User login
Elevate Your Career: AGA Women in GI Regional Workshops Await
As a woman in a dynamic and ever-changing profession, balancing life as a powerhouse physician or scientist is no easy feat.
Expanded to six workshops in 2024, AGA is pleased to offer regionally curated workshops with distinguished speakers at all experience levels to fuel your professional and personal growth. Participate in candid discussions regarding the distinct challenges you face as a woman navigating the 21st century healthcare environment. Derive inspiration from your community and cultivate meaningful connections that will carry you beyond the workshop.
Join us in-person or virtually, whatever fits into your busy schedule. We are also pleased to offer travel grants of up to $300 (per workshop) to help offset the costs of attending this program for one selected individual per region. The travel grant is to support travel and registration fees for early-career women. Additional details for the Maria Leo-Lieber Travel Award may be found in your confirmation email.
Ready to thrive? Register today to attend one of our first workshops or stay tuned for an additional workshop coming near you.
This program is supported by Janssen.
Midwest Regional Workshop
Saturday, Feb. 24, 2024
8 a.m.-3 p.m. CT
University of Chicago, Gleacher Center, Chicago, IL
Deadline to apply for a travel grant: Feb. 9, 2024 Deadline to register: Feb. 16, 2024
Click here to register.
Western Regional Workshop
Saturday, April 27, 2024
8 a.m.-3 p.m. PT
UCLA Luskin Conference Center, Los Angeles, CA
Meet fellow attendees at our pre-workshop networking event on Friday, Apr. 26 from 8 p.m. to 10:30 p.m.
Deadline to apply for a travel grant: April 12, 2024 Deadline to register: April 19, 2024
Click here to register.
As a woman in a dynamic and ever-changing profession, balancing life as a powerhouse physician or scientist is no easy feat.
Expanded to six workshops in 2024, AGA is pleased to offer regionally curated workshops with distinguished speakers at all experience levels to fuel your professional and personal growth. Participate in candid discussions regarding the distinct challenges you face as a woman navigating the 21st century healthcare environment. Derive inspiration from your community and cultivate meaningful connections that will carry you beyond the workshop.
Join us in-person or virtually, whatever fits into your busy schedule. We are also pleased to offer travel grants of up to $300 (per workshop) to help offset the costs of attending this program for one selected individual per region. The travel grant is to support travel and registration fees for early-career women. Additional details for the Maria Leo-Lieber Travel Award may be found in your confirmation email.
Ready to thrive? Register today to attend one of our first workshops or stay tuned for an additional workshop coming near you.
This program is supported by Janssen.
Midwest Regional Workshop
Saturday, Feb. 24, 2024
8 a.m.-3 p.m. CT
University of Chicago, Gleacher Center, Chicago, IL
Deadline to apply for a travel grant: Feb. 9, 2024 Deadline to register: Feb. 16, 2024
Click here to register.
Western Regional Workshop
Saturday, April 27, 2024
8 a.m.-3 p.m. PT
UCLA Luskin Conference Center, Los Angeles, CA
Meet fellow attendees at our pre-workshop networking event on Friday, Apr. 26 from 8 p.m. to 10:30 p.m.
Deadline to apply for a travel grant: April 12, 2024 Deadline to register: April 19, 2024
Click here to register.
As a woman in a dynamic and ever-changing profession, balancing life as a powerhouse physician or scientist is no easy feat.
Expanded to six workshops in 2024, AGA is pleased to offer regionally curated workshops with distinguished speakers at all experience levels to fuel your professional and personal growth. Participate in candid discussions regarding the distinct challenges you face as a woman navigating the 21st century healthcare environment. Derive inspiration from your community and cultivate meaningful connections that will carry you beyond the workshop.
Join us in-person or virtually, whatever fits into your busy schedule. We are also pleased to offer travel grants of up to $300 (per workshop) to help offset the costs of attending this program for one selected individual per region. The travel grant is to support travel and registration fees for early-career women. Additional details for the Maria Leo-Lieber Travel Award may be found in your confirmation email.
Ready to thrive? Register today to attend one of our first workshops or stay tuned for an additional workshop coming near you.
This program is supported by Janssen.
Midwest Regional Workshop
Saturday, Feb. 24, 2024
8 a.m.-3 p.m. CT
University of Chicago, Gleacher Center, Chicago, IL
Deadline to apply for a travel grant: Feb. 9, 2024 Deadline to register: Feb. 16, 2024
Click here to register.
Western Regional Workshop
Saturday, April 27, 2024
8 a.m.-3 p.m. PT
UCLA Luskin Conference Center, Los Angeles, CA
Meet fellow attendees at our pre-workshop networking event on Friday, Apr. 26 from 8 p.m. to 10:30 p.m.
Deadline to apply for a travel grant: April 12, 2024 Deadline to register: April 19, 2024
Click here to register.
ALL: Asparaginase Tx Boosts Survival in AYA Patients
“These findings of a large cohort of adolescents and young adults treated at a variety of U.S. centers confirm the findings of the clinical trial and also provide confidence that patients remaining on this regimen have very excellent 3-year outcomes,” senior author Lori S. Muffly, MD, associate professor of medicine at Stanford University in the Division of Blood and Marrow Transplantation and Cellular Therapy, in Stanford, California, said in an interview.
The study was presented at the American Society of Hematology annual meeting. In the Cancer and Leukemia Group B 10403 trial, the intensive asparaginase pediatric regimen, used in the adult oncology treatment setting, showed benefits in the adolescent and young adult population, with a 3-year event-free survival (EFS) rate of 59% and an overall survival rate of 73%.
Based on the results, the regimen has gained widespread utilization in the United States. However, evidence of the therapy’s safety and efficacy in real-world practice, outside of the controlled clinical trial setting, has been lacking.
To investigate, first author Dr. Muffly, along with coauthor Brandon DaSilva, MD, and colleagues at Stanford University School of Medicine conducted a retrospective analysis of 101 adolescent and young adult patients aged 17 to 40 with newly diagnosed Philadelphia chromosome (Ph)-negative B-cell ALL (B-ALL) or T-cell ALL (T-ALL).
The patients had been treated with the C10403 regimen off-trial at five U.S. centers between October 2012 and July 2020.
The study excluded Ph-positive or Burkitt-type ALL patients, in addition to those who were previously treated, with the exception of treatment with hydroxyurea, steroids, one dose of single-agent therapy, or rituximab for CD20-positive B-ALL. Of the patients, about half, 54%, were between the ages of 20 and 29; 69% were male and 55% were White. Most patients (70%) had B-cell immunophenotype, and among them, 49% had CD20 expression.
Forty percent of patients had normal karyotype; 3% were hypodiploid, 7% were KMT2a-rearranged, and 30% of the 27 patients assessed had Ph-like ALL. CNS involvement was present at diagnosis among 20% (9% with CNS2, 11% with CNS3) and 14% of patients had a mediastinal mass.
Of 71 patients with B-ALL, 16 (23%) received at least one dose of rituximab.
Among the 101 patients who started induction with C10403, 72 (71%) completed induction and continued to consolidation; 51 (50%) continued beyond consolidation, while only 31 (31%) completed the entire C10403 regimen through the end of maintenance.
For the primary outcomes, overall, the rate of induction response, defined as achieving <5% blasts on bone marrow by the end of induction or extended induction, was 91% of whom 54% were measurable residual disease [MRD]-negative (threshold of at least 10–4).
The co-primary endpoint of 3-year event-free survival was 65% and 3-year overall survival was 82.7%.
Two deaths occurred (2%) among patients who were in remission and still receiving treatment.
Overall, 44 patients (44%) were taken off C10403 while in complete remission, including 20 (20%) to receive an allogeneic hematopoietic cell transplant (HCT), 23 (23%) to receive non-HCT alternative treatments including Hyper-CVAD or blinatumomab, and 1 (1%) for patient preference.
Dr. Muffly noted that the 31% of treatment completion is about the same as that seen on the original C10403 trial.
“In clinical practice, there are a variety of reasons that these patients came off therapy — probably the most common reason is for MRD-directed therapy, such as with blinatumomab.”
“We are currently analyzing the results of the patients who came off therapy relative to those who stayed on therapy which will be interesting.”
The slightly higher real-world 3-year EFS and OS (65% and 82.7%, respectively) compared with the outcomes in the clinical trial (59% and 73%, respectively), were “very encouraging,” Dr. Muffly noted.
“A lot has changed and improved in B-ALL for adolescent/young adults since this trial closed to enrollment over 10 years ago,” she explained.
“We have better MRD methods, MRD-directed therapies, and a variety of targeted immunotherapies being used in a variety of ways,” Dr. Muffly said. “The overall outcomes for adolescent/young adult ALL patients are improving and we can see that in this data set.”
Commenting on the study, Catherine Bollard, MD, a pediatric oncologist at Children’s National Hospital in Washington, DC, noted that the study’s retrospective nature is “definitely a major caveat that needs to be considered when evaluating the impact of the data.”
Regarding the relatively low rate of regimen completion, Dr. Bollard said, “I do think the pros still outweigh the cons. But getting patients into a deep complete remission and then evaluating their outcomes after consolidation with HCT or alternative therapy is certainly an important consideration and needs to be studied further in a larger cohort.”
Overall, however, “this ‘real world’ experience validates the use of this regimen outside of the clinical trial setting,” she said.
Dr. Muffly and Dr. Bollard had no disclosures to report. Dr. Bollard is the editor-in-chief of ASH’s journal, Blood Advances.
“These findings of a large cohort of adolescents and young adults treated at a variety of U.S. centers confirm the findings of the clinical trial and also provide confidence that patients remaining on this regimen have very excellent 3-year outcomes,” senior author Lori S. Muffly, MD, associate professor of medicine at Stanford University in the Division of Blood and Marrow Transplantation and Cellular Therapy, in Stanford, California, said in an interview.
The study was presented at the American Society of Hematology annual meeting. In the Cancer and Leukemia Group B 10403 trial, the intensive asparaginase pediatric regimen, used in the adult oncology treatment setting, showed benefits in the adolescent and young adult population, with a 3-year event-free survival (EFS) rate of 59% and an overall survival rate of 73%.
Based on the results, the regimen has gained widespread utilization in the United States. However, evidence of the therapy’s safety and efficacy in real-world practice, outside of the controlled clinical trial setting, has been lacking.
To investigate, first author Dr. Muffly, along with coauthor Brandon DaSilva, MD, and colleagues at Stanford University School of Medicine conducted a retrospective analysis of 101 adolescent and young adult patients aged 17 to 40 with newly diagnosed Philadelphia chromosome (Ph)-negative B-cell ALL (B-ALL) or T-cell ALL (T-ALL).
The patients had been treated with the C10403 regimen off-trial at five U.S. centers between October 2012 and July 2020.
The study excluded Ph-positive or Burkitt-type ALL patients, in addition to those who were previously treated, with the exception of treatment with hydroxyurea, steroids, one dose of single-agent therapy, or rituximab for CD20-positive B-ALL. Of the patients, about half, 54%, were between the ages of 20 and 29; 69% were male and 55% were White. Most patients (70%) had B-cell immunophenotype, and among them, 49% had CD20 expression.
