User login
MRI reliably identifies significant prostate cancer
Prostate cancers that are missed on multiparametric (mp) MRI are small and “not life-threatening,” according to an analysis of data from the Prostate MR Imaging Study (PROMIS).
“Our work suggests that MRI scans of the prostate appear to deliver crucial information about a man’s risk of dying from prostate cancer, even before he has a biopsy,” said Joseph Norris, BM BS, from University College London.
“This may mean that we can finally move prostate cancer to a position in which we can use imaging as the primary tool to direct further investigations, treatment, and prediction of risk,” he told Medscape Medical News.
This is “a position that all other solid organ cancers have reached,” said Norris, who will present the findings at the upcoming virtual European Association of Urology 2020 Congress.
All 576 PROMIS participants underwent an mpMRI scan, a transrectal ultrasonography (TRUS)–guided biopsy, and a template prostate mapping (TPM) biopsy taken at 5-mm intervals across the entire prostate.
PROMIS researchers previously showed that mpMRI had a 93% sensitivity for clinically significant cancer, whereas TRUS biopsy had only a 48% sensitivity, as reported by Medscape Medical News. And they concluded that the use of mpMRI as a first-line diagnostic tool could prevent 27% of all biopsies, which can have serious adverse effects, such as pain, urinary problems, infection, bleeding, and erectile dysfunction.
However, in their study looking at the accuracy of mpMRI and TRUS biopsy, the researchers did not investigate the severity of the 7% of cancers that mpMRI missed. “What if those missed cancers are, in fact, aggressive? That’s what we set out to examine,” Norris explained.
So he and his colleagues conducted a post ad hoc analysis of the PROMIS participants in whom clinically significant cancer had been detected with TPM biopsy to see which of those cancers had been detected with mpMRI. The findings were published online in European Urology.
Cancers met the strict definition of clinically significant if they had a Gleason score of at least 4+3 for a tumor of any length, or a maximum cancer core length (MCCL) greater than 6 mm for a cancer of any grade. They met the less-strict definition if they had a Gleason score of at least 3+4 for a tumor of any length, or a MCCL greater than 4 mm for a cancer of any grade.
In PROMIS, TPM biopsy detected 230 cancers that met the strict definition of clinically significant and 331 that met the less-strict definition.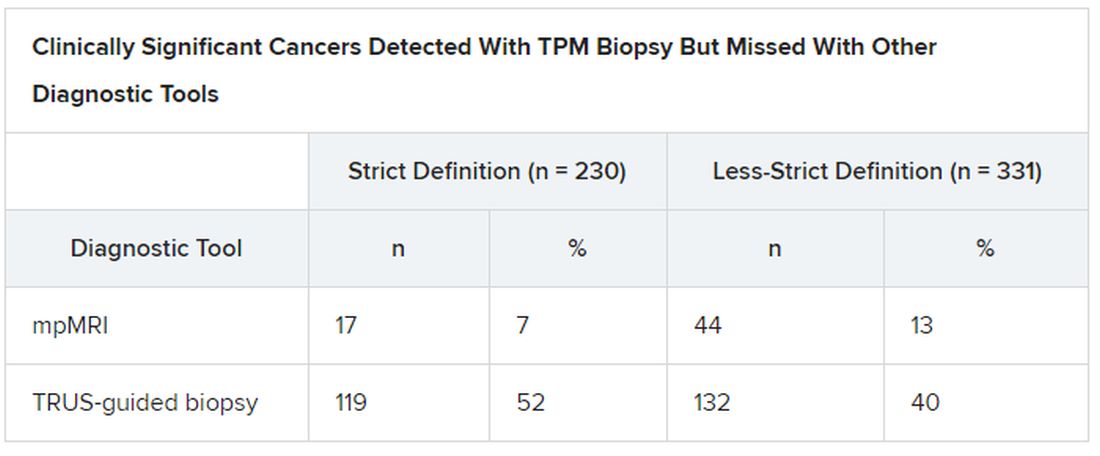
Overall Gleason scores were significantly lower for the 17 strict-definition cancers not detected with 1.5 T mpMRI than for those detected with mpMRI (P = .0007), as were maximum Gleason scores (P < .0001).
Median MCCL was 3 mm shorter for all 17 tumors missed with mpMRI than for those detected with mpMRI (5 vs 8 mm; P < .0001).
mpMRI detected all tumors identified on TPM biopsy that had an overall Gleason score greater than 3+4 (Gleason grades 3 to 5) or a maximum Gleason score greater than 4+3 (Gleason grades 4 and 5).
“This finding is important, given that in PROMIS, no men with an overall Gleason score of 4+3 had cancer missed by MRI, indicating that actually MRI may be able to identify all truly significant cancers,” said Norris.
Adding PSA Density Threshold
To further assess cancers missed on mpMRI, the researchers looked at prostate-specific antigen (PSA) density, calculated as total PSA level (ng/mL) divided by prostate volume (mL).
“We found that if we applied a threshold PSA density to men with normal-looking MRI scans, we could reduce the proportion of missed significant cancer to just 5%. This is exciting; it means we can make MRI an even more effective test for prostate cancer in a very simple way,” Norris reported.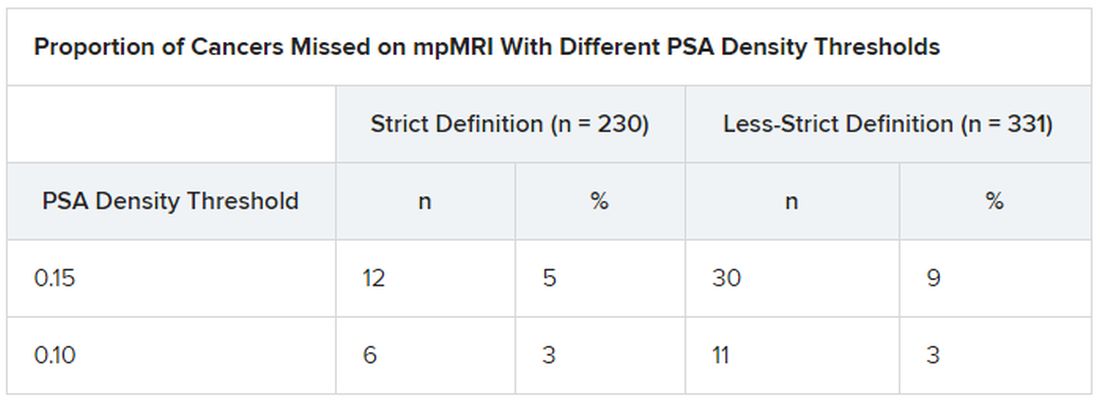
“These data show that no highly aggressive prostate cancers were missed by MRI, either at the level of the whole prostate or at the individual needle level,” said Norris. This should lead to positive outcomes in the long term.
And since the PROMIS data were gathered, MRI technology has improved, he said. The “MRI scanners in PROMIS were 1.5 Tesla,” whereas today’s machines are 3.0 T, which could increase the detection of significant prostate cancer.
In fact, “our analysis here potentially overestimates the amount of undetected disease,” he noted.
Prostate cancer that is not clinically significant is often monitored with active surveillance, so “invisible” cancers missed on mpMRI could actually be looked at in a positive light, he explained.
Variation in technique, interpretation
But the quality of care when it comes to the diagnosis of prostate cancer is not equal everywhere, said Gerald Andriole, MD, from the Washington School of Medicine in St. Louis, Missouri.
“When you get an MRI in a center that doesn’t do a lot of prostate cancer testing, you may not have the best software and you may have a radiologist who is not that experienced,” he told Medscape Medical News. Specialized cancer centers of excellence tend to do a great job finding prostate cancer, “but other centers have high significant-miss rates or high overcall rates.”
“The elephant in the room remains the considerable variation in technique and interobserver interpretation of prostate mpMRI,” write Steven Monda, MD, and Marc Dall’Era, MD, both from UC Davis Health in Sacramento, California, in an editorial that accompanies the new PROMIS analysis.
“These problems must be addressed and remedied in each institution before relying on results from PROMIS to drive changes in clinical practice,” they add.
Norris, Andriole, Monda, and Dall’Era have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Prostate cancers that are missed on multiparametric (mp) MRI are small and “not life-threatening,” according to an analysis of data from the Prostate MR Imaging Study (PROMIS).
“Our work suggests that MRI scans of the prostate appear to deliver crucial information about a man’s risk of dying from prostate cancer, even before he has a biopsy,” said Joseph Norris, BM BS, from University College London.
“This may mean that we can finally move prostate cancer to a position in which we can use imaging as the primary tool to direct further investigations, treatment, and prediction of risk,” he told Medscape Medical News.
This is “a position that all other solid organ cancers have reached,” said Norris, who will present the findings at the upcoming virtual European Association of Urology 2020 Congress.
All 576 PROMIS participants underwent an mpMRI scan, a transrectal ultrasonography (TRUS)–guided biopsy, and a template prostate mapping (TPM) biopsy taken at 5-mm intervals across the entire prostate.
PROMIS researchers previously showed that mpMRI had a 93% sensitivity for clinically significant cancer, whereas TRUS biopsy had only a 48% sensitivity, as reported by Medscape Medical News. And they concluded that the use of mpMRI as a first-line diagnostic tool could prevent 27% of all biopsies, which can have serious adverse effects, such as pain, urinary problems, infection, bleeding, and erectile dysfunction.
However, in their study looking at the accuracy of mpMRI and TRUS biopsy, the researchers did not investigate the severity of the 7% of cancers that mpMRI missed. “What if those missed cancers are, in fact, aggressive? That’s what we set out to examine,” Norris explained.
So he and his colleagues conducted a post ad hoc analysis of the PROMIS participants in whom clinically significant cancer had been detected with TPM biopsy to see which of those cancers had been detected with mpMRI. The findings were published online in European Urology.
Cancers met the strict definition of clinically significant if they had a Gleason score of at least 4+3 for a tumor of any length, or a maximum cancer core length (MCCL) greater than 6 mm for a cancer of any grade. They met the less-strict definition if they had a Gleason score of at least 3+4 for a tumor of any length, or a MCCL greater than 4 mm for a cancer of any grade.
In PROMIS, TPM biopsy detected 230 cancers that met the strict definition of clinically significant and 331 that met the less-strict definition.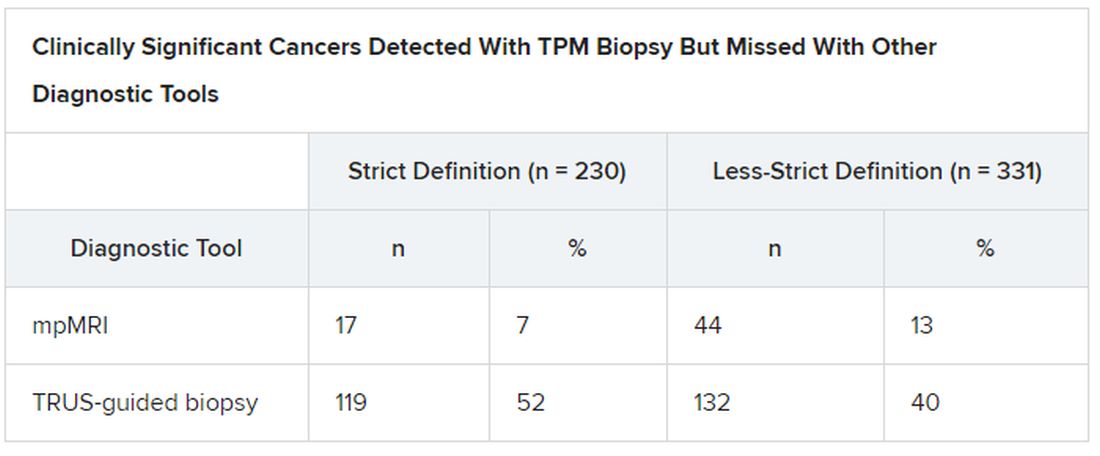
Overall Gleason scores were significantly lower for the 17 strict-definition cancers not detected with 1.5 T mpMRI than for those detected with mpMRI (P = .0007), as were maximum Gleason scores (P < .0001).
Median MCCL was 3 mm shorter for all 17 tumors missed with mpMRI than for those detected with mpMRI (5 vs 8 mm; P < .0001).
mpMRI detected all tumors identified on TPM biopsy that had an overall Gleason score greater than 3+4 (Gleason grades 3 to 5) or a maximum Gleason score greater than 4+3 (Gleason grades 4 and 5).
“This finding is important, given that in PROMIS, no men with an overall Gleason score of 4+3 had cancer missed by MRI, indicating that actually MRI may be able to identify all truly significant cancers,” said Norris.
Adding PSA Density Threshold
To further assess cancers missed on mpMRI, the researchers looked at prostate-specific antigen (PSA) density, calculated as total PSA level (ng/mL) divided by prostate volume (mL).
“We found that if we applied a threshold PSA density to men with normal-looking MRI scans, we could reduce the proportion of missed significant cancer to just 5%. This is exciting; it means we can make MRI an even more effective test for prostate cancer in a very simple way,” Norris reported.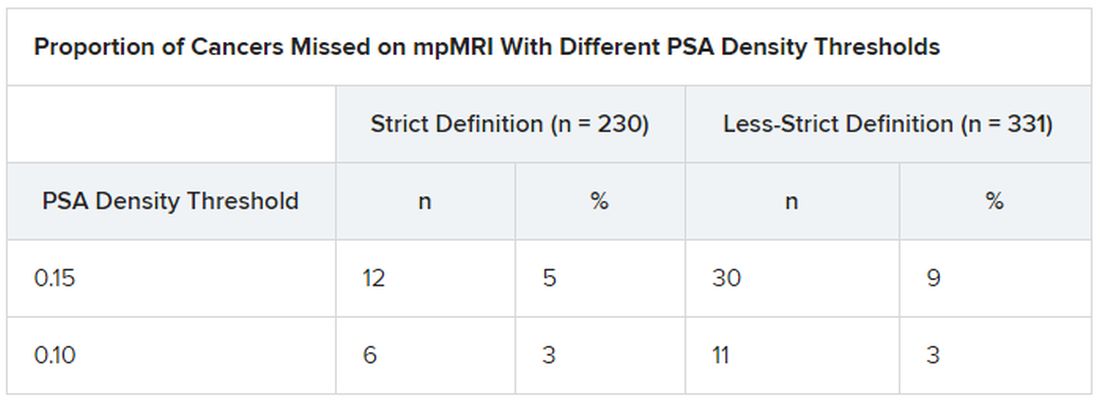
“These data show that no highly aggressive prostate cancers were missed by MRI, either at the level of the whole prostate or at the individual needle level,” said Norris. This should lead to positive outcomes in the long term.
And since the PROMIS data were gathered, MRI technology has improved, he said. The “MRI scanners in PROMIS were 1.5 Tesla,” whereas today’s machines are 3.0 T, which could increase the detection of significant prostate cancer.
In fact, “our analysis here potentially overestimates the amount of undetected disease,” he noted.
Prostate cancer that is not clinically significant is often monitored with active surveillance, so “invisible” cancers missed on mpMRI could actually be looked at in a positive light, he explained.
Variation in technique, interpretation
But the quality of care when it comes to the diagnosis of prostate cancer is not equal everywhere, said Gerald Andriole, MD, from the Washington School of Medicine in St. Louis, Missouri.
“When you get an MRI in a center that doesn’t do a lot of prostate cancer testing, you may not have the best software and you may have a radiologist who is not that experienced,” he told Medscape Medical News. Specialized cancer centers of excellence tend to do a great job finding prostate cancer, “but other centers have high significant-miss rates or high overcall rates.”
“The elephant in the room remains the considerable variation in technique and interobserver interpretation of prostate mpMRI,” write Steven Monda, MD, and Marc Dall’Era, MD, both from UC Davis Health in Sacramento, California, in an editorial that accompanies the new PROMIS analysis.
“These problems must be addressed and remedied in each institution before relying on results from PROMIS to drive changes in clinical practice,” they add.
Norris, Andriole, Monda, and Dall’Era have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Prostate cancers that are missed on multiparametric (mp) MRI are small and “not life-threatening,” according to an analysis of data from the Prostate MR Imaging Study (PROMIS).
“Our work suggests that MRI scans of the prostate appear to deliver crucial information about a man’s risk of dying from prostate cancer, even before he has a biopsy,” said Joseph Norris, BM BS, from University College London.
“This may mean that we can finally move prostate cancer to a position in which we can use imaging as the primary tool to direct further investigations, treatment, and prediction of risk,” he told Medscape Medical News.
This is “a position that all other solid organ cancers have reached,” said Norris, who will present the findings at the upcoming virtual European Association of Urology 2020 Congress.
All 576 PROMIS participants underwent an mpMRI scan, a transrectal ultrasonography (TRUS)–guided biopsy, and a template prostate mapping (TPM) biopsy taken at 5-mm intervals across the entire prostate.
PROMIS researchers previously showed that mpMRI had a 93% sensitivity for clinically significant cancer, whereas TRUS biopsy had only a 48% sensitivity, as reported by Medscape Medical News. And they concluded that the use of mpMRI as a first-line diagnostic tool could prevent 27% of all biopsies, which can have serious adverse effects, such as pain, urinary problems, infection, bleeding, and erectile dysfunction.
However, in their study looking at the accuracy of mpMRI and TRUS biopsy, the researchers did not investigate the severity of the 7% of cancers that mpMRI missed. “What if those missed cancers are, in fact, aggressive? That’s what we set out to examine,” Norris explained.
So he and his colleagues conducted a post ad hoc analysis of the PROMIS participants in whom clinically significant cancer had been detected with TPM biopsy to see which of those cancers had been detected with mpMRI. The findings were published online in European Urology.
Cancers met the strict definition of clinically significant if they had a Gleason score of at least 4+3 for a tumor of any length, or a maximum cancer core length (MCCL) greater than 6 mm for a cancer of any grade. They met the less-strict definition if they had a Gleason score of at least 3+4 for a tumor of any length, or a MCCL greater than 4 mm for a cancer of any grade.
In PROMIS, TPM biopsy detected 230 cancers that met the strict definition of clinically significant and 331 that met the less-strict definition.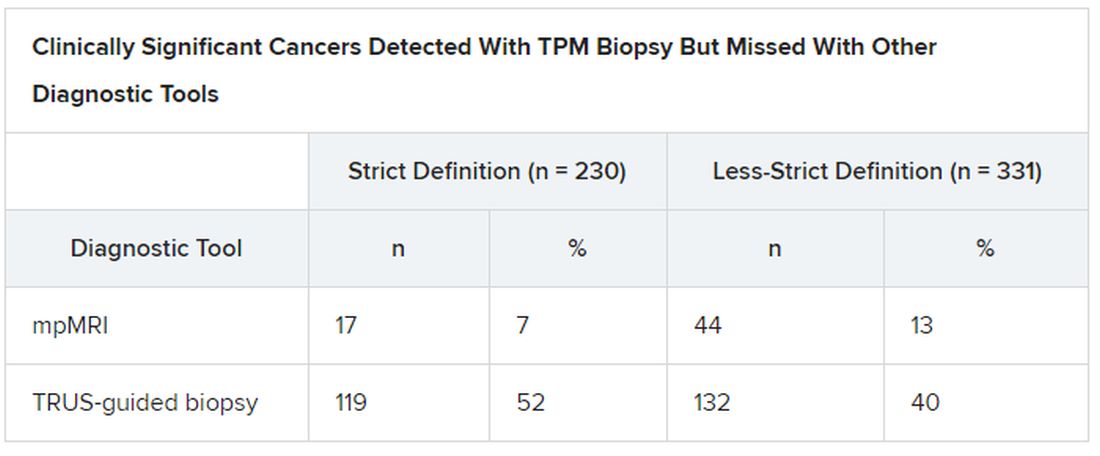
Overall Gleason scores were significantly lower for the 17 strict-definition cancers not detected with 1.5 T mpMRI than for those detected with mpMRI (P = .0007), as were maximum Gleason scores (P < .0001).
