User login
FDA approves injectable treatment for cheek lines, wrinkles
The treatment, marketed as Sculptra, is the first FDA-approved PLLA collagen stimulator that, “when injected into the cheek area, helps stimulate natural collagen production to smooth wrinkles and improve skin quality such as firmness and glow,” according to a press release from the manufacturer, Galderma. Sculptra was first approved for aesthetic use in 2009 in the United States and is now available in more than 40 countries.
With this expanded approval, PLLA-SCA is now indicated for use in people with healthy immune systems for correcting shallow to deep nasolabial fold contour deficiencies, fine lines, and wrinkles in the cheeks and other facial areas.
94% have enduring improvement at 2 years
In a clinical trial, PLLA-SCA achieved the primary efficacy endpoint of at least a 1-grade improvement in wrinkles on both cheeks concurrently at rest and its secondary endpoint of improving cheek wrinkles when smiling for up to 2 years, the company states.
According to Galderma, patients showed aesthetic improvement in cheek wrinkles throughout the study; 96% showed improvement at 3 months, 94% showed improvement at 1 year, and 94% showed improvement at 2 years.
The most common side effects after initial treatment are injection site swelling, tenderness, redness, pain, bruising, bleeding, itching, and lumps, according to the company. Other side effects may include small lumps under the skin that are sometimes noticeable when pressing on the treated area.
PLLA-SCA is available only through a licensed practitioner and should not be used by people allergic to any ingredient of the product or who have a history of keloid formation or hypertrophic scarring. The company notes that safety has not been established in patients who are pregnant, lactating, breastfeeding, or younger than 18.
In its instruction to clinicians, the company warns the treatment should not be injected into the blood vessels “as it may cause vascular occlusion, infarction, or embolic phenomena.”
Skin sores, cysts, pimples, rashes, hives, or infection should be healed completely before injecting the treatment, the company cautions. PLLA-SCA should not be injected into the red area of the lip or in the periorbital area.
A version of this article first appeared on Medscape.com.
The treatment, marketed as Sculptra, is the first FDA-approved PLLA collagen stimulator that, “when injected into the cheek area, helps stimulate natural collagen production to smooth wrinkles and improve skin quality such as firmness and glow,” according to a press release from the manufacturer, Galderma. Sculptra was first approved for aesthetic use in 2009 in the United States and is now available in more than 40 countries.
With this expanded approval, PLLA-SCA is now indicated for use in people with healthy immune systems for correcting shallow to deep nasolabial fold contour deficiencies, fine lines, and wrinkles in the cheeks and other facial areas.
94% have enduring improvement at 2 years
In a clinical trial, PLLA-SCA achieved the primary efficacy endpoint of at least a 1-grade improvement in wrinkles on both cheeks concurrently at rest and its secondary endpoint of improving cheek wrinkles when smiling for up to 2 years, the company states.
According to Galderma, patients showed aesthetic improvement in cheek wrinkles throughout the study; 96% showed improvement at 3 months, 94% showed improvement at 1 year, and 94% showed improvement at 2 years.
The most common side effects after initial treatment are injection site swelling, tenderness, redness, pain, bruising, bleeding, itching, and lumps, according to the company. Other side effects may include small lumps under the skin that are sometimes noticeable when pressing on the treated area.
PLLA-SCA is available only through a licensed practitioner and should not be used by people allergic to any ingredient of the product or who have a history of keloid formation or hypertrophic scarring. The company notes that safety has not been established in patients who are pregnant, lactating, breastfeeding, or younger than 18.
In its instruction to clinicians, the company warns the treatment should not be injected into the blood vessels “as it may cause vascular occlusion, infarction, or embolic phenomena.”
Skin sores, cysts, pimples, rashes, hives, or infection should be healed completely before injecting the treatment, the company cautions. PLLA-SCA should not be injected into the red area of the lip or in the periorbital area.
A version of this article first appeared on Medscape.com.
The treatment, marketed as Sculptra, is the first FDA-approved PLLA collagen stimulator that, “when injected into the cheek area, helps stimulate natural collagen production to smooth wrinkles and improve skin quality such as firmness and glow,” according to a press release from the manufacturer, Galderma. Sculptra was first approved for aesthetic use in 2009 in the United States and is now available in more than 40 countries.
With this expanded approval, PLLA-SCA is now indicated for use in people with healthy immune systems for correcting shallow to deep nasolabial fold contour deficiencies, fine lines, and wrinkles in the cheeks and other facial areas.
94% have enduring improvement at 2 years
In a clinical trial, PLLA-SCA achieved the primary efficacy endpoint of at least a 1-grade improvement in wrinkles on both cheeks concurrently at rest and its secondary endpoint of improving cheek wrinkles when smiling for up to 2 years, the company states.
According to Galderma, patients showed aesthetic improvement in cheek wrinkles throughout the study; 96% showed improvement at 3 months, 94% showed improvement at 1 year, and 94% showed improvement at 2 years.
The most common side effects after initial treatment are injection site swelling, tenderness, redness, pain, bruising, bleeding, itching, and lumps, according to the company. Other side effects may include small lumps under the skin that are sometimes noticeable when pressing on the treated area.
PLLA-SCA is available only through a licensed practitioner and should not be used by people allergic to any ingredient of the product or who have a history of keloid formation or hypertrophic scarring. The company notes that safety has not been established in patients who are pregnant, lactating, breastfeeding, or younger than 18.
In its instruction to clinicians, the company warns the treatment should not be injected into the blood vessels “as it may cause vascular occlusion, infarction, or embolic phenomena.”
Skin sores, cysts, pimples, rashes, hives, or infection should be healed completely before injecting the treatment, the company cautions. PLLA-SCA should not be injected into the red area of the lip or in the periorbital area.
A version of this article first appeared on Medscape.com.
Should youth with type 1 diabetes use closed-loop systems?
Would closed-loop systems be a good option for young patients with type 1 diabetes?
International and French recommendations on closed-loop systems state that the use of an “artificial pancreas” should be reserved for adults who are fully engaged with their treatment. This means that young patients, especially adolescents, who are less likely to comply with treatment and are more likely to experience suboptimal blood glucose control, are often excluded from the use of such systems for managing their diabetes.
Several recent studies seem to call this approach into question.
One such study, which was presented at a Francophone Diabetes Society conference and was published in Nature Communications, showed that adolescents with poorly controlled diabetes who were equipped with closed-loop systems gained IQ points and reasoning capacity and experienced a reduction in edematous tissue in the brain cortex. Furthermore, with the closed-loop system, patients spent 13% more time in a target range, and there was a significant reduction in time spent in hyperglycemia.
In the same vein, a small prospective study published in Diabetes Care showed that the closed-loop system with the Minimed 780G pump improved glycemic control for 20 young patients with type 1 diabetes aged 13-25 years whose diabetes was poorly controlled (hemoglobin A1c ≥ 8.5%). At the end of the 3-month study period, the average A1c had decreased from 10.5% (±2.1%) to 7.6% (±1.1%), an average decrease of 2.9%. The time spent in target A1c, which was set from 0.70 g/L to 1.80 g/L, was increased by almost 40%.
With respect to very young children, a study published in The New England Journal of Medicine also showed a favorable risk-benefit ratio for closed-loop systems. The trial, which enrolled 102 children aged 2 years to less than 6 years who had type 1 diabetes, showed that the amount of time that the glucose level was within the target range during the 13-week study period was higher (+3 hours) for those who had been randomly assigned to receive the hybrid closed-loop system (n = 68) than for those who had received the standard treatment (n = 34), either with an insulin pump or multiple daily injections or a Dexcom G6 continuous glucose monitoring device.
A previous study carried out by the Paris Public Hospital System had already shown that the French Diabeloop system could reduce episodes of hypoglycemia and achieve good glycemic control for prepubescent children (n = 21; aged 6-12 years) with type 1 diabetes in real-life conditions.
Eric Renard, MD, PhD, head of the department of endocrinology and diabetes at Lapeyronie Hospital in Montpellier, France, was not surprised at the findings from the study, especially in adolescents with poorly controlled diabetes.
“We have already seen studies in which those patients who had the most poorly controlled diabetes at the start were the ones who improved the most with the closed-loop system, by at least 20% in terms of time in target. These findings resonate with what I see in my clinic,” said Dr. Renard in an interview.
“In my experience, these young adolescents, who neglected their diabetes when they had no devices to help control it, when they had to inject themselves, et cetera ... well, they’re just not the same people when they’re put on a closed-loop system,” he added. “They rise to the challenge, and for the first time, they succeed without making a huge effort, since the algorithm does what they weren’t doing. It’s astonishing to see near-total engagement in these young people when explaining the technology to them and saying, ‘Let’s give it a go.’ These are the very same youngsters who didn’t want to hear about their diabetes in the past. They are delighted and once again involved in managing their condition.”
That’s why Dr. Renard recommends keeping an open mind when considering treatment options for young patients with poorly controlled type 1 diabetes.
“When young people have very poorly controlled diabetes, they risk having cardiovascular complications and damaging their retinas and kidneys,” he said. “If we can get them from 25% to 45% time in target, even if that hasn’t been easy to achieve, this will help save their blood vessels! The only thing we have to be careful of is that we don’t set up a closed-loop system in someone who doesn’t want one. But, if it can manage to spark the interest of a young patient, in most cases, it’s beneficial.”
This article was translated from the Medscape French edition. A version appeared on Medscape.com.
Would closed-loop systems be a good option for young patients with type 1 diabetes?
International and French recommendations on closed-loop systems state that the use of an “artificial pancreas” should be reserved for adults who are fully engaged with their treatment. This means that young patients, especially adolescents, who are less likely to comply with treatment and are more likely to experience suboptimal blood glucose control, are often excluded from the use of such systems for managing their diabetes.
Several recent studies seem to call this approach into question.
One such study, which was presented at a Francophone Diabetes Society conference and was published in Nature Communications, showed that adolescents with poorly controlled diabetes who were equipped with closed-loop systems gained IQ points and reasoning capacity and experienced a reduction in edematous tissue in the brain cortex. Furthermore, with the closed-loop system, patients spent 13% more time in a target range, and there was a significant reduction in time spent in hyperglycemia.
In the same vein, a small prospective study published in Diabetes Care showed that the closed-loop system with the Minimed 780G pump improved glycemic control for 20 young patients with type 1 diabetes aged 13-25 years whose diabetes was poorly controlled (hemoglobin A1c ≥ 8.5%). At the end of the 3-month study period, the average A1c had decreased from 10.5% (±2.1%) to 7.6% (±1.1%), an average decrease of 2.9%. The time spent in target A1c, which was set from 0.70 g/L to 1.80 g/L, was increased by almost 40%.
With respect to very young children, a study published in The New England Journal of Medicine also showed a favorable risk-benefit ratio for closed-loop systems. The trial, which enrolled 102 children aged 2 years to less than 6 years who had type 1 diabetes, showed that the amount of time that the glucose level was within the target range during the 13-week study period was higher (+3 hours) for those who had been randomly assigned to receive the hybrid closed-loop system (n = 68) than for those who had received the standard treatment (n = 34), either with an insulin pump or multiple daily injections or a Dexcom G6 continuous glucose monitoring device.
A previous study carried out by the Paris Public Hospital System had already shown that the French Diabeloop system could reduce episodes of hypoglycemia and achieve good glycemic control for prepubescent children (n = 21; aged 6-12 years) with type 1 diabetes in real-life conditions.
Eric Renard, MD, PhD, head of the department of endocrinology and diabetes at Lapeyronie Hospital in Montpellier, France, was not surprised at the findings from the study, especially in adolescents with poorly controlled diabetes.
“We have already seen studies in which those patients who had the most poorly controlled diabetes at the start were the ones who improved the most with the closed-loop system, by at least 20% in terms of time in target. These findings resonate with what I see in my clinic,” said Dr. Renard in an interview.
“In my experience, these young adolescents, who neglected their diabetes when they had no devices to help control it, when they had to inject themselves, et cetera ... well, they’re just not the same people when they’re put on a closed-loop system,” he added. “They rise to the challenge, and for the first time, they succeed without making a huge effort, since the algorithm does what they weren’t doing. It’s astonishing to see near-total engagement in these young people when explaining the technology to them and saying, ‘Let’s give it a go.’ These are the very same youngsters who didn’t want to hear about their diabetes in the past. They are delighted and once again involved in managing their condition.”
That’s why Dr. Renard recommends keeping an open mind when considering treatment options for young patients with poorly controlled type 1 diabetes.
“When young people have very poorly controlled diabetes, they risk having cardiovascular complications and damaging their retinas and kidneys,” he said. “If we can get them from 25% to 45% time in target, even if that hasn’t been easy to achieve, this will help save their blood vessels! The only thing we have to be careful of is that we don’t set up a closed-loop system in someone who doesn’t want one. But, if it can manage to spark the interest of a young patient, in most cases, it’s beneficial.”
This article was translated from the Medscape French edition. A version appeared on Medscape.com.
Would closed-loop systems be a good option for young patients with type 1 diabetes?
International and French recommendations on closed-loop systems state that the use of an “artificial pancreas” should be reserved for adults who are fully engaged with their treatment. This means that young patients, especially adolescents, who are less likely to comply with treatment and are more likely to experience suboptimal blood glucose control, are often excluded from the use of such systems for managing their diabetes.
Several recent studies seem to call this approach into question.
One such study, which was presented at a Francophone Diabetes Society conference and was published in Nature Communications, showed that adolescents with poorly controlled diabetes who were equipped with closed-loop systems gained IQ points and reasoning capacity and experienced a reduction in edematous tissue in the brain cortex. Furthermore, with the closed-loop system, patients spent 13% more time in a target range, and there was a significant reduction in time spent in hyperglycemia.
In the same vein, a small prospective study published in Diabetes Care showed that the closed-loop system with the Minimed 780G pump improved glycemic control for 20 young patients with type 1 diabetes aged 13-25 years whose diabetes was poorly controlled (hemoglobin A1c ≥ 8.5%). At the end of the 3-month study period, the average A1c had decreased from 10.5% (±2.1%) to 7.6% (±1.1%), an average decrease of 2.9%. The time spent in target A1c, which was set from 0.70 g/L to 1.80 g/L, was increased by almost 40%.
With respect to very young children, a study published in The New England Journal of Medicine also showed a favorable risk-benefit ratio for closed-loop systems. The trial, which enrolled 102 children aged 2 years to less than 6 years who had type 1 diabetes, showed that the amount of time that the glucose level was within the target range during the 13-week study period was higher (+3 hours) for those who had been randomly assigned to receive the hybrid closed-loop system (n = 68) than for those who had received the standard treatment (n = 34), either with an insulin pump or multiple daily injections or a Dexcom G6 continuous glucose monitoring device.
A previous study carried out by the Paris Public Hospital System had already shown that the French Diabeloop system could reduce episodes of hypoglycemia and achieve good glycemic control for prepubescent children (n = 21; aged 6-12 years) with type 1 diabetes in real-life conditions.
Eric Renard, MD, PhD, head of the department of endocrinology and diabetes at Lapeyronie Hospital in Montpellier, France, was not surprised at the findings from the study, especially in adolescents with poorly controlled diabetes.
“We have already seen studies in which those patients who had the most poorly controlled diabetes at the start were the ones who improved the most with the closed-loop system, by at least 20% in terms of time in target. These findings resonate with what I see in my clinic,” said Dr. Renard in an interview.
“In my experience, these young adolescents, who neglected their diabetes when they had no devices to help control it, when they had to inject themselves, et cetera ... well, they’re just not the same people when they’re put on a closed-loop system,” he added. “They rise to the challenge, and for the first time, they succeed without making a huge effort, since the algorithm does what they weren’t doing. It’s astonishing to see near-total engagement in these young people when explaining the technology to them and saying, ‘Let’s give it a go.’ These are the very same youngsters who didn’t want to hear about their diabetes in the past. They are delighted and once again involved in managing their condition.”
