User login
Multistate opioid crackdown nets indictment against seven physicians
In coordination with federal and state law enforcement, the DOJ charged the defendants for their involvement in the illegal distribution of opioids. At the time that they were charged with the alleged offenses, 12 of the defendants were medical professionals.
The 12 persons in eight federal districts across the country distributed more than 115 million controlled substances, including buprenorphine, clonazepam, dextroamphetamine-amphetamine, hydrocodone, morphine sulfate, oxycodone, oxymorphone, and Suboxone, per the DOJ.
“Doctors and health care professionals are entrusted with prescribing medicine responsibly and in the best interests of their patients. Today’s takedown targets medical providers across the country whose greed drove them to abandon this responsibility in favor of criminal profits,” said Anne Milgram, administrator of the Drug Enforcement Administration.
Medical professionals, others across six states charged
One former nurse, one business manager, and one individual who practiced medicine without a medical credential are among those listed in the indictment. These include the following:
- Eskender Getachew, MD, a Columbus, Ohio, sleep medicine specialist, was charged with unlawful distribution of controlled substances outside the use of professional practice and not for a legitimate medical practice.
- Charles Kistler, DO, an Upper Arlington, Ohio, family practice physician, was charged with unlawful distribution of controlled substances for unlawful prescribing at Midtown Family Practice Clinic in Columbus.
- Yogeshwar Gil, MBBS, a Manchester, Tenn., family medicine doctor and owner of a medical practice, was charged with conspiracy to unlawfully distribute controlled substances and maintaining a drug-involved premises. Dr. Gil was charged in connection with an alleged scheme to distribute opioids and Suboxone outside the usual course of professional practice and without a legitimate medical purpose.
- Contessa Holley, RN, a Pulaski, Tenn., former nurse and clinical director, was charged with wire fraud, aggravated identity theft, and possession of a controlled substance with intent to distribute. She’s alleged to be connected with a scheme to unlawfully obtain opioids by filling fraudulent prescriptions in the names of current and former patients who were in hospice. The indictment alleged that Ms. Holley used the patients’ hospice benefits to cover the opioids’ costs while keeping the drugs for her own use and for further distribution.
- Francene Aretha Gayle, MD, an Orlando, Fla., physician, was charged with conspiracy to unlawfully distribute controlled substances, conspiracy to commit health care fraud, health care fraud, and several substantive counts of illegally issuing opioid prescriptions. Dr. Gayle was charged along with Schara Monique Davis, a Huntsville, Ala.–based business manager. Per the indictment, Dr. Gayle and Ms. Davis operated three medical clinics in Alabama, where Dr. Gayle was the sole physician. The medical clinics billed health insurers for millions of dollars in patient visits that Dr. Gayle had supposedly conducted but during which she was allegedly absent from the clinics; other staff members conducted the visits instead. It’s alleged that Dr. Gayle presigned prescriptions for opioids that were given to patients.
- Robert Taffet, MD, a Haddonfield, N.J., orthopedic surgeon and owner of a medical practice in Sicklerville, N.J., was charged with conspiracy to unlawfully distribute controlled substances. The indictment alleges that he falsified patient files to state that he interacted with patients when he didn’t and that he issued prescriptions for opioids and other controlled substances without assessing the patients in person or by telemedicine. It’s alleged that Dr. Taffett issued prescriptions for more than 179,000 pills that were dispensed by New Jersey pharmacies between April 2020 and December 2021.
- Hau La, MD, a Brentwood, Tenn., family medicine physician and the operator of Absolute Medical Care in Smyrna, Tenn., was charged with sixteen counts of unlawful distribution of a controlled substance. The physician is alleged to have unlawfully prescribed opioids to eight patients outside the usual course of practice and without a legitimate medical purpose.
- Frederick De Mesa, of War, W.Va., practiced as a physician and used a DEA registration number that allowed him to prescribe controlled substances. Mr. De Mesa prescribed these substances without a medical license and didn’t have an active DEA registration number, according to the indictment.
- Loey Kousa, a former internist from Paintsville, Ky., was charged with unlawful distribution of controlled substances, healthcare fraud, and making false statements in connection with the delivery of health care services. The indictment alleges that the former physician issued prescriptions for opioids outside the usual course of professional practice and without a legitimate medical purpose in his capacity as owner and operator of East KY Clinic in Paintsville. He is alleged to have issued the unlawful prescriptions for patients whose treatments were covered by taxpayer-funded programs such as Medicare and Medicaid; he also billed these programs for medically unnecessary procedures for these patients.
Also included in the indictment were Jay Sadrinia, DMD, a Villa Hills, Ky., dentist, who was charged with four counts of illegal distribution of oxycodone and morphine sulfate and one count of illegal distribution of morphine sulfate that resulted in death or serious bodily injury; and Casey Kelleher, an owner-operator of Neighborhood Pharmacy in Boynton Beach, Fla., who allegedly sold large amounts of oxycodone and hydromorphone on the black market.
The Centers for Medicare & Medicaid Services’ Center for Program Integrity has taken six administrative actions against health care providers for their alleged involvement in these offenses, per the DOJ’s announcement.
“Patient care and safety are top priorities for us, and CMS has taken administrative action against six providers to protect critical resources entrusted to Medicare while also safeguarding people with Medicare,” said CMS Administrator Chiquita Brooks-LaSure.
“These actions to combat fraud, waste, and abuse in our federal programs would not be possible without the close and successful partnership of the Centers for Medicare & Medicaid Services, the Department of Justice, and the U.S. Department of Health and Human Services Office of Inspector General,” she added.
A version of this article first appeared on Medscape.com.
In coordination with federal and state law enforcement, the DOJ charged the defendants for their involvement in the illegal distribution of opioids. At the time that they were charged with the alleged offenses, 12 of the defendants were medical professionals.
The 12 persons in eight federal districts across the country distributed more than 115 million controlled substances, including buprenorphine, clonazepam, dextroamphetamine-amphetamine, hydrocodone, morphine sulfate, oxycodone, oxymorphone, and Suboxone, per the DOJ.
“Doctors and health care professionals are entrusted with prescribing medicine responsibly and in the best interests of their patients. Today’s takedown targets medical providers across the country whose greed drove them to abandon this responsibility in favor of criminal profits,” said Anne Milgram, administrator of the Drug Enforcement Administration.
Medical professionals, others across six states charged
One former nurse, one business manager, and one individual who practiced medicine without a medical credential are among those listed in the indictment. These include the following:
- Eskender Getachew, MD, a Columbus, Ohio, sleep medicine specialist, was charged with unlawful distribution of controlled substances outside the use of professional practice and not for a legitimate medical practice.
- Charles Kistler, DO, an Upper Arlington, Ohio, family practice physician, was charged with unlawful distribution of controlled substances for unlawful prescribing at Midtown Family Practice Clinic in Columbus.
- Yogeshwar Gil, MBBS, a Manchester, Tenn., family medicine doctor and owner of a medical practice, was charged with conspiracy to unlawfully distribute controlled substances and maintaining a drug-involved premises. Dr. Gil was charged in connection with an alleged scheme to distribute opioids and Suboxone outside the usual course of professional practice and without a legitimate medical purpose.
- Contessa Holley, RN, a Pulaski, Tenn., former nurse and clinical director, was charged with wire fraud, aggravated identity theft, and possession of a controlled substance with intent to distribute. She’s alleged to be connected with a scheme to unlawfully obtain opioids by filling fraudulent prescriptions in the names of current and former patients who were in hospice. The indictment alleged that Ms. Holley used the patients’ hospice benefits to cover the opioids’ costs while keeping the drugs for her own use and for further distribution.
- Francene Aretha Gayle, MD, an Orlando, Fla., physician, was charged with conspiracy to unlawfully distribute controlled substances, conspiracy to commit health care fraud, health care fraud, and several substantive counts of illegally issuing opioid prescriptions. Dr. Gayle was charged along with Schara Monique Davis, a Huntsville, Ala.–based business manager. Per the indictment, Dr. Gayle and Ms. Davis operated three medical clinics in Alabama, where Dr. Gayle was the sole physician. The medical clinics billed health insurers for millions of dollars in patient visits that Dr. Gayle had supposedly conducted but during which she was allegedly absent from the clinics; other staff members conducted the visits instead. It’s alleged that Dr. Gayle presigned prescriptions for opioids that were given to patients.
- Robert Taffet, MD, a Haddonfield, N.J., orthopedic surgeon and owner of a medical practice in Sicklerville, N.J., was charged with conspiracy to unlawfully distribute controlled substances. The indictment alleges that he falsified patient files to state that he interacted with patients when he didn’t and that he issued prescriptions for opioids and other controlled substances without assessing the patients in person or by telemedicine. It’s alleged that Dr. Taffett issued prescriptions for more than 179,000 pills that were dispensed by New Jersey pharmacies between April 2020 and December 2021.
- Hau La, MD, a Brentwood, Tenn., family medicine physician and the operator of Absolute Medical Care in Smyrna, Tenn., was charged with sixteen counts of unlawful distribution of a controlled substance. The physician is alleged to have unlawfully prescribed opioids to eight patients outside the usual course of practice and without a legitimate medical purpose.
- Frederick De Mesa, of War, W.Va., practiced as a physician and used a DEA registration number that allowed him to prescribe controlled substances. Mr. De Mesa prescribed these substances without a medical license and didn’t have an active DEA registration number, according to the indictment.
- Loey Kousa, a former internist from Paintsville, Ky., was charged with unlawful distribution of controlled substances, healthcare fraud, and making false statements in connection with the delivery of health care services. The indictment alleges that the former physician issued prescriptions for opioids outside the usual course of professional practice and without a legitimate medical purpose in his capacity as owner and operator of East KY Clinic in Paintsville. He is alleged to have issued the unlawful prescriptions for patients whose treatments were covered by taxpayer-funded programs such as Medicare and Medicaid; he also billed these programs for medically unnecessary procedures for these patients.
Also included in the indictment were Jay Sadrinia, DMD, a Villa Hills, Ky., dentist, who was charged with four counts of illegal distribution of oxycodone and morphine sulfate and one count of illegal distribution of morphine sulfate that resulted in death or serious bodily injury; and Casey Kelleher, an owner-operator of Neighborhood Pharmacy in Boynton Beach, Fla., who allegedly sold large amounts of oxycodone and hydromorphone on the black market.
The Centers for Medicare & Medicaid Services’ Center for Program Integrity has taken six administrative actions against health care providers for their alleged involvement in these offenses, per the DOJ’s announcement.
“Patient care and safety are top priorities for us, and CMS has taken administrative action against six providers to protect critical resources entrusted to Medicare while also safeguarding people with Medicare,” said CMS Administrator Chiquita Brooks-LaSure.
“These actions to combat fraud, waste, and abuse in our federal programs would not be possible without the close and successful partnership of the Centers for Medicare & Medicaid Services, the Department of Justice, and the U.S. Department of Health and Human Services Office of Inspector General,” she added.
A version of this article first appeared on Medscape.com.
In coordination with federal and state law enforcement, the DOJ charged the defendants for their involvement in the illegal distribution of opioids. At the time that they were charged with the alleged offenses, 12 of the defendants were medical professionals.
The 12 persons in eight federal districts across the country distributed more than 115 million controlled substances, including buprenorphine, clonazepam, dextroamphetamine-amphetamine, hydrocodone, morphine sulfate, oxycodone, oxymorphone, and Suboxone, per the DOJ.
“Doctors and health care professionals are entrusted with prescribing medicine responsibly and in the best interests of their patients. Today’s takedown targets medical providers across the country whose greed drove them to abandon this responsibility in favor of criminal profits,” said Anne Milgram, administrator of the Drug Enforcement Administration.
Medical professionals, others across six states charged
One former nurse, one business manager, and one individual who practiced medicine without a medical credential are among those listed in the indictment. These include the following:
- Eskender Getachew, MD, a Columbus, Ohio, sleep medicine specialist, was charged with unlawful distribution of controlled substances outside the use of professional practice and not for a legitimate medical practice.
- Charles Kistler, DO, an Upper Arlington, Ohio, family practice physician, was charged with unlawful distribution of controlled substances for unlawful prescribing at Midtown Family Practice Clinic in Columbus.
- Yogeshwar Gil, MBBS, a Manchester, Tenn., family medicine doctor and owner of a medical practice, was charged with conspiracy to unlawfully distribute controlled substances and maintaining a drug-involved premises. Dr. Gil was charged in connection with an alleged scheme to distribute opioids and Suboxone outside the usual course of professional practice and without a legitimate medical purpose.
- Contessa Holley, RN, a Pulaski, Tenn., former nurse and clinical director, was charged with wire fraud, aggravated identity theft, and possession of a controlled substance with intent to distribute. She’s alleged to be connected with a scheme to unlawfully obtain opioids by filling fraudulent prescriptions in the names of current and former patients who were in hospice. The indictment alleged that Ms. Holley used the patients’ hospice benefits to cover the opioids’ costs while keeping the drugs for her own use and for further distribution.
- Francene Aretha Gayle, MD, an Orlando, Fla., physician, was charged with conspiracy to unlawfully distribute controlled substances, conspiracy to commit health care fraud, health care fraud, and several substantive counts of illegally issuing opioid prescriptions. Dr. Gayle was charged along with Schara Monique Davis, a Huntsville, Ala.–based business manager. Per the indictment, Dr. Gayle and Ms. Davis operated three medical clinics in Alabama, where Dr. Gayle was the sole physician. The medical clinics billed health insurers for millions of dollars in patient visits that Dr. Gayle had supposedly conducted but during which she was allegedly absent from the clinics; other staff members conducted the visits instead. It’s alleged that Dr. Gayle presigned prescriptions for opioids that were given to patients.
- Robert Taffet, MD, a Haddonfield, N.J., orthopedic surgeon and owner of a medical practice in Sicklerville, N.J., was charged with conspiracy to unlawfully distribute controlled substances. The indictment alleges that he falsified patient files to state that he interacted with patients when he didn’t and that he issued prescriptions for opioids and other controlled substances without assessing the patients in person or by telemedicine. It’s alleged that Dr. Taffett issued prescriptions for more than 179,000 pills that were dispensed by New Jersey pharmacies between April 2020 and December 2021.
- Hau La, MD, a Brentwood, Tenn., family medicine physician and the operator of Absolute Medical Care in Smyrna, Tenn., was charged with sixteen counts of unlawful distribution of a controlled substance. The physician is alleged to have unlawfully prescribed opioids to eight patients outside the usual course of practice and without a legitimate medical purpose.
- Frederick De Mesa, of War, W.Va., practiced as a physician and used a DEA registration number that allowed him to prescribe controlled substances. Mr. De Mesa prescribed these substances without a medical license and didn’t have an active DEA registration number, according to the indictment.
- Loey Kousa, a former internist from Paintsville, Ky., was charged with unlawful distribution of controlled substances, healthcare fraud, and making false statements in connection with the delivery of health care services. The indictment alleges that the former physician issued prescriptions for opioids outside the usual course of professional practice and without a legitimate medical purpose in his capacity as owner and operator of East KY Clinic in Paintsville. He is alleged to have issued the unlawful prescriptions for patients whose treatments were covered by taxpayer-funded programs such as Medicare and Medicaid; he also billed these programs for medically unnecessary procedures for these patients.