Median MCCL was 3 mm shorter for all 17 tumors missed with mpMRI than for those detected with mpMRI (5 vs 8 mm; P < .0001).
mpMRI detected all tumors identified on TPM biopsy that had an overall Gleason score greater than 3+4 (Gleason grades 3 to 5) or a maximum Gleason score greater than 4+3 (Gleason grades 4 and 5).
“This finding is important, given that in PROMIS, no men with an overall Gleason score of 4+3 had cancer missed by MRI, indicating that actually MRI may be able to identify all truly significant cancers,” said Norris.
Adding PSA Density Threshold
To further assess cancers missed on mpMRI, the researchers looked at prostate-specific antigen (PSA) density, calculated as total PSA level (ng/mL) divided by prostate volume (mL).
“We found that if we applied a threshold PSA density to men with normal-looking MRI scans, we could reduce the proportion of missed significant cancer to just 5%. This is exciting; it means we can make MRI an even more effective test for prostate cancer in a very simple way,” Norris reported.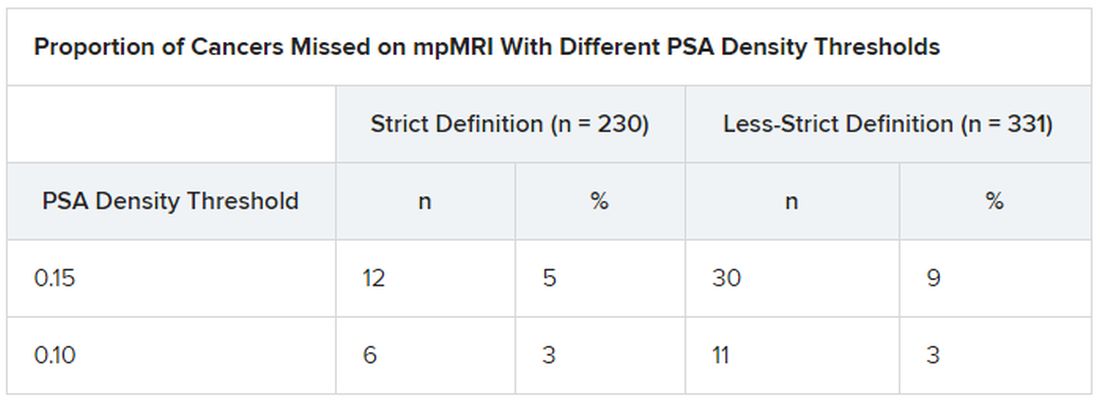
“These data show that no highly aggressive prostate cancers were missed by MRI, either at the level of the whole prostate or at the individual needle level,” said Norris. This should lead to positive outcomes in the long term.
And since the PROMIS data were gathered, MRI technology has improved, he said. The “MRI scanners in PROMIS were 1.5 Tesla,” whereas today’s machines are 3.0 T, which could increase the detection of significant prostate cancer.
In fact, “our analysis here potentially overestimates the amount of undetected disease,” he noted.
Prostate cancer that is not clinically significant is often monitored with active surveillance, so “invisible” cancers missed on mpMRI could actually be looked at in a positive light, he explained.
Variation in technique, interpretation
But the quality of care when it comes to the diagnosis of prostate cancer is not equal everywhere, said Gerald Andriole, MD, from the Washington School of Medicine in St. Louis, Missouri.
“When you get an MRI in a center that doesn’t do a lot of prostate cancer testing, you may not have the best software and you may have a radiologist who is not that experienced,” he told Medscape Medical News. Specialized cancer centers of excellence tend to do a great job finding prostate cancer, “but other centers have high significant-miss rates or high overcall rates.”
“The elephant in the room remains the considerable variation in technique and interobserver interpretation of prostate mpMRI,” write Steven Monda, MD, and Marc Dall’Era, MD, both from UC Davis Health in Sacramento, California, in an editorial that accompanies the new PROMIS analysis.
“These problems must be addressed and remedied in each institution before relying on results from PROMIS to drive changes in clinical practice,” they add.
Norris, Andriole, Monda, and Dall’Era have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Psychiatry trainees subjected to high levels of physical, sexual, verbal abuse from patients
More than 80% of psychiatric trainees have experienced some kind of verbal, physical, or sexual assault from patients, and approximately one-third have been physically attacked multiple times, new survey results show.
Such incidents, said study investigator Victor Pereira-Sanchez, MD, from the department of child and adolescent psychiatry at New York University take a toll on the trainees’ well-being and may ultimately affect the quality of patient care.
“The extent of violence against psychiatric trainees is alarming and calls for the implementation of effective training, prevention, and intervention measures,” Dr. Pereira-Sanchez said in an interview.
The findings were presented at the European Psychiatric Association (EPA) 2020 Congress, which was virtual this year because of the COVID-19 pandemic.
Widespread problem
Violence against health care professionals is widespread among clinicians in EDs with psychiatry trainees “more exposed and vulnerable,” Dr. Pereira-Sanchez said during his presentation.
In 2017, the European Federation of Psychiatric Trainees established a group of researchers to describe “the extent and consequences of violence against psychiatric trainees in Europe and beyond,” he said. The group developed a 15-item questionnaire asking young clinicians about experiences of physical, sexual, and verbal assault at work. The survey was posted online by partner institutions via social media.
A total of 827 psychiatric trainees, the majority of whom were from France and the United Kingdom, completed the survey. Respondents had an average age of 31 years, and 68% were women. On average, respondents had completed 51.3% of their psychiatric training.
with 92.0% reporting verbal assaults, 44.1% physical assaults, and 9.3% sexual assaults. In addition, 14.2% had been assaulted once, 51.9% had been assaulted two to five times, and 33.9% had been assaulted more than five times during their training. Results also showed that assaults were more likely to occur on an inpatient ward (63.4%) or the ED (56.9%), although 37.2% occurred in an outpatient setting and 4.2% in community settings. The majority of respondents (69.0%) did not report their assaults, and 67.3% did not call police or security personnel.
The most common emotions experienced by trainees following an assault were fear, rage, and anxiety. Guilt, sadness, feeling unsupported, and self-doubt were also reported.
Dr. Pereira-Sanchez noted the low rate of reported assaults is likely because trainees view it as “part of the job to get insulted, it’s part of the job to suffer minor physical violence.”
Individuals who did report assaults tended to be those who had been assaulted more than five times and those who felt more anxiety, rage, and fear.
“Basically, those who experience more emotional consequences and physical consequences tend to report more,” he said.
In addition, trainees tended to report assaults if they worked in an institution that provided protocols and training in prevention and management of patient aggression.
However, he added, most respondents reported they were not aware of their center’s protocols with respect to assaults and were not trained in the management or prevention of patient violence.
Management tools key
Commenting on the study in an interview, Renee Binder, MD, professor of psychiatry at University of California, San Francisco, said the findings show that, “when patients are out of control, they may act inappropriately, including verbal, physical, and sexual assaults.”
Consequently, “clinicians should be prepared and have management tools,” said Dr. Binder, who was not involved in the research.
She noted that derogatory statements and racial slurs were included among the verbal assaults, which is particularly common in inpatient units and EDs where “patients may be acutely psychotic or manic and out of control,” she said.
However, Dr. Binder pointed out that the investigators did not separate mild and more severe forms of physical and sexual assault.
“If the authors had more finely separated out the types of physical and sexual assaults, they probably would have found that mild types of assaults are much more common than more severe assaults,” she said.
Dr. Pereira-Sanchez’s fellowship program is funded by Fundacion Alicia Koplowitz. He and Dr. Binder have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
More than 80% of psychiatric trainees have experienced some kind of verbal, physical, or sexual assault from patients, and approximately one-third have been physically attacked multiple times, new survey results show.
Such incidents, said study investigator Victor Pereira-Sanchez, MD, from the department of child and adolescent psychiatry at New York University take a toll on the trainees’ well-being and may ultimately affect the quality of patient care.
“The extent of violence against psychiatric trainees is alarming and calls for the implementation of effective training, prevention, and intervention measures,” Dr. Pereira-Sanchez said in an interview.
The findings were presented at the European Psychiatric Association (EPA) 2020 Congress, which was virtual this year because of the COVID-19 pandemic.
Widespread problem
Violence against health care professionals is widespread among clinicians in EDs with psychiatry trainees “more exposed and vulnerable,” Dr. Pereira-Sanchez said during his presentation.
In 2017, the European Federation of Psychiatric Trainees established a group of researchers to describe “the extent and consequences of violence against psychiatric trainees in Europe and beyond,” he said. The group developed a 15-item questionnaire asking young clinicians about experiences of physical, sexual, and verbal assault at work. The survey was posted online by partner institutions via social media.
A total of 827 psychiatric trainees, the majority of whom were from France and the United Kingdom, completed the survey. Respondents had an average age of 31 years, and 68% were women. On average, respondents had completed 51.3% of their psychiatric training.
with 92.0% reporting verbal assaults, 44.1% physical assaults, and 9.3% sexual assaults. In addition, 14.2% had been assaulted once, 51.9% had been assaulted two to five times, and 33.9% had been assaulted more than five times during their training. Results also showed that assaults were more likely to occur on an inpatient ward (63.4%) or the ED (56.9%), although 37.2% occurred in an outpatient setting and 4.2% in community settings. The majority of respondents (69.0%) did not report their assaults, and 67.3% did not call police or security personnel.
The most common emotions experienced by trainees following an assault were fear, rage, and anxiety. Guilt, sadness, feeling unsupported, and self-doubt were also reported.
Dr. Pereira-Sanchez noted the low rate of reported assaults is likely because trainees view it as “part of the job to get insulted, it’s part of the job to suffer minor physical violence.”
Individuals who did report assaults tended to be those who had been assaulted more than five times and those who felt more anxiety, rage, and fear.
“Basically, those who experience more emotional consequences and physical consequences tend to report more,” he said.
In addition, trainees tended to report assaults if they worked in an institution that provided protocols and training in prevention and management of patient aggression.
However, he added, most respondents reported they were not aware of their center’s protocols with respect to assaults and were not trained in the management or prevention of patient violence.
Management tools key
Commenting on the study in an interview, Renee Binder, MD, professor of psychiatry at University of California, San Francisco, said the findings show that, “when patients are out of control, they may act inappropriately, including verbal, physical, and sexual assaults.”
Consequently, “clinicians should be prepared and have management tools,” said Dr. Binder, who was not involved in the research.
She noted that derogatory statements and racial slurs were included among the verbal assaults, which is particularly common in inpatient units and EDs where “patients may be acutely psychotic or manic and out of control,” she said.
However, Dr. Binder pointed out that the investigators did not separate mild and more severe forms of physical and sexual assault.
“If the authors had more finely separated out the types of physical and sexual assaults, they probably would have found that mild types of assaults are much more common than more severe assaults,” she said.
Dr. Pereira-Sanchez’s fellowship program is funded by Fundacion Alicia Koplowitz. He and Dr. Binder have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
More than 80% of psychiatric trainees have experienced some kind of verbal, physical, or sexual assault from patients, and approximately one-third have been physically attacked multiple times, new survey results show.
Such incidents, said study investigator Victor Pereira-Sanchez, MD, from the department of child and adolescent psychiatry at New York University take a toll on the trainees’ well-being and may ultimately affect the quality of patient care.
“The extent of violence against psychiatric trainees is alarming and calls for the implementation of effective training, prevention, and intervention measures,” Dr. Pereira-Sanchez said in an interview.
The findings were presented at the European Psychiatric Association (EPA) 2020 Congress, which was virtual this year because of the COVID-19 pandemic.
Widespread problem
Violence against health care professionals is widespread among clinicians in EDs with psychiatry trainees “more exposed and vulnerable,” Dr. Pereira-Sanchez said during his presentation.
In 2017, the European Federation of Psychiatric Trainees established a group of researchers to describe “the extent and consequences of violence against psychiatric trainees in Europe and beyond,” he said. The group developed a 15-item questionnaire asking young clinicians about experiences of physical, sexual, and verbal assault at work. The survey was posted online by partner institutions via social media.
A total of 827 psychiatric trainees, the majority of whom were from France and the United Kingdom, completed the survey. Respondents had an average age of 31 years, and 68% were women. On average, respondents had completed 51.3% of their psychiatric training.
with 92.0% reporting verbal assaults, 44.1% physical assaults, and 9.3% sexual assaults. In addition, 14.2% had been assaulted once, 51.9% had been assaulted two to five times, and 33.9% had been assaulted more than five times during their training. Results also showed that assaults were more likely to occur on an inpatient ward (63.4%) or the ED (56.9%), although 37.2% occurred in an outpatient setting and 4.2% in community settings. The majority of respondents (69.0%) did not report their assaults, and 67.3% did not call police or security personnel.
The most common emotions experienced by trainees following an assault were fear, rage, and anxiety. Guilt, sadness, feeling unsupported, and self-doubt were also reported.
Dr. Pereira-Sanchez noted the low rate of reported assaults is likely because trainees view it as “part of the job to get insulted, it’s part of the job to suffer minor physical violence.”
Individuals who did report assaults tended to be those who had been assaulted more than five times and those who felt more anxiety, rage, and fear.
“Basically, those who experience more emotional consequences and physical consequences tend to report more,” he said.
In addition, trainees tended to report assaults if they worked in an institution that provided protocols and training in prevention and management of patient aggression.
However, he added, most respondents reported they were not aware of their center’s protocols with respect to assaults and were not trained in the management or prevention of patient violence.
Management tools key
Commenting on the study in an interview, Renee Binder, MD, professor of psychiatry at University of California, San Francisco, said the findings show that, “when patients are out of control, they may act inappropriately, including verbal, physical, and sexual assaults.”
Consequently, “clinicians should be prepared and have management tools,” said Dr. Binder, who was not involved in the research.
She noted that derogatory statements and racial slurs were included among the verbal assaults, which is particularly common in inpatient units and EDs where “patients may be acutely psychotic or manic and out of control,” she said.
However, Dr. Binder pointed out that the investigators did not separate mild and more severe forms of physical and sexual assault.
“If the authors had more finely separated out the types of physical and sexual assaults, they probably would have found that mild types of assaults are much more common than more severe assaults,” she said.
Dr. Pereira-Sanchez’s fellowship program is funded by Fundacion Alicia Koplowitz. He and Dr. Binder have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Move over supplements, here come medical foods
As the Food and Drug Administration focuses on other issues, companies, both big and small, are looking to boost physician and consumer interest in their “medical foods” – products that fall somewhere between drugs and supplements and promise to mitigate symptoms, or even address underlying pathologies, of a range of diseases.
Manufacturers now market an array of medical foods, ranging from powders and capsules for Alzheimer disease to low-protein spaghetti for chronic kidney disease (CKD). The FDA has not been completely absent; it takes a narrow view of what medical conditions qualify for treatment with food products and has warned some manufacturers that their misbranded products are acting more like unapproved drugs.
By the FDA’s definition, medical food is limited to products that provide crucial therapy for patients with inborn errors of metabolism (IEM). An example is specialized baby formula for infants with phenylketonuria. Unlike supplements, medical foods are supposed to be used under the supervision of a physician. This has prompted some sales reps to turn up in the clinic, and most manufacturers have online approval forms for doctors to sign. Manufacturers, advisers, and regulators were interviewed for a closer look at this burgeoning industry.
The market
The global market for medical foods – about $18 billion in 2019 – is expected to grow steadily in the near future. It is drawing more interest, especially in Europe, where medical foods are more accepted by physicians and consumers, Meghan Donnelly, MS, RDN, said in an interview. She is a registered dietitian who conducts physician outreach in the United States for Flavis, a division of Dr. Schär. That company, based in northern Italy, started out targeting IEMs but now also sells gluten-free foods for celiac disease and low-protein foods for CKD.
It is still a niche market in the United States – and isn’t likely to ever approach the size of the supplement market, according to Marcus Charuvastra, the managing director of Targeted Medical Pharma, which markets Theramine capsules for pain management, among many other products. But it could still be a big win for a manufacturer if they get a small slice of a big market, such as for Alzheimer disease.
Defining medical food
According to an update of the Orphan Drug Act in 1988, a medical food is “a food which is formulated to be consumed or administered enterally under the supervision of a physician and which is intended for the specific dietary management of a disease or condition for which distinctive nutritional requirements, based on recognized scientific principles, are established by medical evaluation.” The FDA issued regulations to accompany that law in 1993 but has since only issued a guidance document that is not legally binding.
Medical foods are not drugs and they are not supplements (the latter are intended only for healthy people). The FDA doesn’t require formal approval of a medical food, but, by law, the ingredients must be generally recognized as safe, and manufacturers must follow good manufacturing practices. However, the agency has taken a narrow view of what conditions require medical foods.
Policing medical foods hasn’t been a priority for the FDA, which is why there has been a proliferation of products that don’t meet the FDA’s view of the statutory definition of medical foods, according to Miriam Guggenheim, a food and drug law attorney in Washington, D.C. The FDA usually takes enforcement action when it sees a risk to the public’s health.
The agency’s stance has led to confusion – among manufacturers, physicians, consumers, and even regulators – making the market a kind of Wild West, according to Paul Hyman, a Washington, D.C.–based attorney who has represented medical food companies.
George A. Burdock, PhD, an Orlando-based regulatory consultant who has worked with medical food makers, believes the FDA will be forced to expand their narrow definition. He foresees a reconsideration of many medical food products in light of an October 2019 White House executive order prohibiting federal agencies from issuing guidance in lieu of rules.
Manufacturers and the FDA differ
One example of a product about which regulators and manufacturers differ is Theramine, which is described as “specially designed to supply the nervous system with the fuel it needs to meet the altered metabolic requirements of chronic pain and inflammatory disorders.”
It is not considered a medical food by the FDA, and the company has had numerous discussions with the agency about their diverging views, according to Mr. Charuvastra. “We’ve had our warning letters and we’ve had our sit downs, and we just had an inspection.”
Targeted Medical Pharma continues to market its products as medical foods but steers away from making any claims that they are like drugs, he said.
Confusion about medical foods has been exposed in the California Workers’ Compensation System by Leslie Wilson, PhD, and colleagues at the University of California, San Francisco. They found that physicians regularly wrote medical food prescriptions for non–FDA-approved uses and that the system reimbursed the majority of the products at a cost of $15.5 million from 2011 to 2013. More than half of these prescriptions were for Theramine.
Dr. Wilson reported that, for most products, no evidence supported effectiveness, and they were frequently mislabeled – for all 36 that were studied, submissions for reimbursement were made using a National Drug Code, an impossibility because medical foods are not drugs, and 14 were labeled “Rx only.”
Big-name companies joining in
The FDA does not keep a list of approved medical foods or manufacturers. Both small businesses and big food companies like Danone, Nestlé, and Abbott are players. Most products are sold online.

In the United States, Danone’s Nutricia division sells formulas and low-protein foods for IEMs. They also sell Ketocal, a powder or ready-to-drink liquid that is pitched as a balanced medical food to simplify and optimize the ketogenic diet for children with intractable epilepsy. Yet the FDA does not include epilepsy among the conditions that medical foods can treat.
Nestlé sells traditional medical foods for IEMs and also markets a range of what it calls nutritional therapies for such conditions as irritable bowel syndrome and dysphagia.
Nestlé is a minority shareholder in Axona, a product originally developed by Accera (Cerecin as of 2018). Jacquelyn Campo, senior director of global communications at Nestlé Health Sciences, said that the company is not actively involved in the operations management of Cerecin. However, on its website, Nestlé touts Axona, which is only available in the United States, as a “medical food” that “is intended for the clinical dietary management of mild to moderate Alzheimer disease.” The Axona site claims that the main ingredient, caprylic triglyceride, is broken down into ketones that provide fuel to treat cerebral hypometabolism, a precursor to Alzheimer disease. In a 2009 study, daily dosing of a preliminary formulation was associated with improved cognitive performance compared with placebo in patients with mild to moderate Alzheimer disease.
