User login
Fetal movement education: Time to change the status quo
Every antepartum record, whether it is on paper or EMR, has a space asking whether the patient feels fetal movement at the visit. Every provider inherently knows that fetal movement is important and worth asking about at each visit. Yet the education for patients about fetal movement and when to alert a provider to changes is not currently standardized in the United States. There is no practice bulletin or guideline from the American College of Obstetricians and Gynecologists and, therefore, there is a wide variation in clinical practice. An Australian study found that 97% of women were asked about fetal movement, but only 62% reported formal education regarding fetal movement. More concerning, only 40% were advised to call immediately if concerned about fetal movement change. A quarter were told to call only if baby moved fewer than 10 times in an hour.1
We have a standardized approach to most aspects of prenatal care. We know what to do if the patient has contractions, or protein in their urine, or an increased blood pressure. Our management and education regarding fetal movement must be standardized as well. In this article I will go through the incorrect education that often is given and the data that do not support this. We need a similar care plan or model for fetal movement education in the United States.
Myth one: Kick counts
When education is done, kick counts are far and away what providers and nurses advise in the clinic and hospital triage when women present with complaint of decreased fetal movement. The standard approach to this is advising the patient to perform a kick count several times per day to check in on the baby and call if less than 10 kicks per hour. This is not bad advice as it may help create awareness for the mom about what is “normal” for her baby and may help her to “check in” on the baby when she is occupied at work or with older children. However, advising that a kick count should be done to reassure a patient about a concerning change in fetal movement is not supported in the literature. A meta-analysis in the February 2020 issue of the Green Journal found that advised kick count monitoring did not significantly reduce stillbirth risk.2 Research shows that most moms will get 10 kicks normally within an hour, but there are no data showing what percentage of moms with perceived decreased fetal movement also will get a “passing” result despite their concern. For example, take a patient who normally feels 50 movements in an hour and is not reassured by 10 movements in an hour, but because she is told that 10 movements is okay, she tries not to worry about the concerning change. Many mothers in the stillbirth community report “passing kick counts” in the days leading up to the diagnosis. We need to move away from kick count education to a much simpler plan. We must tell patients if they are worried about a concerning change in fetal movement, they should call their provider.
Myth 2: Fetuses slow down at the end of pregnancy
There is a very common myth that fetuses slow down at the end of pregnancy, especially once labor has started. A study in the Journal of Physiology continuously monitored term fetuses when mom was both awake and asleep. The study also looked at the effect on fetal heart rate and fetal activity based on different maternal positions. The study found the fetuses spent around 90% of the day with active movements and with reactive nonstress tests (NSTs).3 A 2019 study looking at fetal movement at term and preterm in third-trimester patients illustrated that fetal movement does not decrease in frequency or strength at term. It found that only 6% of patients noted decreased strength and 14% decreased frequency of movements at term. Furthermore, 59% reported an increase in strength, and nearly 39% reported an increase in frequency of fetal movements at term.4 We must educate patients that a change in frequency or strength of movements is not normal or expected, and they must call if concerned about a change.
Myth 3: Try juice, ice water, or food before coming in for evaluation
A common set of advice when a patient calls with a complaint of decreased fetal movement is to suggest a meal or something sugary, although there is little or no evidence to support this. A randomized controlled trial found maternal perception of increased fetal movement was similar among the two groups. Giving something sugary at NST also was not shown in this study to improve reactivity.5 Another randomized, double placebo blind study was done to answer the question of whether glucose via IV helped improve fetal movements and decreased the need for admission for induction or further monitoring. In this study, no difference in outcome is found.6
When a patient calls with decreased fetal movement, advice should be to come and be evaluated, not recommendation of measures like ice water, orange juice, or sugary meal because it is not supported by the literature. This incorrect message also may further the false impression that a baby who is not moving is most likely sleeping or is simply in need of sugar, not that the baby may be at risk for impending stillbirth. The Perinatal Society of Australia and New Zealand and Royal College of Obstetricians and Gynecologists have fetal movement protocol that both discourage this advice and encourage immediate evaluation of patients with complaint of concerning fetal movement change.7,8
Myth 4: An increase in fetal movement is not of concern
I used to believe that increased fetal movement is never of concern. However, the STARS study illustrated that a concerning increase in fetal movement often is noted just before the diagnosis of stillbirth. A single episode of excessively vigorous activity which often is described as frantic or crazy is associated with an odds ratio for stillbirth of 4.3. In the study, 30% of cases reported this, compared with 7% of controls.9 In our practice, we manage mothers who call with this concern the same way as a decreased fetal movement complaint, and bring the mother in immediately for evaluation.
Myth 5: Patients all know that a concerning change in fetal movement is a risk factor for stillbirth
Decreased fetal movement has been associated with an increased OR for stillbirth of 4.51.10 However, patients often do not know of this association. A study in the United States of providers and stillbirth families showed fear of anxiety kept providers from talking about stillbirth and that it still happens. Because of this patients were completely surprised by the diagnosis.11 We tell patients that stillbirth still happens because research by Dr Suzanne Pullen found that 77% of families said they never worried their baby could die outside of the first trimester. Our patients have received this information without increased anxiety and are very appreciative and reassured about the education and protocol (based on the U.K. Saving Babies Lives Care Bundle Version 2) that we have implemented in our practice.
Fact: Fetal movement education guidelines exist and are easy to implement
The practice I am a partner at has been using a formalized method for educating patients about fetal movement over the past year. As mentioned earlier the U.K. and Australia have formal fetal movement education and management guidelines.7,8 Both protocols encourage formal education around 20-24 weeks and education for the patient to call immediately with concerns; the patient should be evaluated within 2 hours of the complaint. The formal education we provide is quite simple. The Star Legacy Foundation (United States) and Still Aware (Australia) have created a simple card to educate patients.
These patient-centric materials were devised from the results of the case/control cohort STARS study by Heazell et al. The STARS study demonstrated that patient report of reduced fetal movement in the 2 weeks prior to loss was associated with an OR of 12.9 for stillbirth, that decreased strength of fetal movement was associated with stillbirth OR of 2.83, and that decreased night time activity was strongly associated with impending stillbirth (74% of cases felt their fetuses died at night).12 This card also addresses sleep position data, supported by a 2018 meta-analysis in the journal Sleep Medicine. The study identified an OR for stillbirth of 2.45 for supine sleepers with LGA or average sized babies. Furthermore, if the baby was SGA and the mother slept supine, the OR for stillbirth increased to 15.66.13
Conclusions
When I think about the patients I have cared for who have presented with a stillborn baby, I think often that they usually presented for a complaint other than decreased fetal movement such as labor check or routine prenatal visit. When asked when they last felt fetal movement they will often say days before. This does not need to happen. Protocols in Norway for fetal movement education have shown that patients call sooner with decreased fetal movement when they have received a formal education.14
Not all stillbirth can be prevented but proper education about fetal movement and not perpetuating dangerous myths about fetal movement, may keep presentations like this from happening. I hope we may soon have a formal protocol for fetal movement education, but until then, I hope some will take these educational tips to heart.
Dr. Heather Florescue is an ob.gyn. in private practice at Women Gynecology and Childbirth Associates in Rochester, NY. She delivers babies at Highland Hospital in Rochester. She has no relevant financial disclosures.
References
1. Aust N Z J Obstet Gynaecol. 2012 Oct;52(5):445-9.
2. Obstet Gynecol. 2020 Feb;135(2):453-62.
3. J Physiol. 2017 Feb 15;595(4):1213-21.
4. PLOS One. 2019 Jun 12. doi: 10.1371/journal.pone.0217583.
5. J Matern Fetal Neonatal Med. 2013 Jun;26(9):915-9.
6. J Perinatol. 2016 Aug;36(8):598-600.
7. Aust N Z J Obstet Gynaecol. 2018 Aug;58(4):463-8.
8. Reduced fetal movements: Green top #57, Royal College of Obstetricians and Gynaecologists.
9. BMC Pregnancy Childb. 2017. doi: 10.1186/s12884-017-1555-6.
10. BMJ Open. 2018. doi: 10.1136/bmjopen-2017-020031.
11. BMC Pregnancy Childb. 2012. doi: 10.1186/1471-2393-12-137.
12. BMC Pregnancy Childb. 2015. doi: 10.1186/s12884-015-0602-4.
13. EClinicalMedicine. 2019 Apr. doi: 10.1016/j.eclinm.2019.03.014.
14. BMC Pregnancy Childb. 2009. doi: 10.1186/1471-2393-9-32.
Every antepartum record, whether it is on paper or EMR, has a space asking whether the patient feels fetal movement at the visit. Every provider inherently knows that fetal movement is important and worth asking about at each visit. Yet the education for patients about fetal movement and when to alert a provider to changes is not currently standardized in the United States. There is no practice bulletin or guideline from the American College of Obstetricians and Gynecologists and, therefore, there is a wide variation in clinical practice. An Australian study found that 97% of women were asked about fetal movement, but only 62% reported formal education regarding fetal movement. More concerning, only 40% were advised to call immediately if concerned about fetal movement change. A quarter were told to call only if baby moved fewer than 10 times in an hour.1
We have a standardized approach to most aspects of prenatal care. We know what to do if the patient has contractions, or protein in their urine, or an increased blood pressure. Our management and education regarding fetal movement must be standardized as well. In this article I will go through the incorrect education that often is given and the data that do not support this. We need a similar care plan or model for fetal movement education in the United States.
Myth one: Kick counts
When education is done, kick counts are far and away what providers and nurses advise in the clinic and hospital triage when women present with complaint of decreased fetal movement. The standard approach to this is advising the patient to perform a kick count several times per day to check in on the baby and call if less than 10 kicks per hour. This is not bad advice as it may help create awareness for the mom about what is “normal” for her baby and may help her to “check in” on the baby when she is occupied at work or with older children. However, advising that a kick count should be done to reassure a patient about a concerning change in fetal movement is not supported in the literature. A meta-analysis in the February 2020 issue of the Green Journal found that advised kick count monitoring did not significantly reduce stillbirth risk.2 Research shows that most moms will get 10 kicks normally within an hour, but there are no data showing what percentage of moms with perceived decreased fetal movement also will get a “passing” result despite their concern. For example, take a patient who normally feels 50 movements in an hour and is not reassured by 10 movements in an hour, but because she is told that 10 movements is okay, she tries not to worry about the concerning change. Many mothers in the stillbirth community report “passing kick counts” in the days leading up to the diagnosis. We need to move away from kick count education to a much simpler plan. We must tell patients if they are worried about a concerning change in fetal movement, they should call their provider.
Myth 2: Fetuses slow down at the end of pregnancy
There is a very common myth that fetuses slow down at the end of pregnancy, especially once labor has started. A study in the Journal of Physiology continuously monitored term fetuses when mom was both awake and asleep. The study also looked at the effect on fetal heart rate and fetal activity based on different maternal positions. The study found the fetuses spent around 90% of the day with active movements and with reactive nonstress tests (NSTs).3 A 2019 study looking at fetal movement at term and preterm in third-trimester patients illustrated that fetal movement does not decrease in frequency or strength at term. It found that only 6% of patients noted decreased strength and 14% decreased frequency of movements at term. Furthermore, 59% reported an increase in strength, and nearly 39% reported an increase in frequency of fetal movements at term.4 We must educate patients that a change in frequency or strength of movements is not normal or expected, and they must call if concerned about a change.
Myth 3: Try juice, ice water, or food before coming in for evaluation
A common set of advice when a patient calls with a complaint of decreased fetal movement is to suggest a meal or something sugary, although there is little or no evidence to support this. A randomized controlled trial found maternal perception of increased fetal movement was similar among the two groups. Giving something sugary at NST also was not shown in this study to improve reactivity.5 Another randomized, double placebo blind study was done to answer the question of whether glucose via IV helped improve fetal movements and decreased the need for admission for induction or further monitoring. In this study, no difference in outcome is found.6
When a patient calls with decreased fetal movement, advice should be to come and be evaluated, not recommendation of measures like ice water, orange juice, or sugary meal because it is not supported by the literature. This incorrect message also may further the false impression that a baby who is not moving is most likely sleeping or is simply in need of sugar, not that the baby may be at risk for impending stillbirth. The Perinatal Society of Australia and New Zealand and Royal College of Obstetricians and Gynecologists have fetal movement protocol that both discourage this advice and encourage immediate evaluation of patients with complaint of concerning fetal movement change.7,8
Myth 4: An increase in fetal movement is not of concern
I used to believe that increased fetal movement is never of concern. However, the STARS study illustrated that a concerning increase in fetal movement often is noted just before the diagnosis of stillbirth. A single episode of excessively vigorous activity which often is described as frantic or crazy is associated with an odds ratio for stillbirth of 4.3. In the study, 30% of cases reported this, compared with 7% of controls.9 In our practice, we manage mothers who call with this concern the same way as a decreased fetal movement complaint, and bring the mother in immediately for evaluation.
Myth 5: Patients all know that a concerning change in fetal movement is a risk factor for stillbirth
Decreased fetal movement has been associated with an increased OR for stillbirth of 4.51.10 However, patients often do not know of this association. A study in the United States of providers and stillbirth families showed fear of anxiety kept providers from talking about stillbirth and that it still happens. Because of this patients were completely surprised by the diagnosis.11 We tell patients that stillbirth still happens because research by Dr Suzanne Pullen found that 77% of families said they never worried their baby could die outside of the first trimester. Our patients have received this information without increased anxiety and are very appreciative and reassured about the education and protocol (based on the U.K. Saving Babies Lives Care Bundle Version 2) that we have implemented in our practice.
Fact: Fetal movement education guidelines exist and are easy to implement
The practice I am a partner at has been using a formalized method for educating patients about fetal movement over the past year. As mentioned earlier the U.K. and Australia have formal fetal movement education and management guidelines.7,8 Both protocols encourage formal education around 20-24 weeks and education for the patient to call immediately with concerns; the patient should be evaluated within 2 hours of the complaint. The formal education we provide is quite simple. The Star Legacy Foundation (United States) and Still Aware (Australia) have created a simple card to educate patients.
These patient-centric materials were devised from the results of the case/control cohort STARS study by Heazell et al. The STARS study demonstrated that patient report of reduced fetal movement in the 2 weeks prior to loss was associated with an OR of 12.9 for stillbirth, that decreased strength of fetal movement was associated with stillbirth OR of 2.83, and that decreased night time activity was strongly associated with impending stillbirth (74% of cases felt their fetuses died at night).12 This card also addresses sleep position data, supported by a 2018 meta-analysis in the journal Sleep Medicine. The study identified an OR for stillbirth of 2.45 for supine sleepers with LGA or average sized babies. Furthermore, if the baby was SGA and the mother slept supine, the OR for stillbirth increased to 15.66.13
Conclusions
When I think about the patients I have cared for who have presented with a stillborn baby, I think often that they usually presented for a complaint other than decreased fetal movement such as labor check or routine prenatal visit. When asked when they last felt fetal movement they will often say days before. This does not need to happen. Protocols in Norway for fetal movement education have shown that patients call sooner with decreased fetal movement when they have received a formal education.14
Not all stillbirth can be prevented but proper education about fetal movement and not perpetuating dangerous myths about fetal movement, may keep presentations like this from happening. I hope we may soon have a formal protocol for fetal movement education, but until then, I hope some will take these educational tips to heart.
Dr. Heather Florescue is an ob.gyn. in private practice at Women Gynecology and Childbirth Associates in Rochester, NY. She delivers babies at Highland Hospital in Rochester. She has no relevant financial disclosures.
References
1. Aust N Z J Obstet Gynaecol. 2012 Oct;52(5):445-9.
2. Obstet Gynecol. 2020 Feb;135(2):453-62.
3. J Physiol. 2017 Feb 15;595(4):1213-21.
4. PLOS One. 2019 Jun 12. doi: 10.1371/journal.pone.0217583.
5. J Matern Fetal Neonatal Med. 2013 Jun;26(9):915-9.
6. J Perinatol. 2016 Aug;36(8):598-600.
7. Aust N Z J Obstet Gynaecol. 2018 Aug;58(4):463-8.
8. Reduced fetal movements: Green top #57, Royal College of Obstetricians and Gynaecologists.
9. BMC Pregnancy Childb. 2017. doi: 10.1186/s12884-017-1555-6.
10. BMJ Open. 2018. doi: 10.1136/bmjopen-2017-020031.
11. BMC Pregnancy Childb. 2012. doi: 10.1186/1471-2393-12-137.
12. BMC Pregnancy Childb. 2015. doi: 10.1186/s12884-015-0602-4.
13. EClinicalMedicine. 2019 Apr. doi: 10.1016/j.eclinm.2019.03.014.
14. BMC Pregnancy Childb. 2009. doi: 10.1186/1471-2393-9-32.
Every antepartum record, whether it is on paper or EMR, has a space asking whether the patient feels fetal movement at the visit. Every provider inherently knows that fetal movement is important and worth asking about at each visit. Yet the education for patients about fetal movement and when to alert a provider to changes is not currently standardized in the United States. There is no practice bulletin or guideline from the American College of Obstetricians and Gynecologists and, therefore, there is a wide variation in clinical practice. An Australian study found that 97% of women were asked about fetal movement, but only 62% reported formal education regarding fetal movement. More concerning, only 40% were advised to call immediately if concerned about fetal movement change. A quarter were told to call only if baby moved fewer than 10 times in an hour.1
We have a standardized approach to most aspects of prenatal care. We know what to do if the patient has contractions, or protein in their urine, or an increased blood pressure. Our management and education regarding fetal movement must be standardized as well. In this article I will go through the incorrect education that often is given and the data that do not support this. We need a similar care plan or model for fetal movement education in the United States.
Myth one: Kick counts
When education is done, kick counts are far and away what providers and nurses advise in the clinic and hospital triage when women present with complaint of decreased fetal movement. The standard approach to this is advising the patient to perform a kick count several times per day to check in on the baby and call if less than 10 kicks per hour. This is not bad advice as it may help create awareness for the mom about what is “normal” for her baby and may help her to “check in” on the baby when she is occupied at work or with older children. However, advising that a kick count should be done to reassure a patient about a concerning change in fetal movement is not supported in the literature. A meta-analysis in the February 2020 issue of the Green Journal found that advised kick count monitoring did not significantly reduce stillbirth risk.2 Research shows that most moms will get 10 kicks normally within an hour, but there are no data showing what percentage of moms with perceived decreased fetal movement also will get a “passing” result despite their concern. For example, take a patient who normally feels 50 movements in an hour and is not reassured by 10 movements in an hour, but because she is told that 10 movements is okay, she tries not to worry about the concerning change. Many mothers in the stillbirth community report “passing kick counts” in the days leading up to the diagnosis. We need to move away from kick count education to a much simpler plan. We must tell patients if they are worried about a concerning change in fetal movement, they should call their provider.
Myth 2: Fetuses slow down at the end of pregnancy
There is a very common myth that fetuses slow down at the end of pregnancy, especially once labor has started. A study in the Journal of Physiology continuously monitored term fetuses when mom was both awake and asleep. The study also looked at the effect on fetal heart rate and fetal activity based on different maternal positions. The study found the fetuses spent around 90% of the day with active movements and with reactive nonstress tests (NSTs).3 A 2019 study looking at fetal movement at term and preterm in third-trimester patients illustrated that fetal movement does not decrease in frequency or strength at term. It found that only 6% of patients noted decreased strength and 14% decreased frequency of movements at term. Furthermore, 59% reported an increase in strength, and nearly 39% reported an increase in frequency of fetal movements at term.4 We must educate patients that a change in frequency or strength of movements is not normal or expected, and they must call if concerned about a change.
Myth 3: Try juice, ice water, or food before coming in for evaluation
A common set of advice when a patient calls with a complaint of decreased fetal movement is to suggest a meal or something sugary, although there is little or no evidence to support this. A randomized controlled trial found maternal perception of increased fetal movement was similar among the two groups. Giving something sugary at NST also was not shown in this study to improve reactivity.5 Another randomized, double placebo blind study was done to answer the question of whether glucose via IV helped improve fetal movements and decreased the need for admission for induction or further monitoring. In this study, no difference in outcome is found.6
When a patient calls with decreased fetal movement, advice should be to come and be evaluated, not recommendation of measures like ice water, orange juice, or sugary meal because it is not supported by the literature. This incorrect message also may further the false impression that a baby who is not moving is most likely sleeping or is simply in need of sugar, not that the baby may be at risk for impending stillbirth. The Perinatal Society of Australia and New Zealand and Royal College of Obstetricians and Gynecologists have fetal movement protocol that both discourage this advice and encourage immediate evaluation of patients with complaint of concerning fetal movement change.7,8
Myth 4: An increase in fetal movement is not of concern
I used to believe that increased fetal movement is never of concern. However, the STARS study illustrated that a concerning increase in fetal movement often is noted just before the diagnosis of stillbirth. A single episode of excessively vigorous activity which often is described as frantic or crazy is associated with an odds ratio for stillbirth of 4.3. In the study, 30% of cases reported this, compared with 7% of controls.9 In our practice, we manage mothers who call with this concern the same way as a decreased fetal movement complaint, and bring the mother in immediately for evaluation.
Myth 5: Patients all know that a concerning change in fetal movement is a risk factor for stillbirth
Decreased fetal movement has been associated with an increased OR for stillbirth of 4.51.10 However, patients often do not know of this association. A study in the United States of providers and stillbirth families showed fear of anxiety kept providers from talking about stillbirth and that it still happens. Because of this patients were completely surprised by the diagnosis.11 We tell patients that stillbirth still happens because research by Dr Suzanne Pullen found that 77% of families said they never worried their baby could die outside of the first trimester. Our patients have received this information without increased anxiety and are very appreciative and reassured about the education and protocol (based on the U.K. Saving Babies Lives Care Bundle Version 2) that we have implemented in our practice.
Fact: Fetal movement education guidelines exist and are easy to implement
The practice I am a partner at has been using a formalized method for educating patients about fetal movement over the past year. As mentioned earlier the U.K. and Australia have formal fetal movement education and management guidelines.7,8 Both protocols encourage formal education around 20-24 weeks and education for the patient to call immediately with concerns; the patient should be evaluated within 2 hours of the complaint. The formal education we provide is quite simple. The Star Legacy Foundation (United States) and Still Aware (Australia) have created a simple card to educate patients.
These patient-centric materials were devised from the results of the case/control cohort STARS study by Heazell et al. The STARS study demonstrated that patient report of reduced fetal movement in the 2 weeks prior to loss was associated with an OR of 12.9 for stillbirth, that decreased strength of fetal movement was associated with stillbirth OR of 2.83, and that decreased night time activity was strongly associated with impending stillbirth (74% of cases felt their fetuses died at night).12 This card also addresses sleep position data, supported by a 2018 meta-analysis in the journal Sleep Medicine. The study identified an OR for stillbirth of 2.45 for supine sleepers with LGA or average sized babies. Furthermore, if the baby was SGA and the mother slept supine, the OR for stillbirth increased to 15.66.13
Conclusions
When I think about the patients I have cared for who have presented with a stillborn baby, I think often that they usually presented for a complaint other than decreased fetal movement such as labor check or routine prenatal visit. When asked when they last felt fetal movement they will often say days before. This does not need to happen. Protocols in Norway for fetal movement education have shown that patients call sooner with decreased fetal movement when they have received a formal education.14
Not all stillbirth can be prevented but proper education about fetal movement and not perpetuating dangerous myths about fetal movement, may keep presentations like this from happening. I hope we may soon have a formal protocol for fetal movement education, but until then, I hope some will take these educational tips to heart.
Dr. Heather Florescue is an ob.gyn. in private practice at Women Gynecology and Childbirth Associates in Rochester, NY. She delivers babies at Highland Hospital in Rochester. She has no relevant financial disclosures.
References
1. Aust N Z J Obstet Gynaecol. 2012 Oct;52(5):445-9.
2. Obstet Gynecol. 2020 Feb;135(2):453-62.
3. J Physiol. 2017 Feb 15;595(4):1213-21.
4. PLOS One. 2019 Jun 12. doi: 10.1371/journal.pone.0217583.
5. J Matern Fetal Neonatal Med. 2013 Jun;26(9):915-9.
6. J Perinatol. 2016 Aug;36(8):598-600.
7. Aust N Z J Obstet Gynaecol. 2018 Aug;58(4):463-8.
8. Reduced fetal movements: Green top #57, Royal College of Obstetricians and Gynaecologists.
9. BMC Pregnancy Childb. 2017. doi: 10.1186/s12884-017-1555-6.
10. BMJ Open. 2018. doi: 10.1136/bmjopen-2017-020031.
11. BMC Pregnancy Childb. 2012. doi: 10.1186/1471-2393-12-137.
12. BMC Pregnancy Childb. 2015. doi: 10.1186/s12884-015-0602-4.
13. EClinicalMedicine. 2019 Apr. doi: 10.1016/j.eclinm.2019.03.014.
14. BMC Pregnancy Childb. 2009. doi: 10.1186/1471-2393-9-32.
How to truly connect with your patients
Introducing the ‘6H model’
I vividly remember the conversation that changed the way I practice medicine today.
During my medicine residency rounds, my attending at a Veterans Affairs hospital stated: “Remember Swati, there are three simple steps to gain your patients’ trust. The three questions they have are: No. 1, who are you? No. 2, are you any good? No. 3, do you really care about me?”
The first two questions are easier to address. The third question requires us bare our authentic human self often hiding behind our white coat and medical degree.
Who are you?
- Introduce yourself (everyone is wearing scrubs/white coats – state your full name and title)
- Describe your role in patient’s care plan
- Hand them your card (your name, photo, and a short description of the role of a hospitalist)
Are you any good?
