User login
Is BMI Underestimating Breast Cancer Risk in Postmenopausal Women?
TOPLINE:
Accurate body fat measures are crucial for effective cancer prevention.
METHODOLOGY:
- Researchers conducted a case-control study including 1033 breast cancer cases and 1143 postmenopausal population controls from the MCC-Spain study.
- Participants were aged 20-85 years. BMI was calculated as the ratio of weight to height squared and categorized using World Health Organization standards: < 25, 25-29.9, 30-34.9, and ≥ 35.
- CUN-BAE was calculated using a specific equation and categorized according to the estimated percentage of body fat: < 35%, 35%-39.9%, 40%-44.9%, and ≥ 45%.
- Odds ratios (ORs) were estimated with 95% CIs for both measures (BMI and CUN-BAE) for breast cancer cases using unconditional logistic regression.
TAKEAWAY:
- Excess body weight attributable to the risk for breast cancer was 23% when assessed using a BMI value > 30 and 38% when assessed using a CUN-BAE value > 40% body fat.
- Hormone receptor stratification showed that these differences in population-attributable fractions were only observed in hormone receptor–positive cases, with an estimated burden of 19.9% for BMI and 41.9% for CUN-BAE.
- The highest categories of CUN-BAE showed an increase in the risk for postmenopausal breast cancer (OR, 2.13 for body fat ≥ 45% compared with the reference category < 35%).
- No similar trend was observed for BMI, as the gradient declined after a BMI ≥ 35.
IN PRACTICE:
“The results of our study indicate that excess body fat is a significant risk factor for hormone receptor–positive breast cancer in postmenopausal women. Our findings suggest that the population impact could be underestimated when using traditional BMI estimates, and that more accurate measures of body fat, such as CUN-BAE, should be considered,” the authors of the study wrote.
SOURCE:
This study was led by Verónica Dávila-Batista, University of Las Palmas de Gran Canaria in Las Palmas de Gran Canaria, Spain. It was published online in Journal of Epidemiology and Community Health.
LIMITATIONS:
The case-control design of the study may have limited the ability to establish causal relationships. BMI was self-reported at the time of the interview for controls and 1 year before diagnosis for cancer cases, which may have introduced recall bias. The formula for CUN-BAE was calculated from a sedentary convenience sample, which may not have been representative of the general population. The small sample size of cases that did not express hormone receptors was another limitation. The study’s findings may not be generalizable to non-White populations as non-White participants were excluded.
DISCLOSURES:
Dávila-Batista disclosed receiving grants from the Carlos III Health Institute. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
Accurate body fat measures are crucial for effective cancer prevention.
METHODOLOGY:
- Researchers conducted a case-control study including 1033 breast cancer cases and 1143 postmenopausal population controls from the MCC-Spain study.
- Participants were aged 20-85 years. BMI was calculated as the ratio of weight to height squared and categorized using World Health Organization standards: < 25, 25-29.9, 30-34.9, and ≥ 35.
- CUN-BAE was calculated using a specific equation and categorized according to the estimated percentage of body fat: < 35%, 35%-39.9%, 40%-44.9%, and ≥ 45%.
- Odds ratios (ORs) were estimated with 95% CIs for both measures (BMI and CUN-BAE) for breast cancer cases using unconditional logistic regression.
TAKEAWAY:
- Excess body weight attributable to the risk for breast cancer was 23% when assessed using a BMI value > 30 and 38% when assessed using a CUN-BAE value > 40% body fat.
- Hormone receptor stratification showed that these differences in population-attributable fractions were only observed in hormone receptor–positive cases, with an estimated burden of 19.9% for BMI and 41.9% for CUN-BAE.
- The highest categories of CUN-BAE showed an increase in the risk for postmenopausal breast cancer (OR, 2.13 for body fat ≥ 45% compared with the reference category < 35%).
- No similar trend was observed for BMI, as the gradient declined after a BMI ≥ 35.
IN PRACTICE:
“The results of our study indicate that excess body fat is a significant risk factor for hormone receptor–positive breast cancer in postmenopausal women. Our findings suggest that the population impact could be underestimated when using traditional BMI estimates, and that more accurate measures of body fat, such as CUN-BAE, should be considered,” the authors of the study wrote.
SOURCE:
This study was led by Verónica Dávila-Batista, University of Las Palmas de Gran Canaria in Las Palmas de Gran Canaria, Spain. It was published online in Journal of Epidemiology and Community Health.
LIMITATIONS:
The case-control design of the study may have limited the ability to establish causal relationships. BMI was self-reported at the time of the interview for controls and 1 year before diagnosis for cancer cases, which may have introduced recall bias. The formula for CUN-BAE was calculated from a sedentary convenience sample, which may not have been representative of the general population. The small sample size of cases that did not express hormone receptors was another limitation. The study’s findings may not be generalizable to non-White populations as non-White participants were excluded.
DISCLOSURES:
Dávila-Batista disclosed receiving grants from the Carlos III Health Institute. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
Accurate body fat measures are crucial for effective cancer prevention.
METHODOLOGY:
- Researchers conducted a case-control study including 1033 breast cancer cases and 1143 postmenopausal population controls from the MCC-Spain study.
- Participants were aged 20-85 years. BMI was calculated as the ratio of weight to height squared and categorized using World Health Organization standards: < 25, 25-29.9, 30-34.9, and ≥ 35.
- CUN-BAE was calculated using a specific equation and categorized according to the estimated percentage of body fat: < 35%, 35%-39.9%, 40%-44.9%, and ≥ 45%.
- Odds ratios (ORs) were estimated with 95% CIs for both measures (BMI and CUN-BAE) for breast cancer cases using unconditional logistic regression.
TAKEAWAY:
- Excess body weight attributable to the risk for breast cancer was 23% when assessed using a BMI value > 30 and 38% when assessed using a CUN-BAE value > 40% body fat.
- Hormone receptor stratification showed that these differences in population-attributable fractions were only observed in hormone receptor–positive cases, with an estimated burden of 19.9% for BMI and 41.9% for CUN-BAE.
- The highest categories of CUN-BAE showed an increase in the risk for postmenopausal breast cancer (OR, 2.13 for body fat ≥ 45% compared with the reference category < 35%).
- No similar trend was observed for BMI, as the gradient declined after a BMI ≥ 35.
IN PRACTICE:
“The results of our study indicate that excess body fat is a significant risk factor for hormone receptor–positive breast cancer in postmenopausal women. Our findings suggest that the population impact could be underestimated when using traditional BMI estimates, and that more accurate measures of body fat, such as CUN-BAE, should be considered,” the authors of the study wrote.
SOURCE:
This study was led by Verónica Dávila-Batista, University of Las Palmas de Gran Canaria in Las Palmas de Gran Canaria, Spain. It was published online in Journal of Epidemiology and Community Health.
LIMITATIONS:
The case-control design of the study may have limited the ability to establish causal relationships. BMI was self-reported at the time of the interview for controls and 1 year before diagnosis for cancer cases, which may have introduced recall bias. The formula for CUN-BAE was calculated from a sedentary convenience sample, which may not have been representative of the general population. The small sample size of cases that did not express hormone receptors was another limitation. The study’s findings may not be generalizable to non-White populations as non-White participants were excluded.
DISCLOSURES:
Dávila-Batista disclosed receiving grants from the Carlos III Health Institute. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
The New Cancer Stats Might Look Like a Death Sentence. They Aren’t.
Cancer is becoming more common in younger generations. Data show that people under 50 are experiencing higher rates of cancer than any generation before them. As a genetic counselor, I hoped these upward trends in early-onset malignancies would slow with a better understanding of risk factors and prevention strategies. Unfortunately, the opposite is happening. Recent findings from the American Cancer Society reveal that the incidence of at least 17 of 34 cancer types is rising among GenX and Millennials.
These statistics are alarming. I appreciate how easy it is for patients to get lost in the headlines about cancer, which may shape how they approach their healthcare. Each year, millions of Americans miss critical cancer screenings, with many citing fear of a positive test result as a leading reason. Others believe, despite the statistics, that cancer is not something they need to worry about until they are older. And then, of course, getting screened is not as easy as it should be.
In my work, I meet with people from both younger and older generations who have either faced cancer themselves or witnessed a loved one experience the disease. One of the most common sentiments I hear from these patients is the desire to catch cancer earlier. My answer is always this: The first and most important step everyone can take is understanding their risk.
For some, knowing they are at increased risk for cancer means starting screenings earlier — sometimes as early as age 25 — or getting screened with a more sensitive test.
This proactive approach is the right one. It also significantly reduces the burden of total and cancer-specific healthcare costs. While screening may carry some potential risks, clinicians can minimize these risks by adhering to evidence-based guidelines, such as those from the American Cancer Society, and ensuring there is appropriate discussion of treatment options when a diagnosis is made.
Normalizing Cancer Risk Assessment and Screening
A detailed cancer risk assessment and education about signs and symptoms should be part of every preventive care visit, regardless of someone’s age. Further, that cancer risk assessment should lead to clear recommendations and support for taking the next steps.
This is where care advocacy and patient navigation come in. Care advocacy can improve outcomes at every stage of the cancer journey, from increasing screening rates to improving quality of life for survivors. I’ve seen first-hand how care advocates help patients overcome hurdles like long wait times for appointments they need, making both screening and diagnostic care easier to access.
Now, with the finalization of a new rule from the Centers for Medicare & Medicaid Services, providers can bill for oncology navigation services that occur under their supervision. This formal recognition of care navigation affirms the value of these services not just clinically but financially as well. It will be through methods like care navigation, targeted outreach, and engaging educational resources — built into and covered by health plans — that patients will feel more in control over their health and have tools to help minimize the effects of cancer on the rest of their lives.
These services benefit healthcare providers as well. Care navigation supports clinical care teams, from primary care providers to oncologists, by ensuring patients are seen before their cancer progresses to a more advanced stage. And even if patients follow screening recommendations for the rest of their lives and never get a positive result, they’ve still gained something invaluable: peace of mind, knowing they’ve taken an active role in their health.
Fighting Fear With Routine
Treating cancer as a normal part of young people’s healthcare means helping them envision the disease as a condition that can be treated, much like a diagnosis of diabetes or high cholesterol. This mindset shift means quickly following up on a concerning symptom or screening result and reducing the time to start treatment if needed. And with treatment options and success rates for some cancers being better than ever, survivorship support must be built into every treatment plan from the start. Before treatment begins, healthcare providers should make time to talk about sometimes-overlooked key topics, such as reproductive options for people whose fertility may be affected by their cancer treatment, about plans for returning to work during or after treatment, and finding the right mental health support.
Where we can’t prevent cancer, both primary care providers and oncologists can work together to help patients receive the right diagnosis and treatment as quickly as possible. Knowing insurance coverage has a direct effect on how early cancer is caught, for example, younger people need support in understanding and accessing benefits and resources that may be available through their existing healthcare channels, like some employer-sponsored health plans. Even if getting treated for cancer is inevitable for some, taking immediate action to get screened when it’s appropriate is the best thing we can do to lessen the impact of these rising cancer incidences across the country. At the end of the day, being afraid of cancer doesn’t decrease the chances of getting sick or dying from it. Proactive screening and early detection do.
Brockman, Genetic Counselor, Color Health, Buffalo, New York, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Cancer is becoming more common in younger generations. Data show that people under 50 are experiencing higher rates of cancer than any generation before them. As a genetic counselor, I hoped these upward trends in early-onset malignancies would slow with a better understanding of risk factors and prevention strategies. Unfortunately, the opposite is happening. Recent findings from the American Cancer Society reveal that the incidence of at least 17 of 34 cancer types is rising among GenX and Millennials.
These statistics are alarming. I appreciate how easy it is for patients to get lost in the headlines about cancer, which may shape how they approach their healthcare. Each year, millions of Americans miss critical cancer screenings, with many citing fear of a positive test result as a leading reason. Others believe, despite the statistics, that cancer is not something they need to worry about until they are older. And then, of course, getting screened is not as easy as it should be.
In my work, I meet with people from both younger and older generations who have either faced cancer themselves or witnessed a loved one experience the disease. One of the most common sentiments I hear from these patients is the desire to catch cancer earlier. My answer is always this: The first and most important step everyone can take is understanding their risk.
For some, knowing they are at increased risk for cancer means starting screenings earlier — sometimes as early as age 25 — or getting screened with a more sensitive test.
This proactive approach is the right one. It also significantly reduces the burden of total and cancer-specific healthcare costs. While screening may carry some potential risks, clinicians can minimize these risks by adhering to evidence-based guidelines, such as those from the American Cancer Society, and ensuring there is appropriate discussion of treatment options when a diagnosis is made.
Normalizing Cancer Risk Assessment and Screening
A detailed cancer risk assessment and education about signs and symptoms should be part of every preventive care visit, regardless of someone’s age. Further, that cancer risk assessment should lead to clear recommendations and support for taking the next steps.
This is where care advocacy and patient navigation come in. Care advocacy can improve outcomes at every stage of the cancer journey, from increasing screening rates to improving quality of life for survivors. I’ve seen first-hand how care advocates help patients overcome hurdles like long wait times for appointments they need, making both screening and diagnostic care easier to access.
Now, with the finalization of a new rule from the Centers for Medicare & Medicaid Services, providers can bill for oncology navigation services that occur under their supervision. This formal recognition of care navigation affirms the value of these services not just clinically but financially as well. It will be through methods like care navigation, targeted outreach, and engaging educational resources — built into and covered by health plans — that patients will feel more in control over their health and have tools to help minimize the effects of cancer on the rest of their lives.
These services benefit healthcare providers as well. Care navigation supports clinical care teams, from primary care providers to oncologists, by ensuring patients are seen before their cancer progresses to a more advanced stage. And even if patients follow screening recommendations for the rest of their lives and never get a positive result, they’ve still gained something invaluable: peace of mind, knowing they’ve taken an active role in their health.
Fighting Fear With Routine
Treating cancer as a normal part of young people’s healthcare means helping them envision the disease as a condition that can be treated, much like a diagnosis of diabetes or high cholesterol. This mindset shift means quickly following up on a concerning symptom or screening result and reducing the time to start treatment if needed. And with treatment options and success rates for some cancers being better than ever, survivorship support must be built into every treatment plan from the start. Before treatment begins, healthcare providers should make time to talk about sometimes-overlooked key topics, such as reproductive options for people whose fertility may be affected by their cancer treatment, about plans for returning to work during or after treatment, and finding the right mental health support.
Where we can’t prevent cancer, both primary care providers and oncologists can work together to help patients receive the right diagnosis and treatment as quickly as possible. Knowing insurance coverage has a direct effect on how early cancer is caught, for example, younger people need support in understanding and accessing benefits and resources that may be available through their existing healthcare channels, like some employer-sponsored health plans. Even if getting treated for cancer is inevitable for some, taking immediate action to get screened when it’s appropriate is the best thing we can do to lessen the impact of these rising cancer incidences across the country. At the end of the day, being afraid of cancer doesn’t decrease the chances of getting sick or dying from it. Proactive screening and early detection do.
Brockman, Genetic Counselor, Color Health, Buffalo, New York, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Cancer is becoming more common in younger generations. Data show that people under 50 are experiencing higher rates of cancer than any generation before them. As a genetic counselor, I hoped these upward trends in early-onset malignancies would slow with a better understanding of risk factors and prevention strategies. Unfortunately, the opposite is happening. Recent findings from the American Cancer Society reveal that the incidence of at least 17 of 34 cancer types is rising among GenX and Millennials.
These statistics are alarming. I appreciate how easy it is for patients to get lost in the headlines about cancer, which may shape how they approach their healthcare. Each year, millions of Americans miss critical cancer screenings, with many citing fear of a positive test result as a leading reason. Others believe, despite the statistics, that cancer is not something they need to worry about until they are older. And then, of course, getting screened is not as easy as it should be.
In my work, I meet with people from both younger and older generations who have either faced cancer themselves or witnessed a loved one experience the disease. One of the most common sentiments I hear from these patients is the desire to catch cancer earlier. My answer is always this: The first and most important step everyone can take is understanding their risk.
For some, knowing they are at increased risk for cancer means starting screenings earlier — sometimes as early as age 25 — or getting screened with a more sensitive test.
This proactive approach is the right one. It also significantly reduces the burden of total and cancer-specific healthcare costs. While screening may carry some potential risks, clinicians can minimize these risks by adhering to evidence-based guidelines, such as those from the American Cancer Society, and ensuring there is appropriate discussion of treatment options when a diagnosis is made.
Normalizing Cancer Risk Assessment and Screening
A detailed cancer risk assessment and education about signs and symptoms should be part of every preventive care visit, regardless of someone’s age. Further, that cancer risk assessment should lead to clear recommendations and support for taking the next steps.
This is where care advocacy and patient navigation come in. Care advocacy can improve outcomes at every stage of the cancer journey, from increasing screening rates to improving quality of life for survivors. I’ve seen first-hand how care advocates help patients overcome hurdles like long wait times for appointments they need, making both screening and diagnostic care easier to access.
Now, with the finalization of a new rule from the Centers for Medicare & Medicaid Services, providers can bill for oncology navigation services that occur under their supervision. This formal recognition of care navigation affirms the value of these services not just clinically but financially as well. It will be through methods like care navigation, targeted outreach, and engaging educational resources — built into and covered by health plans — that patients will feel more in control over their health and have tools to help minimize the effects of cancer on the rest of their lives.
These services benefit healthcare providers as well. Care navigation supports clinical care teams, from primary care providers to oncologists, by ensuring patients are seen before their cancer progresses to a more advanced stage. And even if patients follow screening recommendations for the rest of their lives and never get a positive result, they’ve still gained something invaluable: peace of mind, knowing they’ve taken an active role in their health.
Fighting Fear With Routine
Treating cancer as a normal part of young people’s healthcare means helping them envision the disease as a condition that can be treated, much like a diagnosis of diabetes or high cholesterol. This mindset shift means quickly following up on a concerning symptom or screening result and reducing the time to start treatment if needed. And with treatment options and success rates for some cancers being better than ever, survivorship support must be built into every treatment plan from the start. Before treatment begins, healthcare providers should make time to talk about sometimes-overlooked key topics, such as reproductive options for people whose fertility may be affected by their cancer treatment, about plans for returning to work during or after treatment, and finding the right mental health support.
Where we can’t prevent cancer, both primary care providers and oncologists can work together to help patients receive the right diagnosis and treatment as quickly as possible. Knowing insurance coverage has a direct effect on how early cancer is caught, for example, younger people need support in understanding and accessing benefits and resources that may be available through their existing healthcare channels, like some employer-sponsored health plans. Even if getting treated for cancer is inevitable for some, taking immediate action to get screened when it’s appropriate is the best thing we can do to lessen the impact of these rising cancer incidences across the country. At the end of the day, being afraid of cancer doesn’t decrease the chances of getting sick or dying from it. Proactive screening and early detection do.
Brockman, Genetic Counselor, Color Health, Buffalo, New York, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
How to Treat Cancer While Preserving Fertility
Thanks to the continuously improving treatment options for cancer, the number of cancer survivors is increasing, and a large proportion of survivors is confronted with the long-term effects of cancer treatment. Especially for young patients, the question of the impact of therapy on fertility arises.
