User login
A call for ‘changing the social norms’ on naloxone
SAN DIEGO – Among individuals with a history of injection drug use, more than one-third reported never or sometimes carrying naloxone, while just one in four reported carrying with it them at all times.
Those are key findings from a survey that set out to examine gaps in the naloxone cascade in a sample of people who inject drugs.
“In order to save a life, you have to have the naloxone with you at all times,” lead study author Karin E. Tobin, PhD, said in an interview at the annual meeting of the College on Problems of Drug Dependence.
While emerging research demonstrates the positive impact of opioid overdose education and community naloxone distribution programs to reduce opioid-related overdose deaths, opiate overdose continues to be a major cause of mortality, said Dr. Tobin, who is affiliated with the department of health behavior and society at Johns Hopkins University, Baltimore. “We’ve made a lot of progress in convincing people that naloxone is not addictive, and that it’s not going to cause any harm,” she said. “Now, drug users aren’t afraid to ask for it. Still, we wondered: If everyone knows about naloxone and no one is embarrassed to talk about it, why are people still dying [from opioid overdoses] in Baltimore?”
She and her associates conducted a cross-sectional survey of 353 individuals aged 18 and older in Baltimore who self-reported a lifetime history of injection drug use. The data came from a baseline survey that was conducted as part of a randomized, controlled trial testing the efficacy of a behavioral intervention focused on the Hepatitis C cascade. Individuals were asked to answer questions related to the five steps of the naloxone cascade: awareness (have you ever heard about naloxone?), access (have you ever received naloxone?), training (have you ever been trained to use naloxone?), use (have you ever used naloxone during an opiate overdose?), and possession (how often do you carry naloxone?)
More than half of the survey respondents (65%) were male; mean age was 47 years. For the previous 6 months, more than half of the sample reported the use of crack (64%), heroin (74%), and other injectable drugs (57%), while 90% reported having ever witnessed an overdose – 59% in the prior year alone. Dr. Tobin and her associates found that 90% of respondents had heard about naloxone, 69% had received it, and 60% had been trained to use it. In addition, 37% reported never carrying naloxone, 38% sometimes carried it, 33% said they had used naloxone at some point, and 25% said they always carried it with them.
On multinomial regression analysis, the researchers found that carrying naloxone often or always was significantly associated with the following variables: female sex (odds ratio, 2.77), having ever witnessed an overdose (OR, 1.84), having injected in the past 12 months (OR, 1.75), and having ever used naloxone during an overdose (OR, 4.33). The latter finding is especially important, “because it means that we just have to let people practice using it,” said Dr. Tobin, who noted that more research is needed to understand reasons why injection drug users do not always carry naloxone. “We need to start changing the social norms about carrying naloxone. You never know when it will be useful.”
The National Institute on Drug Abuse supported the study. Dr. Tobin reported having no financial disclosures.
SAN DIEGO – Among individuals with a history of injection drug use, more than one-third reported never or sometimes carrying naloxone, while just one in four reported carrying with it them at all times.
Those are key findings from a survey that set out to examine gaps in the naloxone cascade in a sample of people who inject drugs.
“In order to save a life, you have to have the naloxone with you at all times,” lead study author Karin E. Tobin, PhD, said in an interview at the annual meeting of the College on Problems of Drug Dependence.
While emerging research demonstrates the positive impact of opioid overdose education and community naloxone distribution programs to reduce opioid-related overdose deaths, opiate overdose continues to be a major cause of mortality, said Dr. Tobin, who is affiliated with the department of health behavior and society at Johns Hopkins University, Baltimore. “We’ve made a lot of progress in convincing people that naloxone is not addictive, and that it’s not going to cause any harm,” she said. “Now, drug users aren’t afraid to ask for it. Still, we wondered: If everyone knows about naloxone and no one is embarrassed to talk about it, why are people still dying [from opioid overdoses] in Baltimore?”
She and her associates conducted a cross-sectional survey of 353 individuals aged 18 and older in Baltimore who self-reported a lifetime history of injection drug use. The data came from a baseline survey that was conducted as part of a randomized, controlled trial testing the efficacy of a behavioral intervention focused on the Hepatitis C cascade. Individuals were asked to answer questions related to the five steps of the naloxone cascade: awareness (have you ever heard about naloxone?), access (have you ever received naloxone?), training (have you ever been trained to use naloxone?), use (have you ever used naloxone during an opiate overdose?), and possession (how often do you carry naloxone?)
More than half of the survey respondents (65%) were male; mean age was 47 years. For the previous 6 months, more than half of the sample reported the use of crack (64%), heroin (74%), and other injectable drugs (57%), while 90% reported having ever witnessed an overdose – 59% in the prior year alone. Dr. Tobin and her associates found that 90% of respondents had heard about naloxone, 69% had received it, and 60% had been trained to use it. In addition, 37% reported never carrying naloxone, 38% sometimes carried it, 33% said they had used naloxone at some point, and 25% said they always carried it with them.
On multinomial regression analysis, the researchers found that carrying naloxone often or always was significantly associated with the following variables: female sex (odds ratio, 2.77), having ever witnessed an overdose (OR, 1.84), having injected in the past 12 months (OR, 1.75), and having ever used naloxone during an overdose (OR, 4.33). The latter finding is especially important, “because it means that we just have to let people practice using it,” said Dr. Tobin, who noted that more research is needed to understand reasons why injection drug users do not always carry naloxone. “We need to start changing the social norms about carrying naloxone. You never know when it will be useful.”
The National Institute on Drug Abuse supported the study. Dr. Tobin reported having no financial disclosures.
SAN DIEGO – Among individuals with a history of injection drug use, more than one-third reported never or sometimes carrying naloxone, while just one in four reported carrying with it them at all times.
Those are key findings from a survey that set out to examine gaps in the naloxone cascade in a sample of people who inject drugs.
“In order to save a life, you have to have the naloxone with you at all times,” lead study author Karin E. Tobin, PhD, said in an interview at the annual meeting of the College on Problems of Drug Dependence.
While emerging research demonstrates the positive impact of opioid overdose education and community naloxone distribution programs to reduce opioid-related overdose deaths, opiate overdose continues to be a major cause of mortality, said Dr. Tobin, who is affiliated with the department of health behavior and society at Johns Hopkins University, Baltimore. “We’ve made a lot of progress in convincing people that naloxone is not addictive, and that it’s not going to cause any harm,” she said. “Now, drug users aren’t afraid to ask for it. Still, we wondered: If everyone knows about naloxone and no one is embarrassed to talk about it, why are people still dying [from opioid overdoses] in Baltimore?”
She and her associates conducted a cross-sectional survey of 353 individuals aged 18 and older in Baltimore who self-reported a lifetime history of injection drug use. The data came from a baseline survey that was conducted as part of a randomized, controlled trial testing the efficacy of a behavioral intervention focused on the Hepatitis C cascade. Individuals were asked to answer questions related to the five steps of the naloxone cascade: awareness (have you ever heard about naloxone?), access (have you ever received naloxone?), training (have you ever been trained to use naloxone?), use (have you ever used naloxone during an opiate overdose?), and possession (how often do you carry naloxone?)
More than half of the survey respondents (65%) were male; mean age was 47 years. For the previous 6 months, more than half of the sample reported the use of crack (64%), heroin (74%), and other injectable drugs (57%), while 90% reported having ever witnessed an overdose – 59% in the prior year alone. Dr. Tobin and her associates found that 90% of respondents had heard about naloxone, 69% had received it, and 60% had been trained to use it. In addition, 37% reported never carrying naloxone, 38% sometimes carried it, 33% said they had used naloxone at some point, and 25% said they always carried it with them.
On multinomial regression analysis, the researchers found that carrying naloxone often or always was significantly associated with the following variables: female sex (odds ratio, 2.77), having ever witnessed an overdose (OR, 1.84), having injected in the past 12 months (OR, 1.75), and having ever used naloxone during an overdose (OR, 4.33). The latter finding is especially important, “because it means that we just have to let people practice using it,” said Dr. Tobin, who noted that more research is needed to understand reasons why injection drug users do not always carry naloxone. “We need to start changing the social norms about carrying naloxone. You never know when it will be useful.”
The National Institute on Drug Abuse supported the study. Dr. Tobin reported having no financial disclosures.
AT CPDD 2018
Key clinical point: Increasing possession of naloxone among people who use opiates is essential.
Major finding:. Carrying naloxone often or always was significantly associated with several variables, including female sex (odds ratio, 2.77) and having ever used naloxone during an overdose (OR, 4.33).
Study details: A cross-sectional survey of 353 individuals aged 18 and older in Baltimore who self-reported a lifetime history of injection drug use.
Disclosures: The National Institute on Drug Abuse supported the study. Dr. Tobin reported having no financial disclosures.
Do free meals to physicians affect opioid prescribing?
SAN DIEGO – Physicians who receive gifts and free meals from opioid manufacturers prescribe more opioids than do their counterparts, a new study suggests.
A sampling of doctors who reported marketing payments or gifts prescribed more of the drugs the following year even as their colleagues prescribed fewer. Researchers also found signs of a dose-effect relationship between more free meals received and more opioid medications prescribed.
The findings, presented at the annual meeting of the College on Problems of Drug Dependence and recently published, do not prove a link between free meals and the massive, deadly opioid epidemic. And the purpose of pharmaceutical marketing, of course, is to persuade physicians to prescribe medications, the researchers noted. The report was published in JAMA Internal Medicine.
Still, in light of the opioid epidemic, “there’s a national effort to reduce overprescribing. Our database suggests that the pharmaceutical industry may be a counterforce,” lead author and pediatrician Scott E. Hadland, MD, MPH, of Boston University, said in an interview.
The findings suggest “it doesn’t take much money to get doctors to potentially prescribe more opioids,” he added.
According to data from the Centers for Disease Control and Prevention, a record number of people – 52,404 – died from drug overdoses in 2015, and nearly 13,000 of the deaths were attributable to prescription drugs (natural or semi-synthetic). An estimated 12.5 million people aged 12 and older in 2015, meanwhile, recently had misused prescription pain relievers.
For the new study, Dr. Hadland and his colleagues sought to understand whether opioid marketing in 2014 influenced prescribing in 2015.
The researchers retrospectively tracked 369,139 physicians in a Medicare Part D database who prescribed opioids in 2015 and found that 7% reported receiving opioid marketing – speaking fees ($6.2 million), meals ($1.8 million), travel ($731,000), consulting fees ($290,000), and education ($80,000).
Overall, received marketing.
“The effect is very subtle,” said Dr. Hadland, an addiction medicine specialist at the university. “Nine percent does not seem like a large number, but when you’re talking about hundreds of thousands of physicians, that’s a large number of opioids being prescribed.”
The study takes only Medicare Part D opioid prescriptions into account, and includes only about 42% of the active national physician workforce, he noted.
The researchers linked rising numbers of meals received in 2014 per physician – from 1 to more than 10 – to a steady increase in the number of opioid claims per physician. For example, physicians who received 1 meal made about 150 opioid claims, while those who received more than 10 made more than 700 claims.
As for physician motivations, Dr. Hadland said, he doesn’t believe “this is intentional for most physicians. If you asked the vast majority of physicians in our study, ‘Do you believe marketing is influencing your prescribing?’ most would say no.”
But the findings, he said, still raise questions.
Going forward, researchers plan to study the effect of opioid marketing on public health, he added.
Dr. Hadland reports funding from the National Institute on Drug Abuse, Society for Adolescent Health and Medicine, Thrasher Research Fund, and Academic Pediatric Association. Another author reports funding from NIDA. No additional relevant disclosures were reported.
SOURCE: Hadland SE et al. JAMA Intern Med. 2018 Jun 1;178(6):861-3.
SAN DIEGO – Physicians who receive gifts and free meals from opioid manufacturers prescribe more opioids than do their counterparts, a new study suggests.
A sampling of doctors who reported marketing payments or gifts prescribed more of the drugs the following year even as their colleagues prescribed fewer. Researchers also found signs of a dose-effect relationship between more free meals received and more opioid medications prescribed.
The findings, presented at the annual meeting of the College on Problems of Drug Dependence and recently published, do not prove a link between free meals and the massive, deadly opioid epidemic. And the purpose of pharmaceutical marketing, of course, is to persuade physicians to prescribe medications, the researchers noted. The report was published in JAMA Internal Medicine.
Still, in light of the opioid epidemic, “there’s a national effort to reduce overprescribing. Our database suggests that the pharmaceutical industry may be a counterforce,” lead author and pediatrician Scott E. Hadland, MD, MPH, of Boston University, said in an interview.
The findings suggest “it doesn’t take much money to get doctors to potentially prescribe more opioids,” he added.
According to data from the Centers for Disease Control and Prevention, a record number of people – 52,404 – died from drug overdoses in 2015, and nearly 13,000 of the deaths were attributable to prescription drugs (natural or semi-synthetic). An estimated 12.5 million people aged 12 and older in 2015, meanwhile, recently had misused prescription pain relievers.
For the new study, Dr. Hadland and his colleagues sought to understand whether opioid marketing in 2014 influenced prescribing in 2015.
The researchers retrospectively tracked 369,139 physicians in a Medicare Part D database who prescribed opioids in 2015 and found that 7% reported receiving opioid marketing – speaking fees ($6.2 million), meals ($1.8 million), travel ($731,000), consulting fees ($290,000), and education ($80,000).
Overall, received marketing.
“The effect is very subtle,” said Dr. Hadland, an addiction medicine specialist at the university. “Nine percent does not seem like a large number, but when you’re talking about hundreds of thousands of physicians, that’s a large number of opioids being prescribed.”
The study takes only Medicare Part D opioid prescriptions into account, and includes only about 42% of the active national physician workforce, he noted.
The researchers linked rising numbers of meals received in 2014 per physician – from 1 to more than 10 – to a steady increase in the number of opioid claims per physician. For example, physicians who received 1 meal made about 150 opioid claims, while those who received more than 10 made more than 700 claims.
As for physician motivations, Dr. Hadland said, he doesn’t believe “this is intentional for most physicians. If you asked the vast majority of physicians in our study, ‘Do you believe marketing is influencing your prescribing?’ most would say no.”
But the findings, he said, still raise questions.
Going forward, researchers plan to study the effect of opioid marketing on public health, he added.
Dr. Hadland reports funding from the National Institute on Drug Abuse, Society for Adolescent Health and Medicine, Thrasher Research Fund, and Academic Pediatric Association. Another author reports funding from NIDA. No additional relevant disclosures were reported.
SOURCE: Hadland SE et al. JAMA Intern Med. 2018 Jun 1;178(6):861-3.
SAN DIEGO – Physicians who receive gifts and free meals from opioid manufacturers prescribe more opioids than do their counterparts, a new study suggests.
