User login
FDA OKs Benralizumab for Asthma in Children as Young as 6 Years
Benralizumab is now approved by the US Food and Drug Administration (FDA) for the treatment of asthma in children older than 6 years.
Marketed as Fasenra, the medication first was approved in 2017 for patients aged 12 years or older.
AstraZeneca, which markets the drug, announced the approval for younger patients on April 11.
The expanded indication was supported by a study that showed that the drug functions in the same way with younger children and their adolescent peers. The safety and tolerability were also consistent with the known profile of the medicine, the company said.
For children who weigh ≥ 35 kg, the recommended dose is 30 mg. For patients aged 6-11 years who weigh < 35 kg, a new 10-mg dose will be available, according to the announcement.
The drug, a monoclonal antibody that depletes eosinophils by binding to interleukin 5 receptor alpha on eosinophils, is administered by subcutaneous injection every 4 weeks for the first three doses and then every 8 weeks.
Benralizumab should not be used to treat acute asthma symptoms. Hypersensitivity reasons have occurred after administration of the drug. The most common adverse reactions include headache and pharyngitis.
A version of this article appeared on Medscape.com.
Benralizumab is now approved by the US Food and Drug Administration (FDA) for the treatment of asthma in children older than 6 years.
Marketed as Fasenra, the medication first was approved in 2017 for patients aged 12 years or older.
AstraZeneca, which markets the drug, announced the approval for younger patients on April 11.
The expanded indication was supported by a study that showed that the drug functions in the same way with younger children and their adolescent peers. The safety and tolerability were also consistent with the known profile of the medicine, the company said.
For children who weigh ≥ 35 kg, the recommended dose is 30 mg. For patients aged 6-11 years who weigh < 35 kg, a new 10-mg dose will be available, according to the announcement.
The drug, a monoclonal antibody that depletes eosinophils by binding to interleukin 5 receptor alpha on eosinophils, is administered by subcutaneous injection every 4 weeks for the first three doses and then every 8 weeks.
Benralizumab should not be used to treat acute asthma symptoms. Hypersensitivity reasons have occurred after administration of the drug. The most common adverse reactions include headache and pharyngitis.
A version of this article appeared on Medscape.com.
Benralizumab is now approved by the US Food and Drug Administration (FDA) for the treatment of asthma in children older than 6 years.
Marketed as Fasenra, the medication first was approved in 2017 for patients aged 12 years or older.
AstraZeneca, which markets the drug, announced the approval for younger patients on April 11.
The expanded indication was supported by a study that showed that the drug functions in the same way with younger children and their adolescent peers. The safety and tolerability were also consistent with the known profile of the medicine, the company said.
For children who weigh ≥ 35 kg, the recommended dose is 30 mg. For patients aged 6-11 years who weigh < 35 kg, a new 10-mg dose will be available, according to the announcement.
The drug, a monoclonal antibody that depletes eosinophils by binding to interleukin 5 receptor alpha on eosinophils, is administered by subcutaneous injection every 4 weeks for the first three doses and then every 8 weeks.
Benralizumab should not be used to treat acute asthma symptoms. Hypersensitivity reasons have occurred after administration of the drug. The most common adverse reactions include headache and pharyngitis.
A version of this article appeared on Medscape.com.
Alopecia Areata: Late Responses Complicate Definition of JAK Inhibitor Failure
SAN DIEGO — , according to late breaker data presented at the annual meeting of the American Academy of Dermatology.
Although the majority respond within months, response curves have so far climbed for as long as patients are followed, allowing many with disappointing early results to catch up, according to Rodney D. Sinclair, MD, professor of dermatology at the University of Melbourne, Australia.
His remarks were derived specifically from new long-term follow-up with baricitinib, the first JAK inhibitor approved for AA, but the pattern appears to be similar with ritlecitinib, the only other JAK inhibitor approved for AA, and for several if not all JAK inhibitors in phase 3 AA trials.
“We have had patients on baricitinib where not much was happening at 18 months, but now, at 4 years, they have a SALT score of zero,” Dr. Sinclair reported
A Severity of Alopecia Tool (SALT) score of 0 signifies complete hair regrowth. On a scale with a maximum score of 100 (complete hair loss), a SALT score of 20 or less, signaling clinical success, has been a primary endpoint in many JAK inhibitor trials, including those conducted with baricitinib.
Providing the most recent analysis in patients with severe AA participating in the phase 3 BRAVE-AA1 and BRAVE-AA2 trials of baricitinib, which were published together in 2022, Dr. Sinclair broke the data down into responders, mixed responders, and nonresponders at 52 weeks. The proportion of patients who responded with even longer follow-up were then tallied.
In the as-observed responses over time, the trajectory of response continued to climb through 76 weeks of follow-up in all three groups.
Relative to the 44.5% rate of overall response (SALT ≤ 20 ) at 52 weeks, there was some further growth in every group maintained on JAK inhibitor therapy over longer follow-up. In Dr. Sinclair’s late breaking analysis, this did not include nonresponders, who stopped therapy by week 52, but 78.4% of the combined responders and mixed responders who remained on treatment had reached treatment success at 76 weeks.
Response Curves Climb More Slowly With Severe Alopecia
While improvement in SALT scores was even seen in nonresponders over time as long as they remained on therapy, Dr. Sinclair reported that response curves tended to climb more slowly in those with more severe alopecia at baseline. Yet, they still climbed. For example, 28.1% of those with a baseline SALT score of 95 to 100 had reached treatment success at week 52, but the proportion had climbed to 35.4% by week 76.
The response curves climbed more quickly among those with a SALT score between 50 and 95 at baseline than among those with more severe alopecia, but the differences in SALT scores at 52 weeks and 76 weeks among patients in this range of baseline SALT scores were small.
Basically, “those with a SALT score of 94 did just as well as those with a SALT score of 51 when followed long-term,” he said, noting that this was among several findings that confounded expectations.
Duration of AA was found to be an important prognostic factor, with 4 years emerging as a general threshold separating those with a diminished likelihood of benefit relative to those with a shorter AA duration.
“When the duration of AA is more than 4 years, the response to any JAK inhibitor seems to fall off a cliff,” Dr. Sinclair said.
To clarify this observation, Dr. Sinclair made an analogy between acute and chronic urticaria. Chronicity appears to change the pathophysiology of both urticaria and AA, making durable remissions more difficult to achieve if the inflammatory response was persistently upregulated, he said.
The delayed responses in some patients “suggests that it is not enough to control inflammation for the hair to regrow. You actually have to activate the hair to grow as well as treat the inflammation,” Dr. Sinclair said.
This heterogeneity that has been observed in the speed of AA response to JAK inhibitors might be explained at least in part by the individual differences in hair growth activation. For ritlecitinib, the only other JAK inhibitor approved for AA to date, 62% were categorized as responders in the registration ALLEGRO trials, but only 44% were early responders, meaning SALT scores of ≤ 20 by week 24, according to a summary published last year. Of the remaining 16%, 11% were middle responders, meaning a SALT score of ≤ 20 reached at week 48, and 6% were late responders, meaning a SALT score of ≤ 20 reached at week 96.
In the context of late breaking 68-week data with deuruxolitinib, an oral JAK inhibitor currently under FDA review for treating moderate to severe AA, presented in the same AAD session as Dr. Sinclair’s baricitinib data, Brett King, MD, PhD, associate professor of dermatology, Yale University, New Haven, Connecticut, described similar long-term response curves. At 24 weeks, the SALT ≤ 20 response was achieved in 34.9% of patients, but climbed to 62.8% with continuous therapy over 68 weeks.
The difference between AA and most other inflammatory conditions treated with a JAK inhibitor is that “it takes time to treat,” Dr. King said.
Time Factor Is Important for Response
“What we are learning is that patients keep getting better over time,” Dr. Sinclair said. Asked specifically how long he would treat a patient before giving up, he acknowledged that he used to consider 6 months adequate, but that he has now changed his mind.
“It might be that even 2 years is too short,” he said, although he conceded that a trial of therapy for this long “might be an issue for third-part payers.”
Asked to comment, Melissa Piliang, MD, chair of the department of dermatology at the Cleveland Clinic, agreed with the principle that early responses are not necessarily predictive of complete response.
“In my clinical experience, 6 months is not long enough to assess response,” she told this news organization. “Some patients have hair growth after 18 months to 2 years” of treatment. Additional studies to identify the characteristics and predictors of late response, she said, “would be very helpful, as would trials allowing multiple therapies to simulate real-world practice.”
Like Dr. Sinclair, Dr. Piliang is interested in the possibility of combining a JAK inhibitor with another therapy aimed specially at promoting hair regrowth.
“Using a secondary therapy to stimulate regrowth as an addition to an anti-inflammatory medicine like a JAK inhibitor might speed up response in some patients,” she speculated. Dr. Sinclair reports financial relationships with more than 30 pharmaceutical companies, including Eli Lilly, the manufacturer of baricitinib. Dr. King reports financial relationships with multiple companies, including Concert Pharmaceuticals (consultant and investigator), the manufacturer of deuruxolitinib. Dr. Piliang reports financial relationships with Eli Lilly, Pfizer, and Proctor & Gamble.
SAN DIEGO — , according to late breaker data presented at the annual meeting of the American Academy of Dermatology.
Although the majority respond within months, response curves have so far climbed for as long as patients are followed, allowing many with disappointing early results to catch up, according to Rodney D. Sinclair, MD, professor of dermatology at the University of Melbourne, Australia.
His remarks were derived specifically from new long-term follow-up with baricitinib, the first JAK inhibitor approved for AA, but the pattern appears to be similar with ritlecitinib, the only other JAK inhibitor approved for AA, and for several if not all JAK inhibitors in phase 3 AA trials.
“We have had patients on baricitinib where not much was happening at 18 months, but now, at 4 years, they have a SALT score of zero,” Dr. Sinclair reported
A Severity of Alopecia Tool (SALT) score of 0 signifies complete hair regrowth. On a scale with a maximum score of 100 (complete hair loss), a SALT score of 20 or less, signaling clinical success, has been a primary endpoint in many JAK inhibitor trials, including those conducted with baricitinib.
Providing the most recent analysis in patients with severe AA participating in the phase 3 BRAVE-AA1 and BRAVE-AA2 trials of baricitinib, which were published together in 2022, Dr. Sinclair broke the data down into responders, mixed responders, and nonresponders at 52 weeks. The proportion of patients who responded with even longer follow-up were then tallied.
In the as-observed responses over time, the trajectory of response continued to climb through 76 weeks of follow-up in all three groups.
Relative to the 44.5% rate of overall response (SALT ≤ 20 ) at 52 weeks, there was some further growth in every group maintained on JAK inhibitor therapy over longer follow-up. In Dr. Sinclair’s late breaking analysis, this did not include nonresponders, who stopped therapy by week 52, but 78.4% of the combined responders and mixed responders who remained on treatment had reached treatment success at 76 weeks.
Response Curves Climb More Slowly With Severe Alopecia
While improvement in SALT scores was even seen in nonresponders over time as long as they remained on therapy, Dr. Sinclair reported that response curves tended to climb more slowly in those with more severe alopecia at baseline. Yet, they still climbed. For example, 28.1% of those with a baseline SALT score of 95 to 100 had reached treatment success at week 52, but the proportion had climbed to 35.4% by week 76.
The response curves climbed more quickly among those with a SALT score between 50 and 95 at baseline than among those with more severe alopecia, but the differences in SALT scores at 52 weeks and 76 weeks among patients in this range of baseline SALT scores were small.
Basically, “those with a SALT score of 94 did just as well as those with a SALT score of 51 when followed long-term,” he said, noting that this was among several findings that confounded expectations.
Duration of AA was found to be an important prognostic factor, with 4 years emerging as a general threshold separating those with a diminished likelihood of benefit relative to those with a shorter AA duration.
“When the duration of AA is more than 4 years, the response to any JAK inhibitor seems to fall off a cliff,” Dr. Sinclair said.
To clarify this observation, Dr. Sinclair made an analogy between acute and chronic urticaria. Chronicity appears to change the pathophysiology of both urticaria and AA, making durable remissions more difficult to achieve if the inflammatory response was persistently upregulated, he said.
The delayed responses in some patients “suggests that it is not enough to control inflammation for the hair to regrow. You actually have to activate the hair to grow as well as treat the inflammation,” Dr. Sinclair said.
This heterogeneity that has been observed in the speed of AA response to JAK inhibitors might be explained at least in part by the individual differences in hair growth activation. For ritlecitinib, the only other JAK inhibitor approved for AA to date, 62% were categorized as responders in the registration ALLEGRO trials, but only 44% were early responders, meaning SALT scores of ≤ 20 by week 24, according to a summary published last year. Of the remaining 16%, 11% were middle responders, meaning a SALT score of ≤ 20 reached at week 48, and 6% were late responders, meaning a SALT score of ≤ 20 reached at week 96.
In the context of late breaking 68-week data with deuruxolitinib, an oral JAK inhibitor currently under FDA review for treating moderate to severe AA, presented in the same AAD session as Dr. Sinclair’s baricitinib data, Brett King, MD, PhD, associate professor of dermatology, Yale University, New Haven, Connecticut, described similar long-term response curves. At 24 weeks, the SALT ≤ 20 response was achieved in 34.9% of patients, but climbed to 62.8% with continuous therapy over 68 weeks.
The difference between AA and most other inflammatory conditions treated with a JAK inhibitor is that “it takes time to treat,” Dr. King said.
Time Factor Is Important for Response
“What we are learning is that patients keep getting better over time,” Dr. Sinclair said. Asked specifically how long he would treat a patient before giving up, he acknowledged that he used to consider 6 months adequate, but that he has now changed his mind.
“It might be that even 2 years is too short,” he said, although he conceded that a trial of therapy for this long “might be an issue for third-part payers.”
Asked to comment, Melissa Piliang, MD, chair of the department of dermatology at the Cleveland Clinic, agreed with the principle that early responses are not necessarily predictive of complete response.
“In my clinical experience, 6 months is not long enough to assess response,” she told this news organization. “Some patients have hair growth after 18 months to 2 years” of treatment. Additional studies to identify the characteristics and predictors of late response, she said, “would be very helpful, as would trials allowing multiple therapies to simulate real-world practice.”
Like Dr. Sinclair, Dr. Piliang is interested in the possibility of combining a JAK inhibitor with another therapy aimed specially at promoting hair regrowth.
“Using a secondary therapy to stimulate regrowth as an addition to an anti-inflammatory medicine like a JAK inhibitor might speed up response in some patients,” she speculated. Dr. Sinclair reports financial relationships with more than 30 pharmaceutical companies, including Eli Lilly, the manufacturer of baricitinib. Dr. King reports financial relationships with multiple companies, including Concert Pharmaceuticals (consultant and investigator), the manufacturer of deuruxolitinib. Dr. Piliang reports financial relationships with Eli Lilly, Pfizer, and Proctor & Gamble.
SAN DIEGO — , according to late breaker data presented at the annual meeting of the American Academy of Dermatology.
Although the majority respond within months, response curves have so far climbed for as long as patients are followed, allowing many with disappointing early results to catch up, according to Rodney D. Sinclair, MD, professor of dermatology at the University of Melbourne, Australia.
His remarks were derived specifically from new long-term follow-up with baricitinib, the first JAK inhibitor approved for AA, but the pattern appears to be similar with ritlecitinib, the only other JAK inhibitor approved for AA, and for several if not all JAK inhibitors in phase 3 AA trials.