In 2013, the FDA warned Accera that it was misbranding Axona as a medical food and that the therapeutic claims the company was making would make the product an unapproved drug. Ms. Campo said Nestlé is aware of the agency’s warning, but added, “to our knowledge, Cerecin provided answers to the issues raised by the FDA.”
With the goal of getting drug approval, Accera went on to test a tweaked formulation in a 400-patient randomized, placebo-controlled trial called NOURISH AD that ultimately failed. Nevertheless, Axona is still marketed as a medical food. It costs about $100 for a month’s supply.
Repeated requests for comment from Cerecin were not answered. Danielle Schor, an FDA spokesperson, said the agency will not discuss the status of individual products.
More disputes and insurance coverage
Mary Ann DeMarco, executive director of sales and marketing for the Scottsdale, Ariz.–based medical food maker Primus Pharmaceuticals, said the company believes its products fit within the FDA’s medical foods rubric.
These include Fosteum Plus capsules, which it markets “for the clinical dietary management of the metabolic processes of osteopenia and osteoporosis.” The capsules contain a combination of genistein, zinc, calcium, phosphate, vitamin K2, and vitamin D. As proof of effectiveness, the company cites clinical data on some of the ingredients – not the product itself.
Primus has run afoul of the FDA before when it similarly positioned another product, called Limbrel, as a medical food for osteoarthritis. From 2007 to 2017, the FDA received 194 adverse event reports associated with Limbrel, including reports of drug-induced liver injury, pancreatitis, and hypersensitivity pneumonitis. In December 2017, the agency urged Primus to recall Limbrel, a move that it said was “necessary to protect the public health and welfare.” Primus withdrew the product but laid out a defense of Limbrel on a devoted website.
The FDA would not comment any further, said Ms. Schor. Ms. DeMarco said that Primus is working with the FDA to bring Limbrel back to market.
A lack of insurance coverage – even for approved medical foods for IEMs – has frustrated advocates, parents, and manufacturers. They are putting their weight behind the Medical Nutrition Equity Act, which would mandate public and private payer coverage of medical foods for IEMs and digestive conditions such as Crohn disease. That 2019 House bill has 56 cosponsors; there is no Senate companion bill.
“If you can get reimbursement, it really makes the market,” for Primus and the other manufacturers, Mr. Hyman said.
Primus Pharmaceuticals has launched its own campaign, Cover My Medical Foods, to enlist consumers and others to the cause.
Partnering with advocates
Although its low-protein breads, pastas, and baking products are not considered medical foods by the FDA, Dr. Schär is marketing them as such in the United States. They are trying to make a mark in CKD, according to Ms. Donnelly. She added that Dr. Schär has been successful in Europe, where nutrition therapy is more integrated in the health care system.
In 2019, Flavis and the National Kidney Foundation joined forces to raise awareness of nutritional interventions and to build enthusiasm for the Flavis products. The partnership has now ended, mostly because Flavis could no longer afford it, according to Ms. Donnelly.
“Information on diet and nutrition is the most requested subject matter from the NKF,” said Anthony Gucciardo, senior vice president of strategic partnerships at the foundation. The partnership “has never been necessarily about promoting their products per se; it’s promoting a healthy diet and really a diet specific for CKD.”
The NKF developed cobranded materials on low-protein foods for physicians and a teaching tool they could use with patients. Consumers could access nutrition information and a discount on Flavis products on a dedicated webpage. The foundation didn’t describe the low-protein products as medical foods, said Mr. Gucciardo, even if Flavis promoted them as such.
In patients with CKD, dietary management can help prevent the progression to end-stage renal disease. Although Medicare covers medical nutrition therapy – in which patients receive personalized assessments and dietary advice – uptake is abysmally low, according to a 2018 study.
Dr. Burdock thinks low-protein foods for CKD do meet the FDA’s criteria for a medical food but that the agency might not necessarily agree with him. The FDA would not comment.
Physician beware
When it comes to medical foods, the FDA has often looked the other way because the ingredients may already have been proven safe and the danger to an individual or to the public’s health is relatively low, according to Dr. Burdock and Mr. Hyman.
However, if the agency “feels that a medical food will prevent people from seeking medical care or there is potential to defraud the public, it is justified in taking action against the company,” said Dr. Burdock.
According to Dr. Wilson, the pharmacist who reported on the inappropriate medical food prescriptions in the California system, the FDA could help by creating a list of approved medical foods. Physicians should take time to learn about the difference between medical foods and supplements, she said, adding that they should also not hesitate to “question the veracity of the claims for them.”
Ms. Guggenheim believed doctors need to know that, for the most part, these are not FDA-approved products. She emphasized the importance of evaluating the products and looking at the data of their impact on a disease or condition.
“Many of these companies strongly believe that the products work and help people, so clinicians need to be very data driven,” she said.
A version of this article originally appeared on Medscape.com.
As the Food and Drug Administration focuses on other issues, companies, both big and small, are looking to boost physician and consumer interest in their “medical foods” – products that fall somewhere between drugs and supplements and promise to mitigate symptoms, or even address underlying pathologies, of a range of diseases.
Manufacturers now market an array of medical foods, ranging from powders and capsules for Alzheimer disease to low-protein spaghetti for chronic kidney disease (CKD). The FDA has not been completely absent; it takes a narrow view of what medical conditions qualify for treatment with food products and has warned some manufacturers that their misbranded products are acting more like unapproved drugs.
By the FDA’s definition, medical food is limited to products that provide crucial therapy for patients with inborn errors of metabolism (IEM). An example is specialized baby formula for infants with phenylketonuria. Unlike supplements, medical foods are supposed to be used under the supervision of a physician. This has prompted some sales reps to turn up in the clinic, and most manufacturers have online approval forms for doctors to sign. Manufacturers, advisers, and regulators were interviewed for a closer look at this burgeoning industry.
The market
The global market for medical foods – about $18 billion in 2019 – is expected to grow steadily in the near future. It is drawing more interest, especially in Europe, where medical foods are more accepted by physicians and consumers, Meghan Donnelly, MS, RDN, said in an interview. She is a registered dietitian who conducts physician outreach in the United States for Flavis, a division of Dr. Schär. That company, based in northern Italy, started out targeting IEMs but now also sells gluten-free foods for celiac disease and low-protein foods for CKD.
It is still a niche market in the United States – and isn’t likely to ever approach the size of the supplement market, according to Marcus Charuvastra, the managing director of Targeted Medical Pharma, which markets Theramine capsules for pain management, among many other products. But it could still be a big win for a manufacturer if they get a small slice of a big market, such as for Alzheimer disease.
Defining medical food
According to an update of the Orphan Drug Act in 1988, a medical food is “a food which is formulated to be consumed or administered enterally under the supervision of a physician and which is intended for the specific dietary management of a disease or condition for which distinctive nutritional requirements, based on recognized scientific principles, are established by medical evaluation.” The FDA issued regulations to accompany that law in 1993 but has since only issued a guidance document that is not legally binding.
Medical foods are not drugs and they are not supplements (the latter are intended only for healthy people). The FDA doesn’t require formal approval of a medical food, but, by law, the ingredients must be generally recognized as safe, and manufacturers must follow good manufacturing practices. However, the agency has taken a narrow view of what conditions require medical foods.
Policing medical foods hasn’t been a priority for the FDA, which is why there has been a proliferation of products that don’t meet the FDA’s view of the statutory definition of medical foods, according to Miriam Guggenheim, a food and drug law attorney in Washington, D.C. The FDA usually takes enforcement action when it sees a risk to the public’s health.
The agency’s stance has led to confusion – among manufacturers, physicians, consumers, and even regulators – making the market a kind of Wild West, according to Paul Hyman, a Washington, D.C.–based attorney who has represented medical food companies.
George A. Burdock, PhD, an Orlando-based regulatory consultant who has worked with medical food makers, believes the FDA will be forced to expand their narrow definition. He foresees a reconsideration of many medical food products in light of an October 2019 White House executive order prohibiting federal agencies from issuing guidance in lieu of rules.
Manufacturers and the FDA differ
One example of a product about which regulators and manufacturers differ is Theramine, which is described as “specially designed to supply the nervous system with the fuel it needs to meet the altered metabolic requirements of chronic pain and inflammatory disorders.”
It is not considered a medical food by the FDA, and the company has had numerous discussions with the agency about their diverging views, according to Mr. Charuvastra. “We’ve had our warning letters and we’ve had our sit downs, and we just had an inspection.”
Targeted Medical Pharma continues to market its products as medical foods but steers away from making any claims that they are like drugs, he said.
Confusion about medical foods has been exposed in the California Workers’ Compensation System by Leslie Wilson, PhD, and colleagues at the University of California, San Francisco. They found that physicians regularly wrote medical food prescriptions for non–FDA-approved uses and that the system reimbursed the majority of the products at a cost of $15.5 million from 2011 to 2013. More than half of these prescriptions were for Theramine.
Dr. Wilson reported that, for most products, no evidence supported effectiveness, and they were frequently mislabeled – for all 36 that were studied, submissions for reimbursement were made using a National Drug Code, an impossibility because medical foods are not drugs, and 14 were labeled “Rx only.”
Big-name companies joining in
The FDA does not keep a list of approved medical foods or manufacturers. Both small businesses and big food companies like Danone, Nestlé, and Abbott are players. Most products are sold online.

In the United States, Danone’s Nutricia division sells formulas and low-protein foods for IEMs. They also sell Ketocal, a powder or ready-to-drink liquid that is pitched as a balanced medical food to simplify and optimize the ketogenic diet for children with intractable epilepsy. Yet the FDA does not include epilepsy among the conditions that medical foods can treat.
Nestlé sells traditional medical foods for IEMs and also markets a range of what it calls nutritional therapies for such conditions as irritable bowel syndrome and dysphagia.
Nestlé is a minority shareholder in Axona, a product originally developed by Accera (Cerecin as of 2018). Jacquelyn Campo, senior director of global communications at Nestlé Health Sciences, said that the company is not actively involved in the operations management of Cerecin. However, on its website, Nestlé touts Axona, which is only available in the United States, as a “medical food” that “is intended for the clinical dietary management of mild to moderate Alzheimer disease.” The Axona site claims that the main ingredient, caprylic triglyceride, is broken down into ketones that provide fuel to treat cerebral hypometabolism, a precursor to Alzheimer disease. In a 2009 study, daily dosing of a preliminary formulation was associated with improved cognitive performance compared with placebo in patients with mild to moderate Alzheimer disease.
In 2013, the FDA warned Accera that it was misbranding Axona as a medical food and that the therapeutic claims the company was making would make the product an unapproved drug. Ms. Campo said Nestlé is aware of the agency’s warning, but added, “to our knowledge, Cerecin provided answers to the issues raised by the FDA.”
With the goal of getting drug approval, Accera went on to test a tweaked formulation in a 400-patient randomized, placebo-controlled trial called NOURISH AD that ultimately failed. Nevertheless, Axona is still marketed as a medical food. It costs about $100 for a month’s supply.
Repeated requests for comment from Cerecin were not answered. Danielle Schor, an FDA spokesperson, said the agency will not discuss the status of individual products.
More disputes and insurance coverage
Mary Ann DeMarco, executive director of sales and marketing for the Scottsdale, Ariz.–based medical food maker Primus Pharmaceuticals, said the company believes its products fit within the FDA’s medical foods rubric.
These include Fosteum Plus capsules, which it markets “for the clinical dietary management of the metabolic processes of osteopenia and osteoporosis.” The capsules contain a combination of genistein, zinc, calcium, phosphate, vitamin K2, and vitamin D. As proof of effectiveness, the company cites clinical data on some of the ingredients – not the product itself.
Primus has run afoul of the FDA before when it similarly positioned another product, called Limbrel, as a medical food for osteoarthritis. From 2007 to 2017, the FDA received 194 adverse event reports associated with Limbrel, including reports of drug-induced liver injury, pancreatitis, and hypersensitivity pneumonitis. In December 2017, the agency urged Primus to recall Limbrel, a move that it said was “necessary to protect the public health and welfare.” Primus withdrew the product but laid out a defense of Limbrel on a devoted website.
The FDA would not comment any further, said Ms. Schor. Ms. DeMarco said that Primus is working with the FDA to bring Limbrel back to market.
A lack of insurance coverage – even for approved medical foods for IEMs – has frustrated advocates, parents, and manufacturers. They are putting their weight behind the Medical Nutrition Equity Act, which would mandate public and private payer coverage of medical foods for IEMs and digestive conditions such as Crohn disease. That 2019 House bill has 56 cosponsors; there is no Senate companion bill.
“If you can get reimbursement, it really makes the market,” for Primus and the other manufacturers, Mr. Hyman said.
Primus Pharmaceuticals has launched its own campaign, Cover My Medical Foods, to enlist consumers and others to the cause.
Partnering with advocates
Although its low-protein breads, pastas, and baking products are not considered medical foods by the FDA, Dr. Schär is marketing them as such in the United States. They are trying to make a mark in CKD, according to Ms. Donnelly. She added that Dr. Schär has been successful in Europe, where nutrition therapy is more integrated in the health care system.
In 2019, Flavis and the National Kidney Foundation joined forces to raise awareness of nutritional interventions and to build enthusiasm for the Flavis products. The partnership has now ended, mostly because Flavis could no longer afford it, according to Ms. Donnelly.
“Information on diet and nutrition is the most requested subject matter from the NKF,” said Anthony Gucciardo, senior vice president of strategic partnerships at the foundation. The partnership “has never been necessarily about promoting their products per se; it’s promoting a healthy diet and really a diet specific for CKD.”
The NKF developed cobranded materials on low-protein foods for physicians and a teaching tool they could use with patients. Consumers could access nutrition information and a discount on Flavis products on a dedicated webpage. The foundation didn’t describe the low-protein products as medical foods, said Mr. Gucciardo, even if Flavis promoted them as such.
In patients with CKD, dietary management can help prevent the progression to end-stage renal disease. Although Medicare covers medical nutrition therapy – in which patients receive personalized assessments and dietary advice – uptake is abysmally low, according to a 2018 study.
Dr. Burdock thinks low-protein foods for CKD do meet the FDA’s criteria for a medical food but that the agency might not necessarily agree with him. The FDA would not comment.
Physician beware
When it comes to medical foods, the FDA has often looked the other way because the ingredients may already have been proven safe and the danger to an individual or to the public’s health is relatively low, according to Dr. Burdock and Mr. Hyman.
However, if the agency “feels that a medical food will prevent people from seeking medical care or there is potential to defraud the public, it is justified in taking action against the company,” said Dr. Burdock.
According to Dr. Wilson, the pharmacist who reported on the inappropriate medical food prescriptions in the California system, the FDA could help by creating a list of approved medical foods. Physicians should take time to learn about the difference between medical foods and supplements, she said, adding that they should also not hesitate to “question the veracity of the claims for them.”
Ms. Guggenheim believed doctors need to know that, for the most part, these are not FDA-approved products. She emphasized the importance of evaluating the products and looking at the data of their impact on a disease or condition.
“Many of these companies strongly believe that the products work and help people, so clinicians need to be very data driven,” she said.
A version of this article originally appeared on Medscape.com.
As the Food and Drug Administration focuses on other issues, companies, both big and small, are looking to boost physician and consumer interest in their “medical foods” – products that fall somewhere between drugs and supplements and promise to mitigate symptoms, or even address underlying pathologies, of a range of diseases.
Manufacturers now market an array of medical foods, ranging from powders and capsules for Alzheimer disease to low-protein spaghetti for chronic kidney disease (CKD). The FDA has not been completely absent; it takes a narrow view of what medical conditions qualify for treatment with food products and has warned some manufacturers that their misbranded products are acting more like unapproved drugs.
By the FDA’s definition, medical food is limited to products that provide crucial therapy for patients with inborn errors of metabolism (IEM). An example is specialized baby formula for infants with phenylketonuria. Unlike supplements, medical foods are supposed to be used under the supervision of a physician. This has prompted some sales reps to turn up in the clinic, and most manufacturers have online approval forms for doctors to sign. Manufacturers, advisers, and regulators were interviewed for a closer look at this burgeoning industry.
The market
The global market for medical foods – about $18 billion in 2019 – is expected to grow steadily in the near future. It is drawing more interest, especially in Europe, where medical foods are more accepted by physicians and consumers, Meghan Donnelly, MS, RDN, said in an interview. She is a registered dietitian who conducts physician outreach in the United States for Flavis, a division of Dr. Schär. That company, based in northern Italy, started out targeting IEMs but now also sells gluten-free foods for celiac disease and low-protein foods for CKD.
It is still a niche market in the United States – and isn’t likely to ever approach the size of the supplement market, according to Marcus Charuvastra, the managing director of Targeted Medical Pharma, which markets Theramine capsules for pain management, among many other products. But it could still be a big win for a manufacturer if they get a small slice of a big market, such as for Alzheimer disease.
Defining medical food
According to an update of the Orphan Drug Act in 1988, a medical food is “a food which is formulated to be consumed or administered enterally under the supervision of a physician and which is intended for the specific dietary management of a disease or condition for which distinctive nutritional requirements, based on recognized scientific principles, are established by medical evaluation.” The FDA issued regulations to accompany that law in 1993 but has since only issued a guidance document that is not legally binding.
Medical foods are not drugs and they are not supplements (the latter are intended only for healthy people). The FDA doesn’t require formal approval of a medical food, but, by law, the ingredients must be generally recognized as safe, and manufacturers must follow good manufacturing practices. However, the agency has taken a narrow view of what conditions require medical foods.
Policing medical foods hasn’t been a priority for the FDA, which is why there has been a proliferation of products that don’t meet the FDA’s view of the statutory definition of medical foods, according to Miriam Guggenheim, a food and drug law attorney in Washington, D.C. The FDA usually takes enforcement action when it sees a risk to the public’s health.
The agency’s stance has led to confusion – among manufacturers, physicians, consumers, and even regulators – making the market a kind of Wild West, according to Paul Hyman, a Washington, D.C.–based attorney who has represented medical food companies.
George A. Burdock, PhD, an Orlando-based regulatory consultant who has worked with medical food makers, believes the FDA will be forced to expand their narrow definition. He foresees a reconsideration of many medical food products in light of an October 2019 White House executive order prohibiting federal agencies from issuing guidance in lieu of rules.
Manufacturers and the FDA differ
One example of a product about which regulators and manufacturers differ is Theramine, which is described as “specially designed to supply the nervous system with the fuel it needs to meet the altered metabolic requirements of chronic pain and inflammatory disorders.”
It is not considered a medical food by the FDA, and the company has had numerous discussions with the agency about their diverging views, according to Mr. Charuvastra. “We’ve had our warning letters and we’ve had our sit downs, and we just had an inspection.”
Targeted Medical Pharma continues to market its products as medical foods but steers away from making any claims that they are like drugs, he said.
Confusion about medical foods has been exposed in the California Workers’ Compensation System by Leslie Wilson, PhD, and colleagues at the University of California, San Francisco. They found that physicians regularly wrote medical food prescriptions for non–FDA-approved uses and that the system reimbursed the majority of the products at a cost of $15.5 million from 2011 to 2013. More than half of these prescriptions were for Theramine.
Dr. Wilson reported that, for most products, no evidence supported effectiveness, and they were frequently mislabeled – for all 36 that were studied, submissions for reimbursement were made using a National Drug Code, an impossibility because medical foods are not drugs, and 14 were labeled “Rx only.”
Big-name companies joining in
The FDA does not keep a list of approved medical foods or manufacturers. Both small businesses and big food companies like Danone, Nestlé, and Abbott are players. Most products are sold online.

In the United States, Danone’s Nutricia division sells formulas and low-protein foods for IEMs. They also sell Ketocal, a powder or ready-to-drink liquid that is pitched as a balanced medical food to simplify and optimize the ketogenic diet for children with intractable epilepsy. Yet the FDA does not include epilepsy among the conditions that medical foods can treat.
