Let’s say you’re a patient who’s not doing well, and I do a test and it’s positive; that still means that 20% of the time you will respond.”
He also noted that he coauthored a paper that used decreases in DAS28 to predict nonresponse to certolizumab pegol plus methotrexate with 95% probability in the first 12 weeks of treatment. “That’s closer to what we need,” Dr. Furst said.
However, the MSRC test is a promising sign of where testing for predicting RA therapy is headed, he said. “We are steadily working toward genetic signatures that really are predictive on an individual basis,” Dr. Furst said. “It’s coming; it’s just not here yet.”
Dr. Furst had no relevant financial relationships to disclose. Dr. Soloman is a paid investigator and consultant to Scipher Medicine.
A blood test that uses a patient’s unique genetic signature has shown some ability to predict nonresponse to tumor necrosis factor inhibitors as treatment for rheumatoid arthritis, an observational clinical study has found, but the test’s predictive accuracy was well below 100%.
The test is the blood-based molecular signature response classifier (MSRC) that uses RNA sequencing data based on 23 different biomarkers: 19 RNA transcripts and 4 clinical features. The clinical features are body mass index, gender, patient global assessment, and anticyclic citrullinated protein (anti-CCP) status.
The NETWORK-004 study, published in Rheumatology and Therapy, was able to stratify patients who were likely to respond inadequately to TNFi therapy and could provide patient-specific information to guide therapy choice in RA patients regardless of whether they’ve already been on TNFi therapy. The study evaluated the MSRC test in 504 patients, 391 of whom were treatment naive.
Avoiding ‘fail first’ approach
The idea behind the test is to circumvent the “fail first” approach in finding the right therapy for RA in an individual patient. While the test costs $4,995, Alif Saleh, chief executive officer of Scipher Medicine, which markets the test under the name PrismRA, said in a press release that it has the potential to reduce costs by $19,000 or more per patient per year by avoiding treatments that don’t work. A previous study, which Scipher funded, reported that the test resulted in savings of $7,379 in per-patient costs of ineffective therapy. The same study reported a 25% decrease in costs for ineffective treatments for Medicare-eligible patients.
The price of RA drugs, particularly anti-TNF agents, is hefty and rising. GoodRx has reported that the price of RA drugs increased 92% from 2014 to 2019, and the prices for anti-TNF agents such as etanercept and adalimumab more than doubled in that period. Adalimumab can cost upwards of $84,000 per year while etanercept has a list price of around $72,000 a year. The pharmacy benefit manager WellDyne started covering the test MSRC in February.
Nehad Soloman, MD, a rheumatologist and internist at Midwestern University Arizona College of Osteopathic Medicine in Glendale and a compensated NETWORK-004 investigator, said the MSRC test would be indicated for confirmed RA patients for whom rheumatologists are considering biologic agents, particularly TNFi drugs. “You wouldn’t do it on an RA patient who’s been on several different medications because it doesn’t serve a purpose at that point,” he said.
The potential cost savings may not be the only reason to use the test, Dr. Soloman said. “You don’t want to be dabbling with the wrong drug if there’s another path you can try and save society some money as well as the time and energy it takes to monitor the patients – as well as the patient’s pain,” he said.
How the MSRC test works
The MSRC test detects a signal that’s associated with a high or very high likelihood of inadequate response to TNFi therapies and indicates that the patient is unlikely to achieve low disease activity or remission with TNFi therapies. Response is defined as achieving ACR50 – meaning 50% improvement in American College of Rheumatology response criteria – at 6 months.
Test results are reported on a continuous 1-25 scale, explained Slava Akmaev, PhD, chief technology officer and head of therapeutics at Scipher. “The higher the score, the more likely the patient will have an inadequate response to TNFi therapies and be unable to reach low disease activity; the lower the score, the less likely the patient will have an inadequate response to TNFi therapies,” he said. However, Dr. Akmaev noted that a low score does not ensure a positive response to TNFi therapies.
The MSRC test differs from the multibiomarker disease activity blood test (MBDA; marketed as Vectra by Myriad Genetics) in the number of biomarkers it measures: 19 RNA transcripts vs. 12 serum protein biomarkers in MBDA. The MBDA test is also intended to provide a quantitative, objective measurement of RA disease activity rather than to predict nonresponse to TNFi or other biologics. A number of studies have validated the MBDA test for predicting disease control in RA patients, but not necessarily response to TNFi therapy.
The “high” category threshold of the MSRC test corresponds to an approximate 90% chance of inadequate response to TNFi therapy, or a 10% chance of responding. The “very high” category threshold corresponds to an approximate 95% chance of inadequate response to TNFi therapy, Dr. Akmaev said.
NETWORK-004 used area under the curve (AUC) to measure the accuracy of the MSRC test. An AUC of 1 represents 100% accuracy. Overall, the MSRC had an AUC of 0.64, or 64% accuracy of predicting patients unlikely to respond to TNFi therapy and to achieve ACR50 at 6 months, with an odds ratio of 4.1 (95% confidence interval, 2.0-8.3; P = .0001).
The predictive accuracy went up to 74% with ORs of 3.4-8.8 for additional endpoints at 3 and 6 months (P < .01). Among patients who had already been on TNFi therapy, the predictive accuracy was 83% and associated with ORs of 3.3-26.6 based on ACR, 28-joint Disease Activity Score using C-reactive protein (DAS28-CRP), and Clinical Disease Activity Index (CDAI) metrics.
The investigators also performed an in-cohort cross-validation of the MSRC using baseline blood samples of 245 treatment-naive patients from the CERTAIN study, which yielded a 66% predictive accuracy for the ACR50 outcome at 6 months. Using the 19 RNA transcripts from the test, but not the clinical factors, the predictive accuracy was 62.5%. Using ACR70, CDAI, and DAS28 as measures for 6-month response, the cross-validation analysis of all 23 MSRC features yielded predictive accuracy of 64%-67%.
The study found significant differences in model scores between patients who did and did not have the molecular signal of nonresponse, and the proportion of patients who achieved low disease activity or remission at 6 months based on CDAI and DAS28-CRP measures was greater among those who lacked a molecular signature of nonresponse.
“Those who lack this signature can proceed with TNFi therapy and possibly achieve an increased response rate relative to the unstratified population,” wrote lead study author Stanley B. Cohen, MD, and colleagues.
Daniel E. Furst, MD, emeritus professor at the University of California, Los Angeles, described the design of the NETWORK-004 study as “excellent,” but said that it didn’t overcome potential issues with the MSRC test itself. “The results unfortunately are great for group data but not for individuals, with a predictive area under the curve of 60% to 80%, it really is not that useful,” he said. “Let’s say you’re a patient who’s not doing well, and I do a test and it’s positive; that still means that 20% of the time you will respond.”
He also noted that he coauthored a paper that used decreases in DAS28 to predict nonresponse to certolizumab pegol plus methotrexate with 95% probability in the first 12 weeks of treatment. “That’s closer to what we need,” Dr. Furst said.
However, the MSRC test is a promising sign of where testing for predicting RA therapy is headed, he said. “We are steadily working toward genetic signatures that really are predictive on an individual basis,” Dr. Furst said. “It’s coming; it’s just not here yet.”
Dr. Furst had no relevant financial relationships to disclose. Dr. Soloman is a paid investigator and consultant to Scipher Medicine.
FROM RHEUMATOLOGY AND THERAPY
Tachycardia syndrome may be distinct marker for long COVID
Tachycardia is commonly reported in patients with post-acute COVID-19 syndrome (PACS), also known as long COVID, authors report in a new article. The researchers say tachycardia syndrome should be considered a distinct phenotype.
The study by Marcus Ståhlberg, MD, PhD, of Karolinska University Hospital, Stockholm, and colleagues was published online August 11 in The American Journal of Medicine.
Dr. Ståhlberg told this news organization that although much attention has been paid to cases of clotting and perimyocarditis in patients after COVID, relatively little attention has been paid to tachycardia, despite case reports that show that palpitations are a common complaint.
“We have diagnosed a large number of patients with postural orthostatic tachycardia syndrome [POTS] and other forms of COVID-related tachycardia at our post-COVID outpatient clinic at Karolinska University Hospital and wanted to highlight this phenomenon,” he said.
Between 25% and 50% of patients at the clinic report tachycardia and/or palpitations that last 12 weeks or longer, the authors report.
“Systematic investigations suggest that 9% of Post-acute COVID-19 syndrome patients report palpitations at six months,” the authors write.
The findings also shed light on potential tests and treatments, he said.
“Physicians should be liberal in performing a basic cardiological workup, including an ECG [electrocardiogram], echocardiography, and Holter ECG monitoring in patients complaining of palpitations and/or chest pain,” Dr. Ståhlberg said.
“If orthostatic intolerance is also reported – such as vertigo, nausea, dyspnea – suspicion of POTS should be raised and a head-up tilt test or at least an active standing test should be performed,” he said.
If POTS is confirmed, he said, patients should be offered a heart rate–lowering drug, such as low-dose propranolol or ivabradine. Compression garments, increased fluid intake, and a structured rehabilitation program also help.
“According to our clinical experience, ivabradine can also reduce symptoms in patients with inappropriate sinus tachycardia and post-COVID,” Dr. Ståhlberg said. “Another finding on Holter-ECG to look out for is frequent premature extrasystoles, which could indicate myocarditis and should warrant a cardiac MRI.”
Dr. Ståhlberg said the researchers think the mechanism underlying the tachycardia is autoimmune and that primary SARS-CoV-2 infections trigger an autoimmune response with formation of autoantibodies that can activate receptors regulating blood pressure and heart rate.
Long-lasting symptoms from COVID are prevalent, the authors note, especially in patients who experienced severe forms of the disease.
In the longest follow-up study to date of patients hospitalized with COVID, more than 60% experienced fatigue or muscle weakness 6 months after hospitalization.
PACS should not be considered a single syndrome; the term denotes an array of subsyndromes and phenotypes, the authors write. Typical symptoms include headache, fatigue, dyspnea, and mental fog but can involve multiple organs and systems.
Tachycardia can also be used as a marker to help gauge the severity of long COVID, the authors write.
“[T]achycardia can be considered a universal and easily obtainable quantitative marker of Post-acute COVID-19 syndrome and its severity rather than patient-reported symptoms, blood testing, and thoracic CT-scans,” they write.
An underrecognized complication
Erin D. Michos, MD, MHS, director of women’s cardiovascular health and associate director of preventive cardiology at Johns Hopkins University, Baltimore, said in an interview that she has seen many similar symptoms in the long-COVID patients referred to her practice.
Dr. Michos, who is also an associate professor of medicine and epidemiology, said she’s been receiving a “huge number” of referrals of long-COVID patients with postural tachycardia, inappropriate sinus tachycardia, and POTS.
“I think this is all in the spectrum of autonomic dysfunction that has been recognized a lot since COVID. POTS has been thought to have [a potentially] viral cause that triggers an autoimmune response. Even before COVID, many patients had POTS triggered by a viral infection. The question is whether COVID-related POTS for long COVID is different from other kinds of POTS.”
She says she treats long-COVID patients who complain of elevated heart rates with many of the cardiac workup procedures the authors list and that she treats them in a way similar to the way she treats patients with POTS.
She recommends checking resting oxygen levels and having patients walk the halls and measure their oxygen levels after walking, because their elevated heart rate may be related to ongoing lung injury from COVID.
Eric Adler, MD, a cardiologist with University of San Diego Health, told this news organization that the findings by Dr. Ståhlberg and colleagues are consistent with what he’s seeing in his clinical practice.
Dr. Adler agrees with the authors that tachycardia is an underrecognized complication of long COVID.
He said the article represents further proof that though people may survive COVID, the threat of long-term symptoms, such as heart palpitations, is real and supports the case for vaccinations.
The authors, Dr. Michos, and Dr. Adler have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Tachycardia is commonly reported in patients with post-acute COVID-19 syndrome (PACS), also known as long COVID, authors report in a new article. The researchers say tachycardia syndrome should be considered a distinct phenotype.
The study by Marcus Ståhlberg, MD, PhD, of Karolinska University Hospital, Stockholm, and colleagues was published online August 11 in The American Journal of Medicine.