That’s why Dr. Renard recommends keeping an open mind when considering treatment options for young patients with poorly controlled type 1 diabetes.
“When young people have very poorly controlled diabetes, they risk having cardiovascular complications and damaging their retinas and kidneys,” he said. “If we can get them from 25% to 45% time in target, even if that hasn’t been easy to achieve, this will help save their blood vessels! The only thing we have to be careful of is that we don’t set up a closed-loop system in someone who doesn’t want one. But, if it can manage to spark the interest of a young patient, in most cases, it’s beneficial.”
This article was translated from the Medscape French edition. A version appeared on Medscape.com.
Musculoskeletal disorders prevalent in orchestra musicians
PARIS – For orchestra musicians, performance is everything. So, it’s no wonder that musculoskeletal disorders – a reality for so many of these professionals – are not openly discussed. Physical pain is often pushed aside, unexpressed, until one day the suffering gets to be too much, the ability to play is impacted, and all the effort to keep things under wraps and under control culminates in burnout.
Anne Maugue was one of the speakers at the French College of General Medicine’s 16th Congress of General Medicine. Ms. Maugue is a postdoctoral researcher at Côte d’Azur University, Nice, France. She also plays flute in the Monte-Carlo Philharmonic Orchestra. Through her presentation to the physicians, she sought to raise awareness about MSDs in professional musicians, as well as the associated psychosocial risk factors. “If caught early enough, this pain can often be successfully treated.”
High prevalence
“You’re a violinist in a major symphony orchestra. It’s Sunday night, 8 o’clock, and you’ve just come off the stage. A few minutes ago, you felt a sharp pain in your right arm – a pain that is now, already, overwhelming. The conductor accused you of not being focused, of not concentrating. You know that you have another rehearsal in just a few hours, Monday morning. So, what do you do – other than hope that the pain goes away by then? Where can you turn to get help?”
With this opening scenario, Ms. Maugue was able to immediately orient the attendees to the realities that professional musicians face.
Pain is far from anecdotal. In professional orchestras, its prevalence over 12 months is between 41% and 93%. “An elite athlete has a full training staff they can turn to. An elite musician, on the other hand, usually only has their general practitioner – and that’s assuming the musician even reaches out to get treatment to begin with.
“The fact is that most of the time musicians only care about the pain when it becomes chronic, when it causes discomfort that affects their playing,” said Ms. Maugue.
How, then, does one evaluate this problem? In a Danish study, musicians rated the musculoskeletal problems they had experienced in the preceding 7 days. When the researchers compared those reports with findings from a clinical examination, they found that the examiners were not able to identify which musicians had reported problems. Why? Because a diagnosis does not reflect the severity or the impact, both of which are subjective.
“When faced with pain, the musician’s initial reaction is denial,” said Ms. Maugue. “The pain is often attributed to something other than the physicality of playing their instrument. They then turn to self-care, to colleagues. It’s only much later that they consult a medical professional.”
As a result, the physician is seldom aware of the musician’s psychological distress and has no sense of how long it’s been since the pain first started.
Work environment
Carrying around an instrument all the time and maintaining nonergonomic postures for extended periods are just two of the factors that put professional musicians at risk of physical pain. Not to be forgotten, Ms. Maugue added, are the work-related pressures. Musicians are not immune to issues with their work environment. They can feel like they aren’t getting the resources they need, proper recognition from their leaders, or support from their colleagues. In the end, such feelings can engender a sense of unfairness – and that acts as a stressor that can give rise to MSDs.
Evidence of this phenomenon can be found in the results of a study that Ms. Maugue conducted. Out of 440 French orchestra musicians (44% women), 64% said they had experienced MSD-related pain in the preceding 12 months and 61% in the preceding 7 days.
Using industrial and organizational psychology scales of measurement, Ms. Maugue was able to show, through hierarchical regression, that “emotional exhaustion and MSD-related pain occur when the environment in which people work causes them to feel a sense of unfairness.”
Early detection
Finally, Ms. Maugue encouraged general practitioners to ask every patient whether he or she plays a musical instrument. If the answer is yes, get an idea about any pain that he or she may have been feeling in the back, neck, and upper extremities so that prompt treatment can be given.
“There are other studies underway that are looking to better characterize instrumental activity and to enable more effective management by sports medicine departments,” said Ms. Maugue. “But back to patients with MSDs. It’s important to understand everything about their playing. Where do they practice? How often do they practice? What’s their posture like when they play? What’s the tempo of the music they’re working on? Because what we see in professional musicians is likely to be seen in amateur musicians as well – particularly in young people who study at a conservatory,” where not much is being done to prevent MSDs.
“If professional musicians are given treatment early on, half of them can be permanently cured,” she concluded. “And then, just like elite athletes, they’ll be able to get right back to playing.”
This article was translated from Medscape’s French edition and a version appeared on Medscape.com.
PARIS – For orchestra musicians, performance is everything. So, it’s no wonder that musculoskeletal disorders – a reality for so many of these professionals – are not openly discussed. Physical pain is often pushed aside, unexpressed, until one day the suffering gets to be too much, the ability to play is impacted, and all the effort to keep things under wraps and under control culminates in burnout.
Anne Maugue was one of the speakers at the French College of General Medicine’s 16th Congress of General Medicine. Ms. Maugue is a postdoctoral researcher at Côte d’Azur University, Nice, France. She also plays flute in the Monte-Carlo Philharmonic Orchestra. Through her presentation to the physicians, she sought to raise awareness about MSDs in professional musicians, as well as the associated psychosocial risk factors. “If caught early enough, this pain can often be successfully treated.”
High prevalence
“You’re a violinist in a major symphony orchestra. It’s Sunday night, 8 o’clock, and you’ve just come off the stage. A few minutes ago, you felt a sharp pain in your right arm – a pain that is now, already, overwhelming. The conductor accused you of not being focused, of not concentrating. You know that you have another rehearsal in just a few hours, Monday morning. So, what do you do – other than hope that the pain goes away by then? Where can you turn to get help?”
With this opening scenario, Ms. Maugue was able to immediately orient the attendees to the realities that professional musicians face.
Pain is far from anecdotal. In professional orchestras, its prevalence over 12 months is between 41% and 93%. “An elite athlete has a full training staff they can turn to. An elite musician, on the other hand, usually only has their general practitioner – and that’s assuming the musician even reaches out to get treatment to begin with.
“The fact is that most of the time musicians only care about the pain when it becomes chronic, when it causes discomfort that affects their playing,” said Ms. Maugue.
How, then, does one evaluate this problem? In a Danish study, musicians rated the musculoskeletal problems they had experienced in the preceding 7 days. When the researchers compared those reports with findings from a clinical examination, they found that the examiners were not able to identify which musicians had reported problems. Why? Because a diagnosis does not reflect the severity or the impact, both of which are subjective.
“When faced with pain, the musician’s initial reaction is denial,” said Ms. Maugue. “The pain is often attributed to something other than the physicality of playing their instrument. They then turn to self-care, to colleagues. It’s only much later that they consult a medical professional.”
As a result, the physician is seldom aware of the musician’s psychological distress and has no sense of how long it’s been since the pain first started.
Work environment
Carrying around an instrument all the time and maintaining nonergonomic postures for extended periods are just two of the factors that put professional musicians at risk of physical pain. Not to be forgotten, Ms. Maugue added, are the work-related pressures. Musicians are not immune to issues with their work environment. They can feel like they aren’t getting the resources they need, proper recognition from their leaders, or support from their colleagues. In the end, such feelings can engender a sense of unfairness – and that acts as a stressor that can give rise to MSDs.
Evidence of this phenomenon can be found in the results of a study that Ms. Maugue conducted. Out of 440 French orchestra musicians (44% women), 64% said they had experienced MSD-related pain in the preceding 12 months and 61% in the preceding 7 days.
Using industrial and organizational psychology scales of measurement, Ms. Maugue was able to show, through hierarchical regression, that “emotional exhaustion and MSD-related pain occur when the environment in which people work causes them to feel a sense of unfairness.”
Early detection
Finally, Ms. Maugue encouraged general practitioners to ask every patient whether he or she plays a musical instrument. If the answer is yes, get an idea about any pain that he or she may have been feeling in the back, neck, and upper extremities so that prompt treatment can be given.
“There are other studies underway that are looking to better characterize instrumental activity and to enable more effective management by sports medicine departments,” said Ms. Maugue. “But back to patients with MSDs. It’s important to understand everything about their playing. Where do they practice? How often do they practice? What’s their posture like when they play? What’s the tempo of the music they’re working on? Because what we see in professional musicians is likely to be seen in amateur musicians as well – particularly in young people who study at a conservatory,” where not much is being done to prevent MSDs.
“If professional musicians are given treatment early on, half of them can be permanently cured,” she concluded. “And then, just like elite athletes, they’ll be able to get right back to playing.”
This article was translated from Medscape’s French edition and a version appeared on Medscape.com.
PARIS – For orchestra musicians, performance is everything. So, it’s no wonder that musculoskeletal disorders – a reality for so many of these professionals – are not openly discussed. Physical pain is often pushed aside, unexpressed, until one day the suffering gets to be too much, the ability to play is impacted, and all the effort to keep things under wraps and under control culminates in burnout.
Anne Maugue was one of the speakers at the French College of General Medicine’s 16th Congress of General Medicine. Ms. Maugue is a postdoctoral researcher at Côte d’Azur University, Nice, France. She also plays flute in the Monte-Carlo Philharmonic Orchestra. Through her presentation to the physicians, she sought to raise awareness about MSDs in professional musicians, as well as the associated psychosocial risk factors. “If caught early enough, this pain can often be successfully treated.”
High prevalence
“You’re a violinist in a major symphony orchestra. It’s Sunday night, 8 o’clock, and you’ve just come off the stage. A few minutes ago, you felt a sharp pain in your right arm – a pain that is now, already, overwhelming. The conductor accused you of not being focused, of not concentrating. You know that you have another rehearsal in just a few hours, Monday morning. So, what do you do – other than hope that the pain goes away by then? Where can you turn to get help?”
With this opening scenario, Ms. Maugue was able to immediately orient the attendees to the realities that professional musicians face.
Pain is far from anecdotal. In professional orchestras, its prevalence over 12 months is between 41% and 93%. “An elite athlete has a full training staff they can turn to. An elite musician, on the other hand, usually only has their general practitioner – and that’s assuming the musician even reaches out to get treatment to begin with.
“The fact is that most of the time musicians only care about the pain when it becomes chronic, when it causes discomfort that affects their playing,” said Ms. Maugue.
How, then, does one evaluate this problem? In a Danish study, musicians rated the musculoskeletal problems they had experienced in the preceding 7 days. When the researchers compared those reports with findings from a clinical examination, they found that the examiners were not able to identify which musicians had reported problems. Why? Because a diagnosis does not reflect the severity or the impact, both of which are subjective.
“When faced with pain, the musician’s initial reaction is denial,” said Ms. Maugue. “The pain is often attributed to something other than the physicality of playing their instrument. They then turn to self-care, to colleagues. It’s only much later that they consult a medical professional.”
As a result, the physician is seldom aware of the musician’s psychological distress and has no sense of how long it’s been since the pain first started.
Work environment
Carrying around an instrument all the time and maintaining nonergonomic postures for extended periods are just two of the factors that put professional musicians at risk of physical pain. Not to be forgotten, Ms. Maugue added, are the work-related pressures. Musicians are not immune to issues with their work environment. They can feel like they aren’t getting the resources they need, proper recognition from their leaders, or support from their colleagues. In the end, such feelings can engender a sense of unfairness – and that acts as a stressor that can give rise to MSDs.
Evidence of this phenomenon can be found in the results of a study that Ms. Maugue conducted. Out of 440 French orchestra musicians (44% women), 64% said they had experienced MSD-related pain in the preceding 12 months and 61% in the preceding 7 days.
Using industrial and organizational psychology scales of measurement, Ms. Maugue was able to show, through hierarchical regression, that “emotional exhaustion and MSD-related pain occur when the environment in which people work causes them to feel a sense of unfairness.”
Early detection
Finally, Ms. Maugue encouraged general practitioners to ask every patient whether he or she plays a musical instrument. If the answer is yes, get an idea about any pain that he or she may have been feeling in the back, neck, and upper extremities so that prompt treatment can be given.
“There are other studies underway that are looking to better characterize instrumental activity and to enable more effective management by sports medicine departments,” said Ms. Maugue. “But back to patients with MSDs. It’s important to understand everything about their playing. Where do they practice? How often do they practice? What’s their posture like when they play? What’s the tempo of the music they’re working on? Because what we see in professional musicians is likely to be seen in amateur musicians as well – particularly in young people who study at a conservatory,” where not much is being done to prevent MSDs.
“If professional musicians are given treatment early on, half of them can be permanently cured,” she concluded. “And then, just like elite athletes, they’ll be able to get right back to playing.”
This article was translated from Medscape’s French edition and a version appeared on Medscape.com.
Osteoporosis and osteopenia: Latest treatment recommendations
This transcript has been edited for clarity.
I’m Dr. Neil Skolnik. Today’s topic is the new osteoporosis treatment guidelines issued by the American College of Physicians (ACP). The focus of the guidelines is treatment of osteoporosis. But first, I want to discuss screening.
In its 2018 statement, the U.S. Preventive Services Task Force (USPSTF) says that osteoporosis should be screened for in women older than 65 years of age, and those who are younger who are at increased risk based on a risk assessment tool (usually the FRAX tool). There is not enough evidence to weigh in for or against screening men. The other large organization that weighs in on screening is the Bone Health & Osteoporosis Foundation, which agrees with the USPSTF, but in addition says that we should be screening men over age 70 and men who are younger (age 50 to 69) who have risk factors. We should also screen anyone who has a fracture after low impact or no trauma.
Let’s now go on to the ACP treatment guidelines. Osteoporosis is defined as bone mineral density at the femoral neck or the lumbar spine, or both, with a T score less than -2.5.
For postmenopausal women with osteoporosis, you should use a bisphosphonate as first-line treatment to reduce the risk for future fractures. This is given a strong recommendation based on a high certainty of evidence. Bisphosphonates vs. placebo over 3 years leads to one fewer hip fracture per 150 patients treated and one fewer vertebral fracture per 50 people treated.
All the other recommendations in the guidelines are considered “conditional recommendations” that are correct for most people. But whether they make sense for an individual patient depends upon other details, as well as their values and preferences. For instance, treatment of osteoporosis in men is given a conditional recommendation, not because the evidence suggests that it’s not as effective, but because there is not as much evidence. Initial treatment for a man with osteoporosis is with bisphosphonates. Men do get osteoporosis and account for about 30% of hip fractures. This is not a surprise to anyone who takes care of older adults.
For postmenopausal women or men who you would want to treat but who can’t tolerate a bisphosphonate, then the recommendation is to use a RANK ligand inhibitor. Denosumab can be used as second-line treatment to reduce the risk for fractures. Remember, bisphosphonates and denosumab are antiresorptive drugs, meaning they slow the progression of osteoporosis. The anabolic drugs, on the other hand, such as the sclerostin inhibitor romosozumab and recombinant human parathyroid hormone (PTH) teriparatide, increase bone density. The anabolic agents should be used only in women with primary osteoporosis who are at very high risk for fractures, and use of these agents always needs to be followed by an antiresorptive agent, because otherwise there’s a risk for rebound osteoporosis and an increased risk for vertebral fractures.
