User login
Compared With Interferon, Fingolimod Improves MRI Outcomes of Pediatric MS
NASHVILLE—In patients with pediatric-onset multiple sclerosis (MS), fingolimod significantly reduces MRI activity and slows brain volume loss for as long as two years, compared with interferon beta-1a, according to data described at the 2018 CMSC Annual Meeting.
Analyzing the PARADIGMS Data
PARADIGMS was a double-blind, double-dummy, active-controlled, parallel-group, multicenter study in which patients participated for as long as two years. The investigators randomized patients with pediatric-onset MS (ages 10 through 17) to oral fingolimod or interferon beta-1a. The dose of fingolimod was adjusted for body weight. MRI was performed at baseline and every six months thereafter until the end of the study core phase. A central reading center analyzed the MRI results. The key MRI outcomes were the number of new or newly enlarged T2 lesions and gadolinium-enhancing T1 lesions, annual rate of brain volume change, number of new T1 hypointense lesions, change in total T2 hyperintense lesion volume, and number of combined unique active lesions.
The researchers randomized 107 participants to oral fingolimod and 108 to interferon beta-1a. At baseline, mean age was about 15. Most patients were female. Mean disease duration was one to two years. The average number of relapses in the year before screening was approximately 1.5. Participants had 2.6 to 3.1 gadolinium-enhancing T1 lesions.
Data Support Fingolimod’s Efficacy in Pediatric MS
At the end of the study, fingolimod significantly reduced the annualized rate of new or newly enlarged T2 lesions by 52.6% and the number of gadolinium-enhancing T1 lesions per scan by 66.0%, compared with interferon beta-1a. The odds ratio of freedom from new or newly enlarged T2 lesions was 4.51 in the fingolimod arm, compared with the interferon beta-1a arm. The odds ratio of freedom from gadolinium-enhancing lesions was 3.0 in the fingolimod arm, compared with the interferon beta-1a arm.
Compared with interferon beta-1a, treatment with fingolimod for as long as two years significantly reduced the annualized rate of brain volume change (least squares mean: −0.48 vs −0.80). Fingolimod reduced the annualized rate of new T1 hypointense lesions by 62.8% and the number of combined unique active lesions per scan by 60.7%, compared with interferon beta-1a. Fingolimod also reduced T2 hyperintense lesion volume, compared with interferon beta-1a (percentage change from baseline: 18.4% vs 32.4%).
“The rate of T2-related atrophy [in pediatric MS] is concerning, and I am particularly interested in looking at the extension study data as they come out, and we’ll see if there is a decrease during longer-term treatment,” said Dr. Chitnis.
“These results, overall, along with the efficacy demonstrated on the clinical relapse rate, support the overall benefit of fingolimod in pediatric patients with MS,” she concluded.
—Erik Greb
NASHVILLE—In patients with pediatric-onset multiple sclerosis (MS), fingolimod significantly reduces MRI activity and slows brain volume loss for as long as two years, compared with interferon beta-1a, according to data described at the 2018 CMSC Annual Meeting.
Analyzing the PARADIGMS Data
PARADIGMS was a double-blind, double-dummy, active-controlled, parallel-group, multicenter study in which patients participated for as long as two years. The investigators randomized patients with pediatric-onset MS (ages 10 through 17) to oral fingolimod or interferon beta-1a. The dose of fingolimod was adjusted for body weight. MRI was performed at baseline and every six months thereafter until the end of the study core phase. A central reading center analyzed the MRI results. The key MRI outcomes were the number of new or newly enlarged T2 lesions and gadolinium-enhancing T1 lesions, annual rate of brain volume change, number of new T1 hypointense lesions, change in total T2 hyperintense lesion volume, and number of combined unique active lesions.
The researchers randomized 107 participants to oral fingolimod and 108 to interferon beta-1a. At baseline, mean age was about 15. Most patients were female. Mean disease duration was one to two years. The average number of relapses in the year before screening was approximately 1.5. Participants had 2.6 to 3.1 gadolinium-enhancing T1 lesions.
Data Support Fingolimod’s Efficacy in Pediatric MS
At the end of the study, fingolimod significantly reduced the annualized rate of new or newly enlarged T2 lesions by 52.6% and the number of gadolinium-enhancing T1 lesions per scan by 66.0%, compared with interferon beta-1a. The odds ratio of freedom from new or newly enlarged T2 lesions was 4.51 in the fingolimod arm, compared with the interferon beta-1a arm. The odds ratio of freedom from gadolinium-enhancing lesions was 3.0 in the fingolimod arm, compared with the interferon beta-1a arm.
Compared with interferon beta-1a, treatment with fingolimod for as long as two years significantly reduced the annualized rate of brain volume change (least squares mean: −0.48 vs −0.80). Fingolimod reduced the annualized rate of new T1 hypointense lesions by 62.8% and the number of combined unique active lesions per scan by 60.7%, compared with interferon beta-1a. Fingolimod also reduced T2 hyperintense lesion volume, compared with interferon beta-1a (percentage change from baseline: 18.4% vs 32.4%).
“The rate of T2-related atrophy [in pediatric MS] is concerning, and I am particularly interested in looking at the extension study data as they come out, and we’ll see if there is a decrease during longer-term treatment,” said Dr. Chitnis.
“These results, overall, along with the efficacy demonstrated on the clinical relapse rate, support the overall benefit of fingolimod in pediatric patients with MS,” she concluded.
—Erik Greb
NASHVILLE—In patients with pediatric-onset multiple sclerosis (MS), fingolimod significantly reduces MRI activity and slows brain volume loss for as long as two years, compared with interferon beta-1a, according to data described at the 2018 CMSC Annual Meeting.
Analyzing the PARADIGMS Data
PARADIGMS was a double-blind, double-dummy, active-controlled, parallel-group, multicenter study in which patients participated for as long as two years. The investigators randomized patients with pediatric-onset MS (ages 10 through 17) to oral fingolimod or interferon beta-1a. The dose of fingolimod was adjusted for body weight. MRI was performed at baseline and every six months thereafter until the end of the study core phase. A central reading center analyzed the MRI results. The key MRI outcomes were the number of new or newly enlarged T2 lesions and gadolinium-enhancing T1 lesions, annual rate of brain volume change, number of new T1 hypointense lesions, change in total T2 hyperintense lesion volume, and number of combined unique active lesions.
The researchers randomized 107 participants to oral fingolimod and 108 to interferon beta-1a. At baseline, mean age was about 15. Most patients were female. Mean disease duration was one to two years. The average number of relapses in the year before screening was approximately 1.5. Participants had 2.6 to 3.1 gadolinium-enhancing T1 lesions.
Data Support Fingolimod’s Efficacy in Pediatric MS
At the end of the study, fingolimod significantly reduced the annualized rate of new or newly enlarged T2 lesions by 52.6% and the number of gadolinium-enhancing T1 lesions per scan by 66.0%, compared with interferon beta-1a. The odds ratio of freedom from new or newly enlarged T2 lesions was 4.51 in the fingolimod arm, compared with the interferon beta-1a arm. The odds ratio of freedom from gadolinium-enhancing lesions was 3.0 in the fingolimod arm, compared with the interferon beta-1a arm.
Compared with interferon beta-1a, treatment with fingolimod for as long as two years significantly reduced the annualized rate of brain volume change (least squares mean: −0.48 vs −0.80). Fingolimod reduced the annualized rate of new T1 hypointense lesions by 62.8% and the number of combined unique active lesions per scan by 60.7%, compared with interferon beta-1a. Fingolimod also reduced T2 hyperintense lesion volume, compared with interferon beta-1a (percentage change from baseline: 18.4% vs 32.4%).
“The rate of T2-related atrophy [in pediatric MS] is concerning, and I am particularly interested in looking at the extension study data as they come out, and we’ll see if there is a decrease during longer-term treatment,” said Dr. Chitnis.
“These results, overall, along with the efficacy demonstrated on the clinical relapse rate, support the overall benefit of fingolimod in pediatric patients with MS,” she concluded.
—Erik Greb
Can Exercise Improve Vision in Children With MS?
A positive association was observed between moderate-to-vigorous physical activity and retinal nerve fiber layer thickness in pediatric patients.
NASHVILLE—Moderate-to-vigorous physical activity is positively associated with retinal nerve fiber layer thickness in children with multiple sclerosis (MS), according to research presented at the 2018 CMSC Annual Meeting. This finding may help to support an intervention targeting moderate-to-vigorous physical activity to improve anterior visual pathway integrity in children with MS.
More than one-third of pediatric patients with MS experience optic neuritis, and most experience visual pathway abnormalities, including reductions in the retinal nerve fiber layer and ganglion cell inner-plexiform layer. Previous studies in
To investigate the associations between mild-to-vigorous physical activity, the retinal nerve fiber layer, and the ganglion cell inner-plexiform layer in pediatric patients with MS, Alexander L. Pearson, a medical student at the University of Ottawa in Ontario, and colleagues conducted a cross-sectional study.
The researchers recruited participants from the Pediatric MS and Demyelinating Disorders Center at the Hospital for Sick Children in Toronto. Eligible participants had a diagnosis of MS (according to the International Pediatric MS Study Group consensus definitions) and were younger than 18. Patients with neuroinflammatory abnormalities associated with underlying systemic or neurologic disorders, recurrent neuroinflammatory disorders other than MS, coexisting ocular pathologies, visual acuity ±6 diopters or worse, were excluded.
Participants received standardized visual evaluations, including ocular coherence tomography. Investigators performed evaluations more than 90 days after an optic neuritis episode using a spectral-domain ocular coherence tomography Cirrus scanner. Participants also completed the Godin Leisure-Time Exercise Questionnaire (GLTEQ) more than 30 days after a relapse. This questionnaire was used to calculate the health contribution score.