Dr. Ståhlberg told this news organization that although much attention has been paid to cases of clotting and perimyocarditis in patients after COVID, relatively little attention has been paid to tachycardia, despite case reports that show that palpitations are a common complaint.
“We have diagnosed a large number of patients with postural orthostatic tachycardia syndrome [POTS] and other forms of COVID-related tachycardia at our post-COVID outpatient clinic at Karolinska University Hospital and wanted to highlight this phenomenon,” he said.
Between 25% and 50% of patients at the clinic report tachycardia and/or palpitations that last 12 weeks or longer, the authors report.
“Systematic investigations suggest that 9% of Post-acute COVID-19 syndrome patients report palpitations at six months,” the authors write.
The findings also shed light on potential tests and treatments, he said.
“Physicians should be liberal in performing a basic cardiological workup, including an ECG [electrocardiogram], echocardiography, and Holter ECG monitoring in patients complaining of palpitations and/or chest pain,” Dr. Ståhlberg said.
“If orthostatic intolerance is also reported – such as vertigo, nausea, dyspnea – suspicion of POTS should be raised and a head-up tilt test or at least an active standing test should be performed,” he said.
If POTS is confirmed, he said, patients should be offered a heart rate–lowering drug, such as low-dose propranolol or ivabradine. Compression garments, increased fluid intake, and a structured rehabilitation program also help.
“According to our clinical experience, ivabradine can also reduce symptoms in patients with inappropriate sinus tachycardia and post-COVID,” Dr. Ståhlberg said. “Another finding on Holter-ECG to look out for is frequent premature extrasystoles, which could indicate myocarditis and should warrant a cardiac MRI.”
Dr. Ståhlberg said the researchers think the mechanism underlying the tachycardia is autoimmune and that primary SARS-CoV-2 infections trigger an autoimmune response with formation of autoantibodies that can activate receptors regulating blood pressure and heart rate.
Long-lasting symptoms from COVID are prevalent, the authors note, especially in patients who experienced severe forms of the disease.
In the longest follow-up study to date of patients hospitalized with COVID, more than 60% experienced fatigue or muscle weakness 6 months after hospitalization.
PACS should not be considered a single syndrome; the term denotes an array of subsyndromes and phenotypes, the authors write. Typical symptoms include headache, fatigue, dyspnea, and mental fog but can involve multiple organs and systems.
Tachycardia can also be used as a marker to help gauge the severity of long COVID, the authors write.
“[T]achycardia can be considered a universal and easily obtainable quantitative marker of Post-acute COVID-19 syndrome and its severity rather than patient-reported symptoms, blood testing, and thoracic CT-scans,” they write.
An underrecognized complication
Erin D. Michos, MD, MHS, director of women’s cardiovascular health and associate director of preventive cardiology at Johns Hopkins University, Baltimore, said in an interview that she has seen many similar symptoms in the long-COVID patients referred to her practice.
Dr. Michos, who is also an associate professor of medicine and epidemiology, said she’s been receiving a “huge number” of referrals of long-COVID patients with postural tachycardia, inappropriate sinus tachycardia, and POTS.
“I think this is all in the spectrum of autonomic dysfunction that has been recognized a lot since COVID. POTS has been thought to have [a potentially] viral cause that triggers an autoimmune response. Even before COVID, many patients had POTS triggered by a viral infection. The question is whether COVID-related POTS for long COVID is different from other kinds of POTS.”
She says she treats long-COVID patients who complain of elevated heart rates with many of the cardiac workup procedures the authors list and that she treats them in a way similar to the way she treats patients with POTS.
She recommends checking resting oxygen levels and having patients walk the halls and measure their oxygen levels after walking, because their elevated heart rate may be related to ongoing lung injury from COVID.
Eric Adler, MD, a cardiologist with University of San Diego Health, told this news organization that the findings by Dr. Ståhlberg and colleagues are consistent with what he’s seeing in his clinical practice.
Dr. Adler agrees with the authors that tachycardia is an underrecognized complication of long COVID.
He said the article represents further proof that though people may survive COVID, the threat of long-term symptoms, such as heart palpitations, is real and supports the case for vaccinations.
The authors, Dr. Michos, and Dr. Adler have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Tachycardia is commonly reported in patients with post-acute COVID-19 syndrome (PACS), also known as long COVID, authors report in a new article. The researchers say tachycardia syndrome should be considered a distinct phenotype.
The study by Marcus Ståhlberg, MD, PhD, of Karolinska University Hospital, Stockholm, and colleagues was published online August 11 in The American Journal of Medicine.
Dr. Ståhlberg told this news organization that although much attention has been paid to cases of clotting and perimyocarditis in patients after COVID, relatively little attention has been paid to tachycardia, despite case reports that show that palpitations are a common complaint.
“We have diagnosed a large number of patients with postural orthostatic tachycardia syndrome [POTS] and other forms of COVID-related tachycardia at our post-COVID outpatient clinic at Karolinska University Hospital and wanted to highlight this phenomenon,” he said.
Between 25% and 50% of patients at the clinic report tachycardia and/or palpitations that last 12 weeks or longer, the authors report.
“Systematic investigations suggest that 9% of Post-acute COVID-19 syndrome patients report palpitations at six months,” the authors write.
The findings also shed light on potential tests and treatments, he said.
“Physicians should be liberal in performing a basic cardiological workup, including an ECG [electrocardiogram], echocardiography, and Holter ECG monitoring in patients complaining of palpitations and/or chest pain,” Dr. Ståhlberg said.
“If orthostatic intolerance is also reported – such as vertigo, nausea, dyspnea – suspicion of POTS should be raised and a head-up tilt test or at least an active standing test should be performed,” he said.
If POTS is confirmed, he said, patients should be offered a heart rate–lowering drug, such as low-dose propranolol or ivabradine. Compression garments, increased fluid intake, and a structured rehabilitation program also help.
“According to our clinical experience, ivabradine can also reduce symptoms in patients with inappropriate sinus tachycardia and post-COVID,” Dr. Ståhlberg said. “Another finding on Holter-ECG to look out for is frequent premature extrasystoles, which could indicate myocarditis and should warrant a cardiac MRI.”
Dr. Ståhlberg said the researchers think the mechanism underlying the tachycardia is autoimmune and that primary SARS-CoV-2 infections trigger an autoimmune response with formation of autoantibodies that can activate receptors regulating blood pressure and heart rate.
Long-lasting symptoms from COVID are prevalent, the authors note, especially in patients who experienced severe forms of the disease.
In the longest follow-up study to date of patients hospitalized with COVID, more than 60% experienced fatigue or muscle weakness 6 months after hospitalization.
PACS should not be considered a single syndrome; the term denotes an array of subsyndromes and phenotypes, the authors write. Typical symptoms include headache, fatigue, dyspnea, and mental fog but can involve multiple organs and systems.
Tachycardia can also be used as a marker to help gauge the severity of long COVID, the authors write.
“[T]achycardia can be considered a universal and easily obtainable quantitative marker of Post-acute COVID-19 syndrome and its severity rather than patient-reported symptoms, blood testing, and thoracic CT-scans,” they write.
An underrecognized complication
Erin D. Michos, MD, MHS, director of women’s cardiovascular health and associate director of preventive cardiology at Johns Hopkins University, Baltimore, said in an interview that she has seen many similar symptoms in the long-COVID patients referred to her practice.
Dr. Michos, who is also an associate professor of medicine and epidemiology, said she’s been receiving a “huge number” of referrals of long-COVID patients with postural tachycardia, inappropriate sinus tachycardia, and POTS.
“I think this is all in the spectrum of autonomic dysfunction that has been recognized a lot since COVID. POTS has been thought to have [a potentially] viral cause that triggers an autoimmune response. Even before COVID, many patients had POTS triggered by a viral infection. The question is whether COVID-related POTS for long COVID is different from other kinds of POTS.”
She says she treats long-COVID patients who complain of elevated heart rates with many of the cardiac workup procedures the authors list and that she treats them in a way similar to the way she treats patients with POTS.
She recommends checking resting oxygen levels and having patients walk the halls and measure their oxygen levels after walking, because their elevated heart rate may be related to ongoing lung injury from COVID.
Eric Adler, MD, a cardiologist with University of San Diego Health, told this news organization that the findings by Dr. Ståhlberg and colleagues are consistent with what he’s seeing in his clinical practice.
Dr. Adler agrees with the authors that tachycardia is an underrecognized complication of long COVID.
He said the article represents further proof that though people may survive COVID, the threat of long-term symptoms, such as heart palpitations, is real and supports the case for vaccinations.
The authors, Dr. Michos, and Dr. Adler have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
HM administrators plan for 2021 and beyond
COVID’s impact on practice management
The COVID-19 pandemic has given hospitalists a time to shine. Perhaps few people see – and value – this more than the hospital medicine administrators who work to support them behind the scenes.
“I’m very proud to have been given this opportunity to serve alongside these wonderful hospitalists,” said Elda Dede, FHM, hospital medicine division administrator at the University of Kentucky Healthcare in Lexington, Ky.
As with everything else in U.S. health care, the pandemic has affected hospital medicine administrators planning for 2021 and subsequent years in a big way. Despite all the challenges, some organizations are maintaining equilibrium, while others are even expanding. And intertwined through it all is a bright outlook and a distinct sense of team support.
Pandemic impacts on 2021 planning
Though the Texas Health Physicians Group (THPG) in Fort Worth is part of Texas Health Resources (THR), Ajay Kharbanda, MBA, SFHM, vice president of practice operations at THPG, said that each hospital within the THR system decides who that hospital will contract with for hospitalist services. Because the process is competitive and there’s no guarantee that THPG will get the contract each time, THPG has a large focus on the value they can bring to the hospitals they serve and the patients they care for.
“Having our physicians engaged with their hospital entity leaders was extremely important this year with planning around COVID because multiple hospitals had to create new COVID units,” said Mr. Kharbanda.
With the pressure of not enough volume early in the pandemic, other hospitalist groups were forced to cut back on staffing. “Within our health system, we made the cultural decision not to cancel any shifts or cut back on staffing because we didn’t want our hospitalists to be impacted negatively by things that were out of their control,” Mr. Kharbanda said.
This commitment to their hospitalists paid off when there was a surge of patients during the last quarter of 2020. “We were struggling to ensure there were adequate physicians available to take care of the patients in the hospital, but because we did the right thing by our physicians in the beginning, people did whatever it took to make sure there was enough staffing available for that increased patient volume,” Mr. Kharbanda said.
The first priority for University of Kentucky Healthcare is patient care, said Ms. Dede. Before the pandemic, the health system already had a two-layer jeopardy system in place to deal with scheduling needs in case a staff member couldn’t come in. “For the pandemic, we created six teams with an escalation and de-escalation pattern so that we could be ready to face whatever changes came in,” Ms. Dede said. Thankfully, the community wasn’t hit very hard by COVID-19, so the six new teams ended up being unnecessary, “but we were fully prepared, and everybody was ready to go.”
Making staffing plans amidst all the uncertainty surrounding the pandemic was a big challenge in planning for 2021, said Tiffani Panek, CLHM, SFHM, hospital medicine division administrator at Johns Hopkins School of Medicine, Johns Hopkins Bayview Medical Center, in Baltimore. “We don’t know what next week is going to look like, let alone what two or three months from now is going to look like, so we’ve really had to learn to be flexible,” she said. No longer is there just a Plan A that can be adjusted as needed; now there has to be a Plan B, C, and D as well.
Because the hospital medicine division’s budget is tied to the hospital, Ms. Panek said there hasn’t been a negative impact. “The hospital supports the program and continues to support the program, regardless of COVID,” she said. The health system as a whole did have to reduce benefits and freeze raises temporarily to ensure employees could keep their jobs. However, she said they have been fortunate in that their staff has been able to – and will continue to – stay in place.
As with others, volume fluctuation was an enormous hurdle in 2021 planning, said Larissa Smith, adult hospitalist and palliative care manager at The Salem Health Medical Group, Salem Health Hospitals and Clinics, in Salem, Ore. “It’s really highlighted the continued need for us to be agile in how we structure and operationalize our staffing,” Ms. Smith said. “Adapting to volume fluctuations has been our main focus.”