“We have had patients on baricitinib where not much was happening at 18 months, but now, at 4 years, they have a SALT score of zero,” Dr. Sinclair reported
A Severity of Alopecia Tool (SALT) score of 0 signifies complete hair regrowth. On a scale with a maximum score of 100 (complete hair loss), a SALT score of 20 or less, signaling clinical success, has been a primary endpoint in many JAK inhibitor trials, including those conducted with baricitinib.
Providing the most recent analysis in patients with severe AA participating in the phase 3 BRAVE-AA1 and BRAVE-AA2 trials of baricitinib, which were published together in 2022, Dr. Sinclair broke the data down into responders, mixed responders, and nonresponders at 52 weeks. The proportion of patients who responded with even longer follow-up were then tallied.
In the as-observed responses over time, the trajectory of response continued to climb through 76 weeks of follow-up in all three groups.
Relative to the 44.5% rate of overall response (SALT ≤ 20 ) at 52 weeks, there was some further growth in every group maintained on JAK inhibitor therapy over longer follow-up. In Dr. Sinclair’s late breaking analysis, this did not include nonresponders, who stopped therapy by week 52, but 78.4% of the combined responders and mixed responders who remained on treatment had reached treatment success at 76 weeks.
Response Curves Climb More Slowly With Severe Alopecia
While improvement in SALT scores was even seen in nonresponders over time as long as they remained on therapy, Dr. Sinclair reported that response curves tended to climb more slowly in those with more severe alopecia at baseline. Yet, they still climbed. For example, 28.1% of those with a baseline SALT score of 95 to 100 had reached treatment success at week 52, but the proportion had climbed to 35.4% by week 76.
The response curves climbed more quickly among those with a SALT score between 50 and 95 at baseline than among those with more severe alopecia, but the differences in SALT scores at 52 weeks and 76 weeks among patients in this range of baseline SALT scores were small.
Basically, “those with a SALT score of 94 did just as well as those with a SALT score of 51 when followed long-term,” he said, noting that this was among several findings that confounded expectations.
Duration of AA was found to be an important prognostic factor, with 4 years emerging as a general threshold separating those with a diminished likelihood of benefit relative to those with a shorter AA duration.
“When the duration of AA is more than 4 years, the response to any JAK inhibitor seems to fall off a cliff,” Dr. Sinclair said.
To clarify this observation, Dr. Sinclair made an analogy between acute and chronic urticaria. Chronicity appears to change the pathophysiology of both urticaria and AA, making durable remissions more difficult to achieve if the inflammatory response was persistently upregulated, he said.
The delayed responses in some patients “suggests that it is not enough to control inflammation for the hair to regrow. You actually have to activate the hair to grow as well as treat the inflammation,” Dr. Sinclair said.
This heterogeneity that has been observed in the speed of AA response to JAK inhibitors might be explained at least in part by the individual differences in hair growth activation. For ritlecitinib, the only other JAK inhibitor approved for AA to date, 62% were categorized as responders in the registration ALLEGRO trials, but only 44% were early responders, meaning SALT scores of ≤ 20 by week 24, according to a summary published last year. Of the remaining 16%, 11% were middle responders, meaning a SALT score of ≤ 20 reached at week 48, and 6% were late responders, meaning a SALT score of ≤ 20 reached at week 96.
In the context of late breaking 68-week data with deuruxolitinib, an oral JAK inhibitor currently under FDA review for treating moderate to severe AA, presented in the same AAD session as Dr. Sinclair’s baricitinib data, Brett King, MD, PhD, associate professor of dermatology, Yale University, New Haven, Connecticut, described similar long-term response curves. At 24 weeks, the SALT ≤ 20 response was achieved in 34.9% of patients, but climbed to 62.8% with continuous therapy over 68 weeks.
The difference between AA and most other inflammatory conditions treated with a JAK inhibitor is that “it takes time to treat,” Dr. King said.
Time Factor Is Important for Response
“What we are learning is that patients keep getting better over time,” Dr. Sinclair said. Asked specifically how long he would treat a patient before giving up, he acknowledged that he used to consider 6 months adequate, but that he has now changed his mind.
“It might be that even 2 years is too short,” he said, although he conceded that a trial of therapy for this long “might be an issue for third-part payers.”
Asked to comment, Melissa Piliang, MD, chair of the department of dermatology at the Cleveland Clinic, agreed with the principle that early responses are not necessarily predictive of complete response.
“In my clinical experience, 6 months is not long enough to assess response,” she told this news organization. “Some patients have hair growth after 18 months to 2 years” of treatment. Additional studies to identify the characteristics and predictors of late response, she said, “would be very helpful, as would trials allowing multiple therapies to simulate real-world practice.”
Like Dr. Sinclair, Dr. Piliang is interested in the possibility of combining a JAK inhibitor with another therapy aimed specially at promoting hair regrowth.
“Using a secondary therapy to stimulate regrowth as an addition to an anti-inflammatory medicine like a JAK inhibitor might speed up response in some patients,” she speculated. Dr. Sinclair reports financial relationships with more than 30 pharmaceutical companies, including Eli Lilly, the manufacturer of baricitinib. Dr. King reports financial relationships with multiple companies, including Concert Pharmaceuticals (consultant and investigator), the manufacturer of deuruxolitinib. Dr. Piliang reports financial relationships with Eli Lilly, Pfizer, and Proctor & Gamble.
FROM AAD 2024
A 16-Year-Old Female Presents With Multiple Areas of Hair Loss on the Scalp
KOH analysis of the scales from the scalp areas revealed no fungal elements. Given the observed erythema and scaling, a punch biopsy was conducted. Histopathological examination of the biopsy sample displayed interface inflammation affecting both the infundibular and lower portions of hair follicles. The presence of folliculosebaceous units transitioning from intermediate to terminal size follicles was noted. A perifollicular, peri eccrine, superficial, and deep perivascular lymphoplasmacytic infiltrate was identified, alongside increased dermal mucin, findings consistent with a diagnosis of discoid lupus erythematosus.
Subsequent laboratory investigations were largely unremarkable, except for an elevated ANA titer (1:320, with a speckled pattern). The patient was initiated on a treatment regimen comprising intralesional triamcinolone and oral hydroxychloroquine (Plaquenil).
Discussion
It predominantly affects adults, yet pediatric cases account for 5%-7% of DLE diagnoses, with a significant predominance in females. Pediatric scalp DLE is particularly concerning due to its potential for causing scarring and permanent hair loss, which can significantly impact the psychological wellbeing of affected children.
The pathogenesis of DLE is multifactorial, involving genetic predispositions, environmental factors like UV light exposure, and immunological mechanisms leading to skin damage.
In children, DLE typically presents as well-demarcated, erythematous plaques with scale and follicular plugging, primarily affecting the scalp. Lesions may also exhibit changes in pigmentation, atrophy, and telangiectasia. The scalp involvement often leads to scarring alopecia, which can be distressing for pediatric patients. Unlike systemic lupus erythematosus (SLE), DLE is usually limited to the skin without systemic involvement. The progression of DLE to systemic lupus erythematosus in children has been previously described to be 22.2%. In a recent report of 201 pediatric cases of DLE, 12% of the cases progressed to systemic lupus erythematosus (SLE) and 14.5% had concurrent SLE. The onset of symptoms before the age of 10 years was the only statistically significant predictor for progression to SLE. Pruritus is a common symptom and may be correlated with disease activity.
The differential diagnosis for this patient encompassed a variety of conditions, including tinea capitis, alopecia areata, trichotillomania, and lichen planopilaris, each considered based on clinical presentation but ultimately excluded through clinical, microscopic, and biopsy findings.
Management strategies for pediatric scalp DLE aim at preventing disease progression, minimizing scarring, and addressing aesthetic concerns. These include the use of topical and intralesional corticosteroids, calcineurin inhibitors, and antimalarial agents like hydroxychloroquine, alongside stringent photoprotection to mitigate UV-triggered exacerbations.
Conclusion
The prognosis for pediatric scalp DLE can be favorable with timely and appropriate management, underscoring the importance of early diagnosis and intervention to prevent scarring and hair loss. However, ongoing surveillance is crucial for monitoring potential progression to systemic lupus erythematosus, albeit a low-risk transformation.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
1. George PM and Tunnessen WW. Childhood discoid lupus erythematosus. Arch Dermatol. 1993;129(5):613-617.
2. Hawat T et al. Pediatric discoid lupus erythematosus: Short report. Dermatol Ther. 2022 Jan;35(1):e15170. doi: 10.1111/dth.15170.
3. Arkin LM et al. Practice-based differences in paediatric discoid lupus erythematosus. Br J Dermatol. 2019 Oct;181(4):805-810. doi: 10.1111/bjd.17780.
KOH analysis of the scales from the scalp areas revealed no fungal elements. Given the observed erythema and scaling, a punch biopsy was conducted. Histopathological examination of the biopsy sample displayed interface inflammation affecting both the infundibular and lower portions of hair follicles. The presence of folliculosebaceous units transitioning from intermediate to terminal size follicles was noted. A perifollicular, peri eccrine, superficial, and deep perivascular lymphoplasmacytic infiltrate was identified, alongside increased dermal mucin, findings consistent with a diagnosis of discoid lupus erythematosus.
Subsequent laboratory investigations were largely unremarkable, except for an elevated ANA titer (1:320, with a speckled pattern). The patient was initiated on a treatment regimen comprising intralesional triamcinolone and oral hydroxychloroquine (Plaquenil).
Discussion
It predominantly affects adults, yet pediatric cases account for 5%-7% of DLE diagnoses, with a significant predominance in females. Pediatric scalp DLE is particularly concerning due to its potential for causing scarring and permanent hair loss, which can significantly impact the psychological wellbeing of affected children.
The pathogenesis of DLE is multifactorial, involving genetic predispositions, environmental factors like UV light exposure, and immunological mechanisms leading to skin damage.
In children, DLE typically presents as well-demarcated, erythematous plaques with scale and follicular plugging, primarily affecting the scalp. Lesions may also exhibit changes in pigmentation, atrophy, and telangiectasia. The scalp involvement often leads to scarring alopecia, which can be distressing for pediatric patients. Unlike systemic lupus erythematosus (SLE), DLE is usually limited to the skin without systemic involvement. The progression of DLE to systemic lupus erythematosus in children has been previously described to be 22.2%. In a recent report of 201 pediatric cases of DLE, 12% of the cases progressed to systemic lupus erythematosus (SLE) and 14.5% had concurrent SLE. The onset of symptoms before the age of 10 years was the only statistically significant predictor for progression to SLE. Pruritus is a common symptom and may be correlated with disease activity.
The differential diagnosis for this patient encompassed a variety of conditions, including tinea capitis, alopecia areata, trichotillomania, and lichen planopilaris, each considered based on clinical presentation but ultimately excluded through clinical, microscopic, and biopsy findings.
Management strategies for pediatric scalp DLE aim at preventing disease progression, minimizing scarring, and addressing aesthetic concerns. These include the use of topical and intralesional corticosteroids, calcineurin inhibitors, and antimalarial agents like hydroxychloroquine, alongside stringent photoprotection to mitigate UV-triggered exacerbations.
Conclusion
The prognosis for pediatric scalp DLE can be favorable with timely and appropriate management, underscoring the importance of early diagnosis and intervention to prevent scarring and hair loss. However, ongoing surveillance is crucial for monitoring potential progression to systemic lupus erythematosus, albeit a low-risk transformation.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
1. George PM and Tunnessen WW. Childhood discoid lupus erythematosus. Arch Dermatol. 1993;129(5):613-617.
2. Hawat T et al. Pediatric discoid lupus erythematosus: Short report. Dermatol Ther. 2022 Jan;35(1):e15170. doi: 10.1111/dth.15170.
3. Arkin LM et al. Practice-based differences in paediatric discoid lupus erythematosus. Br J Dermatol. 2019 Oct;181(4):805-810. doi: 10.1111/bjd.17780.
KOH analysis of the scales from the scalp areas revealed no fungal elements. Given the observed erythema and scaling, a punch biopsy was conducted. Histopathological examination of the biopsy sample displayed interface inflammation affecting both the infundibular and lower portions of hair follicles. The presence of folliculosebaceous units transitioning from intermediate to terminal size follicles was noted. A perifollicular, peri eccrine, superficial, and deep perivascular lymphoplasmacytic infiltrate was identified, alongside increased dermal mucin, findings consistent with a diagnosis of discoid lupus erythematosus.
Subsequent laboratory investigations were largely unremarkable, except for an elevated ANA titer (1:320, with a speckled pattern). The patient was initiated on a treatment regimen comprising intralesional triamcinolone and oral hydroxychloroquine (Plaquenil).
Discussion
It predominantly affects adults, yet pediatric cases account for 5%-7% of DLE diagnoses, with a significant predominance in females. Pediatric scalp DLE is particularly concerning due to its potential for causing scarring and permanent hair loss, which can significantly impact the psychological wellbeing of affected children.
The pathogenesis of DLE is multifactorial, involving genetic predispositions, environmental factors like UV light exposure, and immunological mechanisms leading to skin damage.
In children, DLE typically presents as well-demarcated, erythematous plaques with scale and follicular plugging, primarily affecting the scalp. Lesions may also exhibit changes in pigmentation, atrophy, and telangiectasia. The scalp involvement often leads to scarring alopecia, which can be distressing for pediatric patients. Unlike systemic lupus erythematosus (SLE), DLE is usually limited to the skin without systemic involvement. The progression of DLE to systemic lupus erythematosus in children has been previously described to be 22.2%. In a recent report of 201 pediatric cases of DLE, 12% of the cases progressed to systemic lupus erythematosus (SLE) and 14.5% had concurrent SLE. The onset of symptoms before the age of 10 years was the only statistically significant predictor for progression to SLE. Pruritus is a common symptom and may be correlated with disease activity.
The differential diagnosis for this patient encompassed a variety of conditions, including tinea capitis, alopecia areata, trichotillomania, and lichen planopilaris, each considered based on clinical presentation but ultimately excluded through clinical, microscopic, and biopsy findings.
Management strategies for pediatric scalp DLE aim at preventing disease progression, minimizing scarring, and addressing aesthetic concerns. These include the use of topical and intralesional corticosteroids, calcineurin inhibitors, and antimalarial agents like hydroxychloroquine, alongside stringent photoprotection to mitigate UV-triggered exacerbations.
Conclusion
The prognosis for pediatric scalp DLE can be favorable with timely and appropriate management, underscoring the importance of early diagnosis and intervention to prevent scarring and hair loss. However, ongoing surveillance is crucial for monitoring potential progression to systemic lupus erythematosus, albeit a low-risk transformation.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
1. George PM and Tunnessen WW. Childhood discoid lupus erythematosus. Arch Dermatol. 1993;129(5):613-617.
2. Hawat T et al. Pediatric discoid lupus erythematosus: Short report. Dermatol Ther. 2022 Jan;35(1):e15170. doi: 10.1111/dth.15170.
3. Arkin LM et al. Practice-based differences in paediatric discoid lupus erythematosus. Br J Dermatol. 2019 Oct;181(4):805-810. doi: 10.1111/bjd.17780.
Upon physical examination, the patient exhibited several patches of alopecia with accompanying perifollicular scaling, crusting, and erythema on the affected areas. Examination of her face revealed comedones and papules.
Circulating Tumor DNA Predicts Early Treatment Response in Patients With HER2-Positive Cancers
This was the main finding of new data presented by study author Razelle Kurzrock, MD, at the American Association for Cancer Research annual meeting.
