User login
No clear winner in Pfannenstiel vs. vertical incision for high BMI cesareans
DALLAS – though enrollment difficulties limited study numbers, with almost two-thirds of eligible women declining to participate in the surgical trial.
At 6 weeks postdelivery, 21.1% of women who had a vertical incision experienced wound complications, compared with 18.6% of those who had a Pfannenstiel incision, a nonsignificant difference. This was a smaller difference than was seen at 2 weeks postpartum, when 20% of the vertical incision group had wound complications, compared with 10.4% of those who had a Pfannenstiel, also a nonsignificant difference. Maternal and fetal outcomes didn’t differ significantly with the two surgical approaches.
Though there had been several observational studies comparing vertical with Pfannenstiel incisions for cesarean delivery in women with obesity, no randomized, controlled trials had been conducted, and observational study results were mixed, said Dr. Marrs.
Each approach comes with theoretical pros and cons: For women who have a large pannus, the incision site may lie in a moist environment with a low transverse incision, and oxygen tension may be low. However, a Pfannenstiel incision usually will have better cosmesis than will a vertical incision, and generally will result in less postoperative pain.
On the other hand, said Dr. Marrs, vertical incisions can provide improved exposure of the uterus during delivery, and the moist environment underlying the pannus is avoided. However, wound tension may be higher, and subcutaneous thickness is likely to be higher than at the Pfannenstiel incision site.
The study, conducted at two academic medical centers, enrolled women with a body mass index (BMI) of at least 40 kg/m2 at a gestational age of 24 weeks or greater who required cesarean delivery. Consenting women were then randomized to receive Pfannenstiel or vertical incisions.
Women who had clinical chorioamnionitis, whose amniotic membranes had been ruptured for 18 hours or more, or who had placenta accreta were excluded. Also excluded were women with a private physician and those desiring vaginal delivery, said Dr. Marrs, a maternal-fetal medicine fellow at the University of Texas Medical Branch, Galveston.
The study’s primary outcome measure was a composite of wound complications seen within 6 weeks of delivery, including surgical site infection, whether superficial, deep, or involving an organ or tissue space; cellulitis; seroma or hematoma; and wound separation. Other maternal outcomes tracked in the study included postoperative length of stay, transfusion requirement, sepsis, readmission, and death.
Cesarean-specific secondary outcomes included operative time and time from skin incision to delivery, estimated blood loss, and any incidence of hysterectomy through a low transverse incision. Neonatal outcomes included a 5-minute Apgar score of less than 7, umbilical cord pH of less than 7, and neonatal ICU admissions.
Dr. Mars said that the goal enrollment for the study was 300 patients, to ensure adequate statistical power. However, they found enrollment a challenge, with low consent rates during the defined time period from October 2013 to May 2017. They shifted their statistical technique to a Bayesian analysis, taking into account the estimated probability of treatment benefit.
Using this approach, they found a 59% probability that a Pfannenstiel incision would lead to a lower primary outcome rate – a better result – than would a vertical incision. This result just missed the predetermined threshold of 60%, said Dr. Marrs.
Of the 789 women who met the BMI threshold for eligibility assessment, 420 (65%) who passed the screening declined to participate. Of those who consented to participation, an additional 137 women either withdrew consent or failed further screening, leaving 50 women who were randomized to the Pfannenstiel arm and 41 who were randomized to the vertical incision arm.
Baseline characteristics were similar between groups, with a mean maternal age of 30 years in the Pfannenstiel group and 28 years in the vertical incision group. Gestational age at delivery was a mean of 37 weeks in both groups, and mean BMI was 48-50 kg/m2.
Most patients (80%-90%) had public insurance. Diabetes was more common in the Pfannenstiel group (48%) than in the vertical incision cohort (32%). Just over 40% of patients were African American.
Two women in the Pfannenstiel group and three in the vertical incision group did not receive the intended incision. After accounting for patients lost to follow-up by 6 weeks, 43 women who received Pfannenstiel and 38 women who received vertical incisions were available for full evaluation.
Dr. Marrs said that the study, the first randomized trial to address this issue, had several strengths, including its being conducted at two sites with appropriate stratification for the sites. Also, an independent data safety monitoring board and two chart reviewers helped overcome some of the limitations of a surgical study, where complete blinding is impossible.
The Bayesian analysis allowed ascertainment of the probability of treatment benefit despite the lower-than-hoped-for enrollment numbers. The primary weakness of the study, said Dr. Marrs, centered around the low consent rate, which led to a small study that was prematurely terminated.
“It’s difficult to enroll women in a trial that requires random allocation of skin incision, due to their preference to choose their own incision. A larger trial would likewise be challenging, and unlikely to yield different results,” said Dr. Marrs.
Dr. Marrs reported no conflicts of interest.
SOURCE: Marrs CC et al. Am J Obstet Gynecol. 2018 Jan;218:S29.
DALLAS – though enrollment difficulties limited study numbers, with almost two-thirds of eligible women declining to participate in the surgical trial.
At 6 weeks postdelivery, 21.1% of women who had a vertical incision experienced wound complications, compared with 18.6% of those who had a Pfannenstiel incision, a nonsignificant difference. This was a smaller difference than was seen at 2 weeks postpartum, when 20% of the vertical incision group had wound complications, compared with 10.4% of those who had a Pfannenstiel, also a nonsignificant difference. Maternal and fetal outcomes didn’t differ significantly with the two surgical approaches.
Though there had been several observational studies comparing vertical with Pfannenstiel incisions for cesarean delivery in women with obesity, no randomized, controlled trials had been conducted, and observational study results were mixed, said Dr. Marrs.
Each approach comes with theoretical pros and cons: For women who have a large pannus, the incision site may lie in a moist environment with a low transverse incision, and oxygen tension may be low. However, a Pfannenstiel incision usually will have better cosmesis than will a vertical incision, and generally will result in less postoperative pain.
On the other hand, said Dr. Marrs, vertical incisions can provide improved exposure of the uterus during delivery, and the moist environment underlying the pannus is avoided. However, wound tension may be higher, and subcutaneous thickness is likely to be higher than at the Pfannenstiel incision site.
The study, conducted at two academic medical centers, enrolled women with a body mass index (BMI) of at least 40 kg/m2 at a gestational age of 24 weeks or greater who required cesarean delivery. Consenting women were then randomized to receive Pfannenstiel or vertical incisions.
Women who had clinical chorioamnionitis, whose amniotic membranes had been ruptured for 18 hours or more, or who had placenta accreta were excluded. Also excluded were women with a private physician and those desiring vaginal delivery, said Dr. Marrs, a maternal-fetal medicine fellow at the University of Texas Medical Branch, Galveston.
The study’s primary outcome measure was a composite of wound complications seen within 6 weeks of delivery, including surgical site infection, whether superficial, deep, or involving an organ or tissue space; cellulitis; seroma or hematoma; and wound separation. Other maternal outcomes tracked in the study included postoperative length of stay, transfusion requirement, sepsis, readmission, and death.
Cesarean-specific secondary outcomes included operative time and time from skin incision to delivery, estimated blood loss, and any incidence of hysterectomy through a low transverse incision. Neonatal outcomes included a 5-minute Apgar score of less than 7, umbilical cord pH of less than 7, and neonatal ICU admissions.
Dr. Mars said that the goal enrollment for the study was 300 patients, to ensure adequate statistical power. However, they found enrollment a challenge, with low consent rates during the defined time period from October 2013 to May 2017. They shifted their statistical technique to a Bayesian analysis, taking into account the estimated probability of treatment benefit.
Using this approach, they found a 59% probability that a Pfannenstiel incision would lead to a lower primary outcome rate – a better result – than would a vertical incision. This result just missed the predetermined threshold of 60%, said Dr. Marrs.
Of the 789 women who met the BMI threshold for eligibility assessment, 420 (65%) who passed the screening declined to participate. Of those who consented to participation, an additional 137 women either withdrew consent or failed further screening, leaving 50 women who were randomized to the Pfannenstiel arm and 41 who were randomized to the vertical incision arm.
Baseline characteristics were similar between groups, with a mean maternal age of 30 years in the Pfannenstiel group and 28 years in the vertical incision group. Gestational age at delivery was a mean of 37 weeks in both groups, and mean BMI was 48-50 kg/m2.
Most patients (80%-90%) had public insurance. Diabetes was more common in the Pfannenstiel group (48%) than in the vertical incision cohort (32%). Just over 40% of patients were African American.
Two women in the Pfannenstiel group and three in the vertical incision group did not receive the intended incision. After accounting for patients lost to follow-up by 6 weeks, 43 women who received Pfannenstiel and 38 women who received vertical incisions were available for full evaluation.
Dr. Marrs said that the study, the first randomized trial to address this issue, had several strengths, including its being conducted at two sites with appropriate stratification for the sites. Also, an independent data safety monitoring board and two chart reviewers helped overcome some of the limitations of a surgical study, where complete blinding is impossible.
The Bayesian analysis allowed ascertainment of the probability of treatment benefit despite the lower-than-hoped-for enrollment numbers. The primary weakness of the study, said Dr. Marrs, centered around the low consent rate, which led to a small study that was prematurely terminated.
“It’s difficult to enroll women in a trial that requires random allocation of skin incision, due to their preference to choose their own incision. A larger trial would likewise be challenging, and unlikely to yield different results,” said Dr. Marrs.
Dr. Marrs reported no conflicts of interest.
SOURCE: Marrs CC et al. Am J Obstet Gynecol. 2018 Jan;218:S29.
DALLAS – though enrollment difficulties limited study numbers, with almost two-thirds of eligible women declining to participate in the surgical trial.
At 6 weeks postdelivery, 21.1% of women who had a vertical incision experienced wound complications, compared with 18.6% of those who had a Pfannenstiel incision, a nonsignificant difference. This was a smaller difference than was seen at 2 weeks postpartum, when 20% of the vertical incision group had wound complications, compared with 10.4% of those who had a Pfannenstiel, also a nonsignificant difference. Maternal and fetal outcomes didn’t differ significantly with the two surgical approaches.
Though there had been several observational studies comparing vertical with Pfannenstiel incisions for cesarean delivery in women with obesity, no randomized, controlled trials had been conducted, and observational study results were mixed, said Dr. Marrs.
Each approach comes with theoretical pros and cons: For women who have a large pannus, the incision site may lie in a moist environment with a low transverse incision, and oxygen tension may be low. However, a Pfannenstiel incision usually will have better cosmesis than will a vertical incision, and generally will result in less postoperative pain.
On the other hand, said Dr. Marrs, vertical incisions can provide improved exposure of the uterus during delivery, and the moist environment underlying the pannus is avoided. However, wound tension may be higher, and subcutaneous thickness is likely to be higher than at the Pfannenstiel incision site.
The study, conducted at two academic medical centers, enrolled women with a body mass index (BMI) of at least 40 kg/m2 at a gestational age of 24 weeks or greater who required cesarean delivery. Consenting women were then randomized to receive Pfannenstiel or vertical incisions.