A sampling of doctors who reported marketing payments or gifts prescribed more of the drugs the following year even as their colleagues prescribed fewer. Researchers also found signs of a dose-effect relationship between more free meals received and more opioid medications prescribed.
The findings, presented at the annual meeting of the College on Problems of Drug Dependence and recently published, do not prove a link between free meals and the massive, deadly opioid epidemic. And the purpose of pharmaceutical marketing, of course, is to persuade physicians to prescribe medications, the researchers noted. The report was published in JAMA Internal Medicine.
Still, in light of the opioid epidemic, “there’s a national effort to reduce overprescribing. Our database suggests that the pharmaceutical industry may be a counterforce,” lead author and pediatrician Scott E. Hadland, MD, MPH, of Boston University, said in an interview.
The findings suggest “it doesn’t take much money to get doctors to potentially prescribe more opioids,” he added.
According to data from the Centers for Disease Control and Prevention, a record number of people – 52,404 – died from drug overdoses in 2015, and nearly 13,000 of the deaths were attributable to prescription drugs (natural or semi-synthetic). An estimated 12.5 million people aged 12 and older in 2015, meanwhile, recently had misused prescription pain relievers.
For the new study, Dr. Hadland and his colleagues sought to understand whether opioid marketing in 2014 influenced prescribing in 2015.
The researchers retrospectively tracked 369,139 physicians in a Medicare Part D database who prescribed opioids in 2015 and found that 7% reported receiving opioid marketing – speaking fees ($6.2 million), meals ($1.8 million), travel ($731,000), consulting fees ($290,000), and education ($80,000).
Overall, received marketing.
“The effect is very subtle,” said Dr. Hadland, an addiction medicine specialist at the university. “Nine percent does not seem like a large number, but when you’re talking about hundreds of thousands of physicians, that’s a large number of opioids being prescribed.”
The study takes only Medicare Part D opioid prescriptions into account, and includes only about 42% of the active national physician workforce, he noted.
The researchers linked rising numbers of meals received in 2014 per physician – from 1 to more than 10 – to a steady increase in the number of opioid claims per physician. For example, physicians who received 1 meal made about 150 opioid claims, while those who received more than 10 made more than 700 claims.
As for physician motivations, Dr. Hadland said, he doesn’t believe “this is intentional for most physicians. If you asked the vast majority of physicians in our study, ‘Do you believe marketing is influencing your prescribing?’ most would say no.”
But the findings, he said, still raise questions.
Going forward, researchers plan to study the effect of opioid marketing on public health, he added.
Dr. Hadland reports funding from the National Institute on Drug Abuse, Society for Adolescent Health and Medicine, Thrasher Research Fund, and Academic Pediatric Association. Another author reports funding from NIDA. No additional relevant disclosures were reported.
SOURCE: Hadland SE et al. JAMA Intern Med. 2018 Jun 1;178(6):861-3.
REPORTING FROM CPDD 2018
Key clinical point: Opioid marketing appears to affect physician prescribing practices.
Major finding: Physicians who received opioid marketing payments and meals in 2014 prescribed an adjusted 9% more opioids in 2015 than did their opioid-prescribing colleagues.
Study details: Retrospective 2014-2015 analysis of 369,139 opioid-prescribing physicians in a Medicare Part D database.
Disclosures: Dr. Hadland reported funding from the National Institute on Drug Abuse, Society for Adolescent Health and Medicine, Thrasher Research Fund, and Academic Pediatric Association. Another author reported funding from NIDA. No additional relevant disclosures were reported.
Source: Hadland SE et al. JAMA Intern Med. 2018 Jun 1;178(6):861-3.
RBC transfusions with surgery may increase VTE risk
In patients undergoing surgery, RBC transfusions may be associated with the development of new or progressive venous thromboembolism within 30 days of the procedure, results of a recent registry study suggest.
Patients who received perioperative RBC transfusions had significantly higher odds of developing postoperative venous thromboembolism (VTE) overall, as well as higher odds specifically for deep venous thrombosis (DVT) and pulmonary embolism (PE), according to results published in JAMA Surgery.
“In a subset of patients receiving perioperative RBC transfusions, a synergistic and incremental dose-related risk for VTE development may exist,” Dr. Goel and her coauthors wrote.
The analysis was based on prospectively collected North American registry data including 750,937 patients who underwent a surgical procedure in 2014, of which 47,410 (6.3%) received one or more perioperative RBC transfusions. VTE occurred in 6,309 patients (0.8%), of which 4,336 cases were DVT (0.6%) and 2,514 were PE (0.3%).
The patients who received perioperative RBC transfusions had significantly increased odds of developing VTE in the 30-day postoperative period (adjusted odds ratio, 2.1; 95% confidence interval, 2.0-2.3) versus those who had no transfusions, according to results of a multivariable analysis adjusting for age, sex, length of hospital stay, use of mechanical ventilation, and other potentially confounding factors.
Similarly, researchers found transfused patients had higher odds of both DVT (aOR, 2.2; 95% CI, 2.1-2.4), and PE (aOR, 1.9; 95% CI, 1.7-2.1).
Odds of VTE increased significantly along with increasing number of perioperative RBC transfusions from an aOR of 2.1 for those with just one transfusion to 4.5 for those who had three or more transfusion events (P less than .001 for trend), results of a dose-response analysis showed.
The association between RBC transfusions perioperatively and VTE postoperatively remained robust after propensity score matching and was statistically significant in all surgical subspecialties, the researchers reported.
However, they also noted that these results will require validation in prospective cohort studies and randomized clinical trials. “If proven, they underscore the continued need for more stringent and optimal perioperative blood management practices in addition to rigorous VTE prophylaxis in patients undergoing surgery.”
The study was funded in part by grants from the National Institutes of Health and Cornell University. The researchers reported having no conflicts of interest.
SOURCE: Goel R et al. JAMA Surg. 2018 Jun 13. doi: 10.1001/jamasurg.2018.1565.
In patients undergoing surgery, RBC transfusions may be associated with the development of new or progressive venous thromboembolism within 30 days of the procedure, results of a recent registry study suggest.
Patients who received perioperative RBC transfusions had significantly higher odds of developing postoperative venous thromboembolism (VTE) overall, as well as higher odds specifically for deep venous thrombosis (DVT) and pulmonary embolism (PE), according to results published in JAMA Surgery.
“In a subset of patients receiving perioperative RBC transfusions, a synergistic and incremental dose-related risk for VTE development may exist,” Dr. Goel and her coauthors wrote.
The analysis was based on prospectively collected North American registry data including 750,937 patients who underwent a surgical procedure in 2014, of which 47,410 (6.3%) received one or more perioperative RBC transfusions. VTE occurred in 6,309 patients (0.8%), of which 4,336 cases were DVT (0.6%) and 2,514 were PE (0.3%).
The patients who received perioperative RBC transfusions had significantly increased odds of developing VTE in the 30-day postoperative period (adjusted odds ratio, 2.1; 95% confidence interval, 2.0-2.3) versus those who had no transfusions, according to results of a multivariable analysis adjusting for age, sex, length of hospital stay, use of mechanical ventilation, and other potentially confounding factors.
Similarly, researchers found transfused patients had higher odds of both DVT (aOR, 2.2; 95% CI, 2.1-2.4), and PE (aOR, 1.9; 95% CI, 1.7-2.1).
Odds of VTE increased significantly along with increasing number of perioperative RBC transfusions from an aOR of 2.1 for those with just one transfusion to 4.5 for those who had three or more transfusion events (P less than .001 for trend), results of a dose-response analysis showed.
The association between RBC transfusions perioperatively and VTE postoperatively remained robust after propensity score matching and was statistically significant in all surgical subspecialties, the researchers reported.
However, they also noted that these results will require validation in prospective cohort studies and randomized clinical trials. “If proven, they underscore the continued need for more stringent and optimal perioperative blood management practices in addition to rigorous VTE prophylaxis in patients undergoing surgery.”
The study was funded in part by grants from the National Institutes of Health and Cornell University. The researchers reported having no conflicts of interest.
SOURCE: Goel R et al. JAMA Surg. 2018 Jun 13. doi: 10.1001/jamasurg.2018.1565.
In patients undergoing surgery, RBC transfusions may be associated with the development of new or progressive venous thromboembolism within 30 days of the procedure, results of a recent registry study suggest.
Patients who received perioperative RBC transfusions had significantly higher odds of developing postoperative venous thromboembolism (VTE) overall, as well as higher odds specifically for deep venous thrombosis (DVT) and pulmonary embolism (PE), according to results published in JAMA Surgery.
“In a subset of patients receiving perioperative RBC transfusions, a synergistic and incremental dose-related risk for VTE development may exist,” Dr. Goel and her coauthors wrote.
The analysis was based on prospectively collected North American registry data including 750,937 patients who underwent a surgical procedure in 2014, of which 47,410 (6.3%) received one or more perioperative RBC transfusions. VTE occurred in 6,309 patients (0.8%), of which 4,336 cases were DVT (0.6%) and 2,514 were PE (0.3%).
The patients who received perioperative RBC transfusions had significantly increased odds of developing VTE in the 30-day postoperative period (adjusted odds ratio, 2.1; 95% confidence interval, 2.0-2.3) versus those who had no transfusions, according to results of a multivariable analysis adjusting for age, sex, length of hospital stay, use of mechanical ventilation, and other potentially confounding factors.
Similarly, researchers found transfused patients had higher odds of both DVT (aOR, 2.2; 95% CI, 2.1-2.4), and PE (aOR, 1.9; 95% CI, 1.7-2.1).
Odds of VTE increased significantly along with increasing number of perioperative RBC transfusions from an aOR of 2.1 for those with just one transfusion to 4.5 for those who had three or more transfusion events (P less than .001 for trend), results of a dose-response analysis showed.
The association between RBC transfusions perioperatively and VTE postoperatively remained robust after propensity score matching and was statistically significant in all surgical subspecialties, the researchers reported.
However, they also noted that these results will require validation in prospective cohort studies and randomized clinical trials. “If proven, they underscore the continued need for more stringent and optimal perioperative blood management practices in addition to rigorous VTE prophylaxis in patients undergoing surgery.”
The study was funded in part by grants from the National Institutes of Health and Cornell University. The researchers reported having no conflicts of interest.
SOURCE: Goel R et al. JAMA Surg. 2018 Jun 13. doi: 10.1001/jamasurg.2018.1565.
FROM JAMA SURGERY
Key clinical point:
Major finding: Patients who received perioperative RBC transfusions had significantly increased odds of developing VTE in the 30-day postoperative period (adjusted odds ratio, 2.1; 95% confidence interval, 2.0-2.3), compared with patients who did not receive transfusions.
Study details: An analysis of prospectively collected North American registry data including 750,937 patients who underwent a surgical procedure in 2014.
Disclosures: The study was funded in part by grants from the National Institutes of Health and Cornell University, New York. The researchers reported having no conflicts of interest.
Source: Goel R et al. JAMA Surg. 2018 Jun 13. doi: 10.1001/jamasurg.2018.1565.
Giving hospitalists a larger clinical footprint
Sneak Peek: The Hospital Leader blog
“We are playing the same sport, but a different game,” the wise, thoughtful emergency medicine attending physician once told me. “I am playing speed chess – I need to make a move quickly, or I lose – no matter what. My moves have to be right, but they don’t always necessarily need to be the optimal one. I am not always thinking five moves ahead. You guys [in internal medicine] are playing master chess. You have more time, but that means you are trying to always think about the whole game and make the best move possible.”
The pendulum has swung quickly from, “problem #7, chronic anemia: stable but I am not sure it has been worked up before, so I ordered a smear, retic count, and iron panel,” to “problem #1, acute blood loss anemia: now stable after transfusion, seems safe for discharge and GI follow-up.” (NOTE: “Acute blood loss anemia” is a phrase I learned from our “clinical documentation integrity specialist” – I think it gets me “50 CDI points” or something.)
Our job is not merely to work shifts and stabilize patients – there already is a specialty for that, and it is not the one we chose.
Clearly the correct balance is somewhere between the two extremes of “working up everything” and “deferring (nearly) everything to the outpatient setting.”
There are many forces that are contributing to current hospitalist work styles. As the work continues to become more exhaustingly intense and the average number of patients seen by a hospitalist grows impossibly upward, the duration of on-service stints has shortened.
In most settings, long gone are the days of the month-long teaching attending rotation. By day 12, I feel worn and ragged. For “nonteaching” services, hospitalists seem to increasingly treat each day as a separate shift to be covered, oftentimes handing the service back-and-forth every few days, or a week at most. With this structure, who can possibly think about the “whole patient”? Whose patient is this anyways?
Read the full post at hospitalleader.org.
Also on The Hospital Leader …
- How Hospitalists See the Forgotten Victims of Gun Violence by Vineet Arora, MD, MAPP, MHM
- Hospitals, Hospice and SNFs: The Big Deceit by Brad Flansbaum, DO, MPH, MHM
- But He’s a Good Doctor by Leslie Flores, MHA, SFHM
Sneak Peek: The Hospital Leader blog
Sneak Peek: The Hospital Leader blog
“We are playing the same sport, but a different game,” the wise, thoughtful emergency medicine attending physician once told me. “I am playing speed chess – I need to make a move quickly, or I lose – no matter what. My moves have to be right, but they don’t always necessarily need to be the optimal one. I am not always thinking five moves ahead. You guys [in internal medicine] are playing master chess. You have more time, but that means you are trying to always think about the whole game and make the best move possible.”
The pendulum has swung quickly from, “problem #7, chronic anemia: stable but I am not sure it has been worked up before, so I ordered a smear, retic count, and iron panel,” to “problem #1, acute blood loss anemia: now stable after transfusion, seems safe for discharge and GI follow-up.” (NOTE: “Acute blood loss anemia” is a phrase I learned from our “clinical documentation integrity specialist” – I think it gets me “50 CDI points” or something.)
Our job is not merely to work shifts and stabilize patients – there already is a specialty for that, and it is not the one we chose.
Clearly the correct balance is somewhere between the two extremes of “working up everything” and “deferring (nearly) everything to the outpatient setting.”
There are many forces that are contributing to current hospitalist work styles. As the work continues to become more exhaustingly intense and the average number of patients seen by a hospitalist grows impossibly upward, the duration of on-service stints has shortened.
In most settings, long gone are the days of the month-long teaching attending rotation. By day 12, I feel worn and ragged. For “nonteaching” services, hospitalists seem to increasingly treat each day as a separate shift to be covered, oftentimes handing the service back-and-forth every few days, or a week at most. With this structure, who can possibly think about the “whole patient”? Whose patient is this anyways?
Read the full post at hospitalleader.org.
