User login
Mentally ill? Go directly to jail
In the course of researching our book, “Committed: The Battle Over Involuntary Psychiatric Care,” I came to a few very important conclusions. Involuntary commitment can be traumatizing to patients, and it should be done as a last resort when patients are dangerous (generally to themselves, but sometimes toward others) or tormented, and when they can’t be persuaded to get voluntary care. That may sound obvious, but in practice, it doesn’t always work that way. Furthermore, if there is no choice but to hold people against their will, there should be no use of physical force unless it is absolutely necessary to maintain safety, and patients should be treated with kindness and respect. It’s what we’d all want if we were the patient, and it’s not what all patients get.
Knowing that, you can imagine my shock when I saw reporter Mike Anderson’s article “Jail cells await mentally ill in Rapid City” in the Feb. 8, 2017, edition of the Rapid City Journal. Mr. Anderson noted that the Rapid City Regional Hospital was changing its policy on psychiatric admissions. The South Dakota city of 60,000 has a 44-bed psychiatric hospital located 1.5 miles from the main hospital. It is the only inpatient facility for at least 250 miles and serves a total population of approximately 250,000 people. If the unit is full – either because all beds are full or because staffing and acuity issues limit capacity – its policy always has been to admit overflow psychiatric patients to medical beds.
Effective Feb. 1, 2017, we will no longer admit behavioral health patients who do not have acute medical needs to the main hospital when the Behavioral Health facility is at capacity. In these instances, we will expect the County to take custody of patients who are subject to the involuntary mental commitment process, pending an opening at the Behavioral Health unit. It is simply no longer feasible for us to care for behavioral health patients who do not have acute medical needs outside of the Behavioral Health facility. Unless we hear differently, we will contact the Sheriff’s Office to take custody of involuntarily detained persons when the Behavioral Health facility is at capacity.
Also, by way of information, we will no longer admit patients to the Behavioral Health facility who have neurodevelopmental/cognitive disorders such as dementia, Alzheimer’s disease, or Autism Spectrum Disorders. We believe it is in the best interest of all patients to limit the conditions which are appropriate for treatment in our facility.
In other words, if there are no open beds in a psychiatric facility, patients would be transported from the emergency deparment to the Pennington County Jail. The fate of patients with psychiatric issues and dementia or autism was not at all clear.
I spoke with Stephen Manlove, MD, DFAPA. Dr. Manlove has a psychiatric outpatient practice but worked for the Rapid City Regional Hospital for 26 years. He left this past September because he felt the facility had lost sight of its mission to give psychiatric patients excellent care. He also works two mornings a week providing psychiatric treatment at the local jail, a 600-bed facility where 1 in 6 inmates is on psychotropic medications, and an average of 25 inmates at any given time suffer from severe and persistent mental disorders.
“This is obviously a complicated story,” Dr. Manlove noted. “The hospital gave the jail only a few days’ notice. The hospital doesn’t seem to want to invest in this population. They are investing millions of dollars in other projects but can’t find the money to fund psychiatry. Surprisingly, the medical community seems to have accepted this.”
Dr. Manlove noted that the jail is not equipped to offer comprehensive psychiatric treatment, and that inmates are held in cinder block cells with very limited medical supervision.
Kevin Thom, the Pennington County sheriff, was quick to say, “We shouldn’t be criminalizing mental health problems.” While he noted that local statute allows for patients to be held in a jail cell for up to 24 hours if a hospital bed is not available, he commented on the inappropriateness of this and on the brief notice his office was given: “There was no time to figure out a process or alternatives. It’s frustrating.”
Dr. Manlove said he believes that a few patients may have been taken to the jail since the new policy was instituted, but the jail has turned some away. Sheriff Thom said his office had been called to transport a patient and had refused.
I asked what happens when a voluntary patient needs a bed and there is no room. Dr. Manlove replied: “If they are not considered acutely dangerous, I assume they will be told to go to another hospital. If they are acutely dangerous to themselves or others, then a mental health hold would be placed, and they would be sent to jail.”
Of note, the closest hospital with a psychiatric unit is 253 miles away, in Casper, Wyo.
One reason for limiting the type of patients the psychiatric facility will admit may have to do with an effort by the hospital to lower its use of seclusion and restraint. In an article in the Rapid City Journal on Feb. 19, 2017, reporter Chris Huber noted that between July 2015 and July 2016, Rapid City Behavioral Health had seclusion rates 300 times higher than the national average, a fact the hospital attributes to the high acuity needs of autistic patients. Rather than improving its ability to treat these patients, the facility has decided not to accept them.
In June 2016, the Boston Globe Spotlight team began a series called “The Desperate and the Dead” as a way to highlight deficiencies in the Massachusetts public mental health system. The first article was a sensationalized piece about psychiatric patients who kill their family members. The backlash to the stigmatization of psychiatric patients as murderers was huge; a Facebook page set up to accept comments soon had more than 1,300 members, and the entrance to the Globe was blocked by 150 protesters. The response to the Rapid City hospital’s decision to jail people with psychiatric disorders who have committed no crime has been surprisingly quiet; there have been no stories of protests or advocacy outrage. In this egregious stigmatization of those with psychiatric disorders, I had to wonder what they do when the medical beds overflow: Do they send those patients to jail? Of course not. And why would anyone think this is okay?
We know that involuntary care can be traumatizing and that psychiatric care can feel demeaning. On the one hand, there is a call to pass laws to make it easier to treat patients involuntarily. In our polarized world with rising suicide rates, should we be doing everything possible to engage patients in voluntary care? How do we reconcile the fact that a hospital administration can decide that if distressed people seek care, having broken no law, they can be sent to jail? And finally, since suicide rates among physicians remain so high, I’d like to ask this: Would you go to a hospital for treatment if you knew you might end up desperate and alone, receiving no treatment, in a jail cell?
My thanks to Mr. Anderson of the Rapid City Journal, Dr. Manlove, and Sheriff Thom for their help with this article.
Dr. Miller wrote “Committed: The Battle Over Involuntary Psychiatric Care” with Annette Hanson, MD (Baltimore: Johns Hopkins University Press, 2016).
In the course of researching our book, “Committed: The Battle Over Involuntary Psychiatric Care,” I came to a few very important conclusions. Involuntary commitment can be traumatizing to patients, and it should be done as a last resort when patients are dangerous (generally to themselves, but sometimes toward others) or tormented, and when they can’t be persuaded to get voluntary care. That may sound obvious, but in practice, it doesn’t always work that way. Furthermore, if there is no choice but to hold people against their will, there should be no use of physical force unless it is absolutely necessary to maintain safety, and patients should be treated with kindness and respect. It’s what we’d all want if we were the patient, and it’s not what all patients get.
Knowing that, you can imagine my shock when I saw reporter Mike Anderson’s article “Jail cells await mentally ill in Rapid City” in the Feb. 8, 2017, edition of the Rapid City Journal. Mr. Anderson noted that the Rapid City Regional Hospital was changing its policy on psychiatric admissions. The South Dakota city of 60,000 has a 44-bed psychiatric hospital located 1.5 miles from the main hospital. It is the only inpatient facility for at least 250 miles and serves a total population of approximately 250,000 people. If the unit is full – either because all beds are full or because staffing and acuity issues limit capacity – its policy always has been to admit overflow psychiatric patients to medical beds.
Effective Feb. 1, 2017, we will no longer admit behavioral health patients who do not have acute medical needs to the main hospital when the Behavioral Health facility is at capacity. In these instances, we will expect the County to take custody of patients who are subject to the involuntary mental commitment process, pending an opening at the Behavioral Health unit. It is simply no longer feasible for us to care for behavioral health patients who do not have acute medical needs outside of the Behavioral Health facility. Unless we hear differently, we will contact the Sheriff’s Office to take custody of involuntarily detained persons when the Behavioral Health facility is at capacity.
Also, by way of information, we will no longer admit patients to the Behavioral Health facility who have neurodevelopmental/cognitive disorders such as dementia, Alzheimer’s disease, or Autism Spectrum Disorders. We believe it is in the best interest of all patients to limit the conditions which are appropriate for treatment in our facility.
In other words, if there are no open beds in a psychiatric facility, patients would be transported from the emergency deparment to the Pennington County Jail. The fate of patients with psychiatric issues and dementia or autism was not at all clear.
I spoke with Stephen Manlove, MD, DFAPA. Dr. Manlove has a psychiatric outpatient practice but worked for the Rapid City Regional Hospital for 26 years. He left this past September because he felt the facility had lost sight of its mission to give psychiatric patients excellent care. He also works two mornings a week providing psychiatric treatment at the local jail, a 600-bed facility where 1 in 6 inmates is on psychotropic medications, and an average of 25 inmates at any given time suffer from severe and persistent mental disorders.
“This is obviously a complicated story,” Dr. Manlove noted. “The hospital gave the jail only a few days’ notice. The hospital doesn’t seem to want to invest in this population. They are investing millions of dollars in other projects but can’t find the money to fund psychiatry. Surprisingly, the medical community seems to have accepted this.”
Dr. Manlove noted that the jail is not equipped to offer comprehensive psychiatric treatment, and that inmates are held in cinder block cells with very limited medical supervision.
Kevin Thom, the Pennington County sheriff, was quick to say, “We shouldn’t be criminalizing mental health problems.” While he noted that local statute allows for patients to be held in a jail cell for up to 24 hours if a hospital bed is not available, he commented on the inappropriateness of this and on the brief notice his office was given: “There was no time to figure out a process or alternatives. It’s frustrating.”
Dr. Manlove said he believes that a few patients may have been taken to the jail since the new policy was instituted, but the jail has turned some away. Sheriff Thom said his office had been called to transport a patient and had refused.
I asked what happens when a voluntary patient needs a bed and there is no room. Dr. Manlove replied: “If they are not considered acutely dangerous, I assume they will be told to go to another hospital. If they are acutely dangerous to themselves or others, then a mental health hold would be placed, and they would be sent to jail.”
Of note, the closest hospital with a psychiatric unit is 253 miles away, in Casper, Wyo.
One reason for limiting the type of patients the psychiatric facility will admit may have to do with an effort by the hospital to lower its use of seclusion and restraint. In an article in the Rapid City Journal on Feb. 19, 2017, reporter Chris Huber noted that between July 2015 and July 2016, Rapid City Behavioral Health had seclusion rates 300 times higher than the national average, a fact the hospital attributes to the high acuity needs of autistic patients. Rather than improving its ability to treat these patients, the facility has decided not to accept them.
In June 2016, the Boston Globe Spotlight team began a series called “The Desperate and the Dead” as a way to highlight deficiencies in the Massachusetts public mental health system. The first article was a sensationalized piece about psychiatric patients who kill their family members. The backlash to the stigmatization of psychiatric patients as murderers was huge; a Facebook page set up to accept comments soon had more than 1,300 members, and the entrance to the Globe was blocked by 150 protesters. The response to the Rapid City hospital’s decision to jail people with psychiatric disorders who have committed no crime has been surprisingly quiet; there have been no stories of protests or advocacy outrage. In this egregious stigmatization of those with psychiatric disorders, I had to wonder what they do when the medical beds overflow: Do they send those patients to jail? Of course not. And why would anyone think this is okay?
We know that involuntary care can be traumatizing and that psychiatric care can feel demeaning. On the one hand, there is a call to pass laws to make it easier to treat patients involuntarily. In our polarized world with rising suicide rates, should we be doing everything possible to engage patients in voluntary care? How do we reconcile the fact that a hospital administration can decide that if distressed people seek care, having broken no law, they can be sent to jail? And finally, since suicide rates among physicians remain so high, I’d like to ask this: Would you go to a hospital for treatment if you knew you might end up desperate and alone, receiving no treatment, in a jail cell?
My thanks to Mr. Anderson of the Rapid City Journal, Dr. Manlove, and Sheriff Thom for their help with this article.
Dr. Miller wrote “Committed: The Battle Over Involuntary Psychiatric Care” with Annette Hanson, MD (Baltimore: Johns Hopkins University Press, 2016).