Forty percent of patients had normal karyotype; 3% were hypodiploid, 7% were KMT2a-rearranged, and 30% of the 27 patients assessed had Ph-like ALL. CNS involvement was present at diagnosis among 20% (9% with CNS2, 11% with CNS3) and 14% of patients had a mediastinal mass.
Of 71 patients with B-ALL, 16 (23%) received at least one dose of rituximab.
Among the 101 patients who started induction with C10403, 72 (71%) completed induction and continued to consolidation; 51 (50%) continued beyond consolidation, while only 31 (31%) completed the entire C10403 regimen through the end of maintenance.
For the primary outcomes, overall, the rate of induction response, defined as achieving <5% blasts on bone marrow by the end of induction or extended induction, was 91% of whom 54% were measurable residual disease [MRD]-negative (threshold of at least 10–4).
The co-primary endpoint of 3-year event-free survival was 65% and 3-year overall survival was 82.7%.
Two deaths occurred (2%) among patients who were in remission and still receiving treatment.
Overall, 44 patients (44%) were taken off C10403 while in complete remission, including 20 (20%) to receive an allogeneic hematopoietic cell transplant (HCT), 23 (23%) to receive non-HCT alternative treatments including Hyper-CVAD or blinatumomab, and 1 (1%) for patient preference.
Dr. Muffly noted that the 31% of treatment completion is about the same as that seen on the original C10403 trial.
“In clinical practice, there are a variety of reasons that these patients came off therapy — probably the most common reason is for MRD-directed therapy, such as with blinatumomab.”
“We are currently analyzing the results of the patients who came off therapy relative to those who stayed on therapy which will be interesting.”
The slightly higher real-world 3-year EFS and OS (65% and 82.7%, respectively) compared with the outcomes in the clinical trial (59% and 73%, respectively), were “very encouraging,” Dr. Muffly noted.
“A lot has changed and improved in B-ALL for adolescent/young adults since this trial closed to enrollment over 10 years ago,” she explained.
“We have better MRD methods, MRD-directed therapies, and a variety of targeted immunotherapies being used in a variety of ways,” Dr. Muffly said. “The overall outcomes for adolescent/young adult ALL patients are improving and we can see that in this data set.”
Commenting on the study, Catherine Bollard, MD, a pediatric oncologist at Children’s National Hospital in Washington, DC, noted that the study’s retrospective nature is “definitely a major caveat that needs to be considered when evaluating the impact of the data.”
Regarding the relatively low rate of regimen completion, Dr. Bollard said, “I do think the pros still outweigh the cons. But getting patients into a deep complete remission and then evaluating their outcomes after consolidation with HCT or alternative therapy is certainly an important consideration and needs to be studied further in a larger cohort.”
Overall, however, “this ‘real world’ experience validates the use of this regimen outside of the clinical trial setting,” she said.
Dr. Muffly and Dr. Bollard had no disclosures to report. Dr. Bollard is the editor-in-chief of ASH’s journal, Blood Advances.
“These findings of a large cohort of adolescents and young adults treated at a variety of U.S. centers confirm the findings of the clinical trial and also provide confidence that patients remaining on this regimen have very excellent 3-year outcomes,” senior author Lori S. Muffly, MD, associate professor of medicine at Stanford University in the Division of Blood and Marrow Transplantation and Cellular Therapy, in Stanford, California, said in an interview.
The study was presented at the American Society of Hematology annual meeting. In the Cancer and Leukemia Group B 10403 trial, the intensive asparaginase pediatric regimen, used in the adult oncology treatment setting, showed benefits in the adolescent and young adult population, with a 3-year event-free survival (EFS) rate of 59% and an overall survival rate of 73%.
Based on the results, the regimen has gained widespread utilization in the United States. However, evidence of the therapy’s safety and efficacy in real-world practice, outside of the controlled clinical trial setting, has been lacking.
To investigate, first author Dr. Muffly, along with coauthor Brandon DaSilva, MD, and colleagues at Stanford University School of Medicine conducted a retrospective analysis of 101 adolescent and young adult patients aged 17 to 40 with newly diagnosed Philadelphia chromosome (Ph)-negative B-cell ALL (B-ALL) or T-cell ALL (T-ALL).
The patients had been treated with the C10403 regimen off-trial at five U.S. centers between October 2012 and July 2020.
The study excluded Ph-positive or Burkitt-type ALL patients, in addition to those who were previously treated, with the exception of treatment with hydroxyurea, steroids, one dose of single-agent therapy, or rituximab for CD20-positive B-ALL. Of the patients, about half, 54%, were between the ages of 20 and 29; 69% were male and 55% were White. Most patients (70%) had B-cell immunophenotype, and among them, 49% had CD20 expression.
Forty percent of patients had normal karyotype; 3% were hypodiploid, 7% were KMT2a-rearranged, and 30% of the 27 patients assessed had Ph-like ALL. CNS involvement was present at diagnosis among 20% (9% with CNS2, 11% with CNS3) and 14% of patients had a mediastinal mass.
Of 71 patients with B-ALL, 16 (23%) received at least one dose of rituximab.
Among the 101 patients who started induction with C10403, 72 (71%) completed induction and continued to consolidation; 51 (50%) continued beyond consolidation, while only 31 (31%) completed the entire C10403 regimen through the end of maintenance.
For the primary outcomes, overall, the rate of induction response, defined as achieving <5% blasts on bone marrow by the end of induction or extended induction, was 91% of whom 54% were measurable residual disease [MRD]-negative (threshold of at least 10–4).
The co-primary endpoint of 3-year event-free survival was 65% and 3-year overall survival was 82.7%.
Two deaths occurred (2%) among patients who were in remission and still receiving treatment.
Overall, 44 patients (44%) were taken off C10403 while in complete remission, including 20 (20%) to receive an allogeneic hematopoietic cell transplant (HCT), 23 (23%) to receive non-HCT alternative treatments including Hyper-CVAD or blinatumomab, and 1 (1%) for patient preference.
Dr. Muffly noted that the 31% of treatment completion is about the same as that seen on the original C10403 trial.
“In clinical practice, there are a variety of reasons that these patients came off therapy — probably the most common reason is for MRD-directed therapy, such as with blinatumomab.”
“We are currently analyzing the results of the patients who came off therapy relative to those who stayed on therapy which will be interesting.”
The slightly higher real-world 3-year EFS and OS (65% and 82.7%, respectively) compared with the outcomes in the clinical trial (59% and 73%, respectively), were “very encouraging,” Dr. Muffly noted.
“A lot has changed and improved in B-ALL for adolescent/young adults since this trial closed to enrollment over 10 years ago,” she explained.
“We have better MRD methods, MRD-directed therapies, and a variety of targeted immunotherapies being used in a variety of ways,” Dr. Muffly said. “The overall outcomes for adolescent/young adult ALL patients are improving and we can see that in this data set.”
Commenting on the study, Catherine Bollard, MD, a pediatric oncologist at Children’s National Hospital in Washington, DC, noted that the study’s retrospective nature is “definitely a major caveat that needs to be considered when evaluating the impact of the data.”
Regarding the relatively low rate of regimen completion, Dr. Bollard said, “I do think the pros still outweigh the cons. But getting patients into a deep complete remission and then evaluating their outcomes after consolidation with HCT or alternative therapy is certainly an important consideration and needs to be studied further in a larger cohort.”
Overall, however, “this ‘real world’ experience validates the use of this regimen outside of the clinical trial setting,” she said.
Dr. Muffly and Dr. Bollard had no disclosures to report. Dr. Bollard is the editor-in-chief of ASH’s journal, Blood Advances.
FROM ASH 2023
AGA Tech Summit: Bridging the Gap Between Innovation, Industry, and Gastroenterologists
Medicine is transforming at a remarkable pace. It is therefore imperative for the future of the field that physicians understand innovation and collaborate with industry partners. Innovation can be defined as invention, adoption, and diffusion.1 During my training in gastroenterology and advanced fellowships, I learned about multiple endoscopic tools and techniques and became familiar with industry names that I frequently encountered in the endoscopy unit or clinic.
I was nominated to attend the AGA Tech Summit Fellows Program by my advanced endoscopy fellowship program director. A total of 22 fellows from around the United States at various stages of their training and interests in the field of gastroenterology and hepatology were selected for the program through an application process. The program included registration, travel, and accommodations to attend the AGA Tech Summit and Fellows Immersion Day at Medtronic.
The first event in the program was a visit to the Medtronic Santa Clara office, where our initial stop was at the research and development lab. We were introduced to design and biomedical engineers who reviewed with us the extensive testing that devices and endoscopy equipment undergo before coming to the market. These labs have a heavy focus on prototyping and experimentation and exist to promote in-house innovation and inventions.

During the day, we met physicians who shared their journeys on how they developed and advanced their careers in partnership with industry. Our visit also included a session with the business development and strategy manager at Medtronic, who discussed strategy and steps involved in product development — from the inception of an idea, institutional policies, and patents, to industry collaboration, and finally to successful commercialization. During medical school and training, we are focused on appropriately learning and applying medical knowledge to clinical care. The Medtronic Fellows Immersion Day experience offered a different perspective and showed other ways by which clinical knowledge and experience can be used to make an impact, in collaboration with industry and stakeholders. It also highlighted alternative career paths for medical professionals. The evening concluded with a meet and greet with the AGA Center for GI Innovation & Technology (CGIT) members and leadership.