Also included in the indictment were Jay Sadrinia, DMD, a Villa Hills, Ky., dentist, who was charged with four counts of illegal distribution of oxycodone and morphine sulfate and one count of illegal distribution of morphine sulfate that resulted in death or serious bodily injury; and Casey Kelleher, an owner-operator of Neighborhood Pharmacy in Boynton Beach, Fla., who allegedly sold large amounts of oxycodone and hydromorphone on the black market.
The Centers for Medicare & Medicaid Services’ Center for Program Integrity has taken six administrative actions against health care providers for their alleged involvement in these offenses, per the DOJ’s announcement.
“Patient care and safety are top priorities for us, and CMS has taken administrative action against six providers to protect critical resources entrusted to Medicare while also safeguarding people with Medicare,” said CMS Administrator Chiquita Brooks-LaSure.
“These actions to combat fraud, waste, and abuse in our federal programs would not be possible without the close and successful partnership of the Centers for Medicare & Medicaid Services, the Department of Justice, and the U.S. Department of Health and Human Services Office of Inspector General,” she added.
A version of this article first appeared on Medscape.com.
Surgery handoffs still a risky juncture in care – but increasing communication can help
It involved a 70-year-old man who had a history of prostate cancer, obstructive sleep apnea, and hernias. In January, he had a surgery for hernia repair. On the 3rd day after the procedure, he was transferred to the hospital medicine service at about 9 p.m. and was on a patient-controlled pump for pain and had abdominal drains. Because of the extensive surgery and because he had begun to walk shortly after the procedure, he wasn’t on thrombosis prevention medication, Dr. Merli explained at the annual meeting of the American College of Physicians.
The day after his transfer he was walking with a physical therapist when he became short of breath, his oxygen saturation dropped, and his heart rate soared. Bilateral pulmonary emboli were found, along with thrombosis in the right leg.
What was remarkable, Dr. Merli noted, was what the patient’s medical record was lacking.
He added, “I think if we start looking at this at our sites, we may find out that communication needs to be improved, and I believe standardized.”
This situation underscores the continuing need to refine handoffs between surgery and hospital medicine, a point in care that is primed for potential errors, the other panelists noted during the session.
Most important information is often not communicated
A 2010 study in pediatrics that looked at intern-to-intern handoffs found that the most important piece of information wasn’t communicated successfully 60% of the time – in other words, more often than not, the person on the receiving end didn’t really understand that crucial part of the scenario. Since then, the literature has been regularly populated with studies attempting to refine handoff procedures.
Lily Ackermann, MD, hospitalist and clinical associate professor of medicine at Jefferson, said in the session that hospitalists need to be sure to reach out to surgery at important junctures in care.
“I would say the No. 1 biggest mistake we make is not calling the surgery attending directly when clinical questions arise,” she said. “I think this is very important – attending [physician in hospital medicine] to attending [physician in surgery].”
Murray Cohen, MD, director of acute care surgery at Jefferson, said he shared that concern.
“We want to be called, we want to be called for our patients,” he said in the session. “And we’re upset when you don’t call for our patients.”
Hospitalists should discuss blood loss, pain management, management of drains, deep vein thrombosis prevention, nutrition, infectious disease concerns, and timing of vaccines post procedure, Dr. Ackermann said during the presentation,
The panelists also emphasized that understanding the follow-up care that surgery was planning after a procedure is important, and to not just expect surgeons to actively follow a patient. They also reminded hospitalists to look at the wounds and make sure they understand how to handle the wounds going forward. Plus, when transferring a patient to surgery, hospitalists should understand when getting someone to surgery is urgent and not to order unnecessary tests as a formality when time is of the essence, they said.
IPASS: a formalized handoff process
The panelists all spoke highly of a formalized handoff process known as IPASS. This acronym reminds physicians to ask specific questions.
The I represents illness severity and calls for asking: “Is the patient stable or unstable?
The P stands for patient summary and is meant to prompt physicians to seek details about the procedure.
The A is for action list, which is meant to remind the physician to get the post-op plan for neurological, cardiovascular, gastrointestinal, and other areas.
The first S is for situational awareness, and calls for asking: What is the biggest concern over the next 24 hours?
The final S represents synthesis by the receiver, prompting a physician to summarize the information he or she has received about the patient.
Natalie Margules, MD, a clinical instructor and hospitalist at Jefferson who did not present in the session, reiterated the value of the IPASS system. Before it was used for handoffs, she said, “I was never taught anything formalized – basically, just ‘Tell them what’s important.’
Dr. Margules noted that she considers the framework’s call for the synthesis to be one of it most useful parts.
Dr. Merli, Dr. Ackermann, and Dr. Cohen reported no relevant financial disclosures.
It involved a 70-year-old man who had a history of prostate cancer, obstructive sleep apnea, and hernias. In January, he had a surgery for hernia repair. On the 3rd day after the procedure, he was transferred to the hospital medicine service at about 9 p.m. and was on a patient-controlled pump for pain and had abdominal drains. Because of the extensive surgery and because he had begun to walk shortly after the procedure, he wasn’t on thrombosis prevention medication, Dr. Merli explained at the annual meeting of the American College of Physicians.
The day after his transfer he was walking with a physical therapist when he became short of breath, his oxygen saturation dropped, and his heart rate soared. Bilateral pulmonary emboli were found, along with thrombosis in the right leg.
What was remarkable, Dr. Merli noted, was what the patient’s medical record was lacking.
He added, “I think if we start looking at this at our sites, we may find out that communication needs to be improved, and I believe standardized.”
This situation underscores the continuing need to refine handoffs between surgery and hospital medicine, a point in care that is primed for potential errors, the other panelists noted during the session.
Most important information is often not communicated
A 2010 study in pediatrics that looked at intern-to-intern handoffs found that the most important piece of information wasn’t communicated successfully 60% of the time – in other words, more often than not, the person on the receiving end didn’t really understand that crucial part of the scenario. Since then, the literature has been regularly populated with studies attempting to refine handoff procedures.
Lily Ackermann, MD, hospitalist and clinical associate professor of medicine at Jefferson, said in the session that hospitalists need to be sure to reach out to surgery at important junctures in care.
“I would say the No. 1 biggest mistake we make is not calling the surgery attending directly when clinical questions arise,” she said. “I think this is very important – attending [physician in hospital medicine] to attending [physician in surgery].”
Murray Cohen, MD, director of acute care surgery at Jefferson, said he shared that concern.
“We want to be called, we want to be called for our patients,” he said in the session. “And we’re upset when you don’t call for our patients.”
Hospitalists should discuss blood loss, pain management, management of drains, deep vein thrombosis prevention, nutrition, infectious disease concerns, and timing of vaccines post procedure, Dr. Ackermann said during the presentation,
The panelists also emphasized that understanding the follow-up care that surgery was planning after a procedure is important, and to not just expect surgeons to actively follow a patient. They also reminded hospitalists to look at the wounds and make sure they understand how to handle the wounds going forward. Plus, when transferring a patient to surgery, hospitalists should understand when getting someone to surgery is urgent and not to order unnecessary tests as a formality when time is of the essence, they said.
IPASS: a formalized handoff process
The panelists all spoke highly of a formalized handoff process known as IPASS. This acronym reminds physicians to ask specific questions.
The I represents illness severity and calls for asking: “Is the patient stable or unstable?
The P stands for patient summary and is meant to prompt physicians to seek details about the procedure.
The A is for action list, which is meant to remind the physician to get the post-op plan for neurological, cardiovascular, gastrointestinal, and other areas.
The first S is for situational awareness, and calls for asking: What is the biggest concern over the next 24 hours?
The final S represents synthesis by the receiver, prompting a physician to summarize the information he or she has received about the patient.
Natalie Margules, MD, a clinical instructor and hospitalist at Jefferson who did not present in the session, reiterated the value of the IPASS system. Before it was used for handoffs, she said, “I was never taught anything formalized – basically, just ‘Tell them what’s important.’
Dr. Margules noted that she considers the framework’s call for the synthesis to be one of it most useful parts.
Dr. Merli, Dr. Ackermann, and Dr. Cohen reported no relevant financial disclosures.
It involved a 70-year-old man who had a history of prostate cancer, obstructive sleep apnea, and hernias. In January, he had a surgery for hernia repair. On the 3rd day after the procedure, he was transferred to the hospital medicine service at about 9 p.m. and was on a patient-controlled pump for pain and had abdominal drains. Because of the extensive surgery and because he had begun to walk shortly after the procedure, he wasn’t on thrombosis prevention medication, Dr. Merli explained at the annual meeting of the American College of Physicians.
The day after his transfer he was walking with a physical therapist when he became short of breath, his oxygen saturation dropped, and his heart rate soared. Bilateral pulmonary emboli were found, along with thrombosis in the right leg.
What was remarkable, Dr. Merli noted, was what the patient’s medical record was lacking.
He added, “I think if we start looking at this at our sites, we may find out that communication needs to be improved, and I believe standardized.”
This situation underscores the continuing need to refine handoffs between surgery and hospital medicine, a point in care that is primed for potential errors, the other panelists noted during the session.
Most important information is often not communicated
A 2010 study in pediatrics that looked at intern-to-intern handoffs found that the most important piece of information wasn’t communicated successfully 60% of the time – in other words, more often than not, the person on the receiving end didn’t really understand that crucial part of the scenario. Since then, the literature has been regularly populated with studies attempting to refine handoff procedures.
Lily Ackermann, MD, hospitalist and clinical associate professor of medicine at Jefferson, said in the session that hospitalists need to be sure to reach out to surgery at important junctures in care.
“I would say the No. 1 biggest mistake we make is not calling the surgery attending directly when clinical questions arise,” she said. “I think this is very important – attending [physician in hospital medicine] to attending [physician in surgery].”
Murray Cohen, MD, director of acute care surgery at Jefferson, said he shared that concern.
“We want to be called, we want to be called for our patients,” he said in the session. “And we’re upset when you don’t call for our patients.”
Hospitalists should discuss blood loss, pain management, management of drains, deep vein thrombosis prevention, nutrition, infectious disease concerns, and timing of vaccines post procedure, Dr. Ackermann said during the presentation,
The panelists also emphasized that understanding the follow-up care that surgery was planning after a procedure is important, and to not just expect surgeons to actively follow a patient. They also reminded hospitalists to look at the wounds and make sure they understand how to handle the wounds going forward. Plus, when transferring a patient to surgery, hospitalists should understand when getting someone to surgery is urgent and not to order unnecessary tests as a formality when time is of the essence, they said.
IPASS: a formalized handoff process
The panelists all spoke highly of a formalized handoff process known as IPASS. This acronym reminds physicians to ask specific questions.
The I represents illness severity and calls for asking: “Is the patient stable or unstable?
The P stands for patient summary and is meant to prompt physicians to seek details about the procedure.
The A is for action list, which is meant to remind the physician to get the post-op plan for neurological, cardiovascular, gastrointestinal, and other areas.
The first S is for situational awareness, and calls for asking: What is the biggest concern over the next 24 hours?
The final S represents synthesis by the receiver, prompting a physician to summarize the information he or she has received about the patient.
Natalie Margules, MD, a clinical instructor and hospitalist at Jefferson who did not present in the session, reiterated the value of the IPASS system. Before it was used for handoffs, she said, “I was never taught anything formalized – basically, just ‘Tell them what’s important.’
Dr. Margules noted that she considers the framework’s call for the synthesis to be one of it most useful parts.
Dr. Merli, Dr. Ackermann, and Dr. Cohen reported no relevant financial disclosures.
AT INTERNAL MEDICINE 2022
Burnout ‘highly prevalent’ in psychiatrists across the globe
Burnout in psychiatrists is “highly prevalent” across the globe, new research shows.
In a review and meta-analysis of 36 studies and more than 5,000 psychiatrists in European countries, as well as the United States, Australia, New Zealand, India, Turkey, and Thailand,
“Our review showed that regardless of the identification method of burnout, its prevalence among psychiatrists is high and ranges from 25% to 50%,” lead author Kirill Bykov, MD, a PhD candidate at the Peoples’ Friendship University of Russia (RUDN University), Moscow, Russian Federation, told this news organization.
There was a “high heterogeneity of studies in terms of statistics, screening methods, burnout definitions, and cutoff points in the included studies, which necessitates the unification of future research methodology, but not to the detriment of the development of the theoretical background,” Dr. Bykov said.
The findings were published online in the Journal of Affective Disorders.
‘Unresolved problem’
Although burnout is a serious and prevalent problem among health care workers, little research has focused on burnout in mental health workers compared with other professionals, the investigators noted.
A previous systematic review and meta-analysis that focused specifically on burnout in psychiatrists was limited by methodologic concerns, including that the only burnout screening instrument used in the included studies was the full-length (22-item) MBI.
The current researchers surmised that “the integration of different empirical studies of psychiatrists’ burnout prevalence [remained] an unresolved problem.”
Dr. Bykov noted the current review was “investigator-initiated” and was a part of his PhD dissertation.
“Studying the works devoted to the burnout of psychiatrists, I drew attention to the varying prevalence rates of this phenomenon among them. This prompted me to conduct a systematic review of the literature and summarize the available data,” he said.
Unlike the previous review, the current one “does not contain restrictions regarding the place of research, publication language, covered burnout concepts, definitions, and screening instruments. Thus, its results will be helpful for practitioners and scientists around the world,” Dr. Bykov added.
Among the inclusion criteria was that a study should be empirical and quantitative, contain at least 20 practicing psychiatrists as participants, use a valid and reliable burnout screening instrument, have at least one burnout metric extractable specifically with regard to psychiatrists, and have a national survey or a response rate among psychiatrists of 20% or greater.
Qualitative or review articles or studies consisting of psychiatric trainees (such as medical students or residents) or nonpracticing psychiatrists were excluded.
Pooled prevalence
The researchers included 36 studies that comprised 5,481 participants (51.3% were women; mean age, 46.7 years). All studies had from 20 to 1,157 participants. They were employed in an array of settings in 19 countries.
In 22 studies, survey years ranged from 1996 to 2018; 14 studies did not report the year of data collection.
Most studies (75%) used some version of the MBI, and 19 studies used the full-length 22-item MBI Human Service Survey (MBI-HSS) . The survey rates emotional exhaustion (EE), depersonalization (DP), and low personal achievement (PA) on a 7-point Likert scale from 0 (“never”) to 6 (“almost every day”).
Other instruments included the CBI, the 16-item Oldenburg Burnout Inventory, the 21-item Tedium Measure, the 30-item Professional Quality of Life measure, the Rohland et al. Single-Item Measure of Self-Perceived Burnout, and the 21-item Brief Burnout Questionnaire.
Only three studies were free of methodologic limitations. The remaining 33 studies had some problems, such as not reporting the response rate or comparability between responders and nonresponders.
Results showed that the overall prevalence of burnout, as measured by the MBI and the CBI, was 25.9% (range, 11.1%-40.75%) and 50.3% (range, 30.9%-69.8%), respectively.
The pooled prevalence for burnout components is shown in the table.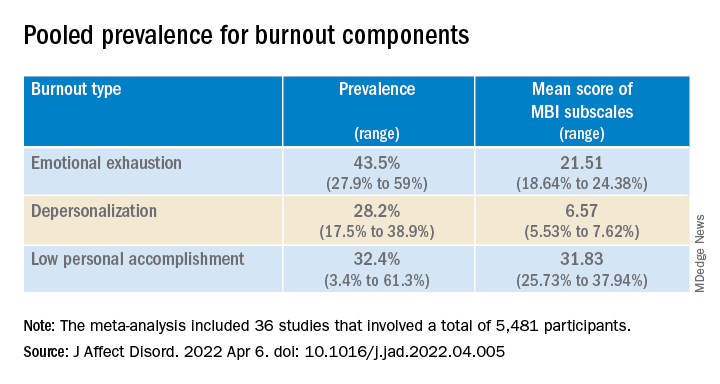
European psychiatrists had lower EE scores (20.82; 95% confidence interval, 7.24-4.41) compared with their non-European counterparts (24.99; 95% CI, 23.05-26.94; P = .045).