Women who had clinical chorioamnionitis, whose amniotic membranes had been ruptured for 18 hours or more, or who had placenta accreta were excluded. Also excluded were women with a private physician and those desiring vaginal delivery, said Dr. Marrs, a maternal-fetal medicine fellow at the University of Texas Medical Branch, Galveston.
The study’s primary outcome measure was a composite of wound complications seen within 6 weeks of delivery, including surgical site infection, whether superficial, deep, or involving an organ or tissue space; cellulitis; seroma or hematoma; and wound separation. Other maternal outcomes tracked in the study included postoperative length of stay, transfusion requirement, sepsis, readmission, and death.
Cesarean-specific secondary outcomes included operative time and time from skin incision to delivery, estimated blood loss, and any incidence of hysterectomy through a low transverse incision. Neonatal outcomes included a 5-minute Apgar score of less than 7, umbilical cord pH of less than 7, and neonatal ICU admissions.
Dr. Mars said that the goal enrollment for the study was 300 patients, to ensure adequate statistical power. However, they found enrollment a challenge, with low consent rates during the defined time period from October 2013 to May 2017. They shifted their statistical technique to a Bayesian analysis, taking into account the estimated probability of treatment benefit.
Using this approach, they found a 59% probability that a Pfannenstiel incision would lead to a lower primary outcome rate – a better result – than would a vertical incision. This result just missed the predetermined threshold of 60%, said Dr. Marrs.
Of the 789 women who met the BMI threshold for eligibility assessment, 420 (65%) who passed the screening declined to participate. Of those who consented to participation, an additional 137 women either withdrew consent or failed further screening, leaving 50 women who were randomized to the Pfannenstiel arm and 41 who were randomized to the vertical incision arm.
Baseline characteristics were similar between groups, with a mean maternal age of 30 years in the Pfannenstiel group and 28 years in the vertical incision group. Gestational age at delivery was a mean of 37 weeks in both groups, and mean BMI was 48-50 kg/m2.
Most patients (80%-90%) had public insurance. Diabetes was more common in the Pfannenstiel group (48%) than in the vertical incision cohort (32%). Just over 40% of patients were African American.
Two women in the Pfannenstiel group and three in the vertical incision group did not receive the intended incision. After accounting for patients lost to follow-up by 6 weeks, 43 women who received Pfannenstiel and 38 women who received vertical incisions were available for full evaluation.
Dr. Marrs said that the study, the first randomized trial to address this issue, had several strengths, including its being conducted at two sites with appropriate stratification for the sites. Also, an independent data safety monitoring board and two chart reviewers helped overcome some of the limitations of a surgical study, where complete blinding is impossible.
The Bayesian analysis allowed ascertainment of the probability of treatment benefit despite the lower-than-hoped-for enrollment numbers. The primary weakness of the study, said Dr. Marrs, centered around the low consent rate, which led to a small study that was prematurely terminated.
“It’s difficult to enroll women in a trial that requires random allocation of skin incision, due to their preference to choose their own incision. A larger trial would likewise be challenging, and unlikely to yield different results,” said Dr. Marrs.
Dr. Marrs reported no conflicts of interest.
SOURCE: Marrs CC et al. Am J Obstet Gynecol. 2018 Jan;218:S29.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: Wound complication rates were similar with Pfannenstiel and vertical incisions in women with obesity.
Major finding: At 6 weeks, 21.1% of vertical incision recipients and 18.6% of Pfannenstiel recipients had wound complications.
Study details: Randomized controlled trial of 91 women with obesity receiving cesarean section.
Disclosures: Dr. Marrs reported no conflicts of interest.
Source: Marrs CC et al. Am J Obstet Gynecol. 2018 Jan;218:S29.
Radiation offers no survival benefit in early lung cancer with positive margins
For patients with early-stage non–small-cell lung cancer (NSCLC) who had positive margins following lobectomy, additional radiation therapy was not associated with a long-term survival benefit in a recent retrospective study.
Positive margins were associated with significantly worse 5-year survival in the study of patients with stage I-II NSCLC, which was published in the Journal of Surgical Research (2018 Mar. doi: 10.1016/j.jss.2017.10.025).
The study is one of the latest to suggest radiation may not be of benefit for treatment of positive margins after surgical resection of lung cancer, according to Brian C. Gulack, MD, MHS, department of surgery, Duke University, Durham, N.C., and his coauthors.
“Our analysis adds important findings to the literature as it focuses specifically on patients undergoing a lobectomy for stage I or II disease,” they wrote.
Adjuvant radiation therapy and re-resection are considered to be two potential treatment options for patients with NSCLC who undergo lobectomy and have positive margins, wrote Dr. Gulack and his coauthors.
However, guidelines from the National Comprehensive Cancer Network recommend re-resection when possible, they added.
The retrospective analysis by Dr. Gulack and his colleagues was based on information in the National Cancer Data Base, which collects data from more than 1,500 hospitals.
The investigators identified 49,563 patients with stage I-II NSCLC who received lobectomy with no induction therapy between 1998 and 2006. Of those patients, 1,934 (3.9%) had positive margins, the authors reported.
Five-year survival was 34.5% for patients with reportedly positive margins, versus 57.2% for patients without positive margins, according to results of an unadjusted analysis.
To evaluate the effects of radiotherapy specifically for treatment of positive margins, the investigators excluded patients who had upstaged disease or who had received palliative radiotherapy. Out of the remaining 1,579 patients, 579 (38.2%) received radiation therapy, according to the report.
In that group, there was no significant difference in likelihood of death associated with radiation treatment (hazard ratio, 1.10, 95% confidence interval, 0.90-1.35).
“Despite the importance of these findings, there is still potential for substantial bias in this retrospective study, and therefore prospective investigation is necessary in order to validate our results,” Dr. Gulack and his colleagues concluded.
Study coauthor Thomas A. D’Amico, MD, reported serving as a consultant for Scanlan, and the rest of the authors had no disclosures.
SOURCE: Gulack et al. J Surg Res 2018 March doi: 10.1016/j.jss.2017.10.025.
For patients with early-stage non–small-cell lung cancer (NSCLC) who had positive margins following lobectomy, additional radiation therapy was not associated with a long-term survival benefit in a recent retrospective study.
Positive margins were associated with significantly worse 5-year survival in the study of patients with stage I-II NSCLC, which was published in the Journal of Surgical Research (2018 Mar. doi: 10.1016/j.jss.2017.10.025).
The study is one of the latest to suggest radiation may not be of benefit for treatment of positive margins after surgical resection of lung cancer, according to Brian C. Gulack, MD, MHS, department of surgery, Duke University, Durham, N.C., and his coauthors.
“Our analysis adds important findings to the literature as it focuses specifically on patients undergoing a lobectomy for stage I or II disease,” they wrote.
Adjuvant radiation therapy and re-resection are considered to be two potential treatment options for patients with NSCLC who undergo lobectomy and have positive margins, wrote Dr. Gulack and his coauthors.
However, guidelines from the National Comprehensive Cancer Network recommend re-resection when possible, they added.
The retrospective analysis by Dr. Gulack and his colleagues was based on information in the National Cancer Data Base, which collects data from more than 1,500 hospitals.
The investigators identified 49,563 patients with stage I-II NSCLC who received lobectomy with no induction therapy between 1998 and 2006. Of those patients, 1,934 (3.9%) had positive margins, the authors reported.
Five-year survival was 34.5% for patients with reportedly positive margins, versus 57.2% for patients without positive margins, according to results of an unadjusted analysis.
To evaluate the effects of radiotherapy specifically for treatment of positive margins, the investigators excluded patients who had upstaged disease or who had received palliative radiotherapy. Out of the remaining 1,579 patients, 579 (38.2%) received radiation therapy, according to the report.
In that group, there was no significant difference in likelihood of death associated with radiation treatment (hazard ratio, 1.10, 95% confidence interval, 0.90-1.35).
“Despite the importance of these findings, there is still potential for substantial bias in this retrospective study, and therefore prospective investigation is necessary in order to validate our results,” Dr. Gulack and his colleagues concluded.
Study coauthor Thomas A. D’Amico, MD, reported serving as a consultant for Scanlan, and the rest of the authors had no disclosures.
SOURCE: Gulack et al. J Surg Res 2018 March doi: 10.1016/j.jss.2017.10.025.
For patients with early-stage non–small-cell lung cancer (NSCLC) who had positive margins following lobectomy, additional radiation therapy was not associated with a long-term survival benefit in a recent retrospective study.
Positive margins were associated with significantly worse 5-year survival in the study of patients with stage I-II NSCLC, which was published in the Journal of Surgical Research (2018 Mar. doi: 10.1016/j.jss.2017.10.025).
The study is one of the latest to suggest radiation may not be of benefit for treatment of positive margins after surgical resection of lung cancer, according to Brian C. Gulack, MD, MHS, department of surgery, Duke University, Durham, N.C., and his coauthors.
“Our analysis adds important findings to the literature as it focuses specifically on patients undergoing a lobectomy for stage I or II disease,” they wrote.
Adjuvant radiation therapy and re-resection are considered to be two potential treatment options for patients with NSCLC who undergo lobectomy and have positive margins, wrote Dr. Gulack and his coauthors.
However, guidelines from the National Comprehensive Cancer Network recommend re-resection when possible, they added.
The retrospective analysis by Dr. Gulack and his colleagues was based on information in the National Cancer Data Base, which collects data from more than 1,500 hospitals.
The investigators identified 49,563 patients with stage I-II NSCLC who received lobectomy with no induction therapy between 1998 and 2006. Of those patients, 1,934 (3.9%) had positive margins, the authors reported.
Five-year survival was 34.5% for patients with reportedly positive margins, versus 57.2% for patients without positive margins, according to results of an unadjusted analysis.
To evaluate the effects of radiotherapy specifically for treatment of positive margins, the investigators excluded patients who had upstaged disease or who had received palliative radiotherapy. Out of the remaining 1,579 patients, 579 (38.2%) received radiation therapy, according to the report.
In that group, there was no significant difference in likelihood of death associated with radiation treatment (hazard ratio, 1.10, 95% confidence interval, 0.90-1.35).
“Despite the importance of these findings, there is still potential for substantial bias in this retrospective study, and therefore prospective investigation is necessary in order to validate our results,” Dr. Gulack and his colleagues concluded.
Study coauthor Thomas A. D’Amico, MD, reported serving as a consultant for Scanlan, and the rest of the authors had no disclosures.
SOURCE: Gulack et al. J Surg Res 2018 March doi: 10.1016/j.jss.2017.10.025.
FROM THE JOURNAL OF SURGICAL RESEARCH
Key clinical point: Additional radiation therapy was not associated with a long-term survival benefit in patients with early-stage non–small-cell lung cancer who had positive margins following lobectomy.
Major finding: There was no significant difference in likelihood of death associated with radiation treatment (hazard ratio, 1.10, 95% CI, 0.90-1.35).
