User login
Texas interventional cardiologist subject of anticompetitive lawsuit
Doctors Hospital of Laredo, Texas, and the Laredo Physicians Group have filed a lawsuit against interventional cardiologist Ricardo Cigarroa, MD, alleging that he engaged in anticompetitive conduct over the availability of cardiologists in Laredo.
Also named in the lawsuit are Cigarroa Heart and Vascular Institute, Laredo Texas Hospital Company (doing business as Laredo Medical Center) and Laredo Physician Associates (LPA).
According to the complaint, in August 2020, Doctors Hospital and Laredo Physicians Group began actively recruiting cardiologists to the city of Laredo.
The complaint states that, with more than 260,000 residents, the city should have a minimum of 20 cardiologists. However, Laredo currently has only eight cardiologists and only six are interventional cardiologists.
The lawsuit alleges that when Dr. Cigarroa got wind of these recruitment efforts, he entered into a conspiracy with the Cigarroa Institute (a cardiology outpatient clinic) and Laredo Medical Center, the largest acute-care hospital in the city, to engage in “anticompetitive and tortious behavior.
“Their conspiracy had a simple but pernicious goal: deprive Doctors Hospital and Physicians Group of the doctors and employees needed to compete and provide interventional cardiology services to the Laredo market,” the complaint reads.
The alleged conspiracy unfolded in multiple steps, it notes, with Dr. Cigarroa issuing threats to Doctors Hospital, Laredo Physicians Group, and prospective interventional cardiologists being recruited.
Through threats and coercion, multiple qualified interventional cardiologists who were interested in joining Laredo Physicians Group, and to whom the group extended employment offers, decided not to join, the complaint states.
It further claims that Dr. Cigarroa, his son, and his nephew – who represent more than half of the interventional cardiologists in Laredo – informed Doctors Hospital that they would “no longer respond” to emergency calls at Doctors Hospital.
The complaint further alleges that after “scaring off competitors and further cementing their dominant market power and position,” the defendants targeted Arthur Santos, MD, Laredo’s only cardiovascular surgeon who was employed by Laredo Physicians Group.
“Defendants successfully induced Dr. Santos to agree to join Defendant Laredo Physicians Associates (LPA), breaching his enforceable noncompete contractual provision,” the complaint states.
The defendants then allegedly induced the cardiothoracic surgery technicians at Doctors Hospital to join Laredo Medical Center (LMC) and work with Dr. Cigarroa and Dr. Santos, the complaint says.
“The conspiracy to monopolize Laredo’s interventional cardiology market is a win-win-win for Defendants. Dr Cigarroa and the clinic avoid competition for interventional cardiological services, while LMC is left as the only provider of acute cardiology services in Laredo, gaining additional patients and corresponding increased revenue,” the complaint reads.
“Meanwhile, Doctors Hospital’s acute-care cardiology program will be threatened with extinction and, critically, Laredo patients are left with higher health care costs and greater health risks and without competitive market alternatives,” it states.
Dr. Cigarroa responds
According to the Laredo Times, in a statement responding to the anticompetitive conduct lawsuit, Dr. Cigarroa said: “This lawsuit is a dispute between a for-profit corporation and a physician who has demonstrated over 30 years of commitment to his patients and patient care in this community.
“It’s unfortunate that the executives [at] Doctors Hospital have chosen to put profit above the well-being of their patients and employees. Their actions confirm that they care more about their bottom line than they do about our residents and reaffirms how disconnected they are from our community,” Dr. Cigarroa said.
“My top priority continues to be the health of all Laredo residents. I will never stop caring for the patients that I love, and I will continue to help save lives,” Dr. Cigarroa said, according to the Times article.
“I am humbled to have received numerous calls of support from many Doctors Hospital employees. Their words of encouragement are a true testament to the strong relationships I have within the medical community,” Dr. Cigarroa added.
A version of this article first appeared on Medscape.com.
Doctors Hospital of Laredo, Texas, and the Laredo Physicians Group have filed a lawsuit against interventional cardiologist Ricardo Cigarroa, MD, alleging that he engaged in anticompetitive conduct over the availability of cardiologists in Laredo.
Also named in the lawsuit are Cigarroa Heart and Vascular Institute, Laredo Texas Hospital Company (doing business as Laredo Medical Center) and Laredo Physician Associates (LPA).
According to the complaint, in August 2020, Doctors Hospital and Laredo Physicians Group began actively recruiting cardiologists to the city of Laredo.
The complaint states that, with more than 260,000 residents, the city should have a minimum of 20 cardiologists. However, Laredo currently has only eight cardiologists and only six are interventional cardiologists.
The lawsuit alleges that when Dr. Cigarroa got wind of these recruitment efforts, he entered into a conspiracy with the Cigarroa Institute (a cardiology outpatient clinic) and Laredo Medical Center, the largest acute-care hospital in the city, to engage in “anticompetitive and tortious behavior.
“Their conspiracy had a simple but pernicious goal: deprive Doctors Hospital and Physicians Group of the doctors and employees needed to compete and provide interventional cardiology services to the Laredo market,” the complaint reads.
The alleged conspiracy unfolded in multiple steps, it notes, with Dr. Cigarroa issuing threats to Doctors Hospital, Laredo Physicians Group, and prospective interventional cardiologists being recruited.
Through threats and coercion, multiple qualified interventional cardiologists who were interested in joining Laredo Physicians Group, and to whom the group extended employment offers, decided not to join, the complaint states.
It further claims that Dr. Cigarroa, his son, and his nephew – who represent more than half of the interventional cardiologists in Laredo – informed Doctors Hospital that they would “no longer respond” to emergency calls at Doctors Hospital.
The complaint further alleges that after “scaring off competitors and further cementing their dominant market power and position,” the defendants targeted Arthur Santos, MD, Laredo’s only cardiovascular surgeon who was employed by Laredo Physicians Group.
“Defendants successfully induced Dr. Santos to agree to join Defendant Laredo Physicians Associates (LPA), breaching his enforceable noncompete contractual provision,” the complaint states.
The defendants then allegedly induced the cardiothoracic surgery technicians at Doctors Hospital to join Laredo Medical Center (LMC) and work with Dr. Cigarroa and Dr. Santos, the complaint says.
“The conspiracy to monopolize Laredo’s interventional cardiology market is a win-win-win for Defendants. Dr Cigarroa and the clinic avoid competition for interventional cardiological services, while LMC is left as the only provider of acute cardiology services in Laredo, gaining additional patients and corresponding increased revenue,” the complaint reads.
“Meanwhile, Doctors Hospital’s acute-care cardiology program will be threatened with extinction and, critically, Laredo patients are left with higher health care costs and greater health risks and without competitive market alternatives,” it states.
Dr. Cigarroa responds
According to the Laredo Times, in a statement responding to the anticompetitive conduct lawsuit, Dr. Cigarroa said: “This lawsuit is a dispute between a for-profit corporation and a physician who has demonstrated over 30 years of commitment to his patients and patient care in this community.
“It’s unfortunate that the executives [at] Doctors Hospital have chosen to put profit above the well-being of their patients and employees. Their actions confirm that they care more about their bottom line than they do about our residents and reaffirms how disconnected they are from our community,” Dr. Cigarroa said.
“My top priority continues to be the health of all Laredo residents. I will never stop caring for the patients that I love, and I will continue to help save lives,” Dr. Cigarroa said, according to the Times article.
“I am humbled to have received numerous calls of support from many Doctors Hospital employees. Their words of encouragement are a true testament to the strong relationships I have within the medical community,” Dr. Cigarroa added.
A version of this article first appeared on Medscape.com.
Doctors Hospital of Laredo, Texas, and the Laredo Physicians Group have filed a lawsuit against interventional cardiologist Ricardo Cigarroa, MD, alleging that he engaged in anticompetitive conduct over the availability of cardiologists in Laredo.
Also named in the lawsuit are Cigarroa Heart and Vascular Institute, Laredo Texas Hospital Company (doing business as Laredo Medical Center) and Laredo Physician Associates (LPA).
According to the complaint, in August 2020, Doctors Hospital and Laredo Physicians Group began actively recruiting cardiologists to the city of Laredo.
The complaint states that, with more than 260,000 residents, the city should have a minimum of 20 cardiologists. However, Laredo currently has only eight cardiologists and only six are interventional cardiologists.
The lawsuit alleges that when Dr. Cigarroa got wind of these recruitment efforts, he entered into a conspiracy with the Cigarroa Institute (a cardiology outpatient clinic) and Laredo Medical Center, the largest acute-care hospital in the city, to engage in “anticompetitive and tortious behavior.
“Their conspiracy had a simple but pernicious goal: deprive Doctors Hospital and Physicians Group of the doctors and employees needed to compete and provide interventional cardiology services to the Laredo market,” the complaint reads.
The alleged conspiracy unfolded in multiple steps, it notes, with Dr. Cigarroa issuing threats to Doctors Hospital, Laredo Physicians Group, and prospective interventional cardiologists being recruited.
Through threats and coercion, multiple qualified interventional cardiologists who were interested in joining Laredo Physicians Group, and to whom the group extended employment offers, decided not to join, the complaint states.
It further claims that Dr. Cigarroa, his son, and his nephew – who represent more than half of the interventional cardiologists in Laredo – informed Doctors Hospital that they would “no longer respond” to emergency calls at Doctors Hospital.
The complaint further alleges that after “scaring off competitors and further cementing their dominant market power and position,” the defendants targeted Arthur Santos, MD, Laredo’s only cardiovascular surgeon who was employed by Laredo Physicians Group.
“Defendants successfully induced Dr. Santos to agree to join Defendant Laredo Physicians Associates (LPA), breaching his enforceable noncompete contractual provision,” the complaint states.
The defendants then allegedly induced the cardiothoracic surgery technicians at Doctors Hospital to join Laredo Medical Center (LMC) and work with Dr. Cigarroa and Dr. Santos, the complaint says.
“The conspiracy to monopolize Laredo’s interventional cardiology market is a win-win-win for Defendants. Dr Cigarroa and the clinic avoid competition for interventional cardiological services, while LMC is left as the only provider of acute cardiology services in Laredo, gaining additional patients and corresponding increased revenue,” the complaint reads.
“Meanwhile, Doctors Hospital’s acute-care cardiology program will be threatened with extinction and, critically, Laredo patients are left with higher health care costs and greater health risks and without competitive market alternatives,” it states.
Dr. Cigarroa responds
According to the Laredo Times, in a statement responding to the anticompetitive conduct lawsuit, Dr. Cigarroa said: “This lawsuit is a dispute between a for-profit corporation and a physician who has demonstrated over 30 years of commitment to his patients and patient care in this community.
“It’s unfortunate that the executives [at] Doctors Hospital have chosen to put profit above the well-being of their patients and employees. Their actions confirm that they care more about their bottom line than they do about our residents and reaffirms how disconnected they are from our community,” Dr. Cigarroa said.
“My top priority continues to be the health of all Laredo residents. I will never stop caring for the patients that I love, and I will continue to help save lives,” Dr. Cigarroa said, according to the Times article.
“I am humbled to have received numerous calls of support from many Doctors Hospital employees. Their words of encouragement are a true testament to the strong relationships I have within the medical community,” Dr. Cigarroa added.
A version of this article first appeared on Medscape.com.
A house divided cannot stand
The United States of America are not united. Politics have polarized the competing monologues and the policy making around vaccines, masks, children returning to school, what children are taught in school, and whether the federal government (or the National Football League) can or should create universal mandates enforcing one extreme of any of those policy disputes. Public health and health care have become so entangled in polarized politics that the role of science has often been pushed aside.
Polarization is not a novel event in the history of governments. The partition of India in 1947 divided most of its Hindu and Muslim inhabitants into separate countries, but that hasn’t stopped the recent resurgence of Hindu nationalism in India. The Thirty Years’ War in Europe sought to decide whether Catholics or Protestants would dominate Western Christianity. Those two sides decided in 1648 that coexistence was wiser than continuing into the abyss of mutual annihilation. Current conflicts between Israelis and Palestinians, between Shia and Sunni Arab states, between China and the Uyghurs, and within Sudan and Ethiopia together demonstrate that polarization to the point of genocide can occur regardless of religion, race, and nationality.
Abraham Lincoln, a lawyer in Illinois with a habit of losing elections, was nominated in 1858 to be the Republican nominee in the U.S. Senate race. His speech accepting the nomination spoke a truth that resonated across the nation and across time. It is known as the House Divided speech. He said: “A house divided against itself cannot stand. I believe this government cannot endure, permanently half slave and half free. I do not expect the Union to be dissolved – I do not expect the house to fall – but I do expect it will cease to be divided. It will become all one thing or all the other.”
The Republican Lincoln, supported by antislavery groups, lost that election to the Democrat Stephen A. Douglas, whose party espoused popular sovereignty and local decision-making about slavery. Lincoln’s acceptance speech propelled him 2 years later to be nominated for and elected President of the United States. Lincoln’s first inaugural address as the President of the United States on March 4, 1861, focused on the issue of division and secession. This time, Lincoln placed much more emphasis on preserving the Union. He specifically renounced any federal efforts to use force to abolish slavery in the states that permitted it. He declared: “I have no purpose, directly or indirectly, to interfere with the institution of slavery in the States where it exists. I believe I have no lawful right to do so, and I have no inclination to do so.”
President Lincoln’s approach might not meet muster in today’s cancel culture. He was facing a precariously divided nation not unlike the current day, so his speech contains insights and wisdom important for today. Lincoln saw government as “a majority held in restraint by constitutional checks and limitations.” I am loath to further quote out of context or paraphrase his masterful words. Go read the original, in its balanced entirety.
I have written previous columns about the importance of taking time to reflect on one’s life and one’s career. Reflection is both a wellness check and a moral compass check. Some call it mindfulness. I lean toward calling it thankfulness and gratitude. Hence, November is a convenient time for pediatricians if flu and respiratory syncytial virus seasons haven’t started.
The Gettysburg Address extols the virtue of dedication. Lincoln’s second inaugural address promotes mercy and forgiveness. His Farewell Address to Springfield in 1861 in a single paragraph captures grief, faith, and hope. Those speeches are my perennial favorites. But this year it is the two aforementioned addresses that must be mined for wisdom.
I advocate vaccine and mask mandates, but I am not enamored with the idea of President Biden using the unchecked power of the executive branch to promulgate a single federal regulation that overreaches into every moderate-size business nationwide. The 1861 inaugural address concurs. Lincoln’s prophecy that division will be solved when one side ultimately wins is not the model I seek. It hasn’t worked for gun control. It hasn’t worked for abortion as we approach the 50th anniversary of Roe v. Wade. The present 50+1 vote majority in the U.S. Senate does not have a mandate to overhaul society, especially when those majorities are transient. One should have the courage to seek change, but beware of creating large divisions with small majorities.
Facebook profits when you meditate in the echo chambers of large, outraged groups. Avoid that. Hebrew tradition has some reflection occurring in groups of two or three, rather than solo. Truth is revealed in community. Voltaire said: “Cherish those who seek the truth but beware of those who find it.” As a scientist, my experience is that humility, skepticism, and a dedication to finding truth have served me well for a lifetime.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
The United States of America are not united. Politics have polarized the competing monologues and the policy making around vaccines, masks, children returning to school, what children are taught in school, and whether the federal government (or the National Football League) can or should create universal mandates enforcing one extreme of any of those policy disputes. Public health and health care have become so entangled in polarized politics that the role of science has often been pushed aside.
Polarization is not a novel event in the history of governments. The partition of India in 1947 divided most of its Hindu and Muslim inhabitants into separate countries, but that hasn’t stopped the recent resurgence of Hindu nationalism in India. The Thirty Years’ War in Europe sought to decide whether Catholics or Protestants would dominate Western Christianity. Those two sides decided in 1648 that coexistence was wiser than continuing into the abyss of mutual annihilation. Current conflicts between Israelis and Palestinians, between Shia and Sunni Arab states, between China and the Uyghurs, and within Sudan and Ethiopia together demonstrate that polarization to the point of genocide can occur regardless of religion, race, and nationality.
Abraham Lincoln, a lawyer in Illinois with a habit of losing elections, was nominated in 1858 to be the Republican nominee in the U.S. Senate race. His speech accepting the nomination spoke a truth that resonated across the nation and across time. It is known as the House Divided speech. He said: “A house divided against itself cannot stand. I believe this government cannot endure, permanently half slave and half free. I do not expect the Union to be dissolved – I do not expect the house to fall – but I do expect it will cease to be divided. It will become all one thing or all the other.”
The Republican Lincoln, supported by antislavery groups, lost that election to the Democrat Stephen A. Douglas, whose party espoused popular sovereignty and local decision-making about slavery. Lincoln’s acceptance speech propelled him 2 years later to be nominated for and elected President of the United States. Lincoln’s first inaugural address as the President of the United States on March 4, 1861, focused on the issue of division and secession. This time, Lincoln placed much more emphasis on preserving the Union. He specifically renounced any federal efforts to use force to abolish slavery in the states that permitted it. He declared: “I have no purpose, directly or indirectly, to interfere with the institution of slavery in the States where it exists. I believe I have no lawful right to do so, and I have no inclination to do so.”
President Lincoln’s approach might not meet muster in today’s cancel culture. He was facing a precariously divided nation not unlike the current day, so his speech contains insights and wisdom important for today. Lincoln saw government as “a majority held in restraint by constitutional checks and limitations.” I am loath to further quote out of context or paraphrase his masterful words. Go read the original, in its balanced entirety.
I have written previous columns about the importance of taking time to reflect on one’s life and one’s career. Reflection is both a wellness check and a moral compass check. Some call it mindfulness. I lean toward calling it thankfulness and gratitude. Hence, November is a convenient time for pediatricians if flu and respiratory syncytial virus seasons haven’t started.
The Gettysburg Address extols the virtue of dedication. Lincoln’s second inaugural address promotes mercy and forgiveness. His Farewell Address to Springfield in 1861 in a single paragraph captures grief, faith, and hope. Those speeches are my perennial favorites. But this year it is the two aforementioned addresses that must be mined for wisdom.
I advocate vaccine and mask mandates, but I am not enamored with the idea of President Biden using the unchecked power of the executive branch to promulgate a single federal regulation that overreaches into every moderate-size business nationwide. The 1861 inaugural address concurs. Lincoln’s prophecy that division will be solved when one side ultimately wins is not the model I seek. It hasn’t worked for gun control. It hasn’t worked for abortion as we approach the 50th anniversary of Roe v. Wade. The present 50+1 vote majority in the U.S. Senate does not have a mandate to overhaul society, especially when those majorities are transient. One should have the courage to seek change, but beware of creating large divisions with small majorities.
Facebook profits when you meditate in the echo chambers of large, outraged groups. Avoid that. Hebrew tradition has some reflection occurring in groups of two or three, rather than solo. Truth is revealed in community. Voltaire said: “Cherish those who seek the truth but beware of those who find it.” As a scientist, my experience is that humility, skepticism, and a dedication to finding truth have served me well for a lifetime.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
The United States of America are not united. Politics have polarized the competing monologues and the policy making around vaccines, masks, children returning to school, what children are taught in school, and whether the federal government (or the National Football League) can or should create universal mandates enforcing one extreme of any of those policy disputes. Public health and health care have become so entangled in polarized politics that the role of science has often been pushed aside.
