User login
What brought me back from the brink of suicide: A physician’s story
William Lynes, MD, had a flourishing medical practice and a fulfilling family life with three children when he first attempted suicide in 1999 at age 45. By 2003, depression and two more suicide attempts led to his early retirement.
In a session at the recent virtual American Psychiatric Association (APA) 2021 annual meeting, Dr. Lynes talked about the challenges of dealing with depression while managing the stresses of a career in medicine. The session in which he spoke was called, “The Suicidal Physician: Narratives From a Physician Who Survived and the Physician Widow of One Who Did Not.”
By writing and speaking about his experiences, he says, he has been able to retain his identity as a physician and avoid obsessive thoughts about suicide. He hopes conversations like these help other physicians feel less alone and enable them to push past stigmas to get the help they need. He suspects they do. More than 600 people joined the APA session, and Dr. Lynes received dozens of thankful messages afterward.
“I love medicine, but intrinsically, the practice of medicine is stressful, and you can’t get away,” said Dr. Lynes, a retired urologist in Temecula, Calif. “As far as feedback, it made me feel like it’s something I should continue to do.”
A way to heal
For Dr. Lynes, his “downward spiral into darkness” began with a series of catastrophic medical events starting in 1998, when he came home from a family vacation in Mexico feeling unwell. He didn’t bother to do anything about it – typical of a physician, he says. Then one night he woke up shaking with chills and fever. Soon he was in the hospital with respiratory failure from septic shock.
Dr. Lynes spent 6 weeks in the intensive care unit, including 4 weeks on a ventilator. He underwent a tracheostomy. He lost 40 pounds and experienced ICU-related delirium. It was a terrifying time, he said. When he tried to return to work 10 months later, he didn’t feel as though he could function normally.
Having once been a driven doctor who worked long hours, he now doubted himself and dreaded giving patients bad news. Spontaneously, he tried to take his own life.
Afterward, he concealed what had happened from everyone except his wife and managed to resume his practice. However, he was unable to regain the enthusiasm he had once had for his work. Although he had experienced depression before, this time it was unrelenting.
He sought help from a psychiatrist, received a diagnosis of bipolar disorder, and began taking medication. Still, he struggled to fulfill his responsibilities. Then in April 2002, he had a snowboarding accident that caused multiple facial fractures and required five operations. When he returned to work this time, he felt like a failure but resisted asking colleagues for help.
A few months later, Dr. Lynes again attempted suicide, which led to another stay in the ICU and more time on a ventilator. Doctors told his family they didn’t think he would survive. When he recovered, he spent time as an inpatient in a psychiatric ward, where he received the first of a series of electroconvulsive therapy sessions. Compounding his anxiety and depression was the inability to come to terms with his life if he were not able to practice medicine.
The next fall, in September 2003, his third suicide attempt took place in his office on a weekend when no one was around. After locking the door, he looked at his reflection in the frame of his medical school diploma. The glass was cracked. “It was dark, it was black, it was cold,” he said. “I can remember seeing my reflection and thinking how disgusted I was.”
For years after that, Dr. Lynes struggled with his sense of self-worth. He hid from the medical system and dreaded doctors’ appointments. Finally in 2016, he found new meaning at a writing conference, where he met a fellow physician whose story was similar to his. She encouraged him to write about his experience. His essay was published in Annals of Internal Medicine that year. “Then I started speaking, and I feel like I’m a physician again,” he said. “That has really healed me quite a bit.”
Why physicians die by suicide
Working in health care can be extremely stressful, even in the best of times, said Michael Myers, MD, a psychiatrist at State University of New York, Brooklyn, and author of the book, “Why Physicians Die By Suicide: Lessons Learned From Their Families and Others Who Cared.”
Years of school and training culminate in a career in which demands are relentless. Societal expectations are high. Many doctors are perfectionists by nature, and physicians tend to feel intense pressure to compete for coveted positions.
Stress starts early in a medical career. A 2016 systematic review and meta-analysis of 183 studies from 43 countries showed that nearly 30% of medical students experienced symptoms of depression and that 11% reported suicidal thoughts, but only 15% sought help.
A 2015 review of 31 studies that involved residents showed that rates of depression remained close to 30% and that about three-quarters of trainees meet criteria for burnout, a type of emotional exhaustion and sense of inadequacy that can result from chronic stress at work.
The stress of medical training appears to be a direct cause of mental health struggles. Rates of depression are higher among those working to become physicians than among their peers of the same age, research shows. In addition, symptoms become more prevalent as people progress through their training.
The COVID-19 pandemic has added stress to an already stressful job. Of more than 2,300 physicians surveyed in August 2020 by the Physicians Foundation, a physicians advocacy organization, 50% indicated that they experienced excessive anger, tearfulness, or anxiety because of the way the pandemic affected their work; 30% felt hopeless or lacking purpose; and 8% had thoughts of self-harm related to the pandemic. Rates of burnout had risen from 40% in 2018 to 58%.
Those problems might be even more acute in places experiencing other types of crises. A 2020 study of 154 emergency department (ED) physicians in Libya, which is in the midst of a civil war, found that 65% were experiencing anxiety, 73% were showing signs of depression, and 68% felt emotionally exhausted.
Every story is different
It is unclear how common suicide is among physicians. One often-repeated estimate is that 300-400 physicians die by suicide each year, but no one is certain how that number was determined, said Dr. Myers, who organized the APA panel.
Studies on suicide are inconsistent, and trends are hard to pinpoint. Anecdotally, he has received just as many calls about physician suicides in the past year as he did before the pandemic started.
Every person is different, and so is every death. Sometimes, career problems have nothing to do with a physician’s suicide, Dr. Myers said. When job stress does play a role, factors are often varied and complex.
After a 35-year career as a double board certified ED physician, Matthew Seaman, MD, retired in January 2017. The same month, a patient filed a complaint against him with the Washington State medical board, which led to an investigation and a lawsuit.
The case was hard on Dr. Seaman, who had continued to work night shifts throughout his career and had won a Hero Award from the American Board of Emergency Medicine, said his wife, Linda Seaman, MD, a family practitioner in Yakima, Wash., who also spoke on the APA panel.
Dr. Seaman said that 2 years after the investigation started, her husband was growing increasingly depressed. In 2019, he testified in a deposition. She said the plaintiff’s attorney “tried every way he could to shame Matt, humiliate Matt, make him believe he was a very bad doctor.” Three days later, he died by suicide at age 62.
Looking back at the year leading up to her husband’s death, Dr. Seaman recognizes multiple obstacles that interfered with her husband’s ability to get help, including frustrating interactions with psychiatrists and the couple’s insurance company.
His identity and experience as a physician also played a role. A couple of months before he died, she tried unsuccessfully to reach his psychiatrist, whose office suggested he go to the ED. However, because he worked as an ED doctor in their small town, he wouldn’t go. Dr. Seaman suspects he was wary of the stigma.
Burnout likely set him up to cave in after decades of work on the front lines, she added. Working in the ED exposes providers to horrific, traumatic cases every day, she said. Physicians learn to suppress their own emotions to deal with what they encounter. Stuffing their feelings can lead to posttraumatic stress. “You just perform,” she said. “You learn to do that.”
A real gift
Whenever Dr. Myers hears stories about doctors who died by suicide or who have written about their mental health struggles to help others, he contacts them. One goal of his own writing and of the conference sessions he organizes is to make it easier for others to share their own stories.
