User login
My palliative care rotation: Lessons of gratitude, mindfulness, and kindness
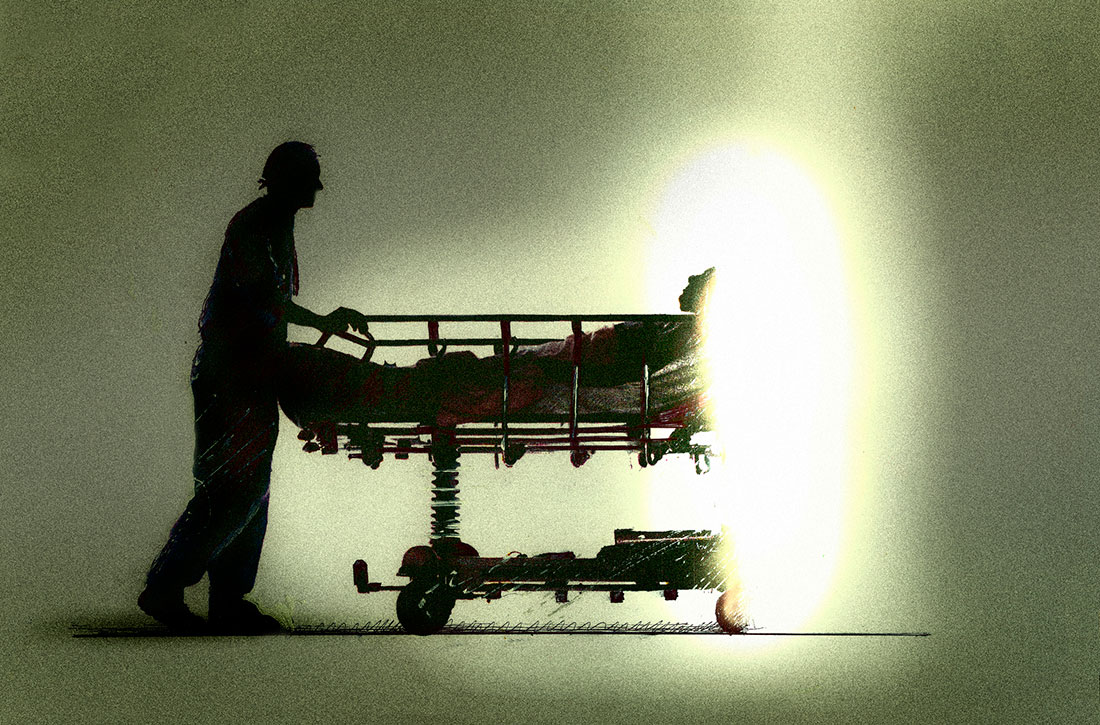
As a psychiatry resident and as a part of consultation-liaison service, I have visited many palliative care patients to assist other physicians in managing psychiatric issues such as depression, anxiety, or delirium. But recently, as the first resident from our Department of Psychiatry who was sent to a palliative care rotation, I followed these patients as a part of a primary palliative care team. Doing so allowed me to see patients from the other side of the bridge.
Palliative care focuses on providing relief from the suffering and stress of a patient’s illness, with the primary goal of improving the quality of life of the patient and their families. The palliative care team works in collaboration with the patient’s other clinicians to provide an extra layer of support. They provide biopsychosociocultural interventions that are in harmony with the needs of the patient rather than the prognosis of the illness. To do so, they first must evaluate the needs of the patient and their family. This is a time-consuming, energy-consuming, emotionally draining job.
During my palliative care rotation, I attended table rounds, bedside rounds, family meetings, long counseling sessions, and disposition planning meetings. This rotation also gave me the opportunity to place my feet in the shoes of a palliative care team and to reflect on how it feels to be the physician of a patient who is dying, which as a psychiatric resident I had seldom experienced. I learned that although working with patients who are dying can cause stress, burnout, and compassion fatigue, it also helps physicians appreciate the little things in life. To appreciate all the blessings we have that we usually take for granted. To practice gratitude. To be kind.
Upon reflection, I learned that the rounds of palliative care are actually mindfulness-based discussions that provide cushions of supportive work, facilitate feelings of being in control, tend to alleviate physical as well as mental suffering, foster clear-sighted hope, and assist in establishing small, subjectively significant, realistic goals for the patient’s immediate future, and to help the patient achieve these goals.
A valuable lesson from a patient
I want to highlight a case of a 65-year-old woman I first visited while I was shadowing my attending, who had been providing palliative care to the patient and her family for several months. The patient was admitted to a tertiary care hospital because cancer had invaded her small bowel and caused mechanical obstruction, resulting in intractable vomiting, abdominal distension, and anorexia. She underwent open laparotomy and ileostomy for symptomatic relief. A nasogastric tube was placed, and she was put on total parenteral nutrition. The day I met her was her third postoperative day. She had been improving significantly, and she wanted to eat. She was missing food. Most of the discussion in the round among my attending, the patient, and her family was centered around how to get to the point where she would be able to eat again and appreciate the taste of biryani.
What my attending did was incredible. After assessing the patient’s needs, he instilled a realistic hope: the hope of tasting food again. The attending, while acknowledging the patient’s apprehensions, respectfully and supportively kept her from wandering into the future, made every possible attempt to bring her attention back to the present moment, and helped her establish goals for the present and her immediate future. My attending was not toxic-positive, forcing his patient to uselessly revisit her current trauma. Instead, he was kind, empathic, and considerate. His primary focus was to understand rather than to be understood, to help her find meaning, and to improve her quality of life—a quality she defined for herself, which was to taste the food of her choice.
That day, when I returned to my working station in the psychiatry ward and had lunch in the break room, I thought, “When I eat, how often do I think about eating?” Mostly I either think about work, tasks, and presentations, or I scroll on social media.
Our taste buds indeed get adapted to repetitive stimulation, but the experience of eating our favorite dish is the naked truth of being alive, and is something that I have been taking for granted for a long time. These are little things in life that I need to appreciate, and learn to cultivate their power.
As a psychiatry resident and as a part of consultation-liaison service, I have visited many palliative care patients to assist other physicians in managing psychiatric issues such as depression, anxiety, or delirium. But recently, as the first resident from our Department of Psychiatry who was sent to a palliative care rotation, I followed these patients as a part of a primary palliative care team. Doing so allowed me to see patients from the other side of the bridge.
Palliative care focuses on providing relief from the suffering and stress of a patient’s illness, with the primary goal of improving the quality of life of the patient and their families. The palliative care team works in collaboration with the patient’s other clinicians to provide an extra layer of support. They provide biopsychosociocultural interventions that are in harmony with the needs of the patient rather than the prognosis of the illness. To do so, they first must evaluate the needs of the patient and their family. This is a time-consuming, energy-consuming, emotionally draining job.
During my palliative care rotation, I attended table rounds, bedside rounds, family meetings, long counseling sessions, and disposition planning meetings. This rotation also gave me the opportunity to place my feet in the shoes of a palliative care team and to reflect on how it feels to be the physician of a patient who is dying, which as a psychiatric resident I had seldom experienced. I learned that although working with patients who are dying can cause stress, burnout, and compassion fatigue, it also helps physicians appreciate the little things in life. To appreciate all the blessings we have that we usually take for granted. To practice gratitude. To be kind.
Upon reflection, I learned that the rounds of palliative care are actually mindfulness-based discussions that provide cushions of supportive work, facilitate feelings of being in control, tend to alleviate physical as well as mental suffering, foster clear-sighted hope, and assist in establishing small, subjectively significant, realistic goals for the patient’s immediate future, and to help the patient achieve these goals.
A valuable lesson from a patient
I want to highlight a case of a 65-year-old woman I first visited while I was shadowing my attending, who had been providing palliative care to the patient and her family for several months. The patient was admitted to a tertiary care hospital because cancer had invaded her small bowel and caused mechanical obstruction, resulting in intractable vomiting, abdominal distension, and anorexia. She underwent open laparotomy and ileostomy for symptomatic relief. A nasogastric tube was placed, and she was put on total parenteral nutrition. The day I met her was her third postoperative day. She had been improving significantly, and she wanted to eat. She was missing food. Most of the discussion in the round among my attending, the patient, and her family was centered around how to get to the point where she would be able to eat again and appreciate the taste of biryani.
What my attending did was incredible. After assessing the patient’s needs, he instilled a realistic hope: the hope of tasting food again. The attending, while acknowledging the patient’s apprehensions, respectfully and supportively kept her from wandering into the future, made every possible attempt to bring her attention back to the present moment, and helped her establish goals for the present and her immediate future. My attending was not toxic-positive, forcing his patient to uselessly revisit her current trauma. Instead, he was kind, empathic, and considerate. His primary focus was to understand rather than to be understood, to help her find meaning, and to improve her quality of life—a quality she defined for herself, which was to taste the food of her choice.
That day, when I returned to my working station in the psychiatry ward and had lunch in the break room, I thought, “When I eat, how often do I think about eating?” Mostly I either think about work, tasks, and presentations, or I scroll on social media.
Our taste buds indeed get adapted to repetitive stimulation, but the experience of eating our favorite dish is the naked truth of being alive, and is something that I have been taking for granted for a long time. These are little things in life that I need to appreciate, and learn to cultivate their power.
As a psychiatry resident and as a part of consultation-liaison service, I have visited many palliative care patients to assist other physicians in managing psychiatric issues such as depression, anxiety, or delirium. But recently, as the first resident from our Department of Psychiatry who was sent to a palliative care rotation, I followed these patients as a part of a primary palliative care team. Doing so allowed me to see patients from the other side of the bridge.
Palliative care focuses on providing relief from the suffering and stress of a patient’s illness, with the primary goal of improving the quality of life of the patient and their families. The palliative care team works in collaboration with the patient’s other clinicians to provide an extra layer of support. They provide biopsychosociocultural interventions that are in harmony with the needs of the patient rather than the prognosis of the illness. To do so, they first must evaluate the needs of the patient and their family. This is a time-consuming, energy-consuming, emotionally draining job.
During my palliative care rotation, I attended table rounds, bedside rounds, family meetings, long counseling sessions, and disposition planning meetings. This rotation also gave me the opportunity to place my feet in the shoes of a palliative care team and to reflect on how it feels to be the physician of a patient who is dying, which as a psychiatric resident I had seldom experienced. I learned that although working with patients who are dying can cause stress, burnout, and compassion fatigue, it also helps physicians appreciate the little things in life. To appreciate all the blessings we have that we usually take for granted. To practice gratitude. To be kind.
Upon reflection, I learned that the rounds of palliative care are actually mindfulness-based discussions that provide cushions of supportive work, facilitate feelings of being in control, tend to alleviate physical as well as mental suffering, foster clear-sighted hope, and assist in establishing small, subjectively significant, realistic goals for the patient’s immediate future, and to help the patient achieve these goals.
A valuable lesson from a patient
I want to highlight a case of a 65-year-old woman I first visited while I was shadowing my attending, who had been providing palliative care to the patient and her family for several months. The patient was admitted to a tertiary care hospital because cancer had invaded her small bowel and caused mechanical obstruction, resulting in intractable vomiting, abdominal distension, and anorexia. She underwent open laparotomy and ileostomy for symptomatic relief. A nasogastric tube was placed, and she was put on total parenteral nutrition. The day I met her was her third postoperative day. She had been improving significantly, and she wanted to eat. She was missing food. Most of the discussion in the round among my attending, the patient, and her family was centered around how to get to the point where she would be able to eat again and appreciate the taste of biryani.
What my attending did was incredible. After assessing the patient’s needs, he instilled a realistic hope: the hope of tasting food again. The attending, while acknowledging the patient’s apprehensions, respectfully and supportively kept her from wandering into the future, made every possible attempt to bring her attention back to the present moment, and helped her establish goals for the present and her immediate future. My attending was not toxic-positive, forcing his patient to uselessly revisit her current trauma. Instead, he was kind, empathic, and considerate. His primary focus was to understand rather than to be understood, to help her find meaning, and to improve her quality of life—a quality she defined for herself, which was to taste the food of her choice.
That day, when I returned to my working station in the psychiatry ward and had lunch in the break room, I thought, “When I eat, how often do I think about eating?” Mostly I either think about work, tasks, and presentations, or I scroll on social media.
Our taste buds indeed get adapted to repetitive stimulation, but the experience of eating our favorite dish is the naked truth of being alive, and is something that I have been taking for granted for a long time. These are little things in life that I need to appreciate, and learn to cultivate their power.
I Never Wanted To Be a Hero
I have been in the business of medicine for more than 15 years and I will never forget the initial surge of the COVID-19 pandemic in Massachusetts.
As a hospitalist, I admitted patients infected with COVID-19, followed them on the floor, and, since I had some experience working in an intensive care unit (ICU), was assigned to cover a “COVID ICU.” This wing of the hospital used to be a fancy orthopedic floor that our institution was lucky enough to have. So began the most life-changing experience in my career as a physician.
In this role, we witness death more than any of us would care to discuss. It comes with the territory, and we never expected this to change once COVID hit. However, so many patients succumbed to this disease, especially during the first surge, which made it difficult to handle emotionally. Patients that fell ill initially stayed isolated at home, optimistic they would turn the corner only to enter the hospital a week later after their conditioned worsened. After requiring a couple of liters of supplemental oxygen in the emergency room, they eventually ended up on a high flow nasal cannula in just a matter of hours.
Patients slowly got sicker and felt more helpless as the days passed, leading us to prescribe drugs that eventually proved to have no benefit. We checked countless inflammatory markers, most of which we were not even sure what to do with. Many times, we hosted a family meeting via FaceTime, holding a patient’s hand in one hand and an iPad in the other to discuss goals of care. Too often, a dark cloud hung over these discussions, a realization that there was not much else we could do.
I have always felt that helping someone have a decent and peaceful death is important, especially when the prognosis is grim, and that patient is suffering. But the sheer number of times this happened during the initial surge of the pandemic was difficult to handle. It felt like I had more of those discussions in 3 months than I did during my entire career as a hospitalist.
We helped plenty of people get better, with some heading home in a week. They thanked us, painted rocks and the sidewalks in front of the hospital displaying messages of gratitude, and sent lunches. Others, though, left the hospital 2 months later with a tube in their stomach so they could receive some form of nutrition and another in their neck to help them breathe.
These struggles were by no means special to me; other hospitalists around the world faced similar situations at one point or another during the pandemic. Working overtime, coming home late, exhausted, undressing in the garage, trying to be there for my 3 kids who were full of energy after a whole day of Zoom and doing the usual kid stuff. My house used to have strict rules about screen time. No more.
The summer months provided a bit of a COVID break, with only 1 or 2 infected patients entering my care. We went to outdoor restaurants and tried to get our lives back to “normal.” As the weather turned cold, however, things went south again. This time no more hydroxychloroquine, a drug used to fight malaria but also treat other autoimmune diseases, as it was proven eventually over many studies that it is not helpful and was potentially harmful. We instead shifted our focus to remdesivir—an antiviral drug that displayed some benefits—tocilizumab, and dexamethasone, anti-inflammatory drugs with the latter providing some positive outcomes on mortality.
Patient survival rates improved slightly, likely due to a combination of factors. We were more experienced at fighting the disease, which led to things in the hospital not being as chaotic and more time available to spend with the patients. Personal protective equipment (PPE) and tests were more readily available, and the population getting hit by the disease changed slightly with fewer elderly people from nursing homes falling ill because of social distancing, other safety measures, or having already fought the disease. Our attention turned instead to more young people that had returned to work and their social lives.
The arrival of the vaccines brought considerable relief. I remember a few decades ago debating and sometimes fighting with friends and family over who was better: Iron Man or Spider-Man. Now I found myself having the same conversation about the Pfizer and Moderna COVID vaccines.
Summer 2021 holds significantly more promise. Most of the adult population is getting vaccinated, and I am very hopeful that we are approaching the end of this nightmare. In June, our office received word that we could remove our masks if we were fully vaccinated. It felt weird, but represented another sign that things are improving. I took my kids to the mall and removed my mask. It felt odd considering how that little blue thing became part of me during the pandemic. It also felt strange to not prescribe a single dose of remdesivir for an entire month.
It feels good—and normal—to care for the patients that we neglected for a year. It has been a needed boost to see patients return to their health care providers for their colonoscopy screenings, mammograms, and managing chronic problems like coronary artery disease, congestive heart failure, or receiving chemotherapy.
I learned plenty from this pandemic and hope I am not alone. I learned to be humble. We started with a drug that was harmful, moved on to a drug that is probably neutral and eventually were able to come up with a drug that seems to decrease mortality at least in some COVID patients. I learned it is fine to try new therapies based on the best data in the hope they result in positive clinical outcomes. However, it is critical that we all keep an eye on the rapidly evolving literature and adjust our behavior accordingly.
I also learned, or relearned, that if people are desperate enough, they will drink bleach to see if it works. Others are convinced that the purpose of vaccination is to inject a microchip allowing ourselves to be tracked by some higher power. I learned that we must take the first step to prepare for the next pandemic by having a decent reserve of PPE.
It is clear synthetic messenger RNA (mRNA) technology is here to stay, and I believe it has a huge potential to change many areas of medicine. mRNA vaccines proved to be much faster to develop and probably much easier to change as the pathogen, in this case coronavirus, changes.
The technology could be used against a variety of infectious diseases to make vaccines against malaria, tuberculosis, HIV, or hepatitis. It can also be very useful for faster vaccine development needed in future possible pandemics such as influenza, Ebola, or severe acute respiratory syndrome. It may also be used for cancer treatment.
As John P. Cooke, MD, PhD, the medical director for the Center of RNA Therapeutics Program at the Houston Methodist Research Institute, said, “Most vaccines today are still viral vaccines – they are inactivated virus, so it’s potentially infectious and you have to have virus on hand. With mRNA, you’re just writing code which is going to tell the cell to make a viral protein – one part of a viral protein to stimulate an immune response. And, here’s the wonderful thing, you don’t even need the virus in hand, just its DNA code.”1
Corresponding author: Dragos Vesbianu, MD, Attending Hospitalist, Newton-Wellesley Hospital, 2014 Washington St, Newton, MA 02462; dragosv@yahoo.com.
Financial dislosures: None.
1. Houston Methodist. Messenger RNA – the Therapy of the Future. Newswise. November 16, 2020. Accessed June 25, 2021. https://www.newswise.com/coronavirus/messenger-rna-the-therapy-of-the-future/
I have been in the business of medicine for more than 15 years and I will never forget the initial surge of the COVID-19 pandemic in Massachusetts.
As a hospitalist, I admitted patients infected with COVID-19, followed them on the floor, and, since I had some experience working in an intensive care unit (ICU), was assigned to cover a “COVID ICU.” This wing of the hospital used to be a fancy orthopedic floor that our institution was lucky enough to have. So began the most life-changing experience in my career as a physician.
In this role, we witness death more than any of us would care to discuss. It comes with the territory, and we never expected this to change once COVID hit. However, so many patients succumbed to this disease, especially during the first surge, which made it difficult to handle emotionally. Patients that fell ill initially stayed isolated at home, optimistic they would turn the corner only to enter the hospital a week later after their conditioned worsened. After requiring a couple of liters of supplemental oxygen in the emergency room, they eventually ended up on a high flow nasal cannula in just a matter of hours.