- Briefly address your professional experience
- Explicitly state all the hard work you have done prior to entering the patient’s room (reviewing past medical records, hand off from ED provider or prior hospitalist)
- State your aim to collaborate with all people involved – their primary care provider, nurse, consultant
“Hello Mrs. Jones, my name is Dr. Swati Mehta. I will be your physician today. As a hospitalist, my role is to take care of your medical needs & worries. I will coordinate with your consultants, primary care physician, and other care teams to get you the answers you need. I have been working at XYZ Hospital for 6 years and have over 12 years of experience in medicine taking care of patients. I have reviewed your medical records, blood work, and x-rays before coming in. How are you feeling today? Do you mind if I ask you a few questions?”
Addressing the third question – Do you really care about me? – is the foundation of every human interaction. Answering this question involves addressing our patients’ many fears: Do you care about what I think is going on with my disease? Will you judge me by my socioeconomic status, gender, color of my skin, or addictions? Am I safe to open up and trust you? Are we equal partners in my health care journey? Do you really care?
A successful connection is achieved when we create a space of psychological safety and mutual respect. Once that happens, our patients open up to let us in their world and become more amenable to our opinion and recommendations. That is when true healing begins.
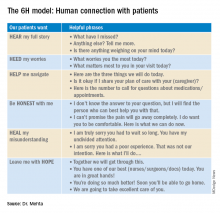
The “6H model” is an aide to form a strong human-centric connection.
The 6H model: Human connection with patients
Looking back at each patient interaction, good or bad, I have had in my almost 2 decades of practicing clinical medicine, the 6H model has brought me closer to my patients. We have formed a bond which has helped them navigate their arduous hospital journey, including medical and financial burdens, social and emotional needs. Utilizing this model, we were fortunate to receive the highest HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) Survey scores for 3 consecutive years while I served as the medical director of a 40-provider hospitalist program in a busy 450-bed hospital in Oregon.
In 2020, we are in the process of embedding the 6H model in several hospitalist programs across California. We are optimistic this intuitive approach will strengthen patient-provider relationships and ultimately improve HCAHPS scores.
To form an authentic connection with our patients doesn’t necessary require a lot of our time. Hardwiring the 6H approach when addressing our patients’ three questions is the key. The answers can change slightly, but the core message remains the same.
While we might not have much influence on all the factors that make or break our patients’ experience, the patient encounter is where we can truly make a difference. Consider using this 6H model in your next clinical shift. Human connection in health care is the need of the hour. Let’s bring “care” back to health care.
Dr. Mehta is director of quality & performance and patient experience at Vituity in Emeryville, Calif., and vice chair of the SHM patient experience committee.
Introducing the ‘6H model’
Introducing the ‘6H model’
I vividly remember the conversation that changed the way I practice medicine today.
During my medicine residency rounds, my attending at a Veterans Affairs hospital stated: “Remember Swati, there are three simple steps to gain your patients’ trust. The three questions they have are: No. 1, who are you? No. 2, are you any good? No. 3, do you really care about me?”
The first two questions are easier to address. The third question requires us bare our authentic human self often hiding behind our white coat and medical degree.
Who are you?
- Introduce yourself (everyone is wearing scrubs/white coats – state your full name and title)
- Describe your role in patient’s care plan
- Hand them your card (your name, photo, and a short description of the role of a hospitalist)
Are you any good?
- Briefly address your professional experience
- Explicitly state all the hard work you have done prior to entering the patient’s room (reviewing past medical records, hand off from ED provider or prior hospitalist)
- State your aim to collaborate with all people involved – their primary care provider, nurse, consultant
“Hello Mrs. Jones, my name is Dr. Swati Mehta. I will be your physician today. As a hospitalist, my role is to take care of your medical needs & worries. I will coordinate with your consultants, primary care physician, and other care teams to get you the answers you need. I have been working at XYZ Hospital for 6 years and have over 12 years of experience in medicine taking care of patients. I have reviewed your medical records, blood work, and x-rays before coming in. How are you feeling today? Do you mind if I ask you a few questions?”
Addressing the third question – Do you really care about me? – is the foundation of every human interaction. Answering this question involves addressing our patients’ many fears: Do you care about what I think is going on with my disease? Will you judge me by my socioeconomic status, gender, color of my skin, or addictions? Am I safe to open up and trust you? Are we equal partners in my health care journey? Do you really care?
A successful connection is achieved when we create a space of psychological safety and mutual respect. Once that happens, our patients open up to let us in their world and become more amenable to our opinion and recommendations. That is when true healing begins.
The “6H model” is an aide to form a strong human-centric connection.
The 6H model: Human connection with patients
Looking back at each patient interaction, good or bad, I have had in my almost 2 decades of practicing clinical medicine, the 6H model has brought me closer to my patients. We have formed a bond which has helped them navigate their arduous hospital journey, including medical and financial burdens, social and emotional needs. Utilizing this model, we were fortunate to receive the highest HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) Survey scores for 3 consecutive years while I served as the medical director of a 40-provider hospitalist program in a busy 450-bed hospital in Oregon.
In 2020, we are in the process of embedding the 6H model in several hospitalist programs across California. We are optimistic this intuitive approach will strengthen patient-provider relationships and ultimately improve HCAHPS scores.
To form an authentic connection with our patients doesn’t necessary require a lot of our time. Hardwiring the 6H approach when addressing our patients’ three questions is the key. The answers can change slightly, but the core message remains the same.
While we might not have much influence on all the factors that make or break our patients’ experience, the patient encounter is where we can truly make a difference. Consider using this 6H model in your next clinical shift. Human connection in health care is the need of the hour. Let’s bring “care” back to health care.
Dr. Mehta is director of quality & performance and patient experience at Vituity in Emeryville, Calif., and vice chair of the SHM patient experience committee.
I vividly remember the conversation that changed the way I practice medicine today.
During my medicine residency rounds, my attending at a Veterans Affairs hospital stated: “Remember Swati, there are three simple steps to gain your patients’ trust. The three questions they have are: No. 1, who are you? No. 2, are you any good? No. 3, do you really care about me?”
The first two questions are easier to address. The third question requires us bare our authentic human self often hiding behind our white coat and medical degree.
Who are you?
- Introduce yourself (everyone is wearing scrubs/white coats – state your full name and title)
- Describe your role in patient’s care plan
- Hand them your card (your name, photo, and a short description of the role of a hospitalist)
Are you any good?
- Briefly address your professional experience
- Explicitly state all the hard work you have done prior to entering the patient’s room (reviewing past medical records, hand off from ED provider or prior hospitalist)
- State your aim to collaborate with all people involved – their primary care provider, nurse, consultant
“Hello Mrs. Jones, my name is Dr. Swati Mehta. I will be your physician today. As a hospitalist, my role is to take care of your medical needs & worries. I will coordinate with your consultants, primary care physician, and other care teams to get you the answers you need. I have been working at XYZ Hospital for 6 years and have over 12 years of experience in medicine taking care of patients. I have reviewed your medical records, blood work, and x-rays before coming in. How are you feeling today? Do you mind if I ask you a few questions?”
Addressing the third question – Do you really care about me? – is the foundation of every human interaction. Answering this question involves addressing our patients’ many fears: Do you care about what I think is going on with my disease? Will you judge me by my socioeconomic status, gender, color of my skin, or addictions? Am I safe to open up and trust you? Are we equal partners in my health care journey? Do you really care?
A successful connection is achieved when we create a space of psychological safety and mutual respect. Once that happens, our patients open up to let us in their world and become more amenable to our opinion and recommendations. That is when true healing begins.
The “6H model” is an aide to form a strong human-centric connection.
The 6H model: Human connection with patients
Looking back at each patient interaction, good or bad, I have had in my almost 2 decades of practicing clinical medicine, the 6H model has brought me closer to my patients. We have formed a bond which has helped them navigate their arduous hospital journey, including medical and financial burdens, social and emotional needs. Utilizing this model, we were fortunate to receive the highest HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) Survey scores for 3 consecutive years while I served as the medical director of a 40-provider hospitalist program in a busy 450-bed hospital in Oregon.
In 2020, we are in the process of embedding the 6H model in several hospitalist programs across California. We are optimistic this intuitive approach will strengthen patient-provider relationships and ultimately improve HCAHPS scores.
To form an authentic connection with our patients doesn’t necessary require a lot of our time. Hardwiring the 6H approach when addressing our patients’ three questions is the key. The answers can change slightly, but the core message remains the same.
While we might not have much influence on all the factors that make or break our patients’ experience, the patient encounter is where we can truly make a difference. Consider using this 6H model in your next clinical shift. Human connection in health care is the need of the hour. Let’s bring “care” back to health care.
Dr. Mehta is director of quality & performance and patient experience at Vituity in Emeryville, Calif., and vice chair of the SHM patient experience committee.
Action and awareness are needed to increase immunization rates
August was National Immunization Awareness Month. ... just in time to address the precipitous drop in immunization delivered during the early months of the pandemic.
In May, the Centers for Disease Control and Prevention reported substantial reductions in vaccine doses ordered through the Vaccines for Children program after the declaration of national emergency because of COVID-19 on March 13. Approximately 2.5 million fewer doses of routine, noninfluenza vaccines were administered between Jan. 6 and April 2020, compared with a similar period last year (MMWR Morb Mortal Wkly Rep. 2020 May 15;69[19]:591-3). Declines in immunization rates were echoed by states and municipalities across the United States. Last month, the health system in which I work reported 40,000 children behind on at least one vaccine.
We all know that, when immunization rates drop, outbreaks of vaccine-preventable diseases follow. In order and that is going to take more than a single month.
Identify patients who’ve missed vaccinations
Simply being open and ready to vaccinate is not enough. The Centers for Disease Control and Prevention urges providers to identify patients who have missed vaccines, and call them to schedule in-person visits. Proactively let parents know about strategies implemented in your office to ensure a safe environment.
Pediatricians are accustomed to an influx of patients in the summer, as parents make sure their children have all of the vaccines required for school attendance. As noted in a Washington Post article from Aug. 4, 2020, schools have traditionally served as a backstop for immunization rates. But as many school districts opt to take education online this fall, the implications for vaccine requirements are unclear. District of Columbia public schools continue to require immunization for virtual school attendance, but it is not clear how easily this can be enforced. To read about how other school districts have chosen to address – or not address – immunization requirements for school, visit the the Immunization Action Coalition’s Repository of Resources for Maintaining Immunization during the COVID-19 Pandemic. The repository links to international, national, and state-level policies and guidance and advocacy materials, including talking points, webinars, press releases, media articles from around the United States and social media posts, as well as telehealth resources.
Get some inspiration to talk about vaccination
Need a little inspiration for talking to parents about vaccines? Check out the CDC’s #HowIRecommend video series. These are short videos, most under a minute in length, that explain the importance of vaccination, how to effectively address questions from parents about vaccine safety, and how clinicians routinely recommend same day vaccination to their patients. These videos are part of the CDC’s National Immunization Awareness Month (NIAM) toolkit for communication with health care professionals. A companion toolkit for communicating with parents and patients contains sample social media messages with graphics, along with educational resources to share with parents.
The “Comprehensive Vaccine Education Program – From Training to Practice,” a free online program offered by the Pediatric Infectious Diseases Society, takes a deeper dive into strategies to combat vaccine misinformation and address vaccine hesitancy. Available modules cover vaccine fundamentals, vaccine safety, clinical manifestations of vaccine-preventable diseases, and communication skills that lead to more effective conversations with patients and parents. The curriculum also includes the newest edition of The Vaccine Handbook app, a comprehensive source of practical information for vaccine providers.
Educate young children about vaccines
Don’t leave young children out of the conversation. Vax-Force is a children’s book that explores how vaccination works inside the human body. Dr. Vaxson the pediatrician explains how trusted doctors and scientists made Vicky the Vaccine. Her mission is to tell Willy the White Blood Cell and his Antibuddies how to find and fight bad-guy germs like measles, tetanus, and polio. The book was written by Kelsey Rowe, MD, while she was a medical student at Saint Louis University School of Medicine. Dr. Rowe, now a pediatric resident, notes, “In a world where anti-vaccination rhetoric threatens the health of our global community, this book’s mission is to teach children and adults alike that getting vaccinations is a safe, effective, and even exciting thing to do.” The book is available for purchase at https://www.vax-force.com/, and a small part of every sale is donated to Unicef USA.
Consider vaccination advocacy in your communities
Vaccinate Your Family, a national, nonprofit organization dedicated to protecting people of all ages from vaccine-preventable diseases, suggests that health care providers need to take an active role in raising immunization rates, not just in their own practices, but in their communities. One way to do this is to submit an opinion piece or letter to the editor to a local newspaper describing why it’s important for parents to make sure their child’s immunizations are current. Those who have never written an opinion-editorial should look at the guidance developed by Voices for Vaccines.
How are we doing?
Early data suggest a rebound in immunization rates in May and June, but that is unlikely to close the gap created by disruptions in health care delivery earlier in the year. Collectively, we need to set ambitious goals. Are we just trying to reach prepandemic immunization levels? In Kentucky, where I practice, only 71% of kids aged 19-45 months had received all doses of seven routinely recommended vaccines (≥4 DTaP doses, ≥3 polio doses, ≥1 MMR dose, Hib full series, ≥3 HepB doses, ≥1 varicella dose, and ≥4 PCV doses) based on 2017 National Immunization Survey data. The Healthy People 2020 target goal is 80%. Only 55% of Kentucky girls aged 13-17 years received at least one dose of HPV vaccine, and rates in boys were even lower. Flu vaccine coverage in children 6 months to 17 years also was 55%. The status quo sets the bar too low. To see how your state is doing, check out the interactive map developed by the American Academy of Pediatrics.
Are we attempting to avoid disaster or can we seize the opportunity to protect more children than ever from vaccine-preventable diseases? The latter would really be something to celebrate.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
August was National Immunization Awareness Month. ... just in time to address the precipitous drop in immunization delivered during the early months of the pandemic.
In May, the Centers for Disease Control and Prevention reported substantial reductions in vaccine doses ordered through the Vaccines for Children program after the declaration of national emergency because of COVID-19 on March 13. Approximately 2.5 million fewer doses of routine, noninfluenza vaccines were administered between Jan. 6 and April 2020, compared with a similar period last year (MMWR Morb Mortal Wkly Rep. 2020 May 15;69[19]:591-3). Declines in immunization rates were echoed by states and municipalities across the United States. Last month, the health system in which I work reported 40,000 children behind on at least one vaccine.
We all know that, when immunization rates drop, outbreaks of vaccine-preventable diseases follow. In order and that is going to take more than a single month.
Identify patients who’ve missed vaccinations
Simply being open and ready to vaccinate is not enough. The Centers for Disease Control and Prevention urges providers to identify patients who have missed vaccines, and call them to schedule in-person visits. Proactively let parents know about strategies implemented in your office to ensure a safe environment.
Pediatricians are accustomed to an influx of patients in the summer, as parents make sure their children have all of the vaccines required for school attendance. As noted in a Washington Post article from Aug. 4, 2020, schools have traditionally served as a backstop for immunization rates. But as many school districts opt to take education online this fall, the implications for vaccine requirements are unclear. District of Columbia public schools continue to require immunization for virtual school attendance, but it is not clear how easily this can be enforced. To read about how other school districts have chosen to address – or not address – immunization requirements for school, visit the the Immunization Action Coalition’s Repository of Resources for Maintaining Immunization during the COVID-19 Pandemic. The repository links to international, national, and state-level policies and guidance and advocacy materials, including talking points, webinars, press releases, media articles from around the United States and social media posts, as well as telehealth resources.
Get some inspiration to talk about vaccination
Need a little inspiration for talking to parents about vaccines? Check out the CDC’s #HowIRecommend video series. These are short videos, most under a minute in length, that explain the importance of vaccination, how to effectively address questions from parents about vaccine safety, and how clinicians routinely recommend same day vaccination to their patients. These videos are part of the CDC’s National Immunization Awareness Month (NIAM) toolkit for communication with health care professionals. A companion toolkit for communicating with parents and patients contains sample social media messages with graphics, along with educational resources to share with parents.
The “Comprehensive Vaccine Education Program – From Training to Practice,” a free online program offered by the Pediatric Infectious Diseases Society, takes a deeper dive into strategies to combat vaccine misinformation and address vaccine hesitancy. Available modules cover vaccine fundamentals, vaccine safety, clinical manifestations of vaccine-preventable diseases, and communication skills that lead to more effective conversations with patients and parents. The curriculum also includes the newest edition of The Vaccine Handbook app, a comprehensive source of practical information for vaccine providers.
Educate young children about vaccines
Don’t leave young children out of the conversation. Vax-Force is a children’s book that explores how vaccination works inside the human body. Dr. Vaxson the pediatrician explains how trusted doctors and scientists made Vicky the Vaccine. Her mission is to tell Willy the White Blood Cell and his Antibuddies how to find and fight bad-guy germs like measles, tetanus, and polio. The book was written by Kelsey Rowe, MD, while she was a medical student at Saint Louis University School of Medicine. Dr. Rowe, now a pediatric resident, notes, “In a world where anti-vaccination rhetoric threatens the health of our global community, this book’s mission is to teach children and adults alike that getting vaccinations is a safe, effective, and even exciting thing to do.” The book is available for purchase at https://www.vax-force.com/, and a small part of every sale is donated to Unicef USA.
Consider vaccination advocacy in your communities
Vaccinate Your Family, a national, nonprofit organization dedicated to protecting people of all ages from vaccine-preventable diseases, suggests that health care providers need to take an active role in raising immunization rates, not just in their own practices, but in their communities. One way to do this is to submit an opinion piece or letter to the editor to a local newspaper describing why it’s important for parents to make sure their child’s immunizations are current. Those who have never written an opinion-editorial should look at the guidance developed by Voices for Vaccines.
How are we doing?
Early data suggest a rebound in immunization rates in May and June, but that is unlikely to close the gap created by disruptions in health care delivery earlier in the year. Collectively, we need to set ambitious goals. Are we just trying to reach prepandemic immunization levels? In Kentucky, where I practice, only 71% of kids aged 19-45 months had received all doses of seven routinely recommended vaccines (≥4 DTaP doses, ≥3 polio doses, ≥1 MMR dose, Hib full series, ≥3 HepB doses, ≥1 varicella dose, and ≥4 PCV doses) based on 2017 National Immunization Survey data. The Healthy People 2020 target goal is 80%. Only 55% of Kentucky girls aged 13-17 years received at least one dose of HPV vaccine, and rates in boys were even lower. Flu vaccine coverage in children 6 months to 17 years also was 55%. The status quo sets the bar too low. To see how your state is doing, check out the interactive map developed by the American Academy of Pediatrics.
Are we attempting to avoid disaster or can we seize the opportunity to protect more children than ever from vaccine-preventable diseases? The latter would really be something to celebrate.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
August was National Immunization Awareness Month. ... just in time to address the precipitous drop in immunization delivered during the early months of the pandemic.
In May, the Centers for Disease Control and Prevention reported substantial reductions in vaccine doses ordered through the Vaccines for Children program after the declaration of national emergency because of COVID-19 on March 13. Approximately 2.5 million fewer doses of routine, noninfluenza vaccines were administered between Jan. 6 and April 2020, compared with a similar period last year (MMWR Morb Mortal Wkly Rep. 2020 May 15;69[19]:591-3). Declines in immunization rates were echoed by states and municipalities across the United States. Last month, the health system in which I work reported 40,000 children behind on at least one vaccine.
We all know that, when immunization rates drop, outbreaks of vaccine-preventable diseases follow. In order and that is going to take more than a single month.
Identify patients who’ve missed vaccinations
Simply being open and ready to vaccinate is not enough. The Centers for Disease Control and Prevention urges providers to identify patients who have missed vaccines, and call them to schedule in-person visits. Proactively let parents know about strategies implemented in your office to ensure a safe environment.
Pediatricians are accustomed to an influx of patients in the summer, as parents make sure their children have all of the vaccines required for school attendance. As noted in a Washington Post article from Aug. 4, 2020, schools have traditionally served as a backstop for immunization rates. But as many school districts opt to take education online this fall, the implications for vaccine requirements are unclear. District of Columbia public schools continue to require immunization for virtual school attendance, but it is not clear how easily this can be enforced. To read about how other school districts have chosen to address – or not address – immunization requirements for school, visit the the Immunization Action Coalition’s Repository of Resources for Maintaining Immunization during the COVID-19 Pandemic. The repository links to international, national, and state-level policies and guidance and advocacy materials, including talking points, webinars, press releases, media articles from around the United States and social media posts, as well as telehealth resources.
Get some inspiration to talk about vaccination
Need a little inspiration for talking to parents about vaccines? Check out the CDC’s #HowIRecommend video series. These are short videos, most under a minute in length, that explain the importance of vaccination, how to effectively address questions from parents about vaccine safety, and how clinicians routinely recommend same day vaccination to their patients. These videos are part of the CDC’s National Immunization Awareness Month (NIAM) toolkit for communication with health care professionals. A companion toolkit for communicating with parents and patients contains sample social media messages with graphics, along with educational resources to share with parents.
The “Comprehensive Vaccine Education Program – From Training to Practice,” a free online program offered by the Pediatric Infectious Diseases Society, takes a deeper dive into strategies to combat vaccine misinformation and address vaccine hesitancy. Available modules cover vaccine fundamentals, vaccine safety, clinical manifestations of vaccine-preventable diseases, and communication skills that lead to more effective conversations with patients and parents. The curriculum also includes the newest edition of The Vaccine Handbook app, a comprehensive source of practical information for vaccine providers.
Educate young children about vaccines
Don’t leave young children out of the conversation. Vax-Force is a children’s book that explores how vaccination works inside the human body. Dr. Vaxson the pediatrician explains how trusted doctors and scientists made Vicky the Vaccine. Her mission is to tell Willy the White Blood Cell and his Antibuddies how to find and fight bad-guy germs like measles, tetanus, and polio. The book was written by Kelsey Rowe, MD, while she was a medical student at Saint Louis University School of Medicine. Dr. Rowe, now a pediatric resident, notes, “In a world where anti-vaccination rhetoric threatens the health of our global community, this book’s mission is to teach children and adults alike that getting vaccinations is a safe, effective, and even exciting thing to do.” The book is available for purchase at https://www.vax-force.com/, and a small part of every sale is donated to Unicef USA.
Consider vaccination advocacy in your communities
Vaccinate Your Family, a national, nonprofit organization dedicated to protecting people of all ages from vaccine-preventable diseases, suggests that health care providers need to take an active role in raising immunization rates, not just in their own practices, but in their communities. One way to do this is to submit an opinion piece or letter to the editor to a local newspaper describing why it’s important for parents to make sure their child’s immunizations are current. Those who have never written an opinion-editorial should look at the guidance developed by Voices for Vaccines.
How are we doing?
Early data suggest a rebound in immunization rates in May and June, but that is unlikely to close the gap created by disruptions in health care delivery earlier in the year. Collectively, we need to set ambitious goals. Are we just trying to reach prepandemic immunization levels? In Kentucky, where I practice, only 71% of kids aged 19-45 months had received all doses of seven routinely recommended vaccines (≥4 DTaP doses, ≥3 polio doses, ≥1 MMR dose, Hib full series, ≥3 HepB doses, ≥1 varicella dose, and ≥4 PCV doses) based on 2017 National Immunization Survey data. The Healthy People 2020 target goal is 80%. Only 55% of Kentucky girls aged 13-17 years received at least one dose of HPV vaccine, and rates in boys were even lower. Flu vaccine coverage in children 6 months to 17 years also was 55%. The status quo sets the bar too low. To see how your state is doing, check out the interactive map developed by the American Academy of Pediatrics.
Are we attempting to avoid disaster or can we seize the opportunity to protect more children than ever from vaccine-preventable diseases? The latter would really be something to celebrate.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
Pandemic effect: Telemedicine is now a ‘must-have’ service
If people try telemedicine, they’ll like telemedicine. And if they want to avoid a doctor’s office, as most people do these days, they’ll try telemedicine. That is the message coming from 1,000 people surveyed for DocASAP, a provider of online patient access and engagement systems.

Here are a couple of numbers: 92% of those who made a telemedicine visit said they were satisfied with the overall appointment experience, and 91% said that they are more likely to schedule a telemedicine visit instead of an in-person appointment. All of the survey respondents had visited a health care provider in the past year, and 40% already had made a telemedicine visit, DocASAP reported.
Puneet Maheshwari, DocASAP cofounder and CEO, said in a statement. “As providers continue to adopt innovative technology to power a more seamless, end-to-end digital consumer experience, I expect telehealth to become fully integrated into overall care management.”
For now, though, COVID-19 is an overriding concern and health care facilities are suspect. When respondents were asked to identify the types of public facilities where they felt safe, hospitals were named by 32%, doctors’ offices by 26%, and ED/urgent care by just 12%, the DocASAP report said. Even public transportation got 13%.
The safest place to be, according to 42% of the respondents? The grocery store.
Of those surveyed, 43% “indicated they will not feel safe entering any health care setting until at least the fall,” the company said. An even higher share of patients, 68%, canceled or postponed an in-person appointment during the pandemic.
“No longer are remote health services viewed as ‘nice to have’ – they are now a must-have care delivery option,” DocASAP said in their report.
Safety concerns involving COVID-19, named by 47% of the sample, were the leading factor that would influence patients’ decision to schedule a telemedicine visit. Insurance coverage was next at 43%, followed by “ease of accessing quality care” at 40%, the report said.
Among those who had made a telemedicine visit, scheduling the appointment was the most satisfying aspect of the experience, according to 54% of respondents, with day-of-appointment wait time next at 38% and quality of the video/audio technology tied with preappointment communication at almost 33%, the survey data show.
Conversely, scheduling the appointment also was declared the most frustrating aspect of the telemedicine experience, although the total in that category was a much lower 29%.
“The pandemic has thrust profound change on every aspect of life, particularly health care. … Innovations – like digital and telehealth solutions – designed to meet patient needs will likely become embedded into the health care delivery system,” DocASAP said.
The survey was commissioned by DocASAP and conducted by marketing research company OnePoll on June 29-30, 2020.
If people try telemedicine, they’ll like telemedicine. And if they want to avoid a doctor’s office, as most people do these days, they’ll try telemedicine. That is the message coming from 1,000 people surveyed for DocASAP, a provider of online patient access and engagement systems.