In the course of researching our book, “Committed: The Battle Over Involuntary Psychiatric Care,” I came to a few very important conclusions. Involuntary commitment can be traumatizing to patients, and it should be done as a last resort when patients are dangerous (generally to themselves, but sometimes toward others) or tormented, and when they can’t be persuaded to get voluntary care. That may sound obvious, but in practice, it doesn’t always work that way. Furthermore, if there is no choice but to hold people against their will, there should be no use of physical force unless it is absolutely necessary to maintain safety, and patients should be treated with kindness and respect. It’s what we’d all want if we were the patient, and it’s not what all patients get.
Knowing that, you can imagine my shock when I saw reporter Mike Anderson’s article “Jail cells await mentally ill in Rapid City” in the Feb. 8, 2017, edition of the Rapid City Journal. Mr. Anderson noted that the Rapid City Regional Hospital was changing its policy on psychiatric admissions. The South Dakota city of 60,000 has a 44-bed psychiatric hospital located 1.5 miles from the main hospital. It is the only inpatient facility for at least 250 miles and serves a total population of approximately 250,000 people. If the unit is full – either because all beds are full or because staffing and acuity issues limit capacity – its policy always has been to admit overflow psychiatric patients to medical beds.
Effective Feb. 1, 2017, we will no longer admit behavioral health patients who do not have acute medical needs to the main hospital when the Behavioral Health facility is at capacity. In these instances, we will expect the County to take custody of patients who are subject to the involuntary mental commitment process, pending an opening at the Behavioral Health unit. It is simply no longer feasible for us to care for behavioral health patients who do not have acute medical needs outside of the Behavioral Health facility. Unless we hear differently, we will contact the Sheriff’s Office to take custody of involuntarily detained persons when the Behavioral Health facility is at capacity.
Also, by way of information, we will no longer admit patients to the Behavioral Health facility who have neurodevelopmental/cognitive disorders such as dementia, Alzheimer’s disease, or Autism Spectrum Disorders. We believe it is in the best interest of all patients to limit the conditions which are appropriate for treatment in our facility.
In other words, if there are no open beds in a psychiatric facility, patients would be transported from the emergency deparment to the Pennington County Jail. The fate of patients with psychiatric issues and dementia or autism was not at all clear.
I spoke with Stephen Manlove, MD, DFAPA. Dr. Manlove has a psychiatric outpatient practice but worked for the Rapid City Regional Hospital for 26 years. He left this past September because he felt the facility had lost sight of its mission to give psychiatric patients excellent care. He also works two mornings a week providing psychiatric treatment at the local jail, a 600-bed facility where 1 in 6 inmates is on psychotropic medications, and an average of 25 inmates at any given time suffer from severe and persistent mental disorders.
“This is obviously a complicated story,” Dr. Manlove noted. “The hospital gave the jail only a few days’ notice. The hospital doesn’t seem to want to invest in this population. They are investing millions of dollars in other projects but can’t find the money to fund psychiatry. Surprisingly, the medical community seems to have accepted this.”
Dr. Manlove noted that the jail is not equipped to offer comprehensive psychiatric treatment, and that inmates are held in cinder block cells with very limited medical supervision.
Kevin Thom, the Pennington County sheriff, was quick to say, “We shouldn’t be criminalizing mental health problems.” While he noted that local statute allows for patients to be held in a jail cell for up to 24 hours if a hospital bed is not available, he commented on the inappropriateness of this and on the brief notice his office was given: “There was no time to figure out a process or alternatives. It’s frustrating.”
Dr. Manlove said he believes that a few patients may have been taken to the jail since the new policy was instituted, but the jail has turned some away. Sheriff Thom said his office had been called to transport a patient and had refused.
I asked what happens when a voluntary patient needs a bed and there is no room. Dr. Manlove replied: “If they are not considered acutely dangerous, I assume they will be told to go to another hospital. If they are acutely dangerous to themselves or others, then a mental health hold would be placed, and they would be sent to jail.”
Of note, the closest hospital with a psychiatric unit is 253 miles away, in Casper, Wyo.
One reason for limiting the type of patients the psychiatric facility will admit may have to do with an effort by the hospital to lower its use of seclusion and restraint. In an article in the Rapid City Journal on Feb. 19, 2017, reporter Chris Huber noted that between July 2015 and July 2016, Rapid City Behavioral Health had seclusion rates 300 times higher than the national average, a fact the hospital attributes to the high acuity needs of autistic patients. Rather than improving its ability to treat these patients, the facility has decided not to accept them.
In June 2016, the Boston Globe Spotlight team began a series called “The Desperate and the Dead” as a way to highlight deficiencies in the Massachusetts public mental health system. The first article was a sensationalized piece about psychiatric patients who kill their family members. The backlash to the stigmatization of psychiatric patients as murderers was huge; a Facebook page set up to accept comments soon had more than 1,300 members, and the entrance to the Globe was blocked by 150 protesters. The response to the Rapid City hospital’s decision to jail people with psychiatric disorders who have committed no crime has been surprisingly quiet; there have been no stories of protests or advocacy outrage. In this egregious stigmatization of those with psychiatric disorders, I had to wonder what they do when the medical beds overflow: Do they send those patients to jail? Of course not. And why would anyone think this is okay?
We know that involuntary care can be traumatizing and that psychiatric care can feel demeaning. On the one hand, there is a call to pass laws to make it easier to treat patients involuntarily. In our polarized world with rising suicide rates, should we be doing everything possible to engage patients in voluntary care? How do we reconcile the fact that a hospital administration can decide that if distressed people seek care, having broken no law, they can be sent to jail? And finally, since suicide rates among physicians remain so high, I’d like to ask this: Would you go to a hospital for treatment if you knew you might end up desperate and alone, receiving no treatment, in a jail cell?
My thanks to Mr. Anderson of the Rapid City Journal, Dr. Manlove, and Sheriff Thom for their help with this article.
Dr. Miller wrote “Committed: The Battle Over Involuntary Psychiatric Care” with Annette Hanson, MD (Baltimore: Johns Hopkins University Press, 2016).
ERCP testing guidelines accurate, but could be improved
Though current American Society for Gastrointestinal Endoscopy guidelines for whether a patient suspected of choledocholithiasis should undergo endoscopic retrograde cholangiopancreatography (ERCP) are accurate, more restrictive criteria would improve specificity and positive predictive value, researchers have determined.
ERCP is a highly effective procedure but is associated with serious, potentially life-threatening risks. Researchers also noted that “adverse events associated with ERCP are a frequent cause of litigation against gastroenterologists,” highlighting the need for decisions driven by data rather than expert opinion (Gastrointest Endosc. 2017 Feb 4. doi: 10.1016/j.gie.2017.01.039).
Society guidelines recommend less invasive testing – such as baseline liver tests and abdominal ultrasound – prior to ERCP to rule out patients who do not need the riskier procedure. From there, the guidelines stratify patients by high, intermediate, or low risk, recommending higher-risk patients (greater than 50% probability of choledocholithiasis) to proceed to ERCP, and lower-risk patients to take more tests first.
Researchers at Sir Run Run Shaw Hospital, Hangzhou, China, studied 2,724 patients with suspected choledocholithiasis. The patients received biochemical testing, abdominal ultrasound, and definitive testing.
The researchers found that the American Society for Gastrointestinal Endoscopy high-risk criteria were able to provide greater than 50% probability that a patient had choledocholithiasis, but that the criteria would still lead to more than a third of patients undergoing unnecessary ERCP.
Two of the tests – abdominal ultrasound, and determining the level of bilirubin to be greater than 4 mg/dL combined with a dilated common bile duct – provided greater specificity and positive predictive value than did the broader society guidelines. Patients who are negative for both of these tests, the researchers recommend, should receive a less invasive magnetic resonance cholangiopancreatography prior to ERCP.
Though current American Society for Gastrointestinal Endoscopy guidelines for whether a patient suspected of choledocholithiasis should undergo endoscopic retrograde cholangiopancreatography (ERCP) are accurate, more restrictive criteria would improve specificity and positive predictive value, researchers have determined.
ERCP is a highly effective procedure but is associated with serious, potentially life-threatening risks. Researchers also noted that “adverse events associated with ERCP are a frequent cause of litigation against gastroenterologists,” highlighting the need for decisions driven by data rather than expert opinion (Gastrointest Endosc. 2017 Feb 4. doi: 10.1016/j.gie.2017.01.039).
Society guidelines recommend less invasive testing – such as baseline liver tests and abdominal ultrasound – prior to ERCP to rule out patients who do not need the riskier procedure. From there, the guidelines stratify patients by high, intermediate, or low risk, recommending higher-risk patients (greater than 50% probability of choledocholithiasis) to proceed to ERCP, and lower-risk patients to take more tests first.
Researchers at Sir Run Run Shaw Hospital, Hangzhou, China, studied 2,724 patients with suspected choledocholithiasis. The patients received biochemical testing, abdominal ultrasound, and definitive testing.
The researchers found that the American Society for Gastrointestinal Endoscopy high-risk criteria were able to provide greater than 50% probability that a patient had choledocholithiasis, but that the criteria would still lead to more than a third of patients undergoing unnecessary ERCP.
Two of the tests – abdominal ultrasound, and determining the level of bilirubin to be greater than 4 mg/dL combined with a dilated common bile duct – provided greater specificity and positive predictive value than did the broader society guidelines. Patients who are negative for both of these tests, the researchers recommend, should receive a less invasive magnetic resonance cholangiopancreatography prior to ERCP.
Though current American Society for Gastrointestinal Endoscopy guidelines for whether a patient suspected of choledocholithiasis should undergo endoscopic retrograde cholangiopancreatography (ERCP) are accurate, more restrictive criteria would improve specificity and positive predictive value, researchers have determined.
ERCP is a highly effective procedure but is associated with serious, potentially life-threatening risks. Researchers also noted that “adverse events associated with ERCP are a frequent cause of litigation against gastroenterologists,” highlighting the need for decisions driven by data rather than expert opinion (Gastrointest Endosc. 2017 Feb 4. doi: 10.1016/j.gie.2017.01.039).
Society guidelines recommend less invasive testing – such as baseline liver tests and abdominal ultrasound – prior to ERCP to rule out patients who do not need the riskier procedure. From there, the guidelines stratify patients by high, intermediate, or low risk, recommending higher-risk patients (greater than 50% probability of choledocholithiasis) to proceed to ERCP, and lower-risk patients to take more tests first.
Researchers at Sir Run Run Shaw Hospital, Hangzhou, China, studied 2,724 patients with suspected choledocholithiasis. The patients received biochemical testing, abdominal ultrasound, and definitive testing.
The researchers found that the American Society for Gastrointestinal Endoscopy high-risk criteria were able to provide greater than 50% probability that a patient had choledocholithiasis, but that the criteria would still lead to more than a third of patients undergoing unnecessary ERCP.
Two of the tests – abdominal ultrasound, and determining the level of bilirubin to be greater than 4 mg/dL combined with a dilated common bile duct – provided greater specificity and positive predictive value than did the broader society guidelines. Patients who are negative for both of these tests, the researchers recommend, should receive a less invasive magnetic resonance cholangiopancreatography prior to ERCP.
FROM GASTROINTESTINAL ENDOSCOPY
Personal finances affect cancer survivors’ medication use
Adult cancer survivors under the age of 65 are more likely to alter their use of prescription drugs for financial reasons than are those without a history of cancer, according to a report published online Feb. 20.