Polarization is not a novel event in the history of governments. The partition of India in 1947 divided most of its Hindu and Muslim inhabitants into separate countries, but that hasn’t stopped the recent resurgence of Hindu nationalism in India. The Thirty Years’ War in Europe sought to decide whether Catholics or Protestants would dominate Western Christianity. Those two sides decided in 1648 that coexistence was wiser than continuing into the abyss of mutual annihilation. Current conflicts between Israelis and Palestinians, between Shia and Sunni Arab states, between China and the Uyghurs, and within Sudan and Ethiopia together demonstrate that polarization to the point of genocide can occur regardless of religion, race, and nationality.
Abraham Lincoln, a lawyer in Illinois with a habit of losing elections, was nominated in 1858 to be the Republican nominee in the U.S. Senate race. His speech accepting the nomination spoke a truth that resonated across the nation and across time. It is known as the House Divided speech. He said: “A house divided against itself cannot stand. I believe this government cannot endure, permanently half slave and half free. I do not expect the Union to be dissolved – I do not expect the house to fall – but I do expect it will cease to be divided. It will become all one thing or all the other.”
The Republican Lincoln, supported by antislavery groups, lost that election to the Democrat Stephen A. Douglas, whose party espoused popular sovereignty and local decision-making about slavery. Lincoln’s acceptance speech propelled him 2 years later to be nominated for and elected President of the United States. Lincoln’s first inaugural address as the President of the United States on March 4, 1861, focused on the issue of division and secession. This time, Lincoln placed much more emphasis on preserving the Union. He specifically renounced any federal efforts to use force to abolish slavery in the states that permitted it. He declared: “I have no purpose, directly or indirectly, to interfere with the institution of slavery in the States where it exists. I believe I have no lawful right to do so, and I have no inclination to do so.”
President Lincoln’s approach might not meet muster in today’s cancel culture. He was facing a precariously divided nation not unlike the current day, so his speech contains insights and wisdom important for today. Lincoln saw government as “a majority held in restraint by constitutional checks and limitations.” I am loath to further quote out of context or paraphrase his masterful words. Go read the original, in its balanced entirety.
I have written previous columns about the importance of taking time to reflect on one’s life and one’s career. Reflection is both a wellness check and a moral compass check. Some call it mindfulness. I lean toward calling it thankfulness and gratitude. Hence, November is a convenient time for pediatricians if flu and respiratory syncytial virus seasons haven’t started.
The Gettysburg Address extols the virtue of dedication. Lincoln’s second inaugural address promotes mercy and forgiveness. His Farewell Address to Springfield in 1861 in a single paragraph captures grief, faith, and hope. Those speeches are my perennial favorites. But this year it is the two aforementioned addresses that must be mined for wisdom.
I advocate vaccine and mask mandates, but I am not enamored with the idea of President Biden using the unchecked power of the executive branch to promulgate a single federal regulation that overreaches into every moderate-size business nationwide. The 1861 inaugural address concurs. Lincoln’s prophecy that division will be solved when one side ultimately wins is not the model I seek. It hasn’t worked for gun control. It hasn’t worked for abortion as we approach the 50th anniversary of Roe v. Wade. The present 50+1 vote majority in the U.S. Senate does not have a mandate to overhaul society, especially when those majorities are transient. One should have the courage to seek change, but beware of creating large divisions with small majorities.
Facebook profits when you meditate in the echo chambers of large, outraged groups. Avoid that. Hebrew tradition has some reflection occurring in groups of two or three, rather than solo. Truth is revealed in community. Voltaire said: “Cherish those who seek the truth but beware of those who find it.” As a scientist, my experience is that humility, skepticism, and a dedication to finding truth have served me well for a lifetime.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
Should you tell your doctor that you’re a doctor?
The question drew spirited debate when urologist Ashley Winter, MD, made a simple, straightforward request on Twitter: “If you are a doctor & you come to an appointment please tell me you are a doctor, not because I will treat you differently but because it’s easier to speak in jargon.”
She later added, “This doesn’t’ mean I would be less patient-focused or emotional with a physician or other [healthcare worker]. Just means that, instead of saying ‘you will have a catheter draining your urine to a bag,’ I can say, ‘you will have a Foley.’ ”
The Tweet followed an encounter with a patient who told Dr. Winter that he was a doctor only after she had gone to some length explaining a surgical procedure in lay terms.
“I explained the surgery, obviously assuming he was an intelligent adult, but using fully layman’s terms,” she said in an interview. The patient then told her that he was a doctor. “I guess I felt this embarrassment — I wouldn’t have treated him differently, but I just could have discussed the procedure with him in more professional terms.”
“To some extent, it was my own fault,” she commented in an interview. “I didn’t take the time to ask [about his work] at the beginning of the consultation, but that’s a fine line, also,” added Dr. Winter, a urologist and sexual medicine physician in Portland, Ore.
“You know that patient is there because they want care from you and it’s not necessarily always at the forefront of importance to be asking them what they do for their work, but alternatively, if you don’t ask then you put them in this position where they have to find a way to go ahead and tell you.”
Several people chimed in on the thread to voice their thoughts on the matter. Some commiserated with Dr. Winter’s experience:
“I took care of a retired cardiologist in the hospital as a second-year resident and honest to god he let me ramble on ‘explaining’ his echo result and never told me. I found out a couple days later and wanted to die,” posted @MaddyAndrewsMD.
Another recalled a similarly embarrassing experience when she “went on and on” discussing headaches with a patient whose husband “was in the corner smirking.”
“They told my attending later [that the] husband was a retired FM doc who practiced medicine longer than I’ve been alive. I wanted to die,” posted @JSinghDO.
Many on the thread, though, were doctors and other healthcare professionals speaking as patients. Some said they didn’t want to disclose their status as a healthcare provider because they felt it affected the care they received.
For example, @drhelenrainford commented: “In my experience my care is less ‘caring’ when they know I am a [doctor]. I get spoken to like they are discussing a patient with me — no empathy just facts and difficult results just blurted out without consideration. Awful awful time as an inpatient …but that’s another story!”
@Dr_B_Ring said: “Nope – You and I speak different jargon – I would want you to speak to me like a human that doesn’t know your jargon. My ego would get in the way of asking about the acronyms I don’t know if you knew I was a fellow physician.”
Conversely, @lozzlemcfozzle said: “Honestly I prefer not to tell my Doctors — I’ve found people skip explanations assuming I ‘know,’ or seem a little nervous when I tell them!”
Others said they felt uncomfortable — pretentious, even — in announcing their status, or worried that they might come across as expecting special care.
“It’s such a tough needle to thread. Want to tell people early but not come off as demanding special treatment, but don’t want to wait too long and it seems like a trap,” said @MDaware.
Twitter user @MsBabyCatcher wrote: “I have a hard time doing this because I don’t want people to think I’m being pretentious or going to micromanage/dictate care.”
Replying to @MsBabyCatcher, @RedStethoscope wrote: “I used to think this too until I got [very poor] care a few times, and was advised by other doctor moms to ‘play the doctor card.’ I have gotten better/more compassionate care by making sure it’s clear that I’m a physician (which is junk, but here we are).”
Several of those responding used the words “tricky” and “awkward,” suggesting a common theme for doctors presenting as patients.
“I struggle with this. My 5-year-old broke her arm this weekend, we spent hours in the ED, of my own hospital, I never mentioned it because I didn’t want to get preferential care. But as they were explaining her type of fracture, it felt awkward and inefficient,” said @lindsay_petty.
To avoid the awkwardness, a number of respondents said they purposefully use medical jargon to open up a conversation rather than just offering up the information that they are a doctor.
Still others offered suggestions on how to broach the subject more directly when presenting as a patient:
‘”Just FYI I’m a X doc but I’m here because I really want your help and advice!” That’s what I usually do,” wrote @drcakefm.
@BeeSting14618 Tweeted: “I usually say ‘I know some of this but I’m here because I want YOUR guidance. Also I may ask dumb questions, and I’ll tell you if a question is asking your opinion or making a request.’”
A few others injected a bit of humor: “I just do the 14-part handshake that only doctors know. Is that not customary?” quipped @Branmiz25.
“Ah yes, that transmits the entire [history of present illness],” replied Dr. Winter.
Jokes aside, the topic is obviously one that touched on a shared experience among healthcare providers, Dr. Winter commented. The Twitter thread she started just “blew up.”
That’s typically a sign that the Tweet is relatable for a lot of people, she said.
“It’s definitely something that all of us as care providers and as patients understand. It’s a funny, awkward thing that can really change an interaction, so we probably all feel pretty strongly about our experiences related to that,” she added.
The debate begs the question: Is there a duty or ethical reason to disclose?
“I definitely think it is very reasonable to disclose that one is a medical professional to another doctor,” medical ethicist Charlotte Blease, PhD, said in an interview. “There are good reasons to believe doing so might make a difference to the quality of communication and transparency.”
If the ability to use medical terminology or jargon more freely improves patient understanding, autonomy, and shared decision-making, then it may be of benefit, said Dr. Blease, a Keane OpenNotes Scholar at Beth Israel Deaconess Medical Center in Boston.
“Since doctors should strive to communicate effectively with every patient and to respect their unique needs and level of understanding, then I see no reason to deny that one is a medic,” she added.”
Knowing how to share the information is another story.
“This is something that affects all of us as physicians — we’re going to be patients at some point, right?” Dr. Winter commented. “But I don’t think how to disclose that is something that was ever brought up in my medical training.”
“Maybe there should just be a discussion of this one day when people are in medical school — maybe in a professionalism course — to broach this topic or look at if there’s any literature on outcomes related to disclosure of status or what are best practices,” she suggested.
A version of this article first appeared on Medscape.com.
The question drew spirited debate when urologist Ashley Winter, MD, made a simple, straightforward request on Twitter: “If you are a doctor & you come to an appointment please tell me you are a doctor, not because I will treat you differently but because it’s easier to speak in jargon.”
She later added, “This doesn’t’ mean I would be less patient-focused or emotional with a physician or other [healthcare worker]. Just means that, instead of saying ‘you will have a catheter draining your urine to a bag,’ I can say, ‘you will have a Foley.’ ”
The Tweet followed an encounter with a patient who told Dr. Winter that he was a doctor only after she had gone to some length explaining a surgical procedure in lay terms.
“I explained the surgery, obviously assuming he was an intelligent adult, but using fully layman’s terms,” she said in an interview. The patient then told her that he was a doctor. “I guess I felt this embarrassment — I wouldn’t have treated him differently, but I just could have discussed the procedure with him in more professional terms.”
“To some extent, it was my own fault,” she commented in an interview. “I didn’t take the time to ask [about his work] at the beginning of the consultation, but that’s a fine line, also,” added Dr. Winter, a urologist and sexual medicine physician in Portland, Ore.
“You know that patient is there because they want care from you and it’s not necessarily always at the forefront of importance to be asking them what they do for their work, but alternatively, if you don’t ask then you put them in this position where they have to find a way to go ahead and tell you.”
Several people chimed in on the thread to voice their thoughts on the matter. Some commiserated with Dr. Winter’s experience:
“I took care of a retired cardiologist in the hospital as a second-year resident and honest to god he let me ramble on ‘explaining’ his echo result and never told me. I found out a couple days later and wanted to die,” posted @MaddyAndrewsMD.
Another recalled a similarly embarrassing experience when she “went on and on” discussing headaches with a patient whose husband “was in the corner smirking.”
“They told my attending later [that the] husband was a retired FM doc who practiced medicine longer than I’ve been alive. I wanted to die,” posted @JSinghDO.
Many on the thread, though, were doctors and other healthcare professionals speaking as patients. Some said they didn’t want to disclose their status as a healthcare provider because they felt it affected the care they received.
For example, @drhelenrainford commented: “In my experience my care is less ‘caring’ when they know I am a [doctor]. I get spoken to like they are discussing a patient with me — no empathy just facts and difficult results just blurted out without consideration. Awful awful time as an inpatient …but that’s another story!”
@Dr_B_Ring said: “Nope – You and I speak different jargon – I would want you to speak to me like a human that doesn’t know your jargon. My ego would get in the way of asking about the acronyms I don’t know if you knew I was a fellow physician.”
Conversely, @lozzlemcfozzle said: “Honestly I prefer not to tell my Doctors — I’ve found people skip explanations assuming I ‘know,’ or seem a little nervous when I tell them!”
Others said they felt uncomfortable — pretentious, even — in announcing their status, or worried that they might come across as expecting special care.
“It’s such a tough needle to thread. Want to tell people early but not come off as demanding special treatment, but don’t want to wait too long and it seems like a trap,” said @MDaware.
Twitter user @MsBabyCatcher wrote: “I have a hard time doing this because I don’t want people to think I’m being pretentious or going to micromanage/dictate care.”
Replying to @MsBabyCatcher, @RedStethoscope wrote: “I used to think this too until I got [very poor] care a few times, and was advised by other doctor moms to ‘play the doctor card.’ I have gotten better/more compassionate care by making sure it’s clear that I’m a physician (which is junk, but here we are).”
Several of those responding used the words “tricky” and “awkward,” suggesting a common theme for doctors presenting as patients.
“I struggle with this. My 5-year-old broke her arm this weekend, we spent hours in the ED, of my own hospital, I never mentioned it because I didn’t want to get preferential care. But as they were explaining her type of fracture, it felt awkward and inefficient,” said @lindsay_petty.
To avoid the awkwardness, a number of respondents said they purposefully use medical jargon to open up a conversation rather than just offering up the information that they are a doctor.
Still others offered suggestions on how to broach the subject more directly when presenting as a patient:
‘”Just FYI I’m a X doc but I’m here because I really want your help and advice!” That’s what I usually do,” wrote @drcakefm.
@BeeSting14618 Tweeted: “I usually say ‘I know some of this but I’m here because I want YOUR guidance. Also I may ask dumb questions, and I’ll tell you if a question is asking your opinion or making a request.’”
A few others injected a bit of humor: “I just do the 14-part handshake that only doctors know. Is that not customary?” quipped @Branmiz25.
“Ah yes, that transmits the entire [history of present illness],” replied Dr. Winter.
Jokes aside, the topic is obviously one that touched on a shared experience among healthcare providers, Dr. Winter commented. The Twitter thread she started just “blew up.”
That’s typically a sign that the Tweet is relatable for a lot of people, she said.
“It’s definitely something that all of us as care providers and as patients understand. It’s a funny, awkward thing that can really change an interaction, so we probably all feel pretty strongly about our experiences related to that,” she added.
The debate begs the question: Is there a duty or ethical reason to disclose?
“I definitely think it is very reasonable to disclose that one is a medical professional to another doctor,” medical ethicist Charlotte Blease, PhD, said in an interview. “There are good reasons to believe doing so might make a difference to the quality of communication and transparency.”
If the ability to use medical terminology or jargon more freely improves patient understanding, autonomy, and shared decision-making, then it may be of benefit, said Dr. Blease, a Keane OpenNotes Scholar at Beth Israel Deaconess Medical Center in Boston.
“Since doctors should strive to communicate effectively with every patient and to respect their unique needs and level of understanding, then I see no reason to deny that one is a medic,” she added.”
Knowing how to share the information is another story.
“This is something that affects all of us as physicians — we’re going to be patients at some point, right?” Dr. Winter commented. “But I don’t think how to disclose that is something that was ever brought up in my medical training.”
“Maybe there should just be a discussion of this one day when people are in medical school — maybe in a professionalism course — to broach this topic or look at if there’s any literature on outcomes related to disclosure of status or what are best practices,” she suggested.
A version of this article first appeared on Medscape.com.
The question drew spirited debate when urologist Ashley Winter, MD, made a simple, straightforward request on Twitter: “If you are a doctor & you come to an appointment please tell me you are a doctor, not because I will treat you differently but because it’s easier to speak in jargon.”
She later added, “This doesn’t’ mean I would be less patient-focused or emotional with a physician or other [healthcare worker]. Just means that, instead of saying ‘you will have a catheter draining your urine to a bag,’ I can say, ‘you will have a Foley.’ ”
The Tweet followed an encounter with a patient who told Dr. Winter that he was a doctor only after she had gone to some length explaining a surgical procedure in lay terms.
“I explained the surgery, obviously assuming he was an intelligent adult, but using fully layman’s terms,” she said in an interview. The patient then told her that he was a doctor. “I guess I felt this embarrassment — I wouldn’t have treated him differently, but I just could have discussed the procedure with him in more professional terms.”
“To some extent, it was my own fault,” she commented in an interview. “I didn’t take the time to ask [about his work] at the beginning of the consultation, but that’s a fine line, also,” added Dr. Winter, a urologist and sexual medicine physician in Portland, Ore.
“You know that patient is there because they want care from you and it’s not necessarily always at the forefront of importance to be asking them what they do for their work, but alternatively, if you don’t ask then you put them in this position where they have to find a way to go ahead and tell you.”
Several people chimed in on the thread to voice their thoughts on the matter. Some commiserated with Dr. Winter’s experience:
“I took care of a retired cardiologist in the hospital as a second-year resident and honest to god he let me ramble on ‘explaining’ his echo result and never told me. I found out a couple days later and wanted to die,” posted @MaddyAndrewsMD.
Another recalled a similarly embarrassing experience when she “went on and on” discussing headaches with a patient whose husband “was in the corner smirking.”
“They told my attending later [that the] husband was a retired FM doc who practiced medicine longer than I’ve been alive. I wanted to die,” posted @JSinghDO.
Many on the thread, though, were doctors and other healthcare professionals speaking as patients. Some said they didn’t want to disclose their status as a healthcare provider because they felt it affected the care they received.
For example, @drhelenrainford commented: “In my experience my care is less ‘caring’ when they know I am a [doctor]. I get spoken to like they are discussing a patient with me — no empathy just facts and difficult results just blurted out without consideration. Awful awful time as an inpatient …but that’s another story!”
@Dr_B_Ring said: “Nope – You and I speak different jargon – I would want you to speak to me like a human that doesn’t know your jargon. My ego would get in the way of asking about the acronyms I don’t know if you knew I was a fellow physician.”
Conversely, @lozzlemcfozzle said: “Honestly I prefer not to tell my Doctors — I’ve found people skip explanations assuming I ‘know,’ or seem a little nervous when I tell them!”
Others said they felt uncomfortable — pretentious, even — in announcing their status, or worried that they might come across as expecting special care.
“It’s such a tough needle to thread. Want to tell people early but not come off as demanding special treatment, but don’t want to wait too long and it seems like a trap,” said @MDaware.
Twitter user @MsBabyCatcher wrote: “I have a hard time doing this because I don’t want people to think I’m being pretentious or going to micromanage/dictate care.”
Replying to @MsBabyCatcher, @RedStethoscope wrote: “I used to think this too until I got [very poor] care a few times, and was advised by other doctor moms to ‘play the doctor card.’ I have gotten better/more compassionate care by making sure it’s clear that I’m a physician (which is junk, but here we are).”
Several of those responding used the words “tricky” and “awkward,” suggesting a common theme for doctors presenting as patients.
“I struggle with this. My 5-year-old broke her arm this weekend, we spent hours in the ED, of my own hospital, I never mentioned it because I didn’t want to get preferential care. But as they were explaining her type of fracture, it felt awkward and inefficient,” said @lindsay_petty.