Now, how about osteopenia? The guidelines recommend that for women over 65 with osteopenia, use an individualized approach influenced by the level of risk for fracture, including increased age, low body weight, current smoking, hip fracture in a parent, fall risk, and a personal history of fracture. The guidelines note that increasing the duration of bisphosphonate therapy beyond 3-5 years does reduce the risk for new vertebral fractures, but it doesn’t reduce the risk for other fractures and it increases the risk for osteonecrosis of the jaw and atypical hip fractures. Therefore, the guidelines say that we should use bisphosphonates only for 3-5 years unless someone is at extremely high risk. It’s also important to note that there’s a fivefold higher risk for atypical femoral fractures among Asian women.
Don’t forget about adequate vitamin D and calcium. And most importantly, don’t forget about exercise, particularly exercise aimed at improving balance and quadriceps strength, which helps prevent falls.
Dr. Skolnik is professor, department of family medicine, Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, and associate director, department of family medicine, Abington (Pa.) Jefferson Health. He disclosed ties with AstraZeneca, Bayer, Boehringer Ingelheim, Eli Lilly, GlaxoSmithKline, Merck, Sanofi, Sanofi Pasteur, and Teva.
A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
I’m Dr. Neil Skolnik. Today’s topic is the new osteoporosis treatment guidelines issued by the American College of Physicians (ACP). The focus of the guidelines is treatment of osteoporosis. But first, I want to discuss screening.
In its 2018 statement, the U.S. Preventive Services Task Force (USPSTF) says that osteoporosis should be screened for in women older than 65 years of age, and those who are younger who are at increased risk based on a risk assessment tool (usually the FRAX tool). There is not enough evidence to weigh in for or against screening men. The other large organization that weighs in on screening is the Bone Health & Osteoporosis Foundation, which agrees with the USPSTF, but in addition says that we should be screening men over age 70 and men who are younger (age 50 to 69) who have risk factors. We should also screen anyone who has a fracture after low impact or no trauma.
Let’s now go on to the ACP treatment guidelines. Osteoporosis is defined as bone mineral density at the femoral neck or the lumbar spine, or both, with a T score less than -2.5.
For postmenopausal women with osteoporosis, you should use a bisphosphonate as first-line treatment to reduce the risk for future fractures. This is given a strong recommendation based on a high certainty of evidence. Bisphosphonates vs. placebo over 3 years leads to one fewer hip fracture per 150 patients treated and one fewer vertebral fracture per 50 people treated.
All the other recommendations in the guidelines are considered “conditional recommendations” that are correct for most people. But whether they make sense for an individual patient depends upon other details, as well as their values and preferences. For instance, treatment of osteoporosis in men is given a conditional recommendation, not because the evidence suggests that it’s not as effective, but because there is not as much evidence. Initial treatment for a man with osteoporosis is with bisphosphonates. Men do get osteoporosis and account for about 30% of hip fractures. This is not a surprise to anyone who takes care of older adults.
For postmenopausal women or men who you would want to treat but who can’t tolerate a bisphosphonate, then the recommendation is to use a RANK ligand inhibitor. Denosumab can be used as second-line treatment to reduce the risk for fractures. Remember, bisphosphonates and denosumab are antiresorptive drugs, meaning they slow the progression of osteoporosis. The anabolic drugs, on the other hand, such as the sclerostin inhibitor romosozumab and recombinant human parathyroid hormone (PTH) teriparatide, increase bone density. The anabolic agents should be used only in women with primary osteoporosis who are at very high risk for fractures, and use of these agents always needs to be followed by an antiresorptive agent, because otherwise there’s a risk for rebound osteoporosis and an increased risk for vertebral fractures.
Now, how about osteopenia? The guidelines recommend that for women over 65 with osteopenia, use an individualized approach influenced by the level of risk for fracture, including increased age, low body weight, current smoking, hip fracture in a parent, fall risk, and a personal history of fracture. The guidelines note that increasing the duration of bisphosphonate therapy beyond 3-5 years does reduce the risk for new vertebral fractures, but it doesn’t reduce the risk for other fractures and it increases the risk for osteonecrosis of the jaw and atypical hip fractures. Therefore, the guidelines say that we should use bisphosphonates only for 3-5 years unless someone is at extremely high risk. It’s also important to note that there’s a fivefold higher risk for atypical femoral fractures among Asian women.
Don’t forget about adequate vitamin D and calcium. And most importantly, don’t forget about exercise, particularly exercise aimed at improving balance and quadriceps strength, which helps prevent falls.
Dr. Skolnik is professor, department of family medicine, Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, and associate director, department of family medicine, Abington (Pa.) Jefferson Health. He disclosed ties with AstraZeneca, Bayer, Boehringer Ingelheim, Eli Lilly, GlaxoSmithKline, Merck, Sanofi, Sanofi Pasteur, and Teva.
A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
I’m Dr. Neil Skolnik. Today’s topic is the new osteoporosis treatment guidelines issued by the American College of Physicians (ACP). The focus of the guidelines is treatment of osteoporosis. But first, I want to discuss screening.
In its 2018 statement, the U.S. Preventive Services Task Force (USPSTF) says that osteoporosis should be screened for in women older than 65 years of age, and those who are younger who are at increased risk based on a risk assessment tool (usually the FRAX tool). There is not enough evidence to weigh in for or against screening men. The other large organization that weighs in on screening is the Bone Health & Osteoporosis Foundation, which agrees with the USPSTF, but in addition says that we should be screening men over age 70 and men who are younger (age 50 to 69) who have risk factors. We should also screen anyone who has a fracture after low impact or no trauma.
Let’s now go on to the ACP treatment guidelines. Osteoporosis is defined as bone mineral density at the femoral neck or the lumbar spine, or both, with a T score less than -2.5.
For postmenopausal women with osteoporosis, you should use a bisphosphonate as first-line treatment to reduce the risk for future fractures. This is given a strong recommendation based on a high certainty of evidence. Bisphosphonates vs. placebo over 3 years leads to one fewer hip fracture per 150 patients treated and one fewer vertebral fracture per 50 people treated.
All the other recommendations in the guidelines are considered “conditional recommendations” that are correct for most people. But whether they make sense for an individual patient depends upon other details, as well as their values and preferences. For instance, treatment of osteoporosis in men is given a conditional recommendation, not because the evidence suggests that it’s not as effective, but because there is not as much evidence. Initial treatment for a man with osteoporosis is with bisphosphonates. Men do get osteoporosis and account for about 30% of hip fractures. This is not a surprise to anyone who takes care of older adults.
For postmenopausal women or men who you would want to treat but who can’t tolerate a bisphosphonate, then the recommendation is to use a RANK ligand inhibitor. Denosumab can be used as second-line treatment to reduce the risk for fractures. Remember, bisphosphonates and denosumab are antiresorptive drugs, meaning they slow the progression of osteoporosis. The anabolic drugs, on the other hand, such as the sclerostin inhibitor romosozumab and recombinant human parathyroid hormone (PTH) teriparatide, increase bone density. The anabolic agents should be used only in women with primary osteoporosis who are at very high risk for fractures, and use of these agents always needs to be followed by an antiresorptive agent, because otherwise there’s a risk for rebound osteoporosis and an increased risk for vertebral fractures.
Now, how about osteopenia? The guidelines recommend that for women over 65 with osteopenia, use an individualized approach influenced by the level of risk for fracture, including increased age, low body weight, current smoking, hip fracture in a parent, fall risk, and a personal history of fracture. The guidelines note that increasing the duration of bisphosphonate therapy beyond 3-5 years does reduce the risk for new vertebral fractures, but it doesn’t reduce the risk for other fractures and it increases the risk for osteonecrosis of the jaw and atypical hip fractures. Therefore, the guidelines say that we should use bisphosphonates only for 3-5 years unless someone is at extremely high risk. It’s also important to note that there’s a fivefold higher risk for atypical femoral fractures among Asian women.
Don’t forget about adequate vitamin D and calcium. And most importantly, don’t forget about exercise, particularly exercise aimed at improving balance and quadriceps strength, which helps prevent falls.
Dr. Skolnik is professor, department of family medicine, Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, and associate director, department of family medicine, Abington (Pa.) Jefferson Health. He disclosed ties with AstraZeneca, Bayer, Boehringer Ingelheim, Eli Lilly, GlaxoSmithKline, Merck, Sanofi, Sanofi Pasteur, and Teva.
A version of this article originally appeared on Medscape.com.
Obesity drugs overpriced, change needed to tackle issue
The lowest available national prices of drugs to treat obesity are up to 20 times higher than the estimated cost of profitable generic versions of the same agents, according to a new analysis.
The findings by Jacob Levi, MBBS, and colleagues were published in Obesity.
“Our study highlights the inequality in pricing that exists for effective antiobesity medications, which are largely unaffordable in most countries,” Dr. Levi, from Royal Free Hospital NHS Trust, London, said in a press release.
“We show that these drugs can actually be produced and sold profitably for low prices,” he summarized. “A public health approach that prioritizes improving access to medications should be adopted, instead of allowing companies to maximize profits,” Dr. Levi urged.
Dr. Levi and colleagues studied the oral agents orlistat, naltrexone/bupropion, topiramate/phentermine, and semaglutide, and subcutaneous liraglutide, semaglutide, and tirzepatide (all approved by the U.S. Food and Drug Administration to treat obesity, except for oral semaglutide and subcutaneous tirzepatide, which are not yet approved to treat obesity in the absence of type 2 diabetes).
“Worldwide, more people are dying from diabetes and clinical obesity than HIV, tuberculosis, and malaria combined now,” senior author Andrew Hill, MD, department of pharmacology and therapeutics, University of Liverpool, England, pointed out.
We need to repeat the low-cost success story with obesity drugs
“Millions of lives have been saved by treating infectious diseases at low cost in poor countries,” Dr. Hill continued. “Now we need to repeat this medical success story, with mass treatment of diabetes and clinical obesity at low prices.”
However, in an accompanying editorial, Eric A. Finkelstein, MD, and Junxing Chay, PhD, Duke-NUS Medical School, Singapore, maintain that “It would be great if everyone had affordable access to all medicines that might improve their health. Yet that is simply not possible, nor will it ever be.”
“What is truly needed is a better way to ration the health care dollars currently available in efforts to maximize population health. That is the challenge ahead not just for [antiobesity medications] but for all treatments,” they say.
“Greater use of cost-effectiveness analysis and direct negotiations, while maintaining the patent system, represents an appropriate approach for allocating scarce health care resources in the United States and beyond,” they continue.
Lowest current patented drug prices vs. estimated generic drug prices
New medications for obesity were highly effective in recent clinical trials, but high prices limit the ability of patients to get these medications, Dr. Levi and colleagues write.
They analyzed prices for obesity drugs in 16 low-, middle-, and high-income countries: Australia, Bangladesh, China, France, Germany, India, Kenya, Morocco, Norway, Peru, Pakistan, South Africa, Turkey, the United Kingdom, the United States, and Vietnam.
The researchers assessed the price of a 30-day supply of each of the studied branded drugs based on the lowest available price (in 2021 U.S. dollars) from multiple online national price databases.
Then they calculated the estimated minimum price of a 30-day supply of a potential generic version of these drugs, which included the cost of the active medicinal ingredients, the excipients (nonactive ingredients), the prefilled injectable device plus needles (for subcutaneous drugs), transportation, 10% profit, and 27% tax on profit.
The national prices of the branded medications for obesity were significantly higher than the estimated minimum prices of potential generic drugs (see Table).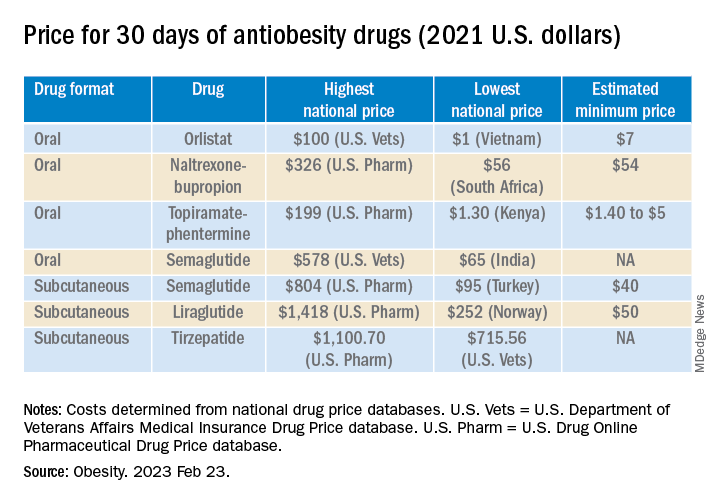
The highest national price for a branded oral drug for obesity vs. the estimated minimum price for a potential generic version was $100 vs. $7 for orlistat, $199 vs. $5 for phentermine/topiramate, and $326 vs. $54 for naltrexone/bupropion, for a 30-day supply.
There was an even greater difference between highest national branded drug price vs. estimated minimum generic drug price for the newer subcutaneously injectable drugs for obesity.
For example, the price of a 30-day course of subcutaneous semaglutide ranged from $804 (United States) to $95 (Turkey), while the estimated minimum potential generic drug price was $40 (which is 20 times lower).
The study was funded by grants from the Make Medicines Affordable/International Treatment Preparedness Coalition and from the National Heart, Lung, and Blood Institute of the National Institutes of Health. Coauthor Francois Venter has reported receiving support from the Bill and Melinda Gates Foundation, U.S. Agency for International Development, Unitaid, SA Medical Research Council, Foundation for Innovative New Diagnostics, the Children’s Investment Fund Foundation, Gilead, ViiV, Mylan, Merck, Adcock Ingram, Aspen, Abbott, Roche, Johnson & Johnson, Sanofi, Virology Education, SA HIV Clinicians Society, and Dira Sengwe. The other authors and Dr. Chay have reported no relevant financial relationships. Dr. Finkelstein has reported receiving support for serving on the WW scientific advisory board and an educational grant unrelated to the present work from Novo Nordisk.
A version of this article first appeared on Medscape.com.
The lowest available national prices of drugs to treat obesity are up to 20 times higher than the estimated cost of profitable generic versions of the same agents, according to a new analysis.
The findings by Jacob Levi, MBBS, and colleagues were published in Obesity.
“Our study highlights the inequality in pricing that exists for effective antiobesity medications, which are largely unaffordable in most countries,” Dr. Levi, from Royal Free Hospital NHS Trust, London, said in a press release.
“We show that these drugs can actually be produced and sold profitably for low prices,” he summarized. “A public health approach that prioritizes improving access to medications should be adopted, instead of allowing companies to maximize profits,” Dr. Levi urged.
Dr. Levi and colleagues studied the oral agents orlistat, naltrexone/bupropion, topiramate/phentermine, and semaglutide, and subcutaneous liraglutide, semaglutide, and tirzepatide (all approved by the U.S. Food and Drug Administration to treat obesity, except for oral semaglutide and subcutaneous tirzepatide, which are not yet approved to treat obesity in the absence of type 2 diabetes).
“Worldwide, more people are dying from diabetes and clinical obesity than HIV, tuberculosis, and malaria combined now,” senior author Andrew Hill, MD, department of pharmacology and therapeutics, University of Liverpool, England, pointed out.
We need to repeat the low-cost success story with obesity drugs
“Millions of lives have been saved by treating infectious diseases at low cost in poor countries,” Dr. Hill continued. “Now we need to repeat this medical success story, with mass treatment of diabetes and clinical obesity at low prices.”
However, in an accompanying editorial, Eric A. Finkelstein, MD, and Junxing Chay, PhD, Duke-NUS Medical School, Singapore, maintain that “It would be great if everyone had affordable access to all medicines that might improve their health. Yet that is simply not possible, nor will it ever be.”
“What is truly needed is a better way to ration the health care dollars currently available in efforts to maximize population health. That is the challenge ahead not just for [antiobesity medications] but for all treatments,” they say.