“We found that on-treatment ctDNA can detect progression before standard-of-care response assessments. These data suggest that monitoring ctDNA can provide clinicians with important prognostic information that may guide treatment decisions,” Dr. Kurzrock, professor at the Medical College of Wisconsin, Milwaukee, said during her presentation.
Commenting on the clinical implications of these findings during an interview, she said the results suggest that ctDNA dynamics provide an early window into predicting response to targeted therapies in patients with HER2-altered cancers, confirming previous findings of the predictive value of ctDNA in other cancer types.
“Such monitoring may be useful in clinical trials and eventually in practice,” she added.
Need for new methods to predict early tumor response
Limitations of standard radiographic tumor assessments present challenges in determining clinical response, particularly for patients receiving targeted therapies.
During her talk, Dr. Kurzrock explained that although targeted therapies are effective for patients with specific molecular alterations, standard imaging assessments fail to uncover molecular-level changes within tumors, limiting the ability of clinicians to accurately assess a patient’s response to targeted therapies.
“In addition to limitations with imaging, patients and physicians want to know as soon as possible whether or not the agents are effective, especially if there are side effects,” Dr. Kurzrock during an interview. She added that monitoring early response may be especially important across tumor types, as HER2 therapies are increasingly being considered in the pan-cancer setting.
Commenting on the potential use of this method in other cancer types with HER2 alterations, Pashtoon Murtaza Kasi, MD, MS, noted that since the study relied on a tumor-informed assay, it would be applicable across diverse tumor types.
“It is less about tissue type but more about that particular patient’s tumor at that instant in time for which a unique barcode is created,” said Dr. Kasi, a medical oncologist at Weill Cornell Medicine, New York, who was not involved in the study.
In an interview, he added that the shedding and biology would affect the assay’s performance for some tissue types.
Design of patient-specific ctDNA assays
In this retrospective study, the researchers examined ctDNA dynamics in 58 patients with various HER2-positive tumor types, including breast, colorectal, and other solid malignancies harboring HER2 alterations. All the patients received combination HER2-targeted therapy with trastuzumab and pertuzumab in the phase 2 basket trial My Pathway (NCT02091141).
By leveraging comprehensive genomic profiling of each patient’s tumor, the researchers designed personalized ctDNA assays, tracking 2-16 tumor-specific genetic variants in the patients’ blood samples. FoundationOne Tracker was used to detect and quantify ctDNA at baseline and the third cycle of therapy (cycle 3 day 1, or C3D1).
During an interview, Dr. Kurzrock explained that FoundationOne Tracker is a personalized ctDNA monitoring assay that allows for the detection of ctDNA in plasma, enabling ongoing liquid-based monitoring and highly sensitive quantification of ctDNA levels as mean tumor molecules per milliliter of plasma.
Among the 52 patients for whom personalized ctDNA assays were successfully designed, 48 (92.3%) had ctDNA data available at baseline, with a median of 100.7 tumor molecules per milliliter of plasma. Most patients (89.6%) were deemed ctDNA-positive, with a median of 119.5 tumor molecules per milliliter of plasma.
Changes in ctDNA levels predict patient survival
The researchers found that patients who experienced a greater than 90% decline in ctDNA levels by the third treatment cycle had significantly longer overall survival (OS) than those with less than 90% ctDNA decline or any increase. According to data presented by Dr. Kurzrock, the median OS was not reached in the group with greater than 90% decline in on-treatment ctDNA levels, versus 9.4 months in the group with less than 90% decline or ctDNA increase (P = .007). These findings held true when the analysis was limited to the 14 patients with colorectal cancer, in which median OS was not reached in the group with greater than 90% decline in on-treatment ctDNA levels, versus 10.2 months in the group with less than 90% decline or ctDNA increase (P = 0.04).
Notably, the prognostic significance of ctDNA changes remained even among patients exhibiting radiographic stable disease, underscoring the limitations of relying solely on anatomic tumor measurements and highlighting the potential for ctDNA monitoring to complement standard clinical assessments. In the subset of patients with radiographic stable disease, those with a greater than 90% ctDNA decline had significantly longer OS than those with less ctDNA reduction (not reached versus 9.4 months; P = .01).
“When used as a complement to imaging, tissue-informed ctDNA monitoring with FoundationOne Tracker can provide more accuracy than imaging alone,” Dr. Kurzrock noted in an interview.
Dr. Kasi echoed Dr. Kurzrock’s enthusiasm regarding the clinical usefulness of these findings, saying, “Not only can you see very early on in whom the ctDNA is going down and clearing, but you can also tell apart within the group who has ‘stable disease’ as to who is deriving more benefit.”
The researchers also observed that increases in on-treatment ctDNA levels often preceded radiographic evidence of disease progression by a median of 1.3 months. These findings highlight the potential for ctDNA monitoring to complement standard clinical assessments, allowing us to detect treatment response and disease progression earlier than what is possible with imaging alone, Dr. Kurzrock explained during her talk. “This early warning signal could allow clinicians to intervene and modify treatment strategies before overt clinical deterioration,” she said.
In an interview, Dr. Kasi highlighted that this high sensitivity and specificity and the short half-life of the tumor-informed ctDNA assay make this liquid biopsy of great clinical value. “The short half-life of a few hours means that if you do an intervention to treat cancer with HER2-directed therapy, you can very quickly assess response to therapy way earlier than traditional radiographic methods.”
Dr. Kasi cautioned, however, that this assay would not capture whether new mutations or HER2 loss occurred at the time of resistance. “A repeat tissue biopsy or a next-generation sequencing-based plasma-only assay would be required for that,” he said.
Implementation of ctDNA monitoring in clinical trials
Dr. Kurzrock acknowledged that further research is needed to validate these results in larger, prospective cohorts before FoundationOne Tracker is adopted in the clinic. She noted, however, that this retrospective analysis, along with results from previous studies, provides a rationale for the use of ctDNA monitoring in clinical trials.
“In some centers like ours, ctDNA monitoring is already part of our standard of care since not only does it help from a physician standpoint to have a more accurate and early assessment of response, but patients also appreciate the information gained from ctDNA dynamics,” Dr. Kasi said in an interview. He explained that when radiographic findings are equivocal, ctDNA monitoring is an additional tool in their toolbox to help guide care.
He noted, however, that the cost is a challenge for implementing ctDNA monitoring as a complementary tool for real-time treatment response monitoring. “For serial monitoring, helping to reduce costs would be important in the long run,” he said in an interview. He added that obtaining sufficient tissue for testing using a tumor-informed assay can present a logistical challenge, at least for the first test. “You need sufficient tissue to make the barcode that you then follow along,” he explained.
“Developing guidelines through systematic studies about testing cadence would also be important. This would help establish whether ctDNA monitoring is helpful,” Dr. Kasi said in an interview. He explained that in some situations, biological variables affect the shedding and detection of ctDNA beyond the assay — in those cases, ctDNA monitoring may not be helpful. “Like any test, it is not meant for every patient or clinical question,” Dr. Kasi concluded.
Dr. Kurzrock and Dr. Kasi reported no relationships with entities whose primary business is producing, marketing, selling, reselling, or distributing healthcare products used by or on patients.
This was the main finding of new data presented by study author Razelle Kurzrock, MD, at the American Association for Cancer Research annual meeting.
“We found that on-treatment ctDNA can detect progression before standard-of-care response assessments. These data suggest that monitoring ctDNA can provide clinicians with important prognostic information that may guide treatment decisions,” Dr. Kurzrock, professor at the Medical College of Wisconsin, Milwaukee, said during her presentation.
Commenting on the clinical implications of these findings during an interview, she said the results suggest that ctDNA dynamics provide an early window into predicting response to targeted therapies in patients with HER2-altered cancers, confirming previous findings of the predictive value of ctDNA in other cancer types.
“Such monitoring may be useful in clinical trials and eventually in practice,” she added.
Need for new methods to predict early tumor response
Limitations of standard radiographic tumor assessments present challenges in determining clinical response, particularly for patients receiving targeted therapies.
During her talk, Dr. Kurzrock explained that although targeted therapies are effective for patients with specific molecular alterations, standard imaging assessments fail to uncover molecular-level changes within tumors, limiting the ability of clinicians to accurately assess a patient’s response to targeted therapies.
“In addition to limitations with imaging, patients and physicians want to know as soon as possible whether or not the agents are effective, especially if there are side effects,” Dr. Kurzrock during an interview. She added that monitoring early response may be especially important across tumor types, as HER2 therapies are increasingly being considered in the pan-cancer setting.
Commenting on the potential use of this method in other cancer types with HER2 alterations, Pashtoon Murtaza Kasi, MD, MS, noted that since the study relied on a tumor-informed assay, it would be applicable across diverse tumor types.
“It is less about tissue type but more about that particular patient’s tumor at that instant in time for which a unique barcode is created,” said Dr. Kasi, a medical oncologist at Weill Cornell Medicine, New York, who was not involved in the study.
In an interview, he added that the shedding and biology would affect the assay’s performance for some tissue types.
Design of patient-specific ctDNA assays
In this retrospective study, the researchers examined ctDNA dynamics in 58 patients with various HER2-positive tumor types, including breast, colorectal, and other solid malignancies harboring HER2 alterations. All the patients received combination HER2-targeted therapy with trastuzumab and pertuzumab in the phase 2 basket trial My Pathway (NCT02091141).
By leveraging comprehensive genomic profiling of each patient’s tumor, the researchers designed personalized ctDNA assays, tracking 2-16 tumor-specific genetic variants in the patients’ blood samples. FoundationOne Tracker was used to detect and quantify ctDNA at baseline and the third cycle of therapy (cycle 3 day 1, or C3D1).
During an interview, Dr. Kurzrock explained that FoundationOne Tracker is a personalized ctDNA monitoring assay that allows for the detection of ctDNA in plasma, enabling ongoing liquid-based monitoring and highly sensitive quantification of ctDNA levels as mean tumor molecules per milliliter of plasma.
Among the 52 patients for whom personalized ctDNA assays were successfully designed, 48 (92.3%) had ctDNA data available at baseline, with a median of 100.7 tumor molecules per milliliter of plasma. Most patients (89.6%) were deemed ctDNA-positive, with a median of 119.5 tumor molecules per milliliter of plasma.
Changes in ctDNA levels predict patient survival
The researchers found that patients who experienced a greater than 90% decline in ctDNA levels by the third treatment cycle had significantly longer overall survival (OS) than those with less than 90% ctDNA decline or any increase. According to data presented by Dr. Kurzrock, the median OS was not reached in the group with greater than 90% decline in on-treatment ctDNA levels, versus 9.4 months in the group with less than 90% decline or ctDNA increase (P = .007). These findings held true when the analysis was limited to the 14 patients with colorectal cancer, in which median OS was not reached in the group with greater than 90% decline in on-treatment ctDNA levels, versus 10.2 months in the group with less than 90% decline or ctDNA increase (P = 0.04).
Notably, the prognostic significance of ctDNA changes remained even among patients exhibiting radiographic stable disease, underscoring the limitations of relying solely on anatomic tumor measurements and highlighting the potential for ctDNA monitoring to complement standard clinical assessments. In the subset of patients with radiographic stable disease, those with a greater than 90% ctDNA decline had significantly longer OS than those with less ctDNA reduction (not reached versus 9.4 months; P = .01).
“When used as a complement to imaging, tissue-informed ctDNA monitoring with FoundationOne Tracker can provide more accuracy than imaging alone,” Dr. Kurzrock noted in an interview.
Dr. Kasi echoed Dr. Kurzrock’s enthusiasm regarding the clinical usefulness of these findings, saying, “Not only can you see very early on in whom the ctDNA is going down and clearing, but you can also tell apart within the group who has ‘stable disease’ as to who is deriving more benefit.”
The researchers also observed that increases in on-treatment ctDNA levels often preceded radiographic evidence of disease progression by a median of 1.3 months. These findings highlight the potential for ctDNA monitoring to complement standard clinical assessments, allowing us to detect treatment response and disease progression earlier than what is possible with imaging alone, Dr. Kurzrock explained during her talk. “This early warning signal could allow clinicians to intervene and modify treatment strategies before overt clinical deterioration,” she said.
In an interview, Dr. Kasi highlighted that this high sensitivity and specificity and the short half-life of the tumor-informed ctDNA assay make this liquid biopsy of great clinical value. “The short half-life of a few hours means that if you do an intervention to treat cancer with HER2-directed therapy, you can very quickly assess response to therapy way earlier than traditional radiographic methods.”
Dr. Kasi cautioned, however, that this assay would not capture whether new mutations or HER2 loss occurred at the time of resistance. “A repeat tissue biopsy or a next-generation sequencing-based plasma-only assay would be required for that,” he said.
Implementation of ctDNA monitoring in clinical trials
Dr. Kurzrock acknowledged that further research is needed to validate these results in larger, prospective cohorts before FoundationOne Tracker is adopted in the clinic. She noted, however, that this retrospective analysis, along with results from previous studies, provides a rationale for the use of ctDNA monitoring in clinical trials.
“In some centers like ours, ctDNA monitoring is already part of our standard of care since not only does it help from a physician standpoint to have a more accurate and early assessment of response, but patients also appreciate the information gained from ctDNA dynamics,” Dr. Kasi said in an interview. He explained that when radiographic findings are equivocal, ctDNA monitoring is an additional tool in their toolbox to help guide care.
He noted, however, that the cost is a challenge for implementing ctDNA monitoring as a complementary tool for real-time treatment response monitoring. “For serial monitoring, helping to reduce costs would be important in the long run,” he said in an interview. He added that obtaining sufficient tissue for testing using a tumor-informed assay can present a logistical challenge, at least for the first test. “You need sufficient tissue to make the barcode that you then follow along,” he explained.
“Developing guidelines through systematic studies about testing cadence would also be important. This would help establish whether ctDNA monitoring is helpful,” Dr. Kasi said in an interview. He explained that in some situations, biological variables affect the shedding and detection of ctDNA beyond the assay — in those cases, ctDNA monitoring may not be helpful. “Like any test, it is not meant for every patient or clinical question,” Dr. Kasi concluded.
Dr. Kurzrock and Dr. Kasi reported no relationships with entities whose primary business is producing, marketing, selling, reselling, or distributing healthcare products used by or on patients.
This was the main finding of new data presented by study author Razelle Kurzrock, MD, at the American Association for Cancer Research annual meeting.
“We found that on-treatment ctDNA can detect progression before standard-of-care response assessments. These data suggest that monitoring ctDNA can provide clinicians with important prognostic information that may guide treatment decisions,” Dr. Kurzrock, professor at the Medical College of Wisconsin, Milwaukee, said during her presentation.
Commenting on the clinical implications of these findings during an interview, she said the results suggest that ctDNA dynamics provide an early window into predicting response to targeted therapies in patients with HER2-altered cancers, confirming previous findings of the predictive value of ctDNA in other cancer types.
“Such monitoring may be useful in clinical trials and eventually in practice,” she added.
Need for new methods to predict early tumor response
Limitations of standard radiographic tumor assessments present challenges in determining clinical response, particularly for patients receiving targeted therapies.
During her talk, Dr. Kurzrock explained that although targeted therapies are effective for patients with specific molecular alterations, standard imaging assessments fail to uncover molecular-level changes within tumors, limiting the ability of clinicians to accurately assess a patient’s response to targeted therapies.
