User login
Breastfeeding practices have improved, but some attitudes are concerning
Pediatricians’ recommendations and practices for breastfeeding have become more closely aligned with American Academy of Pediatrics policy since 1995, but attitudes toward breastfeeding show cause for concern, according to a study.
The percentage of surveyed pediatricians who advise exclusive breastfeeding during the first month rose from 66% in 1995 to 75% in 2014 (P less than .05), reported Lori Feldman-Winter, MD, MPH, of Rowan University, Camden, N.J., and her coauthors (Pediatrics. 2017. doi: 10.1542/peds.2017-1229).
Physicians also were less likely to recommend formula supplementation (12% in 1995; 4.5% in 2014; P less than .05).
In addition, pediatricians in 2014 were significantly more likely to report that their affiliated hospitals had applied to be a baby-friendly hospital (56%), compared with results for 1995 (12%) and 2004 (22%) (P less than .05), the investigators said. The physicians also were more likely to report that their practices were more in line with the “Ten Steps to Successful Breastfeeding” policy.
Despite this general trend toward AAP recommendation–compliant practices, many pediatricians doubt the likelihood of breastfeeding success. Although in 1995, 70% of pediatricians reported that almost any mother can be successful at breastfeeding if she keeps trying, only 56% reported the same in 2014 (P less than .05), Dr. Feldman-Winter and her coauthors said. Similarly, only 50% reported that the benefits of breastfeeding outweigh the difficulties in 2014, compared with 70% in 1995 (P less than .05). This may be in part because younger pediatricians reported less confidence in managing common breastfeeding problems and being able to adequately address parents’ questions about breastfeeding; there was a statistically significant difference between pediatricians younger than 45 years and those 45 years and older (P less than .01).
“Pediatricians have demonstrated a modest decline in attitudes about the potential for breastfeeding success,” the investigators wrote. “Lack of resident support for breastfeeding is apparent among many programs and may set the stage for attitudes about breastfeeding for years to come. There are continued opportunities to enhance training in breastfeeding and participate in breastfeeding management and support.”
The study was funded by the American Academy of Pediatrics and the Maternal and Child Health Bureau, Health Resources and Services Administration, and Department of Health and Human Services. None of the authors reported any financial disclosures.
Despite changes in breastfeeding recommendations and practices as well as numerous initiatives from organizations such as the Centers for Disease Control and Prevention and the Department of Health and Human Services, residency training for breastfeeding is not universal.
The study by Feldman et al. shows some concerning trends toward a lack of belief among pediatricians that the benefits of breastfeeding outweigh the difficulties or inconveniences and toward less confidence in managing breastfeeding. They also indicate that baby-friendly hospitals are providing the required breastfeeding education, but this is only a start.
As the trend toward staffing hospitals with pediatric hospitalists increases, it is essential to remember that ambulatory pediatricians also need breastfeeding education because they are responsible for ongoing follow-up care. Maintenance of certification should include breastfeeding as a “core competency” for general pediatricians as well.
Although this analysis shows progress, “the importance of routine integration of breastfeeding into all aspects of medical education cannot be overstated. Breastfeeding education should be as routine in the curriculum as other preventive health strategies, such as immunization.” Hopefully, future studies will show that pediatricians have the skills, attitudes, and confidence necessary to provide competent support to their patients.
Joan Younger Meek, MD, is the associate dean for graduate medical education and a professor at Florida State University in Tallahassee. Her comments were with the Feldman-Winter et al. article in Pediatrics (2017. doi: 10.1542/peds.2017-2509). She reported no relevant financial disclosures or external funding.
Despite changes in breastfeeding recommendations and practices as well as numerous initiatives from organizations such as the Centers for Disease Control and Prevention and the Department of Health and Human Services, residency training for breastfeeding is not universal.
The study by Feldman et al. shows some concerning trends toward a lack of belief among pediatricians that the benefits of breastfeeding outweigh the difficulties or inconveniences and toward less confidence in managing breastfeeding. They also indicate that baby-friendly hospitals are providing the required breastfeeding education, but this is only a start.
As the trend toward staffing hospitals with pediatric hospitalists increases, it is essential to remember that ambulatory pediatricians also need breastfeeding education because they are responsible for ongoing follow-up care. Maintenance of certification should include breastfeeding as a “core competency” for general pediatricians as well.
Although this analysis shows progress, “the importance of routine integration of breastfeeding into all aspects of medical education cannot be overstated. Breastfeeding education should be as routine in the curriculum as other preventive health strategies, such as immunization.” Hopefully, future studies will show that pediatricians have the skills, attitudes, and confidence necessary to provide competent support to their patients.
Joan Younger Meek, MD, is the associate dean for graduate medical education and a professor at Florida State University in Tallahassee. Her comments were with the Feldman-Winter et al. article in Pediatrics (2017. doi: 10.1542/peds.2017-2509). She reported no relevant financial disclosures or external funding.
Despite changes in breastfeeding recommendations and practices as well as numerous initiatives from organizations such as the Centers for Disease Control and Prevention and the Department of Health and Human Services, residency training for breastfeeding is not universal.
The study by Feldman et al. shows some concerning trends toward a lack of belief among pediatricians that the benefits of breastfeeding outweigh the difficulties or inconveniences and toward less confidence in managing breastfeeding. They also indicate that baby-friendly hospitals are providing the required breastfeeding education, but this is only a start.
As the trend toward staffing hospitals with pediatric hospitalists increases, it is essential to remember that ambulatory pediatricians also need breastfeeding education because they are responsible for ongoing follow-up care. Maintenance of certification should include breastfeeding as a “core competency” for general pediatricians as well.
Although this analysis shows progress, “the importance of routine integration of breastfeeding into all aspects of medical education cannot be overstated. Breastfeeding education should be as routine in the curriculum as other preventive health strategies, such as immunization.” Hopefully, future studies will show that pediatricians have the skills, attitudes, and confidence necessary to provide competent support to their patients.
Joan Younger Meek, MD, is the associate dean for graduate medical education and a professor at Florida State University in Tallahassee. Her comments were with the Feldman-Winter et al. article in Pediatrics (2017. doi: 10.1542/peds.2017-2509). She reported no relevant financial disclosures or external funding.
Pediatricians’ recommendations and practices for breastfeeding have become more closely aligned with American Academy of Pediatrics policy since 1995, but attitudes toward breastfeeding show cause for concern, according to a study.
The percentage of surveyed pediatricians who advise exclusive breastfeeding during the first month rose from 66% in 1995 to 75% in 2014 (P less than .05), reported Lori Feldman-Winter, MD, MPH, of Rowan University, Camden, N.J., and her coauthors (Pediatrics. 2017. doi: 10.1542/peds.2017-1229).
Physicians also were less likely to recommend formula supplementation (12% in 1995; 4.5% in 2014; P less than .05).
In addition, pediatricians in 2014 were significantly more likely to report that their affiliated hospitals had applied to be a baby-friendly hospital (56%), compared with results for 1995 (12%) and 2004 (22%) (P less than .05), the investigators said. The physicians also were more likely to report that their practices were more in line with the “Ten Steps to Successful Breastfeeding” policy.
Despite this general trend toward AAP recommendation–compliant practices, many pediatricians doubt the likelihood of breastfeeding success. Although in 1995, 70% of pediatricians reported that almost any mother can be successful at breastfeeding if she keeps trying, only 56% reported the same in 2014 (P less than .05), Dr. Feldman-Winter and her coauthors said. Similarly, only 50% reported that the benefits of breastfeeding outweigh the difficulties in 2014, compared with 70% in 1995 (P less than .05). This may be in part because younger pediatricians reported less confidence in managing common breastfeeding problems and being able to adequately address parents’ questions about breastfeeding; there was a statistically significant difference between pediatricians younger than 45 years and those 45 years and older (P less than .01).
“Pediatricians have demonstrated a modest decline in attitudes about the potential for breastfeeding success,” the investigators wrote. “Lack of resident support for breastfeeding is apparent among many programs and may set the stage for attitudes about breastfeeding for years to come. There are continued opportunities to enhance training in breastfeeding and participate in breastfeeding management and support.”
The study was funded by the American Academy of Pediatrics and the Maternal and Child Health Bureau, Health Resources and Services Administration, and Department of Health and Human Services. None of the authors reported any financial disclosures.
Pediatricians’ recommendations and practices for breastfeeding have become more closely aligned with American Academy of Pediatrics policy since 1995, but attitudes toward breastfeeding show cause for concern, according to a study.
The percentage of surveyed pediatricians who advise exclusive breastfeeding during the first month rose from 66% in 1995 to 75% in 2014 (P less than .05), reported Lori Feldman-Winter, MD, MPH, of Rowan University, Camden, N.J., and her coauthors (Pediatrics. 2017. doi: 10.1542/peds.2017-1229).
Physicians also were less likely to recommend formula supplementation (12% in 1995; 4.5% in 2014; P less than .05).
In addition, pediatricians in 2014 were significantly more likely to report that their affiliated hospitals had applied to be a baby-friendly hospital (56%), compared with results for 1995 (12%) and 2004 (22%) (P less than .05), the investigators said. The physicians also were more likely to report that their practices were more in line with the “Ten Steps to Successful Breastfeeding” policy.
Despite this general trend toward AAP recommendation–compliant practices, many pediatricians doubt the likelihood of breastfeeding success. Although in 1995, 70% of pediatricians reported that almost any mother can be successful at breastfeeding if she keeps trying, only 56% reported the same in 2014 (P less than .05), Dr. Feldman-Winter and her coauthors said. Similarly, only 50% reported that the benefits of breastfeeding outweigh the difficulties in 2014, compared with 70% in 1995 (P less than .05). This may be in part because younger pediatricians reported less confidence in managing common breastfeeding problems and being able to adequately address parents’ questions about breastfeeding; there was a statistically significant difference between pediatricians younger than 45 years and those 45 years and older (P less than .01).
“Pediatricians have demonstrated a modest decline in attitudes about the potential for breastfeeding success,” the investigators wrote. “Lack of resident support for breastfeeding is apparent among many programs and may set the stage for attitudes about breastfeeding for years to come. There are continued opportunities to enhance training in breastfeeding and participate in breastfeeding management and support.”