Patients slowly got sicker and felt more helpless as the days passed, leading us to prescribe drugs that eventually proved to have no benefit. We checked countless inflammatory markers, most of which we were not even sure what to do with. Many times, we hosted a family meeting via FaceTime, holding a patient’s hand in one hand and an iPad in the other to discuss goals of care. Too often, a dark cloud hung over these discussions, a realization that there was not much else we could do.
I have always felt that helping someone have a decent and peaceful death is important, especially when the prognosis is grim, and that patient is suffering. But the sheer number of times this happened during the initial surge of the pandemic was difficult to handle. It felt like I had more of those discussions in 3 months than I did during my entire career as a hospitalist.
We helped plenty of people get better, with some heading home in a week. They thanked us, painted rocks and the sidewalks in front of the hospital displaying messages of gratitude, and sent lunches. Others, though, left the hospital 2 months later with a tube in their stomach so they could receive some form of nutrition and another in their neck to help them breathe.
These struggles were by no means special to me; other hospitalists around the world faced similar situations at one point or another during the pandemic. Working overtime, coming home late, exhausted, undressing in the garage, trying to be there for my 3 kids who were full of energy after a whole day of Zoom and doing the usual kid stuff. My house used to have strict rules about screen time. No more.
The summer months provided a bit of a COVID break, with only 1 or 2 infected patients entering my care. We went to outdoor restaurants and tried to get our lives back to “normal.” As the weather turned cold, however, things went south again. This time no more hydroxychloroquine, a drug used to fight malaria but also treat other autoimmune diseases, as it was proven eventually over many studies that it is not helpful and was potentially harmful. We instead shifted our focus to remdesivir—an antiviral drug that displayed some benefits—tocilizumab, and dexamethasone, anti-inflammatory drugs with the latter providing some positive outcomes on mortality.
Patient survival rates improved slightly, likely due to a combination of factors. We were more experienced at fighting the disease, which led to things in the hospital not being as chaotic and more time available to spend with the patients. Personal protective equipment (PPE) and tests were more readily available, and the population getting hit by the disease changed slightly with fewer elderly people from nursing homes falling ill because of social distancing, other safety measures, or having already fought the disease. Our attention turned instead to more young people that had returned to work and their social lives.
The arrival of the vaccines brought considerable relief. I remember a few decades ago debating and sometimes fighting with friends and family over who was better: Iron Man or Spider-Man. Now I found myself having the same conversation about the Pfizer and Moderna COVID vaccines.
Summer 2021 holds significantly more promise. Most of the adult population is getting vaccinated, and I am very hopeful that we are approaching the end of this nightmare. In June, our office received word that we could remove our masks if we were fully vaccinated. It felt weird, but represented another sign that things are improving. I took my kids to the mall and removed my mask. It felt odd considering how that little blue thing became part of me during the pandemic. It also felt strange to not prescribe a single dose of remdesivir for an entire month.
It feels good—and normal—to care for the patients that we neglected for a year. It has been a needed boost to see patients return to their health care providers for their colonoscopy screenings, mammograms, and managing chronic problems like coronary artery disease, congestive heart failure, or receiving chemotherapy.
I learned plenty from this pandemic and hope I am not alone. I learned to be humble. We started with a drug that was harmful, moved on to a drug that is probably neutral and eventually were able to come up with a drug that seems to decrease mortality at least in some COVID patients. I learned it is fine to try new therapies based on the best data in the hope they result in positive clinical outcomes. However, it is critical that we all keep an eye on the rapidly evolving literature and adjust our behavior accordingly.
I also learned, or relearned, that if people are desperate enough, they will drink bleach to see if it works. Others are convinced that the purpose of vaccination is to inject a microchip allowing ourselves to be tracked by some higher power. I learned that we must take the first step to prepare for the next pandemic by having a decent reserve of PPE.
It is clear synthetic messenger RNA (mRNA) technology is here to stay, and I believe it has a huge potential to change many areas of medicine. mRNA vaccines proved to be much faster to develop and probably much easier to change as the pathogen, in this case coronavirus, changes.
The technology could be used against a variety of infectious diseases to make vaccines against malaria, tuberculosis, HIV, or hepatitis. It can also be very useful for faster vaccine development needed in future possible pandemics such as influenza, Ebola, or severe acute respiratory syndrome. It may also be used for cancer treatment.
As John P. Cooke, MD, PhD, the medical director for the Center of RNA Therapeutics Program at the Houston Methodist Research Institute, said, “Most vaccines today are still viral vaccines – they are inactivated virus, so it’s potentially infectious and you have to have virus on hand. With mRNA, you’re just writing code which is going to tell the cell to make a viral protein – one part of a viral protein to stimulate an immune response. And, here’s the wonderful thing, you don’t even need the virus in hand, just its DNA code.”1
Corresponding author: Dragos Vesbianu, MD, Attending Hospitalist, Newton-Wellesley Hospital, 2014 Washington St, Newton, MA 02462; dragosv@yahoo.com.
Financial dislosures: None.
I have been in the business of medicine for more than 15 years and I will never forget the initial surge of the COVID-19 pandemic in Massachusetts.
As a hospitalist, I admitted patients infected with COVID-19, followed them on the floor, and, since I had some experience working in an intensive care unit (ICU), was assigned to cover a “COVID ICU.” This wing of the hospital used to be a fancy orthopedic floor that our institution was lucky enough to have. So began the most life-changing experience in my career as a physician.
In this role, we witness death more than any of us would care to discuss. It comes with the territory, and we never expected this to change once COVID hit. However, so many patients succumbed to this disease, especially during the first surge, which made it difficult to handle emotionally. Patients that fell ill initially stayed isolated at home, optimistic they would turn the corner only to enter the hospital a week later after their conditioned worsened. After requiring a couple of liters of supplemental oxygen in the emergency room, they eventually ended up on a high flow nasal cannula in just a matter of hours.
Patients slowly got sicker and felt more helpless as the days passed, leading us to prescribe drugs that eventually proved to have no benefit. We checked countless inflammatory markers, most of which we were not even sure what to do with. Many times, we hosted a family meeting via FaceTime, holding a patient’s hand in one hand and an iPad in the other to discuss goals of care. Too often, a dark cloud hung over these discussions, a realization that there was not much else we could do.
I have always felt that helping someone have a decent and peaceful death is important, especially when the prognosis is grim, and that patient is suffering. But the sheer number of times this happened during the initial surge of the pandemic was difficult to handle. It felt like I had more of those discussions in 3 months than I did during my entire career as a hospitalist.
We helped plenty of people get better, with some heading home in a week. They thanked us, painted rocks and the sidewalks in front of the hospital displaying messages of gratitude, and sent lunches. Others, though, left the hospital 2 months later with a tube in their stomach so they could receive some form of nutrition and another in their neck to help them breathe.
These struggles were by no means special to me; other hospitalists around the world faced similar situations at one point or another during the pandemic. Working overtime, coming home late, exhausted, undressing in the garage, trying to be there for my 3 kids who were full of energy after a whole day of Zoom and doing the usual kid stuff. My house used to have strict rules about screen time. No more.
The summer months provided a bit of a COVID break, with only 1 or 2 infected patients entering my care. We went to outdoor restaurants and tried to get our lives back to “normal.” As the weather turned cold, however, things went south again. This time no more hydroxychloroquine, a drug used to fight malaria but also treat other autoimmune diseases, as it was proven eventually over many studies that it is not helpful and was potentially harmful. We instead shifted our focus to remdesivir—an antiviral drug that displayed some benefits—tocilizumab, and dexamethasone, anti-inflammatory drugs with the latter providing some positive outcomes on mortality.
Patient survival rates improved slightly, likely due to a combination of factors. We were more experienced at fighting the disease, which led to things in the hospital not being as chaotic and more time available to spend with the patients. Personal protective equipment (PPE) and tests were more readily available, and the population getting hit by the disease changed slightly with fewer elderly people from nursing homes falling ill because of social distancing, other safety measures, or having already fought the disease. Our attention turned instead to more young people that had returned to work and their social lives.
The arrival of the vaccines brought considerable relief. I remember a few decades ago debating and sometimes fighting with friends and family over who was better: Iron Man or Spider-Man. Now I found myself having the same conversation about the Pfizer and Moderna COVID vaccines.
Summer 2021 holds significantly more promise. Most of the adult population is getting vaccinated, and I am very hopeful that we are approaching the end of this nightmare. In June, our office received word that we could remove our masks if we were fully vaccinated. It felt weird, but represented another sign that things are improving. I took my kids to the mall and removed my mask. It felt odd considering how that little blue thing became part of me during the pandemic. It also felt strange to not prescribe a single dose of remdesivir for an entire month.
It feels good—and normal—to care for the patients that we neglected for a year. It has been a needed boost to see patients return to their health care providers for their colonoscopy screenings, mammograms, and managing chronic problems like coronary artery disease, congestive heart failure, or receiving chemotherapy.
I learned plenty from this pandemic and hope I am not alone. I learned to be humble. We started with a drug that was harmful, moved on to a drug that is probably neutral and eventually were able to come up with a drug that seems to decrease mortality at least in some COVID patients. I learned it is fine to try new therapies based on the best data in the hope they result in positive clinical outcomes. However, it is critical that we all keep an eye on the rapidly evolving literature and adjust our behavior accordingly.
I also learned, or relearned, that if people are desperate enough, they will drink bleach to see if it works. Others are convinced that the purpose of vaccination is to inject a microchip allowing ourselves to be tracked by some higher power. I learned that we must take the first step to prepare for the next pandemic by having a decent reserve of PPE.
It is clear synthetic messenger RNA (mRNA) technology is here to stay, and I believe it has a huge potential to change many areas of medicine. mRNA vaccines proved to be much faster to develop and probably much easier to change as the pathogen, in this case coronavirus, changes.
The technology could be used against a variety of infectious diseases to make vaccines against malaria, tuberculosis, HIV, or hepatitis. It can also be very useful for faster vaccine development needed in future possible pandemics such as influenza, Ebola, or severe acute respiratory syndrome. It may also be used for cancer treatment.
As John P. Cooke, MD, PhD, the medical director for the Center of RNA Therapeutics Program at the Houston Methodist Research Institute, said, “Most vaccines today are still viral vaccines – they are inactivated virus, so it’s potentially infectious and you have to have virus on hand. With mRNA, you’re just writing code which is going to tell the cell to make a viral protein – one part of a viral protein to stimulate an immune response. And, here’s the wonderful thing, you don’t even need the virus in hand, just its DNA code.”1
Corresponding author: Dragos Vesbianu, MD, Attending Hospitalist, Newton-Wellesley Hospital, 2014 Washington St, Newton, MA 02462; dragosv@yahoo.com.
Financial dislosures: None.
1. Houston Methodist. Messenger RNA – the Therapy of the Future. Newswise. November 16, 2020. Accessed June 25, 2021. https://www.newswise.com/coronavirus/messenger-rna-the-therapy-of-the-future/
1. Houston Methodist. Messenger RNA – the Therapy of the Future. Newswise. November 16, 2020. Accessed June 25, 2021. https://www.newswise.com/coronavirus/messenger-rna-the-therapy-of-the-future/
Nowhere to run and nowhere to hide
Not surprisingly, the pandemic has torn at the already fraying fabric of many families. Cooped up away from friends and the emotional relief valve of school, even children who had been relatively easy to manage in the past have posed disciplinary challenges beyond their parents’ abilities to cope.
In a recent study from the Parenting in Context Lab of the University of Michigan (“Child Discipline During the Covid-19 Pandemic,” Family Snapshots: Life During the Pandemic, American Academy of Pediatrics, June 8 2021) researchers found that one in six parents surveyed (n = 3,000 adults) admitted to spanking. Nearly half of the parents said that they had yelled at or threatened their children.
Five out of six parents reported using what the investigators described as less harsh “positive discipline measures.” Three-quarters of these parents used “explaining” as a strategy and nearly the same number used either time-outs or sent the children to their rooms.
Again, not surprisingly, parents who had experienced at least one adverse childhood experience (ACE) were more than twice as likely to spank. And parents who reported an episode of intimate partner violence (IPV) were more likely to resort to a harsh discipline strategy (yelling, threatening, or spanking).
Over my professional career I’ve spent a lot of time thinking about discipline and I have attempted to summarize my thoughts in a book titled, “How to Say No to Your Toddler” (Simon and Schuster, 2003), that has been published in four languages. Based on my observations, trying to explain to a misbehaving child the error of his ways is generally parental time not well spent. A well-structured time-out, preferably in a separate room with a door closed, is the most effective and safest discipline strategy.
However, as in all of my books, this advice on discipline was colored by the families in my practice and the audience for which I was writing, primarily middle class and upper middle class, reasonably affluent parents who buy books. These are usually folks who have homes in which children often have their own rooms, or where at least there are multiple rooms with doors – spaces to escape when tensions rise. Few of these parents have endured ACEs. Few have they experienced – nor have their children witnessed – IPV.
My advice that parents make only threats that can be safely carried, out such as time-out, and to always follow up on threats and promises, is valid regardless of a family’s socioeconomic situation. However, when it comes to choosing a consequence, my standard recommendation of a time-out can be difficult to follow for a family of six living in a three-room apartment, particularly during pandemic-dictated restrictions and lockdowns.
Of course there are alternatives to time-outs in a separate space, including an extended hug in a parental lap, but these responses require that the parents have been able to compose themselves well enough, and that they have the time. One of the important benefits of time-outs is that they can provide parents the time and space to reassess the situation and consider their role in the conflict. The bottom line is that a time-out is the safest and most effective form of discipline, but it requires space and a parent relatively unburdened of financial or emotional stress. Families without these luxuries are left with few alternatives other than physical or verbal abuse.
The AAP’s Family Snapshot concludes with the observation that “pediatricians and pediatric health care providers can continue to play an important role in supporting positive discipline strategies.” That is a difficult assignment even in prepandemic times, but for those of you working with families who lack the space and time to defuse disciplinary tensions, it is a heroic task.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Not surprisingly, the pandemic has torn at the already fraying fabric of many families. Cooped up away from friends and the emotional relief valve of school, even children who had been relatively easy to manage in the past have posed disciplinary challenges beyond their parents’ abilities to cope.
In a recent study from the Parenting in Context Lab of the University of Michigan (“Child Discipline During the Covid-19 Pandemic,” Family Snapshots: Life During the Pandemic, American Academy of Pediatrics, June 8 2021) researchers found that one in six parents surveyed (n = 3,000 adults) admitted to spanking. Nearly half of the parents said that they had yelled at or threatened their children.
Five out of six parents reported using what the investigators described as less harsh “positive discipline measures.” Three-quarters of these parents used “explaining” as a strategy and nearly the same number used either time-outs or sent the children to their rooms.
Again, not surprisingly, parents who had experienced at least one adverse childhood experience (ACE) were more than twice as likely to spank. And parents who reported an episode of intimate partner violence (IPV) were more likely to resort to a harsh discipline strategy (yelling, threatening, or spanking).
Over my professional career I’ve spent a lot of time thinking about discipline and I have attempted to summarize my thoughts in a book titled, “How to Say No to Your Toddler” (Simon and Schuster, 2003), that has been published in four languages. Based on my observations, trying to explain to a misbehaving child the error of his ways is generally parental time not well spent. A well-structured time-out, preferably in a separate room with a door closed, is the most effective and safest discipline strategy.
However, as in all of my books, this advice on discipline was colored by the families in my practice and the audience for which I was writing, primarily middle class and upper middle class, reasonably affluent parents who buy books. These are usually folks who have homes in which children often have their own rooms, or where at least there are multiple rooms with doors – spaces to escape when tensions rise. Few of these parents have endured ACEs. Few have they experienced – nor have their children witnessed – IPV.
My advice that parents make only threats that can be safely carried, out such as time-out, and to always follow up on threats and promises, is valid regardless of a family’s socioeconomic situation. However, when it comes to choosing a consequence, my standard recommendation of a time-out can be difficult to follow for a family of six living in a three-room apartment, particularly during pandemic-dictated restrictions and lockdowns.
Of course there are alternatives to time-outs in a separate space, including an extended hug in a parental lap, but these responses require that the parents have been able to compose themselves well enough, and that they have the time. One of the important benefits of time-outs is that they can provide parents the time and space to reassess the situation and consider their role in the conflict. The bottom line is that a time-out is the safest and most effective form of discipline, but it requires space and a parent relatively unburdened of financial or emotional stress. Families without these luxuries are left with few alternatives other than physical or verbal abuse.
The AAP’s Family Snapshot concludes with the observation that “pediatricians and pediatric health care providers can continue to play an important role in supporting positive discipline strategies.” That is a difficult assignment even in prepandemic times, but for those of you working with families who lack the space and time to defuse disciplinary tensions, it is a heroic task.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Not surprisingly, the pandemic has torn at the already fraying fabric of many families. Cooped up away from friends and the emotional relief valve of school, even children who had been relatively easy to manage in the past have posed disciplinary challenges beyond their parents’ abilities to cope.
In a recent study from the Parenting in Context Lab of the University of Michigan (“Child Discipline During the Covid-19 Pandemic,” Family Snapshots: Life During the Pandemic, American Academy of Pediatrics, June 8 2021) researchers found that one in six parents surveyed (n = 3,000 adults) admitted to spanking. Nearly half of the parents said that they had yelled at or threatened their children.
Five out of six parents reported using what the investigators described as less harsh “positive discipline measures.” Three-quarters of these parents used “explaining” as a strategy and nearly the same number used either time-outs or sent the children to their rooms.
Again, not surprisingly, parents who had experienced at least one adverse childhood experience (ACE) were more than twice as likely to spank. And parents who reported an episode of intimate partner violence (IPV) were more likely to resort to a harsh discipline strategy (yelling, threatening, or spanking).
Over my professional career I’ve spent a lot of time thinking about discipline and I have attempted to summarize my thoughts in a book titled, “How to Say No to Your Toddler” (Simon and Schuster, 2003), that has been published in four languages. Based on my observations, trying to explain to a misbehaving child the error of his ways is generally parental time not well spent. A well-structured time-out, preferably in a separate room with a door closed, is the most effective and safest discipline strategy.
However, as in all of my books, this advice on discipline was colored by the families in my practice and the audience for which I was writing, primarily middle class and upper middle class, reasonably affluent parents who buy books. These are usually folks who have homes in which children often have their own rooms, or where at least there are multiple rooms with doors – spaces to escape when tensions rise. Few of these parents have endured ACEs. Few have they experienced – nor have their children witnessed – IPV.
My advice that parents make only threats that can be safely carried, out such as time-out, and to always follow up on threats and promises, is valid regardless of a family’s socioeconomic situation. However, when it comes to choosing a consequence, my standard recommendation of a time-out can be difficult to follow for a family of six living in a three-room apartment, particularly during pandemic-dictated restrictions and lockdowns.
Of course there are alternatives to time-outs in a separate space, including an extended hug in a parental lap, but these responses require that the parents have been able to compose themselves well enough, and that they have the time. One of the important benefits of time-outs is that they can provide parents the time and space to reassess the situation and consider their role in the conflict. The bottom line is that a time-out is the safest and most effective form of discipline, but it requires space and a parent relatively unburdened of financial or emotional stress. Families without these luxuries are left with few alternatives other than physical or verbal abuse.
