User login
EEG Basics
ACO Insider: MACRA – don’t let indecision be your biggest decision
By now, most of us have heard of accountable care organizations and bundled payment. But for many of you, the shift to value-based population health management or compensation based on performance hasn’t affected your practice.
You still get paid fee for service. You’ve seen “the next big thing” in health care come and go; you don’t have the capital or spare intellectual bandwidth to make the transformation to value-based care – and as many of you have told me, at the end of the day, you just want to see patients.
There are a lot of reasons to sit on the sidelines a while longer. I get it. But that indecision could result in the biggest decision of your career. But it won’t be your decision – it will be defaulted to others. Why?
Welcome to MACRA – the Medicare Access and CHIP Reauthorization Act. On April 16, 2015, President Obama signed sweeping legislation irrevocably moving the American health care system to value-based payment. The United States Senate and House – Republicans and Democrats – came together to replace the Sustainable Growth Rate formula (SGR) with MACRA.
MACRA represents the end of a long history of perpetually delayed Medicare physician fee schedule cuts that were to be automatically triggered under the punitive SGR formula absent Congress’ annual postponement ritual. After providing for a series of annual physician payment increases, MACRA’s reimbursement methodology transitions to a value-based model that includes two pathways: 1) the Alternative Payment Model (APM), and 2) the Merit-Based Incentive Payment System (MIPS).
APMs include organizations that are focused on providing high-quality and cost-effective care, while also taking on significant financial risk (for example, an ACO).
MACRA highly incentivizes provider participation in APMs. For example, APM participants will receive 5% bonus payments from 2019 to 2024, if they receive a certain percentage of their Medicare revenue through APMs. In addition, providers qualifying as APM participants are excluded from participating in the MIPS model and are subject only to their own quality standards.
Under the MIPS model, provider performance will be evaluated according to established performance standards and used to calculate an adjustment factor that will then determine a provider’s payment for the year.
The performance standards will include the following weighted categories: 1. quality, 2. resource use, 3. clinical practice improvement activities, and 4. meaningful use. Depending on their performance in these categories, providers will receive either a positive adjustment, no adjustment, or a negative adjustment.
In 2022, these adjustments will range from a 9% negative adjustment to a similar positive adjustment. MIPS will apply to all Medicare services and items provided on or after Jan. 1, 2019.
What does this mean to you?
You are going to be reimbursed as if you have embraced value-based population health management, whether you really do or not. The MIPS formula could deny you north of 9% of your payments. Conversely, if you decide to get into an ACO or something similar, you not only don’t get dinged, you receive a 5% bump in fee-for-service compensation and the chance for additional savings payments. Of course, you have to decide to actually engage and lead this care improvement from your medical home. A fake ACO that lets costs rise will be responsible for those increases.
Readers of this column know that the statistics are bearing out the fact that primary care–led ACOs are the best model. The whole premise has changed. Instead of paying for volume and expensive procedures for very sick people, it rewards value – that is the highest quality at the lowest costs – through things in primary care’s wheelhouse: prevention, wellness, care coordination, complex patient management, and medical home care transition management.
In fact, CMS has recognized this by making primary care subspecialties the only ones required to be in the Medicare ACO program and the Medicare Shared Savings Program (MSSP), and recently with its ACO Investment Model, which prioritized ACO advanced infrastructure payments to physician- or small hospital-led ACOs in rural areas.
There are more physician-owned ACOs today than any other kind. If you are part of another type of ACO, such as one driven by a health system or multispecialty practice, don’t despair. They can work, too. But you need to step up and make sure they do.
The price of passivity
MACRA’s shifting of the annual flow of $3 trillion from rewarding volume to rewarding value will, in this author’s estimation, have MACRA easily eclipse the Affordable Care Act in significance. Indecision will not stop your placement in the value-based payment system. Why not control your destiny to achieve your professional and financial goals as leaders of health care? Through indecision, you will be both unprepared and defaulted into the quality and efficiency compensation measurements of MIPS.
MACRA has changed everything. You’ve been asked to lead American health care and get paid to do it. This is not a hard question. Please feel free to contact me directly with questions or comments on how to prepare.
Mr. Bobbitt is a head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He is president of Value Health Partners, LLC, a health care strategic consulting company. He has years of experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at bbobbitt@smithlaw.com or 919-821-6612.
By now, most of us have heard of accountable care organizations and bundled payment. But for many of you, the shift to value-based population health management or compensation based on performance hasn’t affected your practice.
You still get paid fee for service. You’ve seen “the next big thing” in health care come and go; you don’t have the capital or spare intellectual bandwidth to make the transformation to value-based care – and as many of you have told me, at the end of the day, you just want to see patients.
There are a lot of reasons to sit on the sidelines a while longer. I get it. But that indecision could result in the biggest decision of your career. But it won’t be your decision – it will be defaulted to others. Why?
Welcome to MACRA – the Medicare Access and CHIP Reauthorization Act. On April 16, 2015, President Obama signed sweeping legislation irrevocably moving the American health care system to value-based payment. The United States Senate and House – Republicans and Democrats – came together to replace the Sustainable Growth Rate formula (SGR) with MACRA.
MACRA represents the end of a long history of perpetually delayed Medicare physician fee schedule cuts that were to be automatically triggered under the punitive SGR formula absent Congress’ annual postponement ritual. After providing for a series of annual physician payment increases, MACRA’s reimbursement methodology transitions to a value-based model that includes two pathways: 1) the Alternative Payment Model (APM), and 2) the Merit-Based Incentive Payment System (MIPS).
APMs include organizations that are focused on providing high-quality and cost-effective care, while also taking on significant financial risk (for example, an ACO).
MACRA highly incentivizes provider participation in APMs. For example, APM participants will receive 5% bonus payments from 2019 to 2024, if they receive a certain percentage of their Medicare revenue through APMs. In addition, providers qualifying as APM participants are excluded from participating in the MIPS model and are subject only to their own quality standards.
Under the MIPS model, provider performance will be evaluated according to established performance standards and used to calculate an adjustment factor that will then determine a provider’s payment for the year.
The performance standards will include the following weighted categories: 1. quality, 2. resource use, 3. clinical practice improvement activities, and 4. meaningful use. Depending on their performance in these categories, providers will receive either a positive adjustment, no adjustment, or a negative adjustment.
In 2022, these adjustments will range from a 9% negative adjustment to a similar positive adjustment. MIPS will apply to all Medicare services and items provided on or after Jan. 1, 2019.
What does this mean to you?
You are going to be reimbursed as if you have embraced value-based population health management, whether you really do or not. The MIPS formula could deny you north of 9% of your payments. Conversely, if you decide to get into an ACO or something similar, you not only don’t get dinged, you receive a 5% bump in fee-for-service compensation and the chance for additional savings payments. Of course, you have to decide to actually engage and lead this care improvement from your medical home. A fake ACO that lets costs rise will be responsible for those increases.
Readers of this column know that the statistics are bearing out the fact that primary care–led ACOs are the best model. The whole premise has changed. Instead of paying for volume and expensive procedures for very sick people, it rewards value – that is the highest quality at the lowest costs – through things in primary care’s wheelhouse: prevention, wellness, care coordination, complex patient management, and medical home care transition management.
In fact, CMS has recognized this by making primary care subspecialties the only ones required to be in the Medicare ACO program and the Medicare Shared Savings Program (MSSP), and recently with its ACO Investment Model, which prioritized ACO advanced infrastructure payments to physician- or small hospital-led ACOs in rural areas.
There are more physician-owned ACOs today than any other kind. If you are part of another type of ACO, such as one driven by a health system or multispecialty practice, don’t despair. They can work, too. But you need to step up and make sure they do.
The price of passivity
MACRA’s shifting of the annual flow of $3 trillion from rewarding volume to rewarding value will, in this author’s estimation, have MACRA easily eclipse the Affordable Care Act in significance. Indecision will not stop your placement in the value-based payment system. Why not control your destiny to achieve your professional and financial goals as leaders of health care? Through indecision, you will be both unprepared and defaulted into the quality and efficiency compensation measurements of MIPS.
MACRA has changed everything. You’ve been asked to lead American health care and get paid to do it. This is not a hard question. Please feel free to contact me directly with questions or comments on how to prepare.
Mr. Bobbitt is a head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He is president of Value Health Partners, LLC, a health care strategic consulting company. He has years of experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at bbobbitt@smithlaw.com or 919-821-6612.
By now, most of us have heard of accountable care organizations and bundled payment. But for many of you, the shift to value-based population health management or compensation based on performance hasn’t affected your practice.
You still get paid fee for service. You’ve seen “the next big thing” in health care come and go; you don’t have the capital or spare intellectual bandwidth to make the transformation to value-based care – and as many of you have told me, at the end of the day, you just want to see patients.
There are a lot of reasons to sit on the sidelines a while longer. I get it. But that indecision could result in the biggest decision of your career. But it won’t be your decision – it will be defaulted to others. Why?
Welcome to MACRA – the Medicare Access and CHIP Reauthorization Act. On April 16, 2015, President Obama signed sweeping legislation irrevocably moving the American health care system to value-based payment. The United States Senate and House – Republicans and Democrats – came together to replace the Sustainable Growth Rate formula (SGR) with MACRA.
MACRA represents the end of a long history of perpetually delayed Medicare physician fee schedule cuts that were to be automatically triggered under the punitive SGR formula absent Congress’ annual postponement ritual. After providing for a series of annual physician payment increases, MACRA’s reimbursement methodology transitions to a value-based model that includes two pathways: 1) the Alternative Payment Model (APM), and 2) the Merit-Based Incentive Payment System (MIPS).
APMs include organizations that are focused on providing high-quality and cost-effective care, while also taking on significant financial risk (for example, an ACO).
MACRA highly incentivizes provider participation in APMs. For example, APM participants will receive 5% bonus payments from 2019 to 2024, if they receive a certain percentage of their Medicare revenue through APMs. In addition, providers qualifying as APM participants are excluded from participating in the MIPS model and are subject only to their own quality standards.
Under the MIPS model, provider performance will be evaluated according to established performance standards and used to calculate an adjustment factor that will then determine a provider’s payment for the year.
The performance standards will include the following weighted categories: 1. quality, 2. resource use, 3. clinical practice improvement activities, and 4. meaningful use. Depending on their performance in these categories, providers will receive either a positive adjustment, no adjustment, or a negative adjustment.
In 2022, these adjustments will range from a 9% negative adjustment to a similar positive adjustment. MIPS will apply to all Medicare services and items provided on or after Jan. 1, 2019.
What does this mean to you?
You are going to be reimbursed as if you have embraced value-based population health management, whether you really do or not. The MIPS formula could deny you north of 9% of your payments. Conversely, if you decide to get into an ACO or something similar, you not only don’t get dinged, you receive a 5% bump in fee-for-service compensation and the chance for additional savings payments. Of course, you have to decide to actually engage and lead this care improvement from your medical home. A fake ACO that lets costs rise will be responsible for those increases.
Readers of this column know that the statistics are bearing out the fact that primary care–led ACOs are the best model. The whole premise has changed. Instead of paying for volume and expensive procedures for very sick people, it rewards value – that is the highest quality at the lowest costs – through things in primary care’s wheelhouse: prevention, wellness, care coordination, complex patient management, and medical home care transition management.