Also on The Hospital Leader …
- How Hospitalists See the Forgotten Victims of Gun Violence by Vineet Arora, MD, MAPP, MHM
- Hospitals, Hospice and SNFs: The Big Deceit by Brad Flansbaum, DO, MPH, MHM
- But He’s a Good Doctor by Leslie Flores, MHA, SFHM
“We are playing the same sport, but a different game,” the wise, thoughtful emergency medicine attending physician once told me. “I am playing speed chess – I need to make a move quickly, or I lose – no matter what. My moves have to be right, but they don’t always necessarily need to be the optimal one. I am not always thinking five moves ahead. You guys [in internal medicine] are playing master chess. You have more time, but that means you are trying to always think about the whole game and make the best move possible.”
The pendulum has swung quickly from, “problem #7, chronic anemia: stable but I am not sure it has been worked up before, so I ordered a smear, retic count, and iron panel,” to “problem #1, acute blood loss anemia: now stable after transfusion, seems safe for discharge and GI follow-up.” (NOTE: “Acute blood loss anemia” is a phrase I learned from our “clinical documentation integrity specialist” – I think it gets me “50 CDI points” or something.)
Our job is not merely to work shifts and stabilize patients – there already is a specialty for that, and it is not the one we chose.
Clearly the correct balance is somewhere between the two extremes of “working up everything” and “deferring (nearly) everything to the outpatient setting.”
There are many forces that are contributing to current hospitalist work styles. As the work continues to become more exhaustingly intense and the average number of patients seen by a hospitalist grows impossibly upward, the duration of on-service stints has shortened.
In most settings, long gone are the days of the month-long teaching attending rotation. By day 12, I feel worn and ragged. For “nonteaching” services, hospitalists seem to increasingly treat each day as a separate shift to be covered, oftentimes handing the service back-and-forth every few days, or a week at most. With this structure, who can possibly think about the “whole patient”? Whose patient is this anyways?
Read the full post at hospitalleader.org.
Also on The Hospital Leader …
- How Hospitalists See the Forgotten Victims of Gun Violence by Vineet Arora, MD, MAPP, MHM
- Hospitals, Hospice and SNFs: The Big Deceit by Brad Flansbaum, DO, MPH, MHM
- But He’s a Good Doctor by Leslie Flores, MHA, SFHM
Diagnosing pulmonary tuberculosis in the hospital
An uncommon but serious problem in certain populations
Case
A 40-year-old Indian immigrant presented to the emergency department with hemoptysis. He had had an intermittent productive cough for the past 4 weeks with increasing fatigue and lack of appetite. He also had intermittent fever with drenching night sweats. Chest radiograph and CT scan showed a left upper lobe cavitary lesion with infiltrate. He was admitted to the hospital with concern for pneumonia and to rule out possible active pulmonary tuberculosis.
Background
Active pulmonary tuberculosis (APTB) remains an important but often missed diagnosis in hospitalized patients in the Western world.1,2 Because of its relative rarity, the diagnosis of APTB often is delayed in the United States, which can lead hospitalized patients to nosocomial transmission, unnecessary exposures, patient harm,3 and potentially avoidable cost to the health care system.4 The diagnosis and management can be challenging involving isolation needs, sputum clearance, treatment strategy, and criteria for discharge to home.
Diagnosis
Any patient with risk factors presenting with signs and/or symptoms of APTB such as productive cough for more than 4 weeks, night sweats, weight loss, low-grade fevers, upper lobe cavitary lesions, or hemoptysis should be suspected. The diagnostic work-up for APTB should always begin with a thorough medical and social history. A chest radiograph or a CT scan should always be obtained. Risk factors for infection and for progression to active pulmonary TB are listed below.
Risk factors for TB infection:
- Close contacts of a person with APTB.
- Health care workers.
- Immigrants from high-burden countries.
- Homeless people.
- Individuals who have been incarcerated.
- International travelers.
- HIV patients.
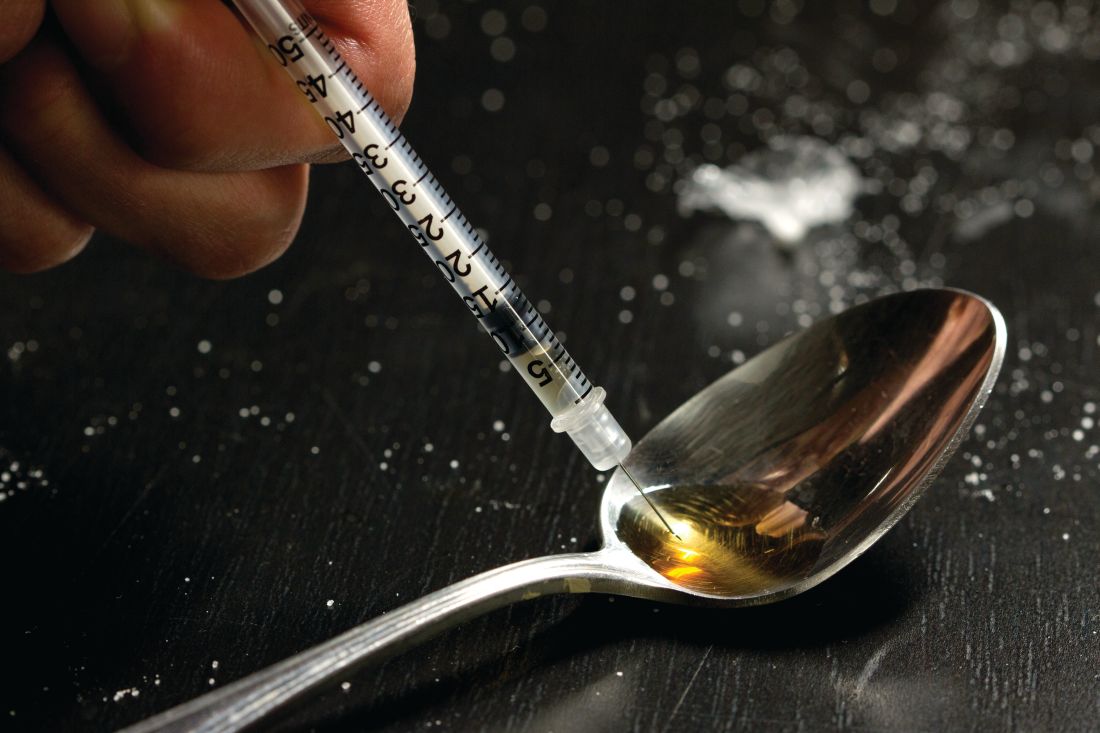
- Intravenous drug users.
Risk factors for progression to APTB:
- HIV infection.
- Intravenous drug use.
- Silicosis.
- Younger than 5 years of age.
- Immunosuppressed.
All patients with suspected or confirmed APTB who cannot be safely discharged home (see discharge considerations below) should be kept in negative-pressure airborne isolation rooms. Isolation can be discontinued once APTB has been ruled out or the patient is determined to be noninfectious based on three consecutive negative sputum smears.
Although rapid and inexpensive, acid-fast bacilli (AFB) smear microscopy has poor sensitivity (45%-80%, with culture-confirmed APTB cases) and poor positive predictive value (50%-80%) for TB in settings in which nontuberculous mycobacteria are commonly isolated. This makes an AFB smear nondiagnostic in the early diagnosis of APTB. The burden of mycobacteria seen in the sputum smear correlates with infectivity.
To improve sensitivity of testing, it is strongly recommended that three AFB smears be completed in 8- to 24-hour intervals and positive smears be accompanied by nucleic acid amplification (NAA) testing.5 If APTB is suspected, but the patient is unable to expectorate, induced sputum samples should be obtained, and, if unable to induce sputum samples, flexible bronchoscopy sampling should be pursued especially for the high-risk populations described above.
The Centers for Disease Control and Prevention recommends that at least one sputum specimen be tested with NAA to expedite the time to diagnosis of APTB. A negative NAA does NOT rule out TB. The turnaround time for this test is about 24-48 hours. NAA has better positive predictive value (greater than 95%) with AFB smear-positive specimens in settings in which nontuberculous mycobacteria are common. The ability to confirm rapidly the presence of Mycobacterium tuberculosis is 50%-80% in AFB smear-negative, culture-positive specimens.6
In patients with clinical or radiologic suspicion of APTB who are unable to produce sputum or have negative sputum smear microscopy results, bronchoscopy is a safe and reliable method for the diagnosis of pulmonary tuberculosis. For the diagnosis of tuberculosis, bronchoalveolar lavage has a sensitivity and specificity of 60% and 100%, respectively. Adding transbronchial biopsy further increases the sensitivity to 84%, and post-bronchoscopy sputum smear microscopy increases the sensitivity to 94%.6
In 2005, the CDC released guidelines for using interferon-gamma release assays (IGRA) to test for M. tuberculosis infection.7 Both tuberculin skin testing (TST) and IGRAs assess lymphocytes’ response to M. tuberculosis. Although these tests can be supportive of a previous tuberculosis infection, they are not diagnostic tests for APTB. Neither an IGRA nor a TST can distinguish latent from active tuberculosis.
Sputum AFB culture remains the preferred method for laboratory confirmation of APTB. Once APTB is confirmed, it is essential for susceptibility testing and genotyping. However, in the absence of a positive culture, APTB can be diagnosed based on signs and symptoms alone in a high-risk patient.
Treatment
A multidisciplinary, patient-centered approach involving the patient, providers, and public health officials is required to accomplish the following treatment goals: eradicating Mycobacterium infection, eliminating the risk of transmission, avoiding the disease, and preventing drug resistance.8
Infectious disease consultation is mandatory in all HIV-positive and suspected or confirmed multidrug-resistant cases. Directly observed therapy is an essential component of APTB treatment to ensure compliance in many situations.
Admission and discharge
Admission to a hospital is not required unless a patient meets criteria for admission independent of APTB diagnosis, or proper risk stratification and assessment cannot be completed in a timely manner. A patient with suspected APTB should be placed in airborne isolation. All staff should wear N95 disposable masks or respirators while inside the patient’s room.9
Discharge considerations are listed below:
- Inform the department of health (DOH).
- Establish proper isolation precautions to minimize exposure.
- Ensure ability to stay at home until DOH and physician determines noninfectivity.
- Educate the patient about length of therapy, directly observed therapy, side effects and importance of compliance.
- Coordinate discharge with the DOH.
- Make sure proper follow-up is scheduled.
Back to the case
Our patient was placed on airborne respiratory isolation immediately upon admission and sputum was sent for AFB. Sputum smear was positive for AFB as well as a positive nucleic acid testing for Mycobacterium tuberculosis. HIV antibody testing was negative. Once the sputum AFB was determined to be positive, the department of health was informed. He was started on the intensive phase of therapy with pyrazinamide, rifampin, ethambutol, and isoniazid along with pyridoxine. He tolerated his medications well and had no immediate reactions. His family and close contacts were screened and advised to be tested.
The patient was discharged after proper follow-up with primary care doctor was scheduled. The department of health arranged for directly observed therapy. He received information about the importance of taking all of his medications and staying at home except for medical visits until the DOH had deemed him to be noninfectious.
Bottom line
APTB in the hospital is an uncommon but serious problem in certain populations. It requires a high index of suspicion and a multidisciplinary approach for effective treatment and prevention of transmission.
Dr. Mallampalli is an attending physician in hospital medicine at Geisinger in Danville, Pa., and clinical assistant professor at Temple University, Philadelphia. Dr. Velidi is an attending physician in hospital medicine at Geisinger. Dr. Courtney is associate director of the department of hospital medicine at Geisinger.
References
1. Miller AC et al. Missed opportunities to diagnose tuberculosis are common among hospitalized patients and patients seen in emergency departments. Open Forum Infectious Diseases. 2015. doi. org/10.1093/ofid/ofv171.
2. Greenaway C et al and the Canadian Collaborative Group in Nosocomial Transmission of Tuberculosis. Delay in diagnosis among hospitalized patients with active tuberculosis–predictors and outcomes. Am J Respir Crit Care Med. 2002 Apr;165:927-33.
3. Medrano BA et al. A missed tuberculosis diagnosis resulting in hospital transmission. Infect Control Hosp Epidemiol. 2014 May;35(5):534-7.
4. Kelly AM et al. Delayed tuberculosis diagnosis and costs of contact investigations for hospital exposure: New York City, 2010-2014. Am J Infect Control. 2017 May 1;45(5):483-6.
5. Lewinsohn DM et al. Official ATS/IDSA/CDC Clinical Practice Guidelines: Diagnosis of tuberculosis in adults and children. Clin Infect Dis. 2017 Jan;64:111-5.
6. Mazurek GH et al. Guidelines for using the QuantiFERON-TB Gold test for detecting Mycobacterium tuberculosis infection, United States. MMWR Recomm Rep. 2005 Dec 16;54(RR-15):49-55.
7. CDC. Trends in tuberculosis – United States, 2010. MMWR Morb Mortal Wkly Rep. 2011 Mar 25;60(11):333-7.
8. Jensen PA et al. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings, 2005. MMWR Recomm Rep. 2005 Dec 30;54(RR-17):1-141.
9. Siegel JD et al and the Health Care Infection Control Practices Advisory Committee. 2007 Guideline for isolation precautions: Preventing transmission of infectious agents in health care settings. Am J Infect Control. 2007 Dec;35(10 Suppl 2):S65-164.
An uncommon but serious problem in certain populations
An uncommon but serious problem in certain populations
Case
A 40-year-old Indian immigrant presented to the emergency department with hemoptysis. He had had an intermittent productive cough for the past 4 weeks with increasing fatigue and lack of appetite. He also had intermittent fever with drenching night sweats. Chest radiograph and CT scan showed a left upper lobe cavitary lesion with infiltrate. He was admitted to the hospital with concern for pneumonia and to rule out possible active pulmonary tuberculosis.
Background
Active pulmonary tuberculosis (APTB) remains an important but often missed diagnosis in hospitalized patients in the Western world.1,2 Because of its relative rarity, the diagnosis of APTB often is delayed in the United States, which can lead hospitalized patients to nosocomial transmission, unnecessary exposures, patient harm,3 and potentially avoidable cost to the health care system.4 The diagnosis and management can be challenging involving isolation needs, sputum clearance, treatment strategy, and criteria for discharge to home.
Diagnosis
Any patient with risk factors presenting with signs and/or symptoms of APTB such as productive cough for more than 4 weeks, night sweats, weight loss, low-grade fevers, upper lobe cavitary lesions, or hemoptysis should be suspected. The diagnostic work-up for APTB should always begin with a thorough medical and social history. A chest radiograph or a CT scan should always be obtained. Risk factors for infection and for progression to active pulmonary TB are listed below.