To prepare for both high and low patient volumes in 2021 and be able to adjust accordingly, The Salem Health Medical Group finalized in December 2020 what they call “team efficiency plans.” These plans consist of four primary areas: surge capacity, low census planning, right providers and right patient collaboration, and right team size.
Ms. Smith is working on the “right providers and right patient collaboration” component with the trauma and acute care, vascular, and general surgery teams to figure out the best ways to utilize hospitalists and specialists. “It’s been really great collaboration,” she said.
Administrative priorities during COVID-19
The pandemic hasn’t changed Ms. Panek’s administrative priorities, which include making sure her staff has whatever they need to do their jobs and that her providers have administrative support. “The work that’s had to be done to fulfill those priorities has changed in light of COVID though,” she said.
For example, she and her staff are all still off site, which she said has been challenging, especially given the lack of preparation they had. “In order to support my staff and to make sure they aren’t getting overwhelmed by being at home, that means my job looks a little bit different, but it doesn’t change my priorities,” said Ms. Panek.
By mid-summer, Ms. Dede said her main priority has been onboarding new team members, which she said is difficult with so many meetings being held virtually. “I’m not walking around the hallways with these people and having opportunities to get feedback about how their onboarding is going, so engaging so many new team members organically into the culture, the vision, the goals of our practice, is a challenge,” she said.
Taking advantage of opportunities for hospital medicine is another administrative priority for Ms. Dede. “For us to be able to take a seat at every possible table where decisions are being made, participate in shaping the strategic vision of the entire institution and be an active player in bringing that vision to life,” she said. “I feel like this is a crucial moment for hospitalists.”
Lean work, which includes the new team efficiency plans, is an administrative priority for Ms. Smith, as it is for the entire organization. “I would say that my biggest priority is just supporting our team,” Ms. Smith said. “We’ve been on a resiliency journey for a couple years.”
Their resiliency work involves periodic team training courtesy of Bryan Sexton, PhD, director of the Duke Center for Healthcare Safety and Quality. The goal of resiliency is to strengthen positive emotion, which enables a quicker recovery when difficulties occur. “I can’t imagine where we would be, this far into the pandemic, without that work,” said Ms. Smith. “I think it has really set us up to weather the storm, literally and figuratively.”
Ensuring the well-being of his provider group’s physicians is a high administrative priority for Mr. Kharbanda. Considering that the work they’ve always done is difficult, and the pandemic has been going on for such a long time, hospitalists are stretched thin. “We are bringing some additional resources to our providers that relate to taking care of themselves and helping them cope with the additional shifts,” Mr. Kharbanda said.
Going forward
The hospital medicine team at University of Kentucky Healthcare was already in the process of planning and adopting a new funds flow model, which increases the budget for HM, when the pandemic hit. “This is actually very good timing for us,” noted Ms. Dede. “We are currently working on building a new incentive model that maximizes engagement and academic productivity for our physicians, which in turn, will allow their careers to flourish and the involvement with enterprise leadership to increase.”
They had also planned to expand their teams and services before the pandemic, so in 2021, they’re hiring “an unprecedented number of hospitalists,” Ms. Dede said.
Mr. Kharbanda said that COVID has shown how much impact hospitalists can have on a hospital’s success, which has further highlighted their value. “Most of our programs are holding steady and we have some growth expected at some of our entities, so for those sites, we are hiring,” he said. Budget-wise, he expected to feel the pandemic’s impact for the first half of 2021, but for the second half, he hopes to return to normal.
Other than some low volumes in the spring, Salem Health has mostly maintained its typical capacities and funds. “Obviously, we don’t have control over external forces that impact health care, but we really try to home in on how we utilize our resources,” said Ms. Smith. “We’re a financially secure organization and I think our lean work really drives that.” The Salem Hospital is currently expanding a building tower to add another 150 beds, giving them more than 600 beds. “That will make us the largest hospital in Oregon,” Ms. Smith said.
Positive takeaways from the pandemic
Ms. Dede feels that hospital medicine has entered the health care spotlight with regard to hospitalists’ role in caring for patients during the pandemic. “Every challenge is an opportunity for growth and an opportunity to show that you know what you’re made of,” she said. “If there was ever doubt that the hospitalists are the beating heart of the hospital, this doubt is now gone. Hospitalists have, and will continue to, shoulder most of the care for COVID patients.”
The pandemic has also presented an opportunity at University of Kentucky Healthcare that helps accomplish both physician and hospital goals. “Hospital medicine is currently being asked to staff units and to participate in leadership committees, so this has been a great opportunity for growth for us,” Ms. Dede said.
The flexibility her team has shown has been a positive outcome for Ms. Panek. “You never really know what you’re going to be capable of doing until you have to do it,” she said. “I’m really proud of my group of administrative staff for how well that they’ve handled this considering it was supposed to be temporary. It’s really shown just how amazing the members of our team are and I think sometimes we take that for granted. COVID has made it so you don’t take things for granted anymore.”
Mr. Kharbanda sees how the pandemic has brought his hospitalist team together. Now, “it’s more like a family,” he said. “I think having the conversations around well-being and family safety were the real value as we learn to survive the pandemic. That was beautiful to see.”
The resiliency work her organization has done has helped Ms. Smith find plenty of positives in the face of the pandemic. “We are really resilient in health care and we can adapt quickly, but also safely,” she said.
Ms. Smith said the pandemic has also brought about changes for the better that will likely be permanent, like having time-saving virtual meetings and working from home. “We’ve put a lot of resources into physical structures and that takes away value from patients,” said Ms. Smith. “If we’re able to shift people in different roles to work from home, that just creates more future value for our community.”
Ms. Dede also sees the potential benefits that stem from people’s newfound comfort with video conferencing. “You can basically have grand rounds presenters from anywhere in the world,” she said. “You don’t have to fly them in, you don’t have to host them and have a whole program for a couple of days. They can talk to your people for an hour from the comfort of their home. I feel that we should take advantage of this too.”
Ms. Dede believes that expanding telehealth options and figuring out how hospitals can maximize that use is a priority right now. “Telehealth has been on the minds of so many hospital medicine practices, but there were still so many questions without answers about how to implement it,” she said. “During the pandemic, we were forced to find those solutions, but a lot of the barriers we are faced with have not been eliminated. I would recommend that groups keep their eyes open for new technological solutions that may empower your expansion into telehealth.”
COVID’s impact on practice management
COVID’s impact on practice management
The COVID-19 pandemic has given hospitalists a time to shine. Perhaps few people see – and value – this more than the hospital medicine administrators who work to support them behind the scenes.
“I’m very proud to have been given this opportunity to serve alongside these wonderful hospitalists,” said Elda Dede, FHM, hospital medicine division administrator at the University of Kentucky Healthcare in Lexington, Ky.
As with everything else in U.S. health care, the pandemic has affected hospital medicine administrators planning for 2021 and subsequent years in a big way. Despite all the challenges, some organizations are maintaining equilibrium, while others are even expanding. And intertwined through it all is a bright outlook and a distinct sense of team support.
Pandemic impacts on 2021 planning
Though the Texas Health Physicians Group (THPG) in Fort Worth is part of Texas Health Resources (THR), Ajay Kharbanda, MBA, SFHM, vice president of practice operations at THPG, said that each hospital within the THR system decides who that hospital will contract with for hospitalist services. Because the process is competitive and there’s no guarantee that THPG will get the contract each time, THPG has a large focus on the value they can bring to the hospitals they serve and the patients they care for.
“Having our physicians engaged with their hospital entity leaders was extremely important this year with planning around COVID because multiple hospitals had to create new COVID units,” said Mr. Kharbanda.
With the pressure of not enough volume early in the pandemic, other hospitalist groups were forced to cut back on staffing. “Within our health system, we made the cultural decision not to cancel any shifts or cut back on staffing because we didn’t want our hospitalists to be impacted negatively by things that were out of their control,” Mr. Kharbanda said.
This commitment to their hospitalists paid off when there was a surge of patients during the last quarter of 2020. “We were struggling to ensure there were adequate physicians available to take care of the patients in the hospital, but because we did the right thing by our physicians in the beginning, people did whatever it took to make sure there was enough staffing available for that increased patient volume,” Mr. Kharbanda said.
The first priority for University of Kentucky Healthcare is patient care, said Ms. Dede. Before the pandemic, the health system already had a two-layer jeopardy system in place to deal with scheduling needs in case a staff member couldn’t come in. “For the pandemic, we created six teams with an escalation and de-escalation pattern so that we could be ready to face whatever changes came in,” Ms. Dede said. Thankfully, the community wasn’t hit very hard by COVID-19, so the six new teams ended up being unnecessary, “but we were fully prepared, and everybody was ready to go.”
Making staffing plans amidst all the uncertainty surrounding the pandemic was a big challenge in planning for 2021, said Tiffani Panek, CLHM, SFHM, hospital medicine division administrator at Johns Hopkins School of Medicine, Johns Hopkins Bayview Medical Center, in Baltimore. “We don’t know what next week is going to look like, let alone what two or three months from now is going to look like, so we’ve really had to learn to be flexible,” she said. No longer is there just a Plan A that can be adjusted as needed; now there has to be a Plan B, C, and D as well.
Because the hospital medicine division’s budget is tied to the hospital, Ms. Panek said there hasn’t been a negative impact. “The hospital supports the program and continues to support the program, regardless of COVID,” she said. The health system as a whole did have to reduce benefits and freeze raises temporarily to ensure employees could keep their jobs. However, she said they have been fortunate in that their staff has been able to – and will continue to – stay in place.
As with others, volume fluctuation was an enormous hurdle in 2021 planning, said Larissa Smith, adult hospitalist and palliative care manager at The Salem Health Medical Group, Salem Health Hospitals and Clinics, in Salem, Ore. “It’s really highlighted the continued need for us to be agile in how we structure and operationalize our staffing,” Ms. Smith said. “Adapting to volume fluctuations has been our main focus.”
To prepare for both high and low patient volumes in 2021 and be able to adjust accordingly, The Salem Health Medical Group finalized in December 2020 what they call “team efficiency plans.” These plans consist of four primary areas: surge capacity, low census planning, right providers and right patient collaboration, and right team size.
Ms. Smith is working on the “right providers and right patient collaboration” component with the trauma and acute care, vascular, and general surgery teams to figure out the best ways to utilize hospitalists and specialists. “It’s been really great collaboration,” she said.
Administrative priorities during COVID-19
The pandemic hasn’t changed Ms. Panek’s administrative priorities, which include making sure her staff has whatever they need to do their jobs and that her providers have administrative support. “The work that’s had to be done to fulfill those priorities has changed in light of COVID though,” she said.
For example, she and her staff are all still off site, which she said has been challenging, especially given the lack of preparation they had. “In order to support my staff and to make sure they aren’t getting overwhelmed by being at home, that means my job looks a little bit different, but it doesn’t change my priorities,” said Ms. Panek.
By mid-summer, Ms. Dede said her main priority has been onboarding new team members, which she said is difficult with so many meetings being held virtually. “I’m not walking around the hallways with these people and having opportunities to get feedback about how their onboarding is going, so engaging so many new team members organically into the culture, the vision, the goals of our practice, is a challenge,” she said.
Taking advantage of opportunities for hospital medicine is another administrative priority for Ms. Dede. “For us to be able to take a seat at every possible table where decisions are being made, participate in shaping the strategic vision of the entire institution and be an active player in bringing that vision to life,” she said. “I feel like this is a crucial moment for hospitalists.”
Lean work, which includes the new team efficiency plans, is an administrative priority for Ms. Smith, as it is for the entire organization. “I would say that my biggest priority is just supporting our team,” Ms. Smith said. “We’ve been on a resiliency journey for a couple years.”
Their resiliency work involves periodic team training courtesy of Bryan Sexton, PhD, director of the Duke Center for Healthcare Safety and Quality. The goal of resiliency is to strengthen positive emotion, which enables a quicker recovery when difficulties occur. “I can’t imagine where we would be, this far into the pandemic, without that work,” said Ms. Smith. “I think it has really set us up to weather the storm, literally and figuratively.”