Nestlé sells traditional medical foods for IEMs and also markets a range of what it calls nutritional therapies for such conditions as irritable bowel syndrome and dysphagia.
Nestlé is a minority shareholder in Axona, a product originally developed by Accera (Cerecin as of 2018). Jacquelyn Campo, senior director of global communications at Nestlé Health Sciences, said that the company is not actively involved in the operations management of Cerecin. However, on its website, Nestlé touts Axona, which is only available in the United States, as a “medical food” that “is intended for the clinical dietary management of mild to moderate Alzheimer disease.” The Axona site claims that the main ingredient, caprylic triglyceride, is broken down into ketones that provide fuel to treat cerebral hypometabolism, a precursor to Alzheimer disease. In a 2009 study, daily dosing of a preliminary formulation was associated with improved cognitive performance compared with placebo in patients with mild to moderate Alzheimer disease.
In 2013, the FDA warned Accera that it was misbranding Axona as a medical food and that the therapeutic claims the company was making would make the product an unapproved drug. Ms. Campo said Nestlé is aware of the agency’s warning, but added, “to our knowledge, Cerecin provided answers to the issues raised by the FDA.”
With the goal of getting drug approval, Accera went on to test a tweaked formulation in a 400-patient randomized, placebo-controlled trial called NOURISH AD that ultimately failed. Nevertheless, Axona is still marketed as a medical food. It costs about $100 for a month’s supply.
Repeated requests for comment from Cerecin were not answered. Danielle Schor, an FDA spokesperson, said the agency will not discuss the status of individual products.
More disputes and insurance coverage
Mary Ann DeMarco, executive director of sales and marketing for the Scottsdale, Ariz.–based medical food maker Primus Pharmaceuticals, said the company believes its products fit within the FDA’s medical foods rubric.
These include Fosteum Plus capsules, which it markets “for the clinical dietary management of the metabolic processes of osteopenia and osteoporosis.” The capsules contain a combination of genistein, zinc, calcium, phosphate, vitamin K2, and vitamin D. As proof of effectiveness, the company cites clinical data on some of the ingredients – not the product itself.
Primus has run afoul of the FDA before when it similarly positioned another product, called Limbrel, as a medical food for osteoarthritis. From 2007 to 2017, the FDA received 194 adverse event reports associated with Limbrel, including reports of drug-induced liver injury, pancreatitis, and hypersensitivity pneumonitis. In December 2017, the agency urged Primus to recall Limbrel, a move that it said was “necessary to protect the public health and welfare.” Primus withdrew the product but laid out a defense of Limbrel on a devoted website.
The FDA would not comment any further, said Ms. Schor. Ms. DeMarco said that Primus is working with the FDA to bring Limbrel back to market.
A lack of insurance coverage – even for approved medical foods for IEMs – has frustrated advocates, parents, and manufacturers. They are putting their weight behind the Medical Nutrition Equity Act, which would mandate public and private payer coverage of medical foods for IEMs and digestive conditions such as Crohn disease. That 2019 House bill has 56 cosponsors; there is no Senate companion bill.
“If you can get reimbursement, it really makes the market,” for Primus and the other manufacturers, Mr. Hyman said.
Primus Pharmaceuticals has launched its own campaign, Cover My Medical Foods, to enlist consumers and others to the cause.
Partnering with advocates
Although its low-protein breads, pastas, and baking products are not considered medical foods by the FDA, Dr. Schär is marketing them as such in the United States. They are trying to make a mark in CKD, according to Ms. Donnelly. She added that Dr. Schär has been successful in Europe, where nutrition therapy is more integrated in the health care system.
In 2019, Flavis and the National Kidney Foundation joined forces to raise awareness of nutritional interventions and to build enthusiasm for the Flavis products. The partnership has now ended, mostly because Flavis could no longer afford it, according to Ms. Donnelly.
“Information on diet and nutrition is the most requested subject matter from the NKF,” said Anthony Gucciardo, senior vice president of strategic partnerships at the foundation. The partnership “has never been necessarily about promoting their products per se; it’s promoting a healthy diet and really a diet specific for CKD.”
The NKF developed cobranded materials on low-protein foods for physicians and a teaching tool they could use with patients. Consumers could access nutrition information and a discount on Flavis products on a dedicated webpage. The foundation didn’t describe the low-protein products as medical foods, said Mr. Gucciardo, even if Flavis promoted them as such.
In patients with CKD, dietary management can help prevent the progression to end-stage renal disease. Although Medicare covers medical nutrition therapy – in which patients receive personalized assessments and dietary advice – uptake is abysmally low, according to a 2018 study.
Dr. Burdock thinks low-protein foods for CKD do meet the FDA’s criteria for a medical food but that the agency might not necessarily agree with him. The FDA would not comment.
Physician beware
When it comes to medical foods, the FDA has often looked the other way because the ingredients may already have been proven safe and the danger to an individual or to the public’s health is relatively low, according to Dr. Burdock and Mr. Hyman.
However, if the agency “feels that a medical food will prevent people from seeking medical care or there is potential to defraud the public, it is justified in taking action against the company,” said Dr. Burdock.
According to Dr. Wilson, the pharmacist who reported on the inappropriate medical food prescriptions in the California system, the FDA could help by creating a list of approved medical foods. Physicians should take time to learn about the difference between medical foods and supplements, she said, adding that they should also not hesitate to “question the veracity of the claims for them.”
Ms. Guggenheim believed doctors need to know that, for the most part, these are not FDA-approved products. She emphasized the importance of evaluating the products and looking at the data of their impact on a disease or condition.
“Many of these companies strongly believe that the products work and help people, so clinicians need to be very data driven,” she said.
A version of this article originally appeared on Medscape.com.
Pediatric News welcomes Margaret Thew to the editorial advisory board
Ms. Thew is the medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee, in addition to working casually among Children’s Wisconsin pediatric urgent cares within the city of Milwaukee and surrounding suburbs. She has published articles on Nexplanon complications and management of the malnourished state of the eating disorder patient. She currently is involved in a longitudinal study on the health and nutrition of high school endurance runners. Ms. Thew has presented her research both nationally and internationally. Her most recent podium presentation was given at the International Conference for Eating Disorders May 2020 on her research working with high school endurance athletes.
Ms. Thew serves on several committees within Children’s Wisconsin including chair of the domestic violence committee and adjunct on the electronic health record provider committee. She is leading a quality improvement project on adolescent confidential care and the judicious use of the adolescent sensitive note. In addition, she is active within her state nursing organizations; she sits on the Wisconsin Nursing Association board as the advanced practice registered nurse director at large.
Ms. Thew was selected and graduated from the exclusive Duke Johnson & Johnson Nurse Leadership Fellowship in 2016 and was selected as the keynote speaker at graduation by her peers. She was asked to speak to this year’s cohort on her accomplishments as a leader at their virtual graduation April 2020.
Ms. Thew received her Doctor of Nursing Practice, Executive Nurse Leadership May 2020 from Concordia University Wisconsin, and her master’s degree in nursing specializing in family practice from the University of Wisconsin–Milwaukee in December 1997. She is presently enrolled in the nurse educator certificate program at Concordia University Wisconsin. She has worked in the department of adolescent medicine specializing in eating disorders and adolescent gynecology for 6 years and was named the medical director in October 2019. In addition to her work in adolescent medicine, she has an extensive history working as a nurse practitioner in pediatric hematology, oncology, and primary care.
Ms. Thew is the medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee, in addition to working casually among Children’s Wisconsin pediatric urgent cares within the city of Milwaukee and surrounding suburbs. She has published articles on Nexplanon complications and management of the malnourished state of the eating disorder patient. She currently is involved in a longitudinal study on the health and nutrition of high school endurance runners. Ms. Thew has presented her research both nationally and internationally. Her most recent podium presentation was given at the International Conference for Eating Disorders May 2020 on her research working with high school endurance athletes.
Ms. Thew serves on several committees within Children’s Wisconsin including chair of the domestic violence committee and adjunct on the electronic health record provider committee. She is leading a quality improvement project on adolescent confidential care and the judicious use of the adolescent sensitive note. In addition, she is active within her state nursing organizations; she sits on the Wisconsin Nursing Association board as the advanced practice registered nurse director at large.
Ms. Thew was selected and graduated from the exclusive Duke Johnson & Johnson Nurse Leadership Fellowship in 2016 and was selected as the keynote speaker at graduation by her peers. She was asked to speak to this year’s cohort on her accomplishments as a leader at their virtual graduation April 2020.
Ms. Thew received her Doctor of Nursing Practice, Executive Nurse Leadership May 2020 from Concordia University Wisconsin, and her master’s degree in nursing specializing in family practice from the University of Wisconsin–Milwaukee in December 1997. She is presently enrolled in the nurse educator certificate program at Concordia University Wisconsin. She has worked in the department of adolescent medicine specializing in eating disorders and adolescent gynecology for 6 years and was named the medical director in October 2019. In addition to her work in adolescent medicine, she has an extensive history working as a nurse practitioner in pediatric hematology, oncology, and primary care.
Ms. Thew is the medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee, in addition to working casually among Children’s Wisconsin pediatric urgent cares within the city of Milwaukee and surrounding suburbs. She has published articles on Nexplanon complications and management of the malnourished state of the eating disorder patient. She currently is involved in a longitudinal study on the health and nutrition of high school endurance runners. Ms. Thew has presented her research both nationally and internationally. Her most recent podium presentation was given at the International Conference for Eating Disorders May 2020 on her research working with high school endurance athletes.
Ms. Thew serves on several committees within Children’s Wisconsin including chair of the domestic violence committee and adjunct on the electronic health record provider committee. She is leading a quality improvement project on adolescent confidential care and the judicious use of the adolescent sensitive note. In addition, she is active within her state nursing organizations; she sits on the Wisconsin Nursing Association board as the advanced practice registered nurse director at large.
Ms. Thew was selected and graduated from the exclusive Duke Johnson & Johnson Nurse Leadership Fellowship in 2016 and was selected as the keynote speaker at graduation by her peers. She was asked to speak to this year’s cohort on her accomplishments as a leader at their virtual graduation April 2020.
Ms. Thew received her Doctor of Nursing Practice, Executive Nurse Leadership May 2020 from Concordia University Wisconsin, and her master’s degree in nursing specializing in family practice from the University of Wisconsin–Milwaukee in December 1997. She is presently enrolled in the nurse educator certificate program at Concordia University Wisconsin. She has worked in the department of adolescent medicine specializing in eating disorders and adolescent gynecology for 6 years and was named the medical director in October 2019. In addition to her work in adolescent medicine, she has an extensive history working as a nurse practitioner in pediatric hematology, oncology, and primary care.
How to not miss something
It’s a mad, mad, mad world. In California, we seem bent on swelling our curve. We’d just begun bringing our patients back into the office. We felt safe, back to business. Then air raid sirens again. Retreat to the Underground. Minimize waiting room waiting, convert to telephone and video. Do what we can to protect our patients and people.
As doctors, we’ve gotten proficient at being triage nurses, examining each appointment request, and sorting who should be seen in person and who could be cared for virtually. We do it for every clinic now.
My 11 a.m. patient last Thursday was an 83-year-old Filipino man with at least a 13-year history of hand dermatitis (based on his long electronic medical record). He had plenty of betamethasone refills. There were even photos of his large, brown hands in his chart. Grandpa hands, calloused by tending his garden and scarred from fixing bikes, building sheds, and doing oil changes for any nephew or niece who asked. The most recent uploads showed a bit of fingertip fissuring, some lichenified plaques. Not much different than they looked after planting persimmon trees a decade ago. I called him early that morning to offer a phone appointment. Perhaps I could save him from venturing out.
“I see that you have an appointment with me in a few hours. If you’d like, I might be able to help you by phone instead.” “Oh, thank you, doc,” he replied. “It’s so kind of you to call. But doc, I think maybe it is better if I come in to see you.” “Are you sure?” “Oh, yes. I will be careful.”
He checked in at 10:45. When I walked into the room he was wearing a face mask and a face shield – good job! He also had a cane and U.S. Navy Destroyer hat. And on the bottom left of his plastic shield was a sticker decal of a U.S. Navy Chief Petty Officer, dress blue insignia. His hands looked just like the photos: no purpura, plenty of lentigines. Fissures, calluses, lichenified plaques. I touched them. In the unaffected areas, his skin was remarkably soft. What stories these hands told. “I was 20 years in the Navy, doc,” he said. “I would have stayed longer but my wife, who’s younger, wanted me back home.” He talked about his nine grandchildren, some of whom went on to join the navy too – but as officers, he noted with pride. Now he spends his days caring for his wife; she has dementia. He can’t stay long because she’s in the waiting room and is likely to get confused if alone for too long.
We quickly reviewed good hand care. I ordered clobetasol ointment. He was pleased; that seemed to work years ago and he was glad to have it again.
So, why did he need to come in? Clearly I could have done this remotely. “Thank you so much for seeing me, doc,” as he stood to walk out. “Proper inspections have to be done in person, right?” Yes, I thought. Otherwise, you might miss something.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
It’s a mad, mad, mad world. In California, we seem bent on swelling our curve. We’d just begun bringing our patients back into the office. We felt safe, back to business. Then air raid sirens again. Retreat to the Underground. Minimize waiting room waiting, convert to telephone and video. Do what we can to protect our patients and people.
As doctors, we’ve gotten proficient at being triage nurses, examining each appointment request, and sorting who should be seen in person and who could be cared for virtually. We do it for every clinic now.
My 11 a.m. patient last Thursday was an 83-year-old Filipino man with at least a 13-year history of hand dermatitis (based on his long electronic medical record). He had plenty of betamethasone refills. There were even photos of his large, brown hands in his chart. Grandpa hands, calloused by tending his garden and scarred from fixing bikes, building sheds, and doing oil changes for any nephew or niece who asked. The most recent uploads showed a bit of fingertip fissuring, some lichenified plaques. Not much different than they looked after planting persimmon trees a decade ago. I called him early that morning to offer a phone appointment. Perhaps I could save him from venturing out.
“I see that you have an appointment with me in a few hours. If you’d like, I might be able to help you by phone instead.” “Oh, thank you, doc,” he replied. “It’s so kind of you to call. But doc, I think maybe it is better if I come in to see you.” “Are you sure?” “Oh, yes. I will be careful.”
He checked in at 10:45. When I walked into the room he was wearing a face mask and a face shield – good job! He also had a cane and U.S. Navy Destroyer hat. And on the bottom left of his plastic shield was a sticker decal of a U.S. Navy Chief Petty Officer, dress blue insignia. His hands looked just like the photos: no purpura, plenty of lentigines. Fissures, calluses, lichenified plaques. I touched them. In the unaffected areas, his skin was remarkably soft. What stories these hands told. “I was 20 years in the Navy, doc,” he said. “I would have stayed longer but my wife, who’s younger, wanted me back home.” He talked about his nine grandchildren, some of whom went on to join the navy too – but as officers, he noted with pride. Now he spends his days caring for his wife; she has dementia. He can’t stay long because she’s in the waiting room and is likely to get confused if alone for too long.
We quickly reviewed good hand care. I ordered clobetasol ointment. He was pleased; that seemed to work years ago and he was glad to have it again.
So, why did he need to come in? Clearly I could have done this remotely. “Thank you so much for seeing me, doc,” as he stood to walk out. “Proper inspections have to be done in person, right?” Yes, I thought. Otherwise, you might miss something.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
It’s a mad, mad, mad world. In California, we seem bent on swelling our curve. We’d just begun bringing our patients back into the office. We felt safe, back to business. Then air raid sirens again. Retreat to the Underground. Minimize waiting room waiting, convert to telephone and video. Do what we can to protect our patients and people.
As doctors, we’ve gotten proficient at being triage nurses, examining each appointment request, and sorting who should be seen in person and who could be cared for virtually. We do it for every clinic now.
My 11 a.m. patient last Thursday was an 83-year-old Filipino man with at least a 13-year history of hand dermatitis (based on his long electronic medical record). He had plenty of betamethasone refills. There were even photos of his large, brown hands in his chart. Grandpa hands, calloused by tending his garden and scarred from fixing bikes, building sheds, and doing oil changes for any nephew or niece who asked. The most recent uploads showed a bit of fingertip fissuring, some lichenified plaques. Not much different than they looked after planting persimmon trees a decade ago. I called him early that morning to offer a phone appointment. Perhaps I could save him from venturing out.
“I see that you have an appointment with me in a few hours. If you’d like, I might be able to help you by phone instead.” “Oh, thank you, doc,” he replied. “It’s so kind of you to call. But doc, I think maybe it is better if I come in to see you.” “Are you sure?” “Oh, yes. I will be careful.”
He checked in at 10:45. When I walked into the room he was wearing a face mask and a face shield – good job! He also had a cane and U.S. Navy Destroyer hat. And on the bottom left of his plastic shield was a sticker decal of a U.S. Navy Chief Petty Officer, dress blue insignia. His hands looked just like the photos: no purpura, plenty of lentigines. Fissures, calluses, lichenified plaques. I touched them. In the unaffected areas, his skin was remarkably soft. What stories these hands told. “I was 20 years in the Navy, doc,” he said. “I would have stayed longer but my wife, who’s younger, wanted me back home.” He talked about his nine grandchildren, some of whom went on to join the navy too – but as officers, he noted with pride. Now he spends his days caring for his wife; she has dementia. He can’t stay long because she’s in the waiting room and is likely to get confused if alone for too long.
We quickly reviewed good hand care. I ordered clobetasol ointment. He was pleased; that seemed to work years ago and he was glad to have it again.
So, why did he need to come in? Clearly I could have done this remotely. “Thank you so much for seeing me, doc,” as he stood to walk out. “Proper inspections have to be done in person, right?” Yes, I thought. Otherwise, you might miss something.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Women suffer less NAFLD but more advanced fibrosis
Women have a lower risk of nonalcoholic fatty liver disease compared with men, but those who do develop the disease are significantly more likely than are men to develop advanced fibrosis, according to data from a meta-analysis of more than 62,000 individuals.
Sex disparity persists in most chronic liver diseases, with more cases and risk of progression reported in men, but the effect of sex on nonalcoholic fatty liver disease (NAFLD) remains unclear, wrote Maya Balakrishnan, MD, of Baylor College of Medicine, Houston, and colleagues. “Knowing whether and how [sex] influences the risk and severity of NAFLD is important for risk stratification, risk modification as well as prognostication,” they said.
In a study published in Clinical Gastroenterology and Hepatology, the researchers conducted a review and meta-analysis of 54 studies, including data from 62,239 patients with NAFLD, 5,428 with nonalcoholic steatohepatitis (NASH), and 6,444 with advanced NAFLD fibrosis.
Overall, women had a 19% lower risk of developing NAFLD compared with men (pooled risk ratio 0.81), a similar risk to men of developing NASH (RR, 1.00), and a 37% increased risk of advanced fibrosis (RR, 1.37) compared with men.
The risk of more severe disease in women increased with age. Among women aged 50 years and older, the risks of NASH and advanced fibrosis were significantly higher, at 17% and 56%, respectively (RR, 1.17 and RR, 1.56). The sex-specific prevalence of advanced fibrosis was not significantly different in patients younger than 50 years.
“Our findings of an increased prevalence of severe phenotypes of NAFLD – NASH and advanced fibrosis – among older women fits well into the current understanding of disease pathogenesis,” the researchers noted.
The findings were limited by several factors, including the cross-sectional nature and heterogeneity of the included studies and lack of data on possible contributions to NASH and NAFLD such as polycystic ovarian syndrome, cumulative use of hormone therapy, and pregnancy, the researchers noted.
However, the results were strengthened by the large patient population. “Given the higher risk of advanced fibrosis observed among women compared to men with NAFLD in our meta-analysis, it is plausible that cirrhosis and its complications may occur with greater frequency among women than in men,” the researchers said. Consequently, women older than 50 years with NAFLD should be evaluated frequently for advanced disease, they noted. In addition, “more focused and intensified efforts may be warranted to target lifestyle modifications and weight loss among young women with NAFLD, particularly in the presence of NASH and/or advanced fibrosis,” the researchers concluded.
