User login
Game over: VTE is a risk in obese, sedentary teens
MONTREAL – It’s well known that airplane passengers, condemned to sit for endless hours in the claustrophobic cabins of the unfriendly skies, are at increased risk for venous thromboembolic events (VTEs). Less well documented, however, is the VTE risk encountered by overweight or obese teens who while their hours away playing video games.
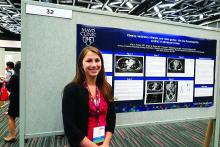
“This is becoming a sedentary-type risk factor,” said Mira A. Kohorst, MD, from the division of pediatric hematology-oncology at the Mayo Clinic in Rochester, Minn.
Dr. Kohorst and her colleagues reported on a small but troubling trend of VTE episodes that they observed in teen boys over the last few years. They refer to obesity, sedentary lifestyle, and gaming as “the new thrombophilia cocktail in adolescent males.”
The reported incidence of pediatric VTE ranges from 0.7 to 4.9 per 100,000 person years, considerably lower than the 1 in 1000 estimated incidences reported in adults. But, thanks to the growing incidence of obesity in children, which more than doubled from 1980 to 2012 and quadrupled in teens age 12-19 years from 5% to 21%, youngsters appear to be catching up in the VTE department, the investigators reported.
“Given the direct mortality rate of 2% [that is] associated with VTE and risk for postthrombotic syndrome of 26%, it is important to understand underlying modifiable risk factors,” they wrote.
To do this, they retrospectively reviewed records of children who presented with VTE in their center.
All play, no exercise
The authors described three cases, including that of an 18-year old boy with a body mass index (BMI) of 37 kg/m2, putting him squarely in the obese category. This lad, who spent 12 or more hours a day playing video games and was sedentary at other times as well, presented with bilateral pulmonary emboli and an associated right lower lobe infarction. Testing for thrombophilia showed that he was heterozygous for factor V Leiden but did not have other coagulation abnormalities. He was started on enoxaparin (Lovenox) and then transitioned to apixaban (Eliquis) for a total of 6 months of thromboprophylaxis. He was counseled about modifying his lifestyle and did not have a recurrence after 14 months of follow-up.
A similarly sedentary 17-year old male with an even higher BMI (39 kg/m2) presented with bilateral basilar pulmonary emboli and infarctions in association with a left femoral deep vein thrombosis. This patients also had factor V Leiden heterozygosity and the May-Thurner (iliac vein compression) syndrome. He was treated for a total of 6 months with warfarin followed by rivaroxaban (Xarelto) and was counseled about lifestyle changes but was unable to lose weight. Eight months after completing therapy, he had a second extensive deep vein thrombosis, this time in his right leg, and was restarted on rivaroxaban.
The third patient, a morbidly obese (BMI 56 kg/m2) 13-year-old boy, presented with left lower lobe pulmonary embolism following 3 weeks of immobility caused by the Guillain-Barré syndrome. As in the other cases, he confessed to a sedentary lifestyle and a predilection for gaming. His father had previously developed a line-associated thrombus. The family declined thrombophilia testing. The patient received 3 months of enoxaparin. He has not been followed since discontinuing therapy.
Move it, kid!
The risk of VTE in adolescent boys, especially obese and extreme gamers who spend most of their waking hours in a chair staring at a screen, is similar to that for adolescent girls who use oral contraceptives, Dr. Kohorst and her colleagues said.
“Many case reports link prolonged ‘gaming’ to thrombosis and fatal pulmonary emboli. Additionally, prolonged television viewing has become a documented risk factor for mortality from pulmonary emboli,” the investigators wrote.
They recommend that clinicians ask adolescents about their gaming and TV-watching habits and encourage them to become more active to lower their risk for VTE.
The study was internally supported. Dr. Kohorst and colleagues reported no relevant disclosures.
MONTREAL – It’s well known that airplane passengers, condemned to sit for endless hours in the claustrophobic cabins of the unfriendly skies, are at increased risk for venous thromboembolic events (VTEs). Less well documented, however, is the VTE risk encountered by overweight or obese teens who while their hours away playing video games.
“This is becoming a sedentary-type risk factor,” said Mira A. Kohorst, MD, from the division of pediatric hematology-oncology at the Mayo Clinic in Rochester, Minn.
Dr. Kohorst and her colleagues reported on a small but troubling trend of VTE episodes that they observed in teen boys over the last few years. They refer to obesity, sedentary lifestyle, and gaming as “the new thrombophilia cocktail in adolescent males.”
The reported incidence of pediatric VTE ranges from 0.7 to 4.9 per 100,000 person years, considerably lower than the 1 in 1000 estimated incidences reported in adults. But, thanks to the growing incidence of obesity in children, which more than doubled from 1980 to 2012 and quadrupled in teens age 12-19 years from 5% to 21%, youngsters appear to be catching up in the VTE department, the investigators reported.
“Given the direct mortality rate of 2% [that is] associated with VTE and risk for postthrombotic syndrome of 26%, it is important to understand underlying modifiable risk factors,” they wrote.
To do this, they retrospectively reviewed records of children who presented with VTE in their center.
All play, no exercise
The authors described three cases, including that of an 18-year old boy with a body mass index (BMI) of 37 kg/m2, putting him squarely in the obese category. This lad, who spent 12 or more hours a day playing video games and was sedentary at other times as well, presented with bilateral pulmonary emboli and an associated right lower lobe infarction. Testing for thrombophilia showed that he was heterozygous for factor V Leiden but did not have other coagulation abnormalities. He was started on enoxaparin (Lovenox) and then transitioned to apixaban (Eliquis) for a total of 6 months of thromboprophylaxis. He was counseled about modifying his lifestyle and did not have a recurrence after 14 months of follow-up.
A similarly sedentary 17-year old male with an even higher BMI (39 kg/m2) presented with bilateral basilar pulmonary emboli and infarctions in association with a left femoral deep vein thrombosis. This patients also had factor V Leiden heterozygosity and the May-Thurner (iliac vein compression) syndrome. He was treated for a total of 6 months with warfarin followed by rivaroxaban (Xarelto) and was counseled about lifestyle changes but was unable to lose weight. Eight months after completing therapy, he had a second extensive deep vein thrombosis, this time in his right leg, and was restarted on rivaroxaban.
The third patient, a morbidly obese (BMI 56 kg/m2) 13-year-old boy, presented with left lower lobe pulmonary embolism following 3 weeks of immobility caused by the Guillain-Barré syndrome. As in the other cases, he confessed to a sedentary lifestyle and a predilection for gaming. His father had previously developed a line-associated thrombus. The family declined thrombophilia testing. The patient received 3 months of enoxaparin. He has not been followed since discontinuing therapy.
Move it, kid!
The risk of VTE in adolescent boys, especially obese and extreme gamers who spend most of their waking hours in a chair staring at a screen, is similar to that for adolescent girls who use oral contraceptives, Dr. Kohorst and her colleagues said.
“Many case reports link prolonged ‘gaming’ to thrombosis and fatal pulmonary emboli. Additionally, prolonged television viewing has become a documented risk factor for mortality from pulmonary emboli,” the investigators wrote.
They recommend that clinicians ask adolescents about their gaming and TV-watching habits and encourage them to become more active to lower their risk for VTE.
The study was internally supported. Dr. Kohorst and colleagues reported no relevant disclosures.
MONTREAL – It’s well known that airplane passengers, condemned to sit for endless hours in the claustrophobic cabins of the unfriendly skies, are at increased risk for venous thromboembolic events (VTEs). Less well documented, however, is the VTE risk encountered by overweight or obese teens who while their hours away playing video games.
“This is becoming a sedentary-type risk factor,” said Mira A. Kohorst, MD, from the division of pediatric hematology-oncology at the Mayo Clinic in Rochester, Minn.
Dr. Kohorst and her colleagues reported on a small but troubling trend of VTE episodes that they observed in teen boys over the last few years. They refer to obesity, sedentary lifestyle, and gaming as “the new thrombophilia cocktail in adolescent males.”
The reported incidence of pediatric VTE ranges from 0.7 to 4.9 per 100,000 person years, considerably lower than the 1 in 1000 estimated incidences reported in adults. But, thanks to the growing incidence of obesity in children, which more than doubled from 1980 to 2012 and quadrupled in teens age 12-19 years from 5% to 21%, youngsters appear to be catching up in the VTE department, the investigators reported.
“Given the direct mortality rate of 2% [that is] associated with VTE and risk for postthrombotic syndrome of 26%, it is important to understand underlying modifiable risk factors,” they wrote.
To do this, they retrospectively reviewed records of children who presented with VTE in their center.
All play, no exercise
The authors described three cases, including that of an 18-year old boy with a body mass index (BMI) of 37 kg/m2, putting him squarely in the obese category. This lad, who spent 12 or more hours a day playing video games and was sedentary at other times as well, presented with bilateral pulmonary emboli and an associated right lower lobe infarction. Testing for thrombophilia showed that he was heterozygous for factor V Leiden but did not have other coagulation abnormalities. He was started on enoxaparin (Lovenox) and then transitioned to apixaban (Eliquis) for a total of 6 months of thromboprophylaxis. He was counseled about modifying his lifestyle and did not have a recurrence after 14 months of follow-up.