Here are a couple of numbers: 92% of those who made a telemedicine visit said they were satisfied with the overall appointment experience, and 91% said that they are more likely to schedule a telemedicine visit instead of an in-person appointment. All of the survey respondents had visited a health care provider in the past year, and 40% already had made a telemedicine visit, DocASAP reported.
Puneet Maheshwari, DocASAP cofounder and CEO, said in a statement. “As providers continue to adopt innovative technology to power a more seamless, end-to-end digital consumer experience, I expect telehealth to become fully integrated into overall care management.”
For now, though, COVID-19 is an overriding concern and health care facilities are suspect. When respondents were asked to identify the types of public facilities where they felt safe, hospitals were named by 32%, doctors’ offices by 26%, and ED/urgent care by just 12%, the DocASAP report said. Even public transportation got 13%.
The safest place to be, according to 42% of the respondents? The grocery store.
Of those surveyed, 43% “indicated they will not feel safe entering any health care setting until at least the fall,” the company said. An even higher share of patients, 68%, canceled or postponed an in-person appointment during the pandemic.
“No longer are remote health services viewed as ‘nice to have’ – they are now a must-have care delivery option,” DocASAP said in their report.
Safety concerns involving COVID-19, named by 47% of the sample, were the leading factor that would influence patients’ decision to schedule a telemedicine visit. Insurance coverage was next at 43%, followed by “ease of accessing quality care” at 40%, the report said.
Among those who had made a telemedicine visit, scheduling the appointment was the most satisfying aspect of the experience, according to 54% of respondents, with day-of-appointment wait time next at 38% and quality of the video/audio technology tied with preappointment communication at almost 33%, the survey data show.
Conversely, scheduling the appointment also was declared the most frustrating aspect of the telemedicine experience, although the total in that category was a much lower 29%.
“The pandemic has thrust profound change on every aspect of life, particularly health care. … Innovations – like digital and telehealth solutions – designed to meet patient needs will likely become embedded into the health care delivery system,” DocASAP said.
The survey was commissioned by DocASAP and conducted by marketing research company OnePoll on June 29-30, 2020.
If people try telemedicine, they’ll like telemedicine. And if they want to avoid a doctor’s office, as most people do these days, they’ll try telemedicine. That is the message coming from 1,000 people surveyed for DocASAP, a provider of online patient access and engagement systems.

Here are a couple of numbers: 92% of those who made a telemedicine visit said they were satisfied with the overall appointment experience, and 91% said that they are more likely to schedule a telemedicine visit instead of an in-person appointment. All of the survey respondents had visited a health care provider in the past year, and 40% already had made a telemedicine visit, DocASAP reported.
Puneet Maheshwari, DocASAP cofounder and CEO, said in a statement. “As providers continue to adopt innovative technology to power a more seamless, end-to-end digital consumer experience, I expect telehealth to become fully integrated into overall care management.”
For now, though, COVID-19 is an overriding concern and health care facilities are suspect. When respondents were asked to identify the types of public facilities where they felt safe, hospitals were named by 32%, doctors’ offices by 26%, and ED/urgent care by just 12%, the DocASAP report said. Even public transportation got 13%.
The safest place to be, according to 42% of the respondents? The grocery store.
Of those surveyed, 43% “indicated they will not feel safe entering any health care setting until at least the fall,” the company said. An even higher share of patients, 68%, canceled or postponed an in-person appointment during the pandemic.
“No longer are remote health services viewed as ‘nice to have’ – they are now a must-have care delivery option,” DocASAP said in their report.
Safety concerns involving COVID-19, named by 47% of the sample, were the leading factor that would influence patients’ decision to schedule a telemedicine visit. Insurance coverage was next at 43%, followed by “ease of accessing quality care” at 40%, the report said.
Among those who had made a telemedicine visit, scheduling the appointment was the most satisfying aspect of the experience, according to 54% of respondents, with day-of-appointment wait time next at 38% and quality of the video/audio technology tied with preappointment communication at almost 33%, the survey data show.
Conversely, scheduling the appointment also was declared the most frustrating aspect of the telemedicine experience, although the total in that category was a much lower 29%.
“The pandemic has thrust profound change on every aspect of life, particularly health care. … Innovations – like digital and telehealth solutions – designed to meet patient needs will likely become embedded into the health care delivery system,” DocASAP said.
The survey was commissioned by DocASAP and conducted by marketing research company OnePoll on June 29-30, 2020.
Back to school: How pediatricians can help LGBTQ youth
September every year means one thing to students across the country: Summer break is over, and it is time to go back to school. For LGBTQ youth, this can be both a blessing and a curse. Schools can be a refuge from being stuck at home with unsupportive family, but it also can mean returning to hallways full of harassment from other students and/or staff. Groups such as a gender-sexuality alliance (GSA) or a chapter of the Gay, Lesbian, and Straight Education Network (GLSEN) can provide a safe space for these students at school. Pediatricians can play an important role in ensuring that their patients know about access to these resources.
Gender-sexuality alliances, or gay-straight alliances as they have been more commonly known, have been around since the late 1980s. The first one was founded at Concord Academy in Massachusetts in 1988 by a straight student who was upset at how her gay classmates were being treated. Today’s GSAs continue this mission to create a welcoming environment for students of all gender identities and sexual orientations to gather, increase awareness on their campus of LGBTQ issues, and make the school environment safer for all students. According to the GSA network, there are over 4,000 active GSAs today in the United States located in 40 states.1
GLSEN was founded in 1990 initially as a network of gay and lesbian educators who wanted to create safer spaces in schools for LGBTQ students. Over the last 30 years, GLSEN continues to support this mission but has expanded into research and advocacy as well. There are currently 43 chapters of GLSEN in 30 states.2 GLSEN sponsors a number of national events throughout the year to raise awareness of LGBTQ issues in schools, including No Name Calling Week and the Day of Silence. Many chapters provide mentoring to local GSAs and volunteering as a mentor can be a great way for pediatricians to become involved in their local schools.
You may be asking yourself, why are GSAs important? According to GLSEN’s 2017 National School Climate Survey, nearly 35% of LGBTQ students missed at least 1 day of school in the previous month because of feeling unsafe, and nearly 57% of students reported hearing homophobic remarks from teachers and staff at their school.3 Around 10% of LGBTQ students reported being physically assaulted based on their sexual orientation and/or gender identity. Those LGBTQ students who experienced discrimination based on their sexual orientation and/or gender identity were more likely to have lower grade point averages and were more likely to be disciplined than those students who had not experienced discrimination.3 The cumulative effect of these negative experiences at school lead a sizable portion of affected students to drop out of school and possibly not pursue postsecondary education. This then leads to decreased job opportunities or career advancement, which could then lead to unemployment or low-wage jobs. Creating safe spaces for education to take place can have a lasting effect on the lives of LGBTQ students.
The 53% of students who reported having a GSA at their school in the National School Climate survey were less likely to report hearing negative comments about LGBTQ students, were less likely to miss school, experienced lower levels of victimization, and reported higher levels of supportive teachers and staff. All of these factors taken together ensure that LGBTQ students are more likely to complete their high school education. Russell B. Toomey, PhD, and colleagues were able to show that LGBTQ students with a perceived effective GSA were two times more likely than those without an effective GSA to attain a college education.4 Research also has shown that the presence of a GSA can have a beneficial impact on reducing bullying in general for all students, whether they identify as LGBTQ or not.5
What active steps can a pediatrician take to support their LGBTQ students? First, If the families run into trouble from the school, have your social workers help them connect with legal resources, as many court cases have established precedent that public schools cannot have a blanket ban on GSAs solely because they focus on LGBTQ issues. Second, if your patient has a GSA at their school and seems to be struggling with his/her sexual orientation and/or gender identity, encourage that student to consider attending their GSA so that they are able to spend time with other students like themselves. Third, as many schools will be starting virtually this year, you can provide your LGBTQ patients with a list of local online groups that students can participate in virtually if their school’s GSA is not meeting (see my LGBTQ Youth Consult column entitled, “Resources for LGBTQ youth during challenging times” at mdedge.com/pediatrics for a few ideas).* Lastly, be an active advocate in your own local school district for the inclusion of comprehensive nondiscrimination policies and the presence of GSAs for students. These small steps can go a long way to helping your LGBTQ patients thrive and succeed in school.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas. Dr. Cooper has no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. gsanetwork.org/mission-vision-history/.
2. www.glsen.org/find_chapter?field_chapter_state_target_id=All.
3. live-glsen-website.pantheonsite.io/sites/default/files/2019-10/GLSEN-2017-National-School-Climate-Survey-NSCS-Full-Report.pdf.
4. Appl Dev Sci. 2011 Nov 7;15(4):175-85.
5.www.usnews.com/news/articles/2016-08-04/gay-straight-alliances-in-schools-pay-off-for-all-students-study-finds.
*This article was updated 8/17/2020.
September every year means one thing to students across the country: Summer break is over, and it is time to go back to school. For LGBTQ youth, this can be both a blessing and a curse. Schools can be a refuge from being stuck at home with unsupportive family, but it also can mean returning to hallways full of harassment from other students and/or staff. Groups such as a gender-sexuality alliance (GSA) or a chapter of the Gay, Lesbian, and Straight Education Network (GLSEN) can provide a safe space for these students at school. Pediatricians can play an important role in ensuring that their patients know about access to these resources.
Gender-sexuality alliances, or gay-straight alliances as they have been more commonly known, have been around since the late 1980s. The first one was founded at Concord Academy in Massachusetts in 1988 by a straight student who was upset at how her gay classmates were being treated. Today’s GSAs continue this mission to create a welcoming environment for students of all gender identities and sexual orientations to gather, increase awareness on their campus of LGBTQ issues, and make the school environment safer for all students. According to the GSA network, there are over 4,000 active GSAs today in the United States located in 40 states.1
GLSEN was founded in 1990 initially as a network of gay and lesbian educators who wanted to create safer spaces in schools for LGBTQ students. Over the last 30 years, GLSEN continues to support this mission but has expanded into research and advocacy as well. There are currently 43 chapters of GLSEN in 30 states.2 GLSEN sponsors a number of national events throughout the year to raise awareness of LGBTQ issues in schools, including No Name Calling Week and the Day of Silence. Many chapters provide mentoring to local GSAs and volunteering as a mentor can be a great way for pediatricians to become involved in their local schools.
You may be asking yourself, why are GSAs important? According to GLSEN’s 2017 National School Climate Survey, nearly 35% of LGBTQ students missed at least 1 day of school in the previous month because of feeling unsafe, and nearly 57% of students reported hearing homophobic remarks from teachers and staff at their school.3 Around 10% of LGBTQ students reported being physically assaulted based on their sexual orientation and/or gender identity. Those LGBTQ students who experienced discrimination based on their sexual orientation and/or gender identity were more likely to have lower grade point averages and were more likely to be disciplined than those students who had not experienced discrimination.3 The cumulative effect of these negative experiences at school lead a sizable portion of affected students to drop out of school and possibly not pursue postsecondary education. This then leads to decreased job opportunities or career advancement, which could then lead to unemployment or low-wage jobs. Creating safe spaces for education to take place can have a lasting effect on the lives of LGBTQ students.
The 53% of students who reported having a GSA at their school in the National School Climate survey were less likely to report hearing negative comments about LGBTQ students, were less likely to miss school, experienced lower levels of victimization, and reported higher levels of supportive teachers and staff. All of these factors taken together ensure that LGBTQ students are more likely to complete their high school education. Russell B. Toomey, PhD, and colleagues were able to show that LGBTQ students with a perceived effective GSA were two times more likely than those without an effective GSA to attain a college education.4 Research also has shown that the presence of a GSA can have a beneficial impact on reducing bullying in general for all students, whether they identify as LGBTQ or not.5
What active steps can a pediatrician take to support their LGBTQ students? First, If the families run into trouble from the school, have your social workers help them connect with legal resources, as many court cases have established precedent that public schools cannot have a blanket ban on GSAs solely because they focus on LGBTQ issues. Second, if your patient has a GSA at their school and seems to be struggling with his/her sexual orientation and/or gender identity, encourage that student to consider attending their GSA so that they are able to spend time with other students like themselves. Third, as many schools will be starting virtually this year, you can provide your LGBTQ patients with a list of local online groups that students can participate in virtually if their school’s GSA is not meeting (see my LGBTQ Youth Consult column entitled, “Resources for LGBTQ youth during challenging times” at mdedge.com/pediatrics for a few ideas).* Lastly, be an active advocate in your own local school district for the inclusion of comprehensive nondiscrimination policies and the presence of GSAs for students. These small steps can go a long way to helping your LGBTQ patients thrive and succeed in school.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas. Dr. Cooper has no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. gsanetwork.org/mission-vision-history/.
2. www.glsen.org/find_chapter?field_chapter_state_target_id=All.
3. live-glsen-website.pantheonsite.io/sites/default/files/2019-10/GLSEN-2017-National-School-Climate-Survey-NSCS-Full-Report.pdf.
4. Appl Dev Sci. 2011 Nov 7;15(4):175-85.
5.www.usnews.com/news/articles/2016-08-04/gay-straight-alliances-in-schools-pay-off-for-all-students-study-finds.
*This article was updated 8/17/2020.
September every year means one thing to students across the country: Summer break is over, and it is time to go back to school. For LGBTQ youth, this can be both a blessing and a curse. Schools can be a refuge from being stuck at home with unsupportive family, but it also can mean returning to hallways full of harassment from other students and/or staff. Groups such as a gender-sexuality alliance (GSA) or a chapter of the Gay, Lesbian, and Straight Education Network (GLSEN) can provide a safe space for these students at school. Pediatricians can play an important role in ensuring that their patients know about access to these resources.
Gender-sexuality alliances, or gay-straight alliances as they have been more commonly known, have been around since the late 1980s. The first one was founded at Concord Academy in Massachusetts in 1988 by a straight student who was upset at how her gay classmates were being treated. Today’s GSAs continue this mission to create a welcoming environment for students of all gender identities and sexual orientations to gather, increase awareness on their campus of LGBTQ issues, and make the school environment safer for all students. According to the GSA network, there are over 4,000 active GSAs today in the United States located in 40 states.1
GLSEN was founded in 1990 initially as a network of gay and lesbian educators who wanted to create safer spaces in schools for LGBTQ students. Over the last 30 years, GLSEN continues to support this mission but has expanded into research and advocacy as well. There are currently 43 chapters of GLSEN in 30 states.2 GLSEN sponsors a number of national events throughout the year to raise awareness of LGBTQ issues in schools, including No Name Calling Week and the Day of Silence. Many chapters provide mentoring to local GSAs and volunteering as a mentor can be a great way for pediatricians to become involved in their local schools.
You may be asking yourself, why are GSAs important? According to GLSEN’s 2017 National School Climate Survey, nearly 35% of LGBTQ students missed at least 1 day of school in the previous month because of feeling unsafe, and nearly 57% of students reported hearing homophobic remarks from teachers and staff at their school.3 Around 10% of LGBTQ students reported being physically assaulted based on their sexual orientation and/or gender identity. Those LGBTQ students who experienced discrimination based on their sexual orientation and/or gender identity were more likely to have lower grade point averages and were more likely to be disciplined than those students who had not experienced discrimination.3 The cumulative effect of these negative experiences at school lead a sizable portion of affected students to drop out of school and possibly not pursue postsecondary education. This then leads to decreased job opportunities or career advancement, which could then lead to unemployment or low-wage jobs. Creating safe spaces for education to take place can have a lasting effect on the lives of LGBTQ students.
The 53% of students who reported having a GSA at their school in the National School Climate survey were less likely to report hearing negative comments about LGBTQ students, were less likely to miss school, experienced lower levels of victimization, and reported higher levels of supportive teachers and staff. All of these factors taken together ensure that LGBTQ students are more likely to complete their high school education. Russell B. Toomey, PhD, and colleagues were able to show that LGBTQ students with a perceived effective GSA were two times more likely than those without an effective GSA to attain a college education.4 Research also has shown that the presence of a GSA can have a beneficial impact on reducing bullying in general for all students, whether they identify as LGBTQ or not.5
What active steps can a pediatrician take to support their LGBTQ students? First, If the families run into trouble from the school, have your social workers help them connect with legal resources, as many court cases have established precedent that public schools cannot have a blanket ban on GSAs solely because they focus on LGBTQ issues. Second, if your patient has a GSA at their school and seems to be struggling with his/her sexual orientation and/or gender identity, encourage that student to consider attending their GSA so that they are able to spend time with other students like themselves. Third, as many schools will be starting virtually this year, you can provide your LGBTQ patients with a list of local online groups that students can participate in virtually if their school’s GSA is not meeting (see my LGBTQ Youth Consult column entitled, “Resources for LGBTQ youth during challenging times” at mdedge.com/pediatrics for a few ideas).* Lastly, be an active advocate in your own local school district for the inclusion of comprehensive nondiscrimination policies and the presence of GSAs for students. These small steps can go a long way to helping your LGBTQ patients thrive and succeed in school.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas. Dr. Cooper has no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. gsanetwork.org/mission-vision-history/.
2. www.glsen.org/find_chapter?field_chapter_state_target_id=All.
3. live-glsen-website.pantheonsite.io/sites/default/files/2019-10/GLSEN-2017-National-School-Climate-Survey-NSCS-Full-Report.pdf.
4. Appl Dev Sci. 2011 Nov 7;15(4):175-85.
5.www.usnews.com/news/articles/2016-08-04/gay-straight-alliances-in-schools-pay-off-for-all-students-study-finds.
*This article was updated 8/17/2020.
Long-lasting COVID-19 symptoms: Patients want answers
Q&A with Dr. Sachin Gupta
For some patients, a bout of COVID-19 may not be over after hospital discharge, acute symptoms subside, or a couple of tests for SARS-CoV-2 come back negative. Those who have reached these milestones of conquering the disease may find that their recovery journey has only begun. Debilitating symptoms such as fatigue, headache, and dyspnea may linger for weeks or longer. Patients with persistent symptoms, often referred to as “long haulers” in reference to the duration of their recovery, are looking for answers about their condition and when their COVID-19 illness will finally resolve.
Long-haul patients organize
What started as an accumulation of anecdotal evidence in social media, blogs, and the mainstream press about slow recovery and long-lasting symptoms of COVID-19 is now the focus of clinical trials in the population of recovering patients. Projects such as the COVID Symptom Study, initiated by the Massachusetts General Hospital, Boston; the Harvard School of Public Health, Boston; King’s College London; and Stanford (Calif.) University, are collecting data on symptoms from millions of patients and will eventually contribute to a better understanding of prolonged recovery.
Patients looking for answers have created groups on social media such as Facebook to exchange information about their experiences (e.g., Survivor Corps, COVID-19 Support Group, COVID-19 Recovered Survivors). Recovering patients have created patient-led research organizations (Body Politic COVID-19 Support Group) to explore persistent symptoms and begin to create data for research.
Some data on lingering symptoms
A small study of 143 previously hospitalized, recovering patients in Italy found that 87.4% of the cohort had at least one persistent symptom 2 months or longer after initial onset and at more than a month after discharge. In this sample, only 5% had been intubated. (JAMA 2020 Jul 9. doi: 10.1001/jama.2020.12603).
One study found that even patients who have had relatively mild symptoms and were not hospitalized can have persistent symptoms. The Centers for Disease Control and Prevention conducted a survey of adults who tested positive for the positive reverse transcription–polymerase chain reaction test for SARS-CoV-2 and found that, among the 292 respondents, 35% were still feeling the impact of the disease 2-3 weeks after testing. Fatigue (71%), cough (61%), and headache (61%) were the most commonly reported symptoms. The survey found that delayed recovery was evident in nearly a quarter of 18- to 34-year-olds and in a third of 35- to 49-year-olds who were not sick enough to require hospitalization (MMWR. 2020 Jul 24. doi: 10.15585/mmwr.mm6930e1).
Sachin Gupta, MD, FCCP, ATSF, a pulmonologist and member of the CHEST Physician editorial advisory board, has treated patients with COVID-19 and shared some of his thoughts on the problem of prolonged symptoms of COVID-19.
Q: Should clinicians expect to see COVID-19 patients who have symptoms persisting weeks after they are diagnosed?
Dr. Gupta: I think clinicians, especially in primary care, are already seeing many patients with lingering symptoms, both respiratory and nonrespiratory related, and debility. A few patients here in the San Francisco Bay Area that I have spoken with 4-6 weeks out from their acute illness have complained of persisting, though improving, fatigue and cough. Early studies are confirming this as a topical issue. There may be other long-lasting sequelae of COVID-19 beyond the common mild lingering symptoms. It will also be important to consider (and get more data on) to what degree asymptomatic patients develop some degree of mild inflammatory and subsequent fibrotic changes in organs like the lungs and heart
Q: How does the recovery phase of COVID-19 compare with recovery from severe influenza or ARDS?
Dr. Gupta: Most prior influenza and acute respiratory distress syndrome (ARDS) studies have provided initial follow-up at 3 months and beyond, so technically speaking, it is a little difficult to compare the symptomatology patterns in the JAMA study of 2 months on follow-up. Nevertheless, the key takeaway is that, even though few patients in the study had ARDS requiring intubation (severe disease), many patients with milder disease had significant lingering symptoms (55% with three or more symptoms) at 2 months.
This fits logically with the premise, which we have some limited data on with ARDS (N Engl J Med. 2003;348:683-93. doi: 10.1056/NEJMoa022450) and severe influenza infection survivors (Nature Sci Rep. 2017;7:17275. doi: 10.1038/s41598-017-17497-6) that varying degrees of the inflammation cascade triggered by certain viruses can lead to changes in important patient-reported outcomes, and objective measures such as pulmonary function over the long term.
Q: What can you do for patients with lingering symptoms of COVID-19 or what can you tell them about their symptoms?
Dr. Gupta: For many patients, there is fear, given the novel nature of the virus/pandemic, that their symptoms may persist long term. Acknowledgment of their symptoms is validating and important for us to recognize as we learn more about the virus. As we are finding, many patients are going online to find answers, after sometimes feeling rushed or dismissed initially in the clinical setting.
In my experience, the bar is fairly high for most patients to reach out to their physicians with complaints of lingering symptoms after acute infection. For the ones who do reach out, they tend to have either a greater constellation of symptoms or higher severity of one or two key symptoms. After assessing and, when appropriate, ruling out secondary infections or newly developed conditions, I shift toward symptom management. I encourage such patients to build up slowly. I suggest they work first on their activities of daily living (bathing, grooming), then their instrumental activities of daily living (cooking, cleaning, checking the mail), and then to engage, based on their tolerance of symptoms, to light purposeful exercise. There are many online resources for at-home exercise activities that I recommend to patients who are more debilitated; some larger centers are beginning to offer some forms of telepulmonary rehab.
Based on what we know about other causes of viral pneumonitis and ARDS, I ask such symptomatic patients to expect a slow, gradual, and in most cases a complete recovery, and depending on the individual case, I recommend pulmonary function tests and imaging that may be helpful to track that progress.
I remind myself, and patients, that our understanding may change as we learn more over time. Checking in at set intervals, even if not in person but through a phone call, can go a long way in a setting where we do not have a specific therapy, other than gradual exercise training, to help these patients recover faster. Reassurance and encouragement are vital for patients who are struggling with the lingering burden of disease and who may find it difficult to return to work or function as usual at home. The final point is to be mindful of our patient’s mental health and, where our reassurance is not enough, to consider appropriate mental health referrals.
Q: Can you handle this kind of problem with telemedicine or which patients with lingering symptoms need to come into the office – or failing that, the ED?
Dr. Gupta: Telemedicine in the outpatient setting provides a helpful tool to assess and manage patients, in my experience, with limited and straightforward complaints. Its scope is limited diagnostically (assessing symptoms and signs) as is its reach (ability to connect with elderly, disabled, or patients without/limited telemedicine access). In many instances, telemedicine limits our ability to connect with patients emotionally and build trust. Many patients who have gone through the acute illness that we see in pulmonary clinic on follow-up are older in age, and for many, video visits are not a practical solution. Telemedicine visits can sometimes present challenges for me as well in terms of thoroughly conveying lifestyle and symptom management strategies. Health literacy is typically easier to gauge and address in person.
For patients with any degree of enduring dyspnea, more so in the acute phase, I recommend home pulse oximetry for monitoring their oxygen saturation if it is financially and technically feasible for them to obtain one. Sending a patient to the ED is an option of last resort, but one that is necessary in some cases. I expect patients with lingering symptoms to tell me that symptoms may be persisting, hopefully gradually improving, and not getting worse. If post–COVID-19 symptoms such as fever, dyspnea, fatigue, or lightheadedness are new or worsening, particularly rapidly, the safest and best option I advise patients is to go to the ED for further assessment and testing. Postviral bacterial pneumonia is something we should consider, and there is some potential for aspergillosis as well.
Q: Do you have any concerns about patients with asthma, chronic obstructive pulmonary disease, or other pulmonary issues having lingering symptoms that may mask exacerbations or may cause exacerbation of their disease?
Dr. Gupta: So far, patients with chronic lung conditions do not appear to have not been disproportionately affected by the pandemic in terms of absolute numbers or percentage wise compared to the general public. I think that sheltering in place has been readily followed by many of these patients, and in addition, I assume better adherence to their maintenance therapies has likely helped. The very few cases of patients with underlying chronic obstructive pulmonary disease and interstitial lung disease that I have seen have fared very poorly when they were diagnosed with COVID-19 in the hospital. There are emerging data about short-term outcomes from severe COVID-19 infection in patients with interstitial lung disease in Europe (medRxiv. 2020 Jul 17. doi: 10.1101/2020.07.15.20152967), and from physicians treating pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension (Ann Am Thorac Soc. 2020 Jul 29. doi: 10.1513/AnnalsATS.202005-521OC). But so far, little has been published on the outcomes of mild disease in these patients with chronic lung disease.
