User login
Pig heart transplants and the ethical challenges that lie ahead
The long-struggling field of cardiac xenotransplantation has had a very good year.
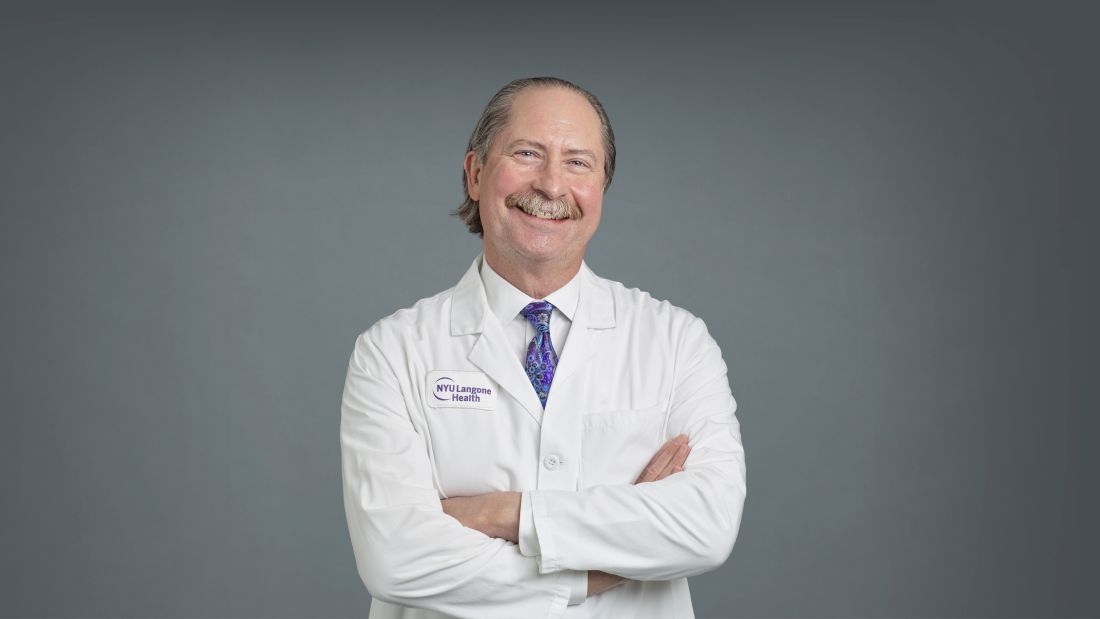
In January, the University of Maryland made history by keeping a 57-year-old man deemed too sick for a human heart transplant alive for 2 months with a genetically engineered pig heart. On July 12, New York University surgeons reported that heart function was “completely normal with excellent contractility” in two brain-dead patients with pig hearts beating in their chests for 72 hours.
The NYU team approached the project with a decedent model in mind and, after discussions with their IRB equivalent, settled on a 72-hour window because that’s the time they typically keep people ventilated when trying to place their organs, explained Robert A. Montgomery, MD, DPhil, director of the NYU Langone Transplant Institute.
“There’s no real ethical argument for that,” he said in an interview. The consideration is what the family is willing to do when trying to balance doing “something very altruistic and good versus having closure.”
Some families have religious beliefs that burial or interment has to occur very rapidly, whereas others, including one of the family donors, were willing to have the research go on much longer, Dr. Montgomery said. Indeed, the next protocol is being written to consider maintaining the bodies for 2-4 weeks.
“People do vary and you have to kind of accommodate that variation,” he said. “For some people, this isn’t going to be what they’re going to want and that’s why you have to go through the consent process.”
Informed authorization
Arthur L. Caplan, PhD, director of medical ethics at the NYU Langone Medical Center, said the Uniform Anatomical Gift Act recognizes an individual’s right to be an organ donor for transplant and research, but it “mentions nothing about maintaining you in a dead state artificially for research purposes.”
“It’s a major shift in what people are thinking about doing when they die or their relatives die,” he said.
Because organ donation is controlled at the state, not federal, level, the possibility of donating organs for xenotransplantation, like medical aid in dying, will vary between states, observed Dr. Caplan. The best way to ensure that patients whose organs are found to be unsuitable for transplantation have the option is to change state laws.
He noted that cases are already springing up where people are requesting postmortem sperm or egg donations without direct consents from the person who died. “So we have this new area opening up of handling the use of the dead body and we need to bring the law into sync with the possibilities that are out there.”
In terms of informed authorization (informed consent is reserved for the living), Dr. Caplan said there should be written evidence the person wanted to be a donor and, while not required by law, all survivors should give their permission and understand what’s going to be done in terms of the experiment, such as the use of animal parts, when the body will be returned, and the possibility of zoonotic viral infection.
“They have to fully accept that the person is dead and we’re just maintaining them artificially,” he said. “There’s no maintaining anyone who’s alive. That’s a source of a lot of confusion.”
Special committees also need to be appointed with voices from people in organ procurement, law, theology, and patient groups to monitor practice to ensure people who have given permission understood the process, that families have their questions answered independent of the research team, and that clear limits are set on how long experiments will last.
As to what those limits should be: “I think in terms of a week or 2,” Dr. Caplan said. “Obviously we could maintain bodies longer and people have. But I think, culturally in our society, going much past that starts to perhaps stress emotionally, psychologically, family and friends about getting closure.”
“I’m not as comfortable when people say things like, ‘How about 2 months?’ ” he said. “That’s a long time to sort of accept the fact that somebody has died but you can’t complete all the things that go along with the death.”
Dr. Caplan is also uncomfortable with the use of one-off emergency authorizations, as used for Maryland resident David Bennett Sr., who was rejected for standard heart transplantation and required mechanical circulatory support to stay alive.
“It’s too premature, I believe, even to try and rescue someone,” he said. “We need to learn more from the deceased models.”
A better model
Dr. Montgomery noted that primates are very imperfect models for predicting what’s going to happen in humans, and that in order to do xenotransplantation in living humans, there are only two pathways – the one-off emergency authorization or a clinical phase 1 trial.
The decedent model, he said, “will make human trials safer because it’s an intermediate step. You don’t have a living human’s life on the line when you’re trying to do iterative changes and improve the procedure.”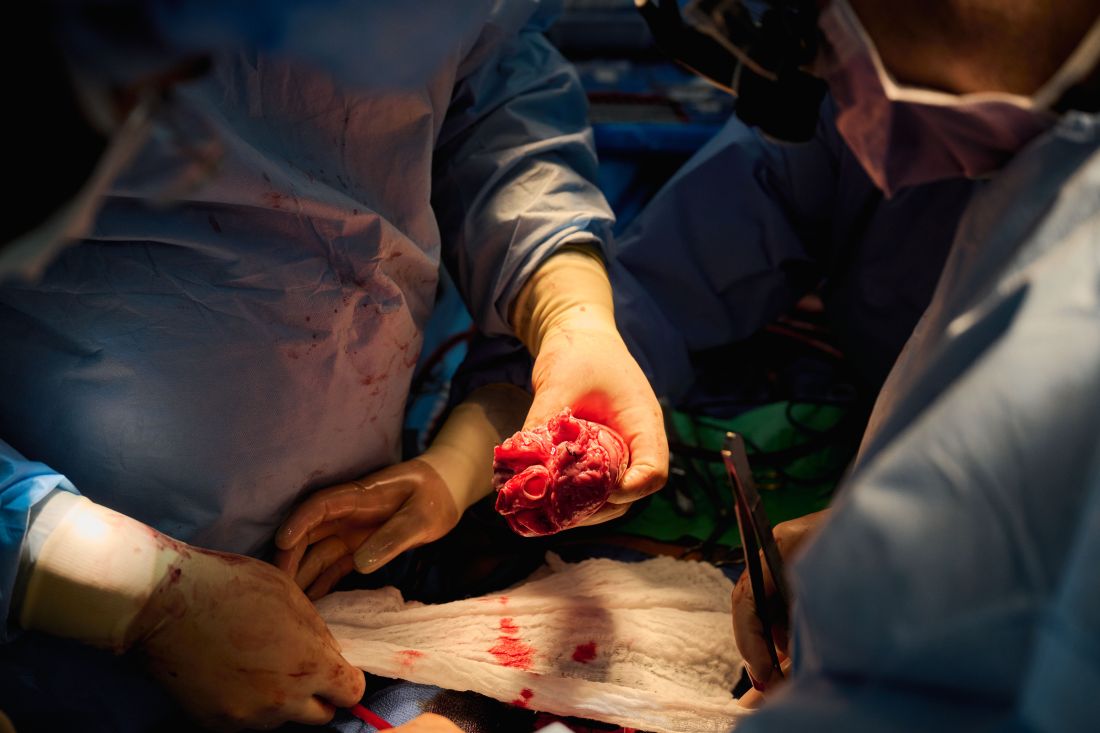
The team, for example, omitted a perfusion pump that was used in the Maryland case and would likely have made its way into phase 1 trials based on baboon data that suggested it was important to have the heart on the pump for hours before it was transplanted, he said. “We didn’t do any of that. We just did it like we would do a regular heart transplant and it started right up, immediately, and started to work.”
The researchers did not release details on the immunosuppression regimen, but noted that, unlike Maryland, they also did not use the experimental anti-CD40 antibody to tamp down the recipients’ immune system.
Although Mr. Bennett’s autopsy did not show any conventional sign of graft rejection, the transplanted pig heart was infected with porcine cytomegalovirus (PCMV) and Mr. Bennett showed traces of DNA from PCMV in his circulation.
Nailing down safety
Dr. Montgomery said he wouldn’t rule out xenotransplantation in a living human, but that the safety issues need to be nailed down. “I think that the tests used on the pig that was the donor for the Bennett case were not sensitive enough for latent virus, and that’s how it slipped through. So there was a bit of going back to the drawing board, really looking at each of the tests, and being sure we had the sensitivity to pick up a latent virus.”
He noted that United Therapeutics, which funded the research and provided the engineered pigs through its subsidiary Revivicor, has created and validated a more sensitive polymerase chain reaction test that covers some 35 different pathogens, microbes, and parasites. NYU has also developed its own platform to repeat the testing and for monitoring after the transplant. “The ones that we’re currently using would have picked up the virus.”
Stuart Russell, MD, a professor of medicine who specializes in advanced HF at Duke University, Durham, N.C., said “the biggest thing from my perspective is those two amazing families that were willing let this happen. ... If 20 years from now, this is what we’re doing, it’s related to these families being this generous at a really tough time in their lives.”
Dr. Russell said he awaits publication of the data on what the pathology of the heart looks like, but that the experiments “help to give us a lot of reassurance that we don’t need to worry about hyperacute rejection,” which by definition is going to happen in the first 24-48 hours.
That said, longer-term data is essential to potential safety issues. Notably, among the 10 genetic modifications made to the pigs, four were porcine gene knockouts, including a growth hormone receptor knockout to prevent abnormal organ growth inside the recipient’s chest. As a result, the organs seem to be small for the age of the pig and just don’t grow that well, admitted Dr. Montgomery, who said they are currently analyzing this with echocardiography.
Dr. Russell said this may create a sizing issue, but also “if you have a heart that’s more stressed in the pig, from the point of being a donor, maybe it’s not as good a heart as if it was growing normally. But that kind of stuff, I think, is going to take more than two cases and longer-term data to sort out.”
Sharon Hunt, MD, professor emerita, Stanford (Calif.) University Medical Center, and past president of the International Society for Heart Lung Transplantation, said it’s not the technical aspects, but the biology of xenotransplantation that’s really daunting.
“It’s not the physical act of doing it, like they needed a bigger heart or a smaller heart. Those are technical problems but they’ll manage them,” she said. “The big problem is biological – and the bottom line is we don’t really know. We may have overcome hyperacute rejection, which is great, but the rest remains to be seen.”
Dr. Hunt, who worked with heart transplantation pioneer Norman Shumway, MD, and spent decades caring for patients after transplantation, said most families will consent to 24 or 48 hours or even a week of experimentation on a brain-dead loved one, but what the transplant community wants to know is whether this is workable for many months.
“So the fact that the xenotransplant works for 72 hours, yeah, that’s groovy. But, you know, the answer is kind of ‘so what,’ ” she said. “I’d like to see this go for months, like they were trying to do in the human in Maryland.”
For phase 1 trials, even longer-term survival with or without rejection or with rejection that’s treatable is needed, Dr. Hunt suggested.
“We haven’t seen that yet. The Maryland people were very valiant but they lost the cause,” she said. “There’s just so much more to do before we have a viable model to start anything like a phase 1 trial. I’d love it if that happens in my lifetime, but I’m not sure it’s going to.”
Dr. Russell and Dr. Hunt reported no relevant financial relationships. Dr. Caplan reported serving as a director, officer, partner, employee, advisor, consultant, or trustee for Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position) and is a contributing author and adviser for Medscape.
A version of this article first appeared on Medscape.com.
The long-struggling field of cardiac xenotransplantation has had a very good year.
In January, the University of Maryland made history by keeping a 57-year-old man deemed too sick for a human heart transplant alive for 2 months with a genetically engineered pig heart. On July 12, New York University surgeons reported that heart function was “completely normal with excellent contractility” in two brain-dead patients with pig hearts beating in their chests for 72 hours.
The NYU team approached the project with a decedent model in mind and, after discussions with their IRB equivalent, settled on a 72-hour window because that’s the time they typically keep people ventilated when trying to place their organs, explained Robert A. Montgomery, MD, DPhil, director of the NYU Langone Transplant Institute.
“There’s no real ethical argument for that,” he said in an interview. The consideration is what the family is willing to do when trying to balance doing “something very altruistic and good versus having closure.”
Some families have religious beliefs that burial or interment has to occur very rapidly, whereas others, including one of the family donors, were willing to have the research go on much longer, Dr. Montgomery said. Indeed, the next protocol is being written to consider maintaining the bodies for 2-4 weeks.
“People do vary and you have to kind of accommodate that variation,” he said. “For some people, this isn’t going to be what they’re going to want and that’s why you have to go through the consent process.”
Informed authorization
Arthur L. Caplan, PhD, director of medical ethics at the NYU Langone Medical Center, said the Uniform Anatomical Gift Act recognizes an individual’s right to be an organ donor for transplant and research, but it “mentions nothing about maintaining you in a dead state artificially for research purposes.”
“It’s a major shift in what people are thinking about doing when they die or their relatives die,” he said.
Because organ donation is controlled at the state, not federal, level, the possibility of donating organs for xenotransplantation, like medical aid in dying, will vary between states, observed Dr. Caplan. The best way to ensure that patients whose organs are found to be unsuitable for transplantation have the option is to change state laws.
He noted that cases are already springing up where people are requesting postmortem sperm or egg donations without direct consents from the person who died. “So we have this new area opening up of handling the use of the dead body and we need to bring the law into sync with the possibilities that are out there.”
In terms of informed authorization (informed consent is reserved for the living), Dr. Caplan said there should be written evidence the person wanted to be a donor and, while not required by law, all survivors should give their permission and understand what’s going to be done in terms of the experiment, such as the use of animal parts, when the body will be returned, and the possibility of zoonotic viral infection.
“They have to fully accept that the person is dead and we’re just maintaining them artificially,” he said. “There’s no maintaining anyone who’s alive. That’s a source of a lot of confusion.”
Special committees also need to be appointed with voices from people in organ procurement, law, theology, and patient groups to monitor practice to ensure people who have given permission understood the process, that families have their questions answered independent of the research team, and that clear limits are set on how long experiments will last.
As to what those limits should be: “I think in terms of a week or 2,” Dr. Caplan said. “Obviously we could maintain bodies longer and people have. But I think, culturally in our society, going much past that starts to perhaps stress emotionally, psychologically, family and friends about getting closure.”
“I’m not as comfortable when people say things like, ‘How about 2 months?’ ” he said. “That’s a long time to sort of accept the fact that somebody has died but you can’t complete all the things that go along with the death.”
Dr. Caplan is also uncomfortable with the use of one-off emergency authorizations, as used for Maryland resident David Bennett Sr., who was rejected for standard heart transplantation and required mechanical circulatory support to stay alive.
“It’s too premature, I believe, even to try and rescue someone,” he said. “We need to learn more from the deceased models.”
A better model
Dr. Montgomery noted that primates are very imperfect models for predicting what’s going to happen in humans, and that in order to do xenotransplantation in living humans, there are only two pathways – the one-off emergency authorization or a clinical phase 1 trial.