A similarly sedentary 17-year old male with an even higher BMI (39 kg/m2) presented with bilateral basilar pulmonary emboli and infarctions in association with a left femoral deep vein thrombosis. This patients also had factor V Leiden heterozygosity and the May-Thurner (iliac vein compression) syndrome. He was treated for a total of 6 months with warfarin followed by rivaroxaban (Xarelto) and was counseled about lifestyle changes but was unable to lose weight. Eight months after completing therapy, he had a second extensive deep vein thrombosis, this time in his right leg, and was restarted on rivaroxaban.
The third patient, a morbidly obese (BMI 56 kg/m2) 13-year-old boy, presented with left lower lobe pulmonary embolism following 3 weeks of immobility caused by the Guillain-Barré syndrome. As in the other cases, he confessed to a sedentary lifestyle and a predilection for gaming. His father had previously developed a line-associated thrombus. The family declined thrombophilia testing. The patient received 3 months of enoxaparin. He has not been followed since discontinuing therapy.
Move it, kid!
The risk of VTE in adolescent boys, especially obese and extreme gamers who spend most of their waking hours in a chair staring at a screen, is similar to that for adolescent girls who use oral contraceptives, Dr. Kohorst and her colleagues said.
“Many case reports link prolonged ‘gaming’ to thrombosis and fatal pulmonary emboli. Additionally, prolonged television viewing has become a documented risk factor for mortality from pulmonary emboli,” the investigators wrote.
They recommend that clinicians ask adolescents about their gaming and TV-watching habits and encourage them to become more active to lower their risk for VTE.
The study was internally supported. Dr. Kohorst and colleagues reported no relevant disclosures.
FROM ASPHO 2017
Key clinical point: Obesity and a sedentary lifestyle are risk factors for venous thromboembolic events in teens, as well as adults.
Major finding: Teen boys who were obese and spent much of their day playing video games presented with VTE.
Data source: Retrospective review and case series.
Disclosures: The study was internally supported. Dr. Kohorst and colleagues reported no relevant disclosures.
Mastectomy unnecessary for some breast cancer recurrences
LAS VEGAS – Although mastectomy is the standard of care for tumor recurrence following lumpectomy and whole breast irradiation, a second lumpectomy with partial breast irradiation is a sound alternative under certain circumstances, according to Manjeet Chadha, MD, professor of radiation oncology and director of the department of radiation oncology at Icahn School of Medicine at Mount Sinai, New York.
It depends on whether the new lesion is a true recurrence, or simply another primary tumor. In the absence of a genetic footprint to compare the two, Dr. Chadha and her colleagues use several of what she called “soft criteria” to make the call and counsel women.
True ipsilateral recurrence of an aggressive tumor tends to happen early, and in the same quadrant. However, if breast cancer recurs more than 3 years after treatment of the primary tumor and in a different quadrant, and if the patient is negative for BRCA mutation, and if the new growth is small, localized on MRI, histologically different from the primary tumor, and likely to be resected with clean margins, Dr. Chadha said she is comfortable offering a second lumpectomy and partial breast radiation – usually multicatheter brachytherapy – to women who do not want a mastectomy.
“Second cancer in a previously irradiated breast is not an uncommon clinical entity. Based on patient preference, the option of repeat breast conservation and reirradiation may be offered selectively as an alternative to mastectomy,” followed by systemic therapy, she said at the annual meeting of the American Society of Breast Surgeons.
“I think all of us across the country are discussing presentations like this in tumor boards,” but it’s not always offered as an option. Sometimes, “the mindset of the treating surgeon is ‘oh, this breast has had radiation; I can’t give radiation again.’ Clearly, whole breast reirradiation is not recommended,” but it seems possible based on a growing body of literature to differentiate new primaries with new biology from true recurrences, and to treat them safely with breast conserving surgery and partial irradiation, she said.
The largest series to date of salvage lumpectomy with multicatheter brachytherapy followed 217 women for a median of 3.9 years. Median tumor size was 1.2 cm. The 5-year local control rate – effectively, the mastectomy-free survival – was 94.4%, and the overall survival was 88.7%, which mirrors the success of first-time lumpectomy with whole breast irradiation, and lends support to the notion that some recurrences are, in fact, entirely new disease. The European team reported excellent or good cosmetic results in 85% of women (Radiother Oncol. 2013 Aug;108[2]:226-31).
The series used high-dose radiation. Dr. Chadha said she and her colleagues have had similar success with low-dose multicatheter brachytherapy, with similarly good aesthetic results. To avoid cosmetic impact, however, she noted it’s important to work with radiation oncologists “mindful of the nuances of what’s needed,” including how far to separate the skin from the radiation.
Brachytherapy has the most support in the literature, but external beam therapy is also an option. “Whatever technique you use, the delineation of the target and the geometric coverage of the lumpectomy cavity [must be] complete in all cases,” she said.
Dr. Chadha had no financial conflicts of interest.
LAS VEGAS – Although mastectomy is the standard of care for tumor recurrence following lumpectomy and whole breast irradiation, a second lumpectomy with partial breast irradiation is a sound alternative under certain circumstances, according to Manjeet Chadha, MD, professor of radiation oncology and director of the department of radiation oncology at Icahn School of Medicine at Mount Sinai, New York.
It depends on whether the new lesion is a true recurrence, or simply another primary tumor. In the absence of a genetic footprint to compare the two, Dr. Chadha and her colleagues use several of what she called “soft criteria” to make the call and counsel women.
True ipsilateral recurrence of an aggressive tumor tends to happen early, and in the same quadrant. However, if breast cancer recurs more than 3 years after treatment of the primary tumor and in a different quadrant, and if the patient is negative for BRCA mutation, and if the new growth is small, localized on MRI, histologically different from the primary tumor, and likely to be resected with clean margins, Dr. Chadha said she is comfortable offering a second lumpectomy and partial breast radiation – usually multicatheter brachytherapy – to women who do not want a mastectomy.
“Second cancer in a previously irradiated breast is not an uncommon clinical entity. Based on patient preference, the option of repeat breast conservation and reirradiation may be offered selectively as an alternative to mastectomy,” followed by systemic therapy, she said at the annual meeting of the American Society of Breast Surgeons.
“I think all of us across the country are discussing presentations like this in tumor boards,” but it’s not always offered as an option. Sometimes, “the mindset of the treating surgeon is ‘oh, this breast has had radiation; I can’t give radiation again.’ Clearly, whole breast reirradiation is not recommended,” but it seems possible based on a growing body of literature to differentiate new primaries with new biology from true recurrences, and to treat them safely with breast conserving surgery and partial irradiation, she said.
The largest series to date of salvage lumpectomy with multicatheter brachytherapy followed 217 women for a median of 3.9 years. Median tumor size was 1.2 cm. The 5-year local control rate – effectively, the mastectomy-free survival – was 94.4%, and the overall survival was 88.7%, which mirrors the success of first-time lumpectomy with whole breast irradiation, and lends support to the notion that some recurrences are, in fact, entirely new disease. The European team reported excellent or good cosmetic results in 85% of women (Radiother Oncol. 2013 Aug;108[2]:226-31).
The series used high-dose radiation. Dr. Chadha said she and her colleagues have had similar success with low-dose multicatheter brachytherapy, with similarly good aesthetic results. To avoid cosmetic impact, however, she noted it’s important to work with radiation oncologists “mindful of the nuances of what’s needed,” including how far to separate the skin from the radiation.
Brachytherapy has the most support in the literature, but external beam therapy is also an option. “Whatever technique you use, the delineation of the target and the geometric coverage of the lumpectomy cavity [must be] complete in all cases,” she said.
Dr. Chadha had no financial conflicts of interest.
LAS VEGAS – Although mastectomy is the standard of care for tumor recurrence following lumpectomy and whole breast irradiation, a second lumpectomy with partial breast irradiation is a sound alternative under certain circumstances, according to Manjeet Chadha, MD, professor of radiation oncology and director of the department of radiation oncology at Icahn School of Medicine at Mount Sinai, New York.
It depends on whether the new lesion is a true recurrence, or simply another primary tumor. In the absence of a genetic footprint to compare the two, Dr. Chadha and her colleagues use several of what she called “soft criteria” to make the call and counsel women.
True ipsilateral recurrence of an aggressive tumor tends to happen early, and in the same quadrant. However, if breast cancer recurs more than 3 years after treatment of the primary tumor and in a different quadrant, and if the patient is negative for BRCA mutation, and if the new growth is small, localized on MRI, histologically different from the primary tumor, and likely to be resected with clean margins, Dr. Chadha said she is comfortable offering a second lumpectomy and partial breast radiation – usually multicatheter brachytherapy – to women who do not want a mastectomy.
“Second cancer in a previously irradiated breast is not an uncommon clinical entity. Based on patient preference, the option of repeat breast conservation and reirradiation may be offered selectively as an alternative to mastectomy,” followed by systemic therapy, she said at the annual meeting of the American Society of Breast Surgeons.