Dose adjustment or modification of the treatment regimen can achieve a lot. But experts at the congress of the European Society for Medical Oncology (ESMO) 2024 noted that knowledge about newer treatment options like immunotherapies is still insufficient.
Therapy Selection
The question of preserving fertility must be considered when deciding on the appropriate treatment, said Matteo Lambertini, MD, PhD, medical oncology consultant at the University of Genoa in Genoa, Italy. “Preserving fertility is also an aim of cancer therapy,” he said.
Lambertini, who is also a member of the ESMO Guideline Group on fertility preservation in cancer patients, referred to the 2020 ESMO guidelines, which list the gonadotoxicity of a substance depending on the treatment regimen and the patient’s age.
Isabelle Demeestere, MD, PhD, director of the research lab for human reproduction at the Erasmus Hospital of the Free University of Brussels in Brussels, Belgium, pointed out the limitations of general guidelines. “Therapies change over time, and a classification must be updated regularly.”
Knowledge gaps related to well-known therapies and many novel options persist. “For many FDA-approved medications, there are either no fertility data or only preclinical data available,” she added.
Chemotherapies and Immunotherapies
Chemotherapies with alkylating or platinum-containing substances are known for their effects on oocytes, follicle maturation, and spermatogenesis, said Demeestere.
Chemotherapy is gonadotoxic and leads to a temporary decrease in sperm quality or temporary azoospermia in men.
These effects, however, can lead to permanent azoospermia and endocrine disorders, depending on the dose, duration, or combination with radiation, said Demeestere.
Cryopreservation of sperm should always be performed before starting treatment. For high-risk patients who are prepubertal, samples of testicular tissue are taken.
In women, chemotherapy affects primordial follicles and follicle maturation through DNA damage. This process results in severe or temporary amenorrhea, a temporary or permanent decrease in egg reserve, and ultimately premature egg insufficiency.
Novel immunotherapies also influence fertility, presumably through interactions of the immune system with the reproductive organs. But insufficient data are available, according to Lambertini, who emphasized that “these data are urgently needed, especially for young patients with cancer.”
In a mouse model, immune checkpoint inhibitors affected ovarian function, and the inflammatory reaction in humans can affect fertility. No long-term data are available for women yet, however, explained Demeestere. The effects of other therapeutics such as PARP, CDK4/6, or tyrosine kinase inhibitors, as well as monoclonal antibodies like trastuzumab, are only seen sporadically.
In the PENELOPE-B phase 3 study, the CDK4/6 inhibitor palbociclib did not affect ovarian function, even though the cyclin-dependent kinases play an important role in mitotic arrest, said Demeestere.
Adjusting the Regimen
In a PET-guided approach, Demeestere’s research team investigated the effects of dose reduction or adjustment of the treatment regimen of procarbazine and cyclophosphamide on the fertility of patients younger than 45 years with advanced Hodgkin lymphoma.
By regularly controlling tumor growth with PET, the treatment could be adjusted so that the effect on egg reserve or spermatogenesis was significantly reduced and loss of fertility could be prevented.
During the 5-year follow-up period, the ovarian function of participating women was assessed by the serum concentration of follicle-stimulating hormone (FSH), estradiol, and anti-Müllerian hormone (AMH) to evaluate egg reserve. In men, testicular function was assessed at the beginning of the study. At the end of treatment, sperm analysis and FSH and testosterone levels were checked.
Demeestere and colleagues demonstrated that dose reduction or altering the treatment regimen for patients who responded early to treatment (determined by PET-guided monitoring) reduced the risk for gonadotoxicity from 46% to 14.5%. That is, the risk was reduced by more than half.
FSH and AMH correlated with the patient’s age and the dose of the alkylating agent. In men, sperm parameters recovered after dose or agent adjustment compared with the unchanged treatment regimen.
Newer results from the PHERGain study in women with early human epidermal growth factor receptor 2–positive breast cancer also provided hope, according to Demeestere. Under PET-guided control, chemotherapy could be reduced.
More Data Needed
The new treatment options pose a challenge to preserving fertility during cancer treatment, said Demeestere.
For new targeted therapies, uniform recommendations cannot be issued because of the lack of data and varying treatment durations. Still, the new therapies are safer than chemotherapy.
The need to collect data on fertility and long-term effects in cancer survivors in clinical studies is also reflected in the literature, according to Demeestere. “There are more review articles on this topic than clinical studies.”
This story was translated from the Medscape German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Thanks to the continuously improving treatment options for cancer, the number of cancer survivors is increasing, and a large proportion of survivors is confronted with the long-term effects of cancer treatment. Especially for young patients, the question of the impact of therapy on fertility arises.
Dose adjustment or modification of the treatment regimen can achieve a lot. But experts at the congress of the European Society for Medical Oncology (ESMO) 2024 noted that knowledge about newer treatment options like immunotherapies is still insufficient.
Therapy Selection
The question of preserving fertility must be considered when deciding on the appropriate treatment, said Matteo Lambertini, MD, PhD, medical oncology consultant at the University of Genoa in Genoa, Italy. “Preserving fertility is also an aim of cancer therapy,” he said.
Lambertini, who is also a member of the ESMO Guideline Group on fertility preservation in cancer patients, referred to the 2020 ESMO guidelines, which list the gonadotoxicity of a substance depending on the treatment regimen and the patient’s age.
Isabelle Demeestere, MD, PhD, director of the research lab for human reproduction at the Erasmus Hospital of the Free University of Brussels in Brussels, Belgium, pointed out the limitations of general guidelines. “Therapies change over time, and a classification must be updated regularly.”
Knowledge gaps related to well-known therapies and many novel options persist. “For many FDA-approved medications, there are either no fertility data or only preclinical data available,” she added.
Chemotherapies and Immunotherapies
Chemotherapies with alkylating or platinum-containing substances are known for their effects on oocytes, follicle maturation, and spermatogenesis, said Demeestere.
Chemotherapy is gonadotoxic and leads to a temporary decrease in sperm quality or temporary azoospermia in men.
These effects, however, can lead to permanent azoospermia and endocrine disorders, depending on the dose, duration, or combination with radiation, said Demeestere.
Cryopreservation of sperm should always be performed before starting treatment. For high-risk patients who are prepubertal, samples of testicular tissue are taken.
In women, chemotherapy affects primordial follicles and follicle maturation through DNA damage. This process results in severe or temporary amenorrhea, a temporary or permanent decrease in egg reserve, and ultimately premature egg insufficiency.
Novel immunotherapies also influence fertility, presumably through interactions of the immune system with the reproductive organs. But insufficient data are available, according to Lambertini, who emphasized that “these data are urgently needed, especially for young patients with cancer.”
In a mouse model, immune checkpoint inhibitors affected ovarian function, and the inflammatory reaction in humans can affect fertility. No long-term data are available for women yet, however, explained Demeestere. The effects of other therapeutics such as PARP, CDK4/6, or tyrosine kinase inhibitors, as well as monoclonal antibodies like trastuzumab, are only seen sporadically.
In the PENELOPE-B phase 3 study, the CDK4/6 inhibitor palbociclib did not affect ovarian function, even though the cyclin-dependent kinases play an important role in mitotic arrest, said Demeestere.
Adjusting the Regimen
In a PET-guided approach, Demeestere’s research team investigated the effects of dose reduction or adjustment of the treatment regimen of procarbazine and cyclophosphamide on the fertility of patients younger than 45 years with advanced Hodgkin lymphoma.
By regularly controlling tumor growth with PET, the treatment could be adjusted so that the effect on egg reserve or spermatogenesis was significantly reduced and loss of fertility could be prevented.
During the 5-year follow-up period, the ovarian function of participating women was assessed by the serum concentration of follicle-stimulating hormone (FSH), estradiol, and anti-Müllerian hormone (AMH) to evaluate egg reserve. In men, testicular function was assessed at the beginning of the study. At the end of treatment, sperm analysis and FSH and testosterone levels were checked.
Demeestere and colleagues demonstrated that dose reduction or altering the treatment regimen for patients who responded early to treatment (determined by PET-guided monitoring) reduced the risk for gonadotoxicity from 46% to 14.5%. That is, the risk was reduced by more than half.
FSH and AMH correlated with the patient’s age and the dose of the alkylating agent. In men, sperm parameters recovered after dose or agent adjustment compared with the unchanged treatment regimen.
Newer results from the PHERGain study in women with early human epidermal growth factor receptor 2–positive breast cancer also provided hope, according to Demeestere. Under PET-guided control, chemotherapy could be reduced.
More Data Needed
The new treatment options pose a challenge to preserving fertility during cancer treatment, said Demeestere.
For new targeted therapies, uniform recommendations cannot be issued because of the lack of data and varying treatment durations. Still, the new therapies are safer than chemotherapy.
The need to collect data on fertility and long-term effects in cancer survivors in clinical studies is also reflected in the literature, according to Demeestere. “There are more review articles on this topic than clinical studies.”
This story was translated from the Medscape German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Thanks to the continuously improving treatment options for cancer, the number of cancer survivors is increasing, and a large proportion of survivors is confronted with the long-term effects of cancer treatment. Especially for young patients, the question of the impact of therapy on fertility arises.
Dose adjustment or modification of the treatment regimen can achieve a lot. But experts at the congress of the European Society for Medical Oncology (ESMO) 2024 noted that knowledge about newer treatment options like immunotherapies is still insufficient.
Therapy Selection
The question of preserving fertility must be considered when deciding on the appropriate treatment, said Matteo Lambertini, MD, PhD, medical oncology consultant at the University of Genoa in Genoa, Italy. “Preserving fertility is also an aim of cancer therapy,” he said.
Lambertini, who is also a member of the ESMO Guideline Group on fertility preservation in cancer patients, referred to the 2020 ESMO guidelines, which list the gonadotoxicity of a substance depending on the treatment regimen and the patient’s age.
Isabelle Demeestere, MD, PhD, director of the research lab for human reproduction at the Erasmus Hospital of the Free University of Brussels in Brussels, Belgium, pointed out the limitations of general guidelines. “Therapies change over time, and a classification must be updated regularly.”
Knowledge gaps related to well-known therapies and many novel options persist. “For many FDA-approved medications, there are either no fertility data or only preclinical data available,” she added.
Chemotherapies and Immunotherapies
Chemotherapies with alkylating or platinum-containing substances are known for their effects on oocytes, follicle maturation, and spermatogenesis, said Demeestere.
Chemotherapy is gonadotoxic and leads to a temporary decrease in sperm quality or temporary azoospermia in men.
These effects, however, can lead to permanent azoospermia and endocrine disorders, depending on the dose, duration, or combination with radiation, said Demeestere.
Cryopreservation of sperm should always be performed before starting treatment. For high-risk patients who are prepubertal, samples of testicular tissue are taken.
In women, chemotherapy affects primordial follicles and follicle maturation through DNA damage. This process results in severe or temporary amenorrhea, a temporary or permanent decrease in egg reserve, and ultimately premature egg insufficiency.
Novel immunotherapies also influence fertility, presumably through interactions of the immune system with the reproductive organs. But insufficient data are available, according to Lambertini, who emphasized that “these data are urgently needed, especially for young patients with cancer.”
In a mouse model, immune checkpoint inhibitors affected ovarian function, and the inflammatory reaction in humans can affect fertility. No long-term data are available for women yet, however, explained Demeestere. The effects of other therapeutics such as PARP, CDK4/6, or tyrosine kinase inhibitors, as well as monoclonal antibodies like trastuzumab, are only seen sporadically.
In the PENELOPE-B phase 3 study, the CDK4/6 inhibitor palbociclib did not affect ovarian function, even though the cyclin-dependent kinases play an important role in mitotic arrest, said Demeestere.
Adjusting the Regimen
In a PET-guided approach, Demeestere’s research team investigated the effects of dose reduction or adjustment of the treatment regimen of procarbazine and cyclophosphamide on the fertility of patients younger than 45 years with advanced Hodgkin lymphoma.
By regularly controlling tumor growth with PET, the treatment could be adjusted so that the effect on egg reserve or spermatogenesis was significantly reduced and loss of fertility could be prevented.
During the 5-year follow-up period, the ovarian function of participating women was assessed by the serum concentration of follicle-stimulating hormone (FSH), estradiol, and anti-Müllerian hormone (AMH) to evaluate egg reserve. In men, testicular function was assessed at the beginning of the study. At the end of treatment, sperm analysis and FSH and testosterone levels were checked.
Demeestere and colleagues demonstrated that dose reduction or altering the treatment regimen for patients who responded early to treatment (determined by PET-guided monitoring) reduced the risk for gonadotoxicity from 46% to 14.5%. That is, the risk was reduced by more than half.
FSH and AMH correlated with the patient’s age and the dose of the alkylating agent. In men, sperm parameters recovered after dose or agent adjustment compared with the unchanged treatment regimen.
Newer results from the PHERGain study in women with early human epidermal growth factor receptor 2–positive breast cancer also provided hope, according to Demeestere. Under PET-guided control, chemotherapy could be reduced.
More Data Needed
The new treatment options pose a challenge to preserving fertility during cancer treatment, said Demeestere.
For new targeted therapies, uniform recommendations cannot be issued because of the lack of data and varying treatment durations. Still, the new therapies are safer than chemotherapy.
The need to collect data on fertility and long-term effects in cancer survivors in clinical studies is also reflected in the literature, according to Demeestere. “There are more review articles on this topic than clinical studies.”
This story was translated from the Medscape German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
ACS: Breast Cancer Incidence Rising, Mortality Disparities Persist
Breast cancer incidence has been on the rise, particularly among White women under age 50, but breast cancer deaths — for some, but not all, populations — have been steadily decreasing, according to a biennial update from the American Cancer Society (ACS).
The ACS update, which underscores the persistence of racial and ethnic disparities in breast cancer incidence and outcomes, noted an overall 1% annual increase in breast cancer incidence from 2012 to 2021. The additional cases were largely composed of localized-stage and hormone receptor (HR)–positive disease, which generally have better prognoses than more advanced and HR–negative disease.
Deaths from breast cancer, however, declined from 1989 to 2022, with an overall drop of 44%. That percentage drop “translates to almost 518,000 fewer women dying from breast cancer in the United States during this time,” Angela N. Giaquinto and ACS colleagues noted in the report, published in CA: A Cancer Journal for Clinicians.
“This progress is the result of advances in treatment and earlier detection through screening,” the authors wrote, while stressing that “these interventions have not been disseminated equally.”
The ACS also published an educational companion — Breast Cancer Facts & Figures 2024-2025 — that provides additional insights about trends in breast cancer and steps needed to bolster prevention, detection, and treatment advances.
Incidence and Mortality
Although the overall annual increase in breast cancer incidence from 2012 to 2021 was 1%, the increase was steeper among women under age 50, at 1.4% annually vs 0.7% among those aged 50 or older.
Asian American/Pacific Islander women had the greatest increases in breast cancer incidence among both age groups, with a 2.7% annual increase for those aged under 50 and a 2.5% increase for those aged 50 or older. This group, however, had the second lowest breast cancer rate in 2000 at 57.4 cases per 100,000 persons, but the highest rate in 2021 at 86.3 cases per 100,000, alongside White women (86.4 cases per 100,000). Black women were not far behind at 81.5 cases per 100,000.
Black women were least likely to be diagnosed with localized-stage breast cancer and most likely to be diagnosed with distant-stage or unstaged cancer, with American Indian/Alaska Native women not far behind.
Despite the rising incidence of breast cancer, death rates from the disease have gone down considerably overall from about 33 deaths per 100,000 women in 1989 to 19 deaths per 100,000 in 2022.
However, not all women have experienced these survival gains equally, Ms. Giaquinto and colleagues noted.
Since 1990, the mortality rate has remained unchanged among American Indian/Alaska Native women. Black women, however, have experienced a 38% higher mortality rate than White women, despite having a 5% lower incidence of breast cancer.
In fact, Black women have the lowest survival of any racial and ethnic group for every breast cancer subtype and stage of disease except localized disease.
Additional key findings from the report:
- In 2024, an estimated 310,720 new invasive breast cancers and 56,500 cases of ductal carcinoma in situ will be diagnosed among women in the United States, and an additional 2790 cases will be diagnosed in men.
- On the mortality front, in 2024, approximately 42,250 women are expected to die of breast cancer; 530 breast cancer deaths are anticipated in men.
- As for the lifetime risk for breast cancer, approximately one in eight women in the United States (13.1%) will be diagnosed with invasive breast cancer; 1 in 43 (2.3%) will die from the disease.
- The 5-year relative survival rate for breast cancer is 91%, but that drops to 86% at 10 years and 81% at 15 years.
- The 5-year relative survival rate is over 99% for breast cancer diagnosed at a localized stage but drops to 87% for regional-stage and 32% for distant-stage disease.
- American Indian/Alaska Native women have a 10% lower breast cancer incidence than White women but 6% higher mortality.
Similar to the ACS report, a recent study published in JAMA Network Open reported rising breast cancer incidence among US women aged 20-49 years of different races in different age groups over the past 2 decades.
The increased incidence of breast cancer in younger women “is an area of concern and an area where we really need to spend more effort trying to understand why,” said lead study author and breast surgeon Adetunji T. Toriola, MD, PhD, MPH, of Washington University in St Louis, Missouri.
Although reproductive and lifestyle factors, such as weight gain, diet, and physical activity, may contribute to the growing breast cancer incidence in younger women — and preliminary findings from Dr. Toriola’s own research suggest that reproductive factors may be a particularly strong driver — environmental factors, including exposure to forever chemicals, may also play a role.
Early-life factors, such as exposure to toxins, remain an underexplored area, Dr. Toriola noted, stressing the importance of teasing out the long-term effects of environmental exposures in puberty and during adolescence.
Overall, the trends observed both in this study and the ACS report highlight the need for enhanced prevention efforts that address racial disparities as well as the rising incidence in young women, said Dr. Toriola, also professor of surgery at the Washington University Institute of Public Health, St Louis.
For now, Dr. Toriola urges women to “engage with mammographic screening as soon as qualified” as per guidelines. Women at average risk should go for screening beginning at age 40, and those with a family history or other risk factors should talk to their physician about earlier screening, he said.
Ms. Giaquinto is employed by the ACS, which receives grants from private and corporate foundations, including foundations associated with companies in the health sector, for research outside of the submitted work. Dr. Toriola reported having no disclosures.
A version of this article first appeared on Medscape.com.
Breast cancer incidence has been on the rise, particularly among White women under age 50, but breast cancer deaths — for some, but not all, populations — have been steadily decreasing, according to a biennial update from the American Cancer Society (ACS).
The ACS update, which underscores the persistence of racial and ethnic disparities in breast cancer incidence and outcomes, noted an overall 1% annual increase in breast cancer incidence from 2012 to 2021. The additional cases were largely composed of localized-stage and hormone receptor (HR)–positive disease, which generally have better prognoses than more advanced and HR–negative disease.
Deaths from breast cancer, however, declined from 1989 to 2022, with an overall drop of 44%. That percentage drop “translates to almost 518,000 fewer women dying from breast cancer in the United States during this time,” Angela N. Giaquinto and ACS colleagues noted in the report, published in CA: A Cancer Journal for Clinicians.
“This progress is the result of advances in treatment and earlier detection through screening,” the authors wrote, while stressing that “these interventions have not been disseminated equally.”