The study was funded by the American Academy of Pediatrics and the Maternal and Child Health Bureau, Health Resources and Services Administration, and Department of Health and Human Services. None of the authors reported any financial disclosures.
FROM PEDIATRICS
Key clinical point:
Major finding: The percentage of surveyed physicians who advise exclusive breastfeeding during the first month rose from 66% in 1995 to 75% in 2014 (P less than .05).
Data source: An analysis of data from three AAP Periodic Surveys of Fellows.
Disclosures: The study was funded by the American Academy of Pediatrics and the Maternal and Child Health Bureau, Health Resources and Services Administration, and Department of Health and Human Services. None of the authors reported any financial disclosures.
Subtle hearing loss after concussion could impair learning
CHICAGO – Children who experience concussion can develop deficits in auditory processing that could impair long-term academic performance and carry implications for return-to-play strategies, according to a study.
Investigators assessed 40 children aged 8-15 years, half of whom experienced concussion. The postconcussion group of 20 children had slower and smaller neural responses to speech, compared with 20 control children, on the noninvasive frequency-following response measure.
“The ability to hear in noise following concussion is impaired in the pediatric population, based on our results, which suggests it might pose additional challenges for classroom learning,” Ms. Thompson said. The study also suggests that auditory function should be considered part of acute and long-term assessment of children post concussion.
Importantly, all participants in the study had normal hearing. “It’s important to know these are very subtle auditory deficits that only emerge if you’re looking for them,” Ms. Thompson said at the annual meeting of the American Academy of Pediatrics.
Children in the concussion group were recruited from the concussion clinic at the Ann and Robert H. Lurie Children’s Hospital of Chicago. Patients were assessed an average of 27 days post injury, with most still symptomatic. The children in the control group had been treated for musculoskeletal injuries. The concussed and control groups were matched for sex and gender.
“We think that these results have implications beyond the classroom,” Ms. Thompson said. “Auditory deficits might increase risk of reinjury if sports are being played in loud, noisy gymnasiums or crowded soccer fields. So this is important to consider with return-to-play strategies.” She added, “There is hope. Auditory processing is a malleable skill, and it can be a useful target for rehabilitation and recovery.”
Ms. Thompson had no relevant financial disclosures. The study was supported by the Knowles Hearing Center.
CHICAGO – Children who experience concussion can develop deficits in auditory processing that could impair long-term academic performance and carry implications for return-to-play strategies, according to a study.
Investigators assessed 40 children aged 8-15 years, half of whom experienced concussion. The postconcussion group of 20 children had slower and smaller neural responses to speech, compared with 20 control children, on the noninvasive frequency-following response measure.
“The ability to hear in noise following concussion is impaired in the pediatric population, based on our results, which suggests it might pose additional challenges for classroom learning,” Ms. Thompson said. The study also suggests that auditory function should be considered part of acute and long-term assessment of children post concussion.
Importantly, all participants in the study had normal hearing. “It’s important to know these are very subtle auditory deficits that only emerge if you’re looking for them,” Ms. Thompson said at the annual meeting of the American Academy of Pediatrics.
Children in the concussion group were recruited from the concussion clinic at the Ann and Robert H. Lurie Children’s Hospital of Chicago. Patients were assessed an average of 27 days post injury, with most still symptomatic. The children in the control group had been treated for musculoskeletal injuries. The concussed and control groups were matched for sex and gender.
“We think that these results have implications beyond the classroom,” Ms. Thompson said. “Auditory deficits might increase risk of reinjury if sports are being played in loud, noisy gymnasiums or crowded soccer fields. So this is important to consider with return-to-play strategies.” She added, “There is hope. Auditory processing is a malleable skill, and it can be a useful target for rehabilitation and recovery.”
Ms. Thompson had no relevant financial disclosures. The study was supported by the Knowles Hearing Center.
CHICAGO – Children who experience concussion can develop deficits in auditory processing that could impair long-term academic performance and carry implications for return-to-play strategies, according to a study.
Investigators assessed 40 children aged 8-15 years, half of whom experienced concussion. The postconcussion group of 20 children had slower and smaller neural responses to speech, compared with 20 control children, on the noninvasive frequency-following response measure.
“The ability to hear in noise following concussion is impaired in the pediatric population, based on our results, which suggests it might pose additional challenges for classroom learning,” Ms. Thompson said. The study also suggests that auditory function should be considered part of acute and long-term assessment of children post concussion.
Importantly, all participants in the study had normal hearing. “It’s important to know these are very subtle auditory deficits that only emerge if you’re looking for them,” Ms. Thompson said at the annual meeting of the American Academy of Pediatrics.
Children in the concussion group were recruited from the concussion clinic at the Ann and Robert H. Lurie Children’s Hospital of Chicago. Patients were assessed an average of 27 days post injury, with most still symptomatic. The children in the control group had been treated for musculoskeletal injuries. The concussed and control groups were matched for sex and gender.
“We think that these results have implications beyond the classroom,” Ms. Thompson said. “Auditory deficits might increase risk of reinjury if sports are being played in loud, noisy gymnasiums or crowded soccer fields. So this is important to consider with return-to-play strategies.” She added, “There is hope. Auditory processing is a malleable skill, and it can be a useful target for rehabilitation and recovery.”
Ms. Thompson had no relevant financial disclosures. The study was supported by the Knowles Hearing Center.
AT AAP 2017
Key clinical point:
Major finding: Children with concussion symptoms performed significantly poorer on the Hearing in Noise Test, compared with nonconcussed peers (P = .001).
Data source: Study of 40 children in a sports medicine tertiary clinic: half experienced concussion and half served as controls.
Disclosures: Ms. Thompson had no relevant financial disclosures. The study was supported by the Knowles Hearing Center.
Combo vaccines improve compliance
, reported Samantha K. Kurosky of RTI Health Solutions, Research Triangle Park, N.C., and her colleagues.
Data from the 2012 National Immunization Survey was used to assess vaccination completion and compliance in 11,561 children age 24-35 months. Most children had providers who were in private practice (58%); about half of the children were enrolled in Medicaid or the Children’s Health Insurance Program (CHIP).
Completion of the full 4:3:1:3:3:1:4 vaccine series (4 DTaP, 3 inactivated polio vaccine [IPV], 1 MMR, 3 or 4 Haemophilus influenzae type b [Hib], 3 hepatitis B, 1 varicella, and 4 pneumococcal conjugate vaccine) was better among those who received combination vaccines, at 69%, compared with children who received single-antigen vaccine only (50%).
Children receiving combination vaccines also had a significantly higher compliance rate for the 4:3:1:3:3:1:4 series, at 24%, compared with those receiving single-antigen vaccines only, at 13% (P less than .001). Of children who received at least one vaccine by 24 months, 86% received at least one combo vaccine.
Children getting at least one combo vaccine were 2.2 times more likely to get all vaccines on time, and 2.4 times more likely to spend less time undervaccinated (less than 7 months), compared with those receiving single-antigen vaccines only, Ms. Kurosky and her associates said.
Previous studies have found that parents who refuse or intentionally delay vaccines often have higher income and are married mothers with college educations. In this study, parents with these demographics tended to have children who received single-antigen–only vaccines – that is, children who were less likely to complete a full vaccine series or have a high compliance rate, they said.
GlaxoSmithKline funded the research.
Read more at Human Vaccines & Immunotherapeutics (2017 Sep 7. doi: 10.1080/21645515.2017.1362515).
, reported Samantha K. Kurosky of RTI Health Solutions, Research Triangle Park, N.C., and her colleagues.
Data from the 2012 National Immunization Survey was used to assess vaccination completion and compliance in 11,561 children age 24-35 months. Most children had providers who were in private practice (58%); about half of the children were enrolled in Medicaid or the Children’s Health Insurance Program (CHIP).
Completion of the full 4:3:1:3:3:1:4 vaccine series (4 DTaP, 3 inactivated polio vaccine [IPV], 1 MMR, 3 or 4 Haemophilus influenzae type b [Hib], 3 hepatitis B, 1 varicella, and 4 pneumococcal conjugate vaccine) was better among those who received combination vaccines, at 69%, compared with children who received single-antigen vaccine only (50%).
Children receiving combination vaccines also had a significantly higher compliance rate for the 4:3:1:3:3:1:4 series, at 24%, compared with those receiving single-antigen vaccines only, at 13% (P less than .001). Of children who received at least one vaccine by 24 months, 86% received at least one combo vaccine.
Children getting at least one combo vaccine were 2.2 times more likely to get all vaccines on time, and 2.4 times more likely to spend less time undervaccinated (less than 7 months), compared with those receiving single-antigen vaccines only, Ms. Kurosky and her associates said.
Previous studies have found that parents who refuse or intentionally delay vaccines often have higher income and are married mothers with college educations. In this study, parents with these demographics tended to have children who received single-antigen–only vaccines – that is, children who were less likely to complete a full vaccine series or have a high compliance rate, they said.
GlaxoSmithKline funded the research.
Read more at Human Vaccines & Immunotherapeutics (2017 Sep 7. doi: 10.1080/21645515.2017.1362515).
, reported Samantha K. Kurosky of RTI Health Solutions, Research Triangle Park, N.C., and her colleagues.
Data from the 2012 National Immunization Survey was used to assess vaccination completion and compliance in 11,561 children age 24-35 months. Most children had providers who were in private practice (58%); about half of the children were enrolled in Medicaid or the Children’s Health Insurance Program (CHIP).
Completion of the full 4:3:1:3:3:1:4 vaccine series (4 DTaP, 3 inactivated polio vaccine [IPV], 1 MMR, 3 or 4 Haemophilus influenzae type b [Hib], 3 hepatitis B, 1 varicella, and 4 pneumococcal conjugate vaccine) was better among those who received combination vaccines, at 69%, compared with children who received single-antigen vaccine only (50%).
Children receiving combination vaccines also had a significantly higher compliance rate for the 4:3:1:3:3:1:4 series, at 24%, compared with those receiving single-antigen vaccines only, at 13% (P less than .001). Of children who received at least one vaccine by 24 months, 86% received at least one combo vaccine.