Q: It’s still early days to know the significance of lingering symptoms. But at what point do you begin to consider the possibility of some kind of relapse? And what is your next move if the symptoms get worse?
Dr. Gupta: COVID-19 recurrence, whether because of reinfection or relapse, is a potential concern but not one that is very commonly seen so far in my purview. Generally, symptoms of post–COVID-19 infection that are lingering trend toward getting better, even if slowly. If post–COVID-19 infection symptoms are progressing (particularly if rapidly), that would be a strong indication to evaluate that patient in the ED (less likely in clinic), reswab them for SARS-CoV-2, and obtain further testing such as blood work and imaging. A significant challenge from a research perspective will be determining if coinfection with another virus is playing a role as we move closer to the fall season.
Q&A with Dr. Sachin Gupta
Q&A with Dr. Sachin Gupta
For some patients, a bout of COVID-19 may not be over after hospital discharge, acute symptoms subside, or a couple of tests for SARS-CoV-2 come back negative. Those who have reached these milestones of conquering the disease may find that their recovery journey has only begun. Debilitating symptoms such as fatigue, headache, and dyspnea may linger for weeks or longer. Patients with persistent symptoms, often referred to as “long haulers” in reference to the duration of their recovery, are looking for answers about their condition and when their COVID-19 illness will finally resolve.
Long-haul patients organize
What started as an accumulation of anecdotal evidence in social media, blogs, and the mainstream press about slow recovery and long-lasting symptoms of COVID-19 is now the focus of clinical trials in the population of recovering patients. Projects such as the COVID Symptom Study, initiated by the Massachusetts General Hospital, Boston; the Harvard School of Public Health, Boston; King’s College London; and Stanford (Calif.) University, are collecting data on symptoms from millions of patients and will eventually contribute to a better understanding of prolonged recovery.
Patients looking for answers have created groups on social media such as Facebook to exchange information about their experiences (e.g., Survivor Corps, COVID-19 Support Group, COVID-19 Recovered Survivors). Recovering patients have created patient-led research organizations (Body Politic COVID-19 Support Group) to explore persistent symptoms and begin to create data for research.
Some data on lingering symptoms
A small study of 143 previously hospitalized, recovering patients in Italy found that 87.4% of the cohort had at least one persistent symptom 2 months or longer after initial onset and at more than a month after discharge. In this sample, only 5% had been intubated. (JAMA 2020 Jul 9. doi: 10.1001/jama.2020.12603).
One study found that even patients who have had relatively mild symptoms and were not hospitalized can have persistent symptoms. The Centers for Disease Control and Prevention conducted a survey of adults who tested positive for the positive reverse transcription–polymerase chain reaction test for SARS-CoV-2 and found that, among the 292 respondents, 35% were still feeling the impact of the disease 2-3 weeks after testing. Fatigue (71%), cough (61%), and headache (61%) were the most commonly reported symptoms. The survey found that delayed recovery was evident in nearly a quarter of 18- to 34-year-olds and in a third of 35- to 49-year-olds who were not sick enough to require hospitalization (MMWR. 2020 Jul 24. doi: 10.15585/mmwr.mm6930e1).
Sachin Gupta, MD, FCCP, ATSF, a pulmonologist and member of the CHEST Physician editorial advisory board, has treated patients with COVID-19 and shared some of his thoughts on the problem of prolonged symptoms of COVID-19.
Q: Should clinicians expect to see COVID-19 patients who have symptoms persisting weeks after they are diagnosed?
Dr. Gupta: I think clinicians, especially in primary care, are already seeing many patients with lingering symptoms, both respiratory and nonrespiratory related, and debility. A few patients here in the San Francisco Bay Area that I have spoken with 4-6 weeks out from their acute illness have complained of persisting, though improving, fatigue and cough. Early studies are confirming this as a topical issue. There may be other long-lasting sequelae of COVID-19 beyond the common mild lingering symptoms. It will also be important to consider (and get more data on) to what degree asymptomatic patients develop some degree of mild inflammatory and subsequent fibrotic changes in organs like the lungs and heart
Q: How does the recovery phase of COVID-19 compare with recovery from severe influenza or ARDS?
Dr. Gupta: Most prior influenza and acute respiratory distress syndrome (ARDS) studies have provided initial follow-up at 3 months and beyond, so technically speaking, it is a little difficult to compare the symptomatology patterns in the JAMA study of 2 months on follow-up. Nevertheless, the key takeaway is that, even though few patients in the study had ARDS requiring intubation (severe disease), many patients with milder disease had significant lingering symptoms (55% with three or more symptoms) at 2 months.
This fits logically with the premise, which we have some limited data on with ARDS (N Engl J Med. 2003;348:683-93. doi: 10.1056/NEJMoa022450) and severe influenza infection survivors (Nature Sci Rep. 2017;7:17275. doi: 10.1038/s41598-017-17497-6) that varying degrees of the inflammation cascade triggered by certain viruses can lead to changes in important patient-reported outcomes, and objective measures such as pulmonary function over the long term.
Q: What can you do for patients with lingering symptoms of COVID-19 or what can you tell them about their symptoms?
Dr. Gupta: For many patients, there is fear, given the novel nature of the virus/pandemic, that their symptoms may persist long term. Acknowledgment of their symptoms is validating and important for us to recognize as we learn more about the virus. As we are finding, many patients are going online to find answers, after sometimes feeling rushed or dismissed initially in the clinical setting.
In my experience, the bar is fairly high for most patients to reach out to their physicians with complaints of lingering symptoms after acute infection. For the ones who do reach out, they tend to have either a greater constellation of symptoms or higher severity of one or two key symptoms. After assessing and, when appropriate, ruling out secondary infections or newly developed conditions, I shift toward symptom management. I encourage such patients to build up slowly. I suggest they work first on their activities of daily living (bathing, grooming), then their instrumental activities of daily living (cooking, cleaning, checking the mail), and then to engage, based on their tolerance of symptoms, to light purposeful exercise. There are many online resources for at-home exercise activities that I recommend to patients who are more debilitated; some larger centers are beginning to offer some forms of telepulmonary rehab.
Based on what we know about other causes of viral pneumonitis and ARDS, I ask such symptomatic patients to expect a slow, gradual, and in most cases a complete recovery, and depending on the individual case, I recommend pulmonary function tests and imaging that may be helpful to track that progress.
I remind myself, and patients, that our understanding may change as we learn more over time. Checking in at set intervals, even if not in person but through a phone call, can go a long way in a setting where we do not have a specific therapy, other than gradual exercise training, to help these patients recover faster. Reassurance and encouragement are vital for patients who are struggling with the lingering burden of disease and who may find it difficult to return to work or function as usual at home. The final point is to be mindful of our patient’s mental health and, where our reassurance is not enough, to consider appropriate mental health referrals.
Q: Can you handle this kind of problem with telemedicine or which patients with lingering symptoms need to come into the office – or failing that, the ED?
Dr. Gupta: Telemedicine in the outpatient setting provides a helpful tool to assess and manage patients, in my experience, with limited and straightforward complaints. Its scope is limited diagnostically (assessing symptoms and signs) as is its reach (ability to connect with elderly, disabled, or patients without/limited telemedicine access). In many instances, telemedicine limits our ability to connect with patients emotionally and build trust. Many patients who have gone through the acute illness that we see in pulmonary clinic on follow-up are older in age, and for many, video visits are not a practical solution. Telemedicine visits can sometimes present challenges for me as well in terms of thoroughly conveying lifestyle and symptom management strategies. Health literacy is typically easier to gauge and address in person.
For patients with any degree of enduring dyspnea, more so in the acute phase, I recommend home pulse oximetry for monitoring their oxygen saturation if it is financially and technically feasible for them to obtain one. Sending a patient to the ED is an option of last resort, but one that is necessary in some cases. I expect patients with lingering symptoms to tell me that symptoms may be persisting, hopefully gradually improving, and not getting worse. If post–COVID-19 symptoms such as fever, dyspnea, fatigue, or lightheadedness are new or worsening, particularly rapidly, the safest and best option I advise patients is to go to the ED for further assessment and testing. Postviral bacterial pneumonia is something we should consider, and there is some potential for aspergillosis as well.
Q: Do you have any concerns about patients with asthma, chronic obstructive pulmonary disease, or other pulmonary issues having lingering symptoms that may mask exacerbations or may cause exacerbation of their disease?
Dr. Gupta: So far, patients with chronic lung conditions do not appear to have not been disproportionately affected by the pandemic in terms of absolute numbers or percentage wise compared to the general public. I think that sheltering in place has been readily followed by many of these patients, and in addition, I assume better adherence to their maintenance therapies has likely helped. The very few cases of patients with underlying chronic obstructive pulmonary disease and interstitial lung disease that I have seen have fared very poorly when they were diagnosed with COVID-19 in the hospital. There are emerging data about short-term outcomes from severe COVID-19 infection in patients with interstitial lung disease in Europe (medRxiv. 2020 Jul 17. doi: 10.1101/2020.07.15.20152967), and from physicians treating pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension (Ann Am Thorac Soc. 2020 Jul 29. doi: 10.1513/AnnalsATS.202005-521OC). But so far, little has been published on the outcomes of mild disease in these patients with chronic lung disease.
Q: It’s still early days to know the significance of lingering symptoms. But at what point do you begin to consider the possibility of some kind of relapse? And what is your next move if the symptoms get worse?
Dr. Gupta: COVID-19 recurrence, whether because of reinfection or relapse, is a potential concern but not one that is very commonly seen so far in my purview. Generally, symptoms of post–COVID-19 infection that are lingering trend toward getting better, even if slowly. If post–COVID-19 infection symptoms are progressing (particularly if rapidly), that would be a strong indication to evaluate that patient in the ED (less likely in clinic), reswab them for SARS-CoV-2, and obtain further testing such as blood work and imaging. A significant challenge from a research perspective will be determining if coinfection with another virus is playing a role as we move closer to the fall season.
For some patients, a bout of COVID-19 may not be over after hospital discharge, acute symptoms subside, or a couple of tests for SARS-CoV-2 come back negative. Those who have reached these milestones of conquering the disease may find that their recovery journey has only begun. Debilitating symptoms such as fatigue, headache, and dyspnea may linger for weeks or longer. Patients with persistent symptoms, often referred to as “long haulers” in reference to the duration of their recovery, are looking for answers about their condition and when their COVID-19 illness will finally resolve.
Long-haul patients organize
What started as an accumulation of anecdotal evidence in social media, blogs, and the mainstream press about slow recovery and long-lasting symptoms of COVID-19 is now the focus of clinical trials in the population of recovering patients. Projects such as the COVID Symptom Study, initiated by the Massachusetts General Hospital, Boston; the Harvard School of Public Health, Boston; King’s College London; and Stanford (Calif.) University, are collecting data on symptoms from millions of patients and will eventually contribute to a better understanding of prolonged recovery.
Patients looking for answers have created groups on social media such as Facebook to exchange information about their experiences (e.g., Survivor Corps, COVID-19 Support Group, COVID-19 Recovered Survivors). Recovering patients have created patient-led research organizations (Body Politic COVID-19 Support Group) to explore persistent symptoms and begin to create data for research.
Some data on lingering symptoms
A small study of 143 previously hospitalized, recovering patients in Italy found that 87.4% of the cohort had at least one persistent symptom 2 months or longer after initial onset and at more than a month after discharge. In this sample, only 5% had been intubated. (JAMA 2020 Jul 9. doi: 10.1001/jama.2020.12603).
One study found that even patients who have had relatively mild symptoms and were not hospitalized can have persistent symptoms. The Centers for Disease Control and Prevention conducted a survey of adults who tested positive for the positive reverse transcription–polymerase chain reaction test for SARS-CoV-2 and found that, among the 292 respondents, 35% were still feeling the impact of the disease 2-3 weeks after testing. Fatigue (71%), cough (61%), and headache (61%) were the most commonly reported symptoms. The survey found that delayed recovery was evident in nearly a quarter of 18- to 34-year-olds and in a third of 35- to 49-year-olds who were not sick enough to require hospitalization (MMWR. 2020 Jul 24. doi: 10.15585/mmwr.mm6930e1).
Sachin Gupta, MD, FCCP, ATSF, a pulmonologist and member of the CHEST Physician editorial advisory board, has treated patients with COVID-19 and shared some of his thoughts on the problem of prolonged symptoms of COVID-19.
Q: Should clinicians expect to see COVID-19 patients who have symptoms persisting weeks after they are diagnosed?
Dr. Gupta: I think clinicians, especially in primary care, are already seeing many patients with lingering symptoms, both respiratory and nonrespiratory related, and debility. A few patients here in the San Francisco Bay Area that I have spoken with 4-6 weeks out from their acute illness have complained of persisting, though improving, fatigue and cough. Early studies are confirming this as a topical issue. There may be other long-lasting sequelae of COVID-19 beyond the common mild lingering symptoms. It will also be important to consider (and get more data on) to what degree asymptomatic patients develop some degree of mild inflammatory and subsequent fibrotic changes in organs like the lungs and heart
Q: How does the recovery phase of COVID-19 compare with recovery from severe influenza or ARDS?
Dr. Gupta: Most prior influenza and acute respiratory distress syndrome (ARDS) studies have provided initial follow-up at 3 months and beyond, so technically speaking, it is a little difficult to compare the symptomatology patterns in the JAMA study of 2 months on follow-up. Nevertheless, the key takeaway is that, even though few patients in the study had ARDS requiring intubation (severe disease), many patients with milder disease had significant lingering symptoms (55% with three or more symptoms) at 2 months.
This fits logically with the premise, which we have some limited data on with ARDS (N Engl J Med. 2003;348:683-93. doi: 10.1056/NEJMoa022450) and severe influenza infection survivors (Nature Sci Rep. 2017;7:17275. doi: 10.1038/s41598-017-17497-6) that varying degrees of the inflammation cascade triggered by certain viruses can lead to changes in important patient-reported outcomes, and objective measures such as pulmonary function over the long term.
Q: What can you do for patients with lingering symptoms of COVID-19 or what can you tell them about their symptoms?
Dr. Gupta: For many patients, there is fear, given the novel nature of the virus/pandemic, that their symptoms may persist long term. Acknowledgment of their symptoms is validating and important for us to recognize as we learn more about the virus. As we are finding, many patients are going online to find answers, after sometimes feeling rushed or dismissed initially in the clinical setting.
In my experience, the bar is fairly high for most patients to reach out to their physicians with complaints of lingering symptoms after acute infection. For the ones who do reach out, they tend to have either a greater constellation of symptoms or higher severity of one or two key symptoms. After assessing and, when appropriate, ruling out secondary infections or newly developed conditions, I shift toward symptom management. I encourage such patients to build up slowly. I suggest they work first on their activities of daily living (bathing, grooming), then their instrumental activities of daily living (cooking, cleaning, checking the mail), and then to engage, based on their tolerance of symptoms, to light purposeful exercise. There are many online resources for at-home exercise activities that I recommend to patients who are more debilitated; some larger centers are beginning to offer some forms of telepulmonary rehab.
Based on what we know about other causes of viral pneumonitis and ARDS, I ask such symptomatic patients to expect a slow, gradual, and in most cases a complete recovery, and depending on the individual case, I recommend pulmonary function tests and imaging that may be helpful to track that progress.
I remind myself, and patients, that our understanding may change as we learn more over time. Checking in at set intervals, even if not in person but through a phone call, can go a long way in a setting where we do not have a specific therapy, other than gradual exercise training, to help these patients recover faster. Reassurance and encouragement are vital for patients who are struggling with the lingering burden of disease and who may find it difficult to return to work or function as usual at home. The final point is to be mindful of our patient’s mental health and, where our reassurance is not enough, to consider appropriate mental health referrals.
Q: Can you handle this kind of problem with telemedicine or which patients with lingering symptoms need to come into the office – or failing that, the ED?
Dr. Gupta: Telemedicine in the outpatient setting provides a helpful tool to assess and manage patients, in my experience, with limited and straightforward complaints. Its scope is limited diagnostically (assessing symptoms and signs) as is its reach (ability to connect with elderly, disabled, or patients without/limited telemedicine access). In many instances, telemedicine limits our ability to connect with patients emotionally and build trust. Many patients who have gone through the acute illness that we see in pulmonary clinic on follow-up are older in age, and for many, video visits are not a practical solution. Telemedicine visits can sometimes present challenges for me as well in terms of thoroughly conveying lifestyle and symptom management strategies. Health literacy is typically easier to gauge and address in person.
For patients with any degree of enduring dyspnea, more so in the acute phase, I recommend home pulse oximetry for monitoring their oxygen saturation if it is financially and technically feasible for them to obtain one. Sending a patient to the ED is an option of last resort, but one that is necessary in some cases. I expect patients with lingering symptoms to tell me that symptoms may be persisting, hopefully gradually improving, and not getting worse. If post–COVID-19 symptoms such as fever, dyspnea, fatigue, or lightheadedness are new or worsening, particularly rapidly, the safest and best option I advise patients is to go to the ED for further assessment and testing. Postviral bacterial pneumonia is something we should consider, and there is some potential for aspergillosis as well.
Q: Do you have any concerns about patients with asthma, chronic obstructive pulmonary disease, or other pulmonary issues having lingering symptoms that may mask exacerbations or may cause exacerbation of their disease?
Dr. Gupta: So far, patients with chronic lung conditions do not appear to have not been disproportionately affected by the pandemic in terms of absolute numbers or percentage wise compared to the general public. I think that sheltering in place has been readily followed by many of these patients, and in addition, I assume better adherence to their maintenance therapies has likely helped. The very few cases of patients with underlying chronic obstructive pulmonary disease and interstitial lung disease that I have seen have fared very poorly when they were diagnosed with COVID-19 in the hospital. There are emerging data about short-term outcomes from severe COVID-19 infection in patients with interstitial lung disease in Europe (medRxiv. 2020 Jul 17. doi: 10.1101/2020.07.15.20152967), and from physicians treating pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension (Ann Am Thorac Soc. 2020 Jul 29. doi: 10.1513/AnnalsATS.202005-521OC). But so far, little has been published on the outcomes of mild disease in these patients with chronic lung disease.
Q: It’s still early days to know the significance of lingering symptoms. But at what point do you begin to consider the possibility of some kind of relapse? And what is your next move if the symptoms get worse?
Dr. Gupta: COVID-19 recurrence, whether because of reinfection or relapse, is a potential concern but not one that is very commonly seen so far in my purview. Generally, symptoms of post–COVID-19 infection that are lingering trend toward getting better, even if slowly. If post–COVID-19 infection symptoms are progressing (particularly if rapidly), that would be a strong indication to evaluate that patient in the ED (less likely in clinic), reswab them for SARS-CoV-2, and obtain further testing such as blood work and imaging. A significant challenge from a research perspective will be determining if coinfection with another virus is playing a role as we move closer to the fall season.
iResident: Virtual care on hospital medicine teaching services during a pandemic
At the start of each shift on his clinical service with rotating internal medicine residents, Benji Mathews, MD, SFHM, now adds a few components to his usual preparation. First, visiting the Minnesota Department of Health and various organizational websites to review the latest COVID-19 updates and guidelines. Next comes checking to see where he needs to pick up the surgical mask and eye protection that he will need to wear through the day. Last, he evaluates which of his patients are in telemedicine-equipped rooms; this last change has fast become a crucial part of working with his resident learners during a pandemic.
During the COVID-19 pandemic, residents and residency programs find themselves in a unique situation. Balancing the educational needs of a training program with the safety of trainees is a challenging task, specifically when taking care of patients who are COVID-19 positive or patients under investigation (PUI). One increasingly available tool that can help protect trainees while continuing to prioritize patient care and medical education is the use of telemedicine for virtual rounding. For our internal medicine residents through the University of Minnesota Internal Medicine Residency program rotating at Regions Hospital in Saint Paul, Minn., we have used video visits to continue our mandate as both health care and education professionals.
Virtual care decision tree
Virtual care can mitigate exposure risk, minimize use of personal protective equipment (PPE), and improve communications with patients and their families. To guide our teaching teams on the optimal situations for telemedicine, we needed to select those patients who would be most appropriate for a virtual visit.
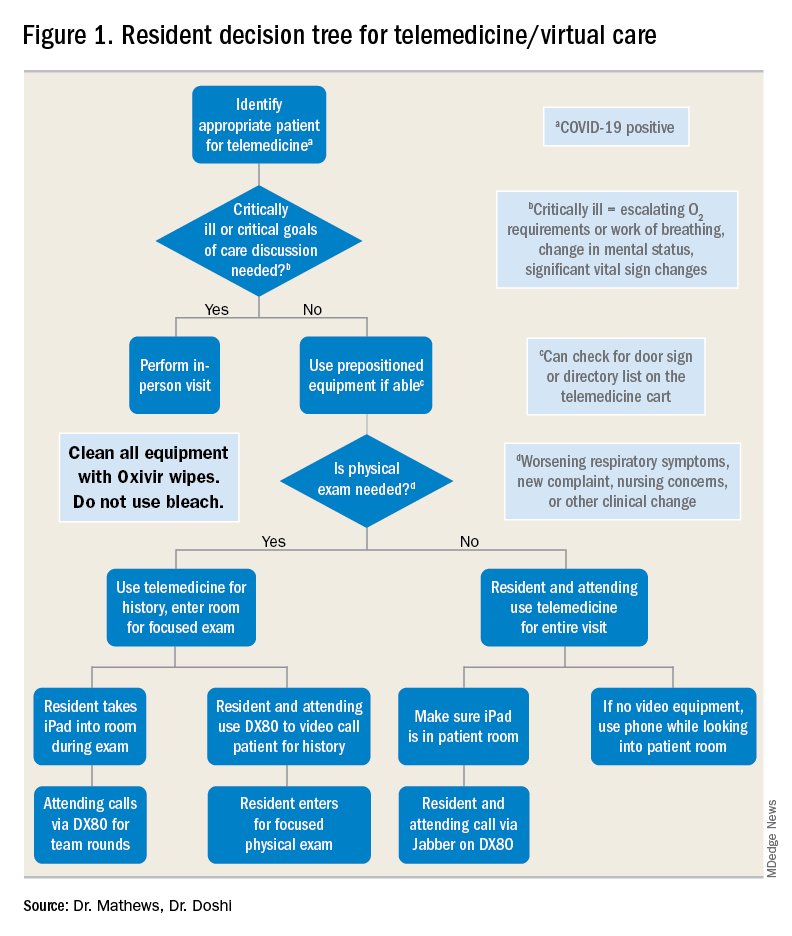
For example, patients with advanced dementia, or intubated in the intensive care unit, would have less utility from a real-time video encounter. Further, we implemented a simple decision tree (Figure 1). First, the team needs to decide whether the patient needs an immediate in-person assessment; for instance, for critically ill patients or those who need end-of-life care discussions, telemedicine would not be an appropriate modality. Next, the decision is made on whether a patient requires an in-person exam at that time. The idea of forgoing the in-person physical exam may run counterintuitive to the core training medical providers undergo, but in certain circumstances telemedicine can still provide the appropriate level of care a patient requires.
Virtual rounding with residents: Pros and cons
Through the course of this pandemic, there have many questions raised regarding how to handle inpatient teaching services: Should resident teams be assigned COVID-19 positives or PUIs? How do you optimize assessing and learning from patients’ conditions that require human touch? Should all members of the teaching team be donning PPE and entering the patient room?
Internal medicine residents in our hospital have been assigned COVID-19 positive and PUI patients. With proper PPE, and donning and doffing practices, residents may continue to learn from this important training opportunity while also optimizing care for patients supplemented by telemedicine. This pandemic has flattened the hierarchy; often residents are teaching their attendings much of the latest literature and best practices around COVID-19. Residents also benefit by joining the organization’s daily virtual interprofessional COVID-19 huddle where they partner with infectious disease, critical care, pharmacy, and other experts to collaborate in the care of these patients.
There have been counterarguments made for residents joining the front lines with COVID-19 patients. Some have conditions that limit them from seeing this subgroup of patients, such as their immune status or other issues. For these residents, we do not assign COVID-19–positive patients. However, they may continue to support in virtually updating COVID-19 patients and their families. A second argument has been the use of PPE. We have implemented telemedicine to limit the total number of exposures and have a protocol for the fewest number of providers possible to see any at-risk or confirmed COVID-19 patient. For example, a resident who sees a COVID-19 patient in person may also be simultaneously virtually supervised by the attending.
Webside manner
The physical exam is only one of several operational considerations when delivering virtual care, whether with a teaching or nonteaching service. One important aspect is the “webside manner” of the provider, the virtual analogue to bedside manner.
Inherent parts of in-person encounters, such as eye contact and allowing for patients to finish their sentences, have added nuances with virtual care. For instance, providers must adjust to looking into the web camera to make eye contact, even though the patient’s face may be on the screen below. Additionally, for patients who are hard of hearing or unfamiliar with video calling, providers must be cognizant of projecting well over an Internet connection and timing responses to avoid overlapping conversation.
Similarly, there are nuances to the virtual physical exam, some specific to care in the COVID-19 era. In our previous virtual care practice, a bedside facilitator assisted in using tools such a digital stethoscope. In contrast, our current practice aims to refine the observational skills of our learners in conjunction with chart review, vital signs, and actively incorporating the patient in the physical exam. This does not mean asking them to auscultate themselves, but is more toward allowing patients to participate in focused evaluations, such as assessing abdominal tenderness or working through range of motion. Remote guidance for virtual exams also extends itself to teaching teams; for example, in our practice, we have been able to conduct bedside ultrasound teaching with in-person team members and a virtual facilitator.
Maskless connections: ‘Face-to-face’ visits with patients
As many hospitalists have witnessed, COVID-19 is so isolating for patients and their families. Patients have limited visitors, and their care team members are aiming to minimize exposures. Those who are entering the rooms wear masks and face shields that limit connecting with patients in a truly “face-to-face” manner. Telemedicine provides a face-to-face encounter that arguably improves upon portions of the traditional in-person encounter during this pandemic, with providers wearing PPE. For medical learners, gaining the interpersonal skills essential for health care professionals has been skewed with pandemic-related limitations; telemedicine can provide a tool to adapt to this unique era and augment this important educational piece.