The AAP’s Family Snapshot concludes with the observation that “pediatricians and pediatric health care providers can continue to play an important role in supporting positive discipline strategies.” That is a difficult assignment even in prepandemic times, but for those of you working with families who lack the space and time to defuse disciplinary tensions, it is a heroic task.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Advice on biopsies, workups, and referrals
Over the next 2 months we will dedicate this column to some general tips and pearls from the perspective of a gynecologic oncologist to guide general obstetrician gynecologists in the workup and management of preinvasive or invasive gynecologic diseases. The goal of these recommendations is to minimize misdiagnosis or delayed diagnosis and avoid unnecessary or untimely referrals.
Perform biopsy, not Pap smears, on visible cervical and vaginal lesions
The purpose of the Pap smear is to screen asymptomatic patients for cervical dysplasia or microscopic invasive disease. Cytology is an unreliable diagnostic tool for visible, symptomatic lesions in large part because of sampling errors, and the lack of architectural information in cytologic versus histopathologic specimens. Invasive lesions can be mischaracterized as preinvasive on a Pap smear. This can result in delayed diagnosis and unnecessary diagnostic procedures. For example, if a visible, abnormal-appearing, cervical lesion is seen during a routine visit and a Pap smear is performed (rather than a biopsy of the mass), the patient may receive an incorrect preliminary diagnosis of “high-grade dysplasia, carcinoma in situ” as it can be difficult to distinguish invasive carcinoma from carcinoma in situ on cytology. If the patient and provider do not understand the limitations of Pap smears in diagnosing invasive cancers, they may be falsely reassured and possibly delay or abstain from follow-up for an excisional procedure. If she does return for the loop electrosurgical excision procedure (LEEP), there might still be unnecessary delays in making referrals and definitive treatment while waiting for results. Radical hysterectomy may not promptly follow because, if performed within 6 weeks of an excisional procedure, it is associated with a significantly higher risk for perioperative complication, and therefore, if the excisional procedure was unnecessary to begin with, there may be additional time lost that need not be.1
Some clinicians avoid biopsy of visible lesions because they are concerned about bleeding complications that might arise in the office. Straightforward strategies to control bleeding are readily available in most gynecology offices, especially those already equipped for procedures such as LEEP and colposcopy. Prior to performing the biopsy, clinicians should ensure that they have supplies such as gauze sponges and ring forceps or packing forceps, silver nitrate, and ferric subsulfate solution (“Monsel’s solution”) close at hand. In the vast majority of cases, direct pressure for 5 minutes with gauze sponges and ferric subsulfate is highly effective at resolving most bleeding from a cervical or vaginal biopsy site. If this does not bring hemostasis, cautery devices or suture can be employed. If all else fails, be prepared to place vaginal packing (always with the insertion of a urinary Foley catheter to prevent urinary retention). In my experience, this is rarely needed.
Wherever possible, visible cervical or vaginal (or vulvar, see below) lesions should be biopsied for histopathology, sampling representative areas of the most concerning portion, in order to minimize misdiagnosis and expedite referral and definitive treatment. For necrotic-appearing lesions I recommend taking multiple samples of the tumor, as necrotic, nonviable tissue can prevent accurate diagnosis of a cancer. In general, Pap smears should be reserved as screening tests for asymptomatic women without visible pathology.
Don’t treat or refer low-grade dysplasia, even if persistent
Increasingly we are understanding that low-grade dysplasia of the lower genital tract (CIN I, VAIN I, VIN I) is less a precursor for cancer, and more a phenomenon of benign HPV-associated changes.2 This HPV change may be chronically persistent, may require years of observation and serial Pap smears, and may be a general nuisance for the patient. However, current guidelines do not recommend intervention for low-grade dysplasia of the lower genital tract.2 Interventions to resect these lesions can result in morbidity, including perineal pain, vaginal scarring, and cervical stenosis or insufficiency. Given the extremely low risk for progression to cancer, these morbidities do not outweigh any small potential benefit.
When I am conferring with patients who have chronic low-grade dysplasia I spend a great deal of time exploring their understanding of the diagnosis and its pathophysiology, their fears, and their expectation regarding “success” of treatment. I spend the time educating them that this is a sequela of chronic viral infection that will not be eradicated with local surgical excisions, that their cancer risk and need for surveillance would persist even if surgical intervention were offered, and that the side effects of treatment would outweigh any benefit from the small risk of cancer or high-grade dysplasia.
In summary, the treatment of choice for persistent low-grade dysplasia of the lower genital tract is comprehensive patient education, not surgical resection or referral to gynecologic oncology.
Repeat sampling if there’s a discordance between imaging and biopsy results
Delay in cancer diagnosis is one of the greatest concerns for front-line gynecology providers. One of the more modifiable strategies to avoid missed or delayed diagnosis is to ensure that there is concordance between clinical findings and testing results. Otherwise said: The results and findings should make sense in aggregate. An example was cited above in which a visible cervical mass demonstrated CIN III on cytologic testing. Another common example is a biopsy result of “scant benign endometrium” in a patient with postmenopausal bleeding and thickened endometrial stripe on ultrasound. In both of these cases there is clear discordance between physical findings and the results of pathology sampling. A pathology report, in all of its black and white certitude, seems like the most reliable source of information. However, always trust your clinical judgment. If the clinical picture is suggesting something far worse than these limited, often random or blind samplings, I recommend repeated or more extensive sampling (for example, dilation and curettage). At the very least, schedule close follow-up with repeated sampling if the symptom or finding persists. The emphasis here is on scheduled follow-up, rather than “p.r.n.,” because a patient who was given a “normal” pathology result to explain her abnormal symptoms may not volunteer that those symptoms are persistent as she may feel that anything sinister was already ruled out. Make certain that you explain the potential for misdiagnosis as the reason for why you would like to see her back shortly to ensure the issue has resolved.
Biopsy vulvar lesions, minimize empiric treatment
Vulvar cancer is notoriously associated with delayed diagnosis. Unfortunately, it is commonplace for gynecologic oncologists to see women who have vulvar cancers that have been empirically treated, sometimes for months or years, with steroids or other topical agents. If a lesion on the vulva is characteristically benign in appearance (such as condyloma or lichen sclerosis), it may be reasonable to start empiric treatment. However, all patients who are treated without biopsy should be rescheduled for a planned follow-up appointment in 2-3 months. If the lesion/area remains unchanged, or worse, the lesion should be biopsied before proceeding with a change in therapy or continued therapy. Once again, don’t rely on patients to return for evaluation if the lesion doesn’t improve. Many patients assume that our first empiric diagnosis is “gospel,” and therefore may not return if the treatment doesn’t work. Meanwhile, providers may assume that patients will know that there is uncertainty in our interpretation and that they will know to report if the initial treatment didn’t work. These assumptions are the recipe for delayed diagnosis. If there is too great a burden on the patient to schedule a return visit because of social or financial reasons then the patient should have a biopsy prior to initiation of treatment. As a rule, empiric treatment is not a good strategy for patients without good access to follow-up.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at obnews@mdedge.com.
References
1. Sullivan S. et al Gynecol Oncol. 2017 Feb;144(2):294-8.
2. Perkins R .et al J Low Genit Tract Dis. 2020 Apr;24(2):102-31.
Over the next 2 months we will dedicate this column to some general tips and pearls from the perspective of a gynecologic oncologist to guide general obstetrician gynecologists in the workup and management of preinvasive or invasive gynecologic diseases. The goal of these recommendations is to minimize misdiagnosis or delayed diagnosis and avoid unnecessary or untimely referrals.
Perform biopsy, not Pap smears, on visible cervical and vaginal lesions
The purpose of the Pap smear is to screen asymptomatic patients for cervical dysplasia or microscopic invasive disease. Cytology is an unreliable diagnostic tool for visible, symptomatic lesions in large part because of sampling errors, and the lack of architectural information in cytologic versus histopathologic specimens. Invasive lesions can be mischaracterized as preinvasive on a Pap smear. This can result in delayed diagnosis and unnecessary diagnostic procedures. For example, if a visible, abnormal-appearing, cervical lesion is seen during a routine visit and a Pap smear is performed (rather than a biopsy of the mass), the patient may receive an incorrect preliminary diagnosis of “high-grade dysplasia, carcinoma in situ” as it can be difficult to distinguish invasive carcinoma from carcinoma in situ on cytology. If the patient and provider do not understand the limitations of Pap smears in diagnosing invasive cancers, they may be falsely reassured and possibly delay or abstain from follow-up for an excisional procedure. If she does return for the loop electrosurgical excision procedure (LEEP), there might still be unnecessary delays in making referrals and definitive treatment while waiting for results. Radical hysterectomy may not promptly follow because, if performed within 6 weeks of an excisional procedure, it is associated with a significantly higher risk for perioperative complication, and therefore, if the excisional procedure was unnecessary to begin with, there may be additional time lost that need not be.1
Some clinicians avoid biopsy of visible lesions because they are concerned about bleeding complications that might arise in the office. Straightforward strategies to control bleeding are readily available in most gynecology offices, especially those already equipped for procedures such as LEEP and colposcopy. Prior to performing the biopsy, clinicians should ensure that they have supplies such as gauze sponges and ring forceps or packing forceps, silver nitrate, and ferric subsulfate solution (“Monsel’s solution”) close at hand. In the vast majority of cases, direct pressure for 5 minutes with gauze sponges and ferric subsulfate is highly effective at resolving most bleeding from a cervical or vaginal biopsy site. If this does not bring hemostasis, cautery devices or suture can be employed. If all else fails, be prepared to place vaginal packing (always with the insertion of a urinary Foley catheter to prevent urinary retention). In my experience, this is rarely needed.
Wherever possible, visible cervical or vaginal (or vulvar, see below) lesions should be biopsied for histopathology, sampling representative areas of the most concerning portion, in order to minimize misdiagnosis and expedite referral and definitive treatment. For necrotic-appearing lesions I recommend taking multiple samples of the tumor, as necrotic, nonviable tissue can prevent accurate diagnosis of a cancer. In general, Pap smears should be reserved as screening tests for asymptomatic women without visible pathology.
Don’t treat or refer low-grade dysplasia, even if persistent
Increasingly we are understanding that low-grade dysplasia of the lower genital tract (CIN I, VAIN I, VIN I) is less a precursor for cancer, and more a phenomenon of benign HPV-associated changes.2 This HPV change may be chronically persistent, may require years of observation and serial Pap smears, and may be a general nuisance for the patient. However, current guidelines do not recommend intervention for low-grade dysplasia of the lower genital tract.2 Interventions to resect these lesions can result in morbidity, including perineal pain, vaginal scarring, and cervical stenosis or insufficiency. Given the extremely low risk for progression to cancer, these morbidities do not outweigh any small potential benefit.
When I am conferring with patients who have chronic low-grade dysplasia I spend a great deal of time exploring their understanding of the diagnosis and its pathophysiology, their fears, and their expectation regarding “success” of treatment. I spend the time educating them that this is a sequela of chronic viral infection that will not be eradicated with local surgical excisions, that their cancer risk and need for surveillance would persist even if surgical intervention were offered, and that the side effects of treatment would outweigh any benefit from the small risk of cancer or high-grade dysplasia.
In summary, the treatment of choice for persistent low-grade dysplasia of the lower genital tract is comprehensive patient education, not surgical resection or referral to gynecologic oncology.
Repeat sampling if there’s a discordance between imaging and biopsy results
Delay in cancer diagnosis is one of the greatest concerns for front-line gynecology providers. One of the more modifiable strategies to avoid missed or delayed diagnosis is to ensure that there is concordance between clinical findings and testing results. Otherwise said: The results and findings should make sense in aggregate. An example was cited above in which a visible cervical mass demonstrated CIN III on cytologic testing. Another common example is a biopsy result of “scant benign endometrium” in a patient with postmenopausal bleeding and thickened endometrial stripe on ultrasound. In both of these cases there is clear discordance between physical findings and the results of pathology sampling. A pathology report, in all of its black and white certitude, seems like the most reliable source of information. However, always trust your clinical judgment. If the clinical picture is suggesting something far worse than these limited, often random or blind samplings, I recommend repeated or more extensive sampling (for example, dilation and curettage). At the very least, schedule close follow-up with repeated sampling if the symptom or finding persists. The emphasis here is on scheduled follow-up, rather than “p.r.n.,” because a patient who was given a “normal” pathology result to explain her abnormal symptoms may not volunteer that those symptoms are persistent as she may feel that anything sinister was already ruled out. Make certain that you explain the potential for misdiagnosis as the reason for why you would like to see her back shortly to ensure the issue has resolved.
Biopsy vulvar lesions, minimize empiric treatment
Vulvar cancer is notoriously associated with delayed diagnosis. Unfortunately, it is commonplace for gynecologic oncologists to see women who have vulvar cancers that have been empirically treated, sometimes for months or years, with steroids or other topical agents. If a lesion on the vulva is characteristically benign in appearance (such as condyloma or lichen sclerosis), it may be reasonable to start empiric treatment. However, all patients who are treated without biopsy should be rescheduled for a planned follow-up appointment in 2-3 months. If the lesion/area remains unchanged, or worse, the lesion should be biopsied before proceeding with a change in therapy or continued therapy. Once again, don’t rely on patients to return for evaluation if the lesion doesn’t improve. Many patients assume that our first empiric diagnosis is “gospel,” and therefore may not return if the treatment doesn’t work. Meanwhile, providers may assume that patients will know that there is uncertainty in our interpretation and that they will know to report if the initial treatment didn’t work. These assumptions are the recipe for delayed diagnosis. If there is too great a burden on the patient to schedule a return visit because of social or financial reasons then the patient should have a biopsy prior to initiation of treatment. As a rule, empiric treatment is not a good strategy for patients without good access to follow-up.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at obnews@mdedge.com.
References
1. Sullivan S. et al Gynecol Oncol. 2017 Feb;144(2):294-8.
2. Perkins R .et al J Low Genit Tract Dis. 2020 Apr;24(2):102-31.
Over the next 2 months we will dedicate this column to some general tips and pearls from the perspective of a gynecologic oncologist to guide general obstetrician gynecologists in the workup and management of preinvasive or invasive gynecologic diseases. The goal of these recommendations is to minimize misdiagnosis or delayed diagnosis and avoid unnecessary or untimely referrals.
Perform biopsy, not Pap smears, on visible cervical and vaginal lesions
The purpose of the Pap smear is to screen asymptomatic patients for cervical dysplasia or microscopic invasive disease. Cytology is an unreliable diagnostic tool for visible, symptomatic lesions in large part because of sampling errors, and the lack of architectural information in cytologic versus histopathologic specimens. Invasive lesions can be mischaracterized as preinvasive on a Pap smear. This can result in delayed diagnosis and unnecessary diagnostic procedures. For example, if a visible, abnormal-appearing, cervical lesion is seen during a routine visit and a Pap smear is performed (rather than a biopsy of the mass), the patient may receive an incorrect preliminary diagnosis of “high-grade dysplasia, carcinoma in situ” as it can be difficult to distinguish invasive carcinoma from carcinoma in situ on cytology. If the patient and provider do not understand the limitations of Pap smears in diagnosing invasive cancers, they may be falsely reassured and possibly delay or abstain from follow-up for an excisional procedure. If she does return for the loop electrosurgical excision procedure (LEEP), there might still be unnecessary delays in making referrals and definitive treatment while waiting for results. Radical hysterectomy may not promptly follow because, if performed within 6 weeks of an excisional procedure, it is associated with a significantly higher risk for perioperative complication, and therefore, if the excisional procedure was unnecessary to begin with, there may be additional time lost that need not be.1
Some clinicians avoid biopsy of visible lesions because they are concerned about bleeding complications that might arise in the office. Straightforward strategies to control bleeding are readily available in most gynecology offices, especially those already equipped for procedures such as LEEP and colposcopy. Prior to performing the biopsy, clinicians should ensure that they have supplies such as gauze sponges and ring forceps or packing forceps, silver nitrate, and ferric subsulfate solution (“Monsel’s solution”) close at hand. In the vast majority of cases, direct pressure for 5 minutes with gauze sponges and ferric subsulfate is highly effective at resolving most bleeding from a cervical or vaginal biopsy site. If this does not bring hemostasis, cautery devices or suture can be employed. If all else fails, be prepared to place vaginal packing (always with the insertion of a urinary Foley catheter to prevent urinary retention). In my experience, this is rarely needed.
Wherever possible, visible cervical or vaginal (or vulvar, see below) lesions should be biopsied for histopathology, sampling representative areas of the most concerning portion, in order to minimize misdiagnosis and expedite referral and definitive treatment. For necrotic-appearing lesions I recommend taking multiple samples of the tumor, as necrotic, nonviable tissue can prevent accurate diagnosis of a cancer. In general, Pap smears should be reserved as screening tests for asymptomatic women without visible pathology.
Don’t treat or refer low-grade dysplasia, even if persistent
Increasingly we are understanding that low-grade dysplasia of the lower genital tract (CIN I, VAIN I, VIN I) is less a precursor for cancer, and more a phenomenon of benign HPV-associated changes.2 This HPV change may be chronically persistent, may require years of observation and serial Pap smears, and may be a general nuisance for the patient. However, current guidelines do not recommend intervention for low-grade dysplasia of the lower genital tract.2 Interventions to resect these lesions can result in morbidity, including perineal pain, vaginal scarring, and cervical stenosis or insufficiency. Given the extremely low risk for progression to cancer, these morbidities do not outweigh any small potential benefit.
When I am conferring with patients who have chronic low-grade dysplasia I spend a great deal of time exploring their understanding of the diagnosis and its pathophysiology, their fears, and their expectation regarding “success” of treatment. I spend the time educating them that this is a sequela of chronic viral infection that will not be eradicated with local surgical excisions, that their cancer risk and need for surveillance would persist even if surgical intervention were offered, and that the side effects of treatment would outweigh any benefit from the small risk of cancer or high-grade dysplasia.
In summary, the treatment of choice for persistent low-grade dysplasia of the lower genital tract is comprehensive patient education, not surgical resection or referral to gynecologic oncology.
Repeat sampling if there’s a discordance between imaging and biopsy results
Delay in cancer diagnosis is one of the greatest concerns for front-line gynecology providers. One of the more modifiable strategies to avoid missed or delayed diagnosis is to ensure that there is concordance between clinical findings and testing results. Otherwise said: The results and findings should make sense in aggregate. An example was cited above in which a visible cervical mass demonstrated CIN III on cytologic testing. Another common example is a biopsy result of “scant benign endometrium” in a patient with postmenopausal bleeding and thickened endometrial stripe on ultrasound. In both of these cases there is clear discordance between physical findings and the results of pathology sampling. A pathology report, in all of its black and white certitude, seems like the most reliable source of information. However, always trust your clinical judgment. If the clinical picture is suggesting something far worse than these limited, often random or blind samplings, I recommend repeated or more extensive sampling (for example, dilation and curettage). At the very least, schedule close follow-up with repeated sampling if the symptom or finding persists. The emphasis here is on scheduled follow-up, rather than “p.r.n.,” because a patient who was given a “normal” pathology result to explain her abnormal symptoms may not volunteer that those symptoms are persistent as she may feel that anything sinister was already ruled out. Make certain that you explain the potential for misdiagnosis as the reason for why you would like to see her back shortly to ensure the issue has resolved.