Study details: A retrospective analysis of data in the National Cancer Data Base including 49,563 patients with stage I-II NSCLC who received lobectomy with no induction therapy between 1998 and 2006.
Disclosures: One study author reported serving as a consultant for Scanlan, and the rest had no disclosures.
Source: Gulack et al. J Surg Res. 2018 Mar. doi: 10.1016/j.jss.2017.10.025.
How to cope after your patient commits suicide
LAS VEGAS – Michael J. Gitlin, MD, was 6 months removed from his psychiatry residency in 1980 when, for the first time, a patient he cared for took his own life.
He was a chronically depressed young man receiving medication and psychotherapy, and had one prior suicide attempt, Dr. Gitlin, now professor of psychiatry and biobehavioral sciences at the University of California, Los Angeles, recalled at an annual psychopharmacology update held by the Nevada Psychiatric Association. “One day he came in and intimated that he was going to kill himself, but not in the near future so as to not upset his parents. I scheduled another visit with him in 2 days and told him, ‘If you’re really having trouble, I’ll put you in the hospital.’ ”
The man never showed for that planned visit. Dr. Gitlin telephoned acquaintances and eventually the police, and through the window of his apartment, they observed his dead body. “That was my first experience, where I began to think, ‘what does this do to us as psychiatrists, and how do we deal with it?’ ”
According to Dr. Gitlin, fewer than 25 papers in the medical literature address the topic of how to cope when a patient takes his or her own life. He considers it ironic, because about 42,000 people in the United States die from suicide each year. “Of that 42,000, a reasonable percentage have seen a health professional, and a little lower percentage a mental health professional, within a number of weeks before the suicide happened,” he said. “Probably 10,000 psychiatrists per year will have this experience.”
The best available literature on the topic shows that about one in six psychiatrists reports having more than five patient suicides during an entire career. “There are two issues here,” Dr. Gitlin said. “One is, because it’s such an infrequent event, nobody has a big enough series to write about. The other issue is, because it’s so infrequent, nobody learns particularly well how to cope with it. You can’t become an oncologist if you’re really phobic and overwhelmed every time a patient dies. But it happens infrequently enough in psychiatry that nobody really masters a way of coping.”
Younger age and lesser clinical experience are most powerful predictors of distress. In fact, over a 3-year training period, about one-third of psychiatry residents will have a patient commit suicide. “Is that because our young colleagues just don’t know what to do and they’re not as thoughtful and as wise, and have as good a judgment as we have and do?” Dr. Gitlin asked. “Of course not. It’s because we give the most ill patients to the people with the least experience. Residents treat much more psychiatrically ill patients, who therefore have a higher risk of suicide.”
Responses are wide-ranging and are similar to other meaningful losses in life. One study found that about 38% of psychiatrists experience levels of distress in the first few weeks after a patient suicide, which is comparable to that of a clinical population (Am J Psychiatry. 2004;161:1442-6). “If you take those same people and follow them out, that level drops rather precipitously, from 38% to 5% or 10%,” Dr. Gitlin said. “That means that it feels like an acute stress reaction. By 6 months, the effect has faded significantly. One-third of psychiatrists will say that when a patient commits suicide, it affects their personal life to some significant degree, and 15% say they thought about retirement. But if you push them on it, only about 3% think about it seriously.”
“And nobody else in this department of board-certified psychiatrists noticed a damn thing. It was all internal, and it was a striking thing. It’s the only time in my life I’ve ever felt that.”
Other reactions include “core responses” of grief, guilt, shame/fear of blame, anger, and relief. “This is not in a variant sequence and not everybody has every one of these feelings,” he emphasized. “If you’ve been working with this person for any extended period of time, you can get attached to them, so you grieve the loss of a person,” he said.
A loss of hope also can occur. “We all imagine that we’re going to help people; a suicide shoves that notion aside,” Dr. Gitlin said. “But in many ways the biggest grief is what I call loss of influence to make a change. I suspect this is truer for younger psychiatrists than for older ones. Early on in our career we all have this feeling that if we do right, if we take good care of the patients, if we’re kind to them and respect boundaries, and we return phone calls, that good things are going to happen. Then you work very hard taking care of a patient as best you can, and they kill themselves on your watch. That changes the equation.”
Another common response when a patient takes his or her own life is a sense of shame. “Think about the cardiologist who loses a patient from heart disease,” said Dr. Gitlin, who also directs the UCLA Mood Disorders Clinic. “Do they feel bad? I assume so. Do they feel a sense of shame? I suspect not. Why do we feel the shame and embarrassment, and they don’t? Even the most hard-core psychopharmacologists among us really don’t believe that it’s just the technical aspects of treatment that make our patients better. It’s us; it’s our relationship with them. That makes the failure of a patient who dies not a clinical failure, but a personal failure. To me, that is the core reason why suicide feels different from an oncologist losing a patient to a disorder that has a known fatality rate.”
A fear of blame, or of being sued, can materialize. So can anger, which can raise complicated questions. For example, are you angry at the patient for committing suicide? Is the family angry? And who are they angry at? Are they angry at you? Are they angry at the hospital? “If it’s in a broader system, let’s say a hospital system, there’s a hierarchy,” Dr. Gitlin said. “Staff could be angry at the ward chief, who could be angry at the attending physician. It can roll downhill. In a complex environment the possibility of projected blame can become a big deal.”
. “In every major religion in the world, when there’s a loss, you rally around the person,” he said. “The rituals of the rallying around differ across cultures and religions, but the rallying around is universal. As humans, we know that it’s much more painful to sit alone with your pain than with the support of family members, friends, loved ones, and community. Find the right person [to confide in]. Not everybody you know will be the right person.”
After the death of a patient from suicide, Dr. Gitlin makes it a point to offer to meet with loved ones. “If you do meet with them, be prepared,” he cautioned. “You don’t know whether the families are a family of interjectors or projectors. Are they going to come in and say, ‘Doctor, thank you so much for doing your best for helping my relative,’ or are they going to come in and say to you, ‘You jerk; my kid died under your care.’ Be prepared for anything that happens in that room.” He also recommends asking the family’s permission to attend the patient’s funeral.
Another helpful coping strategy is to conduct a “psychological autopsy” with colleagues. “Ask what could have been done differently [in the case], not to blame, but to learn,” Dr. Gitlin said. “I have been to some psychological autopsies where it was just ‘Who can be blamed?’ and it was always the youngest person on the totem pole. If the institution can’t get it right psychologically, they shouldn’t do it. That’s more destructive than not doing it at all.”
Maintaining professional boundaries with patients also can help you cope. “We don’t want to put so much into our work with our patients that if it goes bad, we get overwhelmingly devastated,” he said. “Finding that middle ground between blurring boundaries and being too detached is something that every mental health professional should do. Distinguishing between clinical and personal failure is critical. I made a decision some time ago that I want to work with people with prominent psychiatric difficulties. We have some difficult patients, but the philosophical and cognitive relief that I give myself when bad things happen is that I say to myself, ‘I chose to work with sick people. Some of them will die of their illness. I’ll save some, but I can’t save them all.’ There’s a natural mortality rate with mood disorders that is related to suicide, just like 5%-10% of anorexics die from anorexia nervosa. That’s the natural mortality rate of the disease.”
Dr. Gitlin ended his presentation by underscoring the importance of establishing support systems in your workplace or teaching institution. For example, he gives lectures to second-year psychiatry residents at UCLA on the topic of psychiatrist reactions to patient suicide, “because I’m giving them the lecture I wish somebody had given me when I was their age. I and others at UCLA make ourselves available to the residents if and when this happens to them.
“Within our field, most training programs do not deal with this issue as forthrightly as they should. It is our job as the grown-ups in the room to make sure that we do it better. We should be talking with the residents early on about it. Every training institution should have a system set up that when it happens, senior residents help junior residents and faculty is available if a resident is really having trouble dealing with it. Some residencies do this well, and others don’t do it at all.”
Dr. Gitlin reported having no financial disclosures.
LAS VEGAS – Michael J. Gitlin, MD, was 6 months removed from his psychiatry residency in 1980 when, for the first time, a patient he cared for took his own life.
He was a chronically depressed young man receiving medication and psychotherapy, and had one prior suicide attempt, Dr. Gitlin, now professor of psychiatry and biobehavioral sciences at the University of California, Los Angeles, recalled at an annual psychopharmacology update held by the Nevada Psychiatric Association. “One day he came in and intimated that he was going to kill himself, but not in the near future so as to not upset his parents. I scheduled another visit with him in 2 days and told him, ‘If you’re really having trouble, I’ll put you in the hospital.’ ”
The man never showed for that planned visit. Dr. Gitlin telephoned acquaintances and eventually the police, and through the window of his apartment, they observed his dead body. “That was my first experience, where I began to think, ‘what does this do to us as psychiatrists, and how do we deal with it?’ ”
According to Dr. Gitlin, fewer than 25 papers in the medical literature address the topic of how to cope when a patient takes his or her own life. He considers it ironic, because about 42,000 people in the United States die from suicide each year. “Of that 42,000, a reasonable percentage have seen a health professional, and a little lower percentage a mental health professional, within a number of weeks before the suicide happened,” he said. “Probably 10,000 psychiatrists per year will have this experience.”
The best available literature on the topic shows that about one in six psychiatrists reports having more than five patient suicides during an entire career. “There are two issues here,” Dr. Gitlin said. “One is, because it’s such an infrequent event, nobody has a big enough series to write about. The other issue is, because it’s so infrequent, nobody learns particularly well how to cope with it. You can’t become an oncologist if you’re really phobic and overwhelmed every time a patient dies. But it happens infrequently enough in psychiatry that nobody really masters a way of coping.”
Younger age and lesser clinical experience are most powerful predictors of distress. In fact, over a 3-year training period, about one-third of psychiatry residents will have a patient commit suicide. “Is that because our young colleagues just don’t know what to do and they’re not as thoughtful and as wise, and have as good a judgment as we have and do?” Dr. Gitlin asked. “Of course not. It’s because we give the most ill patients to the people with the least experience. Residents treat much more psychiatrically ill patients, who therefore have a higher risk of suicide.”
Responses are wide-ranging and are similar to other meaningful losses in life. One study found that about 38% of psychiatrists experience levels of distress in the first few weeks after a patient suicide, which is comparable to that of a clinical population (Am J Psychiatry. 2004;161:1442-6). “If you take those same people and follow them out, that level drops rather precipitously, from 38% to 5% or 10%,” Dr. Gitlin said. “That means that it feels like an acute stress reaction. By 6 months, the effect has faded significantly. One-third of psychiatrists will say that when a patient commits suicide, it affects their personal life to some significant degree, and 15% say they thought about retirement. But if you push them on it, only about 3% think about it seriously.”
“And nobody else in this department of board-certified psychiatrists noticed a damn thing. It was all internal, and it was a striking thing. It’s the only time in my life I’ve ever felt that.”