In fact, CMS has recognized this by making primary care subspecialties the only ones required to be in the Medicare ACO program and the Medicare Shared Savings Program (MSSP), and recently with its ACO Investment Model, which prioritized ACO advanced infrastructure payments to physician- or small hospital-led ACOs in rural areas.
There are more physician-owned ACOs today than any other kind. If you are part of another type of ACO, such as one driven by a health system or multispecialty practice, don’t despair. They can work, too. But you need to step up and make sure they do.
The price of passivity
MACRA’s shifting of the annual flow of $3 trillion from rewarding volume to rewarding value will, in this author’s estimation, have MACRA easily eclipse the Affordable Care Act in significance. Indecision will not stop your placement in the value-based payment system. Why not control your destiny to achieve your professional and financial goals as leaders of health care? Through indecision, you will be both unprepared and defaulted into the quality and efficiency compensation measurements of MIPS.
MACRA has changed everything. You’ve been asked to lead American health care and get paid to do it. This is not a hard question. Please feel free to contact me directly with questions or comments on how to prepare.
Mr. Bobbitt is a head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He is president of Value Health Partners, LLC, a health care strategic consulting company. He has years of experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at bbobbitt@smithlaw.com or 919-821-6612.
National Harbor - Gateway to Washington, D.C.
For things to see and do while at the Vascular Annual Meeting, consider National Harbor as a gateway port to Washington, D.C., situated just across the Potomac. The famous sights, monuments, museums, and cultural icons in the nation’s capitol are a given for any visitor (visit www.washington.org for a full rundown).
But there are also a lot of lesser known tourist attractions unavailable anywhere else in the country. Medical history buffs, for example, may want to visit the National Musuem of American History, which houses collections of medical science and biotechnology artifacts. And Civil War buffs with access to a car can visit the National Museum of Civil War Medicine in Frederick, Md., about an hour’s drive from National Harbor. Frederick was the site of three Confederate invasions and two major battles.
Cultural events abound during the annual meeting period. Theater goers can attend Shakespeare’s “Taming of the Shrew” or the musical “La Cage aux Folles.” You can attend the DC Jazz Festival or the National Symphony Orchestra’s performance of pieces by Bruckner and Mahler. For more cultural events, visit www.culturalcapitol.com.
For sports lovers, baseball season will be just getting underway and the Washington Nationals will be playing the Philadelphia Phillies on Saturday and Sunday at Nationals Park.
And National Harbor has its own attractions. Hardest to miss is the Capitol Wheel, a giant ferris wheel that soars 180 feet above the Potomac River waterfront, with views of the White House and Capitol, the National Mall, and all the surrounding DC metro area.
To plan your visit, check out www.nationalharbor.com/consumer/entertainment.
For things to see and do while at the Vascular Annual Meeting, consider National Harbor as a gateway port to Washington, D.C., situated just across the Potomac. The famous sights, monuments, museums, and cultural icons in the nation’s capitol are a given for any visitor (visit www.washington.org for a full rundown).
But there are also a lot of lesser known tourist attractions unavailable anywhere else in the country. Medical history buffs, for example, may want to visit the National Musuem of American History, which houses collections of medical science and biotechnology artifacts. And Civil War buffs with access to a car can visit the National Museum of Civil War Medicine in Frederick, Md., about an hour’s drive from National Harbor. Frederick was the site of three Confederate invasions and two major battles.
Cultural events abound during the annual meeting period. Theater goers can attend Shakespeare’s “Taming of the Shrew” or the musical “La Cage aux Folles.” You can attend the DC Jazz Festival or the National Symphony Orchestra’s performance of pieces by Bruckner and Mahler. For more cultural events, visit www.culturalcapitol.com.
For sports lovers, baseball season will be just getting underway and the Washington Nationals will be playing the Philadelphia Phillies on Saturday and Sunday at Nationals Park.
And National Harbor has its own attractions. Hardest to miss is the Capitol Wheel, a giant ferris wheel that soars 180 feet above the Potomac River waterfront, with views of the White House and Capitol, the National Mall, and all the surrounding DC metro area.
To plan your visit, check out www.nationalharbor.com/consumer/entertainment.
For things to see and do while at the Vascular Annual Meeting, consider National Harbor as a gateway port to Washington, D.C., situated just across the Potomac. The famous sights, monuments, museums, and cultural icons in the nation’s capitol are a given for any visitor (visit www.washington.org for a full rundown).
But there are also a lot of lesser known tourist attractions unavailable anywhere else in the country. Medical history buffs, for example, may want to visit the National Musuem of American History, which houses collections of medical science and biotechnology artifacts. And Civil War buffs with access to a car can visit the National Museum of Civil War Medicine in Frederick, Md., about an hour’s drive from National Harbor. Frederick was the site of three Confederate invasions and two major battles.
Cultural events abound during the annual meeting period. Theater goers can attend Shakespeare’s “Taming of the Shrew” or the musical “La Cage aux Folles.” You can attend the DC Jazz Festival or the National Symphony Orchestra’s performance of pieces by Bruckner and Mahler. For more cultural events, visit www.culturalcapitol.com.
For sports lovers, baseball season will be just getting underway and the Washington Nationals will be playing the Philadelphia Phillies on Saturday and Sunday at Nationals Park.
And National Harbor has its own attractions. Hardest to miss is the Capitol Wheel, a giant ferris wheel that soars 180 feet above the Potomac River waterfront, with views of the White House and Capitol, the National Mall, and all the surrounding DC metro area.
To plan your visit, check out www.nationalharbor.com/consumer/entertainment.
What Matters: Fasting and cancer
We are a product of our environment. But we shan’t forget that we are a product of the critical interaction between our environment and our evolutionary biology.
Back when we were roaming the plains searching for food, we likely experienced “forced fasts” (that is, we had no food). Our ancestors who were the best at surviving these periods of scarcity lived to bear us into our current period of staggering abundance. Now, we are the unhealthiest humans in history.
Is part of the answer to our current health problems to return to our roots and ... fast?
In a recent article by Catherine Marinac and her colleagues, patients aged 27-70 years with breast cancer in the Women’s Healthy Eating and Living study were analyzed to uncover the relationship between nightly fasting duration and new primary breast tumors and death (JAMA Oncol. 2016 Mar 31. doi: 10.1001/jamaoncol.2016.0164). Fasting was assessed through use of 24-hour dietary recall.
Fasting less than 13 hours per night was associated with an increased risk of breast cancer, compared with fasting at least 13 hours (hazard ratio, 1.36; 95% confidence interval, 1.05-1.76). Different fasting durations were not associated with breast cancer mortality.
Additional analyses demonstrated that each 2-hour increase in fasting duration was associated with significantly lower hemoglobin A1c levels and a longer duration of nighttime sleep.
The positive health benefits of fasting have become increasingly “discussed,” albeit commonly on websites advertising for fasting cookbooks. Benefits of fasting include weight loss, improved insulin sensitivity, reductions in inflammation, improved cardiovascular risk factors, enhanced brain function, reductions in Alzheimer’s disease symptoms, and extended life span.
Many of these data are preliminary, and some are based upon animal models, such as the prolonged lifespan. In one study, rats undergoing alternate-day fasting lived 83% longer than rats who were not fasted. Interestingly, human data suggest that food consumption on the nonfasting days does not result in caloric consumption to cover the caloric deficit on the fasted day.
I have to admit that I am intrigued. I am not hearing much discussion about fasting among my colleagues – although a lot them skip meals, I know. But nobody is discussing it as a recommendation to appropriately selected patients (for example, not on insulin) to combat obesity and other diseases. I tried to suggest it to a patient the other day, who had a staggering amount of central adiposity, and he laughed at me. Is the thought of skipping eating for a day so anathema to our modern consumptive culture that we can’t even consider it?
Depending on the type of fasting that one is doing, one does not have to count calories on the fasting days, because there aren’t any. That makes it easy.
In a world of abundance and limitless food options, it may seem strange (self-indulgent?) to fast. But perhaps it will be a key to help us continue the species for a couple more generations.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article.
We are a product of our environment. But we shan’t forget that we are a product of the critical interaction between our environment and our evolutionary biology.
Back when we were roaming the plains searching for food, we likely experienced “forced fasts” (that is, we had no food). Our ancestors who were the best at surviving these periods of scarcity lived to bear us into our current period of staggering abundance. Now, we are the unhealthiest humans in history.
Is part of the answer to our current health problems to return to our roots and ... fast?
In a recent article by Catherine Marinac and her colleagues, patients aged 27-70 years with breast cancer in the Women’s Healthy Eating and Living study were analyzed to uncover the relationship between nightly fasting duration and new primary breast tumors and death (JAMA Oncol. 2016 Mar 31. doi: 10.1001/jamaoncol.2016.0164). Fasting was assessed through use of 24-hour dietary recall.
Fasting less than 13 hours per night was associated with an increased risk of breast cancer, compared with fasting at least 13 hours (hazard ratio, 1.36; 95% confidence interval, 1.05-1.76). Different fasting durations were not associated with breast cancer mortality.
Additional analyses demonstrated that each 2-hour increase in fasting duration was associated with significantly lower hemoglobin A1c levels and a longer duration of nighttime sleep.
The positive health benefits of fasting have become increasingly “discussed,” albeit commonly on websites advertising for fasting cookbooks. Benefits of fasting include weight loss, improved insulin sensitivity, reductions in inflammation, improved cardiovascular risk factors, enhanced brain function, reductions in Alzheimer’s disease symptoms, and extended life span.
Many of these data are preliminary, and some are based upon animal models, such as the prolonged lifespan. In one study, rats undergoing alternate-day fasting lived 83% longer than rats who were not fasted. Interestingly, human data suggest that food consumption on the nonfasting days does not result in caloric consumption to cover the caloric deficit on the fasted day.
I have to admit that I am intrigued. I am not hearing much discussion about fasting among my colleagues – although a lot them skip meals, I know. But nobody is discussing it as a recommendation to appropriately selected patients (for example, not on insulin) to combat obesity and other diseases. I tried to suggest it to a patient the other day, who had a staggering amount of central adiposity, and he laughed at me. Is the thought of skipping eating for a day so anathema to our modern consumptive culture that we can’t even consider it?
Depending on the type of fasting that one is doing, one does not have to count calories on the fasting days, because there aren’t any. That makes it easy.
In a world of abundance and limitless food options, it may seem strange (self-indulgent?) to fast. But perhaps it will be a key to help us continue the species for a couple more generations.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article.
We are a product of our environment. But we shan’t forget that we are a product of the critical interaction between our environment and our evolutionary biology.
Back when we were roaming the plains searching for food, we likely experienced “forced fasts” (that is, we had no food). Our ancestors who were the best at surviving these periods of scarcity lived to bear us into our current period of staggering abundance. Now, we are the unhealthiest humans in history.
Is part of the answer to our current health problems to return to our roots and ... fast?
In a recent article by Catherine Marinac and her colleagues, patients aged 27-70 years with breast cancer in the Women’s Healthy Eating and Living study were analyzed to uncover the relationship between nightly fasting duration and new primary breast tumors and death (JAMA Oncol. 2016 Mar 31. doi: 10.1001/jamaoncol.2016.0164). Fasting was assessed through use of 24-hour dietary recall.
Fasting less than 13 hours per night was associated with an increased risk of breast cancer, compared with fasting at least 13 hours (hazard ratio, 1.36; 95% confidence interval, 1.05-1.76). Different fasting durations were not associated with breast cancer mortality.