To avoid the awkwardness, a number of respondents said they purposefully use medical jargon to open up a conversation rather than just offering up the information that they are a doctor.
Still others offered suggestions on how to broach the subject more directly when presenting as a patient:
‘”Just FYI I’m a X doc but I’m here because I really want your help and advice!” That’s what I usually do,” wrote @drcakefm.
@BeeSting14618 Tweeted: “I usually say ‘I know some of this but I’m here because I want YOUR guidance. Also I may ask dumb questions, and I’ll tell you if a question is asking your opinion or making a request.’”
A few others injected a bit of humor: “I just do the 14-part handshake that only doctors know. Is that not customary?” quipped @Branmiz25.
“Ah yes, that transmits the entire [history of present illness],” replied Dr. Winter.
Jokes aside, the topic is obviously one that touched on a shared experience among healthcare providers, Dr. Winter commented. The Twitter thread she started just “blew up.”
That’s typically a sign that the Tweet is relatable for a lot of people, she said.
“It’s definitely something that all of us as care providers and as patients understand. It’s a funny, awkward thing that can really change an interaction, so we probably all feel pretty strongly about our experiences related to that,” she added.
The debate begs the question: Is there a duty or ethical reason to disclose?
“I definitely think it is very reasonable to disclose that one is a medical professional to another doctor,” medical ethicist Charlotte Blease, PhD, said in an interview. “There are good reasons to believe doing so might make a difference to the quality of communication and transparency.”
If the ability to use medical terminology or jargon more freely improves patient understanding, autonomy, and shared decision-making, then it may be of benefit, said Dr. Blease, a Keane OpenNotes Scholar at Beth Israel Deaconess Medical Center in Boston.
“Since doctors should strive to communicate effectively with every patient and to respect their unique needs and level of understanding, then I see no reason to deny that one is a medic,” she added.”
Knowing how to share the information is another story.
“This is something that affects all of us as physicians — we’re going to be patients at some point, right?” Dr. Winter commented. “But I don’t think how to disclose that is something that was ever brought up in my medical training.”
“Maybe there should just be a discussion of this one day when people are in medical school — maybe in a professionalism course — to broach this topic or look at if there’s any literature on outcomes related to disclosure of status or what are best practices,” she suggested.
A version of this article first appeared on Medscape.com.
Aaron Beck: An appreciation
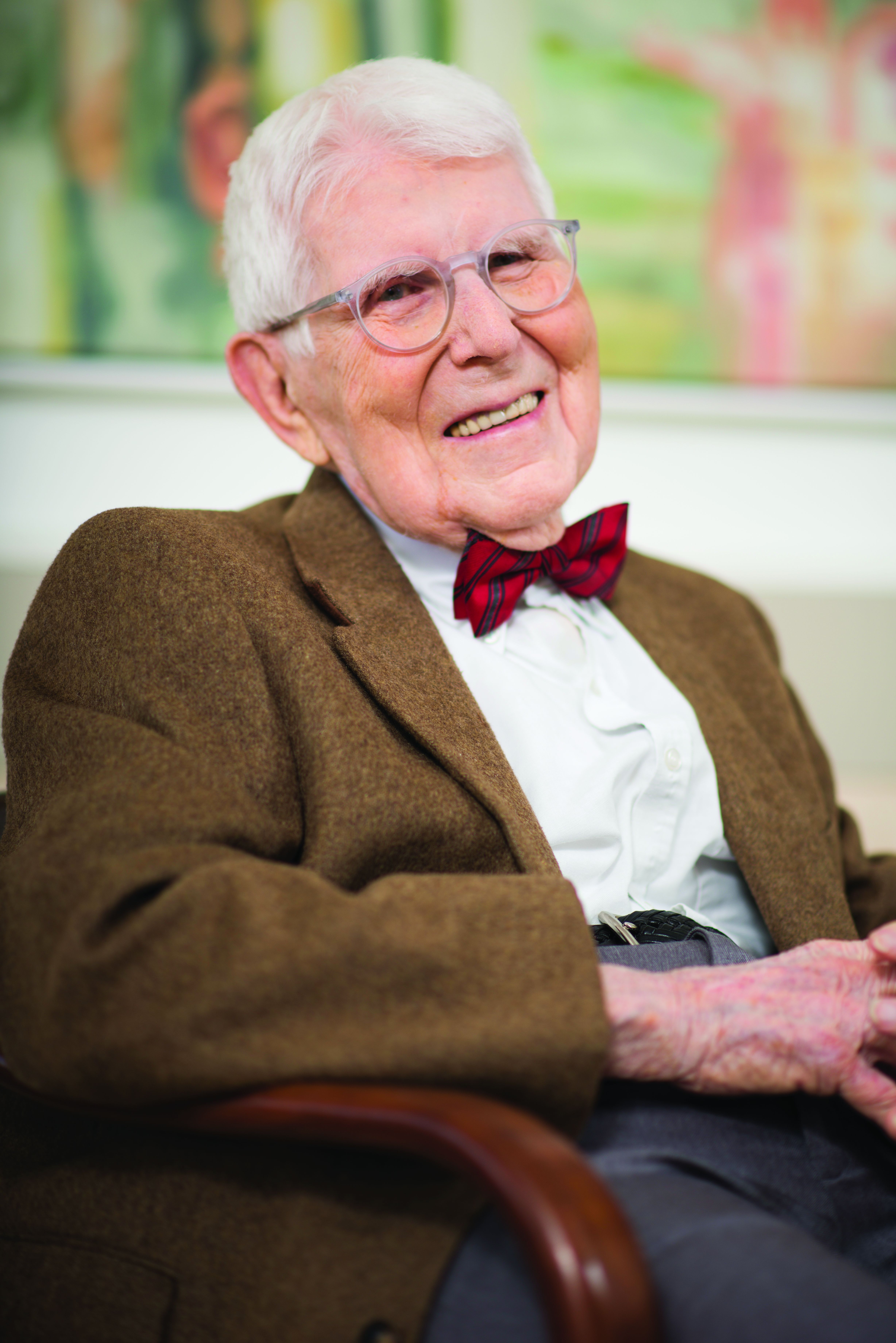
He always dressed the same at conferences: dark suit, white shirt, bright red bow tie.
For all his fame, he was very kind, warmly greeting those who wanted to see him and immediately turning attention toward their research rather than his own. Aaron Beck actually didn’t lecture much; he preferred to roleplay cognitive therapy with an audience member acting as the patient. He would engage in what he called Socratic questioning, or more formally, cognitive restructuring, with warmth and true curiosity:
- What might be another explanation or viewpoint?
- What are the effects of thinking this way?
- Can you think of any evidence that supports the opposite view?
The audience member/patient would benefit not only from thinking about things differently, but also from the captivating interaction with the man, Aaron Temkin Beck, MD, (who went by Tim), youngest child of Jewish immigrants from the Ukraine.
When written up in treatment manuals, cognitive restructuring can seem cold and overly logical, but in person, Dr. Beck made it come to life. This ability to nurture curiosity was a special talent; his friend and fellow cognitive psychologist Donald Meichenbaum, PhD, recalls that even over lunch, he never stopped asking questions, personal and professional, on a wide range of topics.
It is widely accepted that Dr. Beck, who died Nov. 1 at the age of 100 in suburban Philadelphia, was the most important figure in the field of cognitive-behavioral therapy (CBT).
He didn’t invent the field. Behaviorism predated him by generations, founded by figures such as John Watson and B.F. Skinner. Those psychologists set up behaviorism as an alternative to the reigning power of Freudian psychoanalysis, but they ran a distant second.
It wasn’t until Dr. Beck added a new approach, cognitive therapy, to the behavioristic movement that the new mélange, CBT, began to gain traction with clinicians and researchers. Dr. Beck, who had trained in psychiatry, developed his ideas in the 1960s while observing what he believed were limitations in the classic Freudian methods. He recognized that patients had “automatic thoughts,” not just unconscious emotions, when they engaged in Freudian free association, saying whatever came to their minds.
These thoughts often distorted reality, he observed; they were “maladaptive beliefs,” and when they changed, patients’ emotional states improved.
Dr. Beck wasn’t alone. The psychologist Albert Ellis, PhD, in New York, had come to similar conclusions a decade earlier, though with a more coldly logical and challenging style. The prominent British psychologist Hans Eysenck, PhD, had argued strongly that Freudian psychoanalysis was ineffective and that behavioral approaches were better.
Dr. Beck turned the Freudian equation around: Instead of emotion as cause and thought as effect, it was thought which affected emotion, for better or worse. Once you connected behavior as the outcome, you had the essence of CBT: thought, emotion, and behavior – each affecting the other, with thought being the strongest axis of change.
The process wasn’t bloodless. Behaviorists defended their turf against cognitivists, just as much as Freudians rejected both. At one point the behaviorists in the Association for the Advancement of Behavior Therapy tried to expel the advocates of a cognitive approach. Dr. Beck responded by leading the cognitivists in creating a new journal; he emphasized the importance of research being the main mechanism to decide what treatments worked the best.
Putting these ideas out in the 1960s and 1970s, Dr. Beck garnered support from researchers when he manualized the approach. Freudian psychoanalysis was idiosyncratic; it was almost impossible to study empirically, because the therapist would be responding to the unpredictable dreams and memories of patients engaged in free association. Each case was unique.
But CBT was systematic: The same general approach was taken to all patients; the same negative cognitions were found in depression, for instance, like all-or-nothing thinking or overgeneralization. Once manualized, CBT became the standard method of psychotherapy studied with the newly developed method of randomized controlled trials (RCTs).
By the 1980s, RCTs had proven the efficacy of CBT in depression, and the approach took off.
Dr. Beck already had developed a series of rating scales: the Beck Depression Inventory, the Beck Scale for Suicidal Ideation, the Beck Anxiety Inventory, the Beck Hopelessness Scale. Widely used, these scales extended his influence enormously. Copyrighted, they created a new industry of psychological research.
Dr. Beck’s own work was mainly in depression, but his followers extended it everywhere else: anxiety disorders and phobias, eating disorders, substance abuse, bipolar illness, even schizophrenia. Meanwhile, Freudian psychoanalysis fell into a steep decline from which it never recovered.
Some argued that it was abetted by insurance restrictions on psychotherapy, which favored shorter-term CBT; others that its research was biased in its favor because psychotherapy treatments, unlike medications, cannot be blinded; others that its efficacy could not be shown to be specific to its theory, as opposed to the interpersonal relationship between therapist and client.
Still, CBT has transformed psychotherapy and continues to expand its influence. Computer-based CBT has been proven effective, and digital CBT has become a standard approach in many smartphone applications and is central to the claims of multiple new biotechnology companies advocating for digital psychotherapy.
Aaron Beck continued publishing scientific articles to age 98. His last papers reviewed his life’s work. He characteristically gave credit to others, calmly recollected how he traveled away from psychoanalysis, described how his work started and ended in schizophrenia, and noted that the “working relationship with the therapist” remained a key factor for the success of CBT.
That parting comment reminds us that behind all the technology and research stands the kindly man in the dark suit, white shirt, and bright red bow tie, looking at you warmly, asking about your thoughts, and curiously wondering what might be another explanation or viewpoint you hadn’t considered.
Nassir Ghaemi, MD, MPH, is a professor of psychiatry at Tufts Medical Center and a lecturer in psychiatry at Harvard Medical School. He is the author of several general-interest books on psychiatry. A version of this article first appeared on Medscape.com.
He always dressed the same at conferences: dark suit, white shirt, bright red bow tie.
For all his fame, he was very kind, warmly greeting those who wanted to see him and immediately turning attention toward their research rather than his own. Aaron Beck actually didn’t lecture much; he preferred to roleplay cognitive therapy with an audience member acting as the patient. He would engage in what he called Socratic questioning, or more formally, cognitive restructuring, with warmth and true curiosity:
- What might be another explanation or viewpoint?
- What are the effects of thinking this way?
- Can you think of any evidence that supports the opposite view?
The audience member/patient would benefit not only from thinking about things differently, but also from the captivating interaction with the man, Aaron Temkin Beck, MD, (who went by Tim), youngest child of Jewish immigrants from the Ukraine.
When written up in treatment manuals, cognitive restructuring can seem cold and overly logical, but in person, Dr. Beck made it come to life. This ability to nurture curiosity was a special talent; his friend and fellow cognitive psychologist Donald Meichenbaum, PhD, recalls that even over lunch, he never stopped asking questions, personal and professional, on a wide range of topics.
It is widely accepted that Dr. Beck, who died Nov. 1 at the age of 100 in suburban Philadelphia, was the most important figure in the field of cognitive-behavioral therapy (CBT).
He didn’t invent the field. Behaviorism predated him by generations, founded by figures such as John Watson and B.F. Skinner. Those psychologists set up behaviorism as an alternative to the reigning power of Freudian psychoanalysis, but they ran a distant second.
It wasn’t until Dr. Beck added a new approach, cognitive therapy, to the behavioristic movement that the new mélange, CBT, began to gain traction with clinicians and researchers. Dr. Beck, who had trained in psychiatry, developed his ideas in the 1960s while observing what he believed were limitations in the classic Freudian methods. He recognized that patients had “automatic thoughts,” not just unconscious emotions, when they engaged in Freudian free association, saying whatever came to their minds.
These thoughts often distorted reality, he observed; they were “maladaptive beliefs,” and when they changed, patients’ emotional states improved.
Dr. Beck wasn’t alone. The psychologist Albert Ellis, PhD, in New York, had come to similar conclusions a decade earlier, though with a more coldly logical and challenging style. The prominent British psychologist Hans Eysenck, PhD, had argued strongly that Freudian psychoanalysis was ineffective and that behavioral approaches were better.
Dr. Beck turned the Freudian equation around: Instead of emotion as cause and thought as effect, it was thought which affected emotion, for better or worse. Once you connected behavior as the outcome, you had the essence of CBT: thought, emotion, and behavior – each affecting the other, with thought being the strongest axis of change.
The process wasn’t bloodless. Behaviorists defended their turf against cognitivists, just as much as Freudians rejected both. At one point the behaviorists in the Association for the Advancement of Behavior Therapy tried to expel the advocates of a cognitive approach. Dr. Beck responded by leading the cognitivists in creating a new journal; he emphasized the importance of research being the main mechanism to decide what treatments worked the best.
Putting these ideas out in the 1960s and 1970s, Dr. Beck garnered support from researchers when he manualized the approach. Freudian psychoanalysis was idiosyncratic; it was almost impossible to study empirically, because the therapist would be responding to the unpredictable dreams and memories of patients engaged in free association. Each case was unique.
But CBT was systematic: The same general approach was taken to all patients; the same negative cognitions were found in depression, for instance, like all-or-nothing thinking or overgeneralization. Once manualized, CBT became the standard method of psychotherapy studied with the newly developed method of randomized controlled trials (RCTs).
By the 1980s, RCTs had proven the efficacy of CBT in depression, and the approach took off.
Dr. Beck already had developed a series of rating scales: the Beck Depression Inventory, the Beck Scale for Suicidal Ideation, the Beck Anxiety Inventory, the Beck Hopelessness Scale. Widely used, these scales extended his influence enormously. Copyrighted, they created a new industry of psychological research.
Dr. Beck’s own work was mainly in depression, but his followers extended it everywhere else: anxiety disorders and phobias, eating disorders, substance abuse, bipolar illness, even schizophrenia. Meanwhile, Freudian psychoanalysis fell into a steep decline from which it never recovered.
Some argued that it was abetted by insurance restrictions on psychotherapy, which favored shorter-term CBT; others that its research was biased in its favor because psychotherapy treatments, unlike medications, cannot be blinded; others that its efficacy could not be shown to be specific to its theory, as opposed to the interpersonal relationship between therapist and client.
Still, CBT has transformed psychotherapy and continues to expand its influence. Computer-based CBT has been proven effective, and digital CBT has become a standard approach in many smartphone applications and is central to the claims of multiple new biotechnology companies advocating for digital psychotherapy.
Aaron Beck continued publishing scientific articles to age 98. His last papers reviewed his life’s work. He characteristically gave credit to others, calmly recollected how he traveled away from psychoanalysis, described how his work started and ended in schizophrenia, and noted that the “working relationship with the therapist” remained a key factor for the success of CBT.
That parting comment reminds us that behind all the technology and research stands the kindly man in the dark suit, white shirt, and bright red bow tie, looking at you warmly, asking about your thoughts, and curiously wondering what might be another explanation or viewpoint you hadn’t considered.
Nassir Ghaemi, MD, MPH, is a professor of psychiatry at Tufts Medical Center and a lecturer in psychiatry at Harvard Medical School. He is the author of several general-interest books on psychiatry. A version of this article first appeared on Medscape.com.
He always dressed the same at conferences: dark suit, white shirt, bright red bow tie.
For all his fame, he was very kind, warmly greeting those who wanted to see him and immediately turning attention toward their research rather than his own. Aaron Beck actually didn’t lecture much; he preferred to roleplay cognitive therapy with an audience member acting as the patient. He would engage in what he called Socratic questioning, or more formally, cognitive restructuring, with warmth and true curiosity:
- What might be another explanation or viewpoint?
- What are the effects of thinking this way?
- Can you think of any evidence that supports the opposite view?
The audience member/patient would benefit not only from thinking about things differently, but also from the captivating interaction with the man, Aaron Temkin Beck, MD, (who went by Tim), youngest child of Jewish immigrants from the Ukraine.
When written up in treatment manuals, cognitive restructuring can seem cold and overly logical, but in person, Dr. Beck made it come to life. This ability to nurture curiosity was a special talent; his friend and fellow cognitive psychologist Donald Meichenbaum, PhD, recalls that even over lunch, he never stopped asking questions, personal and professional, on a wide range of topics.
It is widely accepted that Dr. Beck, who died Nov. 1 at the age of 100 in suburban Philadelphia, was the most important figure in the field of cognitive-behavioral therapy (CBT).
He didn’t invent the field. Behaviorism predated him by generations, founded by figures such as John Watson and B.F. Skinner. Those psychologists set up behaviorism as an alternative to the reigning power of Freudian psychoanalysis, but they ran a distant second.
It wasn’t until Dr. Beck added a new approach, cognitive therapy, to the behavioristic movement that the new mélange, CBT, began to gain traction with clinicians and researchers. Dr. Beck, who had trained in psychiatry, developed his ideas in the 1960s while observing what he believed were limitations in the classic Freudian methods. He recognized that patients had “automatic thoughts,” not just unconscious emotions, when they engaged in Freudian free association, saying whatever came to their minds.
These thoughts often distorted reality, he observed; they were “maladaptive beliefs,” and when they changed, patients’ emotional states improved.
Dr. Beck wasn’t alone. The psychologist Albert Ellis, PhD, in New York, had come to similar conclusions a decade earlier, though with a more coldly logical and challenging style. The prominent British psychologist Hans Eysenck, PhD, had argued strongly that Freudian psychoanalysis was ineffective and that behavioral approaches were better.
Dr. Beck turned the Freudian equation around: Instead of emotion as cause and thought as effect, it was thought which affected emotion, for better or worse. Once you connected behavior as the outcome, you had the essence of CBT: thought, emotion, and behavior – each affecting the other, with thought being the strongest axis of change.
