User login
Monitoring for Infection in MS Patients
Q) How do you monitor for infection in patients with multiple sclerosis who take disease-modifying therapies?
The answer to this question is “it depends”—on several factors, including current and previous use of disease-modifying therapies (DMTs), concomitant medications, comorbidities, vaccination history, presence of John Cunningham virus (JCV) antibodies (in the case of natalizumab use), and prior or current use of immunosuppressive therapies.
There are many FDA-approved DMTs for multiple sclerosis (MS). Each has a different rate of infection occurring in clinical trials and varying requirements and/or recommendations for safety monitoring. The package inserts for each DMT offer some guidance for clinicians.
Injectable therapies. For two interferon therapies—interferon ß-1b SC and interferon ß-1a—it is recommended to order a complete blood count (CBC), blood chemistry, and liver function tests (LFTs) at baseline, then again at one, three, and six months, and then at clinician discretion thereafter.1,2 For peginterferon ß-1a, ordering a CBC, basic chemistry, and LFTs, at the clinician’s discretion, is advised.3 The package insert for interferon ß-1a IM does not offer specific recommendations for routine safety monitoring.4
The package insert for glatiramer acetate offers no recommendations for routine safety monitoring.5
In patients for whom two or more DMTs have failed to work, the monoclonal antibody daclizumab may be indicated. Compared to placebo and active comparator, this drug was associated with a higher risk for infection in clinical trials. The most commonly observed types were upper respiratory, urinary tract, and viral infections. There are no recommendations for CBC monitoring with daclizumab, but monthly LFTs are required due to increased risk for hepatic injury.6
Oral DMTs. Patients taking fingolimod, teriflunomide, and dimethyl fumarate have increased risk for infection; as a result, there are more safety monitoring recommendations for these medications.7-9
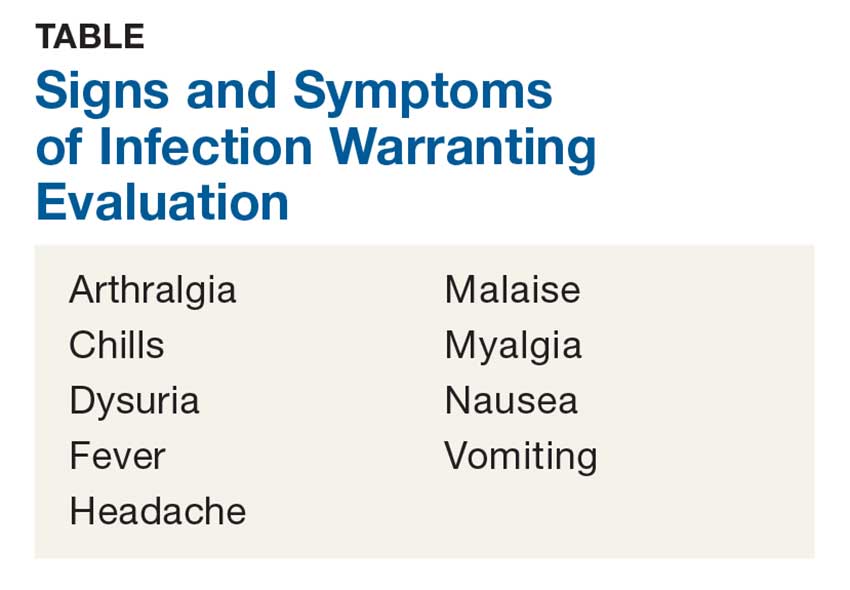
Prior to starting therapy with fingolimod, baseline CBC, blood chemistries, and varicella antibody testing should be done. During therapy, routine CBC testing and LFTs are advised at the clinician’s discretion or if the patient exhibits signs and symptoms of infection (see Table). In clinical trials, fingolimod use was interrupted if the lymphocyte count was sustained at < 200. In rare cases, progressive multifocal leukoencephalopathy (PML) has occurred—so the patient’s age, JCV antibody status, prior use of immunosuppressant therapy, and length of fingolimod treatment should be taken into consideration.7
Patients starting teriflunomide should have baseline LFTs and CBC and tuberculosis (TB) testing (either skin or serum), with subsequent monthly LFTs for the first six months on treatment. Some patients may experience neutropenia, thrombocytopenia, and lymphopenia. As a result, patients may have an increased risk for infection. Safety monitoring is at the clinician’s discretion.8
For patients initiating dimethyl fumarate, a baseline CBC is recommended, to be repeated every six to 12 months thereafter, and/or as clinically indicated. Since lymphopenia may occur, consider interruption of dimethyl fumarate in patients with lymphocyte counts < 0.5 persisting for more than six months. Rare cases of PML have also occurred; at the first suggestive sign or symptom, dimethyl fumarate should be withheld and appropriate diagnostic testing should be completed.9
Infusion therapies. There are four infusion therapies available for MS treatment. Mitoxantrone, though not commonly used, is still available for relapsing and secondary progressive forms of MS. Common infections seen in clinical trials include upper respiratory, urinary tract, and sinus infections. A CBC, including platelets, should be obtained prior to each course of mitoxantrone and again if signs and symptoms of infection develop.10
Natalizumab is an integrin receptor antagonist administered in monthly IV infusions. Patients receiving natalizumab may have increased risk for urinary tract infections, lower respiratory infections, gastroenteritis, vaginitis, and herpes infections. These risks should be monitored at the clinician’s discretion. There have been several cases of PML associated with natalizumab; risk factors include duration of therapy, prior use of immunosuppressants, and presence of JCV antibodies.11
Alemtuzumab is a CD52-directed monoclonal antibody indicated in patients with relapsing forms of MS who have had an inadequate response to at least two DMTs. In clinical trials, subjects had a higher risk for nasopharyngitis, urinary tract infections, upper respiratory infections, sinusitis, herpetic infections, influenza, and bronchitis. Due to the increased risk for infection and secondary autoimmunities, patients are required to have monthly CBC testing, LFTs, and urinalysis for up to 48 months after their last infusion.12
Lastly, ocrelizumab is a CD20-directed cytolytic antibody for the treatment of relapsing and progressive forms of MS. In clinical trials, there was a higher incidence of upper and lower respiratory infections, skin infections, and herpes-related infections. Prior to initiating ocrelizumab, hepatitis B virus screening should be completed. There are no specific recommendations for routine monitoring during therapy, although providers should monitor patients clinically for any signs and symptoms of infection.13
A word of caution: The common signs and symptoms of infection are listed in the Table. If these symptoms are present in your patient, consider ordering diagnostic testing to evaluate for infection.
Symptoms of PML include progressive unilateral weakness, clumsiness of limbs, disturbance of vision, and changes in thinking, memory, and orientation leading to confusion and personality changes. At the first sign or symptom suggestive of PML, the DMT should be discontinued and diagnostic testing performed.
Providers may contact the manufacturer directly for further guidance on DMT surveillance and treatment protocols. —CK
Christen Kutz, PhD, PA-C
Colorado Springs Neurological Associates
1. Betaseron (interferon [b]-1b) [package insert]. Whippany, NJ: Bayer HealthCare Pharmaceuticals; 1993.
2. Rebif (interferon [b]-1a) [package insert]. Rockland, MA: EMD Serono; revised 2015.
3. Plegridy (peginterferon [b]-1a) [package insert]. Cambridge, MA: Biogen Idec; 2013.
4. Avonex (interferon [b] -1a) [package insert]. Cambridge, MA: Biogen Inc.; 1996.
5. Copaxone (glatiramer acetate) [package insert]. Overland Park, KS: Teva Neuroscience; revised 2016.
6. Zinbryta (daclizumab) [package insert]. Cambridge, MA: Biogen Idec; 2016.
7. Gilenya (fingolimod) [package insert]. Hanover, NJ: Novartis; revised 2016.
8. Aubagio (teriflunomide) [package insert]. Cambridge, MA: Genzyme Corporation; revised 2016.
9. Tecfidera (dimethyl fumarate) [package insert]. Cambridge, MA: Biogen Idec; revised 2017.
10. Novantrone (mitoxantrone) [package insert]. Rockland, MA: EMD Serono; 2008.
11. Tysabri (natalizumab) [package insert]. Cambridge, MA: Biogen Idec; revised 2017.
12. Lemtrada (alemtuzumab) [package insert]. Cambridge, MA: Genzyme Corporation; revised 2017.
13. Ocrevus (ocrelizumab) [package insert]. San Francisco, CA: Genentech; 2017.
Q) How do you monitor for infection in patients with multiple sclerosis who take disease-modifying therapies?
The answer to this question is “it depends”—on several factors, including current and previous use of disease-modifying therapies (DMTs), concomitant medications, comorbidities, vaccination history, presence of John Cunningham virus (JCV) antibodies (in the case of natalizumab use), and prior or current use of immunosuppressive therapies.
There are many FDA-approved DMTs for multiple sclerosis (MS). Each has a different rate of infection occurring in clinical trials and varying requirements and/or recommendations for safety monitoring. The package inserts for each DMT offer some guidance for clinicians.
Injectable therapies. For two interferon therapies—interferon ß-1b SC and interferon ß-1a—it is recommended to order a complete blood count (CBC), blood chemistry, and liver function tests (LFTs) at baseline, then again at one, three, and six months, and then at clinician discretion thereafter.1,2 For peginterferon ß-1a, ordering a CBC, basic chemistry, and LFTs, at the clinician’s discretion, is advised.3 The package insert for interferon ß-1a IM does not offer specific recommendations for routine safety monitoring.4
The package insert for glatiramer acetate offers no recommendations for routine safety monitoring.5
In patients for whom two or more DMTs have failed to work, the monoclonal antibody daclizumab may be indicated. Compared to placebo and active comparator, this drug was associated with a higher risk for infection in clinical trials. The most commonly observed types were upper respiratory, urinary tract, and viral infections. There are no recommendations for CBC monitoring with daclizumab, but monthly LFTs are required due to increased risk for hepatic injury.6
Oral DMTs. Patients taking fingolimod, teriflunomide, and dimethyl fumarate have increased risk for infection; as a result, there are more safety monitoring recommendations for these medications.7-9
Prior to starting therapy with fingolimod, baseline CBC, blood chemistries, and varicella antibody testing should be done. During therapy, routine CBC testing and LFTs are advised at the clinician’s discretion or if the patient exhibits signs and symptoms of infection (see Table). In clinical trials, fingolimod use was interrupted if the lymphocyte count was sustained at < 200. In rare cases, progressive multifocal leukoencephalopathy (PML) has occurred—so the patient’s age, JCV antibody status, prior use of immunosuppressant therapy, and length of fingolimod treatment should be taken into consideration.7
Patients starting teriflunomide should have baseline LFTs and CBC and tuberculosis (TB) testing (either skin or serum), with subsequent monthly LFTs for the first six months on treatment. Some patients may experience neutropenia, thrombocytopenia, and lymphopenia. As a result, patients may have an increased risk for infection. Safety monitoring is at the clinician’s discretion.8
For patients initiating dimethyl fumarate, a baseline CBC is recommended, to be repeated every six to 12 months thereafter, and/or as clinically indicated. Since lymphopenia may occur, consider interruption of dimethyl fumarate in patients with lymphocyte counts < 0.5 persisting for more than six months. Rare cases of PML have also occurred; at the first suggestive sign or symptom, dimethyl fumarate should be withheld and appropriate diagnostic testing should be completed.9
Infusion therapies. There are four infusion therapies available for MS treatment. Mitoxantrone, though not commonly used, is still available for relapsing and secondary progressive forms of MS. Common infections seen in clinical trials include upper respiratory, urinary tract, and sinus infections. A CBC, including platelets, should be obtained prior to each course of mitoxantrone and again if signs and symptoms of infection develop.10
Natalizumab is an integrin receptor antagonist administered in monthly IV infusions. Patients receiving natalizumab may have increased risk for urinary tract infections, lower respiratory infections, gastroenteritis, vaginitis, and herpes infections. These risks should be monitored at the clinician’s discretion. There have been several cases of PML associated with natalizumab; risk factors include duration of therapy, prior use of immunosuppressants, and presence of JCV antibodies.11
Alemtuzumab is a CD52-directed monoclonal antibody indicated in patients with relapsing forms of MS who have had an inadequate response to at least two DMTs. In clinical trials, subjects had a higher risk for nasopharyngitis, urinary tract infections, upper respiratory infections, sinusitis, herpetic infections, influenza, and bronchitis. Due to the increased risk for infection and secondary autoimmunities, patients are required to have monthly CBC testing, LFTs, and urinalysis for up to 48 months after their last infusion.12
Lastly, ocrelizumab is a CD20-directed cytolytic antibody for the treatment of relapsing and progressive forms of MS. In clinical trials, there was a higher incidence of upper and lower respiratory infections, skin infections, and herpes-related infections. Prior to initiating ocrelizumab, hepatitis B virus screening should be completed. There are no specific recommendations for routine monitoring during therapy, although providers should monitor patients clinically for any signs and symptoms of infection.13
A word of caution: The common signs and symptoms of infection are listed in the Table. If these symptoms are present in your patient, consider ordering diagnostic testing to evaluate for infection.
Symptoms of PML include progressive unilateral weakness, clumsiness of limbs, disturbance of vision, and changes in thinking, memory, and orientation leading to confusion and personality changes. At the first sign or symptom suggestive of PML, the DMT should be discontinued and diagnostic testing performed.
Providers may contact the manufacturer directly for further guidance on DMT surveillance and treatment protocols. —CK
Christen Kutz, PhD, PA-C
Colorado Springs Neurological Associates
Q) How do you monitor for infection in patients with multiple sclerosis who take disease-modifying therapies?
The answer to this question is “it depends”—on several factors, including current and previous use of disease-modifying therapies (DMTs), concomitant medications, comorbidities, vaccination history, presence of John Cunningham virus (JCV) antibodies (in the case of natalizumab use), and prior or current use of immunosuppressive therapies.
There are many FDA-approved DMTs for multiple sclerosis (MS). Each has a different rate of infection occurring in clinical trials and varying requirements and/or recommendations for safety monitoring. The package inserts for each DMT offer some guidance for clinicians.