Additional analyses demonstrated that each 2-hour increase in fasting duration was associated with significantly lower hemoglobin A1c levels and a longer duration of nighttime sleep.
The positive health benefits of fasting have become increasingly “discussed,” albeit commonly on websites advertising for fasting cookbooks. Benefits of fasting include weight loss, improved insulin sensitivity, reductions in inflammation, improved cardiovascular risk factors, enhanced brain function, reductions in Alzheimer’s disease symptoms, and extended life span.
Many of these data are preliminary, and some are based upon animal models, such as the prolonged lifespan. In one study, rats undergoing alternate-day fasting lived 83% longer than rats who were not fasted. Interestingly, human data suggest that food consumption on the nonfasting days does not result in caloric consumption to cover the caloric deficit on the fasted day.
I have to admit that I am intrigued. I am not hearing much discussion about fasting among my colleagues – although a lot them skip meals, I know. But nobody is discussing it as a recommendation to appropriately selected patients (for example, not on insulin) to combat obesity and other diseases. I tried to suggest it to a patient the other day, who had a staggering amount of central adiposity, and he laughed at me. Is the thought of skipping eating for a day so anathema to our modern consumptive culture that we can’t even consider it?
Depending on the type of fasting that one is doing, one does not have to count calories on the fasting days, because there aren’t any. That makes it easy.
In a world of abundance and limitless food options, it may seem strange (self-indulgent?) to fast. But perhaps it will be a key to help us continue the species for a couple more generations.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article.
Ambulatory blood pressure rules hypertension diagnosis and follow-up
Evidence is becoming overwhelming that ambulatory blood pressure monitoring is the only reliable way to measure blood pressure for both diagnosing hypertension and following patients once they are diagnosed.
Office-based blood pressure measurement is out, be it a one-off reading or a cluster of sequential readings during a single office visit. Ambulatory blood pressure monitoring (ABPM) increasingly is the standard of care.
One recent nail in the coffin of office-based measurement came in a modestly-sized but revealing study reported by Dr. Joyce P. Samuel, a pediatric hypertension specialist at the University of Texas in Houston. She reported her experience directly comparing ambulatory and carefully-done office-based blood pressure measurement in a presentation at the annual meeting of the Pediatric Academic Societies in Baltimore.
Dr. Samuel followed 40 patients age 9-21 years whom she had previously diagnosed with essential hypertension (children with a systolic blood pressure at or above the 95th percentile for sex, age, and height), and repeatedly measured their blood pressures by both ambulatory and office-based readings at 2-week intervals as she searched for the best combination of antihypertensive drugs for each patient. She sent patients home for 24 hours of blood-pressure monitoring with an ambulatory device, and when they returned to her office the next day, she performed an office-based measurement using meticulous technique: Each child was seated and calm, measured on the right arm, with four measurements taken sequentially at about 1 minute intervals with the first reading discarded and the remaining three averaged.
Over the course of several months, she collected 173 paired ambulatory and office-based systolic blood pressure readings from individual patients. Substantial differences between the two forms of measurement were remarkably common. In 20% of the pairs, the ambulatory systolic reading was at least 10 mm Hg higher than the office-based reading, and for some pairs the differences ran as high as 30 mm Hg. In an additional 32% of the paired readings, office-based systolic pressure ran at least 10 mm Hg higher and in some cases as much as 35 mm Hg higher than the ambulatory reading.
Dr. Samuel also analyzed her findings a different way to assess the clinical consequences of these differences based on whether a child’s systolic pressure identified the patient as normotensive, hypertensive, or prehypertensive (a systolic pressure at the 90-94th percentile for the child’s age, sex and height). She found that the diagnoses matched for only 49% of the paired measurements. In 24% of the paired readings, ABPM identified children with hypertension that was not seen with concurrent office-based measurement, cases of masked hypertension. In 17% of the pairs, office-based measurement diagnosed hypertension that was not confirmed by ABPM, cases of white-coat hypertension. The remaining 10% of pairs were mismatched by showing normotensive with one method and prehypertensive with the other method. Dr. Samuel searched for any consistent patterns in these differences and found none. The disparate results with ambulatory and office-based measurements seemed almost random, with no correlation with age, sex, race, the medications patients received, or how many times a patient had already undergone dual blood-pressure monitoring. Individual patients had no meaningful differences between some of their paired measurements but had a meaningful disparity for others.
“We were unable to predict discrepancies,” said Dr. Samuels.
“You can’t get around it, you need ambulatory blood pressure monitoring to make the best diagnosis” of hypertension, she told me. “We need to push to make ambulatory monitoring more available. I am moving toward believing that ambulatory blood pressure monitoring must be routinely done on everyone. This is what the data suggest.”
It’s also where medicine is headed. In 2015, the U.S. Preventative Services Task Force (USPSTF) issued new recommendations for hypertension screening in adults aged 18 years or older, indicating that there was “convincing evidence that ABPM is the best method for diagnosing hypertension,” and the agency further recommended that ABPM is “the reference standard for confirming the diagnosis of hypertension.” Another endorsement of ambulatory blood pressure monitoring came out last year from the International Society for Chronobiology.
Recommendations are not yet as evolved for children. The USPSTF last weighed in on screening kids for hypertension in 2013, and said the evidence as of then was “insufficient” to assess the benefits and harms of screening for hypertension in children and adolescents. That document endorsed careful office-based blood pressure measurement, which highlights how recently expert sentiment has shifted on the issue of measurement. In response to the USPSTF 2013 statement, the American Academy of Pediatrics noted that it continued to back recommendations that are more than a decade old from the National High Blood Pressure Education Program that called for hypertension screening in children starting when they are 3 years old. Neither of these two groups has made any recent statement about the preferred method to measure blood pressure.
On Twitter @mitchelzoler
Evidence is becoming overwhelming that ambulatory blood pressure monitoring is the only reliable way to measure blood pressure for both diagnosing hypertension and following patients once they are diagnosed.
Office-based blood pressure measurement is out, be it a one-off reading or a cluster of sequential readings during a single office visit. Ambulatory blood pressure monitoring (ABPM) increasingly is the standard of care.
One recent nail in the coffin of office-based measurement came in a modestly-sized but revealing study reported by Dr. Joyce P. Samuel, a pediatric hypertension specialist at the University of Texas in Houston. She reported her experience directly comparing ambulatory and carefully-done office-based blood pressure measurement in a presentation at the annual meeting of the Pediatric Academic Societies in Baltimore.
Dr. Samuel followed 40 patients age 9-21 years whom she had previously diagnosed with essential hypertension (children with a systolic blood pressure at or above the 95th percentile for sex, age, and height), and repeatedly measured their blood pressures by both ambulatory and office-based readings at 2-week intervals as she searched for the best combination of antihypertensive drugs for each patient. She sent patients home for 24 hours of blood-pressure monitoring with an ambulatory device, and when they returned to her office the next day, she performed an office-based measurement using meticulous technique: Each child was seated and calm, measured on the right arm, with four measurements taken sequentially at about 1 minute intervals with the first reading discarded and the remaining three averaged.
Over the course of several months, she collected 173 paired ambulatory and office-based systolic blood pressure readings from individual patients. Substantial differences between the two forms of measurement were remarkably common. In 20% of the pairs, the ambulatory systolic reading was at least 10 mm Hg higher than the office-based reading, and for some pairs the differences ran as high as 30 mm Hg. In an additional 32% of the paired readings, office-based systolic pressure ran at least 10 mm Hg higher and in some cases as much as 35 mm Hg higher than the ambulatory reading.
Dr. Samuel also analyzed her findings a different way to assess the clinical consequences of these differences based on whether a child’s systolic pressure identified the patient as normotensive, hypertensive, or prehypertensive (a systolic pressure at the 90-94th percentile for the child’s age, sex and height). She found that the diagnoses matched for only 49% of the paired measurements. In 24% of the paired readings, ABPM identified children with hypertension that was not seen with concurrent office-based measurement, cases of masked hypertension. In 17% of the pairs, office-based measurement diagnosed hypertension that was not confirmed by ABPM, cases of white-coat hypertension. The remaining 10% of pairs were mismatched by showing normotensive with one method and prehypertensive with the other method. Dr. Samuel searched for any consistent patterns in these differences and found none. The disparate results with ambulatory and office-based measurements seemed almost random, with no correlation with age, sex, race, the medications patients received, or how many times a patient had already undergone dual blood-pressure monitoring. Individual patients had no meaningful differences between some of their paired measurements but had a meaningful disparity for others.
“We were unable to predict discrepancies,” said Dr. Samuels.
“You can’t get around it, you need ambulatory blood pressure monitoring to make the best diagnosis” of hypertension, she told me. “We need to push to make ambulatory monitoring more available. I am moving toward believing that ambulatory blood pressure monitoring must be routinely done on everyone. This is what the data suggest.”
It’s also where medicine is headed. In 2015, the U.S. Preventative Services Task Force (USPSTF) issued new recommendations for hypertension screening in adults aged 18 years or older, indicating that there was “convincing evidence that ABPM is the best method for diagnosing hypertension,” and the agency further recommended that ABPM is “the reference standard for confirming the diagnosis of hypertension.” Another endorsement of ambulatory blood pressure monitoring came out last year from the International Society for Chronobiology.
Recommendations are not yet as evolved for children. The USPSTF last weighed in on screening kids for hypertension in 2013, and said the evidence as of then was “insufficient” to assess the benefits and harms of screening for hypertension in children and adolescents. That document endorsed careful office-based blood pressure measurement, which highlights how recently expert sentiment has shifted on the issue of measurement. In response to the USPSTF 2013 statement, the American Academy of Pediatrics noted that it continued to back recommendations that are more than a decade old from the National High Blood Pressure Education Program that called for hypertension screening in children starting when they are 3 years old. Neither of these two groups has made any recent statement about the preferred method to measure blood pressure.
On Twitter @mitchelzoler
Evidence is becoming overwhelming that ambulatory blood pressure monitoring is the only reliable way to measure blood pressure for both diagnosing hypertension and following patients once they are diagnosed.
Office-based blood pressure measurement is out, be it a one-off reading or a cluster of sequential readings during a single office visit. Ambulatory blood pressure monitoring (ABPM) increasingly is the standard of care.
One recent nail in the coffin of office-based measurement came in a modestly-sized but revealing study reported by Dr. Joyce P. Samuel, a pediatric hypertension specialist at the University of Texas in Houston. She reported her experience directly comparing ambulatory and carefully-done office-based blood pressure measurement in a presentation at the annual meeting of the Pediatric Academic Societies in Baltimore.
Dr. Samuel followed 40 patients age 9-21 years whom she had previously diagnosed with essential hypertension (children with a systolic blood pressure at or above the 95th percentile for sex, age, and height), and repeatedly measured their blood pressures by both ambulatory and office-based readings at 2-week intervals as she searched for the best combination of antihypertensive drugs for each patient. She sent patients home for 24 hours of blood-pressure monitoring with an ambulatory device, and when they returned to her office the next day, she performed an office-based measurement using meticulous technique: Each child was seated and calm, measured on the right arm, with four measurements taken sequentially at about 1 minute intervals with the first reading discarded and the remaining three averaged.
