User login
VIDEO: Educational intervention boosts A fib anticoagulation
BARCELONA – A program promoting broader anticoagulation of patients with atrial fibrillation that used education and feedback from practice audits produced a substantial increase in sustained anticoagulant use and cut strokes in a multinational study with almost 2,300 patients in 48 practices.
Among atrial fibrillation (AF) patients who were not on an anticoagulant at baseline (34% of the enrolled group) 48% of patients in the intervention group began anticoagulant treatment and remained on it for a year with intervention compared with 18% of patients in the control arm without the intervention, Christopher B. Granger, MD, said at the annual congress of the European Society of Cardiology.
The intervention, which highlighted to health care providers the opportunity to start their AF patients on anticoagulant treatment, “transforms how care is provided to this population” of AF patients, Dr. Granger said in a video interview. “Doing something like this can have enormous public health implications.”
IMPACT AF (The Clinical Trial to Improve Treatment With Blood Thinners in Patients With Atrial Fibrillation) randomized 2,281 AF patients in 48 practices in five middle-income countries: Argentina, Brazil, China, India, and Romania. Randomization was by practice, and patients were assigned to either usual care or to an intervention that ran educational sessions for patients and providers on the benefits of and best practices for using anticoagulants. The intervention also monitored anticoagulant use by the patients in each practice and gave providers case-by-case feedback on the care patients received. The educational component customized the feedback to focus on overcoming treatment barriers specific for each patient. This audit and feedback process was a key part of the intervention, Dr. Granger said.
In an adjusted analysis, among patients not on an anticoagulant at baseline, the ones managed in practices that received the intervention had a greater than fourfold likelihood of receiving anticoagulant treatment, compared with patients in practices with no intervention. The intervention was especially successful in transitioning patients off of aspirin treatment, considered ineffective for AF stroke prevention, and onto an anticoagulant, most commonly warfarin.
Overall, anticoagulant use rose by 12 percentage points from baseline among patients in the intervention practices and by 3 percentage points over baseline among the control patients, a statistically significant difference for the study’s primary endpoint.
During 1-year follow-up, 11 strokes occurred among patients managed in practices that received the intervention and 21 in those in control practices, a 52% relative hazard reduction linked with the intervention that was statistically significant, Dr. Granger reported. Concurrently with his talk, the results also appeared online (Lancet. 2017. doi: 10.1016/S0140-6736[17]32165-7).
“How will we take what we have learned [in IMPACT AF] and have it available to people who want to replicate this?” asked Dr. Granger. “We have partnered with several national cardiology societies, and we are working with them to optimize the tools and provide the tools we’ve used,” he said. “We will develop a website for people who want to take this information and use it in their practices.” Dr. Granger and his associates also are working with the Food and Drug Administration and other groups to come up with interventions specially designed for U.S. practice.
IMPACT AF received partial funding from Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Daiichi Sankyo, and Pfizer. Dr. Granger has received honoraria and research funding from all of these companies, and also from Janssen and Medtronic.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
IMPACT AF is an important study, with impressive results that confirm the value of integrated atrial fibrillation care. In the study, a comprehensive and continuous educational intervention with 11 distinct components aimed at health care professionals and patients increased the initiation of and adherence to oral anticoagulation in patients with AF. This effect linked with a significantly reduced incidence of strokes.
Digital tools are an important part of the intervention. They provide both information and feedback, and they create a platform that can involve all stakeholders in management of atrial fibrillation. Informing AF patients about their treatment can result in patients who take responsibility for their management. Integrated AF management models can improve continued delivery of chronic care.
Paulus Kirchhof, MD , is a professor and deputy director of the Institute of Cardiovascular Sciences at the University of Birmingham, England. He has received honoraria and research funding from several drug companies. He made these comments as designated discussant for the report.
IMPACT AF is an important study, with impressive results that confirm the value of integrated atrial fibrillation care. In the study, a comprehensive and continuous educational intervention with 11 distinct components aimed at health care professionals and patients increased the initiation of and adherence to oral anticoagulation in patients with AF. This effect linked with a significantly reduced incidence of strokes.
Digital tools are an important part of the intervention. They provide both information and feedback, and they create a platform that can involve all stakeholders in management of atrial fibrillation. Informing AF patients about their treatment can result in patients who take responsibility for their management. Integrated AF management models can improve continued delivery of chronic care.
Paulus Kirchhof, MD , is a professor and deputy director of the Institute of Cardiovascular Sciences at the University of Birmingham, England. He has received honoraria and research funding from several drug companies. He made these comments as designated discussant for the report.
IMPACT AF is an important study, with impressive results that confirm the value of integrated atrial fibrillation care. In the study, a comprehensive and continuous educational intervention with 11 distinct components aimed at health care professionals and patients increased the initiation of and adherence to oral anticoagulation in patients with AF. This effect linked with a significantly reduced incidence of strokes.
Digital tools are an important part of the intervention. They provide both information and feedback, and they create a platform that can involve all stakeholders in management of atrial fibrillation. Informing AF patients about their treatment can result in patients who take responsibility for their management. Integrated AF management models can improve continued delivery of chronic care.
Paulus Kirchhof, MD , is a professor and deputy director of the Institute of Cardiovascular Sciences at the University of Birmingham, England. He has received honoraria and research funding from several drug companies. He made these comments as designated discussant for the report.
BARCELONA – A program promoting broader anticoagulation of patients with atrial fibrillation that used education and feedback from practice audits produced a substantial increase in sustained anticoagulant use and cut strokes in a multinational study with almost 2,300 patients in 48 practices.
Among atrial fibrillation (AF) patients who were not on an anticoagulant at baseline (34% of the enrolled group) 48% of patients in the intervention group began anticoagulant treatment and remained on it for a year with intervention compared with 18% of patients in the control arm without the intervention, Christopher B. Granger, MD, said at the annual congress of the European Society of Cardiology.
The intervention, which highlighted to health care providers the opportunity to start their AF patients on anticoagulant treatment, “transforms how care is provided to this population” of AF patients, Dr. Granger said in a video interview. “Doing something like this can have enormous public health implications.”
IMPACT AF (The Clinical Trial to Improve Treatment With Blood Thinners in Patients With Atrial Fibrillation) randomized 2,281 AF patients in 48 practices in five middle-income countries: Argentina, Brazil, China, India, and Romania. Randomization was by practice, and patients were assigned to either usual care or to an intervention that ran educational sessions for patients and providers on the benefits of and best practices for using anticoagulants. The intervention also monitored anticoagulant use by the patients in each practice and gave providers case-by-case feedback on the care patients received. The educational component customized the feedback to focus on overcoming treatment barriers specific for each patient. This audit and feedback process was a key part of the intervention, Dr. Granger said.
In an adjusted analysis, among patients not on an anticoagulant at baseline, the ones managed in practices that received the intervention had a greater than fourfold likelihood of receiving anticoagulant treatment, compared with patients in practices with no intervention. The intervention was especially successful in transitioning patients off of aspirin treatment, considered ineffective for AF stroke prevention, and onto an anticoagulant, most commonly warfarin.
Overall, anticoagulant use rose by 12 percentage points from baseline among patients in the intervention practices and by 3 percentage points over baseline among the control patients, a statistically significant difference for the study’s primary endpoint.
During 1-year follow-up, 11 strokes occurred among patients managed in practices that received the intervention and 21 in those in control practices, a 52% relative hazard reduction linked with the intervention that was statistically significant, Dr. Granger reported. Concurrently with his talk, the results also appeared online (Lancet. 2017. doi: 10.1016/S0140-6736[17]32165-7).
“How will we take what we have learned [in IMPACT AF] and have it available to people who want to replicate this?” asked Dr. Granger. “We have partnered with several national cardiology societies, and we are working with them to optimize the tools and provide the tools we’ve used,” he said. “We will develop a website for people who want to take this information and use it in their practices.” Dr. Granger and his associates also are working with the Food and Drug Administration and other groups to come up with interventions specially designed for U.S. practice.
IMPACT AF received partial funding from Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Daiichi Sankyo, and Pfizer. Dr. Granger has received honoraria and research funding from all of these companies, and also from Janssen and Medtronic.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
BARCELONA – A program promoting broader anticoagulation of patients with atrial fibrillation that used education and feedback from practice audits produced a substantial increase in sustained anticoagulant use and cut strokes in a multinational study with almost 2,300 patients in 48 practices.
Among atrial fibrillation (AF) patients who were not on an anticoagulant at baseline (34% of the enrolled group) 48% of patients in the intervention group began anticoagulant treatment and remained on it for a year with intervention compared with 18% of patients in the control arm without the intervention, Christopher B. Granger, MD, said at the annual congress of the European Society of Cardiology.
The intervention, which highlighted to health care providers the opportunity to start their AF patients on anticoagulant treatment, “transforms how care is provided to this population” of AF patients, Dr. Granger said in a video interview. “Doing something like this can have enormous public health implications.”
IMPACT AF (The Clinical Trial to Improve Treatment With Blood Thinners in Patients With Atrial Fibrillation) randomized 2,281 AF patients in 48 practices in five middle-income countries: Argentina, Brazil, China, India, and Romania. Randomization was by practice, and patients were assigned to either usual care or to an intervention that ran educational sessions for patients and providers on the benefits of and best practices for using anticoagulants. The intervention also monitored anticoagulant use by the patients in each practice and gave providers case-by-case feedback on the care patients received. The educational component customized the feedback to focus on overcoming treatment barriers specific for each patient. This audit and feedback process was a key part of the intervention, Dr. Granger said.
In an adjusted analysis, among patients not on an anticoagulant at baseline, the ones managed in practices that received the intervention had a greater than fourfold likelihood of receiving anticoagulant treatment, compared with patients in practices with no intervention. The intervention was especially successful in transitioning patients off of aspirin treatment, considered ineffective for AF stroke prevention, and onto an anticoagulant, most commonly warfarin.
Overall, anticoagulant use rose by 12 percentage points from baseline among patients in the intervention practices and by 3 percentage points over baseline among the control patients, a statistically significant difference for the study’s primary endpoint.
During 1-year follow-up, 11 strokes occurred among patients managed in practices that received the intervention and 21 in those in control practices, a 52% relative hazard reduction linked with the intervention that was statistically significant, Dr. Granger reported. Concurrently with his talk, the results also appeared online (Lancet. 2017. doi: 10.1016/S0140-6736[17]32165-7).
“How will we take what we have learned [in IMPACT AF] and have it available to people who want to replicate this?” asked Dr. Granger. “We have partnered with several national cardiology societies, and we are working with them to optimize the tools and provide the tools we’ve used,” he said. “We will develop a website for people who want to take this information and use it in their practices.” Dr. Granger and his associates also are working with the Food and Drug Administration and other groups to come up with interventions specially designed for U.S. practice.
IMPACT AF received partial funding from Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Daiichi Sankyo, and Pfizer. Dr. Granger has received honoraria and research funding from all of these companies, and also from Janssen and Medtronic.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
AT THE ESC CONGRESS 2017
Key clinical point:
Major finding: Anticoagulation rose by 12 percentage points from baseline with intervention and by 3 percentage points among controls.
Data source: IMPACT AF, which randomized 2,281 AF patients for 1 year at 48 centers in five middle-income countries.
Disclosures: IMPACT AF received partial funding from Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Daiichi Sankyo, and Pfizer. Dr. Granger has received honoraria and research funding from all of these companies, and also from Janssen and Medtronic.
E-cigarettes most popular among youngest adults
Over 15% of adults have used electronic cigarettes at some time, and about 3% reported current use when they were surveyed in 2016, according to the Centers for Disease Control and Prevention.
When those numbers are broken down by age group, the youngest adults are the most likely e-cigarette users: 23.5% of those aged 18-24 years had ever vaped and 4.5% were currently vaping either every day or on some days, the CDC reported (MMWR. 2017;66[33]:892).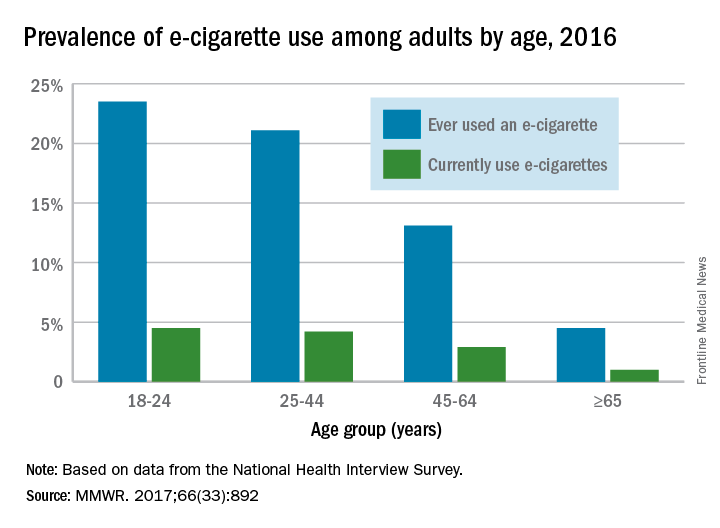
Over 15% of adults have used electronic cigarettes at some time, and about 3% reported current use when they were surveyed in 2016, according to the Centers for Disease Control and Prevention.