Ensuring the well-being of his provider group’s physicians is a high administrative priority for Mr. Kharbanda. Considering that the work they’ve always done is difficult, and the pandemic has been going on for such a long time, hospitalists are stretched thin. “We are bringing some additional resources to our providers that relate to taking care of themselves and helping them cope with the additional shifts,” Mr. Kharbanda said.
Going forward
The hospital medicine team at University of Kentucky Healthcare was already in the process of planning and adopting a new funds flow model, which increases the budget for HM, when the pandemic hit. “This is actually very good timing for us,” noted Ms. Dede. “We are currently working on building a new incentive model that maximizes engagement and academic productivity for our physicians, which in turn, will allow their careers to flourish and the involvement with enterprise leadership to increase.”
They had also planned to expand their teams and services before the pandemic, so in 2021, they’re hiring “an unprecedented number of hospitalists,” Ms. Dede said.
Mr. Kharbanda said that COVID has shown how much impact hospitalists can have on a hospital’s success, which has further highlighted their value. “Most of our programs are holding steady and we have some growth expected at some of our entities, so for those sites, we are hiring,” he said. Budget-wise, he expected to feel the pandemic’s impact for the first half of 2021, but for the second half, he hopes to return to normal.
Other than some low volumes in the spring, Salem Health has mostly maintained its typical capacities and funds. “Obviously, we don’t have control over external forces that impact health care, but we really try to home in on how we utilize our resources,” said Ms. Smith. “We’re a financially secure organization and I think our lean work really drives that.” The Salem Hospital is currently expanding a building tower to add another 150 beds, giving them more than 600 beds. “That will make us the largest hospital in Oregon,” Ms. Smith said.
Positive takeaways from the pandemic
Ms. Dede feels that hospital medicine has entered the health care spotlight with regard to hospitalists’ role in caring for patients during the pandemic. “Every challenge is an opportunity for growth and an opportunity to show that you know what you’re made of,” she said. “If there was ever doubt that the hospitalists are the beating heart of the hospital, this doubt is now gone. Hospitalists have, and will continue to, shoulder most of the care for COVID patients.”
The pandemic has also presented an opportunity at University of Kentucky Healthcare that helps accomplish both physician and hospital goals. “Hospital medicine is currently being asked to staff units and to participate in leadership committees, so this has been a great opportunity for growth for us,” Ms. Dede said.
The flexibility her team has shown has been a positive outcome for Ms. Panek. “You never really know what you’re going to be capable of doing until you have to do it,” she said. “I’m really proud of my group of administrative staff for how well that they’ve handled this considering it was supposed to be temporary. It’s really shown just how amazing the members of our team are and I think sometimes we take that for granted. COVID has made it so you don’t take things for granted anymore.”
Mr. Kharbanda sees how the pandemic has brought his hospitalist team together. Now, “it’s more like a family,” he said. “I think having the conversations around well-being and family safety were the real value as we learn to survive the pandemic. That was beautiful to see.”
The resiliency work her organization has done has helped Ms. Smith find plenty of positives in the face of the pandemic. “We are really resilient in health care and we can adapt quickly, but also safely,” she said.
Ms. Smith said the pandemic has also brought about changes for the better that will likely be permanent, like having time-saving virtual meetings and working from home. “We’ve put a lot of resources into physical structures and that takes away value from patients,” said Ms. Smith. “If we’re able to shift people in different roles to work from home, that just creates more future value for our community.”
Ms. Dede also sees the potential benefits that stem from people’s newfound comfort with video conferencing. “You can basically have grand rounds presenters from anywhere in the world,” she said. “You don’t have to fly them in, you don’t have to host them and have a whole program for a couple of days. They can talk to your people for an hour from the comfort of their home. I feel that we should take advantage of this too.”
Ms. Dede believes that expanding telehealth options and figuring out how hospitals can maximize that use is a priority right now. “Telehealth has been on the minds of so many hospital medicine practices, but there were still so many questions without answers about how to implement it,” she said. “During the pandemic, we were forced to find those solutions, but a lot of the barriers we are faced with have not been eliminated. I would recommend that groups keep their eyes open for new technological solutions that may empower your expansion into telehealth.”
The COVID-19 pandemic has given hospitalists a time to shine. Perhaps few people see – and value – this more than the hospital medicine administrators who work to support them behind the scenes.
“I’m very proud to have been given this opportunity to serve alongside these wonderful hospitalists,” said Elda Dede, FHM, hospital medicine division administrator at the University of Kentucky Healthcare in Lexington, Ky.
As with everything else in U.S. health care, the pandemic has affected hospital medicine administrators planning for 2021 and subsequent years in a big way. Despite all the challenges, some organizations are maintaining equilibrium, while others are even expanding. And intertwined through it all is a bright outlook and a distinct sense of team support.
Pandemic impacts on 2021 planning
Though the Texas Health Physicians Group (THPG) in Fort Worth is part of Texas Health Resources (THR), Ajay Kharbanda, MBA, SFHM, vice president of practice operations at THPG, said that each hospital within the THR system decides who that hospital will contract with for hospitalist services. Because the process is competitive and there’s no guarantee that THPG will get the contract each time, THPG has a large focus on the value they can bring to the hospitals they serve and the patients they care for.
“Having our physicians engaged with their hospital entity leaders was extremely important this year with planning around COVID because multiple hospitals had to create new COVID units,” said Mr. Kharbanda.
With the pressure of not enough volume early in the pandemic, other hospitalist groups were forced to cut back on staffing. “Within our health system, we made the cultural decision not to cancel any shifts or cut back on staffing because we didn’t want our hospitalists to be impacted negatively by things that were out of their control,” Mr. Kharbanda said.
This commitment to their hospitalists paid off when there was a surge of patients during the last quarter of 2020. “We were struggling to ensure there were adequate physicians available to take care of the patients in the hospital, but because we did the right thing by our physicians in the beginning, people did whatever it took to make sure there was enough staffing available for that increased patient volume,” Mr. Kharbanda said.
The first priority for University of Kentucky Healthcare is patient care, said Ms. Dede. Before the pandemic, the health system already had a two-layer jeopardy system in place to deal with scheduling needs in case a staff member couldn’t come in. “For the pandemic, we created six teams with an escalation and de-escalation pattern so that we could be ready to face whatever changes came in,” Ms. Dede said. Thankfully, the community wasn’t hit very hard by COVID-19, so the six new teams ended up being unnecessary, “but we were fully prepared, and everybody was ready to go.”
Making staffing plans amidst all the uncertainty surrounding the pandemic was a big challenge in planning for 2021, said Tiffani Panek, CLHM, SFHM, hospital medicine division administrator at Johns Hopkins School of Medicine, Johns Hopkins Bayview Medical Center, in Baltimore. “We don’t know what next week is going to look like, let alone what two or three months from now is going to look like, so we’ve really had to learn to be flexible,” she said. No longer is there just a Plan A that can be adjusted as needed; now there has to be a Plan B, C, and D as well.
Because the hospital medicine division’s budget is tied to the hospital, Ms. Panek said there hasn’t been a negative impact. “The hospital supports the program and continues to support the program, regardless of COVID,” she said. The health system as a whole did have to reduce benefits and freeze raises temporarily to ensure employees could keep their jobs. However, she said they have been fortunate in that their staff has been able to – and will continue to – stay in place.
As with others, volume fluctuation was an enormous hurdle in 2021 planning, said Larissa Smith, adult hospitalist and palliative care manager at The Salem Health Medical Group, Salem Health Hospitals and Clinics, in Salem, Ore. “It’s really highlighted the continued need for us to be agile in how we structure and operationalize our staffing,” Ms. Smith said. “Adapting to volume fluctuations has been our main focus.”
To prepare for both high and low patient volumes in 2021 and be able to adjust accordingly, The Salem Health Medical Group finalized in December 2020 what they call “team efficiency plans.” These plans consist of four primary areas: surge capacity, low census planning, right providers and right patient collaboration, and right team size.
Ms. Smith is working on the “right providers and right patient collaboration” component with the trauma and acute care, vascular, and general surgery teams to figure out the best ways to utilize hospitalists and specialists. “It’s been really great collaboration,” she said.
Administrative priorities during COVID-19
The pandemic hasn’t changed Ms. Panek’s administrative priorities, which include making sure her staff has whatever they need to do their jobs and that her providers have administrative support. “The work that’s had to be done to fulfill those priorities has changed in light of COVID though,” she said.
For example, she and her staff are all still off site, which she said has been challenging, especially given the lack of preparation they had. “In order to support my staff and to make sure they aren’t getting overwhelmed by being at home, that means my job looks a little bit different, but it doesn’t change my priorities,” said Ms. Panek.
By mid-summer, Ms. Dede said her main priority has been onboarding new team members, which she said is difficult with so many meetings being held virtually. “I’m not walking around the hallways with these people and having opportunities to get feedback about how their onboarding is going, so engaging so many new team members organically into the culture, the vision, the goals of our practice, is a challenge,” she said.
Taking advantage of opportunities for hospital medicine is another administrative priority for Ms. Dede. “For us to be able to take a seat at every possible table where decisions are being made, participate in shaping the strategic vision of the entire institution and be an active player in bringing that vision to life,” she said. “I feel like this is a crucial moment for hospitalists.”
Lean work, which includes the new team efficiency plans, is an administrative priority for Ms. Smith, as it is for the entire organization. “I would say that my biggest priority is just supporting our team,” Ms. Smith said. “We’ve been on a resiliency journey for a couple years.”
Their resiliency work involves periodic team training courtesy of Bryan Sexton, PhD, director of the Duke Center for Healthcare Safety and Quality. The goal of resiliency is to strengthen positive emotion, which enables a quicker recovery when difficulties occur. “I can’t imagine where we would be, this far into the pandemic, without that work,” said Ms. Smith. “I think it has really set us up to weather the storm, literally and figuratively.”
Ensuring the well-being of his provider group’s physicians is a high administrative priority for Mr. Kharbanda. Considering that the work they’ve always done is difficult, and the pandemic has been going on for such a long time, hospitalists are stretched thin. “We are bringing some additional resources to our providers that relate to taking care of themselves and helping them cope with the additional shifts,” Mr. Kharbanda said.
Going forward
The hospital medicine team at University of Kentucky Healthcare was already in the process of planning and adopting a new funds flow model, which increases the budget for HM, when the pandemic hit. “This is actually very good timing for us,” noted Ms. Dede. “We are currently working on building a new incentive model that maximizes engagement and academic productivity for our physicians, which in turn, will allow their careers to flourish and the involvement with enterprise leadership to increase.”
They had also planned to expand their teams and services before the pandemic, so in 2021, they’re hiring “an unprecedented number of hospitalists,” Ms. Dede said.
Mr. Kharbanda said that COVID has shown how much impact hospitalists can have on a hospital’s success, which has further highlighted their value. “Most of our programs are holding steady and we have some growth expected at some of our entities, so for those sites, we are hiring,” he said. Budget-wise, he expected to feel the pandemic’s impact for the first half of 2021, but for the second half, he hopes to return to normal.
Other than some low volumes in the spring, Salem Health has mostly maintained its typical capacities and funds. “Obviously, we don’t have control over external forces that impact health care, but we really try to home in on how we utilize our resources,” said Ms. Smith. “We’re a financially secure organization and I think our lean work really drives that.” The Salem Hospital is currently expanding a building tower to add another 150 beds, giving them more than 600 beds. “That will make us the largest hospital in Oregon,” Ms. Smith said.
Positive takeaways from the pandemic
Ms. Dede feels that hospital medicine has entered the health care spotlight with regard to hospitalists’ role in caring for patients during the pandemic. “Every challenge is an opportunity for growth and an opportunity to show that you know what you’re made of,” she said. “If there was ever doubt that the hospitalists are the beating heart of the hospital, this doubt is now gone. Hospitalists have, and will continue to, shoulder most of the care for COVID patients.”
