User login
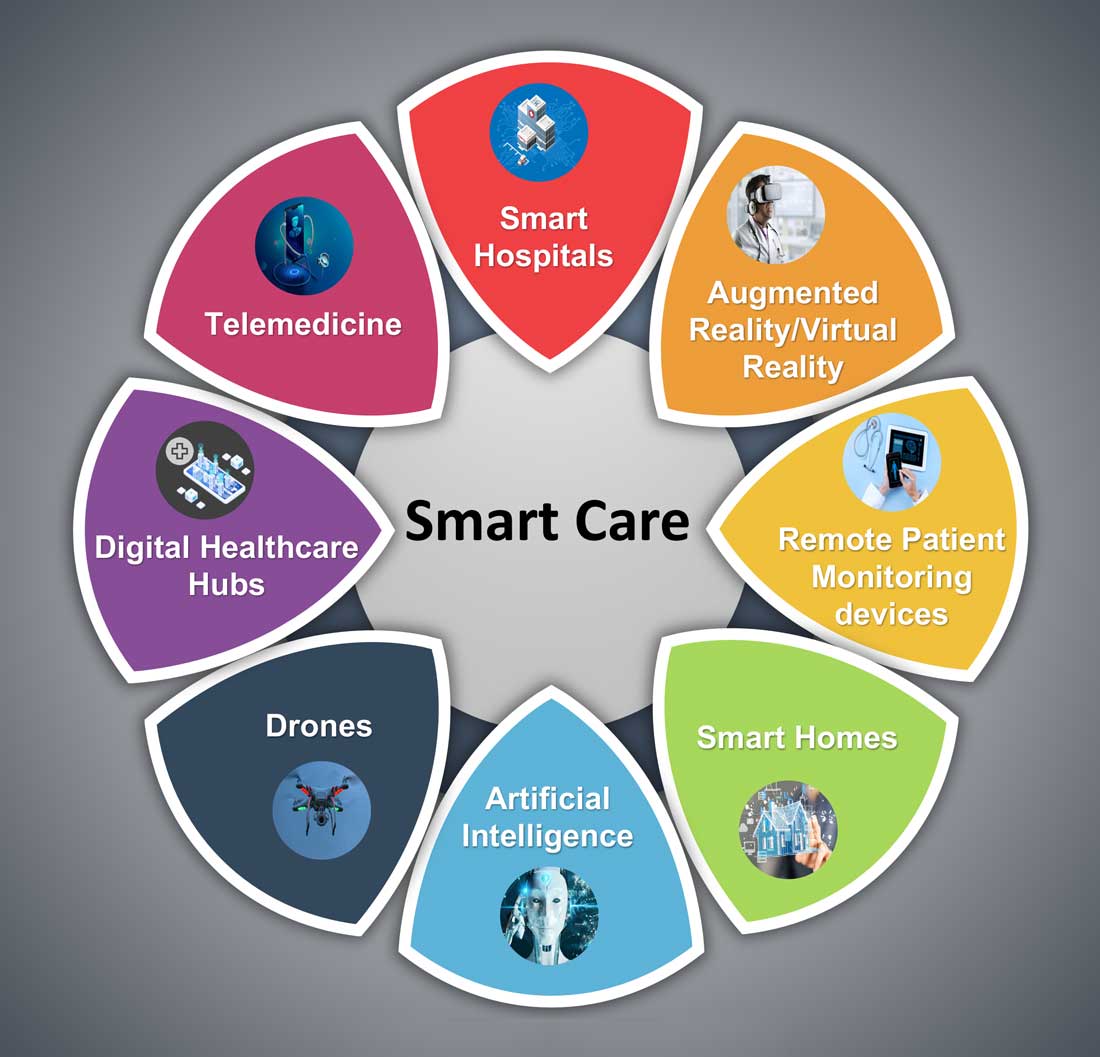
Hospital medicine and the future of smart care
People often overestimate what will happen in the next two years and underestimate what will happen in ten. – Bill Gates
The COVID-19 pandemic set in motion a series of innovations catalyzing the digital transformation of the health care landscape.
Telemedicine use exploded over the last 12 months to the point that it has almost become ubiquitous. With that, we saw a rapid proliferation of wearables and remote patient monitoring devices. Thanks to virtual care, care delivery is no longer strictly dependent on having onsite specialists, and care itself is not confined to the boundaries of hospitals or doctors’ offices anymore.
We saw the formation of the digital front door and the emergence of new virtual care sites like virtual urgent care, virtual home health, virtual office visits, virtual hospital at home that allowed clinical care to be delivered safely outside the boundaries of hospitals. Nonclinical public places like gyms, schools, and community centers were being transformed into virtual health care portals that brought care closer to the people.
Inside the hospital, we saw a fusion of traditional inpatient care and virtual care. Onsite hospital teams embraced telemedicine during the pandemic for various reasons; to conserve personal protective equipment (PPE), limit exposure, boost care capacity, improve access to specialists at distant sites, and bring family memberse to “webside” who cannot be at a patient’s bedside.
In clinical trials as well, virtual care is a welcome change. According to one survey1, most trial participants favored the use of telehealth services for clinical trials, as these helped them stay engaged, compliant, monitored, and on track while remaining at home. Furthermore, we are seeing the integration of artificial intelligence (AI) into telehealth, whether it is to aid physicians in clinical decision-making or to generate reminders to help patients with chronic disease management. However, this integration is only beginning to scratch the surface of the combination of two technologies’ real potential.
What’s next?
Based on these trends, it should be no surprise that digital health will become a vital sign for health care organizations.
The next 12 to 24 months will set new standards for digital health and play a significant role in defining the next generation of virtual care. There are projections that global health care industry revenues will exceed $2.6 trillion by 2025, with AI and telehealth playing a prominent role in this growth.2 According to estimates, telehealth itself will be a $175 billion market by 2026 and approximately one in three patient encounters will go virtual.3,4 Moreover, virtual care will continue to make exciting transformations, helping to make quality care accessible to everyone in innovative ways. For example, the University of Cincinnati has recently developed a pilot project using a drone equipped with video technology, artificial intelligence, sensors, and first aid kits to go to hard-to-reach areas to deliver care via telemedicine.5
Smart hospitals
In coming years, we can expect the integration of AI, augmented reality (AR), and virtual reality (VR) into telemedicine at lightning speed – and at a much larger scale – that will enable surgeons from different parts of the globe to perform procedures remotely and more precisely.
AI is already gaining traction in different fields within health care – whether it’s predicting length of stay in the ICU, or assisting in triage decisions, or reading radiological images, to name just a few. The Mayo Clinic is using AI and computer-aided decision-making tools to predict the risk of surgery and potential post-op complications, which could allow even better collaboration between medical and surgical teams. We hear about the “X-ray” vision offered to proceduralists using HoloLens – mixed reality smartglasses – a technology that enables them to perform procedures more precisely. Others project that there will be more sensors and voice recognition tools in the OR that will be used to gather data to develop intelligent algorithms, and to build a safety net for interventionalists that can notify them of potential hazards or accidental sterile field breaches. The insights gained will be used to create best practices and even allow some procedures to be performed outside the traditional OR setting.
Additionally, we are seeing the development of “smart” patient rooms. For example, one health system in Florida is working on deploying Amazon Alexa in 2,500 patient rooms to allow patients to connect more easily to their care team members. In the not-so-distant future, smart hospitals with smart patient rooms and smart ORs equipped with telemedicine, AI, AR, mixed reality, and computer-aided decision-making tools will no longer be an exception.
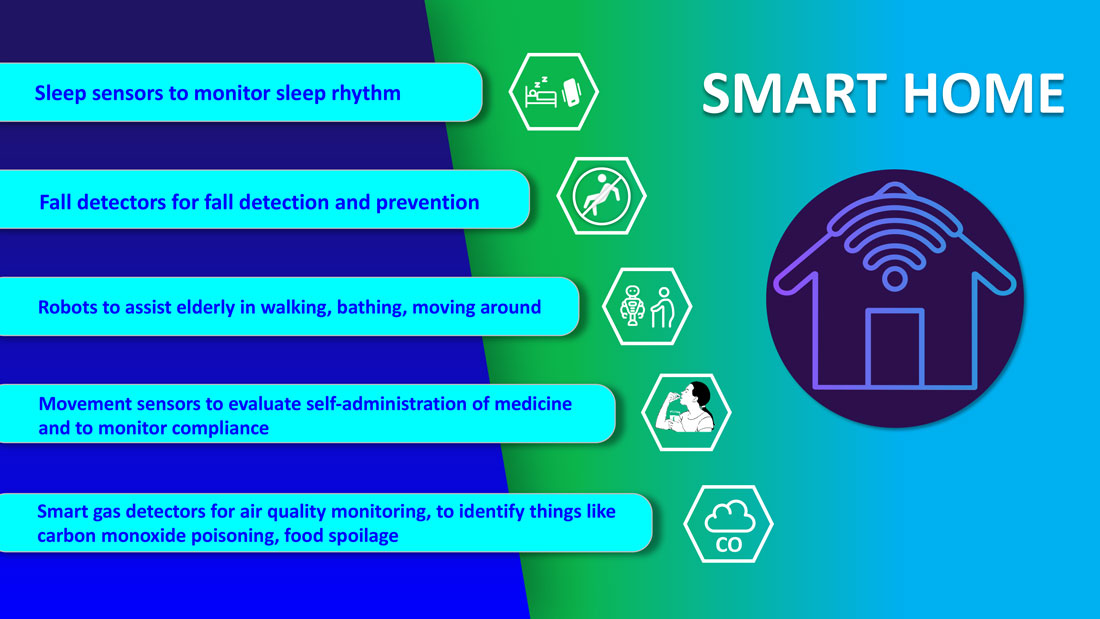
Smart homes for smart care
Smart homes with technologies like gas detectors, movement sensors, and sleep sensors will continue to evolve. According to one estimate, the global smart home health care market was $8.7 billion in 2019, and is expected to be $96.2 billion by 2030.6
Smart technologies will have applications in fall detection and prevention, evaluation of self-administration of medicine, sleep rhythm monitoring, air quality monitoring for the detection of abnormal gas levels, and identification of things like carbon monoxide poisoning or food spoilage. In coming years, expect to see more virtual medical homes and digital health care complexes. Patients, from the convenience of their homes, might be able to connect to a suite of caregivers, all working collaboratively to provide more coordinated, effective care. The “hospital at home” model that started with six hospitals has already grown to over 100 hospitals across 29 states. The shift from onsite specialists to onscreen specialists will continue, providing greater access to specialized services.
With these emerging trends, it can be anticipated that much acute care will be provided to patients outside the hospital – either under the hospital at home model, via drone technology using telemedicine, through smart devices in smart homes, or via wearables and artificial intelligence. Hence, hospitals’ configuration in the future will be much different and more compact than currently, and many hospitals will be reserved for trauma patients, casualties of natural disasters, higher acuity diseases requiring complex procedures, and other emergencies.
The role of hospitalists has evolved over the years and is still evolving. It should be no surprise if, in the future, we work alongside a digital hospitalist twin to provide better and more personalized care to our patients. Change is uncomfortable but it is inevitable. When COVID hit, we were forced to find innovative ways to deliver care to our patients. One thing is for certain: post-pandemic (AD, or After Disease) we are not going back to a Before COVID (BC) state in terms of virtual care. With the new dawn of digital era, the crucial questions to address will be: What will the future role of a hospitalist look like? How can we leverage technology and embrace our flexibility to adapt to these trends? How can we apply the lessons learned during the pandemic to propel hospital medicine into the future? And is it time to rethink our role and even reclassify ourselves – from hospitalists to Acute Care Experts (ACE) or Primary Acute Care Physicians?
Dr. Zia is a hospitalist, physician advisor, and founder of Virtual Hospitalist - a telemedicine company with a 360-degree care model for hospital patients.
References
1. www.subjectwell.com/news/data-shows-a-majority-of-patients-remain-interested-in-clinical-trials-during-the-coronavirus-pandemic/
2. ww2.frost.com/news/press-releases/technology-innovations-and-virtual-consultations-drive-healthcare-2025/
3. www.gminsights.com/industry-analysis/telemedicine-market
4. www.healthcareitnews.com/blog/frost-sullivans-top-10-predictions-healthcare-2021
5. www.uc.edu/news/articles/2021/03/virtual-medicine--new-uc-telehealth-drone-makes-house-calls.html
6. www.psmarketresearch.com/market-analysis/smart-home-healthcare-market
People often overestimate what will happen in the next two years and underestimate what will happen in ten. – Bill Gates
The COVID-19 pandemic set in motion a series of innovations catalyzing the digital transformation of the health care landscape.
Telemedicine use exploded over the last 12 months to the point that it has almost become ubiquitous. With that, we saw a rapid proliferation of wearables and remote patient monitoring devices. Thanks to virtual care, care delivery is no longer strictly dependent on having onsite specialists, and care itself is not confined to the boundaries of hospitals or doctors’ offices anymore.
We saw the formation of the digital front door and the emergence of new virtual care sites like virtual urgent care, virtual home health, virtual office visits, virtual hospital at home that allowed clinical care to be delivered safely outside the boundaries of hospitals. Nonclinical public places like gyms, schools, and community centers were being transformed into virtual health care portals that brought care closer to the people.
Inside the hospital, we saw a fusion of traditional inpatient care and virtual care. Onsite hospital teams embraced telemedicine during the pandemic for various reasons; to conserve personal protective equipment (PPE), limit exposure, boost care capacity, improve access to specialists at distant sites, and bring family memberse to “webside” who cannot be at a patient’s bedside.
In clinical trials as well, virtual care is a welcome change. According to one survey1, most trial participants favored the use of telehealth services for clinical trials, as these helped them stay engaged, compliant, monitored, and on track while remaining at home. Furthermore, we are seeing the integration of artificial intelligence (AI) into telehealth, whether it is to aid physicians in clinical decision-making or to generate reminders to help patients with chronic disease management. However, this integration is only beginning to scratch the surface of the combination of two technologies’ real potential.
What’s next?
Based on these trends, it should be no surprise that digital health will become a vital sign for health care organizations.
The next 12 to 24 months will set new standards for digital health and play a significant role in defining the next generation of virtual care. There are projections that global health care industry revenues will exceed $2.6 trillion by 2025, with AI and telehealth playing a prominent role in this growth.2 According to estimates, telehealth itself will be a $175 billion market by 2026 and approximately one in three patient encounters will go virtual.3,4 Moreover, virtual care will continue to make exciting transformations, helping to make quality care accessible to everyone in innovative ways. For example, the University of Cincinnati has recently developed a pilot project using a drone equipped with video technology, artificial intelligence, sensors, and first aid kits to go to hard-to-reach areas to deliver care via telemedicine.5
Smart hospitals
In coming years, we can expect the integration of AI, augmented reality (AR), and virtual reality (VR) into telemedicine at lightning speed – and at a much larger scale – that will enable surgeons from different parts of the globe to perform procedures remotely and more precisely.
AI is already gaining traction in different fields within health care – whether it’s predicting length of stay in the ICU, or assisting in triage decisions, or reading radiological images, to name just a few. The Mayo Clinic is using AI and computer-aided decision-making tools to predict the risk of surgery and potential post-op complications, which could allow even better collaboration between medical and surgical teams. We hear about the “X-ray” vision offered to proceduralists using HoloLens – mixed reality smartglasses – a technology that enables them to perform procedures more precisely. Others project that there will be more sensors and voice recognition tools in the OR that will be used to gather data to develop intelligent algorithms, and to build a safety net for interventionalists that can notify them of potential hazards or accidental sterile field breaches. The insights gained will be used to create best practices and even allow some procedures to be performed outside the traditional OR setting.
Additionally, we are seeing the development of “smart” patient rooms. For example, one health system in Florida is working on deploying Amazon Alexa in 2,500 patient rooms to allow patients to connect more easily to their care team members. In the not-so-distant future, smart hospitals with smart patient rooms and smart ORs equipped with telemedicine, AI, AR, mixed reality, and computer-aided decision-making tools will no longer be an exception.
Smart homes for smart care
Smart homes with technologies like gas detectors, movement sensors, and sleep sensors will continue to evolve. According to one estimate, the global smart home health care market was $8.7 billion in 2019, and is expected to be $96.2 billion by 2030.6
Smart technologies will have applications in fall detection and prevention, evaluation of self-administration of medicine, sleep rhythm monitoring, air quality monitoring for the detection of abnormal gas levels, and identification of things like carbon monoxide poisoning or food spoilage. In coming years, expect to see more virtual medical homes and digital health care complexes. Patients, from the convenience of their homes, might be able to connect to a suite of caregivers, all working collaboratively to provide more coordinated, effective care. The “hospital at home” model that started with six hospitals has already grown to over 100 hospitals across 29 states. The shift from onsite specialists to onscreen specialists will continue, providing greater access to specialized services.
With these emerging trends, it can be anticipated that much acute care will be provided to patients outside the hospital – either under the hospital at home model, via drone technology using telemedicine, through smart devices in smart homes, or via wearables and artificial intelligence. Hence, hospitals’ configuration in the future will be much different and more compact than currently, and many hospitals will be reserved for trauma patients, casualties of natural disasters, higher acuity diseases requiring complex procedures, and other emergencies.
The role of hospitalists has evolved over the years and is still evolving. It should be no surprise if, in the future, we work alongside a digital hospitalist twin to provide better and more personalized care to our patients. Change is uncomfortable but it is inevitable. When COVID hit, we were forced to find innovative ways to deliver care to our patients. One thing is for certain: post-pandemic (AD, or After Disease) we are not going back to a Before COVID (BC) state in terms of virtual care. With the new dawn of digital era, the crucial questions to address will be: What will the future role of a hospitalist look like? How can we leverage technology and embrace our flexibility to adapt to these trends? How can we apply the lessons learned during the pandemic to propel hospital medicine into the future? And is it time to rethink our role and even reclassify ourselves – from hospitalists to Acute Care Experts (ACE) or Primary Acute Care Physicians?
Dr. Zia is a hospitalist, physician advisor, and founder of Virtual Hospitalist - a telemedicine company with a 360-degree care model for hospital patients.
References
1. www.subjectwell.com/news/data-shows-a-majority-of-patients-remain-interested-in-clinical-trials-during-the-coronavirus-pandemic/
2. ww2.frost.com/news/press-releases/technology-innovations-and-virtual-consultations-drive-healthcare-2025/
3. www.gminsights.com/industry-analysis/telemedicine-market
4. www.healthcareitnews.com/blog/frost-sullivans-top-10-predictions-healthcare-2021
5. www.uc.edu/news/articles/2021/03/virtual-medicine--new-uc-telehealth-drone-makes-house-calls.html
6. www.psmarketresearch.com/market-analysis/smart-home-healthcare-market
People often overestimate what will happen in the next two years and underestimate what will happen in ten. – Bill Gates
The COVID-19 pandemic set in motion a series of innovations catalyzing the digital transformation of the health care landscape.
Telemedicine use exploded over the last 12 months to the point that it has almost become ubiquitous. With that, we saw a rapid proliferation of wearables and remote patient monitoring devices. Thanks to virtual care, care delivery is no longer strictly dependent on having onsite specialists, and care itself is not confined to the boundaries of hospitals or doctors’ offices anymore.
We saw the formation of the digital front door and the emergence of new virtual care sites like virtual urgent care, virtual home health, virtual office visits, virtual hospital at home that allowed clinical care to be delivered safely outside the boundaries of hospitals. Nonclinical public places like gyms, schools, and community centers were being transformed into virtual health care portals that brought care closer to the people.
Inside the hospital, we saw a fusion of traditional inpatient care and virtual care. Onsite hospital teams embraced telemedicine during the pandemic for various reasons; to conserve personal protective equipment (PPE), limit exposure, boost care capacity, improve access to specialists at distant sites, and bring family memberse to “webside” who cannot be at a patient’s bedside.
In clinical trials as well, virtual care is a welcome change. According to one survey1, most trial participants favored the use of telehealth services for clinical trials, as these helped them stay engaged, compliant, monitored, and on track while remaining at home. Furthermore, we are seeing the integration of artificial intelligence (AI) into telehealth, whether it is to aid physicians in clinical decision-making or to generate reminders to help patients with chronic disease management. However, this integration is only beginning to scratch the surface of the combination of two technologies’ real potential.
What’s next?
Based on these trends, it should be no surprise that digital health will become a vital sign for health care organizations.
The next 12 to 24 months will set new standards for digital health and play a significant role in defining the next generation of virtual care. There are projections that global health care industry revenues will exceed $2.6 trillion by 2025, with AI and telehealth playing a prominent role in this growth.2 According to estimates, telehealth itself will be a $175 billion market by 2026 and approximately one in three patient encounters will go virtual.3,4 Moreover, virtual care will continue to make exciting transformations, helping to make quality care accessible to everyone in innovative ways. For example, the University of Cincinnati has recently developed a pilot project using a drone equipped with video technology, artificial intelligence, sensors, and first aid kits to go to hard-to-reach areas to deliver care via telemedicine.5
Smart hospitals
In coming years, we can expect the integration of AI, augmented reality (AR), and virtual reality (VR) into telemedicine at lightning speed – and at a much larger scale – that will enable surgeons from different parts of the globe to perform procedures remotely and more precisely.