“I tell them, first of all, their courage and honesty is a real gift, and they’re saving lives,” he said. “There are so many suffering doctors out there who think that they’re the only one.”
Public conversations such as those that occurred in the APA session also offer opportunities to share advice, including Dr. Myers’ recommendation that doctors be sure they have a primary care physician of their own.
Many don’t, he says, because they say they are too busy, they can treat their own symptoms, or they can self-refer to specialists when needed. But physicians don’t always recognize symptoms of depression in themselves, and when mental health problems arise, they may not seek help or treat themselves appropriately.
A primary care physician can be the first person to recognize a mental health problem and refer a patient for mental health care, said Dr. Myers, whose latest book, “Becoming a Doctors’ Doctor: A Memoir,” explores his experiences treating doctors with burnout and other mental health problems.
Whether they have a primary care doctor or not, he suggests that physicians talk to anyone they trust – a social worker, a religious leader, or a family member who can then help them find the right sort of care.
In the United States, around-the-clock help is available through the National Suicide Prevention Lifeline at 800-273-8255. A psychiatrist-run hotline specifically for physicians is available at 888-409-0141. “Reach out and get some help,” Dr. Myers said. “Just don’t do it alone.”
Dr. Lynes advocates setting boundaries between life and work. He has also benefited from writing about his experiences. A blog or a diary can help physicians process their feelings, he said. His 2016 essay marked a major turning point in his life, giving his life meaning in helping others.
“Since I wrote that article, I can’t tell you how much better I am,” he said. “Now, I’m not embarrassed to be around physicians. I actually consider myself a physician. I didn’t for many, many years. So, I’m doing pretty well.”
A version of this article first appeared on Medscape.com.
William Lynes, MD, had a flourishing medical practice and a fulfilling family life with three children when he first attempted suicide in 1999 at age 45. By 2003, depression and two more suicide attempts led to his early retirement.
In a session at the recent virtual American Psychiatric Association (APA) 2021 annual meeting, Dr. Lynes talked about the challenges of dealing with depression while managing the stresses of a career in medicine. The session in which he spoke was called, “The Suicidal Physician: Narratives From a Physician Who Survived and the Physician Widow of One Who Did Not.”
By writing and speaking about his experiences, he says, he has been able to retain his identity as a physician and avoid obsessive thoughts about suicide. He hopes conversations like these help other physicians feel less alone and enable them to push past stigmas to get the help they need. He suspects they do. More than 600 people joined the APA session, and Dr. Lynes received dozens of thankful messages afterward.
“I love medicine, but intrinsically, the practice of medicine is stressful, and you can’t get away,” said Dr. Lynes, a retired urologist in Temecula, Calif. “As far as feedback, it made me feel like it’s something I should continue to do.”
A way to heal
For Dr. Lynes, his “downward spiral into darkness” began with a series of catastrophic medical events starting in 1998, when he came home from a family vacation in Mexico feeling unwell. He didn’t bother to do anything about it – typical of a physician, he says. Then one night he woke up shaking with chills and fever. Soon he was in the hospital with respiratory failure from septic shock.
Dr. Lynes spent 6 weeks in the intensive care unit, including 4 weeks on a ventilator. He underwent a tracheostomy. He lost 40 pounds and experienced ICU-related delirium. It was a terrifying time, he said. When he tried to return to work 10 months later, he didn’t feel as though he could function normally.
Having once been a driven doctor who worked long hours, he now doubted himself and dreaded giving patients bad news. Spontaneously, he tried to take his own life.
Afterward, he concealed what had happened from everyone except his wife and managed to resume his practice. However, he was unable to regain the enthusiasm he had once had for his work. Although he had experienced depression before, this time it was unrelenting.
He sought help from a psychiatrist, received a diagnosis of bipolar disorder, and began taking medication. Still, he struggled to fulfill his responsibilities. Then in April 2002, he had a snowboarding accident that caused multiple facial fractures and required five operations. When he returned to work this time, he felt like a failure but resisted asking colleagues for help.
A few months later, Dr. Lynes again attempted suicide, which led to another stay in the ICU and more time on a ventilator. Doctors told his family they didn’t think he would survive. When he recovered, he spent time as an inpatient in a psychiatric ward, where he received the first of a series of electroconvulsive therapy sessions. Compounding his anxiety and depression was the inability to come to terms with his life if he were not able to practice medicine.
The next fall, in September 2003, his third suicide attempt took place in his office on a weekend when no one was around. After locking the door, he looked at his reflection in the frame of his medical school diploma. The glass was cracked. “It was dark, it was black, it was cold,” he said. “I can remember seeing my reflection and thinking how disgusted I was.”
For years after that, Dr. Lynes struggled with his sense of self-worth. He hid from the medical system and dreaded doctors’ appointments. Finally in 2016, he found new meaning at a writing conference, where he met a fellow physician whose story was similar to his. She encouraged him to write about his experience. His essay was published in Annals of Internal Medicine that year. “Then I started speaking, and I feel like I’m a physician again,” he said. “That has really healed me quite a bit.”
Why physicians die by suicide
Working in health care can be extremely stressful, even in the best of times, said Michael Myers, MD, a psychiatrist at State University of New York, Brooklyn, and author of the book, “Why Physicians Die By Suicide: Lessons Learned From Their Families and Others Who Cared.”
Years of school and training culminate in a career in which demands are relentless. Societal expectations are high. Many doctors are perfectionists by nature, and physicians tend to feel intense pressure to compete for coveted positions.
Stress starts early in a medical career. A 2016 systematic review and meta-analysis of 183 studies from 43 countries showed that nearly 30% of medical students experienced symptoms of depression and that 11% reported suicidal thoughts, but only 15% sought help.
A 2015 review of 31 studies that involved residents showed that rates of depression remained close to 30% and that about three-quarters of trainees meet criteria for burnout, a type of emotional exhaustion and sense of inadequacy that can result from chronic stress at work.
The stress of medical training appears to be a direct cause of mental health struggles. Rates of depression are higher among those working to become physicians than among their peers of the same age, research shows. In addition, symptoms become more prevalent as people progress through their training.
The COVID-19 pandemic has added stress to an already stressful job. Of more than 2,300 physicians surveyed in August 2020 by the Physicians Foundation, a physicians advocacy organization, 50% indicated that they experienced excessive anger, tearfulness, or anxiety because of the way the pandemic affected their work; 30% felt hopeless or lacking purpose; and 8% had thoughts of self-harm related to the pandemic. Rates of burnout had risen from 40% in 2018 to 58%.
Those problems might be even more acute in places experiencing other types of crises. A 2020 study of 154 emergency department (ED) physicians in Libya, which is in the midst of a civil war, found that 65% were experiencing anxiety, 73% were showing signs of depression, and 68% felt emotionally exhausted.
Every story is different
It is unclear how common suicide is among physicians. One often-repeated estimate is that 300-400 physicians die by suicide each year, but no one is certain how that number was determined, said Dr. Myers, who organized the APA panel.
Studies on suicide are inconsistent, and trends are hard to pinpoint. Anecdotally, he has received just as many calls about physician suicides in the past year as he did before the pandemic started.
Every person is different, and so is every death. Sometimes, career problems have nothing to do with a physician’s suicide, Dr. Myers said. When job stress does play a role, factors are often varied and complex.
After a 35-year career as a double board certified ED physician, Matthew Seaman, MD, retired in January 2017. The same month, a patient filed a complaint against him with the Washington State medical board, which led to an investigation and a lawsuit.