“In addition to limitations with imaging, patients and physicians want to know as soon as possible whether or not the agents are effective, especially if there are side effects,” Dr. Kurzrock during an interview. She added that monitoring early response may be especially important across tumor types, as HER2 therapies are increasingly being considered in the pan-cancer setting.
Commenting on the potential use of this method in other cancer types with HER2 alterations, Pashtoon Murtaza Kasi, MD, MS, noted that since the study relied on a tumor-informed assay, it would be applicable across diverse tumor types.
“It is less about tissue type but more about that particular patient’s tumor at that instant in time for which a unique barcode is created,” said Dr. Kasi, a medical oncologist at Weill Cornell Medicine, New York, who was not involved in the study.
In an interview, he added that the shedding and biology would affect the assay’s performance for some tissue types.
Design of patient-specific ctDNA assays
In this retrospective study, the researchers examined ctDNA dynamics in 58 patients with various HER2-positive tumor types, including breast, colorectal, and other solid malignancies harboring HER2 alterations. All the patients received combination HER2-targeted therapy with trastuzumab and pertuzumab in the phase 2 basket trial My Pathway (NCT02091141).
By leveraging comprehensive genomic profiling of each patient’s tumor, the researchers designed personalized ctDNA assays, tracking 2-16 tumor-specific genetic variants in the patients’ blood samples. FoundationOne Tracker was used to detect and quantify ctDNA at baseline and the third cycle of therapy (cycle 3 day 1, or C3D1).
During an interview, Dr. Kurzrock explained that FoundationOne Tracker is a personalized ctDNA monitoring assay that allows for the detection of ctDNA in plasma, enabling ongoing liquid-based monitoring and highly sensitive quantification of ctDNA levels as mean tumor molecules per milliliter of plasma.
Among the 52 patients for whom personalized ctDNA assays were successfully designed, 48 (92.3%) had ctDNA data available at baseline, with a median of 100.7 tumor molecules per milliliter of plasma. Most patients (89.6%) were deemed ctDNA-positive, with a median of 119.5 tumor molecules per milliliter of plasma.
Changes in ctDNA levels predict patient survival
The researchers found that patients who experienced a greater than 90% decline in ctDNA levels by the third treatment cycle had significantly longer overall survival (OS) than those with less than 90% ctDNA decline or any increase. According to data presented by Dr. Kurzrock, the median OS was not reached in the group with greater than 90% decline in on-treatment ctDNA levels, versus 9.4 months in the group with less than 90% decline or ctDNA increase (P = .007). These findings held true when the analysis was limited to the 14 patients with colorectal cancer, in which median OS was not reached in the group with greater than 90% decline in on-treatment ctDNA levels, versus 10.2 months in the group with less than 90% decline or ctDNA increase (P = 0.04).
Notably, the prognostic significance of ctDNA changes remained even among patients exhibiting radiographic stable disease, underscoring the limitations of relying solely on anatomic tumor measurements and highlighting the potential for ctDNA monitoring to complement standard clinical assessments. In the subset of patients with radiographic stable disease, those with a greater than 90% ctDNA decline had significantly longer OS than those with less ctDNA reduction (not reached versus 9.4 months; P = .01).
“When used as a complement to imaging, tissue-informed ctDNA monitoring with FoundationOne Tracker can provide more accuracy than imaging alone,” Dr. Kurzrock noted in an interview.
Dr. Kasi echoed Dr. Kurzrock’s enthusiasm regarding the clinical usefulness of these findings, saying, “Not only can you see very early on in whom the ctDNA is going down and clearing, but you can also tell apart within the group who has ‘stable disease’ as to who is deriving more benefit.”
The researchers also observed that increases in on-treatment ctDNA levels often preceded radiographic evidence of disease progression by a median of 1.3 months. These findings highlight the potential for ctDNA monitoring to complement standard clinical assessments, allowing us to detect treatment response and disease progression earlier than what is possible with imaging alone, Dr. Kurzrock explained during her talk. “This early warning signal could allow clinicians to intervene and modify treatment strategies before overt clinical deterioration,” she said.
In an interview, Dr. Kasi highlighted that this high sensitivity and specificity and the short half-life of the tumor-informed ctDNA assay make this liquid biopsy of great clinical value. “The short half-life of a few hours means that if you do an intervention to treat cancer with HER2-directed therapy, you can very quickly assess response to therapy way earlier than traditional radiographic methods.”
Dr. Kasi cautioned, however, that this assay would not capture whether new mutations or HER2 loss occurred at the time of resistance. “A repeat tissue biopsy or a next-generation sequencing-based plasma-only assay would be required for that,” he said.
Implementation of ctDNA monitoring in clinical trials
Dr. Kurzrock acknowledged that further research is needed to validate these results in larger, prospective cohorts before FoundationOne Tracker is adopted in the clinic. She noted, however, that this retrospective analysis, along with results from previous studies, provides a rationale for the use of ctDNA monitoring in clinical trials.
“In some centers like ours, ctDNA monitoring is already part of our standard of care since not only does it help from a physician standpoint to have a more accurate and early assessment of response, but patients also appreciate the information gained from ctDNA dynamics,” Dr. Kasi said in an interview. He explained that when radiographic findings are equivocal, ctDNA monitoring is an additional tool in their toolbox to help guide care.
He noted, however, that the cost is a challenge for implementing ctDNA monitoring as a complementary tool for real-time treatment response monitoring. “For serial monitoring, helping to reduce costs would be important in the long run,” he said in an interview. He added that obtaining sufficient tissue for testing using a tumor-informed assay can present a logistical challenge, at least for the first test. “You need sufficient tissue to make the barcode that you then follow along,” he explained.
“Developing guidelines through systematic studies about testing cadence would also be important. This would help establish whether ctDNA monitoring is helpful,” Dr. Kasi said in an interview. He explained that in some situations, biological variables affect the shedding and detection of ctDNA beyond the assay — in those cases, ctDNA monitoring may not be helpful. “Like any test, it is not meant for every patient or clinical question,” Dr. Kasi concluded.
Dr. Kurzrock and Dr. Kasi reported no relationships with entities whose primary business is producing, marketing, selling, reselling, or distributing healthcare products used by or on patients.
FROM AACR 2024
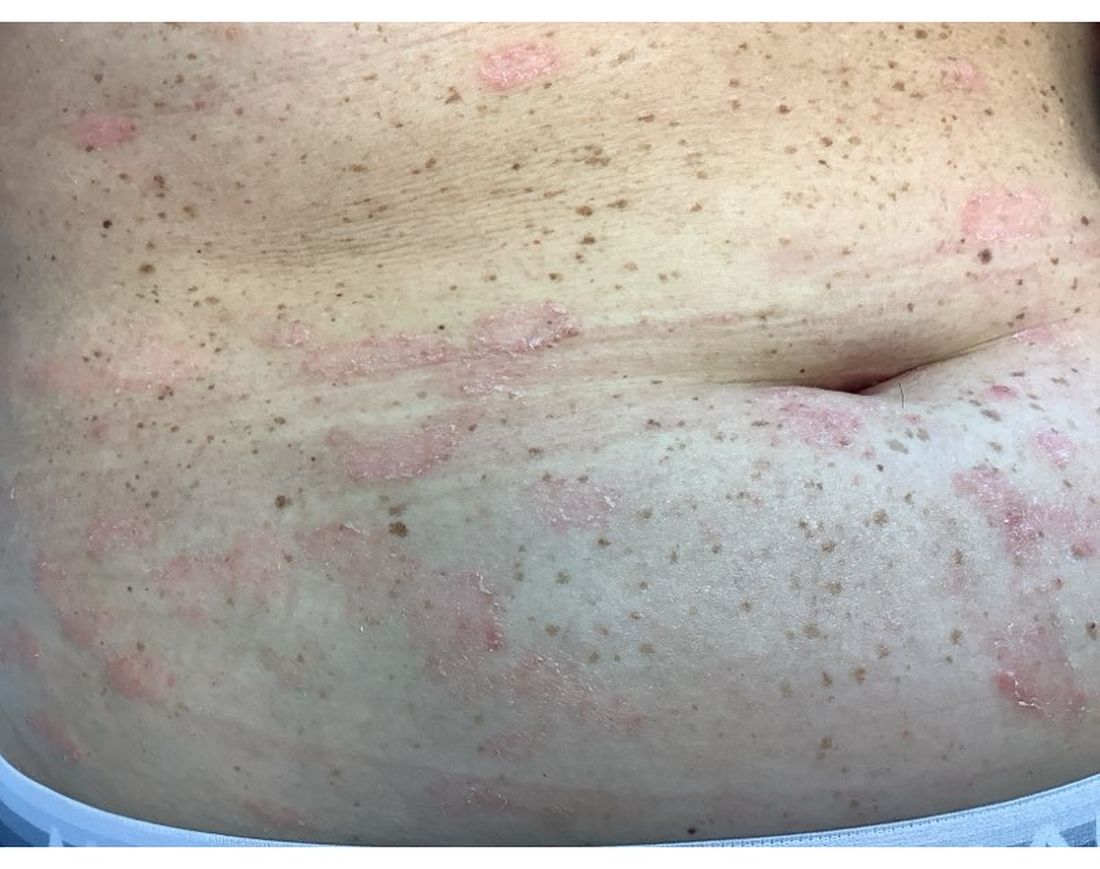
A 30-Year-Old White Female Presented With a 4-Month History of Scaly, Erythematous Patches and Plaques on Her Trunk and Extremities
Tumor necrosis factor (TNF)-alpha inhibitors are used to treat a variety of autoimmune conditions including psoriasis, psoriatic arthritis, rheumatoid arthritis (RA), spondyloarthritis, and inflammatory bowel disease (IBD). Interestingly, they have also been observed to cause paradoxical psoriasis with an incidence between 0.6%-5.3%, most commonly occurring in patients with underlying Crohn’s disease and rheumatoid arthritis (RA). Infliximab is the most common TNF inhibitor associated with this condition (52.6%-62.6% of cases) followed by etanercept (12%-29%). .
Psoriasis is traditionally divided into two types. Patients with type I psoriasis have a family history, develop symptoms before the age of 40 and are often positive for HLA-Cw6. Type II psoriasis is not related to HLA-Cw6, lacks a family history, and typically manifests after age 40. Psoriatic lesions are well-defined, erythematous plaques with silvery scales most commonly appearing on extensor surfaces and the scalp. Variants include nail psoriasis, pustular psoriasis, inverse psoriasis, and guttate psoriasis.
Although psoriasis is typically a clinical diagnosis, histologic examination may be used to differentiate from other dermatoses if necessary. The lesions of TNF inhibitor-induced psoriasis characteristically display patterns similar to primary psoriasis, including parakeratosis, microabscesses, and rete ridges. Eosinophilic hypersensitivity reactions and features overlapping with eczematous hypersensitivity (psoriasiform dermatitis) may also be present.
The pathogenesis of this condition is not well understood, but theories include a variety of immune processes including interferon overproduction, interleukin and T-cell activation, and the presence of an infectious nidus. Classical psoriasis is related to type 1 interferon release, so theoretically, immunosuppression caused by TNF inhibitor treatment may permit uncontrolled production of interferons, resulting in psoriatic lesions. Another theory is that interleukin (IL)-23, a pro-inflammatory cytokine, promotes activation of T-helper 17 (Th17) cells. Th17 cells are part of the pathogenesis of primary psoriasis and other inflammatory conditions, such as RA and inflammatory bowel disease. Of note, individuals with gastrointestinal inflammatory diseases are already known to be at a greater risk for developing psoriasis. Immunosuppression caused by a TNF inhibitor may leave patients more susceptible to other infections, which may induce psoriatic plaques.
There are multiple approaches to treatment depending on the severity of the disease. If the psoriatic eruption is mild, the medication may be continued. This “treat-through” method is often considered when stopping the current immunotherapy would cause the patient significant issues. Moderate to severe cases of TNF inhibitor-induced psoriasis may warrant switching TNF inhibitor therapy or completely changing the drug class used in the treatment of the underlying autoimmune condition. Additional treatments include topical and oral steroids, UV therapy, methotrexate, cyclosporine, and acitretin.
This case and the photo were submitted by Lucas Shapiro, BS, of Nova Southeastern University College of Osteopathic Medicine, Fort Lauderdale, Florida, and Leon S. Maratchi, MD, Gastro Health, Hollywood, Florida. The column was edited by Donna Bilu Martin, MD.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
1. Li SJ et al. J Psoriasis Psoriatic Arthritis. 2019 Apr;4(2):70-80. doi: 10.1177/2475530318810851.
2. Lu J and Lu Y. J Transl Autoimmun. 2023 Sep 6:7:100211. doi: 10.1016/j.jtauto.2023.100211.
3. Nair PA and Badri T. Psoriasis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: www.ncbi.nlm.nih.gov/books/NBK448194/
Tumor necrosis factor (TNF)-alpha inhibitors are used to treat a variety of autoimmune conditions including psoriasis, psoriatic arthritis, rheumatoid arthritis (RA), spondyloarthritis, and inflammatory bowel disease (IBD). Interestingly, they have also been observed to cause paradoxical psoriasis with an incidence between 0.6%-5.3%, most commonly occurring in patients with underlying Crohn’s disease and rheumatoid arthritis (RA). Infliximab is the most common TNF inhibitor associated with this condition (52.6%-62.6% of cases) followed by etanercept (12%-29%). .
Psoriasis is traditionally divided into two types. Patients with type I psoriasis have a family history, develop symptoms before the age of 40 and are often positive for HLA-Cw6. Type II psoriasis is not related to HLA-Cw6, lacks a family history, and typically manifests after age 40. Psoriatic lesions are well-defined, erythematous plaques with silvery scales most commonly appearing on extensor surfaces and the scalp. Variants include nail psoriasis, pustular psoriasis, inverse psoriasis, and guttate psoriasis.
Although psoriasis is typically a clinical diagnosis, histologic examination may be used to differentiate from other dermatoses if necessary. The lesions of TNF inhibitor-induced psoriasis characteristically display patterns similar to primary psoriasis, including parakeratosis, microabscesses, and rete ridges. Eosinophilic hypersensitivity reactions and features overlapping with eczematous hypersensitivity (psoriasiform dermatitis) may also be present.
The pathogenesis of this condition is not well understood, but theories include a variety of immune processes including interferon overproduction, interleukin and T-cell activation, and the presence of an infectious nidus. Classical psoriasis is related to type 1 interferon release, so theoretically, immunosuppression caused by TNF inhibitor treatment may permit uncontrolled production of interferons, resulting in psoriatic lesions. Another theory is that interleukin (IL)-23, a pro-inflammatory cytokine, promotes activation of T-helper 17 (Th17) cells. Th17 cells are part of the pathogenesis of primary psoriasis and other inflammatory conditions, such as RA and inflammatory bowel disease. Of note, individuals with gastrointestinal inflammatory diseases are already known to be at a greater risk for developing psoriasis. Immunosuppression caused by a TNF inhibitor may leave patients more susceptible to other infections, which may induce psoriatic plaques.
There are multiple approaches to treatment depending on the severity of the disease. If the psoriatic eruption is mild, the medication may be continued. This “treat-through” method is often considered when stopping the current immunotherapy would cause the patient significant issues. Moderate to severe cases of TNF inhibitor-induced psoriasis may warrant switching TNF inhibitor therapy or completely changing the drug class used in the treatment of the underlying autoimmune condition. Additional treatments include topical and oral steroids, UV therapy, methotrexate, cyclosporine, and acitretin.