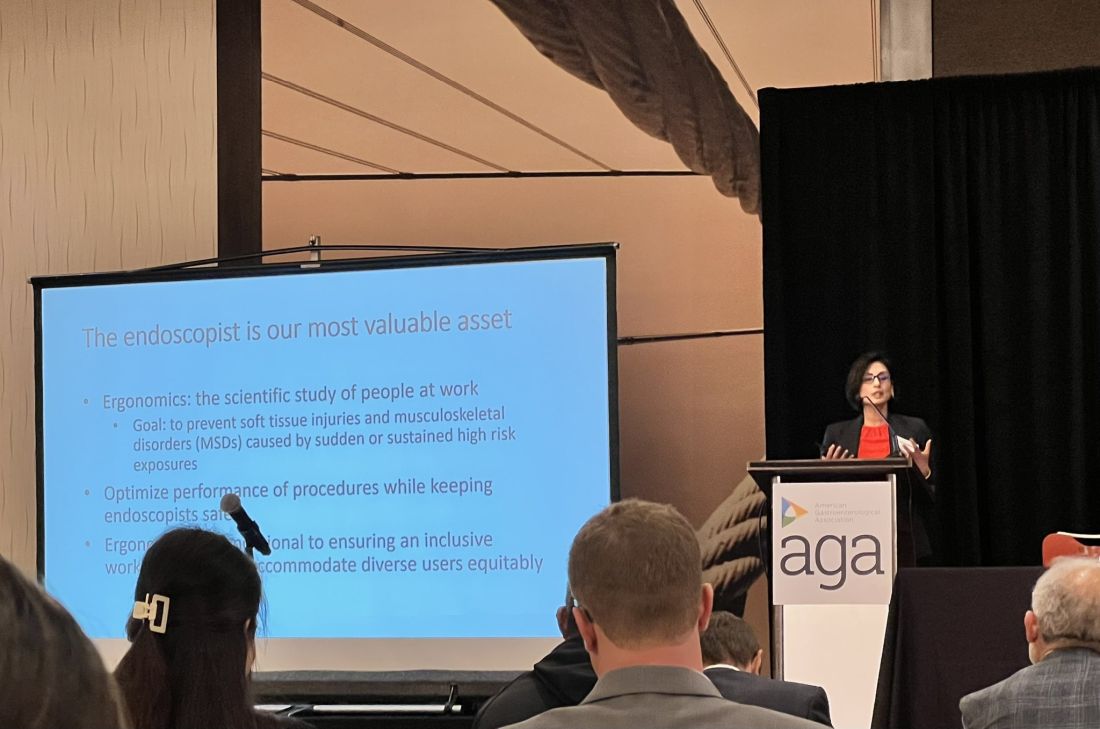
The AGA Tech Summit was unlike any conference I have been to in my 13 years of training in medicine (which included mostly clinically focused scientific meetings). Sessions involved ergonomics, applications of artificial intelligence, advances in imaging, environmental endoscopy, the role of the FDA, and innovations around the world. The audience included but was not limited to industry executives, AGA CGIT leadership, physician innovators, gastroenterologists, venture capitalists, and others. Attendees represented the diversity of our field in terms of organizational structures and backgrounds. This resulted in an opportunity to hear and learn different perspectives about products, emerging technology, and the costs involved for physicians, industry, and patients.
The final session of the summit, the AGA Shark Tank, was perhaps the most intriguing one of all. The session showcased landscape-changing technology to AGA investors and venture capitalists. The participants presented their own pitches and faced the sharks (judges). The winner received additional funding, tailored guidance from the AGA CGIT committee, partnering opportunities with interested parties, and the opportunity to represent AGA Shark Tank at the Digestive Disease Week (DDW).
The AGA Tech Summit Fellows Program is a learning platform that not only helps you find your niche in the world of GI innovation but also equips you with resources and connections to make an impact. It is also a great way to infuse new ideas into your practice or research. As healthcare professionals, we must create a culture where innovation can flourish, and where staff and patients feel empowered to contribute to the innovation process and help make change happen — to me, the AGA Tech Summit is one such avenue.
Reference
1. Kelly CJ and Young AJ. Promoting innovation in healthcare. Future Healthc J. 2017 Jun. doi: 10.7861/futurehosp.4-2-121.
Dr. Umar is Assistant Professor of Medicine, Section of Gastroenterology and Hepatology, Baylor College of Medicine, Houston, Texas, and a staff physician at Michael E. DeBakey VA Medical Center, Houston. Dr. Umar has no relevant financial conflicts and is on X, formerly Twitter, @shifaumarMD.
Medicine is transforming at a remarkable pace. It is therefore imperative for the future of the field that physicians understand innovation and collaborate with industry partners. Innovation can be defined as invention, adoption, and diffusion.1 During my training in gastroenterology and advanced fellowships, I learned about multiple endoscopic tools and techniques and became familiar with industry names that I frequently encountered in the endoscopy unit or clinic.
I was nominated to attend the AGA Tech Summit Fellows Program by my advanced endoscopy fellowship program director. A total of 22 fellows from around the United States at various stages of their training and interests in the field of gastroenterology and hepatology were selected for the program through an application process. The program included registration, travel, and accommodations to attend the AGA Tech Summit and Fellows Immersion Day at Medtronic.
The first event in the program was a visit to the Medtronic Santa Clara office, where our initial stop was at the research and development lab. We were introduced to design and biomedical engineers who reviewed with us the extensive testing that devices and endoscopy equipment undergo before coming to the market. These labs have a heavy focus on prototyping and experimentation and exist to promote in-house innovation and inventions.

During the day, we met physicians who shared their journeys on how they developed and advanced their careers in partnership with industry. Our visit also included a session with the business development and strategy manager at Medtronic, who discussed strategy and steps involved in product development — from the inception of an idea, institutional policies, and patents, to industry collaboration, and finally to successful commercialization. During medical school and training, we are focused on appropriately learning and applying medical knowledge to clinical care. The Medtronic Fellows Immersion Day experience offered a different perspective and showed other ways by which clinical knowledge and experience can be used to make an impact, in collaboration with industry and stakeholders. It also highlighted alternative career paths for medical professionals. The evening concluded with a meet and greet with the AGA Center for GI Innovation & Technology (CGIT) members and leadership.
The AGA Tech Summit was unlike any conference I have been to in my 13 years of training in medicine (which included mostly clinically focused scientific meetings). Sessions involved ergonomics, applications of artificial intelligence, advances in imaging, environmental endoscopy, the role of the FDA, and innovations around the world. The audience included but was not limited to industry executives, AGA CGIT leadership, physician innovators, gastroenterologists, venture capitalists, and others. Attendees represented the diversity of our field in terms of organizational structures and backgrounds. This resulted in an opportunity to hear and learn different perspectives about products, emerging technology, and the costs involved for physicians, industry, and patients.
The final session of the summit, the AGA Shark Tank, was perhaps the most intriguing one of all. The session showcased landscape-changing technology to AGA investors and venture capitalists. The participants presented their own pitches and faced the sharks (judges). The winner received additional funding, tailored guidance from the AGA CGIT committee, partnering opportunities with interested parties, and the opportunity to represent AGA Shark Tank at the Digestive Disease Week (DDW).
The AGA Tech Summit Fellows Program is a learning platform that not only helps you find your niche in the world of GI innovation but also equips you with resources and connections to make an impact. It is also a great way to infuse new ideas into your practice or research. As healthcare professionals, we must create a culture where innovation can flourish, and where staff and patients feel empowered to contribute to the innovation process and help make change happen — to me, the AGA Tech Summit is one such avenue.
Reference
1. Kelly CJ and Young AJ. Promoting innovation in healthcare. Future Healthc J. 2017 Jun. doi: 10.7861/futurehosp.4-2-121.
Dr. Umar is Assistant Professor of Medicine, Section of Gastroenterology and Hepatology, Baylor College of Medicine, Houston, Texas, and a staff physician at Michael E. DeBakey VA Medical Center, Houston. Dr. Umar has no relevant financial conflicts and is on X, formerly Twitter, @shifaumarMD.
Medicine is transforming at a remarkable pace. It is therefore imperative for the future of the field that physicians understand innovation and collaborate with industry partners. Innovation can be defined as invention, adoption, and diffusion.1 During my training in gastroenterology and advanced fellowships, I learned about multiple endoscopic tools and techniques and became familiar with industry names that I frequently encountered in the endoscopy unit or clinic.
I was nominated to attend the AGA Tech Summit Fellows Program by my advanced endoscopy fellowship program director. A total of 22 fellows from around the United States at various stages of their training and interests in the field of gastroenterology and hepatology were selected for the program through an application process. The program included registration, travel, and accommodations to attend the AGA Tech Summit and Fellows Immersion Day at Medtronic.
The first event in the program was a visit to the Medtronic Santa Clara office, where our initial stop was at the research and development lab. We were introduced to design and biomedical engineers who reviewed with us the extensive testing that devices and endoscopy equipment undergo before coming to the market. These labs have a heavy focus on prototyping and experimentation and exist to promote in-house innovation and inventions.

During the day, we met physicians who shared their journeys on how they developed and advanced their careers in partnership with industry. Our visit also included a session with the business development and strategy manager at Medtronic, who discussed strategy and steps involved in product development — from the inception of an idea, institutional policies, and patents, to industry collaboration, and finally to successful commercialization. During medical school and training, we are focused on appropriately learning and applying medical knowledge to clinical care. The Medtronic Fellows Immersion Day experience offered a different perspective and showed other ways by which clinical knowledge and experience can be used to make an impact, in collaboration with industry and stakeholders. It also highlighted alternative career paths for medical professionals. The evening concluded with a meet and greet with the AGA Center for GI Innovation & Technology (CGIT) members and leadership.
The AGA Tech Summit was unlike any conference I have been to in my 13 years of training in medicine (which included mostly clinically focused scientific meetings). Sessions involved ergonomics, applications of artificial intelligence, advances in imaging, environmental endoscopy, the role of the FDA, and innovations around the world. The audience included but was not limited to industry executives, AGA CGIT leadership, physician innovators, gastroenterologists, venture capitalists, and others. Attendees represented the diversity of our field in terms of organizational structures and backgrounds. This resulted in an opportunity to hear and learn different perspectives about products, emerging technology, and the costs involved for physicians, industry, and patients.
The final session of the summit, the AGA Shark Tank, was perhaps the most intriguing one of all. The session showcased landscape-changing technology to AGA investors and venture capitalists. The participants presented their own pitches and faced the sharks (judges). The winner received additional funding, tailored guidance from the AGA CGIT committee, partnering opportunities with interested parties, and the opportunity to represent AGA Shark Tank at the Digestive Disease Week (DDW).
The AGA Tech Summit Fellows Program is a learning platform that not only helps you find your niche in the world of GI innovation but also equips you with resources and connections to make an impact. It is also a great way to infuse new ideas into your practice or research. As healthcare professionals, we must create a culture where innovation can flourish, and where staff and patients feel empowered to contribute to the innovation process and help make change happen — to me, the AGA Tech Summit is one such avenue.
Reference
1. Kelly CJ and Young AJ. Promoting innovation in healthcare. Future Healthc J. 2017 Jun. doi: 10.7861/futurehosp.4-2-121.
Dr. Umar is Assistant Professor of Medicine, Section of Gastroenterology and Hepatology, Baylor College of Medicine, Houston, Texas, and a staff physician at Michael E. DeBakey VA Medical Center, Houston. Dr. Umar has no relevant financial conflicts and is on X, formerly Twitter, @shifaumarMD.
AGA Legacy Society Members Sustain GI Research
Research creates successful practices. Patients benefit from GI research daily in practices. Scientists are working hard to develop new treatments, therapies and discover cures to advance the field and better patient care. But they can’t do this without research funding.
They recognize the value that research has had in their profession, both in academic medicine and in private practice, and are showing their appreciation by giving back.
“I give back because I have a firsthand knowledge of what it will mean to a young investigator’s career,” said Shrikant Anant, PhD, AGAF, University of Kansas, AGA Legacy Society member. “I was propelled in my career when I received the 2002 AGA Research Scholar Award from the AGA Research Foundation. The funds helped me develop my independent research that led to many NIH grants and, associated with it, career advancement. I still vividly remember the day I received the notice of award and how my whole life changed. Today, I am proud to be a donor myself because I know it is making a difference on yet another young investigator.”