‘Carry the hope’
In a comment, Christine Crawford, MD, associate medical director of the National Alliance on Mental Illness (NAMI), said she was surprised the burnout numbers weren’t higher.
Many colleagues she interacts with “have been experiencing pretty significant burnout that has only been exacerbated by the pandemic and ever-growing demand for mental health providers, and there aren’t enough to meet that demand,” said Dr. Crawford, a psychiatrist at Boston Medical Center’s Outpatient Child and Adolescent Psychiatry Clinic and at Codman Square Health Center. She was not involved with the current research.
Dr. Crawford noted that much of the data was from Europeans. Speaking to the experience of U.S.-based psychiatrists, she said there is a “greater appreciation for what we do as mental health providers, due to the growing conversations around mental health and normalizing mental health conditions.”
On the other hand, there is “a lack of parity in reimbursement rates. Although the general public values mental health, the medical system doesn’t value mental health providers in the same way as physicians in other specialties,” Dr. Crawford said. Feeling devalued can contribute to burnout, she added.
One way to counter burnout is to remember “that our role is to carry the hope. We can be hopeful for the patient that the treatment will work or the medications can provide some relief,” Dr. Crawford noted.
Psychiatrists “may need to hold on tightly to that hope because we may not receive that instant gratification from the patient or receive praise or see the change from the patient during that time, which can be challenging,” she said.
“But it’s important for us to keep in mind that, even in that moment when the patient can’t see it, we can work alongside the patient to create the vision of hope and what it will look like in the future,” said Dr. Crawford.
In the 2022 Medscape Psychiatrist Lifestyle, Happiness & Burnout Report, an annual online survey of Medscape member physicians, 47% of respondents reported burnout – which was up from 42% the previous year.
The investigators received no funding for this work. They and Dr. Crawford report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Burnout in psychiatrists is “highly prevalent” across the globe, new research shows.
In a review and meta-analysis of 36 studies and more than 5,000 psychiatrists in European countries, as well as the United States, Australia, New Zealand, India, Turkey, and Thailand,
“Our review showed that regardless of the identification method of burnout, its prevalence among psychiatrists is high and ranges from 25% to 50%,” lead author Kirill Bykov, MD, a PhD candidate at the Peoples’ Friendship University of Russia (RUDN University), Moscow, Russian Federation, told this news organization.
There was a “high heterogeneity of studies in terms of statistics, screening methods, burnout definitions, and cutoff points in the included studies, which necessitates the unification of future research methodology, but not to the detriment of the development of the theoretical background,” Dr. Bykov said.
The findings were published online in the Journal of Affective Disorders.
‘Unresolved problem’
Although burnout is a serious and prevalent problem among health care workers, little research has focused on burnout in mental health workers compared with other professionals, the investigators noted.
A previous systematic review and meta-analysis that focused specifically on burnout in psychiatrists was limited by methodologic concerns, including that the only burnout screening instrument used in the included studies was the full-length (22-item) MBI.
The current researchers surmised that “the integration of different empirical studies of psychiatrists’ burnout prevalence [remained] an unresolved problem.”
Dr. Bykov noted the current review was “investigator-initiated” and was a part of his PhD dissertation.
“Studying the works devoted to the burnout of psychiatrists, I drew attention to the varying prevalence rates of this phenomenon among them. This prompted me to conduct a systematic review of the literature and summarize the available data,” he said.
Unlike the previous review, the current one “does not contain restrictions regarding the place of research, publication language, covered burnout concepts, definitions, and screening instruments. Thus, its results will be helpful for practitioners and scientists around the world,” Dr. Bykov added.
Among the inclusion criteria was that a study should be empirical and quantitative, contain at least 20 practicing psychiatrists as participants, use a valid and reliable burnout screening instrument, have at least one burnout metric extractable specifically with regard to psychiatrists, and have a national survey or a response rate among psychiatrists of 20% or greater.
Qualitative or review articles or studies consisting of psychiatric trainees (such as medical students or residents) or nonpracticing psychiatrists were excluded.
Pooled prevalence
The researchers included 36 studies that comprised 5,481 participants (51.3% were women; mean age, 46.7 years). All studies had from 20 to 1,157 participants. They were employed in an array of settings in 19 countries.
In 22 studies, survey years ranged from 1996 to 2018; 14 studies did not report the year of data collection.
Most studies (75%) used some version of the MBI, and 19 studies used the full-length 22-item MBI Human Service Survey (MBI-HSS) . The survey rates emotional exhaustion (EE), depersonalization (DP), and low personal achievement (PA) on a 7-point Likert scale from 0 (“never”) to 6 (“almost every day”).
Other instruments included the CBI, the 16-item Oldenburg Burnout Inventory, the 21-item Tedium Measure, the 30-item Professional Quality of Life measure, the Rohland et al. Single-Item Measure of Self-Perceived Burnout, and the 21-item Brief Burnout Questionnaire.
Only three studies were free of methodologic limitations. The remaining 33 studies had some problems, such as not reporting the response rate or comparability between responders and nonresponders.
Results showed that the overall prevalence of burnout, as measured by the MBI and the CBI, was 25.9% (range, 11.1%-40.75%) and 50.3% (range, 30.9%-69.8%), respectively.
The pooled prevalence for burnout components is shown in the table.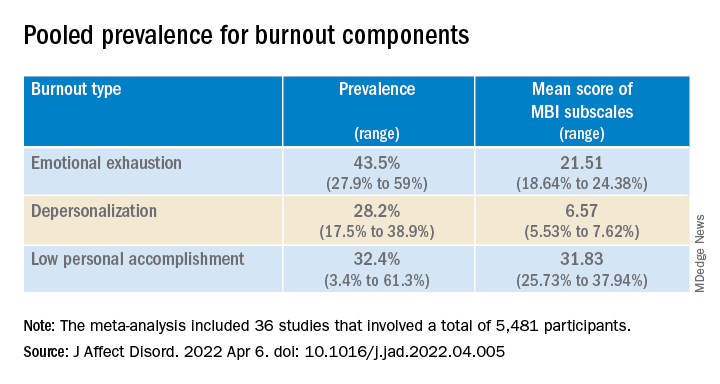
European psychiatrists had lower EE scores (20.82; 95% confidence interval, 7.24-4.41) compared with their non-European counterparts (24.99; 95% CI, 23.05-26.94; P = .045).
‘Carry the hope’
In a comment, Christine Crawford, MD, associate medical director of the National Alliance on Mental Illness (NAMI), said she was surprised the burnout numbers weren’t higher.
Many colleagues she interacts with “have been experiencing pretty significant burnout that has only been exacerbated by the pandemic and ever-growing demand for mental health providers, and there aren’t enough to meet that demand,” said Dr. Crawford, a psychiatrist at Boston Medical Center’s Outpatient Child and Adolescent Psychiatry Clinic and at Codman Square Health Center. She was not involved with the current research.
Dr. Crawford noted that much of the data was from Europeans. Speaking to the experience of U.S.-based psychiatrists, she said there is a “greater appreciation for what we do as mental health providers, due to the growing conversations around mental health and normalizing mental health conditions.”
On the other hand, there is “a lack of parity in reimbursement rates. Although the general public values mental health, the medical system doesn’t value mental health providers in the same way as physicians in other specialties,” Dr. Crawford said. Feeling devalued can contribute to burnout, she added.
One way to counter burnout is to remember “that our role is to carry the hope. We can be hopeful for the patient that the treatment will work or the medications can provide some relief,” Dr. Crawford noted.
Psychiatrists “may need to hold on tightly to that hope because we may not receive that instant gratification from the patient or receive praise or see the change from the patient during that time, which can be challenging,” she said.
“But it’s important for us to keep in mind that, even in that moment when the patient can’t see it, we can work alongside the patient to create the vision of hope and what it will look like in the future,” said Dr. Crawford.
In the 2022 Medscape Psychiatrist Lifestyle, Happiness & Burnout Report, an annual online survey of Medscape member physicians, 47% of respondents reported burnout – which was up from 42% the previous year.
The investigators received no funding for this work. They and Dr. Crawford report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Burnout in psychiatrists is “highly prevalent” across the globe, new research shows.
In a review and meta-analysis of 36 studies and more than 5,000 psychiatrists in European countries, as well as the United States, Australia, New Zealand, India, Turkey, and Thailand,
“Our review showed that regardless of the identification method of burnout, its prevalence among psychiatrists is high and ranges from 25% to 50%,” lead author Kirill Bykov, MD, a PhD candidate at the Peoples’ Friendship University of Russia (RUDN University), Moscow, Russian Federation, told this news organization.
There was a “high heterogeneity of studies in terms of statistics, screening methods, burnout definitions, and cutoff points in the included studies, which necessitates the unification of future research methodology, but not to the detriment of the development of the theoretical background,” Dr. Bykov said.
The findings were published online in the Journal of Affective Disorders.
‘Unresolved problem’
Although burnout is a serious and prevalent problem among health care workers, little research has focused on burnout in mental health workers compared with other professionals, the investigators noted.
A previous systematic review and meta-analysis that focused specifically on burnout in psychiatrists was limited by methodologic concerns, including that the only burnout screening instrument used in the included studies was the full-length (22-item) MBI.
The current researchers surmised that “the integration of different empirical studies of psychiatrists’ burnout prevalence [remained] an unresolved problem.”
Dr. Bykov noted the current review was “investigator-initiated” and was a part of his PhD dissertation.
“Studying the works devoted to the burnout of psychiatrists, I drew attention to the varying prevalence rates of this phenomenon among them. This prompted me to conduct a systematic review of the literature and summarize the available data,” he said.
Unlike the previous review, the current one “does not contain restrictions regarding the place of research, publication language, covered burnout concepts, definitions, and screening instruments. Thus, its results will be helpful for practitioners and scientists around the world,” Dr. Bykov added.
Among the inclusion criteria was that a study should be empirical and quantitative, contain at least 20 practicing psychiatrists as participants, use a valid and reliable burnout screening instrument, have at least one burnout metric extractable specifically with regard to psychiatrists, and have a national survey or a response rate among psychiatrists of 20% or greater.
Qualitative or review articles or studies consisting of psychiatric trainees (such as medical students or residents) or nonpracticing psychiatrists were excluded.
Pooled prevalence
The researchers included 36 studies that comprised 5,481 participants (51.3% were women; mean age, 46.7 years). All studies had from 20 to 1,157 participants. They were employed in an array of settings in 19 countries.
In 22 studies, survey years ranged from 1996 to 2018; 14 studies did not report the year of data collection.
Most studies (75%) used some version of the MBI, and 19 studies used the full-length 22-item MBI Human Service Survey (MBI-HSS) . The survey rates emotional exhaustion (EE), depersonalization (DP), and low personal achievement (PA) on a 7-point Likert scale from 0 (“never”) to 6 (“almost every day”).
Other instruments included the CBI, the 16-item Oldenburg Burnout Inventory, the 21-item Tedium Measure, the 30-item Professional Quality of Life measure, the Rohland et al. Single-Item Measure of Self-Perceived Burnout, and the 21-item Brief Burnout Questionnaire.
Only three studies were free of methodologic limitations. The remaining 33 studies had some problems, such as not reporting the response rate or comparability between responders and nonresponders.
Results showed that the overall prevalence of burnout, as measured by the MBI and the CBI, was 25.9% (range, 11.1%-40.75%) and 50.3% (range, 30.9%-69.8%), respectively.
The pooled prevalence for burnout components is shown in the table.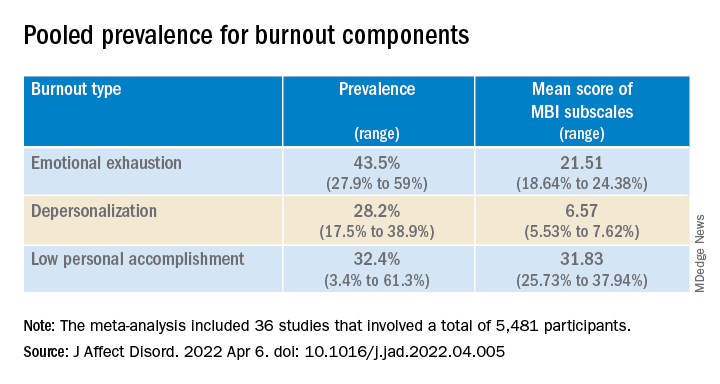
European psychiatrists had lower EE scores (20.82; 95% confidence interval, 7.24-4.41) compared with their non-European counterparts (24.99; 95% CI, 23.05-26.94; P = .045).
‘Carry the hope’
In a comment, Christine Crawford, MD, associate medical director of the National Alliance on Mental Illness (NAMI), said she was surprised the burnout numbers weren’t higher.
Many colleagues she interacts with “have been experiencing pretty significant burnout that has only been exacerbated by the pandemic and ever-growing demand for mental health providers, and there aren’t enough to meet that demand,” said Dr. Crawford, a psychiatrist at Boston Medical Center’s Outpatient Child and Adolescent Psychiatry Clinic and at Codman Square Health Center. She was not involved with the current research.
Dr. Crawford noted that much of the data was from Europeans. Speaking to the experience of U.S.-based psychiatrists, she said there is a “greater appreciation for what we do as mental health providers, due to the growing conversations around mental health and normalizing mental health conditions.”
On the other hand, there is “a lack of parity in reimbursement rates. Although the general public values mental health, the medical system doesn’t value mental health providers in the same way as physicians in other specialties,” Dr. Crawford said. Feeling devalued can contribute to burnout, she added.
One way to counter burnout is to remember “that our role is to carry the hope. We can be hopeful for the patient that the treatment will work or the medications can provide some relief,” Dr. Crawford noted.
Psychiatrists “may need to hold on tightly to that hope because we may not receive that instant gratification from the patient or receive praise or see the change from the patient during that time, which can be challenging,” she said.
“But it’s important for us to keep in mind that, even in that moment when the patient can’t see it, we can work alongside the patient to create the vision of hope and what it will look like in the future,” said Dr. Crawford.
In the 2022 Medscape Psychiatrist Lifestyle, Happiness & Burnout Report, an annual online survey of Medscape member physicians, 47% of respondents reported burnout – which was up from 42% the previous year.
The investigators received no funding for this work. They and Dr. Crawford report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF AFFECTIVE DISORDERS
Abortion politics lead to power struggles over family planning grants
BOZEMAN, Mont. – In a busy downtown coffee shop, a drawing of a ski lift with intrauterine devices for chairs draws the eyes of sleepy customers getting their morning underway with a caffeine jolt.
The flyer touts the services of Bridgercare, a nonprofit reproductive health clinic a few miles up the road. The clinic offers wellness exams, birth control, and LGBTQ+ services – and, starting in April, it oversees the state’s multimillion-dollar share of federal family planning program funding.
In March, Bridgercare beat out the state health department to become administrator of Montana’s $2.3 million Title X program, which helps pay for family planning and preventive health services. The organization applied for the grant because its leaders were concerned about a new state law that sought to restrict which local providers are funded.