Among nonelderly adults, 31.6% of those who had been diagnosed within the previous 2 years and 27.9% of those who had been diagnosed 2 or more years earlier reported a change in prescription drug use for financial reasons, compared with 21.4% of adults without a history of cancer, said Zhiyuan Zheng, PhD, of the American Cancer Society, Atlanta, and his associates (Cancer 2017 Feb 20. doi: 10.1002/cncr.30560).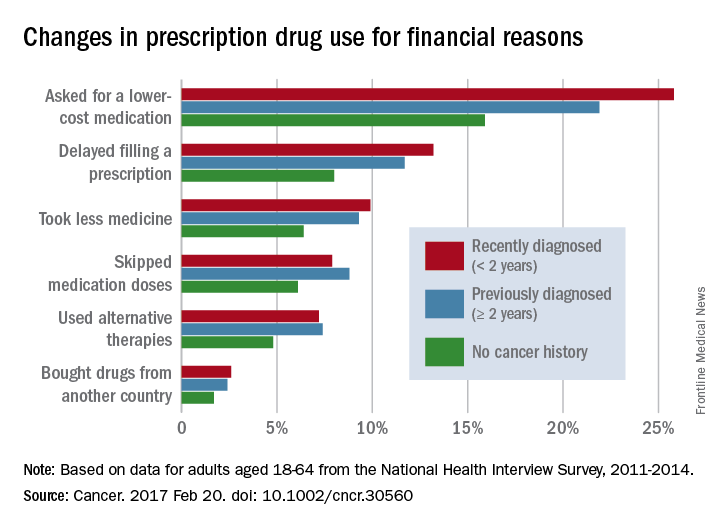
The differences between cancer survivors and those with no cancer history were much smaller for those aged 65 years and over: 24.9% of recent survivors and 21.8% of previous survivors changed their behavior for financial reasons, compared with 20.4% for those with no history of cancer, according to the analysis of data from the National Health Interview Survey for 2011-2014.
No funding source for the study was disclosed, and the investigators did not make any disclosures of conflicts of interest.
Adult cancer survivors under the age of 65 are more likely to alter their use of prescription drugs for financial reasons than are those without a history of cancer, according to a report published online Feb. 20.
Among nonelderly adults, 31.6% of those who had been diagnosed within the previous 2 years and 27.9% of those who had been diagnosed 2 or more years earlier reported a change in prescription drug use for financial reasons, compared with 21.4% of adults without a history of cancer, said Zhiyuan Zheng, PhD, of the American Cancer Society, Atlanta, and his associates (Cancer 2017 Feb 20. doi: 10.1002/cncr.30560).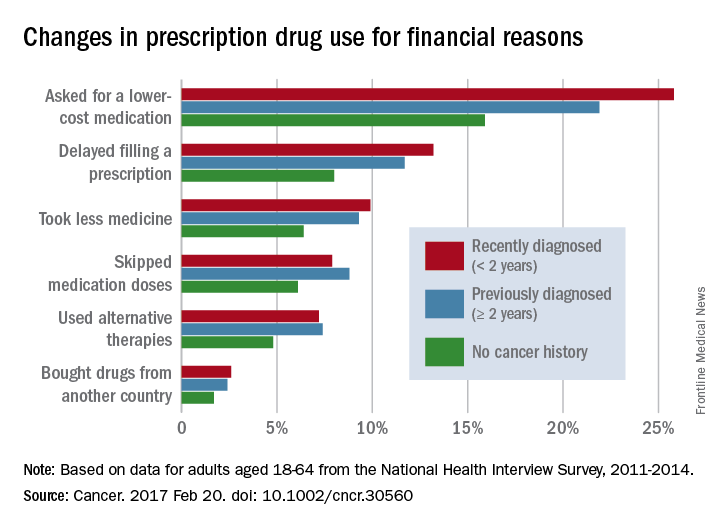
The differences between cancer survivors and those with no cancer history were much smaller for those aged 65 years and over: 24.9% of recent survivors and 21.8% of previous survivors changed their behavior for financial reasons, compared with 20.4% for those with no history of cancer, according to the analysis of data from the National Health Interview Survey for 2011-2014.
No funding source for the study was disclosed, and the investigators did not make any disclosures of conflicts of interest.
Adult cancer survivors under the age of 65 are more likely to alter their use of prescription drugs for financial reasons than are those without a history of cancer, according to a report published online Feb. 20.
Among nonelderly adults, 31.6% of those who had been diagnosed within the previous 2 years and 27.9% of those who had been diagnosed 2 or more years earlier reported a change in prescription drug use for financial reasons, compared with 21.4% of adults without a history of cancer, said Zhiyuan Zheng, PhD, of the American Cancer Society, Atlanta, and his associates (Cancer 2017 Feb 20. doi: 10.1002/cncr.30560).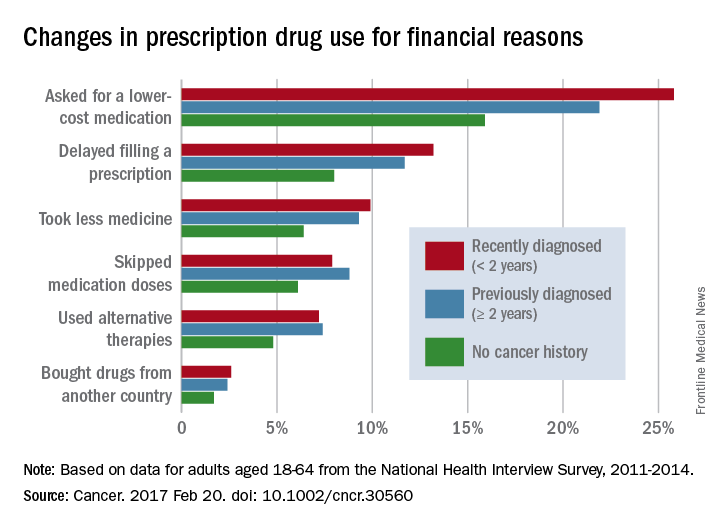
The differences between cancer survivors and those with no cancer history were much smaller for those aged 65 years and over: 24.9% of recent survivors and 21.8% of previous survivors changed their behavior for financial reasons, compared with 20.4% for those with no history of cancer, according to the analysis of data from the National Health Interview Survey for 2011-2014.
No funding source for the study was disclosed, and the investigators did not make any disclosures of conflicts of interest.
FROM CANCER
Testosterone Trials’ cardiac, cognitive results disappoint
Testosterone treatment may have beneficial effects on unexplained anemia or bone density in men with age-related low testosterone, but at the cost of an increase in coronary artery plaque and with no benefit on cognitive function, new research suggests.
The results of four of the seven Testosterone Trials were published Feb. 21 in JAMA and JAMA Internal Medicine, adding to a growing body of research on the impact of testosterone supplementation but without finding clear evidence of an overall benefit.
In the double-blind, multicenter Anemia Trial, 788 men aged 65 years or older with average testosterone levels of less than 275 ng/dL were allocated to 12 months of testosterone gel or placebo. The group included 126 individuals with a hemoglobin level at or below 12.7 g/dL (JAMA Intern Med. 2017 Feb 21. doi: 10.1001/jamainternmed.2016.9540).
The study found that significantly more men who received testosterone treatment experienced increases in hemoglobin concentration of 1 g/dL or more above baseline, compared with those who received the placebo gel (54% vs. 15%; 95% CI 3.7-277.8; P = .002).
This effect was seen in men with known causes of anemia, such as myelodysplasia, iron deficiency, B12 deficiency, or chronic inflammation or disease; in men with anemia of unknown case; and in men who weren’t anemic.
After 12 months, more than half of the testosterone-treated men who started the study with unexplained anemia were no longer anemic, compared with around one-quarter of the placebo-treated men (58.3% vs. 22.2%). The men treated with placebo also had lower average hemoglobin level changes, compared with those treated with testosterone.
“Increases in hemoglobin levels were positively and significantly associated with participants’ global impression of change in overall health and energy,” wrote Cindy N. Roy, PhD, of Johns Hopkins University, Baltimore, and her coauthors.
Bone mineral density
A second trial examined the effect of 12 months of testosterone gel or placebo on bone mineral density in a group of 211 men with average testosterone concentrations less than 275 ng/L (JAMA Intern Med. 2017 Feb 21. doi: 10.1001/jamainternmed.2016.9539). The treatment increased median serum concentrations of total testosterone, free testosterone, and estradiol to within the normal ranges for young men.
The study showed significantly greater increases – measured by quantitative computed tomography – with testosterone treatment, compared with placebo, in spine trabecular, spine peripheral, hip trabecular, and peripheral volumetric bone mineral density, as well as in mean estimated strength of spine trabecular bone, spine peripheral bone, and hip trabecular and peripheral bone.
For the primary outcome of mean lumbar spine trabecular volumetric bone mineral density, testosterone treatment was associated with a mean increase of 7.5%, compared with a 0.8% increase with placebo.
Researchers also noted that the magnitude of the increase in spine trabecular bone mineral density from baseline was significantly associated with changes in total testosterone and estradiol.
However, there were no significant differences in fracture rate, with six fractures reported in each group during the year of treatment. In the observation year after treatment, three fractures were reported in the testosterone arm and four in the placebo arm.
“These results are unequivocal compared with prior studies of the effect of testosterone treatment on bone in older men, in spite of treatment limited to 1 year, perhaps because the mean pretreatment testosterone level was lower and the sample size larger than in prior studies, and because the primary outcome in this trial was vBMD by QCT,” wrote Peter J. Snyder, MD, of the University of Pennsylvania, Philadelphia, and his coauthors.
Coronary artery plaque
However, a third trial – this one in 170 men with low testosterone and symptoms suggestive of hypogonadism – found significantly greater increases in noncalcified plaque volume, median total plaque volume, and median coronary artery calcification score among the 88 men assigned to 12 months of testosterone gel, compared with those assigned to placebo.
The men treated with testosterone showed a mean increase in noncalcified coronary artery plaque volume of 40 mm3, compared with 4 mm3 in men given the placebo gel, and a mean increase in total plaque volume of 57 mm3 with testosterone and 21 mm3 with placebo (JAMA. 2017 Feb 21;317[7]:708-16).
There were no significant differences between the groups in change to coronary artery calcium score, and there were no adverse cardiovascular events reported in either group, despite the fact that around half the participants had severe atherosclerosis at baseline.
“The increase in coronary artery noncalcified and total plaque volumes in men treated with testosterone is concerning, because any limitation of the vascular lumen could be considered deleterious,” wrote Matthew J. Budoff, MD, of the Los Angeles Biomedical Research Institute, Torrance, Calif., and his coauthors. “The clinical significance of these increases could depend on the differential effects of testosterone on the individual components of noncalcified plaque.”
However, the investigators pointed out that the trial was neither large enough nor long enough to draw conclusions about the cardiovascular risks of testosterone treatment, and they called for larger studies to explore the association.
Cognitive function
The fourth study looked at mean change in cognitive function from baseline in 493 men with a serum testosterone level less than 275 ng/dL, impaired sexual function, physical function, or vitality, and who met the criteria for age-associated memory impairment. Half the participants were assigned to 12 months of testosterone gel, and half were assigned to placebo gel (JAMA. 2017 Feb 21;317[7]:717-27).
Researchers found no significant differences between the two groups from baseline to 6 months and 12 months in mean change in delayed paragraph recall score, visual memory, executive function, or spatial ability.
“The lack of association between testosterone treatment and cognition was apparent across all cognitive domains assessed among men with [age-associated memory impairment], in spite of an increase in circulating total and free testosterone concentrations in the testosterone group to levels typical of men aged 19-40 years,” wrote Susan M. Resnick, PhD, of the National Institute on Aging, and her coauthors.
The Testosterone Trials were supported by the National Institute on Aging, the National Heart, Lung, and Blood Institute, the National Institute of Neurological Diseases and Stroke, the National Institute of Child Health and Human Development, and AbbVie, which also provided the AndroGel, and placebo gel. Authors from the trials declared a range of funding, consultancies, and other support from the pharmaceutical industry, including AbbVie. One author declared a pending patent for a free testosterone calculator.
Today, 8 decades since the first clinical use of testosterone, the sole unequivocal indication for testosterone treatment is as replacement therapy for men with pathological hypogonadism (i.e., organic disorders of the reproductive system). Yet despite no proven new indications, global testosterone sales increased 100-fold over the last 3 decades, including increases of 40-fold in Canada and 10-fold in the United States from 2000 to 2011.
Overall, the findings from subtrials of the TTrials do not materially change the unfavorable balance of safety and efficacy to initiate testosterone treatment for age-related hypogonadism. With the results of the studies by Resnick et al. and by Budoff et al. in this issue of JAMA, the hopes for testosterone-led rejuvenation for older men are dimmed and disappointed if not yet finally dashed.