The ACS also published an educational companion — Breast Cancer Facts & Figures 2024-2025 — that provides additional insights about trends in breast cancer and steps needed to bolster prevention, detection, and treatment advances.
Incidence and Mortality
Although the overall annual increase in breast cancer incidence from 2012 to 2021 was 1%, the increase was steeper among women under age 50, at 1.4% annually vs 0.7% among those aged 50 or older.
Asian American/Pacific Islander women had the greatest increases in breast cancer incidence among both age groups, with a 2.7% annual increase for those aged under 50 and a 2.5% increase for those aged 50 or older. This group, however, had the second lowest breast cancer rate in 2000 at 57.4 cases per 100,000 persons, but the highest rate in 2021 at 86.3 cases per 100,000, alongside White women (86.4 cases per 100,000). Black women were not far behind at 81.5 cases per 100,000.
Black women were least likely to be diagnosed with localized-stage breast cancer and most likely to be diagnosed with distant-stage or unstaged cancer, with American Indian/Alaska Native women not far behind.
Despite the rising incidence of breast cancer, death rates from the disease have gone down considerably overall from about 33 deaths per 100,000 women in 1989 to 19 deaths per 100,000 in 2022.
However, not all women have experienced these survival gains equally, Ms. Giaquinto and colleagues noted.
Since 1990, the mortality rate has remained unchanged among American Indian/Alaska Native women. Black women, however, have experienced a 38% higher mortality rate than White women, despite having a 5% lower incidence of breast cancer.
In fact, Black women have the lowest survival of any racial and ethnic group for every breast cancer subtype and stage of disease except localized disease.
Additional key findings from the report:
- In 2024, an estimated 310,720 new invasive breast cancers and 56,500 cases of ductal carcinoma in situ will be diagnosed among women in the United States, and an additional 2790 cases will be diagnosed in men.
- On the mortality front, in 2024, approximately 42,250 women are expected to die of breast cancer; 530 breast cancer deaths are anticipated in men.
- As for the lifetime risk for breast cancer, approximately one in eight women in the United States (13.1%) will be diagnosed with invasive breast cancer; 1 in 43 (2.3%) will die from the disease.
- The 5-year relative survival rate for breast cancer is 91%, but that drops to 86% at 10 years and 81% at 15 years.
- The 5-year relative survival rate is over 99% for breast cancer diagnosed at a localized stage but drops to 87% for regional-stage and 32% for distant-stage disease.
- American Indian/Alaska Native women have a 10% lower breast cancer incidence than White women but 6% higher mortality.
Similar to the ACS report, a recent study published in JAMA Network Open reported rising breast cancer incidence among US women aged 20-49 years of different races in different age groups over the past 2 decades.
The increased incidence of breast cancer in younger women “is an area of concern and an area where we really need to spend more effort trying to understand why,” said lead study author and breast surgeon Adetunji T. Toriola, MD, PhD, MPH, of Washington University in St Louis, Missouri.
Although reproductive and lifestyle factors, such as weight gain, diet, and physical activity, may contribute to the growing breast cancer incidence in younger women — and preliminary findings from Dr. Toriola’s own research suggest that reproductive factors may be a particularly strong driver — environmental factors, including exposure to forever chemicals, may also play a role.
Early-life factors, such as exposure to toxins, remain an underexplored area, Dr. Toriola noted, stressing the importance of teasing out the long-term effects of environmental exposures in puberty and during adolescence.
Overall, the trends observed both in this study and the ACS report highlight the need for enhanced prevention efforts that address racial disparities as well as the rising incidence in young women, said Dr. Toriola, also professor of surgery at the Washington University Institute of Public Health, St Louis.
For now, Dr. Toriola urges women to “engage with mammographic screening as soon as qualified” as per guidelines. Women at average risk should go for screening beginning at age 40, and those with a family history or other risk factors should talk to their physician about earlier screening, he said.
Ms. Giaquinto is employed by the ACS, which receives grants from private and corporate foundations, including foundations associated with companies in the health sector, for research outside of the submitted work. Dr. Toriola reported having no disclosures.
A version of this article first appeared on Medscape.com.
Breast cancer incidence has been on the rise, particularly among White women under age 50, but breast cancer deaths — for some, but not all, populations — have been steadily decreasing, according to a biennial update from the American Cancer Society (ACS).
The ACS update, which underscores the persistence of racial and ethnic disparities in breast cancer incidence and outcomes, noted an overall 1% annual increase in breast cancer incidence from 2012 to 2021. The additional cases were largely composed of localized-stage and hormone receptor (HR)–positive disease, which generally have better prognoses than more advanced and HR–negative disease.
Deaths from breast cancer, however, declined from 1989 to 2022, with an overall drop of 44%. That percentage drop “translates to almost 518,000 fewer women dying from breast cancer in the United States during this time,” Angela N. Giaquinto and ACS colleagues noted in the report, published in CA: A Cancer Journal for Clinicians.
“This progress is the result of advances in treatment and earlier detection through screening,” the authors wrote, while stressing that “these interventions have not been disseminated equally.”
The ACS also published an educational companion — Breast Cancer Facts & Figures 2024-2025 — that provides additional insights about trends in breast cancer and steps needed to bolster prevention, detection, and treatment advances.
Incidence and Mortality
Although the overall annual increase in breast cancer incidence from 2012 to 2021 was 1%, the increase was steeper among women under age 50, at 1.4% annually vs 0.7% among those aged 50 or older.
Asian American/Pacific Islander women had the greatest increases in breast cancer incidence among both age groups, with a 2.7% annual increase for those aged under 50 and a 2.5% increase for those aged 50 or older. This group, however, had the second lowest breast cancer rate in 2000 at 57.4 cases per 100,000 persons, but the highest rate in 2021 at 86.3 cases per 100,000, alongside White women (86.4 cases per 100,000). Black women were not far behind at 81.5 cases per 100,000.
Black women were least likely to be diagnosed with localized-stage breast cancer and most likely to be diagnosed with distant-stage or unstaged cancer, with American Indian/Alaska Native women not far behind.
Despite the rising incidence of breast cancer, death rates from the disease have gone down considerably overall from about 33 deaths per 100,000 women in 1989 to 19 deaths per 100,000 in 2022.
However, not all women have experienced these survival gains equally, Ms. Giaquinto and colleagues noted.
Since 1990, the mortality rate has remained unchanged among American Indian/Alaska Native women. Black women, however, have experienced a 38% higher mortality rate than White women, despite having a 5% lower incidence of breast cancer.
In fact, Black women have the lowest survival of any racial and ethnic group for every breast cancer subtype and stage of disease except localized disease.
Additional key findings from the report:
- In 2024, an estimated 310,720 new invasive breast cancers and 56,500 cases of ductal carcinoma in situ will be diagnosed among women in the United States, and an additional 2790 cases will be diagnosed in men.
- On the mortality front, in 2024, approximately 42,250 women are expected to die of breast cancer; 530 breast cancer deaths are anticipated in men.
- As for the lifetime risk for breast cancer, approximately one in eight women in the United States (13.1%) will be diagnosed with invasive breast cancer; 1 in 43 (2.3%) will die from the disease.
- The 5-year relative survival rate for breast cancer is 91%, but that drops to 86% at 10 years and 81% at 15 years.
- The 5-year relative survival rate is over 99% for breast cancer diagnosed at a localized stage but drops to 87% for regional-stage and 32% for distant-stage disease.
- American Indian/Alaska Native women have a 10% lower breast cancer incidence than White women but 6% higher mortality.
Similar to the ACS report, a recent study published in JAMA Network Open reported rising breast cancer incidence among US women aged 20-49 years of different races in different age groups over the past 2 decades.
The increased incidence of breast cancer in younger women “is an area of concern and an area where we really need to spend more effort trying to understand why,” said lead study author and breast surgeon Adetunji T. Toriola, MD, PhD, MPH, of Washington University in St Louis, Missouri.
Although reproductive and lifestyle factors, such as weight gain, diet, and physical activity, may contribute to the growing breast cancer incidence in younger women — and preliminary findings from Dr. Toriola’s own research suggest that reproductive factors may be a particularly strong driver — environmental factors, including exposure to forever chemicals, may also play a role.
Early-life factors, such as exposure to toxins, remain an underexplored area, Dr. Toriola noted, stressing the importance of teasing out the long-term effects of environmental exposures in puberty and during adolescence.
Overall, the trends observed both in this study and the ACS report highlight the need for enhanced prevention efforts that address racial disparities as well as the rising incidence in young women, said Dr. Toriola, also professor of surgery at the Washington University Institute of Public Health, St Louis.
For now, Dr. Toriola urges women to “engage with mammographic screening as soon as qualified” as per guidelines. Women at average risk should go for screening beginning at age 40, and those with a family history or other risk factors should talk to their physician about earlier screening, he said.
Ms. Giaquinto is employed by the ACS, which receives grants from private and corporate foundations, including foundations associated with companies in the health sector, for research outside of the submitted work. Dr. Toriola reported having no disclosures.
A version of this article first appeared on Medscape.com.
The Biology of ‘Precancer’: Stopping Cancer Before It Starts
Some breast cancer types are more likely than others to recur. Researchers have known this for more than a decade.
But they have long wondered why.
“How did those tumor types arise?” said Christina Curtis, PhD, a professor of medicine, genetics and biomedical data science at Stanford University in California. “They’re all breast cancers. They’re all estrogen receptor positive. But these groups are different. When did they become different, and how is that determined?”
Dr. Curtis and colleagues are finally starting to answer these questions. They recently broke new ground in a study linking differences in cancer-related genes to disease subtype and aggressiveness.
DNA inherited from our parents is known as the germline genome. It affects whether the immune system attacks or retreats when confronted with variations that may lead to breast cancer.
“It turns out, the germline genome sculpts tumor evolution,” said Dr. Curtis.
The study is part of a growing effort to understand “precancer” — the critical period after cells have started to grow abnormally but before they’ve developed into cancer — a research trend that could trigger a decisive shift in how cancer treatments are realized. Therapeutics could be designed on the basis of the biology of these precancerous cells.
While biotech start-ups push new tests to catch cancer early, researchers like Dr. Curtis hope to stop cancer before it even starts.
“This is a really exciting area of research,” said Susan Domchek, MD, executive director of the Basser Center for BRCA at the University of Pennsylvania, Philadelphia, who was not involved in the study. “What we hope for is that, over time, we’re going to have more and more biologically driven interception.”
‘We’re Basically Unearthing the Dark Matter of the Human Genome’
Of course, we already have mechanical ways of heading off cancer, like having a precancerous polyp removed. But for the Stanford researchers, biologic interception is the goal. They hope to figure out how to use the immune system to stop the cancer.
In their study, they looked at DNA variabilities known as somatic aberrations or single-nucleotide protein sequences (SNPs). The HER2 gene, for example, can contain SNPs — possibly affecting how the HER2 protein regulates breast cell growth and division.
“There’s been a huge effort through genomewide association studies to link SNPs to cancer outcomes and risk,” Dr. Curtis said.
Focusing on people with a genetic predisposition for breast cancer, Dr. Curtis used machine learning to show that these variabilities can occur in specific epitopes (protein features that can trigger an immune response).
They also found that heightened variability can show up in a region of the genome called the human leukocyte antigen (HLA). Each HLA molecule can contain many epitopes.
“We developed a whole new algorithm to compute this ‘germline epitope burden,’ ” Dr. Curtis said. “We’re basically unearthing the dark matter of the human genome to ask about the interplay between SNPs and HLA class one presentation.”
These aberration-rich regions can grab the immune system’s attention. Sometimes the immune system identifies and eradicates those epitopes.
In that case: “I have immunosurveillance. I’ve cured my cancer,” said Nora Disis, PhD, director of the Cancer Vaccine Institute and a professor of medicine at the University of Washington, Seattle. Dr. Disis was not involved in the study.
But other times, the immune system finds a way around the high “epitope burden,” and the tumors become more aggressive and immunosuppressive. That’s when cancer forms.
This suggests a “critical juncture between preinvasive and invasive disease,” Dr. Curtis said.
And that “critical juncture” may very well be the optimal time for intervention.
The Precancer Push
Stanford’s findings add information to prior biomarkers and may provide a way to identify “bad-acting tumors” from a simple blood draw measuring germline epitope burden, Dr. Curtis said. Looking further ahead, “this also reveals a new source of epitopes that might be immunogenic and might be informative for the development of vaccines.”
Many labs are trying to understand the biology of precancer and exploring possible vaccines.
The National Cancer Institute’s Human Tumor Atlas Network is building three-dimensional models of the evolution from precancerous to advanced disease. And researchers at the Cancer Vaccine Institute at the University of Washington are developing a vaccine for a precancerous lesion linked to many ovarian cancers.
Dr. Domchek’s research explores whether breast cancers caused by mutations in the BRCA 1 and 2 genes can be intercepted at very early stages. In a clinical trial of healthy people with those mutations, Dr. Domchek and colleagues are attempting to “rev up the immune system to tackle telomerase,” an enzyme that’s over-expressed in 95% of cancers. The hope is for this experimental vaccine to lower their risk of developing cancer.
At the Fred Hutch Cancer Center, Seattle, Ming Yu, PhD, is studying how senescent cells affect immune cells in precancer. As cells age and stop dividing, she said, they can accumulate and create a “tumor-promoting microenvironment” in older people.
Dr. Yu has found that the antiaging drug rapamycin can eliminate those “zombie cells” in mice. She’s studying whether the “cleanup” can help prevent cancer and expects results in a few months.
In the years and decades to come, all of this could lead to a new era in cancer treatment.
“Most drug development starts with people with advanced cancer and then goes into the earlier and earlier spaces,” said Dr. Domchek. “But it may be that we’re thinking about it all wrong and that you really have to understand the unique biology of early lesions to go after them.”
A version of this article first appeared on Medscape.com.
Some breast cancer types are more likely than others to recur. Researchers have known this for more than a decade.
But they have long wondered why.
“How did those tumor types arise?” said Christina Curtis, PhD, a professor of medicine, genetics and biomedical data science at Stanford University in California. “They’re all breast cancers. They’re all estrogen receptor positive. But these groups are different. When did they become different, and how is that determined?”
Dr. Curtis and colleagues are finally starting to answer these questions. They recently broke new ground in a study linking differences in cancer-related genes to disease subtype and aggressiveness.
DNA inherited from our parents is known as the germline genome. It affects whether the immune system attacks or retreats when confronted with variations that may lead to breast cancer.
“It turns out, the germline genome sculpts tumor evolution,” said Dr. Curtis.
The study is part of a growing effort to understand “precancer” — the critical period after cells have started to grow abnormally but before they’ve developed into cancer — a research trend that could trigger a decisive shift in how cancer treatments are realized. Therapeutics could be designed on the basis of the biology of these precancerous cells.
While biotech start-ups push new tests to catch cancer early, researchers like Dr. Curtis hope to stop cancer before it even starts.
“This is a really exciting area of research,” said Susan Domchek, MD, executive director of the Basser Center for BRCA at the University of Pennsylvania, Philadelphia, who was not involved in the study. “What we hope for is that, over time, we’re going to have more and more biologically driven interception.”
‘We’re Basically Unearthing the Dark Matter of the Human Genome’
Of course, we already have mechanical ways of heading off cancer, like having a precancerous polyp removed. But for the Stanford researchers, biologic interception is the goal. They hope to figure out how to use the immune system to stop the cancer.
In their study, they looked at DNA variabilities known as somatic aberrations or single-nucleotide protein sequences (SNPs). The HER2 gene, for example, can contain SNPs — possibly affecting how the HER2 protein regulates breast cell growth and division.
“There’s been a huge effort through genomewide association studies to link SNPs to cancer outcomes and risk,” Dr. Curtis said.
Focusing on people with a genetic predisposition for breast cancer, Dr. Curtis used machine learning to show that these variabilities can occur in specific epitopes (protein features that can trigger an immune response).
They also found that heightened variability can show up in a region of the genome called the human leukocyte antigen (HLA). Each HLA molecule can contain many epitopes.
“We developed a whole new algorithm to compute this ‘germline epitope burden,’ ” Dr. Curtis said. “We’re basically unearthing the dark matter of the human genome to ask about the interplay between SNPs and HLA class one presentation.”
These aberration-rich regions can grab the immune system’s attention. Sometimes the immune system identifies and eradicates those epitopes.
In that case: “I have immunosurveillance. I’ve cured my cancer,” said Nora Disis, PhD, director of the Cancer Vaccine Institute and a professor of medicine at the University of Washington, Seattle. Dr. Disis was not involved in the study.
But other times, the immune system finds a way around the high “epitope burden,” and the tumors become more aggressive and immunosuppressive. That’s when cancer forms.
This suggests a “critical juncture between preinvasive and invasive disease,” Dr. Curtis said.
And that “critical juncture” may very well be the optimal time for intervention.
The Precancer Push
Stanford’s findings add information to prior biomarkers and may provide a way to identify “bad-acting tumors” from a simple blood draw measuring germline epitope burden, Dr. Curtis said. Looking further ahead, “this also reveals a new source of epitopes that might be immunogenic and might be informative for the development of vaccines.”
Many labs are trying to understand the biology of precancer and exploring possible vaccines.
The National Cancer Institute’s Human Tumor Atlas Network is building three-dimensional models of the evolution from precancerous to advanced disease. And researchers at the Cancer Vaccine Institute at the University of Washington are developing a vaccine for a precancerous lesion linked to many ovarian cancers.
Dr. Domchek’s research explores whether breast cancers caused by mutations in the BRCA 1 and 2 genes can be intercepted at very early stages. In a clinical trial of healthy people with those mutations, Dr. Domchek and colleagues are attempting to “rev up the immune system to tackle telomerase,” an enzyme that’s over-expressed in 95% of cancers. The hope is for this experimental vaccine to lower their risk of developing cancer.
At the Fred Hutch Cancer Center, Seattle, Ming Yu, PhD, is studying how senescent cells affect immune cells in precancer. As cells age and stop dividing, she said, they can accumulate and create a “tumor-promoting microenvironment” in older people.
Dr. Yu has found that the antiaging drug rapamycin can eliminate those “zombie cells” in mice. She’s studying whether the “cleanup” can help prevent cancer and expects results in a few months.
In the years and decades to come, all of this could lead to a new era in cancer treatment.
“Most drug development starts with people with advanced cancer and then goes into the earlier and earlier spaces,” said Dr. Domchek. “But it may be that we’re thinking about it all wrong and that you really have to understand the unique biology of early lesions to go after them.”
A version of this article first appeared on Medscape.com.
Some breast cancer types are more likely than others to recur. Researchers have known this for more than a decade.
But they have long wondered why.
“How did those tumor types arise?” said Christina Curtis, PhD, a professor of medicine, genetics and biomedical data science at Stanford University in California. “They’re all breast cancers. They’re all estrogen receptor positive. But these groups are different. When did they become different, and how is that determined?”
Dr. Curtis and colleagues are finally starting to answer these questions. They recently broke new ground in a study linking differences in cancer-related genes to disease subtype and aggressiveness.
DNA inherited from our parents is known as the germline genome. It affects whether the immune system attacks or retreats when confronted with variations that may lead to breast cancer.
“It turns out, the germline genome sculpts tumor evolution,” said Dr. Curtis.