When those numbers are broken down by age group, the youngest adults are the most likely e-cigarette users: 23.5% of those aged 18-24 years had ever vaped and 4.5% were currently vaping either every day or on some days, the CDC reported (MMWR. 2017;66[33]:892).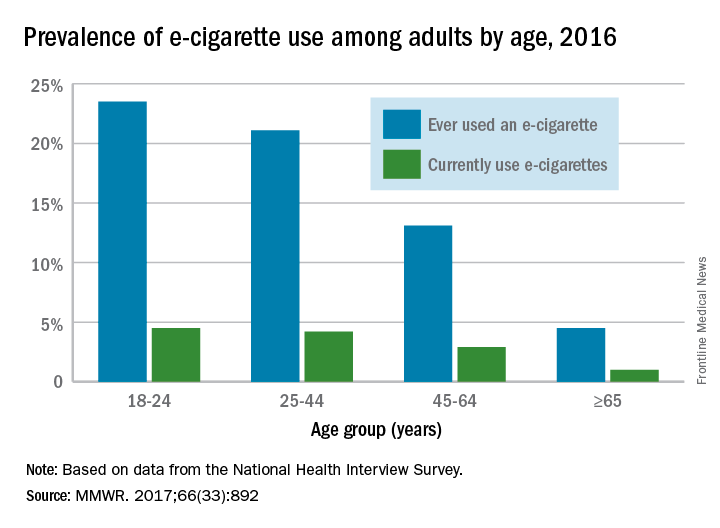
Over 15% of adults have used electronic cigarettes at some time, and about 3% reported current use when they were surveyed in 2016, according to the Centers for Disease Control and Prevention.
When those numbers are broken down by age group, the youngest adults are the most likely e-cigarette users: 23.5% of those aged 18-24 years had ever vaped and 4.5% were currently vaping either every day or on some days, the CDC reported (MMWR. 2017;66[33]:892).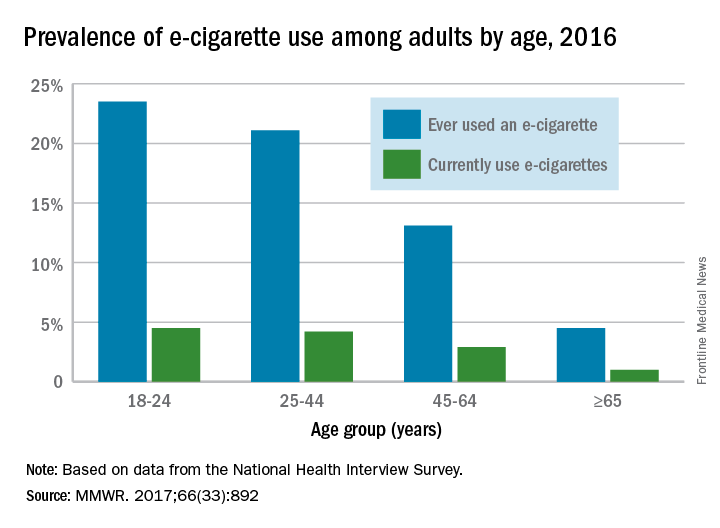
FROM MMWR
Wound expert: Consider hyperbaric oxygen therapy for diabetic foot ulcers
SAN DIEGO – Hyperbaric oxygen therapy, a mainstay of wound care, has a long and controversial history as a treatment for diabetic foot ulcers. Conflicting studies have spawned plenty of debate, and the most recent Cochrane Library review of existing research didn’t shed much light on the value of the treatment because the evidence was weak (Cochrane Database Syst Rev. 2015 Jun 24;[6]:CD004123).
But William H. Tettelbach, MD, a wound care specialist, told an audience at the annual scientific sessions of the American Diabetic Association that hyperbaric treatments are worth a try in certain cases. And he brought evidence to prove it – a 2015 report he coauthored that reviewed studies and offered clinical practice guidelines for hyperbaric oxygen therapy for the treatment of diabetic foot ulcers (DFUs) (Undersea Hyperb Med. 2015 May-Jun;42[3]:205-47).
In an interview, Dr. Tettelbach discussed ideal candidates for the treatment and offered clinical advice to endocrinologists.
Question: What did your review of research tell you about the value of hyperbaric oxygen treatment for DFUs?
Answer: We came to the same conclusion that most of the papers have indicated over the years: Hyperbaric oxygen is effective and attains goals such as reducing rates of amputation in a select population of diabetic ulcer patients.
Patients who have Wagner grade 3 or greater ulcers or admitted for surgery due to a septic diabetic foot benefit from an evaluation by a hyperbaric medicine–trained physician and treatment when indicated. There is evidence and years of clinical experience indicating that these patients benefit and have improved outcomes when evaluated and treated appropriately with hyperbaric oxygen therapy.
In the United States, hyperbaric oxygen therapy is not indicated in Wagner grade 2, 1 or 0 diabetic foot ulcers, the ulcers that involve soft tissue but not deep structure like bone.
Q: Why has there been so much controversy over the value of this treatment?
A: In the past, there have been problems with commercial outpatient wound centers that are heavily driven by profits. Financial margins in wound care clinics can be tight, and the need to remain profitable has at times resulted in patients being treated inappropriately with hyperbaric oxygen therapy (Adv Skin Wound Care. 2017 Apr;30[4]:181-90).
Q: Why does hyperbaric oxygen treatment work in some cases?
A: When you place a patient in a hyperbaric chamber where they breathe 100% oxygen under pressure, you increase the percentage of oxygen in the blood. At such a high percentage, oxygen saturates the plasma versus just being carried by red blood cells, thereby allowing the oxygen to penetrate farther into hypoxic tissues. By increasing the oxygen, you have the ability to make the environment unfavorable for rapid proliferation of anaerobic or microaerophilic bacteria that do not survive a highly oxygen-rich environment. Increasing tissue oxygen tension to 30 mm Hg or greater increases the macrophages’ ability to have an oxidative burst needed to kill bacteria. Furthermore, there are antibiotics that require certain levels of oxygen for transport across the bacterial cell wall.
Q: What should physicians understand about hyperbaric oxygen therapy for DFUs?
A: Overall, hyperbaric practitioners need to be more selective in identifying and treating patients according to what the evidence supports. Poorly designed trials with misleading results should not drive medical decisions. We should revisit diabetic foot ulcers through well-thought-out studies that target those who would benefit as suggested by current evidence. Prior trials have been heavily weighted with Wagner grade 1 and 2 candidates or ischemic diabetic ulcers that are not revascularized. These are biased toward poor outcomes since the current evidence does not strongly support treating these types of individuals with adjunctive hyperbaric oxygen therapy (Ont Health Technol Assess Ser. 2017 May 12;17[5]:1-142. eCollection 2017).
Q: What conditions should trigger endocrinologists to think about hyperbaric oxygen therapy for their DFU patients?
A: Candidates for the therapy include diabetic ulcers that have persisted for longer than 30 days, since these ulcers are at a significantly higher risk of a complicating infection, along with those that have failed treatment or are becoming more symptomatic over time (Undersea Hyperb Med. 2017 Mar-Apr;44[2]:157-60).
At that point, it might make sense to refer those patients to a wound and hyperbaric specialist for further evaluation and management, especially to a wound center that offers hyperbaric oxygen therapy.
These wound centers can be found in smaller towns. But some folks will have to travel, perhaps to a wound center at a hospital that has room and board like they do for cancer patients.
Q: What about treatment after surgery?
A: Using hyperbariatric oxygen therapy to treat inpatients with septic diabetic foot ulcers – Wagner grade 3 or higher – immediately after surgery may reduce length of stay as well as lower the risk of requiring multiple surgical debridements.
Q: What are the best-case scenarios for treatment?
A: A significant portion of what we do is limb preservation. Hyperbaric oxygen therapy often can help save a digit, forefoot, or even an extremity.
But it’s not something that just happens overnight. It’s a long-term process. Underlying complicating osteomyelitis may require up to 40-60 adjunctive hyperbaric oxygen treatments, 5 days a week with weekends off, along with concurrent antibiotics, wound care, and vascular interventions when indicated.
Q: Is insurance ever an issue for this treatment?
A: Typically, not if one follows the indications set by the Centers for Medicare & Medicaid Services and the Undersea and Hyperbaric Medical Society.
Medicare lists 15 medical indications that it will cover, and a majority of commercial insurers will cover the same 15 indications and possibly more. But commercial insurers may require prior authorization of medical necessity before preceding with hyperbaric oxygen therapy (Diving Hyperb Med. 2016 Sep;46[3]:133-4).
SAN DIEGO – Hyperbaric oxygen therapy, a mainstay of wound care, has a long and controversial history as a treatment for diabetic foot ulcers. Conflicting studies have spawned plenty of debate, and the most recent Cochrane Library review of existing research didn’t shed much light on the value of the treatment because the evidence was weak (Cochrane Database Syst Rev. 2015 Jun 24;[6]:CD004123).
But William H. Tettelbach, MD, a wound care specialist, told an audience at the annual scientific sessions of the American Diabetic Association that hyperbaric treatments are worth a try in certain cases. And he brought evidence to prove it – a 2015 report he coauthored that reviewed studies and offered clinical practice guidelines for hyperbaric oxygen therapy for the treatment of diabetic foot ulcers (DFUs) (Undersea Hyperb Med. 2015 May-Jun;42[3]:205-47).
In an interview, Dr. Tettelbach discussed ideal candidates for the treatment and offered clinical advice to endocrinologists.
Question: What did your review of research tell you about the value of hyperbaric oxygen treatment for DFUs?
Answer: We came to the same conclusion that most of the papers have indicated over the years: Hyperbaric oxygen is effective and attains goals such as reducing rates of amputation in a select population of diabetic ulcer patients.
Patients who have Wagner grade 3 or greater ulcers or admitted for surgery due to a septic diabetic foot benefit from an evaluation by a hyperbaric medicine–trained physician and treatment when indicated. There is evidence and years of clinical experience indicating that these patients benefit and have improved outcomes when evaluated and treated appropriately with hyperbaric oxygen therapy.
In the United States, hyperbaric oxygen therapy is not indicated in Wagner grade 2, 1 or 0 diabetic foot ulcers, the ulcers that involve soft tissue but not deep structure like bone.
Q: Why has there been so much controversy over the value of this treatment?
A: In the past, there have been problems with commercial outpatient wound centers that are heavily driven by profits. Financial margins in wound care clinics can be tight, and the need to remain profitable has at times resulted in patients being treated inappropriately with hyperbaric oxygen therapy (Adv Skin Wound Care. 2017 Apr;30[4]:181-90).
Q: Why does hyperbaric oxygen treatment work in some cases?
A: When you place a patient in a hyperbaric chamber where they breathe 100% oxygen under pressure, you increase the percentage of oxygen in the blood. At such a high percentage, oxygen saturates the plasma versus just being carried by red blood cells, thereby allowing the oxygen to penetrate farther into hypoxic tissues. By increasing the oxygen, you have the ability to make the environment unfavorable for rapid proliferation of anaerobic or microaerophilic bacteria that do not survive a highly oxygen-rich environment. Increasing tissue oxygen tension to 30 mm Hg or greater increases the macrophages’ ability to have an oxidative burst needed to kill bacteria. Furthermore, there are antibiotics that require certain levels of oxygen for transport across the bacterial cell wall.
Q: What should physicians understand about hyperbaric oxygen therapy for DFUs?
A: Overall, hyperbaric practitioners need to be more selective in identifying and treating patients according to what the evidence supports. Poorly designed trials with misleading results should not drive medical decisions. We should revisit diabetic foot ulcers through well-thought-out studies that target those who would benefit as suggested by current evidence. Prior trials have been heavily weighted with Wagner grade 1 and 2 candidates or ischemic diabetic ulcers that are not revascularized. These are biased toward poor outcomes since the current evidence does not strongly support treating these types of individuals with adjunctive hyperbaric oxygen therapy (Ont Health Technol Assess Ser. 2017 May 12;17[5]:1-142. eCollection 2017).
Q: What conditions should trigger endocrinologists to think about hyperbaric oxygen therapy for their DFU patients?
A: Candidates for the therapy include diabetic ulcers that have persisted for longer than 30 days, since these ulcers are at a significantly higher risk of a complicating infection, along with those that have failed treatment or are becoming more symptomatic over time (Undersea Hyperb Med. 2017 Mar-Apr;44[2]:157-60).
At that point, it might make sense to refer those patients to a wound and hyperbaric specialist for further evaluation and management, especially to a wound center that offers hyperbaric oxygen therapy.
These wound centers can be found in smaller towns. But some folks will have to travel, perhaps to a wound center at a hospital that has room and board like they do for cancer patients.
Q: What about treatment after surgery?
A: Using hyperbariatric oxygen therapy to treat inpatients with septic diabetic foot ulcers – Wagner grade 3 or higher – immediately after surgery may reduce length of stay as well as lower the risk of requiring multiple surgical debridements.
Q: What are the best-case scenarios for treatment?
A: A significant portion of what we do is limb preservation. Hyperbaric oxygen therapy often can help save a digit, forefoot, or even an extremity.
But it’s not something that just happens overnight. It’s a long-term process. Underlying complicating osteomyelitis may require up to 40-60 adjunctive hyperbaric oxygen treatments, 5 days a week with weekends off, along with concurrent antibiotics, wound care, and vascular interventions when indicated.
Q: Is insurance ever an issue for this treatment?
A: Typically, not if one follows the indications set by the Centers for Medicare & Medicaid Services and the Undersea and Hyperbaric Medical Society.
Medicare lists 15 medical indications that it will cover, and a majority of commercial insurers will cover the same 15 indications and possibly more. But commercial insurers may require prior authorization of medical necessity before preceding with hyperbaric oxygen therapy (Diving Hyperb Med. 2016 Sep;46[3]:133-4).