Injectable therapies. For two interferon therapies—interferon ß-1b SC and interferon ß-1a—it is recommended to order a complete blood count (CBC), blood chemistry, and liver function tests (LFTs) at baseline, then again at one, three, and six months, and then at clinician discretion thereafter.1,2 For peginterferon ß-1a, ordering a CBC, basic chemistry, and LFTs, at the clinician’s discretion, is advised.3 The package insert for interferon ß-1a IM does not offer specific recommendations for routine safety monitoring.4
The package insert for glatiramer acetate offers no recommendations for routine safety monitoring.5
In patients for whom two or more DMTs have failed to work, the monoclonal antibody daclizumab may be indicated. Compared to placebo and active comparator, this drug was associated with a higher risk for infection in clinical trials. The most commonly observed types were upper respiratory, urinary tract, and viral infections. There are no recommendations for CBC monitoring with daclizumab, but monthly LFTs are required due to increased risk for hepatic injury.6
Oral DMTs. Patients taking fingolimod, teriflunomide, and dimethyl fumarate have increased risk for infection; as a result, there are more safety monitoring recommendations for these medications.7-9
Prior to starting therapy with fingolimod, baseline CBC, blood chemistries, and varicella antibody testing should be done. During therapy, routine CBC testing and LFTs are advised at the clinician’s discretion or if the patient exhibits signs and symptoms of infection (see Table). In clinical trials, fingolimod use was interrupted if the lymphocyte count was sustained at < 200. In rare cases, progressive multifocal leukoencephalopathy (PML) has occurred—so the patient’s age, JCV antibody status, prior use of immunosuppressant therapy, and length of fingolimod treatment should be taken into consideration.7
Patients starting teriflunomide should have baseline LFTs and CBC and tuberculosis (TB) testing (either skin or serum), with subsequent monthly LFTs for the first six months on treatment. Some patients may experience neutropenia, thrombocytopenia, and lymphopenia. As a result, patients may have an increased risk for infection. Safety monitoring is at the clinician’s discretion.8
For patients initiating dimethyl fumarate, a baseline CBC is recommended, to be repeated every six to 12 months thereafter, and/or as clinically indicated. Since lymphopenia may occur, consider interruption of dimethyl fumarate in patients with lymphocyte counts < 0.5 persisting for more than six months. Rare cases of PML have also occurred; at the first suggestive sign or symptom, dimethyl fumarate should be withheld and appropriate diagnostic testing should be completed.9
Infusion therapies. There are four infusion therapies available for MS treatment. Mitoxantrone, though not commonly used, is still available for relapsing and secondary progressive forms of MS. Common infections seen in clinical trials include upper respiratory, urinary tract, and sinus infections. A CBC, including platelets, should be obtained prior to each course of mitoxantrone and again if signs and symptoms of infection develop.10
Natalizumab is an integrin receptor antagonist administered in monthly IV infusions. Patients receiving natalizumab may have increased risk for urinary tract infections, lower respiratory infections, gastroenteritis, vaginitis, and herpes infections. These risks should be monitored at the clinician’s discretion. There have been several cases of PML associated with natalizumab; risk factors include duration of therapy, prior use of immunosuppressants, and presence of JCV antibodies.11
Alemtuzumab is a CD52-directed monoclonal antibody indicated in patients with relapsing forms of MS who have had an inadequate response to at least two DMTs. In clinical trials, subjects had a higher risk for nasopharyngitis, urinary tract infections, upper respiratory infections, sinusitis, herpetic infections, influenza, and bronchitis. Due to the increased risk for infection and secondary autoimmunities, patients are required to have monthly CBC testing, LFTs, and urinalysis for up to 48 months after their last infusion.12
Lastly, ocrelizumab is a CD20-directed cytolytic antibody for the treatment of relapsing and progressive forms of MS. In clinical trials, there was a higher incidence of upper and lower respiratory infections, skin infections, and herpes-related infections. Prior to initiating ocrelizumab, hepatitis B virus screening should be completed. There are no specific recommendations for routine monitoring during therapy, although providers should monitor patients clinically for any signs and symptoms of infection.13
A word of caution: The common signs and symptoms of infection are listed in the Table. If these symptoms are present in your patient, consider ordering diagnostic testing to evaluate for infection.
Symptoms of PML include progressive unilateral weakness, clumsiness of limbs, disturbance of vision, and changes in thinking, memory, and orientation leading to confusion and personality changes. At the first sign or symptom suggestive of PML, the DMT should be discontinued and diagnostic testing performed.
Providers may contact the manufacturer directly for further guidance on DMT surveillance and treatment protocols. —CK
Christen Kutz, PhD, PA-C
Colorado Springs Neurological Associates
1. Betaseron (interferon [b]-1b) [package insert]. Whippany, NJ: Bayer HealthCare Pharmaceuticals; 1993.
2. Rebif (interferon [b]-1a) [package insert]. Rockland, MA: EMD Serono; revised 2015.
3. Plegridy (peginterferon [b]-1a) [package insert]. Cambridge, MA: Biogen Idec; 2013.
4. Avonex (interferon [b] -1a) [package insert]. Cambridge, MA: Biogen Inc.; 1996.
5. Copaxone (glatiramer acetate) [package insert]. Overland Park, KS: Teva Neuroscience; revised 2016.
6. Zinbryta (daclizumab) [package insert]. Cambridge, MA: Biogen Idec; 2016.
7. Gilenya (fingolimod) [package insert]. Hanover, NJ: Novartis; revised 2016.
8. Aubagio (teriflunomide) [package insert]. Cambridge, MA: Genzyme Corporation; revised 2016.
9. Tecfidera (dimethyl fumarate) [package insert]. Cambridge, MA: Biogen Idec; revised 2017.
10. Novantrone (mitoxantrone) [package insert]. Rockland, MA: EMD Serono; 2008.
11. Tysabri (natalizumab) [package insert]. Cambridge, MA: Biogen Idec; revised 2017.
12. Lemtrada (alemtuzumab) [package insert]. Cambridge, MA: Genzyme Corporation; revised 2017.
13. Ocrevus (ocrelizumab) [package insert]. San Francisco, CA: Genentech; 2017.
1. Betaseron (interferon [b]-1b) [package insert]. Whippany, NJ: Bayer HealthCare Pharmaceuticals; 1993.
2. Rebif (interferon [b]-1a) [package insert]. Rockland, MA: EMD Serono; revised 2015.
3. Plegridy (peginterferon [b]-1a) [package insert]. Cambridge, MA: Biogen Idec; 2013.
4. Avonex (interferon [b] -1a) [package insert]. Cambridge, MA: Biogen Inc.; 1996.
5. Copaxone (glatiramer acetate) [package insert]. Overland Park, KS: Teva Neuroscience; revised 2016.
6. Zinbryta (daclizumab) [package insert]. Cambridge, MA: Biogen Idec; 2016.
7. Gilenya (fingolimod) [package insert]. Hanover, NJ: Novartis; revised 2016.
8. Aubagio (teriflunomide) [package insert]. Cambridge, MA: Genzyme Corporation; revised 2016.
9. Tecfidera (dimethyl fumarate) [package insert]. Cambridge, MA: Biogen Idec; revised 2017.
10. Novantrone (mitoxantrone) [package insert]. Rockland, MA: EMD Serono; 2008.
11. Tysabri (natalizumab) [package insert]. Cambridge, MA: Biogen Idec; revised 2017.
12. Lemtrada (alemtuzumab) [package insert]. Cambridge, MA: Genzyme Corporation; revised 2017.
13. Ocrevus (ocrelizumab) [package insert]. San Francisco, CA: Genentech; 2017.
Managing schizophrenia as a chronic disease linked to better outcomes
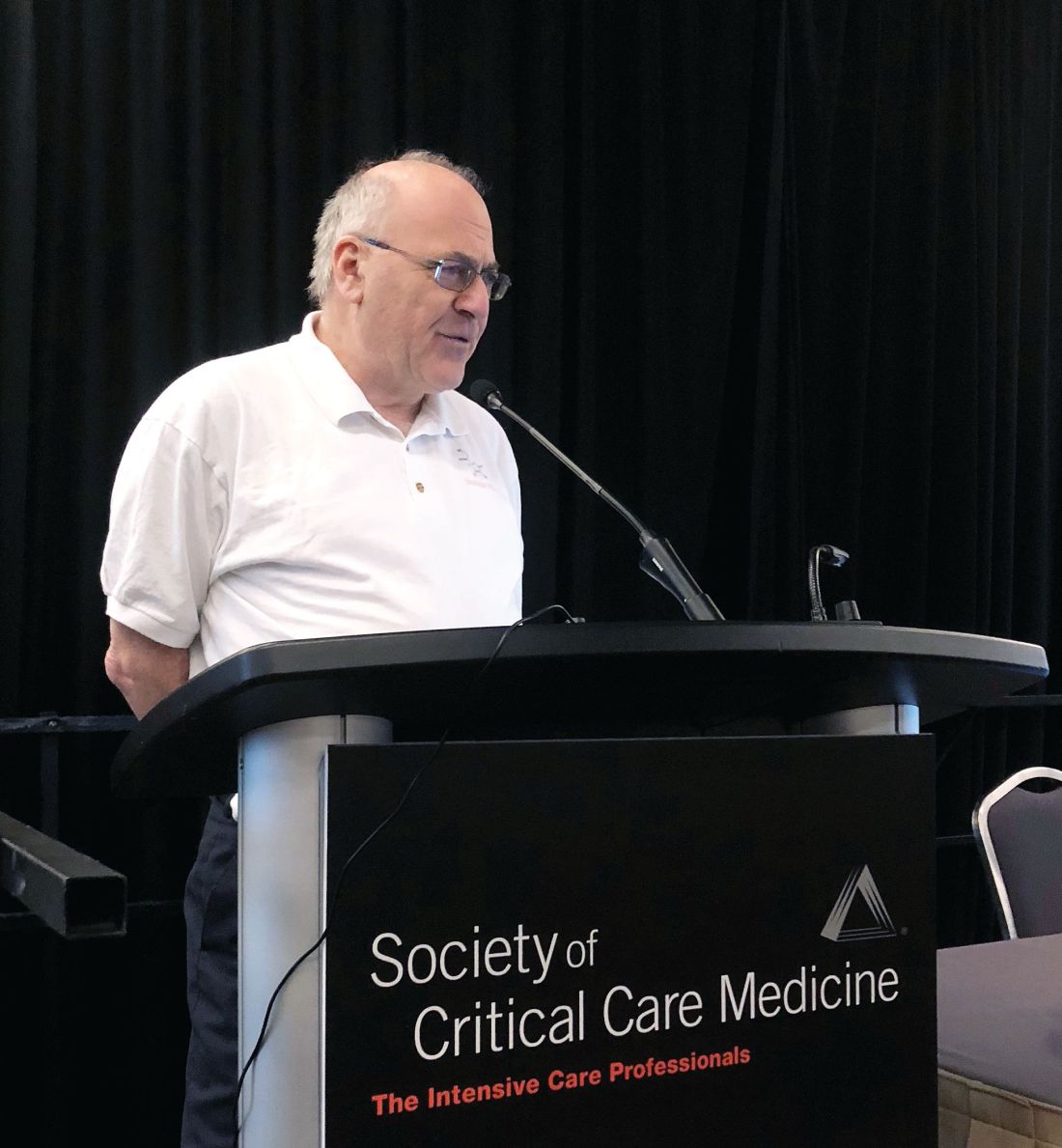
TAMPA – The secret to optimal long-term disease control in schizophrenia is to implement the same type of continuous and close management provided to other chronic diseases, like hypertension or inflammatory bowel disease, according to a lecture delivered at the annual meeting of the American College of Psychiatrists.
In the Dean Award Lecture – a talk characterized as “a stroll through the long-term understanding of the treatment of schizophrenia” – Ira D. Glick, MD, said that, although antipsychotics provide the foundation of disease control, patients and families need to understand and respect disease chronicity.
“In the last 5 or 6 years, I did something that no one has ever done before. I looked at the outcomes of patients treated for decades,” Dr. Glick recounted. Specifically, he contacted patients who had been in his care for up to 50 years. In “this naturalistic study,” he specifically asked the patients to rate their adherence to antipsychotics and to provide a global assessment of their life satisfaction, both on a scale of 1-10.
“What I found in a relatively large sample was that the more adherent patients were to their medication, the more likely they were to report adequate satisfaction with their life,” Dr. Glick said. For those who were not adherent, life in general “has been a disaster.”
This finding is not entirely surprising given the power of antipsychotics to change thinking. However, for those engaged in the immediate task of controlling acute symptoms, the importance of chronicity might not be given adequate emphasis. This requires educating patients and their families about the need to embark on lifetime treatment, Dr. Glick said. Like a diagnosis of diabetes, a diagnosis of schizophrenia means constant vigilance for manifestations of disease and appropriate adjustments of therapy to improve long-term outcomes.
Since evaluating the relationship between medication adherence and long-term outcomes in patients with schizophrenia treated at Stanford, the same type of evaluation was conducted with population samples from the Veterans Affairs system and from China. The data “show exactly the same thing,” Dr. Glick said.
It is important to use every available resource in helping patients recognize and deal with schizophrenia chronicity.
Earlier in his career, Dr. Glick participated in a randomized clinical trial of hospitalization for patients with schizophrenia. Recounting that experience, he reported that he was struck by the improvement in outcomes among patients who grasped that schizophrenia must be approached as a chronic disease.
“Once the patient understood what they had, they were much more apt to be adherent and to stay on their medication for their lifetime,” Dr. Glick reported. Although there is evidence that identifying an effective antipsychotic is key to disease control, “you have to talk to the patient, not just throw a medicine at them,” he said. This makes educating patients and families the key step in embarking on indefinite, close disease monitoring.
Control of schizophrenia over time is likely to vary as symptoms wax and wane, but this is true of other chronic disease processes. Diabetes, for example, requires frequent monitoring for and adjustment of blood glucose. Often medications for diabetes must be intensified or switched. The monitoring and management of schizophrenia is analogous.
One strategy for improving control of schizophrenia is to educate patients about this concept. Approaching schizophrenia as a chronic illness like other diseases that require lifetime drugs will help reduce the crises and the adverse effects associated with nonadherence to tight management, Dr. Glick maintained.
Dr. Glick reported financial relationships with Forum Pharmaceuticals, Johnson & Johnson, Neurocrine, Sunovion, and Teva.
TAMPA – The secret to optimal long-term disease control in schizophrenia is to implement the same type of continuous and close management provided to other chronic diseases, like hypertension or inflammatory bowel disease, according to a lecture delivered at the annual meeting of the American College of Psychiatrists.
In the Dean Award Lecture – a talk characterized as “a stroll through the long-term understanding of the treatment of schizophrenia” – Ira D. Glick, MD, said that, although antipsychotics provide the foundation of disease control, patients and families need to understand and respect disease chronicity.