The decedent model, he said, “will make human trials safer because it’s an intermediate step. You don’t have a living human’s life on the line when you’re trying to do iterative changes and improve the procedure.”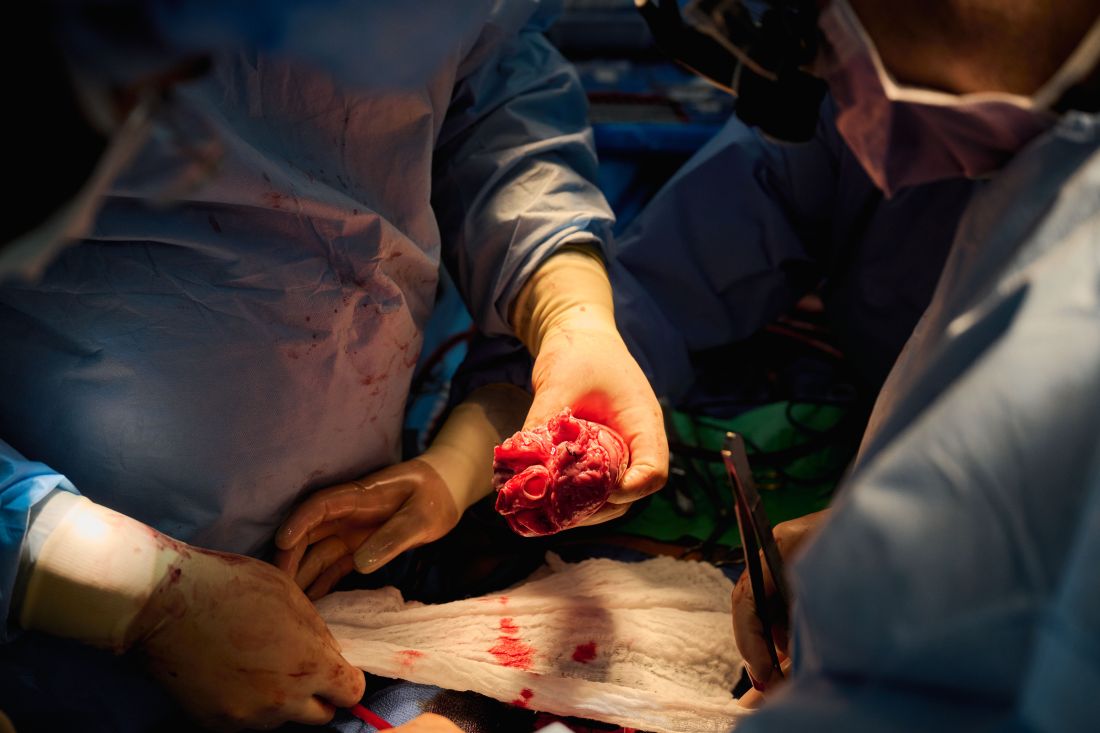
The team, for example, omitted a perfusion pump that was used in the Maryland case and would likely have made its way into phase 1 trials based on baboon data that suggested it was important to have the heart on the pump for hours before it was transplanted, he said. “We didn’t do any of that. We just did it like we would do a regular heart transplant and it started right up, immediately, and started to work.”
The researchers did not release details on the immunosuppression regimen, but noted that, unlike Maryland, they also did not use the experimental anti-CD40 antibody to tamp down the recipients’ immune system.
Although Mr. Bennett’s autopsy did not show any conventional sign of graft rejection, the transplanted pig heart was infected with porcine cytomegalovirus (PCMV) and Mr. Bennett showed traces of DNA from PCMV in his circulation.
Nailing down safety
Dr. Montgomery said he wouldn’t rule out xenotransplantation in a living human, but that the safety issues need to be nailed down. “I think that the tests used on the pig that was the donor for the Bennett case were not sensitive enough for latent virus, and that’s how it slipped through. So there was a bit of going back to the drawing board, really looking at each of the tests, and being sure we had the sensitivity to pick up a latent virus.”
He noted that United Therapeutics, which funded the research and provided the engineered pigs through its subsidiary Revivicor, has created and validated a more sensitive polymerase chain reaction test that covers some 35 different pathogens, microbes, and parasites. NYU has also developed its own platform to repeat the testing and for monitoring after the transplant. “The ones that we’re currently using would have picked up the virus.”
Stuart Russell, MD, a professor of medicine who specializes in advanced HF at Duke University, Durham, N.C., said “the biggest thing from my perspective is those two amazing families that were willing let this happen. ... If 20 years from now, this is what we’re doing, it’s related to these families being this generous at a really tough time in their lives.”
Dr. Russell said he awaits publication of the data on what the pathology of the heart looks like, but that the experiments “help to give us a lot of reassurance that we don’t need to worry about hyperacute rejection,” which by definition is going to happen in the first 24-48 hours.
That said, longer-term data is essential to potential safety issues. Notably, among the 10 genetic modifications made to the pigs, four were porcine gene knockouts, including a growth hormone receptor knockout to prevent abnormal organ growth inside the recipient’s chest. As a result, the organs seem to be small for the age of the pig and just don’t grow that well, admitted Dr. Montgomery, who said they are currently analyzing this with echocardiography.
Dr. Russell said this may create a sizing issue, but also “if you have a heart that’s more stressed in the pig, from the point of being a donor, maybe it’s not as good a heart as if it was growing normally. But that kind of stuff, I think, is going to take more than two cases and longer-term data to sort out.”
Sharon Hunt, MD, professor emerita, Stanford (Calif.) University Medical Center, and past president of the International Society for Heart Lung Transplantation, said it’s not the technical aspects, but the biology of xenotransplantation that’s really daunting.
“It’s not the physical act of doing it, like they needed a bigger heart or a smaller heart. Those are technical problems but they’ll manage them,” she said. “The big problem is biological – and the bottom line is we don’t really know. We may have overcome hyperacute rejection, which is great, but the rest remains to be seen.”
Dr. Hunt, who worked with heart transplantation pioneer Norman Shumway, MD, and spent decades caring for patients after transplantation, said most families will consent to 24 or 48 hours or even a week of experimentation on a brain-dead loved one, but what the transplant community wants to know is whether this is workable for many months.
“So the fact that the xenotransplant works for 72 hours, yeah, that’s groovy. But, you know, the answer is kind of ‘so what,’ ” she said. “I’d like to see this go for months, like they were trying to do in the human in Maryland.”
For phase 1 trials, even longer-term survival with or without rejection or with rejection that’s treatable is needed, Dr. Hunt suggested.
“We haven’t seen that yet. The Maryland people were very valiant but they lost the cause,” she said. “There’s just so much more to do before we have a viable model to start anything like a phase 1 trial. I’d love it if that happens in my lifetime, but I’m not sure it’s going to.”
Dr. Russell and Dr. Hunt reported no relevant financial relationships. Dr. Caplan reported serving as a director, officer, partner, employee, advisor, consultant, or trustee for Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position) and is a contributing author and adviser for Medscape.
A version of this article first appeared on Medscape.com.
The long-struggling field of cardiac xenotransplantation has had a very good year.
In January, the University of Maryland made history by keeping a 57-year-old man deemed too sick for a human heart transplant alive for 2 months with a genetically engineered pig heart. On July 12, New York University surgeons reported that heart function was “completely normal with excellent contractility” in two brain-dead patients with pig hearts beating in their chests for 72 hours.
The NYU team approached the project with a decedent model in mind and, after discussions with their IRB equivalent, settled on a 72-hour window because that’s the time they typically keep people ventilated when trying to place their organs, explained Robert A. Montgomery, MD, DPhil, director of the NYU Langone Transplant Institute.
“There’s no real ethical argument for that,” he said in an interview. The consideration is what the family is willing to do when trying to balance doing “something very altruistic and good versus having closure.”
Some families have religious beliefs that burial or interment has to occur very rapidly, whereas others, including one of the family donors, were willing to have the research go on much longer, Dr. Montgomery said. Indeed, the next protocol is being written to consider maintaining the bodies for 2-4 weeks.
“People do vary and you have to kind of accommodate that variation,” he said. “For some people, this isn’t going to be what they’re going to want and that’s why you have to go through the consent process.”
Informed authorization
Arthur L. Caplan, PhD, director of medical ethics at the NYU Langone Medical Center, said the Uniform Anatomical Gift Act recognizes an individual’s right to be an organ donor for transplant and research, but it “mentions nothing about maintaining you in a dead state artificially for research purposes.”
“It’s a major shift in what people are thinking about doing when they die or their relatives die,” he said.
Because organ donation is controlled at the state, not federal, level, the possibility of donating organs for xenotransplantation, like medical aid in dying, will vary between states, observed Dr. Caplan. The best way to ensure that patients whose organs are found to be unsuitable for transplantation have the option is to change state laws.
He noted that cases are already springing up where people are requesting postmortem sperm or egg donations without direct consents from the person who died. “So we have this new area opening up of handling the use of the dead body and we need to bring the law into sync with the possibilities that are out there.”
In terms of informed authorization (informed consent is reserved for the living), Dr. Caplan said there should be written evidence the person wanted to be a donor and, while not required by law, all survivors should give their permission and understand what’s going to be done in terms of the experiment, such as the use of animal parts, when the body will be returned, and the possibility of zoonotic viral infection.
“They have to fully accept that the person is dead and we’re just maintaining them artificially,” he said. “There’s no maintaining anyone who’s alive. That’s a source of a lot of confusion.”
Special committees also need to be appointed with voices from people in organ procurement, law, theology, and patient groups to monitor practice to ensure people who have given permission understood the process, that families have their questions answered independent of the research team, and that clear limits are set on how long experiments will last.
As to what those limits should be: “I think in terms of a week or 2,” Dr. Caplan said. “Obviously we could maintain bodies longer and people have. But I think, culturally in our society, going much past that starts to perhaps stress emotionally, psychologically, family and friends about getting closure.”
“I’m not as comfortable when people say things like, ‘How about 2 months?’ ” he said. “That’s a long time to sort of accept the fact that somebody has died but you can’t complete all the things that go along with the death.”
Dr. Caplan is also uncomfortable with the use of one-off emergency authorizations, as used for Maryland resident David Bennett Sr., who was rejected for standard heart transplantation and required mechanical circulatory support to stay alive.
“It’s too premature, I believe, even to try and rescue someone,” he said. “We need to learn more from the deceased models.”
A better model
Dr. Montgomery noted that primates are very imperfect models for predicting what’s going to happen in humans, and that in order to do xenotransplantation in living humans, there are only two pathways – the one-off emergency authorization or a clinical phase 1 trial.
The decedent model, he said, “will make human trials safer because it’s an intermediate step. You don’t have a living human’s life on the line when you’re trying to do iterative changes and improve the procedure.”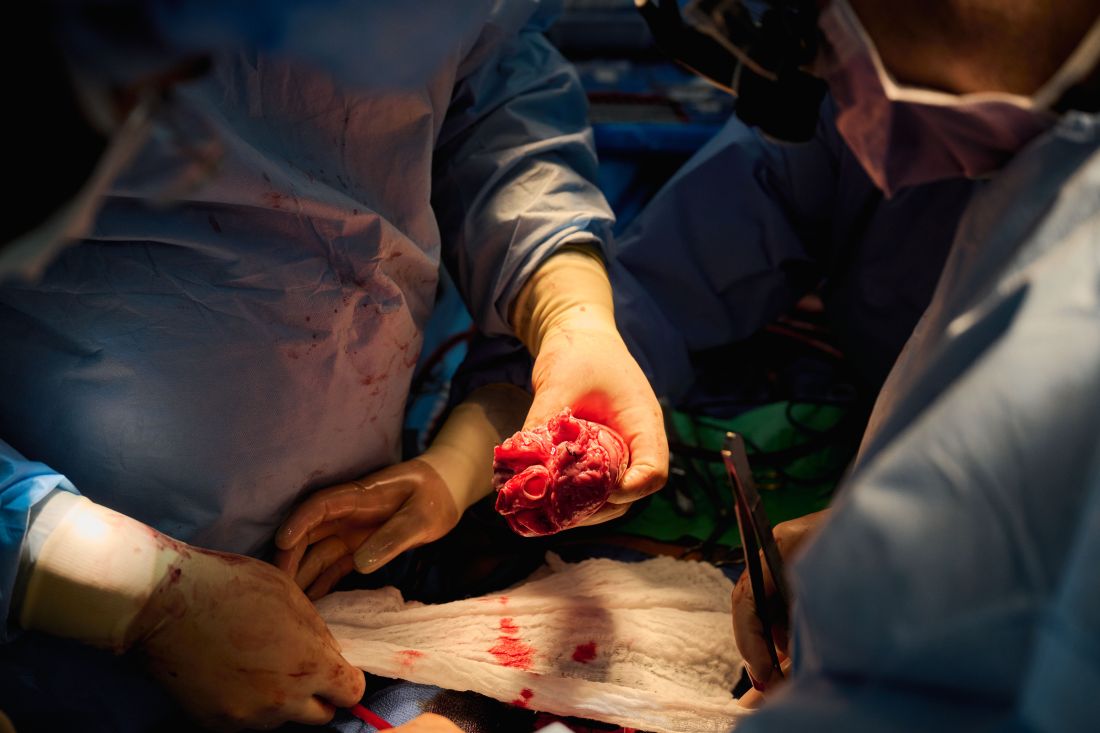
The team, for example, omitted a perfusion pump that was used in the Maryland case and would likely have made its way into phase 1 trials based on baboon data that suggested it was important to have the heart on the pump for hours before it was transplanted, he said. “We didn’t do any of that. We just did it like we would do a regular heart transplant and it started right up, immediately, and started to work.”
The researchers did not release details on the immunosuppression regimen, but noted that, unlike Maryland, they also did not use the experimental anti-CD40 antibody to tamp down the recipients’ immune system.
Although Mr. Bennett’s autopsy did not show any conventional sign of graft rejection, the transplanted pig heart was infected with porcine cytomegalovirus (PCMV) and Mr. Bennett showed traces of DNA from PCMV in his circulation.
Nailing down safety
Dr. Montgomery said he wouldn’t rule out xenotransplantation in a living human, but that the safety issues need to be nailed down. “I think that the tests used on the pig that was the donor for the Bennett case were not sensitive enough for latent virus, and that’s how it slipped through. So there was a bit of going back to the drawing board, really looking at each of the tests, and being sure we had the sensitivity to pick up a latent virus.”
He noted that United Therapeutics, which funded the research and provided the engineered pigs through its subsidiary Revivicor, has created and validated a more sensitive polymerase chain reaction test that covers some 35 different pathogens, microbes, and parasites. NYU has also developed its own platform to repeat the testing and for monitoring after the transplant. “The ones that we’re currently using would have picked up the virus.”
Stuart Russell, MD, a professor of medicine who specializes in advanced HF at Duke University, Durham, N.C., said “the biggest thing from my perspective is those two amazing families that were willing let this happen. ... If 20 years from now, this is what we’re doing, it’s related to these families being this generous at a really tough time in their lives.”
Dr. Russell said he awaits publication of the data on what the pathology of the heart looks like, but that the experiments “help to give us a lot of reassurance that we don’t need to worry about hyperacute rejection,” which by definition is going to happen in the first 24-48 hours.
That said, longer-term data is essential to potential safety issues. Notably, among the 10 genetic modifications made to the pigs, four were porcine gene knockouts, including a growth hormone receptor knockout to prevent abnormal organ growth inside the recipient’s chest. As a result, the organs seem to be small for the age of the pig and just don’t grow that well, admitted Dr. Montgomery, who said they are currently analyzing this with echocardiography.
Dr. Russell said this may create a sizing issue, but also “if you have a heart that’s more stressed in the pig, from the point of being a donor, maybe it’s not as good a heart as if it was growing normally. But that kind of stuff, I think, is going to take more than two cases and longer-term data to sort out.”
Sharon Hunt, MD, professor emerita, Stanford (Calif.) University Medical Center, and past president of the International Society for Heart Lung Transplantation, said it’s not the technical aspects, but the biology of xenotransplantation that’s really daunting.
“It’s not the physical act of doing it, like they needed a bigger heart or a smaller heart. Those are technical problems but they’ll manage them,” she said. “The big problem is biological – and the bottom line is we don’t really know. We may have overcome hyperacute rejection, which is great, but the rest remains to be seen.”
Dr. Hunt, who worked with heart transplantation pioneer Norman Shumway, MD, and spent decades caring for patients after transplantation, said most families will consent to 24 or 48 hours or even a week of experimentation on a brain-dead loved one, but what the transplant community wants to know is whether this is workable for many months.
“So the fact that the xenotransplant works for 72 hours, yeah, that’s groovy. But, you know, the answer is kind of ‘so what,’ ” she said. “I’d like to see this go for months, like they were trying to do in the human in Maryland.”
For phase 1 trials, even longer-term survival with or without rejection or with rejection that’s treatable is needed, Dr. Hunt suggested.
“We haven’t seen that yet. The Maryland people were very valiant but they lost the cause,” she said. “There’s just so much more to do before we have a viable model to start anything like a phase 1 trial. I’d love it if that happens in my lifetime, but I’m not sure it’s going to.”