The study is part of a growing effort to understand “precancer” — the critical period after cells have started to grow abnormally but before they’ve developed into cancer — a research trend that could trigger a decisive shift in how cancer treatments are realized. Therapeutics could be designed on the basis of the biology of these precancerous cells.
While biotech start-ups push new tests to catch cancer early, researchers like Dr. Curtis hope to stop cancer before it even starts.
“This is a really exciting area of research,” said Susan Domchek, MD, executive director of the Basser Center for BRCA at the University of Pennsylvania, Philadelphia, who was not involved in the study. “What we hope for is that, over time, we’re going to have more and more biologically driven interception.”
‘We’re Basically Unearthing the Dark Matter of the Human Genome’
Of course, we already have mechanical ways of heading off cancer, like having a precancerous polyp removed. But for the Stanford researchers, biologic interception is the goal. They hope to figure out how to use the immune system to stop the cancer.
In their study, they looked at DNA variabilities known as somatic aberrations or single-nucleotide protein sequences (SNPs). The HER2 gene, for example, can contain SNPs — possibly affecting how the HER2 protein regulates breast cell growth and division.
“There’s been a huge effort through genomewide association studies to link SNPs to cancer outcomes and risk,” Dr. Curtis said.
Focusing on people with a genetic predisposition for breast cancer, Dr. Curtis used machine learning to show that these variabilities can occur in specific epitopes (protein features that can trigger an immune response).
They also found that heightened variability can show up in a region of the genome called the human leukocyte antigen (HLA). Each HLA molecule can contain many epitopes.
“We developed a whole new algorithm to compute this ‘germline epitope burden,’ ” Dr. Curtis said. “We’re basically unearthing the dark matter of the human genome to ask about the interplay between SNPs and HLA class one presentation.”
These aberration-rich regions can grab the immune system’s attention. Sometimes the immune system identifies and eradicates those epitopes.
In that case: “I have immunosurveillance. I’ve cured my cancer,” said Nora Disis, PhD, director of the Cancer Vaccine Institute and a professor of medicine at the University of Washington, Seattle. Dr. Disis was not involved in the study.
But other times, the immune system finds a way around the high “epitope burden,” and the tumors become more aggressive and immunosuppressive. That’s when cancer forms.
This suggests a “critical juncture between preinvasive and invasive disease,” Dr. Curtis said.
And that “critical juncture” may very well be the optimal time for intervention.
The Precancer Push
Stanford’s findings add information to prior biomarkers and may provide a way to identify “bad-acting tumors” from a simple blood draw measuring germline epitope burden, Dr. Curtis said. Looking further ahead, “this also reveals a new source of epitopes that might be immunogenic and might be informative for the development of vaccines.”
Many labs are trying to understand the biology of precancer and exploring possible vaccines.
The National Cancer Institute’s Human Tumor Atlas Network is building three-dimensional models of the evolution from precancerous to advanced disease. And researchers at the Cancer Vaccine Institute at the University of Washington are developing a vaccine for a precancerous lesion linked to many ovarian cancers.
Dr. Domchek’s research explores whether breast cancers caused by mutations in the BRCA 1 and 2 genes can be intercepted at very early stages. In a clinical trial of healthy people with those mutations, Dr. Domchek and colleagues are attempting to “rev up the immune system to tackle telomerase,” an enzyme that’s over-expressed in 95% of cancers. The hope is for this experimental vaccine to lower their risk of developing cancer.
At the Fred Hutch Cancer Center, Seattle, Ming Yu, PhD, is studying how senescent cells affect immune cells in precancer. As cells age and stop dividing, she said, they can accumulate and create a “tumor-promoting microenvironment” in older people.
Dr. Yu has found that the antiaging drug rapamycin can eliminate those “zombie cells” in mice. She’s studying whether the “cleanup” can help prevent cancer and expects results in a few months.
In the years and decades to come, all of this could lead to a new era in cancer treatment.
“Most drug development starts with people with advanced cancer and then goes into the earlier and earlier spaces,” said Dr. Domchek. “But it may be that we’re thinking about it all wrong and that you really have to understand the unique biology of early lesions to go after them.”
A version of this article first appeared on Medscape.com.
Facial Angioedema, Rash, and “Mastitis” in a 31-Year-Old Female
A previously healthy 31-year-old female active-duty Navy sailor working as a calibration technician developed a painful, erythematous, pruritic, indurated plaque on her left breast. The sailor was not lactating and had no known family history of malignancy. Initially, she was treated by her primary care practitioner for presumed mastitis with oral cephalexin and then with oral clindamycin with no symptom improvement. About 2 weeks after the completion of both antibiotic courses, she developed angioedema and periorbital edema (Figure 1), requiring highdose corticosteroids and antihistamines with a corticosteroid course of prednisone 40 mg daily tapered to 10 mg daily over 12 days and diphenhydramine 25 mg to use up to 4 times daily. Workup for both was acquired and hereditary angioedema was unremarkable. Two months later, the patient developed patches of alopecia, oral ulcerations, and hypopigmented plaques with a peripheral hyperpigmented rim on the central face and bilateral conchal bowls (Figure 2). She also developed hypopigmented papules with peripheral hyperpigmentation on the bilateral dorsal hands overlying the metacarpal and proximal interphalangeal joints, which eventually ulcerated (Figure 3). Laboratory evaluation, including tests for creatine kinase, aldolase, transaminases, lactate dehydrogenase, and autoantibodies (antiJo-1, anti-Mi-2, anti-MDA-5, anti-TIF-1, anti-NXP-2, and anti-SAEP), were unremarkable. A punch biopsy from a papule on the right dorsal hand showed superficial perivascular lymphohistiocytic inflammation with a subtle focal increase in dermal mucin, highlighted by the colloidal iron stain. Further evaluation of the left breast plaque revealed ER/PR+ HER2- stage IIIB inflammatory breast cancer.

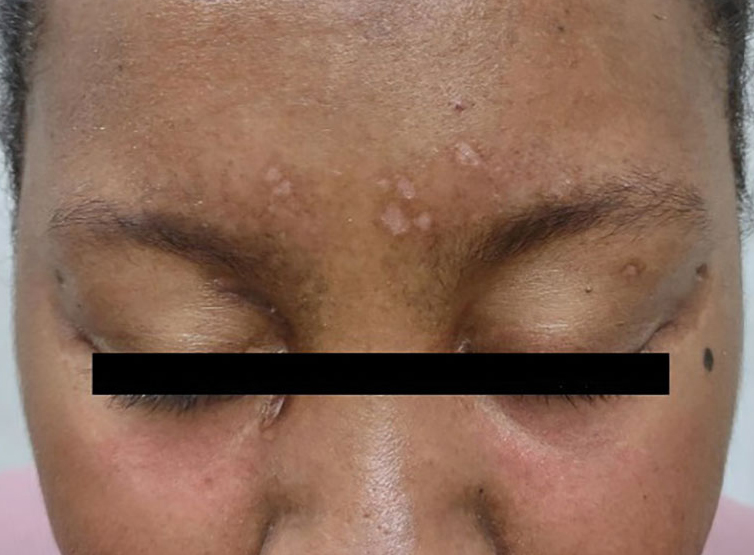

DISCUSSION
Based on the clinical presentation and diagnosis of inflammatory breast cancer, the patient was diagnosed with paraneoplastic clinically amyopathic dermatomyositis (CADM). She was treated for her breast cancer with an initial chemotherapy regimen consisting of dose-dense cyclophosphamide and doxorubicin followed by paclitaxel. The patient underwent a mastectomy, axillary lymph node dissection, and 25 sessions of radiation therapy, and is currently continuing therapy with anastrozole 1 mg daily and ovarian suppression with leuprorelin 11.25 mg every 3 months. For the severe angioedema and dermatomyositis-like cutaneous findings, the patient was continued on high-dose corticosteroids at prednisone 60 mg daily with a prolonged taper to prednisone 10 mg daily. After about 10 months, she transitioned from prednisone 10 mg daily to hydrocortisone 30 mg daily and is currently tapering her hydrocortisone dosing. She was additionally started on monthly intravenous immunoglobulin, hydroxychloroquine 300 mg daily, and amlodipine 5 mg daily. The ulcerated papules on her hands were treated with topical clobetasol 0.05% ointment applied daily, topical tacrolimus 0.1% ointment applied daily, and multiple intralesional triamcinolone 5 mg/mL injections. With this regimen, the patient experienced significant improvement in her cutaneous symptoms.
CADM is a rare autoimmune inflammatory disease featuring classic dermatomyositis-like cutaneous findings such as a heliotrope rash and Gottron papules. Ulcerative Gottron papules are less common than the typical erythematous papules and are associated more strongly with amyopathic disease.1 Paraneoplastic myositis poses a diagnostic challenge because it presents like an idiopathic dermatomyositis and often has a heterogeneous clinical presentation with additional manifestations, including periorbital edema, myalgias, dysphagia, and shortness of breath. If clinically suspected, laboratory tests (eg, creatine kinase, aldolase, transaminases, and lactate dehydrogenase) can assist in diagnosing paraneoplastic myositis. Additionally, serologic testing for autoantibodies such as anti-CADM-140, anti-Jo-1, anti-Mi-2, antiMDA-5, anti-TIF-1, anti-NXP-2, and antiSAE can assist the diagnosis and predict disease phenotype.1,2
Malignancy can precede, occur during, or develop after the diagnosis of CADM.3 Malignancies most often associated with CADM include ovarian, breast, and lung cancers.4 Despite the strong correlation with malignancy, there are currently no screening guidelines for malignancy upon inflammatory myositis diagnosis. Therefore, it is important to consider the entirety of a patient’s clinical presentation in establishing further evaluation in the initial diagnostic workup.
There are numerous systemic complications associated with inflammatory myositis and imaging modalities can help to rule out some of these conditions. CADM is strongly associated with the development of interstitial lung disease, so chest radiography and pulmonary function testing are often checked.1 Though cardiac and esophageal involvement are more commonly associated with classic dermatomyositis, it may be useful to obtain an electrocardiogram to rule out conduction abnormalities from myocardial involvement, along with esophageal manometry to evaluate for esophageal dysmotility.1,5
In the management of paraneoplastic CADM, the underlying malignancy should be treated first.6 If symptoms persist after the cancer is in remission, then CADM is treated with immunosuppressive medications such as methotrexate, mycophenolate mofetil, or azathioprine. Physical therapy can also provide further symptom relief for those suffering from proximal weakness.
CONCLUSIONS
Presumed mastitis, angioedema, and eczematous lesions for this patient were dermatologic manifestations of an underlying inflammatory breast cancer. This case highlights the importance of early recognition, the diagnosis of CADM and awareness of its association with underlying malignancy, especially within the primary care setting where most skin concerns are addressed. Early clinical suspicion and a swift diagnostic workup can further optimize multidisciplinary management, which is often required to treat malignancies.
- Cao H, Xia Q, Pan M, et al. Gottron papules and gottron sign with ulceration: a distinctive cutaneous feature in a subset of patients with classic dermatomyositis and clinically amyopathic dermatomyositis. J Rheumatol. 2016;43(9):1735-1742. doi:10.3899/jrheum.160024
- Satoh M, Tanaka S, Ceribelli A, Calise SJ, Chan EK. A comprehensive overview on myositis-specific antibodies: new and old biomarkers in idiopathic inflammatory myopathy. Clin Rev Allergy Immunol. 2017;52(1):1-19. doi:10.1007/s12016-015-8510-y
- Zahr ZA, Baer AN. Malignancy in myositis. Curr Rheumatol Rep. 2011;13(3):208-215. doi:10.1007/s11926-011-0169-7
- Udkoff J, Cohen PR. Amyopathic dermatomyositis: a concise review of clinical manifestations and associated malignancies. Am J Clin Dermatol. 2016;17(5): 509-518. doi:10.1007/s40257-016-0199-z
- Fathi M, Lundberg IE, Tornling G. Pulmonary complications of polymyositis and dermatomyositis. Semin Respir Crit Care Med. 2007;28(4):451-458. doi:10.1055/s-2007-985666
- Hendren E, Vinik O, Faragalla H, Haq R. Breast cancer and dermatomyositis: a case study and literature review. Curr Oncol. 2017;24(5):e429-e433. doi:10.3747/co.24.3696
A previously healthy 31-year-old female active-duty Navy sailor working as a calibration technician developed a painful, erythematous, pruritic, indurated plaque on her left breast. The sailor was not lactating and had no known family history of malignancy. Initially, she was treated by her primary care practitioner for presumed mastitis with oral cephalexin and then with oral clindamycin with no symptom improvement. About 2 weeks after the completion of both antibiotic courses, she developed angioedema and periorbital edema (Figure 1), requiring highdose corticosteroids and antihistamines with a corticosteroid course of prednisone 40 mg daily tapered to 10 mg daily over 12 days and diphenhydramine 25 mg to use up to 4 times daily. Workup for both was acquired and hereditary angioedema was unremarkable. Two months later, the patient developed patches of alopecia, oral ulcerations, and hypopigmented plaques with a peripheral hyperpigmented rim on the central face and bilateral conchal bowls (Figure 2). She also developed hypopigmented papules with peripheral hyperpigmentation on the bilateral dorsal hands overlying the metacarpal and proximal interphalangeal joints, which eventually ulcerated (Figure 3). Laboratory evaluation, including tests for creatine kinase, aldolase, transaminases, lactate dehydrogenase, and autoantibodies (antiJo-1, anti-Mi-2, anti-MDA-5, anti-TIF-1, anti-NXP-2, and anti-SAEP), were unremarkable. A punch biopsy from a papule on the right dorsal hand showed superficial perivascular lymphohistiocytic inflammation with a subtle focal increase in dermal mucin, highlighted by the colloidal iron stain. Further evaluation of the left breast plaque revealed ER/PR+ HER2- stage IIIB inflammatory breast cancer.

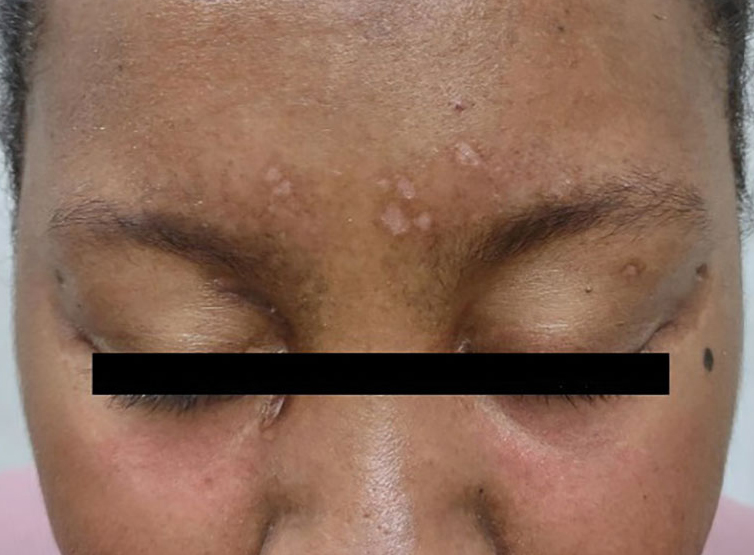

DISCUSSION
Based on the clinical presentation and diagnosis of inflammatory breast cancer, the patient was diagnosed with paraneoplastic clinically amyopathic dermatomyositis (CADM). She was treated for her breast cancer with an initial chemotherapy regimen consisting of dose-dense cyclophosphamide and doxorubicin followed by paclitaxel. The patient underwent a mastectomy, axillary lymph node dissection, and 25 sessions of radiation therapy, and is currently continuing therapy with anastrozole 1 mg daily and ovarian suppression with leuprorelin 11.25 mg every 3 months. For the severe angioedema and dermatomyositis-like cutaneous findings, the patient was continued on high-dose corticosteroids at prednisone 60 mg daily with a prolonged taper to prednisone 10 mg daily. After about 10 months, she transitioned from prednisone 10 mg daily to hydrocortisone 30 mg daily and is currently tapering her hydrocortisone dosing. She was additionally started on monthly intravenous immunoglobulin, hydroxychloroquine 300 mg daily, and amlodipine 5 mg daily. The ulcerated papules on her hands were treated with topical clobetasol 0.05% ointment applied daily, topical tacrolimus 0.1% ointment applied daily, and multiple intralesional triamcinolone 5 mg/mL injections. With this regimen, the patient experienced significant improvement in her cutaneous symptoms.
CADM is a rare autoimmune inflammatory disease featuring classic dermatomyositis-like cutaneous findings such as a heliotrope rash and Gottron papules. Ulcerative Gottron papules are less common than the typical erythematous papules and are associated more strongly with amyopathic disease.1 Paraneoplastic myositis poses a diagnostic challenge because it presents like an idiopathic dermatomyositis and often has a heterogeneous clinical presentation with additional manifestations, including periorbital edema, myalgias, dysphagia, and shortness of breath. If clinically suspected, laboratory tests (eg, creatine kinase, aldolase, transaminases, and lactate dehydrogenase) can assist in diagnosing paraneoplastic myositis. Additionally, serologic testing for autoantibodies such as anti-CADM-140, anti-Jo-1, anti-Mi-2, antiMDA-5, anti-TIF-1, anti-NXP-2, and antiSAE can assist the diagnosis and predict disease phenotype.1,2
Malignancy can precede, occur during, or develop after the diagnosis of CADM.3 Malignancies most often associated with CADM include ovarian, breast, and lung cancers.4 Despite the strong correlation with malignancy, there are currently no screening guidelines for malignancy upon inflammatory myositis diagnosis. Therefore, it is important to consider the entirety of a patient’s clinical presentation in establishing further evaluation in the initial diagnostic workup.
There are numerous systemic complications associated with inflammatory myositis and imaging modalities can help to rule out some of these conditions. CADM is strongly associated with the development of interstitial lung disease, so chest radiography and pulmonary function testing are often checked.1 Though cardiac and esophageal involvement are more commonly associated with classic dermatomyositis, it may be useful to obtain an electrocardiogram to rule out conduction abnormalities from myocardial involvement, along with esophageal manometry to evaluate for esophageal dysmotility.1,5
In the management of paraneoplastic CADM, the underlying malignancy should be treated first.6 If symptoms persist after the cancer is in remission, then CADM is treated with immunosuppressive medications such as methotrexate, mycophenolate mofetil, or azathioprine. Physical therapy can also provide further symptom relief for those suffering from proximal weakness.
CONCLUSIONS
Presumed mastitis, angioedema, and eczematous lesions for this patient were dermatologic manifestations of an underlying inflammatory breast cancer. This case highlights the importance of early recognition, the diagnosis of CADM and awareness of its association with underlying malignancy, especially within the primary care setting where most skin concerns are addressed. Early clinical suspicion and a swift diagnostic workup can further optimize multidisciplinary management, which is often required to treat malignancies.