“In the last 5 or 6 years, I did something that no one has ever done before. I looked at the outcomes of patients treated for decades,” Dr. Glick recounted. Specifically, he contacted patients who had been in his care for up to 50 years. In “this naturalistic study,” he specifically asked the patients to rate their adherence to antipsychotics and to provide a global assessment of their life satisfaction, both on a scale of 1-10.
“What I found in a relatively large sample was that the more adherent patients were to their medication, the more likely they were to report adequate satisfaction with their life,” Dr. Glick said. For those who were not adherent, life in general “has been a disaster.”
This finding is not entirely surprising given the power of antipsychotics to change thinking. However, for those engaged in the immediate task of controlling acute symptoms, the importance of chronicity might not be given adequate emphasis. This requires educating patients and their families about the need to embark on lifetime treatment, Dr. Glick said. Like a diagnosis of diabetes, a diagnosis of schizophrenia means constant vigilance for manifestations of disease and appropriate adjustments of therapy to improve long-term outcomes.
Since evaluating the relationship between medication adherence and long-term outcomes in patients with schizophrenia treated at Stanford, the same type of evaluation was conducted with population samples from the Veterans Affairs system and from China. The data “show exactly the same thing,” Dr. Glick said.
It is important to use every available resource in helping patients recognize and deal with schizophrenia chronicity.
Earlier in his career, Dr. Glick participated in a randomized clinical trial of hospitalization for patients with schizophrenia. Recounting that experience, he reported that he was struck by the improvement in outcomes among patients who grasped that schizophrenia must be approached as a chronic disease.
“Once the patient understood what they had, they were much more apt to be adherent and to stay on their medication for their lifetime,” Dr. Glick reported. Although there is evidence that identifying an effective antipsychotic is key to disease control, “you have to talk to the patient, not just throw a medicine at them,” he said. This makes educating patients and families the key step in embarking on indefinite, close disease monitoring.
Control of schizophrenia over time is likely to vary as symptoms wax and wane, but this is true of other chronic disease processes. Diabetes, for example, requires frequent monitoring for and adjustment of blood glucose. Often medications for diabetes must be intensified or switched. The monitoring and management of schizophrenia is analogous.
One strategy for improving control of schizophrenia is to educate patients about this concept. Approaching schizophrenia as a chronic illness like other diseases that require lifetime drugs will help reduce the crises and the adverse effects associated with nonadherence to tight management, Dr. Glick maintained.
Dr. Glick reported financial relationships with Forum Pharmaceuticals, Johnson & Johnson, Neurocrine, Sunovion, and Teva.
TAMPA – The secret to optimal long-term disease control in schizophrenia is to implement the same type of continuous and close management provided to other chronic diseases, like hypertension or inflammatory bowel disease, according to a lecture delivered at the annual meeting of the American College of Psychiatrists.
In the Dean Award Lecture – a talk characterized as “a stroll through the long-term understanding of the treatment of schizophrenia” – Ira D. Glick, MD, said that, although antipsychotics provide the foundation of disease control, patients and families need to understand and respect disease chronicity.
“In the last 5 or 6 years, I did something that no one has ever done before. I looked at the outcomes of patients treated for decades,” Dr. Glick recounted. Specifically, he contacted patients who had been in his care for up to 50 years. In “this naturalistic study,” he specifically asked the patients to rate their adherence to antipsychotics and to provide a global assessment of their life satisfaction, both on a scale of 1-10.
“What I found in a relatively large sample was that the more adherent patients were to their medication, the more likely they were to report adequate satisfaction with their life,” Dr. Glick said. For those who were not adherent, life in general “has been a disaster.”
This finding is not entirely surprising given the power of antipsychotics to change thinking. However, for those engaged in the immediate task of controlling acute symptoms, the importance of chronicity might not be given adequate emphasis. This requires educating patients and their families about the need to embark on lifetime treatment, Dr. Glick said. Like a diagnosis of diabetes, a diagnosis of schizophrenia means constant vigilance for manifestations of disease and appropriate adjustments of therapy to improve long-term outcomes.
Since evaluating the relationship between medication adherence and long-term outcomes in patients with schizophrenia treated at Stanford, the same type of evaluation was conducted with population samples from the Veterans Affairs system and from China. The data “show exactly the same thing,” Dr. Glick said.
It is important to use every available resource in helping patients recognize and deal with schizophrenia chronicity.
Earlier in his career, Dr. Glick participated in a randomized clinical trial of hospitalization for patients with schizophrenia. Recounting that experience, he reported that he was struck by the improvement in outcomes among patients who grasped that schizophrenia must be approached as a chronic disease.
“Once the patient understood what they had, they were much more apt to be adherent and to stay on their medication for their lifetime,” Dr. Glick reported. Although there is evidence that identifying an effective antipsychotic is key to disease control, “you have to talk to the patient, not just throw a medicine at them,” he said. This makes educating patients and families the key step in embarking on indefinite, close disease monitoring.
Control of schizophrenia over time is likely to vary as symptoms wax and wane, but this is true of other chronic disease processes. Diabetes, for example, requires frequent monitoring for and adjustment of blood glucose. Often medications for diabetes must be intensified or switched. The monitoring and management of schizophrenia is analogous.
One strategy for improving control of schizophrenia is to educate patients about this concept. Approaching schizophrenia as a chronic illness like other diseases that require lifetime drugs will help reduce the crises and the adverse effects associated with nonadherence to tight management, Dr. Glick maintained.
Dr. Glick reported financial relationships with Forum Pharmaceuticals, Johnson & Johnson, Neurocrine, Sunovion, and Teva.
REPORTING FROM THE COLLEGE 2018
Review finds some evidence of efficacy for nonpharmacological acne therapies
A systematic review of 33 studies evaluating nonpharmacological treatments for acne provided what was described as “circumstantial” evidence of efficacy by the authors who conducted the analysis.
The 33 studies evaluated three types of treatments: laser-based and light-based treatments (20), chemical peels (11), and fractional microneedling radiofrequency (2); most were associated with significant reductions in acne lesions in the studies. The evidence for efficacy was “strong” for glycolic acid at concentrations from 10% to 40%, and “moderate” for amino fruit acids at concentrations of 20%-60%, for intense pulsed light (IPL: 400-700 and 870-1,200 nm), and for the diode laser 1450 nm, according to F.M.C. de Vries, MD, of the department of dermatology, Radboud University, Nijmegen, the Netherlands, and coauthors.
However, they added, “although a high rate of statistically significant results was found in most of the studies, indicating efficacy of nonpharmacological therapies, the low methodological quality of the included studies made it difficult to draw clear conclusions.” Most of the studies were limited by factors that included a small number of enrolled participants, short follow-up, and lack of or possibly inadequate blinding in participants and/or clinicians.
Their review of three electronic databases (MEDLINE, Cochrane library, CINAHL) identified the 33 studies evaluating these treatments in 1,404 participants with acne, published between January 2000 and May 2017, which met their inclusion criteria.
Most of the studies on laser- and light-based treatments found a “significant reduction in acne lesions,” including eight that had a control group. However, with two exceptions, “suboptimal methodologic quality of the majority of these studies resulted in limited evidence of efficacy,” they added. The exceptions were two studies that were the basis of their “moderate” rating for IPL and the diode laser: a randomized study of IPL (40-700 and 870-1,200 nm, 100 ms, 20 J/cm2, 20 ms, 18 J/cm2), which found that treatment with IPL resulted in a significant reduction in papules, pustules, and comedones, compared with controls; and a randomized controlled study that found that treatment with a diode laser (1,450 nm, 9.5-11.0 J/cm2, 29-30 ms) resulted in reductions in inflammatory acne that were statistically significant.
The agents studied in the 11 chemical peel trials included salicylic acid, glycolic acid, Jessner solution, trichloroacetic acid, mandelic acid, amino fruit acid, and lipohydroxy acids. “Strong evidence of efficacy” was evident in two studies of glycolic acid (10% and 40% concentrations), which were double-blind, randomized, placebo-controlled studies that were of “high methodological quality,” the authors wrote.
Both studies of fractional microneedling radiofrequency, which were split-face randomized controlled studies, found statistically significant effects of treatment on inflammatory and noninflammatory acne in one study, and a “substantial” reduction in papules and pustules, compared with baseline in the other study. But this evidence was considered limited, because of the “suboptimal methodological quality” of both studies, they noted.
Erythema, pain (described as “tolerable”), purpura, edema, and hyperpigmentation were among the most common adverse effects associated with the nonpharmacological treatments and were described as mild and transient in most cases.
The review provided “circumstantial evidence for nonpharmacological therapies in the treatment of acne vulgaris” and “has created order and structure in resulting outcomes in which a first step towards future research is generated,” the authors concluded. “The large amount of studies performed in the area of acne treatment and the frequent application of these therapies in daily practice indicates a great interest in this topic and the urgent demand for effective nonpharmacological treatment options for acne in addition to the use of conventional therapies,” they added.
The authors had no disclosures. Of the six authors, Dr. de Vries and three other authors are affiliated with HU University of Applied Sciences, Utrecht, the Netherlands, which funded the study.
emechcatie@frontlinemedcom.com
SOURCE: de Vries FMC et al. J Eur Acad Dermatol Venereol. 2018 Feb 14. doi: 10.1111/jdv.14881.
A systematic review of 33 studies evaluating nonpharmacological treatments for acne provided what was described as “circumstantial” evidence of efficacy by the authors who conducted the analysis.
The 33 studies evaluated three types of treatments: laser-based and light-based treatments (20), chemical peels (11), and fractional microneedling radiofrequency (2); most were associated with significant reductions in acne lesions in the studies. The evidence for efficacy was “strong” for glycolic acid at concentrations from 10% to 40%, and “moderate” for amino fruit acids at concentrations of 20%-60%, for intense pulsed light (IPL: 400-700 and 870-1,200 nm), and for the diode laser 1450 nm, according to F.M.C. de Vries, MD, of the department of dermatology, Radboud University, Nijmegen, the Netherlands, and coauthors.
However, they added, “although a high rate of statistically significant results was found in most of the studies, indicating efficacy of nonpharmacological therapies, the low methodological quality of the included studies made it difficult to draw clear conclusions.” Most of the studies were limited by factors that included a small number of enrolled participants, short follow-up, and lack of or possibly inadequate blinding in participants and/or clinicians.
Their review of three electronic databases (MEDLINE, Cochrane library, CINAHL) identified the 33 studies evaluating these treatments in 1,404 participants with acne, published between January 2000 and May 2017, which met their inclusion criteria.
Most of the studies on laser- and light-based treatments found a “significant reduction in acne lesions,” including eight that had a control group. However, with two exceptions, “suboptimal methodologic quality of the majority of these studies resulted in limited evidence of efficacy,” they added. The exceptions were two studies that were the basis of their “moderate” rating for IPL and the diode laser: a randomized study of IPL (40-700 and 870-1,200 nm, 100 ms, 20 J/cm2, 20 ms, 18 J/cm2), which found that treatment with IPL resulted in a significant reduction in papules, pustules, and comedones, compared with controls; and a randomized controlled study that found that treatment with a diode laser (1,450 nm, 9.5-11.0 J/cm2, 29-30 ms) resulted in reductions in inflammatory acne that were statistically significant.
The agents studied in the 11 chemical peel trials included salicylic acid, glycolic acid, Jessner solution, trichloroacetic acid, mandelic acid, amino fruit acid, and lipohydroxy acids. “Strong evidence of efficacy” was evident in two studies of glycolic acid (10% and 40% concentrations), which were double-blind, randomized, placebo-controlled studies that were of “high methodological quality,” the authors wrote.
Both studies of fractional microneedling radiofrequency, which were split-face randomized controlled studies, found statistically significant effects of treatment on inflammatory and noninflammatory acne in one study, and a “substantial” reduction in papules and pustules, compared with baseline in the other study. But this evidence was considered limited, because of the “suboptimal methodological quality” of both studies, they noted.
Erythema, pain (described as “tolerable”), purpura, edema, and hyperpigmentation were among the most common adverse effects associated with the nonpharmacological treatments and were described as mild and transient in most cases.
The review provided “circumstantial evidence for nonpharmacological therapies in the treatment of acne vulgaris” and “has created order and structure in resulting outcomes in which a first step towards future research is generated,” the authors concluded. “The large amount of studies performed in the area of acne treatment and the frequent application of these therapies in daily practice indicates a great interest in this topic and the urgent demand for effective nonpharmacological treatment options for acne in addition to the use of conventional therapies,” they added.
The authors had no disclosures. Of the six authors, Dr. de Vries and three other authors are affiliated with HU University of Applied Sciences, Utrecht, the Netherlands, which funded the study.
emechcatie@frontlinemedcom.com
SOURCE: de Vries FMC et al. J Eur Acad Dermatol Venereol. 2018 Feb 14. doi: 10.1111/jdv.14881.
A systematic review of 33 studies evaluating nonpharmacological treatments for acne provided what was described as “circumstantial” evidence of efficacy by the authors who conducted the analysis.
The 33 studies evaluated three types of treatments: laser-based and light-based treatments (20), chemical peels (11), and fractional microneedling radiofrequency (2); most were associated with significant reductions in acne lesions in the studies. The evidence for efficacy was “strong” for glycolic acid at concentrations from 10% to 40%, and “moderate” for amino fruit acids at concentrations of 20%-60%, for intense pulsed light (IPL: 400-700 and 870-1,200 nm), and for the diode laser 1450 nm, according to F.M.C. de Vries, MD, of the department of dermatology, Radboud University, Nijmegen, the Netherlands, and coauthors.
However, they added, “although a high rate of statistically significant results was found in most of the studies, indicating efficacy of nonpharmacological therapies, the low methodological quality of the included studies made it difficult to draw clear conclusions.” Most of the studies were limited by factors that included a small number of enrolled participants, short follow-up, and lack of or possibly inadequate blinding in participants and/or clinicians.
Their review of three electronic databases (MEDLINE, Cochrane library, CINAHL) identified the 33 studies evaluating these treatments in 1,404 participants with acne, published between January 2000 and May 2017, which met their inclusion criteria.
Most of the studies on laser- and light-based treatments found a “significant reduction in acne lesions,” including eight that had a control group. However, with two exceptions, “suboptimal methodologic quality of the majority of these studies resulted in limited evidence of efficacy,” they added. The exceptions were two studies that were the basis of their “moderate” rating for IPL and the diode laser: a randomized study of IPL (40-700 and 870-1,200 nm, 100 ms, 20 J/cm2, 20 ms, 18 J/cm2), which found that treatment with IPL resulted in a significant reduction in papules, pustules, and comedones, compared with controls; and a randomized controlled study that found that treatment with a diode laser (1,450 nm, 9.5-11.0 J/cm2, 29-30 ms) resulted in reductions in inflammatory acne that were statistically significant.