Limitations, equity, and technological considerations
Realistically, the virtual exam during COVID-19 does have its limitations. An important part of virtual care and teaching services is instilling the appropriate times for use of telemedicine. If a patient has a clinical change (such as increase in FiO2 requirements) or other clinical need, there should be no hesitation for learners to conduct in-person assessments with appropriate PPE.
Nonexam indications are just as important – for example, if a patient requires extensive goals of care counseling, we recommend this not be done virtually. Other indications may vary between organizations; in our practice, we suggest at least one in-person assessment on the initial and discharge hospital days. Regardless of the specific indications, a successful virtual inpatient teaching service must be predicated on outlining the appropriate uses of telemedicine.
In the United States, there are already health care disparities for people of color and non–English speakers. If there is not a careful consideration for these marginalized groups, their health disparities could be further exacerbated – not just around COVID-19, but also for other inpatient conditions where telemedicine is being used. Groups whose equity must be thoughtfully managed include those who do not speak English and those who do not have access to smartphones or the Internet. Our HealthPartners organization has implemented the integration of interpreters for virtual three-way connections with patients and their clinicians to help mitigate this for non–English speakers. Additionally, utilizing easy-to-use tablets and telemedicine-capable carts has helped patients overcome technology barriers.
Last, the members of the teaching team must know the essential technical aspects of the technology they are using. Robust information technology (IT) support is also needed, but no matter how simple the equipment may be, staff and trainees must know how to both operate it and handle basic troubleshooting (such as audio or video disconnections). This also dovetails with the important element of on-boarding other members of the care team. In our practice, nursing staff, chaplains, interpreters, and dietitians also use virtual care as part of their workflow. However, even if it is used only by the teaching team, orienting other care team members will limit technical problems such as equipment being turned off or moved out of position.
Prior to the COVID-19 pandemic, telemedicine adoption was limited because of lack of awareness, barriers in training, understanding, and narrow beliefs regarding the innovation. The COVID-19 pandemic has resulted in a remarkable increase in the provision of telemedicine services in the inpatient hospital medicine services. Importantly, it is, and should be, a developing part of the education and training for health care learners. This pandemic has underscored the need for providing telemedicine services that will likely long outlast this crisis, and to support our health care learners in being effective “iResidents” on our care teams.
Takeaways
- The future of graduate medical education involves virtual care.
The COVID-19 pandemic response has demonstrated that virtual care plays an instrumental part in patient care, and its effects will not dissipate when the pandemic is done. The curriculum for health care trainees should incorporate telemedicine competencies so that they may more effectively leverage this technology for improving care delivery.
- Selection of telemedicine patients must be stratified.
In order to obtain the highest utility for medical learners on telemedicine, there needs to be a clear decision process for which patients can be seen virtually. This involves both clinical criteria, such as avoiding virtual care for end-of-life discussions, and patient criteria, such as those who are hard of hearing.
- Virtual communication requires new communication skills.
Seeing patients via telemedicine mandates a different skill set than in-person communication. Learners must improve their “webside manner” in order to build the patient-provider relationship. Instilling these tools can pay dividends in settings where telemedicine has high yield, such as maskless communication during a pandemic.
- Health disparities could be further exacerbated by telemedicine and should not be overlooked.
Equity in access to health care applies to telemedicine as it does to many other elements. There are multiple groups that can suffer from disparities, such as patients who need interpreters, or those who have lower technological literacy and access to digital devices. Creating awareness of these pitfalls in virtual care can help medical learners recognize and support in creative solutions for these factors.
Dr. Mathews is chief, hospital medicine, at Regions Hospital, HealthPartners, St. Paul, Minn. Dr. Doshi is telemedicine director, hospital medicine, HealthPartners.
At the start of each shift on his clinical service with rotating internal medicine residents, Benji Mathews, MD, SFHM, now adds a few components to his usual preparation. First, visiting the Minnesota Department of Health and various organizational websites to review the latest COVID-19 updates and guidelines. Next comes checking to see where he needs to pick up the surgical mask and eye protection that he will need to wear through the day. Last, he evaluates which of his patients are in telemedicine-equipped rooms; this last change has fast become a crucial part of working with his resident learners during a pandemic.
During the COVID-19 pandemic, residents and residency programs find themselves in a unique situation. Balancing the educational needs of a training program with the safety of trainees is a challenging task, specifically when taking care of patients who are COVID-19 positive or patients under investigation (PUI). One increasingly available tool that can help protect trainees while continuing to prioritize patient care and medical education is the use of telemedicine for virtual rounding. For our internal medicine residents through the University of Minnesota Internal Medicine Residency program rotating at Regions Hospital in Saint Paul, Minn., we have used video visits to continue our mandate as both health care and education professionals.
Virtual care decision tree
Virtual care can mitigate exposure risk, minimize use of personal protective equipment (PPE), and improve communications with patients and their families. To guide our teaching teams on the optimal situations for telemedicine, we needed to select those patients who would be most appropriate for a virtual visit.
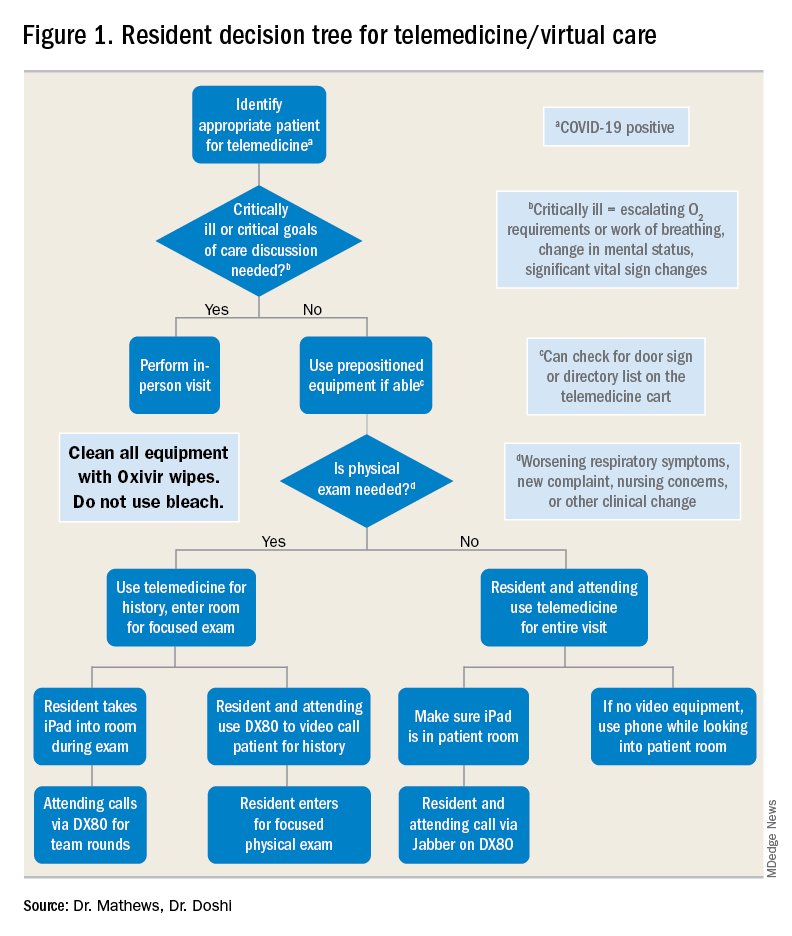
For example, patients with advanced dementia, or intubated in the intensive care unit, would have less utility from a real-time video encounter. Further, we implemented a simple decision tree (Figure 1). First, the team needs to decide whether the patient needs an immediate in-person assessment; for instance, for critically ill patients or those who need end-of-life care discussions, telemedicine would not be an appropriate modality. Next, the decision is made on whether a patient requires an in-person exam at that time. The idea of forgoing the in-person physical exam may run counterintuitive to the core training medical providers undergo, but in certain circumstances telemedicine can still provide the appropriate level of care a patient requires.
Virtual rounding with residents: Pros and cons
Through the course of this pandemic, there have many questions raised regarding how to handle inpatient teaching services: Should resident teams be assigned COVID-19 positives or PUIs? How do you optimize assessing and learning from patients’ conditions that require human touch? Should all members of the teaching team be donning PPE and entering the patient room?
Internal medicine residents in our hospital have been assigned COVID-19 positive and PUI patients. With proper PPE, and donning and doffing practices, residents may continue to learn from this important training opportunity while also optimizing care for patients supplemented by telemedicine. This pandemic has flattened the hierarchy; often residents are teaching their attendings much of the latest literature and best practices around COVID-19. Residents also benefit by joining the organization’s daily virtual interprofessional COVID-19 huddle where they partner with infectious disease, critical care, pharmacy, and other experts to collaborate in the care of these patients.
There have been counterarguments made for residents joining the front lines with COVID-19 patients. Some have conditions that limit them from seeing this subgroup of patients, such as their immune status or other issues. For these residents, we do not assign COVID-19–positive patients. However, they may continue to support in virtually updating COVID-19 patients and their families. A second argument has been the use of PPE. We have implemented telemedicine to limit the total number of exposures and have a protocol for the fewest number of providers possible to see any at-risk or confirmed COVID-19 patient. For example, a resident who sees a COVID-19 patient in person may also be simultaneously virtually supervised by the attending.
Webside manner
The physical exam is only one of several operational considerations when delivering virtual care, whether with a teaching or nonteaching service. One important aspect is the “webside manner” of the provider, the virtual analogue to bedside manner.
Inherent parts of in-person encounters, such as eye contact and allowing for patients to finish their sentences, have added nuances with virtual care. For instance, providers must adjust to looking into the web camera to make eye contact, even though the patient’s face may be on the screen below. Additionally, for patients who are hard of hearing or unfamiliar with video calling, providers must be cognizant of projecting well over an Internet connection and timing responses to avoid overlapping conversation.
Similarly, there are nuances to the virtual physical exam, some specific to care in the COVID-19 era. In our previous virtual care practice, a bedside facilitator assisted in using tools such a digital stethoscope. In contrast, our current practice aims to refine the observational skills of our learners in conjunction with chart review, vital signs, and actively incorporating the patient in the physical exam. This does not mean asking them to auscultate themselves, but is more toward allowing patients to participate in focused evaluations, such as assessing abdominal tenderness or working through range of motion. Remote guidance for virtual exams also extends itself to teaching teams; for example, in our practice, we have been able to conduct bedside ultrasound teaching with in-person team members and a virtual facilitator.
Maskless connections: ‘Face-to-face’ visits with patients
As many hospitalists have witnessed, COVID-19 is so isolating for patients and their families. Patients have limited visitors, and their care team members are aiming to minimize exposures. Those who are entering the rooms wear masks and face shields that limit connecting with patients in a truly “face-to-face” manner. Telemedicine provides a face-to-face encounter that arguably improves upon portions of the traditional in-person encounter during this pandemic, with providers wearing PPE. For medical learners, gaining the interpersonal skills essential for health care professionals has been skewed with pandemic-related limitations; telemedicine can provide a tool to adapt to this unique era and augment this important educational piece.
Limitations, equity, and technological considerations
Realistically, the virtual exam during COVID-19 does have its limitations. An important part of virtual care and teaching services is instilling the appropriate times for use of telemedicine. If a patient has a clinical change (such as increase in FiO2 requirements) or other clinical need, there should be no hesitation for learners to conduct in-person assessments with appropriate PPE.
Nonexam indications are just as important – for example, if a patient requires extensive goals of care counseling, we recommend this not be done virtually. Other indications may vary between organizations; in our practice, we suggest at least one in-person assessment on the initial and discharge hospital days. Regardless of the specific indications, a successful virtual inpatient teaching service must be predicated on outlining the appropriate uses of telemedicine.
In the United States, there are already health care disparities for people of color and non–English speakers. If there is not a careful consideration for these marginalized groups, their health disparities could be further exacerbated – not just around COVID-19, but also for other inpatient conditions where telemedicine is being used. Groups whose equity must be thoughtfully managed include those who do not speak English and those who do not have access to smartphones or the Internet. Our HealthPartners organization has implemented the integration of interpreters for virtual three-way connections with patients and their clinicians to help mitigate this for non–English speakers. Additionally, utilizing easy-to-use tablets and telemedicine-capable carts has helped patients overcome technology barriers.
Last, the members of the teaching team must know the essential technical aspects of the technology they are using. Robust information technology (IT) support is also needed, but no matter how simple the equipment may be, staff and trainees must know how to both operate it and handle basic troubleshooting (such as audio or video disconnections). This also dovetails with the important element of on-boarding other members of the care team. In our practice, nursing staff, chaplains, interpreters, and dietitians also use virtual care as part of their workflow. However, even if it is used only by the teaching team, orienting other care team members will limit technical problems such as equipment being turned off or moved out of position.
Prior to the COVID-19 pandemic, telemedicine adoption was limited because of lack of awareness, barriers in training, understanding, and narrow beliefs regarding the innovation. The COVID-19 pandemic has resulted in a remarkable increase in the provision of telemedicine services in the inpatient hospital medicine services. Importantly, it is, and should be, a developing part of the education and training for health care learners. This pandemic has underscored the need for providing telemedicine services that will likely long outlast this crisis, and to support our health care learners in being effective “iResidents” on our care teams.
Takeaways
- The future of graduate medical education involves virtual care.
The COVID-19 pandemic response has demonstrated that virtual care plays an instrumental part in patient care, and its effects will not dissipate when the pandemic is done. The curriculum for health care trainees should incorporate telemedicine competencies so that they may more effectively leverage this technology for improving care delivery.
- Selection of telemedicine patients must be stratified.
In order to obtain the highest utility for medical learners on telemedicine, there needs to be a clear decision process for which patients can be seen virtually. This involves both clinical criteria, such as avoiding virtual care for end-of-life discussions, and patient criteria, such as those who are hard of hearing.
- Virtual communication requires new communication skills.
Seeing patients via telemedicine mandates a different skill set than in-person communication. Learners must improve their “webside manner” in order to build the patient-provider relationship. Instilling these tools can pay dividends in settings where telemedicine has high yield, such as maskless communication during a pandemic.
- Health disparities could be further exacerbated by telemedicine and should not be overlooked.
Equity in access to health care applies to telemedicine as it does to many other elements. There are multiple groups that can suffer from disparities, such as patients who need interpreters, or those who have lower technological literacy and access to digital devices. Creating awareness of these pitfalls in virtual care can help medical learners recognize and support in creative solutions for these factors.
Dr. Mathews is chief, hospital medicine, at Regions Hospital, HealthPartners, St. Paul, Minn. Dr. Doshi is telemedicine director, hospital medicine, HealthPartners.
At the start of each shift on his clinical service with rotating internal medicine residents, Benji Mathews, MD, SFHM, now adds a few components to his usual preparation. First, visiting the Minnesota Department of Health and various organizational websites to review the latest COVID-19 updates and guidelines. Next comes checking to see where he needs to pick up the surgical mask and eye protection that he will need to wear through the day. Last, he evaluates which of his patients are in telemedicine-equipped rooms; this last change has fast become a crucial part of working with his resident learners during a pandemic.
During the COVID-19 pandemic, residents and residency programs find themselves in a unique situation. Balancing the educational needs of a training program with the safety of trainees is a challenging task, specifically when taking care of patients who are COVID-19 positive or patients under investigation (PUI). One increasingly available tool that can help protect trainees while continuing to prioritize patient care and medical education is the use of telemedicine for virtual rounding. For our internal medicine residents through the University of Minnesota Internal Medicine Residency program rotating at Regions Hospital in Saint Paul, Minn., we have used video visits to continue our mandate as both health care and education professionals.
Virtual care decision tree
Virtual care can mitigate exposure risk, minimize use of personal protective equipment (PPE), and improve communications with patients and their families. To guide our teaching teams on the optimal situations for telemedicine, we needed to select those patients who would be most appropriate for a virtual visit.
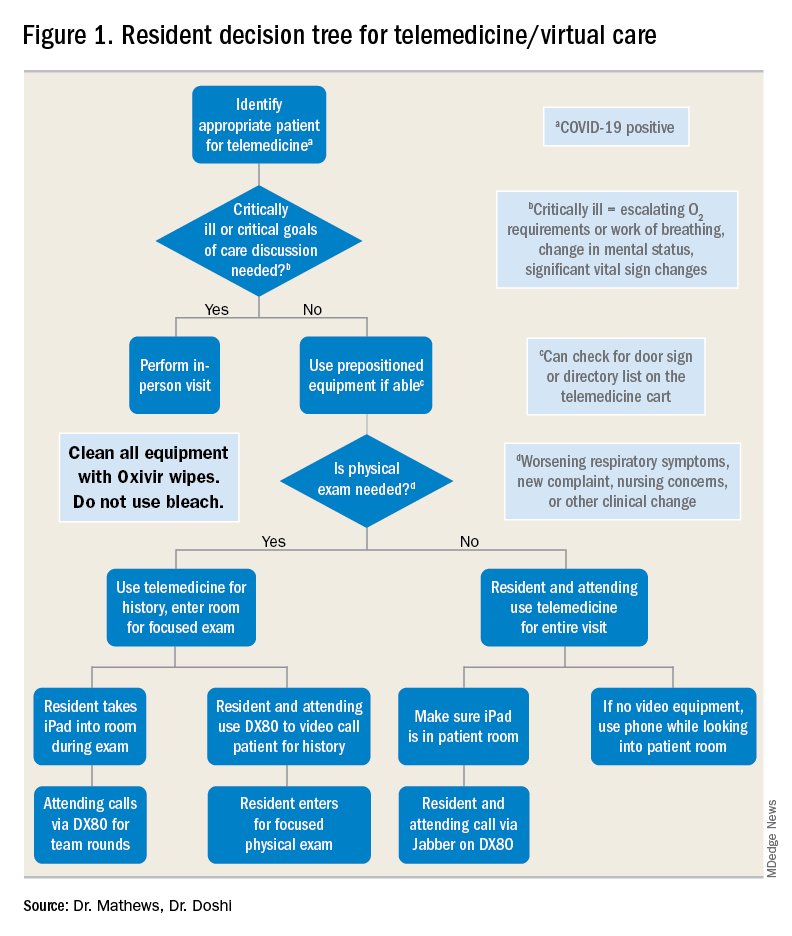
For example, patients with advanced dementia, or intubated in the intensive care unit, would have less utility from a real-time video encounter. Further, we implemented a simple decision tree (Figure 1). First, the team needs to decide whether the patient needs an immediate in-person assessment; for instance, for critically ill patients or those who need end-of-life care discussions, telemedicine would not be an appropriate modality. Next, the decision is made on whether a patient requires an in-person exam at that time. The idea of forgoing the in-person physical exam may run counterintuitive to the core training medical providers undergo, but in certain circumstances telemedicine can still provide the appropriate level of care a patient requires.
Virtual rounding with residents: Pros and cons
Through the course of this pandemic, there have many questions raised regarding how to handle inpatient teaching services: Should resident teams be assigned COVID-19 positives or PUIs? How do you optimize assessing and learning from patients’ conditions that require human touch? Should all members of the teaching team be donning PPE and entering the patient room?
Internal medicine residents in our hospital have been assigned COVID-19 positive and PUI patients. With proper PPE, and donning and doffing practices, residents may continue to learn from this important training opportunity while also optimizing care for patients supplemented by telemedicine. This pandemic has flattened the hierarchy; often residents are teaching their attendings much of the latest literature and best practices around COVID-19. Residents also benefit by joining the organization’s daily virtual interprofessional COVID-19 huddle where they partner with infectious disease, critical care, pharmacy, and other experts to collaborate in the care of these patients.
There have been counterarguments made for residents joining the front lines with COVID-19 patients. Some have conditions that limit them from seeing this subgroup of patients, such as their immune status or other issues. For these residents, we do not assign COVID-19–positive patients. However, they may continue to support in virtually updating COVID-19 patients and their families. A second argument has been the use of PPE. We have implemented telemedicine to limit the total number of exposures and have a protocol for the fewest number of providers possible to see any at-risk or confirmed COVID-19 patient. For example, a resident who sees a COVID-19 patient in person may also be simultaneously virtually supervised by the attending.
Webside manner
The physical exam is only one of several operational considerations when delivering virtual care, whether with a teaching or nonteaching service. One important aspect is the “webside manner” of the provider, the virtual analogue to bedside manner.
Inherent parts of in-person encounters, such as eye contact and allowing for patients to finish their sentences, have added nuances with virtual care. For instance, providers must adjust to looking into the web camera to make eye contact, even though the patient’s face may be on the screen below. Additionally, for patients who are hard of hearing or unfamiliar with video calling, providers must be cognizant of projecting well over an Internet connection and timing responses to avoid overlapping conversation.
Similarly, there are nuances to the virtual physical exam, some specific to care in the COVID-19 era. In our previous virtual care practice, a bedside facilitator assisted in using tools such a digital stethoscope. In contrast, our current practice aims to refine the observational skills of our learners in conjunction with chart review, vital signs, and actively incorporating the patient in the physical exam. This does not mean asking them to auscultate themselves, but is more toward allowing patients to participate in focused evaluations, such as assessing abdominal tenderness or working through range of motion. Remote guidance for virtual exams also extends itself to teaching teams; for example, in our practice, we have been able to conduct bedside ultrasound teaching with in-person team members and a virtual facilitator.
Maskless connections: ‘Face-to-face’ visits with patients
As many hospitalists have witnessed, COVID-19 is so isolating for patients and their families. Patients have limited visitors, and their care team members are aiming to minimize exposures. Those who are entering the rooms wear masks and face shields that limit connecting with patients in a truly “face-to-face” manner. Telemedicine provides a face-to-face encounter that arguably improves upon portions of the traditional in-person encounter during this pandemic, with providers wearing PPE. For medical learners, gaining the interpersonal skills essential for health care professionals has been skewed with pandemic-related limitations; telemedicine can provide a tool to adapt to this unique era and augment this important educational piece.
Limitations, equity, and technological considerations
Realistically, the virtual exam during COVID-19 does have its limitations. An important part of virtual care and teaching services is instilling the appropriate times for use of telemedicine. If a patient has a clinical change (such as increase in FiO2 requirements) or other clinical need, there should be no hesitation for learners to conduct in-person assessments with appropriate PPE.
Nonexam indications are just as important – for example, if a patient requires extensive goals of care counseling, we recommend this not be done virtually. Other indications may vary between organizations; in our practice, we suggest at least one in-person assessment on the initial and discharge hospital days. Regardless of the specific indications, a successful virtual inpatient teaching service must be predicated on outlining the appropriate uses of telemedicine.
In the United States, there are already health care disparities for people of color and non–English speakers. If there is not a careful consideration for these marginalized groups, their health disparities could be further exacerbated – not just around COVID-19, but also for other inpatient conditions where telemedicine is being used. Groups whose equity must be thoughtfully managed include those who do not speak English and those who do not have access to smartphones or the Internet. Our HealthPartners organization has implemented the integration of interpreters for virtual three-way connections with patients and their clinicians to help mitigate this for non–English speakers. Additionally, utilizing easy-to-use tablets and telemedicine-capable carts has helped patients overcome technology barriers.
Last, the members of the teaching team must know the essential technical aspects of the technology they are using. Robust information technology (IT) support is also needed, but no matter how simple the equipment may be, staff and trainees must know how to both operate it and handle basic troubleshooting (such as audio or video disconnections). This also dovetails with the important element of on-boarding other members of the care team. In our practice, nursing staff, chaplains, interpreters, and dietitians also use virtual care as part of their workflow. However, even if it is used only by the teaching team, orienting other care team members will limit technical problems such as equipment being turned off or moved out of position.
Prior to the COVID-19 pandemic, telemedicine adoption was limited because of lack of awareness, barriers in training, understanding, and narrow beliefs regarding the innovation. The COVID-19 pandemic has resulted in a remarkable increase in the provision of telemedicine services in the inpatient hospital medicine services. Importantly, it is, and should be, a developing part of the education and training for health care learners. This pandemic has underscored the need for providing telemedicine services that will likely long outlast this crisis, and to support our health care learners in being effective “iResidents” on our care teams.
Takeaways
- The future of graduate medical education involves virtual care.
The COVID-19 pandemic response has demonstrated that virtual care plays an instrumental part in patient care, and its effects will not dissipate when the pandemic is done. The curriculum for health care trainees should incorporate telemedicine competencies so that they may more effectively leverage this technology for improving care delivery.
- Selection of telemedicine patients must be stratified.
In order to obtain the highest utility for medical learners on telemedicine, there needs to be a clear decision process for which patients can be seen virtually. This involves both clinical criteria, such as avoiding virtual care for end-of-life discussions, and patient criteria, such as those who are hard of hearing.
- Virtual communication requires new communication skills.
Seeing patients via telemedicine mandates a different skill set than in-person communication. Learners must improve their “webside manner” in order to build the patient-provider relationship. Instilling these tools can pay dividends in settings where telemedicine has high yield, such as maskless communication during a pandemic.
- Health disparities could be further exacerbated by telemedicine and should not be overlooked.
Equity in access to health care applies to telemedicine as it does to many other elements. There are multiple groups that can suffer from disparities, such as patients who need interpreters, or those who have lower technological literacy and access to digital devices. Creating awareness of these pitfalls in virtual care can help medical learners recognize and support in creative solutions for these factors.
Dr. Mathews is chief, hospital medicine, at Regions Hospital, HealthPartners, St. Paul, Minn. Dr. Doshi is telemedicine director, hospital medicine, HealthPartners.
Artificial intelligence matches cancer genotypes to patient phenotypes
Precision medicine is driven by technologies such as rapid genome sequencing and artificial intelligence (AI), according to a presentation at the AACR virtual meeting II.
AI can be applied to the sequencing information derived from advanced cancers to make highly personalized treatment recommendations for patients, said Olivier Elemento, PhD, of Weill Cornell Medicine, New York.
Dr. Elemento described such work during the opening plenary session of the meeting.