“Greater use of cost-effectiveness analysis and direct negotiations, while maintaining the patent system, represents an appropriate approach for allocating scarce health care resources in the United States and beyond,” they continue.
Lowest current patented drug prices vs. estimated generic drug prices
New medications for obesity were highly effective in recent clinical trials, but high prices limit the ability of patients to get these medications, Dr. Levi and colleagues write.
They analyzed prices for obesity drugs in 16 low-, middle-, and high-income countries: Australia, Bangladesh, China, France, Germany, India, Kenya, Morocco, Norway, Peru, Pakistan, South Africa, Turkey, the United Kingdom, the United States, and Vietnam.
The researchers assessed the price of a 30-day supply of each of the studied branded drugs based on the lowest available price (in 2021 U.S. dollars) from multiple online national price databases.
Then they calculated the estimated minimum price of a 30-day supply of a potential generic version of these drugs, which included the cost of the active medicinal ingredients, the excipients (nonactive ingredients), the prefilled injectable device plus needles (for subcutaneous drugs), transportation, 10% profit, and 27% tax on profit.
The national prices of the branded medications for obesity were significantly higher than the estimated minimum prices of potential generic drugs (see Table).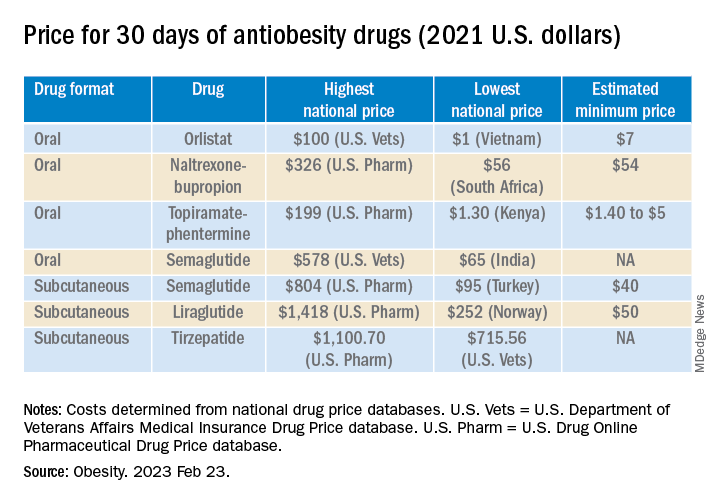
The highest national price for a branded oral drug for obesity vs. the estimated minimum price for a potential generic version was $100 vs. $7 for orlistat, $199 vs. $5 for phentermine/topiramate, and $326 vs. $54 for naltrexone/bupropion, for a 30-day supply.
There was an even greater difference between highest national branded drug price vs. estimated minimum generic drug price for the newer subcutaneously injectable drugs for obesity.
For example, the price of a 30-day course of subcutaneous semaglutide ranged from $804 (United States) to $95 (Turkey), while the estimated minimum potential generic drug price was $40 (which is 20 times lower).
The study was funded by grants from the Make Medicines Affordable/International Treatment Preparedness Coalition and from the National Heart, Lung, and Blood Institute of the National Institutes of Health. Coauthor Francois Venter has reported receiving support from the Bill and Melinda Gates Foundation, U.S. Agency for International Development, Unitaid, SA Medical Research Council, Foundation for Innovative New Diagnostics, the Children’s Investment Fund Foundation, Gilead, ViiV, Mylan, Merck, Adcock Ingram, Aspen, Abbott, Roche, Johnson & Johnson, Sanofi, Virology Education, SA HIV Clinicians Society, and Dira Sengwe. The other authors and Dr. Chay have reported no relevant financial relationships. Dr. Finkelstein has reported receiving support for serving on the WW scientific advisory board and an educational grant unrelated to the present work from Novo Nordisk.
A version of this article first appeared on Medscape.com.
The lowest available national prices of drugs to treat obesity are up to 20 times higher than the estimated cost of profitable generic versions of the same agents, according to a new analysis.
The findings by Jacob Levi, MBBS, and colleagues were published in Obesity.
“Our study highlights the inequality in pricing that exists for effective antiobesity medications, which are largely unaffordable in most countries,” Dr. Levi, from Royal Free Hospital NHS Trust, London, said in a press release.
“We show that these drugs can actually be produced and sold profitably for low prices,” he summarized. “A public health approach that prioritizes improving access to medications should be adopted, instead of allowing companies to maximize profits,” Dr. Levi urged.
Dr. Levi and colleagues studied the oral agents orlistat, naltrexone/bupropion, topiramate/phentermine, and semaglutide, and subcutaneous liraglutide, semaglutide, and tirzepatide (all approved by the U.S. Food and Drug Administration to treat obesity, except for oral semaglutide and subcutaneous tirzepatide, which are not yet approved to treat obesity in the absence of type 2 diabetes).
“Worldwide, more people are dying from diabetes and clinical obesity than HIV, tuberculosis, and malaria combined now,” senior author Andrew Hill, MD, department of pharmacology and therapeutics, University of Liverpool, England, pointed out.
We need to repeat the low-cost success story with obesity drugs
“Millions of lives have been saved by treating infectious diseases at low cost in poor countries,” Dr. Hill continued. “Now we need to repeat this medical success story, with mass treatment of diabetes and clinical obesity at low prices.”
However, in an accompanying editorial, Eric A. Finkelstein, MD, and Junxing Chay, PhD, Duke-NUS Medical School, Singapore, maintain that “It would be great if everyone had affordable access to all medicines that might improve their health. Yet that is simply not possible, nor will it ever be.”
“What is truly needed is a better way to ration the health care dollars currently available in efforts to maximize population health. That is the challenge ahead not just for [antiobesity medications] but for all treatments,” they say.
“Greater use of cost-effectiveness analysis and direct negotiations, while maintaining the patent system, represents an appropriate approach for allocating scarce health care resources in the United States and beyond,” they continue.
Lowest current patented drug prices vs. estimated generic drug prices
New medications for obesity were highly effective in recent clinical trials, but high prices limit the ability of patients to get these medications, Dr. Levi and colleagues write.
They analyzed prices for obesity drugs in 16 low-, middle-, and high-income countries: Australia, Bangladesh, China, France, Germany, India, Kenya, Morocco, Norway, Peru, Pakistan, South Africa, Turkey, the United Kingdom, the United States, and Vietnam.
The researchers assessed the price of a 30-day supply of each of the studied branded drugs based on the lowest available price (in 2021 U.S. dollars) from multiple online national price databases.
Then they calculated the estimated minimum price of a 30-day supply of a potential generic version of these drugs, which included the cost of the active medicinal ingredients, the excipients (nonactive ingredients), the prefilled injectable device plus needles (for subcutaneous drugs), transportation, 10% profit, and 27% tax on profit.
The national prices of the branded medications for obesity were significantly higher than the estimated minimum prices of potential generic drugs (see Table).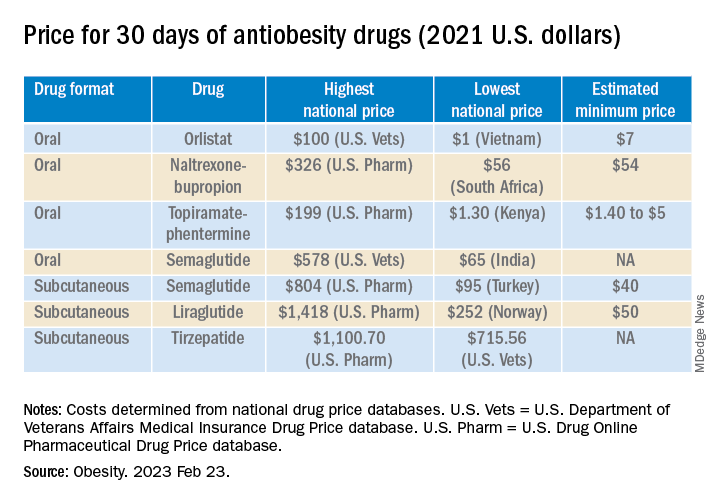
The highest national price for a branded oral drug for obesity vs. the estimated minimum price for a potential generic version was $100 vs. $7 for orlistat, $199 vs. $5 for phentermine/topiramate, and $326 vs. $54 for naltrexone/bupropion, for a 30-day supply.
There was an even greater difference between highest national branded drug price vs. estimated minimum generic drug price for the newer subcutaneously injectable drugs for obesity.
For example, the price of a 30-day course of subcutaneous semaglutide ranged from $804 (United States) to $95 (Turkey), while the estimated minimum potential generic drug price was $40 (which is 20 times lower).
The study was funded by grants from the Make Medicines Affordable/International Treatment Preparedness Coalition and from the National Heart, Lung, and Blood Institute of the National Institutes of Health. Coauthor Francois Venter has reported receiving support from the Bill and Melinda Gates Foundation, U.S. Agency for International Development, Unitaid, SA Medical Research Council, Foundation for Innovative New Diagnostics, the Children’s Investment Fund Foundation, Gilead, ViiV, Mylan, Merck, Adcock Ingram, Aspen, Abbott, Roche, Johnson & Johnson, Sanofi, Virology Education, SA HIV Clinicians Society, and Dira Sengwe. The other authors and Dr. Chay have reported no relevant financial relationships. Dr. Finkelstein has reported receiving support for serving on the WW scientific advisory board and an educational grant unrelated to the present work from Novo Nordisk.
A version of this article first appeared on Medscape.com.
Novel strategy could improve heart transplant allocation
Prediction models that incorporate more than just treatment status could rank order heart transplant candidates by urgency more effectively than the current system, a modeling study suggests.
Since 2018, the U.S. heart transplant allocation system has ranked heart candidates according to six treatment-based “statuses” (up from three used previously), ignoring many objective patient characteristics, the authors write.
Their study showed no significant difference in survival between statuses four and six, and status five had lower survival than status four.
“We expected multivariable prediction models to outperform the six-status system when it comes to rank ordering patients by how likely they are to die on the wait list (medical urgency),” William F. Parker, MD, MS, PhD, of the University of Chicago, told this news organization.
“However, we were surprised to see that the statuses were out of order,” he said. “Status five patients are more urgent than status three or status four patients,” mainly because most are in renal failure and listed for multiorgan transplantation with a kidney.
Objective physiologic measurements, such as glomerular filtration rate (GFR), had high variable importance, offering a minimally invasive measurement with predictive power in assessing medical urgency. Therefore, including GFR and other variables such as extracorporeal membrane oxygenation (ECMO) could improve the accuracy of the allocation system in identifying the most medically urgent candidates, Dr. Parker and colleagues suggest.
The study was published online in JACC: Heart Failure.
‘Moderate ability’ to rank order
The investigators assessed the effectiveness of the standard six-status ranking system and several novel prediction models in identifying the most urgent heart transplant candidates. The primary outcome was death before receipt of a heart transplant.
The final data set contained 32,294 candidates (mean age, 53 years; 74%, men); 27,200 made up the prepolicy training set and 5,094 were included in the postpolicy test set.
The team evaluated the accuracy of the six-status system using Harrell’s C-index and log-rank tests of Kaplan-Meier estimated survival by status for candidates listed after the policy change (November 2018 to March 2020) in the Scientific Registry of Transplant Recipients data set.
They then developed Cox proportional hazards models and random survival forest models using prepolicy data (2010-2017). Predictor variables included age, diagnosis, laboratory measurements, hemodynamics, and supportive treatment at the time of listing.
They found that the six-status ranking at listing has had “moderate ability” to rank order candidates.
As Dr. Parker indicated, statuses four and six had no significant difference in survival, and status five had lower survival than status four.
The investigators’ multivariable prediction models derived with prepolicy data ranked candidates correctly more often than the six-status rankings. Objective physiologic measurements, such as GFR and ECMO, were identified as having significant importance with regard to ranking by urgency.
“The novel prediction models we developed … could be implemented by the Organ Procurement and Transplantation Network (OPTN) as allocation policy and would be better than the status quo,” Dr. Parker said. “However, I think we could do even better using the newer data collected after 2018.”
Modifications underway
The OPTN Heart Transplantation Committee is currently working on developing a new framework for allocating deceased donor hearts called Continuous Distribution.
“The six-tiered system works well, and it better stratifies the most medically urgent candidates than the previous allocation framework,” the leadership of the United Network for Organ Sharing Heart Transplantation Committee, including Chair Richard C. Daly, MD, Mayo Clinic; Vice-Chair Jondavid Menteer, MD, University of Southern California, Los Angeles; and former Chair Shelley Hall, MD, Baylor University Medical Center, told this news organization.
“That said, it is always appropriate to review and adjust variables that affect the medical urgency attribute for heart allocation.”
The new framework will change how patients are prioritized, they said. “Continuous distribution will consider all patient factors, including medical urgency, together to determine the order of an organ offer, and no single factor will decide an organ match.
“The goal is to increase fairness by moving to a points-based allocation framework that allows candidates to be compared using a single score composed of multiple factors.
“Furthermore,” they added, “continuous distribution provides a framework that will allow modifications of the criteria defining medical urgency (and other attributes of allocation) to a finer degree than the current policy. … Once continuous distribution is in place and the OPTN has policy monitoring data, the committee may consider and model different ways of defining medical urgency.”
Kiran K. Khush, MD, of Stanford (Calif.) University School of Medicine, coauthor of a related commentary, elaborated. “The composite allocation score (CAS) will consist of a ‘points-based system,’ in which candidates will be assigned points based on (1) medical urgency, (2) anticipated posttransplant survival, (3) candidate biology (eg., special characteristics that may result in higher prioritization, such as blood type O and allosensitization), (4) access (eg., prior living donor, pediatric patient), and (5) placement efficacy (travel, proximity).”
Candidates will be assigned points based on these categories, and will be rank ordered for each donor offer.
Dr. Khush and colleagues propose that a multivariable model – such as the ones described in the study – would be the best way to assign points for medical urgency.
“This system will be more equitable than the current system,” Dr. Khush said, “because it will better prioritize the sickest candidates while improving access for patients who are currently at a disadvantage [for example, blood O, highly sensitized patients], and will also remove artificial geographic boundaries [for example, the current 500-mile rule for heart allocation].”
Going further
Jesse D. Schold, PhD, of the University of Colorado at Denver, Aurora, raises concerns about other aspects of the heart allocation system in another related commentary.
“One big issue with our data in transplantation … is that, while it is very comprehensive for capturing transplant candidates and recipients, there is no data collection for patients and processes of care for patients prior to wait list placement,” he told this news organization. This phase of care is subject to wide variation in practice, he said, “and is likely as important as any to patients – the ability to be referred, evaluated, and placed on a waiting list.”
Report cards that measure quality of care after wait list placement ignore key phases prior to wait list placement, he said. “This may have the unintended consequences of limiting access to care and to the waiting list for patients perceived to be at higher risk, or the use of higher-risk donors, despite their potential survival advantage.
“In contrast,” he said, “quality report cards that incentivize treatment for all patients who may benefit would likely have a greater beneficial impact on patients with end-organ disease.”
There is also significant risk of underlying differences in patient populations between centers, despite the use of multivariable models, he added. This heterogeneity “may not be reflected accurately in the report cards [which] have significant impact for regulatory review, private payer contracting, and center reputation.”
Some of these concerns may be addressed in the new OPTN Modernization Initiative, according to David Bowman, a public affairs specialist at the Health Resources and Services Administration. One of the goals of the initiative “is to ensure that the OPTN Board of Directors is high functioning, has greater independence, and represents the diversity of communities served by the OPTN,” he told this news organization. “Strengthened governance will lead to effective policy development and implementation, and enhanced transparency and accountability of the process.”
Addressing another concern about the system, Savitri Fedson, MD, of the Michael E. DeBakey VA Medical Center and Baylor College of Medicine, Houston, wonders in a related editorial whether organ donors and recipients should know more about each other, and if so, could that reverse the ongoing downward trend in organ acceptance?
