User login
News and Views that Matter to Pediatricians
The leading independent newspaper covering news and commentary in pediatrics.
Pertussis Cases Spike in November
Six times as many cases of pertussis were reported in the United States for the week ending November 16, 2024, as the same week in 2023, according to new data from the Centers for Disease Control and Prevention (CDC).
Of the 434 cases reported for the week ending November 16, 2024, a majority (109) occurred in the East North Central region, mostly in Ohio (93). Another 70 cases occurred in the West North Central region, with 32 cases and 37 cases in Missouri and Nebraska, respectively.
None of the 75 cases in the Middle Atlantic region occurred in New Jersey or New York City; 38 were reported elsewhere in New York, and 37 in Pennsylvania. The South Atlantic region reported 55 cases, including 29 in Florida. The East South Central and West South Central regions reported 11 and 20 cases, respectively. The Mountain and Pacific regions reported 31 (20 in Arizona) and 47 (20 in Washington State) cases, respectively.
The CDC tracks pertussis cases through a national surveillance system, but many cases are likely unrecognized and unreported, according to the CDC.
Although vaccines for pertussis (whooping cough) provide protection, their effectiveness decreases over time, and the CDC expects rates to increase in vaccinated and unvaccinated populations as case levels rebound with the lifting of pandemic mitigation strategies such as masking and remote learning.
Recent CDC data reported by Medscape Medical News showed an association between lower vaccination rates and 2024’s uptick in pertussis cases.
A version of this article first appeared on Medscape.com.
Six times as many cases of pertussis were reported in the United States for the week ending November 16, 2024, as the same week in 2023, according to new data from the Centers for Disease Control and Prevention (CDC).
Of the 434 cases reported for the week ending November 16, 2024, a majority (109) occurred in the East North Central region, mostly in Ohio (93). Another 70 cases occurred in the West North Central region, with 32 cases and 37 cases in Missouri and Nebraska, respectively.
None of the 75 cases in the Middle Atlantic region occurred in New Jersey or New York City; 38 were reported elsewhere in New York, and 37 in Pennsylvania. The South Atlantic region reported 55 cases, including 29 in Florida. The East South Central and West South Central regions reported 11 and 20 cases, respectively. The Mountain and Pacific regions reported 31 (20 in Arizona) and 47 (20 in Washington State) cases, respectively.
The CDC tracks pertussis cases through a national surveillance system, but many cases are likely unrecognized and unreported, according to the CDC.
Although vaccines for pertussis (whooping cough) provide protection, their effectiveness decreases over time, and the CDC expects rates to increase in vaccinated and unvaccinated populations as case levels rebound with the lifting of pandemic mitigation strategies such as masking and remote learning.
Recent CDC data reported by Medscape Medical News showed an association between lower vaccination rates and 2024’s uptick in pertussis cases.
A version of this article first appeared on Medscape.com.
Six times as many cases of pertussis were reported in the United States for the week ending November 16, 2024, as the same week in 2023, according to new data from the Centers for Disease Control and Prevention (CDC).
Of the 434 cases reported for the week ending November 16, 2024, a majority (109) occurred in the East North Central region, mostly in Ohio (93). Another 70 cases occurred in the West North Central region, with 32 cases and 37 cases in Missouri and Nebraska, respectively.
None of the 75 cases in the Middle Atlantic region occurred in New Jersey or New York City; 38 were reported elsewhere in New York, and 37 in Pennsylvania. The South Atlantic region reported 55 cases, including 29 in Florida. The East South Central and West South Central regions reported 11 and 20 cases, respectively. The Mountain and Pacific regions reported 31 (20 in Arizona) and 47 (20 in Washington State) cases, respectively.
The CDC tracks pertussis cases through a national surveillance system, but many cases are likely unrecognized and unreported, according to the CDC.
Although vaccines for pertussis (whooping cough) provide protection, their effectiveness decreases over time, and the CDC expects rates to increase in vaccinated and unvaccinated populations as case levels rebound with the lifting of pandemic mitigation strategies such as masking and remote learning.
Recent CDC data reported by Medscape Medical News showed an association between lower vaccination rates and 2024’s uptick in pertussis cases.
A version of this article first appeared on Medscape.com.
There Are ‘Four Pillars of Acne Pathogenesis’: Make Sure Treatment Hits as Many as Possible
LAS VEGAS — For clinicians who rely on generic tretinoin 0.5% as their go-to treatment for patients with acne, Shanna Miranti, MPAS, PA-C, offers some straightforward advice: You can do better.
“Friends don’t let friends write generic tretinoin only because there are so many better options out there,” Miranti, who practices dermatology in Naples, Florida, said at the Society of Dermatology Physician Associates (SDPA) 22nd Annual Fall Dermatology Conference. “Don’t get lazy; your patients deserve better.”
In her wide-ranging presentation, Miranti described the four pillars of acne pathogenesis as increased sebum production caused by androgens, follicular hyperkeratinization in the pilosebaceous unit, colonization by Cutibacterium acnes (formerly Proprionibacterium acnes), and inflammation. Acne “starts with androgens, but this is a cascade, so you have to find treatment options that hit as many of these four pillars as possible,” Miranti explained. “If you’re only using generic tretinoin, you’re only hitting maybe two of the four pillars at best.”
She then discussed the best treatment options for each pillar:
Follicular plugging and hyperkeratinization. Topical retinoids, including tretinoin, adapalene, tazarotene, and trifarotene, are highly effective for this issue. Systemic isotretinoin is also a strong option. For patients who are pregnant or trying to conceive, azelaic acid is a helpful alternative.
Excessive sebum production and androgens. “This may be the genesis of when acne begins — during puberty,” Miranti said. “With rising androgens comes rising amounts of sebum.” The only topical treatment that specifically targets this is clascoterone (Winlevi), which should be applied twice daily. For systemic management of excessive sebum, isotretinoin is highly effective. In women, spironolactone (50 mg daily, or split into two doses) and oral contraceptives are also options.
Inflammation. Topical options include retinoids, antibiotics, benzoyl peroxide (BPO), topical dapsone, azelaic acid, and clascoterone. Systemic options include isotretinoin; the antibiotics doxycycline, minocycline, and sarecycline; spironolactone; and oral contraceptives. “So, when you see patients with intense inflammation, and they’re starting to get post-inflammatory erythema or post-inflammatory hyperpigmentation, you need something to address this inflammatory problem,” she noted.
C acnes. Topical treatment options include BPO and antibiotics. However, topical antibiotics should never be used alone, Miranti said; they must always be combined with BPO to prevent bacterial resistance. Oral options include sarecycline, “which has a low propensity for antibiotic resistance and spares the gut microbiome to some degree,” and the “old-school” antibiotics doxycycline, minocycline, and tetracycline. “But all oral antibiotics should be used concomitantly with BPO,” she added.
Regardless of which treatment is chosen for any pillar, Miranti emphasized that monotherapy with a single agent is often insufficient. “Historically, we have combined therapies to treat the multiple causes of acne,” she said. “The average number of acne products used per patient is 2.53, but that’s also the average number of copays. We have to be conscious of that. If you are a mom with four kids who are on acne medication, you want to minimize your copay burden. So, if you can find a topical medication that hits three out of the four pillars of acne pathogenesis, that would be fantastic.” The only topical that targets excess sebum is clascoterone, she noted, and the only medication that hits all four pillars is isotretinoin.
In October 2023, the Food and Drug Administration approved a once-daily topical gel for patients aged 12 years or older that contains clindamycin 1.2%, adapalene 0.15%, and BPO 3.1%. The first-ever triple combination therapy, known as Cabtreo, was released to pharmacies in March 2024. In a phase 2 trial, researchers randomized 394 patients aged 9 years or older with moderate to severe acne to once-daily IDP-126, one of three dyad combination gels, or vehicle gel for 12 weeks. Patients in the Cabtreo arm achieved significantly greater lesion reductions than those in the vehicle arm (inflammatory: 78.3% vs 45.1%; noninflammatory: 70.0% vs 37.6%; P < .001 for both). They also experienced lesion reductions that were 9.2%-16.6% greater than those observed with any of the dyad combination gels. Miranti characterized the study results as “pretty phenomenal,” noting that the ease of use makes Cabtreo stand out as a treatment option. “Simplicity drives compliance, and compliance drives results,” she said. “This is one product to apply once a day. Any of you who have a teenage son like me, you know it is hard to get them to brush their teeth twice a day, let alone take medicine before they leave the house in the morning. This can be a home run for a lot of patients, and not just our teenagers. Adult females have done very well with this medication.”
In a network meta-analysis, researchers reviewed 221 randomized controlled trials to compare the efficacy of pharmacologic treatment for acne. The most effective treatment in reducing inflammatory and noninflammatory lesions was oral isotretinoin, followed by Cabtreo.
Miranti disclosed being a speaker, consultant, and/or an advisory board member for Arcutis Biotherapeutics, Bausch Health, Dermavant Sciences, Galderma, Incyte, LEO Pharma, Eli Lilly, Sun Pharma, Swift USA, and Verrica Pharmaceuticals.
A version of this article first appeared on Medscape.com.
LAS VEGAS — For clinicians who rely on generic tretinoin 0.5% as their go-to treatment for patients with acne, Shanna Miranti, MPAS, PA-C, offers some straightforward advice: You can do better.
“Friends don’t let friends write generic tretinoin only because there are so many better options out there,” Miranti, who practices dermatology in Naples, Florida, said at the Society of Dermatology Physician Associates (SDPA) 22nd Annual Fall Dermatology Conference. “Don’t get lazy; your patients deserve better.”
In her wide-ranging presentation, Miranti described the four pillars of acne pathogenesis as increased sebum production caused by androgens, follicular hyperkeratinization in the pilosebaceous unit, colonization by Cutibacterium acnes (formerly Proprionibacterium acnes), and inflammation. Acne “starts with androgens, but this is a cascade, so you have to find treatment options that hit as many of these four pillars as possible,” Miranti explained. “If you’re only using generic tretinoin, you’re only hitting maybe two of the four pillars at best.”
She then discussed the best treatment options for each pillar:
Follicular plugging and hyperkeratinization. Topical retinoids, including tretinoin, adapalene, tazarotene, and trifarotene, are highly effective for this issue. Systemic isotretinoin is also a strong option. For patients who are pregnant or trying to conceive, azelaic acid is a helpful alternative.
Excessive sebum production and androgens. “This may be the genesis of when acne begins — during puberty,” Miranti said. “With rising androgens comes rising amounts of sebum.” The only topical treatment that specifically targets this is clascoterone (Winlevi), which should be applied twice daily. For systemic management of excessive sebum, isotretinoin is highly effective. In women, spironolactone (50 mg daily, or split into two doses) and oral contraceptives are also options.
Inflammation. Topical options include retinoids, antibiotics, benzoyl peroxide (BPO), topical dapsone, azelaic acid, and clascoterone. Systemic options include isotretinoin; the antibiotics doxycycline, minocycline, and sarecycline; spironolactone; and oral contraceptives. “So, when you see patients with intense inflammation, and they’re starting to get post-inflammatory erythema or post-inflammatory hyperpigmentation, you need something to address this inflammatory problem,” she noted.
C acnes. Topical treatment options include BPO and antibiotics. However, topical antibiotics should never be used alone, Miranti said; they must always be combined with BPO to prevent bacterial resistance. Oral options include sarecycline, “which has a low propensity for antibiotic resistance and spares the gut microbiome to some degree,” and the “old-school” antibiotics doxycycline, minocycline, and tetracycline. “But all oral antibiotics should be used concomitantly with BPO,” she added.
Regardless of which treatment is chosen for any pillar, Miranti emphasized that monotherapy with a single agent is often insufficient. “Historically, we have combined therapies to treat the multiple causes of acne,” she said. “The average number of acne products used per patient is 2.53, but that’s also the average number of copays. We have to be conscious of that. If you are a mom with four kids who are on acne medication, you want to minimize your copay burden. So, if you can find a topical medication that hits three out of the four pillars of acne pathogenesis, that would be fantastic.” The only topical that targets excess sebum is clascoterone, she noted, and the only medication that hits all four pillars is isotretinoin.
In October 2023, the Food and Drug Administration approved a once-daily topical gel for patients aged 12 years or older that contains clindamycin 1.2%, adapalene 0.15%, and BPO 3.1%. The first-ever triple combination therapy, known as Cabtreo, was released to pharmacies in March 2024. In a phase 2 trial, researchers randomized 394 patients aged 9 years or older with moderate to severe acne to once-daily IDP-126, one of three dyad combination gels, or vehicle gel for 12 weeks. Patients in the Cabtreo arm achieved significantly greater lesion reductions than those in the vehicle arm (inflammatory: 78.3% vs 45.1%; noninflammatory: 70.0% vs 37.6%; P < .001 for both). They also experienced lesion reductions that were 9.2%-16.6% greater than those observed with any of the dyad combination gels. Miranti characterized the study results as “pretty phenomenal,” noting that the ease of use makes Cabtreo stand out as a treatment option. “Simplicity drives compliance, and compliance drives results,” she said. “This is one product to apply once a day. Any of you who have a teenage son like me, you know it is hard to get them to brush their teeth twice a day, let alone take medicine before they leave the house in the morning. This can be a home run for a lot of patients, and not just our teenagers. Adult females have done very well with this medication.”
In a network meta-analysis, researchers reviewed 221 randomized controlled trials to compare the efficacy of pharmacologic treatment for acne. The most effective treatment in reducing inflammatory and noninflammatory lesions was oral isotretinoin, followed by Cabtreo.
Miranti disclosed being a speaker, consultant, and/or an advisory board member for Arcutis Biotherapeutics, Bausch Health, Dermavant Sciences, Galderma, Incyte, LEO Pharma, Eli Lilly, Sun Pharma, Swift USA, and Verrica Pharmaceuticals.
A version of this article first appeared on Medscape.com.
LAS VEGAS — For clinicians who rely on generic tretinoin 0.5% as their go-to treatment for patients with acne, Shanna Miranti, MPAS, PA-C, offers some straightforward advice: You can do better.
“Friends don’t let friends write generic tretinoin only because there are so many better options out there,” Miranti, who practices dermatology in Naples, Florida, said at the Society of Dermatology Physician Associates (SDPA) 22nd Annual Fall Dermatology Conference. “Don’t get lazy; your patients deserve better.”
In her wide-ranging presentation, Miranti described the four pillars of acne pathogenesis as increased sebum production caused by androgens, follicular hyperkeratinization in the pilosebaceous unit, colonization by Cutibacterium acnes (formerly Proprionibacterium acnes), and inflammation. Acne “starts with androgens, but this is a cascade, so you have to find treatment options that hit as many of these four pillars as possible,” Miranti explained. “If you’re only using generic tretinoin, you’re only hitting maybe two of the four pillars at best.”
She then discussed the best treatment options for each pillar:
Follicular plugging and hyperkeratinization. Topical retinoids, including tretinoin, adapalene, tazarotene, and trifarotene, are highly effective for this issue. Systemic isotretinoin is also a strong option. For patients who are pregnant or trying to conceive, azelaic acid is a helpful alternative.
Excessive sebum production and androgens. “This may be the genesis of when acne begins — during puberty,” Miranti said. “With rising androgens comes rising amounts of sebum.” The only topical treatment that specifically targets this is clascoterone (Winlevi), which should be applied twice daily. For systemic management of excessive sebum, isotretinoin is highly effective. In women, spironolactone (50 mg daily, or split into two doses) and oral contraceptives are also options.