A previously healthy 31-year-old female active-duty Navy sailor working as a calibration technician developed a painful, erythematous, pruritic, indurated plaque on her left breast. The sailor was not lactating and had no known family history of malignancy. Initially, she was treated by her primary care practitioner for presumed mastitis with oral cephalexin and then with oral clindamycin with no symptom improvement. About 2 weeks after the completion of both antibiotic courses, she developed angioedema and periorbital edema (Figure 1), requiring highdose corticosteroids and antihistamines with a corticosteroid course of prednisone 40 mg daily tapered to 10 mg daily over 12 days and diphenhydramine 25 mg to use up to 4 times daily. Workup for both was acquired and hereditary angioedema was unremarkable. Two months later, the patient developed patches of alopecia, oral ulcerations, and hypopigmented plaques with a peripheral hyperpigmented rim on the central face and bilateral conchal bowls (Figure 2). She also developed hypopigmented papules with peripheral hyperpigmentation on the bilateral dorsal hands overlying the metacarpal and proximal interphalangeal joints, which eventually ulcerated (Figure 3). Laboratory evaluation, including tests for creatine kinase, aldolase, transaminases, lactate dehydrogenase, and autoantibodies (antiJo-1, anti-Mi-2, anti-MDA-5, anti-TIF-1, anti-NXP-2, and anti-SAEP), were unremarkable. A punch biopsy from a papule on the right dorsal hand showed superficial perivascular lymphohistiocytic inflammation with a subtle focal increase in dermal mucin, highlighted by the colloidal iron stain. Further evaluation of the left breast plaque revealed ER/PR+ HER2- stage IIIB inflammatory breast cancer.

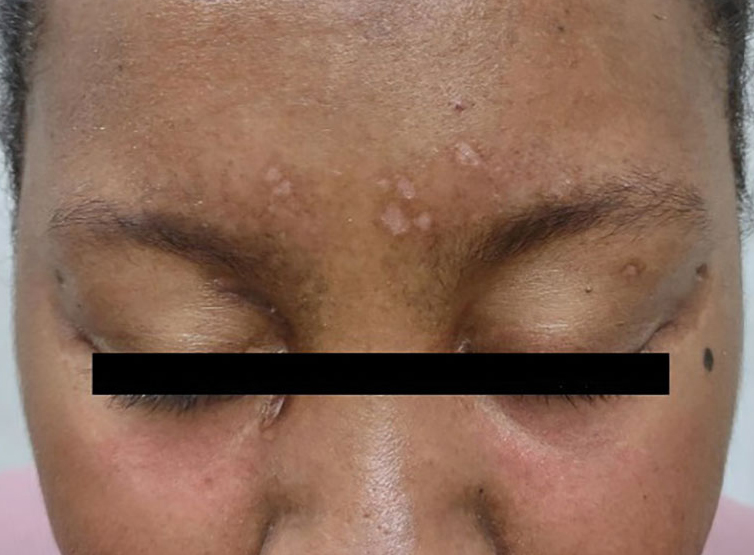

DISCUSSION
Based on the clinical presentation and diagnosis of inflammatory breast cancer, the patient was diagnosed with paraneoplastic clinically amyopathic dermatomyositis (CADM). She was treated for her breast cancer with an initial chemotherapy regimen consisting of dose-dense cyclophosphamide and doxorubicin followed by paclitaxel. The patient underwent a mastectomy, axillary lymph node dissection, and 25 sessions of radiation therapy, and is currently continuing therapy with anastrozole 1 mg daily and ovarian suppression with leuprorelin 11.25 mg every 3 months. For the severe angioedema and dermatomyositis-like cutaneous findings, the patient was continued on high-dose corticosteroids at prednisone 60 mg daily with a prolonged taper to prednisone 10 mg daily. After about 10 months, she transitioned from prednisone 10 mg daily to hydrocortisone 30 mg daily and is currently tapering her hydrocortisone dosing. She was additionally started on monthly intravenous immunoglobulin, hydroxychloroquine 300 mg daily, and amlodipine 5 mg daily. The ulcerated papules on her hands were treated with topical clobetasol 0.05% ointment applied daily, topical tacrolimus 0.1% ointment applied daily, and multiple intralesional triamcinolone 5 mg/mL injections. With this regimen, the patient experienced significant improvement in her cutaneous symptoms.
CADM is a rare autoimmune inflammatory disease featuring classic dermatomyositis-like cutaneous findings such as a heliotrope rash and Gottron papules. Ulcerative Gottron papules are less common than the typical erythematous papules and are associated more strongly with amyopathic disease.1 Paraneoplastic myositis poses a diagnostic challenge because it presents like an idiopathic dermatomyositis and often has a heterogeneous clinical presentation with additional manifestations, including periorbital edema, myalgias, dysphagia, and shortness of breath. If clinically suspected, laboratory tests (eg, creatine kinase, aldolase, transaminases, and lactate dehydrogenase) can assist in diagnosing paraneoplastic myositis. Additionally, serologic testing for autoantibodies such as anti-CADM-140, anti-Jo-1, anti-Mi-2, antiMDA-5, anti-TIF-1, anti-NXP-2, and antiSAE can assist the diagnosis and predict disease phenotype.1,2
Malignancy can precede, occur during, or develop after the diagnosis of CADM.3 Malignancies most often associated with CADM include ovarian, breast, and lung cancers.4 Despite the strong correlation with malignancy, there are currently no screening guidelines for malignancy upon inflammatory myositis diagnosis. Therefore, it is important to consider the entirety of a patient’s clinical presentation in establishing further evaluation in the initial diagnostic workup.
There are numerous systemic complications associated with inflammatory myositis and imaging modalities can help to rule out some of these conditions. CADM is strongly associated with the development of interstitial lung disease, so chest radiography and pulmonary function testing are often checked.1 Though cardiac and esophageal involvement are more commonly associated with classic dermatomyositis, it may be useful to obtain an electrocardiogram to rule out conduction abnormalities from myocardial involvement, along with esophageal manometry to evaluate for esophageal dysmotility.1,5
In the management of paraneoplastic CADM, the underlying malignancy should be treated first.6 If symptoms persist after the cancer is in remission, then CADM is treated with immunosuppressive medications such as methotrexate, mycophenolate mofetil, or azathioprine. Physical therapy can also provide further symptom relief for those suffering from proximal weakness.
CONCLUSIONS
Presumed mastitis, angioedema, and eczematous lesions for this patient were dermatologic manifestations of an underlying inflammatory breast cancer. This case highlights the importance of early recognition, the diagnosis of CADM and awareness of its association with underlying malignancy, especially within the primary care setting where most skin concerns are addressed. Early clinical suspicion and a swift diagnostic workup can further optimize multidisciplinary management, which is often required to treat malignancies.
- Cao H, Xia Q, Pan M, et al. Gottron papules and gottron sign with ulceration: a distinctive cutaneous feature in a subset of patients with classic dermatomyositis and clinically amyopathic dermatomyositis. J Rheumatol. 2016;43(9):1735-1742. doi:10.3899/jrheum.160024
- Satoh M, Tanaka S, Ceribelli A, Calise SJ, Chan EK. A comprehensive overview on myositis-specific antibodies: new and old biomarkers in idiopathic inflammatory myopathy. Clin Rev Allergy Immunol. 2017;52(1):1-19. doi:10.1007/s12016-015-8510-y
- Zahr ZA, Baer AN. Malignancy in myositis. Curr Rheumatol Rep. 2011;13(3):208-215. doi:10.1007/s11926-011-0169-7
- Udkoff J, Cohen PR. Amyopathic dermatomyositis: a concise review of clinical manifestations and associated malignancies. Am J Clin Dermatol. 2016;17(5): 509-518. doi:10.1007/s40257-016-0199-z
- Fathi M, Lundberg IE, Tornling G. Pulmonary complications of polymyositis and dermatomyositis. Semin Respir Crit Care Med. 2007;28(4):451-458. doi:10.1055/s-2007-985666
- Hendren E, Vinik O, Faragalla H, Haq R. Breast cancer and dermatomyositis: a case study and literature review. Curr Oncol. 2017;24(5):e429-e433. doi:10.3747/co.24.3696
- Cao H, Xia Q, Pan M, et al. Gottron papules and gottron sign with ulceration: a distinctive cutaneous feature in a subset of patients with classic dermatomyositis and clinically amyopathic dermatomyositis. J Rheumatol. 2016;43(9):1735-1742. doi:10.3899/jrheum.160024
- Satoh M, Tanaka S, Ceribelli A, Calise SJ, Chan EK. A comprehensive overview on myositis-specific antibodies: new and old biomarkers in idiopathic inflammatory myopathy. Clin Rev Allergy Immunol. 2017;52(1):1-19. doi:10.1007/s12016-015-8510-y
- Zahr ZA, Baer AN. Malignancy in myositis. Curr Rheumatol Rep. 2011;13(3):208-215. doi:10.1007/s11926-011-0169-7
- Udkoff J, Cohen PR. Amyopathic dermatomyositis: a concise review of clinical manifestations and associated malignancies. Am J Clin Dermatol. 2016;17(5): 509-518. doi:10.1007/s40257-016-0199-z
- Fathi M, Lundberg IE, Tornling G. Pulmonary complications of polymyositis and dermatomyositis. Semin Respir Crit Care Med. 2007;28(4):451-458. doi:10.1055/s-2007-985666
- Hendren E, Vinik O, Faragalla H, Haq R. Breast cancer and dermatomyositis: a case study and literature review. Curr Oncol. 2017;24(5):e429-e433. doi:10.3747/co.24.3696
‘Cancer Doesn’t Wait’: How Prior Authorization Harms Care
Fantine Giap, MD, sat across from a 21-year-old with a rare sarcoma at the base of her skull.
Despite the large tumor, nestled in a sensitive area, the Boston-based radiation oncologist could envision a bright future for her patient.
She and the other members of the patient’s care team had an impressive cancer-fighting arsenal at her fingertips. The team had recommended surgery, followed by proton therapy — a sophisticated tool able to deliver concentrated, razor-focused radiation to the once apple-sized growth, while sparing the fragile brain stem, optic nerve, and spinal cord.
Surgery went as planned. But as the days and weeks wore on and insurance prior authorization for the proton therapy never came, the tumor roared back, leading to more surgeries and more complications. Ultimately, the young woman needed a tracheostomy and a feeding tube.
By the time insurance said yes, more than 1 year from her initial visit, the future the team had envisioned seemed out of reach.
“Unfortunately for this patient, it went from a potentially curable situation to a likely not curable situation,” recalled Dr. Giap, a clinician at Massachusetts General Hospital and instructor at Harvard Medical School, Boston. “I wanted to cry every day that she waited.’’
While a stark example, such insurance delays are not uncommon, according to new research published in JAMA Network Open.
Other studies have found that number to be even higher, with more than 86% of prior authorization requests ultimately approved with few changes.
‘’It gives you the idea that this entire process might be a little futile — that it’s just wasting people’s time,’’ said Fumiko Chino, MD, coauthor on the JAMA study and now an assistant professor in radiation oncology at MD Anderson Cancer Center in Houston. ‘’The problem is cancer doesn’t wait for bureaucracy.’’
Barriers at Every Step
As Dr. Chino and her study coauthors explained, advancements like intensity-modulated radiation therapy and stereotactic radiosurgery have allowed a new generation of specialists to treat previously untreatable cancers in ways that maximize tumor-killing power while minimizing collateral damage. But these tools require sophisticated planning, imaging, simulations and execution — all of which are subject to increased insurance scrutiny.
‘’We face barriers pretty much every step of the way for every patient,’’ said Dr. Chino.
To investigate how such barriers impact care, Dr. Chino and colleagues at Memorial Sloan Kettering Cancer Center — where she worked until July — looked at 206 cases in which payers denied prior authorization for radiation therapy from November 1, 2021 to December 8, 2022.
The team found that 62% were ultimately approved without any change to technique or dose, while 28% were authorized, but with lower doses or less sophisticated techniques. Four people, however, never got authorization at all — three abandoned treatment altogether, and one sought treatment at another institution.
Treatment delays ranged from 1 day to 49 days. Eighty-three patients died.
Would some of them have lived if it weren’t for prior authorization?
Dr. Chino cannot say for sure, but did note that certain cancers, like cervical cancer, can grow so quickly that every day of delayed treatment makes them harder to control.
Patients with metastatic or late-stage cancers are often denied more aggressive treatments by insurers who, in essence, “assume that they are going to die from their disease anyway,” Dr. Chino said.
She views this as tragically shortsighted.
‘’There’s actually a strong body of evidence to show that if you treat even metastatic stage IV diseases aggressively, you can prolong not just quality of life but also quantity,’’ she said.
In cases where the cancer is more localized and insurance mandates lower doses or cheaper techniques, the consequences can be equally heartbreaking.
‘’It’s like saying instead of taking an extra-strength Tylenol you can only have a baby aspirin,’’ she said. ‘’Their pain is less likely to be controlled, their disease is less likely to be controlled, and they are more likely to need retreatment.’’
Prior authorization delays can also significantly stress patients at the most vulnerable point of their lives.
In another recent study, Dr. Chino found that 69% of patients with cancer reported prior authorization-related delays in care, with one-third waiting a month or longer. One in five never got the care their doctors recommended, and 20% reported spending more than 11 hours on the phone haggling with their insurance companies.
Most patients rated the process as ‘’bad’’ or ‘’horrible,’’ and said it fueled anxiety.
Such delays can be hard on clinicians and the healthcare system too.
One 2022 study found that a typical academic radiation oncology practice spent about a half-million dollars per year seeking insurance preauthorization. Nationally, that number exceeds $40 million.
Then there is the burnout factor.
Dr. Giap, an early-career physician who specializes in rare, aggressive sarcomas, works at an institution that helped pioneer proton therapy. She says it pains her to tell a desperate patient, like the 21-year-old, who has traveled to her from out of state that they have to wait.
‘’Knowing that the majority of the cases are ultimately approved and that this wait is often unnecessary makes it even tougher,’’ she said.
Dr. Chino, a breast cancer specialist, has taken to warning patients before the alarming insurance letter arrives in the mail that their insurance may delay authorizing their care. But she tells patients that she will do everything she can to fight for them and develops a back-up plan to pivot to quickly, if needed.
‘’No one goes into medicine to spend their time talking to insurance companies,’’ said Dr. Chino.
The national trade group, America’s Health Insurance Plans (AHIP), did not return repeated requests for an interview for this story. But their official position, as stated on their website, is that “prior authorization is one of many tools health insurance providers use to promote safe, timely, evidence-based, affordable, and efficient care.”
Both Dr. Giap and Dr. Chino believe that prior authorization was developed with good intentions: to save healthcare costs and rein in treatments that don’t necessarily benefit patients.
But, in their specialty, the burden has proliferated to a point that Dr. Chino characterizes as ‘’unconscionable.’’
She believes that policy changes like the proposed Improving Seniors’ Timely Access to Care Act — which would require real-time decisions for procedures that are routinely approved — could go a long way in improving patient care.
Meanwhile, Dr. Giap said, more research and professional guidelines are necessary to bolster insurance company confidence in newer technologies, particularly for rare cancers.
Her patient ultimately got her proton therapy and is ‘’doing relatively well, all things considered.’’
But not all the stories end like this.
Dr. Chino will never forget a patient with a cancer growing so rapidly she could see it protruding through her chest wall. She called for an urgent PET scan to see where else in the body the cancer might be brewing and rushed the planning process for radiation therapy, both of which faced prior authorization barriers. That scan — which ultimately showed the cancer had spread — was delayed for months.*
If the team had had those imaging results upfront, she said, they would have recommended a completely different course of treatment.
And her patient might be alive today.
‘’Unfortunately,” Dr. Chino said, “the people with the very worst prior authorization stories aren’t here anymore to tell you about them.”
*Correction, 10/4/24: An earlier version of this article erroneously stated that Dr. Chino called for surgery for her patient. She actually called for a PET scan and an urgent radiation start.
A version of this article first appeared on Medscape.com.
Fantine Giap, MD, sat across from a 21-year-old with a rare sarcoma at the base of her skull.
Despite the large tumor, nestled in a sensitive area, the Boston-based radiation oncologist could envision a bright future for her patient.
She and the other members of the patient’s care team had an impressive cancer-fighting arsenal at her fingertips. The team had recommended surgery, followed by proton therapy — a sophisticated tool able to deliver concentrated, razor-focused radiation to the once apple-sized growth, while sparing the fragile brain stem, optic nerve, and spinal cord.
Surgery went as planned. But as the days and weeks wore on and insurance prior authorization for the proton therapy never came, the tumor roared back, leading to more surgeries and more complications. Ultimately, the young woman needed a tracheostomy and a feeding tube.
By the time insurance said yes, more than 1 year from her initial visit, the future the team had envisioned seemed out of reach.
“Unfortunately for this patient, it went from a potentially curable situation to a likely not curable situation,” recalled Dr. Giap, a clinician at Massachusetts General Hospital and instructor at Harvard Medical School, Boston. “I wanted to cry every day that she waited.’’
While a stark example, such insurance delays are not uncommon, according to new research published in JAMA Network Open.
Other studies have found that number to be even higher, with more than 86% of prior authorization requests ultimately approved with few changes.
‘’It gives you the idea that this entire process might be a little futile — that it’s just wasting people’s time,’’ said Fumiko Chino, MD, coauthor on the JAMA study and now an assistant professor in radiation oncology at MD Anderson Cancer Center in Houston. ‘’The problem is cancer doesn’t wait for bureaucracy.’’
Barriers at Every Step
As Dr. Chino and her study coauthors explained, advancements like intensity-modulated radiation therapy and stereotactic radiosurgery have allowed a new generation of specialists to treat previously untreatable cancers in ways that maximize tumor-killing power while minimizing collateral damage. But these tools require sophisticated planning, imaging, simulations and execution — all of which are subject to increased insurance scrutiny.
‘’We face barriers pretty much every step of the way for every patient,’’ said Dr. Chino.
To investigate how such barriers impact care, Dr. Chino and colleagues at Memorial Sloan Kettering Cancer Center — where she worked until July — looked at 206 cases in which payers denied prior authorization for radiation therapy from November 1, 2021 to December 8, 2022.
The team found that 62% were ultimately approved without any change to technique or dose, while 28% were authorized, but with lower doses or less sophisticated techniques. Four people, however, never got authorization at all — three abandoned treatment altogether, and one sought treatment at another institution.
Treatment delays ranged from 1 day to 49 days. Eighty-three patients died.
Would some of them have lived if it weren’t for prior authorization?
Dr. Chino cannot say for sure, but did note that certain cancers, like cervical cancer, can grow so quickly that every day of delayed treatment makes them harder to control.
Patients with metastatic or late-stage cancers are often denied more aggressive treatments by insurers who, in essence, “assume that they are going to die from their disease anyway,” Dr. Chino said.
She views this as tragically shortsighted.
‘’There’s actually a strong body of evidence to show that if you treat even metastatic stage IV diseases aggressively, you can prolong not just quality of life but also quantity,’’ she said.
In cases where the cancer is more localized and insurance mandates lower doses or cheaper techniques, the consequences can be equally heartbreaking.
‘’It’s like saying instead of taking an extra-strength Tylenol you can only have a baby aspirin,’’ she said. ‘’Their pain is less likely to be controlled, their disease is less likely to be controlled, and they are more likely to need retreatment.’’
Prior authorization delays can also significantly stress patients at the most vulnerable point of their lives.
In another recent study, Dr. Chino found that 69% of patients with cancer reported prior authorization-related delays in care, with one-third waiting a month or longer. One in five never got the care their doctors recommended, and 20% reported spending more than 11 hours on the phone haggling with their insurance companies.
Most patients rated the process as ‘’bad’’ or ‘’horrible,’’ and said it fueled anxiety.