What is happening in Montana is the latest example of an ongoing power struggle between nonprofits and conservative-leaning states over who receives federal family planning money. That has intensified in recent years as the Title X program has increasingly become entangled with the politics of abortion.
This year, the federal government set aside $257 million for family planning and preventive care. The providers that get that funding often serve families with low incomes, and Title X is one of the few federal programs in which people without legal permission to be in the United States can participate.
“The program permeates into communities that otherwise would be unreached by public health efforts,” said Rebecca Kreitzer, an associate professor of public policy at the University of North Carolina at Chapel Hill.
The Montana Department of Public Health and Human Services controlled the distribution of the state’s Title X funds for decades. Bridgercare sought the administrator role to circumvent a Republican-sponsored law passed last year that required the state to prioritize the money for local health departments and federally qualified health centers. That would have put the nonprofit – which doesn’t provide abortion procedures – and similar organizations at the bottom of the list. The law also banned clinics that perform abortions from receiving Title X funds from the state health department.
Bridgercare Executive Director Stephanie McDowell said the group applied for the grant to try to protect the program from decisions coming out of the state capitol. “Because of the politicization of Title X, we’re seeing how it’s run, swinging back and forth based on partisan leadership,” Ms. McDowell said.
A U.S. Department of Health & Human Services spokesperson, Tara Broido, didn’t answer a question about whether the agency intentionally awarded grants to nonprofits to avoid state politics. Instead, she said in a statement that applicants were evaluated in a competitive process by a panel of independent reviewers based on criteria to deliver high-quality, client-centered services.
Federal law prohibits the money from being used to perform abortions. But it can cover other services provided by groups that offer abortions – the largest and best-known by far is Planned Parenthood. In recent years, conservative politicians have tried to keep such providers from receiving Title X funding.
In some cases, contraception has entered the debate around which family planning services government should help fund. Some abortion opponents have raised concerns that long-lasting forms of birth control, such as IUDs, lead to abortions. Those claims are disputed by reproductive health experts.
In 2019, the Trump administration introduced several new rules for Title X, including disqualifying from receiving the funding family planning clinics that also offered abortion services or referrals. Many clinics across the nation left the program instead of conforming to the rules. Simultaneously, the spread of COVID-19 interrupted routine care. The number of patients served by Title X plummeted.
The Biden administration reversed most of those rules, including allowing providers with abortion services back into the Title X program. States also try to influence the funding’s reach, either through legislation or budget rules.
The current Title X funding cycle is 5 years, and the amount of money available each year could shift based on the state’s network of providers or federal budget changes. Jon Ebelt, a spokesperson for the Montana Department of Public Health and Human Services, didn’t answer when asked whether the state planned to reapply to administer the funding in 2027. He said the department was disappointed with the Biden administration’s “refusal” to renew the state’s funding.
“We recognize, however, that recent proabortion federal rule changes have distorted Title X and conflict with Montana law,” he said.
Conservative states have been tangling with nonprofits and the federal government over Title X funding for more than a decade. In 2011, during the Obama administration, Texas whittled down the state’s family planning spending and prioritized sending the federal money to general primary care providers over reproductive health clinics. As a result, 25% of family planning clinics in Texas closed. In 2013, a nonprofit now called Every Body Texas joined the competition to distribute the state’s Title X dollars and won.
“Filling and rebuilding those holes have taken this last decade, essentially,” said Berna Mason, director of service delivery improvement for Every Body Texas.
In 2019, the governor of Nebraska proposed a budget that would have prohibited the money from going to any organization that provided abortions or referred patients for abortions outside of an emergency. It also would have required that funding recipients be legally and financially separate from such clinics, a restriction that would have gone further than the Trump administration’s rules. Afterward, a family planning council won the right to administer Title X money.
In 2017, the nonprofit Arizona Family Health Partnership lost its status as that state’s only Title X administrator when the state health department was given 25% of the funding to deliver to providers. That came after Arizona lawmakers ordered the department to apply for the funds and distribute them first to state- or county-owned clinics, with the remaining money going to primary care facilities. The change was backed by groups that were opposed to abortion, and reproductive health care providers saw it as an attempt to weaken clinics that offer abortion services.
However, the state left nearly all the money it received untouched, and although it’s still required by law to apply for Title X funding, it hasn’t received a portion of the grant since.
Bré Thomas, CEO of Arizona Family Health Partnership, said that, even though the nonprofit is the sole administrator of the Title X funding again, the threat remains that some or all could be taken away because of politics. “We’re at the will of who’s in charge,” Ms. Thomas said.
Nonprofits say they have an advantage over state agencies in expanding services because they have more flexibility in fundraising and fewer administrative hurdles.
In April, Mississippi nonprofit Converge took over administration of Title X funds, a role the state had held for decades. The organization’s founders said they weren’t worried that conservative politicians would restrict access to services but simply believed they could do a better job. “Service quality was very low, and it was very hard to get appointments,” said cofounder Danielle Lampton.
A Mississippi State Department of Health spokesperson, Liz Sharlot, said the agency looks forward to working with Converge.
In Montana, Bridgercare plans to restore funding to Planned Parenthood clinics that have been cut off from the program since 2019, recruit more health centers to participate, and expand the program’s reach in rural, frontier, and tribal communities using telehealth services, Ms. McDowell said.
The organization’s goal is to increase the number of patients benefiting from the federal program by at least 10% in each year of the 5-year grant cycle. The clinic also plans to apply to keep its Title X role beyond this grant.
“In 5 years, our grant application should be a clear front-runner for funding,” she said. “It’s less about ‘How do we beat someone in 5 years?’ And more about ‘How do we grow this program to serve patients?’”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
BOZEMAN, Mont. – In a busy downtown coffee shop, a drawing of a ski lift with intrauterine devices for chairs draws the eyes of sleepy customers getting their morning underway with a caffeine jolt.
The flyer touts the services of Bridgercare, a nonprofit reproductive health clinic a few miles up the road. The clinic offers wellness exams, birth control, and LGBTQ+ services – and, starting in April, it oversees the state’s multimillion-dollar share of federal family planning program funding.
In March, Bridgercare beat out the state health department to become administrator of Montana’s $2.3 million Title X program, which helps pay for family planning and preventive health services. The organization applied for the grant because its leaders were concerned about a new state law that sought to restrict which local providers are funded.
What is happening in Montana is the latest example of an ongoing power struggle between nonprofits and conservative-leaning states over who receives federal family planning money. That has intensified in recent years as the Title X program has increasingly become entangled with the politics of abortion.
This year, the federal government set aside $257 million for family planning and preventive care. The providers that get that funding often serve families with low incomes, and Title X is one of the few federal programs in which people without legal permission to be in the United States can participate.
“The program permeates into communities that otherwise would be unreached by public health efforts,” said Rebecca Kreitzer, an associate professor of public policy at the University of North Carolina at Chapel Hill.
The Montana Department of Public Health and Human Services controlled the distribution of the state’s Title X funds for decades. Bridgercare sought the administrator role to circumvent a Republican-sponsored law passed last year that required the state to prioritize the money for local health departments and federally qualified health centers. That would have put the nonprofit – which doesn’t provide abortion procedures – and similar organizations at the bottom of the list. The law also banned clinics that perform abortions from receiving Title X funds from the state health department.
Bridgercare Executive Director Stephanie McDowell said the group applied for the grant to try to protect the program from decisions coming out of the state capitol. “Because of the politicization of Title X, we’re seeing how it’s run, swinging back and forth based on partisan leadership,” Ms. McDowell said.
A U.S. Department of Health & Human Services spokesperson, Tara Broido, didn’t answer a question about whether the agency intentionally awarded grants to nonprofits to avoid state politics. Instead, she said in a statement that applicants were evaluated in a competitive process by a panel of independent reviewers based on criteria to deliver high-quality, client-centered services.
Federal law prohibits the money from being used to perform abortions. But it can cover other services provided by groups that offer abortions – the largest and best-known by far is Planned Parenthood. In recent years, conservative politicians have tried to keep such providers from receiving Title X funding.
In some cases, contraception has entered the debate around which family planning services government should help fund. Some abortion opponents have raised concerns that long-lasting forms of birth control, such as IUDs, lead to abortions. Those claims are disputed by reproductive health experts.
In 2019, the Trump administration introduced several new rules for Title X, including disqualifying from receiving the funding family planning clinics that also offered abortion services or referrals. Many clinics across the nation left the program instead of conforming to the rules. Simultaneously, the spread of COVID-19 interrupted routine care. The number of patients served by Title X plummeted.
The Biden administration reversed most of those rules, including allowing providers with abortion services back into the Title X program. States also try to influence the funding’s reach, either through legislation or budget rules.
The current Title X funding cycle is 5 years, and the amount of money available each year could shift based on the state’s network of providers or federal budget changes. Jon Ebelt, a spokesperson for the Montana Department of Public Health and Human Services, didn’t answer when asked whether the state planned to reapply to administer the funding in 2027. He said the department was disappointed with the Biden administration’s “refusal” to renew the state’s funding.
“We recognize, however, that recent proabortion federal rule changes have distorted Title X and conflict with Montana law,” he said.
Conservative states have been tangling with nonprofits and the federal government over Title X funding for more than a decade. In 2011, during the Obama administration, Texas whittled down the state’s family planning spending and prioritized sending the federal money to general primary care providers over reproductive health clinics. As a result, 25% of family planning clinics in Texas closed. In 2013, a nonprofit now called Every Body Texas joined the competition to distribute the state’s Title X dollars and won.
“Filling and rebuilding those holes have taken this last decade, essentially,” said Berna Mason, director of service delivery improvement for Every Body Texas.
In 2019, the governor of Nebraska proposed a budget that would have prohibited the money from going to any organization that provided abortions or referred patients for abortions outside of an emergency. It also would have required that funding recipients be legally and financially separate from such clinics, a restriction that would have gone further than the Trump administration’s rules. Afterward, a family planning council won the right to administer Title X money.
In 2017, the nonprofit Arizona Family Health Partnership lost its status as that state’s only Title X administrator when the state health department was given 25% of the funding to deliver to providers. That came after Arizona lawmakers ordered the department to apply for the funds and distribute them first to state- or county-owned clinics, with the remaining money going to primary care facilities. The change was backed by groups that were opposed to abortion, and reproductive health care providers saw it as an attempt to weaken clinics that offer abortion services.
However, the state left nearly all the money it received untouched, and although it’s still required by law to apply for Title X funding, it hasn’t received a portion of the grant since.
Bré Thomas, CEO of Arizona Family Health Partnership, said that, even though the nonprofit is the sole administrator of the Title X funding again, the threat remains that some or all could be taken away because of politics. “We’re at the will of who’s in charge,” Ms. Thomas said.
Nonprofits say they have an advantage over state agencies in expanding services because they have more flexibility in fundraising and fewer administrative hurdles.
In April, Mississippi nonprofit Converge took over administration of Title X funds, a role the state had held for decades. The organization’s founders said they weren’t worried that conservative politicians would restrict access to services but simply believed they could do a better job. “Service quality was very low, and it was very hard to get appointments,” said cofounder Danielle Lampton.
A Mississippi State Department of Health spokesperson, Liz Sharlot, said the agency looks forward to working with Converge.
In Montana, Bridgercare plans to restore funding to Planned Parenthood clinics that have been cut off from the program since 2019, recruit more health centers to participate, and expand the program’s reach in rural, frontier, and tribal communities using telehealth services, Ms. McDowell said.
The organization’s goal is to increase the number of patients benefiting from the federal program by at least 10% in each year of the 5-year grant cycle. The clinic also plans to apply to keep its Title X role beyond this grant.
“In 5 years, our grant application should be a clear front-runner for funding,” she said. “It’s less about ‘How do we beat someone in 5 years?’ And more about ‘How do we grow this program to serve patients?’”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
BOZEMAN, Mont. – In a busy downtown coffee shop, a drawing of a ski lift with intrauterine devices for chairs draws the eyes of sleepy customers getting their morning underway with a caffeine jolt.
The flyer touts the services of Bridgercare, a nonprofit reproductive health clinic a few miles up the road. The clinic offers wellness exams, birth control, and LGBTQ+ services – and, starting in April, it oversees the state’s multimillion-dollar share of federal family planning program funding.
In March, Bridgercare beat out the state health department to become administrator of Montana’s $2.3 million Title X program, which helps pay for family planning and preventive health services. The organization applied for the grant because its leaders were concerned about a new state law that sought to restrict which local providers are funded.
What is happening in Montana is the latest example of an ongoing power struggle between nonprofits and conservative-leaning states over who receives federal family planning money. That has intensified in recent years as the Title X program has increasingly become entangled with the politics of abortion.
This year, the federal government set aside $257 million for family planning and preventive care. The providers that get that funding often serve families with low incomes, and Title X is one of the few federal programs in which people without legal permission to be in the United States can participate.
“The program permeates into communities that otherwise would be unreached by public health efforts,” said Rebecca Kreitzer, an associate professor of public policy at the University of North Carolina at Chapel Hill.
The Montana Department of Public Health and Human Services controlled the distribution of the state’s Title X funds for decades. Bridgercare sought the administrator role to circumvent a Republican-sponsored law passed last year that required the state to prioritize the money for local health departments and federally qualified health centers. That would have put the nonprofit – which doesn’t provide abortion procedures – and similar organizations at the bottom of the list. The law also banned clinics that perform abortions from receiving Title X funds from the state health department.
Bridgercare Executive Director Stephanie McDowell said the group applied for the grant to try to protect the program from decisions coming out of the state capitol. “Because of the politicization of Title X, we’re seeing how it’s run, swinging back and forth based on partisan leadership,” Ms. McDowell said.
A U.S. Department of Health & Human Services spokesperson, Tara Broido, didn’t answer a question about whether the agency intentionally awarded grants to nonprofits to avoid state politics. Instead, she said in a statement that applicants were evaluated in a competitive process by a panel of independent reviewers based on criteria to deliver high-quality, client-centered services.
Federal law prohibits the money from being used to perform abortions. But it can cover other services provided by groups that offer abortions – the largest and best-known by far is Planned Parenthood. In recent years, conservative politicians have tried to keep such providers from receiving Title X funding.
In some cases, contraception has entered the debate around which family planning services government should help fund. Some abortion opponents have raised concerns that long-lasting forms of birth control, such as IUDs, lead to abortions. Those claims are disputed by reproductive health experts.
In 2019, the Trump administration introduced several new rules for Title X, including disqualifying from receiving the funding family planning clinics that also offered abortion services or referrals. Many clinics across the nation left the program instead of conforming to the rules. Simultaneously, the spread of COVID-19 interrupted routine care. The number of patients served by Title X plummeted.
The Biden administration reversed most of those rules, including allowing providers with abortion services back into the Title X program. States also try to influence the funding’s reach, either through legislation or budget rules.
The current Title X funding cycle is 5 years, and the amount of money available each year could shift based on the state’s network of providers or federal budget changes. Jon Ebelt, a spokesperson for the Montana Department of Public Health and Human Services, didn’t answer when asked whether the state planned to reapply to administer the funding in 2027. He said the department was disappointed with the Biden administration’s “refusal” to renew the state’s funding.
“We recognize, however, that recent proabortion federal rule changes have distorted Title X and conflict with Montana law,” he said.
Conservative states have been tangling with nonprofits and the federal government over Title X funding for more than a decade. In 2011, during the Obama administration, Texas whittled down the state’s family planning spending and prioritized sending the federal money to general primary care providers over reproductive health clinics. As a result, 25% of family planning clinics in Texas closed. In 2013, a nonprofit now called Every Body Texas joined the competition to distribute the state’s Title X dollars and won.
