User login
Pheochromocytoma linked to higher risk of postop complications
LAS VEGAS – Patients with pheochromocytoma are likely to have preoperative comorbidities that predispose them to postoperative cardiopulmonary complications, leading to a longer length of stay and greater hospital charges.
A 5-year national database review found high rates of chronic lung disease and malignant hypertension among these patients, Punam P. Parikh, MD, said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“They are also at an increased risk for vascular injury during surgery, perhaps because these tumors are so vascular in nature, and associated intraoperative blood transfusion,” said Dr. Parikh of the University of Miami. Postoperatively, patients with pheochromocytoma are twice as likely to experience respiratory complications and almost eight times as likely to experience cardiac complications as patients with other hormonally active adrenal tumors.
Dr. Parikh queried the National Inpatient Sample to find patients who underwent adrenalectomy for the rare adrenal tumor from 2006 to 2011. Of 27,312 patients who had adrenalectomy during the 5-year period, 22% had hormonally active adrenal tumors. Of these, just 1.4% (85) were pheochromocytoma. Other hormonally active adrenal tumors were Conn’s syndrome (65%) and Cushing’s syndrome (33%).
A number of comorbidities were significantly more common among pheochromocytoma patients than among those with Conn’s and Cushing’s syndromes, including congestive heart failure (12% vs. 4% in the other syndromes) and malignant hypertension (5% vs. 3% and 0.3%, respectively). A third of pheochromocytoma patients also had diabetes.
The rate of intraoperative complications was significantly higher in these patients (22%) than in those with Conn’s and Cushing’s (11% and 17%). Vascular injury occurred in 6% vs. 2% and 4%, respectively. Almost a quarter of pheochromocytoma patients (21%) needed an intraoperative transfusion, compared with 2% of Conn’s patients and 3% of Cushing’s patients.
There were also more postoperative complications among pheochromocytoma patients than Conn’s or Cushing’s patients, including cardiac (6% vs. 0.4% and 0.6%) and pulmonary complications (17% vs. 6% and 9%).
Not surprisingly, Dr. Parikh said, pheochromocytoma patients had longer hospital stays (5 days), compared with patients with the other tumors (3 days). Hospital charges were also higher for those with pheochromocytoma ($50,000) than those with Conn’s or Cushing’s ($35,500 and $46,334, respectively).
A multivariate analysis concluded that pheochromocytoma was an independent risk factor for intraoperative blood transfusion (odds ratio, 4.2), postoperative cardiac complications (OR, 7.6), and postoperative respiratory complications (OR, 1.9).
Dr. Parikh suggested that patients with pheochromocytoma could benefit from some preoperative preparation.
“Because of these issues, these high-risk patients should undergo appropriate preoperative medical optimization in preparation for their adrenalectomy,” she noted.
She had no financial disclosures.
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
LAS VEGAS – Patients with pheochromocytoma are likely to have preoperative comorbidities that predispose them to postoperative cardiopulmonary complications, leading to a longer length of stay and greater hospital charges.
A 5-year national database review found high rates of chronic lung disease and malignant hypertension among these patients, Punam P. Parikh, MD, said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“They are also at an increased risk for vascular injury during surgery, perhaps because these tumors are so vascular in nature, and associated intraoperative blood transfusion,” said Dr. Parikh of the University of Miami. Postoperatively, patients with pheochromocytoma are twice as likely to experience respiratory complications and almost eight times as likely to experience cardiac complications as patients with other hormonally active adrenal tumors.
Dr. Parikh queried the National Inpatient Sample to find patients who underwent adrenalectomy for the rare adrenal tumor from 2006 to 2011. Of 27,312 patients who had adrenalectomy during the 5-year period, 22% had hormonally active adrenal tumors. Of these, just 1.4% (85) were pheochromocytoma. Other hormonally active adrenal tumors were Conn’s syndrome (65%) and Cushing’s syndrome (33%).
A number of comorbidities were significantly more common among pheochromocytoma patients than among those with Conn’s and Cushing’s syndromes, including congestive heart failure (12% vs. 4% in the other syndromes) and malignant hypertension (5% vs. 3% and 0.3%, respectively). A third of pheochromocytoma patients also had diabetes.
The rate of intraoperative complications was significantly higher in these patients (22%) than in those with Conn’s and Cushing’s (11% and 17%). Vascular injury occurred in 6% vs. 2% and 4%, respectively. Almost a quarter of pheochromocytoma patients (21%) needed an intraoperative transfusion, compared with 2% of Conn’s patients and 3% of Cushing’s patients.
There were also more postoperative complications among pheochromocytoma patients than Conn’s or Cushing’s patients, including cardiac (6% vs. 0.4% and 0.6%) and pulmonary complications (17% vs. 6% and 9%).
Not surprisingly, Dr. Parikh said, pheochromocytoma patients had longer hospital stays (5 days), compared with patients with the other tumors (3 days). Hospital charges were also higher for those with pheochromocytoma ($50,000) than those with Conn’s or Cushing’s ($35,500 and $46,334, respectively).
A multivariate analysis concluded that pheochromocytoma was an independent risk factor for intraoperative blood transfusion (odds ratio, 4.2), postoperative cardiac complications (OR, 7.6), and postoperative respiratory complications (OR, 1.9).
Dr. Parikh suggested that patients with pheochromocytoma could benefit from some preoperative preparation.
“Because of these issues, these high-risk patients should undergo appropriate preoperative medical optimization in preparation for their adrenalectomy,” she noted.
She had no financial disclosures.
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
LAS VEGAS – Patients with pheochromocytoma are likely to have preoperative comorbidities that predispose them to postoperative cardiopulmonary complications, leading to a longer length of stay and greater hospital charges.
A 5-year national database review found high rates of chronic lung disease and malignant hypertension among these patients, Punam P. Parikh, MD, said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“They are also at an increased risk for vascular injury during surgery, perhaps because these tumors are so vascular in nature, and associated intraoperative blood transfusion,” said Dr. Parikh of the University of Miami. Postoperatively, patients with pheochromocytoma are twice as likely to experience respiratory complications and almost eight times as likely to experience cardiac complications as patients with other hormonally active adrenal tumors.
Dr. Parikh queried the National Inpatient Sample to find patients who underwent adrenalectomy for the rare adrenal tumor from 2006 to 2011. Of 27,312 patients who had adrenalectomy during the 5-year period, 22% had hormonally active adrenal tumors. Of these, just 1.4% (85) were pheochromocytoma. Other hormonally active adrenal tumors were Conn’s syndrome (65%) and Cushing’s syndrome (33%).
A number of comorbidities were significantly more common among pheochromocytoma patients than among those with Conn’s and Cushing’s syndromes, including congestive heart failure (12% vs. 4% in the other syndromes) and malignant hypertension (5% vs. 3% and 0.3%, respectively). A third of pheochromocytoma patients also had diabetes.
The rate of intraoperative complications was significantly higher in these patients (22%) than in those with Conn’s and Cushing’s (11% and 17%). Vascular injury occurred in 6% vs. 2% and 4%, respectively. Almost a quarter of pheochromocytoma patients (21%) needed an intraoperative transfusion, compared with 2% of Conn’s patients and 3% of Cushing’s patients.
There were also more postoperative complications among pheochromocytoma patients than Conn’s or Cushing’s patients, including cardiac (6% vs. 0.4% and 0.6%) and pulmonary complications (17% vs. 6% and 9%).
Not surprisingly, Dr. Parikh said, pheochromocytoma patients had longer hospital stays (5 days), compared with patients with the other tumors (3 days). Hospital charges were also higher for those with pheochromocytoma ($50,000) than those with Conn’s or Cushing’s ($35,500 and $46,334, respectively).
A multivariate analysis concluded that pheochromocytoma was an independent risk factor for intraoperative blood transfusion (odds ratio, 4.2), postoperative cardiac complications (OR, 7.6), and postoperative respiratory complications (OR, 1.9).
Dr. Parikh suggested that patients with pheochromocytoma could benefit from some preoperative preparation.
“Because of these issues, these high-risk patients should undergo appropriate preoperative medical optimization in preparation for their adrenalectomy,” she noted.
She had no financial disclosures.
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
AT THE ACADEMIC SURGICAL CONGRESS
Key clinical point: that predispose them to postoperative complications and prolonged hospital stays.
Major finding: Pheochromocytoma patients had more postoperative complications than Conn’s or Cushing’s patients, including cardiac (6% vs. 0.4% and 0.6%) and pulmonary complications (17% vs. 6% and 9%).
Data source: The database review comprised more than 27,000 patients with adrenal tumors.
Disclosures: Dr. Parikh had no financial disclosures.
The two faces of mitral regurgitation
SNOWMASS, COLO. – Primary mitral regurgitation and secondary mitral regurgitation may sound a lot alike, but they are in fact starkly different diseases, Blase A. Carabello, MD, said at the Annual Cardiovascular Conference at Snowmass.
“They are almost entirely different in their etiologies, in their pathophysiologies, and in their therapies,” according to Dr. Carabello, professor of medicine and chief of cardiology at East Carolina University in Greenville, N.C.
“On the other hand, if you fix the valve, you fix the disease,” he said.
In contrast, in secondary MR, the dysfunctional valve is a result of the ventricular problem, not its cause.
“In secondary MR, it’s the ventricle that made the valve sick. It’s the regional wall motion abnormalities, the displacement of the papillary muscles, and the dilation of the mitral annulus that pulls the mitral valve apart and prevents it from coapting,” he explained.
Dr. Carabello, who was on the writing committee for the current American College of Cardiology/American Heart Association guidelines on management of valvular heart disease (Circulation. 2014 Jun 10;129[23]:e521-643), highlighted other key distinctions between the two diseases.
Primary MR
“Primary MR, unlike aortic regurgitation, is not well tolerated. Early repair is key,” the cardiologist stressed.
The ACC/AHA guidelines emphasize the importance of early referral for surgery for primary MR because of surgery’s proven survival benefit. The triggers for surgery, as described in the guidelines, are easy to remember, namely, “symptoms/60/50/40.” That is, it’s time to move on to surgery when any of the following occurs: The patient becomes even mildly symptomatic, the left ventricular ejection fraction (LVEF) drops to 60%, the pulmonary artery pressure climbs to 50 mm Hg, or the LV end-systolic dimension reaches 40 mm.
Dr. Carabello said he believes those surgical thresholds are conservative, and it’s best to make the surgical referral when a patient approaches one or more of those triggers, but before actually reaching them.
“That’s the way I practice: Don’t wait for any of those things. Just get it done. One advantage to early repair is the patient can’t get lost to follow-up. They’re repaired, and they can’t take it out,” he said.
It’s possible that the next iteration of the guidelines will utilize stricter thresholds for surgery. French investigators have shown that surgery for primary MR achieves a significantly higher rate of normal LV function if the operation occurs when patients have an LVEF of 64% or more and an LV end-systolic dimension of less than 37 mm (Eur J Echocardiogr. 2011 Sep;12[9]:702-10). So far, though, there hasn’t been a confirmatory study.
“I think the normal EF in primary MR is about 70%. By the time the EF in a patient with primary MR gets down into the 50s, you’re looking at an extraordinarily sick ventricle,” according to Dr. Carabello.
The impetus for including the “symptoms/60/50/40” surgical triggers in the guidelines is to encourage physicians to make the surgical referral earlier than has often been the case. Too frequently, the surgical referral is delayed until damage to the ventricle is irreversible, with a resultant worsened prognosis.
“The natural history is such that, from the time a patient with severe primary MR enters your office to the annual mortality risk reaching 50% is only about 5 years. So if you’re going to do watchful waiting, fine, but remember: You don’t have all that long to watch and wait before something bad happens to these folks,” the cardiologist cautioned.
He added that it’s possible that, in the future, cardiac biomarkers will be utilized to help predict the long-term mortality risk of patients under medical management of their primary MR. In a recent study of 1,331 patients with primary MR, the investigators showed that the ratio of B-type natriuretic peptide (BNP) to the upper limit of normal BNP, adjusted for age and sex, was a powerful independent predictor of this risk (J Am Coll Cardiol. 2016 Sep 20;68[12]:1297-307).
The guidelines state that mitral valve repair is preferable to replacement as long as the heart team determines there’s at least a 95% chance of a durable repair. That’s because the operative mortality associated with replacement is significantly higher than with repair.
Secondary MR
Unlike in primary MR, it’s unclear whether surgery prolongs life for patients with secondary MR, or if mitral repair is superior to replacement. Thus, the current guidelines recommend surgery only for patients who are still severely symptomatic despite maximal guideline-directed medical therapy for heart failure as well as cardiac resynchronization therapy, provided they have a conduction system abnormality and qualify for the device therapy.
“If you’ve done all that and they’re still sick, I think that surgery or the MitraClip may benefit them very much,” Dr. Carabello said.
In the United States, the MitraClip transcatheter device is approved only for the treatment of primary MR in inoperable patients. But in the rest of the world, roughly three-quarters of these devices are used for treatment of secondary MR. That potential indication is currently under study in the United States in the phase III COAPT trial (Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients With Functional Mitral Regurgitation).
“In the acute setting, the changes in hemodynamic variables and left ventricular performance that occur with the MitraClip are quite dramatic, with a marked decrease in wedge pressure and a markedly increased stroke volume, which is what it’s supposed to do. So I’m encouraged. We’ll wait for the results of the COAPT trial, which I believe is likely to demonstrate a reduction in hospitalizations and certainly an improvement in patient symptoms. But I doubt very much that we’ll ever see a change in lifespan because the ventricle is still sick, and we in 2017 have not found a way yet to revive a sick ventricle. It’s unlikely that fixing the MR will do so,” according to Dr. Carabello.
He reported serving on a data safety monitoring board for Edwards Lifesciences.
SNOWMASS, COLO. – Primary mitral regurgitation and secondary mitral regurgitation may sound a lot alike, but they are in fact starkly different diseases, Blase A. Carabello, MD, said at the Annual Cardiovascular Conference at Snowmass.
“They are almost entirely different in their etiologies, in their pathophysiologies, and in their therapies,” according to Dr. Carabello, professor of medicine and chief of cardiology at East Carolina University in Greenville, N.C.
“On the other hand, if you fix the valve, you fix the disease,” he said.
In contrast, in secondary MR, the dysfunctional valve is a result of the ventricular problem, not its cause.
“In secondary MR, it’s the ventricle that made the valve sick. It’s the regional wall motion abnormalities, the displacement of the papillary muscles, and the dilation of the mitral annulus that pulls the mitral valve apart and prevents it from coapting,” he explained.
Dr. Carabello, who was on the writing committee for the current American College of Cardiology/American Heart Association guidelines on management of valvular heart disease (Circulation. 2014 Jun 10;129[23]:e521-643), highlighted other key distinctions between the two diseases.