Dr. Elemento advocated for whole-genome sequencing (WGS) of metastatic sites, as it can reveal “branched evolution” as tumors progress from localized to metastatic (Nat Genet. 2016 Dec;48[12]:1490-9).
The metastases share common mutations with the primaries from which they arise but also develop their own mutational profiles, which facilitate site-of-origin-agnostic, predictive treatment choices.
As examples, Dr. Elemento mentioned HER2 amplification found in a patient with urothelial cancer (J Natl Compr Canc Netw. 2019 Mar 1;17[3]:194-200) and a patient with uterine serous carcinoma (Gynecol Oncol Rep. 2019 Feb 21;28:54-7), both of whom experienced long-lasting remissions to HER2-targeted therapy.
Dr. Elemento also noted that WGS can reveal complex structural variants in lung adenocarcinomas that lack alterations in the RTK/RAS/RAF pathway (unpublished data).
Application of machine learning
One study suggested that microRNA expression and machine learning can be used to identify malignant thyroid lesions (Clin Cancer Res. 2012 Apr 1;18[7]:2032-8). The approach diagnosed malignant lesions with 90% accuracy, 100% sensitivity, and 86% specificity.
Dr. Elemento and colleagues used a similar approach to predict response to immunotherapy in melanoma (unpublished data).
The idea was to mine the cancer genome and transcriptome, allowing for identification of signals from neoantigens, immune gene expression, immune cell composition, and T-cell receptor repertoires, Dr. Elemento said. Integrating these signals with clinical outcome data via machine learning technology enabled the researchers to predict immunotherapy response in malignant melanoma with nearly 90% accuracy.
AI and image analysis
Studies have indicated that AI can be applied to medical images to improve diagnosis and treatment. The approach has been shown to:
- Facilitate correct diagnoses of malignant skin lesions (Nature. 2017 Feb 2;542[7639]:115-8).
- Distinguish lung adenocarcinoma from squamous cell cancer with 100% accuracy (EBioMedicine. 2018 Jan;27:317-28).
- Recognize distinct breast cancer subtypes (ductal, lobular, mucinous, papillary) and biomarkers (bioRxiv 242818. doi: 10.1101/242818; EBioMedicine. 2018 Jan;27:317-28)
- Predict mesothelioma prognosis (Nat Med. 2019 Oct;25[10]:1519-25).
- Predict prostate biopsy results (unpublished data) and calculate Gleason scores that can predict survival in prostate cancer patients (AACR 2020, Abstract 867).
Drug development through applied AI
In another study, Dr. Elemento and colleagues used a Bayesian machine learning approach to predict targets of molecules without a known mechanism of action (Nat Commun. 2019 Nov 19;10[1]:5221).
The method involved using data on gene expression profiles, cell line viability, side effects in animals, and structures of the molecules. The researchers applied this method to a large library of orphan small molecules and found it could predict targets in about 40% of cases.
Of 24 AI-predicted microtubule-targeting molecules, 14 depolymerized microtubules in the lab. Five of these molecules were effective in cell lines that were resistant to other microtubule-targeted drugs.
Dr. Elemento went on to describe how Oncoceutics was developing an antineoplastic agent called ONC201, but the company lacked information about the agent’s target. Using AI, the target was identified as dopamine receptor 2 (DRD2; Clin Cancer Res. 2019 Apr 1;25[7]:2305-13).
With that information, Oncoceutics initiated trials of ONC201 in tumors expressing high levels of DRD2, including a highly resistant glioma (J Neurooncol. 2019 Oct;145[1]:97-105). Responses were seen, and ONC201 is now being tested against other DRD2-expressing cancers.
Challenges to acknowledge
Potential benefits of AI in the clinic are exciting, but there are many bench-to-bedside challenges.
A clinically obvious example of AI’s applications is radiographic image analysis. There is no biologic rationale for our RECIST “cut values” for partial response, minimal response, and stable disease.
If AI can measure subtle changes on imaging that correlate with tumor biology (i.e., radiomics), we stand a better chance of predicting treatment outcomes than we can with conventional measurements of shrinkage of arbitrarily selected “target lesions.”
A tremendous amount of work is needed to build the required large image banks. During that time, AI will only improve – and without the human risks of fatigue, inconsistency, or burnout.
Those human frailties notwithstanding, AI cannot substitute for the key discussions between patient and clinician regarding goals of care, trade-offs of risks and benefits, and shared decision-making regarding management options.
At least initially (but painfully), complex technologies like WGS and digital image analysis via AI may further disadvantage patients who are medically disadvantaged by geography or socioeconomic circumstances.
In the discussion period, AACR President Antoni Ribas, MD, of University of California, Los Angeles, asked whether AI can simulate crosstalk between gene pathways so that unique treatment combinations can be identified. Dr. Elemento said those simulations are the subject of ongoing investigation.
The theme of the opening plenary session at the AACR virtual meeting II was “Turning Science into Life-Saving Care.” Applications of AI to optimize personalized use of genomics, digital image analysis, and drug development show great promise for being among the technologies that can help to realize AACR’s thematic vision.
Dr. Elemento disclosed relationships with Volastra Therapeutics, OneThree Biotech, Owkin, Freenome, Genetic Intelligence, Acuamark Diagnostics, Eli Lilly, Janssen, and Sanofi.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Precision medicine is driven by technologies such as rapid genome sequencing and artificial intelligence (AI), according to a presentation at the AACR virtual meeting II.
AI can be applied to the sequencing information derived from advanced cancers to make highly personalized treatment recommendations for patients, said Olivier Elemento, PhD, of Weill Cornell Medicine, New York.
Dr. Elemento described such work during the opening plenary session of the meeting.
Dr. Elemento advocated for whole-genome sequencing (WGS) of metastatic sites, as it can reveal “branched evolution” as tumors progress from localized to metastatic (Nat Genet. 2016 Dec;48[12]:1490-9).
The metastases share common mutations with the primaries from which they arise but also develop their own mutational profiles, which facilitate site-of-origin-agnostic, predictive treatment choices.
As examples, Dr. Elemento mentioned HER2 amplification found in a patient with urothelial cancer (J Natl Compr Canc Netw. 2019 Mar 1;17[3]:194-200) and a patient with uterine serous carcinoma (Gynecol Oncol Rep. 2019 Feb 21;28:54-7), both of whom experienced long-lasting remissions to HER2-targeted therapy.
Dr. Elemento also noted that WGS can reveal complex structural variants in lung adenocarcinomas that lack alterations in the RTK/RAS/RAF pathway (unpublished data).
Application of machine learning
One study suggested that microRNA expression and machine learning can be used to identify malignant thyroid lesions (Clin Cancer Res. 2012 Apr 1;18[7]:2032-8). The approach diagnosed malignant lesions with 90% accuracy, 100% sensitivity, and 86% specificity.
Dr. Elemento and colleagues used a similar approach to predict response to immunotherapy in melanoma (unpublished data).
The idea was to mine the cancer genome and transcriptome, allowing for identification of signals from neoantigens, immune gene expression, immune cell composition, and T-cell receptor repertoires, Dr. Elemento said. Integrating these signals with clinical outcome data via machine learning technology enabled the researchers to predict immunotherapy response in malignant melanoma with nearly 90% accuracy.
AI and image analysis
Studies have indicated that AI can be applied to medical images to improve diagnosis and treatment. The approach has been shown to:
- Facilitate correct diagnoses of malignant skin lesions (Nature. 2017 Feb 2;542[7639]:115-8).
- Distinguish lung adenocarcinoma from squamous cell cancer with 100% accuracy (EBioMedicine. 2018 Jan;27:317-28).
- Recognize distinct breast cancer subtypes (ductal, lobular, mucinous, papillary) and biomarkers (bioRxiv 242818. doi: 10.1101/242818; EBioMedicine. 2018 Jan;27:317-28)
- Predict mesothelioma prognosis (Nat Med. 2019 Oct;25[10]:1519-25).
- Predict prostate biopsy results (unpublished data) and calculate Gleason scores that can predict survival in prostate cancer patients (AACR 2020, Abstract 867).
Drug development through applied AI
In another study, Dr. Elemento and colleagues used a Bayesian machine learning approach to predict targets of molecules without a known mechanism of action (Nat Commun. 2019 Nov 19;10[1]:5221).
The method involved using data on gene expression profiles, cell line viability, side effects in animals, and structures of the molecules. The researchers applied this method to a large library of orphan small molecules and found it could predict targets in about 40% of cases.
Of 24 AI-predicted microtubule-targeting molecules, 14 depolymerized microtubules in the lab. Five of these molecules were effective in cell lines that were resistant to other microtubule-targeted drugs.
Dr. Elemento went on to describe how Oncoceutics was developing an antineoplastic agent called ONC201, but the company lacked information about the agent’s target. Using AI, the target was identified as dopamine receptor 2 (DRD2; Clin Cancer Res. 2019 Apr 1;25[7]:2305-13).
With that information, Oncoceutics initiated trials of ONC201 in tumors expressing high levels of DRD2, including a highly resistant glioma (J Neurooncol. 2019 Oct;145[1]:97-105). Responses were seen, and ONC201 is now being tested against other DRD2-expressing cancers.
Challenges to acknowledge
Potential benefits of AI in the clinic are exciting, but there are many bench-to-bedside challenges.
A clinically obvious example of AI’s applications is radiographic image analysis. There is no biologic rationale for our RECIST “cut values” for partial response, minimal response, and stable disease.
If AI can measure subtle changes on imaging that correlate with tumor biology (i.e., radiomics), we stand a better chance of predicting treatment outcomes than we can with conventional measurements of shrinkage of arbitrarily selected “target lesions.”
A tremendous amount of work is needed to build the required large image banks. During that time, AI will only improve – and without the human risks of fatigue, inconsistency, or burnout.
Those human frailties notwithstanding, AI cannot substitute for the key discussions between patient and clinician regarding goals of care, trade-offs of risks and benefits, and shared decision-making regarding management options.
At least initially (but painfully), complex technologies like WGS and digital image analysis via AI may further disadvantage patients who are medically disadvantaged by geography or socioeconomic circumstances.
In the discussion period, AACR President Antoni Ribas, MD, of University of California, Los Angeles, asked whether AI can simulate crosstalk between gene pathways so that unique treatment combinations can be identified. Dr. Elemento said those simulations are the subject of ongoing investigation.
The theme of the opening plenary session at the AACR virtual meeting II was “Turning Science into Life-Saving Care.” Applications of AI to optimize personalized use of genomics, digital image analysis, and drug development show great promise for being among the technologies that can help to realize AACR’s thematic vision.
Dr. Elemento disclosed relationships with Volastra Therapeutics, OneThree Biotech, Owkin, Freenome, Genetic Intelligence, Acuamark Diagnostics, Eli Lilly, Janssen, and Sanofi.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Precision medicine is driven by technologies such as rapid genome sequencing and artificial intelligence (AI), according to a presentation at the AACR virtual meeting II.
AI can be applied to the sequencing information derived from advanced cancers to make highly personalized treatment recommendations for patients, said Olivier Elemento, PhD, of Weill Cornell Medicine, New York.
Dr. Elemento described such work during the opening plenary session of the meeting.
Dr. Elemento advocated for whole-genome sequencing (WGS) of metastatic sites, as it can reveal “branched evolution” as tumors progress from localized to metastatic (Nat Genet. 2016 Dec;48[12]:1490-9).
The metastases share common mutations with the primaries from which they arise but also develop their own mutational profiles, which facilitate site-of-origin-agnostic, predictive treatment choices.
As examples, Dr. Elemento mentioned HER2 amplification found in a patient with urothelial cancer (J Natl Compr Canc Netw. 2019 Mar 1;17[3]:194-200) and a patient with uterine serous carcinoma (Gynecol Oncol Rep. 2019 Feb 21;28:54-7), both of whom experienced long-lasting remissions to HER2-targeted therapy.
Dr. Elemento also noted that WGS can reveal complex structural variants in lung adenocarcinomas that lack alterations in the RTK/RAS/RAF pathway (unpublished data).
Application of machine learning
One study suggested that microRNA expression and machine learning can be used to identify malignant thyroid lesions (Clin Cancer Res. 2012 Apr 1;18[7]:2032-8). The approach diagnosed malignant lesions with 90% accuracy, 100% sensitivity, and 86% specificity.
Dr. Elemento and colleagues used a similar approach to predict response to immunotherapy in melanoma (unpublished data).
The idea was to mine the cancer genome and transcriptome, allowing for identification of signals from neoantigens, immune gene expression, immune cell composition, and T-cell receptor repertoires, Dr. Elemento said. Integrating these signals with clinical outcome data via machine learning technology enabled the researchers to predict immunotherapy response in malignant melanoma with nearly 90% accuracy.
AI and image analysis
Studies have indicated that AI can be applied to medical images to improve diagnosis and treatment. The approach has been shown to:
- Facilitate correct diagnoses of malignant skin lesions (Nature. 2017 Feb 2;542[7639]:115-8).
- Distinguish lung adenocarcinoma from squamous cell cancer with 100% accuracy (EBioMedicine. 2018 Jan;27:317-28).
- Recognize distinct breast cancer subtypes (ductal, lobular, mucinous, papillary) and biomarkers (bioRxiv 242818. doi: 10.1101/242818; EBioMedicine. 2018 Jan;27:317-28)
- Predict mesothelioma prognosis (Nat Med. 2019 Oct;25[10]:1519-25).
- Predict prostate biopsy results (unpublished data) and calculate Gleason scores that can predict survival in prostate cancer patients (AACR 2020, Abstract 867).
Drug development through applied AI
In another study, Dr. Elemento and colleagues used a Bayesian machine learning approach to predict targets of molecules without a known mechanism of action (Nat Commun. 2019 Nov 19;10[1]:5221).
The method involved using data on gene expression profiles, cell line viability, side effects in animals, and structures of the molecules. The researchers applied this method to a large library of orphan small molecules and found it could predict targets in about 40% of cases.
Of 24 AI-predicted microtubule-targeting molecules, 14 depolymerized microtubules in the lab. Five of these molecules were effective in cell lines that were resistant to other microtubule-targeted drugs.
Dr. Elemento went on to describe how Oncoceutics was developing an antineoplastic agent called ONC201, but the company lacked information about the agent’s target. Using AI, the target was identified as dopamine receptor 2 (DRD2; Clin Cancer Res. 2019 Apr 1;25[7]:2305-13).
With that information, Oncoceutics initiated trials of ONC201 in tumors expressing high levels of DRD2, including a highly resistant glioma (J Neurooncol. 2019 Oct;145[1]:97-105). Responses were seen, and ONC201 is now being tested against other DRD2-expressing cancers.
Challenges to acknowledge
Potential benefits of AI in the clinic are exciting, but there are many bench-to-bedside challenges.
A clinically obvious example of AI’s applications is radiographic image analysis. There is no biologic rationale for our RECIST “cut values” for partial response, minimal response, and stable disease.
If AI can measure subtle changes on imaging that correlate with tumor biology (i.e., radiomics), we stand a better chance of predicting treatment outcomes than we can with conventional measurements of shrinkage of arbitrarily selected “target lesions.”
A tremendous amount of work is needed to build the required large image banks. During that time, AI will only improve – and without the human risks of fatigue, inconsistency, or burnout.
Those human frailties notwithstanding, AI cannot substitute for the key discussions between patient and clinician regarding goals of care, trade-offs of risks and benefits, and shared decision-making regarding management options.
At least initially (but painfully), complex technologies like WGS and digital image analysis via AI may further disadvantage patients who are medically disadvantaged by geography or socioeconomic circumstances.
In the discussion period, AACR President Antoni Ribas, MD, of University of California, Los Angeles, asked whether AI can simulate crosstalk between gene pathways so that unique treatment combinations can be identified. Dr. Elemento said those simulations are the subject of ongoing investigation.
The theme of the opening plenary session at the AACR virtual meeting II was “Turning Science into Life-Saving Care.” Applications of AI to optimize personalized use of genomics, digital image analysis, and drug development show great promise for being among the technologies that can help to realize AACR’s thematic vision.
Dr. Elemento disclosed relationships with Volastra Therapeutics, OneThree Biotech, Owkin, Freenome, Genetic Intelligence, Acuamark Diagnostics, Eli Lilly, Janssen, and Sanofi.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
FROM AACR 2020
Telemedicine in primary care
How to effectively utilize this tool
By now it is well known that the COVID-19 pandemic has significantly disrupted primary care. Office visits and revenues have precipitously dropped as physicians and patients alike fear in-person visits may increase their risks of contracting the virus. However, telemedicine has emerged as a lifeline of sorts for many practices, enabling them to conduct visits and maintain contact with patients.
Telemedicine is likely to continue to serve as a tool for primary care providers to improve access to convenient, cost-effective, high-quality care after the pandemic. Another benefit of telemedicine is it can help maintain a portion of a practice’s revenue stream for physicians during uncertain times.
Indeed, the nation has seen recent progress toward telemedicine parity, which refers to the concept of reimbursing providers’ telehealth visits at the same rates as similar in-person visits.
A challenge to adopting telemedicine is that it calls for adjusting established workflows for in-person encounters. A practice cannot simply replicate in-person processes to work for telehealth. While both in-person and virtual visits require adherence to HIPAA, for example, how you actually protect patient privacy will call for different measures. Harking back to the early days of EMR implementation, one does not need to like the telemedicine platform or process, but come to terms with the fact that it is a tool that is here to stay to deliver patient care.
Treat your practice like a laboratory
Adoption may vary between practices depending on many factors, including clinicians’ comfort with technology, clinical tolerance and triage rules for nontouch encounters, state regulations, and more. Every provider group should begin experimenting with telemedicine in specific ways that make sense for them.
One physician may practice telemedicine full-time while the rest abstain, or perhaps the practice prefers to offer telemedicine services during specific hours on specific days. Don’t be afraid to start slowly when you’re trying something new – but do get started with telehealth. It will increasingly be a mainstream medium and more patients will come to expect it.
Train the entire team
Many primary care practices do not enjoy the resources of an information technology team, so all team members essentially need to learn the new skill of telemedicine usage, in addition to assisting patients. That can’t happen without staff buy-in, so it is essential that everyone from the office manager to medical assistants have the training they need to make the technology work. Juggling schedules for telehealth and in-office, activating an account through email, starting and joining a telehealth meeting, and preparing a patient for a visit are just a handful of basic tasks your staff should be trained to do to contribute to the successful integration of telehealth.
Educate and encourage patients to use telehealth
While unfamiliarity with technology may represent a roadblock for some patients, others resist telemedicine simply because no one has explained to them why it’s so important and the benefits it can hold for them. Education and communication are critical, including the sometimes painstaking work of slowly walking patients through the process of performing important functions on the telemedicine app. By providing them with some friendly coaching, patients won’t feel lost or abandoned during what for some may be an unfamiliar and frustrating process.
Manage more behavioral health
Different states and health plans incentivize primary practices for integrating behavioral health into their offerings. Rather than dismiss this addition to your own practice as too cumbersome to take on, I would recommend using telehealth to expand behavioral health care services.
If your practice is working toward a team-based, interdisciplinary approach to care delivery, behavioral health is a critical component. While other elements of this “whole person” health care may be better suited for an office visit, the vast majority of behavioral health services can be delivered virtually.
To decide if your patient may benefit from behavioral health care, the primary care provider (PCP) can conduct a screening via telehealth. Once the screening is complete, the PCP can discuss results and refer the patient to a mental health professional – all via telehealth. While patients may be reluctant to receive behavioral health treatment, perhaps because of stigma or inexperience, they may appreciate the telemedicine option as they can remain in the comfort and familiarity of their homes.
Collaborative Care is both an in-person and virtual model that allows PCP practices to offer behavioral health services in a cost effective way by utilizing a psychiatrist as a “consultant” to the practice as opposed to hiring a full-time psychiatrist. All services within the Collaborative Care Model can be offered via telehealth, and all major insurance providers reimburse primary care providers for delivering Collaborative Care.
When PCPs provide behavioral health treatment as an “extension” of the primary care service offerings, the stigma is reduced and more patients are willing to accept the care they need.
Many areas of the country suffer from a lack of access to behavioral health specialists. In rural counties, for example, the nearest therapist may be located over an hour away. By integrating behavioral telehealth services into your practice’s offerings, you can remove geographic and transportation obstacles to care for your patient population.
Doing this can lead to providing more culturally competent care. It’s important that you’re able to offer mental health services to your patients from a professional with a similar ethnic or racial background. Language barriers and cultural differences may limit a provider’s ability to treat a patient, particularly if the patient faces health disparities related to race or ethnicity. If your practice needs to look outside of your community to tap into a more diverse pool of providers to better meet your patients’ needs, telehealth makes it easier to do that.
Adopting telemedicine for consultative patient visits offers primary care a path toward restoring patient volume and hope for a postpandemic future.
Mark Stephan, MD, is chief medical officer at Equality Health, a whole-health delivery system. He practiced family medicine for 19 years, including hospital medicine and obstetrics in rural and urban settings. Dr. Stephan has no conflicts related to the content of this piece.
How to effectively utilize this tool
How to effectively utilize this tool
By now it is well known that the COVID-19 pandemic has significantly disrupted primary care. Office visits and revenues have precipitously dropped as physicians and patients alike fear in-person visits may increase their risks of contracting the virus. However, telemedicine has emerged as a lifeline of sorts for many practices, enabling them to conduct visits and maintain contact with patients.
Telemedicine is likely to continue to serve as a tool for primary care providers to improve access to convenient, cost-effective, high-quality care after the pandemic. Another benefit of telemedicine is it can help maintain a portion of a practice’s revenue stream for physicians during uncertain times.
Indeed, the nation has seen recent progress toward telemedicine parity, which refers to the concept of reimbursing providers’ telehealth visits at the same rates as similar in-person visits.
A challenge to adopting telemedicine is that it calls for adjusting established workflows for in-person encounters. A practice cannot simply replicate in-person processes to work for telehealth. While both in-person and virtual visits require adherence to HIPAA, for example, how you actually protect patient privacy will call for different measures. Harking back to the early days of EMR implementation, one does not need to like the telemedicine platform or process, but come to terms with the fact that it is a tool that is here to stay to deliver patient care.
Treat your practice like a laboratory
Adoption may vary between practices depending on many factors, including clinicians’ comfort with technology, clinical tolerance and triage rules for nontouch encounters, state regulations, and more. Every provider group should begin experimenting with telemedicine in specific ways that make sense for them.
One physician may practice telemedicine full-time while the rest abstain, or perhaps the practice prefers to offer telemedicine services during specific hours on specific days. Don’t be afraid to start slowly when you’re trying something new – but do get started with telehealth. It will increasingly be a mainstream medium and more patients will come to expect it.
Train the entire team
Many primary care practices do not enjoy the resources of an information technology team, so all team members essentially need to learn the new skill of telemedicine usage, in addition to assisting patients. That can’t happen without staff buy-in, so it is essential that everyone from the office manager to medical assistants have the training they need to make the technology work. Juggling schedules for telehealth and in-office, activating an account through email, starting and joining a telehealth meeting, and preparing a patient for a visit are just a handful of basic tasks your staff should be trained to do to contribute to the successful integration of telehealth.
Educate and encourage patients to use telehealth
While unfamiliarity with technology may represent a roadblock for some patients, others resist telemedicine simply because no one has explained to them why it’s so important and the benefits it can hold for them. Education and communication are critical, including the sometimes painstaking work of slowly walking patients through the process of performing important functions on the telemedicine app. By providing them with some friendly coaching, patients won’t feel lost or abandoned during what for some may be an unfamiliar and frustrating process.
Manage more behavioral health
Different states and health plans incentivize primary practices for integrating behavioral health into their offerings. Rather than dismiss this addition to your own practice as too cumbersome to take on, I would recommend using telehealth to expand behavioral health care services.
If your practice is working toward a team-based, interdisciplinary approach to care delivery, behavioral health is a critical component. While other elements of this “whole person” health care may be better suited for an office visit, the vast majority of behavioral health services can be delivered virtually.
To decide if your patient may benefit from behavioral health care, the primary care provider (PCP) can conduct a screening via telehealth. Once the screening is complete, the PCP can discuss results and refer the patient to a mental health professional – all via telehealth. While patients may be reluctant to receive behavioral health treatment, perhaps because of stigma or inexperience, they may appreciate the telemedicine option as they can remain in the comfort and familiarity of their homes.
Collaborative Care is both an in-person and virtual model that allows PCP practices to offer behavioral health services in a cost effective way by utilizing a psychiatrist as a “consultant” to the practice as opposed to hiring a full-time psychiatrist. All services within the Collaborative Care Model can be offered via telehealth, and all major insurance providers reimburse primary care providers for delivering Collaborative Care.
When PCPs provide behavioral health treatment as an “extension” of the primary care service offerings, the stigma is reduced and more patients are willing to accept the care they need.
Many areas of the country suffer from a lack of access to behavioral health specialists. In rural counties, for example, the nearest therapist may be located over an hour away. By integrating behavioral telehealth services into your practice’s offerings, you can remove geographic and transportation obstacles to care for your patient population.
Doing this can lead to providing more culturally competent care. It’s important that you’re able to offer mental health services to your patients from a professional with a similar ethnic or racial background. Language barriers and cultural differences may limit a provider’s ability to treat a patient, particularly if the patient faces health disparities related to race or ethnicity. If your practice needs to look outside of your community to tap into a more diverse pool of providers to better meet your patients’ needs, telehealth makes it easier to do that.
Adopting telemedicine for consultative patient visits offers primary care a path toward restoring patient volume and hope for a postpandemic future.
Mark Stephan, MD, is chief medical officer at Equality Health, a whole-health delivery system. He practiced family medicine for 19 years, including hospital medicine and obstetrics in rural and urban settings. Dr. Stephan has no conflicts related to the content of this piece.
By now it is well known that the COVID-19 pandemic has significantly disrupted primary care. Office visits and revenues have precipitously dropped as physicians and patients alike fear in-person visits may increase their risks of contracting the virus. However, telemedicine has emerged as a lifeline of sorts for many practices, enabling them to conduct visits and maintain contact with patients.