Biopsy vulvar lesions, minimize empiric treatment
Vulvar cancer is notoriously associated with delayed diagnosis. Unfortunately, it is commonplace for gynecologic oncologists to see women who have vulvar cancers that have been empirically treated, sometimes for months or years, with steroids or other topical agents. If a lesion on the vulva is characteristically benign in appearance (such as condyloma or lichen sclerosis), it may be reasonable to start empiric treatment. However, all patients who are treated without biopsy should be rescheduled for a planned follow-up appointment in 2-3 months. If the lesion/area remains unchanged, or worse, the lesion should be biopsied before proceeding with a change in therapy or continued therapy. Once again, don’t rely on patients to return for evaluation if the lesion doesn’t improve. Many patients assume that our first empiric diagnosis is “gospel,” and therefore may not return if the treatment doesn’t work. Meanwhile, providers may assume that patients will know that there is uncertainty in our interpretation and that they will know to report if the initial treatment didn’t work. These assumptions are the recipe for delayed diagnosis. If there is too great a burden on the patient to schedule a return visit because of social or financial reasons then the patient should have a biopsy prior to initiation of treatment. As a rule, empiric treatment is not a good strategy for patients without good access to follow-up.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at obnews@mdedge.com.
References
1. Sullivan S. et al Gynecol Oncol. 2017 Feb;144(2):294-8.
2. Perkins R .et al J Low Genit Tract Dis. 2020 Apr;24(2):102-31.
Fibroids: Is surgery the only management approach?
Two chronic gynecologic conditions notably affect a woman’s quality of life (QoL), including fertility – one is endometriosis, and the other is a fibroid uterus. For a benign tumor, fibroids have an impressive prevalence found in approximately 50%-60% of women during their reproductive years. By menopause, it is estimated that 70% of woman have a fibroid, yet the true incidence is unknown given that only 25% of women experience symptoms bothersome enough to warrant intervention. This month’s article reviews the burden of fibroids and the latest management options that may potentially avoid surgery.
Background
Fibroids are monoclonal tumors of uterine smooth muscle that originate from the myometrium. Risk factors include family history, being premenopausal, increasing time since last delivery, obesity, and hypertension (ACOG Practice Bulletin no. 228 Jun 2021: Obstet Gynecol. 2021 Jun 1;137[6]:e100-e15) but oral hormonal contraception, depot medroxyprogesterone acetate (MPA), and increased parity reduce the risk of fibroids. Compared with White women, Black women have a 2-3 times higher prevalence of fibroids, develop them at a younger age, and present with larger fibroids.
The FIGO leiomyoma classification is the agreed upon system for identifying fibroid location. Symptoms are all too familiar to gynecologists, with life-threatening hemorrhage with severe anemia being the most feared, particularly for FIGO types 1-5. Transvaginal ultrasound is the simplest imaging tool for evaluation.
Fibroids and fertility
Fibroids can impair fertility in several ways: alteration of local anatomy, including the detrimental effects of abnormal uterine bleeding; functional changes by increasing uterine contractions and impairing endometrium and myometrial blood supply; and changes to the local hormonal environment that could impair egg/sperm transport, or embryo implantation (Hum Reprod Update. 2017;22:665-86).
Prior to consideration of surgery, saline infusion sonogram can determine the degree of impact on the endometrium, which is most applicable to the infertility patient, but can also allow guidance toward the appropriate surgical approach.
Treatment options – medical
Management of fibroids is based on a woman’s age, desire for fertility, symptoms, and location of the fibroid(s). Expectant observation of a woman with fibroids may be a reasonable approach, provided the lack of symptoms impairing QoL and of anemia. Typically, there is no change in fibroid size during the short term, considered less than 1 year. Regarding fertility, studies are heterogeneous so there is no definitive conclusion that fibroids impair natural fertility (Reprod Biomed Online. 2021;43:100-10). Spontaneous regression, defined by a reduction in fibroid volume of greater than 20%, has been noted to occur in 7.0% of fibroids (Curr Obstet Gynecol Rep. 2018;7[3]:117-21).
When fertility is not desired, medical management of fibroids is the initial conservative approach. GnRH agonists have been utilized for temporary relief of menometrorrhagia because of fibroids and to reduce their volume, particularly preoperatively. However, extended treatment can induce bone mineral density loss. Add-back therapy (tibolone, raloxifene, estriol, and ipriflavone) is of value in reducing bone loss while MPA and tibolone may manage vasomotor symptoms. More recently, the use of a GnRH antagonist (elagolix) along with add-back therapy has been approved for up to 24 months by the Food and Drug Administration and has demonstrated a more than 50% amenorrhea rate at 12 months (Obstet Gynecol. 2020;135:1313-26).
Progesterone plays an important role in fibroid growth, but the mechanism is unclear. Although not FDA approved, selective progesterone receptor modulators (SPRM) act directly on fibroid size reduction at the level of the pituitary to induce amenorrhea through inhibition of ovulation. Also, more than one course of SPRMs can provide benefit for bleeding control and volume reduction. The SPRM ulipristal acetate for four courses of 3 months demonstrated 73.5% of patients experienced a fibroid volume reduction of greater than 25% and were amenorrheic (Fertil Steril. 2017;108:416-25). GnRH agonists or SPRMs may benefit women if the fibroid is larger than 3 cm or anemia exists, thereby precluding immediate surgery.
Other medication options include the levonorgestrel IUD, combined hormonal contraceptives, and tranexamic acid – all of which have limited data on effective results of treating abnormal uterine bleeding.
Treatment options – surgical
Fibroids are the most common reason for hysterectomy as they are the contributing indication in approximately one-third of surgeries. When future fertility is desired, current surgical options include hysteroscopic and laparoscopic (including robotic) myomectomy. Hysteroscopy is the standard approach for FIGO type 1 fibroids and can also manage some type 2 fibroids provided they are less than 3 cm and the latter is greater than 5 mm from the serosa. Type 2 fibroids may benefit from a “two-step” removal to allow the myometrium to contract and extrude the fibroid. In light of the risk of fluid overload with nonelectrolyte solutions that enable the use of monopolar cautery, many procedures are now performed with bipolar cautery or morcellators.
Laparoscopy (including robotic) has outcomes similar to those of laparotomy although the risk of uterine rupture with the former requires careful attention to thorough closure of the myometrial defect. Robotic myomectomy has outcomes similar to those of standard laparoscopy with less blood loss, but operating times may be prolonged (Best Pract Res Clin Obstet Gynaecol. 2018;46:113-9).
The rate of myomectomy is reported to be 9.2 per 10,000 woman-years in Black women and 1.3 per 10,000 woman years in White women (Fertil Steril 2017;108;416-25). The rate of recurrence after myomectomy can be as great as 60% when patients are followed up to 5 years. Intramural fibroids greater than 2.85 cm and not distorting the uterine cavity may decrease in vitro fertilization (IVF) success (Fertil Steril 2014;101:716-21).
Noninvasive treatment modalities
Uterine artery embolization (UAE) is the most popular minimally invasive alternative to surgical myomectomy. Risks include postembolization syndrome (pain, fever, nausea, leukocytosis, and occasionally malaise), infection, and damage to fertility. Rarely, loss of ovarian function can occur, particularly in women above age 45. Because of the disruption of uterine blood flow, UAE increases the risk of accelerating ovarian aging and infertility as well as atrophic endometrium. In addition, pregnancy complications are increased including miscarriage, preterm labor, and postpartum hemorrhage. There is debate regarding the need for cesarean section at time of delivery given the potential for weakening of the uterine wall following UAE.
High-intensity focused ultrasound (HIFU) is guided by ultrasound or MRI and involves a high-energy-density ultrasound wave passing through the skin. The wave is absorbed and transformed into heat, causing the tissue protein to coagulate, and to be absorbed by the body. The procedure is scarless, carries a minimal risk of infection, and offers less pain compared with traditional approaches. However, HIFU is time consuming, and skin burns and unintentional tissue injury are a risk. A meta-analysis demonstrated improved symptoms of fibroids at 6 and 12 months (J Min Invasive Gynecol. 2021 in press).
Ultrasound-guided microwave ablation (MWA) uses an ablative electrode that is directly inserted into the target tissue via transcutaneous or transcervical approach via ultrasound guidance using microwave to produce heat for tissue coagulation necrosis. The advantages of MWA compared with HIFU and RFA are a higher tissue temperature, larger ablation volume, shorter operating time, less pain and no adverse major events (J Min Invasive Gynecol. 2021, in press).
Conclusion
The current literature cannot conclude that fibroids reduce the likelihood of achieving pregnancy with or without fertility treatment, based on a specific size, number, or location (not including submucosal or cavity-distorting intramural fibroids). Definitive evidence on the efficacy of myomectomy to improve fertility remains limited. Hysteroscopic myomectomy presumably improves pregnancy rates, but there is uncertainty as to its role in reducing miscarriage. Novel nonsurgical modalities are available and are expected to continue being developed but clarity on fertility outcomes is needed.
Dr. Trolice is director of Fertility CARE – The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando. He has no conflicts of interests. Please contact him at obnews@mdedge.com.
Two chronic gynecologic conditions notably affect a woman’s quality of life (QoL), including fertility – one is endometriosis, and the other is a fibroid uterus. For a benign tumor, fibroids have an impressive prevalence found in approximately 50%-60% of women during their reproductive years. By menopause, it is estimated that 70% of woman have a fibroid, yet the true incidence is unknown given that only 25% of women experience symptoms bothersome enough to warrant intervention. This month’s article reviews the burden of fibroids and the latest management options that may potentially avoid surgery.
Background
Fibroids are monoclonal tumors of uterine smooth muscle that originate from the myometrium. Risk factors include family history, being premenopausal, increasing time since last delivery, obesity, and hypertension (ACOG Practice Bulletin no. 228 Jun 2021: Obstet Gynecol. 2021 Jun 1;137[6]:e100-e15) but oral hormonal contraception, depot medroxyprogesterone acetate (MPA), and increased parity reduce the risk of fibroids. Compared with White women, Black women have a 2-3 times higher prevalence of fibroids, develop them at a younger age, and present with larger fibroids.
The FIGO leiomyoma classification is the agreed upon system for identifying fibroid location. Symptoms are all too familiar to gynecologists, with life-threatening hemorrhage with severe anemia being the most feared, particularly for FIGO types 1-5. Transvaginal ultrasound is the simplest imaging tool for evaluation.
Fibroids and fertility
Fibroids can impair fertility in several ways: alteration of local anatomy, including the detrimental effects of abnormal uterine bleeding; functional changes by increasing uterine contractions and impairing endometrium and myometrial blood supply; and changes to the local hormonal environment that could impair egg/sperm transport, or embryo implantation (Hum Reprod Update. 2017;22:665-86).
Prior to consideration of surgery, saline infusion sonogram can determine the degree of impact on the endometrium, which is most applicable to the infertility patient, but can also allow guidance toward the appropriate surgical approach.
Treatment options – medical
Management of fibroids is based on a woman’s age, desire for fertility, symptoms, and location of the fibroid(s). Expectant observation of a woman with fibroids may be a reasonable approach, provided the lack of symptoms impairing QoL and of anemia. Typically, there is no change in fibroid size during the short term, considered less than 1 year. Regarding fertility, studies are heterogeneous so there is no definitive conclusion that fibroids impair natural fertility (Reprod Biomed Online. 2021;43:100-10). Spontaneous regression, defined by a reduction in fibroid volume of greater than 20%, has been noted to occur in 7.0% of fibroids (Curr Obstet Gynecol Rep. 2018;7[3]:117-21).
When fertility is not desired, medical management of fibroids is the initial conservative approach. GnRH agonists have been utilized for temporary relief of menometrorrhagia because of fibroids and to reduce their volume, particularly preoperatively. However, extended treatment can induce bone mineral density loss. Add-back therapy (tibolone, raloxifene, estriol, and ipriflavone) is of value in reducing bone loss while MPA and tibolone may manage vasomotor symptoms. More recently, the use of a GnRH antagonist (elagolix) along with add-back therapy has been approved for up to 24 months by the Food and Drug Administration and has demonstrated a more than 50% amenorrhea rate at 12 months (Obstet Gynecol. 2020;135:1313-26).
Progesterone plays an important role in fibroid growth, but the mechanism is unclear. Although not FDA approved, selective progesterone receptor modulators (SPRM) act directly on fibroid size reduction at the level of the pituitary to induce amenorrhea through inhibition of ovulation. Also, more than one course of SPRMs can provide benefit for bleeding control and volume reduction. The SPRM ulipristal acetate for four courses of 3 months demonstrated 73.5% of patients experienced a fibroid volume reduction of greater than 25% and were amenorrheic (Fertil Steril. 2017;108:416-25). GnRH agonists or SPRMs may benefit women if the fibroid is larger than 3 cm or anemia exists, thereby precluding immediate surgery.
Other medication options include the levonorgestrel IUD, combined hormonal contraceptives, and tranexamic acid – all of which have limited data on effective results of treating abnormal uterine bleeding.
Treatment options – surgical
Fibroids are the most common reason for hysterectomy as they are the contributing indication in approximately one-third of surgeries. When future fertility is desired, current surgical options include hysteroscopic and laparoscopic (including robotic) myomectomy. Hysteroscopy is the standard approach for FIGO type 1 fibroids and can also manage some type 2 fibroids provided they are less than 3 cm and the latter is greater than 5 mm from the serosa. Type 2 fibroids may benefit from a “two-step” removal to allow the myometrium to contract and extrude the fibroid. In light of the risk of fluid overload with nonelectrolyte solutions that enable the use of monopolar cautery, many procedures are now performed with bipolar cautery or morcellators.
Laparoscopy (including robotic) has outcomes similar to those of laparotomy although the risk of uterine rupture with the former requires careful attention to thorough closure of the myometrial defect. Robotic myomectomy has outcomes similar to those of standard laparoscopy with less blood loss, but operating times may be prolonged (Best Pract Res Clin Obstet Gynaecol. 2018;46:113-9).
The rate of myomectomy is reported to be 9.2 per 10,000 woman-years in Black women and 1.3 per 10,000 woman years in White women (Fertil Steril 2017;108;416-25). The rate of recurrence after myomectomy can be as great as 60% when patients are followed up to 5 years. Intramural fibroids greater than 2.85 cm and not distorting the uterine cavity may decrease in vitro fertilization (IVF) success (Fertil Steril 2014;101:716-21).
Noninvasive treatment modalities
Uterine artery embolization (UAE) is the most popular minimally invasive alternative to surgical myomectomy. Risks include postembolization syndrome (pain, fever, nausea, leukocytosis, and occasionally malaise), infection, and damage to fertility. Rarely, loss of ovarian function can occur, particularly in women above age 45. Because of the disruption of uterine blood flow, UAE increases the risk of accelerating ovarian aging and infertility as well as atrophic endometrium. In addition, pregnancy complications are increased including miscarriage, preterm labor, and postpartum hemorrhage. There is debate regarding the need for cesarean section at time of delivery given the potential for weakening of the uterine wall following UAE.
High-intensity focused ultrasound (HIFU) is guided by ultrasound or MRI and involves a high-energy-density ultrasound wave passing through the skin. The wave is absorbed and transformed into heat, causing the tissue protein to coagulate, and to be absorbed by the body. The procedure is scarless, carries a minimal risk of infection, and offers less pain compared with traditional approaches. However, HIFU is time consuming, and skin burns and unintentional tissue injury are a risk. A meta-analysis demonstrated improved symptoms of fibroids at 6 and 12 months (J Min Invasive Gynecol. 2021 in press).
Ultrasound-guided microwave ablation (MWA) uses an ablative electrode that is directly inserted into the target tissue via transcutaneous or transcervical approach via ultrasound guidance using microwave to produce heat for tissue coagulation necrosis. The advantages of MWA compared with HIFU and RFA are a higher tissue temperature, larger ablation volume, shorter operating time, less pain and no adverse major events (J Min Invasive Gynecol. 2021, in press).
Conclusion
The current literature cannot conclude that fibroids reduce the likelihood of achieving pregnancy with or without fertility treatment, based on a specific size, number, or location (not including submucosal or cavity-distorting intramural fibroids). Definitive evidence on the efficacy of myomectomy to improve fertility remains limited. Hysteroscopic myomectomy presumably improves pregnancy rates, but there is uncertainty as to its role in reducing miscarriage. Novel nonsurgical modalities are available and are expected to continue being developed but clarity on fertility outcomes is needed.
Dr. Trolice is director of Fertility CARE – The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando. He has no conflicts of interests. Please contact him at obnews@mdedge.com.
Two chronic gynecologic conditions notably affect a woman’s quality of life (QoL), including fertility – one is endometriosis, and the other is a fibroid uterus. For a benign tumor, fibroids have an impressive prevalence found in approximately 50%-60% of women during their reproductive years. By menopause, it is estimated that 70% of woman have a fibroid, yet the true incidence is unknown given that only 25% of women experience symptoms bothersome enough to warrant intervention. This month’s article reviews the burden of fibroids and the latest management options that may potentially avoid surgery.
Background
Fibroids are monoclonal tumors of uterine smooth muscle that originate from the myometrium. Risk factors include family history, being premenopausal, increasing time since last delivery, obesity, and hypertension (ACOG Practice Bulletin no. 228 Jun 2021: Obstet Gynecol. 2021 Jun 1;137[6]:e100-e15) but oral hormonal contraception, depot medroxyprogesterone acetate (MPA), and increased parity reduce the risk of fibroids. Compared with White women, Black women have a 2-3 times higher prevalence of fibroids, develop them at a younger age, and present with larger fibroids.
The FIGO leiomyoma classification is the agreed upon system for identifying fibroid location. Symptoms are all too familiar to gynecologists, with life-threatening hemorrhage with severe anemia being the most feared, particularly for FIGO types 1-5. Transvaginal ultrasound is the simplest imaging tool for evaluation.
Fibroids and fertility
Fibroids can impair fertility in several ways: alteration of local anatomy, including the detrimental effects of abnormal uterine bleeding; functional changes by increasing uterine contractions and impairing endometrium and myometrial blood supply; and changes to the local hormonal environment that could impair egg/sperm transport, or embryo implantation (Hum Reprod Update. 2017;22:665-86).
Prior to consideration of surgery, saline infusion sonogram can determine the degree of impact on the endometrium, which is most applicable to the infertility patient, but can also allow guidance toward the appropriate surgical approach.
Treatment options – medical
Management of fibroids is based on a woman’s age, desire for fertility, symptoms, and location of the fibroid(s). Expectant observation of a woman with fibroids may be a reasonable approach, provided the lack of symptoms impairing QoL and of anemia. Typically, there is no change in fibroid size during the short term, considered less than 1 year. Regarding fertility, studies are heterogeneous so there is no definitive conclusion that fibroids impair natural fertility (Reprod Biomed Online. 2021;43:100-10). Spontaneous regression, defined by a reduction in fibroid volume of greater than 20%, has been noted to occur in 7.0% of fibroids (Curr Obstet Gynecol Rep. 2018;7[3]:117-21).