Over the course of several months, she collected 173 paired ambulatory and office-based systolic blood pressure readings from individual patients. Substantial differences between the two forms of measurement were remarkably common. In 20% of the pairs, the ambulatory systolic reading was at least 10 mm Hg higher than the office-based reading, and for some pairs the differences ran as high as 30 mm Hg. In an additional 32% of the paired readings, office-based systolic pressure ran at least 10 mm Hg higher and in some cases as much as 35 mm Hg higher than the ambulatory reading.
Dr. Samuel also analyzed her findings a different way to assess the clinical consequences of these differences based on whether a child’s systolic pressure identified the patient as normotensive, hypertensive, or prehypertensive (a systolic pressure at the 90-94th percentile for the child’s age, sex and height). She found that the diagnoses matched for only 49% of the paired measurements. In 24% of the paired readings, ABPM identified children with hypertension that was not seen with concurrent office-based measurement, cases of masked hypertension. In 17% of the pairs, office-based measurement diagnosed hypertension that was not confirmed by ABPM, cases of white-coat hypertension. The remaining 10% of pairs were mismatched by showing normotensive with one method and prehypertensive with the other method. Dr. Samuel searched for any consistent patterns in these differences and found none. The disparate results with ambulatory and office-based measurements seemed almost random, with no correlation with age, sex, race, the medications patients received, or how many times a patient had already undergone dual blood-pressure monitoring. Individual patients had no meaningful differences between some of their paired measurements but had a meaningful disparity for others.
“We were unable to predict discrepancies,” said Dr. Samuels.
“You can’t get around it, you need ambulatory blood pressure monitoring to make the best diagnosis” of hypertension, she told me. “We need to push to make ambulatory monitoring more available. I am moving toward believing that ambulatory blood pressure monitoring must be routinely done on everyone. This is what the data suggest.”
It’s also where medicine is headed. In 2015, the U.S. Preventative Services Task Force (USPSTF) issued new recommendations for hypertension screening in adults aged 18 years or older, indicating that there was “convincing evidence that ABPM is the best method for diagnosing hypertension,” and the agency further recommended that ABPM is “the reference standard for confirming the diagnosis of hypertension.” Another endorsement of ambulatory blood pressure monitoring came out last year from the International Society for Chronobiology.
Recommendations are not yet as evolved for children. The USPSTF last weighed in on screening kids for hypertension in 2013, and said the evidence as of then was “insufficient” to assess the benefits and harms of screening for hypertension in children and adolescents. That document endorsed careful office-based blood pressure measurement, which highlights how recently expert sentiment has shifted on the issue of measurement. In response to the USPSTF 2013 statement, the American Academy of Pediatrics noted that it continued to back recommendations that are more than a decade old from the National High Blood Pressure Education Program that called for hypertension screening in children starting when they are 3 years old. Neither of these two groups has made any recent statement about the preferred method to measure blood pressure.
On Twitter @mitchelzoler
Candida linked to sex-specific schizophrenia symptoms
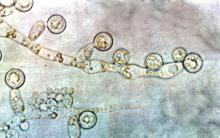
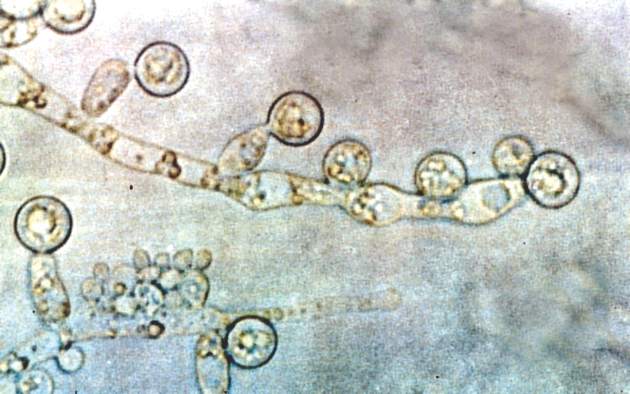
Exposure to Candida albicans significantly increased the odds of a schizophrenia diagnosis in men, according to case-control data from two cohorts of 947 adults.
“Fungal pathogens have not been extensively evaluated in studies of psychiatric disorders,” wrote Dr. Emily G. Severance of Johns Hopkins University in Baltimore, and her colleagues, in njp (Nature Partner Journals) Schizophrenia.
The researchers compared C. albicans IgG levels of individuals with schizophrenia and bipolar disorder with controls and found no diagnostic differences. However, stratification by sex showed a significantly increased risk of schizophrenia in men with elevated C. albicans IgG levels, with a ninefold increase in risk at the highest of three levels of seropositivity (odds ratio, 9.53). Elevated C. albicans levels in males with bipolar disorder were attributed to a history of homelessness.
C. albicans antibodies in women were not significantly different between groups. However, C. albicans was significantly associated with cognitive impairment in women with schizophrenia vs. control women (OR, 1.12), but no such difference was noted in men.
High levels of C. albicans antibodies were associated with comorbid gastrointestinal, genitourinary, and neoplastic conditions among individuals with psychiatric disorders overall.
“It may be premature to list this pathogen as a risk factor for disease causation, but its status as a comorbidity requires clinical attention,” the researchers wrote. “In the long term, more research is required to understand the mechanisms that trigger pathogenicity of fungal commensals and how this might impact brain function in psychiatric disorders.”
The findings were published in npj Schizophrenia. Read the full study here (npj Schizophrenia 2016 May 4. doi: 10.1038/npjschz.2016.18).
Exposure to Candida albicans significantly increased the odds of a schizophrenia diagnosis in men, according to case-control data from two cohorts of 947 adults.
“Fungal pathogens have not been extensively evaluated in studies of psychiatric disorders,” wrote Dr. Emily G. Severance of Johns Hopkins University in Baltimore, and her colleagues, in njp (Nature Partner Journals) Schizophrenia.
The researchers compared C. albicans IgG levels of individuals with schizophrenia and bipolar disorder with controls and found no diagnostic differences. However, stratification by sex showed a significantly increased risk of schizophrenia in men with elevated C. albicans IgG levels, with a ninefold increase in risk at the highest of three levels of seropositivity (odds ratio, 9.53). Elevated C. albicans levels in males with bipolar disorder were attributed to a history of homelessness.
C. albicans antibodies in women were not significantly different between groups. However, C. albicans was significantly associated with cognitive impairment in women with schizophrenia vs. control women (OR, 1.12), but no such difference was noted in men.
High levels of C. albicans antibodies were associated with comorbid gastrointestinal, genitourinary, and neoplastic conditions among individuals with psychiatric disorders overall.
“It may be premature to list this pathogen as a risk factor for disease causation, but its status as a comorbidity requires clinical attention,” the researchers wrote. “In the long term, more research is required to understand the mechanisms that trigger pathogenicity of fungal commensals and how this might impact brain function in psychiatric disorders.”
The findings were published in npj Schizophrenia. Read the full study here (npj Schizophrenia 2016 May 4. doi: 10.1038/npjschz.2016.18).
Exposure to Candida albicans significantly increased the odds of a schizophrenia diagnosis in men, according to case-control data from two cohorts of 947 adults.
“Fungal pathogens have not been extensively evaluated in studies of psychiatric disorders,” wrote Dr. Emily G. Severance of Johns Hopkins University in Baltimore, and her colleagues, in njp (Nature Partner Journals) Schizophrenia.
The researchers compared C. albicans IgG levels of individuals with schizophrenia and bipolar disorder with controls and found no diagnostic differences. However, stratification by sex showed a significantly increased risk of schizophrenia in men with elevated C. albicans IgG levels, with a ninefold increase in risk at the highest of three levels of seropositivity (odds ratio, 9.53). Elevated C. albicans levels in males with bipolar disorder were attributed to a history of homelessness.
C. albicans antibodies in women were not significantly different between groups. However, C. albicans was significantly associated with cognitive impairment in women with schizophrenia vs. control women (OR, 1.12), but no such difference was noted in men.
High levels of C. albicans antibodies were associated with comorbid gastrointestinal, genitourinary, and neoplastic conditions among individuals with psychiatric disorders overall.
“It may be premature to list this pathogen as a risk factor for disease causation, but its status as a comorbidity requires clinical attention,” the researchers wrote. “In the long term, more research is required to understand the mechanisms that trigger pathogenicity of fungal commensals and how this might impact brain function in psychiatric disorders.”
The findings were published in npj Schizophrenia. Read the full study here (npj Schizophrenia 2016 May 4. doi: 10.1038/npjschz.2016.18).
FROM NPJ SCHIZOPHRENIA
Welcome from the Vascular Quality Initiative
I am pleased to welcome you to the first Vascular Quality Initiative (VQI) Annual Meeting (VQI@VAM), which will be held on June 8th, in conjunction with this year’s Vascular Annual Meeting at Gaylord National Resort & Convention Center. We have scheduled a full day program of practical QI sessions, including presentations from both QI leaders and VQI members who will be sharing their experiences in sessions designed to benefit both vascular specialists and quality improvement professionals.
We are very fortunate to have two QI experts joining us – Dr. Michael Englesbe from the Michigan Surgical Quality Collaborative and Dr. Ted James from the University of Vermont – who will provide their perspectives on how we can drive quality with the VQI registries. Dr. Englesbe, as our keynote speaker, and Dr. James, our quality expert, will be addressing the practicalities, opportunities, and challenges of using registry data for quality improvement. Dr. James will also be moderating case study discussion with centers from across the country to help VQI members use the QI tools and VQI data effectively in their own practices. All the sessions are geared to demonstrating practical QI skills so that attendees can leverage their own VQI data and reporting, and discuss solutions. Registration and a $100 fee are required.
Overall, I believe that the Annual Meeting will create a valuable opportunity for both vascular specialists and quality improvement staff to see how participation in VQI can help improve the day-to-day quality of vascular care for patients. By taking a team approach, those who attend will be able to share a combination of best practice, collaboration, and benchmarking. Data managers will gain deeper insights into the value of reporting and analytics, and practitioners will able to compare their experiences with others.
This inaugural VQI Annual Meeting is an important part of our road map to the next level for the Vascular Quality Initiative’s development. It allows us to directly reach our base of over 2,800 physicians to introduce new approaches, such as tracking long-term follow-up and better measurement of the quality of vascular care, which will increase our effectiveness as practitioners.
Over the years of development of the VQI, we’ve seen the value of quality improvement data and analytics for the VQI in our practices. Now we’ve developed a valuable body of VQI-based real world experience to draw upon, which we will demonstrate at this event and going forward. I look forward to seeing you at the Gaylord National Resort & Convention Center on June 8th for VQI@VAM.
Dr. Larry Kraiss
Chair, SVS PSO Governing Council
I am pleased to welcome you to the first Vascular Quality Initiative (VQI) Annual Meeting (VQI@VAM), which will be held on June 8th, in conjunction with this year’s Vascular Annual Meeting at Gaylord National Resort & Convention Center. We have scheduled a full day program of practical QI sessions, including presentations from both QI leaders and VQI members who will be sharing their experiences in sessions designed to benefit both vascular specialists and quality improvement professionals.
We are very fortunate to have two QI experts joining us – Dr. Michael Englesbe from the Michigan Surgical Quality Collaborative and Dr. Ted James from the University of Vermont – who will provide their perspectives on how we can drive quality with the VQI registries. Dr. Englesbe, as our keynote speaker, and Dr. James, our quality expert, will be addressing the practicalities, opportunities, and challenges of using registry data for quality improvement. Dr. James will also be moderating case study discussion with centers from across the country to help VQI members use the QI tools and VQI data effectively in their own practices. All the sessions are geared to demonstrating practical QI skills so that attendees can leverage their own VQI data and reporting, and discuss solutions. Registration and a $100 fee are required.
