User login
ED visits by young patients trended up in California
Children’s and adolescents’ use of emergency departments rose markedly in the late 2000s, a sharp contrast from their steady or decreasing rates of ED use throughout the 1990s and early 2000s, according to a Research Letter to the Editor published online Oct. 14 in JAMA.
The recent uptick in pediatric ED visits also contrasts with a notable decline in adult ED use during the same time period. “These findings suggest that the drivers for ED use differ significantly between youths and adults, and that policies regarding insurance expansion” – that is, coverage through the Affordable Care Act – “may also have varying effects,” said Dr. Renee Y. Hsia of the department of emergency medicine, University of California, San Francisco, and San Francisco General Hospital, and her associates.
They performed a retrospective analysis using a database recording all ED visits by children and adolescents up to 18 years of age to general hospitals across California between 2005 and 2010. The overall number of visits rose from 2.5 million to 2.8 million per year during that period, an increase of 11%. The fastest increase in rates of ED use occurred among uninsured youths, who showed a 23% rise. The rate rose 15% among privately insured youths and 7% among youths covered by Medicaid, the investigators said (JAMA 2014;312:1587-8).
“The divergence from older trends in ED use among youths may also reflect the increasingly central role of the ED in the U.S. health care system, especially during a period of severe economic recession, and could signal an overall deterioration in access to primary care across payer groups, or that even privately insured youths with greater access to primary care physicians are being directed to the ED for care,” Dr. Hsia and her associates said.
Children’s and adolescents’ use of emergency departments rose markedly in the late 2000s, a sharp contrast from their steady or decreasing rates of ED use throughout the 1990s and early 2000s, according to a Research Letter to the Editor published online Oct. 14 in JAMA.
The recent uptick in pediatric ED visits also contrasts with a notable decline in adult ED use during the same time period. “These findings suggest that the drivers for ED use differ significantly between youths and adults, and that policies regarding insurance expansion” – that is, coverage through the Affordable Care Act – “may also have varying effects,” said Dr. Renee Y. Hsia of the department of emergency medicine, University of California, San Francisco, and San Francisco General Hospital, and her associates.
They performed a retrospective analysis using a database recording all ED visits by children and adolescents up to 18 years of age to general hospitals across California between 2005 and 2010. The overall number of visits rose from 2.5 million to 2.8 million per year during that period, an increase of 11%. The fastest increase in rates of ED use occurred among uninsured youths, who showed a 23% rise. The rate rose 15% among privately insured youths and 7% among youths covered by Medicaid, the investigators said (JAMA 2014;312:1587-8).
“The divergence from older trends in ED use among youths may also reflect the increasingly central role of the ED in the U.S. health care system, especially during a period of severe economic recession, and could signal an overall deterioration in access to primary care across payer groups, or that even privately insured youths with greater access to primary care physicians are being directed to the ED for care,” Dr. Hsia and her associates said.
Children’s and adolescents’ use of emergency departments rose markedly in the late 2000s, a sharp contrast from their steady or decreasing rates of ED use throughout the 1990s and early 2000s, according to a Research Letter to the Editor published online Oct. 14 in JAMA.
The recent uptick in pediatric ED visits also contrasts with a notable decline in adult ED use during the same time period. “These findings suggest that the drivers for ED use differ significantly between youths and adults, and that policies regarding insurance expansion” – that is, coverage through the Affordable Care Act – “may also have varying effects,” said Dr. Renee Y. Hsia of the department of emergency medicine, University of California, San Francisco, and San Francisco General Hospital, and her associates.
They performed a retrospective analysis using a database recording all ED visits by children and adolescents up to 18 years of age to general hospitals across California between 2005 and 2010. The overall number of visits rose from 2.5 million to 2.8 million per year during that period, an increase of 11%. The fastest increase in rates of ED use occurred among uninsured youths, who showed a 23% rise. The rate rose 15% among privately insured youths and 7% among youths covered by Medicaid, the investigators said (JAMA 2014;312:1587-8).
“The divergence from older trends in ED use among youths may also reflect the increasingly central role of the ED in the U.S. health care system, especially during a period of severe economic recession, and could signal an overall deterioration in access to primary care across payer groups, or that even privately insured youths with greater access to primary care physicians are being directed to the ED for care,” Dr. Hsia and her associates said.
Key clinical point: Children’s and adolescents’ use of emergency departments increased markedly across all payer categories between 2005 and 2010 in California.
Major finding: Youths’ use of EDs statewide rose 11% overall, 23% among the uninsured, 15% among the privately insured, and 7% among those covered by Medicaid in the late 2000s.
Data source: A retrospective analysis of all 2-3 million annual visits to California EDs by children up to age 18 in 2005-2010.
Disclosures: This study was primarily supported by the California HealthCare Foundation, with additional support from the National Center for Advancing Translational Sciences, the National Institutes of Health, the University of California, and the Robert Wood Johnson Foundation. Dr. Hsia and her associates reported having no financial disclosures.
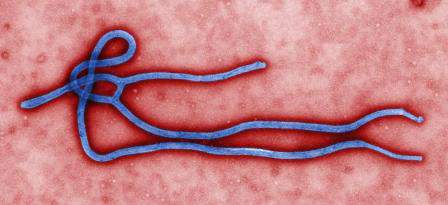
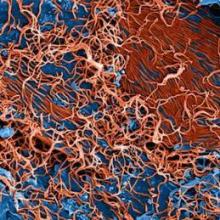
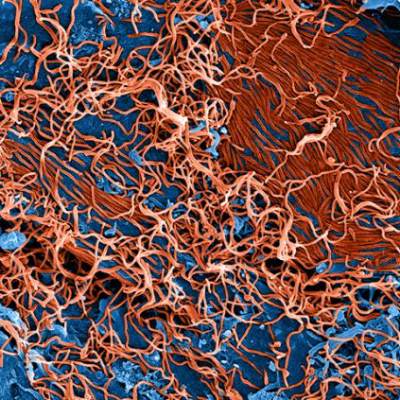
CDC: Breaches at Liberia hospital likely led to HCW infections
An investigation into a cluster of five health care workers infected with Ebola virus while treating patients at a designated center in Monrovia, Liberia, has revealed no common source or chain of transmission, according to a report published by the Centers for Disease Control and Prevention.
Nonetheless, the investigators, led by the CDC’s Dr. Joseph D. Forrester, found several opportunities for transmission at the hospital and treatment center during an on-site evaluation conducted in late July 2014. All five infections occurred over a 2-week period ending July 29.
Potential means of transmission included exposure to patients with undetected Ebola infection in the emergency department (before they could be transferred to the hospital’s Ebola treatment unit); inadequate or inconsistent use of personal protective equipment, particularly during or after cleaning; and transmission of Ebola virus from one health care worker (HCW) to another, Dr. Forrester and his colleagues report in an early release of the Oct. 14 Morbidity and Mortality Weekly Report (MMWR 2014;63).
Two of the five health care workers who became ill died as a result of their infections.
Opportunities for transmission to the HCWs identified by Dr. Forrester and his colleagues included a patient with unrecognized Ebola who died in the emergency department, potentially exposing HCWs there. They also found that HCWs were not being monitored for fever or other symptoms, and that some had cleaned grossly contaminated surfaces without adequate protective equipment.
“None of the information collected suggested a mode of Ebola virus transmission that had not previously been described,” the investigators wrote in their analysis.
They noted as limitations of their study that interviews had not been conducted in a standardized format, and that one of the HCWs had died before investigators could conduct an interview, forcing them to rely on information provided by that individual’s colleagues.
In the same issue of MMWR, Dr. Satish K. Pillai of the CDC and his colleagues described an incident management system (IMS) implemented by Liberian health officials in consultation with the CDC. The system is designed to enhance the speed and effectiveness of the chain of command structure governing the Ebola response. It is modeled after IMSs that have been used by state and government agencies in the United States.
Changes to the Liberian system include the appointment of an incident manager in charge of setting the goals of the response. The system also creates additional staff positions to improve the logistical, financial, and administrative components of the response.
The Liberian Ministry of Health and Social Welfare will continue working with the CDC for the next 6-9 months to refine the Ebola response to IMS, Dr. Pillai and his colleagues noted. “The findings in this report might also be useful in other settings where IMS has not been used previously and is being considered for the first time,” they said.
An investigation into a cluster of five health care workers infected with Ebola virus while treating patients at a designated center in Monrovia, Liberia, has revealed no common source or chain of transmission, according to a report published by the Centers for Disease Control and Prevention.
Nonetheless, the investigators, led by the CDC’s Dr. Joseph D. Forrester, found several opportunities for transmission at the hospital and treatment center during an on-site evaluation conducted in late July 2014. All five infections occurred over a 2-week period ending July 29.
Potential means of transmission included exposure to patients with undetected Ebola infection in the emergency department (before they could be transferred to the hospital’s Ebola treatment unit); inadequate or inconsistent use of personal protective equipment, particularly during or after cleaning; and transmission of Ebola virus from one health care worker (HCW) to another, Dr. Forrester and his colleagues report in an early release of the Oct. 14 Morbidity and Mortality Weekly Report (MMWR 2014;63).