The AGA Legacy Society boasts 161 members. AGA Legacy Society members see the promise the future holds and are committed to furthering research in gastroenterology and hepatology through their generous donations.
AGA members who make gifts at the AGA Legacy Society level anytime before Digestive Disease Week® (DDW) 2024 will receive an invitation to the AGA Research Foundation Benefactor’s Event in Washington, D.C. Individuals interested in learning more about the AGA Legacy Society membership may contact foundation@gastro.org or visit https://foundation.gastro.org/our-donors/aga-legacy-society/ for more information about the AGA Legacy Society.
Research creates successful practices. Patients benefit from GI research daily in practices. Scientists are working hard to develop new treatments, therapies and discover cures to advance the field and better patient care. But they can’t do this without research funding.
They recognize the value that research has had in their profession, both in academic medicine and in private practice, and are showing their appreciation by giving back.
“I give back because I have a firsthand knowledge of what it will mean to a young investigator’s career,” said Shrikant Anant, PhD, AGAF, University of Kansas, AGA Legacy Society member. “I was propelled in my career when I received the 2002 AGA Research Scholar Award from the AGA Research Foundation. The funds helped me develop my independent research that led to many NIH grants and, associated with it, career advancement. I still vividly remember the day I received the notice of award and how my whole life changed. Today, I am proud to be a donor myself because I know it is making a difference on yet another young investigator.”
The AGA Legacy Society boasts 161 members. AGA Legacy Society members see the promise the future holds and are committed to furthering research in gastroenterology and hepatology through their generous donations.
AGA members who make gifts at the AGA Legacy Society level anytime before Digestive Disease Week® (DDW) 2024 will receive an invitation to the AGA Research Foundation Benefactor’s Event in Washington, D.C. Individuals interested in learning more about the AGA Legacy Society membership may contact foundation@gastro.org or visit https://foundation.gastro.org/our-donors/aga-legacy-society/ for more information about the AGA Legacy Society.
Research creates successful practices. Patients benefit from GI research daily in practices. Scientists are working hard to develop new treatments, therapies and discover cures to advance the field and better patient care. But they can’t do this without research funding.
They recognize the value that research has had in their profession, both in academic medicine and in private practice, and are showing their appreciation by giving back.
“I give back because I have a firsthand knowledge of what it will mean to a young investigator’s career,” said Shrikant Anant, PhD, AGAF, University of Kansas, AGA Legacy Society member. “I was propelled in my career when I received the 2002 AGA Research Scholar Award from the AGA Research Foundation. The funds helped me develop my independent research that led to many NIH grants and, associated with it, career advancement. I still vividly remember the day I received the notice of award and how my whole life changed. Today, I am proud to be a donor myself because I know it is making a difference on yet another young investigator.”
The AGA Legacy Society boasts 161 members. AGA Legacy Society members see the promise the future holds and are committed to furthering research in gastroenterology and hepatology through their generous donations.
AGA members who make gifts at the AGA Legacy Society level anytime before Digestive Disease Week® (DDW) 2024 will receive an invitation to the AGA Research Foundation Benefactor’s Event in Washington, D.C. Individuals interested in learning more about the AGA Legacy Society membership may contact foundation@gastro.org or visit https://foundation.gastro.org/our-donors/aga-legacy-society/ for more information about the AGA Legacy Society.
What’s the Real Prevalence of Conjunctivitis in AD Patients Treated With Dupilumab?
Those are key findings from an analysis of published trials of dupilumab for AD and other conditions that study author Matthew Zirwas, MD, presented during a late-breaking abstract session at the Revolutionizing Atopic Dermatitis (RAD) Virtual Conference.
Adults with AD have a significant and disease severity–dependent increased risk of developing ocular surface diseases, including conjunctivitis and keratitis, compared with the general population and independent of any drug effect, according to Dr. Zirwas, a dermatologist with Probity Medical Research of Columbus, Ohio.
Dupilumab inhibits signaling of interleukin (IL)-4 and IL-13, which drive type 2 inflammatory diseases such as AD, asthma, chronic rhinosinusitis with nasal polyposis (CRSwNP), eosinophilic esophagitis (EoE), prurigo nodularis (PN), and chronic spontaneous urticaria (CSU).
In randomized, placebo-controlled trials of dupilumab in patients with moderate to severe AD, conjunctivitis was reported in more patients who received dupilumab treatment than in placebo-treated patients.
“When it comes to dupilumab-induced conjunctivitis, we have a good idea of the etiology, but the question of how frequently it occurs versus how frequently the conjunctivitis is unrelated to dupilumab is an interesting one,” he said. “How often is it clinically meaningful? What is it that is so unique about AD patients? We’ve all heard that it is a unique adverse event that only happens to people with AD and not to people using dupilumab for other indications. Where it gets interesting to me is how do we differentiate the cases that are dupilumab induced versus the cases that are just part of the underlying AD process?”
For their analysis, Dr. Zirwas and co-authors reviewed the incidence of conjunctivitis adverse events in patients from 15 completed, randomized, double-blind placebo-controlled trials evaluating dupilumab in AD, asthma, CRSwNP, EoE, PN, and CSU, along with the severity and resolution of conjunctivitis events in adults with AD.
Of the 15 trials, 7 were conducted in patients with AD: 4 in adults, 1 in adolescents, 1 in school-aged children, and 1 in preschoolers. One of the AD trials, LIBERTY AD CHRONOS, extends 52 weeks. The remaining eight trials of patients with asthma, CRSwNP, EoE, PN, and CSU lasted 24-52 weeks.
In the non-AD trials, the researchers observed that conjunctivitis rates were generally in the 1%-3% range, with less pronounced or no differences between the dupilumab and placebo groups. In the AD trials, conjunctivitis rates were higher in patients receiving dupilumab, compared with those receiving placebo across age groups.
In the 16-week SOLO 1 & 2 and AD-1021 monotherapy trials, 12 conjunctivitis events occurred in 517 patients who received placebo (2%), compared with 103 of 1047 patients (9.84%) who received dupilumab. Of the dupilumab-associated conjunctivitis cases, 80 (78%) patients recovered by the end of the trials. Of the 23 cases of conjunctivitis that did not recover or dropped out of the trial, 15 were among the 529 patients who received 300 mg dupilumab once every 2 weeks (q2w) (3%) and eight were among the 518 who received 300 mg dupilumab once weekly (qw) (2%).
In the 52-week LIBERTY AD CHRONOS trial, 29 conjunctivitis events occurred in 315 patients who received placebo plus topical corticosteroid (TCS) (9%), compared with 113 of 425 patients (27%) who received dupilumab plus TCS. Of these, 103 (91%) recovered by the end of the trial. Of the 11 patients with conjunctivitis who did not recover or dropped out of the trial, 3 were among the 110 patients who received 300 mg dupilumab q2w plus TCS (3%), and 8 were among the 315 who received 300 mg dupilumab qw plus TCS (3%).
“When I look at all of this data, I think that about 2% of people treated with dupilumab are going to get clinically very meaningful conjunctivitis that may be therapy limiting,” Dr. Zirwas concluded. “The vast majority of those cases appear to happen in the first 16 weeks. This is just not something we see in cases of patients treated with dupilumab treated for other reasons.”
Following his presentation, a meeting attendee asked Dr. Zirwas if conjunctivitis occurs more often in patients with facial dermatitis. “My perception is that it happens more often in people who have facial or eyelid dermatitis, but I’ve seen it in plenty of people who didn’t have any facial or eyelid dermatitis,” he said. “I have seen more conjunctivitis in people with more severe AD and more severe atopic comorbidities. That is anecdotal. The data that I have seen has been back and forth on this topic.”
Dr. Zirwas disclosed that he is a speaker and consultant for Sanofi, Regeneron, Leo, Lilly, Galderma, Pfizer, and AbbVie. Several of his co-authors work for Regeneron Pharmaceuticals.
Those are key findings from an analysis of published trials of dupilumab for AD and other conditions that study author Matthew Zirwas, MD, presented during a late-breaking abstract session at the Revolutionizing Atopic Dermatitis (RAD) Virtual Conference.
Adults with AD have a significant and disease severity–dependent increased risk of developing ocular surface diseases, including conjunctivitis and keratitis, compared with the general population and independent of any drug effect, according to Dr. Zirwas, a dermatologist with Probity Medical Research of Columbus, Ohio.
Dupilumab inhibits signaling of interleukin (IL)-4 and IL-13, which drive type 2 inflammatory diseases such as AD, asthma, chronic rhinosinusitis with nasal polyposis (CRSwNP), eosinophilic esophagitis (EoE), prurigo nodularis (PN), and chronic spontaneous urticaria (CSU).
In randomized, placebo-controlled trials of dupilumab in patients with moderate to severe AD, conjunctivitis was reported in more patients who received dupilumab treatment than in placebo-treated patients.
“When it comes to dupilumab-induced conjunctivitis, we have a good idea of the etiology, but the question of how frequently it occurs versus how frequently the conjunctivitis is unrelated to dupilumab is an interesting one,” he said. “How often is it clinically meaningful? What is it that is so unique about AD patients? We’ve all heard that it is a unique adverse event that only happens to people with AD and not to people using dupilumab for other indications. Where it gets interesting to me is how do we differentiate the cases that are dupilumab induced versus the cases that are just part of the underlying AD process?”
For their analysis, Dr. Zirwas and co-authors reviewed the incidence of conjunctivitis adverse events in patients from 15 completed, randomized, double-blind placebo-controlled trials evaluating dupilumab in AD, asthma, CRSwNP, EoE, PN, and CSU, along with the severity and resolution of conjunctivitis events in adults with AD.
Of the 15 trials, 7 were conducted in patients with AD: 4 in adults, 1 in adolescents, 1 in school-aged children, and 1 in preschoolers. One of the AD trials, LIBERTY AD CHRONOS, extends 52 weeks. The remaining eight trials of patients with asthma, CRSwNP, EoE, PN, and CSU lasted 24-52 weeks.
In the non-AD trials, the researchers observed that conjunctivitis rates were generally in the 1%-3% range, with less pronounced or no differences between the dupilumab and placebo groups. In the AD trials, conjunctivitis rates were higher in patients receiving dupilumab, compared with those receiving placebo across age groups.
In the 16-week SOLO 1 & 2 and AD-1021 monotherapy trials, 12 conjunctivitis events occurred in 517 patients who received placebo (2%), compared with 103 of 1047 patients (9.84%) who received dupilumab. Of the dupilumab-associated conjunctivitis cases, 80 (78%) patients recovered by the end of the trials. Of the 23 cases of conjunctivitis that did not recover or dropped out of the trial, 15 were among the 529 patients who received 300 mg dupilumab once every 2 weeks (q2w) (3%) and eight were among the 518 who received 300 mg dupilumab once weekly (qw) (2%).