When fertility is not desired, medical management of fibroids is the initial conservative approach. GnRH agonists have been utilized for temporary relief of menometrorrhagia because of fibroids and to reduce their volume, particularly preoperatively. However, extended treatment can induce bone mineral density loss. Add-back therapy (tibolone, raloxifene, estriol, and ipriflavone) is of value in reducing bone loss while MPA and tibolone may manage vasomotor symptoms. More recently, the use of a GnRH antagonist (elagolix) along with add-back therapy has been approved for up to 24 months by the Food and Drug Administration and has demonstrated a more than 50% amenorrhea rate at 12 months (Obstet Gynecol. 2020;135:1313-26).
Progesterone plays an important role in fibroid growth, but the mechanism is unclear. Although not FDA approved, selective progesterone receptor modulators (SPRM) act directly on fibroid size reduction at the level of the pituitary to induce amenorrhea through inhibition of ovulation. Also, more than one course of SPRMs can provide benefit for bleeding control and volume reduction. The SPRM ulipristal acetate for four courses of 3 months demonstrated 73.5% of patients experienced a fibroid volume reduction of greater than 25% and were amenorrheic (Fertil Steril. 2017;108:416-25). GnRH agonists or SPRMs may benefit women if the fibroid is larger than 3 cm or anemia exists, thereby precluding immediate surgery.
Other medication options include the levonorgestrel IUD, combined hormonal contraceptives, and tranexamic acid – all of which have limited data on effective results of treating abnormal uterine bleeding.
Treatment options – surgical
Fibroids are the most common reason for hysterectomy as they are the contributing indication in approximately one-third of surgeries. When future fertility is desired, current surgical options include hysteroscopic and laparoscopic (including robotic) myomectomy. Hysteroscopy is the standard approach for FIGO type 1 fibroids and can also manage some type 2 fibroids provided they are less than 3 cm and the latter is greater than 5 mm from the serosa. Type 2 fibroids may benefit from a “two-step” removal to allow the myometrium to contract and extrude the fibroid. In light of the risk of fluid overload with nonelectrolyte solutions that enable the use of monopolar cautery, many procedures are now performed with bipolar cautery or morcellators.
Laparoscopy (including robotic) has outcomes similar to those of laparotomy although the risk of uterine rupture with the former requires careful attention to thorough closure of the myometrial defect. Robotic myomectomy has outcomes similar to those of standard laparoscopy with less blood loss, but operating times may be prolonged (Best Pract Res Clin Obstet Gynaecol. 2018;46:113-9).
The rate of myomectomy is reported to be 9.2 per 10,000 woman-years in Black women and 1.3 per 10,000 woman years in White women (Fertil Steril 2017;108;416-25). The rate of recurrence after myomectomy can be as great as 60% when patients are followed up to 5 years. Intramural fibroids greater than 2.85 cm and not distorting the uterine cavity may decrease in vitro fertilization (IVF) success (Fertil Steril 2014;101:716-21).
Noninvasive treatment modalities
Uterine artery embolization (UAE) is the most popular minimally invasive alternative to surgical myomectomy. Risks include postembolization syndrome (pain, fever, nausea, leukocytosis, and occasionally malaise), infection, and damage to fertility. Rarely, loss of ovarian function can occur, particularly in women above age 45. Because of the disruption of uterine blood flow, UAE increases the risk of accelerating ovarian aging and infertility as well as atrophic endometrium. In addition, pregnancy complications are increased including miscarriage, preterm labor, and postpartum hemorrhage. There is debate regarding the need for cesarean section at time of delivery given the potential for weakening of the uterine wall following UAE.
High-intensity focused ultrasound (HIFU) is guided by ultrasound or MRI and involves a high-energy-density ultrasound wave passing through the skin. The wave is absorbed and transformed into heat, causing the tissue protein to coagulate, and to be absorbed by the body. The procedure is scarless, carries a minimal risk of infection, and offers less pain compared with traditional approaches. However, HIFU is time consuming, and skin burns and unintentional tissue injury are a risk. A meta-analysis demonstrated improved symptoms of fibroids at 6 and 12 months (J Min Invasive Gynecol. 2021 in press).
Ultrasound-guided microwave ablation (MWA) uses an ablative electrode that is directly inserted into the target tissue via transcutaneous or transcervical approach via ultrasound guidance using microwave to produce heat for tissue coagulation necrosis. The advantages of MWA compared with HIFU and RFA are a higher tissue temperature, larger ablation volume, shorter operating time, less pain and no adverse major events (J Min Invasive Gynecol. 2021, in press).
Conclusion
The current literature cannot conclude that fibroids reduce the likelihood of achieving pregnancy with or without fertility treatment, based on a specific size, number, or location (not including submucosal or cavity-distorting intramural fibroids). Definitive evidence on the efficacy of myomectomy to improve fertility remains limited. Hysteroscopic myomectomy presumably improves pregnancy rates, but there is uncertainty as to its role in reducing miscarriage. Novel nonsurgical modalities are available and are expected to continue being developed but clarity on fertility outcomes is needed.
Dr. Trolice is director of Fertility CARE – The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando. He has no conflicts of interests. Please contact him at obnews@mdedge.com.
Animal-assisted therapy could boost patients’ mental health
For me, vacation planning brings with it a bit of anxiety and stress – particularly as we navigate the many uncertainties around COVID-19.
Not only must my husband and I think about our own safety, we also have to make sure that our beloved dog, Samson, gets the proper care while we are away.
My husband adopted Samson, an 11-year-old mixed-breed rescue, when he was just a year old. He’s an important part of our family.
So, when booking our hotel room and flights, we also had to find someone we trust to care for Samson in our absence. Family members are not always an option, so we often rely on pet-sitting apps. We looked through profile after profile, contacted sitters, and interrogated them as if we were looking for care for a tiny human.
Eventually, we found a service that allows owners to use a mobile app that provides updates about how their pets are faring. While we were away, the sitter sent daily photos and videos of Samson that put our minds at ease.
As a registered nurse who works in an ICU, my own anxiety about leaving Samson reminded me about my patients’ reservations about leaving their pets during hospitalizations. Many of them share the same kinds of anxieties when they are separated from their beloved pets. Hospital visits are rarely planned. I have cared for patients who expressed concerns about their pets being home alone and needing to coordinate pet care. In some cases – to alleviate those patients’ anxieties – I have helped them contact friends and family members to assist with care.
Pets’ popularity grows in U.S.
According to the 2019-2020 National Pet Owners Survey, about 67% of U.S. households own a pet – which translates to about 84.9 million homes. During the height of COVID, Americans also acquired a greater number of smaller pets.1 In addition, when social restrictions increased, the demand for dog adoptions and the desire to serve as foster owners rose significantly.2 Last Chance Animal Rescue of Waldorf, Md., reportedly saw the adoption of dogs rise from 30%-40% in 2020. Another animal rescue operation, Lucky Dog, of Arlington, Va., in 2020 helped about 3,385 pets find adoption, up from about 1,800 in 2019.3 About two-thirds of all American households and roughly half of elderly individuals own pets.4
I am not surprised by those numbers. In my nursing practice, I face many stress-related factors, such as alternating day and night shifts, 12-hour shifts, strenuous physical work, and the psychological strain of attending to ill and dying patients. Interacting with Samson helps relieve that stress. The motion of petting Samson helps calm my heart rate and decreases my anxiety. In addition, Samson makes me smile – and excites almost all the people I interact with while he’s around. Of course, I’m not objective, but I view Samson’s impact on people as a symbol of the power of animal-assisted therapy (AAT).
AAT, defined as “the positive interaction between an animal and a patient within a therapeutic framework,”has proven to be an effective intervention for adults with intellectual disabilities who experience anxiety in an observational study.5 The intervention also has helped reduce cortisol levels in a study of nurses in physical medicine, internal medicine, and long-term care.6 Since most patient hospital stays are unplanned, there is a need to introduce AAT into hospital care. This would lessen anxiety in patients concerning their pets’ welfare.
We know that long-term hospital stays often cause adverse psychosocial effects on patients. Such stays can result in “hospitalization syndrome,” which is characterized by a gradual loss of cognition and orientation, an unwillingness to maintain contact with others or to engage in group therapy, and a loss of interest in their surroundings.7 The common causes for this syndrome are infection, medication, isolation, response to surgery, and dehydration. A consequence can be a permanent change in cognitive function or psychological impairment. However, my experience of practicing nursing for years has led me to discover that pets as an external stimulus can prevent the syndrome’s onset. This is because a large percentage of hospitalized patients have pets, and contact with a pet reminds them of home and the memories they share at home.
Introducing animal therapy into health care facilities could boost patients’ mental health – and ease their anxiety – by acting as a bridge between their present circumstances and the lives they have outside the establishment.
References
1. American Pet Owners Association. Will the COVID Pet Spike Last? State of the industry presentation. 2021 Mar 24.
2. Morgan L et al. Humanit Soc Sci Comm. 2020 Nov 24;7(144). doi: 10.1057/S41599-020-00649-x.
3. Hedgpeth D. So many pets have been adopted during the pandemic that shelters are running out. Washington Post. 2021 Jan 6.
4. Cherniack EP and Cherniack AR. Curr Gerontol Geriatr Res. 2014. doi: 10.1155/2014/623203.
5. Giuliani F and Jacquemettaz M. Eur J Integ Med. 2017 Sep;14;13-9.
6. Machová K et al. Int J Environ Res and Public Health. 2019 Oct;16(19):3670.
7. Machová K et al. Int J Environ Res Public Health. 2012 Apr;16(8):1362.
Ms. Scott is a registered nurse specializing in critical care and also has experience in nursing leadership. She has 8 years of experience in cardiothoracic ICUs. Ms. Scott received a bachelor of science in nursing degree from Queens University of Charlotte (N.C.), and a master of business administration in health care administration from the University of North Alabama, Florence. She has no conflicts of interest.
For me, vacation planning brings with it a bit of anxiety and stress – particularly as we navigate the many uncertainties around COVID-19.
Not only must my husband and I think about our own safety, we also have to make sure that our beloved dog, Samson, gets the proper care while we are away.
My husband adopted Samson, an 11-year-old mixed-breed rescue, when he was just a year old. He’s an important part of our family.
So, when booking our hotel room and flights, we also had to find someone we trust to care for Samson in our absence. Family members are not always an option, so we often rely on pet-sitting apps. We looked through profile after profile, contacted sitters, and interrogated them as if we were looking for care for a tiny human.
Eventually, we found a service that allows owners to use a mobile app that provides updates about how their pets are faring. While we were away, the sitter sent daily photos and videos of Samson that put our minds at ease.
As a registered nurse who works in an ICU, my own anxiety about leaving Samson reminded me about my patients’ reservations about leaving their pets during hospitalizations. Many of them share the same kinds of anxieties when they are separated from their beloved pets. Hospital visits are rarely planned. I have cared for patients who expressed concerns about their pets being home alone and needing to coordinate pet care. In some cases – to alleviate those patients’ anxieties – I have helped them contact friends and family members to assist with care.
Pets’ popularity grows in U.S.
According to the 2019-2020 National Pet Owners Survey, about 67% of U.S. households own a pet – which translates to about 84.9 million homes. During the height of COVID, Americans also acquired a greater number of smaller pets.1 In addition, when social restrictions increased, the demand for dog adoptions and the desire to serve as foster owners rose significantly.2 Last Chance Animal Rescue of Waldorf, Md., reportedly saw the adoption of dogs rise from 30%-40% in 2020. Another animal rescue operation, Lucky Dog, of Arlington, Va., in 2020 helped about 3,385 pets find adoption, up from about 1,800 in 2019.3 About two-thirds of all American households and roughly half of elderly individuals own pets.4
I am not surprised by those numbers. In my nursing practice, I face many stress-related factors, such as alternating day and night shifts, 12-hour shifts, strenuous physical work, and the psychological strain of attending to ill and dying patients. Interacting with Samson helps relieve that stress. The motion of petting Samson helps calm my heart rate and decreases my anxiety. In addition, Samson makes me smile – and excites almost all the people I interact with while he’s around. Of course, I’m not objective, but I view Samson’s impact on people as a symbol of the power of animal-assisted therapy (AAT).
AAT, defined as “the positive interaction between an animal and a patient within a therapeutic framework,”has proven to be an effective intervention for adults with intellectual disabilities who experience anxiety in an observational study.5 The intervention also has helped reduce cortisol levels in a study of nurses in physical medicine, internal medicine, and long-term care.6 Since most patient hospital stays are unplanned, there is a need to introduce AAT into hospital care. This would lessen anxiety in patients concerning their pets’ welfare.
We know that long-term hospital stays often cause adverse psychosocial effects on patients. Such stays can result in “hospitalization syndrome,” which is characterized by a gradual loss of cognition and orientation, an unwillingness to maintain contact with others or to engage in group therapy, and a loss of interest in their surroundings.7 The common causes for this syndrome are infection, medication, isolation, response to surgery, and dehydration. A consequence can be a permanent change in cognitive function or psychological impairment. However, my experience of practicing nursing for years has led me to discover that pets as an external stimulus can prevent the syndrome’s onset. This is because a large percentage of hospitalized patients have pets, and contact with a pet reminds them of home and the memories they share at home.
Introducing animal therapy into health care facilities could boost patients’ mental health – and ease their anxiety – by acting as a bridge between their present circumstances and the lives they have outside the establishment.
References
1. American Pet Owners Association. Will the COVID Pet Spike Last? State of the industry presentation. 2021 Mar 24.
2. Morgan L et al. Humanit Soc Sci Comm. 2020 Nov 24;7(144). doi: 10.1057/S41599-020-00649-x.
3. Hedgpeth D. So many pets have been adopted during the pandemic that shelters are running out. Washington Post. 2021 Jan 6.
4. Cherniack EP and Cherniack AR. Curr Gerontol Geriatr Res. 2014. doi: 10.1155/2014/623203.
5. Giuliani F and Jacquemettaz M. Eur J Integ Med. 2017 Sep;14;13-9.
6. Machová K et al. Int J Environ Res and Public Health. 2019 Oct;16(19):3670.
7. Machová K et al. Int J Environ Res Public Health. 2012 Apr;16(8):1362.
Ms. Scott is a registered nurse specializing in critical care and also has experience in nursing leadership. She has 8 years of experience in cardiothoracic ICUs. Ms. Scott received a bachelor of science in nursing degree from Queens University of Charlotte (N.C.), and a master of business administration in health care administration from the University of North Alabama, Florence. She has no conflicts of interest.
For me, vacation planning brings with it a bit of anxiety and stress – particularly as we navigate the many uncertainties around COVID-19.
Not only must my husband and I think about our own safety, we also have to make sure that our beloved dog, Samson, gets the proper care while we are away.
My husband adopted Samson, an 11-year-old mixed-breed rescue, when he was just a year old. He’s an important part of our family.
So, when booking our hotel room and flights, we also had to find someone we trust to care for Samson in our absence. Family members are not always an option, so we often rely on pet-sitting apps. We looked through profile after profile, contacted sitters, and interrogated them as if we were looking for care for a tiny human.
Eventually, we found a service that allows owners to use a mobile app that provides updates about how their pets are faring. While we were away, the sitter sent daily photos and videos of Samson that put our minds at ease.
As a registered nurse who works in an ICU, my own anxiety about leaving Samson reminded me about my patients’ reservations about leaving their pets during hospitalizations. Many of them share the same kinds of anxieties when they are separated from their beloved pets. Hospital visits are rarely planned. I have cared for patients who expressed concerns about their pets being home alone and needing to coordinate pet care. In some cases – to alleviate those patients’ anxieties – I have helped them contact friends and family members to assist with care.
Pets’ popularity grows in U.S.
According to the 2019-2020 National Pet Owners Survey, about 67% of U.S. households own a pet – which translates to about 84.9 million homes. During the height of COVID, Americans also acquired a greater number of smaller pets.1 In addition, when social restrictions increased, the demand for dog adoptions and the desire to serve as foster owners rose significantly.2 Last Chance Animal Rescue of Waldorf, Md., reportedly saw the adoption of dogs rise from 30%-40% in 2020. Another animal rescue operation, Lucky Dog, of Arlington, Va., in 2020 helped about 3,385 pets find adoption, up from about 1,800 in 2019.3 About two-thirds of all American households and roughly half of elderly individuals own pets.4
I am not surprised by those numbers. In my nursing practice, I face many stress-related factors, such as alternating day and night shifts, 12-hour shifts, strenuous physical work, and the psychological strain of attending to ill and dying patients. Interacting with Samson helps relieve that stress. The motion of petting Samson helps calm my heart rate and decreases my anxiety. In addition, Samson makes me smile – and excites almost all the people I interact with while he’s around. Of course, I’m not objective, but I view Samson’s impact on people as a symbol of the power of animal-assisted therapy (AAT).
AAT, defined as “the positive interaction between an animal and a patient within a therapeutic framework,”has proven to be an effective intervention for adults with intellectual disabilities who experience anxiety in an observational study.5 The intervention also has helped reduce cortisol levels in a study of nurses in physical medicine, internal medicine, and long-term care.6 Since most patient hospital stays are unplanned, there is a need to introduce AAT into hospital care. This would lessen anxiety in patients concerning their pets’ welfare.
We know that long-term hospital stays often cause adverse psychosocial effects on patients. Such stays can result in “hospitalization syndrome,” which is characterized by a gradual loss of cognition and orientation, an unwillingness to maintain contact with others or to engage in group therapy, and a loss of interest in their surroundings.7 The common causes for this syndrome are infection, medication, isolation, response to surgery, and dehydration. A consequence can be a permanent change in cognitive function or psychological impairment. However, my experience of practicing nursing for years has led me to discover that pets as an external stimulus can prevent the syndrome’s onset. This is because a large percentage of hospitalized patients have pets, and contact with a pet reminds them of home and the memories they share at home.
Introducing animal therapy into health care facilities could boost patients’ mental health – and ease their anxiety – by acting as a bridge between their present circumstances and the lives they have outside the establishment.
References
1. American Pet Owners Association. Will the COVID Pet Spike Last? State of the industry presentation. 2021 Mar 24.
2. Morgan L et al. Humanit Soc Sci Comm. 2020 Nov 24;7(144). doi: 10.1057/S41599-020-00649-x.
3. Hedgpeth D. So many pets have been adopted during the pandemic that shelters are running out. Washington Post. 2021 Jan 6.
4. Cherniack EP and Cherniack AR. Curr Gerontol Geriatr Res. 2014. doi: 10.1155/2014/623203.
5. Giuliani F and Jacquemettaz M. Eur J Integ Med. 2017 Sep;14;13-9.
6. Machová K et al. Int J Environ Res and Public Health. 2019 Oct;16(19):3670.
7. Machová K et al. Int J Environ Res Public Health. 2012 Apr;16(8):1362.
Ms. Scott is a registered nurse specializing in critical care and also has experience in nursing leadership. She has 8 years of experience in cardiothoracic ICUs. Ms. Scott received a bachelor of science in nursing degree from Queens University of Charlotte (N.C.), and a master of business administration in health care administration from the University of North Alabama, Florence. She has no conflicts of interest.
The febrile infant: New AAP guidance for the first 2 months of life
Sixteen years in the making, the American Academy of Pediatrics just released a new clinical practice guideline (CPG), “Evaluation and Management of Well-Appearing Febrile Infants 8-60 Days Old”. The recommendations were derived from interpretations of sequential studies in young, febrile, but well-appearing infants that covered invasive bacterial infection (IBI) incidence, diagnostic modalities, and treatment during the first 2 months of life, further refining approaches to evaluation and empirical treatment.