Risk factors for TB infection:
- Close contacts of a person with APTB.
- Health care workers.
- Immigrants from high-burden countries.
- Homeless people.
- Individuals who have been incarcerated.
- International travelers.
- HIV patients.
- Intravenous drug users.
Risk factors for progression to APTB:
- HIV infection.
- Intravenous drug use.
- Silicosis.
- Younger than 5 years of age.
- Immunosuppressed.
All patients with suspected or confirmed APTB who cannot be safely discharged home (see discharge considerations below) should be kept in negative-pressure airborne isolation rooms. Isolation can be discontinued once APTB has been ruled out or the patient is determined to be noninfectious based on three consecutive negative sputum smears.
Although rapid and inexpensive, acid-fast bacilli (AFB) smear microscopy has poor sensitivity (45%-80%, with culture-confirmed APTB cases) and poor positive predictive value (50%-80%) for TB in settings in which nontuberculous mycobacteria are commonly isolated. This makes an AFB smear nondiagnostic in the early diagnosis of APTB. The burden of mycobacteria seen in the sputum smear correlates with infectivity.
To improve sensitivity of testing, it is strongly recommended that three AFB smears be completed in 8- to 24-hour intervals and positive smears be accompanied by nucleic acid amplification (NAA) testing.5 If APTB is suspected, but the patient is unable to expectorate, induced sputum samples should be obtained, and, if unable to induce sputum samples, flexible bronchoscopy sampling should be pursued especially for the high-risk populations described above.
The Centers for Disease Control and Prevention recommends that at least one sputum specimen be tested with NAA to expedite the time to diagnosis of APTB. A negative NAA does NOT rule out TB. The turnaround time for this test is about 24-48 hours. NAA has better positive predictive value (greater than 95%) with AFB smear-positive specimens in settings in which nontuberculous mycobacteria are common. The ability to confirm rapidly the presence of Mycobacterium tuberculosis is 50%-80% in AFB smear-negative, culture-positive specimens.6
In patients with clinical or radiologic suspicion of APTB who are unable to produce sputum or have negative sputum smear microscopy results, bronchoscopy is a safe and reliable method for the diagnosis of pulmonary tuberculosis. For the diagnosis of tuberculosis, bronchoalveolar lavage has a sensitivity and specificity of 60% and 100%, respectively. Adding transbronchial biopsy further increases the sensitivity to 84%, and post-bronchoscopy sputum smear microscopy increases the sensitivity to 94%.6
In 2005, the CDC released guidelines for using interferon-gamma release assays (IGRA) to test for M. tuberculosis infection.7 Both tuberculin skin testing (TST) and IGRAs assess lymphocytes’ response to M. tuberculosis. Although these tests can be supportive of a previous tuberculosis infection, they are not diagnostic tests for APTB. Neither an IGRA nor a TST can distinguish latent from active tuberculosis.
Sputum AFB culture remains the preferred method for laboratory confirmation of APTB. Once APTB is confirmed, it is essential for susceptibility testing and genotyping. However, in the absence of a positive culture, APTB can be diagnosed based on signs and symptoms alone in a high-risk patient.
Treatment
A multidisciplinary, patient-centered approach involving the patient, providers, and public health officials is required to accomplish the following treatment goals: eradicating Mycobacterium infection, eliminating the risk of transmission, avoiding the disease, and preventing drug resistance.8
Infectious disease consultation is mandatory in all HIV-positive and suspected or confirmed multidrug-resistant cases. Directly observed therapy is an essential component of APTB treatment to ensure compliance in many situations.
Admission and discharge
Admission to a hospital is not required unless a patient meets criteria for admission independent of APTB diagnosis, or proper risk stratification and assessment cannot be completed in a timely manner. A patient with suspected APTB should be placed in airborne isolation. All staff should wear N95 disposable masks or respirators while inside the patient’s room.9
Discharge considerations are listed below:
- Inform the department of health (DOH).
- Establish proper isolation precautions to minimize exposure.
- Ensure ability to stay at home until DOH and physician determines noninfectivity.
- Educate the patient about length of therapy, directly observed therapy, side effects and importance of compliance.
- Coordinate discharge with the DOH.
- Make sure proper follow-up is scheduled.
Back to the case
Our patient was placed on airborne respiratory isolation immediately upon admission and sputum was sent for AFB. Sputum smear was positive for AFB as well as a positive nucleic acid testing for Mycobacterium tuberculosis. HIV antibody testing was negative. Once the sputum AFB was determined to be positive, the department of health was informed. He was started on the intensive phase of therapy with pyrazinamide, rifampin, ethambutol, and isoniazid along with pyridoxine. He tolerated his medications well and had no immediate reactions. His family and close contacts were screened and advised to be tested.
The patient was discharged after proper follow-up with primary care doctor was scheduled. The department of health arranged for directly observed therapy. He received information about the importance of taking all of his medications and staying at home except for medical visits until the DOH had deemed him to be noninfectious.
Bottom line
APTB in the hospital is an uncommon but serious problem in certain populations. It requires a high index of suspicion and a multidisciplinary approach for effective treatment and prevention of transmission.
Dr. Mallampalli is an attending physician in hospital medicine at Geisinger in Danville, Pa., and clinical assistant professor at Temple University, Philadelphia. Dr. Velidi is an attending physician in hospital medicine at Geisinger. Dr. Courtney is associate director of the department of hospital medicine at Geisinger.
References
1. Miller AC et al. Missed opportunities to diagnose tuberculosis are common among hospitalized patients and patients seen in emergency departments. Open Forum Infectious Diseases. 2015. doi. org/10.1093/ofid/ofv171.
2. Greenaway C et al and the Canadian Collaborative Group in Nosocomial Transmission of Tuberculosis. Delay in diagnosis among hospitalized patients with active tuberculosis–predictors and outcomes. Am J Respir Crit Care Med. 2002 Apr;165:927-33.
3. Medrano BA et al. A missed tuberculosis diagnosis resulting in hospital transmission. Infect Control Hosp Epidemiol. 2014 May;35(5):534-7.
4. Kelly AM et al. Delayed tuberculosis diagnosis and costs of contact investigations for hospital exposure: New York City, 2010-2014. Am J Infect Control. 2017 May 1;45(5):483-6.
5. Lewinsohn DM et al. Official ATS/IDSA/CDC Clinical Practice Guidelines: Diagnosis of tuberculosis in adults and children. Clin Infect Dis. 2017 Jan;64:111-5.
6. Mazurek GH et al. Guidelines for using the QuantiFERON-TB Gold test for detecting Mycobacterium tuberculosis infection, United States. MMWR Recomm Rep. 2005 Dec 16;54(RR-15):49-55.
7. CDC. Trends in tuberculosis – United States, 2010. MMWR Morb Mortal Wkly Rep. 2011 Mar 25;60(11):333-7.
8. Jensen PA et al. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings, 2005. MMWR Recomm Rep. 2005 Dec 30;54(RR-17):1-141.
9. Siegel JD et al and the Health Care Infection Control Practices Advisory Committee. 2007 Guideline for isolation precautions: Preventing transmission of infectious agents in health care settings. Am J Infect Control. 2007 Dec;35(10 Suppl 2):S65-164.
Case
A 40-year-old Indian immigrant presented to the emergency department with hemoptysis. He had had an intermittent productive cough for the past 4 weeks with increasing fatigue and lack of appetite. He also had intermittent fever with drenching night sweats. Chest radiograph and CT scan showed a left upper lobe cavitary lesion with infiltrate. He was admitted to the hospital with concern for pneumonia and to rule out possible active pulmonary tuberculosis.
Background
Active pulmonary tuberculosis (APTB) remains an important but often missed diagnosis in hospitalized patients in the Western world.1,2 Because of its relative rarity, the diagnosis of APTB often is delayed in the United States, which can lead hospitalized patients to nosocomial transmission, unnecessary exposures, patient harm,3 and potentially avoidable cost to the health care system.4 The diagnosis and management can be challenging involving isolation needs, sputum clearance, treatment strategy, and criteria for discharge to home.
Diagnosis
Any patient with risk factors presenting with signs and/or symptoms of APTB such as productive cough for more than 4 weeks, night sweats, weight loss, low-grade fevers, upper lobe cavitary lesions, or hemoptysis should be suspected. The diagnostic work-up for APTB should always begin with a thorough medical and social history. A chest radiograph or a CT scan should always be obtained. Risk factors for infection and for progression to active pulmonary TB are listed below.
Risk factors for TB infection:
- Close contacts of a person with APTB.
- Health care workers.
- Immigrants from high-burden countries.
- Homeless people.
- Individuals who have been incarcerated.
- International travelers.
- HIV patients.
- Intravenous drug users.
Risk factors for progression to APTB:
- HIV infection.
- Intravenous drug use.
- Silicosis.
- Younger than 5 years of age.
- Immunosuppressed.
All patients with suspected or confirmed APTB who cannot be safely discharged home (see discharge considerations below) should be kept in negative-pressure airborne isolation rooms. Isolation can be discontinued once APTB has been ruled out or the patient is determined to be noninfectious based on three consecutive negative sputum smears.
Although rapid and inexpensive, acid-fast bacilli (AFB) smear microscopy has poor sensitivity (45%-80%, with culture-confirmed APTB cases) and poor positive predictive value (50%-80%) for TB in settings in which nontuberculous mycobacteria are commonly isolated. This makes an AFB smear nondiagnostic in the early diagnosis of APTB. The burden of mycobacteria seen in the sputum smear correlates with infectivity.
To improve sensitivity of testing, it is strongly recommended that three AFB smears be completed in 8- to 24-hour intervals and positive smears be accompanied by nucleic acid amplification (NAA) testing.5 If APTB is suspected, but the patient is unable to expectorate, induced sputum samples should be obtained, and, if unable to induce sputum samples, flexible bronchoscopy sampling should be pursued especially for the high-risk populations described above.
The Centers for Disease Control and Prevention recommends that at least one sputum specimen be tested with NAA to expedite the time to diagnosis of APTB. A negative NAA does NOT rule out TB. The turnaround time for this test is about 24-48 hours. NAA has better positive predictive value (greater than 95%) with AFB smear-positive specimens in settings in which nontuberculous mycobacteria are common. The ability to confirm rapidly the presence of Mycobacterium tuberculosis is 50%-80% in AFB smear-negative, culture-positive specimens.6
In patients with clinical or radiologic suspicion of APTB who are unable to produce sputum or have negative sputum smear microscopy results, bronchoscopy is a safe and reliable method for the diagnosis of pulmonary tuberculosis. For the diagnosis of tuberculosis, bronchoalveolar lavage has a sensitivity and specificity of 60% and 100%, respectively. Adding transbronchial biopsy further increases the sensitivity to 84%, and post-bronchoscopy sputum smear microscopy increases the sensitivity to 94%.6
In 2005, the CDC released guidelines for using interferon-gamma release assays (IGRA) to test for M. tuberculosis infection.7 Both tuberculin skin testing (TST) and IGRAs assess lymphocytes’ response to M. tuberculosis. Although these tests can be supportive of a previous tuberculosis infection, they are not diagnostic tests for APTB. Neither an IGRA nor a TST can distinguish latent from active tuberculosis.
Sputum AFB culture remains the preferred method for laboratory confirmation of APTB. Once APTB is confirmed, it is essential for susceptibility testing and genotyping. However, in the absence of a positive culture, APTB can be diagnosed based on signs and symptoms alone in a high-risk patient.
Treatment
A multidisciplinary, patient-centered approach involving the patient, providers, and public health officials is required to accomplish the following treatment goals: eradicating Mycobacterium infection, eliminating the risk of transmission, avoiding the disease, and preventing drug resistance.8
Infectious disease consultation is mandatory in all HIV-positive and suspected or confirmed multidrug-resistant cases. Directly observed therapy is an essential component of APTB treatment to ensure compliance in many situations.
Admission and discharge
Admission to a hospital is not required unless a patient meets criteria for admission independent of APTB diagnosis, or proper risk stratification and assessment cannot be completed in a timely manner. A patient with suspected APTB should be placed in airborne isolation. All staff should wear N95 disposable masks or respirators while inside the patient’s room.9
Discharge considerations are listed below:
- Inform the department of health (DOH).
- Establish proper isolation precautions to minimize exposure.
- Ensure ability to stay at home until DOH and physician determines noninfectivity.
- Educate the patient about length of therapy, directly observed therapy, side effects and importance of compliance.
- Coordinate discharge with the DOH.
- Make sure proper follow-up is scheduled.
Back to the case
Our patient was placed on airborne respiratory isolation immediately upon admission and sputum was sent for AFB. Sputum smear was positive for AFB as well as a positive nucleic acid testing for Mycobacterium tuberculosis. HIV antibody testing was negative. Once the sputum AFB was determined to be positive, the department of health was informed. He was started on the intensive phase of therapy with pyrazinamide, rifampin, ethambutol, and isoniazid along with pyridoxine. He tolerated his medications well and had no immediate reactions. His family and close contacts were screened and advised to be tested.
The patient was discharged after proper follow-up with primary care doctor was scheduled. The department of health arranged for directly observed therapy. He received information about the importance of taking all of his medications and staying at home except for medical visits until the DOH had deemed him to be noninfectious.
Bottom line
APTB in the hospital is an uncommon but serious problem in certain populations. It requires a high index of suspicion and a multidisciplinary approach for effective treatment and prevention of transmission.
Dr. Mallampalli is an attending physician in hospital medicine at Geisinger in Danville, Pa., and clinical assistant professor at Temple University, Philadelphia. Dr. Velidi is an attending physician in hospital medicine at Geisinger. Dr. Courtney is associate director of the department of hospital medicine at Geisinger.
References
1. Miller AC et al. Missed opportunities to diagnose tuberculosis are common among hospitalized patients and patients seen in emergency departments. Open Forum Infectious Diseases. 2015. doi. org/10.1093/ofid/ofv171.
2. Greenaway C et al and the Canadian Collaborative Group in Nosocomial Transmission of Tuberculosis. Delay in diagnosis among hospitalized patients with active tuberculosis–predictors and outcomes. Am J Respir Crit Care Med. 2002 Apr;165:927-33.
3. Medrano BA et al. A missed tuberculosis diagnosis resulting in hospital transmission. Infect Control Hosp Epidemiol. 2014 May;35(5):534-7.
4. Kelly AM et al. Delayed tuberculosis diagnosis and costs of contact investigations for hospital exposure: New York City, 2010-2014. Am J Infect Control. 2017 May 1;45(5):483-6.
5. Lewinsohn DM et al. Official ATS/IDSA/CDC Clinical Practice Guidelines: Diagnosis of tuberculosis in adults and children. Clin Infect Dis. 2017 Jan;64:111-5.