The case was hard on Dr. Seaman, who had continued to work night shifts throughout his career and had won a Hero Award from the American Board of Emergency Medicine, said his wife, Linda Seaman, MD, a family practitioner in Yakima, Wash., who also spoke on the APA panel.
Dr. Seaman said that 2 years after the investigation started, her husband was growing increasingly depressed. In 2019, he testified in a deposition. She said the plaintiff’s attorney “tried every way he could to shame Matt, humiliate Matt, make him believe he was a very bad doctor.” Three days later, he died by suicide at age 62.
Looking back at the year leading up to her husband’s death, Dr. Seaman recognizes multiple obstacles that interfered with her husband’s ability to get help, including frustrating interactions with psychiatrists and the couple’s insurance company.
His identity and experience as a physician also played a role. A couple of months before he died, she tried unsuccessfully to reach his psychiatrist, whose office suggested he go to the ED. However, because he worked as an ED doctor in their small town, he wouldn’t go. Dr. Seaman suspects he was wary of the stigma.
Burnout likely set him up to cave in after decades of work on the front lines, she added. Working in the ED exposes providers to horrific, traumatic cases every day, she said. Physicians learn to suppress their own emotions to deal with what they encounter. Stuffing their feelings can lead to posttraumatic stress. “You just perform,” she said. “You learn to do that.”
A real gift
Whenever Dr. Myers hears stories about doctors who died by suicide or who have written about their mental health struggles to help others, he contacts them. One goal of his own writing and of the conference sessions he organizes is to make it easier for others to share their own stories.
“I tell them, first of all, their courage and honesty is a real gift, and they’re saving lives,” he said. “There are so many suffering doctors out there who think that they’re the only one.”
Public conversations such as those that occurred in the APA session also offer opportunities to share advice, including Dr. Myers’ recommendation that doctors be sure they have a primary care physician of their own.
Many don’t, he says, because they say they are too busy, they can treat their own symptoms, or they can self-refer to specialists when needed. But physicians don’t always recognize symptoms of depression in themselves, and when mental health problems arise, they may not seek help or treat themselves appropriately.
A primary care physician can be the first person to recognize a mental health problem and refer a patient for mental health care, said Dr. Myers, whose latest book, “Becoming a Doctors’ Doctor: A Memoir,” explores his experiences treating doctors with burnout and other mental health problems.
Whether they have a primary care doctor or not, he suggests that physicians talk to anyone they trust – a social worker, a religious leader, or a family member who can then help them find the right sort of care.
In the United States, around-the-clock help is available through the National Suicide Prevention Lifeline at 800-273-8255. A psychiatrist-run hotline specifically for physicians is available at 888-409-0141. “Reach out and get some help,” Dr. Myers said. “Just don’t do it alone.”
Dr. Lynes advocates setting boundaries between life and work. He has also benefited from writing about his experiences. A blog or a diary can help physicians process their feelings, he said. His 2016 essay marked a major turning point in his life, giving his life meaning in helping others.
“Since I wrote that article, I can’t tell you how much better I am,” he said. “Now, I’m not embarrassed to be around physicians. I actually consider myself a physician. I didn’t for many, many years. So, I’m doing pretty well.”
A version of this article first appeared on Medscape.com.
William Lynes, MD, had a flourishing medical practice and a fulfilling family life with three children when he first attempted suicide in 1999 at age 45. By 2003, depression and two more suicide attempts led to his early retirement.
In a session at the recent virtual American Psychiatric Association (APA) 2021 annual meeting, Dr. Lynes talked about the challenges of dealing with depression while managing the stresses of a career in medicine. The session in which he spoke was called, “The Suicidal Physician: Narratives From a Physician Who Survived and the Physician Widow of One Who Did Not.”
By writing and speaking about his experiences, he says, he has been able to retain his identity as a physician and avoid obsessive thoughts about suicide. He hopes conversations like these help other physicians feel less alone and enable them to push past stigmas to get the help they need. He suspects they do. More than 600 people joined the APA session, and Dr. Lynes received dozens of thankful messages afterward.
“I love medicine, but intrinsically, the practice of medicine is stressful, and you can’t get away,” said Dr. Lynes, a retired urologist in Temecula, Calif. “As far as feedback, it made me feel like it’s something I should continue to do.”
A way to heal
For Dr. Lynes, his “downward spiral into darkness” began with a series of catastrophic medical events starting in 1998, when he came home from a family vacation in Mexico feeling unwell. He didn’t bother to do anything about it – typical of a physician, he says. Then one night he woke up shaking with chills and fever. Soon he was in the hospital with respiratory failure from septic shock.
Dr. Lynes spent 6 weeks in the intensive care unit, including 4 weeks on a ventilator. He underwent a tracheostomy. He lost 40 pounds and experienced ICU-related delirium. It was a terrifying time, he said. When he tried to return to work 10 months later, he didn’t feel as though he could function normally.
Having once been a driven doctor who worked long hours, he now doubted himself and dreaded giving patients bad news. Spontaneously, he tried to take his own life.
Afterward, he concealed what had happened from everyone except his wife and managed to resume his practice. However, he was unable to regain the enthusiasm he had once had for his work. Although he had experienced depression before, this time it was unrelenting.
He sought help from a psychiatrist, received a diagnosis of bipolar disorder, and began taking medication. Still, he struggled to fulfill his responsibilities. Then in April 2002, he had a snowboarding accident that caused multiple facial fractures and required five operations. When he returned to work this time, he felt like a failure but resisted asking colleagues for help.
A few months later, Dr. Lynes again attempted suicide, which led to another stay in the ICU and more time on a ventilator. Doctors told his family they didn’t think he would survive. When he recovered, he spent time as an inpatient in a psychiatric ward, where he received the first of a series of electroconvulsive therapy sessions. Compounding his anxiety and depression was the inability to come to terms with his life if he were not able to practice medicine.
The next fall, in September 2003, his third suicide attempt took place in his office on a weekend when no one was around. After locking the door, he looked at his reflection in the frame of his medical school diploma. The glass was cracked. “It was dark, it was black, it was cold,” he said. “I can remember seeing my reflection and thinking how disgusted I was.”
For years after that, Dr. Lynes struggled with his sense of self-worth. He hid from the medical system and dreaded doctors’ appointments. Finally in 2016, he found new meaning at a writing conference, where he met a fellow physician whose story was similar to his. She encouraged him to write about his experience. His essay was published in Annals of Internal Medicine that year. “Then I started speaking, and I feel like I’m a physician again,” he said. “That has really healed me quite a bit.”
Why physicians die by suicide
Working in health care can be extremely stressful, even in the best of times, said Michael Myers, MD, a psychiatrist at State University of New York, Brooklyn, and author of the book, “Why Physicians Die By Suicide: Lessons Learned From Their Families and Others Who Cared.”
Years of school and training culminate in a career in which demands are relentless. Societal expectations are high. Many doctors are perfectionists by nature, and physicians tend to feel intense pressure to compete for coveted positions.
Stress starts early in a medical career. A 2016 systematic review and meta-analysis of 183 studies from 43 countries showed that nearly 30% of medical students experienced symptoms of depression and that 11% reported suicidal thoughts, but only 15% sought help.
A 2015 review of 31 studies that involved residents showed that rates of depression remained close to 30% and that about three-quarters of trainees meet criteria for burnout, a type of emotional exhaustion and sense of inadequacy that can result from chronic stress at work.