Primary MR
“Primary MR, unlike aortic regurgitation, is not well tolerated. Early repair is key,” the cardiologist stressed.
The ACC/AHA guidelines emphasize the importance of early referral for surgery for primary MR because of surgery’s proven survival benefit. The triggers for surgery, as described in the guidelines, are easy to remember, namely, “symptoms/60/50/40.” That is, it’s time to move on to surgery when any of the following occurs: The patient becomes even mildly symptomatic, the left ventricular ejection fraction (LVEF) drops to 60%, the pulmonary artery pressure climbs to 50 mm Hg, or the LV end-systolic dimension reaches 40 mm.
Dr. Carabello said he believes those surgical thresholds are conservative, and it’s best to make the surgical referral when a patient approaches one or more of those triggers, but before actually reaching them.
“That’s the way I practice: Don’t wait for any of those things. Just get it done. One advantage to early repair is the patient can’t get lost to follow-up. They’re repaired, and they can’t take it out,” he said.
It’s possible that the next iteration of the guidelines will utilize stricter thresholds for surgery. French investigators have shown that surgery for primary MR achieves a significantly higher rate of normal LV function if the operation occurs when patients have an LVEF of 64% or more and an LV end-systolic dimension of less than 37 mm (Eur J Echocardiogr. 2011 Sep;12[9]:702-10). So far, though, there hasn’t been a confirmatory study.
“I think the normal EF in primary MR is about 70%. By the time the EF in a patient with primary MR gets down into the 50s, you’re looking at an extraordinarily sick ventricle,” according to Dr. Carabello.
The impetus for including the “symptoms/60/50/40” surgical triggers in the guidelines is to encourage physicians to make the surgical referral earlier than has often been the case. Too frequently, the surgical referral is delayed until damage to the ventricle is irreversible, with a resultant worsened prognosis.
“The natural history is such that, from the time a patient with severe primary MR enters your office to the annual mortality risk reaching 50% is only about 5 years. So if you’re going to do watchful waiting, fine, but remember: You don’t have all that long to watch and wait before something bad happens to these folks,” the cardiologist cautioned.
He added that it’s possible that, in the future, cardiac biomarkers will be utilized to help predict the long-term mortality risk of patients under medical management of their primary MR. In a recent study of 1,331 patients with primary MR, the investigators showed that the ratio of B-type natriuretic peptide (BNP) to the upper limit of normal BNP, adjusted for age and sex, was a powerful independent predictor of this risk (J Am Coll Cardiol. 2016 Sep 20;68[12]:1297-307).
The guidelines state that mitral valve repair is preferable to replacement as long as the heart team determines there’s at least a 95% chance of a durable repair. That’s because the operative mortality associated with replacement is significantly higher than with repair.
Secondary MR
Unlike in primary MR, it’s unclear whether surgery prolongs life for patients with secondary MR, or if mitral repair is superior to replacement. Thus, the current guidelines recommend surgery only for patients who are still severely symptomatic despite maximal guideline-directed medical therapy for heart failure as well as cardiac resynchronization therapy, provided they have a conduction system abnormality and qualify for the device therapy.
“If you’ve done all that and they’re still sick, I think that surgery or the MitraClip may benefit them very much,” Dr. Carabello said.
In the United States, the MitraClip transcatheter device is approved only for the treatment of primary MR in inoperable patients. But in the rest of the world, roughly three-quarters of these devices are used for treatment of secondary MR. That potential indication is currently under study in the United States in the phase III COAPT trial (Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients With Functional Mitral Regurgitation).
“In the acute setting, the changes in hemodynamic variables and left ventricular performance that occur with the MitraClip are quite dramatic, with a marked decrease in wedge pressure and a markedly increased stroke volume, which is what it’s supposed to do. So I’m encouraged. We’ll wait for the results of the COAPT trial, which I believe is likely to demonstrate a reduction in hospitalizations and certainly an improvement in patient symptoms. But I doubt very much that we’ll ever see a change in lifespan because the ventricle is still sick, and we in 2017 have not found a way yet to revive a sick ventricle. It’s unlikely that fixing the MR will do so,” according to Dr. Carabello.
He reported serving on a data safety monitoring board for Edwards Lifesciences.
SNOWMASS, COLO. – Primary mitral regurgitation and secondary mitral regurgitation may sound a lot alike, but they are in fact starkly different diseases, Blase A. Carabello, MD, said at the Annual Cardiovascular Conference at Snowmass.
“They are almost entirely different in their etiologies, in their pathophysiologies, and in their therapies,” according to Dr. Carabello, professor of medicine and chief of cardiology at East Carolina University in Greenville, N.C.
“On the other hand, if you fix the valve, you fix the disease,” he said.
In contrast, in secondary MR, the dysfunctional valve is a result of the ventricular problem, not its cause.
“In secondary MR, it’s the ventricle that made the valve sick. It’s the regional wall motion abnormalities, the displacement of the papillary muscles, and the dilation of the mitral annulus that pulls the mitral valve apart and prevents it from coapting,” he explained.
Dr. Carabello, who was on the writing committee for the current American College of Cardiology/American Heart Association guidelines on management of valvular heart disease (Circulation. 2014 Jun 10;129[23]:e521-643), highlighted other key distinctions between the two diseases.
Primary MR
“Primary MR, unlike aortic regurgitation, is not well tolerated. Early repair is key,” the cardiologist stressed.
The ACC/AHA guidelines emphasize the importance of early referral for surgery for primary MR because of surgery’s proven survival benefit. The triggers for surgery, as described in the guidelines, are easy to remember, namely, “symptoms/60/50/40.” That is, it’s time to move on to surgery when any of the following occurs: The patient becomes even mildly symptomatic, the left ventricular ejection fraction (LVEF) drops to 60%, the pulmonary artery pressure climbs to 50 mm Hg, or the LV end-systolic dimension reaches 40 mm.
Dr. Carabello said he believes those surgical thresholds are conservative, and it’s best to make the surgical referral when a patient approaches one or more of those triggers, but before actually reaching them.
“That’s the way I practice: Don’t wait for any of those things. Just get it done. One advantage to early repair is the patient can’t get lost to follow-up. They’re repaired, and they can’t take it out,” he said.
It’s possible that the next iteration of the guidelines will utilize stricter thresholds for surgery. French investigators have shown that surgery for primary MR achieves a significantly higher rate of normal LV function if the operation occurs when patients have an LVEF of 64% or more and an LV end-systolic dimension of less than 37 mm (Eur J Echocardiogr. 2011 Sep;12[9]:702-10). So far, though, there hasn’t been a confirmatory study.
“I think the normal EF in primary MR is about 70%. By the time the EF in a patient with primary MR gets down into the 50s, you’re looking at an extraordinarily sick ventricle,” according to Dr. Carabello.
The impetus for including the “symptoms/60/50/40” surgical triggers in the guidelines is to encourage physicians to make the surgical referral earlier than has often been the case. Too frequently, the surgical referral is delayed until damage to the ventricle is irreversible, with a resultant worsened prognosis.
“The natural history is such that, from the time a patient with severe primary MR enters your office to the annual mortality risk reaching 50% is only about 5 years. So if you’re going to do watchful waiting, fine, but remember: You don’t have all that long to watch and wait before something bad happens to these folks,” the cardiologist cautioned.
He added that it’s possible that, in the future, cardiac biomarkers will be utilized to help predict the long-term mortality risk of patients under medical management of their primary MR. In a recent study of 1,331 patients with primary MR, the investigators showed that the ratio of B-type natriuretic peptide (BNP) to the upper limit of normal BNP, adjusted for age and sex, was a powerful independent predictor of this risk (J Am Coll Cardiol. 2016 Sep 20;68[12]:1297-307).
The guidelines state that mitral valve repair is preferable to replacement as long as the heart team determines there’s at least a 95% chance of a durable repair. That’s because the operative mortality associated with replacement is significantly higher than with repair.
Secondary MR
Unlike in primary MR, it’s unclear whether surgery prolongs life for patients with secondary MR, or if mitral repair is superior to replacement. Thus, the current guidelines recommend surgery only for patients who are still severely symptomatic despite maximal guideline-directed medical therapy for heart failure as well as cardiac resynchronization therapy, provided they have a conduction system abnormality and qualify for the device therapy.
“If you’ve done all that and they’re still sick, I think that surgery or the MitraClip may benefit them very much,” Dr. Carabello said.
In the United States, the MitraClip transcatheter device is approved only for the treatment of primary MR in inoperable patients. But in the rest of the world, roughly three-quarters of these devices are used for treatment of secondary MR. That potential indication is currently under study in the United States in the phase III COAPT trial (Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients With Functional Mitral Regurgitation).
“In the acute setting, the changes in hemodynamic variables and left ventricular performance that occur with the MitraClip are quite dramatic, with a marked decrease in wedge pressure and a markedly increased stroke volume, which is what it’s supposed to do. So I’m encouraged. We’ll wait for the results of the COAPT trial, which I believe is likely to demonstrate a reduction in hospitalizations and certainly an improvement in patient symptoms. But I doubt very much that we’ll ever see a change in lifespan because the ventricle is still sick, and we in 2017 have not found a way yet to revive a sick ventricle. It’s unlikely that fixing the MR will do so,” according to Dr. Carabello.
He reported serving on a data safety monitoring board for Edwards Lifesciences.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Model illustrates progression to MDS, AML
Researchers say they have created a model that shows the step-by-step progression from normal blood cells to acute myeloid leukemia (AML).
The team generated induced pluripotent stem cell (iPSC) lines capturing disease stages that included preleukemia, low-risk myelodysplastic syndrome (MDS), high-risk MDS, and AML.
The researchers then used CRISPR/Cas9 genome editing to induce disease progression and reversal.
And they used the iPSCs to uncover disease-stage-specific effects of 2 drugs.
Eirini P. Papapetrou, MD, PhD, of the Icahn School of Medicine at Mount Sinai in New York, New York, and her colleagues described this work in Cell Stem Cell.
The researchers first explained how they generated patient-derived iPSCs that represented familial predisposition to myeloid malignancy, low-risk and high-risk MDS, and AML.
By studying these iPSC lines, the team uncovered “a phenotypic road map of disease progression” that led to a “serially transplantable leukemia.”
“We are encouraged by the discovery that it was possible to generate potent, engraftable leukemia derived from AML induced pluripotent stem cells,” said study author Michael G. Kharas, PhD, of the Icahn School of Medicine at Mount Sinai.
The researchers also showed that they could revert a high-risk MDS iPSC line to a premalignant state by correcting a chromosome 7q deletion.
And they could force progression in a preleukemic iPSC line. The team induced progression to low-risk MDS by inactivating the second GATA2 allele and progression to high-risk MDS by deleting chromosome 7q.
“This work shows that integrated patient cell reprogramming and cancer genetics is a powerful way to dissect cancer progression,” Dr Kharas said.
The researchers reported that, ultimately, they were able to model the stepwise progression of normal cells to preleukemia and MDS by sequentially introducing genetic lesions associated with earlier and later disease stages (ASXL1 truncation and chromosome 7q deletion, respectively).
“The new model will empower investigation into the cellular and molecular events underlying the development of leukemia in ways that were not possible before,” Dr Papapetrou said.
She added that the group’s findings provide a framework to aid investigation into disease mechanisms, events driving progression, and drug responses.
In fact, the researchers did use hematopoietic progenitor cells (HPCs) derived from their iPSCs to analyze the disease-stage-specific effects of 2 drugs—5-azacytidine and rigosertib.
The team said they found evidence to suggest that 5-azacytidine may work in low-risk MDS by affecting differentiation, and the drug’s main therapeutic action in high-risk MDS might be mediated through selective inhibition of the MDS clone.
The researchers tested rigosertib in HPCs derived from 2 AML lines (from the same patient) that captured 2 different disease stages. One line was derived from the dominant clone (del 7q), and the other was derived from a KRAS-mutated subclone.
The team found that HPCs derived from the KRAS-mutated line demonstrated “marked sensitivity” to rigosertib, but the other HPCs were “marginally affected.” ![]()
Researchers say they have created a model that shows the step-by-step progression from normal blood cells to acute myeloid leukemia (AML).
The team generated induced pluripotent stem cell (iPSC) lines capturing disease stages that included preleukemia, low-risk myelodysplastic syndrome (MDS), high-risk MDS, and AML.
The researchers then used CRISPR/Cas9 genome editing to induce disease progression and reversal.
And they used the iPSCs to uncover disease-stage-specific effects of 2 drugs.
Eirini P. Papapetrou, MD, PhD, of the Icahn School of Medicine at Mount Sinai in New York, New York, and her colleagues described this work in Cell Stem Cell.
The researchers first explained how they generated patient-derived iPSCs that represented familial predisposition to myeloid malignancy, low-risk and high-risk MDS, and AML.
By studying these iPSC lines, the team uncovered “a phenotypic road map of disease progression” that led to a “serially transplantable leukemia.”
“We are encouraged by the discovery that it was possible to generate potent, engraftable leukemia derived from AML induced pluripotent stem cells,” said study author Michael G. Kharas, PhD, of the Icahn School of Medicine at Mount Sinai.
The researchers also showed that they could revert a high-risk MDS iPSC line to a premalignant state by correcting a chromosome 7q deletion.
And they could force progression in a preleukemic iPSC line. The team induced progression to low-risk MDS by inactivating the second GATA2 allele and progression to high-risk MDS by deleting chromosome 7q.
“This work shows that integrated patient cell reprogramming and cancer genetics is a powerful way to dissect cancer progression,” Dr Kharas said.
The researchers reported that, ultimately, they were able to model the stepwise progression of normal cells to preleukemia and MDS by sequentially introducing genetic lesions associated with earlier and later disease stages (ASXL1 truncation and chromosome 7q deletion, respectively).
“The new model will empower investigation into the cellular and molecular events underlying the development of leukemia in ways that were not possible before,” Dr Papapetrou said.
She added that the group’s findings provide a framework to aid investigation into disease mechanisms, events driving progression, and drug responses.
In fact, the researchers did use hematopoietic progenitor cells (HPCs) derived from their iPSCs to analyze the disease-stage-specific effects of 2 drugs—5-azacytidine and rigosertib.
The team said they found evidence to suggest that 5-azacytidine may work in low-risk MDS by affecting differentiation, and the drug’s main therapeutic action in high-risk MDS might be mediated through selective inhibition of the MDS clone.
The researchers tested rigosertib in HPCs derived from 2 AML lines (from the same patient) that captured 2 different disease stages. One line was derived from the dominant clone (del 7q), and the other was derived from a KRAS-mutated subclone.