Conducting the study at this time was important because of conjectures of sex-based differences in NAFLD prevalence and NAFLD progression, Dr. Balakrishnan said in an interview. “However, the findings from studies conducted across different study populations have been disparate. Therefore, it was important to perform a systematic review and meta-analysis to determine whether there are differences in NAFLD and NAFLD severity risk between the [sexes],” she said.
Dr. Balakrishnan said she was surprised by the higher risk of severe NASH fibrosis in women compared with men once NAFLD is established. “This was surprising and sets NAFLD apart from other highly prevalent chronic liver disease etiologies,” she said. “Other common liver diseases, for example hepatitis B and hepatitis C, tend to be more common among men and tend to progress more rapidly, and tend to be more severe among men compared to women,” she noted.
The take-home message for clinicians is that NAFLD is at least equally, if not more, aggressive in women compared with men, and should be evaluated with equal aggressiveness, Dr. Balakrishnan emphasized. “Moreover, in the future we may expect to see the burden of cirrhosis distributed more equally among women and men than we have to date. This has implications for liver disease screening and women’s health,” she said. The next steps for research are to determine the specific reasons for the higher risk of NAFLD fibrosis in women compared with men, she added.
The study was supported in part by the National Institutes of Health. The researchers had no financial conflicts to disclose.
SOURCE: Balakrishnan M et al. Clin Gastroenterol Hepatol. 2020 Apr 30. doi: 10.1016/j.cgh.2020.04.067.
Women have a lower risk of nonalcoholic fatty liver disease compared with men, but those who do develop the disease are significantly more likely than are men to develop advanced fibrosis, according to data from a meta-analysis of more than 62,000 individuals.
Sex disparity persists in most chronic liver diseases, with more cases and risk of progression reported in men, but the effect of sex on nonalcoholic fatty liver disease (NAFLD) remains unclear, wrote Maya Balakrishnan, MD, of Baylor College of Medicine, Houston, and colleagues. “Knowing whether and how [sex] influences the risk and severity of NAFLD is important for risk stratification, risk modification as well as prognostication,” they said.
In a study published in Clinical Gastroenterology and Hepatology, the researchers conducted a review and meta-analysis of 54 studies, including data from 62,239 patients with NAFLD, 5,428 with nonalcoholic steatohepatitis (NASH), and 6,444 with advanced NAFLD fibrosis.
Overall, women had a 19% lower risk of developing NAFLD compared with men (pooled risk ratio 0.81), a similar risk to men of developing NASH (RR, 1.00), and a 37% increased risk of advanced fibrosis (RR, 1.37) compared with men.
The risk of more severe disease in women increased with age. Among women aged 50 years and older, the risks of NASH and advanced fibrosis were significantly higher, at 17% and 56%, respectively (RR, 1.17 and RR, 1.56). The sex-specific prevalence of advanced fibrosis was not significantly different in patients younger than 50 years.
“Our findings of an increased prevalence of severe phenotypes of NAFLD – NASH and advanced fibrosis – among older women fits well into the current understanding of disease pathogenesis,” the researchers noted.
The findings were limited by several factors, including the cross-sectional nature and heterogeneity of the included studies and lack of data on possible contributions to NASH and NAFLD such as polycystic ovarian syndrome, cumulative use of hormone therapy, and pregnancy, the researchers noted.
However, the results were strengthened by the large patient population. “Given the higher risk of advanced fibrosis observed among women compared to men with NAFLD in our meta-analysis, it is plausible that cirrhosis and its complications may occur with greater frequency among women than in men,” the researchers said. Consequently, women older than 50 years with NAFLD should be evaluated frequently for advanced disease, they noted. In addition, “more focused and intensified efforts may be warranted to target lifestyle modifications and weight loss among young women with NAFLD, particularly in the presence of NASH and/or advanced fibrosis,” the researchers concluded.
Conducting the study at this time was important because of conjectures of sex-based differences in NAFLD prevalence and NAFLD progression, Dr. Balakrishnan said in an interview. “However, the findings from studies conducted across different study populations have been disparate. Therefore, it was important to perform a systematic review and meta-analysis to determine whether there are differences in NAFLD and NAFLD severity risk between the [sexes],” she said.
Dr. Balakrishnan said she was surprised by the higher risk of severe NASH fibrosis in women compared with men once NAFLD is established. “This was surprising and sets NAFLD apart from other highly prevalent chronic liver disease etiologies,” she said. “Other common liver diseases, for example hepatitis B and hepatitis C, tend to be more common among men and tend to progress more rapidly, and tend to be more severe among men compared to women,” she noted.
The take-home message for clinicians is that NAFLD is at least equally, if not more, aggressive in women compared with men, and should be evaluated with equal aggressiveness, Dr. Balakrishnan emphasized. “Moreover, in the future we may expect to see the burden of cirrhosis distributed more equally among women and men than we have to date. This has implications for liver disease screening and women’s health,” she said. The next steps for research are to determine the specific reasons for the higher risk of NAFLD fibrosis in women compared with men, she added.
The study was supported in part by the National Institutes of Health. The researchers had no financial conflicts to disclose.
SOURCE: Balakrishnan M et al. Clin Gastroenterol Hepatol. 2020 Apr 30. doi: 10.1016/j.cgh.2020.04.067.
Women have a lower risk of nonalcoholic fatty liver disease compared with men, but those who do develop the disease are significantly more likely than are men to develop advanced fibrosis, according to data from a meta-analysis of more than 62,000 individuals.
Sex disparity persists in most chronic liver diseases, with more cases and risk of progression reported in men, but the effect of sex on nonalcoholic fatty liver disease (NAFLD) remains unclear, wrote Maya Balakrishnan, MD, of Baylor College of Medicine, Houston, and colleagues. “Knowing whether and how [sex] influences the risk and severity of NAFLD is important for risk stratification, risk modification as well as prognostication,” they said.
In a study published in Clinical Gastroenterology and Hepatology, the researchers conducted a review and meta-analysis of 54 studies, including data from 62,239 patients with NAFLD, 5,428 with nonalcoholic steatohepatitis (NASH), and 6,444 with advanced NAFLD fibrosis.
Overall, women had a 19% lower risk of developing NAFLD compared with men (pooled risk ratio 0.81), a similar risk to men of developing NASH (RR, 1.00), and a 37% increased risk of advanced fibrosis (RR, 1.37) compared with men.
The risk of more severe disease in women increased with age. Among women aged 50 years and older, the risks of NASH and advanced fibrosis were significantly higher, at 17% and 56%, respectively (RR, 1.17 and RR, 1.56). The sex-specific prevalence of advanced fibrosis was not significantly different in patients younger than 50 years.
“Our findings of an increased prevalence of severe phenotypes of NAFLD – NASH and advanced fibrosis – among older women fits well into the current understanding of disease pathogenesis,” the researchers noted.
The findings were limited by several factors, including the cross-sectional nature and heterogeneity of the included studies and lack of data on possible contributions to NASH and NAFLD such as polycystic ovarian syndrome, cumulative use of hormone therapy, and pregnancy, the researchers noted.
However, the results were strengthened by the large patient population. “Given the higher risk of advanced fibrosis observed among women compared to men with NAFLD in our meta-analysis, it is plausible that cirrhosis and its complications may occur with greater frequency among women than in men,” the researchers said. Consequently, women older than 50 years with NAFLD should be evaluated frequently for advanced disease, they noted. In addition, “more focused and intensified efforts may be warranted to target lifestyle modifications and weight loss among young women with NAFLD, particularly in the presence of NASH and/or advanced fibrosis,” the researchers concluded.
Conducting the study at this time was important because of conjectures of sex-based differences in NAFLD prevalence and NAFLD progression, Dr. Balakrishnan said in an interview. “However, the findings from studies conducted across different study populations have been disparate. Therefore, it was important to perform a systematic review and meta-analysis to determine whether there are differences in NAFLD and NAFLD severity risk between the [sexes],” she said.
Dr. Balakrishnan said she was surprised by the higher risk of severe NASH fibrosis in women compared with men once NAFLD is established. “This was surprising and sets NAFLD apart from other highly prevalent chronic liver disease etiologies,” she said. “Other common liver diseases, for example hepatitis B and hepatitis C, tend to be more common among men and tend to progress more rapidly, and tend to be more severe among men compared to women,” she noted.
The take-home message for clinicians is that NAFLD is at least equally, if not more, aggressive in women compared with men, and should be evaluated with equal aggressiveness, Dr. Balakrishnan emphasized. “Moreover, in the future we may expect to see the burden of cirrhosis distributed more equally among women and men than we have to date. This has implications for liver disease screening and women’s health,” she said. The next steps for research are to determine the specific reasons for the higher risk of NAFLD fibrosis in women compared with men, she added.
The study was supported in part by the National Institutes of Health. The researchers had no financial conflicts to disclose.
SOURCE: Balakrishnan M et al. Clin Gastroenterol Hepatol. 2020 Apr 30. doi: 10.1016/j.cgh.2020.04.067.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Characterization of norovirus immunity in nonsecretor adults might provide vaccine model for children
Among nonsecretors – individuals who express a less diverse array of fucosylated histoblood group antigen carbohydrates (HBGAs) and consequently are less susceptible to some norovirus strains – natural infection with norovirus strain GII.2 induced cellular and antibody immunity that lasted for at least 30 days for T cells, monocytes, and dendritic cells and for at least 180 days for blocking antibodies, researchers reported.
“Multiple cellular lineages expressing interferon-gamma and tumor necrosis factor [TNF]–alpha dominated the response. Both T-cell and B-cell responses were cross-reactive with other GII strains, but not GI strains,” Lisa C. Lindesmith of the University of North Carolina, Chapel Hill, and her associates wrote in Cellular and Molecular Gastroenterology and Hepatology. The researchers also found that bile salts enable GII.2 to bind HBGAs produced by nonsecretors. “[I]n addition to HBGAs, one or more specific components of bile also is likely to be an essential co-factor for human norovirus attachment and infection,” the researchers wrote.
Susceptibility to norovirus depends on whether individuals express secretor enzyme, which is encoded by the FUT2 gene. Nonsecretors (who are FUT2–/–) express less varied HBGA, are susceptible to fewer norovirus strains, and are resistant to the predominant norovirus strain, GII.4. “Because future human norovirus vaccines will comprise GII.4 antigen, and because secretor phenotype impacts GII.4 infection and immunity, nonsecretors may mimic young children immunologically in response to GII.4 vaccination,” the researchers explained. But until now, most vaccines have focused on adult secretors, they said.
Their study focused on a familial norovirus outbreak in Chapel Hill that was the first to be characterized among nonsecretors who were naturally infected with norovirus GII.2. Four adults provided blood samples, and one provided a stool sample from which the researchers isolated and cloned the G11.2 capsid gene sequence. They used neutralization assays to study serologic immunity and flow cytometry to assess cellular activation and cytokine production in blood samples from the four cases and from seven healthy donors.
Norovirus GII.2 infection activated both innate and adaptive immunity and typical production of antiviral helper T cell (Th)1 and Th2 cytokines. The cellular immune response lasted at least 30 days, “long after symptom resolution,” the investigators wrote.
Compared with healthy donors, blood specimens from infected nonsecretors showed increases in non-class-switched memory, transitional B cells, and plasmablast B cells, and both naive and memory B cells also were positive for activation markers for at least 30 days after infection. Activated interferon-gamma+ T cells, natural killer cells, TNF-alpha+ monocytes, IL-10+, TNF-alpha+ myeloid dendritic cells, and TNF plasmacytoid dendritic cells also persisted for at least 30 days. Cross-reactive GII immunity was evident for at least 180 days. “GII.2 infection boosted cross-reactive blocking antibodies to GII.3, GII.14, and GII.17, as well as T-cell responses to GII.4, despite the lack of clear serologic evidence of previous GII.4 exposure,” the investigators wrote.
Based on prior reports that bile enhances norovirus growth or ligand binding, they inoculated specimens with chenodeoxycholic acid (CDCA) and glycochenodeoxycholic acid (GCDCA), pig bile, ox bile, or human bile. “Strikingly, the addition of bile enabled GII.2 Chapel Hill outbreak virus-like particle to bind to saliva from the four nonsecretor donors,” the researchers wrote. Bile acids “may override the genetic advantage of less-diverse HBGA expression in nonsecretors by improving the avidity of GII.2 binding to nonsecretor HBGAs, potentially paving the way for infection.” However, bile salts did not enable the GII.2 strain to replicate in human intestinal enteroid cells, which suggests that additional factors play into how norovirus enters human cells, according to the researchers.
The findings, they wrote, “support development of within-genogroup, cross-reactive antibody and T-cell immunity, key outcomes that may provide the foundation for eliciting broad immune responses after GII.4 vaccination in individuals with limited GII.4 immunity, including young children.”
The National Institutes of Health, the Wellcome Trust, the Centers for Disease Control and Prevention, and a Cancer Center Core support provided funding. Ms. Lindesmith and her associates reported having no relevant conflicts of interest.
SOURCE: Lindesmith LC et al. Cell Molec Gastroenterol Hepatol. 2020;10:245-67.
Noroviruses belonging to genogroup II.4 are the leading cause of acute gastroenteritis, but our understanding of norovirus immunity remains incomplete. Most studies have focused on humoral responses and have shown that antibodies may be short lived, strain specific, and not always protective against rechallenge. On the other hand, human innate and T-cell immunity have received little attention despite evidence from the mouse norovirus model that they are critical for limiting viral spread and clearing antigen.
In this study, Lindesmith et al. conducted broad phenotypic and functional analysis of innate and adaptive immune responses following infection with a GII.2 strain of norovirus. Their cohort consists of “nonsecretors,” subjects who express a limited repertoire of histoblood group antigens and are therefore naturally resistant to GII.4 infection. Since nonsecretors have no pre-existing immunity against GII.4 viruses, this system enables the authors to test cross-reactivity of GII.2-specific T cells against GII.4 virus-like particles (VLPs).
The authors showed broad immune activation against natural norovirus infection. Following GII.2 infection, T-cell responses persist for at least a month and, importantly, are cross-reactive against GII.4 VLPs. These findings suggest that T cells may target conserved viral epitopes and play an important role in long-term protection against reinfection.
Developing an effective norovirus vaccine will require a detailed understanding of immune correlates of protection, and this study is a step in the right direction. In future work, tracking epitope-specific T cells must further define the phenotype, functionality, and localization of the norovirus T-cell repertoire.
Vesselin Tomov, MD, PhD, is assistant professor of medicine at the Hospital of the University of Pennsylvania, Philadelphia. He has no conflicts of interest.
Noroviruses belonging to genogroup II.4 are the leading cause of acute gastroenteritis, but our understanding of norovirus immunity remains incomplete. Most studies have focused on humoral responses and have shown that antibodies may be short lived, strain specific, and not always protective against rechallenge. On the other hand, human innate and T-cell immunity have received little attention despite evidence from the mouse norovirus model that they are critical for limiting viral spread and clearing antigen.
In this study, Lindesmith et al. conducted broad phenotypic and functional analysis of innate and adaptive immune responses following infection with a GII.2 strain of norovirus. Their cohort consists of “nonsecretors,” subjects who express a limited repertoire of histoblood group antigens and are therefore naturally resistant to GII.4 infection. Since nonsecretors have no pre-existing immunity against GII.4 viruses, this system enables the authors to test cross-reactivity of GII.2-specific T cells against GII.4 virus-like particles (VLPs).
The authors showed broad immune activation against natural norovirus infection. Following GII.2 infection, T-cell responses persist for at least a month and, importantly, are cross-reactive against GII.4 VLPs. These findings suggest that T cells may target conserved viral epitopes and play an important role in long-term protection against reinfection.
Developing an effective norovirus vaccine will require a detailed understanding of immune correlates of protection, and this study is a step in the right direction. In future work, tracking epitope-specific T cells must further define the phenotype, functionality, and localization of the norovirus T-cell repertoire.
Vesselin Tomov, MD, PhD, is assistant professor of medicine at the Hospital of the University of Pennsylvania, Philadelphia. He has no conflicts of interest.
Noroviruses belonging to genogroup II.4 are the leading cause of acute gastroenteritis, but our understanding of norovirus immunity remains incomplete. Most studies have focused on humoral responses and have shown that antibodies may be short lived, strain specific, and not always protective against rechallenge. On the other hand, human innate and T-cell immunity have received little attention despite evidence from the mouse norovirus model that they are critical for limiting viral spread and clearing antigen.
In this study, Lindesmith et al. conducted broad phenotypic and functional analysis of innate and adaptive immune responses following infection with a GII.2 strain of norovirus. Their cohort consists of “nonsecretors,” subjects who express a limited repertoire of histoblood group antigens and are therefore naturally resistant to GII.4 infection. Since nonsecretors have no pre-existing immunity against GII.4 viruses, this system enables the authors to test cross-reactivity of GII.2-specific T cells against GII.4 virus-like particles (VLPs).
The authors showed broad immune activation against natural norovirus infection. Following GII.2 infection, T-cell responses persist for at least a month and, importantly, are cross-reactive against GII.4 VLPs. These findings suggest that T cells may target conserved viral epitopes and play an important role in long-term protection against reinfection.
Developing an effective norovirus vaccine will require a detailed understanding of immune correlates of protection, and this study is a step in the right direction. In future work, tracking epitope-specific T cells must further define the phenotype, functionality, and localization of the norovirus T-cell repertoire.
Vesselin Tomov, MD, PhD, is assistant professor of medicine at the Hospital of the University of Pennsylvania, Philadelphia. He has no conflicts of interest.
Among nonsecretors – individuals who express a less diverse array of fucosylated histoblood group antigen carbohydrates (HBGAs) and consequently are less susceptible to some norovirus strains – natural infection with norovirus strain GII.2 induced cellular and antibody immunity that lasted for at least 30 days for T cells, monocytes, and dendritic cells and for at least 180 days for blocking antibodies, researchers reported.
“Multiple cellular lineages expressing interferon-gamma and tumor necrosis factor [TNF]–alpha dominated the response. Both T-cell and B-cell responses were cross-reactive with other GII strains, but not GI strains,” Lisa C. Lindesmith of the University of North Carolina, Chapel Hill, and her associates wrote in Cellular and Molecular Gastroenterology and Hepatology. The researchers also found that bile salts enable GII.2 to bind HBGAs produced by nonsecretors. “[I]n addition to HBGAs, one or more specific components of bile also is likely to be an essential co-factor for human norovirus attachment and infection,” the researchers wrote.
Susceptibility to norovirus depends on whether individuals express secretor enzyme, which is encoded by the FUT2 gene. Nonsecretors (who are FUT2–/–) express less varied HBGA, are susceptible to fewer norovirus strains, and are resistant to the predominant norovirus strain, GII.4. “Because future human norovirus vaccines will comprise GII.4 antigen, and because secretor phenotype impacts GII.4 infection and immunity, nonsecretors may mimic young children immunologically in response to GII.4 vaccination,” the researchers explained. But until now, most vaccines have focused on adult secretors, they said.
Their study focused on a familial norovirus outbreak in Chapel Hill that was the first to be characterized among nonsecretors who were naturally infected with norovirus GII.2. Four adults provided blood samples, and one provided a stool sample from which the researchers isolated and cloned the G11.2 capsid gene sequence. They used neutralization assays to study serologic immunity and flow cytometry to assess cellular activation and cytokine production in blood samples from the four cases and from seven healthy donors.
Norovirus GII.2 infection activated both innate and adaptive immunity and typical production of antiviral helper T cell (Th)1 and Th2 cytokines. The cellular immune response lasted at least 30 days, “long after symptom resolution,” the investigators wrote.