AI is already gaining traction in different fields within health care – whether it’s predicting length of stay in the ICU, or assisting in triage decisions, or reading radiological images, to name just a few. The Mayo Clinic is using AI and computer-aided decision-making tools to predict the risk of surgery and potential post-op complications, which could allow even better collaboration between medical and surgical teams. We hear about the “X-ray” vision offered to proceduralists using HoloLens – mixed reality smartglasses – a technology that enables them to perform procedures more precisely. Others project that there will be more sensors and voice recognition tools in the OR that will be used to gather data to develop intelligent algorithms, and to build a safety net for interventionalists that can notify them of potential hazards or accidental sterile field breaches. The insights gained will be used to create best practices and even allow some procedures to be performed outside the traditional OR setting.
Additionally, we are seeing the development of “smart” patient rooms. For example, one health system in Florida is working on deploying Amazon Alexa in 2,500 patient rooms to allow patients to connect more easily to their care team members. In the not-so-distant future, smart hospitals with smart patient rooms and smart ORs equipped with telemedicine, AI, AR, mixed reality, and computer-aided decision-making tools will no longer be an exception.
Smart homes for smart care
Smart homes with technologies like gas detectors, movement sensors, and sleep sensors will continue to evolve. According to one estimate, the global smart home health care market was $8.7 billion in 2019, and is expected to be $96.2 billion by 2030.6
Smart technologies will have applications in fall detection and prevention, evaluation of self-administration of medicine, sleep rhythm monitoring, air quality monitoring for the detection of abnormal gas levels, and identification of things like carbon monoxide poisoning or food spoilage. In coming years, expect to see more virtual medical homes and digital health care complexes. Patients, from the convenience of their homes, might be able to connect to a suite of caregivers, all working collaboratively to provide more coordinated, effective care. The “hospital at home” model that started with six hospitals has already grown to over 100 hospitals across 29 states. The shift from onsite specialists to onscreen specialists will continue, providing greater access to specialized services.
With these emerging trends, it can be anticipated that much acute care will be provided to patients outside the hospital – either under the hospital at home model, via drone technology using telemedicine, through smart devices in smart homes, or via wearables and artificial intelligence. Hence, hospitals’ configuration in the future will be much different and more compact than currently, and many hospitals will be reserved for trauma patients, casualties of natural disasters, higher acuity diseases requiring complex procedures, and other emergencies.
The role of hospitalists has evolved over the years and is still evolving. It should be no surprise if, in the future, we work alongside a digital hospitalist twin to provide better and more personalized care to our patients. Change is uncomfortable but it is inevitable. When COVID hit, we were forced to find innovative ways to deliver care to our patients. One thing is for certain: post-pandemic (AD, or After Disease) we are not going back to a Before COVID (BC) state in terms of virtual care. With the new dawn of digital era, the crucial questions to address will be: What will the future role of a hospitalist look like? How can we leverage technology and embrace our flexibility to adapt to these trends? How can we apply the lessons learned during the pandemic to propel hospital medicine into the future? And is it time to rethink our role and even reclassify ourselves – from hospitalists to Acute Care Experts (ACE) or Primary Acute Care Physicians?
Dr. Zia is a hospitalist, physician advisor, and founder of Virtual Hospitalist - a telemedicine company with a 360-degree care model for hospital patients.
References
1. www.subjectwell.com/news/data-shows-a-majority-of-patients-remain-interested-in-clinical-trials-during-the-coronavirus-pandemic/
2. ww2.frost.com/news/press-releases/technology-innovations-and-virtual-consultations-drive-healthcare-2025/
3. www.gminsights.com/industry-analysis/telemedicine-market
4. www.healthcareitnews.com/blog/frost-sullivans-top-10-predictions-healthcare-2021
5. www.uc.edu/news/articles/2021/03/virtual-medicine--new-uc-telehealth-drone-makes-house-calls.html
6. www.psmarketresearch.com/market-analysis/smart-home-healthcare-market
Vaccine mandates, passports, and Kant
Houston Methodist Hospital in June 2021 enforced an April mandate that all its employees, about 26,000 of them, must be vaccinated against COVID-19. In the following weeks, many other large health care systems adopted a similar employer mandate.
Compliance with Houston Methodist’s mandate has been very high at nearly 99%. There were some deferrals, mostly because of pregnancy. There were some “medical and personal” exemptions for less than 1% of employees. The reasons for those personal exemptions have not been made public. A lawsuit by 117 employees objecting to the vaccine mandate was dismissed by a federal district judge on June 12.
Objections to the vaccine mandate have rarely involved religious-based conscientious objections, which need to be accommodated differently, legally and ethically. The objections have been disagreements on the science. As a politician said decades ago: “People are entitled to their own opinions, but not their own facts.” A medical institution is an excellent organization for determining the risks and benefits of vaccination. The judge dismissing the case was very critical of the characterizations used by the plaintiffs.
The vaccine mandate has strong ethical support from both the universalizability principle of Kant and a consequentialist analysis. The U.S. Equal Employment Opportunity Commission on May 28, 2021, released technical assistance that has generally been interpreted to support an employer’s right to set vaccine requirements. HIPAA does not forbid an employer from asking about vaccination, but the EEOC guidance reminds employers that if they do ask, employers have legal obligations to protect the health information and keep it separate from other personnel files.
In the past few years, many hospitals and clinics have adopted mandates for influenza vaccines. In many children’s hospitals staff have been required to have chicken pox vaccines (or, as in my case, titers showing immunity from the real thing – I’m old) since the early 2000s. Measles titers (again, mine were acquired naturally – I still remember the illness and recommend against that) and TB status are occasionally required for locum tenens positions. I keep copies of these labs alongside copies of my diplomas. To me, the COVID-19 mandate is not capricious.
Some people have pointed out that the COVID-19 vaccines are not fully Food and Drug Administration approved. They are used under an emergency use authorization. Any traction that distinction might have had ethically and scientifically in November 2020 has disappeared with the experience of 9 months and 300 million doses in the United States. Dr. Fauci on July 11, 2021, said: “These vaccines are as good as officially approved with all the I’s dotted and the T’s crossed.”
On July 12, 2021, French President Macron, facing a resurgence of the pandemic because of the delta variant, announced a national vaccine mandate for all health care workers. He also announced plans to require proof of vaccination (or prior disease) in order to enter amusement parks, restaurants, and other public facilities. The ethics of his plans have been debated by ethicists and politicians for months under the rubric of a “vaccine passport.” England has required proof of vaccination or a recent negative COVID-19 test before entering soccer stadiums. In the United States, some localities, particularly those where the local politicians are against the vaccine, have passed laws proscribing the creation of these passport-like restrictions. Elsewhere, many businesses have already started to exclude customers who are not vaccinated. Airlines, hotels, and cruise ships are at the forefront of this. Society has started to create consequences for not getting the vaccine. President Macron indicated that the goal was now to put restrictions on the unvaccinated rather than on everyone.
Pediatricians are experts on the importance of consequences for misbehavior and refusals. It is a frequent topic of conversation with parents of toddlers and teenagers. Consequences are ethical, just, and effective ways of promoting safe and fair behavior. At this point, the public has been educated about the disease and the vaccines. In the United States, there has been ample access to the vaccine. It is time to enforce consequences.
Daily vaccination rates in the United States have slowed to 25% of the peak rates. The reasons for hesitancy have been analyzed in many publications. Further public education hasn’t been productive, so empathic listening has been urged to overcome hesitancy. (A similar program has long been advocated to deal with hesitancy for teenage HPV vaccines.) President Biden on July 6, 2021, proposed a program of going door to door to overcome resistance.
The world is in a race between vaccines and the delta variant. The Delta variant is moving the finish line, with some French epidemiologists advising President Macron that this more contagious variant may require a 90% vaccination level to achieve herd immunity. Israel has started giving a third booster shot in select situations and Pfizer is considering the idea. I agree with providing education, using empathic listening, and improving access. Those are all reasonable, even necessary, strategies. But at this point, I anchor my suggestions with the same advice pediatricians have long given to parents. Set rules and create consequences for misbehavior.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. He has no financial disclosures. Email him at pdnews@mdedge.com.
Houston Methodist Hospital in June 2021 enforced an April mandate that all its employees, about 26,000 of them, must be vaccinated against COVID-19. In the following weeks, many other large health care systems adopted a similar employer mandate.
Compliance with Houston Methodist’s mandate has been very high at nearly 99%. There were some deferrals, mostly because of pregnancy. There were some “medical and personal” exemptions for less than 1% of employees. The reasons for those personal exemptions have not been made public. A lawsuit by 117 employees objecting to the vaccine mandate was dismissed by a federal district judge on June 12.
Objections to the vaccine mandate have rarely involved religious-based conscientious objections, which need to be accommodated differently, legally and ethically. The objections have been disagreements on the science. As a politician said decades ago: “People are entitled to their own opinions, but not their own facts.” A medical institution is an excellent organization for determining the risks and benefits of vaccination. The judge dismissing the case was very critical of the characterizations used by the plaintiffs.
The vaccine mandate has strong ethical support from both the universalizability principle of Kant and a consequentialist analysis. The U.S. Equal Employment Opportunity Commission on May 28, 2021, released technical assistance that has generally been interpreted to support an employer’s right to set vaccine requirements. HIPAA does not forbid an employer from asking about vaccination, but the EEOC guidance reminds employers that if they do ask, employers have legal obligations to protect the health information and keep it separate from other personnel files.
In the past few years, many hospitals and clinics have adopted mandates for influenza vaccines. In many children’s hospitals staff have been required to have chicken pox vaccines (or, as in my case, titers showing immunity from the real thing – I’m old) since the early 2000s. Measles titers (again, mine were acquired naturally – I still remember the illness and recommend against that) and TB status are occasionally required for locum tenens positions. I keep copies of these labs alongside copies of my diplomas. To me, the COVID-19 mandate is not capricious.
Some people have pointed out that the COVID-19 vaccines are not fully Food and Drug Administration approved. They are used under an emergency use authorization. Any traction that distinction might have had ethically and scientifically in November 2020 has disappeared with the experience of 9 months and 300 million doses in the United States. Dr. Fauci on July 11, 2021, said: “These vaccines are as good as officially approved with all the I’s dotted and the T’s crossed.”
On July 12, 2021, French President Macron, facing a resurgence of the pandemic because of the delta variant, announced a national vaccine mandate for all health care workers. He also announced plans to require proof of vaccination (or prior disease) in order to enter amusement parks, restaurants, and other public facilities. The ethics of his plans have been debated by ethicists and politicians for months under the rubric of a “vaccine passport.” England has required proof of vaccination or a recent negative COVID-19 test before entering soccer stadiums. In the United States, some localities, particularly those where the local politicians are against the vaccine, have passed laws proscribing the creation of these passport-like restrictions. Elsewhere, many businesses have already started to exclude customers who are not vaccinated. Airlines, hotels, and cruise ships are at the forefront of this. Society has started to create consequences for not getting the vaccine. President Macron indicated that the goal was now to put restrictions on the unvaccinated rather than on everyone.
Pediatricians are experts on the importance of consequences for misbehavior and refusals. It is a frequent topic of conversation with parents of toddlers and teenagers. Consequences are ethical, just, and effective ways of promoting safe and fair behavior. At this point, the public has been educated about the disease and the vaccines. In the United States, there has been ample access to the vaccine. It is time to enforce consequences.
Daily vaccination rates in the United States have slowed to 25% of the peak rates. The reasons for hesitancy have been analyzed in many publications. Further public education hasn’t been productive, so empathic listening has been urged to overcome hesitancy. (A similar program has long been advocated to deal with hesitancy for teenage HPV vaccines.) President Biden on July 6, 2021, proposed a program of going door to door to overcome resistance.
The world is in a race between vaccines and the delta variant. The Delta variant is moving the finish line, with some French epidemiologists advising President Macron that this more contagious variant may require a 90% vaccination level to achieve herd immunity. Israel has started giving a third booster shot in select situations and Pfizer is considering the idea. I agree with providing education, using empathic listening, and improving access. Those are all reasonable, even necessary, strategies. But at this point, I anchor my suggestions with the same advice pediatricians have long given to parents. Set rules and create consequences for misbehavior.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. He has no financial disclosures. Email him at pdnews@mdedge.com.
Houston Methodist Hospital in June 2021 enforced an April mandate that all its employees, about 26,000 of them, must be vaccinated against COVID-19. In the following weeks, many other large health care systems adopted a similar employer mandate.
Compliance with Houston Methodist’s mandate has been very high at nearly 99%. There were some deferrals, mostly because of pregnancy. There were some “medical and personal” exemptions for less than 1% of employees. The reasons for those personal exemptions have not been made public. A lawsuit by 117 employees objecting to the vaccine mandate was dismissed by a federal district judge on June 12.
Objections to the vaccine mandate have rarely involved religious-based conscientious objections, which need to be accommodated differently, legally and ethically. The objections have been disagreements on the science. As a politician said decades ago: “People are entitled to their own opinions, but not their own facts.” A medical institution is an excellent organization for determining the risks and benefits of vaccination. The judge dismissing the case was very critical of the characterizations used by the plaintiffs.
The vaccine mandate has strong ethical support from both the universalizability principle of Kant and a consequentialist analysis. The U.S. Equal Employment Opportunity Commission on May 28, 2021, released technical assistance that has generally been interpreted to support an employer’s right to set vaccine requirements. HIPAA does not forbid an employer from asking about vaccination, but the EEOC guidance reminds employers that if they do ask, employers have legal obligations to protect the health information and keep it separate from other personnel files.
In the past few years, many hospitals and clinics have adopted mandates for influenza vaccines. In many children’s hospitals staff have been required to have chicken pox vaccines (or, as in my case, titers showing immunity from the real thing – I’m old) since the early 2000s. Measles titers (again, mine were acquired naturally – I still remember the illness and recommend against that) and TB status are occasionally required for locum tenens positions. I keep copies of these labs alongside copies of my diplomas. To me, the COVID-19 mandate is not capricious.
Some people have pointed out that the COVID-19 vaccines are not fully Food and Drug Administration approved. They are used under an emergency use authorization. Any traction that distinction might have had ethically and scientifically in November 2020 has disappeared with the experience of 9 months and 300 million doses in the United States. Dr. Fauci on July 11, 2021, said: “These vaccines are as good as officially approved with all the I’s dotted and the T’s crossed.”
On July 12, 2021, French President Macron, facing a resurgence of the pandemic because of the delta variant, announced a national vaccine mandate for all health care workers. He also announced plans to require proof of vaccination (or prior disease) in order to enter amusement parks, restaurants, and other public facilities. The ethics of his plans have been debated by ethicists and politicians for months under the rubric of a “vaccine passport.” England has required proof of vaccination or a recent negative COVID-19 test before entering soccer stadiums. In the United States, some localities, particularly those where the local politicians are against the vaccine, have passed laws proscribing the creation of these passport-like restrictions. Elsewhere, many businesses have already started to exclude customers who are not vaccinated. Airlines, hotels, and cruise ships are at the forefront of this. Society has started to create consequences for not getting the vaccine. President Macron indicated that the goal was now to put restrictions on the unvaccinated rather than on everyone.
Pediatricians are experts on the importance of consequences for misbehavior and refusals. It is a frequent topic of conversation with parents of toddlers and teenagers. Consequences are ethical, just, and effective ways of promoting safe and fair behavior. At this point, the public has been educated about the disease and the vaccines. In the United States, there has been ample access to the vaccine. It is time to enforce consequences.
Daily vaccination rates in the United States have slowed to 25% of the peak rates. The reasons for hesitancy have been analyzed in many publications. Further public education hasn’t been productive, so empathic listening has been urged to overcome hesitancy. (A similar program has long been advocated to deal with hesitancy for teenage HPV vaccines.) President Biden on July 6, 2021, proposed a program of going door to door to overcome resistance.
The world is in a race between vaccines and the delta variant. The Delta variant is moving the finish line, with some French epidemiologists advising President Macron that this more contagious variant may require a 90% vaccination level to achieve herd immunity. Israel has started giving a third booster shot in select situations and Pfizer is considering the idea. I agree with providing education, using empathic listening, and improving access. Those are all reasonable, even necessary, strategies. But at this point, I anchor my suggestions with the same advice pediatricians have long given to parents. Set rules and create consequences for misbehavior.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. He has no financial disclosures. Email him at pdnews@mdedge.com.
Dogs know their humans, but humans don’t know expiration dates
An extreme price to pay for immortality
We know that men don’t live as long as women, but the reasons aren’t entirely clear. However, some New Zealand scientists have a thought on the subject, thanks to a sheep called Shrek.
The researchers were inspired by a famous old sheep who escaped captivity, but was captured 6 years later at the age of 10. The sheep then lived 6 more years, far beyond the lifespan of a normal sheep, capturing the hearts and minds of Kiwis everywhere. Look, it’s New Zealand, sheep are life, so it’s only natural the country got attached. Scientists from the University of Otago suspected that Shrek lived such a long life because he was castrated.
So they undertook a study of sheep, and lo and behold, sheep that were castrated lived significantly longer than their uncastrated kin, thanks to a slowing of their epigenetic clocks – the DNA aged noticeably slower in the castrated sheep.
Although the research can most immediately be applied to the improvement of the New Zealand sheep industry, the implication for humanity is also apparent. Want to live longer? Get rid of the testosterone. An extreme solution to be sure. As previously reported in this column, researchers wanted to torture our mouths to get us to lose weight, and now they want to castrate people for longer life. What exactly is going on down there in New Zealand?
Man’s best mind reader
There are a lot of reasons why dogs are sometimes called “man’s best friend,” but the root of it may actually have something to do with how easily we communicate with each other. Researchers dug deeper and fetched something that Fido is born with, but his wild wolf cousin isn’t.
That something is known as the “theory of mind” ability. Have you noticed that when you point and tell dogs to grab a leash or toy, they react as if they understood the language you spoke? Researchers from Duke University wondered if this ability is a canine thing or just a domesticated dog thing.
They compared 44 canine puppies and 37 wolf pups between 5 and 18 weeks old. The wolf pups were taken into human homes and raised with a great amount of human interaction, while the dog pups were left with their mothers and raised with less human interaction.
All the puppies were then put through multiple tests. In one test, they were given clues to find a treat under a bowl. In another test, a block of wood was placed next to the treat as a physical marker. During yet another test, researchers pointed to the food directly.
The researchers discovered that the dog puppies knew where the treat was every time, while their wild relatives didn’t.
“This study really solidifies the evidence that the social genius of dogs is a product of domestication,” senior author Brian Hare said in a separate statement.
The domestication hypothesis theorizes that dogs picked up the human social cues through thousands of years of interaction. The more friendly and cooperative a wolf was with humans, the more likely it was to survive and pass on those same traits and practices. Even within the study, the dog puppies were 30 times more likely to approach a stranger than were the wolf pups.
You may think your dog understands everything you say, but it’s actually body language that Fido is most fluent in.
I’m not a dentist, but I play one on TikTok
In last week’s column, it was garlic cloves up the nose to treat a cold. This week, TikTok brings us a new way to whiten teeth.
Familiar with the Mr. Clean Magic Eraser? If not, we’ll save you the trouble of Googling it: Check it out here and here.
Have you heard anything about using it to clean your teeth? No, neither did we, and we did a lot of Googling. Proctor & Gamble, which makes the Magic Eraser, goes so far as to say on the package: “Do not use on skin or other parts of the body. Using on skin will likely cause abrasions.” (The warning is actually in all caps, but we are stylistically forbidden by our editorial overlords to do that.)
But it’s magic, right? How can you not use it on your teeth? Enter TikTok. Heather Dunn posted a video in which she rubbed a bit of a Magic Eraser on her teeth – being careful to avoid her gums, because you can never be too careful – “as the product squeaked back and forth,” the Miami Herald reported. The video has almost 256,000 likes so far.
“Yeah, your teeth are white because you scrubbed all the enamel off them. So don’t do this,” Dr. Benjamin Winters, aka the Bentist, said in a YouTube video that has 105,000 likes.
In this race for common sense, common sense is losing. Please help the Bentist restore sanity to the dental world by liking his video. It would make Mr. Clean happy.
Don’t let an expiration date boss you around
Surely you’ve been there: It’s Taco Tuesday and you’re rummaging through the refrigerator to find that shredded cheese you’re sure you have. Jackpot! You find it, but realize it’s probably been in the refrigerator for a while. You open the bag, it smells and looks fine, but the expiration date was 2 days ago. Now you have a decision to make. Maybe you’ll be fine, or maybe you’ll risk food poisoning right before your brother’s wedding.
But here’s the truth: Americans throw away perfectly good food every day. The average American family throws out $1,365 to $2,275 worth of food a year, according to a 2013 study.
