User login
Combo antifungal/corticosteroid creams contraindicated in children
Don’t use combination antifungal/corticosteroid medications in children or for treating diaper dermatitis, warned Chikoti M. Wheat, MD, of Johns Hopkins University, Baltimore, and her associates.
Lotrisone is a combination product with a high-potency topical corticosteroid, betamethasone dipropionate 0.05% cream, and a topical antifungal agent, clotrimazole 1% cream. The Food and Drug Administration does not recommend it for the population and indication mentioned above, yet it is often used so off-label, Dr. Wheat and her associates said. Mycolog-II, a combination antifungal/corticosteroid with nystatin, an antiyeast agent, and triamcinolone, a medium-potency topical steroid, was taken off the market in 2015, but patients may still have some that they are inclined to use (J Pediatr. 2017. doi: 0.1016/j.jpeds.2017.03.031).
In a study of 9,797 patients aged 0-14 years who were prescribed either Lotrisone or Mycolog-II creams from 2007 to 2014, pediatricians were most likely to prescribe the combination creams (mean, 810 patients), followed by family physicians (mean, 309 patients), and dermatologists (mean, 49 patients). No pediatric dermatologists prescribed either cream.
Why are these combination creams being used?
Sometimes a fungal infection induces an inflammatory dermatitis. In these cases the use of both an antifungal and a corticosteroid with careful monitoring can benefit the patient, the researchers said. “Research, however, has shown that when combination antifungal/corticosteroid agents are used for fungal infections, they not only result in high rates of recurrence of fungal infections but also have greater side effect profiles.”
Also, in 1984, Lotrisone was approved by the FDA for treating tinea corporis, tinea pedis, and tinea cruris in patients older than 12 years. However, lack of efficacy and severe adverse effects including hypothalamic-pituitary-adrenal axis suppression, Cushing syndrome, hyperglycemia, hirsutism, delayed growth, and skin atrophy led the FDA to recommend that Lotrisone not be prescribed for patients younger than 17 years and not be prescribed to treat diaper dermatitis.
So what should you do?
Dr. Wheat and her associates recommend a single-agent topical antifungal to treat superficial fungal infection. If there is intense itching due to infection-induced dermatitis, add a low- or medium-potency topical corticosteroid for just 7-10 days.
For diaper dermatitis with a confirmed secondary fungal infection, they recommend a topical antifungal agent in combination with a barrier cream. “If intense inflammatory changes are present, a low- to medium-potency topical corticosteroid can be used up to twice daily and tapered over 1-2 weeks with careful monitoring,” they said.
Dr. Wheat and her associates declared they had no conflicts of interest.
cnellist@frontlinemedcom.com
Don’t use combination antifungal/corticosteroid medications in children or for treating diaper dermatitis, warned Chikoti M. Wheat, MD, of Johns Hopkins University, Baltimore, and her associates.
Lotrisone is a combination product with a high-potency topical corticosteroid, betamethasone dipropionate 0.05% cream, and a topical antifungal agent, clotrimazole 1% cream. The Food and Drug Administration does not recommend it for the population and indication mentioned above, yet it is often used so off-label, Dr. Wheat and her associates said. Mycolog-II, a combination antifungal/corticosteroid with nystatin, an antiyeast agent, and triamcinolone, a medium-potency topical steroid, was taken off the market in 2015, but patients may still have some that they are inclined to use (J Pediatr. 2017. doi: 0.1016/j.jpeds.2017.03.031).
In a study of 9,797 patients aged 0-14 years who were prescribed either Lotrisone or Mycolog-II creams from 2007 to 2014, pediatricians were most likely to prescribe the combination creams (mean, 810 patients), followed by family physicians (mean, 309 patients), and dermatologists (mean, 49 patients). No pediatric dermatologists prescribed either cream.
Why are these combination creams being used?
Sometimes a fungal infection induces an inflammatory dermatitis. In these cases the use of both an antifungal and a corticosteroid with careful monitoring can benefit the patient, the researchers said. “Research, however, has shown that when combination antifungal/corticosteroid agents are used for fungal infections, they not only result in high rates of recurrence of fungal infections but also have greater side effect profiles.”
Also, in 1984, Lotrisone was approved by the FDA for treating tinea corporis, tinea pedis, and tinea cruris in patients older than 12 years. However, lack of efficacy and severe adverse effects including hypothalamic-pituitary-adrenal axis suppression, Cushing syndrome, hyperglycemia, hirsutism, delayed growth, and skin atrophy led the FDA to recommend that Lotrisone not be prescribed for patients younger than 17 years and not be prescribed to treat diaper dermatitis.
So what should you do?
Dr. Wheat and her associates recommend a single-agent topical antifungal to treat superficial fungal infection. If there is intense itching due to infection-induced dermatitis, add a low- or medium-potency topical corticosteroid for just 7-10 days.
For diaper dermatitis with a confirmed secondary fungal infection, they recommend a topical antifungal agent in combination with a barrier cream. “If intense inflammatory changes are present, a low- to medium-potency topical corticosteroid can be used up to twice daily and tapered over 1-2 weeks with careful monitoring,” they said.
Dr. Wheat and her associates declared they had no conflicts of interest.
cnellist@frontlinemedcom.com
Don’t use combination antifungal/corticosteroid medications in children or for treating diaper dermatitis, warned Chikoti M. Wheat, MD, of Johns Hopkins University, Baltimore, and her associates.
Lotrisone is a combination product with a high-potency topical corticosteroid, betamethasone dipropionate 0.05% cream, and a topical antifungal agent, clotrimazole 1% cream. The Food and Drug Administration does not recommend it for the population and indication mentioned above, yet it is often used so off-label, Dr. Wheat and her associates said. Mycolog-II, a combination antifungal/corticosteroid with nystatin, an antiyeast agent, and triamcinolone, a medium-potency topical steroid, was taken off the market in 2015, but patients may still have some that they are inclined to use (J Pediatr. 2017. doi: 0.1016/j.jpeds.2017.03.031).
In a study of 9,797 patients aged 0-14 years who were prescribed either Lotrisone or Mycolog-II creams from 2007 to 2014, pediatricians were most likely to prescribe the combination creams (mean, 810 patients), followed by family physicians (mean, 309 patients), and dermatologists (mean, 49 patients). No pediatric dermatologists prescribed either cream.
Why are these combination creams being used?
Sometimes a fungal infection induces an inflammatory dermatitis. In these cases the use of both an antifungal and a corticosteroid with careful monitoring can benefit the patient, the researchers said. “Research, however, has shown that when combination antifungal/corticosteroid agents are used for fungal infections, they not only result in high rates of recurrence of fungal infections but also have greater side effect profiles.”
Also, in 1984, Lotrisone was approved by the FDA for treating tinea corporis, tinea pedis, and tinea cruris in patients older than 12 years. However, lack of efficacy and severe adverse effects including hypothalamic-pituitary-adrenal axis suppression, Cushing syndrome, hyperglycemia, hirsutism, delayed growth, and skin atrophy led the FDA to recommend that Lotrisone not be prescribed for patients younger than 17 years and not be prescribed to treat diaper dermatitis.
So what should you do?
Dr. Wheat and her associates recommend a single-agent topical antifungal to treat superficial fungal infection. If there is intense itching due to infection-induced dermatitis, add a low- or medium-potency topical corticosteroid for just 7-10 days.
For diaper dermatitis with a confirmed secondary fungal infection, they recommend a topical antifungal agent in combination with a barrier cream. “If intense inflammatory changes are present, a low- to medium-potency topical corticosteroid can be used up to twice daily and tapered over 1-2 weeks with careful monitoring,” they said.
Dr. Wheat and her associates declared they had no conflicts of interest.
cnellist@frontlinemedcom.com
FROM THE JOURNAL OF PEDIATRICS
Key clinical point:
Major finding: Pediatricians were most likely to prescribe the combination creams (mean, 810 patients), followed by family physicians (mean, 309 patients), dermatologists (mean, 49 patients), and pediatric dermatologists (none).
Data source: A study of 9,797 patients aged 0-14 years who were prescribed either Lotrisone or Mycolog-II creams from 2007 to 2014.
Disclosures: Dr. Wheat and her associates declared they had no conflicts of interest.
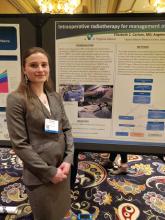
Intraoperative radiation looks good for DCIS
LAS VEGAS – Intraoperative radiation therapy (IORT) is effective in patients with ductal carcinoma in situ (DCIS), and bilateral digital mammography and breast MRI effectively predicted which patients would be most suited for the procedure, according to a nonrandomized study.
The TARGIT-A trial showed that IORT was noninferior to external beam radiation therapy in women with early-stage breast cancer (Lancet. 2014 Feb 15;383:603-13), but the technique hasn’t been tested in DCIS patients.
The researchers conducted a prospective, nonrandomized study of DCIS in women who underwent core biopsy between February 2012 and July 2016 at Virginia Mason Medical Center. Those who elected breast conserving therapy were assessed for IORT using bilateral digital mammography and contrast enhanced MRI.
For criteria, the researchers selected patients over age 44 years with unifocal DCIS and a lesion size of up to 3.0 cm. Physicians recommended additional therapy when the pathology report revealed DCIS larger than 3 cm and/or margins of up to 2 mm.
Of the 57 patients initially enrolled, 7 were found to have invasive disease and were excluded. Another eight patients were excluded because of margins, tumor size, or multifocal disease, and were recommended for additional treatment.
The remaining 42 patients with DCIS were treated with IORT. At a mean follow-up time of 32 months, the researchers observed no local recurrences, and no Radiation Therapy Oncology Group grade 3 or 4 complications were reported.
Hyperpigmentation occurred more often in the IORT group, at 40% (17 of 42 patients), than in the additional treatment group, at 13% (1 of 8), a nonsignificant difference. The hyperpigmentation tended to be minimal and focused on the surgical scar. There were no differences between the groups with respect to superficial wound separation, infection, seroma, fat necrosis, transient radiation dermatitis, or rib fracture.
“Our conclusions are that are selection criteria with mammography and MRI are effective in identifying patients who are appropriate for IORT, and importantly, at 32 months follow-up, no patients had recurrences, so we’re not negatively impacting oncological outcome,” said Dr. Carlson.
The fact that eight patients were recommended for additional treatment based on margins, a disease span greater than 3 cm, or multifocal disease “is actually quite heartening because it implies that the mammogram and the MRI are quite effective at identifying patients that met our criteria,” said Dr. Carlson.
The study is small and had no control group, but Dr. Carlson is confident of the results. “We didn’t do a randomized trial because we believed strongly that IORT will be effective in these patients with good cosmesis. When you compare it to local recurrence rates in the TARGIT-A trial, we’re still doing quite well, so to some extent that can be used as a baseline benchmark,” she said.