“Filling and rebuilding those holes have taken this last decade, essentially,” said Berna Mason, director of service delivery improvement for Every Body Texas.
In 2019, the governor of Nebraska proposed a budget that would have prohibited the money from going to any organization that provided abortions or referred patients for abortions outside of an emergency. It also would have required that funding recipients be legally and financially separate from such clinics, a restriction that would have gone further than the Trump administration’s rules. Afterward, a family planning council won the right to administer Title X money.
In 2017, the nonprofit Arizona Family Health Partnership lost its status as that state’s only Title X administrator when the state health department was given 25% of the funding to deliver to providers. That came after Arizona lawmakers ordered the department to apply for the funds and distribute them first to state- or county-owned clinics, with the remaining money going to primary care facilities. The change was backed by groups that were opposed to abortion, and reproductive health care providers saw it as an attempt to weaken clinics that offer abortion services.
However, the state left nearly all the money it received untouched, and although it’s still required by law to apply for Title X funding, it hasn’t received a portion of the grant since.
Bré Thomas, CEO of Arizona Family Health Partnership, said that, even though the nonprofit is the sole administrator of the Title X funding again, the threat remains that some or all could be taken away because of politics. “We’re at the will of who’s in charge,” Ms. Thomas said.
Nonprofits say they have an advantage over state agencies in expanding services because they have more flexibility in fundraising and fewer administrative hurdles.
In April, Mississippi nonprofit Converge took over administration of Title X funds, a role the state had held for decades. The organization’s founders said they weren’t worried that conservative politicians would restrict access to services but simply believed they could do a better job. “Service quality was very low, and it was very hard to get appointments,” said cofounder Danielle Lampton.
A Mississippi State Department of Health spokesperson, Liz Sharlot, said the agency looks forward to working with Converge.
In Montana, Bridgercare plans to restore funding to Planned Parenthood clinics that have been cut off from the program since 2019, recruit more health centers to participate, and expand the program’s reach in rural, frontier, and tribal communities using telehealth services, Ms. McDowell said.
The organization’s goal is to increase the number of patients benefiting from the federal program by at least 10% in each year of the 5-year grant cycle. The clinic also plans to apply to keep its Title X role beyond this grant.
“In 5 years, our grant application should be a clear front-runner for funding,” she said. “It’s less about ‘How do we beat someone in 5 years?’ And more about ‘How do we grow this program to serve patients?’”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Supreme Court appears ready to overturn Roe
to the news outlet Politico.
The draft opinion, written by Justice Samuel Alito, outlines ways a presumed majority of the nine justices believes the 1973 ruling in Roe v. Wade was incorrect. If signed by a majority of the court, the ruling would eliminate the protections for abortion rights that Roe provided and give the 50 states the power to legislate abortion.
“We hold that Roe and Casey must be overruled,” Justice Alito writes in the draft. “It is time to heed the Constitution and return the issue of abortion to the people’s elected representatives.”
While a final ruling was not expected from the court until June, the leaked draft – a nearly unprecedented breach of the court’s internal workings – gives a strong signal of the court’s five most conservative members’ decisions. During oral arguments in the case in December, conservative justices appeared prepared to undo at least part of the country’s abortion protections.
President Joe Biden said his administration was already preparing for a potential ruling that struck down federal abortion protections.
The White House, he said in a statement, is working on a “response to the continued attack on abortion and reproductive rights, under a variety of possible outcomes in the cases pending before the Supreme Court. We will be ready when any ruling is issued.”
But if the draft opinion becomes final, he said the fight will move to the states.
“It will fall on our nation’s elected officials at all levels of government to protect a woman’s right to choose,” he said. “And it will fall on voters to elect pro-choice officials this November.”
With more pro-abortion rights members of Congress, it would be possible to pass federal legislation protecting abortion rights, “which I will work to pass and sign into law.”
Should the Alito draft become law, its first impact would be to allow a Mississippi law that bans abortions after 15 weeks to take effect.
But quickly after that, abortions would become illegal in many states. Several conservative-leaning states, mostly in the South and Midwest, have already passed laws severely restricting abortions well beyond what Roe allowed. Should Roe be overturned then, those laws would take effect without the threat of lengthy lawsuits or rulings from lower-court judges who have blocked them.
Nearly half of the states, mostly in the Northeast and West, would likely allow abortion to continue in some way. In fact, several states, including Colorado and Vermont, have already passed laws granting the right to an abortion into state law.
The leaked draft, however, is still a draft, meaning it remains possible Roe survives. Anthony Kreis, PhD, a professor of law at Georgia State University, says that could have been the point of whoever leaked the draft.
“It suggests to me that whoever leaked it knew that public outrage was the last resort to stopping the court from overturning Roe v. Wade and letting states ban all abortions,” Dr. Kreis said. “The danger that abortions won’t be legal in most of the country is very real.”
A version of this article first appeared on WebMD.com.
This article was updated 5/3/22.
to the news outlet Politico.
The draft opinion, written by Justice Samuel Alito, outlines ways a presumed majority of the nine justices believes the 1973 ruling in Roe v. Wade was incorrect. If signed by a majority of the court, the ruling would eliminate the protections for abortion rights that Roe provided and give the 50 states the power to legislate abortion.
“We hold that Roe and Casey must be overruled,” Justice Alito writes in the draft. “It is time to heed the Constitution and return the issue of abortion to the people’s elected representatives.”
While a final ruling was not expected from the court until June, the leaked draft – a nearly unprecedented breach of the court’s internal workings – gives a strong signal of the court’s five most conservative members’ decisions. During oral arguments in the case in December, conservative justices appeared prepared to undo at least part of the country’s abortion protections.
President Joe Biden said his administration was already preparing for a potential ruling that struck down federal abortion protections.
The White House, he said in a statement, is working on a “response to the continued attack on abortion and reproductive rights, under a variety of possible outcomes in the cases pending before the Supreme Court. We will be ready when any ruling is issued.”
But if the draft opinion becomes final, he said the fight will move to the states.
“It will fall on our nation’s elected officials at all levels of government to protect a woman’s right to choose,” he said. “And it will fall on voters to elect pro-choice officials this November.”
With more pro-abortion rights members of Congress, it would be possible to pass federal legislation protecting abortion rights, “which I will work to pass and sign into law.”
Should the Alito draft become law, its first impact would be to allow a Mississippi law that bans abortions after 15 weeks to take effect.
But quickly after that, abortions would become illegal in many states. Several conservative-leaning states, mostly in the South and Midwest, have already passed laws severely restricting abortions well beyond what Roe allowed. Should Roe be overturned then, those laws would take effect without the threat of lengthy lawsuits or rulings from lower-court judges who have blocked them.
Nearly half of the states, mostly in the Northeast and West, would likely allow abortion to continue in some way. In fact, several states, including Colorado and Vermont, have already passed laws granting the right to an abortion into state law.
The leaked draft, however, is still a draft, meaning it remains possible Roe survives. Anthony Kreis, PhD, a professor of law at Georgia State University, says that could have been the point of whoever leaked the draft.
“It suggests to me that whoever leaked it knew that public outrage was the last resort to stopping the court from overturning Roe v. Wade and letting states ban all abortions,” Dr. Kreis said. “The danger that abortions won’t be legal in most of the country is very real.”
A version of this article first appeared on WebMD.com.
This article was updated 5/3/22.
to the news outlet Politico.
The draft opinion, written by Justice Samuel Alito, outlines ways a presumed majority of the nine justices believes the 1973 ruling in Roe v. Wade was incorrect. If signed by a majority of the court, the ruling would eliminate the protections for abortion rights that Roe provided and give the 50 states the power to legislate abortion.
“We hold that Roe and Casey must be overruled,” Justice Alito writes in the draft. “It is time to heed the Constitution and return the issue of abortion to the people’s elected representatives.”
While a final ruling was not expected from the court until June, the leaked draft – a nearly unprecedented breach of the court’s internal workings – gives a strong signal of the court’s five most conservative members’ decisions. During oral arguments in the case in December, conservative justices appeared prepared to undo at least part of the country’s abortion protections.
President Joe Biden said his administration was already preparing for a potential ruling that struck down federal abortion protections.
The White House, he said in a statement, is working on a “response to the continued attack on abortion and reproductive rights, under a variety of possible outcomes in the cases pending before the Supreme Court. We will be ready when any ruling is issued.”
But if the draft opinion becomes final, he said the fight will move to the states.
“It will fall on our nation’s elected officials at all levels of government to protect a woman’s right to choose,” he said. “And it will fall on voters to elect pro-choice officials this November.”
With more pro-abortion rights members of Congress, it would be possible to pass federal legislation protecting abortion rights, “which I will work to pass and sign into law.”
Should the Alito draft become law, its first impact would be to allow a Mississippi law that bans abortions after 15 weeks to take effect.
But quickly after that, abortions would become illegal in many states. Several conservative-leaning states, mostly in the South and Midwest, have already passed laws severely restricting abortions well beyond what Roe allowed. Should Roe be overturned then, those laws would take effect without the threat of lengthy lawsuits or rulings from lower-court judges who have blocked them.
Nearly half of the states, mostly in the Northeast and West, would likely allow abortion to continue in some way. In fact, several states, including Colorado and Vermont, have already passed laws granting the right to an abortion into state law.
The leaked draft, however, is still a draft, meaning it remains possible Roe survives. Anthony Kreis, PhD, a professor of law at Georgia State University, says that could have been the point of whoever leaked the draft.
“It suggests to me that whoever leaked it knew that public outrage was the last resort to stopping the court from overturning Roe v. Wade and letting states ban all abortions,” Dr. Kreis said. “The danger that abortions won’t be legal in most of the country is very real.”
A version of this article first appeared on WebMD.com.
This article was updated 5/3/22.
A tip of the cap
“It was my wife’s walker, and I’ve never used one before. Sorry that I keep bumping into things.”
He was in his early 70s, recently widowed. He hadn’t needed a walker until yesterday, and his son had gotten it out of the garage where they’d just stowed it away. I showed him how to change the height setting on it so he didn’t have to lean so far over.
His daughter was a longstanding patient of mine, and now she and her brother were worried about their dad. He’d been so healthy for years, taking care of their mother as she declined with cancer. Now, 2 months since her death, he’d started going downhill. He’d been, understandably, depressed and had lost some weight. A few weeks ago he’d had some nonspecific upper respiratory crud, and now they were worried he wasn’t eating. He’d gotten progressively weaker in the last few days, leading to their getting out the walker.
I knew my patient for several years. She wasn’t given to panicking, and was worried about her dad. By this time, I was too. Twenty-eight years of neurology training and practice puts you on the edge for some things. The “Spidey Sense,” as I’ve always called it, was tingling.
It took a very quick neurologic exam to find what I needed. He was indeed weak, had decreased distal sensation, and was completely areflexic. It was time to take the most-dreaded outpatient neurology gamble: The direct office-to-ER admission.
I told his daughter to take him to the nearby ER and scribbled a note that said “Probable Guillain-Barré. Needs urgent workup.” They were somewhat taken aback, as they had dinner plans that night, but his daughter knew me well enough to know that I don’t pull fire alarms for fun.
As soon as they’d left I called the ER doctor and told her what was coming. My hospital days ended 2 years ago, but I wanted to do everything I could to make sure the right ball was rolling.
Then my part was over. I had other patients waiting, tests to review, phone calls to make.
This is where the anxiety began. Nobody wants to be the person who cries wolf, or admits “dumps.” I’ve been on both sides of admissions, and bashing outpatient docs for unnecessary hospital referrals is a perennial pastime of inpatient care.
I was sure of my actions, but as the hours crept by some doubt came in. What if he got to the hospital and suddenly wasn’t weak? Or it was all from a medication error he’d made at home?
No one wants to claim they saw a flare when there wasn’t one, or get the reputation of being past their game. I was worried about the patient, but also began to worry I’d screwed up and missed something else.
I finished the day and went home. After closing out my usual end-of-the-day stuff I logged into the hospital system to see what was going on.
Normal cervical spine MRI. Spinal fluid had zero cells and elevated protein.
I breathed a sigh of relief and relaxed back into my chair. I’d made the right call. The hospital neurologist had ordered IVIG. The patient would hopefully recover. No one would think I’d screwed up a potentially serious case. And, somewhere in the back of my mind, the Sherlock Holmes inside every neurologist tipped his deerstalker cap at me and gave a slight nod.
There’s the relief of having done the right thing for the patient, having made the correct diagnosis, and, at the end of the day, being reassured that (some days at least) I still know what I’m doing.
It’s those feelings that brought me here and still keep me going.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“It was my wife’s walker, and I’ve never used one before. Sorry that I keep bumping into things.”
He was in his early 70s, recently widowed. He hadn’t needed a walker until yesterday, and his son had gotten it out of the garage where they’d just stowed it away. I showed him how to change the height setting on it so he didn’t have to lean so far over.
His daughter was a longstanding patient of mine, and now she and her brother were worried about their dad. He’d been so healthy for years, taking care of their mother as she declined with cancer. Now, 2 months since her death, he’d started going downhill. He’d been, understandably, depressed and had lost some weight. A few weeks ago he’d had some nonspecific upper respiratory crud, and now they were worried he wasn’t eating. He’d gotten progressively weaker in the last few days, leading to their getting out the walker.
I knew my patient for several years. She wasn’t given to panicking, and was worried about her dad. By this time, I was too. Twenty-eight years of neurology training and practice puts you on the edge for some things. The “Spidey Sense,” as I’ve always called it, was tingling.
It took a very quick neurologic exam to find what I needed. He was indeed weak, had decreased distal sensation, and was completely areflexic. It was time to take the most-dreaded outpatient neurology gamble: The direct office-to-ER admission.
I told his daughter to take him to the nearby ER and scribbled a note that said “Probable Guillain-Barré. Needs urgent workup.” They were somewhat taken aback, as they had dinner plans that night, but his daughter knew me well enough to know that I don’t pull fire alarms for fun.
As soon as they’d left I called the ER doctor and told her what was coming. My hospital days ended 2 years ago, but I wanted to do everything I could to make sure the right ball was rolling.
Then my part was over. I had other patients waiting, tests to review, phone calls to make.
This is where the anxiety began. Nobody wants to be the person who cries wolf, or admits “dumps.” I’ve been on both sides of admissions, and bashing outpatient docs for unnecessary hospital referrals is a perennial pastime of inpatient care.
I was sure of my actions, but as the hours crept by some doubt came in. What if he got to the hospital and suddenly wasn’t weak? Or it was all from a medication error he’d made at home?
No one wants to claim they saw a flare when there wasn’t one, or get the reputation of being past their game. I was worried about the patient, but also began to worry I’d screwed up and missed something else.
I finished the day and went home. After closing out my usual end-of-the-day stuff I logged into the hospital system to see what was going on.
Normal cervical spine MRI. Spinal fluid had zero cells and elevated protein.
I breathed a sigh of relief and relaxed back into my chair. I’d made the right call. The hospital neurologist had ordered IVIG. The patient would hopefully recover. No one would think I’d screwed up a potentially serious case. And, somewhere in the back of my mind, the Sherlock Holmes inside every neurologist tipped his deerstalker cap at me and gave a slight nod.
There’s the relief of having done the right thing for the patient, having made the correct diagnosis, and, at the end of the day, being reassured that (some days at least) I still know what I’m doing.