The stress of medical training appears to be a direct cause of mental health struggles. Rates of depression are higher among those working to become physicians than among their peers of the same age, research shows. In addition, symptoms become more prevalent as people progress through their training.
The COVID-19 pandemic has added stress to an already stressful job. Of more than 2,300 physicians surveyed in August 2020 by the Physicians Foundation, a physicians advocacy organization, 50% indicated that they experienced excessive anger, tearfulness, or anxiety because of the way the pandemic affected their work; 30% felt hopeless or lacking purpose; and 8% had thoughts of self-harm related to the pandemic. Rates of burnout had risen from 40% in 2018 to 58%.
Those problems might be even more acute in places experiencing other types of crises. A 2020 study of 154 emergency department (ED) physicians in Libya, which is in the midst of a civil war, found that 65% were experiencing anxiety, 73% were showing signs of depression, and 68% felt emotionally exhausted.
Every story is different
It is unclear how common suicide is among physicians. One often-repeated estimate is that 300-400 physicians die by suicide each year, but no one is certain how that number was determined, said Dr. Myers, who organized the APA panel.
Studies on suicide are inconsistent, and trends are hard to pinpoint. Anecdotally, he has received just as many calls about physician suicides in the past year as he did before the pandemic started.
Every person is different, and so is every death. Sometimes, career problems have nothing to do with a physician’s suicide, Dr. Myers said. When job stress does play a role, factors are often varied and complex.
After a 35-year career as a double board certified ED physician, Matthew Seaman, MD, retired in January 2017. The same month, a patient filed a complaint against him with the Washington State medical board, which led to an investigation and a lawsuit.
The case was hard on Dr. Seaman, who had continued to work night shifts throughout his career and had won a Hero Award from the American Board of Emergency Medicine, said his wife, Linda Seaman, MD, a family practitioner in Yakima, Wash., who also spoke on the APA panel.
Dr. Seaman said that 2 years after the investigation started, her husband was growing increasingly depressed. In 2019, he testified in a deposition. She said the plaintiff’s attorney “tried every way he could to shame Matt, humiliate Matt, make him believe he was a very bad doctor.” Three days later, he died by suicide at age 62.
Looking back at the year leading up to her husband’s death, Dr. Seaman recognizes multiple obstacles that interfered with her husband’s ability to get help, including frustrating interactions with psychiatrists and the couple’s insurance company.
His identity and experience as a physician also played a role. A couple of months before he died, she tried unsuccessfully to reach his psychiatrist, whose office suggested he go to the ED. However, because he worked as an ED doctor in their small town, he wouldn’t go. Dr. Seaman suspects he was wary of the stigma.
Burnout likely set him up to cave in after decades of work on the front lines, she added. Working in the ED exposes providers to horrific, traumatic cases every day, she said. Physicians learn to suppress their own emotions to deal with what they encounter. Stuffing their feelings can lead to posttraumatic stress. “You just perform,” she said. “You learn to do that.”
A real gift
Whenever Dr. Myers hears stories about doctors who died by suicide or who have written about their mental health struggles to help others, he contacts them. One goal of his own writing and of the conference sessions he organizes is to make it easier for others to share their own stories.
“I tell them, first of all, their courage and honesty is a real gift, and they’re saving lives,” he said. “There are so many suffering doctors out there who think that they’re the only one.”
Public conversations such as those that occurred in the APA session also offer opportunities to share advice, including Dr. Myers’ recommendation that doctors be sure they have a primary care physician of their own.
Many don’t, he says, because they say they are too busy, they can treat their own symptoms, or they can self-refer to specialists when needed. But physicians don’t always recognize symptoms of depression in themselves, and when mental health problems arise, they may not seek help or treat themselves appropriately.
A primary care physician can be the first person to recognize a mental health problem and refer a patient for mental health care, said Dr. Myers, whose latest book, “Becoming a Doctors’ Doctor: A Memoir,” explores his experiences treating doctors with burnout and other mental health problems.
Whether they have a primary care doctor or not, he suggests that physicians talk to anyone they trust – a social worker, a religious leader, or a family member who can then help them find the right sort of care.
In the United States, around-the-clock help is available through the National Suicide Prevention Lifeline at 800-273-8255. A psychiatrist-run hotline specifically for physicians is available at 888-409-0141. “Reach out and get some help,” Dr. Myers said. “Just don’t do it alone.”
Dr. Lynes advocates setting boundaries between life and work. He has also benefited from writing about his experiences. A blog or a diary can help physicians process their feelings, he said. His 2016 essay marked a major turning point in his life, giving his life meaning in helping others.
“Since I wrote that article, I can’t tell you how much better I am,” he said. “Now, I’m not embarrassed to be around physicians. I actually consider myself a physician. I didn’t for many, many years. So, I’m doing pretty well.”
A version of this article first appeared on Medscape.com.
APA, AMA, others move to stop insurer from overturning mental health claims ruling
The American Psychiatric Association has joined with the American Medical Association and other medical societies to oppose United Behavioral Health’s (UBH) request that a court throw out a ruling that found the insurer unfairly denied tens of thousands of claims for mental health and substance use disorder services.
Wit v. United Behavioral Health, in litigation since 2014, is being closely watched by clinicians, patients, providers, and attorneys.
Reena Kapoor, MD, chair of the APA’s Committee on Judicial Action, said in an interview that the APA is hopeful that “whatever the court says about UBH should be applicable to all insurance companies that are providing employer-sponsored health benefits.”
In a friend of the court (amicus curiae) brief, the APA, AMA, the California Medical Association, Southern California Psychiatric Society, Northern California Psychiatric Society, Orange County Psychiatric Society, Central California Psychiatric Society, and San Diego Psychiatric Society argue that “despite the availability of professionally developed, evidence-based guidelines embodying generally accepted standards of care for mental health and substance use disorders, managed care organizations commonly base coverage decisions on internally developed ‘level of care guidelines’ that are inappropriately restrictive.”
The guidelines “may lead to denial of coverage for treatment that is recommended by a patient’s physician and even cut off coverage when treatment is already being delivered,” said the groups.
The U.S. Department of Labor also filed a brief in support of the plaintiffs who are suing UBH. Those individuals suffered injury when they were denied coverage, said the federal agency, which regulates employer-sponsored insurance plans.
California Attorney General Rob Bonta also made an amicus filing supporting the plaintiffs.
“When insurers limit access to this critical care, they leave Californians who need it feeling as if they have no other option than to try to cope alone,” said Mr. Bonta in a statement.
‘Discrimination must end’
Mr. Bonta said he agreed with a 2019 ruling by the U.S. District Court for the Northern District of California that UBH had violated its fiduciary duties by wrongfully using its internally developed coverage determination guidelines and level of care guidelines to deny care.
The court also found that UBH’s medically necessary criteria meant that only “acute” episodes would be covered. Instead, said the court last November, chronic and comorbid conditions should always be treated, according to Maureen Gammon and Kathleen Rosenow of Willis Towers Watson, a risk advisor.
In November, the same Northern California District Court ruled on the remedies it would require of United, including that the insurer reprocess more than 67,000 claims. UBH was also barred indefinitely from using any of its guidelines to make coverage determinations. Instead, it was ordered to make determinations “consistent with generally accepted standards of care,” and consistent with state laws.
The District Court denied a request by UBH to put a hold on the claims reprocessing until it appealed the overall case. But the Ninth Circuit Court of Appeals in February granted that request.
Then, in March, United appealed the District Court’s overall ruling, claiming that the plaintiffs had not proven harm.