The process wasn’t bloodless. Behaviorists defended their turf against cognitivists, just as much as Freudians rejected both. At one point the behaviorists in the Association for the Advancement of Behavior Therapy tried to expel the advocates of a cognitive approach. Dr. Beck responded by leading the cognitivists in creating a new journal; he emphasized the importance of research being the main mechanism to decide what treatments worked the best.
Putting these ideas out in the 1960s and 1970s, Dr. Beck garnered support from researchers when he manualized the approach. Freudian psychoanalysis was idiosyncratic; it was almost impossible to study empirically, because the therapist would be responding to the unpredictable dreams and memories of patients engaged in free association. Each case was unique.
But CBT was systematic: The same general approach was taken to all patients; the same negative cognitions were found in depression, for instance, like all-or-nothing thinking or overgeneralization. Once manualized, CBT became the standard method of psychotherapy studied with the newly developed method of randomized controlled trials (RCTs).
By the 1980s, RCTs had proven the efficacy of CBT in depression, and the approach took off.
Dr. Beck already had developed a series of rating scales: the Beck Depression Inventory, the Beck Scale for Suicidal Ideation, the Beck Anxiety Inventory, the Beck Hopelessness Scale. Widely used, these scales extended his influence enormously. Copyrighted, they created a new industry of psychological research.
Dr. Beck’s own work was mainly in depression, but his followers extended it everywhere else: anxiety disorders and phobias, eating disorders, substance abuse, bipolar illness, even schizophrenia. Meanwhile, Freudian psychoanalysis fell into a steep decline from which it never recovered.
Some argued that it was abetted by insurance restrictions on psychotherapy, which favored shorter-term CBT; others that its research was biased in its favor because psychotherapy treatments, unlike medications, cannot be blinded; others that its efficacy could not be shown to be specific to its theory, as opposed to the interpersonal relationship between therapist and client.
Still, CBT has transformed psychotherapy and continues to expand its influence. Computer-based CBT has been proven effective, and digital CBT has become a standard approach in many smartphone applications and is central to the claims of multiple new biotechnology companies advocating for digital psychotherapy.
Aaron Beck continued publishing scientific articles to age 98. His last papers reviewed his life’s work. He characteristically gave credit to others, calmly recollected how he traveled away from psychoanalysis, described how his work started and ended in schizophrenia, and noted that the “working relationship with the therapist” remained a key factor for the success of CBT.
That parting comment reminds us that behind all the technology and research stands the kindly man in the dark suit, white shirt, and bright red bow tie, looking at you warmly, asking about your thoughts, and curiously wondering what might be another explanation or viewpoint you hadn’t considered.
Nassir Ghaemi, MD, MPH, is a professor of psychiatry at Tufts Medical Center and a lecturer in psychiatry at Harvard Medical School. He is the author of several general-interest books on psychiatry. A version of this article first appeared on Medscape.com.
From bored to springboard
A weekend, for most of us in solo practice, doesn’t really signify time off from work. It just means we’re not seeing patients at the office.
There’s always business stuff to do like payroll and paying bills, records to review, the never-ending forms for a million things, and all the other stuff there never seems to be enough time to do on weekdays.
This weekend I started attacking the pile after dinner on Friday and found myself done by Saturday afternoon, which is rare. Usually I spend the better part of a weekend at my desk.
And then, unexpectedly faced with an empty desk, I found myself wondering what to do next.
Boredom is one of the odder human conditions. I have no idea if any other animal experiences it. Certainly, at least for us, there are more ways to entertain ourselves now than there ever have been – TV, Netflix, phone games, TikTok, books, just to name a few.
But do we always have to be entertained? Many great scientists have said that world-changing ideas have come to them when they weren’t working, such as while showering or riding to work. Leo Szilard was crossing a London street in 1933 when he suddenly saw how a nuclear chain reaction would be self-sustaining once initiated. Fortunately he wasn’t hit by a car in the process.
But I’m not Szilard. So I rationalized a reason not to exercise and sat on the couch with a book.
The remarkable human brain doesn’t shut down easily. With nothing else to do, most mammals tend do doze off. But not us. Our brains are always on, trying to think of the next goal, the next move, the next whatever.
Having nothing to do sounds like a great idea, until you have nothing to do. It may be fine for a few days, but after a while you realize there’s only so long you can stare at the waves or mountains before your mind turns back to “what’s next.” Many patients tell me how retirement sounded good until they got there and then found themselves volunteering or taking new jobs just to keep busy.
This isn’t a bad thing. Being bored is probably constructive. Without realizing it we use it to form new ideas and start new plans.
Maybe this is why we are where we are. Perhaps it’s this feature that pushed the development of intelligence further and led us to form civilizations.
It’s how we keep moving forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A weekend, for most of us in solo practice, doesn’t really signify time off from work. It just means we’re not seeing patients at the office.
There’s always business stuff to do like payroll and paying bills, records to review, the never-ending forms for a million things, and all the other stuff there never seems to be enough time to do on weekdays.
This weekend I started attacking the pile after dinner on Friday and found myself done by Saturday afternoon, which is rare. Usually I spend the better part of a weekend at my desk.
And then, unexpectedly faced with an empty desk, I found myself wondering what to do next.
Boredom is one of the odder human conditions. I have no idea if any other animal experiences it. Certainly, at least for us, there are more ways to entertain ourselves now than there ever have been – TV, Netflix, phone games, TikTok, books, just to name a few.
But do we always have to be entertained? Many great scientists have said that world-changing ideas have come to them when they weren’t working, such as while showering or riding to work. Leo Szilard was crossing a London street in 1933 when he suddenly saw how a nuclear chain reaction would be self-sustaining once initiated. Fortunately he wasn’t hit by a car in the process.
But I’m not Szilard. So I rationalized a reason not to exercise and sat on the couch with a book.
The remarkable human brain doesn’t shut down easily. With nothing else to do, most mammals tend do doze off. But not us. Our brains are always on, trying to think of the next goal, the next move, the next whatever.
Having nothing to do sounds like a great idea, until you have nothing to do. It may be fine for a few days, but after a while you realize there’s only so long you can stare at the waves or mountains before your mind turns back to “what’s next.” Many patients tell me how retirement sounded good until they got there and then found themselves volunteering or taking new jobs just to keep busy.
This isn’t a bad thing. Being bored is probably constructive. Without realizing it we use it to form new ideas and start new plans.
Maybe this is why we are where we are. Perhaps it’s this feature that pushed the development of intelligence further and led us to form civilizations.
It’s how we keep moving forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A weekend, for most of us in solo practice, doesn’t really signify time off from work. It just means we’re not seeing patients at the office.
There’s always business stuff to do like payroll and paying bills, records to review, the never-ending forms for a million things, and all the other stuff there never seems to be enough time to do on weekdays.
This weekend I started attacking the pile after dinner on Friday and found myself done by Saturday afternoon, which is rare. Usually I spend the better part of a weekend at my desk.
And then, unexpectedly faced with an empty desk, I found myself wondering what to do next.
Boredom is one of the odder human conditions. I have no idea if any other animal experiences it. Certainly, at least for us, there are more ways to entertain ourselves now than there ever have been – TV, Netflix, phone games, TikTok, books, just to name a few.
But do we always have to be entertained? Many great scientists have said that world-changing ideas have come to them when they weren’t working, such as while showering or riding to work. Leo Szilard was crossing a London street in 1933 when he suddenly saw how a nuclear chain reaction would be self-sustaining once initiated. Fortunately he wasn’t hit by a car in the process.
But I’m not Szilard. So I rationalized a reason not to exercise and sat on the couch with a book.
The remarkable human brain doesn’t shut down easily. With nothing else to do, most mammals tend do doze off. But not us. Our brains are always on, trying to think of the next goal, the next move, the next whatever.
Having nothing to do sounds like a great idea, until you have nothing to do. It may be fine for a few days, but after a while you realize there’s only so long you can stare at the waves or mountains before your mind turns back to “what’s next.” Many patients tell me how retirement sounded good until they got there and then found themselves volunteering or taking new jobs just to keep busy.
This isn’t a bad thing. Being bored is probably constructive. Without realizing it we use it to form new ideas and start new plans.
Maybe this is why we are where we are. Perhaps it’s this feature that pushed the development of intelligence further and led us to form civilizations.
It’s how we keep moving forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Practicing telepsychiatry: Include backup plans, ground rules
For psychiatrists embarking on a telemedicine consultation, it might be helpful to review a checklist of steps that will reduce the risk of problems when things go wrong, according to an overview of the dangers at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sponsored by Medscape Live.
Ideally, telepsychiatry will function much like an inpatient office visit, but the dynamics differ – as do the things that can go wrong, according to Sanjay Gupta, MD, chief medical officer, BryLin Behavioral Health System, Buffalo, N.Y. “Issues can arise suddenly. You need contingency planning.”
At the outset, psychiatrists should establish the location of the patient. This is necessary at every telemedicine encounter. With a remote device, a patient could be essentially anywhere on Earth. Patients might not even remember to mention that they are vacationing in Australia.
The location of the patient is important in the event of an unexpected crisis. This is not only relevant to an unstable patient at risk of dangerous behavior, such as actively attempting suicide, but to patients who have a seizure or some other emergency that inhibits communication. , and this requires confirming that the patient is where he or she was expected to be.
In addition, there should be a plan for technological failure. As everyone knows, these failures, such as dysfunction of a device, a poor connection, or an Internet outage, can happen at any time. Both the clinician and the patient can derive reassurance from at least one if not two or more plans to reconnect in the event of these failures.
The visit should also begin with questions that will establish the patient has a sense of adequate privacy. This is one of the most common obstacles to an effective telemedicine consultation. Dr. Gupta pointed out that phone or computer cameras do not typically permit the clinician to exclude the presence of another individual sitting even a few feet away from the patient. With spouses and children nearby, there might be a tenuous sense of privacy even if they are unlikely to overhear the telemedicine visit.
One strategy that can be used to assess the patient’s level of comfort is to ask for a description of the patient’s surroundings and any other people at the location. Dr. Gupta also said it is appropriate to establish ground rules about recording of the session, which has its own potential to inhibit the interaction.
Warning that some form of consent to a telemedicine visit is mandatory in most states, Dr. Gupta also cautioned that a formal identification check is appropriate for a first-time visit. The risk of an individual offering a false identification is likely to be low, but it can be eliminated entirely by a protocol that verifies consent and identify before the clinical work begins.
Because of the importance of engaging patients quickly, Dr. Gupta called the first few minutes of a telemedicine visit “crucial.” By initiating the visit with a warm and respectful tone, by relaying a competent and professional appearance, and by establishing an atmosphere that encourages communication, the initial minutes of the call can set a tone that facilitates an effective visit.
Simple and established telehealth etiquette strategies should be employed, according to Dr. Gupta. He suggested paying attention to such issues as lighting, background, and camera position. Descriptions of what constitutes adequate lighting and background are easily obtained on free how-to websites, but the goal is to provide patients with a nondistracting and clear view of the clinician.
During a telemedicine visit, the clinician’s focus should remain on the patient, according to Dr. Gupta. He advised against taking notes or documenting the visit on an electronic health record during the course of the visit. Rather, he advised positioning the camera in a way that the patient feels eye contact is being made.
“It can be helpful to periodically summarize what the patient has said to demonstrate that you are fully engaged,” Dr. Gupta suggested.
Telemedicine is very effective for many but not all patients. Some, such as those with active psychosis, are not suited to this approach, but others are simply uncomfortable with this form of communication. Dr. Gupta suggested that clinicians should be mindful of the advantages and the limitations of telepsychiatry.
Ultimately, Dr. Gupta believes that the substantial expansion of telepsychiatry that took place during the COVID-19 pandemic is likely to persist when the pandemic ends, even if many of the changes that permitted its expansion, such as a relaxation of HIPPA requirements, are withdrawn. However, parity reimbursement for visits offered by telemedicine relative to those that are face-to-face, which greatly facilitated the growth of telepsychiatry, is not guaranteed, so this remains an unanswered question.
“The question is what will happen to the billing codes when we see COVID-19 in the rearview mirror, and the answer is that no one knows,” he said.
Uncertainty about future use
Other experts in this field agreed. James (Jay) H. Shore, MD, MPH, director of telemedicine, Helen and Arthur E. Johnson Depression Center, University of Colorado at Denver, Aurora, has long been an advocate for the value of telepsychiatry for reaching patients with limited psychosocial services. The attention drawn to this practice by the COVID-19 pandemic has been welcome, but he does not know how it will affect the future.
“There is too much uncertainty in the system to make a good prediction of where this may end up,” he said.
It is not just reimbursement that is at risk, according to Peter Yellowlees, MBBS, MD, chief wellness officer at the University of California, Davis. Also a longtime advocate of telepsychiatry, particularly to reach the underserved, Dr. Yellowlees pointed out that the ability to prescribe controlled substances through telemedicine and the ability to consult with patients across state lines might also be in jeopardy if and when rules for telemedicine are revisited after the pandemic.
“Many organizations are lobbying to make the pandemic changes permanent because they greatly support telemedicine delivery,” Dr. Yellowlees said, but agreed about the uncertainty regarding what policy makers will do.
Jayasudha Gude, MD, who is completing her residency in psychiatry at Zucker Hillside Hospital, Northwell Health, New York, recently led a literature review evaluating the needs and viability of telepsychiatry during and after the COVID-19 era (Cureus. 2021 Aug;13:e16974). Based on the benefits she identified in her review, she said, “I would definitely want to advocate for the continued use of telepsychiatry after the pandemic is over.” She hopes that psychiatrists who now have experience in this area will join her.
“I am hopeful that a lot of mental health providers will also be advocating since they have experience, and many will want to continue its use,” she said. Medscape Live and this news organization are owned by the same parent company. Dr. Gupta, Dr. Shore, Dr. Yellowlees, and Dr. Gude reported no potential conflicts of interest.
For psychiatrists embarking on a telemedicine consultation, it might be helpful to review a checklist of steps that will reduce the risk of problems when things go wrong, according to an overview of the dangers at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sponsored by Medscape Live.
Ideally, telepsychiatry will function much like an inpatient office visit, but the dynamics differ – as do the things that can go wrong, according to Sanjay Gupta, MD, chief medical officer, BryLin Behavioral Health System, Buffalo, N.Y. “Issues can arise suddenly. You need contingency planning.”
At the outset, psychiatrists should establish the location of the patient. This is necessary at every telemedicine encounter. With a remote device, a patient could be essentially anywhere on Earth. Patients might not even remember to mention that they are vacationing in Australia.
The location of the patient is important in the event of an unexpected crisis. This is not only relevant to an unstable patient at risk of dangerous behavior, such as actively attempting suicide, but to patients who have a seizure or some other emergency that inhibits communication. , and this requires confirming that the patient is where he or she was expected to be.
In addition, there should be a plan for technological failure. As everyone knows, these failures, such as dysfunction of a device, a poor connection, or an Internet outage, can happen at any time. Both the clinician and the patient can derive reassurance from at least one if not two or more plans to reconnect in the event of these failures.
The visit should also begin with questions that will establish the patient has a sense of adequate privacy. This is one of the most common obstacles to an effective telemedicine consultation. Dr. Gupta pointed out that phone or computer cameras do not typically permit the clinician to exclude the presence of another individual sitting even a few feet away from the patient. With spouses and children nearby, there might be a tenuous sense of privacy even if they are unlikely to overhear the telemedicine visit.
One strategy that can be used to assess the patient’s level of comfort is to ask for a description of the patient’s surroundings and any other people at the location. Dr. Gupta also said it is appropriate to establish ground rules about recording of the session, which has its own potential to inhibit the interaction.
Warning that some form of consent to a telemedicine visit is mandatory in most states, Dr. Gupta also cautioned that a formal identification check is appropriate for a first-time visit. The risk of an individual offering a false identification is likely to be low, but it can be eliminated entirely by a protocol that verifies consent and identify before the clinical work begins.
Because of the importance of engaging patients quickly, Dr. Gupta called the first few minutes of a telemedicine visit “crucial.” By initiating the visit with a warm and respectful tone, by relaying a competent and professional appearance, and by establishing an atmosphere that encourages communication, the initial minutes of the call can set a tone that facilitates an effective visit.
Simple and established telehealth etiquette strategies should be employed, according to Dr. Gupta. He suggested paying attention to such issues as lighting, background, and camera position. Descriptions of what constitutes adequate lighting and background are easily obtained on free how-to websites, but the goal is to provide patients with a nondistracting and clear view of the clinician.
During a telemedicine visit, the clinician’s focus should remain on the patient, according to Dr. Gupta. He advised against taking notes or documenting the visit on an electronic health record during the course of the visit. Rather, he advised positioning the camera in a way that the patient feels eye contact is being made.
“It can be helpful to periodically summarize what the patient has said to demonstrate that you are fully engaged,” Dr. Gupta suggested.
Telemedicine is very effective for many but not all patients. Some, such as those with active psychosis, are not suited to this approach, but others are simply uncomfortable with this form of communication. Dr. Gupta suggested that clinicians should be mindful of the advantages and the limitations of telepsychiatry.
Ultimately, Dr. Gupta believes that the substantial expansion of telepsychiatry that took place during the COVID-19 pandemic is likely to persist when the pandemic ends, even if many of the changes that permitted its expansion, such as a relaxation of HIPPA requirements, are withdrawn. However, parity reimbursement for visits offered by telemedicine relative to those that are face-to-face, which greatly facilitated the growth of telepsychiatry, is not guaranteed, so this remains an unanswered question.
“The question is what will happen to the billing codes when we see COVID-19 in the rearview mirror, and the answer is that no one knows,” he said.
Uncertainty about future use
Other experts in this field agreed. James (Jay) H. Shore, MD, MPH, director of telemedicine, Helen and Arthur E. Johnson Depression Center, University of Colorado at Denver, Aurora, has long been an advocate for the value of telepsychiatry for reaching patients with limited psychosocial services. The attention drawn to this practice by the COVID-19 pandemic has been welcome, but he does not know how it will affect the future.
“There is too much uncertainty in the system to make a good prediction of where this may end up,” he said.
It is not just reimbursement that is at risk, according to Peter Yellowlees, MBBS, MD, chief wellness officer at the University of California, Davis. Also a longtime advocate of telepsychiatry, particularly to reach the underserved, Dr. Yellowlees pointed out that the ability to prescribe controlled substances through telemedicine and the ability to consult with patients across state lines might also be in jeopardy if and when rules for telemedicine are revisited after the pandemic.
“Many organizations are lobbying to make the pandemic changes permanent because they greatly support telemedicine delivery,” Dr. Yellowlees said, but agreed about the uncertainty regarding what policy makers will do.
Jayasudha Gude, MD, who is completing her residency in psychiatry at Zucker Hillside Hospital, Northwell Health, New York, recently led a literature review evaluating the needs and viability of telepsychiatry during and after the COVID-19 era (Cureus. 2021 Aug;13:e16974). Based on the benefits she identified in her review, she said, “I would definitely want to advocate for the continued use of telepsychiatry after the pandemic is over.” She hopes that psychiatrists who now have experience in this area will join her.
“I am hopeful that a lot of mental health providers will also be advocating since they have experience, and many will want to continue its use,” she said. Medscape Live and this news organization are owned by the same parent company. Dr. Gupta, Dr. Shore, Dr. Yellowlees, and Dr. Gude reported no potential conflicts of interest.