Generalized linear models were used to assess the associations between moderate-to-vigorous physical activity, the retinal nerve fiber layer, and the ganglion cell inner-plexiform layer when controlling for sex, number of optic neuritis episodes, disease duration at time of ocular coherence tomography, and within-subject correlation between eyes. Bonferroni correction was used to adjust for multiple comparisons.
Thirty patients participated in this study; 23 were female. Ocular coherence tomography was performed at a mean age of 15.7 (range, 10.6–18.0) and a median of 1.9 years from disease onset. The median retinal nerve fiber layer was 90 μm, and the median ganglion cell inner-plexiform layer was 73.5 μm. The median amount of moderate-to-vigorous physical activity was 26.5 metabolic equivalents per week.
The research team found that moderate-to-vigorous physical activity was positively associated with retinal nerve fiber layer thickness. Although the retinal nerve fiber layer and ganglion cell inner-plexiform layer were moderately correlated, moderate-to-vigorous physical activity was not associated with the ganglion cell inner-plexiform layer, said the authors.
“Next steps include a trial using mild-to-vigorous physical activity to improve anterior visual pathway integrity in children with MS,” the researchers concluded.
A positive association was observed between moderate-to-vigorous physical activity and retinal nerve fiber layer thickness in pediatric patients.
A positive association was observed between moderate-to-vigorous physical activity and retinal nerve fiber layer thickness in pediatric patients.
NASHVILLE—Moderate-to-vigorous physical activity is positively associated with retinal nerve fiber layer thickness in children with multiple sclerosis (MS), according to research presented at the 2018 CMSC Annual Meeting. This finding may help to support an intervention targeting moderate-to-vigorous physical activity to improve anterior visual pathway integrity in children with MS.
More than one-third of pediatric patients with MS experience optic neuritis, and most experience visual pathway abnormalities, including reductions in the retinal nerve fiber layer and ganglion cell inner-plexiform layer. Previous studies in
To investigate the associations between mild-to-vigorous physical activity, the retinal nerve fiber layer, and the ganglion cell inner-plexiform layer in pediatric patients with MS, Alexander L. Pearson, a medical student at the University of Ottawa in Ontario, and colleagues conducted a cross-sectional study.
The researchers recruited participants from the Pediatric MS and Demyelinating Disorders Center at the Hospital for Sick Children in Toronto. Eligible participants had a diagnosis of MS (according to the International Pediatric MS Study Group consensus definitions) and were younger than 18. Patients with neuroinflammatory abnormalities associated with underlying systemic or neurologic disorders, recurrent neuroinflammatory disorders other than MS, coexisting ocular pathologies, visual acuity ±6 diopters or worse, were excluded.
Participants received standardized visual evaluations, including ocular coherence tomography. Investigators performed evaluations more than 90 days after an optic neuritis episode using a spectral-domain ocular coherence tomography Cirrus scanner. Participants also completed the Godin Leisure-Time Exercise Questionnaire (GLTEQ) more than 30 days after a relapse. This questionnaire was used to calculate the health contribution score.
Generalized linear models were used to assess the associations between moderate-to-vigorous physical activity, the retinal nerve fiber layer, and the ganglion cell inner-plexiform layer when controlling for sex, number of optic neuritis episodes, disease duration at time of ocular coherence tomography, and within-subject correlation between eyes. Bonferroni correction was used to adjust for multiple comparisons.
Thirty patients participated in this study; 23 were female. Ocular coherence tomography was performed at a mean age of 15.7 (range, 10.6–18.0) and a median of 1.9 years from disease onset. The median retinal nerve fiber layer was 90 μm, and the median ganglion cell inner-plexiform layer was 73.5 μm. The median amount of moderate-to-vigorous physical activity was 26.5 metabolic equivalents per week.
The research team found that moderate-to-vigorous physical activity was positively associated with retinal nerve fiber layer thickness. Although the retinal nerve fiber layer and ganglion cell inner-plexiform layer were moderately correlated, moderate-to-vigorous physical activity was not associated with the ganglion cell inner-plexiform layer, said the authors.
“Next steps include a trial using mild-to-vigorous physical activity to improve anterior visual pathway integrity in children with MS,” the researchers concluded.
NASHVILLE—Moderate-to-vigorous physical activity is positively associated with retinal nerve fiber layer thickness in children with multiple sclerosis (MS), according to research presented at the 2018 CMSC Annual Meeting. This finding may help to support an intervention targeting moderate-to-vigorous physical activity to improve anterior visual pathway integrity in children with MS.
More than one-third of pediatric patients with MS experience optic neuritis, and most experience visual pathway abnormalities, including reductions in the retinal nerve fiber layer and ganglion cell inner-plexiform layer. Previous studies in
To investigate the associations between mild-to-vigorous physical activity, the retinal nerve fiber layer, and the ganglion cell inner-plexiform layer in pediatric patients with MS, Alexander L. Pearson, a medical student at the University of Ottawa in Ontario, and colleagues conducted a cross-sectional study.
The researchers recruited participants from the Pediatric MS and Demyelinating Disorders Center at the Hospital for Sick Children in Toronto. Eligible participants had a diagnosis of MS (according to the International Pediatric MS Study Group consensus definitions) and were younger than 18. Patients with neuroinflammatory abnormalities associated with underlying systemic or neurologic disorders, recurrent neuroinflammatory disorders other than MS, coexisting ocular pathologies, visual acuity ±6 diopters or worse, were excluded.
Participants received standardized visual evaluations, including ocular coherence tomography. Investigators performed evaluations more than 90 days after an optic neuritis episode using a spectral-domain ocular coherence tomography Cirrus scanner. Participants also completed the Godin Leisure-Time Exercise Questionnaire (GLTEQ) more than 30 days after a relapse. This questionnaire was used to calculate the health contribution score.
Generalized linear models were used to assess the associations between moderate-to-vigorous physical activity, the retinal nerve fiber layer, and the ganglion cell inner-plexiform layer when controlling for sex, number of optic neuritis episodes, disease duration at time of ocular coherence tomography, and within-subject correlation between eyes. Bonferroni correction was used to adjust for multiple comparisons.
Thirty patients participated in this study; 23 were female. Ocular coherence tomography was performed at a mean age of 15.7 (range, 10.6–18.0) and a median of 1.9 years from disease onset. The median retinal nerve fiber layer was 90 μm, and the median ganglion cell inner-plexiform layer was 73.5 μm. The median amount of moderate-to-vigorous physical activity was 26.5 metabolic equivalents per week.
The research team found that moderate-to-vigorous physical activity was positively associated with retinal nerve fiber layer thickness. Although the retinal nerve fiber layer and ganglion cell inner-plexiform layer were moderately correlated, moderate-to-vigorous physical activity was not associated with the ganglion cell inner-plexiform layer, said the authors.
“Next steps include a trial using mild-to-vigorous physical activity to improve anterior visual pathway integrity in children with MS,” the researchers concluded.
More Frequent Dosing of Interferon Beta-1a May Benefit Patients With MS With Breakthrough Disease
NASHVILLE—Patients with multiple sclerosis (MS) with breakthrough disease may benefit from intramuscular interferon beta 1-a treatment twice per week, according to research described at the 2018 CMSC Annual Meeting. “Advantages to using an intramuscular interferon beta 1-a preparation include no skin reactions and a lower incidence of interferon neutralizing antibodies,” said Robert W. Baumhefner, MD, a neurologist at the Veteran Affairs West Los Angeles Medical Center.
Previous clinical trials have suggested a dose-response effect for interferon beta in MS. The European Interferon Beta-1a Dose Comparison Study, however, found no change in efficacy with just doubling the standard dose of intramuscular interferon beta-1a once per week. This may not be the same as increasing the frequency of intramuscular interferon administration, said Baumhefner. In addition, none of the previous studies have information on patients with breakthrough disease on standard-dose intramuscular interferon beta-1a switched to twice-weekly dosing.
Dr. Baumhefner conducted a retrospective observational study of patients MS with breakthrough disease receiving intramuscular interferon beta 1-a once per week who were switched to intramuscular interferon beta 1-a twice per week.
A total of 107 patients with MS were started on intramuscular interferon beta 1-a from 1995 to 2015 at the MS clinic of the VA West Los Angeles Medical Center. Of these, 59 patients with breakthrough disease were switched to twice-weekly intramuscular interferon beta-1a. There was adequate follow-up for at least two years for 52 of these patients. In addition, participants were followed up an average of every four months.
At each visit, an interval history of any relapse; scores on the Incapacity Status Scale, Functional Systems Scale, and Expanded Disability Status Scale (EDSS); and a proprietary graded neurologic examination were obtained. Annual MRI of the brain using a contrast-enhanced MS protocol was obtained in most patients. Baumhefner defined breakthrough disease as continued clinical relapses, new T2 or enhanced lesions on MRI, or worsening of EDSS or neurologic examination.
Of the 52 patients with adequate follow-up, 26 had no further breakthrough disease for 14 months or longer (range, 14-192 months). Five patients did not tolerate the increase in frequency of administration. Interferon beta neutralizing antibody testing was performed on 25 patients while they were receiving twice-weekly dosing. One patient who failed twice-weekly interferon beta had consistently elevated titers on two determinations (4%). African American patients, those with a higher EDSS score when switching, and patients with a longer duration of stability on weekly dosed treatment may be less likely to respond, the researcher concluded.
NASHVILLE—Patients with multiple sclerosis (MS) with breakthrough disease may benefit from intramuscular interferon beta 1-a treatment twice per week, according to research described at the 2018 CMSC Annual Meeting. “Advantages to using an intramuscular interferon beta 1-a preparation include no skin reactions and a lower incidence of interferon neutralizing antibodies,” said Robert W. Baumhefner, MD, a neurologist at the Veteran Affairs West Los Angeles Medical Center.
Previous clinical trials have suggested a dose-response effect for interferon beta in MS. The European Interferon Beta-1a Dose Comparison Study, however, found no change in efficacy with just doubling the standard dose of intramuscular interferon beta-1a once per week. This may not be the same as increasing the frequency of intramuscular interferon administration, said Baumhefner. In addition, none of the previous studies have information on patients with breakthrough disease on standard-dose intramuscular interferon beta-1a switched to twice-weekly dosing.