“I think all of us across the country are discussing presentations like this in tumor boards,” but it’s not always offered as an option. Sometimes, “the mindset of the treating surgeon is ‘oh, this breast has had radiation; I can’t give radiation again.’ Clearly, whole breast reirradiation is not recommended,” but it seems possible based on a growing body of literature to differentiate new primaries with new biology from true recurrences, and to treat them safely with breast conserving surgery and partial irradiation, she said.
The largest series to date of salvage lumpectomy with multicatheter brachytherapy followed 217 women for a median of 3.9 years. Median tumor size was 1.2 cm. The 5-year local control rate – effectively, the mastectomy-free survival – was 94.4%, and the overall survival was 88.7%, which mirrors the success of first-time lumpectomy with whole breast irradiation, and lends support to the notion that some recurrences are, in fact, entirely new disease. The European team reported excellent or good cosmetic results in 85% of women (Radiother Oncol. 2013 Aug;108[2]:226-31).
The series used high-dose radiation. Dr. Chadha said she and her colleagues have had similar success with low-dose multicatheter brachytherapy, with similarly good aesthetic results. To avoid cosmetic impact, however, she noted it’s important to work with radiation oncologists “mindful of the nuances of what’s needed,” including how far to separate the skin from the radiation.
Brachytherapy has the most support in the literature, but external beam therapy is also an option. “Whatever technique you use, the delineation of the target and the geometric coverage of the lumpectomy cavity [must be] complete in all cases,” she said.
Dr. Chadha had no financial conflicts of interest.
EXPERT ANALYSIS FROM ASBS 2017
Could refractory T-ALL be daratumumab’s next frontier?
MONTREAL – Daratumumab may do for patients with T-cell acute lymphoblastic leukemia (T-ALL) what it has done for those with multiple myeloma. That, at least, is the hope of a team of investigators who are conducting preclinical studies and planning human trials of the CD38 inhibitor in leukemia.
“We believe daratumumab significantly inhibits disease progression as shown in our different [patient-derived xenograft] models,” said Karen L. Bride, MD, of Children’s Hospital of Philadelphia.
The Food and Drug Administration approved daratumumab (Darzalex) in November 2015 for the treatment of patients with multiple myeloma who had received at least three prior lines of therapy. They then amended the approval last fall to “at least one prior medicine.”
When added to a standard regimen of bortezomib and dexamethasone in patients with relapsed or refractory multiple myeloma in the phase III CASTOR trial, daratumumab reduced the risk of disease progression or death by 61% with little increase in toxicity.
The drug is believed to work against multiple myeloma through both an on-target (anti-CD38) mechanism, and through off-target promotion of increases in T-helper cells, cytotoxic T-lymphocytes, T-cell function response, and T-cell receptor clonality (Blood. 2016 Jan. doi: 10.1182/blood-2015-12-687749).
CD38 in T-ALL
Dr. Bride and her colleagues hope to bring daratumumab’s anti-CD38 action to bear on relapsed or refractory T-ALL.
“One of the reasons this is particularly challenging is that we find T-ALL is clinically and genetically heterogeneous,” she said. “With a number of different genetic mutations that have been identified, there are certainly some potentially targetable pathways. However, finding an appropriate target that can be broadly applicable is still needed.”
CD38 may be one such target. It is expressed at relatively high levels on both T-ALL and B-precursor ALL blasts but at only low levels on normal immune cells.
The investigators first used flow cytometry to measure CD38 levels in samples from 10 patients with early T-cell precursor (ETP) T-ALL and 11 with non-ETP disease, both at diagnosis and after 1 month of induction chemotherapy. CD38 expression was detectable in all of the samples and did not change significantly after chemotherapy, suggesting that CD38 was indeed a valid target in T-ALL.
They then grafted primary ALL blasts from patients with ETP-ALL and non-ETP-ALL into mice and randomly assigned them to be treated for 3 to 5 weeks with daratumumab or to serve as controls. The mice were initially treated after they developed more than 1% of peripheral blood blasts.
Daratumumab-treated models had significant reductions in disease burden as measured by blasts in both peripheral blood (P = .0112) and spleen (P = .0003).
There were six responses to daratumumab in the seven treated mice grafted with ETP-ALL and no cases of toxicity. Among the eight mice with non-ETP ALL, however, there was only one response, and five animals became moribund roughly 1 hour after injection.
The investigators could not find an explanation for these reactions either on necropsy or pathology studies.
“We hypothesized that there was potentially massive tumor lysis syndrome being experienced by the mice, and, as a consequence, they were becoming moribund,” Dr. Bride said.
In subsequent experiments, they have begun introducing the drug within 5 days of adoptive transfer, prior to full engraftment. This is akin to treating during a minimal residual disease phase, she said.
Despite the observed but unexplained toxicities in some animals, “our data are promising enough that we’re hopeful that we will open a phase I/II trial of daratumumab starting next year,” Dr. Bride said.
Not so fast
However, a pediatric hematologist/oncologist who was not involved in the study said in an interview that Dr. Bride and her colleagues would be wise not to proceed too quickly into human trials, at least until the potential toxicities of daratumumab in T-ALL have been more fully elucidated.
“I found it very striking that the mice responded the way they did, and that was just from receiving the drug. So, there is something else that’s going on, and I think it behooves them to investigate further. It’s not that I’m skeptical about the activity of the drug; I just don’t want studies to be shut down because the investigators didn’t have the best trial design,” said Valerie I. Brown, MD.
Dr. Brown, director of experimental therapeutics at Penn State Health Milton S. Hershey (Penn.) Medical Center, was a comoderator of the session where Dr. Bride presented the study findings.
Asked about her response to Dr. Brown’s comments in an interview, Dr. Bride said that “because of the success of daratumumab in humans already, I think I’m a bit less worried about this agent. You can’t necessarily translate exactly across diseases, but I do think it’s very promising, and I don’t think [the toxicity] is a reason to pull back.”
The study was supported by grants from the Leukemia and Lymphoma Society and the National Institutes of Health. Janssen donated the daratumumab. Dr. Bride and Dr. Brown reported no conflicts of interest to disclose.
MONTREAL – Daratumumab may do for patients with T-cell acute lymphoblastic leukemia (T-ALL) what it has done for those with multiple myeloma. That, at least, is the hope of a team of investigators who are conducting preclinical studies and planning human trials of the CD38 inhibitor in leukemia.
“We believe daratumumab significantly inhibits disease progression as shown in our different [patient-derived xenograft] models,” said Karen L. Bride, MD, of Children’s Hospital of Philadelphia.
The Food and Drug Administration approved daratumumab (Darzalex) in November 2015 for the treatment of patients with multiple myeloma who had received at least three prior lines of therapy. They then amended the approval last fall to “at least one prior medicine.”
When added to a standard regimen of bortezomib and dexamethasone in patients with relapsed or refractory multiple myeloma in the phase III CASTOR trial, daratumumab reduced the risk of disease progression or death by 61% with little increase in toxicity.
The drug is believed to work against multiple myeloma through both an on-target (anti-CD38) mechanism, and through off-target promotion of increases in T-helper cells, cytotoxic T-lymphocytes, T-cell function response, and T-cell receptor clonality (Blood. 2016 Jan. doi: 10.1182/blood-2015-12-687749).
CD38 in T-ALL
Dr. Bride and her colleagues hope to bring daratumumab’s anti-CD38 action to bear on relapsed or refractory T-ALL.
“One of the reasons this is particularly challenging is that we find T-ALL is clinically and genetically heterogeneous,” she said. “With a number of different genetic mutations that have been identified, there are certainly some potentially targetable pathways. However, finding an appropriate target that can be broadly applicable is still needed.”
CD38 may be one such target. It is expressed at relatively high levels on both T-ALL and B-precursor ALL blasts but at only low levels on normal immune cells.
The investigators first used flow cytometry to measure CD38 levels in samples from 10 patients with early T-cell precursor (ETP) T-ALL and 11 with non-ETP disease, both at diagnosis and after 1 month of induction chemotherapy. CD38 expression was detectable in all of the samples and did not change significantly after chemotherapy, suggesting that CD38 was indeed a valid target in T-ALL.
They then grafted primary ALL blasts from patients with ETP-ALL and non-ETP-ALL into mice and randomly assigned them to be treated for 3 to 5 weeks with daratumumab or to serve as controls. The mice were initially treated after they developed more than 1% of peripheral blood blasts.
Daratumumab-treated models had significant reductions in disease burden as measured by blasts in both peripheral blood (P = .0112) and spleen (P = .0003).
There were six responses to daratumumab in the seven treated mice grafted with ETP-ALL and no cases of toxicity. Among the eight mice with non-ETP ALL, however, there was only one response, and five animals became moribund roughly 1 hour after injection.
The investigators could not find an explanation for these reactions either on necropsy or pathology studies.
“We hypothesized that there was potentially massive tumor lysis syndrome being experienced by the mice, and, as a consequence, they were becoming moribund,” Dr. Bride said.
In subsequent experiments, they have begun introducing the drug within 5 days of adoptive transfer, prior to full engraftment. This is akin to treating during a minimal residual disease phase, she said.
Despite the observed but unexplained toxicities in some animals, “our data are promising enough that we’re hopeful that we will open a phase I/II trial of daratumumab starting next year,” Dr. Bride said.