Dr. Russell and Dr. Hunt reported no relevant financial relationships. Dr. Caplan reported serving as a director, officer, partner, employee, advisor, consultant, or trustee for Johnson & Johnson’s Panel for Compassionate Drug Use (unpaid position) and is a contributing author and adviser for Medscape.
A version of this article first appeared on Medscape.com.
Who’s in charge here? Rheumatologists battle local Medicare policies threatening access, practice sustainability
Rheumatologists who administer medications in their office for Medicare patients, specifically those that are infused, have in recent years encountered problems providing certain medication formulations as well as coding and billing for their administration. In attempting to resolve these issues, rheumatologists and their professional organizations have found themselves caught in a morass of Medicare agency “ping-pong,” where it is unclear who the decision makers are.
The private health care insurers that process medical claims for Medicare beneficiaries, called A/B Medicare Administrative Contractors or more commonly known as MACs, are the operational intermediary between the Centers for Medicare & Medicaid Services’ fee-for-service program and the physicians enrolled in it. The country is divided into 12 sections, each with a MAC that has jurisdiction over that area. Among other things, the MACs establish local coverage and payment policies based on their understanding of CMS’ rules, regulations, and the Medicare statute, and therein lies the problem: When a physician has a question on a policy or decision that was made by a MAC, it is very difficult to determine the origins of the issue and who can address the problem. It’s a lot of “running in circles” between the MACs and CMS headquarters, hoping that someone will take the time to listen to your concern, but more importantly, work toward resolving the problem.
Who can address problems?
Meaningful, solutions-driven engagement with the MACs and CMS has become frustrating for physicians and advocacy organizations attempting to address a host of problems. The two issues alluded to above include the Self-Administered Drug Exclusion List (SAD List), which excludes certain Part B medication formulations from coverage under certain conditions and the “down coding” of certain infusion administration codes when specific drugs are delivered. These problems are compounded by the curtailment of physician stakeholder input via Contractor Advisory Committees (CACs). Each state has its own CAC, but the CAC meetings have been restructured as a result of the 21st Century Cures Act, and ultimately eradicated the involvement of these physician advisers in policy development at the local level.
This has left many of rheumatology representatives to the CACs demoralized and generally unhappy about certain decisions being made without their input. There is also inconsistency in terms of coverage and payment policies throughout the country. For example, in one MAC jurisdiction, a certain medication may be on the SAD List and excluded from Part B coverage, meaning beneficiary access is only available through Part D (and assuming they can afford it), while in an adjacent MAC jurisdiction, both formulations are covered.
The Coalition of State Rheumatology Organizations, along with the American College of Rheumatology and other specialty groups, is attempting to address these issues from many different angles. There is not enough space to explain the nuances of local coverage policy development, but the timeline below highlights the long and winding road that we have travelled to resolve these issues.
- February 2021: CSRO meets with CMS’ Coverage and Analysis Group (CAG) to raise concerns about ustekinumab (Stelara) and its inclusion on the SAD List.
- April 2021: CSRO follows up with CMS’ CAG on SAD List concerns in a letter.
- May 2021: Most MACs issue or revise local coverage articles, or “billing and coding” articles, that down code the administration of certain biologic medications, with some expanding the list of biologic medications subject to the policy, prompting a strong response from CSRO.
- September 2021: CSRO meets with multijurisdictional MAC Contract Medical Director (CMD) work group to discuss down coding, SAD List, and physician/CAC engagement.
- October 2021: At the suggestion of the CMDs, CSRO re-engages with CMS’ CAG to raise concerns about down-coding policies and physician/CAC engagement, and continue the SAD List discussion.
- November 2021: CSRO is connected with CMS’ “payment ombudsman” on down coding and the SAD List.
- January 2022: CSRO signs on to multispecialty coalition effort aimed at improving local coverage and payment policy and restoring the importance of the CAC.
- February 2022: CSRO participates in CMS CAG meeting with multispecialty coalition, raising concerns about the down-coding and SAD List policies.
- March/April 2022: Through its coalition partner, the Alliance of Specialty Medicine, CSRO meets with the principal deputy CMS administrator and raises awareness to these issues.
- May 2022: CSRO participates in follow-up discussion with CMS’ CAG as part of multispecialty coalition, reiterating concerns about the down coding and SAD List policies. With the assistance of the CMS’ Office of the Administrator, CSRO meets with CMS’ Center for Program Integrity to seek a “pause” in down-coding policies for certain biologic medications.
- June 2022: CMS notifies CSRO of a “temporary pause” in medical review while the agency reviews various manuals and policies to determine the appropriate steps forward. To assist the agency, CSRO works with practices to develop a resource that CMS can use to establish criteria for determining when a medication warrants use of complex drug administration codes. CSRO re-engages with multijurisdictional MAC CMD workgroup to continue discussions on SAD List.
- July 2022: CSRO meets with new multijurisdictional MAC CMD workgroup focused on improving the process for developing local coverage and payment policy.
Our dialogue with CMS leadership and staff continues. In the most recent communication, staff in the CMS administrator’s office informed us that the issue is complicated and crosses several different parts of the agency, and they are still determining next steps.
The rheumatology community’s journey toward solving the challenges facing practices and patients is emblematic of the communication problem between provider groups and the CMS-MAC establishment. While we understand this is how bureaucracy works, it is not to the benefit of Medicare beneficiaries to have a system that is so difficult to navigate, even by the best of the regulatory gurus. This is not an indictment of any specific group but a call to action on the part of the government and their contractors to create a clear, transparent path to getting answers when we have a problem.
And by the way, we do have another meeting with yet another CMS “center” regarding the SAD List in August.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is president of the CSRO, past chair of the Alliance for Safe Biologic Medicines, and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at rhnews@mdedge.com.
Rheumatologists who administer medications in their office for Medicare patients, specifically those that are infused, have in recent years encountered problems providing certain medication formulations as well as coding and billing for their administration. In attempting to resolve these issues, rheumatologists and their professional organizations have found themselves caught in a morass of Medicare agency “ping-pong,” where it is unclear who the decision makers are.
The private health care insurers that process medical claims for Medicare beneficiaries, called A/B Medicare Administrative Contractors or more commonly known as MACs, are the operational intermediary between the Centers for Medicare & Medicaid Services’ fee-for-service program and the physicians enrolled in it. The country is divided into 12 sections, each with a MAC that has jurisdiction over that area. Among other things, the MACs establish local coverage and payment policies based on their understanding of CMS’ rules, regulations, and the Medicare statute, and therein lies the problem: When a physician has a question on a policy or decision that was made by a MAC, it is very difficult to determine the origins of the issue and who can address the problem. It’s a lot of “running in circles” between the MACs and CMS headquarters, hoping that someone will take the time to listen to your concern, but more importantly, work toward resolving the problem.
Who can address problems?
Meaningful, solutions-driven engagement with the MACs and CMS has become frustrating for physicians and advocacy organizations attempting to address a host of problems. The two issues alluded to above include the Self-Administered Drug Exclusion List (SAD List), which excludes certain Part B medication formulations from coverage under certain conditions and the “down coding” of certain infusion administration codes when specific drugs are delivered. These problems are compounded by the curtailment of physician stakeholder input via Contractor Advisory Committees (CACs). Each state has its own CAC, but the CAC meetings have been restructured as a result of the 21st Century Cures Act, and ultimately eradicated the involvement of these physician advisers in policy development at the local level.
This has left many of rheumatology representatives to the CACs demoralized and generally unhappy about certain decisions being made without their input. There is also inconsistency in terms of coverage and payment policies throughout the country. For example, in one MAC jurisdiction, a certain medication may be on the SAD List and excluded from Part B coverage, meaning beneficiary access is only available through Part D (and assuming they can afford it), while in an adjacent MAC jurisdiction, both formulations are covered.
The Coalition of State Rheumatology Organizations, along with the American College of Rheumatology and other specialty groups, is attempting to address these issues from many different angles. There is not enough space to explain the nuances of local coverage policy development, but the timeline below highlights the long and winding road that we have travelled to resolve these issues.
- February 2021: CSRO meets with CMS’ Coverage and Analysis Group (CAG) to raise concerns about ustekinumab (Stelara) and its inclusion on the SAD List.
- April 2021: CSRO follows up with CMS’ CAG on SAD List concerns in a letter.
- May 2021: Most MACs issue or revise local coverage articles, or “billing and coding” articles, that down code the administration of certain biologic medications, with some expanding the list of biologic medications subject to the policy, prompting a strong response from CSRO.
- September 2021: CSRO meets with multijurisdictional MAC Contract Medical Director (CMD) work group to discuss down coding, SAD List, and physician/CAC engagement.
- October 2021: At the suggestion of the CMDs, CSRO re-engages with CMS’ CAG to raise concerns about down-coding policies and physician/CAC engagement, and continue the SAD List discussion.
- November 2021: CSRO is connected with CMS’ “payment ombudsman” on down coding and the SAD List.
- January 2022: CSRO signs on to multispecialty coalition effort aimed at improving local coverage and payment policy and restoring the importance of the CAC.
- February 2022: CSRO participates in CMS CAG meeting with multispecialty coalition, raising concerns about the down-coding and SAD List policies.
- March/April 2022: Through its coalition partner, the Alliance of Specialty Medicine, CSRO meets with the principal deputy CMS administrator and raises awareness to these issues.
- May 2022: CSRO participates in follow-up discussion with CMS’ CAG as part of multispecialty coalition, reiterating concerns about the down coding and SAD List policies. With the assistance of the CMS’ Office of the Administrator, CSRO meets with CMS’ Center for Program Integrity to seek a “pause” in down-coding policies for certain biologic medications.
- June 2022: CMS notifies CSRO of a “temporary pause” in medical review while the agency reviews various manuals and policies to determine the appropriate steps forward. To assist the agency, CSRO works with practices to develop a resource that CMS can use to establish criteria for determining when a medication warrants use of complex drug administration codes. CSRO re-engages with multijurisdictional MAC CMD workgroup to continue discussions on SAD List.
- July 2022: CSRO meets with new multijurisdictional MAC CMD workgroup focused on improving the process for developing local coverage and payment policy.
Our dialogue with CMS leadership and staff continues. In the most recent communication, staff in the CMS administrator’s office informed us that the issue is complicated and crosses several different parts of the agency, and they are still determining next steps.
The rheumatology community’s journey toward solving the challenges facing practices and patients is emblematic of the communication problem between provider groups and the CMS-MAC establishment. While we understand this is how bureaucracy works, it is not to the benefit of Medicare beneficiaries to have a system that is so difficult to navigate, even by the best of the regulatory gurus. This is not an indictment of any specific group but a call to action on the part of the government and their contractors to create a clear, transparent path to getting answers when we have a problem.
And by the way, we do have another meeting with yet another CMS “center” regarding the SAD List in August.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is president of the CSRO, past chair of the Alliance for Safe Biologic Medicines, and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at rhnews@mdedge.com.
Rheumatologists who administer medications in their office for Medicare patients, specifically those that are infused, have in recent years encountered problems providing certain medication formulations as well as coding and billing for their administration. In attempting to resolve these issues, rheumatologists and their professional organizations have found themselves caught in a morass of Medicare agency “ping-pong,” where it is unclear who the decision makers are.
The private health care insurers that process medical claims for Medicare beneficiaries, called A/B Medicare Administrative Contractors or more commonly known as MACs, are the operational intermediary between the Centers for Medicare & Medicaid Services’ fee-for-service program and the physicians enrolled in it. The country is divided into 12 sections, each with a MAC that has jurisdiction over that area. Among other things, the MACs establish local coverage and payment policies based on their understanding of CMS’ rules, regulations, and the Medicare statute, and therein lies the problem: When a physician has a question on a policy or decision that was made by a MAC, it is very difficult to determine the origins of the issue and who can address the problem. It’s a lot of “running in circles” between the MACs and CMS headquarters, hoping that someone will take the time to listen to your concern, but more importantly, work toward resolving the problem.
Who can address problems?
Meaningful, solutions-driven engagement with the MACs and CMS has become frustrating for physicians and advocacy organizations attempting to address a host of problems. The two issues alluded to above include the Self-Administered Drug Exclusion List (SAD List), which excludes certain Part B medication formulations from coverage under certain conditions and the “down coding” of certain infusion administration codes when specific drugs are delivered. These problems are compounded by the curtailment of physician stakeholder input via Contractor Advisory Committees (CACs). Each state has its own CAC, but the CAC meetings have been restructured as a result of the 21st Century Cures Act, and ultimately eradicated the involvement of these physician advisers in policy development at the local level.
This has left many of rheumatology representatives to the CACs demoralized and generally unhappy about certain decisions being made without their input. There is also inconsistency in terms of coverage and payment policies throughout the country. For example, in one MAC jurisdiction, a certain medication may be on the SAD List and excluded from Part B coverage, meaning beneficiary access is only available through Part D (and assuming they can afford it), while in an adjacent MAC jurisdiction, both formulations are covered.
The Coalition of State Rheumatology Organizations, along with the American College of Rheumatology and other specialty groups, is attempting to address these issues from many different angles. There is not enough space to explain the nuances of local coverage policy development, but the timeline below highlights the long and winding road that we have travelled to resolve these issues.
- February 2021: CSRO meets with CMS’ Coverage and Analysis Group (CAG) to raise concerns about ustekinumab (Stelara) and its inclusion on the SAD List.
- April 2021: CSRO follows up with CMS’ CAG on SAD List concerns in a letter.
- May 2021: Most MACs issue or revise local coverage articles, or “billing and coding” articles, that down code the administration of certain biologic medications, with some expanding the list of biologic medications subject to the policy, prompting a strong response from CSRO.
- September 2021: CSRO meets with multijurisdictional MAC Contract Medical Director (CMD) work group to discuss down coding, SAD List, and physician/CAC engagement.
- October 2021: At the suggestion of the CMDs, CSRO re-engages with CMS’ CAG to raise concerns about down-coding policies and physician/CAC engagement, and continue the SAD List discussion.
- November 2021: CSRO is connected with CMS’ “payment ombudsman” on down coding and the SAD List.
- January 2022: CSRO signs on to multispecialty coalition effort aimed at improving local coverage and payment policy and restoring the importance of the CAC.
- February 2022: CSRO participates in CMS CAG meeting with multispecialty coalition, raising concerns about the down-coding and SAD List policies.
- March/April 2022: Through its coalition partner, the Alliance of Specialty Medicine, CSRO meets with the principal deputy CMS administrator and raises awareness to these issues.
- May 2022: CSRO participates in follow-up discussion with CMS’ CAG as part of multispecialty coalition, reiterating concerns about the down coding and SAD List policies. With the assistance of the CMS’ Office of the Administrator, CSRO meets with CMS’ Center for Program Integrity to seek a “pause” in down-coding policies for certain biologic medications.
- June 2022: CMS notifies CSRO of a “temporary pause” in medical review while the agency reviews various manuals and policies to determine the appropriate steps forward. To assist the agency, CSRO works with practices to develop a resource that CMS can use to establish criteria for determining when a medication warrants use of complex drug administration codes. CSRO re-engages with multijurisdictional MAC CMD workgroup to continue discussions on SAD List.
- July 2022: CSRO meets with new multijurisdictional MAC CMD workgroup focused on improving the process for developing local coverage and payment policy.
Our dialogue with CMS leadership and staff continues. In the most recent communication, staff in the CMS administrator’s office informed us that the issue is complicated and crosses several different parts of the agency, and they are still determining next steps.
The rheumatology community’s journey toward solving the challenges facing practices and patients is emblematic of the communication problem between provider groups and the CMS-MAC establishment. While we understand this is how bureaucracy works, it is not to the benefit of Medicare beneficiaries to have a system that is so difficult to navigate, even by the best of the regulatory gurus. This is not an indictment of any specific group but a call to action on the part of the government and their contractors to create a clear, transparent path to getting answers when we have a problem.
And by the way, we do have another meeting with yet another CMS “center” regarding the SAD List in August.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is president of the CSRO, past chair of the Alliance for Safe Biologic Medicines, and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at rhnews@mdedge.com.
Job market for physicians, advanced practitioners rebounds after COVID-19 slump: Report
After a year of uncertainty and decline because of the COVID-19 pandemic, according to a recently released report from Merritt Hawkins, the physician search division of AMN Healthcare.
The study is based on an analysis of job search and consulting assignments that the firm conducted on behalf of its health care organization clients from April 1, 2021, to March 31, 2022.
“Search engagements were down a little over 30% in 2020, but by the end of 2021, everything started spiking dramatically to the point of where we were at a 34-year high,” Michael Belkin, divisional vice president with Merritt Hawkins, told this news organization. “The pendulum has gone all the way back. People are more interested in going out and seeing their physicians.”