Truthfully, expiration dates are not for buyers, rather they’re for stores to have an idea of their stock’s freshness. Emily Broad Leib, director of the Harvard Law School Food and Policy Clinic and lead author of the 2013 study, told Vox that manufacturers use the dates as a way of “protecting the brand” to keep consumers from eating food that’s just a little past its peak.
With approximately 40 million people in the United States concerned about where their next meal is coming from, the Vox article noted, we need to reevaluate our system. Our national misunderstanding of expiration labels is hurting both suppliers and consumers because perfectly good food is wasted.
Sure, there is always that chance that something might be a little funky after a certain amount of time, but all in all, food probably stays fresh a lot longer than we think. Don’t always judge the shredded cheese by its expiration date.
An extreme price to pay for immortality
We know that men don’t live as long as women, but the reasons aren’t entirely clear. However, some New Zealand scientists have a thought on the subject, thanks to a sheep called Shrek.
The researchers were inspired by a famous old sheep who escaped captivity, but was captured 6 years later at the age of 10. The sheep then lived 6 more years, far beyond the lifespan of a normal sheep, capturing the hearts and minds of Kiwis everywhere. Look, it’s New Zealand, sheep are life, so it’s only natural the country got attached. Scientists from the University of Otago suspected that Shrek lived such a long life because he was castrated.
So they undertook a study of sheep, and lo and behold, sheep that were castrated lived significantly longer than their uncastrated kin, thanks to a slowing of their epigenetic clocks – the DNA aged noticeably slower in the castrated sheep.
Although the research can most immediately be applied to the improvement of the New Zealand sheep industry, the implication for humanity is also apparent. Want to live longer? Get rid of the testosterone. An extreme solution to be sure. As previously reported in this column, researchers wanted to torture our mouths to get us to lose weight, and now they want to castrate people for longer life. What exactly is going on down there in New Zealand?
Man’s best mind reader
There are a lot of reasons why dogs are sometimes called “man’s best friend,” but the root of it may actually have something to do with how easily we communicate with each other. Researchers dug deeper and fetched something that Fido is born with, but his wild wolf cousin isn’t.
That something is known as the “theory of mind” ability. Have you noticed that when you point and tell dogs to grab a leash or toy, they react as if they understood the language you spoke? Researchers from Duke University wondered if this ability is a canine thing or just a domesticated dog thing.
They compared 44 canine puppies and 37 wolf pups between 5 and 18 weeks old. The wolf pups were taken into human homes and raised with a great amount of human interaction, while the dog pups were left with their mothers and raised with less human interaction.
All the puppies were then put through multiple tests. In one test, they were given clues to find a treat under a bowl. In another test, a block of wood was placed next to the treat as a physical marker. During yet another test, researchers pointed to the food directly.
The researchers discovered that the dog puppies knew where the treat was every time, while their wild relatives didn’t.
“This study really solidifies the evidence that the social genius of dogs is a product of domestication,” senior author Brian Hare said in a separate statement.
The domestication hypothesis theorizes that dogs picked up the human social cues through thousands of years of interaction. The more friendly and cooperative a wolf was with humans, the more likely it was to survive and pass on those same traits and practices. Even within the study, the dog puppies were 30 times more likely to approach a stranger than were the wolf pups.
You may think your dog understands everything you say, but it’s actually body language that Fido is most fluent in.
I’m not a dentist, but I play one on TikTok
In last week’s column, it was garlic cloves up the nose to treat a cold. This week, TikTok brings us a new way to whiten teeth.
Familiar with the Mr. Clean Magic Eraser? If not, we’ll save you the trouble of Googling it: Check it out here and here.
Have you heard anything about using it to clean your teeth? No, neither did we, and we did a lot of Googling. Proctor & Gamble, which makes the Magic Eraser, goes so far as to say on the package: “Do not use on skin or other parts of the body. Using on skin will likely cause abrasions.” (The warning is actually in all caps, but we are stylistically forbidden by our editorial overlords to do that.)
But it’s magic, right? How can you not use it on your teeth? Enter TikTok. Heather Dunn posted a video in which she rubbed a bit of a Magic Eraser on her teeth – being careful to avoid her gums, because you can never be too careful – “as the product squeaked back and forth,” the Miami Herald reported. The video has almost 256,000 likes so far.
“Yeah, your teeth are white because you scrubbed all the enamel off them. So don’t do this,” Dr. Benjamin Winters, aka the Bentist, said in a YouTube video that has 105,000 likes.
In this race for common sense, common sense is losing. Please help the Bentist restore sanity to the dental world by liking his video. It would make Mr. Clean happy.
Don’t let an expiration date boss you around
Surely you’ve been there: It’s Taco Tuesday and you’re rummaging through the refrigerator to find that shredded cheese you’re sure you have. Jackpot! You find it, but realize it’s probably been in the refrigerator for a while. You open the bag, it smells and looks fine, but the expiration date was 2 days ago. Now you have a decision to make. Maybe you’ll be fine, or maybe you’ll risk food poisoning right before your brother’s wedding.
But here’s the truth: Americans throw away perfectly good food every day. The average American family throws out $1,365 to $2,275 worth of food a year, according to a 2013 study.
Truthfully, expiration dates are not for buyers, rather they’re for stores to have an idea of their stock’s freshness. Emily Broad Leib, director of the Harvard Law School Food and Policy Clinic and lead author of the 2013 study, told Vox that manufacturers use the dates as a way of “protecting the brand” to keep consumers from eating food that’s just a little past its peak.
With approximately 40 million people in the United States concerned about where their next meal is coming from, the Vox article noted, we need to reevaluate our system. Our national misunderstanding of expiration labels is hurting both suppliers and consumers because perfectly good food is wasted.
Sure, there is always that chance that something might be a little funky after a certain amount of time, but all in all, food probably stays fresh a lot longer than we think. Don’t always judge the shredded cheese by its expiration date.
An extreme price to pay for immortality
We know that men don’t live as long as women, but the reasons aren’t entirely clear. However, some New Zealand scientists have a thought on the subject, thanks to a sheep called Shrek.
The researchers were inspired by a famous old sheep who escaped captivity, but was captured 6 years later at the age of 10. The sheep then lived 6 more years, far beyond the lifespan of a normal sheep, capturing the hearts and minds of Kiwis everywhere. Look, it’s New Zealand, sheep are life, so it’s only natural the country got attached. Scientists from the University of Otago suspected that Shrek lived such a long life because he was castrated.
So they undertook a study of sheep, and lo and behold, sheep that were castrated lived significantly longer than their uncastrated kin, thanks to a slowing of their epigenetic clocks – the DNA aged noticeably slower in the castrated sheep.
Although the research can most immediately be applied to the improvement of the New Zealand sheep industry, the implication for humanity is also apparent. Want to live longer? Get rid of the testosterone. An extreme solution to be sure. As previously reported in this column, researchers wanted to torture our mouths to get us to lose weight, and now they want to castrate people for longer life. What exactly is going on down there in New Zealand?
Man’s best mind reader
There are a lot of reasons why dogs are sometimes called “man’s best friend,” but the root of it may actually have something to do with how easily we communicate with each other. Researchers dug deeper and fetched something that Fido is born with, but his wild wolf cousin isn’t.
That something is known as the “theory of mind” ability. Have you noticed that when you point and tell dogs to grab a leash or toy, they react as if they understood the language you spoke? Researchers from Duke University wondered if this ability is a canine thing or just a domesticated dog thing.
They compared 44 canine puppies and 37 wolf pups between 5 and 18 weeks old. The wolf pups were taken into human homes and raised with a great amount of human interaction, while the dog pups were left with their mothers and raised with less human interaction.
All the puppies were then put through multiple tests. In one test, they were given clues to find a treat under a bowl. In another test, a block of wood was placed next to the treat as a physical marker. During yet another test, researchers pointed to the food directly.
The researchers discovered that the dog puppies knew where the treat was every time, while their wild relatives didn’t.
“This study really solidifies the evidence that the social genius of dogs is a product of domestication,” senior author Brian Hare said in a separate statement.
The domestication hypothesis theorizes that dogs picked up the human social cues through thousands of years of interaction. The more friendly and cooperative a wolf was with humans, the more likely it was to survive and pass on those same traits and practices. Even within the study, the dog puppies were 30 times more likely to approach a stranger than were the wolf pups.
You may think your dog understands everything you say, but it’s actually body language that Fido is most fluent in.
I’m not a dentist, but I play one on TikTok
In last week’s column, it was garlic cloves up the nose to treat a cold. This week, TikTok brings us a new way to whiten teeth.
Familiar with the Mr. Clean Magic Eraser? If not, we’ll save you the trouble of Googling it: Check it out here and here.
Have you heard anything about using it to clean your teeth? No, neither did we, and we did a lot of Googling. Proctor & Gamble, which makes the Magic Eraser, goes so far as to say on the package: “Do not use on skin or other parts of the body. Using on skin will likely cause abrasions.” (The warning is actually in all caps, but we are stylistically forbidden by our editorial overlords to do that.)
But it’s magic, right? How can you not use it on your teeth? Enter TikTok. Heather Dunn posted a video in which she rubbed a bit of a Magic Eraser on her teeth – being careful to avoid her gums, because you can never be too careful – “as the product squeaked back and forth,” the Miami Herald reported. The video has almost 256,000 likes so far.
“Yeah, your teeth are white because you scrubbed all the enamel off them. So don’t do this,” Dr. Benjamin Winters, aka the Bentist, said in a YouTube video that has 105,000 likes.
In this race for common sense, common sense is losing. Please help the Bentist restore sanity to the dental world by liking his video. It would make Mr. Clean happy.
Don’t let an expiration date boss you around
Surely you’ve been there: It’s Taco Tuesday and you’re rummaging through the refrigerator to find that shredded cheese you’re sure you have. Jackpot! You find it, but realize it’s probably been in the refrigerator for a while. You open the bag, it smells and looks fine, but the expiration date was 2 days ago. Now you have a decision to make. Maybe you’ll be fine, or maybe you’ll risk food poisoning right before your brother’s wedding.
But here’s the truth: Americans throw away perfectly good food every day. The average American family throws out $1,365 to $2,275 worth of food a year, according to a 2013 study.
Truthfully, expiration dates are not for buyers, rather they’re for stores to have an idea of their stock’s freshness. Emily Broad Leib, director of the Harvard Law School Food and Policy Clinic and lead author of the 2013 study, told Vox that manufacturers use the dates as a way of “protecting the brand” to keep consumers from eating food that’s just a little past its peak.
With approximately 40 million people in the United States concerned about where their next meal is coming from, the Vox article noted, we need to reevaluate our system. Our national misunderstanding of expiration labels is hurting both suppliers and consumers because perfectly good food is wasted.
Sure, there is always that chance that something might be a little funky after a certain amount of time, but all in all, food probably stays fresh a lot longer than we think. Don’t always judge the shredded cheese by its expiration date.
Denial or a call to action?
Now that everyone in my family has been vaccinated, we’re starting to do more.
Last week we met my mom and some of her (vaccinated) friends for dinner at a local restaurant. Except for picking up takeout, I hadn’t been to one since early March 2020.
During the usual chatting about jobs, music, my kids, and trips we were thinking about, one of her friends suddenly said: “That’s funny.”
I asked him what was funny, and he said: “My left vision suddenly went dark.”
It only takes a fraction of a second to shift into doctor mode. I asked a few pointed questions and did a quick neuroscan for asymmetries, slurred speech, the things that, after 23 years, have become second nature.
It resolved after about 30 seconds. He clearly didn’t think it was anything to be alarmed about. He’s intelligent and well educated, but not a doctor. I wasn’t going to let it go, and quietly spoke to him a short while later. He may not be my patient, but pushing him in the needed direction is the right thing to do.
I’ve gotten him to the right doctors now, and the ball is rolling, but I keep thinking about it. If I hadn’t been there it’s likely nothing would have been done. In fact, he seemed to think it was more amusing than potentially serious.
Medical blogs and doctors’ lounge stories are full of similar anecdotes, where we wonder why people don’t take such things seriously. We tend to view such people as stupid and/or ignorant.
Yet, this gentleman is neither. I’ve known him since childhood. He’s smart, well educated, and well read. He’s not a medical person, though.
In reality, I don’t think doctors or nurses are any better. I suspect that’s more human nature, which is hard to override regardless of training.
But maybe it’s time to start giving these people, like my family friend, a pass, with the realization that denial and different training are part of being human, and not something to be poked fun at.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Now that everyone in my family has been vaccinated, we’re starting to do more.
Last week we met my mom and some of her (vaccinated) friends for dinner at a local restaurant. Except for picking up takeout, I hadn’t been to one since early March 2020.
During the usual chatting about jobs, music, my kids, and trips we were thinking about, one of her friends suddenly said: “That’s funny.”
I asked him what was funny, and he said: “My left vision suddenly went dark.”
It only takes a fraction of a second to shift into doctor mode. I asked a few pointed questions and did a quick neuroscan for asymmetries, slurred speech, the things that, after 23 years, have become second nature.
It resolved after about 30 seconds. He clearly didn’t think it was anything to be alarmed about. He’s intelligent and well educated, but not a doctor. I wasn’t going to let it go, and quietly spoke to him a short while later. He may not be my patient, but pushing him in the needed direction is the right thing to do.
I’ve gotten him to the right doctors now, and the ball is rolling, but I keep thinking about it. If I hadn’t been there it’s likely nothing would have been done. In fact, he seemed to think it was more amusing than potentially serious.
Medical blogs and doctors’ lounge stories are full of similar anecdotes, where we wonder why people don’t take such things seriously. We tend to view such people as stupid and/or ignorant.
Yet, this gentleman is neither. I’ve known him since childhood. He’s smart, well educated, and well read. He’s not a medical person, though.
In reality, I don’t think doctors or nurses are any better. I suspect that’s more human nature, which is hard to override regardless of training.
But maybe it’s time to start giving these people, like my family friend, a pass, with the realization that denial and different training are part of being human, and not something to be poked fun at.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Now that everyone in my family has been vaccinated, we’re starting to do more.
Last week we met my mom and some of her (vaccinated) friends for dinner at a local restaurant. Except for picking up takeout, I hadn’t been to one since early March 2020.
During the usual chatting about jobs, music, my kids, and trips we were thinking about, one of her friends suddenly said: “That’s funny.”
I asked him what was funny, and he said: “My left vision suddenly went dark.”
It only takes a fraction of a second to shift into doctor mode. I asked a few pointed questions and did a quick neuroscan for asymmetries, slurred speech, the things that, after 23 years, have become second nature.
It resolved after about 30 seconds. He clearly didn’t think it was anything to be alarmed about. He’s intelligent and well educated, but not a doctor. I wasn’t going to let it go, and quietly spoke to him a short while later. He may not be my patient, but pushing him in the needed direction is the right thing to do.
I’ve gotten him to the right doctors now, and the ball is rolling, but I keep thinking about it. If I hadn’t been there it’s likely nothing would have been done. In fact, he seemed to think it was more amusing than potentially serious.
Medical blogs and doctors’ lounge stories are full of similar anecdotes, where we wonder why people don’t take such things seriously. We tend to view such people as stupid and/or ignorant.
Yet, this gentleman is neither. I’ve known him since childhood. He’s smart, well educated, and well read. He’s not a medical person, though.
In reality, I don’t think doctors or nurses are any better. I suspect that’s more human nature, which is hard to override regardless of training.
But maybe it’s time to start giving these people, like my family friend, a pass, with the realization that denial and different training are part of being human, and not something to be poked fun at.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Are there some things we might want to keep from the COVID experience?
As your patients return to your offices for annual exams and sports physicals before the school year starts, everyone will still be processing the challenges, losses, and grief that have marked end of the COVID experience. There will be questions about the safety of vaccines for younger children, whether foreign travel is now a reasonable option, and about how best to help children – school age and teenagers, vulnerable and secure – get their footing socially and academically in the new school year. But dig a little, and you may hear about the silver linings of this past year: children who enjoyed having more time with their parents, parents who were with their families rather than in a car commuting for hours a day or traveling many days a month, grocery deliveries that eased the parent’s workload, adolescents who were able to pull back from overscheduled days, and opportunities for calm conversations that occurred quite naturally during nightly family dinners. Office visits present a dual opportunity to review – what were the psychological costs of COVID and what were positive personal and family adaptations to COVID they may want to continue as the pandemic ends?
Family dinner: Whether because sports practice was suspended, schooling was virtual, or working was at home, many families returned to eating dinner together during the pandemic year. Nightly dinners are a simple but powerful routine allowing all members of a family to reconnect and recharge together, and they are often the first things to disappear in the face of school, sports, and work demands. Research over the past several decades has demonstrated that regular family dinners are associated with better academic performance and higher self-esteem in children. They are also associated with lower rates of depression, substance abuse, eating disorders, and pregnancy in adolescents. Finally, they are associated with better cardiovascular health and lower rates of obesity in both youth and parents. The response is dose dependent, with more regular dinners leading to better outcomes. The food can be simple, what matters most is that the tone is warm, sharing, and curious, not rigid and controlling. Families can be an essential source of support as they help put events and feelings into context, giving them meaning or a framework based on the parents’ past, values, or perspective and on the family’s cultural history. Everyone benefits as family members cope with small and large setbacks, share values, and celebrate one another’s small and large successes. The return of the family dinner table, as often as is reasonable, is one “consequence” of COVID that families should try to preserve.
Consistent virtual family visits: Many families managed the cancellation of holiday visits or supported elderly relatives by connecting with family virtually. For some families, a weekly Zoom call came to function like a weekly family dinner with cousins and grandparents. Not only do these regular video calls protect elderly relatives from loneliness and isolation, but they also made it very easy for extended families to stay connected. Children cannot have too many caring adults around them, and regular calls mean that aunts, uncles, and grandparents can be an enthusiastic audience for their achievements and can offer perspective and guidance when needed. Staying connected without having to manage hours of travel makes it easy to build and maintain these family connections, creating bonds that will be deeper and stronger. Like family dinner, regular virtual gatherings with extended family are unequivocally beneficial for younger and older children and a valuable legacy of COVID.
Lowering the pressure: Many children struggled to stay engaged with virtual school and deeply missed time with friends or in activities like woodshop, soccer, or theater. But many other children had a chance to slow down from a relentless schedule of school, homework, sports, clubs, music lessons, tutoring, and on and on. For these children, many of whom are intensely ambitious and were not willing to voluntarily give up any activities, the forced slowdown of COVID has offered a new perspective on how they might manage their time. The COVID slowdown shone a light on the value of spending enough time in an activity to really learn it, and then choosing which activities to continue to explore and master, while opening time to explore new activities. There was also more time for “senseless fun,” activities that do not lead to achievement or recognition, but are simply fun, e.g., playing video games, splashing in a pool, or surfing the web. This process is critical to healthy development in early and later adolescence, and for many driven teenagers, it has been replaced by a tightly packed schedule of activities they felt they “should” be doing. If these young people hear from you that not only does the COVID pace feel better, but it can also contribute to better health and more meaningful learning and engagement, they may adopt a more thoughtful and intentional approach to managing their most precious asset – their time. Your discussion about prioritizing healthy exercise, virtual visits with friends, hobbies, or even senseless fun might reset the pressure gauge from high to moderate.
Homework help: Many children (and teenagers) found that their parents became an important source of academic support during the year of virtual school. While few parents welcomed the chance to master calculus, it is powerful for parents to know what their children are facing at school and for children to know that their parents are available to help them when they face a challenge. When parents can bear uncertainty, frustration, and even failure alongside their children, they help their children to cultivate tenacity and resilience, whether or not they can help them with a chemistry problem. Some parents will have special skills like knowing a language, being a good writer, or an academic expertise related to their work. But what matters more is working out how to help, not pressure or argue – how to share knowledge in a pleasurable manner. While it is important for children to have access to teachers and tutors with the knowledge and skills to help them learn specific subjects, the positive presence and involvement of their parents can make a valuable contribution to their psychological and educational development.
New ritual: Over the past 16 months, families found many creative ways to pass time together, from evening walks to reading aloud, listening to music, and even mastering new card games. The family evenings of a century earlier, when family members listened together to radio programs, practiced music, or played board games, seemed to have returned. While everyone could still escape to their own space to be on a screen activity alone, solitary computer time was leavened by collective time. Families may have rediscovered joy in shared recreation, exploration, or diversion. This kind of family time is a reward in itself, but it also deepens a child’s connections to everyone in their family. Such time provides lessons in how to turn boredom into something meaningful and even fun. COVID forced families inward and gave them more time. There were many costs including illness, deaths of friends and relatives, loss of time with peers, missed activities and milestones, and an impaired education. However, many of the coerced adaptations had a silver lining or unanticipated benefit. Keeping some of those benefits post COVID could enhance the lives of every member of the family.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@mdedge.com.
