User login
Putting a number on biologic DMARD costs
Annual medical costs for patients with rheumatoid arthritis were almost three times higher for those who used biologic disease-modifying antirheumatic drugs (bDMARDs), compared with those who used any treatment regimen, according to meta-analysis of 12 studies conducted since bDMARDs were introduced in 1999.
RA patients who used bDMARDs had an average direct cost of $36,053 per year, which was 2.9 times higher than the $12,509 in annual direct medical costs for all RA patients on any treatment regimen. Proportionately, the difference was even greater for RA-specific care, with the annual cost of bDMARD care ($20,262) 5.4 times higher than that of all treatment regimens ($3,723), reported Andrew Hresko and his associates at Brigham and Women’s Hospital, Boston.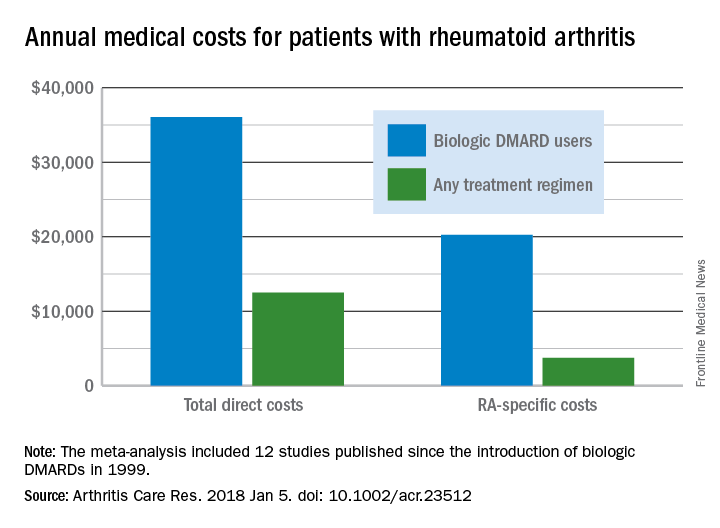
Funding for the study was supported through a grant from the National Institutes of Health. Mr. Hresko was supported by a fellowship from Tufts University. One of his associates receives research support from grants to his hospital from Amgen, Pfizer, Eli Lilly, AstraZeneca, Genentech, Bristol Myers Squibb, and Corrona. The third investigator is now an employee of Amgen but was not during the study.
SOURCE: Hresko A et al. Arthritis Care Res. 2018 Jan 5. doi: 10.1002/acr.23512.
Annual medical costs for patients with rheumatoid arthritis were almost three times higher for those who used biologic disease-modifying antirheumatic drugs (bDMARDs), compared with those who used any treatment regimen, according to meta-analysis of 12 studies conducted since bDMARDs were introduced in 1999.
RA patients who used bDMARDs had an average direct cost of $36,053 per year, which was 2.9 times higher than the $12,509 in annual direct medical costs for all RA patients on any treatment regimen. Proportionately, the difference was even greater for RA-specific care, with the annual cost of bDMARD care ($20,262) 5.4 times higher than that of all treatment regimens ($3,723), reported Andrew Hresko and his associates at Brigham and Women’s Hospital, Boston.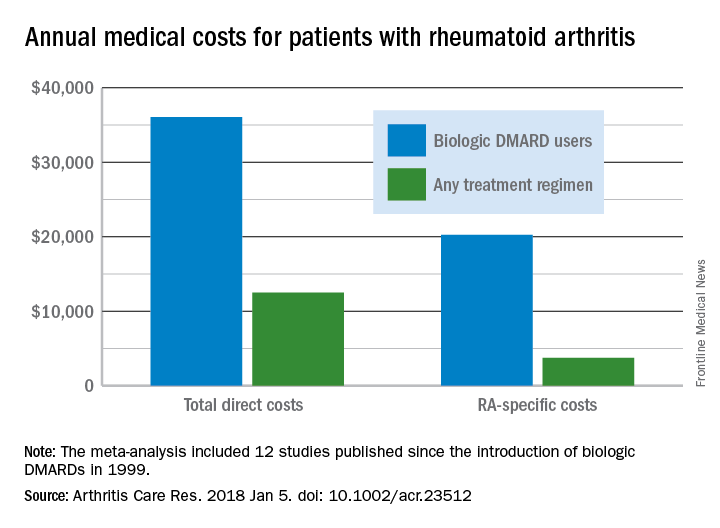
Funding for the study was supported through a grant from the National Institutes of Health. Mr. Hresko was supported by a fellowship from Tufts University. One of his associates receives research support from grants to his hospital from Amgen, Pfizer, Eli Lilly, AstraZeneca, Genentech, Bristol Myers Squibb, and Corrona. The third investigator is now an employee of Amgen but was not during the study.
SOURCE: Hresko A et al. Arthritis Care Res. 2018 Jan 5. doi: 10.1002/acr.23512.
Annual medical costs for patients with rheumatoid arthritis were almost three times higher for those who used biologic disease-modifying antirheumatic drugs (bDMARDs), compared with those who used any treatment regimen, according to meta-analysis of 12 studies conducted since bDMARDs were introduced in 1999.
RA patients who used bDMARDs had an average direct cost of $36,053 per year, which was 2.9 times higher than the $12,509 in annual direct medical costs for all RA patients on any treatment regimen. Proportionately, the difference was even greater for RA-specific care, with the annual cost of bDMARD care ($20,262) 5.4 times higher than that of all treatment regimens ($3,723), reported Andrew Hresko and his associates at Brigham and Women’s Hospital, Boston.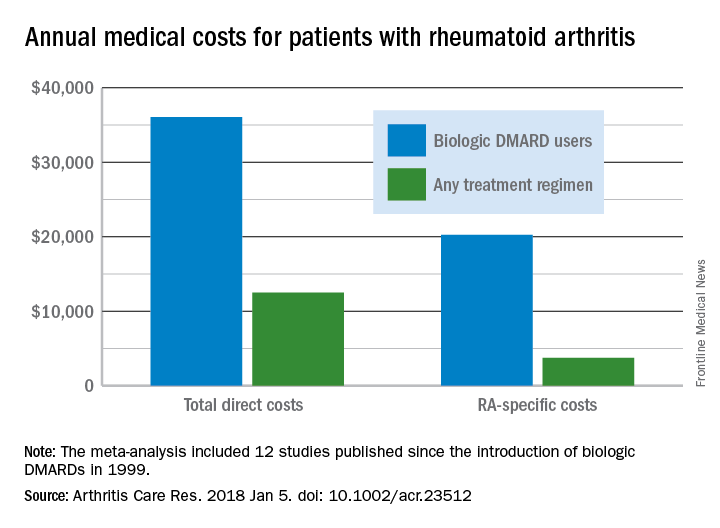
Funding for the study was supported through a grant from the National Institutes of Health. Mr. Hresko was supported by a fellowship from Tufts University. One of his associates receives research support from grants to his hospital from Amgen, Pfizer, Eli Lilly, AstraZeneca, Genentech, Bristol Myers Squibb, and Corrona. The third investigator is now an employee of Amgen but was not during the study.
SOURCE: Hresko A et al. Arthritis Care Res. 2018 Jan 5. doi: 10.1002/acr.23512.
FROM ARTHRITIS CARE & RESEARCH
Finance Committee votes on Azar HHS nomination
With a Senate Finance Committee vote of 15 to 12, Alex Azar’s nomination for secretary of Health & Human Services has been sent to the full Senate for consideration.
Finance Committee Chairman Orrin Hatch (R-Utah) said at a Jan. 17 hearing that “by any objective account, Mr. Azar is very well qualified for this important position. He has close to two decades of experience, the right expertise, and sound judgment.”
Most recently, Mr. Azar served as president of Eli Lilly’s U.S. operations from 2012 to 2017 after joining the company in 2007. His drug industry ties have raised concerns that the agency’s regulatory actions would be favorable to pharmaceutical manufacturers at the expense of patients. However, at his confirmation hearing, Mr. Azar noted that he would be willing to investigate government drug price negotiations for Medicare Part B drugs.
The top Democrat on the Finance Committee, Sen. Ron Wyden (D-Ore.) voted against Mr. Azar’s nomination, noting that President Trump “famously said, his words, in the 2016 campaign, ‘price-hiking drug companies were getting away with murder.’ The President has now nominated a drug company executive with a documented history of raising drug prices.”
Sen. Wyden noted that prices of many commonly prescribed drugs “more than doubled under [Mr. Azar’s] watch” while no drugs saw a decline in pricing.
With a Senate Finance Committee vote of 15 to 12, Alex Azar’s nomination for secretary of Health & Human Services has been sent to the full Senate for consideration.
Finance Committee Chairman Orrin Hatch (R-Utah) said at a Jan. 17 hearing that “by any objective account, Mr. Azar is very well qualified for this important position. He has close to two decades of experience, the right expertise, and sound judgment.”
Most recently, Mr. Azar served as president of Eli Lilly’s U.S. operations from 2012 to 2017 after joining the company in 2007. His drug industry ties have raised concerns that the agency’s regulatory actions would be favorable to pharmaceutical manufacturers at the expense of patients. However, at his confirmation hearing, Mr. Azar noted that he would be willing to investigate government drug price negotiations for Medicare Part B drugs.
The top Democrat on the Finance Committee, Sen. Ron Wyden (D-Ore.) voted against Mr. Azar’s nomination, noting that President Trump “famously said, his words, in the 2016 campaign, ‘price-hiking drug companies were getting away with murder.’ The President has now nominated a drug company executive with a documented history of raising drug prices.”
Sen. Wyden noted that prices of many commonly prescribed drugs “more than doubled under [Mr. Azar’s] watch” while no drugs saw a decline in pricing.
With a Senate Finance Committee vote of 15 to 12, Alex Azar’s nomination for secretary of Health & Human Services has been sent to the full Senate for consideration.
Finance Committee Chairman Orrin Hatch (R-Utah) said at a Jan. 17 hearing that “by any objective account, Mr. Azar is very well qualified for this important position. He has close to two decades of experience, the right expertise, and sound judgment.”