Children getting at least one combo vaccine were 2.2 times more likely to get all vaccines on time, and 2.4 times more likely to spend less time undervaccinated (less than 7 months), compared with those receiving single-antigen vaccines only, Ms. Kurosky and her associates said.
Previous studies have found that parents who refuse or intentionally delay vaccines often have higher income and are married mothers with college educations. In this study, parents with these demographics tended to have children who received single-antigen–only vaccines – that is, children who were less likely to complete a full vaccine series or have a high compliance rate, they said.
GlaxoSmithKline funded the research.
Read more at Human Vaccines & Immunotherapeutics (2017 Sep 7. doi: 10.1080/21645515.2017.1362515).
FROM HUMAN VACCINES & IMMUNOTHERAPEUTICS
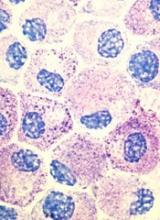
CHMP recommends approval of generic imatinib
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended granting marketing authorization for Imatinib Teva B.V., a generic of Glivec.
The recommendation is that Imatinib Teva B.V. be approved to treat chronic myeloid leukemia (CML), acute lymphoblastic leukemia (ALL), hypereosinophilic syndrome (HES), chronic eosinophilic leukemia (CEL), myelodysplastic syndromes (MDS), myeloproliferative neoplasms (MPNs), gastrointestinal stromal tumors (GIST), and dermatofibrosarcoma protuberans (DFSP).
The European Commission typically adheres to the CHMP’s recommendations and delivers its final decision within 67 days of the CHMP’s recommendation.
The European Commission’s decision will be applicable to the entire European Economic Area—all member states of the European Union plus Iceland, Liechtenstein, and Norway.
If approved, Imatinib Teva B.V. will be available as capsules and film-coated tablets (100 mg and 400 mg). And it will be authorized:
- As monotherapy for pediatric patients with newly diagnosed, Philadelphia-chromosome-positive (Ph+) CML for whom bone marrow transplant is not considered the first line of treatment.
- As monotherapy for pediatric patients with Ph+ CML in chronic phase after failure of interferon-alpha therapy or in accelerated phase or blast crisis.
- As monotherapy for adults with Ph+ CML in blast crisis.
- Integrated with chemotherapy to treat adult and pediatric patients with newly diagnosed, Ph+ ALL.
- As monotherapy for adults with relapsed or refractory Ph+ ALL.
- As monotherapy for adults with MDS/MPNs associated with platelet-derived growth factor receptor gene re-arrangements.
- As monotherapy for adults with advanced HES and/or CEL with FIP1L1-PDGFRα rearrangement.
- As monotherapy for adults with Kit- (CD117-) positive, unresectable and/or metastatic malignant GISTs.
- For the adjuvant treatment of adults who are at significant risk of relapse following resection of Kit-positive GIST. Patients who have a low or very low risk of recurrence should not receive adjuvant treatment.
- As monotherapy for adults with unresectable DFSP and adults with recurrent and/or metastatic DFSP who are not eligible for surgery.
The CHMP said studies have demonstrated the satisfactory quality of Imatinib Teva B.V. and its bioequivalence to the reference product, Glivec.
In adult and pediatric patients, the effectiveness of imatinib is based on:
- Overall hematologic and cytogenetic response rates and progression-free survival in CML
- Hematologic and cytogenetic response rates in Ph+ ALL and MDS/MPNs
- Hematologic response rates in HES/CEL
- Objective response rates in adults with unresectable and/or metastatic GIST and DFSP
- Recurrence-free survival in adjuvant GIST.
The experience with imatinib in patients with MDS/MPNs associated with PDGFR gene re-arrangements is very limited. There are no controlled trials demonstrating a clinical benefit or increased survival for these diseases. ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended granting marketing authorization for Imatinib Teva B.V., a generic of Glivec.
The recommendation is that Imatinib Teva B.V. be approved to treat chronic myeloid leukemia (CML), acute lymphoblastic leukemia (ALL), hypereosinophilic syndrome (HES), chronic eosinophilic leukemia (CEL), myelodysplastic syndromes (MDS), myeloproliferative neoplasms (MPNs), gastrointestinal stromal tumors (GIST), and dermatofibrosarcoma protuberans (DFSP).
The European Commission typically adheres to the CHMP’s recommendations and delivers its final decision within 67 days of the CHMP’s recommendation.
The European Commission’s decision will be applicable to the entire European Economic Area—all member states of the European Union plus Iceland, Liechtenstein, and Norway.
If approved, Imatinib Teva B.V. will be available as capsules and film-coated tablets (100 mg and 400 mg). And it will be authorized:
- As monotherapy for pediatric patients with newly diagnosed, Philadelphia-chromosome-positive (Ph+) CML for whom bone marrow transplant is not considered the first line of treatment.
- As monotherapy for pediatric patients with Ph+ CML in chronic phase after failure of interferon-alpha therapy or in accelerated phase or blast crisis.
- As monotherapy for adults with Ph+ CML in blast crisis.
- Integrated with chemotherapy to treat adult and pediatric patients with newly diagnosed, Ph+ ALL.
- As monotherapy for adults with relapsed or refractory Ph+ ALL.
- As monotherapy for adults with MDS/MPNs associated with platelet-derived growth factor receptor gene re-arrangements.
- As monotherapy for adults with advanced HES and/or CEL with FIP1L1-PDGFRα rearrangement.
- As monotherapy for adults with Kit- (CD117-) positive, unresectable and/or metastatic malignant GISTs.
- For the adjuvant treatment of adults who are at significant risk of relapse following resection of Kit-positive GIST. Patients who have a low or very low risk of recurrence should not receive adjuvant treatment.
- As monotherapy for adults with unresectable DFSP and adults with recurrent and/or metastatic DFSP who are not eligible for surgery.
The CHMP said studies have demonstrated the satisfactory quality of Imatinib Teva B.V. and its bioequivalence to the reference product, Glivec.
In adult and pediatric patients, the effectiveness of imatinib is based on:
- Overall hematologic and cytogenetic response rates and progression-free survival in CML
- Hematologic and cytogenetic response rates in Ph+ ALL and MDS/MPNs
- Hematologic response rates in HES/CEL
- Objective response rates in adults with unresectable and/or metastatic GIST and DFSP
- Recurrence-free survival in adjuvant GIST.
The experience with imatinib in patients with MDS/MPNs associated with PDGFR gene re-arrangements is very limited. There are no controlled trials demonstrating a clinical benefit or increased survival for these diseases. ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended granting marketing authorization for Imatinib Teva B.V., a generic of Glivec.
The recommendation is that Imatinib Teva B.V. be approved to treat chronic myeloid leukemia (CML), acute lymphoblastic leukemia (ALL), hypereosinophilic syndrome (HES), chronic eosinophilic leukemia (CEL), myelodysplastic syndromes (MDS), myeloproliferative neoplasms (MPNs), gastrointestinal stromal tumors (GIST), and dermatofibrosarcoma protuberans (DFSP).
The European Commission typically adheres to the CHMP’s recommendations and delivers its final decision within 67 days of the CHMP’s recommendation.
The European Commission’s decision will be applicable to the entire European Economic Area—all member states of the European Union plus Iceland, Liechtenstein, and Norway.
If approved, Imatinib Teva B.V. will be available as capsules and film-coated tablets (100 mg and 400 mg). And it will be authorized:
- As monotherapy for pediatric patients with newly diagnosed, Philadelphia-chromosome-positive (Ph+) CML for whom bone marrow transplant is not considered the first line of treatment.
- As monotherapy for pediatric patients with Ph+ CML in chronic phase after failure of interferon-alpha therapy or in accelerated phase or blast crisis.
- As monotherapy for adults with Ph+ CML in blast crisis.
- Integrated with chemotherapy to treat adult and pediatric patients with newly diagnosed, Ph+ ALL.
- As monotherapy for adults with relapsed or refractory Ph+ ALL.
- As monotherapy for adults with MDS/MPNs associated with platelet-derived growth factor receptor gene re-arrangements.
- As monotherapy for adults with advanced HES and/or CEL with FIP1L1-PDGFRα rearrangement.
- As monotherapy for adults with Kit- (CD117-) positive, unresectable and/or metastatic malignant GISTs.
- For the adjuvant treatment of adults who are at significant risk of relapse following resection of Kit-positive GIST. Patients who have a low or very low risk of recurrence should not receive adjuvant treatment.
- As monotherapy for adults with unresectable DFSP and adults with recurrent and/or metastatic DFSP who are not eligible for surgery.
The CHMP said studies have demonstrated the satisfactory quality of Imatinib Teva B.V. and its bioequivalence to the reference product, Glivec.
In adult and pediatric patients, the effectiveness of imatinib is based on:
- Overall hematologic and cytogenetic response rates and progression-free survival in CML
- Hematologic and cytogenetic response rates in Ph+ ALL and MDS/MPNs
- Hematologic response rates in HES/CEL
- Objective response rates in adults with unresectable and/or metastatic GIST and DFSP
- Recurrence-free survival in adjuvant GIST.
The experience with imatinib in patients with MDS/MPNs associated with PDGFR gene re-arrangements is very limited. There are no controlled trials demonstrating a clinical benefit or increased survival for these diseases. ![]()
CHMP advocates refusal of application for SM drug
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended refusal of the marketing authorization for masitinib (Masipro).
Masitinib is a tyrosine kinase inhibitor being developed by AB Science to treat adults with smoldering or indolent severe systemic mastocytosis (SM).
To support the application for masitinib, AB Science presented data from a study involving 135 SM patients who had severe symptoms, including at least one of the following: itching, hot flashes, depression, and tiredness.
Researchers compared masitinib to placebo in these patients, looking for improvements in any of the symptoms during the first 24 weeks of treatment.
The CHMP said it was concerned about the reliability of the study results because a routine good clinical practice inspection at the study sites revealed serious failings in the way the study had been conducted.
In addition, major changes were made to the study design while the study was underway, which made the results difficult to interpret.
Finally, data on the safety of masitinib were limited. And the CHMP was concerned about side effects, including neutropenia and harmful effects on the skin and liver, which were particularly relevant because masitinib was intended to be used long-term.