For psychiatrists embarking on a telemedicine consultation, it might be helpful to review a checklist of steps that will reduce the risk of problems when things go wrong, according to an overview of the dangers at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sponsored by Medscape Live.
Ideally, telepsychiatry will function much like an inpatient office visit, but the dynamics differ – as do the things that can go wrong, according to Sanjay Gupta, MD, chief medical officer, BryLin Behavioral Health System, Buffalo, N.Y. “Issues can arise suddenly. You need contingency planning.”
At the outset, psychiatrists should establish the location of the patient. This is necessary at every telemedicine encounter. With a remote device, a patient could be essentially anywhere on Earth. Patients might not even remember to mention that they are vacationing in Australia.
The location of the patient is important in the event of an unexpected crisis. This is not only relevant to an unstable patient at risk of dangerous behavior, such as actively attempting suicide, but to patients who have a seizure or some other emergency that inhibits communication. , and this requires confirming that the patient is where he or she was expected to be.
In addition, there should be a plan for technological failure. As everyone knows, these failures, such as dysfunction of a device, a poor connection, or an Internet outage, can happen at any time. Both the clinician and the patient can derive reassurance from at least one if not two or more plans to reconnect in the event of these failures.
The visit should also begin with questions that will establish the patient has a sense of adequate privacy. This is one of the most common obstacles to an effective telemedicine consultation. Dr. Gupta pointed out that phone or computer cameras do not typically permit the clinician to exclude the presence of another individual sitting even a few feet away from the patient. With spouses and children nearby, there might be a tenuous sense of privacy even if they are unlikely to overhear the telemedicine visit.
One strategy that can be used to assess the patient’s level of comfort is to ask for a description of the patient’s surroundings and any other people at the location. Dr. Gupta also said it is appropriate to establish ground rules about recording of the session, which has its own potential to inhibit the interaction.
Warning that some form of consent to a telemedicine visit is mandatory in most states, Dr. Gupta also cautioned that a formal identification check is appropriate for a first-time visit. The risk of an individual offering a false identification is likely to be low, but it can be eliminated entirely by a protocol that verifies consent and identify before the clinical work begins.
Because of the importance of engaging patients quickly, Dr. Gupta called the first few minutes of a telemedicine visit “crucial.” By initiating the visit with a warm and respectful tone, by relaying a competent and professional appearance, and by establishing an atmosphere that encourages communication, the initial minutes of the call can set a tone that facilitates an effective visit.
Simple and established telehealth etiquette strategies should be employed, according to Dr. Gupta. He suggested paying attention to such issues as lighting, background, and camera position. Descriptions of what constitutes adequate lighting and background are easily obtained on free how-to websites, but the goal is to provide patients with a nondistracting and clear view of the clinician.
During a telemedicine visit, the clinician’s focus should remain on the patient, according to Dr. Gupta. He advised against taking notes or documenting the visit on an electronic health record during the course of the visit. Rather, he advised positioning the camera in a way that the patient feels eye contact is being made.
“It can be helpful to periodically summarize what the patient has said to demonstrate that you are fully engaged,” Dr. Gupta suggested.
Telemedicine is very effective for many but not all patients. Some, such as those with active psychosis, are not suited to this approach, but others are simply uncomfortable with this form of communication. Dr. Gupta suggested that clinicians should be mindful of the advantages and the limitations of telepsychiatry.
Ultimately, Dr. Gupta believes that the substantial expansion of telepsychiatry that took place during the COVID-19 pandemic is likely to persist when the pandemic ends, even if many of the changes that permitted its expansion, such as a relaxation of HIPPA requirements, are withdrawn. However, parity reimbursement for visits offered by telemedicine relative to those that are face-to-face, which greatly facilitated the growth of telepsychiatry, is not guaranteed, so this remains an unanswered question.
“The question is what will happen to the billing codes when we see COVID-19 in the rearview mirror, and the answer is that no one knows,” he said.
Uncertainty about future use
Other experts in this field agreed. James (Jay) H. Shore, MD, MPH, director of telemedicine, Helen and Arthur E. Johnson Depression Center, University of Colorado at Denver, Aurora, has long been an advocate for the value of telepsychiatry for reaching patients with limited psychosocial services. The attention drawn to this practice by the COVID-19 pandemic has been welcome, but he does not know how it will affect the future.
“There is too much uncertainty in the system to make a good prediction of where this may end up,” he said.
It is not just reimbursement that is at risk, according to Peter Yellowlees, MBBS, MD, chief wellness officer at the University of California, Davis. Also a longtime advocate of telepsychiatry, particularly to reach the underserved, Dr. Yellowlees pointed out that the ability to prescribe controlled substances through telemedicine and the ability to consult with patients across state lines might also be in jeopardy if and when rules for telemedicine are revisited after the pandemic.
“Many organizations are lobbying to make the pandemic changes permanent because they greatly support telemedicine delivery,” Dr. Yellowlees said, but agreed about the uncertainty regarding what policy makers will do.
Jayasudha Gude, MD, who is completing her residency in psychiatry at Zucker Hillside Hospital, Northwell Health, New York, recently led a literature review evaluating the needs and viability of telepsychiatry during and after the COVID-19 era (Cureus. 2021 Aug;13:e16974). Based on the benefits she identified in her review, she said, “I would definitely want to advocate for the continued use of telepsychiatry after the pandemic is over.” She hopes that psychiatrists who now have experience in this area will join her.
“I am hopeful that a lot of mental health providers will also be advocating since they have experience, and many will want to continue its use,” she said. Medscape Live and this news organization are owned by the same parent company. Dr. Gupta, Dr. Shore, Dr. Yellowlees, and Dr. Gude reported no potential conflicts of interest.
FROM PSYCHOPHARMACOLOGY UPDATE
Texas practitioners see increased interest in birth control since near-total abortion ban
In September, when Texas’ near-total abortion ban took effect, Planned Parenthood clinics in the Lone Star State started offering every patient who walked in information on Senate Bill 8, as well as emergency contraception, condoms, and two pregnancy tests. The plan is to distribute 22,000 “empowerment kits” this year.
“We felt it was very important for patients to have as many tools on hand to help them meet this really onerous law,” said Elizabeth Cardwell, lead clinician at Planned Parenthood of Greater Texas, which has 24 clinics across the northern and central regions of the state and provides care to tens of thousands of people annually.
Most of their patients – who tend to be uninsured and have annual household incomes of less than $25,000 – had not known about SB 8 the first several weeks after implementation, said Dr. Cardwell. But once they learned about it, patients seemed to rush to get on birth control, she said.
SB 8 allows private citizens, in Texas or elsewhere, to sue anyone who performs an abortion in the state or who “aided or abetted” someone getting an abortion once fetal cardiac activity is detected. This is generally around six weeks, before most people know they’re pregnant. It’s had a chilling effect in Texas, where access to abortion was already limited.
Medical staffs are doubling down on educating patients about birth control. They recognize the strategy isn’t foolproof but are desperate to prevent unintended pregnancies, nearly half of which nationwide end in abortion.
“It’s more important now than it ever has been,” said Dr. Cardwell. “I’ve been in abortion care 30-plus years, and my go-to line was ‘You’ve got plenty of time. You don’t have to feel rushed. Talk with your partner. Talk with your family,’” she said. “Now we don’t have that luxury.”
Patients, too, seem to feel a sense of urgency. During September, according to data from Planned Parenthood of Greater Texas, medical staff provided patients with some form of birth control — for example, pill packs, Depo-Provera shots or IUD implant insertions – in more than 3,750 visits, 5% more than in Sept. 2020.
Dr. Jennifer Liedtke, a family physician in West Texas, said she and her nurse practitioners explain SB 8 to every patient who comes to their private practice and saw a 20% increase in requests for long-acting reversible contraceptive methods, known as LARCs, in September.
LARCs, a category that includes intrauterine devices and hormonal implants, have become increasingly appealing because they are 99% effective at preventing pregnancy and last several years. They are also simpler than the pill, which needs to be taken daily, or the vaginal ring, which needs to be changed monthly.
Still, LARCs are not everyone’s preferred method. For example, inserting an IUD can be painful.
A doctor’s office is one of the few opportunities for reliable birth control education. Texas law doesn’t require schools to teach sex education, and if they do, educators must stress abstinence as the preferred birth control method. Some doctors opt to explain abortion access in the state when naming birth control options.
Dr. Liedtke is used to having to explain new laws passed by the Texas legislature. “It happens all the time,” she said. But the controversy surrounding SB 8 confuses patients all the more as the law works its way through the court system with differing rulings, one of which briefly blocked the measure. The U.S. Supreme Court heard related arguments Nov. 1.
“People just don’t understand,” said Dr. Liedtke. “It was tied up for 48 hours, so they are like, ‘It’s not a law anymore?’ Well, no, technically it is.”
Not all providers are able to talk freely about abortion access. In 2019, the Trump administration barred providers that participate in the federally funded family planning program, Title X, from mentioning abortion care to patients, even if patients themselves raise questions. In early October, the Biden administration reversed that rule. The change will kick in this month. Planned Parenthood can discuss SB 8 in Texas because Texas affiliates do not receive Title X dollars.
Dr. Lindsey Vasquez of Legacy Community Health, the largest federally qualified health center in Texas and a recipient of Title X dollars, said she and other staff members have not discussed abortion or SB 8 because they also must juggle a variety of other priorities. Legacy’s patients are underserved, she said. A majority live at or below the federal poverty level.
Nearly two years into the Covid-19 pandemic, “we’re literally maximizing those visits,” Dr. Vasquez said. Their jobs go beyond offering reproductive care. “We’re making sure they have food resources, that they have their housing stable,” she said. “We really are trying to make sure that all of their needs are met because we know for these types of populations – patients that we serve – this may be our only moment that we get to meet them.”
Specialized family planning clinics that receive Title X dollars do have proactive conversations about contraceptive methods, according to Every Body Texas, the Title X grantee for the state.
Discussions of long-acting reversible contraception must be handled with sensitivity because these forms of birth control have a questionable history among certain populations, primarily lower-income patients. In the 1990s, lawmakers in several states, including Texas, introduced bills to offer cash assistance recipients financial incentives to get an implant or mandate insertion for people on government benefits, a move seen as reproductive coercion.
“It’s important for a client to get on the contraceptive method of their choice,” said Mimi Garcia, communications director for Every Body Texas. “Some people will just say, ‘Let’s get everyone on IUDs’ or ‘Let’s get everybody on hormonal implants’ because those are the most effective methods. ... That’s not something that’s going to work for [every] individual. ... Either they don’t agree with it philosophically, or they don’t like how it makes their body feel.”
It’s a nuanced subject for providers to broach, so some suggest starting the conversation by asking the patient about their future.
“The best question to ask is ‘When do you want to have another baby?’” said Dr. Liedtke. And then if they say, ‘Oh, gosh, I’m not even sure I want to have more kids’ or ‘Five or six years from now,’ then we start talking LARCs. ... But if it’s like, ‘Man, I really want to start trying in a year,’ then I don’t talk to them about putting one of those in.”
The Biden administration expected more demand for birth control in Texas, so Health & Human Services Secretary Xavier Becerra announced in mid-September that Every Body Texas would receive additional Title X funding, as would local providers experiencing an influx of clients as a result of SB 8.
But providers said improved access to contraception will not blunt the law’s effects. It will not protect patients who want to get pregnant but ultimately decide on abortion because they receive a diagnosis of a serious complication, their relationship status changes, or they lose financial or social support, said Dr. Elissa Serapio, an OB-GYN in the Rio Grande Valley and a fellow with Physicians for Reproductive Health.
“It’s the very best that we can do,” said Dr. Cardwell, of Planned Parenthood of Greater Texas. “There’s no 100% effective method of birth control.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
In September, when Texas’ near-total abortion ban took effect, Planned Parenthood clinics in the Lone Star State started offering every patient who walked in information on Senate Bill 8, as well as emergency contraception, condoms, and two pregnancy tests. The plan is to distribute 22,000 “empowerment kits” this year.
“We felt it was very important for patients to have as many tools on hand to help them meet this really onerous law,” said Elizabeth Cardwell, lead clinician at Planned Parenthood of Greater Texas, which has 24 clinics across the northern and central regions of the state and provides care to tens of thousands of people annually.
Most of their patients – who tend to be uninsured and have annual household incomes of less than $25,000 – had not known about SB 8 the first several weeks after implementation, said Dr. Cardwell. But once they learned about it, patients seemed to rush to get on birth control, she said.
SB 8 allows private citizens, in Texas or elsewhere, to sue anyone who performs an abortion in the state or who “aided or abetted” someone getting an abortion once fetal cardiac activity is detected. This is generally around six weeks, before most people know they’re pregnant. It’s had a chilling effect in Texas, where access to abortion was already limited.
Medical staffs are doubling down on educating patients about birth control. They recognize the strategy isn’t foolproof but are desperate to prevent unintended pregnancies, nearly half of which nationwide end in abortion.
“It’s more important now than it ever has been,” said Dr. Cardwell. “I’ve been in abortion care 30-plus years, and my go-to line was ‘You’ve got plenty of time. You don’t have to feel rushed. Talk with your partner. Talk with your family,’” she said. “Now we don’t have that luxury.”
Patients, too, seem to feel a sense of urgency. During September, according to data from Planned Parenthood of Greater Texas, medical staff provided patients with some form of birth control — for example, pill packs, Depo-Provera shots or IUD implant insertions – in more than 3,750 visits, 5% more than in Sept. 2020.
Dr. Jennifer Liedtke, a family physician in West Texas, said she and her nurse practitioners explain SB 8 to every patient who comes to their private practice and saw a 20% increase in requests for long-acting reversible contraceptive methods, known as LARCs, in September.
LARCs, a category that includes intrauterine devices and hormonal implants, have become increasingly appealing because they are 99% effective at preventing pregnancy and last several years. They are also simpler than the pill, which needs to be taken daily, or the vaginal ring, which needs to be changed monthly.
Still, LARCs are not everyone’s preferred method. For example, inserting an IUD can be painful.
A doctor’s office is one of the few opportunities for reliable birth control education. Texas law doesn’t require schools to teach sex education, and if they do, educators must stress abstinence as the preferred birth control method. Some doctors opt to explain abortion access in the state when naming birth control options.
Dr. Liedtke is used to having to explain new laws passed by the Texas legislature. “It happens all the time,” she said. But the controversy surrounding SB 8 confuses patients all the more as the law works its way through the court system with differing rulings, one of which briefly blocked the measure. The U.S. Supreme Court heard related arguments Nov. 1.
“People just don’t understand,” said Dr. Liedtke. “It was tied up for 48 hours, so they are like, ‘It’s not a law anymore?’ Well, no, technically it is.”
Not all providers are able to talk freely about abortion access. In 2019, the Trump administration barred providers that participate in the federally funded family planning program, Title X, from mentioning abortion care to patients, even if patients themselves raise questions. In early October, the Biden administration reversed that rule. The change will kick in this month. Planned Parenthood can discuss SB 8 in Texas because Texas affiliates do not receive Title X dollars.
Dr. Lindsey Vasquez of Legacy Community Health, the largest federally qualified health center in Texas and a recipient of Title X dollars, said she and other staff members have not discussed abortion or SB 8 because they also must juggle a variety of other priorities. Legacy’s patients are underserved, she said. A majority live at or below the federal poverty level.
Nearly two years into the Covid-19 pandemic, “we’re literally maximizing those visits,” Dr. Vasquez said. Their jobs go beyond offering reproductive care. “We’re making sure they have food resources, that they have their housing stable,” she said. “We really are trying to make sure that all of their needs are met because we know for these types of populations – patients that we serve – this may be our only moment that we get to meet them.”
Specialized family planning clinics that receive Title X dollars do have proactive conversations about contraceptive methods, according to Every Body Texas, the Title X grantee for the state.
Discussions of long-acting reversible contraception must be handled with sensitivity because these forms of birth control have a questionable history among certain populations, primarily lower-income patients. In the 1990s, lawmakers in several states, including Texas, introduced bills to offer cash assistance recipients financial incentives to get an implant or mandate insertion for people on government benefits, a move seen as reproductive coercion.
“It’s important for a client to get on the contraceptive method of their choice,” said Mimi Garcia, communications director for Every Body Texas. “Some people will just say, ‘Let’s get everyone on IUDs’ or ‘Let’s get everybody on hormonal implants’ because those are the most effective methods. ... That’s not something that’s going to work for [every] individual. ... Either they don’t agree with it philosophically, or they don’t like how it makes their body feel.”
It’s a nuanced subject for providers to broach, so some suggest starting the conversation by asking the patient about their future.
“The best question to ask is ‘When do you want to have another baby?’” said Dr. Liedtke. And then if they say, ‘Oh, gosh, I’m not even sure I want to have more kids’ or ‘Five or six years from now,’ then we start talking LARCs. ... But if it’s like, ‘Man, I really want to start trying in a year,’ then I don’t talk to them about putting one of those in.”
The Biden administration expected more demand for birth control in Texas, so Health & Human Services Secretary Xavier Becerra announced in mid-September that Every Body Texas would receive additional Title X funding, as would local providers experiencing an influx of clients as a result of SB 8.
But providers said improved access to contraception will not blunt the law’s effects. It will not protect patients who want to get pregnant but ultimately decide on abortion because they receive a diagnosis of a serious complication, their relationship status changes, or they lose financial or social support, said Dr. Elissa Serapio, an OB-GYN in the Rio Grande Valley and a fellow with Physicians for Reproductive Health.
“It’s the very best that we can do,” said Dr. Cardwell, of Planned Parenthood of Greater Texas. “There’s no 100% effective method of birth control.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
In September, when Texas’ near-total abortion ban took effect, Planned Parenthood clinics in the Lone Star State started offering every patient who walked in information on Senate Bill 8, as well as emergency contraception, condoms, and two pregnancy tests. The plan is to distribute 22,000 “empowerment kits” this year.
“We felt it was very important for patients to have as many tools on hand to help them meet this really onerous law,” said Elizabeth Cardwell, lead clinician at Planned Parenthood of Greater Texas, which has 24 clinics across the northern and central regions of the state and provides care to tens of thousands of people annually.
Most of their patients – who tend to be uninsured and have annual household incomes of less than $25,000 – had not known about SB 8 the first several weeks after implementation, said Dr. Cardwell. But once they learned about it, patients seemed to rush to get on birth control, she said.
SB 8 allows private citizens, in Texas or elsewhere, to sue anyone who performs an abortion in the state or who “aided or abetted” someone getting an abortion once fetal cardiac activity is detected. This is generally around six weeks, before most people know they’re pregnant. It’s had a chilling effect in Texas, where access to abortion was already limited.
Medical staffs are doubling down on educating patients about birth control. They recognize the strategy isn’t foolproof but are desperate to prevent unintended pregnancies, nearly half of which nationwide end in abortion.
“It’s more important now than it ever has been,” said Dr. Cardwell. “I’ve been in abortion care 30-plus years, and my go-to line was ‘You’ve got plenty of time. You don’t have to feel rushed. Talk with your partner. Talk with your family,’” she said. “Now we don’t have that luxury.”