This case and the photo were submitted by Lucas Shapiro, BS, of Nova Southeastern University College of Osteopathic Medicine, Fort Lauderdale, Florida, and Leon S. Maratchi, MD, Gastro Health, Hollywood, Florida. The column was edited by Donna Bilu Martin, MD.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
1. Li SJ et al. J Psoriasis Psoriatic Arthritis. 2019 Apr;4(2):70-80. doi: 10.1177/2475530318810851.
2. Lu J and Lu Y. J Transl Autoimmun. 2023 Sep 6:7:100211. doi: 10.1016/j.jtauto.2023.100211.
3. Nair PA and Badri T. Psoriasis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: www.ncbi.nlm.nih.gov/books/NBK448194/
Tumor necrosis factor (TNF)-alpha inhibitors are used to treat a variety of autoimmune conditions including psoriasis, psoriatic arthritis, rheumatoid arthritis (RA), spondyloarthritis, and inflammatory bowel disease (IBD). Interestingly, they have also been observed to cause paradoxical psoriasis with an incidence between 0.6%-5.3%, most commonly occurring in patients with underlying Crohn’s disease and rheumatoid arthritis (RA). Infliximab is the most common TNF inhibitor associated with this condition (52.6%-62.6% of cases) followed by etanercept (12%-29%). .
Psoriasis is traditionally divided into two types. Patients with type I psoriasis have a family history, develop symptoms before the age of 40 and are often positive for HLA-Cw6. Type II psoriasis is not related to HLA-Cw6, lacks a family history, and typically manifests after age 40. Psoriatic lesions are well-defined, erythematous plaques with silvery scales most commonly appearing on extensor surfaces and the scalp. Variants include nail psoriasis, pustular psoriasis, inverse psoriasis, and guttate psoriasis.
Although psoriasis is typically a clinical diagnosis, histologic examination may be used to differentiate from other dermatoses if necessary. The lesions of TNF inhibitor-induced psoriasis characteristically display patterns similar to primary psoriasis, including parakeratosis, microabscesses, and rete ridges. Eosinophilic hypersensitivity reactions and features overlapping with eczematous hypersensitivity (psoriasiform dermatitis) may also be present.
The pathogenesis of this condition is not well understood, but theories include a variety of immune processes including interferon overproduction, interleukin and T-cell activation, and the presence of an infectious nidus. Classical psoriasis is related to type 1 interferon release, so theoretically, immunosuppression caused by TNF inhibitor treatment may permit uncontrolled production of interferons, resulting in psoriatic lesions. Another theory is that interleukin (IL)-23, a pro-inflammatory cytokine, promotes activation of T-helper 17 (Th17) cells. Th17 cells are part of the pathogenesis of primary psoriasis and other inflammatory conditions, such as RA and inflammatory bowel disease. Of note, individuals with gastrointestinal inflammatory diseases are already known to be at a greater risk for developing psoriasis. Immunosuppression caused by a TNF inhibitor may leave patients more susceptible to other infections, which may induce psoriatic plaques.
There are multiple approaches to treatment depending on the severity of the disease. If the psoriatic eruption is mild, the medication may be continued. This “treat-through” method is often considered when stopping the current immunotherapy would cause the patient significant issues. Moderate to severe cases of TNF inhibitor-induced psoriasis may warrant switching TNF inhibitor therapy or completely changing the drug class used in the treatment of the underlying autoimmune condition. Additional treatments include topical and oral steroids, UV therapy, methotrexate, cyclosporine, and acitretin.
This case and the photo were submitted by Lucas Shapiro, BS, of Nova Southeastern University College of Osteopathic Medicine, Fort Lauderdale, Florida, and Leon S. Maratchi, MD, Gastro Health, Hollywood, Florida. The column was edited by Donna Bilu Martin, MD.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
1. Li SJ et al. J Psoriasis Psoriatic Arthritis. 2019 Apr;4(2):70-80. doi: 10.1177/2475530318810851.
2. Lu J and Lu Y. J Transl Autoimmun. 2023 Sep 6:7:100211. doi: 10.1016/j.jtauto.2023.100211.
3. Nair PA and Badri T. Psoriasis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: www.ncbi.nlm.nih.gov/books/NBK448194/
Mild Hidradenitis Suppurativa: Positive Results Reported for Topical Therapy
SAN DIEGO — cream, in a phase 2 trial.
“HS is a chronic, recurring inflammatory skin disease that is associated with painful inflammatory modules and abscesses,” said presenting author Martina J. Porter, MD, a dermatologist at Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, Massachusetts. Dr. Porter presented the data during a late-breaking session at the annual meeting of the American Academy of Dermatology.
“Over time, these patients may progress to having tunnels, ulcerations, malodorous discharge, and permanent scarring,” she said. “Currently, there are no approved therapies for milder HS, and the standard treatments that we apply in clinical practice are often inadequate.”
Ruxolitinib is a selective Janus kinase (JAK) 1/JAK2 inhibitor that has demonstrated efficacy in other inflammatory and autoimmune skin diseases. Ruxolitinib cream, 1.5%, is approved for treating mild to moderate atopic dermatitis and nonsegmental vitiligo in patients ages 12 years and older.
The phase 2 double-blind, vehicle-controlled trial evaluated the efficacy and safety of ruxolitinib cream for mild HS. Researchers assigned 69 adults with Hurley stage I or II HS to receive 1.5% ruxolitinib cream or vehicle cream twice daily for 16 weeks. The primary endpoint was the change from baseline in AN count at week 16. To be eligible, patients had to have an AN count between 3 and 10.
“This is much more mild than what we have seen in any systemic therapy trials,” Dr. Porter said. “And, if patients had 3 lesions, they all needed to be in one anatomic area, but if they had 4-10 lesions, they had to have two anatomic areas involved. Also, no patients with active draining tunnels were allowed in the study.”
Of the 69 patients, 34 received ruxolitinib cream and 35 received vehicle. About 51% of patients in the vehicle arm were Black and 34% were White, while about 32% of patients in the ruxolitinib arm were Black and 56% were White.
The mean age of patients overall was 29 years, and about half the patients in both study arms had Hurley stage I disease, while the other half had Hurley stage II disease. Their average AN count ranged between 5.3 and 5.6 — mostly inflammatory nodules and few abscesses. Patients were not allowed to receive any type of intervention or rescue therapy during the study.
Dr. Porter reported that the least square mean change in AN count from baseline to week 16 was -2.42 in the vehicle arm vs -3.61 in the ruxolitinib cream arm (P <.05). The proportion of patients who achieved a 50% decrease in AN count was 79.2% in the ruxolitinib cream arm, compared with 56.5% of patients in the vehicle arm, respectively. More patients in the ruxolitinib cream arm achieved a 75% decrease in AN count (54.2% vs 25%), a 90% decrease in AN count (20.8 vs 12.5%), and a 100% decrease in AN count (20.8% vs 12.5%).
In other findings, 79.2% of patients in the ruxolitinib cream arm achieved a Hidradenitis Suppurativa Clinical Response score from baseline through week 16, compared with 50% of those in the vehicle group. The International Hidradenitis Suppurativa Severity Score System results favored the ruxolitinib cream arm (-4.46 vs -2.66 in the vehicle arm). Skin Pain and Itch numeric rating scale scores were moderate at baseline and improved similarly in both groups during the study.
Ruxolitinib cream was generally well tolerated over 16 weeks. No serious treatment-emergent adverse events were reported. The most common adverse event reported in the ruxolitinib cream group was COVID-19 and nasopharyngitis (two cases each) and one case of an application site reaction.
“Twice-daily 1.5% ruxolitinib cream was effective in patients with milder HS,” Dr. Porter concluded. “Modifications to our traditionally accepted clinical endpoints may be needed in studies of patients with milder HS.”
Jennifer L. Hsiao, MD, a dermatologist who directs the HS clinic at the University of Southern California, Los Angeles, who was asked to comment on the results, characterized the study as exciting for several reasons.
“First, with the global push in recent years to increase HS awareness, I am already seeing more patients earlier in their disease course with milder disease, and there is currently a gap in approved therapies for this patient population,” she told this news organization.
“Second, patients are very interested in topical therapies for HS and are thrilled whenever they learn that topical options are under investigation. This study had small patient numbers, but it was encouraging to see the positive results for ruxolitinib cream and that the treatment appeared well-tolerated.”
The trial was sponsored by the Incyte Corporation. Dr. Porter disclosed that she has received consulting fees from AbbVie, Alumis, Eli Lilly, Incyte, Janssen, Novartis, Pfizer, Prometheus Laboratories, Sanofi, Sonoma Biotherapeutics, Trifecta Clinical, and UCB. Dr. Hsiao disclosed that she is a member of the board of directors for the HS Foundation. She has also served as a consultant for AbbVie, Aclaris, Boehringer Ingelheim, Incyte, Novartis, and UCB; as a speaker for AbbVie, Novartis, and UCB; and as an investigator for Amgen, Boehringer Ingelheim, and Incyte.
A version of this article appeared on Medscape.com .
SAN DIEGO — cream, in a phase 2 trial.
“HS is a chronic, recurring inflammatory skin disease that is associated with painful inflammatory modules and abscesses,” said presenting author Martina J. Porter, MD, a dermatologist at Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, Massachusetts. Dr. Porter presented the data during a late-breaking session at the annual meeting of the American Academy of Dermatology.
“Over time, these patients may progress to having tunnels, ulcerations, malodorous discharge, and permanent scarring,” she said. “Currently, there are no approved therapies for milder HS, and the standard treatments that we apply in clinical practice are often inadequate.”
Ruxolitinib is a selective Janus kinase (JAK) 1/JAK2 inhibitor that has demonstrated efficacy in other inflammatory and autoimmune skin diseases. Ruxolitinib cream, 1.5%, is approved for treating mild to moderate atopic dermatitis and nonsegmental vitiligo in patients ages 12 years and older.
The phase 2 double-blind, vehicle-controlled trial evaluated the efficacy and safety of ruxolitinib cream for mild HS. Researchers assigned 69 adults with Hurley stage I or II HS to receive 1.5% ruxolitinib cream or vehicle cream twice daily for 16 weeks. The primary endpoint was the change from baseline in AN count at week 16. To be eligible, patients had to have an AN count between 3 and 10.
“This is much more mild than what we have seen in any systemic therapy trials,” Dr. Porter said. “And, if patients had 3 lesions, they all needed to be in one anatomic area, but if they had 4-10 lesions, they had to have two anatomic areas involved. Also, no patients with active draining tunnels were allowed in the study.”
Of the 69 patients, 34 received ruxolitinib cream and 35 received vehicle. About 51% of patients in the vehicle arm were Black and 34% were White, while about 32% of patients in the ruxolitinib arm were Black and 56% were White.
The mean age of patients overall was 29 years, and about half the patients in both study arms had Hurley stage I disease, while the other half had Hurley stage II disease. Their average AN count ranged between 5.3 and 5.6 — mostly inflammatory nodules and few abscesses. Patients were not allowed to receive any type of intervention or rescue therapy during the study.
Dr. Porter reported that the least square mean change in AN count from baseline to week 16 was -2.42 in the vehicle arm vs -3.61 in the ruxolitinib cream arm (P <.05). The proportion of patients who achieved a 50% decrease in AN count was 79.2% in the ruxolitinib cream arm, compared with 56.5% of patients in the vehicle arm, respectively. More patients in the ruxolitinib cream arm achieved a 75% decrease in AN count (54.2% vs 25%), a 90% decrease in AN count (20.8 vs 12.5%), and a 100% decrease in AN count (20.8% vs 12.5%).
In other findings, 79.2% of patients in the ruxolitinib cream arm achieved a Hidradenitis Suppurativa Clinical Response score from baseline through week 16, compared with 50% of those in the vehicle group. The International Hidradenitis Suppurativa Severity Score System results favored the ruxolitinib cream arm (-4.46 vs -2.66 in the vehicle arm). Skin Pain and Itch numeric rating scale scores were moderate at baseline and improved similarly in both groups during the study.
Ruxolitinib cream was generally well tolerated over 16 weeks. No serious treatment-emergent adverse events were reported. The most common adverse event reported in the ruxolitinib cream group was COVID-19 and nasopharyngitis (two cases each) and one case of an application site reaction.
“Twice-daily 1.5% ruxolitinib cream was effective in patients with milder HS,” Dr. Porter concluded. “Modifications to our traditionally accepted clinical endpoints may be needed in studies of patients with milder HS.”
Jennifer L. Hsiao, MD, a dermatologist who directs the HS clinic at the University of Southern California, Los Angeles, who was asked to comment on the results, characterized the study as exciting for several reasons.
“First, with the global push in recent years to increase HS awareness, I am already seeing more patients earlier in their disease course with milder disease, and there is currently a gap in approved therapies for this patient population,” she told this news organization.
“Second, patients are very interested in topical therapies for HS and are thrilled whenever they learn that topical options are under investigation. This study had small patient numbers, but it was encouraging to see the positive results for ruxolitinib cream and that the treatment appeared well-tolerated.”
The trial was sponsored by the Incyte Corporation. Dr. Porter disclosed that she has received consulting fees from AbbVie, Alumis, Eli Lilly, Incyte, Janssen, Novartis, Pfizer, Prometheus Laboratories, Sanofi, Sonoma Biotherapeutics, Trifecta Clinical, and UCB. Dr. Hsiao disclosed that she is a member of the board of directors for the HS Foundation. She has also served as a consultant for AbbVie, Aclaris, Boehringer Ingelheim, Incyte, Novartis, and UCB; as a speaker for AbbVie, Novartis, and UCB; and as an investigator for Amgen, Boehringer Ingelheim, and Incyte.
A version of this article appeared on Medscape.com .
SAN DIEGO — cream, in a phase 2 trial.
“HS is a chronic, recurring inflammatory skin disease that is associated with painful inflammatory modules and abscesses,” said presenting author Martina J. Porter, MD, a dermatologist at Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, Massachusetts. Dr. Porter presented the data during a late-breaking session at the annual meeting of the American Academy of Dermatology.
“Over time, these patients may progress to having tunnels, ulcerations, malodorous discharge, and permanent scarring,” she said. “Currently, there are no approved therapies for milder HS, and the standard treatments that we apply in clinical practice are often inadequate.”
Ruxolitinib is a selective Janus kinase (JAK) 1/JAK2 inhibitor that has demonstrated efficacy in other inflammatory and autoimmune skin diseases. Ruxolitinib cream, 1.5%, is approved for treating mild to moderate atopic dermatitis and nonsegmental vitiligo in patients ages 12 years and older.
The phase 2 double-blind, vehicle-controlled trial evaluated the efficacy and safety of ruxolitinib cream for mild HS. Researchers assigned 69 adults with Hurley stage I or II HS to receive 1.5% ruxolitinib cream or vehicle cream twice daily for 16 weeks. The primary endpoint was the change from baseline in AN count at week 16. To be eligible, patients had to have an AN count between 3 and 10.
“This is much more mild than what we have seen in any systemic therapy trials,” Dr. Porter said. “And, if patients had 3 lesions, they all needed to be in one anatomic area, but if they had 4-10 lesions, they had to have two anatomic areas involved. Also, no patients with active draining tunnels were allowed in the study.”
Of the 69 patients, 34 received ruxolitinib cream and 35 received vehicle. About 51% of patients in the vehicle arm were Black and 34% were White, while about 32% of patients in the ruxolitinib arm were Black and 56% were White.