As your patients return to your offices for annual exams and sports physicals before the school year starts, everyone will still be processing the challenges, losses, and grief that have marked end of the COVID experience. There will be questions about the safety of vaccines for younger children, whether foreign travel is now a reasonable option, and about how best to help children – school age and teenagers, vulnerable and secure – get their footing socially and academically in the new school year. But dig a little, and you may hear about the silver linings of this past year: children who enjoyed having more time with their parents, parents who were with their families rather than in a car commuting for hours a day or traveling many days a month, grocery deliveries that eased the parent’s workload, adolescents who were able to pull back from overscheduled days, and opportunities for calm conversations that occurred quite naturally during nightly family dinners. Office visits present a dual opportunity to review – what were the psychological costs of COVID and what were positive personal and family adaptations to COVID they may want to continue as the pandemic ends?
Family dinner: Whether because sports practice was suspended, schooling was virtual, or working was at home, many families returned to eating dinner together during the pandemic year. Nightly dinners are a simple but powerful routine allowing all members of a family to reconnect and recharge together, and they are often the first things to disappear in the face of school, sports, and work demands. Research over the past several decades has demonstrated that regular family dinners are associated with better academic performance and higher self-esteem in children. They are also associated with lower rates of depression, substance abuse, eating disorders, and pregnancy in adolescents. Finally, they are associated with better cardiovascular health and lower rates of obesity in both youth and parents. The response is dose dependent, with more regular dinners leading to better outcomes. The food can be simple, what matters most is that the tone is warm, sharing, and curious, not rigid and controlling. Families can be an essential source of support as they help put events and feelings into context, giving them meaning or a framework based on the parents’ past, values, or perspective and on the family’s cultural history. Everyone benefits as family members cope with small and large setbacks, share values, and celebrate one another’s small and large successes. The return of the family dinner table, as often as is reasonable, is one “consequence” of COVID that families should try to preserve.
Consistent virtual family visits: Many families managed the cancellation of holiday visits or supported elderly relatives by connecting with family virtually. For some families, a weekly Zoom call came to function like a weekly family dinner with cousins and grandparents. Not only do these regular video calls protect elderly relatives from loneliness and isolation, but they also made it very easy for extended families to stay connected. Children cannot have too many caring adults around them, and regular calls mean that aunts, uncles, and grandparents can be an enthusiastic audience for their achievements and can offer perspective and guidance when needed. Staying connected without having to manage hours of travel makes it easy to build and maintain these family connections, creating bonds that will be deeper and stronger. Like family dinner, regular virtual gatherings with extended family are unequivocally beneficial for younger and older children and a valuable legacy of COVID.
Lowering the pressure: Many children struggled to stay engaged with virtual school and deeply missed time with friends or in activities like woodshop, soccer, or theater. But many other children had a chance to slow down from a relentless schedule of school, homework, sports, clubs, music lessons, tutoring, and on and on. For these children, many of whom are intensely ambitious and were not willing to voluntarily give up any activities, the forced slowdown of COVID has offered a new perspective on how they might manage their time. The COVID slowdown shone a light on the value of spending enough time in an activity to really learn it, and then choosing which activities to continue to explore and master, while opening time to explore new activities. There was also more time for “senseless fun,” activities that do not lead to achievement or recognition, but are simply fun, e.g., playing video games, splashing in a pool, or surfing the web. This process is critical to healthy development in early and later adolescence, and for many driven teenagers, it has been replaced by a tightly packed schedule of activities they felt they “should” be doing. If these young people hear from you that not only does the COVID pace feel better, but it can also contribute to better health and more meaningful learning and engagement, they may adopt a more thoughtful and intentional approach to managing their most precious asset – their time. Your discussion about prioritizing healthy exercise, virtual visits with friends, hobbies, or even senseless fun might reset the pressure gauge from high to moderate.
Homework help: Many children (and teenagers) found that their parents became an important source of academic support during the year of virtual school. While few parents welcomed the chance to master calculus, it is powerful for parents to know what their children are facing at school and for children to know that their parents are available to help them when they face a challenge. When parents can bear uncertainty, frustration, and even failure alongside their children, they help their children to cultivate tenacity and resilience, whether or not they can help them with a chemistry problem. Some parents will have special skills like knowing a language, being a good writer, or an academic expertise related to their work. But what matters more is working out how to help, not pressure or argue – how to share knowledge in a pleasurable manner. While it is important for children to have access to teachers and tutors with the knowledge and skills to help them learn specific subjects, the positive presence and involvement of their parents can make a valuable contribution to their psychological and educational development.
New ritual: Over the past 16 months, families found many creative ways to pass time together, from evening walks to reading aloud, listening to music, and even mastering new card games. The family evenings of a century earlier, when family members listened together to radio programs, practiced music, or played board games, seemed to have returned. While everyone could still escape to their own space to be on a screen activity alone, solitary computer time was leavened by collective time. Families may have rediscovered joy in shared recreation, exploration, or diversion. This kind of family time is a reward in itself, but it also deepens a child’s connections to everyone in their family. Such time provides lessons in how to turn boredom into something meaningful and even fun. COVID forced families inward and gave them more time. There were many costs including illness, deaths of friends and relatives, loss of time with peers, missed activities and milestones, and an impaired education. However, many of the coerced adaptations had a silver lining or unanticipated benefit. Keeping some of those benefits post COVID could enhance the lives of every member of the family.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@mdedge.com.
As your patients return to your offices for annual exams and sports physicals before the school year starts, everyone will still be processing the challenges, losses, and grief that have marked end of the COVID experience. There will be questions about the safety of vaccines for younger children, whether foreign travel is now a reasonable option, and about how best to help children – school age and teenagers, vulnerable and secure – get their footing socially and academically in the new school year. But dig a little, and you may hear about the silver linings of this past year: children who enjoyed having more time with their parents, parents who were with their families rather than in a car commuting for hours a day or traveling many days a month, grocery deliveries that eased the parent’s workload, adolescents who were able to pull back from overscheduled days, and opportunities for calm conversations that occurred quite naturally during nightly family dinners. Office visits present a dual opportunity to review – what were the psychological costs of COVID and what were positive personal and family adaptations to COVID they may want to continue as the pandemic ends?
Family dinner: Whether because sports practice was suspended, schooling was virtual, or working was at home, many families returned to eating dinner together during the pandemic year. Nightly dinners are a simple but powerful routine allowing all members of a family to reconnect and recharge together, and they are often the first things to disappear in the face of school, sports, and work demands. Research over the past several decades has demonstrated that regular family dinners are associated with better academic performance and higher self-esteem in children. They are also associated with lower rates of depression, substance abuse, eating disorders, and pregnancy in adolescents. Finally, they are associated with better cardiovascular health and lower rates of obesity in both youth and parents. The response is dose dependent, with more regular dinners leading to better outcomes. The food can be simple, what matters most is that the tone is warm, sharing, and curious, not rigid and controlling. Families can be an essential source of support as they help put events and feelings into context, giving them meaning or a framework based on the parents’ past, values, or perspective and on the family’s cultural history. Everyone benefits as family members cope with small and large setbacks, share values, and celebrate one another’s small and large successes. The return of the family dinner table, as often as is reasonable, is one “consequence” of COVID that families should try to preserve.
Consistent virtual family visits: Many families managed the cancellation of holiday visits or supported elderly relatives by connecting with family virtually. For some families, a weekly Zoom call came to function like a weekly family dinner with cousins and grandparents. Not only do these regular video calls protect elderly relatives from loneliness and isolation, but they also made it very easy for extended families to stay connected. Children cannot have too many caring adults around them, and regular calls mean that aunts, uncles, and grandparents can be an enthusiastic audience for their achievements and can offer perspective and guidance when needed. Staying connected without having to manage hours of travel makes it easy to build and maintain these family connections, creating bonds that will be deeper and stronger. Like family dinner, regular virtual gatherings with extended family are unequivocally beneficial for younger and older children and a valuable legacy of COVID.
Lowering the pressure: Many children struggled to stay engaged with virtual school and deeply missed time with friends or in activities like woodshop, soccer, or theater. But many other children had a chance to slow down from a relentless schedule of school, homework, sports, clubs, music lessons, tutoring, and on and on. For these children, many of whom are intensely ambitious and were not willing to voluntarily give up any activities, the forced slowdown of COVID has offered a new perspective on how they might manage their time. The COVID slowdown shone a light on the value of spending enough time in an activity to really learn it, and then choosing which activities to continue to explore and master, while opening time to explore new activities. There was also more time for “senseless fun,” activities that do not lead to achievement or recognition, but are simply fun, e.g., playing video games, splashing in a pool, or surfing the web. This process is critical to healthy development in early and later adolescence, and for many driven teenagers, it has been replaced by a tightly packed schedule of activities they felt they “should” be doing. If these young people hear from you that not only does the COVID pace feel better, but it can also contribute to better health and more meaningful learning and engagement, they may adopt a more thoughtful and intentional approach to managing their most precious asset – their time. Your discussion about prioritizing healthy exercise, virtual visits with friends, hobbies, or even senseless fun might reset the pressure gauge from high to moderate.
Homework help: Many children (and teenagers) found that their parents became an important source of academic support during the year of virtual school. While few parents welcomed the chance to master calculus, it is powerful for parents to know what their children are facing at school and for children to know that their parents are available to help them when they face a challenge. When parents can bear uncertainty, frustration, and even failure alongside their children, they help their children to cultivate tenacity and resilience, whether or not they can help them with a chemistry problem. Some parents will have special skills like knowing a language, being a good writer, or an academic expertise related to their work. But what matters more is working out how to help, not pressure or argue – how to share knowledge in a pleasurable manner. While it is important for children to have access to teachers and tutors with the knowledge and skills to help them learn specific subjects, the positive presence and involvement of their parents can make a valuable contribution to their psychological and educational development.
New ritual: Over the past 16 months, families found many creative ways to pass time together, from evening walks to reading aloud, listening to music, and even mastering new card games. The family evenings of a century earlier, when family members listened together to radio programs, practiced music, or played board games, seemed to have returned. While everyone could still escape to their own space to be on a screen activity alone, solitary computer time was leavened by collective time. Families may have rediscovered joy in shared recreation, exploration, or diversion. This kind of family time is a reward in itself, but it also deepens a child’s connections to everyone in their family. Such time provides lessons in how to turn boredom into something meaningful and even fun. COVID forced families inward and gave them more time. There were many costs including illness, deaths of friends and relatives, loss of time with peers, missed activities and milestones, and an impaired education. However, many of the coerced adaptations had a silver lining or unanticipated benefit. Keeping some of those benefits post COVID could enhance the lives of every member of the family.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@mdedge.com.
Trans youth in sports
Over the last several years, the United States has seen a substantial increase in proposed legislation directed toward transgender individuals, particularly youth.1 One type of this legislation aims to prevent participation of transgender girls on female sports teams. While at first glance these bills may seem like common sense protections, in reality they are based on little evidence and serve to further marginalize an already-vulnerable population.
The majority of the population, and thus the majority of athletes, are cisgender.2 According a limited data set from the 2017 Youth Risk Behavior Survey, only 1.8% of high school students identify as transgender.3,4 Overall, this is a very small percentage and it is unlikely that all of them, or even a majority, participate in athletics. In fact, many transgender individuals avoid athletics as it worsens their dysphoria. Winners are no more likely to be transgender than cisgender.
While proponents of this legislation say that trans women have an unfair advantage because of elevated testosterone levels (and thus theoretically increased muscle mass), there is no clear relationship between higher testosterone levels in athletes and improved athletic performance.2 In fact, there are plenty of sports in which a smaller physique may be beneficial, such as gymnastics. A systematic review showed “no direct or consistent research suggesting transgender female individuals ... have an athletic advantage at any stage of their transition.”5 Furthermore, trans women are not the only women with elevated testosterone levels. Many cisgender women who have polycystic ovary syndrome or a disorder of sexual differentiation can have higher levels of testosterone and theoretically may have higher muscle mass. Who is to decide which team would be most appropriate for them? Is the plan to require a karyotype, other genetic testing, or an invasive physical exam for every young athlete? Even if the concern is with regards to testosterone levels and muscle mass, this ignores that fact that appropriate medical intervention for transgender adolescents will alter these attributes. If a transgender girl began gonadotropin-releasing hormone agonists early in puberty, she is unlikely to have increased muscle mass or a higher testosterone level than a cisgender girl. Those trans girls who take estradiol also experience a decrease in muscle mass. Additionally, adolescents grow and develop at different rates – surely there is already significant variability among hormone levels, muscle mass, sexual maturity ratings, and ability among individual athletes, regardless of gender identity? The argument that trans women should be excluded based on a theoretical genetic advantage is reminiscent of the argument that Black athletes should be excluded because of genetic advantage. Just as with cisgender athletes, transgender athletes will naturally vary in ability.6
In addition, there are many places and organizations that already have trans-inclusive policies in place for sports, yet we have not seen transgender individuals dominate their peers. In the 8 years since implementation of a trans-inclusive sports policy in California, a trans woman has never dominated a sport.7 The same is true for Canada since the institution of their policy 2 years ago. While transgender people can participate in the Olympics, this year marks the first time a trans woman has ever qualified (Laurel Hubbard, New Zealand, women’s weightlifting). The lack of transgender Olympians may be in part because of problematic requirements (such as duration of hormone therapy and surgery requirements) for transgender individuals, which may be so onerous that they are functionally excluded.2,5
In reality, athletes are improving over time and the performance gap between genders is shrinking. For example, in 1970 Mark Spitz swam the 100-meter freestyle in 51.94 seconds, a time that has now been surpassed by both men and women, such as Sarah Sjöström (women’s world record holder at 51.71 seconds). Athletes’ physical attributes are often less important than their training and dedication to their sport.
More importantly, this discussion raises the philosophical question of the purpose of athletics for youth and young adults. Winning and good performance can – though rarely – lead to college scholarships and professional careers, the biggest benefit of athletics comes from participation. We encourage youth to play sports not to win, but to learn about leadership, dedication, and collegiality, as well as for the health benefits of exercise. Inclusion in sports and other extracurricular activities improves depression, anxiety, and suicide rates. In fact, participation in sports has been associated with improved grades, greater homework completion, higher educational and occupational aspirations, and improved self-esteem.8-12 Excluding a population that already experiences such drastic marginalization will cause more damage. Values of nondiscrimination and inclusion should be promoted among all student athletes, rather than “other-ism.”
Forcing trans women to compete with men will worsen their dysphoria and further ostracize the most vulnerable, giving credence to those that believe they are not “real women.” Allowing transgender individuals to play on the team consistent with their gender identity is appropriate, not only for scientific reasons but also for humanitarian ones. Such laws are based not on evidence, but on discrimination. Not only do trans women not do better than cisgender women in sports, but such proposed legislation also ignores the normal variability among individuals as well as the intense training and dedication involved in becoming a top athlete. Limiting trans women’s participation in sports does not raise up cisgender women, but rather brings us all down. Please advocate for your patients to participate in athletics in accordance with their gender identity to promote both their physical and emotional well-being.
Dr. Lawlis is assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures.
References
1. Cooper MB. Pediatric News. 2020 Dec 11, 2020.
2. Turban J. Scientific American. 2021 May 21.
3. Redfield RR et al. Morbid Mortal Wkly Rep. 2018;67(8):1-11.
4. Johns MM et al. Morbid Mortal Wkly Rep. 2019;68(3):67-71.
5. Jones BA et al. Sports Med (Auckland, New Zealand). 2017;47(4):701-16.
6. Strangio C et al. ACLU News. 2020 Apr 30.
7. Strauss L. USA Today. 2021 Apr 9.
8. Darling N et al. J Leisure Res. 2005;37(1):51-76.
9. Fredricks JA et al. Dev Psych. 2006;42(4):698-713.
10. Marsh HW et al. J Sport Exerc Psychol. 2003;25(2):205.
11. Nelson MC et al. Pediatrics. 2006;117(4):1281-90.
12. Ortega FB et al. Int J Obes. 2008;32(1):1-11.
Over the last several years, the United States has seen a substantial increase in proposed legislation directed toward transgender individuals, particularly youth.1 One type of this legislation aims to prevent participation of transgender girls on female sports teams. While at first glance these bills may seem like common sense protections, in reality they are based on little evidence and serve to further marginalize an already-vulnerable population.
The majority of the population, and thus the majority of athletes, are cisgender.2 According a limited data set from the 2017 Youth Risk Behavior Survey, only 1.8% of high school students identify as transgender.3,4 Overall, this is a very small percentage and it is unlikely that all of them, or even a majority, participate in athletics. In fact, many transgender individuals avoid athletics as it worsens their dysphoria. Winners are no more likely to be transgender than cisgender.
While proponents of this legislation say that trans women have an unfair advantage because of elevated testosterone levels (and thus theoretically increased muscle mass), there is no clear relationship between higher testosterone levels in athletes and improved athletic performance.2 In fact, there are plenty of sports in which a smaller physique may be beneficial, such as gymnastics. A systematic review showed “no direct or consistent research suggesting transgender female individuals ... have an athletic advantage at any stage of their transition.”5 Furthermore, trans women are not the only women with elevated testosterone levels. Many cisgender women who have polycystic ovary syndrome or a disorder of sexual differentiation can have higher levels of testosterone and theoretically may have higher muscle mass. Who is to decide which team would be most appropriate for them? Is the plan to require a karyotype, other genetic testing, or an invasive physical exam for every young athlete? Even if the concern is with regards to testosterone levels and muscle mass, this ignores that fact that appropriate medical intervention for transgender adolescents will alter these attributes. If a transgender girl began gonadotropin-releasing hormone agonists early in puberty, she is unlikely to have increased muscle mass or a higher testosterone level than a cisgender girl. Those trans girls who take estradiol also experience a decrease in muscle mass. Additionally, adolescents grow and develop at different rates – surely there is already significant variability among hormone levels, muscle mass, sexual maturity ratings, and ability among individual athletes, regardless of gender identity? The argument that trans women should be excluded based on a theoretical genetic advantage is reminiscent of the argument that Black athletes should be excluded because of genetic advantage. Just as with cisgender athletes, transgender athletes will naturally vary in ability.6
In addition, there are many places and organizations that already have trans-inclusive policies in place for sports, yet we have not seen transgender individuals dominate their peers. In the 8 years since implementation of a trans-inclusive sports policy in California, a trans woman has never dominated a sport.7 The same is true for Canada since the institution of their policy 2 years ago. While transgender people can participate in the Olympics, this year marks the first time a trans woman has ever qualified (Laurel Hubbard, New Zealand, women’s weightlifting). The lack of transgender Olympians may be in part because of problematic requirements (such as duration of hormone therapy and surgery requirements) for transgender individuals, which may be so onerous that they are functionally excluded.2,5
In reality, athletes are improving over time and the performance gap between genders is shrinking. For example, in 1970 Mark Spitz swam the 100-meter freestyle in 51.94 seconds, a time that has now been surpassed by both men and women, such as Sarah Sjöström (women’s world record holder at 51.71 seconds). Athletes’ physical attributes are often less important than their training and dedication to their sport.
More importantly, this discussion raises the philosophical question of the purpose of athletics for youth and young adults. Winning and good performance can – though rarely – lead to college scholarships and professional careers, the biggest benefit of athletics comes from participation. We encourage youth to play sports not to win, but to learn about leadership, dedication, and collegiality, as well as for the health benefits of exercise. Inclusion in sports and other extracurricular activities improves depression, anxiety, and suicide rates. In fact, participation in sports has been associated with improved grades, greater homework completion, higher educational and occupational aspirations, and improved self-esteem.8-12 Excluding a population that already experiences such drastic marginalization will cause more damage. Values of nondiscrimination and inclusion should be promoted among all student athletes, rather than “other-ism.”
Forcing trans women to compete with men will worsen their dysphoria and further ostracize the most vulnerable, giving credence to those that believe they are not “real women.” Allowing transgender individuals to play on the team consistent with their gender identity is appropriate, not only for scientific reasons but also for humanitarian ones. Such laws are based not on evidence, but on discrimination. Not only do trans women not do better than cisgender women in sports, but such proposed legislation also ignores the normal variability among individuals as well as the intense training and dedication involved in becoming a top athlete. Limiting trans women’s participation in sports does not raise up cisgender women, but rather brings us all down. Please advocate for your patients to participate in athletics in accordance with their gender identity to promote both their physical and emotional well-being.
Dr. Lawlis is assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures.
References
1. Cooper MB. Pediatric News. 2020 Dec 11, 2020.
2. Turban J. Scientific American. 2021 May 21.
3. Redfield RR et al. Morbid Mortal Wkly Rep. 2018;67(8):1-11.
4. Johns MM et al. Morbid Mortal Wkly Rep. 2019;68(3):67-71.
5. Jones BA et al. Sports Med (Auckland, New Zealand). 2017;47(4):701-16.
6. Strangio C et al. ACLU News. 2020 Apr 30.
7. Strauss L. USA Today. 2021 Apr 9.
8. Darling N et al. J Leisure Res. 2005;37(1):51-76.
9. Fredricks JA et al. Dev Psych. 2006;42(4):698-713.
10. Marsh HW et al. J Sport Exerc Psychol. 2003;25(2):205.
11. Nelson MC et al. Pediatrics. 2006;117(4):1281-90.
12. Ortega FB et al. Int J Obes. 2008;32(1):1-11.
Over the last several years, the United States has seen a substantial increase in proposed legislation directed toward transgender individuals, particularly youth.1 One type of this legislation aims to prevent participation of transgender girls on female sports teams. While at first glance these bills may seem like common sense protections, in reality they are based on little evidence and serve to further marginalize an already-vulnerable population.