Inflammation. Topical options include retinoids, antibiotics, benzoyl peroxide (BPO), topical dapsone, azelaic acid, and clascoterone. Systemic options include isotretinoin; the antibiotics doxycycline, minocycline, and sarecycline; spironolactone; and oral contraceptives. “So, when you see patients with intense inflammation, and they’re starting to get post-inflammatory erythema or post-inflammatory hyperpigmentation, you need something to address this inflammatory problem,” she noted.
C acnes. Topical treatment options include BPO and antibiotics. However, topical antibiotics should never be used alone, Miranti said; they must always be combined with BPO to prevent bacterial resistance. Oral options include sarecycline, “which has a low propensity for antibiotic resistance and spares the gut microbiome to some degree,” and the “old-school” antibiotics doxycycline, minocycline, and tetracycline. “But all oral antibiotics should be used concomitantly with BPO,” she added.
Regardless of which treatment is chosen for any pillar, Miranti emphasized that monotherapy with a single agent is often insufficient. “Historically, we have combined therapies to treat the multiple causes of acne,” she said. “The average number of acne products used per patient is 2.53, but that’s also the average number of copays. We have to be conscious of that. If you are a mom with four kids who are on acne medication, you want to minimize your copay burden. So, if you can find a topical medication that hits three out of the four pillars of acne pathogenesis, that would be fantastic.” The only topical that targets excess sebum is clascoterone, she noted, and the only medication that hits all four pillars is isotretinoin.
In October 2023, the Food and Drug Administration approved a once-daily topical gel for patients aged 12 years or older that contains clindamycin 1.2%, adapalene 0.15%, and BPO 3.1%. The first-ever triple combination therapy, known as Cabtreo, was released to pharmacies in March 2024. In a phase 2 trial, researchers randomized 394 patients aged 9 years or older with moderate to severe acne to once-daily IDP-126, one of three dyad combination gels, or vehicle gel for 12 weeks. Patients in the Cabtreo arm achieved significantly greater lesion reductions than those in the vehicle arm (inflammatory: 78.3% vs 45.1%; noninflammatory: 70.0% vs 37.6%; P < .001 for both). They also experienced lesion reductions that were 9.2%-16.6% greater than those observed with any of the dyad combination gels. Miranti characterized the study results as “pretty phenomenal,” noting that the ease of use makes Cabtreo stand out as a treatment option. “Simplicity drives compliance, and compliance drives results,” she said. “This is one product to apply once a day. Any of you who have a teenage son like me, you know it is hard to get them to brush their teeth twice a day, let alone take medicine before they leave the house in the morning. This can be a home run for a lot of patients, and not just our teenagers. Adult females have done very well with this medication.”
In a network meta-analysis, researchers reviewed 221 randomized controlled trials to compare the efficacy of pharmacologic treatment for acne. The most effective treatment in reducing inflammatory and noninflammatory lesions was oral isotretinoin, followed by Cabtreo.
Miranti disclosed being a speaker, consultant, and/or an advisory board member for Arcutis Biotherapeutics, Bausch Health, Dermavant Sciences, Galderma, Incyte, LEO Pharma, Eli Lilly, Sun Pharma, Swift USA, and Verrica Pharmaceuticals.
A version of this article first appeared on Medscape.com.
FROM SDPA 2024
Flu Vaccine Guards Household Contacts of Infected People
TOPLINE:
Vaccination lowers the risk of contracting the infection among household contacts.
METHODOLOGY:
- Researchers conducted a prospective cohort study of data between 2017 and 2020 to determine the estimated effectiveness of influenza vaccines in preventing secondary infections in household contacts.
- Overall, 699 people were primary contacts, or the first in a household to get infected (median age, 13 years; 54.5% women); there were 1581 household contacts (median age, 31 years; 52.7% women), and both groups were followed for 7 days.
- Participants collected daily symptom diaries and nasal swabs during the follow-up period.
- Participants also submitted their history of influenza vaccination; 50.1% of household contacts had received a shot at least 14 days before the first case of disease onset in the household.
- The risk for secondary infection and vaccine effectiveness in preventing infection among household contacts was estimated overall and by virus type, subtype, and lineage.
TAKEAWAY:
- Nearly half (48.2%) of primary cases were from children and teens between ages 5 and 17 years.
- Overall, 22% household contacts had laboratory-confirmed influenza during follow-up, of which 7% were asymptomatic.
- The overall risk for secondary infection among unvaccinated household contacts was 18.8%, with the highest risk observed among children younger than age 5 years (29.9%).
- The overall effectiveness of influenza vaccines in preventing laboratory-confirmed infections among household contacts was 21% (95% CI, 1.4%-36.7%).
- The vaccine demonstrated specific protection against influenza B infection (56.4%; 95% CI, 30.1%-72.8%), particularly among those between ages 5 and 17 years.
IN PRACTICE:
“Although complementary preventive strategies to prevent influenza in household settings may be considered, seasonal influenza vaccination is the primary strategy recommended for prevention of influenza illness and its complications,” the authors wrote.
SOURCE:
The study was led by Carlos G. Grijalva, MD, MPH, of Vanderbilt University Medical Center in Nashville, Tennessee, and was published online in JAMA Network Open.
LIMITATIONS:
The recruitment of infected individuals from clinical testing pools may have limited the generalizability of the risk for secondary infection in households in which the primary case had a milder or asymptomatic infection. The study was unable to assess the effectiveness of specific vaccine formulations, such as those receiving high doses. The stratification of estimates by influenza subtypes and lineages was challenging because of small cell sizes.
DISCLOSURES:
This study was supported by grants from the Centers for Disease Control and Prevention (CDC) and authors reported support from grants from the National Institute Of Allergy And Infectious Diseases. Some authors reported contracts, receiving personal fees and grants from the CDC and various pharmaceutical companies such as Merck and Sanofi.
This article was created using several editorial tools, including artificial intelligence, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Vaccination lowers the risk of contracting the infection among household contacts.
METHODOLOGY:
- Researchers conducted a prospective cohort study of data between 2017 and 2020 to determine the estimated effectiveness of influenza vaccines in preventing secondary infections in household contacts.
- Overall, 699 people were primary contacts, or the first in a household to get infected (median age, 13 years; 54.5% women); there were 1581 household contacts (median age, 31 years; 52.7% women), and both groups were followed for 7 days.
- Participants collected daily symptom diaries and nasal swabs during the follow-up period.
- Participants also submitted their history of influenza vaccination; 50.1% of household contacts had received a shot at least 14 days before the first case of disease onset in the household.
- The risk for secondary infection and vaccine effectiveness in preventing infection among household contacts was estimated overall and by virus type, subtype, and lineage.
TAKEAWAY:
- Nearly half (48.2%) of primary cases were from children and teens between ages 5 and 17 years.
- Overall, 22% household contacts had laboratory-confirmed influenza during follow-up, of which 7% were asymptomatic.
- The overall risk for secondary infection among unvaccinated household contacts was 18.8%, with the highest risk observed among children younger than age 5 years (29.9%).
- The overall effectiveness of influenza vaccines in preventing laboratory-confirmed infections among household contacts was 21% (95% CI, 1.4%-36.7%).
- The vaccine demonstrated specific protection against influenza B infection (56.4%; 95% CI, 30.1%-72.8%), particularly among those between ages 5 and 17 years.
IN PRACTICE:
“Although complementary preventive strategies to prevent influenza in household settings may be considered, seasonal influenza vaccination is the primary strategy recommended for prevention of influenza illness and its complications,” the authors wrote.
SOURCE:
The study was led by Carlos G. Grijalva, MD, MPH, of Vanderbilt University Medical Center in Nashville, Tennessee, and was published online in JAMA Network Open.
LIMITATIONS:
The recruitment of infected individuals from clinical testing pools may have limited the generalizability of the risk for secondary infection in households in which the primary case had a milder or asymptomatic infection. The study was unable to assess the effectiveness of specific vaccine formulations, such as those receiving high doses. The stratification of estimates by influenza subtypes and lineages was challenging because of small cell sizes.
DISCLOSURES:
This study was supported by grants from the Centers for Disease Control and Prevention (CDC) and authors reported support from grants from the National Institute Of Allergy And Infectious Diseases. Some authors reported contracts, receiving personal fees and grants from the CDC and various pharmaceutical companies such as Merck and Sanofi.
This article was created using several editorial tools, including artificial intelligence, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Vaccination lowers the risk of contracting the infection among household contacts.
METHODOLOGY:
- Researchers conducted a prospective cohort study of data between 2017 and 2020 to determine the estimated effectiveness of influenza vaccines in preventing secondary infections in household contacts.
- Overall, 699 people were primary contacts, or the first in a household to get infected (median age, 13 years; 54.5% women); there were 1581 household contacts (median age, 31 years; 52.7% women), and both groups were followed for 7 days.
- Participants collected daily symptom diaries and nasal swabs during the follow-up period.
- Participants also submitted their history of influenza vaccination; 50.1% of household contacts had received a shot at least 14 days before the first case of disease onset in the household.
- The risk for secondary infection and vaccine effectiveness in preventing infection among household contacts was estimated overall and by virus type, subtype, and lineage.
TAKEAWAY:
- Nearly half (48.2%) of primary cases were from children and teens between ages 5 and 17 years.
- Overall, 22% household contacts had laboratory-confirmed influenza during follow-up, of which 7% were asymptomatic.
- The overall risk for secondary infection among unvaccinated household contacts was 18.8%, with the highest risk observed among children younger than age 5 years (29.9%).
- The overall effectiveness of influenza vaccines in preventing laboratory-confirmed infections among household contacts was 21% (95% CI, 1.4%-36.7%).
- The vaccine demonstrated specific protection against influenza B infection (56.4%; 95% CI, 30.1%-72.8%), particularly among those between ages 5 and 17 years.
IN PRACTICE:
“Although complementary preventive strategies to prevent influenza in household settings may be considered, seasonal influenza vaccination is the primary strategy recommended for prevention of influenza illness and its complications,” the authors wrote.
SOURCE:
The study was led by Carlos G. Grijalva, MD, MPH, of Vanderbilt University Medical Center in Nashville, Tennessee, and was published online in JAMA Network Open.
LIMITATIONS:
The recruitment of infected individuals from clinical testing pools may have limited the generalizability of the risk for secondary infection in households in which the primary case had a milder or asymptomatic infection. The study was unable to assess the effectiveness of specific vaccine formulations, such as those receiving high doses. The stratification of estimates by influenza subtypes and lineages was challenging because of small cell sizes.
DISCLOSURES:
This study was supported by grants from the Centers for Disease Control and Prevention (CDC) and authors reported support from grants from the National Institute Of Allergy And Infectious Diseases. Some authors reported contracts, receiving personal fees and grants from the CDC and various pharmaceutical companies such as Merck and Sanofi.
This article was created using several editorial tools, including artificial intelligence, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
AMR Could Surpass Cancer as Leading Cause of Death by 2050
Antimicrobial resistance (AMR) is globally recognized as one of the greatest health threats of the 21st century, responsible for 1.27 million deaths annually. “According to the WHO, if no measures are taken promptly, AMR could lead to more deaths than cancer by 2050,” Arnaud Marchant, MD, PhD, director of the European Plotkin Institute for Vaccinology at Université libre de Bruxelles (EPIV-ULB), Anderlecht, Belgium, said in an interview with MediQuality, part of the Medscape Professional Network. “This is a huge problem, and vaccination could be part of the solution.”
EPIV-ULB marked the start of the World AMR Awareness Week (November 18-24) with an event highlighting the critical role of vaccination to counter the rise for resistant pathogens. During the event, MediQuality interviewed Marchant, along with several other experts in the field.
Antibiotics Losing Effectiveness
Marc Van Ranst, PhD, virologist at Rega Institute KU Leuven in Leuven, Belgium, echoed Marchant’s concerns. He noted that “an increasing number of bacteria are becoming resistant to more antibiotics.” “While antibiotics were once miracle drugs, they have now stopped — or almost stopped — working against certain bacteria. Although we are discovering more effective therapies, bacterial infections are increasingly likely to worsen due to AMR.”
Van Ranst issued a stark warning: “If this trend continues, it is entirely reasonable to predict that in 25 years, some antibiotics will become useless, certain bacterial infections will be much harder to treat, and deaths will outnumber those caused by cancer. It’s worth noting, however, that as cancer treatments improve, cancer-related deaths are expected to decline, further highlighting the growing burden of AMR-related fatalities.”
Viruses, Vaccines, and Resistance
Van Ranst emphasized that while AMR primarily involves bacteria, viral infections and vaccination against them also play a role in addressing the issue. “When vaccines prevent illness, they reduce the need for unnecessary antibiotic use. In the past, antibiotics were frequently prescribed for respiratory infections — typically caused by viruses — leading to misuse and heightened resistance. By preventing viral infections through vaccines, we reduce inappropriate antibiotic prescriptions and, subsequently, AMR.”
Strategic Areas of Focus
To maximize the impact of vaccination in combating AMR, Belgium must prioritize several strategic areas, according to EPIV-ULB. “Expanding vaccination coverage for recommended vaccines is crucial to effectively preventing the spread of resistant pathogens,” said Marchant.
“Innovation and development of new vaccines are also essential, including targeted research into vaccines for infections that are currently unavoidable through other means. Enhancing epidemiological surveillance through national data collection and analysis will further clarify the impact of vaccines on AMR and inform policy decisions.”
EPIV-ULB underscored the importance of educating the public and healthcare professionals. “Public awareness is essential to addressing vaccine hesitancy by providing clear information on the importance of prevention,” Marchant explained. “Healthcare professional training must also improve, encouraging preventive practices and judicious antibiotic use. Furthermore, additional research is necessary to fill data gaps and develop predictive models that can guide vaccine development in the future.”
Role of Vaccination
According to EPIV-ULB, Belgium needs a strengthened national strategy to address AMR effectively. “Complementary solutions are increasingly important as antimicrobials lose efficacy and treatments become more complex,” Marchant said. “Vaccination offers a proactive and effective preventive solution, directly and indirectly reducing the spread of resistant pathogens.”
Vaccines combat AMR through various mechanisms. “They prevent diseases such as pneumococcal pneumonia and meningitis, reducing the need for antibiotics to treat these infections,” Marchant explained. “Additionally, vaccination lowers inappropriate antibiotic use by preventing viral infections, reducing the risk of overprescribing antibiotics in cases where they are unnecessary. Lastly, herd immunity from vaccination slows the circulation of resistant pathogens, limiting their spread.”
Van Ranst urged healthcare professionals to prioritize vaccinating at-risk populations as identified by Belgium’s Superior Health Council. These include the elderly with underlying conditions and pregnant women, especially for influenza vaccines. University Hospitals Leuven in Belgium, also conducts annual vaccination campaigns for its staff, combining flu and COVID vaccines to increase uptake.
A Global Challenge
Marc Noppen, MD, PhD, director of University Hospital Brussels, Belgium, emphasized the complexity of AMR as a global issue. “The problem isn’t solely due to human antibiotic use; it also stems from veterinary medicine, plant breeding, and animal husbandry. This is a multifactorial, worldwide issue that requires public awareness. Improved vaccination strategies are one way to address AMR, particularly in this post-COVID era of heightened skepticism toward vaccines,” he explained.