SAN DIEGO – Hyperbaric oxygen therapy, a mainstay of wound care, has a long and controversial history as a treatment for diabetic foot ulcers. Conflicting studies have spawned plenty of debate, and the most recent Cochrane Library review of existing research didn’t shed much light on the value of the treatment because the evidence was weak (Cochrane Database Syst Rev. 2015 Jun 24;[6]:CD004123).
But William H. Tettelbach, MD, a wound care specialist, told an audience at the annual scientific sessions of the American Diabetic Association that hyperbaric treatments are worth a try in certain cases. And he brought evidence to prove it – a 2015 report he coauthored that reviewed studies and offered clinical practice guidelines for hyperbaric oxygen therapy for the treatment of diabetic foot ulcers (DFUs) (Undersea Hyperb Med. 2015 May-Jun;42[3]:205-47).
In an interview, Dr. Tettelbach discussed ideal candidates for the treatment and offered clinical advice to endocrinologists.
Question: What did your review of research tell you about the value of hyperbaric oxygen treatment for DFUs?
Answer: We came to the same conclusion that most of the papers have indicated over the years: Hyperbaric oxygen is effective and attains goals such as reducing rates of amputation in a select population of diabetic ulcer patients.
Patients who have Wagner grade 3 or greater ulcers or admitted for surgery due to a septic diabetic foot benefit from an evaluation by a hyperbaric medicine–trained physician and treatment when indicated. There is evidence and years of clinical experience indicating that these patients benefit and have improved outcomes when evaluated and treated appropriately with hyperbaric oxygen therapy.
In the United States, hyperbaric oxygen therapy is not indicated in Wagner grade 2, 1 or 0 diabetic foot ulcers, the ulcers that involve soft tissue but not deep structure like bone.
Q: Why has there been so much controversy over the value of this treatment?
A: In the past, there have been problems with commercial outpatient wound centers that are heavily driven by profits. Financial margins in wound care clinics can be tight, and the need to remain profitable has at times resulted in patients being treated inappropriately with hyperbaric oxygen therapy (Adv Skin Wound Care. 2017 Apr;30[4]:181-90).
Q: Why does hyperbaric oxygen treatment work in some cases?
A: When you place a patient in a hyperbaric chamber where they breathe 100% oxygen under pressure, you increase the percentage of oxygen in the blood. At such a high percentage, oxygen saturates the plasma versus just being carried by red blood cells, thereby allowing the oxygen to penetrate farther into hypoxic tissues. By increasing the oxygen, you have the ability to make the environment unfavorable for rapid proliferation of anaerobic or microaerophilic bacteria that do not survive a highly oxygen-rich environment. Increasing tissue oxygen tension to 30 mm Hg or greater increases the macrophages’ ability to have an oxidative burst needed to kill bacteria. Furthermore, there are antibiotics that require certain levels of oxygen for transport across the bacterial cell wall.
Q: What should physicians understand about hyperbaric oxygen therapy for DFUs?
A: Overall, hyperbaric practitioners need to be more selective in identifying and treating patients according to what the evidence supports. Poorly designed trials with misleading results should not drive medical decisions. We should revisit diabetic foot ulcers through well-thought-out studies that target those who would benefit as suggested by current evidence. Prior trials have been heavily weighted with Wagner grade 1 and 2 candidates or ischemic diabetic ulcers that are not revascularized. These are biased toward poor outcomes since the current evidence does not strongly support treating these types of individuals with adjunctive hyperbaric oxygen therapy (Ont Health Technol Assess Ser. 2017 May 12;17[5]:1-142. eCollection 2017).
Q: What conditions should trigger endocrinologists to think about hyperbaric oxygen therapy for their DFU patients?
A: Candidates for the therapy include diabetic ulcers that have persisted for longer than 30 days, since these ulcers are at a significantly higher risk of a complicating infection, along with those that have failed treatment or are becoming more symptomatic over time (Undersea Hyperb Med. 2017 Mar-Apr;44[2]:157-60).
At that point, it might make sense to refer those patients to a wound and hyperbaric specialist for further evaluation and management, especially to a wound center that offers hyperbaric oxygen therapy.
These wound centers can be found in smaller towns. But some folks will have to travel, perhaps to a wound center at a hospital that has room and board like they do for cancer patients.
Q: What about treatment after surgery?
A: Using hyperbariatric oxygen therapy to treat inpatients with septic diabetic foot ulcers – Wagner grade 3 or higher – immediately after surgery may reduce length of stay as well as lower the risk of requiring multiple surgical debridements.
Q: What are the best-case scenarios for treatment?
A: A significant portion of what we do is limb preservation. Hyperbaric oxygen therapy often can help save a digit, forefoot, or even an extremity.
But it’s not something that just happens overnight. It’s a long-term process. Underlying complicating osteomyelitis may require up to 40-60 adjunctive hyperbaric oxygen treatments, 5 days a week with weekends off, along with concurrent antibiotics, wound care, and vascular interventions when indicated.
Q: Is insurance ever an issue for this treatment?
A: Typically, not if one follows the indications set by the Centers for Medicare & Medicaid Services and the Undersea and Hyperbaric Medical Society.
Medicare lists 15 medical indications that it will cover, and a majority of commercial insurers will cover the same 15 indications and possibly more. But commercial insurers may require prior authorization of medical necessity before preceding with hyperbaric oxygen therapy (Diving Hyperb Med. 2016 Sep;46[3]:133-4).
EXPERT ANALYSIS AT THE ADA ANNUAL SCIENTIFIC SESSIONS
MONARCH 3: Abemaciclib plus AI boosts PFS in HR+/HER2- breast cancer
Madrid – A combination of the investigational cyclin-dependent kinase 4/6 (CDK4/6) agent abemaciclib and a nonsteroidal aromatase inhibitor (AI) was associated with a near doubling of progression-free survival in postmenopausal women with previously untreated hormone-receptor positive, human epidermal growth factor receptor 2–negative (HR+/HER2-) advanced breast cancer.
At a planned 18-month interim analysis of the MONARCH 3 trial, the median investigator-assessed progression free survival (PFS), the primary endpoint, had not been reached for 328 patients assigned to receive abemaciclib with either anastrozole (Arimidex) or letrozole (Femara). In contrast, the median PFS for 165 patients assigned to an AI and a placebo was 14.7 months, translating into a hazard ratio (HR) of 0.543 (P = .000021), reported Angelo Di Leo, MD, of Hospital of Prato, Istituto Toscano Tumori, Prato, Italy.
“Abemaciclib in combination with a nonsteroidal aromatase inhibitor is superior to a nonsteroidal aromatase inhibitor alone in terms of progression-free survival, but also in terms of the objective response rate as the initial treatment of HER2-negative, endocrine sensitive advanced breast cancer,” he said at a briefing prior to his presentation of the data in a presidential symposium at the European Society for Medical Oncology Congress.
The efficacy of abemaciclib was consistently seen across all subgroups.
“However, we have observed that the patients deriving the largest benefit from abemaciclib are those who have adverse prognostic factors such as, for instance, the presence of liver metastases, or the fact the disease has relapsed only after a few years from the end of adjuvant endocrine therapy,” he added.
The study was stopped for efficacy at the interim analysis.
Abemaciclib has previously been shown to be active as a monotherapy in treatment-refractory HR+/HER2- breast cancer, and in combination with fulvestrant (Faslodex) in patients who had disease progression on endocrine therapy.
Dr. Di Leo and his colleagues enrolled 493 postmenopausal women with metastatic or locally recurrent HR+/HER2- breast cancer who had not received systemic therapy in this setting. Patients who had prior neoadjuvant or adjuvant endocrine therapy were allowed if they had a disease-free interval of more than 1 year since completing endocrine therapy, The patients also had to have good performance status (Eastern Cooperative Oncology Group PS score 1 or less).
They were randomly assigned on a 2:1 basis to receive abemaciclib 150 mg b.i.d. on a continuous schedule plus either anastrozole 1 mg or letrozole 2.5 mg daily until disease progression, or to placebo plus either of the two AIs.
In addition to the superior PFS with abemaciclib added to an AI, as noted before, the CDK4/6 inhibitor was associated with a significantly better objective response rate (ORR), at 48.2% compared with 34.5% for placebo (P = .002). Among patients with measurable disease at baseline, the respective ORRs were 59.2% and 43.8% (P = .004). The clinical benefit rate in this subgroup was also better with abemaciclib, at 79.3% vs. 69.2% (P = .024).
In exploratory subgroup analyses, the investigators found that patients who had indicators of poor prognosis seemed to derive “substantial” benefit from the addition of abemaciclib. However, in an exploratory analysis in patients with disease only in bone, the investigators found that adding abemaciclib did not appear to improve PFS, suggesting that this subgroup could be treated effectively with endocrine therapy alone. Dr. Di Leo cautioned against overinterpreting this finding however, as only 109 patients had bone-only disease.
The safety analysis showed that patients were able to tolerate the combination fairly well. The incidence of grade 3 or 4 neutropenia was 21.1% with the combination compared with 1.2% with placebo, and grade 3 diarrhea occurred in 9.5% vs. 1.2% (no grade 4 diarrhea in either arm). The diarrhea tended to occur early in therapy and could be managed with dose adjustments and antidiarrheal medications, Dr. Di Leo said.
“What we would like to ask is, is this a practice-changing study? Do the results change standard first-line endocrine-based therapy, and then do these results change who we give endocrine therapy to?,” said invited discussant Nicholas Turner, PhD, of The Royal Marsden Hospital in London.
“The study stopped at the reported interim analysis, so at the moment the abemaciclib arm hasn’t reached the median PFS, but we can anticipate that with further follow-up we will see approximately a year improvement in median PFS by the addition of abemaciclib, which is really a substantial improvement in PFS for these patients. And importantly, this benefit was confirmed by a blinded independent central review of the investigator PFS,” he said.
Eli Lilly funded MONARCH 3. Dr. Di Leo and Dr. Turner reported receiving honoraria from the company.
Madrid – A combination of the investigational cyclin-dependent kinase 4/6 (CDK4/6) agent abemaciclib and a nonsteroidal aromatase inhibitor (AI) was associated with a near doubling of progression-free survival in postmenopausal women with previously untreated hormone-receptor positive, human epidermal growth factor receptor 2–negative (HR+/HER2-) advanced breast cancer.
At a planned 18-month interim analysis of the MONARCH 3 trial, the median investigator-assessed progression free survival (PFS), the primary endpoint, had not been reached for 328 patients assigned to receive abemaciclib with either anastrozole (Arimidex) or letrozole (Femara). In contrast, the median PFS for 165 patients assigned to an AI and a placebo was 14.7 months, translating into a hazard ratio (HR) of 0.543 (P = .000021), reported Angelo Di Leo, MD, of Hospital of Prato, Istituto Toscano Tumori, Prato, Italy.
“Abemaciclib in combination with a nonsteroidal aromatase inhibitor is superior to a nonsteroidal aromatase inhibitor alone in terms of progression-free survival, but also in terms of the objective response rate as the initial treatment of HER2-negative, endocrine sensitive advanced breast cancer,” he said at a briefing prior to his presentation of the data in a presidential symposium at the European Society for Medical Oncology Congress.
The efficacy of abemaciclib was consistently seen across all subgroups.
“However, we have observed that the patients deriving the largest benefit from abemaciclib are those who have adverse prognostic factors such as, for instance, the presence of liver metastases, or the fact the disease has relapsed only after a few years from the end of adjuvant endocrine therapy,” he added.
The study was stopped for efficacy at the interim analysis.
Abemaciclib has previously been shown to be active as a monotherapy in treatment-refractory HR+/HER2- breast cancer, and in combination with fulvestrant (Faslodex) in patients who had disease progression on endocrine therapy.
Dr. Di Leo and his colleagues enrolled 493 postmenopausal women with metastatic or locally recurrent HR+/HER2- breast cancer who had not received systemic therapy in this setting. Patients who had prior neoadjuvant or adjuvant endocrine therapy were allowed if they had a disease-free interval of more than 1 year since completing endocrine therapy, The patients also had to have good performance status (Eastern Cooperative Oncology Group PS score 1 or less).
They were randomly assigned on a 2:1 basis to receive abemaciclib 150 mg b.i.d. on a continuous schedule plus either anastrozole 1 mg or letrozole 2.5 mg daily until disease progression, or to placebo plus either of the two AIs.
In addition to the superior PFS with abemaciclib added to an AI, as noted before, the CDK4/6 inhibitor was associated with a significantly better objective response rate (ORR), at 48.2% compared with 34.5% for placebo (P = .002). Among patients with measurable disease at baseline, the respective ORRs were 59.2% and 43.8% (P = .004). The clinical benefit rate in this subgroup was also better with abemaciclib, at 79.3% vs. 69.2% (P = .024).
In exploratory subgroup analyses, the investigators found that patients who had indicators of poor prognosis seemed to derive “substantial” benefit from the addition of abemaciclib. However, in an exploratory analysis in patients with disease only in bone, the investigators found that adding abemaciclib did not appear to improve PFS, suggesting that this subgroup could be treated effectively with endocrine therapy alone. Dr. Di Leo cautioned against overinterpreting this finding however, as only 109 patients had bone-only disease.
The safety analysis showed that patients were able to tolerate the combination fairly well. The incidence of grade 3 or 4 neutropenia was 21.1% with the combination compared with 1.2% with placebo, and grade 3 diarrhea occurred in 9.5% vs. 1.2% (no grade 4 diarrhea in either arm). The diarrhea tended to occur early in therapy and could be managed with dose adjustments and antidiarrheal medications, Dr. Di Leo said.