The agents studied in the 11 chemical peel trials included salicylic acid, glycolic acid, Jessner solution, trichloroacetic acid, mandelic acid, amino fruit acid, and lipohydroxy acids. “Strong evidence of efficacy” was evident in two studies of glycolic acid (10% and 40% concentrations), which were double-blind, randomized, placebo-controlled studies that were of “high methodological quality,” the authors wrote.
Both studies of fractional microneedling radiofrequency, which were split-face randomized controlled studies, found statistically significant effects of treatment on inflammatory and noninflammatory acne in one study, and a “substantial” reduction in papules and pustules, compared with baseline in the other study. But this evidence was considered limited, because of the “suboptimal methodological quality” of both studies, they noted.
Erythema, pain (described as “tolerable”), purpura, edema, and hyperpigmentation were among the most common adverse effects associated with the nonpharmacological treatments and were described as mild and transient in most cases.
The review provided “circumstantial evidence for nonpharmacological therapies in the treatment of acne vulgaris” and “has created order and structure in resulting outcomes in which a first step towards future research is generated,” the authors concluded. “The large amount of studies performed in the area of acne treatment and the frequent application of these therapies in daily practice indicates a great interest in this topic and the urgent demand for effective nonpharmacological treatment options for acne in addition to the use of conventional therapies,” they added.
The authors had no disclosures. Of the six authors, Dr. de Vries and three other authors are affiliated with HU University of Applied Sciences, Utrecht, the Netherlands, which funded the study.
emechcatie@frontlinemedcom.com
SOURCE: de Vries FMC et al. J Eur Acad Dermatol Venereol. 2018 Feb 14. doi: 10.1111/jdv.14881.
FROM THE JOURNAL OF THE EUROPEAN ACADEMY OF DERMATOLOGY AND VENEREOLOGY
Key clinical point: Certain nonpharmacological acne treatments are effective but better data are needed.
Major finding: There is moderate to strong evidence of efficacy for glycolic acid, IPL, and the diode laser in treating acne.
Study details: A systematic review of 33 studies evaluating nonpharmacological treatments in 1,404 participants with acne.
Disclosures: The authors had no disclosures; three of the six authors are affiliated with HU University of Applied Sciences, Utrecht, which funded the study.
Source: de Vries FMC et al. J Eur Acad Dermatol Venereol. 2018 Feb 14. doi: 10.1111/jdv.14881.
Climate change is worsening allergies, expert says
ORLANDO – Climate change is not just eroding coastlines and threatening seaside cities and taking lives with increasingly powerful hurricanes, but appears to be contributing to increases in allergy and asthma, an expert told the audience at the joint congress of the American Academy of Allergy, Asthma and Immunology and the World Asthma Organization.
Longer pollen seasons, allergens unleashed by felled trees and ripped-up plants, mold growth following floods, and irritants launched into the air by wildfires are some of the concerns that should be alarming physicians and policy makers, said Nelson A. Rosario, MD, PhD, professor of pediatrics at Federal University of Paraná (Brazil).
And evidence suggests that his fellow allergists and their patients agree.
A 2015 international survey found that 80% of rhinitis patients blamed climate change for contributing to their symptoms.
Only 11% said that climate change wasn’t relevant at all. Asked how patients have been affected by climate change, about two-thirds said “increased care for allergic sensitization and symptoms on exposure to plants or mold.”
Science supports these views, Dr. Rosario said.
A 2011 study of North American pollen seasons found that some cities had significant increases of 11-27 days, compared with 15 years before.
And a 2017 review noted the impacts of the consequences of climate change, from increased allergies due to heavy precipitation events, asthma prompted by intense tropical cyclones, and allergic conditions caused by extremely high sea levels.
Dr. Rosario suggested that, rather than wait for official agencies to take action, physicians need to adapt and help their patients adapt. A team of doctors wrote in 2013 that while “improved governmental controls” could lead to cleaner air, they “meet strong opposition because of their effect on business and productivity.” So, they said, the allergy community should adjust, by “anticipating the needs of patients and by adopting practices and research methods to meet changing environmental conditions.”
Dr. Rosario urged physicians to think of the climate-change effects on allergy and asthma as a “collective action” problem, not an individual one.
“The consequences will come,” he said. “There must be international cooperation.”
ORLANDO – Climate change is not just eroding coastlines and threatening seaside cities and taking lives with increasingly powerful hurricanes, but appears to be contributing to increases in allergy and asthma, an expert told the audience at the joint congress of the American Academy of Allergy, Asthma and Immunology and the World Asthma Organization.
Longer pollen seasons, allergens unleashed by felled trees and ripped-up plants, mold growth following floods, and irritants launched into the air by wildfires are some of the concerns that should be alarming physicians and policy makers, said Nelson A. Rosario, MD, PhD, professor of pediatrics at Federal University of Paraná (Brazil).
And evidence suggests that his fellow allergists and their patients agree.
A 2015 international survey found that 80% of rhinitis patients blamed climate change for contributing to their symptoms.
Only 11% said that climate change wasn’t relevant at all. Asked how patients have been affected by climate change, about two-thirds said “increased care for allergic sensitization and symptoms on exposure to plants or mold.”
Science supports these views, Dr. Rosario said.
A 2011 study of North American pollen seasons found that some cities had significant increases of 11-27 days, compared with 15 years before.
And a 2017 review noted the impacts of the consequences of climate change, from increased allergies due to heavy precipitation events, asthma prompted by intense tropical cyclones, and allergic conditions caused by extremely high sea levels.
Dr. Rosario suggested that, rather than wait for official agencies to take action, physicians need to adapt and help their patients adapt. A team of doctors wrote in 2013 that while “improved governmental controls” could lead to cleaner air, they “meet strong opposition because of their effect on business and productivity.” So, they said, the allergy community should adjust, by “anticipating the needs of patients and by adopting practices and research methods to meet changing environmental conditions.”
Dr. Rosario urged physicians to think of the climate-change effects on allergy and asthma as a “collective action” problem, not an individual one.
“The consequences will come,” he said. “There must be international cooperation.”
ORLANDO – Climate change is not just eroding coastlines and threatening seaside cities and taking lives with increasingly powerful hurricanes, but appears to be contributing to increases in allergy and asthma, an expert told the audience at the joint congress of the American Academy of Allergy, Asthma and Immunology and the World Asthma Organization.
Longer pollen seasons, allergens unleashed by felled trees and ripped-up plants, mold growth following floods, and irritants launched into the air by wildfires are some of the concerns that should be alarming physicians and policy makers, said Nelson A. Rosario, MD, PhD, professor of pediatrics at Federal University of Paraná (Brazil).
And evidence suggests that his fellow allergists and their patients agree.
A 2015 international survey found that 80% of rhinitis patients blamed climate change for contributing to their symptoms.
Only 11% said that climate change wasn’t relevant at all. Asked how patients have been affected by climate change, about two-thirds said “increased care for allergic sensitization and symptoms on exposure to plants or mold.”
Science supports these views, Dr. Rosario said.
A 2011 study of North American pollen seasons found that some cities had significant increases of 11-27 days, compared with 15 years before.
And a 2017 review noted the impacts of the consequences of climate change, from increased allergies due to heavy precipitation events, asthma prompted by intense tropical cyclones, and allergic conditions caused by extremely high sea levels.
Dr. Rosario suggested that, rather than wait for official agencies to take action, physicians need to adapt and help their patients adapt. A team of doctors wrote in 2013 that while “improved governmental controls” could lead to cleaner air, they “meet strong opposition because of their effect on business and productivity.” So, they said, the allergy community should adjust, by “anticipating the needs of patients and by adopting practices and research methods to meet changing environmental conditions.”
Dr. Rosario urged physicians to think of the climate-change effects on allergy and asthma as a “collective action” problem, not an individual one.
“The consequences will come,” he said. “There must be international cooperation.”
EXPERT ANALYSIS FROM AAAAI/WAO JOINT CONGRESS
MEC plus ixazomib looks promising in relapsed/refractory AML
ATLANTA – Mitoxantrone, etoposide, and cytarabine (MEC) in combination with the second-generation proteasome inhibitor ixazomib was well tolerated and effective in a phase 1 expansion study of patients with relapsed or refractory acute myeloid leukemia.
The overall response rate in 30 patients enrolled in the study and treated with the novel combination was 53%; 11 patients had a complete response (CR), and 5 had a complete response with incomplete blood count recovery (CRi). The median overall survival was 4.9 months, Anjali S. Advani, MD, reported at the annual meeting of the American Society of Hematology.
Thirteen patients proceeded to allogeneic hematopoietic cell transplant (AHCT), and one received a donor lymphocyte infusion. Seven of these 14 patients are alive with a median follow-up of 14.5 months, said Dr. Advani of Taussig Cancer Institute, Cleveland Clinic.
The patients, who had a median age of 58 years (range of 18-70 years), were eligible for the study if they had relapsed/refractory acute myeloid leukemia (AML), adequate organ function, and cardiac ejection fraction of at least 45%. The median time from initial diagnosis to enrollment was 7.6 months.
Eight patients had a history of an antecedent hematologic disorder; 14 were in their first relapse; and 13 had disease that was refractory to their last treatment. Two had received a prior AHCT; seven had FLT3 internal tandem duplication (ITD) mutations indicative of particularly poor prognosis; and seven had adverse cytogenetics, she said.
They received one cycle of the therapy, which included 8mg/m2 of mitoxantrone, 80 mg/m2 of etoposide, and 1,000 mg/m2 of cytarabine given intravenously on days 1-6, plus ixazomib at doses of 1 mg (27 patients) or 2 mg (3 patients) given orally on days 1, 4, 8, and 11. An additional 18 patients were treated at the maximum tolerated dose (1 mg, as determined in phase 1 of the trial), Dr. Advani said.
The treatment was well tolerated in most patients. Grade 3-5 nonhematologic toxicities occurred in at least 15% of patients and included infection in 74%, febrile neutropenia in 85%, hypotension in 18%, hypoxia in 19%, mucositis in 15%, hypokalemia in 33%, and hypoalbuminemia in 30%, she said. The early mortality rate was 10%.
Of note, prior studies have demonstrated that the number of mutations in DNMT3A, TP53, ASXL1, and NRAS is associated with a worse response to salvage therapy. Of 21 patients in the current study who had available data, 10 patients had at least one of these mutations, and 8 of those 10 patients achieved CR or CRi, Dr. Advani said.
“To identify a signature predictive of response to treatment, we performed RNA sequencing on pretreatment samples from 17 patients, and on posttreatment samples from 11 patients,” she said. “We found that genes were differentially expressed between resistant and responding patients in 314 genes in the pretreatment samples, in 217 genes in the posttreatment samples, and in 72 genes at both time points.”
Gene set enrichment analysis identified significantly differentially expressed genes clustering in heme-metabolism and erythroblast differentiation, inflammatory response, cytokine/STAT signaling, nuclear factor-kappa beta (NF-kappaB), and hypoxia. Two genes – gamma-interferon–inducible lysosomal thiol reductase (IFI30) and retinoic acid–related orphan receptor A (ROR-alpha) – were found to be significantly different between responding and resistant patients, and could potentially classify response, she noted.
“IFI30, which may increase the levels of antioxidants and lead to a decreased ER [endoplasmic reticulum] stress response to therapy, was more highly expressed in resistant patients, and ROR-alpha, a tumor-suppressor gene, was down regulated in resistant patients,” she said.
Ixazomib was combined with the AML salvage regimen MEC in this study because proteasome inhibitors like ixazomib induce cell death in AML cells through inhibition of NF-kappaB, and also increase chemosensitivity to anthracyclines and cytarabines, Dr. Advani explained.
The findings are encouraging and suggest that results from gene expression profiling may help identify resistant patients and provide further therapeutic targets, she said, noting that in vitro studies are planned to clarify whether the use of ROR-alpha agonists may help sensitize resistant cells to treatment.
Dr. Advani reported receiving research funding from Takeda/Millenium, and serving as a consultant for Pfizer.
ATLANTA – Mitoxantrone, etoposide, and cytarabine (MEC) in combination with the second-generation proteasome inhibitor ixazomib was well tolerated and effective in a phase 1 expansion study of patients with relapsed or refractory acute myeloid leukemia.
The overall response rate in 30 patients enrolled in the study and treated with the novel combination was 53%; 11 patients had a complete response (CR), and 5 had a complete response with incomplete blood count recovery (CRi). The median overall survival was 4.9 months, Anjali S. Advani, MD, reported at the annual meeting of the American Society of Hematology.
Thirteen patients proceeded to allogeneic hematopoietic cell transplant (AHCT), and one received a donor lymphocyte infusion. Seven of these 14 patients are alive with a median follow-up of 14.5 months, said Dr. Advani of Taussig Cancer Institute, Cleveland Clinic.
The patients, who had a median age of 58 years (range of 18-70 years), were eligible for the study if they had relapsed/refractory acute myeloid leukemia (AML), adequate organ function, and cardiac ejection fraction of at least 45%. The median time from initial diagnosis to enrollment was 7.6 months.
Eight patients had a history of an antecedent hematologic disorder; 14 were in their first relapse; and 13 had disease that was refractory to their last treatment. Two had received a prior AHCT; seven had FLT3 internal tandem duplication (ITD) mutations indicative of particularly poor prognosis; and seven had adverse cytogenetics, she said.
They received one cycle of the therapy, which included 8mg/m2 of mitoxantrone, 80 mg/m2 of etoposide, and 1,000 mg/m2 of cytarabine given intravenously on days 1-6, plus ixazomib at doses of 1 mg (27 patients) or 2 mg (3 patients) given orally on days 1, 4, 8, and 11. An additional 18 patients were treated at the maximum tolerated dose (1 mg, as determined in phase 1 of the trial), Dr. Advani said.
The treatment was well tolerated in most patients. Grade 3-5 nonhematologic toxicities occurred in at least 15% of patients and included infection in 74%, febrile neutropenia in 85%, hypotension in 18%, hypoxia in 19%, mucositis in 15%, hypokalemia in 33%, and hypoalbuminemia in 30%, she said. The early mortality rate was 10%.
Of note, prior studies have demonstrated that the number of mutations in DNMT3A, TP53, ASXL1, and NRAS is associated with a worse response to salvage therapy. Of 21 patients in the current study who had available data, 10 patients had at least one of these mutations, and 8 of those 10 patients achieved CR or CRi, Dr. Advani said.