Two of the five health care workers who became ill died as a result of their infections.
Opportunities for transmission to the HCWs identified by Dr. Forrester and his colleagues included a patient with unrecognized Ebola who died in the emergency department, potentially exposing HCWs there. They also found that HCWs were not being monitored for fever or other symptoms, and that some had cleaned grossly contaminated surfaces without adequate protective equipment.
“None of the information collected suggested a mode of Ebola virus transmission that had not previously been described,” the investigators wrote in their analysis.
They noted as limitations of their study that interviews had not been conducted in a standardized format, and that one of the HCWs had died before investigators could conduct an interview, forcing them to rely on information provided by that individual’s colleagues.
In the same issue of MMWR, Dr. Satish K. Pillai of the CDC and his colleagues described an incident management system (IMS) implemented by Liberian health officials in consultation with the CDC. The system is designed to enhance the speed and effectiveness of the chain of command structure governing the Ebola response. It is modeled after IMSs that have been used by state and government agencies in the United States.
Changes to the Liberian system include the appointment of an incident manager in charge of setting the goals of the response. The system also creates additional staff positions to improve the logistical, financial, and administrative components of the response.
The Liberian Ministry of Health and Social Welfare will continue working with the CDC for the next 6-9 months to refine the Ebola response to IMS, Dr. Pillai and his colleagues noted. “The findings in this report might also be useful in other settings where IMS has not been used previously and is being considered for the first time,” they said.
An investigation into a cluster of five health care workers infected with Ebola virus while treating patients at a designated center in Monrovia, Liberia, has revealed no common source or chain of transmission, according to a report published by the Centers for Disease Control and Prevention.
Nonetheless, the investigators, led by the CDC’s Dr. Joseph D. Forrester, found several opportunities for transmission at the hospital and treatment center during an on-site evaluation conducted in late July 2014. All five infections occurred over a 2-week period ending July 29.
Potential means of transmission included exposure to patients with undetected Ebola infection in the emergency department (before they could be transferred to the hospital’s Ebola treatment unit); inadequate or inconsistent use of personal protective equipment, particularly during or after cleaning; and transmission of Ebola virus from one health care worker (HCW) to another, Dr. Forrester and his colleagues report in an early release of the Oct. 14 Morbidity and Mortality Weekly Report (MMWR 2014;63).
Two of the five health care workers who became ill died as a result of their infections.
Opportunities for transmission to the HCWs identified by Dr. Forrester and his colleagues included a patient with unrecognized Ebola who died in the emergency department, potentially exposing HCWs there. They also found that HCWs were not being monitored for fever or other symptoms, and that some had cleaned grossly contaminated surfaces without adequate protective equipment.
“None of the information collected suggested a mode of Ebola virus transmission that had not previously been described,” the investigators wrote in their analysis.
They noted as limitations of their study that interviews had not been conducted in a standardized format, and that one of the HCWs had died before investigators could conduct an interview, forcing them to rely on information provided by that individual’s colleagues.
In the same issue of MMWR, Dr. Satish K. Pillai of the CDC and his colleagues described an incident management system (IMS) implemented by Liberian health officials in consultation with the CDC. The system is designed to enhance the speed and effectiveness of the chain of command structure governing the Ebola response. It is modeled after IMSs that have been used by state and government agencies in the United States.
Changes to the Liberian system include the appointment of an incident manager in charge of setting the goals of the response. The system also creates additional staff positions to improve the logistical, financial, and administrative components of the response.
The Liberian Ministry of Health and Social Welfare will continue working with the CDC for the next 6-9 months to refine the Ebola response to IMS, Dr. Pillai and his colleagues noted. “The findings in this report might also be useful in other settings where IMS has not been used previously and is being considered for the first time,” they said.
CDC chief: Overuse of protective clothing may have increased Ebola transmission risk
The use of protective clothing by hospital staff has become the focus of an investigation as to how a Texas nurse became infected while caring for a patient with Ebola, health officials said on Oct. 13.
Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention, said in a press conference that the agency had spent the past 24 hours investigating potential avenues of transmission at the hospital, Texas Health Presbyterian in Dallas.
Dr. Frieden said that health care workers treating Thomas Eric Duncan, the Ebola patient who died at the hospital on Oct. 8, had been using positive air pressure respirators, suggesting that that the likelihood of their having inhaled infectious material while attending to Mr. Duncan was low. Nor was there evidence of a needlestick, he said.
Health care workers treating patients with Ebola “have to go in and out” of isolation multiple times during the course of a day, Dr. Frieden said. “One of the things we’ve found is that sometimes health care workers think more is better and may put on additional sets of gloves or additional coverings, and that may end up paradoxically making things less safe, because it may be difficult to remove those layers and it inadvertently increases risk. We don’t know that happened here, but that’s one of the things we’ve been addressing.”
CDC investigators at Texas Health Presbyterian, where the nurse is bring treated, “are now watching as [health care workers] are putting on and taking off protective garb. … We are looking hard at the infection control practices and making sure they are even more stringent,” Dr. Frieden said.
Dr. Frieden noted that investigators were preparing for the possibility of more cases among health care workers who had contact with Mr. Duncan while he was isolated and treated at the hospital. Dr. Frieden added that “a large number” of health care workers at the Texas hospital potentially had contact with the patient besides the nurse known to be infected, and that the effort to identify and monitor all of them was still ongoing.
“We would not be surprised if we see more cases” in the coming days, Dr. Frieden said.
The use of protective clothing by hospital staff has become the focus of an investigation as to how a Texas nurse became infected while caring for a patient with Ebola, health officials said on Oct. 13.
Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention, said in a press conference that the agency had spent the past 24 hours investigating potential avenues of transmission at the hospital, Texas Health Presbyterian in Dallas.
Dr. Frieden said that health care workers treating Thomas Eric Duncan, the Ebola patient who died at the hospital on Oct. 8, had been using positive air pressure respirators, suggesting that that the likelihood of their having inhaled infectious material while attending to Mr. Duncan was low. Nor was there evidence of a needlestick, he said.
Health care workers treating patients with Ebola “have to go in and out” of isolation multiple times during the course of a day, Dr. Frieden said. “One of the things we’ve found is that sometimes health care workers think more is better and may put on additional sets of gloves or additional coverings, and that may end up paradoxically making things less safe, because it may be difficult to remove those layers and it inadvertently increases risk. We don’t know that happened here, but that’s one of the things we’ve been addressing.”
CDC investigators at Texas Health Presbyterian, where the nurse is bring treated, “are now watching as [health care workers] are putting on and taking off protective garb. … We are looking hard at the infection control practices and making sure they are even more stringent,” Dr. Frieden said.
Dr. Frieden noted that investigators were preparing for the possibility of more cases among health care workers who had contact with Mr. Duncan while he was isolated and treated at the hospital. Dr. Frieden added that “a large number” of health care workers at the Texas hospital potentially had contact with the patient besides the nurse known to be infected, and that the effort to identify and monitor all of them was still ongoing.
“We would not be surprised if we see more cases” in the coming days, Dr. Frieden said.
The use of protective clothing by hospital staff has become the focus of an investigation as to how a Texas nurse became infected while caring for a patient with Ebola, health officials said on Oct. 13.
Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention, said in a press conference that the agency had spent the past 24 hours investigating potential avenues of transmission at the hospital, Texas Health Presbyterian in Dallas.
Dr. Frieden said that health care workers treating Thomas Eric Duncan, the Ebola patient who died at the hospital on Oct. 8, had been using positive air pressure respirators, suggesting that that the likelihood of their having inhaled infectious material while attending to Mr. Duncan was low. Nor was there evidence of a needlestick, he said.
Health care workers treating patients with Ebola “have to go in and out” of isolation multiple times during the course of a day, Dr. Frieden said. “One of the things we’ve found is that sometimes health care workers think more is better and may put on additional sets of gloves or additional coverings, and that may end up paradoxically making things less safe, because it may be difficult to remove those layers and it inadvertently increases risk. We don’t know that happened here, but that’s one of the things we’ve been addressing.”
CDC investigators at Texas Health Presbyterian, where the nurse is bring treated, “are now watching as [health care workers] are putting on and taking off protective garb. … We are looking hard at the infection control practices and making sure they are even more stringent,” Dr. Frieden said.
Dr. Frieden noted that investigators were preparing for the possibility of more cases among health care workers who had contact with Mr. Duncan while he was isolated and treated at the hospital. Dr. Frieden added that “a large number” of health care workers at the Texas hospital potentially had contact with the patient besides the nurse known to be infected, and that the effort to identify and monitor all of them was still ongoing.
“We would not be surprised if we see more cases” in the coming days, Dr. Frieden said.