LAS VEGAS – Intraoperative radiation therapy (IORT) is effective in patients with ductal carcinoma in situ (DCIS), and bilateral digital mammography and breast MRI effectively predicted which patients would be most suited for the procedure, according to a nonrandomized study.
The TARGIT-A trial showed that IORT was noninferior to external beam radiation therapy in women with early-stage breast cancer (Lancet. 2014 Feb 15;383:603-13), but the technique hasn’t been tested in DCIS patients.
The researchers conducted a prospective, nonrandomized study of DCIS in women who underwent core biopsy between February 2012 and July 2016 at Virginia Mason Medical Center. Those who elected breast conserving therapy were assessed for IORT using bilateral digital mammography and contrast enhanced MRI.
For criteria, the researchers selected patients over age 44 years with unifocal DCIS and a lesion size of up to 3.0 cm. Physicians recommended additional therapy when the pathology report revealed DCIS larger than 3 cm and/or margins of up to 2 mm.
Of the 57 patients initially enrolled, 7 were found to have invasive disease and were excluded. Another eight patients were excluded because of margins, tumor size, or multifocal disease, and were recommended for additional treatment.
The remaining 42 patients with DCIS were treated with IORT. At a mean follow-up time of 32 months, the researchers observed no local recurrences, and no Radiation Therapy Oncology Group grade 3 or 4 complications were reported.
Hyperpigmentation occurred more often in the IORT group, at 40% (17 of 42 patients), than in the additional treatment group, at 13% (1 of 8), a nonsignificant difference. The hyperpigmentation tended to be minimal and focused on the surgical scar. There were no differences between the groups with respect to superficial wound separation, infection, seroma, fat necrosis, transient radiation dermatitis, or rib fracture.
“Our conclusions are that are selection criteria with mammography and MRI are effective in identifying patients who are appropriate for IORT, and importantly, at 32 months follow-up, no patients had recurrences, so we’re not negatively impacting oncological outcome,” said Dr. Carlson.
The fact that eight patients were recommended for additional treatment based on margins, a disease span greater than 3 cm, or multifocal disease “is actually quite heartening because it implies that the mammogram and the MRI are quite effective at identifying patients that met our criteria,” said Dr. Carlson.
The study is small and had no control group, but Dr. Carlson is confident of the results. “We didn’t do a randomized trial because we believed strongly that IORT will be effective in these patients with good cosmesis. When you compare it to local recurrence rates in the TARGIT-A trial, we’re still doing quite well, so to some extent that can be used as a baseline benchmark,” she said.
LAS VEGAS – Intraoperative radiation therapy (IORT) is effective in patients with ductal carcinoma in situ (DCIS), and bilateral digital mammography and breast MRI effectively predicted which patients would be most suited for the procedure, according to a nonrandomized study.
The TARGIT-A trial showed that IORT was noninferior to external beam radiation therapy in women with early-stage breast cancer (Lancet. 2014 Feb 15;383:603-13), but the technique hasn’t been tested in DCIS patients.
The researchers conducted a prospective, nonrandomized study of DCIS in women who underwent core biopsy between February 2012 and July 2016 at Virginia Mason Medical Center. Those who elected breast conserving therapy were assessed for IORT using bilateral digital mammography and contrast enhanced MRI.
For criteria, the researchers selected patients over age 44 years with unifocal DCIS and a lesion size of up to 3.0 cm. Physicians recommended additional therapy when the pathology report revealed DCIS larger than 3 cm and/or margins of up to 2 mm.
Of the 57 patients initially enrolled, 7 were found to have invasive disease and were excluded. Another eight patients were excluded because of margins, tumor size, or multifocal disease, and were recommended for additional treatment.
The remaining 42 patients with DCIS were treated with IORT. At a mean follow-up time of 32 months, the researchers observed no local recurrences, and no Radiation Therapy Oncology Group grade 3 or 4 complications were reported.
Hyperpigmentation occurred more often in the IORT group, at 40% (17 of 42 patients), than in the additional treatment group, at 13% (1 of 8), a nonsignificant difference. The hyperpigmentation tended to be minimal and focused on the surgical scar. There were no differences between the groups with respect to superficial wound separation, infection, seroma, fat necrosis, transient radiation dermatitis, or rib fracture.
“Our conclusions are that are selection criteria with mammography and MRI are effective in identifying patients who are appropriate for IORT, and importantly, at 32 months follow-up, no patients had recurrences, so we’re not negatively impacting oncological outcome,” said Dr. Carlson.
The fact that eight patients were recommended for additional treatment based on margins, a disease span greater than 3 cm, or multifocal disease “is actually quite heartening because it implies that the mammogram and the MRI are quite effective at identifying patients that met our criteria,” said Dr. Carlson.
The study is small and had no control group, but Dr. Carlson is confident of the results. “We didn’t do a randomized trial because we believed strongly that IORT will be effective in these patients with good cosmesis. When you compare it to local recurrence rates in the TARGIT-A trial, we’re still doing quite well, so to some extent that can be used as a baseline benchmark,” she said.
AT ASBS 2017
Key clinical point: Intraoperative radiation appears safe and effective, and is more convenient than postoperative radiation.
Major finding: There were no ductal carcinoma in situ recurrences at a median 32 months’ follow-up.
Data source: Uncontrolled, prospective study of 42 patients.
Disclosures: The study was funded by the National Institutes of Health. Dr. Carlson reported having no financial disclosures.
Sexual dysfunction, depression common in endometriosis patients
VANCOUVER – Endometriosis is associated with an increased risk of a range of sexual dysfunctions, and depression and anxiety are also common, according to a study conducted in Brazilian women.
Depression and anxiety were so common that the study itself had to be altered. Almost a third of participants were excluded from the study due to depressive symptoms. So many, in fact, that the researchers decided to include patients with mild to moderate depression and anxiety, and ultimately exclude only those with severe symptoms.
The final sample included 254 women with endometriosis and 329 control subjects between 18 and 45 years old. They all had an active sex life in the previous 6 months, and were heterosexual.
Forty-three percent of women in the endometriosis group had sexual dysfunction, compared with 18% in the control group (P less than .001), as measured by the Female Sexual Quotient. They also had higher rates of individual types of sexual dysfunction, including sexual desire dysfunction (25% vs. 16%; P = .007); sexual arousal dysfunction (16% vs. 4%; P less than .001); pain during intercourse/sex dysfunction (46% vs. 16%; P less than .001); and orgasm and/or sexual satisfaction dysfunction (30% vs. 13%; P less than .001).
The researchers also examined the relationship between sexual dysfunction and psychological factors, and found statistically significant positive associations with anxiety and depression.
The underlying psychological issues are of particular concern to Dr. Fairbanks. “It’s the main step to begin anything with them. We have to know if they have anxiety and depression or not,” she said.
Her team now asks patients with endometriosis about their sex life in order to establish a baseline that can be referred to. “After 1 year, 2 years, 5 years, we reapply the questionnaire to show them that their sexual life was not so good in the beginning.”
The study was eye-opening to Lori Brotto, PhD, professor of gynecology at the University of British Columbia, Vancouver, who was a discussant at the session. “The call to action is for doctors to really pay attention to sexual dysfunction, even though that might not be the primary issue that brings the patient to them,” Dr. Brotto said.
The high rates of depression and anxiety also suggest a need for a more rounded approach to endometriosis treatment. “A physician may think, ‘we’ll treat the endometriosis, and all other parts of her should improve as well.’ This study suggests that primarily physical interventions may not be sufficient for addressing something like sexual health, which is really mind and body together,” said Dr. Brotto.
The study was not funded. Dr. Fairbanks and Dr. Brotto reported having no relevant financial disclosures.
VANCOUVER – Endometriosis is associated with an increased risk of a range of sexual dysfunctions, and depression and anxiety are also common, according to a study conducted in Brazilian women.
Depression and anxiety were so common that the study itself had to be altered. Almost a third of participants were excluded from the study due to depressive symptoms. So many, in fact, that the researchers decided to include patients with mild to moderate depression and anxiety, and ultimately exclude only those with severe symptoms.
The final sample included 254 women with endometriosis and 329 control subjects between 18 and 45 years old. They all had an active sex life in the previous 6 months, and were heterosexual.
Forty-three percent of women in the endometriosis group had sexual dysfunction, compared with 18% in the control group (P less than .001), as measured by the Female Sexual Quotient. They also had higher rates of individual types of sexual dysfunction, including sexual desire dysfunction (25% vs. 16%; P = .007); sexual arousal dysfunction (16% vs. 4%; P less than .001); pain during intercourse/sex dysfunction (46% vs. 16%; P less than .001); and orgasm and/or sexual satisfaction dysfunction (30% vs. 13%; P less than .001).
The researchers also examined the relationship between sexual dysfunction and psychological factors, and found statistically significant positive associations with anxiety and depression.
The underlying psychological issues are of particular concern to Dr. Fairbanks. “It’s the main step to begin anything with them. We have to know if they have anxiety and depression or not,” she said.
Her team now asks patients with endometriosis about their sex life in order to establish a baseline that can be referred to. “After 1 year, 2 years, 5 years, we reapply the questionnaire to show them that their sexual life was not so good in the beginning.”
The study was eye-opening to Lori Brotto, PhD, professor of gynecology at the University of British Columbia, Vancouver, who was a discussant at the session. “The call to action is for doctors to really pay attention to sexual dysfunction, even though that might not be the primary issue that brings the patient to them,” Dr. Brotto said.
The high rates of depression and anxiety also suggest a need for a more rounded approach to endometriosis treatment. “A physician may think, ‘we’ll treat the endometriosis, and all other parts of her should improve as well.’ This study suggests that primarily physical interventions may not be sufficient for addressing something like sexual health, which is really mind and body together,” said Dr. Brotto.
The study was not funded. Dr. Fairbanks and Dr. Brotto reported having no relevant financial disclosures.
VANCOUVER – Endometriosis is associated with an increased risk of a range of sexual dysfunctions, and depression and anxiety are also common, according to a study conducted in Brazilian women.
Depression and anxiety were so common that the study itself had to be altered. Almost a third of participants were excluded from the study due to depressive symptoms. So many, in fact, that the researchers decided to include patients with mild to moderate depression and anxiety, and ultimately exclude only those with severe symptoms.
The final sample included 254 women with endometriosis and 329 control subjects between 18 and 45 years old. They all had an active sex life in the previous 6 months, and were heterosexual.
Forty-three percent of women in the endometriosis group had sexual dysfunction, compared with 18% in the control group (P less than .001), as measured by the Female Sexual Quotient. They also had higher rates of individual types of sexual dysfunction, including sexual desire dysfunction (25% vs. 16%; P = .007); sexual arousal dysfunction (16% vs. 4%; P less than .001); pain during intercourse/sex dysfunction (46% vs. 16%; P less than .001); and orgasm and/or sexual satisfaction dysfunction (30% vs. 13%; P less than .001).