Overall, I believe that the Annual Meeting will create a valuable opportunity for both vascular specialists and quality improvement staff to see how participation in VQI can help improve the day-to-day quality of vascular care for patients. By taking a team approach, those who attend will be able to share a combination of best practice, collaboration, and benchmarking. Data managers will gain deeper insights into the value of reporting and analytics, and practitioners will able to compare their experiences with others.
This inaugural VQI Annual Meeting is an important part of our road map to the next level for the Vascular Quality Initiative’s development. It allows us to directly reach our base of over 2,800 physicians to introduce new approaches, such as tracking long-term follow-up and better measurement of the quality of vascular care, which will increase our effectiveness as practitioners.
Over the years of development of the VQI, we’ve seen the value of quality improvement data and analytics for the VQI in our practices. Now we’ve developed a valuable body of VQI-based real world experience to draw upon, which we will demonstrate at this event and going forward. I look forward to seeing you at the Gaylord National Resort & Convention Center on June 8th for VQI@VAM.
Dr. Larry Kraiss
Chair, SVS PSO Governing Council
I am pleased to welcome you to the first Vascular Quality Initiative (VQI) Annual Meeting (VQI@VAM), which will be held on June 8th, in conjunction with this year’s Vascular Annual Meeting at Gaylord National Resort & Convention Center. We have scheduled a full day program of practical QI sessions, including presentations from both QI leaders and VQI members who will be sharing their experiences in sessions designed to benefit both vascular specialists and quality improvement professionals.
We are very fortunate to have two QI experts joining us – Dr. Michael Englesbe from the Michigan Surgical Quality Collaborative and Dr. Ted James from the University of Vermont – who will provide their perspectives on how we can drive quality with the VQI registries. Dr. Englesbe, as our keynote speaker, and Dr. James, our quality expert, will be addressing the practicalities, opportunities, and challenges of using registry data for quality improvement. Dr. James will also be moderating case study discussion with centers from across the country to help VQI members use the QI tools and VQI data effectively in their own practices. All the sessions are geared to demonstrating practical QI skills so that attendees can leverage their own VQI data and reporting, and discuss solutions. Registration and a $100 fee are required.
Overall, I believe that the Annual Meeting will create a valuable opportunity for both vascular specialists and quality improvement staff to see how participation in VQI can help improve the day-to-day quality of vascular care for patients. By taking a team approach, those who attend will be able to share a combination of best practice, collaboration, and benchmarking. Data managers will gain deeper insights into the value of reporting and analytics, and practitioners will able to compare their experiences with others.
This inaugural VQI Annual Meeting is an important part of our road map to the next level for the Vascular Quality Initiative’s development. It allows us to directly reach our base of over 2,800 physicians to introduce new approaches, such as tracking long-term follow-up and better measurement of the quality of vascular care, which will increase our effectiveness as practitioners.
Over the years of development of the VQI, we’ve seen the value of quality improvement data and analytics for the VQI in our practices. Now we’ve developed a valuable body of VQI-based real world experience to draw upon, which we will demonstrate at this event and going forward. I look forward to seeing you at the Gaylord National Resort & Convention Center on June 8th for VQI@VAM.
Dr. Larry Kraiss
Chair, SVS PSO Governing Council
SFA-Popliteal Claudication: What’s Appropriate Care?
In past years the Crawford Critical Issues Symposium has served as a forum in which nonclinical issues took center stage. At the 2016 Vascular Annual Meeting, Dr. Ron Fairman of the University of Pennsylvania Health System will take the symposium in a clinical direction with an issue that, he says, highlights critical questions about appropriateness of care. Titled “In Search of Clarity,” speakers will talk about interventions for claudication in the superficial femoral-popliteal arteries. This year’s lineup will address the role of medical management and exercise, along with the choice, cost, and durability of common interventions.
Speakers will be:
Dr. Mary McDermott of Northwestern University, on exercise;
Dr. Elizabeth Ratchford, Johns Hopkins University on medical management;
Dr. Michael Conte, of the University of California San Francisco, on understanding data sets, durability, and guidelines;
Dr. Peter Schneider of Kaiser Permanente on how claudication is approached in a system outside the traditional fee-for-service model;
Dr. Dennis Gable of Texas Vascular Associates on approaches to claudication in the community practice setting; and
Dr. Robert Zwolak of Dartmouth-Hitchcock Medical Center on the financial aspects, including hidden costs.
VC: Why did you choose claudication as this year’s key theme?
Dr. Fairman: There is probably no other subject that touches more on appropriateness of care than interventions for claudication, and if you look at how patients are managed across the country, there probably is no greater area of disparity. One of the most significant aspects of treating patients with expensive interventions for claudication is frequently the lack of durability. We often see patients in the office who present for a second opinion who already have undergone multiple invasive interventions over a 1- to 2-year period, all resulting in short-term improvement followed by – frighteningly – a much more serious set of symptoms than they started with. And this is fostered by a reimbursement system that demonstrates a willingness to reimburse physicians and hospitals for procedures that have little durability.
VC: Is there too much of a leap in the vascular community to invasive interventions?
Dr. Fairman: I believe that the members of our society understand that before a patient is considered for an invasive intervention for claudication, they should undergo exercise training and optimization of their medical status – but there are challenges associated with that. How do you do get a patient connected to a training regimen? Have all the patient’s risk factors been effectively addressed? Have they quit smoking? Is their blood sugar under control? We view ourselves as a unique specialty that offers comprehensive care of patients with vascular disease. We don’t just do surgery and procedures, but we have the ability to offer the entire package. We also understand by virtue of our training the natural history of the anatomic lesions we are treating. It is essential that physicians look at the whole patient before planning an intervention, and this forum should help us think more about that.
VC: What’s missing from a research perspective that might shed light on when intervention is needed and which interventions to perform?
Dr. Fairman: We need studies comparing durability of interventions with longer follow-up; 1 year is not enough. Dr. Conte will address what the available large data sets show in terms of durability. We need real-world data that compare technologies for claudication. We all have biases about technology based on our own experiences, but many of us struggle in selecting from the very many interventional options available to treat our patients. In addition, physician reimbursement typically increases from simple balloon angioplasty, to placement of a stent, to atherectomy.
VC: What other cost and reimbursement issues do you expect to deal with during the symposium?
I’m interested in Dr. Schneider’s perspective practicing in a health system that is a non–fee-for-service model. How does he make day-to-day decisions about using technology? Dr. Zwolek will talk about the financial side, not only in terms of physician reimbursement, but how physicians should view the expensive disposable inventory that they use when treating patients with claudication. This relates to hospital or facility reimbursement and issues related to margin. Regrettably, given the time constraints of this program, we were unable to secure speakers representing the viewpoints and perspectives of CMS [the Centers for Medicare and Medicaid Services] and the FDA [Food and Drug Administration].
In past years the Crawford Critical Issues Symposium has served as a forum in which nonclinical issues took center stage. At the 2016 Vascular Annual Meeting, Dr. Ron Fairman of the University of Pennsylvania Health System will take the symposium in a clinical direction with an issue that, he says, highlights critical questions about appropriateness of care. Titled “In Search of Clarity,” speakers will talk about interventions for claudication in the superficial femoral-popliteal arteries. This year’s lineup will address the role of medical management and exercise, along with the choice, cost, and durability of common interventions.
Speakers will be:
Dr. Mary McDermott of Northwestern University, on exercise;
Dr. Elizabeth Ratchford, Johns Hopkins University on medical management;
Dr. Michael Conte, of the University of California San Francisco, on understanding data sets, durability, and guidelines;
Dr. Peter Schneider of Kaiser Permanente on how claudication is approached in a system outside the traditional fee-for-service model;
Dr. Dennis Gable of Texas Vascular Associates on approaches to claudication in the community practice setting; and
Dr. Robert Zwolak of Dartmouth-Hitchcock Medical Center on the financial aspects, including hidden costs.
VC: Why did you choose claudication as this year’s key theme?
Dr. Fairman: There is probably no other subject that touches more on appropriateness of care than interventions for claudication, and if you look at how patients are managed across the country, there probably is no greater area of disparity. One of the most significant aspects of treating patients with expensive interventions for claudication is frequently the lack of durability. We often see patients in the office who present for a second opinion who already have undergone multiple invasive interventions over a 1- to 2-year period, all resulting in short-term improvement followed by – frighteningly – a much more serious set of symptoms than they started with. And this is fostered by a reimbursement system that demonstrates a willingness to reimburse physicians and hospitals for procedures that have little durability.
VC: Is there too much of a leap in the vascular community to invasive interventions?
Dr. Fairman: I believe that the members of our society understand that before a patient is considered for an invasive intervention for claudication, they should undergo exercise training and optimization of their medical status – but there are challenges associated with that. How do you do get a patient connected to a training regimen? Have all the patient’s risk factors been effectively addressed? Have they quit smoking? Is their blood sugar under control? We view ourselves as a unique specialty that offers comprehensive care of patients with vascular disease. We don’t just do surgery and procedures, but we have the ability to offer the entire package. We also understand by virtue of our training the natural history of the anatomic lesions we are treating. It is essential that physicians look at the whole patient before planning an intervention, and this forum should help us think more about that.
VC: What’s missing from a research perspective that might shed light on when intervention is needed and which interventions to perform?
Dr. Fairman: We need studies comparing durability of interventions with longer follow-up; 1 year is not enough. Dr. Conte will address what the available large data sets show in terms of durability. We need real-world data that compare technologies for claudication. We all have biases about technology based on our own experiences, but many of us struggle in selecting from the very many interventional options available to treat our patients. In addition, physician reimbursement typically increases from simple balloon angioplasty, to placement of a stent, to atherectomy.
VC: What other cost and reimbursement issues do you expect to deal with during the symposium?
I’m interested in Dr. Schneider’s perspective practicing in a health system that is a non–fee-for-service model. How does he make day-to-day decisions about using technology? Dr. Zwolek will talk about the financial side, not only in terms of physician reimbursement, but how physicians should view the expensive disposable inventory that they use when treating patients with claudication. This relates to hospital or facility reimbursement and issues related to margin. Regrettably, given the time constraints of this program, we were unable to secure speakers representing the viewpoints and perspectives of CMS [the Centers for Medicare and Medicaid Services] and the FDA [Food and Drug Administration].
In past years the Crawford Critical Issues Symposium has served as a forum in which nonclinical issues took center stage. At the 2016 Vascular Annual Meeting, Dr. Ron Fairman of the University of Pennsylvania Health System will take the symposium in a clinical direction with an issue that, he says, highlights critical questions about appropriateness of care. Titled “In Search of Clarity,” speakers will talk about interventions for claudication in the superficial femoral-popliteal arteries. This year’s lineup will address the role of medical management and exercise, along with the choice, cost, and durability of common interventions.
Speakers will be:
Dr. Mary McDermott of Northwestern University, on exercise;
Dr. Elizabeth Ratchford, Johns Hopkins University on medical management;
Dr. Michael Conte, of the University of California San Francisco, on understanding data sets, durability, and guidelines;
Dr. Peter Schneider of Kaiser Permanente on how claudication is approached in a system outside the traditional fee-for-service model;
Dr. Dennis Gable of Texas Vascular Associates on approaches to claudication in the community practice setting; and
Dr. Robert Zwolak of Dartmouth-Hitchcock Medical Center on the financial aspects, including hidden costs.