Not so fast
However, a pediatric hematologist/oncologist who was not involved in the study said in an interview that Dr. Bride and her colleagues would be wise not to proceed too quickly into human trials, at least until the potential toxicities of daratumumab in T-ALL have been more fully elucidated.
“I found it very striking that the mice responded the way they did, and that was just from receiving the drug. So, there is something else that’s going on, and I think it behooves them to investigate further. It’s not that I’m skeptical about the activity of the drug; I just don’t want studies to be shut down because the investigators didn’t have the best trial design,” said Valerie I. Brown, MD.
Dr. Brown, director of experimental therapeutics at Penn State Health Milton S. Hershey (Penn.) Medical Center, was a comoderator of the session where Dr. Bride presented the study findings.
Asked about her response to Dr. Brown’s comments in an interview, Dr. Bride said that “because of the success of daratumumab in humans already, I think I’m a bit less worried about this agent. You can’t necessarily translate exactly across diseases, but I do think it’s very promising, and I don’t think [the toxicity] is a reason to pull back.”
The study was supported by grants from the Leukemia and Lymphoma Society and the National Institutes of Health. Janssen donated the daratumumab. Dr. Bride and Dr. Brown reported no conflicts of interest to disclose.
MONTREAL – Daratumumab may do for patients with T-cell acute lymphoblastic leukemia (T-ALL) what it has done for those with multiple myeloma. That, at least, is the hope of a team of investigators who are conducting preclinical studies and planning human trials of the CD38 inhibitor in leukemia.
“We believe daratumumab significantly inhibits disease progression as shown in our different [patient-derived xenograft] models,” said Karen L. Bride, MD, of Children’s Hospital of Philadelphia.
The Food and Drug Administration approved daratumumab (Darzalex) in November 2015 for the treatment of patients with multiple myeloma who had received at least three prior lines of therapy. They then amended the approval last fall to “at least one prior medicine.”
When added to a standard regimen of bortezomib and dexamethasone in patients with relapsed or refractory multiple myeloma in the phase III CASTOR trial, daratumumab reduced the risk of disease progression or death by 61% with little increase in toxicity.
The drug is believed to work against multiple myeloma through both an on-target (anti-CD38) mechanism, and through off-target promotion of increases in T-helper cells, cytotoxic T-lymphocytes, T-cell function response, and T-cell receptor clonality (Blood. 2016 Jan. doi: 10.1182/blood-2015-12-687749).
CD38 in T-ALL
Dr. Bride and her colleagues hope to bring daratumumab’s anti-CD38 action to bear on relapsed or refractory T-ALL.
“One of the reasons this is particularly challenging is that we find T-ALL is clinically and genetically heterogeneous,” she said. “With a number of different genetic mutations that have been identified, there are certainly some potentially targetable pathways. However, finding an appropriate target that can be broadly applicable is still needed.”
CD38 may be one such target. It is expressed at relatively high levels on both T-ALL and B-precursor ALL blasts but at only low levels on normal immune cells.
The investigators first used flow cytometry to measure CD38 levels in samples from 10 patients with early T-cell precursor (ETP) T-ALL and 11 with non-ETP disease, both at diagnosis and after 1 month of induction chemotherapy. CD38 expression was detectable in all of the samples and did not change significantly after chemotherapy, suggesting that CD38 was indeed a valid target in T-ALL.
They then grafted primary ALL blasts from patients with ETP-ALL and non-ETP-ALL into mice and randomly assigned them to be treated for 3 to 5 weeks with daratumumab or to serve as controls. The mice were initially treated after they developed more than 1% of peripheral blood blasts.
Daratumumab-treated models had significant reductions in disease burden as measured by blasts in both peripheral blood (P = .0112) and spleen (P = .0003).
There were six responses to daratumumab in the seven treated mice grafted with ETP-ALL and no cases of toxicity. Among the eight mice with non-ETP ALL, however, there was only one response, and five animals became moribund roughly 1 hour after injection.
The investigators could not find an explanation for these reactions either on necropsy or pathology studies.
“We hypothesized that there was potentially massive tumor lysis syndrome being experienced by the mice, and, as a consequence, they were becoming moribund,” Dr. Bride said.
In subsequent experiments, they have begun introducing the drug within 5 days of adoptive transfer, prior to full engraftment. This is akin to treating during a minimal residual disease phase, she said.
Despite the observed but unexplained toxicities in some animals, “our data are promising enough that we’re hopeful that we will open a phase I/II trial of daratumumab starting next year,” Dr. Bride said.
Not so fast
However, a pediatric hematologist/oncologist who was not involved in the study said in an interview that Dr. Bride and her colleagues would be wise not to proceed too quickly into human trials, at least until the potential toxicities of daratumumab in T-ALL have been more fully elucidated.
“I found it very striking that the mice responded the way they did, and that was just from receiving the drug. So, there is something else that’s going on, and I think it behooves them to investigate further. It’s not that I’m skeptical about the activity of the drug; I just don’t want studies to be shut down because the investigators didn’t have the best trial design,” said Valerie I. Brown, MD.
Dr. Brown, director of experimental therapeutics at Penn State Health Milton S. Hershey (Penn.) Medical Center, was a comoderator of the session where Dr. Bride presented the study findings.
Asked about her response to Dr. Brown’s comments in an interview, Dr. Bride said that “because of the success of daratumumab in humans already, I think I’m a bit less worried about this agent. You can’t necessarily translate exactly across diseases, but I do think it’s very promising, and I don’t think [the toxicity] is a reason to pull back.”
The study was supported by grants from the Leukemia and Lymphoma Society and the National Institutes of Health. Janssen donated the daratumumab. Dr. Bride and Dr. Brown reported no conflicts of interest to disclose.
Key clinical point: CD38 may be a valid target for therapy against relapsed/refractory T-cell acute lymphoblastic leukemia.
Major finding: Six of seven models of early T-precursor T-ALL responded to daratumumab injections.
Data source: In vitro and in vivo studies evaluating the potential of daratumumab for treatment of T-ALL.
Disclosures: The study was supported by grants from the Leukemia and Lymphoma Society and the National Institutes of Health. Janssen donated the daratumumab. Dr. Bride and Dr. Brown reported having no conflicts of interest.
Elder abuse: Strong social support prevents associated psychopathology
SAN FRANCISCO – Victims of elder abuse who have perceived strong social support from family or friends are “completely inoculated” against the otherwise dramatically increased risk of trauma-related psychopathology that pertains to mistreated seniors who lack such support, according to Ron Acierno, PhD.
Dr. Acierno, professor of nursing at the Medical University of South Carolina in Charleston, presented 8-year follow-up data from the National Elder Mistreatment Study, the largest study of elder abuse ever conducted in the United States.
The National Elder Mistreatment Study involved 5,777 randomly selected community-dwelling older adults who, in 2008, participated in structured interviews assessing whether they had experienced physical, psychological, sexual, or neglectful mistreatment. The study made headlines by documenting an unexpectedly high 11% rate of elder mistreatment within the previous 12 months (Am J Public Health. 2010 Feb;100[2]:292-7).
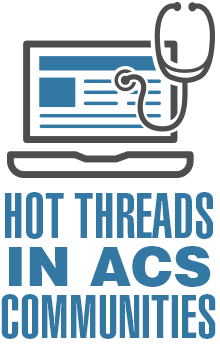
Eight years later, Dr. Acierno and his coinvestigators were able to recontact 173 of the original 684 abused elders, as well as 602 nonabused controls for structured interviews assessing their current mental health. At that point, the participants averaged 84.9 years of age.
Striking differences in mental health status based on elder abuse history were documented. The prevalences of depression, generalized anxiety disorder, and posttraumatic stress disorder were 13%, 7%, and 8%, respectively, in the elder abuse group, compared with 5%, 1%, and 1% in the nonabused controls. Of the group subjected to abuse 8 years earlier, 40% were categorized at follow-up as “in poor health,” compared with 23% of controls.
More importantly, high social support essentially erased the elder abuse group’s increased risk (see graphic), Dr. Acierno said.
The National Elder Mistreatment Study was funded by the National Institute of Justice, the National Institute on Aging, and the Archstone Foundation. Dr. Acierno reported having no financial conflicts.
SAN FRANCISCO – Victims of elder abuse who have perceived strong social support from family or friends are “completely inoculated” against the otherwise dramatically increased risk of trauma-related psychopathology that pertains to mistreated seniors who lack such support, according to Ron Acierno, PhD.