In the 52-week LIBERTY AD CHRONOS trial, 29 conjunctivitis events occurred in 315 patients who received placebo plus topical corticosteroid (TCS) (9%), compared with 113 of 425 patients (27%) who received dupilumab plus TCS. Of these, 103 (91%) recovered by the end of the trial. Of the 11 patients with conjunctivitis who did not recover or dropped out of the trial, 3 were among the 110 patients who received 300 mg dupilumab q2w plus TCS (3%), and 8 were among the 315 who received 300 mg dupilumab qw plus TCS (3%).
“When I look at all of this data, I think that about 2% of people treated with dupilumab are going to get clinically very meaningful conjunctivitis that may be therapy limiting,” Dr. Zirwas concluded. “The vast majority of those cases appear to happen in the first 16 weeks. This is just not something we see in cases of patients treated with dupilumab treated for other reasons.”
Following his presentation, a meeting attendee asked Dr. Zirwas if conjunctivitis occurs more often in patients with facial dermatitis. “My perception is that it happens more often in people who have facial or eyelid dermatitis, but I’ve seen it in plenty of people who didn’t have any facial or eyelid dermatitis,” he said. “I have seen more conjunctivitis in people with more severe AD and more severe atopic comorbidities. That is anecdotal. The data that I have seen has been back and forth on this topic.”
Dr. Zirwas disclosed that he is a speaker and consultant for Sanofi, Regeneron, Leo, Lilly, Galderma, Pfizer, and AbbVie. Several of his co-authors work for Regeneron Pharmaceuticals.
Those are key findings from an analysis of published trials of dupilumab for AD and other conditions that study author Matthew Zirwas, MD, presented during a late-breaking abstract session at the Revolutionizing Atopic Dermatitis (RAD) Virtual Conference.
Adults with AD have a significant and disease severity–dependent increased risk of developing ocular surface diseases, including conjunctivitis and keratitis, compared with the general population and independent of any drug effect, according to Dr. Zirwas, a dermatologist with Probity Medical Research of Columbus, Ohio.
Dupilumab inhibits signaling of interleukin (IL)-4 and IL-13, which drive type 2 inflammatory diseases such as AD, asthma, chronic rhinosinusitis with nasal polyposis (CRSwNP), eosinophilic esophagitis (EoE), prurigo nodularis (PN), and chronic spontaneous urticaria (CSU).
In randomized, placebo-controlled trials of dupilumab in patients with moderate to severe AD, conjunctivitis was reported in more patients who received dupilumab treatment than in placebo-treated patients.
“When it comes to dupilumab-induced conjunctivitis, we have a good idea of the etiology, but the question of how frequently it occurs versus how frequently the conjunctivitis is unrelated to dupilumab is an interesting one,” he said. “How often is it clinically meaningful? What is it that is so unique about AD patients? We’ve all heard that it is a unique adverse event that only happens to people with AD and not to people using dupilumab for other indications. Where it gets interesting to me is how do we differentiate the cases that are dupilumab induced versus the cases that are just part of the underlying AD process?”
For their analysis, Dr. Zirwas and co-authors reviewed the incidence of conjunctivitis adverse events in patients from 15 completed, randomized, double-blind placebo-controlled trials evaluating dupilumab in AD, asthma, CRSwNP, EoE, PN, and CSU, along with the severity and resolution of conjunctivitis events in adults with AD.
Of the 15 trials, 7 were conducted in patients with AD: 4 in adults, 1 in adolescents, 1 in school-aged children, and 1 in preschoolers. One of the AD trials, LIBERTY AD CHRONOS, extends 52 weeks. The remaining eight trials of patients with asthma, CRSwNP, EoE, PN, and CSU lasted 24-52 weeks.
In the non-AD trials, the researchers observed that conjunctivitis rates were generally in the 1%-3% range, with less pronounced or no differences between the dupilumab and placebo groups. In the AD trials, conjunctivitis rates were higher in patients receiving dupilumab, compared with those receiving placebo across age groups.
In the 16-week SOLO 1 & 2 and AD-1021 monotherapy trials, 12 conjunctivitis events occurred in 517 patients who received placebo (2%), compared with 103 of 1047 patients (9.84%) who received dupilumab. Of the dupilumab-associated conjunctivitis cases, 80 (78%) patients recovered by the end of the trials. Of the 23 cases of conjunctivitis that did not recover or dropped out of the trial, 15 were among the 529 patients who received 300 mg dupilumab once every 2 weeks (q2w) (3%) and eight were among the 518 who received 300 mg dupilumab once weekly (qw) (2%).
In the 52-week LIBERTY AD CHRONOS trial, 29 conjunctivitis events occurred in 315 patients who received placebo plus topical corticosteroid (TCS) (9%), compared with 113 of 425 patients (27%) who received dupilumab plus TCS. Of these, 103 (91%) recovered by the end of the trial. Of the 11 patients with conjunctivitis who did not recover or dropped out of the trial, 3 were among the 110 patients who received 300 mg dupilumab q2w plus TCS (3%), and 8 were among the 315 who received 300 mg dupilumab qw plus TCS (3%).
“When I look at all of this data, I think that about 2% of people treated with dupilumab are going to get clinically very meaningful conjunctivitis that may be therapy limiting,” Dr. Zirwas concluded. “The vast majority of those cases appear to happen in the first 16 weeks. This is just not something we see in cases of patients treated with dupilumab treated for other reasons.”
Following his presentation, a meeting attendee asked Dr. Zirwas if conjunctivitis occurs more often in patients with facial dermatitis. “My perception is that it happens more often in people who have facial or eyelid dermatitis, but I’ve seen it in plenty of people who didn’t have any facial or eyelid dermatitis,” he said. “I have seen more conjunctivitis in people with more severe AD and more severe atopic comorbidities. That is anecdotal. The data that I have seen has been back and forth on this topic.”
Dr. Zirwas disclosed that he is a speaker and consultant for Sanofi, Regeneron, Leo, Lilly, Galderma, Pfizer, and AbbVie. Several of his co-authors work for Regeneron Pharmaceuticals.
FROM RAD 2023
2024 Gut Microbiota for Health World Summit Explores the Clinical Impacts of the Microbiome
Join global experts in-person or online as they gather for the 2024 Gut Microbiota for Health World Summit (GMFH) on March 23-24, 2024, in Washington, DC.
This meeting brings together an international and multidisciplinary community of GI clinicians, dietitians, and researchers to discuss personalized approaches to modifying the gut microbiome to improve health and treat disease.
This year’s program will explore:
- Better health through the gut microbiome.
- Big data and the gut microbiome.
- Human-derived to synthetic communities.
- Bringing new microbiome-based products to market.
Early-career faculty and trainees are encouraged to submit abstracts for presentation during the reception. Five $1,000 abstract prizes are available for top-scoring submissions.
Register here.
Join global experts in-person or online as they gather for the 2024 Gut Microbiota for Health World Summit (GMFH) on March 23-24, 2024, in Washington, DC.
This meeting brings together an international and multidisciplinary community of GI clinicians, dietitians, and researchers to discuss personalized approaches to modifying the gut microbiome to improve health and treat disease.
This year’s program will explore:
- Better health through the gut microbiome.
- Big data and the gut microbiome.
- Human-derived to synthetic communities.
- Bringing new microbiome-based products to market.
Early-career faculty and trainees are encouraged to submit abstracts for presentation during the reception. Five $1,000 abstract prizes are available for top-scoring submissions.
Register here.
Join global experts in-person or online as they gather for the 2024 Gut Microbiota for Health World Summit (GMFH) on March 23-24, 2024, in Washington, DC.
This meeting brings together an international and multidisciplinary community of GI clinicians, dietitians, and researchers to discuss personalized approaches to modifying the gut microbiome to improve health and treat disease.
This year’s program will explore:
- Better health through the gut microbiome.
- Big data and the gut microbiome.
- Human-derived to synthetic communities.
- Bringing new microbiome-based products to market.
Early-career faculty and trainees are encouraged to submit abstracts for presentation during the reception. Five $1,000 abstract prizes are available for top-scoring submissions.
Register here.
Announcing AGA Journal Social Media Editors
AGA journals have welcomed new social media editors for Clinical Gastroenterology and Hepatology (CGH), Cellular and Molecular Gastroenterology and Hepatology (CMGH), Techniques and Innovations in Gastrointestinal Endoscopy (TIGE) and Gastro Hep Advances (GHA).
Clinical Gastroenterology and Hepatology (CGH)
Joseph Sleiman, MD
University of Pittsburgh Medical Center
Dr. Sleiman’s research interests include inflammatory bowel disease (IBD), immunotherapy-induced colitis, Lynch Syndrome surveillance strategies and machine learning for GI research purposes.
Follow Dr. Sleiman
Cellular and Molecular Gastroenterology and Hepatology (CMGH)
Lindsey Kennedy, PhD
Indiana University School of Medicine
Dr. Kennedy’s research interests include the cellular crosstalk and pathological mechanisms regulating biliary and liver damage in cholestatic disorders, such as primary sclerosing cholangitis (PSC) and primary biliary cholangitis (PBC).
Follow Dr. Kennedy
Techniques and Innovations in Gastrointestinal Endoscopy (TIGE)
Judy Trieu, MD, MPH
Washington University Physicians
Dr. Trieu specializes in interventional endoscopy and general gastroenterology.
Follow Dr. Trieu
Gastro Hep Advances (GHA)
Shida Haghighat, MD, MPH
University of Miami
Dr. Haghighat’s research interests center around the prevention and screening of gastrointestinal cancers.
Follow Dr. Haghihat
AGA journals have welcomed new social media editors for Clinical Gastroenterology and Hepatology (CGH), Cellular and Molecular Gastroenterology and Hepatology (CMGH), Techniques and Innovations in Gastrointestinal Endoscopy (TIGE) and Gastro Hep Advances (GHA).
Clinical Gastroenterology and Hepatology (CGH)
Joseph Sleiman, MD
University of Pittsburgh Medical Center
Dr. Sleiman’s research interests include inflammatory bowel disease (IBD), immunotherapy-induced colitis, Lynch Syndrome surveillance strategies and machine learning for GI research purposes.
Follow Dr. Sleiman
Cellular and Molecular Gastroenterology and Hepatology (CMGH)
Lindsey Kennedy, PhD
Indiana University School of Medicine
Dr. Kennedy’s research interests include the cellular crosstalk and pathological mechanisms regulating biliary and liver damage in cholestatic disorders, such as primary sclerosing cholangitis (PSC) and primary biliary cholangitis (PBC).
Follow Dr. Kennedy
Techniques and Innovations in Gastrointestinal Endoscopy (TIGE)
Judy Trieu, MD, MPH
Washington University Physicians
Dr. Trieu specializes in interventional endoscopy and general gastroenterology.
Follow Dr. Trieu
Gastro Hep Advances (GHA)
Shida Haghighat, MD, MPH
University of Miami
Dr. Haghighat’s research interests center around the prevention and screening of gastrointestinal cancers.
Follow Dr. Haghihat
AGA journals have welcomed new social media editors for Clinical Gastroenterology and Hepatology (CGH), Cellular and Molecular Gastroenterology and Hepatology (CMGH), Techniques and Innovations in Gastrointestinal Endoscopy (TIGE) and Gastro Hep Advances (GHA).