“What we would like to ask is, is this a practice-changing study? Do the results change standard first-line endocrine-based therapy, and then do these results change who we give endocrine therapy to?,” said invited discussant Nicholas Turner, PhD, of The Royal Marsden Hospital in London.
“The study stopped at the reported interim analysis, so at the moment the abemaciclib arm hasn’t reached the median PFS, but we can anticipate that with further follow-up we will see approximately a year improvement in median PFS by the addition of abemaciclib, which is really a substantial improvement in PFS for these patients. And importantly, this benefit was confirmed by a blinded independent central review of the investigator PFS,” he said.
Eli Lilly funded MONARCH 3. Dr. Di Leo and Dr. Turner reported receiving honoraria from the company.
Madrid – A combination of the investigational cyclin-dependent kinase 4/6 (CDK4/6) agent abemaciclib and a nonsteroidal aromatase inhibitor (AI) was associated with a near doubling of progression-free survival in postmenopausal women with previously untreated hormone-receptor positive, human epidermal growth factor receptor 2–negative (HR+/HER2-) advanced breast cancer.
At a planned 18-month interim analysis of the MONARCH 3 trial, the median investigator-assessed progression free survival (PFS), the primary endpoint, had not been reached for 328 patients assigned to receive abemaciclib with either anastrozole (Arimidex) or letrozole (Femara). In contrast, the median PFS for 165 patients assigned to an AI and a placebo was 14.7 months, translating into a hazard ratio (HR) of 0.543 (P = .000021), reported Angelo Di Leo, MD, of Hospital of Prato, Istituto Toscano Tumori, Prato, Italy.
“Abemaciclib in combination with a nonsteroidal aromatase inhibitor is superior to a nonsteroidal aromatase inhibitor alone in terms of progression-free survival, but also in terms of the objective response rate as the initial treatment of HER2-negative, endocrine sensitive advanced breast cancer,” he said at a briefing prior to his presentation of the data in a presidential symposium at the European Society for Medical Oncology Congress.
The efficacy of abemaciclib was consistently seen across all subgroups.
“However, we have observed that the patients deriving the largest benefit from abemaciclib are those who have adverse prognostic factors such as, for instance, the presence of liver metastases, or the fact the disease has relapsed only after a few years from the end of adjuvant endocrine therapy,” he added.
The study was stopped for efficacy at the interim analysis.
Abemaciclib has previously been shown to be active as a monotherapy in treatment-refractory HR+/HER2- breast cancer, and in combination with fulvestrant (Faslodex) in patients who had disease progression on endocrine therapy.
Dr. Di Leo and his colleagues enrolled 493 postmenopausal women with metastatic or locally recurrent HR+/HER2- breast cancer who had not received systemic therapy in this setting. Patients who had prior neoadjuvant or adjuvant endocrine therapy were allowed if they had a disease-free interval of more than 1 year since completing endocrine therapy, The patients also had to have good performance status (Eastern Cooperative Oncology Group PS score 1 or less).
They were randomly assigned on a 2:1 basis to receive abemaciclib 150 mg b.i.d. on a continuous schedule plus either anastrozole 1 mg or letrozole 2.5 mg daily until disease progression, or to placebo plus either of the two AIs.
In addition to the superior PFS with abemaciclib added to an AI, as noted before, the CDK4/6 inhibitor was associated with a significantly better objective response rate (ORR), at 48.2% compared with 34.5% for placebo (P = .002). Among patients with measurable disease at baseline, the respective ORRs were 59.2% and 43.8% (P = .004). The clinical benefit rate in this subgroup was also better with abemaciclib, at 79.3% vs. 69.2% (P = .024).
In exploratory subgroup analyses, the investigators found that patients who had indicators of poor prognosis seemed to derive “substantial” benefit from the addition of abemaciclib. However, in an exploratory analysis in patients with disease only in bone, the investigators found that adding abemaciclib did not appear to improve PFS, suggesting that this subgroup could be treated effectively with endocrine therapy alone. Dr. Di Leo cautioned against overinterpreting this finding however, as only 109 patients had bone-only disease.
The safety analysis showed that patients were able to tolerate the combination fairly well. The incidence of grade 3 or 4 neutropenia was 21.1% with the combination compared with 1.2% with placebo, and grade 3 diarrhea occurred in 9.5% vs. 1.2% (no grade 4 diarrhea in either arm). The diarrhea tended to occur early in therapy and could be managed with dose adjustments and antidiarrheal medications, Dr. Di Leo said.
“What we would like to ask is, is this a practice-changing study? Do the results change standard first-line endocrine-based therapy, and then do these results change who we give endocrine therapy to?,” said invited discussant Nicholas Turner, PhD, of The Royal Marsden Hospital in London.
“The study stopped at the reported interim analysis, so at the moment the abemaciclib arm hasn’t reached the median PFS, but we can anticipate that with further follow-up we will see approximately a year improvement in median PFS by the addition of abemaciclib, which is really a substantial improvement in PFS for these patients. And importantly, this benefit was confirmed by a blinded independent central review of the investigator PFS,” he said.
Eli Lilly funded MONARCH 3. Dr. Di Leo and Dr. Turner reported receiving honoraria from the company.
AT ESMO 2017
Key clinical point: Adding the CDK4/6 inhibitor abemaciclib to an aromatase inhibitor significantly improved progression-free survival in the frontline for postmenopausal women with HR+/HER2- breast cancer.
Major finding: Median PFS was not reached with abemaciclib and letrozole or anastrozole, vs. 14.7 months for a placebo plus aromatase inhibitor.
Data source: Randomized phase 3 trial of 493 postmenopausal women with metastatic or locally recurrent HR+/HER2- breast cancer.
Disclosures: Eli Lilly funded MONARCH 3. Dr. Di Leo and Dr. Turner reported receiving honoraria from the company.
Alopecia patients share their struggles
SILVER SPRING, MD. – Alopecia areata patients struggle as much, if not more so, with the social and emotional challenges of the disease as with the physical challenges, according to patients and others who spoke at a public meeting on alopecia areata patient-focused drug development.
Alopecia areata affects as many as 6.8 million individuals in the United States, according to the National Alopecia Areata Foundation (NAAF). However, the particulars of alopecia can vary widely from one person to another; some patients experience total hair loss (alopecia universalis), while others retain eyebrows, eyelashes, or some body hair.
The FDA meeting, held on Sept. 11, is part of the agency’s patient-focused drug development initiative. “We wanted to hear the broader patient’s voice,” Theresa M. Mullin, PhD, director of the FDA’s Office of Strategic Programs, said in her opening remarks. Gary Sherwood, communications director for NAAF, said that the meeting was the culmination of a 5-year effort, begun in 2012 when alopecia areata was named as one of 39 disease categories under consideration for such a meeting. “It is too early to know what the exact results will be … but if the past is any indication, they may be significant. The meeting held with psoriasis yielded FDA approval of a treatment previously denied,” he added in an interview.
Two panel presentations featured patients who discussed their experiences with alopecia; each was followed by a discussion period where patients and family members in the audience were invited to share their experiences.
The “Health Effects and Daily Impacts” panel allowed several patients and their family members the opportunity to identify specific issues that may surprise clinicians.
“One thing I learned was how much the patients are bothered by sweating of the scalp; this can affect what type of head covering, hair piece, or hat/helmet they are able to wear, and thus limits activities,” Dr. Marathe continued. “This is not something I had focused on previously. I will be more inclined to ask about sweating and offer treatments, such as scalp botulinum toxin or aluminum chloride now that I have been alerted to this concern. Also, the challenges of facial makeup such as pencil for eyebrows was another thing that the FDA session brought home for me; I’m more inclined to suggest things such as microblading for eyebrows, or to try treatments like latanoprost for eyebrows/lashes.”
The second panel, “Current Approaches to Treatment,” included a different group of patients who shared stories of treatments that had been successful and those that had not. “The patients at the FDA meeting expressed very eloquently what our patients feel – different treatments may work temporarily and then stop working, which leads to a roller coaster of emotions of hope and disappointment,” A. Yasmine Kirkorian, MD, also a dermatologist at Children’s National Health System, said in an interview. “Patients and physicians would be interested in a treatment option with a track record for predictable efficacy with durable and sustained hair regrowth and minimal side effects.”
Dr. Marathe noted that in her experience, those who develop alopecia totalis or universalis at a younger age tend to have more recalcitrant disease. “It is still very hard for me to predict which children will regrow their hair spontaneously, or with topical therapies, versus those with more resistant disease. I hope that continued study will allow us to offer a more realistic prognosis for these patients,” she said.
Discussion after the treatment panel included testimonials from patients who reported successful treatment with tofacitinib (Xeljanz), a Janus kinase inhibitor approved for rheumatoid arthritis, which is not approved for treatment of alopecia.
“I absolutely agree with the focus on JAK inhibitors and increasing our understanding of how they work, as well as what some of the long-term effects are,” said Dr. Marathe. “The better we are able to target the pathogenesis of this condition, the more easily we can treat in a more focused fashion and reduce side effects,” but more clinical trials are needed to determine safety and efficacy for children and teens, she noted.
One of her hesitations in prescribing tofacitinib to her patients is that she cannot provide them with a sense of how long they will need to be on the treatment. “Current data show that the hair growth on the medication is usually lost upon stopping it; the question I still struggle with is whether it is realistic to put a 4- or 5-year-old on a medication that has no estimated or anticipated stop date,” she said.
As for what she offers patients in terms of resources for emotional support, Dr. Kirkorian said the psychosocial aspects of alopecia areata are always discussed at patient visits. “Psychosocial needs vary based on age, personality, and personal philosophy. We offer the gamut of outside resources from local support groups, the National Alopecia Areata Foundation, referral to psychology/psychiatry and, very importantly, referral to Camp Discovery. Children have told us across the board how important and meaningful it was to them to be able to just be themselves around other children who look like them.”
Dr. Marathe and Dr. Kirkorian were attendees at the meeting; they had no relevant disclosures. They are members of the Dermatology News Editorial Advisory Board.
SILVER SPRING, MD. – Alopecia areata patients struggle as much, if not more so, with the social and emotional challenges of the disease as with the physical challenges, according to patients and others who spoke at a public meeting on alopecia areata patient-focused drug development.
Alopecia areata affects as many as 6.8 million individuals in the United States, according to the National Alopecia Areata Foundation (NAAF). However, the particulars of alopecia can vary widely from one person to another; some patients experience total hair loss (alopecia universalis), while others retain eyebrows, eyelashes, or some body hair.
The FDA meeting, held on Sept. 11, is part of the agency’s patient-focused drug development initiative. “We wanted to hear the broader patient’s voice,” Theresa M. Mullin, PhD, director of the FDA’s Office of Strategic Programs, said in her opening remarks. Gary Sherwood, communications director for NAAF, said that the meeting was the culmination of a 5-year effort, begun in 2012 when alopecia areata was named as one of 39 disease categories under consideration for such a meeting. “It is too early to know what the exact results will be … but if the past is any indication, they may be significant. The meeting held with psoriasis yielded FDA approval of a treatment previously denied,” he added in an interview.
Two panel presentations featured patients who discussed their experiences with alopecia; each was followed by a discussion period where patients and family members in the audience were invited to share their experiences.
The “Health Effects and Daily Impacts” panel allowed several patients and their family members the opportunity to identify specific issues that may surprise clinicians.
“One thing I learned was how much the patients are bothered by sweating of the scalp; this can affect what type of head covering, hair piece, or hat/helmet they are able to wear, and thus limits activities,” Dr. Marathe continued. “This is not something I had focused on previously. I will be more inclined to ask about sweating and offer treatments, such as scalp botulinum toxin or aluminum chloride now that I have been alerted to this concern. Also, the challenges of facial makeup such as pencil for eyebrows was another thing that the FDA session brought home for me; I’m more inclined to suggest things such as microblading for eyebrows, or to try treatments like latanoprost for eyebrows/lashes.”
The second panel, “Current Approaches to Treatment,” included a different group of patients who shared stories of treatments that had been successful and those that had not. “The patients at the FDA meeting expressed very eloquently what our patients feel – different treatments may work temporarily and then stop working, which leads to a roller coaster of emotions of hope and disappointment,” A. Yasmine Kirkorian, MD, also a dermatologist at Children’s National Health System, said in an interview. “Patients and physicians would be interested in a treatment option with a track record for predictable efficacy with durable and sustained hair regrowth and minimal side effects.”
Dr. Marathe noted that in her experience, those who develop alopecia totalis or universalis at a younger age tend to have more recalcitrant disease. “It is still very hard for me to predict which children will regrow their hair spontaneously, or with topical therapies, versus those with more resistant disease. I hope that continued study will allow us to offer a more realistic prognosis for these patients,” she said.
Discussion after the treatment panel included testimonials from patients who reported successful treatment with tofacitinib (Xeljanz), a Janus kinase inhibitor approved for rheumatoid arthritis, which is not approved for treatment of alopecia.
“I absolutely agree with the focus on JAK inhibitors and increasing our understanding of how they work, as well as what some of the long-term effects are,” said Dr. Marathe. “The better we are able to target the pathogenesis of this condition, the more easily we can treat in a more focused fashion and reduce side effects,” but more clinical trials are needed to determine safety and efficacy for children and teens, she noted.