Dr. Acierno, professor of nursing at the Medical University of South Carolina in Charleston, presented 8-year follow-up data from the National Elder Mistreatment Study, the largest study of elder abuse ever conducted in the United States.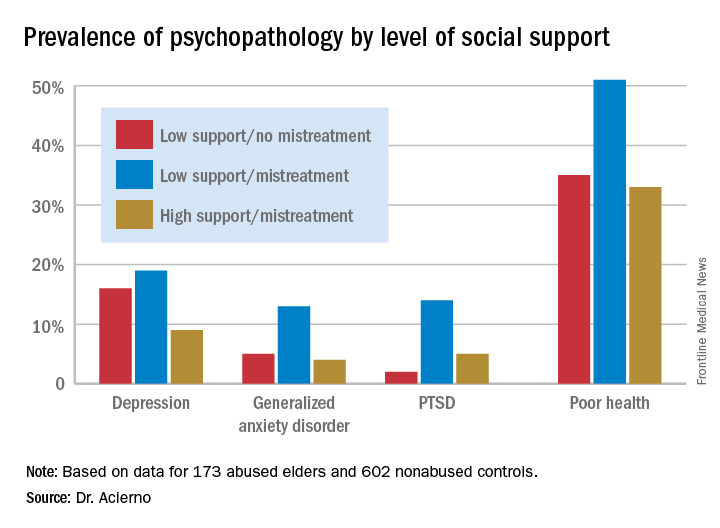
The National Elder Mistreatment Study involved 5,777 randomly selected community-dwelling older adults who, in 2008, participated in structured interviews assessing whether they had experienced physical, psychological, sexual, or neglectful mistreatment. The study made headlines by documenting an unexpectedly high 11% rate of elder mistreatment within the previous 12 months (Am J Public Health. 2010 Feb;100[2]:292-7).
Eight years later, Dr. Acierno and his coinvestigators were able to recontact 173 of the original 684 abused elders, as well as 602 nonabused controls for structured interviews assessing their current mental health. At that point, the participants averaged 84.9 years of age.
Striking differences in mental health status based on elder abuse history were documented. The prevalences of depression, generalized anxiety disorder, and posttraumatic stress disorder were 13%, 7%, and 8%, respectively, in the elder abuse group, compared with 5%, 1%, and 1% in the nonabused controls. Of the group subjected to abuse 8 years earlier, 40% were categorized at follow-up as “in poor health,” compared with 23% of controls.
More importantly, high social support essentially erased the elder abuse group’s increased risk (see graphic), Dr. Acierno said.
The National Elder Mistreatment Study was funded by the National Institute of Justice, the National Institute on Aging, and the Archstone Foundation. Dr. Acierno reported having no financial conflicts.
SAN FRANCISCO – Victims of elder abuse who have perceived strong social support from family or friends are “completely inoculated” against the otherwise dramatically increased risk of trauma-related psychopathology that pertains to mistreated seniors who lack such support, according to Ron Acierno, PhD.
Dr. Acierno, professor of nursing at the Medical University of South Carolina in Charleston, presented 8-year follow-up data from the National Elder Mistreatment Study, the largest study of elder abuse ever conducted in the United States.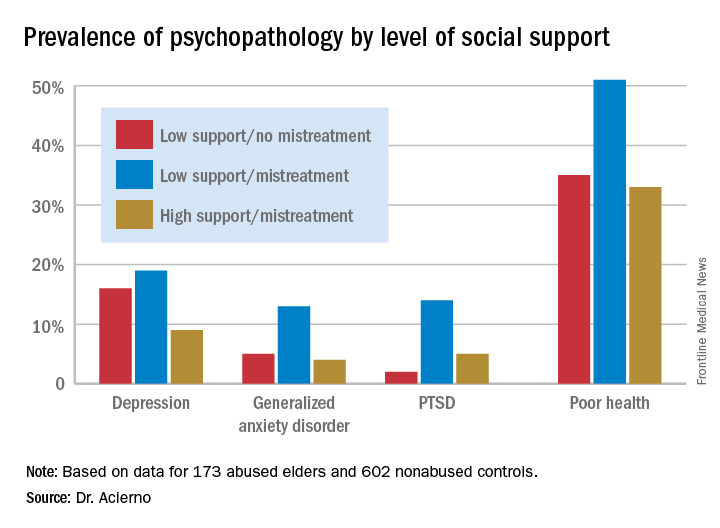
The National Elder Mistreatment Study involved 5,777 randomly selected community-dwelling older adults who, in 2008, participated in structured interviews assessing whether they had experienced physical, psychological, sexual, or neglectful mistreatment. The study made headlines by documenting an unexpectedly high 11% rate of elder mistreatment within the previous 12 months (Am J Public Health. 2010 Feb;100[2]:292-7).
Eight years later, Dr. Acierno and his coinvestigators were able to recontact 173 of the original 684 abused elders, as well as 602 nonabused controls for structured interviews assessing their current mental health. At that point, the participants averaged 84.9 years of age.
Striking differences in mental health status based on elder abuse history were documented. The prevalences of depression, generalized anxiety disorder, and posttraumatic stress disorder were 13%, 7%, and 8%, respectively, in the elder abuse group, compared with 5%, 1%, and 1% in the nonabused controls. Of the group subjected to abuse 8 years earlier, 40% were categorized at follow-up as “in poor health,” compared with 23% of controls.
More importantly, high social support essentially erased the elder abuse group’s increased risk (see graphic), Dr. Acierno said.
The National Elder Mistreatment Study was funded by the National Institute of Justice, the National Institute on Aging, and the Archstone Foundation. Dr. Acierno reported having no financial conflicts.
AT THE ANXIETY AND DEPRESSION CONFERENCE 2017
Key clinical point:
Major finding: Having a strong social support network virtually eliminated the otherwise sharply increased risk of trauma-related psychopathology in victims of elder abuse.
Data source: An 8-year follow-up report on the mental health status of participants in the largest study of elder mistreatment in US history.
Disclosures: The National Elder Mistreatment Study was funded by the National Institute of Justice, the National Institute on Aging, and the Archstone Foundation. The presenter reported having no financial conflicts.
Study identifies gaps in surgical trainees’ readiness
PHILADELPHIA – The question of how prepared general surgery residents are to operate independently after their training is longstanding, but clear definitions of competency and readiness have been elusive. A consortium of general surgery residencies has developed a metric for assessing surgeon readiness, but what the metric revealed may be a cause for concern for the surgical profession.
Brian C. George, MD, of the University of Michigan, Ann Arbor, reported at the annual meeting of the American Surgical Association on results of a study designed to measure the autonomy and readiness for independent practice of residents at 14 general surgery programs.
The study found that in the final 6 months of training, 96% of residents were rated competent by their observers to perform a straightforward appendectomy on their own, but only 71% were rated the same for partial colectomy, Dr. George said.
The participating general surgery attendings rated residents according to three scales (J Surg Educ. 2016;73:e118-130):
•“Performance” scale to measure readiness for independent practice, with competence defined as practice-ready and exceptional performance.
• “Zwisch” scale, named after Jay Zwischenberger, MD, FACS, of the University of Kentucky, to assess the amount of autonomy granted to a resident by the supervising surgical attending.
• “Complexity” scale to measure the patient-related complexity of the case at hand.
The study used a smartphone-based app, SIMPL, to collect data from September 2015 through December 2016. In evaluating performance, 437 observers provided 8,526 different ratings of 522 residents.
In a subset analysis, the study authors focused on the 132 operations the Surgical Council on Resident Education considers the core procedures of general surgery and found that 77% of fifth-year residents were rated as competent. Further restricting the analysis to residents in their final 6 months of training performing the five most commonly rated core procedures – appendectomy, cholecystectomy, ventral hernia repair, inguinal/femoral hernia repair, and partial colectomy – the researchers found that competency ranged from a high of 96% for appendectomy to a low of 71% for partial colectomy.
“If you combine all five procedures into one category, on average the residents are rated competent 84% of the time during the last 6 months of training,” Dr. George said. “But what’s really interesting – and I think this is probably the most important result for this study – is that looking at just the less-frequently rated core procedures and excluding the top five, residents are deemed competent in the last 6 months of training for 74% of those observed procedures.”
According to the Zwisch” scale to measure autonomy, residents in their last 6 months of training displayed what Dr. George termed “meaningful autonomy” in 77% of their observed operations for the core procedures. “Interestingly,” he added, “they were observed to have maximum autonomy, which is the supervision-only level, for 33% of all observed procedures.”
The researchers did an adjusted analysis to account for confounding factors such as the stringency of individual raters and patient complexity. “Using this type of analysis, the likelihood that a typical trainee rated by a typical attendee would be deemed competent by the end of training for a relatively straightforward laparoscopy appendectomy is 97%,” Dr. George said. “For a difficult laparoscopic appendectomy, by the end of training, they’re likely to be deemed competent 92% of time.” In the adjusted analysis, for a straightforward partial colectomy the raters predicted trainees to be competent 91.8% of time, but only 81.8% of the time for a complicated partial colectomy. “For less-frequently performed core procedures, there are many for which residents are likely to be deemed competent at a much lower level,” Dr. George added.
In discussing the study, Ara Darzi, MD, of St. Mary’s Hospital, London, called the methodology “unique and commendable,” and asked “Would you make the case to say we should increase the number of years of trainees from PG5 to PG6 or at least make your fellowships compulsory?”
Dr. George answered that 80% of general surgery residents already go into fellowships. “Whether it’s required or not is above my pay grade,” he said. “I hope not. Five years is already a big ask for a lot of medical students who are considering this profession. If we increase the training requirements, we’re going to have a supply problem that we will then need to address. We will be trading one problem for another.” He later added “The 20,000 hours of surgical residency should be enough to train a general surgeon to competence – its up to us to figure out how.”
The following organizations supported the research: American Board of Surgery, Association for Surgical Education, Association for Program Directors in Surgery, Massachusetts General Hospital, Northwestern University, Indiana University, and the members of the Procedural Learning and Safety Collaborative.