Most recently, Mr. Azar served as president of Eli Lilly’s U.S. operations from 2012 to 2017 after joining the company in 2007. His drug industry ties have raised concerns that the agency’s regulatory actions would be favorable to pharmaceutical manufacturers at the expense of patients. However, at his confirmation hearing, Mr. Azar noted that he would be willing to investigate government drug price negotiations for Medicare Part B drugs.
The top Democrat on the Finance Committee, Sen. Ron Wyden (D-Ore.) voted against Mr. Azar’s nomination, noting that President Trump “famously said, his words, in the 2016 campaign, ‘price-hiking drug companies were getting away with murder.’ The President has now nominated a drug company executive with a documented history of raising drug prices.”
Sen. Wyden noted that prices of many commonly prescribed drugs “more than doubled under [Mr. Azar’s] watch” while no drugs saw a decline in pricing.
REPORTING FROM A SENATE FINANCE COMMITTEE HEARING
Mood changes reported in cases of methotrexate use for dermatologic disease
, said Trisha Bhat and Carrie C. Coughlin, MD, both of Washington University, St. Louis.
Neurotoxicity with low-dose methotrexate often has been described when used to treat rheumatologic disease, the investigators said, but not in the dermatologic literature – although CNS symptoms such as dizziness and headache have been described in both.
An 8-year-old girl with psoriasis vulgaris and no prior psychiatric history began weekly subcutaneous methotrexate 12.5 mg (0.23 mg/kg) with folic acid supplementation 6 days per week after failing topical therapy. Her parents noticed severe irritability right away and fluctuating mood changes over the next 2 months. At first, she was angry and unsettled, with depressed mood; her irritability became less frequent later, but she said she wanted to hurt someone else. After stopping methotrexate, her mood returned to normal within 2 weeks.
It is unclear how methotrexate affects mood, but recent evidence suggests that abnormalities in synaptic plasticity are involved in mood changes, and there is evidence that mice treated with methotrexate show changes in synaptic plasticity. Methotrexate also increases extracellular adenosine, which affects neuronal excitability and synaptic plasticity, Ms. Bhat and Dr. Coughlin observed. Methotrexate also affects glucose metabolism in rats, and regional metabolic disturbances occur in a number of psychiatric disorders.
Read more at Pediatric Dermatology (2018 Jan 9. doi: 10.1111/pde.13406).
, said Trisha Bhat and Carrie C. Coughlin, MD, both of Washington University, St. Louis.
Neurotoxicity with low-dose methotrexate often has been described when used to treat rheumatologic disease, the investigators said, but not in the dermatologic literature – although CNS symptoms such as dizziness and headache have been described in both.
An 8-year-old girl with psoriasis vulgaris and no prior psychiatric history began weekly subcutaneous methotrexate 12.5 mg (0.23 mg/kg) with folic acid supplementation 6 days per week after failing topical therapy. Her parents noticed severe irritability right away and fluctuating mood changes over the next 2 months. At first, she was angry and unsettled, with depressed mood; her irritability became less frequent later, but she said she wanted to hurt someone else. After stopping methotrexate, her mood returned to normal within 2 weeks.
It is unclear how methotrexate affects mood, but recent evidence suggests that abnormalities in synaptic plasticity are involved in mood changes, and there is evidence that mice treated with methotrexate show changes in synaptic plasticity. Methotrexate also increases extracellular adenosine, which affects neuronal excitability and synaptic plasticity, Ms. Bhat and Dr. Coughlin observed. Methotrexate also affects glucose metabolism in rats, and regional metabolic disturbances occur in a number of psychiatric disorders.
Read more at Pediatric Dermatology (2018 Jan 9. doi: 10.1111/pde.13406).
, said Trisha Bhat and Carrie C. Coughlin, MD, both of Washington University, St. Louis.
Neurotoxicity with low-dose methotrexate often has been described when used to treat rheumatologic disease, the investigators said, but not in the dermatologic literature – although CNS symptoms such as dizziness and headache have been described in both.
An 8-year-old girl with psoriasis vulgaris and no prior psychiatric history began weekly subcutaneous methotrexate 12.5 mg (0.23 mg/kg) with folic acid supplementation 6 days per week after failing topical therapy. Her parents noticed severe irritability right away and fluctuating mood changes over the next 2 months. At first, she was angry and unsettled, with depressed mood; her irritability became less frequent later, but she said she wanted to hurt someone else. After stopping methotrexate, her mood returned to normal within 2 weeks.
It is unclear how methotrexate affects mood, but recent evidence suggests that abnormalities in synaptic plasticity are involved in mood changes, and there is evidence that mice treated with methotrexate show changes in synaptic plasticity. Methotrexate also increases extracellular adenosine, which affects neuronal excitability and synaptic plasticity, Ms. Bhat and Dr. Coughlin observed. Methotrexate also affects glucose metabolism in rats, and regional metabolic disturbances occur in a number of psychiatric disorders.
Read more at Pediatric Dermatology (2018 Jan 9. doi: 10.1111/pde.13406).
FROM PEDIATRIC DERMATOLOGY
FDA grants priority review to CAR T-cell therapy for DLBCL
The Food and Drug Administration has granted a priority review for the CAR T-cell therapy tisagenlecleucel suspension, formerly CTL019, for the treatment of adult patients with relapsed or refractory diffuse large B-cell lymphoma who are ineligible for or relapsed after autologous stem cell transplant.
The current application is based on a 6-month primary analysis from the single-arm, phase 2 JULIET clinical trial in adult patients with relapsed or refractory diffuse large B-cell lymphoma. According to results presented at ASH 2017, among 81 patients followed for at least 3 months before data cutoff, best overall response rate was 53%, and 40% had a complete response. Cytokine release syndrome (all grades) occurred in 58% of infused patients. Other grade 3 or 4 adverse events included neurologic toxicities, cytopenias lasting more than 28 days, infections, and febrile neutropenia.
Tisagenlecleucel suspension is marketed as Kymriah by Novartis.
The Food and Drug Administration has granted a priority review for the CAR T-cell therapy tisagenlecleucel suspension, formerly CTL019, for the treatment of adult patients with relapsed or refractory diffuse large B-cell lymphoma who are ineligible for or relapsed after autologous stem cell transplant.
The current application is based on a 6-month primary analysis from the single-arm, phase 2 JULIET clinical trial in adult patients with relapsed or refractory diffuse large B-cell lymphoma. According to results presented at ASH 2017, among 81 patients followed for at least 3 months before data cutoff, best overall response rate was 53%, and 40% had a complete response. Cytokine release syndrome (all grades) occurred in 58% of infused patients. Other grade 3 or 4 adverse events included neurologic toxicities, cytopenias lasting more than 28 days, infections, and febrile neutropenia.
Tisagenlecleucel suspension is marketed as Kymriah by Novartis.
The Food and Drug Administration has granted a priority review for the CAR T-cell therapy tisagenlecleucel suspension, formerly CTL019, for the treatment of adult patients with relapsed or refractory diffuse large B-cell lymphoma who are ineligible for or relapsed after autologous stem cell transplant.
The current application is based on a 6-month primary analysis from the single-arm, phase 2 JULIET clinical trial in adult patients with relapsed or refractory diffuse large B-cell lymphoma. According to results presented at ASH 2017, among 81 patients followed for at least 3 months before data cutoff, best overall response rate was 53%, and 40% had a complete response. Cytokine release syndrome (all grades) occurred in 58% of infused patients. Other grade 3 or 4 adverse events included neurologic toxicities, cytopenias lasting more than 28 days, infections, and febrile neutropenia.
Tisagenlecleucel suspension is marketed as Kymriah by Novartis.
FDA approves injection treatment for low-risk APL
The Food and Drug Administration announced the approval of arsenic trioxide injection (Trisenox) in combination with tretinoin for the treatment of adults with newly diagnosed, low-risk acute promyelocytic leukemia (APL) characterized by t(15;17) translocation or PML/RAR-alpha gene expression.
The expanded indication was granted by the FDA on Jan. 12 after priority review. It is based on published studies and a review of Teva’s global safety database for arsenic trioxide.
A recent randomized, phase 3 trial compared tretinoin plus arsenic trioxide with tretinoin plus chemotherapy as first-line treatment for APL (J Clin Oncol. 2017 Feb 20;35[6]:605-12). It found that 100% of 127 patients in the tretinoin plus arsenic trioxide arm achieved complete remission, compared with 97% of 136 patients in the tretinoin plus chemotherapy arm. After a median follow-up of 40.6 months, the event-free survival at 50 months for patients in the tretinoin/arsenic trioxide arm was 97.3% vs. 80% for tretinoin/chemotherapy (P = .001).
The arsenic trioxide injection carries a boxed warning for differentiation syndrome and cardiac conduction abnormalities.
The Food and Drug Administration announced the approval of arsenic trioxide injection (Trisenox) in combination with tretinoin for the treatment of adults with newly diagnosed, low-risk acute promyelocytic leukemia (APL) characterized by t(15;17) translocation or PML/RAR-alpha gene expression.
The expanded indication was granted by the FDA on Jan. 12 after priority review. It is based on published studies and a review of Teva’s global safety database for arsenic trioxide.
A recent randomized, phase 3 trial compared tretinoin plus arsenic trioxide with tretinoin plus chemotherapy as first-line treatment for APL (J Clin Oncol. 2017 Feb 20;35[6]:605-12). It found that 100% of 127 patients in the tretinoin plus arsenic trioxide arm achieved complete remission, compared with 97% of 136 patients in the tretinoin plus chemotherapy arm. After a median follow-up of 40.6 months, the event-free survival at 50 months for patients in the tretinoin/arsenic trioxide arm was 97.3% vs. 80% for tretinoin/chemotherapy (P = .001).
The arsenic trioxide injection carries a boxed warning for differentiation syndrome and cardiac conduction abnormalities.
The Food and Drug Administration announced the approval of arsenic trioxide injection (Trisenox) in combination with tretinoin for the treatment of adults with newly diagnosed, low-risk acute promyelocytic leukemia (APL) characterized by t(15;17) translocation or PML/RAR-alpha gene expression.