One of her hesitations in prescribing tofacitinib to her patients is that she cannot provide them with a sense of how long they will need to be on the treatment. “Current data show that the hair growth on the medication is usually lost upon stopping it; the question I still struggle with is whether it is realistic to put a 4- or 5-year-old on a medication that has no estimated or anticipated stop date,” she said.
As for what she offers patients in terms of resources for emotional support, Dr. Kirkorian said the psychosocial aspects of alopecia areata are always discussed at patient visits. “Psychosocial needs vary based on age, personality, and personal philosophy. We offer the gamut of outside resources from local support groups, the National Alopecia Areata Foundation, referral to psychology/psychiatry and, very importantly, referral to Camp Discovery. Children have told us across the board how important and meaningful it was to them to be able to just be themselves around other children who look like them.”
Dr. Marathe and Dr. Kirkorian were attendees at the meeting; they had no relevant disclosures. They are members of the Dermatology News Editorial Advisory Board.
SILVER SPRING, MD. – Alopecia areata patients struggle as much, if not more so, with the social and emotional challenges of the disease as with the physical challenges, according to patients and others who spoke at a public meeting on alopecia areata patient-focused drug development.
Alopecia areata affects as many as 6.8 million individuals in the United States, according to the National Alopecia Areata Foundation (NAAF). However, the particulars of alopecia can vary widely from one person to another; some patients experience total hair loss (alopecia universalis), while others retain eyebrows, eyelashes, or some body hair.
The FDA meeting, held on Sept. 11, is part of the agency’s patient-focused drug development initiative. “We wanted to hear the broader patient’s voice,” Theresa M. Mullin, PhD, director of the FDA’s Office of Strategic Programs, said in her opening remarks. Gary Sherwood, communications director for NAAF, said that the meeting was the culmination of a 5-year effort, begun in 2012 when alopecia areata was named as one of 39 disease categories under consideration for such a meeting. “It is too early to know what the exact results will be … but if the past is any indication, they may be significant. The meeting held with psoriasis yielded FDA approval of a treatment previously denied,” he added in an interview.
Two panel presentations featured patients who discussed their experiences with alopecia; each was followed by a discussion period where patients and family members in the audience were invited to share their experiences.
The “Health Effects and Daily Impacts” panel allowed several patients and their family members the opportunity to identify specific issues that may surprise clinicians.
“One thing I learned was how much the patients are bothered by sweating of the scalp; this can affect what type of head covering, hair piece, or hat/helmet they are able to wear, and thus limits activities,” Dr. Marathe continued. “This is not something I had focused on previously. I will be more inclined to ask about sweating and offer treatments, such as scalp botulinum toxin or aluminum chloride now that I have been alerted to this concern. Also, the challenges of facial makeup such as pencil for eyebrows was another thing that the FDA session brought home for me; I’m more inclined to suggest things such as microblading for eyebrows, or to try treatments like latanoprost for eyebrows/lashes.”
The second panel, “Current Approaches to Treatment,” included a different group of patients who shared stories of treatments that had been successful and those that had not. “The patients at the FDA meeting expressed very eloquently what our patients feel – different treatments may work temporarily and then stop working, which leads to a roller coaster of emotions of hope and disappointment,” A. Yasmine Kirkorian, MD, also a dermatologist at Children’s National Health System, said in an interview. “Patients and physicians would be interested in a treatment option with a track record for predictable efficacy with durable and sustained hair regrowth and minimal side effects.”
Dr. Marathe noted that in her experience, those who develop alopecia totalis or universalis at a younger age tend to have more recalcitrant disease. “It is still very hard for me to predict which children will regrow their hair spontaneously, or with topical therapies, versus those with more resistant disease. I hope that continued study will allow us to offer a more realistic prognosis for these patients,” she said.
Discussion after the treatment panel included testimonials from patients who reported successful treatment with tofacitinib (Xeljanz), a Janus kinase inhibitor approved for rheumatoid arthritis, which is not approved for treatment of alopecia.
“I absolutely agree with the focus on JAK inhibitors and increasing our understanding of how they work, as well as what some of the long-term effects are,” said Dr. Marathe. “The better we are able to target the pathogenesis of this condition, the more easily we can treat in a more focused fashion and reduce side effects,” but more clinical trials are needed to determine safety and efficacy for children and teens, she noted.
One of her hesitations in prescribing tofacitinib to her patients is that she cannot provide them with a sense of how long they will need to be on the treatment. “Current data show that the hair growth on the medication is usually lost upon stopping it; the question I still struggle with is whether it is realistic to put a 4- or 5-year-old on a medication that has no estimated or anticipated stop date,” she said.
As for what she offers patients in terms of resources for emotional support, Dr. Kirkorian said the psychosocial aspects of alopecia areata are always discussed at patient visits. “Psychosocial needs vary based on age, personality, and personal philosophy. We offer the gamut of outside resources from local support groups, the National Alopecia Areata Foundation, referral to psychology/psychiatry and, very importantly, referral to Camp Discovery. Children have told us across the board how important and meaningful it was to them to be able to just be themselves around other children who look like them.”
Dr. Marathe and Dr. Kirkorian were attendees at the meeting; they had no relevant disclosures. They are members of the Dermatology News Editorial Advisory Board.
AT AN FDA PUBLIC MEETING
Calcitonin-to-CEA ratio predicts medullary thyroid cancer survival
BOSTON – The ratio of serum calcitonin to the serum level of carcinoembryonic antigen in patients with medullary thyroid cancer can predict which patients have a better chance for survival following thyroidectomy, based on retrospective findings from 164 presurgical patients at one U.S. center.
A lower serum calcitonin–to–serum carcinoembryonic antigen (CEA) ratio following thyroidectomy is a second marker of good postsurgical survival, Tania Jaber, MD, said at the World Congress on Thyroid Cancer.
“Patients want to know whether surgery will cure them, and we have had no prognostic markers to predict this. Depending on the ratio, we can now tell patients whether or not they have a good chance of cure,” said Dr. Jaber, an endocrinological oncologist at MD Anderson in Houston. “Surgery remains the standard of care, so the ratio does not affect the decision of whether to undergo surgery, but it helps patients know what to expect” after surgery, she said in an interview.
“If their ratio is favorable it can be reassuring, and if their ratio is unfavorable it helps set expectations. We are also studying whether the ratio can be a marker for the need for systemic therapy following surgery. Right now, our prognostic tools for medullary thyroid cancer are very limited, so any additional information we can give patients based on their calcitonin-to-CEA ratio is very valuable.”
Her study included 164 patients treated at MD Anderson who had their serum drawn before thyroidectomy, and 187 patients with specimens taken 3-9 months after surgery. Median patient follow-up after surgery was 5 years. Calcitonin levels were measured as pg/mL and CEA levels as ng/mL; despite this difference in unit size the researchers calculated the ratios by a direct numerical comparison that ignored the units.
Among the preoperative patients and specifically among those with a low serum CEA level of less than 25 ng/ML a calcitonin-to-CEA ratio of less than 43 had the best survival rate, Dr. Jaber reported. Among preoperative patients with a CEA level of 25 ng/mL or greater a ratio of less than 18 flagged patients with the best survival rate following thyroidectomy.
Among postoperative patients the ratios that linked with better survival also depended on the CEA level. In patients with a low postoperative CEA a ratio of less than 149 linked with better survival. In patients with a high CEA level a ratio of less than 12 linked with better postoperative survival.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
BOSTON – The ratio of serum calcitonin to the serum level of carcinoembryonic antigen in patients with medullary thyroid cancer can predict which patients have a better chance for survival following thyroidectomy, based on retrospective findings from 164 presurgical patients at one U.S. center.
A lower serum calcitonin–to–serum carcinoembryonic antigen (CEA) ratio following thyroidectomy is a second marker of good postsurgical survival, Tania Jaber, MD, said at the World Congress on Thyroid Cancer.
“Patients want to know whether surgery will cure them, and we have had no prognostic markers to predict this. Depending on the ratio, we can now tell patients whether or not they have a good chance of cure,” said Dr. Jaber, an endocrinological oncologist at MD Anderson in Houston. “Surgery remains the standard of care, so the ratio does not affect the decision of whether to undergo surgery, but it helps patients know what to expect” after surgery, she said in an interview.
“If their ratio is favorable it can be reassuring, and if their ratio is unfavorable it helps set expectations. We are also studying whether the ratio can be a marker for the need for systemic therapy following surgery. Right now, our prognostic tools for medullary thyroid cancer are very limited, so any additional information we can give patients based on their calcitonin-to-CEA ratio is very valuable.”
Her study included 164 patients treated at MD Anderson who had their serum drawn before thyroidectomy, and 187 patients with specimens taken 3-9 months after surgery. Median patient follow-up after surgery was 5 years. Calcitonin levels were measured as pg/mL and CEA levels as ng/mL; despite this difference in unit size the researchers calculated the ratios by a direct numerical comparison that ignored the units.
Among the preoperative patients and specifically among those with a low serum CEA level of less than 25 ng/ML a calcitonin-to-CEA ratio of less than 43 had the best survival rate, Dr. Jaber reported. Among preoperative patients with a CEA level of 25 ng/mL or greater a ratio of less than 18 flagged patients with the best survival rate following thyroidectomy.
Among postoperative patients the ratios that linked with better survival also depended on the CEA level. In patients with a low postoperative CEA a ratio of less than 149 linked with better survival. In patients with a high CEA level a ratio of less than 12 linked with better postoperative survival.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
BOSTON – The ratio of serum calcitonin to the serum level of carcinoembryonic antigen in patients with medullary thyroid cancer can predict which patients have a better chance for survival following thyroidectomy, based on retrospective findings from 164 presurgical patients at one U.S. center.
A lower serum calcitonin–to–serum carcinoembryonic antigen (CEA) ratio following thyroidectomy is a second marker of good postsurgical survival, Tania Jaber, MD, said at the World Congress on Thyroid Cancer.
“Patients want to know whether surgery will cure them, and we have had no prognostic markers to predict this. Depending on the ratio, we can now tell patients whether or not they have a good chance of cure,” said Dr. Jaber, an endocrinological oncologist at MD Anderson in Houston. “Surgery remains the standard of care, so the ratio does not affect the decision of whether to undergo surgery, but it helps patients know what to expect” after surgery, she said in an interview.
“If their ratio is favorable it can be reassuring, and if their ratio is unfavorable it helps set expectations. We are also studying whether the ratio can be a marker for the need for systemic therapy following surgery. Right now, our prognostic tools for medullary thyroid cancer are very limited, so any additional information we can give patients based on their calcitonin-to-CEA ratio is very valuable.”
Her study included 164 patients treated at MD Anderson who had their serum drawn before thyroidectomy, and 187 patients with specimens taken 3-9 months after surgery. Median patient follow-up after surgery was 5 years. Calcitonin levels were measured as pg/mL and CEA levels as ng/mL; despite this difference in unit size the researchers calculated the ratios by a direct numerical comparison that ignored the units.
Among the preoperative patients and specifically among those with a low serum CEA level of less than 25 ng/ML a calcitonin-to-CEA ratio of less than 43 had the best survival rate, Dr. Jaber reported. Among preoperative patients with a CEA level of 25 ng/mL or greater a ratio of less than 18 flagged patients with the best survival rate following thyroidectomy.
Among postoperative patients the ratios that linked with better survival also depended on the CEA level. In patients with a low postoperative CEA a ratio of less than 149 linked with better survival. In patients with a high CEA level a ratio of less than 12 linked with better postoperative survival.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
AT WCTC 2017
Key clinical point:
Major finding: Presurgery, a calcitonin-to-CEA ratio below 18 was linked with superior survival in patients whose CEA was at least 25 ng/Ml.
Data source: A single-center, retrospective study with 164 patients assessed before thyroidectomy and 187 assessed after surgery.
Disclosures: Dr. Jaber had no disclosures.
How to give a talk
I have to give a talk. Get this – the topic is how to give a good talk. Very meta.
I’ve given a hundred or so presentations in my career, including a couple of TEDx talks. With each one, I try to get a little better. Effective speaking is always simple but never easy. Let me share with you a few things I’ve learned.
Even if you don’t want to become a TEDMED phenom, you should know a few fundamentals. Giving good talks enhances your reputation and can jump-start your practice or career. For any talk, you must master three things: preparation, content, and delivery.
Just as we choose movies with actors we like, people choose speakers they want to see. Who you are matters. If you are introduced by an emcee, then be sure he or she bills you as a star. However, don’t try to be someone you aren’t – If I gave a talk on robotic prostate surgery, I’d be sure to lose no matter how witty I was. That’s why writing your own intro can sometimes be your best option.
Next up: content. It’s the king of speaking as well as marketing. Although you can pick up points for style, if you want to be remembered, you have to deliver something worth remembering. This starts with your preparation. Resist the temptation to focus exclusively on your slides. As in writing, it is best to brainstorm what you want to cover, then outline your ideas, then fill in content with slides.
Most presentations require visuals; however, there are times when you can do without. Go for it! Nothing is more freeing or more intimate than you one-on-one with your audience. If you must have slides, then follow the one-idea one-slide rule. Slides crammed with information actually detract from your presentation. Here’s a tip: Write only what you can fit with a marker on a Post-it pad. Then, laying out the Post-its, you can rearrange slides getting a feel for the flow or argument of the talk.
Did you ever wonder why headlines like, “Why I never use this suture” and “How I cut my EMR documentation time in half” work so well? They tap into a core human instinct: curiosity. Your opening should introduce some sense of wonder. What is she going to share? Really, how does he do that? Starting with a problem and taking them to a solution is also a great game plan that will often yield success.