Other reactions include “core responses” of grief, guilt, shame/fear of blame, anger, and relief. “This is not in a variant sequence and not everybody has every one of these feelings,” he emphasized. “If you’ve been working with this person for any extended period of time, you can get attached to them, so you grieve the loss of a person,” he said.
A loss of hope also can occur. “We all imagine that we’re going to help people; a suicide shoves that notion aside,” Dr. Gitlin said. “But in many ways the biggest grief is what I call loss of influence to make a change. I suspect this is truer for younger psychiatrists than for older ones. Early on in our career we all have this feeling that if we do right, if we take good care of the patients, if we’re kind to them and respect boundaries, and we return phone calls, that good things are going to happen. Then you work very hard taking care of a patient as best you can, and they kill themselves on your watch. That changes the equation.”
Another common response when a patient takes his or her own life is a sense of shame. “Think about the cardiologist who loses a patient from heart disease,” said Dr. Gitlin, who also directs the UCLA Mood Disorders Clinic. “Do they feel bad? I assume so. Do they feel a sense of shame? I suspect not. Why do we feel the shame and embarrassment, and they don’t? Even the most hard-core psychopharmacologists among us really don’t believe that it’s just the technical aspects of treatment that make our patients better. It’s us; it’s our relationship with them. That makes the failure of a patient who dies not a clinical failure, but a personal failure. To me, that is the core reason why suicide feels different from an oncologist losing a patient to a disorder that has a known fatality rate.”
A fear of blame, or of being sued, can materialize. So can anger, which can raise complicated questions. For example, are you angry at the patient for committing suicide? Is the family angry? And who are they angry at? Are they angry at you? Are they angry at the hospital? “If it’s in a broader system, let’s say a hospital system, there’s a hierarchy,” Dr. Gitlin said. “Staff could be angry at the ward chief, who could be angry at the attending physician. It can roll downhill. In a complex environment the possibility of projected blame can become a big deal.”
. “In every major religion in the world, when there’s a loss, you rally around the person,” he said. “The rituals of the rallying around differ across cultures and religions, but the rallying around is universal. As humans, we know that it’s much more painful to sit alone with your pain than with the support of family members, friends, loved ones, and community. Find the right person [to confide in]. Not everybody you know will be the right person.”
After the death of a patient from suicide, Dr. Gitlin makes it a point to offer to meet with loved ones. “If you do meet with them, be prepared,” he cautioned. “You don’t know whether the families are a family of interjectors or projectors. Are they going to come in and say, ‘Doctor, thank you so much for doing your best for helping my relative,’ or are they going to come in and say to you, ‘You jerk; my kid died under your care.’ Be prepared for anything that happens in that room.” He also recommends asking the family’s permission to attend the patient’s funeral.
Another helpful coping strategy is to conduct a “psychological autopsy” with colleagues. “Ask what could have been done differently [in the case], not to blame, but to learn,” Dr. Gitlin said. “I have been to some psychological autopsies where it was just ‘Who can be blamed?’ and it was always the youngest person on the totem pole. If the institution can’t get it right psychologically, they shouldn’t do it. That’s more destructive than not doing it at all.”
Maintaining professional boundaries with patients also can help you cope. “We don’t want to put so much into our work with our patients that if it goes bad, we get overwhelmingly devastated,” he said. “Finding that middle ground between blurring boundaries and being too detached is something that every mental health professional should do. Distinguishing between clinical and personal failure is critical. I made a decision some time ago that I want to work with people with prominent psychiatric difficulties. We have some difficult patients, but the philosophical and cognitive relief that I give myself when bad things happen is that I say to myself, ‘I chose to work with sick people. Some of them will die of their illness. I’ll save some, but I can’t save them all.’ There’s a natural mortality rate with mood disorders that is related to suicide, just like 5%-10% of anorexics die from anorexia nervosa. That’s the natural mortality rate of the disease.”
Dr. Gitlin ended his presentation by underscoring the importance of establishing support systems in your workplace or teaching institution. For example, he gives lectures to second-year psychiatry residents at UCLA on the topic of psychiatrist reactions to patient suicide, “because I’m giving them the lecture I wish somebody had given me when I was their age. I and others at UCLA make ourselves available to the residents if and when this happens to them.
“Within our field, most training programs do not deal with this issue as forthrightly as they should. It is our job as the grown-ups in the room to make sure that we do it better. We should be talking with the residents early on about it. Every training institution should have a system set up that when it happens, senior residents help junior residents and faculty is available if a resident is really having trouble dealing with it. Some residencies do this well, and others don’t do it at all.”
Dr. Gitlin reported having no financial disclosures.
LAS VEGAS – Michael J. Gitlin, MD, was 6 months removed from his psychiatry residency in 1980 when, for the first time, a patient he cared for took his own life.
He was a chronically depressed young man receiving medication and psychotherapy, and had one prior suicide attempt, Dr. Gitlin, now professor of psychiatry and biobehavioral sciences at the University of California, Los Angeles, recalled at an annual psychopharmacology update held by the Nevada Psychiatric Association. “One day he came in and intimated that he was going to kill himself, but not in the near future so as to not upset his parents. I scheduled another visit with him in 2 days and told him, ‘If you’re really having trouble, I’ll put you in the hospital.’ ”
The man never showed for that planned visit. Dr. Gitlin telephoned acquaintances and eventually the police, and through the window of his apartment, they observed his dead body. “That was my first experience, where I began to think, ‘what does this do to us as psychiatrists, and how do we deal with it?’ ”
According to Dr. Gitlin, fewer than 25 papers in the medical literature address the topic of how to cope when a patient takes his or her own life. He considers it ironic, because about 42,000 people in the United States die from suicide each year. “Of that 42,000, a reasonable percentage have seen a health professional, and a little lower percentage a mental health professional, within a number of weeks before the suicide happened,” he said. “Probably 10,000 psychiatrists per year will have this experience.”
The best available literature on the topic shows that about one in six psychiatrists reports having more than five patient suicides during an entire career. “There are two issues here,” Dr. Gitlin said. “One is, because it’s such an infrequent event, nobody has a big enough series to write about. The other issue is, because it’s so infrequent, nobody learns particularly well how to cope with it. You can’t become an oncologist if you’re really phobic and overwhelmed every time a patient dies. But it happens infrequently enough in psychiatry that nobody really masters a way of coping.”
Younger age and lesser clinical experience are most powerful predictors of distress. In fact, over a 3-year training period, about one-third of psychiatry residents will have a patient commit suicide. “Is that because our young colleagues just don’t know what to do and they’re not as thoughtful and as wise, and have as good a judgment as we have and do?” Dr. Gitlin asked. “Of course not. It’s because we give the most ill patients to the people with the least experience. Residents treat much more psychiatrically ill patients, who therefore have a higher risk of suicide.”
Responses are wide-ranging and are similar to other meaningful losses in life. One study found that about 38% of psychiatrists experience levels of distress in the first few weeks after a patient suicide, which is comparable to that of a clinical population (Am J Psychiatry. 2004;161:1442-6). “If you take those same people and follow them out, that level drops rather precipitously, from 38% to 5% or 10%,” Dr. Gitlin said. “That means that it feels like an acute stress reaction. By 6 months, the effect has faded significantly. One-third of psychiatrists will say that when a patient commits suicide, it affects their personal life to some significant degree, and 15% say they thought about retirement. But if you push them on it, only about 3% think about it seriously.”
“And nobody else in this department of board-certified psychiatrists noticed a damn thing. It was all internal, and it was a striking thing. It’s the only time in my life I’ve ever felt that.”
Other reactions include “core responses” of grief, guilt, shame/fear of blame, anger, and relief. “This is not in a variant sequence and not everybody has every one of these feelings,” he emphasized. “If you’ve been working with this person for any extended period of time, you can get attached to them, so you grieve the loss of a person,” he said.
A loss of hope also can occur. “We all imagine that we’re going to help people; a suicide shoves that notion aside,” Dr. Gitlin said. “But in many ways the biggest grief is what I call loss of influence to make a change. I suspect this is truer for younger psychiatrists than for older ones. Early on in our career we all have this feeling that if we do right, if we take good care of the patients, if we’re kind to them and respect boundaries, and we return phone calls, that good things are going to happen. Then you work very hard taking care of a patient as best you can, and they kill themselves on your watch. That changes the equation.”
Another common response when a patient takes his or her own life is a sense of shame. “Think about the cardiologist who loses a patient from heart disease,” said Dr. Gitlin, who also directs the UCLA Mood Disorders Clinic. “Do they feel bad? I assume so. Do they feel a sense of shame? I suspect not. Why do we feel the shame and embarrassment, and they don’t? Even the most hard-core psychopharmacologists among us really don’t believe that it’s just the technical aspects of treatment that make our patients better. It’s us; it’s our relationship with them. That makes the failure of a patient who dies not a clinical failure, but a personal failure. To me, that is the core reason why suicide feels different from an oncologist losing a patient to a disorder that has a known fatality rate.”
A fear of blame, or of being sued, can materialize. So can anger, which can raise complicated questions. For example, are you angry at the patient for committing suicide? Is the family angry? And who are they angry at? Are they angry at you? Are they angry at the hospital? “If it’s in a broader system, let’s say a hospital system, there’s a hierarchy,” Dr. Gitlin said. “Staff could be angry at the ward chief, who could be angry at the attending physician. It can roll downhill. In a complex environment the possibility of projected blame can become a big deal.”
. “In every major religion in the world, when there’s a loss, you rally around the person,” he said. “The rituals of the rallying around differ across cultures and religions, but the rallying around is universal. As humans, we know that it’s much more painful to sit alone with your pain than with the support of family members, friends, loved ones, and community. Find the right person [to confide in]. Not everybody you know will be the right person.”
After the death of a patient from suicide, Dr. Gitlin makes it a point to offer to meet with loved ones. “If you do meet with them, be prepared,” he cautioned. “You don’t know whether the families are a family of interjectors or projectors. Are they going to come in and say, ‘Doctor, thank you so much for doing your best for helping my relative,’ or are they going to come in and say to you, ‘You jerk; my kid died under your care.’ Be prepared for anything that happens in that room.” He also recommends asking the family’s permission to attend the patient’s funeral.
Another helpful coping strategy is to conduct a “psychological autopsy” with colleagues. “Ask what could have been done differently [in the case], not to blame, but to learn,” Dr. Gitlin said. “I have been to some psychological autopsies where it was just ‘Who can be blamed?’ and it was always the youngest person on the totem pole. If the institution can’t get it right psychologically, they shouldn’t do it. That’s more destructive than not doing it at all.”