6. Mazurek GH et al. Guidelines for using the QuantiFERON-TB Gold test for detecting Mycobacterium tuberculosis infection, United States. MMWR Recomm Rep. 2005 Dec 16;54(RR-15):49-55.
7. CDC. Trends in tuberculosis – United States, 2010. MMWR Morb Mortal Wkly Rep. 2011 Mar 25;60(11):333-7.
8. Jensen PA et al. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings, 2005. MMWR Recomm Rep. 2005 Dec 30;54(RR-17):1-141.
9. Siegel JD et al and the Health Care Infection Control Practices Advisory Committee. 2007 Guideline for isolation precautions: Preventing transmission of infectious agents in health care settings. Am J Infect Control. 2007 Dec;35(10 Suppl 2):S65-164.
hs-cTnT test tied to fewer reinfarctions but no survival benefit
The introduction of the new high-sensitivity cardiac troponin T (hs-cTnT) test was linked with an 11% decrease in reinfarctions but showed no evidence of improving survival in a large longitudinal cohort study.
Over an average of 3.9 years of follow-up, the adjusted risk of all-cause mortality was identical whether patients’ initial MI was diagnosed with the new troponin test or the conventional one, reported Maria Odqvist, MD, of South Alvsborg Hospital, Boras, Sweden, and her associates. “As hs-cTn assays become widely available and clinicians gain experience interpreting the results, more work is needed to enhance clinical reasoning and implementation to improve patient outcomes,” the researchers wrote in the Journal of the American College of Cardiology.
High-sensitivity cardiac troponin T assays detect acute coronary syndrome more rapidly than their conventional predecessors. However, hs-cTnT’s higher sensitivity comes with lost specificity and hence has raised concerns about potentially wasting health care resources. Some clinicians have asked whether the new test is worthwhile and how to maximize its benefits.
The study, which included nearly 88,000 patients with initial MI from the Swedish National Patient Registry, spanned 2009-2013, when 73% of Swedish acute care hospitals transitioned from conventional troponin tests (cTn) to hs-cTnT. After adjustment for factors such as age, sex, location, chronic kidney disease, cardiovascular history, and prescriptions, Dr. Odqvist and her associates compared each test types’ risks of death, reinfarction, coronary angiography, and revascularization among patients diagnosed.
In all, 47,133 (54%) patients’ initial MI was diagnosed with cTn while 46% were diagnosed with hs-cTnT. Overall, the rate of MI rose by 5% during the 90 days after hospitals implemented hs-cTnT, compared with the 90 days before. But hospitals used varying hs-cTnT thresholds for MI, which might explain why some hospitals initially observed a marked initial decrease in MI while others saw a relatively large increase, the investigators wrote.
There were 15,766 reinfarctions over an average of 3.1 years of follow-up. Although there was no difference in all-cause mortality, risk of reinfarction was 11% lower among patients diagnosed using hs-cTnT, compared with those diagnosed by cTn.
At the hospital level, coronary angiography and revascularization became only slightly more common during the 3 months after hospitals switched to hs-cTnT, the researchers wrote. However, patients whose MIs were diagnosed with hs-cTnT were 16% more likely to undergo coronary angiography and 13% more likely to undergo revascularization within the next 30 days, compared with patients diagnosed with cTn. Patients diagnosed with hs-cTnT also were more likely to receive statins, but trends in other prescriptions did not change.
The Swedish Heart-Lung Foundation funded one investigator. Dr. Odqvist and one coinvestigator reported having no relevant conflicts of interest. Senior author Martin J. Holzmann, MD, PhD, disclosed ties to Actelion and Pfizer. Two other coinvestigators disclosed ties to Roche, Gilead, Janssen, Abbvie, CTI Bipharma, GlaxoSmithKline, Abbott Laboratories, and AstraZeneca, and Fiomi Diagnostics.
SOURCE: Odqvist M et al. J Am Coll Cardiol. 2018 Jun 12;71(23):2616-24
It’s unclear why reinfarctions were 11% lower after MI was diagnosed with high-sensitivity cardiac troponin (hs-cTn) assays instead of conventional troponin tests in this study.
Use of evidence-based medicines changed only slightly after hospitals implemented the switch. It is tempting to associate the reduction in reinfarction with increased use of angiography and revascularization, but this may be too simplistic. Intervention might have most benefited patients whom conventional troponin assay would have missed. Shifts in medication compliance or rehabilitation might also have been factors.
Used appropriately, hs-cTnT assays can more rapidly rule MI in or out, shorten emergency department stays, and cut costs. Based on the Swedish experience, the increase in MI diagnoses will be modest and manageable. Nonetheless, we will need to develop strategies to manage patients with myonecrosis from etiologies other than MI that will be detected using hs-cTn assays.
L. Kristin Newby, MD, MHS , and Angela Lowenstern, MD , of Duke University in Durham, N.C., made these comments in an accompanying editorial (J Am Coll Cardiol. 2018;71:625-7). Dr. Newby has received consulting honoraria from Roche Diagnostics, Ortho-Clinical Diagnostics, and Philips Healthcare. Dr. Lowenstern is supported by a National Institutes of Health training grant to Duke University .
It’s unclear why reinfarctions were 11% lower after MI was diagnosed with high-sensitivity cardiac troponin (hs-cTn) assays instead of conventional troponin tests in this study.
Use of evidence-based medicines changed only slightly after hospitals implemented the switch. It is tempting to associate the reduction in reinfarction with increased use of angiography and revascularization, but this may be too simplistic. Intervention might have most benefited patients whom conventional troponin assay would have missed. Shifts in medication compliance or rehabilitation might also have been factors.
Used appropriately, hs-cTnT assays can more rapidly rule MI in or out, shorten emergency department stays, and cut costs. Based on the Swedish experience, the increase in MI diagnoses will be modest and manageable. Nonetheless, we will need to develop strategies to manage patients with myonecrosis from etiologies other than MI that will be detected using hs-cTn assays.
L. Kristin Newby, MD, MHS , and Angela Lowenstern, MD , of Duke University in Durham, N.C., made these comments in an accompanying editorial (J Am Coll Cardiol. 2018;71:625-7). Dr. Newby has received consulting honoraria from Roche Diagnostics, Ortho-Clinical Diagnostics, and Philips Healthcare. Dr. Lowenstern is supported by a National Institutes of Health training grant to Duke University .
It’s unclear why reinfarctions were 11% lower after MI was diagnosed with high-sensitivity cardiac troponin (hs-cTn) assays instead of conventional troponin tests in this study.
Use of evidence-based medicines changed only slightly after hospitals implemented the switch. It is tempting to associate the reduction in reinfarction with increased use of angiography and revascularization, but this may be too simplistic. Intervention might have most benefited patients whom conventional troponin assay would have missed. Shifts in medication compliance or rehabilitation might also have been factors.
Used appropriately, hs-cTnT assays can more rapidly rule MI in or out, shorten emergency department stays, and cut costs. Based on the Swedish experience, the increase in MI diagnoses will be modest and manageable. Nonetheless, we will need to develop strategies to manage patients with myonecrosis from etiologies other than MI that will be detected using hs-cTn assays.
L. Kristin Newby, MD, MHS , and Angela Lowenstern, MD , of Duke University in Durham, N.C., made these comments in an accompanying editorial (J Am Coll Cardiol. 2018;71:625-7). Dr. Newby has received consulting honoraria from Roche Diagnostics, Ortho-Clinical Diagnostics, and Philips Healthcare. Dr. Lowenstern is supported by a National Institutes of Health training grant to Duke University .
The introduction of the new high-sensitivity cardiac troponin T (hs-cTnT) test was linked with an 11% decrease in reinfarctions but showed no evidence of improving survival in a large longitudinal cohort study.
Over an average of 3.9 years of follow-up, the adjusted risk of all-cause mortality was identical whether patients’ initial MI was diagnosed with the new troponin test or the conventional one, reported Maria Odqvist, MD, of South Alvsborg Hospital, Boras, Sweden, and her associates. “As hs-cTn assays become widely available and clinicians gain experience interpreting the results, more work is needed to enhance clinical reasoning and implementation to improve patient outcomes,” the researchers wrote in the Journal of the American College of Cardiology.
High-sensitivity cardiac troponin T assays detect acute coronary syndrome more rapidly than their conventional predecessors. However, hs-cTnT’s higher sensitivity comes with lost specificity and hence has raised concerns about potentially wasting health care resources. Some clinicians have asked whether the new test is worthwhile and how to maximize its benefits.
The study, which included nearly 88,000 patients with initial MI from the Swedish National Patient Registry, spanned 2009-2013, when 73% of Swedish acute care hospitals transitioned from conventional troponin tests (cTn) to hs-cTnT. After adjustment for factors such as age, sex, location, chronic kidney disease, cardiovascular history, and prescriptions, Dr. Odqvist and her associates compared each test types’ risks of death, reinfarction, coronary angiography, and revascularization among patients diagnosed.
In all, 47,133 (54%) patients’ initial MI was diagnosed with cTn while 46% were diagnosed with hs-cTnT. Overall, the rate of MI rose by 5% during the 90 days after hospitals implemented hs-cTnT, compared with the 90 days before. But hospitals used varying hs-cTnT thresholds for MI, which might explain why some hospitals initially observed a marked initial decrease in MI while others saw a relatively large increase, the investigators wrote.
There were 15,766 reinfarctions over an average of 3.1 years of follow-up. Although there was no difference in all-cause mortality, risk of reinfarction was 11% lower among patients diagnosed using hs-cTnT, compared with those diagnosed by cTn.
At the hospital level, coronary angiography and revascularization became only slightly more common during the 3 months after hospitals switched to hs-cTnT, the researchers wrote. However, patients whose MIs were diagnosed with hs-cTnT were 16% more likely to undergo coronary angiography and 13% more likely to undergo revascularization within the next 30 days, compared with patients diagnosed with cTn. Patients diagnosed with hs-cTnT also were more likely to receive statins, but trends in other prescriptions did not change.
The Swedish Heart-Lung Foundation funded one investigator. Dr. Odqvist and one coinvestigator reported having no relevant conflicts of interest. Senior author Martin J. Holzmann, MD, PhD, disclosed ties to Actelion and Pfizer. Two other coinvestigators disclosed ties to Roche, Gilead, Janssen, Abbvie, CTI Bipharma, GlaxoSmithKline, Abbott Laboratories, and AstraZeneca, and Fiomi Diagnostics.
SOURCE: Odqvist M et al. J Am Coll Cardiol. 2018 Jun 12;71(23):2616-24
The introduction of the new high-sensitivity cardiac troponin T (hs-cTnT) test was linked with an 11% decrease in reinfarctions but showed no evidence of improving survival in a large longitudinal cohort study.
Over an average of 3.9 years of follow-up, the adjusted risk of all-cause mortality was identical whether patients’ initial MI was diagnosed with the new troponin test or the conventional one, reported Maria Odqvist, MD, of South Alvsborg Hospital, Boras, Sweden, and her associates. “As hs-cTn assays become widely available and clinicians gain experience interpreting the results, more work is needed to enhance clinical reasoning and implementation to improve patient outcomes,” the researchers wrote in the Journal of the American College of Cardiology.
High-sensitivity cardiac troponin T assays detect acute coronary syndrome more rapidly than their conventional predecessors. However, hs-cTnT’s higher sensitivity comes with lost specificity and hence has raised concerns about potentially wasting health care resources. Some clinicians have asked whether the new test is worthwhile and how to maximize its benefits.
The study, which included nearly 88,000 patients with initial MI from the Swedish National Patient Registry, spanned 2009-2013, when 73% of Swedish acute care hospitals transitioned from conventional troponin tests (cTn) to hs-cTnT. After adjustment for factors such as age, sex, location, chronic kidney disease, cardiovascular history, and prescriptions, Dr. Odqvist and her associates compared each test types’ risks of death, reinfarction, coronary angiography, and revascularization among patients diagnosed.
In all, 47,133 (54%) patients’ initial MI was diagnosed with cTn while 46% were diagnosed with hs-cTnT. Overall, the rate of MI rose by 5% during the 90 days after hospitals implemented hs-cTnT, compared with the 90 days before. But hospitals used varying hs-cTnT thresholds for MI, which might explain why some hospitals initially observed a marked initial decrease in MI while others saw a relatively large increase, the investigators wrote.
There were 15,766 reinfarctions over an average of 3.1 years of follow-up. Although there was no difference in all-cause mortality, risk of reinfarction was 11% lower among patients diagnosed using hs-cTnT, compared with those diagnosed by cTn.
At the hospital level, coronary angiography and revascularization became only slightly more common during the 3 months after hospitals switched to hs-cTnT, the researchers wrote. However, patients whose MIs were diagnosed with hs-cTnT were 16% more likely to undergo coronary angiography and 13% more likely to undergo revascularization within the next 30 days, compared with patients diagnosed with cTn. Patients diagnosed with hs-cTnT also were more likely to receive statins, but trends in other prescriptions did not change.
The Swedish Heart-Lung Foundation funded one investigator. Dr. Odqvist and one coinvestigator reported having no relevant conflicts of interest. Senior author Martin J. Holzmann, MD, PhD, disclosed ties to Actelion and Pfizer. Two other coinvestigators disclosed ties to Roche, Gilead, Janssen, Abbvie, CTI Bipharma, GlaxoSmithKline, Abbott Laboratories, and AstraZeneca, and Fiomi Diagnostics.
SOURCE: Odqvist M et al. J Am Coll Cardiol. 2018 Jun 12;71(23):2616-24
FROM JACC
Key clinical point: The introduction of the new high-sensitivity cardiac troponin T test was associated with an 11% decrease in reinfarctions but showed no evidence of improving survival.
Major finding: Over an average of 3.9 years of follow-up, the adjusted risk of all-cause mortality was identical whether patients’ initial MI was diagnosed with the new troponin test or with the conventional one.
Study details: National cohort study of 87,879 patients with first myocardial infarction, 2009-2013.
Disclosures: Dr. Odqvist and one coinvestigator had no relevant disclosures. Senior author Martin J. Holzmann, MD, PhD, disclosed ties to Actelion and Pfizer. Two other coinvestigators disclosed ties to Roche, Gilead, Janssen, AbbVie, CTI Biopharma, GlaxoSmithKline, Abbott Laboratories, and AstraZeneca, and Fiomi Diagnostics.
Source: Odqvist M et al. J Am Coll Cardiol. 2018 Jun 12;71(23):2616-24.
High-dose opioid prescribing linked to heroin use risk among U.S. veterans
SAN DIEGO – High-dose opioid prescribing is associated with an increased risk of heroin use among U.S. veterans, a prospective study showed.