Malpractice premiums remained flat in 2014
Malpractice premiums for physicians stayed mostly the same in 2014, with 65% of liability insurance rates remaining steady nationwide, according to the Medical Liability Monitor’s annual survey and analysis of premiums nationwide.
Ongoing trends of slow lawsuit frequency and low plaintiff payouts are contributing to the steady market, said Chad C. Karls, editor of the 2014 Annual Rate Survey and a principal and consulting actuary for Milliman in Brookfield, Wis.
“We certainly do see those very large verdicts in the industry, but when we take it across all claims, the vast majority don’t have a verdict attached to them,” Mr. Karls said in an interview. “The vast majority get settled. That average claim has remained relatively stable.”
Unchanging insurance rates, however, can mean payment misery or relief depending on where physicians practice. Internists in southern Florida will pay a high of $47,707 for malpractice insurance this year, while their counterparts in South Dakota will pay just $3,697. For ob.gyns., malpractice insurance is priciest in the New York counties of Nassau and Suffolk, where they will pay $214,999 in malpractice premiums this year. But in Central California, ob.gyns. will pay just $16,240. General surgeons in southern Florida will dish out $190,829 in premiums in 2014, while Wisconsin surgeons will pay $10,868.
Premiums did increase in some areas in 2014. Indiana physicians saw the highest increase at 4.5%. Nevada doctors experienced a 34.8% decrease in premiums, by far the largest drop among states. (See map.) Nevada’s average percent change was driven by two companies that reported high rate decreases, the survey noted. (Acquisitions by some Nevada insurers may have affected the numbers.)
In general, Nevada’s large rate decline is not surprising, said Dr. Warren Volker, trustee-at-large for the Clark County (Nev.) Medical Society and chair of Premiere Physician Insurance Company in Nevada. Doctors in the state have experienced a stable medical liability climate for the last decade, he said.
“Our premiums have gone down dramatically, across the board,” Dr. Volker said in an interview. “Physicians have enjoyed cost savings as long as they have a good history.”
He attributed the declines to tort reform passed in 2002, including a $350,000 noneconomic damages cap in medical malpractice cases. Since then, the number of lawsuit filings has gone down and competition among liability insurers has increased, he said.
Legal reforms such as Nevada’s have probably contributed to the overall decrease in lawsuit frequency and payout severity across the country, Mr. Karls said. Patient safety initiatives and better risk management within medical practices also may be having an impact.
It remains to be seen how the Affordable Care Act will affect medical liability premiums. So far, industry analysts have not seen a definitive impact on medical malpractice insurance rates from the law, Mr. Karls said. The law could ultimately help lower liability claims if the ACA results in more proactive, preventive approaches to medical errors and less acute care, but in the short term, more patients covered under the ACA could mean a rise in lawsuits and, thus, premiums.
There are “more people getting care from the same number of health providers,” he said. “That puts additional pressure on an already strained system. Short term, the impact of the ACA could lead to additional [malpractice] claims.”
As for states with extremely high insurance rates, Dr. Volker does not see premium relief any time soon. He expects the trend of practice mergers and acquisitions to continue as more physicians seek to escape high premium costs and regulatory burdens.
“I think what you’re going to see in the hotbeds is more migration,” said Dr. Volker, who is licensed to practice in Nevada, California, Florida, and Arizona. “More doctors [will be] giving up their individual practices and joining larger groups.”
The MLM survey, published in October, gathered July 1 premium data from the major medical malpractice insurers and examines rates for mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
On Twitter @legal_med
Malpractice premiums for physicians stayed mostly the same in 2014, with 65% of liability insurance rates remaining steady nationwide, according to the Medical Liability Monitor’s annual survey and analysis of premiums nationwide.
Ongoing trends of slow lawsuit frequency and low plaintiff payouts are contributing to the steady market, said Chad C. Karls, editor of the 2014 Annual Rate Survey and a principal and consulting actuary for Milliman in Brookfield, Wis.
“We certainly do see those very large verdicts in the industry, but when we take it across all claims, the vast majority don’t have a verdict attached to them,” Mr. Karls said in an interview. “The vast majority get settled. That average claim has remained relatively stable.”
Unchanging insurance rates, however, can mean payment misery or relief depending on where physicians practice. Internists in southern Florida will pay a high of $47,707 for malpractice insurance this year, while their counterparts in South Dakota will pay just $3,697. For ob.gyns., malpractice insurance is priciest in the New York counties of Nassau and Suffolk, where they will pay $214,999 in malpractice premiums this year. But in Central California, ob.gyns. will pay just $16,240. General surgeons in southern Florida will dish out $190,829 in premiums in 2014, while Wisconsin surgeons will pay $10,868.
Premiums did increase in some areas in 2014. Indiana physicians saw the highest increase at 4.5%. Nevada doctors experienced a 34.8% decrease in premiums, by far the largest drop among states. (See map.) Nevada’s average percent change was driven by two companies that reported high rate decreases, the survey noted. (Acquisitions by some Nevada insurers may have affected the numbers.)
In general, Nevada’s large rate decline is not surprising, said Dr. Warren Volker, trustee-at-large for the Clark County (Nev.) Medical Society and chair of Premiere Physician Insurance Company in Nevada. Doctors in the state have experienced a stable medical liability climate for the last decade, he said.
“Our premiums have gone down dramatically, across the board,” Dr. Volker said in an interview. “Physicians have enjoyed cost savings as long as they have a good history.”
He attributed the declines to tort reform passed in 2002, including a $350,000 noneconomic damages cap in medical malpractice cases. Since then, the number of lawsuit filings has gone down and competition among liability insurers has increased, he said.
Legal reforms such as Nevada’s have probably contributed to the overall decrease in lawsuit frequency and payout severity across the country, Mr. Karls said. Patient safety initiatives and better risk management within medical practices also may be having an impact.
It remains to be seen how the Affordable Care Act will affect medical liability premiums. So far, industry analysts have not seen a definitive impact on medical malpractice insurance rates from the law, Mr. Karls said. The law could ultimately help lower liability claims if the ACA results in more proactive, preventive approaches to medical errors and less acute care, but in the short term, more patients covered under the ACA could mean a rise in lawsuits and, thus, premiums.
There are “more people getting care from the same number of health providers,” he said. “That puts additional pressure on an already strained system. Short term, the impact of the ACA could lead to additional [malpractice] claims.”
As for states with extremely high insurance rates, Dr. Volker does not see premium relief any time soon. He expects the trend of practice mergers and acquisitions to continue as more physicians seek to escape high premium costs and regulatory burdens.
“I think what you’re going to see in the hotbeds is more migration,” said Dr. Volker, who is licensed to practice in Nevada, California, Florida, and Arizona. “More doctors [will be] giving up their individual practices and joining larger groups.”
The MLM survey, published in October, gathered July 1 premium data from the major medical malpractice insurers and examines rates for mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
On Twitter @legal_med
Malpractice premiums for physicians stayed mostly the same in 2014, with 65% of liability insurance rates remaining steady nationwide, according to the Medical Liability Monitor’s annual survey and analysis of premiums nationwide.
Ongoing trends of slow lawsuit frequency and low plaintiff payouts are contributing to the steady market, said Chad C. Karls, editor of the 2014 Annual Rate Survey and a principal and consulting actuary for Milliman in Brookfield, Wis.
“We certainly do see those very large verdicts in the industry, but when we take it across all claims, the vast majority don’t have a verdict attached to them,” Mr. Karls said in an interview. “The vast majority get settled. That average claim has remained relatively stable.”
Unchanging insurance rates, however, can mean payment misery or relief depending on where physicians practice. Internists in southern Florida will pay a high of $47,707 for malpractice insurance this year, while their counterparts in South Dakota will pay just $3,697. For ob.gyns., malpractice insurance is priciest in the New York counties of Nassau and Suffolk, where they will pay $214,999 in malpractice premiums this year. But in Central California, ob.gyns. will pay just $16,240. General surgeons in southern Florida will dish out $190,829 in premiums in 2014, while Wisconsin surgeons will pay $10,868.
Premiums did increase in some areas in 2014. Indiana physicians saw the highest increase at 4.5%. Nevada doctors experienced a 34.8% decrease in premiums, by far the largest drop among states. (See map.) Nevada’s average percent change was driven by two companies that reported high rate decreases, the survey noted. (Acquisitions by some Nevada insurers may have affected the numbers.)
In general, Nevada’s large rate decline is not surprising, said Dr. Warren Volker, trustee-at-large for the Clark County (Nev.) Medical Society and chair of Premiere Physician Insurance Company in Nevada. Doctors in the state have experienced a stable medical liability climate for the last decade, he said.
“Our premiums have gone down dramatically, across the board,” Dr. Volker said in an interview. “Physicians have enjoyed cost savings as long as they have a good history.”
He attributed the declines to tort reform passed in 2002, including a $350,000 noneconomic damages cap in medical malpractice cases. Since then, the number of lawsuit filings has gone down and competition among liability insurers has increased, he said.