Dr. Baumhefner conducted a retrospective observational study of patients MS with breakthrough disease receiving intramuscular interferon beta 1-a once per week who were switched to intramuscular interferon beta 1-a twice per week.
A total of 107 patients with MS were started on intramuscular interferon beta 1-a from 1995 to 2015 at the MS clinic of the VA West Los Angeles Medical Center. Of these, 59 patients with breakthrough disease were switched to twice-weekly intramuscular interferon beta-1a. There was adequate follow-up for at least two years for 52 of these patients. In addition, participants were followed up an average of every four months.
At each visit, an interval history of any relapse; scores on the Incapacity Status Scale, Functional Systems Scale, and Expanded Disability Status Scale (EDSS); and a proprietary graded neurologic examination were obtained. Annual MRI of the brain using a contrast-enhanced MS protocol was obtained in most patients. Baumhefner defined breakthrough disease as continued clinical relapses, new T2 or enhanced lesions on MRI, or worsening of EDSS or neurologic examination.
Of the 52 patients with adequate follow-up, 26 had no further breakthrough disease for 14 months or longer (range, 14-192 months). Five patients did not tolerate the increase in frequency of administration. Interferon beta neutralizing antibody testing was performed on 25 patients while they were receiving twice-weekly dosing. One patient who failed twice-weekly interferon beta had consistently elevated titers on two determinations (4%). African American patients, those with a higher EDSS score when switching, and patients with a longer duration of stability on weekly dosed treatment may be less likely to respond, the researcher concluded.
NASHVILLE—Patients with multiple sclerosis (MS) with breakthrough disease may benefit from intramuscular interferon beta 1-a treatment twice per week, according to research described at the 2018 CMSC Annual Meeting. “Advantages to using an intramuscular interferon beta 1-a preparation include no skin reactions and a lower incidence of interferon neutralizing antibodies,” said Robert W. Baumhefner, MD, a neurologist at the Veteran Affairs West Los Angeles Medical Center.
Previous clinical trials have suggested a dose-response effect for interferon beta in MS. The European Interferon Beta-1a Dose Comparison Study, however, found no change in efficacy with just doubling the standard dose of intramuscular interferon beta-1a once per week. This may not be the same as increasing the frequency of intramuscular interferon administration, said Baumhefner. In addition, none of the previous studies have information on patients with breakthrough disease on standard-dose intramuscular interferon beta-1a switched to twice-weekly dosing.
Dr. Baumhefner conducted a retrospective observational study of patients MS with breakthrough disease receiving intramuscular interferon beta 1-a once per week who were switched to intramuscular interferon beta 1-a twice per week.
A total of 107 patients with MS were started on intramuscular interferon beta 1-a from 1995 to 2015 at the MS clinic of the VA West Los Angeles Medical Center. Of these, 59 patients with breakthrough disease were switched to twice-weekly intramuscular interferon beta-1a. There was adequate follow-up for at least two years for 52 of these patients. In addition, participants were followed up an average of every four months.
At each visit, an interval history of any relapse; scores on the Incapacity Status Scale, Functional Systems Scale, and Expanded Disability Status Scale (EDSS); and a proprietary graded neurologic examination were obtained. Annual MRI of the brain using a contrast-enhanced MS protocol was obtained in most patients. Baumhefner defined breakthrough disease as continued clinical relapses, new T2 or enhanced lesions on MRI, or worsening of EDSS or neurologic examination.
Of the 52 patients with adequate follow-up, 26 had no further breakthrough disease for 14 months or longer (range, 14-192 months). Five patients did not tolerate the increase in frequency of administration. Interferon beta neutralizing antibody testing was performed on 25 patients while they were receiving twice-weekly dosing. One patient who failed twice-weekly interferon beta had consistently elevated titers on two determinations (4%). African American patients, those with a higher EDSS score when switching, and patients with a longer duration of stability on weekly dosed treatment may be less likely to respond, the researcher concluded.
Ocrelizumab’s Benefits on Confirmed Disability Improvement Persist in Open-Label Extension
This outcome remains more likely in patients who started on ocrelizumab than in those who switched to it from interferon beta.
NASHVILLE—The benefits of ocrelizumab on 24-week confirmed disability improvement, which were demonstrated in two-year, double-blind, controlled trials, were maintained for two years in an open-label extension study in patients with relapsing-remitting multiple sclerosis (MS), according to data described at the 2018 CMSC Annual Meeting.
The 96-week, double-blind, controlled periods of the OPERA I and II trials demonstrated the efficacy and safety of ocrelizumab in relapsing-remitting MS. Upon completion of the controlled treatment periods, all patients were eligible to enter an open-label extension phase during which they would receive ocrelizumab. Robert T. Naismith, MD, Associate Professor of Neurology at Washington University School of Medicine in St. Louis, and colleagues reviewed data from this extension phase to assess the effect of switching to ocrelizumab or maintaining ocrelizumab therapy on the proportion of patients experiencing disability improvement.
Difference Between Groups Endured
During the controlled treatment period, patients received IV ocrelizumab (600 mg) every 24 weeks or subcutaneous interferon beta-1a (44 μg) three times weekly for 96 weeks. At the start of the open-label extension period, patients continued ocrelizumab or were switched from interferon beta-1a to ocrelizumab. Disability improvement compared with baseline was defined as a reduction in Expanded Disability Status Scale (EDSS) score of 1.0 or more points for patients with a baseline EDSS score from 2.0 to 5.5, or a reduction of 0.5 or more points for patients with a baseline EDSS score greater than 5.5. Time to onset of 24-week confirmed disability improvement was analyzed in patients with a baseline EDSS score of 2.0 or greater.
More than 89% of patients who entered the open-label extension period completed two years of the open-label extension. The group that started and continued ocrelizumab (n = 454), compared with the group that switched from interferon beta-1a to ocrelizumab (n = 419), had a higher proportion of patients with 24-week confirmed disability improvement in the year before the switch (16.8% vs 13.3%). At year 1 of the extension, the group that started and continued ocrelizumab included 399 participants, and 20.6% had 24-week confirmed disability improvement, compared with 16.6% of the group that switched from interferon beta-1a to ocrelizumab, which included 366 participants. At year 2, the former group included 363 patients, and 23.7% had 24-week confirmed disability improvement. The latter group included 339 participants, and 18.9% of them achieved this outcome.
Analyzing Four Years of Treatment
When the investigators examined data for four years of treatment (ie, the double-blind and extension phases), they observed that between 20% and 25% of patients with an EDSS score of 2 or more who received ocrelizumab had improvement in EDSS score. When they examined patients with EDSS scores lower than 2, the results were similar. “This [finding] parallels some of the effects that we see in clinical efficacy, based upon a reduction in MRI parameters such as T1 and T2 lesions,” said Dr. Naismith.
“What we are seeing, especially with some of our high-efficacy therapies, is that patients come back and report that they are feeling better in subsequent visits. I admit, I never tell patients that this is an expectation they should have…. But it is always nice to hear from a patient that they are doing better in some tangible way in their lives,” Dr. Naismith concluded.
—Erik Greb
This outcome remains more likely in patients who started on ocrelizumab than in those who switched to it from interferon beta.
This outcome remains more likely in patients who started on ocrelizumab than in those who switched to it from interferon beta.
NASHVILLE—The benefits of ocrelizumab on 24-week confirmed disability improvement, which were demonstrated in two-year, double-blind, controlled trials, were maintained for two years in an open-label extension study in patients with relapsing-remitting multiple sclerosis (MS), according to data described at the 2018 CMSC Annual Meeting.
The 96-week, double-blind, controlled periods of the OPERA I and II trials demonstrated the efficacy and safety of ocrelizumab in relapsing-remitting MS. Upon completion of the controlled treatment periods, all patients were eligible to enter an open-label extension phase during which they would receive ocrelizumab. Robert T. Naismith, MD, Associate Professor of Neurology at Washington University School of Medicine in St. Louis, and colleagues reviewed data from this extension phase to assess the effect of switching to ocrelizumab or maintaining ocrelizumab therapy on the proportion of patients experiencing disability improvement.
Difference Between Groups Endured
During the controlled treatment period, patients received IV ocrelizumab (600 mg) every 24 weeks or subcutaneous interferon beta-1a (44 μg) three times weekly for 96 weeks. At the start of the open-label extension period, patients continued ocrelizumab or were switched from interferon beta-1a to ocrelizumab. Disability improvement compared with baseline was defined as a reduction in Expanded Disability Status Scale (EDSS) score of 1.0 or more points for patients with a baseline EDSS score from 2.0 to 5.5, or a reduction of 0.5 or more points for patients with a baseline EDSS score greater than 5.5. Time to onset of 24-week confirmed disability improvement was analyzed in patients with a baseline EDSS score of 2.0 or greater.
More than 89% of patients who entered the open-label extension period completed two years of the open-label extension. The group that started and continued ocrelizumab (n = 454), compared with the group that switched from interferon beta-1a to ocrelizumab (n = 419), had a higher proportion of patients with 24-week confirmed disability improvement in the year before the switch (16.8% vs 13.3%). At year 1 of the extension, the group that started and continued ocrelizumab included 399 participants, and 20.6% had 24-week confirmed disability improvement, compared with 16.6% of the group that switched from interferon beta-1a to ocrelizumab, which included 366 participants. At year 2, the former group included 363 patients, and 23.7% had 24-week confirmed disability improvement. The latter group included 339 participants, and 18.9% of them achieved this outcome.
Analyzing Four Years of Treatment
When the investigators examined data for four years of treatment (ie, the double-blind and extension phases), they observed that between 20% and 25% of patients with an EDSS score of 2 or more who received ocrelizumab had improvement in EDSS score. When they examined patients with EDSS scores lower than 2, the results were similar. “This [finding] parallels some of the effects that we see in clinical efficacy, based upon a reduction in MRI parameters such as T1 and T2 lesions,” said Dr. Naismith.