The researchers also examined the relationship between sexual dysfunction and psychological factors, and found statistically significant positive associations with anxiety and depression.
The underlying psychological issues are of particular concern to Dr. Fairbanks. “It’s the main step to begin anything with them. We have to know if they have anxiety and depression or not,” she said.
Her team now asks patients with endometriosis about their sex life in order to establish a baseline that can be referred to. “After 1 year, 2 years, 5 years, we reapply the questionnaire to show them that their sexual life was not so good in the beginning.”
The study was eye-opening to Lori Brotto, PhD, professor of gynecology at the University of British Columbia, Vancouver, who was a discussant at the session. “The call to action is for doctors to really pay attention to sexual dysfunction, even though that might not be the primary issue that brings the patient to them,” Dr. Brotto said.
The high rates of depression and anxiety also suggest a need for a more rounded approach to endometriosis treatment. “A physician may think, ‘we’ll treat the endometriosis, and all other parts of her should improve as well.’ This study suggests that primarily physical interventions may not be sufficient for addressing something like sexual health, which is really mind and body together,” said Dr. Brotto.
The study was not funded. Dr. Fairbanks and Dr. Brotto reported having no relevant financial disclosures.
AT WCE 2017
Key clinical point: Sexual dysfunction is common but not always addressed by clinicians.
Major finding: Women with endometriosis had more than doubled risk of sexual dysfunction.
Data source: Forty-three percent of the endometriosis group had dysfunction, compared with 17.6% of controls.
Disclosures: The study was not funded. Dr. Fairbanks and Dr. Brotto reported having no relevant financial disclosures.
Meconium-stained amniotic fluid linked to postcesarean SSI
SAN DIEGO – Meconium-stained amniotic fluid may increased risk of surgical site infections following a cesarean delivery, results from a large analysis showed.
Surgical site infection (SSI) occurs in 3%-9% of patients who have a cesarean delivery, and many require hospitalization or further surgery, lead study author Andrea Snyder, MD, PhD, said at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. Risk factors for SSI included chorioamnionitis, obesity, preeclampsia, preterm premature rupture of membranes, nulliparity, or emergency cesarean. Current management for avoiding SSIs includes prophylactic antibiotics, antiseptic skin, and vaginal prep.
In an effort to test the hypothesis that meconium-stained fluid is an independent risk factor associated with an increased risk of postcesarean SSI, she and her associates evaluated a subset of 25,220 women from the Maternal-Fetal Medicine Units Network cesarean registry who were treated at 19 different institutions. Their mean age was 27 years, they were all attempting labor or induction of labor, were all singleton pregnancies, and all had cesarean deliveries.
Of the 25,220 patients studied, 5,883 (23%) had MSAF. The researchers found that the incidence of SSI was 11.9% among patients who had MSAF, compared with an incidence of 8.9% among patients who did not, a difference that reached statistical significance (P less than .001). After using a multivariable logistic regression model to control for confounders including chorioamnionitis, diabetes, intrauterine pressure catheter placement, tobacco use, length of labor, length of rupture, preeclampsia, and obesity, the association between MSAF and SSI persisted (odds ratio, 1.25; confidence interval, 1.12-1.39; P less than .001).
Advantages of the study, she said, include the fact that it was a large population of patients treated at multiple institutions, “so it should be very generalizable to most practices. We also controlled for many known factors associated with SSI.” Dr. Snyder acknowledged certain limitations of the study, including the fact that the data do not show causation and that there is no further information about the SSIs. “Were those associated with meconium less or more severe SSIs?” she asked. “Does the increase in risk confer an increased risk of severe infectious morbidity? Where do we go from here and what do we do with this information? At this point we don’t have any way of preventing meconium.”
A 2014 Cochrane review found that, while prophylactic antibiotics for patients with MSAF did not decrease the risk of postpartum endometriosis, it did decrease the risk of chorioamnionitis. “But would it help decrease the risk of SSIs? We have no idea,” Dr. Snyder asked. “Would continuing antibiotics after delivery help reduce wound infections? We don’t do that routinely in a C-section, but maybe that would make sense for patients that are higher risk.” She reported having no financial disclosures.
dbrunk@frontlinemedcom.com
SAN DIEGO – Meconium-stained amniotic fluid may increased risk of surgical site infections following a cesarean delivery, results from a large analysis showed.
Surgical site infection (SSI) occurs in 3%-9% of patients who have a cesarean delivery, and many require hospitalization or further surgery, lead study author Andrea Snyder, MD, PhD, said at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. Risk factors for SSI included chorioamnionitis, obesity, preeclampsia, preterm premature rupture of membranes, nulliparity, or emergency cesarean. Current management for avoiding SSIs includes prophylactic antibiotics, antiseptic skin, and vaginal prep.
In an effort to test the hypothesis that meconium-stained fluid is an independent risk factor associated with an increased risk of postcesarean SSI, she and her associates evaluated a subset of 25,220 women from the Maternal-Fetal Medicine Units Network cesarean registry who were treated at 19 different institutions. Their mean age was 27 years, they were all attempting labor or induction of labor, were all singleton pregnancies, and all had cesarean deliveries.
Of the 25,220 patients studied, 5,883 (23%) had MSAF. The researchers found that the incidence of SSI was 11.9% among patients who had MSAF, compared with an incidence of 8.9% among patients who did not, a difference that reached statistical significance (P less than .001). After using a multivariable logistic regression model to control for confounders including chorioamnionitis, diabetes, intrauterine pressure catheter placement, tobacco use, length of labor, length of rupture, preeclampsia, and obesity, the association between MSAF and SSI persisted (odds ratio, 1.25; confidence interval, 1.12-1.39; P less than .001).
Advantages of the study, she said, include the fact that it was a large population of patients treated at multiple institutions, “so it should be very generalizable to most practices. We also controlled for many known factors associated with SSI.” Dr. Snyder acknowledged certain limitations of the study, including the fact that the data do not show causation and that there is no further information about the SSIs. “Were those associated with meconium less or more severe SSIs?” she asked. “Does the increase in risk confer an increased risk of severe infectious morbidity? Where do we go from here and what do we do with this information? At this point we don’t have any way of preventing meconium.”
A 2014 Cochrane review found that, while prophylactic antibiotics for patients with MSAF did not decrease the risk of postpartum endometriosis, it did decrease the risk of chorioamnionitis. “But would it help decrease the risk of SSIs? We have no idea,” Dr. Snyder asked. “Would continuing antibiotics after delivery help reduce wound infections? We don’t do that routinely in a C-section, but maybe that would make sense for patients that are higher risk.” She reported having no financial disclosures.
dbrunk@frontlinemedcom.com
SAN DIEGO – Meconium-stained amniotic fluid may increased risk of surgical site infections following a cesarean delivery, results from a large analysis showed.
Surgical site infection (SSI) occurs in 3%-9% of patients who have a cesarean delivery, and many require hospitalization or further surgery, lead study author Andrea Snyder, MD, PhD, said at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. Risk factors for SSI included chorioamnionitis, obesity, preeclampsia, preterm premature rupture of membranes, nulliparity, or emergency cesarean. Current management for avoiding SSIs includes prophylactic antibiotics, antiseptic skin, and vaginal prep.
In an effort to test the hypothesis that meconium-stained fluid is an independent risk factor associated with an increased risk of postcesarean SSI, she and her associates evaluated a subset of 25,220 women from the Maternal-Fetal Medicine Units Network cesarean registry who were treated at 19 different institutions. Their mean age was 27 years, they were all attempting labor or induction of labor, were all singleton pregnancies, and all had cesarean deliveries.
Of the 25,220 patients studied, 5,883 (23%) had MSAF. The researchers found that the incidence of SSI was 11.9% among patients who had MSAF, compared with an incidence of 8.9% among patients who did not, a difference that reached statistical significance (P less than .001). After using a multivariable logistic regression model to control for confounders including chorioamnionitis, diabetes, intrauterine pressure catheter placement, tobacco use, length of labor, length of rupture, preeclampsia, and obesity, the association between MSAF and SSI persisted (odds ratio, 1.25; confidence interval, 1.12-1.39; P less than .001).
Advantages of the study, she said, include the fact that it was a large population of patients treated at multiple institutions, “so it should be very generalizable to most practices. We also controlled for many known factors associated with SSI.” Dr. Snyder acknowledged certain limitations of the study, including the fact that the data do not show causation and that there is no further information about the SSIs. “Were those associated with meconium less or more severe SSIs?” she asked. “Does the increase in risk confer an increased risk of severe infectious morbidity? Where do we go from here and what do we do with this information? At this point we don’t have any way of preventing meconium.”
A 2014 Cochrane review found that, while prophylactic antibiotics for patients with MSAF did not decrease the risk of postpartum endometriosis, it did decrease the risk of chorioamnionitis. “But would it help decrease the risk of SSIs? We have no idea,” Dr. Snyder asked. “Would continuing antibiotics after delivery help reduce wound infections? We don’t do that routinely in a C-section, but maybe that would make sense for patients that are higher risk.” She reported having no financial disclosures.
dbrunk@frontlinemedcom.com
AT ACOG 2017
Key clinical point:
Major finding: The incidence of SSI was 11.9% in patients who had meconium-stained amniotic fluid, compared with an incidence of 8.9% in patients who did not, a difference that reached statistical significance (P less than .001).
Data source: A subset analysis of 25,220 women from the Maternal-Fetal Medicine Networks Cesarean Registry who were treated at 19 different institutions.
Disclosures: Dr. Snyder reported having no financial disclosures.
Ibrutinib response in CLL/SLL less affected by select risk factors
NEW YORK – Risk factors associated with poor outcomes in chronic lymphocytic leukemia/small lymphocytic leukemia patients treated with standard therapies appear to have less relevance with ibrutinib treatment, according to an integrated analysis of data from the randomized, phase III RESONATE, RESONATE 2, and HELIOS trials.
In the combined analysis, at a median follow-up of 21 months, progression-free survival (PFS), overall survival (OS), overall response rate (ORR), and complete response rate (CRR) were better in ibrutinib-treated patients than in comparator-treated patients – and, in the ibrutinib-treated patients, the outcomes did not differ based on the adverse genomic factors examined, Thomas J. Kipps, MD, PhD, said at the annual International Workshop on Chronic Lymphocytic Leukemia.
The trials compared well with each other, but differed in terms of number of prior therapies received by patients, he said. Furthermore, the analysis did not examine the effect of del(17p); patients with that deletion were included only in the RESONATE trial.
In RESONATE, ibrutinib was superior to ofatumumab in relapsed/refractory CLL/SLL. In RESONATE 2, ibrutinib was superior to chlorambucil in treatment-naive patients with CLL/SLL. In HELIOS, ibrutinib with bendamustine/rituximab was superior to placebo with bendamustine/rituximab in patients with relapsed/refractory CLL/SLL.