VC: Why did you choose claudication as this year’s key theme?
Dr. Fairman: There is probably no other subject that touches more on appropriateness of care than interventions for claudication, and if you look at how patients are managed across the country, there probably is no greater area of disparity. One of the most significant aspects of treating patients with expensive interventions for claudication is frequently the lack of durability. We often see patients in the office who present for a second opinion who already have undergone multiple invasive interventions over a 1- to 2-year period, all resulting in short-term improvement followed by – frighteningly – a much more serious set of symptoms than they started with. And this is fostered by a reimbursement system that demonstrates a willingness to reimburse physicians and hospitals for procedures that have little durability.
VC: Is there too much of a leap in the vascular community to invasive interventions?
Dr. Fairman: I believe that the members of our society understand that before a patient is considered for an invasive intervention for claudication, they should undergo exercise training and optimization of their medical status – but there are challenges associated with that. How do you do get a patient connected to a training regimen? Have all the patient’s risk factors been effectively addressed? Have they quit smoking? Is their blood sugar under control? We view ourselves as a unique specialty that offers comprehensive care of patients with vascular disease. We don’t just do surgery and procedures, but we have the ability to offer the entire package. We also understand by virtue of our training the natural history of the anatomic lesions we are treating. It is essential that physicians look at the whole patient before planning an intervention, and this forum should help us think more about that.
VC: What’s missing from a research perspective that might shed light on when intervention is needed and which interventions to perform?
Dr. Fairman: We need studies comparing durability of interventions with longer follow-up; 1 year is not enough. Dr. Conte will address what the available large data sets show in terms of durability. We need real-world data that compare technologies for claudication. We all have biases about technology based on our own experiences, but many of us struggle in selecting from the very many interventional options available to treat our patients. In addition, physician reimbursement typically increases from simple balloon angioplasty, to placement of a stent, to atherectomy.
VC: What other cost and reimbursement issues do you expect to deal with during the symposium?
I’m interested in Dr. Schneider’s perspective practicing in a health system that is a non–fee-for-service model. How does he make day-to-day decisions about using technology? Dr. Zwolek will talk about the financial side, not only in terms of physician reimbursement, but how physicians should view the expensive disposable inventory that they use when treating patients with claudication. This relates to hospital or facility reimbursement and issues related to margin. Regrettably, given the time constraints of this program, we were unable to secure speakers representing the viewpoints and perspectives of CMS [the Centers for Medicare and Medicaid Services] and the FDA [Food and Drug Administration].
Vascular Annual Meeting: A ‘Must-Attend’ Event
Our nation’s capital is the perfect venue for the pre-eminent vascular surgical educational and social meeting of the year – the 2016 SVS Vascular Annual Meeting on June 8-11.
This year’s meeting will be the most educationally jam-packed and stimulating annual meeting in our Society’s 70-year history, and a “must-attend” event for all serious health care professionals caring for patients with circulatory disease who want to succeed in our rapidly changing and challenging health care system and economy.
Recognizing that the majority of vascular surgical care in the United States is delivered in the community by nonacademic surgeons, our Program Committee, under the direction of my leadership team, has focused the Annual Meeting on the practical educational needs of our community practice SVS members. This includes the latest clinical research and results of evolving endovascular therapeutic interventions, “how-to” videos, focused hands-on training sessions, postgraduate courses geared to the contemporary practicing vascular surgeon and named lectureships delivered by visionary international leaders such as Dr. Frank Veith, the Homans Lecturer.
Here is just some of what you’ll experience this year: Hands-on training and sessions focused on topics such as the multidisciplinary management of the diabetic foot; the impact on vascular surgery practices of changing reimbursement models; contemporary management of intermittent claudication; and much, much more.
• More presentations and clinically focused sessions than ever before, with real-time audience interaction with the speakers and panelists to enhance the educational experience.
• CME and self-assessment credits to satisfy your MOC requirements in a user-friendly fashion in one meeting.
• An extensive offering of industry-sponsored educational presentations focused on “what is next,” to keep you ahead of the competition.
• Events for our growing roster of international guests, including International Forum, International Fast Talk, and the International Reception.
• The interactive “Vascular LIVE,” showcasing the latest technology.
• Social events to mingle and chat with your colleagues and international vascular leaders.
The Gaylord National Resort & Convention Center is a spectacular luxury property on the Potomac River in National Harbor, just outside Washington, D.C., and a ferry ride across the river from historic Old Town Alexandria, Va.
Registration is open and ahead of last year’s pace! Check the VAM housing link online for hotel availability and www.vsweb.org/VAM2016 for more information. I look forward to welcoming you to Washington, D.C., in June to celebrate our specialty and to learn together.
Bruce A. Perler, M.D.
SVS President
Our nation’s capital is the perfect venue for the pre-eminent vascular surgical educational and social meeting of the year – the 2016 SVS Vascular Annual Meeting on June 8-11.
This year’s meeting will be the most educationally jam-packed and stimulating annual meeting in our Society’s 70-year history, and a “must-attend” event for all serious health care professionals caring for patients with circulatory disease who want to succeed in our rapidly changing and challenging health care system and economy.
Recognizing that the majority of vascular surgical care in the United States is delivered in the community by nonacademic surgeons, our Program Committee, under the direction of my leadership team, has focused the Annual Meeting on the practical educational needs of our community practice SVS members. This includes the latest clinical research and results of evolving endovascular therapeutic interventions, “how-to” videos, focused hands-on training sessions, postgraduate courses geared to the contemporary practicing vascular surgeon and named lectureships delivered by visionary international leaders such as Dr. Frank Veith, the Homans Lecturer.
Here is just some of what you’ll experience this year: Hands-on training and sessions focused on topics such as the multidisciplinary management of the diabetic foot; the impact on vascular surgery practices of changing reimbursement models; contemporary management of intermittent claudication; and much, much more.
• More presentations and clinically focused sessions than ever before, with real-time audience interaction with the speakers and panelists to enhance the educational experience.
• CME and self-assessment credits to satisfy your MOC requirements in a user-friendly fashion in one meeting.
• An extensive offering of industry-sponsored educational presentations focused on “what is next,” to keep you ahead of the competition.
• Events for our growing roster of international guests, including International Forum, International Fast Talk, and the International Reception.
• The interactive “Vascular LIVE,” showcasing the latest technology.
• Social events to mingle and chat with your colleagues and international vascular leaders.
The Gaylord National Resort & Convention Center is a spectacular luxury property on the Potomac River in National Harbor, just outside Washington, D.C., and a ferry ride across the river from historic Old Town Alexandria, Va.
Registration is open and ahead of last year’s pace! Check the VAM housing link online for hotel availability and www.vsweb.org/VAM2016 for more information. I look forward to welcoming you to Washington, D.C., in June to celebrate our specialty and to learn together.
Bruce A. Perler, M.D.
SVS President
Our nation’s capital is the perfect venue for the pre-eminent vascular surgical educational and social meeting of the year – the 2016 SVS Vascular Annual Meeting on June 8-11.
This year’s meeting will be the most educationally jam-packed and stimulating annual meeting in our Society’s 70-year history, and a “must-attend” event for all serious health care professionals caring for patients with circulatory disease who want to succeed in our rapidly changing and challenging health care system and economy.
Recognizing that the majority of vascular surgical care in the United States is delivered in the community by nonacademic surgeons, our Program Committee, under the direction of my leadership team, has focused the Annual Meeting on the practical educational needs of our community practice SVS members. This includes the latest clinical research and results of evolving endovascular therapeutic interventions, “how-to” videos, focused hands-on training sessions, postgraduate courses geared to the contemporary practicing vascular surgeon and named lectureships delivered by visionary international leaders such as Dr. Frank Veith, the Homans Lecturer.
Here is just some of what you’ll experience this year: Hands-on training and sessions focused on topics such as the multidisciplinary management of the diabetic foot; the impact on vascular surgery practices of changing reimbursement models; contemporary management of intermittent claudication; and much, much more.
• More presentations and clinically focused sessions than ever before, with real-time audience interaction with the speakers and panelists to enhance the educational experience.
• CME and self-assessment credits to satisfy your MOC requirements in a user-friendly fashion in one meeting.
• An extensive offering of industry-sponsored educational presentations focused on “what is next,” to keep you ahead of the competition.
• Events for our growing roster of international guests, including International Forum, International Fast Talk, and the International Reception.
• The interactive “Vascular LIVE,” showcasing the latest technology.
• Social events to mingle and chat with your colleagues and international vascular leaders.
The Gaylord National Resort & Convention Center is a spectacular luxury property on the Potomac River in National Harbor, just outside Washington, D.C., and a ferry ride across the river from historic Old Town Alexandria, Va.
Registration is open and ahead of last year’s pace! Check the VAM housing link online for hotel availability and www.vsweb.org/VAM2016 for more information. I look forward to welcoming you to Washington, D.C., in June to celebrate our specialty and to learn together.
Bruce A. Perler, M.D.
SVS President
DACA: High Court ruling could squash dreams of becoming a doctor
Growing up, Denisse Rojas Marquez rarely visited the doctor. As undocumented immigrants from Mexico, her family viewed medical care as a luxury and sought it only in emergencies.
“I would always wait until it was very severe to see a doctor,” said Ms. Rojas Marquez, who came to the United States as a toddler. “That’s still a mentality I have to train myself out of. Growing up, going to the doctor meant very expensive bills and navigating through very complex systems.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
At 26, Ms. Rojas Marquez is determined to become a physician and help bridge the gap between undocumented immigrants and medical care. She is close to making that dream a reality because of a 2012 policy called the Deferred Action for Childhood Arrivals (DACA), which protects undocumented immigrants brought to the United States as children from deportation and offers access to work authorization. The policy enabled Ms. Rojas Marquez to become one of the first undocumented students to attend the Icahn School of Medicine at Mount Sinai in New York.
But the fate of Ms. Rojas Marquez’s medical education is in flux as the U.S. Supreme Court considers protections for undocumented immigrants in the case of Texas v. United States. In dispute is the constitutionality of two of President Obama’s immigration policies: the Deferred Action for Parents of Americans and Lawful Permanent Residents (DAPA) and expanded DACA. The former protects undocumented immigrants who are parents of U.S. citizens from deportation, if they meet certain criteria. The second extends work authorization under the original DACA program from 2 years to 3 years and broadens age requirements.
Texas and 25 other states have sued over the programs, arguing the president does not have the authority to issue the new immigration policies, and that the programs violate the Constitution as well as the Administrative Procedure Act for notice-and-comment rule making. High court justices heard oral arguments April 18.
The ruling could impact the growing number of medical students with DACA status across the country, and jeopardize the funding invested in their training. Sixty-one medical schools now accept applications from DACA applicants, according to data from the Association of American Medical Colleges (AAMC). In 2015, 46 students with DACA status applied to U.S. medical schools and 20 were enrolled. In 2016, more than double (112) applied, although enrollment data will not be available until year’s end. Neither AAMC nor the National Resident Matching Program collect data on residents with DACA status.