“Despite evidence linking increased risk of opioid use disorder with specific opioid prescribing patterns, the relationship between these practices and heroin use is less understood,” researchers led by Geetanjoli Banerjee wrote in an abstract presented during the annual meeting of the College on Problems of Drug Dependence. “Understanding the relationship between prescription opioid use and initiation of heroin use among veterans is particularly important, as this population has both a higher underlying prevalence of substance abuse disorders and pain conditions.”
Ms. Banerjee, a graduate student at Brown University, Providence, R.I., and her associates examined data from 3,570 individuals enrolled in the Veterans Aging Cohort Study without nonmedical use or prescription opioids or heroin use in the year prior to baseline, and who received more than one prescription opioid from the VA during follow-up. between 2002 and 2012.
Among the 3,833 eligible participants, the proportion who were prescribed high-dose opioids (defined as a morphine equivalent daily dose of 90 mg or greater) did not change significantly between 2002 and 2012, and ranged from 4.4% to 5.9% (P = .22). The researchers also found that the 10-year incidence rate of recent heroin use was 8.15 event per 1,000 person-years. The time to recent heroin use differed significantly between participants with and without prior receipt of a high-dose prescription at baseline (P less than .001). Multivariable Cox regression analysis showed that prior receipt of a high-dose opioid prescription was associated with recent heroin use (adjusted hazard ratio, 2.54).
“Among patients who report no past year illicit use of opioids at baseline and who are receiving prescription opioids from the VA, receipt of high-dose prescription opioid increased the risk of subsequent heroin use,” the researchers concluded. “Patients receiving high-dose opioids, ages 50-56, with a history of HCV infection, injecting, opioid use disorder, or recent stimulant use should be screened for heroin use.”
They acknowledged certain limitations of the study, including its self-reported design and the fact that VA pharmacy data do not capture opioid prescriptions filled outside of the VA.
The study was funded by the National Institute on Alcohol Abuse and Alcoholism and the National Institute on Drug Abuse. Ms. Banerjee reported having no financial disclosures.
SAN DIEGO – High-dose opioid prescribing is associated with an increased risk of heroin use among U.S. veterans, a prospective study showed.
“Despite evidence linking increased risk of opioid use disorder with specific opioid prescribing patterns, the relationship between these practices and heroin use is less understood,” researchers led by Geetanjoli Banerjee wrote in an abstract presented during the annual meeting of the College on Problems of Drug Dependence. “Understanding the relationship between prescription opioid use and initiation of heroin use among veterans is particularly important, as this population has both a higher underlying prevalence of substance abuse disorders and pain conditions.”
Ms. Banerjee, a graduate student at Brown University, Providence, R.I., and her associates examined data from 3,570 individuals enrolled in the Veterans Aging Cohort Study without nonmedical use or prescription opioids or heroin use in the year prior to baseline, and who received more than one prescription opioid from the VA during follow-up. between 2002 and 2012.
Among the 3,833 eligible participants, the proportion who were prescribed high-dose opioids (defined as a morphine equivalent daily dose of 90 mg or greater) did not change significantly between 2002 and 2012, and ranged from 4.4% to 5.9% (P = .22). The researchers also found that the 10-year incidence rate of recent heroin use was 8.15 event per 1,000 person-years. The time to recent heroin use differed significantly between participants with and without prior receipt of a high-dose prescription at baseline (P less than .001). Multivariable Cox regression analysis showed that prior receipt of a high-dose opioid prescription was associated with recent heroin use (adjusted hazard ratio, 2.54).
“Among patients who report no past year illicit use of opioids at baseline and who are receiving prescription opioids from the VA, receipt of high-dose prescription opioid increased the risk of subsequent heroin use,” the researchers concluded. “Patients receiving high-dose opioids, ages 50-56, with a history of HCV infection, injecting, opioid use disorder, or recent stimulant use should be screened for heroin use.”
They acknowledged certain limitations of the study, including its self-reported design and the fact that VA pharmacy data do not capture opioid prescriptions filled outside of the VA.
The study was funded by the National Institute on Alcohol Abuse and Alcoholism and the National Institute on Drug Abuse. Ms. Banerjee reported having no financial disclosures.
SAN DIEGO – High-dose opioid prescribing is associated with an increased risk of heroin use among U.S. veterans, a prospective study showed.
“Despite evidence linking increased risk of opioid use disorder with specific opioid prescribing patterns, the relationship between these practices and heroin use is less understood,” researchers led by Geetanjoli Banerjee wrote in an abstract presented during the annual meeting of the College on Problems of Drug Dependence. “Understanding the relationship between prescription opioid use and initiation of heroin use among veterans is particularly important, as this population has both a higher underlying prevalence of substance abuse disorders and pain conditions.”
Ms. Banerjee, a graduate student at Brown University, Providence, R.I., and her associates examined data from 3,570 individuals enrolled in the Veterans Aging Cohort Study without nonmedical use or prescription opioids or heroin use in the year prior to baseline, and who received more than one prescription opioid from the VA during follow-up. between 2002 and 2012.
Among the 3,833 eligible participants, the proportion who were prescribed high-dose opioids (defined as a morphine equivalent daily dose of 90 mg or greater) did not change significantly between 2002 and 2012, and ranged from 4.4% to 5.9% (P = .22). The researchers also found that the 10-year incidence rate of recent heroin use was 8.15 event per 1,000 person-years. The time to recent heroin use differed significantly between participants with and without prior receipt of a high-dose prescription at baseline (P less than .001). Multivariable Cox regression analysis showed that prior receipt of a high-dose opioid prescription was associated with recent heroin use (adjusted hazard ratio, 2.54).
“Among patients who report no past year illicit use of opioids at baseline and who are receiving prescription opioids from the VA, receipt of high-dose prescription opioid increased the risk of subsequent heroin use,” the researchers concluded. “Patients receiving high-dose opioids, ages 50-56, with a history of HCV infection, injecting, opioid use disorder, or recent stimulant use should be screened for heroin use.”
They acknowledged certain limitations of the study, including its self-reported design and the fact that VA pharmacy data do not capture opioid prescriptions filled outside of the VA.
The study was funded by the National Institute on Alcohol Abuse and Alcoholism and the National Institute on Drug Abuse. Ms. Banerjee reported having no financial disclosures.
REPORTING CPDD 2018
Key clinical point: Screen patients who receive high-dose opioids and meet several other criteria for heroin use.
Major finding:. On multivariate Cox regression, prior prescription of high-dose opioids was an independent predictor of recent heroin use (adjusted hazard ratio, 2.54).
Study details: A prospective analysis of 3,833 participants in the Veterans Aging Cohort Study.
Disclosures: The study was funded by the National Institute on Alcohol Abuse and Alcoholism and the National Institute on Drug Abuse. Ms. Banerjee reported having no financial disclosures.
USPSTF: Don’t add ECG for cardio risk assessment
Adding electrocardiography screening to standard cardiovascular disease assessment is not necessary for asymptomatic, low-risk adults, according to final recommendations from the U.S. Preventive Services Task Force.
In the statement published June 12 in JAMA, the USPSTF gave a D recommendation against using ECG screening to evaluate cardiovascular disease risk in asymptomatic, low-risk individuals and issued a statement that current evidence is inadequate (I statement) to evaluate the harms versus benefits of additional ECG for asymptomatic individuals who may be at medium to high risk for future cardiovascular events.
The Task Force concluded that the potential harms of screening ECG outweigh or equal potential benefits in the asymptomatic low-risk population. However, they noted clinical considerations for screening in moderate to high-risk individuals including the potential for more intensive medical management in those identified as higher risk after an ECG, balanced by the potential for harms from medication side effects or follow-up procedures.
Treatment for asymptomatic adults at increased risk for CVD may include lipid-lowering medications, tobacco cessation, and lifestyle modifications regarding diet and exercise, according to the Task Force, and guidelines already exist for many of these factors.
ECG screening could reclassify individuals as higher or lower risk, which could potentially improve health outcomes, wrote Daniel E. Jonas, MD, of the University of North Carolina, Chapel Hill, and his colleagues in the evidence report accompanying the recommendations. The researchers reviewed data from 16 studies including 77,140 individuals. However, the strength of evidence was low for the value of ECG to reclassify individuals, and no improvements in health outcomes were noted, even in high-risk populations such as diabetes patients, the researchers said.
In particular, no significant improvement from additional exercise ECG occurred in a pair of randomized controlled trials including 1,151 individuals, they noted.
The final recommendation reflects the 2017 draft statement and the 2012 final recommendation statement. The full recommendation statement is available online in JAMA and on the Task Force website.
The research was funded by the Agency for Healthcare Research and Quality under a grant from the U.S. Department of Health and Human Services. The researchers had no financial conflicts to disclose.
SOURCES: Jonas D et al. JAMA. 2018 Jun 12;319(22):2315-28; Curry S et al. JAMA. 2018 Jun 12;319(22):2308-14.
The conclusions reached by the USPSTF were warranted, based on the latest research, but may be modified by future information as the science evolves.
In contrast to the 2004 and 2012 task force statements, which were focused on coronary heart disease events, the current analysis used a measure of cardiovascular events, defined as the composite of coronary heart disease, cerebrovascular disease, and peripheral artery disease. Given that ECG parameters usually reflect the presence of coronary heart disease, their value as a predictor of cardiovascular disease in asymptomatic adults may be limited.
The evidence reviewed by the USPSTF shows that ECG screening of low-risk individuals is unlikely to prevent CVD; however, the assessment of risk remains a challenge and puts the decision on physicians based on individual risk factors. It would be an overstatement of current knowledge to conclude that patients at the higher end of the intermediate to high-risk classification would benefit from routine ECG testing with repeated measures over time,” he said.
However, risk factors aside, one special population to be considered for ECG screening is competitive athletes. Screening athletes is common in many countries, though somewhat controversial in the United States, despite its increasing use by professional and college sports team. More research is needed on the value of resting and exercise ECG as markers of CVD risk, and new data may lead researchers to reassess the value of ECG procedures and use them for improved risk classification.
Robert J. Myerburg, MD, an electrophysiologist at the University of Miami, made these comments in an editorial accompanying the article (JAMA. 2018 June 12;319[2]:2277-9). He had no financial conflicts to disclose.
The conclusions reached by the USPSTF were warranted, based on the latest research, but may be modified by future information as the science evolves.
In contrast to the 2004 and 2012 task force statements, which were focused on coronary heart disease events, the current analysis used a measure of cardiovascular events, defined as the composite of coronary heart disease, cerebrovascular disease, and peripheral artery disease. Given that ECG parameters usually reflect the presence of coronary heart disease, their value as a predictor of cardiovascular disease in asymptomatic adults may be limited.
The evidence reviewed by the USPSTF shows that ECG screening of low-risk individuals is unlikely to prevent CVD; however, the assessment of risk remains a challenge and puts the decision on physicians based on individual risk factors. It would be an overstatement of current knowledge to conclude that patients at the higher end of the intermediate to high-risk classification would benefit from routine ECG testing with repeated measures over time,” he said.
However, risk factors aside, one special population to be considered for ECG screening is competitive athletes. Screening athletes is common in many countries, though somewhat controversial in the United States, despite its increasing use by professional and college sports team. More research is needed on the value of resting and exercise ECG as markers of CVD risk, and new data may lead researchers to reassess the value of ECG procedures and use them for improved risk classification.
Robert J. Myerburg, MD, an electrophysiologist at the University of Miami, made these comments in an editorial accompanying the article (JAMA. 2018 June 12;319[2]:2277-9). He had no financial conflicts to disclose.
The conclusions reached by the USPSTF were warranted, based on the latest research, but may be modified by future information as the science evolves.
In contrast to the 2004 and 2012 task force statements, which were focused on coronary heart disease events, the current analysis used a measure of cardiovascular events, defined as the composite of coronary heart disease, cerebrovascular disease, and peripheral artery disease. Given that ECG parameters usually reflect the presence of coronary heart disease, their value as a predictor of cardiovascular disease in asymptomatic adults may be limited.
The evidence reviewed by the USPSTF shows that ECG screening of low-risk individuals is unlikely to prevent CVD; however, the assessment of risk remains a challenge and puts the decision on physicians based on individual risk factors. It would be an overstatement of current knowledge to conclude that patients at the higher end of the intermediate to high-risk classification would benefit from routine ECG testing with repeated measures over time,” he said.
However, risk factors aside, one special population to be considered for ECG screening is competitive athletes. Screening athletes is common in many countries, though somewhat controversial in the United States, despite its increasing use by professional and college sports team. More research is needed on the value of resting and exercise ECG as markers of CVD risk, and new data may lead researchers to reassess the value of ECG procedures and use them for improved risk classification.
Robert J. Myerburg, MD, an electrophysiologist at the University of Miami, made these comments in an editorial accompanying the article (JAMA. 2018 June 12;319[2]:2277-9). He had no financial conflicts to disclose.
Adding electrocardiography screening to standard cardiovascular disease assessment is not necessary for asymptomatic, low-risk adults, according to final recommendations from the U.S. Preventive Services Task Force.
In the statement published June 12 in JAMA, the USPSTF gave a D recommendation against using ECG screening to evaluate cardiovascular disease risk in asymptomatic, low-risk individuals and issued a statement that current evidence is inadequate (I statement) to evaluate the harms versus benefits of additional ECG for asymptomatic individuals who may be at medium to high risk for future cardiovascular events.
The Task Force concluded that the potential harms of screening ECG outweigh or equal potential benefits in the asymptomatic low-risk population. However, they noted clinical considerations for screening in moderate to high-risk individuals including the potential for more intensive medical management in those identified as higher risk after an ECG, balanced by the potential for harms from medication side effects or follow-up procedures.
Treatment for asymptomatic adults at increased risk for CVD may include lipid-lowering medications, tobacco cessation, and lifestyle modifications regarding diet and exercise, according to the Task Force, and guidelines already exist for many of these factors.
ECG screening could reclassify individuals as higher or lower risk, which could potentially improve health outcomes, wrote Daniel E. Jonas, MD, of the University of North Carolina, Chapel Hill, and his colleagues in the evidence report accompanying the recommendations. The researchers reviewed data from 16 studies including 77,140 individuals. However, the strength of evidence was low for the value of ECG to reclassify individuals, and no improvements in health outcomes were noted, even in high-risk populations such as diabetes patients, the researchers said.
In particular, no significant improvement from additional exercise ECG occurred in a pair of randomized controlled trials including 1,151 individuals, they noted.
The final recommendation reflects the 2017 draft statement and the 2012 final recommendation statement. The full recommendation statement is available online in JAMA and on the Task Force website.
The research was funded by the Agency for Healthcare Research and Quality under a grant from the U.S. Department of Health and Human Services. The researchers had no financial conflicts to disclose.