Neither Dr. George nor Dr. Darzi had any relevant financial disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 137th Annual Meeting, April 2017, in Philadelphia, Pennsylvania, is to be published in Annals of Surgery pending editorial review.
PHILADELPHIA – The question of how prepared general surgery residents are to operate independently after their training is longstanding, but clear definitions of competency and readiness have been elusive. A consortium of general surgery residencies has developed a metric for assessing surgeon readiness, but what the metric revealed may be a cause for concern for the surgical profession.
Brian C. George, MD, of the University of Michigan, Ann Arbor, reported at the annual meeting of the American Surgical Association on results of a study designed to measure the autonomy and readiness for independent practice of residents at 14 general surgery programs.
The study found that in the final 6 months of training, 96% of residents were rated competent by their observers to perform a straightforward appendectomy on their own, but only 71% were rated the same for partial colectomy, Dr. George said.
The participating general surgery attendings rated residents according to three scales (J Surg Educ. 2016;73:e118-130):
•“Performance” scale to measure readiness for independent practice, with competence defined as practice-ready and exceptional performance.
• “Zwisch” scale, named after Jay Zwischenberger, MD, FACS, of the University of Kentucky, to assess the amount of autonomy granted to a resident by the supervising surgical attending.
• “Complexity” scale to measure the patient-related complexity of the case at hand.
The study used a smartphone-based app, SIMPL, to collect data from September 2015 through December 2016. In evaluating performance, 437 observers provided 8,526 different ratings of 522 residents.
In a subset analysis, the study authors focused on the 132 operations the Surgical Council on Resident Education considers the core procedures of general surgery and found that 77% of fifth-year residents were rated as competent. Further restricting the analysis to residents in their final 6 months of training performing the five most commonly rated core procedures – appendectomy, cholecystectomy, ventral hernia repair, inguinal/femoral hernia repair, and partial colectomy – the researchers found that competency ranged from a high of 96% for appendectomy to a low of 71% for partial colectomy.
“If you combine all five procedures into one category, on average the residents are rated competent 84% of the time during the last 6 months of training,” Dr. George said. “But what’s really interesting – and I think this is probably the most important result for this study – is that looking at just the less-frequently rated core procedures and excluding the top five, residents are deemed competent in the last 6 months of training for 74% of those observed procedures.”
According to the Zwisch” scale to measure autonomy, residents in their last 6 months of training displayed what Dr. George termed “meaningful autonomy” in 77% of their observed operations for the core procedures. “Interestingly,” he added, “they were observed to have maximum autonomy, which is the supervision-only level, for 33% of all observed procedures.”
The researchers did an adjusted analysis to account for confounding factors such as the stringency of individual raters and patient complexity. “Using this type of analysis, the likelihood that a typical trainee rated by a typical attendee would be deemed competent by the end of training for a relatively straightforward laparoscopy appendectomy is 97%,” Dr. George said. “For a difficult laparoscopic appendectomy, by the end of training, they’re likely to be deemed competent 92% of time.” In the adjusted analysis, for a straightforward partial colectomy the raters predicted trainees to be competent 91.8% of time, but only 81.8% of the time for a complicated partial colectomy. “For less-frequently performed core procedures, there are many for which residents are likely to be deemed competent at a much lower level,” Dr. George added.
In discussing the study, Ara Darzi, MD, of St. Mary’s Hospital, London, called the methodology “unique and commendable,” and asked “Would you make the case to say we should increase the number of years of trainees from PG5 to PG6 or at least make your fellowships compulsory?”
Dr. George answered that 80% of general surgery residents already go into fellowships. “Whether it’s required or not is above my pay grade,” he said. “I hope not. Five years is already a big ask for a lot of medical students who are considering this profession. If we increase the training requirements, we’re going to have a supply problem that we will then need to address. We will be trading one problem for another.” He later added “The 20,000 hours of surgical residency should be enough to train a general surgeon to competence – its up to us to figure out how.”
The following organizations supported the research: American Board of Surgery, Association for Surgical Education, Association for Program Directors in Surgery, Massachusetts General Hospital, Northwestern University, Indiana University, and the members of the Procedural Learning and Safety Collaborative.
Neither Dr. George nor Dr. Darzi had any relevant financial disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 137th Annual Meeting, April 2017, in Philadelphia, Pennsylvania, is to be published in Annals of Surgery pending editorial review.
PHILADELPHIA – The question of how prepared general surgery residents are to operate independently after their training is longstanding, but clear definitions of competency and readiness have been elusive. A consortium of general surgery residencies has developed a metric for assessing surgeon readiness, but what the metric revealed may be a cause for concern for the surgical profession.
Brian C. George, MD, of the University of Michigan, Ann Arbor, reported at the annual meeting of the American Surgical Association on results of a study designed to measure the autonomy and readiness for independent practice of residents at 14 general surgery programs.
The study found that in the final 6 months of training, 96% of residents were rated competent by their observers to perform a straightforward appendectomy on their own, but only 71% were rated the same for partial colectomy, Dr. George said.
The participating general surgery attendings rated residents according to three scales (J Surg Educ. 2016;73:e118-130):
•“Performance” scale to measure readiness for independent practice, with competence defined as practice-ready and exceptional performance.
• “Zwisch” scale, named after Jay Zwischenberger, MD, FACS, of the University of Kentucky, to assess the amount of autonomy granted to a resident by the supervising surgical attending.
• “Complexity” scale to measure the patient-related complexity of the case at hand.
The study used a smartphone-based app, SIMPL, to collect data from September 2015 through December 2016. In evaluating performance, 437 observers provided 8,526 different ratings of 522 residents.
In a subset analysis, the study authors focused on the 132 operations the Surgical Council on Resident Education considers the core procedures of general surgery and found that 77% of fifth-year residents were rated as competent. Further restricting the analysis to residents in their final 6 months of training performing the five most commonly rated core procedures – appendectomy, cholecystectomy, ventral hernia repair, inguinal/femoral hernia repair, and partial colectomy – the researchers found that competency ranged from a high of 96% for appendectomy to a low of 71% for partial colectomy.
“If you combine all five procedures into one category, on average the residents are rated competent 84% of the time during the last 6 months of training,” Dr. George said. “But what’s really interesting – and I think this is probably the most important result for this study – is that looking at just the less-frequently rated core procedures and excluding the top five, residents are deemed competent in the last 6 months of training for 74% of those observed procedures.”
According to the Zwisch” scale to measure autonomy, residents in their last 6 months of training displayed what Dr. George termed “meaningful autonomy” in 77% of their observed operations for the core procedures. “Interestingly,” he added, “they were observed to have maximum autonomy, which is the supervision-only level, for 33% of all observed procedures.”
The researchers did an adjusted analysis to account for confounding factors such as the stringency of individual raters and patient complexity. “Using this type of analysis, the likelihood that a typical trainee rated by a typical attendee would be deemed competent by the end of training for a relatively straightforward laparoscopy appendectomy is 97%,” Dr. George said. “For a difficult laparoscopic appendectomy, by the end of training, they’re likely to be deemed competent 92% of time.” In the adjusted analysis, for a straightforward partial colectomy the raters predicted trainees to be competent 91.8% of time, but only 81.8% of the time for a complicated partial colectomy. “For less-frequently performed core procedures, there are many for which residents are likely to be deemed competent at a much lower level,” Dr. George added.
In discussing the study, Ara Darzi, MD, of St. Mary’s Hospital, London, called the methodology “unique and commendable,” and asked “Would you make the case to say we should increase the number of years of trainees from PG5 to PG6 or at least make your fellowships compulsory?”
Dr. George answered that 80% of general surgery residents already go into fellowships. “Whether it’s required or not is above my pay grade,” he said. “I hope not. Five years is already a big ask for a lot of medical students who are considering this profession. If we increase the training requirements, we’re going to have a supply problem that we will then need to address. We will be trading one problem for another.” He later added “The 20,000 hours of surgical residency should be enough to train a general surgeon to competence – its up to us to figure out how.”
The following organizations supported the research: American Board of Surgery, Association for Surgical Education, Association for Program Directors in Surgery, Massachusetts General Hospital, Northwestern University, Indiana University, and the members of the Procedural Learning and Safety Collaborative.
Neither Dr. George nor Dr. Darzi had any relevant financial disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 137th Annual Meeting, April 2017, in Philadelphia, Pennsylvania, is to be published in Annals of Surgery pending editorial review.
AT THE ASA ANNUAL MEETING
Key clinical point: General surgery residents are often but not universally ready to independently perform core surgical procedures upon completion of surgical training.
Major finding: In the last 6 months of training, residents were rated competent 84% of the time in performing the five leading core procedures and 64% of the time for less-frequently performed procedures.
Data source: Ratings of 437 of 8,526 different observations of 522 residents at 14 institutions of the Procedural Learning and Safety Collaborative.
Disclosures: Dr. George and his coauthors reported having no financial disclosures.
How Often Is Optic Neuritis Misdiagnosed?