In the new multivariate analysis of the pooled data from these trials – adjusting for the four genomic risk factors and age, sex, ECOG performance status, cytopenia, lactate dehydrogenase (LDH), bulky disease, and number of prior therapies – only having had one or more vs. no prior therapies, and having two or more vs. one prior therapies was associated with shorter PFS and OS in ibrutinib-treated patients, with a trend toward significance.
In comparator-treated patients, however, unmutated IGHV, del(11q), complex karyotype, male sex, two or more prior therapies, and bulky disease all were associated with significantly shorter PFS. Complex karyotype, male sex, bulky disease, ECOG performance status greater than 1, and elevated LDH were associated with significantly shorter OS.
“We need to debate on what the significance of this is and how that can be incorporated into our idea about first-line therapies,” said Dr. Kipps, who was an investigator in both RESONATE trials and is a professor of medicine at the University of California, San Diego.
In univariate analysis of data from ibrutinib-treated patients, unmutated IGHV, del(11q), trisomy 12, and complex karyotype were generally not associated with shorter PFS, OS, or lower ORR or CRR.
Overall survival with and without unmutated IGHV was 78% and 84%, respectively; with and without trisomy 12 was 82% and 80%, respectively; and with and without complex karyotype was 77% and 78%, respectively.
ORR, for example, was comparable in the presence (90%) and absence (89%) of unmutated IGHV in ibrutinib-treated patients, as was CRR, at 29% and 26%, respectively.
In the presence and absence of trisomy 12, ORR was 85% and 91%, respectively; CRR was 33% and 22%.
In the presence and absence of complex karyotype, ORR was 88% and 89%, respectively, and CRR was 18% and 24%.
In the presence and absence of del(11q), ORR was 91% and 90%, respectively, and CRR was 22% and 27%.
The only difference that reached statistical significance was the complete response rate with trisomy 12, which favored the presence of trisomy 12.
Interestingly, the ibrutinib-treated patients with del(11q) had a trend toward longer PFS and OS, compared with those without del(11q), said Dr. Kipps.
At 36 months, PFS was 74% with the presence of del(11q) and 68% with the absence of del(11q) (hazard ratio, 0.73 vs. 1.88 in comparator-treated patients), and overall survival at 42 months was 80% in patients with del(11q) and 78% in those without del(11q) (HR, 0.73), Dr. Kipps said.
“The [finding in the] patients with the complex karyotype was a bit surprising, and I think this requires further analysis,” he said, explaining that complex karyotype actually was associated with a shorter PFS in patients treated on the comparator arm, and that this finding conflicts with earlier data.
The findings suggest ibrutinib-treated patients with trisomy 12, for reasons that are unclear, had a significantly higher complete response rate, but not greater PFS or OS vs. those without trisomy 12, Dr. Kipps said.
“It’s also interesting that ... unmutated antibody genes or del(11q) or complex karyotype were adverse prognostic factors in patients treated with comparator treatments, but not necessarily in patients treated with ibrutinib-based therapy,” he said.
Furthermore, although a prior phase II study involving heavily pretreated patients suggested that del(11q) may have adverse prognostic influence on PFS, that finding may not be borne out in patients with fewer lines of prior therapy.
The findings suggest that genomic risk factors associated with poor outcomes with initial chemoimmunotherapy may be less apparent in patients treated with ibrutinib.
“I think this is important, because it may then turn a prognostic factor into a predictive factor, meaning, a predictor of adverse outcomes for a given type of therapy as opposed to adverse prognostic value overall,” he concluded.
Ibrutinib (Imbruvica, Pharmacyclics) was approved by the Food and Drug Administration in January 2015 for the treatment of CLL after previous therapy. Dr. Kipps has received research funding from and/or served as a consultant or advisor for AbbVie, Genentech, Gilead, and Pharmacyclics, an AbbVie company.
sworcester@frontlinemedcom.com
NEW YORK – Risk factors associated with poor outcomes in chronic lymphocytic leukemia/small lymphocytic leukemia patients treated with standard therapies appear to have less relevance with ibrutinib treatment, according to an integrated analysis of data from the randomized, phase III RESONATE, RESONATE 2, and HELIOS trials.
In the combined analysis, at a median follow-up of 21 months, progression-free survival (PFS), overall survival (OS), overall response rate (ORR), and complete response rate (CRR) were better in ibrutinib-treated patients than in comparator-treated patients – and, in the ibrutinib-treated patients, the outcomes did not differ based on the adverse genomic factors examined, Thomas J. Kipps, MD, PhD, said at the annual International Workshop on Chronic Lymphocytic Leukemia.
The trials compared well with each other, but differed in terms of number of prior therapies received by patients, he said. Furthermore, the analysis did not examine the effect of del(17p); patients with that deletion were included only in the RESONATE trial.
In RESONATE, ibrutinib was superior to ofatumumab in relapsed/refractory CLL/SLL. In RESONATE 2, ibrutinib was superior to chlorambucil in treatment-naive patients with CLL/SLL. In HELIOS, ibrutinib with bendamustine/rituximab was superior to placebo with bendamustine/rituximab in patients with relapsed/refractory CLL/SLL.
In the new multivariate analysis of the pooled data from these trials – adjusting for the four genomic risk factors and age, sex, ECOG performance status, cytopenia, lactate dehydrogenase (LDH), bulky disease, and number of prior therapies – only having had one or more vs. no prior therapies, and having two or more vs. one prior therapies was associated with shorter PFS and OS in ibrutinib-treated patients, with a trend toward significance.
In comparator-treated patients, however, unmutated IGHV, del(11q), complex karyotype, male sex, two or more prior therapies, and bulky disease all were associated with significantly shorter PFS. Complex karyotype, male sex, bulky disease, ECOG performance status greater than 1, and elevated LDH were associated with significantly shorter OS.
“We need to debate on what the significance of this is and how that can be incorporated into our idea about first-line therapies,” said Dr. Kipps, who was an investigator in both RESONATE trials and is a professor of medicine at the University of California, San Diego.
In univariate analysis of data from ibrutinib-treated patients, unmutated IGHV, del(11q), trisomy 12, and complex karyotype were generally not associated with shorter PFS, OS, or lower ORR or CRR.
Overall survival with and without unmutated IGHV was 78% and 84%, respectively; with and without trisomy 12 was 82% and 80%, respectively; and with and without complex karyotype was 77% and 78%, respectively.
ORR, for example, was comparable in the presence (90%) and absence (89%) of unmutated IGHV in ibrutinib-treated patients, as was CRR, at 29% and 26%, respectively.
In the presence and absence of trisomy 12, ORR was 85% and 91%, respectively; CRR was 33% and 22%.
In the presence and absence of complex karyotype, ORR was 88% and 89%, respectively, and CRR was 18% and 24%.
In the presence and absence of del(11q), ORR was 91% and 90%, respectively, and CRR was 22% and 27%.
The only difference that reached statistical significance was the complete response rate with trisomy 12, which favored the presence of trisomy 12.
Interestingly, the ibrutinib-treated patients with del(11q) had a trend toward longer PFS and OS, compared with those without del(11q), said Dr. Kipps.
At 36 months, PFS was 74% with the presence of del(11q) and 68% with the absence of del(11q) (hazard ratio, 0.73 vs. 1.88 in comparator-treated patients), and overall survival at 42 months was 80% in patients with del(11q) and 78% in those without del(11q) (HR, 0.73), Dr. Kipps said.
“The [finding in the] patients with the complex karyotype was a bit surprising, and I think this requires further analysis,” he said, explaining that complex karyotype actually was associated with a shorter PFS in patients treated on the comparator arm, and that this finding conflicts with earlier data.
The findings suggest ibrutinib-treated patients with trisomy 12, for reasons that are unclear, had a significantly higher complete response rate, but not greater PFS or OS vs. those without trisomy 12, Dr. Kipps said.
“It’s also interesting that ... unmutated antibody genes or del(11q) or complex karyotype were adverse prognostic factors in patients treated with comparator treatments, but not necessarily in patients treated with ibrutinib-based therapy,” he said.
Furthermore, although a prior phase II study involving heavily pretreated patients suggested that del(11q) may have adverse prognostic influence on PFS, that finding may not be borne out in patients with fewer lines of prior therapy.
The findings suggest that genomic risk factors associated with poor outcomes with initial chemoimmunotherapy may be less apparent in patients treated with ibrutinib.
“I think this is important, because it may then turn a prognostic factor into a predictive factor, meaning, a predictor of adverse outcomes for a given type of therapy as opposed to adverse prognostic value overall,” he concluded.
Ibrutinib (Imbruvica, Pharmacyclics) was approved by the Food and Drug Administration in January 2015 for the treatment of CLL after previous therapy. Dr. Kipps has received research funding from and/or served as a consultant or advisor for AbbVie, Genentech, Gilead, and Pharmacyclics, an AbbVie company.
sworcester@frontlinemedcom.com
NEW YORK – Risk factors associated with poor outcomes in chronic lymphocytic leukemia/small lymphocytic leukemia patients treated with standard therapies appear to have less relevance with ibrutinib treatment, according to an integrated analysis of data from the randomized, phase III RESONATE, RESONATE 2, and HELIOS trials.
In the combined analysis, at a median follow-up of 21 months, progression-free survival (PFS), overall survival (OS), overall response rate (ORR), and complete response rate (CRR) were better in ibrutinib-treated patients than in comparator-treated patients – and, in the ibrutinib-treated patients, the outcomes did not differ based on the adverse genomic factors examined, Thomas J. Kipps, MD, PhD, said at the annual International Workshop on Chronic Lymphocytic Leukemia.
The trials compared well with each other, but differed in terms of number of prior therapies received by patients, he said. Furthermore, the analysis did not examine the effect of del(17p); patients with that deletion were included only in the RESONATE trial.
In RESONATE, ibrutinib was superior to ofatumumab in relapsed/refractory CLL/SLL. In RESONATE 2, ibrutinib was superior to chlorambucil in treatment-naive patients with CLL/SLL. In HELIOS, ibrutinib with bendamustine/rituximab was superior to placebo with bendamustine/rituximab in patients with relapsed/refractory CLL/SLL.
In the new multivariate analysis of the pooled data from these trials – adjusting for the four genomic risk factors and age, sex, ECOG performance status, cytopenia, lactate dehydrogenase (LDH), bulky disease, and number of prior therapies – only having had one or more vs. no prior therapies, and having two or more vs. one prior therapies was associated with shorter PFS and OS in ibrutinib-treated patients, with a trend toward significance.
In comparator-treated patients, however, unmutated IGHV, del(11q), complex karyotype, male sex, two or more prior therapies, and bulky disease all were associated with significantly shorter PFS. Complex karyotype, male sex, bulky disease, ECOG performance status greater than 1, and elevated LDH were associated with significantly shorter OS.