Demand for physicians was suppressed during the peak of the pandemic, as many hospitals curtailed elective procedures and many patients refrained from entering a medical facility. A large backlog of patients needing care subsequently developed.
This, combined with an aging population and widespread chronic medical conditions, has caused a strong surge in demand for physicians and advanced practitioners, according to the report.
In addition to the volume of searches increasing, physician starting salaries have rebounded from the COVID-19 downturn.
Average starting salaries of 14 physician specialties tracked in 2021/2022 increased, while only 3 decreased. Orthopedic surgeons were offered an average of $565,000 to start, exclusive of signing bonuses and other incentives, up from $546,000 the previous year. Urologists were offered an average of $510,000 to start, up from $497,000; gastroenterologists were offered $474,000, up from $453,000; while radiologists were offered $455,000, up from $401,000.
Similarly, a recent Medscape study based on responses from more than 13,000 U.S. physicians across 29 specialties found that income for all physician specialists increased, with otolaryngologists, gastroenterologists, and dermatologists experiencing the greatest gains.
A new reality
While the job market for physicians and advanced practitioners has seemingly recovered, there are many differences between today’s working environment for clinicians and what existed during the pandemic.
First, specialists are now stepping into the spotlight, a position that primary care clinicians previously held. The majority of Merritt Hawkins’ search engagements (64%) in 2021/2022 were for physician specialists, including cardiologists, gastroenterologists, orthopedic surgeons, neurologists, oncologists, and others. Only 17% of the search engagements were for primary care physicians, down from 18% in 2020/2021 and 20% in 2019/2020.
“We’ve seen specialties bounce back faster. Of course, you’ve got the aging population; you’ve got people that want that specialized care,” Mr. Belkin said.
Advanced practitioners also are playing a more significant role in the postpandemic word. In fact, 19% of Merritt Hawkins’ search engagements were for advanced practitioners, including nurse practitioners (NPs), physician assistants, and certified registered nurse anesthetists, up from 18% the previous year and just 13% the year prior to that, indicating growing demand for nonphysician providers.
NPs, in fact, topped the list of most requested search engagements, underscoring a shift from traditional physician office-based primary care delivery settings toward “convenient care” settings such as urgent care centers and retail clinics that are largely staffed by NPs and other advanced practitioners.
Advanced practitioners are taking on more responsibility for primary care simply because there is a large number of these professionals ready to take on the challenge.
The health care industry was “not able to produce enough primary care physicians over the last decade. So advanced practitioners, I believe, have slowly started to work alongside those primary care physicians. In a lot of areas such as your retail space, your CVS, your Walmart, your Walgreens, your standalone urgent cares, they’ve stepped up,” Mr. Belkin said.
Advanced practitioners also are providing the convenience that consumers are increasingly demanding.
“We are a society that wants things immediately ... but it’s still a challenge to schedule an appointment with a physician. However, it’s less of a challenge to get into a retail clinic or an urgent care center or to schedule something through telehealth,” Mr. Belkin noted.
More than just money
With the job market strong, the challenge for health care organizations is to create competitive recruiting packages. Sure enough, 92% of candidates were offered signing bonuses in 2021/2022 compared with just 61% in 2020/2021.
The financial incentives, however, might not be enough. In this environment, health care organizations need to go beyond simply offering competitive salaries to new recruits. For example, clinicians are seeking flexibility, as many potential hires are seeking remote positions. In fact, 18% of radiology search engagements were for teleradiologists, while 15% of its search engagements for psychiatrists were for telepsychiatrists in 2021/2022.
“Right now, quality of life is a very important factor. It’s work-life balance. It’s sensitivity to the stresses that we just experienced over the last 2.5 years,” Mr. Belkin concluded. “There’s more sensitivity around the culture of the organizations. What’s the leadership like? How did the organization handle the pandemic? How do they respond?”
A version of this article first appeared on Medscape.com.
After a year of uncertainty and decline because of the COVID-19 pandemic, according to a recently released report from Merritt Hawkins, the physician search division of AMN Healthcare.
The study is based on an analysis of job search and consulting assignments that the firm conducted on behalf of its health care organization clients from April 1, 2021, to March 31, 2022.
“Search engagements were down a little over 30% in 2020, but by the end of 2021, everything started spiking dramatically to the point of where we were at a 34-year high,” Michael Belkin, divisional vice president with Merritt Hawkins, told this news organization. “The pendulum has gone all the way back. People are more interested in going out and seeing their physicians.”
Demand for physicians was suppressed during the peak of the pandemic, as many hospitals curtailed elective procedures and many patients refrained from entering a medical facility. A large backlog of patients needing care subsequently developed.
This, combined with an aging population and widespread chronic medical conditions, has caused a strong surge in demand for physicians and advanced practitioners, according to the report.
In addition to the volume of searches increasing, physician starting salaries have rebounded from the COVID-19 downturn.
Average starting salaries of 14 physician specialties tracked in 2021/2022 increased, while only 3 decreased. Orthopedic surgeons were offered an average of $565,000 to start, exclusive of signing bonuses and other incentives, up from $546,000 the previous year. Urologists were offered an average of $510,000 to start, up from $497,000; gastroenterologists were offered $474,000, up from $453,000; while radiologists were offered $455,000, up from $401,000.
Similarly, a recent Medscape study based on responses from more than 13,000 U.S. physicians across 29 specialties found that income for all physician specialists increased, with otolaryngologists, gastroenterologists, and dermatologists experiencing the greatest gains.
A new reality
While the job market for physicians and advanced practitioners has seemingly recovered, there are many differences between today’s working environment for clinicians and what existed during the pandemic.
First, specialists are now stepping into the spotlight, a position that primary care clinicians previously held. The majority of Merritt Hawkins’ search engagements (64%) in 2021/2022 were for physician specialists, including cardiologists, gastroenterologists, orthopedic surgeons, neurologists, oncologists, and others. Only 17% of the search engagements were for primary care physicians, down from 18% in 2020/2021 and 20% in 2019/2020.
“We’ve seen specialties bounce back faster. Of course, you’ve got the aging population; you’ve got people that want that specialized care,” Mr. Belkin said.
Advanced practitioners also are playing a more significant role in the postpandemic word. In fact, 19% of Merritt Hawkins’ search engagements were for advanced practitioners, including nurse practitioners (NPs), physician assistants, and certified registered nurse anesthetists, up from 18% the previous year and just 13% the year prior to that, indicating growing demand for nonphysician providers.
NPs, in fact, topped the list of most requested search engagements, underscoring a shift from traditional physician office-based primary care delivery settings toward “convenient care” settings such as urgent care centers and retail clinics that are largely staffed by NPs and other advanced practitioners.
Advanced practitioners are taking on more responsibility for primary care simply because there is a large number of these professionals ready to take on the challenge.
The health care industry was “not able to produce enough primary care physicians over the last decade. So advanced practitioners, I believe, have slowly started to work alongside those primary care physicians. In a lot of areas such as your retail space, your CVS, your Walmart, your Walgreens, your standalone urgent cares, they’ve stepped up,” Mr. Belkin said.
Advanced practitioners also are providing the convenience that consumers are increasingly demanding.
“We are a society that wants things immediately ... but it’s still a challenge to schedule an appointment with a physician. However, it’s less of a challenge to get into a retail clinic or an urgent care center or to schedule something through telehealth,” Mr. Belkin noted.
More than just money
With the job market strong, the challenge for health care organizations is to create competitive recruiting packages. Sure enough, 92% of candidates were offered signing bonuses in 2021/2022 compared with just 61% in 2020/2021.
The financial incentives, however, might not be enough. In this environment, health care organizations need to go beyond simply offering competitive salaries to new recruits. For example, clinicians are seeking flexibility, as many potential hires are seeking remote positions. In fact, 18% of radiology search engagements were for teleradiologists, while 15% of its search engagements for psychiatrists were for telepsychiatrists in 2021/2022.
“Right now, quality of life is a very important factor. It’s work-life balance. It’s sensitivity to the stresses that we just experienced over the last 2.5 years,” Mr. Belkin concluded. “There’s more sensitivity around the culture of the organizations. What’s the leadership like? How did the organization handle the pandemic? How do they respond?”
A version of this article first appeared on Medscape.com.
After a year of uncertainty and decline because of the COVID-19 pandemic, according to a recently released report from Merritt Hawkins, the physician search division of AMN Healthcare.
The study is based on an analysis of job search and consulting assignments that the firm conducted on behalf of its health care organization clients from April 1, 2021, to March 31, 2022.
“Search engagements were down a little over 30% in 2020, but by the end of 2021, everything started spiking dramatically to the point of where we were at a 34-year high,” Michael Belkin, divisional vice president with Merritt Hawkins, told this news organization. “The pendulum has gone all the way back. People are more interested in going out and seeing their physicians.”
Demand for physicians was suppressed during the peak of the pandemic, as many hospitals curtailed elective procedures and many patients refrained from entering a medical facility. A large backlog of patients needing care subsequently developed.
This, combined with an aging population and widespread chronic medical conditions, has caused a strong surge in demand for physicians and advanced practitioners, according to the report.
In addition to the volume of searches increasing, physician starting salaries have rebounded from the COVID-19 downturn.
Average starting salaries of 14 physician specialties tracked in 2021/2022 increased, while only 3 decreased. Orthopedic surgeons were offered an average of $565,000 to start, exclusive of signing bonuses and other incentives, up from $546,000 the previous year. Urologists were offered an average of $510,000 to start, up from $497,000; gastroenterologists were offered $474,000, up from $453,000; while radiologists were offered $455,000, up from $401,000.
Similarly, a recent Medscape study based on responses from more than 13,000 U.S. physicians across 29 specialties found that income for all physician specialists increased, with otolaryngologists, gastroenterologists, and dermatologists experiencing the greatest gains.
A new reality
While the job market for physicians and advanced practitioners has seemingly recovered, there are many differences between today’s working environment for clinicians and what existed during the pandemic.
First, specialists are now stepping into the spotlight, a position that primary care clinicians previously held. The majority of Merritt Hawkins’ search engagements (64%) in 2021/2022 were for physician specialists, including cardiologists, gastroenterologists, orthopedic surgeons, neurologists, oncologists, and others. Only 17% of the search engagements were for primary care physicians, down from 18% in 2020/2021 and 20% in 2019/2020.
“We’ve seen specialties bounce back faster. Of course, you’ve got the aging population; you’ve got people that want that specialized care,” Mr. Belkin said.
Advanced practitioners also are playing a more significant role in the postpandemic word. In fact, 19% of Merritt Hawkins’ search engagements were for advanced practitioners, including nurse practitioners (NPs), physician assistants, and certified registered nurse anesthetists, up from 18% the previous year and just 13% the year prior to that, indicating growing demand for nonphysician providers.
NPs, in fact, topped the list of most requested search engagements, underscoring a shift from traditional physician office-based primary care delivery settings toward “convenient care” settings such as urgent care centers and retail clinics that are largely staffed by NPs and other advanced practitioners.
Advanced practitioners are taking on more responsibility for primary care simply because there is a large number of these professionals ready to take on the challenge.
The health care industry was “not able to produce enough primary care physicians over the last decade. So advanced practitioners, I believe, have slowly started to work alongside those primary care physicians. In a lot of areas such as your retail space, your CVS, your Walmart, your Walgreens, your standalone urgent cares, they’ve stepped up,” Mr. Belkin said.
Advanced practitioners also are providing the convenience that consumers are increasingly demanding.
“We are a society that wants things immediately ... but it’s still a challenge to schedule an appointment with a physician. However, it’s less of a challenge to get into a retail clinic or an urgent care center or to schedule something through telehealth,” Mr. Belkin noted.
More than just money
With the job market strong, the challenge for health care organizations is to create competitive recruiting packages. Sure enough, 92% of candidates were offered signing bonuses in 2021/2022 compared with just 61% in 2020/2021.
The financial incentives, however, might not be enough. In this environment, health care organizations need to go beyond simply offering competitive salaries to new recruits. For example, clinicians are seeking flexibility, as many potential hires are seeking remote positions. In fact, 18% of radiology search engagements were for teleradiologists, while 15% of its search engagements for psychiatrists were for telepsychiatrists in 2021/2022.
“Right now, quality of life is a very important factor. It’s work-life balance. It’s sensitivity to the stresses that we just experienced over the last 2.5 years,” Mr. Belkin concluded. “There’s more sensitivity around the culture of the organizations. What’s the leadership like? How did the organization handle the pandemic? How do they respond?”
A version of this article first appeared on Medscape.com.
What are your weaknesses?
In a video posted to TikTok by the comedian Will Flanary, MD, better known to his followers as Dr. Glaucomflecken, he imitates a neurosurgical residency interview. With glasses perched on the bridge of his nose, Dr. Glaucomflecken poses as the attending, asking: “What are your weaknesses?”
The residency applicant answers without hesitation: “My physiological need for sleep.” “What are your strengths?” The resident replies with the hard, steely stare of the determined and uninitiated: “My desire to eliminate my physiological need for sleep.”
If you follow Dr. Glaucomflecken on Twitter, you might know the skit I’m referencing. For many physicians and physicians-in-training, what makes the satire successful is its reflection of reality.
Many things have changed in medicine since his time, but the tired trope of the sleepless surgeon hangs on. Undaunted, I spent my second and third year of medical school accumulating accolades, conducting research, and connecting with mentors with the singular goal of joining the surgical ranks.
Midway through my third year, I completed a month-long surgical subinternship designed to give students a taste of what life would look like as an intern. I loved the operating room; it felt like the difference between being on dry land and being underwater. There were fewer distractions – your patient in the spotlight while everything else receded to the shadows.
However, as the month wore on, something stronger took hold. I couldn’t keep my eyes open in the darkened operating rooms and had to decline stools, fearing that I would fall asleep if I sat down.
On early morning prerounds, it’s 4:50 a.m. when I glance at the clock and pull back the curtain, already apologizing. My patient rolls over, flashing a wry smile. “Do you ever go home?” I’ve seen residents respond to this exact question in various ways. I live here. Yes. No. Soon. Not enough. My partner doesn’t think so.
There are days and, yes, years when we are led to believe this is what we live for: to be constantly available to our patients. It feels like a hollow victory when the patient, 2 days out from a total colectomy, begins to worry about your personal life. I ask her how she slept (not enough), any fevers (no), vomiting (no), urinating (I pause – she has a catheter).
My favorite part of these early morning rounds is the pause in my scripted litany of questions to listen to heart and lungs. It never fails to feel sacred: Patients become so quiet and still that I can’t help but think they have faith in me. Without prompting, she slides the back of her hospital gown forward like a curtain, already taking deep breaths so I can hear her lungs.
I look outside. The streetlights are still on, and from the seventh-floor window, I can watch staff making their way through the sliding double-doors, just beyond the yellowed pools of streetlight. I smile. I love medicine. I’m so tired.
For many in medicine, we are treated, and thus behave, as though our ability to manipulate physiology should also apply within the borders of our bodies: commanding less sleep, food, or bathroom breaks.
It places health care workers solidly in the realm of superhuman, living beyond one’s corporeal needs. The pandemic only heightened this misappropriation – adding hero and setting out a pedestal for health care workers to make their ungainly ascent. This kind of unsolicited admiration implicitly implies inhumanness, an otherness.
What would it look like if we started treating ourselves less like physicians and more like patients? I wish I was offering a solution, but really this is just a story.
To students rising through the ranks of medical training, identify what it is you need early and often. I can count on one hand how many physicians I’ve seen take a lunch break – even 10 minutes. Embrace hard work and self-preservation equally. My hope is that if enough of us take this path, it just might become a matter of course.
Dr. Meffert is a resident in the department of emergency medicine, MedStar Georgetown University Hospital, Washington Hospital Center, Washington. Dr. Meffert disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a video posted to TikTok by the comedian Will Flanary, MD, better known to his followers as Dr. Glaucomflecken, he imitates a neurosurgical residency interview. With glasses perched on the bridge of his nose, Dr. Glaucomflecken poses as the attending, asking: “What are your weaknesses?”
The residency applicant answers without hesitation: “My physiological need for sleep.” “What are your strengths?” The resident replies with the hard, steely stare of the determined and uninitiated: “My desire to eliminate my physiological need for sleep.”
If you follow Dr. Glaucomflecken on Twitter, you might know the skit I’m referencing. For many physicians and physicians-in-training, what makes the satire successful is its reflection of reality.
Many things have changed in medicine since his time, but the tired trope of the sleepless surgeon hangs on. Undaunted, I spent my second and third year of medical school accumulating accolades, conducting research, and connecting with mentors with the singular goal of joining the surgical ranks.
Midway through my third year, I completed a month-long surgical subinternship designed to give students a taste of what life would look like as an intern. I loved the operating room; it felt like the difference between being on dry land and being underwater. There were fewer distractions – your patient in the spotlight while everything else receded to the shadows.