A high court ruling in favor of the states could lead to DACA’s undoing, said Michael M. Hethmon, an attorney for the Immigration Reform Law Institute in Washington, D.C. The institute issued a brief to the Supreme Court in support of Texas.
If Texas prevails, “it’ll be a matter of weeks before a similar challenge will be levied against DACA and a number of other related programs,” Mr. Hethmon said in an interview. “There will be no more legal justification for those programs that exist.”
Saving talent or wasting money?
Loyola University in Chicago has accepted more students with DACA status than any other U.S. medical school. The reasons are simple, said Mark Kuczewski, Ph.D., chair of medical education at Loyola’s Stritch School of Medicine.
“We’re in the business of taking outstanding students,” Dr. Kuczewski said in an interview. “If the student is outstanding, we want them in our applicant pool. Second, being bilingual and bicultural is extremely important. We have patient populations out there that are diverse and underserved. We want to utilize this talent.”
In the fall of 2014, Stritch enrolled seven medical students with DACA status; in 2014, they doubled that enrollment. The students competed on the same playing field as other applicants and received no special treatment, Dr. Kuczewski said.
DACA students do pose funding challenges, he acknowledged. Although the students are protected from deportation and receive work authorization, they don’t qualify for federal student loans. Medical schools must find unique ways to help DACA students finance their education. A major Catholic health system provides student loan packages for several DACA students at Stritch, Dr. Kuczewski said. DACA students can also apply for financial assistance through an AAMC assistance program.
“Medical students use copious amounts of federal student loans,” he said. “Somehow the school has to make up that difference. We’ve found partners, but they don’t have infinite capacity, so we have to keep going back and finding new partners each year.”
The University of California, San Francisco, also has opened its doors to DACA students. Now in his third year, Jirayut New Latthivongskorn is UCSF’s first undocumented medical student. His education is financed by grants, private funding, and donations, said Mr. Latthivongskorn who came to the United States from Thailand when he was 9 years old. He is cofounder of Pre-Health Dreamers, a network of undocumented students who plan to pursue medical careers.
Before DACA granted his entry into UCSF, Mr. Latthivongskorn was accustomed to barriers because of his undocumented status, including having to turn down a nearly full-ride scholarship from the University of California, Davis, after high school.
“It was devastating,” Mr. Latthivongskorn said in an interview. “It was one of the very first times where I felt different and thought, ‘This is not going to work. You are undocumented.’”
Mr. Latthivongskorn and his family scraped together money for him to complete his undergraduate degree at the University of California, Berkeley. California has since passed the DREAM Act, a law that allows undocumented immigrants to receive private scholarships funded through public universities.
Not everyone believes undocumented immigrants should get the chance to become U.S. physicians. Dr. Jane M. Orient, executive director of the Association of American Physicians and Surgeons, argued that undocumented immigrants are not the answer to curbing the physician shortage.
“In a country that’s supposed to be ruled by law, it seems incomprehensible that people who are violating the law should be given privileges over people who are here legally,” she said in an interview. “We desperately do need more physicians, but we should not be blocking Americans from having this opportunity.”
Dr. Shirie Leng, a Boston anesthesiologist, said DACA is promising in theory, but falls short in practical application.
“There’s no particular reason why [undocumented students] wouldn’t make great doctors,” said Dr. Leng. “The problem is funding related. You can give kids all the opportunity you want, but if you can’t pay for it, that seems to me to be the biggest sticking point.”
Basing admission policies on programs that are vulnerable could end poorly for schools and students, Dr. Leng added.
If DACA is revoked, “it’s not just a waste of money for the school, but a waste of time for the kids,” she said.
Protections hinge on Supreme Court … and next president
During oral arguments earlier this month, justices appeared to disagree on whether DAPA and expanded DACA were properly executed.
Associate Justice Anthony M. Kennedy indicated that the normal order of government policy making had been “turned upside down,” by the creation of the programs. Associate Justice Sonia Sotomayor, meanwhile, noted that immigration policies with broader reaches have been similarly instituted in the past.
A ruling for the government would mean the president can use his executive power to enact policies that run contrary to immigration laws already in place, said Mr. Hethmon, the D.C. attorney. Current immigration laws trump informal agency discretion and do not allow for the government’s “arbitrary and capricious creation of a massive classification of nonstatus alien beneficiaries,” Mr. Hethmon wrote in his high court brief.
A decision that favors Texas would unravel opportunities for undocumented immigrants and prevent their ability to contribute to society, said Ignacia Rodriguez, a legal fellow at the National Immigration Law Center, which authored a brief in support of the government.
“What’s at stake is providing a stable environment for U.S. citizen children to grow, and providing people with the opportunity and tools to be able to contribute to the workforce [and] to the economy,” she said in an interview. “This is a payoff for everybody, not just those receiving the benefit.”
Regardless of what the Supreme Court decides, the next president could have the last word, according Ashley C. Parrish, a Washington D.C. attorney who cowrote a brief in support of the states. Mr. Parrish takes no position on the merits of the immigration programs, but rather, he is concerned with the administration’s failure to follow the Administrative Procedure Act’s requirements for notice-and-comment rule making.
“If the program were adopted as a legal rule after notice and comment, it could not be changed without going through a new notice-and-comment process,” he said. “If it is just a bare statement of policy, it can be changed at any time, without notice to anyone. The next administration could say, ‘Thank you for coming out of the shadows; we are now going to deport all of you.’ ”
Among the Democrats running for president, former Secretary of State Hillary Clinton has said she will defend DACA and Sen. Bernie Sanders (I-Vt.) has said he supports DACA and DAPA, and plans to expand them if elected.
Conversely, presumed Republican presidential nominee Donald Trump has indicated he would rescind DACA and related programs if elected.
After spending most of her life terrified of deportation, Ms. Rojas Marquez said she is not wasting time worrying about the Supreme Court’s decision or whether the next president will overturn the policy. She is keeping her studies foremost in her mind and the goal of becoming a doctor firmly in her heart.
“I have always lived with what-ifs,” she said. “This time around, I’m not going to be living in fear of the removing of DACA, because I wouldn’t have made it this far if I always lived in fear. My plan is no matter what happens, I’m going to finish medical school, and from there, I pray that I will be able to practice in the U.S.”
The Supreme Court is expected to issue its decision by June.
On Twitter @legal_med
Growing up, Denisse Rojas Marquez rarely visited the doctor. As undocumented immigrants from Mexico, her family viewed medical care as a luxury and sought it only in emergencies.
“I would always wait until it was very severe to see a doctor,” said Ms. Rojas Marquez, who came to the United States as a toddler. “That’s still a mentality I have to train myself out of. Growing up, going to the doctor meant very expensive bills and navigating through very complex systems.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
At 26, Ms. Rojas Marquez is determined to become a physician and help bridge the gap between undocumented immigrants and medical care. She is close to making that dream a reality because of a 2012 policy called the Deferred Action for Childhood Arrivals (DACA), which protects undocumented immigrants brought to the United States as children from deportation and offers access to work authorization. The policy enabled Ms. Rojas Marquez to become one of the first undocumented students to attend the Icahn School of Medicine at Mount Sinai in New York.
But the fate of Ms. Rojas Marquez’s medical education is in flux as the U.S. Supreme Court considers protections for undocumented immigrants in the case of Texas v. United States. In dispute is the constitutionality of two of President Obama’s immigration policies: the Deferred Action for Parents of Americans and Lawful Permanent Residents (DAPA) and expanded DACA. The former protects undocumented immigrants who are parents of U.S. citizens from deportation, if they meet certain criteria. The second extends work authorization under the original DACA program from 2 years to 3 years and broadens age requirements.
Texas and 25 other states have sued over the programs, arguing the president does not have the authority to issue the new immigration policies, and that the programs violate the Constitution as well as the Administrative Procedure Act for notice-and-comment rule making. High court justices heard oral arguments April 18.
The ruling could impact the growing number of medical students with DACA status across the country, and jeopardize the funding invested in their training. Sixty-one medical schools now accept applications from DACA applicants, according to data from the Association of American Medical Colleges (AAMC). In 2015, 46 students with DACA status applied to U.S. medical schools and 20 were enrolled. In 2016, more than double (112) applied, although enrollment data will not be available until year’s end. Neither AAMC nor the National Resident Matching Program collect data on residents with DACA status.
A high court ruling in favor of the states could lead to DACA’s undoing, said Michael M. Hethmon, an attorney for the Immigration Reform Law Institute in Washington, D.C. The institute issued a brief to the Supreme Court in support of Texas.
If Texas prevails, “it’ll be a matter of weeks before a similar challenge will be levied against DACA and a number of other related programs,” Mr. Hethmon said in an interview. “There will be no more legal justification for those programs that exist.”
Saving talent or wasting money?
Loyola University in Chicago has accepted more students with DACA status than any other U.S. medical school. The reasons are simple, said Mark Kuczewski, Ph.D., chair of medical education at Loyola’s Stritch School of Medicine.
“We’re in the business of taking outstanding students,” Dr. Kuczewski said in an interview. “If the student is outstanding, we want them in our applicant pool. Second, being bilingual and bicultural is extremely important. We have patient populations out there that are diverse and underserved. We want to utilize this talent.”
In the fall of 2014, Stritch enrolled seven medical students with DACA status; in 2014, they doubled that enrollment. The students competed on the same playing field as other applicants and received no special treatment, Dr. Kuczewski said.
DACA students do pose funding challenges, he acknowledged. Although the students are protected from deportation and receive work authorization, they don’t qualify for federal student loans. Medical schools must find unique ways to help DACA students finance their education. A major Catholic health system provides student loan packages for several DACA students at Stritch, Dr. Kuczewski said. DACA students can also apply for financial assistance through an AAMC assistance program.
“Medical students use copious amounts of federal student loans,” he said. “Somehow the school has to make up that difference. We’ve found partners, but they don’t have infinite capacity, so we have to keep going back and finding new partners each year.”
The University of California, San Francisco, also has opened its doors to DACA students. Now in his third year, Jirayut New Latthivongskorn is UCSF’s first undocumented medical student. His education is financed by grants, private funding, and donations, said Mr. Latthivongskorn who came to the United States from Thailand when he was 9 years old. He is cofounder of Pre-Health Dreamers, a network of undocumented students who plan to pursue medical careers.
Before DACA granted his entry into UCSF, Mr. Latthivongskorn was accustomed to barriers because of his undocumented status, including having to turn down a nearly full-ride scholarship from the University of California, Davis, after high school.
“It was devastating,” Mr. Latthivongskorn said in an interview. “It was one of the very first times where I felt different and thought, ‘This is not going to work. You are undocumented.’”
Mr. Latthivongskorn and his family scraped together money for him to complete his undergraduate degree at the University of California, Berkeley. California has since passed the DREAM Act, a law that allows undocumented immigrants to receive private scholarships funded through public universities.
Not everyone believes undocumented immigrants should get the chance to become U.S. physicians. Dr. Jane M. Orient, executive director of the Association of American Physicians and Surgeons, argued that undocumented immigrants are not the answer to curbing the physician shortage.
“In a country that’s supposed to be ruled by law, it seems incomprehensible that people who are violating the law should be given privileges over people who are here legally,” she said in an interview. “We desperately do need more physicians, but we should not be blocking Americans from having this opportunity.”
Dr. Shirie Leng, a Boston anesthesiologist, said DACA is promising in theory, but falls short in practical application.