The expanded indication was granted by the FDA on Jan. 12 after priority review. It is based on published studies and a review of Teva’s global safety database for arsenic trioxide.
A recent randomized, phase 3 trial compared tretinoin plus arsenic trioxide with tretinoin plus chemotherapy as first-line treatment for APL (J Clin Oncol. 2017 Feb 20;35[6]:605-12). It found that 100% of 127 patients in the tretinoin plus arsenic trioxide arm achieved complete remission, compared with 97% of 136 patients in the tretinoin plus chemotherapy arm. After a median follow-up of 40.6 months, the event-free survival at 50 months for patients in the tretinoin/arsenic trioxide arm was 97.3% vs. 80% for tretinoin/chemotherapy (P = .001).
The arsenic trioxide injection carries a boxed warning for differentiation syndrome and cardiac conduction abnormalities.
Clinical rule decreased pediatric trauma CT scans
ORLANDO – A according to a study presented at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
With values for five clinical variables, the prediction rule would eliminate the need to subject some patients to unwarranted radiation exposure, which has become a growing health and financial concern for medical institutions.
“CT utilization rates in pediatric blunt trauma are very high, at a rate of 40%-60%, despite a relatively low incidence of intra-abdominal injury after abdominal trauma,” according to presenter Chase A. Arbra, MD, of the department of surgery at the Medical University of South Carolina, Charleston. “With increasing concerns regarding the cost and radiation exposure in children, our group is focusing on research to safely avoid these unnecessary scans.”
The rule, developed by the Pediatric Surgery Research Collaborative (PedSRC), evaluates abdominal wall trauma and tenderness, complaint of abdominal pain, aspartate aminotransferase level greater than 200 U/L, abnormal pancreatic enzymes, and abnormal chest x-rays to determine a patient’s risk of having an intra-abdominal injury (IAI). If none of the five variables in a patient is abnormal, the finding is considered negative and the patient is considered to be at very low risk for having an IAI or an IAI requiring acute intervention (IAI-I).
Investigators studied 2,435 pediatric blunt trauma patients with all five clinical variables documented within 6 hours of arrival, using data gathered from the Pediatric Emergency Care Applied Research Network.
Patients were an average of 9.4 years old, with an IAI rate of 9.7% (n = 235) and an IAI-I rate of 2.5% (n = 60); 61.1% of the patients had a CT scan.
Prediction sensitivity of the method was 97.5% for IAI and 100% for IAI-I, said Dr. Arbra. Negative predictive value for the model was 99.3% for IAI and 100% for IAI-I.
Patients who were found to have aspartate aminotransferase level greater than 200 U/L were at the highest risk of IAI (52.6%) and IAI-I (11.9%), according to investigators. One-third of the test population was found to be at very low risk after using the prediction model, according to Dr. Arbra, with 46.8% of them still undergoing a CT scan. Of those tested, six patients had IAI that was not predicted by the model, three of whom were intubated. Because CT scans were not required and there was no follow-up after discharge, investigators are not able to determine if any minor IAI was missed.
Despite these limitations, the highly sensitive rule shows great promise, according to Dr. Arbra.
“Patients with 0-5 variables, even patients who were involved in a high impact mechanism, could potentially forgo CT scans safely.”
A closer look at the 26 patients who only had abdominal pain showed that only 1 had IAI, suggesting that patients with only abdominal pain could be safely observed with only serial exams, according to Dr. Arbra.
Investigators plan to conduct a prospective study that will include older patients.
Dr. Arbra concluded, “The rule could potentially help centers to determine who could avoid imaging prior to transfer and potentially could one day be used to see who could be discharged.”
Dr. Arbra reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
SOURCE: Arbra CA. EAST Scientific Assembly 2018, paper #7.
ORLANDO – A according to a study presented at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
With values for five clinical variables, the prediction rule would eliminate the need to subject some patients to unwarranted radiation exposure, which has become a growing health and financial concern for medical institutions.
“CT utilization rates in pediatric blunt trauma are very high, at a rate of 40%-60%, despite a relatively low incidence of intra-abdominal injury after abdominal trauma,” according to presenter Chase A. Arbra, MD, of the department of surgery at the Medical University of South Carolina, Charleston. “With increasing concerns regarding the cost and radiation exposure in children, our group is focusing on research to safely avoid these unnecessary scans.”
The rule, developed by the Pediatric Surgery Research Collaborative (PedSRC), evaluates abdominal wall trauma and tenderness, complaint of abdominal pain, aspartate aminotransferase level greater than 200 U/L, abnormal pancreatic enzymes, and abnormal chest x-rays to determine a patient’s risk of having an intra-abdominal injury (IAI). If none of the five variables in a patient is abnormal, the finding is considered negative and the patient is considered to be at very low risk for having an IAI or an IAI requiring acute intervention (IAI-I).
Investigators studied 2,435 pediatric blunt trauma patients with all five clinical variables documented within 6 hours of arrival, using data gathered from the Pediatric Emergency Care Applied Research Network.
Patients were an average of 9.4 years old, with an IAI rate of 9.7% (n = 235) and an IAI-I rate of 2.5% (n = 60); 61.1% of the patients had a CT scan.
Prediction sensitivity of the method was 97.5% for IAI and 100% for IAI-I, said Dr. Arbra. Negative predictive value for the model was 99.3% for IAI and 100% for IAI-I.
Patients who were found to have aspartate aminotransferase level greater than 200 U/L were at the highest risk of IAI (52.6%) and IAI-I (11.9%), according to investigators. One-third of the test population was found to be at very low risk after using the prediction model, according to Dr. Arbra, with 46.8% of them still undergoing a CT scan. Of those tested, six patients had IAI that was not predicted by the model, three of whom were intubated. Because CT scans were not required and there was no follow-up after discharge, investigators are not able to determine if any minor IAI was missed.
Despite these limitations, the highly sensitive rule shows great promise, according to Dr. Arbra.
“Patients with 0-5 variables, even patients who were involved in a high impact mechanism, could potentially forgo CT scans safely.”
A closer look at the 26 patients who only had abdominal pain showed that only 1 had IAI, suggesting that patients with only abdominal pain could be safely observed with only serial exams, according to Dr. Arbra.
Investigators plan to conduct a prospective study that will include older patients.
Dr. Arbra concluded, “The rule could potentially help centers to determine who could avoid imaging prior to transfer and potentially could one day be used to see who could be discharged.”
Dr. Arbra reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
SOURCE: Arbra CA. EAST Scientific Assembly 2018, paper #7.
ORLANDO – A according to a study presented at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
With values for five clinical variables, the prediction rule would eliminate the need to subject some patients to unwarranted radiation exposure, which has become a growing health and financial concern for medical institutions.
“CT utilization rates in pediatric blunt trauma are very high, at a rate of 40%-60%, despite a relatively low incidence of intra-abdominal injury after abdominal trauma,” according to presenter Chase A. Arbra, MD, of the department of surgery at the Medical University of South Carolina, Charleston. “With increasing concerns regarding the cost and radiation exposure in children, our group is focusing on research to safely avoid these unnecessary scans.”
The rule, developed by the Pediatric Surgery Research Collaborative (PedSRC), evaluates abdominal wall trauma and tenderness, complaint of abdominal pain, aspartate aminotransferase level greater than 200 U/L, abnormal pancreatic enzymes, and abnormal chest x-rays to determine a patient’s risk of having an intra-abdominal injury (IAI). If none of the five variables in a patient is abnormal, the finding is considered negative and the patient is considered to be at very low risk for having an IAI or an IAI requiring acute intervention (IAI-I).
Investigators studied 2,435 pediatric blunt trauma patients with all five clinical variables documented within 6 hours of arrival, using data gathered from the Pediatric Emergency Care Applied Research Network.
Patients were an average of 9.4 years old, with an IAI rate of 9.7% (n = 235) and an IAI-I rate of 2.5% (n = 60); 61.1% of the patients had a CT scan.
Prediction sensitivity of the method was 97.5% for IAI and 100% for IAI-I, said Dr. Arbra. Negative predictive value for the model was 99.3% for IAI and 100% for IAI-I.
Patients who were found to have aspartate aminotransferase level greater than 200 U/L were at the highest risk of IAI (52.6%) and IAI-I (11.9%), according to investigators. One-third of the test population was found to be at very low risk after using the prediction model, according to Dr. Arbra, with 46.8% of them still undergoing a CT scan. Of those tested, six patients had IAI that was not predicted by the model, three of whom were intubated. Because CT scans were not required and there was no follow-up after discharge, investigators are not able to determine if any minor IAI was missed.
Despite these limitations, the highly sensitive rule shows great promise, according to Dr. Arbra.
“Patients with 0-5 variables, even patients who were involved in a high impact mechanism, could potentially forgo CT scans safely.”
A closer look at the 26 patients who only had abdominal pain showed that only 1 had IAI, suggesting that patients with only abdominal pain could be safely observed with only serial exams, according to Dr. Arbra.
Investigators plan to conduct a prospective study that will include older patients.
Dr. Arbra concluded, “The rule could potentially help centers to determine who could avoid imaging prior to transfer and potentially could one day be used to see who could be discharged.”
Dr. Arbra reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
SOURCE: Arbra CA. EAST Scientific Assembly 2018, paper #7.
REPORTING FROM EAST 2018
Key clinical point: New prediction model successfully identified patients with intra-abdominal injury (IAI) and IAI patients who require acute intervention (IAI-I).
Major finding: The test had a negative predictive value of 99.3% in IAI patients and 100% in IAI-I patients when either had no abnormalities.
Study details: Prospective study of 2,345 pediatric patients with IAI or IAI-I, the data for which was collected from the Pediatric Emergency Care Applied Research Network.
Disclosures: Dr. Arbra reported no relevant financial disclosures.
Source: Arbra CA. EAST Scientific Assembly 2018, paper #7.