Legal reforms such as Nevada’s have probably contributed to the overall decrease in lawsuit frequency and payout severity across the country, Mr. Karls said. Patient safety initiatives and better risk management within medical practices also may be having an impact.
It remains to be seen how the Affordable Care Act will affect medical liability premiums. So far, industry analysts have not seen a definitive impact on medical malpractice insurance rates from the law, Mr. Karls said. The law could ultimately help lower liability claims if the ACA results in more proactive, preventive approaches to medical errors and less acute care, but in the short term, more patients covered under the ACA could mean a rise in lawsuits and, thus, premiums.
There are “more people getting care from the same number of health providers,” he said. “That puts additional pressure on an already strained system. Short term, the impact of the ACA could lead to additional [malpractice] claims.”
As for states with extremely high insurance rates, Dr. Volker does not see premium relief any time soon. He expects the trend of practice mergers and acquisitions to continue as more physicians seek to escape high premium costs and regulatory burdens.
“I think what you’re going to see in the hotbeds is more migration,” said Dr. Volker, who is licensed to practice in Nevada, California, Florida, and Arizona. “More doctors [will be] giving up their individual practices and joining larger groups.”
The MLM survey, published in October, gathered July 1 premium data from the major medical malpractice insurers and examines rates for mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
On Twitter @legal_med
CDC: ‘Breach’ responsible for Dallas health care worker’s Ebola infection
CDC officials are “deeply concerned” that a health care worker in Dallas has tested positive for Ebola virus as a result of contact with Thomas Duncan, the index patient from Liberia who died Oct 8.
In an emergency press conference Oct. 12, Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention, blamed what he called a breach of protocol for the infection.
However, Dr. Frieden said that investigators had yet to identify any specific breach of protocol at Texas Presbyterian Hospital, Dallas. He pointed to two procedures performed on Mr. Duncan – respiratory intubation and kidney dialysis – as having the potential to have spread infection to the health care worker.
Additional health care workers treating Mr. Duncan are being closely monitored along with all of Mr. Duncan’s contacts both before and after admission, Dr. Frieden said.
“Unfortunately, it is possible that we will see additional cases of Ebola,” he said.
The CDC is mulling a policy in which procedures performed on Ebola patients would be limited to those deemed “essential.” Pressed to explain, Dr. Frieden said that for example, blood draws to monitor electrolytes could be limited to one per day, down from three, to reduce potential for exposure.
Dr. Frieden also cited the need to reduce the number of health care workers caring for patients with Ebola.
The news of an infected health care worker at Texas Presbyterian Hospital, Dallas, which initially failed to isolate Mr. Duncan, drew questions as to whether suspected Ebola infection cases should be transferred to special treatment centers with isolation units instead of being treated for locally.
Dr. Frieden said that it was important that all hospitals be ready to diagnose and isolate Ebola patients safely. “We can’t have any hospital let its guard down,” he said, adding that the CDC has not ruled out transferring Ebola patients to specially equipped centers for treatment.
Confirmatory results for the health care worker were expected later Oct. 12, Dr. Frieden said. The health care worker had been self-monitoring for symptoms as instructed, when she presented with a low-grade fever, and viral levels that Dr. Frieden said appeared to be low. The health care worker only reported having a single contact following the first appearance of symptoms.
Dr. Frieden said that the agency was continuing to investigate the 48 contacts of Mr. Duncan before his isolation and admission to the hospital and that it had opened another investigation into his post-admission contacts.
“It’s deeply concerning that this occurred,” Dr. Frieden said, but he added that the case “doesn’t change the bottom line, which is that we know how to break the chain of transmission” though prompt diagnosis and isolation and notification of contacts.
This new infection signifies a further need to “ramp up infection control” in the hospital setting, he said. “We know how Ebola spreads, we know how to stop it, but this reemphasizes how meticulous we have to be.”
CDC officials are “deeply concerned” that a health care worker in Dallas has tested positive for Ebola virus as a result of contact with Thomas Duncan, the index patient from Liberia who died Oct 8.
In an emergency press conference Oct. 12, Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention, blamed what he called a breach of protocol for the infection.
However, Dr. Frieden said that investigators had yet to identify any specific breach of protocol at Texas Presbyterian Hospital, Dallas. He pointed to two procedures performed on Mr. Duncan – respiratory intubation and kidney dialysis – as having the potential to have spread infection to the health care worker.
Additional health care workers treating Mr. Duncan are being closely monitored along with all of Mr. Duncan’s contacts both before and after admission, Dr. Frieden said.
“Unfortunately, it is possible that we will see additional cases of Ebola,” he said.
The CDC is mulling a policy in which procedures performed on Ebola patients would be limited to those deemed “essential.” Pressed to explain, Dr. Frieden said that for example, blood draws to monitor electrolytes could be limited to one per day, down from three, to reduce potential for exposure.
Dr. Frieden also cited the need to reduce the number of health care workers caring for patients with Ebola.
The news of an infected health care worker at Texas Presbyterian Hospital, Dallas, which initially failed to isolate Mr. Duncan, drew questions as to whether suspected Ebola infection cases should be transferred to special treatment centers with isolation units instead of being treated for locally.
Dr. Frieden said that it was important that all hospitals be ready to diagnose and isolate Ebola patients safely. “We can’t have any hospital let its guard down,” he said, adding that the CDC has not ruled out transferring Ebola patients to specially equipped centers for treatment.
Confirmatory results for the health care worker were expected later Oct. 12, Dr. Frieden said. The health care worker had been self-monitoring for symptoms as instructed, when she presented with a low-grade fever, and viral levels that Dr. Frieden said appeared to be low. The health care worker only reported having a single contact following the first appearance of symptoms.
Dr. Frieden said that the agency was continuing to investigate the 48 contacts of Mr. Duncan before his isolation and admission to the hospital and that it had opened another investigation into his post-admission contacts.
“It’s deeply concerning that this occurred,” Dr. Frieden said, but he added that the case “doesn’t change the bottom line, which is that we know how to break the chain of transmission” though prompt diagnosis and isolation and notification of contacts.
This new infection signifies a further need to “ramp up infection control” in the hospital setting, he said. “We know how Ebola spreads, we know how to stop it, but this reemphasizes how meticulous we have to be.”
CDC officials are “deeply concerned” that a health care worker in Dallas has tested positive for Ebola virus as a result of contact with Thomas Duncan, the index patient from Liberia who died Oct 8.
In an emergency press conference Oct. 12, Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention, blamed what he called a breach of protocol for the infection.
However, Dr. Frieden said that investigators had yet to identify any specific breach of protocol at Texas Presbyterian Hospital, Dallas. He pointed to two procedures performed on Mr. Duncan – respiratory intubation and kidney dialysis – as having the potential to have spread infection to the health care worker.
Additional health care workers treating Mr. Duncan are being closely monitored along with all of Mr. Duncan’s contacts both before and after admission, Dr. Frieden said.
“Unfortunately, it is possible that we will see additional cases of Ebola,” he said.
The CDC is mulling a policy in which procedures performed on Ebola patients would be limited to those deemed “essential.” Pressed to explain, Dr. Frieden said that for example, blood draws to monitor electrolytes could be limited to one per day, down from three, to reduce potential for exposure.
Dr. Frieden also cited the need to reduce the number of health care workers caring for patients with Ebola.
The news of an infected health care worker at Texas Presbyterian Hospital, Dallas, which initially failed to isolate Mr. Duncan, drew questions as to whether suspected Ebola infection cases should be transferred to special treatment centers with isolation units instead of being treated for locally.
Dr. Frieden said that it was important that all hospitals be ready to diagnose and isolate Ebola patients safely. “We can’t have any hospital let its guard down,” he said, adding that the CDC has not ruled out transferring Ebola patients to specially equipped centers for treatment.
Confirmatory results for the health care worker were expected later Oct. 12, Dr. Frieden said. The health care worker had been self-monitoring for symptoms as instructed, when she presented with a low-grade fever, and viral levels that Dr. Frieden said appeared to be low. The health care worker only reported having a single contact following the first appearance of symptoms.
Dr. Frieden said that the agency was continuing to investigate the 48 contacts of Mr. Duncan before his isolation and admission to the hospital and that it had opened another investigation into his post-admission contacts.
“It’s deeply concerning that this occurred,” Dr. Frieden said, but he added that the case “doesn’t change the bottom line, which is that we know how to break the chain of transmission” though prompt diagnosis and isolation and notification of contacts.
This new infection signifies a further need to “ramp up infection control” in the hospital setting, he said. “We know how Ebola spreads, we know how to stop it, but this reemphasizes how meticulous we have to be.”
First drug-coated angioplasty balloon approved for PAD
A drug-coated angioplasty balloon catheter has been approved for treating peripheral artery disease, the first such device approved for this use, the Food and Drug Administration announced on October 10.