“We need to debate on what the significance of this is and how that can be incorporated into our idea about first-line therapies,” said Dr. Kipps, who was an investigator in both RESONATE trials and is a professor of medicine at the University of California, San Diego.
In univariate analysis of data from ibrutinib-treated patients, unmutated IGHV, del(11q), trisomy 12, and complex karyotype were generally not associated with shorter PFS, OS, or lower ORR or CRR.
Overall survival with and without unmutated IGHV was 78% and 84%, respectively; with and without trisomy 12 was 82% and 80%, respectively; and with and without complex karyotype was 77% and 78%, respectively.
ORR, for example, was comparable in the presence (90%) and absence (89%) of unmutated IGHV in ibrutinib-treated patients, as was CRR, at 29% and 26%, respectively.
In the presence and absence of trisomy 12, ORR was 85% and 91%, respectively; CRR was 33% and 22%.
In the presence and absence of complex karyotype, ORR was 88% and 89%, respectively, and CRR was 18% and 24%.
In the presence and absence of del(11q), ORR was 91% and 90%, respectively, and CRR was 22% and 27%.
The only difference that reached statistical significance was the complete response rate with trisomy 12, which favored the presence of trisomy 12.
Interestingly, the ibrutinib-treated patients with del(11q) had a trend toward longer PFS and OS, compared with those without del(11q), said Dr. Kipps.
At 36 months, PFS was 74% with the presence of del(11q) and 68% with the absence of del(11q) (hazard ratio, 0.73 vs. 1.88 in comparator-treated patients), and overall survival at 42 months was 80% in patients with del(11q) and 78% in those without del(11q) (HR, 0.73), Dr. Kipps said.
“The [finding in the] patients with the complex karyotype was a bit surprising, and I think this requires further analysis,” he said, explaining that complex karyotype actually was associated with a shorter PFS in patients treated on the comparator arm, and that this finding conflicts with earlier data.
The findings suggest ibrutinib-treated patients with trisomy 12, for reasons that are unclear, had a significantly higher complete response rate, but not greater PFS or OS vs. those without trisomy 12, Dr. Kipps said.
“It’s also interesting that ... unmutated antibody genes or del(11q) or complex karyotype were adverse prognostic factors in patients treated with comparator treatments, but not necessarily in patients treated with ibrutinib-based therapy,” he said.
Furthermore, although a prior phase II study involving heavily pretreated patients suggested that del(11q) may have adverse prognostic influence on PFS, that finding may not be borne out in patients with fewer lines of prior therapy.
The findings suggest that genomic risk factors associated with poor outcomes with initial chemoimmunotherapy may be less apparent in patients treated with ibrutinib.
“I think this is important, because it may then turn a prognostic factor into a predictive factor, meaning, a predictor of adverse outcomes for a given type of therapy as opposed to adverse prognostic value overall,” he concluded.
Ibrutinib (Imbruvica, Pharmacyclics) was approved by the Food and Drug Administration in January 2015 for the treatment of CLL after previous therapy. Dr. Kipps has received research funding from and/or served as a consultant or advisor for AbbVie, Genentech, Gilead, and Pharmacyclics, an AbbVie company.
sworcester@frontlinemedcom.com
AT THE IWCLL MEETING
Key clinical point:
Major finding: In ibrutinib-treated patients, overall survival with and without unmutated IGHV was 78% and 84%, respectively; with and without trisomy 12 was 82% and 80%, respectively; and with and without complex karyotype was 77% and 78%, respectively.
Data source: A pooled analysis of data from 1,210 patients from three randomized phase III trials.
Disclosures: Dr. Kipps has received research funding from and/or served as a consultant or advisor for AbbVie, Genentech, Gilead, and Pharmacyclics, an AbbVie company.
Novel Lotus valve outperforms CoreValve in REPRISE III
PARIS – The investigational mechanically expandable Lotus valve system for transcatheter aortic valve replacement proved significantly more effective than the commercially available CoreValve platform in patients with severe aortic stenosis deemed at high or extreme surgical risk in the randomized pivotal phase III REPRISE III trial, Ted E. Feldman, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The 1-year composite primary effectiveness endpoint comprised of all-cause mortality, disabling stroke, and moderate or greater paravalvular leak (PVL) occurred in 17% of patients randomized to the Lotus transcatheter aortic valve replacement (TAVR) device, compared with 29% of those in the CoreValve group, said Dr. Feldman, director of the cardiac catheterization laboratory at NorthShore University HealthSystem in Evanston, Ill.
A key finding was that the Lotus valve group had a 1-year rate of moderate or greater PVL of just 2% as assessed in a central core lab, compared with an 11% rate in patients randomized to the classic CoreValve or the subsequent-generation Evolut R device, he observed.
“With the Lotus valve there was no or only trace PVL in over 85% of patients. This is probably even more important than the low rate of moderate or severe PVL. The valve really does result in virtually no PVL in the vast majority of patients. That’s unique to this platform,” the cardiologist said in an interview.
The unprecedented low rate of moderate or severe PVL at 1 year postprocedure is attributable to the polymer seal delivered via the Lotus system for that express purpose, he explained.
REPRISE III was the first large randomized comparative clinical trial featuring two TAVR valves, an event that reflects the rapid expansion of the field. All previous major trials had compared TAVR with surgical aortic valve replacement.
REPRISE III randomized 912 TAVR patients at 55 centers 2:1 to the Lotus valve in its 23-, 25-, or 27-mm configurations or to a CoreValve at 26, 29, or 31 mm. Roughly half of the CoreValve group got the newer repositionable and retrievable Evolut R valve, while the earlier enrollees received the nonrepositionable classic CoreValve.
The Lotus valve group proved noninferior to the CoreValve recipients for the primary safety endpoint, a 30-day composite of all-cause mortality, stroke, major or life-threatening bleeding, major vascular complications, and stage 2 or 3 acute kidney injury. The rates were 20.3% in the Lotus arm and 17.2% with CoreValve.
The 1-year rate of disabling stroke was 3.6% in the Lotus group versus 7.3% in the CoreValve group. Dr. Feldman downplayed the importance of this difference, even though it was statistically significant. The Lotus valve performed as expected, but the disabling stroke rate in the CoreValve group was higher than in earlier studies for reasons unknown, most likely simply the play of chance, he said.
“I think the real message here is that the Lotus valve performed very well,” the cardiologist said. “There have been concerns that repositioning the valve into a better position during the deployment process might create excess stroke. It appears clear that’s not the case.”
The ability to reposition the Lotus device resulted in a significantly lower rate of repeat procedures at 1 year: 0.2% versus 2% with the CoreValve, as well as zero cases of aortic valve malposition and valve-in-valve deployment.
The need for a new pacemaker within 30 days after TAVR was strikingly more common in the Lotus valve group: 36%, compared with 20% with the CoreValve. Dr. Feldman attributed the high new pacemaker rate in the Lotus arm partly to the operators’ limited experience with the novel valve along with the fact that REPRISE III used a first-iteration device deployment mechanism. An improved deployment mechanism designed to minimize problematic contact with the left ventricular outflow tract was developed too late for inclusion in the trial. But in a recent European study using this proprietary deployment system, known as Depth Guard, the new pacemaker rate was below 20%.
The learning curve for the new Lotus valve system is “not at all challenging,” according to the cardiologist. He noted that U.S. operators participating in REPRISE III, who had no prior experience with the device, were allowed only two initial cases in order to gain experience; after that, every patient counted in the clinical trial results.
The REPRISE III results will be offered to the Food and Drug Administration to support regulatory approval of the device in high-surgical-risk patients. Dr. Feldman said Boston Scientific plans to conduct an additional clinical trial of the Lotus valve, this time in intermediate-risk patients, with the goal of gaining an expanded indication. This, too, will be a head-to-head comparison with a commercially available TAVR valve, probably the Edwards Sapien 3 valve.
REPRISE III was sponsored by Boston Scientific. Dr. Feldman reported serving as a consultant to that company, Abbott, and Edwards Lifesciences, and having received institutional research grants from those companies as well.
bjancin@frontlinemedcom.com
PARIS – The investigational mechanically expandable Lotus valve system for transcatheter aortic valve replacement proved significantly more effective than the commercially available CoreValve platform in patients with severe aortic stenosis deemed at high or extreme surgical risk in the randomized pivotal phase III REPRISE III trial, Ted E. Feldman, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The 1-year composite primary effectiveness endpoint comprised of all-cause mortality, disabling stroke, and moderate or greater paravalvular leak (PVL) occurred in 17% of patients randomized to the Lotus transcatheter aortic valve replacement (TAVR) device, compared with 29% of those in the CoreValve group, said Dr. Feldman, director of the cardiac catheterization laboratory at NorthShore University HealthSystem in Evanston, Ill.
A key finding was that the Lotus valve group had a 1-year rate of moderate or greater PVL of just 2% as assessed in a central core lab, compared with an 11% rate in patients randomized to the classic CoreValve or the subsequent-generation Evolut R device, he observed.
“With the Lotus valve there was no or only trace PVL in over 85% of patients. This is probably even more important than the low rate of moderate or severe PVL. The valve really does result in virtually no PVL in the vast majority of patients. That’s unique to this platform,” the cardiologist said in an interview.
The unprecedented low rate of moderate or severe PVL at 1 year postprocedure is attributable to the polymer seal delivered via the Lotus system for that express purpose, he explained.
REPRISE III was the first large randomized comparative clinical trial featuring two TAVR valves, an event that reflects the rapid expansion of the field. All previous major trials had compared TAVR with surgical aortic valve replacement.
REPRISE III randomized 912 TAVR patients at 55 centers 2:1 to the Lotus valve in its 23-, 25-, or 27-mm configurations or to a CoreValve at 26, 29, or 31 mm. Roughly half of the CoreValve group got the newer repositionable and retrievable Evolut R valve, while the earlier enrollees received the nonrepositionable classic CoreValve.
The Lotus valve group proved noninferior to the CoreValve recipients for the primary safety endpoint, a 30-day composite of all-cause mortality, stroke, major or life-threatening bleeding, major vascular complications, and stage 2 or 3 acute kidney injury. The rates were 20.3% in the Lotus arm and 17.2% with CoreValve.
The 1-year rate of disabling stroke was 3.6% in the Lotus group versus 7.3% in the CoreValve group. Dr. Feldman downplayed the importance of this difference, even though it was statistically significant. The Lotus valve performed as expected, but the disabling stroke rate in the CoreValve group was higher than in earlier studies for reasons unknown, most likely simply the play of chance, he said.
“I think the real message here is that the Lotus valve performed very well,” the cardiologist said. “There have been concerns that repositioning the valve into a better position during the deployment process might create excess stroke. It appears clear that’s not the case.”
The ability to reposition the Lotus device resulted in a significantly lower rate of repeat procedures at 1 year: 0.2% versus 2% with the CoreValve, as well as zero cases of aortic valve malposition and valve-in-valve deployment.