David J. Handelsman, MD, is from the ANZAC Research Institute, University of Sydney and Concord Hospital, Australia. These comments are taken from an editorial (JAMA 2017 Feb 21;317:699-701). Dr. Handelsman reported grants from Lawley Pharmaceuticals and Besins Healthcare and serving as a medical expert in testosterone litigation.
Today, 8 decades since the first clinical use of testosterone, the sole unequivocal indication for testosterone treatment is as replacement therapy for men with pathological hypogonadism (i.e., organic disorders of the reproductive system). Yet despite no proven new indications, global testosterone sales increased 100-fold over the last 3 decades, including increases of 40-fold in Canada and 10-fold in the United States from 2000 to 2011.
Overall, the findings from subtrials of the TTrials do not materially change the unfavorable balance of safety and efficacy to initiate testosterone treatment for age-related hypogonadism. With the results of the studies by Resnick et al. and by Budoff et al. in this issue of JAMA, the hopes for testosterone-led rejuvenation for older men are dimmed and disappointed if not yet finally dashed.
David J. Handelsman, MD, is from the ANZAC Research Institute, University of Sydney and Concord Hospital, Australia. These comments are taken from an editorial (JAMA 2017 Feb 21;317:699-701). Dr. Handelsman reported grants from Lawley Pharmaceuticals and Besins Healthcare and serving as a medical expert in testosterone litigation.
Today, 8 decades since the first clinical use of testosterone, the sole unequivocal indication for testosterone treatment is as replacement therapy for men with pathological hypogonadism (i.e., organic disorders of the reproductive system). Yet despite no proven new indications, global testosterone sales increased 100-fold over the last 3 decades, including increases of 40-fold in Canada and 10-fold in the United States from 2000 to 2011.
Overall, the findings from subtrials of the TTrials do not materially change the unfavorable balance of safety and efficacy to initiate testosterone treatment for age-related hypogonadism. With the results of the studies by Resnick et al. and by Budoff et al. in this issue of JAMA, the hopes for testosterone-led rejuvenation for older men are dimmed and disappointed if not yet finally dashed.
David J. Handelsman, MD, is from the ANZAC Research Institute, University of Sydney and Concord Hospital, Australia. These comments are taken from an editorial (JAMA 2017 Feb 21;317:699-701). Dr. Handelsman reported grants from Lawley Pharmaceuticals and Besins Healthcare and serving as a medical expert in testosterone litigation.
Testosterone treatment may have beneficial effects on unexplained anemia or bone density in men with age-related low testosterone, but at the cost of an increase in coronary artery plaque and with no benefit on cognitive function, new research suggests.
The results of four of the seven Testosterone Trials were published Feb. 21 in JAMA and JAMA Internal Medicine, adding to a growing body of research on the impact of testosterone supplementation but without finding clear evidence of an overall benefit.
In the double-blind, multicenter Anemia Trial, 788 men aged 65 years or older with average testosterone levels of less than 275 ng/dL were allocated to 12 months of testosterone gel or placebo. The group included 126 individuals with a hemoglobin level at or below 12.7 g/dL (JAMA Intern Med. 2017 Feb 21. doi: 10.1001/jamainternmed.2016.9540).
The study found that significantly more men who received testosterone treatment experienced increases in hemoglobin concentration of 1 g/dL or more above baseline, compared with those who received the placebo gel (54% vs. 15%; 95% CI 3.7-277.8; P = .002).
This effect was seen in men with known causes of anemia, such as myelodysplasia, iron deficiency, B12 deficiency, or chronic inflammation or disease; in men with anemia of unknown case; and in men who weren’t anemic.
After 12 months, more than half of the testosterone-treated men who started the study with unexplained anemia were no longer anemic, compared with around one-quarter of the placebo-treated men (58.3% vs. 22.2%). The men treated with placebo also had lower average hemoglobin level changes, compared with those treated with testosterone.
“Increases in hemoglobin levels were positively and significantly associated with participants’ global impression of change in overall health and energy,” wrote Cindy N. Roy, PhD, of Johns Hopkins University, Baltimore, and her coauthors.
Bone mineral density
A second trial examined the effect of 12 months of testosterone gel or placebo on bone mineral density in a group of 211 men with average testosterone concentrations less than 275 ng/L (JAMA Intern Med. 2017 Feb 21. doi: 10.1001/jamainternmed.2016.9539). The treatment increased median serum concentrations of total testosterone, free testosterone, and estradiol to within the normal ranges for young men.
The study showed significantly greater increases – measured by quantitative computed tomography – with testosterone treatment, compared with placebo, in spine trabecular, spine peripheral, hip trabecular, and peripheral volumetric bone mineral density, as well as in mean estimated strength of spine trabecular bone, spine peripheral bone, and hip trabecular and peripheral bone.
For the primary outcome of mean lumbar spine trabecular volumetric bone mineral density, testosterone treatment was associated with a mean increase of 7.5%, compared with a 0.8% increase with placebo.
Researchers also noted that the magnitude of the increase in spine trabecular bone mineral density from baseline was significantly associated with changes in total testosterone and estradiol.
However, there were no significant differences in fracture rate, with six fractures reported in each group during the year of treatment. In the observation year after treatment, three fractures were reported in the testosterone arm and four in the placebo arm.
“These results are unequivocal compared with prior studies of the effect of testosterone treatment on bone in older men, in spite of treatment limited to 1 year, perhaps because the mean pretreatment testosterone level was lower and the sample size larger than in prior studies, and because the primary outcome in this trial was vBMD by QCT,” wrote Peter J. Snyder, MD, of the University of Pennsylvania, Philadelphia, and his coauthors.
Coronary artery plaque
However, a third trial – this one in 170 men with low testosterone and symptoms suggestive of hypogonadism – found significantly greater increases in noncalcified plaque volume, median total plaque volume, and median coronary artery calcification score among the 88 men assigned to 12 months of testosterone gel, compared with those assigned to placebo.
The men treated with testosterone showed a mean increase in noncalcified coronary artery plaque volume of 40 mm3, compared with 4 mm3 in men given the placebo gel, and a mean increase in total plaque volume of 57 mm3 with testosterone and 21 mm3 with placebo (JAMA. 2017 Feb 21;317[7]:708-16).
There were no significant differences between the groups in change to coronary artery calcium score, and there were no adverse cardiovascular events reported in either group, despite the fact that around half the participants had severe atherosclerosis at baseline.
“The increase in coronary artery noncalcified and total plaque volumes in men treated with testosterone is concerning, because any limitation of the vascular lumen could be considered deleterious,” wrote Matthew J. Budoff, MD, of the Los Angeles Biomedical Research Institute, Torrance, Calif., and his coauthors. “The clinical significance of these increases could depend on the differential effects of testosterone on the individual components of noncalcified plaque.”
However, the investigators pointed out that the trial was neither large enough nor long enough to draw conclusions about the cardiovascular risks of testosterone treatment, and they called for larger studies to explore the association.
Cognitive function
The fourth study looked at mean change in cognitive function from baseline in 493 men with a serum testosterone level less than 275 ng/dL, impaired sexual function, physical function, or vitality, and who met the criteria for age-associated memory impairment. Half the participants were assigned to 12 months of testosterone gel, and half were assigned to placebo gel (JAMA. 2017 Feb 21;317[7]:717-27).
Researchers found no significant differences between the two groups from baseline to 6 months and 12 months in mean change in delayed paragraph recall score, visual memory, executive function, or spatial ability.
“The lack of association between testosterone treatment and cognition was apparent across all cognitive domains assessed among men with [age-associated memory impairment], in spite of an increase in circulating total and free testosterone concentrations in the testosterone group to levels typical of men aged 19-40 years,” wrote Susan M. Resnick, PhD, of the National Institute on Aging, and her coauthors.
The Testosterone Trials were supported by the National Institute on Aging, the National Heart, Lung, and Blood Institute, the National Institute of Neurological Diseases and Stroke, the National Institute of Child Health and Human Development, and AbbVie, which also provided the AndroGel, and placebo gel. Authors from the trials declared a range of funding, consultancies, and other support from the pharmaceutical industry, including AbbVie. One author declared a pending patent for a free testosterone calculator.
Testosterone treatment may have beneficial effects on unexplained anemia or bone density in men with age-related low testosterone, but at the cost of an increase in coronary artery plaque and with no benefit on cognitive function, new research suggests.
The results of four of the seven Testosterone Trials were published Feb. 21 in JAMA and JAMA Internal Medicine, adding to a growing body of research on the impact of testosterone supplementation but without finding clear evidence of an overall benefit.
In the double-blind, multicenter Anemia Trial, 788 men aged 65 years or older with average testosterone levels of less than 275 ng/dL were allocated to 12 months of testosterone gel or placebo. The group included 126 individuals with a hemoglobin level at or below 12.7 g/dL (JAMA Intern Med. 2017 Feb 21. doi: 10.1001/jamainternmed.2016.9540).
The study found that significantly more men who received testosterone treatment experienced increases in hemoglobin concentration of 1 g/dL or more above baseline, compared with those who received the placebo gel (54% vs. 15%; 95% CI 3.7-277.8; P = .002).
This effect was seen in men with known causes of anemia, such as myelodysplasia, iron deficiency, B12 deficiency, or chronic inflammation or disease; in men with anemia of unknown case; and in men who weren’t anemic.
After 12 months, more than half of the testosterone-treated men who started the study with unexplained anemia were no longer anemic, compared with around one-quarter of the placebo-treated men (58.3% vs. 22.2%). The men treated with placebo also had lower average hemoglobin level changes, compared with those treated with testosterone.
“Increases in hemoglobin levels were positively and significantly associated with participants’ global impression of change in overall health and energy,” wrote Cindy N. Roy, PhD, of Johns Hopkins University, Baltimore, and her coauthors.
Bone mineral density
A second trial examined the effect of 12 months of testosterone gel or placebo on bone mineral density in a group of 211 men with average testosterone concentrations less than 275 ng/L (JAMA Intern Med. 2017 Feb 21. doi: 10.1001/jamainternmed.2016.9539). The treatment increased median serum concentrations of total testosterone, free testosterone, and estradiol to within the normal ranges for young men.
The study showed significantly greater increases – measured by quantitative computed tomography – with testosterone treatment, compared with placebo, in spine trabecular, spine peripheral, hip trabecular, and peripheral volumetric bone mineral density, as well as in mean estimated strength of spine trabecular bone, spine peripheral bone, and hip trabecular and peripheral bone.
For the primary outcome of mean lumbar spine trabecular volumetric bone mineral density, testosterone treatment was associated with a mean increase of 7.5%, compared with a 0.8% increase with placebo.
Researchers also noted that the magnitude of the increase in spine trabecular bone mineral density from baseline was significantly associated with changes in total testosterone and estradiol.
However, there were no significant differences in fracture rate, with six fractures reported in each group during the year of treatment. In the observation year after treatment, three fractures were reported in the testosterone arm and four in the placebo arm.
“These results are unequivocal compared with prior studies of the effect of testosterone treatment on bone in older men, in spite of treatment limited to 1 year, perhaps because the mean pretreatment testosterone level was lower and the sample size larger than in prior studies, and because the primary outcome in this trial was vBMD by QCT,” wrote Peter J. Snyder, MD, of the University of Pennsylvania, Philadelphia, and his coauthors.
Coronary artery plaque
However, a third trial – this one in 170 men with low testosterone and symptoms suggestive of hypogonadism – found significantly greater increases in noncalcified plaque volume, median total plaque volume, and median coronary artery calcification score among the 88 men assigned to 12 months of testosterone gel, compared with those assigned to placebo.
The men treated with testosterone showed a mean increase in noncalcified coronary artery plaque volume of 40 mm3, compared with 4 mm3 in men given the placebo gel, and a mean increase in total plaque volume of 57 mm3 with testosterone and 21 mm3 with placebo (JAMA. 2017 Feb 21;317[7]:708-16).
There were no significant differences between the groups in change to coronary artery calcium score, and there were no adverse cardiovascular events reported in either group, despite the fact that around half the participants had severe atherosclerosis at baseline.
“The increase in coronary artery noncalcified and total plaque volumes in men treated with testosterone is concerning, because any limitation of the vascular lumen could be considered deleterious,” wrote Matthew J. Budoff, MD, of the Los Angeles Biomedical Research Institute, Torrance, Calif., and his coauthors. “The clinical significance of these increases could depend on the differential effects of testosterone on the individual components of noncalcified plaque.”