Pediatricians have long had solid information to help assess the risk for IBI among febrile infants aged 0-3 months, but there has been an ongoing desire to further refine the suggested evaluation of these very young infants. A study of febrile infants from the Pediatric Research in Office Settings network along with subsequent evidence has identified the first 3 weeks of life as the period of highest risk for IBI, with risk declining in a graded fashion aged between 22 and 56 days.
Critical caveats
First, some caveats. Infants 0-7 days are not addressed in the CPG, and all should be treated as high risk and receive full IBI evaluation according to newborn protocols. Second, the recommendations apply only to “well-appearing” infants. Any ill-appearing infant should be treated as high risk and receive full IBI evaluation and begun on empirical antimicrobials. Third, even though the CPG deals with infants as young as 8-21 days old, the recommendations are to treat all infants in this age group as high risk, even if well-appearing, and complete full IBI evaluation and empirical therapy while awaiting results. Fourth, these guidelines apply only to infants born at 37 weeks’ gestation or more. Finally, the new CPG action statements are meant to be recommendations rather than a standard of medical care, leaving some leeway for clinician interpretation of individual patient scenarios. Where appropriate, parents’ values and preferences should be incorporated as part of shared decision-making.
The CPG divides young, febrile infants into three cohorts based on age:
- 8-21 days old
- 22-28 days old
- 29-60 days old
Age 8-21 days
For well-appearing febrile infants 8-21 days old, the CPG recommends a complete IBI evaluation that includes urine, blood, and cerebrospinal fluid (CSF) for culture, approaching all infants in this cohort as high risk. Inflammatory markers may be obtained, but the evidence is not comprehensive enough to evaluate their role in decision-making for this age group. A two-step urine evaluation method (urine analysis followed by culture if the urine analysis looks concerning) is not recommended for infants aged 8-21 days. Urine samples for culture from these young infants should be obtained by catheterization or suprapubic aspiration.
The CPG recommends drawing blood cultures and CSF by lumbar puncture from this cohort. These infants should be admitted to the hospital, treated empirically with antimicrobials, and actively monitored. However, if the cultures are negative at 24-36 hours, the clinician should discontinue antimicrobials and discharge the infant if there is no other reason for continued hospitalization.
Age 22-28 days
Well-appearing, febrile infants 22-28 days old are in an intermediate-risk zone. The recommendation for infants in this cohort is to obtain a urine specimen by catheterization or suprapubic aspiration for both urine analysis and culture. Clinicians may consider obtaining urine samples for analysis noninvasively (e.g., urine bag) in this cohort, but this is not the preferred method.
Blood culture should be obtained from all infants in this group. Inflammatory markers can help clinicians identify infants at greater risk for IBI, including meningitis. Previous data suggested that inflammatory markers such as serum white blood cell counts greater than 11,000/mcL, a serum absolute neutrophil count of greater than 4,000/mcL, and elevated C-reactive protein and procalcitonin levels could help providers identify febrile infants with true IBI. A 2008 study demonstrated that procalcitonin had the best receiver operating characteristic curve in regard to predicting IBI in young febrile infants. Other research backed up that finding and identified cutoff values for procalcitonin levels greater than 1.0 ng/mL. The CPG recommends considering a procalcitonin value of 0.5 ng/mL or higher as positive, indicating that the infant is at greater risk for IBI and potentially should undergo an expanded IBI workup. Therefore, in infants aged 22-28 days, inflammatory markers can play a role in deciding whether to perform a lumbar puncture.
Many more nuanced recommendations for whether to and how to empirically treat with antimicrobials in this cohort can be found in the CPG, including whether to manage in the hospital or at home. Treatment recommendations vary greatly for this cohort on the basis of the tests obtained and whether tests were positive or negative at the initial evaluation.
Age 29-60 days
The CPG will be most helpful when clinicians are faced with well-appearing, febrile infants in the 29- to 60-day age group. As with the other groups, a urine evaluation is recommended; however, the CPG suggests that the two-step approach – obtaining a urine analysis by a noninvasive method and only obtaining culture if the urine analysis is positive – is reasonable. This means that a bag or free-flowing urine specimen would be appropriate for urinalysis, followed by catheterization/suprapubic aspiration if a culture is necessary. This would save approximately 90% of infants from invasive urine collection. Regardless, only catheter or suprapubic specimens are appropriate for urine culture.
The CPG also recommends that clinicians obtain blood culture on all of these infants. Inflammatory markers should be assessed in this cohort because avoiding lumbar puncture for CSF culture would be appropriate in this cohort if the inflammatory markers are negative. If CSF is obtained in this age cohort, enterovirus testing should be added to the testing regimen. Again, for any infant considered at higher risk for IBI on the basis of screening tests, the CPG recommends a 24- to 36-hour rule-out period with empirical antimicrobial treatment and active monitoring in the hospital.
Summary
The recommended approach for febrile infants 8-21 days old is relatively aggressive, with urine, blood, and CSF evaluation for IBI. Clinicians gain some leeway for infants age 22-28 days, but the guidelines recommend a more flexible approach to evaluating well-appearing, febrile infants age 29-60 days, when a two-step urine evaluation and inflammatory marker assessment can help clinicians and parents have a better discussion about the risk-benefit trade-offs of more aggressive testing and empirical treatment.
The author would like to thank Ken Roberts, MD, for his review and helpful comments on this summary of the CPG highlights. Summary points of the CPG were presented by the writing group at the 2021 Pediatric Academic Societies meeting.
William T. Basco, Jr, MD, MS, is a professor of pediatrics at the Medical University of South Carolina, Charleston, and director of the division of general pediatrics. He is an active health services researcher and has published more than 60 manuscripts in the peer-reviewed literature.
A version of this article first appeared on Medscape.com.
Sixteen years in the making, the American Academy of Pediatrics just released a new clinical practice guideline (CPG), “Evaluation and Management of Well-Appearing Febrile Infants 8-60 Days Old”. The recommendations were derived from interpretations of sequential studies in young, febrile, but well-appearing infants that covered invasive bacterial infection (IBI) incidence, diagnostic modalities, and treatment during the first 2 months of life, further refining approaches to evaluation and empirical treatment.
Pediatricians have long had solid information to help assess the risk for IBI among febrile infants aged 0-3 months, but there has been an ongoing desire to further refine the suggested evaluation of these very young infants. A study of febrile infants from the Pediatric Research in Office Settings network along with subsequent evidence has identified the first 3 weeks of life as the period of highest risk for IBI, with risk declining in a graded fashion aged between 22 and 56 days.
Critical caveats
First, some caveats. Infants 0-7 days are not addressed in the CPG, and all should be treated as high risk and receive full IBI evaluation according to newborn protocols. Second, the recommendations apply only to “well-appearing” infants. Any ill-appearing infant should be treated as high risk and receive full IBI evaluation and begun on empirical antimicrobials. Third, even though the CPG deals with infants as young as 8-21 days old, the recommendations are to treat all infants in this age group as high risk, even if well-appearing, and complete full IBI evaluation and empirical therapy while awaiting results. Fourth, these guidelines apply only to infants born at 37 weeks’ gestation or more. Finally, the new CPG action statements are meant to be recommendations rather than a standard of medical care, leaving some leeway for clinician interpretation of individual patient scenarios. Where appropriate, parents’ values and preferences should be incorporated as part of shared decision-making.
The CPG divides young, febrile infants into three cohorts based on age:
- 8-21 days old
- 22-28 days old
- 29-60 days old
Age 8-21 days
For well-appearing febrile infants 8-21 days old, the CPG recommends a complete IBI evaluation that includes urine, blood, and cerebrospinal fluid (CSF) for culture, approaching all infants in this cohort as high risk. Inflammatory markers may be obtained, but the evidence is not comprehensive enough to evaluate their role in decision-making for this age group. A two-step urine evaluation method (urine analysis followed by culture if the urine analysis looks concerning) is not recommended for infants aged 8-21 days. Urine samples for culture from these young infants should be obtained by catheterization or suprapubic aspiration.
The CPG recommends drawing blood cultures and CSF by lumbar puncture from this cohort. These infants should be admitted to the hospital, treated empirically with antimicrobials, and actively monitored. However, if the cultures are negative at 24-36 hours, the clinician should discontinue antimicrobials and discharge the infant if there is no other reason for continued hospitalization.
Age 22-28 days
Well-appearing, febrile infants 22-28 days old are in an intermediate-risk zone. The recommendation for infants in this cohort is to obtain a urine specimen by catheterization or suprapubic aspiration for both urine analysis and culture. Clinicians may consider obtaining urine samples for analysis noninvasively (e.g., urine bag) in this cohort, but this is not the preferred method.
Blood culture should be obtained from all infants in this group. Inflammatory markers can help clinicians identify infants at greater risk for IBI, including meningitis. Previous data suggested that inflammatory markers such as serum white blood cell counts greater than 11,000/mcL, a serum absolute neutrophil count of greater than 4,000/mcL, and elevated C-reactive protein and procalcitonin levels could help providers identify febrile infants with true IBI. A 2008 study demonstrated that procalcitonin had the best receiver operating characteristic curve in regard to predicting IBI in young febrile infants. Other research backed up that finding and identified cutoff values for procalcitonin levels greater than 1.0 ng/mL. The CPG recommends considering a procalcitonin value of 0.5 ng/mL or higher as positive, indicating that the infant is at greater risk for IBI and potentially should undergo an expanded IBI workup. Therefore, in infants aged 22-28 days, inflammatory markers can play a role in deciding whether to perform a lumbar puncture.
Many more nuanced recommendations for whether to and how to empirically treat with antimicrobials in this cohort can be found in the CPG, including whether to manage in the hospital or at home. Treatment recommendations vary greatly for this cohort on the basis of the tests obtained and whether tests were positive or negative at the initial evaluation.
Age 29-60 days
The CPG will be most helpful when clinicians are faced with well-appearing, febrile infants in the 29- to 60-day age group. As with the other groups, a urine evaluation is recommended; however, the CPG suggests that the two-step approach – obtaining a urine analysis by a noninvasive method and only obtaining culture if the urine analysis is positive – is reasonable. This means that a bag or free-flowing urine specimen would be appropriate for urinalysis, followed by catheterization/suprapubic aspiration if a culture is necessary. This would save approximately 90% of infants from invasive urine collection. Regardless, only catheter or suprapubic specimens are appropriate for urine culture.
The CPG also recommends that clinicians obtain blood culture on all of these infants. Inflammatory markers should be assessed in this cohort because avoiding lumbar puncture for CSF culture would be appropriate in this cohort if the inflammatory markers are negative. If CSF is obtained in this age cohort, enterovirus testing should be added to the testing regimen. Again, for any infant considered at higher risk for IBI on the basis of screening tests, the CPG recommends a 24- to 36-hour rule-out period with empirical antimicrobial treatment and active monitoring in the hospital.
Summary
The recommended approach for febrile infants 8-21 days old is relatively aggressive, with urine, blood, and CSF evaluation for IBI. Clinicians gain some leeway for infants age 22-28 days, but the guidelines recommend a more flexible approach to evaluating well-appearing, febrile infants age 29-60 days, when a two-step urine evaluation and inflammatory marker assessment can help clinicians and parents have a better discussion about the risk-benefit trade-offs of more aggressive testing and empirical treatment.
The author would like to thank Ken Roberts, MD, for his review and helpful comments on this summary of the CPG highlights. Summary points of the CPG were presented by the writing group at the 2021 Pediatric Academic Societies meeting.
William T. Basco, Jr, MD, MS, is a professor of pediatrics at the Medical University of South Carolina, Charleston, and director of the division of general pediatrics. He is an active health services researcher and has published more than 60 manuscripts in the peer-reviewed literature.
A version of this article first appeared on Medscape.com.
Sixteen years in the making, the American Academy of Pediatrics just released a new clinical practice guideline (CPG), “Evaluation and Management of Well-Appearing Febrile Infants 8-60 Days Old”. The recommendations were derived from interpretations of sequential studies in young, febrile, but well-appearing infants that covered invasive bacterial infection (IBI) incidence, diagnostic modalities, and treatment during the first 2 months of life, further refining approaches to evaluation and empirical treatment.
Pediatricians have long had solid information to help assess the risk for IBI among febrile infants aged 0-3 months, but there has been an ongoing desire to further refine the suggested evaluation of these very young infants. A study of febrile infants from the Pediatric Research in Office Settings network along with subsequent evidence has identified the first 3 weeks of life as the period of highest risk for IBI, with risk declining in a graded fashion aged between 22 and 56 days.
Critical caveats
First, some caveats. Infants 0-7 days are not addressed in the CPG, and all should be treated as high risk and receive full IBI evaluation according to newborn protocols. Second, the recommendations apply only to “well-appearing” infants. Any ill-appearing infant should be treated as high risk and receive full IBI evaluation and begun on empirical antimicrobials. Third, even though the CPG deals with infants as young as 8-21 days old, the recommendations are to treat all infants in this age group as high risk, even if well-appearing, and complete full IBI evaluation and empirical therapy while awaiting results. Fourth, these guidelines apply only to infants born at 37 weeks’ gestation or more. Finally, the new CPG action statements are meant to be recommendations rather than a standard of medical care, leaving some leeway for clinician interpretation of individual patient scenarios. Where appropriate, parents’ values and preferences should be incorporated as part of shared decision-making.
The CPG divides young, febrile infants into three cohorts based on age:
- 8-21 days old
- 22-28 days old
- 29-60 days old
Age 8-21 days
For well-appearing febrile infants 8-21 days old, the CPG recommends a complete IBI evaluation that includes urine, blood, and cerebrospinal fluid (CSF) for culture, approaching all infants in this cohort as high risk. Inflammatory markers may be obtained, but the evidence is not comprehensive enough to evaluate their role in decision-making for this age group. A two-step urine evaluation method (urine analysis followed by culture if the urine analysis looks concerning) is not recommended for infants aged 8-21 days. Urine samples for culture from these young infants should be obtained by catheterization or suprapubic aspiration.
The CPG recommends drawing blood cultures and CSF by lumbar puncture from this cohort. These infants should be admitted to the hospital, treated empirically with antimicrobials, and actively monitored. However, if the cultures are negative at 24-36 hours, the clinician should discontinue antimicrobials and discharge the infant if there is no other reason for continued hospitalization.
Age 22-28 days
Well-appearing, febrile infants 22-28 days old are in an intermediate-risk zone. The recommendation for infants in this cohort is to obtain a urine specimen by catheterization or suprapubic aspiration for both urine analysis and culture. Clinicians may consider obtaining urine samples for analysis noninvasively (e.g., urine bag) in this cohort, but this is not the preferred method.
Blood culture should be obtained from all infants in this group. Inflammatory markers can help clinicians identify infants at greater risk for IBI, including meningitis. Previous data suggested that inflammatory markers such as serum white blood cell counts greater than 11,000/mcL, a serum absolute neutrophil count of greater than 4,000/mcL, and elevated C-reactive protein and procalcitonin levels could help providers identify febrile infants with true IBI. A 2008 study demonstrated that procalcitonin had the best receiver operating characteristic curve in regard to predicting IBI in young febrile infants. Other research backed up that finding and identified cutoff values for procalcitonin levels greater than 1.0 ng/mL. The CPG recommends considering a procalcitonin value of 0.5 ng/mL or higher as positive, indicating that the infant is at greater risk for IBI and potentially should undergo an expanded IBI workup. Therefore, in infants aged 22-28 days, inflammatory markers can play a role in deciding whether to perform a lumbar puncture.
Many more nuanced recommendations for whether to and how to empirically treat with antimicrobials in this cohort can be found in the CPG, including whether to manage in the hospital or at home. Treatment recommendations vary greatly for this cohort on the basis of the tests obtained and whether tests were positive or negative at the initial evaluation.
Age 29-60 days
The CPG will be most helpful when clinicians are faced with well-appearing, febrile infants in the 29- to 60-day age group. As with the other groups, a urine evaluation is recommended; however, the CPG suggests that the two-step approach – obtaining a urine analysis by a noninvasive method and only obtaining culture if the urine analysis is positive – is reasonable. This means that a bag or free-flowing urine specimen would be appropriate for urinalysis, followed by catheterization/suprapubic aspiration if a culture is necessary. This would save approximately 90% of infants from invasive urine collection. Regardless, only catheter or suprapubic specimens are appropriate for urine culture.
The CPG also recommends that clinicians obtain blood culture on all of these infants. Inflammatory markers should be assessed in this cohort because avoiding lumbar puncture for CSF culture would be appropriate in this cohort if the inflammatory markers are negative. If CSF is obtained in this age cohort, enterovirus testing should be added to the testing regimen. Again, for any infant considered at higher risk for IBI on the basis of screening tests, the CPG recommends a 24- to 36-hour rule-out period with empirical antimicrobial treatment and active monitoring in the hospital.
Summary
The recommended approach for febrile infants 8-21 days old is relatively aggressive, with urine, blood, and CSF evaluation for IBI. Clinicians gain some leeway for infants age 22-28 days, but the guidelines recommend a more flexible approach to evaluating well-appearing, febrile infants age 29-60 days, when a two-step urine evaluation and inflammatory marker assessment can help clinicians and parents have a better discussion about the risk-benefit trade-offs of more aggressive testing and empirical treatment.
The author would like to thank Ken Roberts, MD, for his review and helpful comments on this summary of the CPG highlights. Summary points of the CPG were presented by the writing group at the 2021 Pediatric Academic Societies meeting.
William T. Basco, Jr, MD, MS, is a professor of pediatrics at the Medical University of South Carolina, Charleston, and director of the division of general pediatrics. He is an active health services researcher and has published more than 60 manuscripts in the peer-reviewed literature.
A version of this article first appeared on Medscape.com.
The ADA and hearing-impaired patients
A recent claim against a New Jersey physician attracted considerable attention in both the medical and legal communities, not only because it resulted in a substantial jury award, but because that award was not covered by malpractice insurance.
It is a good reminder for the rest of us: This case involved a charge of discrimination against a hearing-impaired patient – which meant the physician not only had to fund his own defense, but was personally responsible for the $400,000 award against him.
The Americans with Disabilities Act (ADA) was designed to protect individuals with various disabilities against discrimination in various public situations – including, specifically, “the professional office of a health care professional.”
When the disability is impaired hearing, the law requires physicians to provide any “auxiliary aids and services” that might be necessary to insure clear communication between doctor and patient. In the vast majority of such situations, a pad and pencil will satisfy that requirement. But occasionally it does not, particularly when complex medical concepts are involved; and in such cases, as the New Jersey trial demonstrated, failure to make the necessary extra effort can be very expensive.
The claim involved a hearing-impaired patient with lupus erythematosus under treatment by a rheumatologist. For almost 2 years the patient’s partner and her daughter provided translation; but that arrangement was inadequate, she testified, because her partner and daughter were unfamiliar with medical terminology and she was “unable to understand and participate in her care,” which left her “unaware of risks and available alternatives.”
She repeatedly requested that the rheumatologist provide an American Sign Language interpreter for her office visits. He refused on grounds that the cost of an interpreter would exceed the payment he would receive for the visits, which made it an “undue financial burden,” and therefore exempt from ADA requirements.