Marie-Lise Verschelden from Pfizer highlighted the need for cooperation across the healthcare sector. “Belgium is fortunate to have a fantastic ecosystem of academics, clinicians, and industry experts. Collaboration, including government involvement, is critical to advancing our efforts. At Pfizer, we continue to develop new vaccines and technologies, and the COVID crisis has reinforced the critical role of vaccination in combating AMR. Through our vaccine portfolio and ongoing developments, we are well-positioned to contribute significantly to this global challenge.”
Elisabeth Van Damme from GSK reiterated that AMR is a global issue requiring joint efforts. “Existing vaccines are underutilized. Vaccination protects against certain infectious diseases, reducing the need for antibiotics. Antibiotics, in turn, are sometimes prescribed incorrectly, especially for viral infections they cannot treat. At GSK, we are already developing new vaccines to meet future needs.”
Vaccination remains a cornerstone in the fight against AMR. As pathogens grow increasingly resistant to antibiotics, coordinated efforts and innovative vaccine development are essential to mitigating this global health crisis.
This story was translated and adapted from MediQuality using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Antimicrobial resistance (AMR) is globally recognized as one of the greatest health threats of the 21st century, responsible for 1.27 million deaths annually. “According to the WHO, if no measures are taken promptly, AMR could lead to more deaths than cancer by 2050,” Arnaud Marchant, MD, PhD, director of the European Plotkin Institute for Vaccinology at Université libre de Bruxelles (EPIV-ULB), Anderlecht, Belgium, said in an interview with MediQuality, part of the Medscape Professional Network. “This is a huge problem, and vaccination could be part of the solution.”
EPIV-ULB marked the start of the World AMR Awareness Week (November 18-24) with an event highlighting the critical role of vaccination to counter the rise for resistant pathogens. During the event, MediQuality interviewed Marchant, along with several other experts in the field.
Antibiotics Losing Effectiveness
Marc Van Ranst, PhD, virologist at Rega Institute KU Leuven in Leuven, Belgium, echoed Marchant’s concerns. He noted that “an increasing number of bacteria are becoming resistant to more antibiotics.” “While antibiotics were once miracle drugs, they have now stopped — or almost stopped — working against certain bacteria. Although we are discovering more effective therapies, bacterial infections are increasingly likely to worsen due to AMR.”
Van Ranst issued a stark warning: “If this trend continues, it is entirely reasonable to predict that in 25 years, some antibiotics will become useless, certain bacterial infections will be much harder to treat, and deaths will outnumber those caused by cancer. It’s worth noting, however, that as cancer treatments improve, cancer-related deaths are expected to decline, further highlighting the growing burden of AMR-related fatalities.”
Viruses, Vaccines, and Resistance
Van Ranst emphasized that while AMR primarily involves bacteria, viral infections and vaccination against them also play a role in addressing the issue. “When vaccines prevent illness, they reduce the need for unnecessary antibiotic use. In the past, antibiotics were frequently prescribed for respiratory infections — typically caused by viruses — leading to misuse and heightened resistance. By preventing viral infections through vaccines, we reduce inappropriate antibiotic prescriptions and, subsequently, AMR.”
Strategic Areas of Focus
To maximize the impact of vaccination in combating AMR, Belgium must prioritize several strategic areas, according to EPIV-ULB. “Expanding vaccination coverage for recommended vaccines is crucial to effectively preventing the spread of resistant pathogens,” said Marchant.
“Innovation and development of new vaccines are also essential, including targeted research into vaccines for infections that are currently unavoidable through other means. Enhancing epidemiological surveillance through national data collection and analysis will further clarify the impact of vaccines on AMR and inform policy decisions.”
EPIV-ULB underscored the importance of educating the public and healthcare professionals. “Public awareness is essential to addressing vaccine hesitancy by providing clear information on the importance of prevention,” Marchant explained. “Healthcare professional training must also improve, encouraging preventive practices and judicious antibiotic use. Furthermore, additional research is necessary to fill data gaps and develop predictive models that can guide vaccine development in the future.”
Role of Vaccination
According to EPIV-ULB, Belgium needs a strengthened national strategy to address AMR effectively. “Complementary solutions are increasingly important as antimicrobials lose efficacy and treatments become more complex,” Marchant said. “Vaccination offers a proactive and effective preventive solution, directly and indirectly reducing the spread of resistant pathogens.”
Vaccines combat AMR through various mechanisms. “They prevent diseases such as pneumococcal pneumonia and meningitis, reducing the need for antibiotics to treat these infections,” Marchant explained. “Additionally, vaccination lowers inappropriate antibiotic use by preventing viral infections, reducing the risk of overprescribing antibiotics in cases where they are unnecessary. Lastly, herd immunity from vaccination slows the circulation of resistant pathogens, limiting their spread.”
Van Ranst urged healthcare professionals to prioritize vaccinating at-risk populations as identified by Belgium’s Superior Health Council. These include the elderly with underlying conditions and pregnant women, especially for influenza vaccines. University Hospitals Leuven in Belgium, also conducts annual vaccination campaigns for its staff, combining flu and COVID vaccines to increase uptake.
A Global Challenge
Marc Noppen, MD, PhD, director of University Hospital Brussels, Belgium, emphasized the complexity of AMR as a global issue. “The problem isn’t solely due to human antibiotic use; it also stems from veterinary medicine, plant breeding, and animal husbandry. This is a multifactorial, worldwide issue that requires public awareness. Improved vaccination strategies are one way to address AMR, particularly in this post-COVID era of heightened skepticism toward vaccines,” he explained.
Marie-Lise Verschelden from Pfizer highlighted the need for cooperation across the healthcare sector. “Belgium is fortunate to have a fantastic ecosystem of academics, clinicians, and industry experts. Collaboration, including government involvement, is critical to advancing our efforts. At Pfizer, we continue to develop new vaccines and technologies, and the COVID crisis has reinforced the critical role of vaccination in combating AMR. Through our vaccine portfolio and ongoing developments, we are well-positioned to contribute significantly to this global challenge.”
Elisabeth Van Damme from GSK reiterated that AMR is a global issue requiring joint efforts. “Existing vaccines are underutilized. Vaccination protects against certain infectious diseases, reducing the need for antibiotics. Antibiotics, in turn, are sometimes prescribed incorrectly, especially for viral infections they cannot treat. At GSK, we are already developing new vaccines to meet future needs.”
Vaccination remains a cornerstone in the fight against AMR. As pathogens grow increasingly resistant to antibiotics, coordinated efforts and innovative vaccine development are essential to mitigating this global health crisis.
This story was translated and adapted from MediQuality using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Antimicrobial resistance (AMR) is globally recognized as one of the greatest health threats of the 21st century, responsible for 1.27 million deaths annually. “According to the WHO, if no measures are taken promptly, AMR could lead to more deaths than cancer by 2050,” Arnaud Marchant, MD, PhD, director of the European Plotkin Institute for Vaccinology at Université libre de Bruxelles (EPIV-ULB), Anderlecht, Belgium, said in an interview with MediQuality, part of the Medscape Professional Network. “This is a huge problem, and vaccination could be part of the solution.”
EPIV-ULB marked the start of the World AMR Awareness Week (November 18-24) with an event highlighting the critical role of vaccination to counter the rise for resistant pathogens. During the event, MediQuality interviewed Marchant, along with several other experts in the field.
Antibiotics Losing Effectiveness
Marc Van Ranst, PhD, virologist at Rega Institute KU Leuven in Leuven, Belgium, echoed Marchant’s concerns. He noted that “an increasing number of bacteria are becoming resistant to more antibiotics.” “While antibiotics were once miracle drugs, they have now stopped — or almost stopped — working against certain bacteria. Although we are discovering more effective therapies, bacterial infections are increasingly likely to worsen due to AMR.”
Van Ranst issued a stark warning: “If this trend continues, it is entirely reasonable to predict that in 25 years, some antibiotics will become useless, certain bacterial infections will be much harder to treat, and deaths will outnumber those caused by cancer. It’s worth noting, however, that as cancer treatments improve, cancer-related deaths are expected to decline, further highlighting the growing burden of AMR-related fatalities.”
Viruses, Vaccines, and Resistance
Van Ranst emphasized that while AMR primarily involves bacteria, viral infections and vaccination against them also play a role in addressing the issue. “When vaccines prevent illness, they reduce the need for unnecessary antibiotic use. In the past, antibiotics were frequently prescribed for respiratory infections — typically caused by viruses — leading to misuse and heightened resistance. By preventing viral infections through vaccines, we reduce inappropriate antibiotic prescriptions and, subsequently, AMR.”
Strategic Areas of Focus
To maximize the impact of vaccination in combating AMR, Belgium must prioritize several strategic areas, according to EPIV-ULB. “Expanding vaccination coverage for recommended vaccines is crucial to effectively preventing the spread of resistant pathogens,” said Marchant.
“Innovation and development of new vaccines are also essential, including targeted research into vaccines for infections that are currently unavoidable through other means. Enhancing epidemiological surveillance through national data collection and analysis will further clarify the impact of vaccines on AMR and inform policy decisions.”
EPIV-ULB underscored the importance of educating the public and healthcare professionals. “Public awareness is essential to addressing vaccine hesitancy by providing clear information on the importance of prevention,” Marchant explained. “Healthcare professional training must also improve, encouraging preventive practices and judicious antibiotic use. Furthermore, additional research is necessary to fill data gaps and develop predictive models that can guide vaccine development in the future.”
Role of Vaccination
According to EPIV-ULB, Belgium needs a strengthened national strategy to address AMR effectively. “Complementary solutions are increasingly important as antimicrobials lose efficacy and treatments become more complex,” Marchant said. “Vaccination offers a proactive and effective preventive solution, directly and indirectly reducing the spread of resistant pathogens.”
Vaccines combat AMR through various mechanisms. “They prevent diseases such as pneumococcal pneumonia and meningitis, reducing the need for antibiotics to treat these infections,” Marchant explained. “Additionally, vaccination lowers inappropriate antibiotic use by preventing viral infections, reducing the risk of overprescribing antibiotics in cases where they are unnecessary. Lastly, herd immunity from vaccination slows the circulation of resistant pathogens, limiting their spread.”
Van Ranst urged healthcare professionals to prioritize vaccinating at-risk populations as identified by Belgium’s Superior Health Council. These include the elderly with underlying conditions and pregnant women, especially for influenza vaccines. University Hospitals Leuven in Belgium, also conducts annual vaccination campaigns for its staff, combining flu and COVID vaccines to increase uptake.
A Global Challenge
Marc Noppen, MD, PhD, director of University Hospital Brussels, Belgium, emphasized the complexity of AMR as a global issue. “The problem isn’t solely due to human antibiotic use; it also stems from veterinary medicine, plant breeding, and animal husbandry. This is a multifactorial, worldwide issue that requires public awareness. Improved vaccination strategies are one way to address AMR, particularly in this post-COVID era of heightened skepticism toward vaccines,” he explained.
Marie-Lise Verschelden from Pfizer highlighted the need for cooperation across the healthcare sector. “Belgium is fortunate to have a fantastic ecosystem of academics, clinicians, and industry experts. Collaboration, including government involvement, is critical to advancing our efforts. At Pfizer, we continue to develop new vaccines and technologies, and the COVID crisis has reinforced the critical role of vaccination in combating AMR. Through our vaccine portfolio and ongoing developments, we are well-positioned to contribute significantly to this global challenge.”
Elisabeth Van Damme from GSK reiterated that AMR is a global issue requiring joint efforts. “Existing vaccines are underutilized. Vaccination protects against certain infectious diseases, reducing the need for antibiotics. Antibiotics, in turn, are sometimes prescribed incorrectly, especially for viral infections they cannot treat. At GSK, we are already developing new vaccines to meet future needs.”
Vaccination remains a cornerstone in the fight against AMR. As pathogens grow increasingly resistant to antibiotics, coordinated efforts and innovative vaccine development are essential to mitigating this global health crisis.
This story was translated and adapted from MediQuality using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Watch That Attitude: Is There Ageism in Healthcare?
People are living longer in Europe. Life expectancy increased on the continent by around 12 years between 1960 and 2022. And despite slower progress during the COVID-19 pandemic, the trend appears to be continuing.
Not only are Europeans living longer, their fertility rates are declining. This means that the number of people aged 75-84 years is projected to grow in Europe a full 56.1% by 2050, while the population younger than 55 years is expected to fall by 13.5%.
This means that attitudes toward age need to change, and fast — even among healthcare professionals.
Healthcare Is Not Exempt From Ageist Attitudes
A systematic review published in the journal PLOS ONE in 2020 found that age was a determinant factor in dictating who received certain medical procedures or treatments. For example, a study of 9105 hospitalized patients found that healthcare providers were significantly more likely to withhold life-sustaining treatments from older patients. Another study found evidence that older people are excluded from clinical trials, even when the trials are for diseases that appear later in life, like Parkinson’s.
“In healthcare, there are different levels of ageism,” explained Hannah Swift, PhD, reader in social and organizational psychology at the University of Kent in the United Kingdom.
Ageism is embedded in the laws, rules, and practices of institutions, she explained. This became especially obvious during the pandemic, when health professionals had to decide who to treat, possibly using age as a proxy for making some of these decisions, she said.
“When you categorize people, you might be using stereotypes, assumptions, and expectations about age and that age group to make those decisions, and that’s where errors can occur.”
She added that ageist attitudes also become apparent at the interpersonal level by using patronizing language or offering unnecessary help to older people based on assumptions about their cognitive and physical abilities.
“Older age is often wrongly associated with declining levels of health and activity,” said Ittay Mannheim, PhD, guest postdoctoral researcher on aging and ageism at the Open University of the Netherlands. “However, older adults are a very diverse group, varying widely in many aspects, including health conditions. This stereotype can influence how healthcare professionals interact with them, assuming frailty or memory issues simply based on age. It’s important to recognize that being older doesn’t necessarily mean being ill.”
Mannheim’s research found that healthcare professionals often stand in the way of older people using technology-based treatments due to negative attitudes towards age. “So, actually, a barrier to using these technologies could be that healthcare professionals don’t think that someone can use it or won’t even offer it because someone looks old or is old,” he said.
The Impacts
Discrimination impacts the physical, mental, and social well-being of its victims. This includes attitudes towards age.
The PLOS ONE review of research on the global reach of ageism found that experienced or self-determined ageism was associated with significantly worse health outcomes across all countries examined. The same research team calculated that an estimated 6.3 million cases of depression worldwide are linked to ageism.
Other research has found that exposure to negative age stereotyping impacts willingness to adopt a healthy lifestyle in addition to increasing the risk for cardiovascular events.
What Can Be Done?
“Healthcare professionals frequently interact with older adults at their most vulnerable, which can reinforce negative stereotypes of older people being vulnerable or ill,” said Swift. “However, not all older adults fit these stereotypes. Many can live well and independently. Perhaps healthcare education should include reminders of the diverse experiences of older individuals rather than solely focusing on the moments when they require help.”
Research indicates that although progress has been made in geriatric training and the care of older individuals by healthcare education institutions, improved education and training are still needed at all levels of geriatric healthcare, including hospital administrators, physicians, nurses, personal caregivers, and associated health professions.