“To identify a signature predictive of response to treatment, we performed RNA sequencing on pretreatment samples from 17 patients, and on posttreatment samples from 11 patients,” she said. “We found that genes were differentially expressed between resistant and responding patients in 314 genes in the pretreatment samples, in 217 genes in the posttreatment samples, and in 72 genes at both time points.”
Gene set enrichment analysis identified significantly differentially expressed genes clustering in heme-metabolism and erythroblast differentiation, inflammatory response, cytokine/STAT signaling, nuclear factor-kappa beta (NF-kappaB), and hypoxia. Two genes – gamma-interferon–inducible lysosomal thiol reductase (IFI30) and retinoic acid–related orphan receptor A (ROR-alpha) – were found to be significantly different between responding and resistant patients, and could potentially classify response, she noted.
“IFI30, which may increase the levels of antioxidants and lead to a decreased ER [endoplasmic reticulum] stress response to therapy, was more highly expressed in resistant patients, and ROR-alpha, a tumor-suppressor gene, was down regulated in resistant patients,” she said.
Ixazomib was combined with the AML salvage regimen MEC in this study because proteasome inhibitors like ixazomib induce cell death in AML cells through inhibition of NF-kappaB, and also increase chemosensitivity to anthracyclines and cytarabines, Dr. Advani explained.
The findings are encouraging and suggest that results from gene expression profiling may help identify resistant patients and provide further therapeutic targets, she said, noting that in vitro studies are planned to clarify whether the use of ROR-alpha agonists may help sensitize resistant cells to treatment.
Dr. Advani reported receiving research funding from Takeda/Millenium, and serving as a consultant for Pfizer.
ATLANTA – Mitoxantrone, etoposide, and cytarabine (MEC) in combination with the second-generation proteasome inhibitor ixazomib was well tolerated and effective in a phase 1 expansion study of patients with relapsed or refractory acute myeloid leukemia.
The overall response rate in 30 patients enrolled in the study and treated with the novel combination was 53%; 11 patients had a complete response (CR), and 5 had a complete response with incomplete blood count recovery (CRi). The median overall survival was 4.9 months, Anjali S. Advani, MD, reported at the annual meeting of the American Society of Hematology.
Thirteen patients proceeded to allogeneic hematopoietic cell transplant (AHCT), and one received a donor lymphocyte infusion. Seven of these 14 patients are alive with a median follow-up of 14.5 months, said Dr. Advani of Taussig Cancer Institute, Cleveland Clinic.
The patients, who had a median age of 58 years (range of 18-70 years), were eligible for the study if they had relapsed/refractory acute myeloid leukemia (AML), adequate organ function, and cardiac ejection fraction of at least 45%. The median time from initial diagnosis to enrollment was 7.6 months.
Eight patients had a history of an antecedent hematologic disorder; 14 were in their first relapse; and 13 had disease that was refractory to their last treatment. Two had received a prior AHCT; seven had FLT3 internal tandem duplication (ITD) mutations indicative of particularly poor prognosis; and seven had adverse cytogenetics, she said.
They received one cycle of the therapy, which included 8mg/m2 of mitoxantrone, 80 mg/m2 of etoposide, and 1,000 mg/m2 of cytarabine given intravenously on days 1-6, plus ixazomib at doses of 1 mg (27 patients) or 2 mg (3 patients) given orally on days 1, 4, 8, and 11. An additional 18 patients were treated at the maximum tolerated dose (1 mg, as determined in phase 1 of the trial), Dr. Advani said.
The treatment was well tolerated in most patients. Grade 3-5 nonhematologic toxicities occurred in at least 15% of patients and included infection in 74%, febrile neutropenia in 85%, hypotension in 18%, hypoxia in 19%, mucositis in 15%, hypokalemia in 33%, and hypoalbuminemia in 30%, she said. The early mortality rate was 10%.
Of note, prior studies have demonstrated that the number of mutations in DNMT3A, TP53, ASXL1, and NRAS is associated with a worse response to salvage therapy. Of 21 patients in the current study who had available data, 10 patients had at least one of these mutations, and 8 of those 10 patients achieved CR or CRi, Dr. Advani said.
“To identify a signature predictive of response to treatment, we performed RNA sequencing on pretreatment samples from 17 patients, and on posttreatment samples from 11 patients,” she said. “We found that genes were differentially expressed between resistant and responding patients in 314 genes in the pretreatment samples, in 217 genes in the posttreatment samples, and in 72 genes at both time points.”
Gene set enrichment analysis identified significantly differentially expressed genes clustering in heme-metabolism and erythroblast differentiation, inflammatory response, cytokine/STAT signaling, nuclear factor-kappa beta (NF-kappaB), and hypoxia. Two genes – gamma-interferon–inducible lysosomal thiol reductase (IFI30) and retinoic acid–related orphan receptor A (ROR-alpha) – were found to be significantly different between responding and resistant patients, and could potentially classify response, she noted.
“IFI30, which may increase the levels of antioxidants and lead to a decreased ER [endoplasmic reticulum] stress response to therapy, was more highly expressed in resistant patients, and ROR-alpha, a tumor-suppressor gene, was down regulated in resistant patients,” she said.
Ixazomib was combined with the AML salvage regimen MEC in this study because proteasome inhibitors like ixazomib induce cell death in AML cells through inhibition of NF-kappaB, and also increase chemosensitivity to anthracyclines and cytarabines, Dr. Advani explained.
The findings are encouraging and suggest that results from gene expression profiling may help identify resistant patients and provide further therapeutic targets, she said, noting that in vitro studies are planned to clarify whether the use of ROR-alpha agonists may help sensitize resistant cells to treatment.
Dr. Advani reported receiving research funding from Takeda/Millenium, and serving as a consultant for Pfizer.
REPORTING FROM ASH 2017
Key clinical point: Major finding: The overall response rate was 53%.
Study details: A phase 1 trial involving 30 patients.
Disclosures: Dr. Advani reported receiving research funding from Takeda/Millenium, and serving as a consultant for Pfizer.
Source: Advani A et al. ASH 2017, Abstract 150.
AHRQ Practice Toolbox: Practice transformation
This is the seventh in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Thus far, this series has discussed topics such as shared decision making, team-based care, and integrating behavioral health and primary care. All of these are important topics, but this raises the question, “How do I make the changes to my practice?” This month’s article discusses AHRQ’s resources for transforming your practice to be able to better introduce these advances.
Building capacity for quality improvement in primary care. Primary care practices often benefit from external support and assistance while they develop the capacity to carry out quality improvement activities as an integral part of their work. These resources describe approaches and supports that are needed to build QI capacity in primary care.
Care coordination. The main goal of care coordination is to meet patients’ needs and preferences in the delivery of high-quality, high-value health care. This means that the patient’s needs and preferences are known and communicated at the right time to the right people, which results in safe, appropriate, and effective care. AHRQ’s resources in this area offer examples of care coordination approaches and activities, as well as guidance and models for understanding and measuring patients’ perceptions of care coordination.
Improvement approaches related to patient engagement and support. Several different types of resources related to patient engagement are available. These include the what, why, and how of self-management support, implementing health literacy universal precautions, and engaging patients and families in patient safety efforts.
AHRQ’s Primary Care YouTube channel offers videos from clinical staff, researchers, and others describing their work in many of these areas.
While the goal of practice transformation is the improvement of patient care and patient outcomes, patient and staff satisfaction (including issues regarding provider burnout) must not be lost in the process. The Clinician & Group Survey of the Consumer Assessment of Healthcare Providers and Systems assesses patient experiences with health care providers and staff in doctors’ offices. Survey results can be used to improve care provided by individual providers, sites of care, medical groups, or provider networks, as well as equip consumers with information they can use to choose physicians and other health care providers, physician practices, or medical groups. The survey includes standardized questionnaires for adults and children. The adult questionnaire can be used in both primary care and specialty care settings; the child questionnaire is designed for primary care settings but could be adapted for specialty care. Users can also add supplemental items to customize their questionnaires.
For many practices, working with a practice facilitator will be a big part of the transformation. Practice facilitation is an evidence-based approach to quality improvement in primary care practices. It will be discussed at length next month. In addition, in July and August, we will discuss optimizing health information technology and workflow in your practice.
Dr. Genevro is a health scientist at AHRQ. Dr. Ganiats is the director of the National Center for Excellence in Primary Care Research at AHRQ.
This is the seventh in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Thus far, this series has discussed topics such as shared decision making, team-based care, and integrating behavioral health and primary care. All of these are important topics, but this raises the question, “How do I make the changes to my practice?” This month’s article discusses AHRQ’s resources for transforming your practice to be able to better introduce these advances.
Building capacity for quality improvement in primary care. Primary care practices often benefit from external support and assistance while they develop the capacity to carry out quality improvement activities as an integral part of their work. These resources describe approaches and supports that are needed to build QI capacity in primary care.
Care coordination. The main goal of care coordination is to meet patients’ needs and preferences in the delivery of high-quality, high-value health care. This means that the patient’s needs and preferences are known and communicated at the right time to the right people, which results in safe, appropriate, and effective care. AHRQ’s resources in this area offer examples of care coordination approaches and activities, as well as guidance and models for understanding and measuring patients’ perceptions of care coordination.
Improvement approaches related to patient engagement and support. Several different types of resources related to patient engagement are available. These include the what, why, and how of self-management support, implementing health literacy universal precautions, and engaging patients and families in patient safety efforts.
AHRQ’s Primary Care YouTube channel offers videos from clinical staff, researchers, and others describing their work in many of these areas.
While the goal of practice transformation is the improvement of patient care and patient outcomes, patient and staff satisfaction (including issues regarding provider burnout) must not be lost in the process. The Clinician & Group Survey of the Consumer Assessment of Healthcare Providers and Systems assesses patient experiences with health care providers and staff in doctors’ offices. Survey results can be used to improve care provided by individual providers, sites of care, medical groups, or provider networks, as well as equip consumers with information they can use to choose physicians and other health care providers, physician practices, or medical groups. The survey includes standardized questionnaires for adults and children. The adult questionnaire can be used in both primary care and specialty care settings; the child questionnaire is designed for primary care settings but could be adapted for specialty care. Users can also add supplemental items to customize their questionnaires.
For many practices, working with a practice facilitator will be a big part of the transformation. Practice facilitation is an evidence-based approach to quality improvement in primary care practices. It will be discussed at length next month. In addition, in July and August, we will discuss optimizing health information technology and workflow in your practice.
Dr. Genevro is a health scientist at AHRQ. Dr. Ganiats is the director of the National Center for Excellence in Primary Care Research at AHRQ.
This is the seventh in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Thus far, this series has discussed topics such as shared decision making, team-based care, and integrating behavioral health and primary care. All of these are important topics, but this raises the question, “How do I make the changes to my practice?” This month’s article discusses AHRQ’s resources for transforming your practice to be able to better introduce these advances.
Building capacity for quality improvement in primary care. Primary care practices often benefit from external support and assistance while they develop the capacity to carry out quality improvement activities as an integral part of their work. These resources describe approaches and supports that are needed to build QI capacity in primary care.
Care coordination. The main goal of care coordination is to meet patients’ needs and preferences in the delivery of high-quality, high-value health care. This means that the patient’s needs and preferences are known and communicated at the right time to the right people, which results in safe, appropriate, and effective care. AHRQ’s resources in this area offer examples of care coordination approaches and activities, as well as guidance and models for understanding and measuring patients’ perceptions of care coordination.
Improvement approaches related to patient engagement and support. Several different types of resources related to patient engagement are available. These include the what, why, and how of self-management support, implementing health literacy universal precautions, and engaging patients and families in patient safety efforts.
AHRQ’s Primary Care YouTube channel offers videos from clinical staff, researchers, and others describing their work in many of these areas.
While the goal of practice transformation is the improvement of patient care and patient outcomes, patient and staff satisfaction (including issues regarding provider burnout) must not be lost in the process. The Clinician & Group Survey of the Consumer Assessment of Healthcare Providers and Systems assesses patient experiences with health care providers and staff in doctors’ offices. Survey results can be used to improve care provided by individual providers, sites of care, medical groups, or provider networks, as well as equip consumers with information they can use to choose physicians and other health care providers, physician practices, or medical groups. The survey includes standardized questionnaires for adults and children. The adult questionnaire can be used in both primary care and specialty care settings; the child questionnaire is designed for primary care settings but could be adapted for specialty care. Users can also add supplemental items to customize their questionnaires.
For many practices, working with a practice facilitator will be a big part of the transformation. Practice facilitation is an evidence-based approach to quality improvement in primary care practices. It will be discussed at length next month. In addition, in July and August, we will discuss optimizing health information technology and workflow in your practice.
Dr. Genevro is a health scientist at AHRQ. Dr. Ganiats is the director of the National Center for Excellence in Primary Care Research at AHRQ.
Xeljanz: FDA panel recommends ulcerative colitis indication
SILVER SPRING, MD. – Federal advisors to the Food and Drug Administration on March 8 voted unanimously to recommend approval of an additional indication for tofacitinib (Xeljanz), this time for ulcerative colitis.
Members of the Gastrointestinal Drugs Advisory Committee unanimously voted to recommend two different dosing regimens: 10 mg twice daily for 16 weeks in patients who have not experienced a therapeutic benefit after 8 weeks of treatment, as well as 10 mg twice daily for patients who have an inadequate or loss of response to TNF-blocker therapy, based on the results of several phase 3 clinical trials.
The recommended ulcerative colitis (UC) indication was based on the OCTAVE trials (N Engl J Med 2017;376:1723-36), including a phase 2 study, two identical phase 3 induction trials (OCTAVE Induction 1 and OCTAVE Induction 2), a 53-week, phase 3 maintenance trial (OCTAVE Sustain), and an open-label extension study.
The induction trials enrolled a total of 1,139 patients with moderate to severe UC. Patients in both studies were administered tofacitinib 10 mg twice daily or placebo and were assessed after 8 weeks to judge clinical response. Patients in both studies displayed notable remission rates (18.5% and 16.6%), compared with placebo, according to Eric Maller, MD, executive director of the UC development program at Pfizer.*
Patients who did not achieve remission, but showed some clinical response (decrease in Mayo score of at least 3 points), were then enrolled in the 53-week OCTAVE Sustain, where they were randomized to receive tofacitinib 10 mg twice daily, 5 mg twice daily, or placebo.
During maintenance treatment, both 5 mg and 10 mg doses demonstrated substantial treatment benefits, with 32.4% and 41.0% of patients achieving remission, an increase of 22.0% and 30.7%, compared with placebo, respectively.