SOURCES: Jonas D et al. JAMA. 2018 Jun 12;319(22):2315-28; Curry S et al. JAMA. 2018 Jun 12;319(22):2308-14.
Adding electrocardiography screening to standard cardiovascular disease assessment is not necessary for asymptomatic, low-risk adults, according to final recommendations from the U.S. Preventive Services Task Force.
In the statement published June 12 in JAMA, the USPSTF gave a D recommendation against using ECG screening to evaluate cardiovascular disease risk in asymptomatic, low-risk individuals and issued a statement that current evidence is inadequate (I statement) to evaluate the harms versus benefits of additional ECG for asymptomatic individuals who may be at medium to high risk for future cardiovascular events.
The Task Force concluded that the potential harms of screening ECG outweigh or equal potential benefits in the asymptomatic low-risk population. However, they noted clinical considerations for screening in moderate to high-risk individuals including the potential for more intensive medical management in those identified as higher risk after an ECG, balanced by the potential for harms from medication side effects or follow-up procedures.
Treatment for asymptomatic adults at increased risk for CVD may include lipid-lowering medications, tobacco cessation, and lifestyle modifications regarding diet and exercise, according to the Task Force, and guidelines already exist for many of these factors.
ECG screening could reclassify individuals as higher or lower risk, which could potentially improve health outcomes, wrote Daniel E. Jonas, MD, of the University of North Carolina, Chapel Hill, and his colleagues in the evidence report accompanying the recommendations. The researchers reviewed data from 16 studies including 77,140 individuals. However, the strength of evidence was low for the value of ECG to reclassify individuals, and no improvements in health outcomes were noted, even in high-risk populations such as diabetes patients, the researchers said.
In particular, no significant improvement from additional exercise ECG occurred in a pair of randomized controlled trials including 1,151 individuals, they noted.
The final recommendation reflects the 2017 draft statement and the 2012 final recommendation statement. The full recommendation statement is available online in JAMA and on the Task Force website.
The research was funded by the Agency for Healthcare Research and Quality under a grant from the U.S. Department of Health and Human Services. The researchers had no financial conflicts to disclose.
SOURCES: Jonas D et al. JAMA. 2018 Jun 12;319(22):2315-28; Curry S et al. JAMA. 2018 Jun 12;319(22):2308-14.
FROM JAMA
Key clinical point:
Major finding: Two randomized controlled trials including 1,151 individuals found no significant improvement from additional exercise ECG.
Study details: Researchers reviewed data from 16 studies including 77,140 individuals.
Disclosures: The research was funded by the Agency for Healthcare Research and Quality under a grant from the U.S. Department of Health & Human Services. The researchers had no financial conflicts to disclose.
Sources: Jonas D et al. JAMA.2018;319[22]:2315-28; Curry S et al. JAMA.2018;319[22]:2308-14.
DOAC’s edge over warfarin fades with low adherence
BOSTON – The direct acting oral anticoagulants boost patient adherence compared with warfarin anticoagulation, but when patients did not adhere to their regimens, those prescribed a new, direct-acting oral anticoagulant had worse outcomes than did patients on warfarin – even patients poorly adherent with warfarin – based on data from more than 80,000 U.S. patients.
Among low-adherence patients, defined as those with adherence rates of 40%-80% based on prescriptions filled, patients with nonvalvular atrial fibrillation and a CHA2DS2-VASc score of at least 2 and treated with warfarin had a 3.37/100 patient-years rate of thromboembolic events–driven hospitalizations or emergency department visits, compared with a 4.05/100 patient-years rate among low-adherence patients receiving a direct-acting oral anticoagulant (DOAC), Dhanunjaya Lakkireddy, MD, said at the annual scientific sessions of the Heart Rhythm Society. The incidence of strokes of any kind was also lower in the low-adherence warfarin patients compared with the low-adherence DOAC patients, although the relationship flipped for hemorrhagic strokes and bleeds, which were more common in the warfarin patients.
In contrast, when patients were adherent, taking more than 80% of their prescribed drug, the performance of the DOACs generally surpassed that of warfarin. In an analysis adjusted for several demographic and clinical confounders, and when compared with patients adherent to a warfarin regimen, those adherent to a DOAC had a 7% lower rate of thromboembolic events, a 36% lower rate of hemorrhagic strokes, an 8% lower rate of any stroke, and a 10% lower rate of bleeds (excluding hemorrhagic strokes), all statistically significant differences, reported Dr. Lakkireddy, medical director of the Kansas City Heart Rhythm Institute in Overland Park, Kan.
The message from this analysis is the importance of maximizing patient adherence, Dr. Lakkireddy said.
“We should not make the false assumption that putting a patient on a DOAC will take care of everything. We need to make it a habit to make sure patients are taking their pills,” he said in an interview. “We were surprised. Our assumption was that the DOACs were more forgiving than warfarin” in poorly compliant patients. “We need to make talking about adherence with patients routine.”
The results also documented that adherence to therapy is better with a DOAC, with a 74% rate of good adherence among the nearly 41,000 patients in the database prescribed a DOAC compared with a 63% rate of good compliance among the more than 42,000 patients prescribed warfarin.
“It’s ironic that we might think low-adherence patients should go on warfarin. That’s sort of backwards,” said Andrew D. Krahn, MD, a cardiac electrophysiologist and professor of medicine at the University of British Columbia in Vancouver. “It’s not biologically plausible” to predict that less adherent patients would do better on warfarin, he noted.
The study run by Dr. Lakkireddy and his associates used data collected by IBM Watson Health Market Scan from about 4 million Medicare patients and 47 million American residents with private insurance during 2012-2016. They focused on the more than 600,000 patients prescribed an anticoagulant during 2014 and 2015, and then narrowed the study group down to just over 83,000 adults with nonvalvular atrial fibrillation, a CHA2DS2-VASc score of 2 or more. The patients’ average age was about 74 years.
Dr. Lakkireddy has been a consultant to or has received research support from Biosense Webster, Boehringer Ingelheim, Bristol Myers Squibb, EstechPharma, Janssen, Pfizer, SentreHeart, and St. Jude. Dr. Krahn has been a consultant to Medtronic and has received research support from Medtronic and Boston Scientific.
SOURCE: Lakkireddy D et al. Heart Rhythm 2018, Abstract B-LBCT02-03.
What is clear from this analysis is that adherence to oral anticoagulant regimens is something we need to address. It would help if we could determine why patients are not well adherent, but regardless of the cause, changing patient behavior and improving adherence will require better patient education and better integration of medical care toward better adherence.
This study has several obvious limitations, including its reliance on an administrative database that does not allow for adjudication of outcomes. The analysis presented so far is also limited by not breaking down the direct-acting oral anticoagulant into individual drugs, and without propensity-score matching of the two treatment subgroups.
We must be very alert to the possibility for confounding by indication in a real-world dataset like this. For example, the stroke rate we see in the patients treated with a DOAC may be affected by clinicians who preferentially prescribed one of the direct-acting drugs to patients who had what they thought was a high stroke risk because they felt these drugs might work better for stroke prevention than warfarin.
What is also notable in the results is that, even among the patients with good adherence, the event and adverse effects rates remained high. Among the highly adherent patients the thromboembolic event rate was greater than 3% per year in both the warfarin and direct-acting drug groups, the stroke rate was also greater than 3% per year in both subgroups, and bleeding events occurred at rates of greater than 4% per year among the patients treated with direct-acting drugs and greater than 5% per year in the warfarin group.
Hein Heidbuchel, MD, professor of medicine and chair of cardiology at the University of Antwerp, Belgium, made these comments as designated discussant for the study. He had no current disclosures.
What is clear from this analysis is that adherence to oral anticoagulant regimens is something we need to address. It would help if we could determine why patients are not well adherent, but regardless of the cause, changing patient behavior and improving adherence will require better patient education and better integration of medical care toward better adherence.
This study has several obvious limitations, including its reliance on an administrative database that does not allow for adjudication of outcomes. The analysis presented so far is also limited by not breaking down the direct-acting oral anticoagulant into individual drugs, and without propensity-score matching of the two treatment subgroups.
We must be very alert to the possibility for confounding by indication in a real-world dataset like this. For example, the stroke rate we see in the patients treated with a DOAC may be affected by clinicians who preferentially prescribed one of the direct-acting drugs to patients who had what they thought was a high stroke risk because they felt these drugs might work better for stroke prevention than warfarin.
What is also notable in the results is that, even among the patients with good adherence, the event and adverse effects rates remained high. Among the highly adherent patients the thromboembolic event rate was greater than 3% per year in both the warfarin and direct-acting drug groups, the stroke rate was also greater than 3% per year in both subgroups, and bleeding events occurred at rates of greater than 4% per year among the patients treated with direct-acting drugs and greater than 5% per year in the warfarin group.
Hein Heidbuchel, MD, professor of medicine and chair of cardiology at the University of Antwerp, Belgium, made these comments as designated discussant for the study. He had no current disclosures.
What is clear from this analysis is that adherence to oral anticoagulant regimens is something we need to address. It would help if we could determine why patients are not well adherent, but regardless of the cause, changing patient behavior and improving adherence will require better patient education and better integration of medical care toward better adherence.
This study has several obvious limitations, including its reliance on an administrative database that does not allow for adjudication of outcomes. The analysis presented so far is also limited by not breaking down the direct-acting oral anticoagulant into individual drugs, and without propensity-score matching of the two treatment subgroups.
We must be very alert to the possibility for confounding by indication in a real-world dataset like this. For example, the stroke rate we see in the patients treated with a DOAC may be affected by clinicians who preferentially prescribed one of the direct-acting drugs to patients who had what they thought was a high stroke risk because they felt these drugs might work better for stroke prevention than warfarin.
What is also notable in the results is that, even among the patients with good adherence, the event and adverse effects rates remained high. Among the highly adherent patients the thromboembolic event rate was greater than 3% per year in both the warfarin and direct-acting drug groups, the stroke rate was also greater than 3% per year in both subgroups, and bleeding events occurred at rates of greater than 4% per year among the patients treated with direct-acting drugs and greater than 5% per year in the warfarin group.
Hein Heidbuchel, MD, professor of medicine and chair of cardiology at the University of Antwerp, Belgium, made these comments as designated discussant for the study. He had no current disclosures.
BOSTON – The direct acting oral anticoagulants boost patient adherence compared with warfarin anticoagulation, but when patients did not adhere to their regimens, those prescribed a new, direct-acting oral anticoagulant had worse outcomes than did patients on warfarin – even patients poorly adherent with warfarin – based on data from more than 80,000 U.S. patients.
Among low-adherence patients, defined as those with adherence rates of 40%-80% based on prescriptions filled, patients with nonvalvular atrial fibrillation and a CHA2DS2-VASc score of at least 2 and treated with warfarin had a 3.37/100 patient-years rate of thromboembolic events–driven hospitalizations or emergency department visits, compared with a 4.05/100 patient-years rate among low-adherence patients receiving a direct-acting oral anticoagulant (DOAC), Dhanunjaya Lakkireddy, MD, said at the annual scientific sessions of the Heart Rhythm Society. The incidence of strokes of any kind was also lower in the low-adherence warfarin patients compared with the low-adherence DOAC patients, although the relationship flipped for hemorrhagic strokes and bleeds, which were more common in the warfarin patients.
In contrast, when patients were adherent, taking more than 80% of their prescribed drug, the performance of the DOACs generally surpassed that of warfarin. In an analysis adjusted for several demographic and clinical confounders, and when compared with patients adherent to a warfarin regimen, those adherent to a DOAC had a 7% lower rate of thromboembolic events, a 36% lower rate of hemorrhagic strokes, an 8% lower rate of any stroke, and a 10% lower rate of bleeds (excluding hemorrhagic strokes), all statistically significant differences, reported Dr. Lakkireddy, medical director of the Kansas City Heart Rhythm Institute in Overland Park, Kan.
The message from this analysis is the importance of maximizing patient adherence, Dr. Lakkireddy said.
“We should not make the false assumption that putting a patient on a DOAC will take care of everything. We need to make it a habit to make sure patients are taking their pills,” he said in an interview. “We were surprised. Our assumption was that the DOACs were more forgiving than warfarin” in poorly compliant patients. “We need to make talking about adherence with patients routine.”
The results also documented that adherence to therapy is better with a DOAC, with a 74% rate of good adherence among the nearly 41,000 patients in the database prescribed a DOAC compared with a 63% rate of good compliance among the more than 42,000 patients prescribed warfarin.
“It’s ironic that we might think low-adherence patients should go on warfarin. That’s sort of backwards,” said Andrew D. Krahn, MD, a cardiac electrophysiologist and professor of medicine at the University of British Columbia in Vancouver. “It’s not biologically plausible” to predict that less adherent patients would do better on warfarin, he noted.
The study run by Dr. Lakkireddy and his associates used data collected by IBM Watson Health Market Scan from about 4 million Medicare patients and 47 million American residents with private insurance during 2012-2016. They focused on the more than 600,000 patients prescribed an anticoagulant during 2014 and 2015, and then narrowed the study group down to just over 83,000 adults with nonvalvular atrial fibrillation, a CHA2DS2-VASc score of 2 or more. The patients’ average age was about 74 years.
Dr. Lakkireddy has been a consultant to or has received research support from Biosense Webster, Boehringer Ingelheim, Bristol Myers Squibb, EstechPharma, Janssen, Pfizer, SentreHeart, and St. Jude. Dr. Krahn has been a consultant to Medtronic and has received research support from Medtronic and Boston Scientific.
SOURCE: Lakkireddy D et al. Heart Rhythm 2018, Abstract B-LBCT02-03.
BOSTON – The direct acting oral anticoagulants boost patient adherence compared with warfarin anticoagulation, but when patients did not adhere to their regimens, those prescribed a new, direct-acting oral anticoagulant had worse outcomes than did patients on warfarin – even patients poorly adherent with warfarin – based on data from more than 80,000 U.S. patients.
Among low-adherence patients, defined as those with adherence rates of 40%-80% based on prescriptions filled, patients with nonvalvular atrial fibrillation and a CHA2DS2-VASc score of at least 2 and treated with warfarin had a 3.37/100 patient-years rate of thromboembolic events–driven hospitalizations or emergency department visits, compared with a 4.05/100 patient-years rate among low-adherence patients receiving a direct-acting oral anticoagulant (DOAC), Dhanunjaya Lakkireddy, MD, said at the annual scientific sessions of the Heart Rhythm Society. The incidence of strokes of any kind was also lower in the low-adherence warfarin patients compared with the low-adherence DOAC patients, although the relationship flipped for hemorrhagic strokes and bleeds, which were more common in the warfarin patients.