“Generally speaking, what healthcare professionals learn about aging tends to focus more on the biological aspects,” said Mannheim. “However, they may not fully understand what it means to be old or how to interact with older individuals, especially regarding technology. It is important to raise awareness about ageism because, in my experience working with healthcare professionals, even a single workshop on ageism can have a profound impact. Participants often respond with surprise, saying something like, ‘Wow, I never thought about this before.’”
Mannheim said that training healthcare providers to understand the aging process better could help to reduce any biases they might have and better prepare them to respond more adequately to the needs of older patients.
“We cannot devalue the lives of older people simply because they are older. It is crucial for all of us, especially governments, to acknowledge our responsibility to protect and promote human rights for individuals of all ages. If we fail to do this, the strategies we’ve witnessed during this pandemic will be repeated in the future,” said Nena Georgantzi, PhD, Barcelona-based human rights manager at AGE Platform Europe, an EU network of organizations of and for older people.
A version of this article appeared on Medscape.com.
People are living longer in Europe. Life expectancy increased on the continent by around 12 years between 1960 and 2022. And despite slower progress during the COVID-19 pandemic, the trend appears to be continuing.
Not only are Europeans living longer, their fertility rates are declining. This means that the number of people aged 75-84 years is projected to grow in Europe a full 56.1% by 2050, while the population younger than 55 years is expected to fall by 13.5%.
This means that attitudes toward age need to change, and fast — even among healthcare professionals.
Healthcare Is Not Exempt From Ageist Attitudes
A systematic review published in the journal PLOS ONE in 2020 found that age was a determinant factor in dictating who received certain medical procedures or treatments. For example, a study of 9105 hospitalized patients found that healthcare providers were significantly more likely to withhold life-sustaining treatments from older patients. Another study found evidence that older people are excluded from clinical trials, even when the trials are for diseases that appear later in life, like Parkinson’s.
“In healthcare, there are different levels of ageism,” explained Hannah Swift, PhD, reader in social and organizational psychology at the University of Kent in the United Kingdom.
Ageism is embedded in the laws, rules, and practices of institutions, she explained. This became especially obvious during the pandemic, when health professionals had to decide who to treat, possibly using age as a proxy for making some of these decisions, she said.
“When you categorize people, you might be using stereotypes, assumptions, and expectations about age and that age group to make those decisions, and that’s where errors can occur.”
She added that ageist attitudes also become apparent at the interpersonal level by using patronizing language or offering unnecessary help to older people based on assumptions about their cognitive and physical abilities.
“Older age is often wrongly associated with declining levels of health and activity,” said Ittay Mannheim, PhD, guest postdoctoral researcher on aging and ageism at the Open University of the Netherlands. “However, older adults are a very diverse group, varying widely in many aspects, including health conditions. This stereotype can influence how healthcare professionals interact with them, assuming frailty or memory issues simply based on age. It’s important to recognize that being older doesn’t necessarily mean being ill.”
Mannheim’s research found that healthcare professionals often stand in the way of older people using technology-based treatments due to negative attitudes towards age. “So, actually, a barrier to using these technologies could be that healthcare professionals don’t think that someone can use it or won’t even offer it because someone looks old or is old,” he said.
The Impacts
Discrimination impacts the physical, mental, and social well-being of its victims. This includes attitudes towards age.
The PLOS ONE review of research on the global reach of ageism found that experienced or self-determined ageism was associated with significantly worse health outcomes across all countries examined. The same research team calculated that an estimated 6.3 million cases of depression worldwide are linked to ageism.
Other research has found that exposure to negative age stereotyping impacts willingness to adopt a healthy lifestyle in addition to increasing the risk for cardiovascular events.
What Can Be Done?
“Healthcare professionals frequently interact with older adults at their most vulnerable, which can reinforce negative stereotypes of older people being vulnerable or ill,” said Swift. “However, not all older adults fit these stereotypes. Many can live well and independently. Perhaps healthcare education should include reminders of the diverse experiences of older individuals rather than solely focusing on the moments when they require help.”
Research indicates that although progress has been made in geriatric training and the care of older individuals by healthcare education institutions, improved education and training are still needed at all levels of geriatric healthcare, including hospital administrators, physicians, nurses, personal caregivers, and associated health professions.
“Generally speaking, what healthcare professionals learn about aging tends to focus more on the biological aspects,” said Mannheim. “However, they may not fully understand what it means to be old or how to interact with older individuals, especially regarding technology. It is important to raise awareness about ageism because, in my experience working with healthcare professionals, even a single workshop on ageism can have a profound impact. Participants often respond with surprise, saying something like, ‘Wow, I never thought about this before.’”
Mannheim said that training healthcare providers to understand the aging process better could help to reduce any biases they might have and better prepare them to respond more adequately to the needs of older patients.
“We cannot devalue the lives of older people simply because they are older. It is crucial for all of us, especially governments, to acknowledge our responsibility to protect and promote human rights for individuals of all ages. If we fail to do this, the strategies we’ve witnessed during this pandemic will be repeated in the future,” said Nena Georgantzi, PhD, Barcelona-based human rights manager at AGE Platform Europe, an EU network of organizations of and for older people.
A version of this article appeared on Medscape.com.
People are living longer in Europe. Life expectancy increased on the continent by around 12 years between 1960 and 2022. And despite slower progress during the COVID-19 pandemic, the trend appears to be continuing.
Not only are Europeans living longer, their fertility rates are declining. This means that the number of people aged 75-84 years is projected to grow in Europe a full 56.1% by 2050, while the population younger than 55 years is expected to fall by 13.5%.
This means that attitudes toward age need to change, and fast — even among healthcare professionals.
Healthcare Is Not Exempt From Ageist Attitudes
A systematic review published in the journal PLOS ONE in 2020 found that age was a determinant factor in dictating who received certain medical procedures or treatments. For example, a study of 9105 hospitalized patients found that healthcare providers were significantly more likely to withhold life-sustaining treatments from older patients. Another study found evidence that older people are excluded from clinical trials, even when the trials are for diseases that appear later in life, like Parkinson’s.
“In healthcare, there are different levels of ageism,” explained Hannah Swift, PhD, reader in social and organizational psychology at the University of Kent in the United Kingdom.
Ageism is embedded in the laws, rules, and practices of institutions, she explained. This became especially obvious during the pandemic, when health professionals had to decide who to treat, possibly using age as a proxy for making some of these decisions, she said.
“When you categorize people, you might be using stereotypes, assumptions, and expectations about age and that age group to make those decisions, and that’s where errors can occur.”
She added that ageist attitudes also become apparent at the interpersonal level by using patronizing language or offering unnecessary help to older people based on assumptions about their cognitive and physical abilities.
“Older age is often wrongly associated with declining levels of health and activity,” said Ittay Mannheim, PhD, guest postdoctoral researcher on aging and ageism at the Open University of the Netherlands. “However, older adults are a very diverse group, varying widely in many aspects, including health conditions. This stereotype can influence how healthcare professionals interact with them, assuming frailty or memory issues simply based on age. It’s important to recognize that being older doesn’t necessarily mean being ill.”
Mannheim’s research found that healthcare professionals often stand in the way of older people using technology-based treatments due to negative attitudes towards age. “So, actually, a barrier to using these technologies could be that healthcare professionals don’t think that someone can use it or won’t even offer it because someone looks old or is old,” he said.
The Impacts
Discrimination impacts the physical, mental, and social well-being of its victims. This includes attitudes towards age.
The PLOS ONE review of research on the global reach of ageism found that experienced or self-determined ageism was associated with significantly worse health outcomes across all countries examined. The same research team calculated that an estimated 6.3 million cases of depression worldwide are linked to ageism.
Other research has found that exposure to negative age stereotyping impacts willingness to adopt a healthy lifestyle in addition to increasing the risk for cardiovascular events.
What Can Be Done?
“Healthcare professionals frequently interact with older adults at their most vulnerable, which can reinforce negative stereotypes of older people being vulnerable or ill,” said Swift. “However, not all older adults fit these stereotypes. Many can live well and independently. Perhaps healthcare education should include reminders of the diverse experiences of older individuals rather than solely focusing on the moments when they require help.”
Research indicates that although progress has been made in geriatric training and the care of older individuals by healthcare education institutions, improved education and training are still needed at all levels of geriatric healthcare, including hospital administrators, physicians, nurses, personal caregivers, and associated health professions.
“Generally speaking, what healthcare professionals learn about aging tends to focus more on the biological aspects,” said Mannheim. “However, they may not fully understand what it means to be old or how to interact with older individuals, especially regarding technology. It is important to raise awareness about ageism because, in my experience working with healthcare professionals, even a single workshop on ageism can have a profound impact. Participants often respond with surprise, saying something like, ‘Wow, I never thought about this before.’”
Mannheim said that training healthcare providers to understand the aging process better could help to reduce any biases they might have and better prepare them to respond more adequately to the needs of older patients.
“We cannot devalue the lives of older people simply because they are older. It is crucial for all of us, especially governments, to acknowledge our responsibility to protect and promote human rights for individuals of all ages. If we fail to do this, the strategies we’ve witnessed during this pandemic will be repeated in the future,” said Nena Georgantzi, PhD, Barcelona-based human rights manager at AGE Platform Europe, an EU network of organizations of and for older people.
A version of this article appeared on Medscape.com.
Study Finds Different Survival Rates for Hidradenitis Suppurativa Treatments in Children
results from a small single-center study showed.
A previous study found that overall drug survival of adalimumab and infliximab in adults with HS at 12 and 24 months was 56.3% and 30.5%, and 58.3% and 48.6%, respectively. “They also found that older age, longer disease duration, higher body mass index (BMI), and surgery during treatment are associated with increased drug survival,” Robyn Guo, a third-year medical student at Duke University, Durham, North Carolina, told this news organization following the annual Symposium on Hidradenitis Suppurativa Advances, where the study was presented during an oral abstract session. “To our knowledge, the drug survival of biologic therapies in pediatric HS patients has not been previously investigated.”
Adalimumab and infliximab are tumor necrosis factor blockers approved for multiple indications; adalimumab is approved for treating moderate to severe HS in patients aged 12 years or older. Infliximab is not approved for HS but is used to treat the disease.
To determine the drug survival of adalimumab and infliximab in pediatric patients with HS and whether patient comorbidities and HS lesion location are associated with length of biologic survival in pediatric patients with HS, Guo and colleagues used Kaplan-Meier survival curves to calculate biologic survival at 12 and 24 months following biologic initiation and Cox proportional hazards regression to analyze potential factors associated with biologic survival. The study population included 49 pediatric patients in the adalimumab cohort and 11 in the infliximab cohort.
The researchers found that drug survival for adalimumab was 90.6% at 12 months (95% CI, 83.0%-98.8%) and 78.3% at 24 months (95% CI, 67.7%-90.6%), while drug survival for infliximab was 54.5% at 12 months (95% CI, 31.8%-93.6%) and 36.4% at 24 months, an overall difference that reached statistical significance (P = .0009). “Our data suggests that adalimumab survival is significantly higher than infliximab survival in pediatric HS patients,” Guo said.
On univariate Cox regression analysis, gluteal HS lesions were associated with shorter adalimumab survival, and obesity was associated with longer infliximab survival.
The researchers acknowledged certain limitations of their study, including the small sample size and that unadjusted Cox regression analysis did not account for baseline HS severity, biologic therapy dosing, and concomitant medication use. Also, there were patients in both cohorts who were not biologic-naive: Two in the adalimumab cohort were previously treated with infliximab, and five patients in the infliximab cohort were previously treated with adalimumab.
“We plan on conducting further analysis using adjusted Cox regression analysis to account for baseline disease severity measured by Hurley stage, BMI, medication dosing, and concomitant medication use,” Guo said.
The researchers reported having no financial disclosures.
A version of this article appeared on Medscape.com.
results from a small single-center study showed.
A previous study found that overall drug survival of adalimumab and infliximab in adults with HS at 12 and 24 months was 56.3% and 30.5%, and 58.3% and 48.6%, respectively. “They also found that older age, longer disease duration, higher body mass index (BMI), and surgery during treatment are associated with increased drug survival,” Robyn Guo, a third-year medical student at Duke University, Durham, North Carolina, told this news organization following the annual Symposium on Hidradenitis Suppurativa Advances, where the study was presented during an oral abstract session. “To our knowledge, the drug survival of biologic therapies in pediatric HS patients has not been previously investigated.”
Adalimumab and infliximab are tumor necrosis factor blockers approved for multiple indications; adalimumab is approved for treating moderate to severe HS in patients aged 12 years or older. Infliximab is not approved for HS but is used to treat the disease.
To determine the drug survival of adalimumab and infliximab in pediatric patients with HS and whether patient comorbidities and HS lesion location are associated with length of biologic survival in pediatric patients with HS, Guo and colleagues used Kaplan-Meier survival curves to calculate biologic survival at 12 and 24 months following biologic initiation and Cox proportional hazards regression to analyze potential factors associated with biologic survival. The study population included 49 pediatric patients in the adalimumab cohort and 11 in the infliximab cohort.
The researchers found that drug survival for adalimumab was 90.6% at 12 months (95% CI, 83.0%-98.8%) and 78.3% at 24 months (95% CI, 67.7%-90.6%), while drug survival for infliximab was 54.5% at 12 months (95% CI, 31.8%-93.6%) and 36.4% at 24 months, an overall difference that reached statistical significance (P = .0009). “Our data suggests that adalimumab survival is significantly higher than infliximab survival in pediatric HS patients,” Guo said.
On univariate Cox regression analysis, gluteal HS lesions were associated with shorter adalimumab survival, and obesity was associated with longer infliximab survival.
The researchers acknowledged certain limitations of their study, including the small sample size and that unadjusted Cox regression analysis did not account for baseline HS severity, biologic therapy dosing, and concomitant medication use. Also, there were patients in both cohorts who were not biologic-naive: Two in the adalimumab cohort were previously treated with infliximab, and five patients in the infliximab cohort were previously treated with adalimumab.
“We plan on conducting further analysis using adjusted Cox regression analysis to account for baseline disease severity measured by Hurley stage, BMI, medication dosing, and concomitant medication use,” Guo said.
The researchers reported having no financial disclosures.
A version of this article appeared on Medscape.com.
results from a small single-center study showed.
A previous study found that overall drug survival of adalimumab and infliximab in adults with HS at 12 and 24 months was 56.3% and 30.5%, and 58.3% and 48.6%, respectively. “They also found that older age, longer disease duration, higher body mass index (BMI), and surgery during treatment are associated with increased drug survival,” Robyn Guo, a third-year medical student at Duke University, Durham, North Carolina, told this news organization following the annual Symposium on Hidradenitis Suppurativa Advances, where the study was presented during an oral abstract session. “To our knowledge, the drug survival of biologic therapies in pediatric HS patients has not been previously investigated.”
Adalimumab and infliximab are tumor necrosis factor blockers approved for multiple indications; adalimumab is approved for treating moderate to severe HS in patients aged 12 years or older. Infliximab is not approved for HS but is used to treat the disease.
To determine the drug survival of adalimumab and infliximab in pediatric patients with HS and whether patient comorbidities and HS lesion location are associated with length of biologic survival in pediatric patients with HS, Guo and colleagues used Kaplan-Meier survival curves to calculate biologic survival at 12 and 24 months following biologic initiation and Cox proportional hazards regression to analyze potential factors associated with biologic survival. The study population included 49 pediatric patients in the adalimumab cohort and 11 in the infliximab cohort.