The majority of the population, and thus the majority of athletes, are cisgender.2 According a limited data set from the 2017 Youth Risk Behavior Survey, only 1.8% of high school students identify as transgender.3,4 Overall, this is a very small percentage and it is unlikely that all of them, or even a majority, participate in athletics. In fact, many transgender individuals avoid athletics as it worsens their dysphoria. Winners are no more likely to be transgender than cisgender.
While proponents of this legislation say that trans women have an unfair advantage because of elevated testosterone levels (and thus theoretically increased muscle mass), there is no clear relationship between higher testosterone levels in athletes and improved athletic performance.2 In fact, there are plenty of sports in which a smaller physique may be beneficial, such as gymnastics. A systematic review showed “no direct or consistent research suggesting transgender female individuals ... have an athletic advantage at any stage of their transition.”5 Furthermore, trans women are not the only women with elevated testosterone levels. Many cisgender women who have polycystic ovary syndrome or a disorder of sexual differentiation can have higher levels of testosterone and theoretically may have higher muscle mass. Who is to decide which team would be most appropriate for them? Is the plan to require a karyotype, other genetic testing, or an invasive physical exam for every young athlete? Even if the concern is with regards to testosterone levels and muscle mass, this ignores that fact that appropriate medical intervention for transgender adolescents will alter these attributes. If a transgender girl began gonadotropin-releasing hormone agonists early in puberty, she is unlikely to have increased muscle mass or a higher testosterone level than a cisgender girl. Those trans girls who take estradiol also experience a decrease in muscle mass. Additionally, adolescents grow and develop at different rates – surely there is already significant variability among hormone levels, muscle mass, sexual maturity ratings, and ability among individual athletes, regardless of gender identity? The argument that trans women should be excluded based on a theoretical genetic advantage is reminiscent of the argument that Black athletes should be excluded because of genetic advantage. Just as with cisgender athletes, transgender athletes will naturally vary in ability.6
In addition, there are many places and organizations that already have trans-inclusive policies in place for sports, yet we have not seen transgender individuals dominate their peers. In the 8 years since implementation of a trans-inclusive sports policy in California, a trans woman has never dominated a sport.7 The same is true for Canada since the institution of their policy 2 years ago. While transgender people can participate in the Olympics, this year marks the first time a trans woman has ever qualified (Laurel Hubbard, New Zealand, women’s weightlifting). The lack of transgender Olympians may be in part because of problematic requirements (such as duration of hormone therapy and surgery requirements) for transgender individuals, which may be so onerous that they are functionally excluded.2,5
In reality, athletes are improving over time and the performance gap between genders is shrinking. For example, in 1970 Mark Spitz swam the 100-meter freestyle in 51.94 seconds, a time that has now been surpassed by both men and women, such as Sarah Sjöström (women’s world record holder at 51.71 seconds). Athletes’ physical attributes are often less important than their training and dedication to their sport.
More importantly, this discussion raises the philosophical question of the purpose of athletics for youth and young adults. Winning and good performance can – though rarely – lead to college scholarships and professional careers, the biggest benefit of athletics comes from participation. We encourage youth to play sports not to win, but to learn about leadership, dedication, and collegiality, as well as for the health benefits of exercise. Inclusion in sports and other extracurricular activities improves depression, anxiety, and suicide rates. In fact, participation in sports has been associated with improved grades, greater homework completion, higher educational and occupational aspirations, and improved self-esteem.8-12 Excluding a population that already experiences such drastic marginalization will cause more damage. Values of nondiscrimination and inclusion should be promoted among all student athletes, rather than “other-ism.”
Forcing trans women to compete with men will worsen their dysphoria and further ostracize the most vulnerable, giving credence to those that believe they are not “real women.” Allowing transgender individuals to play on the team consistent with their gender identity is appropriate, not only for scientific reasons but also for humanitarian ones. Such laws are based not on evidence, but on discrimination. Not only do trans women not do better than cisgender women in sports, but such proposed legislation also ignores the normal variability among individuals as well as the intense training and dedication involved in becoming a top athlete. Limiting trans women’s participation in sports does not raise up cisgender women, but rather brings us all down. Please advocate for your patients to participate in athletics in accordance with their gender identity to promote both their physical and emotional well-being.
Dr. Lawlis is assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures.
References
1. Cooper MB. Pediatric News. 2020 Dec 11, 2020.
2. Turban J. Scientific American. 2021 May 21.
3. Redfield RR et al. Morbid Mortal Wkly Rep. 2018;67(8):1-11.
4. Johns MM et al. Morbid Mortal Wkly Rep. 2019;68(3):67-71.
5. Jones BA et al. Sports Med (Auckland, New Zealand). 2017;47(4):701-16.
6. Strangio C et al. ACLU News. 2020 Apr 30.
7. Strauss L. USA Today. 2021 Apr 9.
8. Darling N et al. J Leisure Res. 2005;37(1):51-76.
9. Fredricks JA et al. Dev Psych. 2006;42(4):698-713.
10. Marsh HW et al. J Sport Exerc Psychol. 2003;25(2):205.
11. Nelson MC et al. Pediatrics. 2006;117(4):1281-90.
12. Ortega FB et al. Int J Obes. 2008;32(1):1-11.
Does optimal iron absorption include vitamin C?
Her blood work shows a hematocrit level of 32, a mean corpuscular volume of 77, a platelet count of 390,000, and a ferritin level of 5.
What would you recommend for iron replacement?
A. FeSO4 325 mg three times a day with vitamin C
B. FeSO4 325 mg daily with vitamin C
C. FeSO4 325 mg every other day
Recommendations and supporting research
I think I would start with choice C, FeSO4 every other day.
Treatment of iron deficiency with oral iron has traditionally been done by giving 150-200 mg of elemental iron (which is equal to three 325 mg tablets of iron sulfate).1 This dosing regimen has considerable gastrointestinal side effects. Recent evidence has shown that iron absorption is diminished the more frequently it is given.
Stoffel and colleagues found that fractional iron absorption was higher in iron-deficient women who were given iron every other day, compared with those who received daily iron.2 They also found that the more frequently iron was administered, the higher the hepcidin levels were, and the lower the iron absorption.
Karacok and colleagues studied every other day iron versus daily iron for the treatment of iron-deficiency anemia of pregnancy.3 A total of 217 women completed randomization and participated in the study, with all women receiving 100 mg of elemental iron, either daily (111) or every other day (106). There was no significant difference in increase in ferritin levels, or hemoglobin increase between the groups. The daily iron group had more gastrointestinal symptoms (41.4%) than the every other day iron group (15.1%) (P < .0057).
Düzen Oflas and colleagues looked at the same question in nonpregnant women with iron deficiency anemia.4 Study patients either received 80 mg iron sulfate twice a day, 80 mg once a day, or 80 mg every other day. There was no statistically significant difference in hemoglobin improvement between groups, but the group that received twice a day dosing of iron had statistically significantly higher ferritin levels than the daily or every other day iron groups. This improvement in ferritin levels came at a cost, though, as 68% of patients in the twice daily iron group had gastrointestinal symptoms, compared with only 10% in the every other day iron group (P < .01).
Vitamin C is often recommended to be taken with iron to promote absorption. The evidence for this practice is scant, and dates back almost 50 years.5,6
Cook and Reddy found there was no significant difference in mean iron absorption among the three dietary periods studied in 12 patients despite a range of mean daily intakes of dietary vitamin C of 51-247 mg/d.7
Hunt and colleagues studied 25 non pregnant, healthy women with low ferritin levels.8 The women’s meals were supplemented with vitamin C (500 mg, three times a day) for 5 of the 10 weeks, in a double-blind, crossover design. Vitamin C supplementation did not lead to a difference in iron absorption, lab indices of iron deficiency, or the biological half-life of iron.
Li and colleagues looked at the effect of vitamin C supplementation on iron levels in women with iron deficiency anemia.9 A total of 440 women were recruited, with 432 completing the trial. Women were randomized to receive iron supplements plus vitamin C or iron supplements only. Their findings were that oral iron supplements alone were equivalent to oral iron supplements plus vitamin C in improving hemoglobin recovery and iron absorption.
Bottom line
Less frequent administration of iron supplements (every other day) is as effective as more frequent administration, with less GI symptoms. Also, adding vitamin C does not appear to improve absorption of iron supplements.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at imnews@mdedge.com.
References
1. 1. Fairbanks VF and Beutler E. Iron deficiency, in “Williams Textbook of Hematology, 6th ed.” (New York: McGraw-Hill, 2001).
2. Stoffel N et al. Lancet Haematology. 2017;4: e524-33.
3. Karakoc G et al. J Matern Fetal Neonatal Med. 2021 Apr 18:1-5
4. Düzen Oflas N et al. Intern Med J. 2020 Jul;50(7):854-8
5. Cook JD and Monsen ER. Am J Clin Nutr. 1977;30:235-41.
6. Hallberg L etal. Hum Nutr Appl Nutr. 1986;40: 97-113.
7. Cook JD and Reddy M. Am J Clin Nutr. 2001;73:93-8.
8. Hunt JR et al. Am J Clin Nutr. 1994 Jun;59(6):1381-5.
9. Li N et al. JAMA Netw Open. 2020 Nov 2;3(11):e2023644.
Her blood work shows a hematocrit level of 32, a mean corpuscular volume of 77, a platelet count of 390,000, and a ferritin level of 5.
What would you recommend for iron replacement?
A. FeSO4 325 mg three times a day with vitamin C
B. FeSO4 325 mg daily with vitamin C
C. FeSO4 325 mg every other day
Recommendations and supporting research
I think I would start with choice C, FeSO4 every other day.
Treatment of iron deficiency with oral iron has traditionally been done by giving 150-200 mg of elemental iron (which is equal to three 325 mg tablets of iron sulfate).1 This dosing regimen has considerable gastrointestinal side effects. Recent evidence has shown that iron absorption is diminished the more frequently it is given.
Stoffel and colleagues found that fractional iron absorption was higher in iron-deficient women who were given iron every other day, compared with those who received daily iron.2 They also found that the more frequently iron was administered, the higher the hepcidin levels were, and the lower the iron absorption.
Karacok and colleagues studied every other day iron versus daily iron for the treatment of iron-deficiency anemia of pregnancy.3 A total of 217 women completed randomization and participated in the study, with all women receiving 100 mg of elemental iron, either daily (111) or every other day (106). There was no significant difference in increase in ferritin levels, or hemoglobin increase between the groups. The daily iron group had more gastrointestinal symptoms (41.4%) than the every other day iron group (15.1%) (P < .0057).
Düzen Oflas and colleagues looked at the same question in nonpregnant women with iron deficiency anemia.4 Study patients either received 80 mg iron sulfate twice a day, 80 mg once a day, or 80 mg every other day. There was no statistically significant difference in hemoglobin improvement between groups, but the group that received twice a day dosing of iron had statistically significantly higher ferritin levels than the daily or every other day iron groups. This improvement in ferritin levels came at a cost, though, as 68% of patients in the twice daily iron group had gastrointestinal symptoms, compared with only 10% in the every other day iron group (P < .01).
Vitamin C is often recommended to be taken with iron to promote absorption. The evidence for this practice is scant, and dates back almost 50 years.5,6
Cook and Reddy found there was no significant difference in mean iron absorption among the three dietary periods studied in 12 patients despite a range of mean daily intakes of dietary vitamin C of 51-247 mg/d.7
Hunt and colleagues studied 25 non pregnant, healthy women with low ferritin levels.8 The women’s meals were supplemented with vitamin C (500 mg, three times a day) for 5 of the 10 weeks, in a double-blind, crossover design. Vitamin C supplementation did not lead to a difference in iron absorption, lab indices of iron deficiency, or the biological half-life of iron.
Li and colleagues looked at the effect of vitamin C supplementation on iron levels in women with iron deficiency anemia.9 A total of 440 women were recruited, with 432 completing the trial. Women were randomized to receive iron supplements plus vitamin C or iron supplements only. Their findings were that oral iron supplements alone were equivalent to oral iron supplements plus vitamin C in improving hemoglobin recovery and iron absorption.
Bottom line
Less frequent administration of iron supplements (every other day) is as effective as more frequent administration, with less GI symptoms. Also, adding vitamin C does not appear to improve absorption of iron supplements.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at imnews@mdedge.com.
References
1. 1. Fairbanks VF and Beutler E. Iron deficiency, in “Williams Textbook of Hematology, 6th ed.” (New York: McGraw-Hill, 2001).
2. Stoffel N et al. Lancet Haematology. 2017;4: e524-33.
3. Karakoc G et al. J Matern Fetal Neonatal Med. 2021 Apr 18:1-5
4. Düzen Oflas N et al. Intern Med J. 2020 Jul;50(7):854-8
5. Cook JD and Monsen ER. Am J Clin Nutr. 1977;30:235-41.
6. Hallberg L etal. Hum Nutr Appl Nutr. 1986;40: 97-113.
7. Cook JD and Reddy M. Am J Clin Nutr. 2001;73:93-8.
8. Hunt JR et al. Am J Clin Nutr. 1994 Jun;59(6):1381-5.
9. Li N et al. JAMA Netw Open. 2020 Nov 2;3(11):e2023644.
Her blood work shows a hematocrit level of 32, a mean corpuscular volume of 77, a platelet count of 390,000, and a ferritin level of 5.
What would you recommend for iron replacement?
A. FeSO4 325 mg three times a day with vitamin C
B. FeSO4 325 mg daily with vitamin C
C. FeSO4 325 mg every other day
Recommendations and supporting research
I think I would start with choice C, FeSO4 every other day.
Treatment of iron deficiency with oral iron has traditionally been done by giving 150-200 mg of elemental iron (which is equal to three 325 mg tablets of iron sulfate).1 This dosing regimen has considerable gastrointestinal side effects. Recent evidence has shown that iron absorption is diminished the more frequently it is given.
Stoffel and colleagues found that fractional iron absorption was higher in iron-deficient women who were given iron every other day, compared with those who received daily iron.2 They also found that the more frequently iron was administered, the higher the hepcidin levels were, and the lower the iron absorption.
Karacok and colleagues studied every other day iron versus daily iron for the treatment of iron-deficiency anemia of pregnancy.3 A total of 217 women completed randomization and participated in the study, with all women receiving 100 mg of elemental iron, either daily (111) or every other day (106). There was no significant difference in increase in ferritin levels, or hemoglobin increase between the groups. The daily iron group had more gastrointestinal symptoms (41.4%) than the every other day iron group (15.1%) (P < .0057).
Düzen Oflas and colleagues looked at the same question in nonpregnant women with iron deficiency anemia.4 Study patients either received 80 mg iron sulfate twice a day, 80 mg once a day, or 80 mg every other day. There was no statistically significant difference in hemoglobin improvement between groups, but the group that received twice a day dosing of iron had statistically significantly higher ferritin levels than the daily or every other day iron groups. This improvement in ferritin levels came at a cost, though, as 68% of patients in the twice daily iron group had gastrointestinal symptoms, compared with only 10% in the every other day iron group (P < .01).
Vitamin C is often recommended to be taken with iron to promote absorption. The evidence for this practice is scant, and dates back almost 50 years.5,6
Cook and Reddy found there was no significant difference in mean iron absorption among the three dietary periods studied in 12 patients despite a range of mean daily intakes of dietary vitamin C of 51-247 mg/d.7
Hunt and colleagues studied 25 non pregnant, healthy women with low ferritin levels.8 The women’s meals were supplemented with vitamin C (500 mg, three times a day) for 5 of the 10 weeks, in a double-blind, crossover design. Vitamin C supplementation did not lead to a difference in iron absorption, lab indices of iron deficiency, or the biological half-life of iron.
Li and colleagues looked at the effect of vitamin C supplementation on iron levels in women with iron deficiency anemia.9 A total of 440 women were recruited, with 432 completing the trial. Women were randomized to receive iron supplements plus vitamin C or iron supplements only. Their findings were that oral iron supplements alone were equivalent to oral iron supplements plus vitamin C in improving hemoglobin recovery and iron absorption.
Bottom line
Less frequent administration of iron supplements (every other day) is as effective as more frequent administration, with less GI symptoms. Also, adding vitamin C does not appear to improve absorption of iron supplements.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at imnews@mdedge.com.
References
1. 1. Fairbanks VF and Beutler E. Iron deficiency, in “Williams Textbook of Hematology, 6th ed.” (New York: McGraw-Hill, 2001).
2. Stoffel N et al. Lancet Haematology. 2017;4: e524-33.
3. Karakoc G et al. J Matern Fetal Neonatal Med. 2021 Apr 18:1-5
4. Düzen Oflas N et al. Intern Med J. 2020 Jul;50(7):854-8
5. Cook JD and Monsen ER. Am J Clin Nutr. 1977;30:235-41.
6. Hallberg L etal. Hum Nutr Appl Nutr. 1986;40: 97-113.
7. Cook JD and Reddy M. Am J Clin Nutr. 2001;73:93-8.
8. Hunt JR et al. Am J Clin Nutr. 1994 Jun;59(6):1381-5.
9. Li N et al. JAMA Netw Open. 2020 Nov 2;3(11):e2023644.
“Enough English” to be at risk
A hectic Friday morning at the hospital seemed less stressful amid morning greetings and humor from colleagues. In a team room full of hospitalists, life and death are often discussed in detail, ranging from medical discussions to joys and frustrations of the day to philosophy, politics, and more. It is almost impossible to miss something interesting.
People breaking into their native languages over the phone call from home always make me smile. The mention of a “complicated Indian patient unable to use interpreter” caught my attention.
My friend and colleague asked if I would be willing to take over the patient since I could speak Hindi. I was doubtful if I would add anything to make a meaningful difference, given the patient wasn’t even participating in a conversation. However, my colleague’s concern for the patient and faith in me was enough to say, “Sure, let me add her to my list.”
At the bedside, it felt like a classic “acute on chronic” hot mess situation. The patient presented with a generalized rash, anasarca, renal failure, multifocal pneumonia, and delirium. All I could gather from the patient were some incomprehensible words that sounded like Hindi. I called the family to obtain some history and to provide updates. Her son was excited to hear from me, and it didn’t take him long to guess that I was from India. But that could still mean that I might speak any of the twenty-two or more Indian languages.
Answering my questions one by one in perfectly understandable English, he was short and sweet. Suspicious of missing out on details, I offered hesitantly, “You could speak in Hindi with me.” Then came a flood of information with the details, concerns, questions, and what was lost in the translation.
We all attend to patients and families with limited English proficiency (LEP), immigrants, and nonimmigrants. LEP is a term used to describe individuals who do not speak English as their primary language and have a limited ability to read, speak, write, or understand English.1 Recent data from the American Community Survey (2005-2009) reports that 8.6% of the population (24 million Americans) have LEP.2 It’s a large and growing population that needs help overcoming language barriers and the appropriate use of professional medical interpreter services – a backbone to safe, quality, and cost-effective patient care.
The following day at bedside rounds, the nurse reported that the patient was looking and responding better. She could cooperate with interpreter services and could speak “some English.” Over the years, one thing that sounds more alarming than “no English” is “some English” or “enough English.” Around noon I received a page that the patient was refusing intravenous Lasix. At the bedside, however, the patient seemed unaware of the perceived refusal. Further discussions with the nurse lead to a familiar culprit, a relatively common gesture in South Asian cultures, a head bobble or shake.
The nurse reported that the patient shook her head side to side, seemed upset, and said “NO” when trying to administer the medication. On the other hand, the patient reported that she was upset to be at the hospital but had “NO” problem with the medicine.
My patient’s “some English” was indeed “enough English” to put her at risk due to medical error, which is highly likely when patients or providers can speak or understand a language to “get by” or to “make do.” Like my patient, the LEP patient population is more likely to experience medical errors, longer hospital stays, hospital-acquired complications, surgical delays, and readmissions. They are also less likely to receive preventive care, have access to regular care, or be satisfied with their care. They are much more likely to have adverse effects from drug complications, poor understanding of diagnoses, a greater risk of being misunderstood by their physicians or ancillary staff, and less likely to follow physician instructions.3-5 One study analyzed over 1,000 adverse-incident reports from six Joint Commission-accredited hospitals for LEP and English-speaking patients and found that 49% of LEP patients experienced physical harm versus 29.5% of English-speaking patients.6
I updated the patient’s LEP status that was missing in the chart, likely due to altered mental status at the time of admission. Reliable language and English proficiency data are usually entered at the patient’s point of entry with documentation of the language services required during the patient-provider encounter. The U.S. Census Bureau’s operational definition for LEP is a patient’s self-assessed ability to speak English less than “very well,” but how well it correlates with a patient’s actual English ability needs more study. Also, one’s self-assessed perception of ability might vary day to day, and language ability, by itself, is not static; it can differ from moment to moment and situation to situation. It may be easier to understand words in English when the situation is simple and less stressful than when things are complicated and stressful.