Therefore, the CHMP concluded the benefits of masitinib do not appear to outweigh the risks, and the committee recommended the drug be refused marketing authorization.
The CHMP informed AB Science of this negative opinion in May, and the company asked the committee to re-examine its opinion. However, the CHMP ultimately concluded that masitinib should be refused marketing authorization.
AB Science said this decision does not have any consequences for patients in clinical trials or compassionate use programs of masitinib.
The company also said it intends to initiate a confirmatory study in patients with smoldering or indolent severe SM that is unresponsive to optimal symptomatic treatment in order to confirm the results from the first pivotal study. ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended refusal of the marketing authorization for masitinib (Masipro).
Masitinib is a tyrosine kinase inhibitor being developed by AB Science to treat adults with smoldering or indolent severe systemic mastocytosis (SM).
To support the application for masitinib, AB Science presented data from a study involving 135 SM patients who had severe symptoms, including at least one of the following: itching, hot flashes, depression, and tiredness.
Researchers compared masitinib to placebo in these patients, looking for improvements in any of the symptoms during the first 24 weeks of treatment.
The CHMP said it was concerned about the reliability of the study results because a routine good clinical practice inspection at the study sites revealed serious failings in the way the study had been conducted.
In addition, major changes were made to the study design while the study was underway, which made the results difficult to interpret.
Finally, data on the safety of masitinib were limited. And the CHMP was concerned about side effects, including neutropenia and harmful effects on the skin and liver, which were particularly relevant because masitinib was intended to be used long-term.
Therefore, the CHMP concluded the benefits of masitinib do not appear to outweigh the risks, and the committee recommended the drug be refused marketing authorization.
The CHMP informed AB Science of this negative opinion in May, and the company asked the committee to re-examine its opinion. However, the CHMP ultimately concluded that masitinib should be refused marketing authorization.
AB Science said this decision does not have any consequences for patients in clinical trials or compassionate use programs of masitinib.
The company also said it intends to initiate a confirmatory study in patients with smoldering or indolent severe SM that is unresponsive to optimal symptomatic treatment in order to confirm the results from the first pivotal study. ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended refusal of the marketing authorization for masitinib (Masipro).
Masitinib is a tyrosine kinase inhibitor being developed by AB Science to treat adults with smoldering or indolent severe systemic mastocytosis (SM).
To support the application for masitinib, AB Science presented data from a study involving 135 SM patients who had severe symptoms, including at least one of the following: itching, hot flashes, depression, and tiredness.
Researchers compared masitinib to placebo in these patients, looking for improvements in any of the symptoms during the first 24 weeks of treatment.
The CHMP said it was concerned about the reliability of the study results because a routine good clinical practice inspection at the study sites revealed serious failings in the way the study had been conducted.
In addition, major changes were made to the study design while the study was underway, which made the results difficult to interpret.
Finally, data on the safety of masitinib were limited. And the CHMP was concerned about side effects, including neutropenia and harmful effects on the skin and liver, which were particularly relevant because masitinib was intended to be used long-term.
Therefore, the CHMP concluded the benefits of masitinib do not appear to outweigh the risks, and the committee recommended the drug be refused marketing authorization.
The CHMP informed AB Science of this negative opinion in May, and the company asked the committee to re-examine its opinion. However, the CHMP ultimately concluded that masitinib should be refused marketing authorization.
AB Science said this decision does not have any consequences for patients in clinical trials or compassionate use programs of masitinib.
The company also said it intends to initiate a confirmatory study in patients with smoldering or indolent severe SM that is unresponsive to optimal symptomatic treatment in order to confirm the results from the first pivotal study. ![]()
Tattooing and piercing are no longer taboo, but health concerns persist
Educate adolescents about the potential medical complications and social consequences of tattooing and body piercing as their popularity rises, an American Academy of Pediatrics clinical report recommends.
The most common complications post tattooing are bacterial and viral infections, and inflammation at the site of the tattoo. Rarely, more serious complications can arise in the form of endocarditis, gangrene, and amputations. Postprocedure care is important in preventing most complications: “Reputable tattoo parlors and piercing salons should provide a long list of do’s and don’ts on how to care for the area that was worked on, and what signs might indicate a problem,” Cora C. Breuner, MD, chairperson of the AAP Committee on Adolescence and coauthor of the report, said in a press statement. The clinical report was presented at the AAP annual meeting in Chicago and simultaneously published in the journal Pediatrics (2017 Sep 18. doi: 10.1542/peds.2017-1962).
Data concerning adolescent tattooing and piercing vary by source and age, but there is a distinct trend of adolescents getting or having an interest in body modification. In samples of adolescents attending clinics at ages 12-22 years, 10%-23% had tattoos and 27%-42% had body piercing (other than the earlobe); rates were higher among girls vs. boys and among older vs. young adolescents. “Of students with current piercings, high-ear cartilage (53%) was the most common visible piercing, followed by navel (38%), tongue (13%), and nipple and genital (9%) piercings” according to the report.
A concern that many adolescents and young adults may not consider is how tattoos affect society’s perception of tattooed and pierced people. A 2008 study found that 29% of people surveyed thought tattooed people were more likely to engage in deviant behavior; this belief had decreased to 24% by 2012 , according to a Harris Poll.
While society at large may appear more accepting of tattooed individuals, employers may be less open to hiring them. According to an executive career coach, “37% of human resource managers cite tattoos as the third physical attribute likely to limit career potential” with non-ear piercings in the top two barriers to career advancement (Am J Nurs. 2012;112[5]:15). In a 2014 survey of 2,675 people, 76% thought that tattoos and/or piercings had hurt their chances of getting a job, and 39% thought employees with tattoos and/or body piercings reflect poorly on their employers. Also, 42% of those surveyed felt visible tattoos are inappropriate at work, with 55% felt the same about body piercings.
“In most cases, teens just enjoy the look of the tattoo or piercing, but we do advise them to talk any decision over with their parents or another adult first,” David Levine, MD, coauthor of the AAP report, said in a press statement. “They may not realize how expensive it is to remove a tattoo, or how a piercing on your tongue might result in a chipped tooth.”
Laser removal of tattoos can range from $49 to $300 per square inch of treatment area, according to the report.
Some tips from the report
- You should advise adolescent patients to assess sanitary and hygienic practices of the tattoo parlors and tattoo artists, including: “use of new, disposable gloves; removal of the new needle and equipment from a sealed, sterile container; and the use of fresh, unused ink poured into a new, disposable container with each new client.”
- You should advise adolescents with tattoos to come to the office if there are signs and symptoms of infection .
- Lesions that appear to grow and/or change within a tattoo suggest a neoplasm.
- You should familiarize yourself with local laws and regulations related to tattooing so you can inform patients and parents.
- Counsel adolescents about the implications of visible tattoos on jobs.
- Use antibiotic agents with good coverage against Pseudomonas and Staphylococcus species (such as fluoroquinolones) to treat piercing-associated infections of the auricular cartilage.
- Recommend removing all jewelry during contact sports. If jewelry interferes with mouth guards or protective equipment, it should be removed before play. Have patients remove nipple jewelry prior to breastfeeding.
The authors have no relevant financial disclosures.
Educate adolescents about the potential medical complications and social consequences of tattooing and body piercing as their popularity rises, an American Academy of Pediatrics clinical report recommends.
The most common complications post tattooing are bacterial and viral infections, and inflammation at the site of the tattoo. Rarely, more serious complications can arise in the form of endocarditis, gangrene, and amputations. Postprocedure care is important in preventing most complications: “Reputable tattoo parlors and piercing salons should provide a long list of do’s and don’ts on how to care for the area that was worked on, and what signs might indicate a problem,” Cora C. Breuner, MD, chairperson of the AAP Committee on Adolescence and coauthor of the report, said in a press statement. The clinical report was presented at the AAP annual meeting in Chicago and simultaneously published in the journal Pediatrics (2017 Sep 18. doi: 10.1542/peds.2017-1962).
Data concerning adolescent tattooing and piercing vary by source and age, but there is a distinct trend of adolescents getting or having an interest in body modification. In samples of adolescents attending clinics at ages 12-22 years, 10%-23% had tattoos and 27%-42% had body piercing (other than the earlobe); rates were higher among girls vs. boys and among older vs. young adolescents. “Of students with current piercings, high-ear cartilage (53%) was the most common visible piercing, followed by navel (38%), tongue (13%), and nipple and genital (9%) piercings” according to the report.
A concern that many adolescents and young adults may not consider is how tattoos affect society’s perception of tattooed and pierced people. A 2008 study found that 29% of people surveyed thought tattooed people were more likely to engage in deviant behavior; this belief had decreased to 24% by 2012 , according to a Harris Poll.
While society at large may appear more accepting of tattooed individuals, employers may be less open to hiring them. According to an executive career coach, “37% of human resource managers cite tattoos as the third physical attribute likely to limit career potential” with non-ear piercings in the top two barriers to career advancement (Am J Nurs. 2012;112[5]:15). In a 2014 survey of 2,675 people, 76% thought that tattoos and/or piercings had hurt their chances of getting a job, and 39% thought employees with tattoos and/or body piercings reflect poorly on their employers. Also, 42% of those surveyed felt visible tattoos are inappropriate at work, with 55% felt the same about body piercings.
“In most cases, teens just enjoy the look of the tattoo or piercing, but we do advise them to talk any decision over with their parents or another adult first,” David Levine, MD, coauthor of the AAP report, said in a press statement. “They may not realize how expensive it is to remove a tattoo, or how a piercing on your tongue might result in a chipped tooth.”
Laser removal of tattoos can range from $49 to $300 per square inch of treatment area, according to the report.
Some tips from the report
- You should advise adolescent patients to assess sanitary and hygienic practices of the tattoo parlors and tattoo artists, including: “use of new, disposable gloves; removal of the new needle and equipment from a sealed, sterile container; and the use of fresh, unused ink poured into a new, disposable container with each new client.”
- You should advise adolescents with tattoos to come to the office if there are signs and symptoms of infection .
- Lesions that appear to grow and/or change within a tattoo suggest a neoplasm.
- You should familiarize yourself with local laws and regulations related to tattooing so you can inform patients and parents.