The mean age of patients overall was 29 years, and about half the patients in both study arms had Hurley stage I disease, while the other half had Hurley stage II disease. Their average AN count ranged between 5.3 and 5.6 — mostly inflammatory nodules and few abscesses. Patients were not allowed to receive any type of intervention or rescue therapy during the study.
Dr. Porter reported that the least square mean change in AN count from baseline to week 16 was -2.42 in the vehicle arm vs -3.61 in the ruxolitinib cream arm (P <.05). The proportion of patients who achieved a 50% decrease in AN count was 79.2% in the ruxolitinib cream arm, compared with 56.5% of patients in the vehicle arm, respectively. More patients in the ruxolitinib cream arm achieved a 75% decrease in AN count (54.2% vs 25%), a 90% decrease in AN count (20.8 vs 12.5%), and a 100% decrease in AN count (20.8% vs 12.5%).
In other findings, 79.2% of patients in the ruxolitinib cream arm achieved a Hidradenitis Suppurativa Clinical Response score from baseline through week 16, compared with 50% of those in the vehicle group. The International Hidradenitis Suppurativa Severity Score System results favored the ruxolitinib cream arm (-4.46 vs -2.66 in the vehicle arm). Skin Pain and Itch numeric rating scale scores were moderate at baseline and improved similarly in both groups during the study.
Ruxolitinib cream was generally well tolerated over 16 weeks. No serious treatment-emergent adverse events were reported. The most common adverse event reported in the ruxolitinib cream group was COVID-19 and nasopharyngitis (two cases each) and one case of an application site reaction.
“Twice-daily 1.5% ruxolitinib cream was effective in patients with milder HS,” Dr. Porter concluded. “Modifications to our traditionally accepted clinical endpoints may be needed in studies of patients with milder HS.”
Jennifer L. Hsiao, MD, a dermatologist who directs the HS clinic at the University of Southern California, Los Angeles, who was asked to comment on the results, characterized the study as exciting for several reasons.
“First, with the global push in recent years to increase HS awareness, I am already seeing more patients earlier in their disease course with milder disease, and there is currently a gap in approved therapies for this patient population,” she told this news organization.
“Second, patients are very interested in topical therapies for HS and are thrilled whenever they learn that topical options are under investigation. This study had small patient numbers, but it was encouraging to see the positive results for ruxolitinib cream and that the treatment appeared well-tolerated.”
The trial was sponsored by the Incyte Corporation. Dr. Porter disclosed that she has received consulting fees from AbbVie, Alumis, Eli Lilly, Incyte, Janssen, Novartis, Pfizer, Prometheus Laboratories, Sanofi, Sonoma Biotherapeutics, Trifecta Clinical, and UCB. Dr. Hsiao disclosed that she is a member of the board of directors for the HS Foundation. She has also served as a consultant for AbbVie, Aclaris, Boehringer Ingelheim, Incyte, Novartis, and UCB; as a speaker for AbbVie, Novartis, and UCB; and as an investigator for Amgen, Boehringer Ingelheim, and Incyte.
A version of this article appeared on Medscape.com .
FROM AAD 2024
Study Identifies Several Factors That Influence Longterm Antibiotic Prescribing for Acne
to follow them, according to the authors of a recently published study.
“This study explored why dermatologists still prescribe a good number of long-term antibiotics for people with acne,” the study’s senior author Howa Yeung, MD, MSc, assistant professor of dermatology at Emory University, Atlanta, said in an interview. “And we found a lot of reasons.” The study was published online in JAMA Dermatology.
Using online surveys and semi-structured video interviews of 30 dermatologists, infectious disease physicians with expertise in antimicrobial stewardship, dermatology residents, and nonphysician clinicians, the investigators assessed respondents’ knowledge and attitudes regarding long-term antibiotics in acne. Salient themes impacting long-term antibiotic prescriptions included the following:
- A perceived dearth of evidence to justify changes in practice.
- Difficulties with iPLEDGE, the Risk Evaluation and Mitigation Strategy (REMS) for managing the teratogenic risks associated with isotretinoin, and with discussing oral contraceptives.
- “Navigating” discussions with about tapering-off of antibiotics.
- Challenging patient demands.
- A lack of effective tools for monitoring progress in antibiotic stewardship.
“It’s surprising there are so many barriers that make it difficult for dermatologists to stick with the guidelines even if they want to,” said Dr. Yeung, a coauthor of the recently released updated American Academy of Dermatology (AAD) acne management guidelines.
A dermatologist who wants to stop systemic antibiotics within 3 months may not know how to do so, he explained, or high demand for appointments may prevent timely follow-ups.
A major reason why dermatologists struggle to limit long-term antibiotic use is that there are very few substitutes that are perceived to work as well, said David J. Margolis, MD, PhD, who was not involved with the study and was asked to comment on the results. He is professor of epidemiology and dermatology at the University of Pennsylvania, Philadelphia.
“Part of the reason antibiotics are being used to treat acne is that they’re effective, and effective for severe disease,” he said. The alternatives, which are mostly topicals, said Dr. Margolis, do not work as well for moderate to severe disease or, with isotretinoin, involve time-consuming hurdles. Dr. Margolis said that he often hears such concerns from individual dermatologists. “But it’s helpful to see these in a well-organized, well-reported qualitative study.”
Infectious disease specialists surveyed considered limiting long-term antibiotic use as extremely important, while several dermatologists “argued that other specialties ‘underestimate the impact acne has on people’s lives,’ ” the authors wrote. Other respondents prioritized making the right choice for the patient at hand.
Although guidelines were never meant to be black and white, Dr. Yeung said, it is crucial to target the goal of tapering off after about 3-4 months — a cutoff with which guidelines from groups including the AAD, the Japanese Dermatological Association in guidelines from 2016, and 2017, respectively, and others concur.
He added, “Some folks believe that if the oral antibiotic is working, why stop? We need to develop evidence to show that reducing oral antibiotic use is important to our patients, not just to a theoretical problem of antibiotic resistance in society.” For example, in a study published in The Lancet in 2004, patients who used strictly topical regimens achieved efficacy similar to that of those who used only oral antibiotics.
In addition, some clinicians worried that limiting antibiotics could reduce patient satisfaction, spurring switches to other providers. However, he and the other authors of the JAMA Dermatology study noted that in a survey of patients with acne published in the Journal of Clinical and Aesthetic Dermatology in 2019, 76.9% said they would be “very or extremely likely” to use effective antibiotic-free treatments if offered.
Because most respondents were highly aware of the importance of antibiotic stewardship, Dr. Yeung said, additional passive education is not necessarily the answer. “It will take a concerted effort by our national societies to come up with resources and solutions for individual dermatologists to overcome some of these larger barriers.” Such solutions could range from training in communication and shared decision-making to implementing systems that provide individualized feedback to support antibiotic stewardship.
Many ongoing studies are examining antibiotic stewardship, Dr. Margolis said in the interview. However, he added, dermatologists’ idea of long-term use is 3 months, versus 1 month or less in other specialties. “Moreover, dermatology patients tend to be much healthier individuals and are rarely hospitalized, so there may be some issues comparing the ongoing studies to individuals with acne.” Future research will need to account for such differences, he said.
The study was funded by an American Acne & Rosacea Society Clinical Research Award. Dr. Yeung is associate editor of JAMA Dermatology. Dr. Margolis has received a National Institutes of Health grant to study doxycycline versus spironolactone in acne.
to follow them, according to the authors of a recently published study.
“This study explored why dermatologists still prescribe a good number of long-term antibiotics for people with acne,” the study’s senior author Howa Yeung, MD, MSc, assistant professor of dermatology at Emory University, Atlanta, said in an interview. “And we found a lot of reasons.” The study was published online in JAMA Dermatology.
Using online surveys and semi-structured video interviews of 30 dermatologists, infectious disease physicians with expertise in antimicrobial stewardship, dermatology residents, and nonphysician clinicians, the investigators assessed respondents’ knowledge and attitudes regarding long-term antibiotics in acne. Salient themes impacting long-term antibiotic prescriptions included the following:
- A perceived dearth of evidence to justify changes in practice.
- Difficulties with iPLEDGE, the Risk Evaluation and Mitigation Strategy (REMS) for managing the teratogenic risks associated with isotretinoin, and with discussing oral contraceptives.
- “Navigating” discussions with about tapering-off of antibiotics.
- Challenging patient demands.
- A lack of effective tools for monitoring progress in antibiotic stewardship.
“It’s surprising there are so many barriers that make it difficult for dermatologists to stick with the guidelines even if they want to,” said Dr. Yeung, a coauthor of the recently released updated American Academy of Dermatology (AAD) acne management guidelines.
A dermatologist who wants to stop systemic antibiotics within 3 months may not know how to do so, he explained, or high demand for appointments may prevent timely follow-ups.
A major reason why dermatologists struggle to limit long-term antibiotic use is that there are very few substitutes that are perceived to work as well, said David J. Margolis, MD, PhD, who was not involved with the study and was asked to comment on the results. He is professor of epidemiology and dermatology at the University of Pennsylvania, Philadelphia.
“Part of the reason antibiotics are being used to treat acne is that they’re effective, and effective for severe disease,” he said. The alternatives, which are mostly topicals, said Dr. Margolis, do not work as well for moderate to severe disease or, with isotretinoin, involve time-consuming hurdles. Dr. Margolis said that he often hears such concerns from individual dermatologists. “But it’s helpful to see these in a well-organized, well-reported qualitative study.”
Infectious disease specialists surveyed considered limiting long-term antibiotic use as extremely important, while several dermatologists “argued that other specialties ‘underestimate the impact acne has on people’s lives,’ ” the authors wrote. Other respondents prioritized making the right choice for the patient at hand.
Although guidelines were never meant to be black and white, Dr. Yeung said, it is crucial to target the goal of tapering off after about 3-4 months — a cutoff with which guidelines from groups including the AAD, the Japanese Dermatological Association in guidelines from 2016, and 2017, respectively, and others concur.
He added, “Some folks believe that if the oral antibiotic is working, why stop? We need to develop evidence to show that reducing oral antibiotic use is important to our patients, not just to a theoretical problem of antibiotic resistance in society.” For example, in a study published in The Lancet in 2004, patients who used strictly topical regimens achieved efficacy similar to that of those who used only oral antibiotics.
In addition, some clinicians worried that limiting antibiotics could reduce patient satisfaction, spurring switches to other providers. However, he and the other authors of the JAMA Dermatology study noted that in a survey of patients with acne published in the Journal of Clinical and Aesthetic Dermatology in 2019, 76.9% said they would be “very or extremely likely” to use effective antibiotic-free treatments if offered.
Because most respondents were highly aware of the importance of antibiotic stewardship, Dr. Yeung said, additional passive education is not necessarily the answer. “It will take a concerted effort by our national societies to come up with resources and solutions for individual dermatologists to overcome some of these larger barriers.” Such solutions could range from training in communication and shared decision-making to implementing systems that provide individualized feedback to support antibiotic stewardship.
Many ongoing studies are examining antibiotic stewardship, Dr. Margolis said in the interview. However, he added, dermatologists’ idea of long-term use is 3 months, versus 1 month or less in other specialties. “Moreover, dermatology patients tend to be much healthier individuals and are rarely hospitalized, so there may be some issues comparing the ongoing studies to individuals with acne.” Future research will need to account for such differences, he said.
The study was funded by an American Acne & Rosacea Society Clinical Research Award. Dr. Yeung is associate editor of JAMA Dermatology. Dr. Margolis has received a National Institutes of Health grant to study doxycycline versus spironolactone in acne.
to follow them, according to the authors of a recently published study.
“This study explored why dermatologists still prescribe a good number of long-term antibiotics for people with acne,” the study’s senior author Howa Yeung, MD, MSc, assistant professor of dermatology at Emory University, Atlanta, said in an interview. “And we found a lot of reasons.” The study was published online in JAMA Dermatology.
Using online surveys and semi-structured video interviews of 30 dermatologists, infectious disease physicians with expertise in antimicrobial stewardship, dermatology residents, and nonphysician clinicians, the investigators assessed respondents’ knowledge and attitudes regarding long-term antibiotics in acne. Salient themes impacting long-term antibiotic prescriptions included the following:
- A perceived dearth of evidence to justify changes in practice.
- Difficulties with iPLEDGE, the Risk Evaluation and Mitigation Strategy (REMS) for managing the teratogenic risks associated with isotretinoin, and with discussing oral contraceptives.
- “Navigating” discussions with about tapering-off of antibiotics.
- Challenging patient demands.
- A lack of effective tools for monitoring progress in antibiotic stewardship.
“It’s surprising there are so many barriers that make it difficult for dermatologists to stick with the guidelines even if they want to,” said Dr. Yeung, a coauthor of the recently released updated American Academy of Dermatology (AAD) acne management guidelines.
A dermatologist who wants to stop systemic antibiotics within 3 months may not know how to do so, he explained, or high demand for appointments may prevent timely follow-ups.
A major reason why dermatologists struggle to limit long-term antibiotic use is that there are very few substitutes that are perceived to work as well, said David J. Margolis, MD, PhD, who was not involved with the study and was asked to comment on the results. He is professor of epidemiology and dermatology at the University of Pennsylvania, Philadelphia.
“Part of the reason antibiotics are being used to treat acne is that they’re effective, and effective for severe disease,” he said. The alternatives, which are mostly topicals, said Dr. Margolis, do not work as well for moderate to severe disease or, with isotretinoin, involve time-consuming hurdles. Dr. Margolis said that he often hears such concerns from individual dermatologists. “But it’s helpful to see these in a well-organized, well-reported qualitative study.”
Infectious disease specialists surveyed considered limiting long-term antibiotic use as extremely important, while several dermatologists “argued that other specialties ‘underestimate the impact acne has on people’s lives,’ ” the authors wrote. Other respondents prioritized making the right choice for the patient at hand.
Although guidelines were never meant to be black and white, Dr. Yeung said, it is crucial to target the goal of tapering off after about 3-4 months — a cutoff with which guidelines from groups including the AAD, the Japanese Dermatological Association in guidelines from 2016, and 2017, respectively, and others concur.
He added, “Some folks believe that if the oral antibiotic is working, why stop? We need to develop evidence to show that reducing oral antibiotic use is important to our patients, not just to a theoretical problem of antibiotic resistance in society.” For example, in a study published in The Lancet in 2004, patients who used strictly topical regimens achieved efficacy similar to that of those who used only oral antibiotics.
In addition, some clinicians worried that limiting antibiotics could reduce patient satisfaction, spurring switches to other providers. However, he and the other authors of the JAMA Dermatology study noted that in a survey of patients with acne published in the Journal of Clinical and Aesthetic Dermatology in 2019, 76.9% said they would be “very or extremely likely” to use effective antibiotic-free treatments if offered.
Because most respondents were highly aware of the importance of antibiotic stewardship, Dr. Yeung said, additional passive education is not necessarily the answer. “It will take a concerted effort by our national societies to come up with resources and solutions for individual dermatologists to overcome some of these larger barriers.” Such solutions could range from training in communication and shared decision-making to implementing systems that provide individualized feedback to support antibiotic stewardship.
Many ongoing studies are examining antibiotic stewardship, Dr. Margolis said in the interview. However, he added, dermatologists’ idea of long-term use is 3 months, versus 1 month or less in other specialties. “Moreover, dermatology patients tend to be much healthier individuals and are rarely hospitalized, so there may be some issues comparing the ongoing studies to individuals with acne.” Future research will need to account for such differences, he said.