The device is the Lutonix 035 Drug Coated Balloon Percutaneous Transluminal Angioplasty Catheter (Lutonix DCB), manufactured by Lutonix; its outer surface is coated with paclitaxel, “which may help to prevent” restenosis after the angioplasty procedure, according to the FDA statement announcing the approval. “The clinical data show that Lutonix DCB may be more effective than traditional balloon angioplasty at helping to prevent further blockage in the artery,” Dr. William Maisel, deputy director for science and chief scientist in the FDA’s Center for Devices and Radiological Health, said in the statement.
Approval was based on the results of three clinical trials and nonclinical testing:
• A randomized, multicenter study of 101 people in Europe, which found that after 6 months, no further treatment for PAD was needed in almost 72% of the patients treated with Lutonix DCB, compared with almost 50% of those treated with conventional balloon angioplasty.
• A single-blind, multicenter, randomized study of 476 people in the United States and Europe, which found that 65% of those randomized to treatment with Lutonix DCB had no restenosis at 12 months, compared with roughly 53% of those randomized to treatment with conventional balloon angioplasty.
• A single-arm, ongoing study that is further evaluating safety and effectiveness in 657 people treated with the device in the United States and Europe, which, at the time of approval, “show that there have been no unanticipated device- or drug-related adverse events,” the FDA said.
These studies also indicated that the safety of Lutonix DCB was comparable to conventional balloon angioplasty. The most common major adverse events included additional intervention, pain as a result of poor blood flow, narrowing of arteries that were not treated, chest pain, and abnormal growth of tissue.
Contraindications include women who are breastfeeding, pregnant, or plan to become pregnant; and men who plan to father children.
The company is required by the FDA to conduct two postapproval studies, the ongoing 5-year study of 657 patients, and a randomized, single-blind, multicenter study that will evaluate safety and effectiveness of the device in women in the United States, “due to differences in observed outcomes in this group as compared to outcomes for the general study population,” according to the FDA.
The device was reviewed at an FDA advisory panel meeting in June.
A drug-coated angioplasty balloon catheter has been approved for treating peripheral artery disease, the first such device approved for this use, the Food and Drug Administration announced on October 10.
The device is the Lutonix 035 Drug Coated Balloon Percutaneous Transluminal Angioplasty Catheter (Lutonix DCB), manufactured by Lutonix; its outer surface is coated with paclitaxel, “which may help to prevent” restenosis after the angioplasty procedure, according to the FDA statement announcing the approval. “The clinical data show that Lutonix DCB may be more effective than traditional balloon angioplasty at helping to prevent further blockage in the artery,” Dr. William Maisel, deputy director for science and chief scientist in the FDA’s Center for Devices and Radiological Health, said in the statement.
Approval was based on the results of three clinical trials and nonclinical testing:
• A randomized, multicenter study of 101 people in Europe, which found that after 6 months, no further treatment for PAD was needed in almost 72% of the patients treated with Lutonix DCB, compared with almost 50% of those treated with conventional balloon angioplasty.
• A single-blind, multicenter, randomized study of 476 people in the United States and Europe, which found that 65% of those randomized to treatment with Lutonix DCB had no restenosis at 12 months, compared with roughly 53% of those randomized to treatment with conventional balloon angioplasty.
• A single-arm, ongoing study that is further evaluating safety and effectiveness in 657 people treated with the device in the United States and Europe, which, at the time of approval, “show that there have been no unanticipated device- or drug-related adverse events,” the FDA said.
These studies also indicated that the safety of Lutonix DCB was comparable to conventional balloon angioplasty. The most common major adverse events included additional intervention, pain as a result of poor blood flow, narrowing of arteries that were not treated, chest pain, and abnormal growth of tissue.
Contraindications include women who are breastfeeding, pregnant, or plan to become pregnant; and men who plan to father children.
The company is required by the FDA to conduct two postapproval studies, the ongoing 5-year study of 657 patients, and a randomized, single-blind, multicenter study that will evaluate safety and effectiveness of the device in women in the United States, “due to differences in observed outcomes in this group as compared to outcomes for the general study population,” according to the FDA.
The device was reviewed at an FDA advisory panel meeting in June.
A drug-coated angioplasty balloon catheter has been approved for treating peripheral artery disease, the first such device approved for this use, the Food and Drug Administration announced on October 10.
The device is the Lutonix 035 Drug Coated Balloon Percutaneous Transluminal Angioplasty Catheter (Lutonix DCB), manufactured by Lutonix; its outer surface is coated with paclitaxel, “which may help to prevent” restenosis after the angioplasty procedure, according to the FDA statement announcing the approval. “The clinical data show that Lutonix DCB may be more effective than traditional balloon angioplasty at helping to prevent further blockage in the artery,” Dr. William Maisel, deputy director for science and chief scientist in the FDA’s Center for Devices and Radiological Health, said in the statement.
Approval was based on the results of three clinical trials and nonclinical testing:
• A randomized, multicenter study of 101 people in Europe, which found that after 6 months, no further treatment for PAD was needed in almost 72% of the patients treated with Lutonix DCB, compared with almost 50% of those treated with conventional balloon angioplasty.
• A single-blind, multicenter, randomized study of 476 people in the United States and Europe, which found that 65% of those randomized to treatment with Lutonix DCB had no restenosis at 12 months, compared with roughly 53% of those randomized to treatment with conventional balloon angioplasty.
• A single-arm, ongoing study that is further evaluating safety and effectiveness in 657 people treated with the device in the United States and Europe, which, at the time of approval, “show that there have been no unanticipated device- or drug-related adverse events,” the FDA said.
These studies also indicated that the safety of Lutonix DCB was comparable to conventional balloon angioplasty. The most common major adverse events included additional intervention, pain as a result of poor blood flow, narrowing of arteries that were not treated, chest pain, and abnormal growth of tissue.
Contraindications include women who are breastfeeding, pregnant, or plan to become pregnant; and men who plan to father children.
The company is required by the FDA to conduct two postapproval studies, the ongoing 5-year study of 657 patients, and a randomized, single-blind, multicenter study that will evaluate safety and effectiveness of the device in women in the United States, “due to differences in observed outcomes in this group as compared to outcomes for the general study population,” according to the FDA.
The device was reviewed at an FDA advisory panel meeting in June.
To stop Ebola, think about it, identify, isolate, diagnose
Thomas Eric Duncan, a Liberian man who has become the face of Ebola in the United States, died on Wednesday morning at Texas Health Presbyterian Hospital, more than a week after he became the first person to be diagnosed with the virus here.
His body will be handled and cremated in accordance to the Centers for Disease Control and Prevention guidelines, said the Texas Department of State Health Services in a statement.
Mr. Duncan’s death further highlights “what a deadly enemy Ebola is and how important it is to protect Americans and to stop Ebola at its source in West Africa,” said CDC Director Dr. Thomas Frieden, in an afternoon news briefing on Wednesday.
Like more than 36,000 individuals leaving West Africa in the last 2 months, Mr. Duncan filled out a questionnaire and had his temperature taken before he boarded a plane to visit his family in Dallas.
For more layers of protection, federal officials ramped up their efforts on Wednesday by adding entry screening for those arriving from the affected West African countries at five U.S. airports
New York’s JFK International Airport, Washington-Dulles, Newark, Chicago-O’Hare, and Atlanta International airports receive more than 94% of travelers from Guinea, Liberia, and Sierra Leone. Passengers arriving from the three affected countries to these airports will be screened there. If they have symptoms or are suspected of having exposure to Ebola, they will be referred to a public health authority. Travelers with no symptoms will be asked to provide contact information and to complete a daily temperature log. The screening will begin as early as this Saturday.
CDC has also issued level 3 travel advisories for Guinea, Liberia, Sierra Leone, asking Americans to avoid nonessential trips to these regions.
Meanwhile, health professionals should be thinking about the possibility of Ebola and be able to identify who might have it and isolate and test them.
“Identification, diagnosis, and safe care needs to be on top of the minds right now for health care professionals,” said Dr. Frieden.
The American freelance journalist who contracted the virus in Liberia and is hospitalized in Nebraska has received blood transfusion from another American, Dr. Kent Brantly, who survived the virus.
Another patient who was suspected of having Ebola and was hospitalized at the National Institutes of Health Clinical Center was released on Tuesday, October 7, without a positive diagnosis. He continues to be monitored.
Nearly 50 individuals in Texas who have had definite or possible contact with Mr. Duncan will continue to be monitored for 21 days. None have shown any symptoms.
Since March, there have been 8,033 cases of Ebola in Guinea, Liberia, Nigeria, Senegal, Sierra Leone, and the United States, including 3,879 deaths, according to the latest numbers from the World Health Organization.
Dr. Frieden once again emphasized that isolating the affected West African countries is not the answer to stopping the Ebola threat.
“As long as Ebola is spreading in Africa, it will remain a risk in the United States,” he said.
Helpful links:
Information for health care workers
Latest outbreak information in West Africa
Center for Infectious Disease Research and Policy
American College of Emergency Physicians
On Twitter @naseemmiller
Thomas Eric Duncan, a Liberian man who has become the face of Ebola in the United States, died on Wednesday morning at Texas Health Presbyterian Hospital, more than a week after he became the first person to be diagnosed with the virus here.