Telemedicine is likely to continue to serve as a tool for primary care providers to improve access to convenient, cost-effective, high-quality care after the pandemic. Another benefit of telemedicine is it can help maintain a portion of a practice’s revenue stream for physicians during uncertain times.
Indeed, the nation has seen recent progress toward telemedicine parity, which refers to the concept of reimbursing providers’ telehealth visits at the same rates as similar in-person visits.
A challenge to adopting telemedicine is that it calls for adjusting established workflows for in-person encounters. A practice cannot simply replicate in-person processes to work for telehealth. While both in-person and virtual visits require adherence to HIPAA, for example, how you actually protect patient privacy will call for different measures. Harking back to the early days of EMR implementation, one does not need to like the telemedicine platform or process, but come to terms with the fact that it is a tool that is here to stay to deliver patient care.
Treat your practice like a laboratory
Adoption may vary between practices depending on many factors, including clinicians’ comfort with technology, clinical tolerance and triage rules for nontouch encounters, state regulations, and more. Every provider group should begin experimenting with telemedicine in specific ways that make sense for them.
One physician may practice telemedicine full-time while the rest abstain, or perhaps the practice prefers to offer telemedicine services during specific hours on specific days. Don’t be afraid to start slowly when you’re trying something new – but do get started with telehealth. It will increasingly be a mainstream medium and more patients will come to expect it.
Train the entire team
Many primary care practices do not enjoy the resources of an information technology team, so all team members essentially need to learn the new skill of telemedicine usage, in addition to assisting patients. That can’t happen without staff buy-in, so it is essential that everyone from the office manager to medical assistants have the training they need to make the technology work. Juggling schedules for telehealth and in-office, activating an account through email, starting and joining a telehealth meeting, and preparing a patient for a visit are just a handful of basic tasks your staff should be trained to do to contribute to the successful integration of telehealth.
Educate and encourage patients to use telehealth
While unfamiliarity with technology may represent a roadblock for some patients, others resist telemedicine simply because no one has explained to them why it’s so important and the benefits it can hold for them. Education and communication are critical, including the sometimes painstaking work of slowly walking patients through the process of performing important functions on the telemedicine app. By providing them with some friendly coaching, patients won’t feel lost or abandoned during what for some may be an unfamiliar and frustrating process.
Manage more behavioral health
Different states and health plans incentivize primary practices for integrating behavioral health into their offerings. Rather than dismiss this addition to your own practice as too cumbersome to take on, I would recommend using telehealth to expand behavioral health care services.
If your practice is working toward a team-based, interdisciplinary approach to care delivery, behavioral health is a critical component. While other elements of this “whole person” health care may be better suited for an office visit, the vast majority of behavioral health services can be delivered virtually.
To decide if your patient may benefit from behavioral health care, the primary care provider (PCP) can conduct a screening via telehealth. Once the screening is complete, the PCP can discuss results and refer the patient to a mental health professional – all via telehealth. While patients may be reluctant to receive behavioral health treatment, perhaps because of stigma or inexperience, they may appreciate the telemedicine option as they can remain in the comfort and familiarity of their homes.
Collaborative Care is both an in-person and virtual model that allows PCP practices to offer behavioral health services in a cost effective way by utilizing a psychiatrist as a “consultant” to the practice as opposed to hiring a full-time psychiatrist. All services within the Collaborative Care Model can be offered via telehealth, and all major insurance providers reimburse primary care providers for delivering Collaborative Care.
When PCPs provide behavioral health treatment as an “extension” of the primary care service offerings, the stigma is reduced and more patients are willing to accept the care they need.
Many areas of the country suffer from a lack of access to behavioral health specialists. In rural counties, for example, the nearest therapist may be located over an hour away. By integrating behavioral telehealth services into your practice’s offerings, you can remove geographic and transportation obstacles to care for your patient population.
Doing this can lead to providing more culturally competent care. It’s important that you’re able to offer mental health services to your patients from a professional with a similar ethnic or racial background. Language barriers and cultural differences may limit a provider’s ability to treat a patient, particularly if the patient faces health disparities related to race or ethnicity. If your practice needs to look outside of your community to tap into a more diverse pool of providers to better meet your patients’ needs, telehealth makes it easier to do that.
Adopting telemedicine for consultative patient visits offers primary care a path toward restoring patient volume and hope for a postpandemic future.
Mark Stephan, MD, is chief medical officer at Equality Health, a whole-health delivery system. He practiced family medicine for 19 years, including hospital medicine and obstetrics in rural and urban settings. Dr. Stephan has no conflicts related to the content of this piece.
Children’s doctors in the world of adults
Pediatric hospitalists venture into COVID-19 adult care
The memories I have from the few nights spent in the adult pop-up cardiac intensive care unit are pouring in as I sit down to tell this story. I am a pediatric hospitalist at Columbia University NewYork-Presbyterian Morgan Stanley Children’s Hospital. I usually take care of sick, hospitalized children. However, in these extraordinary times, I have joined an army of colleagues taking care of adult patients with COVID-19.
Almost all these patients had tracheostomies connected to ventilators, as well as acute-on-chronic cardiac issues. They were often delirious and unable to speak, and always alone. I was happy to help our adult colleagues, but I was also afraid. I was scared to make a mistake that could be detrimental to my patient, even though I knew well that ICU residents, fellows, and attendings were just a phone call away.
I felt like Alice in Wonderland, initially too small compared with her environment, and the next minute hunched, giant, and still clearly displaced. Except I was not dreaming or watching a movie. There was no white rabbit to chase. The situation was serious and emotionally challenging. I imagined that each patient was the dearest member of my family: my mother, my father, my aunt or uncle. I took pleasure in sharing smiles while asking the patients how they were feeling, and I touched their hands, even though much of my face was covered and there were gloves on my hands.
The year 2020 has been surreal. People have had to find their own way of pushing through the unknown and unexpected. For a start, I would never in a million years have imagined using phrases like pop-up ICU.1 I was signing an admission note for a 90-year-old lady with acute-on-chronic congestive heart failure and acute respiratory hypoxemic failure and there, at the bottom of the note, was my name, followed by an odd remark: “pediatric hospital medicine.” That is what happened in New York City in 2020: Many unexpected events took place.
This article represents a virtual conversation with three other pediatric hospitalists who, under different sets of circumstances, did the same thing: took care of adult patients. I hope that the answers to the questions I asked make you pause, reflect, and learn from the experiences described.
Would you describe the usual environment where you practice pediatric hospital medicine?
Julie Dunbar, MD: I am a full-time pediatric hospitalist at the Children’s Hospital at Montefiore, a tertiary care academic children’s hospital in the Bronx. A typical day on service involves staffing up to 14 patients, up to 21 years old, on a teaching service with residents and physician assistants. We normally staff the hospital in two shifts – day and evening – until 11:00 at night. We are situated at the heart of a medically underserved area, and our hospital system cares for about one-third of the total population of the Bronx.
L. Nell Hodo, MD: I work at Kravis Children’s Hospital at the Mount Sinai Hospital, in Manhattan at the juncture of the Upper East Side and Harlem. Our usual hospital medicine environment is the general ward/floor in a nested children’s hospital within an adult hospital. We have about 32 non-ICU beds, and the patients are managed by a combination of hospitalists, general pediatricians, and specialist attendings. All patients are on resident teams. We have a comanagement model in which the primary attending for surgical patients is always a pediatric attending (hospitalist or specialist).
Avital M. Fischer, MD: NewYork-Presbyterian Morgan Stanley Children’s Hospital is a quaternary care center – where children from the area receive subspecialty care – as well as, functionally, a community hospital for the Washington Heights area. Therefore, we always have an interesting mix of general pediatric inpatient medicine including patients with complex medical conditions, rare diseases, postoperative conditions, and undiagnosed illnesses on our wards. We are a children’s hospital, connected to a larger adult hospital system. Pediatric hospitalists cover two pediatric wards, team-staffed by residents, and a progressive care unit, staffed by nurse practitioners. There is usually evening coverage until 11 p.m.
How did this change when New York became the U.S. epicenter of the SARS-CoV-2 pandemic? Was the transition to taking care of adult patients gradual or sudden? Were you deployed to a different hospital or part of the hospital? How prepared did you feel?
Dr. Dunbar: We experienced the COVID-19 pandemic like much of the rest of New York City – it started as a slow and uncertain process, and then it hit us all at once. In initial conversations, like everyone else, we did not know exactly what was coming. We started with small changes like working from home on nonclinical days and canceling family-centered rounds to conserve personal protective equipment (PPE). In mid-March, we were still expecting that redeployment to adult floors was a highly unlikely scenario. We made work-from-home schedules and planned projects we would work on while social distancing. We planned journal clubs about emerging evidence on COVID-19. However, things happened fast, and many of these plans were scrapped.
On Saturday, March 28, we closed the main floor of the children’s hospital because so few pediatric patients were being admitted. Two days later, we admitted our first cohort of adult COVID-19 patients, all more than 30 years old. They were transferred en masse from an outside hospital emergency department that desperately needed our beds. They arrived all at once, and they all required respiratory support. At the last hospitalist division meeting before the adults arrived, we had time for only one priority set of information, and so we chose end-of-life care. We reviewed scripts for advance care planning and logistics of death certificates. As fast as things changed for us, they changed even faster for the patients. Most were relatively healthy people who rather suddenly found themselves isolated, on oxygen, dictating their final wishes to pediatricians in full protective gear. Many, many patients got better, and of course, several spent their last moments with us. One physician assistant, who works closely with the hospitalists, spent the last 5 hours of an elderly patient’s life holding her hand and helping her FaceTime with family.
For the most part, the patients came to us. We worked with our own colleagues and our own nurses, on our own territory. A few of my colleagues were briefly redeployed to a series of conference rooms that were used for several weeks as overflow space for more stable COVID-19 patients. Staffing by the pediatrics teams was so robust, with willing volunteers from every corner of the children’s hospital, that we were not needed for long.
During the early days, there was no clinical pathway to follow to care for COVID-19 patients – it didn’t exist for this novel and variable disease. We created a platform to share documents and resources in real time as they became available to us. We used group texts and emails to learn from our experiences and encourage one another. Importantly, no one was afraid to ask for help, and we relied on our adult colleagues when patients started to decompensate. Adult critical care came to our aid for all rapid responses for patients older than 30. Pediatric critical care, in their infinite flexibility, was responsible for anyone younger.
Dr. Hodo: We had a variety of changes. The first thing was the deployment of many of our attendings (hospital medicine, ICU, outpatient, and subspecialists) and residents to the adult side to work on medical COVID-19 units or in the many ICUs (some new “pop-up” units in former medical units, postanesthesia care units, and so on).2 On the adult floor we had “COVID teams,” which had an attending and two frontline providers; one of these three people was an internal medicine faculty member or resident. Residents from other specialties (emergency medicine, family medicine) were pulled off pediatric assignments in pediatric wards, PICUs, and EDs, so pediatric residents not originally assigned to inpatient rotations were sent to cover these core pediatric areas. The remaining pediatric faculty backfilled the pediatric services – so the remaining ICU docs did more shifts to cover ICU; the undeployed specialists took more inpatient service or clinic time, and so on. Outpatient pediatrics covered the inpatient pediatric service for the 3 weeks when most of the hospitalists were deployed.
We had one pediatric unit, which was a unit with equipment that made it capable of having ICU patients or floor patients, that was designated a COVID-19 unit. Most COVID-19 patients were there. Some were also in negative-pressure rooms on other floors or in the unit directly above the COVID-19 unit. Some adult patients came to the unit in the pediatric hospital but not as many as initially expected, and most were young adults in their 20s. So rather than adult patients coming to pediatrics, our experience was more that pediatricians went to the adult side.
The transition to adult care for physicians was variable in its suddenness. Most people had at least 48 hours’ notice, whereas some had as much as a week. Most of our department members deployed within the hospital complex of which we are a part, though a few went to other sites in the health system. Some were deployed into administrative or support roles in the system, rather than patient-facing roles. I felt, I would say, reasonably prepared. I trained in family medicine, though I have been exclusively in pediatrics for the past 7 years. I felt rusty, for sure, but perhaps not quite as out of my element as others. In preparation, I read a lot about COVID, reviewed some adult medicine topics provided by the medicine department, used the resources on the Pediatric Overflow Planning Contingency Response Network (POPCoRN), including an Advanced Cardiac Life Support review, and was able to shadow on a COVID-19 unit before I actually started – that was incredibly helpful. I also had the opportunity to speak about that shadowing experience in a department meeting, which I hope was helpful for others.
Dr. Fischer: Our whole focus for a relatively short time shifted to how to take care of adults within the children’s hospital. Although we had some time to prepare – the ICU was the first unit to take adults, so we knew they would come to the floor – it still felt quick. We took adult patients onto the general pediatrics floor from both the emergency department and the ICU. We took adults mostly with COVID-19, but we did have some young adults admitted for other reasons too. Those of us who were on service during this time collaborated closely, sharing what we learned and even joining one another on rounds to provide support. We basically would “teach it forward” as we learned. We also had adult providers available by phone for questions, and our pediatric subspecialists were readily available for consults and would reach out to their adult counterparts for support. Some of the hospitalists were reaching out to POPCoRN, and some were attending an ACLS crash course prior to getting on service.
What was hardest about this experience for you?
Dr. Dunbar: For me, one of the hardest aspects of dealing with COVID-19 was the unknown. In every aspect of professional life and clinical care, there were unanswered questions. What’s the best way to care for these patients? What prognoses can we give their loved ones? How can I help when it seems like there’s so little I can offer? Will we run out of PPE? As doctors, what behaviors most endanger our friends and family when we go home after work? When will things start to get better?
Dr. Hodo: For me, the week or two before being notified of the deployment was the worst and hardest time. The uncertainty about if I would be called or no, and to do what? And where? I was trying to read everything there was on management, what little was known about treatment, and so on. Once I received notification of a start date, that allowed me to focus on very clear endpoints and knowledge items (for example, reviewing ACLS algorithms) and to do things I knew would help me settle and be more effective (like shadowing).
Dr. Fischer: It was a lot of new. Not only were we taking care of a population that we hadn’t cared for since medical school (adults), but we were facing a disease process that was also new to everyone. We were learning on our feet, while at the same time providing guidance to our house staff.
What have you learned about yourself that you did not know before?
Dr. Dunbar: I was surprised to learn how much I liked caring for adult patients. The fear I felt immediately before they arrived dissipated fairly quickly after they arrived. The opportunity to address their chronic conditions while supporting them in an acute illness took me back to many of the fundamentals of medicine that I hadn’t thought much about since medical school. I liked that they could speak up to tell us how they were feeling, both physically and emotionally, so that we could address their needs and allow them to participate in their own care. Some of my favorite patients kept detailed histories of their own C-reactive protein values and oxygen levels to show they were active participants in their own recovery.
I was worried that these adult patients would be offended or scared to learn that they were being cared for by pediatricians, but at no point did anyone ask me why they were not assigned to an adult hospitalist. They saw us only as doctors and nurses, and they were grateful for our care. One 65-year-old U.S. Army veteran told me that his nurse had told him to take a shower and make his bed. “She treated me just like a 5-year-old kid. And I loved it!” he said.
Dr. Hodo: I don’t know that I was totally unaware of these things, but I will say that I had partially forgotten them: I really like adult medicine, and I love geriatrics. I like high-energy and high-stress situations … at least occasionally! I feel very comfortable discussing end-of-life decisions and death. I cope with personal stress by helping and supporting others – patients, team members, colleagues, neighbors. I risk not taking enough time for myself and have to remind myself to do so.
Dr. Fischer: I actually loved taking care of adults. It felt like there was a different kind of patient-doctor relationship to be had, and it was interesting to get to know people who had jobs and families of their own – essentially a different type of story than you typically hear taking care of children.
Were there any silver linings in this situation? How did you grow personally through this experience? What do we need to do better going forward as a profession and a community?
Dr. Dunbar: The part that I hope will stay with me is the memory of how we came together as clinicians to fight a common invisible enemy. The teamwork was unprecedented. Our day-to-day goals were simple and straightforward: do what needed to be done to help as many New Yorkers as possible. Our team made themselves available for last-minute meetings and shift changes without complaint. We practiced a type of medicine that prioritized patient comfort, flexibility, and compassionate care. We ordered methadone and insulin and antihypertensives – brand new experiences for us, but we figured it out. We worked through novel clinical problems together because there was no textbook to read.
Our colleagues from other specialties and different levels of experience stepped up to join us on overnight shifts, and we welcomed them. With the help of an ad hoc palliative care team, we improved how we listened to patients’ own self-directed needs. We reached across the aisle to our internal medicine and adult hospitalist colleagues to refresh our memories on chronic conditions, and they always answered the phone. I hope we always remember who we were during this crisis, because we were ourselves at our most generous.
Dr. Hodo: This was an unexpected but great opportunity to meet physicians, nurses, and staff in different departments and sections of the hospital from my own. I am hopeful that this experience will help us in the future with multidisciplinary work and breaking down silos that isolate specialties and units in the hospital.
I feel (and this is probably weird) invigorated by this experience. It feels good to have been able to help when I was needed. Even though there are a lot of things in adult hospital medicine I do not know, I know I did my best, asked for help when I needed it, and asked for feedback regularly from the medicine residents and nurses I worked with. I know I supported my team and my colleagues to the best of my ability through stressful and sometimes upsetting and emotionally draining times.
As a profession, we can continue to remember the value of the multidisciplinary team and the value of listening to, and making space for, different voices to be heard. We can reconsider the traditional, rigid hierarchy in medicine and medical education that can stifle creative thought and innovative ideas. We can remember that the people “at the top” of the pyramid can always learn something from those “at the bottom.” We can see the ways that department and discipline and specialty can help us but also sometimes hinder, and seek involvement in programs and discussions that unite and pool resources and skills. And, most of all, we can try, every day we are at work, to put the patients’ and families’ needs first – and when we leave work, to turn that around, and put ourselves and our loved ones in that prime position.
As a community, we also can work on thinking communally – that, after all, is the entire point of the wearing of masks in public and social distancing. It is as much about you as about me! We can try to hold on to some of this perspective of the greater good and appreciation for the work others do that makes our lives better and easier. It is not only health care workers who deserve a round of applause every day; it is every person who did something today that benefited someone else, be that giving extra space in a line, wearing a mask in a store, delivering food to an elder, teaching a class over Zoom, or simply minimizing time outside the house. It is every person who thought about the community at or near the same level of priority that they thought about themselves.
Dr. Fischer: It was a very challenging situation, but because our adult patients in the children’s hospital were relatively young with fewer comorbidities, we got to see people get well. I took care of one man with renal failure who we thought would be on dialysis for the rest of his life. By the end of my first week on service, he had begun to regain kidney function. It was amazing. I think most frontline providers caring for adults in this pandemic have had to face significant morbidity and mortality. I felt lucky that we were able to care for patients who generally got better.
I recently read the article published in the Journal of Pediatrics laying out how the Children’s Hospital at Montefiore adapted an entire pediatric floor to caring for adults.3 This example of recognition of need, quick preparation, and collaboration both within the children’s hospital and with the adult hospital was admirable. I also feel that at the beginning of this pandemic, there was a glimmer that the failure of our health care system to cover everyone and the repercussions of this failure would be drawn into sharp relief. I hope that this understanding of the importance of universal coverage persists beyond the pandemic.
Dr. Giordano is assistant professor of pediatrics at Columbia University and a pediatric hospitalist at NewYork-Presbyterian Morgan Stanley Children’s Hospital with an interest in surgical comanagement. She serves on the Society of Hospital Medicine’s Pediatric Special Interest Group Executive Committee and is the chair of the Education Subcommittee. She is also an advisory board member for the New York/Westchester SHM Chapter.
References
1. Kumaraiah D et al. Innovative ICU physician care models: Covid-19 pandemic at NewYork-Presbyterian. NEJM Catal. 2020 Apr 28. doi: 10.1056/CAT.20.0158.
2. Kim MK et al. A primer for clinician deployment to the medicine floors from an epicenter of Covid-19. NEJM Catal. 2020 May 4. doi: 10.1056/CAT.20.0180.
3. Philips K, et al. Rapid Implementation of an Adult COVID-19 Unit in a Children’s Hospital. J Pediatr. 2020. doi: 10.1016/j.jpeds.2020.04.060.
Pediatric hospitalists venture into COVID-19 adult care
Pediatric hospitalists venture into COVID-19 adult care
The memories I have from the few nights spent in the adult pop-up cardiac intensive care unit are pouring in as I sit down to tell this story. I am a pediatric hospitalist at Columbia University NewYork-Presbyterian Morgan Stanley Children’s Hospital. I usually take care of sick, hospitalized children. However, in these extraordinary times, I have joined an army of colleagues taking care of adult patients with COVID-19.
Almost all these patients had tracheostomies connected to ventilators, as well as acute-on-chronic cardiac issues. They were often delirious and unable to speak, and always alone. I was happy to help our adult colleagues, but I was also afraid. I was scared to make a mistake that could be detrimental to my patient, even though I knew well that ICU residents, fellows, and attendings were just a phone call away.
I felt like Alice in Wonderland, initially too small compared with her environment, and the next minute hunched, giant, and still clearly displaced. Except I was not dreaming or watching a movie. There was no white rabbit to chase. The situation was serious and emotionally challenging. I imagined that each patient was the dearest member of my family: my mother, my father, my aunt or uncle. I took pleasure in sharing smiles while asking the patients how they were feeling, and I touched their hands, even though much of my face was covered and there were gloves on my hands.
The year 2020 has been surreal. People have had to find their own way of pushing through the unknown and unexpected. For a start, I would never in a million years have imagined using phrases like pop-up ICU.1 I was signing an admission note for a 90-year-old lady with acute-on-chronic congestive heart failure and acute respiratory hypoxemic failure and there, at the bottom of the note, was my name, followed by an odd remark: “pediatric hospital medicine.” That is what happened in New York City in 2020: Many unexpected events took place.
This article represents a virtual conversation with three other pediatric hospitalists who, under different sets of circumstances, did the same thing: took care of adult patients. I hope that the answers to the questions I asked make you pause, reflect, and learn from the experiences described.
Would you describe the usual environment where you practice pediatric hospital medicine?
Julie Dunbar, MD: I am a full-time pediatric hospitalist at the Children’s Hospital at Montefiore, a tertiary care academic children’s hospital in the Bronx. A typical day on service involves staffing up to 14 patients, up to 21 years old, on a teaching service with residents and physician assistants. We normally staff the hospital in two shifts – day and evening – until 11:00 at night. We are situated at the heart of a medically underserved area, and our hospital system cares for about one-third of the total population of the Bronx.
L. Nell Hodo, MD: I work at Kravis Children’s Hospital at the Mount Sinai Hospital, in Manhattan at the juncture of the Upper East Side and Harlem. Our usual hospital medicine environment is the general ward/floor in a nested children’s hospital within an adult hospital. We have about 32 non-ICU beds, and the patients are managed by a combination of hospitalists, general pediatricians, and specialist attendings. All patients are on resident teams. We have a comanagement model in which the primary attending for surgical patients is always a pediatric attending (hospitalist or specialist).
Avital M. Fischer, MD: NewYork-Presbyterian Morgan Stanley Children’s Hospital is a quaternary care center – where children from the area receive subspecialty care – as well as, functionally, a community hospital for the Washington Heights area. Therefore, we always have an interesting mix of general pediatric inpatient medicine including patients with complex medical conditions, rare diseases, postoperative conditions, and undiagnosed illnesses on our wards. We are a children’s hospital, connected to a larger adult hospital system. Pediatric hospitalists cover two pediatric wards, team-staffed by residents, and a progressive care unit, staffed by nurse practitioners. There is usually evening coverage until 11 p.m.
How did this change when New York became the U.S. epicenter of the SARS-CoV-2 pandemic? Was the transition to taking care of adult patients gradual or sudden? Were you deployed to a different hospital or part of the hospital? How prepared did you feel?
Dr. Dunbar: We experienced the COVID-19 pandemic like much of the rest of New York City – it started as a slow and uncertain process, and then it hit us all at once. In initial conversations, like everyone else, we did not know exactly what was coming. We started with small changes like working from home on nonclinical days and canceling family-centered rounds to conserve personal protective equipment (PPE). In mid-March, we were still expecting that redeployment to adult floors was a highly unlikely scenario. We made work-from-home schedules and planned projects we would work on while social distancing. We planned journal clubs about emerging evidence on COVID-19. However, things happened fast, and many of these plans were scrapped.
On Saturday, March 28, we closed the main floor of the children’s hospital because so few pediatric patients were being admitted. Two days later, we admitted our first cohort of adult COVID-19 patients, all more than 30 years old. They were transferred en masse from an outside hospital emergency department that desperately needed our beds. They arrived all at once, and they all required respiratory support. At the last hospitalist division meeting before the adults arrived, we had time for only one priority set of information, and so we chose end-of-life care. We reviewed scripts for advance care planning and logistics of death certificates. As fast as things changed for us, they changed even faster for the patients. Most were relatively healthy people who rather suddenly found themselves isolated, on oxygen, dictating their final wishes to pediatricians in full protective gear. Many, many patients got better, and of course, several spent their last moments with us. One physician assistant, who works closely with the hospitalists, spent the last 5 hours of an elderly patient’s life holding her hand and helping her FaceTime with family.
For the most part, the patients came to us. We worked with our own colleagues and our own nurses, on our own territory. A few of my colleagues were briefly redeployed to a series of conference rooms that were used for several weeks as overflow space for more stable COVID-19 patients. Staffing by the pediatrics teams was so robust, with willing volunteers from every corner of the children’s hospital, that we were not needed for long.