Patients, too, seem to feel a sense of urgency. During September, according to data from Planned Parenthood of Greater Texas, medical staff provided patients with some form of birth control — for example, pill packs, Depo-Provera shots or IUD implant insertions – in more than 3,750 visits, 5% more than in Sept. 2020.
Dr. Jennifer Liedtke, a family physician in West Texas, said she and her nurse practitioners explain SB 8 to every patient who comes to their private practice and saw a 20% increase in requests for long-acting reversible contraceptive methods, known as LARCs, in September.
LARCs, a category that includes intrauterine devices and hormonal implants, have become increasingly appealing because they are 99% effective at preventing pregnancy and last several years. They are also simpler than the pill, which needs to be taken daily, or the vaginal ring, which needs to be changed monthly.
Still, LARCs are not everyone’s preferred method. For example, inserting an IUD can be painful.
A doctor’s office is one of the few opportunities for reliable birth control education. Texas law doesn’t require schools to teach sex education, and if they do, educators must stress abstinence as the preferred birth control method. Some doctors opt to explain abortion access in the state when naming birth control options.
Dr. Liedtke is used to having to explain new laws passed by the Texas legislature. “It happens all the time,” she said. But the controversy surrounding SB 8 confuses patients all the more as the law works its way through the court system with differing rulings, one of which briefly blocked the measure. The U.S. Supreme Court heard related arguments Nov. 1.
“People just don’t understand,” said Dr. Liedtke. “It was tied up for 48 hours, so they are like, ‘It’s not a law anymore?’ Well, no, technically it is.”
Not all providers are able to talk freely about abortion access. In 2019, the Trump administration barred providers that participate in the federally funded family planning program, Title X, from mentioning abortion care to patients, even if patients themselves raise questions. In early October, the Biden administration reversed that rule. The change will kick in this month. Planned Parenthood can discuss SB 8 in Texas because Texas affiliates do not receive Title X dollars.
Dr. Lindsey Vasquez of Legacy Community Health, the largest federally qualified health center in Texas and a recipient of Title X dollars, said she and other staff members have not discussed abortion or SB 8 because they also must juggle a variety of other priorities. Legacy’s patients are underserved, she said. A majority live at or below the federal poverty level.
Nearly two years into the Covid-19 pandemic, “we’re literally maximizing those visits,” Dr. Vasquez said. Their jobs go beyond offering reproductive care. “We’re making sure they have food resources, that they have their housing stable,” she said. “We really are trying to make sure that all of their needs are met because we know for these types of populations – patients that we serve – this may be our only moment that we get to meet them.”
Specialized family planning clinics that receive Title X dollars do have proactive conversations about contraceptive methods, according to Every Body Texas, the Title X grantee for the state.
Discussions of long-acting reversible contraception must be handled with sensitivity because these forms of birth control have a questionable history among certain populations, primarily lower-income patients. In the 1990s, lawmakers in several states, including Texas, introduced bills to offer cash assistance recipients financial incentives to get an implant or mandate insertion for people on government benefits, a move seen as reproductive coercion.
“It’s important for a client to get on the contraceptive method of their choice,” said Mimi Garcia, communications director for Every Body Texas. “Some people will just say, ‘Let’s get everyone on IUDs’ or ‘Let’s get everybody on hormonal implants’ because those are the most effective methods. ... That’s not something that’s going to work for [every] individual. ... Either they don’t agree with it philosophically, or they don’t like how it makes their body feel.”
It’s a nuanced subject for providers to broach, so some suggest starting the conversation by asking the patient about their future.
“The best question to ask is ‘When do you want to have another baby?’” said Dr. Liedtke. And then if they say, ‘Oh, gosh, I’m not even sure I want to have more kids’ or ‘Five or six years from now,’ then we start talking LARCs. ... But if it’s like, ‘Man, I really want to start trying in a year,’ then I don’t talk to them about putting one of those in.”
The Biden administration expected more demand for birth control in Texas, so Health & Human Services Secretary Xavier Becerra announced in mid-September that Every Body Texas would receive additional Title X funding, as would local providers experiencing an influx of clients as a result of SB 8.
But providers said improved access to contraception will not blunt the law’s effects. It will not protect patients who want to get pregnant but ultimately decide on abortion because they receive a diagnosis of a serious complication, their relationship status changes, or they lose financial or social support, said Dr. Elissa Serapio, an OB-GYN in the Rio Grande Valley and a fellow with Physicians for Reproductive Health.
“It’s the very best that we can do,” said Dr. Cardwell, of Planned Parenthood of Greater Texas. “There’s no 100% effective method of birth control.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
COVID-19 has brought more complex, longer office visits
Evidence of this came from the latest Primary Care Collaborative (PCC) survey, which found that primary care clinicians are seeing more complex patients requiring longer appointments in the wake of COVID-19.
The PCC with the Larry A. Green Center regularly surveys primary care clinicians. This round of questions came August 14-17 and included 1,263 respondents from 49 states, the District of Columbia, and two territories.
More than 7 in 10 (71%) respondents said their patients are more complex and nearly the same percentage said appointments are taking more time.
Ann Greiner, president and CEO of the PCC, said in an interview that 55% of respondents reported that clinicians are struggling to keep up with pent-up demand after patients have delayed or canceled care. Sixty-five percent in the survey said they had seen a rise in children’s mental health issues, and 58% said they were unsure how to help their patients with long COVID.
In addition, primary care clinicians are having repeated conversations with patients on why they should get a vaccine and which one.
“I think that’s adding to the complexity. There is a lot going on here with patient trust,” Ms. Greiner said.
‘We’re going to be playing catch-up’
Jacqueline Fincher, MD, an internist in Thompson, Ga., said in an interview that appointments have gotten longer and more complex in the wake of the pandemic – “no question.”
The immediate past president of the American College of Physicians is seeing patients with chronic disease that has gone untreated for sometimes a year or more, she said.
“Their blood pressure was not under good control, they were under more stress, their sugars were up and weren’t being followed as closely for conditions such as congestive heart failure,” she said.
Dr. Fincher, who works in a rural practice 40 miles from Augusta, Ga., with her physician husband and two other physicians, said patients are ready to come back in, “but I don’t have enough slots for them.”
She said she prioritizes what to help patients with first and schedules the next tier for the next appointment, but added, “honestly, over the next 2 years we’re going to be playing catch-up.”
At the same time, the CDC has estimated that 45% of U.S. adults are at increased risk for complications from COVID-19 because of cardiovascular disease, diabetes, respiratory disease, hypertension, or cancer. Rates ranged from 19.8% for people 18-29 years old to 80.7% for people over 80 years of age.
Long COVID could overwhelm existing health care capacity
Primary care physicians are also having to diagnose sometimes “invisible” symptoms after people have recovered from acute COVID-19 infection. Diagnosing takes intent listening to patients who describe symptoms that tests can’t confirm.
As this news organization has previously reported, half of COVID-19 survivors report postacute sequelae of COVID-19 (PASC) lasting longer than 6 months.
“These long-term PASC effects occur on a scale that could overwhelm existing health care capacity, particularly in low- and middle-income countries,” the authors wrote.
Anxiety, depression ‘have gone off the charts’
Danielle Loeb, MD, MPH, associate professor of internal medicine at the University of Colorado in Denver, who studies complexity in primary care, said in the wake of COVID-19, more patients have developed “new, serious anxiety.”
“That got extremely exacerbated during the pandemic. Anxiety and depression have gone off the charts,” said Dr. Loeb, who prefers the pronoun “they.”
Dr. Loeb cares for a large number of transgender patients. As offices reopen, some patients are having trouble reintegrating into the workplace and resuming social contacts. The primary care doctor says appointments can get longer because of the need to complete tasks, such as filling out forms for Family Medical Leave Act for those not yet ready to return to work.
COVID-19–related fears are keeping many patients from coming into the office, Dr. Loeb said, either from fear of exposure or because they have mental health issues that keep them from feeling safe leaving the house.
“That really affects my ability to care for them,” they said.
Loss of employment in the pandemic or fear of job loss and subsequent changing of insurance has complicated primary care in terms of treatment and administrative tasks, according to Dr. Loeb.
To help treat patients with acute mental health issues and manage other patients, Dr. Loeb’s practice has brought in a social worker and a therapist.
Team-based care is key in the survival of primary care practices, though providing that is difficult in the smaller clinics because of the critical mass of patients needed to make it viable, they said.
“It’s the only answer. It’s the only way you don’t drown,” Dr. Loeb added. “I’m not drowning, and I credit that to my clinic having the help to support the mental health piece of things.”
Rethinking workflow
Tricia McGinnis, MPP, MPH, executive vice president of the nonprofit Center for Health Care Strategies (CHCS) says complexity has forced rethinking workflow.
“A lot of the trends we’re seeing in primary care were there pre-COVID, but COVID has exacerbated those trends,” she said in an interview.
“The good news ... is that it was already becoming clear that primary care needed to provide basic mental health services and integrate with behavioral health. It had also become clear that effective primary care needed to address social issues that keep patients from accessing health care,” she said.
Expanding care teams, as Dr. Loeb mentioned, is a key strategy, according to Ms. McGinnis. Potential teams would include the clinical staff, but also social workers and community health workers – people who come from the community primary care is serving who can help build trust with patients and connect the patient to the primary care team.
“There’s a lot that needs to happen that the clinician doesn’t need to do,” she said.
Telehealth can be a big factor in coordinating the team, Ms. McGinnis added.
“It’s thinking less about who’s doing the work, but more about the work that needs to be done to keep people healthy. Then let’s think about the type of workers best suited to perform those tasks,” she said.
As for reimbursing more complex care, population-based, up-front capitated payments linked to high-quality care and better outcomes will need to replace fee-for-service models, according to Ms. McGinnis.
That will provide reliable incomes for primary care offices, but also flexibility in how each patient with different levels of complexity is managed, she said.
Ms. Greiner, Dr. Fincher, Dr. Loeb, and Ms. McGinnis have no relevant financial relationships.
Evidence of this came from the latest Primary Care Collaborative (PCC) survey, which found that primary care clinicians are seeing more complex patients requiring longer appointments in the wake of COVID-19.
The PCC with the Larry A. Green Center regularly surveys primary care clinicians. This round of questions came August 14-17 and included 1,263 respondents from 49 states, the District of Columbia, and two territories.
More than 7 in 10 (71%) respondents said their patients are more complex and nearly the same percentage said appointments are taking more time.
Ann Greiner, president and CEO of the PCC, said in an interview that 55% of respondents reported that clinicians are struggling to keep up with pent-up demand after patients have delayed or canceled care. Sixty-five percent in the survey said they had seen a rise in children’s mental health issues, and 58% said they were unsure how to help their patients with long COVID.
In addition, primary care clinicians are having repeated conversations with patients on why they should get a vaccine and which one.
“I think that’s adding to the complexity. There is a lot going on here with patient trust,” Ms. Greiner said.
‘We’re going to be playing catch-up’
Jacqueline Fincher, MD, an internist in Thompson, Ga., said in an interview that appointments have gotten longer and more complex in the wake of the pandemic – “no question.”
The immediate past president of the American College of Physicians is seeing patients with chronic disease that has gone untreated for sometimes a year or more, she said.
“Their blood pressure was not under good control, they were under more stress, their sugars were up and weren’t being followed as closely for conditions such as congestive heart failure,” she said.
Dr. Fincher, who works in a rural practice 40 miles from Augusta, Ga., with her physician husband and two other physicians, said patients are ready to come back in, “but I don’t have enough slots for them.”
She said she prioritizes what to help patients with first and schedules the next tier for the next appointment, but added, “honestly, over the next 2 years we’re going to be playing catch-up.”
At the same time, the CDC has estimated that 45% of U.S. adults are at increased risk for complications from COVID-19 because of cardiovascular disease, diabetes, respiratory disease, hypertension, or cancer. Rates ranged from 19.8% for people 18-29 years old to 80.7% for people over 80 years of age.
Long COVID could overwhelm existing health care capacity
Primary care physicians are also having to diagnose sometimes “invisible” symptoms after people have recovered from acute COVID-19 infection. Diagnosing takes intent listening to patients who describe symptoms that tests can’t confirm.
As this news organization has previously reported, half of COVID-19 survivors report postacute sequelae of COVID-19 (PASC) lasting longer than 6 months.
“These long-term PASC effects occur on a scale that could overwhelm existing health care capacity, particularly in low- and middle-income countries,” the authors wrote.
Anxiety, depression ‘have gone off the charts’
Danielle Loeb, MD, MPH, associate professor of internal medicine at the University of Colorado in Denver, who studies complexity in primary care, said in the wake of COVID-19, more patients have developed “new, serious anxiety.”
“That got extremely exacerbated during the pandemic. Anxiety and depression have gone off the charts,” said Dr. Loeb, who prefers the pronoun “they.”
Dr. Loeb cares for a large number of transgender patients. As offices reopen, some patients are having trouble reintegrating into the workplace and resuming social contacts. The primary care doctor says appointments can get longer because of the need to complete tasks, such as filling out forms for Family Medical Leave Act for those not yet ready to return to work.
COVID-19–related fears are keeping many patients from coming into the office, Dr. Loeb said, either from fear of exposure or because they have mental health issues that keep them from feeling safe leaving the house.
“That really affects my ability to care for them,” they said.
Loss of employment in the pandemic or fear of job loss and subsequent changing of insurance has complicated primary care in terms of treatment and administrative tasks, according to Dr. Loeb.
To help treat patients with acute mental health issues and manage other patients, Dr. Loeb’s practice has brought in a social worker and a therapist.
Team-based care is key in the survival of primary care practices, though providing that is difficult in the smaller clinics because of the critical mass of patients needed to make it viable, they said.
“It’s the only answer. It’s the only way you don’t drown,” Dr. Loeb added. “I’m not drowning, and I credit that to my clinic having the help to support the mental health piece of things.”
Rethinking workflow
Tricia McGinnis, MPP, MPH, executive vice president of the nonprofit Center for Health Care Strategies (CHCS) says complexity has forced rethinking workflow.
“A lot of the trends we’re seeing in primary care were there pre-COVID, but COVID has exacerbated those trends,” she said in an interview.
“The good news ... is that it was already becoming clear that primary care needed to provide basic mental health services and integrate with behavioral health. It had also become clear that effective primary care needed to address social issues that keep patients from accessing health care,” she said.
Expanding care teams, as Dr. Loeb mentioned, is a key strategy, according to Ms. McGinnis. Potential teams would include the clinical staff, but also social workers and community health workers – people who come from the community primary care is serving who can help build trust with patients and connect the patient to the primary care team.
“There’s a lot that needs to happen that the clinician doesn’t need to do,” she said.
Telehealth can be a big factor in coordinating the team, Ms. McGinnis added.
“It’s thinking less about who’s doing the work, but more about the work that needs to be done to keep people healthy. Then let’s think about the type of workers best suited to perform those tasks,” she said.
As for reimbursing more complex care, population-based, up-front capitated payments linked to high-quality care and better outcomes will need to replace fee-for-service models, according to Ms. McGinnis.
That will provide reliable incomes for primary care offices, but also flexibility in how each patient with different levels of complexity is managed, she said.
Ms. Greiner, Dr. Fincher, Dr. Loeb, and Ms. McGinnis have no relevant financial relationships.
Evidence of this came from the latest Primary Care Collaborative (PCC) survey, which found that primary care clinicians are seeing more complex patients requiring longer appointments in the wake of COVID-19.
The PCC with the Larry A. Green Center regularly surveys primary care clinicians. This round of questions came August 14-17 and included 1,263 respondents from 49 states, the District of Columbia, and two territories.
More than 7 in 10 (71%) respondents said their patients are more complex and nearly the same percentage said appointments are taking more time.
Ann Greiner, president and CEO of the PCC, said in an interview that 55% of respondents reported that clinicians are struggling to keep up with pent-up demand after patients have delayed or canceled care. Sixty-five percent in the survey said they had seen a rise in children’s mental health issues, and 58% said they were unsure how to help their patients with long COVID.
In addition, primary care clinicians are having repeated conversations with patients on why they should get a vaccine and which one.
“I think that’s adding to the complexity. There is a lot going on here with patient trust,” Ms. Greiner said.
‘We’re going to be playing catch-up’
Jacqueline Fincher, MD, an internist in Thompson, Ga., said in an interview that appointments have gotten longer and more complex in the wake of the pandemic – “no question.”
The immediate past president of the American College of Physicians is seeing patients with chronic disease that has gone untreated for sometimes a year or more, she said.
“Their blood pressure was not under good control, they were under more stress, their sugars were up and weren’t being followed as closely for conditions such as congestive heart failure,” she said.
Dr. Fincher, who works in a rural practice 40 miles from Augusta, Ga., with her physician husband and two other physicians, said patients are ready to come back in, “but I don’t have enough slots for them.”
She said she prioritizes what to help patients with first and schedules the next tier for the next appointment, but added, “honestly, over the next 2 years we’re going to be playing catch-up.”
At the same time, the CDC has estimated that 45% of U.S. adults are at increased risk for complications from COVID-19 because of cardiovascular disease, diabetes, respiratory disease, hypertension, or cancer. Rates ranged from 19.8% for people 18-29 years old to 80.7% for people over 80 years of age.
Long COVID could overwhelm existing health care capacity
Primary care physicians are also having to diagnose sometimes “invisible” symptoms after people have recovered from acute COVID-19 infection. Diagnosing takes intent listening to patients who describe symptoms that tests can’t confirm.
As this news organization has previously reported, half of COVID-19 survivors report postacute sequelae of COVID-19 (PASC) lasting longer than 6 months.
“These long-term PASC effects occur on a scale that could overwhelm existing health care capacity, particularly in low- and middle-income countries,” the authors wrote.
Anxiety, depression ‘have gone off the charts’
Danielle Loeb, MD, MPH, associate professor of internal medicine at the University of Colorado in Denver, who studies complexity in primary care, said in the wake of COVID-19, more patients have developed “new, serious anxiety.”
“That got extremely exacerbated during the pandemic. Anxiety and depression have gone off the charts,” said Dr. Loeb, who prefers the pronoun “they.”
Dr. Loeb cares for a large number of transgender patients. As offices reopen, some patients are having trouble reintegrating into the workplace and resuming social contacts. The primary care doctor says appointments can get longer because of the need to complete tasks, such as filling out forms for Family Medical Leave Act for those not yet ready to return to work.
COVID-19–related fears are keeping many patients from coming into the office, Dr. Loeb said, either from fear of exposure or because they have mental health issues that keep them from feeling safe leaving the house.
“That really affects my ability to care for them,” they said.
Loss of employment in the pandemic or fear of job loss and subsequent changing of insurance has complicated primary care in terms of treatment and administrative tasks, according to Dr. Loeb.
To help treat patients with acute mental health issues and manage other patients, Dr. Loeb’s practice has brought in a social worker and a therapist.
Team-based care is key in the survival of primary care practices, though providing that is difficult in the smaller clinics because of the critical mass of patients needed to make it viable, they said.
“It’s the only answer. It’s the only way you don’t drown,” Dr. Loeb added. “I’m not drowning, and I credit that to my clinic having the help to support the mental health piece of things.”
Rethinking workflow
Tricia McGinnis, MPP, MPH, executive vice president of the nonprofit Center for Health Care Strategies (CHCS) says complexity has forced rethinking workflow.