Such delays can be hard on clinicians and the healthcare system too.
One 2022 study found that a typical academic radiation oncology practice spent about a half-million dollars per year seeking insurance preauthorization. Nationally, that number exceeds $40 million.
Then there is the burnout factor.
Dr. Giap, an early-career physician who specializes in rare, aggressive sarcomas, works at an institution that helped pioneer proton therapy. She says it pains her to tell a desperate patient, like the 21-year-old, who has traveled to her from out of state that they have to wait.
‘’Knowing that the majority of the cases are ultimately approved and that this wait is often unnecessary makes it even tougher,’’ she said.
Dr. Chino, a breast cancer specialist, has taken to warning patients before the alarming insurance letter arrives in the mail that their insurance may delay authorizing their care. But she tells patients that she will do everything she can to fight for them and develops a back-up plan to pivot to quickly, if needed.
‘’No one goes into medicine to spend their time talking to insurance companies,’’ said Dr. Chino.
The national trade group, America’s Health Insurance Plans (AHIP), did not return repeated requests for an interview for this story. But their official position, as stated on their website, is that “prior authorization is one of many tools health insurance providers use to promote safe, timely, evidence-based, affordable, and efficient care.”
Both Dr. Giap and Dr. Chino believe that prior authorization was developed with good intentions: to save healthcare costs and rein in treatments that don’t necessarily benefit patients.
But, in their specialty, the burden has proliferated to a point that Dr. Chino characterizes as ‘’unconscionable.’’
She believes that policy changes like the proposed Improving Seniors’ Timely Access to Care Act — which would require real-time decisions for procedures that are routinely approved — could go a long way in improving patient care.
Meanwhile, Dr. Giap said, more research and professional guidelines are necessary to bolster insurance company confidence in newer technologies, particularly for rare cancers.
Her patient ultimately got her proton therapy and is ‘’doing relatively well, all things considered.’’
But not all the stories end like this.
Dr. Chino will never forget a patient with a cancer growing so rapidly she could see it protruding through her chest wall. She called for an urgent PET scan to see where else in the body the cancer might be brewing and rushed the planning process for radiation therapy, both of which faced prior authorization barriers. That scan — which ultimately showed the cancer had spread — was delayed for months.*
If the team had had those imaging results upfront, she said, they would have recommended a completely different course of treatment.
And her patient might be alive today.
‘’Unfortunately,” Dr. Chino said, “the people with the very worst prior authorization stories aren’t here anymore to tell you about them.”
*Correction, 10/4/24: An earlier version of this article erroneously stated that Dr. Chino called for surgery for her patient. She actually called for a PET scan and an urgent radiation start.
A version of this article first appeared on Medscape.com.
Fantine Giap, MD, sat across from a 21-year-old with a rare sarcoma at the base of her skull.
Despite the large tumor, nestled in a sensitive area, the Boston-based radiation oncologist could envision a bright future for her patient.
She and the other members of the patient’s care team had an impressive cancer-fighting arsenal at her fingertips. The team had recommended surgery, followed by proton therapy — a sophisticated tool able to deliver concentrated, razor-focused radiation to the once apple-sized growth, while sparing the fragile brain stem, optic nerve, and spinal cord.
Surgery went as planned. But as the days and weeks wore on and insurance prior authorization for the proton therapy never came, the tumor roared back, leading to more surgeries and more complications. Ultimately, the young woman needed a tracheostomy and a feeding tube.
By the time insurance said yes, more than 1 year from her initial visit, the future the team had envisioned seemed out of reach.
“Unfortunately for this patient, it went from a potentially curable situation to a likely not curable situation,” recalled Dr. Giap, a clinician at Massachusetts General Hospital and instructor at Harvard Medical School, Boston. “I wanted to cry every day that she waited.’’
While a stark example, such insurance delays are not uncommon, according to new research published in JAMA Network Open.
Other studies have found that number to be even higher, with more than 86% of prior authorization requests ultimately approved with few changes.
‘’It gives you the idea that this entire process might be a little futile — that it’s just wasting people’s time,’’ said Fumiko Chino, MD, coauthor on the JAMA study and now an assistant professor in radiation oncology at MD Anderson Cancer Center in Houston. ‘’The problem is cancer doesn’t wait for bureaucracy.’’
Barriers at Every Step
As Dr. Chino and her study coauthors explained, advancements like intensity-modulated radiation therapy and stereotactic radiosurgery have allowed a new generation of specialists to treat previously untreatable cancers in ways that maximize tumor-killing power while minimizing collateral damage. But these tools require sophisticated planning, imaging, simulations and execution — all of which are subject to increased insurance scrutiny.
‘’We face barriers pretty much every step of the way for every patient,’’ said Dr. Chino.
To investigate how such barriers impact care, Dr. Chino and colleagues at Memorial Sloan Kettering Cancer Center — where she worked until July — looked at 206 cases in which payers denied prior authorization for radiation therapy from November 1, 2021 to December 8, 2022.
The team found that 62% were ultimately approved without any change to technique or dose, while 28% were authorized, but with lower doses or less sophisticated techniques. Four people, however, never got authorization at all — three abandoned treatment altogether, and one sought treatment at another institution.
Treatment delays ranged from 1 day to 49 days. Eighty-three patients died.
Would some of them have lived if it weren’t for prior authorization?
Dr. Chino cannot say for sure, but did note that certain cancers, like cervical cancer, can grow so quickly that every day of delayed treatment makes them harder to control.
Patients with metastatic or late-stage cancers are often denied more aggressive treatments by insurers who, in essence, “assume that they are going to die from their disease anyway,” Dr. Chino said.
She views this as tragically shortsighted.
‘’There’s actually a strong body of evidence to show that if you treat even metastatic stage IV diseases aggressively, you can prolong not just quality of life but also quantity,’’ she said.
In cases where the cancer is more localized and insurance mandates lower doses or cheaper techniques, the consequences can be equally heartbreaking.
‘’It’s like saying instead of taking an extra-strength Tylenol you can only have a baby aspirin,’’ she said. ‘’Their pain is less likely to be controlled, their disease is less likely to be controlled, and they are more likely to need retreatment.’’
Prior authorization delays can also significantly stress patients at the most vulnerable point of their lives.
In another recent study, Dr. Chino found that 69% of patients with cancer reported prior authorization-related delays in care, with one-third waiting a month or longer. One in five never got the care their doctors recommended, and 20% reported spending more than 11 hours on the phone haggling with their insurance companies.
Most patients rated the process as ‘’bad’’ or ‘’horrible,’’ and said it fueled anxiety.
Such delays can be hard on clinicians and the healthcare system too.
One 2022 study found that a typical academic radiation oncology practice spent about a half-million dollars per year seeking insurance preauthorization. Nationally, that number exceeds $40 million.
Then there is the burnout factor.
Dr. Giap, an early-career physician who specializes in rare, aggressive sarcomas, works at an institution that helped pioneer proton therapy. She says it pains her to tell a desperate patient, like the 21-year-old, who has traveled to her from out of state that they have to wait.
‘’Knowing that the majority of the cases are ultimately approved and that this wait is often unnecessary makes it even tougher,’’ she said.
Dr. Chino, a breast cancer specialist, has taken to warning patients before the alarming insurance letter arrives in the mail that their insurance may delay authorizing their care. But she tells patients that she will do everything she can to fight for them and develops a back-up plan to pivot to quickly, if needed.
‘’No one goes into medicine to spend their time talking to insurance companies,’’ said Dr. Chino.
The national trade group, America’s Health Insurance Plans (AHIP), did not return repeated requests for an interview for this story. But their official position, as stated on their website, is that “prior authorization is one of many tools health insurance providers use to promote safe, timely, evidence-based, affordable, and efficient care.”
Both Dr. Giap and Dr. Chino believe that prior authorization was developed with good intentions: to save healthcare costs and rein in treatments that don’t necessarily benefit patients.
But, in their specialty, the burden has proliferated to a point that Dr. Chino characterizes as ‘’unconscionable.’’
She believes that policy changes like the proposed Improving Seniors’ Timely Access to Care Act — which would require real-time decisions for procedures that are routinely approved — could go a long way in improving patient care.
Meanwhile, Dr. Giap said, more research and professional guidelines are necessary to bolster insurance company confidence in newer technologies, particularly for rare cancers.
Her patient ultimately got her proton therapy and is ‘’doing relatively well, all things considered.’’
But not all the stories end like this.
Dr. Chino will never forget a patient with a cancer growing so rapidly she could see it protruding through her chest wall. She called for an urgent PET scan to see where else in the body the cancer might be brewing and rushed the planning process for radiation therapy, both of which faced prior authorization barriers. That scan — which ultimately showed the cancer had spread — was delayed for months.*
If the team had had those imaging results upfront, she said, they would have recommended a completely different course of treatment.
And her patient might be alive today.
‘’Unfortunately,” Dr. Chino said, “the people with the very worst prior authorization stories aren’t here anymore to tell you about them.”
*Correction, 10/4/24: An earlier version of this article erroneously stated that Dr. Chino called for surgery for her patient. She actually called for a PET scan and an urgent radiation start.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Popular Weight Loss Drugs Now for Patients With Cancer?
Demand for new weight loss drugs has surged over the past few years.
Led by the antiobesity drugs semaglutide (Wegovy) and tirzepatide (Zepbound), these popular medications — more commonly known as glucagon-like peptide 1 (GLP-1) agonists — have become game changers for shedding excess pounds.
Aside from obesity indications, both drugs have been approved to treat type 2 diabetes under different brand names and have a growing list of other potential benefits, such as reducing inflammation and depression.
While there’s limited data to support the use of GLP-1 agonists for weight loss in cancer, some oncologists have begun carefully integrating the antiobesity agents into care and studying their effects in this patient population.
The reason: Research suggests that obesity can reduce the effectiveness of cancer therapies, especially in patients with breast cancer, and can increase the risk for treatment-related side effects.
The idea is that managing patients’ weight will improve their cancer outcomes, explained Lajos Pusztai, MD, PhD, a breast cancer specialist and professor of medicine at Yale School of Medicine in New Haven, Connecticut.
Although Dr. Pusztai and his oncology peers at Yale don’t yet use GPL-1 agonists, Neil Iyengar, MD, and colleagues have begun doing so to help some patients with breast cancer manage their weight. Dr. Iyengar estimates that a few hundred — almost 40% — of his patients are on the antiobesity drugs.
“For a patient who has really tried to reduce their weight and who is in the obese range, that’s where I think the use of these medications can be considered,” said Dr. Iyengar, a breast cancer oncologist at Memorial Sloan Kettering Cancer Center in New York City.
Why GLP-1s in Cancer?
GLP-1 is a hormone that the small intestine releases after eating. GLP-1 agonists work by mimicking GLP-1 to trigger the release of insulin and reduce the production of glucagon — two processes that help regulate blood sugar.
These agents, such as Wegovy (or Ozempic when prescribed for diabetes), also slow gastric emptying and can make people feel fuller longer.
Zebound (or Mounjaro for type 2 diabetes) is considered a dual GLP-1 and glucose-dependent insulinotropic polypeptide agonist, which may enhance its weight loss benefits.
In practice, however, these drugs can increase nausea and vomiting from chemotherapy, so Dr. Iyengar typically has patients use them afterwards, during maintenance treatment.
Oncologists don’t prescribe the drugs themselves but instead refer patients to endocrinologists or weight management centers that then write the prescriptions. Taking these drugs involves weekly subcutaneous injections patients can administer themselves.
Endocrinologist Emily Gallagher, MD, PhD, of Mount Sinai Hospital in New York City, estimates she has prescribed the antiobesity drugs to a few hundred patients with cancer and, like Dr. Iyengar, uses the drugs during maintenance treatment with hormone therapy for breast cancer. She also has used these agents in patients with prostate and endometrial cancers and has found the drugs can help counter steroid weight gain in multiple myeloma.
But, to date, the evidence for using GPL-1 agonists in cancer remains limited and the practice has not yet become widespread.
Research largely comes down to a few small retrospective studies in patients with breast cancer receiving aromatase inhibitors. Although no safety issues have emerged so far, these initial reports suggest that the drugs lead to significantly less weight loss in patients with cancer compared to the general population.
Dr. Iyengar led one recent study, presented at the 2024 annual meeting of the American Society of Clinical Oncology, in which he and his team assessed outcomes in 75 women with breast cancer who received a GLP-1 agonist. Almost 80% of patients had diabetes, and 60% received hormone therapy, most commonly an aromatase inhibitor. Patients’ median body mass index (BMI) at baseline was 34 kg/m2 (range, 23-50 kg/m2).
From baseline, patients lost 6.2 kg, on average, or about 5% of their total body weight, 12 months after initiating GLP-1 therapy.
In contrast, phase 3 trials show much higher mean weight loss — about two times — in patients without cancer.
Another recent study also reported modest weight loss results in patients with breast cancer undergoing endocrine therapy. The researchers reported that, at 12 months, Wegovy led to 4.34% reduction in BMI, compared with a 14% change reported in the general population. Zebound, however, was associated with a 2.31% BMI increase overall — though some patients did experience a decrease — compared with a 15% reduction in the general population.
“These findings indicate a substantially reduced weight loss efficacy in breast cancer patients on endocrine therapy compared to the general population,” the authors concluded.
It’s unclear why the drugs appear to not work as well in patients with cancer. It’s possible that hormone therapy or metabolic changes interfere with their effectiveness, given that some cancer therapies lead to weight gain. Steroids and hormone therapies, for instance, often increase appetite, and some treatments can slow patients’ metabolism or lead to fatigue, which can make it harder to exercise.
Patients with cancer may need a higher dose of GLP-1 agonists to achieve similar weight loss to the general population, Dr. Iyengar noted.
However, Dr. Gallagher said, in her own experience, she hasn’t found the drugs to be less effective in patients with cancer, especially the newer agents, like Wegovy and Zepbound.
As for safety, Wegovy and Zepbound both carry a black box warning for thyroid C-cell tumors, including medullary thyroid carcinoma. (Recent research, however, has found that GLP-1 agonists do not increase thyroid cancer risk).
These antiobesity agents are also contraindicated in patients with a personal or family history of medullary thyroid carcinoma and in patients who have multiple endocrine neoplasia syndrome type 2, which is associated with medullary thyroid carcinoma.
Dr. Gallagher hasn’t seen any secondary tumors — thyroid or otherwise — in her patients with cancer, but she follows the labeling contraindications. Dr. Iyengar also noted that more recent and larger data sets have shown no impact on this risk, which may not actually exist, he said
Dr. Gallagher remains cautious about using GPL-1 agonists in patients who have had bariatric surgery because these agents can compound the slower gastric emptying and intestinal transit from surgery, potentially leading to gastrointestinal obstructions.
Looking ahead, GPL-1 manufacturers are interested in adding cancer indications to the drug labeling. Both Dr. Iyengar and Dr. Gallagher said their institutions are in talks with companies to participate in large, multicenter, global phase 3 trials.
Dr. Iyengar welcomes the efforts, not only to test the effectiveness of GPL-1 agonists in oncology but also to “nail down” their safety in cancer.
“I don’t think that there’s mechanistically anything that’s particularly worrisome,” and current observations suggest that these drugs are likely to be safe, Dr. Iyengar said. Even so, “GLP-1 agonists do a lot of things that we don’t fully understand yet.”
The bigger challenge, Dr. Iyengar noted, is that companies will have to show a sizable benefit to using these drugs in patients with cancer to get the Food and Drug Administration’s approval. And to move the needle on cancer-specific outcomes, these antiobesity drugs will need to demonstrate significant, durable weight loss in patients with cancer.
But if these drugs can do that, “I think it’s going to be one of the biggest advances in medicine and oncology given the obesity and cancer epidemic,” Dr. Iyengar said.
Dr. Iyengar has adviser and/or researcher ties with companies that make or are developing GPL-1 agonists, including AstraZeneca, Novartis, Gilead, and Pfizer. Dr. Gallagher is a consultant for Novartis, Flare Therapeutics, Reactive Biosciences, and Seagen.
A version of this article first appeared on Medscape.com.
Demand for new weight loss drugs has surged over the past few years.
Led by the antiobesity drugs semaglutide (Wegovy) and tirzepatide (Zepbound), these popular medications — more commonly known as glucagon-like peptide 1 (GLP-1) agonists — have become game changers for shedding excess pounds.
Aside from obesity indications, both drugs have been approved to treat type 2 diabetes under different brand names and have a growing list of other potential benefits, such as reducing inflammation and depression.
While there’s limited data to support the use of GLP-1 agonists for weight loss in cancer, some oncologists have begun carefully integrating the antiobesity agents into care and studying their effects in this patient population.
The reason: Research suggests that obesity can reduce the effectiveness of cancer therapies, especially in patients with breast cancer, and can increase the risk for treatment-related side effects.
The idea is that managing patients’ weight will improve their cancer outcomes, explained Lajos Pusztai, MD, PhD, a breast cancer specialist and professor of medicine at Yale School of Medicine in New Haven, Connecticut.
Although Dr. Pusztai and his oncology peers at Yale don’t yet use GPL-1 agonists, Neil Iyengar, MD, and colleagues have begun doing so to help some patients with breast cancer manage their weight. Dr. Iyengar estimates that a few hundred — almost 40% — of his patients are on the antiobesity drugs.
“For a patient who has really tried to reduce their weight and who is in the obese range, that’s where I think the use of these medications can be considered,” said Dr. Iyengar, a breast cancer oncologist at Memorial Sloan Kettering Cancer Center in New York City.
Why GLP-1s in Cancer?
GLP-1 is a hormone that the small intestine releases after eating. GLP-1 agonists work by mimicking GLP-1 to trigger the release of insulin and reduce the production of glucagon — two processes that help regulate blood sugar.
These agents, such as Wegovy (or Ozempic when prescribed for diabetes), also slow gastric emptying and can make people feel fuller longer.
Zebound (or Mounjaro for type 2 diabetes) is considered a dual GLP-1 and glucose-dependent insulinotropic polypeptide agonist, which may enhance its weight loss benefits.
In practice, however, these drugs can increase nausea and vomiting from chemotherapy, so Dr. Iyengar typically has patients use them afterwards, during maintenance treatment.
Oncologists don’t prescribe the drugs themselves but instead refer patients to endocrinologists or weight management centers that then write the prescriptions. Taking these drugs involves weekly subcutaneous injections patients can administer themselves.
Endocrinologist Emily Gallagher, MD, PhD, of Mount Sinai Hospital in New York City, estimates she has prescribed the antiobesity drugs to a few hundred patients with cancer and, like Dr. Iyengar, uses the drugs during maintenance treatment with hormone therapy for breast cancer. She also has used these agents in patients with prostate and endometrial cancers and has found the drugs can help counter steroid weight gain in multiple myeloma.
But, to date, the evidence for using GPL-1 agonists in cancer remains limited and the practice has not yet become widespread.
Research largely comes down to a few small retrospective studies in patients with breast cancer receiving aromatase inhibitors. Although no safety issues have emerged so far, these initial reports suggest that the drugs lead to significantly less weight loss in patients with cancer compared to the general population.