But the undue-burden exemption is not automatic; it must be demonstrated in court. And the jury decided the rheumatologist’s annual income of $425,000 rendered the cost of an interpreter quite affordable.
The lessons are clear: Physicians must take antidiscrimination laws seriously, particularly when uninsurable issues are involved; and we must be constantly aware of the needs of disabled patients, to be sure their care is not substantially different from that of any other patient.
In the case of hearing-impaired or deaf patients, it is important to remember that forms of communication that are quite adequate for most are not appropriate for some. Lip reading, written notes, and the use of family members as interpreters may be perfectly acceptable to one patient and unsuitable for another.
If the patient agrees to written notes and lip reading, as most do, you need to remember to speak slowly, and to write down critical information to avoid any miscommunications. And as always, it is crucial to document all communication, as well as the methods used for that communication – specifically including the fact that the patient agreed to those forms of communication. Documentation, as I’ve often said, is like garlic: There is no such thing as too much of it.
Should a patient not agree that written notes are sufficient, other alternatives can be offered: computer transcription, assistive listening devices, videotext displays (often available in hospitals), and telecommunication devices such as TTY and TDD. But if the patient rejects all of those options and continues to insist on a professional interpreter, the precedent set by the New Jersey case suggests that you need to acquiesce, even if the interpreter’s fee exceeds the visit reimbursement – and the ADA prohibits you from passing your cost along to the patient. But any such cost will be far less than a noninsured judgment against you.
If you must go that route, make sure the interpreter you hire is familiar with medical terminology, and is not acquainted or related to the patient (for HIPAA reasons). Your state may have an online registry of available interpreters, or your hospital may have a sign language interpreter on its staff that they might allow you to “borrow.”
The good news is several states have responded to this issue by introducing legislation that would require health insurance carriers to pay for the cost of interpreters, although none, as of this writing, have yet become law.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
A recent claim against a New Jersey physician attracted considerable attention in both the medical and legal communities, not only because it resulted in a substantial jury award, but because that award was not covered by malpractice insurance.
It is a good reminder for the rest of us: This case involved a charge of discrimination against a hearing-impaired patient – which meant the physician not only had to fund his own defense, but was personally responsible for the $400,000 award against him.
The Americans with Disabilities Act (ADA) was designed to protect individuals with various disabilities against discrimination in various public situations – including, specifically, “the professional office of a health care professional.”
When the disability is impaired hearing, the law requires physicians to provide any “auxiliary aids and services” that might be necessary to insure clear communication between doctor and patient. In the vast majority of such situations, a pad and pencil will satisfy that requirement. But occasionally it does not, particularly when complex medical concepts are involved; and in such cases, as the New Jersey trial demonstrated, failure to make the necessary extra effort can be very expensive.
The claim involved a hearing-impaired patient with lupus erythematosus under treatment by a rheumatologist. For almost 2 years the patient’s partner and her daughter provided translation; but that arrangement was inadequate, she testified, because her partner and daughter were unfamiliar with medical terminology and she was “unable to understand and participate in her care,” which left her “unaware of risks and available alternatives.”
She repeatedly requested that the rheumatologist provide an American Sign Language interpreter for her office visits. He refused on grounds that the cost of an interpreter would exceed the payment he would receive for the visits, which made it an “undue financial burden,” and therefore exempt from ADA requirements.
But the undue-burden exemption is not automatic; it must be demonstrated in court. And the jury decided the rheumatologist’s annual income of $425,000 rendered the cost of an interpreter quite affordable.
The lessons are clear: Physicians must take antidiscrimination laws seriously, particularly when uninsurable issues are involved; and we must be constantly aware of the needs of disabled patients, to be sure their care is not substantially different from that of any other patient.
In the case of hearing-impaired or deaf patients, it is important to remember that forms of communication that are quite adequate for most are not appropriate for some. Lip reading, written notes, and the use of family members as interpreters may be perfectly acceptable to one patient and unsuitable for another.
If the patient agrees to written notes and lip reading, as most do, you need to remember to speak slowly, and to write down critical information to avoid any miscommunications. And as always, it is crucial to document all communication, as well as the methods used for that communication – specifically including the fact that the patient agreed to those forms of communication. Documentation, as I’ve often said, is like garlic: There is no such thing as too much of it.
Should a patient not agree that written notes are sufficient, other alternatives can be offered: computer transcription, assistive listening devices, videotext displays (often available in hospitals), and telecommunication devices such as TTY and TDD. But if the patient rejects all of those options and continues to insist on a professional interpreter, the precedent set by the New Jersey case suggests that you need to acquiesce, even if the interpreter’s fee exceeds the visit reimbursement – and the ADA prohibits you from passing your cost along to the patient. But any such cost will be far less than a noninsured judgment against you.
If you must go that route, make sure the interpreter you hire is familiar with medical terminology, and is not acquainted or related to the patient (for HIPAA reasons). Your state may have an online registry of available interpreters, or your hospital may have a sign language interpreter on its staff that they might allow you to “borrow.”
The good news is several states have responded to this issue by introducing legislation that would require health insurance carriers to pay for the cost of interpreters, although none, as of this writing, have yet become law.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
A recent claim against a New Jersey physician attracted considerable attention in both the medical and legal communities, not only because it resulted in a substantial jury award, but because that award was not covered by malpractice insurance.
It is a good reminder for the rest of us: This case involved a charge of discrimination against a hearing-impaired patient – which meant the physician not only had to fund his own defense, but was personally responsible for the $400,000 award against him.
The Americans with Disabilities Act (ADA) was designed to protect individuals with various disabilities against discrimination in various public situations – including, specifically, “the professional office of a health care professional.”
When the disability is impaired hearing, the law requires physicians to provide any “auxiliary aids and services” that might be necessary to insure clear communication between doctor and patient. In the vast majority of such situations, a pad and pencil will satisfy that requirement. But occasionally it does not, particularly when complex medical concepts are involved; and in such cases, as the New Jersey trial demonstrated, failure to make the necessary extra effort can be very expensive.
The claim involved a hearing-impaired patient with lupus erythematosus under treatment by a rheumatologist. For almost 2 years the patient’s partner and her daughter provided translation; but that arrangement was inadequate, she testified, because her partner and daughter were unfamiliar with medical terminology and she was “unable to understand and participate in her care,” which left her “unaware of risks and available alternatives.”
She repeatedly requested that the rheumatologist provide an American Sign Language interpreter for her office visits. He refused on grounds that the cost of an interpreter would exceed the payment he would receive for the visits, which made it an “undue financial burden,” and therefore exempt from ADA requirements.
But the undue-burden exemption is not automatic; it must be demonstrated in court. And the jury decided the rheumatologist’s annual income of $425,000 rendered the cost of an interpreter quite affordable.
The lessons are clear: Physicians must take antidiscrimination laws seriously, particularly when uninsurable issues are involved; and we must be constantly aware of the needs of disabled patients, to be sure their care is not substantially different from that of any other patient.
In the case of hearing-impaired or deaf patients, it is important to remember that forms of communication that are quite adequate for most are not appropriate for some. Lip reading, written notes, and the use of family members as interpreters may be perfectly acceptable to one patient and unsuitable for another.
If the patient agrees to written notes and lip reading, as most do, you need to remember to speak slowly, and to write down critical information to avoid any miscommunications. And as always, it is crucial to document all communication, as well as the methods used for that communication – specifically including the fact that the patient agreed to those forms of communication. Documentation, as I’ve often said, is like garlic: There is no such thing as too much of it.
Should a patient not agree that written notes are sufficient, other alternatives can be offered: computer transcription, assistive listening devices, videotext displays (often available in hospitals), and telecommunication devices such as TTY and TDD. But if the patient rejects all of those options and continues to insist on a professional interpreter, the precedent set by the New Jersey case suggests that you need to acquiesce, even if the interpreter’s fee exceeds the visit reimbursement – and the ADA prohibits you from passing your cost along to the patient. But any such cost will be far less than a noninsured judgment against you.
If you must go that route, make sure the interpreter you hire is familiar with medical terminology, and is not acquainted or related to the patient (for HIPAA reasons). Your state may have an online registry of available interpreters, or your hospital may have a sign language interpreter on its staff that they might allow you to “borrow.”
The good news is several states have responded to this issue by introducing legislation that would require health insurance carriers to pay for the cost of interpreters, although none, as of this writing, have yet become law.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
When patients demand vaccinated health care providers
Should a hospital or medical practice fulfill a patient’s request to be treated or cared for only by vaccinated health care providers?The answer is yes, in a perfect world. Patients should feel assured that their health care providers – clinicians and caregivers – are not exposing them to infectious diseases.But issues are being raised – subquestions that need to be answered to understand the current situation and assist health care employers in their decision-making:
- Must health care employers ensure that their employees are vaccinated?
- Can health care employers require that their employees be vaccinated?
- Do employees have any rights to refuse vaccination or to refuse to supply their employer with their vaccination status?
- Can a health care employer terminate an employee who refuses vaccination?
- Does a patient have a legal right to a vaccinated health care provider?
At present, federal policy says that employers may, but are not required to, insist that employees be vaccinated. The currently prevailing state case law says that hospitals and other employers can require staff to be vaccinated and can terminate employees who refuse vaccination. In June, a Texas court dismissed a case in which 117 employees sued a hospital for requiring that employees be vaccinated. More cases are pending in other states, and there may be differing decisions in other states and on appeal.
State laws enacted years ago also weigh in on employer obligations. In at least one state, Oregon, employers of health care providers may not require vaccination, even though other employers may. Other states have laws about what an employer may or may not require of an employee regarding vaccination, and some have introduced laws which are pending.
So, in most states, health care employers may, not must, require that employees be vaccinated. In most states, hospitals and medical practices may terminate employees who refuse vaccination. However, employers should research the laws of their own states before requiring vaccinations and before terminating employees who are not vaccinated.
The issue of employer mandates is complicated further by the practicality that, in some areas of the country, health care providers are in scarce supply. Employers don’t want to lose the providers they have.
And there are additional questions about how certain federal laws affect the situation. Federal law that may apply includes:
- U.S. Food and Drug Administration regulation on approval of vaccines
- The Americans With Disabilities Act (ADA)
- The Health Insurance Portability and Accountability Act of 1996, which protects sensitive patient health information from being disclosed without the patient’s consent
- Civil rights laws
- Patients’ rights
FDA. Some health care providers who refuse vaccination argue that employers have no legal right to require a vaccine that is not fully approved by the FDA. COVID-19 vaccinations have emergency use authorization – something less than full approval. Courts have not yet ruled on this issue.
ADA. Some attorneys believe that honoring a patient’s request to be attended only by a vaccinated health care provider can implicate the ADA. However, the ADA doesn’t protect healthy individuals who don’t want to be vaccinated. The ADA protects the person who, because of their disability, shouldn’t get the vaccination. If an employer mandates vaccination, the employer must, under the ADA, consider requests for exemptions from disabled individuals. However, even when an employee has a disability that may qualify the employee for an exemption to the vaccination requirement, an employer may argue that giving an exemption would be a direct threat to the safety of others; in that case, the ADA may require that the disabled employee and hospital work something out. A compromise might be that the unvaccinated disabled individual would not provide direct patient care or would wear a mask and maintain physical distance.
HIPAA. Some argue that federal privacy law enters into the discussion, maintaining that health care employers can’t disclose employees’ vaccination status under HIPAA. That is not true. Employers are not “covered entities” under HIPAA. It is health care providers who are precluded under HIPAA from disclosing a patient’s personal information. So, if an employer were to ask an employee’s health care provider about the employee’s vaccination status, the health care provider could disclose that status only if the employee consented to the disclosure. An employer may ask an employee for the employee’s proof of vaccination card. However, employers must not ask for unnecessary details that might reveal disability information protected by the ADA.
Civil rights law. Civil rights laws may protect certain individuals from employment consequences of refusing vaccination. Specifically, individuals with sincerely held religious convictions against vaccinations are protected from retaliation by employers for refusing vaccination, under the Constitutional right of freedom of religion. The individual without sincerely held religious convictions against vaccinations and without a relevant disability doesn’t have legal remedies under civil rights laws.
Civil rights laws may apply if employers don’t apply their vaccination requirements to all employees equally. That is, employers can’t require vaccinations of some employees but not others.
Patients’ rights. Legal protections for patients who want a vaccinated health care provider are nowhere to be seen, at this time. It is unlikely that a single patient will be able to convince a hospital or medical practice to require that its staff be vaccinated. However, if a patient becomes infected with COVID-19 and can prove that the illness is causally related to interacting with an unvaccinated health care worker, the patient may have a case against the employer. The legal theory would be malpractice or negligence under informed consent law: That is, the patient did not consent to be treated by an unvaccinated person.
Employer options
So, what can health care employers do? They have three options:
- Require vaccination of all employees, independent contractors, and other providers who have privileges to see patients. Then, as long as the employer enforces the vaccination mandate, the employer can tell patients that all providers are vaccinated.
- Not require that employees and others with access to patients be vaccinated, and if a patient requests to be seen only by vaccinated providers, provide that patient with a vaccinated provider. It is especially important that health care employers take care with patients who are unvaccinated and who have been advised not to be vaccinated because of a medical condition. Both the patient and the health care employer would be protected best by avoiding having two unvaccinated individuals interact. Masks and physical distancing may decrease the risk.
- Not require that employees be vaccinated and refuse to guarantee that providers are vaccinated. To avoid risk for future lawsuits, employers should inform patients that there is no assurance that providers are vaccinated. That leaves it to each patient to ask individual providers about the provider’s vaccination status. If a patient doesn’t like a provider’s answer, then the patient has the right to leave. It’s not clear that the patient has a legal right to stay and demand a vaccinated provider.
Option three is problematic for a number of reasons. Patients aren’t always in a position to query each provider who enters the room about vaccination status. Patients may be sedated or too ill to exert that effort. And it puts supervisors in the position of having to mediate situations where a patient wants to leave against medical advice but the option of staying may also be dangerous.
Health care employers should discuss the options with their legal counsel before deciding which option to adopt.
A version of this article first appeared on Medscape.com.
Should a hospital or medical practice fulfill a patient’s request to be treated or cared for only by vaccinated health care providers?The answer is yes, in a perfect world. Patients should feel assured that their health care providers – clinicians and caregivers – are not exposing them to infectious diseases.But issues are being raised – subquestions that need to be answered to understand the current situation and assist health care employers in their decision-making:
- Must health care employers ensure that their employees are vaccinated?
- Can health care employers require that their employees be vaccinated?
- Do employees have any rights to refuse vaccination or to refuse to supply their employer with their vaccination status?
- Can a health care employer terminate an employee who refuses vaccination?
- Does a patient have a legal right to a vaccinated health care provider?
At present, federal policy says that employers may, but are not required to, insist that employees be vaccinated. The currently prevailing state case law says that hospitals and other employers can require staff to be vaccinated and can terminate employees who refuse vaccination. In June, a Texas court dismissed a case in which 117 employees sued a hospital for requiring that employees be vaccinated. More cases are pending in other states, and there may be differing decisions in other states and on appeal.
State laws enacted years ago also weigh in on employer obligations. In at least one state, Oregon, employers of health care providers may not require vaccination, even though other employers may. Other states have laws about what an employer may or may not require of an employee regarding vaccination, and some have introduced laws which are pending.
So, in most states, health care employers may, not must, require that employees be vaccinated. In most states, hospitals and medical practices may terminate employees who refuse vaccination. However, employers should research the laws of their own states before requiring vaccinations and before terminating employees who are not vaccinated.
The issue of employer mandates is complicated further by the practicality that, in some areas of the country, health care providers are in scarce supply. Employers don’t want to lose the providers they have.
And there are additional questions about how certain federal laws affect the situation. Federal law that may apply includes:
- U.S. Food and Drug Administration regulation on approval of vaccines
- The Americans With Disabilities Act (ADA)
- The Health Insurance Portability and Accountability Act of 1996, which protects sensitive patient health information from being disclosed without the patient’s consent
- Civil rights laws
- Patients’ rights
FDA. Some health care providers who refuse vaccination argue that employers have no legal right to require a vaccine that is not fully approved by the FDA. COVID-19 vaccinations have emergency use authorization – something less than full approval. Courts have not yet ruled on this issue.
ADA. Some attorneys believe that honoring a patient’s request to be attended only by a vaccinated health care provider can implicate the ADA. However, the ADA doesn’t protect healthy individuals who don’t want to be vaccinated. The ADA protects the person who, because of their disability, shouldn’t get the vaccination. If an employer mandates vaccination, the employer must, under the ADA, consider requests for exemptions from disabled individuals. However, even when an employee has a disability that may qualify the employee for an exemption to the vaccination requirement, an employer may argue that giving an exemption would be a direct threat to the safety of others; in that case, the ADA may require that the disabled employee and hospital work something out. A compromise might be that the unvaccinated disabled individual would not provide direct patient care or would wear a mask and maintain physical distance.
HIPAA. Some argue that federal privacy law enters into the discussion, maintaining that health care employers can’t disclose employees’ vaccination status under HIPAA. That is not true. Employers are not “covered entities” under HIPAA. It is health care providers who are precluded under HIPAA from disclosing a patient’s personal information. So, if an employer were to ask an employee’s health care provider about the employee’s vaccination status, the health care provider could disclose that status only if the employee consented to the disclosure. An employer may ask an employee for the employee’s proof of vaccination card. However, employers must not ask for unnecessary details that might reveal disability information protected by the ADA.
Civil rights law. Civil rights laws may protect certain individuals from employment consequences of refusing vaccination. Specifically, individuals with sincerely held religious convictions against vaccinations are protected from retaliation by employers for refusing vaccination, under the Constitutional right of freedom of religion. The individual without sincerely held religious convictions against vaccinations and without a relevant disability doesn’t have legal remedies under civil rights laws.
Civil rights laws may apply if employers don’t apply their vaccination requirements to all employees equally. That is, employers can’t require vaccinations of some employees but not others.
Patients’ rights. Legal protections for patients who want a vaccinated health care provider are nowhere to be seen, at this time. It is unlikely that a single patient will be able to convince a hospital or medical practice to require that its staff be vaccinated. However, if a patient becomes infected with COVID-19 and can prove that the illness is causally related to interacting with an unvaccinated health care worker, the patient may have a case against the employer. The legal theory would be malpractice or negligence under informed consent law: That is, the patient did not consent to be treated by an unvaccinated person.
Employer options
So, what can health care employers do? They have three options:
- Require vaccination of all employees, independent contractors, and other providers who have privileges to see patients. Then, as long as the employer enforces the vaccination mandate, the employer can tell patients that all providers are vaccinated.
- Not require that employees and others with access to patients be vaccinated, and if a patient requests to be seen only by vaccinated providers, provide that patient with a vaccinated provider. It is especially important that health care employers take care with patients who are unvaccinated and who have been advised not to be vaccinated because of a medical condition. Both the patient and the health care employer would be protected best by avoiding having two unvaccinated individuals interact. Masks and physical distancing may decrease the risk.
- Not require that employees be vaccinated and refuse to guarantee that providers are vaccinated. To avoid risk for future lawsuits, employers should inform patients that there is no assurance that providers are vaccinated. That leaves it to each patient to ask individual providers about the provider’s vaccination status. If a patient doesn’t like a provider’s answer, then the patient has the right to leave. It’s not clear that the patient has a legal right to stay and demand a vaccinated provider.