Compared with healthy donors, blood specimens from infected nonsecretors showed increases in non-class-switched memory, transitional B cells, and plasmablast B cells, and both naive and memory B cells also were positive for activation markers for at least 30 days after infection. Activated interferon-gamma+ T cells, natural killer cells, TNF-alpha+ monocytes, IL-10+, TNF-alpha+ myeloid dendritic cells, and TNF plasmacytoid dendritic cells also persisted for at least 30 days. Cross-reactive GII immunity was evident for at least 180 days. “GII.2 infection boosted cross-reactive blocking antibodies to GII.3, GII.14, and GII.17, as well as T-cell responses to GII.4, despite the lack of clear serologic evidence of previous GII.4 exposure,” the investigators wrote.
Based on prior reports that bile enhances norovirus growth or ligand binding, they inoculated specimens with chenodeoxycholic acid (CDCA) and glycochenodeoxycholic acid (GCDCA), pig bile, ox bile, or human bile. “Strikingly, the addition of bile enabled GII.2 Chapel Hill outbreak virus-like particle to bind to saliva from the four nonsecretor donors,” the researchers wrote. Bile acids “may override the genetic advantage of less-diverse HBGA expression in nonsecretors by improving the avidity of GII.2 binding to nonsecretor HBGAs, potentially paving the way for infection.” However, bile salts did not enable the GII.2 strain to replicate in human intestinal enteroid cells, which suggests that additional factors play into how norovirus enters human cells, according to the researchers.
The findings, they wrote, “support development of within-genogroup, cross-reactive antibody and T-cell immunity, key outcomes that may provide the foundation for eliciting broad immune responses after GII.4 vaccination in individuals with limited GII.4 immunity, including young children.”
The National Institutes of Health, the Wellcome Trust, the Centers for Disease Control and Prevention, and a Cancer Center Core support provided funding. Ms. Lindesmith and her associates reported having no relevant conflicts of interest.
SOURCE: Lindesmith LC et al. Cell Molec Gastroenterol Hepatol. 2020;10:245-67.
Among nonsecretors – individuals who express a less diverse array of fucosylated histoblood group antigen carbohydrates (HBGAs) and consequently are less susceptible to some norovirus strains – natural infection with norovirus strain GII.2 induced cellular and antibody immunity that lasted for at least 30 days for T cells, monocytes, and dendritic cells and for at least 180 days for blocking antibodies, researchers reported.
“Multiple cellular lineages expressing interferon-gamma and tumor necrosis factor [TNF]–alpha dominated the response. Both T-cell and B-cell responses were cross-reactive with other GII strains, but not GI strains,” Lisa C. Lindesmith of the University of North Carolina, Chapel Hill, and her associates wrote in Cellular and Molecular Gastroenterology and Hepatology. The researchers also found that bile salts enable GII.2 to bind HBGAs produced by nonsecretors. “[I]n addition to HBGAs, one or more specific components of bile also is likely to be an essential co-factor for human norovirus attachment and infection,” the researchers wrote.
Susceptibility to norovirus depends on whether individuals express secretor enzyme, which is encoded by the FUT2 gene. Nonsecretors (who are FUT2–/–) express less varied HBGA, are susceptible to fewer norovirus strains, and are resistant to the predominant norovirus strain, GII.4. “Because future human norovirus vaccines will comprise GII.4 antigen, and because secretor phenotype impacts GII.4 infection and immunity, nonsecretors may mimic young children immunologically in response to GII.4 vaccination,” the researchers explained. But until now, most vaccines have focused on adult secretors, they said.
Their study focused on a familial norovirus outbreak in Chapel Hill that was the first to be characterized among nonsecretors who were naturally infected with norovirus GII.2. Four adults provided blood samples, and one provided a stool sample from which the researchers isolated and cloned the G11.2 capsid gene sequence. They used neutralization assays to study serologic immunity and flow cytometry to assess cellular activation and cytokine production in blood samples from the four cases and from seven healthy donors.
Norovirus GII.2 infection activated both innate and adaptive immunity and typical production of antiviral helper T cell (Th)1 and Th2 cytokines. The cellular immune response lasted at least 30 days, “long after symptom resolution,” the investigators wrote.
Compared with healthy donors, blood specimens from infected nonsecretors showed increases in non-class-switched memory, transitional B cells, and plasmablast B cells, and both naive and memory B cells also were positive for activation markers for at least 30 days after infection. Activated interferon-gamma+ T cells, natural killer cells, TNF-alpha+ monocytes, IL-10+, TNF-alpha+ myeloid dendritic cells, and TNF plasmacytoid dendritic cells also persisted for at least 30 days. Cross-reactive GII immunity was evident for at least 180 days. “GII.2 infection boosted cross-reactive blocking antibodies to GII.3, GII.14, and GII.17, as well as T-cell responses to GII.4, despite the lack of clear serologic evidence of previous GII.4 exposure,” the investigators wrote.
Based on prior reports that bile enhances norovirus growth or ligand binding, they inoculated specimens with chenodeoxycholic acid (CDCA) and glycochenodeoxycholic acid (GCDCA), pig bile, ox bile, or human bile. “Strikingly, the addition of bile enabled GII.2 Chapel Hill outbreak virus-like particle to bind to saliva from the four nonsecretor donors,” the researchers wrote. Bile acids “may override the genetic advantage of less-diverse HBGA expression in nonsecretors by improving the avidity of GII.2 binding to nonsecretor HBGAs, potentially paving the way for infection.” However, bile salts did not enable the GII.2 strain to replicate in human intestinal enteroid cells, which suggests that additional factors play into how norovirus enters human cells, according to the researchers.
The findings, they wrote, “support development of within-genogroup, cross-reactive antibody and T-cell immunity, key outcomes that may provide the foundation for eliciting broad immune responses after GII.4 vaccination in individuals with limited GII.4 immunity, including young children.”
The National Institutes of Health, the Wellcome Trust, the Centers for Disease Control and Prevention, and a Cancer Center Core support provided funding. Ms. Lindesmith and her associates reported having no relevant conflicts of interest.
SOURCE: Lindesmith LC et al. Cell Molec Gastroenterol Hepatol. 2020;10:245-67.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
Creating a student-staffed family call line to alleviate clinical burden
The coronavirus pandemic has fundamentally altered American health care. At our academic medical center in Brooklyn, a large safety net institution, clinical year medical students are normally integral members of the team consistent with the model of “value-added medical education.”1 With the suspension of clinical rotations on March 13, 2020, a key part of the workforce was suddenly withdrawn while demand skyrocketed.
In response, students self-organized into numerous remote support projects, including the project described below.
Under infection control regulations, a “no-visitor” policy was instituted. Concurrently, the dramatic increase in patient volume left clinicians unable to regularly update patients’ families. To address this gap, a family contact line was created.
A dedicated phone number was distributed to key hospital personnel to share with families seeking information. The work flow for returning calls is shown in the figure. After verifying patient information and the caller’s relation, students provide updates based on chart review. Calls are prefaced with the disclaimer that students are not part of the treatment team and can only give information that is accessible via the electronic medical record.
Students created a phone script in conjunction with faculty, as well as a referral system for those seeking specific information from other departments. This script undergoes daily revision after the student huddle to address new issues. Flow of information is bidirectional: students relay patient updates as well as quarantine precautions and obtain past medical history. This proved essential during the surge of patients, unknown to the hospital and frequently altered, arriving by ambulance. Students document these conversations in the EMR, including family concerns and whether immediate provider follow-up is needed.
Two key limitations were quickly addressed: First, patients requiring ICU-level care have fluctuating courses, and an update based solely on chart review is insufficient. In response, students worked with intensivist teams to create a dedicated call line staffed by providers.
Second, conversations regarding goals of care and end of life concerns were beyond students’ scope. Together with palliative care teams, students developed criteria for flagging families for follow-up by a consulting palliative care attending.
Through working the call line, students received a crash course in empathetically communicating over the phone. Particularly during the worst of the surge, families were afraid and often frustrated at the lack of communication up to that point. Navigating these emotions, learning how to update family members while removed from the teams, and educating callers on quarantine precautions and other concerns was a valuable learning experience.
As students, we have been exposed to many of the realities of communicating as a physician. Relaying updates and prognosis to family while also providing emotional support is not something we are taught in medical school, but is something we will be expected to handle our first night on the wards as an intern. This experience has prepared us well for that and has illuminated missing parts of the medical school curriculum we are working on emphasizing moving forward.
Over the first 2 weeks, students put in 848 volunteer-hours, making 1,438 calls which reached 1,114 different families. We hope our experience proves instructive for other academic medical centers facing similar concerns in coming months. This model allows medical students to be directly involved in patient care during this crisis and shifts these time-intensive conversations away from overwhelmed primary medical teams.
Reference
1. Gonzalo JD et al. Value-added clinical systems learning roles for 355 medical students that transform education and health: A guide for building partnerships between 356 medical schools and health systems. Acad Med. 2017;92(5):602-7.
Ms. Jaiman is an MD candidate at State University of New York, Brooklyn and a PhD candidate at the National Center of Biological Sciences in Bangalore, India. Mr. Hessburg is an MD/PhD candidate at State University of New York, Brooklyn. Dr. Egelko is a recent graduate of State University of New York, Brooklyn.
The coronavirus pandemic has fundamentally altered American health care. At our academic medical center in Brooklyn, a large safety net institution, clinical year medical students are normally integral members of the team consistent with the model of “value-added medical education.”1 With the suspension of clinical rotations on March 13, 2020, a key part of the workforce was suddenly withdrawn while demand skyrocketed.
In response, students self-organized into numerous remote support projects, including the project described below.
Under infection control regulations, a “no-visitor” policy was instituted. Concurrently, the dramatic increase in patient volume left clinicians unable to regularly update patients’ families. To address this gap, a family contact line was created.
A dedicated phone number was distributed to key hospital personnel to share with families seeking information. The work flow for returning calls is shown in the figure. After verifying patient information and the caller’s relation, students provide updates based on chart review. Calls are prefaced with the disclaimer that students are not part of the treatment team and can only give information that is accessible via the electronic medical record.
Students created a phone script in conjunction with faculty, as well as a referral system for those seeking specific information from other departments. This script undergoes daily revision after the student huddle to address new issues. Flow of information is bidirectional: students relay patient updates as well as quarantine precautions and obtain past medical history. This proved essential during the surge of patients, unknown to the hospital and frequently altered, arriving by ambulance. Students document these conversations in the EMR, including family concerns and whether immediate provider follow-up is needed.
Two key limitations were quickly addressed: First, patients requiring ICU-level care have fluctuating courses, and an update based solely on chart review is insufficient. In response, students worked with intensivist teams to create a dedicated call line staffed by providers.
Second, conversations regarding goals of care and end of life concerns were beyond students’ scope. Together with palliative care teams, students developed criteria for flagging families for follow-up by a consulting palliative care attending.
Through working the call line, students received a crash course in empathetically communicating over the phone. Particularly during the worst of the surge, families were afraid and often frustrated at the lack of communication up to that point. Navigating these emotions, learning how to update family members while removed from the teams, and educating callers on quarantine precautions and other concerns was a valuable learning experience.
As students, we have been exposed to many of the realities of communicating as a physician. Relaying updates and prognosis to family while also providing emotional support is not something we are taught in medical school, but is something we will be expected to handle our first night on the wards as an intern. This experience has prepared us well for that and has illuminated missing parts of the medical school curriculum we are working on emphasizing moving forward.
Over the first 2 weeks, students put in 848 volunteer-hours, making 1,438 calls which reached 1,114 different families. We hope our experience proves instructive for other academic medical centers facing similar concerns in coming months. This model allows medical students to be directly involved in patient care during this crisis and shifts these time-intensive conversations away from overwhelmed primary medical teams.
Reference
1. Gonzalo JD et al. Value-added clinical systems learning roles for 355 medical students that transform education and health: A guide for building partnerships between 356 medical schools and health systems. Acad Med. 2017;92(5):602-7.
Ms. Jaiman is an MD candidate at State University of New York, Brooklyn and a PhD candidate at the National Center of Biological Sciences in Bangalore, India. Mr. Hessburg is an MD/PhD candidate at State University of New York, Brooklyn. Dr. Egelko is a recent graduate of State University of New York, Brooklyn.
The coronavirus pandemic has fundamentally altered American health care. At our academic medical center in Brooklyn, a large safety net institution, clinical year medical students are normally integral members of the team consistent with the model of “value-added medical education.”1 With the suspension of clinical rotations on March 13, 2020, a key part of the workforce was suddenly withdrawn while demand skyrocketed.
In response, students self-organized into numerous remote support projects, including the project described below.
Under infection control regulations, a “no-visitor” policy was instituted. Concurrently, the dramatic increase in patient volume left clinicians unable to regularly update patients’ families. To address this gap, a family contact line was created.
A dedicated phone number was distributed to key hospital personnel to share with families seeking information. The work flow for returning calls is shown in the figure. After verifying patient information and the caller’s relation, students provide updates based on chart review. Calls are prefaced with the disclaimer that students are not part of the treatment team and can only give information that is accessible via the electronic medical record.
Students created a phone script in conjunction with faculty, as well as a referral system for those seeking specific information from other departments. This script undergoes daily revision after the student huddle to address new issues. Flow of information is bidirectional: students relay patient updates as well as quarantine precautions and obtain past medical history. This proved essential during the surge of patients, unknown to the hospital and frequently altered, arriving by ambulance. Students document these conversations in the EMR, including family concerns and whether immediate provider follow-up is needed.
Two key limitations were quickly addressed: First, patients requiring ICU-level care have fluctuating courses, and an update based solely on chart review is insufficient. In response, students worked with intensivist teams to create a dedicated call line staffed by providers.
Second, conversations regarding goals of care and end of life concerns were beyond students’ scope. Together with palliative care teams, students developed criteria for flagging families for follow-up by a consulting palliative care attending.
Through working the call line, students received a crash course in empathetically communicating over the phone. Particularly during the worst of the surge, families were afraid and often frustrated at the lack of communication up to that point. Navigating these emotions, learning how to update family members while removed from the teams, and educating callers on quarantine precautions and other concerns was a valuable learning experience.
As students, we have been exposed to many of the realities of communicating as a physician. Relaying updates and prognosis to family while also providing emotional support is not something we are taught in medical school, but is something we will be expected to handle our first night on the wards as an intern. This experience has prepared us well for that and has illuminated missing parts of the medical school curriculum we are working on emphasizing moving forward.
Over the first 2 weeks, students put in 848 volunteer-hours, making 1,438 calls which reached 1,114 different families. We hope our experience proves instructive for other academic medical centers facing similar concerns in coming months. This model allows medical students to be directly involved in patient care during this crisis and shifts these time-intensive conversations away from overwhelmed primary medical teams.
Reference
1. Gonzalo JD et al. Value-added clinical systems learning roles for 355 medical students that transform education and health: A guide for building partnerships between 356 medical schools and health systems. Acad Med. 2017;92(5):602-7.
Ms. Jaiman is an MD candidate at State University of New York, Brooklyn and a PhD candidate at the National Center of Biological Sciences in Bangalore, India. Mr. Hessburg is an MD/PhD candidate at State University of New York, Brooklyn. Dr. Egelko is a recent graduate of State University of New York, Brooklyn.
The wheels on the bus take lung cancer screening to rural areas
Results from a pilot study, published online July 13 in The Annals of Thoracic Surgery, show that the scheme is both practical and financially sustainable.
During a 10-month test run, the mobile unit screened 548 individuals at 104 sites. Five lung cancers (four of which were early stage) and a type B thymoma were discovered, and all of these individuals went on to have treatment.
Significant pulmonary findings were also discovered in 52 individuals, who were advised to undergo further testing, as well as significant nonpulmonary findings in 152 individuals (of whom 13 required further testing, but none went on to have treatment). These findings included severe coronary disease and thyroid abnormalities.
The bus reached the estimated financial break-even point of 428 scans, but future economic viability of such a program will likely rely on additional revenue from the treatment of patients with incidental findings from low-dose CT screens, acknowledged the authors, led by James R. Headrick Jr, MD, MBA, from the University of Tennessee College of Medicine in Chattanooga.
The real value of the Breathe Easy program, however, comes from bringing both patient education and lung cancer screening services to a high-risk population who might otherwise be overlooked, Headrick said in an interview with Medscape Medical News.
“We were all excited when lung screening was approved, and we got the recommendation from the United States Preventive Services Task Force [USPSTF], and the Centers for Medicare & Medicaid Services signed off on it, and we sat in our offices and clinics and hospitals — and nobody showed up. We were thinking, ‘Wow, we have this simple test, the easiest screening tool in the world, and nobody’s coming,’ “ he said.
“There was certainly an educational issue that needed to be solved,” he continued, “but we were also dealing with a population that had been told that if they smoked and didn’t live life well, there was a 100% chance they were going to get lung cancer and die,” he said.
The individuals screened in the program were very heavy smokers.
The mean pack-years of smoking was 41 — 11 pack-years higher than the minimum recommended under current lung cancer screening guidelines, and 21 pack-years higher than that recently recommended under proposed low-dose CT screening guidelines by the USPSTF.
Albert Rizzo, MD, chief medical officer for the American Lung Association, who was not involved in the study, told Medscape Medical News any initiative that can expand lung cancer screening is welcome, particularly when a program may be self-sustaining.
“The interesting part of this article included the downstream revenue to help make something like this viable,” Rizzo said. “Just doing the scans is probably not going to cover the cost of the mobile unit itself, but if you take into account that other things are being found in addition to lung cancer, such as coronary abnormalities, then it becomes more cost-effective, especially if those patients are then treated at the site where the mobile unit is coming from,” he said.
Starting at square one
The first mobile CT scanner was launched in Nagano Prefecture, a rural area in Japan, in 1996. Since then, mobile screening units, primarily mounted on tractor trailers, have brought screening to centralized areas, such as shopping mall parking lots. The Levine Cancer Institute in Charlotte, North Carolina, also has a mobile CT-screening unit mounted in a modified box truck.
For Headrick and colleagues the goal was not to reinvent the wheel, but to see if a mobile lung cancer screening program could improve access and also pay for itself in a time of parsimonious support for preventive medicine.
Their first challenge was the mobile unit itself.
“CT scanners are sensitive, complex electrical machines that require climate control and a level environment to operate. Historically, they have been placed in tractor trailers and parked on level concrete slabs connected to external power supplies. We needed mobility, self-leveling, independent power, climate control, patient comfort, and drivability,” they wrote.
They assembled a team of engineers from CT and vehicle makers, and input was also provided by a thoracic surgeon, pulmonologist, radiologist, CT technician, and driver with a commercial driver’s license. Together, they designed and built the bus over 8 months. Funds for the total cost of the prototype vehicle ($650,000) came from two local nonprofit foundations. The estimated cost for a commercial version of the same vehicle was $850,000.
The Breathe Easy pilot began operation in early 2018, with the initial plan to drive the bus within a 2-hour radius of CHI Memorial Hospital, Chattanooga, Tennessee, to avoid overnight trips. The radius was later shortened to 1.5 hours when operators realized it was a burden for patients with significant screening findings to travel to as much as 4 hours (round trip) to Chattanooga for further testing.
Each screening visit takes about 15 minutes.
Cancer and other significant findings
As noted before, the bus traveled to 104 sites over 10 months, and 548 patients with a mean age of 62 were screened. Five lung cancers were identified, including two stage 1A, one stage 1A2, one stage 1B, and one stage 3A.
Two patients with early stage disease underwent stereotactic body radiation therapy, and two underwent minimally invasive surgery (a segmentectomy and a lobectomy). The patient with stage 3A disease underwent curative chemotherapy and radiation therapy. One patient with a type B1 thymoma underwent robotic-assisted thoracoscopic resection with en bloc pericardial resection and reconstruction.
A total of 51 patients had a significant pulmonary finding of Lung CT Screening Reporting and Data System (Lung-RADS) 3 or 4 and were advised to follow up with further testing, but 17 patients in this group did not pursue further testing. Of these 17 patients, 15 had been screened in a health clinic for the homeless at a rural site.