Dr. Iyengar led one recent study, presented at the 2024 annual meeting of the American Society of Clinical Oncology, in which he and his team assessed outcomes in 75 women with breast cancer who received a GLP-1 agonist. Almost 80% of patients had diabetes, and 60% received hormone therapy, most commonly an aromatase inhibitor. Patients’ median body mass index (BMI) at baseline was 34 kg/m2 (range, 23-50 kg/m2).
From baseline, patients lost 6.2 kg, on average, or about 5% of their total body weight, 12 months after initiating GLP-1 therapy.
In contrast, phase 3 trials show much higher mean weight loss — about two times — in patients without cancer.
Another recent study also reported modest weight loss results in patients with breast cancer undergoing endocrine therapy. The researchers reported that, at 12 months, Wegovy led to 4.34% reduction in BMI, compared with a 14% change reported in the general population. Zebound, however, was associated with a 2.31% BMI increase overall — though some patients did experience a decrease — compared with a 15% reduction in the general population.
“These findings indicate a substantially reduced weight loss efficacy in breast cancer patients on endocrine therapy compared to the general population,” the authors concluded.
It’s unclear why the drugs appear to not work as well in patients with cancer. It’s possible that hormone therapy or metabolic changes interfere with their effectiveness, given that some cancer therapies lead to weight gain. Steroids and hormone therapies, for instance, often increase appetite, and some treatments can slow patients’ metabolism or lead to fatigue, which can make it harder to exercise.
Patients with cancer may need a higher dose of GLP-1 agonists to achieve similar weight loss to the general population, Dr. Iyengar noted.
However, Dr. Gallagher said, in her own experience, she hasn’t found the drugs to be less effective in patients with cancer, especially the newer agents, like Wegovy and Zepbound.
As for safety, Wegovy and Zepbound both carry a black box warning for thyroid C-cell tumors, including medullary thyroid carcinoma. (Recent research, however, has found that GLP-1 agonists do not increase thyroid cancer risk).
These antiobesity agents are also contraindicated in patients with a personal or family history of medullary thyroid carcinoma and in patients who have multiple endocrine neoplasia syndrome type 2, which is associated with medullary thyroid carcinoma.
Dr. Gallagher hasn’t seen any secondary tumors — thyroid or otherwise — in her patients with cancer, but she follows the labeling contraindications. Dr. Iyengar also noted that more recent and larger data sets have shown no impact on this risk, which may not actually exist, he said
Dr. Gallagher remains cautious about using GPL-1 agonists in patients who have had bariatric surgery because these agents can compound the slower gastric emptying and intestinal transit from surgery, potentially leading to gastrointestinal obstructions.
Looking ahead, GPL-1 manufacturers are interested in adding cancer indications to the drug labeling. Both Dr. Iyengar and Dr. Gallagher said their institutions are in talks with companies to participate in large, multicenter, global phase 3 trials.
Dr. Iyengar welcomes the efforts, not only to test the effectiveness of GPL-1 agonists in oncology but also to “nail down” their safety in cancer.
“I don’t think that there’s mechanistically anything that’s particularly worrisome,” and current observations suggest that these drugs are likely to be safe, Dr. Iyengar said. Even so, “GLP-1 agonists do a lot of things that we don’t fully understand yet.”
The bigger challenge, Dr. Iyengar noted, is that companies will have to show a sizable benefit to using these drugs in patients with cancer to get the Food and Drug Administration’s approval. And to move the needle on cancer-specific outcomes, these antiobesity drugs will need to demonstrate significant, durable weight loss in patients with cancer.
But if these drugs can do that, “I think it’s going to be one of the biggest advances in medicine and oncology given the obesity and cancer epidemic,” Dr. Iyengar said.
Dr. Iyengar has adviser and/or researcher ties with companies that make or are developing GPL-1 agonists, including AstraZeneca, Novartis, Gilead, and Pfizer. Dr. Gallagher is a consultant for Novartis, Flare Therapeutics, Reactive Biosciences, and Seagen.
A version of this article first appeared on Medscape.com.
Demand for new weight loss drugs has surged over the past few years.
Led by the antiobesity drugs semaglutide (Wegovy) and tirzepatide (Zepbound), these popular medications — more commonly known as glucagon-like peptide 1 (GLP-1) agonists — have become game changers for shedding excess pounds.
Aside from obesity indications, both drugs have been approved to treat type 2 diabetes under different brand names and have a growing list of other potential benefits, such as reducing inflammation and depression.
While there’s limited data to support the use of GLP-1 agonists for weight loss in cancer, some oncologists have begun carefully integrating the antiobesity agents into care and studying their effects in this patient population.
The reason: Research suggests that obesity can reduce the effectiveness of cancer therapies, especially in patients with breast cancer, and can increase the risk for treatment-related side effects.
The idea is that managing patients’ weight will improve their cancer outcomes, explained Lajos Pusztai, MD, PhD, a breast cancer specialist and professor of medicine at Yale School of Medicine in New Haven, Connecticut.
Although Dr. Pusztai and his oncology peers at Yale don’t yet use GPL-1 agonists, Neil Iyengar, MD, and colleagues have begun doing so to help some patients with breast cancer manage their weight. Dr. Iyengar estimates that a few hundred — almost 40% — of his patients are on the antiobesity drugs.
“For a patient who has really tried to reduce their weight and who is in the obese range, that’s where I think the use of these medications can be considered,” said Dr. Iyengar, a breast cancer oncologist at Memorial Sloan Kettering Cancer Center in New York City.
Why GLP-1s in Cancer?
GLP-1 is a hormone that the small intestine releases after eating. GLP-1 agonists work by mimicking GLP-1 to trigger the release of insulin and reduce the production of glucagon — two processes that help regulate blood sugar.
These agents, such as Wegovy (or Ozempic when prescribed for diabetes), also slow gastric emptying and can make people feel fuller longer.
Zebound (or Mounjaro for type 2 diabetes) is considered a dual GLP-1 and glucose-dependent insulinotropic polypeptide agonist, which may enhance its weight loss benefits.
In practice, however, these drugs can increase nausea and vomiting from chemotherapy, so Dr. Iyengar typically has patients use them afterwards, during maintenance treatment.
Oncologists don’t prescribe the drugs themselves but instead refer patients to endocrinologists or weight management centers that then write the prescriptions. Taking these drugs involves weekly subcutaneous injections patients can administer themselves.
Endocrinologist Emily Gallagher, MD, PhD, of Mount Sinai Hospital in New York City, estimates she has prescribed the antiobesity drugs to a few hundred patients with cancer and, like Dr. Iyengar, uses the drugs during maintenance treatment with hormone therapy for breast cancer. She also has used these agents in patients with prostate and endometrial cancers and has found the drugs can help counter steroid weight gain in multiple myeloma.
But, to date, the evidence for using GPL-1 agonists in cancer remains limited and the practice has not yet become widespread.
Research largely comes down to a few small retrospective studies in patients with breast cancer receiving aromatase inhibitors. Although no safety issues have emerged so far, these initial reports suggest that the drugs lead to significantly less weight loss in patients with cancer compared to the general population.
Dr. Iyengar led one recent study, presented at the 2024 annual meeting of the American Society of Clinical Oncology, in which he and his team assessed outcomes in 75 women with breast cancer who received a GLP-1 agonist. Almost 80% of patients had diabetes, and 60% received hormone therapy, most commonly an aromatase inhibitor. Patients’ median body mass index (BMI) at baseline was 34 kg/m2 (range, 23-50 kg/m2).
From baseline, patients lost 6.2 kg, on average, or about 5% of their total body weight, 12 months after initiating GLP-1 therapy.
In contrast, phase 3 trials show much higher mean weight loss — about two times — in patients without cancer.
Another recent study also reported modest weight loss results in patients with breast cancer undergoing endocrine therapy. The researchers reported that, at 12 months, Wegovy led to 4.34% reduction in BMI, compared with a 14% change reported in the general population. Zebound, however, was associated with a 2.31% BMI increase overall — though some patients did experience a decrease — compared with a 15% reduction in the general population.
“These findings indicate a substantially reduced weight loss efficacy in breast cancer patients on endocrine therapy compared to the general population,” the authors concluded.
It’s unclear why the drugs appear to not work as well in patients with cancer. It’s possible that hormone therapy or metabolic changes interfere with their effectiveness, given that some cancer therapies lead to weight gain. Steroids and hormone therapies, for instance, often increase appetite, and some treatments can slow patients’ metabolism or lead to fatigue, which can make it harder to exercise.
Patients with cancer may need a higher dose of GLP-1 agonists to achieve similar weight loss to the general population, Dr. Iyengar noted.
However, Dr. Gallagher said, in her own experience, she hasn’t found the drugs to be less effective in patients with cancer, especially the newer agents, like Wegovy and Zepbound.
As for safety, Wegovy and Zepbound both carry a black box warning for thyroid C-cell tumors, including medullary thyroid carcinoma. (Recent research, however, has found that GLP-1 agonists do not increase thyroid cancer risk).
These antiobesity agents are also contraindicated in patients with a personal or family history of medullary thyroid carcinoma and in patients who have multiple endocrine neoplasia syndrome type 2, which is associated with medullary thyroid carcinoma.
Dr. Gallagher hasn’t seen any secondary tumors — thyroid or otherwise — in her patients with cancer, but she follows the labeling contraindications. Dr. Iyengar also noted that more recent and larger data sets have shown no impact on this risk, which may not actually exist, he said
Dr. Gallagher remains cautious about using GPL-1 agonists in patients who have had bariatric surgery because these agents can compound the slower gastric emptying and intestinal transit from surgery, potentially leading to gastrointestinal obstructions.
Looking ahead, GPL-1 manufacturers are interested in adding cancer indications to the drug labeling. Both Dr. Iyengar and Dr. Gallagher said their institutions are in talks with companies to participate in large, multicenter, global phase 3 trials.
Dr. Iyengar welcomes the efforts, not only to test the effectiveness of GPL-1 agonists in oncology but also to “nail down” their safety in cancer.
“I don’t think that there’s mechanistically anything that’s particularly worrisome,” and current observations suggest that these drugs are likely to be safe, Dr. Iyengar said. Even so, “GLP-1 agonists do a lot of things that we don’t fully understand yet.”
The bigger challenge, Dr. Iyengar noted, is that companies will have to show a sizable benefit to using these drugs in patients with cancer to get the Food and Drug Administration’s approval. And to move the needle on cancer-specific outcomes, these antiobesity drugs will need to demonstrate significant, durable weight loss in patients with cancer.
But if these drugs can do that, “I think it’s going to be one of the biggest advances in medicine and oncology given the obesity and cancer epidemic,” Dr. Iyengar said.
Dr. Iyengar has adviser and/or researcher ties with companies that make or are developing GPL-1 agonists, including AstraZeneca, Novartis, Gilead, and Pfizer. Dr. Gallagher is a consultant for Novartis, Flare Therapeutics, Reactive Biosciences, and Seagen.
A version of this article first appeared on Medscape.com.
Does Medicare Advantage Offer Higher-Value Chemotherapy?
TOPLINE:
METHODOLOGY:
- Private Medicare Advantage plans enroll more than half of the Medicare population, but it is unknown if or how the cost restrictions they impose affect chemotherapy, which accounts for a large portion of cancer care costs.
- Researchers conducted a cohort study using national Medicare data from January 2015 to December 2019 to look at Medicare Advantage enrollment and treatment patterns for patients with cancer receiving chemotherapy.
- The study included 96,501 Medicare Advantage enrollees and 206,274 traditional Medicare beneficiaries who initiated chemotherapy between January 2016 and December 2019 (mean age, ~73 years; ~56% women; Hispanic individuals, 15% and 8%; Black individuals, 15% and 8%; and White individuals, 75% and 86%, respectively).
- Resource use and care quality were measured during a 6-month period following chemotherapy initiation, and survival days were measured 18 months after beginning chemotherapy.
- Resource use measures included hospital inpatient services, outpatient care, prescription drugs, hospice services, and chemotherapy services. Quality measures included chemotherapy-related emergency visits and hospital admissions, as well as avoidable emergency visits and preventable hospitalizations.
TAKEAWAY:
- Medicare Advantage plans had lower resource use than traditional Medicare per enrollee with cancer undergoing chemotherapy ($8718 lower; 95% CI, $8343-$9094).
- The lower resource use was largely caused by fewer chemotherapy visits and less expensive chemotherapy per visit in Medicare Advantage plans ($5032 lower; 95% CI, $4772-$5293).
- Medicare Advantage enrollees had 2.5 percentage points fewer chemotherapy-related emergency department visits and 0.7 percentage points fewer chemotherapy-related hospitalizations than traditional Medicare beneficiaries.
- There was no clinically meaningful difference in survival between Medicare Advantage and traditional Medicare beneficiaries during the 18 months following chemotherapy initiation.
IN PRACTICE:
“Our new finding is that MA [Medicare Advantage] plans had lower resource use than TM [traditional Medicare] among enrollees with cancer undergoing chemotherapy — a serious condition managed by specialists and requiring expensive treatments. This suggests that MA’s cost advantages over TM are not limited to conditions for which low-cost primary care management can avoid costly services,” the authors wrote.
SOURCE:
The study was led by Yamini Kalidindi, PhD, McDermott+ Consulting, Washington, DC. It was published online on September 20, 2024, in JAMA Network Open (doi: 10.1001/jamanetworkopen.2024.34707), with a commentary.
LIMITATIONS:
The study’s findings may be affected by unobserved patient characteristics despite the use of inverse-probability weighting. The exclusion of Medicare Advantage enrollees in contracts with incomplete encounter data limits the generalizability of the results. The study does not apply to beneficiaries without Part D drug coverage. Quality measures were limited to those available from claims and encounter data, lacking information on patients’ cancer stage. The 18-month measure of survival might not adequately capture survival differences associated with early-stage cancers. The study did not measure whether patient care followed recommended guidelines.
DISCLOSURES:
Various authors reported grants from the National Institute on Aging, the National Institutes of Health, The Commonwealth Fund, Arnold Ventures, the National Cancer Institute, the Department of Defense, and the National Institute of Health Care Management. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Private Medicare Advantage plans enroll more than half of the Medicare population, but it is unknown if or how the cost restrictions they impose affect chemotherapy, which accounts for a large portion of cancer care costs.
- Researchers conducted a cohort study using national Medicare data from January 2015 to December 2019 to look at Medicare Advantage enrollment and treatment patterns for patients with cancer receiving chemotherapy.
- The study included 96,501 Medicare Advantage enrollees and 206,274 traditional Medicare beneficiaries who initiated chemotherapy between January 2016 and December 2019 (mean age, ~73 years; ~56% women; Hispanic individuals, 15% and 8%; Black individuals, 15% and 8%; and White individuals, 75% and 86%, respectively).
- Resource use and care quality were measured during a 6-month period following chemotherapy initiation, and survival days were measured 18 months after beginning chemotherapy.
- Resource use measures included hospital inpatient services, outpatient care, prescription drugs, hospice services, and chemotherapy services. Quality measures included chemotherapy-related emergency visits and hospital admissions, as well as avoidable emergency visits and preventable hospitalizations.
TAKEAWAY:
- Medicare Advantage plans had lower resource use than traditional Medicare per enrollee with cancer undergoing chemotherapy ($8718 lower; 95% CI, $8343-$9094).
- The lower resource use was largely caused by fewer chemotherapy visits and less expensive chemotherapy per visit in Medicare Advantage plans ($5032 lower; 95% CI, $4772-$5293).
- Medicare Advantage enrollees had 2.5 percentage points fewer chemotherapy-related emergency department visits and 0.7 percentage points fewer chemotherapy-related hospitalizations than traditional Medicare beneficiaries.
- There was no clinically meaningful difference in survival between Medicare Advantage and traditional Medicare beneficiaries during the 18 months following chemotherapy initiation.
IN PRACTICE:
“Our new finding is that MA [Medicare Advantage] plans had lower resource use than TM [traditional Medicare] among enrollees with cancer undergoing chemotherapy — a serious condition managed by specialists and requiring expensive treatments. This suggests that MA’s cost advantages over TM are not limited to conditions for which low-cost primary care management can avoid costly services,” the authors wrote.
SOURCE:
The study was led by Yamini Kalidindi, PhD, McDermott+ Consulting, Washington, DC. It was published online on September 20, 2024, in JAMA Network Open (doi: 10.1001/jamanetworkopen.2024.34707), with a commentary.
LIMITATIONS:
The study’s findings may be affected by unobserved patient characteristics despite the use of inverse-probability weighting. The exclusion of Medicare Advantage enrollees in contracts with incomplete encounter data limits the generalizability of the results. The study does not apply to beneficiaries without Part D drug coverage. Quality measures were limited to those available from claims and encounter data, lacking information on patients’ cancer stage. The 18-month measure of survival might not adequately capture survival differences associated with early-stage cancers. The study did not measure whether patient care followed recommended guidelines.
DISCLOSURES:
Various authors reported grants from the National Institute on Aging, the National Institutes of Health, The Commonwealth Fund, Arnold Ventures, the National Cancer Institute, the Department of Defense, and the National Institute of Health Care Management. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Private Medicare Advantage plans enroll more than half of the Medicare population, but it is unknown if or how the cost restrictions they impose affect chemotherapy, which accounts for a large portion of cancer care costs.
- Researchers conducted a cohort study using national Medicare data from January 2015 to December 2019 to look at Medicare Advantage enrollment and treatment patterns for patients with cancer receiving chemotherapy.
- The study included 96,501 Medicare Advantage enrollees and 206,274 traditional Medicare beneficiaries who initiated chemotherapy between January 2016 and December 2019 (mean age, ~73 years; ~56% women; Hispanic individuals, 15% and 8%; Black individuals, 15% and 8%; and White individuals, 75% and 86%, respectively).
- Resource use and care quality were measured during a 6-month period following chemotherapy initiation, and survival days were measured 18 months after beginning chemotherapy.
- Resource use measures included hospital inpatient services, outpatient care, prescription drugs, hospice services, and chemotherapy services. Quality measures included chemotherapy-related emergency visits and hospital admissions, as well as avoidable emergency visits and preventable hospitalizations.
TAKEAWAY:
- Medicare Advantage plans had lower resource use than traditional Medicare per enrollee with cancer undergoing chemotherapy ($8718 lower; 95% CI, $8343-$9094).
- The lower resource use was largely caused by fewer chemotherapy visits and less expensive chemotherapy per visit in Medicare Advantage plans ($5032 lower; 95% CI, $4772-$5293).
- Medicare Advantage enrollees had 2.5 percentage points fewer chemotherapy-related emergency department visits and 0.7 percentage points fewer chemotherapy-related hospitalizations than traditional Medicare beneficiaries.
- There was no clinically meaningful difference in survival between Medicare Advantage and traditional Medicare beneficiaries during the 18 months following chemotherapy initiation.
IN PRACTICE:
“Our new finding is that MA [Medicare Advantage] plans had lower resource use than TM [traditional Medicare] among enrollees with cancer undergoing chemotherapy — a serious condition managed by specialists and requiring expensive treatments. This suggests that MA’s cost advantages over TM are not limited to conditions for which low-cost primary care management can avoid costly services,” the authors wrote.
SOURCE:
The study was led by Yamini Kalidindi, PhD, McDermott+ Consulting, Washington, DC. It was published online on September 20, 2024, in JAMA Network Open (doi: 10.1001/jamanetworkopen.2024.34707), with a commentary.