The researchers found that drug survival for adalimumab was 90.6% at 12 months (95% CI, 83.0%-98.8%) and 78.3% at 24 months (95% CI, 67.7%-90.6%), while drug survival for infliximab was 54.5% at 12 months (95% CI, 31.8%-93.6%) and 36.4% at 24 months, an overall difference that reached statistical significance (P = .0009). “Our data suggests that adalimumab survival is significantly higher than infliximab survival in pediatric HS patients,” Guo said.
On univariate Cox regression analysis, gluteal HS lesions were associated with shorter adalimumab survival, and obesity was associated with longer infliximab survival.
The researchers acknowledged certain limitations of their study, including the small sample size and that unadjusted Cox regression analysis did not account for baseline HS severity, biologic therapy dosing, and concomitant medication use. Also, there were patients in both cohorts who were not biologic-naive: Two in the adalimumab cohort were previously treated with infliximab, and five patients in the infliximab cohort were previously treated with adalimumab.
“We plan on conducting further analysis using adjusted Cox regression analysis to account for baseline disease severity measured by Hurley stage, BMI, medication dosing, and concomitant medication use,” Guo said.
The researchers reported having no financial disclosures.
A version of this article appeared on Medscape.com.
FROM SDPA 24
Varicella Outbreaks: 2022-2024
Practitioners providing care to children are familiar with the childhood immunization schedule and routinely administer varicella vaccine at the 12-month and 4- to 5-year visits. However, when is the last time most of us or any of the current trainees have seen a case?
Briefly, varicella is a highly contagious disease caused by varicella-zoster virus (VZV). It is characterized by a generalized pruritic erythematous rash in various stages of development beginning as macules, progressing to papules, and ultimately becoming vesicular lesions on an erythematous base (“dewdrop on a rose petal”) and resolves with crusting of the lesion (Figure 1). It has an incubation period of 10-21 days with symptoms usually developing within 14-16 days after exposure. The vesicular rash must be differentiated from enterovirus, Staphylococcus aureus, contact dermatitis, or insect bites, which initially may be difficult. Approximately 50% of children can have symptoms including fever, malaise, anorexia, headache, and occasionally, mild abdominal pain in the 24-48 hours prior to the appearance of rash. Lesions usually first appear on the scalp, face, or trunk in successive crops over several days. A person with varicella has lesions in various stages.
In a normal host, new vesicle formation usually stops within 4 days, and most lesions have fully crusted by day 6. VZV establishes latency in sensory ganglia and may reactivate years or decades later to cause herpes zoster (HZ). Most healthy children with varicella recover without sequelae so the disease is generally regarded as benign. However, varicella can lead to serious complications and deaths in healthy as well as immunocompromised persons.
Complications of Varicella: bacterial superinfection of skin lesions most often with Streptococcus pyogenes or S aureus manifested as cellulitis, myositis, or necrotizing fasciitis; neurologic complications include cerebellar ataxia and encephalitis with the latter seen most often in adults. Pneumonia occurs most often in adults, especially those infected during pregnancy. Another concern, infection during the first 20 weeks of pregnancy can lead to fetal death or severe birth defects, including limb hypoplasia, cutaneous scarring, ocular abnormalities, and central nervous system damage (congenital varicella syndrome).
The risk for development of severe disseminated disease was first noted in the 1960s as treatments for leukemia in children improved. They were surviving their cancer only to develop severe and often fatal varicella. Today it is recognized that development of disseminated disease is a risk for all infected persons with impaired T cell function, malignancies, HIV, or receiving immunosuppressive therapy.
Reye’s syndrome is rarely seen today since taking salicylates while infected with VZV was identified as a predisposing factor for development.
VZV is only found in humans and transmission is person to person or airborne. The secondary household attack rate is approximately 90%. In contrast, the secondary attack rates in classrooms may be as low as 12%-33%. Transmission rates in the tropics for unexplained reasons are also lower.
Vaccine History: Why do we rarely see this disease anymore? Varicella, a live attenuated vaccine, was developed in 1974 by Dr. Michiaki Takahashi. It remains the only vaccine directed against a herpes group virus. In 1979, the Collaborative Varicella Vaccine Study Group was established at the National Institutes of Health (NIH) and additional safety and efficacy trials were conducted in the United States initially in leukemic patients in remission and later in healthy children, which supported Takahashi’s data. Licensure of varicella vaccine was granted in 1995. That same year, due to continuing disease and societal burden, the United States was the first country to incorporate varicella into the routine childhood immunization schedule, which resulted in significant reductions in cases. To further improve control of varicella, in 2007 vaccine recommendations were revised and a routine two-dose schedule was implemented. The impact of varicella disease pre- and post-vaccine licensure is illustrated in Figure 2. Not listed, is that in the pre-vaccine era, there were approximately 44 cases of congenital varicella syndrome annually.
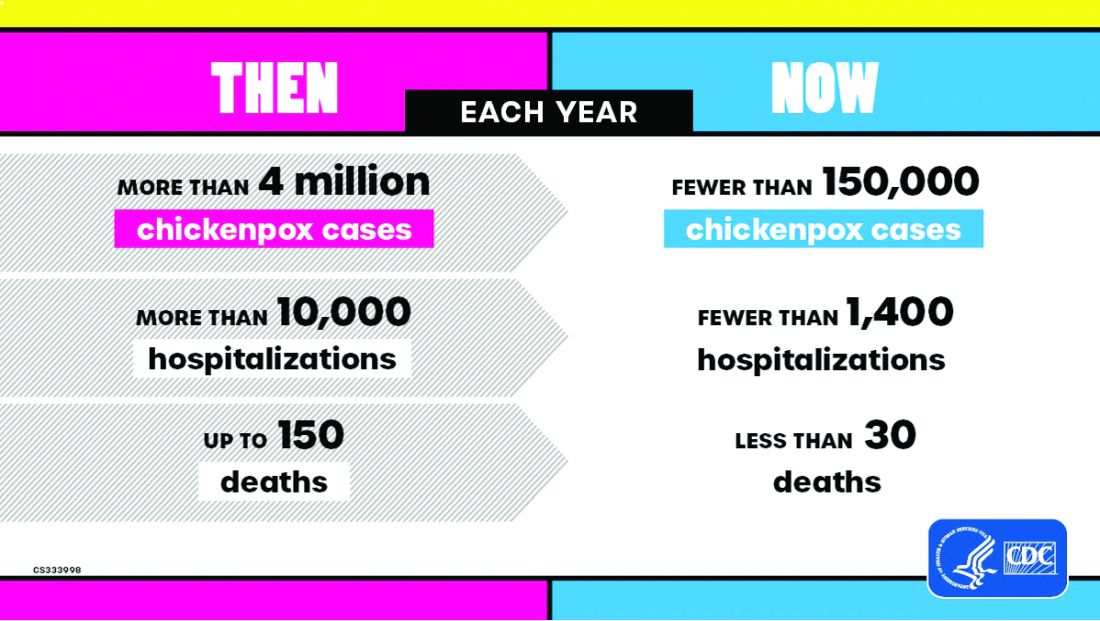
As of 2023 only 23% (45/195) of nations routinely administer this vaccine and 4% (8/195) have restricted recommendations. The remaining 73% of countries do not offer the vaccine, including all countries on the African continent, and Cuba, Guatemala, Haiti, Honduras, India, Jordan, Lebanon, Philippines, Portugal, and Venezuela to list a few.
Varicella Outbreak: In October 2022, New York City (NYC) identified a varicella outbreak primarily involving persons who recently migrated from Central and South America and lived in a shelter in NYC or residential facility (n = 105); the outbreak is ongoing. As of March 8, 2024, 873 cases (53%) were among children aged 4-18 years and 91.9% had no documentation of varicella vaccine at time of symptom onset. There were 28 hospitalizations, and no deaths reported. The most common sources of transmission were the residential facilities (41.3%) and importation or possible importation (39.4%). School transmission accounted for only 1.2% of cases.
Most migrants arrived from countries where varicella vaccination is not part of the routine childhood immunization schedule. Although most cases occurred in children, almost 30% occurred in adults. Many of the migrants arrived from tropical countries where susceptibility rates are also higher in adults. This outbreak is a reminder of the importance of limiting disease transmission by maintaining high vaccination rates. To curtail this outbreak, approximately 27,000 doses of varicella vaccine were administered to the arriving migrants. In addition, MMR, COVID-19, influenza, and all routine pediatric vaccines required for school entry were administered. Temporary closure of the residential facilities were required. Education was provided to residents regarding immunizations as well as assistance to help them establish a primary care home. Multiple agencies were mobilized to successfully coordinate these efforts.
Take Home Message
1. Each country has its own routine immunization schedule. It may not include all vaccines recommended in the US schedule. When questioned I’m frequently told that immunizations are up to date, only to review records and find they are not, especially when it is related to MMR. It is often administered at 9 months and/or MR or MM is administered depending on the country. As reported here, varicella is a routine vaccine in only 45 countries.
2.
3. Once an outbreak has been identified, the infrastructure to manage and contain it must already be established. In most instances there will be a need for a rapid and often large-scale effort involving multiple agencies including local health care providers.
4. Not all diseases are reportable. Only deaths by varicella are nationally notifiable. Otherwise, cases are reported voluntarily. As of November 2, 2024, there have been 5,157 cases of varicella reported, excluding any cases from NYC.
Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
Suggested Reading
CDC. Nationally Notifiable Infectious Diseases and Conditions, United States: Weekly Tables. https://wonder.cdc.gov/nndss/nndss_weekly_tables_menu.asp.
Graham KA et al. Varicella Outbreak Among Recent Arrivals to New York City, 2022-2024. MMWR Morb Mortal Wkly Rep. 2024 May 30;73(21):478-483. doi: 10.15585/mmwr.mm7321a1.
Marin M et al. Health and Economic Impact of the United States Varicella Vaccination Program, 1996-2020. J Infect Dis. 2022 Oct 21;226(Suppl 4):S463-S469. doi: 10.1093/infdis/jiac271.
Varicella-Zoster Virus Infections in Kimberkin DW et al, eds. Red Book: 2024 Report of the Committee on Infectious Diseases, 33rd Edition. American Academy of Pediatrics, 2024:938-951. https://www.aap.org/Red-Book-2024-Report-of-the-Committee-on-Infectious-Diseases-33rd-Edition-Paperback?srsltid=AfmBOoqyF60rR9ZwQ5jA8AouNhtRRTyPLnc_r7HWw7JVYV8v33Hr2vQS.
Practitioners providing care to children are familiar with the childhood immunization schedule and routinely administer varicella vaccine at the 12-month and 4- to 5-year visits. However, when is the last time most of us or any of the current trainees have seen a case?
Briefly, varicella is a highly contagious disease caused by varicella-zoster virus (VZV). It is characterized by a generalized pruritic erythematous rash in various stages of development beginning as macules, progressing to papules, and ultimately becoming vesicular lesions on an erythematous base (“dewdrop on a rose petal”) and resolves with crusting of the lesion (Figure 1). It has an incubation period of 10-21 days with symptoms usually developing within 14-16 days after exposure. The vesicular rash must be differentiated from enterovirus, Staphylococcus aureus, contact dermatitis, or insect bites, which initially may be difficult. Approximately 50% of children can have symptoms including fever, malaise, anorexia, headache, and occasionally, mild abdominal pain in the 24-48 hours prior to the appearance of rash. Lesions usually first appear on the scalp, face, or trunk in successive crops over several days. A person with varicella has lesions in various stages.
In a normal host, new vesicle formation usually stops within 4 days, and most lesions have fully crusted by day 6. VZV establishes latency in sensory ganglia and may reactivate years or decades later to cause herpes zoster (HZ). Most healthy children with varicella recover without sequelae so the disease is generally regarded as benign. However, varicella can lead to serious complications and deaths in healthy as well as immunocompromised persons.
Complications of Varicella: bacterial superinfection of skin lesions most often with Streptococcus pyogenes or S aureus manifested as cellulitis, myositis, or necrotizing fasciitis; neurologic complications include cerebellar ataxia and encephalitis with the latter seen most often in adults. Pneumonia occurs most often in adults, especially those infected during pregnancy. Another concern, infection during the first 20 weeks of pregnancy can lead to fetal death or severe birth defects, including limb hypoplasia, cutaneous scarring, ocular abnormalities, and central nervous system damage (congenital varicella syndrome).
The risk for development of severe disseminated disease was first noted in the 1960s as treatments for leukemia in children improved. They were surviving their cancer only to develop severe and often fatal varicella. Today it is recognized that development of disseminated disease is a risk for all infected persons with impaired T cell function, malignancies, HIV, or receiving immunosuppressive therapy.
Reye’s syndrome is rarely seen today since taking salicylates while infected with VZV was identified as a predisposing factor for development.
VZV is only found in humans and transmission is person to person or airborne. The secondary household attack rate is approximately 90%. In contrast, the secondary attack rates in classrooms may be as low as 12%-33%. Transmission rates in the tropics for unexplained reasons are also lower.
Vaccine History: Why do we rarely see this disease anymore? Varicella, a live attenuated vaccine, was developed in 1974 by Dr. Michiaki Takahashi. It remains the only vaccine directed against a herpes group virus. In 1979, the Collaborative Varicella Vaccine Study Group was established at the National Institutes of Health (NIH) and additional safety and efficacy trials were conducted in the United States initially in leukemic patients in remission and later in healthy children, which supported Takahashi’s data. Licensure of varicella vaccine was granted in 1995. That same year, due to continuing disease and societal burden, the United States was the first country to incorporate varicella into the routine childhood immunization schedule, which resulted in significant reductions in cases. To further improve control of varicella, in 2007 vaccine recommendations were revised and a routine two-dose schedule was implemented. The impact of varicella disease pre- and post-vaccine licensure is illustrated in Figure 2. Not listed, is that in the pre-vaccine era, there were approximately 44 cases of congenital varicella syndrome annually.
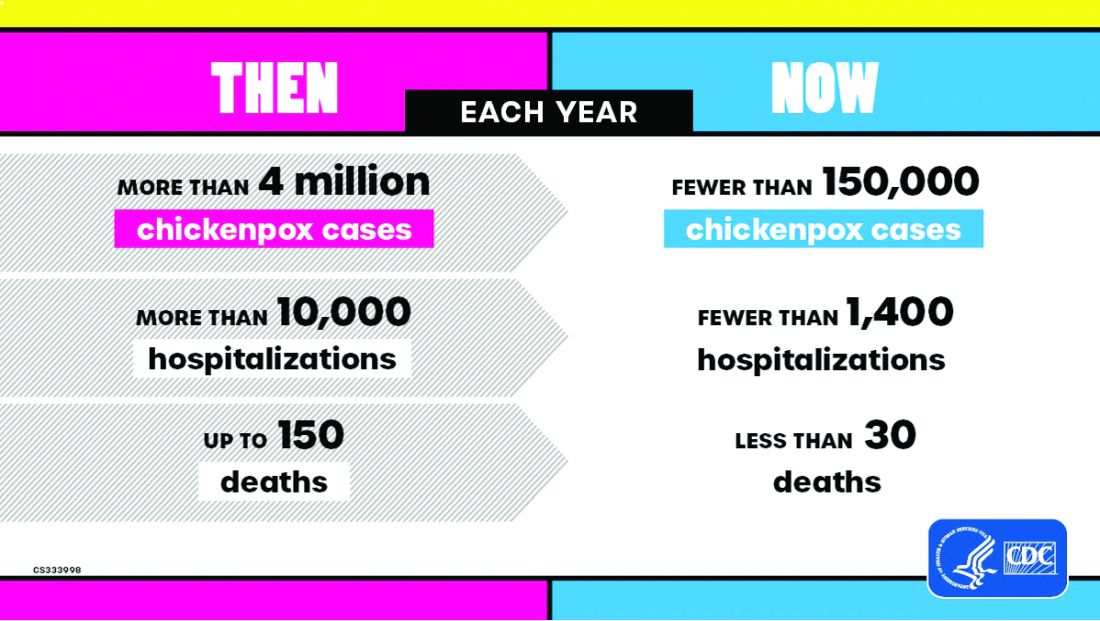
As of 2023 only 23% (45/195) of nations routinely administer this vaccine and 4% (8/195) have restricted recommendations. The remaining 73% of countries do not offer the vaccine, including all countries on the African continent, and Cuba, Guatemala, Haiti, Honduras, India, Jordan, Lebanon, Philippines, Portugal, and Venezuela to list a few.