Maintaining professional boundaries with patients also can help you cope. “We don’t want to put so much into our work with our patients that if it goes bad, we get overwhelmingly devastated,” he said. “Finding that middle ground between blurring boundaries and being too detached is something that every mental health professional should do. Distinguishing between clinical and personal failure is critical. I made a decision some time ago that I want to work with people with prominent psychiatric difficulties. We have some difficult patients, but the philosophical and cognitive relief that I give myself when bad things happen is that I say to myself, ‘I chose to work with sick people. Some of them will die of their illness. I’ll save some, but I can’t save them all.’ There’s a natural mortality rate with mood disorders that is related to suicide, just like 5%-10% of anorexics die from anorexia nervosa. That’s the natural mortality rate of the disease.”
Dr. Gitlin ended his presentation by underscoring the importance of establishing support systems in your workplace or teaching institution. For example, he gives lectures to second-year psychiatry residents at UCLA on the topic of psychiatrist reactions to patient suicide, “because I’m giving them the lecture I wish somebody had given me when I was their age. I and others at UCLA make ourselves available to the residents if and when this happens to them.
“Within our field, most training programs do not deal with this issue as forthrightly as they should. It is our job as the grown-ups in the room to make sure that we do it better. We should be talking with the residents early on about it. Every training institution should have a system set up that when it happens, senior residents help junior residents and faculty is available if a resident is really having trouble dealing with it. Some residencies do this well, and others don’t do it at all.”
Dr. Gitlin reported having no financial disclosures.
EXPERT ANALYSIS AT NPA 2018
Critical illness-related corticosteroid insufficiency guidelines explained
SAN ANTONIO – When corticosteroids are used for septic shock, the dose should be low to moderate, the timing should be early, and the duration should be at least 3 days, said a speaker at the Critical Care Congress sponsored by the Society for Critical Care.
Dosing, timing, and duration are “three critical questions” critical care specialists face that are answered by the new critical illness–related corticosteroid insufficiency (CIRCI) guidelines, continued Stephen M. Pastores, MD, a cochair of the task force that developed guidelines for the diagnosis and management of CIRCI in critically ill patients.
During his presentation, Dr. Pastores limited his remarks to discussion of sepsis and septic shock with corticosteroids. He cautioned that, despite careful deliberations by the panel, the level of evidence behind some of the recommendations was “low to moderate and never high” and that not all task force members agreed with all recommendations.
“There were a lot of back and forth disagreements behind these recommendations,” said Dr. Pastores, who is the director of the critical care medicine fellowship training and research programs at Memorial Sloan Kettering Cancer Center, New York. “We only required 80% of the panelists to agree that these were the recommendations and statements that we were going to go by.”
The guidelines recommend against the use of corticosteroids in adult patients who have sepsis without shock, Dr. Pastores noted.
In contrast,
In an analysis of available data from randomized clinical trials including patients with septic shock, corticosteroids significantly reduced 28-day mortality when compared with placebo, Dr. Pastores said.
That survival benefit seems to be dependent on several factors: dose of the corticosteroids (hydrocortisone less than 400 mg/day), longer duration (at least 3 or more days), and severity of sepsis. “The more severe the sepsis, the more septic shock the patient was in, the more likely the corticosteroids were likely to help those patients,” Dr. Pastores explained.
Accordingly, the guidelines further suggest using long-course, low-dose corticosteroid treatment, namely intravenous hydrocortisone at no more than 400 mg/day for at least 3 days.
The expert panel specifically recommended hydrocortisone as the corticosteroid of choice in this setting, according to Dr. Pastores. That recommendation was based in part on a recent systematic review and meta-analysis showing that hydrocortisone, given as a bolus or an infusion, was more likely than placebo or methylprednisolone to result in shock reversal.
Dr. Pastores reported disclosures related to Theravance Biopharma, Bayer HealthCare Pharmaceuticals, Spectral Diagnostics, and Asahi-Kasei.
SAN ANTONIO – When corticosteroids are used for septic shock, the dose should be low to moderate, the timing should be early, and the duration should be at least 3 days, said a speaker at the Critical Care Congress sponsored by the Society for Critical Care.
Dosing, timing, and duration are “three critical questions” critical care specialists face that are answered by the new critical illness–related corticosteroid insufficiency (CIRCI) guidelines, continued Stephen M. Pastores, MD, a cochair of the task force that developed guidelines for the diagnosis and management of CIRCI in critically ill patients.
During his presentation, Dr. Pastores limited his remarks to discussion of sepsis and septic shock with corticosteroids. He cautioned that, despite careful deliberations by the panel, the level of evidence behind some of the recommendations was “low to moderate and never high” and that not all task force members agreed with all recommendations.
“There were a lot of back and forth disagreements behind these recommendations,” said Dr. Pastores, who is the director of the critical care medicine fellowship training and research programs at Memorial Sloan Kettering Cancer Center, New York. “We only required 80% of the panelists to agree that these were the recommendations and statements that we were going to go by.”
The guidelines recommend against the use of corticosteroids in adult patients who have sepsis without shock, Dr. Pastores noted.
In contrast,
In an analysis of available data from randomized clinical trials including patients with septic shock, corticosteroids significantly reduced 28-day mortality when compared with placebo, Dr. Pastores said.
That survival benefit seems to be dependent on several factors: dose of the corticosteroids (hydrocortisone less than 400 mg/day), longer duration (at least 3 or more days), and severity of sepsis. “The more severe the sepsis, the more septic shock the patient was in, the more likely the corticosteroids were likely to help those patients,” Dr. Pastores explained.
Accordingly, the guidelines further suggest using long-course, low-dose corticosteroid treatment, namely intravenous hydrocortisone at no more than 400 mg/day for at least 3 days.
The expert panel specifically recommended hydrocortisone as the corticosteroid of choice in this setting, according to Dr. Pastores. That recommendation was based in part on a recent systematic review and meta-analysis showing that hydrocortisone, given as a bolus or an infusion, was more likely than placebo or methylprednisolone to result in shock reversal.
Dr. Pastores reported disclosures related to Theravance Biopharma, Bayer HealthCare Pharmaceuticals, Spectral Diagnostics, and Asahi-Kasei.
SAN ANTONIO – When corticosteroids are used for septic shock, the dose should be low to moderate, the timing should be early, and the duration should be at least 3 days, said a speaker at the Critical Care Congress sponsored by the Society for Critical Care.
Dosing, timing, and duration are “three critical questions” critical care specialists face that are answered by the new critical illness–related corticosteroid insufficiency (CIRCI) guidelines, continued Stephen M. Pastores, MD, a cochair of the task force that developed guidelines for the diagnosis and management of CIRCI in critically ill patients.
During his presentation, Dr. Pastores limited his remarks to discussion of sepsis and septic shock with corticosteroids. He cautioned that, despite careful deliberations by the panel, the level of evidence behind some of the recommendations was “low to moderate and never high” and that not all task force members agreed with all recommendations.
“There were a lot of back and forth disagreements behind these recommendations,” said Dr. Pastores, who is the director of the critical care medicine fellowship training and research programs at Memorial Sloan Kettering Cancer Center, New York. “We only required 80% of the panelists to agree that these were the recommendations and statements that we were going to go by.”
The guidelines recommend against the use of corticosteroids in adult patients who have sepsis without shock, Dr. Pastores noted.
In contrast,
In an analysis of available data from randomized clinical trials including patients with septic shock, corticosteroids significantly reduced 28-day mortality when compared with placebo, Dr. Pastores said.
That survival benefit seems to be dependent on several factors: dose of the corticosteroids (hydrocortisone less than 400 mg/day), longer duration (at least 3 or more days), and severity of sepsis. “The more severe the sepsis, the more septic shock the patient was in, the more likely the corticosteroids were likely to help those patients,” Dr. Pastores explained.
Accordingly, the guidelines further suggest using long-course, low-dose corticosteroid treatment, namely intravenous hydrocortisone at no more than 400 mg/day for at least 3 days.
The expert panel specifically recommended hydrocortisone as the corticosteroid of choice in this setting, according to Dr. Pastores. That recommendation was based in part on a recent systematic review and meta-analysis showing that hydrocortisone, given as a bolus or an infusion, was more likely than placebo or methylprednisolone to result in shock reversal.
Dr. Pastores reported disclosures related to Theravance Biopharma, Bayer HealthCare Pharmaceuticals, Spectral Diagnostics, and Asahi-Kasei.
EXPERT ANALYSIS FROM THE CCC47
Revascularization in paraplegics best performed with PCI
WASHINGTON – When paraplegics and quadriplegics have an acute MI and are candidates for revascularization, they should be treated preferentially with a percutaneous coronary intervention, according to data presented at the 2018 Cardiovascular Research Technologies meeting.
When compared 30 days after revascularization, the rates of major adverse cardiovascular events (MACE) following coronary artery bypass grafting (CABG) were 22% in the group with paraplegia or quadriplegia versus only 3.5% in those without loss of limb function. For percutaneous coronary intervention (PCI), the rates were 6% versus 2%, respectively, reported Xuming Dai, MD, PhD, an interventional cardiologist and assistant professor at the University of North Carolina at Chapel Hill.
“There are no guidelines, no studies. I could not even find a case report,” Dr. Dai recounted.
As a result, he initiated his own study, looking for such cases in the New York State Inpatient Database, in which there were 1,400 patients with paraplegia or quadriplegia and more than 400,000 without these limb impairments who had presented with acute MI over the period of study. After comparing outcomes in these two groups, a subsequent analysis was performed in which each patient with paraplegia/quadriplegia was matched by propensity scoring to five patients from the database without paraplegia/quadriplegia.
Notably, patients with paraplegia/quadriplegia were found to represent a small but steady proportion of acute MI cases. With only modest variation, the rate hovered around 0.2%-0.3% of cases per year.
“The patients with paraplegia or quadriplegia tended to be somewhat younger [67 vs. 70 years of age; P less than .001], have more comorbidities, and were more likely to be enrolled in Medicare,” Dr. Dai reported.
Of patients in the database without paraplegia/quadriplegia, 56% received medical therapy alone and 14% underwent catheterization but were not revascularized. Of the 31% who were revascularized, 82% underwent PCI, and the remainder underwent CABG.
Among those with paraplegia/quadriplegia, 83.7% were managed medically and 7.2% underwent catheterization but no revascularization. Of the 9.1% who were revascularized, 7.2% underwent PCI and 1.9% underwent CABG.
When evaluated with propensity scoring, the differences in outcomes between those with or without paraplegia/quadriplegia were more modest, but MACE rates after CABG remained significantly higher (8.4% vs. 3.5%; P = .02). In contrast, the difference in MACE rates after propensity matching was no longer significantly higher in the paraplegia/quadriplegia group treated with PCI (4.4% vs. 2.0%; P = .46).
When CABG was compared to PCI among those with paraplegia/quadriplegia, the rate of in-hospital mortality was almost four times higher (9.5% vs. 2.5; P less than.01). Paraplegic/quadriplegic patients treated with CABG also had longer lengths of hospital stay and incurred higher treatment costs, according to Dr. Dai.
The moderator of the session at which these data were presented, Scott Schurmer, MD, chief of cardiology at Texas Tech Health Sciences Center, Lubbock, cautioned about the limitations of propensity scoring. He also suggested that PCI, based on concern for potential comorbidities in patients with paraplegia and quadriplegia, would likely be the choice of many physicians even without these data.