BOSTON—Misdiagnosing optic neuritis may expose patients to risks associated with undergoing MRI with a contrast agent, lumbar puncture, and high-dose steroid treatment. It also costs patients and hospitals time and money. Leanne Stunkel, MD, a neurology resident at Washington University in St. Louis, and her colleagues observed a 60% misdiagnosis rate of optic neuritis among patients who were referred to their neuro-ophthalmology clinic, according to a study presented at the 69th Annual Meeting of the American Academy of Neurology.
“The most common [diagnostic] errors were overreliance on a single item of history and failure to consider alternative diagnoses,” said Dr. Stunkel.
Optic neuritis is an acute inflammatory demyelinating condition of the optic nerve. Presenting symptoms include acute or subacute vision loss, pain with eye movement, and changes in color vision, especially affecting the color red, said Dr. Stunkel. Many patients who were referred to their tertiary care clinic for optic neuritis turned out to have other conditions, which prompted the researchers to find out more about optic neuritis misdiagnosis.
Previous studies found a misdiagnosis rate of between 10% and 40%, but none of these studies examined which errors led to these misdiagnoses. To determine how often optic neuritis is misdiagnosed and which diagnostic errors play a role, and to identify diagnoses commonly mistaken for optic neuritis, Dr. Stunkel and colleagues performed a retrospective chart review.
The researchers reviewed new patient encounters between January 2014 and October 2016 to identify patients referred with a diagnosis of optic neuritis. Experienced neuro-ophthalmologists determined the final diagnosis. The researchers then applied the Diagnosis Error Evaluation and Research (DEER) taxonomy tool to identify diagnostic errors in cases in which the patient did not have optic neuritis.
A total of 122 patients were referred for optic neuritis during the study period. Only 40% of these patients were diagnosed with optic neuritis, and 60% of patients had alternative diagnoses. The most common alternative diagnoses were headache with eye pain and visual symptoms (22%), functional visual loss (19%), and other optic neuropathies (16%).
In addition, 15% of patients had retinal or macular problems rather than pathology of the optic nerve. Other diagnoses included neoplasms, congenital disk abnormalities, and inflammatory conditions that affected other parts of the eye.
The most common diagnostic errors were from problems eliciting or interpreting the history (33%). “We saw an overreliance on history of risk factors such as multiple sclerosis or other inflammatory disorders and some failure to elicit the fact that these were brief stereotyped episodes of vision loss, like in a migraine aura,” said Dr. Stunkel.
Twenty-one percent of diagnostic errors were due to errors interpreting physical exam findings, and 14% of errors were due to misinterpretation of diagnostic tests. Finally, 32% of diagnostic errors resulted from failure to consider alternative diagnoses. Of patients who did not have optic neuritis, 17% had already received a lumbar puncture, 17% had received a contrast MRI that turned out to be negative, and 11 patients had inappropriately received IV steroids, said Dr. Stunkel.
Some of the study limitations include that the DEER category assignments were subjective, and that not every referral for optic neuritis was included in the study due to limitations of the clinic’s electronic medical records system, said Dr. Stunkel.
—Erica Tricarico
BOSTON—Misdiagnosing optic neuritis may expose patients to risks associated with undergoing MRI with a contrast agent, lumbar puncture, and high-dose steroid treatment. It also costs patients and hospitals time and money. Leanne Stunkel, MD, a neurology resident at Washington University in St. Louis, and her colleagues observed a 60% misdiagnosis rate of optic neuritis among patients who were referred to their neuro-ophthalmology clinic, according to a study presented at the 69th Annual Meeting of the American Academy of Neurology.
“The most common [diagnostic] errors were overreliance on a single item of history and failure to consider alternative diagnoses,” said Dr. Stunkel.
Optic neuritis is an acute inflammatory demyelinating condition of the optic nerve. Presenting symptoms include acute or subacute vision loss, pain with eye movement, and changes in color vision, especially affecting the color red, said Dr. Stunkel. Many patients who were referred to their tertiary care clinic for optic neuritis turned out to have other conditions, which prompted the researchers to find out more about optic neuritis misdiagnosis.
Previous studies found a misdiagnosis rate of between 10% and 40%, but none of these studies examined which errors led to these misdiagnoses. To determine how often optic neuritis is misdiagnosed and which diagnostic errors play a role, and to identify diagnoses commonly mistaken for optic neuritis, Dr. Stunkel and colleagues performed a retrospective chart review.
The researchers reviewed new patient encounters between January 2014 and October 2016 to identify patients referred with a diagnosis of optic neuritis. Experienced neuro-ophthalmologists determined the final diagnosis. The researchers then applied the Diagnosis Error Evaluation and Research (DEER) taxonomy tool to identify diagnostic errors in cases in which the patient did not have optic neuritis.
A total of 122 patients were referred for optic neuritis during the study period. Only 40% of these patients were diagnosed with optic neuritis, and 60% of patients had alternative diagnoses. The most common alternative diagnoses were headache with eye pain and visual symptoms (22%), functional visual loss (19%), and other optic neuropathies (16%).
In addition, 15% of patients had retinal or macular problems rather than pathology of the optic nerve. Other diagnoses included neoplasms, congenital disk abnormalities, and inflammatory conditions that affected other parts of the eye.
The most common diagnostic errors were from problems eliciting or interpreting the history (33%). “We saw an overreliance on history of risk factors such as multiple sclerosis or other inflammatory disorders and some failure to elicit the fact that these were brief stereotyped episodes of vision loss, like in a migraine aura,” said Dr. Stunkel.
Twenty-one percent of diagnostic errors were due to errors interpreting physical exam findings, and 14% of errors were due to misinterpretation of diagnostic tests. Finally, 32% of diagnostic errors resulted from failure to consider alternative diagnoses. Of patients who did not have optic neuritis, 17% had already received a lumbar puncture, 17% had received a contrast MRI that turned out to be negative, and 11 patients had inappropriately received IV steroids, said Dr. Stunkel.
Some of the study limitations include that the DEER category assignments were subjective, and that not every referral for optic neuritis was included in the study due to limitations of the clinic’s electronic medical records system, said Dr. Stunkel.
—Erica Tricarico
BOSTON—Misdiagnosing optic neuritis may expose patients to risks associated with undergoing MRI with a contrast agent, lumbar puncture, and high-dose steroid treatment. It also costs patients and hospitals time and money. Leanne Stunkel, MD, a neurology resident at Washington University in St. Louis, and her colleagues observed a 60% misdiagnosis rate of optic neuritis among patients who were referred to their neuro-ophthalmology clinic, according to a study presented at the 69th Annual Meeting of the American Academy of Neurology.
“The most common [diagnostic] errors were overreliance on a single item of history and failure to consider alternative diagnoses,” said Dr. Stunkel.
Optic neuritis is an acute inflammatory demyelinating condition of the optic nerve. Presenting symptoms include acute or subacute vision loss, pain with eye movement, and changes in color vision, especially affecting the color red, said Dr. Stunkel. Many patients who were referred to their tertiary care clinic for optic neuritis turned out to have other conditions, which prompted the researchers to find out more about optic neuritis misdiagnosis.
Previous studies found a misdiagnosis rate of between 10% and 40%, but none of these studies examined which errors led to these misdiagnoses. To determine how often optic neuritis is misdiagnosed and which diagnostic errors play a role, and to identify diagnoses commonly mistaken for optic neuritis, Dr. Stunkel and colleagues performed a retrospective chart review.
The researchers reviewed new patient encounters between January 2014 and October 2016 to identify patients referred with a diagnosis of optic neuritis. Experienced neuro-ophthalmologists determined the final diagnosis. The researchers then applied the Diagnosis Error Evaluation and Research (DEER) taxonomy tool to identify diagnostic errors in cases in which the patient did not have optic neuritis.
A total of 122 patients were referred for optic neuritis during the study period. Only 40% of these patients were diagnosed with optic neuritis, and 60% of patients had alternative diagnoses. The most common alternative diagnoses were headache with eye pain and visual symptoms (22%), functional visual loss (19%), and other optic neuropathies (16%).
In addition, 15% of patients had retinal or macular problems rather than pathology of the optic nerve. Other diagnoses included neoplasms, congenital disk abnormalities, and inflammatory conditions that affected other parts of the eye.
The most common diagnostic errors were from problems eliciting or interpreting the history (33%). “We saw an overreliance on history of risk factors such as multiple sclerosis or other inflammatory disorders and some failure to elicit the fact that these were brief stereotyped episodes of vision loss, like in a migraine aura,” said Dr. Stunkel.
Twenty-one percent of diagnostic errors were due to errors interpreting physical exam findings, and 14% of errors were due to misinterpretation of diagnostic tests. Finally, 32% of diagnostic errors resulted from failure to consider alternative diagnoses. Of patients who did not have optic neuritis, 17% had already received a lumbar puncture, 17% had received a contrast MRI that turned out to be negative, and 11 patients had inappropriately received IV steroids, said Dr. Stunkel.
Some of the study limitations include that the DEER category assignments were subjective, and that not every referral for optic neuritis was included in the study due to limitations of the clinic’s electronic medical records system, said Dr. Stunkel.