- Counsel adolescents about the implications of visible tattoos on jobs.
- Use antibiotic agents with good coverage against Pseudomonas and Staphylococcus species (such as fluoroquinolones) to treat piercing-associated infections of the auricular cartilage.
- Recommend removing all jewelry during contact sports. If jewelry interferes with mouth guards or protective equipment, it should be removed before play. Have patients remove nipple jewelry prior to breastfeeding.
The authors have no relevant financial disclosures.
Educate adolescents about the potential medical complications and social consequences of tattooing and body piercing as their popularity rises, an American Academy of Pediatrics clinical report recommends.
The most common complications post tattooing are bacterial and viral infections, and inflammation at the site of the tattoo. Rarely, more serious complications can arise in the form of endocarditis, gangrene, and amputations. Postprocedure care is important in preventing most complications: “Reputable tattoo parlors and piercing salons should provide a long list of do’s and don’ts on how to care for the area that was worked on, and what signs might indicate a problem,” Cora C. Breuner, MD, chairperson of the AAP Committee on Adolescence and coauthor of the report, said in a press statement. The clinical report was presented at the AAP annual meeting in Chicago and simultaneously published in the journal Pediatrics (2017 Sep 18. doi: 10.1542/peds.2017-1962).
Data concerning adolescent tattooing and piercing vary by source and age, but there is a distinct trend of adolescents getting or having an interest in body modification. In samples of adolescents attending clinics at ages 12-22 years, 10%-23% had tattoos and 27%-42% had body piercing (other than the earlobe); rates were higher among girls vs. boys and among older vs. young adolescents. “Of students with current piercings, high-ear cartilage (53%) was the most common visible piercing, followed by navel (38%), tongue (13%), and nipple and genital (9%) piercings” according to the report.
A concern that many adolescents and young adults may not consider is how tattoos affect society’s perception of tattooed and pierced people. A 2008 study found that 29% of people surveyed thought tattooed people were more likely to engage in deviant behavior; this belief had decreased to 24% by 2012 , according to a Harris Poll.
While society at large may appear more accepting of tattooed individuals, employers may be less open to hiring them. According to an executive career coach, “37% of human resource managers cite tattoos as the third physical attribute likely to limit career potential” with non-ear piercings in the top two barriers to career advancement (Am J Nurs. 2012;112[5]:15). In a 2014 survey of 2,675 people, 76% thought that tattoos and/or piercings had hurt their chances of getting a job, and 39% thought employees with tattoos and/or body piercings reflect poorly on their employers. Also, 42% of those surveyed felt visible tattoos are inappropriate at work, with 55% felt the same about body piercings.
“In most cases, teens just enjoy the look of the tattoo or piercing, but we do advise them to talk any decision over with their parents or another adult first,” David Levine, MD, coauthor of the AAP report, said in a press statement. “They may not realize how expensive it is to remove a tattoo, or how a piercing on your tongue might result in a chipped tooth.”
Laser removal of tattoos can range from $49 to $300 per square inch of treatment area, according to the report.
Some tips from the report
- You should advise adolescent patients to assess sanitary and hygienic practices of the tattoo parlors and tattoo artists, including: “use of new, disposable gloves; removal of the new needle and equipment from a sealed, sterile container; and the use of fresh, unused ink poured into a new, disposable container with each new client.”
- You should advise adolescents with tattoos to come to the office if there are signs and symptoms of infection .
- Lesions that appear to grow and/or change within a tattoo suggest a neoplasm.
- You should familiarize yourself with local laws and regulations related to tattooing so you can inform patients and parents.
- Counsel adolescents about the implications of visible tattoos on jobs.
- Use antibiotic agents with good coverage against Pseudomonas and Staphylococcus species (such as fluoroquinolones) to treat piercing-associated infections of the auricular cartilage.
- Recommend removing all jewelry during contact sports. If jewelry interferes with mouth guards or protective equipment, it should be removed before play. Have patients remove nipple jewelry prior to breastfeeding.
The authors have no relevant financial disclosures.
FROM AAP 2017
Oral Cues to Disease
1. A 21-year-old man complains of prolonged diarrhea with steady abdominal pain and recent weight loss. He also reports painful knee and hip joints and generalized fatigue. Physical exam reveals fissure-like ulcerations of the mandibular buccal vestibule and localized abdominal pain with fullness in the right lower quadrant.
Diagnosis: Crohn disease can affect the gastrointestinal tract anywhere from the mouth to the anus, and can manifest with oral findings that may not correlate with abdominal symptoms (eg, mucosal cobble stoning, mucosal tags, deep linear ulcerations, gingival hyperplasia, lip fissuring, aphthous ulcers, angular cheilitis). Other features may include diffuse, painless swelling of the lips and mucosal erythema.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
2. Over the past few months, this 43-year-old woman has had multiple severely painful, slow-healing oral ulcers, resulting in the erosion of the lower lip. She reports pain on swallowing and occasional bloody nose after blowing in the morning.
Diagnosis: Vesiculo-bullous lesions in the mouth may be seen with pemphigus vulgaris or bullous pemphigoid. Pemphigus vulgaris, an autoimmune intraepithelial blistering disease, often manifests as flaccid bullae or painful ulcerations in the oral cavity prior to the onset of skin lesions.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
3. A 26-year-old woman presents with fever and fatigue, as well as arthralgia in her hands. Upon examination, she has a malar rash and lichenoid inflammation of the buccal mucosa. She has a family history of autoimmune disorders.
Diagnosis: Oral findings suggestive of systemic or discoid lupus erythematosus may greatly resemble those of oral lichen planus.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
4. This 14-year-old girl is concerned about the multiple ecchymoses and thrombi in her mouth. She feels fatigued and has a fever. Her history includes a tendency to bruise easily, menorrhagia, and a recent infection treated with vancomycin. Physical exam is notable for retinal hemorrhages and jaundice.
Diagnosis: Thrombocytopenia purpura may manifest with oral petechiae, purpura, oral hematomas, or hemorrhagic bullae.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
1. A 21-year-old man complains of prolonged diarrhea with steady abdominal pain and recent weight loss. He also reports painful knee and hip joints and generalized fatigue. Physical exam reveals fissure-like ulcerations of the mandibular buccal vestibule and localized abdominal pain with fullness in the right lower quadrant.
Diagnosis: Crohn disease can affect the gastrointestinal tract anywhere from the mouth to the anus, and can manifest with oral findings that may not correlate with abdominal symptoms (eg, mucosal cobble stoning, mucosal tags, deep linear ulcerations, gingival hyperplasia, lip fissuring, aphthous ulcers, angular cheilitis). Other features may include diffuse, painless swelling of the lips and mucosal erythema.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
2. Over the past few months, this 43-year-old woman has had multiple severely painful, slow-healing oral ulcers, resulting in the erosion of the lower lip. She reports pain on swallowing and occasional bloody nose after blowing in the morning.
Diagnosis: Vesiculo-bullous lesions in the mouth may be seen with pemphigus vulgaris or bullous pemphigoid. Pemphigus vulgaris, an autoimmune intraepithelial blistering disease, often manifests as flaccid bullae or painful ulcerations in the oral cavity prior to the onset of skin lesions.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
3. A 26-year-old woman presents with fever and fatigue, as well as arthralgia in her hands. Upon examination, she has a malar rash and lichenoid inflammation of the buccal mucosa. She has a family history of autoimmune disorders.
Diagnosis: Oral findings suggestive of systemic or discoid lupus erythematosus may greatly resemble those of oral lichen planus.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
4. This 14-year-old girl is concerned about the multiple ecchymoses and thrombi in her mouth. She feels fatigued and has a fever. Her history includes a tendency to bruise easily, menorrhagia, and a recent infection treated with vancomycin. Physical exam is notable for retinal hemorrhages and jaundice.
Diagnosis: Thrombocytopenia purpura may manifest with oral petechiae, purpura, oral hematomas, or hemorrhagic bullae.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
1. A 21-year-old man complains of prolonged diarrhea with steady abdominal pain and recent weight loss. He also reports painful knee and hip joints and generalized fatigue. Physical exam reveals fissure-like ulcerations of the mandibular buccal vestibule and localized abdominal pain with fullness in the right lower quadrant.
Diagnosis: Crohn disease can affect the gastrointestinal tract anywhere from the mouth to the anus, and can manifest with oral findings that may not correlate with abdominal symptoms (eg, mucosal cobble stoning, mucosal tags, deep linear ulcerations, gingival hyperplasia, lip fissuring, aphthous ulcers, angular cheilitis). Other features may include diffuse, painless swelling of the lips and mucosal erythema.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
2. Over the past few months, this 43-year-old woman has had multiple severely painful, slow-healing oral ulcers, resulting in the erosion of the lower lip. She reports pain on swallowing and occasional bloody nose after blowing in the morning.
Diagnosis: Vesiculo-bullous lesions in the mouth may be seen with pemphigus vulgaris or bullous pemphigoid. Pemphigus vulgaris, an autoimmune intraepithelial blistering disease, often manifests as flaccid bullae or painful ulcerations in the oral cavity prior to the onset of skin lesions.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
3. A 26-year-old woman presents with fever and fatigue, as well as arthralgia in her hands. Upon examination, she has a malar rash and lichenoid inflammation of the buccal mucosa. She has a family history of autoimmune disorders.
Diagnosis: Oral findings suggestive of systemic or discoid lupus erythematosus may greatly resemble those of oral lichen planus.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
4. This 14-year-old girl is concerned about the multiple ecchymoses and thrombi in her mouth. She feels fatigued and has a fever. Her history includes a tendency to bruise easily, menorrhagia, and a recent infection treated with vancomycin. Physical exam is notable for retinal hemorrhages and jaundice.
Diagnosis: Thrombocytopenia purpura may manifest with oral petechiae, purpura, oral hematomas, or hemorrhagic bullae.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
COPD in Primary Care
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CONCEPTT: Continuous glucose monitoring during pregnancy benefits baby
LISBON – , according to the investigators of a prospective, multicenter, randomized, controlled study who found that it improved a number of neonatal outcomes.