His body will be handled and cremated in accordance to the Centers for Disease Control and Prevention guidelines, said the Texas Department of State Health Services in a statement.
Mr. Duncan’s death further highlights “what a deadly enemy Ebola is and how important it is to protect Americans and to stop Ebola at its source in West Africa,” said CDC Director Dr. Thomas Frieden, in an afternoon news briefing on Wednesday.
Like more than 36,000 individuals leaving West Africa in the last 2 months, Mr. Duncan filled out a questionnaire and had his temperature taken before he boarded a plane to visit his family in Dallas.
For more layers of protection, federal officials ramped up their efforts on Wednesday by adding entry screening for those arriving from the affected West African countries at five U.S. airports
New York’s JFK International Airport, Washington-Dulles, Newark, Chicago-O’Hare, and Atlanta International airports receive more than 94% of travelers from Guinea, Liberia, and Sierra Leone. Passengers arriving from the three affected countries to these airports will be screened there. If they have symptoms or are suspected of having exposure to Ebola, they will be referred to a public health authority. Travelers with no symptoms will be asked to provide contact information and to complete a daily temperature log. The screening will begin as early as this Saturday.
CDC has also issued level 3 travel advisories for Guinea, Liberia, Sierra Leone, asking Americans to avoid nonessential trips to these regions.
Meanwhile, health professionals should be thinking about the possibility of Ebola and be able to identify who might have it and isolate and test them.
“Identification, diagnosis, and safe care needs to be on top of the minds right now for health care professionals,” said Dr. Frieden.
The American freelance journalist who contracted the virus in Liberia and is hospitalized in Nebraska has received blood transfusion from another American, Dr. Kent Brantly, who survived the virus.
Another patient who was suspected of having Ebola and was hospitalized at the National Institutes of Health Clinical Center was released on Tuesday, October 7, without a positive diagnosis. He continues to be monitored.
Nearly 50 individuals in Texas who have had definite or possible contact with Mr. Duncan will continue to be monitored for 21 days. None have shown any symptoms.
Since March, there have been 8,033 cases of Ebola in Guinea, Liberia, Nigeria, Senegal, Sierra Leone, and the United States, including 3,879 deaths, according to the latest numbers from the World Health Organization.
Dr. Frieden once again emphasized that isolating the affected West African countries is not the answer to stopping the Ebola threat.
“As long as Ebola is spreading in Africa, it will remain a risk in the United States,” he said.
Helpful links:
Information for health care workers
Latest outbreak information in West Africa
Center for Infectious Disease Research and Policy
American College of Emergency Physicians
On Twitter @naseemmiller
Thomas Eric Duncan, a Liberian man who has become the face of Ebola in the United States, died on Wednesday morning at Texas Health Presbyterian Hospital, more than a week after he became the first person to be diagnosed with the virus here.
His body will be handled and cremated in accordance to the Centers for Disease Control and Prevention guidelines, said the Texas Department of State Health Services in a statement.
Mr. Duncan’s death further highlights “what a deadly enemy Ebola is and how important it is to protect Americans and to stop Ebola at its source in West Africa,” said CDC Director Dr. Thomas Frieden, in an afternoon news briefing on Wednesday.
Like more than 36,000 individuals leaving West Africa in the last 2 months, Mr. Duncan filled out a questionnaire and had his temperature taken before he boarded a plane to visit his family in Dallas.
For more layers of protection, federal officials ramped up their efforts on Wednesday by adding entry screening for those arriving from the affected West African countries at five U.S. airports
New York’s JFK International Airport, Washington-Dulles, Newark, Chicago-O’Hare, and Atlanta International airports receive more than 94% of travelers from Guinea, Liberia, and Sierra Leone. Passengers arriving from the three affected countries to these airports will be screened there. If they have symptoms or are suspected of having exposure to Ebola, they will be referred to a public health authority. Travelers with no symptoms will be asked to provide contact information and to complete a daily temperature log. The screening will begin as early as this Saturday.
CDC has also issued level 3 travel advisories for Guinea, Liberia, Sierra Leone, asking Americans to avoid nonessential trips to these regions.
Meanwhile, health professionals should be thinking about the possibility of Ebola and be able to identify who might have it and isolate and test them.
“Identification, diagnosis, and safe care needs to be on top of the minds right now for health care professionals,” said Dr. Frieden.
The American freelance journalist who contracted the virus in Liberia and is hospitalized in Nebraska has received blood transfusion from another American, Dr. Kent Brantly, who survived the virus.
Another patient who was suspected of having Ebola and was hospitalized at the National Institutes of Health Clinical Center was released on Tuesday, October 7, without a positive diagnosis. He continues to be monitored.
Nearly 50 individuals in Texas who have had definite or possible contact with Mr. Duncan will continue to be monitored for 21 days. None have shown any symptoms.
Since March, there have been 8,033 cases of Ebola in Guinea, Liberia, Nigeria, Senegal, Sierra Leone, and the United States, including 3,879 deaths, according to the latest numbers from the World Health Organization.
Dr. Frieden once again emphasized that isolating the affected West African countries is not the answer to stopping the Ebola threat.
“As long as Ebola is spreading in Africa, it will remain a risk in the United States,” he said.
Helpful links:
Information for health care workers
Latest outbreak information in West Africa
Center for Infectious Disease Research and Policy
American College of Emergency Physicians
On Twitter @naseemmiller
FROM A CDC TELEBRIEFING
CDC director: Expect long Ebola fight
The enemy is a virus, and the fight will be long and hard, but the tried and true public health measures will stop the spread of Ebola, said Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention.
“The main point is to suspect Ebola and isolate it,” said Dr. Frieden during an Oct. 7 news briefing. You don’t need a fancy unit for infection control, he said. All you need is a private room with its own bathroom, and meticulous attention to details and protocols.
Federal officials are also planning to announce increased safety measures for travelers in the upcoming days.
In the past 2 months, CDC teams have screened more than 36,000 airplane passengers coming from West Africa, officials said. More than 70 have been stopped from boarding the planes, although there are no signs that any of them developed Ebola.
Meanwhile, Thomas Eric Duncan, the first person to be diagnosed with Ebola in the United States, remains in critical but stable condition. “He is on a ventilator and receiving kidney dialysis. His liver function, which declined over the weekend, has improved, but doctors caution that this could vary in coming days,” according to a statement from Texas Health Presbyterian Hospital, Dallas, where he is in isolation. He is still receiving the investigational drug brincidofovir.
Another American, a freelance journalist who tested positive for Ebola in Liberia and is now in isolation in Omaha, Nebraska, also is receiving the investigational drug.
Dr. Frieden said that no more ZMapp is available.
Federal and Texas health officials continue to monitor 48 individuals, 10 of whom have had definite contact with Mr. Duncan. None have shown any signs or symptoms of Ebola so far.
In Spain, a nurse who was caring for Ebola patients there became the first patient to contract Ebola outside of the affected West African countries. U.S. health officials said Oct. 7 that the case highlights the importance of meticulous attention to detail, teamwork, and careful attention to protocols.
Dr. Frieden said that there are some signs of progress in West Africa. The number of cases in some parts of Liberia has dropped, partly because there are enough isolation beds and because of improvements in burial practice safety, but there’s no way to know when the epidemic will be under control and come to an end.
So far, there’s no sign that the Ebola Zaire virus strain has mutated or become airborne, officials said.
Since Mr. Duncan was diagnosed with Ebola in Texas last week, federal health officials and President Barack Obama have stressed that isolating the affected West African countries is not the answer.
“One of our cardinal rules in medicine is do no harm,” said Dr. Frieden. Impeding the ability to control Ebola in West Africa will only increase the challenge of controlling the spread of the virus, he said.
On Twitter @naseemmiller
The enemy is a virus, and the fight will be long and hard, but the tried and true public health measures will stop the spread of Ebola, said Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention.
“The main point is to suspect Ebola and isolate it,” said Dr. Frieden during an Oct. 7 news briefing. You don’t need a fancy unit for infection control, he said. All you need is a private room with its own bathroom, and meticulous attention to details and protocols.
Federal officials are also planning to announce increased safety measures for travelers in the upcoming days.
In the past 2 months, CDC teams have screened more than 36,000 airplane passengers coming from West Africa, officials said. More than 70 have been stopped from boarding the planes, although there are no signs that any of them developed Ebola.
Meanwhile, Thomas Eric Duncan, the first person to be diagnosed with Ebola in the United States, remains in critical but stable condition. “He is on a ventilator and receiving kidney dialysis. His liver function, which declined over the weekend, has improved, but doctors caution that this could vary in coming days,” according to a statement from Texas Health Presbyterian Hospital, Dallas, where he is in isolation. He is still receiving the investigational drug brincidofovir.
Another American, a freelance journalist who tested positive for Ebola in Liberia and is now in isolation in Omaha, Nebraska, also is receiving the investigational drug.