However, as the month wore on, something stronger took hold. I couldn’t keep my eyes open in the darkened operating rooms and had to decline stools, fearing that I would fall asleep if I sat down.
On early morning prerounds, it’s 4:50 a.m. when I glance at the clock and pull back the curtain, already apologizing. My patient rolls over, flashing a wry smile. “Do you ever go home?” I’ve seen residents respond to this exact question in various ways. I live here. Yes. No. Soon. Not enough. My partner doesn’t think so.
There are days and, yes, years when we are led to believe this is what we live for: to be constantly available to our patients. It feels like a hollow victory when the patient, 2 days out from a total colectomy, begins to worry about your personal life. I ask her how she slept (not enough), any fevers (no), vomiting (no), urinating (I pause – she has a catheter).
My favorite part of these early morning rounds is the pause in my scripted litany of questions to listen to heart and lungs. It never fails to feel sacred: Patients become so quiet and still that I can’t help but think they have faith in me. Without prompting, she slides the back of her hospital gown forward like a curtain, already taking deep breaths so I can hear her lungs.
I look outside. The streetlights are still on, and from the seventh-floor window, I can watch staff making their way through the sliding double-doors, just beyond the yellowed pools of streetlight. I smile. I love medicine. I’m so tired.
For many in medicine, we are treated, and thus behave, as though our ability to manipulate physiology should also apply within the borders of our bodies: commanding less sleep, food, or bathroom breaks.
It places health care workers solidly in the realm of superhuman, living beyond one’s corporeal needs. The pandemic only heightened this misappropriation – adding hero and setting out a pedestal for health care workers to make their ungainly ascent. This kind of unsolicited admiration implicitly implies inhumanness, an otherness.
What would it look like if we started treating ourselves less like physicians and more like patients? I wish I was offering a solution, but really this is just a story.
To students rising through the ranks of medical training, identify what it is you need early and often. I can count on one hand how many physicians I’ve seen take a lunch break – even 10 minutes. Embrace hard work and self-preservation equally. My hope is that if enough of us take this path, it just might become a matter of course.
Dr. Meffert is a resident in the department of emergency medicine, MedStar Georgetown University Hospital, Washington Hospital Center, Washington. Dr. Meffert disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a video posted to TikTok by the comedian Will Flanary, MD, better known to his followers as Dr. Glaucomflecken, he imitates a neurosurgical residency interview. With glasses perched on the bridge of his nose, Dr. Glaucomflecken poses as the attending, asking: “What are your weaknesses?”
The residency applicant answers without hesitation: “My physiological need for sleep.” “What are your strengths?” The resident replies with the hard, steely stare of the determined and uninitiated: “My desire to eliminate my physiological need for sleep.”
If you follow Dr. Glaucomflecken on Twitter, you might know the skit I’m referencing. For many physicians and physicians-in-training, what makes the satire successful is its reflection of reality.
Many things have changed in medicine since his time, but the tired trope of the sleepless surgeon hangs on. Undaunted, I spent my second and third year of medical school accumulating accolades, conducting research, and connecting with mentors with the singular goal of joining the surgical ranks.
Midway through my third year, I completed a month-long surgical subinternship designed to give students a taste of what life would look like as an intern. I loved the operating room; it felt like the difference between being on dry land and being underwater. There were fewer distractions – your patient in the spotlight while everything else receded to the shadows.
However, as the month wore on, something stronger took hold. I couldn’t keep my eyes open in the darkened operating rooms and had to decline stools, fearing that I would fall asleep if I sat down.
On early morning prerounds, it’s 4:50 a.m. when I glance at the clock and pull back the curtain, already apologizing. My patient rolls over, flashing a wry smile. “Do you ever go home?” I’ve seen residents respond to this exact question in various ways. I live here. Yes. No. Soon. Not enough. My partner doesn’t think so.
There are days and, yes, years when we are led to believe this is what we live for: to be constantly available to our patients. It feels like a hollow victory when the patient, 2 days out from a total colectomy, begins to worry about your personal life. I ask her how she slept (not enough), any fevers (no), vomiting (no), urinating (I pause – she has a catheter).
My favorite part of these early morning rounds is the pause in my scripted litany of questions to listen to heart and lungs. It never fails to feel sacred: Patients become so quiet and still that I can’t help but think they have faith in me. Without prompting, she slides the back of her hospital gown forward like a curtain, already taking deep breaths so I can hear her lungs.
I look outside. The streetlights are still on, and from the seventh-floor window, I can watch staff making their way through the sliding double-doors, just beyond the yellowed pools of streetlight. I smile. I love medicine. I’m so tired.
For many in medicine, we are treated, and thus behave, as though our ability to manipulate physiology should also apply within the borders of our bodies: commanding less sleep, food, or bathroom breaks.
It places health care workers solidly in the realm of superhuman, living beyond one’s corporeal needs. The pandemic only heightened this misappropriation – adding hero and setting out a pedestal for health care workers to make their ungainly ascent. This kind of unsolicited admiration implicitly implies inhumanness, an otherness.
What would it look like if we started treating ourselves less like physicians and more like patients? I wish I was offering a solution, but really this is just a story.
To students rising through the ranks of medical training, identify what it is you need early and often. I can count on one hand how many physicians I’ve seen take a lunch break – even 10 minutes. Embrace hard work and self-preservation equally. My hope is that if enough of us take this path, it just might become a matter of course.
Dr. Meffert is a resident in the department of emergency medicine, MedStar Georgetown University Hospital, Washington Hospital Center, Washington. Dr. Meffert disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Former nurses of historic Black hospital sue to preserve its legacy
A training facility for Black doctors and nurses in St. Louis, which was the only public hospital for Black community from the late 1930s through the mid-1950s, has been at the center of many contentious community protests over the years and is facing another.
A federal lawsuit was filed recently by the nurses’ alumni of Homer G. Phillips Hospital against a St. Louis developer who is using the hospital’s name for a small for-profit urgent care health facility.
Homer G. Phillips was a St. Louis attorney and civic leader who joined with other Black leaders in 1922 to gain money for a hospital that would serve the Black community, according to online sources. He didn’t live to see the hospital named in his honor completed in 1937.
The former Homer G. Phillips Hospital closed in 1979 despite the community’s outcry at that time, according to The Missouri Independent. The building sat vacant for many years before being converted into a senior center, Yvonne Jones, alumni president, said in an interview.
She said of the new health center, which hasn’t opened yet, “We are not against the facility; we want to protect the name and legacy” of the original hospital, which remains at the heart of the historic St. Louis Black community.
At press time, the developer and his attorneys had not returned this news organization’s request for comment.
Having a new center with the name of the iconic hospital would mean that “the goodwill and the pride it represents has been usurped,” said Zenobia Thompson, who served as head nurse of Homer G. Phillips and is now the co-chair of the Change the Name Coalition. It formed last year after Ms. Thompson and others noticed a sign posted at the site of the new health center that lists it as the Homer G. Phillips Hospital, with a trademark symbol that the nurses say it doesn’t have a right to.
The coalition, which meets weekly, sponsored a petition and has been protesting at the site of the new center twice a month, Ms. Thompson said.
“We wrote a letter to [developer] Paul McKee that the legacy not be trivialized for commercial reasons,” Ms. Thompson said.
Richard Voytas, attorney for the alumni group, said in an interview that the developer did not ask permission from the nurses to use the trademark and he didn’t know if the nurses will grant that permission now. “If they [the developers] use the name, it is very important that they honor the Homer G. Phillips legacy,” Mr. Voytas said.
Honoring a legacy or taking advantage of a name?
In her new book, Climbing the Ladder, Chasing the Dream: A History of Homer G. Phillips Hospital, author Candace O’Connor cites the importance of the hospital’s heritage.
“Several nurses came from rural, impoverished backgrounds and went on to get jobs all across the country,” Ms. O’Connor wrote in the book. “Because all you had to do was say, ‘I’m from Homer Phillips,’ and they would say ‘you’re hired.’ It didn’t just change the nurse. It created opportunities for whole families.”
The area where the hospital remains once boasted a grocery store, high school, college, ice cream shop, and renowned Black churches, some of which still exist as historical sites. “They built up the area for Blacks who couldn’t go anywhere else,” Ms. Jones said.
In the suit, the alumni group describes itself as a 100-year-old philanthropic organization that brought healthcare to St. Louis’ historically underserved Black community and remains very active in the area today in fundraising and community outreach efforts. The group has been fighting with the developers since learning in 2019 about the proposed use of the name that is “confusingly similar” to the trademark and immediately voiced its objections via lawsuit, demanding that another name be chosen, stating:
“…in its name and efforts to market its for-profit urgent care facility immediately within plaintiff’s primary market to directly compete with plaintiff for name recognition and goodwill, only increases the likelihood of consumer confusion and, upon information and belief, represents an effort by defendants’ to pass off their products and services as those offered by plaintiff and its members.”
“Defendants stated purpose in using the mark, or a phrase confusingly similar to the mark, for its name is to ‘honor’ the name of Homer G. Phillips and to ‘emulate his spirit andtenacity in serving the health care needs of North St. Louis,’” the suit continues.
The St. Louis Board of Aldermen passed a resolution in December calling the use of the name for the new health center an “inappropriate cultural appropriation.” Mayor Tishaura Jones and Congresswoman Cori Bush followed that with a joint statement: “Profiting off of Homer G. Phillips’ name on a small 3-bed facility that will fail to meet the needs of the most vulnerable in our communities is an insult to Homer G. Phillips’ legacy and the Black community.”
The alumni group is requesting a jury trial and damages to be determined at trial, three times the defendant’s profits or plaintiffs’ damages, whichever is greater, along with attorneys’ fees and interest.
A version of this article first appeared on Medscape.com.
A training facility for Black doctors and nurses in St. Louis, which was the only public hospital for Black community from the late 1930s through the mid-1950s, has been at the center of many contentious community protests over the years and is facing another.
A federal lawsuit was filed recently by the nurses’ alumni of Homer G. Phillips Hospital against a St. Louis developer who is using the hospital’s name for a small for-profit urgent care health facility.
Homer G. Phillips was a St. Louis attorney and civic leader who joined with other Black leaders in 1922 to gain money for a hospital that would serve the Black community, according to online sources. He didn’t live to see the hospital named in his honor completed in 1937.
The former Homer G. Phillips Hospital closed in 1979 despite the community’s outcry at that time, according to The Missouri Independent. The building sat vacant for many years before being converted into a senior center, Yvonne Jones, alumni president, said in an interview.
She said of the new health center, which hasn’t opened yet, “We are not against the facility; we want to protect the name and legacy” of the original hospital, which remains at the heart of the historic St. Louis Black community.
At press time, the developer and his attorneys had not returned this news organization’s request for comment.
Having a new center with the name of the iconic hospital would mean that “the goodwill and the pride it represents has been usurped,” said Zenobia Thompson, who served as head nurse of Homer G. Phillips and is now the co-chair of the Change the Name Coalition. It formed last year after Ms. Thompson and others noticed a sign posted at the site of the new health center that lists it as the Homer G. Phillips Hospital, with a trademark symbol that the nurses say it doesn’t have a right to.
The coalition, which meets weekly, sponsored a petition and has been protesting at the site of the new center twice a month, Ms. Thompson said.
“We wrote a letter to [developer] Paul McKee that the legacy not be trivialized for commercial reasons,” Ms. Thompson said.
Richard Voytas, attorney for the alumni group, said in an interview that the developer did not ask permission from the nurses to use the trademark and he didn’t know if the nurses will grant that permission now. “If they [the developers] use the name, it is very important that they honor the Homer G. Phillips legacy,” Mr. Voytas said.
Honoring a legacy or taking advantage of a name?
In her new book, Climbing the Ladder, Chasing the Dream: A History of Homer G. Phillips Hospital, author Candace O’Connor cites the importance of the hospital’s heritage.
“Several nurses came from rural, impoverished backgrounds and went on to get jobs all across the country,” Ms. O’Connor wrote in the book. “Because all you had to do was say, ‘I’m from Homer Phillips,’ and they would say ‘you’re hired.’ It didn’t just change the nurse. It created opportunities for whole families.”
The area where the hospital remains once boasted a grocery store, high school, college, ice cream shop, and renowned Black churches, some of which still exist as historical sites. “They built up the area for Blacks who couldn’t go anywhere else,” Ms. Jones said.
In the suit, the alumni group describes itself as a 100-year-old philanthropic organization that brought healthcare to St. Louis’ historically underserved Black community and remains very active in the area today in fundraising and community outreach efforts. The group has been fighting with the developers since learning in 2019 about the proposed use of the name that is “confusingly similar” to the trademark and immediately voiced its objections via lawsuit, demanding that another name be chosen, stating:
“…in its name and efforts to market its for-profit urgent care facility immediately within plaintiff’s primary market to directly compete with plaintiff for name recognition and goodwill, only increases the likelihood of consumer confusion and, upon information and belief, represents an effort by defendants’ to pass off their products and services as those offered by plaintiff and its members.”
“Defendants stated purpose in using the mark, or a phrase confusingly similar to the mark, for its name is to ‘honor’ the name of Homer G. Phillips and to ‘emulate his spirit andtenacity in serving the health care needs of North St. Louis,’” the suit continues.
The St. Louis Board of Aldermen passed a resolution in December calling the use of the name for the new health center an “inappropriate cultural appropriation.” Mayor Tishaura Jones and Congresswoman Cori Bush followed that with a joint statement: “Profiting off of Homer G. Phillips’ name on a small 3-bed facility that will fail to meet the needs of the most vulnerable in our communities is an insult to Homer G. Phillips’ legacy and the Black community.”
The alumni group is requesting a jury trial and damages to be determined at trial, three times the defendant’s profits or plaintiffs’ damages, whichever is greater, along with attorneys’ fees and interest.
A version of this article first appeared on Medscape.com.
A training facility for Black doctors and nurses in St. Louis, which was the only public hospital for Black community from the late 1930s through the mid-1950s, has been at the center of many contentious community protests over the years and is facing another.
A federal lawsuit was filed recently by the nurses’ alumni of Homer G. Phillips Hospital against a St. Louis developer who is using the hospital’s name for a small for-profit urgent care health facility.
Homer G. Phillips was a St. Louis attorney and civic leader who joined with other Black leaders in 1922 to gain money for a hospital that would serve the Black community, according to online sources. He didn’t live to see the hospital named in his honor completed in 1937.
The former Homer G. Phillips Hospital closed in 1979 despite the community’s outcry at that time, according to The Missouri Independent. The building sat vacant for many years before being converted into a senior center, Yvonne Jones, alumni president, said in an interview.
She said of the new health center, which hasn’t opened yet, “We are not against the facility; we want to protect the name and legacy” of the original hospital, which remains at the heart of the historic St. Louis Black community.
At press time, the developer and his attorneys had not returned this news organization’s request for comment.
Having a new center with the name of the iconic hospital would mean that “the goodwill and the pride it represents has been usurped,” said Zenobia Thompson, who served as head nurse of Homer G. Phillips and is now the co-chair of the Change the Name Coalition. It formed last year after Ms. Thompson and others noticed a sign posted at the site of the new health center that lists it as the Homer G. Phillips Hospital, with a trademark symbol that the nurses say it doesn’t have a right to.
The coalition, which meets weekly, sponsored a petition and has been protesting at the site of the new center twice a month, Ms. Thompson said.
“We wrote a letter to [developer] Paul McKee that the legacy not be trivialized for commercial reasons,” Ms. Thompson said.
Richard Voytas, attorney for the alumni group, said in an interview that the developer did not ask permission from the nurses to use the trademark and he didn’t know if the nurses will grant that permission now. “If they [the developers] use the name, it is very important that they honor the Homer G. Phillips legacy,” Mr. Voytas said.
Honoring a legacy or taking advantage of a name?
In her new book, Climbing the Ladder, Chasing the Dream: A History of Homer G. Phillips Hospital, author Candace O’Connor cites the importance of the hospital’s heritage.
“Several nurses came from rural, impoverished backgrounds and went on to get jobs all across the country,” Ms. O’Connor wrote in the book. “Because all you had to do was say, ‘I’m from Homer Phillips,’ and they would say ‘you’re hired.’ It didn’t just change the nurse. It created opportunities for whole families.”
The area where the hospital remains once boasted a grocery store, high school, college, ice cream shop, and renowned Black churches, some of which still exist as historical sites. “They built up the area for Blacks who couldn’t go anywhere else,” Ms. Jones said.