With a definition of LEP rather vague and the term somewhat derogatory, its meaning is open to interpretation. One study found that though speaking English less than “very well” was the most sensitive measure for identifying all of the patients who reported that they were unable to communicate effectively with their physicians, it was also the least specific.7 This lower specificity could lead to misclassification of some patients as LEP who are, in fact, able to effectively communicate in English with their physicians. This type of misclassification might lead to costly language assistance and carry the potential to cause conflicts between patient and provider. Telling a patient or family that they may have a “limited English proficiency” when they have believed otherwise and feel confident about their skills may come as a challenge. Some patients may also pretend to understand English to avoid being embarrassed about their linguistic abilities or perceive that they might be judged on their abilities in general.
Exiting the room, I gently reminded the RN to use the interpreter services. “Who has never been guilty of using an ad hoc interpreter or rushing through a long interpreter phone call due to time constraints?” I thought. A study from 2011 found that 43% of hospitalized patients with LEP had communicated without an interpreter present during admission, and 40% had communicated without an interpreter present after admission.8 In other words, a system in place does not mean service in use. But, the use of a trained interpreter is not only an obligation for care providers but a right for patients as per legal requirements of Title VI of the Civil Rights Act and the Standards for Culturally and Linguistically Appropriate Services (CLAS) by the Department of Health and Human Services’ (HSS) Office of Minority Health.9 In January 2010, The Joint Commission released a set of new and revised standards for patient-centered communication as part of an initiative to advance effective communication, cultural competence, and patient- and family-centered care.
Despite the requirements and availability of qualified medical interpreter services, there are multiple perceived and experienced barriers to the use of interpreter services. The most common one is that what comes as a free service for patients is a time commitment for providers. A long list of patients, acuity of the situation, and ease of use/availability of translation aids can change the calculus. One may be able to bill a prolonged service code (99354-99357) in addition to the appropriate E/M code, although a patient cannot be billed for the actual service provided by the interpreter. Longstanding CMS policy also permits reimbursement for translation/interpretation activities, so long as they are not included and paid for as part of the rate for direct service.10
The patient, however, insisted that she would rather have her son as the interpreter on the 3-way over the phone (OPI) conference call for interpretation. “He speaks good English and knows my medical history well,” she said. I counseled the patient on the benefits of using interpreter services and explained how to use the call button light and the visual aids.
Placing emphasis on educating patients about the benefits of using, and risks of not using, interpreter services is as essential as emphasizing that care providers use the services. Some patients may voluntarily choose to provide their own interpreter. Use of family members, friends, or unqualified staff as interpreters is one of the most commonly reported causes of errors by frontline staff. Using in-language collateral may help these patients understand how medical interpretation may create a better patient experience and outcome. A short factsheet, in different languages, on qualified interpreters’ expected benefits: meaning-for-meaning communication, impartiality, medical privacy, and improved patient safety and satisfaction, can also come in handy.
However, if the patient still refuses, providers should document the refusal of the offer of free language services, the name of the interpreter designated by the patient, the interpreter’s relationship to the LEP person, and the time or portions of the patient encounter that the interpreter’s services were used. Yet, language interpretation alone can be inadequate without document translation. According to one study, despite the availability of on-site professional interpreter services, hospitalized patients who do not speak English are less likely to have signed consent forms in their medical records.11 Health care professionals, therefore, need well-translated documents to treat LEP patients. Translated documents of consent forms for medical procedures, post-discharge instructions, prescription and medical device labels, and drug usage information may enhance informed decision making, safety and reduce stress and medical errors.
An unpopular and underused service needs it all: availability, convenience, monitoring, reporting, and team effort. Due to the sheer unpopularity and underuse of interpreter services, institutions should enhance ease of availability, monitor the use and quality of interpreter services, and optimize reporting of language-related errors. Ease of availability goes hand in hand with tapping local resources. Over the years, and even more so during the pandemic, in-person interpretation has transitioned to telephonic or video interpretation due to availability, safety, and cost issues. There are challenges in translating a language, and the absence of a visual channel adds another layer of complexity.
The current body of evidence does not indicate a superior interpreting method. Still, in one study providers and interpreters exposed to all three methods were more critical of remote methods and preferred videoconferencing to the telephone as a remote method. The significantly shorter phone interviews raised questions about the prospects of miscommunication in telephonic interpretation, given the absence of a visual channel.12
One way to bypass language barriers is to recognize the value added by hiring and training bilingual health care providers and fostering cultural competence. International medical graduates in many parts of the country aid in closing language barriers. Language-concordant care enhances trust between patients and physicians, optimizes health outcomes, and advances health equity for diverse populations.13-15 The presence of bilingual providers means more effective and timelier communication and improved patient satisfaction. But, according to a Doximity study, there is a significant “language gap” between those languages spoken by physicians and their patients.16 Hospitals, therefore, should assess, qualify, and incentivize staff who can serve as on-site medical interpreters for patients as a means to facilitate language concordant care for LEP patients.
The Agency of Healthcare Research and Quality (AHRQ) also has a guide on how hospitals can better identify, report, monitor, and prevent medical errors in patients with LEP. Included is the TeamSTEPPS LEP module to help develop and deploy a customized plan to train staff in teamwork skills and lead a medical teamwork improvement initiative.17
“Without my family, I was scared that nobody would understand me”
Back to the case. My patient was recovering well, and I was tying up loose ends on the switch day for the hospitalist teams.
“You will likely be discharged in a couple of days,” I said. She and the family were grateful and satisfied with the care. She had used the interpreter services and also received ethnocultural and language concordant and culturally competent care. Reducing language barriers is one of the crucial ways to reduce racial and ethnic disparities in quality of care and health outcomes, and it starts – in many cases – with identifying LEP patients. Proper use and monitoring of interpreter services, reporting language-related errors, hiring and testing bilingual staff’s language proficiency, and educating staff on cultural awareness are essential strategies for caring for LEP patients.
At my weeks’ end, in my handoff note to the incoming providers, I highlighted: “Patient will benefit from a Hindi speaking provider, Limited English Proficiency.”
Dr. Saigal is a hospitalist and clinical assistant professor of medicine in the division of hospital medicine at the Ohio State University Wexner Medical Center, Columbus.
References
1. Questions and Answers. Limited English Proficiency: A federal interagency website. www.lep.gov/commonly-asked-questions.
2. United States Census Bureau. Percent of people 5 years and over who speak English less than ‘very well’. www.census.gov/library/visualizations/interactive/people-that-speak-english-less-than-very-well.html.
3. Jacobs EA, et al. Overcoming language barriers in health care: Costs and benefits of interpreter services. Am J Public Health. 2004;94(5):866–869. doi: 10.2105/ajph.94.5.866.
4. Gandhi TK, et al. Drug complications in outpatients. J Gen Intern Med. 2000;15(3):149–154. doi: 10.1046/j.1525-1497.2000.04199.x.
5. Karliner LS, et al. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42(2):727–754. doi: 10.1111/j.1475-6773.2006.00629.x.
6. Divi C, et al. Language proficiency and adverse events in US hospitals: a pilot study. Int J Qual Health Care. 2007 Apr;19(2):60-7. doi: 10.1093/intqhc/mzl069.
7. Karliner LS, et al. Identification of limited English proficient patients in clinical care. J Gen Intern Med. 2008;23(10):1555-1560. doi:10.1007/s11606-008-0693-y.
8. Schenker Y, et al. Patterns of interpreter use for hospitalized patients with limited English proficiency. J Gen Intern Med. 2011 Jul;26(7):712-7. doi: 10.1007/s11606-010-1619-z.
9. Office of Minority Health, US Department of Health and Human Services. National Standards for Culturally and Linguistically Appropriate Services in Health Care: Final Report. Washington, DC: US Department of Health and Human Services; 2001. https://minorityhealth.hhs.gov/assets/pdf/checked/finalreport.pdf.
10. www.medicaid.gov/medicaid/financial-management/medicaid-administrative-claiming/translation-and-interpretation-services/index.html
11. Schenker Y, et al. The Impact of Language Barriers on Documentation of Informed Consent at a Hospital with On-Site Interpreter Services. J Gen Intern Med. 2007 Nov;22 Suppl 2(Suppl 2):294-9. doi: 10.1007/s11606-007-0359-1.
12. Locatis C, et al. Comparing in-person, video, and telephonic medical interpretation. J Gen Intern Med. 2010;25(4):345-350. doi:10.1007/s11606-009-1236-x.
13. Dunlap JL, et al. The effects of language concordant care on patient satisfaction and clinical understanding for Hispanic pediatric surgery patients. J Pediatr Surg. 2015 Sep;50(9):1586-9. doi: 10.1016/j.jpedsurg.2014.12.020.
14. Diamond L, et al. A Systematic Review of the Impact of Patient–Physician Non-English Language Concordance on Quality of Care and Outcomes. J Gen Intern Med. 2019 Aug;34(8):1591-1606. doi: 10.1007/s11606-019-04847-5.
15. Ngo-Metzger Q, et al. Providing high-quality care for limited English proficient patients: the importance of language concordance and interpreter use. J Gen Intern Med. 2007 Nov;22 Suppl 2(Suppl 2):324-30. doi: 10.1007/s11606-007-0340-z.
16. https://press.doximity.com/articles/first-ever-national-study-to-examine-different-languages-spoken-by-us-doctors.
17. Agency for Healthcare Research and Quality. Patients with Limited English Proficiency. www.ahrq.gov/teamstepps/lep/index.html.
A hectic Friday morning at the hospital seemed less stressful amid morning greetings and humor from colleagues. In a team room full of hospitalists, life and death are often discussed in detail, ranging from medical discussions to joys and frustrations of the day to philosophy, politics, and more. It is almost impossible to miss something interesting.
People breaking into their native languages over the phone call from home always make me smile. The mention of a “complicated Indian patient unable to use interpreter” caught my attention.
My friend and colleague asked if I would be willing to take over the patient since I could speak Hindi. I was doubtful if I would add anything to make a meaningful difference, given the patient wasn’t even participating in a conversation. However, my colleague’s concern for the patient and faith in me was enough to say, “Sure, let me add her to my list.”
At the bedside, it felt like a classic “acute on chronic” hot mess situation. The patient presented with a generalized rash, anasarca, renal failure, multifocal pneumonia, and delirium. All I could gather from the patient were some incomprehensible words that sounded like Hindi. I called the family to obtain some history and to provide updates. Her son was excited to hear from me, and it didn’t take him long to guess that I was from India. But that could still mean that I might speak any of the twenty-two or more Indian languages.
Answering my questions one by one in perfectly understandable English, he was short and sweet. Suspicious of missing out on details, I offered hesitantly, “You could speak in Hindi with me.” Then came a flood of information with the details, concerns, questions, and what was lost in the translation.
We all attend to patients and families with limited English proficiency (LEP), immigrants, and nonimmigrants. LEP is a term used to describe individuals who do not speak English as their primary language and have a limited ability to read, speak, write, or understand English.1 Recent data from the American Community Survey (2005-2009) reports that 8.6% of the population (24 million Americans) have LEP.2 It’s a large and growing population that needs help overcoming language barriers and the appropriate use of professional medical interpreter services – a backbone to safe, quality, and cost-effective patient care.
The following day at bedside rounds, the nurse reported that the patient was looking and responding better. She could cooperate with interpreter services and could speak “some English.” Over the years, one thing that sounds more alarming than “no English” is “some English” or “enough English.” Around noon I received a page that the patient was refusing intravenous Lasix. At the bedside, however, the patient seemed unaware of the perceived refusal. Further discussions with the nurse lead to a familiar culprit, a relatively common gesture in South Asian cultures, a head bobble or shake.
The nurse reported that the patient shook her head side to side, seemed upset, and said “NO” when trying to administer the medication. On the other hand, the patient reported that she was upset to be at the hospital but had “NO” problem with the medicine.
My patient’s “some English” was indeed “enough English” to put her at risk due to medical error, which is highly likely when patients or providers can speak or understand a language to “get by” or to “make do.” Like my patient, the LEP patient population is more likely to experience medical errors, longer hospital stays, hospital-acquired complications, surgical delays, and readmissions. They are also less likely to receive preventive care, have access to regular care, or be satisfied with their care. They are much more likely to have adverse effects from drug complications, poor understanding of diagnoses, a greater risk of being misunderstood by their physicians or ancillary staff, and less likely to follow physician instructions.3-5 One study analyzed over 1,000 adverse-incident reports from six Joint Commission-accredited hospitals for LEP and English-speaking patients and found that 49% of LEP patients experienced physical harm versus 29.5% of English-speaking patients.6
I updated the patient’s LEP status that was missing in the chart, likely due to altered mental status at the time of admission. Reliable language and English proficiency data are usually entered at the patient’s point of entry with documentation of the language services required during the patient-provider encounter. The U.S. Census Bureau’s operational definition for LEP is a patient’s self-assessed ability to speak English less than “very well,” but how well it correlates with a patient’s actual English ability needs more study. Also, one’s self-assessed perception of ability might vary day to day, and language ability, by itself, is not static; it can differ from moment to moment and situation to situation. It may be easier to understand words in English when the situation is simple and less stressful than when things are complicated and stressful.
With a definition of LEP rather vague and the term somewhat derogatory, its meaning is open to interpretation. One study found that though speaking English less than “very well” was the most sensitive measure for identifying all of the patients who reported that they were unable to communicate effectively with their physicians, it was also the least specific.7 This lower specificity could lead to misclassification of some patients as LEP who are, in fact, able to effectively communicate in English with their physicians. This type of misclassification might lead to costly language assistance and carry the potential to cause conflicts between patient and provider. Telling a patient or family that they may have a “limited English proficiency” when they have believed otherwise and feel confident about their skills may come as a challenge. Some patients may also pretend to understand English to avoid being embarrassed about their linguistic abilities or perceive that they might be judged on their abilities in general.
Exiting the room, I gently reminded the RN to use the interpreter services. “Who has never been guilty of using an ad hoc interpreter or rushing through a long interpreter phone call due to time constraints?” I thought. A study from 2011 found that 43% of hospitalized patients with LEP had communicated without an interpreter present during admission, and 40% had communicated without an interpreter present after admission.8 In other words, a system in place does not mean service in use. But, the use of a trained interpreter is not only an obligation for care providers but a right for patients as per legal requirements of Title VI of the Civil Rights Act and the Standards for Culturally and Linguistically Appropriate Services (CLAS) by the Department of Health and Human Services’ (HSS) Office of Minority Health.9 In January 2010, The Joint Commission released a set of new and revised standards for patient-centered communication as part of an initiative to advance effective communication, cultural competence, and patient- and family-centered care.
Despite the requirements and availability of qualified medical interpreter services, there are multiple perceived and experienced barriers to the use of interpreter services. The most common one is that what comes as a free service for patients is a time commitment for providers. A long list of patients, acuity of the situation, and ease of use/availability of translation aids can change the calculus. One may be able to bill a prolonged service code (99354-99357) in addition to the appropriate E/M code, although a patient cannot be billed for the actual service provided by the interpreter. Longstanding CMS policy also permits reimbursement for translation/interpretation activities, so long as they are not included and paid for as part of the rate for direct service.10
The patient, however, insisted that she would rather have her son as the interpreter on the 3-way over the phone (OPI) conference call for interpretation. “He speaks good English and knows my medical history well,” she said. I counseled the patient on the benefits of using interpreter services and explained how to use the call button light and the visual aids.
Placing emphasis on educating patients about the benefits of using, and risks of not using, interpreter services is as essential as emphasizing that care providers use the services. Some patients may voluntarily choose to provide their own interpreter. Use of family members, friends, or unqualified staff as interpreters is one of the most commonly reported causes of errors by frontline staff. Using in-language collateral may help these patients understand how medical interpretation may create a better patient experience and outcome. A short factsheet, in different languages, on qualified interpreters’ expected benefits: meaning-for-meaning communication, impartiality, medical privacy, and improved patient safety and satisfaction, can also come in handy.
However, if the patient still refuses, providers should document the refusal of the offer of free language services, the name of the interpreter designated by the patient, the interpreter’s relationship to the LEP person, and the time or portions of the patient encounter that the interpreter’s services were used. Yet, language interpretation alone can be inadequate without document translation. According to one study, despite the availability of on-site professional interpreter services, hospitalized patients who do not speak English are less likely to have signed consent forms in their medical records.11 Health care professionals, therefore, need well-translated documents to treat LEP patients. Translated documents of consent forms for medical procedures, post-discharge instructions, prescription and medical device labels, and drug usage information may enhance informed decision making, safety and reduce stress and medical errors.
An unpopular and underused service needs it all: availability, convenience, monitoring, reporting, and team effort. Due to the sheer unpopularity and underuse of interpreter services, institutions should enhance ease of availability, monitor the use and quality of interpreter services, and optimize reporting of language-related errors. Ease of availability goes hand in hand with tapping local resources. Over the years, and even more so during the pandemic, in-person interpretation has transitioned to telephonic or video interpretation due to availability, safety, and cost issues. There are challenges in translating a language, and the absence of a visual channel adds another layer of complexity.
The current body of evidence does not indicate a superior interpreting method. Still, in one study providers and interpreters exposed to all three methods were more critical of remote methods and preferred videoconferencing to the telephone as a remote method. The significantly shorter phone interviews raised questions about the prospects of miscommunication in telephonic interpretation, given the absence of a visual channel.12
One way to bypass language barriers is to recognize the value added by hiring and training bilingual health care providers and fostering cultural competence. International medical graduates in many parts of the country aid in closing language barriers. Language-concordant care enhances trust between patients and physicians, optimizes health outcomes, and advances health equity for diverse populations.13-15 The presence of bilingual providers means more effective and timelier communication and improved patient satisfaction. But, according to a Doximity study, there is a significant “language gap” between those languages spoken by physicians and their patients.16 Hospitals, therefore, should assess, qualify, and incentivize staff who can serve as on-site medical interpreters for patients as a means to facilitate language concordant care for LEP patients.
The Agency of Healthcare Research and Quality (AHRQ) also has a guide on how hospitals can better identify, report, monitor, and prevent medical errors in patients with LEP. Included is the TeamSTEPPS LEP module to help develop and deploy a customized plan to train staff in teamwork skills and lead a medical teamwork improvement initiative.17
“Without my family, I was scared that nobody would understand me”
Back to the case. My patient was recovering well, and I was tying up loose ends on the switch day for the hospitalist teams.
“You will likely be discharged in a couple of days,” I said. She and the family were grateful and satisfied with the care. She had used the interpreter services and also received ethnocultural and language concordant and culturally competent care. Reducing language barriers is one of the crucial ways to reduce racial and ethnic disparities in quality of care and health outcomes, and it starts – in many cases – with identifying LEP patients. Proper use and monitoring of interpreter services, reporting language-related errors, hiring and testing bilingual staff’s language proficiency, and educating staff on cultural awareness are essential strategies for caring for LEP patients.
At my weeks’ end, in my handoff note to the incoming providers, I highlighted: “Patient will benefit from a Hindi speaking provider, Limited English Proficiency.”
Dr. Saigal is a hospitalist and clinical assistant professor of medicine in the division of hospital medicine at the Ohio State University Wexner Medical Center, Columbus.
References
1. Questions and Answers. Limited English Proficiency: A federal interagency website. www.lep.gov/commonly-asked-questions.
2. United States Census Bureau. Percent of people 5 years and over who speak English less than ‘very well’. www.census.gov/library/visualizations/interactive/people-that-speak-english-less-than-very-well.html.
3. Jacobs EA, et al. Overcoming language barriers in health care: Costs and benefits of interpreter services. Am J Public Health. 2004;94(5):866–869. doi: 10.2105/ajph.94.5.866.
4. Gandhi TK, et al. Drug complications in outpatients. J Gen Intern Med. 2000;15(3):149–154. doi: 10.1046/j.1525-1497.2000.04199.x.
5. Karliner LS, et al. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42(2):727–754. doi: 10.1111/j.1475-6773.2006.00629.x.
6. Divi C, et al. Language proficiency and adverse events in US hospitals: a pilot study. Int J Qual Health Care. 2007 Apr;19(2):60-7. doi: 10.1093/intqhc/mzl069.
7. Karliner LS, et al. Identification of limited English proficient patients in clinical care. J Gen Intern Med. 2008;23(10):1555-1560. doi:10.1007/s11606-008-0693-y.
8. Schenker Y, et al. Patterns of interpreter use for hospitalized patients with limited English proficiency. J Gen Intern Med. 2011 Jul;26(7):712-7. doi: 10.1007/s11606-010-1619-z.
9. Office of Minority Health, US Department of Health and Human Services. National Standards for Culturally and Linguistically Appropriate Services in Health Care: Final Report. Washington, DC: US Department of Health and Human Services; 2001. https://minorityhealth.hhs.gov/assets/pdf/checked/finalreport.pdf.