It’s those feelings that brought me here and still keep me going.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“It was my wife’s walker, and I’ve never used one before. Sorry that I keep bumping into things.”
He was in his early 70s, recently widowed. He hadn’t needed a walker until yesterday, and his son had gotten it out of the garage where they’d just stowed it away. I showed him how to change the height setting on it so he didn’t have to lean so far over.
His daughter was a longstanding patient of mine, and now she and her brother were worried about their dad. He’d been so healthy for years, taking care of their mother as she declined with cancer. Now, 2 months since her death, he’d started going downhill. He’d been, understandably, depressed and had lost some weight. A few weeks ago he’d had some nonspecific upper respiratory crud, and now they were worried he wasn’t eating. He’d gotten progressively weaker in the last few days, leading to their getting out the walker.
I knew my patient for several years. She wasn’t given to panicking, and was worried about her dad. By this time, I was too. Twenty-eight years of neurology training and practice puts you on the edge for some things. The “Spidey Sense,” as I’ve always called it, was tingling.
It took a very quick neurologic exam to find what I needed. He was indeed weak, had decreased distal sensation, and was completely areflexic. It was time to take the most-dreaded outpatient neurology gamble: The direct office-to-ER admission.
I told his daughter to take him to the nearby ER and scribbled a note that said “Probable Guillain-Barré. Needs urgent workup.” They were somewhat taken aback, as they had dinner plans that night, but his daughter knew me well enough to know that I don’t pull fire alarms for fun.
As soon as they’d left I called the ER doctor and told her what was coming. My hospital days ended 2 years ago, but I wanted to do everything I could to make sure the right ball was rolling.
Then my part was over. I had other patients waiting, tests to review, phone calls to make.
This is where the anxiety began. Nobody wants to be the person who cries wolf, or admits “dumps.” I’ve been on both sides of admissions, and bashing outpatient docs for unnecessary hospital referrals is a perennial pastime of inpatient care.
I was sure of my actions, but as the hours crept by some doubt came in. What if he got to the hospital and suddenly wasn’t weak? Or it was all from a medication error he’d made at home?
No one wants to claim they saw a flare when there wasn’t one, or get the reputation of being past their game. I was worried about the patient, but also began to worry I’d screwed up and missed something else.
I finished the day and went home. After closing out my usual end-of-the-day stuff I logged into the hospital system to see what was going on.
Normal cervical spine MRI. Spinal fluid had zero cells and elevated protein.
I breathed a sigh of relief and relaxed back into my chair. I’d made the right call. The hospital neurologist had ordered IVIG. The patient would hopefully recover. No one would think I’d screwed up a potentially serious case. And, somewhere in the back of my mind, the Sherlock Holmes inside every neurologist tipped his deerstalker cap at me and gave a slight nod.
There’s the relief of having done the right thing for the patient, having made the correct diagnosis, and, at the end of the day, being reassured that (some days at least) I still know what I’m doing.
It’s those feelings that brought me here and still keep me going.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
How to ‘cybersecure’ your practice
The health care sector is not immune from cybersecurity attacks (malicious attempts to access or damage a computer or network system). Between October 2019 and October 2021, 857 data breaches were reported to the United States Department of Health and Human Services.1 The 3 main types of breaches reported were theft, hacking/IT incident, or unauthorized access/disclosure.1 Health care has become a common target due to the availability of valuable patient information (health, personal, and financial), the industry’s financial stability and resource capacity, and network susceptibility.2 The top 2 cybersecurity threats facing physician practices are:
- ransomware attacks, in which an external party uses a type of malicious software (malware) that prevents you from accessing your computer files, systems, or networks, and demands you pay a ransom for their return.
- employee-related threats, such as the theft or destruction of sensitive information by a disgruntled employee.3
The financial implications of health care–related cybersecurity threats coupled with exposure to potential litigation associated with breaches of confidentiality result in a need to “cybersecure” your practice.2 In this article, I outline steps to take to protect your practice against such threats. Although the recommendations I provide will increase your practice’s cybersecurity fortification, they are not exhaustive, and you may need to consult with an IT specialist to help protect your data and network.
Improve your network protection. A broadband internet connection is always operating, which makes it continuously susceptible to cybersecurity attacks. Install a firewall (a network security system that monitors and controls network traffic and permits or blocks traffic based on a defined set of rules) between your practice’s internal computer network and the internet.4 For maximum protection, enable all available firewall settings in your operating software.2 Prevent unauthorized access by ensuring that all network passwords are strong (ie, they include a combination of uppercase and lowercase letters, numbers, and symbols). Consider using different networks for online communication and for storing sensitive information.2 Create separate Wi-Fi networks for your practice and for your patients, and use unique passwords for each that are not easily guessed.4 If you or your employees use a virtual private network (VPN) to remotely access your practice’s network, ensure that all devices used to do so (cell phones, tablets, etc) are encrypted and secured with strong passwords.
Reduce employee-related threats. Not every employee in your practice will need to access to your patients’ clinical or financial data. Limiting employee access to sensitive clinical or financial data can reduce the risks of employee-related cybersecurity threats.3 In addition, restrict an employee’s ability to install software on computers and other devices that belong to your practice.2
Frequently incorporate cybersecurity training, such as teaching your employees about the risks of clicking on links and attachments in emails and how to identify phishing attacks (in which an individual sends a fraudulent communication that appears to come from a reputable source in order to trick the recipient into revealing financial information, system credentials, or other sensitive data).2,3 Use multifactor authentication to verify an employee’s login identity, and change passwords often. Reinforce these policies at staff meetings and educate new employees about this process.3 If you need to fire an employee, consider deploying cybersurveillance software to monitor the behavior of all employees before the employee is terminated.3 Once the employee has been terminated, change all logins and passwords.
1. U.S. Department of Health and Human Services. Office for Civil Rights. Breach portal: Notice to the Secretary of HHS breach of unsecured protected health information. Accessed December 26, 2021. https://ocrportal.hhs.gov/ocr/breach/breach_report.jsf
2. Umali G. How to safeguard your practice from cybersecurity threats. Psychiatric News. 2021;56(12):23.
3. Cryts A. Top two cybersecurity threats facing physician practices. Physicians Practice. March 13, 2020. Accessed December 26, 2021. https://www.physicianspractice.com/view/top-two-cybersecurity-threats-facing-physician-practices
4. American Medical Association. Protect your practice and patients from cybersecurity threats. 2017. Accessed December 26, 2021. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/government/advocacy/network-security.pdf
The health care sector is not immune from cybersecurity attacks (malicious attempts to access or damage a computer or network system). Between October 2019 and October 2021, 857 data breaches were reported to the United States Department of Health and Human Services.1 The 3 main types of breaches reported were theft, hacking/IT incident, or unauthorized access/disclosure.1 Health care has become a common target due to the availability of valuable patient information (health, personal, and financial), the industry’s financial stability and resource capacity, and network susceptibility.2 The top 2 cybersecurity threats facing physician practices are:
- ransomware attacks, in which an external party uses a type of malicious software (malware) that prevents you from accessing your computer files, systems, or networks, and demands you pay a ransom for their return.
- employee-related threats, such as the theft or destruction of sensitive information by a disgruntled employee.3
The financial implications of health care–related cybersecurity threats coupled with exposure to potential litigation associated with breaches of confidentiality result in a need to “cybersecure” your practice.2 In this article, I outline steps to take to protect your practice against such threats. Although the recommendations I provide will increase your practice’s cybersecurity fortification, they are not exhaustive, and you may need to consult with an IT specialist to help protect your data and network.
Improve your network protection. A broadband internet connection is always operating, which makes it continuously susceptible to cybersecurity attacks. Install a firewall (a network security system that monitors and controls network traffic and permits or blocks traffic based on a defined set of rules) between your practice’s internal computer network and the internet.4 For maximum protection, enable all available firewall settings in your operating software.2 Prevent unauthorized access by ensuring that all network passwords are strong (ie, they include a combination of uppercase and lowercase letters, numbers, and symbols). Consider using different networks for online communication and for storing sensitive information.2 Create separate Wi-Fi networks for your practice and for your patients, and use unique passwords for each that are not easily guessed.4 If you or your employees use a virtual private network (VPN) to remotely access your practice’s network, ensure that all devices used to do so (cell phones, tablets, etc) are encrypted and secured with strong passwords.
Reduce employee-related threats. Not every employee in your practice will need to access to your patients’ clinical or financial data. Limiting employee access to sensitive clinical or financial data can reduce the risks of employee-related cybersecurity threats.3 In addition, restrict an employee’s ability to install software on computers and other devices that belong to your practice.2
Frequently incorporate cybersecurity training, such as teaching your employees about the risks of clicking on links and attachments in emails and how to identify phishing attacks (in which an individual sends a fraudulent communication that appears to come from a reputable source in order to trick the recipient into revealing financial information, system credentials, or other sensitive data).2,3 Use multifactor authentication to verify an employee’s login identity, and change passwords often. Reinforce these policies at staff meetings and educate new employees about this process.3 If you need to fire an employee, consider deploying cybersurveillance software to monitor the behavior of all employees before the employee is terminated.3 Once the employee has been terminated, change all logins and passwords.
The health care sector is not immune from cybersecurity attacks (malicious attempts to access or damage a computer or network system). Between October 2019 and October 2021, 857 data breaches were reported to the United States Department of Health and Human Services.1 The 3 main types of breaches reported were theft, hacking/IT incident, or unauthorized access/disclosure.1 Health care has become a common target due to the availability of valuable patient information (health, personal, and financial), the industry’s financial stability and resource capacity, and network susceptibility.2 The top 2 cybersecurity threats facing physician practices are:
- ransomware attacks, in which an external party uses a type of malicious software (malware) that prevents you from accessing your computer files, systems, or networks, and demands you pay a ransom for their return.
- employee-related threats, such as the theft or destruction of sensitive information by a disgruntled employee.3
The financial implications of health care–related cybersecurity threats coupled with exposure to potential litigation associated with breaches of confidentiality result in a need to “cybersecure” your practice.2 In this article, I outline steps to take to protect your practice against such threats. Although the recommendations I provide will increase your practice’s cybersecurity fortification, they are not exhaustive, and you may need to consult with an IT specialist to help protect your data and network.
Improve your network protection. A broadband internet connection is always operating, which makes it continuously susceptible to cybersecurity attacks. Install a firewall (a network security system that monitors and controls network traffic and permits or blocks traffic based on a defined set of rules) between your practice’s internal computer network and the internet.4 For maximum protection, enable all available firewall settings in your operating software.2 Prevent unauthorized access by ensuring that all network passwords are strong (ie, they include a combination of uppercase and lowercase letters, numbers, and symbols). Consider using different networks for online communication and for storing sensitive information.2 Create separate Wi-Fi networks for your practice and for your patients, and use unique passwords for each that are not easily guessed.4 If you or your employees use a virtual private network (VPN) to remotely access your practice’s network, ensure that all devices used to do so (cell phones, tablets, etc) are encrypted and secured with strong passwords.
Reduce employee-related threats. Not every employee in your practice will need to access to your patients’ clinical or financial data. Limiting employee access to sensitive clinical or financial data can reduce the risks of employee-related cybersecurity threats.3 In addition, restrict an employee’s ability to install software on computers and other devices that belong to your practice.2
Frequently incorporate cybersecurity training, such as teaching your employees about the risks of clicking on links and attachments in emails and how to identify phishing attacks (in which an individual sends a fraudulent communication that appears to come from a reputable source in order to trick the recipient into revealing financial information, system credentials, or other sensitive data).2,3 Use multifactor authentication to verify an employee’s login identity, and change passwords often. Reinforce these policies at staff meetings and educate new employees about this process.3 If you need to fire an employee, consider deploying cybersurveillance software to monitor the behavior of all employees before the employee is terminated.3 Once the employee has been terminated, change all logins and passwords.
1. U.S. Department of Health and Human Services. Office for Civil Rights. Breach portal: Notice to the Secretary of HHS breach of unsecured protected health information. Accessed December 26, 2021. https://ocrportal.hhs.gov/ocr/breach/breach_report.jsf
2. Umali G. How to safeguard your practice from cybersecurity threats. Psychiatric News. 2021;56(12):23.
3. Cryts A. Top two cybersecurity threats facing physician practices. Physicians Practice. March 13, 2020. Accessed December 26, 2021. https://www.physicianspractice.com/view/top-two-cybersecurity-threats-facing-physician-practices
4. American Medical Association. Protect your practice and patients from cybersecurity threats. 2017. Accessed December 26, 2021. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/government/advocacy/network-security.pdf
1. U.S. Department of Health and Human Services. Office for Civil Rights. Breach portal: Notice to the Secretary of HHS breach of unsecured protected health information. Accessed December 26, 2021. https://ocrportal.hhs.gov/ocr/breach/breach_report.jsf
2. Umali G. How to safeguard your practice from cybersecurity threats. Psychiatric News. 2021;56(12):23.
3. Cryts A. Top two cybersecurity threats facing physician practices. Physicians Practice. March 13, 2020. Accessed December 26, 2021. https://www.physicianspractice.com/view/top-two-cybersecurity-threats-facing-physician-practices
4. American Medical Association. Protect your practice and patients from cybersecurity threats. 2017. Accessed December 26, 2021. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/government/advocacy/network-security.pdf
How to communicate effectively with patients when tension is high
“At my hospital, it was such a big thing to make sure that families are called,” said Dr. Nwankwo, in an interview following a session on compassionate communication at the annual meeting of the American College of Physicians. “So you have 19 patients, and you have to call almost every family to update them. And then you call, and they say, ‘Call this person as well.’ You feel like you’re at your wit’s end a lot of times.”
Sometimes, she has had to dig deep to find the empathy for patients that she knows her patients deserve.
“You really want to care by thinking about where is this patient coming from? What’s going on in their lives? And not just label them a difficult patient,” she said.
Become curious
Auguste Fortin, MD, MPH, offered advice for handling patient interactions under these kinds of circumstances, while serving as a moderator during the session.
“When the going gets tough, turn to wonder.” Become curious about why a patient might be feeling the way they are, he said.
Dr. Fortin, professor of internal medicine at Yale University, New Haven, Conn., said using the ADOBE acronym, has helped him more effectively communicate with his patients. This tool cues him to keep the following in mind: acknowledge, discover, opportunity, boundary setting, and extend.
He went on to explain to the audience why thinking about these terms is useful when interacting with patients.
First, acknowledge the feelings of the patient. Noting that a patient is angry, perhaps counterintuitively, helps, he said. In fact, not acknowledging the anger “throws gasoline on the fire.”
Then, discover the cause of their emotion. Saying "tell me more" and "help me understand" can be powerful tools, he noted.
Next, take this as an opportunity for empathy – especially important to remember when you’re being verbally attacked.
Boundary setting is important, because it lets the patient know that the conversation won’t continue unless they show the same respect the physician is showing, he said.
Finally, physicians can extend the system of support by asking others – such as colleagues or security – for help.
Use the NURS guide to show empathy
Dr. Fortin said he uses the “NURS” guide or calling to mind “name, express, respect, and support” to show empathy:
This involves naming a patient’s emotion; expressing understanding, with phrases like "I can see how you could be …"; showing respect, acknowledging a patient is going through a lot; and offering support, by saying something like, "Let’s see what we can do together to get to the bottom of this," he explained.
“My lived experience in using [these] in this order is that by the end of it, the patient cannot stay mad at me,” Dr. Fortin said.
“It’s really quite remarkable,” he added.