The team found that HPCs derived from the KRAS-mutated line demonstrated “marked sensitivity” to rigosertib, but the other HPCs were “marginally affected.” ![]()
Researchers say they have created a model that shows the step-by-step progression from normal blood cells to acute myeloid leukemia (AML).
The team generated induced pluripotent stem cell (iPSC) lines capturing disease stages that included preleukemia, low-risk myelodysplastic syndrome (MDS), high-risk MDS, and AML.
The researchers then used CRISPR/Cas9 genome editing to induce disease progression and reversal.
And they used the iPSCs to uncover disease-stage-specific effects of 2 drugs.
Eirini P. Papapetrou, MD, PhD, of the Icahn School of Medicine at Mount Sinai in New York, New York, and her colleagues described this work in Cell Stem Cell.
The researchers first explained how they generated patient-derived iPSCs that represented familial predisposition to myeloid malignancy, low-risk and high-risk MDS, and AML.
By studying these iPSC lines, the team uncovered “a phenotypic road map of disease progression” that led to a “serially transplantable leukemia.”
“We are encouraged by the discovery that it was possible to generate potent, engraftable leukemia derived from AML induced pluripotent stem cells,” said study author Michael G. Kharas, PhD, of the Icahn School of Medicine at Mount Sinai.
The researchers also showed that they could revert a high-risk MDS iPSC line to a premalignant state by correcting a chromosome 7q deletion.
And they could force progression in a preleukemic iPSC line. The team induced progression to low-risk MDS by inactivating the second GATA2 allele and progression to high-risk MDS by deleting chromosome 7q.
“This work shows that integrated patient cell reprogramming and cancer genetics is a powerful way to dissect cancer progression,” Dr Kharas said.
The researchers reported that, ultimately, they were able to model the stepwise progression of normal cells to preleukemia and MDS by sequentially introducing genetic lesions associated with earlier and later disease stages (ASXL1 truncation and chromosome 7q deletion, respectively).
“The new model will empower investigation into the cellular and molecular events underlying the development of leukemia in ways that were not possible before,” Dr Papapetrou said.
She added that the group’s findings provide a framework to aid investigation into disease mechanisms, events driving progression, and drug responses.
In fact, the researchers did use hematopoietic progenitor cells (HPCs) derived from their iPSCs to analyze the disease-stage-specific effects of 2 drugs—5-azacytidine and rigosertib.
The team said they found evidence to suggest that 5-azacytidine may work in low-risk MDS by affecting differentiation, and the drug’s main therapeutic action in high-risk MDS might be mediated through selective inhibition of the MDS clone.
The researchers tested rigosertib in HPCs derived from 2 AML lines (from the same patient) that captured 2 different disease stages. One line was derived from the dominant clone (del 7q), and the other was derived from a KRAS-mutated subclone.
The team found that HPCs derived from the KRAS-mutated line demonstrated “marked sensitivity” to rigosertib, but the other HPCs were “marginally affected.” ![]()
Pertussis susceptibility estimates call for public health push
, according to results of research by Lana Childs and Robert A. Bednarczyk, PhD.
There were 32,971 pertussis cases reported in 2014, a 15% increase over 2013; most cases occurred in children who were too young to be fully vaccinated and in preadolescents with waning immunity from their vaccines. In the United States, vaccine coverage during childhood tends to be high overall, but DTaP coverage (84% in 2014) “remains lower than coverage for other childhood vaccinations,” they noted.
“These findings emphasize the need for public health professionals to continue efforts to increase DTaP vaccine coverage in children and Tdap coverage in pregnant women, plan for potential outbreaks, and maintain immunity levels needed to prevent the spread of pertussis.” the investigators concluded.
Read more at (Ped Inf Dis J. 2017. doi: 10.1097/INF.0000000000001537).
, according to results of research by Lana Childs and Robert A. Bednarczyk, PhD.
There were 32,971 pertussis cases reported in 2014, a 15% increase over 2013; most cases occurred in children who were too young to be fully vaccinated and in preadolescents with waning immunity from their vaccines. In the United States, vaccine coverage during childhood tends to be high overall, but DTaP coverage (84% in 2014) “remains lower than coverage for other childhood vaccinations,” they noted.
“These findings emphasize the need for public health professionals to continue efforts to increase DTaP vaccine coverage in children and Tdap coverage in pregnant women, plan for potential outbreaks, and maintain immunity levels needed to prevent the spread of pertussis.” the investigators concluded.
Read more at (Ped Inf Dis J. 2017. doi: 10.1097/INF.0000000000001537).
, according to results of research by Lana Childs and Robert A. Bednarczyk, PhD.
There were 32,971 pertussis cases reported in 2014, a 15% increase over 2013; most cases occurred in children who were too young to be fully vaccinated and in preadolescents with waning immunity from their vaccines. In the United States, vaccine coverage during childhood tends to be high overall, but DTaP coverage (84% in 2014) “remains lower than coverage for other childhood vaccinations,” they noted.
“These findings emphasize the need for public health professionals to continue efforts to increase DTaP vaccine coverage in children and Tdap coverage in pregnant women, plan for potential outbreaks, and maintain immunity levels needed to prevent the spread of pertussis.” the investigators concluded.
Read more at (Ped Inf Dis J. 2017. doi: 10.1097/INF.0000000000001537).
FROM THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
One-third of micropapillary thyroid cancer found to be multifocal
LAS VEGAS – Micropapillary thyroid carcinoma may not be as indolent as generally thought, according to the findings of a retrospective study of thyroidectomy cases.
A review of 213 patients diagnosed with the cancer found that 34% of them had multifocal disease, and 14%, metastatic disease, Maggie Bosley reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
Ms. Bosley presented a review of 213 consecutive patients who underwent thyroidectomy from 2007 to 2015, and were found to have micropapillary thyroid cancer. She reviewed the pathology reports for tumor size, presence or absence of metastases in the central and lateral node basins, and multifocality.
Most of the patients (88%) were women, with an average age of 56 years, although the range was wide (18-89 years).
About a third of the patients (73; 34%) had multifocal disease. This was bilateral in 21 (29%). Metastasis to the central nodes was present in 31 patients (14%); 4 of these patients also had positive lateral neck node metastases (2%).
“Approximately 13% of patients with node metastasis also required selective lateral neck dissections,” Ms. Bosley said.
She noted that, in 2015, the American Thyroid Association published a set of guidelines for diagnosing and treating micropapillary cancer. The guidelines suggest that most of these cancers can be safely followed with ultrasound exams, if there is no extrathyroid extension or nodal metastasis.
“However, ultrasound surveillance [quality] is very operator dependent,” Ms. Bosley said. Technician skill “could potentially impact the quality of surveillance.”
She had no relevant financial declarations.
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
LAS VEGAS – Micropapillary thyroid carcinoma may not be as indolent as generally thought, according to the findings of a retrospective study of thyroidectomy cases.
A review of 213 patients diagnosed with the cancer found that 34% of them had multifocal disease, and 14%, metastatic disease, Maggie Bosley reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
Ms. Bosley presented a review of 213 consecutive patients who underwent thyroidectomy from 2007 to 2015, and were found to have micropapillary thyroid cancer. She reviewed the pathology reports for tumor size, presence or absence of metastases in the central and lateral node basins, and multifocality.
Most of the patients (88%) were women, with an average age of 56 years, although the range was wide (18-89 years).
About a third of the patients (73; 34%) had multifocal disease. This was bilateral in 21 (29%). Metastasis to the central nodes was present in 31 patients (14%); 4 of these patients also had positive lateral neck node metastases (2%).
“Approximately 13% of patients with node metastasis also required selective lateral neck dissections,” Ms. Bosley said.
She noted that, in 2015, the American Thyroid Association published a set of guidelines for diagnosing and treating micropapillary cancer. The guidelines suggest that most of these cancers can be safely followed with ultrasound exams, if there is no extrathyroid extension or nodal metastasis.
“However, ultrasound surveillance [quality] is very operator dependent,” Ms. Bosley said. Technician skill “could potentially impact the quality of surveillance.”
She had no relevant financial declarations.
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
LAS VEGAS – Micropapillary thyroid carcinoma may not be as indolent as generally thought, according to the findings of a retrospective study of thyroidectomy cases.
A review of 213 patients diagnosed with the cancer found that 34% of them had multifocal disease, and 14%, metastatic disease, Maggie Bosley reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
Ms. Bosley presented a review of 213 consecutive patients who underwent thyroidectomy from 2007 to 2015, and were found to have micropapillary thyroid cancer. She reviewed the pathology reports for tumor size, presence or absence of metastases in the central and lateral node basins, and multifocality.
Most of the patients (88%) were women, with an average age of 56 years, although the range was wide (18-89 years).
About a third of the patients (73; 34%) had multifocal disease. This was bilateral in 21 (29%). Metastasis to the central nodes was present in 31 patients (14%); 4 of these patients also had positive lateral neck node metastases (2%).
“Approximately 13% of patients with node metastasis also required selective lateral neck dissections,” Ms. Bosley said.
She noted that, in 2015, the American Thyroid Association published a set of guidelines for diagnosing and treating micropapillary cancer. The guidelines suggest that most of these cancers can be safely followed with ultrasound exams, if there is no extrathyroid extension or nodal metastasis.
“However, ultrasound surveillance [quality] is very operator dependent,” Ms. Bosley said. Technician skill “could potentially impact the quality of surveillance.”
She had no relevant financial declarations.
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
AT THE ACADEMIC SURGICAL CONGRESS
Key clinical point:
Major finding: Micropapillary thyroid cancer was metastatic in 14% of cases.
Data source: A review involving 213 patients.
Disclosures: Ms. Bosley had no relevant financial disclosures.
IgG4-related disease can strike any organ system
SNOWMASS, COLO. – Progress in the understanding and treatment of immunoglobulin G4–related disease is occurring “at lightning speed,” John H. Stone, MD, said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
Eight or nine years ago no one had heard of immunoglobulin G4–related disease (IgG4-RD). Today, because of the broad swath the disease cuts, it’s a hot research topic in every subspecialty of medicine as well as surgery, pathology, and radiology.
This new understanding of IgG4-RD, he added, is opening the door to novel treatments.
“This is not a new disease. It was there when we were all in medical school, and for hundreds of years before that. But it’s really only in the last decade that we have come to understand that the disease can affect literally every organ system in the body with syndromes that we once thought were isolated organ-specific syndromes but we now recognize are part of a multiorgan disease currently called IgG4-related disease,” the rheumatologist said.
IgG4-RD is an immune-mediated fibroinflammatory condition characterized histopathologically by three hallmark features in involved tissue: obliterative phlebitis, storiform fibrosis, and a dense lymphoplasmacytic infiltrate.
Clinically, IgG4-RD often presents as a mass lesion that can affect any organ.
“I have many patients who’ve undergone modified Whipple procedures because they were thought to have adenocarcinoma of the pancreas,” according to Dr. Stone.
Other common presentations include Riedel’s thyroiditis, autoimmune pancreatitis, sclerosing cholangitis, sialadenitis, dacryoadenitis, periaortitis, an eosinophilic rash, and pseudotumor of the lung, lymph nodes, or orbits.
“Retroperitoneal fibrosis is a common and underappreciated manifestation. It may be the most common subsyndrome associated with IgG4-related disease,” he observed.
Another common presentation involves atopic disease – asthma, allergic rhinitis, eczema, eosinophilia, nasal polyps – developing out of the blue in middle age or later life. This observation led some other investigators to posit that IgG4-RD is a T-helper type 2–driven disease, an assertion debunked by Dr. Stone and coworkers (Allergy. 2014 Feb;69[2]:269-72).
Dr. Stone and his coinvestigators have published the largest series of patients with biopsy-proven IgG4-RD reported to date (Arthritis Rheumatol. 2015 Sep; 67[9]:2466-75). The average age at disease onset was 50 years. Of note, multiorgan involvement was the norm: 24% of patients had two organs involved, and 38% had three or more.
Analysis of this large patient series has led Dr. Stone to a surprising conclusion about the nature of IgG4-RD: “We have greatly overemphasized the importance of IgG4 in this condition,” he asserted.
Indeed, a mere 51% of the patients with clinically active untreated IgG4-RD in his series had an elevated serum IgG level. Dr. Stone characterized IgG4 as “kind of a wimpy antibody” incapable of driving the disease process because it is a noninflammatory immunoglobulin. This has led to speculation that IgG4 functions as what he termed an “antigen sink,” attempting to bind antigen at sites of inflammation.
But while an elevated serum IgG4 is of limited utility for diagnostic purposes, Dr. Stone and coworkers have demonstrated that it is of value as a predictor of relapse. Among patients with a treatment-induced remission, those in the top quartile in terms of baseline pretreatment serum IgG4 were 6.2-fold more likely to relapse (Rheumatology [Oxford]. 2016 Jun;55[6]:1000-8).
“This is a very useful marker for patients who are going to need chronic ongoing therapy. The notion of putting such patients on steroids for months and years is not appealing,” he said.
Levels of circulating plasmablasts as measured by peripheral blood flow cytometry, especially IgG4-positive plasmablasts, have proven much more helpful than serum IgG4 levels as a diagnostic tool, a reliable biomarker of disease activity, and a therapeutic target. Levels of these short-lived CD19+CD38+CD27+ plasmablasts are enormously elevated independent of serum IgG4 in patients with active IgG4-RD.
“One of the questions I’m most often asked is whether IgG4-related disease is a premalignant condition. My answer is no. The plasmablast expansion is oligoclonal, not polyclonal,” Dr. Stone continued.
He described IgG4-RD as “a continuous dance between T cells and B cells.” The latest thinking regarding pathogenesis is that type 2 T follicular helper cells activate B cells, which become memory B cells or plasmablasts. These activated B cells and plasmablasts present antigen to CD4+ cytotoxic T cells at sites of disease. Dr. Stone and his coinvestigators recently identified these CD4+ cytotoxic T cells as a novel population of clonally expanded T cells with SLAMF7 as a surface marker. The cells secrete interferon-gamma, interleukin-1, and transforming growth factor-beta, all of which are capable of driving the intense fibrosis characteristic of IgG4-RD. In addition, these CD4+ cytotoxic T cells secrete granzyme B and perforin, previously thought to be released mainly by natural killer T cells.
Joint American College of Rheumatology/European League Against Rheumatism classification criteria for the disease are expected to be finalized this winter at the Third International Symposium on IgG4-Related Diseases.
Treatment with rituxumab
Glucocorticoids remain the first-line therapy in IgG4-related disease, but it’s essential to bear in mind that their long-term efficacy in this immune-mediated fibroinflammatory disease is the exception rather than the rule, Dr. Stone said at the symposium.
Dr. Stone was a coauthor of an international expert consensus statement on the treatment of IgG4-related disease (IgG4-RD), which emphasized that point (Arthritis Rheumatol. 2015 Jul;67[7]:1688-99).