Influenza vaccination of pregnant women needs surveillance
Seasonal influenza vaccine is specifically recommended for women who are or who might become pregnant in the flu season. This special population is targeted for vaccination because pregnant women are at increased risks of serious complications if infected with influenza virus. Despite this recommendation, recent evidence indicates that still fewer than 50% of women in the United States are vaccinated during pregnancy (MMWR Morb Mortal Wkly Rep. 2016 Dec 9;65[48]:1370-3).
Potential reasons for this lack of uptake are concerns about safety of the vaccine for mothers and fetuses (Vaccine. 2012 Dec 17;31[1]:213-8). This has highlighted the need for systematic safety surveillance for influenza vaccination with each subsequent seasonal formulation. To that end, season-specific studies of birth and infant outcomes since the 2009 season have been conducted; findings have been generally reassuring (Vaccine. 2016 Aug 17;34[37]:4443-9; Vaccine. 2016 Aug 17;34[37]:4450-9).
The authors found a doubling of risk for spontaneous abortion within that 28-day exposure window, but no association if the vaccination took place outside that period. This was in contrast to null findings for a similar analysis that the same group had conducted for vaccination in the 2005-2006 and 2006-2007 seasons. Of further interest, the authors noted even higher risks among women who had also been vaccinated for influenza in the previous season (adjusted odds ratio, 7.7; 95% confidence interval, 2.2-27.3). The highest odds ratios were among women who had been vaccinated in the 2010-2011 season and had also been vaccinated with monovalent pandemic H1N1 vaccine in the 2009-2010 season (aOR, 32.5; 95% CI, 2.9-359.0).
The VSD findings raise interesting questions about the biologic plausibility of strain-specific risks for spontaneous abortion, and risks of receiving a second vaccine containing the same strain in a subsequent season. However, this study should be interpreted with caution. With respect to the overall finding of a doubling of risk for spontaneous abortion, this is inconsistent with previous studies. A systematic review of 19 observational studies, 14 of which included exposure to the 2009 monovalent pandemic H1N1 strain, noted hazard ratios or odds ratios for spontaneous abortion ranging from 0.45 to 1.23 and 95% confidence intervals that crossed or were below the null (Vaccine. 2015 Apr 27;33[18]:2108-17). More recently, the Vaccines and Medications in Pregnancy Surveillance System investigators evaluated spontaneous abortion in pregnancies exposed to influenza vaccine over four seasons from 2010 to 2014 and found an overall hazard ratio of 1.09 (95% CI, 0.49-2.40).
However, there are a number of limitations that must be considered. Many previous studies, including the VSD analysis, could have had misclassification of exposure, especially in recent years when vaccines are often received in nontraditional settings. The VSD study findings could have been influenced by unmeasured confounding. For example, there could be differential vaccine uptake in women with comorbidities that are also associated with spontaneous abortion, such as subfertility and psychiatric disorders.
In summary, at present the data viewed as a whole do not support a change to the current recommendation that pregnant women be vaccinated for influenza regardless of trimester. However, these data do call for continued surveillance for the safety of each seasonal formulation of influenza vaccine, and for further exploration of the association between repeat vaccination and spontaneous abortion in other datasets.
Dr. Chambers is professor of pediatrics and director of clinical research at Rady Children’s Hospital and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is also director of MotherToBaby California, a past president of the Organization of Teratology Information Specialists, and past president of the Teratology Society. She has no direct conflicts of interest to disclose, but has received grant funding to study influenza vaccine from the Biomedical Advanced Research and Development Authority (BARDA) in the Department of Health and Human Services, and from Seqirus Corporation.
Seasonal influenza vaccine is specifically recommended for women who are or who might become pregnant in the flu season. This special population is targeted for vaccination because pregnant women are at increased risks of serious complications if infected with influenza virus. Despite this recommendation, recent evidence indicates that still fewer than 50% of women in the United States are vaccinated during pregnancy (MMWR Morb Mortal Wkly Rep. 2016 Dec 9;65[48]:1370-3).
Potential reasons for this lack of uptake are concerns about safety of the vaccine for mothers and fetuses (Vaccine. 2012 Dec 17;31[1]:213-8). This has highlighted the need for systematic safety surveillance for influenza vaccination with each subsequent seasonal formulation. To that end, season-specific studies of birth and infant outcomes since the 2009 season have been conducted; findings have been generally reassuring (Vaccine. 2016 Aug 17;34[37]:4443-9; Vaccine. 2016 Aug 17;34[37]:4450-9).
The authors found a doubling of risk for spontaneous abortion within that 28-day exposure window, but no association if the vaccination took place outside that period. This was in contrast to null findings for a similar analysis that the same group had conducted for vaccination in the 2005-2006 and 2006-2007 seasons. Of further interest, the authors noted even higher risks among women who had also been vaccinated for influenza in the previous season (adjusted odds ratio, 7.7; 95% confidence interval, 2.2-27.3). The highest odds ratios were among women who had been vaccinated in the 2010-2011 season and had also been vaccinated with monovalent pandemic H1N1 vaccine in the 2009-2010 season (aOR, 32.5; 95% CI, 2.9-359.0).
The VSD findings raise interesting questions about the biologic plausibility of strain-specific risks for spontaneous abortion, and risks of receiving a second vaccine containing the same strain in a subsequent season. However, this study should be interpreted with caution. With respect to the overall finding of a doubling of risk for spontaneous abortion, this is inconsistent with previous studies. A systematic review of 19 observational studies, 14 of which included exposure to the 2009 monovalent pandemic H1N1 strain, noted hazard ratios or odds ratios for spontaneous abortion ranging from 0.45 to 1.23 and 95% confidence intervals that crossed or were below the null (Vaccine. 2015 Apr 27;33[18]:2108-17). More recently, the Vaccines and Medications in Pregnancy Surveillance System investigators evaluated spontaneous abortion in pregnancies exposed to influenza vaccine over four seasons from 2010 to 2014 and found an overall hazard ratio of 1.09 (95% CI, 0.49-2.40).
However, there are a number of limitations that must be considered. Many previous studies, including the VSD analysis, could have had misclassification of exposure, especially in recent years when vaccines are often received in nontraditional settings. The VSD study findings could have been influenced by unmeasured confounding. For example, there could be differential vaccine uptake in women with comorbidities that are also associated with spontaneous abortion, such as subfertility and psychiatric disorders.
In summary, at present the data viewed as a whole do not support a change to the current recommendation that pregnant women be vaccinated for influenza regardless of trimester. However, these data do call for continued surveillance for the safety of each seasonal formulation of influenza vaccine, and for further exploration of the association between repeat vaccination and spontaneous abortion in other datasets.
Dr. Chambers is professor of pediatrics and director of clinical research at Rady Children’s Hospital and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is also director of MotherToBaby California, a past president of the Organization of Teratology Information Specialists, and past president of the Teratology Society. She has no direct conflicts of interest to disclose, but has received grant funding to study influenza vaccine from the Biomedical Advanced Research and Development Authority (BARDA) in the Department of Health and Human Services, and from Seqirus Corporation.
Seasonal influenza vaccine is specifically recommended for women who are or who might become pregnant in the flu season. This special population is targeted for vaccination because pregnant women are at increased risks of serious complications if infected with influenza virus. Despite this recommendation, recent evidence indicates that still fewer than 50% of women in the United States are vaccinated during pregnancy (MMWR Morb Mortal Wkly Rep. 2016 Dec 9;65[48]:1370-3).
Potential reasons for this lack of uptake are concerns about safety of the vaccine for mothers and fetuses (Vaccine. 2012 Dec 17;31[1]:213-8). This has highlighted the need for systematic safety surveillance for influenza vaccination with each subsequent seasonal formulation. To that end, season-specific studies of birth and infant outcomes since the 2009 season have been conducted; findings have been generally reassuring (Vaccine. 2016 Aug 17;34[37]:4443-9; Vaccine. 2016 Aug 17;34[37]:4450-9).
The authors found a doubling of risk for spontaneous abortion within that 28-day exposure window, but no association if the vaccination took place outside that period. This was in contrast to null findings for a similar analysis that the same group had conducted for vaccination in the 2005-2006 and 2006-2007 seasons. Of further interest, the authors noted even higher risks among women who had also been vaccinated for influenza in the previous season (adjusted odds ratio, 7.7; 95% confidence interval, 2.2-27.3). The highest odds ratios were among women who had been vaccinated in the 2010-2011 season and had also been vaccinated with monovalent pandemic H1N1 vaccine in the 2009-2010 season (aOR, 32.5; 95% CI, 2.9-359.0).
The VSD findings raise interesting questions about the biologic plausibility of strain-specific risks for spontaneous abortion, and risks of receiving a second vaccine containing the same strain in a subsequent season. However, this study should be interpreted with caution. With respect to the overall finding of a doubling of risk for spontaneous abortion, this is inconsistent with previous studies. A systematic review of 19 observational studies, 14 of which included exposure to the 2009 monovalent pandemic H1N1 strain, noted hazard ratios or odds ratios for spontaneous abortion ranging from 0.45 to 1.23 and 95% confidence intervals that crossed or were below the null (Vaccine. 2015 Apr 27;33[18]:2108-17). More recently, the Vaccines and Medications in Pregnancy Surveillance System investigators evaluated spontaneous abortion in pregnancies exposed to influenza vaccine over four seasons from 2010 to 2014 and found an overall hazard ratio of 1.09 (95% CI, 0.49-2.40).
However, there are a number of limitations that must be considered. Many previous studies, including the VSD analysis, could have had misclassification of exposure, especially in recent years when vaccines are often received in nontraditional settings. The VSD study findings could have been influenced by unmeasured confounding. For example, there could be differential vaccine uptake in women with comorbidities that are also associated with spontaneous abortion, such as subfertility and psychiatric disorders.
In summary, at present the data viewed as a whole do not support a change to the current recommendation that pregnant women be vaccinated for influenza regardless of trimester. However, these data do call for continued surveillance for the safety of each seasonal formulation of influenza vaccine, and for further exploration of the association between repeat vaccination and spontaneous abortion in other datasets.