The need for a new pacemaker within 30 days after TAVR was strikingly more common in the Lotus valve group: 36%, compared with 20% with the CoreValve. Dr. Feldman attributed the high new pacemaker rate in the Lotus arm partly to the operators’ limited experience with the novel valve along with the fact that REPRISE III used a first-iteration device deployment mechanism. An improved deployment mechanism designed to minimize problematic contact with the left ventricular outflow tract was developed too late for inclusion in the trial. But in a recent European study using this proprietary deployment system, known as Depth Guard, the new pacemaker rate was below 20%.
The learning curve for the new Lotus valve system is “not at all challenging,” according to the cardiologist. He noted that U.S. operators participating in REPRISE III, who had no prior experience with the device, were allowed only two initial cases in order to gain experience; after that, every patient counted in the clinical trial results.
The REPRISE III results will be offered to the Food and Drug Administration to support regulatory approval of the device in high-surgical-risk patients. Dr. Feldman said Boston Scientific plans to conduct an additional clinical trial of the Lotus valve, this time in intermediate-risk patients, with the goal of gaining an expanded indication. This, too, will be a head-to-head comparison with a commercially available TAVR valve, probably the Edwards Sapien 3 valve.
REPRISE III was sponsored by Boston Scientific. Dr. Feldman reported serving as a consultant to that company, Abbott, and Edwards Lifesciences, and having received institutional research grants from those companies as well.
bjancin@frontlinemedcom.com
PARIS – The investigational mechanically expandable Lotus valve system for transcatheter aortic valve replacement proved significantly more effective than the commercially available CoreValve platform in patients with severe aortic stenosis deemed at high or extreme surgical risk in the randomized pivotal phase III REPRISE III trial, Ted E. Feldman, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The 1-year composite primary effectiveness endpoint comprised of all-cause mortality, disabling stroke, and moderate or greater paravalvular leak (PVL) occurred in 17% of patients randomized to the Lotus transcatheter aortic valve replacement (TAVR) device, compared with 29% of those in the CoreValve group, said Dr. Feldman, director of the cardiac catheterization laboratory at NorthShore University HealthSystem in Evanston, Ill.
A key finding was that the Lotus valve group had a 1-year rate of moderate or greater PVL of just 2% as assessed in a central core lab, compared with an 11% rate in patients randomized to the classic CoreValve or the subsequent-generation Evolut R device, he observed.
“With the Lotus valve there was no or only trace PVL in over 85% of patients. This is probably even more important than the low rate of moderate or severe PVL. The valve really does result in virtually no PVL in the vast majority of patients. That’s unique to this platform,” the cardiologist said in an interview.
The unprecedented low rate of moderate or severe PVL at 1 year postprocedure is attributable to the polymer seal delivered via the Lotus system for that express purpose, he explained.
REPRISE III was the first large randomized comparative clinical trial featuring two TAVR valves, an event that reflects the rapid expansion of the field. All previous major trials had compared TAVR with surgical aortic valve replacement.
REPRISE III randomized 912 TAVR patients at 55 centers 2:1 to the Lotus valve in its 23-, 25-, or 27-mm configurations or to a CoreValve at 26, 29, or 31 mm. Roughly half of the CoreValve group got the newer repositionable and retrievable Evolut R valve, while the earlier enrollees received the nonrepositionable classic CoreValve.
The Lotus valve group proved noninferior to the CoreValve recipients for the primary safety endpoint, a 30-day composite of all-cause mortality, stroke, major or life-threatening bleeding, major vascular complications, and stage 2 or 3 acute kidney injury. The rates were 20.3% in the Lotus arm and 17.2% with CoreValve.
The 1-year rate of disabling stroke was 3.6% in the Lotus group versus 7.3% in the CoreValve group. Dr. Feldman downplayed the importance of this difference, even though it was statistically significant. The Lotus valve performed as expected, but the disabling stroke rate in the CoreValve group was higher than in earlier studies for reasons unknown, most likely simply the play of chance, he said.
“I think the real message here is that the Lotus valve performed very well,” the cardiologist said. “There have been concerns that repositioning the valve into a better position during the deployment process might create excess stroke. It appears clear that’s not the case.”
The ability to reposition the Lotus device resulted in a significantly lower rate of repeat procedures at 1 year: 0.2% versus 2% with the CoreValve, as well as zero cases of aortic valve malposition and valve-in-valve deployment.
The need for a new pacemaker within 30 days after TAVR was strikingly more common in the Lotus valve group: 36%, compared with 20% with the CoreValve. Dr. Feldman attributed the high new pacemaker rate in the Lotus arm partly to the operators’ limited experience with the novel valve along with the fact that REPRISE III used a first-iteration device deployment mechanism. An improved deployment mechanism designed to minimize problematic contact with the left ventricular outflow tract was developed too late for inclusion in the trial. But in a recent European study using this proprietary deployment system, known as Depth Guard, the new pacemaker rate was below 20%.
The learning curve for the new Lotus valve system is “not at all challenging,” according to the cardiologist. He noted that U.S. operators participating in REPRISE III, who had no prior experience with the device, were allowed only two initial cases in order to gain experience; after that, every patient counted in the clinical trial results.
The REPRISE III results will be offered to the Food and Drug Administration to support regulatory approval of the device in high-surgical-risk patients. Dr. Feldman said Boston Scientific plans to conduct an additional clinical trial of the Lotus valve, this time in intermediate-risk patients, with the goal of gaining an expanded indication. This, too, will be a head-to-head comparison with a commercially available TAVR valve, probably the Edwards Sapien 3 valve.
REPRISE III was sponsored by Boston Scientific. Dr. Feldman reported serving as a consultant to that company, Abbott, and Edwards Lifesciences, and having received institutional research grants from those companies as well.
bjancin@frontlinemedcom.com
AT EUROPCR
Key clinical point:
Major finding: The rate of the 1-year composite primary effectiveness endpoint comprised of all-cause mortality, disabling stroke, and moderate or greater paravalvular leak was 17% in patients randomized to the investigational Lotus transcatheter aortic valve replacement system, compared with 29% in recipients of the CoreValve.
Data source: REPRISE III, a prospective, multicenter, international clinical trial randomized 912 patients with severe aortic stenosis who were at high surgical risk to TAVR with the investigational Lotus valve or a commercially available CoreValve.
Disclosures: REPRISE III was sponsored by Boston Scientific. The study presenter reported serving as a consultant to that company as well as for Abbott and Edwards Lifesciences. He has also received institutional research grants from those companies.
Consider S. pyogenes in cases of pediatric intertrigo
Beefy-red, well demarcated lesions in skin folds without satellite lesions are the clinical signs of intertrigo, and Streptococcus pyogenes may be the cause, said Anca Chiriac, MD, PhD, of Apollonia University, Iasi, Romania, and her associates.
Intertrigo is frequently misdiagnosed in young children, and S. pyogenes skin infections often are misdiagnosed or overlooked. A case series of six children under 9 years of age was discussed in which the children presented with intense erythematous patches that often were pruritic occurring around the anus, in and around the umbilicus, on the vulva, in the intertriginous folds of the neck, in the toe web, and in the antecubital fossa.
The skin lesions often were misdiagnosed as contact dermatitis or atopic dermatitis or a fungal infection, and in several cases they were treated with potent corticosteroids, which aggravated the problem, or a topical antifungal, which had no effect. Swabs for bacterial culture identified S. pyogenes, and courses of oral antibiotics such as penicillin, amoxicillin, or ceftriaxone led to rapid improvement.
S. pyogenes skin infections complications include septicemia, arthritis, osteomyelitis, pneumonia, and toxic shock syndrome. “It is our practice to perform urinalysis because of the risk of poststreptococcal glomerulonephritis,” Dr. Chiriac and her associates said. They recommended penicillin or cephalosporin in age-related doses, or erythromycin or clindamycin if children are allergic to penicillin.
Read more at (J Pediatr. 2017 May;184:230-1).
cnellist@frontlinemedcom.com
Beefy-red, well demarcated lesions in skin folds without satellite lesions are the clinical signs of intertrigo, and Streptococcus pyogenes may be the cause, said Anca Chiriac, MD, PhD, of Apollonia University, Iasi, Romania, and her associates.
Intertrigo is frequently misdiagnosed in young children, and S. pyogenes skin infections often are misdiagnosed or overlooked. A case series of six children under 9 years of age was discussed in which the children presented with intense erythematous patches that often were pruritic occurring around the anus, in and around the umbilicus, on the vulva, in the intertriginous folds of the neck, in the toe web, and in the antecubital fossa.
The skin lesions often were misdiagnosed as contact dermatitis or atopic dermatitis or a fungal infection, and in several cases they were treated with potent corticosteroids, which aggravated the problem, or a topical antifungal, which had no effect. Swabs for bacterial culture identified S. pyogenes, and courses of oral antibiotics such as penicillin, amoxicillin, or ceftriaxone led to rapid improvement.
S. pyogenes skin infections complications include septicemia, arthritis, osteomyelitis, pneumonia, and toxic shock syndrome. “It is our practice to perform urinalysis because of the risk of poststreptococcal glomerulonephritis,” Dr. Chiriac and her associates said. They recommended penicillin or cephalosporin in age-related doses, or erythromycin or clindamycin if children are allergic to penicillin.
Read more at (J Pediatr. 2017 May;184:230-1).
cnellist@frontlinemedcom.com
Beefy-red, well demarcated lesions in skin folds without satellite lesions are the clinical signs of intertrigo, and Streptococcus pyogenes may be the cause, said Anca Chiriac, MD, PhD, of Apollonia University, Iasi, Romania, and her associates.
Intertrigo is frequently misdiagnosed in young children, and S. pyogenes skin infections often are misdiagnosed or overlooked. A case series of six children under 9 years of age was discussed in which the children presented with intense erythematous patches that often were pruritic occurring around the anus, in and around the umbilicus, on the vulva, in the intertriginous folds of the neck, in the toe web, and in the antecubital fossa.
The skin lesions often were misdiagnosed as contact dermatitis or atopic dermatitis or a fungal infection, and in several cases they were treated with potent corticosteroids, which aggravated the problem, or a topical antifungal, which had no effect. Swabs for bacterial culture identified S. pyogenes, and courses of oral antibiotics such as penicillin, amoxicillin, or ceftriaxone led to rapid improvement.
S. pyogenes skin infections complications include septicemia, arthritis, osteomyelitis, pneumonia, and toxic shock syndrome. “It is our practice to perform urinalysis because of the risk of poststreptococcal glomerulonephritis,” Dr. Chiriac and her associates said. They recommended penicillin or cephalosporin in age-related doses, or erythromycin or clindamycin if children are allergic to penicillin.
Read more at (J Pediatr. 2017 May;184:230-1).
cnellist@frontlinemedcom.com
FROM THE JOURNAL OF PEDIATRICS
SFDA approves product for hemophilia A
The Saudi Food & Drug Authority (SFDA) in the Kingdom of Saudi Arabia has approved efmoroctocog alfa (Elocta®), a recombinant human factor VIII Fc-fusion protein, for the treatment of hemophilia A.