“I typically start with prednisone at 40 mg/day, and there’s a dramatic response in these patients. Then I taper them off after 2-3 months. If 2-3 months doesn’t put them into a long-term sustained remission, it’s time to go to something else,” said Dr. Stone.
So what’s the next move, then, after steroids fail? Dr. Stone was a pioneer in the strikingly successful use of B cell depletion via rituximab (Rituxan) in patients with IgG4-RD. First he and his coinvestigators demonstrated that this off-label use of rituximab led to rapid clinical and histologic improvement (Ann Rheum Dis. 2015 Jun; 74[6]:1171-7), then they showed it also causes levels of circulating plasmablasts, serum IgG4, and biomarkers of fibrosis to plunge, suggesting B cell depletion may halt the destructive process of collagen deposition that characterizes this immune-related disease (Ann Rheum Dis. 2015 Dec;74[12]:2236-43). They have also reported that patients with very elevated baseline serum IgG4 levels are at more than sixfold increased risk of relapse at a median of 244 days from their first rituximab infusion (Rheumatology [Oxford]. 2016 Jun;55[6]:1000-8).
The success with rituximab is just one example of how improved understanding of the pathophysiology of IgG4-RD has opened the door to novel treatments. Dr. Stone is the lead investigator in an ongoing phase II, open-label study in which 15 patients with active IgG4-RD will receive intravenous XmAb5871 every 2 weeks for 6 months to evaluate the effect on the IgG4-RD Responder Index. XmAb5871 is a monoclonal antibody that binds to CD19 and FCgammaRIIb in order to downregulate activated B cells and plasmablasts. It is also being developed for treatment of systemic lupus erythematosus.
Dr. Stone and his coinvestigators are working on a therapeutic approach to IgG4-RD that targets antigen presentation by activated B cells to CD4+ cytotoxic T cells at sites of disease. These CD4+ cytotoxic T cells contain signaling lymphocyte activation molecule F7 (SLAMF7) as a surface marker. Elotuzumab (Empliciti), an immunostimulatory humanized monoclonal antibody targeting SLAMF7, is already on the market for treatment of multiple myeloma, he noted.
Dr. Stone reported receiving IgG4-RD-related research funding from and serving as a consultant to Genentech and Xencor, which is developing XmAb5871.
SNOWMASS, COLO. – Progress in the understanding and treatment of immunoglobulin G4–related disease is occurring “at lightning speed,” John H. Stone, MD, said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
Eight or nine years ago no one had heard of immunoglobulin G4–related disease (IgG4-RD). Today, because of the broad swath the disease cuts, it’s a hot research topic in every subspecialty of medicine as well as surgery, pathology, and radiology.
This new understanding of IgG4-RD, he added, is opening the door to novel treatments.
“This is not a new disease. It was there when we were all in medical school, and for hundreds of years before that. But it’s really only in the last decade that we have come to understand that the disease can affect literally every organ system in the body with syndromes that we once thought were isolated organ-specific syndromes but we now recognize are part of a multiorgan disease currently called IgG4-related disease,” the rheumatologist said.
IgG4-RD is an immune-mediated fibroinflammatory condition characterized histopathologically by three hallmark features in involved tissue: obliterative phlebitis, storiform fibrosis, and a dense lymphoplasmacytic infiltrate.
Clinically, IgG4-RD often presents as a mass lesion that can affect any organ.
“I have many patients who’ve undergone modified Whipple procedures because they were thought to have adenocarcinoma of the pancreas,” according to Dr. Stone.
Other common presentations include Riedel’s thyroiditis, autoimmune pancreatitis, sclerosing cholangitis, sialadenitis, dacryoadenitis, periaortitis, an eosinophilic rash, and pseudotumor of the lung, lymph nodes, or orbits.
“Retroperitoneal fibrosis is a common and underappreciated manifestation. It may be the most common subsyndrome associated with IgG4-related disease,” he observed.
Another common presentation involves atopic disease – asthma, allergic rhinitis, eczema, eosinophilia, nasal polyps – developing out of the blue in middle age or later life. This observation led some other investigators to posit that IgG4-RD is a T-helper type 2–driven disease, an assertion debunked by Dr. Stone and coworkers (Allergy. 2014 Feb;69[2]:269-72).
Dr. Stone and his coinvestigators have published the largest series of patients with biopsy-proven IgG4-RD reported to date (Arthritis Rheumatol. 2015 Sep; 67[9]:2466-75). The average age at disease onset was 50 years. Of note, multiorgan involvement was the norm: 24% of patients had two organs involved, and 38% had three or more.
Analysis of this large patient series has led Dr. Stone to a surprising conclusion about the nature of IgG4-RD: “We have greatly overemphasized the importance of IgG4 in this condition,” he asserted.
Indeed, a mere 51% of the patients with clinically active untreated IgG4-RD in his series had an elevated serum IgG level. Dr. Stone characterized IgG4 as “kind of a wimpy antibody” incapable of driving the disease process because it is a noninflammatory immunoglobulin. This has led to speculation that IgG4 functions as what he termed an “antigen sink,” attempting to bind antigen at sites of inflammation.
But while an elevated serum IgG4 is of limited utility for diagnostic purposes, Dr. Stone and coworkers have demonstrated that it is of value as a predictor of relapse. Among patients with a treatment-induced remission, those in the top quartile in terms of baseline pretreatment serum IgG4 were 6.2-fold more likely to relapse (Rheumatology [Oxford]. 2016 Jun;55[6]:1000-8).
“This is a very useful marker for patients who are going to need chronic ongoing therapy. The notion of putting such patients on steroids for months and years is not appealing,” he said.
Levels of circulating plasmablasts as measured by peripheral blood flow cytometry, especially IgG4-positive plasmablasts, have proven much more helpful than serum IgG4 levels as a diagnostic tool, a reliable biomarker of disease activity, and a therapeutic target. Levels of these short-lived CD19+CD38+CD27+ plasmablasts are enormously elevated independent of serum IgG4 in patients with active IgG4-RD.
“One of the questions I’m most often asked is whether IgG4-related disease is a premalignant condition. My answer is no. The plasmablast expansion is oligoclonal, not polyclonal,” Dr. Stone continued.
He described IgG4-RD as “a continuous dance between T cells and B cells.” The latest thinking regarding pathogenesis is that type 2 T follicular helper cells activate B cells, which become memory B cells or plasmablasts. These activated B cells and plasmablasts present antigen to CD4+ cytotoxic T cells at sites of disease. Dr. Stone and his coinvestigators recently identified these CD4+ cytotoxic T cells as a novel population of clonally expanded T cells with SLAMF7 as a surface marker. The cells secrete interferon-gamma, interleukin-1, and transforming growth factor-beta, all of which are capable of driving the intense fibrosis characteristic of IgG4-RD. In addition, these CD4+ cytotoxic T cells secrete granzyme B and perforin, previously thought to be released mainly by natural killer T cells.
Joint American College of Rheumatology/European League Against Rheumatism classification criteria for the disease are expected to be finalized this winter at the Third International Symposium on IgG4-Related Diseases.
Treatment with rituxumab
Glucocorticoids remain the first-line therapy in IgG4-related disease, but it’s essential to bear in mind that their long-term efficacy in this immune-mediated fibroinflammatory disease is the exception rather than the rule, Dr. Stone said at the symposium.
Dr. Stone was a coauthor of an international expert consensus statement on the treatment of IgG4-related disease (IgG4-RD), which emphasized that point (Arthritis Rheumatol. 2015 Jul;67[7]:1688-99).
“I typically start with prednisone at 40 mg/day, and there’s a dramatic response in these patients. Then I taper them off after 2-3 months. If 2-3 months doesn’t put them into a long-term sustained remission, it’s time to go to something else,” said Dr. Stone.
So what’s the next move, then, after steroids fail? Dr. Stone was a pioneer in the strikingly successful use of B cell depletion via rituximab (Rituxan) in patients with IgG4-RD. First he and his coinvestigators demonstrated that this off-label use of rituximab led to rapid clinical and histologic improvement (Ann Rheum Dis. 2015 Jun; 74[6]:1171-7), then they showed it also causes levels of circulating plasmablasts, serum IgG4, and biomarkers of fibrosis to plunge, suggesting B cell depletion may halt the destructive process of collagen deposition that characterizes this immune-related disease (Ann Rheum Dis. 2015 Dec;74[12]:2236-43). They have also reported that patients with very elevated baseline serum IgG4 levels are at more than sixfold increased risk of relapse at a median of 244 days from their first rituximab infusion (Rheumatology [Oxford]. 2016 Jun;55[6]:1000-8).
The success with rituximab is just one example of how improved understanding of the pathophysiology of IgG4-RD has opened the door to novel treatments. Dr. Stone is the lead investigator in an ongoing phase II, open-label study in which 15 patients with active IgG4-RD will receive intravenous XmAb5871 every 2 weeks for 6 months to evaluate the effect on the IgG4-RD Responder Index. XmAb5871 is a monoclonal antibody that binds to CD19 and FCgammaRIIb in order to downregulate activated B cells and plasmablasts. It is also being developed for treatment of systemic lupus erythematosus.
Dr. Stone and his coinvestigators are working on a therapeutic approach to IgG4-RD that targets antigen presentation by activated B cells to CD4+ cytotoxic T cells at sites of disease. These CD4+ cytotoxic T cells contain signaling lymphocyte activation molecule F7 (SLAMF7) as a surface marker. Elotuzumab (Empliciti), an immunostimulatory humanized monoclonal antibody targeting SLAMF7, is already on the market for treatment of multiple myeloma, he noted.
Dr. Stone reported receiving IgG4-RD-related research funding from and serving as a consultant to Genentech and Xencor, which is developing XmAb5871.
SNOWMASS, COLO. – Progress in the understanding and treatment of immunoglobulin G4–related disease is occurring “at lightning speed,” John H. Stone, MD, said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
Eight or nine years ago no one had heard of immunoglobulin G4–related disease (IgG4-RD). Today, because of the broad swath the disease cuts, it’s a hot research topic in every subspecialty of medicine as well as surgery, pathology, and radiology.
This new understanding of IgG4-RD, he added, is opening the door to novel treatments.
“This is not a new disease. It was there when we were all in medical school, and for hundreds of years before that. But it’s really only in the last decade that we have come to understand that the disease can affect literally every organ system in the body with syndromes that we once thought were isolated organ-specific syndromes but we now recognize are part of a multiorgan disease currently called IgG4-related disease,” the rheumatologist said.
IgG4-RD is an immune-mediated fibroinflammatory condition characterized histopathologically by three hallmark features in involved tissue: obliterative phlebitis, storiform fibrosis, and a dense lymphoplasmacytic infiltrate.
Clinically, IgG4-RD often presents as a mass lesion that can affect any organ.
“I have many patients who’ve undergone modified Whipple procedures because they were thought to have adenocarcinoma of the pancreas,” according to Dr. Stone.
Other common presentations include Riedel’s thyroiditis, autoimmune pancreatitis, sclerosing cholangitis, sialadenitis, dacryoadenitis, periaortitis, an eosinophilic rash, and pseudotumor of the lung, lymph nodes, or orbits.
“Retroperitoneal fibrosis is a common and underappreciated manifestation. It may be the most common subsyndrome associated with IgG4-related disease,” he observed.
Another common presentation involves atopic disease – asthma, allergic rhinitis, eczema, eosinophilia, nasal polyps – developing out of the blue in middle age or later life. This observation led some other investigators to posit that IgG4-RD is a T-helper type 2–driven disease, an assertion debunked by Dr. Stone and coworkers (Allergy. 2014 Feb;69[2]:269-72).
Dr. Stone and his coinvestigators have published the largest series of patients with biopsy-proven IgG4-RD reported to date (Arthritis Rheumatol. 2015 Sep; 67[9]:2466-75). The average age at disease onset was 50 years. Of note, multiorgan involvement was the norm: 24% of patients had two organs involved, and 38% had three or more.
Analysis of this large patient series has led Dr. Stone to a surprising conclusion about the nature of IgG4-RD: “We have greatly overemphasized the importance of IgG4 in this condition,” he asserted.
Indeed, a mere 51% of the patients with clinically active untreated IgG4-RD in his series had an elevated serum IgG level. Dr. Stone characterized IgG4 as “kind of a wimpy antibody” incapable of driving the disease process because it is a noninflammatory immunoglobulin. This has led to speculation that IgG4 functions as what he termed an “antigen sink,” attempting to bind antigen at sites of inflammation.
But while an elevated serum IgG4 is of limited utility for diagnostic purposes, Dr. Stone and coworkers have demonstrated that it is of value as a predictor of relapse. Among patients with a treatment-induced remission, those in the top quartile in terms of baseline pretreatment serum IgG4 were 6.2-fold more likely to relapse (Rheumatology [Oxford]. 2016 Jun;55[6]:1000-8).
“This is a very useful marker for patients who are going to need chronic ongoing therapy. The notion of putting such patients on steroids for months and years is not appealing,” he said.
Levels of circulating plasmablasts as measured by peripheral blood flow cytometry, especially IgG4-positive plasmablasts, have proven much more helpful than serum IgG4 levels as a diagnostic tool, a reliable biomarker of disease activity, and a therapeutic target. Levels of these short-lived CD19+CD38+CD27+ plasmablasts are enormously elevated independent of serum IgG4 in patients with active IgG4-RD.
“One of the questions I’m most often asked is whether IgG4-related disease is a premalignant condition. My answer is no. The plasmablast expansion is oligoclonal, not polyclonal,” Dr. Stone continued.
He described IgG4-RD as “a continuous dance between T cells and B cells.” The latest thinking regarding pathogenesis is that type 2 T follicular helper cells activate B cells, which become memory B cells or plasmablasts. These activated B cells and plasmablasts present antigen to CD4+ cytotoxic T cells at sites of disease. Dr. Stone and his coinvestigators recently identified these CD4+ cytotoxic T cells as a novel population of clonally expanded T cells with SLAMF7 as a surface marker. The cells secrete interferon-gamma, interleukin-1, and transforming growth factor-beta, all of which are capable of driving the intense fibrosis characteristic of IgG4-RD. In addition, these CD4+ cytotoxic T cells secrete granzyme B and perforin, previously thought to be released mainly by natural killer T cells.
Joint American College of Rheumatology/European League Against Rheumatism classification criteria for the disease are expected to be finalized this winter at the Third International Symposium on IgG4-Related Diseases.
Treatment with rituxumab
Glucocorticoids remain the first-line therapy in IgG4-related disease, but it’s essential to bear in mind that their long-term efficacy in this immune-mediated fibroinflammatory disease is the exception rather than the rule, Dr. Stone said at the symposium.