“A lot of the trends we’re seeing in primary care were there pre-COVID, but COVID has exacerbated those trends,” she said in an interview.
“The good news ... is that it was already becoming clear that primary care needed to provide basic mental health services and integrate with behavioral health. It had also become clear that effective primary care needed to address social issues that keep patients from accessing health care,” she said.
Expanding care teams, as Dr. Loeb mentioned, is a key strategy, according to Ms. McGinnis. Potential teams would include the clinical staff, but also social workers and community health workers – people who come from the community primary care is serving who can help build trust with patients and connect the patient to the primary care team.
“There’s a lot that needs to happen that the clinician doesn’t need to do,” she said.
Telehealth can be a big factor in coordinating the team, Ms. McGinnis added.
“It’s thinking less about who’s doing the work, but more about the work that needs to be done to keep people healthy. Then let’s think about the type of workers best suited to perform those tasks,” she said.
As for reimbursing more complex care, population-based, up-front capitated payments linked to high-quality care and better outcomes will need to replace fee-for-service models, according to Ms. McGinnis.
That will provide reliable incomes for primary care offices, but also flexibility in how each patient with different levels of complexity is managed, she said.
Ms. Greiner, Dr. Fincher, Dr. Loeb, and Ms. McGinnis have no relevant financial relationships.
Pharma rep admits to money laundering, obstruction of justice
Pharma rep admits to health care fraud, money laundering, and more
Mr. Camarda pleaded guilty in federal court to one count of conspiracy to commit healthcare fraud and one count of conspiracy to obstruct justice and engage in money laundering.
Mr. Camarda, 39, of Holmdel, N. J., created a side business called Dynasty Capital LLC to independently market medical products and services for other companies, including compounded prescription medications for specialty pharmacies, according to the U.S. Department of Justice.
Mr. Camarda learned that certain local government employees had insurance coverage for these compounded medications and discovered that certain compounded medications were reimbursed up to thousands of dollars for a 1-month supply. Mr. Camarda recruited individuals with insurance coverage to fraudulently obtain medically unnecessary compounded medications.
He marketed compounded medications for several pharmacies. As part of his arrangements with the compounding pharmacies and his conspirators, Mr. Camarda was paid a percentage of the insurance payments received for prescriptions arranged by him and those working for him.
Mr. Camarda received more than $2.2 million in payments for the prescriptions he and those working with him arranged. Mr. Camarda and his recruits caused more than $3.4 million in fraudulent claims to be submitted to the pharmacy benefits administrator for compounded medications.
He is due to be sentenced in November and faces up to 15 years in prison plus $500,000 in fines.
Home health care and hospice agency owner defrauds Medicare for $31 million
Akop Atoyan, 48, of Glendale, Calif., pleaded guilty to one count of conspiracy to commit healthcare fraud and one count of conspiracy to pay and receive healthcare kickbacks.
According to the U.S. Department of Justice, Mr. Atoyan and his wife, Liana Karapetyan, owned and controlled home healthcare and hospice agencies in the greater Sacramento area: ANG Health Care Inc, Excel Home Healthcare Inc, and Excel Hospice Inc. Mr. Atoyan and Ms. Karapetyan certified to Medicare that their agencies would not pay kickbacks in exchange for Medicare beneficiary referrals.
Officials claim Mr. Atoyan and Ms. Karapetyan paid and directed others to pay kickbacks to multiple individuals for beneficiary referrals, including employees of healthcare facilities, as well as employees’ spouses. In total, Mr. Atoyan, Ms. Karapetyan, and others caused the agencies to submit over 8,000 claims to Medicare for the cost of home healthcare and hospice services. Medicare was billed about $31 million.
As part of his guilty plea, Mr. Atoyan agreed to pay about $2.5 million in restitution to the U.S. Department of Health and Human Services. He also agreed to forfeit that amount to the United States.
Medical clinic owner sentenced to jail for Medicaid fraud
Larry Lance Crawford, 49, of Las Vegas, was sentenced in a Medicaid fraud case involving the failure to maintain adequate records to substantiate claims submitted to Nevada Medicaid.
The Nevada Attorney General’s Office announced that Mr. Crawford was given 364 days in jail and was ordered to pay $50,000.00 in restitution.
The Medicaid Fraud Control Unit received information that Mr. Crawford, the owner of Dynamic Future, was using his business to submit false claims for services that were never provided to Medicaid recipients. The investigation revealed that Mr. Crawford failed to maintain records to support the services that were allegedly provided.
A version of this article first appeared on Medscape.com.
Pharma rep admits to health care fraud, money laundering, and more
Mr. Camarda pleaded guilty in federal court to one count of conspiracy to commit healthcare fraud and one count of conspiracy to obstruct justice and engage in money laundering.
Mr. Camarda, 39, of Holmdel, N. J., created a side business called Dynasty Capital LLC to independently market medical products and services for other companies, including compounded prescription medications for specialty pharmacies, according to the U.S. Department of Justice.
Mr. Camarda learned that certain local government employees had insurance coverage for these compounded medications and discovered that certain compounded medications were reimbursed up to thousands of dollars for a 1-month supply. Mr. Camarda recruited individuals with insurance coverage to fraudulently obtain medically unnecessary compounded medications.
He marketed compounded medications for several pharmacies. As part of his arrangements with the compounding pharmacies and his conspirators, Mr. Camarda was paid a percentage of the insurance payments received for prescriptions arranged by him and those working for him.
Mr. Camarda received more than $2.2 million in payments for the prescriptions he and those working with him arranged. Mr. Camarda and his recruits caused more than $3.4 million in fraudulent claims to be submitted to the pharmacy benefits administrator for compounded medications.
He is due to be sentenced in November and faces up to 15 years in prison plus $500,000 in fines.
Home health care and hospice agency owner defrauds Medicare for $31 million
Akop Atoyan, 48, of Glendale, Calif., pleaded guilty to one count of conspiracy to commit healthcare fraud and one count of conspiracy to pay and receive healthcare kickbacks.
According to the U.S. Department of Justice, Mr. Atoyan and his wife, Liana Karapetyan, owned and controlled home healthcare and hospice agencies in the greater Sacramento area: ANG Health Care Inc, Excel Home Healthcare Inc, and Excel Hospice Inc. Mr. Atoyan and Ms. Karapetyan certified to Medicare that their agencies would not pay kickbacks in exchange for Medicare beneficiary referrals.
Officials claim Mr. Atoyan and Ms. Karapetyan paid and directed others to pay kickbacks to multiple individuals for beneficiary referrals, including employees of healthcare facilities, as well as employees’ spouses. In total, Mr. Atoyan, Ms. Karapetyan, and others caused the agencies to submit over 8,000 claims to Medicare for the cost of home healthcare and hospice services. Medicare was billed about $31 million.
As part of his guilty plea, Mr. Atoyan agreed to pay about $2.5 million in restitution to the U.S. Department of Health and Human Services. He also agreed to forfeit that amount to the United States.
Medical clinic owner sentenced to jail for Medicaid fraud
Larry Lance Crawford, 49, of Las Vegas, was sentenced in a Medicaid fraud case involving the failure to maintain adequate records to substantiate claims submitted to Nevada Medicaid.
The Nevada Attorney General’s Office announced that Mr. Crawford was given 364 days in jail and was ordered to pay $50,000.00 in restitution.
The Medicaid Fraud Control Unit received information that Mr. Crawford, the owner of Dynamic Future, was using his business to submit false claims for services that were never provided to Medicaid recipients. The investigation revealed that Mr. Crawford failed to maintain records to support the services that were allegedly provided.
A version of this article first appeared on Medscape.com.
Pharma rep admits to health care fraud, money laundering, and more
Mr. Camarda pleaded guilty in federal court to one count of conspiracy to commit healthcare fraud and one count of conspiracy to obstruct justice and engage in money laundering.
Mr. Camarda, 39, of Holmdel, N. J., created a side business called Dynasty Capital LLC to independently market medical products and services for other companies, including compounded prescription medications for specialty pharmacies, according to the U.S. Department of Justice.
Mr. Camarda learned that certain local government employees had insurance coverage for these compounded medications and discovered that certain compounded medications were reimbursed up to thousands of dollars for a 1-month supply. Mr. Camarda recruited individuals with insurance coverage to fraudulently obtain medically unnecessary compounded medications.
He marketed compounded medications for several pharmacies. As part of his arrangements with the compounding pharmacies and his conspirators, Mr. Camarda was paid a percentage of the insurance payments received for prescriptions arranged by him and those working for him.
Mr. Camarda received more than $2.2 million in payments for the prescriptions he and those working with him arranged. Mr. Camarda and his recruits caused more than $3.4 million in fraudulent claims to be submitted to the pharmacy benefits administrator for compounded medications.
He is due to be sentenced in November and faces up to 15 years in prison plus $500,000 in fines.
Home health care and hospice agency owner defrauds Medicare for $31 million
Akop Atoyan, 48, of Glendale, Calif., pleaded guilty to one count of conspiracy to commit healthcare fraud and one count of conspiracy to pay and receive healthcare kickbacks.
According to the U.S. Department of Justice, Mr. Atoyan and his wife, Liana Karapetyan, owned and controlled home healthcare and hospice agencies in the greater Sacramento area: ANG Health Care Inc, Excel Home Healthcare Inc, and Excel Hospice Inc. Mr. Atoyan and Ms. Karapetyan certified to Medicare that their agencies would not pay kickbacks in exchange for Medicare beneficiary referrals.
Officials claim Mr. Atoyan and Ms. Karapetyan paid and directed others to pay kickbacks to multiple individuals for beneficiary referrals, including employees of healthcare facilities, as well as employees’ spouses. In total, Mr. Atoyan, Ms. Karapetyan, and others caused the agencies to submit over 8,000 claims to Medicare for the cost of home healthcare and hospice services. Medicare was billed about $31 million.
As part of his guilty plea, Mr. Atoyan agreed to pay about $2.5 million in restitution to the U.S. Department of Health and Human Services. He also agreed to forfeit that amount to the United States.
Medical clinic owner sentenced to jail for Medicaid fraud
Larry Lance Crawford, 49, of Las Vegas, was sentenced in a Medicaid fraud case involving the failure to maintain adequate records to substantiate claims submitted to Nevada Medicaid.
The Nevada Attorney General’s Office announced that Mr. Crawford was given 364 days in jail and was ordered to pay $50,000.00 in restitution.
The Medicaid Fraud Control Unit received information that Mr. Crawford, the owner of Dynamic Future, was using his business to submit false claims for services that were never provided to Medicaid recipients. The investigation revealed that Mr. Crawford failed to maintain records to support the services that were allegedly provided.
A version of this article first appeared on Medscape.com.
‘Residents’ Viewpoint’ revisited
We are currently republishing an installment of this column as part of our continuing celebration of Family Practice News’s 50th anniversary.
Bruce A. Bagley, MD, wrote the first batch of these columns, when he was chief resident in family medicine at St. Joseph’s Hospital, Syracuse, N.Y. Joseph E. Scherger, MD, was the second writer for Family Practice News’s monthly “Residents’ Viewpoint.” At the time Dr. Scherger became a columnist, he was a 26-year-old, 2nd-year family practice resident at the Family Medical Center, University Hospital, University of Washington, Seattle.
Dr. Scherger’s first column was published on Feb. 5, 1977. We are republishing his “Residents’ Viewpoint” from June 15, 1977 (see below) and a new column by Victoria Persampiere, DO, who is currently a 2nd-year resident in the family medicine program at Abington Jefferson Health. (See “My experience as a family medicine resident in 2021” after Dr. Scherger’s column.).
We hope you will enjoy comparing and contrasting the experiences of a resident practicing family medicine today to those of a resident practicing family medicine nearly 4½ decades ago.To learn about Dr. Scherger’s current practice and long career, you can read his profile on the cover of the September 2021 issue of Family Practice News or on MDedge.com/FamilyMedicine in our “Family Practice News 50th Anniversary” section.
Art of medicine or deception?
Originally published in Family Practice News on June 15, 1977.
In medical school I learned the science of medicine. There I diligently studied the basic sciences and gained a thorough understanding of the pathophysiology of disease. In the clinical years I learned to apply this knowledge to a wide variety of interesting patients who came to the academic center.
Yet, when I started my family practice residency, I lacked the ability to care for patients. Though I could take a thorough history, perform a complete physical examination, and diagnose and treat specific illnesses, I had little idea how to satisfy patients by meeting their needs.
The art of medicine is the nonscientific part of a successful doctor-patient interaction. For a doctor-patient interaction to be successful, not only must the illness be appropriately addressed, but both patient and physician must be satisfied.
In the university environment, the art of medicine often gets inadequate attention. Indeed, most academic physicians think that only scientific medicine exists and that patients should be satisfied with a sophisticated approach to their problems. Some patients are satisfied, but many are disgruntled. It is not unusual for a patient, after a $1,000 work-up, to go to a family physician or chiropractor for satisfaction.
I was eager to discover the art of medicine at its finest during my rotation away from the university in a rural community. During these 2 months I looked for the pearls of wisdom that allowed community physicians to be so successful. I found that a very explicit technique was used by some physicians to achieve not only satisfaction but adoration from their patients. Unfortunately, this technique is dishonest.
Early in my community experience I was impressed by how often patients told me a doctor had saved them. I heard such statements as “Dr. X saved my leg,” or “Dr. X saved my life.” I know that it does occur, but not as often as I was hearing it.
Investigating these statements I found such stories as, “One day l twisted my ankle very badly, and it became quite swollen. My doctor told me 1 could lose my leg from this but that he would take x-rays, put my leg in an Ace bandage, and give me crutches. In 3 days I was well. I am so thankful he saved my leg.”
And, “One day I had a temperature of 104. All of my muscles ached, my head hurt, and I had a terrible sore throat and cough. My doctor told me l could die from this, but he gave me a medicine and made me stay home. I was sick for about 2 weeks, but I got better. He saved my life.”
Is the art of medicine the art of deception? This horrifying thought actually came to me after hearing several such stories, but I learned that most of the physicians involved in such stories were not well respected by their colleagues.
I learned many honest techniques for successfully caring for patients. The several family physicians with whom I worked, all clinical instructors associated with my residency, were impeccably honest and taught me to combine compassion and efficiency.
Despite learning many positive techniques and having good role models, I left the community experience somewhat saddened by the lack of integrity that can exist in the profession. I was naive in believing that all the nonscientific aspects of medicine that made patients happy must be good.
By experiencing deception, I learned why quackery continues to flourish despite the widespread availability of honest medical care. Most significantly, I learned the importance of a sometimes frustrating humility; my patients with sprained ankles and influenza will not believe I saved their lives.
My experience as a family medicine resident in 2021
I did not get a medical school graduation; I was one of the many thousands of newly graduated students who simply left their 4th-year rotation sites one chilly day in March 2020 and just never went back. My medical school education didn’t end with me walking triumphantly across the stage – a first-generation college student finally achieving the greatest dream in her life. Instead, it ended with a Zoom “graduation” and a cross-country move from Georgia to Pennsylvania amidst the greatest pandemic in recent memory. To say my impostor syndrome was bad would be an understatement.
Residency in the COVID-19 era
The joy and the draw to family medicine for me has always been the broad scope of conditions that we see and treat. From day 1, however, much of my residency has been devoted to one very small subset of patients – those with COVID-19. At one point, our hospital was so strained that our family medicine program had to run a second inpatient service alongside our usual five-resident service team just to provide care to everybody. Patients were in the hallways. The ER was packed to the gills. We were sleepless, terrified, unvaccinated, and desperate to help our patients survive a disease that was incompletely understood, with very few tools in our toolbox to combat it.
I distinctly remember sitting in the workroom with a coresident of mine, our faces seemingly permanently lined from wearing N95s all shift, and saying to him, “I worry I will be a bad family medicine physician. I worry I haven’t seen enough, other than COVID.” It was midway through my intern year; the days were short, so I was driving to and from the hospital in chilly darkness. My patients, like many around the country, were doing poorly. Vaccines seemed like a promise too good to be true. Worst of all: Those of us who were interns, who had no triumphant podium moment to end our medical school education, were suffering with an intense sense of impostor syndrome, which was strengthened by every “there is nothing else we can offer your loved one at this time” conversation we had. My apprehension about not having seen a wider breadth of medicine during my training is a sentiment still widely shared by COVID-era residents.
Luckily, my coresident was supportive.
“We’re going to be great family medicine physicians,” he said. “We’re learning the hard stuff – the bread and butter of FM – up-front. You’ll see.”
In some ways, I think he was right. Clinical skills, empathy, humility, and forging strong relationships are at the center of every family medicine physician’s heart; my generation has had to learn these skills early and under pressure. Sometimes, there are no answers. Sometimes, the best thing a family doctor can do for a patient is to hear them, understand them, and hold their hand.
‘We watched Cinderella together’
Shortly after that conversation with my coresident, I had a particular case which moved me. This gentleman with intellectual disability and COVID had been declining steadily since his admission to the hospital. He was isolated from everybody he knew and loved, but it did not dampen his spirits. He was cheerful to every person who entered his room, clad in their shrouds of PPE, which more often than not felt more like mourning garb than protective wear. I remember very little about this patient’s clinical picture – the COVID, the superimposed pneumonia, the repeated intubations. What I do remember is he loved the Disney classic Cinderella. I knew this because I developed a very close relationship with his family during the course of his hospitalization. Amidst the torrential onslaught of patients, I made sure to call families every day – not because I wanted to, but because my mentors and attendings and coresidents had all drilled into me from day 1 that we are family medicine, and a large part of our role is to advocate for our patients, and to communicate with their loved ones. So I called. I learned a lot about him; his likes, his dislikes, his close bond with his siblings, and of course his lifelong love for Cinderella. On the last week of my ICU rotation, my patient passed peacefully. His nurse and I were bedside. We held his hand. We told him his family loved him. We watched Cinderella together on an iPad encased in protective plastic.
My next rotation was an outpatient one and it looked more like the “bread and butter” of family medicine. But as I whisked in and out of patient rooms, attending to patients with diabetes, with depression, with pain, I could not stop thinking about my hospitalized patients who my coresidents had assumed care of. Each exam room I entered, I rather morbidly thought “this patient could be next on our hospital service.” Without realizing it, I made more of an effort to get to know each patient holistically. I learned who they were as people. I found myself writing small, medically low-yield details in the chart: “Margaret loves to sing in her church choir;” “Katherine is a self-published author.”
I learned from my attendings. As I sat at the precepting table with them, observing their conversations about patients, their collective decades of experience were apparent.
“I’ve been seeing this patient every few weeks since I was a resident,” said one of my attendings.
“I don’t even see my parents that often,” I thought.
The depth of her relationship with, understanding of, and compassion for this patient struck me deeply. This was why I went into family medicine. My attending knew her patients; they were not faceless unknowns in a hospital gown to her. She would have known to play Cinderella for them in the end.
This is a unique time for trainees. We have been challenged, terrified, overwhelmed, and heartbroken. But at no point have we been isolated. We’ve had the generations of doctors before us to lead the way, to teach us the “hard stuff.” We’ve had senior residents to lean on, who have taken us aside and told us, “I can do the goals-of-care talk today; you need a break.” While the plague seems to have passed over our hospital for now, it has left behind a class of family medicine residents who are proud to carry on our specialty’s long tradition of compassionate, empathetic, lifelong care. “We care for all life stages, from cradle to grave,” says every family medicine physician.