“What we are seeing, especially with some of our high-efficacy therapies, is that patients come back and report that they are feeling better in subsequent visits. I admit, I never tell patients that this is an expectation they should have…. But it is always nice to hear from a patient that they are doing better in some tangible way in their lives,” Dr. Naismith concluded.
—Erik Greb
NASHVILLE—The benefits of ocrelizumab on 24-week confirmed disability improvement, which were demonstrated in two-year, double-blind, controlled trials, were maintained for two years in an open-label extension study in patients with relapsing-remitting multiple sclerosis (MS), according to data described at the 2018 CMSC Annual Meeting.
The 96-week, double-blind, controlled periods of the OPERA I and II trials demonstrated the efficacy and safety of ocrelizumab in relapsing-remitting MS. Upon completion of the controlled treatment periods, all patients were eligible to enter an open-label extension phase during which they would receive ocrelizumab. Robert T. Naismith, MD, Associate Professor of Neurology at Washington University School of Medicine in St. Louis, and colleagues reviewed data from this extension phase to assess the effect of switching to ocrelizumab or maintaining ocrelizumab therapy on the proportion of patients experiencing disability improvement.
Difference Between Groups Endured
During the controlled treatment period, patients received IV ocrelizumab (600 mg) every 24 weeks or subcutaneous interferon beta-1a (44 μg) three times weekly for 96 weeks. At the start of the open-label extension period, patients continued ocrelizumab or were switched from interferon beta-1a to ocrelizumab. Disability improvement compared with baseline was defined as a reduction in Expanded Disability Status Scale (EDSS) score of 1.0 or more points for patients with a baseline EDSS score from 2.0 to 5.5, or a reduction of 0.5 or more points for patients with a baseline EDSS score greater than 5.5. Time to onset of 24-week confirmed disability improvement was analyzed in patients with a baseline EDSS score of 2.0 or greater.
More than 89% of patients who entered the open-label extension period completed two years of the open-label extension. The group that started and continued ocrelizumab (n = 454), compared with the group that switched from interferon beta-1a to ocrelizumab (n = 419), had a higher proportion of patients with 24-week confirmed disability improvement in the year before the switch (16.8% vs 13.3%). At year 1 of the extension, the group that started and continued ocrelizumab included 399 participants, and 20.6% had 24-week confirmed disability improvement, compared with 16.6% of the group that switched from interferon beta-1a to ocrelizumab, which included 366 participants. At year 2, the former group included 363 patients, and 23.7% had 24-week confirmed disability improvement. The latter group included 339 participants, and 18.9% of them achieved this outcome.
Analyzing Four Years of Treatment
When the investigators examined data for four years of treatment (ie, the double-blind and extension phases), they observed that between 20% and 25% of patients with an EDSS score of 2 or more who received ocrelizumab had improvement in EDSS score. When they examined patients with EDSS scores lower than 2, the results were similar. “This [finding] parallels some of the effects that we see in clinical efficacy, based upon a reduction in MRI parameters such as T1 and T2 lesions,” said Dr. Naismith.
“What we are seeing, especially with some of our high-efficacy therapies, is that patients come back and report that they are feeling better in subsequent visits. I admit, I never tell patients that this is an expectation they should have…. But it is always nice to hear from a patient that they are doing better in some tangible way in their lives,” Dr. Naismith concluded.
—Erik Greb
Hip pain predicts arthritis mortality beyond comorbidities
Also today, COPD patient subset gains no benefit from low-dose theophylline, Barrett’s segment length and low-grade dysplasia are tied to an increased risk of neoplastic progression, and the vestibular/oculomotor component of concussions warrants more attention.
Listen to the MDedge Daily News podcast for all the details on today’s top news.
Also today, COPD patient subset gains no benefit from low-dose theophylline, Barrett’s segment length and low-grade dysplasia are tied to an increased risk of neoplastic progression, and the vestibular/oculomotor component of concussions warrants more attention.
Listen to the MDedge Daily News podcast for all the details on today’s top news.
Also today, COPD patient subset gains no benefit from low-dose theophylline, Barrett’s segment length and low-grade dysplasia are tied to an increased risk of neoplastic progression, and the vestibular/oculomotor component of concussions warrants more attention.
Listen to the MDedge Daily News podcast for all the details on today’s top news.
Geriatric assessments improve oncologist-patient communications
CHICAGO – Elderly cancer patients have better communication with their oncologists and report greater satisfaction with their care when the oncologists are provided with geriatric assessment summaries prior to the patient visit.
Although “satisfaction” can be subjective, the conclusion about the benefit of previsit geriatric assessments is objective, reported Supriya Gupta Mohile, MD, of the University of Rochester, New York.
“Physicians often don’t know patients’ and caregivers’ age-related concerns, such as concerns about memory or concerns about falling. Many patients and caregivers do not ask about age-related concerns, because of their unclear understanding of the relevance of those issues to an oncology clinical encounter,” she added.
The aim of the researchers was to see whether communication between physicians and their elderly patients could be improved, and patient support needs addressed, with the aid of the Geriatric Assessment (GA), a multidisciplinary diagnostic and treatment instrument.
The GA evaluates patients in the domains of functional status, objective physical performance, comorbidities, cognition, nutritional status, psychological status, and social support, and identifies vulnerabilities that could be addressed by specific interventions.
For example, patients with suboptimal physical performance may trigger recommendations for fall prevention and a review of medications that could increase fall risk. For patients with decrements in functional status, recommendations may include physical therapy, safety evaluation, and/or vision assessment.
Each domain independently predicts morbidity and/or mortality in older patients.
The investigators enrolled 31 oncology practices in the National Cancer Institute’s Community Oncology Research Program that were treating patients aged 70 or older with advanced solid tumors or lymphoma. Patients who were enrolled had at least one impaired GA domain. In all, 542 patients across the sites were enrolled.
All patients in each arm completed the GA.
Randomization was by practice, with practices in arm 1 randomized to receive GA intervention results. Oncologists in this trial arm were provided with a GA summary and list of recommended GA-guided interventions.
Practices in arm 2 (controls) did not receive summaries or lists of recommendations, but oncologists were notified if patients had clinically significant depression or cognitive impairment.
In the intervention group, patients completed all assessments within 30 minutes, and less than 10 minutes of practice staff time was required for administration of objective tests.
The investigators made audio recordings and transcripts of clinic visits after GA in both arms, with two blinded coders evaluating quality of communication and plans for follow-up interventions. Patients were surveyed by telephone about their satisfaction, via the Health Care Climate Questionnaire (HCCQ) and the same instrument modified for age-related concerns (HCCQ-age).
“We found that patients enrolled in the study had a high prevalence of impairments of Geriatric Assessment domains, ranging from over 90% for physical performance, to 25% for psychological status, mainly depression. Of note, more than 30% of patients ... screened positive for cognitive impairment.” Dr. Mohile said.
For the coprimary endpoint of communication about age-related concerns, the mean number of discussions was 7.74 in the GA arm, compared with 4.24 in the control arm, a difference of 3.5 (P less than .0001).
Arm 1 was rated as having more discussions with higher-quality communications (mean 4.42 vs. 2.47, P less than .0001), and had more discussions leading to an intervention (3.08 vs. 1.15, P less than .0001).
Patients in arm 1 consistently rated their satisfaction with communication (the other coprimary endpoint) higher than did patients in arm 2, at both baseline, 4-6 weeks after the visit, and 3 months after the visit.
“This is a very important study that I think is likely to have a direct impact on the care of older patients with cancer,” ASCO expert Joshua A. Jones, MD, of the University of Pennsylvania, Philadelphia, said at the meeting.
“This study shows in a randomized fashion that we can, with a simple intervention, improve communication about what’s really important to older patients with cancer,” he said. “We have interventions, things like physical therapy, things like counseling, supports that can be provided to patients and families as they are thinking through treatment decisions, helping us to provide the most appropriate care for these individuals.”
SOURCE: Mohile SG et al. ASCO 2018, abstract LBA10003.
CHICAGO – Elderly cancer patients have better communication with their oncologists and report greater satisfaction with their care when the oncologists are provided with geriatric assessment summaries prior to the patient visit.
Although “satisfaction” can be subjective, the conclusion about the benefit of previsit geriatric assessments is objective, reported Supriya Gupta Mohile, MD, of the University of Rochester, New York.
“Physicians often don’t know patients’ and caregivers’ age-related concerns, such as concerns about memory or concerns about falling. Many patients and caregivers do not ask about age-related concerns, because of their unclear understanding of the relevance of those issues to an oncology clinical encounter,” she added.
The aim of the researchers was to see whether communication between physicians and their elderly patients could be improved, and patient support needs addressed, with the aid of the Geriatric Assessment (GA), a multidisciplinary diagnostic and treatment instrument.
The GA evaluates patients in the domains of functional status, objective physical performance, comorbidities, cognition, nutritional status, psychological status, and social support, and identifies vulnerabilities that could be addressed by specific interventions.
For example, patients with suboptimal physical performance may trigger recommendations for fall prevention and a review of medications that could increase fall risk. For patients with decrements in functional status, recommendations may include physical therapy, safety evaluation, and/or vision assessment.
Each domain independently predicts morbidity and/or mortality in older patients.
The investigators enrolled 31 oncology practices in the National Cancer Institute’s Community Oncology Research Program that were treating patients aged 70 or older with advanced solid tumors or lymphoma. Patients who were enrolled had at least one impaired GA domain. In all, 542 patients across the sites were enrolled.
All patients in each arm completed the GA.
Randomization was by practice, with practices in arm 1 randomized to receive GA intervention results. Oncologists in this trial arm were provided with a GA summary and list of recommended GA-guided interventions.
Practices in arm 2 (controls) did not receive summaries or lists of recommendations, but oncologists were notified if patients had clinically significant depression or cognitive impairment.