Dr. Stone was a coauthor of an international expert consensus statement on the treatment of IgG4-related disease (IgG4-RD), which emphasized that point (Arthritis Rheumatol. 2015 Jul;67[7]:1688-99).
“I typically start with prednisone at 40 mg/day, and there’s a dramatic response in these patients. Then I taper them off after 2-3 months. If 2-3 months doesn’t put them into a long-term sustained remission, it’s time to go to something else,” said Dr. Stone.
So what’s the next move, then, after steroids fail? Dr. Stone was a pioneer in the strikingly successful use of B cell depletion via rituximab (Rituxan) in patients with IgG4-RD. First he and his coinvestigators demonstrated that this off-label use of rituximab led to rapid clinical and histologic improvement (Ann Rheum Dis. 2015 Jun; 74[6]:1171-7), then they showed it also causes levels of circulating plasmablasts, serum IgG4, and biomarkers of fibrosis to plunge, suggesting B cell depletion may halt the destructive process of collagen deposition that characterizes this immune-related disease (Ann Rheum Dis. 2015 Dec;74[12]:2236-43). They have also reported that patients with very elevated baseline serum IgG4 levels are at more than sixfold increased risk of relapse at a median of 244 days from their first rituximab infusion (Rheumatology [Oxford]. 2016 Jun;55[6]:1000-8).
The success with rituximab is just one example of how improved understanding of the pathophysiology of IgG4-RD has opened the door to novel treatments. Dr. Stone is the lead investigator in an ongoing phase II, open-label study in which 15 patients with active IgG4-RD will receive intravenous XmAb5871 every 2 weeks for 6 months to evaluate the effect on the IgG4-RD Responder Index. XmAb5871 is a monoclonal antibody that binds to CD19 and FCgammaRIIb in order to downregulate activated B cells and plasmablasts. It is also being developed for treatment of systemic lupus erythematosus.
Dr. Stone and his coinvestigators are working on a therapeutic approach to IgG4-RD that targets antigen presentation by activated B cells to CD4+ cytotoxic T cells at sites of disease. These CD4+ cytotoxic T cells contain signaling lymphocyte activation molecule F7 (SLAMF7) as a surface marker. Elotuzumab (Empliciti), an immunostimulatory humanized monoclonal antibody targeting SLAMF7, is already on the market for treatment of multiple myeloma, he noted.
Dr. Stone reported receiving IgG4-RD-related research funding from and serving as a consultant to Genentech and Xencor, which is developing XmAb5871.
EXPERT ANALYSIS FROM THE WINTER RHEUMATOLOGY SYMPOSIUM
Twenty-five states at highest flu activity level
Flu activity in the United States continued to increase as half of the states reached the highest level of influenza-like illness (ILI) activity in the week ending Feb. 11, according to the Centers for Disease Control and Prevention.
For the week, the 25 states at level 10 on the CDC’s 1-10 scale of ILI activity were joined in the high range by Illinois and Kentucky at level 9 and Iowa at level 8, the CDC reported. The previous week, there were 23 states in the high range.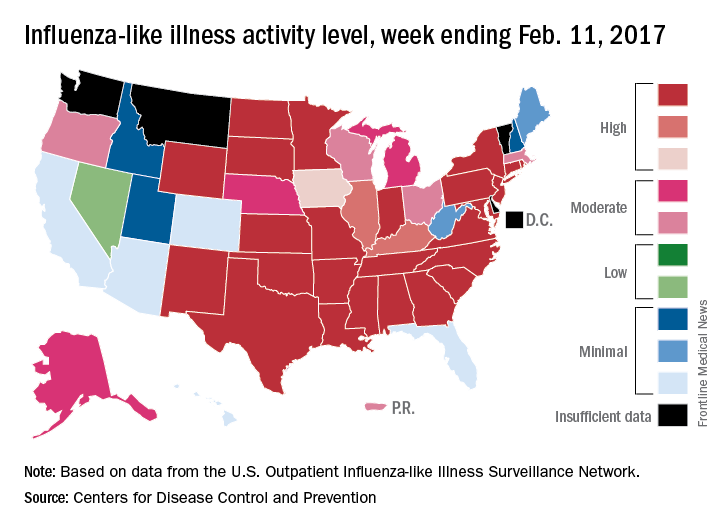
Of the nine flu-related pediatric deaths reported to the CDC during the latest week, eight occurred in earlier weeks. For the 2016-2017 season so far, 29 flu-related pediatric deaths have been reported, the CDC said.
Flu activity in the United States continued to increase as half of the states reached the highest level of influenza-like illness (ILI) activity in the week ending Feb. 11, according to the Centers for Disease Control and Prevention.
For the week, the 25 states at level 10 on the CDC’s 1-10 scale of ILI activity were joined in the high range by Illinois and Kentucky at level 9 and Iowa at level 8, the CDC reported. The previous week, there were 23 states in the high range.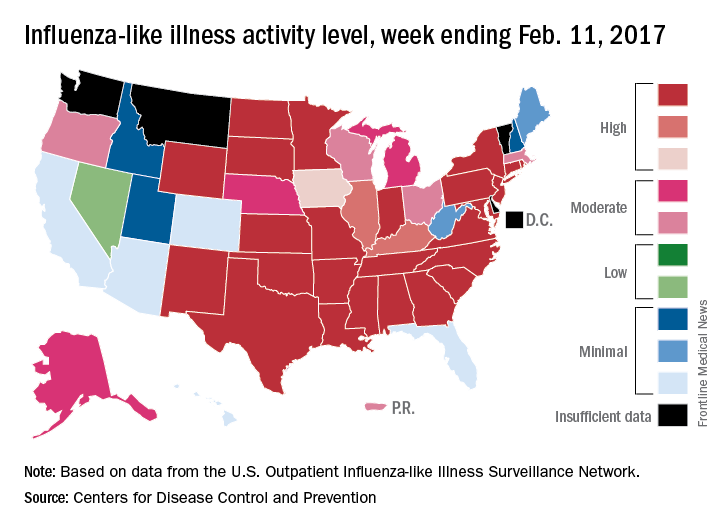
Of the nine flu-related pediatric deaths reported to the CDC during the latest week, eight occurred in earlier weeks. For the 2016-2017 season so far, 29 flu-related pediatric deaths have been reported, the CDC said.
Flu activity in the United States continued to increase as half of the states reached the highest level of influenza-like illness (ILI) activity in the week ending Feb. 11, according to the Centers for Disease Control and Prevention.
For the week, the 25 states at level 10 on the CDC’s 1-10 scale of ILI activity were joined in the high range by Illinois and Kentucky at level 9 and Iowa at level 8, the CDC reported. The previous week, there were 23 states in the high range.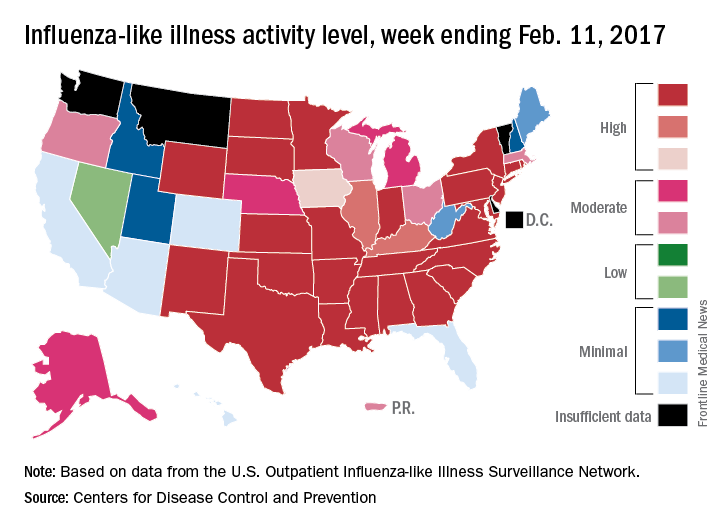
Of the nine flu-related pediatric deaths reported to the CDC during the latest week, eight occurred in earlier weeks. For the 2016-2017 season so far, 29 flu-related pediatric deaths have been reported, the CDC said.
Treating psychopathology in developmentally disabled tricky
LAS VEGAS – Individuals with intellectual disability experience behavioral and psychiatric illness at higher rates than the general population, according to Bryan H. King, MD.
“Increasingly, these individuals are showing up in all of our clinical practices,” Dr. King said at an annual psychopharmacology update held by the Nevada Psychiatric Association. “In this area, it’s not so much that the population doesn’t experience psychiatric illness, but the diagnosis can be challenging because the presentation of symptoms may be different. For someone who can’t articulate whether they’re feeling anxious, fearful, or nervous, it’s more challenging to make a diagnosis.”
More than 10 years ago, researchers from the University of North Carolina at Chapel Hill compared health disparities between adults with developmental disabilities in North Carolina and adults in the state with other disabilities and adults without disabilities (Public Health Rep. 2004;114[4]:418-26). They found those in the developmental disability group had a similar or greater risk of having high blood pressure, cardiovascular disease, diabetes, and chronic pain, compared with nondisabled adults. In addition, 24% of adults in the developmental disability group reported having either no one to talk to about personal things or often felt lonely.
A more recent, large national study found that, compared with adults with no autism diagnoses, those diagnosed with autism had significantly increased rates for all psychiatric disorders, including depression, anxiety, bipolar disorder, obsessive-compulsive disorder, schizophrenia (a more than 20-fold increased rate), and suicide attempts (Autism. 2015;19[7]:814-23). In addition, nearly all medical conditions such as obesity and dyslipidemia were significantly more common in adults with autism.
Results from a separate study of 371 adults with intellectual disabilities found that 40% had at least one mental health disorder and 45% had at least one moderate or severe behavior problem (Soc Psychiatry Psychiatr Epidemiol. 2016;51:767-76). In addition, the highest ratios of unmet to met need were found with respect to sexuality issues and with respect to mental health problems.
Once a diagnosis is made, Dr. King said patients who have developmental disabilities should be treated in the same way as patients who do not. “There is a tremendous amount of heterogeneity in this population,” he said. “If you are confident that you have someone before you who has depression, the treatment for depression is going to proceed in the same ways it does for someone without the condition. Let that guide the way for medications you are going to use.”
In a recent edition of Current Opinion in Psychiatry, authors Na Young Ji, MD, and Robert L. Findling, MD, reviewed current evidence-based pharmacotherapy options for mental health problems in people with intellectual disability (Curr Opin Psychiatry. 2016;29:103-25). Their five key points were:
1. “Antipsychotics, particularly risperidone, appear to be effective in reducing problem behaviors associated with intellectual disability.
2. “For attention-deficit/hyperactivity disorder symptoms, methylphenidate has been shown to be effective, and atomoxetine and alpha-agonists might be beneficial.
3. “Lithium might be effective in reducing aggression. Evidence for the use of antiepileptic drugs, anxiolytics, and naltrexone for management of problem behaviors is insufficient to draw conclusions.
4. “Antidepressants are often poorly tolerated and do not appear to be effective in decreasing repetitive or stereotypic behaviors associated with intellectual disability.
5. “Melatonin appears to improve sleep in people with intellectual disability.”
Dr. King noted that the data for using lithium in people with intellectual disability “are very old. There’s been nothing recent to help us fine-tune the indications.” He said naltrexone is among the best studied in this population, “especially for self-injurious behavior. The two large placebo-controlled trials were negative. In my own clinical experience, I have not seen it helpful.”
Dr. King disclosed that he has received research funding from the National Institutes of Health, Janssen, and Roche. He also is a consultant for Care Management Technologies and Neurotrope.
LAS VEGAS – Individuals with intellectual disability experience behavioral and psychiatric illness at higher rates than the general population, according to Bryan H. King, MD.
“Increasingly, these individuals are showing up in all of our clinical practices,” Dr. King said at an annual psychopharmacology update held by the Nevada Psychiatric Association. “In this area, it’s not so much that the population doesn’t experience psychiatric illness, but the diagnosis can be challenging because the presentation of symptoms may be different. For someone who can’t articulate whether they’re feeling anxious, fearful, or nervous, it’s more challenging to make a diagnosis.”
More than 10 years ago, researchers from the University of North Carolina at Chapel Hill compared health disparities between adults with developmental disabilities in North Carolina and adults in the state with other disabilities and adults without disabilities (Public Health Rep. 2004;114[4]:418-26). They found those in the developmental disability group had a similar or greater risk of having high blood pressure, cardiovascular disease, diabetes, and chronic pain, compared with nondisabled adults. In addition, 24% of adults in the developmental disability group reported having either no one to talk to about personal things or often felt lonely.
A more recent, large national study found that, compared with adults with no autism diagnoses, those diagnosed with autism had significantly increased rates for all psychiatric disorders, including depression, anxiety, bipolar disorder, obsessive-compulsive disorder, schizophrenia (a more than 20-fold increased rate), and suicide attempts (Autism. 2015;19[7]:814-23). In addition, nearly all medical conditions such as obesity and dyslipidemia were significantly more common in adults with autism.
Results from a separate study of 371 adults with intellectual disabilities found that 40% had at least one mental health disorder and 45% had at least one moderate or severe behavior problem (Soc Psychiatry Psychiatr Epidemiol. 2016;51:767-76). In addition, the highest ratios of unmet to met need were found with respect to sexuality issues and with respect to mental health problems.
Once a diagnosis is made, Dr. King said patients who have developmental disabilities should be treated in the same way as patients who do not. “There is a tremendous amount of heterogeneity in this population,” he said. “If you are confident that you have someone before you who has depression, the treatment for depression is going to proceed in the same ways it does for someone without the condition. Let that guide the way for medications you are going to use.”
In a recent edition of Current Opinion in Psychiatry, authors Na Young Ji, MD, and Robert L. Findling, MD, reviewed current evidence-based pharmacotherapy options for mental health problems in people with intellectual disability (Curr Opin Psychiatry. 2016;29:103-25). Their five key points were:
1. “Antipsychotics, particularly risperidone, appear to be effective in reducing problem behaviors associated with intellectual disability.
2. “For attention-deficit/hyperactivity disorder symptoms, methylphenidate has been shown to be effective, and atomoxetine and alpha-agonists might be beneficial.
3. “Lithium might be effective in reducing aggression. Evidence for the use of antiepileptic drugs, anxiolytics, and naltrexone for management of problem behaviors is insufficient to draw conclusions.
4. “Antidepressants are often poorly tolerated and do not appear to be effective in decreasing repetitive or stereotypic behaviors associated with intellectual disability.
5. “Melatonin appears to improve sleep in people with intellectual disability.”
Dr. King noted that the data for using lithium in people with intellectual disability “are very old. There’s been nothing recent to help us fine-tune the indications.” He said naltrexone is among the best studied in this population, “especially for self-injurious behavior. The two large placebo-controlled trials were negative. In my own clinical experience, I have not seen it helpful.”