Although some organizations are in favor of sharing more information, Dr. Fedson notes that “less information may have the greater benefit.” She writes, “We might realize that the simplest approach is often the best: a fulsome thank you for the donor’s gift that is willingly given to a stranger without expectation of payment, and on the recipient side, the knowledge that an organ is of good quality.
“The transplant patient can be comforted with the understanding that the risk of disease transmission, while not zero, is low, and that their survival following acceptance of an organ is better than languishing on a waiting list.”
The study received no commercial funding. Dr. Parker, Dr. Khush, Dr. Schold, and Dr. Fedson report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Prediction models that incorporate more than just treatment status could rank order heart transplant candidates by urgency more effectively than the current system, a modeling study suggests.
Since 2018, the U.S. heart transplant allocation system has ranked heart candidates according to six treatment-based “statuses” (up from three used previously), ignoring many objective patient characteristics, the authors write.
Their study showed no significant difference in survival between statuses four and six, and status five had lower survival than status four.
“We expected multivariable prediction models to outperform the six-status system when it comes to rank ordering patients by how likely they are to die on the wait list (medical urgency),” William F. Parker, MD, MS, PhD, of the University of Chicago, told this news organization.
“However, we were surprised to see that the statuses were out of order,” he said. “Status five patients are more urgent than status three or status four patients,” mainly because most are in renal failure and listed for multiorgan transplantation with a kidney.
Objective physiologic measurements, such as glomerular filtration rate (GFR), had high variable importance, offering a minimally invasive measurement with predictive power in assessing medical urgency. Therefore, including GFR and other variables such as extracorporeal membrane oxygenation (ECMO) could improve the accuracy of the allocation system in identifying the most medically urgent candidates, Dr. Parker and colleagues suggest.
The study was published online in JACC: Heart Failure.
‘Moderate ability’ to rank order
The investigators assessed the effectiveness of the standard six-status ranking system and several novel prediction models in identifying the most urgent heart transplant candidates. The primary outcome was death before receipt of a heart transplant.
The final data set contained 32,294 candidates (mean age, 53 years; 74%, men); 27,200 made up the prepolicy training set and 5,094 were included in the postpolicy test set.
The team evaluated the accuracy of the six-status system using Harrell’s C-index and log-rank tests of Kaplan-Meier estimated survival by status for candidates listed after the policy change (November 2018 to March 2020) in the Scientific Registry of Transplant Recipients data set.
They then developed Cox proportional hazards models and random survival forest models using prepolicy data (2010-2017). Predictor variables included age, diagnosis, laboratory measurements, hemodynamics, and supportive treatment at the time of listing.
They found that the six-status ranking at listing has had “moderate ability” to rank order candidates.
As Dr. Parker indicated, statuses four and six had no significant difference in survival, and status five had lower survival than status four.
The investigators’ multivariable prediction models derived with prepolicy data ranked candidates correctly more often than the six-status rankings. Objective physiologic measurements, such as GFR and ECMO, were identified as having significant importance with regard to ranking by urgency.
“The novel prediction models we developed … could be implemented by the Organ Procurement and Transplantation Network (OPTN) as allocation policy and would be better than the status quo,” Dr. Parker said. “However, I think we could do even better using the newer data collected after 2018.”
Modifications underway
The OPTN Heart Transplantation Committee is currently working on developing a new framework for allocating deceased donor hearts called Continuous Distribution.
“The six-tiered system works well, and it better stratifies the most medically urgent candidates than the previous allocation framework,” the leadership of the United Network for Organ Sharing Heart Transplantation Committee, including Chair Richard C. Daly, MD, Mayo Clinic; Vice-Chair Jondavid Menteer, MD, University of Southern California, Los Angeles; and former Chair Shelley Hall, MD, Baylor University Medical Center, told this news organization.
“That said, it is always appropriate to review and adjust variables that affect the medical urgency attribute for heart allocation.”
The new framework will change how patients are prioritized, they said. “Continuous distribution will consider all patient factors, including medical urgency, together to determine the order of an organ offer, and no single factor will decide an organ match.
“The goal is to increase fairness by moving to a points-based allocation framework that allows candidates to be compared using a single score composed of multiple factors.
“Furthermore,” they added, “continuous distribution provides a framework that will allow modifications of the criteria defining medical urgency (and other attributes of allocation) to a finer degree than the current policy. … Once continuous distribution is in place and the OPTN has policy monitoring data, the committee may consider and model different ways of defining medical urgency.”
Kiran K. Khush, MD, of Stanford (Calif.) University School of Medicine, coauthor of a related commentary, elaborated. “The composite allocation score (CAS) will consist of a ‘points-based system,’ in which candidates will be assigned points based on (1) medical urgency, (2) anticipated posttransplant survival, (3) candidate biology (eg., special characteristics that may result in higher prioritization, such as blood type O and allosensitization), (4) access (eg., prior living donor, pediatric patient), and (5) placement efficacy (travel, proximity).”
Candidates will be assigned points based on these categories, and will be rank ordered for each donor offer.
Dr. Khush and colleagues propose that a multivariable model – such as the ones described in the study – would be the best way to assign points for medical urgency.
“This system will be more equitable than the current system,” Dr. Khush said, “because it will better prioritize the sickest candidates while improving access for patients who are currently at a disadvantage [for example, blood O, highly sensitized patients], and will also remove artificial geographic boundaries [for example, the current 500-mile rule for heart allocation].”
Going further
Jesse D. Schold, PhD, of the University of Colorado at Denver, Aurora, raises concerns about other aspects of the heart allocation system in another related commentary.
“One big issue with our data in transplantation … is that, while it is very comprehensive for capturing transplant candidates and recipients, there is no data collection for patients and processes of care for patients prior to wait list placement,” he told this news organization. This phase of care is subject to wide variation in practice, he said, “and is likely as important as any to patients – the ability to be referred, evaluated, and placed on a waiting list.”
Report cards that measure quality of care after wait list placement ignore key phases prior to wait list placement, he said. “This may have the unintended consequences of limiting access to care and to the waiting list for patients perceived to be at higher risk, or the use of higher-risk donors, despite their potential survival advantage.
“In contrast,” he said, “quality report cards that incentivize treatment for all patients who may benefit would likely have a greater beneficial impact on patients with end-organ disease.”
There is also significant risk of underlying differences in patient populations between centers, despite the use of multivariable models, he added. This heterogeneity “may not be reflected accurately in the report cards [which] have significant impact for regulatory review, private payer contracting, and center reputation.”
Some of these concerns may be addressed in the new OPTN Modernization Initiative, according to David Bowman, a public affairs specialist at the Health Resources and Services Administration. One of the goals of the initiative “is to ensure that the OPTN Board of Directors is high functioning, has greater independence, and represents the diversity of communities served by the OPTN,” he told this news organization. “Strengthened governance will lead to effective policy development and implementation, and enhanced transparency and accountability of the process.”
Addressing another concern about the system, Savitri Fedson, MD, of the Michael E. DeBakey VA Medical Center and Baylor College of Medicine, Houston, wonders in a related editorial whether organ donors and recipients should know more about each other, and if so, could that reverse the ongoing downward trend in organ acceptance?
Although some organizations are in favor of sharing more information, Dr. Fedson notes that “less information may have the greater benefit.” She writes, “We might realize that the simplest approach is often the best: a fulsome thank you for the donor’s gift that is willingly given to a stranger without expectation of payment, and on the recipient side, the knowledge that an organ is of good quality.
“The transplant patient can be comforted with the understanding that the risk of disease transmission, while not zero, is low, and that their survival following acceptance of an organ is better than languishing on a waiting list.”
The study received no commercial funding. Dr. Parker, Dr. Khush, Dr. Schold, and Dr. Fedson report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Prediction models that incorporate more than just treatment status could rank order heart transplant candidates by urgency more effectively than the current system, a modeling study suggests.
Since 2018, the U.S. heart transplant allocation system has ranked heart candidates according to six treatment-based “statuses” (up from three used previously), ignoring many objective patient characteristics, the authors write.
Their study showed no significant difference in survival between statuses four and six, and status five had lower survival than status four.
“We expected multivariable prediction models to outperform the six-status system when it comes to rank ordering patients by how likely they are to die on the wait list (medical urgency),” William F. Parker, MD, MS, PhD, of the University of Chicago, told this news organization.
“However, we were surprised to see that the statuses were out of order,” he said. “Status five patients are more urgent than status three or status four patients,” mainly because most are in renal failure and listed for multiorgan transplantation with a kidney.
Objective physiologic measurements, such as glomerular filtration rate (GFR), had high variable importance, offering a minimally invasive measurement with predictive power in assessing medical urgency. Therefore, including GFR and other variables such as extracorporeal membrane oxygenation (ECMO) could improve the accuracy of the allocation system in identifying the most medically urgent candidates, Dr. Parker and colleagues suggest.
The study was published online in JACC: Heart Failure.
‘Moderate ability’ to rank order
The investigators assessed the effectiveness of the standard six-status ranking system and several novel prediction models in identifying the most urgent heart transplant candidates. The primary outcome was death before receipt of a heart transplant.
The final data set contained 32,294 candidates (mean age, 53 years; 74%, men); 27,200 made up the prepolicy training set and 5,094 were included in the postpolicy test set.
The team evaluated the accuracy of the six-status system using Harrell’s C-index and log-rank tests of Kaplan-Meier estimated survival by status for candidates listed after the policy change (November 2018 to March 2020) in the Scientific Registry of Transplant Recipients data set.
They then developed Cox proportional hazards models and random survival forest models using prepolicy data (2010-2017). Predictor variables included age, diagnosis, laboratory measurements, hemodynamics, and supportive treatment at the time of listing.
They found that the six-status ranking at listing has had “moderate ability” to rank order candidates.
As Dr. Parker indicated, statuses four and six had no significant difference in survival, and status five had lower survival than status four.
The investigators’ multivariable prediction models derived with prepolicy data ranked candidates correctly more often than the six-status rankings. Objective physiologic measurements, such as GFR and ECMO, were identified as having significant importance with regard to ranking by urgency.
“The novel prediction models we developed … could be implemented by the Organ Procurement and Transplantation Network (OPTN) as allocation policy and would be better than the status quo,” Dr. Parker said. “However, I think we could do even better using the newer data collected after 2018.”
Modifications underway
The OPTN Heart Transplantation Committee is currently working on developing a new framework for allocating deceased donor hearts called Continuous Distribution.
“The six-tiered system works well, and it better stratifies the most medically urgent candidates than the previous allocation framework,” the leadership of the United Network for Organ Sharing Heart Transplantation Committee, including Chair Richard C. Daly, MD, Mayo Clinic; Vice-Chair Jondavid Menteer, MD, University of Southern California, Los Angeles; and former Chair Shelley Hall, MD, Baylor University Medical Center, told this news organization.
“That said, it is always appropriate to review and adjust variables that affect the medical urgency attribute for heart allocation.”
The new framework will change how patients are prioritized, they said. “Continuous distribution will consider all patient factors, including medical urgency, together to determine the order of an organ offer, and no single factor will decide an organ match.
“The goal is to increase fairness by moving to a points-based allocation framework that allows candidates to be compared using a single score composed of multiple factors.
“Furthermore,” they added, “continuous distribution provides a framework that will allow modifications of the criteria defining medical urgency (and other attributes of allocation) to a finer degree than the current policy. … Once continuous distribution is in place and the OPTN has policy monitoring data, the committee may consider and model different ways of defining medical urgency.”
Kiran K. Khush, MD, of Stanford (Calif.) University School of Medicine, coauthor of a related commentary, elaborated. “The composite allocation score (CAS) will consist of a ‘points-based system,’ in which candidates will be assigned points based on (1) medical urgency, (2) anticipated posttransplant survival, (3) candidate biology (eg., special characteristics that may result in higher prioritization, such as blood type O and allosensitization), (4) access (eg., prior living donor, pediatric patient), and (5) placement efficacy (travel, proximity).”
Candidates will be assigned points based on these categories, and will be rank ordered for each donor offer.
Dr. Khush and colleagues propose that a multivariable model – such as the ones described in the study – would be the best way to assign points for medical urgency.
“This system will be more equitable than the current system,” Dr. Khush said, “because it will better prioritize the sickest candidates while improving access for patients who are currently at a disadvantage [for example, blood O, highly sensitized patients], and will also remove artificial geographic boundaries [for example, the current 500-mile rule for heart allocation].”
Going further
Jesse D. Schold, PhD, of the University of Colorado at Denver, Aurora, raises concerns about other aspects of the heart allocation system in another related commentary.
“One big issue with our data in transplantation … is that, while it is very comprehensive for capturing transplant candidates and recipients, there is no data collection for patients and processes of care for patients prior to wait list placement,” he told this news organization. This phase of care is subject to wide variation in practice, he said, “and is likely as important as any to patients – the ability to be referred, evaluated, and placed on a waiting list.”
Report cards that measure quality of care after wait list placement ignore key phases prior to wait list placement, he said. “This may have the unintended consequences of limiting access to care and to the waiting list for patients perceived to be at higher risk, or the use of higher-risk donors, despite their potential survival advantage.
“In contrast,” he said, “quality report cards that incentivize treatment for all patients who may benefit would likely have a greater beneficial impact on patients with end-organ disease.”
There is also significant risk of underlying differences in patient populations between centers, despite the use of multivariable models, he added. This heterogeneity “may not be reflected accurately in the report cards [which] have significant impact for regulatory review, private payer contracting, and center reputation.”
Some of these concerns may be addressed in the new OPTN Modernization Initiative, according to David Bowman, a public affairs specialist at the Health Resources and Services Administration. One of the goals of the initiative “is to ensure that the OPTN Board of Directors is high functioning, has greater independence, and represents the diversity of communities served by the OPTN,” he told this news organization. “Strengthened governance will lead to effective policy development and implementation, and enhanced transparency and accountability of the process.”
Addressing another concern about the system, Savitri Fedson, MD, of the Michael E. DeBakey VA Medical Center and Baylor College of Medicine, Houston, wonders in a related editorial whether organ donors and recipients should know more about each other, and if so, could that reverse the ongoing downward trend in organ acceptance?
Although some organizations are in favor of sharing more information, Dr. Fedson notes that “less information may have the greater benefit.” She writes, “We might realize that the simplest approach is often the best: a fulsome thank you for the donor’s gift that is willingly given to a stranger without expectation of payment, and on the recipient side, the knowledge that an organ is of good quality.
“The transplant patient can be comforted with the understanding that the risk of disease transmission, while not zero, is low, and that their survival following acceptance of an organ is better than languishing on a waiting list.”
The study received no commercial funding. Dr. Parker, Dr. Khush, Dr. Schold, and Dr. Fedson report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JACC: HEART FAILURE
Erratic sleep, lack of activity tied to worsening schizophrenia symptoms
The findings also showed that people with schizophrenia spectrum disorders (SSDs) who lived in residential facilities experienced rigid routines, which correlated with a higher degree of negative symptoms.
The rigid routines were problematic for the patients living in residential settings, lead investigator Fabio Ferrarelli, MD, PhD, told this news organization. Dr. Ferrarelli is an associate professor of psychiatry at the University of Pittsburgh.
“Engaging in different activities at different times in activities associated with motivation and social interaction – this helps to ameliorate difficult-to-treat negative symptoms,” he said.
The findings were published online in Molecular Psychiatry.
Need to increase activity levels
While there is no shortage of research on sleep disturbances among people with schizophrenia, research focusing specifically on rest-activity rhythm disturbances and their relationships to symptoms of schizophrenia has been limited by small sample sizes or the lack of a control group, the investigators note.