In the open-label Continuous Glucose Monitoring in Pregnant Women with Type 1 Diabetes(CONCEPTT) study, infants born to mothers who had used continuous glucose monitoring (CGM) versus those who had not had a 49% lower chance of being large for gestational age (53% vs. 69%, odds ratio [OR] 0.51, P = .0210) and were 52% less likely to need neonatal intensive care lasting for longer than 24 hours (27% vs. 43%, OR 0.48, P = .0157).
Neonates born to mothers who used CGM during their pregnancy were also less likely to experience hypoglycemia (15% vs. 28%, OR 0.45, P = .0250) and were able to leave the hospital with their mother 1 day earlier (P = .0091) than those born to mothers who did not use CGM.However, these were secondary outcomes of the study, which first looked at how CGM affected the glycemic profile of the mother.“To the best of our knowledge, this is the first trial to demonstrate a benefit of CGM on health outcomes beyond glucose control,” Helen Murphy, MD, one of the CONCEPTT trial’s two principal investigators, said at the annual meeting of the European Association for the Study of Diabetes.
“We would suggest, on the back of these data, that CGM should be offered to all pregnant women with type 1 diabetes using intensive insulin therapy during the first trimester,” Dr. Murphy said, adding that results of the study were simultaneously published online in the Lancet (2017 Sept. 15. doi. 10.1016/S0140-6736(17)32400-5).
“The CONCEPTT study will change the future for pregnant women with diabetes,” commented Elisabeth Mathiesen, MD, who was the EASD’s invited discussant for the study, and who congratulated the investigators for “a well performed study” and being “brave,” as “performing a RCT [randomized controlled trial] in pregnancy is not easy”.
Satish Garg, MD, and Sarit Polsky, MD, of the Barbara Davis Center for Diabetes at the University of Colorado, Denver, agreed in an editorial (Lancet 2017; Sept. 12. doi: 10.1016/S0140-6736(17)32449-2) accompanying the published article that the study findings were clinically important.
“We believe that the CONCEPTT results support CGM use during pregnancy for all women with type 1 diabetes,” they wrote, adding that the mother’s “time in [glycated hemoglobin, HbA1C] range might become an important measure in pregnancies with type 1 diabetes.”
Dr. Garg and Dr. Polsky also suggested that endocrine and obstetric medical societies take note and perhaps revise accordingly their guidelines on the use of CGM during pregnancy in diabetic women.
CONCEPTT involved 325 women with type 1 diabetes; 215 were pregnant at the time of enrollment, and 110 were planning on becoming pregnant in the near future.
Co-principal investigator Denice Feig, MD, of Sinai Health System in Toronto, explained that women were eligible for inclusion in the trial if they had type 1 diabetes for at least 1 year, were aged between 18 and 40 years, and had been using daily insulin delivered by either an insulin pump or multiple daily injections (MDI). At enrollment, the participants’ insulin regimen had to been stable for at least 4 weeks before randomization to CGM with capillary glucose monitoring or capillary glucose monitoring alone and their glycemic control had to be suboptimal.
Two groups of women were studied: a “pre-pregnancy group” of women who were planning on pregnancy and wanted to optimize their glycemic control before conception, and a “pregnancy group” of women in their first trimester (less than 14 weeks’ gestation) who were due to have a live, singleton birth as confirmed by ultrasound.
The primary outcome of the trial was the change in HbA1C from baseline to 34 weeks, with pre-specified secondary outcomes of various CGM measures, neoneonatal outcomes, and patient-reported outcomes.
Pregnant women using CGM had lower HbA1C levels during the trial than women who did not have CGM monitoring, although the difference was small (–0.19%, P = .0207).
The use of CGM was associated with more time spent in target HbA1C range (68% of women using CMG vs. 61% of those not using CGM, P = .0034), with less time being hyperglycemic (27% vs. 37%, P = .0279) and comparable rates of hypoglycemia (17 vs. 21 episodes) and time spent being hypoglycemic (2% vs. 4%, P = .10).“The CGM effects were very comparable among insulin pump and MDI users and across 31 international sites,” Dr. Murphy summarized, although she noted that there was no consistent benefit of using CGM seen in women who were planning a pregnancy. Dr. Feig noted that the strengths of the study were the large sample size and that CGM was used continuously from the first trimester until delivery. Women using both pumps and MDI were included at multiple centers and countries, and HbA1C was centrally assessed, with detailed CGM measures used in an exclusively type 1 diabetes population.“Of note, one needed to treat only six women with CGM to prevent one episode of large for gestational age,” Dr. Feig reported. “One needed to treat only eight women to prevent one neonatal hypoglycemia, and six women to prevent one NICU [neonatal intensive care unit] admission over 24 hours.”
There were some limitations, of course, including: around 20% of women had missing data on their HbA1C level; women using CGM also made more unscheduled visits to their health care providers although there are no data on the frequency of self-monitoring of blood glucose or frequency of insulin bolus dosing; and the study was open label.
In her independent précis of the trial, Dr. Mathiesen, professor of endocrinology and chief physician managing pregnant women with diabetes at the Rigshospitalet University Hospital in Copenhagen, noted that there were some other downsides to using CGM in the study.
The CONCEPTT study was funded by the Juvenile Diabetes Research Foundation, the Canadian Clinical Trial Network, the National Institute for Health Research, the Center for Mother, Infant, and Child Research, and the Jaeb Center for Health Research. Medtronic also supported the study by providing the CGM sensors and systems at a reduced cost. Dr. Feig declared she had no competing interests. Dr. Murphy disclosed sitting on an advisory board for Medtronic and receiving personal fees from Novo Nordisk and Roche, unrelated to the current study. Dr. Mathiesen was the invited EASD independent commentator for the trial and did not give any disclosures. Dr. Garg has received advisory board consulting fees and research grants from Medtronic and several other pharmaceutical companies specializing in diabetes care. Dr. Polsky has received research funding from DexCom for diabetes device use in patients with diabetes paid directly to the University of Denver.
LISBON – , according to the investigators of a prospective, multicenter, randomized, controlled study who found that it improved a number of neonatal outcomes.
In the open-label Continuous Glucose Monitoring in Pregnant Women with Type 1 Diabetes(CONCEPTT) study, infants born to mothers who had used continuous glucose monitoring (CGM) versus those who had not had a 49% lower chance of being large for gestational age (53% vs. 69%, odds ratio [OR] 0.51, P = .0210) and were 52% less likely to need neonatal intensive care lasting for longer than 24 hours (27% vs. 43%, OR 0.48, P = .0157).
Neonates born to mothers who used CGM during their pregnancy were also less likely to experience hypoglycemia (15% vs. 28%, OR 0.45, P = .0250) and were able to leave the hospital with their mother 1 day earlier (P = .0091) than those born to mothers who did not use CGM.However, these were secondary outcomes of the study, which first looked at how CGM affected the glycemic profile of the mother.“To the best of our knowledge, this is the first trial to demonstrate a benefit of CGM on health outcomes beyond glucose control,” Helen Murphy, MD, one of the CONCEPTT trial’s two principal investigators, said at the annual meeting of the European Association for the Study of Diabetes.
“We would suggest, on the back of these data, that CGM should be offered to all pregnant women with type 1 diabetes using intensive insulin therapy during the first trimester,” Dr. Murphy said, adding that results of the study were simultaneously published online in the Lancet (2017 Sept. 15. doi. 10.1016/S0140-6736(17)32400-5).
“The CONCEPTT study will change the future for pregnant women with diabetes,” commented Elisabeth Mathiesen, MD, who was the EASD’s invited discussant for the study, and who congratulated the investigators for “a well performed study” and being “brave,” as “performing a RCT [randomized controlled trial] in pregnancy is not easy”.
Satish Garg, MD, and Sarit Polsky, MD, of the Barbara Davis Center for Diabetes at the University of Colorado, Denver, agreed in an editorial (Lancet 2017; Sept. 12. doi: 10.1016/S0140-6736(17)32449-2) accompanying the published article that the study findings were clinically important.
“We believe that the CONCEPTT results support CGM use during pregnancy for all women with type 1 diabetes,” they wrote, adding that the mother’s “time in [glycated hemoglobin, HbA1C] range might become an important measure in pregnancies with type 1 diabetes.”
Dr. Garg and Dr. Polsky also suggested that endocrine and obstetric medical societies take note and perhaps revise accordingly their guidelines on the use of CGM during pregnancy in diabetic women.
CONCEPTT involved 325 women with type 1 diabetes; 215 were pregnant at the time of enrollment, and 110 were planning on becoming pregnant in the near future.
Co-principal investigator Denice Feig, MD, of Sinai Health System in Toronto, explained that women were eligible for inclusion in the trial if they had type 1 diabetes for at least 1 year, were aged between 18 and 40 years, and had been using daily insulin delivered by either an insulin pump or multiple daily injections (MDI). At enrollment, the participants’ insulin regimen had to been stable for at least 4 weeks before randomization to CGM with capillary glucose monitoring or capillary glucose monitoring alone and their glycemic control had to be suboptimal.
Two groups of women were studied: a “pre-pregnancy group” of women who were planning on pregnancy and wanted to optimize their glycemic control before conception, and a “pregnancy group” of women in their first trimester (less than 14 weeks’ gestation) who were due to have a live, singleton birth as confirmed by ultrasound.
The primary outcome of the trial was the change in HbA1C from baseline to 34 weeks, with pre-specified secondary outcomes of various CGM measures, neoneonatal outcomes, and patient-reported outcomes.
Pregnant women using CGM had lower HbA1C levels during the trial than women who did not have CGM monitoring, although the difference was small (–0.19%, P = .0207).
The use of CGM was associated with more time spent in target HbA1C range (68% of women using CMG vs. 61% of those not using CGM, P = .0034), with less time being hyperglycemic (27% vs. 37%, P = .0279) and comparable rates of hypoglycemia (17 vs. 21 episodes) and time spent being hypoglycemic (2% vs. 4%, P = .10).“The CGM effects were very comparable among insulin pump and MDI users and across 31 international sites,” Dr. Murphy summarized, although she noted that there was no consistent benefit of using CGM seen in women who were planning a pregnancy. Dr. Feig noted that the strengths of the study were the large sample size and that CGM was used continuously from the first trimester until delivery. Women using both pumps and MDI were included at multiple centers and countries, and HbA1C was centrally assessed, with detailed CGM measures used in an exclusively type 1 diabetes population.“Of note, one needed to treat only six women with CGM to prevent one episode of large for gestational age,” Dr. Feig reported. “One needed to treat only eight women to prevent one neonatal hypoglycemia, and six women to prevent one NICU [neonatal intensive care unit] admission over 24 hours.”