In the suit, the alumni group describes itself as a 100-year-old philanthropic organization that brought healthcare to St. Louis’ historically underserved Black community and remains very active in the area today in fundraising and community outreach efforts. The group has been fighting with the developers since learning in 2019 about the proposed use of the name that is “confusingly similar” to the trademark and immediately voiced its objections via lawsuit, demanding that another name be chosen, stating:
“…in its name and efforts to market its for-profit urgent care facility immediately within plaintiff’s primary market to directly compete with plaintiff for name recognition and goodwill, only increases the likelihood of consumer confusion and, upon information and belief, represents an effort by defendants’ to pass off their products and services as those offered by plaintiff and its members.”
“Defendants stated purpose in using the mark, or a phrase confusingly similar to the mark, for its name is to ‘honor’ the name of Homer G. Phillips and to ‘emulate his spirit andtenacity in serving the health care needs of North St. Louis,’” the suit continues.
The St. Louis Board of Aldermen passed a resolution in December calling the use of the name for the new health center an “inappropriate cultural appropriation.” Mayor Tishaura Jones and Congresswoman Cori Bush followed that with a joint statement: “Profiting off of Homer G. Phillips’ name on a small 3-bed facility that will fail to meet the needs of the most vulnerable in our communities is an insult to Homer G. Phillips’ legacy and the Black community.”
The alumni group is requesting a jury trial and damages to be determined at trial, three times the defendant’s profits or plaintiffs’ damages, whichever is greater, along with attorneys’ fees and interest.
A version of this article first appeared on Medscape.com.
Cardiologists’ incomes bounce back from pandemic: Survey
The financial struggles created by the pandemic have eased somewhat, but physicians are still facing an array of challenges, including increased workloads and longer hours. All in all, however, things seem to be looking up.
More than 13,000 physicians in more than 29 specialties shared information about their incomes and other aspects of their careers in a survey conducted by Medscape. The responses showed a trend back to something like normal after the initial blow of the COVID-19 pandemic.
As the profession began to recover from the pandemic, cardiologists reported that their incomes increased in 2021, reaching an average of $490,000 for the year, up from $459,000 the previous year. This was in keeping with physicians in other specialties. “Compensation for most physicians is trending back up, as demands for physicians accelerates,” said James Taylor, group president and chief operating officer of AMN Healthcare’s Physician & Leadership Solutions Division. “The market for physicians has done a complete 180 over just 7 or 8 months.” And though inflation is on everyone’s mind these days, rising salaries have helped physicians keep up with rising prices.
Despite the increase in income (and the accompanying increased workload), nearly 30% of cardiologists have taken on extra work, most of that being medical work, but a few did report unrelated side hustles. This may be due not to a shortfall in income, but rather to a desire to pad the coffers for the future. Lauren Podnos, a financial planner with Wealth Care, a firm that specializes in working with physicians and other health care professionals, points out that many physicians like to build wealth as quickly as possible as a hedge against possible burnout later on. “With physicians,” she said, “we work to get to the point where they have the freedom to do whatever they want – cut back and work part-time or transition into another career – so if they do burn out, they have other options.”
Though physician pay rose overall, not all cardiologists enjoyed a boost in income. However, those who did lose ground did not always lay the blame on COVID-19: General pay cuts were mentioned, for example. For physicians overall, a gender pay gap still remains, with men averaging $373,000 per year, in contrast to women who make $282,000. With more women moving into higher-paying specialties, the gap has narrowed somewhat in recent years, and industry leaders are making efforts to accelerate that trend. “A great many of the specialty organizations have efforts underway not just to increase the number of women in specialties but also to address gender pay gaps and bias in evaluations during residency and fellowship,” said Ron Holder, chief operating officer of the Medical Group Management Association (MGMA).
Incentive bonuses helped bump up income as well. Overall, 57% of physicians receive some kind of incentive bonus; the average for cardiologists was $85,000 last year, up from $71,000 the prior year. While such bonuses can certainly help the bottom line, they’re not always an unmitigated good. A 2021 study found that incentive programs can cause people to prioritize time spent at work and with work colleagues at the expense of family and personal relationships, a potentially troubling finding with so many physicians struggling with depression and burnout. “There’s been a lot of previous evidence showing that the more time we spend with our loved ones the happier we are,” said Julia Hur, PhD, assistant professor of management and organizations at New York University’s Stern School of Business, and lead author of the study. “The core argument of this study is about attention, and performance incentives create an attentional fixation on money,” she said, “causing people to spend more time with work colleagues and people who are helpful to their careers. And that takes away from time for family and friends.”
Still rewarding
Getting paid well is one thing; feeling that you’re being paid well is another. Only 57% of cardiologists who responded to the survey said they felt they were fairly compensated for their work. This puts them at roughly the middle of the pack of specialties. Contrast that with physicians in public health and preventive medicine who topped the charts on this one, with 72% of these doctors feeling that they were being paid fairly for their work.
However, cardiology did rank at the top of specialties whose members said they would choose medicine if they had a chance to do it again, though that number was down from the previous year (81% in 2021 versus 86% in 2020). Of cardiologists surveyed, 88% would choose cardiology if they got a do-over.
Cardiologists spend an average of 16.4 hours each week on paperwork and administration. That’s only slightly higher than the average for all specialties, about 15.5 hours a week. Despite billing hassles and low reimbursement rates, 80% of cardiologists polled say they plan to continue taking new and existing Medicare and Medicaid patients. Though 17% said they could or would drop low-paying insurers, 83% said they could not do that for business, ethical, or other reasons.
Despite its many headaches, medicine is still a rewarding profession. The most rewarding aspects cited by cardiologists were relationships with patients (34%), being good at their work (23%), and knowing they’re making the world a better place (21%). Though this is mostly in line with previous surveys, in recent years physicians have increasingly cited making the world a better place as a key motivation and reward.
The most challenging part of the job? This will not come as a surprise: Having so many rules and regulations. This was the reason given by 26% of respondents. But a close second – at 21% – was having to work long hours. One positive development is that cardiologists are making peace with their EHR systems. Only 10% said this was the most challenging part of the job (the same percentage that cited dealing with difficult patients as most challenging).
The financial struggles created by the pandemic have eased somewhat, but physicians are still facing an array of challenges, including increased workloads and longer hours. All in all, however, things seem to be looking up.
More than 13,000 physicians in more than 29 specialties shared information about their incomes and other aspects of their careers in a survey conducted by Medscape. The responses showed a trend back to something like normal after the initial blow of the COVID-19 pandemic.
As the profession began to recover from the pandemic, cardiologists reported that their incomes increased in 2021, reaching an average of $490,000 for the year, up from $459,000 the previous year. This was in keeping with physicians in other specialties. “Compensation for most physicians is trending back up, as demands for physicians accelerates,” said James Taylor, group president and chief operating officer of AMN Healthcare’s Physician & Leadership Solutions Division. “The market for physicians has done a complete 180 over just 7 or 8 months.” And though inflation is on everyone’s mind these days, rising salaries have helped physicians keep up with rising prices.
Despite the increase in income (and the accompanying increased workload), nearly 30% of cardiologists have taken on extra work, most of that being medical work, but a few did report unrelated side hustles. This may be due not to a shortfall in income, but rather to a desire to pad the coffers for the future. Lauren Podnos, a financial planner with Wealth Care, a firm that specializes in working with physicians and other health care professionals, points out that many physicians like to build wealth as quickly as possible as a hedge against possible burnout later on. “With physicians,” she said, “we work to get to the point where they have the freedom to do whatever they want – cut back and work part-time or transition into another career – so if they do burn out, they have other options.”
Though physician pay rose overall, not all cardiologists enjoyed a boost in income. However, those who did lose ground did not always lay the blame on COVID-19: General pay cuts were mentioned, for example. For physicians overall, a gender pay gap still remains, with men averaging $373,000 per year, in contrast to women who make $282,000. With more women moving into higher-paying specialties, the gap has narrowed somewhat in recent years, and industry leaders are making efforts to accelerate that trend. “A great many of the specialty organizations have efforts underway not just to increase the number of women in specialties but also to address gender pay gaps and bias in evaluations during residency and fellowship,” said Ron Holder, chief operating officer of the Medical Group Management Association (MGMA).
Incentive bonuses helped bump up income as well. Overall, 57% of physicians receive some kind of incentive bonus; the average for cardiologists was $85,000 last year, up from $71,000 the prior year. While such bonuses can certainly help the bottom line, they’re not always an unmitigated good. A 2021 study found that incentive programs can cause people to prioritize time spent at work and with work colleagues at the expense of family and personal relationships, a potentially troubling finding with so many physicians struggling with depression and burnout. “There’s been a lot of previous evidence showing that the more time we spend with our loved ones the happier we are,” said Julia Hur, PhD, assistant professor of management and organizations at New York University’s Stern School of Business, and lead author of the study. “The core argument of this study is about attention, and performance incentives create an attentional fixation on money,” she said, “causing people to spend more time with work colleagues and people who are helpful to their careers. And that takes away from time for family and friends.”
Still rewarding
Getting paid well is one thing; feeling that you’re being paid well is another. Only 57% of cardiologists who responded to the survey said they felt they were fairly compensated for their work. This puts them at roughly the middle of the pack of specialties. Contrast that with physicians in public health and preventive medicine who topped the charts on this one, with 72% of these doctors feeling that they were being paid fairly for their work.
However, cardiology did rank at the top of specialties whose members said they would choose medicine if they had a chance to do it again, though that number was down from the previous year (81% in 2021 versus 86% in 2020). Of cardiologists surveyed, 88% would choose cardiology if they got a do-over.
Cardiologists spend an average of 16.4 hours each week on paperwork and administration. That’s only slightly higher than the average for all specialties, about 15.5 hours a week. Despite billing hassles and low reimbursement rates, 80% of cardiologists polled say they plan to continue taking new and existing Medicare and Medicaid patients. Though 17% said they could or would drop low-paying insurers, 83% said they could not do that for business, ethical, or other reasons.
Despite its many headaches, medicine is still a rewarding profession. The most rewarding aspects cited by cardiologists were relationships with patients (34%), being good at their work (23%), and knowing they’re making the world a better place (21%). Though this is mostly in line with previous surveys, in recent years physicians have increasingly cited making the world a better place as a key motivation and reward.
The most challenging part of the job? This will not come as a surprise: Having so many rules and regulations. This was the reason given by 26% of respondents. But a close second – at 21% – was having to work long hours. One positive development is that cardiologists are making peace with their EHR systems. Only 10% said this was the most challenging part of the job (the same percentage that cited dealing with difficult patients as most challenging).
The financial struggles created by the pandemic have eased somewhat, but physicians are still facing an array of challenges, including increased workloads and longer hours. All in all, however, things seem to be looking up.
More than 13,000 physicians in more than 29 specialties shared information about their incomes and other aspects of their careers in a survey conducted by Medscape. The responses showed a trend back to something like normal after the initial blow of the COVID-19 pandemic.
As the profession began to recover from the pandemic, cardiologists reported that their incomes increased in 2021, reaching an average of $490,000 for the year, up from $459,000 the previous year. This was in keeping with physicians in other specialties. “Compensation for most physicians is trending back up, as demands for physicians accelerates,” said James Taylor, group president and chief operating officer of AMN Healthcare’s Physician & Leadership Solutions Division. “The market for physicians has done a complete 180 over just 7 or 8 months.” And though inflation is on everyone’s mind these days, rising salaries have helped physicians keep up with rising prices.
Despite the increase in income (and the accompanying increased workload), nearly 30% of cardiologists have taken on extra work, most of that being medical work, but a few did report unrelated side hustles. This may be due not to a shortfall in income, but rather to a desire to pad the coffers for the future. Lauren Podnos, a financial planner with Wealth Care, a firm that specializes in working with physicians and other health care professionals, points out that many physicians like to build wealth as quickly as possible as a hedge against possible burnout later on. “With physicians,” she said, “we work to get to the point where they have the freedom to do whatever they want – cut back and work part-time or transition into another career – so if they do burn out, they have other options.”
Though physician pay rose overall, not all cardiologists enjoyed a boost in income. However, those who did lose ground did not always lay the blame on COVID-19: General pay cuts were mentioned, for example. For physicians overall, a gender pay gap still remains, with men averaging $373,000 per year, in contrast to women who make $282,000. With more women moving into higher-paying specialties, the gap has narrowed somewhat in recent years, and industry leaders are making efforts to accelerate that trend. “A great many of the specialty organizations have efforts underway not just to increase the number of women in specialties but also to address gender pay gaps and bias in evaluations during residency and fellowship,” said Ron Holder, chief operating officer of the Medical Group Management Association (MGMA).
Incentive bonuses helped bump up income as well. Overall, 57% of physicians receive some kind of incentive bonus; the average for cardiologists was $85,000 last year, up from $71,000 the prior year. While such bonuses can certainly help the bottom line, they’re not always an unmitigated good. A 2021 study found that incentive programs can cause people to prioritize time spent at work and with work colleagues at the expense of family and personal relationships, a potentially troubling finding with so many physicians struggling with depression and burnout. “There’s been a lot of previous evidence showing that the more time we spend with our loved ones the happier we are,” said Julia Hur, PhD, assistant professor of management and organizations at New York University’s Stern School of Business, and lead author of the study. “The core argument of this study is about attention, and performance incentives create an attentional fixation on money,” she said, “causing people to spend more time with work colleagues and people who are helpful to their careers. And that takes away from time for family and friends.”
Still rewarding
Getting paid well is one thing; feeling that you’re being paid well is another. Only 57% of cardiologists who responded to the survey said they felt they were fairly compensated for their work. This puts them at roughly the middle of the pack of specialties. Contrast that with physicians in public health and preventive medicine who topped the charts on this one, with 72% of these doctors feeling that they were being paid fairly for their work.
However, cardiology did rank at the top of specialties whose members said they would choose medicine if they had a chance to do it again, though that number was down from the previous year (81% in 2021 versus 86% in 2020). Of cardiologists surveyed, 88% would choose cardiology if they got a do-over.
Cardiologists spend an average of 16.4 hours each week on paperwork and administration. That’s only slightly higher than the average for all specialties, about 15.5 hours a week. Despite billing hassles and low reimbursement rates, 80% of cardiologists polled say they plan to continue taking new and existing Medicare and Medicaid patients. Though 17% said they could or would drop low-paying insurers, 83% said they could not do that for business, ethical, or other reasons.
Despite its many headaches, medicine is still a rewarding profession. The most rewarding aspects cited by cardiologists were relationships with patients (34%), being good at their work (23%), and knowing they’re making the world a better place (21%). Though this is mostly in line with previous surveys, in recent years physicians have increasingly cited making the world a better place as a key motivation and reward.
The most challenging part of the job? This will not come as a surprise: Having so many rules and regulations. This was the reason given by 26% of respondents. But a close second – at 21% – was having to work long hours. One positive development is that cardiologists are making peace with their EHR systems. Only 10% said this was the most challenging part of the job (the same percentage that cited dealing with difficult patients as most challenging).
‘I shall harm’
I was quite sure I had multiple sclerosis when I was a medical student. I first noticed symptoms during my neurology rotation. All the signs were there: Fatigue that was getting worse in the North Carolina heat (Uhthoff sign!). A tingle running down my neck (Lhermitte sign!). Blurry vision late at night while studying pathways in Lange Neurology. “Didn’t cousin Amy have MS?” I asked my Mom. I started researching which medical specialties didn’t require dexterity. My left eyelid began twitching and didn’t stop until I rotated to ob.gyn.
Fortunately, it was not multiple sclerosis I had, but rather nosophobia, also known as Medical Student’s Disease. The combination of intense study of symptoms, spotty knowledge of diagnoses, and grade anxiety makes nosophobia common in med students. Despite its name, it doesn’t afflict only doctors. Patients often come to us convinced they have a disease but without reason. So unshakable is their belief that multiple visits are often required to disabuse them of their self-diagnosis. I sometimes have to remind myself to appear concerned even when a “melanoma” is a freckle so small I can barely see it with a dermatoscope. Or a “genital wart” is a hair follicle that looks exactly like the hundreds on the patient’s scrotum. Tougher though, are the treatment-avoiders: patients whose imagined side effects lead them to stop or refuse treatment.
I recently saw a middle-aged man with erythroderma so severe he looked like a ghillie suit of scale. He had a lifelong history of atopic dermatitis and a 2-year history of avoiding treatments. At some point, he tried all the usual remedies: cyclosporine, methotrexate, azathioprine, light therapy, boxes of topicals. The last treatment had been dupilumab, which he tried for a few weeks. “Why did you stop that one?” I asked. The injections were making him go blind, he explained. “Not blurry? Blind?” I asked. Yes, he could not see at all after each injection. Perhaps he might have dry eyes or keratitis? Sure. But blindness? It seemed an unreasonable concern. Further discussion revealed that intolerance to medication side effects was why he had stopped all his other treatments.