The study was funded by an American Acne & Rosacea Society Clinical Research Award. Dr. Yeung is associate editor of JAMA Dermatology. Dr. Margolis has received a National Institutes of Health grant to study doxycycline versus spironolactone in acne.
FROM JAMA DERMATOLOGY
Androgenetic Alopecia: Study Finds Efficacy of Topical and Oral Minoxidil Similar
Oral minoxidil, 5 mg once a day, “did not demonstrate superiority” over topical minoxidil, 5%, applied twice a day, after 24 weeks, reported Mariana Alvares Penha, MD, of the department of dermatology at São Paulo State University, in Botucatu, Brazil, and coauthors. Their randomized, controlled, double-blind study was published online in JAMA Dermatology.
Topical minoxidil is approved by the US Food and Drug Administration (FDA) for androgenetic alopecia (AGA), but there has been increasing interest worldwide in the use of low-dose oral minoxidil, a vasodilator approved as an antihypertensive, as an alternative treatment.
The trial “is important information that’s never been elucidated before,” Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington, said in an interview. The data, he added, can be used to reassure patients who do not want to take the oral form of the drug that a topical is just as effective.
“This study does let us counsel patients better and really give them the evidence,” said Shari Lipner, MD, PhD, associate professor of clinical dermatology at Weill Cornell Medicine, New York, who was also asked to comment on the results.
Both Dr. Lipner and Dr. Friedman said the study was well-designed.
The investigators enrolled 90 men aged 18-55; 68 completed the trial. Most had mild to moderate AGA. Men were excluded if they had received treatment for alopecia in the previous 6 months, a history of hair transplant, cardiopathy, nephropathy, dermatoses involving the scalp, any clinical conditions causing hair loss, or hypersensitivity to minoxidil.
They were randomized to receive either 5 mg of oral minoxidil a day, plus a placebo solution to apply to the scalp, or topical minoxidil solution (5%) applied twice a day plus placebo capsules. They were told to take a capsule at bedtime and to apply 1 mL of the solution to dry hair in the morning and at night.
The final analysis included 35 men in the topical group and 33 in the oral group (mean age, 36.6 years). Seven people in the topical group and 11 in the oral group were not able to attend the final appointment at 24 weeks. Three additional patients in the topical group dropped out for insomnia, hair shedding, and scalp eczema, while one dropped out of the oral group because of headache.
At 24 weeks, the percentage increase in terminal hair density in the oral minoxidil group was 27% higher (P = .005) in the vertex and 13% higher (P = .15) in the frontal scalp, compared with the topical-treated group.
Total hair density increased by 2% in the oral group compared with topical treatment in the vertex and decreased by 0.2% in the frontal area compared with topical treatment. None of these differences were statistically significant.
Three dermatologists blinded to the treatments, who analyzed photographs, determined that 60% of the men in the oral group and 48% in the topical group had clinical improvement in the frontal area, which was not statistically significant. More orally-treated patients had improvement in the vertex area: 70% compared with 46% of those on topical treatment (P = .04).
Hypertrichosis, Headache
Of the original 90 patients in the trial, more men taking oral minoxidil had hypertrichosis: 49% compared with 25% in the topical formulation group. Headache was also more common among those on oral minoxidil: six cases (14%) vs. one case (2%) among those on topical minoxidil. There was no difference in mean arterial blood pressure or resting heart rate between the two groups. Transient hair loss was more common with topical treatment, but it was not significant.
Dr. Friedman said that the study results would not change how he practices, but that it would give him data to use to inform patients who do not want to take oral minoxidil. He generally prescribes the oral form, unless patients do not want to take it or there is a medical contraindication, which he said is rare.
“I personally think oral is superior to topical,” mainly “because the patient’s actually using it,” said Dr. Friedman. “They’re more likely to take a pill a day versus apply something topically twice a day,” he added.
Both Dr. Lipner and Dr. Friedman said that they doubted that individuals could — or would want to — follow the twice-daily topical regimen used in the trial.
“In real life, not in the clinical trial scenario, it may be very hard for patients to comply with putting on the topical minoxidil twice a day or even once a day,” Dr. Lipner said.
However, she continues to prescribe more topical minoxidil than oral, because she believes “there’s less potential for side effects.” For patients who can adhere to the topical regimen, the study shows that they will get results, said Dr. Lipner.
Dr. Friedman, however, said that for patients who are looking at a lifetime of medication, “an oral will always win out on a topical to the scalp from an adherence perspective.”
The study was supported by the Brazilian Dermatology Society Support Fund. Dr. Penha reported receiving grants from the fund; no other disclosures were reported. Dr. Friedman and Dr. Lipner reported no conflicts related to minoxidil.
Oral minoxidil, 5 mg once a day, “did not demonstrate superiority” over topical minoxidil, 5%, applied twice a day, after 24 weeks, reported Mariana Alvares Penha, MD, of the department of dermatology at São Paulo State University, in Botucatu, Brazil, and coauthors. Their randomized, controlled, double-blind study was published online in JAMA Dermatology.
Topical minoxidil is approved by the US Food and Drug Administration (FDA) for androgenetic alopecia (AGA), but there has been increasing interest worldwide in the use of low-dose oral minoxidil, a vasodilator approved as an antihypertensive, as an alternative treatment.
The trial “is important information that’s never been elucidated before,” Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington, said in an interview. The data, he added, can be used to reassure patients who do not want to take the oral form of the drug that a topical is just as effective.
“This study does let us counsel patients better and really give them the evidence,” said Shari Lipner, MD, PhD, associate professor of clinical dermatology at Weill Cornell Medicine, New York, who was also asked to comment on the results.
Both Dr. Lipner and Dr. Friedman said the study was well-designed.
The investigators enrolled 90 men aged 18-55; 68 completed the trial. Most had mild to moderate AGA. Men were excluded if they had received treatment for alopecia in the previous 6 months, a history of hair transplant, cardiopathy, nephropathy, dermatoses involving the scalp, any clinical conditions causing hair loss, or hypersensitivity to minoxidil.
They were randomized to receive either 5 mg of oral minoxidil a day, plus a placebo solution to apply to the scalp, or topical minoxidil solution (5%) applied twice a day plus placebo capsules. They were told to take a capsule at bedtime and to apply 1 mL of the solution to dry hair in the morning and at night.
The final analysis included 35 men in the topical group and 33 in the oral group (mean age, 36.6 years). Seven people in the topical group and 11 in the oral group were not able to attend the final appointment at 24 weeks. Three additional patients in the topical group dropped out for insomnia, hair shedding, and scalp eczema, while one dropped out of the oral group because of headache.
At 24 weeks, the percentage increase in terminal hair density in the oral minoxidil group was 27% higher (P = .005) in the vertex and 13% higher (P = .15) in the frontal scalp, compared with the topical-treated group.
Total hair density increased by 2% in the oral group compared with topical treatment in the vertex and decreased by 0.2% in the frontal area compared with topical treatment. None of these differences were statistically significant.
Three dermatologists blinded to the treatments, who analyzed photographs, determined that 60% of the men in the oral group and 48% in the topical group had clinical improvement in the frontal area, which was not statistically significant. More orally-treated patients had improvement in the vertex area: 70% compared with 46% of those on topical treatment (P = .04).
Hypertrichosis, Headache
Of the original 90 patients in the trial, more men taking oral minoxidil had hypertrichosis: 49% compared with 25% in the topical formulation group. Headache was also more common among those on oral minoxidil: six cases (14%) vs. one case (2%) among those on topical minoxidil. There was no difference in mean arterial blood pressure or resting heart rate between the two groups. Transient hair loss was more common with topical treatment, but it was not significant.
Dr. Friedman said that the study results would not change how he practices, but that it would give him data to use to inform patients who do not want to take oral minoxidil. He generally prescribes the oral form, unless patients do not want to take it or there is a medical contraindication, which he said is rare.
“I personally think oral is superior to topical,” mainly “because the patient’s actually using it,” said Dr. Friedman. “They’re more likely to take a pill a day versus apply something topically twice a day,” he added.
Both Dr. Lipner and Dr. Friedman said that they doubted that individuals could — or would want to — follow the twice-daily topical regimen used in the trial.
“In real life, not in the clinical trial scenario, it may be very hard for patients to comply with putting on the topical minoxidil twice a day or even once a day,” Dr. Lipner said.
However, she continues to prescribe more topical minoxidil than oral, because she believes “there’s less potential for side effects.” For patients who can adhere to the topical regimen, the study shows that they will get results, said Dr. Lipner.
Dr. Friedman, however, said that for patients who are looking at a lifetime of medication, “an oral will always win out on a topical to the scalp from an adherence perspective.”
The study was supported by the Brazilian Dermatology Society Support Fund. Dr. Penha reported receiving grants from the fund; no other disclosures were reported. Dr. Friedman and Dr. Lipner reported no conflicts related to minoxidil.
Oral minoxidil, 5 mg once a day, “did not demonstrate superiority” over topical minoxidil, 5%, applied twice a day, after 24 weeks, reported Mariana Alvares Penha, MD, of the department of dermatology at São Paulo State University, in Botucatu, Brazil, and coauthors. Their randomized, controlled, double-blind study was published online in JAMA Dermatology.
Topical minoxidil is approved by the US Food and Drug Administration (FDA) for androgenetic alopecia (AGA), but there has been increasing interest worldwide in the use of low-dose oral minoxidil, a vasodilator approved as an antihypertensive, as an alternative treatment.
The trial “is important information that’s never been elucidated before,” Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington, said in an interview. The data, he added, can be used to reassure patients who do not want to take the oral form of the drug that a topical is just as effective.
“This study does let us counsel patients better and really give them the evidence,” said Shari Lipner, MD, PhD, associate professor of clinical dermatology at Weill Cornell Medicine, New York, who was also asked to comment on the results.
Both Dr. Lipner and Dr. Friedman said the study was well-designed.
The investigators enrolled 90 men aged 18-55; 68 completed the trial. Most had mild to moderate AGA. Men were excluded if they had received treatment for alopecia in the previous 6 months, a history of hair transplant, cardiopathy, nephropathy, dermatoses involving the scalp, any clinical conditions causing hair loss, or hypersensitivity to minoxidil.
They were randomized to receive either 5 mg of oral minoxidil a day, plus a placebo solution to apply to the scalp, or topical minoxidil solution (5%) applied twice a day plus placebo capsules. They were told to take a capsule at bedtime and to apply 1 mL of the solution to dry hair in the morning and at night.
The final analysis included 35 men in the topical group and 33 in the oral group (mean age, 36.6 years). Seven people in the topical group and 11 in the oral group were not able to attend the final appointment at 24 weeks. Three additional patients in the topical group dropped out for insomnia, hair shedding, and scalp eczema, while one dropped out of the oral group because of headache.
At 24 weeks, the percentage increase in terminal hair density in the oral minoxidil group was 27% higher (P = .005) in the vertex and 13% higher (P = .15) in the frontal scalp, compared with the topical-treated group.
Total hair density increased by 2% in the oral group compared with topical treatment in the vertex and decreased by 0.2% in the frontal area compared with topical treatment. None of these differences were statistically significant.
Three dermatologists blinded to the treatments, who analyzed photographs, determined that 60% of the men in the oral group and 48% in the topical group had clinical improvement in the frontal area, which was not statistically significant. More orally-treated patients had improvement in the vertex area: 70% compared with 46% of those on topical treatment (P = .04).
Hypertrichosis, Headache
Of the original 90 patients in the trial, more men taking oral minoxidil had hypertrichosis: 49% compared with 25% in the topical formulation group. Headache was also more common among those on oral minoxidil: six cases (14%) vs. one case (2%) among those on topical minoxidil. There was no difference in mean arterial blood pressure or resting heart rate between the two groups. Transient hair loss was more common with topical treatment, but it was not significant.
Dr. Friedman said that the study results would not change how he practices, but that it would give him data to use to inform patients who do not want to take oral minoxidil. He generally prescribes the oral form, unless patients do not want to take it or there is a medical contraindication, which he said is rare.
“I personally think oral is superior to topical,” mainly “because the patient’s actually using it,” said Dr. Friedman. “They’re more likely to take a pill a day versus apply something topically twice a day,” he added.
Both Dr. Lipner and Dr. Friedman said that they doubted that individuals could — or would want to — follow the twice-daily topical regimen used in the trial.
“In real life, not in the clinical trial scenario, it may be very hard for patients to comply with putting on the topical minoxidil twice a day or even once a day,” Dr. Lipner said.
However, she continues to prescribe more topical minoxidil than oral, because she believes “there’s less potential for side effects.” For patients who can adhere to the topical regimen, the study shows that they will get results, said Dr. Lipner.
Dr. Friedman, however, said that for patients who are looking at a lifetime of medication, “an oral will always win out on a topical to the scalp from an adherence perspective.”
The study was supported by the Brazilian Dermatology Society Support Fund. Dr. Penha reported receiving grants from the fund; no other disclosures were reported. Dr. Friedman and Dr. Lipner reported no conflicts related to minoxidil.
FROM JAMA DERMATOLOGY
Bimekizumab Under FDA Review for Hidradenitis Suppurativa
On April 4, 2024, the US .
The agency also accepted a second sBLA for a bimekizumab-bkzx 2-mL device.
The developments were announced in a press release from UCB, the manufacturer of bimekizumab-bkzx (Bimzelx), which was first approved in the United States in October 2023 for the treatment of moderate to severe plaque psoriasis in adults who are candidates for systemic therapy or phototherapy.
According to the press release, acceptance of the sBLA was based on results from two phase 3 studies known as BE HEARD I and BE HEARD II, which found that bimekizumab-bkzx showed clinically meaningful improvements compared with placebo at week 16 and were sustained to week 48. If approved, this would be the first HS approval for bimekizumab-bkzx worldwide. In the European Union, it is approved for treating adults with psoriatic arthritis and axial spondyloarthritis, in addition to moderate to severe psoriasis.
According to the company, approval of the 2-mL injection device would mean that patients would have an alternative one-injection regimen option; currently, one dose for psoriasis is administered as two 1-mL injections. Full US prescribing information for bimekizumab-bkzx can be found here.
A version of this article first appeared on Medscape.com.
On April 4, 2024, the US .
The agency also accepted a second sBLA for a bimekizumab-bkzx 2-mL device.
The developments were announced in a press release from UCB, the manufacturer of bimekizumab-bkzx (Bimzelx), which was first approved in the United States in October 2023 for the treatment of moderate to severe plaque psoriasis in adults who are candidates for systemic therapy or phototherapy.
According to the press release, acceptance of the sBLA was based on results from two phase 3 studies known as BE HEARD I and BE HEARD II, which found that bimekizumab-bkzx showed clinically meaningful improvements compared with placebo at week 16 and were sustained to week 48. If approved, this would be the first HS approval for bimekizumab-bkzx worldwide. In the European Union, it is approved for treating adults with psoriatic arthritis and axial spondyloarthritis, in addition to moderate to severe psoriasis.
According to the company, approval of the 2-mL injection device would mean that patients would have an alternative one-injection regimen option; currently, one dose for psoriasis is administered as two 1-mL injections. Full US prescribing information for bimekizumab-bkzx can be found here.
A version of this article first appeared on Medscape.com.
On April 4, 2024, the US .
The agency also accepted a second sBLA for a bimekizumab-bkzx 2-mL device.
The developments were announced in a press release from UCB, the manufacturer of bimekizumab-bkzx (Bimzelx), which was first approved in the United States in October 2023 for the treatment of moderate to severe plaque psoriasis in adults who are candidates for systemic therapy or phototherapy.