Dr. Chambers is professor of pediatrics and director of clinical research at Rady Children’s Hospital and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is also director of MotherToBaby California, a past president of the Organization of Teratology Information Specialists, and past president of the Teratology Society. She has no direct conflicts of interest to disclose, but has received grant funding to study influenza vaccine from the Biomedical Advanced Research and Development Authority (BARDA) in the Department of Health and Human Services, and from Seqirus Corporation.
Carotid stenting isn’t safer than endarterectomy with contralateral carotid occlusion
CHICAGO – Carotid angioplasty and stenting (CAS) isn’t associated with a lower 30-day stroke risk than carotid endarterectomy (CEA) for revascularization of the internal carotid artery in patients with contralateral carotid occlusion, Leila Mureebe, MD, said at a symposium on vascular surgery sponsored by Northwestern University, Chicago.
The reported prevalence of contralateral carotid occlusion (CCO) in patients undergoing revascularization for carotid artery disease is 3%-15%. Of late Dr. Mureebe has been particularly interested in two questions regarding CCO in patients undergoing revascularization of their other carotid artery: Is CCO truly a risk factor for perioperative stroke? And if so, can this risk be mitigated by the choice of procedure?
To answer the first question, Dr. Mureebe and her coinvestigators performed a meta-analysis of eight representative studies published between 1994 and 2012; they determined that CCO in patients undergoing CEA was indeed associated with a near doubling of perioperative stroke risk, compared with that of patients without CCO.
In order to learn whether CAS mitigates this risk, she and her coworkers analyzed the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database for the period between 2011 and 2015, in which they identified 15,619 fully documented CEA and 496 CAS.
“This NSQIP data is not just academic medical centers or big centers. I think it’s a pretty good look at what’s actually being done in the real world today,” according to Dr. Mureebe.
The analysis showed that CCO has already had an effect on practice. A higher proportion of patients with CCO now undergo stenting as opposed to endarterectomy. Only 4.6% of all CEAs were done in patients with CCO, compared with 11.5% of CAS procedures. Moreover, the majority of revascularizations in the setting of CCO were performed in patients with asymptomatic disease: 57% of all CEA and 53% of the CAS. The CAS finding was surprising given that reimbursement for CAS is at present limited to symptomatic patients at high surgical risk who have a significant internal carotid artery stenosis, Dr. Mureebe observed.
The 30-day stroke rate in patients with CCO was 3.22% after CEA and 1.75% after CAS, a difference that wasn’t statistically significant. In patients without CCO, the stroke rate was 2.03% after CEA and 2.96% after CAS.
Next, the investigators analyzed differences in stroke rates according to symptom status. Among patients with CCO and preprocedural transient ischemic attack, stroke, or transient monocular blindness who underwent CEA, the 30-day stroke risk associated with CEA was 5.2%, a significantly higher rate than the 2.1% rate seen in patients without symptoms. The number of patients with CCO undergoing CAS was too small to draw conclusions regarding possible differences in stroke risk based upon symptom status.
In the NSQIP database, patients with CCO had higher prevalences of heart failure, hypertension, and smoking. For this reason, Dr. Mureebe said she suspects CCO is a surrogate for greater atherosclerotic disease burden and not an independent risk factor for periprocedural stroke. If future studies of the minimally invasive transcarotid artery revascularization procedure also show a higher rate of bad outcomes in patients with CCO, that would further support the hypothesis that CCO is a marker of higher atherosclerotic disease burden, Dr. Mureebe said.
A limitation of the NSQIP database is that it captures only those CAS cases done in operating rooms. “Maybe patients undergoing CAS in the OR are different from those undergoing CAS in a radiologic suite or cath lab,” she noted.
Dr. Mureebe reported having no financial conflicts of interest regarding her presentation.
bjancin@frontlinemedcom.com
SOURCE: Mureebe L. 42nd Annual Northwestern Vascular Symposium.
CHICAGO – Carotid angioplasty and stenting (CAS) isn’t associated with a lower 30-day stroke risk than carotid endarterectomy (CEA) for revascularization of the internal carotid artery in patients with contralateral carotid occlusion, Leila Mureebe, MD, said at a symposium on vascular surgery sponsored by Northwestern University, Chicago.
The reported prevalence of contralateral carotid occlusion (CCO) in patients undergoing revascularization for carotid artery disease is 3%-15%. Of late Dr. Mureebe has been particularly interested in two questions regarding CCO in patients undergoing revascularization of their other carotid artery: Is CCO truly a risk factor for perioperative stroke? And if so, can this risk be mitigated by the choice of procedure?
To answer the first question, Dr. Mureebe and her coinvestigators performed a meta-analysis of eight representative studies published between 1994 and 2012; they determined that CCO in patients undergoing CEA was indeed associated with a near doubling of perioperative stroke risk, compared with that of patients without CCO.
In order to learn whether CAS mitigates this risk, she and her coworkers analyzed the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database for the period between 2011 and 2015, in which they identified 15,619 fully documented CEA and 496 CAS.
“This NSQIP data is not just academic medical centers or big centers. I think it’s a pretty good look at what’s actually being done in the real world today,” according to Dr. Mureebe.
The analysis showed that CCO has already had an effect on practice. A higher proportion of patients with CCO now undergo stenting as opposed to endarterectomy. Only 4.6% of all CEAs were done in patients with CCO, compared with 11.5% of CAS procedures. Moreover, the majority of revascularizations in the setting of CCO were performed in patients with asymptomatic disease: 57% of all CEA and 53% of the CAS. The CAS finding was surprising given that reimbursement for CAS is at present limited to symptomatic patients at high surgical risk who have a significant internal carotid artery stenosis, Dr. Mureebe observed.
The 30-day stroke rate in patients with CCO was 3.22% after CEA and 1.75% after CAS, a difference that wasn’t statistically significant. In patients without CCO, the stroke rate was 2.03% after CEA and 2.96% after CAS.
Next, the investigators analyzed differences in stroke rates according to symptom status. Among patients with CCO and preprocedural transient ischemic attack, stroke, or transient monocular blindness who underwent CEA, the 30-day stroke risk associated with CEA was 5.2%, a significantly higher rate than the 2.1% rate seen in patients without symptoms. The number of patients with CCO undergoing CAS was too small to draw conclusions regarding possible differences in stroke risk based upon symptom status.
In the NSQIP database, patients with CCO had higher prevalences of heart failure, hypertension, and smoking. For this reason, Dr. Mureebe said she suspects CCO is a surrogate for greater atherosclerotic disease burden and not an independent risk factor for periprocedural stroke. If future studies of the minimally invasive transcarotid artery revascularization procedure also show a higher rate of bad outcomes in patients with CCO, that would further support the hypothesis that CCO is a marker of higher atherosclerotic disease burden, Dr. Mureebe said.
A limitation of the NSQIP database is that it captures only those CAS cases done in operating rooms. “Maybe patients undergoing CAS in the OR are different from those undergoing CAS in a radiologic suite or cath lab,” she noted.
Dr. Mureebe reported having no financial conflicts of interest regarding her presentation.
bjancin@frontlinemedcom.com
SOURCE: Mureebe L. 42nd Annual Northwestern Vascular Symposium.
CHICAGO – Carotid angioplasty and stenting (CAS) isn’t associated with a lower 30-day stroke risk than carotid endarterectomy (CEA) for revascularization of the internal carotid artery in patients with contralateral carotid occlusion, Leila Mureebe, MD, said at a symposium on vascular surgery sponsored by Northwestern University, Chicago.
The reported prevalence of contralateral carotid occlusion (CCO) in patients undergoing revascularization for carotid artery disease is 3%-15%. Of late Dr. Mureebe has been particularly interested in two questions regarding CCO in patients undergoing revascularization of their other carotid artery: Is CCO truly a risk factor for perioperative stroke? And if so, can this risk be mitigated by the choice of procedure?
To answer the first question, Dr. Mureebe and her coinvestigators performed a meta-analysis of eight representative studies published between 1994 and 2012; they determined that CCO in patients undergoing CEA was indeed associated with a near doubling of perioperative stroke risk, compared with that of patients without CCO.
In order to learn whether CAS mitigates this risk, she and her coworkers analyzed the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database for the period between 2011 and 2015, in which they identified 15,619 fully documented CEA and 496 CAS.
“This NSQIP data is not just academic medical centers or big centers. I think it’s a pretty good look at what’s actually being done in the real world today,” according to Dr. Mureebe.
The analysis showed that CCO has already had an effect on practice. A higher proportion of patients with CCO now undergo stenting as opposed to endarterectomy. Only 4.6% of all CEAs were done in patients with CCO, compared with 11.5% of CAS procedures. Moreover, the majority of revascularizations in the setting of CCO were performed in patients with asymptomatic disease: 57% of all CEA and 53% of the CAS. The CAS finding was surprising given that reimbursement for CAS is at present limited to symptomatic patients at high surgical risk who have a significant internal carotid artery stenosis, Dr. Mureebe observed.
The 30-day stroke rate in patients with CCO was 3.22% after CEA and 1.75% after CAS, a difference that wasn’t statistically significant. In patients without CCO, the stroke rate was 2.03% after CEA and 2.96% after CAS.
Next, the investigators analyzed differences in stroke rates according to symptom status. Among patients with CCO and preprocedural transient ischemic attack, stroke, or transient monocular blindness who underwent CEA, the 30-day stroke risk associated with CEA was 5.2%, a significantly higher rate than the 2.1% rate seen in patients without symptoms. The number of patients with CCO undergoing CAS was too small to draw conclusions regarding possible differences in stroke risk based upon symptom status.
In the NSQIP database, patients with CCO had higher prevalences of heart failure, hypertension, and smoking. For this reason, Dr. Mureebe said she suspects CCO is a surrogate for greater atherosclerotic disease burden and not an independent risk factor for periprocedural stroke. If future studies of the minimally invasive transcarotid artery revascularization procedure also show a higher rate of bad outcomes in patients with CCO, that would further support the hypothesis that CCO is a marker of higher atherosclerotic disease burden, Dr. Mureebe said.
A limitation of the NSQIP database is that it captures only those CAS cases done in operating rooms. “Maybe patients undergoing CAS in the OR are different from those undergoing CAS in a radiologic suite or cath lab,” she noted.