10. www.medicaid.gov/medicaid/financial-management/medicaid-administrative-claiming/translation-and-interpretation-services/index.html
11. Schenker Y, et al. The Impact of Language Barriers on Documentation of Informed Consent at a Hospital with On-Site Interpreter Services. J Gen Intern Med. 2007 Nov;22 Suppl 2(Suppl 2):294-9. doi: 10.1007/s11606-007-0359-1.
12. Locatis C, et al. Comparing in-person, video, and telephonic medical interpretation. J Gen Intern Med. 2010;25(4):345-350. doi:10.1007/s11606-009-1236-x.
13. Dunlap JL, et al. The effects of language concordant care on patient satisfaction and clinical understanding for Hispanic pediatric surgery patients. J Pediatr Surg. 2015 Sep;50(9):1586-9. doi: 10.1016/j.jpedsurg.2014.12.020.
14. Diamond L, et al. A Systematic Review of the Impact of Patient–Physician Non-English Language Concordance on Quality of Care and Outcomes. J Gen Intern Med. 2019 Aug;34(8):1591-1606. doi: 10.1007/s11606-019-04847-5.
15. Ngo-Metzger Q, et al. Providing high-quality care for limited English proficient patients: the importance of language concordance and interpreter use. J Gen Intern Med. 2007 Nov;22 Suppl 2(Suppl 2):324-30. doi: 10.1007/s11606-007-0340-z.
16. https://press.doximity.com/articles/first-ever-national-study-to-examine-different-languages-spoken-by-us-doctors.
17. Agency for Healthcare Research and Quality. Patients with Limited English Proficiency. www.ahrq.gov/teamstepps/lep/index.html.
A hectic Friday morning at the hospital seemed less stressful amid morning greetings and humor from colleagues. In a team room full of hospitalists, life and death are often discussed in detail, ranging from medical discussions to joys and frustrations of the day to philosophy, politics, and more. It is almost impossible to miss something interesting.
People breaking into their native languages over the phone call from home always make me smile. The mention of a “complicated Indian patient unable to use interpreter” caught my attention.
My friend and colleague asked if I would be willing to take over the patient since I could speak Hindi. I was doubtful if I would add anything to make a meaningful difference, given the patient wasn’t even participating in a conversation. However, my colleague’s concern for the patient and faith in me was enough to say, “Sure, let me add her to my list.”
At the bedside, it felt like a classic “acute on chronic” hot mess situation. The patient presented with a generalized rash, anasarca, renal failure, multifocal pneumonia, and delirium. All I could gather from the patient were some incomprehensible words that sounded like Hindi. I called the family to obtain some history and to provide updates. Her son was excited to hear from me, and it didn’t take him long to guess that I was from India. But that could still mean that I might speak any of the twenty-two or more Indian languages.
Answering my questions one by one in perfectly understandable English, he was short and sweet. Suspicious of missing out on details, I offered hesitantly, “You could speak in Hindi with me.” Then came a flood of information with the details, concerns, questions, and what was lost in the translation.
We all attend to patients and families with limited English proficiency (LEP), immigrants, and nonimmigrants. LEP is a term used to describe individuals who do not speak English as their primary language and have a limited ability to read, speak, write, or understand English.1 Recent data from the American Community Survey (2005-2009) reports that 8.6% of the population (24 million Americans) have LEP.2 It’s a large and growing population that needs help overcoming language barriers and the appropriate use of professional medical interpreter services – a backbone to safe, quality, and cost-effective patient care.
The following day at bedside rounds, the nurse reported that the patient was looking and responding better. She could cooperate with interpreter services and could speak “some English.” Over the years, one thing that sounds more alarming than “no English” is “some English” or “enough English.” Around noon I received a page that the patient was refusing intravenous Lasix. At the bedside, however, the patient seemed unaware of the perceived refusal. Further discussions with the nurse lead to a familiar culprit, a relatively common gesture in South Asian cultures, a head bobble or shake.
The nurse reported that the patient shook her head side to side, seemed upset, and said “NO” when trying to administer the medication. On the other hand, the patient reported that she was upset to be at the hospital but had “NO” problem with the medicine.
My patient’s “some English” was indeed “enough English” to put her at risk due to medical error, which is highly likely when patients or providers can speak or understand a language to “get by” or to “make do.” Like my patient, the LEP patient population is more likely to experience medical errors, longer hospital stays, hospital-acquired complications, surgical delays, and readmissions. They are also less likely to receive preventive care, have access to regular care, or be satisfied with their care. They are much more likely to have adverse effects from drug complications, poor understanding of diagnoses, a greater risk of being misunderstood by their physicians or ancillary staff, and less likely to follow physician instructions.3-5 One study analyzed over 1,000 adverse-incident reports from six Joint Commission-accredited hospitals for LEP and English-speaking patients and found that 49% of LEP patients experienced physical harm versus 29.5% of English-speaking patients.6
I updated the patient’s LEP status that was missing in the chart, likely due to altered mental status at the time of admission. Reliable language and English proficiency data are usually entered at the patient’s point of entry with documentation of the language services required during the patient-provider encounter. The U.S. Census Bureau’s operational definition for LEP is a patient’s self-assessed ability to speak English less than “very well,” but how well it correlates with a patient’s actual English ability needs more study. Also, one’s self-assessed perception of ability might vary day to day, and language ability, by itself, is not static; it can differ from moment to moment and situation to situation. It may be easier to understand words in English when the situation is simple and less stressful than when things are complicated and stressful.
With a definition of LEP rather vague and the term somewhat derogatory, its meaning is open to interpretation. One study found that though speaking English less than “very well” was the most sensitive measure for identifying all of the patients who reported that they were unable to communicate effectively with their physicians, it was also the least specific.7 This lower specificity could lead to misclassification of some patients as LEP who are, in fact, able to effectively communicate in English with their physicians. This type of misclassification might lead to costly language assistance and carry the potential to cause conflicts between patient and provider. Telling a patient or family that they may have a “limited English proficiency” when they have believed otherwise and feel confident about their skills may come as a challenge. Some patients may also pretend to understand English to avoid being embarrassed about their linguistic abilities or perceive that they might be judged on their abilities in general.
Exiting the room, I gently reminded the RN to use the interpreter services. “Who has never been guilty of using an ad hoc interpreter or rushing through a long interpreter phone call due to time constraints?” I thought. A study from 2011 found that 43% of hospitalized patients with LEP had communicated without an interpreter present during admission, and 40% had communicated without an interpreter present after admission.8 In other words, a system in place does not mean service in use. But, the use of a trained interpreter is not only an obligation for care providers but a right for patients as per legal requirements of Title VI of the Civil Rights Act and the Standards for Culturally and Linguistically Appropriate Services (CLAS) by the Department of Health and Human Services’ (HSS) Office of Minority Health.9 In January 2010, The Joint Commission released a set of new and revised standards for patient-centered communication as part of an initiative to advance effective communication, cultural competence, and patient- and family-centered care.
Despite the requirements and availability of qualified medical interpreter services, there are multiple perceived and experienced barriers to the use of interpreter services. The most common one is that what comes as a free service for patients is a time commitment for providers. A long list of patients, acuity of the situation, and ease of use/availability of translation aids can change the calculus. One may be able to bill a prolonged service code (99354-99357) in addition to the appropriate E/M code, although a patient cannot be billed for the actual service provided by the interpreter. Longstanding CMS policy also permits reimbursement for translation/interpretation activities, so long as they are not included and paid for as part of the rate for direct service.10
The patient, however, insisted that she would rather have her son as the interpreter on the 3-way over the phone (OPI) conference call for interpretation. “He speaks good English and knows my medical history well,” she said. I counseled the patient on the benefits of using interpreter services and explained how to use the call button light and the visual aids.
Placing emphasis on educating patients about the benefits of using, and risks of not using, interpreter services is as essential as emphasizing that care providers use the services. Some patients may voluntarily choose to provide their own interpreter. Use of family members, friends, or unqualified staff as interpreters is one of the most commonly reported causes of errors by frontline staff. Using in-language collateral may help these patients understand how medical interpretation may create a better patient experience and outcome. A short factsheet, in different languages, on qualified interpreters’ expected benefits: meaning-for-meaning communication, impartiality, medical privacy, and improved patient safety and satisfaction, can also come in handy.
However, if the patient still refuses, providers should document the refusal of the offer of free language services, the name of the interpreter designated by the patient, the interpreter’s relationship to the LEP person, and the time or portions of the patient encounter that the interpreter’s services were used. Yet, language interpretation alone can be inadequate without document translation. According to one study, despite the availability of on-site professional interpreter services, hospitalized patients who do not speak English are less likely to have signed consent forms in their medical records.11 Health care professionals, therefore, need well-translated documents to treat LEP patients. Translated documents of consent forms for medical procedures, post-discharge instructions, prescription and medical device labels, and drug usage information may enhance informed decision making, safety and reduce stress and medical errors.
An unpopular and underused service needs it all: availability, convenience, monitoring, reporting, and team effort. Due to the sheer unpopularity and underuse of interpreter services, institutions should enhance ease of availability, monitor the use and quality of interpreter services, and optimize reporting of language-related errors. Ease of availability goes hand in hand with tapping local resources. Over the years, and even more so during the pandemic, in-person interpretation has transitioned to telephonic or video interpretation due to availability, safety, and cost issues. There are challenges in translating a language, and the absence of a visual channel adds another layer of complexity.
The current body of evidence does not indicate a superior interpreting method. Still, in one study providers and interpreters exposed to all three methods were more critical of remote methods and preferred videoconferencing to the telephone as a remote method. The significantly shorter phone interviews raised questions about the prospects of miscommunication in telephonic interpretation, given the absence of a visual channel.12
One way to bypass language barriers is to recognize the value added by hiring and training bilingual health care providers and fostering cultural competence. International medical graduates in many parts of the country aid in closing language barriers. Language-concordant care enhances trust between patients and physicians, optimizes health outcomes, and advances health equity for diverse populations.13-15 The presence of bilingual providers means more effective and timelier communication and improved patient satisfaction. But, according to a Doximity study, there is a significant “language gap” between those languages spoken by physicians and their patients.16 Hospitals, therefore, should assess, qualify, and incentivize staff who can serve as on-site medical interpreters for patients as a means to facilitate language concordant care for LEP patients.
The Agency of Healthcare Research and Quality (AHRQ) also has a guide on how hospitals can better identify, report, monitor, and prevent medical errors in patients with LEP. Included is the TeamSTEPPS LEP module to help develop and deploy a customized plan to train staff in teamwork skills and lead a medical teamwork improvement initiative.17
“Without my family, I was scared that nobody would understand me”
Back to the case. My patient was recovering well, and I was tying up loose ends on the switch day for the hospitalist teams.
“You will likely be discharged in a couple of days,” I said. She and the family were grateful and satisfied with the care. She had used the interpreter services and also received ethnocultural and language concordant and culturally competent care. Reducing language barriers is one of the crucial ways to reduce racial and ethnic disparities in quality of care and health outcomes, and it starts – in many cases – with identifying LEP patients. Proper use and monitoring of interpreter services, reporting language-related errors, hiring and testing bilingual staff’s language proficiency, and educating staff on cultural awareness are essential strategies for caring for LEP patients.
At my weeks’ end, in my handoff note to the incoming providers, I highlighted: “Patient will benefit from a Hindi speaking provider, Limited English Proficiency.”
Dr. Saigal is a hospitalist and clinical assistant professor of medicine in the division of hospital medicine at the Ohio State University Wexner Medical Center, Columbus.
References
1. Questions and Answers. Limited English Proficiency: A federal interagency website. www.lep.gov/commonly-asked-questions.
2. United States Census Bureau. Percent of people 5 years and over who speak English less than ‘very well’. www.census.gov/library/visualizations/interactive/people-that-speak-english-less-than-very-well.html.
3. Jacobs EA, et al. Overcoming language barriers in health care: Costs and benefits of interpreter services. Am J Public Health. 2004;94(5):866–869. doi: 10.2105/ajph.94.5.866.
4. Gandhi TK, et al. Drug complications in outpatients. J Gen Intern Med. 2000;15(3):149–154. doi: 10.1046/j.1525-1497.2000.04199.x.
5. Karliner LS, et al. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42(2):727–754. doi: 10.1111/j.1475-6773.2006.00629.x.
6. Divi C, et al. Language proficiency and adverse events in US hospitals: a pilot study. Int J Qual Health Care. 2007 Apr;19(2):60-7. doi: 10.1093/intqhc/mzl069.
7. Karliner LS, et al. Identification of limited English proficient patients in clinical care. J Gen Intern Med. 2008;23(10):1555-1560. doi:10.1007/s11606-008-0693-y.
8. Schenker Y, et al. Patterns of interpreter use for hospitalized patients with limited English proficiency. J Gen Intern Med. 2011 Jul;26(7):712-7. doi: 10.1007/s11606-010-1619-z.
9. Office of Minority Health, US Department of Health and Human Services. National Standards for Culturally and Linguistically Appropriate Services in Health Care: Final Report. Washington, DC: US Department of Health and Human Services; 2001. https://minorityhealth.hhs.gov/assets/pdf/checked/finalreport.pdf.
10. www.medicaid.gov/medicaid/financial-management/medicaid-administrative-claiming/translation-and-interpretation-services/index.html
11. Schenker Y, et al. The Impact of Language Barriers on Documentation of Informed Consent at a Hospital with On-Site Interpreter Services. J Gen Intern Med. 2007 Nov;22 Suppl 2(Suppl 2):294-9. doi: 10.1007/s11606-007-0359-1.
12. Locatis C, et al. Comparing in-person, video, and telephonic medical interpretation. J Gen Intern Med. 2010;25(4):345-350. doi:10.1007/s11606-009-1236-x.
13. Dunlap JL, et al. The effects of language concordant care on patient satisfaction and clinical understanding for Hispanic pediatric surgery patients. J Pediatr Surg. 2015 Sep;50(9):1586-9. doi: 10.1016/j.jpedsurg.2014.12.020.
14. Diamond L, et al. A Systematic Review of the Impact of Patient–Physician Non-English Language Concordance on Quality of Care and Outcomes. J Gen Intern Med. 2019 Aug;34(8):1591-1606. doi: 10.1007/s11606-019-04847-5.
15. Ngo-Metzger Q, et al. Providing high-quality care for limited English proficient patients: the importance of language concordance and interpreter use. J Gen Intern Med. 2007 Nov;22 Suppl 2(Suppl 2):324-30. doi: 10.1007/s11606-007-0340-z.
16. https://press.doximity.com/articles/first-ever-national-study-to-examine-different-languages-spoken-by-us-doctors.
17. Agency for Healthcare Research and Quality. Patients with Limited English Proficiency. www.ahrq.gov/teamstepps/lep/index.html.
Respiratory infection– and asthma-prone children
Some children are more susceptible to viral and bacterial respiratory infections in the first few years of life than others. However, the factors contributing to this susceptibility are incompletely understood. The pathogenesis, development, severity, and clinical outcomes of respiratory infections are largely dependent on the resident composition of the nasopharyngeal microbiome and immune defense.1
Respiratory infections caused by bacteria and/or viruses are a leading cause of death in children in the United States and worldwide. The well-recognized, predominant causative bacteria are Streptococcus pneumoniae (pneumococcus), nontypeable Haemophilus influenzae (Hflu), and Moraxella catarrhalis (Mcat). Respiratory infections caused by these pathogens result in considerable morbidity, mortality, and account for high health care costs. The clinical and laboratory group that I lead in Rochester, N.Y., has been studying acute otitis media (AOM) etiology, epidemiology, pathogenesis, prevention, and treatment for over 3 decades. Our research findings are likely applicable and generalizable to understanding the pathogenesis and immune response to other infectious diseases induced by pneumococcus, Hflu, and Mcat since they are also key pathogens causing sinusitis and lung infections.
Previous immunologic analysis of children with AOM by our group provided clarity in differences between infection-prone children manifest as otitis prone (OP; often referred to in our publications as stringently defined OP because of the stringent diagnostic requirement of tympanocentesis-proven etiology of infection) and non-OP children. We showed that about 90% of OP children have deficient immune responses following nasopharyngeal colonization and AOM, demonstrated by inadequate innate responses and adaptive immune responses.2 Many of these children also showed an increased propensity to viral upper respiratory infection and 30% fail to produce protective antibody responses after injection of routine pediatric vaccines.3,4
In this column, I want to share new information regarding differences in the nasopharyngeal microbiome of children who are respiratory infection prone versus those who are non–respiratory infection prone and children with asthma versus those who do not exhibit that clinical phenotype. We performed a retrospective analysis of clinical samples collected from 358 children, aged 6 months to 5 years, from our prospectively enrolled cohort in Rochester, N.Y., to determine associations between AOM and other childhood respiratory illnesses and nasopharyngeal microbiota. In order to define subgroups of children within the cohort, we used a statistical method called unsupervised clustering analysis to see if relatively unique groups of children could be discerned. The overall cohort successfully clustered into two groups, showing marked differences in the prevalence of respiratory infections and asthma.5 We termed the two clinical phenotypes infection and asthma prone (n = 99, 28% of the children) and non–infection and asthma prone (n = 259, 72% of the children). Infection- and asthma-prone children were significantly more likely to experience recurrent AOM, influenza, sinusitis, pneumonia, asthma, and allergic rhinitis, compared with non–infection- and asthma-prone children (Figure).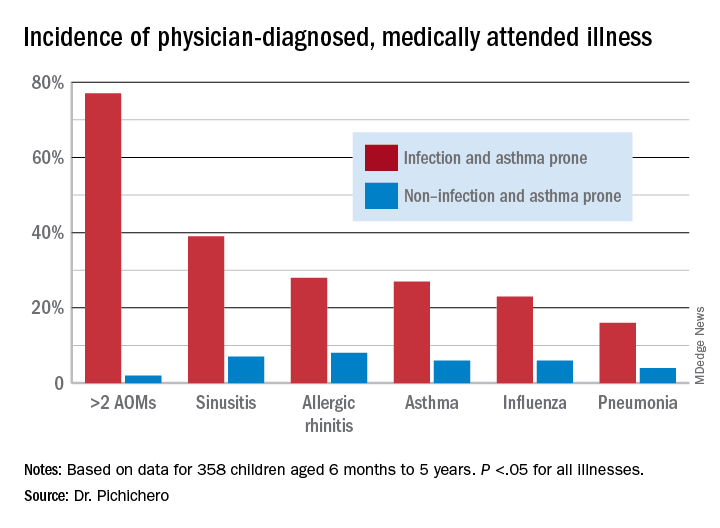
The two groups did not experience significantly different rates of eczema, food allergy, skin infections, urinary tract infections, or acute gastroenteritis, suggesting a common thread involving the respiratory tract that did not cross over to the gastrointestinal, skin, or urinary tract. We found that age at first nasopharyngeal colonization with any of the three bacterial respiratory pathogens (pneumococcus, Hflu, or Mcat) was significantly associated with the respiratory infection– and asthma-prone clinical phenotype. Specifically, respiratory infection– and asthma-prone children experienced colonization at a significantly earlier age than nonprone children did for all three bacteria. In an analysis of individual conditions, early Mcat colonization significantly associated with pneumonia, sinusitis, and asthma susceptibility; Hflu with pneumonia, sinusitis, influenza, and allergic rhinitis; and pneumococcus with sinusitis.
Since early colonization with the three bacterial respiratory pathogens was strongly associated with respiratory illnesses and asthma, nasopharyngeal microbiome analysis was performed on an available subset of samples. Bacterial diversity trended lower in infection- and asthma-prone children, consistent with dysbiosis in the respiratory infection– and asthma-prone clinical phenotype. Nine different bacteria genera were found to be differentially abundant when comparing respiratory infection– and asthma-prone and nonprone children, pointing the way to possible interventions to make the respiratory infection– and asthma-prone child nasopharyngeal microbiome more like the nonprone child.
As I have written previously in this column, recent accumulating data have shed light on the importance of the human microbiome in modulating immune homeostasis and disease susceptibility.6 My group is working toward generating new knowledge for the long-term goal of identifying new therapeutic strategies to facilitate a protective, diverse nasopharyngeal microbiome (with appropriately tuned intranasal probiotics) to prevent respiratory pathogen colonization and/or subsequent progression to respiratory infection and asthma. Also, vaccines directed against colonization-enhancing members of the microbiome may provide a means to indirectly control respiratory pathogen nasopharyngeal colonization.