In the intervention group, patients completed all assessments within 30 minutes, and less than 10 minutes of practice staff time was required for administration of objective tests.
The investigators made audio recordings and transcripts of clinic visits after GA in both arms, with two blinded coders evaluating quality of communication and plans for follow-up interventions. Patients were surveyed by telephone about their satisfaction, via the Health Care Climate Questionnaire (HCCQ) and the same instrument modified for age-related concerns (HCCQ-age).
“We found that patients enrolled in the study had a high prevalence of impairments of Geriatric Assessment domains, ranging from over 90% for physical performance, to 25% for psychological status, mainly depression. Of note, more than 30% of patients ... screened positive for cognitive impairment.” Dr. Mohile said.
For the coprimary endpoint of communication about age-related concerns, the mean number of discussions was 7.74 in the GA arm, compared with 4.24 in the control arm, a difference of 3.5 (P less than .0001).
Arm 1 was rated as having more discussions with higher-quality communications (mean 4.42 vs. 2.47, P less than .0001), and had more discussions leading to an intervention (3.08 vs. 1.15, P less than .0001).
Patients in arm 1 consistently rated their satisfaction with communication (the other coprimary endpoint) higher than did patients in arm 2, at both baseline, 4-6 weeks after the visit, and 3 months after the visit.
“This is a very important study that I think is likely to have a direct impact on the care of older patients with cancer,” ASCO expert Joshua A. Jones, MD, of the University of Pennsylvania, Philadelphia, said at the meeting.
“This study shows in a randomized fashion that we can, with a simple intervention, improve communication about what’s really important to older patients with cancer,” he said. “We have interventions, things like physical therapy, things like counseling, supports that can be provided to patients and families as they are thinking through treatment decisions, helping us to provide the most appropriate care for these individuals.”
SOURCE: Mohile SG et al. ASCO 2018, abstract LBA10003.
CHICAGO – Elderly cancer patients have better communication with their oncologists and report greater satisfaction with their care when the oncologists are provided with geriatric assessment summaries prior to the patient visit.
Although “satisfaction” can be subjective, the conclusion about the benefit of previsit geriatric assessments is objective, reported Supriya Gupta Mohile, MD, of the University of Rochester, New York.
“Physicians often don’t know patients’ and caregivers’ age-related concerns, such as concerns about memory or concerns about falling. Many patients and caregivers do not ask about age-related concerns, because of their unclear understanding of the relevance of those issues to an oncology clinical encounter,” she added.
The aim of the researchers was to see whether communication between physicians and their elderly patients could be improved, and patient support needs addressed, with the aid of the Geriatric Assessment (GA), a multidisciplinary diagnostic and treatment instrument.
The GA evaluates patients in the domains of functional status, objective physical performance, comorbidities, cognition, nutritional status, psychological status, and social support, and identifies vulnerabilities that could be addressed by specific interventions.
For example, patients with suboptimal physical performance may trigger recommendations for fall prevention and a review of medications that could increase fall risk. For patients with decrements in functional status, recommendations may include physical therapy, safety evaluation, and/or vision assessment.
Each domain independently predicts morbidity and/or mortality in older patients.
The investigators enrolled 31 oncology practices in the National Cancer Institute’s Community Oncology Research Program that were treating patients aged 70 or older with advanced solid tumors or lymphoma. Patients who were enrolled had at least one impaired GA domain. In all, 542 patients across the sites were enrolled.
All patients in each arm completed the GA.
Randomization was by practice, with practices in arm 1 randomized to receive GA intervention results. Oncologists in this trial arm were provided with a GA summary and list of recommended GA-guided interventions.
Practices in arm 2 (controls) did not receive summaries or lists of recommendations, but oncologists were notified if patients had clinically significant depression or cognitive impairment.
In the intervention group, patients completed all assessments within 30 minutes, and less than 10 minutes of practice staff time was required for administration of objective tests.
The investigators made audio recordings and transcripts of clinic visits after GA in both arms, with two blinded coders evaluating quality of communication and plans for follow-up interventions. Patients were surveyed by telephone about their satisfaction, via the Health Care Climate Questionnaire (HCCQ) and the same instrument modified for age-related concerns (HCCQ-age).
“We found that patients enrolled in the study had a high prevalence of impairments of Geriatric Assessment domains, ranging from over 90% for physical performance, to 25% for psychological status, mainly depression. Of note, more than 30% of patients ... screened positive for cognitive impairment.” Dr. Mohile said.
For the coprimary endpoint of communication about age-related concerns, the mean number of discussions was 7.74 in the GA arm, compared with 4.24 in the control arm, a difference of 3.5 (P less than .0001).
Arm 1 was rated as having more discussions with higher-quality communications (mean 4.42 vs. 2.47, P less than .0001), and had more discussions leading to an intervention (3.08 vs. 1.15, P less than .0001).
Patients in arm 1 consistently rated their satisfaction with communication (the other coprimary endpoint) higher than did patients in arm 2, at both baseline, 4-6 weeks after the visit, and 3 months after the visit.
“This is a very important study that I think is likely to have a direct impact on the care of older patients with cancer,” ASCO expert Joshua A. Jones, MD, of the University of Pennsylvania, Philadelphia, said at the meeting.
“This study shows in a randomized fashion that we can, with a simple intervention, improve communication about what’s really important to older patients with cancer,” he said. “We have interventions, things like physical therapy, things like counseling, supports that can be provided to patients and families as they are thinking through treatment decisions, helping us to provide the most appropriate care for these individuals.”
SOURCE: Mohile SG et al. ASCO 2018, abstract LBA10003.
REPORTING FROM ASCO 2018
Key clinical point: Geriatric cancer patients may have age-related concerns that they don’t bring up during an oncology visit, but that could affect their care.
Major finding: Patients whose oncologists received geriatric assessment results had significantly more and higher quality discussions of age-related concerns, and were significantly more satisfied with their communications at follow-up.
Study details: Cluster randomized controlled trial comprising 542 patients aged 70 and older from 31 community oncology sites.
Disclosures: The National Cancer Institute funded the study. Dr. Mohile disclosed a consulting/advisory role with Seattle Genetics. Dr. Jones reported no conflicts of interest relevant to the study.
Source: Mohile SG et al. ASCO 2018, abstract LBA10003.
Trachelectomy rate for early-stage cervical cancer rises to 17% in younger women
based on a recent analysis of the National Cancer Database.
Of 15,150 patients analyzed, the vast majority (97.1%) underwent hysterectomy, but trachelectomy performance increased from 1.5% (95% confidence interval, 0.8%-2.2%; P less than .001) in 2004 to 3.8% (95% CI, 2.7%-4.8%; P less than .001) by 2014. The increase was mostly seen among women younger than 30 years old. In that group, trachelectomy increased from 4.6% (95% CI, 1.0%-8.2%; P less than .001) in 2004 to 17% (95% CI, 10.2%-23.7%; P less than .001) in 2014. Rates among women aged 30-49 years were relatively stable over the same period.
“A possible explanation for this rise in trachelectomy is the trend in delayed childbearing in women in the United States,” wrote Rosa R. Cui, MD, a resident at Columbia University, New York, and her coauthors.
In the analysis, mortality risk and 5-year survival rates were similar between the two procedures. Overall cohort 5-year survival was nearly identical with hysterectomy and trachelectomy at 92.4% and 92.3%, respectively. For stages IA2, IB1, and IB not specified, tumor stage was not associated with differences in 5-year survival for the two procedures. As few patients with stage IB2 tumors received trachelectomy, that data was excluded from the analysis.
Though increasing tumor size made trachelectomy less likely, 30% of patients in the study who underwent trachelectomy had a tumor greater than 2 cm in diameter, and 4% had a tumor greater than 4 cm in diameter. The researchers noted studies published in the past few years suggest abdominal radical trachelectomy may be a safe option for larger tumors, compared with vaginal trachelectomy. In the current analysis, they did not find a statistically significant decrease in survival for trachelectomy patients with tumors greater than 2 cm in diameter, but the sample size was small.
“The trachelectomy procedure has evolved significantly since it was initially described and now encompasses several approaches,” and can be performed more or less conservatively depending on the diagnosis “without compromising outcomes,” wrote Dr. Cui and her coauthors.
The researchers noted that the National Cancer Database does not have data on fertility outcomes, a possible focus of future studies of trachelectomy.
Two coauthors disclosed grants and a fellowship from the National Cancer Institute, and others disclosed consulting for several pharmaceutical companies including Pfizer, Teva, and Eisai.
SOURCE: Cui RR et al. Obstet Gynecol. 2018 Jun;131(6):1085-94.
based on a recent analysis of the National Cancer Database.
Of 15,150 patients analyzed, the vast majority (97.1%) underwent hysterectomy, but trachelectomy performance increased from 1.5% (95% confidence interval, 0.8%-2.2%; P less than .001) in 2004 to 3.8% (95% CI, 2.7%-4.8%; P less than .001) by 2014. The increase was mostly seen among women younger than 30 years old. In that group, trachelectomy increased from 4.6% (95% CI, 1.0%-8.2%; P less than .001) in 2004 to 17% (95% CI, 10.2%-23.7%; P less than .001) in 2014. Rates among women aged 30-49 years were relatively stable over the same period.
“A possible explanation for this rise in trachelectomy is the trend in delayed childbearing in women in the United States,” wrote Rosa R. Cui, MD, a resident at Columbia University, New York, and her coauthors.
In the analysis, mortality risk and 5-year survival rates were similar between the two procedures. Overall cohort 5-year survival was nearly identical with hysterectomy and trachelectomy at 92.4% and 92.3%, respectively. For stages IA2, IB1, and IB not specified, tumor stage was not associated with differences in 5-year survival for the two procedures. As few patients with stage IB2 tumors received trachelectomy, that data was excluded from the analysis.