“There’s no particular reason why [undocumented students] wouldn’t make great doctors,” said Dr. Leng. “The problem is funding related. You can give kids all the opportunity you want, but if you can’t pay for it, that seems to me to be the biggest sticking point.”
Basing admission policies on programs that are vulnerable could end poorly for schools and students, Dr. Leng added.
If DACA is revoked, “it’s not just a waste of money for the school, but a waste of time for the kids,” she said.
Protections hinge on Supreme Court … and next president
During oral arguments earlier this month, justices appeared to disagree on whether DAPA and expanded DACA were properly executed.
Associate Justice Anthony M. Kennedy indicated that the normal order of government policy making had been “turned upside down,” by the creation of the programs. Associate Justice Sonia Sotomayor, meanwhile, noted that immigration policies with broader reaches have been similarly instituted in the past.
A ruling for the government would mean the president can use his executive power to enact policies that run contrary to immigration laws already in place, said Mr. Hethmon, the D.C. attorney. Current immigration laws trump informal agency discretion and do not allow for the government’s “arbitrary and capricious creation of a massive classification of nonstatus alien beneficiaries,” Mr. Hethmon wrote in his high court brief.
A decision that favors Texas would unravel opportunities for undocumented immigrants and prevent their ability to contribute to society, said Ignacia Rodriguez, a legal fellow at the National Immigration Law Center, which authored a brief in support of the government.
“What’s at stake is providing a stable environment for U.S. citizen children to grow, and providing people with the opportunity and tools to be able to contribute to the workforce [and] to the economy,” she said in an interview. “This is a payoff for everybody, not just those receiving the benefit.”
Regardless of what the Supreme Court decides, the next president could have the last word, according Ashley C. Parrish, a Washington D.C. attorney who cowrote a brief in support of the states. Mr. Parrish takes no position on the merits of the immigration programs, but rather, he is concerned with the administration’s failure to follow the Administrative Procedure Act’s requirements for notice-and-comment rule making.
“If the program were adopted as a legal rule after notice and comment, it could not be changed without going through a new notice-and-comment process,” he said. “If it is just a bare statement of policy, it can be changed at any time, without notice to anyone. The next administration could say, ‘Thank you for coming out of the shadows; we are now going to deport all of you.’ ”
Among the Democrats running for president, former Secretary of State Hillary Clinton has said she will defend DACA and Sen. Bernie Sanders (I-Vt.) has said he supports DACA and DAPA, and plans to expand them if elected.
Conversely, presumed Republican presidential nominee Donald Trump has indicated he would rescind DACA and related programs if elected.
After spending most of her life terrified of deportation, Ms. Rojas Marquez said she is not wasting time worrying about the Supreme Court’s decision or whether the next president will overturn the policy. She is keeping her studies foremost in her mind and the goal of becoming a doctor firmly in her heart.
“I have always lived with what-ifs,” she said. “This time around, I’m not going to be living in fear of the removing of DACA, because I wouldn’t have made it this far if I always lived in fear. My plan is no matter what happens, I’m going to finish medical school, and from there, I pray that I will be able to practice in the U.S.”
The Supreme Court is expected to issue its decision by June.
On Twitter @legal_med
Growing up, Denisse Rojas Marquez rarely visited the doctor. As undocumented immigrants from Mexico, her family viewed medical care as a luxury and sought it only in emergencies.
“I would always wait until it was very severe to see a doctor,” said Ms. Rojas Marquez, who came to the United States as a toddler. “That’s still a mentality I have to train myself out of. Growing up, going to the doctor meant very expensive bills and navigating through very complex systems.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
At 26, Ms. Rojas Marquez is determined to become a physician and help bridge the gap between undocumented immigrants and medical care. She is close to making that dream a reality because of a 2012 policy called the Deferred Action for Childhood Arrivals (DACA), which protects undocumented immigrants brought to the United States as children from deportation and offers access to work authorization. The policy enabled Ms. Rojas Marquez to become one of the first undocumented students to attend the Icahn School of Medicine at Mount Sinai in New York.
But the fate of Ms. Rojas Marquez’s medical education is in flux as the U.S. Supreme Court considers protections for undocumented immigrants in the case of Texas v. United States. In dispute is the constitutionality of two of President Obama’s immigration policies: the Deferred Action for Parents of Americans and Lawful Permanent Residents (DAPA) and expanded DACA. The former protects undocumented immigrants who are parents of U.S. citizens from deportation, if they meet certain criteria. The second extends work authorization under the original DACA program from 2 years to 3 years and broadens age requirements.
Texas and 25 other states have sued over the programs, arguing the president does not have the authority to issue the new immigration policies, and that the programs violate the Constitution as well as the Administrative Procedure Act for notice-and-comment rule making. High court justices heard oral arguments April 18.
The ruling could impact the growing number of medical students with DACA status across the country, and jeopardize the funding invested in their training. Sixty-one medical schools now accept applications from DACA applicants, according to data from the Association of American Medical Colleges (AAMC). In 2015, 46 students with DACA status applied to U.S. medical schools and 20 were enrolled. In 2016, more than double (112) applied, although enrollment data will not be available until year’s end. Neither AAMC nor the National Resident Matching Program collect data on residents with DACA status.
A high court ruling in favor of the states could lead to DACA’s undoing, said Michael M. Hethmon, an attorney for the Immigration Reform Law Institute in Washington, D.C. The institute issued a brief to the Supreme Court in support of Texas.
If Texas prevails, “it’ll be a matter of weeks before a similar challenge will be levied against DACA and a number of other related programs,” Mr. Hethmon said in an interview. “There will be no more legal justification for those programs that exist.”
Saving talent or wasting money?
Loyola University in Chicago has accepted more students with DACA status than any other U.S. medical school. The reasons are simple, said Mark Kuczewski, Ph.D., chair of medical education at Loyola’s Stritch School of Medicine.
“We’re in the business of taking outstanding students,” Dr. Kuczewski said in an interview. “If the student is outstanding, we want them in our applicant pool. Second, being bilingual and bicultural is extremely important. We have patient populations out there that are diverse and underserved. We want to utilize this talent.”
In the fall of 2014, Stritch enrolled seven medical students with DACA status; in 2014, they doubled that enrollment. The students competed on the same playing field as other applicants and received no special treatment, Dr. Kuczewski said.
DACA students do pose funding challenges, he acknowledged. Although the students are protected from deportation and receive work authorization, they don’t qualify for federal student loans. Medical schools must find unique ways to help DACA students finance their education. A major Catholic health system provides student loan packages for several DACA students at Stritch, Dr. Kuczewski said. DACA students can also apply for financial assistance through an AAMC assistance program.
“Medical students use copious amounts of federal student loans,” he said. “Somehow the school has to make up that difference. We’ve found partners, but they don’t have infinite capacity, so we have to keep going back and finding new partners each year.”
The University of California, San Francisco, also has opened its doors to DACA students. Now in his third year, Jirayut New Latthivongskorn is UCSF’s first undocumented medical student. His education is financed by grants, private funding, and donations, said Mr. Latthivongskorn who came to the United States from Thailand when he was 9 years old. He is cofounder of Pre-Health Dreamers, a network of undocumented students who plan to pursue medical careers.
Before DACA granted his entry into UCSF, Mr. Latthivongskorn was accustomed to barriers because of his undocumented status, including having to turn down a nearly full-ride scholarship from the University of California, Davis, after high school.
“It was devastating,” Mr. Latthivongskorn said in an interview. “It was one of the very first times where I felt different and thought, ‘This is not going to work. You are undocumented.’”
Mr. Latthivongskorn and his family scraped together money for him to complete his undergraduate degree at the University of California, Berkeley. California has since passed the DREAM Act, a law that allows undocumented immigrants to receive private scholarships funded through public universities.
Not everyone believes undocumented immigrants should get the chance to become U.S. physicians. Dr. Jane M. Orient, executive director of the Association of American Physicians and Surgeons, argued that undocumented immigrants are not the answer to curbing the physician shortage.
“In a country that’s supposed to be ruled by law, it seems incomprehensible that people who are violating the law should be given privileges over people who are here legally,” she said in an interview. “We desperately do need more physicians, but we should not be blocking Americans from having this opportunity.”
Dr. Shirie Leng, a Boston anesthesiologist, said DACA is promising in theory, but falls short in practical application.
“There’s no particular reason why [undocumented students] wouldn’t make great doctors,” said Dr. Leng. “The problem is funding related. You can give kids all the opportunity you want, but if you can’t pay for it, that seems to me to be the biggest sticking point.”
Basing admission policies on programs that are vulnerable could end poorly for schools and students, Dr. Leng added.
If DACA is revoked, “it’s not just a waste of money for the school, but a waste of time for the kids,” she said.
Protections hinge on Supreme Court … and next president
During oral arguments earlier this month, justices appeared to disagree on whether DAPA and expanded DACA were properly executed.
Associate Justice Anthony M. Kennedy indicated that the normal order of government policy making had been “turned upside down,” by the creation of the programs. Associate Justice Sonia Sotomayor, meanwhile, noted that immigration policies with broader reaches have been similarly instituted in the past.
A ruling for the government would mean the president can use his executive power to enact policies that run contrary to immigration laws already in place, said Mr. Hethmon, the D.C. attorney. Current immigration laws trump informal agency discretion and do not allow for the government’s “arbitrary and capricious creation of a massive classification of nonstatus alien beneficiaries,” Mr. Hethmon wrote in his high court brief.
A decision that favors Texas would unravel opportunities for undocumented immigrants and prevent their ability to contribute to society, said Ignacia Rodriguez, a legal fellow at the National Immigration Law Center, which authored a brief in support of the government.
“What’s at stake is providing a stable environment for U.S. citizen children to grow, and providing people with the opportunity and tools to be able to contribute to the workforce [and] to the economy,” she said in an interview. “This is a payoff for everybody, not just those receiving the benefit.”
Regardless of what the Supreme Court decides, the next president could have the last word, according Ashley C. Parrish, a Washington D.C. attorney who cowrote a brief in support of the states. Mr. Parrish takes no position on the merits of the immigration programs, but rather, he is concerned with the administration’s failure to follow the Administrative Procedure Act’s requirements for notice-and-comment rule making.
“If the program were adopted as a legal rule after notice and comment, it could not be changed without going through a new notice-and-comment process,” he said. “If it is just a bare statement of policy, it can be changed at any time, without notice to anyone. The next administration could say, ‘Thank you for coming out of the shadows; we are now going to deport all of you.’ ”
Among the Democrats running for president, former Secretary of State Hillary Clinton has said she will defend DACA and Sen. Bernie Sanders (I-Vt.) has said he supports DACA and DAPA, and plans to expand them if elected.
Conversely, presumed Republican presidential nominee Donald Trump has indicated he would rescind DACA and related programs if elected.
After spending most of her life terrified of deportation, Ms. Rojas Marquez said she is not wasting time worrying about the Supreme Court’s decision or whether the next president will overturn the policy. She is keeping her studies foremost in her mind and the goal of becoming a doctor firmly in her heart.
“I have always lived with what-ifs,” she said. “This time around, I’m not going to be living in fear of the removing of DACA, because I wouldn’t have made it this far if I always lived in fear. My plan is no matter what happens, I’m going to finish medical school, and from there, I pray that I will be able to practice in the U.S.”
The Supreme Court is expected to issue its decision by June.
On Twitter @legal_med