Dr. Dai reported no financial relationships to disclose.
SOURCE: Dai X. CRT 2018.
WASHINGTON – When paraplegics and quadriplegics have an acute MI and are candidates for revascularization, they should be treated preferentially with a percutaneous coronary intervention, according to data presented at the 2018 Cardiovascular Research Technologies meeting.
When compared 30 days after revascularization, the rates of major adverse cardiovascular events (MACE) following coronary artery bypass grafting (CABG) were 22% in the group with paraplegia or quadriplegia versus only 3.5% in those without loss of limb function. For percutaneous coronary intervention (PCI), the rates were 6% versus 2%, respectively, reported Xuming Dai, MD, PhD, an interventional cardiologist and assistant professor at the University of North Carolina at Chapel Hill.
“There are no guidelines, no studies. I could not even find a case report,” Dr. Dai recounted.
As a result, he initiated his own study, looking for such cases in the New York State Inpatient Database, in which there were 1,400 patients with paraplegia or quadriplegia and more than 400,000 without these limb impairments who had presented with acute MI over the period of study. After comparing outcomes in these two groups, a subsequent analysis was performed in which each patient with paraplegia/quadriplegia was matched by propensity scoring to five patients from the database without paraplegia/quadriplegia.
Notably, patients with paraplegia/quadriplegia were found to represent a small but steady proportion of acute MI cases. With only modest variation, the rate hovered around 0.2%-0.3% of cases per year.
“The patients with paraplegia or quadriplegia tended to be somewhat younger [67 vs. 70 years of age; P less than .001], have more comorbidities, and were more likely to be enrolled in Medicare,” Dr. Dai reported.
Of patients in the database without paraplegia/quadriplegia, 56% received medical therapy alone and 14% underwent catheterization but were not revascularized. Of the 31% who were revascularized, 82% underwent PCI, and the remainder underwent CABG.
Among those with paraplegia/quadriplegia, 83.7% were managed medically and 7.2% underwent catheterization but no revascularization. Of the 9.1% who were revascularized, 7.2% underwent PCI and 1.9% underwent CABG.
When evaluated with propensity scoring, the differences in outcomes between those with or without paraplegia/quadriplegia were more modest, but MACE rates after CABG remained significantly higher (8.4% vs. 3.5%; P = .02). In contrast, the difference in MACE rates after propensity matching was no longer significantly higher in the paraplegia/quadriplegia group treated with PCI (4.4% vs. 2.0%; P = .46).
When CABG was compared to PCI among those with paraplegia/quadriplegia, the rate of in-hospital mortality was almost four times higher (9.5% vs. 2.5; P less than.01). Paraplegic/quadriplegic patients treated with CABG also had longer lengths of hospital stay and incurred higher treatment costs, according to Dr. Dai.
The moderator of the session at which these data were presented, Scott Schurmer, MD, chief of cardiology at Texas Tech Health Sciences Center, Lubbock, cautioned about the limitations of propensity scoring. He also suggested that PCI, based on concern for potential comorbidities in patients with paraplegia and quadriplegia, would likely be the choice of many physicians even without these data.
Dr. Dai reported no financial relationships to disclose.
SOURCE: Dai X. CRT 2018.
WASHINGTON – When paraplegics and quadriplegics have an acute MI and are candidates for revascularization, they should be treated preferentially with a percutaneous coronary intervention, according to data presented at the 2018 Cardiovascular Research Technologies meeting.
When compared 30 days after revascularization, the rates of major adverse cardiovascular events (MACE) following coronary artery bypass grafting (CABG) were 22% in the group with paraplegia or quadriplegia versus only 3.5% in those without loss of limb function. For percutaneous coronary intervention (PCI), the rates were 6% versus 2%, respectively, reported Xuming Dai, MD, PhD, an interventional cardiologist and assistant professor at the University of North Carolina at Chapel Hill.
“There are no guidelines, no studies. I could not even find a case report,” Dr. Dai recounted.
As a result, he initiated his own study, looking for such cases in the New York State Inpatient Database, in which there were 1,400 patients with paraplegia or quadriplegia and more than 400,000 without these limb impairments who had presented with acute MI over the period of study. After comparing outcomes in these two groups, a subsequent analysis was performed in which each patient with paraplegia/quadriplegia was matched by propensity scoring to five patients from the database without paraplegia/quadriplegia.
Notably, patients with paraplegia/quadriplegia were found to represent a small but steady proportion of acute MI cases. With only modest variation, the rate hovered around 0.2%-0.3% of cases per year.
“The patients with paraplegia or quadriplegia tended to be somewhat younger [67 vs. 70 years of age; P less than .001], have more comorbidities, and were more likely to be enrolled in Medicare,” Dr. Dai reported.
Of patients in the database without paraplegia/quadriplegia, 56% received medical therapy alone and 14% underwent catheterization but were not revascularized. Of the 31% who were revascularized, 82% underwent PCI, and the remainder underwent CABG.
Among those with paraplegia/quadriplegia, 83.7% were managed medically and 7.2% underwent catheterization but no revascularization. Of the 9.1% who were revascularized, 7.2% underwent PCI and 1.9% underwent CABG.
When evaluated with propensity scoring, the differences in outcomes between those with or without paraplegia/quadriplegia were more modest, but MACE rates after CABG remained significantly higher (8.4% vs. 3.5%; P = .02). In contrast, the difference in MACE rates after propensity matching was no longer significantly higher in the paraplegia/quadriplegia group treated with PCI (4.4% vs. 2.0%; P = .46).
When CABG was compared to PCI among those with paraplegia/quadriplegia, the rate of in-hospital mortality was almost four times higher (9.5% vs. 2.5; P less than.01). Paraplegic/quadriplegic patients treated with CABG also had longer lengths of hospital stay and incurred higher treatment costs, according to Dr. Dai.
The moderator of the session at which these data were presented, Scott Schurmer, MD, chief of cardiology at Texas Tech Health Sciences Center, Lubbock, cautioned about the limitations of propensity scoring. He also suggested that PCI, based on concern for potential comorbidities in patients with paraplegia and quadriplegia, would likely be the choice of many physicians even without these data.
Dr. Dai reported no financial relationships to disclose.
SOURCE: Dai X. CRT 2018.
AT THE 2018 CRT MEETING
Key clinical point:
Major finding: Major adverse cardiovascular events at 30 days were lower after PCI than coronary artery bypass grafting (6% vs. 22%).
Data source: A nonrandomized retrospective analysis.
Disclosures: Dr. Dai reported no financial relationships to disclose. Source: Dai X. CRT 2018.
Buy the IBD, get the comorbidity for free
Chronic conditions, such as arthritis and respiratory disease, are significantly more common in adults with inflammatory bowel disease than in those without IBD, according to the Centers for Disease Control and Prevention.
The age-adjusted prevalence of arthritis in adults with IBD is 36.3%, compared with 21.1% for those without IBD, and the prevalence of respiratory disease is 27.3% for IBD patients and 16.6% for non-IBD patients, CDC investigators reported in the Morbidity and Mortality Weekly Report.
Other comorbid chronic conditions with a significantly higher prevalence in patients with IBD than in those without were ulcer (26% vs. 5.5%), cardiovascular disease (19.2% vs. 12%), and cancer (13.7% vs. 8.1%), said Fang Xu, PhD, of the CDC’s National Center for Chronic Disease Prevention and Health Promotion and associates.
Serious psychological distress in the past 30 days was significantly more prevalent in adults with IBD (7.4%) than in those without it (3.4%), and those with IBD were also significantly more likely to report averaging less than 7 hours of sleep than were those without IBD (38.2% vs. 32.2%), according to their analysis of the 2015 and 2016 National Health Interview Surveys.
“Given the disease’s complexity and the effects of chronic conditions and symptoms, optimal IBD care might require a multidisciplinary approach that includes gastroenterologists, preventive medicine specialists, and other medical practitioners,” the investigators wrote.
SOURCE: Xu F et al. MMWR. 2018 Feb 16;67(6);190-5.
Chronic conditions, such as arthritis and respiratory disease, are significantly more common in adults with inflammatory bowel disease than in those without IBD, according to the Centers for Disease Control and Prevention.
The age-adjusted prevalence of arthritis in adults with IBD is 36.3%, compared with 21.1% for those without IBD, and the prevalence of respiratory disease is 27.3% for IBD patients and 16.6% for non-IBD patients, CDC investigators reported in the Morbidity and Mortality Weekly Report.
Other comorbid chronic conditions with a significantly higher prevalence in patients with IBD than in those without were ulcer (26% vs. 5.5%), cardiovascular disease (19.2% vs. 12%), and cancer (13.7% vs. 8.1%), said Fang Xu, PhD, of the CDC’s National Center for Chronic Disease Prevention and Health Promotion and associates.
Serious psychological distress in the past 30 days was significantly more prevalent in adults with IBD (7.4%) than in those without it (3.4%), and those with IBD were also significantly more likely to report averaging less than 7 hours of sleep than were those without IBD (38.2% vs. 32.2%), according to their analysis of the 2015 and 2016 National Health Interview Surveys.
“Given the disease’s complexity and the effects of chronic conditions and symptoms, optimal IBD care might require a multidisciplinary approach that includes gastroenterologists, preventive medicine specialists, and other medical practitioners,” the investigators wrote.
SOURCE: Xu F et al. MMWR. 2018 Feb 16;67(6);190-5.
Chronic conditions, such as arthritis and respiratory disease, are significantly more common in adults with inflammatory bowel disease than in those without IBD, according to the Centers for Disease Control and Prevention.
The age-adjusted prevalence of arthritis in adults with IBD is 36.3%, compared with 21.1% for those without IBD, and the prevalence of respiratory disease is 27.3% for IBD patients and 16.6% for non-IBD patients, CDC investigators reported in the Morbidity and Mortality Weekly Report.
Other comorbid chronic conditions with a significantly higher prevalence in patients with IBD than in those without were ulcer (26% vs. 5.5%), cardiovascular disease (19.2% vs. 12%), and cancer (13.7% vs. 8.1%), said Fang Xu, PhD, of the CDC’s National Center for Chronic Disease Prevention and Health Promotion and associates.
Serious psychological distress in the past 30 days was significantly more prevalent in adults with IBD (7.4%) than in those without it (3.4%), and those with IBD were also significantly more likely to report averaging less than 7 hours of sleep than were those without IBD (38.2% vs. 32.2%), according to their analysis of the 2015 and 2016 National Health Interview Surveys.
“Given the disease’s complexity and the effects of chronic conditions and symptoms, optimal IBD care might require a multidisciplinary approach that includes gastroenterologists, preventive medicine specialists, and other medical practitioners,” the investigators wrote.
SOURCE: Xu F et al. MMWR. 2018 Feb 16;67(6);190-5.