In contrast, when patients were adherent, taking more than 80% of their prescribed drug, the performance of the DOACs generally surpassed that of warfarin. In an analysis adjusted for several demographic and clinical confounders, and when compared with patients adherent to a warfarin regimen, those adherent to a DOAC had a 7% lower rate of thromboembolic events, a 36% lower rate of hemorrhagic strokes, an 8% lower rate of any stroke, and a 10% lower rate of bleeds (excluding hemorrhagic strokes), all statistically significant differences, reported Dr. Lakkireddy, medical director of the Kansas City Heart Rhythm Institute in Overland Park, Kan.
The message from this analysis is the importance of maximizing patient adherence, Dr. Lakkireddy said.
“We should not make the false assumption that putting a patient on a DOAC will take care of everything. We need to make it a habit to make sure patients are taking their pills,” he said in an interview. “We were surprised. Our assumption was that the DOACs were more forgiving than warfarin” in poorly compliant patients. “We need to make talking about adherence with patients routine.”
The results also documented that adherence to therapy is better with a DOAC, with a 74% rate of good adherence among the nearly 41,000 patients in the database prescribed a DOAC compared with a 63% rate of good compliance among the more than 42,000 patients prescribed warfarin.
“It’s ironic that we might think low-adherence patients should go on warfarin. That’s sort of backwards,” said Andrew D. Krahn, MD, a cardiac electrophysiologist and professor of medicine at the University of British Columbia in Vancouver. “It’s not biologically plausible” to predict that less adherent patients would do better on warfarin, he noted.
The study run by Dr. Lakkireddy and his associates used data collected by IBM Watson Health Market Scan from about 4 million Medicare patients and 47 million American residents with private insurance during 2012-2016. They focused on the more than 600,000 patients prescribed an anticoagulant during 2014 and 2015, and then narrowed the study group down to just over 83,000 adults with nonvalvular atrial fibrillation, a CHA2DS2-VASc score of 2 or more. The patients’ average age was about 74 years.
Dr. Lakkireddy has been a consultant to or has received research support from Biosense Webster, Boehringer Ingelheim, Bristol Myers Squibb, EstechPharma, Janssen, Pfizer, SentreHeart, and St. Jude. Dr. Krahn has been a consultant to Medtronic and has received research support from Medtronic and Boston Scientific.
SOURCE: Lakkireddy D et al. Heart Rhythm 2018, Abstract B-LBCT02-03.
REPORTING FROM HEART RHYTHM 2018
Key clinical point: Good adherence is needed for direct-acting oral anticoagulants to outperform warfarin.
Major finding: Thromboembolic events in low-adherence patients were 4.05/100 patient years with a DOAC and 3.37/100 patient years with warfarin.
Study details: Analysis of 83,168 insured U.S. atrial fibrillation patients treated with an oral anticoagulant in 2014-2015.
Disclosures: Dr. Lakkireddy has been a consultant to or has received research support from Biosense Webster, Boehringer Ingelheim, Bristol Myers Squibb, EstechPharma, Janssen, Pfizer, SentreHeart, and St. Jude. Dr. Krahn has been a consultant to Medtronic and has received research support from Medtronic and Boston Scientific.
Source: Lakkireddy D et al. Heart Rhythm 2018, Abstract B-LBCT02-03.
NIH launches HEAL Initiative to combat opioid crisis
The NIH HEAL (Helping to End Addiction Long-term) Initiative aims to bring together agencies across the federal government, as well as academic institutions, private industry, and patient advocates to find new solutions to address the current national health emergency.
“There are 15 initiatives altogether that are being put out that we think are pretty bold and should make a big difference in our understanding of what to do about this national public health crisis,” NIH Director Francis Collins, MD, said in an interview.
HEAL will investigate ways to reformulate existing treatments for opioid use disorder (OUD), to improve efficacy and extend their availability to more patients.
“Although there are effective medications for OUD (methadone, buprenorphine, and naltrexone), only a small percentage of individuals in the United States who would benefit receive these medications,” according to an editorial introducing the NIH HEAL Initiative published in JAMA (doi:10.1001/jama.2018.8826). “Even among those who have initiated these medications, about half will relapse within 6 months.”
The editorial was authored by Dr. Collins, Walter J. Koroshetz, MD, director of the National Institute of Neurological Disorders and Stroke, and Nora Volkow, MD, director of the National Institute on Drug Abuse.
For example, the current formulation of naltrexone lasts about a month within the body, Dr. Collins said in an interview. “If we had a 6-month version of that, I think it would be much more effective because oftentimes the relapses happen after a month or so, before people have fully gotten themselves on the ground.”
Better overdose antidotes are needed as well, he said, particularly for fentanyl overdose. “Narcan may not be strong enough for those long-lasting and very potent opioids like fentanyl,” he said.
HEAL also will seek a better understanding of neonatal opioid withdrawal syndrome (NOWS), also referred to as neonatal abstinence syndrome, which has become alarmingly common as more women of childbearing potential struggle with opioid addiction.
“Innovative methods to identify and treat newborns exposed to opioids, often along with other drugs, have the potential to improve both short- and long-term developmental outcomes in such children,” Dr. Collins and colleagues noted. “To determine better approaches, HEAL will expand Advancing Clinical Trials in Neonatal Opioid Withdrawal Syndrome (ACT NOW). This pilot study is designed to assess the prevalence of NOWS, understand current approaches to managing NOWS , and develop common approaches for larger-scale studies that will determine best practices for clinical care of infants with NOWS throughout the country.”
HEAL efforts also seek to find integrated approaches to OUD treatment.
“One particularly bold element is to put together a number of pilot projects that enable bringing together all of the ways in which we are trying to turn this epidemic around by making it possible to assess whether individuals who are addicted can be successfully treated and maintained in abstinence for long periods of time,” Dr. Collins said. “Right now, the success is not so great.
“Suppose we brought together all of the treatment programs – the primary care facilities, the emergency rooms, the fire departments, the social work experts, the health departments in the states, the local communities, the criminal justice system. We brought together all of those players in a research design where we can really see what was working. Could we do a lot more to turn this around than basically doing one of those at a time? There is this multisite idea of a national research effort, still somewhat in development, but to do integration of all of these efforts. I am pretty excited about that one.”
In looking for better ways to treat pain safely and effectively, “we need to understand how it is that people transition from acute pain to chronic pain … and what can we do increase the likelihood of recovery from acute pain without making that transition,” Dr. Collins said. “Then we need to identify additional novel targets for developing pain therapies, both devices and pharmaceuticals. We need better means of testing those ideas.”
In addition to gaining a better understanding of chronic pain, HEAL aims to investigate new nonaddictive pain treatments and find ways to expedite those treatments through the clinical pipeline, according to Dr. Collins and colleagues.
HEAL “lays the foundation for an innovative therapy-development pipeline through a planned new public-private partnership. In collaboration with biopharmaceutical groups, the Food and Drug Administration, and the Foundation for the NIH, the NIH will collect and evaluate treatment assets from academia and biopharmaceutical and device companies to coordinate and accelerate the development of effective treatments for pain and addiction,” they wrote.
SOURCE: Collins F et al, JAMA doi: 10.1001/jama.2018.8826.
The NIH HEAL (Helping to End Addiction Long-term) Initiative aims to bring together agencies across the federal government, as well as academic institutions, private industry, and patient advocates to find new solutions to address the current national health emergency.
“There are 15 initiatives altogether that are being put out that we think are pretty bold and should make a big difference in our understanding of what to do about this national public health crisis,” NIH Director Francis Collins, MD, said in an interview.
HEAL will investigate ways to reformulate existing treatments for opioid use disorder (OUD), to improve efficacy and extend their availability to more patients.
“Although there are effective medications for OUD (methadone, buprenorphine, and naltrexone), only a small percentage of individuals in the United States who would benefit receive these medications,” according to an editorial introducing the NIH HEAL Initiative published in JAMA (doi:10.1001/jama.2018.8826). “Even among those who have initiated these medications, about half will relapse within 6 months.”
The editorial was authored by Dr. Collins, Walter J. Koroshetz, MD, director of the National Institute of Neurological Disorders and Stroke, and Nora Volkow, MD, director of the National Institute on Drug Abuse.
For example, the current formulation of naltrexone lasts about a month within the body, Dr. Collins said in an interview. “If we had a 6-month version of that, I think it would be much more effective because oftentimes the relapses happen after a month or so, before people have fully gotten themselves on the ground.”
Better overdose antidotes are needed as well, he said, particularly for fentanyl overdose. “Narcan may not be strong enough for those long-lasting and very potent opioids like fentanyl,” he said.
HEAL also will seek a better understanding of neonatal opioid withdrawal syndrome (NOWS), also referred to as neonatal abstinence syndrome, which has become alarmingly common as more women of childbearing potential struggle with opioid addiction.
“Innovative methods to identify and treat newborns exposed to opioids, often along with other drugs, have the potential to improve both short- and long-term developmental outcomes in such children,” Dr. Collins and colleagues noted. “To determine better approaches, HEAL will expand Advancing Clinical Trials in Neonatal Opioid Withdrawal Syndrome (ACT NOW). This pilot study is designed to assess the prevalence of NOWS, understand current approaches to managing NOWS , and develop common approaches for larger-scale studies that will determine best practices for clinical care of infants with NOWS throughout the country.”
HEAL efforts also seek to find integrated approaches to OUD treatment.
“One particularly bold element is to put together a number of pilot projects that enable bringing together all of the ways in which we are trying to turn this epidemic around by making it possible to assess whether individuals who are addicted can be successfully treated and maintained in abstinence for long periods of time,” Dr. Collins said. “Right now, the success is not so great.
“Suppose we brought together all of the treatment programs – the primary care facilities, the emergency rooms, the fire departments, the social work experts, the health departments in the states, the local communities, the criminal justice system. We brought together all of those players in a research design where we can really see what was working. Could we do a lot more to turn this around than basically doing one of those at a time? There is this multisite idea of a national research effort, still somewhat in development, but to do integration of all of these efforts. I am pretty excited about that one.”
In looking for better ways to treat pain safely and effectively, “we need to understand how it is that people transition from acute pain to chronic pain … and what can we do increase the likelihood of recovery from acute pain without making that transition,” Dr. Collins said. “Then we need to identify additional novel targets for developing pain therapies, both devices and pharmaceuticals. We need better means of testing those ideas.”
In addition to gaining a better understanding of chronic pain, HEAL aims to investigate new nonaddictive pain treatments and find ways to expedite those treatments through the clinical pipeline, according to Dr. Collins and colleagues.
HEAL “lays the foundation for an innovative therapy-development pipeline through a planned new public-private partnership. In collaboration with biopharmaceutical groups, the Food and Drug Administration, and the Foundation for the NIH, the NIH will collect and evaluate treatment assets from academia and biopharmaceutical and device companies to coordinate and accelerate the development of effective treatments for pain and addiction,” they wrote.
SOURCE: Collins F et al, JAMA doi: 10.1001/jama.2018.8826.
The NIH HEAL (Helping to End Addiction Long-term) Initiative aims to bring together agencies across the federal government, as well as academic institutions, private industry, and patient advocates to find new solutions to address the current national health emergency.
“There are 15 initiatives altogether that are being put out that we think are pretty bold and should make a big difference in our understanding of what to do about this national public health crisis,” NIH Director Francis Collins, MD, said in an interview.
HEAL will investigate ways to reformulate existing treatments for opioid use disorder (OUD), to improve efficacy and extend their availability to more patients.
“Although there are effective medications for OUD (methadone, buprenorphine, and naltrexone), only a small percentage of individuals in the United States who would benefit receive these medications,” according to an editorial introducing the NIH HEAL Initiative published in JAMA (doi:10.1001/jama.2018.8826). “Even among those who have initiated these medications, about half will relapse within 6 months.”
The editorial was authored by Dr. Collins, Walter J. Koroshetz, MD, director of the National Institute of Neurological Disorders and Stroke, and Nora Volkow, MD, director of the National Institute on Drug Abuse.
For example, the current formulation of naltrexone lasts about a month within the body, Dr. Collins said in an interview. “If we had a 6-month version of that, I think it would be much more effective because oftentimes the relapses happen after a month or so, before people have fully gotten themselves on the ground.”
Better overdose antidotes are needed as well, he said, particularly for fentanyl overdose. “Narcan may not be strong enough for those long-lasting and very potent opioids like fentanyl,” he said.
HEAL also will seek a better understanding of neonatal opioid withdrawal syndrome (NOWS), also referred to as neonatal abstinence syndrome, which has become alarmingly common as more women of childbearing potential struggle with opioid addiction.
“Innovative methods to identify and treat newborns exposed to opioids, often along with other drugs, have the potential to improve both short- and long-term developmental outcomes in such children,” Dr. Collins and colleagues noted. “To determine better approaches, HEAL will expand Advancing Clinical Trials in Neonatal Opioid Withdrawal Syndrome (ACT NOW). This pilot study is designed to assess the prevalence of NOWS, understand current approaches to managing NOWS , and develop common approaches for larger-scale studies that will determine best practices for clinical care of infants with NOWS throughout the country.”
HEAL efforts also seek to find integrated approaches to OUD treatment.
“One particularly bold element is to put together a number of pilot projects that enable bringing together all of the ways in which we are trying to turn this epidemic around by making it possible to assess whether individuals who are addicted can be successfully treated and maintained in abstinence for long periods of time,” Dr. Collins said. “Right now, the success is not so great.
“Suppose we brought together all of the treatment programs – the primary care facilities, the emergency rooms, the fire departments, the social work experts, the health departments in the states, the local communities, the criminal justice system. We brought together all of those players in a research design where we can really see what was working. Could we do a lot more to turn this around than basically doing one of those at a time? There is this multisite idea of a national research effort, still somewhat in development, but to do integration of all of these efforts. I am pretty excited about that one.”
In looking for better ways to treat pain safely and effectively, “we need to understand how it is that people transition from acute pain to chronic pain … and what can we do increase the likelihood of recovery from acute pain without making that transition,” Dr. Collins said. “Then we need to identify additional novel targets for developing pain therapies, both devices and pharmaceuticals. We need better means of testing those ideas.”
In addition to gaining a better understanding of chronic pain, HEAL aims to investigate new nonaddictive pain treatments and find ways to expedite those treatments through the clinical pipeline, according to Dr. Collins and colleagues.
HEAL “lays the foundation for an innovative therapy-development pipeline through a planned new public-private partnership. In collaboration with biopharmaceutical groups, the Food and Drug Administration, and the Foundation for the NIH, the NIH will collect and evaluate treatment assets from academia and biopharmaceutical and device companies to coordinate and accelerate the development of effective treatments for pain and addiction,” they wrote.
SOURCE: Collins F et al, JAMA doi: 10.1001/jama.2018.8826.
FROM JAMA