Dr. Frieden said that no more ZMapp is available.
Federal and Texas health officials continue to monitor 48 individuals, 10 of whom have had definite contact with Mr. Duncan. None have shown any signs or symptoms of Ebola so far.
In Spain, a nurse who was caring for Ebola patients there became the first patient to contract Ebola outside of the affected West African countries. U.S. health officials said Oct. 7 that the case highlights the importance of meticulous attention to detail, teamwork, and careful attention to protocols.
Dr. Frieden said that there are some signs of progress in West Africa. The number of cases in some parts of Liberia has dropped, partly because there are enough isolation beds and because of improvements in burial practice safety, but there’s no way to know when the epidemic will be under control and come to an end.
So far, there’s no sign that the Ebola Zaire virus strain has mutated or become airborne, officials said.
Since Mr. Duncan was diagnosed with Ebola in Texas last week, federal health officials and President Barack Obama have stressed that isolating the affected West African countries is not the answer.
“One of our cardinal rules in medicine is do no harm,” said Dr. Frieden. Impeding the ability to control Ebola in West Africa will only increase the challenge of controlling the spread of the virus, he said.
On Twitter @naseemmiller
The enemy is a virus, and the fight will be long and hard, but the tried and true public health measures will stop the spread of Ebola, said Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention.
“The main point is to suspect Ebola and isolate it,” said Dr. Frieden during an Oct. 7 news briefing. You don’t need a fancy unit for infection control, he said. All you need is a private room with its own bathroom, and meticulous attention to details and protocols.
Federal officials are also planning to announce increased safety measures for travelers in the upcoming days.
In the past 2 months, CDC teams have screened more than 36,000 airplane passengers coming from West Africa, officials said. More than 70 have been stopped from boarding the planes, although there are no signs that any of them developed Ebola.
Meanwhile, Thomas Eric Duncan, the first person to be diagnosed with Ebola in the United States, remains in critical but stable condition. “He is on a ventilator and receiving kidney dialysis. His liver function, which declined over the weekend, has improved, but doctors caution that this could vary in coming days,” according to a statement from Texas Health Presbyterian Hospital, Dallas, where he is in isolation. He is still receiving the investigational drug brincidofovir.
Another American, a freelance journalist who tested positive for Ebola in Liberia and is now in isolation in Omaha, Nebraska, also is receiving the investigational drug.
Dr. Frieden said that no more ZMapp is available.
Federal and Texas health officials continue to monitor 48 individuals, 10 of whom have had definite contact with Mr. Duncan. None have shown any signs or symptoms of Ebola so far.
In Spain, a nurse who was caring for Ebola patients there became the first patient to contract Ebola outside of the affected West African countries. U.S. health officials said Oct. 7 that the case highlights the importance of meticulous attention to detail, teamwork, and careful attention to protocols.
Dr. Frieden said that there are some signs of progress in West Africa. The number of cases in some parts of Liberia has dropped, partly because there are enough isolation beds and because of improvements in burial practice safety, but there’s no way to know when the epidemic will be under control and come to an end.
So far, there’s no sign that the Ebola Zaire virus strain has mutated or become airborne, officials said.
Since Mr. Duncan was diagnosed with Ebola in Texas last week, federal health officials and President Barack Obama have stressed that isolating the affected West African countries is not the answer.
“One of our cardinal rules in medicine is do no harm,” said Dr. Frieden. Impeding the ability to control Ebola in West Africa will only increase the challenge of controlling the spread of the virus, he said.
On Twitter @naseemmiller
FROM A CDC TELEBRIEFING
Cardiology Collaboration in Washington, DC
Six teams from 4 medical schools convened in the Washington, DC VAMC (DCVAMC) on Friday, September 12, 2014, at the 2nd Annual Fall Meeting of the Association of VA Heart Providers (AVAHeart) to present their latest research findings and professional experiences in managing an array of cardiovascular diseases. About half the registered attendees were from the DC area, but the scope of the presenters’ reach went far beyond the walls of the Freedom Auditorium.
The presenters all discussed poignant hypotheses for best treating their VA cardiology patients. Peter Kokkinos, PhD, director of the Lifestyle Intervention for Veterans (LIVe) program at the DCVAMC, investigated exercise as an alternative to statins in patients who can’t tolerate statins as well as in those whose atrial stiffness, for example, can be alleviated after just 4 weeks of moderate exercise.
Michael Franz, MD, PhD, is currently engaged in a new VA co-op study assessing quality of life issues surrounding implantable cardioverter-defibrillator (ICD) implantation in patients aged > 70 years. The DCVAMC study is the “brainchild” of Steven Singh, MD, and is also being conducted by Hans Moore, MD.
But that is just a piece of the bigger picture this organization has in mind for VA cardiology providers. Since the incorporation of AVAHeart less than 2 years ago, the group has aimed “to improve the care of our nation’s veterans with cardiovascular diseases through provider education and collaboration.”
AVAHeart is led by President Pamela Steele, MD; with Vice President Hans Moore, MD; Vice President Pendleton Alexander, MD; Secretary David Lu, MD; and Treasurer Muriel Kneib, PA-C.
Peripheral discussions during the meeting included how the VA struggles with patient recruitment numbers for vital studies as well as the difficulty in attaining certain technologies for trials.
For information on AVAHeart, its mission, membership, and meetings, visit http://avaheart.org.
Six teams from 4 medical schools convened in the Washington, DC VAMC (DCVAMC) on Friday, September 12, 2014, at the 2nd Annual Fall Meeting of the Association of VA Heart Providers (AVAHeart) to present their latest research findings and professional experiences in managing an array of cardiovascular diseases. About half the registered attendees were from the DC area, but the scope of the presenters’ reach went far beyond the walls of the Freedom Auditorium.
The presenters all discussed poignant hypotheses for best treating their VA cardiology patients. Peter Kokkinos, PhD, director of the Lifestyle Intervention for Veterans (LIVe) program at the DCVAMC, investigated exercise as an alternative to statins in patients who can’t tolerate statins as well as in those whose atrial stiffness, for example, can be alleviated after just 4 weeks of moderate exercise.
Michael Franz, MD, PhD, is currently engaged in a new VA co-op study assessing quality of life issues surrounding implantable cardioverter-defibrillator (ICD) implantation in patients aged > 70 years. The DCVAMC study is the “brainchild” of Steven Singh, MD, and is also being conducted by Hans Moore, MD.
But that is just a piece of the bigger picture this organization has in mind for VA cardiology providers. Since the incorporation of AVAHeart less than 2 years ago, the group has aimed “to improve the care of our nation’s veterans with cardiovascular diseases through provider education and collaboration.”
AVAHeart is led by President Pamela Steele, MD; with Vice President Hans Moore, MD; Vice President Pendleton Alexander, MD; Secretary David Lu, MD; and Treasurer Muriel Kneib, PA-C.
Peripheral discussions during the meeting included how the VA struggles with patient recruitment numbers for vital studies as well as the difficulty in attaining certain technologies for trials.
For information on AVAHeart, its mission, membership, and meetings, visit http://avaheart.org.
Six teams from 4 medical schools convened in the Washington, DC VAMC (DCVAMC) on Friday, September 12, 2014, at the 2nd Annual Fall Meeting of the Association of VA Heart Providers (AVAHeart) to present their latest research findings and professional experiences in managing an array of cardiovascular diseases. About half the registered attendees were from the DC area, but the scope of the presenters’ reach went far beyond the walls of the Freedom Auditorium.
The presenters all discussed poignant hypotheses for best treating their VA cardiology patients. Peter Kokkinos, PhD, director of the Lifestyle Intervention for Veterans (LIVe) program at the DCVAMC, investigated exercise as an alternative to statins in patients who can’t tolerate statins as well as in those whose atrial stiffness, for example, can be alleviated after just 4 weeks of moderate exercise.
Michael Franz, MD, PhD, is currently engaged in a new VA co-op study assessing quality of life issues surrounding implantable cardioverter-defibrillator (ICD) implantation in patients aged > 70 years. The DCVAMC study is the “brainchild” of Steven Singh, MD, and is also being conducted by Hans Moore, MD.
But that is just a piece of the bigger picture this organization has in mind for VA cardiology providers. Since the incorporation of AVAHeart less than 2 years ago, the group has aimed “to improve the care of our nation’s veterans with cardiovascular diseases through provider education and collaboration.”
AVAHeart is led by President Pamela Steele, MD; with Vice President Hans Moore, MD; Vice President Pendleton Alexander, MD; Secretary David Lu, MD; and Treasurer Muriel Kneib, PA-C.
Peripheral discussions during the meeting included how the VA struggles with patient recruitment numbers for vital studies as well as the difficulty in attaining certain technologies for trials.
For information on AVAHeart, its mission, membership, and meetings, visit http://avaheart.org.
Liberia improves Ebola response tactics
Liberian health officials have stepped up their ability to respond to the ongoing Ebola epidemic, improving facilities and boosting personnel to help meet the crisis.