There were some limitations, of course, including: around 20% of women had missing data on their HbA1C level; women using CGM also made more unscheduled visits to their health care providers although there are no data on the frequency of self-monitoring of blood glucose or frequency of insulin bolus dosing; and the study was open label.
In her independent précis of the trial, Dr. Mathiesen, professor of endocrinology and chief physician managing pregnant women with diabetes at the Rigshospitalet University Hospital in Copenhagen, noted that there were some other downsides to using CGM in the study.
The CONCEPTT study was funded by the Juvenile Diabetes Research Foundation, the Canadian Clinical Trial Network, the National Institute for Health Research, the Center for Mother, Infant, and Child Research, and the Jaeb Center for Health Research. Medtronic also supported the study by providing the CGM sensors and systems at a reduced cost. Dr. Feig declared she had no competing interests. Dr. Murphy disclosed sitting on an advisory board for Medtronic and receiving personal fees from Novo Nordisk and Roche, unrelated to the current study. Dr. Mathiesen was the invited EASD independent commentator for the trial and did not give any disclosures. Dr. Garg has received advisory board consulting fees and research grants from Medtronic and several other pharmaceutical companies specializing in diabetes care. Dr. Polsky has received research funding from DexCom for diabetes device use in patients with diabetes paid directly to the University of Denver.
LISBON – , according to the investigators of a prospective, multicenter, randomized, controlled study who found that it improved a number of neonatal outcomes.
In the open-label Continuous Glucose Monitoring in Pregnant Women with Type 1 Diabetes(CONCEPTT) study, infants born to mothers who had used continuous glucose monitoring (CGM) versus those who had not had a 49% lower chance of being large for gestational age (53% vs. 69%, odds ratio [OR] 0.51, P = .0210) and were 52% less likely to need neonatal intensive care lasting for longer than 24 hours (27% vs. 43%, OR 0.48, P = .0157).
Neonates born to mothers who used CGM during their pregnancy were also less likely to experience hypoglycemia (15% vs. 28%, OR 0.45, P = .0250) and were able to leave the hospital with their mother 1 day earlier (P = .0091) than those born to mothers who did not use CGM.However, these were secondary outcomes of the study, which first looked at how CGM affected the glycemic profile of the mother.“To the best of our knowledge, this is the first trial to demonstrate a benefit of CGM on health outcomes beyond glucose control,” Helen Murphy, MD, one of the CONCEPTT trial’s two principal investigators, said at the annual meeting of the European Association for the Study of Diabetes.
“We would suggest, on the back of these data, that CGM should be offered to all pregnant women with type 1 diabetes using intensive insulin therapy during the first trimester,” Dr. Murphy said, adding that results of the study were simultaneously published online in the Lancet (2017 Sept. 15. doi. 10.1016/S0140-6736(17)32400-5).
“The CONCEPTT study will change the future for pregnant women with diabetes,” commented Elisabeth Mathiesen, MD, who was the EASD’s invited discussant for the study, and who congratulated the investigators for “a well performed study” and being “brave,” as “performing a RCT [randomized controlled trial] in pregnancy is not easy”.
Satish Garg, MD, and Sarit Polsky, MD, of the Barbara Davis Center for Diabetes at the University of Colorado, Denver, agreed in an editorial (Lancet 2017; Sept. 12. doi: 10.1016/S0140-6736(17)32449-2) accompanying the published article that the study findings were clinically important.
“We believe that the CONCEPTT results support CGM use during pregnancy for all women with type 1 diabetes,” they wrote, adding that the mother’s “time in [glycated hemoglobin, HbA1C] range might become an important measure in pregnancies with type 1 diabetes.”
Dr. Garg and Dr. Polsky also suggested that endocrine and obstetric medical societies take note and perhaps revise accordingly their guidelines on the use of CGM during pregnancy in diabetic women.
CONCEPTT involved 325 women with type 1 diabetes; 215 were pregnant at the time of enrollment, and 110 were planning on becoming pregnant in the near future.
Co-principal investigator Denice Feig, MD, of Sinai Health System in Toronto, explained that women were eligible for inclusion in the trial if they had type 1 diabetes for at least 1 year, were aged between 18 and 40 years, and had been using daily insulin delivered by either an insulin pump or multiple daily injections (MDI). At enrollment, the participants’ insulin regimen had to been stable for at least 4 weeks before randomization to CGM with capillary glucose monitoring or capillary glucose monitoring alone and their glycemic control had to be suboptimal.
Two groups of women were studied: a “pre-pregnancy group” of women who were planning on pregnancy and wanted to optimize their glycemic control before conception, and a “pregnancy group” of women in their first trimester (less than 14 weeks’ gestation) who were due to have a live, singleton birth as confirmed by ultrasound.
The primary outcome of the trial was the change in HbA1C from baseline to 34 weeks, with pre-specified secondary outcomes of various CGM measures, neoneonatal outcomes, and patient-reported outcomes.
Pregnant women using CGM had lower HbA1C levels during the trial than women who did not have CGM monitoring, although the difference was small (–0.19%, P = .0207).
The use of CGM was associated with more time spent in target HbA1C range (68% of women using CMG vs. 61% of those not using CGM, P = .0034), with less time being hyperglycemic (27% vs. 37%, P = .0279) and comparable rates of hypoglycemia (17 vs. 21 episodes) and time spent being hypoglycemic (2% vs. 4%, P = .10).“The CGM effects were very comparable among insulin pump and MDI users and across 31 international sites,” Dr. Murphy summarized, although she noted that there was no consistent benefit of using CGM seen in women who were planning a pregnancy. Dr. Feig noted that the strengths of the study were the large sample size and that CGM was used continuously from the first trimester until delivery. Women using both pumps and MDI were included at multiple centers and countries, and HbA1C was centrally assessed, with detailed CGM measures used in an exclusively type 1 diabetes population.“Of note, one needed to treat only six women with CGM to prevent one episode of large for gestational age,” Dr. Feig reported. “One needed to treat only eight women to prevent one neonatal hypoglycemia, and six women to prevent one NICU [neonatal intensive care unit] admission over 24 hours.”
There were some limitations, of course, including: around 20% of women had missing data on their HbA1C level; women using CGM also made more unscheduled visits to their health care providers although there are no data on the frequency of self-monitoring of blood glucose or frequency of insulin bolus dosing; and the study was open label.
In her independent précis of the trial, Dr. Mathiesen, professor of endocrinology and chief physician managing pregnant women with diabetes at the Rigshospitalet University Hospital in Copenhagen, noted that there were some other downsides to using CGM in the study.
The CONCEPTT study was funded by the Juvenile Diabetes Research Foundation, the Canadian Clinical Trial Network, the National Institute for Health Research, the Center for Mother, Infant, and Child Research, and the Jaeb Center for Health Research. Medtronic also supported the study by providing the CGM sensors and systems at a reduced cost. Dr. Feig declared she had no competing interests. Dr. Murphy disclosed sitting on an advisory board for Medtronic and receiving personal fees from Novo Nordisk and Roche, unrelated to the current study. Dr. Mathiesen was the invited EASD independent commentator for the trial and did not give any disclosures. Dr. Garg has received advisory board consulting fees and research grants from Medtronic and several other pharmaceutical companies specializing in diabetes care. Dr. Polsky has received research funding from DexCom for diabetes device use in patients with diabetes paid directly to the University of Denver.
AT EASD 2017
Key clinical point: Continuous glucose monitoring should be offered to women with type 1 diabetes on intensive insulin therapy during their pregnancy.
Major finding: Neonatal outcomes were significantly better if women used CGM while they were pregnant than if they did not. Some maternal outcomes were also improved.
Data source: CONCEPTT: a prospective, multicenter, open-label, randomized controlled trial of 325 women with type 1 diabetes: 215 were pregnant; 110 were planning a pregnancy.
Disclosures: The study was funded by the Juvenile Diabetes Research Foundation, the Canadian Clinical Trial Network, the National Institute for Health Research, the Center for Mother, Infant, and Child Research, and the Jaeb Center for Health Research. Medtronic also supported the study by providing the CGM sensors and systems at a reduced cost. One of the study presenters disclosed sitting on an advisory board for Medtronic.
How can pediatricians help prevent preschool expulsions?
CHICAGO –
Young African American boys are particularly at risk, said Claire Lerner, a senior parenting specialist with the nonprofit organization Zero to Three in Washington.
Speaking at the annual meeting of the American Academy of Pediatrics, Ms. Lerner cited data from 2005 showing that 10.4% of prekindergarten (preK) teachers had expelled at least one child for behavior problems during the previous year, yielding a preK expulsion rate of 6.7 per 1,000 students. This contrasts with a K-12 expulsion rate of 2.1 per 1,000 students.
“What I would say to you is that if a parent, or school, or caregiver comes to you and says, ‘The teacher’s concerned about X,’ don’t dismiss it. I cannot tell you how many times parents have come to me and said, ‘Well, the pediatrician says he’s totally fine. He’s just two.’”
This is not to blame pediatricians, said Ms. Lerner. Rather, “it’s to help you remember that teachers are smart, and they’re with these kids in a natural environment all day long. ...You are seeing such a random, finite, artificial experience in that room that you don’t see what’s going on in the classroom.” The child’s interactions with other children -- usually the impetus for disciplinary action -- will not necessarily be apparent in the pediatrician’s office.
Often, said Ms. Lerner, the child in question isn’t picking up on verbal and physical clues from other children, leading to behavior that’s seen as inappropriate or aggressive by other children -- and by staff. “A lot of these kids have motor planning problems, meaning they don’t know how to take their idea and execute it, so they’re the ones who are knocking down towers, and in kids’ faces. ...Those are the things that I’m talking about that are very unlikely to be picked up in a pediatric well-child visit,” she said.