Dr. King disclosed that he has received research funding from the National Institutes of Health, Janssen, and Roche. He also is a consultant for Care Management Technologies and Neurotrope.
LAS VEGAS – Individuals with intellectual disability experience behavioral and psychiatric illness at higher rates than the general population, according to Bryan H. King, MD.
“Increasingly, these individuals are showing up in all of our clinical practices,” Dr. King said at an annual psychopharmacology update held by the Nevada Psychiatric Association. “In this area, it’s not so much that the population doesn’t experience psychiatric illness, but the diagnosis can be challenging because the presentation of symptoms may be different. For someone who can’t articulate whether they’re feeling anxious, fearful, or nervous, it’s more challenging to make a diagnosis.”
More than 10 years ago, researchers from the University of North Carolina at Chapel Hill compared health disparities between adults with developmental disabilities in North Carolina and adults in the state with other disabilities and adults without disabilities (Public Health Rep. 2004;114[4]:418-26). They found those in the developmental disability group had a similar or greater risk of having high blood pressure, cardiovascular disease, diabetes, and chronic pain, compared with nondisabled adults. In addition, 24% of adults in the developmental disability group reported having either no one to talk to about personal things or often felt lonely.
A more recent, large national study found that, compared with adults with no autism diagnoses, those diagnosed with autism had significantly increased rates for all psychiatric disorders, including depression, anxiety, bipolar disorder, obsessive-compulsive disorder, schizophrenia (a more than 20-fold increased rate), and suicide attempts (Autism. 2015;19[7]:814-23). In addition, nearly all medical conditions such as obesity and dyslipidemia were significantly more common in adults with autism.
Results from a separate study of 371 adults with intellectual disabilities found that 40% had at least one mental health disorder and 45% had at least one moderate or severe behavior problem (Soc Psychiatry Psychiatr Epidemiol. 2016;51:767-76). In addition, the highest ratios of unmet to met need were found with respect to sexuality issues and with respect to mental health problems.
Once a diagnosis is made, Dr. King said patients who have developmental disabilities should be treated in the same way as patients who do not. “There is a tremendous amount of heterogeneity in this population,” he said. “If you are confident that you have someone before you who has depression, the treatment for depression is going to proceed in the same ways it does for someone without the condition. Let that guide the way for medications you are going to use.”
In a recent edition of Current Opinion in Psychiatry, authors Na Young Ji, MD, and Robert L. Findling, MD, reviewed current evidence-based pharmacotherapy options for mental health problems in people with intellectual disability (Curr Opin Psychiatry. 2016;29:103-25). Their five key points were:
1. “Antipsychotics, particularly risperidone, appear to be effective in reducing problem behaviors associated with intellectual disability.
2. “For attention-deficit/hyperactivity disorder symptoms, methylphenidate has been shown to be effective, and atomoxetine and alpha-agonists might be beneficial.
3. “Lithium might be effective in reducing aggression. Evidence for the use of antiepileptic drugs, anxiolytics, and naltrexone for management of problem behaviors is insufficient to draw conclusions.
4. “Antidepressants are often poorly tolerated and do not appear to be effective in decreasing repetitive or stereotypic behaviors associated with intellectual disability.
5. “Melatonin appears to improve sleep in people with intellectual disability.”
Dr. King noted that the data for using lithium in people with intellectual disability “are very old. There’s been nothing recent to help us fine-tune the indications.” He said naltrexone is among the best studied in this population, “especially for self-injurious behavior. The two large placebo-controlled trials were negative. In my own clinical experience, I have not seen it helpful.”
Dr. King disclosed that he has received research funding from the National Institutes of Health, Janssen, and Roche. He also is a consultant for Care Management Technologies and Neurotrope.
EXPERT ANALYSIS AT THE NPA PSYCHOPHARMACOLOGY UPDATE
Lupus Erythematosus Tumidus of the Scalp Masquerading as Alopecia Areata
Lupus erythematosus tumidus (LET) is a relatively rare condition but may simply be underdiagnosed in the literature. It presents as urticarialike papules and plaques in sun-exposed areas, characterized by induration and erythema. Lesions occur on the face, neck, upper extremities, and trunk and heal without scarring.1,2 Rarely, lesions can show fine scaling and associated pruritus, but most often the lesions are asymptomatic.3
Case Report
A 45-year-old woman presented with 2 asymptomatic self-described bald spots on the top of the head of 2 months’ duration. The patient denied prior treatment of the lesions and noted one patch was resolving. She reported no involvement of the eyebrows, eyelashes, and axillary and pubic hair. A review of systems was negative. The patient denied personal or family history of lupus, thyroid disease, or vitiligo.
Clinical examination revealed a 1.1-cm round patch of nonscarring alopecia on the right vertex scalp and a 0.9-cm round patch of nonscarring alopecia with moderate hair regrowth on the left vertex scalp. There was no erythema, scaling, or induration. The rest of the scalp was normal in appearance and the eyebrows and eyelashes were uninvolved. The patient was diagnosed with alopecia areata and was treated with 10 mg/mL of intralesional triamcinolone once monthly for 4 months.
The patient initially showed improvement with moderate hair regrowth. After 4 months of treatment, she developed 3 new 1- to 1.5-cm erythematous alopecic patches on the vertex scalp and had worsening in the initial patches (Figure 1). Given the resistance to standard therapy and the onset of multiple new areas with evidence of inflammatory involvement, a punch biopsy was performed. Histopathologic examination revealed a fairly unremarkable epidermis and a dense dermal inflammatory infiltrate that was present both in the superficial and deep dermis (Figure 2). The inflammatory cells, which appeared to be predominantly comprised of lymphocytes, had a predilection for the vasculature but also were observed within the interstitial dermis. Additionally, mucin appeared to be slightly increased in the deep dermis. The lymphocytic phenotype was confirmed by immunohistochemical studies for CD20 and CD3. The most likely possibilities for this reaction pattern were LET, Jessner lymphocytic infiltrate of the skin (JLIS), gyrate erythema, and lymphoma; however, the immunohistochemical studies effectively ruled out lymphoma. Additionally, there was pronounced dermal mucin noted in the specimen. The patient was diagnosed with LET of the scalp based on the constellation of findings.

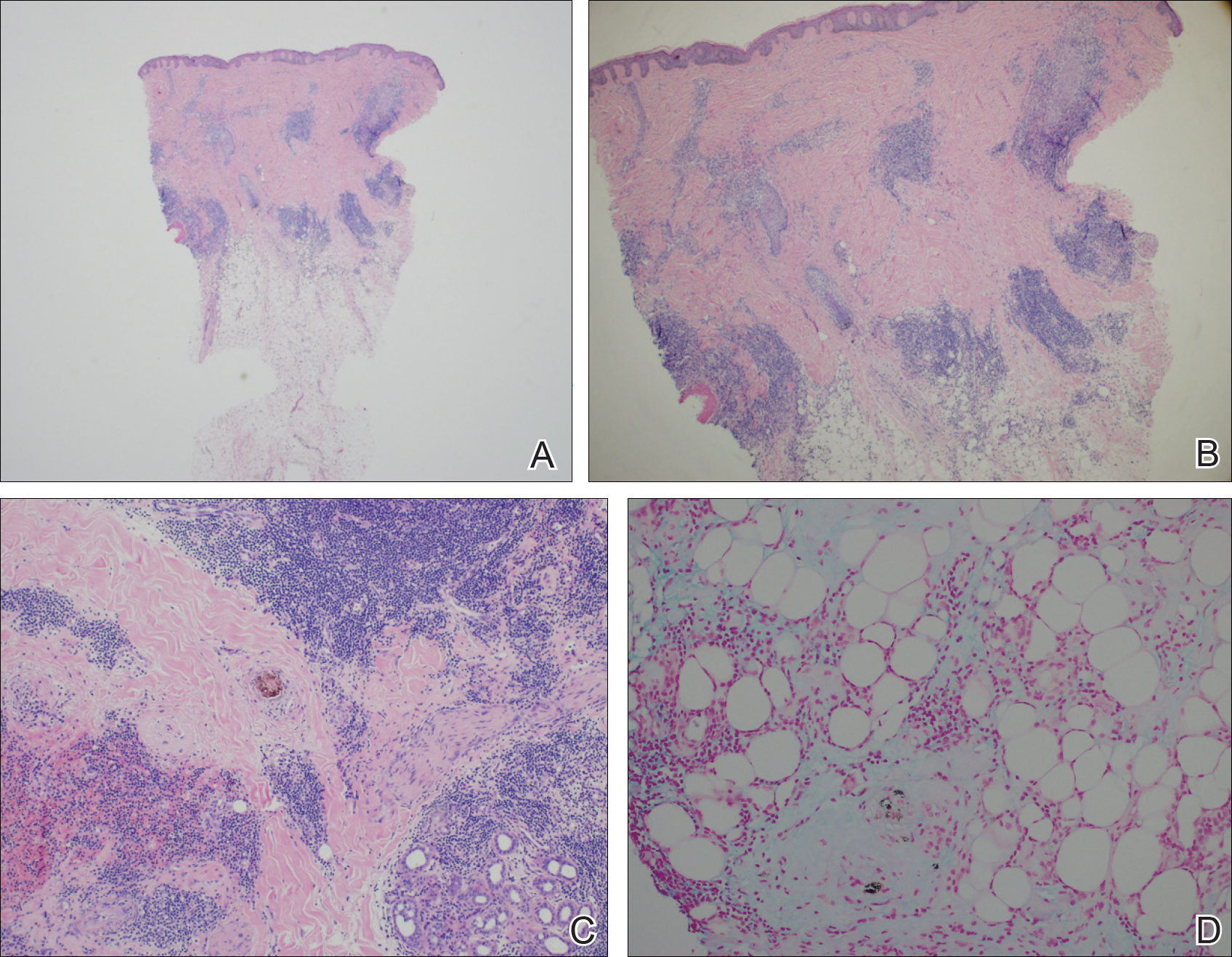
Comment
The classification of LET as a single unique entity or disease process sui generis has been in flux in the last decade. Its similarities to JLIS and other forms of chronic cutaneous lupus erythematosus (CCLE) have brought debate.4-6 In 1930, Gougerot and Burnier7 documented the first case of LET in the literature, describing smooth, infiltrated, erythematous lesions with no desquamation or other superficial changes seen in 5 patients.
In 2000, interest in LET and other forms of CCLE was increasing, and reports in the literature paralleled. That year, Kuhn et al4 reported 40 cases of LET, characterizing the clinical and histological features of each case to demonstrate that LET should be separate from other forms of CCLE. Until then, it is likely that many lesions that should have been classified as LET were instead classified as various forms of CCLE. The investigators maintained that LET also should be distinct from JLIS because it is associated with UV exposure.4 Kuhn et al8 reviewed phototesting in 60 patients with LET in 2001 and confirmed this subset was the most photosensitive type of lupus erythematosus.
In general, the histopathologic and immunohistochemical studies in LET and JLIS can be quite similar. Relatively distinguishing histopathologic findings in JLIS include no evidence of epidermal atrophy, basal vacuolar change, or follicular plugging, as well as negative immunofluorescence studies. Both entities show a predominantly T-cell population with a smaller component of B cells and thus a distinction cannot be made based on relative proportions of T and B cells in lesions.2
In 2003, Alexiades-Armenakas et al6 determined immunohistochemical criteria for LET, finding a predominance of T cells and more CD4 lymphocytes than CD8 lymphocytes with a mean ratio of roughly 3 to 1. Their study results maintained LET should be classified as a form of CCLE due to the chronicity of the lesions, the serologic profile with negative anti–double-stranded DNA, anticentromere, anti-Smith, anti-Ro/Sjögren syndrome antigen A, anti-La/Sjögren syndrome antigen B, and anti-nuclear ribonucleoprotein antibodies and the rare association with systemic disease.6 This conclusion was further solidified by a review published that same year citing unique histopathological features when compared to subacute cutaneous LE and discoid lupus erythematosus.5
This case illustrates the importance of histologic evaluation in determining the correct diagnosis in a patient with alopecia areata recalcitrant to treatment. Including LET in the differential of alopecic patches on the scalp could prove beneficial for patients, as LET responds well to antimalarial drugs and photoprotection.9 This patient had a normal antinuclear antibody panel and no signs or symptoms of systemic lupus. It was recommended that she avoid sun exposure and begin treatment with hydroxychloroquine but she declined. At a follow-up visit 6 months later she reported the lesions had improved, but a permanent wig had been sewn over the area, so it could not be examined.
- Lee L, Werth V. Rheumatologic disease. In: Bolognia JL, Jorizzo JL, Rapini RP, eds. Dermatology. Vol 2. 3rd ed. Mosby Elsevier; 2008:615-629.
- Weedon D. The lichenoid reaction pattern. In: Weedon D. Skin Pathology. 2nd ed. Edinburgh, Scotland: Churchill Livingstone; 2002:35-70.
- Dekle CL, Mannes KD, Davis LS, et al. Lupus tumidus. J Am Acad Dermatol. 1999;41:250-253.
- Kuhn A, Richter-Hintz D, Oslislo C, et al. Lupus erythematosus tumidus—a neglected subset of cutaneous lupus erythematosus: report of 40 cases. Arch Dermatol. 2000;136:1033-1041.
- Kuhn A, Sonntag M, Ruzicka T, et al. Histopathologic findings in lupus erythematosus tumidus: review of 80 patients. J Am Acad Dermatol. 2003;48:901-908.
- Alexiades-Armenakas MR, Baldassano M, Bince B, et al. Tumid lupus erythematosus: criteria for classification with immunohistochemical analysis. Arthritis Rheum. 2003;49:494-500.
- Gougerot H, Burnier R. Lupuse rythe mateux “tumidus.” Bull Soc Fr Dermatol Syph. 1930;37:1291-1292.
- Kuhn A, Sonntag M, Richter-Hintz D, et al. Phototesting in lupus erythematosus tumidus—review of 60 patients. Photochem Photobiol. 2001;73:532-536.
- Cozzani E, Christana K, Rongioletti F, et al. Lupus erythematosus tumidus: clinical, histopathological and serological aspects and therapy response of 21 patients. Eur J Dermatol. 2010;20:797-801.
Lupus erythematosus tumidus (LET) is a relatively rare condition but may simply be underdiagnosed in the literature. It presents as urticarialike papules and plaques in sun-exposed areas, characterized by induration and erythema. Lesions occur on the face, neck, upper extremities, and trunk and heal without scarring.1,2 Rarely, lesions can show fine scaling and associated pruritus, but most often the lesions are asymptomatic.3
Case Report
A 45-year-old woman presented with 2 asymptomatic self-described bald spots on the top of the head of 2 months’ duration. The patient denied prior treatment of the lesions and noted one patch was resolving. She reported no involvement of the eyebrows, eyelashes, and axillary and pubic hair. A review of systems was negative. The patient denied personal or family history of lupus, thyroid disease, or vitiligo.