The U.S. Chamber of Commerce has filed a brief in support of United, agreeing with its arguments.
However, the APA and other clinician groups said there is no question of harm.
“Failure to provide appropriate levels of care for treatment of mental illness and substance use disorders leads to relapse, overdose, transmission of infectious diseases, and death,” said APA CEO and Medical Director Saul Levin, MD, MPA, in a statement.
APA President Vivian Pender, MD, said guidelines that “are overly focused on stabilizing acute symptoms of mental health and substance use disorders” are not treating the underlying disease. “When the injury is physical, insurers treat the underlying disease and not just the symptoms. Discrimination against patients with mental illness must end,” she said.
No court has ever recognized the type of claims reprocessing ordered by the District Court judge, said attorneys Nathaniel Cohen and Joseph Laska of Manatt, Phelps & Phillips, in an analysis of the case.
Mr. Cohen and Mr. Laska write. “Practitioners, health plans, and health insurers would be wise to track UBH’s long-awaited appeal to the Ninth Circuit.”
This article first appeared on Medscape.com.
The American Psychiatric Association has joined with the American Medical Association and other medical societies to oppose United Behavioral Health’s (UBH) request that a court throw out a ruling that found the insurer unfairly denied tens of thousands of claims for mental health and substance use disorder services.
Wit v. United Behavioral Health, in litigation since 2014, is being closely watched by clinicians, patients, providers, and attorneys.
Reena Kapoor, MD, chair of the APA’s Committee on Judicial Action, said in an interview that the APA is hopeful that “whatever the court says about UBH should be applicable to all insurance companies that are providing employer-sponsored health benefits.”
In a friend of the court (amicus curiae) brief, the APA, AMA, the California Medical Association, Southern California Psychiatric Society, Northern California Psychiatric Society, Orange County Psychiatric Society, Central California Psychiatric Society, and San Diego Psychiatric Society argue that “despite the availability of professionally developed, evidence-based guidelines embodying generally accepted standards of care for mental health and substance use disorders, managed care organizations commonly base coverage decisions on internally developed ‘level of care guidelines’ that are inappropriately restrictive.”
The guidelines “may lead to denial of coverage for treatment that is recommended by a patient’s physician and even cut off coverage when treatment is already being delivered,” said the groups.
The U.S. Department of Labor also filed a brief in support of the plaintiffs who are suing UBH. Those individuals suffered injury when they were denied coverage, said the federal agency, which regulates employer-sponsored insurance plans.
California Attorney General Rob Bonta also made an amicus filing supporting the plaintiffs.
“When insurers limit access to this critical care, they leave Californians who need it feeling as if they have no other option than to try to cope alone,” said Mr. Bonta in a statement.
‘Discrimination must end’
Mr. Bonta said he agreed with a 2019 ruling by the U.S. District Court for the Northern District of California that UBH had violated its fiduciary duties by wrongfully using its internally developed coverage determination guidelines and level of care guidelines to deny care.
The court also found that UBH’s medically necessary criteria meant that only “acute” episodes would be covered. Instead, said the court last November, chronic and comorbid conditions should always be treated, according to Maureen Gammon and Kathleen Rosenow of Willis Towers Watson, a risk advisor.
In November, the same Northern California District Court ruled on the remedies it would require of United, including that the insurer reprocess more than 67,000 claims. UBH was also barred indefinitely from using any of its guidelines to make coverage determinations. Instead, it was ordered to make determinations “consistent with generally accepted standards of care,” and consistent with state laws.
The District Court denied a request by UBH to put a hold on the claims reprocessing until it appealed the overall case. But the Ninth Circuit Court of Appeals in February granted that request.
Then, in March, United appealed the District Court’s overall ruling, claiming that the plaintiffs had not proven harm.
The U.S. Chamber of Commerce has filed a brief in support of United, agreeing with its arguments.
However, the APA and other clinician groups said there is no question of harm.
“Failure to provide appropriate levels of care for treatment of mental illness and substance use disorders leads to relapse, overdose, transmission of infectious diseases, and death,” said APA CEO and Medical Director Saul Levin, MD, MPA, in a statement.
APA President Vivian Pender, MD, said guidelines that “are overly focused on stabilizing acute symptoms of mental health and substance use disorders” are not treating the underlying disease. “When the injury is physical, insurers treat the underlying disease and not just the symptoms. Discrimination against patients with mental illness must end,” she said.
No court has ever recognized the type of claims reprocessing ordered by the District Court judge, said attorneys Nathaniel Cohen and Joseph Laska of Manatt, Phelps & Phillips, in an analysis of the case.
Mr. Cohen and Mr. Laska write. “Practitioners, health plans, and health insurers would be wise to track UBH’s long-awaited appeal to the Ninth Circuit.”
This article first appeared on Medscape.com.
The American Psychiatric Association has joined with the American Medical Association and other medical societies to oppose United Behavioral Health’s (UBH) request that a court throw out a ruling that found the insurer unfairly denied tens of thousands of claims for mental health and substance use disorder services.
Wit v. United Behavioral Health, in litigation since 2014, is being closely watched by clinicians, patients, providers, and attorneys.
Reena Kapoor, MD, chair of the APA’s Committee on Judicial Action, said in an interview that the APA is hopeful that “whatever the court says about UBH should be applicable to all insurance companies that are providing employer-sponsored health benefits.”
In a friend of the court (amicus curiae) brief, the APA, AMA, the California Medical Association, Southern California Psychiatric Society, Northern California Psychiatric Society, Orange County Psychiatric Society, Central California Psychiatric Society, and San Diego Psychiatric Society argue that “despite the availability of professionally developed, evidence-based guidelines embodying generally accepted standards of care for mental health and substance use disorders, managed care organizations commonly base coverage decisions on internally developed ‘level of care guidelines’ that are inappropriately restrictive.”
The guidelines “may lead to denial of coverage for treatment that is recommended by a patient’s physician and even cut off coverage when treatment is already being delivered,” said the groups.
The U.S. Department of Labor also filed a brief in support of the plaintiffs who are suing UBH. Those individuals suffered injury when they were denied coverage, said the federal agency, which regulates employer-sponsored insurance plans.
California Attorney General Rob Bonta also made an amicus filing supporting the plaintiffs.
“When insurers limit access to this critical care, they leave Californians who need it feeling as if they have no other option than to try to cope alone,” said Mr. Bonta in a statement.
‘Discrimination must end’
Mr. Bonta said he agreed with a 2019 ruling by the U.S. District Court for the Northern District of California that UBH had violated its fiduciary duties by wrongfully using its internally developed coverage determination guidelines and level of care guidelines to deny care.
The court also found that UBH’s medically necessary criteria meant that only “acute” episodes would be covered. Instead, said the court last November, chronic and comorbid conditions should always be treated, according to Maureen Gammon and Kathleen Rosenow of Willis Towers Watson, a risk advisor.
In November, the same Northern California District Court ruled on the remedies it would require of United, including that the insurer reprocess more than 67,000 claims. UBH was also barred indefinitely from using any of its guidelines to make coverage determinations. Instead, it was ordered to make determinations “consistent with generally accepted standards of care,” and consistent with state laws.
The District Court denied a request by UBH to put a hold on the claims reprocessing until it appealed the overall case. But the Ninth Circuit Court of Appeals in February granted that request.
Then, in March, United appealed the District Court’s overall ruling, claiming that the plaintiffs had not proven harm.
The U.S. Chamber of Commerce has filed a brief in support of United, agreeing with its arguments.