Varicella Outbreak: In October 2022, New York City (NYC) identified a varicella outbreak primarily involving persons who recently migrated from Central and South America and lived in a shelter in NYC or residential facility (n = 105); the outbreak is ongoing. As of March 8, 2024, 873 cases (53%) were among children aged 4-18 years and 91.9% had no documentation of varicella vaccine at time of symptom onset. There were 28 hospitalizations, and no deaths reported. The most common sources of transmission were the residential facilities (41.3%) and importation or possible importation (39.4%). School transmission accounted for only 1.2% of cases.
Most migrants arrived from countries where varicella vaccination is not part of the routine childhood immunization schedule. Although most cases occurred in children, almost 30% occurred in adults. Many of the migrants arrived from tropical countries where susceptibility rates are also higher in adults. This outbreak is a reminder of the importance of limiting disease transmission by maintaining high vaccination rates. To curtail this outbreak, approximately 27,000 doses of varicella vaccine were administered to the arriving migrants. In addition, MMR, COVID-19, influenza, and all routine pediatric vaccines required for school entry were administered. Temporary closure of the residential facilities were required. Education was provided to residents regarding immunizations as well as assistance to help them establish a primary care home. Multiple agencies were mobilized to successfully coordinate these efforts.
Take Home Message
1. Each country has its own routine immunization schedule. It may not include all vaccines recommended in the US schedule. When questioned I’m frequently told that immunizations are up to date, only to review records and find they are not, especially when it is related to MMR. It is often administered at 9 months and/or MR or MM is administered depending on the country. As reported here, varicella is a routine vaccine in only 45 countries.
2.
3. Once an outbreak has been identified, the infrastructure to manage and contain it must already be established. In most instances there will be a need for a rapid and often large-scale effort involving multiple agencies including local health care providers.
4. Not all diseases are reportable. Only deaths by varicella are nationally notifiable. Otherwise, cases are reported voluntarily. As of November 2, 2024, there have been 5,157 cases of varicella reported, excluding any cases from NYC.
Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
Suggested Reading
CDC. Nationally Notifiable Infectious Diseases and Conditions, United States: Weekly Tables. https://wonder.cdc.gov/nndss/nndss_weekly_tables_menu.asp.
Graham KA et al. Varicella Outbreak Among Recent Arrivals to New York City, 2022-2024. MMWR Morb Mortal Wkly Rep. 2024 May 30;73(21):478-483. doi: 10.15585/mmwr.mm7321a1.
Marin M et al. Health and Economic Impact of the United States Varicella Vaccination Program, 1996-2020. J Infect Dis. 2022 Oct 21;226(Suppl 4):S463-S469. doi: 10.1093/infdis/jiac271.
Varicella-Zoster Virus Infections in Kimberkin DW et al, eds. Red Book: 2024 Report of the Committee on Infectious Diseases, 33rd Edition. American Academy of Pediatrics, 2024:938-951. https://www.aap.org/Red-Book-2024-Report-of-the-Committee-on-Infectious-Diseases-33rd-Edition-Paperback?srsltid=AfmBOoqyF60rR9ZwQ5jA8AouNhtRRTyPLnc_r7HWw7JVYV8v33Hr2vQS.
Practitioners providing care to children are familiar with the childhood immunization schedule and routinely administer varicella vaccine at the 12-month and 4- to 5-year visits. However, when is the last time most of us or any of the current trainees have seen a case?
Briefly, varicella is a highly contagious disease caused by varicella-zoster virus (VZV). It is characterized by a generalized pruritic erythematous rash in various stages of development beginning as macules, progressing to papules, and ultimately becoming vesicular lesions on an erythematous base (“dewdrop on a rose petal”) and resolves with crusting of the lesion (Figure 1). It has an incubation period of 10-21 days with symptoms usually developing within 14-16 days after exposure. The vesicular rash must be differentiated from enterovirus, Staphylococcus aureus, contact dermatitis, or insect bites, which initially may be difficult. Approximately 50% of children can have symptoms including fever, malaise, anorexia, headache, and occasionally, mild abdominal pain in the 24-48 hours prior to the appearance of rash. Lesions usually first appear on the scalp, face, or trunk in successive crops over several days. A person with varicella has lesions in various stages.
In a normal host, new vesicle formation usually stops within 4 days, and most lesions have fully crusted by day 6. VZV establishes latency in sensory ganglia and may reactivate years or decades later to cause herpes zoster (HZ). Most healthy children with varicella recover without sequelae so the disease is generally regarded as benign. However, varicella can lead to serious complications and deaths in healthy as well as immunocompromised persons.
Complications of Varicella: bacterial superinfection of skin lesions most often with Streptococcus pyogenes or S aureus manifested as cellulitis, myositis, or necrotizing fasciitis; neurologic complications include cerebellar ataxia and encephalitis with the latter seen most often in adults. Pneumonia occurs most often in adults, especially those infected during pregnancy. Another concern, infection during the first 20 weeks of pregnancy can lead to fetal death or severe birth defects, including limb hypoplasia, cutaneous scarring, ocular abnormalities, and central nervous system damage (congenital varicella syndrome).
The risk for development of severe disseminated disease was first noted in the 1960s as treatments for leukemia in children improved. They were surviving their cancer only to develop severe and often fatal varicella. Today it is recognized that development of disseminated disease is a risk for all infected persons with impaired T cell function, malignancies, HIV, or receiving immunosuppressive therapy.
Reye’s syndrome is rarely seen today since taking salicylates while infected with VZV was identified as a predisposing factor for development.
VZV is only found in humans and transmission is person to person or airborne. The secondary household attack rate is approximately 90%. In contrast, the secondary attack rates in classrooms may be as low as 12%-33%. Transmission rates in the tropics for unexplained reasons are also lower.
Vaccine History: Why do we rarely see this disease anymore? Varicella, a live attenuated vaccine, was developed in 1974 by Dr. Michiaki Takahashi. It remains the only vaccine directed against a herpes group virus. In 1979, the Collaborative Varicella Vaccine Study Group was established at the National Institutes of Health (NIH) and additional safety and efficacy trials were conducted in the United States initially in leukemic patients in remission and later in healthy children, which supported Takahashi’s data. Licensure of varicella vaccine was granted in 1995. That same year, due to continuing disease and societal burden, the United States was the first country to incorporate varicella into the routine childhood immunization schedule, which resulted in significant reductions in cases. To further improve control of varicella, in 2007 vaccine recommendations were revised and a routine two-dose schedule was implemented. The impact of varicella disease pre- and post-vaccine licensure is illustrated in Figure 2. Not listed, is that in the pre-vaccine era, there were approximately 44 cases of congenital varicella syndrome annually.
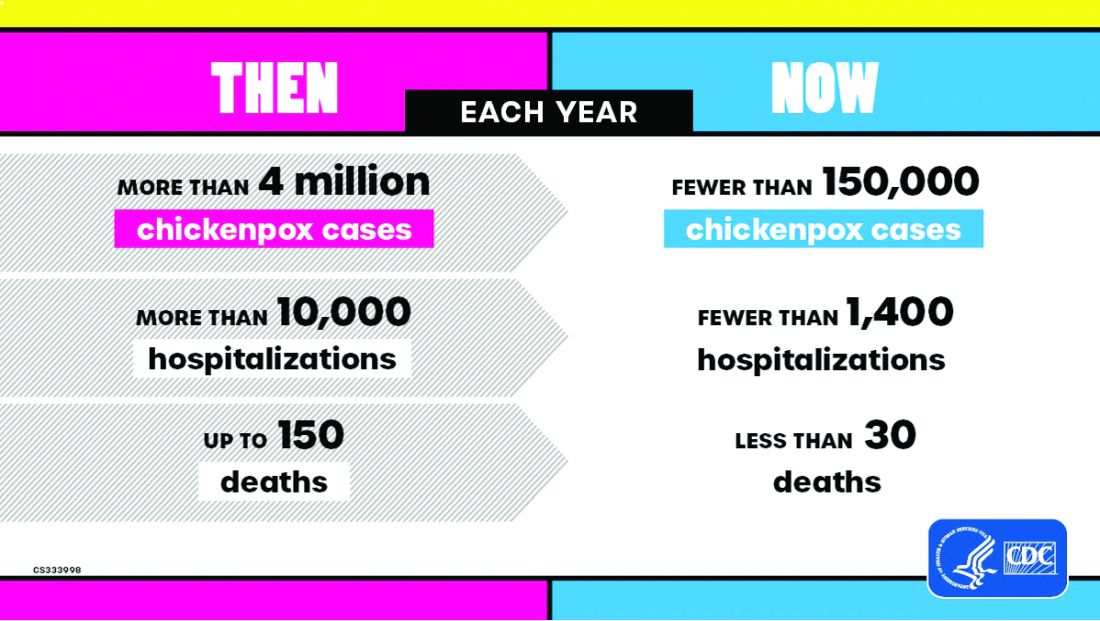
As of 2023 only 23% (45/195) of nations routinely administer this vaccine and 4% (8/195) have restricted recommendations. The remaining 73% of countries do not offer the vaccine, including all countries on the African continent, and Cuba, Guatemala, Haiti, Honduras, India, Jordan, Lebanon, Philippines, Portugal, and Venezuela to list a few.
Varicella Outbreak: In October 2022, New York City (NYC) identified a varicella outbreak primarily involving persons who recently migrated from Central and South America and lived in a shelter in NYC or residential facility (n = 105); the outbreak is ongoing. As of March 8, 2024, 873 cases (53%) were among children aged 4-18 years and 91.9% had no documentation of varicella vaccine at time of symptom onset. There were 28 hospitalizations, and no deaths reported. The most common sources of transmission were the residential facilities (41.3%) and importation or possible importation (39.4%). School transmission accounted for only 1.2% of cases.
Most migrants arrived from countries where varicella vaccination is not part of the routine childhood immunization schedule. Although most cases occurred in children, almost 30% occurred in adults. Many of the migrants arrived from tropical countries where susceptibility rates are also higher in adults. This outbreak is a reminder of the importance of limiting disease transmission by maintaining high vaccination rates. To curtail this outbreak, approximately 27,000 doses of varicella vaccine were administered to the arriving migrants. In addition, MMR, COVID-19, influenza, and all routine pediatric vaccines required for school entry were administered. Temporary closure of the residential facilities were required. Education was provided to residents regarding immunizations as well as assistance to help them establish a primary care home. Multiple agencies were mobilized to successfully coordinate these efforts.
Take Home Message
1. Each country has its own routine immunization schedule. It may not include all vaccines recommended in the US schedule. When questioned I’m frequently told that immunizations are up to date, only to review records and find they are not, especially when it is related to MMR. It is often administered at 9 months and/or MR or MM is administered depending on the country. As reported here, varicella is a routine vaccine in only 45 countries.
2.
3. Once an outbreak has been identified, the infrastructure to manage and contain it must already be established. In most instances there will be a need for a rapid and often large-scale effort involving multiple agencies including local health care providers.
4. Not all diseases are reportable. Only deaths by varicella are nationally notifiable. Otherwise, cases are reported voluntarily. As of November 2, 2024, there have been 5,157 cases of varicella reported, excluding any cases from NYC.
Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
Suggested Reading
CDC. Nationally Notifiable Infectious Diseases and Conditions, United States: Weekly Tables. https://wonder.cdc.gov/nndss/nndss_weekly_tables_menu.asp.
Graham KA et al. Varicella Outbreak Among Recent Arrivals to New York City, 2022-2024. MMWR Morb Mortal Wkly Rep. 2024 May 30;73(21):478-483. doi: 10.15585/mmwr.mm7321a1.
Marin M et al. Health and Economic Impact of the United States Varicella Vaccination Program, 1996-2020. J Infect Dis. 2022 Oct 21;226(Suppl 4):S463-S469. doi: 10.1093/infdis/jiac271.
Varicella-Zoster Virus Infections in Kimberkin DW et al, eds. Red Book: 2024 Report of the Committee on Infectious Diseases, 33rd Edition. American Academy of Pediatrics, 2024:938-951. https://www.aap.org/Red-Book-2024-Report-of-the-Committee-on-Infectious-Diseases-33rd-Edition-Paperback?srsltid=AfmBOoqyF60rR9ZwQ5jA8AouNhtRRTyPLnc_r7HWw7JVYV8v33Hr2vQS.
Exercise or Inactivity?
The answer one gets often depends on how one crafts the question. For example, Jeffrey D. Johnson PhD, a professor of communications at Portland State University in Oregon has found that if patients are asked “Is there something else you would like to address today?” 80% had their unmet questions addressed. However, if the question was worded “Is there anything else ...?” Very few had their unmet concerns addressed.
I recently encountered two studies that provide another striking example of how differently structured questions aimed at same topic can result in dramatically different results. In this case both studies used one database, the UK Biobank cohort study which contains “de-identified genetic, lifestyle, and health information” collected from a half million adults in the UK. A subgroup of nearly 90,000 who had undergone a week long activity measurement using a wrist accelerometer was the focus of both groups of investigators who asked the same broad question “What is the relationship between physical activity and disease?”
The first study I found has already received some publicity in the lay press and dealt with those individuals who, for a variety of reasons, pack all of their exercise into just a few days, usually the weekend, aka weekend warriors. The investigators found that when compared with generally inactive individuals those who were able to achieve activity volumes that met current guidelines were at lower risk for more than 200 diseases, particularly those that were cardiac based. I guess that shouldn’t surprise us. The finding that has received most of the publicity to date in the lay press was that “Associations were similar whether the activity followed a weekend warrior pattern or was spread out evenly through the week.”
The second study, using the same database, found that those individuals who spent more than 10.6 hours per day sitting had 60% an increased risk of heart failure and cardiovascular related death. And, here’s the real news, that risk remained even in people who were otherwise physically active.
I suspect these two groups of investigators, both associated with Harvard-related institutions, knew of each other’s work and would agree that their findings are not incompatible. However, it is interesting that, when presented with the same database, one group chose to focus its attention on the exercise end of the spectrum while the other looked at the effect of inactivity.
I have always tried to include a “healthy” amount of exercise in my day. However, more recently my professional interest has been drawn to the increasing number of studies I read that deal with the risks of inactivity and sedentarism. For example, just in the last 2 years I have written about a study in children that showed that sedentary time is responsible for 70% of the total increase in cholesterol as children advance into young adulthood. Another study in adults found that every 2-hour increase in sedentary behavior was associated with a 12% decrease in the patient’s likelihood of achieving healthy aging.