Clinical Gastroenterology and Hepatology (CGH)
Joseph Sleiman, MD
University of Pittsburgh Medical Center
Dr. Sleiman’s research interests include inflammatory bowel disease (IBD), immunotherapy-induced colitis, Lynch Syndrome surveillance strategies and machine learning for GI research purposes.
Follow Dr. Sleiman
Cellular and Molecular Gastroenterology and Hepatology (CMGH)
Lindsey Kennedy, PhD
Indiana University School of Medicine
Dr. Kennedy’s research interests include the cellular crosstalk and pathological mechanisms regulating biliary and liver damage in cholestatic disorders, such as primary sclerosing cholangitis (PSC) and primary biliary cholangitis (PBC).
Follow Dr. Kennedy
Techniques and Innovations in Gastrointestinal Endoscopy (TIGE)
Judy Trieu, MD, MPH
Washington University Physicians
Dr. Trieu specializes in interventional endoscopy and general gastroenterology.
Follow Dr. Trieu
Gastro Hep Advances (GHA)
Shida Haghighat, MD, MPH
University of Miami
Dr. Haghighat’s research interests center around the prevention and screening of gastrointestinal cancers.
Follow Dr. Haghihat
How an Obesity Drug Could Help Alcohol Use Disorder
The glucagon-like peptide 1 (GLP-1) receptor agonist semaglutide has made headlines as a US Food and Drug Administration (FDA)–approved treatment for type 2 diabetes (Ozempic) and obesity (Wegovy).
Recently,
“There is some really interesting preclinical research in rodents and monkeys that shows that GLP-1 agonist molecules, like semaglutide, have the effect of reducing the consumption of not just food, but also alcohol, nicotine, cocaine and amphetamines,” Kyle Simmons, PhD, professor of pharmacology and physiology at Oklahoma State University Center for Health Sciences in Tulsa, said in an interview.
Some of that early research was conducted by Elisabet Jerlhag Holm, PhD, and colleagues at University of Gothenburg, Sweden.
“We have worked on GLP-1 and alcohol since 2012, and observe promising effects,” Holm told this news organization.
Her team published two studies earlier this year — one in one in Frontiers in Pharmacology and the other in eBioMedicine — demonstrating that semaglutide, in low doses, reduces alcohol intake in male and female rats.
“We have shown that semaglutide binds to the nucleus accumbens — an area of the brain associated with reward. We have also shown that semaglutide alters the dopamine metabolism when alcohol is on board. This provides a tentative mechanism,” Dr. Holm said.
First Human Data
The preclinical data fueled interest in testing the value of the GLP-1 agonist in patient populations with addiction.
Dr. Simmons and colleagues have now published what is believed to be the first evidence in humans that semaglutide specifically reduces the symptoms of alcohol use disorder (AUD).
In a report published online on November 27 in The Journal of Clinical Psychiatry, they describe six patients (of whom five are female; mean age, 43 years) who received semaglutide treatment in the course of pharmacotherapy for weight loss.
All six screened positive for AUD on the Alcohol Use Disorders Identification Test (AUDIT), and all six showed significant improvement in their alcohol-related symptoms after starting semaglutide.
An AUDIT score > 8 is considered positive. The mean AUDIT score at baseline was 14. It fell to 4.5 on average after semaglutide treatment. The mean 9.5-point decrease in AUDIT scores with semaglutide was statistically significant (P < .001).
The patients were followed up from a few weeks to almost 9 months, and all of them had a reduction in AUD symptoms. At the various follow-up time points, all six patients had AUDIT scores consistent with “low-risk” drinking.
Strong Response at Low Doses
“There was a very strong response, even at a very low dose,” lead author Jesse Richards, DO, director of obesity medicine and assistant professor of medicine University of Oklahoma School of Community Medicine, Tulsa, said in an interview.
Three patients were treated with 0.5 mg of semaglutide weekly, two with 0.25 mg weekly, and one with 1 mg weekly. These doses are lower than those currently approved for treatment of type 2 diabetes and obesity.
Dr. Holm is not surprised by the results in these six patients. “Based on our preclinical data, this outcome is expected. The data are promising and bigger studies needed,” she said.
Simmons is currently leading a randomized placebo-controlled trial to further test the impact of semaglutide on AUD.
The STAR (Semaglutide Therapy for Alcohol Reduction) study is funded by the Hardesty Family Foundation and Oklahoma State University Center for Health Sciences.
A sister study is also currently underway in Baltimore, funded by the National Institute on Drug Abuse.
Hopefully, these studies will be able to “definitively tell us whether semaglutide is safe and effective for treatment” for AUD, Dr. Simmons said in a statement.
Despite being a major cause of preventable death worldwide, AUD currently has only three FDA-approved pharmacotherapies. However, there has been limited uptake of these drugs.
“There remains a significant treatment gap and need for new and novel or perhaps better tolerated or different mechanism treatment options for patients,” Dr. Richards said.
The preclinical and early clinical data provide a “signal” of a treatment effect for semaglutide in AUD, Dr. Richards said. The randomized controlled trials now underway should be concluding in the next 1-2 years, “at which point we’ll have a much better sense of the safety and efficacy of this drug for AUD,” he said.
The case series had no specific funding. Dr. Richards is on speakers bureaus for Rhythm Pharmaceuticals and Novo Nordisk and is on an advisory board for Rhythm Pharmaceuticals. Simmons is the recipient of a grant from the Hardesty Family Foundation to support an ongoing clinical trial of semaglutide in the treatment of AUD. Dr. Holm has no relevant disclosures.
A version of this article appeared on Medscape.com.
The glucagon-like peptide 1 (GLP-1) receptor agonist semaglutide has made headlines as a US Food and Drug Administration (FDA)–approved treatment for type 2 diabetes (Ozempic) and obesity (Wegovy).
Recently,
“There is some really interesting preclinical research in rodents and monkeys that shows that GLP-1 agonist molecules, like semaglutide, have the effect of reducing the consumption of not just food, but also alcohol, nicotine, cocaine and amphetamines,” Kyle Simmons, PhD, professor of pharmacology and physiology at Oklahoma State University Center for Health Sciences in Tulsa, said in an interview.
Some of that early research was conducted by Elisabet Jerlhag Holm, PhD, and colleagues at University of Gothenburg, Sweden.
“We have worked on GLP-1 and alcohol since 2012, and observe promising effects,” Holm told this news organization.
Her team published two studies earlier this year — one in one in Frontiers in Pharmacology and the other in eBioMedicine — demonstrating that semaglutide, in low doses, reduces alcohol intake in male and female rats.
“We have shown that semaglutide binds to the nucleus accumbens — an area of the brain associated with reward. We have also shown that semaglutide alters the dopamine metabolism when alcohol is on board. This provides a tentative mechanism,” Dr. Holm said.
First Human Data
The preclinical data fueled interest in testing the value of the GLP-1 agonist in patient populations with addiction.
Dr. Simmons and colleagues have now published what is believed to be the first evidence in humans that semaglutide specifically reduces the symptoms of alcohol use disorder (AUD).
In a report published online on November 27 in The Journal of Clinical Psychiatry, they describe six patients (of whom five are female; mean age, 43 years) who received semaglutide treatment in the course of pharmacotherapy for weight loss.
All six screened positive for AUD on the Alcohol Use Disorders Identification Test (AUDIT), and all six showed significant improvement in their alcohol-related symptoms after starting semaglutide.
An AUDIT score > 8 is considered positive. The mean AUDIT score at baseline was 14. It fell to 4.5 on average after semaglutide treatment. The mean 9.5-point decrease in AUDIT scores with semaglutide was statistically significant (P < .001).
The patients were followed up from a few weeks to almost 9 months, and all of them had a reduction in AUD symptoms. At the various follow-up time points, all six patients had AUDIT scores consistent with “low-risk” drinking.
Strong Response at Low Doses
“There was a very strong response, even at a very low dose,” lead author Jesse Richards, DO, director of obesity medicine and assistant professor of medicine University of Oklahoma School of Community Medicine, Tulsa, said in an interview.
Three patients were treated with 0.5 mg of semaglutide weekly, two with 0.25 mg weekly, and one with 1 mg weekly. These doses are lower than those currently approved for treatment of type 2 diabetes and obesity.
Dr. Holm is not surprised by the results in these six patients. “Based on our preclinical data, this outcome is expected. The data are promising and bigger studies needed,” she said.
Simmons is currently leading a randomized placebo-controlled trial to further test the impact of semaglutide on AUD.
The STAR (Semaglutide Therapy for Alcohol Reduction) study is funded by the Hardesty Family Foundation and Oklahoma State University Center for Health Sciences.
A sister study is also currently underway in Baltimore, funded by the National Institute on Drug Abuse.
Hopefully, these studies will be able to “definitively tell us whether semaglutide is safe and effective for treatment” for AUD, Dr. Simmons said in a statement.
Despite being a major cause of preventable death worldwide, AUD currently has only three FDA-approved pharmacotherapies. However, there has been limited uptake of these drugs.
“There remains a significant treatment gap and need for new and novel or perhaps better tolerated or different mechanism treatment options for patients,” Dr. Richards said.
The preclinical and early clinical data provide a “signal” of a treatment effect for semaglutide in AUD, Dr. Richards said. The randomized controlled trials now underway should be concluding in the next 1-2 years, “at which point we’ll have a much better sense of the safety and efficacy of this drug for AUD,” he said.
The case series had no specific funding. Dr. Richards is on speakers bureaus for Rhythm Pharmaceuticals and Novo Nordisk and is on an advisory board for Rhythm Pharmaceuticals. Simmons is the recipient of a grant from the Hardesty Family Foundation to support an ongoing clinical trial of semaglutide in the treatment of AUD. Dr. Holm has no relevant disclosures.
A version of this article appeared on Medscape.com.
The glucagon-like peptide 1 (GLP-1) receptor agonist semaglutide has made headlines as a US Food and Drug Administration (FDA)–approved treatment for type 2 diabetes (Ozempic) and obesity (Wegovy).
Recently,
“There is some really interesting preclinical research in rodents and monkeys that shows that GLP-1 agonist molecules, like semaglutide, have the effect of reducing the consumption of not just food, but also alcohol, nicotine, cocaine and amphetamines,” Kyle Simmons, PhD, professor of pharmacology and physiology at Oklahoma State University Center for Health Sciences in Tulsa, said in an interview.
Some of that early research was conducted by Elisabet Jerlhag Holm, PhD, and colleagues at University of Gothenburg, Sweden.
“We have worked on GLP-1 and alcohol since 2012, and observe promising effects,” Holm told this news organization.
Her team published two studies earlier this year — one in one in Frontiers in Pharmacology and the other in eBioMedicine — demonstrating that semaglutide, in low doses, reduces alcohol intake in male and female rats.
“We have shown that semaglutide binds to the nucleus accumbens — an area of the brain associated with reward. We have also shown that semaglutide alters the dopamine metabolism when alcohol is on board. This provides a tentative mechanism,” Dr. Holm said.