According to the press release, acceptance of the sBLA was based on results from two phase 3 studies known as BE HEARD I and BE HEARD II, which found that bimekizumab-bkzx showed clinically meaningful improvements compared with placebo at week 16 and were sustained to week 48. If approved, this would be the first HS approval for bimekizumab-bkzx worldwide. In the European Union, it is approved for treating adults with psoriatic arthritis and axial spondyloarthritis, in addition to moderate to severe psoriasis.
According to the company, approval of the 2-mL injection device would mean that patients would have an alternative one-injection regimen option; currently, one dose for psoriasis is administered as two 1-mL injections. Full US prescribing information for bimekizumab-bkzx can be found here.
A version of this article first appeared on Medscape.com.
Delirium Linked to a Threefold Increased Risk for Dementia
, new research showed.
Incident dementia risk was more than three times higher in those who experienced just one episode of delirium, with each additional episode linked to a further 20% increase in dementia risk. The association was strongest in men.
Patients with delirium also had a 39% higher mortality risk than those with no history of delirium.
“We have known for a long time that delirium is dangerous, and this provides evidence that it’s even more dangerous than perhaps we had appreciated,” said study investigator Emily H. Gordon, PhD, MBBS, a geriatrician and senior lecturer at the University of Queensland, Brisbane, Australia.
“But we also know delirium is preventable. There are no excuses anymore; we really need to work together to improve the hospital system, to implement what are known to be effective interventions,” she added.
The findings were published online in The BMJ.
Close Matching
Prior studies that suggested an association between delirium and dementia were relatively small with short follow-up and varied in their adjustment for confounders. They also didn’t account for the competing risk for death, researchers noted.
Investigators used a linked New South Wales (NSW) statewide dataset that includes records of care episodes from all NSW hospitals as well as personal, administrative, clinical, and death information.
The study included an eligible sample of 626,467 older adults without dementia at baseline with at least one hospital admission between 2009 and 2014. For these patients, researchers calculated a hospital frailty risk score and collected other information including primary diagnosis and mean length of hospital stay and stay in the intensive care unit. From diagnostic codes, they categorized patients into no delirium and delirium groups and determined the number of delirium episodes.
Investigators matched patients in the delirium group to patients with no delirium according to characteristics with potential to confound the association between delirium and risk for dementia, including age, gender, frailty, reason for hospitalization, and length of stay in hospital and intensive care.
The matched study sample included 55,211 (mean age, 83 years) each in the delirium and the no delirium groups. Despite matching, the length of hospital stay for the index episode was longer for the delirium group than the no delirium group (mean, 9 days vs 6 days).
The primary outcomes were death and incident dementia, determined via diagnostic codes. During a follow-up of 5.25 years, 58% of patients died, and 17% had a new dementia diagnosis.
Among patients with at least one episode of delirium, the rate of incident dementia was 3.4 times higher than in those without delirium. After accounting for the competing risk for death, incident dementia risk remained three times higher among the delirium group (hazard ratio [HR], 3.00; 95% CI, 2.91-3.10).
This association was stronger for men than women (HR, 3.17 and 2.88, respectively; P = .004).
Sex Differences
The study is thought to be the first to identify a difference between sexes in dementia risk and delirium, Dr. Gordon said. It’s possible delirium in men is more severe in intensity or lasts longer than in women, or the male brain is, for whatever reason, more vulnerable to the effects of delirium, said Dr. Gordon. But she stressed these are only theories.
Investigators also found a mortality rate 1.4 times higher in the delirium group versus those without delirium, equating to a 39% increased risk for death (HR, 1.39; 95% CI, 1.37-1.41). The risk was similar for men and women (interaction P = .62).
When researchers categorized delirium by number of episodes, they found each additional episode was associated with a 10% increased risk for death (HR, 1.10; 95% CI, 1.09-1.12).
In addition to its large size, long follow-up, and close matching, what sets this new study apart from previous research is it accounted for the competing risk for death, said Dr. Gordon.
“This is really important because you’re not going to get dementia if you die, and in this population, the rate of death is incredibly high,” she said. “If we just assume people who died didn’t get dementia, then that screws the results.”
Causal Link?
For those who experienced at least one episode of delirium within the first 12 months, each additional episode of delirium was associated with a 20% increased risk for dementia (HR, 1.20; 95% CI, 1.18-1.23).
That dose-response association suggests a causal link between the two, Dr. Gordon said.
“The number one way to prove causality is to do a randomized controlled trial,” which isn’t feasible with delirium, she said. “By demonstrating a dose-response relationship suggests that it could be a causal pathway.”
Exact mechanisms linking delirium with dementia are unclear. Delirium might uncover preexisting or preclinical dementia, or it might cause dementia by accelerating underlying neuropathologic processes or de novo mechanisms, the authors noted.
Study limitations included the potential for residual confounding from unmeasured variables in the matching criteria. Delirium and dementia diagnoses depended on clinical coding of medical information recorded in the administrative dataset, and under-coding of dementia during hospitalization is well-recognized.
Although the study controlled for length of stay in hospital and in intensive care, this may not have fully captured differences in severity of medical conditions. Data about the duration and severity of delirium episodes were also unavailable, which limited the dose-response analysis.
Commenting on the findings, Christopher Weber, PhD, Alzheimer’s Association as director of Global Science Initiatives, said the results are consistent with other research on the association between delirium and incidents of dementia.
The increased risk for dementia following delirium in males is “an interesting finding,” said Dr. Weber. “This suggests a need for more research to understand the impact of sex differences in delirium, as well as research to see if preventing incidents of delirium could ultimately reduce rates of dementia.”
The study received support from the National Health and Medical Research Council: Partnership Centre for Health System Sustainability. Dr. Gordon and Dr. Weber reported no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
, new research showed.
Incident dementia risk was more than three times higher in those who experienced just one episode of delirium, with each additional episode linked to a further 20% increase in dementia risk. The association was strongest in men.
Patients with delirium also had a 39% higher mortality risk than those with no history of delirium.
“We have known for a long time that delirium is dangerous, and this provides evidence that it’s even more dangerous than perhaps we had appreciated,” said study investigator Emily H. Gordon, PhD, MBBS, a geriatrician and senior lecturer at the University of Queensland, Brisbane, Australia.
“But we also know delirium is preventable. There are no excuses anymore; we really need to work together to improve the hospital system, to implement what are known to be effective interventions,” she added.
The findings were published online in The BMJ.
Close Matching
Prior studies that suggested an association between delirium and dementia were relatively small with short follow-up and varied in their adjustment for confounders. They also didn’t account for the competing risk for death, researchers noted.
Investigators used a linked New South Wales (NSW) statewide dataset that includes records of care episodes from all NSW hospitals as well as personal, administrative, clinical, and death information.
The study included an eligible sample of 626,467 older adults without dementia at baseline with at least one hospital admission between 2009 and 2014. For these patients, researchers calculated a hospital frailty risk score and collected other information including primary diagnosis and mean length of hospital stay and stay in the intensive care unit. From diagnostic codes, they categorized patients into no delirium and delirium groups and determined the number of delirium episodes.
Investigators matched patients in the delirium group to patients with no delirium according to characteristics with potential to confound the association between delirium and risk for dementia, including age, gender, frailty, reason for hospitalization, and length of stay in hospital and intensive care.
The matched study sample included 55,211 (mean age, 83 years) each in the delirium and the no delirium groups. Despite matching, the length of hospital stay for the index episode was longer for the delirium group than the no delirium group (mean, 9 days vs 6 days).
The primary outcomes were death and incident dementia, determined via diagnostic codes. During a follow-up of 5.25 years, 58% of patients died, and 17% had a new dementia diagnosis.
Among patients with at least one episode of delirium, the rate of incident dementia was 3.4 times higher than in those without delirium. After accounting for the competing risk for death, incident dementia risk remained three times higher among the delirium group (hazard ratio [HR], 3.00; 95% CI, 2.91-3.10).
This association was stronger for men than women (HR, 3.17 and 2.88, respectively; P = .004).
Sex Differences
The study is thought to be the first to identify a difference between sexes in dementia risk and delirium, Dr. Gordon said. It’s possible delirium in men is more severe in intensity or lasts longer than in women, or the male brain is, for whatever reason, more vulnerable to the effects of delirium, said Dr. Gordon. But she stressed these are only theories.
Investigators also found a mortality rate 1.4 times higher in the delirium group versus those without delirium, equating to a 39% increased risk for death (HR, 1.39; 95% CI, 1.37-1.41). The risk was similar for men and women (interaction P = .62).
When researchers categorized delirium by number of episodes, they found each additional episode was associated with a 10% increased risk for death (HR, 1.10; 95% CI, 1.09-1.12).
In addition to its large size, long follow-up, and close matching, what sets this new study apart from previous research is it accounted for the competing risk for death, said Dr. Gordon.
“This is really important because you’re not going to get dementia if you die, and in this population, the rate of death is incredibly high,” she said. “If we just assume people who died didn’t get dementia, then that screws the results.”
Causal Link?
For those who experienced at least one episode of delirium within the first 12 months, each additional episode of delirium was associated with a 20% increased risk for dementia (HR, 1.20; 95% CI, 1.18-1.23).
That dose-response association suggests a causal link between the two, Dr. Gordon said.
“The number one way to prove causality is to do a randomized controlled trial,” which isn’t feasible with delirium, she said. “By demonstrating a dose-response relationship suggests that it could be a causal pathway.”
Exact mechanisms linking delirium with dementia are unclear. Delirium might uncover preexisting or preclinical dementia, or it might cause dementia by accelerating underlying neuropathologic processes or de novo mechanisms, the authors noted.
Study limitations included the potential for residual confounding from unmeasured variables in the matching criteria. Delirium and dementia diagnoses depended on clinical coding of medical information recorded in the administrative dataset, and under-coding of dementia during hospitalization is well-recognized.
Although the study controlled for length of stay in hospital and in intensive care, this may not have fully captured differences in severity of medical conditions. Data about the duration and severity of delirium episodes were also unavailable, which limited the dose-response analysis.
Commenting on the findings, Christopher Weber, PhD, Alzheimer’s Association as director of Global Science Initiatives, said the results are consistent with other research on the association between delirium and incidents of dementia.
The increased risk for dementia following delirium in males is “an interesting finding,” said Dr. Weber. “This suggests a need for more research to understand the impact of sex differences in delirium, as well as research to see if preventing incidents of delirium could ultimately reduce rates of dementia.”
The study received support from the National Health and Medical Research Council: Partnership Centre for Health System Sustainability. Dr. Gordon and Dr. Weber reported no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
, new research showed.
Incident dementia risk was more than three times higher in those who experienced just one episode of delirium, with each additional episode linked to a further 20% increase in dementia risk. The association was strongest in men.
Patients with delirium also had a 39% higher mortality risk than those with no history of delirium.
“We have known for a long time that delirium is dangerous, and this provides evidence that it’s even more dangerous than perhaps we had appreciated,” said study investigator Emily H. Gordon, PhD, MBBS, a geriatrician and senior lecturer at the University of Queensland, Brisbane, Australia.
“But we also know delirium is preventable. There are no excuses anymore; we really need to work together to improve the hospital system, to implement what are known to be effective interventions,” she added.
The findings were published online in The BMJ.
Close Matching
Prior studies that suggested an association between delirium and dementia were relatively small with short follow-up and varied in their adjustment for confounders. They also didn’t account for the competing risk for death, researchers noted.
Investigators used a linked New South Wales (NSW) statewide dataset that includes records of care episodes from all NSW hospitals as well as personal, administrative, clinical, and death information.
The study included an eligible sample of 626,467 older adults without dementia at baseline with at least one hospital admission between 2009 and 2014. For these patients, researchers calculated a hospital frailty risk score and collected other information including primary diagnosis and mean length of hospital stay and stay in the intensive care unit. From diagnostic codes, they categorized patients into no delirium and delirium groups and determined the number of delirium episodes.
Investigators matched patients in the delirium group to patients with no delirium according to characteristics with potential to confound the association between delirium and risk for dementia, including age, gender, frailty, reason for hospitalization, and length of stay in hospital and intensive care.
The matched study sample included 55,211 (mean age, 83 years) each in the delirium and the no delirium groups. Despite matching, the length of hospital stay for the index episode was longer for the delirium group than the no delirium group (mean, 9 days vs 6 days).
The primary outcomes were death and incident dementia, determined via diagnostic codes. During a follow-up of 5.25 years, 58% of patients died, and 17% had a new dementia diagnosis.
Among patients with at least one episode of delirium, the rate of incident dementia was 3.4 times higher than in those without delirium. After accounting for the competing risk for death, incident dementia risk remained three times higher among the delirium group (hazard ratio [HR], 3.00; 95% CI, 2.91-3.10).
This association was stronger for men than women (HR, 3.17 and 2.88, respectively; P = .004).
Sex Differences
The study is thought to be the first to identify a difference between sexes in dementia risk and delirium, Dr. Gordon said. It’s possible delirium in men is more severe in intensity or lasts longer than in women, or the male brain is, for whatever reason, more vulnerable to the effects of delirium, said Dr. Gordon. But she stressed these are only theories.
Investigators also found a mortality rate 1.4 times higher in the delirium group versus those without delirium, equating to a 39% increased risk for death (HR, 1.39; 95% CI, 1.37-1.41). The risk was similar for men and women (interaction P = .62).
When researchers categorized delirium by number of episodes, they found each additional episode was associated with a 10% increased risk for death (HR, 1.10; 95% CI, 1.09-1.12).
In addition to its large size, long follow-up, and close matching, what sets this new study apart from previous research is it accounted for the competing risk for death, said Dr. Gordon.
“This is really important because you’re not going to get dementia if you die, and in this population, the rate of death is incredibly high,” she said. “If we just assume people who died didn’t get dementia, then that screws the results.”
Causal Link?
For those who experienced at least one episode of delirium within the first 12 months, each additional episode of delirium was associated with a 20% increased risk for dementia (HR, 1.20; 95% CI, 1.18-1.23).
That dose-response association suggests a causal link between the two, Dr. Gordon said.
“The number one way to prove causality is to do a randomized controlled trial,” which isn’t feasible with delirium, she said. “By demonstrating a dose-response relationship suggests that it could be a causal pathway.”
Exact mechanisms linking delirium with dementia are unclear. Delirium might uncover preexisting or preclinical dementia, or it might cause dementia by accelerating underlying neuropathologic processes or de novo mechanisms, the authors noted.
Study limitations included the potential for residual confounding from unmeasured variables in the matching criteria. Delirium and dementia diagnoses depended on clinical coding of medical information recorded in the administrative dataset, and under-coding of dementia during hospitalization is well-recognized.
Although the study controlled for length of stay in hospital and in intensive care, this may not have fully captured differences in severity of medical conditions. Data about the duration and severity of delirium episodes were also unavailable, which limited the dose-response analysis.
Commenting on the findings, Christopher Weber, PhD, Alzheimer’s Association as director of Global Science Initiatives, said the results are consistent with other research on the association between delirium and incidents of dementia.
The increased risk for dementia following delirium in males is “an interesting finding,” said Dr. Weber. “This suggests a need for more research to understand the impact of sex differences in delirium, as well as research to see if preventing incidents of delirium could ultimately reduce rates of dementia.”
The study received support from the National Health and Medical Research Council: Partnership Centre for Health System Sustainability. Dr. Gordon and Dr. Weber reported no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
FROM THE BMJ