If I were asked to place relative values on these two studies, I would say that the study highlighting the risk of prolonged sitting is potentially far more relevant to the population at large, which is for the most part sedentary. Of course, while I have no data to support my contention, I see the weekend warrior population as a niche group.
So what are the take-home messages from these two studies? One is for the weekend warrior. “You can take some comfort in the results that support your exercise schedule but don’t feel too comfortable about it if most of the week you are sitting at a desk.”
For the rest of us — It’s beginning to feel like we should be including accelerometers in our regular diagnostic and therapeutic weaponry. Sending home patients with a Holter cardiac monitor has become commonplace. We should be sending more folks home with accelerometers or asking the more affluent to share the data from their smart watches. “You’ve been bragging about your “steps. Show me your sitting time.”
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
The answer one gets often depends on how one crafts the question. For example, Jeffrey D. Johnson PhD, a professor of communications at Portland State University in Oregon has found that if patients are asked “Is there something else you would like to address today?” 80% had their unmet questions addressed. However, if the question was worded “Is there anything else ...?” Very few had their unmet concerns addressed.
I recently encountered two studies that provide another striking example of how differently structured questions aimed at same topic can result in dramatically different results. In this case both studies used one database, the UK Biobank cohort study which contains “de-identified genetic, lifestyle, and health information” collected from a half million adults in the UK. A subgroup of nearly 90,000 who had undergone a week long activity measurement using a wrist accelerometer was the focus of both groups of investigators who asked the same broad question “What is the relationship between physical activity and disease?”
The first study I found has already received some publicity in the lay press and dealt with those individuals who, for a variety of reasons, pack all of their exercise into just a few days, usually the weekend, aka weekend warriors. The investigators found that when compared with generally inactive individuals those who were able to achieve activity volumes that met current guidelines were at lower risk for more than 200 diseases, particularly those that were cardiac based. I guess that shouldn’t surprise us. The finding that has received most of the publicity to date in the lay press was that “Associations were similar whether the activity followed a weekend warrior pattern or was spread out evenly through the week.”
The second study, using the same database, found that those individuals who spent more than 10.6 hours per day sitting had 60% an increased risk of heart failure and cardiovascular related death. And, here’s the real news, that risk remained even in people who were otherwise physically active.
I suspect these two groups of investigators, both associated with Harvard-related institutions, knew of each other’s work and would agree that their findings are not incompatible. However, it is interesting that, when presented with the same database, one group chose to focus its attention on the exercise end of the spectrum while the other looked at the effect of inactivity.
I have always tried to include a “healthy” amount of exercise in my day. However, more recently my professional interest has been drawn to the increasing number of studies I read that deal with the risks of inactivity and sedentarism. For example, just in the last 2 years I have written about a study in children that showed that sedentary time is responsible for 70% of the total increase in cholesterol as children advance into young adulthood. Another study in adults found that every 2-hour increase in sedentary behavior was associated with a 12% decrease in the patient’s likelihood of achieving healthy aging.
If I were asked to place relative values on these two studies, I would say that the study highlighting the risk of prolonged sitting is potentially far more relevant to the population at large, which is for the most part sedentary. Of course, while I have no data to support my contention, I see the weekend warrior population as a niche group.
So what are the take-home messages from these two studies? One is for the weekend warrior. “You can take some comfort in the results that support your exercise schedule but don’t feel too comfortable about it if most of the week you are sitting at a desk.”
For the rest of us — It’s beginning to feel like we should be including accelerometers in our regular diagnostic and therapeutic weaponry. Sending home patients with a Holter cardiac monitor has become commonplace. We should be sending more folks home with accelerometers or asking the more affluent to share the data from their smart watches. “You’ve been bragging about your “steps. Show me your sitting time.”
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
The answer one gets often depends on how one crafts the question. For example, Jeffrey D. Johnson PhD, a professor of communications at Portland State University in Oregon has found that if patients are asked “Is there something else you would like to address today?” 80% had their unmet questions addressed. However, if the question was worded “Is there anything else ...?” Very few had their unmet concerns addressed.
I recently encountered two studies that provide another striking example of how differently structured questions aimed at same topic can result in dramatically different results. In this case both studies used one database, the UK Biobank cohort study which contains “de-identified genetic, lifestyle, and health information” collected from a half million adults in the UK. A subgroup of nearly 90,000 who had undergone a week long activity measurement using a wrist accelerometer was the focus of both groups of investigators who asked the same broad question “What is the relationship between physical activity and disease?”
The first study I found has already received some publicity in the lay press and dealt with those individuals who, for a variety of reasons, pack all of their exercise into just a few days, usually the weekend, aka weekend warriors. The investigators found that when compared with generally inactive individuals those who were able to achieve activity volumes that met current guidelines were at lower risk for more than 200 diseases, particularly those that were cardiac based. I guess that shouldn’t surprise us. The finding that has received most of the publicity to date in the lay press was that “Associations were similar whether the activity followed a weekend warrior pattern or was spread out evenly through the week.”
The second study, using the same database, found that those individuals who spent more than 10.6 hours per day sitting had 60% an increased risk of heart failure and cardiovascular related death. And, here’s the real news, that risk remained even in people who were otherwise physically active.
I suspect these two groups of investigators, both associated with Harvard-related institutions, knew of each other’s work and would agree that their findings are not incompatible. However, it is interesting that, when presented with the same database, one group chose to focus its attention on the exercise end of the spectrum while the other looked at the effect of inactivity.
I have always tried to include a “healthy” amount of exercise in my day. However, more recently my professional interest has been drawn to the increasing number of studies I read that deal with the risks of inactivity and sedentarism. For example, just in the last 2 years I have written about a study in children that showed that sedentary time is responsible for 70% of the total increase in cholesterol as children advance into young adulthood. Another study in adults found that every 2-hour increase in sedentary behavior was associated with a 12% decrease in the patient’s likelihood of achieving healthy aging.
If I were asked to place relative values on these two studies, I would say that the study highlighting the risk of prolonged sitting is potentially far more relevant to the population at large, which is for the most part sedentary. Of course, while I have no data to support my contention, I see the weekend warrior population as a niche group.
So what are the take-home messages from these two studies? One is for the weekend warrior. “You can take some comfort in the results that support your exercise schedule but don’t feel too comfortable about it if most of the week you are sitting at a desk.”
For the rest of us — It’s beginning to feel like we should be including accelerometers in our regular diagnostic and therapeutic weaponry. Sending home patients with a Holter cardiac monitor has become commonplace. We should be sending more folks home with accelerometers or asking the more affluent to share the data from their smart watches. “You’ve been bragging about your “steps. Show me your sitting time.”
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Nodding Off While Feeding an Infant
In a recent survey of 1259 mothers published in the journal Pediatrics, 28% reported they had fallen asleep while feeding their babies, and 83% of those mothers reported that the sleep was unplanned. Although the study sample was small, the investigators found that sociodemographic factors did not increase the odds that a mother would fall asleep while feeding.
These numbers are not surprising, but nonetheless they are concerning because co-sleeping is a known risk factor for sudden unexplained infant death (SUID). Every parent will tell you during the first 6 months of their adventure in parenting they didn’t get enough sleep. In fact some will tell you that sleep deprivation was their chronic state for the child’s first year.
Falling asleep easily at times and places not intended for sleep is the primary symptom of sleep deprivation. SUID is the most tragic event associated with parental sleep deprivation, but it is certainly not the only one. Overtired parents are more likely to be involved in accidents and are more likely to make poor decisions, particularly those regarding how to respond to a crying or misbehaving child.
The investigators found that 24% of mothers who reported that their usual nighttime feeding location was a chair or sofa (14%). Not surprisingly, mothers who fed in chairs were less likely to fall asleep while feeding. Many of these mothers reported that they chose the chair because they thought they would be less likely to fall asleep and/or disturb other family members. One wonders how we should interpret these numbers in light of other research that has found it is “relatively less hazardous to fall asleep with an infant in the adult bed than on a chair or sofa.” Had these chair feeding mothers made the better choice under the circumstances? It would take a much larger and more granular study to answer that question.
Mothers who exclusively breastfed were more likely to fall asleep feeding than were those who partially breastfed or used formula. The investigators postulated that the infants of mothers who exclusively breastfed may have required more feedings because breast milk is more easily and quickly digested. I know this is a common explanation, but in my experience I have found that exclusively breastfed infants often use nursing as pacification and a sleep trigger and spend more time at the breast regardless of how quickly they emptied their stomachs.
This study also examined the effect of repeated educational interventions and support and found that mothers who received an intervention based on safe sleep practices were less likely to fall asleep while feeding than were the mothers who had received the intervention focused on exclusive breastfeeding value and barriers to its adoption.
Education is one avenue, particularly when it includes the mother’s partner who can play an important role as standby lifeguard to make sure the mother doesn’t fall asleep. Obviously, this is easier said than done because when there is a new baby in the house sleep deprivation is usually a shared experience.
Although I believe that my family is on the verge of gifting me a smartwatch to protect me from my own misadventures, I don’t have any personal experience with these wonders of modern technology. However, I suspect with very little tweaking a wearable sensor could be easily programmed to detect when a mother is beginning to fall asleep while she is feeding her infant. A smartwatch would be an expensive intervention and is unlikely to filter down to economically challenged families. On the other hand, this paper has reinforced our suspicions that sleep-deprived infant feeding is a significant problem. A subsidized loaner program for those families that can’t afford a smartwatch is an option that should be considered.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
In a recent survey of 1259 mothers published in the journal Pediatrics, 28% reported they had fallen asleep while feeding their babies, and 83% of those mothers reported that the sleep was unplanned. Although the study sample was small, the investigators found that sociodemographic factors did not increase the odds that a mother would fall asleep while feeding.
These numbers are not surprising, but nonetheless they are concerning because co-sleeping is a known risk factor for sudden unexplained infant death (SUID). Every parent will tell you during the first 6 months of their adventure in parenting they didn’t get enough sleep. In fact some will tell you that sleep deprivation was their chronic state for the child’s first year.
Falling asleep easily at times and places not intended for sleep is the primary symptom of sleep deprivation. SUID is the most tragic event associated with parental sleep deprivation, but it is certainly not the only one. Overtired parents are more likely to be involved in accidents and are more likely to make poor decisions, particularly those regarding how to respond to a crying or misbehaving child.
The investigators found that 24% of mothers who reported that their usual nighttime feeding location was a chair or sofa (14%). Not surprisingly, mothers who fed in chairs were less likely to fall asleep while feeding. Many of these mothers reported that they chose the chair because they thought they would be less likely to fall asleep and/or disturb other family members. One wonders how we should interpret these numbers in light of other research that has found it is “relatively less hazardous to fall asleep with an infant in the adult bed than on a chair or sofa.” Had these chair feeding mothers made the better choice under the circumstances? It would take a much larger and more granular study to answer that question.
Mothers who exclusively breastfed were more likely to fall asleep feeding than were those who partially breastfed or used formula. The investigators postulated that the infants of mothers who exclusively breastfed may have required more feedings because breast milk is more easily and quickly digested. I know this is a common explanation, but in my experience I have found that exclusively breastfed infants often use nursing as pacification and a sleep trigger and spend more time at the breast regardless of how quickly they emptied their stomachs.
This study also examined the effect of repeated educational interventions and support and found that mothers who received an intervention based on safe sleep practices were less likely to fall asleep while feeding than were the mothers who had received the intervention focused on exclusive breastfeeding value and barriers to its adoption.
Education is one avenue, particularly when it includes the mother’s partner who can play an important role as standby lifeguard to make sure the mother doesn’t fall asleep. Obviously, this is easier said than done because when there is a new baby in the house sleep deprivation is usually a shared experience.
Although I believe that my family is on the verge of gifting me a smartwatch to protect me from my own misadventures, I don’t have any personal experience with these wonders of modern technology. However, I suspect with very little tweaking a wearable sensor could be easily programmed to detect when a mother is beginning to fall asleep while she is feeding her infant. A smartwatch would be an expensive intervention and is unlikely to filter down to economically challenged families. On the other hand, this paper has reinforced our suspicions that sleep-deprived infant feeding is a significant problem. A subsidized loaner program for those families that can’t afford a smartwatch is an option that should be considered.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
In a recent survey of 1259 mothers published in the journal Pediatrics, 28% reported they had fallen asleep while feeding their babies, and 83% of those mothers reported that the sleep was unplanned. Although the study sample was small, the investigators found that sociodemographic factors did not increase the odds that a mother would fall asleep while feeding.
These numbers are not surprising, but nonetheless they are concerning because co-sleeping is a known risk factor for sudden unexplained infant death (SUID). Every parent will tell you during the first 6 months of their adventure in parenting they didn’t get enough sleep. In fact some will tell you that sleep deprivation was their chronic state for the child’s first year.
Falling asleep easily at times and places not intended for sleep is the primary symptom of sleep deprivation. SUID is the most tragic event associated with parental sleep deprivation, but it is certainly not the only one. Overtired parents are more likely to be involved in accidents and are more likely to make poor decisions, particularly those regarding how to respond to a crying or misbehaving child.
The investigators found that 24% of mothers who reported that their usual nighttime feeding location was a chair or sofa (14%). Not surprisingly, mothers who fed in chairs were less likely to fall asleep while feeding. Many of these mothers reported that they chose the chair because they thought they would be less likely to fall asleep and/or disturb other family members. One wonders how we should interpret these numbers in light of other research that has found it is “relatively less hazardous to fall asleep with an infant in the adult bed than on a chair or sofa.” Had these chair feeding mothers made the better choice under the circumstances? It would take a much larger and more granular study to answer that question.
Mothers who exclusively breastfed were more likely to fall asleep feeding than were those who partially breastfed or used formula. The investigators postulated that the infants of mothers who exclusively breastfed may have required more feedings because breast milk is more easily and quickly digested. I know this is a common explanation, but in my experience I have found that exclusively breastfed infants often use nursing as pacification and a sleep trigger and spend more time at the breast regardless of how quickly they emptied their stomachs.
This study also examined the effect of repeated educational interventions and support and found that mothers who received an intervention based on safe sleep practices were less likely to fall asleep while feeding than were the mothers who had received the intervention focused on exclusive breastfeeding value and barriers to its adoption.
Education is one avenue, particularly when it includes the mother’s partner who can play an important role as standby lifeguard to make sure the mother doesn’t fall asleep. Obviously, this is easier said than done because when there is a new baby in the house sleep deprivation is usually a shared experience.
Although I believe that my family is on the verge of gifting me a smartwatch to protect me from my own misadventures, I don’t have any personal experience with these wonders of modern technology. However, I suspect with very little tweaking a wearable sensor could be easily programmed to detect when a mother is beginning to fall asleep while she is feeding her infant. A smartwatch would be an expensive intervention and is unlikely to filter down to economically challenged families. On the other hand, this paper has reinforced our suspicions that sleep-deprived infant feeding is a significant problem. A subsidized loaner program for those families that can’t afford a smartwatch is an option that should be considered.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Trump Nominations for US Health Agencies Spark Controversy, Criticism, Praise
President-elect Donald Trump’s vision for the nation’s top health agencies is coming into focus with three nominations announced Nov. 22 that drew both criticism and praise:
- Surgeon and health researcher Martin A. Makary, MD, MPH, to lead the US Food and Drug Administration (FDA).