The pandemic has also presented an opportunity at University of Kentucky Healthcare that helps accomplish both physician and hospital goals. “Hospital medicine is currently being asked to staff units and to participate in leadership committees, so this has been a great opportunity for growth for us,” Ms. Dede said.
The flexibility her team has shown has been a positive outcome for Ms. Panek. “You never really know what you’re going to be capable of doing until you have to do it,” she said. “I’m really proud of my group of administrative staff for how well that they’ve handled this considering it was supposed to be temporary. It’s really shown just how amazing the members of our team are and I think sometimes we take that for granted. COVID has made it so you don’t take things for granted anymore.”
Mr. Kharbanda sees how the pandemic has brought his hospitalist team together. Now, “it’s more like a family,” he said. “I think having the conversations around well-being and family safety were the real value as we learn to survive the pandemic. That was beautiful to see.”
The resiliency work her organization has done has helped Ms. Smith find plenty of positives in the face of the pandemic. “We are really resilient in health care and we can adapt quickly, but also safely,” she said.
Ms. Smith said the pandemic has also brought about changes for the better that will likely be permanent, like having time-saving virtual meetings and working from home. “We’ve put a lot of resources into physical structures and that takes away value from patients,” said Ms. Smith. “If we’re able to shift people in different roles to work from home, that just creates more future value for our community.”
Ms. Dede also sees the potential benefits that stem from people’s newfound comfort with video conferencing. “You can basically have grand rounds presenters from anywhere in the world,” she said. “You don’t have to fly them in, you don’t have to host them and have a whole program for a couple of days. They can talk to your people for an hour from the comfort of their home. I feel that we should take advantage of this too.”
Ms. Dede believes that expanding telehealth options and figuring out how hospitals can maximize that use is a priority right now. “Telehealth has been on the minds of so many hospital medicine practices, but there were still so many questions without answers about how to implement it,” she said. “During the pandemic, we were forced to find those solutions, but a lot of the barriers we are faced with have not been eliminated. I would recommend that groups keep their eyes open for new technological solutions that may empower your expansion into telehealth.”
Survey: Family medicine adds wealth, but higher net worth skews male
.
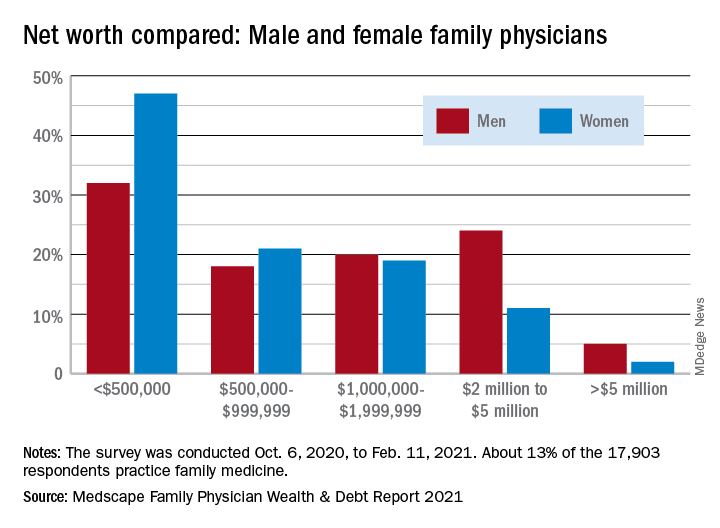
In early 2020, in a survey done before the pandemic, family physicians reported average earnings of $234,000. In 2021, with months of pandemic behind them, survey data show that family physicians averaged $236,000 in earnings.
“Although many medical offices were closed for a period of time in 2020, some physicians made use of the Paycheck Protection Program; others cut staff, renegotiated leases, switched to telephysician visits, and made other cost-cutting changes that kept earnings on par,” Medscape’s Christine Lehman wrote.
Their net worth – total wealth accounting for all financial assets and debts – did even better in 2021. More family physicians are worth $1 million to $5 million in 2021, compared with last year (38% vs. 33%), more are worth over $5 million (4% vs. 3%), and fewer FPs are worth less than $1 million (60% vs. 65%), according to Medscape’s annual wealth and debt report.
“The rise in home prices is certainly a factor,” Joel Greenwald, MD, CFP, a wealth management adviser for physicians, said in an interview.
“Definitely, the rise in the stock market played a large role; the S&P 500 finished the year up over 18%. Finally, I’ve seen clients ... cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on,” said Dr. Greenwald of St. Louis Park, Minn.
Wealth disparities between male, female family physicians
The wealth disparities that exist among family physicians get somewhat realigned, however, when viewed through the lens of physician gender. The higher-worth segments of the specialty skew rather heavily male: Five percent of male FPs are worth over $5 million versus 2% of females, and 24% of men are worth $2 million to $5 million versus 11% of women, based on data from the 13% of survey respondents (n = 17,903) who practice family medicine.
Zooming out from the world of family practice to the universe of all physicians shows that FPs are closer to allergists and immunologists than to dermatologists when it comes to share of practitioners with net worth over $5 million. That macro view puts allergy/immunology at 2%, family medicine at 4%, and dermatology at 28%. Meanwhile, family physicians’ 40% share of those worth under $500,000 is at the high end of a range in which oncologists are lowest at 16%.
Medical school and other debt
Another area where FPs find themselves looking down on most specialties is medical school debt. Only emergency medicine has more physicians (33%) paying off their school loans than family medicine (31%), while infectious disease has the fewest (12%), according to the Medscape survey, which was conducted Oct. 6, 2020, to Feb. 11, 2021.
Larger proportions of family physicians are paying off credit card debt (30%), car loans (44%), and mortgages on primary residences (67%), while 10% said that they are not paying off debts. Nonpayment of those debts was an issue for 9% of FPs who said that they missed payments on mortgages or other bills because of the COVID-19 pandemic. Almost all FPs said that they live either within (48%) or below (46%) their means, Medscape reported.
“There are certainly folks who believe that as long as they pay off their credit card each month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” Dr. Greenwald said. “I would say that living within one’s means is having a 3- to 6-month emergency fund; saving at least 20% of gross income toward retirement; adequately funding 529 college accounts; and, for younger docs, paying down high-interest-rate debt at a good clip.”
.
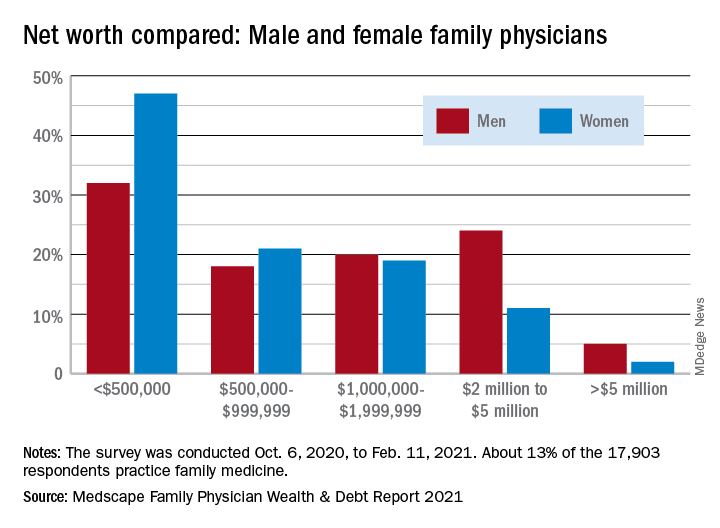
In early 2020, in a survey done before the pandemic, family physicians reported average earnings of $234,000. In 2021, with months of pandemic behind them, survey data show that family physicians averaged $236,000 in earnings.
“Although many medical offices were closed for a period of time in 2020, some physicians made use of the Paycheck Protection Program; others cut staff, renegotiated leases, switched to telephysician visits, and made other cost-cutting changes that kept earnings on par,” Medscape’s Christine Lehman wrote.
Their net worth – total wealth accounting for all financial assets and debts – did even better in 2021. More family physicians are worth $1 million to $5 million in 2021, compared with last year (38% vs. 33%), more are worth over $5 million (4% vs. 3%), and fewer FPs are worth less than $1 million (60% vs. 65%), according to Medscape’s annual wealth and debt report.
“The rise in home prices is certainly a factor,” Joel Greenwald, MD, CFP, a wealth management adviser for physicians, said in an interview.
“Definitely, the rise in the stock market played a large role; the S&P 500 finished the year up over 18%. Finally, I’ve seen clients ... cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on,” said Dr. Greenwald of St. Louis Park, Minn.
Wealth disparities between male, female family physicians
The wealth disparities that exist among family physicians get somewhat realigned, however, when viewed through the lens of physician gender. The higher-worth segments of the specialty skew rather heavily male: Five percent of male FPs are worth over $5 million versus 2% of females, and 24% of men are worth $2 million to $5 million versus 11% of women, based on data from the 13% of survey respondents (n = 17,903) who practice family medicine.
Zooming out from the world of family practice to the universe of all physicians shows that FPs are closer to allergists and immunologists than to dermatologists when it comes to share of practitioners with net worth over $5 million. That macro view puts allergy/immunology at 2%, family medicine at 4%, and dermatology at 28%. Meanwhile, family physicians’ 40% share of those worth under $500,000 is at the high end of a range in which oncologists are lowest at 16%.
Medical school and other debt
Another area where FPs find themselves looking down on most specialties is medical school debt. Only emergency medicine has more physicians (33%) paying off their school loans than family medicine (31%), while infectious disease has the fewest (12%), according to the Medscape survey, which was conducted Oct. 6, 2020, to Feb. 11, 2021.
Larger proportions of family physicians are paying off credit card debt (30%), car loans (44%), and mortgages on primary residences (67%), while 10% said that they are not paying off debts. Nonpayment of those debts was an issue for 9% of FPs who said that they missed payments on mortgages or other bills because of the COVID-19 pandemic. Almost all FPs said that they live either within (48%) or below (46%) their means, Medscape reported.
“There are certainly folks who believe that as long as they pay off their credit card each month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” Dr. Greenwald said. “I would say that living within one’s means is having a 3- to 6-month emergency fund; saving at least 20% of gross income toward retirement; adequately funding 529 college accounts; and, for younger docs, paying down high-interest-rate debt at a good clip.”
.
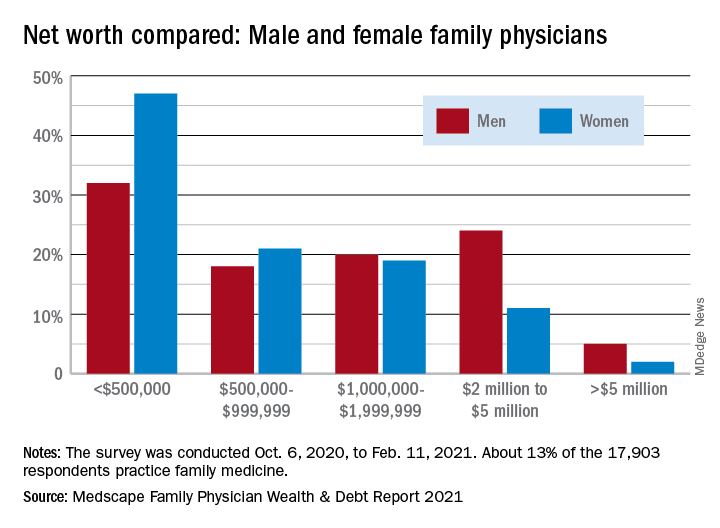
In early 2020, in a survey done before the pandemic, family physicians reported average earnings of $234,000. In 2021, with months of pandemic behind them, survey data show that family physicians averaged $236,000 in earnings.
“Although many medical offices were closed for a period of time in 2020, some physicians made use of the Paycheck Protection Program; others cut staff, renegotiated leases, switched to telephysician visits, and made other cost-cutting changes that kept earnings on par,” Medscape’s Christine Lehman wrote.
Their net worth – total wealth accounting for all financial assets and debts – did even better in 2021. More family physicians are worth $1 million to $5 million in 2021, compared with last year (38% vs. 33%), more are worth over $5 million (4% vs. 3%), and fewer FPs are worth less than $1 million (60% vs. 65%), according to Medscape’s annual wealth and debt report.