Dr. Mureebe reported having no financial conflicts of interest regarding her presentation.
bjancin@frontlinemedcom.com
SOURCE: Mureebe L. 42nd Annual Northwestern Vascular Symposium.
EXPERT ANALYSIS FROM THE NORTHWESTERN VASCULAR SYMPOSIUM
Insulin delivery devices now covered under Part D
Older Americans will now have access to insulin delivery devices under Part D of Medicare coverage, according to guidance issued by the Centers for Medicare & Medicaid Services (CMS). The CMS guidance clarified that devices not previously covered under Medicare Part B will be covered under Part D of the prescription drug program. As a result, older Americans will now have access to a wider range of insulin delivery devices.
Insulin delivery devices help patients manage blood sugar levels effectively. The devices prevent dangerous blood sugar fluctuations that can lead to complications like hypoglycemia.
In the guidance, the CMS wrote: “With the introduction of new insulin delivery devices to the market, questions have arisen about Part D coverage for these products. Specifically, we have been asked whether newer insulin delivery devices that are not covered under Medicare Part B meet the Part D definition of ‘medical supplies associated with the injection of insulin. … The examples that were previously provided were never intended to be an exhaustive list of products that could be covered under Part D. Instead, they represented our understanding of the types of medical supplies associated with the injection of insulin that were available at the time.”
Since then, new delivery devices have been introduced to market “in the form of both mechanical and electronic insulin pumps” that are not covered under the Medicare Part B durable medical equipment (DME) benefit.
“We expect that technology will continue to advance and that ‘medical supplies associated with the injection of insulin’ will become significantly more sophisticated,” wrote the CMS. “As new products become available, Part D sponsors may evaluate these products for formulary placement and medical necessity and, subject to Part D coverage determination and appeals requirements, allow access and restrict use accordingly.”
According to the guidance, Part D will cover supplies “that are alternatives to insulin syringes,” and the CMS will not require insurers who offer Part D plan coverage to include these on their formularies. If these alternatives are included on formularies, sponsors may use utilization management criteria for the products.
In a statement praising the CMS’s decision, the Endocrine Society wrote: “This opens the door for older Americans to gain coverage for devices such as the Omnipod insulin management system, a popular insulin pump system. Until the new guidance was issued, Omnipod was the only FDA [Food and Drug Administration]–approved insulin pump system not covered by Medicare. Previously, people with diabetes who qualified for Medicare at age 65 had to pay out of pocket to continue using the Omnipod, and many lost access to the device.”
Robert Lash, MD, chief professional and clinical affairs officer for the Endocrine Society, said in an interview that the new CMS guidance "gives physicians and people with diabetes access to a wider range of technology options, since some people with type 1 diabetes prefer the Omnipod’s tubing-free design because it makes it easier to participate in sports and safer to work in certain environments.
“Before this guidance was issued, those patients had to switch pumps or revert to insulin injections when they turned 65 years old. We are pleased this guidance will open the door to greater choice” for patients, said Dr. Lash.
The CMS’s decision on insulin delivery devices follows a decision last year to cover continuous glucose monitors (CGMs) through Medicare. Last week, the CMS also announced it will provide coverage for the Abbott Freestyle Libre CGM, a welcome move for patients seeking additional choices.
This article was revised 1/18/18.
Older Americans will now have access to insulin delivery devices under Part D of Medicare coverage, according to guidance issued by the Centers for Medicare & Medicaid Services (CMS). The CMS guidance clarified that devices not previously covered under Medicare Part B will be covered under Part D of the prescription drug program. As a result, older Americans will now have access to a wider range of insulin delivery devices.
Insulin delivery devices help patients manage blood sugar levels effectively. The devices prevent dangerous blood sugar fluctuations that can lead to complications like hypoglycemia.
In the guidance, the CMS wrote: “With the introduction of new insulin delivery devices to the market, questions have arisen about Part D coverage for these products. Specifically, we have been asked whether newer insulin delivery devices that are not covered under Medicare Part B meet the Part D definition of ‘medical supplies associated with the injection of insulin. … The examples that were previously provided were never intended to be an exhaustive list of products that could be covered under Part D. Instead, they represented our understanding of the types of medical supplies associated with the injection of insulin that were available at the time.”
Since then, new delivery devices have been introduced to market “in the form of both mechanical and electronic insulin pumps” that are not covered under the Medicare Part B durable medical equipment (DME) benefit.
“We expect that technology will continue to advance and that ‘medical supplies associated with the injection of insulin’ will become significantly more sophisticated,” wrote the CMS. “As new products become available, Part D sponsors may evaluate these products for formulary placement and medical necessity and, subject to Part D coverage determination and appeals requirements, allow access and restrict use accordingly.”
According to the guidance, Part D will cover supplies “that are alternatives to insulin syringes,” and the CMS will not require insurers who offer Part D plan coverage to include these on their formularies. If these alternatives are included on formularies, sponsors may use utilization management criteria for the products.
In a statement praising the CMS’s decision, the Endocrine Society wrote: “This opens the door for older Americans to gain coverage for devices such as the Omnipod insulin management system, a popular insulin pump system. Until the new guidance was issued, Omnipod was the only FDA [Food and Drug Administration]–approved insulin pump system not covered by Medicare. Previously, people with diabetes who qualified for Medicare at age 65 had to pay out of pocket to continue using the Omnipod, and many lost access to the device.”
Robert Lash, MD, chief professional and clinical affairs officer for the Endocrine Society, said in an interview that the new CMS guidance "gives physicians and people with diabetes access to a wider range of technology options, since some people with type 1 diabetes prefer the Omnipod’s tubing-free design because it makes it easier to participate in sports and safer to work in certain environments.
“Before this guidance was issued, those patients had to switch pumps or revert to insulin injections when they turned 65 years old. We are pleased this guidance will open the door to greater choice” for patients, said Dr. Lash.
The CMS’s decision on insulin delivery devices follows a decision last year to cover continuous glucose monitors (CGMs) through Medicare. Last week, the CMS also announced it will provide coverage for the Abbott Freestyle Libre CGM, a welcome move for patients seeking additional choices.
This article was revised 1/18/18.
Older Americans will now have access to insulin delivery devices under Part D of Medicare coverage, according to guidance issued by the Centers for Medicare & Medicaid Services (CMS). The CMS guidance clarified that devices not previously covered under Medicare Part B will be covered under Part D of the prescription drug program. As a result, older Americans will now have access to a wider range of insulin delivery devices.
Insulin delivery devices help patients manage blood sugar levels effectively. The devices prevent dangerous blood sugar fluctuations that can lead to complications like hypoglycemia.
In the guidance, the CMS wrote: “With the introduction of new insulin delivery devices to the market, questions have arisen about Part D coverage for these products. Specifically, we have been asked whether newer insulin delivery devices that are not covered under Medicare Part B meet the Part D definition of ‘medical supplies associated with the injection of insulin. … The examples that were previously provided were never intended to be an exhaustive list of products that could be covered under Part D. Instead, they represented our understanding of the types of medical supplies associated with the injection of insulin that were available at the time.”
Since then, new delivery devices have been introduced to market “in the form of both mechanical and electronic insulin pumps” that are not covered under the Medicare Part B durable medical equipment (DME) benefit.
“We expect that technology will continue to advance and that ‘medical supplies associated with the injection of insulin’ will become significantly more sophisticated,” wrote the CMS. “As new products become available, Part D sponsors may evaluate these products for formulary placement and medical necessity and, subject to Part D coverage determination and appeals requirements, allow access and restrict use accordingly.”
According to the guidance, Part D will cover supplies “that are alternatives to insulin syringes,” and the CMS will not require insurers who offer Part D plan coverage to include these on their formularies. If these alternatives are included on formularies, sponsors may use utilization management criteria for the products.
In a statement praising the CMS’s decision, the Endocrine Society wrote: “This opens the door for older Americans to gain coverage for devices such as the Omnipod insulin management system, a popular insulin pump system. Until the new guidance was issued, Omnipod was the only FDA [Food and Drug Administration]–approved insulin pump system not covered by Medicare. Previously, people with diabetes who qualified for Medicare at age 65 had to pay out of pocket to continue using the Omnipod, and many lost access to the device.”
Robert Lash, MD, chief professional and clinical affairs officer for the Endocrine Society, said in an interview that the new CMS guidance "gives physicians and people with diabetes access to a wider range of technology options, since some people with type 1 diabetes prefer the Omnipod’s tubing-free design because it makes it easier to participate in sports and safer to work in certain environments.
“Before this guidance was issued, those patients had to switch pumps or revert to insulin injections when they turned 65 years old. We are pleased this guidance will open the door to greater choice” for patients, said Dr. Lash.
The CMS’s decision on insulin delivery devices follows a decision last year to cover continuous glucose monitors (CGMs) through Medicare. Last week, the CMS also announced it will provide coverage for the Abbott Freestyle Libre CGM, a welcome move for patients seeking additional choices.
This article was revised 1/18/18.
Pathological video game use can be ‘life-dominating’
SAN DIEGO – As a medical student, David L. Atkinson, MD, learned about a group of five adult men who played EverQuest, which bills itself as a 3D online world that “offers endless excitement, adventure, battle, and discovery.” They shared an apartment in Austin, Tex., and rotated which one would hold a full-time job while the other four spent their waking hours playing EverQuest.
“It was a little concerning,” recalled Dr. Atkinson, now a psychiatrist and the medical director of the teen recovery program at Children’s Health, Dallas. “EverQuest had a button in the game where you could order a pizza without interrupting your game play. Pathological video game use can be incredibly life-dominating.”
Many terms are used for pathological video game use, including problematic video game use, gaming disorder, and Internet gaming disorder, which is the term used in section III of DSM-5. Whether chronic video game use is a societal problem or an individual problem “is a very big question,” Dr. Atkinson said. “When we look at some of the prevalence data from Monitoring the Future, we have seen reductions in all kinds of substance use. We have seen reductions in teenage motor vehicle accidents and in teen pregnancy. If kids are playing video games and they’re all getting out of shape, that’s a cultural challenge. A clinician, though, may advocate against it as part of good health care.