However, the APA and other clinician groups said there is no question of harm.
“Failure to provide appropriate levels of care for treatment of mental illness and substance use disorders leads to relapse, overdose, transmission of infectious diseases, and death,” said APA CEO and Medical Director Saul Levin, MD, MPA, in a statement.
APA President Vivian Pender, MD, said guidelines that “are overly focused on stabilizing acute symptoms of mental health and substance use disorders” are not treating the underlying disease. “When the injury is physical, insurers treat the underlying disease and not just the symptoms. Discrimination against patients with mental illness must end,” she said.
No court has ever recognized the type of claims reprocessing ordered by the District Court judge, said attorneys Nathaniel Cohen and Joseph Laska of Manatt, Phelps & Phillips, in an analysis of the case.
Mr. Cohen and Mr. Laska write. “Practitioners, health plans, and health insurers would be wise to track UBH’s long-awaited appeal to the Ninth Circuit.”
This article first appeared on Medscape.com.
No-cancel culture: How telehealth is making it easier to keep that therapy session
When the COVID-19 pandemic forced behavioral health providers to stop seeing patients in person and instead hold therapy sessions remotely, the switch produced an unintended, positive consequence: Fewer patients skipped appointments.
That had long been a problem in mental health care. Some outpatient programs previously had no-show rates as high as 60%, according to several studies.
Only 9% of psychiatrists reported that all patients kept their appointments before the pandemic, according to an American Psychiatric Association report. Once providers switched to telepsychiatry, that number increased to 32%.
Not only that, but providers and patients say teletherapy has largely been an effective lifeline for people struggling with anxiety, depression, and other psychological issues during an extraordinarily difficult time, even though it created a new set of challenges.
Many providers say they plan to continue offering teletherapy after the pandemic. Some states are making permanent the temporary pandemic rules that allow providers to be reimbursed at the same rates as for in-person visits, which is welcome news to practitioners who take patients’ insurance.
“We are in a mental health crisis right now, so more people are struggling and may be more open to accessing services,” said psychologist Allison Dempsey, PhD, associate professor at University of Colorado at Denver, Aurora. “It’s much easier to connect from your living room.”
The problem for patients who didn’t show up was often as simple as a canceled ride, said Jody Long, a clinical social worker who studied the 60% rate of no-shows or late cancellations at the University of Tennessee Health Science Center psychiatric clinic in Memphis.
But sometimes it was the health problem itself. Mr. Long remembers seeing a first-time patient drive around the parking lot and then exit. The patient later called and told Mr. Long, “I just could not get out of the car; please forgive me and reschedule me.”
Mr. Long, now an assistant professor at Jacksonville (Ala.) State University, said that incident changed his perspective. “I realized when you’re having panic attacks or anxiety attacks or suffering from major depressive disorder, it’s hard,” he said. “It’s like you have built up these walls for protection and then all of a sudden you’re having to let these walls down.”
Absences strain providers whose bosses set billing and productivity expectations and those in private practice who lose billable hours, said Dr. Dempsey, who directs a program to provide mental health care for families of babies with serious medical complications. Psychotherapists often overbooked patients with the expectation that some would not show up.
Now Dr. Dempsey and colleagues no longer need to overbook. When patients don’t show up, staffers can sometimes contact a patient right away and hold the session. Other times, they can reschedule them for later that day or a different day.
And telepsychiatry performs as well as, if not better than, face-to-face delivery of mental health services, according to a World Journal of Psychiatry review of 452 studies.
Virtual visits can also save patients money, because they might not need to travel, take time off work, or pay for child care, said Jay Shore, MD, MPH, chairperson of the American Psychiatric Association’s telepsychiatry committee and a psychiatrist at the University of Colorado.
Dr. Shore started examining the potential of video conferencing to reach rural patients in the late ’90s and concluded that patients and providers can virtually build rapport, which he said is fundamental for effective therapy and medicine management.
But before the pandemic, almost 64% of psychiatrists had never used telehealth, according to the psychiatric association. Amid widespread skepticism, providers then had to do “10 years of implementations in 10 days,” said Dr. Shore, who has consulted with Dr. Dempsey and other providers.
Dr. Dempsey and colleagues faced a steep learning curve. She said she recently held a video therapy session with a mother who “seemed very out of it” before disappearing from the screen while her baby was crying.
She wondered if the patient’s exit was related to the stress of new motherhood or “something more concerning,” like addiction. She thinks she might have better understood the woman’s condition had they been in the same room. The patient called Dr. Dempsey’s team that night and told them she had relapsed into drug use and been taken to the emergency room. The mental health providers directed her to a treatment program, Dr. Dempsey said.
“We spent a lot of time reviewing what happened with that case and thinking about what we need to do differently,” Dr. Dempsey said.
Providers now routinely ask for the name of someone to call if they lose a connection and can no longer reach the patient.
In another session, Dr. Dempsey noticed that a patient seemed guarded and saw her partner hovering in the background. She said she worried about the possibility of domestic violence or “some other form of controlling behavior.”
In such cases, Dr. Dempsey called after the appointments or sent the patients secure messages to their online health portal. She asked if they felt safe and suggested they talk in person.
Such inability to maintain privacy remains a concern.
In a Walmart parking lot recently, psychologist Kristy Keefe, PsyD, of Western Illinois University, Macomb, heard a patient talking with her therapist from her car. Dr. Keefe said she wondered if the patient “had no other safe place to go to.”
To avoid that scenario, Dr. Keefe does 30-minute consultations with patients before their first telehealth appointment. She asks if they have space to talk where no one can overhear them and makes sure they have sufficient internet access and know how to use video conferencing.
To ensure that she, too, was prepared, Dr. Keefe upgraded her WiFi router, purchased two white-noise machines to drown out her conversations, and placed a stop sign on her door during appointments so her 5-year-old son knew she was seeing patients.
Dr. Keefe concluded that audio alone sometimes works better than video, which often lags. Over the phone, she and her psychology students “got really sensitive to tone fluctuations” in a patient’s voice and were better able to “pick up the emotion” than with video conferencing.
With those telehealth visits, her 20% no-show rate evaporated.
Kate Barnes, a 29-year-old middle school teacher in Fayetteville, Ark., who struggles with anxiety and depression, also has found visits easier by phone than by Zoom, because she doesn’t feel like a spotlight is on her.
“I can focus more on what I want to say,” she said.
In one of Dr. Keefe’s video sessions, though, a patient reached out, touched the camera and started to cry as she said how appreciative she was that someone was there, Dr. Keefe recalled.
“I am so very thankful that they had something in this terrible time of loss and trauma and isolation,” said Dr. Keefe.
Demand for mental health services will likely continue even after the lifting of all COVID restrictions. according to data from the U.S. Census Bureau and the National Health Interview Survey.
“That is not going to go away with snapping our fingers,” Dr. Dempsey said.
After the pandemic, Dr. Shore said, providers should review data from the past year and determine when virtual care or in-person care is more effective. He also said the health care industry needs to work to bridge the digital divide that exists because of lack of access to devices and broadband internet.
Even though Ms. Barnes said she did not see teletherapy as less effective than in-person therapy, she would like to return to seeing her therapist in person.
“When you are in person with someone, you can pick up on their body language better,” she said. “It’s a lot harder over a video call to do that.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
When the COVID-19 pandemic forced behavioral health providers to stop seeing patients in person and instead hold therapy sessions remotely, the switch produced an unintended, positive consequence: Fewer patients skipped appointments.