Nocebo, from the Latin “I shall harm,” is the dark counterpart to the placebo. Patients experience imagined, or even real, adverse effects because they believe the treatment is causing them harm. This is true even though that treatment might not be having any unwanted physiologic effect. Statins are a good example. Studies have shown that most patient-reported side effects of statins are in fact nocebo effects rather than a result of pharmacologic causes.
Yet, many patients on statins report muscle pain or other concerns as unbearable. As a consequence, some patients who might have benefited from statins might be missing out on the protective gains. as compared with bad outcomes that occurred from not taking action. It’s frustrating when there’s a standard of care treatment, but our patient can’t get past their fear of harm to try it.
Despite my recommendations, my eczema patient insisted on continuing his nontreatment rather than take any risks with treatments for now. There are ways I might help, but I expect it will require additional visits to build trust. Today, the best I can do is to understand and respect him. At least he doesn’t think he has a genital wart – I’m not sure how I’d treat it if he did.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
I was quite sure I had multiple sclerosis when I was a medical student. I first noticed symptoms during my neurology rotation. All the signs were there: Fatigue that was getting worse in the North Carolina heat (Uhthoff sign!). A tingle running down my neck (Lhermitte sign!). Blurry vision late at night while studying pathways in Lange Neurology. “Didn’t cousin Amy have MS?” I asked my Mom. I started researching which medical specialties didn’t require dexterity. My left eyelid began twitching and didn’t stop until I rotated to ob.gyn.
Fortunately, it was not multiple sclerosis I had, but rather nosophobia, also known as Medical Student’s Disease. The combination of intense study of symptoms, spotty knowledge of diagnoses, and grade anxiety makes nosophobia common in med students. Despite its name, it doesn’t afflict only doctors. Patients often come to us convinced they have a disease but without reason. So unshakable is their belief that multiple visits are often required to disabuse them of their self-diagnosis. I sometimes have to remind myself to appear concerned even when a “melanoma” is a freckle so small I can barely see it with a dermatoscope. Or a “genital wart” is a hair follicle that looks exactly like the hundreds on the patient’s scrotum. Tougher though, are the treatment-avoiders: patients whose imagined side effects lead them to stop or refuse treatment.
I recently saw a middle-aged man with erythroderma so severe he looked like a ghillie suit of scale. He had a lifelong history of atopic dermatitis and a 2-year history of avoiding treatments. At some point, he tried all the usual remedies: cyclosporine, methotrexate, azathioprine, light therapy, boxes of topicals. The last treatment had been dupilumab, which he tried for a few weeks. “Why did you stop that one?” I asked. The injections were making him go blind, he explained. “Not blurry? Blind?” I asked. Yes, he could not see at all after each injection. Perhaps he might have dry eyes or keratitis? Sure. But blindness? It seemed an unreasonable concern. Further discussion revealed that intolerance to medication side effects was why he had stopped all his other treatments.
Nocebo, from the Latin “I shall harm,” is the dark counterpart to the placebo. Patients experience imagined, or even real, adverse effects because they believe the treatment is causing them harm. This is true even though that treatment might not be having any unwanted physiologic effect. Statins are a good example. Studies have shown that most patient-reported side effects of statins are in fact nocebo effects rather than a result of pharmacologic causes.
Yet, many patients on statins report muscle pain or other concerns as unbearable. As a consequence, some patients who might have benefited from statins might be missing out on the protective gains. as compared with bad outcomes that occurred from not taking action. It’s frustrating when there’s a standard of care treatment, but our patient can’t get past their fear of harm to try it.
Despite my recommendations, my eczema patient insisted on continuing his nontreatment rather than take any risks with treatments for now. There are ways I might help, but I expect it will require additional visits to build trust. Today, the best I can do is to understand and respect him. At least he doesn’t think he has a genital wart – I’m not sure how I’d treat it if he did.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
I was quite sure I had multiple sclerosis when I was a medical student. I first noticed symptoms during my neurology rotation. All the signs were there: Fatigue that was getting worse in the North Carolina heat (Uhthoff sign!). A tingle running down my neck (Lhermitte sign!). Blurry vision late at night while studying pathways in Lange Neurology. “Didn’t cousin Amy have MS?” I asked my Mom. I started researching which medical specialties didn’t require dexterity. My left eyelid began twitching and didn’t stop until I rotated to ob.gyn.
Fortunately, it was not multiple sclerosis I had, but rather nosophobia, also known as Medical Student’s Disease. The combination of intense study of symptoms, spotty knowledge of diagnoses, and grade anxiety makes nosophobia common in med students. Despite its name, it doesn’t afflict only doctors. Patients often come to us convinced they have a disease but without reason. So unshakable is their belief that multiple visits are often required to disabuse them of their self-diagnosis. I sometimes have to remind myself to appear concerned even when a “melanoma” is a freckle so small I can barely see it with a dermatoscope. Or a “genital wart” is a hair follicle that looks exactly like the hundreds on the patient’s scrotum. Tougher though, are the treatment-avoiders: patients whose imagined side effects lead them to stop or refuse treatment.
I recently saw a middle-aged man with erythroderma so severe he looked like a ghillie suit of scale. He had a lifelong history of atopic dermatitis and a 2-year history of avoiding treatments. At some point, he tried all the usual remedies: cyclosporine, methotrexate, azathioprine, light therapy, boxes of topicals. The last treatment had been dupilumab, which he tried for a few weeks. “Why did you stop that one?” I asked. The injections were making him go blind, he explained. “Not blurry? Blind?” I asked. Yes, he could not see at all after each injection. Perhaps he might have dry eyes or keratitis? Sure. But blindness? It seemed an unreasonable concern. Further discussion revealed that intolerance to medication side effects was why he had stopped all his other treatments.
Nocebo, from the Latin “I shall harm,” is the dark counterpart to the placebo. Patients experience imagined, or even real, adverse effects because they believe the treatment is causing them harm. This is true even though that treatment might not be having any unwanted physiologic effect. Statins are a good example. Studies have shown that most patient-reported side effects of statins are in fact nocebo effects rather than a result of pharmacologic causes.
Yet, many patients on statins report muscle pain or other concerns as unbearable. As a consequence, some patients who might have benefited from statins might be missing out on the protective gains. as compared with bad outcomes that occurred from not taking action. It’s frustrating when there’s a standard of care treatment, but our patient can’t get past their fear of harm to try it.
Despite my recommendations, my eczema patient insisted on continuing his nontreatment rather than take any risks with treatments for now. There are ways I might help, but I expect it will require additional visits to build trust. Today, the best I can do is to understand and respect him. At least he doesn’t think he has a genital wart – I’m not sure how I’d treat it if he did.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
In some states, voters will get to decide the future of abortion rights
As states grapple with the future of abortion in the United States, Michigan, California, and Vermont could become the first states to let voters decide whether the right to abortion should be written into the state constitution.
In Michigan, a proposed constitutional amendment would override a 90-year-old state law that makes abortion a felony even in cases of rape or incest. The U.S. Supreme Court’s overturning of Roe v. Wade could revive that abortion ban – and has galvanized abortion-rights advocates to secure new protections.
Some of the momentum is coming from activists getting involved for the first time.
“I wanted to do something, but I had no political experience or really any experience in activism,” said Amanda Mazur, who lives in rural northwestern Michigan. “But I thought, ‘Maybe I can volunteer and just offer something tangible to the movement.’”
Michigan organizers like Ms. Mazur submitted more than 750,000 signatures – a record number, they said – to state election officials in hopes of having the amendment appear on the November ballot.
If just over half those signatures are validated, Michigan voters will decide whether to amend the state’s constitution to guarantee broad individual rights to “reproductive freedom” that would cover abortion, contraception, and fertility treatments. It would also prevent the state from regulating abortions later in pregnancy if the patient’s “physical or mental health” is at risk.
The ballot initiative has the backing of medical groups like the American College of Obstetricians and Gynecologists, while conservative groups have called it radical and dangerous, claiming it would “allow late-term abortions for practically any reason.”
In California, the push to expand abortion access starts from a very different vantage point: The right to abortion is protected in state statute. And voters will be asked whether they want to enshrine it in the constitution. Proposition 1, which will be on the ballot in November, would prohibit the state from interfering with Californians’ reproductive health decisions, including those related to abortion or contraception.
“I want to know for sure that that right is protected,” state Sen. Toni Atkins (D-Calif.), the Democratic leader in the Senate and lead author of the amendment, said at a legislative hearing in June. “We are protecting ourselves from future courts and future politicians.”
The amendment is one strategy that several California lawmakers are pursuing to protect abortion access in the state. Gov. Gavin Newsom, a Democrat, has signed legislation to eliminate out-of-pocket expenses for abortion for most Californians and to protect California providers that offer abortion services from lawsuits in other states. The recent state budget deal also includes $200 million for reproductive and abortion care.
Earlier in July, Vermont Gov. Phil Scott, a Republican, announced that Proposal 5 will be on the November ballot. He said in a statement: “In Vermont, we solidified the right to choose in law, and now Vermonters have the opportunity to further protect that right in our constitution.”
For Ms. Mazur, the desire to “do something” started in 2017, when she and her husband gave their daughter, then 2 years old, some happy news: She was going to be a big sister. The family was thrilled.
But then doctors told Ms. Mazur something was wrong.
“I found out halfway through the pregnancy that the baby my husband and I hoped for suffered from a rare and life-limiting genetic condition,” Ms. Mazur said. “We ultimately made the compassionate choice to end the pregnancy for my well-being, and for the well-being of our family, and the life of what we thought would be our child.”
Devastated, Ms. Mazur turned to a national online support group and met people having similar experiences. But many group members said they were having a tough time finding a way to terminate their pregnancies.
“It really broke my heart that you’re going through this already devastating experience but have to travel far away from your home across the country ... [and] advocate for yourself like crazy just to get care that you have decided with your doctor is best for you,” Ms. Mazur said.
At the time, abortion rights in Michigan seemed pretty stable, but Ms. Mazur’s political awakening found an outlet this year.
Reproductive Freedom for All, a petition group backed by the American Civil Liberties Union of Michigan and Planned Parenthood Advocates of Michigan, was gathering signatures for the constitutional amendment to enshrine abortion protections in state law. The effort took on new urgency in May after a draft of the Supreme Court’s decision in Dobbs v. Jackson Women’s Health Organization was leaked and then published.
“Folks realized that this big, scary thing that they did not think would happen might actually happen,” said Jessica Ayoub, a field organizer with the ACLU of Michigan.
Some Michiganders were registering to vote just to be eligible to sign the petition. Jaynie Hoerauf, a 62-year-old attorney in Farwell, drove 40 miles to attend a rally where she knew she could sign it.
“A bunch of us were so ticked off [about Roe being overturned], and we were talking about it. And I was like, ‘I’m just going to go on and find where I can sign the stupid petition,’” Ms. Hoerauf said.
Activists on both sides of the abortion-rights debate expect to spend millions of dollars. They predict that donations will pour in from outside Michigan and that voters in other states will be watching.
“This is just the start of our fight,” Ms. Ayoub said. “We know that it is a long road to November.”
KHN correspondent Rachel Bluth contributed to this report. This story is part of a partnership that includes Michigan Radio, NPR, and KHN. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
As states grapple with the future of abortion in the United States, Michigan, California, and Vermont could become the first states to let voters decide whether the right to abortion should be written into the state constitution.
In Michigan, a proposed constitutional amendment would override a 90-year-old state law that makes abortion a felony even in cases of rape or incest. The U.S. Supreme Court’s overturning of Roe v. Wade could revive that abortion ban – and has galvanized abortion-rights advocates to secure new protections.
Some of the momentum is coming from activists getting involved for the first time.
“I wanted to do something, but I had no political experience or really any experience in activism,” said Amanda Mazur, who lives in rural northwestern Michigan. “But I thought, ‘Maybe I can volunteer and just offer something tangible to the movement.’”
Michigan organizers like Ms. Mazur submitted more than 750,000 signatures – a record number, they said – to state election officials in hopes of having the amendment appear on the November ballot.
If just over half those signatures are validated, Michigan voters will decide whether to amend the state’s constitution to guarantee broad individual rights to “reproductive freedom” that would cover abortion, contraception, and fertility treatments. It would also prevent the state from regulating abortions later in pregnancy if the patient’s “physical or mental health” is at risk.
The ballot initiative has the backing of medical groups like the American College of Obstetricians and Gynecologists, while conservative groups have called it radical and dangerous, claiming it would “allow late-term abortions for practically any reason.”
In California, the push to expand abortion access starts from a very different vantage point: The right to abortion is protected in state statute. And voters will be asked whether they want to enshrine it in the constitution. Proposition 1, which will be on the ballot in November, would prohibit the state from interfering with Californians’ reproductive health decisions, including those related to abortion or contraception.
“I want to know for sure that that right is protected,” state Sen. Toni Atkins (D-Calif.), the Democratic leader in the Senate and lead author of the amendment, said at a legislative hearing in June. “We are protecting ourselves from future courts and future politicians.”
The amendment is one strategy that several California lawmakers are pursuing to protect abortion access in the state. Gov. Gavin Newsom, a Democrat, has signed legislation to eliminate out-of-pocket expenses for abortion for most Californians and to protect California providers that offer abortion services from lawsuits in other states. The recent state budget deal also includes $200 million for reproductive and abortion care.
Earlier in July, Vermont Gov. Phil Scott, a Republican, announced that Proposal 5 will be on the November ballot. He said in a statement: “In Vermont, we solidified the right to choose in law, and now Vermonters have the opportunity to further protect that right in our constitution.”
For Ms. Mazur, the desire to “do something” started in 2017, when she and her husband gave their daughter, then 2 years old, some happy news: She was going to be a big sister. The family was thrilled.
But then doctors told Ms. Mazur something was wrong.
“I found out halfway through the pregnancy that the baby my husband and I hoped for suffered from a rare and life-limiting genetic condition,” Ms. Mazur said. “We ultimately made the compassionate choice to end the pregnancy for my well-being, and for the well-being of our family, and the life of what we thought would be our child.”
Devastated, Ms. Mazur turned to a national online support group and met people having similar experiences. But many group members said they were having a tough time finding a way to terminate their pregnancies.
“It really broke my heart that you’re going through this already devastating experience but have to travel far away from your home across the country ... [and] advocate for yourself like crazy just to get care that you have decided with your doctor is best for you,” Ms. Mazur said.
At the time, abortion rights in Michigan seemed pretty stable, but Ms. Mazur’s political awakening found an outlet this year.
Reproductive Freedom for All, a petition group backed by the American Civil Liberties Union of Michigan and Planned Parenthood Advocates of Michigan, was gathering signatures for the constitutional amendment to enshrine abortion protections in state law. The effort took on new urgency in May after a draft of the Supreme Court’s decision in Dobbs v. Jackson Women’s Health Organization was leaked and then published.
“Folks realized that this big, scary thing that they did not think would happen might actually happen,” said Jessica Ayoub, a field organizer with the ACLU of Michigan.
Some Michiganders were registering to vote just to be eligible to sign the petition. Jaynie Hoerauf, a 62-year-old attorney in Farwell, drove 40 miles to attend a rally where she knew she could sign it.
“A bunch of us were so ticked off [about Roe being overturned], and we were talking about it. And I was like, ‘I’m just going to go on and find where I can sign the stupid petition,’” Ms. Hoerauf said.
Activists on both sides of the abortion-rights debate expect to spend millions of dollars. They predict that donations will pour in from outside Michigan and that voters in other states will be watching.
“This is just the start of our fight,” Ms. Ayoub said. “We know that it is a long road to November.”
KHN correspondent Rachel Bluth contributed to this report. This story is part of a partnership that includes Michigan Radio, NPR, and KHN. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
As states grapple with the future of abortion in the United States, Michigan, California, and Vermont could become the first states to let voters decide whether the right to abortion should be written into the state constitution.
In Michigan, a proposed constitutional amendment would override a 90-year-old state law that makes abortion a felony even in cases of rape or incest. The U.S. Supreme Court’s overturning of Roe v. Wade could revive that abortion ban – and has galvanized abortion-rights advocates to secure new protections.
Some of the momentum is coming from activists getting involved for the first time.
“I wanted to do something, but I had no political experience or really any experience in activism,” said Amanda Mazur, who lives in rural northwestern Michigan. “But I thought, ‘Maybe I can volunteer and just offer something tangible to the movement.’”
Michigan organizers like Ms. Mazur submitted more than 750,000 signatures – a record number, they said – to state election officials in hopes of having the amendment appear on the November ballot.
If just over half those signatures are validated, Michigan voters will decide whether to amend the state’s constitution to guarantee broad individual rights to “reproductive freedom” that would cover abortion, contraception, and fertility treatments. It would also prevent the state from regulating abortions later in pregnancy if the patient’s “physical or mental health” is at risk.