When it comes to slides, be clean and concise. Taking a cue from wildly popular TED talks, use images and art instead of words. Use sentence fragments, not sentences, and limit content to the width of the slide (no easy feat). Sometimes you need the slide to prompt your talking point. Put only the data or fact you need and leave the rest at the bottom in your notes section.
Humor is almost always a good idea and more difficult to execute than most realize. Cartoons with captions don’t work. I know that’s hard for many of you to hear, but it’s true. Delete them from your decks. Go ahead, I’ll wait.
Instead, try finding something relevant to the audience that only they will find funny. Inside jokes not only have a higher chance of success, but will also help you bond with your audience. A joke about ICD10 as it relates to neurology is better than the funniest Calvin and Hobbes strip. Self-deprecating humor is always appreciated. I’m not among the gifted who can come up with a great one-liner on the spot. It’s OK to plan it ahead.
Once you’ve got your talk built, it’s time to run it. This is hard, as it requires planning to have your content done in time to rehearse. Find the discipline to do it. The first time you run it, you’ll likely realize that 1/3 of the content needs to be cut. Cut it. Indeed, plan to run 10% less than the time allotted. Leave your audience wanting for more rather than wishing for less.
As I’ve learned, your talking points and slides will always be most appreciated in your own head. Keeping to time shows your respect for your audience and makes you appear polished.
The day of, get to the venue well ahead of time and check the sound, lights, and temperature. All of your preparation will be for naught if they can’t hear you, see your slides, or feel their fingers due to the frigid AC.
One of the reasons I love giving talks is because they are live. You and your audience are intimately engaged, and like any conversation, you’ll sense how it’s going. Are they looking at you or at their phones? Do they seem bored? Do they laugh easily, even when you weren’t expecting them to? Observe what is happening and adjust your performance accordingly. Are you losing them? Pause. Let them catch up. Are you putting them to sleep? Pick up the pace. Try that bit of humor now.
Your delivery is critical to your success. If you’re on the dais and behind the podium of a large audience, then be big, Greek theatre big, which means bigger facial expressions and bigger arm and hand gestures. Vary the tone and pace of your voice. Speed it up to build excitement. Slow down and lower your pitch for gravity and authority. Pause for 3-4 seconds to create suspense and drama.
Leave time for discussion when possible. Invite the audience to engage by asking, What do you think? Finally, on the plane ride home, or even as you walk back from the auditorium to your clinic, think about your presentation: What worked? What fell flat? What roused the audience? How can you deliver it better next time?
Even if it didn’t go well, remember, there’s always next week. It’s on to Cincinnati.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@frontlinemedcom.com.
I have to give a talk. Get this – the topic is how to give a good talk. Very meta.
I’ve given a hundred or so presentations in my career, including a couple of TEDx talks. With each one, I try to get a little better. Effective speaking is always simple but never easy. Let me share with you a few things I’ve learned.
Even if you don’t want to become a TEDMED phenom, you should know a few fundamentals. Giving good talks enhances your reputation and can jump-start your practice or career. For any talk, you must master three things: preparation, content, and delivery.
Just as we choose movies with actors we like, people choose speakers they want to see. Who you are matters. If you are introduced by an emcee, then be sure he or she bills you as a star. However, don’t try to be someone you aren’t – If I gave a talk on robotic prostate surgery, I’d be sure to lose no matter how witty I was. That’s why writing your own intro can sometimes be your best option.
Next up: content. It’s the king of speaking as well as marketing. Although you can pick up points for style, if you want to be remembered, you have to deliver something worth remembering. This starts with your preparation. Resist the temptation to focus exclusively on your slides. As in writing, it is best to brainstorm what you want to cover, then outline your ideas, then fill in content with slides.
Most presentations require visuals; however, there are times when you can do without. Go for it! Nothing is more freeing or more intimate than you one-on-one with your audience. If you must have slides, then follow the one-idea one-slide rule. Slides crammed with information actually detract from your presentation. Here’s a tip: Write only what you can fit with a marker on a Post-it pad. Then, laying out the Post-its, you can rearrange slides getting a feel for the flow or argument of the talk.
Did you ever wonder why headlines like, “Why I never use this suture” and “How I cut my EMR documentation time in half” work so well? They tap into a core human instinct: curiosity. Your opening should introduce some sense of wonder. What is she going to share? Really, how does he do that? Starting with a problem and taking them to a solution is also a great game plan that will often yield success.
When it comes to slides, be clean and concise. Taking a cue from wildly popular TED talks, use images and art instead of words. Use sentence fragments, not sentences, and limit content to the width of the slide (no easy feat). Sometimes you need the slide to prompt your talking point. Put only the data or fact you need and leave the rest at the bottom in your notes section.
Humor is almost always a good idea and more difficult to execute than most realize. Cartoons with captions don’t work. I know that’s hard for many of you to hear, but it’s true. Delete them from your decks. Go ahead, I’ll wait.
Instead, try finding something relevant to the audience that only they will find funny. Inside jokes not only have a higher chance of success, but will also help you bond with your audience. A joke about ICD10 as it relates to neurology is better than the funniest Calvin and Hobbes strip. Self-deprecating humor is always appreciated. I’m not among the gifted who can come up with a great one-liner on the spot. It’s OK to plan it ahead.
Once you’ve got your talk built, it’s time to run it. This is hard, as it requires planning to have your content done in time to rehearse. Find the discipline to do it. The first time you run it, you’ll likely realize that 1/3 of the content needs to be cut. Cut it. Indeed, plan to run 10% less than the time allotted. Leave your audience wanting for more rather than wishing for less.
As I’ve learned, your talking points and slides will always be most appreciated in your own head. Keeping to time shows your respect for your audience and makes you appear polished.
The day of, get to the venue well ahead of time and check the sound, lights, and temperature. All of your preparation will be for naught if they can’t hear you, see your slides, or feel their fingers due to the frigid AC.
One of the reasons I love giving talks is because they are live. You and your audience are intimately engaged, and like any conversation, you’ll sense how it’s going. Are they looking at you or at their phones? Do they seem bored? Do they laugh easily, even when you weren’t expecting them to? Observe what is happening and adjust your performance accordingly. Are you losing them? Pause. Let them catch up. Are you putting them to sleep? Pick up the pace. Try that bit of humor now.
Your delivery is critical to your success. If you’re on the dais and behind the podium of a large audience, then be big, Greek theatre big, which means bigger facial expressions and bigger arm and hand gestures. Vary the tone and pace of your voice. Speed it up to build excitement. Slow down and lower your pitch for gravity and authority. Pause for 3-4 seconds to create suspense and drama.
Leave time for discussion when possible. Invite the audience to engage by asking, What do you think? Finally, on the plane ride home, or even as you walk back from the auditorium to your clinic, think about your presentation: What worked? What fell flat? What roused the audience? How can you deliver it better next time?
Even if it didn’t go well, remember, there’s always next week. It’s on to Cincinnati.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@frontlinemedcom.com.
I have to give a talk. Get this – the topic is how to give a good talk. Very meta.
I’ve given a hundred or so presentations in my career, including a couple of TEDx talks. With each one, I try to get a little better. Effective speaking is always simple but never easy. Let me share with you a few things I’ve learned.
Even if you don’t want to become a TEDMED phenom, you should know a few fundamentals. Giving good talks enhances your reputation and can jump-start your practice or career. For any talk, you must master three things: preparation, content, and delivery.
Just as we choose movies with actors we like, people choose speakers they want to see. Who you are matters. If you are introduced by an emcee, then be sure he or she bills you as a star. However, don’t try to be someone you aren’t – If I gave a talk on robotic prostate surgery, I’d be sure to lose no matter how witty I was. That’s why writing your own intro can sometimes be your best option.
Next up: content. It’s the king of speaking as well as marketing. Although you can pick up points for style, if you want to be remembered, you have to deliver something worth remembering. This starts with your preparation. Resist the temptation to focus exclusively on your slides. As in writing, it is best to brainstorm what you want to cover, then outline your ideas, then fill in content with slides.
Most presentations require visuals; however, there are times when you can do without. Go for it! Nothing is more freeing or more intimate than you one-on-one with your audience. If you must have slides, then follow the one-idea one-slide rule. Slides crammed with information actually detract from your presentation. Here’s a tip: Write only what you can fit with a marker on a Post-it pad. Then, laying out the Post-its, you can rearrange slides getting a feel for the flow or argument of the talk.
Did you ever wonder why headlines like, “Why I never use this suture” and “How I cut my EMR documentation time in half” work so well? They tap into a core human instinct: curiosity. Your opening should introduce some sense of wonder. What is she going to share? Really, how does he do that? Starting with a problem and taking them to a solution is also a great game plan that will often yield success.
When it comes to slides, be clean and concise. Taking a cue from wildly popular TED talks, use images and art instead of words. Use sentence fragments, not sentences, and limit content to the width of the slide (no easy feat). Sometimes you need the slide to prompt your talking point. Put only the data or fact you need and leave the rest at the bottom in your notes section.
Humor is almost always a good idea and more difficult to execute than most realize. Cartoons with captions don’t work. I know that’s hard for many of you to hear, but it’s true. Delete them from your decks. Go ahead, I’ll wait.
Instead, try finding something relevant to the audience that only they will find funny. Inside jokes not only have a higher chance of success, but will also help you bond with your audience. A joke about ICD10 as it relates to neurology is better than the funniest Calvin and Hobbes strip. Self-deprecating humor is always appreciated. I’m not among the gifted who can come up with a great one-liner on the spot. It’s OK to plan it ahead.
Once you’ve got your talk built, it’s time to run it. This is hard, as it requires planning to have your content done in time to rehearse. Find the discipline to do it. The first time you run it, you’ll likely realize that 1/3 of the content needs to be cut. Cut it. Indeed, plan to run 10% less than the time allotted. Leave your audience wanting for more rather than wishing for less.
As I’ve learned, your talking points and slides will always be most appreciated in your own head. Keeping to time shows your respect for your audience and makes you appear polished.
The day of, get to the venue well ahead of time and check the sound, lights, and temperature. All of your preparation will be for naught if they can’t hear you, see your slides, or feel their fingers due to the frigid AC.
One of the reasons I love giving talks is because they are live. You and your audience are intimately engaged, and like any conversation, you’ll sense how it’s going. Are they looking at you or at their phones? Do they seem bored? Do they laugh easily, even when you weren’t expecting them to? Observe what is happening and adjust your performance accordingly. Are you losing them? Pause. Let them catch up. Are you putting them to sleep? Pick up the pace. Try that bit of humor now.
Your delivery is critical to your success. If you’re on the dais and behind the podium of a large audience, then be big, Greek theatre big, which means bigger facial expressions and bigger arm and hand gestures. Vary the tone and pace of your voice. Speed it up to build excitement. Slow down and lower your pitch for gravity and authority. Pause for 3-4 seconds to create suspense and drama.
Leave time for discussion when possible. Invite the audience to engage by asking, What do you think? Finally, on the plane ride home, or even as you walk back from the auditorium to your clinic, think about your presentation: What worked? What fell flat? What roused the audience? How can you deliver it better next time?
Even if it didn’t go well, remember, there’s always next week. It’s on to Cincinnati.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@frontlinemedcom.com.
GERD postop relapse rates highest in women, older adults
Healthy men younger than 45 years have the lowest risk of relapse after reflux surgery compared with other demographic subgroups, according to data from a population-based study of 2,655 adults in Sweden. The findings were published online in JAMA.
“Cohort studies have shown a high risk of recurrent symptoms of GERD after surgery, which may have contributed to the decline in the use of antireflux surgery,” but long-term reflux recurrence rates and potential risk factors have not been well studied, wrote John Maret-Ouda, MD, and colleagues at the Karolinska Institutet in Stockholm, Sweden.
Overall, 18% of the patients suffered a reflux relapse; 84% of these were prescribed long-term medication, and 16% underwent additional surgery.
The highest relapse rates occurred among women, older patients, and those with comorbid conditions. Reflux occurred in 22% of women vs. 14% of men (hazard ratio 1.57), and the hazard ratio was 1.41 for patients aged 61 years and older compared with those aged 45 years and younger. Patients with one or more comorbidities were approximately one-third more likely to have a recurrence of reflux, compared with those who had no comorbidities (hazard ratio 1.36).
Approximately 4% of patients reported complications; the most common complication was infection (1.1%), followed by bleeding (0.9%), and esophageal perforation (0.9%).
The recurrence rate of 18% is low compared with other studies, the researchers noted. Possible reasons for the difference include the population-based design of the current study, which meant that no patients were lost to follow-up, as well as the recent time period, “in which laparoscopic antireflux surgery has become more centralized to expert centers where selection of patients might be stricter and the quality of surgery might be higher,” they wrote.
The study findings were limited by several factors including clinical variations on coding, lack of data on certain confounding variables including body mass index and smoking, and a lack of control GERD patients who did not undergo antireflux surgery, the researchers said. The results suggest that the benefits of laparoscopic antireflux surgery may be diminished by the potential for recurrent GERD, they added.
The Swedish Research Council funded the study. The researchers had no financial conflicts to disclose.