FROM MMWR
Death rate steady with pediatric early warning system
SAN ANTONIO – , but did not reduce the rate of all-cause hospital mortality, according to results of a large, multicenter trial.
Taken together, the findings of the trial do not support the use of the Bedside Pediatric Early Warning System (BedsidePEWS) to reduce hospital mortality, noted investigator Christopher S. Parshuram, MBChB, DPhil, during a presentation at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
The multicenter randomized cluster study, called the EPOCH trial, included 21 hospitals in seven countries that provided inpatient pediatric care. Ten of the hospitals delivered the BedsidePEWS intervention, while the remaining 11 provided usual care. The study data included 144,539 patient discharges comprising 559,443 patient days. Enrollment began Feb. 28, 2011, and ended on June 21, 2015.
For the BedsidePEWS group, all-cause hospital mortality was 1.93 per 1,000 patient discharges, versus 1.56 per 1,000 patient discharges for usual care (adjusted odds ratio, 1.01; 95% confidence interval, 0.61-1.69; P = .96), according to a report on this study that was published in JAMA.
However, the BedsidePEWS group had a significant improvement in the secondary outcome of significant clinical deterioration events, a composite outcome reflecting late ICU admissions.
In the BedsidePEWS group, the rate of significant clinical deterioration events was 0.50 per 1,000 patient-days, compared with 0.84 per 1,000 patient-days at hospitals with usual care (adjusted rate ratio, 0.77; 95% CI, 0.61-0.97; P = .03), the investigators wrote.
The goal of the EPOCH trial was to determine whether BedsidePEWS could reduce rates of all-cause hospital mortality and significant clinical deterioration among hospitalized children, according to the researchers.
“The BedsidePEWS versus usual care did improve processes of care and early detection of critical illness, aligned with the notion of providing the right care, right now,” Dr. Parshuram, associate professor of critical care medicine and pediatrics at the University of Toronto, said during his presentation at the meeting. “Certainly more vital signs were documented, and anecdotally there were reports of culture change.
“However, when we looked further, there was no difference in hospital mortality, nor hospital resource utilization,” Dr. Parshuram added.
The Canadian Institutes of Health Research funded the study. Dr. Parshuram is an inventor of BedsidePEWS and owns shares in a company that is commercializing it.
SOURCE: Parshuram et al. JAMA. 2018 Feb 27. doi: 10.1001/jama.2018.0948.
SAN ANTONIO – , but did not reduce the rate of all-cause hospital mortality, according to results of a large, multicenter trial.
Taken together, the findings of the trial do not support the use of the Bedside Pediatric Early Warning System (BedsidePEWS) to reduce hospital mortality, noted investigator Christopher S. Parshuram, MBChB, DPhil, during a presentation at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
The multicenter randomized cluster study, called the EPOCH trial, included 21 hospitals in seven countries that provided inpatient pediatric care. Ten of the hospitals delivered the BedsidePEWS intervention, while the remaining 11 provided usual care. The study data included 144,539 patient discharges comprising 559,443 patient days. Enrollment began Feb. 28, 2011, and ended on June 21, 2015.
For the BedsidePEWS group, all-cause hospital mortality was 1.93 per 1,000 patient discharges, versus 1.56 per 1,000 patient discharges for usual care (adjusted odds ratio, 1.01; 95% confidence interval, 0.61-1.69; P = .96), according to a report on this study that was published in JAMA.
However, the BedsidePEWS group had a significant improvement in the secondary outcome of significant clinical deterioration events, a composite outcome reflecting late ICU admissions.
In the BedsidePEWS group, the rate of significant clinical deterioration events was 0.50 per 1,000 patient-days, compared with 0.84 per 1,000 patient-days at hospitals with usual care (adjusted rate ratio, 0.77; 95% CI, 0.61-0.97; P = .03), the investigators wrote.
The goal of the EPOCH trial was to determine whether BedsidePEWS could reduce rates of all-cause hospital mortality and significant clinical deterioration among hospitalized children, according to the researchers.
“The BedsidePEWS versus usual care did improve processes of care and early detection of critical illness, aligned with the notion of providing the right care, right now,” Dr. Parshuram, associate professor of critical care medicine and pediatrics at the University of Toronto, said during his presentation at the meeting. “Certainly more vital signs were documented, and anecdotally there were reports of culture change.
“However, when we looked further, there was no difference in hospital mortality, nor hospital resource utilization,” Dr. Parshuram added.
The Canadian Institutes of Health Research funded the study. Dr. Parshuram is an inventor of BedsidePEWS and owns shares in a company that is commercializing it.
SOURCE: Parshuram et al. JAMA. 2018 Feb 27. doi: 10.1001/jama.2018.0948.
SAN ANTONIO – , but did not reduce the rate of all-cause hospital mortality, according to results of a large, multicenter trial.
Taken together, the findings of the trial do not support the use of the Bedside Pediatric Early Warning System (BedsidePEWS) to reduce hospital mortality, noted investigator Christopher S. Parshuram, MBChB, DPhil, during a presentation at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
The multicenter randomized cluster study, called the EPOCH trial, included 21 hospitals in seven countries that provided inpatient pediatric care. Ten of the hospitals delivered the BedsidePEWS intervention, while the remaining 11 provided usual care. The study data included 144,539 patient discharges comprising 559,443 patient days. Enrollment began Feb. 28, 2011, and ended on June 21, 2015.
For the BedsidePEWS group, all-cause hospital mortality was 1.93 per 1,000 patient discharges, versus 1.56 per 1,000 patient discharges for usual care (adjusted odds ratio, 1.01; 95% confidence interval, 0.61-1.69; P = .96), according to a report on this study that was published in JAMA.
However, the BedsidePEWS group had a significant improvement in the secondary outcome of significant clinical deterioration events, a composite outcome reflecting late ICU admissions.
In the BedsidePEWS group, the rate of significant clinical deterioration events was 0.50 per 1,000 patient-days, compared with 0.84 per 1,000 patient-days at hospitals with usual care (adjusted rate ratio, 0.77; 95% CI, 0.61-0.97; P = .03), the investigators wrote.
The goal of the EPOCH trial was to determine whether BedsidePEWS could reduce rates of all-cause hospital mortality and significant clinical deterioration among hospitalized children, according to the researchers.
“The BedsidePEWS versus usual care did improve processes of care and early detection of critical illness, aligned with the notion of providing the right care, right now,” Dr. Parshuram, associate professor of critical care medicine and pediatrics at the University of Toronto, said during his presentation at the meeting. “Certainly more vital signs were documented, and anecdotally there were reports of culture change.
“However, when we looked further, there was no difference in hospital mortality, nor hospital resource utilization,” Dr. Parshuram added.
The Canadian Institutes of Health Research funded the study. Dr. Parshuram is an inventor of BedsidePEWS and owns shares in a company that is commercializing it.
SOURCE: Parshuram et al. JAMA. 2018 Feb 27. doi: 10.1001/jama.2018.0948.
REPORTING FROM CCC47
Key clinical point: Use of a pediatric early warning system (BedsidePEWS) did not reduce rates of all-cause hospital mortality among hospitalized children, compared with usual care, but did reduce rates of significant clinical deterioration events.
Major finding: For hospitals implementing BedsidePEWS, all-cause hospital mortality was 1.93 per 1,000 patient discharges, versus 1.56 per 1,000 at hospitals with usual care (adjusted odds ratio, 1.01; 95% confidence interval, 0.61-1.69; P = .96).
Study details: A multicenter cluster randomized trial of 144,539 patient discharges from 21 hospitals in seven countries providing pediatric care.
Disclosures: The Canadian Institutes of Health Research funded the study. Dr. Parshuram is an inventor of BedsidePEWS and owns shares in a company that is commercializing it.
Source: Parshuram et al. JAMA. 2018 Feb 27. doi: 10.1001/jama.2018.0948.
Opioid prescriptions got shorter in 2017
Use of opioids was down among enrollees of all types of payers in 2017, while the use of drugs to treat opioid dependence went up for three of the four payer categories, according to pharmacy benefits manager Express Scripts.
The days’ worth of opioids dispensed per person per year was down 16.6% from 2016 to 2017 for enrollees with plans on the health exchanges received managed by Express Scripts. Medicaid patients received 16% fewer days’ worth, patients with commercial plans received 10.3% fewer days’ worth, and Medicare patients received 4.9% fewer days’ worth, Express Scripts said in its 2017 Drug Trend Report, which was based on data for 34.3 million members of pharmacy benefits plans the company administers.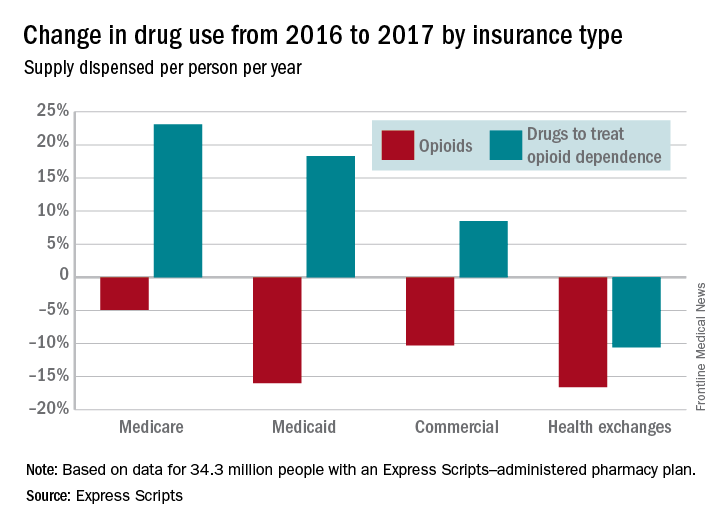
Plans that participated in Express Scripts’ Advanced Opioid Management solution, which was launched in September, experienced “a 60% reduction in the average days’ supply per initial fill, from 18.6 days to just 7.5 days,” according to the report.
Use of opioids was down among enrollees of all types of payers in 2017, while the use of drugs to treat opioid dependence went up for three of the four payer categories, according to pharmacy benefits manager Express Scripts.