LIMITATIONS:
The study’s findings may be affected by unobserved patient characteristics despite the use of inverse-probability weighting. The exclusion of Medicare Advantage enrollees in contracts with incomplete encounter data limits the generalizability of the results. The study does not apply to beneficiaries without Part D drug coverage. Quality measures were limited to those available from claims and encounter data, lacking information on patients’ cancer stage. The 18-month measure of survival might not adequately capture survival differences associated with early-stage cancers. The study did not measure whether patient care followed recommended guidelines.
DISCLOSURES:
Various authors reported grants from the National Institute on Aging, the National Institutes of Health, The Commonwealth Fund, Arnold Ventures, the National Cancer Institute, the Department of Defense, and the National Institute of Health Care Management. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
AACR Cancer Progress Report: Big Strides and Big Gaps
The AACR’s 216-page report — an annual endeavor now in its 14th year — focused on the “tremendous” strides made in cancer care, prevention, and early detection and highlighted areas where more research and attention are warranted.
One key area is funding. For the first time since 2016, federal funding for the National Institutes of Health (NIH) and National Cancer Institute (NCI) decreased in the past year. The cuts followed nearly a decade of funding increases that saw the NIH budget expand by nearly $15 billion, and that allowed for a “rapid pace and broad scope” of advances in cancer, AACR’s chief executive officer Margaret Foti, MD, PhD, said during a press briefing.
These recent cuts “threaten to curtail the medical progress seen in recent years and stymie future advancements,” said Dr. Foti, who called on Congress to commit to funding cancer research at significant and consistent levels to “maintain the momentum of progress against cancer.”
Inside the Report: Big Progress
Overall, advances in prevention, early detection, and treatment have helped catch more cancers earlier and save lives.
According to the AACR report, the age-adjusted overall cancer death rate in the United States fell by 33% between 1991 and 2021, meaning about 4.1 million cancer deaths were averted. The overall cancer death rate for children and adolescents has declined by 24% in the past 2 decades. The 5-year relative survival rate for children diagnosed with cancer in the US has improved from 58% for those diagnosed in the mid-1970s to 85% for those diagnosed between 2013 and 2019.
The past fiscal year has seen many new approvals for cancer drugs, diagnostics, and screening tests. From July 1, 2023, to June 30, 2024, the Food and Drug Administration (FDA) approved 15 new anticancer therapeutics, as well as 15 new indications for previously approved agents, one new imaging agent, several artificial intelligence (AI) tools to improve early cancer detection and diagnosis, and two minimally invasive tests for assessing inherited cancer risk or early cancer detection, according to the report.
“Cancer diagnostics are becoming more sophisticated,” AACR president Patricia M. LoRusso, DO, PhD, said during the briefing. “New technologies, such as spatial transcriptomics, are helping us study tumors at a cellular level, and helping to unveil things that we did not initially even begin to understand or think of. AI-based approaches are beginning to transform cancer detection, diagnosis, clinical decision-making, and treatment response monitoring.”
The report also highlights the significant progress in many childhood and adolescent/young adult cancers, Dr. LoRusso noted. These include FDA approvals for two new molecularly targeted therapeutics: tovorafenib for children with certain types of brain tumor and repotrectinib for children with a wide array of cancer types that have a specific genetic alteration known as NTRK gene fusion. It also includes an expanded approval for eflornithine to reduce the risk for relapse in children with high-risk neuroblastoma.
“Decades — decades — of basic research discoveries, have led to these clinical breakthroughs,” she stressed. “These gains against cancer are because of the rapid progress in our ability to decode the cancer genome, which has opened new and innovative avenues for drug development.”
The Gaps
Even with progress in cancer prevention, early detection, and treatment, cancer remains a significant issue.
“In 2024, it is estimated that more than 2 million new cases of cancer will be diagnosed in the United States. More than 611,000 people will die from the disease,” according to the report.
The 2024 report shows that incidence rates for some cancers are increasing in the United States, including vaccine-preventable cancers such as human papillomavirus (HPV)–associated oral cancers and, in young adults, cervical cancers. A recent analysis also found that overall cervical cancer incidence among women aged 30-34 years increased by 2.5% a year between 2012 and 2019.
Furthermore, despite clear evidence demonstrating that the HPV vaccine reduces cervical cancer incidence, uptake has remained poor, with only 38.6% of US children and adolescents aged 9-17 years receiving at least one dose of the vaccine in 2022.
Early-onset cancers are also increasing. Rates of breast, colorectal, and other cancers are on the rise in adults younger than 50 years, the report noted.
The report also pointed to data that 40% of all cancer cases in the United States can be attributed to preventable factors, such as smoking, excess body weight, and alcohol. However, our understanding of these risk factors has improved. Excessive levels of alcohol consumption have, for instance, been shown to increase the risk for six different types of cancer: certain types of head and neck cancer, esophageal squamous cell carcinoma, and breast, colorectal, liver, and stomach cancers.
Financial toxicity remains prevalent as well.
The report explains that financial hardship following a cancer diagnosis is widespread, and the effects can last for years. In fact, more than 40% of patients can spend their entire life savings within the first 2 years of cancer treatment. Among adult survivors of childhood cancers, 20.7% had trouble paying their medical bills, 29.9% said they had been sent to debt collection for unpaid bills, 14.1% had forgone medical care, and 26.8% could not afford nutritious meals.
For young cancer survivors, the lifetime costs associated with a diagnosis of cancer are substantial, reaching an average of $259,324 per person.
On a global level, it is estimated that from 2020 to 2050, the cumulative economic burden of cancer will be $25.2 trillion.
The Path Forward
Despite these challenges, Dr. LoRusso said, “it is unquestionable that we are in a time of unparalleled opportunities in cancer research.
“I am excited about what the future holds for cancer research, and especially for patient care,” she said.
However, funding commitments are needed to avoid impeding this momentum and losing a “talented and creative young workforce” that has brought new ideas and new technologies to the table.
Continued robust funding will help “to markedly improve cancer care, increase cancer survivorship, spur economic growth, and maintain the United States’ position as the global leader in science and medical research,” she added.
The AACR report specifically calls on Congress to:
- Appropriate at least $51.3 billion in fiscal year 2025 for the base budget of the NIH and at least $7.934 billion for the NCI.
- Provide $3.6 billion in dedicated funding for Cancer Moonshot activities through fiscal year 2026 in addition to other funding, consistent with the President’s fiscal year 2025 budget.
- Appropriate at least $472.4 million in fiscal year 2025 for the CDC’s Division of Cancer Prevention to support comprehensive cancer control, central cancer registries, and screening and awareness programs for specific cancers.
- Allocate $55 million in funding for the Oncology Center of Excellence at FDA in fiscal year 2025 to provide regulators with the staff and tools necessary to conduct expedited review of cancer-related medical products.
By working together with Congress and other stakeholders, “we will be able to accelerate the pace of progress and make major strides toward the lifesaving goal of preventing and curing all cancers at the earliest possible time,” Dr. Foti said. “I believe if we do that ... one day we will win this war on cancer.”
A version of this article first appeared on Medscape.com.
The AACR’s 216-page report — an annual endeavor now in its 14th year — focused on the “tremendous” strides made in cancer care, prevention, and early detection and highlighted areas where more research and attention are warranted.
One key area is funding. For the first time since 2016, federal funding for the National Institutes of Health (NIH) and National Cancer Institute (NCI) decreased in the past year. The cuts followed nearly a decade of funding increases that saw the NIH budget expand by nearly $15 billion, and that allowed for a “rapid pace and broad scope” of advances in cancer, AACR’s chief executive officer Margaret Foti, MD, PhD, said during a press briefing.
These recent cuts “threaten to curtail the medical progress seen in recent years and stymie future advancements,” said Dr. Foti, who called on Congress to commit to funding cancer research at significant and consistent levels to “maintain the momentum of progress against cancer.”
Inside the Report: Big Progress
Overall, advances in prevention, early detection, and treatment have helped catch more cancers earlier and save lives.
According to the AACR report, the age-adjusted overall cancer death rate in the United States fell by 33% between 1991 and 2021, meaning about 4.1 million cancer deaths were averted. The overall cancer death rate for children and adolescents has declined by 24% in the past 2 decades. The 5-year relative survival rate for children diagnosed with cancer in the US has improved from 58% for those diagnosed in the mid-1970s to 85% for those diagnosed between 2013 and 2019.
The past fiscal year has seen many new approvals for cancer drugs, diagnostics, and screening tests. From July 1, 2023, to June 30, 2024, the Food and Drug Administration (FDA) approved 15 new anticancer therapeutics, as well as 15 new indications for previously approved agents, one new imaging agent, several artificial intelligence (AI) tools to improve early cancer detection and diagnosis, and two minimally invasive tests for assessing inherited cancer risk or early cancer detection, according to the report.
“Cancer diagnostics are becoming more sophisticated,” AACR president Patricia M. LoRusso, DO, PhD, said during the briefing. “New technologies, such as spatial transcriptomics, are helping us study tumors at a cellular level, and helping to unveil things that we did not initially even begin to understand or think of. AI-based approaches are beginning to transform cancer detection, diagnosis, clinical decision-making, and treatment response monitoring.”
The report also highlights the significant progress in many childhood and adolescent/young adult cancers, Dr. LoRusso noted. These include FDA approvals for two new molecularly targeted therapeutics: tovorafenib for children with certain types of brain tumor and repotrectinib for children with a wide array of cancer types that have a specific genetic alteration known as NTRK gene fusion. It also includes an expanded approval for eflornithine to reduce the risk for relapse in children with high-risk neuroblastoma.
“Decades — decades — of basic research discoveries, have led to these clinical breakthroughs,” she stressed. “These gains against cancer are because of the rapid progress in our ability to decode the cancer genome, which has opened new and innovative avenues for drug development.”
The Gaps
Even with progress in cancer prevention, early detection, and treatment, cancer remains a significant issue.
“In 2024, it is estimated that more than 2 million new cases of cancer will be diagnosed in the United States. More than 611,000 people will die from the disease,” according to the report.
The 2024 report shows that incidence rates for some cancers are increasing in the United States, including vaccine-preventable cancers such as human papillomavirus (HPV)–associated oral cancers and, in young adults, cervical cancers. A recent analysis also found that overall cervical cancer incidence among women aged 30-34 years increased by 2.5% a year between 2012 and 2019.
Furthermore, despite clear evidence demonstrating that the HPV vaccine reduces cervical cancer incidence, uptake has remained poor, with only 38.6% of US children and adolescents aged 9-17 years receiving at least one dose of the vaccine in 2022.
Early-onset cancers are also increasing. Rates of breast, colorectal, and other cancers are on the rise in adults younger than 50 years, the report noted.
The report also pointed to data that 40% of all cancer cases in the United States can be attributed to preventable factors, such as smoking, excess body weight, and alcohol. However, our understanding of these risk factors has improved. Excessive levels of alcohol consumption have, for instance, been shown to increase the risk for six different types of cancer: certain types of head and neck cancer, esophageal squamous cell carcinoma, and breast, colorectal, liver, and stomach cancers.
Financial toxicity remains prevalent as well.
The report explains that financial hardship following a cancer diagnosis is widespread, and the effects can last for years. In fact, more than 40% of patients can spend their entire life savings within the first 2 years of cancer treatment. Among adult survivors of childhood cancers, 20.7% had trouble paying their medical bills, 29.9% said they had been sent to debt collection for unpaid bills, 14.1% had forgone medical care, and 26.8% could not afford nutritious meals.
For young cancer survivors, the lifetime costs associated with a diagnosis of cancer are substantial, reaching an average of $259,324 per person.
On a global level, it is estimated that from 2020 to 2050, the cumulative economic burden of cancer will be $25.2 trillion.
The Path Forward
Despite these challenges, Dr. LoRusso said, “it is unquestionable that we are in a time of unparalleled opportunities in cancer research.
“I am excited about what the future holds for cancer research, and especially for patient care,” she said.
However, funding commitments are needed to avoid impeding this momentum and losing a “talented and creative young workforce” that has brought new ideas and new technologies to the table.
Continued robust funding will help “to markedly improve cancer care, increase cancer survivorship, spur economic growth, and maintain the United States’ position as the global leader in science and medical research,” she added.
The AACR report specifically calls on Congress to:
- Appropriate at least $51.3 billion in fiscal year 2025 for the base budget of the NIH and at least $7.934 billion for the NCI.
- Provide $3.6 billion in dedicated funding for Cancer Moonshot activities through fiscal year 2026 in addition to other funding, consistent with the President’s fiscal year 2025 budget.
- Appropriate at least $472.4 million in fiscal year 2025 for the CDC’s Division of Cancer Prevention to support comprehensive cancer control, central cancer registries, and screening and awareness programs for specific cancers.
- Allocate $55 million in funding for the Oncology Center of Excellence at FDA in fiscal year 2025 to provide regulators with the staff and tools necessary to conduct expedited review of cancer-related medical products.
By working together with Congress and other stakeholders, “we will be able to accelerate the pace of progress and make major strides toward the lifesaving goal of preventing and curing all cancers at the earliest possible time,” Dr. Foti said. “I believe if we do that ... one day we will win this war on cancer.”
A version of this article first appeared on Medscape.com.
The AACR’s 216-page report — an annual endeavor now in its 14th year — focused on the “tremendous” strides made in cancer care, prevention, and early detection and highlighted areas where more research and attention are warranted.
One key area is funding. For the first time since 2016, federal funding for the National Institutes of Health (NIH) and National Cancer Institute (NCI) decreased in the past year. The cuts followed nearly a decade of funding increases that saw the NIH budget expand by nearly $15 billion, and that allowed for a “rapid pace and broad scope” of advances in cancer, AACR’s chief executive officer Margaret Foti, MD, PhD, said during a press briefing.
These recent cuts “threaten to curtail the medical progress seen in recent years and stymie future advancements,” said Dr. Foti, who called on Congress to commit to funding cancer research at significant and consistent levels to “maintain the momentum of progress against cancer.”
Inside the Report: Big Progress
Overall, advances in prevention, early detection, and treatment have helped catch more cancers earlier and save lives.
According to the AACR report, the age-adjusted overall cancer death rate in the United States fell by 33% between 1991 and 2021, meaning about 4.1 million cancer deaths were averted. The overall cancer death rate for children and adolescents has declined by 24% in the past 2 decades. The 5-year relative survival rate for children diagnosed with cancer in the US has improved from 58% for those diagnosed in the mid-1970s to 85% for those diagnosed between 2013 and 2019.
The past fiscal year has seen many new approvals for cancer drugs, diagnostics, and screening tests. From July 1, 2023, to June 30, 2024, the Food and Drug Administration (FDA) approved 15 new anticancer therapeutics, as well as 15 new indications for previously approved agents, one new imaging agent, several artificial intelligence (AI) tools to improve early cancer detection and diagnosis, and two minimally invasive tests for assessing inherited cancer risk or early cancer detection, according to the report.
“Cancer diagnostics are becoming more sophisticated,” AACR president Patricia M. LoRusso, DO, PhD, said during the briefing. “New technologies, such as spatial transcriptomics, are helping us study tumors at a cellular level, and helping to unveil things that we did not initially even begin to understand or think of. AI-based approaches are beginning to transform cancer detection, diagnosis, clinical decision-making, and treatment response monitoring.”
The report also highlights the significant progress in many childhood and adolescent/young adult cancers, Dr. LoRusso noted. These include FDA approvals for two new molecularly targeted therapeutics: tovorafenib for children with certain types of brain tumor and repotrectinib for children with a wide array of cancer types that have a specific genetic alteration known as NTRK gene fusion. It also includes an expanded approval for eflornithine to reduce the risk for relapse in children with high-risk neuroblastoma.
“Decades — decades — of basic research discoveries, have led to these clinical breakthroughs,” she stressed. “These gains against cancer are because of the rapid progress in our ability to decode the cancer genome, which has opened new and innovative avenues for drug development.”
The Gaps
Even with progress in cancer prevention, early detection, and treatment, cancer remains a significant issue.
“In 2024, it is estimated that more than 2 million new cases of cancer will be diagnosed in the United States. More than 611,000 people will die from the disease,” according to the report.
The 2024 report shows that incidence rates for some cancers are increasing in the United States, including vaccine-preventable cancers such as human papillomavirus (HPV)–associated oral cancers and, in young adults, cervical cancers. A recent analysis also found that overall cervical cancer incidence among women aged 30-34 years increased by 2.5% a year between 2012 and 2019.
Furthermore, despite clear evidence demonstrating that the HPV vaccine reduces cervical cancer incidence, uptake has remained poor, with only 38.6% of US children and adolescents aged 9-17 years receiving at least one dose of the vaccine in 2022.
Early-onset cancers are also increasing. Rates of breast, colorectal, and other cancers are on the rise in adults younger than 50 years, the report noted.
The report also pointed to data that 40% of all cancer cases in the United States can be attributed to preventable factors, such as smoking, excess body weight, and alcohol. However, our understanding of these risk factors has improved. Excessive levels of alcohol consumption have, for instance, been shown to increase the risk for six different types of cancer: certain types of head and neck cancer, esophageal squamous cell carcinoma, and breast, colorectal, liver, and stomach cancers.
Financial toxicity remains prevalent as well.
The report explains that financial hardship following a cancer diagnosis is widespread, and the effects can last for years. In fact, more than 40% of patients can spend their entire life savings within the first 2 years of cancer treatment. Among adult survivors of childhood cancers, 20.7% had trouble paying their medical bills, 29.9% said they had been sent to debt collection for unpaid bills, 14.1% had forgone medical care, and 26.8% could not afford nutritious meals.
For young cancer survivors, the lifetime costs associated with a diagnosis of cancer are substantial, reaching an average of $259,324 per person.
On a global level, it is estimated that from 2020 to 2050, the cumulative economic burden of cancer will be $25.2 trillion.
The Path Forward
Despite these challenges, Dr. LoRusso said, “it is unquestionable that we are in a time of unparalleled opportunities in cancer research.
“I am excited about what the future holds for cancer research, and especially for patient care,” she said.
However, funding commitments are needed to avoid impeding this momentum and losing a “talented and creative young workforce” that has brought new ideas and new technologies to the table.
Continued robust funding will help “to markedly improve cancer care, increase cancer survivorship, spur economic growth, and maintain the United States’ position as the global leader in science and medical research,” she added.
The AACR report specifically calls on Congress to:
- Appropriate at least $51.3 billion in fiscal year 2025 for the base budget of the NIH and at least $7.934 billion for the NCI.
- Provide $3.6 billion in dedicated funding for Cancer Moonshot activities through fiscal year 2026 in addition to other funding, consistent with the President’s fiscal year 2025 budget.
- Appropriate at least $472.4 million in fiscal year 2025 for the CDC’s Division of Cancer Prevention to support comprehensive cancer control, central cancer registries, and screening and awareness programs for specific cancers.
- Allocate $55 million in funding for the Oncology Center of Excellence at FDA in fiscal year 2025 to provide regulators with the staff and tools necessary to conduct expedited review of cancer-related medical products.
By working together with Congress and other stakeholders, “we will be able to accelerate the pace of progress and make major strides toward the lifesaving goal of preventing and curing all cancers at the earliest possible time,” Dr. Foti said. “I believe if we do that ... one day we will win this war on cancer.”
A version of this article first appeared on Medscape.com.