Steps for nonviolent communication
Rebecca Andrews, MD, MS, another moderator for the session, offered these steps for “nonviolent communication”:
- Observing the situation without blame or judgment.
- Telling the person how this situation makes you feel.
- Connecting with a need of the other person.
- Making a request that is specific and based on action, rather than a request not to do something, such as "Would you be willing to … ?"
Dr. Andrews, who is professor of medicine at the University of Connecticut, Farmington, said this approach has worked well for her, both in interactions with patients and in her personal life.
“It is evidence based that compassion actually makes care better,” she noted.
Varun Jain, MD, a member of the audience, expressed gratitude to the session’s speakers for teaching him something that he had not learned in medical school or residency.
“Every week you will have one or two people who will be labeled as ‘difficult,’ ” and it was nice to have some proven advice on how to handle these tough interactions, said the hospitalist at St. Francis Hospital in Hartford, Conn.
“We never got any actual training on this, and we were expected to know this because we are just physicians, and physicians are expected to be compassionate,” Dr. Jain said. “No one taught us how to have compassion.”
Dr. Fortin and Dr. Andrews disclosed no relevant financial relationships.
“At my hospital, it was such a big thing to make sure that families are called,” said Dr. Nwankwo, in an interview following a session on compassionate communication at the annual meeting of the American College of Physicians. “So you have 19 patients, and you have to call almost every family to update them. And then you call, and they say, ‘Call this person as well.’ You feel like you’re at your wit’s end a lot of times.”
Sometimes, she has had to dig deep to find the empathy for patients that she knows her patients deserve.
“You really want to care by thinking about where is this patient coming from? What’s going on in their lives? And not just label them a difficult patient,” she said.
Become curious
Auguste Fortin, MD, MPH, offered advice for handling patient interactions under these kinds of circumstances, while serving as a moderator during the session.
“When the going gets tough, turn to wonder.” Become curious about why a patient might be feeling the way they are, he said.
Dr. Fortin, professor of internal medicine at Yale University, New Haven, Conn., said using the ADOBE acronym, has helped him more effectively communicate with his patients. This tool cues him to keep the following in mind: acknowledge, discover, opportunity, boundary setting, and extend.
He went on to explain to the audience why thinking about these terms is useful when interacting with patients.
First, acknowledge the feelings of the patient. Noting that a patient is angry, perhaps counterintuitively, helps, he said. In fact, not acknowledging the anger “throws gasoline on the fire.”
Then, discover the cause of their emotion. Saying "tell me more" and "help me understand" can be powerful tools, he noted.
Next, take this as an opportunity for empathy – especially important to remember when you’re being verbally attacked.
Boundary setting is important, because it lets the patient know that the conversation won’t continue unless they show the same respect the physician is showing, he said.
Finally, physicians can extend the system of support by asking others – such as colleagues or security – for help.
Use the NURS guide to show empathy
Dr. Fortin said he uses the “NURS” guide or calling to mind “name, express, respect, and support” to show empathy:
This involves naming a patient’s emotion; expressing understanding, with phrases like "I can see how you could be …"; showing respect, acknowledging a patient is going through a lot; and offering support, by saying something like, "Let’s see what we can do together to get to the bottom of this," he explained.
“My lived experience in using [these] in this order is that by the end of it, the patient cannot stay mad at me,” Dr. Fortin said.
“It’s really quite remarkable,” he added.
Steps for nonviolent communication
Rebecca Andrews, MD, MS, another moderator for the session, offered these steps for “nonviolent communication”:
- Observing the situation without blame or judgment.
- Telling the person how this situation makes you feel.
- Connecting with a need of the other person.
- Making a request that is specific and based on action, rather than a request not to do something, such as "Would you be willing to … ?"
Dr. Andrews, who is professor of medicine at the University of Connecticut, Farmington, said this approach has worked well for her, both in interactions with patients and in her personal life.
“It is evidence based that compassion actually makes care better,” she noted.
Varun Jain, MD, a member of the audience, expressed gratitude to the session’s speakers for teaching him something that he had not learned in medical school or residency.
“Every week you will have one or two people who will be labeled as ‘difficult,’ ” and it was nice to have some proven advice on how to handle these tough interactions, said the hospitalist at St. Francis Hospital in Hartford, Conn.
“We never got any actual training on this, and we were expected to know this because we are just physicians, and physicians are expected to be compassionate,” Dr. Jain said. “No one taught us how to have compassion.”
Dr. Fortin and Dr. Andrews disclosed no relevant financial relationships.
“At my hospital, it was such a big thing to make sure that families are called,” said Dr. Nwankwo, in an interview following a session on compassionate communication at the annual meeting of the American College of Physicians. “So you have 19 patients, and you have to call almost every family to update them. And then you call, and they say, ‘Call this person as well.’ You feel like you’re at your wit’s end a lot of times.”
Sometimes, she has had to dig deep to find the empathy for patients that she knows her patients deserve.
“You really want to care by thinking about where is this patient coming from? What’s going on in their lives? And not just label them a difficult patient,” she said.
Become curious
Auguste Fortin, MD, MPH, offered advice for handling patient interactions under these kinds of circumstances, while serving as a moderator during the session.
“When the going gets tough, turn to wonder.” Become curious about why a patient might be feeling the way they are, he said.
Dr. Fortin, professor of internal medicine at Yale University, New Haven, Conn., said using the ADOBE acronym, has helped him more effectively communicate with his patients. This tool cues him to keep the following in mind: acknowledge, discover, opportunity, boundary setting, and extend.
He went on to explain to the audience why thinking about these terms is useful when interacting with patients.
First, acknowledge the feelings of the patient. Noting that a patient is angry, perhaps counterintuitively, helps, he said. In fact, not acknowledging the anger “throws gasoline on the fire.”
Then, discover the cause of their emotion. Saying "tell me more" and "help me understand" can be powerful tools, he noted.
Next, take this as an opportunity for empathy – especially important to remember when you’re being verbally attacked.
Boundary setting is important, because it lets the patient know that the conversation won’t continue unless they show the same respect the physician is showing, he said.
Finally, physicians can extend the system of support by asking others – such as colleagues or security – for help.
Use the NURS guide to show empathy
Dr. Fortin said he uses the “NURS” guide or calling to mind “name, express, respect, and support” to show empathy:
This involves naming a patient’s emotion; expressing understanding, with phrases like "I can see how you could be …"; showing respect, acknowledging a patient is going through a lot; and offering support, by saying something like, "Let’s see what we can do together to get to the bottom of this," he explained.
“My lived experience in using [these] in this order is that by the end of it, the patient cannot stay mad at me,” Dr. Fortin said.
“It’s really quite remarkable,” he added.
Steps for nonviolent communication
Rebecca Andrews, MD, MS, another moderator for the session, offered these steps for “nonviolent communication”:
- Observing the situation without blame or judgment.
- Telling the person how this situation makes you feel.
- Connecting with a need of the other person.
- Making a request that is specific and based on action, rather than a request not to do something, such as "Would you be willing to … ?"
Dr. Andrews, who is professor of medicine at the University of Connecticut, Farmington, said this approach has worked well for her, both in interactions with patients and in her personal life.
“It is evidence based that compassion actually makes care better,” she noted.
Varun Jain, MD, a member of the audience, expressed gratitude to the session’s speakers for teaching him something that he had not learned in medical school or residency.
“Every week you will have one or two people who will be labeled as ‘difficult,’ ” and it was nice to have some proven advice on how to handle these tough interactions, said the hospitalist at St. Francis Hospital in Hartford, Conn.
“We never got any actual training on this, and we were expected to know this because we are just physicians, and physicians are expected to be compassionate,” Dr. Jain said. “No one taught us how to have compassion.”
Dr. Fortin and Dr. Andrews disclosed no relevant financial relationships.
AT INTERNAL MEDICINE 2022
Homelessness seems to have greater link to death than common diseases, says physician
On a return visit about 10 years later, Dr. Perri went to the park and inquired about the men.
“I came to the horrible realization that all of these people were dead. All of them in 10 years,” he continued, speaking to an audience at the annual meeting of the American College of Physicians.
People experiencing homelessness don’t have to have such a grim health outlook, said Dr. Perri, who is medical director of the Center for Inclusion Health at the Allegheny Health Network in Pittsburgh.
During his talk, filled with jarring statistics on the health plight of those who struggle to stay sheltered, Dr. Perri said that many of the things that sicken and kill these people are the same things that sicken and kill others – liver disease, congestive heart failure, substance abuse. But the system isn’t equipped to handle the problems.
“Their needs are actually straightforward, they’re easy to describe,” he declared. “They’re known quantities. But the way that our systems respond, or don’t respond, to that creates the complexity. It’s the systems that are complex.”
Morbidity, mortality rates ‘go off a cliff’
A 2017 study in The Lancet compared morbidity and mortality in high-income countries, grouping people by their “level of deprivation.” The morbidity and mortality ticked higher with each deprivation level, but skyrocketed – nearly 10 times higher – for the group that included those experiencing homelessness or imprisonment, sex workers, and those with substance use disorders. As Dr. Perri put it, the rates “go off a cliff.”
Studies by the Boston Healthcare for the Homeless program have tracked mortality, and from 1988 to 1993 the average age at death was 47, so, “if you died while homeless, you probably died young.” Moreover, from their first contact to receive care through the program, to their death, only 25 months had elapsed.
“If there’s going to be an effective health care intervention, an acute one at least, you’ve got to get cracking,” Dr. Perri said.
Age at death has improved somewhat over time but drug overdose has become a much more common cause, Dr. Perri noted.
“There is utilitarian value in learning from people experiencing homelessness,” he said.
The same program looked at a high-risk cohort of 199 – those who went unsheltered for more than 6 months,were age 60 or older, or had certain serious health conditions, such as cirrhosis, substance abuse, and AIDS. A third of these people died within 5 years.
“There aren’t any other common diseases that I’m aware of that have statistics like that,” he said.
These people had an average of 31 emergency department visits a year and accounted for 871 hospitalizations. The estimated cost per-person, per-year was $22,000, while the average annual rent for a one-bedroom in Boston was $10,000.
“We’re hemorrhaging utilization around this population,” Dr. Perri said. “Maybe it makes sense to invest in something else other than acute health care. It’s not really yielding very much return on investment.”
Street medicine could be the answer
Housing First, a program to provide housing without the need to meet preconditions such as sobriety or passing background checks, has had a nonsignificant effect on mortality, substance use disorders, and mental health but has improved self-reported health status and quality of life. Analyses of the program suggest that better interventions are needed, Dr. Perri said.
Street medicine could be an answer, he said. Teams of medical staff go to where the people are, and the concept is intended as a continuous, cost-effective, flexible approach to care. Lehigh Valley Street Medicine in Pennsylvania has reported a reduction in emergency department visits and hospitalizations, Dr. Perri said. The programs are still too new to gauge the effect on actual health outcomes, but they hold the promise of being able to do so, he continued.
Curiosity about those experiencing homeless is a key first step in improving care, he said. The HOUSED BEDS tool, developed in Los Angeles, can help guide clinicians through their interactions with patients who do not have homes.
Dr. Perri said it is “enlightening” when you “express interest, genuine curiosity, about other people’s experiences.”
Catherine Kiley, MD, a retired internal medicine physician who volunteers as a preceptor for medical students in Cincinnati, said there is a void when it comes to teaching students about those experiencing homelessness.
“I don’t think there’s much of this type of discussion that they’re exposed to as part of medical education,” Dr. Kiley said. “Their experiences over time, as with most of medicine, will inform them.”
But the findings shared in the session show “how great the need is to speak out, speak up, about patients as people, and what they have to teach us.”
Dr. Perri disclosed no relevant financial relationships.
On a return visit about 10 years later, Dr. Perri went to the park and inquired about the men.
“I came to the horrible realization that all of these people were dead. All of them in 10 years,” he continued, speaking to an audience at the annual meeting of the American College of Physicians.
People experiencing homelessness don’t have to have such a grim health outlook, said Dr. Perri, who is medical director of the Center for Inclusion Health at the Allegheny Health Network in Pittsburgh.
During his talk, filled with jarring statistics on the health plight of those who struggle to stay sheltered, Dr. Perri said that many of the things that sicken and kill these people are the same things that sicken and kill others – liver disease, congestive heart failure, substance abuse. But the system isn’t equipped to handle the problems.
“Their needs are actually straightforward, they’re easy to describe,” he declared. “They’re known quantities. But the way that our systems respond, or don’t respond, to that creates the complexity. It’s the systems that are complex.”
Morbidity, mortality rates ‘go off a cliff’
A 2017 study in The Lancet compared morbidity and mortality in high-income countries, grouping people by their “level of deprivation.” The morbidity and mortality ticked higher with each deprivation level, but skyrocketed – nearly 10 times higher – for the group that included those experiencing homelessness or imprisonment, sex workers, and those with substance use disorders. As Dr. Perri put it, the rates “go off a cliff.”
Studies by the Boston Healthcare for the Homeless program have tracked mortality, and from 1988 to 1993 the average age at death was 47, so, “if you died while homeless, you probably died young.” Moreover, from their first contact to receive care through the program, to their death, only 25 months had elapsed.
“If there’s going to be an effective health care intervention, an acute one at least, you’ve got to get cracking,” Dr. Perri said.
Age at death has improved somewhat over time but drug overdose has become a much more common cause, Dr. Perri noted.
“There is utilitarian value in learning from people experiencing homelessness,” he said.
The same program looked at a high-risk cohort of 199 – those who went unsheltered for more than 6 months,were age 60 or older, or had certain serious health conditions, such as cirrhosis, substance abuse, and AIDS. A third of these people died within 5 years.
“There aren’t any other common diseases that I’m aware of that have statistics like that,” he said.
These people had an average of 31 emergency department visits a year and accounted for 871 hospitalizations. The estimated cost per-person, per-year was $22,000, while the average annual rent for a one-bedroom in Boston was $10,000.
“We’re hemorrhaging utilization around this population,” Dr. Perri said. “Maybe it makes sense to invest in something else other than acute health care. It’s not really yielding very much return on investment.”
Street medicine could be the answer
Housing First, a program to provide housing without the need to meet preconditions such as sobriety or passing background checks, has had a nonsignificant effect on mortality, substance use disorders, and mental health but has improved self-reported health status and quality of life. Analyses of the program suggest that better interventions are needed, Dr. Perri said.
Street medicine could be an answer, he said. Teams of medical staff go to where the people are, and the concept is intended as a continuous, cost-effective, flexible approach to care. Lehigh Valley Street Medicine in Pennsylvania has reported a reduction in emergency department visits and hospitalizations, Dr. Perri said. The programs are still too new to gauge the effect on actual health outcomes, but they hold the promise of being able to do so, he continued.
Curiosity about those experiencing homeless is a key first step in improving care, he said. The HOUSED BEDS tool, developed in Los Angeles, can help guide clinicians through their interactions with patients who do not have homes.
Dr. Perri said it is “enlightening” when you “express interest, genuine curiosity, about other people’s experiences.”
Catherine Kiley, MD, a retired internal medicine physician who volunteers as a preceptor for medical students in Cincinnati, said there is a void when it comes to teaching students about those experiencing homelessness.
“I don’t think there’s much of this type of discussion that they’re exposed to as part of medical education,” Dr. Kiley said. “Their experiences over time, as with most of medicine, will inform them.”
But the findings shared in the session show “how great the need is to speak out, speak up, about patients as people, and what they have to teach us.”