As part of the maintenance study, Pfizer analyzed patients with or without prior TNF-blocker failure. This analysis revealed that patients who had previously failed TNF-blocker therapy experienced a greater treatment benefit than those who had not. While the benefit was noticeable in both dosage groups, patients taking the 10-mg dose experienced the greatest benefit, with 70% increase in remission rates, 39% increase in mucosal healing, and 75% increase in steroid-free remission among baseline remitters, compared with patients in the 5-mg group, Dr. Maller said.
Researchers also looked at a subgroup of 295 patients as part of an open-label extension study who had no clinical response to tofacitinib 10 mg twice daily after 8 weeks and subsequently treated them for an additional 8 weeks. After the additional 8 weeks of treatment, over half (51.2%) displayed clinical responses and 8.6% were in remission.
“This is a desperate patient population. These are impressive results,” stated Darrell Pardi, MD, vice chair of the advisory committee and professor of medicine at the Mayo Clinic, Rochester, Minn.
Serious adverse events were seen in 4% of tofacitinib-treated patients in the induction trials, compared with 6% of placebo-treated, according to Lesley Hanes, MD, medical officer with the FDA Center for Drug Evaluation and Research.
Adverse events appeared to be dose dependent, with risk of deaths and malignancies (excluding nonmelanoma skin cancer), opportunistic infections, herpes zoster infection (HZ), “possible” drug-induced liver injury, and cardiovascular and thromboembolic events more common with the 10-mg dose, Dr. Hanes said.
“I think the safety concerns, though, they are dose dependent, the difference between the 5 [mg] and 10 [mg] were not large,” according to Dr. Pardi. “Several of these are mitigatable by dermatologic exam or, hopefully, a vaccine.”
Several of the advisory committee members submitted conflict of interest waivers. Chair and vice chair Jean-Pierre Raufman, MD, and Darrell Pardi, MD, disclosed funding from competing pharmaceutical manufacturers.
*This article was updated on March 12, 2018.
SILVER SPRING, MD. – Federal advisors to the Food and Drug Administration on March 8 voted unanimously to recommend approval of an additional indication for tofacitinib (Xeljanz), this time for ulcerative colitis.
Members of the Gastrointestinal Drugs Advisory Committee unanimously voted to recommend two different dosing regimens: 10 mg twice daily for 16 weeks in patients who have not experienced a therapeutic benefit after 8 weeks of treatment, as well as 10 mg twice daily for patients who have an inadequate or loss of response to TNF-blocker therapy, based on the results of several phase 3 clinical trials.
The recommended ulcerative colitis (UC) indication was based on the OCTAVE trials (N Engl J Med 2017;376:1723-36), including a phase 2 study, two identical phase 3 induction trials (OCTAVE Induction 1 and OCTAVE Induction 2), a 53-week, phase 3 maintenance trial (OCTAVE Sustain), and an open-label extension study.
The induction trials enrolled a total of 1,139 patients with moderate to severe UC. Patients in both studies were administered tofacitinib 10 mg twice daily or placebo and were assessed after 8 weeks to judge clinical response. Patients in both studies displayed notable remission rates (18.5% and 16.6%), compared with placebo, according to Eric Maller, MD, executive director of the UC development program at Pfizer.*
Patients who did not achieve remission, but showed some clinical response (decrease in Mayo score of at least 3 points), were then enrolled in the 53-week OCTAVE Sustain, where they were randomized to receive tofacitinib 10 mg twice daily, 5 mg twice daily, or placebo.
During maintenance treatment, both 5 mg and 10 mg doses demonstrated substantial treatment benefits, with 32.4% and 41.0% of patients achieving remission, an increase of 22.0% and 30.7%, compared with placebo, respectively.
As part of the maintenance study, Pfizer analyzed patients with or without prior TNF-blocker failure. This analysis revealed that patients who had previously failed TNF-blocker therapy experienced a greater treatment benefit than those who had not. While the benefit was noticeable in both dosage groups, patients taking the 10-mg dose experienced the greatest benefit, with 70% increase in remission rates, 39% increase in mucosal healing, and 75% increase in steroid-free remission among baseline remitters, compared with patients in the 5-mg group, Dr. Maller said.
Researchers also looked at a subgroup of 295 patients as part of an open-label extension study who had no clinical response to tofacitinib 10 mg twice daily after 8 weeks and subsequently treated them for an additional 8 weeks. After the additional 8 weeks of treatment, over half (51.2%) displayed clinical responses and 8.6% were in remission.
“This is a desperate patient population. These are impressive results,” stated Darrell Pardi, MD, vice chair of the advisory committee and professor of medicine at the Mayo Clinic, Rochester, Minn.
Serious adverse events were seen in 4% of tofacitinib-treated patients in the induction trials, compared with 6% of placebo-treated, according to Lesley Hanes, MD, medical officer with the FDA Center for Drug Evaluation and Research.
Adverse events appeared to be dose dependent, with risk of deaths and malignancies (excluding nonmelanoma skin cancer), opportunistic infections, herpes zoster infection (HZ), “possible” drug-induced liver injury, and cardiovascular and thromboembolic events more common with the 10-mg dose, Dr. Hanes said.
“I think the safety concerns, though, they are dose dependent, the difference between the 5 [mg] and 10 [mg] were not large,” according to Dr. Pardi. “Several of these are mitigatable by dermatologic exam or, hopefully, a vaccine.”
Several of the advisory committee members submitted conflict of interest waivers. Chair and vice chair Jean-Pierre Raufman, MD, and Darrell Pardi, MD, disclosed funding from competing pharmaceutical manufacturers.
*This article was updated on March 12, 2018.
SILVER SPRING, MD. – Federal advisors to the Food and Drug Administration on March 8 voted unanimously to recommend approval of an additional indication for tofacitinib (Xeljanz), this time for ulcerative colitis.
Members of the Gastrointestinal Drugs Advisory Committee unanimously voted to recommend two different dosing regimens: 10 mg twice daily for 16 weeks in patients who have not experienced a therapeutic benefit after 8 weeks of treatment, as well as 10 mg twice daily for patients who have an inadequate or loss of response to TNF-blocker therapy, based on the results of several phase 3 clinical trials.
The recommended ulcerative colitis (UC) indication was based on the OCTAVE trials (N Engl J Med 2017;376:1723-36), including a phase 2 study, two identical phase 3 induction trials (OCTAVE Induction 1 and OCTAVE Induction 2), a 53-week, phase 3 maintenance trial (OCTAVE Sustain), and an open-label extension study.
The induction trials enrolled a total of 1,139 patients with moderate to severe UC. Patients in both studies were administered tofacitinib 10 mg twice daily or placebo and were assessed after 8 weeks to judge clinical response. Patients in both studies displayed notable remission rates (18.5% and 16.6%), compared with placebo, according to Eric Maller, MD, executive director of the UC development program at Pfizer.*
Patients who did not achieve remission, but showed some clinical response (decrease in Mayo score of at least 3 points), were then enrolled in the 53-week OCTAVE Sustain, where they were randomized to receive tofacitinib 10 mg twice daily, 5 mg twice daily, or placebo.
During maintenance treatment, both 5 mg and 10 mg doses demonstrated substantial treatment benefits, with 32.4% and 41.0% of patients achieving remission, an increase of 22.0% and 30.7%, compared with placebo, respectively.
As part of the maintenance study, Pfizer analyzed patients with or without prior TNF-blocker failure. This analysis revealed that patients who had previously failed TNF-blocker therapy experienced a greater treatment benefit than those who had not. While the benefit was noticeable in both dosage groups, patients taking the 10-mg dose experienced the greatest benefit, with 70% increase in remission rates, 39% increase in mucosal healing, and 75% increase in steroid-free remission among baseline remitters, compared with patients in the 5-mg group, Dr. Maller said.
Researchers also looked at a subgroup of 295 patients as part of an open-label extension study who had no clinical response to tofacitinib 10 mg twice daily after 8 weeks and subsequently treated them for an additional 8 weeks. After the additional 8 weeks of treatment, over half (51.2%) displayed clinical responses and 8.6% were in remission.
“This is a desperate patient population. These are impressive results,” stated Darrell Pardi, MD, vice chair of the advisory committee and professor of medicine at the Mayo Clinic, Rochester, Minn.
Serious adverse events were seen in 4% of tofacitinib-treated patients in the induction trials, compared with 6% of placebo-treated, according to Lesley Hanes, MD, medical officer with the FDA Center for Drug Evaluation and Research.
Adverse events appeared to be dose dependent, with risk of deaths and malignancies (excluding nonmelanoma skin cancer), opportunistic infections, herpes zoster infection (HZ), “possible” drug-induced liver injury, and cardiovascular and thromboembolic events more common with the 10-mg dose, Dr. Hanes said.
“I think the safety concerns, though, they are dose dependent, the difference between the 5 [mg] and 10 [mg] were not large,” according to Dr. Pardi. “Several of these are mitigatable by dermatologic exam or, hopefully, a vaccine.”
Several of the advisory committee members submitted conflict of interest waivers. Chair and vice chair Jean-Pierre Raufman, MD, and Darrell Pardi, MD, disclosed funding from competing pharmaceutical manufacturers.
*This article was updated on March 12, 2018.
REPORTING FROM AN FDA ADVISORY COMMITTEE MEETING
Dr. Paul E. Marik proclaims end to corticosteroid monotherapy for sepsis
SAN ANTONIO – While critical care specialists await more data on a so-called sepsis cocktail with varying degrees of hope and skepticism, Paul E. Marik, MD, FCCP, has proclaimed the dawning of a new era.
Dr. Marik became a celebrity in the critical care medicine community after he and his colleagues reported the results of his retrospective study evaluating the combination of hydrocortisone, vitamin C, and thiamine for treatment of severe sepsis and septic shock (Chest. 2017 June. doi: 10.1016/j.chest.2016.11.036).
Since this study, several physicians have already been putting Dr. Marik’s method to practice, the investigator and audience members noted during a session at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
in his presentation at the meeting.
These comments echoed Dr. Marik’s May 2017 editorial in Critical Care Medicine, in which he suggested that critically ill and injured patients may benefit from combination therapy with hydrocortisone and vitamin C (Crit Care Med 2017 May;45[5]910-1).
That editorial was quickly followed by the report on Dr. Marik and colleagues’ before-after study, in which hospital mortality was 8.5%, versus 0.4% in the treatment and control groups, respectively (P less than .001). This finding led the investigators to suggest that intravenous vitamin C administered along with corticosteroids and thiamine is “effective” in reducing mortality, in their paper published in CHEST®.
During Dr. Marik’s presentation at the meeting, he noted that he had been “misquoted” with regard to the finality of his study’s results. The final line of the CHEST® paper reads, “Additional studies are required to confirm these preliminary findings,” he emphasized.
Nevertheless, Dr. Marik alluded to a “big paradigm shift” in the treatment of sepsis.
“Our experience has been echoed by now hundreds, if not thousands, of clinicians across the world,” said Dr. Marik, chief of the division of pulmonary and critical care medicine, Eastern Virginia Medical School, Norfolk.
He recounted an anecdotal case submitted by “Josh from Ohio” describing an elderly man who was “started on cocktail and within a day his pressor requirements melted away and he was extubated.” Quoting “Josh from Ohio,” Dr. Mark continued, “Tomorrow he will probably leave the ICU with no residual organ dysfunction, no volume overload, (and) no ICU complications.”
Eddy Gutierrez, MD, of Jacksonville, Fla., noted in a question-and-answer period that he has had “positive results” with a similar approach.
“When we first learned about the vitamin C and the ‘Marik protocol,’ so to speak, I was in fellowship and I got laughed at,” Dr. Gutierrez said. “Nobody would let me try it.”
Others are taking a wait-and-see approach.
Greg S. Martin, MD, secretary of the Society of Critical Care Medicine, said in an interview that there are “at least two schools of thought” among critical care specialists regarding the use of hydrocortisone, vitamin C, and thiamine for treatment of sepsis and septic shock.
“One school of thought is that this is incredibly important if this is even fractionally as effective as what [Dr. Marik] showed, because we have not found an effective therapy for sepsis,” said Dr. Martin, associate professor of medicine at Grady Memorial Hospital, Atlanta.
“The contrarian approach is to say, ‘yes, but this seems remarkably unlikely to be as effective as what he has shown,’ ” Dr. Martin added. “Particularly in sepsis, people are very skeptical of whether a drug or a drug combination is going to be as effective when you really get down to a high-quality randomized controlled trial that would be the definitive level of evidence.”
The wait may not be long for at least some data. Multiple clinical trials are recruiting or planned, according to Dr. Marik. These included a 140-patient U.S. randomized, double-blind trial of vitamin C, hydrocortisone, and thiamine vs. placebo that started in February 2018 and is expected to be completed by February 2019, according to the study’s ClinicalTrials.gov listing.
“The good news is some people think this is of value,” Dr. Marik said.
As part of his presentation, Dr. Marik reported a disclosure related to Baxter (advisory board).
SAN ANTONIO – While critical care specialists await more data on a so-called sepsis cocktail with varying degrees of hope and skepticism, Paul E. Marik, MD, FCCP, has proclaimed the dawning of a new era.
Dr. Marik became a celebrity in the critical care medicine community after he and his colleagues reported the results of his retrospective study evaluating the combination of hydrocortisone, vitamin C, and thiamine for treatment of severe sepsis and septic shock (Chest. 2017 June. doi: 10.1016/j.chest.2016.11.036).
Since this study, several physicians have already been putting Dr. Marik’s method to practice, the investigator and audience members noted during a session at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
in his presentation at the meeting.
These comments echoed Dr. Marik’s May 2017 editorial in Critical Care Medicine, in which he suggested that critically ill and injured patients may benefit from combination therapy with hydrocortisone and vitamin C (Crit Care Med 2017 May;45[5]910-1).
That editorial was quickly followed by the report on Dr. Marik and colleagues’ before-after study, in which hospital mortality was 8.5%, versus 0.4% in the treatment and control groups, respectively (P less than .001). This finding led the investigators to suggest that intravenous vitamin C administered along with corticosteroids and thiamine is “effective” in reducing mortality, in their paper published in CHEST®.
During Dr. Marik’s presentation at the meeting, he noted that he had been “misquoted” with regard to the finality of his study’s results. The final line of the CHEST® paper reads, “Additional studies are required to confirm these preliminary findings,” he emphasized.
Nevertheless, Dr. Marik alluded to a “big paradigm shift” in the treatment of sepsis.