That had long been a problem in mental health care. Some outpatient programs previously had no-show rates as high as 60%, according to several studies.
Only 9% of psychiatrists reported that all patients kept their appointments before the pandemic, according to an American Psychiatric Association report. Once providers switched to telepsychiatry, that number increased to 32%.
Not only that, but providers and patients say teletherapy has largely been an effective lifeline for people struggling with anxiety, depression, and other psychological issues during an extraordinarily difficult time, even though it created a new set of challenges.
Many providers say they plan to continue offering teletherapy after the pandemic. Some states are making permanent the temporary pandemic rules that allow providers to be reimbursed at the same rates as for in-person visits, which is welcome news to practitioners who take patients’ insurance.
“We are in a mental health crisis right now, so more people are struggling and may be more open to accessing services,” said psychologist Allison Dempsey, PhD, associate professor at University of Colorado at Denver, Aurora. “It’s much easier to connect from your living room.”
The problem for patients who didn’t show up was often as simple as a canceled ride, said Jody Long, a clinical social worker who studied the 60% rate of no-shows or late cancellations at the University of Tennessee Health Science Center psychiatric clinic in Memphis.
But sometimes it was the health problem itself. Mr. Long remembers seeing a first-time patient drive around the parking lot and then exit. The patient later called and told Mr. Long, “I just could not get out of the car; please forgive me and reschedule me.”
Mr. Long, now an assistant professor at Jacksonville (Ala.) State University, said that incident changed his perspective. “I realized when you’re having panic attacks or anxiety attacks or suffering from major depressive disorder, it’s hard,” he said. “It’s like you have built up these walls for protection and then all of a sudden you’re having to let these walls down.”
Absences strain providers whose bosses set billing and productivity expectations and those in private practice who lose billable hours, said Dr. Dempsey, who directs a program to provide mental health care for families of babies with serious medical complications. Psychotherapists often overbooked patients with the expectation that some would not show up.
Now Dr. Dempsey and colleagues no longer need to overbook. When patients don’t show up, staffers can sometimes contact a patient right away and hold the session. Other times, they can reschedule them for later that day or a different day.
And telepsychiatry performs as well as, if not better than, face-to-face delivery of mental health services, according to a World Journal of Psychiatry review of 452 studies.
Virtual visits can also save patients money, because they might not need to travel, take time off work, or pay for child care, said Jay Shore, MD, MPH, chairperson of the American Psychiatric Association’s telepsychiatry committee and a psychiatrist at the University of Colorado.
Dr. Shore started examining the potential of video conferencing to reach rural patients in the late ’90s and concluded that patients and providers can virtually build rapport, which he said is fundamental for effective therapy and medicine management.
But before the pandemic, almost 64% of psychiatrists had never used telehealth, according to the psychiatric association. Amid widespread skepticism, providers then had to do “10 years of implementations in 10 days,” said Dr. Shore, who has consulted with Dr. Dempsey and other providers.
Dr. Dempsey and colleagues faced a steep learning curve. She said she recently held a video therapy session with a mother who “seemed very out of it” before disappearing from the screen while her baby was crying.
She wondered if the patient’s exit was related to the stress of new motherhood or “something more concerning,” like addiction. She thinks she might have better understood the woman’s condition had they been in the same room. The patient called Dr. Dempsey’s team that night and told them she had relapsed into drug use and been taken to the emergency room. The mental health providers directed her to a treatment program, Dr. Dempsey said.
“We spent a lot of time reviewing what happened with that case and thinking about what we need to do differently,” Dr. Dempsey said.
Providers now routinely ask for the name of someone to call if they lose a connection and can no longer reach the patient.
In another session, Dr. Dempsey noticed that a patient seemed guarded and saw her partner hovering in the background. She said she worried about the possibility of domestic violence or “some other form of controlling behavior.”
In such cases, Dr. Dempsey called after the appointments or sent the patients secure messages to their online health portal. She asked if they felt safe and suggested they talk in person.
Such inability to maintain privacy remains a concern.
In a Walmart parking lot recently, psychologist Kristy Keefe, PsyD, of Western Illinois University, Macomb, heard a patient talking with her therapist from her car. Dr. Keefe said she wondered if the patient “had no other safe place to go to.”
To avoid that scenario, Dr. Keefe does 30-minute consultations with patients before their first telehealth appointment. She asks if they have space to talk where no one can overhear them and makes sure they have sufficient internet access and know how to use video conferencing.
To ensure that she, too, was prepared, Dr. Keefe upgraded her WiFi router, purchased two white-noise machines to drown out her conversations, and placed a stop sign on her door during appointments so her 5-year-old son knew she was seeing patients.
Dr. Keefe concluded that audio alone sometimes works better than video, which often lags. Over the phone, she and her psychology students “got really sensitive to tone fluctuations” in a patient’s voice and were better able to “pick up the emotion” than with video conferencing.
With those telehealth visits, her 20% no-show rate evaporated.
Kate Barnes, a 29-year-old middle school teacher in Fayetteville, Ark., who struggles with anxiety and depression, also has found visits easier by phone than by Zoom, because she doesn’t feel like a spotlight is on her.
“I can focus more on what I want to say,” she said.
In one of Dr. Keefe’s video sessions, though, a patient reached out, touched the camera and started to cry as she said how appreciative she was that someone was there, Dr. Keefe recalled.
“I am so very thankful that they had something in this terrible time of loss and trauma and isolation,” said Dr. Keefe.
Demand for mental health services will likely continue even after the lifting of all COVID restrictions. according to data from the U.S. Census Bureau and the National Health Interview Survey.
“That is not going to go away with snapping our fingers,” Dr. Dempsey said.
After the pandemic, Dr. Shore said, providers should review data from the past year and determine when virtual care or in-person care is more effective. He also said the health care industry needs to work to bridge the digital divide that exists because of lack of access to devices and broadband internet.
Even though Ms. Barnes said she did not see teletherapy as less effective than in-person therapy, she would like to return to seeing her therapist in person.
“When you are in person with someone, you can pick up on their body language better,” she said. “It’s a lot harder over a video call to do that.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
When the COVID-19 pandemic forced behavioral health providers to stop seeing patients in person and instead hold therapy sessions remotely, the switch produced an unintended, positive consequence: Fewer patients skipped appointments.
That had long been a problem in mental health care. Some outpatient programs previously had no-show rates as high as 60%, according to several studies.
Only 9% of psychiatrists reported that all patients kept their appointments before the pandemic, according to an American Psychiatric Association report. Once providers switched to telepsychiatry, that number increased to 32%.
Not only that, but providers and patients say teletherapy has largely been an effective lifeline for people struggling with anxiety, depression, and other psychological issues during an extraordinarily difficult time, even though it created a new set of challenges.
Many providers say they plan to continue offering teletherapy after the pandemic. Some states are making permanent the temporary pandemic rules that allow providers to be reimbursed at the same rates as for in-person visits, which is welcome news to practitioners who take patients’ insurance.
“We are in a mental health crisis right now, so more people are struggling and may be more open to accessing services,” said psychologist Allison Dempsey, PhD, associate professor at University of Colorado at Denver, Aurora. “It’s much easier to connect from your living room.”
The problem for patients who didn’t show up was often as simple as a canceled ride, said Jody Long, a clinical social worker who studied the 60% rate of no-shows or late cancellations at the University of Tennessee Health Science Center psychiatric clinic in Memphis.