Dr. Perri disclosed no relevant financial relationships.
On a return visit about 10 years later, Dr. Perri went to the park and inquired about the men.
“I came to the horrible realization that all of these people were dead. All of them in 10 years,” he continued, speaking to an audience at the annual meeting of the American College of Physicians.
People experiencing homelessness don’t have to have such a grim health outlook, said Dr. Perri, who is medical director of the Center for Inclusion Health at the Allegheny Health Network in Pittsburgh.
During his talk, filled with jarring statistics on the health plight of those who struggle to stay sheltered, Dr. Perri said that many of the things that sicken and kill these people are the same things that sicken and kill others – liver disease, congestive heart failure, substance abuse. But the system isn’t equipped to handle the problems.
“Their needs are actually straightforward, they’re easy to describe,” he declared. “They’re known quantities. But the way that our systems respond, or don’t respond, to that creates the complexity. It’s the systems that are complex.”
Morbidity, mortality rates ‘go off a cliff’
A 2017 study in The Lancet compared morbidity and mortality in high-income countries, grouping people by their “level of deprivation.” The morbidity and mortality ticked higher with each deprivation level, but skyrocketed – nearly 10 times higher – for the group that included those experiencing homelessness or imprisonment, sex workers, and those with substance use disorders. As Dr. Perri put it, the rates “go off a cliff.”
Studies by the Boston Healthcare for the Homeless program have tracked mortality, and from 1988 to 1993 the average age at death was 47, so, “if you died while homeless, you probably died young.” Moreover, from their first contact to receive care through the program, to their death, only 25 months had elapsed.
“If there’s going to be an effective health care intervention, an acute one at least, you’ve got to get cracking,” Dr. Perri said.
Age at death has improved somewhat over time but drug overdose has become a much more common cause, Dr. Perri noted.
“There is utilitarian value in learning from people experiencing homelessness,” he said.
The same program looked at a high-risk cohort of 199 – those who went unsheltered for more than 6 months,were age 60 or older, or had certain serious health conditions, such as cirrhosis, substance abuse, and AIDS. A third of these people died within 5 years.
“There aren’t any other common diseases that I’m aware of that have statistics like that,” he said.
These people had an average of 31 emergency department visits a year and accounted for 871 hospitalizations. The estimated cost per-person, per-year was $22,000, while the average annual rent for a one-bedroom in Boston was $10,000.
“We’re hemorrhaging utilization around this population,” Dr. Perri said. “Maybe it makes sense to invest in something else other than acute health care. It’s not really yielding very much return on investment.”
Street medicine could be the answer
Housing First, a program to provide housing without the need to meet preconditions such as sobriety or passing background checks, has had a nonsignificant effect on mortality, substance use disorders, and mental health but has improved self-reported health status and quality of life. Analyses of the program suggest that better interventions are needed, Dr. Perri said.
Street medicine could be an answer, he said. Teams of medical staff go to where the people are, and the concept is intended as a continuous, cost-effective, flexible approach to care. Lehigh Valley Street Medicine in Pennsylvania has reported a reduction in emergency department visits and hospitalizations, Dr. Perri said. The programs are still too new to gauge the effect on actual health outcomes, but they hold the promise of being able to do so, he continued.
Curiosity about those experiencing homeless is a key first step in improving care, he said. The HOUSED BEDS tool, developed in Los Angeles, can help guide clinicians through their interactions with patients who do not have homes.
Dr. Perri said it is “enlightening” when you “express interest, genuine curiosity, about other people’s experiences.”
Catherine Kiley, MD, a retired internal medicine physician who volunteers as a preceptor for medical students in Cincinnati, said there is a void when it comes to teaching students about those experiencing homelessness.
“I don’t think there’s much of this type of discussion that they’re exposed to as part of medical education,” Dr. Kiley said. “Their experiences over time, as with most of medicine, will inform them.”
But the findings shared in the session show “how great the need is to speak out, speak up, about patients as people, and what they have to teach us.”
Dr. Perri disclosed no relevant financial relationships.
REPORTING FROM INTERNAL MEDICINE 2022
How to address social determinants of health, according to expert panel
This patient is on prednisone for her RA because she can’t afford better drugs, and she has been occasionally skipping her insulin, Dr. Candler said during her presentation, at the annual meeting of the American College of Physicians
Plus, her first language is Turkish, and she’s missed many doctor appointments because she lives too far from the center-city clinics, said Dr. Candler, who is the care team medical director at Iora Primary Care in Houston.
How are this woman’s needs supposed to be met in a fee-for-service system that allows medical staff 15 to 30 minutes to help solve her problems?
Potential regulatory fixes
A panel of experts talked about potential policies and regulatory fixes that take into account the impact of “social determinants of health.” Some of these are gaining traction, but there is still a huge gap between how medicine in practiced in the United States and the health needs of people in the community, the panelists said.
The ACO REACH (Realizing Equity, Access and Community Health) model is a recent step forward, said Josh Liao, MD, MSc, associate chair for health systems at the University of Washington, Seattle. The accountable care organization model pays doctors more for caring for Medicare patients in underserved communities.
“To me, it represents that at least we’re moving in the direction where we’re acknowledging directly that social environment matters,” he said.
The American College of Physicians’ Medical Practice and Quality Committee helped improve payment for telehealth, an important step for equity to the underserved, said William Fox, MD, at Fox and Brantley Internal Medicine in Charlottesville, Va., and chair of the committee for ACP’s Virginia chapter. But many policies require much more work, he said.
One aim is getting to universal health coverage – 31 million people in the United States still don’t have health insurance, a number that is greatly improved since the Affordable Care Act but has plateaued recently.
Another is to invest more in primary care – which accounts for about 5% of spending even though 35% of patient visits are to primary care.
Dr. Fox said the U.S. system also needs to evolve beyond fee-for-service, invest in information technology to bridge the gap between the access for the rich and poor, continue to expand telehealth, and reform payment programs to recognize social factors.
“The current finance system and the quality payment program are focused on downstream impacts of poor health,” Dr. Fox said.
Primary care needs to shed the expectation that it must show that it reduces costs in order to be valued, he continued. Care sometimes is necessary but doesn’t reduce cost. Also, cost reduction is often seen in the long run, but studied only in the short term, and therefore the evidence for cost reduction can be elusive.
What can internists do to help?
Dr. Candler said internal medicine physicians can do their part by collecting data on patients and staff and measuring outcomes to identify disparities. Additionally, they could run their practices with community and cultural needs in mind, she said.
“Some of that might mean hiring differently. Think about it – if you’re in a position to start building new practices, go where they need you,” Dr. Candler explained. “It might mean a little bit more of a commute for you. But your patients are already doing that with their untreated cataracts, so who’s safer on the roads?”
George Abraham, MD, MPH – president of ACP and professor of medicine at the University of Massachusetts , Boston, who did not present in the session – suggested physicians should be looking at their own practice style, location, and the way their practice runs, and see where there are opportunities to be more in touch.
“I’m sure we all have practices where we have a diverse patient population,” he said. What doctors can do is to specifically focus on their minority population and ask: ‘What do they experience that others don’t experience as my patient coming into my office?’ he said.
Dr. Abraham, who received his medical degree in India and is ACP’s first president who is an international medical graduate, pointed to ACP’s emphasis on diversifying the internal medicine workforce to reflect the communities.
Recent measures have included the creation of an ACP international medical graduate task force and establishing an antiharassment policy and reporting process.
“The conversation has started a lot more,” he said.
Dr. Candler reports financial relationships with Abbott, AbbVie, Johnson & Johnson, Merck, Medtronic, Pfizer, and other companies. She is also a member of the editorial advisory board of Internal Medicine News. Dr. Fox reports financial relationships with Obagi Cosmeceuticals. Dr. Liao reports financial relationships with Eli Lilly, Gilead, Johnson & Johnson, Novavax, and other companies. Dr. Abraham reports no relevant financial relationships.
This patient is on prednisone for her RA because she can’t afford better drugs, and she has been occasionally skipping her insulin, Dr. Candler said during her presentation, at the annual meeting of the American College of Physicians
Plus, her first language is Turkish, and she’s missed many doctor appointments because she lives too far from the center-city clinics, said Dr. Candler, who is the care team medical director at Iora Primary Care in Houston.
How are this woman’s needs supposed to be met in a fee-for-service system that allows medical staff 15 to 30 minutes to help solve her problems?
Potential regulatory fixes
A panel of experts talked about potential policies and regulatory fixes that take into account the impact of “social determinants of health.” Some of these are gaining traction, but there is still a huge gap between how medicine in practiced in the United States and the health needs of people in the community, the panelists said.
The ACO REACH (Realizing Equity, Access and Community Health) model is a recent step forward, said Josh Liao, MD, MSc, associate chair for health systems at the University of Washington, Seattle. The accountable care organization model pays doctors more for caring for Medicare patients in underserved communities.
“To me, it represents that at least we’re moving in the direction where we’re acknowledging directly that social environment matters,” he said.
The American College of Physicians’ Medical Practice and Quality Committee helped improve payment for telehealth, an important step for equity to the underserved, said William Fox, MD, at Fox and Brantley Internal Medicine in Charlottesville, Va., and chair of the committee for ACP’s Virginia chapter. But many policies require much more work, he said.
One aim is getting to universal health coverage – 31 million people in the United States still don’t have health insurance, a number that is greatly improved since the Affordable Care Act but has plateaued recently.
Another is to invest more in primary care – which accounts for about 5% of spending even though 35% of patient visits are to primary care.
Dr. Fox said the U.S. system also needs to evolve beyond fee-for-service, invest in information technology to bridge the gap between the access for the rich and poor, continue to expand telehealth, and reform payment programs to recognize social factors.
“The current finance system and the quality payment program are focused on downstream impacts of poor health,” Dr. Fox said.
Primary care needs to shed the expectation that it must show that it reduces costs in order to be valued, he continued. Care sometimes is necessary but doesn’t reduce cost. Also, cost reduction is often seen in the long run, but studied only in the short term, and therefore the evidence for cost reduction can be elusive.
What can internists do to help?
Dr. Candler said internal medicine physicians can do their part by collecting data on patients and staff and measuring outcomes to identify disparities. Additionally, they could run their practices with community and cultural needs in mind, she said.
“Some of that might mean hiring differently. Think about it – if you’re in a position to start building new practices, go where they need you,” Dr. Candler explained. “It might mean a little bit more of a commute for you. But your patients are already doing that with their untreated cataracts, so who’s safer on the roads?”
George Abraham, MD, MPH – president of ACP and professor of medicine at the University of Massachusetts , Boston, who did not present in the session – suggested physicians should be looking at their own practice style, location, and the way their practice runs, and see where there are opportunities to be more in touch.
“I’m sure we all have practices where we have a diverse patient population,” he said. What doctors can do is to specifically focus on their minority population and ask: ‘What do they experience that others don’t experience as my patient coming into my office?’ he said.
Dr. Abraham, who received his medical degree in India and is ACP’s first president who is an international medical graduate, pointed to ACP’s emphasis on diversifying the internal medicine workforce to reflect the communities.
Recent measures have included the creation of an ACP international medical graduate task force and establishing an antiharassment policy and reporting process.
“The conversation has started a lot more,” he said.
Dr. Candler reports financial relationships with Abbott, AbbVie, Johnson & Johnson, Merck, Medtronic, Pfizer, and other companies. She is also a member of the editorial advisory board of Internal Medicine News. Dr. Fox reports financial relationships with Obagi Cosmeceuticals. Dr. Liao reports financial relationships with Eli Lilly, Gilead, Johnson & Johnson, Novavax, and other companies. Dr. Abraham reports no relevant financial relationships.
This patient is on prednisone for her RA because she can’t afford better drugs, and she has been occasionally skipping her insulin, Dr. Candler said during her presentation, at the annual meeting of the American College of Physicians
Plus, her first language is Turkish, and she’s missed many doctor appointments because she lives too far from the center-city clinics, said Dr. Candler, who is the care team medical director at Iora Primary Care in Houston.
How are this woman’s needs supposed to be met in a fee-for-service system that allows medical staff 15 to 30 minutes to help solve her problems?
Potential regulatory fixes
A panel of experts talked about potential policies and regulatory fixes that take into account the impact of “social determinants of health.” Some of these are gaining traction, but there is still a huge gap between how medicine in practiced in the United States and the health needs of people in the community, the panelists said.
The ACO REACH (Realizing Equity, Access and Community Health) model is a recent step forward, said Josh Liao, MD, MSc, associate chair for health systems at the University of Washington, Seattle. The accountable care organization model pays doctors more for caring for Medicare patients in underserved communities.
“To me, it represents that at least we’re moving in the direction where we’re acknowledging directly that social environment matters,” he said.
The American College of Physicians’ Medical Practice and Quality Committee helped improve payment for telehealth, an important step for equity to the underserved, said William Fox, MD, at Fox and Brantley Internal Medicine in Charlottesville, Va., and chair of the committee for ACP’s Virginia chapter. But many policies require much more work, he said.
One aim is getting to universal health coverage – 31 million people in the United States still don’t have health insurance, a number that is greatly improved since the Affordable Care Act but has plateaued recently.
Another is to invest more in primary care – which accounts for about 5% of spending even though 35% of patient visits are to primary care.
Dr. Fox said the U.S. system also needs to evolve beyond fee-for-service, invest in information technology to bridge the gap between the access for the rich and poor, continue to expand telehealth, and reform payment programs to recognize social factors.
“The current finance system and the quality payment program are focused on downstream impacts of poor health,” Dr. Fox said.
Primary care needs to shed the expectation that it must show that it reduces costs in order to be valued, he continued. Care sometimes is necessary but doesn’t reduce cost. Also, cost reduction is often seen in the long run, but studied only in the short term, and therefore the evidence for cost reduction can be elusive.
What can internists do to help?
Dr. Candler said internal medicine physicians can do their part by collecting data on patients and staff and measuring outcomes to identify disparities. Additionally, they could run their practices with community and cultural needs in mind, she said.
“Some of that might mean hiring differently. Think about it – if you’re in a position to start building new practices, go where they need you,” Dr. Candler explained. “It might mean a little bit more of a commute for you. But your patients are already doing that with their untreated cataracts, so who’s safer on the roads?”
George Abraham, MD, MPH – president of ACP and professor of medicine at the University of Massachusetts , Boston, who did not present in the session – suggested physicians should be looking at their own practice style, location, and the way their practice runs, and see where there are opportunities to be more in touch.
“I’m sure we all have practices where we have a diverse patient population,” he said. What doctors can do is to specifically focus on their minority population and ask: ‘What do they experience that others don’t experience as my patient coming into my office?’ he said.
Dr. Abraham, who received his medical degree in India and is ACP’s first president who is an international medical graduate, pointed to ACP’s emphasis on diversifying the internal medicine workforce to reflect the communities.
Recent measures have included the creation of an ACP international medical graduate task force and establishing an antiharassment policy and reporting process.
“The conversation has started a lot more,” he said.
Dr. Candler reports financial relationships with Abbott, AbbVie, Johnson & Johnson, Merck, Medtronic, Pfizer, and other companies. She is also a member of the editorial advisory board of Internal Medicine News. Dr. Fox reports financial relationships with Obagi Cosmeceuticals. Dr. Liao reports financial relationships with Eli Lilly, Gilead, Johnson & Johnson, Novavax, and other companies. Dr. Abraham reports no relevant financial relationships.
AT INTERNAL MEDICINE 2022