During the early days, there was no clinical pathway to follow to care for COVID-19 patients – it didn’t exist for this novel and variable disease. We created a platform to share documents and resources in real time as they became available to us. We used group texts and emails to learn from our experiences and encourage one another. Importantly, no one was afraid to ask for help, and we relied on our adult colleagues when patients started to decompensate. Adult critical care came to our aid for all rapid responses for patients older than 30. Pediatric critical care, in their infinite flexibility, was responsible for anyone younger.
Dr. Hodo: We had a variety of changes. The first thing was the deployment of many of our attendings (hospital medicine, ICU, outpatient, and subspecialists) and residents to the adult side to work on medical COVID-19 units or in the many ICUs (some new “pop-up” units in former medical units, postanesthesia care units, and so on).2 On the adult floor we had “COVID teams,” which had an attending and two frontline providers; one of these three people was an internal medicine faculty member or resident. Residents from other specialties (emergency medicine, family medicine) were pulled off pediatric assignments in pediatric wards, PICUs, and EDs, so pediatric residents not originally assigned to inpatient rotations were sent to cover these core pediatric areas. The remaining pediatric faculty backfilled the pediatric services – so the remaining ICU docs did more shifts to cover ICU; the undeployed specialists took more inpatient service or clinic time, and so on. Outpatient pediatrics covered the inpatient pediatric service for the 3 weeks when most of the hospitalists were deployed.
We had one pediatric unit, which was a unit with equipment that made it capable of having ICU patients or floor patients, that was designated a COVID-19 unit. Most COVID-19 patients were there. Some were also in negative-pressure rooms on other floors or in the unit directly above the COVID-19 unit. Some adult patients came to the unit in the pediatric hospital but not as many as initially expected, and most were young adults in their 20s. So rather than adult patients coming to pediatrics, our experience was more that pediatricians went to the adult side.
The transition to adult care for physicians was variable in its suddenness. Most people had at least 48 hours’ notice, whereas some had as much as a week. Most of our department members deployed within the hospital complex of which we are a part, though a few went to other sites in the health system. Some were deployed into administrative or support roles in the system, rather than patient-facing roles. I felt, I would say, reasonably prepared. I trained in family medicine, though I have been exclusively in pediatrics for the past 7 years. I felt rusty, for sure, but perhaps not quite as out of my element as others. In preparation, I read a lot about COVID, reviewed some adult medicine topics provided by the medicine department, used the resources on the Pediatric Overflow Planning Contingency Response Network (POPCoRN), including an Advanced Cardiac Life Support review, and was able to shadow on a COVID-19 unit before I actually started – that was incredibly helpful. I also had the opportunity to speak about that shadowing experience in a department meeting, which I hope was helpful for others.
Dr. Fischer: Our whole focus for a relatively short time shifted to how to take care of adults within the children’s hospital. Although we had some time to prepare – the ICU was the first unit to take adults, so we knew they would come to the floor – it still felt quick. We took adult patients onto the general pediatrics floor from both the emergency department and the ICU. We took adults mostly with COVID-19, but we did have some young adults admitted for other reasons too. Those of us who were on service during this time collaborated closely, sharing what we learned and even joining one another on rounds to provide support. We basically would “teach it forward” as we learned. We also had adult providers available by phone for questions, and our pediatric subspecialists were readily available for consults and would reach out to their adult counterparts for support. Some of the hospitalists were reaching out to POPCoRN, and some were attending an ACLS crash course prior to getting on service.
What was hardest about this experience for you?
Dr. Dunbar: For me, one of the hardest aspects of dealing with COVID-19 was the unknown. In every aspect of professional life and clinical care, there were unanswered questions. What’s the best way to care for these patients? What prognoses can we give their loved ones? How can I help when it seems like there’s so little I can offer? Will we run out of PPE? As doctors, what behaviors most endanger our friends and family when we go home after work? When will things start to get better?
Dr. Hodo: For me, the week or two before being notified of the deployment was the worst and hardest time. The uncertainty about if I would be called or no, and to do what? And where? I was trying to read everything there was on management, what little was known about treatment, and so on. Once I received notification of a start date, that allowed me to focus on very clear endpoints and knowledge items (for example, reviewing ACLS algorithms) and to do things I knew would help me settle and be more effective (like shadowing).
Dr. Fischer: It was a lot of new. Not only were we taking care of a population that we hadn’t cared for since medical school (adults), but we were facing a disease process that was also new to everyone. We were learning on our feet, while at the same time providing guidance to our house staff.
What have you learned about yourself that you did not know before?
Dr. Dunbar: I was surprised to learn how much I liked caring for adult patients. The fear I felt immediately before they arrived dissipated fairly quickly after they arrived. The opportunity to address their chronic conditions while supporting them in an acute illness took me back to many of the fundamentals of medicine that I hadn’t thought much about since medical school. I liked that they could speak up to tell us how they were feeling, both physically and emotionally, so that we could address their needs and allow them to participate in their own care. Some of my favorite patients kept detailed histories of their own C-reactive protein values and oxygen levels to show they were active participants in their own recovery.
I was worried that these adult patients would be offended or scared to learn that they were being cared for by pediatricians, but at no point did anyone ask me why they were not assigned to an adult hospitalist. They saw us only as doctors and nurses, and they were grateful for our care. One 65-year-old U.S. Army veteran told me that his nurse had told him to take a shower and make his bed. “She treated me just like a 5-year-old kid. And I loved it!” he said.
Dr. Hodo: I don’t know that I was totally unaware of these things, but I will say that I had partially forgotten them: I really like adult medicine, and I love geriatrics. I like high-energy and high-stress situations … at least occasionally! I feel very comfortable discussing end-of-life decisions and death. I cope with personal stress by helping and supporting others – patients, team members, colleagues, neighbors. I risk not taking enough time for myself and have to remind myself to do so.
Dr. Fischer: I actually loved taking care of adults. It felt like there was a different kind of patient-doctor relationship to be had, and it was interesting to get to know people who had jobs and families of their own – essentially a different type of story than you typically hear taking care of children.
Were there any silver linings in this situation? How did you grow personally through this experience? What do we need to do better going forward as a profession and a community?
Dr. Dunbar: The part that I hope will stay with me is the memory of how we came together as clinicians to fight a common invisible enemy. The teamwork was unprecedented. Our day-to-day goals were simple and straightforward: do what needed to be done to help as many New Yorkers as possible. Our team made themselves available for last-minute meetings and shift changes without complaint. We practiced a type of medicine that prioritized patient comfort, flexibility, and compassionate care. We ordered methadone and insulin and antihypertensives – brand new experiences for us, but we figured it out. We worked through novel clinical problems together because there was no textbook to read.
Our colleagues from other specialties and different levels of experience stepped up to join us on overnight shifts, and we welcomed them. With the help of an ad hoc palliative care team, we improved how we listened to patients’ own self-directed needs. We reached across the aisle to our internal medicine and adult hospitalist colleagues to refresh our memories on chronic conditions, and they always answered the phone. I hope we always remember who we were during this crisis, because we were ourselves at our most generous.
Dr. Hodo: This was an unexpected but great opportunity to meet physicians, nurses, and staff in different departments and sections of the hospital from my own. I am hopeful that this experience will help us in the future with multidisciplinary work and breaking down silos that isolate specialties and units in the hospital.
I feel (and this is probably weird) invigorated by this experience. It feels good to have been able to help when I was needed. Even though there are a lot of things in adult hospital medicine I do not know, I know I did my best, asked for help when I needed it, and asked for feedback regularly from the medicine residents and nurses I worked with. I know I supported my team and my colleagues to the best of my ability through stressful and sometimes upsetting and emotionally draining times.
As a profession, we can continue to remember the value of the multidisciplinary team and the value of listening to, and making space for, different voices to be heard. We can reconsider the traditional, rigid hierarchy in medicine and medical education that can stifle creative thought and innovative ideas. We can remember that the people “at the top” of the pyramid can always learn something from those “at the bottom.” We can see the ways that department and discipline and specialty can help us but also sometimes hinder, and seek involvement in programs and discussions that unite and pool resources and skills. And, most of all, we can try, every day we are at work, to put the patients’ and families’ needs first – and when we leave work, to turn that around, and put ourselves and our loved ones in that prime position.
As a community, we also can work on thinking communally – that, after all, is the entire point of the wearing of masks in public and social distancing. It is as much about you as about me! We can try to hold on to some of this perspective of the greater good and appreciation for the work others do that makes our lives better and easier. It is not only health care workers who deserve a round of applause every day; it is every person who did something today that benefited someone else, be that giving extra space in a line, wearing a mask in a store, delivering food to an elder, teaching a class over Zoom, or simply minimizing time outside the house. It is every person who thought about the community at or near the same level of priority that they thought about themselves.
Dr. Fischer: It was a very challenging situation, but because our adult patients in the children’s hospital were relatively young with fewer comorbidities, we got to see people get well. I took care of one man with renal failure who we thought would be on dialysis for the rest of his life. By the end of my first week on service, he had begun to regain kidney function. It was amazing. I think most frontline providers caring for adults in this pandemic have had to face significant morbidity and mortality. I felt lucky that we were able to care for patients who generally got better.
I recently read the article published in the Journal of Pediatrics laying out how the Children’s Hospital at Montefiore adapted an entire pediatric floor to caring for adults.3 This example of recognition of need, quick preparation, and collaboration both within the children’s hospital and with the adult hospital was admirable. I also feel that at the beginning of this pandemic, there was a glimmer that the failure of our health care system to cover everyone and the repercussions of this failure would be drawn into sharp relief. I hope that this understanding of the importance of universal coverage persists beyond the pandemic.
Dr. Giordano is assistant professor of pediatrics at Columbia University and a pediatric hospitalist at NewYork-Presbyterian Morgan Stanley Children’s Hospital with an interest in surgical comanagement. She serves on the Society of Hospital Medicine’s Pediatric Special Interest Group Executive Committee and is the chair of the Education Subcommittee. She is also an advisory board member for the New York/Westchester SHM Chapter.
References
1. Kumaraiah D et al. Innovative ICU physician care models: Covid-19 pandemic at NewYork-Presbyterian. NEJM Catal. 2020 Apr 28. doi: 10.1056/CAT.20.0158.
2. Kim MK et al. A primer for clinician deployment to the medicine floors from an epicenter of Covid-19. NEJM Catal. 2020 May 4. doi: 10.1056/CAT.20.0180.
3. Philips K, et al. Rapid Implementation of an Adult COVID-19 Unit in a Children’s Hospital. J Pediatr. 2020. doi: 10.1016/j.jpeds.2020.04.060.
The memories I have from the few nights spent in the adult pop-up cardiac intensive care unit are pouring in as I sit down to tell this story. I am a pediatric hospitalist at Columbia University NewYork-Presbyterian Morgan Stanley Children’s Hospital. I usually take care of sick, hospitalized children. However, in these extraordinary times, I have joined an army of colleagues taking care of adult patients with COVID-19.
Almost all these patients had tracheostomies connected to ventilators, as well as acute-on-chronic cardiac issues. They were often delirious and unable to speak, and always alone. I was happy to help our adult colleagues, but I was also afraid. I was scared to make a mistake that could be detrimental to my patient, even though I knew well that ICU residents, fellows, and attendings were just a phone call away.
I felt like Alice in Wonderland, initially too small compared with her environment, and the next minute hunched, giant, and still clearly displaced. Except I was not dreaming or watching a movie. There was no white rabbit to chase. The situation was serious and emotionally challenging. I imagined that each patient was the dearest member of my family: my mother, my father, my aunt or uncle. I took pleasure in sharing smiles while asking the patients how they were feeling, and I touched their hands, even though much of my face was covered and there were gloves on my hands.
The year 2020 has been surreal. People have had to find their own way of pushing through the unknown and unexpected. For a start, I would never in a million years have imagined using phrases like pop-up ICU.1 I was signing an admission note for a 90-year-old lady with acute-on-chronic congestive heart failure and acute respiratory hypoxemic failure and there, at the bottom of the note, was my name, followed by an odd remark: “pediatric hospital medicine.” That is what happened in New York City in 2020: Many unexpected events took place.
This article represents a virtual conversation with three other pediatric hospitalists who, under different sets of circumstances, did the same thing: took care of adult patients. I hope that the answers to the questions I asked make you pause, reflect, and learn from the experiences described.
Would you describe the usual environment where you practice pediatric hospital medicine?
Julie Dunbar, MD: I am a full-time pediatric hospitalist at the Children’s Hospital at Montefiore, a tertiary care academic children’s hospital in the Bronx. A typical day on service involves staffing up to 14 patients, up to 21 years old, on a teaching service with residents and physician assistants. We normally staff the hospital in two shifts – day and evening – until 11:00 at night. We are situated at the heart of a medically underserved area, and our hospital system cares for about one-third of the total population of the Bronx.
L. Nell Hodo, MD: I work at Kravis Children’s Hospital at the Mount Sinai Hospital, in Manhattan at the juncture of the Upper East Side and Harlem. Our usual hospital medicine environment is the general ward/floor in a nested children’s hospital within an adult hospital. We have about 32 non-ICU beds, and the patients are managed by a combination of hospitalists, general pediatricians, and specialist attendings. All patients are on resident teams. We have a comanagement model in which the primary attending for surgical patients is always a pediatric attending (hospitalist or specialist).
Avital M. Fischer, MD: NewYork-Presbyterian Morgan Stanley Children’s Hospital is a quaternary care center – where children from the area receive subspecialty care – as well as, functionally, a community hospital for the Washington Heights area. Therefore, we always have an interesting mix of general pediatric inpatient medicine including patients with complex medical conditions, rare diseases, postoperative conditions, and undiagnosed illnesses on our wards. We are a children’s hospital, connected to a larger adult hospital system. Pediatric hospitalists cover two pediatric wards, team-staffed by residents, and a progressive care unit, staffed by nurse practitioners. There is usually evening coverage until 11 p.m.
How did this change when New York became the U.S. epicenter of the SARS-CoV-2 pandemic? Was the transition to taking care of adult patients gradual or sudden? Were you deployed to a different hospital or part of the hospital? How prepared did you feel?
Dr. Dunbar: We experienced the COVID-19 pandemic like much of the rest of New York City – it started as a slow and uncertain process, and then it hit us all at once. In initial conversations, like everyone else, we did not know exactly what was coming. We started with small changes like working from home on nonclinical days and canceling family-centered rounds to conserve personal protective equipment (PPE). In mid-March, we were still expecting that redeployment to adult floors was a highly unlikely scenario. We made work-from-home schedules and planned projects we would work on while social distancing. We planned journal clubs about emerging evidence on COVID-19. However, things happened fast, and many of these plans were scrapped.
On Saturday, March 28, we closed the main floor of the children’s hospital because so few pediatric patients were being admitted. Two days later, we admitted our first cohort of adult COVID-19 patients, all more than 30 years old. They were transferred en masse from an outside hospital emergency department that desperately needed our beds. They arrived all at once, and they all required respiratory support. At the last hospitalist division meeting before the adults arrived, we had time for only one priority set of information, and so we chose end-of-life care. We reviewed scripts for advance care planning and logistics of death certificates. As fast as things changed for us, they changed even faster for the patients. Most were relatively healthy people who rather suddenly found themselves isolated, on oxygen, dictating their final wishes to pediatricians in full protective gear. Many, many patients got better, and of course, several spent their last moments with us. One physician assistant, who works closely with the hospitalists, spent the last 5 hours of an elderly patient’s life holding her hand and helping her FaceTime with family.
For the most part, the patients came to us. We worked with our own colleagues and our own nurses, on our own territory. A few of my colleagues were briefly redeployed to a series of conference rooms that were used for several weeks as overflow space for more stable COVID-19 patients. Staffing by the pediatrics teams was so robust, with willing volunteers from every corner of the children’s hospital, that we were not needed for long.
During the early days, there was no clinical pathway to follow to care for COVID-19 patients – it didn’t exist for this novel and variable disease. We created a platform to share documents and resources in real time as they became available to us. We used group texts and emails to learn from our experiences and encourage one another. Importantly, no one was afraid to ask for help, and we relied on our adult colleagues when patients started to decompensate. Adult critical care came to our aid for all rapid responses for patients older than 30. Pediatric critical care, in their infinite flexibility, was responsible for anyone younger.
Dr. Hodo: We had a variety of changes. The first thing was the deployment of many of our attendings (hospital medicine, ICU, outpatient, and subspecialists) and residents to the adult side to work on medical COVID-19 units or in the many ICUs (some new “pop-up” units in former medical units, postanesthesia care units, and so on).2 On the adult floor we had “COVID teams,” which had an attending and two frontline providers; one of these three people was an internal medicine faculty member or resident. Residents from other specialties (emergency medicine, family medicine) were pulled off pediatric assignments in pediatric wards, PICUs, and EDs, so pediatric residents not originally assigned to inpatient rotations were sent to cover these core pediatric areas. The remaining pediatric faculty backfilled the pediatric services – so the remaining ICU docs did more shifts to cover ICU; the undeployed specialists took more inpatient service or clinic time, and so on. Outpatient pediatrics covered the inpatient pediatric service for the 3 weeks when most of the hospitalists were deployed.
We had one pediatric unit, which was a unit with equipment that made it capable of having ICU patients or floor patients, that was designated a COVID-19 unit. Most COVID-19 patients were there. Some were also in negative-pressure rooms on other floors or in the unit directly above the COVID-19 unit. Some adult patients came to the unit in the pediatric hospital but not as many as initially expected, and most were young adults in their 20s. So rather than adult patients coming to pediatrics, our experience was more that pediatricians went to the adult side.
The transition to adult care for physicians was variable in its suddenness. Most people had at least 48 hours’ notice, whereas some had as much as a week. Most of our department members deployed within the hospital complex of which we are a part, though a few went to other sites in the health system. Some were deployed into administrative or support roles in the system, rather than patient-facing roles. I felt, I would say, reasonably prepared. I trained in family medicine, though I have been exclusively in pediatrics for the past 7 years. I felt rusty, for sure, but perhaps not quite as out of my element as others. In preparation, I read a lot about COVID, reviewed some adult medicine topics provided by the medicine department, used the resources on the Pediatric Overflow Planning Contingency Response Network (POPCoRN), including an Advanced Cardiac Life Support review, and was able to shadow on a COVID-19 unit before I actually started – that was incredibly helpful. I also had the opportunity to speak about that shadowing experience in a department meeting, which I hope was helpful for others.
Dr. Fischer: Our whole focus for a relatively short time shifted to how to take care of adults within the children’s hospital. Although we had some time to prepare – the ICU was the first unit to take adults, so we knew they would come to the floor – it still felt quick. We took adult patients onto the general pediatrics floor from both the emergency department and the ICU. We took adults mostly with COVID-19, but we did have some young adults admitted for other reasons too. Those of us who were on service during this time collaborated closely, sharing what we learned and even joining one another on rounds to provide support. We basically would “teach it forward” as we learned. We also had adult providers available by phone for questions, and our pediatric subspecialists were readily available for consults and would reach out to their adult counterparts for support. Some of the hospitalists were reaching out to POPCoRN, and some were attending an ACLS crash course prior to getting on service.
What was hardest about this experience for you?
Dr. Dunbar: For me, one of the hardest aspects of dealing with COVID-19 was the unknown. In every aspect of professional life and clinical care, there were unanswered questions. What’s the best way to care for these patients? What prognoses can we give their loved ones? How can I help when it seems like there’s so little I can offer? Will we run out of PPE? As doctors, what behaviors most endanger our friends and family when we go home after work? When will things start to get better?
Dr. Hodo: For me, the week or two before being notified of the deployment was the worst and hardest time. The uncertainty about if I would be called or no, and to do what? And where? I was trying to read everything there was on management, what little was known about treatment, and so on. Once I received notification of a start date, that allowed me to focus on very clear endpoints and knowledge items (for example, reviewing ACLS algorithms) and to do things I knew would help me settle and be more effective (like shadowing).
Dr. Fischer: It was a lot of new. Not only were we taking care of a population that we hadn’t cared for since medical school (adults), but we were facing a disease process that was also new to everyone. We were learning on our feet, while at the same time providing guidance to our house staff.
What have you learned about yourself that you did not know before?
Dr. Dunbar: I was surprised to learn how much I liked caring for adult patients. The fear I felt immediately before they arrived dissipated fairly quickly after they arrived. The opportunity to address their chronic conditions while supporting them in an acute illness took me back to many of the fundamentals of medicine that I hadn’t thought much about since medical school. I liked that they could speak up to tell us how they were feeling, both physically and emotionally, so that we could address their needs and allow them to participate in their own care. Some of my favorite patients kept detailed histories of their own C-reactive protein values and oxygen levels to show they were active participants in their own recovery.
I was worried that these adult patients would be offended or scared to learn that they were being cared for by pediatricians, but at no point did anyone ask me why they were not assigned to an adult hospitalist. They saw us only as doctors and nurses, and they were grateful for our care. One 65-year-old U.S. Army veteran told me that his nurse had told him to take a shower and make his bed. “She treated me just like a 5-year-old kid. And I loved it!” he said.
Dr. Hodo: I don’t know that I was totally unaware of these things, but I will say that I had partially forgotten them: I really like adult medicine, and I love geriatrics. I like high-energy and high-stress situations … at least occasionally! I feel very comfortable discussing end-of-life decisions and death. I cope with personal stress by helping and supporting others – patients, team members, colleagues, neighbors. I risk not taking enough time for myself and have to remind myself to do so.
Dr. Fischer: I actually loved taking care of adults. It felt like there was a different kind of patient-doctor relationship to be had, and it was interesting to get to know people who had jobs and families of their own – essentially a different type of story than you typically hear taking care of children.
Were there any silver linings in this situation? How did you grow personally through this experience? What do we need to do better going forward as a profession and a community?
Dr. Dunbar: The part that I hope will stay with me is the memory of how we came together as clinicians to fight a common invisible enemy. The teamwork was unprecedented. Our day-to-day goals were simple and straightforward: do what needed to be done to help as many New Yorkers as possible. Our team made themselves available for last-minute meetings and shift changes without complaint. We practiced a type of medicine that prioritized patient comfort, flexibility, and compassionate care. We ordered methadone and insulin and antihypertensives – brand new experiences for us, but we figured it out. We worked through novel clinical problems together because there was no textbook to read.
Our colleagues from other specialties and different levels of experience stepped up to join us on overnight shifts, and we welcomed them. With the help of an ad hoc palliative care team, we improved how we listened to patients’ own self-directed needs. We reached across the aisle to our internal medicine and adult hospitalist colleagues to refresh our memories on chronic conditions, and they always answered the phone. I hope we always remember who we were during this crisis, because we were ourselves at our most generous.
Dr. Hodo: This was an unexpected but great opportunity to meet physicians, nurses, and staff in different departments and sections of the hospital from my own. I am hopeful that this experience will help us in the future with multidisciplinary work and breaking down silos that isolate specialties and units in the hospital.
I feel (and this is probably weird) invigorated by this experience. It feels good to have been able to help when I was needed. Even though there are a lot of things in adult hospital medicine I do not know, I know I did my best, asked for help when I needed it, and asked for feedback regularly from the medicine residents and nurses I worked with. I know I supported my team and my colleagues to the best of my ability through stressful and sometimes upsetting and emotionally draining times.
As a profession, we can continue to remember the value of the multidisciplinary team and the value of listening to, and making space for, different voices to be heard. We can reconsider the traditional, rigid hierarchy in medicine and medical education that can stifle creative thought and innovative ideas. We can remember that the people “at the top” of the pyramid can always learn something from those “at the bottom.” We can see the ways that department and discipline and specialty can help us but also sometimes hinder, and seek involvement in programs and discussions that unite and pool resources and skills. And, most of all, we can try, every day we are at work, to put the patients’ and families’ needs first – and when we leave work, to turn that around, and put ourselves and our loved ones in that prime position.
As a community, we also can work on thinking communally – that, after all, is the entire point of the wearing of masks in public and social distancing. It is as much about you as about me! We can try to hold on to some of this perspective of the greater good and appreciation for the work others do that makes our lives better and easier. It is not only health care workers who deserve a round of applause every day; it is every person who did something today that benefited someone else, be that giving extra space in a line, wearing a mask in a store, delivering food to an elder, teaching a class over Zoom, or simply minimizing time outside the house. It is every person who thought about the community at or near the same level of priority that they thought about themselves.
Dr. Fischer: It was a very challenging situation, but because our adult patients in the children’s hospital were relatively young with fewer comorbidities, we got to see people get well. I took care of one man with renal failure who we thought would be on dialysis for the rest of his life. By the end of my first week on service, he had begun to regain kidney function. It was amazing. I think most frontline providers caring for adults in this pandemic have had to face significant morbidity and mortality. I felt lucky that we were able to care for patients who generally got better.
I recently read the article published in the Journal of Pediatrics laying out how the Children’s Hospital at Montefiore adapted an entire pediatric floor to caring for adults.3 This example of recognition of need, quick preparation, and collaboration both within the children’s hospital and with the adult hospital was admirable. I also feel that at the beginning of this pandemic, there was a glimmer that the failure of our health care system to cover everyone and the repercussions of this failure would be drawn into sharp relief. I hope that this understanding of the importance of universal coverage persists beyond the pandemic.
Dr. Giordano is assistant professor of pediatrics at Columbia University and a pediatric hospitalist at NewYork-Presbyterian Morgan Stanley Children’s Hospital with an interest in surgical comanagement. She serves on the Society of Hospital Medicine’s Pediatric Special Interest Group Executive Committee and is the chair of the Education Subcommittee. She is also an advisory board member for the New York/Westchester SHM Chapter.
References
1. Kumaraiah D et al. Innovative ICU physician care models: Covid-19 pandemic at NewYork-Presbyterian. NEJM Catal. 2020 Apr 28. doi: 10.1056/CAT.20.0158.
2. Kim MK et al. A primer for clinician deployment to the medicine floors from an epicenter of Covid-19. NEJM Catal. 2020 May 4. doi: 10.1056/CAT.20.0180.
3. Philips K, et al. Rapid Implementation of an Adult COVID-19 Unit in a Children’s Hospital. J Pediatr. 2020. doi: 10.1016/j.jpeds.2020.04.060.