“For instance, underage drinking in some American subcultures is normative. It doesn’t mean it’s a good idea.”
Most youth do not develop addictive behavior from playing games like EverQuest. “Substance use and gaming are different,” Dr. Atkinson said. “The amount of time spent at the expense of other things is one of the primary harms of video gaming, but financial concerns are not irrelevant. The new Star Wars Battlefront game would cost $2,100 if someone were to buy all of the available extras for the video game. Otherwise, it would take several hundred hours of game play to achieve all of these unlocked features.” While video games do not induce supraphysiologic dopamine release in the way drugs like cocaine do, the addictive potential is measured by an equation of reward versus effort. Obtaining a video game is not dependent upon social interactions, unlike drug use in states where the drug in question is illegal. In fact, the fewer social connections, the greater the risk of developing a video game use disorder.
“The perception of harm of video game addiction is very low, and parents do not consider the potential for developing an addiction before they buy a computer, handheld device, or video game console,” he said. “It is viewed as something that has to be limited ... not as something that is impossible to limit.” However, when parents begin to detect problems, they often find themselves unable to control their children’s or teens’ use of gaming, according to Dr. Atkinson.
In the DSM-5, Internet gaming disorder is defined as being preoccupied with games and withdrawn when not playing them, including irritability, anxiety, and sadness. Tolerance manifests as needing to spend more time playing the game. Typically, gamers cannot reduce their use despite effort, and there is a loss of interest in other activities and hobbies, Dr. Atkinson said. They may continue to engage in overuse of games despite knowing it’s a problem; they may lie about usage, may use games to escape anxiety or guilt, and may have lost or risked lose or risk relationships or career opportunities because of games.
“Not all gamers will do all of these things,” he emphasized. “For example, some gamers have disordered use and lose interest in other things, but don’t lie about it.” DSM-5 criteria also note that the video gaming itself must cause clinically significant impairment and must not be a manifestation of another disorder.
Tools aimed at helping in the diagnosis include the Problem Video Game Playing Questionnaire, the Internet Gaming Disorder Scale, the Internet Gaming Disorder Scale–Short-Form, the Problematic Online Gaming Questionnaire, the Game Addiction Scale, and the Electronic Gaming Motives Questionnaire, which measures enhancement, coping, social, and self-gratification motives.
According to Dr. Atkinson, 90% of children in Japan, Korea, North America, and Europe play video games. However, the prevalence of Internet gaming disorder is estimated to be 1% in the United States, 1.14% in Germany, and 5.9% in South Korea. Males have higher rates of pathological video game use, while afflicted females tend to have more problems. Pathological gaming use is associated with high levels of previous truancy and few leisure activities. It’s also associated with depression, poor impulse control, narcissistic traits, high anxiety, poor social competence, and less religiosity.
“The overlap with depression is very interesting,” Dr. Atkinson said. “ When they get rejected in a peer group or for a job, they tend to take it harder than people who don’t game. The gaming world is a place where you can be safe from rejection. If your credit card goes through, you’re allowed in.”
Anhedonia is another factor within the clinical syndrome of depression that is associated with video game use. A nationwide community sample of individuals in Korea showed that gaming and depression have their overlap most strongly with the “escape from negative emotions” model (J Nerv Ment Dis. 2017;205[7]:568-73). Other associated problems include greater obesity; metabolic indicators, such as high triglycerides and cholesterol; and sleep deprivation. Chronic gamers also tend to have less social support, less health promotion, and heightened social phobia. “When you’re gaming all the time, you’re going to have less opportunity to engage in an exposure paradigm to help you get over your social phobia,” Dr. Atkinson said. “Problem gamers are also more likely to have pathological use of pornography, poor impulse control, and ADHD symptoms.”
Studies of biobehavioral characteristics of those with pathological video game use suggest that there is a decreased dopamine striatal response (Neurosci Biobehav Rev. 2017 Apr;75:314-30). They also suggest decreased functional connectivity across areas of the brain, including decreased resting-state functional connectivity between ventral tegmental area and the nucleus accumbens, and lower tonic dopamine firing.
Parental management training can be successful at setting gaming limits in children under 12 years of age, he said. Pathological video game use is associated with physiologic stress in the family problem-solving task. One study of a brief 3-week family therapy intervention as measured by functional MRI showed that improvement in perceived family cohesion was associated with an increase in the activity of the caudate nucleus in response to the gamer’s viewing images of family cohesion and was inversely correlated with changes in online game playing time (Psychiatry Res. 2012 May 31;202[2]:126-31). “Bringing the family together may give them something to do besides gaming,” Dr. Atkinson said. “That can help them put games in a more balanced perspective.”
The largest evidence base supports cognitive-behavioral therapy for Internet gaming disorder, but there is insufficient evidence to make a clear statement of benefit (Clin Psychol Rev. 2017 Jun;54:123-33). Gaming-related cognitions accounted for a large portion of the variance in treatment response.
“Does the gaming cause the thoughts? Or do the thoughts cause the gaming?” Dr. Atkinson asked. “The cognitive model of CBT would tell you there’s a bidirectional relationship.”
As for medications, bupropion has been shown to reduce online gaming in depressed individuals, and escitalopram also may be efficacious. One comparative analysis showed that there were greater effects from using bupropion than for using escitalopram (Clin Psychopharmacol Neurosci. 2017 Nov 30;15[4]:361-8). Methylphenidate also has been shown to reduce online gaming (Compr Psychiatry. 2009 May-Jun;50[3]:251-6).
Parents who take video games away from their children often are met with a burst of aggression. “There’s an attempt to reestablish dominance in the situation, to obtain the old reinforcer or to reestablish control,” Dr. Atkinson said. “It’s different from tapering a drug; this is something that you have to plan for. Tapering video games is difficult to do. If the kid plays longer than they’re supposed to, what do you do then? You may have a fight to discontinue the video game. That’s one of the practical problems.”
Dr. Atkinson reported having no financial disclosures.
SOURCE: Atkinson DL. AAAP 2017.
SAN DIEGO – As a medical student, David L. Atkinson, MD, learned about a group of five adult men who played EverQuest, which bills itself as a 3D online world that “offers endless excitement, adventure, battle, and discovery.” They shared an apartment in Austin, Tex., and rotated which one would hold a full-time job while the other four spent their waking hours playing EverQuest.
“It was a little concerning,” recalled Dr. Atkinson, now a psychiatrist and the medical director of the teen recovery program at Children’s Health, Dallas. “EverQuest had a button in the game where you could order a pizza without interrupting your game play. Pathological video game use can be incredibly life-dominating.”
Many terms are used for pathological video game use, including problematic video game use, gaming disorder, and Internet gaming disorder, which is the term used in section III of DSM-5. Whether chronic video game use is a societal problem or an individual problem “is a very big question,” Dr. Atkinson said. “When we look at some of the prevalence data from Monitoring the Future, we have seen reductions in all kinds of substance use. We have seen reductions in teenage motor vehicle accidents and in teen pregnancy. If kids are playing video games and they’re all getting out of shape, that’s a cultural challenge. A clinician, though, may advocate against it as part of good health care.
“For instance, underage drinking in some American subcultures is normative. It doesn’t mean it’s a good idea.”
Most youth do not develop addictive behavior from playing games like EverQuest. “Substance use and gaming are different,” Dr. Atkinson said. “The amount of time spent at the expense of other things is one of the primary harms of video gaming, but financial concerns are not irrelevant. The new Star Wars Battlefront game would cost $2,100 if someone were to buy all of the available extras for the video game. Otherwise, it would take several hundred hours of game play to achieve all of these unlocked features.” While video games do not induce supraphysiologic dopamine release in the way drugs like cocaine do, the addictive potential is measured by an equation of reward versus effort. Obtaining a video game is not dependent upon social interactions, unlike drug use in states where the drug in question is illegal. In fact, the fewer social connections, the greater the risk of developing a video game use disorder.
“The perception of harm of video game addiction is very low, and parents do not consider the potential for developing an addiction before they buy a computer, handheld device, or video game console,” he said. “It is viewed as something that has to be limited ... not as something that is impossible to limit.” However, when parents begin to detect problems, they often find themselves unable to control their children’s or teens’ use of gaming, according to Dr. Atkinson.
In the DSM-5, Internet gaming disorder is defined as being preoccupied with games and withdrawn when not playing them, including irritability, anxiety, and sadness. Tolerance manifests as needing to spend more time playing the game. Typically, gamers cannot reduce their use despite effort, and there is a loss of interest in other activities and hobbies, Dr. Atkinson said. They may continue to engage in overuse of games despite knowing it’s a problem; they may lie about usage, may use games to escape anxiety or guilt, and may have lost or risked lose or risk relationships or career opportunities because of games.
“Not all gamers will do all of these things,” he emphasized. “For example, some gamers have disordered use and lose interest in other things, but don’t lie about it.” DSM-5 criteria also note that the video gaming itself must cause clinically significant impairment and must not be a manifestation of another disorder.
Tools aimed at helping in the diagnosis include the Problem Video Game Playing Questionnaire, the Internet Gaming Disorder Scale, the Internet Gaming Disorder Scale–Short-Form, the Problematic Online Gaming Questionnaire, the Game Addiction Scale, and the Electronic Gaming Motives Questionnaire, which measures enhancement, coping, social, and self-gratification motives.
According to Dr. Atkinson, 90% of children in Japan, Korea, North America, and Europe play video games. However, the prevalence of Internet gaming disorder is estimated to be 1% in the United States, 1.14% in Germany, and 5.9% in South Korea. Males have higher rates of pathological video game use, while afflicted females tend to have more problems. Pathological gaming use is associated with high levels of previous truancy and few leisure activities. It’s also associated with depression, poor impulse control, narcissistic traits, high anxiety, poor social competence, and less religiosity.
“The overlap with depression is very interesting,” Dr. Atkinson said. “ When they get rejected in a peer group or for a job, they tend to take it harder than people who don’t game. The gaming world is a place where you can be safe from rejection. If your credit card goes through, you’re allowed in.”