However, the investigators pointed out that the trial was neither large enough nor long enough to draw conclusions about the cardiovascular risks of testosterone treatment, and they called for larger studies to explore the association.
Cognitive function
The fourth study looked at mean change in cognitive function from baseline in 493 men with a serum testosterone level less than 275 ng/dL, impaired sexual function, physical function, or vitality, and who met the criteria for age-associated memory impairment. Half the participants were assigned to 12 months of testosterone gel, and half were assigned to placebo gel (JAMA. 2017 Feb 21;317[7]:717-27).
Researchers found no significant differences between the two groups from baseline to 6 months and 12 months in mean change in delayed paragraph recall score, visual memory, executive function, or spatial ability.
“The lack of association between testosterone treatment and cognition was apparent across all cognitive domains assessed among men with [age-associated memory impairment], in spite of an increase in circulating total and free testosterone concentrations in the testosterone group to levels typical of men aged 19-40 years,” wrote Susan M. Resnick, PhD, of the National Institute on Aging, and her coauthors.
The Testosterone Trials were supported by the National Institute on Aging, the National Heart, Lung, and Blood Institute, the National Institute of Neurological Diseases and Stroke, the National Institute of Child Health and Human Development, and AbbVie, which also provided the AndroGel, and placebo gel. Authors from the trials declared a range of funding, consultancies, and other support from the pharmaceutical industry, including AbbVie. One author declared a pending patent for a free testosterone calculator.
FROM JAMA AND JAMA INTERNAL MEDICINE
Key clinical point: Testosterone treatment may have beneficial effects on unexplained anemia or bone density in men with age-related low testosterone, but at the cost of an increase in coronary artery plaque and with no benefit for cognitive function.
Major finding: Testosterone treatment was associated with significantly greater increases in bone mineral density, hemoglobin, and noncalcified coronary artery plaque, compared with placebo, but no significant effects on cognitive function.
Data source: The Testosterone Trials in men aged 65 years or older with age-related testosterone decline.
Disclosures: The Testosterone Trials were supported by the National Institute on Aging, the National Heart, Lung, and Blood Institute, the National Institute of Neurological Diseases and Stroke, the National Institute of Child Health and Human Development, and AbbVie, which provided the AndroGel and placebo gel. Authors from the trials declared a range of funding, consultancies, and other support from the pharmaceutical industry, including AbbVie. One author declared a pending patent for a free testosterone calculator.
Comparison of immunosuppressants for early diffuse systemic sclerosis yields mixed results
Placing patients who have early diffuse cutaneous systemic sclerosis (dcSSc ) on an immunosuppressant regimen can have a beneficial, but not necessarily sustainable, impact, according to findings from the European Scleroderma Observational Study.
“At present, there is no drug known to favorably influence disease course [because] randomized controlled trials have historically been confounded by disease rarity [and] strict entry criteria,” wrote the study investigators – led by Ariane L. Herrick, MD, of the University of Manchester (England). They sought to get around the lack of randomized, controlled trial data by comparing observational data on “the effectiveness of standard treatment approaches [in] the early management of patients with dcSSc.”
The patients receiving methotrexate had a target dose of 20-25 mg/week, either orally or subcutaneously. Patients on MMF were given two 500-mg doses a day for 2 weeks, then two 1-g doses daily. Cyclophosphamide regimens varied based on the centers, with some patients receiving one IV 500-mg/m2 dose monthly for 6-12 months and others receiving a daily dose of 1-2 mg/kg/day orally for 12 months, with most being transferred later to maintenance with methotrexate, MMF, or azathioprine. All patients underwent assessment at baseline and then every 3 months for the trial duration of 24 months; however, because the study occurred during 2010-2014 and some patients were recruited in 2013, those who joined after September 2013 were followed for only 12-24 months. Of the 326 subjects enrolled, 276 completed 12 months of follow-up and 234 completed 24 months (Ann Rheum Dis. 2017 Feb 10. doi: 10.1136/annrheumdis-2016-210503).
After weighting the 12-month outcomes between the groups by equalizing the distribution of confounding variables, all groups experienced a significant reduction in the study’s primary outcome measure, the modified Rodnan skin score (mRSS), which can range from 0 to 51. From a median baseline mRSS of 21 (interquartile range of 16-27), the mRSS for the methotrexate group fell 4.0 (IQR −5.2 to −2.7), for those on MMF it dropped 4.1 (IQR −5.3 to −2.9), for the cyclophosphamide group it decreased 3.3 (IQR −4.9 to −1.7), and for those on no immunosuppressants it dropped 2.2 (IQR −4.0 to −0.3). There were no significant differences between the groups.
Although none of the treatments had a significant effect on improving forced vital capacity (FVC) or carbon monoxide–diffusing capacity in the groups overall, the subgroup of patients with confirmed or suspected pulmonary fibrosis showed a significant difference in the rate of change over time for FVC in patients who were initially prescribed cyclophosphamide (7.4% absolute increase), but not for MMF (3.2% increase), methotrexate (2.0% decrease), or no immunosuppressant (4.0% increase). The investigators noted that this finding “confirms the relative effectiveness of cyclophosphamide in patients with pulmonary fibrosis.”
At 24 months, there were no significant differences in mortality between the four groups. After weighting, the predicted survival rates were 94% for methotrexate, 89% for MMF, 90% for cyclophosphamide, and 84% for those with no immunosuppressants. All three immunosuppressants also showed no significant difference in terms of tolerability. At this point in time, the rate of adherence to the initial protocol was comparable between the groups: 76% for methotrexate, 80% for MMF, 79% for cyclophosphamide, and 73% for those not taking an immunosuppressant, although 10 who started without an immunosuppressant later started one.
“An important point when interpreting our findings (and therefore a note of caution) is that the ‘no immunosuppressant’ group was not a control group,” Dr. Herrick and her coauthors wrote. “Patients in this group had a longer disease duration than the other three groups and were more likely to have renal involvement.”
Nevertheless, the authors contend that these findings carry a strong take-home message for clinicians: “There is a weak signal to support using immunosuppressants for early dcSSc (and in particular cyclophosphamide for patients with pulmonary fibrosis). However, it is clear that there remains a pressing need for the development of more effective and targeted treatments.”
The study was funded by a grant from the European League Against Rheumatism’s Orphan Disease Program, and additional support from Scleroderma and Raynaud’s UK. Dr. Herrick disclosed relationships with Actelion, Apricus, and GlaxoSmithKline; her coauthors disclosed numerous financial relationships of their own.
Placing patients who have early diffuse cutaneous systemic sclerosis (dcSSc ) on an immunosuppressant regimen can have a beneficial, but not necessarily sustainable, impact, according to findings from the European Scleroderma Observational Study.
“At present, there is no drug known to favorably influence disease course [because] randomized controlled trials have historically been confounded by disease rarity [and] strict entry criteria,” wrote the study investigators – led by Ariane L. Herrick, MD, of the University of Manchester (England). They sought to get around the lack of randomized, controlled trial data by comparing observational data on “the effectiveness of standard treatment approaches [in] the early management of patients with dcSSc.”
The patients receiving methotrexate had a target dose of 20-25 mg/week, either orally or subcutaneously. Patients on MMF were given two 500-mg doses a day for 2 weeks, then two 1-g doses daily. Cyclophosphamide regimens varied based on the centers, with some patients receiving one IV 500-mg/m2 dose monthly for 6-12 months and others receiving a daily dose of 1-2 mg/kg/day orally for 12 months, with most being transferred later to maintenance with methotrexate, MMF, or azathioprine. All patients underwent assessment at baseline and then every 3 months for the trial duration of 24 months; however, because the study occurred during 2010-2014 and some patients were recruited in 2013, those who joined after September 2013 were followed for only 12-24 months. Of the 326 subjects enrolled, 276 completed 12 months of follow-up and 234 completed 24 months (Ann Rheum Dis. 2017 Feb 10. doi: 10.1136/annrheumdis-2016-210503).
After weighting the 12-month outcomes between the groups by equalizing the distribution of confounding variables, all groups experienced a significant reduction in the study’s primary outcome measure, the modified Rodnan skin score (mRSS), which can range from 0 to 51. From a median baseline mRSS of 21 (interquartile range of 16-27), the mRSS for the methotrexate group fell 4.0 (IQR −5.2 to −2.7), for those on MMF it dropped 4.1 (IQR −5.3 to −2.9), for the cyclophosphamide group it decreased 3.3 (IQR −4.9 to −1.7), and for those on no immunosuppressants it dropped 2.2 (IQR −4.0 to −0.3). There were no significant differences between the groups.
Although none of the treatments had a significant effect on improving forced vital capacity (FVC) or carbon monoxide–diffusing capacity in the groups overall, the subgroup of patients with confirmed or suspected pulmonary fibrosis showed a significant difference in the rate of change over time for FVC in patients who were initially prescribed cyclophosphamide (7.4% absolute increase), but not for MMF (3.2% increase), methotrexate (2.0% decrease), or no immunosuppressant (4.0% increase). The investigators noted that this finding “confirms the relative effectiveness of cyclophosphamide in patients with pulmonary fibrosis.”
At 24 months, there were no significant differences in mortality between the four groups. After weighting, the predicted survival rates were 94% for methotrexate, 89% for MMF, 90% for cyclophosphamide, and 84% for those with no immunosuppressants. All three immunosuppressants also showed no significant difference in terms of tolerability. At this point in time, the rate of adherence to the initial protocol was comparable between the groups: 76% for methotrexate, 80% for MMF, 79% for cyclophosphamide, and 73% for those not taking an immunosuppressant, although 10 who started without an immunosuppressant later started one.
“An important point when interpreting our findings (and therefore a note of caution) is that the ‘no immunosuppressant’ group was not a control group,” Dr. Herrick and her coauthors wrote. “Patients in this group had a longer disease duration than the other three groups and were more likely to have renal involvement.”
Nevertheless, the authors contend that these findings carry a strong take-home message for clinicians: “There is a weak signal to support using immunosuppressants for early dcSSc (and in particular cyclophosphamide for patients with pulmonary fibrosis). However, it is clear that there remains a pressing need for the development of more effective and targeted treatments.”
The study was funded by a grant from the European League Against Rheumatism’s Orphan Disease Program, and additional support from Scleroderma and Raynaud’s UK. Dr. Herrick disclosed relationships with Actelion, Apricus, and GlaxoSmithKline; her coauthors disclosed numerous financial relationships of their own.
Placing patients who have early diffuse cutaneous systemic sclerosis (dcSSc ) on an immunosuppressant regimen can have a beneficial, but not necessarily sustainable, impact, according to findings from the European Scleroderma Observational Study.
“At present, there is no drug known to favorably influence disease course [because] randomized controlled trials have historically been confounded by disease rarity [and] strict entry criteria,” wrote the study investigators – led by Ariane L. Herrick, MD, of the University of Manchester (England). They sought to get around the lack of randomized, controlled trial data by comparing observational data on “the effectiveness of standard treatment approaches [in] the early management of patients with dcSSc.”
The patients receiving methotrexate had a target dose of 20-25 mg/week, either orally or subcutaneously. Patients on MMF were given two 500-mg doses a day for 2 weeks, then two 1-g doses daily. Cyclophosphamide regimens varied based on the centers, with some patients receiving one IV 500-mg/m2 dose monthly for 6-12 months and others receiving a daily dose of 1-2 mg/kg/day orally for 12 months, with most being transferred later to maintenance with methotrexate, MMF, or azathioprine. All patients underwent assessment at baseline and then every 3 months for the trial duration of 24 months; however, because the study occurred during 2010-2014 and some patients were recruited in 2013, those who joined after September 2013 were followed for only 12-24 months. Of the 326 subjects enrolled, 276 completed 12 months of follow-up and 234 completed 24 months (Ann Rheum Dis. 2017 Feb 10. doi: 10.1136/annrheumdis-2016-210503).