“The evidence tells us that gender and race matter” in preschool suspensions and expulsions, said Ms. Lerner, noting that black preschool children are 3.6 times as likely as white children to be given an out-of-school suspension.
Black boys, she said, are 19% of male preschool attendees but make up 45% of the preschool children who receive out-of-school suspensions. Black girls make up 20% of female preschool attendees, but 54% of preschool girls who receive out-of-school suspensions are black.
In public preschools, 78% of those suspended are boys, though they make up just 54% of the attendees.
Aside from the home and work disruption caused by these suspensions, Ms. Lerner said that later outcomes are much worse for young students who are expelled or suspended, stacking the deck further against success. Rates of dropping out of high school, grade retention, and incarceration may be up to 10 times higher for these children.
Many school-related factors, including a higher child-teacher ratio and a longer school day, are associated with higher rates of preschool expulsion. Also, teachers who report more job stress are more likely to mete out suspensions or expulsions. By contrast, the availability of behavioral consultations reduces the risk of expulsion.
Within the realistic constraints of a busy pediatric practice, what can a physician do?
At the very least, said Ms. Lerner, pay attention when a parent comes to you and says, “My child’s getting in trouble in the classroom, and I’m afraid he’s going to get kicked out.” At that point, she said, the pediatrician should get in touch with the school. An approach that can be used in communicating with the school is to say, “We’re not seeing that, but we want to learn more,” said Ms. Lerner.
Just the fact that a pediatrician or his or her team members would reach out to the teacher for collaboration helps the teacher and school or daycare center realize that the family is taking the concerns seriously, said Ms. Lerner. “I will tell you that even just that phone call changes what happens for that kid,” she said.
Facilitating appropriate behavioral and mental health evaluations allows those professionals to become part of the problem-solving team for the child, school, and family.
Physicians can also help children and families by being familiar with the Americans with Disabilities Act safeguards for children with an Individualized Education Program (IEP) or a 504 Plan and making sure that families know about these protections.
Within the larger context of the school district and the community, a pediatrician’s voice can be a powerful advocacy tool to lobby against zero tolerance policies, and for stronger prevention and outreach strategies to help avoid out-of-school suspensions and expulsions for the very young. “There are things you can do -- starting tomorrow -- that will change the course for these children,” said Ms. Lerner.
Ms. Lerner is employed by Zero to Three. She reported no conflicts of interest.
CHICAGO –
Young African American boys are particularly at risk, said Claire Lerner, a senior parenting specialist with the nonprofit organization Zero to Three in Washington.
Speaking at the annual meeting of the American Academy of Pediatrics, Ms. Lerner cited data from 2005 showing that 10.4% of prekindergarten (preK) teachers had expelled at least one child for behavior problems during the previous year, yielding a preK expulsion rate of 6.7 per 1,000 students. This contrasts with a K-12 expulsion rate of 2.1 per 1,000 students.
“What I would say to you is that if a parent, or school, or caregiver comes to you and says, ‘The teacher’s concerned about X,’ don’t dismiss it. I cannot tell you how many times parents have come to me and said, ‘Well, the pediatrician says he’s totally fine. He’s just two.’”
This is not to blame pediatricians, said Ms. Lerner. Rather, “it’s to help you remember that teachers are smart, and they’re with these kids in a natural environment all day long. ...You are seeing such a random, finite, artificial experience in that room that you don’t see what’s going on in the classroom.” The child’s interactions with other children -- usually the impetus for disciplinary action -- will not necessarily be apparent in the pediatrician’s office.
Often, said Ms. Lerner, the child in question isn’t picking up on verbal and physical clues from other children, leading to behavior that’s seen as inappropriate or aggressive by other children -- and by staff. “A lot of these kids have motor planning problems, meaning they don’t know how to take their idea and execute it, so they’re the ones who are knocking down towers, and in kids’ faces. ...Those are the things that I’m talking about that are very unlikely to be picked up in a pediatric well-child visit,” she said.
“The evidence tells us that gender and race matter” in preschool suspensions and expulsions, said Ms. Lerner, noting that black preschool children are 3.6 times as likely as white children to be given an out-of-school suspension.
Black boys, she said, are 19% of male preschool attendees but make up 45% of the preschool children who receive out-of-school suspensions. Black girls make up 20% of female preschool attendees, but 54% of preschool girls who receive out-of-school suspensions are black.
In public preschools, 78% of those suspended are boys, though they make up just 54% of the attendees.
Aside from the home and work disruption caused by these suspensions, Ms. Lerner said that later outcomes are much worse for young students who are expelled or suspended, stacking the deck further against success. Rates of dropping out of high school, grade retention, and incarceration may be up to 10 times higher for these children.
Many school-related factors, including a higher child-teacher ratio and a longer school day, are associated with higher rates of preschool expulsion. Also, teachers who report more job stress are more likely to mete out suspensions or expulsions. By contrast, the availability of behavioral consultations reduces the risk of expulsion.
Within the realistic constraints of a busy pediatric practice, what can a physician do?
At the very least, said Ms. Lerner, pay attention when a parent comes to you and says, “My child’s getting in trouble in the classroom, and I’m afraid he’s going to get kicked out.” At that point, she said, the pediatrician should get in touch with the school. An approach that can be used in communicating with the school is to say, “We’re not seeing that, but we want to learn more,” said Ms. Lerner.
Just the fact that a pediatrician or his or her team members would reach out to the teacher for collaboration helps the teacher and school or daycare center realize that the family is taking the concerns seriously, said Ms. Lerner. “I will tell you that even just that phone call changes what happens for that kid,” she said.
Facilitating appropriate behavioral and mental health evaluations allows those professionals to become part of the problem-solving team for the child, school, and family.
Physicians can also help children and families by being familiar with the Americans with Disabilities Act safeguards for children with an Individualized Education Program (IEP) or a 504 Plan and making sure that families know about these protections.
Within the larger context of the school district and the community, a pediatrician’s voice can be a powerful advocacy tool to lobby against zero tolerance policies, and for stronger prevention and outreach strategies to help avoid out-of-school suspensions and expulsions for the very young. “There are things you can do -- starting tomorrow -- that will change the course for these children,” said Ms. Lerner.
Ms. Lerner is employed by Zero to Three. She reported no conflicts of interest.
CHICAGO –
Young African American boys are particularly at risk, said Claire Lerner, a senior parenting specialist with the nonprofit organization Zero to Three in Washington.
Speaking at the annual meeting of the American Academy of Pediatrics, Ms. Lerner cited data from 2005 showing that 10.4% of prekindergarten (preK) teachers had expelled at least one child for behavior problems during the previous year, yielding a preK expulsion rate of 6.7 per 1,000 students. This contrasts with a K-12 expulsion rate of 2.1 per 1,000 students.
“What I would say to you is that if a parent, or school, or caregiver comes to you and says, ‘The teacher’s concerned about X,’ don’t dismiss it. I cannot tell you how many times parents have come to me and said, ‘Well, the pediatrician says he’s totally fine. He’s just two.’”
This is not to blame pediatricians, said Ms. Lerner. Rather, “it’s to help you remember that teachers are smart, and they’re with these kids in a natural environment all day long. ...You are seeing such a random, finite, artificial experience in that room that you don’t see what’s going on in the classroom.” The child’s interactions with other children -- usually the impetus for disciplinary action -- will not necessarily be apparent in the pediatrician’s office.
Often, said Ms. Lerner, the child in question isn’t picking up on verbal and physical clues from other children, leading to behavior that’s seen as inappropriate or aggressive by other children -- and by staff. “A lot of these kids have motor planning problems, meaning they don’t know how to take their idea and execute it, so they’re the ones who are knocking down towers, and in kids’ faces. ...Those are the things that I’m talking about that are very unlikely to be picked up in a pediatric well-child visit,” she said.
“The evidence tells us that gender and race matter” in preschool suspensions and expulsions, said Ms. Lerner, noting that black preschool children are 3.6 times as likely as white children to be given an out-of-school suspension.
Black boys, she said, are 19% of male preschool attendees but make up 45% of the preschool children who receive out-of-school suspensions. Black girls make up 20% of female preschool attendees, but 54% of preschool girls who receive out-of-school suspensions are black.
In public preschools, 78% of those suspended are boys, though they make up just 54% of the attendees.
Aside from the home and work disruption caused by these suspensions, Ms. Lerner said that later outcomes are much worse for young students who are expelled or suspended, stacking the deck further against success. Rates of dropping out of high school, grade retention, and incarceration may be up to 10 times higher for these children.
Many school-related factors, including a higher child-teacher ratio and a longer school day, are associated with higher rates of preschool expulsion. Also, teachers who report more job stress are more likely to mete out suspensions or expulsions. By contrast, the availability of behavioral consultations reduces the risk of expulsion.
Within the realistic constraints of a busy pediatric practice, what can a physician do?
At the very least, said Ms. Lerner, pay attention when a parent comes to you and says, “My child’s getting in trouble in the classroom, and I’m afraid he’s going to get kicked out.” At that point, she said, the pediatrician should get in touch with the school. An approach that can be used in communicating with the school is to say, “We’re not seeing that, but we want to learn more,” said Ms. Lerner.
Just the fact that a pediatrician or his or her team members would reach out to the teacher for collaboration helps the teacher and school or daycare center realize that the family is taking the concerns seriously, said Ms. Lerner. “I will tell you that even just that phone call changes what happens for that kid,” she said.
Facilitating appropriate behavioral and mental health evaluations allows those professionals to become part of the problem-solving team for the child, school, and family.
Physicians can also help children and families by being familiar with the Americans with Disabilities Act safeguards for children with an Individualized Education Program (IEP) or a 504 Plan and making sure that families know about these protections.
Within the larger context of the school district and the community, a pediatrician’s voice can be a powerful advocacy tool to lobby against zero tolerance policies, and for stronger prevention and outreach strategies to help avoid out-of-school suspensions and expulsions for the very young. “There are things you can do -- starting tomorrow -- that will change the course for these children,” said Ms. Lerner.
Ms. Lerner is employed by Zero to Three. She reported no conflicts of interest.
EXPERT ANALYSIS FROM AAP 2017