Though increasing tumor size made trachelectomy less likely, 30% of patients in the study who underwent trachelectomy had a tumor greater than 2 cm in diameter, and 4% had a tumor greater than 4 cm in diameter. The researchers noted studies published in the past few years suggest abdominal radical trachelectomy may be a safe option for larger tumors, compared with vaginal trachelectomy. In the current analysis, they did not find a statistically significant decrease in survival for trachelectomy patients with tumors greater than 2 cm in diameter, but the sample size was small.
“The trachelectomy procedure has evolved significantly since it was initially described and now encompasses several approaches,” and can be performed more or less conservatively depending on the diagnosis “without compromising outcomes,” wrote Dr. Cui and her coauthors.
The researchers noted that the National Cancer Database does not have data on fertility outcomes, a possible focus of future studies of trachelectomy.
Two coauthors disclosed grants and a fellowship from the National Cancer Institute, and others disclosed consulting for several pharmaceutical companies including Pfizer, Teva, and Eisai.
SOURCE: Cui RR et al. Obstet Gynecol. 2018 Jun;131(6):1085-94.
based on a recent analysis of the National Cancer Database.
Of 15,150 patients analyzed, the vast majority (97.1%) underwent hysterectomy, but trachelectomy performance increased from 1.5% (95% confidence interval, 0.8%-2.2%; P less than .001) in 2004 to 3.8% (95% CI, 2.7%-4.8%; P less than .001) by 2014. The increase was mostly seen among women younger than 30 years old. In that group, trachelectomy increased from 4.6% (95% CI, 1.0%-8.2%; P less than .001) in 2004 to 17% (95% CI, 10.2%-23.7%; P less than .001) in 2014. Rates among women aged 30-49 years were relatively stable over the same period.
“A possible explanation for this rise in trachelectomy is the trend in delayed childbearing in women in the United States,” wrote Rosa R. Cui, MD, a resident at Columbia University, New York, and her coauthors.
In the analysis, mortality risk and 5-year survival rates were similar between the two procedures. Overall cohort 5-year survival was nearly identical with hysterectomy and trachelectomy at 92.4% and 92.3%, respectively. For stages IA2, IB1, and IB not specified, tumor stage was not associated with differences in 5-year survival for the two procedures. As few patients with stage IB2 tumors received trachelectomy, that data was excluded from the analysis.
Though increasing tumor size made trachelectomy less likely, 30% of patients in the study who underwent trachelectomy had a tumor greater than 2 cm in diameter, and 4% had a tumor greater than 4 cm in diameter. The researchers noted studies published in the past few years suggest abdominal radical trachelectomy may be a safe option for larger tumors, compared with vaginal trachelectomy. In the current analysis, they did not find a statistically significant decrease in survival for trachelectomy patients with tumors greater than 2 cm in diameter, but the sample size was small.
“The trachelectomy procedure has evolved significantly since it was initially described and now encompasses several approaches,” and can be performed more or less conservatively depending on the diagnosis “without compromising outcomes,” wrote Dr. Cui and her coauthors.
The researchers noted that the National Cancer Database does not have data on fertility outcomes, a possible focus of future studies of trachelectomy.
Two coauthors disclosed grants and a fellowship from the National Cancer Institute, and others disclosed consulting for several pharmaceutical companies including Pfizer, Teva, and Eisai.
SOURCE: Cui RR et al. Obstet Gynecol. 2018 Jun;131(6):1085-94.
FROM OBSTETRICS & GYNECOLOGY
What is causing my patients’ macrocytosis?
A 56-year-old man presents for his annual physical. He brings in blood work done for all employees in his workplace (he is an aerospace engineer), and wants to talk about the lab that has an asterisk by it. All his labs are normal, except that his mean corpuscular volume (MCV) is 101. His hematocrit (HCT) is 42. He has no symptoms and a normal physical exam.
What test or tests would most likely be abnormal?
A. Thyroid-stimulating hormone.
B. Vitamin B12/folate.
C. Testosterone.
D. Gamma-glutamyl-transferase (GGT).
The finding of macrocytosis is fairly common in primary care, estimated to be found in 3% of complete blood count results.1 Most students in medical school quickly learn that vitamin B12 and folate deficiency can cause macrocytic anemias. The standard workups for patients with macrocytosis began and ended with checking vitamin B12 and folate levels, which are usually normal in the vast majority of patients with macrocytosis.
For this patient, the correct answer would be an abnormal GGT, because chronic moderate to heavy alcohol use can raise GGT levels, as well as MCVs.
Dr. David Savage and colleagues evaluated the etiology of macrocytosis in 300 consecutive hospitalized patients with macrocytosis.2 They found that the most common causes were medications, alcohol, liver disease, and reticulocytosis. The study was done in New York and was published in 2000, so zidovudine (AZT) was a common medication cause of the macrocytosis. This medication is much less commonly used today. Zidovudine causes macrocytosis in more than 80% of patients who take it. They also found in the study that very high MCVs (> 120) were most commonly associated with vitamin B12 deficiency.
Dr. Kaija Seppä and colleagues looked at all outpatients who had a blood count done over an 8-month period. A total of 9,527 blood counts were ordered, and 287 (3%) had macrocytosis.1 Further workup was done for 113 of the patients. The most common cause found for macrocytosis was alcohol abuse, in 74 (65%) of the patients (80% of the men and 36% of the women). No cause of the macrocytosis was found in 24 (21%) of the patients.
Dr. A. Wymer and colleagues looked at 2,800 adult outpatients who had complete blood counts. A total of 138 (3.7%) had macrocytosis, with 128 of these patients having charts that could be reviewed.3 A total of 73 patients had a workup for their macrocytosis. Alcohol was the diagnostic cause of the macrocytosis in 47 (64%). Only five of the patients had B12 deficiency (7%).
Dr. Seppä and colleagues also reported on hematologic morphologic features in nonanemic patients with macrocytosis due to alcohol abuse or vitamin B12 deficiency.4 They studied 136 patients with alcohol abuse and normal B12 levels, and 18 patients with pernicious anemia. The combination of a low red cell count or a high red cell distribution width with a normal platelet count was found in 94.4% of the vitamin-deficient patients but in only 14.6% of the abusers.
Pearl:
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the university. Contact Dr. Paauw at dpaauw@uw.edu.
References
1. J Stud Alcohol. 1996 Jan;57(1):97-100.
2. Am J Med Sci. 2000 Jun;319(6):343-52.
3. J Gen Intern Med. 1990 May-Jun;5(3):192-7.
4. Alcohol. 1993 Sep-Oct;10(5):343-7.
5. South Med J. 2013 Feb;106(2):121-5.
A 56-year-old man presents for his annual physical. He brings in blood work done for all employees in his workplace (he is an aerospace engineer), and wants to talk about the lab that has an asterisk by it. All his labs are normal, except that his mean corpuscular volume (MCV) is 101. His hematocrit (HCT) is 42. He has no symptoms and a normal physical exam.
What test or tests would most likely be abnormal?
A. Thyroid-stimulating hormone.
B. Vitamin B12/folate.
C. Testosterone.
D. Gamma-glutamyl-transferase (GGT).
The finding of macrocytosis is fairly common in primary care, estimated to be found in 3% of complete blood count results.1 Most students in medical school quickly learn that vitamin B12 and folate deficiency can cause macrocytic anemias. The standard workups for patients with macrocytosis began and ended with checking vitamin B12 and folate levels, which are usually normal in the vast majority of patients with macrocytosis.
For this patient, the correct answer would be an abnormal GGT, because chronic moderate to heavy alcohol use can raise GGT levels, as well as MCVs.
Dr. David Savage and colleagues evaluated the etiology of macrocytosis in 300 consecutive hospitalized patients with macrocytosis.2 They found that the most common causes were medications, alcohol, liver disease, and reticulocytosis. The study was done in New York and was published in 2000, so zidovudine (AZT) was a common medication cause of the macrocytosis. This medication is much less commonly used today. Zidovudine causes macrocytosis in more than 80% of patients who take it. They also found in the study that very high MCVs (> 120) were most commonly associated with vitamin B12 deficiency.
Dr. Kaija Seppä and colleagues looked at all outpatients who had a blood count done over an 8-month period. A total of 9,527 blood counts were ordered, and 287 (3%) had macrocytosis.1 Further workup was done for 113 of the patients. The most common cause found for macrocytosis was alcohol abuse, in 74 (65%) of the patients (80% of the men and 36% of the women). No cause of the macrocytosis was found in 24 (21%) of the patients.
Dr. A. Wymer and colleagues looked at 2,800 adult outpatients who had complete blood counts. A total of 138 (3.7%) had macrocytosis, with 128 of these patients having charts that could be reviewed.3 A total of 73 patients had a workup for their macrocytosis. Alcohol was the diagnostic cause of the macrocytosis in 47 (64%). Only five of the patients had B12 deficiency (7%).
Dr. Seppä and colleagues also reported on hematologic morphologic features in nonanemic patients with macrocytosis due to alcohol abuse or vitamin B12 deficiency.4 They studied 136 patients with alcohol abuse and normal B12 levels, and 18 patients with pernicious anemia. The combination of a low red cell count or a high red cell distribution width with a normal platelet count was found in 94.4% of the vitamin-deficient patients but in only 14.6% of the abusers.
Pearl:
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the university. Contact Dr. Paauw at dpaauw@uw.edu.
References
1. J Stud Alcohol. 1996 Jan;57(1):97-100.
2. Am J Med Sci. 2000 Jun;319(6):343-52.
3. J Gen Intern Med. 1990 May-Jun;5(3):192-7.
4. Alcohol. 1993 Sep-Oct;10(5):343-7.
5. South Med J. 2013 Feb;106(2):121-5.
A 56-year-old man presents for his annual physical. He brings in blood work done for all employees in his workplace (he is an aerospace engineer), and wants to talk about the lab that has an asterisk by it. All his labs are normal, except that his mean corpuscular volume (MCV) is 101. His hematocrit (HCT) is 42. He has no symptoms and a normal physical exam.
What test or tests would most likely be abnormal?