After weighting the 12-month outcomes between the groups by equalizing the distribution of confounding variables, all groups experienced a significant reduction in the study’s primary outcome measure, the modified Rodnan skin score (mRSS), which can range from 0 to 51. From a median baseline mRSS of 21 (interquartile range of 16-27), the mRSS for the methotrexate group fell 4.0 (IQR −5.2 to −2.7), for those on MMF it dropped 4.1 (IQR −5.3 to −2.9), for the cyclophosphamide group it decreased 3.3 (IQR −4.9 to −1.7), and for those on no immunosuppressants it dropped 2.2 (IQR −4.0 to −0.3). There were no significant differences between the groups.
Although none of the treatments had a significant effect on improving forced vital capacity (FVC) or carbon monoxide–diffusing capacity in the groups overall, the subgroup of patients with confirmed or suspected pulmonary fibrosis showed a significant difference in the rate of change over time for FVC in patients who were initially prescribed cyclophosphamide (7.4% absolute increase), but not for MMF (3.2% increase), methotrexate (2.0% decrease), or no immunosuppressant (4.0% increase). The investigators noted that this finding “confirms the relative effectiveness of cyclophosphamide in patients with pulmonary fibrosis.”
At 24 months, there were no significant differences in mortality between the four groups. After weighting, the predicted survival rates were 94% for methotrexate, 89% for MMF, 90% for cyclophosphamide, and 84% for those with no immunosuppressants. All three immunosuppressants also showed no significant difference in terms of tolerability. At this point in time, the rate of adherence to the initial protocol was comparable between the groups: 76% for methotrexate, 80% for MMF, 79% for cyclophosphamide, and 73% for those not taking an immunosuppressant, although 10 who started without an immunosuppressant later started one.
“An important point when interpreting our findings (and therefore a note of caution) is that the ‘no immunosuppressant’ group was not a control group,” Dr. Herrick and her coauthors wrote. “Patients in this group had a longer disease duration than the other three groups and were more likely to have renal involvement.”
Nevertheless, the authors contend that these findings carry a strong take-home message for clinicians: “There is a weak signal to support using immunosuppressants for early dcSSc (and in particular cyclophosphamide for patients with pulmonary fibrosis). However, it is clear that there remains a pressing need for the development of more effective and targeted treatments.”
The study was funded by a grant from the European League Against Rheumatism’s Orphan Disease Program, and additional support from Scleroderma and Raynaud’s UK. Dr. Herrick disclosed relationships with Actelion, Apricus, and GlaxoSmithKline; her coauthors disclosed numerous financial relationships of their own.
FROM ANNALS OF THE RHEUMATIC DISEASES
Key clinical point:
Major finding: Subjects taking no immunosuppressants showed significant reduction in mRSS over 12 months (2.2; IQR, −4.0 to −0.3), but no significant difference in survival rates over 24 months.
Data source: A prospective, observational cohort study of 326 dcSSc patients recruited in 2010-2014.
Disclosures: Funded by EULAR and Scleroderma and Raynaud’s UK. Authors reported numerous financial relationships.
Infections boost postop wound dehiscence risk
SAN DIEGO – Pre- and postsurgical infections top the list of factors in putting patients at risk of wound dehiscence after laparotomy, a database study has found.
Before surgery, a contaminated or dirty wound and sepsis doubled the risk of a post-laparotomy dehiscence, Anam Pal*, MD, said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
After surgery, a deep wound infection raised the risk by more than four times, and a superficial wound infection almost tripled the risk, said Dr. Pal, a second-year surgical resident at Hofstra Northwell School of Medicine at Staten Island University Hospital Program, New York.*
“Since infections are the strongest predictors, we need more aggressive efforts to prevent surgical site infections in these patients,” she said. Any patient who displays these risk factors should have retention sutures placed during closing as an extra measure of precaution against the potentially devastating complication.
Dr. Pal said the time is right for a new risk model of wound dehiscence after abdominal laparotomy. The existing predictive tool is almost 20 years old and was validated in the Veterans Affairs Surgical Quality Improvement Program database.
“This risk score was created using patient data gathered from 1996 to 1998 on the VA population. We know that this group is older and sicker than the general population,” she said. In fact, she ran that calculation on her own dataset and found that it “grossly overestimated” the risk of wound dehiscence in a general population. “This raises questions about the generalizability of that score.”
Among the 18,306 exploratory laparotomies in Dr. Pal’s dataset, there were 275 cases of wound dehiscence, for a rate of 1.5%.
There were striking baseline differences between the patient groups, she noted. Generally, patients with wound dehiscence were sicker and frailer than those without. “There was significantly more smoking, chronic obstructive pulmonary disease, diabetes, pneumonia and ventilator placement, obesity, and disseminated malignancy.”
She also noted significantly higher rates of wound infection and steroid use. Patients with dehiscence were significantly less likely to have lost weight during the 6 months before their laparotomy as well.
They were more likely to have sepsis or septic shock, to present emergently, and to have had a surgery within the 30 days prior. Functionally, they were significantly more likely to be rated as “totally dependent.”
A multivariate analysis identified six preoperative and four postoperative risk factors:
Preoperative
• Contaminated/dirty wound – odds ratio 2.00.
• Sepsis/septic shock – OR 1.85.
• Totally dependent status – OR 1.8.
• Male gender – OR 1.6.
• ASA class 3 or greater – OR 1.4.
• Smoking – OR 1.3.
• Weight loss protective – OR 0.44.
Postoperative
• Deep wound infection – OR 4.25.
• Superficial wound infection – OR 2.76.
• Reintubation – OR 2.38.
• Deep space infection – OR 1.67.
The investigators then split the data randomly into a 75% training cohort and 25% validation cohort. A receiver operator curve analysis determined that both cohorts had an AUC of around 0.70, meaning that the model was a moderate-good predictor of wound dehiscence.
“Our predictive model is just as good as the one that was developed 20 years ago,” and potentially, more appropriate for a general population, Dr. Pal concluded.
She had no financial disclosures.
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
*An earlier version of this article misstated Dr. Pal's name and affiliation.
SAN DIEGO – Pre- and postsurgical infections top the list of factors in putting patients at risk of wound dehiscence after laparotomy, a database study has found.
Before surgery, a contaminated or dirty wound and sepsis doubled the risk of a post-laparotomy dehiscence, Anam Pal*, MD, said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
After surgery, a deep wound infection raised the risk by more than four times, and a superficial wound infection almost tripled the risk, said Dr. Pal, a second-year surgical resident at Hofstra Northwell School of Medicine at Staten Island University Hospital Program, New York.*
“Since infections are the strongest predictors, we need more aggressive efforts to prevent surgical site infections in these patients,” she said. Any patient who displays these risk factors should have retention sutures placed during closing as an extra measure of precaution against the potentially devastating complication.
Dr. Pal said the time is right for a new risk model of wound dehiscence after abdominal laparotomy. The existing predictive tool is almost 20 years old and was validated in the Veterans Affairs Surgical Quality Improvement Program database.
“This risk score was created using patient data gathered from 1996 to 1998 on the VA population. We know that this group is older and sicker than the general population,” she said. In fact, she ran that calculation on her own dataset and found that it “grossly overestimated” the risk of wound dehiscence in a general population. “This raises questions about the generalizability of that score.”
Among the 18,306 exploratory laparotomies in Dr. Pal’s dataset, there were 275 cases of wound dehiscence, for a rate of 1.5%.
There were striking baseline differences between the patient groups, she noted. Generally, patients with wound dehiscence were sicker and frailer than those without. “There was significantly more smoking, chronic obstructive pulmonary disease, diabetes, pneumonia and ventilator placement, obesity, and disseminated malignancy.”
She also noted significantly higher rates of wound infection and steroid use. Patients with dehiscence were significantly less likely to have lost weight during the 6 months before their laparotomy as well.
They were more likely to have sepsis or septic shock, to present emergently, and to have had a surgery within the 30 days prior. Functionally, they were significantly more likely to be rated as “totally dependent.”
A multivariate analysis identified six preoperative and four postoperative risk factors:
Preoperative
• Contaminated/dirty wound – odds ratio 2.00.
• Sepsis/septic shock – OR 1.85.
• Totally dependent status – OR 1.8.
• Male gender – OR 1.6.
• ASA class 3 or greater – OR 1.4.
• Smoking – OR 1.3.
• Weight loss protective – OR 0.44.
Postoperative
• Deep wound infection – OR 4.25.
• Superficial wound infection – OR 2.76.
• Reintubation – OR 2.38.
• Deep space infection – OR 1.67.
The investigators then split the data randomly into a 75% training cohort and 25% validation cohort. A receiver operator curve analysis determined that both cohorts had an AUC of around 0.70, meaning that the model was a moderate-good predictor of wound dehiscence.
“Our predictive model is just as good as the one that was developed 20 years ago,” and potentially, more appropriate for a general population, Dr. Pal concluded.
She had no financial disclosures.
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
*An earlier version of this article misstated Dr. Pal's name and affiliation.
SAN DIEGO – Pre- and postsurgical infections top the list of factors in putting patients at risk of wound dehiscence after laparotomy, a database study has found.
Before surgery, a contaminated or dirty wound and sepsis doubled the risk of a post-laparotomy dehiscence, Anam Pal*, MD, said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
After surgery, a deep wound infection raised the risk by more than four times, and a superficial wound infection almost tripled the risk, said Dr. Pal, a second-year surgical resident at Hofstra Northwell School of Medicine at Staten Island University Hospital Program, New York.*
“Since infections are the strongest predictors, we need more aggressive efforts to prevent surgical site infections in these patients,” she said. Any patient who displays these risk factors should have retention sutures placed during closing as an extra measure of precaution against the potentially devastating complication.
Dr. Pal said the time is right for a new risk model of wound dehiscence after abdominal laparotomy. The existing predictive tool is almost 20 years old and was validated in the Veterans Affairs Surgical Quality Improvement Program database.
“This risk score was created using patient data gathered from 1996 to 1998 on the VA population. We know that this group is older and sicker than the general population,” she said. In fact, she ran that calculation on her own dataset and found that it “grossly overestimated” the risk of wound dehiscence in a general population. “This raises questions about the generalizability of that score.”
Among the 18,306 exploratory laparotomies in Dr. Pal’s dataset, there were 275 cases of wound dehiscence, for a rate of 1.5%.
There were striking baseline differences between the patient groups, she noted. Generally, patients with wound dehiscence were sicker and frailer than those without. “There was significantly more smoking, chronic obstructive pulmonary disease, diabetes, pneumonia and ventilator placement, obesity, and disseminated malignancy.”
She also noted significantly higher rates of wound infection and steroid use. Patients with dehiscence were significantly less likely to have lost weight during the 6 months before their laparotomy as well.
They were more likely to have sepsis or septic shock, to present emergently, and to have had a surgery within the 30 days prior. Functionally, they were significantly more likely to be rated as “totally dependent.”
A multivariate analysis identified six preoperative and four postoperative risk factors:
Preoperative
• Contaminated/dirty wound – odds ratio 2.00.
• Sepsis/septic shock – OR 1.85.
• Totally dependent status – OR 1.8.
• Male gender – OR 1.6.
• ASA class 3 or greater – OR 1.4.
• Smoking – OR 1.3.
• Weight loss protective – OR 0.44.
Postoperative
• Deep wound infection – OR 4.25.
• Superficial wound infection – OR 2.76.
• Reintubation – OR 2.38.
• Deep space infection – OR 1.67.
The investigators then split the data randomly into a 75% training cohort and 25% validation cohort. A receiver operator curve analysis determined that both cohorts had an AUC of around 0.70, meaning that the model was a moderate-good predictor of wound dehiscence.
“Our predictive model is just as good as the one that was developed 20 years ago,” and potentially, more appropriate for a general population, Dr. Pal concluded.
She had no financial disclosures.
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
*An earlier version of this article misstated Dr. Pal's name and affiliation.
AT THE ACADEMIC SURGICAL CONGRESS
Key clinical point:
Major finding: Deep wound infection quadrupled the risk of wound dehiscence and superficial wound infection almost tripled it.
Data source: The ACS NSQIP review comprised more than 18,000 operations.
Disclosures: Dr. Pal had no financial disclosures.