Clinical examination revealed a 1.1-cm round patch of nonscarring alopecia on the right vertex scalp and a 0.9-cm round patch of nonscarring alopecia with moderate hair regrowth on the left vertex scalp. There was no erythema, scaling, or induration. The rest of the scalp was normal in appearance and the eyebrows and eyelashes were uninvolved. The patient was diagnosed with alopecia areata and was treated with 10 mg/mL of intralesional triamcinolone once monthly for 4 months.
The patient initially showed improvement with moderate hair regrowth. After 4 months of treatment, she developed 3 new 1- to 1.5-cm erythematous alopecic patches on the vertex scalp and had worsening in the initial patches (Figure 1). Given the resistance to standard therapy and the onset of multiple new areas with evidence of inflammatory involvement, a punch biopsy was performed. Histopathologic examination revealed a fairly unremarkable epidermis and a dense dermal inflammatory infiltrate that was present both in the superficial and deep dermis (Figure 2). The inflammatory cells, which appeared to be predominantly comprised of lymphocytes, had a predilection for the vasculature but also were observed within the interstitial dermis. Additionally, mucin appeared to be slightly increased in the deep dermis. The lymphocytic phenotype was confirmed by immunohistochemical studies for CD20 and CD3. The most likely possibilities for this reaction pattern were LET, Jessner lymphocytic infiltrate of the skin (JLIS), gyrate erythema, and lymphoma; however, the immunohistochemical studies effectively ruled out lymphoma. Additionally, there was pronounced dermal mucin noted in the specimen. The patient was diagnosed with LET of the scalp based on the constellation of findings.

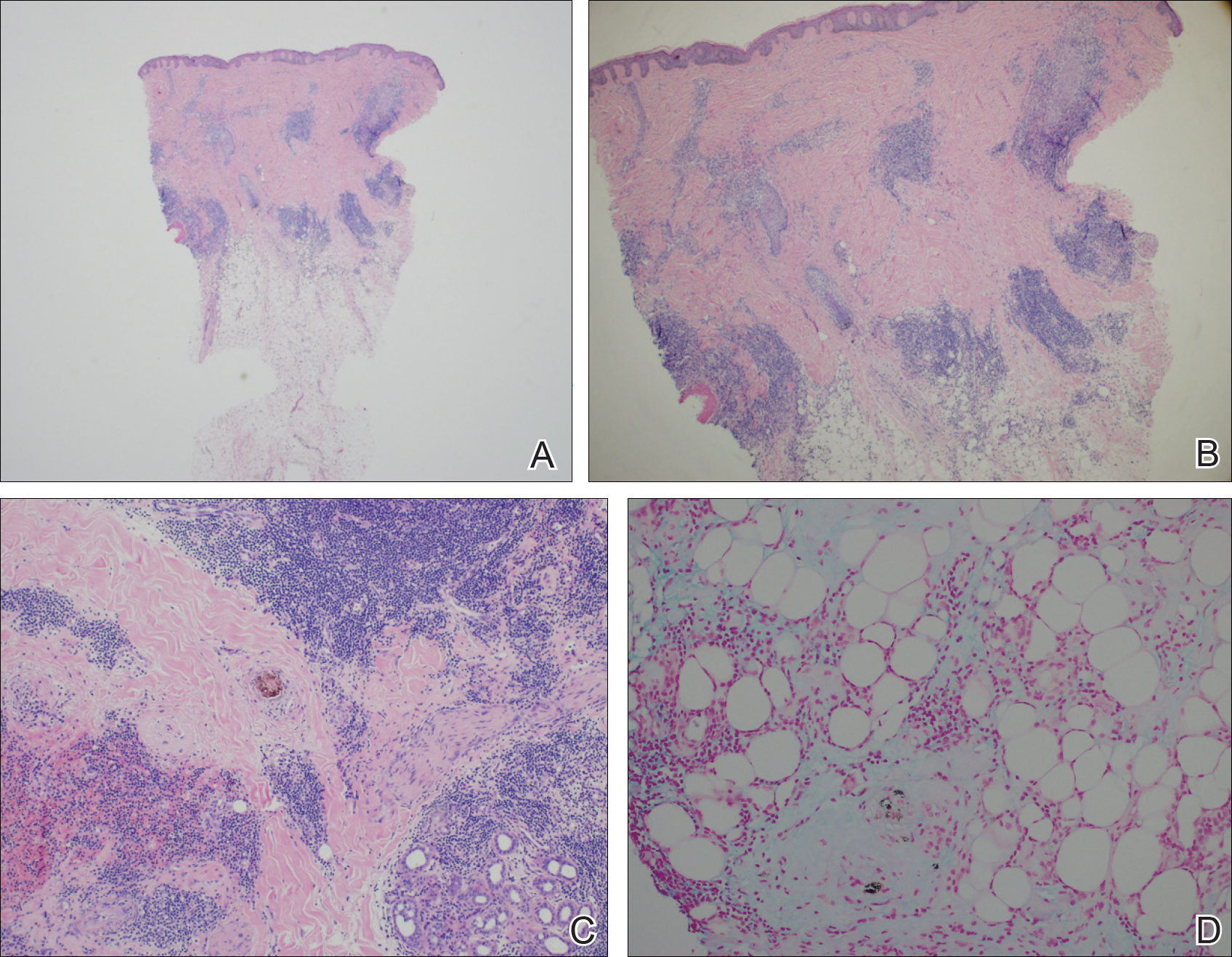
Comment
The classification of LET as a single unique entity or disease process sui generis has been in flux in the last decade. Its similarities to JLIS and other forms of chronic cutaneous lupus erythematosus (CCLE) have brought debate.4-6 In 1930, Gougerot and Burnier7 documented the first case of LET in the literature, describing smooth, infiltrated, erythematous lesions with no desquamation or other superficial changes seen in 5 patients.
In 2000, interest in LET and other forms of CCLE was increasing, and reports in the literature paralleled. That year, Kuhn et al4 reported 40 cases of LET, characterizing the clinical and histological features of each case to demonstrate that LET should be separate from other forms of CCLE. Until then, it is likely that many lesions that should have been classified as LET were instead classified as various forms of CCLE. The investigators maintained that LET also should be distinct from JLIS because it is associated with UV exposure.4 Kuhn et al8 reviewed phototesting in 60 patients with LET in 2001 and confirmed this subset was the most photosensitive type of lupus erythematosus.
In general, the histopathologic and immunohistochemical studies in LET and JLIS can be quite similar. Relatively distinguishing histopathologic findings in JLIS include no evidence of epidermal atrophy, basal vacuolar change, or follicular plugging, as well as negative immunofluorescence studies. Both entities show a predominantly T-cell population with a smaller component of B cells and thus a distinction cannot be made based on relative proportions of T and B cells in lesions.2
In 2003, Alexiades-Armenakas et al6 determined immunohistochemical criteria for LET, finding a predominance of T cells and more CD4 lymphocytes than CD8 lymphocytes with a mean ratio of roughly 3 to 1. Their study results maintained LET should be classified as a form of CCLE due to the chronicity of the lesions, the serologic profile with negative anti–double-stranded DNA, anticentromere, anti-Smith, anti-Ro/Sjögren syndrome antigen A, anti-La/Sjögren syndrome antigen B, and anti-nuclear ribonucleoprotein antibodies and the rare association with systemic disease.6 This conclusion was further solidified by a review published that same year citing unique histopathological features when compared to subacute cutaneous LE and discoid lupus erythematosus.5
This case illustrates the importance of histologic evaluation in determining the correct diagnosis in a patient with alopecia areata recalcitrant to treatment. Including LET in the differential of alopecic patches on the scalp could prove beneficial for patients, as LET responds well to antimalarial drugs and photoprotection.9 This patient had a normal antinuclear antibody panel and no signs or symptoms of systemic lupus. It was recommended that she avoid sun exposure and begin treatment with hydroxychloroquine but she declined. At a follow-up visit 6 months later she reported the lesions had improved, but a permanent wig had been sewn over the area, so it could not be examined.
Lupus erythematosus tumidus (LET) is a relatively rare condition but may simply be underdiagnosed in the literature. It presents as urticarialike papules and plaques in sun-exposed areas, characterized by induration and erythema. Lesions occur on the face, neck, upper extremities, and trunk and heal without scarring.1,2 Rarely, lesions can show fine scaling and associated pruritus, but most often the lesions are asymptomatic.3
Case Report
A 45-year-old woman presented with 2 asymptomatic self-described bald spots on the top of the head of 2 months’ duration. The patient denied prior treatment of the lesions and noted one patch was resolving. She reported no involvement of the eyebrows, eyelashes, and axillary and pubic hair. A review of systems was negative. The patient denied personal or family history of lupus, thyroid disease, or vitiligo.
Clinical examination revealed a 1.1-cm round patch of nonscarring alopecia on the right vertex scalp and a 0.9-cm round patch of nonscarring alopecia with moderate hair regrowth on the left vertex scalp. There was no erythema, scaling, or induration. The rest of the scalp was normal in appearance and the eyebrows and eyelashes were uninvolved. The patient was diagnosed with alopecia areata and was treated with 10 mg/mL of intralesional triamcinolone once monthly for 4 months.
The patient initially showed improvement with moderate hair regrowth. After 4 months of treatment, she developed 3 new 1- to 1.5-cm erythematous alopecic patches on the vertex scalp and had worsening in the initial patches (Figure 1). Given the resistance to standard therapy and the onset of multiple new areas with evidence of inflammatory involvement, a punch biopsy was performed. Histopathologic examination revealed a fairly unremarkable epidermis and a dense dermal inflammatory infiltrate that was present both in the superficial and deep dermis (Figure 2). The inflammatory cells, which appeared to be predominantly comprised of lymphocytes, had a predilection for the vasculature but also were observed within the interstitial dermis. Additionally, mucin appeared to be slightly increased in the deep dermis. The lymphocytic phenotype was confirmed by immunohistochemical studies for CD20 and CD3. The most likely possibilities for this reaction pattern were LET, Jessner lymphocytic infiltrate of the skin (JLIS), gyrate erythema, and lymphoma; however, the immunohistochemical studies effectively ruled out lymphoma. Additionally, there was pronounced dermal mucin noted in the specimen. The patient was diagnosed with LET of the scalp based on the constellation of findings.

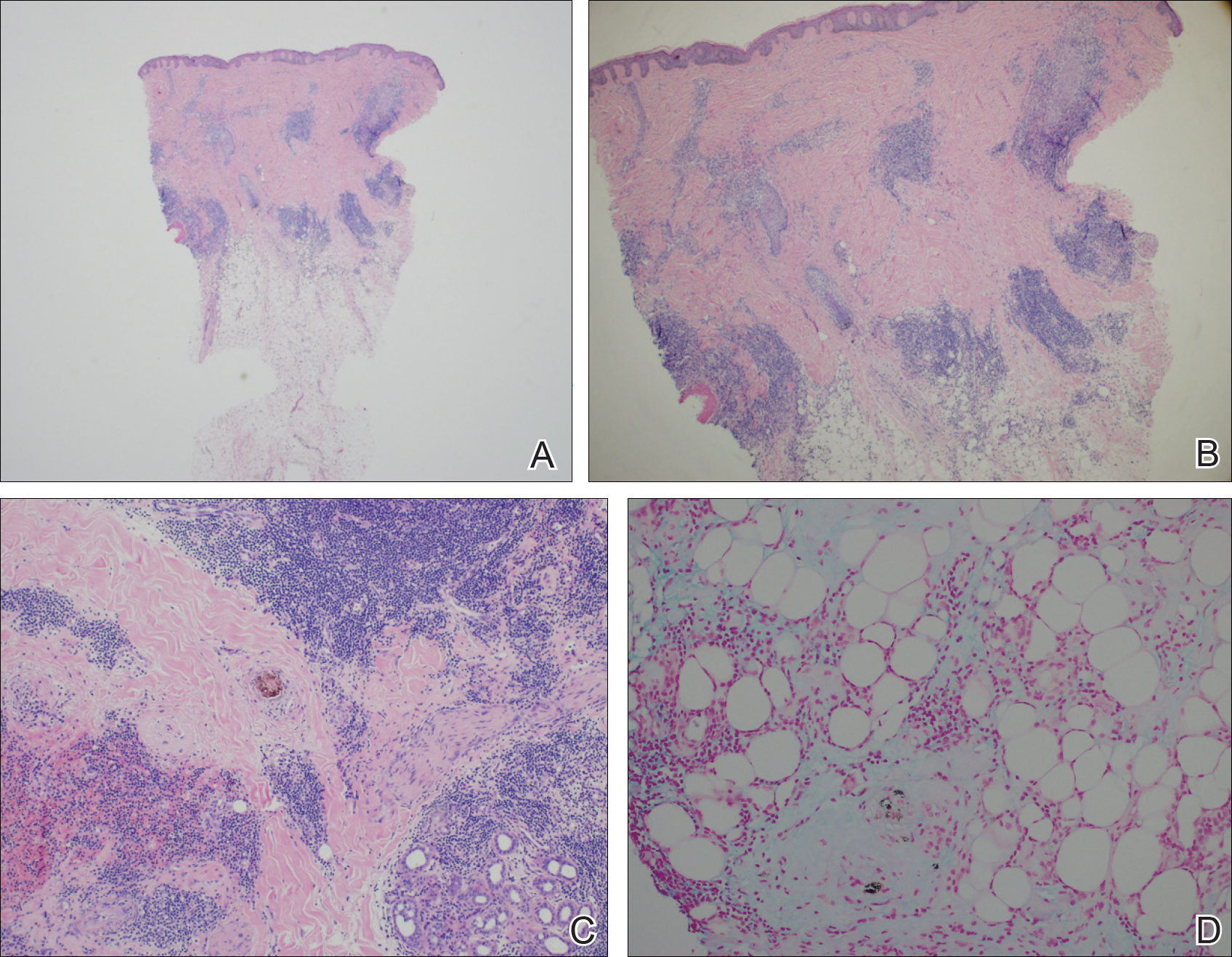
Comment
The classification of LET as a single unique entity or disease process sui generis has been in flux in the last decade. Its similarities to JLIS and other forms of chronic cutaneous lupus erythematosus (CCLE) have brought debate.4-6 In 1930, Gougerot and Burnier7 documented the first case of LET in the literature, describing smooth, infiltrated, erythematous lesions with no desquamation or other superficial changes seen in 5 patients.