Significant nonpulmonary findings included moderate to severe coronary artery disease in 101 patients, abdominal findings in 15, thyroid abnormalities in 14, other thoracic findings in 10, and ascending aortic dilatation in 9. Of the 152 patients with nonpulmonary findings, only 13 required further testing and none required treatment.
Revisions, improvements, and priorities
The Breathe Easy bus has been in operation for more than 2 years, performing an average of approximately 100 screenings per month, with a goal of 200. The bus continued to operate throughout the COVID-19 pandemic because many patients viewed it as a safer alternative to a hospital visit, Headrick said.
Design changes planned to improve performance of the bus include a stronger chassis and structural components, as well as swapping out the 16-slice CT unit for a specially designed 64-slice mobile unit that can be operated with an iPad and provide gated coronary calcium scores.
When challenged about whether the cost of lung cancer screening is the best use of limited resources, Headrick said, “if it’s not, then when we need to go back to the drawing board and jump-start lung cancer screening.”
“When I spent a year in 2014-2015 trying to talk to radio stations, news stations, media, nobody really cared about lung cancer screening,” he said. “But as soon as I had this shiny object, which is the bus, which we labeled as the easiest and most valuable doctor visit, people had an interest.”
The pilot study was supported by local nonprofit foundations through the CHI Memorial Foundation.
This article first appeared on Medscape.com.
Results from a pilot study, published online July 13 in The Annals of Thoracic Surgery, show that the scheme is both practical and financially sustainable.
During a 10-month test run, the mobile unit screened 548 individuals at 104 sites. Five lung cancers (four of which were early stage) and a type B thymoma were discovered, and all of these individuals went on to have treatment.
Significant pulmonary findings were also discovered in 52 individuals, who were advised to undergo further testing, as well as significant nonpulmonary findings in 152 individuals (of whom 13 required further testing, but none went on to have treatment). These findings included severe coronary disease and thyroid abnormalities.
The bus reached the estimated financial break-even point of 428 scans, but future economic viability of such a program will likely rely on additional revenue from the treatment of patients with incidental findings from low-dose CT screens, acknowledged the authors, led by James R. Headrick Jr, MD, MBA, from the University of Tennessee College of Medicine in Chattanooga.
The real value of the Breathe Easy program, however, comes from bringing both patient education and lung cancer screening services to a high-risk population who might otherwise be overlooked, Headrick said in an interview with Medscape Medical News.
“We were all excited when lung screening was approved, and we got the recommendation from the United States Preventive Services Task Force [USPSTF], and the Centers for Medicare & Medicaid Services signed off on it, and we sat in our offices and clinics and hospitals — and nobody showed up. We were thinking, ‘Wow, we have this simple test, the easiest screening tool in the world, and nobody’s coming,’ “ he said.
“There was certainly an educational issue that needed to be solved,” he continued, “but we were also dealing with a population that had been told that if they smoked and didn’t live life well, there was a 100% chance they were going to get lung cancer and die,” he said.
The individuals screened in the program were very heavy smokers.
The mean pack-years of smoking was 41 — 11 pack-years higher than the minimum recommended under current lung cancer screening guidelines, and 21 pack-years higher than that recently recommended under proposed low-dose CT screening guidelines by the USPSTF.
Albert Rizzo, MD, chief medical officer for the American Lung Association, who was not involved in the study, told Medscape Medical News any initiative that can expand lung cancer screening is welcome, particularly when a program may be self-sustaining.
“The interesting part of this article included the downstream revenue to help make something like this viable,” Rizzo said. “Just doing the scans is probably not going to cover the cost of the mobile unit itself, but if you take into account that other things are being found in addition to lung cancer, such as coronary abnormalities, then it becomes more cost-effective, especially if those patients are then treated at the site where the mobile unit is coming from,” he said.
Starting at square one
The first mobile CT scanner was launched in Nagano Prefecture, a rural area in Japan, in 1996. Since then, mobile screening units, primarily mounted on tractor trailers, have brought screening to centralized areas, such as shopping mall parking lots. The Levine Cancer Institute in Charlotte, North Carolina, also has a mobile CT-screening unit mounted in a modified box truck.
For Headrick and colleagues the goal was not to reinvent the wheel, but to see if a mobile lung cancer screening program could improve access and also pay for itself in a time of parsimonious support for preventive medicine.
Their first challenge was the mobile unit itself.
“CT scanners are sensitive, complex electrical machines that require climate control and a level environment to operate. Historically, they have been placed in tractor trailers and parked on level concrete slabs connected to external power supplies. We needed mobility, self-leveling, independent power, climate control, patient comfort, and drivability,” they wrote.
They assembled a team of engineers from CT and vehicle makers, and input was also provided by a thoracic surgeon, pulmonologist, radiologist, CT technician, and driver with a commercial driver’s license. Together, they designed and built the bus over 8 months. Funds for the total cost of the prototype vehicle ($650,000) came from two local nonprofit foundations. The estimated cost for a commercial version of the same vehicle was $850,000.
The Breathe Easy pilot began operation in early 2018, with the initial plan to drive the bus within a 2-hour radius of CHI Memorial Hospital, Chattanooga, Tennessee, to avoid overnight trips. The radius was later shortened to 1.5 hours when operators realized it was a burden for patients with significant screening findings to travel to as much as 4 hours (round trip) to Chattanooga for further testing.
Each screening visit takes about 15 minutes.
Cancer and other significant findings
As noted before, the bus traveled to 104 sites over 10 months, and 548 patients with a mean age of 62 were screened. Five lung cancers were identified, including two stage 1A, one stage 1A2, one stage 1B, and one stage 3A.
Two patients with early stage disease underwent stereotactic body radiation therapy, and two underwent minimally invasive surgery (a segmentectomy and a lobectomy). The patient with stage 3A disease underwent curative chemotherapy and radiation therapy. One patient with a type B1 thymoma underwent robotic-assisted thoracoscopic resection with en bloc pericardial resection and reconstruction.
A total of 51 patients had a significant pulmonary finding of Lung CT Screening Reporting and Data System (Lung-RADS) 3 or 4 and were advised to follow up with further testing, but 17 patients in this group did not pursue further testing. Of these 17 patients, 15 had been screened in a health clinic for the homeless at a rural site.
Significant nonpulmonary findings included moderate to severe coronary artery disease in 101 patients, abdominal findings in 15, thyroid abnormalities in 14, other thoracic findings in 10, and ascending aortic dilatation in 9. Of the 152 patients with nonpulmonary findings, only 13 required further testing and none required treatment.
Revisions, improvements, and priorities
The Breathe Easy bus has been in operation for more than 2 years, performing an average of approximately 100 screenings per month, with a goal of 200. The bus continued to operate throughout the COVID-19 pandemic because many patients viewed it as a safer alternative to a hospital visit, Headrick said.
Design changes planned to improve performance of the bus include a stronger chassis and structural components, as well as swapping out the 16-slice CT unit for a specially designed 64-slice mobile unit that can be operated with an iPad and provide gated coronary calcium scores.
When challenged about whether the cost of lung cancer screening is the best use of limited resources, Headrick said, “if it’s not, then when we need to go back to the drawing board and jump-start lung cancer screening.”
“When I spent a year in 2014-2015 trying to talk to radio stations, news stations, media, nobody really cared about lung cancer screening,” he said. “But as soon as I had this shiny object, which is the bus, which we labeled as the easiest and most valuable doctor visit, people had an interest.”
The pilot study was supported by local nonprofit foundations through the CHI Memorial Foundation.
This article first appeared on Medscape.com.
Results from a pilot study, published online July 13 in The Annals of Thoracic Surgery, show that the scheme is both practical and financially sustainable.
During a 10-month test run, the mobile unit screened 548 individuals at 104 sites. Five lung cancers (four of which were early stage) and a type B thymoma were discovered, and all of these individuals went on to have treatment.
Significant pulmonary findings were also discovered in 52 individuals, who were advised to undergo further testing, as well as significant nonpulmonary findings in 152 individuals (of whom 13 required further testing, but none went on to have treatment). These findings included severe coronary disease and thyroid abnormalities.
The bus reached the estimated financial break-even point of 428 scans, but future economic viability of such a program will likely rely on additional revenue from the treatment of patients with incidental findings from low-dose CT screens, acknowledged the authors, led by James R. Headrick Jr, MD, MBA, from the University of Tennessee College of Medicine in Chattanooga.
The real value of the Breathe Easy program, however, comes from bringing both patient education and lung cancer screening services to a high-risk population who might otherwise be overlooked, Headrick said in an interview with Medscape Medical News.
“We were all excited when lung screening was approved, and we got the recommendation from the United States Preventive Services Task Force [USPSTF], and the Centers for Medicare & Medicaid Services signed off on it, and we sat in our offices and clinics and hospitals — and nobody showed up. We were thinking, ‘Wow, we have this simple test, the easiest screening tool in the world, and nobody’s coming,’ “ he said.
“There was certainly an educational issue that needed to be solved,” he continued, “but we were also dealing with a population that had been told that if they smoked and didn’t live life well, there was a 100% chance they were going to get lung cancer and die,” he said.
The individuals screened in the program were very heavy smokers.
The mean pack-years of smoking was 41 — 11 pack-years higher than the minimum recommended under current lung cancer screening guidelines, and 21 pack-years higher than that recently recommended under proposed low-dose CT screening guidelines by the USPSTF.
Albert Rizzo, MD, chief medical officer for the American Lung Association, who was not involved in the study, told Medscape Medical News any initiative that can expand lung cancer screening is welcome, particularly when a program may be self-sustaining.
“The interesting part of this article included the downstream revenue to help make something like this viable,” Rizzo said. “Just doing the scans is probably not going to cover the cost of the mobile unit itself, but if you take into account that other things are being found in addition to lung cancer, such as coronary abnormalities, then it becomes more cost-effective, especially if those patients are then treated at the site where the mobile unit is coming from,” he said.
Starting at square one
The first mobile CT scanner was launched in Nagano Prefecture, a rural area in Japan, in 1996. Since then, mobile screening units, primarily mounted on tractor trailers, have brought screening to centralized areas, such as shopping mall parking lots. The Levine Cancer Institute in Charlotte, North Carolina, also has a mobile CT-screening unit mounted in a modified box truck.
For Headrick and colleagues the goal was not to reinvent the wheel, but to see if a mobile lung cancer screening program could improve access and also pay for itself in a time of parsimonious support for preventive medicine.
Their first challenge was the mobile unit itself.
“CT scanners are sensitive, complex electrical machines that require climate control and a level environment to operate. Historically, they have been placed in tractor trailers and parked on level concrete slabs connected to external power supplies. We needed mobility, self-leveling, independent power, climate control, patient comfort, and drivability,” they wrote.
They assembled a team of engineers from CT and vehicle makers, and input was also provided by a thoracic surgeon, pulmonologist, radiologist, CT technician, and driver with a commercial driver’s license. Together, they designed and built the bus over 8 months. Funds for the total cost of the prototype vehicle ($650,000) came from two local nonprofit foundations. The estimated cost for a commercial version of the same vehicle was $850,000.
The Breathe Easy pilot began operation in early 2018, with the initial plan to drive the bus within a 2-hour radius of CHI Memorial Hospital, Chattanooga, Tennessee, to avoid overnight trips. The radius was later shortened to 1.5 hours when operators realized it was a burden for patients with significant screening findings to travel to as much as 4 hours (round trip) to Chattanooga for further testing.
Each screening visit takes about 15 minutes.
Cancer and other significant findings
As noted before, the bus traveled to 104 sites over 10 months, and 548 patients with a mean age of 62 were screened. Five lung cancers were identified, including two stage 1A, one stage 1A2, one stage 1B, and one stage 3A.
Two patients with early stage disease underwent stereotactic body radiation therapy, and two underwent minimally invasive surgery (a segmentectomy and a lobectomy). The patient with stage 3A disease underwent curative chemotherapy and radiation therapy. One patient with a type B1 thymoma underwent robotic-assisted thoracoscopic resection with en bloc pericardial resection and reconstruction.
A total of 51 patients had a significant pulmonary finding of Lung CT Screening Reporting and Data System (Lung-RADS) 3 or 4 and were advised to follow up with further testing, but 17 patients in this group did not pursue further testing. Of these 17 patients, 15 had been screened in a health clinic for the homeless at a rural site.
Significant nonpulmonary findings included moderate to severe coronary artery disease in 101 patients, abdominal findings in 15, thyroid abnormalities in 14, other thoracic findings in 10, and ascending aortic dilatation in 9. Of the 152 patients with nonpulmonary findings, only 13 required further testing and none required treatment.
Revisions, improvements, and priorities
The Breathe Easy bus has been in operation for more than 2 years, performing an average of approximately 100 screenings per month, with a goal of 200. The bus continued to operate throughout the COVID-19 pandemic because many patients viewed it as a safer alternative to a hospital visit, Headrick said.
Design changes planned to improve performance of the bus include a stronger chassis and structural components, as well as swapping out the 16-slice CT unit for a specially designed 64-slice mobile unit that can be operated with an iPad and provide gated coronary calcium scores.
When challenged about whether the cost of lung cancer screening is the best use of limited resources, Headrick said, “if it’s not, then when we need to go back to the drawing board and jump-start lung cancer screening.”
“When I spent a year in 2014-2015 trying to talk to radio stations, news stations, media, nobody really cared about lung cancer screening,” he said. “But as soon as I had this shiny object, which is the bus, which we labeled as the easiest and most valuable doctor visit, people had an interest.”
The pilot study was supported by local nonprofit foundations through the CHI Memorial Foundation.
This article first appeared on Medscape.com.
Revisiting Xanax amid the coronavirus crisis
One of the more alarming trends that has emerged during the coronavirus crisis is the concomitant rise in the use of benzodiazepines, such as Xanax. It has been reported that at-risk individuals began seeking prescription anxiolytics as early as mid-February with a consequent peak of 34% the following month, coinciding with the World Health Organization’s declaration of a global pandemic.1
Consistent with the available literature indicating that women are twice as likely to be affected by anxiety disorders, the prescription spikes were almost double when compared with those of their male counterparts.2 The pandemic has instilled a sense of fear in people, leading to social repercussions, such as estrangement, insomnia, and paranoia for at-risk populations.3,4
“Benzos” are commonly prescribed to help people sleep or to assist them in overcoming a host of anxiety disorders. The rapid onset of effects make Xanax a desirable and efficacious benzodiazepine.5 The use of these medications might not be an immediate cause for concern because patients might be taking it as intended. Nevertheless, clinicians are shying away from medical management in favor of counseling or therapy.
Dangerous trends
Numerous factors might contribute to this grim scenario, including patient dependence on benzodiazepines, paranoia about engaging with health care professionals because of fear tied to potential COVID-19 exposure, and/or increased access to illicit counterfeit pills from drug dealers or the dark web markets.
Lessons can be gleaned from the most extensive dark web drug busts in Britain’s history, in which a deluge of “pharmaceutical grade” Xanax pills made it to the hands of drug dealers and consumers between 2015 and 2017.6 A similar phenomenon emerged stateside.7 Virtually indistinguishable from recognized 2-mg Xanax pills, these fake pills posed a serious challenge to forensic scientists.8 The threat of overdose is very real for users targeted by the counterfeit Xanax trade, especially since those at risk often bypass professional health care guidelines.
In broad daylight, the drug dealers ran their operations revolving around two fake Xanax products: a primary knockoff and a limited edition – and vastly more potent “Red Devil” variant that was intentionally dyed for branding purposes. Because the “Red Devil” formulations contained 2.5 times the dose of the 2-mg pill, it had even more pronounced tolerance, dependence, and withdrawal effects (for example, panic attacks, anxiety, and/or hallucinations) – fatal consequences for users involved in consuming other drugs, such as alcohol or opioids. Preexisting drug users tend to gravitate toward benzodiazepines, such as alprazolam (Xanax), perhaps in part, because of its relatively rapid onset of action. Xanax also is known for inducing proeuphoric states at higher doses, hence the appeal of the “Red Devil” pills.
Benzodiazepines, as a class of drugs, facilitate the neurotransmitter gamma-aminobutryric acid’s (GABA) effect on the brain, producing anxiolytic, hypnotic, and/or anticonvulsant states within the user.9 Unbeknownst to numerous users is the fact that drugs such as alcohol and opioids, like Xanax, also serve as respiratory depressants, overriding the brain’s governance of the breathing mechanism. This, in turn, leads to unintended overdose deaths, even among seasoned drug seekers.
Overdose deaths have been steadily climbing over the years because it is common for some users to consume alcohol while being on Xanax therapy – without realizing that both substances are depressants and that taking them together can lead to side effects such as respiratory depression.
Forensic cases also have revealed that preexisting opioid consumers were drawn to Xanax; the drug’s potent mechanism of action would likely appeal to habituated users. A typical behavioral pattern has emerged among users and must be addressed. According to Australian Professor Shane Darke: “So they take their Xanax, they take their painkiller, then they get drunk, that could be enough to kill them.”
Fatalities are more likely when benzodiazepines are combined with other drug classes or if the existing supply is contaminated or laced (for example, with fentanyl).8
As far as deaths by accidental benzodiazepine overdose are concerned, a similar epidemic has been recorded in the United States. In 2013, almost one-third of all prescription overdose deaths can be attributed to the use of benzodiazepines (for example, Xanax, Valium, and Ativan). However, media attention has been considerably muted, especially when compared with that of narcotic abuse. This is even more puzzling when taking into account that three-quarters of benzodiazepine mortalities co-occur within the context of narcotic consumption. Substance Abuse and Mental Health Services Administration data confirm the ubiquitous nature of benzodiazepine (such as alprazolam) coprescriptions, accounting for roughly half of the 176,000 emergency department cases for 2011. The Centers for Disease Control and Prevention noted that there was a 67% increase in benzodiazepine prescriptions between 1996 and 2013, which warranted more stringent regulations for this particular class of drugs.
In 2016, the CDC issued new guidelines for opioid use acknowledging the danger of benzodiazepine coprescriptions. Food and Drug Administration “black box” warnings now grace the prescriptions of both of these drug classes.10 This trend remains on an upward trajectory, even more so during the pandemic, as there are 9.7 million prescriptions of anxiolytics/hypnotics such as Xanax, Ativan, and Klonopin in the United States as of March 2020, which represents a 10% increase over the previous year. , as well as the implementation of urine drug screening monitoring for drug adherence/compliance and diversion in those with suspected benzodiazepine addiction or a history of polysubstance abuse.11,12
Clinical correlates
For patients who present acutely with Xanax toxicity in the emergency room setting, we will need to initially stabilize the vital signs and address the ongoing symptoms. It is advisable to arrange health care accommodations for patients with physical dependence to monitor and treat their withdrawal symptoms. The patient should be enrolled in a comprehensive addiction facility after undergoing formal detoxification; a tapered treatment protocol will need to be implemented because quitting “cold turkey” can lead to convulsions and, in some cases, death. Patient education, talk therapy, and alternatives to benzodiazepines should be discussed with the clinician.13,145
However, to truly address the elephant in the room, we will need to consider institutional reforms to prevent a similar situation from arising in the future. Primary care physician shortages are compounded by changes in insurance policies. Nurses and physician assistants will need to be trained to manage benzodiazepine prescriptions. If there are community shortages in physicians, patients might turn to illegal means to secure their benzodiazepine supply, and it is imperative that we have the necessary fellowship and education programs to educate nonphysician health care clinicians with benzodiazepine management. Because physicians were prescribing benzodiazepines liberally, the Prescription Drug Monitoring Programs (PDMP) was enacted to monitor physician practices. Unfortunately, this ultimately intimidated physicians and effectively curbed reasonable physician prescribing patterns. It might be necessary to revisit existing prescription monitoring programs, encourage drug evaluations and guidelines based on evidence-based medicine and embrace telemedicine in order to facilitate patient-physician communication.