“Our experience has been echoed by now hundreds, if not thousands, of clinicians across the world,” said Dr. Marik, chief of the division of pulmonary and critical care medicine, Eastern Virginia Medical School, Norfolk.
He recounted an anecdotal case submitted by “Josh from Ohio” describing an elderly man who was “started on cocktail and within a day his pressor requirements melted away and he was extubated.” Quoting “Josh from Ohio,” Dr. Mark continued, “Tomorrow he will probably leave the ICU with no residual organ dysfunction, no volume overload, (and) no ICU complications.”
Eddy Gutierrez, MD, of Jacksonville, Fla., noted in a question-and-answer period that he has had “positive results” with a similar approach.
“When we first learned about the vitamin C and the ‘Marik protocol,’ so to speak, I was in fellowship and I got laughed at,” Dr. Gutierrez said. “Nobody would let me try it.”
Others are taking a wait-and-see approach.
Greg S. Martin, MD, secretary of the Society of Critical Care Medicine, said in an interview that there are “at least two schools of thought” among critical care specialists regarding the use of hydrocortisone, vitamin C, and thiamine for treatment of sepsis and septic shock.
“One school of thought is that this is incredibly important if this is even fractionally as effective as what [Dr. Marik] showed, because we have not found an effective therapy for sepsis,” said Dr. Martin, associate professor of medicine at Grady Memorial Hospital, Atlanta.
“The contrarian approach is to say, ‘yes, but this seems remarkably unlikely to be as effective as what he has shown,’ ” Dr. Martin added. “Particularly in sepsis, people are very skeptical of whether a drug or a drug combination is going to be as effective when you really get down to a high-quality randomized controlled trial that would be the definitive level of evidence.”
The wait may not be long for at least some data. Multiple clinical trials are recruiting or planned, according to Dr. Marik. These included a 140-patient U.S. randomized, double-blind trial of vitamin C, hydrocortisone, and thiamine vs. placebo that started in February 2018 and is expected to be completed by February 2019, according to the study’s ClinicalTrials.gov listing.
“The good news is some people think this is of value,” Dr. Marik said.
As part of his presentation, Dr. Marik reported a disclosure related to Baxter (advisory board).
SAN ANTONIO – While critical care specialists await more data on a so-called sepsis cocktail with varying degrees of hope and skepticism, Paul E. Marik, MD, FCCP, has proclaimed the dawning of a new era.
Dr. Marik became a celebrity in the critical care medicine community after he and his colleagues reported the results of his retrospective study evaluating the combination of hydrocortisone, vitamin C, and thiamine for treatment of severe sepsis and septic shock (Chest. 2017 June. doi: 10.1016/j.chest.2016.11.036).
Since this study, several physicians have already been putting Dr. Marik’s method to practice, the investigator and audience members noted during a session at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
in his presentation at the meeting.
These comments echoed Dr. Marik’s May 2017 editorial in Critical Care Medicine, in which he suggested that critically ill and injured patients may benefit from combination therapy with hydrocortisone and vitamin C (Crit Care Med 2017 May;45[5]910-1).
That editorial was quickly followed by the report on Dr. Marik and colleagues’ before-after study, in which hospital mortality was 8.5%, versus 0.4% in the treatment and control groups, respectively (P less than .001). This finding led the investigators to suggest that intravenous vitamin C administered along with corticosteroids and thiamine is “effective” in reducing mortality, in their paper published in CHEST®.
During Dr. Marik’s presentation at the meeting, he noted that he had been “misquoted” with regard to the finality of his study’s results. The final line of the CHEST® paper reads, “Additional studies are required to confirm these preliminary findings,” he emphasized.
Nevertheless, Dr. Marik alluded to a “big paradigm shift” in the treatment of sepsis.
“Our experience has been echoed by now hundreds, if not thousands, of clinicians across the world,” said Dr. Marik, chief of the division of pulmonary and critical care medicine, Eastern Virginia Medical School, Norfolk.
He recounted an anecdotal case submitted by “Josh from Ohio” describing an elderly man who was “started on cocktail and within a day his pressor requirements melted away and he was extubated.” Quoting “Josh from Ohio,” Dr. Mark continued, “Tomorrow he will probably leave the ICU with no residual organ dysfunction, no volume overload, (and) no ICU complications.”
Eddy Gutierrez, MD, of Jacksonville, Fla., noted in a question-and-answer period that he has had “positive results” with a similar approach.
“When we first learned about the vitamin C and the ‘Marik protocol,’ so to speak, I was in fellowship and I got laughed at,” Dr. Gutierrez said. “Nobody would let me try it.”
Others are taking a wait-and-see approach.
Greg S. Martin, MD, secretary of the Society of Critical Care Medicine, said in an interview that there are “at least two schools of thought” among critical care specialists regarding the use of hydrocortisone, vitamin C, and thiamine for treatment of sepsis and septic shock.
“One school of thought is that this is incredibly important if this is even fractionally as effective as what [Dr. Marik] showed, because we have not found an effective therapy for sepsis,” said Dr. Martin, associate professor of medicine at Grady Memorial Hospital, Atlanta.
“The contrarian approach is to say, ‘yes, but this seems remarkably unlikely to be as effective as what he has shown,’ ” Dr. Martin added. “Particularly in sepsis, people are very skeptical of whether a drug or a drug combination is going to be as effective when you really get down to a high-quality randomized controlled trial that would be the definitive level of evidence.”
The wait may not be long for at least some data. Multiple clinical trials are recruiting or planned, according to Dr. Marik. These included a 140-patient U.S. randomized, double-blind trial of vitamin C, hydrocortisone, and thiamine vs. placebo that started in February 2018 and is expected to be completed by February 2019, according to the study’s ClinicalTrials.gov listing.
“The good news is some people think this is of value,” Dr. Marik said.
As part of his presentation, Dr. Marik reported a disclosure related to Baxter (advisory board).
REPORTING FROM CCC47
Postmenopausal women: Walk farther and faster to reduce heart failure risk
Brisk walking for at least 40 minutes two or three times a week reduced the risk of heart failure by approximately 25% in postmenopausal women, according to data from more that 89,000 participants in the Women’s Health Initiative.
The benefits of walking are well understood, said Somwail Rasla, MD, of Saint Vincent Hospital in Worcester, Mass., but he and his colleagues focused for the first time on how the speed, frequency, and duration of walking affected health in older women who may be less likely to visit a gym or engage in a formal exercise program.
The researchers followed the women, aged 50-79 years, for approximately 10 years.
Overall, the risk of heart failure was 20%-25% less for women who walked at least twice a week than it was for women who walked less frequently. In addition, women who walked for at least 40 minutes per walk had a 21%-25% lower heart failure risk than did those who walked less than 40 minutes per walk.
Pace mattered as well, Dr. Rasla pointed out. Women walking at an average pace and a fast pace had, respectively, 26% and 38% lower heart failure risk, compared with women who walked at a casual pace.
The researchers measured the women’s energy expenditure using the Metabolic Equivalent of Task (MET), a value calculated using the women’s self-reports of their walking frequency, duration, and speed. The results were similar across different age groups, ethnicities, and baseline body weight, which suggests the findings can be generalized to apply to most women. “I think we could give the same advice [about walking] to women up to age 79,” said Dr. Rasla.
The findings were limited by the use of self-reports, Dr. Rasla noted. However, the results suggest that walking can be a valuable and accessible form of exercise for older women, he said.
The Women’s Health Initiative is sponsored by the National Institutes of Health. The investigators reported no relevant conflicts of interest.
SOURCE: Rasla S et al. ACC 18, Poster 1315M-03.
Brisk walking for at least 40 minutes two or three times a week reduced the risk of heart failure by approximately 25% in postmenopausal women, according to data from more that 89,000 participants in the Women’s Health Initiative.
The benefits of walking are well understood, said Somwail Rasla, MD, of Saint Vincent Hospital in Worcester, Mass., but he and his colleagues focused for the first time on how the speed, frequency, and duration of walking affected health in older women who may be less likely to visit a gym or engage in a formal exercise program.
The researchers followed the women, aged 50-79 years, for approximately 10 years.
Overall, the risk of heart failure was 20%-25% less for women who walked at least twice a week than it was for women who walked less frequently. In addition, women who walked for at least 40 minutes per walk had a 21%-25% lower heart failure risk than did those who walked less than 40 minutes per walk.
Pace mattered as well, Dr. Rasla pointed out. Women walking at an average pace and a fast pace had, respectively, 26% and 38% lower heart failure risk, compared with women who walked at a casual pace.
The researchers measured the women’s energy expenditure using the Metabolic Equivalent of Task (MET), a value calculated using the women’s self-reports of their walking frequency, duration, and speed. The results were similar across different age groups, ethnicities, and baseline body weight, which suggests the findings can be generalized to apply to most women. “I think we could give the same advice [about walking] to women up to age 79,” said Dr. Rasla.
The findings were limited by the use of self-reports, Dr. Rasla noted. However, the results suggest that walking can be a valuable and accessible form of exercise for older women, he said.
The Women’s Health Initiative is sponsored by the National Institutes of Health. The investigators reported no relevant conflicts of interest.
SOURCE: Rasla S et al. ACC 18, Poster 1315M-03.
Brisk walking for at least 40 minutes two or three times a week reduced the risk of heart failure by approximately 25% in postmenopausal women, according to data from more that 89,000 participants in the Women’s Health Initiative.
The benefits of walking are well understood, said Somwail Rasla, MD, of Saint Vincent Hospital in Worcester, Mass., but he and his colleagues focused for the first time on how the speed, frequency, and duration of walking affected health in older women who may be less likely to visit a gym or engage in a formal exercise program.
The researchers followed the women, aged 50-79 years, for approximately 10 years.
Overall, the risk of heart failure was 20%-25% less for women who walked at least twice a week than it was for women who walked less frequently. In addition, women who walked for at least 40 minutes per walk had a 21%-25% lower heart failure risk than did those who walked less than 40 minutes per walk.
Pace mattered as well, Dr. Rasla pointed out. Women walking at an average pace and a fast pace had, respectively, 26% and 38% lower heart failure risk, compared with women who walked at a casual pace.
The researchers measured the women’s energy expenditure using the Metabolic Equivalent of Task (MET), a value calculated using the women’s self-reports of their walking frequency, duration, and speed. The results were similar across different age groups, ethnicities, and baseline body weight, which suggests the findings can be generalized to apply to most women. “I think we could give the same advice [about walking] to women up to age 79,” said Dr. Rasla.
The findings were limited by the use of self-reports, Dr. Rasla noted. However, the results suggest that walking can be a valuable and accessible form of exercise for older women, he said.
The Women’s Health Initiative is sponsored by the National Institutes of Health. The investigators reported no relevant conflicts of interest.
SOURCE: Rasla S et al. ACC 18, Poster 1315M-03.
FROM ACC18
Key clinical point: Urge older female patients to walk briskly at least twice a week.
Major finding: Patients with a fast pace had a 38% lower risk of heart failure.
Study details: A long-term, national observational study of 89,270 women.
Disclosures: The Women’s Health Initiative is sponsored by the National Institutes of Health. The investigators reported no relevant conflicts of interest.
Source: Rasla S et al. ACC 18, Poster 1315M-03.
Best options for treating relapsed/refractory PTCL
LA JOLLA, CALIF. – When patients with peripheral T-cell lymphoma (PTCL) experience relapse, consider an allogeneic stem cell transplant or clinical trial, investigators advised.
Patients with relapsed PTCL have generally dismal outcomes, with a median progression-free survival (PFS) of 3.7 months and a median overall survival (OS) of just 6.5 months, according to one study (J Clin Oncol. 2013 Jun 1;31[16]:1970-6).
“Clearly the problem with most of the relapsed PTCL [cases] is that they don’t achieve a good response to salvage therapy. If they do, then they have much better chance of doing well,” she said at the annual T-cell Lymphoma Forum.
She outlined her center’s approach for treating patients with relapsed or refractory PTCL, following a case presentation by Royal Marsden fellow Matthew Cross, MD.
Complex disease, multiple therapies
The patient was a 71-year-old woman who in 2007 had a diagnosis of asymptomatic stage 4A follicular lymphoma managed with observation; in 2010, she was diagnosed with a CD30-positive PTCL not otherwise specified with ongoing low-level bone marrow involvement with follicular lymphoma.
She initially was treated elsewhere with R-CHOP chemotherapy (cyclophosphamide, doxorubicin, vincristine, and prednisone plus rituximab) and had a response after four cycles; however, she had progression with new intra-abdominal nodal sites by the sixth cycle and then was started on two cycles of ESHAP (etoposide, methylprednisolone, high-dose cytarabine, and cisplatin), but she had further progression by May 2011 and opted to forgo additional treatment.
By July 2011, however, she became highly symptomatic with new pruritic rashes on her legs, abdominal pain, and distention. She was referred to the Royal Marsden Hospital, where she was eventually diagnosed with angioimmunoblastic T-cell lymphoma (AITL) with an Epstein-Barr virus–negative clonal large B-cell proliferation in her bone marrow.
She was treated with gemcitabine plus methylprednisolone and prophylactic intrathecal methotrexate and had an “excellent clinical and radiological response,” Dr. Cross said.
A subsequent bone marrow biopsy showed marked hypocellularity but no evidence of either T-cell of B-cell lymphomas.
An autologous stem cell transplant was planned, but two attempts at harvesting peripheral blood stem cells – including one with plerixafor (Mozobil) – failed, and a PET scan within 3 months showed signs of early progression.
In April 2012, the patient was started on romidepsin (Istodax) and had a 1-year remission. But in April 2013, a repeat biopsy again showed CD30-positive AITL. Based on the CD30 positivity, the patient was started on brentuximab vedotin (Adcetris) in May 2013. She was observed to have progression in inguinal nodes in January 2014; she was treated with local radiotherapy and continued on brentuximab but had further progression in June 2014. At that time, she had additional gemcitabine-based combination chemotherapy and had stable disease for 10 months.
In March 2015, she received lenalidomide for further progression but could not tolerate the drug. She died in September 2015, 5 years after diagnosis and 4.5 years after frontline therapy failed.
Therapeutic rationale
Dr. Dearden walked through the choices that she, along with Dr. Cross and their colleagues, made in treating the patient. They chose gemcitabine-based regimens for salvage therapy because of the drug’s efficacy across various forms on non-Hodgkin and Hodgkin lymphoma, she said.
However, a randomized, phase 3, noninferiority trial in the United Kingdom comparing GEM-P (gemcitabine, cisplatin, and methylprednisolone) with CHOP for first-line therapy of PTCL was halted at the interim analysis because GEM-P had not meet the primary endpoint, she said. Results of that trial have not been published to date.