In 2000, interest in LET and other forms of CCLE was increasing, and reports in the literature paralleled. That year, Kuhn et al4 reported 40 cases of LET, characterizing the clinical and histological features of each case to demonstrate that LET should be separate from other forms of CCLE. Until then, it is likely that many lesions that should have been classified as LET were instead classified as various forms of CCLE. The investigators maintained that LET also should be distinct from JLIS because it is associated with UV exposure.4 Kuhn et al8 reviewed phototesting in 60 patients with LET in 2001 and confirmed this subset was the most photosensitive type of lupus erythematosus.
In general, the histopathologic and immunohistochemical studies in LET and JLIS can be quite similar. Relatively distinguishing histopathologic findings in JLIS include no evidence of epidermal atrophy, basal vacuolar change, or follicular plugging, as well as negative immunofluorescence studies. Both entities show a predominantly T-cell population with a smaller component of B cells and thus a distinction cannot be made based on relative proportions of T and B cells in lesions.2
In 2003, Alexiades-Armenakas et al6 determined immunohistochemical criteria for LET, finding a predominance of T cells and more CD4 lymphocytes than CD8 lymphocytes with a mean ratio of roughly 3 to 1. Their study results maintained LET should be classified as a form of CCLE due to the chronicity of the lesions, the serologic profile with negative anti–double-stranded DNA, anticentromere, anti-Smith, anti-Ro/Sjögren syndrome antigen A, anti-La/Sjögren syndrome antigen B, and anti-nuclear ribonucleoprotein antibodies and the rare association with systemic disease.6 This conclusion was further solidified by a review published that same year citing unique histopathological features when compared to subacute cutaneous LE and discoid lupus erythematosus.5
This case illustrates the importance of histologic evaluation in determining the correct diagnosis in a patient with alopecia areata recalcitrant to treatment. Including LET in the differential of alopecic patches on the scalp could prove beneficial for patients, as LET responds well to antimalarial drugs and photoprotection.9 This patient had a normal antinuclear antibody panel and no signs or symptoms of systemic lupus. It was recommended that she avoid sun exposure and begin treatment with hydroxychloroquine but she declined. At a follow-up visit 6 months later she reported the lesions had improved, but a permanent wig had been sewn over the area, so it could not be examined.
- Lee L, Werth V. Rheumatologic disease. In: Bolognia JL, Jorizzo JL, Rapini RP, eds. Dermatology. Vol 2. 3rd ed. Mosby Elsevier; 2008:615-629.
- Weedon D. The lichenoid reaction pattern. In: Weedon D. Skin Pathology. 2nd ed. Edinburgh, Scotland: Churchill Livingstone; 2002:35-70.
- Dekle CL, Mannes KD, Davis LS, et al. Lupus tumidus. J Am Acad Dermatol. 1999;41:250-253.
- Kuhn A, Richter-Hintz D, Oslislo C, et al. Lupus erythematosus tumidus—a neglected subset of cutaneous lupus erythematosus: report of 40 cases. Arch Dermatol. 2000;136:1033-1041.
- Kuhn A, Sonntag M, Ruzicka T, et al. Histopathologic findings in lupus erythematosus tumidus: review of 80 patients. J Am Acad Dermatol. 2003;48:901-908.
- Alexiades-Armenakas MR, Baldassano M, Bince B, et al. Tumid lupus erythematosus: criteria for classification with immunohistochemical analysis. Arthritis Rheum. 2003;49:494-500.
- Gougerot H, Burnier R. Lupuse rythe mateux “tumidus.” Bull Soc Fr Dermatol Syph. 1930;37:1291-1292.
- Kuhn A, Sonntag M, Richter-Hintz D, et al. Phototesting in lupus erythematosus tumidus—review of 60 patients. Photochem Photobiol. 2001;73:532-536.
- Cozzani E, Christana K, Rongioletti F, et al. Lupus erythematosus tumidus: clinical, histopathological and serological aspects and therapy response of 21 patients. Eur J Dermatol. 2010;20:797-801.
- Lee L, Werth V. Rheumatologic disease. In: Bolognia JL, Jorizzo JL, Rapini RP, eds. Dermatology. Vol 2. 3rd ed. Mosby Elsevier; 2008:615-629.
- Weedon D. The lichenoid reaction pattern. In: Weedon D. Skin Pathology. 2nd ed. Edinburgh, Scotland: Churchill Livingstone; 2002:35-70.
- Dekle CL, Mannes KD, Davis LS, et al. Lupus tumidus. J Am Acad Dermatol. 1999;41:250-253.
- Kuhn A, Richter-Hintz D, Oslislo C, et al. Lupus erythematosus tumidus—a neglected subset of cutaneous lupus erythematosus: report of 40 cases. Arch Dermatol. 2000;136:1033-1041.
- Kuhn A, Sonntag M, Ruzicka T, et al. Histopathologic findings in lupus erythematosus tumidus: review of 80 patients. J Am Acad Dermatol. 2003;48:901-908.
- Alexiades-Armenakas MR, Baldassano M, Bince B, et al. Tumid lupus erythematosus: criteria for classification with immunohistochemical analysis. Arthritis Rheum. 2003;49:494-500.
- Gougerot H, Burnier R. Lupuse rythe mateux “tumidus.” Bull Soc Fr Dermatol Syph. 1930;37:1291-1292.
- Kuhn A, Sonntag M, Richter-Hintz D, et al. Phototesting in lupus erythematosus tumidus—review of 60 patients. Photochem Photobiol. 2001;73:532-536.
- Cozzani E, Christana K, Rongioletti F, et al. Lupus erythematosus tumidus: clinical, histopathological and serological aspects and therapy response of 21 patients. Eur J Dermatol. 2010;20:797-801.
Practice Points
- Lupus erythematosus tumidus (LET) of the scalp can mimic alopecia areata on clinical presentation.
- A unique variant of chronic cutaneous lupus erythematosus, LET presents in sun-exposed areas without any corresponding systemic signs.
- Lupus erythematosus tumidus may respond well to antimalarial drugs.
Collaborative care aids seniors’ mild depression
A collaborative care model significantly mitigated mild depression in adults aged 65 and older, compared with usual care in the short term, based on data from 705 patients. The findings were published online Feb. 21.
“There is limited research about older people with mild depressive disorders who have insufficient levels of depressive symptoms to meet diagnostic criteria (called subclinical, subthreshold, or subsyndromal depression) but also reduced quality of life and function,” wrote Simon Gilbody, PhD, of the University of York (England) and colleagues. However, subthreshold depression increases the risk of a severe depressive illness, the researchers added.
Overall, patients in the collaborative care group improved from an average score of 7.8 at baseline to 5.4 after 4 months; the usual care group improved from an average of 7.8 at baseline to 6.7 at 4 months. The difference in scores persisted at 12 months in the secondary analysis (JAMA. 2017;317:728-37. doi: 10.1001/jama.2017.0130). “For populations with case-level depression, a successful treatment outcome has been defined as 5 points on the PHQ-9,” the researchers noted. “This magnitude of benefit was not observed in either group of the trial when comparing scores before and after treatment, although this result would be anticipated given the lower baseline PHQ-9 scores in populations with subthreshold depression.’
The study participants came from 32 primary care practices in northern England; the average age was 77 years, and 58% were women.
The results were limited by several factors, including the absence of a standardized interview to diagnose depression, differences in retention and attrition between groups, and the absence of long-term follow-up, “and further research is needed to assess longer-term efficacy,” the researchers said.
Neither Dr. Gilbody nor his colleagues had financial conflicts to disclose.
The CASPER trial “provides the first evidence that collaborative care may benefit patients with subthreshold depression,” Kurt Kroenke, MD, wrote in an accompanying editorial. In addition to the improvements on the Patient Health Questionnaire and the reduction in risk of progression to threshold level depression, the findings further support the use of behavioral activation, which was the core treatment in the study, he said. “Strong evidence for the effectiveness of behavioral activation was provided by the recent COBRA trial. … and behavioral activation was found to be noninferior to cognitive-behavioral therapy for the outcome of depression,” he wrote. However, more research is needed before clinicians routinely expand treatment beyond major depression to include subthreshold depression, Dr. Kroenke noted. Key factors include the variable rate of progression from subthreshold depression to major depression, the duration and context of subthreshold depression, patient preferences, and the possible role of antidepressants, he noted. However, the CASPER findings show “new evidence that collaborative care improves outcomes for at least some patients with subthreshold depression,” Dr. Kroenke said. “Patients with persistent symptoms, functional impairment, and a desire for treatment may particularly benefit,” he added (JAMA. 2017;317:702-4).
Kurt Kroenke, MD, is affiliated with the VA Health Services Research and Development Service Center for Health Communication and Information, Regenstrief Institute and Indiana University, both in Indianapolis. He had no financial conflicts to disclose.
The CASPER trial “provides the first evidence that collaborative care may benefit patients with subthreshold depression,” Kurt Kroenke, MD, wrote in an accompanying editorial. In addition to the improvements on the Patient Health Questionnaire and the reduction in risk of progression to threshold level depression, the findings further support the use of behavioral activation, which was the core treatment in the study, he said. “Strong evidence for the effectiveness of behavioral activation was provided by the recent COBRA trial. … and behavioral activation was found to be noninferior to cognitive-behavioral therapy for the outcome of depression,” he wrote. However, more research is needed before clinicians routinely expand treatment beyond major depression to include subthreshold depression, Dr. Kroenke noted. Key factors include the variable rate of progression from subthreshold depression to major depression, the duration and context of subthreshold depression, patient preferences, and the possible role of antidepressants, he noted. However, the CASPER findings show “new evidence that collaborative care improves outcomes for at least some patients with subthreshold depression,” Dr. Kroenke said. “Patients with persistent symptoms, functional impairment, and a desire for treatment may particularly benefit,” he added (JAMA. 2017;317:702-4).
Kurt Kroenke, MD, is affiliated with the VA Health Services Research and Development Service Center for Health Communication and Information, Regenstrief Institute and Indiana University, both in Indianapolis. He had no financial conflicts to disclose.
The CASPER trial “provides the first evidence that collaborative care may benefit patients with subthreshold depression,” Kurt Kroenke, MD, wrote in an accompanying editorial. In addition to the improvements on the Patient Health Questionnaire and the reduction in risk of progression to threshold level depression, the findings further support the use of behavioral activation, which was the core treatment in the study, he said. “Strong evidence for the effectiveness of behavioral activation was provided by the recent COBRA trial. … and behavioral activation was found to be noninferior to cognitive-behavioral therapy for the outcome of depression,” he wrote. However, more research is needed before clinicians routinely expand treatment beyond major depression to include subthreshold depression, Dr. Kroenke noted. Key factors include the variable rate of progression from subthreshold depression to major depression, the duration and context of subthreshold depression, patient preferences, and the possible role of antidepressants, he noted. However, the CASPER findings show “new evidence that collaborative care improves outcomes for at least some patients with subthreshold depression,” Dr. Kroenke said. “Patients with persistent symptoms, functional impairment, and a desire for treatment may particularly benefit,” he added (JAMA. 2017;317:702-4).
Kurt Kroenke, MD, is affiliated with the VA Health Services Research and Development Service Center for Health Communication and Information, Regenstrief Institute and Indiana University, both in Indianapolis. He had no financial conflicts to disclose.
A collaborative care model significantly mitigated mild depression in adults aged 65 and older, compared with usual care in the short term, based on data from 705 patients. The findings were published online Feb. 21.
“There is limited research about older people with mild depressive disorders who have insufficient levels of depressive symptoms to meet diagnostic criteria (called subclinical, subthreshold, or subsyndromal depression) but also reduced quality of life and function,” wrote Simon Gilbody, PhD, of the University of York (England) and colleagues. However, subthreshold depression increases the risk of a severe depressive illness, the researchers added.
Overall, patients in the collaborative care group improved from an average score of 7.8 at baseline to 5.4 after 4 months; the usual care group improved from an average of 7.8 at baseline to 6.7 at 4 months. The difference in scores persisted at 12 months in the secondary analysis (JAMA. 2017;317:728-37. doi: 10.1001/jama.2017.0130). “For populations with case-level depression, a successful treatment outcome has been defined as 5 points on the PHQ-9,” the researchers noted. “This magnitude of benefit was not observed in either group of the trial when comparing scores before and after treatment, although this result would be anticipated given the lower baseline PHQ-9 scores in populations with subthreshold depression.’
The study participants came from 32 primary care practices in northern England; the average age was 77 years, and 58% were women.
The results were limited by several factors, including the absence of a standardized interview to diagnose depression, differences in retention and attrition between groups, and the absence of long-term follow-up, “and further research is needed to assess longer-term efficacy,” the researchers said.
Neither Dr. Gilbody nor his colleagues had financial conflicts to disclose.
A collaborative care model significantly mitigated mild depression in adults aged 65 and older, compared with usual care in the short term, based on data from 705 patients. The findings were published online Feb. 21.
“There is limited research about older people with mild depressive disorders who have insufficient levels of depressive symptoms to meet diagnostic criteria (called subclinical, subthreshold, or subsyndromal depression) but also reduced quality of life and function,” wrote Simon Gilbody, PhD, of the University of York (England) and colleagues. However, subthreshold depression increases the risk of a severe depressive illness, the researchers added.
Overall, patients in the collaborative care group improved from an average score of 7.8 at baseline to 5.4 after 4 months; the usual care group improved from an average of 7.8 at baseline to 6.7 at 4 months. The difference in scores persisted at 12 months in the secondary analysis (JAMA. 2017;317:728-37. doi: 10.1001/jama.2017.0130). “For populations with case-level depression, a successful treatment outcome has been defined as 5 points on the PHQ-9,” the researchers noted. “This magnitude of benefit was not observed in either group of the trial when comparing scores before and after treatment, although this result would be anticipated given the lower baseline PHQ-9 scores in populations with subthreshold depression.’
The study participants came from 32 primary care practices in northern England; the average age was 77 years, and 58% were women.
The results were limited by several factors, including the absence of a standardized interview to diagnose depression, differences in retention and attrition between groups, and the absence of long-term follow-up, “and further research is needed to assess longer-term efficacy,” the researchers said.
Neither Dr. Gilbody nor his colleagues had financial conflicts to disclose.
FROM JAMA
Key clinical point: Collaborative care reduced subthreshold depression in older adults, compared with usual care after 4 months.
Major finding: Older adults with subthreshold depression who received collaborative care had lower depression scores on the Patient Health Questionnaire than those who received usual care after 4 months (average scores 5.4 and 6.7, respectively).
Data source: A randomized trial of 705 adults aged 65 years and older with subthreshold depression.
Disclosures: The researchers had no financial conflicts to disclose.