To address this research gap, the investigators recruited 230 patients with SSD from participating residential facilities and communities throughout Italy. The participants included 108 healthy control participants, 54 community-dwelling patients with SSD who were receiving outpatient services, and 68 patients with SSD who were living in residential facilities.
All participants wore an actigraph for 7 consecutive days so that investigators could monitor sleep-wake patterns.
Compared with healthy control participants, both SSD groups had more total sleep time and spent more time resting or being passive (P < .001). In contrast, healthy control participants were much more active.
Part of the explanation for this may be that most of the control participants had jobs or attended school. In addition, the investigators note that many medications used to treat SSD can be highly sedating, causing some patients to sleep up to 15 hours per day.
Among residential participants with SSD, there was a higher level of inter-daily stability and higher daily rest-activity-rest fragmentation than occurred among healthy control participants or community-dwelling patients with SSD (P < .001). There was also a higher level of negative symptoms among residential participants with SSD than among the community-dwelling group with SSD.
When the findings were taken together, Dr. Ferrarelli and his team interpreted them to mean that inter-daily stability could reflect premature aging or neurodegenerative processes in patients with more severe forms of schizophrenia.
Another explanation could be that the rigid routine of the residential facility was making negative symptoms worse, Dr. Ferrarelli said. It is important to add variety into the mix – getting people to engage in different activities at different times of day would likely help residential SSD patients overcome negative symptoms of the disorder.
Although participants were recruited in Italy, Dr. Ferrarelli said he believes the findings are generalizable.
Bidirectional relationship?
Commenting on the findings, Matcheri Keshavan, MD, professor of psychiatry at Harvard Medical School in Boston, said the results are consistent with “well-known clinical observations that SSD patients tend to spend more time in bed and have more dysregulated sleep.
“Negative symptoms are also common, especially in residential patients. However, it is difficult to determine causality, as we do not know whether excessive sleepiness and decreased physical activity cause negative symptoms, or vice versa, or whether this is a bidirectional relationship,” Dr. Keshavan said.
He emphasized that physical exercise is known to increase sleep quality for people with mental illness and may also improve negative symptoms. “A useful approach in clinical practice is to increase activity levels, especially physical activities like walking and gardening.”
Dr. Keshavan said he would like to see future research that focuses on whether an intervention such as aerobic exercise would improve sleep quality as well as negative symptoms.
He also said that future research should ideally examine the characteristics of sleep alterations in schizophrenia.
“For example, while sleep duration is increased in schizophrenia, studies suggest that time spent in deep sleep is reduced; sleep spindles, which are important for consolidating memory during sleep, are also reduced. Correcting these deficits may improve negative symptoms and cognitive deficits,” he added.
The study was funded by the Italian Ministry of Health and the National Institute of Mental Health. There were no conflicts of interest.
A version of this article first appeared on Medscape.com.
The findings also showed that people with schizophrenia spectrum disorders (SSDs) who lived in residential facilities experienced rigid routines, which correlated with a higher degree of negative symptoms.
The rigid routines were problematic for the patients living in residential settings, lead investigator Fabio Ferrarelli, MD, PhD, told this news organization. Dr. Ferrarelli is an associate professor of psychiatry at the University of Pittsburgh.
“Engaging in different activities at different times in activities associated with motivation and social interaction – this helps to ameliorate difficult-to-treat negative symptoms,” he said.
The findings were published online in Molecular Psychiatry.
Need to increase activity levels
While there is no shortage of research on sleep disturbances among people with schizophrenia, research focusing specifically on rest-activity rhythm disturbances and their relationships to symptoms of schizophrenia has been limited by small sample sizes or the lack of a control group, the investigators note.
To address this research gap, the investigators recruited 230 patients with SSD from participating residential facilities and communities throughout Italy. The participants included 108 healthy control participants, 54 community-dwelling patients with SSD who were receiving outpatient services, and 68 patients with SSD who were living in residential facilities.
All participants wore an actigraph for 7 consecutive days so that investigators could monitor sleep-wake patterns.
Compared with healthy control participants, both SSD groups had more total sleep time and spent more time resting or being passive (P < .001). In contrast, healthy control participants were much more active.
Part of the explanation for this may be that most of the control participants had jobs or attended school. In addition, the investigators note that many medications used to treat SSD can be highly sedating, causing some patients to sleep up to 15 hours per day.
Among residential participants with SSD, there was a higher level of inter-daily stability and higher daily rest-activity-rest fragmentation than occurred among healthy control participants or community-dwelling patients with SSD (P < .001). There was also a higher level of negative symptoms among residential participants with SSD than among the community-dwelling group with SSD.
When the findings were taken together, Dr. Ferrarelli and his team interpreted them to mean that inter-daily stability could reflect premature aging or neurodegenerative processes in patients with more severe forms of schizophrenia.
Another explanation could be that the rigid routine of the residential facility was making negative symptoms worse, Dr. Ferrarelli said. It is important to add variety into the mix – getting people to engage in different activities at different times of day would likely help residential SSD patients overcome negative symptoms of the disorder.
Although participants were recruited in Italy, Dr. Ferrarelli said he believes the findings are generalizable.
Bidirectional relationship?
Commenting on the findings, Matcheri Keshavan, MD, professor of psychiatry at Harvard Medical School in Boston, said the results are consistent with “well-known clinical observations that SSD patients tend to spend more time in bed and have more dysregulated sleep.
“Negative symptoms are also common, especially in residential patients. However, it is difficult to determine causality, as we do not know whether excessive sleepiness and decreased physical activity cause negative symptoms, or vice versa, or whether this is a bidirectional relationship,” Dr. Keshavan said.
He emphasized that physical exercise is known to increase sleep quality for people with mental illness and may also improve negative symptoms. “A useful approach in clinical practice is to increase activity levels, especially physical activities like walking and gardening.”
Dr. Keshavan said he would like to see future research that focuses on whether an intervention such as aerobic exercise would improve sleep quality as well as negative symptoms.
He also said that future research should ideally examine the characteristics of sleep alterations in schizophrenia.
“For example, while sleep duration is increased in schizophrenia, studies suggest that time spent in deep sleep is reduced; sleep spindles, which are important for consolidating memory during sleep, are also reduced. Correcting these deficits may improve negative symptoms and cognitive deficits,” he added.
The study was funded by the Italian Ministry of Health and the National Institute of Mental Health. There were no conflicts of interest.
A version of this article first appeared on Medscape.com.
The findings also showed that people with schizophrenia spectrum disorders (SSDs) who lived in residential facilities experienced rigid routines, which correlated with a higher degree of negative symptoms.
The rigid routines were problematic for the patients living in residential settings, lead investigator Fabio Ferrarelli, MD, PhD, told this news organization. Dr. Ferrarelli is an associate professor of psychiatry at the University of Pittsburgh.
“Engaging in different activities at different times in activities associated with motivation and social interaction – this helps to ameliorate difficult-to-treat negative symptoms,” he said.
The findings were published online in Molecular Psychiatry.
Need to increase activity levels
While there is no shortage of research on sleep disturbances among people with schizophrenia, research focusing specifically on rest-activity rhythm disturbances and their relationships to symptoms of schizophrenia has been limited by small sample sizes or the lack of a control group, the investigators note.
To address this research gap, the investigators recruited 230 patients with SSD from participating residential facilities and communities throughout Italy. The participants included 108 healthy control participants, 54 community-dwelling patients with SSD who were receiving outpatient services, and 68 patients with SSD who were living in residential facilities.
All participants wore an actigraph for 7 consecutive days so that investigators could monitor sleep-wake patterns.
Compared with healthy control participants, both SSD groups had more total sleep time and spent more time resting or being passive (P < .001). In contrast, healthy control participants were much more active.
Part of the explanation for this may be that most of the control participants had jobs or attended school. In addition, the investigators note that many medications used to treat SSD can be highly sedating, causing some patients to sleep up to 15 hours per day.
Among residential participants with SSD, there was a higher level of inter-daily stability and higher daily rest-activity-rest fragmentation than occurred among healthy control participants or community-dwelling patients with SSD (P < .001). There was also a higher level of negative symptoms among residential participants with SSD than among the community-dwelling group with SSD.
When the findings were taken together, Dr. Ferrarelli and his team interpreted them to mean that inter-daily stability could reflect premature aging or neurodegenerative processes in patients with more severe forms of schizophrenia.
Another explanation could be that the rigid routine of the residential facility was making negative symptoms worse, Dr. Ferrarelli said. It is important to add variety into the mix – getting people to engage in different activities at different times of day would likely help residential SSD patients overcome negative symptoms of the disorder.
Although participants were recruited in Italy, Dr. Ferrarelli said he believes the findings are generalizable.
Bidirectional relationship?
Commenting on the findings, Matcheri Keshavan, MD, professor of psychiatry at Harvard Medical School in Boston, said the results are consistent with “well-known clinical observations that SSD patients tend to spend more time in bed and have more dysregulated sleep.
“Negative symptoms are also common, especially in residential patients. However, it is difficult to determine causality, as we do not know whether excessive sleepiness and decreased physical activity cause negative symptoms, or vice versa, or whether this is a bidirectional relationship,” Dr. Keshavan said.
He emphasized that physical exercise is known to increase sleep quality for people with mental illness and may also improve negative symptoms. “A useful approach in clinical practice is to increase activity levels, especially physical activities like walking and gardening.”
Dr. Keshavan said he would like to see future research that focuses on whether an intervention such as aerobic exercise would improve sleep quality as well as negative symptoms.
He also said that future research should ideally examine the characteristics of sleep alterations in schizophrenia.
“For example, while sleep duration is increased in schizophrenia, studies suggest that time spent in deep sleep is reduced; sleep spindles, which are important for consolidating memory during sleep, are also reduced. Correcting these deficits may improve negative symptoms and cognitive deficits,” he added.
The study was funded by the Italian Ministry of Health and the National Institute of Mental Health. There were no conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM MOLECULAR PSYCHIATRY
Harnessing ChatGPT to improve liver disease outcomes
ChatGPT, an artificial intelligence (AI) chatbot, may be helpful for patients with cirrhosis or hepatocellular carcinoma (HCC) and their clinicians by generating easy-to-understand information about the disease, a new study suggests.
; however, the majority of the correct responses were labeled by clinician specialists as “correct but inadequate,” according to the study findings.
The AI tool can also provide empathetic and practical advice to patients and caregivers but falls short in its ability to provide tailored recommendations, the researchers said.
“Patients with cirrhosis and/or liver cancer and their caregivers often have unmet needs and insufficient knowledge about managing and preventing complications of their disease. We found ChatGPT – while it has limitations – can help empower patients and improve health literacy for different populations,” study investigator Brennan Spiegel, MD, director of health services research at Cedars-Sinai, Los Angeles, said in a news release.
The study was published online in Clinical and Molecular Hepatology.
Adjunctive health literacy tool
ChatGPT (Chat Generative Pre-Trained Transformer), developed by OpenAI, is a natural language processing tool that allows users to have personalized conversations with an AI bot capable of providing detailed responses to any question posed.
It has already seen several potential applications in the medical field, but the Cedars-Sinai study is one of the first to examine the chatbot’s ability to answer clinically oriented, disease-specific questions correctly and compare its performance to that of physicians.
The investigators asked ChatGPT 164 questions relevant to patients with cirrhosis and/or HCC across five categories – basic knowledge, diagnosis, treatment, lifestyle, and preventive medicine. The chatbot’s answers were graded independently by two liver transplant specialists.
Overall, ChatGPT answered about 77% of the questions correctly, generating high levels of accuracy in 91 questions across the categories, the researchers reported.
ChatGPT regurgitated extensive knowledge of cirrhosis (79% correct) and HCC (74% correct), but only small proportions were deemed by specialists to be comprehensive (47% in cirrhosis, 41% in HCC).
The chatbot performed better in basic knowledge, lifestyle, and treatment than in the domains of diagnosis and preventive medicine.
The specialists grading ChatGPT felt that 75% of its answers for questions on basic knowledge, treatment, and lifestyle were comprehensive or correct but inadequate. The corresponding percentages for diagnosis and preventive medicine were lower (67% and 50%, respectively). No responses from ChatGPT were graded as completely incorrect.
Responses deemed by the specialists to be “mixed with correct and incorrect/outdated data” were 22% for basic knowledge, 33% for diagnosis, 25% for treatment, 18% for lifestyle, and 50% for preventive medicine.
No substitute for specialists
The investigators also tested ChatGPT on cirrhosis quality measures recommended by the American Association for the Study of Liver Diseases and contained in two published questionnaires. ChatGPT answered 77% of the relevant questions correctly but failed to specify decision-making cutoffs and treatment durations.
ChatGPT also lacked knowledge of variations in regional guidelines, such as HCC screening criteria, but it did offer “practical and multifaceted” advice to patients and caregivers about next steps and adjusting to a new diagnosis.
“We believe ChatGPT to be a very useful adjunctive tool for physicians – not a replacement – but adjunctive tool that provides access to reliable and accurate health information that is easy for many to understand,” Dr. Spiegel said in the news release. “We hope that this can help physicians to empower patients and improve health literacy for patients facing challenging conditions such as cirrhosis and liver cancer.”
ChatGPT could enhance clinician workflow by helping to draft a framework for each tailored question asked by patients and caregivers, the researchers wrote.
“Given the high proportion of either comprehensive or correct but inadequate responses and expected continued improvement over time, we foresee that physicians would only need to revise ChatGPT’s responses to best answer patient queries,” they wrote. “This may not only improve the efficiency of physicians but also decrease the overall cost and burden on the healthcare system.”
In addition, ChatGPT could empower patients to be better informed about their care, the researchers noted.
“This allows for patient-led care and facilitates efficient shared decision-making by providing patients with an additional source of information,” they added.
The study had no specific funding. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ChatGPT, an artificial intelligence (AI) chatbot, may be helpful for patients with cirrhosis or hepatocellular carcinoma (HCC) and their clinicians by generating easy-to-understand information about the disease, a new study suggests.
; however, the majority of the correct responses were labeled by clinician specialists as “correct but inadequate,” according to the study findings.
The AI tool can also provide empathetic and practical advice to patients and caregivers but falls short in its ability to provide tailored recommendations, the researchers said.
“Patients with cirrhosis and/or liver cancer and their caregivers often have unmet needs and insufficient knowledge about managing and preventing complications of their disease. We found ChatGPT – while it has limitations – can help empower patients and improve health literacy for different populations,” study investigator Brennan Spiegel, MD, director of health services research at Cedars-Sinai, Los Angeles, said in a news release.
The study was published online in Clinical and Molecular Hepatology.
Adjunctive health literacy tool
ChatGPT (Chat Generative Pre-Trained Transformer), developed by OpenAI, is a natural language processing tool that allows users to have personalized conversations with an AI bot capable of providing detailed responses to any question posed.
It has already seen several potential applications in the medical field, but the Cedars-Sinai study is one of the first to examine the chatbot’s ability to answer clinically oriented, disease-specific questions correctly and compare its performance to that of physicians.
The investigators asked ChatGPT 164 questions relevant to patients with cirrhosis and/or HCC across five categories – basic knowledge, diagnosis, treatment, lifestyle, and preventive medicine. The chatbot’s answers were graded independently by two liver transplant specialists.
Overall, ChatGPT answered about 77% of the questions correctly, generating high levels of accuracy in 91 questions across the categories, the researchers reported.
ChatGPT regurgitated extensive knowledge of cirrhosis (79% correct) and HCC (74% correct), but only small proportions were deemed by specialists to be comprehensive (47% in cirrhosis, 41% in HCC).
The chatbot performed better in basic knowledge, lifestyle, and treatment than in the domains of diagnosis and preventive medicine.
The specialists grading ChatGPT felt that 75% of its answers for questions on basic knowledge, treatment, and lifestyle were comprehensive or correct but inadequate. The corresponding percentages for diagnosis and preventive medicine were lower (67% and 50%, respectively). No responses from ChatGPT were graded as completely incorrect.