The ballot initiative has the backing of medical groups like the American College of Obstetricians and Gynecologists, while conservative groups have called it radical and dangerous, claiming it would “allow late-term abortions for practically any reason.”
In California, the push to expand abortion access starts from a very different vantage point: The right to abortion is protected in state statute. And voters will be asked whether they want to enshrine it in the constitution. Proposition 1, which will be on the ballot in November, would prohibit the state from interfering with Californians’ reproductive health decisions, including those related to abortion or contraception.
“I want to know for sure that that right is protected,” state Sen. Toni Atkins (D-Calif.), the Democratic leader in the Senate and lead author of the amendment, said at a legislative hearing in June. “We are protecting ourselves from future courts and future politicians.”
The amendment is one strategy that several California lawmakers are pursuing to protect abortion access in the state. Gov. Gavin Newsom, a Democrat, has signed legislation to eliminate out-of-pocket expenses for abortion for most Californians and to protect California providers that offer abortion services from lawsuits in other states. The recent state budget deal also includes $200 million for reproductive and abortion care.
Earlier in July, Vermont Gov. Phil Scott, a Republican, announced that Proposal 5 will be on the November ballot. He said in a statement: “In Vermont, we solidified the right to choose in law, and now Vermonters have the opportunity to further protect that right in our constitution.”
For Ms. Mazur, the desire to “do something” started in 2017, when she and her husband gave their daughter, then 2 years old, some happy news: She was going to be a big sister. The family was thrilled.
But then doctors told Ms. Mazur something was wrong.
“I found out halfway through the pregnancy that the baby my husband and I hoped for suffered from a rare and life-limiting genetic condition,” Ms. Mazur said. “We ultimately made the compassionate choice to end the pregnancy for my well-being, and for the well-being of our family, and the life of what we thought would be our child.”
Devastated, Ms. Mazur turned to a national online support group and met people having similar experiences. But many group members said they were having a tough time finding a way to terminate their pregnancies.
“It really broke my heart that you’re going through this already devastating experience but have to travel far away from your home across the country ... [and] advocate for yourself like crazy just to get care that you have decided with your doctor is best for you,” Ms. Mazur said.
At the time, abortion rights in Michigan seemed pretty stable, but Ms. Mazur’s political awakening found an outlet this year.
Reproductive Freedom for All, a petition group backed by the American Civil Liberties Union of Michigan and Planned Parenthood Advocates of Michigan, was gathering signatures for the constitutional amendment to enshrine abortion protections in state law. The effort took on new urgency in May after a draft of the Supreme Court’s decision in Dobbs v. Jackson Women’s Health Organization was leaked and then published.
“Folks realized that this big, scary thing that they did not think would happen might actually happen,” said Jessica Ayoub, a field organizer with the ACLU of Michigan.
Some Michiganders were registering to vote just to be eligible to sign the petition. Jaynie Hoerauf, a 62-year-old attorney in Farwell, drove 40 miles to attend a rally where she knew she could sign it.
“A bunch of us were so ticked off [about Roe being overturned], and we were talking about it. And I was like, ‘I’m just going to go on and find where I can sign the stupid petition,’” Ms. Hoerauf said.
Activists on both sides of the abortion-rights debate expect to spend millions of dollars. They predict that donations will pour in from outside Michigan and that voters in other states will be watching.
“This is just the start of our fight,” Ms. Ayoub said. “We know that it is a long road to November.”
KHN correspondent Rachel Bluth contributed to this report. This story is part of a partnership that includes Michigan Radio, NPR, and KHN. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
The shell game
The shell game is probably the world’s oldest confidence game, going back 2,000-3,000 years. You still see people getting lured into it in cities today.
It’s also played, albeit legally, in physician offices and pharmacies around the country.
You know, the ones piled up in your sample cabinet. Get a month free of Whateveritscalled to try and/or have your copay reduced to $0 or something reasonably low. All, of course, subject to terms and conditions in the small print and that of your insurance carrier. Your mileage may vary.
In my experience these things often don’t work as well as advertised. Sometimes it’s because the patient doesn’t understand how to use them, other times because their pharmacy doesn’t want to have anything to do with the cards, and still other times because their insurance has some exclusion against them.
But they do sometimes work ... until they don’t. Sometimes, out of the blue, they’ll stop. Maybe there was an insurance change, or the pharmacy policy changed, or the manufacturer’s program changed, or the offer expired. I usually don’t know and rarely find out.
So the shell game begins. The patients call multiple pharmacies, trying to find one that may be able to honor the coupons. Then they call my office and ask me to switch the script. So I do. They they go to the pharmacy. Sometimes they can get the script, sometimes not. If not, they move to another pharmacy and call my office to switch it again. Wash, rinse, repeat.
Other times it’s more complicated. They want a new card for each try, so they show up at my office asking for one (usually they can be downloaded online so some try that. Others do both). Like pebbles under a shell, the prescriptions and cards get switched from pharmacy to pharmacy.
This isn’t exclusive to manufacturers’ copay cards. I see the same phenomenon with GoodRx and similar cost-saving programs. People move scripts around to find the best deal. It may be helping them, but it certainly doesn’t help me and my staff as we try to keep up, or the badly overworked pharmacy staff.
I’ve even had some patients take the audacious step of asking me to write a script in the name of their spouses so they can double their supply. Obviously, such requests are refused. I’m not going to play that game.
I understand new drugs are costly, and often outside the reach of many patients today. I know the manufacturers are trying to get their products tried, or even make them more affordable for those who need it.
But, in many cases, this becomes (unintentionally or intentionally; I’m not sure) a shell game. Legal, perhaps, but still equally frustrating for all of us who are trying to keep up with it.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The shell game is probably the world’s oldest confidence game, going back 2,000-3,000 years. You still see people getting lured into it in cities today.
It’s also played, albeit legally, in physician offices and pharmacies around the country.
You know, the ones piled up in your sample cabinet. Get a month free of Whateveritscalled to try and/or have your copay reduced to $0 or something reasonably low. All, of course, subject to terms and conditions in the small print and that of your insurance carrier. Your mileage may vary.
In my experience these things often don’t work as well as advertised. Sometimes it’s because the patient doesn’t understand how to use them, other times because their pharmacy doesn’t want to have anything to do with the cards, and still other times because their insurance has some exclusion against them.
But they do sometimes work ... until they don’t. Sometimes, out of the blue, they’ll stop. Maybe there was an insurance change, or the pharmacy policy changed, or the manufacturer’s program changed, or the offer expired. I usually don’t know and rarely find out.
So the shell game begins. The patients call multiple pharmacies, trying to find one that may be able to honor the coupons. Then they call my office and ask me to switch the script. So I do. They they go to the pharmacy. Sometimes they can get the script, sometimes not. If not, they move to another pharmacy and call my office to switch it again. Wash, rinse, repeat.
Other times it’s more complicated. They want a new card for each try, so they show up at my office asking for one (usually they can be downloaded online so some try that. Others do both). Like pebbles under a shell, the prescriptions and cards get switched from pharmacy to pharmacy.
This isn’t exclusive to manufacturers’ copay cards. I see the same phenomenon with GoodRx and similar cost-saving programs. People move scripts around to find the best deal. It may be helping them, but it certainly doesn’t help me and my staff as we try to keep up, or the badly overworked pharmacy staff.
I’ve even had some patients take the audacious step of asking me to write a script in the name of their spouses so they can double their supply. Obviously, such requests are refused. I’m not going to play that game.
I understand new drugs are costly, and often outside the reach of many patients today. I know the manufacturers are trying to get their products tried, or even make them more affordable for those who need it.
But, in many cases, this becomes (unintentionally or intentionally; I’m not sure) a shell game. Legal, perhaps, but still equally frustrating for all of us who are trying to keep up with it.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The shell game is probably the world’s oldest confidence game, going back 2,000-3,000 years. You still see people getting lured into it in cities today.
It’s also played, albeit legally, in physician offices and pharmacies around the country.
You know, the ones piled up in your sample cabinet. Get a month free of Whateveritscalled to try and/or have your copay reduced to $0 or something reasonably low. All, of course, subject to terms and conditions in the small print and that of your insurance carrier. Your mileage may vary.
In my experience these things often don’t work as well as advertised. Sometimes it’s because the patient doesn’t understand how to use them, other times because their pharmacy doesn’t want to have anything to do with the cards, and still other times because their insurance has some exclusion against them.
But they do sometimes work ... until they don’t. Sometimes, out of the blue, they’ll stop. Maybe there was an insurance change, or the pharmacy policy changed, or the manufacturer’s program changed, or the offer expired. I usually don’t know and rarely find out.
So the shell game begins. The patients call multiple pharmacies, trying to find one that may be able to honor the coupons. Then they call my office and ask me to switch the script. So I do. They they go to the pharmacy. Sometimes they can get the script, sometimes not. If not, they move to another pharmacy and call my office to switch it again. Wash, rinse, repeat.
Other times it’s more complicated. They want a new card for each try, so they show up at my office asking for one (usually they can be downloaded online so some try that. Others do both). Like pebbles under a shell, the prescriptions and cards get switched from pharmacy to pharmacy.
This isn’t exclusive to manufacturers’ copay cards. I see the same phenomenon with GoodRx and similar cost-saving programs. People move scripts around to find the best deal. It may be helping them, but it certainly doesn’t help me and my staff as we try to keep up, or the badly overworked pharmacy staff.
I’ve even had some patients take the audacious step of asking me to write a script in the name of their spouses so they can double their supply. Obviously, such requests are refused. I’m not going to play that game.
I understand new drugs are costly, and often outside the reach of many patients today. I know the manufacturers are trying to get their products tried, or even make them more affordable for those who need it.
But, in many cases, this becomes (unintentionally or intentionally; I’m not sure) a shell game. Legal, perhaps, but still equally frustrating for all of us who are trying to keep up with it.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Commentary: Reversal of Roe v. Wade affects adolescents
The Supreme Court decision to strike down the 50-year ruling on Roe v. Wade, which allowed legal abortion, will affect all patients and families seeking care in pediatric and adolescent medicine clinics. Regardless of how you view abortion, the reality is your adolescent female patients and their parents will seek your counsel.
The overturning of Roe has resulted in much confusion for both patients and providers. The overall effect of this decision in Wisconsin is yet to be known but currently we have had to create road maps to direct adolescent patients who experience an unplanned pregnancy and wish to abort. Unfortunately, these road maps include only resources out of state or online. Providing adolescents confidential care may be challenged as the teens may need to disclose the unplanned pregnancy to an adult to access resources.
Providers remain unsettled regarding their risk of assisting an adolescent who discloses an unplanned pregnancy. Recently, many questions arose regarding dispensing Plan B and the risk to prescribers. Communication was needed to assure providers that Plan B is contraception and at this time contraception remains legal in our state.
Daily I educate adolescent females on the risks of unplanned pregnancy and what the Supreme Court decision will mean to them if they become pregnant. Unfortunately, many teens do not understand the ruling and how this decision affects them personally. Education is needed today more than ever regarding pregnancy prevention.
The recent AAP policy statement reaffirms its position that the rights of adolescents to seek confidential care when considering abortion must be protected.1 It further reaffirms access to safe and legal abortion is a core tenant of sexual and reproductive health care.
A recent article published in AAP News by Elise D. Berlan, MD, “AAP’s teen reproductive health policies reaffirm right to comprehensive care,” further advises on the role of the pediatric provider.2 Pediatric providers should continue offering option counseling for pregnant adolescents, be prepared to provide accurate information regarding these options with awareness that some options such as the IUD may no longer be available, remain supportive of the decision they choose, and encourage discussion with a family member to support their decisions. It is imperative that we familiarize ourselves with the abortion policies in our states, advocate to prevent government interference with the patient-doctor relationship, and recognize the impact restrictive abortion has regarding marginalized individuals, she stated. Finally we must recognize our own bias regarding option counseling and refer appropriately to another professional if we are unable to confidently offer guidance.
Ms. Thew is the medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee.
References
1. AAP Committee on Adolescence. Pediatrics. 2022. doi: 10.1542/peds.2022-058780.
2. Berlan ED. AAP’s teen reproductive health policies reaffirm right to comprehensive care. 2022. AAP News.
The Supreme Court decision to strike down the 50-year ruling on Roe v. Wade, which allowed legal abortion, will affect all patients and families seeking care in pediatric and adolescent medicine clinics. Regardless of how you view abortion, the reality is your adolescent female patients and their parents will seek your counsel.
The overturning of Roe has resulted in much confusion for both patients and providers. The overall effect of this decision in Wisconsin is yet to be known but currently we have had to create road maps to direct adolescent patients who experience an unplanned pregnancy and wish to abort. Unfortunately, these road maps include only resources out of state or online. Providing adolescents confidential care may be challenged as the teens may need to disclose the unplanned pregnancy to an adult to access resources.
Providers remain unsettled regarding their risk of assisting an adolescent who discloses an unplanned pregnancy. Recently, many questions arose regarding dispensing Plan B and the risk to prescribers. Communication was needed to assure providers that Plan B is contraception and at this time contraception remains legal in our state.
Daily I educate adolescent females on the risks of unplanned pregnancy and what the Supreme Court decision will mean to them if they become pregnant. Unfortunately, many teens do not understand the ruling and how this decision affects them personally. Education is needed today more than ever regarding pregnancy prevention.
The recent AAP policy statement reaffirms its position that the rights of adolescents to seek confidential care when considering abortion must be protected.1 It further reaffirms access to safe and legal abortion is a core tenant of sexual and reproductive health care.
A recent article published in AAP News by Elise D. Berlan, MD, “AAP’s teen reproductive health policies reaffirm right to comprehensive care,” further advises on the role of the pediatric provider.2 Pediatric providers should continue offering option counseling for pregnant adolescents, be prepared to provide accurate information regarding these options with awareness that some options such as the IUD may no longer be available, remain supportive of the decision they choose, and encourage discussion with a family member to support their decisions. It is imperative that we familiarize ourselves with the abortion policies in our states, advocate to prevent government interference with the patient-doctor relationship, and recognize the impact restrictive abortion has regarding marginalized individuals, she stated. Finally we must recognize our own bias regarding option counseling and refer appropriately to another professional if we are unable to confidently offer guidance.
Ms. Thew is the medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee.
References
1. AAP Committee on Adolescence. Pediatrics. 2022. doi: 10.1542/peds.2022-058780.
2. Berlan ED. AAP’s teen reproductive health policies reaffirm right to comprehensive care. 2022. AAP News.
The Supreme Court decision to strike down the 50-year ruling on Roe v. Wade, which allowed legal abortion, will affect all patients and families seeking care in pediatric and adolescent medicine clinics. Regardless of how you view abortion, the reality is your adolescent female patients and their parents will seek your counsel.
The overturning of Roe has resulted in much confusion for both patients and providers. The overall effect of this decision in Wisconsin is yet to be known but currently we have had to create road maps to direct adolescent patients who experience an unplanned pregnancy and wish to abort. Unfortunately, these road maps include only resources out of state or online. Providing adolescents confidential care may be challenged as the teens may need to disclose the unplanned pregnancy to an adult to access resources.
Providers remain unsettled regarding their risk of assisting an adolescent who discloses an unplanned pregnancy. Recently, many questions arose regarding dispensing Plan B and the risk to prescribers. Communication was needed to assure providers that Plan B is contraception and at this time contraception remains legal in our state.
Daily I educate adolescent females on the risks of unplanned pregnancy and what the Supreme Court decision will mean to them if they become pregnant. Unfortunately, many teens do not understand the ruling and how this decision affects them personally. Education is needed today more than ever regarding pregnancy prevention.
The recent AAP policy statement reaffirms its position that the rights of adolescents to seek confidential care when considering abortion must be protected.1 It further reaffirms access to safe and legal abortion is a core tenant of sexual and reproductive health care.
A recent article published in AAP News by Elise D. Berlan, MD, “AAP’s teen reproductive health policies reaffirm right to comprehensive care,” further advises on the role of the pediatric provider.2 Pediatric providers should continue offering option counseling for pregnant adolescents, be prepared to provide accurate information regarding these options with awareness that some options such as the IUD may no longer be available, remain supportive of the decision they choose, and encourage discussion with a family member to support their decisions. It is imperative that we familiarize ourselves with the abortion policies in our states, advocate to prevent government interference with the patient-doctor relationship, and recognize the impact restrictive abortion has regarding marginalized individuals, she stated. Finally we must recognize our own bias regarding option counseling and refer appropriately to another professional if we are unable to confidently offer guidance.
Ms. Thew is the medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee.
References
1. AAP Committee on Adolescence. Pediatrics. 2022. doi: 10.1542/peds.2022-058780.
2. Berlan ED. AAP’s teen reproductive health policies reaffirm right to comprehensive care. 2022. AAP News.