My class, for better or for worse, has cared more often for patients in the twilight of their lives, and while it has been hard, I believe it has made us all better doctors. Now, when I hold a newborn in my arms for a well-child check, I am exceptionally grateful – for the opportunities I have been given, for new beginnings amidst so much sadness, and for the great privilege of being a family medicine physician. ■
Dr. Persampiere is a second-year resident in the family medicine residency program at Abington (Pa.) Jefferson Health. You can contact her directly at victoria.persampiere@jefferson.edu or via fpnews@mdedge.com.
klennon@mdedge.com
We are currently republishing an installment of this column as part of our continuing celebration of Family Practice News’s 50th anniversary.
Bruce A. Bagley, MD, wrote the first batch of these columns, when he was chief resident in family medicine at St. Joseph’s Hospital, Syracuse, N.Y. Joseph E. Scherger, MD, was the second writer for Family Practice News’s monthly “Residents’ Viewpoint.” At the time Dr. Scherger became a columnist, he was a 26-year-old, 2nd-year family practice resident at the Family Medical Center, University Hospital, University of Washington, Seattle.
Dr. Scherger’s first column was published on Feb. 5, 1977. We are republishing his “Residents’ Viewpoint” from June 15, 1977 (see below) and a new column by Victoria Persampiere, DO, who is currently a 2nd-year resident in the family medicine program at Abington Jefferson Health. (See “My experience as a family medicine resident in 2021” after Dr. Scherger’s column.).
We hope you will enjoy comparing and contrasting the experiences of a resident practicing family medicine today to those of a resident practicing family medicine nearly 4½ decades ago.To learn about Dr. Scherger’s current practice and long career, you can read his profile on the cover of the September 2021 issue of Family Practice News or on MDedge.com/FamilyMedicine in our “Family Practice News 50th Anniversary” section.
Art of medicine or deception?
Originally published in Family Practice News on June 15, 1977.
In medical school I learned the science of medicine. There I diligently studied the basic sciences and gained a thorough understanding of the pathophysiology of disease. In the clinical years I learned to apply this knowledge to a wide variety of interesting patients who came to the academic center.
Yet, when I started my family practice residency, I lacked the ability to care for patients. Though I could take a thorough history, perform a complete physical examination, and diagnose and treat specific illnesses, I had little idea how to satisfy patients by meeting their needs.
The art of medicine is the nonscientific part of a successful doctor-patient interaction. For a doctor-patient interaction to be successful, not only must the illness be appropriately addressed, but both patient and physician must be satisfied.
In the university environment, the art of medicine often gets inadequate attention. Indeed, most academic physicians think that only scientific medicine exists and that patients should be satisfied with a sophisticated approach to their problems. Some patients are satisfied, but many are disgruntled. It is not unusual for a patient, after a $1,000 work-up, to go to a family physician or chiropractor for satisfaction.
I was eager to discover the art of medicine at its finest during my rotation away from the university in a rural community. During these 2 months I looked for the pearls of wisdom that allowed community physicians to be so successful. I found that a very explicit technique was used by some physicians to achieve not only satisfaction but adoration from their patients. Unfortunately, this technique is dishonest.
Early in my community experience I was impressed by how often patients told me a doctor had saved them. I heard such statements as “Dr. X saved my leg,” or “Dr. X saved my life.” I know that it does occur, but not as often as I was hearing it.
Investigating these statements I found such stories as, “One day l twisted my ankle very badly, and it became quite swollen. My doctor told me 1 could lose my leg from this but that he would take x-rays, put my leg in an Ace bandage, and give me crutches. In 3 days I was well. I am so thankful he saved my leg.”
And, “One day I had a temperature of 104. All of my muscles ached, my head hurt, and I had a terrible sore throat and cough. My doctor told me l could die from this, but he gave me a medicine and made me stay home. I was sick for about 2 weeks, but I got better. He saved my life.”
Is the art of medicine the art of deception? This horrifying thought actually came to me after hearing several such stories, but I learned that most of the physicians involved in such stories were not well respected by their colleagues.
I learned many honest techniques for successfully caring for patients. The several family physicians with whom I worked, all clinical instructors associated with my residency, were impeccably honest and taught me to combine compassion and efficiency.
Despite learning many positive techniques and having good role models, I left the community experience somewhat saddened by the lack of integrity that can exist in the profession. I was naive in believing that all the nonscientific aspects of medicine that made patients happy must be good.
By experiencing deception, I learned why quackery continues to flourish despite the widespread availability of honest medical care. Most significantly, I learned the importance of a sometimes frustrating humility; my patients with sprained ankles and influenza will not believe I saved their lives.
My experience as a family medicine resident in 2021
I did not get a medical school graduation; I was one of the many thousands of newly graduated students who simply left their 4th-year rotation sites one chilly day in March 2020 and just never went back. My medical school education didn’t end with me walking triumphantly across the stage – a first-generation college student finally achieving the greatest dream in her life. Instead, it ended with a Zoom “graduation” and a cross-country move from Georgia to Pennsylvania amidst the greatest pandemic in recent memory. To say my impostor syndrome was bad would be an understatement.
Residency in the COVID-19 era
The joy and the draw to family medicine for me has always been the broad scope of conditions that we see and treat. From day 1, however, much of my residency has been devoted to one very small subset of patients – those with COVID-19. At one point, our hospital was so strained that our family medicine program had to run a second inpatient service alongside our usual five-resident service team just to provide care to everybody. Patients were in the hallways. The ER was packed to the gills. We were sleepless, terrified, unvaccinated, and desperate to help our patients survive a disease that was incompletely understood, with very few tools in our toolbox to combat it.
I distinctly remember sitting in the workroom with a coresident of mine, our faces seemingly permanently lined from wearing N95s all shift, and saying to him, “I worry I will be a bad family medicine physician. I worry I haven’t seen enough, other than COVID.” It was midway through my intern year; the days were short, so I was driving to and from the hospital in chilly darkness. My patients, like many around the country, were doing poorly. Vaccines seemed like a promise too good to be true. Worst of all: Those of us who were interns, who had no triumphant podium moment to end our medical school education, were suffering with an intense sense of impostor syndrome, which was strengthened by every “there is nothing else we can offer your loved one at this time” conversation we had. My apprehension about not having seen a wider breadth of medicine during my training is a sentiment still widely shared by COVID-era residents.
Luckily, my coresident was supportive.
“We’re going to be great family medicine physicians,” he said. “We’re learning the hard stuff – the bread and butter of FM – up-front. You’ll see.”
In some ways, I think he was right. Clinical skills, empathy, humility, and forging strong relationships are at the center of every family medicine physician’s heart; my generation has had to learn these skills early and under pressure. Sometimes, there are no answers. Sometimes, the best thing a family doctor can do for a patient is to hear them, understand them, and hold their hand.
‘We watched Cinderella together’
Shortly after that conversation with my coresident, I had a particular case which moved me. This gentleman with intellectual disability and COVID had been declining steadily since his admission to the hospital. He was isolated from everybody he knew and loved, but it did not dampen his spirits. He was cheerful to every person who entered his room, clad in their shrouds of PPE, which more often than not felt more like mourning garb than protective wear. I remember very little about this patient’s clinical picture – the COVID, the superimposed pneumonia, the repeated intubations. What I do remember is he loved the Disney classic Cinderella. I knew this because I developed a very close relationship with his family during the course of his hospitalization. Amidst the torrential onslaught of patients, I made sure to call families every day – not because I wanted to, but because my mentors and attendings and coresidents had all drilled into me from day 1 that we are family medicine, and a large part of our role is to advocate for our patients, and to communicate with their loved ones. So I called. I learned a lot about him; his likes, his dislikes, his close bond with his siblings, and of course his lifelong love for Cinderella. On the last week of my ICU rotation, my patient passed peacefully. His nurse and I were bedside. We held his hand. We told him his family loved him. We watched Cinderella together on an iPad encased in protective plastic.
My next rotation was an outpatient one and it looked more like the “bread and butter” of family medicine. But as I whisked in and out of patient rooms, attending to patients with diabetes, with depression, with pain, I could not stop thinking about my hospitalized patients who my coresidents had assumed care of. Each exam room I entered, I rather morbidly thought “this patient could be next on our hospital service.” Without realizing it, I made more of an effort to get to know each patient holistically. I learned who they were as people. I found myself writing small, medically low-yield details in the chart: “Margaret loves to sing in her church choir;” “Katherine is a self-published author.”
I learned from my attendings. As I sat at the precepting table with them, observing their conversations about patients, their collective decades of experience were apparent.
“I’ve been seeing this patient every few weeks since I was a resident,” said one of my attendings.
“I don’t even see my parents that often,” I thought.
The depth of her relationship with, understanding of, and compassion for this patient struck me deeply. This was why I went into family medicine. My attending knew her patients; they were not faceless unknowns in a hospital gown to her. She would have known to play Cinderella for them in the end.
This is a unique time for trainees. We have been challenged, terrified, overwhelmed, and heartbroken. But at no point have we been isolated. We’ve had the generations of doctors before us to lead the way, to teach us the “hard stuff.” We’ve had senior residents to lean on, who have taken us aside and told us, “I can do the goals-of-care talk today; you need a break.” While the plague seems to have passed over our hospital for now, it has left behind a class of family medicine residents who are proud to carry on our specialty’s long tradition of compassionate, empathetic, lifelong care. “We care for all life stages, from cradle to grave,” says every family medicine physician.
My class, for better or for worse, has cared more often for patients in the twilight of their lives, and while it has been hard, I believe it has made us all better doctors. Now, when I hold a newborn in my arms for a well-child check, I am exceptionally grateful – for the opportunities I have been given, for new beginnings amidst so much sadness, and for the great privilege of being a family medicine physician. ■
Dr. Persampiere is a second-year resident in the family medicine residency program at Abington (Pa.) Jefferson Health. You can contact her directly at victoria.persampiere@jefferson.edu or via fpnews@mdedge.com.
klennon@mdedge.com
We are currently republishing an installment of this column as part of our continuing celebration of Family Practice News’s 50th anniversary.
Bruce A. Bagley, MD, wrote the first batch of these columns, when he was chief resident in family medicine at St. Joseph’s Hospital, Syracuse, N.Y. Joseph E. Scherger, MD, was the second writer for Family Practice News’s monthly “Residents’ Viewpoint.” At the time Dr. Scherger became a columnist, he was a 26-year-old, 2nd-year family practice resident at the Family Medical Center, University Hospital, University of Washington, Seattle.
Dr. Scherger’s first column was published on Feb. 5, 1977. We are republishing his “Residents’ Viewpoint” from June 15, 1977 (see below) and a new column by Victoria Persampiere, DO, who is currently a 2nd-year resident in the family medicine program at Abington Jefferson Health. (See “My experience as a family medicine resident in 2021” after Dr. Scherger’s column.).
We hope you will enjoy comparing and contrasting the experiences of a resident practicing family medicine today to those of a resident practicing family medicine nearly 4½ decades ago.To learn about Dr. Scherger’s current practice and long career, you can read his profile on the cover of the September 2021 issue of Family Practice News or on MDedge.com/FamilyMedicine in our “Family Practice News 50th Anniversary” section.
Art of medicine or deception?
Originally published in Family Practice News on June 15, 1977.
In medical school I learned the science of medicine. There I diligently studied the basic sciences and gained a thorough understanding of the pathophysiology of disease. In the clinical years I learned to apply this knowledge to a wide variety of interesting patients who came to the academic center.
Yet, when I started my family practice residency, I lacked the ability to care for patients. Though I could take a thorough history, perform a complete physical examination, and diagnose and treat specific illnesses, I had little idea how to satisfy patients by meeting their needs.
The art of medicine is the nonscientific part of a successful doctor-patient interaction. For a doctor-patient interaction to be successful, not only must the illness be appropriately addressed, but both patient and physician must be satisfied.
In the university environment, the art of medicine often gets inadequate attention. Indeed, most academic physicians think that only scientific medicine exists and that patients should be satisfied with a sophisticated approach to their problems. Some patients are satisfied, but many are disgruntled. It is not unusual for a patient, after a $1,000 work-up, to go to a family physician or chiropractor for satisfaction.
I was eager to discover the art of medicine at its finest during my rotation away from the university in a rural community. During these 2 months I looked for the pearls of wisdom that allowed community physicians to be so successful. I found that a very explicit technique was used by some physicians to achieve not only satisfaction but adoration from their patients. Unfortunately, this technique is dishonest.
Early in my community experience I was impressed by how often patients told me a doctor had saved them. I heard such statements as “Dr. X saved my leg,” or “Dr. X saved my life.” I know that it does occur, but not as often as I was hearing it.
Investigating these statements I found such stories as, “One day l twisted my ankle very badly, and it became quite swollen. My doctor told me 1 could lose my leg from this but that he would take x-rays, put my leg in an Ace bandage, and give me crutches. In 3 days I was well. I am so thankful he saved my leg.”
And, “One day I had a temperature of 104. All of my muscles ached, my head hurt, and I had a terrible sore throat and cough. My doctor told me l could die from this, but he gave me a medicine and made me stay home. I was sick for about 2 weeks, but I got better. He saved my life.”
Is the art of medicine the art of deception? This horrifying thought actually came to me after hearing several such stories, but I learned that most of the physicians involved in such stories were not well respected by their colleagues.
I learned many honest techniques for successfully caring for patients. The several family physicians with whom I worked, all clinical instructors associated with my residency, were impeccably honest and taught me to combine compassion and efficiency.
Despite learning many positive techniques and having good role models, I left the community experience somewhat saddened by the lack of integrity that can exist in the profession. I was naive in believing that all the nonscientific aspects of medicine that made patients happy must be good.
By experiencing deception, I learned why quackery continues to flourish despite the widespread availability of honest medical care. Most significantly, I learned the importance of a sometimes frustrating humility; my patients with sprained ankles and influenza will not believe I saved their lives.
My experience as a family medicine resident in 2021
I did not get a medical school graduation; I was one of the many thousands of newly graduated students who simply left their 4th-year rotation sites one chilly day in March 2020 and just never went back. My medical school education didn’t end with me walking triumphantly across the stage – a first-generation college student finally achieving the greatest dream in her life. Instead, it ended with a Zoom “graduation” and a cross-country move from Georgia to Pennsylvania amidst the greatest pandemic in recent memory. To say my impostor syndrome was bad would be an understatement.
Residency in the COVID-19 era
The joy and the draw to family medicine for me has always been the broad scope of conditions that we see and treat. From day 1, however, much of my residency has been devoted to one very small subset of patients – those with COVID-19. At one point, our hospital was so strained that our family medicine program had to run a second inpatient service alongside our usual five-resident service team just to provide care to everybody. Patients were in the hallways. The ER was packed to the gills. We were sleepless, terrified, unvaccinated, and desperate to help our patients survive a disease that was incompletely understood, with very few tools in our toolbox to combat it.
I distinctly remember sitting in the workroom with a coresident of mine, our faces seemingly permanently lined from wearing N95s all shift, and saying to him, “I worry I will be a bad family medicine physician. I worry I haven’t seen enough, other than COVID.” It was midway through my intern year; the days were short, so I was driving to and from the hospital in chilly darkness. My patients, like many around the country, were doing poorly. Vaccines seemed like a promise too good to be true. Worst of all: Those of us who were interns, who had no triumphant podium moment to end our medical school education, were suffering with an intense sense of impostor syndrome, which was strengthened by every “there is nothing else we can offer your loved one at this time” conversation we had. My apprehension about not having seen a wider breadth of medicine during my training is a sentiment still widely shared by COVID-era residents.
Luckily, my coresident was supportive.
“We’re going to be great family medicine physicians,” he said. “We’re learning the hard stuff – the bread and butter of FM – up-front. You’ll see.”
In some ways, I think he was right. Clinical skills, empathy, humility, and forging strong relationships are at the center of every family medicine physician’s heart; my generation has had to learn these skills early and under pressure. Sometimes, there are no answers. Sometimes, the best thing a family doctor can do for a patient is to hear them, understand them, and hold their hand.
‘We watched Cinderella together’
Shortly after that conversation with my coresident, I had a particular case which moved me. This gentleman with intellectual disability and COVID had been declining steadily since his admission to the hospital. He was isolated from everybody he knew and loved, but it did not dampen his spirits. He was cheerful to every person who entered his room, clad in their shrouds of PPE, which more often than not felt more like mourning garb than protective wear. I remember very little about this patient’s clinical picture – the COVID, the superimposed pneumonia, the repeated intubations. What I do remember is he loved the Disney classic Cinderella. I knew this because I developed a very close relationship with his family during the course of his hospitalization. Amidst the torrential onslaught of patients, I made sure to call families every day – not because I wanted to, but because my mentors and attendings and coresidents had all drilled into me from day 1 that we are family medicine, and a large part of our role is to advocate for our patients, and to communicate with their loved ones. So I called. I learned a lot about him; his likes, his dislikes, his close bond with his siblings, and of course his lifelong love for Cinderella. On the last week of my ICU rotation, my patient passed peacefully. His nurse and I were bedside. We held his hand. We told him his family loved him. We watched Cinderella together on an iPad encased in protective plastic.
My next rotation was an outpatient one and it looked more like the “bread and butter” of family medicine. But as I whisked in and out of patient rooms, attending to patients with diabetes, with depression, with pain, I could not stop thinking about my hospitalized patients who my coresidents had assumed care of. Each exam room I entered, I rather morbidly thought “this patient could be next on our hospital service.” Without realizing it, I made more of an effort to get to know each patient holistically. I learned who they were as people. I found myself writing small, medically low-yield details in the chart: “Margaret loves to sing in her church choir;” “Katherine is a self-published author.”
I learned from my attendings. As I sat at the precepting table with them, observing their conversations about patients, their collective decades of experience were apparent.
“I’ve been seeing this patient every few weeks since I was a resident,” said one of my attendings.
“I don’t even see my parents that often,” I thought.
The depth of her relationship with, understanding of, and compassion for this patient struck me deeply. This was why I went into family medicine. My attending knew her patients; they were not faceless unknowns in a hospital gown to her. She would have known to play Cinderella for them in the end.
This is a unique time for trainees. We have been challenged, terrified, overwhelmed, and heartbroken. But at no point have we been isolated. We’ve had the generations of doctors before us to lead the way, to teach us the “hard stuff.” We’ve had senior residents to lean on, who have taken us aside and told us, “I can do the goals-of-care talk today; you need a break.” While the plague seems to have passed over our hospital for now, it has left behind a class of family medicine residents who are proud to carry on our specialty’s long tradition of compassionate, empathetic, lifelong care. “We care for all life stages, from cradle to grave,” says every family medicine physician.
My class, for better or for worse, has cared more often for patients in the twilight of their lives, and while it has been hard, I believe it has made us all better doctors. Now, when I hold a newborn in my arms for a well-child check, I am exceptionally grateful – for the opportunities I have been given, for new beginnings amidst so much sadness, and for the great privilege of being a family medicine physician. ■
Dr. Persampiere is a second-year resident in the family medicine residency program at Abington (Pa.) Jefferson Health. You can contact her directly at victoria.persampiere@jefferson.edu or via fpnews@mdedge.com.
klennon@mdedge.com