“The rise in home prices is certainly a factor,” Joel Greenwald, MD, CFP, a wealth management adviser for physicians, said in an interview.
“Definitely, the rise in the stock market played a large role; the S&P 500 finished the year up over 18%. Finally, I’ve seen clients ... cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on,” said Dr. Greenwald of St. Louis Park, Minn.
Wealth disparities between male, female family physicians
The wealth disparities that exist among family physicians get somewhat realigned, however, when viewed through the lens of physician gender. The higher-worth segments of the specialty skew rather heavily male: Five percent of male FPs are worth over $5 million versus 2% of females, and 24% of men are worth $2 million to $5 million versus 11% of women, based on data from the 13% of survey respondents (n = 17,903) who practice family medicine.
Zooming out from the world of family practice to the universe of all physicians shows that FPs are closer to allergists and immunologists than to dermatologists when it comes to share of practitioners with net worth over $5 million. That macro view puts allergy/immunology at 2%, family medicine at 4%, and dermatology at 28%. Meanwhile, family physicians’ 40% share of those worth under $500,000 is at the high end of a range in which oncologists are lowest at 16%.
Medical school and other debt
Another area where FPs find themselves looking down on most specialties is medical school debt. Only emergency medicine has more physicians (33%) paying off their school loans than family medicine (31%), while infectious disease has the fewest (12%), according to the Medscape survey, which was conducted Oct. 6, 2020, to Feb. 11, 2021.
Larger proportions of family physicians are paying off credit card debt (30%), car loans (44%), and mortgages on primary residences (67%), while 10% said that they are not paying off debts. Nonpayment of those debts was an issue for 9% of FPs who said that they missed payments on mortgages or other bills because of the COVID-19 pandemic. Almost all FPs said that they live either within (48%) or below (46%) their means, Medscape reported.
“There are certainly folks who believe that as long as they pay off their credit card each month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” Dr. Greenwald said. “I would say that living within one’s means is having a 3- to 6-month emergency fund; saving at least 20% of gross income toward retirement; adequately funding 529 college accounts; and, for younger docs, paying down high-interest-rate debt at a good clip.”
Survey: Internists gain wealth, pay off debt
a Medscape survey shows.
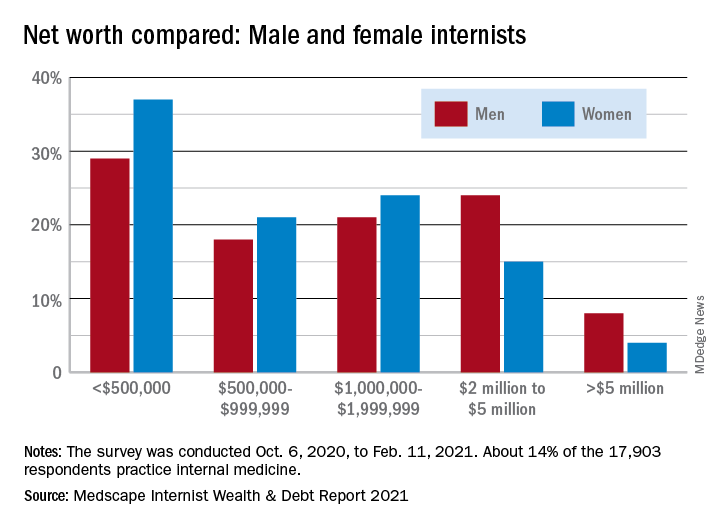
More internists are worth $1 million to $5 million in 2021, compared with last year (42% vs. 37%), more are worth over $5 million (6% vs. 5%), and fewer internists are worth less than $1 million (52% vs. 58%), according to Medscape’s annual wealth and debt report.
“The rise in home prices is certainly a factor,” Joel Greenwald, MD, CFP, a wealth management adviser for physicians, said in an interview.
“Definitely the rise in the stock market played a large role; the S&P 500 finished the year up over 18%. Finally, I’ve seen clients ... cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on,” said Dr. Greenwald of St. Louis Park, Minn.
Wealth disparities between male and female internists
The wealth disparities that exist among internists get somewhat realigned, however, when viewed through the lens of physician gender. The higher-worth segments of the specialty skew rather heavily male: 8% of male internists are worth over $5 million versus 4% of females, and 24% of men are worth $2 million to $5 million but only 15% of women, based on data from the 14% of survey respondents (n = 17,903) who practice internal medicine.
Zooming out from the world of internal medicine to the universe of all physicians shows that internists are closer to allergists and immunologists than to dermatologists when it comes to share of practitioners with net worth over $5 million. That macro view puts allergy/immunology at 2%, internal medicine at 6%, and dermatology at 28%. Meanwhile, internists’ 33% share of those worth under $500,000 is lower than family medicine’s 40% but higher than oncologists’ 16%.
Medical school and other debt
Continuing the comparison with all specialties, internists are doing somewhat better at paying off school loans. Among those responding to the survey, 20% are still paying off their medical school debt, closer to the low of 12% for infectious disease specialists than the high of 33% for the emergency physicians, according to the Medscape report.
Larger proportions of internists are paying off credit card debt (26%), car loans (35%), and mortgages on primary residences (61%), while 13% said that they are not paying off debts. Nonpayment of those debts was an issue for 11% of internists who said that they missed payments on mortgages or other bills because of the COVID pandemic.
Almost all internists said that they live either within (50%) or below (44%) their means, Medscape reported.
“There are certainly folks who believe that as long as they pay off their credit card each month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” Dr. Greenwald said. “I would say that living within one’s means is having a 3- to 6-months emergency fund; saving at least 20% of gross income toward retirement; adequately funding 529 college accounts; and, for younger docs, paying down high-interest-rate debt at a good clip.”
a Medscape survey shows.
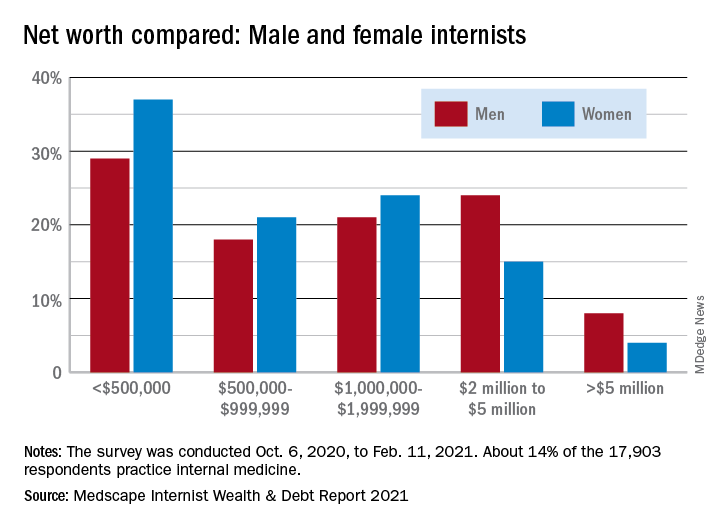
More internists are worth $1 million to $5 million in 2021, compared with last year (42% vs. 37%), more are worth over $5 million (6% vs. 5%), and fewer internists are worth less than $1 million (52% vs. 58%), according to Medscape’s annual wealth and debt report.
“The rise in home prices is certainly a factor,” Joel Greenwald, MD, CFP, a wealth management adviser for physicians, said in an interview.
“Definitely the rise in the stock market played a large role; the S&P 500 finished the year up over 18%. Finally, I’ve seen clients ... cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on,” said Dr. Greenwald of St. Louis Park, Minn.
Wealth disparities between male and female internists
The wealth disparities that exist among internists get somewhat realigned, however, when viewed through the lens of physician gender. The higher-worth segments of the specialty skew rather heavily male: 8% of male internists are worth over $5 million versus 4% of females, and 24% of men are worth $2 million to $5 million but only 15% of women, based on data from the 14% of survey respondents (n = 17,903) who practice internal medicine.
Zooming out from the world of internal medicine to the universe of all physicians shows that internists are closer to allergists and immunologists than to dermatologists when it comes to share of practitioners with net worth over $5 million. That macro view puts allergy/immunology at 2%, internal medicine at 6%, and dermatology at 28%. Meanwhile, internists’ 33% share of those worth under $500,000 is lower than family medicine’s 40% but higher than oncologists’ 16%.
Medical school and other debt
Continuing the comparison with all specialties, internists are doing somewhat better at paying off school loans. Among those responding to the survey, 20% are still paying off their medical school debt, closer to the low of 12% for infectious disease specialists than the high of 33% for the emergency physicians, according to the Medscape report.
Larger proportions of internists are paying off credit card debt (26%), car loans (35%), and mortgages on primary residences (61%), while 13% said that they are not paying off debts. Nonpayment of those debts was an issue for 11% of internists who said that they missed payments on mortgages or other bills because of the COVID pandemic.
Almost all internists said that they live either within (50%) or below (44%) their means, Medscape reported.
“There are certainly folks who believe that as long as they pay off their credit card each month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” Dr. Greenwald said. “I would say that living within one’s means is having a 3- to 6-months emergency fund; saving at least 20% of gross income toward retirement; adequately funding 529 college accounts; and, for younger docs, paying down high-interest-rate debt at a good clip.”
a Medscape survey shows.
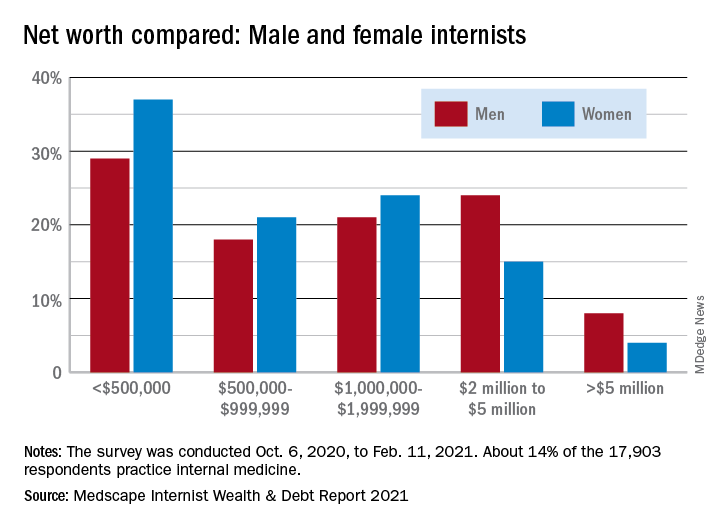
More internists are worth $1 million to $5 million in 2021, compared with last year (42% vs. 37%), more are worth over $5 million (6% vs. 5%), and fewer internists are worth less than $1 million (52% vs. 58%), according to Medscape’s annual wealth and debt report.
“The rise in home prices is certainly a factor,” Joel Greenwald, MD, CFP, a wealth management adviser for physicians, said in an interview.
“Definitely the rise in the stock market played a large role; the S&P 500 finished the year up over 18%. Finally, I’ve seen clients ... cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on,” said Dr. Greenwald of St. Louis Park, Minn.
Wealth disparities between male and female internists
The wealth disparities that exist among internists get somewhat realigned, however, when viewed through the lens of physician gender. The higher-worth segments of the specialty skew rather heavily male: 8% of male internists are worth over $5 million versus 4% of females, and 24% of men are worth $2 million to $5 million but only 15% of women, based on data from the 14% of survey respondents (n = 17,903) who practice internal medicine.
Zooming out from the world of internal medicine to the universe of all physicians shows that internists are closer to allergists and immunologists than to dermatologists when it comes to share of practitioners with net worth over $5 million. That macro view puts allergy/immunology at 2%, internal medicine at 6%, and dermatology at 28%. Meanwhile, internists’ 33% share of those worth under $500,000 is lower than family medicine’s 40% but higher than oncologists’ 16%.
Medical school and other debt
Continuing the comparison with all specialties, internists are doing somewhat better at paying off school loans. Among those responding to the survey, 20% are still paying off their medical school debt, closer to the low of 12% for infectious disease specialists than the high of 33% for the emergency physicians, according to the Medscape report.