Mycobacterium tuberculosis: Overcoming one obstacle on the road to elimination
March 24 is World TB Day. It was on this date in 1882 that physician Robert Koch announced the discovery of Mycobacterium tuberculosis, the causative agent of tuberculosis. Worldwide, activities are planned to raise awareness of TB and to support initiatives for prevention, better control, and ultimately the elimination of this disease.
Globally in 2015, the World Health Organization estimated there were 10.4 million new cases of TB, including 1 million in children. Data from the United States reveal that after 20 years of annual decline, the incidence of TB has plateaued. In 2015, 9,563 cases of TB disease were reported, including 440 cases in children less than 15 years of age. While the overall incidence was 3 cases per 100,000, the incidence among foreign-born persons was 15.1 cases per 100,000. There were 3,201 cases (33.5%) among U.S.-born individuals. Foreign-born persons accounted for 66.2% of cases; however, the majority of those cases were diagnosed several years after their arrival in the United States. The top five countries of origin of these individuals were China, India, Mexico, the Philippines, and Vietnam. In contrast, only one-quarter of all pediatric cases occurred in foreign-born children. Four states (California, Florida, New York, and Texas) reported more than 500 cases each in 2015, as they have for the last 7 consecutive years. In 2015, these states accounted for slightly more than half (4,839) of all cases (MMWR 2016 Mar 25;65[11]:273-8).
Why as pediatricians should we be concerned? TB in a child is a sentinel event and represents recent or ongoing transmission. Young children who are infected are more likely to progress to TB disease and develop severe manifestations such as miliary TB or meningitis. Children less than 4 years old and those with certain underlying disorders, including those with an immunodeficiency or who are receiving immunosuppressive agents, also are at greater risk for progression from infection to disease. Other predictors of disease progression include diagnosis of the infection within the past 2 years, use of chemotherapy and high-dose corticosteroids, as well as certain cancers, diabetes, and chronic renal failure.
Once infected, most children and adolescents remain asymptomatic. If disease occurs, symptoms develop 1-6 months after infection and include fever, cough, weight loss or failure to thrive, night sweats, and chills. Chest radiographic findings are nonspecific. Infiltrates and intrathoracic lymph node enlargement may or may not be present. However, our goal is to diagnose at-risk children with infection, treat them, and avoid their progression to TB disease.
Screening tests
The interferon-gamma release assay is a blood test that has a greater specificity than TST and requires only one visit. A positive test is seen in both latent TB infection and TB disease. There is no cross-reaction with BCG. This is the ideal test for prior BCG recipients and others who are unlikely to return for TST readings and are at least 5 years of age.
A chest radiograph is required to differentiate latent TB infection from TB disease. Latent TB infection is diagnosed when there is an absence of parenchymal disease, opacification, or intrathoracic adenopathy.
Treatment of latent TB infection versus TB disease is beyond the scope of this article. Consultation with an infectious disease expert is recommended.
For additional information and resources, go to www.cdc.gov/tb, and for a sample TB risk assessment tool, go to www.cdc.gov/tb/publications/ltbi/appendixa.htm.
As we mark the passing of another World TB Day, we have one goal – to identify, screen, and treat children and adolescents at risk for latent TB infection and help eliminate future cases of TB disease.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
March 24 is World TB Day. It was on this date in 1882 that physician Robert Koch announced the discovery of Mycobacterium tuberculosis, the causative agent of tuberculosis. Worldwide, activities are planned to raise awareness of TB and to support initiatives for prevention, better control, and ultimately the elimination of this disease.
Globally in 2015, the World Health Organization estimated there were 10.4 million new cases of TB, including 1 million in children. Data from the United States reveal that after 20 years of annual decline, the incidence of TB has plateaued. In 2015, 9,563 cases of TB disease were reported, including 440 cases in children less than 15 years of age. While the overall incidence was 3 cases per 100,000, the incidence among foreign-born persons was 15.1 cases per 100,000. There were 3,201 cases (33.5%) among U.S.-born individuals. Foreign-born persons accounted for 66.2% of cases; however, the majority of those cases were diagnosed several years after their arrival in the United States. The top five countries of origin of these individuals were China, India, Mexico, the Philippines, and Vietnam. In contrast, only one-quarter of all pediatric cases occurred in foreign-born children. Four states (California, Florida, New York, and Texas) reported more than 500 cases each in 2015, as they have for the last 7 consecutive years. In 2015, these states accounted for slightly more than half (4,839) of all cases (MMWR 2016 Mar 25;65[11]:273-8).
Why as pediatricians should we be concerned? TB in a child is a sentinel event and represents recent or ongoing transmission. Young children who are infected are more likely to progress to TB disease and develop severe manifestations such as miliary TB or meningitis. Children less than 4 years old and those with certain underlying disorders, including those with an immunodeficiency or who are receiving immunosuppressive agents, also are at greater risk for progression from infection to disease. Other predictors of disease progression include diagnosis of the infection within the past 2 years, use of chemotherapy and high-dose corticosteroids, as well as certain cancers, diabetes, and chronic renal failure.
Once infected, most children and adolescents remain asymptomatic. If disease occurs, symptoms develop 1-6 months after infection and include fever, cough, weight loss or failure to thrive, night sweats, and chills. Chest radiographic findings are nonspecific. Infiltrates and intrathoracic lymph node enlargement may or may not be present. However, our goal is to diagnose at-risk children with infection, treat them, and avoid their progression to TB disease.
Screening tests
The interferon-gamma release assay is a blood test that has a greater specificity than TST and requires only one visit. A positive test is seen in both latent TB infection and TB disease. There is no cross-reaction with BCG. This is the ideal test for prior BCG recipients and others who are unlikely to return for TST readings and are at least 5 years of age.
A chest radiograph is required to differentiate latent TB infection from TB disease. Latent TB infection is diagnosed when there is an absence of parenchymal disease, opacification, or intrathoracic adenopathy.
Treatment of latent TB infection versus TB disease is beyond the scope of this article. Consultation with an infectious disease expert is recommended.
For additional information and resources, go to www.cdc.gov/tb, and for a sample TB risk assessment tool, go to www.cdc.gov/tb/publications/ltbi/appendixa.htm.
As we mark the passing of another World TB Day, we have one goal – to identify, screen, and treat children and adolescents at risk for latent TB infection and help eliminate future cases of TB disease.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
March 24 is World TB Day. It was on this date in 1882 that physician Robert Koch announced the discovery of Mycobacterium tuberculosis, the causative agent of tuberculosis. Worldwide, activities are planned to raise awareness of TB and to support initiatives for prevention, better control, and ultimately the elimination of this disease.
Globally in 2015, the World Health Organization estimated there were 10.4 million new cases of TB, including 1 million in children. Data from the United States reveal that after 20 years of annual decline, the incidence of TB has plateaued. In 2015, 9,563 cases of TB disease were reported, including 440 cases in children less than 15 years of age. While the overall incidence was 3 cases per 100,000, the incidence among foreign-born persons was 15.1 cases per 100,000. There were 3,201 cases (33.5%) among U.S.-born individuals. Foreign-born persons accounted for 66.2% of cases; however, the majority of those cases were diagnosed several years after their arrival in the United States. The top five countries of origin of these individuals were China, India, Mexico, the Philippines, and Vietnam. In contrast, only one-quarter of all pediatric cases occurred in foreign-born children. Four states (California, Florida, New York, and Texas) reported more than 500 cases each in 2015, as they have for the last 7 consecutive years. In 2015, these states accounted for slightly more than half (4,839) of all cases (MMWR 2016 Mar 25;65[11]:273-8).
Why as pediatricians should we be concerned? TB in a child is a sentinel event and represents recent or ongoing transmission. Young children who are infected are more likely to progress to TB disease and develop severe manifestations such as miliary TB or meningitis. Children less than 4 years old and those with certain underlying disorders, including those with an immunodeficiency or who are receiving immunosuppressive agents, also are at greater risk for progression from infection to disease. Other predictors of disease progression include diagnosis of the infection within the past 2 years, use of chemotherapy and high-dose corticosteroids, as well as certain cancers, diabetes, and chronic renal failure.
Once infected, most children and adolescents remain asymptomatic. If disease occurs, symptoms develop 1-6 months after infection and include fever, cough, weight loss or failure to thrive, night sweats, and chills. Chest radiographic findings are nonspecific. Infiltrates and intrathoracic lymph node enlargement may or may not be present. However, our goal is to diagnose at-risk children with infection, treat them, and avoid their progression to TB disease.
Screening tests
The interferon-gamma release assay is a blood test that has a greater specificity than TST and requires only one visit. A positive test is seen in both latent TB infection and TB disease. There is no cross-reaction with BCG. This is the ideal test for prior BCG recipients and others who are unlikely to return for TST readings and are at least 5 years of age.
A chest radiograph is required to differentiate latent TB infection from TB disease. Latent TB infection is diagnosed when there is an absence of parenchymal disease, opacification, or intrathoracic adenopathy.
Treatment of latent TB infection versus TB disease is beyond the scope of this article. Consultation with an infectious disease expert is recommended.
For additional information and resources, go to www.cdc.gov/tb, and for a sample TB risk assessment tool, go to www.cdc.gov/tb/publications/ltbi/appendixa.htm.
As we mark the passing of another World TB Day, we have one goal – to identify, screen, and treat children and adolescents at risk for latent TB infection and help eliminate future cases of TB disease.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
Hot Threads in ACS Communities
Your colleagues already have a lot to say in 2017. Here are the top discussion threads in ACS Communities just prior to press time (communities in which the threads appear are listed in parentheses):
1. Music in the OR. (General Surgery)
2. Nephrologist to surgeon in 3 months! (General Surgery)
3. MACRA. (Advocacy)
4. Mini-fellowship – or how to “brush up” on trauma? (General Surgery)
5. Trauma/PEG for intubated polytrauma patient. (Trauma Surgery)
6. Students observing in OR. (General Surgery)
7. Pediatric appendectomy. (General Surgery)
8. Call-bladders. (General Surgery)
9. Physician rehabilitation. (General Surgery)
10. Letters to ACS Fellows, Members and Members of Congress. (Vascular Surgery)
To join communities, log in to ACS Communities at http://acscommunities.facs.org/home, go to “Browse All Communities” near the top of any page, and click the blue “Join” button next to the community you’d like to join. If you have any questions, please send them to acscommunities@facs.org.
Your colleagues already have a lot to say in 2017. Here are the top discussion threads in ACS Communities just prior to press time (communities in which the threads appear are listed in parentheses):
1. Music in the OR. (General Surgery)
2. Nephrologist to surgeon in 3 months! (General Surgery)
3. MACRA. (Advocacy)
4. Mini-fellowship – or how to “brush up” on trauma? (General Surgery)
5. Trauma/PEG for intubated polytrauma patient. (Trauma Surgery)
6. Students observing in OR. (General Surgery)
7. Pediatric appendectomy. (General Surgery)
8. Call-bladders. (General Surgery)
9. Physician rehabilitation. (General Surgery)
10. Letters to ACS Fellows, Members and Members of Congress. (Vascular Surgery)
To join communities, log in to ACS Communities at http://acscommunities.facs.org/home, go to “Browse All Communities” near the top of any page, and click the blue “Join” button next to the community you’d like to join. If you have any questions, please send them to acscommunities@facs.org.
Your colleagues already have a lot to say in 2017. Here are the top discussion threads in ACS Communities just prior to press time (communities in which the threads appear are listed in parentheses):
1. Music in the OR. (General Surgery)
2. Nephrologist to surgeon in 3 months! (General Surgery)
3. MACRA. (Advocacy)
4. Mini-fellowship – or how to “brush up” on trauma? (General Surgery)
5. Trauma/PEG for intubated polytrauma patient. (Trauma Surgery)
6. Students observing in OR. (General Surgery)
7. Pediatric appendectomy. (General Surgery)
8. Call-bladders. (General Surgery)
9. Physician rehabilitation. (General Surgery)
10. Letters to ACS Fellows, Members and Members of Congress. (Vascular Surgery)
To join communities, log in to ACS Communities at http://acscommunities.facs.org/home, go to “Browse All Communities” near the top of any page, and click the blue “Join” button next to the community you’d like to join. If you have any questions, please send them to acscommunities@facs.org.