“The operation can be performed with a relatively low rate of morbidity and a very low mortality rate,” Stuart J. Spechler, MD, wrote in an editorial. “Although findings regarding GERD symptom relief and patient satisfaction based on medication usage data should be interpreted with caution, the observation that more than 80% of patients did not restart antireflux medications after laparoscopic antireflux surgery suggests that the operation provided long-lasting relief of GERD symptoms for most patients,” he said. Although surgery is not a permanent cure for all patients with GERD, “the ever-increasing number of proposed [proton pump inhibitor] risks has caused the greatest concern among clinicians and their patients,” said Dr. Spechler. “Whether the greater than 80% possibility of long-term freedom from PPIs and their associated risks warrants the 4% risk of acute surgical complications and the 17.7% risk of GERD recurrence is a decision that individual patients should make after a detailed discussion of these risks and benefits with their physicians,” he said. However, the study findings suggest “that laparoscopic antireflux surgery might be an especially appealing option for young and otherwise healthy men, who seem to have the lowest rate of GERD recurrence after antireflux surgery and who otherwise would likely require decades of PPI treatment without the operation,” he wrote (JAMA 2017;318:913-5).
Dr. Spechler is affiliated with Baylor University in Dallas. He disclosed serving as a consultant for Ironwood Pharmaceuticals and Takeda Pharmaceuticals, and funding support from the National Institutes of Health.
“The operation can be performed with a relatively low rate of morbidity and a very low mortality rate,” Stuart J. Spechler, MD, wrote in an editorial. “Although findings regarding GERD symptom relief and patient satisfaction based on medication usage data should be interpreted with caution, the observation that more than 80% of patients did not restart antireflux medications after laparoscopic antireflux surgery suggests that the operation provided long-lasting relief of GERD symptoms for most patients,” he said. Although surgery is not a permanent cure for all patients with GERD, “the ever-increasing number of proposed [proton pump inhibitor] risks has caused the greatest concern among clinicians and their patients,” said Dr. Spechler. “Whether the greater than 80% possibility of long-term freedom from PPIs and their associated risks warrants the 4% risk of acute surgical complications and the 17.7% risk of GERD recurrence is a decision that individual patients should make after a detailed discussion of these risks and benefits with their physicians,” he said. However, the study findings suggest “that laparoscopic antireflux surgery might be an especially appealing option for young and otherwise healthy men, who seem to have the lowest rate of GERD recurrence after antireflux surgery and who otherwise would likely require decades of PPI treatment without the operation,” he wrote (JAMA 2017;318:913-5).
Dr. Spechler is affiliated with Baylor University in Dallas. He disclosed serving as a consultant for Ironwood Pharmaceuticals and Takeda Pharmaceuticals, and funding support from the National Institutes of Health.
“The operation can be performed with a relatively low rate of morbidity and a very low mortality rate,” Stuart J. Spechler, MD, wrote in an editorial. “Although findings regarding GERD symptom relief and patient satisfaction based on medication usage data should be interpreted with caution, the observation that more than 80% of patients did not restart antireflux medications after laparoscopic antireflux surgery suggests that the operation provided long-lasting relief of GERD symptoms for most patients,” he said. Although surgery is not a permanent cure for all patients with GERD, “the ever-increasing number of proposed [proton pump inhibitor] risks has caused the greatest concern among clinicians and their patients,” said Dr. Spechler. “Whether the greater than 80% possibility of long-term freedom from PPIs and their associated risks warrants the 4% risk of acute surgical complications and the 17.7% risk of GERD recurrence is a decision that individual patients should make after a detailed discussion of these risks and benefits with their physicians,” he said. However, the study findings suggest “that laparoscopic antireflux surgery might be an especially appealing option for young and otherwise healthy men, who seem to have the lowest rate of GERD recurrence after antireflux surgery and who otherwise would likely require decades of PPI treatment without the operation,” he wrote (JAMA 2017;318:913-5).
Dr. Spechler is affiliated with Baylor University in Dallas. He disclosed serving as a consultant for Ironwood Pharmaceuticals and Takeda Pharmaceuticals, and funding support from the National Institutes of Health.
Healthy men younger than 45 years have the lowest risk of relapse after reflux surgery compared with other demographic subgroups, according to data from a population-based study of 2,655 adults in Sweden. The findings were published online in JAMA.
“Cohort studies have shown a high risk of recurrent symptoms of GERD after surgery, which may have contributed to the decline in the use of antireflux surgery,” but long-term reflux recurrence rates and potential risk factors have not been well studied, wrote John Maret-Ouda, MD, and colleagues at the Karolinska Institutet in Stockholm, Sweden.
Overall, 18% of the patients suffered a reflux relapse; 84% of these were prescribed long-term medication, and 16% underwent additional surgery.
The highest relapse rates occurred among women, older patients, and those with comorbid conditions. Reflux occurred in 22% of women vs. 14% of men (hazard ratio 1.57), and the hazard ratio was 1.41 for patients aged 61 years and older compared with those aged 45 years and younger. Patients with one or more comorbidities were approximately one-third more likely to have a recurrence of reflux, compared with those who had no comorbidities (hazard ratio 1.36).
Approximately 4% of patients reported complications; the most common complication was infection (1.1%), followed by bleeding (0.9%), and esophageal perforation (0.9%).
The recurrence rate of 18% is low compared with other studies, the researchers noted. Possible reasons for the difference include the population-based design of the current study, which meant that no patients were lost to follow-up, as well as the recent time period, “in which laparoscopic antireflux surgery has become more centralized to expert centers where selection of patients might be stricter and the quality of surgery might be higher,” they wrote.
The study findings were limited by several factors including clinical variations on coding, lack of data on certain confounding variables including body mass index and smoking, and a lack of control GERD patients who did not undergo antireflux surgery, the researchers said. The results suggest that the benefits of laparoscopic antireflux surgery may be diminished by the potential for recurrent GERD, they added.
The Swedish Research Council funded the study. The researchers had no financial conflicts to disclose.
Healthy men younger than 45 years have the lowest risk of relapse after reflux surgery compared with other demographic subgroups, according to data from a population-based study of 2,655 adults in Sweden. The findings were published online in JAMA.
“Cohort studies have shown a high risk of recurrent symptoms of GERD after surgery, which may have contributed to the decline in the use of antireflux surgery,” but long-term reflux recurrence rates and potential risk factors have not been well studied, wrote John Maret-Ouda, MD, and colleagues at the Karolinska Institutet in Stockholm, Sweden.
Overall, 18% of the patients suffered a reflux relapse; 84% of these were prescribed long-term medication, and 16% underwent additional surgery.
The highest relapse rates occurred among women, older patients, and those with comorbid conditions. Reflux occurred in 22% of women vs. 14% of men (hazard ratio 1.57), and the hazard ratio was 1.41 for patients aged 61 years and older compared with those aged 45 years and younger. Patients with one or more comorbidities were approximately one-third more likely to have a recurrence of reflux, compared with those who had no comorbidities (hazard ratio 1.36).
Approximately 4% of patients reported complications; the most common complication was infection (1.1%), followed by bleeding (0.9%), and esophageal perforation (0.9%).
The recurrence rate of 18% is low compared with other studies, the researchers noted. Possible reasons for the difference include the population-based design of the current study, which meant that no patients were lost to follow-up, as well as the recent time period, “in which laparoscopic antireflux surgery has become more centralized to expert centers where selection of patients might be stricter and the quality of surgery might be higher,” they wrote.
The study findings were limited by several factors including clinical variations on coding, lack of data on certain confounding variables including body mass index and smoking, and a lack of control GERD patients who did not undergo antireflux surgery, the researchers said. The results suggest that the benefits of laparoscopic antireflux surgery may be diminished by the potential for recurrent GERD, they added.
The Swedish Research Council funded the study. The researchers had no financial conflicts to disclose.
FROM JAMA
Key clinical point: Young men were less likely than were other demographic groups to experience recurrence of gastroesophageal reflux after surgery.
Major finding: Overall, 18% of 2,655 adults who underwent reflux surgery experienced recurrent reflux requiring long-term medication or additional surgery.
Data source: A population-based, retrospective cohort study of reflux surgery patients in Sweden.
Disclosures: The Swedish Research Council supported the study.
The AHRQ Practice Tool Box
This is the first in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Primary care providers deal with a multitude of challenging clinical issues (e.g., providing first contact and preventive care, diagnosis in the undifferentiated patient, care of patients with chronic illness and multiple chronic conditions, keeping up with the literature) while managing a rapidly changing and often difficult health care environment. Despite this complexity and these challenges, primary care clinicians and health care systems strive to provide high-quality health care – i.e., care that is safe, effective, patient centered, timely, efficient, and equitable.
The Agency for Healthcare Research and Quality (AHRQ), a subdivision of the U.S. Department of Health & Human Services, recognizes that revitalizing this nation’s primary care system is critical to achieving quality health care. To that end, the agency is committed to helping you improve the care you deliver by offering the latest information, providing evidence syntheses, developing tools for improving primary care practice, and generating data and measures to track and improve performance in primary care.
AHRQ established the National Center for Excellence in Primary Care Research (NCEPCR) to be its intellectual home for primary care research. It is the agency’s vehicle for communicating the evidence from AHRQ’s research – and information about how this evidence can be used to improve health and primary health care – to researchers, primary care professionals, health care decision makers, patients, and families.
Electronic resources for daily practice
Every day you rely on guidelines for handling issues that range from prevention to caring for those with multiple chronic conditions. Two of AHRQ’s tools make the use of these guidelines easier.
First, the Electronic Prevention Services Selector (ePSS) is a free application that allows you to search or browse U.S. Preventive Services Task Force recommendations on the Web, a PDA, or a mobile device. You can enter patient-specific information (for example, age, sex, smoking status) to get customized information for your patient. The ePSS brings information on clinical preventive services – recommendations, clinical considerations, and selected practice tools – to the point of care. You can sign up for notifications when there are updates.
The National Guideline Clearinghouse (NGC) provides health professionals with a tool for obtaining objective, detailed information on evidence-based clinical practice guidelines. After you enter a condition onto the webpage, the site offers key information on guidelines related to that condition – including relevant FDA drug safety alerts – and flags guidelines addressing multiple chronic conditions. The site lets you readily compare different guidelines on the same topic.
Like all of AHRQ’s tools and resources, the ePSS and NGC are freely available. These and other tools can be found at the NCEPCR website.
Dr. Bierman is the director of the Center for Evidence and Practice Improvement at AHRQ. Dr. Ganiats is the director for the National Center for Excellence in Primary Care Research at AHRQ.
This is the first in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Primary care providers deal with a multitude of challenging clinical issues (e.g., providing first contact and preventive care, diagnosis in the undifferentiated patient, care of patients with chronic illness and multiple chronic conditions, keeping up with the literature) while managing a rapidly changing and often difficult health care environment. Despite this complexity and these challenges, primary care clinicians and health care systems strive to provide high-quality health care – i.e., care that is safe, effective, patient centered, timely, efficient, and equitable.
The Agency for Healthcare Research and Quality (AHRQ), a subdivision of the U.S. Department of Health & Human Services, recognizes that revitalizing this nation’s primary care system is critical to achieving quality health care. To that end, the agency is committed to helping you improve the care you deliver by offering the latest information, providing evidence syntheses, developing tools for improving primary care practice, and generating data and measures to track and improve performance in primary care.
AHRQ established the National Center for Excellence in Primary Care Research (NCEPCR) to be its intellectual home for primary care research. It is the agency’s vehicle for communicating the evidence from AHRQ’s research – and information about how this evidence can be used to improve health and primary health care – to researchers, primary care professionals, health care decision makers, patients, and families.
Electronic resources for daily practice
Every day you rely on guidelines for handling issues that range from prevention to caring for those with multiple chronic conditions. Two of AHRQ’s tools make the use of these guidelines easier.
First, the Electronic Prevention Services Selector (ePSS) is a free application that allows you to search or browse U.S. Preventive Services Task Force recommendations on the Web, a PDA, or a mobile device. You can enter patient-specific information (for example, age, sex, smoking status) to get customized information for your patient. The ePSS brings information on clinical preventive services – recommendations, clinical considerations, and selected practice tools – to the point of care. You can sign up for notifications when there are updates.
The National Guideline Clearinghouse (NGC) provides health professionals with a tool for obtaining objective, detailed information on evidence-based clinical practice guidelines. After you enter a condition onto the webpage, the site offers key information on guidelines related to that condition – including relevant FDA drug safety alerts – and flags guidelines addressing multiple chronic conditions. The site lets you readily compare different guidelines on the same topic.
Like all of AHRQ’s tools and resources, the ePSS and NGC are freely available. These and other tools can be found at the NCEPCR website.
Dr. Bierman is the director of the Center for Evidence and Practice Improvement at AHRQ. Dr. Ganiats is the director for the National Center for Excellence in Primary Care Research at AHRQ.
This is the first in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Primary care providers deal with a multitude of challenging clinical issues (e.g., providing first contact and preventive care, diagnosis in the undifferentiated patient, care of patients with chronic illness and multiple chronic conditions, keeping up with the literature) while managing a rapidly changing and often difficult health care environment. Despite this complexity and these challenges, primary care clinicians and health care systems strive to provide high-quality health care – i.e., care that is safe, effective, patient centered, timely, efficient, and equitable.
The Agency for Healthcare Research and Quality (AHRQ), a subdivision of the U.S. Department of Health & Human Services, recognizes that revitalizing this nation’s primary care system is critical to achieving quality health care. To that end, the agency is committed to helping you improve the care you deliver by offering the latest information, providing evidence syntheses, developing tools for improving primary care practice, and generating data and measures to track and improve performance in primary care.