Responses deemed by the specialists to be “mixed with correct and incorrect/outdated data” were 22% for basic knowledge, 33% for diagnosis, 25% for treatment, 18% for lifestyle, and 50% for preventive medicine.
No substitute for specialists
The investigators also tested ChatGPT on cirrhosis quality measures recommended by the American Association for the Study of Liver Diseases and contained in two published questionnaires. ChatGPT answered 77% of the relevant questions correctly but failed to specify decision-making cutoffs and treatment durations.
ChatGPT also lacked knowledge of variations in regional guidelines, such as HCC screening criteria, but it did offer “practical and multifaceted” advice to patients and caregivers about next steps and adjusting to a new diagnosis.
“We believe ChatGPT to be a very useful adjunctive tool for physicians – not a replacement – but adjunctive tool that provides access to reliable and accurate health information that is easy for many to understand,” Dr. Spiegel said in the news release. “We hope that this can help physicians to empower patients and improve health literacy for patients facing challenging conditions such as cirrhosis and liver cancer.”
ChatGPT could enhance clinician workflow by helping to draft a framework for each tailored question asked by patients and caregivers, the researchers wrote.
“Given the high proportion of either comprehensive or correct but inadequate responses and expected continued improvement over time, we foresee that physicians would only need to revise ChatGPT’s responses to best answer patient queries,” they wrote. “This may not only improve the efficiency of physicians but also decrease the overall cost and burden on the healthcare system.”
In addition, ChatGPT could empower patients to be better informed about their care, the researchers noted.
“This allows for patient-led care and facilitates efficient shared decision-making by providing patients with an additional source of information,” they added.
The study had no specific funding. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ChatGPT, an artificial intelligence (AI) chatbot, may be helpful for patients with cirrhosis or hepatocellular carcinoma (HCC) and their clinicians by generating easy-to-understand information about the disease, a new study suggests.
; however, the majority of the correct responses were labeled by clinician specialists as “correct but inadequate,” according to the study findings.
The AI tool can also provide empathetic and practical advice to patients and caregivers but falls short in its ability to provide tailored recommendations, the researchers said.
“Patients with cirrhosis and/or liver cancer and their caregivers often have unmet needs and insufficient knowledge about managing and preventing complications of their disease. We found ChatGPT – while it has limitations – can help empower patients and improve health literacy for different populations,” study investigator Brennan Spiegel, MD, director of health services research at Cedars-Sinai, Los Angeles, said in a news release.
The study was published online in Clinical and Molecular Hepatology.
Adjunctive health literacy tool
ChatGPT (Chat Generative Pre-Trained Transformer), developed by OpenAI, is a natural language processing tool that allows users to have personalized conversations with an AI bot capable of providing detailed responses to any question posed.
It has already seen several potential applications in the medical field, but the Cedars-Sinai study is one of the first to examine the chatbot’s ability to answer clinically oriented, disease-specific questions correctly and compare its performance to that of physicians.
The investigators asked ChatGPT 164 questions relevant to patients with cirrhosis and/or HCC across five categories – basic knowledge, diagnosis, treatment, lifestyle, and preventive medicine. The chatbot’s answers were graded independently by two liver transplant specialists.
Overall, ChatGPT answered about 77% of the questions correctly, generating high levels of accuracy in 91 questions across the categories, the researchers reported.
ChatGPT regurgitated extensive knowledge of cirrhosis (79% correct) and HCC (74% correct), but only small proportions were deemed by specialists to be comprehensive (47% in cirrhosis, 41% in HCC).
The chatbot performed better in basic knowledge, lifestyle, and treatment than in the domains of diagnosis and preventive medicine.
The specialists grading ChatGPT felt that 75% of its answers for questions on basic knowledge, treatment, and lifestyle were comprehensive or correct but inadequate. The corresponding percentages for diagnosis and preventive medicine were lower (67% and 50%, respectively). No responses from ChatGPT were graded as completely incorrect.
Responses deemed by the specialists to be “mixed with correct and incorrect/outdated data” were 22% for basic knowledge, 33% for diagnosis, 25% for treatment, 18% for lifestyle, and 50% for preventive medicine.
No substitute for specialists
The investigators also tested ChatGPT on cirrhosis quality measures recommended by the American Association for the Study of Liver Diseases and contained in two published questionnaires. ChatGPT answered 77% of the relevant questions correctly but failed to specify decision-making cutoffs and treatment durations.
ChatGPT also lacked knowledge of variations in regional guidelines, such as HCC screening criteria, but it did offer “practical and multifaceted” advice to patients and caregivers about next steps and adjusting to a new diagnosis.
“We believe ChatGPT to be a very useful adjunctive tool for physicians – not a replacement – but adjunctive tool that provides access to reliable and accurate health information that is easy for many to understand,” Dr. Spiegel said in the news release. “We hope that this can help physicians to empower patients and improve health literacy for patients facing challenging conditions such as cirrhosis and liver cancer.”
ChatGPT could enhance clinician workflow by helping to draft a framework for each tailored question asked by patients and caregivers, the researchers wrote.
“Given the high proportion of either comprehensive or correct but inadequate responses and expected continued improvement over time, we foresee that physicians would only need to revise ChatGPT’s responses to best answer patient queries,” they wrote. “This may not only improve the efficiency of physicians but also decrease the overall cost and burden on the healthcare system.”
In addition, ChatGPT could empower patients to be better informed about their care, the researchers noted.
“This allows for patient-led care and facilitates efficient shared decision-making by providing patients with an additional source of information,” they added.
The study had no specific funding. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CLINICAL AND MOLECULAR HEPATOLOGY
Unawareness of memory slips could indicate risk for Alzheimer’s
Everyone’s memory fades to some extent as we age, but not everyone will develop Alzheimer’s disease. Screening the most likely people to develop Alzheimer’s remains an ongoing challenge, as some people present only unambiguous symptoms once their disease is advanced.
A new study in JAMA Network Open suggests that one early clue is found in people’s own self-perception of their memory skills. People who are more aware of their own declining memory capacity are less likely to develop Alzheimer’s, the study suggests.
“Some people are very aware of changes in their memory, but many people are unaware,” said study author Patrizia Vannini, PhD, a neurologist at Brigham and Women’s Hospital in Boston. There are gradations of unawareness of memory loss, Dr. Vannini said, from complete unawareness that anything is wrong, to a partial unawareness that memory is declining.
The study compared the records of 436 participants in the Alzheimer’s Disease Neuroimaging Initiative, an Alzheimer’s research institute housed at the University of Southern California. More than 90% of the participants were White, and generally had a college education. Their average age was 75 years, and 53% of participants were women.
Dr. Vannini and colleagues tracked people whose cognitive function was normal at the beginning of the study, based on the Clinical Dementia Rating. Throughout the course of the study, which included data from 2010 to 2021, 91 of the 436 participants experienced a sustained decline in their Clinical Dementia Rating scores, indicating a risk for eventual Alzheimer’s, whereas the other participants held steady.
The people who declined in cognitive function were less aware of slips in their memory, as assessed by discrepancies between people’s self-reports of their own memory skills and the perceptions of someone in their lives. For this part of the study, Dr. Vannini and colleagues used the Everyday Cognition Questionnaire, which evaluates memory tasks such as shopping without a grocery list or recalling conversations from a few days ago. Both the participant and the study partner rated their performance on such tasks compared to 10 years earlier. Those who were less aware of their memory slips were more likely to experience declines in the Clinical Dementia Rating, compared with people with a heightened concern about memory loss (as measured by being more concerned about memory decline than their study partners).
“Partial or complete unawareness is often related to delayed diagnosis of Alzheimer’s, because the patient is unaware they are having problems,” Dr. Vannini said, adding that this is associated with a poorer prognosis as well.
Implications for clinicians
Soo Borson, MD, professor of clinical family medicine at the University of Southern California and coleader of a CDC-funded early dementia detection center at New York University, pointed out that sometimes people are genuinely unaware that their memory is declining, while at other times they know it all too well but say everything is fine when a doctor asks about their current memory status. That may be because people fear the label of “Alzheimer’s,” Dr. Borson suggested, or simply because they don’t want to start a protracted diagnostic pathway that could involve lots of tests and time.
Dr. Borson, who was not involved in the study, noted that the population was predominantly White and well-educated, and by definition included people who were concerned enough about potential memory loss to become part of an Alzheimer’s research network. This limits the generalizability of this study’s results to other populations, Dr. Borson said.
Despite that limitation, in Dr. Borson’s view the study points to the continued importance of clinicians (ideally a primary care doctor who knows the patient well) engaging with patients about their brain health once they reach midlife. A doctor could ask if patients have noticed a decline in their thinking or memory over the last year, for example, or a more open-ended question about any memory concerns.
Although some patients may choose to withhold concerns about their memory, Dr. Borson acknowledged, the overall thrust of these questions is to provide a safe space for patients to air their concerns if they so choose. In some cases it would be appropriate to do a simple memory test on the spot, and then proceed accordingly – either for further tests if something of concern emerges, or to reassure the patient if the test doesn’t yield anything of note. In the latter case some patients will still want further tests for additional reassurance, and Dr. Borson thinks doctors should facilitate that request even if in their own judgment nothing is wrong.
“This is not like testing for impaired kidney function by doing a serum creatinine test,” Dr. Borson said. While the orientation of the health care system is toward quick and easy answers for everything, detecting possible dementia eludes such an approach.
Dr. Vannini reports funding from the National Institutes of Health National Institute on Aging. Dr. Borson reported no disclosures.
Everyone’s memory fades to some extent as we age, but not everyone will develop Alzheimer’s disease. Screening the most likely people to develop Alzheimer’s remains an ongoing challenge, as some people present only unambiguous symptoms once their disease is advanced.
A new study in JAMA Network Open suggests that one early clue is found in people’s own self-perception of their memory skills. People who are more aware of their own declining memory capacity are less likely to develop Alzheimer’s, the study suggests.
“Some people are very aware of changes in their memory, but many people are unaware,” said study author Patrizia Vannini, PhD, a neurologist at Brigham and Women’s Hospital in Boston. There are gradations of unawareness of memory loss, Dr. Vannini said, from complete unawareness that anything is wrong, to a partial unawareness that memory is declining.
The study compared the records of 436 participants in the Alzheimer’s Disease Neuroimaging Initiative, an Alzheimer’s research institute housed at the University of Southern California. More than 90% of the participants were White, and generally had a college education. Their average age was 75 years, and 53% of participants were women.
Dr. Vannini and colleagues tracked people whose cognitive function was normal at the beginning of the study, based on the Clinical Dementia Rating. Throughout the course of the study, which included data from 2010 to 2021, 91 of the 436 participants experienced a sustained decline in their Clinical Dementia Rating scores, indicating a risk for eventual Alzheimer’s, whereas the other participants held steady.
The people who declined in cognitive function were less aware of slips in their memory, as assessed by discrepancies between people’s self-reports of their own memory skills and the perceptions of someone in their lives. For this part of the study, Dr. Vannini and colleagues used the Everyday Cognition Questionnaire, which evaluates memory tasks such as shopping without a grocery list or recalling conversations from a few days ago. Both the participant and the study partner rated their performance on such tasks compared to 10 years earlier. Those who were less aware of their memory slips were more likely to experience declines in the Clinical Dementia Rating, compared with people with a heightened concern about memory loss (as measured by being more concerned about memory decline than their study partners).
“Partial or complete unawareness is often related to delayed diagnosis of Alzheimer’s, because the patient is unaware they are having problems,” Dr. Vannini said, adding that this is associated with a poorer prognosis as well.
Implications for clinicians
Soo Borson, MD, professor of clinical family medicine at the University of Southern California and coleader of a CDC-funded early dementia detection center at New York University, pointed out that sometimes people are genuinely unaware that their memory is declining, while at other times they know it all too well but say everything is fine when a doctor asks about their current memory status. That may be because people fear the label of “Alzheimer’s,” Dr. Borson suggested, or simply because they don’t want to start a protracted diagnostic pathway that could involve lots of tests and time.
Dr. Borson, who was not involved in the study, noted that the population was predominantly White and well-educated, and by definition included people who were concerned enough about potential memory loss to become part of an Alzheimer’s research network. This limits the generalizability of this study’s results to other populations, Dr. Borson said.
Despite that limitation, in Dr. Borson’s view the study points to the continued importance of clinicians (ideally a primary care doctor who knows the patient well) engaging with patients about their brain health once they reach midlife. A doctor could ask if patients have noticed a decline in their thinking or memory over the last year, for example, or a more open-ended question about any memory concerns.
Although some patients may choose to withhold concerns about their memory, Dr. Borson acknowledged, the overall thrust of these questions is to provide a safe space for patients to air their concerns if they so choose. In some cases it would be appropriate to do a simple memory test on the spot, and then proceed accordingly – either for further tests if something of concern emerges, or to reassure the patient if the test doesn’t yield anything of note. In the latter case some patients will still want further tests for additional reassurance, and Dr. Borson thinks doctors should facilitate that request even if in their own judgment nothing is wrong.
“This is not like testing for impaired kidney function by doing a serum creatinine test,” Dr. Borson said. While the orientation of the health care system is toward quick and easy answers for everything, detecting possible dementia eludes such an approach.
Dr. Vannini reports funding from the National Institutes of Health National Institute on Aging. Dr. Borson reported no disclosures.
Everyone’s memory fades to some extent as we age, but not everyone will develop Alzheimer’s disease. Screening the most likely people to develop Alzheimer’s remains an ongoing challenge, as some people present only unambiguous symptoms once their disease is advanced.
A new study in JAMA Network Open suggests that one early clue is found in people’s own self-perception of their memory skills. People who are more aware of their own declining memory capacity are less likely to develop Alzheimer’s, the study suggests.
“Some people are very aware of changes in their memory, but many people are unaware,” said study author Patrizia Vannini, PhD, a neurologist at Brigham and Women’s Hospital in Boston. There are gradations of unawareness of memory loss, Dr. Vannini said, from complete unawareness that anything is wrong, to a partial unawareness that memory is declining.
The study compared the records of 436 participants in the Alzheimer’s Disease Neuroimaging Initiative, an Alzheimer’s research institute housed at the University of Southern California. More than 90% of the participants were White, and generally had a college education. Their average age was 75 years, and 53% of participants were women.
Dr. Vannini and colleagues tracked people whose cognitive function was normal at the beginning of the study, based on the Clinical Dementia Rating. Throughout the course of the study, which included data from 2010 to 2021, 91 of the 436 participants experienced a sustained decline in their Clinical Dementia Rating scores, indicating a risk for eventual Alzheimer’s, whereas the other participants held steady.
The people who declined in cognitive function were less aware of slips in their memory, as assessed by discrepancies between people’s self-reports of their own memory skills and the perceptions of someone in their lives. For this part of the study, Dr. Vannini and colleagues used the Everyday Cognition Questionnaire, which evaluates memory tasks such as shopping without a grocery list or recalling conversations from a few days ago. Both the participant and the study partner rated their performance on such tasks compared to 10 years earlier. Those who were less aware of their memory slips were more likely to experience declines in the Clinical Dementia Rating, compared with people with a heightened concern about memory loss (as measured by being more concerned about memory decline than their study partners).
“Partial or complete unawareness is often related to delayed diagnosis of Alzheimer’s, because the patient is unaware they are having problems,” Dr. Vannini said, adding that this is associated with a poorer prognosis as well.
Implications for clinicians
Soo Borson, MD, professor of clinical family medicine at the University of Southern California and coleader of a CDC-funded early dementia detection center at New York University, pointed out that sometimes people are genuinely unaware that their memory is declining, while at other times they know it all too well but say everything is fine when a doctor asks about their current memory status. That may be because people fear the label of “Alzheimer’s,” Dr. Borson suggested, or simply because they don’t want to start a protracted diagnostic pathway that could involve lots of tests and time.