Larger proportions of internists are paying off credit card debt (26%), car loans (35%), and mortgages on primary residences (61%), while 13% said that they are not paying off debts. Nonpayment of those debts was an issue for 11% of internists who said that they missed payments on mortgages or other bills because of the COVID pandemic.
Almost all internists said that they live either within (50%) or below (44%) their means, Medscape reported.
“There are certainly folks who believe that as long as they pay off their credit card each month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” Dr. Greenwald said. “I would say that living within one’s means is having a 3- to 6-months emergency fund; saving at least 20% of gross income toward retirement; adequately funding 529 college accounts; and, for younger docs, paying down high-interest-rate debt at a good clip.”
Low glycemic diet improves A1c, other risk factors in diabetes
A diet rich in vegetables and low in carbs – a so-called low glycemic index (GI) diet – is associated with clinically significant benefits beyond those provided by existing medications for people with type 1 and type 2 diabetes, compared with a higher glycemic diet, findings from a new meta-analysis show.
“Although the effects were small, which is not surprising in clinical trials in nutrition, they were clinically meaningful improvements for which our certainty in the effects were moderate to high,” first author Laura Chiavaroli, PhD, of the department of nutritional sciences, Temerty Faculty of Medicine, University of Toronto, said in an interview.
The GI rates foods on the basis of how quickly they affect blood glucose levels.
Fruits, vegetables, and whole grains have a low GI. They also help to regulate blood sugar levels. Such foods are linked to a reduced risk for heart disease among people with diabetes.
But guidelines on this – such as those from the European Association for the Study of Diabetes – reflect research published more than 15 years ago, before several key trials were published.
Dr. Chiavaroli and colleagues identified 27 randomized controlled trials – the most recent of which was published in May 2021 – that involved a total of 1,617 adults with type 1 or 2 diabetes. For the patients in these trials, diabetes was moderately controlled with glucose-lowering drugs or insulin. All of the included trials examined the effects of a low GI diet or a low glycemic load (GL) diet for people with diabetes over a period 3 or more weeks. The majority of patients in the studies were overweight or had obesity, and they were largely middle-aged.
The meta-analysis, which included new data, was published Aug. 5 in The BMJ. The study “expands the number of relevant intermediate cardiometabolic outcomes, and assesses the certainty of the evidence using GRADE [grading of recommendations assessment, development, and evaluation],” Dr. Chiavaroli and colleagues noted.
“The available evidence provides a good indication of the likely benefit in this population and supports existing recommendations for the use of low GI dietary patterns in the management of diabetes,” they emphasized.
Improvements in A1c, fasting glucose, cholesterol, and triglycerides
Overall, compared with people who consumed diets with higher GI/GL ratings, for those who consumed lower glycemic diets, glycemic control was significantly improved, as reflected in A1c level, which was the primary outcome of the study (mean difference, –0.31%; P < .001).
This “would meet the threshold of ≥ 0.3% reduction in HbA1c proposed by the European Medicines Agency as clinically relevant for risk reduction of diabetic complications,” the authors noted.
Those who consumed low glycemic diets also showed improvements in secondary outcomes, including fasting glucose level, which was reduced by 0.36 mmol/L (–6.5 mg/dL), a 6% reduction in low-density cholesterol (LDL-C) (–0.17 mmol/L), and a fall in triglyceride levels (–0.09 mmol/L).
They also lost marginally more body weight, at –0.66 kg (–1.5 pounds). Body mass index was lower by –0.38, and inflammation was reduced (C-reactive protein, –.41 mg/L; all P < .05).
No significant differences were observed between the groups in blood insulin level, high-density lipoprotein cholesterol level, waist circumference, or blood pressure.
Three of the studies showed that participants developed a preference for the low GI diet. “In recent years, there has been a growing interest in whole-food plant-based diets, and there are more options, for example, for pulse-based products,” Dr. Chiavaroli said.
This meta-analysis should support the recommendation of the low-glycemic diet, particularly among people with diabetes, she reiterated.
Will larger randomized trial show effect on outcomes?
The authors noted, however, that to determine whether these small improvements in intermediate cardiometabolic risk factors observed with low GI diets translate to reductions in cardiovascular disease, nephropathy, and retinopathy among people with diabetes, larger randomized trials are needed.
One such trial, the Low Glycemic Index Diet for Type 2 Diabetics, includes 169 high-risk patients with type 2 diabetes and subclinical atherosclerosis. The investigators are evaluating the effect of a low GI diet on the progression of atherosclerosis, as assessed by vascular MRI over 3 years.
“We await the results,” they said.
The study received funding from the Diabetes and Nutrition Study Group of the European Association for the Study of Diabetes (EASD) as part of the development of the EASD Clinical Practice Guidelines for Nutrition Therapy. The study was also supported by the Canadian Institutes of Health Research through the Canada-wide Human Nutrition Trialists’ Network. The Diet, Digestive Tract, and Disease (3D) Center, which is funded through the Canada Foundation for Innovation and the Ministry of Research and Innovation’s Ontario Research Fund, provided the infrastructure for the study.
A version of this article first appeared on Medscape.com.
A diet rich in vegetables and low in carbs – a so-called low glycemic index (GI) diet – is associated with clinically significant benefits beyond those provided by existing medications for people with type 1 and type 2 diabetes, compared with a higher glycemic diet, findings from a new meta-analysis show.
“Although the effects were small, which is not surprising in clinical trials in nutrition, they were clinically meaningful improvements for which our certainty in the effects were moderate to high,” first author Laura Chiavaroli, PhD, of the department of nutritional sciences, Temerty Faculty of Medicine, University of Toronto, said in an interview.
The GI rates foods on the basis of how quickly they affect blood glucose levels.
Fruits, vegetables, and whole grains have a low GI. They also help to regulate blood sugar levels. Such foods are linked to a reduced risk for heart disease among people with diabetes.
But guidelines on this – such as those from the European Association for the Study of Diabetes – reflect research published more than 15 years ago, before several key trials were published.
Dr. Chiavaroli and colleagues identified 27 randomized controlled trials – the most recent of which was published in May 2021 – that involved a total of 1,617 adults with type 1 or 2 diabetes. For the patients in these trials, diabetes was moderately controlled with glucose-lowering drugs or insulin. All of the included trials examined the effects of a low GI diet or a low glycemic load (GL) diet for people with diabetes over a period 3 or more weeks. The majority of patients in the studies were overweight or had obesity, and they were largely middle-aged.
The meta-analysis, which included new data, was published Aug. 5 in The BMJ. The study “expands the number of relevant intermediate cardiometabolic outcomes, and assesses the certainty of the evidence using GRADE [grading of recommendations assessment, development, and evaluation],” Dr. Chiavaroli and colleagues noted.
“The available evidence provides a good indication of the likely benefit in this population and supports existing recommendations for the use of low GI dietary patterns in the management of diabetes,” they emphasized.
Improvements in A1c, fasting glucose, cholesterol, and triglycerides
Overall, compared with people who consumed diets with higher GI/GL ratings, for those who consumed lower glycemic diets, glycemic control was significantly improved, as reflected in A1c level, which was the primary outcome of the study (mean difference, –0.31%; P < .001).
This “would meet the threshold of ≥ 0.3% reduction in HbA1c proposed by the European Medicines Agency as clinically relevant for risk reduction of diabetic complications,” the authors noted.
Those who consumed low glycemic diets also showed improvements in secondary outcomes, including fasting glucose level, which was reduced by 0.36 mmol/L (–6.5 mg/dL), a 6% reduction in low-density cholesterol (LDL-C) (–0.17 mmol/L), and a fall in triglyceride levels (–0.09 mmol/L).
They also lost marginally more body weight, at –0.66 kg (–1.5 pounds). Body mass index was lower by –0.38, and inflammation was reduced (C-reactive protein, –.41 mg/L; all P < .05).
No significant differences were observed between the groups in blood insulin level, high-density lipoprotein cholesterol level, waist circumference, or blood pressure.
Three of the studies showed that participants developed a preference for the low GI diet. “In recent years, there has been a growing interest in whole-food plant-based diets, and there are more options, for example, for pulse-based products,” Dr. Chiavaroli said.
This meta-analysis should support the recommendation of the low-glycemic diet, particularly among people with diabetes, she reiterated.
Will larger randomized trial show effect on outcomes?
The authors noted, however, that to determine whether these small improvements in intermediate cardiometabolic risk factors observed with low GI diets translate to reductions in cardiovascular disease, nephropathy, and retinopathy among people with diabetes, larger randomized trials are needed.
One such trial, the Low Glycemic Index Diet for Type 2 Diabetics, includes 169 high-risk patients with type 2 diabetes and subclinical atherosclerosis. The investigators are evaluating the effect of a low GI diet on the progression of atherosclerosis, as assessed by vascular MRI over 3 years.
“We await the results,” they said.
The study received funding from the Diabetes and Nutrition Study Group of the European Association for the Study of Diabetes (EASD) as part of the development of the EASD Clinical Practice Guidelines for Nutrition Therapy. The study was also supported by the Canadian Institutes of Health Research through the Canada-wide Human Nutrition Trialists’ Network. The Diet, Digestive Tract, and Disease (3D) Center, which is funded through the Canada Foundation for Innovation and the Ministry of Research and Innovation’s Ontario Research Fund, provided the infrastructure for the study.
A version of this article first appeared on Medscape.com.
A diet rich in vegetables and low in carbs – a so-called low glycemic index (GI) diet – is associated with clinically significant benefits beyond those provided by existing medications for people with type 1 and type 2 diabetes, compared with a higher glycemic diet, findings from a new meta-analysis show.
“Although the effects were small, which is not surprising in clinical trials in nutrition, they were clinically meaningful improvements for which our certainty in the effects were moderate to high,” first author Laura Chiavaroli, PhD, of the department of nutritional sciences, Temerty Faculty of Medicine, University of Toronto, said in an interview.
The GI rates foods on the basis of how quickly they affect blood glucose levels.
Fruits, vegetables, and whole grains have a low GI. They also help to regulate blood sugar levels. Such foods are linked to a reduced risk for heart disease among people with diabetes.
But guidelines on this – such as those from the European Association for the Study of Diabetes – reflect research published more than 15 years ago, before several key trials were published.
Dr. Chiavaroli and colleagues identified 27 randomized controlled trials – the most recent of which was published in May 2021 – that involved a total of 1,617 adults with type 1 or 2 diabetes. For the patients in these trials, diabetes was moderately controlled with glucose-lowering drugs or insulin. All of the included trials examined the effects of a low GI diet or a low glycemic load (GL) diet for people with diabetes over a period 3 or more weeks. The majority of patients in the studies were overweight or had obesity, and they were largely middle-aged.
The meta-analysis, which included new data, was published Aug. 5 in The BMJ. The study “expands the number of relevant intermediate cardiometabolic outcomes, and assesses the certainty of the evidence using GRADE [grading of recommendations assessment, development, and evaluation],” Dr. Chiavaroli and colleagues noted.
“The available evidence provides a good indication of the likely benefit in this population and supports existing recommendations for the use of low GI dietary patterns in the management of diabetes,” they emphasized.
Improvements in A1c, fasting glucose, cholesterol, and triglycerides
Overall, compared with people who consumed diets with higher GI/GL ratings, for those who consumed lower glycemic diets, glycemic control was significantly improved, as reflected in A1c level, which was the primary outcome of the study (mean difference, –0.31%; P < .001).
This “would meet the threshold of ≥ 0.3% reduction in HbA1c proposed by the European Medicines Agency as clinically relevant for risk reduction of diabetic complications,” the authors noted.
Those who consumed low glycemic diets also showed improvements in secondary outcomes, including fasting glucose level, which was reduced by 0.36 mmol/L (–6.5 mg/dL), a 6% reduction in low-density cholesterol (LDL-C) (–0.17 mmol/L), and a fall in triglyceride levels (–0.09 mmol/L).
They also lost marginally more body weight, at –0.66 kg (–1.5 pounds). Body mass index was lower by –0.38, and inflammation was reduced (C-reactive protein, –.41 mg/L; all P < .05).
No significant differences were observed between the groups in blood insulin level, high-density lipoprotein cholesterol level, waist circumference, or blood pressure.