—Erica Tricarico
Hot Threads in ACS Communities
Here are the top discussion threads in ACS Communities just prior to press time (all of these threads are from the General Surgery community):
1. Potential Florida legislation prohibiting maintenance of certification requirements
2. My proposal for changing MOC
3. Surgical training and ethics in the ’50s/’60s
4. Timing of cholecystectomy in severe gallstone pancreatitis
5. GOO (Gastric Outlet Obstruction) – What would you do?
6. Transv colon cancer, abdominal aortic aneurysm
7. Catheter migration
8. Cholecystectomy after endoscopic retrograde cholangiopancreatography for choledocholithiasis
9. Cecal mass and concomitant distal sigmoid large polyp
10. Feeding after perforated ulcer/Graham patch
To join communities, log in to ACS Communities at http://acscommunities.facs.org/home, go to “Browse All Communities” near the top of any page, and click the blue “Join” button next to the community you’d like to join. If you have any questions, please send them to acscommunities@facs.org.
Here are the top discussion threads in ACS Communities just prior to press time (all of these threads are from the General Surgery community):
1. Potential Florida legislation prohibiting maintenance of certification requirements
2. My proposal for changing MOC
3. Surgical training and ethics in the ’50s/’60s
4. Timing of cholecystectomy in severe gallstone pancreatitis
5. GOO (Gastric Outlet Obstruction) – What would you do?
6. Transv colon cancer, abdominal aortic aneurysm
7. Catheter migration
8. Cholecystectomy after endoscopic retrograde cholangiopancreatography for choledocholithiasis
9. Cecal mass and concomitant distal sigmoid large polyp
10. Feeding after perforated ulcer/Graham patch
To join communities, log in to ACS Communities at http://acscommunities.facs.org/home, go to “Browse All Communities” near the top of any page, and click the blue “Join” button next to the community you’d like to join. If you have any questions, please send them to acscommunities@facs.org.
Here are the top discussion threads in ACS Communities just prior to press time (all of these threads are from the General Surgery community):
1. Potential Florida legislation prohibiting maintenance of certification requirements
2. My proposal for changing MOC
3. Surgical training and ethics in the ’50s/’60s
4. Timing of cholecystectomy in severe gallstone pancreatitis
5. GOO (Gastric Outlet Obstruction) – What would you do?
6. Transv colon cancer, abdominal aortic aneurysm
7. Catheter migration
8. Cholecystectomy after endoscopic retrograde cholangiopancreatography for choledocholithiasis
9. Cecal mass and concomitant distal sigmoid large polyp
10. Feeding after perforated ulcer/Graham patch
To join communities, log in to ACS Communities at http://acscommunities.facs.org/home, go to “Browse All Communities” near the top of any page, and click the blue “Join” button next to the community you’d like to join. If you have any questions, please send them to acscommunities@facs.org.
Fewer adults unaware of their hypertension
Hypertension awareness has improved significantly in adults since 2002, according to the National Center for Health Statistics.
The percentage of adults aged 18-39 years who had hypertension but reported not being told about it by a health care provider dropped 36% from 1999-2002, when it was 48.3%, to 2011-2014, when it was down to 30.8%. For adults aged 40-59 years, 26.6% were unaware of their hypertension in 1999-2002, compared with 17.4% in 2011-2014, a relative decrease of almost 35%. The decline was an even larger 55% for those aged 60 years and over – from 27.6% in 1999-2002 to 12.5% in 2011-2014, the NCHS reported.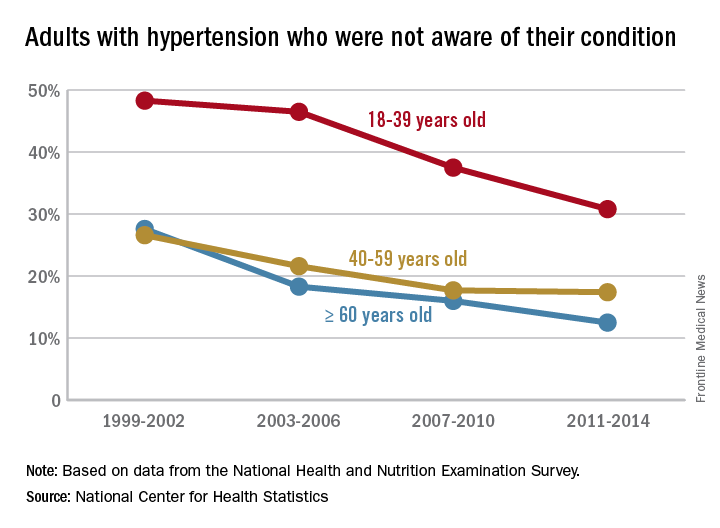
Hypertension awareness has improved significantly in adults since 2002, according to the National Center for Health Statistics.
The percentage of adults aged 18-39 years who had hypertension but reported not being told about it by a health care provider dropped 36% from 1999-2002, when it was 48.3%, to 2011-2014, when it was down to 30.8%. For adults aged 40-59 years, 26.6% were unaware of their hypertension in 1999-2002, compared with 17.4% in 2011-2014, a relative decrease of almost 35%. The decline was an even larger 55% for those aged 60 years and over – from 27.6% in 1999-2002 to 12.5% in 2011-2014, the NCHS reported.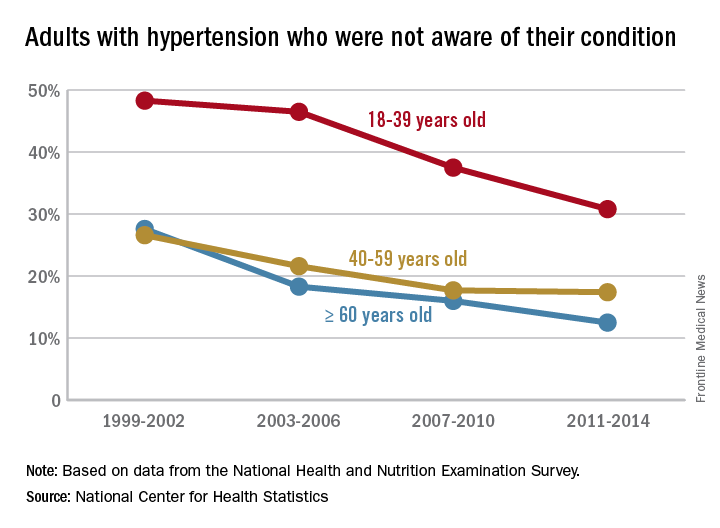
Hypertension awareness has improved significantly in adults since 2002, according to the National Center for Health Statistics.
The percentage of adults aged 18-39 years who had hypertension but reported not being told about it by a health care provider dropped 36% from 1999-2002, when it was 48.3%, to 2011-2014, when it was down to 30.8%. For adults aged 40-59 years, 26.6% were unaware of their hypertension in 1999-2002, compared with 17.4% in 2011-2014, a relative decrease of almost 35%. The decline was an even larger 55% for those aged 60 years and over – from 27.6% in 1999-2002 to 12.5% in 2011-2014, the NCHS reported.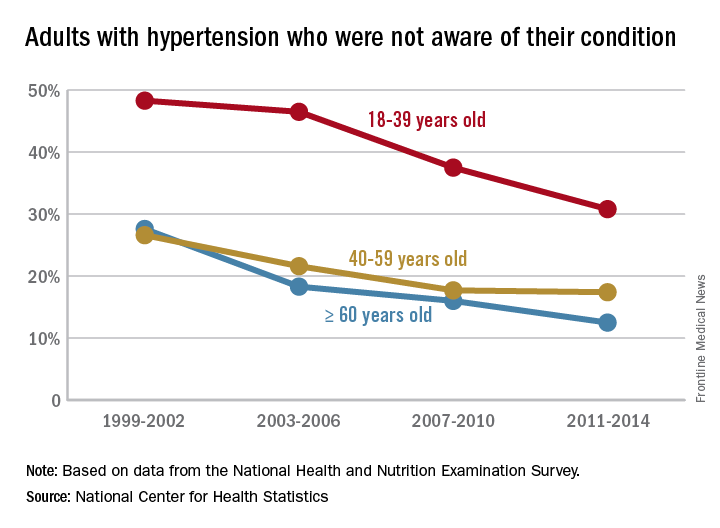
Bacterial vaginosis: Meet patients' needs with effective diagnosis and treatment
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Editorial Note
The first Skin of Color column, "Diversity in Dermatology: A Society Devoted to Skin of Color," produced in collaboration with the Skin of Color Society appears on page 322. This column will be published quarterly and will serve to increase the knowledge available to dermatologists to help improve delivery of care to this underserved population.
Look for Skin of Color columns in upcoming issues of Cutis.
The first Skin of Color column, "Diversity in Dermatology: A Society Devoted to Skin of Color," produced in collaboration with the Skin of Color Society appears on page 322. This column will be published quarterly and will serve to increase the knowledge available to dermatologists to help improve delivery of care to this underserved population.
Look for Skin of Color columns in upcoming issues of Cutis.
The first Skin of Color column, "Diversity in Dermatology: A Society Devoted to Skin of Color," produced in collaboration with the Skin of Color Society appears on page 322. This column will be published quarterly and will serve to increase the knowledge available to dermatologists to help improve delivery of care to this underserved population.
Look for Skin of Color columns in upcoming issues of Cutis.