As of now, it is too early to prescribe Xanax routinely for ongoing anxiety experienced during the coronavirus crisis, and several physicians are cautious about prescribing antianxiety medications for more than a few months.17 Surprisingly, researchers in Barcelona have even explored the role of Xanax as potentially inhibiting Mpro, the primary protease of coronavirus, thereby forestalling the virus’s ability to replicate.16 However, it is worth noting that, given the preliminary nature of the results, any attempts at conclusively integrating Xanax within the context of coronavirus therapy would be premature.
References
1. Luhby T. Anti-anxiety medication prescriptions up 34% since coronavirus. CNN. 2020 Apr 16.
2. Women and Anxiety. Anxiety and Depression Association of America.
3. Shigemura J et al. Psychiatry Clin Neurosci. 2012 Apr 7;74(4):281-2.
4. Petersen A. More people are taking drugs for anxiety and insomnia, and doctors are worried. The Wall Street Journal. 2020 May 25.
5. Downey M. Xanax overdose and related deaths. National Drug & Alcohol Research Centre. UNSW Sydney.
6. Bryant B. Fake Xanax: The UK’s biggest ever dark net drugs bust. BBC. 2018 Mar 10.
7. Reinberg S. Fatal overdoses rising from sedatives like Valium, Xanax. HealthDay. 2016 Feb.
8. Is counterfeit Xanax dangerous? American Addiction Centers. Updated 2018 Nov 14.
9. McLaren E. Xanax history and statistics. Drugabuse.com.
10. Benzodiazepines and opioids. National Institute on Drug Abuse. 2018 Mar 15.
11. Choudhry Z et al. J Psychiatry. 2015;18(5). doi: 10.4172/2378-5756.1000319.
12. Islam FA et al. Current Psychiatry. 2018 Dec 17(12):43-4.
13. Adams M. Xanax death rate on the rise. White Sands Treatment. 2017 Sept.NEED LINK
14. Storrs C. Benzodiazepine overdose deaths soared in recent years, study finds. CNN. 2016 Feb. 18.
15. Hanscom DA. Plan A – Thrive and survive COVID-19. Back in Control. 2020.
16. Smith C. Xanax, a common anxiety medication, might actually block coronavirus. BGR. 2020 May 29.
Dr. Islam is a medical adviser for the International Maternal and Child Health Foundation (IMCHF), Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Islam disclosed no relevant financial relationships.
Mr. Choudhry is a research assistant at the IMCHF. He has no disclosures.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF and is Mr. Choudhry’s father. He has no disclosures.
One of the more alarming trends that has emerged during the coronavirus crisis is the concomitant rise in the use of benzodiazepines, such as Xanax. It has been reported that at-risk individuals began seeking prescription anxiolytics as early as mid-February with a consequent peak of 34% the following month, coinciding with the World Health Organization’s declaration of a global pandemic.1
Consistent with the available literature indicating that women are twice as likely to be affected by anxiety disorders, the prescription spikes were almost double when compared with those of their male counterparts.2 The pandemic has instilled a sense of fear in people, leading to social repercussions, such as estrangement, insomnia, and paranoia for at-risk populations.3,4
“Benzos” are commonly prescribed to help people sleep or to assist them in overcoming a host of anxiety disorders. The rapid onset of effects make Xanax a desirable and efficacious benzodiazepine.5 The use of these medications might not be an immediate cause for concern because patients might be taking it as intended. Nevertheless, clinicians are shying away from medical management in favor of counseling or therapy.
Dangerous trends
Numerous factors might contribute to this grim scenario, including patient dependence on benzodiazepines, paranoia about engaging with health care professionals because of fear tied to potential COVID-19 exposure, and/or increased access to illicit counterfeit pills from drug dealers or the dark web markets.
Lessons can be gleaned from the most extensive dark web drug busts in Britain’s history, in which a deluge of “pharmaceutical grade” Xanax pills made it to the hands of drug dealers and consumers between 2015 and 2017.6 A similar phenomenon emerged stateside.7 Virtually indistinguishable from recognized 2-mg Xanax pills, these fake pills posed a serious challenge to forensic scientists.8 The threat of overdose is very real for users targeted by the counterfeit Xanax trade, especially since those at risk often bypass professional health care guidelines.
In broad daylight, the drug dealers ran their operations revolving around two fake Xanax products: a primary knockoff and a limited edition – and vastly more potent “Red Devil” variant that was intentionally dyed for branding purposes. Because the “Red Devil” formulations contained 2.5 times the dose of the 2-mg pill, it had even more pronounced tolerance, dependence, and withdrawal effects (for example, panic attacks, anxiety, and/or hallucinations) – fatal consequences for users involved in consuming other drugs, such as alcohol or opioids. Preexisting drug users tend to gravitate toward benzodiazepines, such as alprazolam (Xanax), perhaps in part, because of its relatively rapid onset of action. Xanax also is known for inducing proeuphoric states at higher doses, hence the appeal of the “Red Devil” pills.
Benzodiazepines, as a class of drugs, facilitate the neurotransmitter gamma-aminobutryric acid’s (GABA) effect on the brain, producing anxiolytic, hypnotic, and/or anticonvulsant states within the user.9 Unbeknownst to numerous users is the fact that drugs such as alcohol and opioids, like Xanax, also serve as respiratory depressants, overriding the brain’s governance of the breathing mechanism. This, in turn, leads to unintended overdose deaths, even among seasoned drug seekers.
Overdose deaths have been steadily climbing over the years because it is common for some users to consume alcohol while being on Xanax therapy – without realizing that both substances are depressants and that taking them together can lead to side effects such as respiratory depression.
Forensic cases also have revealed that preexisting opioid consumers were drawn to Xanax; the drug’s potent mechanism of action would likely appeal to habituated users. A typical behavioral pattern has emerged among users and must be addressed. According to Australian Professor Shane Darke: “So they take their Xanax, they take their painkiller, then they get drunk, that could be enough to kill them.”
Fatalities are more likely when benzodiazepines are combined with other drug classes or if the existing supply is contaminated or laced (for example, with fentanyl).8
As far as deaths by accidental benzodiazepine overdose are concerned, a similar epidemic has been recorded in the United States. In 2013, almost one-third of all prescription overdose deaths can be attributed to the use of benzodiazepines (for example, Xanax, Valium, and Ativan). However, media attention has been considerably muted, especially when compared with that of narcotic abuse. This is even more puzzling when taking into account that three-quarters of benzodiazepine mortalities co-occur within the context of narcotic consumption. Substance Abuse and Mental Health Services Administration data confirm the ubiquitous nature of benzodiazepine (such as alprazolam) coprescriptions, accounting for roughly half of the 176,000 emergency department cases for 2011. The Centers for Disease Control and Prevention noted that there was a 67% increase in benzodiazepine prescriptions between 1996 and 2013, which warranted more stringent regulations for this particular class of drugs.
In 2016, the CDC issued new guidelines for opioid use acknowledging the danger of benzodiazepine coprescriptions. Food and Drug Administration “black box” warnings now grace the prescriptions of both of these drug classes.10 This trend remains on an upward trajectory, even more so during the pandemic, as there are 9.7 million prescriptions of anxiolytics/hypnotics such as Xanax, Ativan, and Klonopin in the United States as of March 2020, which represents a 10% increase over the previous year. , as well as the implementation of urine drug screening monitoring for drug adherence/compliance and diversion in those with suspected benzodiazepine addiction or a history of polysubstance abuse.11,12
Clinical correlates
For patients who present acutely with Xanax toxicity in the emergency room setting, we will need to initially stabilize the vital signs and address the ongoing symptoms. It is advisable to arrange health care accommodations for patients with physical dependence to monitor and treat their withdrawal symptoms. The patient should be enrolled in a comprehensive addiction facility after undergoing formal detoxification; a tapered treatment protocol will need to be implemented because quitting “cold turkey” can lead to convulsions and, in some cases, death. Patient education, talk therapy, and alternatives to benzodiazepines should be discussed with the clinician.13,145
However, to truly address the elephant in the room, we will need to consider institutional reforms to prevent a similar situation from arising in the future. Primary care physician shortages are compounded by changes in insurance policies. Nurses and physician assistants will need to be trained to manage benzodiazepine prescriptions. If there are community shortages in physicians, patients might turn to illegal means to secure their benzodiazepine supply, and it is imperative that we have the necessary fellowship and education programs to educate nonphysician health care clinicians with benzodiazepine management. Because physicians were prescribing benzodiazepines liberally, the Prescription Drug Monitoring Programs (PDMP) was enacted to monitor physician practices. Unfortunately, this ultimately intimidated physicians and effectively curbed reasonable physician prescribing patterns. It might be necessary to revisit existing prescription monitoring programs, encourage drug evaluations and guidelines based on evidence-based medicine and embrace telemedicine in order to facilitate patient-physician communication.
As of now, it is too early to prescribe Xanax routinely for ongoing anxiety experienced during the coronavirus crisis, and several physicians are cautious about prescribing antianxiety medications for more than a few months.17 Surprisingly, researchers in Barcelona have even explored the role of Xanax as potentially inhibiting Mpro, the primary protease of coronavirus, thereby forestalling the virus’s ability to replicate.16 However, it is worth noting that, given the preliminary nature of the results, any attempts at conclusively integrating Xanax within the context of coronavirus therapy would be premature.
References
1. Luhby T. Anti-anxiety medication prescriptions up 34% since coronavirus. CNN. 2020 Apr 16.
2. Women and Anxiety. Anxiety and Depression Association of America.
3. Shigemura J et al. Psychiatry Clin Neurosci. 2012 Apr 7;74(4):281-2.
4. Petersen A. More people are taking drugs for anxiety and insomnia, and doctors are worried. The Wall Street Journal. 2020 May 25.
5. Downey M. Xanax overdose and related deaths. National Drug & Alcohol Research Centre. UNSW Sydney.
6. Bryant B. Fake Xanax: The UK’s biggest ever dark net drugs bust. BBC. 2018 Mar 10.
7. Reinberg S. Fatal overdoses rising from sedatives like Valium, Xanax. HealthDay. 2016 Feb.
8. Is counterfeit Xanax dangerous? American Addiction Centers. Updated 2018 Nov 14.
9. McLaren E. Xanax history and statistics. Drugabuse.com.
10. Benzodiazepines and opioids. National Institute on Drug Abuse. 2018 Mar 15.
11. Choudhry Z et al. J Psychiatry. 2015;18(5). doi: 10.4172/2378-5756.1000319.
12. Islam FA et al. Current Psychiatry. 2018 Dec 17(12):43-4.
13. Adams M. Xanax death rate on the rise. White Sands Treatment. 2017 Sept.NEED LINK
14. Storrs C. Benzodiazepine overdose deaths soared in recent years, study finds. CNN. 2016 Feb. 18.
15. Hanscom DA. Plan A – Thrive and survive COVID-19. Back in Control. 2020.
16. Smith C. Xanax, a common anxiety medication, might actually block coronavirus. BGR. 2020 May 29.
Dr. Islam is a medical adviser for the International Maternal and Child Health Foundation (IMCHF), Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Islam disclosed no relevant financial relationships.
Mr. Choudhry is a research assistant at the IMCHF. He has no disclosures.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF and is Mr. Choudhry’s father. He has no disclosures.
One of the more alarming trends that has emerged during the coronavirus crisis is the concomitant rise in the use of benzodiazepines, such as Xanax. It has been reported that at-risk individuals began seeking prescription anxiolytics as early as mid-February with a consequent peak of 34% the following month, coinciding with the World Health Organization’s declaration of a global pandemic.1
Consistent with the available literature indicating that women are twice as likely to be affected by anxiety disorders, the prescription spikes were almost double when compared with those of their male counterparts.2 The pandemic has instilled a sense of fear in people, leading to social repercussions, such as estrangement, insomnia, and paranoia for at-risk populations.3,4
“Benzos” are commonly prescribed to help people sleep or to assist them in overcoming a host of anxiety disorders. The rapid onset of effects make Xanax a desirable and efficacious benzodiazepine.5 The use of these medications might not be an immediate cause for concern because patients might be taking it as intended. Nevertheless, clinicians are shying away from medical management in favor of counseling or therapy.
Dangerous trends
Numerous factors might contribute to this grim scenario, including patient dependence on benzodiazepines, paranoia about engaging with health care professionals because of fear tied to potential COVID-19 exposure, and/or increased access to illicit counterfeit pills from drug dealers or the dark web markets.
Lessons can be gleaned from the most extensive dark web drug busts in Britain’s history, in which a deluge of “pharmaceutical grade” Xanax pills made it to the hands of drug dealers and consumers between 2015 and 2017.6 A similar phenomenon emerged stateside.7 Virtually indistinguishable from recognized 2-mg Xanax pills, these fake pills posed a serious challenge to forensic scientists.8 The threat of overdose is very real for users targeted by the counterfeit Xanax trade, especially since those at risk often bypass professional health care guidelines.
In broad daylight, the drug dealers ran their operations revolving around two fake Xanax products: a primary knockoff and a limited edition – and vastly more potent “Red Devil” variant that was intentionally dyed for branding purposes. Because the “Red Devil” formulations contained 2.5 times the dose of the 2-mg pill, it had even more pronounced tolerance, dependence, and withdrawal effects (for example, panic attacks, anxiety, and/or hallucinations) – fatal consequences for users involved in consuming other drugs, such as alcohol or opioids. Preexisting drug users tend to gravitate toward benzodiazepines, such as alprazolam (Xanax), perhaps in part, because of its relatively rapid onset of action. Xanax also is known for inducing proeuphoric states at higher doses, hence the appeal of the “Red Devil” pills.
Benzodiazepines, as a class of drugs, facilitate the neurotransmitter gamma-aminobutryric acid’s (GABA) effect on the brain, producing anxiolytic, hypnotic, and/or anticonvulsant states within the user.9 Unbeknownst to numerous users is the fact that drugs such as alcohol and opioids, like Xanax, also serve as respiratory depressants, overriding the brain’s governance of the breathing mechanism. This, in turn, leads to unintended overdose deaths, even among seasoned drug seekers.
Overdose deaths have been steadily climbing over the years because it is common for some users to consume alcohol while being on Xanax therapy – without realizing that both substances are depressants and that taking them together can lead to side effects such as respiratory depression.
Forensic cases also have revealed that preexisting opioid consumers were drawn to Xanax; the drug’s potent mechanism of action would likely appeal to habituated users. A typical behavioral pattern has emerged among users and must be addressed. According to Australian Professor Shane Darke: “So they take their Xanax, they take their painkiller, then they get drunk, that could be enough to kill them.”
Fatalities are more likely when benzodiazepines are combined with other drug classes or if the existing supply is contaminated or laced (for example, with fentanyl).8
As far as deaths by accidental benzodiazepine overdose are concerned, a similar epidemic has been recorded in the United States. In 2013, almost one-third of all prescription overdose deaths can be attributed to the use of benzodiazepines (for example, Xanax, Valium, and Ativan). However, media attention has been considerably muted, especially when compared with that of narcotic abuse. This is even more puzzling when taking into account that three-quarters of benzodiazepine mortalities co-occur within the context of narcotic consumption. Substance Abuse and Mental Health Services Administration data confirm the ubiquitous nature of benzodiazepine (such as alprazolam) coprescriptions, accounting for roughly half of the 176,000 emergency department cases for 2011. The Centers for Disease Control and Prevention noted that there was a 67% increase in benzodiazepine prescriptions between 1996 and 2013, which warranted more stringent regulations for this particular class of drugs.
In 2016, the CDC issued new guidelines for opioid use acknowledging the danger of benzodiazepine coprescriptions. Food and Drug Administration “black box” warnings now grace the prescriptions of both of these drug classes.10 This trend remains on an upward trajectory, even more so during the pandemic, as there are 9.7 million prescriptions of anxiolytics/hypnotics such as Xanax, Ativan, and Klonopin in the United States as of March 2020, which represents a 10% increase over the previous year. , as well as the implementation of urine drug screening monitoring for drug adherence/compliance and diversion in those with suspected benzodiazepine addiction or a history of polysubstance abuse.11,12
Clinical correlates
For patients who present acutely with Xanax toxicity in the emergency room setting, we will need to initially stabilize the vital signs and address the ongoing symptoms. It is advisable to arrange health care accommodations for patients with physical dependence to monitor and treat their withdrawal symptoms. The patient should be enrolled in a comprehensive addiction facility after undergoing formal detoxification; a tapered treatment protocol will need to be implemented because quitting “cold turkey” can lead to convulsions and, in some cases, death. Patient education, talk therapy, and alternatives to benzodiazepines should be discussed with the clinician.13,145
However, to truly address the elephant in the room, we will need to consider institutional reforms to prevent a similar situation from arising in the future. Primary care physician shortages are compounded by changes in insurance policies. Nurses and physician assistants will need to be trained to manage benzodiazepine prescriptions. If there are community shortages in physicians, patients might turn to illegal means to secure their benzodiazepine supply, and it is imperative that we have the necessary fellowship and education programs to educate nonphysician health care clinicians with benzodiazepine management. Because physicians were prescribing benzodiazepines liberally, the Prescription Drug Monitoring Programs (PDMP) was enacted to monitor physician practices. Unfortunately, this ultimately intimidated physicians and effectively curbed reasonable physician prescribing patterns. It might be necessary to revisit existing prescription monitoring programs, encourage drug evaluations and guidelines based on evidence-based medicine and embrace telemedicine in order to facilitate patient-physician communication.
As of now, it is too early to prescribe Xanax routinely for ongoing anxiety experienced during the coronavirus crisis, and several physicians are cautious about prescribing antianxiety medications for more than a few months.17 Surprisingly, researchers in Barcelona have even explored the role of Xanax as potentially inhibiting Mpro, the primary protease of coronavirus, thereby forestalling the virus’s ability to replicate.16 However, it is worth noting that, given the preliminary nature of the results, any attempts at conclusively integrating Xanax within the context of coronavirus therapy would be premature.
References
1. Luhby T. Anti-anxiety medication prescriptions up 34% since coronavirus. CNN. 2020 Apr 16.
2. Women and Anxiety. Anxiety and Depression Association of America.
3. Shigemura J et al. Psychiatry Clin Neurosci. 2012 Apr 7;74(4):281-2.
4. Petersen A. More people are taking drugs for anxiety and insomnia, and doctors are worried. The Wall Street Journal. 2020 May 25.
5. Downey M. Xanax overdose and related deaths. National Drug & Alcohol Research Centre. UNSW Sydney.
6. Bryant B. Fake Xanax: The UK’s biggest ever dark net drugs bust. BBC. 2018 Mar 10.
7. Reinberg S. Fatal overdoses rising from sedatives like Valium, Xanax. HealthDay. 2016 Feb.
8. Is counterfeit Xanax dangerous? American Addiction Centers. Updated 2018 Nov 14.
9. McLaren E. Xanax history and statistics. Drugabuse.com.
10. Benzodiazepines and opioids. National Institute on Drug Abuse. 2018 Mar 15.
11. Choudhry Z et al. J Psychiatry. 2015;18(5). doi: 10.4172/2378-5756.1000319.
12. Islam FA et al. Current Psychiatry. 2018 Dec 17(12):43-4.
13. Adams M. Xanax death rate on the rise. White Sands Treatment. 2017 Sept.NEED LINK
14. Storrs C. Benzodiazepine overdose deaths soared in recent years, study finds. CNN. 2016 Feb. 18.
15. Hanscom DA. Plan A – Thrive and survive COVID-19. Back in Control. 2020.
16. Smith C. Xanax, a common anxiety medication, might actually block coronavirus. BGR. 2020 May 29.
Dr. Islam is a medical adviser for the International Maternal and Child Health Foundation (IMCHF), Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Islam disclosed no relevant financial relationships.
Mr. Choudhry is a research assistant at the IMCHF. He has no disclosures.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF and is Mr. Choudhry’s father. He has no disclosures.