Three of the studies showed that participants developed a preference for the low GI diet. “In recent years, there has been a growing interest in whole-food plant-based diets, and there are more options, for example, for pulse-based products,” Dr. Chiavaroli said.
This meta-analysis should support the recommendation of the low-glycemic diet, particularly among people with diabetes, she reiterated.
Will larger randomized trial show effect on outcomes?
The authors noted, however, that to determine whether these small improvements in intermediate cardiometabolic risk factors observed with low GI diets translate to reductions in cardiovascular disease, nephropathy, and retinopathy among people with diabetes, larger randomized trials are needed.
One such trial, the Low Glycemic Index Diet for Type 2 Diabetics, includes 169 high-risk patients with type 2 diabetes and subclinical atherosclerosis. The investigators are evaluating the effect of a low GI diet on the progression of atherosclerosis, as assessed by vascular MRI over 3 years.
“We await the results,” they said.
The study received funding from the Diabetes and Nutrition Study Group of the European Association for the Study of Diabetes (EASD) as part of the development of the EASD Clinical Practice Guidelines for Nutrition Therapy. The study was also supported by the Canadian Institutes of Health Research through the Canada-wide Human Nutrition Trialists’ Network. The Diet, Digestive Tract, and Disease (3D) Center, which is funded through the Canada Foundation for Innovation and the Ministry of Research and Innovation’s Ontario Research Fund, provided the infrastructure for the study.
A version of this article first appeared on Medscape.com.
Obesity leads to depression via social and metabolic factors
New research provides further evidence that a high body mass index (BMI) leads to depressed mood and poor well-being via social and physical factors.
Obesity and depression are “major global health challenges; our findings suggest that reducing obesity will lower depression and improve well-being,” co–lead author Jessica O’Loughlin, PhD student, University of Exeter Medical School, United Kingdom, told this news organization.
“Doctors should consider both the biological consequences of having a higher BMI as well as the social implications when treating patients with obesity in order to help reduce the odds of them developing depression,” Ms. O’Loughlin added.
The study was published online July 16 in Human Molecular Genetics.
Large body of evidence
A large body of evidence indicates that higher BMI leads to depression.
Ms. O’Loughlin and colleagues leveraged genetic data from more than 145,000 individuals in the UK Biobank and Mendelian randomization to determine whether the causal link between high BMI and depression is the result of psychosocial pathways, physical pathways, or both.
The analysis showed that a genetically determined 1 standard deviation higher BMI (4.6 kg/m2) was associated with higher likelihood of depression (odds ratio, 1.50; 95% confidence interval, 1.15-1.95) and lower well-being (beta, -0.15; 95% CI, -0.26 to -0.04).
Using genetics to distinguish metabolic and psychosocial effects, the results also indicate that, even in the absence of adverse metabolic effects, “higher adiposity remains causal to depression and lowers wellbeing,” the researchers report.
“ and when using genetic variants that make you fatter but metabolically healthier (favorable adiposity genetic variants),” said Ms. O’Loughlin.
“Although we can’t tell which factor plays a bigger role in the adiposity-depression relationship, our analysis suggests that both physical and social factors (e.g., social stigma) play a role in the relationship between higher BMI and higher odds of depression,” she added.
In contrast, there was little evidence that higher BMI in the presence or absence of adverse metabolic consequences causes generalized anxiety disorder.
“Finding ways to support people to lose weight could benefit their mental health as well as their physical health,” co–lead author Francesco Casanova, PhD, with the University of Exeter, said in a statement.
Unexpected finding
Reached for comment, Samoon Ahmad, MD, professor, department of psychiatry, New York University, said that “multiple studies have shown a correlation between stress, obesity, inflammation, overall well-being, and psychiatric disorders, particularly depressive and anxiety disorders.”
He said this new study is important for three reasons.
“The first is the cohort size. There were over 145,000 participants involved in the study, which is significant and serves to make its conclusions stronger,” Dr. Ahmad noted.
“The second point is that the authors found that the correlation between higher adiposity and depression and lower well-being scores occurred even in patients without adverse metabolic effects,” he said in an interview.
“Of note, obesity significantly increases the risk of developing type 2 diabetes, hypertension, and a host of other illnesses as well as inflammatory conditions, which can all have a negative impact on quality of life. Consequently, these can contribute to depression as well as anxiety,” Dr. Ahmad added.
“Interestingly, what this study suggests is that even people without these additional stressors are reporting higher rates of depression and lower scores of well-being, while higher adiposity is the common denominator,” he noted.
“Third, the paper found little to no correlation between higher adiposity and generalized anxiety disorder. This comes as a complete surprise because anxiety and depression are very common comorbidities,” Dr. Ahmad said.
“Moreover, numerous studies as well as clinical data suggest that obesity leads to chronic inflammation, which in turn is associated with less favorable metabolic profiles, and that anxiety and depressive disorders may in some way be psychiatric manifestations of inflammation. To see one but not the other was quite an unexpected finding,” Dr. Ahmad said.
The study was funded by the Academy of Medical Sciences. Ms. O’Loughlin, Dr. Casanova, and Dr. Ahmad have disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
New research provides further evidence that a high body mass index (BMI) leads to depressed mood and poor well-being via social and physical factors.
Obesity and depression are “major global health challenges; our findings suggest that reducing obesity will lower depression and improve well-being,” co–lead author Jessica O’Loughlin, PhD student, University of Exeter Medical School, United Kingdom, told this news organization.
“Doctors should consider both the biological consequences of having a higher BMI as well as the social implications when treating patients with obesity in order to help reduce the odds of them developing depression,” Ms. O’Loughlin added.
The study was published online July 16 in Human Molecular Genetics.
Large body of evidence
A large body of evidence indicates that higher BMI leads to depression.
Ms. O’Loughlin and colleagues leveraged genetic data from more than 145,000 individuals in the UK Biobank and Mendelian randomization to determine whether the causal link between high BMI and depression is the result of psychosocial pathways, physical pathways, or both.
The analysis showed that a genetically determined 1 standard deviation higher BMI (4.6 kg/m2) was associated with higher likelihood of depression (odds ratio, 1.50; 95% confidence interval, 1.15-1.95) and lower well-being (beta, -0.15; 95% CI, -0.26 to -0.04).
Using genetics to distinguish metabolic and psychosocial effects, the results also indicate that, even in the absence of adverse metabolic effects, “higher adiposity remains causal to depression and lowers wellbeing,” the researchers report.
“ and when using genetic variants that make you fatter but metabolically healthier (favorable adiposity genetic variants),” said Ms. O’Loughlin.
“Although we can’t tell which factor plays a bigger role in the adiposity-depression relationship, our analysis suggests that both physical and social factors (e.g., social stigma) play a role in the relationship between higher BMI and higher odds of depression,” she added.
In contrast, there was little evidence that higher BMI in the presence or absence of adverse metabolic consequences causes generalized anxiety disorder.
“Finding ways to support people to lose weight could benefit their mental health as well as their physical health,” co–lead author Francesco Casanova, PhD, with the University of Exeter, said in a statement.
Unexpected finding
Reached for comment, Samoon Ahmad, MD, professor, department of psychiatry, New York University, said that “multiple studies have shown a correlation between stress, obesity, inflammation, overall well-being, and psychiatric disorders, particularly depressive and anxiety disorders.”
He said this new study is important for three reasons.
“The first is the cohort size. There were over 145,000 participants involved in the study, which is significant and serves to make its conclusions stronger,” Dr. Ahmad noted.
“The second point is that the authors found that the correlation between higher adiposity and depression and lower well-being scores occurred even in patients without adverse metabolic effects,” he said in an interview.
“Of note, obesity significantly increases the risk of developing type 2 diabetes, hypertension, and a host of other illnesses as well as inflammatory conditions, which can all have a negative impact on quality of life. Consequently, these can contribute to depression as well as anxiety,” Dr. Ahmad added.
“Interestingly, what this study suggests is that even people without these additional stressors are reporting higher rates of depression and lower scores of well-being, while higher adiposity is the common denominator,” he noted.
“Third, the paper found little to no correlation between higher adiposity and generalized anxiety disorder. This comes as a complete surprise because anxiety and depression are very common comorbidities,” Dr. Ahmad said.
“Moreover, numerous studies as well as clinical data suggest that obesity leads to chronic inflammation, which in turn is associated with less favorable metabolic profiles, and that anxiety and depressive disorders may in some way be psychiatric manifestations of inflammation. To see one but not the other was quite an unexpected finding,” Dr. Ahmad said.
The study was funded by the Academy of Medical Sciences. Ms. O’Loughlin, Dr. Casanova, and Dr. Ahmad have disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
New research provides further evidence that a high body mass index (BMI) leads to depressed mood and poor well-being via social and physical factors.
Obesity and depression are “major global health challenges; our findings suggest that reducing obesity will lower depression and improve well-being,” co–lead author Jessica O’Loughlin, PhD student, University of Exeter Medical School, United Kingdom, told this news organization.
“Doctors should consider both the biological consequences of having a higher BMI as well as the social implications when treating patients with obesity in order to help reduce the odds of them developing depression,” Ms. O’Loughlin added.
The study was published online July 16 in Human Molecular Genetics.
Large body of evidence
A large body of evidence indicates that higher BMI leads to depression.
Ms. O’Loughlin and colleagues leveraged genetic data from more than 145,000 individuals in the UK Biobank and Mendelian randomization to determine whether the causal link between high BMI and depression is the result of psychosocial pathways, physical pathways, or both.
The analysis showed that a genetically determined 1 standard deviation higher BMI (4.6 kg/m2) was associated with higher likelihood of depression (odds ratio, 1.50; 95% confidence interval, 1.15-1.95) and lower well-being (beta, -0.15; 95% CI, -0.26 to -0.04).
Using genetics to distinguish metabolic and psychosocial effects, the results also indicate that, even in the absence of adverse metabolic effects, “higher adiposity remains causal to depression and lowers wellbeing,” the researchers report.
“ and when using genetic variants that make you fatter but metabolically healthier (favorable adiposity genetic variants),” said Ms. O’Loughlin.
“Although we can’t tell which factor plays a bigger role in the adiposity-depression relationship, our analysis suggests that both physical and social factors (e.g., social stigma) play a role in the relationship between higher BMI and higher odds of depression,” she added.
In contrast, there was little evidence that higher BMI in the presence or absence of adverse metabolic consequences causes generalized anxiety disorder.
“Finding ways to support people to lose weight could benefit their mental health as well as their physical health,” co–lead author Francesco Casanova, PhD, with the University of Exeter, said in a statement.
Unexpected finding
Reached for comment, Samoon Ahmad, MD, professor, department of psychiatry, New York University, said that “multiple studies have shown a correlation between stress, obesity, inflammation, overall well-being, and psychiatric disorders, particularly depressive and anxiety disorders.”
He said this new study is important for three reasons.
“The first is the cohort size. There were over 145,000 participants involved in the study, which is significant and serves to make its conclusions stronger,” Dr. Ahmad noted.
“The second point is that the authors found that the correlation between higher adiposity and depression and lower well-being scores occurred even in patients without adverse metabolic effects,” he said in an interview.
“Of note, obesity significantly increases the risk of developing type 2 diabetes, hypertension, and a host of other illnesses as well as inflammatory conditions, which can all have a negative impact on quality of life. Consequently, these can contribute to depression as well as anxiety,” Dr. Ahmad added.
“Interestingly, what this study suggests is that even people without these additional stressors are reporting higher rates of depression and lower scores of well-being, while higher adiposity is the common denominator,” he noted.
“Third, the paper found little to no correlation between higher adiposity and generalized anxiety disorder. This comes as a complete surprise because anxiety and depression are very common comorbidities,” Dr. Ahmad said.
“Moreover, numerous studies as well as clinical data suggest that obesity leads to chronic inflammation, which in turn is associated with less favorable metabolic profiles, and that anxiety and depressive disorders may in some way be psychiatric manifestations of inflammation. To see one but not the other was quite an unexpected finding,” Dr. Ahmad said.
The study was funded by the Academy of Medical Sciences. Ms. O’Loughlin, Dr. Casanova, and Dr. Ahmad have disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.