The days’ worth of opioids dispensed per person per year was down 16.6% from 2016 to 2017 for enrollees with plans on the health exchanges received managed by Express Scripts. Medicaid patients received 16% fewer days’ worth, patients with commercial plans received 10.3% fewer days’ worth, and Medicare patients received 4.9% fewer days’ worth, Express Scripts said in its 2017 Drug Trend Report, which was based on data for 34.3 million members of pharmacy benefits plans the company administers.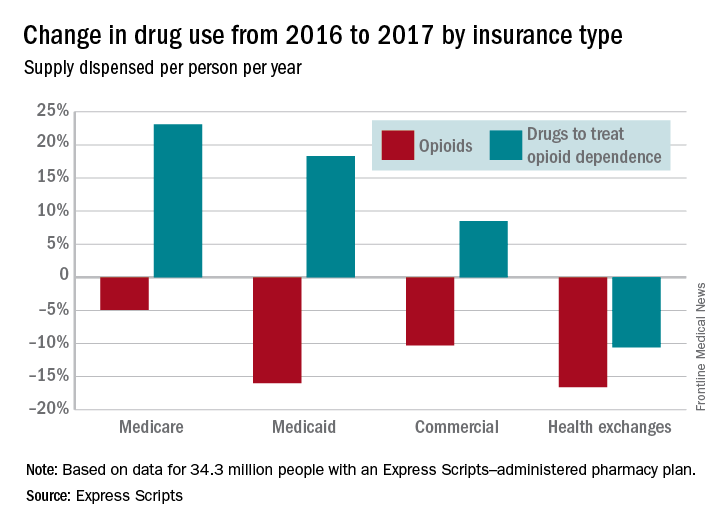
Plans that participated in Express Scripts’ Advanced Opioid Management solution, which was launched in September, experienced “a 60% reduction in the average days’ supply per initial fill, from 18.6 days to just 7.5 days,” according to the report.
Use of opioids was down among enrollees of all types of payers in 2017, while the use of drugs to treat opioid dependence went up for three of the four payer categories, according to pharmacy benefits manager Express Scripts.
The days’ worth of opioids dispensed per person per year was down 16.6% from 2016 to 2017 for enrollees with plans on the health exchanges received managed by Express Scripts. Medicaid patients received 16% fewer days’ worth, patients with commercial plans received 10.3% fewer days’ worth, and Medicare patients received 4.9% fewer days’ worth, Express Scripts said in its 2017 Drug Trend Report, which was based on data for 34.3 million members of pharmacy benefits plans the company administers.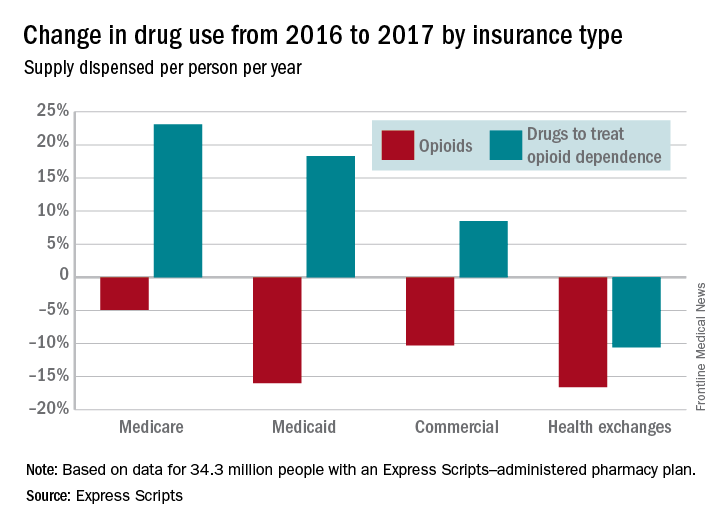
Plans that participated in Express Scripts’ Advanced Opioid Management solution, which was launched in September, experienced “a 60% reduction in the average days’ supply per initial fill, from 18.6 days to just 7.5 days,” according to the report.
Hemophilia A treatment gains approval in Europe
The European Commission has approved emicizumab for routine prophylaxis of bleeding episodes in adults and children with hemophilia A with factor VIII inhibitors.
The European Medicines Agency’s Committee for Medicinal Products for Human Use recommended granting marketing authorization to emicizumab (Hemlibra) in January 2018 and it was approved by the Food and Drug Administration in November 2017.
The approvals are based on findings from the HAVEN 1 trial (in 109 adults and adolescents) and the HAVEN 2 trial (in children younger than age 12 years), according to the drug’s maker, Roche. In HAVEN 1 (NCT02622321), emicizumab showed a significant reduction in treatment bleeds (87%), compared with no prophylaxis. And the drug reduced treated bleeds by 79%, compared with previous treatment with bypassing agent prophylaxis. An interim analysis of HAVEN 2 (NCT02795767) of 23 children, showed that 87% of children who received emicizumab prophylaxis had zero treated bleeds, according to Roche.
The European Commission has approved emicizumab for routine prophylaxis of bleeding episodes in adults and children with hemophilia A with factor VIII inhibitors.
The European Medicines Agency’s Committee for Medicinal Products for Human Use recommended granting marketing authorization to emicizumab (Hemlibra) in January 2018 and it was approved by the Food and Drug Administration in November 2017.
The approvals are based on findings from the HAVEN 1 trial (in 109 adults and adolescents) and the HAVEN 2 trial (in children younger than age 12 years), according to the drug’s maker, Roche. In HAVEN 1 (NCT02622321), emicizumab showed a significant reduction in treatment bleeds (87%), compared with no prophylaxis. And the drug reduced treated bleeds by 79%, compared with previous treatment with bypassing agent prophylaxis. An interim analysis of HAVEN 2 (NCT02795767) of 23 children, showed that 87% of children who received emicizumab prophylaxis had zero treated bleeds, according to Roche.
The European Commission has approved emicizumab for routine prophylaxis of bleeding episodes in adults and children with hemophilia A with factor VIII inhibitors.
The European Medicines Agency’s Committee for Medicinal Products for Human Use recommended granting marketing authorization to emicizumab (Hemlibra) in January 2018 and it was approved by the Food and Drug Administration in November 2017.
The approvals are based on findings from the HAVEN 1 trial (in 109 adults and adolescents) and the HAVEN 2 trial (in children younger than age 12 years), according to the drug’s maker, Roche. In HAVEN 1 (NCT02622321), emicizumab showed a significant reduction in treatment bleeds (87%), compared with no prophylaxis. And the drug reduced treated bleeds by 79%, compared with previous treatment with bypassing agent prophylaxis. An interim analysis of HAVEN 2 (NCT02795767) of 23 children, showed that 87% of children who received emicizumab prophylaxis had zero treated bleeds, according to Roche.
Finding a groove helps patients move
Listening to uptempo music significantly improved patients’ compared with patients who didn’t listen to music, according to data from a randomized trial of 127 patients.
Exercise stress tests are frequently recommended to evaluate patients for heart disease, but many patients don’t work hard enough to reach a useful level of exertion, Waseem Shami, MD, of Texas Tech University in El Paso, said in a web briefing in advance of the annual meeting of the American College of Cardiology.
The group of patients that listened to lively music averaged 55 seconds longer exercise time, compared with the no-music control group, Dr. Shami said. The average exercise time was 505.8 seconds in the music group and 455.2 in the control group (P = .045).
Dr. Shami and his colleagues randomized 67 adults scheduled for cardiac stress tests to listen to music during the test and 60 controls to undergo the test without music. The average age of the patients was 53 years, and 61% and 67% of those in the music and control groups, respectively, were women. Demographic characteristics and variables, including resting heart rate and blood pressure, were similar between the music and control groups.
In a clinical setting, the use of music may help reduce unnecessary stress testing, which is deemed unsuccessful if the patient doesn’t exercise hard enough to achieve a target heart rate. “Perhaps this motivational tool can help us make stress testing more valuable,” said Dr. Shami. The results were limited by the relatively small study population and the fact that the researchers, not the patients, chose the music, Dr. Shami said.
More research is needed in a larger trial, and “allowing patients to choose their own music might make an even bigger difference,” he noted. Also, patients’ discomfort with exercising in general and exercising in public may have impacted the results, he said.
Moderator Martha Gulati, MD, of the University of Arizona, Phoenix, noted that an area for future research might be to do a cardiac stress test without and without music on the same person, with the patient serving as his or her own control.
Dr. Shami had no relevant financial conflicts to disclose.
Listening to uptempo music significantly improved patients’ compared with patients who didn’t listen to music, according to data from a randomized trial of 127 patients.
Exercise stress tests are frequently recommended to evaluate patients for heart disease, but many patients don’t work hard enough to reach a useful level of exertion, Waseem Shami, MD, of Texas Tech University in El Paso, said in a web briefing in advance of the annual meeting of the American College of Cardiology.
The group of patients that listened to lively music averaged 55 seconds longer exercise time, compared with the no-music control group, Dr. Shami said. The average exercise time was 505.8 seconds in the music group and 455.2 in the control group (P = .045).
Dr. Shami and his colleagues randomized 67 adults scheduled for cardiac stress tests to listen to music during the test and 60 controls to undergo the test without music. The average age of the patients was 53 years, and 61% and 67% of those in the music and control groups, respectively, were women. Demographic characteristics and variables, including resting heart rate and blood pressure, were similar between the music and control groups.
In a clinical setting, the use of music may help reduce unnecessary stress testing, which is deemed unsuccessful if the patient doesn’t exercise hard enough to achieve a target heart rate. “Perhaps this motivational tool can help us make stress testing more valuable,” said Dr. Shami. The results were limited by the relatively small study population and the fact that the researchers, not the patients, chose the music, Dr. Shami said.
More research is needed in a larger trial, and “allowing patients to choose their own music might make an even bigger difference,” he noted. Also, patients’ discomfort with exercising in general and exercising in public may have impacted the results, he said.
Moderator Martha Gulati, MD, of the University of Arizona, Phoenix, noted that an area for future research might be to do a cardiac stress test without and without music on the same person, with the patient serving as his or her own control.
Dr. Shami had no relevant financial conflicts to disclose.
Listening to uptempo music significantly improved patients’ compared with patients who didn’t listen to music, according to data from a randomized trial of 127 patients.
Exercise stress tests are frequently recommended to evaluate patients for heart disease, but many patients don’t work hard enough to reach a useful level of exertion, Waseem Shami, MD, of Texas Tech University in El Paso, said in a web briefing in advance of the annual meeting of the American College of Cardiology.
The group of patients that listened to lively music averaged 55 seconds longer exercise time, compared with the no-music control group, Dr. Shami said. The average exercise time was 505.8 seconds in the music group and 455.2 in the control group (P = .045).
Dr. Shami and his colleagues randomized 67 adults scheduled for cardiac stress tests to listen to music during the test and 60 controls to undergo the test without music. The average age of the patients was 53 years, and 61% and 67% of those in the music and control groups, respectively, were women. Demographic characteristics and variables, including resting heart rate and blood pressure, were similar between the music and control groups.
In a clinical setting, the use of music may help reduce unnecessary stress testing, which is deemed unsuccessful if the patient doesn’t exercise hard enough to achieve a target heart rate. “Perhaps this motivational tool can help us make stress testing more valuable,” said Dr. Shami. The results were limited by the relatively small study population and the fact that the researchers, not the patients, chose the music, Dr. Shami said.
More research is needed in a larger trial, and “allowing patients to choose their own music might make an even bigger difference,” he noted. Also, patients’ discomfort with exercising in general and exercising in public may have impacted the results, he said.
Moderator Martha Gulati, MD, of the University of Arizona, Phoenix, noted that an area for future research might be to do a cardiac stress test without and without music on the same person, with the patient serving as his or her own control.
Dr. Shami had no relevant financial conflicts to disclose.
FROM ACC 18