Option three is problematic for a number of reasons. Patients aren’t always in a position to query each provider who enters the room about vaccination status. Patients may be sedated or too ill to exert that effort. And it puts supervisors in the position of having to mediate situations where a patient wants to leave against medical advice but the option of staying may also be dangerous.
Health care employers should discuss the options with their legal counsel before deciding which option to adopt.
A version of this article first appeared on Medscape.com.
Should a hospital or medical practice fulfill a patient’s request to be treated or cared for only by vaccinated health care providers?The answer is yes, in a perfect world. Patients should feel assured that their health care providers – clinicians and caregivers – are not exposing them to infectious diseases.But issues are being raised – subquestions that need to be answered to understand the current situation and assist health care employers in their decision-making:
- Must health care employers ensure that their employees are vaccinated?
- Can health care employers require that their employees be vaccinated?
- Do employees have any rights to refuse vaccination or to refuse to supply their employer with their vaccination status?
- Can a health care employer terminate an employee who refuses vaccination?
- Does a patient have a legal right to a vaccinated health care provider?
At present, federal policy says that employers may, but are not required to, insist that employees be vaccinated. The currently prevailing state case law says that hospitals and other employers can require staff to be vaccinated and can terminate employees who refuse vaccination. In June, a Texas court dismissed a case in which 117 employees sued a hospital for requiring that employees be vaccinated. More cases are pending in other states, and there may be differing decisions in other states and on appeal.
State laws enacted years ago also weigh in on employer obligations. In at least one state, Oregon, employers of health care providers may not require vaccination, even though other employers may. Other states have laws about what an employer may or may not require of an employee regarding vaccination, and some have introduced laws which are pending.
So, in most states, health care employers may, not must, require that employees be vaccinated. In most states, hospitals and medical practices may terminate employees who refuse vaccination. However, employers should research the laws of their own states before requiring vaccinations and before terminating employees who are not vaccinated.
The issue of employer mandates is complicated further by the practicality that, in some areas of the country, health care providers are in scarce supply. Employers don’t want to lose the providers they have.
And there are additional questions about how certain federal laws affect the situation. Federal law that may apply includes:
- U.S. Food and Drug Administration regulation on approval of vaccines
- The Americans With Disabilities Act (ADA)
- The Health Insurance Portability and Accountability Act of 1996, which protects sensitive patient health information from being disclosed without the patient’s consent
- Civil rights laws
- Patients’ rights
FDA. Some health care providers who refuse vaccination argue that employers have no legal right to require a vaccine that is not fully approved by the FDA. COVID-19 vaccinations have emergency use authorization – something less than full approval. Courts have not yet ruled on this issue.
ADA. Some attorneys believe that honoring a patient’s request to be attended only by a vaccinated health care provider can implicate the ADA. However, the ADA doesn’t protect healthy individuals who don’t want to be vaccinated. The ADA protects the person who, because of their disability, shouldn’t get the vaccination. If an employer mandates vaccination, the employer must, under the ADA, consider requests for exemptions from disabled individuals. However, even when an employee has a disability that may qualify the employee for an exemption to the vaccination requirement, an employer may argue that giving an exemption would be a direct threat to the safety of others; in that case, the ADA may require that the disabled employee and hospital work something out. A compromise might be that the unvaccinated disabled individual would not provide direct patient care or would wear a mask and maintain physical distance.
HIPAA. Some argue that federal privacy law enters into the discussion, maintaining that health care employers can’t disclose employees’ vaccination status under HIPAA. That is not true. Employers are not “covered entities” under HIPAA. It is health care providers who are precluded under HIPAA from disclosing a patient’s personal information. So, if an employer were to ask an employee’s health care provider about the employee’s vaccination status, the health care provider could disclose that status only if the employee consented to the disclosure. An employer may ask an employee for the employee’s proof of vaccination card. However, employers must not ask for unnecessary details that might reveal disability information protected by the ADA.
Civil rights law. Civil rights laws may protect certain individuals from employment consequences of refusing vaccination. Specifically, individuals with sincerely held religious convictions against vaccinations are protected from retaliation by employers for refusing vaccination, under the Constitutional right of freedom of religion. The individual without sincerely held religious convictions against vaccinations and without a relevant disability doesn’t have legal remedies under civil rights laws.
Civil rights laws may apply if employers don’t apply their vaccination requirements to all employees equally. That is, employers can’t require vaccinations of some employees but not others.
Patients’ rights. Legal protections for patients who want a vaccinated health care provider are nowhere to be seen, at this time. It is unlikely that a single patient will be able to convince a hospital or medical practice to require that its staff be vaccinated. However, if a patient becomes infected with COVID-19 and can prove that the illness is causally related to interacting with an unvaccinated health care worker, the patient may have a case against the employer. The legal theory would be malpractice or negligence under informed consent law: That is, the patient did not consent to be treated by an unvaccinated person.
Employer options
So, what can health care employers do? They have three options:
- Require vaccination of all employees, independent contractors, and other providers who have privileges to see patients. Then, as long as the employer enforces the vaccination mandate, the employer can tell patients that all providers are vaccinated.
- Not require that employees and others with access to patients be vaccinated, and if a patient requests to be seen only by vaccinated providers, provide that patient with a vaccinated provider. It is especially important that health care employers take care with patients who are unvaccinated and who have been advised not to be vaccinated because of a medical condition. Both the patient and the health care employer would be protected best by avoiding having two unvaccinated individuals interact. Masks and physical distancing may decrease the risk.
- Not require that employees be vaccinated and refuse to guarantee that providers are vaccinated. To avoid risk for future lawsuits, employers should inform patients that there is no assurance that providers are vaccinated. That leaves it to each patient to ask individual providers about the provider’s vaccination status. If a patient doesn’t like a provider’s answer, then the patient has the right to leave. It’s not clear that the patient has a legal right to stay and demand a vaccinated provider.
Option three is problematic for a number of reasons. Patients aren’t always in a position to query each provider who enters the room about vaccination status. Patients may be sedated or too ill to exert that effort. And it puts supervisors in the position of having to mediate situations where a patient wants to leave against medical advice but the option of staying may also be dangerous.
Health care employers should discuss the options with their legal counsel before deciding which option to adopt.
A version of this article first appeared on Medscape.com.
Legislative wins set groundwork for future success
I receive updates and stories every day from rheumatologists and their offices regarding the egregious behavior of various health care entities that profit off patients and harm them in the process. If you know me, you know I’m willing to tell and retell horror stories of pharmacy benefit managers (PBMs), especially of how they construct formularies for the most profit, again, harming patients in the process. It’s critical to serve as a voice to counter the PBM trade group, the Pharmaceutical Care Management Association, which continues to extol how PBMs are essentially saving our country billions ... one restrictive formulary at a time.
It does seem that we are constantly fighting against something:
- Patients arbitrarily being switched to completely different medications to “save” money. These “savings” are pocketed by the middlemen, not the patients or the employers paying for the coverage.
- Copay cards for medications that have no lower-cost alternative. These fill the coffers of the health plans without patients getting credit toward their deductible.
- Mandating that patients move from receiving their infusions under the watchful eye of their rheumatologist’s office to home infusion. This has been shown to be more dangerous for our patients.
- Wasting hours on prior authorization paperwork for needed medication. We know that these are nearly always approved, and thereby delay treatment unnecessarily.
By now you might wonder: “Where is the good news?” In spite of the daily barrage of battles that come our way, rheumatologists continue to do good and improve the lives of our patients. I would go as far as to say that we are prospering in spite of the challenges. Why? Because every day there are wins. Seeing that smile for the first time on the face of a patient who finally has answers and a treatment plan for their newly diagnosed RA. Walking out of the exam room and having patients and their parents give you a hug. Helping a dad be able to walk his daughter down the aisle with ease. On the clinical front, I don’t have to tell you: We score wins every single day.
There is good news on the advocacy side, too. In my own state of Louisiana, this legislative session, we passed a number of bills that are beneficial to our patients, including a bill to stop the aforementioned attacks on copay assistance by state regulated payers. We even blocked one that the Rheumatology Alliance of Louisiana felt would be harmful to our patients. The wins this session follow wins during the previous session, including passage of new and updated laws to put more prescribing power back in the hands of physicians when medication access is unnecessarily restricted by step therapy. While there has been some doubt as to whether these state laws actually work, I can attest that the new Louisiana step therapy law has allowed stable patients to remain on their medication in a number of specialties, including rheumatology and ophthalmology.
My own state of Louisiana is not the only one where the rheumatology community has seen legislative successes, and that speaks to the strength of the network that rheumatologists have built within their states and across the country, as well as our passion for our patients. Just 3 years after the emergence of accumulator programs, 11 states have already seen fit to curtail their use (Arizona, Arkansas, Connecticut, Georgia, Illinois, Kentucky, Louisiana, Oklahoma, Tennessee, Virginia, and West Virginia), and over 20 states considered adopting similar legislation this year. Reforms to the use of step therapy continue their drumbeat across the country, with three more states (Arkansas, Nebraska, and Oregon) having bills signed into law this year. West Virginia took a bold step to reduce patient out-of-pocket costs at the point of sale by an amount commensurate with 100% of rebates received by a PBM. These material policy wins demonstrate how we continue to successfully chip away at the opacity of PBMs and the rebate system, which is truly at the root of so many of the issues affecting our patients’ care.
At the federal level, rheumatologists engage both with Congress and the administration to ensure that our patients’ voices are represented against very well funded and organized forces like insurers and PBMs. Rheumatologists weighed in on issues ranging from Medicaid payment policy, to copay accumulators in the exchanges, to creating transparency and fixing misaligned incentives in the pharmaceutical supply chain. We drive coalition engagement on issues of shared interest with other specialty and provider groups, such as extending a moratorium on Medicare sequestration. We also engage on narrow issues as they arise: For example, I personally testified before Congress that any proposed limitations on pharmaceutical samples must consider the fact that these samples can provide a critical bridge for patients waiting for their insurers to approve their needed medication. And, perhaps most importantly, we have defeated misguided and potentially devastating Part B payment reform models from the Innovation Center three separate times.
There is more work to be done. And to make it easier to find “Rheum for Action” in your daily work, the Coalition of State Rheumatology Organizations has tools on our website that summarize legislation and facilitate engagement with policy makers, including thank you messages to those who supported our priorities to celebrate the good news this year.
So yes, there is good news now, and more to come! I am optimistic that we will continue to see these advocacy wins, which will help to ensure that those hugs we share with our patients will continue long into the future.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is President of the CSRO, chair of the Alliance for Safe Biologic Medicines, and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at rhnews@mdedge.com.
I receive updates and stories every day from rheumatologists and their offices regarding the egregious behavior of various health care entities that profit off patients and harm them in the process. If you know me, you know I’m willing to tell and retell horror stories of pharmacy benefit managers (PBMs), especially of how they construct formularies for the most profit, again, harming patients in the process. It’s critical to serve as a voice to counter the PBM trade group, the Pharmaceutical Care Management Association, which continues to extol how PBMs are essentially saving our country billions ... one restrictive formulary at a time.
It does seem that we are constantly fighting against something:
- Patients arbitrarily being switched to completely different medications to “save” money. These “savings” are pocketed by the middlemen, not the patients or the employers paying for the coverage.
- Copay cards for medications that have no lower-cost alternative. These fill the coffers of the health plans without patients getting credit toward their deductible.
- Mandating that patients move from receiving their infusions under the watchful eye of their rheumatologist’s office to home infusion. This has been shown to be more dangerous for our patients.
- Wasting hours on prior authorization paperwork for needed medication. We know that these are nearly always approved, and thereby delay treatment unnecessarily.
By now you might wonder: “Where is the good news?” In spite of the daily barrage of battles that come our way, rheumatologists continue to do good and improve the lives of our patients. I would go as far as to say that we are prospering in spite of the challenges. Why? Because every day there are wins. Seeing that smile for the first time on the face of a patient who finally has answers and a treatment plan for their newly diagnosed RA. Walking out of the exam room and having patients and their parents give you a hug. Helping a dad be able to walk his daughter down the aisle with ease. On the clinical front, I don’t have to tell you: We score wins every single day.
There is good news on the advocacy side, too. In my own state of Louisiana, this legislative session, we passed a number of bills that are beneficial to our patients, including a bill to stop the aforementioned attacks on copay assistance by state regulated payers. We even blocked one that the Rheumatology Alliance of Louisiana felt would be harmful to our patients. The wins this session follow wins during the previous session, including passage of new and updated laws to put more prescribing power back in the hands of physicians when medication access is unnecessarily restricted by step therapy. While there has been some doubt as to whether these state laws actually work, I can attest that the new Louisiana step therapy law has allowed stable patients to remain on their medication in a number of specialties, including rheumatology and ophthalmology.
My own state of Louisiana is not the only one where the rheumatology community has seen legislative successes, and that speaks to the strength of the network that rheumatologists have built within their states and across the country, as well as our passion for our patients. Just 3 years after the emergence of accumulator programs, 11 states have already seen fit to curtail their use (Arizona, Arkansas, Connecticut, Georgia, Illinois, Kentucky, Louisiana, Oklahoma, Tennessee, Virginia, and West Virginia), and over 20 states considered adopting similar legislation this year. Reforms to the use of step therapy continue their drumbeat across the country, with three more states (Arkansas, Nebraska, and Oregon) having bills signed into law this year. West Virginia took a bold step to reduce patient out-of-pocket costs at the point of sale by an amount commensurate with 100% of rebates received by a PBM. These material policy wins demonstrate how we continue to successfully chip away at the opacity of PBMs and the rebate system, which is truly at the root of so many of the issues affecting our patients’ care.
At the federal level, rheumatologists engage both with Congress and the administration to ensure that our patients’ voices are represented against very well funded and organized forces like insurers and PBMs. Rheumatologists weighed in on issues ranging from Medicaid payment policy, to copay accumulators in the exchanges, to creating transparency and fixing misaligned incentives in the pharmaceutical supply chain. We drive coalition engagement on issues of shared interest with other specialty and provider groups, such as extending a moratorium on Medicare sequestration. We also engage on narrow issues as they arise: For example, I personally testified before Congress that any proposed limitations on pharmaceutical samples must consider the fact that these samples can provide a critical bridge for patients waiting for their insurers to approve their needed medication. And, perhaps most importantly, we have defeated misguided and potentially devastating Part B payment reform models from the Innovation Center three separate times.
There is more work to be done. And to make it easier to find “Rheum for Action” in your daily work, the Coalition of State Rheumatology Organizations has tools on our website that summarize legislation and facilitate engagement with policy makers, including thank you messages to those who supported our priorities to celebrate the good news this year.
So yes, there is good news now, and more to come! I am optimistic that we will continue to see these advocacy wins, which will help to ensure that those hugs we share with our patients will continue long into the future.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is President of the CSRO, chair of the Alliance for Safe Biologic Medicines, and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at rhnews@mdedge.com.
I receive updates and stories every day from rheumatologists and their offices regarding the egregious behavior of various health care entities that profit off patients and harm them in the process. If you know me, you know I’m willing to tell and retell horror stories of pharmacy benefit managers (PBMs), especially of how they construct formularies for the most profit, again, harming patients in the process. It’s critical to serve as a voice to counter the PBM trade group, the Pharmaceutical Care Management Association, which continues to extol how PBMs are essentially saving our country billions ... one restrictive formulary at a time.
It does seem that we are constantly fighting against something:
- Patients arbitrarily being switched to completely different medications to “save” money. These “savings” are pocketed by the middlemen, not the patients or the employers paying for the coverage.
- Copay cards for medications that have no lower-cost alternative. These fill the coffers of the health plans without patients getting credit toward their deductible.
- Mandating that patients move from receiving their infusions under the watchful eye of their rheumatologist’s office to home infusion. This has been shown to be more dangerous for our patients.
- Wasting hours on prior authorization paperwork for needed medication. We know that these are nearly always approved, and thereby delay treatment unnecessarily.
By now you might wonder: “Where is the good news?” In spite of the daily barrage of battles that come our way, rheumatologists continue to do good and improve the lives of our patients. I would go as far as to say that we are prospering in spite of the challenges. Why? Because every day there are wins. Seeing that smile for the first time on the face of a patient who finally has answers and a treatment plan for their newly diagnosed RA. Walking out of the exam room and having patients and their parents give you a hug. Helping a dad be able to walk his daughter down the aisle with ease. On the clinical front, I don’t have to tell you: We score wins every single day.
There is good news on the advocacy side, too. In my own state of Louisiana, this legislative session, we passed a number of bills that are beneficial to our patients, including a bill to stop the aforementioned attacks on copay assistance by state regulated payers. We even blocked one that the Rheumatology Alliance of Louisiana felt would be harmful to our patients. The wins this session follow wins during the previous session, including passage of new and updated laws to put more prescribing power back in the hands of physicians when medication access is unnecessarily restricted by step therapy. While there has been some doubt as to whether these state laws actually work, I can attest that the new Louisiana step therapy law has allowed stable patients to remain on their medication in a number of specialties, including rheumatology and ophthalmology.
My own state of Louisiana is not the only one where the rheumatology community has seen legislative successes, and that speaks to the strength of the network that rheumatologists have built within their states and across the country, as well as our passion for our patients. Just 3 years after the emergence of accumulator programs, 11 states have already seen fit to curtail their use (Arizona, Arkansas, Connecticut, Georgia, Illinois, Kentucky, Louisiana, Oklahoma, Tennessee, Virginia, and West Virginia), and over 20 states considered adopting similar legislation this year. Reforms to the use of step therapy continue their drumbeat across the country, with three more states (Arkansas, Nebraska, and Oregon) having bills signed into law this year. West Virginia took a bold step to reduce patient out-of-pocket costs at the point of sale by an amount commensurate with 100% of rebates received by a PBM. These material policy wins demonstrate how we continue to successfully chip away at the opacity of PBMs and the rebate system, which is truly at the root of so many of the issues affecting our patients’ care.
At the federal level, rheumatologists engage both with Congress and the administration to ensure that our patients’ voices are represented against very well funded and organized forces like insurers and PBMs. Rheumatologists weighed in on issues ranging from Medicaid payment policy, to copay accumulators in the exchanges, to creating transparency and fixing misaligned incentives in the pharmaceutical supply chain. We drive coalition engagement on issues of shared interest with other specialty and provider groups, such as extending a moratorium on Medicare sequestration. We also engage on narrow issues as they arise: For example, I personally testified before Congress that any proposed limitations on pharmaceutical samples must consider the fact that these samples can provide a critical bridge for patients waiting for their insurers to approve their needed medication. And, perhaps most importantly, we have defeated misguided and potentially devastating Part B payment reform models from the Innovation Center three separate times.
There is more work to be done. And to make it easier to find “Rheum for Action” in your daily work, the Coalition of State Rheumatology Organizations has tools on our website that summarize legislation and facilitate engagement with policy makers, including thank you messages to those who supported our priorities to celebrate the good news this year.
So yes, there is good news now, and more to come! I am optimistic that we will continue to see these advocacy wins, which will help to ensure that those hugs we share with our patients will continue long into the future.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is President of the CSRO, chair of the Alliance for Safe Biologic Medicines, and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at rhnews@mdedge.com.