First Human Data
The preclinical data fueled interest in testing the value of the GLP-1 agonist in patient populations with addiction.
Dr. Simmons and colleagues have now published what is believed to be the first evidence in humans that semaglutide specifically reduces the symptoms of alcohol use disorder (AUD).
In a report published online on November 27 in The Journal of Clinical Psychiatry, they describe six patients (of whom five are female; mean age, 43 years) who received semaglutide treatment in the course of pharmacotherapy for weight loss.
All six screened positive for AUD on the Alcohol Use Disorders Identification Test (AUDIT), and all six showed significant improvement in their alcohol-related symptoms after starting semaglutide.
An AUDIT score > 8 is considered positive. The mean AUDIT score at baseline was 14. It fell to 4.5 on average after semaglutide treatment. The mean 9.5-point decrease in AUDIT scores with semaglutide was statistically significant (P < .001).
The patients were followed up from a few weeks to almost 9 months, and all of them had a reduction in AUD symptoms. At the various follow-up time points, all six patients had AUDIT scores consistent with “low-risk” drinking.
Strong Response at Low Doses
“There was a very strong response, even at a very low dose,” lead author Jesse Richards, DO, director of obesity medicine and assistant professor of medicine University of Oklahoma School of Community Medicine, Tulsa, said in an interview.
Three patients were treated with 0.5 mg of semaglutide weekly, two with 0.25 mg weekly, and one with 1 mg weekly. These doses are lower than those currently approved for treatment of type 2 diabetes and obesity.
Dr. Holm is not surprised by the results in these six patients. “Based on our preclinical data, this outcome is expected. The data are promising and bigger studies needed,” she said.
Simmons is currently leading a randomized placebo-controlled trial to further test the impact of semaglutide on AUD.
The STAR (Semaglutide Therapy for Alcohol Reduction) study is funded by the Hardesty Family Foundation and Oklahoma State University Center for Health Sciences.
A sister study is also currently underway in Baltimore, funded by the National Institute on Drug Abuse.
Hopefully, these studies will be able to “definitively tell us whether semaglutide is safe and effective for treatment” for AUD, Dr. Simmons said in a statement.
Despite being a major cause of preventable death worldwide, AUD currently has only three FDA-approved pharmacotherapies. However, there has been limited uptake of these drugs.
“There remains a significant treatment gap and need for new and novel or perhaps better tolerated or different mechanism treatment options for patients,” Dr. Richards said.
The preclinical and early clinical data provide a “signal” of a treatment effect for semaglutide in AUD, Dr. Richards said. The randomized controlled trials now underway should be concluding in the next 1-2 years, “at which point we’ll have a much better sense of the safety and efficacy of this drug for AUD,” he said.
The case series had no specific funding. Dr. Richards is on speakers bureaus for Rhythm Pharmaceuticals and Novo Nordisk and is on an advisory board for Rhythm Pharmaceuticals. Simmons is the recipient of a grant from the Hardesty Family Foundation to support an ongoing clinical trial of semaglutide in the treatment of AUD. Dr. Holm has no relevant disclosures.
A version of this article appeared on Medscape.com.
Too Little and Too Late with Obesity Prevention
As we begin to find our way in the new world of obesity management, questions continue to surface more quickly than answers. This isn’t surprising, as we are being asked to view obesity as a disease when for decades the general consensus has been that overweight people are simply will power deficient.
Are the new drugs as effective as we are told by the patients and physicians who have had some experience using and prescribing them? Will they continue to be effective in the very long run? Will their safety record hold up over time? And for those of us in pediatrics, what will be their role for children? As a group we tend to be cautious about drugs that haven’t been thoroughly tested in children. How many years will it take before we feel comfortable with obesity drugs? And, of course, we should be asking ourselves the same questions about bariatric surgery.
Fortunately, while the media spotlight has been focused on the treatment arm of our obesity strategy, there are still some folks looking at what has been up to now the discouraging prospects for prevention. The U.S. Preventive Services Task Force (USPSTF) has recently released a draft of its recommendations that includes evidence supporting the effectiveness of “intensive behavioral interventions” (defined as a minimum of 26 hours of counseling). In reviewing data from nearly 60 randomized controlled trials, which included more than 10,000 children, the task force found that It should be noted that the USPSTF gave the intervention package only a B grade, which means that the agency found evidence of high certainty of a moderate benefit over an unspecified time period. Certainly, not a ringing endorsement.
While I think we must applaud the diligent efforts of the task force and its commitment to prevention, I fear that the strategy is too little too late. That being said, I am willing to accept the idea that targeting age 6 for intensive counseling may qualify for the better-late-than-never category. The task force acknowledges that procuring the resources given our already understaffed mental health clinics is going to be difficult and expensive. I would add that it will be so costly in time and money as to be unrealistic.
Based on my observations of thousands of children, the scaffolding of habits, diet, and preference for inactivity that underly obesity has already been laid by age 6. Are we prepared to shoulder our already overburdened school systems in an attempt to reconfigure this foundation of an obesogenic lifestyle? An effort on this scale after children have been sent off to first grade is doomed to failure.
A recent review of data reported by the CDC and reviewed in the journal Pediatrics reveals that about 2% of children receiving federal assistance from the WIC program are severely obese. It is probably safe to say that these preschoolers represent just the tip of a very concerning iceberg.
By waiting until age 6, we would increase the risk of further stigmatizing the obese child. What will he tell his peers when he is taken out of school or misses a playdate because he has to meet with his “obesity counselor”?
If we are going to take obesity prevention seriously and spend time and money in counseling, doesn’t it make more sense to invest this effort on the parents and the home situation when the child is still under their influence? We must be prepared to unwrap and employ an “intensive behavioral package” the first time we see evidence that the child’s growth chart is heading in an unhealthy direction.
This won’t always be easy. I can recall seeing a 4-year-old whose weight had risen dramatically from her previous curve in the year since her 3-year checkup. The answer became obvious when I discovered that her grandmother, for whom baking was a passion, had taken over as her daycare provider. Arriving at a solution that kept the family on speaking terms took some tact, but it was one of my rare successes in obesity prevention. And, it worked because of early intervention.
Thank you USPSTF, but 6 years is too late.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
As we begin to find our way in the new world of obesity management, questions continue to surface more quickly than answers. This isn’t surprising, as we are being asked to view obesity as a disease when for decades the general consensus has been that overweight people are simply will power deficient.
Are the new drugs as effective as we are told by the patients and physicians who have had some experience using and prescribing them? Will they continue to be effective in the very long run? Will their safety record hold up over time? And for those of us in pediatrics, what will be their role for children? As a group we tend to be cautious about drugs that haven’t been thoroughly tested in children. How many years will it take before we feel comfortable with obesity drugs? And, of course, we should be asking ourselves the same questions about bariatric surgery.
Fortunately, while the media spotlight has been focused on the treatment arm of our obesity strategy, there are still some folks looking at what has been up to now the discouraging prospects for prevention. The U.S. Preventive Services Task Force (USPSTF) has recently released a draft of its recommendations that includes evidence supporting the effectiveness of “intensive behavioral interventions” (defined as a minimum of 26 hours of counseling). In reviewing data from nearly 60 randomized controlled trials, which included more than 10,000 children, the task force found that It should be noted that the USPSTF gave the intervention package only a B grade, which means that the agency found evidence of high certainty of a moderate benefit over an unspecified time period. Certainly, not a ringing endorsement.
While I think we must applaud the diligent efforts of the task force and its commitment to prevention, I fear that the strategy is too little too late. That being said, I am willing to accept the idea that targeting age 6 for intensive counseling may qualify for the better-late-than-never category. The task force acknowledges that procuring the resources given our already understaffed mental health clinics is going to be difficult and expensive. I would add that it will be so costly in time and money as to be unrealistic.
Based on my observations of thousands of children, the scaffolding of habits, diet, and preference for inactivity that underly obesity has already been laid by age 6. Are we prepared to shoulder our already overburdened school systems in an attempt to reconfigure this foundation of an obesogenic lifestyle? An effort on this scale after children have been sent off to first grade is doomed to failure.
A recent review of data reported by the CDC and reviewed in the journal Pediatrics reveals that about 2% of children receiving federal assistance from the WIC program are severely obese. It is probably safe to say that these preschoolers represent just the tip of a very concerning iceberg.
By waiting until age 6, we would increase the risk of further stigmatizing the obese child. What will he tell his peers when he is taken out of school or misses a playdate because he has to meet with his “obesity counselor”?
If we are going to take obesity prevention seriously and spend time and money in counseling, doesn’t it make more sense to invest this effort on the parents and the home situation when the child is still under their influence? We must be prepared to unwrap and employ an “intensive behavioral package” the first time we see evidence that the child’s growth chart is heading in an unhealthy direction.
This won’t always be easy. I can recall seeing a 4-year-old whose weight had risen dramatically from her previous curve in the year since her 3-year checkup. The answer became obvious when I discovered that her grandmother, for whom baking was a passion, had taken over as her daycare provider. Arriving at a solution that kept the family on speaking terms took some tact, but it was one of my rare successes in obesity prevention. And, it worked because of early intervention.
Thank you USPSTF, but 6 years is too late.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
As we begin to find our way in the new world of obesity management, questions continue to surface more quickly than answers. This isn’t surprising, as we are being asked to view obesity as a disease when for decades the general consensus has been that overweight people are simply will power deficient.
Are the new drugs as effective as we are told by the patients and physicians who have had some experience using and prescribing them? Will they continue to be effective in the very long run? Will their safety record hold up over time? And for those of us in pediatrics, what will be their role for children? As a group we tend to be cautious about drugs that haven’t been thoroughly tested in children. How many years will it take before we feel comfortable with obesity drugs? And, of course, we should be asking ourselves the same questions about bariatric surgery.
Fortunately, while the media spotlight has been focused on the treatment arm of our obesity strategy, there are still some folks looking at what has been up to now the discouraging prospects for prevention. The U.S. Preventive Services Task Force (USPSTF) has recently released a draft of its recommendations that includes evidence supporting the effectiveness of “intensive behavioral interventions” (defined as a minimum of 26 hours of counseling). In reviewing data from nearly 60 randomized controlled trials, which included more than 10,000 children, the task force found that It should be noted that the USPSTF gave the intervention package only a B grade, which means that the agency found evidence of high certainty of a moderate benefit over an unspecified time period. Certainly, not a ringing endorsement.
While I think we must applaud the diligent efforts of the task force and its commitment to prevention, I fear that the strategy is too little too late. That being said, I am willing to accept the idea that targeting age 6 for intensive counseling may qualify for the better-late-than-never category. The task force acknowledges that procuring the resources given our already understaffed mental health clinics is going to be difficult and expensive. I would add that it will be so costly in time and money as to be unrealistic.