A. Thyroid-stimulating hormone.
B. Vitamin B12/folate.
C. Testosterone.
D. Gamma-glutamyl-transferase (GGT).
The finding of macrocytosis is fairly common in primary care, estimated to be found in 3% of complete blood count results.1 Most students in medical school quickly learn that vitamin B12 and folate deficiency can cause macrocytic anemias. The standard workups for patients with macrocytosis began and ended with checking vitamin B12 and folate levels, which are usually normal in the vast majority of patients with macrocytosis.
For this patient, the correct answer would be an abnormal GGT, because chronic moderate to heavy alcohol use can raise GGT levels, as well as MCVs.
Dr. David Savage and colleagues evaluated the etiology of macrocytosis in 300 consecutive hospitalized patients with macrocytosis.2 They found that the most common causes were medications, alcohol, liver disease, and reticulocytosis. The study was done in New York and was published in 2000, so zidovudine (AZT) was a common medication cause of the macrocytosis. This medication is much less commonly used today. Zidovudine causes macrocytosis in more than 80% of patients who take it. They also found in the study that very high MCVs (> 120) were most commonly associated with vitamin B12 deficiency.
Dr. Kaija Seppä and colleagues looked at all outpatients who had a blood count done over an 8-month period. A total of 9,527 blood counts were ordered, and 287 (3%) had macrocytosis.1 Further workup was done for 113 of the patients. The most common cause found for macrocytosis was alcohol abuse, in 74 (65%) of the patients (80% of the men and 36% of the women). No cause of the macrocytosis was found in 24 (21%) of the patients.
Dr. A. Wymer and colleagues looked at 2,800 adult outpatients who had complete blood counts. A total of 138 (3.7%) had macrocytosis, with 128 of these patients having charts that could be reviewed.3 A total of 73 patients had a workup for their macrocytosis. Alcohol was the diagnostic cause of the macrocytosis in 47 (64%). Only five of the patients had B12 deficiency (7%).
Dr. Seppä and colleagues also reported on hematologic morphologic features in nonanemic patients with macrocytosis due to alcohol abuse or vitamin B12 deficiency.4 They studied 136 patients with alcohol abuse and normal B12 levels, and 18 patients with pernicious anemia. The combination of a low red cell count or a high red cell distribution width with a normal platelet count was found in 94.4% of the vitamin-deficient patients but in only 14.6% of the abusers.
Pearl:
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the university. Contact Dr. Paauw at dpaauw@uw.edu.
References
1. J Stud Alcohol. 1996 Jan;57(1):97-100.
2. Am J Med Sci. 2000 Jun;319(6):343-52.
3. J Gen Intern Med. 1990 May-Jun;5(3):192-7.
4. Alcohol. 1993 Sep-Oct;10(5):343-7.
5. South Med J. 2013 Feb;106(2):121-5.
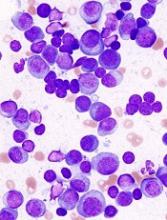
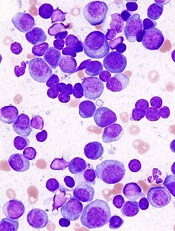
Encouraging early results for CB-derived NK cells in MM
CHICAGO—Cord blood (CB) is a viable source of natural killer (NK) cells for adoptive cellular therapy for multiple myeloma (MM), according to a speaker at the 2018 ASCO Annual Meeting.
Ex-vivo expanded cord blood NK cells were well tolerated without significant graft-versus-host disease (GVHD) or cytokine release syndrome (CRS) in a phase 2 study.
Nina Shah, MD, of the University of California San Francisco, reported these results as abstract 8006.*
The phase 2 study (NCT01729091) included 33 patients with symptomatic MM who were appropriate candidates for autologous stem cell transplant (ASCT).
For each patient, investigators chose cord blood units with at least a 4/6 match at HLA-A, -B and –DR.
Prior to the autologous graft, patients received lenalidomide and melphalan. Lenalidomide was given based on preclinical data suggesting synergy between that immunomodulatory agent and NK cells, Dr Shah said.
Patients were a median age of 59 (range, 25 – 72), 36% had a history of progressive disease or relapse, and 73% had adverse cytogenetics/FISH, were ISS III, or had a history of progressive disease or relapse.
Results
Dr Shah observed that in a generally high-risk population, responses to treatment with cord blood NK cells in the setting of ASCT were “encouraging,” with 79% of patients achieving very good partial response (VGPR) or better.
Twenty-one patients (64%) achieved a complete response (CR) or near CR. And 61% achieved minimal residual disease (MRD) negativity by day 100.
Patients had an estimated 3-year progression-free survival of 52%.
Three patients died, all from disease progression, and 13 patients have progressed.
The investigators observed no infusional toxicities, no GVHD, no CRS, and no neurotoxicity.
One patient experienced graft failure and was rescued with an autologous back-up graft.
"We are able to detect the donor-derived NK cells up to 13 days after infusion,” Dr Shah said, “but I think a more sensitive analysis with flow chimerism will not only allow us to detect more patients, but also better interrogate them to truly understand the in vivo phenotype and activation status of these cells."
Dr Shah indicated she and her colleagues became interested in studying cord blood for NK cell therapy because it is a known source of hematopoietic cells that is immediately available, does not require donor manipulation, and has more flexibility in genetic matching.
Previously, Dr Shah and colleagues conducted a phase 1 study, in which 12 patients received cord blood NK cells up to a dose of 1 x 108 NK cells/kg. “This was determined to be adequate and safe to move on to the phase 2,” she said.
Despite encouraging results, more research needs to be done, according to Dr Shah. “I don't think this is the end-all, be-all for NK cell therapy.”
Some future directions include combination with antibody therapy, improving NK persistence in vivo using cytokine manipulation, and possibly engineering chimeric antigen receptor (CAR)-modified NK cells, Dr Shah observed.
It’s also possible that HLA match may not be needed: “If that is the case, we will truly have an off-the-shelf source of NK cells that we can apply more readily to various patients,” she said.
The study was supported by Celgene Corporation, Stading-Younger Cancer Research Foundation, and the MD Anderson High-Risk Multiple Myeloma Moonshot Project.
*Data in the presentation differ from the abstract.
CHICAGO—Cord blood (CB) is a viable source of natural killer (NK) cells for adoptive cellular therapy for multiple myeloma (MM), according to a speaker at the 2018 ASCO Annual Meeting.
Ex-vivo expanded cord blood NK cells were well tolerated without significant graft-versus-host disease (GVHD) or cytokine release syndrome (CRS) in a phase 2 study.
Nina Shah, MD, of the University of California San Francisco, reported these results as abstract 8006.*
The phase 2 study (NCT01729091) included 33 patients with symptomatic MM who were appropriate candidates for autologous stem cell transplant (ASCT).
For each patient, investigators chose cord blood units with at least a 4/6 match at HLA-A, -B and –DR.
Prior to the autologous graft, patients received lenalidomide and melphalan. Lenalidomide was given based on preclinical data suggesting synergy between that immunomodulatory agent and NK cells, Dr Shah said.
Patients were a median age of 59 (range, 25 – 72), 36% had a history of progressive disease or relapse, and 73% had adverse cytogenetics/FISH, were ISS III, or had a history of progressive disease or relapse.
Results
Dr Shah observed that in a generally high-risk population, responses to treatment with cord blood NK cells in the setting of ASCT were “encouraging,” with 79% of patients achieving very good partial response (VGPR) or better.
Twenty-one patients (64%) achieved a complete response (CR) or near CR. And 61% achieved minimal residual disease (MRD) negativity by day 100.
Patients had an estimated 3-year progression-free survival of 52%.
Three patients died, all from disease progression, and 13 patients have progressed.
The investigators observed no infusional toxicities, no GVHD, no CRS, and no neurotoxicity.
One patient experienced graft failure and was rescued with an autologous back-up graft.
"We are able to detect the donor-derived NK cells up to 13 days after infusion,” Dr Shah said, “but I think a more sensitive analysis with flow chimerism will not only allow us to detect more patients, but also better interrogate them to truly understand the in vivo phenotype and activation status of these cells."
Dr Shah indicated she and her colleagues became interested in studying cord blood for NK cell therapy because it is a known source of hematopoietic cells that is immediately available, does not require donor manipulation, and has more flexibility in genetic matching.
Previously, Dr Shah and colleagues conducted a phase 1 study, in which 12 patients received cord blood NK cells up to a dose of 1 x 108 NK cells/kg. “This was determined to be adequate and safe to move on to the phase 2,” she said.
Despite encouraging results, more research needs to be done, according to Dr Shah. “I don't think this is the end-all, be-all for NK cell therapy.”
Some future directions include combination with antibody therapy, improving NK persistence in vivo using cytokine manipulation, and possibly engineering chimeric antigen receptor (CAR)-modified NK cells, Dr Shah observed.
It’s also possible that HLA match may not be needed: “If that is the case, we will truly have an off-the-shelf source of NK cells that we can apply more readily to various patients,” she said.
The study was supported by Celgene Corporation, Stading-Younger Cancer Research Foundation, and the MD Anderson High-Risk Multiple Myeloma Moonshot Project.
*Data in the presentation differ from the abstract.
CHICAGO—Cord blood (CB) is a viable source of natural killer (NK) cells for adoptive cellular therapy for multiple myeloma (MM), according to a speaker at the 2018 ASCO Annual Meeting.
Ex-vivo expanded cord blood NK cells were well tolerated without significant graft-versus-host disease (GVHD) or cytokine release syndrome (CRS) in a phase 2 study.
Nina Shah, MD, of the University of California San Francisco, reported these results as abstract 8006.*
The phase 2 study (NCT01729091) included 33 patients with symptomatic MM who were appropriate candidates for autologous stem cell transplant (ASCT).
For each patient, investigators chose cord blood units with at least a 4/6 match at HLA-A, -B and –DR.