Efmoroctocog alfa is indicated for both on-demand treatment and prophylaxis in hemophilia A patients of all ages.
It is the first extended half-life and recombinant factor VIII Fc fusion protein therapy approved for the treatment of hemophilia A in Saudi Arabia.
The SFDA’s approval of efmoroctocog alfa was based on data from a pair of phase 3 studies: A-LONG and Kids A-LONG.
A-LONG
The A-LONG study included 165 previously treated males 12 years of age and older with severe hemophilia A. Researchers evaluated individualized and weekly prophylaxis to reduce or prevent bleeding episodes and on-demand dosing to treat bleeding episodes.
Prophylaxis with efmoroctocog alfa resulted in low annualized bleeding rates, and a majority of bleeding episodes were controlled with a single injection of efmoroctocog alfa.
None of the patients developed neutralizing antibodies, efmoroctocog alfa was considered well-tolerated, and the product had a prolonged half-life when compared with recombinant factor VIII.
Kids A-LONG
The Kids A-LONG study included 71 boys (younger than 12) with severe hemophilia A who had at least 50 prior exposure days to factor VIII therapies.
The children saw their median annualized bleeding rate decrease with efmoroctocog alfa, and close to half of the children did not have any bleeding episodes while they were receiving efmoroctocog alfa.
None of the patients developed inhibitors, and researchers said adverse events were typical of a pediatric hemophilia population.
Efmoroctocog alfa is being developed and commercialized by Sobi and Bioverativ. ![]()
The Saudi Food & Drug Authority (SFDA) in the Kingdom of Saudi Arabia has approved efmoroctocog alfa (Elocta®), a recombinant human factor VIII Fc-fusion protein, for the treatment of hemophilia A.
Efmoroctocog alfa is indicated for both on-demand treatment and prophylaxis in hemophilia A patients of all ages.
It is the first extended half-life and recombinant factor VIII Fc fusion protein therapy approved for the treatment of hemophilia A in Saudi Arabia.
The SFDA’s approval of efmoroctocog alfa was based on data from a pair of phase 3 studies: A-LONG and Kids A-LONG.
A-LONG
The A-LONG study included 165 previously treated males 12 years of age and older with severe hemophilia A. Researchers evaluated individualized and weekly prophylaxis to reduce or prevent bleeding episodes and on-demand dosing to treat bleeding episodes.
Prophylaxis with efmoroctocog alfa resulted in low annualized bleeding rates, and a majority of bleeding episodes were controlled with a single injection of efmoroctocog alfa.
None of the patients developed neutralizing antibodies, efmoroctocog alfa was considered well-tolerated, and the product had a prolonged half-life when compared with recombinant factor VIII.
Kids A-LONG
The Kids A-LONG study included 71 boys (younger than 12) with severe hemophilia A who had at least 50 prior exposure days to factor VIII therapies.
The children saw their median annualized bleeding rate decrease with efmoroctocog alfa, and close to half of the children did not have any bleeding episodes while they were receiving efmoroctocog alfa.
None of the patients developed inhibitors, and researchers said adverse events were typical of a pediatric hemophilia population.
Efmoroctocog alfa is being developed and commercialized by Sobi and Bioverativ. ![]()
The Saudi Food & Drug Authority (SFDA) in the Kingdom of Saudi Arabia has approved efmoroctocog alfa (Elocta®), a recombinant human factor VIII Fc-fusion protein, for the treatment of hemophilia A.
Efmoroctocog alfa is indicated for both on-demand treatment and prophylaxis in hemophilia A patients of all ages.
It is the first extended half-life and recombinant factor VIII Fc fusion protein therapy approved for the treatment of hemophilia A in Saudi Arabia.
The SFDA’s approval of efmoroctocog alfa was based on data from a pair of phase 3 studies: A-LONG and Kids A-LONG.
A-LONG
The A-LONG study included 165 previously treated males 12 years of age and older with severe hemophilia A. Researchers evaluated individualized and weekly prophylaxis to reduce or prevent bleeding episodes and on-demand dosing to treat bleeding episodes.
Prophylaxis with efmoroctocog alfa resulted in low annualized bleeding rates, and a majority of bleeding episodes were controlled with a single injection of efmoroctocog alfa.
None of the patients developed neutralizing antibodies, efmoroctocog alfa was considered well-tolerated, and the product had a prolonged half-life when compared with recombinant factor VIII.
Kids A-LONG
The Kids A-LONG study included 71 boys (younger than 12) with severe hemophilia A who had at least 50 prior exposure days to factor VIII therapies.
The children saw their median annualized bleeding rate decrease with efmoroctocog alfa, and close to half of the children did not have any bleeding episodes while they were receiving efmoroctocog alfa.
None of the patients developed inhibitors, and researchers said adverse events were typical of a pediatric hemophilia population.
Efmoroctocog alfa is being developed and commercialized by Sobi and Bioverativ. ![]()
Positive node risk defined for elderly breast cancer patients
LAS VEGAS – In women aged 70 years or older with hormone receptor–positive invasive breast cancer, their tumor size, grade, and histology – but not human epidermal growth factor receptor–2 status – predicted nodal positivity, according to a retrospective analysis.
Investigators at the Mayo Clinic, Rochester, Minn., reviewed 52,532 women in the National Cancer Database from 2010 to 2013 who were at least 70 years old with hormone receptor–positive invasive breast cancer and clinically node negative disease, who had axillary surgery performed. Two-thirds of the cohort was used to identify risk factors, and the remaining third to validate them. About 16% in both groups had cancer in their axillary lymph nodes.
On multivariate analysis, higher clinical T stage, higher grade, and invasive lobular and invasive mammary histology were all associated with positive nodes. Although significant on univariate analysis, age (P = .57) and HER2 status (P = .32) fell out on multivariate analysis.
Nodal positivity was more than five times as likely with clinical T2 tumors, compared with T1a tumors, and far less likely for patients with invasive mucinous carcinoma than for those with invasive ductal carcinoma.
The team expects to release a nomogram for general use in clinical practice to predict the risk of positive nodes for various combinations of tumor size, grade, and histology in older women. When the model predicted a less than 10% chance of node positive disease, the actual rate in the validation set was around 5.5%. When it predicted a 30%-39% chance, the actual rate was 32.6%. The area under the receiver operating characteristic curve was 0.7 in both the development and validation sets, indicating good discrimination.
The work grew out of an effort to implement the Society of Surgical Oncologists’ recommendation not to do routine sentinel node biopsies in clinically node negative, hormone receptor–positive invasive breast cancer in women over the age of 70 years, a recommendation the group made as part of its contribution to the Choosing Wisely campaign.
“After the guideline was released, we were sitting in the clinic thinking how to apply it to our patients,” lead investigator Jessemae Welsh, MD, a surgeon at the Mayo Clinic, said at the American Society of Breast Surgeons annual meeting.
The problem is that nodal positivity is important to know for other aspects of care, including regional nodal irradiation and duration of systemic hormone therapy, and axillary lymph node staging might still be indicated if older women are truly at high risk. “We [wanted] to develop a multivariate model that gives a precise estimate of nodal risk,” to help “patients and surgeons to decide together based on an individual risk” how best to proceed. Also, a prediction of low risk “can help reassure patients that they will do well without axillary surgery,” she said.
Mayo’s nomogram is unique in that it focuses specifically on women 70 years and older. Development of previous nomograms incorporated older women, but did not focus on them specifically, Dr. Welsh said.
Dr. Welsh said she had no relevant disclosures.
aotto@frontlinemedcom.com
LAS VEGAS – In women aged 70 years or older with hormone receptor–positive invasive breast cancer, their tumor size, grade, and histology – but not human epidermal growth factor receptor–2 status – predicted nodal positivity, according to a retrospective analysis.
Investigators at the Mayo Clinic, Rochester, Minn., reviewed 52,532 women in the National Cancer Database from 2010 to 2013 who were at least 70 years old with hormone receptor–positive invasive breast cancer and clinically node negative disease, who had axillary surgery performed. Two-thirds of the cohort was used to identify risk factors, and the remaining third to validate them. About 16% in both groups had cancer in their axillary lymph nodes.
On multivariate analysis, higher clinical T stage, higher grade, and invasive lobular and invasive mammary histology were all associated with positive nodes. Although significant on univariate analysis, age (P = .57) and HER2 status (P = .32) fell out on multivariate analysis.
Nodal positivity was more than five times as likely with clinical T2 tumors, compared with T1a tumors, and far less likely for patients with invasive mucinous carcinoma than for those with invasive ductal carcinoma.
The team expects to release a nomogram for general use in clinical practice to predict the risk of positive nodes for various combinations of tumor size, grade, and histology in older women. When the model predicted a less than 10% chance of node positive disease, the actual rate in the validation set was around 5.5%. When it predicted a 30%-39% chance, the actual rate was 32.6%. The area under the receiver operating characteristic curve was 0.7 in both the development and validation sets, indicating good discrimination.
The work grew out of an effort to implement the Society of Surgical Oncologists’ recommendation not to do routine sentinel node biopsies in clinically node negative, hormone receptor–positive invasive breast cancer in women over the age of 70 years, a recommendation the group made as part of its contribution to the Choosing Wisely campaign.
“After the guideline was released, we were sitting in the clinic thinking how to apply it to our patients,” lead investigator Jessemae Welsh, MD, a surgeon at the Mayo Clinic, said at the American Society of Breast Surgeons annual meeting.
The problem is that nodal positivity is important to know for other aspects of care, including regional nodal irradiation and duration of systemic hormone therapy, and axillary lymph node staging might still be indicated if older women are truly at high risk. “We [wanted] to develop a multivariate model that gives a precise estimate of nodal risk,” to help “patients and surgeons to decide together based on an individual risk” how best to proceed. Also, a prediction of low risk “can help reassure patients that they will do well without axillary surgery,” she said.
Mayo’s nomogram is unique in that it focuses specifically on women 70 years and older. Development of previous nomograms incorporated older women, but did not focus on them specifically, Dr. Welsh said.
Dr. Welsh said she had no relevant disclosures.
aotto@frontlinemedcom.com
LAS VEGAS – In women aged 70 years or older with hormone receptor–positive invasive breast cancer, their tumor size, grade, and histology – but not human epidermal growth factor receptor–2 status – predicted nodal positivity, according to a retrospective analysis.
Investigators at the Mayo Clinic, Rochester, Minn., reviewed 52,532 women in the National Cancer Database from 2010 to 2013 who were at least 70 years old with hormone receptor–positive invasive breast cancer and clinically node negative disease, who had axillary surgery performed. Two-thirds of the cohort was used to identify risk factors, and the remaining third to validate them. About 16% in both groups had cancer in their axillary lymph nodes.