In response to last spring’s increasing cases in more populous areas of the country, officials undertook a facilities and personnel assessment in four rural counties in the southeast. Conducted in August, the review found serious problems with the ability to effectively respond to any developing Ebola threat, Dr. Joseph Forrester and his colleagues wrote in the Oct. 7 issue of the Morbidity and Mortality Weekly Report (2014;63:1-3).
Each of the four reviewed counties contained one referral hospital; the region had previously been served by six physicians, but three of these had fled the county because of the epidemic, said Dr. Forrester, an infectious disease specialist with the Centers for Disease Control and Prevention.
In two hospitals, nursing staff had ceased coming to work; in another, workers were still providing care despite not having been paid for 3 months. Nursing students, aides, and community volunteers were providing much of basic medical care, and even responding to obstetric and surgical emergencies.
Even the most basic supplies were depleted or absent. There were few hand-washing stations, and most of these consisted of a simple water jug. Soap, bleach, and alcohol hand gels were rare. There were only rudimentary isolation facilities in two counties, and neither of these had water, electricity, or waste disposal. Communication between the hospitals and county health officials was via cell phone or radio, with little Internet connectivity. About half of the local health care facilities had no communications at all and required site visits for assessment. Only one ambulance served the entire four-county region. There was little or no protective equipment for those who would work with patients.
Although each county had an Ebola task force, problems with transportation, communication, and resources limited their effectiveness. Health care workers had not received proper training for Ebola patient care or case investigation, including how to trace patient contacts.
Since the assessment, however, things have improved, Dr. Forrester and his coauthors wrote. Health officials in one county were able to identify their first patient – a woman who died during a spontaneous abortion on Aug. 3. She had apparently been infected in Monrovia after attending a funeral. Shortly thereafter, patient 2 was diagnosed – a man who had participated in the community funeral of patient 1 and who was attempting to flee to another Liberian county. “He was sent back ... and later reported to have died of laboratory-confirmed Ebola. This was the first evidence of secondary transmission of Ebola in southeast Liberia,” the team noted.
Since August, additional cases have surfaced in southeast Liberia, but the region is better prepared to cope with them. Local health officials have been trained in surveillance, infection control and prevention, and safe burial practices. There are regular, coordinated task force meetings. Additional ambulances are available; there are plans to establish three specialized treatment centers.
“Still,” the researchers wrote, “obstacles to prevent the spread of Ebola remain, and personal protective equipment, sufficient personnel for effective contact tracing and case management, efficient patient transport, and regional diagnostic laboratory capabilities are urgently needed.”
The latest updates, including case counts, on the 2014 Ebola outbreak in West Africa are available at http://www.cdc.gov/vhf/Ebola/outbreaks/guinea/index.html. The most up-to-date clinical guidelines on the 2014 Ebola outbreak in West Africa are available at http://www.cdc.gov/vhf/ebola/hcp/index.html.
On Twitter @alz_gal
Liberian health officials have stepped up their ability to respond to the ongoing Ebola epidemic, improving facilities and boosting personnel to help meet the crisis.
In response to last spring’s increasing cases in more populous areas of the country, officials undertook a facilities and personnel assessment in four rural counties in the southeast. Conducted in August, the review found serious problems with the ability to effectively respond to any developing Ebola threat, Dr. Joseph Forrester and his colleagues wrote in the Oct. 7 issue of the Morbidity and Mortality Weekly Report (2014;63:1-3).
Each of the four reviewed counties contained one referral hospital; the region had previously been served by six physicians, but three of these had fled the county because of the epidemic, said Dr. Forrester, an infectious disease specialist with the Centers for Disease Control and Prevention.
In two hospitals, nursing staff had ceased coming to work; in another, workers were still providing care despite not having been paid for 3 months. Nursing students, aides, and community volunteers were providing much of basic medical care, and even responding to obstetric and surgical emergencies.
Even the most basic supplies were depleted or absent. There were few hand-washing stations, and most of these consisted of a simple water jug. Soap, bleach, and alcohol hand gels were rare. There were only rudimentary isolation facilities in two counties, and neither of these had water, electricity, or waste disposal. Communication between the hospitals and county health officials was via cell phone or radio, with little Internet connectivity. About half of the local health care facilities had no communications at all and required site visits for assessment. Only one ambulance served the entire four-county region. There was little or no protective equipment for those who would work with patients.
Although each county had an Ebola task force, problems with transportation, communication, and resources limited their effectiveness. Health care workers had not received proper training for Ebola patient care or case investigation, including how to trace patient contacts.
Since the assessment, however, things have improved, Dr. Forrester and his coauthors wrote. Health officials in one county were able to identify their first patient – a woman who died during a spontaneous abortion on Aug. 3. She had apparently been infected in Monrovia after attending a funeral. Shortly thereafter, patient 2 was diagnosed – a man who had participated in the community funeral of patient 1 and who was attempting to flee to another Liberian county. “He was sent back ... and later reported to have died of laboratory-confirmed Ebola. This was the first evidence of secondary transmission of Ebola in southeast Liberia,” the team noted.
Since August, additional cases have surfaced in southeast Liberia, but the region is better prepared to cope with them. Local health officials have been trained in surveillance, infection control and prevention, and safe burial practices. There are regular, coordinated task force meetings. Additional ambulances are available; there are plans to establish three specialized treatment centers.
“Still,” the researchers wrote, “obstacles to prevent the spread of Ebola remain, and personal protective equipment, sufficient personnel for effective contact tracing and case management, efficient patient transport, and regional diagnostic laboratory capabilities are urgently needed.”
The latest updates, including case counts, on the 2014 Ebola outbreak in West Africa are available at http://www.cdc.gov/vhf/Ebola/outbreaks/guinea/index.html. The most up-to-date clinical guidelines on the 2014 Ebola outbreak in West Africa are available at http://www.cdc.gov/vhf/ebola/hcp/index.html.
On Twitter @alz_gal
Liberian health officials have stepped up their ability to respond to the ongoing Ebola epidemic, improving facilities and boosting personnel to help meet the crisis.
In response to last spring’s increasing cases in more populous areas of the country, officials undertook a facilities and personnel assessment in four rural counties in the southeast. Conducted in August, the review found serious problems with the ability to effectively respond to any developing Ebola threat, Dr. Joseph Forrester and his colleagues wrote in the Oct. 7 issue of the Morbidity and Mortality Weekly Report (2014;63:1-3).
Each of the four reviewed counties contained one referral hospital; the region had previously been served by six physicians, but three of these had fled the county because of the epidemic, said Dr. Forrester, an infectious disease specialist with the Centers for Disease Control and Prevention.
In two hospitals, nursing staff had ceased coming to work; in another, workers were still providing care despite not having been paid for 3 months. Nursing students, aides, and community volunteers were providing much of basic medical care, and even responding to obstetric and surgical emergencies.
Even the most basic supplies were depleted or absent. There were few hand-washing stations, and most of these consisted of a simple water jug. Soap, bleach, and alcohol hand gels were rare. There were only rudimentary isolation facilities in two counties, and neither of these had water, electricity, or waste disposal. Communication between the hospitals and county health officials was via cell phone or radio, with little Internet connectivity. About half of the local health care facilities had no communications at all and required site visits for assessment. Only one ambulance served the entire four-county region. There was little or no protective equipment for those who would work with patients.
Although each county had an Ebola task force, problems with transportation, communication, and resources limited their effectiveness. Health care workers had not received proper training for Ebola patient care or case investigation, including how to trace patient contacts.
Since the assessment, however, things have improved, Dr. Forrester and his coauthors wrote. Health officials in one county were able to identify their first patient – a woman who died during a spontaneous abortion on Aug. 3. She had apparently been infected in Monrovia after attending a funeral. Shortly thereafter, patient 2 was diagnosed – a man who had participated in the community funeral of patient 1 and who was attempting to flee to another Liberian county. “He was sent back ... and later reported to have died of laboratory-confirmed Ebola. This was the first evidence of secondary transmission of Ebola in southeast Liberia,” the team noted.
Since August, additional cases have surfaced in southeast Liberia, but the region is better prepared to cope with them. Local health officials have been trained in surveillance, infection control and prevention, and safe burial practices. There are regular, coordinated task force meetings. Additional ambulances are available; there are plans to establish three specialized treatment centers.
“Still,” the researchers wrote, “obstacles to prevent the spread of Ebola remain, and personal protective equipment, sufficient personnel for effective contact tracing and case management, efficient patient transport, and regional diagnostic laboratory capabilities are urgently needed.”
The latest updates, including case counts, on the 2014 Ebola outbreak in West Africa are available at http://www.cdc.gov/vhf/Ebola/outbreaks/guinea/index.html. The most up-to-date clinical guidelines on the 2014 Ebola outbreak in West Africa are available at http://www.cdc.gov/vhf/ebola/hcp/index.html.
On Twitter @alz_gal
FROM THE MMWR