Based on my observations of thousands of children, the scaffolding of habits, diet, and preference for inactivity that underly obesity has already been laid by age 6. Are we prepared to shoulder our already overburdened school systems in an attempt to reconfigure this foundation of an obesogenic lifestyle? An effort on this scale after children have been sent off to first grade is doomed to failure.
A recent review of data reported by the CDC and reviewed in the journal Pediatrics reveals that about 2% of children receiving federal assistance from the WIC program are severely obese. It is probably safe to say that these preschoolers represent just the tip of a very concerning iceberg.
By waiting until age 6, we would increase the risk of further stigmatizing the obese child. What will he tell his peers when he is taken out of school or misses a playdate because he has to meet with his “obesity counselor”?
If we are going to take obesity prevention seriously and spend time and money in counseling, doesn’t it make more sense to invest this effort on the parents and the home situation when the child is still under their influence? We must be prepared to unwrap and employ an “intensive behavioral package” the first time we see evidence that the child’s growth chart is heading in an unhealthy direction.
This won’t always be easy. I can recall seeing a 4-year-old whose weight had risen dramatically from her previous curve in the year since her 3-year checkup. The answer became obvious when I discovered that her grandmother, for whom baking was a passion, had taken over as her daycare provider. Arriving at a solution that kept the family on speaking terms took some tact, but it was one of my rare successes in obesity prevention. And, it worked because of early intervention.
Thank you USPSTF, but 6 years is too late.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Can a Healthy Gut Microbiome Prevent Kidney Stones?
TOPLINE:
Gut and urinary microbiota alterations appear to play key roles in the development of kidney stones, suggesting that
Kidney stones are commonly formed by calcium oxalate produced by the body, but the findings suggest that in efforts to better understand the formation and prevention of the stones, focus should shift away from the long-held focus on specific gut bacterium, such as Oxalobacter formigenesm,to apparent systems-level microbial imbalances.
METHODOLOGY:
- The authors evaluated the gut, urinary, and oral microbiota of 83 patients having kidney stones surgically removed at St. Joseph’s Hospital in London, Ontario, and compared them to 30 healthy controls recruited between August 2015 and January 2019.
- Analysis using measures including shotgun metagenomic sequencing were used to identify specific gut bacteria and the genetic capabilities of the bacteria, and simpler sequencing was conducted using oral and urinary microbiota samples.
- Patients had no antibiotic exposure within the previous 90 days.
TAKEAWAY:
- Significant differences were observed in disturbances in microbiota in all three microbiomes among those who did and did not form kidney stones.
- Patients who formed kidney stones also showed more antibiotic-resistant genes, suggesting greater exposure to antimicrobials.
- Those who had formed kidney stones had reduced taxonomic and functional diversity compared with healthy controls.
- Core functional bioenergetic pathways had been replaced with virulence-associated gene markers in gut and urinary microbiota in those with kidney stones.
- And community network microbiota had collapsed among those with kidney stones.
- “These multisite microbial community shifts may be the result of deleterious environmental factors including antibiotic exposure,” the authors speculated.
- However, no differences were observed between the cohorts in terms of oxalate metabolism — commonly considered a culprit in kidney stone formation.
IN PRACTICE:
- “We found not only that those who got kidney stones had an unhealthy microbiome, including a gut microbiome that was more likely to excrete toxins to the kidneys, but also that they were antibiotic resistant,” explains senior author Jeremy Burton, PhD, the Lawson Scientist and Research Chair of Human Microbiome and Probiotics at St. Joseph’s Health Care London, in a press statement.
- “We conclude that multisite microbiota alteration is a hallmark of stone formation, and kidney stone disease treatment should consider microbial functional restoration and the avoidance of aberrant modulators such as poor diet and antibiotics, where applicable, to prevent stone recurrence,” the authors further wrote in the study.
- “Based on these findings, we suggest that the historic emphasis put on O formigenes and other direct oxalate-handling taxa should be discontinued in favor of mechanistic study into the apparent systems-level microbial imbalances in kidney stone formers,” they said.
SOURCE:
The study was published in Microbiome.
It was conducted by the first author Kait F. Al, PhD, of the department of microbiology and immunology, The University of Western Ontario, London, and colleagues.
LIMITATIONS:
The sampling techniques used in the study provide relative compositional but not absolute abundance information, and the sequencing methods do not provide taxonomic annotation to the species level in all cases.
“For this reason, as well as the problematic nature of comparison across sequencing methodologies, caution should be taken when comparing these data and taxonomic annotations in future studies,” the authors noted.
Furthermore, as the study was observational, causality of stone disease cannot be established to the differences detected between the microbiota of healthy control individuals and those with kidney stones.
DISCLOSURES:
The authors had no disclosures to report.
A version of this article appeared on Medscape.com.
TOPLINE:
Gut and urinary microbiota alterations appear to play key roles in the development of kidney stones, suggesting that
Kidney stones are commonly formed by calcium oxalate produced by the body, but the findings suggest that in efforts to better understand the formation and prevention of the stones, focus should shift away from the long-held focus on specific gut bacterium, such as Oxalobacter formigenesm,to apparent systems-level microbial imbalances.
METHODOLOGY:
- The authors evaluated the gut, urinary, and oral microbiota of 83 patients having kidney stones surgically removed at St. Joseph’s Hospital in London, Ontario, and compared them to 30 healthy controls recruited between August 2015 and January 2019.
- Analysis using measures including shotgun metagenomic sequencing were used to identify specific gut bacteria and the genetic capabilities of the bacteria, and simpler sequencing was conducted using oral and urinary microbiota samples.
- Patients had no antibiotic exposure within the previous 90 days.
TAKEAWAY:
- Significant differences were observed in disturbances in microbiota in all three microbiomes among those who did and did not form kidney stones.
- Patients who formed kidney stones also showed more antibiotic-resistant genes, suggesting greater exposure to antimicrobials.
- Those who had formed kidney stones had reduced taxonomic and functional diversity compared with healthy controls.
- Core functional bioenergetic pathways had been replaced with virulence-associated gene markers in gut and urinary microbiota in those with kidney stones.
- And community network microbiota had collapsed among those with kidney stones.
- “These multisite microbial community shifts may be the result of deleterious environmental factors including antibiotic exposure,” the authors speculated.
- However, no differences were observed between the cohorts in terms of oxalate metabolism — commonly considered a culprit in kidney stone formation.
IN PRACTICE:
- “We found not only that those who got kidney stones had an unhealthy microbiome, including a gut microbiome that was more likely to excrete toxins to the kidneys, but also that they were antibiotic resistant,” explains senior author Jeremy Burton, PhD, the Lawson Scientist and Research Chair of Human Microbiome and Probiotics at St. Joseph’s Health Care London, in a press statement.
- “We conclude that multisite microbiota alteration is a hallmark of stone formation, and kidney stone disease treatment should consider microbial functional restoration and the avoidance of aberrant modulators such as poor diet and antibiotics, where applicable, to prevent stone recurrence,” the authors further wrote in the study.
- “Based on these findings, we suggest that the historic emphasis put on O formigenes and other direct oxalate-handling taxa should be discontinued in favor of mechanistic study into the apparent systems-level microbial imbalances in kidney stone formers,” they said.
SOURCE:
The study was published in Microbiome.
It was conducted by the first author Kait F. Al, PhD, of the department of microbiology and immunology, The University of Western Ontario, London, and colleagues.
LIMITATIONS:
The sampling techniques used in the study provide relative compositional but not absolute abundance information, and the sequencing methods do not provide taxonomic annotation to the species level in all cases.
“For this reason, as well as the problematic nature of comparison across sequencing methodologies, caution should be taken when comparing these data and taxonomic annotations in future studies,” the authors noted.
Furthermore, as the study was observational, causality of stone disease cannot be established to the differences detected between the microbiota of healthy control individuals and those with kidney stones.
DISCLOSURES:
The authors had no disclosures to report.
A version of this article appeared on Medscape.com.
TOPLINE:
Gut and urinary microbiota alterations appear to play key roles in the development of kidney stones, suggesting that
Kidney stones are commonly formed by calcium oxalate produced by the body, but the findings suggest that in efforts to better understand the formation and prevention of the stones, focus should shift away from the long-held focus on specific gut bacterium, such as Oxalobacter formigenesm,to apparent systems-level microbial imbalances.
METHODOLOGY:
- The authors evaluated the gut, urinary, and oral microbiota of 83 patients having kidney stones surgically removed at St. Joseph’s Hospital in London, Ontario, and compared them to 30 healthy controls recruited between August 2015 and January 2019.
- Analysis using measures including shotgun metagenomic sequencing were used to identify specific gut bacteria and the genetic capabilities of the bacteria, and simpler sequencing was conducted using oral and urinary microbiota samples.
- Patients had no antibiotic exposure within the previous 90 days.
TAKEAWAY:
- Significant differences were observed in disturbances in microbiota in all three microbiomes among those who did and did not form kidney stones.
- Patients who formed kidney stones also showed more antibiotic-resistant genes, suggesting greater exposure to antimicrobials.
- Those who had formed kidney stones had reduced taxonomic and functional diversity compared with healthy controls.
- Core functional bioenergetic pathways had been replaced with virulence-associated gene markers in gut and urinary microbiota in those with kidney stones.
- And community network microbiota had collapsed among those with kidney stones.
- “These multisite microbial community shifts may be the result of deleterious environmental factors including antibiotic exposure,” the authors speculated.
- However, no differences were observed between the cohorts in terms of oxalate metabolism — commonly considered a culprit in kidney stone formation.
IN PRACTICE:
- “We found not only that those who got kidney stones had an unhealthy microbiome, including a gut microbiome that was more likely to excrete toxins to the kidneys, but also that they were antibiotic resistant,” explains senior author Jeremy Burton, PhD, the Lawson Scientist and Research Chair of Human Microbiome and Probiotics at St. Joseph’s Health Care London, in a press statement.
- “We conclude that multisite microbiota alteration is a hallmark of stone formation, and kidney stone disease treatment should consider microbial functional restoration and the avoidance of aberrant modulators such as poor diet and antibiotics, where applicable, to prevent stone recurrence,” the authors further wrote in the study.
- “Based on these findings, we suggest that the historic emphasis put on O formigenes and other direct oxalate-handling taxa should be discontinued in favor of mechanistic study into the apparent systems-level microbial imbalances in kidney stone formers,” they said.
SOURCE:
The study was published in Microbiome.
It was conducted by the first author Kait F. Al, PhD, of the department of microbiology and immunology, The University of Western Ontario, London, and colleagues.
LIMITATIONS:
The sampling techniques used in the study provide relative compositional but not absolute abundance information, and the sequencing methods do not provide taxonomic annotation to the species level in all cases.
“For this reason, as well as the problematic nature of comparison across sequencing methodologies, caution should be taken when comparing these data and taxonomic annotations in future studies,” the authors noted.
Furthermore, as the study was observational, causality of stone disease cannot be established to the differences detected between the microbiota of healthy control individuals and those with kidney stones.
DISCLOSURES:
The authors had no disclosures to report.
A version of this article appeared on Medscape.com.