Anhedonia is another factor within the clinical syndrome of depression that is associated with video game use. A nationwide community sample of individuals in Korea showed that gaming and depression have their overlap most strongly with the “escape from negative emotions” model (J Nerv Ment Dis. 2017;205[7]:568-73). Other associated problems include greater obesity; metabolic indicators, such as high triglycerides and cholesterol; and sleep deprivation. Chronic gamers also tend to have less social support, less health promotion, and heightened social phobia. “When you’re gaming all the time, you’re going to have less opportunity to engage in an exposure paradigm to help you get over your social phobia,” Dr. Atkinson said. “Problem gamers are also more likely to have pathological use of pornography, poor impulse control, and ADHD symptoms.”
Studies of biobehavioral characteristics of those with pathological video game use suggest that there is a decreased dopamine striatal response (Neurosci Biobehav Rev. 2017 Apr;75:314-30). They also suggest decreased functional connectivity across areas of the brain, including decreased resting-state functional connectivity between ventral tegmental area and the nucleus accumbens, and lower tonic dopamine firing.
Parental management training can be successful at setting gaming limits in children under 12 years of age, he said. Pathological video game use is associated with physiologic stress in the family problem-solving task. One study of a brief 3-week family therapy intervention as measured by functional MRI showed that improvement in perceived family cohesion was associated with an increase in the activity of the caudate nucleus in response to the gamer’s viewing images of family cohesion and was inversely correlated with changes in online game playing time (Psychiatry Res. 2012 May 31;202[2]:126-31). “Bringing the family together may give them something to do besides gaming,” Dr. Atkinson said. “That can help them put games in a more balanced perspective.”
The largest evidence base supports cognitive-behavioral therapy for Internet gaming disorder, but there is insufficient evidence to make a clear statement of benefit (Clin Psychol Rev. 2017 Jun;54:123-33). Gaming-related cognitions accounted for a large portion of the variance in treatment response.
“Does the gaming cause the thoughts? Or do the thoughts cause the gaming?” Dr. Atkinson asked. “The cognitive model of CBT would tell you there’s a bidirectional relationship.”
As for medications, bupropion has been shown to reduce online gaming in depressed individuals, and escitalopram also may be efficacious. One comparative analysis showed that there were greater effects from using bupropion than for using escitalopram (Clin Psychopharmacol Neurosci. 2017 Nov 30;15[4]:361-8). Methylphenidate also has been shown to reduce online gaming (Compr Psychiatry. 2009 May-Jun;50[3]:251-6).
Parents who take video games away from their children often are met with a burst of aggression. “There’s an attempt to reestablish dominance in the situation, to obtain the old reinforcer or to reestablish control,” Dr. Atkinson said. “It’s different from tapering a drug; this is something that you have to plan for. Tapering video games is difficult to do. If the kid plays longer than they’re supposed to, what do you do then? You may have a fight to discontinue the video game. That’s one of the practical problems.”
Dr. Atkinson reported having no financial disclosures.
SOURCE: Atkinson DL. AAAP 2017.
SAN DIEGO – As a medical student, David L. Atkinson, MD, learned about a group of five adult men who played EverQuest, which bills itself as a 3D online world that “offers endless excitement, adventure, battle, and discovery.” They shared an apartment in Austin, Tex., and rotated which one would hold a full-time job while the other four spent their waking hours playing EverQuest.
“It was a little concerning,” recalled Dr. Atkinson, now a psychiatrist and the medical director of the teen recovery program at Children’s Health, Dallas. “EverQuest had a button in the game where you could order a pizza without interrupting your game play. Pathological video game use can be incredibly life-dominating.”
Many terms are used for pathological video game use, including problematic video game use, gaming disorder, and Internet gaming disorder, which is the term used in section III of DSM-5. Whether chronic video game use is a societal problem or an individual problem “is a very big question,” Dr. Atkinson said. “When we look at some of the prevalence data from Monitoring the Future, we have seen reductions in all kinds of substance use. We have seen reductions in teenage motor vehicle accidents and in teen pregnancy. If kids are playing video games and they’re all getting out of shape, that’s a cultural challenge. A clinician, though, may advocate against it as part of good health care.
“For instance, underage drinking in some American subcultures is normative. It doesn’t mean it’s a good idea.”
Most youth do not develop addictive behavior from playing games like EverQuest. “Substance use and gaming are different,” Dr. Atkinson said. “The amount of time spent at the expense of other things is one of the primary harms of video gaming, but financial concerns are not irrelevant. The new Star Wars Battlefront game would cost $2,100 if someone were to buy all of the available extras for the video game. Otherwise, it would take several hundred hours of game play to achieve all of these unlocked features.” While video games do not induce supraphysiologic dopamine release in the way drugs like cocaine do, the addictive potential is measured by an equation of reward versus effort. Obtaining a video game is not dependent upon social interactions, unlike drug use in states where the drug in question is illegal. In fact, the fewer social connections, the greater the risk of developing a video game use disorder.
“The perception of harm of video game addiction is very low, and parents do not consider the potential for developing an addiction before they buy a computer, handheld device, or video game console,” he said. “It is viewed as something that has to be limited ... not as something that is impossible to limit.” However, when parents begin to detect problems, they often find themselves unable to control their children’s or teens’ use of gaming, according to Dr. Atkinson.
In the DSM-5, Internet gaming disorder is defined as being preoccupied with games and withdrawn when not playing them, including irritability, anxiety, and sadness. Tolerance manifests as needing to spend more time playing the game. Typically, gamers cannot reduce their use despite effort, and there is a loss of interest in other activities and hobbies, Dr. Atkinson said. They may continue to engage in overuse of games despite knowing it’s a problem; they may lie about usage, may use games to escape anxiety or guilt, and may have lost or risked lose or risk relationships or career opportunities because of games.
“Not all gamers will do all of these things,” he emphasized. “For example, some gamers have disordered use and lose interest in other things, but don’t lie about it.” DSM-5 criteria also note that the video gaming itself must cause clinically significant impairment and must not be a manifestation of another disorder.
Tools aimed at helping in the diagnosis include the Problem Video Game Playing Questionnaire, the Internet Gaming Disorder Scale, the Internet Gaming Disorder Scale–Short-Form, the Problematic Online Gaming Questionnaire, the Game Addiction Scale, and the Electronic Gaming Motives Questionnaire, which measures enhancement, coping, social, and self-gratification motives.
According to Dr. Atkinson, 90% of children in Japan, Korea, North America, and Europe play video games. However, the prevalence of Internet gaming disorder is estimated to be 1% in the United States, 1.14% in Germany, and 5.9% in South Korea. Males have higher rates of pathological video game use, while afflicted females tend to have more problems. Pathological gaming use is associated with high levels of previous truancy and few leisure activities. It’s also associated with depression, poor impulse control, narcissistic traits, high anxiety, poor social competence, and less religiosity.
“The overlap with depression is very interesting,” Dr. Atkinson said. “ When they get rejected in a peer group or for a job, they tend to take it harder than people who don’t game. The gaming world is a place where you can be safe from rejection. If your credit card goes through, you’re allowed in.”
Anhedonia is another factor within the clinical syndrome of depression that is associated with video game use. A nationwide community sample of individuals in Korea showed that gaming and depression have their overlap most strongly with the “escape from negative emotions” model (J Nerv Ment Dis. 2017;205[7]:568-73). Other associated problems include greater obesity; metabolic indicators, such as high triglycerides and cholesterol; and sleep deprivation. Chronic gamers also tend to have less social support, less health promotion, and heightened social phobia. “When you’re gaming all the time, you’re going to have less opportunity to engage in an exposure paradigm to help you get over your social phobia,” Dr. Atkinson said. “Problem gamers are also more likely to have pathological use of pornography, poor impulse control, and ADHD symptoms.”
Studies of biobehavioral characteristics of those with pathological video game use suggest that there is a decreased dopamine striatal response (Neurosci Biobehav Rev. 2017 Apr;75:314-30). They also suggest decreased functional connectivity across areas of the brain, including decreased resting-state functional connectivity between ventral tegmental area and the nucleus accumbens, and lower tonic dopamine firing.
Parental management training can be successful at setting gaming limits in children under 12 years of age, he said. Pathological video game use is associated with physiologic stress in the family problem-solving task. One study of a brief 3-week family therapy intervention as measured by functional MRI showed that improvement in perceived family cohesion was associated with an increase in the activity of the caudate nucleus in response to the gamer’s viewing images of family cohesion and was inversely correlated with changes in online game playing time (Psychiatry Res. 2012 May 31;202[2]:126-31). “Bringing the family together may give them something to do besides gaming,” Dr. Atkinson said. “That can help them put games in a more balanced perspective.”
The largest evidence base supports cognitive-behavioral therapy for Internet gaming disorder, but there is insufficient evidence to make a clear statement of benefit (Clin Psychol Rev. 2017 Jun;54:123-33). Gaming-related cognitions accounted for a large portion of the variance in treatment response.
“Does the gaming cause the thoughts? Or do the thoughts cause the gaming?” Dr. Atkinson asked. “The cognitive model of CBT would tell you there’s a bidirectional relationship.”
As for medications, bupropion has been shown to reduce online gaming in depressed individuals, and escitalopram also may be efficacious. One comparative analysis showed that there were greater effects from using bupropion than for using escitalopram (Clin Psychopharmacol Neurosci. 2017 Nov 30;15[4]:361-8). Methylphenidate also has been shown to reduce online gaming (Compr Psychiatry. 2009 May-Jun;50[3]:251-6).
Parents who take video games away from their children often are met with a burst of aggression. “There’s an attempt to reestablish dominance in the situation, to obtain the old reinforcer or to reestablish control,” Dr. Atkinson said. “It’s different from tapering a drug; this is something that you have to plan for. Tapering video games is difficult to do. If the kid plays longer than they’re supposed to, what do you do then? You may have a fight to discontinue the video game. That’s one of the practical problems.”
Dr. Atkinson reported having no financial disclosures.
SOURCE: Atkinson DL. AAAP 2017.
REPORTING FROM AAAP