Dr. Pichichero is a specialist in pediatric infectious diseases and director of the Research Institute at Rochester (N.Y.) General Hospital. He has no conflicts to declare. Contact him at pdnews@mdedge.com
References
1. Man WH et al. Nat Rev Microbiol. 2017;15(5):259-70.
2. Pichichero ME. J Infect. 2020;80(6):614-22.
3. Ren D et al. Clin Infect Dis. 2019;68(9):1566-74.
4. Pichichero ME et al. Pediatr Infect Dis J. 2013;32(11):1163-8.
5. Chapman T et al. PLoS One. 2020 Dec 11;15(12).
6. Blaser MJ. The microbiome revolution. J Clin Invest. 2014;124:4162-5.
Some children are more susceptible to viral and bacterial respiratory infections in the first few years of life than others. However, the factors contributing to this susceptibility are incompletely understood. The pathogenesis, development, severity, and clinical outcomes of respiratory infections are largely dependent on the resident composition of the nasopharyngeal microbiome and immune defense.1
Respiratory infections caused by bacteria and/or viruses are a leading cause of death in children in the United States and worldwide. The well-recognized, predominant causative bacteria are Streptococcus pneumoniae (pneumococcus), nontypeable Haemophilus influenzae (Hflu), and Moraxella catarrhalis (Mcat). Respiratory infections caused by these pathogens result in considerable morbidity, mortality, and account for high health care costs. The clinical and laboratory group that I lead in Rochester, N.Y., has been studying acute otitis media (AOM) etiology, epidemiology, pathogenesis, prevention, and treatment for over 3 decades. Our research findings are likely applicable and generalizable to understanding the pathogenesis and immune response to other infectious diseases induced by pneumococcus, Hflu, and Mcat since they are also key pathogens causing sinusitis and lung infections.
Previous immunologic analysis of children with AOM by our group provided clarity in differences between infection-prone children manifest as otitis prone (OP; often referred to in our publications as stringently defined OP because of the stringent diagnostic requirement of tympanocentesis-proven etiology of infection) and non-OP children. We showed that about 90% of OP children have deficient immune responses following nasopharyngeal colonization and AOM, demonstrated by inadequate innate responses and adaptive immune responses.2 Many of these children also showed an increased propensity to viral upper respiratory infection and 30% fail to produce protective antibody responses after injection of routine pediatric vaccines.3,4
In this column, I want to share new information regarding differences in the nasopharyngeal microbiome of children who are respiratory infection prone versus those who are non–respiratory infection prone and children with asthma versus those who do not exhibit that clinical phenotype. We performed a retrospective analysis of clinical samples collected from 358 children, aged 6 months to 5 years, from our prospectively enrolled cohort in Rochester, N.Y., to determine associations between AOM and other childhood respiratory illnesses and nasopharyngeal microbiota. In order to define subgroups of children within the cohort, we used a statistical method called unsupervised clustering analysis to see if relatively unique groups of children could be discerned. The overall cohort successfully clustered into two groups, showing marked differences in the prevalence of respiratory infections and asthma.5 We termed the two clinical phenotypes infection and asthma prone (n = 99, 28% of the children) and non–infection and asthma prone (n = 259, 72% of the children). Infection- and asthma-prone children were significantly more likely to experience recurrent AOM, influenza, sinusitis, pneumonia, asthma, and allergic rhinitis, compared with non–infection- and asthma-prone children (Figure).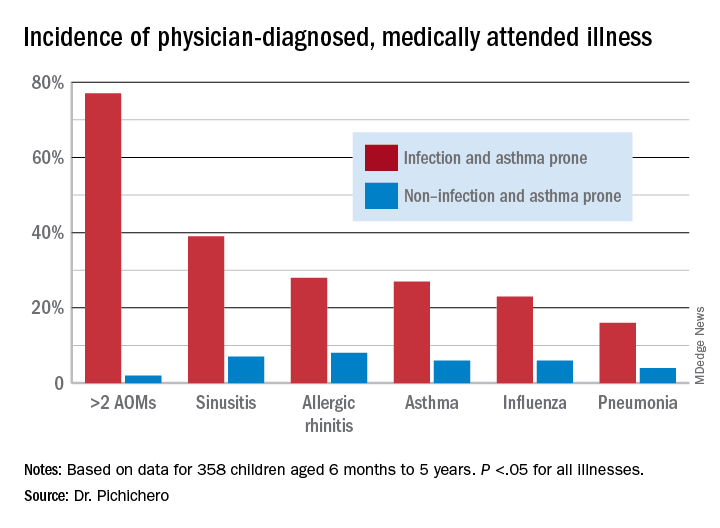
The two groups did not experience significantly different rates of eczema, food allergy, skin infections, urinary tract infections, or acute gastroenteritis, suggesting a common thread involving the respiratory tract that did not cross over to the gastrointestinal, skin, or urinary tract. We found that age at first nasopharyngeal colonization with any of the three bacterial respiratory pathogens (pneumococcus, Hflu, or Mcat) was significantly associated with the respiratory infection– and asthma-prone clinical phenotype. Specifically, respiratory infection– and asthma-prone children experienced colonization at a significantly earlier age than nonprone children did for all three bacteria. In an analysis of individual conditions, early Mcat colonization significantly associated with pneumonia, sinusitis, and asthma susceptibility; Hflu with pneumonia, sinusitis, influenza, and allergic rhinitis; and pneumococcus with sinusitis.
Since early colonization with the three bacterial respiratory pathogens was strongly associated with respiratory illnesses and asthma, nasopharyngeal microbiome analysis was performed on an available subset of samples. Bacterial diversity trended lower in infection- and asthma-prone children, consistent with dysbiosis in the respiratory infection– and asthma-prone clinical phenotype. Nine different bacteria genera were found to be differentially abundant when comparing respiratory infection– and asthma-prone and nonprone children, pointing the way to possible interventions to make the respiratory infection– and asthma-prone child nasopharyngeal microbiome more like the nonprone child.
As I have written previously in this column, recent accumulating data have shed light on the importance of the human microbiome in modulating immune homeostasis and disease susceptibility.6 My group is working toward generating new knowledge for the long-term goal of identifying new therapeutic strategies to facilitate a protective, diverse nasopharyngeal microbiome (with appropriately tuned intranasal probiotics) to prevent respiratory pathogen colonization and/or subsequent progression to respiratory infection and asthma. Also, vaccines directed against colonization-enhancing members of the microbiome may provide a means to indirectly control respiratory pathogen nasopharyngeal colonization.
Dr. Pichichero is a specialist in pediatric infectious diseases and director of the Research Institute at Rochester (N.Y.) General Hospital. He has no conflicts to declare. Contact him at pdnews@mdedge.com
References
1. Man WH et al. Nat Rev Microbiol. 2017;15(5):259-70.
2. Pichichero ME. J Infect. 2020;80(6):614-22.
3. Ren D et al. Clin Infect Dis. 2019;68(9):1566-74.
4. Pichichero ME et al. Pediatr Infect Dis J. 2013;32(11):1163-8.
5. Chapman T et al. PLoS One. 2020 Dec 11;15(12).
6. Blaser MJ. The microbiome revolution. J Clin Invest. 2014;124:4162-5.
Some children are more susceptible to viral and bacterial respiratory infections in the first few years of life than others. However, the factors contributing to this susceptibility are incompletely understood. The pathogenesis, development, severity, and clinical outcomes of respiratory infections are largely dependent on the resident composition of the nasopharyngeal microbiome and immune defense.1
Respiratory infections caused by bacteria and/or viruses are a leading cause of death in children in the United States and worldwide. The well-recognized, predominant causative bacteria are Streptococcus pneumoniae (pneumococcus), nontypeable Haemophilus influenzae (Hflu), and Moraxella catarrhalis (Mcat). Respiratory infections caused by these pathogens result in considerable morbidity, mortality, and account for high health care costs. The clinical and laboratory group that I lead in Rochester, N.Y., has been studying acute otitis media (AOM) etiology, epidemiology, pathogenesis, prevention, and treatment for over 3 decades. Our research findings are likely applicable and generalizable to understanding the pathogenesis and immune response to other infectious diseases induced by pneumococcus, Hflu, and Mcat since they are also key pathogens causing sinusitis and lung infections.
Previous immunologic analysis of children with AOM by our group provided clarity in differences between infection-prone children manifest as otitis prone (OP; often referred to in our publications as stringently defined OP because of the stringent diagnostic requirement of tympanocentesis-proven etiology of infection) and non-OP children. We showed that about 90% of OP children have deficient immune responses following nasopharyngeal colonization and AOM, demonstrated by inadequate innate responses and adaptive immune responses.2 Many of these children also showed an increased propensity to viral upper respiratory infection and 30% fail to produce protective antibody responses after injection of routine pediatric vaccines.3,4
In this column, I want to share new information regarding differences in the nasopharyngeal microbiome of children who are respiratory infection prone versus those who are non–respiratory infection prone and children with asthma versus those who do not exhibit that clinical phenotype. We performed a retrospective analysis of clinical samples collected from 358 children, aged 6 months to 5 years, from our prospectively enrolled cohort in Rochester, N.Y., to determine associations between AOM and other childhood respiratory illnesses and nasopharyngeal microbiota. In order to define subgroups of children within the cohort, we used a statistical method called unsupervised clustering analysis to see if relatively unique groups of children could be discerned. The overall cohort successfully clustered into two groups, showing marked differences in the prevalence of respiratory infections and asthma.5 We termed the two clinical phenotypes infection and asthma prone (n = 99, 28% of the children) and non–infection and asthma prone (n = 259, 72% of the children). Infection- and asthma-prone children were significantly more likely to experience recurrent AOM, influenza, sinusitis, pneumonia, asthma, and allergic rhinitis, compared with non–infection- and asthma-prone children (Figure).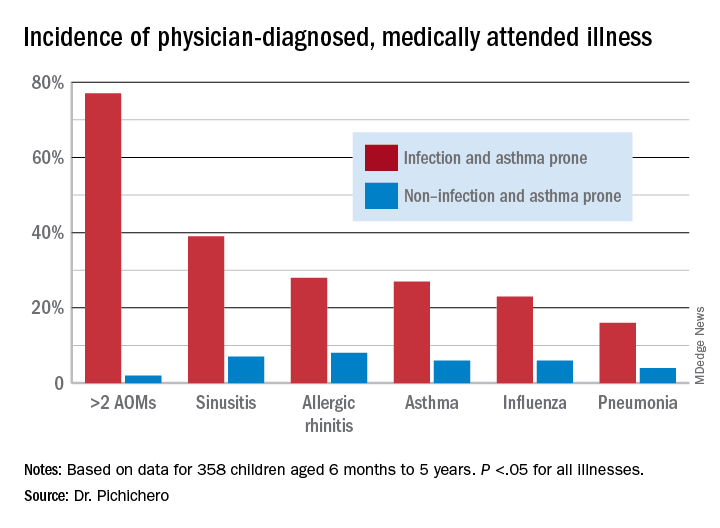
The two groups did not experience significantly different rates of eczema, food allergy, skin infections, urinary tract infections, or acute gastroenteritis, suggesting a common thread involving the respiratory tract that did not cross over to the gastrointestinal, skin, or urinary tract. We found that age at first nasopharyngeal colonization with any of the three bacterial respiratory pathogens (pneumococcus, Hflu, or Mcat) was significantly associated with the respiratory infection– and asthma-prone clinical phenotype. Specifically, respiratory infection– and asthma-prone children experienced colonization at a significantly earlier age than nonprone children did for all three bacteria. In an analysis of individual conditions, early Mcat colonization significantly associated with pneumonia, sinusitis, and asthma susceptibility; Hflu with pneumonia, sinusitis, influenza, and allergic rhinitis; and pneumococcus with sinusitis.
Since early colonization with the three bacterial respiratory pathogens was strongly associated with respiratory illnesses and asthma, nasopharyngeal microbiome analysis was performed on an available subset of samples. Bacterial diversity trended lower in infection- and asthma-prone children, consistent with dysbiosis in the respiratory infection– and asthma-prone clinical phenotype. Nine different bacteria genera were found to be differentially abundant when comparing respiratory infection– and asthma-prone and nonprone children, pointing the way to possible interventions to make the respiratory infection– and asthma-prone child nasopharyngeal microbiome more like the nonprone child.
As I have written previously in this column, recent accumulating data have shed light on the importance of the human microbiome in modulating immune homeostasis and disease susceptibility.6 My group is working toward generating new knowledge for the long-term goal of identifying new therapeutic strategies to facilitate a protective, diverse nasopharyngeal microbiome (with appropriately tuned intranasal probiotics) to prevent respiratory pathogen colonization and/or subsequent progression to respiratory infection and asthma. Also, vaccines directed against colonization-enhancing members of the microbiome may provide a means to indirectly control respiratory pathogen nasopharyngeal colonization.
Dr. Pichichero is a specialist in pediatric infectious diseases and director of the Research Institute at Rochester (N.Y.) General Hospital. He has no conflicts to declare. Contact him at pdnews@mdedge.com
References
1. Man WH et al. Nat Rev Microbiol. 2017;15(5):259-70.
2. Pichichero ME. J Infect. 2020;80(6):614-22.
3. Ren D et al. Clin Infect Dis. 2019;68(9):1566-74.
4. Pichichero ME et al. Pediatr Infect Dis J. 2013;32(11):1163-8.
5. Chapman T et al. PLoS One. 2020 Dec 11;15(12).
6. Blaser MJ. The microbiome revolution. J Clin Invest. 2014;124:4162-5.
‘If only you knew’
Patient:
Alone in the Emergency Dept, breathless, I wait for you
“The Hospitalist will admit you” says the nurse, “she will come in a few.”
Muffled voices – masked faces bustle in & out of the room
Loud beeping machines & the rushed pace, fill me with gloom
You walk in the room, lean in to introduce
You tell me your name and what you will do
For a moment I’m more than a diagnosis, an H&P,
and then the fleeting connection passes, can’t you see?
You listen, seem hurried, but I think you care
Would you sit with me while my story I share?
Physician:
I do see you, I feel your fear & anguish
A moment to know you too, is all that I wish
How do I convince you that I truly care?
When, with all my tasks I have only minutes to spare
Patient:
You diligently ask questions from your checklist of H.P.I.,
Finalizing the diagnosis, when I hear your pager beep.
An admission awaits I know, but please sit by my side
Could we make our new-found meeting, a little more deep?
Physician:
The minute our day begins, it’s go-go-go
There isn’t a second to pause, inhale, or be slow
Missed lunch, it’s 6 p.m., bite to eat I dare?
My shift ended 3 hrs. back but I’m still here
Notes, DC summaries, calls to your PCP
Advocating for you, is more than a job to me.
Tirelessly I work, giving patients my all
Drained, exhausted yet, for you, standing tall
Our bond albeit short lived, is very important to me
Watching you get better each day, is fulfilling for me!
Patient:
You take time to ask about my family, about what I like to do
I tell you all about Beatles & my sweet grandkids
You sit & ask me “what matters most to you”
I reply: getting well for the wedding of my daughter “Sue”
Physician:
I sense loneliness engulfing you at times
Your fear and anxiety, I promise to help overcome
I will help you navigate this complex hospital stay
Together we will fight this virus or anything that comes our way
Each passing minute the line between doctor and patient disappears
That’s when we win over this virus, and hope replaces fear
Patient:
Every day you come see me, tell me my numbers are improving
I notice your warm and kind eyes behind that stifling mask
When they light up as you tell me I’m going home soon
I feel assured I mean more to you, than a mere task
Physician:
Each day I visit, together we hum “here comes the sun”
I too open up and share with you, my favorite Beatles song
Our visits cover much more than clinical medicine
True connection & mutual soul healing begins, before long.
Patient:
Today is the day, grateful to go home,
My body may be healed due to all the medicine & potions,
But my bruised soul was healed due to all your kind emotions.
Time to bid adieu Dear Doc – If I meet you at our local grocery store,
I promise I’ll remember those kind eyes, and wave
After all, you stood between me and death
I’m indebted to you, it’s my life that you did save!
Dr. Mehta is a hospitalist and director of quality and performance and patient experience at Vituity in Emeryville, Calif. She is chair of the SHM patient experience executive council and executive board member of the SHM San Francisco Bay Area chapter.
Patient:
Alone in the Emergency Dept, breathless, I wait for you
“The Hospitalist will admit you” says the nurse, “she will come in a few.”
Muffled voices – masked faces bustle in & out of the room
Loud beeping machines & the rushed pace, fill me with gloom
You walk in the room, lean in to introduce
You tell me your name and what you will do
For a moment I’m more than a diagnosis, an H&P,
and then the fleeting connection passes, can’t you see?
You listen, seem hurried, but I think you care
Would you sit with me while my story I share?
Physician:
I do see you, I feel your fear & anguish
A moment to know you too, is all that I wish
How do I convince you that I truly care?
When, with all my tasks I have only minutes to spare
Patient:
You diligently ask questions from your checklist of H.P.I.,
Finalizing the diagnosis, when I hear your pager beep.
An admission awaits I know, but please sit by my side
Could we make our new-found meeting, a little more deep?
Physician:
The minute our day begins, it’s go-go-go
There isn’t a second to pause, inhale, or be slow
Missed lunch, it’s 6 p.m., bite to eat I dare?
My shift ended 3 hrs. back but I’m still here
Notes, DC summaries, calls to your PCP
Advocating for you, is more than a job to me.
Tirelessly I work, giving patients my all
Drained, exhausted yet, for you, standing tall
Our bond albeit short lived, is very important to me
Watching you get better each day, is fulfilling for me!
Patient:
You take time to ask about my family, about what I like to do
I tell you all about Beatles & my sweet grandkids
You sit & ask me “what matters most to you”
I reply: getting well for the wedding of my daughter “Sue”
Physician:
I sense loneliness engulfing you at times
Your fear and anxiety, I promise to help overcome
I will help you navigate this complex hospital stay
Together we will fight this virus or anything that comes our way
Each passing minute the line between doctor and patient disappears
That’s when we win over this virus, and hope replaces fear
Patient:
Every day you come see me, tell me my numbers are improving
I notice your warm and kind eyes behind that stifling mask
When they light up as you tell me I’m going home soon
I feel assured I mean more to you, than a mere task
Physician:
Each day I visit, together we hum “here comes the sun”
I too open up and share with you, my favorite Beatles song
Our visits cover much more than clinical medicine
True connection & mutual soul healing begins, before long.
Patient:
Today is the day, grateful to go home,
My body may be healed due to all the medicine & potions,
But my bruised soul was healed due to all your kind emotions.
Time to bid adieu Dear Doc – If I meet you at our local grocery store,
I promise I’ll remember those kind eyes, and wave
After all, you stood between me and death
I’m indebted to you, it’s my life that you did save!
Dr. Mehta is a hospitalist and director of quality and performance and patient experience at Vituity in Emeryville, Calif. She is chair of the SHM patient experience executive council and executive board member of the SHM San Francisco Bay Area chapter.
Patient:
Alone in the Emergency Dept, breathless, I wait for you
“The Hospitalist will admit you” says the nurse, “she will come in a few.”
Muffled voices – masked faces bustle in & out of the room
Loud beeping machines & the rushed pace, fill me with gloom
You walk in the room, lean in to introduce
You tell me your name and what you will do
For a moment I’m more than a diagnosis, an H&P,
and then the fleeting connection passes, can’t you see?
You listen, seem hurried, but I think you care
Would you sit with me while my story I share?
Physician:
I do see you, I feel your fear & anguish
A moment to know you too, is all that I wish
How do I convince you that I truly care?
When, with all my tasks I have only minutes to spare
Patient:
You diligently ask questions from your checklist of H.P.I.,
Finalizing the diagnosis, when I hear your pager beep.
An admission awaits I know, but please sit by my side
Could we make our new-found meeting, a little more deep?
Physician:
The minute our day begins, it’s go-go-go
There isn’t a second to pause, inhale, or be slow
Missed lunch, it’s 6 p.m., bite to eat I dare?
My shift ended 3 hrs. back but I’m still here
Notes, DC summaries, calls to your PCP
Advocating for you, is more than a job to me.
Tirelessly I work, giving patients my all
Drained, exhausted yet, for you, standing tall
Our bond albeit short lived, is very important to me
Watching you get better each day, is fulfilling for me!
Patient:
You take time to ask about my family, about what I like to do
I tell you all about Beatles & my sweet grandkids
You sit & ask me “what matters most to you”
I reply: getting well for the wedding of my daughter “Sue”
Physician:
I sense loneliness engulfing you at times
Your fear and anxiety, I promise to help overcome
I will help you navigate this complex hospital stay
Together we will fight this virus or anything that comes our way
Each passing minute the line between doctor and patient disappears
That’s when we win over this virus, and hope replaces fear
Patient:
Every day you come see me, tell me my numbers are improving
I notice your warm and kind eyes behind that stifling mask
When they light up as you tell me I’m going home soon
I feel assured I mean more to you, than a mere task
Physician:
Each day I visit, together we hum “here comes the sun”
I too open up and share with you, my favorite Beatles song
Our visits cover much more than clinical medicine
True connection & mutual soul healing begins, before long.
Patient:
Today is the day, grateful to go home,
My body may be healed due to all the medicine & potions,
But my bruised soul was healed due to all your kind emotions.
Time to bid adieu Dear Doc – If I meet you at our local grocery store,
I promise I’ll remember those kind eyes, and wave
After all, you stood between me and death
I’m indebted to you, it’s my life that you did save!
Dr. Mehta is a hospitalist and director of quality and performance and patient experience at Vituity in Emeryville, Calif. She is chair of the SHM patient experience executive council and executive board member of the SHM San Francisco Bay Area chapter.