- Former Republican congressman and physician David J. Weldon, MD, for director of the US Centers for Disease Control and Prevention (CDC).
- Fox News contributor Janette Nesheiwat, MD, for surgeon general.
Earlier in November, Trump nominated vaccine skeptic and former presidential candidate Robert F. Kennedy Jr. to lead the US Department of Health and Human Services (HHS).
Here’s what to know about the latest nominees, who, like Kennedy, must be confirmed by the US Senate.
Martin A. Makary
Currently a professor at the Johns Hopkins School of Medicine and chief of islet transplant surgery at Johns Hopkins Hospital, Makary co-invented in 2006 a surgery checklist that became a widely-used patient safety tool.
As a US FDA commissioner, Makary would preside over a $6.5 billion agency with more than 18,000 employees. The agency, part of HHS, oversees human and animal drugs and vaccines, medical devices, food, tobacco and other products. Some of Makary’s views align closely with those of HHS nominee Kennedy.
Makary is also chief medical officer of telehealth platform Sesame.
Makary was primarily known as a health researcher and author of books about price transparency and the cost of health care until the COVID-19 pandemic, when he became an outspoken critic of the federal response, lambasting restrictions and mandates advocated by the CDC and other public health officials.
In 2023, Makary told the House Select Subcommittee on the COVID Pandemic that federal officials had ignored what he called “natural immunity.” Studies have shown that natural immunity is “at least as effective as vaccinated immunity, and probably better,” testified Makary.
Makary called for an overhaul of the US FDA in a 2021 Fox News opinion, saying that its culture was “defined by counterproductive rigidity and a refusal to adapt.”
Blind Spots, his most recent book, takes on what he calls “medical dogma” and challenges conventional views on subjects ranging from the microbiome to marijuana to cancer prevention, hormone replacement therapy, antibiotics and peanut allergies.
In an interview he posted to X, Makary blames inappropriate use of antibiotics for a variety of childhood illnesses. He cites increases in obesity, learning disabilities, attention deficit disorder, asthma, celiac disease, ulcerative colitis and Crohn’s disease as all potentially causally related to antibiotics given in childhood.
Makary is an advisor to two conservative think tanks, the Foundation for Research on Equal Opportunity, and to Paragon Health Institute, begun in 2021 by two former top officials in the previous Trump administration.
Makary would “cut the bureaucratic red tape at the agency to make sure Americans get the medical cures and treatments they deserve,” Trump said on his social media platform, Truth Social, and in a press release.
While Los Angeles Times owner and physician-entrepreneur Patrick Soon-Shiong, MBBCh, MSc, praised the nomination of Makary (and the two other nominees) as “inspired,” other physicians criticized Makary for his anti-COVID mandate views and “fear-mongering” over COVID vaccine side effects.
Janette Nesheiwat
As surgeon general, Nesheiwat would serve as the top “health communicator in chief” and oversee the 6000 member US Public Health Service Commissioned Corps.
She is a frequent medical contributor to Fox News and serves as a medical director for a group of urgent care clinics in New York. She received her medical degree from the American University of the Caribbean School of Medicine and completed a family medicine residency at the University of Arkansas for Medical Sciences. She is board-certified in family medicine.
Nesheiwat sells vitamin supplements on her website and in December will publish a book on “miracles in medicine” and her Christian faith.
Trump said in a statement that Nesheiwat “is a fierce advocate and strong communicator for preventive medicine and public health. She is committed to ensuring that Americans have access to affordable, quality healthcare, and believes in empowering individuals to take charge of their health to live longer, healthier lives.”
While Nesheiwat was critical of COVID mandates, she voiced more support for COVID vaccines and mask-wearing during the pandemic than her fellow nominees, leading some Trump supporters to criticize her nomination.
“A good appointment, happy about this: I got to know @DoctorJanette during the pandemic, exchanging information. She is very smart, thoughtful, interested in learning, and a compassionate doctor, and…a truly nice person,” noted vaccine researcher Peter Hotez, MD, PhD, said on X.
David J. Weldon
If confirmed, former congressman Weldon would oversee the sprawling CDC, an agency with a roughly $17 billion budget, 15,000 employees or contractors, and numerous centers covering everything from health statistics to vaccines to epidemiology.
After earning his medical degree from the University at Buffalo School of Medicine, Weldon served in the US Army and US Army reserve. The Republican later served for 14 years in Congress representing Florida’s 15th district, which covers the Tampa region.
He now practices as an internist in Brevard County, Florida.
In Congress, Weldon raised concerns about the safety of some vaccines and promoted the false narrative that a former vaccine ingredient, thimerosal, caused autism, the Washington Post reported. Thimerosal has not been used in child vaccines for more than two decades. He also introduced a bill to move vaccine safety oversight from the CDC to an independent agency within HHS.
Trump said in a statement that Weldon “will proudly restore the CDC to its true purpose, and will work to end the Chronic Disease Epidemic.”
But some physicians criticized Weldon for what they called his anti-vaccine views.
A version of this article first appeared on Medscape.com.
President-elect Donald Trump’s vision for the nation’s top health agencies is coming into focus with three nominations announced Nov. 22 that drew both criticism and praise:
- Surgeon and health researcher Martin A. Makary, MD, MPH, to lead the US Food and Drug Administration (FDA).
- Former Republican congressman and physician David J. Weldon, MD, for director of the US Centers for Disease Control and Prevention (CDC).
- Fox News contributor Janette Nesheiwat, MD, for surgeon general.
Earlier in November, Trump nominated vaccine skeptic and former presidential candidate Robert F. Kennedy Jr. to lead the US Department of Health and Human Services (HHS).
Here’s what to know about the latest nominees, who, like Kennedy, must be confirmed by the US Senate.
Martin A. Makary
Currently a professor at the Johns Hopkins School of Medicine and chief of islet transplant surgery at Johns Hopkins Hospital, Makary co-invented in 2006 a surgery checklist that became a widely-used patient safety tool.
As a US FDA commissioner, Makary would preside over a $6.5 billion agency with more than 18,000 employees. The agency, part of HHS, oversees human and animal drugs and vaccines, medical devices, food, tobacco and other products. Some of Makary’s views align closely with those of HHS nominee Kennedy.
Makary is also chief medical officer of telehealth platform Sesame.
Makary was primarily known as a health researcher and author of books about price transparency and the cost of health care until the COVID-19 pandemic, when he became an outspoken critic of the federal response, lambasting restrictions and mandates advocated by the CDC and other public health officials.
In 2023, Makary told the House Select Subcommittee on the COVID Pandemic that federal officials had ignored what he called “natural immunity.” Studies have shown that natural immunity is “at least as effective as vaccinated immunity, and probably better,” testified Makary.
Makary called for an overhaul of the US FDA in a 2021 Fox News opinion, saying that its culture was “defined by counterproductive rigidity and a refusal to adapt.”
Blind Spots, his most recent book, takes on what he calls “medical dogma” and challenges conventional views on subjects ranging from the microbiome to marijuana to cancer prevention, hormone replacement therapy, antibiotics and peanut allergies.
In an interview he posted to X, Makary blames inappropriate use of antibiotics for a variety of childhood illnesses. He cites increases in obesity, learning disabilities, attention deficit disorder, asthma, celiac disease, ulcerative colitis and Crohn’s disease as all potentially causally related to antibiotics given in childhood.
Makary is an advisor to two conservative think tanks, the Foundation for Research on Equal Opportunity, and to Paragon Health Institute, begun in 2021 by two former top officials in the previous Trump administration.
Makary would “cut the bureaucratic red tape at the agency to make sure Americans get the medical cures and treatments they deserve,” Trump said on his social media platform, Truth Social, and in a press release.
While Los Angeles Times owner and physician-entrepreneur Patrick Soon-Shiong, MBBCh, MSc, praised the nomination of Makary (and the two other nominees) as “inspired,” other physicians criticized Makary for his anti-COVID mandate views and “fear-mongering” over COVID vaccine side effects.
Janette Nesheiwat
As surgeon general, Nesheiwat would serve as the top “health communicator in chief” and oversee the 6000 member US Public Health Service Commissioned Corps.
She is a frequent medical contributor to Fox News and serves as a medical director for a group of urgent care clinics in New York. She received her medical degree from the American University of the Caribbean School of Medicine and completed a family medicine residency at the University of Arkansas for Medical Sciences. She is board-certified in family medicine.
Nesheiwat sells vitamin supplements on her website and in December will publish a book on “miracles in medicine” and her Christian faith.
Trump said in a statement that Nesheiwat “is a fierce advocate and strong communicator for preventive medicine and public health. She is committed to ensuring that Americans have access to affordable, quality healthcare, and believes in empowering individuals to take charge of their health to live longer, healthier lives.”
While Nesheiwat was critical of COVID mandates, she voiced more support for COVID vaccines and mask-wearing during the pandemic than her fellow nominees, leading some Trump supporters to criticize her nomination.
“A good appointment, happy about this: I got to know @DoctorJanette during the pandemic, exchanging information. She is very smart, thoughtful, interested in learning, and a compassionate doctor, and…a truly nice person,” noted vaccine researcher Peter Hotez, MD, PhD, said on X.
David J. Weldon
If confirmed, former congressman Weldon would oversee the sprawling CDC, an agency with a roughly $17 billion budget, 15,000 employees or contractors, and numerous centers covering everything from health statistics to vaccines to epidemiology.
After earning his medical degree from the University at Buffalo School of Medicine, Weldon served in the US Army and US Army reserve. The Republican later served for 14 years in Congress representing Florida’s 15th district, which covers the Tampa region.
He now practices as an internist in Brevard County, Florida.
In Congress, Weldon raised concerns about the safety of some vaccines and promoted the false narrative that a former vaccine ingredient, thimerosal, caused autism, the Washington Post reported. Thimerosal has not been used in child vaccines for more than two decades. He also introduced a bill to move vaccine safety oversight from the CDC to an independent agency within HHS.
Trump said in a statement that Weldon “will proudly restore the CDC to its true purpose, and will work to end the Chronic Disease Epidemic.”
But some physicians criticized Weldon for what they called his anti-vaccine views.
A version of this article first appeared on Medscape.com.
President-elect Donald Trump’s vision for the nation’s top health agencies is coming into focus with three nominations announced Nov. 22 that drew both criticism and praise:
- Surgeon and health researcher Martin A. Makary, MD, MPH, to lead the US Food and Drug Administration (FDA).
- Former Republican congressman and physician David J. Weldon, MD, for director of the US Centers for Disease Control and Prevention (CDC).
- Fox News contributor Janette Nesheiwat, MD, for surgeon general.
Earlier in November, Trump nominated vaccine skeptic and former presidential candidate Robert F. Kennedy Jr. to lead the US Department of Health and Human Services (HHS).
Here’s what to know about the latest nominees, who, like Kennedy, must be confirmed by the US Senate.
Martin A. Makary
Currently a professor at the Johns Hopkins School of Medicine and chief of islet transplant surgery at Johns Hopkins Hospital, Makary co-invented in 2006 a surgery checklist that became a widely-used patient safety tool.
As a US FDA commissioner, Makary would preside over a $6.5 billion agency with more than 18,000 employees. The agency, part of HHS, oversees human and animal drugs and vaccines, medical devices, food, tobacco and other products. Some of Makary’s views align closely with those of HHS nominee Kennedy.
Makary is also chief medical officer of telehealth platform Sesame.
Makary was primarily known as a health researcher and author of books about price transparency and the cost of health care until the COVID-19 pandemic, when he became an outspoken critic of the federal response, lambasting restrictions and mandates advocated by the CDC and other public health officials.
In 2023, Makary told the House Select Subcommittee on the COVID Pandemic that federal officials had ignored what he called “natural immunity.” Studies have shown that natural immunity is “at least as effective as vaccinated immunity, and probably better,” testified Makary.
Makary called for an overhaul of the US FDA in a 2021 Fox News opinion, saying that its culture was “defined by counterproductive rigidity and a refusal to adapt.”
Blind Spots, his most recent book, takes on what he calls “medical dogma” and challenges conventional views on subjects ranging from the microbiome to marijuana to cancer prevention, hormone replacement therapy, antibiotics and peanut allergies.
In an interview he posted to X, Makary blames inappropriate use of antibiotics for a variety of childhood illnesses. He cites increases in obesity, learning disabilities, attention deficit disorder, asthma, celiac disease, ulcerative colitis and Crohn’s disease as all potentially causally related to antibiotics given in childhood.
Makary is an advisor to two conservative think tanks, the Foundation for Research on Equal Opportunity, and to Paragon Health Institute, begun in 2021 by two former top officials in the previous Trump administration.
Makary would “cut the bureaucratic red tape at the agency to make sure Americans get the medical cures and treatments they deserve,” Trump said on his social media platform, Truth Social, and in a press release.
While Los Angeles Times owner and physician-entrepreneur Patrick Soon-Shiong, MBBCh, MSc, praised the nomination of Makary (and the two other nominees) as “inspired,” other physicians criticized Makary for his anti-COVID mandate views and “fear-mongering” over COVID vaccine side effects.
Janette Nesheiwat
As surgeon general, Nesheiwat would serve as the top “health communicator in chief” and oversee the 6000 member US Public Health Service Commissioned Corps.
She is a frequent medical contributor to Fox News and serves as a medical director for a group of urgent care clinics in New York. She received her medical degree from the American University of the Caribbean School of Medicine and completed a family medicine residency at the University of Arkansas for Medical Sciences. She is board-certified in family medicine.
Nesheiwat sells vitamin supplements on her website and in December will publish a book on “miracles in medicine” and her Christian faith.
Trump said in a statement that Nesheiwat “is a fierce advocate and strong communicator for preventive medicine and public health. She is committed to ensuring that Americans have access to affordable, quality healthcare, and believes in empowering individuals to take charge of their health to live longer, healthier lives.”
While Nesheiwat was critical of COVID mandates, she voiced more support for COVID vaccines and mask-wearing during the pandemic than her fellow nominees, leading some Trump supporters to criticize her nomination.
“A good appointment, happy about this: I got to know @DoctorJanette during the pandemic, exchanging information. She is very smart, thoughtful, interested in learning, and a compassionate doctor, and…a truly nice person,” noted vaccine researcher Peter Hotez, MD, PhD, said on X.
David J. Weldon
If confirmed, former congressman Weldon would oversee the sprawling CDC, an agency with a roughly $17 billion budget, 15,000 employees or contractors, and numerous centers covering everything from health statistics to vaccines to epidemiology.
After earning his medical degree from the University at Buffalo School of Medicine, Weldon served in the US Army and US Army reserve. The Republican later served for 14 years in Congress representing Florida’s 15th district, which covers the Tampa region.
He now practices as an internist in Brevard County, Florida.
In Congress, Weldon raised concerns about the safety of some vaccines and promoted the false narrative that a former vaccine ingredient, thimerosal, caused autism, the Washington Post reported. Thimerosal has not been used in child vaccines for more than two decades. He also introduced a bill to move vaccine safety oversight from the CDC to an independent agency within HHS.
Trump said in a statement that Weldon “will proudly restore the CDC to its true purpose, and will work to end the Chronic Disease Epidemic.”
But some physicians criticized Weldon for what they called his anti-vaccine views.
A version of this article first appeared on Medscape.com.