“Clearly, if it’s the patients who do well, often it’s because they achieve a good enough remission to be able to proceed to some sort of consolidation therapy with autologous or allogeneic stem cell transplants, and I think auto-graft is probably accepted for the younger, fitter patients with relapsed chemo-sensitive disease,” she said.
Three-year survival rates for autologous hematopoietic stem cell transplantation range from 36% to 58% and are better than those seen with chemotherapy alone, she said.
“The problem of course is that not many patients receive the planned auto-graft, even if that’s the intention, either because of failure to respond to salvage regimen or early disease progression, which happens before the transplant is able to take place,” she said,
A reasonable alternative for patients with relapsed/refractory PTCL is allogeneic transplantation, as shown in a 2008 study.
Among 77 patients – 57 of whom had received myeloablative conditioning, 31 of whom were in complete remission, and 26 of whom had partial response at the time of transplants – the 5-year treatment-related mortality rate was 33%. However, the 5-year event-free and overall survival rates were 53% and 57%, respectively. Patients with AITL had especially good outcomes (J Clin Oncol. 2008 May 10;26[14]:2264-71).
“In an ideal world, if our patient had been a suitable candidate for an allo-transplant, it’s what we would have tried to undertake,” Dr. Dearden said.
Dr. Dearden recommended that all patients with relapsed or refractory PTCL be considered for clinical trials. For fit patients in first relapse, combination platinum-based chemotherapy followed by autologous or allogeneic transplant may be effective.
For patients not eligible for transplant or with chemotherapy-refractory disease, she recommended trying the following monotherapy approaches: pralatrexate for patients with PTCL not otherwise specified, histone deacetylase inhibitors or 5-azacytidine for AITL, brentuximab vedotin for anaplastic large cell lymphoma, and pembrolizumab for natural killer/T-cell lymphomas.
Although two lines of intensive chemotherapy had failed the case patient within 6 months of diagnosis, she still survived for 5 years with sequential monotherapies, Dr. Dearden noted.
“I use to say to her, ‘You just need to stay one drug ahead of your disease.’ And she was well, she had a very good quality of life for a period of time, and if you can deliver a treatment that is effective for a patient, it will extend their survival,” Dr. Dearden said.
The T-cell Lymphoma Forum is held by Jonathan Wood & Associates, which is owned by the same company as this news organization. Dr. Dearden has consulted for MedImmune, Infinity Pharmaceuticals, Janssen, Gilead Sciences, and Roche, and has received honoraria from Janssen and Gilead. Dr. Cross reported no having no financial disclosures.
LA JOLLA, CALIF. – When patients with peripheral T-cell lymphoma (PTCL) experience relapse, consider an allogeneic stem cell transplant or clinical trial, investigators advised.
Patients with relapsed PTCL have generally dismal outcomes, with a median progression-free survival (PFS) of 3.7 months and a median overall survival (OS) of just 6.5 months, according to one study (J Clin Oncol. 2013 Jun 1;31[16]:1970-6).
“Clearly the problem with most of the relapsed PTCL [cases] is that they don’t achieve a good response to salvage therapy. If they do, then they have much better chance of doing well,” she said at the annual T-cell Lymphoma Forum.
She outlined her center’s approach for treating patients with relapsed or refractory PTCL, following a case presentation by Royal Marsden fellow Matthew Cross, MD.
Complex disease, multiple therapies
The patient was a 71-year-old woman who in 2007 had a diagnosis of asymptomatic stage 4A follicular lymphoma managed with observation; in 2010, she was diagnosed with a CD30-positive PTCL not otherwise specified with ongoing low-level bone marrow involvement with follicular lymphoma.
She initially was treated elsewhere with R-CHOP chemotherapy (cyclophosphamide, doxorubicin, vincristine, and prednisone plus rituximab) and had a response after four cycles; however, she had progression with new intra-abdominal nodal sites by the sixth cycle and then was started on two cycles of ESHAP (etoposide, methylprednisolone, high-dose cytarabine, and cisplatin), but she had further progression by May 2011 and opted to forgo additional treatment.
By July 2011, however, she became highly symptomatic with new pruritic rashes on her legs, abdominal pain, and distention. She was referred to the Royal Marsden Hospital, where she was eventually diagnosed with angioimmunoblastic T-cell lymphoma (AITL) with an Epstein-Barr virus–negative clonal large B-cell proliferation in her bone marrow.
She was treated with gemcitabine plus methylprednisolone and prophylactic intrathecal methotrexate and had an “excellent clinical and radiological response,” Dr. Cross said.
A subsequent bone marrow biopsy showed marked hypocellularity but no evidence of either T-cell of B-cell lymphomas.
An autologous stem cell transplant was planned, but two attempts at harvesting peripheral blood stem cells – including one with plerixafor (Mozobil) – failed, and a PET scan within 3 months showed signs of early progression.
In April 2012, the patient was started on romidepsin (Istodax) and had a 1-year remission. But in April 2013, a repeat biopsy again showed CD30-positive AITL. Based on the CD30 positivity, the patient was started on brentuximab vedotin (Adcetris) in May 2013. She was observed to have progression in inguinal nodes in January 2014; she was treated with local radiotherapy and continued on brentuximab but had further progression in June 2014. At that time, she had additional gemcitabine-based combination chemotherapy and had stable disease for 10 months.
In March 2015, she received lenalidomide for further progression but could not tolerate the drug. She died in September 2015, 5 years after diagnosis and 4.5 years after frontline therapy failed.
Therapeutic rationale
Dr. Dearden walked through the choices that she, along with Dr. Cross and their colleagues, made in treating the patient. They chose gemcitabine-based regimens for salvage therapy because of the drug’s efficacy across various forms on non-Hodgkin and Hodgkin lymphoma, she said.
However, a randomized, phase 3, noninferiority trial in the United Kingdom comparing GEM-P (gemcitabine, cisplatin, and methylprednisolone) with CHOP for first-line therapy of PTCL was halted at the interim analysis because GEM-P had not meet the primary endpoint, she said. Results of that trial have not been published to date.
“Clearly, if it’s the patients who do well, often it’s because they achieve a good enough remission to be able to proceed to some sort of consolidation therapy with autologous or allogeneic stem cell transplants, and I think auto-graft is probably accepted for the younger, fitter patients with relapsed chemo-sensitive disease,” she said.
Three-year survival rates for autologous hematopoietic stem cell transplantation range from 36% to 58% and are better than those seen with chemotherapy alone, she said.
“The problem of course is that not many patients receive the planned auto-graft, even if that’s the intention, either because of failure to respond to salvage regimen or early disease progression, which happens before the transplant is able to take place,” she said,
A reasonable alternative for patients with relapsed/refractory PTCL is allogeneic transplantation, as shown in a 2008 study.
Among 77 patients – 57 of whom had received myeloablative conditioning, 31 of whom were in complete remission, and 26 of whom had partial response at the time of transplants – the 5-year treatment-related mortality rate was 33%. However, the 5-year event-free and overall survival rates were 53% and 57%, respectively. Patients with AITL had especially good outcomes (J Clin Oncol. 2008 May 10;26[14]:2264-71).
“In an ideal world, if our patient had been a suitable candidate for an allo-transplant, it’s what we would have tried to undertake,” Dr. Dearden said.
Dr. Dearden recommended that all patients with relapsed or refractory PTCL be considered for clinical trials. For fit patients in first relapse, combination platinum-based chemotherapy followed by autologous or allogeneic transplant may be effective.
For patients not eligible for transplant or with chemotherapy-refractory disease, she recommended trying the following monotherapy approaches: pralatrexate for patients with PTCL not otherwise specified, histone deacetylase inhibitors or 5-azacytidine for AITL, brentuximab vedotin for anaplastic large cell lymphoma, and pembrolizumab for natural killer/T-cell lymphomas.
Although two lines of intensive chemotherapy had failed the case patient within 6 months of diagnosis, she still survived for 5 years with sequential monotherapies, Dr. Dearden noted.
“I use to say to her, ‘You just need to stay one drug ahead of your disease.’ And she was well, she had a very good quality of life for a period of time, and if you can deliver a treatment that is effective for a patient, it will extend their survival,” Dr. Dearden said.
The T-cell Lymphoma Forum is held by Jonathan Wood & Associates, which is owned by the same company as this news organization. Dr. Dearden has consulted for MedImmune, Infinity Pharmaceuticals, Janssen, Gilead Sciences, and Roche, and has received honoraria from Janssen and Gilead. Dr. Cross reported no having no financial disclosures.
LA JOLLA, CALIF. – When patients with peripheral T-cell lymphoma (PTCL) experience relapse, consider an allogeneic stem cell transplant or clinical trial, investigators advised.
Patients with relapsed PTCL have generally dismal outcomes, with a median progression-free survival (PFS) of 3.7 months and a median overall survival (OS) of just 6.5 months, according to one study (J Clin Oncol. 2013 Jun 1;31[16]:1970-6).
“Clearly the problem with most of the relapsed PTCL [cases] is that they don’t achieve a good response to salvage therapy. If they do, then they have much better chance of doing well,” she said at the annual T-cell Lymphoma Forum.
She outlined her center’s approach for treating patients with relapsed or refractory PTCL, following a case presentation by Royal Marsden fellow Matthew Cross, MD.
Complex disease, multiple therapies
The patient was a 71-year-old woman who in 2007 had a diagnosis of asymptomatic stage 4A follicular lymphoma managed with observation; in 2010, she was diagnosed with a CD30-positive PTCL not otherwise specified with ongoing low-level bone marrow involvement with follicular lymphoma.
She initially was treated elsewhere with R-CHOP chemotherapy (cyclophosphamide, doxorubicin, vincristine, and prednisone plus rituximab) and had a response after four cycles; however, she had progression with new intra-abdominal nodal sites by the sixth cycle and then was started on two cycles of ESHAP (etoposide, methylprednisolone, high-dose cytarabine, and cisplatin), but she had further progression by May 2011 and opted to forgo additional treatment.
By July 2011, however, she became highly symptomatic with new pruritic rashes on her legs, abdominal pain, and distention. She was referred to the Royal Marsden Hospital, where she was eventually diagnosed with angioimmunoblastic T-cell lymphoma (AITL) with an Epstein-Barr virus–negative clonal large B-cell proliferation in her bone marrow.
She was treated with gemcitabine plus methylprednisolone and prophylactic intrathecal methotrexate and had an “excellent clinical and radiological response,” Dr. Cross said.
A subsequent bone marrow biopsy showed marked hypocellularity but no evidence of either T-cell of B-cell lymphomas.
An autologous stem cell transplant was planned, but two attempts at harvesting peripheral blood stem cells – including one with plerixafor (Mozobil) – failed, and a PET scan within 3 months showed signs of early progression.
In April 2012, the patient was started on romidepsin (Istodax) and had a 1-year remission. But in April 2013, a repeat biopsy again showed CD30-positive AITL. Based on the CD30 positivity, the patient was started on brentuximab vedotin (Adcetris) in May 2013. She was observed to have progression in inguinal nodes in January 2014; she was treated with local radiotherapy and continued on brentuximab but had further progression in June 2014. At that time, she had additional gemcitabine-based combination chemotherapy and had stable disease for 10 months.
In March 2015, she received lenalidomide for further progression but could not tolerate the drug. She died in September 2015, 5 years after diagnosis and 4.5 years after frontline therapy failed.
Therapeutic rationale
Dr. Dearden walked through the choices that she, along with Dr. Cross and their colleagues, made in treating the patient. They chose gemcitabine-based regimens for salvage therapy because of the drug’s efficacy across various forms on non-Hodgkin and Hodgkin lymphoma, she said.
However, a randomized, phase 3, noninferiority trial in the United Kingdom comparing GEM-P (gemcitabine, cisplatin, and methylprednisolone) with CHOP for first-line therapy of PTCL was halted at the interim analysis because GEM-P had not meet the primary endpoint, she said. Results of that trial have not been published to date.
“Clearly, if it’s the patients who do well, often it’s because they achieve a good enough remission to be able to proceed to some sort of consolidation therapy with autologous or allogeneic stem cell transplants, and I think auto-graft is probably accepted for the younger, fitter patients with relapsed chemo-sensitive disease,” she said.
Three-year survival rates for autologous hematopoietic stem cell transplantation range from 36% to 58% and are better than those seen with chemotherapy alone, she said.
“The problem of course is that not many patients receive the planned auto-graft, even if that’s the intention, either because of failure to respond to salvage regimen or early disease progression, which happens before the transplant is able to take place,” she said,
A reasonable alternative for patients with relapsed/refractory PTCL is allogeneic transplantation, as shown in a 2008 study.
Among 77 patients – 57 of whom had received myeloablative conditioning, 31 of whom were in complete remission, and 26 of whom had partial response at the time of transplants – the 5-year treatment-related mortality rate was 33%. However, the 5-year event-free and overall survival rates were 53% and 57%, respectively. Patients with AITL had especially good outcomes (J Clin Oncol. 2008 May 10;26[14]:2264-71).
“In an ideal world, if our patient had been a suitable candidate for an allo-transplant, it’s what we would have tried to undertake,” Dr. Dearden said.
Dr. Dearden recommended that all patients with relapsed or refractory PTCL be considered for clinical trials. For fit patients in first relapse, combination platinum-based chemotherapy followed by autologous or allogeneic transplant may be effective.
For patients not eligible for transplant or with chemotherapy-refractory disease, she recommended trying the following monotherapy approaches: pralatrexate for patients with PTCL not otherwise specified, histone deacetylase inhibitors or 5-azacytidine for AITL, brentuximab vedotin for anaplastic large cell lymphoma, and pembrolizumab for natural killer/T-cell lymphomas.
Although two lines of intensive chemotherapy had failed the case patient within 6 months of diagnosis, she still survived for 5 years with sequential monotherapies, Dr. Dearden noted.
“I use to say to her, ‘You just need to stay one drug ahead of your disease.’ And she was well, she had a very good quality of life for a period of time, and if you can deliver a treatment that is effective for a patient, it will extend their survival,” Dr. Dearden said.
The T-cell Lymphoma Forum is held by Jonathan Wood & Associates, which is owned by the same company as this news organization. Dr. Dearden has consulted for MedImmune, Infinity Pharmaceuticals, Janssen, Gilead Sciences, and Roche, and has received honoraria from Janssen and Gilead. Dr. Cross reported no having no financial disclosures.
EXPERT ANALYSIS FROM TCLF 2018