On multivariate analysis, higher clinical T stage, higher grade, and invasive lobular and invasive mammary histology were all associated with positive nodes. Although significant on univariate analysis, age (P = .57) and HER2 status (P = .32) fell out on multivariate analysis.
Nodal positivity was more than five times as likely with clinical T2 tumors, compared with T1a tumors, and far less likely for patients with invasive mucinous carcinoma than for those with invasive ductal carcinoma.
The team expects to release a nomogram for general use in clinical practice to predict the risk of positive nodes for various combinations of tumor size, grade, and histology in older women. When the model predicted a less than 10% chance of node positive disease, the actual rate in the validation set was around 5.5%. When it predicted a 30%-39% chance, the actual rate was 32.6%. The area under the receiver operating characteristic curve was 0.7 in both the development and validation sets, indicating good discrimination.
The work grew out of an effort to implement the Society of Surgical Oncologists’ recommendation not to do routine sentinel node biopsies in clinically node negative, hormone receptor–positive invasive breast cancer in women over the age of 70 years, a recommendation the group made as part of its contribution to the Choosing Wisely campaign.
“After the guideline was released, we were sitting in the clinic thinking how to apply it to our patients,” lead investigator Jessemae Welsh, MD, a surgeon at the Mayo Clinic, said at the American Society of Breast Surgeons annual meeting.
The problem is that nodal positivity is important to know for other aspects of care, including regional nodal irradiation and duration of systemic hormone therapy, and axillary lymph node staging might still be indicated if older women are truly at high risk. “We [wanted] to develop a multivariate model that gives a precise estimate of nodal risk,” to help “patients and surgeons to decide together based on an individual risk” how best to proceed. Also, a prediction of low risk “can help reassure patients that they will do well without axillary surgery,” she said.
Mayo’s nomogram is unique in that it focuses specifically on women 70 years and older. Development of previous nomograms incorporated older women, but did not focus on them specifically, Dr. Welsh said.
Dr. Welsh said she had no relevant disclosures.
aotto@frontlinemedcom.com
AT ASBS 2017
Key clinical point:
Major finding: On multivariate analysis, higher clinical T stage, higher grade, and invasive lobular and invasive mammary histology were all associated with positive nodes.
Data source: An analysis of data from 52,532 women in the National Cancer Database during 2010-2013.
Disclosures: The lead investigator had no disclosures.
Forgo axillary dissection for single suspicious node on ultrasound
LAS VEGAS – About half of breast cancer patients without palpable lymphadenopathy but with preoperative ultrasound-guided, biopsy-proven axillary lymph node metastases have N1 disease, according to a review of 129 women.
Among the 30 women with a primary tumor 2 cm or smaller and only one abnormal lymph node on axillary ultrasound, 22 (73%) had metastases limited to the one lymph node, suggesting that such patients “may undergo ... sentinel lymph node biopsy” instead of a complete axillary lymph node dissection (ALND), the investigators concluded.
The problem that has come up in clinical practice is that axillary ultrasound is now a routine part of breast cancer workup, but the original trial didn’t address ultrasound, said senior investigator Rubie Sue Jackson, MD, at the annual meeting of the American Society of Breast Surgeons. As a result, “surgeons don’t know what to do with an ultrasound-detected suspicious node. I think a lot of surgeons, if they detect a positive lymph node by ultrasound, even if it’s nonpalpable, would not consider the patient a candidate for sentinel lymph node biopsy. Our data suggest that many of these patients are being overtreated if they have an upfront axillary lymph node dissection,” she said.
The 129 women had 1-3 suspicious, nonpalpable nodes on ultrasound that turned out to have metastatic disease on needle biopsy. They all had subsequent ALNDs.
On final pathology, 67 women (52%) had only one metastatic node. For those women, a sentinel lymph node biopsy was likely all that they required. “They probably did not benefit from having an ALND,” said Dr. Jackson, a breast surgeon at the Anne Arundel Medical Center in Annapolis, Md. The other 62 women (48%) had N2-3 disease.
A primary tumor sized 2 cm or smaller (P = .012); nonlobular histology (P = .013), and having only one suspicious nonpalpable node on ultrasound (P = .008) were all associated with NI disease. Of the women who met the criteria, only eight (27%) had N 2-3 disease (P = .007).
“Patients meeting the three criteria are particularly unlikely to have three or more positive sentinel lymph nodes” and require subsequent ALND. “You don’t need to do a complete axillary lymph node dissection upfront, as long as they are getting a lumpectomy and whole breast radiation,” Dr. Jackson said.
These days at Anne Arundel, “we do the axillary ultrasound, we biopsy the lymph node if it looks suspicious, but we don’t feel forced to do an ALND. If a patient has tumor biology that’s likely to be highly responsive, we do upfront chemotherapy. If they have luminal tumor biology that’s not going to be very responsive to neoadjuvant therapy,” with one or two suspicious nodes, “and they are planning to get breast conserving therapy, I would do a sentinel lymph node biopsy and x-ray the specimen to make sure that I’ve retrieved the clip,” she said.
Dr. Jackson didn’t have any disclosures, and there was no industry funding for the work.
aotto@frontlinemedcom.com
LAS VEGAS – About half of breast cancer patients without palpable lymphadenopathy but with preoperative ultrasound-guided, biopsy-proven axillary lymph node metastases have N1 disease, according to a review of 129 women.
Among the 30 women with a primary tumor 2 cm or smaller and only one abnormal lymph node on axillary ultrasound, 22 (73%) had metastases limited to the one lymph node, suggesting that such patients “may undergo ... sentinel lymph node biopsy” instead of a complete axillary lymph node dissection (ALND), the investigators concluded.
The problem that has come up in clinical practice is that axillary ultrasound is now a routine part of breast cancer workup, but the original trial didn’t address ultrasound, said senior investigator Rubie Sue Jackson, MD, at the annual meeting of the American Society of Breast Surgeons. As a result, “surgeons don’t know what to do with an ultrasound-detected suspicious node. I think a lot of surgeons, if they detect a positive lymph node by ultrasound, even if it’s nonpalpable, would not consider the patient a candidate for sentinel lymph node biopsy. Our data suggest that many of these patients are being overtreated if they have an upfront axillary lymph node dissection,” she said.
The 129 women had 1-3 suspicious, nonpalpable nodes on ultrasound that turned out to have metastatic disease on needle biopsy. They all had subsequent ALNDs.
On final pathology, 67 women (52%) had only one metastatic node. For those women, a sentinel lymph node biopsy was likely all that they required. “They probably did not benefit from having an ALND,” said Dr. Jackson, a breast surgeon at the Anne Arundel Medical Center in Annapolis, Md. The other 62 women (48%) had N2-3 disease.
A primary tumor sized 2 cm or smaller (P = .012); nonlobular histology (P = .013), and having only one suspicious nonpalpable node on ultrasound (P = .008) were all associated with NI disease. Of the women who met the criteria, only eight (27%) had N 2-3 disease (P = .007).
“Patients meeting the three criteria are particularly unlikely to have three or more positive sentinel lymph nodes” and require subsequent ALND. “You don’t need to do a complete axillary lymph node dissection upfront, as long as they are getting a lumpectomy and whole breast radiation,” Dr. Jackson said.
These days at Anne Arundel, “we do the axillary ultrasound, we biopsy the lymph node if it looks suspicious, but we don’t feel forced to do an ALND. If a patient has tumor biology that’s likely to be highly responsive, we do upfront chemotherapy. If they have luminal tumor biology that’s not going to be very responsive to neoadjuvant therapy,” with one or two suspicious nodes, “and they are planning to get breast conserving therapy, I would do a sentinel lymph node biopsy and x-ray the specimen to make sure that I’ve retrieved the clip,” she said.
Dr. Jackson didn’t have any disclosures, and there was no industry funding for the work.
aotto@frontlinemedcom.com
LAS VEGAS – About half of breast cancer patients without palpable lymphadenopathy but with preoperative ultrasound-guided, biopsy-proven axillary lymph node metastases have N1 disease, according to a review of 129 women.
Among the 30 women with a primary tumor 2 cm or smaller and only one abnormal lymph node on axillary ultrasound, 22 (73%) had metastases limited to the one lymph node, suggesting that such patients “may undergo ... sentinel lymph node biopsy” instead of a complete axillary lymph node dissection (ALND), the investigators concluded.
The problem that has come up in clinical practice is that axillary ultrasound is now a routine part of breast cancer workup, but the original trial didn’t address ultrasound, said senior investigator Rubie Sue Jackson, MD, at the annual meeting of the American Society of Breast Surgeons. As a result, “surgeons don’t know what to do with an ultrasound-detected suspicious node. I think a lot of surgeons, if they detect a positive lymph node by ultrasound, even if it’s nonpalpable, would not consider the patient a candidate for sentinel lymph node biopsy. Our data suggest that many of these patients are being overtreated if they have an upfront axillary lymph node dissection,” she said.
The 129 women had 1-3 suspicious, nonpalpable nodes on ultrasound that turned out to have metastatic disease on needle biopsy. They all had subsequent ALNDs.
On final pathology, 67 women (52%) had only one metastatic node. For those women, a sentinel lymph node biopsy was likely all that they required. “They probably did not benefit from having an ALND,” said Dr. Jackson, a breast surgeon at the Anne Arundel Medical Center in Annapolis, Md. The other 62 women (48%) had N2-3 disease.
A primary tumor sized 2 cm or smaller (P = .012); nonlobular histology (P = .013), and having only one suspicious nonpalpable node on ultrasound (P = .008) were all associated with NI disease. Of the women who met the criteria, only eight (27%) had N 2-3 disease (P = .007).
“Patients meeting the three criteria are particularly unlikely to have three or more positive sentinel lymph nodes” and require subsequent ALND. “You don’t need to do a complete axillary lymph node dissection upfront, as long as they are getting a lumpectomy and whole breast radiation,” Dr. Jackson said.
These days at Anne Arundel, “we do the axillary ultrasound, we biopsy the lymph node if it looks suspicious, but we don’t feel forced to do an ALND. If a patient has tumor biology that’s likely to be highly responsive, we do upfront chemotherapy. If they have luminal tumor biology that’s not going to be very responsive to neoadjuvant therapy,” with one or two suspicious nodes, “and they are planning to get breast conserving therapy, I would do a sentinel lymph node biopsy and x-ray the specimen to make sure that I’ve retrieved the clip,” she said.
Dr. Jackson didn’t have any disclosures, and there was no industry funding for the work.
aotto@frontlinemedcom.com
AT ASBS 2017
Key clinical point:
Major finding: Among the 30 women with tumors 2 cm or smaller, and only one abnormal lymph node on axillary ultrasound, 22 (73%) had metastasis limited to the one lymph node.
Data source: A review of 129 women with breast cancer.
Disclosures: There was no industry funding, and the senior investigator had no disclosures.