Dr. Borson, who was not involved in the study, noted that the population was predominantly White and well-educated, and by definition included people who were concerned enough about potential memory loss to become part of an Alzheimer’s research network. This limits the generalizability of this study’s results to other populations, Dr. Borson said.
Despite that limitation, in Dr. Borson’s view the study points to the continued importance of clinicians (ideally a primary care doctor who knows the patient well) engaging with patients about their brain health once they reach midlife. A doctor could ask if patients have noticed a decline in their thinking or memory over the last year, for example, or a more open-ended question about any memory concerns.
Although some patients may choose to withhold concerns about their memory, Dr. Borson acknowledged, the overall thrust of these questions is to provide a safe space for patients to air their concerns if they so choose. In some cases it would be appropriate to do a simple memory test on the spot, and then proceed accordingly – either for further tests if something of concern emerges, or to reassure the patient if the test doesn’t yield anything of note. In the latter case some patients will still want further tests for additional reassurance, and Dr. Borson thinks doctors should facilitate that request even if in their own judgment nothing is wrong.
“This is not like testing for impaired kidney function by doing a serum creatinine test,” Dr. Borson said. While the orientation of the health care system is toward quick and easy answers for everything, detecting possible dementia eludes such an approach.
Dr. Vannini reports funding from the National Institutes of Health National Institute on Aging. Dr. Borson reported no disclosures.
FROM JAMA NETWORK OPEN
Drug combo improves recurrence-free survival after HCC resection
ORLANDO – Patients with hepatocellular carcinoma (HCC) who undergo surgery or thermal ablation with curative intent are at high risk for recurrence, but currently, no adjuvant therapy standard of care exists for these patients.
New findings signal a promising option for these patients. The combination of the immune checkpoint inhibitor atezolizumab (Tecentriq) and the angiogenesis inhibitor bevacizumab (Avastin) was associated with a significant improvement in recurrence-free survival, compared with active surveillance, and represents the first option to show efficacy in the adjuvant setting following surgical resection of HCCs for patients at high risk for recurrence.
among patients who received the combination therapy in comparison with active surveillance. However, the overall survival data remain immature.
The data come from an interim analysis of the IMbrave050 trial, which was presented at the annual meeting of the American Association for Cancer Research.
“Atezolizumab plus bevacizumab may be a practice-changing adjuvant treatment options for patients with high-risk HCC,” said lead investigator Pierce Chow, MBBS, PhD, codirector of the National Cancer Centre Singapore Comprehensive Liver Cancer Clinic. He presented the results in an oral abstract session at the meeting. The combination “may also change clinical indications for surgical resection” because clinicians may be more likely to consider resection for patients at extremely high risk for recurrence if the risk of recurrence can be reduced with this combination.
In the previous IMbrave150 trial, the combination of atezolizumab and bevacizumab significantly improved outcomes for patients with high-risk and non–high-risk unresectable HCC, compared with the standard of care sorafenib (Nexavar).
In that trial, the median overall survival in the intention-to-treat population was 19.2 months for patients who received atezolizumab-bevacizumab versus 13.4 months for patients who received sorafenib (P = .0009).
The combination was also associated with improvements in progression-free survival and objective response rates, compared with sorafenib.
On the basis of these results, the IMbrave050 investigators explored whether the same benefits would occur for patients with resectable disease considered to be at high risk for recurrence owing to tumor size, vascular invasion, or poor tumor differentiation. The trial compared the combination for 334 patients with active surveillance, also for 334 patients, in the adjuvant setting.
Patients were considered good candidates for thermal ablation if they had a single tumor greater than 2 cm, but not larger than 5 cm in its longest dimension, or if they had four or fewer tumors, all of which were no larger than 5 cm. For all other patients, surgical resection was recommended.
The median age of the patients was 60. For about half of patients in each arm, the expression level of programmed death–ligand-1 (PD-L1) was 1% or higher.
After a median follow-up of 17.4 months, the 12-month recurrence-free survival rate, as assessed by independent review, was 78% for patients in the treatment arm, compared with 65% for patients who were assigned to active surveillance (hazard ratio, 0.72; P = .012). This finding was generally consistent across clinical subgroups, including groups based on age, sex, race/ethnicity, performance status, PD-L1 expression, number of high-risk features, Barcelona Clinic Liver Cancer stage, cancer etiology, procedure type, microvascular invasion, or tumor numbers and size.
Of 133 patients on active surveillance who experienced a protocol-defined recurrence event, 81 (61%) crossed over to the atezolizumab/bevacizumab arm.
The overall survival benefit of the combination therapy was less clear. Dr. Chow called the overall survival data “highly immature” at the time of data cutoff.
Overall, 47 patients died – 7 more in the combination arm (27 vs. 20). More specifically, 17 patients in the combination arm and 16 on active surveillance died from progressive disease; 6 patients in the treatment arm versus 1 on surveillance died from adverse events. The remaining deaths were attributed to other causes. Two deaths in the combination arm were considered treatment related, one from esophageal varices hemorrhage, and the other from ischemic stroke.
Dr. Chow said a number of deaths attributed to HCC recurrence was similar between the groups. There were three COVID-19–related deaths within 1 year of randomization, all in the combination arm.
As for adverse events, the safety of the combination was largely consistent with that reported in the IMbrave150 trial. Nearly all patients experienced at least one adverse event. Treatment-related grade 3 or 4 adverse events occurred in 34.9% of patients in the combination group, and serious treatment-related events occurred in 13.3%.
The most common adverse events of any grade were proteinuria, hypertension, decreased platelet count, increases in liver enzyme level, hypothyroidism, arthralgia, pruritus, rash, increase in serum bilirubin level, and fever.
Invited discussant Stephen L. Chan, MD, from the Chinese University of Hong Kong, said the study was “definitely” relevant to clinicians and addresses “a very important unmet need.”
Dr. Chan noted that he thinks this combination will “likely” be practice changing, given the improvement in recurrence-free survival, but “certainly we need more data to guide us in patient selection.”
The study was funded by F. Hoffman–La Roche. Dr. Chow has consulting for and has received honoraria and grant/research support from Roche and others. Dr. Chan has received honoraria from Roche and consulting fees and grant/research support from others.
A version of this article first appeared on Medscape.com.
ORLANDO – Patients with hepatocellular carcinoma (HCC) who undergo surgery or thermal ablation with curative intent are at high risk for recurrence, but currently, no adjuvant therapy standard of care exists for these patients.
New findings signal a promising option for these patients. The combination of the immune checkpoint inhibitor atezolizumab (Tecentriq) and the angiogenesis inhibitor bevacizumab (Avastin) was associated with a significant improvement in recurrence-free survival, compared with active surveillance, and represents the first option to show efficacy in the adjuvant setting following surgical resection of HCCs for patients at high risk for recurrence.
among patients who received the combination therapy in comparison with active surveillance. However, the overall survival data remain immature.
The data come from an interim analysis of the IMbrave050 trial, which was presented at the annual meeting of the American Association for Cancer Research.
“Atezolizumab plus bevacizumab may be a practice-changing adjuvant treatment options for patients with high-risk HCC,” said lead investigator Pierce Chow, MBBS, PhD, codirector of the National Cancer Centre Singapore Comprehensive Liver Cancer Clinic. He presented the results in an oral abstract session at the meeting. The combination “may also change clinical indications for surgical resection” because clinicians may be more likely to consider resection for patients at extremely high risk for recurrence if the risk of recurrence can be reduced with this combination.
In the previous IMbrave150 trial, the combination of atezolizumab and bevacizumab significantly improved outcomes for patients with high-risk and non–high-risk unresectable HCC, compared with the standard of care sorafenib (Nexavar).
In that trial, the median overall survival in the intention-to-treat population was 19.2 months for patients who received atezolizumab-bevacizumab versus 13.4 months for patients who received sorafenib (P = .0009).
The combination was also associated with improvements in progression-free survival and objective response rates, compared with sorafenib.
On the basis of these results, the IMbrave050 investigators explored whether the same benefits would occur for patients with resectable disease considered to be at high risk for recurrence owing to tumor size, vascular invasion, or poor tumor differentiation. The trial compared the combination for 334 patients with active surveillance, also for 334 patients, in the adjuvant setting.
Patients were considered good candidates for thermal ablation if they had a single tumor greater than 2 cm, but not larger than 5 cm in its longest dimension, or if they had four or fewer tumors, all of which were no larger than 5 cm. For all other patients, surgical resection was recommended.
The median age of the patients was 60. For about half of patients in each arm, the expression level of programmed death–ligand-1 (PD-L1) was 1% or higher.
After a median follow-up of 17.4 months, the 12-month recurrence-free survival rate, as assessed by independent review, was 78% for patients in the treatment arm, compared with 65% for patients who were assigned to active surveillance (hazard ratio, 0.72; P = .012). This finding was generally consistent across clinical subgroups, including groups based on age, sex, race/ethnicity, performance status, PD-L1 expression, number of high-risk features, Barcelona Clinic Liver Cancer stage, cancer etiology, procedure type, microvascular invasion, or tumor numbers and size.
Of 133 patients on active surveillance who experienced a protocol-defined recurrence event, 81 (61%) crossed over to the atezolizumab/bevacizumab arm.
The overall survival benefit of the combination therapy was less clear. Dr. Chow called the overall survival data “highly immature” at the time of data cutoff.
Overall, 47 patients died – 7 more in the combination arm (27 vs. 20). More specifically, 17 patients in the combination arm and 16 on active surveillance died from progressive disease; 6 patients in the treatment arm versus 1 on surveillance died from adverse events. The remaining deaths were attributed to other causes. Two deaths in the combination arm were considered treatment related, one from esophageal varices hemorrhage, and the other from ischemic stroke.
Dr. Chow said a number of deaths attributed to HCC recurrence was similar between the groups. There were three COVID-19–related deaths within 1 year of randomization, all in the combination arm.
As for adverse events, the safety of the combination was largely consistent with that reported in the IMbrave150 trial. Nearly all patients experienced at least one adverse event. Treatment-related grade 3 or 4 adverse events occurred in 34.9% of patients in the combination group, and serious treatment-related events occurred in 13.3%.
The most common adverse events of any grade were proteinuria, hypertension, decreased platelet count, increases in liver enzyme level, hypothyroidism, arthralgia, pruritus, rash, increase in serum bilirubin level, and fever.
Invited discussant Stephen L. Chan, MD, from the Chinese University of Hong Kong, said the study was “definitely” relevant to clinicians and addresses “a very important unmet need.”
Dr. Chan noted that he thinks this combination will “likely” be practice changing, given the improvement in recurrence-free survival, but “certainly we need more data to guide us in patient selection.”
The study was funded by F. Hoffman–La Roche. Dr. Chow has consulting for and has received honoraria and grant/research support from Roche and others. Dr. Chan has received honoraria from Roche and consulting fees and grant/research support from others.
A version of this article first appeared on Medscape.com.
ORLANDO – Patients with hepatocellular carcinoma (HCC) who undergo surgery or thermal ablation with curative intent are at high risk for recurrence, but currently, no adjuvant therapy standard of care exists for these patients.
New findings signal a promising option for these patients. The combination of the immune checkpoint inhibitor atezolizumab (Tecentriq) and the angiogenesis inhibitor bevacizumab (Avastin) was associated with a significant improvement in recurrence-free survival, compared with active surveillance, and represents the first option to show efficacy in the adjuvant setting following surgical resection of HCCs for patients at high risk for recurrence.
among patients who received the combination therapy in comparison with active surveillance. However, the overall survival data remain immature.
The data come from an interim analysis of the IMbrave050 trial, which was presented at the annual meeting of the American Association for Cancer Research.
“Atezolizumab plus bevacizumab may be a practice-changing adjuvant treatment options for patients with high-risk HCC,” said lead investigator Pierce Chow, MBBS, PhD, codirector of the National Cancer Centre Singapore Comprehensive Liver Cancer Clinic. He presented the results in an oral abstract session at the meeting. The combination “may also change clinical indications for surgical resection” because clinicians may be more likely to consider resection for patients at extremely high risk for recurrence if the risk of recurrence can be reduced with this combination.
In the previous IMbrave150 trial, the combination of atezolizumab and bevacizumab significantly improved outcomes for patients with high-risk and non–high-risk unresectable HCC, compared with the standard of care sorafenib (Nexavar).
In that trial, the median overall survival in the intention-to-treat population was 19.2 months for patients who received atezolizumab-bevacizumab versus 13.4 months for patients who received sorafenib (P = .0009).
The combination was also associated with improvements in progression-free survival and objective response rates, compared with sorafenib.
On the basis of these results, the IMbrave050 investigators explored whether the same benefits would occur for patients with resectable disease considered to be at high risk for recurrence owing to tumor size, vascular invasion, or poor tumor differentiation. The trial compared the combination for 334 patients with active surveillance, also for 334 patients, in the adjuvant setting.
Patients were considered good candidates for thermal ablation if they had a single tumor greater than 2 cm, but not larger than 5 cm in its longest dimension, or if they had four or fewer tumors, all of which were no larger than 5 cm. For all other patients, surgical resection was recommended.
The median age of the patients was 60. For about half of patients in each arm, the expression level of programmed death–ligand-1 (PD-L1) was 1% or higher.
After a median follow-up of 17.4 months, the 12-month recurrence-free survival rate, as assessed by independent review, was 78% for patients in the treatment arm, compared with 65% for patients who were assigned to active surveillance (hazard ratio, 0.72; P = .012). This finding was generally consistent across clinical subgroups, including groups based on age, sex, race/ethnicity, performance status, PD-L1 expression, number of high-risk features, Barcelona Clinic Liver Cancer stage, cancer etiology, procedure type, microvascular invasion, or tumor numbers and size.
Of 133 patients on active surveillance who experienced a protocol-defined recurrence event, 81 (61%) crossed over to the atezolizumab/bevacizumab arm.
The overall survival benefit of the combination therapy was less clear. Dr. Chow called the overall survival data “highly immature” at the time of data cutoff.
Overall, 47 patients died – 7 more in the combination arm (27 vs. 20). More specifically, 17 patients in the combination arm and 16 on active surveillance died from progressive disease; 6 patients in the treatment arm versus 1 on surveillance died from adverse events. The remaining deaths were attributed to other causes. Two deaths in the combination arm were considered treatment related, one from esophageal varices hemorrhage, and the other from ischemic stroke.
Dr. Chow said a number of deaths attributed to HCC recurrence was similar between the groups. There were three COVID-19–related deaths within 1 year of randomization, all in the combination arm.
As for adverse events, the safety of the combination was largely consistent with that reported in the IMbrave150 trial. Nearly all patients experienced at least one adverse event. Treatment-related grade 3 or 4 adverse events occurred in 34.9% of patients in the combination group, and serious treatment-related events occurred in 13.3%.
The most common adverse events of any grade were proteinuria, hypertension, decreased platelet count, increases in liver enzyme level, hypothyroidism, arthralgia, pruritus, rash, increase in serum bilirubin level, and fever.
Invited discussant Stephen L. Chan, MD, from the Chinese University of Hong Kong, said the study was “definitely” relevant to clinicians and addresses “a very important unmet need.”
Dr. Chan noted that he thinks this combination will “likely” be practice changing, given the improvement in recurrence-free survival, but “certainly we need more data to guide us in patient selection.”
The study was funded by F. Hoffman–La Roche. Dr. Chow has consulting for and has received honoraria and grant/research support from Roche and others. Dr. Chan has received honoraria from Roche and consulting fees and grant/research support from others.
A version of this article first appeared on Medscape.com.
AT AACR 2023