Prior to the autologous graft, patients received lenalidomide and melphalan. Lenalidomide was given based on preclinical data suggesting synergy between that immunomodulatory agent and NK cells, Dr Shah said.
Patients were a median age of 59 (range, 25 – 72), 36% had a history of progressive disease or relapse, and 73% had adverse cytogenetics/FISH, were ISS III, or had a history of progressive disease or relapse.
Results
Dr Shah observed that in a generally high-risk population, responses to treatment with cord blood NK cells in the setting of ASCT were “encouraging,” with 79% of patients achieving very good partial response (VGPR) or better.
Twenty-one patients (64%) achieved a complete response (CR) or near CR. And 61% achieved minimal residual disease (MRD) negativity by day 100.
Patients had an estimated 3-year progression-free survival of 52%.
Three patients died, all from disease progression, and 13 patients have progressed.
The investigators observed no infusional toxicities, no GVHD, no CRS, and no neurotoxicity.
One patient experienced graft failure and was rescued with an autologous back-up graft.
"We are able to detect the donor-derived NK cells up to 13 days after infusion,” Dr Shah said, “but I think a more sensitive analysis with flow chimerism will not only allow us to detect more patients, but also better interrogate them to truly understand the in vivo phenotype and activation status of these cells."
Dr Shah indicated she and her colleagues became interested in studying cord blood for NK cell therapy because it is a known source of hematopoietic cells that is immediately available, does not require donor manipulation, and has more flexibility in genetic matching.
Previously, Dr Shah and colleagues conducted a phase 1 study, in which 12 patients received cord blood NK cells up to a dose of 1 x 108 NK cells/kg. “This was determined to be adequate and safe to move on to the phase 2,” she said.
Despite encouraging results, more research needs to be done, according to Dr Shah. “I don't think this is the end-all, be-all for NK cell therapy.”
Some future directions include combination with antibody therapy, improving NK persistence in vivo using cytokine manipulation, and possibly engineering chimeric antigen receptor (CAR)-modified NK cells, Dr Shah observed.
It’s also possible that HLA match may not be needed: “If that is the case, we will truly have an off-the-shelf source of NK cells that we can apply more readily to various patients,” she said.
The study was supported by Celgene Corporation, Stading-Younger Cancer Research Foundation, and the MD Anderson High-Risk Multiple Myeloma Moonshot Project.
*Data in the presentation differ from the abstract.
CAR T-cell technology making headway in MM
Chimeric antigen receptor (CAR) T-cell technology has been successfully used in the treatment of hematologic malignancies such as leukemias and lymphomas. Now, this technology has come to the forefront in multiple myeloma (MM).
Researchers at the National Cancer Institute, led by James N. Kochenderfer, MD, generated CAR T cells expressing the B-cell maturation antigen (BCMA), which is uniquely found on MM cells.
In the first in humans study, 24 patients received CAR-BCMA T cells at doses ranging between 0.3 and 3 x 106 CAR+ T cells/kg. Sixteen patients were treated at the highest dose. These patients had a median of 9.5 lines of prior therapy and 63% were refractory to their last treatment.
Thirteen patients had responses that were either partial or better and the overall response rate was 81%. Median event-free survival was 31 weeks. At the time of the report, 6 patients still have ongoing responses.
Patient cases
The report highlights a case study of a patient who had a large abdominal mass that resolved on computed tomography imaging, with λ light chains decreasing dramatically and becoming undetectable after CAR T-cell infusion. Recovery of normal plasma cells was noticeable with λ chain increases, but the ratio of κ to λ ratio remained normal 6 months after CAR T-cell infusion.
Using immunohistochemistry staining of CS138 before and 2 months after CAR-BMCA infusion, the researchers found effective depletion in bone marrow plasma cells in patients who were evaluated.
In patients who responded to treatment, decline in serum BCMA was also observed. However, in a patient who later progressed, BCMA increases were seen, leading the researchers to suggest that BCMA may be a tumor marker for MM.
The researchers noted that peak levels of CAR T cells occurred between 7 and 14 days after infusion and highest levels were seen in patients who showed antimyeloma responses.
Toxicity
CAR T-cell technology is also associated with accompanying toxicities.
At the highest dose, cytokine release syndrome (CRS) was a substantial toxicity especially in 2 patients who had a significant MM burden: in one case 80% of bone marrow cells were MM plasma cells and in the other the MM burden was 90%.
Six of the 16 patients required vasopressor support for hypotension and 1 patient required mechanical ventilation. The researchers noted that CRS of grade 3/4 was seen in patients who had a higher MM plasma cell burden.
The researchers indicated there is room for improvement. “The importance of persistence of CAR T cells in treating MM requires additional study,” they stated.
The sometimes low or absence of BCMA expression on MM cells may prompt the search for other antigens. “Treatment outcomes varied substantially between patients, and much room for improvement remains in improving the durability of antimyeloma responses and in reducing toxicity,” they concluded.
The researchers reported their findings in the Journal of Clinical Oncology.
Chimeric antigen receptor (CAR) T-cell technology has been successfully used in the treatment of hematologic malignancies such as leukemias and lymphomas. Now, this technology has come to the forefront in multiple myeloma (MM).
Researchers at the National Cancer Institute, led by James N. Kochenderfer, MD, generated CAR T cells expressing the B-cell maturation antigen (BCMA), which is uniquely found on MM cells.
In the first in humans study, 24 patients received CAR-BCMA T cells at doses ranging between 0.3 and 3 x 106 CAR+ T cells/kg. Sixteen patients were treated at the highest dose. These patients had a median of 9.5 lines of prior therapy and 63% were refractory to their last treatment.
Thirteen patients had responses that were either partial or better and the overall response rate was 81%. Median event-free survival was 31 weeks. At the time of the report, 6 patients still have ongoing responses.
Patient cases
The report highlights a case study of a patient who had a large abdominal mass that resolved on computed tomography imaging, with λ light chains decreasing dramatically and becoming undetectable after CAR T-cell infusion. Recovery of normal plasma cells was noticeable with λ chain increases, but the ratio of κ to λ ratio remained normal 6 months after CAR T-cell infusion.
Using immunohistochemistry staining of CS138 before and 2 months after CAR-BMCA infusion, the researchers found effective depletion in bone marrow plasma cells in patients who were evaluated.
In patients who responded to treatment, decline in serum BCMA was also observed. However, in a patient who later progressed, BCMA increases were seen, leading the researchers to suggest that BCMA may be a tumor marker for MM.
The researchers noted that peak levels of CAR T cells occurred between 7 and 14 days after infusion and highest levels were seen in patients who showed antimyeloma responses.
Toxicity
CAR T-cell technology is also associated with accompanying toxicities.
At the highest dose, cytokine release syndrome (CRS) was a substantial toxicity especially in 2 patients who had a significant MM burden: in one case 80% of bone marrow cells were MM plasma cells and in the other the MM burden was 90%.
Six of the 16 patients required vasopressor support for hypotension and 1 patient required mechanical ventilation. The researchers noted that CRS of grade 3/4 was seen in patients who had a higher MM plasma cell burden.
The researchers indicated there is room for improvement. “The importance of persistence of CAR T cells in treating MM requires additional study,” they stated.
The sometimes low or absence of BCMA expression on MM cells may prompt the search for other antigens. “Treatment outcomes varied substantially between patients, and much room for improvement remains in improving the durability of antimyeloma responses and in reducing toxicity,” they concluded.
The researchers reported their findings in the Journal of Clinical Oncology.
Chimeric antigen receptor (CAR) T-cell technology has been successfully used in the treatment of hematologic malignancies such as leukemias and lymphomas. Now, this technology has come to the forefront in multiple myeloma (MM).
Researchers at the National Cancer Institute, led by James N. Kochenderfer, MD, generated CAR T cells expressing the B-cell maturation antigen (BCMA), which is uniquely found on MM cells.
In the first in humans study, 24 patients received CAR-BCMA T cells at doses ranging between 0.3 and 3 x 106 CAR+ T cells/kg. Sixteen patients were treated at the highest dose. These patients had a median of 9.5 lines of prior therapy and 63% were refractory to their last treatment.
Thirteen patients had responses that were either partial or better and the overall response rate was 81%. Median event-free survival was 31 weeks. At the time of the report, 6 patients still have ongoing responses.
Patient cases
The report highlights a case study of a patient who had a large abdominal mass that resolved on computed tomography imaging, with λ light chains decreasing dramatically and becoming undetectable after CAR T-cell infusion. Recovery of normal plasma cells was noticeable with λ chain increases, but the ratio of κ to λ ratio remained normal 6 months after CAR T-cell infusion.
Using immunohistochemistry staining of CS138 before and 2 months after CAR-BMCA infusion, the researchers found effective depletion in bone marrow plasma cells in patients who were evaluated.
In patients who responded to treatment, decline in serum BCMA was also observed. However, in a patient who later progressed, BCMA increases were seen, leading the researchers to suggest that BCMA may be a tumor marker for MM.
The researchers noted that peak levels of CAR T cells occurred between 7 and 14 days after infusion and highest levels were seen in patients who showed antimyeloma responses.
Toxicity
CAR T-cell technology is also associated with accompanying toxicities.
At the highest dose, cytokine release syndrome (CRS) was a substantial toxicity especially in 2 patients who had a significant MM burden: in one case 80% of bone marrow cells were MM plasma cells and in the other the MM burden was 90%.
Six of the 16 patients required vasopressor support for hypotension and 1 patient required mechanical ventilation. The researchers noted that CRS of grade 3/4 was seen in patients who had a higher MM plasma cell burden.
The researchers indicated there is room for improvement. “The importance of persistence of CAR T cells in treating MM requires additional study,” they stated.
The sometimes low or absence of BCMA expression on MM cells may prompt the search for other antigens. “Treatment outcomes varied substantially between patients, and much room for improvement remains in improving the durability of antimyeloma responses and in reducing toxicity,” they concluded.
The researchers reported their findings in the Journal of Clinical Oncology.