Your colleagues already have a lot to say in 2017. Here are the top discussion threads in ACS Communities just prior to press time
FDA confirms complications from intragastric balloons
Complications from overinflation and acute pancreatitis can create problems for obesity patients treated with intragastric balloons, according to a statement from the Food and Drug Administration. In a letter to health care providers published on February 9, 2017, the FDA warned of the two specific issues that have been the subject of multiple adverse event reports.
“We recommend that you closely monitor patients with these devices for these adverse events, and to submit reports to help us better understand any complications from the use of these obesity treatment devices,” the letter said.
Most of the overinflation reports involved the Orbera Intragastric Balloon System (Apollo Endosurgery) that uses a single balloon, although some reports involved the ReShape Integrated Dual Balloon System (ReShape Medical) that uses two balloons. Neither product mentions overinflation risk in its labeling. “At this moment there is not enough information to determine what is causing the balloon to overinflate,” according to the FDA letter.
A separate set of adverse event reports noted the development of acute pancreatitis caused when the balloons compressed other gastrointestinal structures. Both the Orbera and ReShape products were associated with pancreatitis, although neither lists pancreatitis as a potential complication on their labels. Pancreatitis was reported as early as 3 days after implantation, and symptoms included severe back and abdominal pain.
The FDA letter recommends that health care providers consider overinflation and pancreatitis in their differential diagnoses of obesity patients with intragastric balloons who present with the symptoms described, and to report any type of serious adverse events associated with intragastric balloons to the FDA through the MedWatch program. For more information about reporting adverse events to the FDA, visit the MedWatch site.
Complications from overinflation and acute pancreatitis can create problems for obesity patients treated with intragastric balloons, according to a statement from the Food and Drug Administration. In a letter to health care providers published on February 9, 2017, the FDA warned of the two specific issues that have been the subject of multiple adverse event reports.
“We recommend that you closely monitor patients with these devices for these adverse events, and to submit reports to help us better understand any complications from the use of these obesity treatment devices,” the letter said.
Most of the overinflation reports involved the Orbera Intragastric Balloon System (Apollo Endosurgery) that uses a single balloon, although some reports involved the ReShape Integrated Dual Balloon System (ReShape Medical) that uses two balloons. Neither product mentions overinflation risk in its labeling. “At this moment there is not enough information to determine what is causing the balloon to overinflate,” according to the FDA letter.
A separate set of adverse event reports noted the development of acute pancreatitis caused when the balloons compressed other gastrointestinal structures. Both the Orbera and ReShape products were associated with pancreatitis, although neither lists pancreatitis as a potential complication on their labels. Pancreatitis was reported as early as 3 days after implantation, and symptoms included severe back and abdominal pain.
The FDA letter recommends that health care providers consider overinflation and pancreatitis in their differential diagnoses of obesity patients with intragastric balloons who present with the symptoms described, and to report any type of serious adverse events associated with intragastric balloons to the FDA through the MedWatch program. For more information about reporting adverse events to the FDA, visit the MedWatch site.
Complications from overinflation and acute pancreatitis can create problems for obesity patients treated with intragastric balloons, according to a statement from the Food and Drug Administration. In a letter to health care providers published on February 9, 2017, the FDA warned of the two specific issues that have been the subject of multiple adverse event reports.
“We recommend that you closely monitor patients with these devices for these adverse events, and to submit reports to help us better understand any complications from the use of these obesity treatment devices,” the letter said.
Most of the overinflation reports involved the Orbera Intragastric Balloon System (Apollo Endosurgery) that uses a single balloon, although some reports involved the ReShape Integrated Dual Balloon System (ReShape Medical) that uses two balloons. Neither product mentions overinflation risk in its labeling. “At this moment there is not enough information to determine what is causing the balloon to overinflate,” according to the FDA letter.
A separate set of adverse event reports noted the development of acute pancreatitis caused when the balloons compressed other gastrointestinal structures. Both the Orbera and ReShape products were associated with pancreatitis, although neither lists pancreatitis as a potential complication on their labels. Pancreatitis was reported as early as 3 days after implantation, and symptoms included severe back and abdominal pain.
The FDA letter recommends that health care providers consider overinflation and pancreatitis in their differential diagnoses of obesity patients with intragastric balloons who present with the symptoms described, and to report any type of serious adverse events associated with intragastric balloons to the FDA through the MedWatch program. For more information about reporting adverse events to the FDA, visit the MedWatch site.
What I wish I knew when I started my internship
In my first year of residency I faced a steep learning curve. I learned a lot about psychiatry, but I learned so much more about myself. If I had known then what I know now, my internship would have been smoother and more enjoyable.
Be organized. Create systems to remember your patients’ information and your to-do list. I have templates of progress notes, psychiatry assessments, mental status assessments, “rounds sheets” (a sheet listing every patient on my floor, including their diagnoses, laboratories, medications, and other notes). Although my system involves lots of paper, I like it. Make a system that works for you. Go out and have fun. I know you are tired, you haven’t slept, and your apartment is a mess, but you won’t remember that time you went home, did laundry, and went to bed early. You will remember the fun night when you and other interns went out and explored the city.
Unplug from medicine. Nothing is more boring than working for 12 hours, only to go out for drinks with coworkers and talk about work. Although you need to vent, life is more than medicine. Find time for something else. Read a book, play a video game, hang out with people who are not doctors. I started a monthly book club with other women around my age. Make some time for something other than your profession.
Reach out to your senior colleagues. I was so concerned about making a good first impression that I didn’t share my concerns with others. I kept my head low because I always blame myself first when something is wrong.
During an off-service rotation, I was unable to finish my shift because I had food poisoning. To make up for that uncompleted shift, the chief from that service gave me 2 extra night shifts. I found the measure extreme, but thought it was my fault for going home early. A few days later, the Psychiatry Chief Resident approached me, after he had seen my schedule and spoke with the other chief because he found the situation unfair. He was reaching out to me saying, “We’ve got your back.” I realized that it wasn’t always my fault, and I could speak up when there was an issue. I was fortunate to have seniors and chiefs who looked out for me. I always found support, good advice, and respect for my feelings.
If you have questions or concerns, are anxious, or feel something is wrong, approach a senior or the chief. They were in your shoes once and will give you their best advice.
Medicine is different in the United States. As an international medica
People understand that you are from another country. At the beginning, I used Google to search for everything, and then I realized that my 2 wonderful students didn’t think less of me because I didn’t know what BKA (below knee amputation) means. Do not be ashamed if you don’t know how things work in a different country. You will find people who are willing to help you; you will learn, and it will be a minor thing a year from now.
Keep your support system. It was 3
If you moved away from home for residency, you are surrounded by new faces and far from the people you are comfortable with. Do not lose touch with them because you never know when you might need them the most. I had a hard road getting to where I am now, and many people helped me. You have to be there for them, too; a text message takes 30 seconds, and an e-mail, 1 minute.
Remember, you need to take care of yourself before taking care of others. No matter how much the MD or DO degree makes you feel like a superhero, you are still human.
In my first year of residency I faced a steep learning curve. I learned a lot about psychiatry, but I learned so much more about myself. If I had known then what I know now, my internship would have been smoother and more enjoyable.
Be organized. Create systems to remember your patients’ information and your to-do list. I have templates of progress notes, psychiatry assessments, mental status assessments, “rounds sheets” (a sheet listing every patient on my floor, including their diagnoses, laboratories, medications, and other notes). Although my system involves lots of paper, I like it. Make a system that works for you. Go out and have fun. I know you are tired, you haven’t slept, and your apartment is a mess, but you won’t remember that time you went home, did laundry, and went to bed early. You will remember the fun night when you and other interns went out and explored the city.
Unplug from medicine. Nothing is more boring than working for 12 hours, only to go out for drinks with coworkers and talk about work. Although you need to vent, life is more than medicine. Find time for something else. Read a book, play a video game, hang out with people who are not doctors. I started a monthly book club with other women around my age. Make some time for something other than your profession.
Reach out to your senior colleagues. I was so concerned about making a good first impression that I didn’t share my concerns with others. I kept my head low because I always blame myself first when something is wrong.
During an off-service rotation, I was unable to finish my shift because I had food poisoning. To make up for that uncompleted shift, the chief from that service gave me 2 extra night shifts. I found the measure extreme, but thought it was my fault for going home early. A few days later, the Psychiatry Chief Resident approached me, after he had seen my schedule and spoke with the other chief because he found the situation unfair. He was reaching out to me saying, “We’ve got your back.” I realized that it wasn’t always my fault, and I could speak up when there was an issue. I was fortunate to have seniors and chiefs who looked out for me. I always found support, good advice, and respect for my feelings.
If you have questions or concerns, are anxious, or feel something is wrong, approach a senior or the chief. They were in your shoes once and will give you their best advice.
Medicine is different in the United States. As an international medica
People understand that you are from another country. At the beginning, I used Google to search for everything, and then I realized that my 2 wonderful students didn’t think less of me because I didn’t know what BKA (below knee amputation) means. Do not be ashamed if you don’t know how things work in a different country. You will find people who are willing to help you; you will learn, and it will be a minor thing a year from now.
Keep your support system. It was 3
If you moved away from home for residency, you are surrounded by new faces and far from the people you are comfortable with. Do not lose touch with them because you never know when you might need them the most. I had a hard road getting to where I am now, and many people helped me. You have to be there for them, too; a text message takes 30 seconds, and an e-mail, 1 minute.
Remember, you need to take care of yourself before taking care of others. No matter how much the MD or DO degree makes you feel like a superhero, you are still human.
In my first year of residency I faced a steep learning curve. I learned a lot about psychiatry, but I learned so much more about myself. If I had known then what I know now, my internship would have been smoother and more enjoyable.
Be organized. Create systems to remember your patients’ information and your to-do list. I have templates of progress notes, psychiatry assessments, mental status assessments, “rounds sheets” (a sheet listing every patient on my floor, including their diagnoses, laboratories, medications, and other notes). Although my system involves lots of paper, I like it. Make a system that works for you. Go out and have fun. I know you are tired, you haven’t slept, and your apartment is a mess, but you won’t remember that time you went home, did laundry, and went to bed early. You will remember the fun night when you and other interns went out and explored the city.
Unplug from medicine. Nothing is more boring than working for 12 hours, only to go out for drinks with coworkers and talk about work. Although you need to vent, life is more than medicine. Find time for something else. Read a book, play a video game, hang out with people who are not doctors. I started a monthly book club with other women around my age. Make some time for something other than your profession.
Reach out to your senior colleagues. I was so concerned about making a good first impression that I didn’t share my concerns with others. I kept my head low because I always blame myself first when something is wrong.
During an off-service rotation, I was unable to finish my shift because I had food poisoning. To make up for that uncompleted shift, the chief from that service gave me 2 extra night shifts. I found the measure extreme, but thought it was my fault for going home early. A few days later, the Psychiatry Chief Resident approached me, after he had seen my schedule and spoke with the other chief because he found the situation unfair. He was reaching out to me saying, “We’ve got your back.” I realized that it wasn’t always my fault, and I could speak up when there was an issue. I was fortunate to have seniors and chiefs who looked out for me. I always found support, good advice, and respect for my feelings.
If you have questions or concerns, are anxious, or feel something is wrong, approach a senior or the chief. They were in your shoes once and will give you their best advice.
Medicine is different in the United States. As an international medica
People understand that you are from another country. At the beginning, I used Google to search for everything, and then I realized that my 2 wonderful students didn’t think less of me because I didn’t know what BKA (below knee amputation) means. Do not be ashamed if you don’t know how things work in a different country. You will find people who are willing to help you; you will learn, and it will be a minor thing a year from now.
Keep your support system. It was 3
If you moved away from home for residency, you are surrounded by new faces and far from the people you are comfortable with. Do not lose touch with them because you never know when you might need them the most. I had a hard road getting to where I am now, and many people helped me. You have to be there for them, too; a text message takes 30 seconds, and an e-mail, 1 minute.
Remember, you need to take care of yourself before taking care of others. No matter how much the MD or DO degree makes you feel like a superhero, you are still human.