AHRQ established the National Center for Excellence in Primary Care Research (NCEPCR) to be its intellectual home for primary care research. It is the agency’s vehicle for communicating the evidence from AHRQ’s research – and information about how this evidence can be used to improve health and primary health care – to researchers, primary care professionals, health care decision makers, patients, and families.
Electronic resources for daily practice
Every day you rely on guidelines for handling issues that range from prevention to caring for those with multiple chronic conditions. Two of AHRQ’s tools make the use of these guidelines easier.
First, the Electronic Prevention Services Selector (ePSS) is a free application that allows you to search or browse U.S. Preventive Services Task Force recommendations on the Web, a PDA, or a mobile device. You can enter patient-specific information (for example, age, sex, smoking status) to get customized information for your patient. The ePSS brings information on clinical preventive services – recommendations, clinical considerations, and selected practice tools – to the point of care. You can sign up for notifications when there are updates.
The National Guideline Clearinghouse (NGC) provides health professionals with a tool for obtaining objective, detailed information on evidence-based clinical practice guidelines. After you enter a condition onto the webpage, the site offers key information on guidelines related to that condition – including relevant FDA drug safety alerts – and flags guidelines addressing multiple chronic conditions. The site lets you readily compare different guidelines on the same topic.
Like all of AHRQ’s tools and resources, the ePSS and NGC are freely available. These and other tools can be found at the NCEPCR website.
Dr. Bierman is the director of the Center for Evidence and Practice Improvement at AHRQ. Dr. Ganiats is the director for the National Center for Excellence in Primary Care Research at AHRQ.
Statins linked to lower death rates in COPD
Receiving a statin prescription within a year after diagnosis of chronic obstructive pulmonary disease was associated with a 21% decrease in the subsequent risk of all-cause mortality and a 45% drop in risk of pulmonary mortality, according to the results of a large retrospective administrative database study.
The findings belie those of the recent Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) trial, in which daily simvastatin (40 mg) did not affect exacerbation rates or time to first exacerbation in high-risk COPD patients, wrote Adam Raymakers, MSc, a doctoral candidate at the University of British Columbia, Vancouver, and his associates. Their study was observational, but the association between statin use and decreased mortality “persisted across several measures of statin exposure,” they wrote. “Our findings, in conjunction with previously reported evidence, suggests that there may be a specific subtype of COPD patients that may benefit from statin use.” The study appears in the September issue of Chest (2017;152;486-93).
To further explore the question, the researchers analyzed linked health databases from nearly 40,000 patients aged 50 years and older who had received at least three prescriptions for an anticholinergic or a short-acting beta agonist in 12 months some time between 1998 and 2007. The first prescription was considered the date of COPD “diagnosis.” The average age of the patients was 71 years; 55% were female.
A total of 7,775 patients (19.6%) who met this definition of incident COPD were prescribed a statin at least once during the subsequent year. These patients had a significantly reduced risk of subsequent all-cause mortality in univariate and multivariate analyses, with hazard ratios of 0.79 (95% confidence intervals, 0.68 to 0.91; P less than .002). Statins also showed a protective effect against pulmonary mortality, with univariate and multivariate hazard ratios of 0.52 (P = .01) and 0.55 (P = .03), respectively.
The protective effect of statins held up when the investigators narrowed the exposure period to 6 months after COPD diagnosis and when they expanded it to 18 months. Exposure to statins for 80% of the 1-year window after COPD diagnosis – a proxy for statin adherence – also led to a reduced risk of all-cause mortality, but the 95% confidence interval for the hazard ratio did not reach statistical significance (0.71 to 1.01; P = .06).
The most common prescription was for atorvastatin (49%), usually for 90 days (23%), 100 days (20%), or 30 days (15%), the researchers said. While the “possibility of the ‘healthy user’ or the ‘healthy adherer’ cannot be ignored,” they adjusted for other prescriptions, comorbidities, and income level, which should have helped eliminate this effect, they added. However, they lacked data on smoking and lung function assessments, both of which are “important confounders and contributors to mortality,” they acknowledged.
Canadian Institutes of Health Research supported the study. One coinvestigator disclosed consulting relationships with Teva, Pfizer, and Novartis. The others had no conflicts of interest.
Despite [its] limitations, the study results are intriguing and in line with findings from other retrospective cohorts. How then can we reconcile the apparent benefits observed in retrospective studies with the lack of clinical effect seen in prospective trials, particularly the Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) study? Could it be that both negative and positive studies are “correct”? Prospective studies have thus far not been adequately powered for mortality as an endpoint. Perhaps the choice of the particular statin matters? While STATCOPE involved simvastatin, the majority of the cohort reported by Raymakers et al. received atorvastatin. [Or perhaps] the negative results of STATCOPE could be related to careful selection of study participants with a low burden of systemic inflammation.
This most recent study reinforces the idea that statins may play a beneficial role in COPD, but it isn’t clear which patients to target for therapy. It is unlikely that the findings by Raymakers et al. will reverse recent recommendations by the American College of Chest Physicians and Canadian Thoracic Society against the use of statins for the purpose of prevention of COPD exacerbations, but the suggestion of survival advantage related to statins certainly may breathe new life into an enthusiasm greatly tempered by STATCOPE.
Or Kalchiem-Dekel, MD, and Robert M. Reed, MD, are at the pulmonary and critical care medicine division, University of Maryland, Baltimore. Neither editorialist had conflicts of interest (Chest. 2017;152:456-7. doi: 10.1016/j.chest.2017.04.156).
Despite [its] limitations, the study results are intriguing and in line with findings from other retrospective cohorts. How then can we reconcile the apparent benefits observed in retrospective studies with the lack of clinical effect seen in prospective trials, particularly the Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) study? Could it be that both negative and positive studies are “correct”? Prospective studies have thus far not been adequately powered for mortality as an endpoint. Perhaps the choice of the particular statin matters? While STATCOPE involved simvastatin, the majority of the cohort reported by Raymakers et al. received atorvastatin. [Or perhaps] the negative results of STATCOPE could be related to careful selection of study participants with a low burden of systemic inflammation.
This most recent study reinforces the idea that statins may play a beneficial role in COPD, but it isn’t clear which patients to target for therapy. It is unlikely that the findings by Raymakers et al. will reverse recent recommendations by the American College of Chest Physicians and Canadian Thoracic Society against the use of statins for the purpose of prevention of COPD exacerbations, but the suggestion of survival advantage related to statins certainly may breathe new life into an enthusiasm greatly tempered by STATCOPE.
Or Kalchiem-Dekel, MD, and Robert M. Reed, MD, are at the pulmonary and critical care medicine division, University of Maryland, Baltimore. Neither editorialist had conflicts of interest (Chest. 2017;152:456-7. doi: 10.1016/j.chest.2017.04.156).
Despite [its] limitations, the study results are intriguing and in line with findings from other retrospective cohorts. How then can we reconcile the apparent benefits observed in retrospective studies with the lack of clinical effect seen in prospective trials, particularly the Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) study? Could it be that both negative and positive studies are “correct”? Prospective studies have thus far not been adequately powered for mortality as an endpoint. Perhaps the choice of the particular statin matters? While STATCOPE involved simvastatin, the majority of the cohort reported by Raymakers et al. received atorvastatin. [Or perhaps] the negative results of STATCOPE could be related to careful selection of study participants with a low burden of systemic inflammation.
This most recent study reinforces the idea that statins may play a beneficial role in COPD, but it isn’t clear which patients to target for therapy. It is unlikely that the findings by Raymakers et al. will reverse recent recommendations by the American College of Chest Physicians and Canadian Thoracic Society against the use of statins for the purpose of prevention of COPD exacerbations, but the suggestion of survival advantage related to statins certainly may breathe new life into an enthusiasm greatly tempered by STATCOPE.
Or Kalchiem-Dekel, MD, and Robert M. Reed, MD, are at the pulmonary and critical care medicine division, University of Maryland, Baltimore. Neither editorialist had conflicts of interest (Chest. 2017;152:456-7. doi: 10.1016/j.chest.2017.04.156).
Receiving a statin prescription within a year after diagnosis of chronic obstructive pulmonary disease was associated with a 21% decrease in the subsequent risk of all-cause mortality and a 45% drop in risk of pulmonary mortality, according to the results of a large retrospective administrative database study.
The findings belie those of the recent Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) trial, in which daily simvastatin (40 mg) did not affect exacerbation rates or time to first exacerbation in high-risk COPD patients, wrote Adam Raymakers, MSc, a doctoral candidate at the University of British Columbia, Vancouver, and his associates. Their study was observational, but the association between statin use and decreased mortality “persisted across several measures of statin exposure,” they wrote. “Our findings, in conjunction with previously reported evidence, suggests that there may be a specific subtype of COPD patients that may benefit from statin use.” The study appears in the September issue of Chest (2017;152;486-93).
To further explore the question, the researchers analyzed linked health databases from nearly 40,000 patients aged 50 years and older who had received at least three prescriptions for an anticholinergic or a short-acting beta agonist in 12 months some time between 1998 and 2007. The first prescription was considered the date of COPD “diagnosis.” The average age of the patients was 71 years; 55% were female.
A total of 7,775 patients (19.6%) who met this definition of incident COPD were prescribed a statin at least once during the subsequent year. These patients had a significantly reduced risk of subsequent all-cause mortality in univariate and multivariate analyses, with hazard ratios of 0.79 (95% confidence intervals, 0.68 to 0.91; P less than .002). Statins also showed a protective effect against pulmonary mortality, with univariate and multivariate hazard ratios of 0.52 (P = .01) and 0.55 (P = .03), respectively.
The protective effect of statins held up when the investigators narrowed the exposure period to 6 months after COPD diagnosis and when they expanded it to 18 months. Exposure to statins for 80% of the 1-year window after COPD diagnosis – a proxy for statin adherence – also led to a reduced risk of all-cause mortality, but the 95% confidence interval for the hazard ratio did not reach statistical significance (0.71 to 1.01; P = .06).
The most common prescription was for atorvastatin (49%), usually for 90 days (23%), 100 days (20%), or 30 days (15%), the researchers said. While the “possibility of the ‘healthy user’ or the ‘healthy adherer’ cannot be ignored,” they adjusted for other prescriptions, comorbidities, and income level, which should have helped eliminate this effect, they added. However, they lacked data on smoking and lung function assessments, both of which are “important confounders and contributors to mortality,” they acknowledged.
Canadian Institutes of Health Research supported the study. One coinvestigator disclosed consulting relationships with Teva, Pfizer, and Novartis. The others had no conflicts of interest.
Receiving a statin prescription within a year after diagnosis of chronic obstructive pulmonary disease was associated with a 21% decrease in the subsequent risk of all-cause mortality and a 45% drop in risk of pulmonary mortality, according to the results of a large retrospective administrative database study.
The findings belie those of the recent Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) trial, in which daily simvastatin (40 mg) did not affect exacerbation rates or time to first exacerbation in high-risk COPD patients, wrote Adam Raymakers, MSc, a doctoral candidate at the University of British Columbia, Vancouver, and his associates. Their study was observational, but the association between statin use and decreased mortality “persisted across several measures of statin exposure,” they wrote. “Our findings, in conjunction with previously reported evidence, suggests that there may be a specific subtype of COPD patients that may benefit from statin use.” The study appears in the September issue of Chest (2017;152;486-93).
To further explore the question, the researchers analyzed linked health databases from nearly 40,000 patients aged 50 years and older who had received at least three prescriptions for an anticholinergic or a short-acting beta agonist in 12 months some time between 1998 and 2007. The first prescription was considered the date of COPD “diagnosis.” The average age of the patients was 71 years; 55% were female.
A total of 7,775 patients (19.6%) who met this definition of incident COPD were prescribed a statin at least once during the subsequent year. These patients had a significantly reduced risk of subsequent all-cause mortality in univariate and multivariate analyses, with hazard ratios of 0.79 (95% confidence intervals, 0.68 to 0.91; P less than .002). Statins also showed a protective effect against pulmonary mortality, with univariate and multivariate hazard ratios of 0.52 (P = .01) and 0.55 (P = .03), respectively.
The protective effect of statins held up when the investigators narrowed the exposure period to 6 months after COPD diagnosis and when they expanded it to 18 months. Exposure to statins for 80% of the 1-year window after COPD diagnosis – a proxy for statin adherence – also led to a reduced risk of all-cause mortality, but the 95% confidence interval for the hazard ratio did not reach statistical significance (0.71 to 1.01; P = .06).
The most common prescription was for atorvastatin (49%), usually for 90 days (23%), 100 days (20%), or 30 days (15%), the researchers said. While the “possibility of the ‘healthy user’ or the ‘healthy adherer’ cannot be ignored,” they adjusted for other prescriptions, comorbidities, and income level, which should have helped eliminate this effect, they added. However, they lacked data on smoking and lung function assessments, both of which are “important confounders and contributors to mortality,” they acknowledged.
Canadian Institutes of Health Research supported the study. One coinvestigator disclosed consulting relationships with Teva, Pfizer, and Novartis. The others had no conflicts of interest.
FROM CHEST
Key clinical point: Statins might reduce the risk of death among patients with chronic obstructive pulmonary disease.
Major finding: Statin use was associated with a 21% decrease in risk of all-cause mortality and a 45% decrease in risk of pulmonary mortality.
Data source: A retrospective cohort study of 39,678 patients with COPD, including 7,775 prescribed statins.
Disclosures: Canadian Institutes of Health Research supported the study. One coinvestigator disclosed consulting relationships with Teva, Pfizer, and Novartis. The others had no conflicts of interest.