But sometimes it was the health problem itself. Mr. Long remembers seeing a first-time patient drive around the parking lot and then exit. The patient later called and told Mr. Long, “I just could not get out of the car; please forgive me and reschedule me.”
Mr. Long, now an assistant professor at Jacksonville (Ala.) State University, said that incident changed his perspective. “I realized when you’re having panic attacks or anxiety attacks or suffering from major depressive disorder, it’s hard,” he said. “It’s like you have built up these walls for protection and then all of a sudden you’re having to let these walls down.”
Absences strain providers whose bosses set billing and productivity expectations and those in private practice who lose billable hours, said Dr. Dempsey, who directs a program to provide mental health care for families of babies with serious medical complications. Psychotherapists often overbooked patients with the expectation that some would not show up.
Now Dr. Dempsey and colleagues no longer need to overbook. When patients don’t show up, staffers can sometimes contact a patient right away and hold the session. Other times, they can reschedule them for later that day or a different day.
And telepsychiatry performs as well as, if not better than, face-to-face delivery of mental health services, according to a World Journal of Psychiatry review of 452 studies.
Virtual visits can also save patients money, because they might not need to travel, take time off work, or pay for child care, said Jay Shore, MD, MPH, chairperson of the American Psychiatric Association’s telepsychiatry committee and a psychiatrist at the University of Colorado.
Dr. Shore started examining the potential of video conferencing to reach rural patients in the late ’90s and concluded that patients and providers can virtually build rapport, which he said is fundamental for effective therapy and medicine management.
But before the pandemic, almost 64% of psychiatrists had never used telehealth, according to the psychiatric association. Amid widespread skepticism, providers then had to do “10 years of implementations in 10 days,” said Dr. Shore, who has consulted with Dr. Dempsey and other providers.
Dr. Dempsey and colleagues faced a steep learning curve. She said she recently held a video therapy session with a mother who “seemed very out of it” before disappearing from the screen while her baby was crying.
She wondered if the patient’s exit was related to the stress of new motherhood or “something more concerning,” like addiction. She thinks she might have better understood the woman’s condition had they been in the same room. The patient called Dr. Dempsey’s team that night and told them she had relapsed into drug use and been taken to the emergency room. The mental health providers directed her to a treatment program, Dr. Dempsey said.
“We spent a lot of time reviewing what happened with that case and thinking about what we need to do differently,” Dr. Dempsey said.
Providers now routinely ask for the name of someone to call if they lose a connection and can no longer reach the patient.
In another session, Dr. Dempsey noticed that a patient seemed guarded and saw her partner hovering in the background. She said she worried about the possibility of domestic violence or “some other form of controlling behavior.”
In such cases, Dr. Dempsey called after the appointments or sent the patients secure messages to their online health portal. She asked if they felt safe and suggested they talk in person.
Such inability to maintain privacy remains a concern.
In a Walmart parking lot recently, psychologist Kristy Keefe, PsyD, of Western Illinois University, Macomb, heard a patient talking with her therapist from her car. Dr. Keefe said she wondered if the patient “had no other safe place to go to.”
To avoid that scenario, Dr. Keefe does 30-minute consultations with patients before their first telehealth appointment. She asks if they have space to talk where no one can overhear them and makes sure they have sufficient internet access and know how to use video conferencing.
To ensure that she, too, was prepared, Dr. Keefe upgraded her WiFi router, purchased two white-noise machines to drown out her conversations, and placed a stop sign on her door during appointments so her 5-year-old son knew she was seeing patients.
Dr. Keefe concluded that audio alone sometimes works better than video, which often lags. Over the phone, she and her psychology students “got really sensitive to tone fluctuations” in a patient’s voice and were better able to “pick up the emotion” than with video conferencing.
With those telehealth visits, her 20% no-show rate evaporated.
Kate Barnes, a 29-year-old middle school teacher in Fayetteville, Ark., who struggles with anxiety and depression, also has found visits easier by phone than by Zoom, because she doesn’t feel like a spotlight is on her.
“I can focus more on what I want to say,” she said.
In one of Dr. Keefe’s video sessions, though, a patient reached out, touched the camera and started to cry as she said how appreciative she was that someone was there, Dr. Keefe recalled.
“I am so very thankful that they had something in this terrible time of loss and trauma and isolation,” said Dr. Keefe.
Demand for mental health services will likely continue even after the lifting of all COVID restrictions. according to data from the U.S. Census Bureau and the National Health Interview Survey.
“That is not going to go away with snapping our fingers,” Dr. Dempsey said.
After the pandemic, Dr. Shore said, providers should review data from the past year and determine when virtual care or in-person care is more effective. He also said the health care industry needs to work to bridge the digital divide that exists because of lack of access to devices and broadband internet.
Even though Ms. Barnes said she did not see teletherapy as less effective than in-person therapy, she would like to return to seeing her therapist in person.
“When you are in person with someone, you can pick up on their body language better,” she said. “It’s a lot harder over a video call to do that.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Cardiologists’ pay increases, despite COVID-19 impacts
Despite the huge challenges of COVID-19, including a drop in patient visits, cardiologists reported an average increase in income in 2020 and remain among the top earners in medicine, according to the 2021 Medscape Cardiologist Compensation Report.
Although 46% of cardiologists reported some decline in compensation, average cardiologist income was $459,000 in 2020 – up from $438,000 in 2019.
Cardiologist pay is the third highest of all specialties in the overall 2021 Medscape Physician Compensation Report, which covers U.S. physicians as a whole and almost 18,000 physicians in 29 specialties.
Only plastic surgeons ($526,000) and orthopedists ($511,000) earned more than cardiologists in 2020.
On average among cardiologists, self-employment yields a somewhat higher paycheck than does being employed ($477,000 vs. $450,000).
Just like in last year’s report, nearly two-thirds (61%) of cardiologists overall say they feel fairly compensated.
The average incentive bonus payment for cardiologists in 2020 was 14% of total salary, about the same as last year. Two-thirds of cardiologists who earn an incentive bonus achieve more than three-quarters of their potential annual payment, up from 55% the prior year.
COVID challenges and the road back
The vast majority (92%) of cardiologists who saw a drop in income last year cited COVID-related issues such as job loss, working fewer hours, and seeing fewer patients.
Close to half (48%) of cardiologists who suffered financial or practice-related ill effects as a result of the pandemic expect their income to return to normal this year; 38% believe it will take 2 to 3 years. Notably, 45% of physicians overall said the pandemic did not cause them financial or practice-related harm.
Physician work hours generally declined for at least some time during the pandemic – and some physicians were furloughed – but most are now working about the same number of hours they did prior to COVID-19.
Cardiologists are back working an average of 57 hours per week. Perhaps not surprising, intensivists, infectious disease physicians, and public health/preventive medicine physicians are pulling longer hours now, about 6 or 7 more per week than before.
Although working about the same number of hours per week now as they did before the pandemic, physicians overall are typically seeing fewer patients because of time spent on medical office safety protocols, answering COVID-19–related questions and other factors.
Cardiologists are seeing an average decline in weekly patient visits of about 6% – from 77 to 72 patients. Pediatricians are experiencing the largest average declines – from 78 patients per week prior to 64 now, an 18% drop.
Among self-employed cardiologists, 43% believe that a drop in patient volume of up to one-quarter is permanent.
Most cardiologists remain happy at work
Despite COVID-19 and other professional challenges, most cardiologists (and physicians overall) continue to find their work rewarding.
Cardiologists say the most rewarding aspect of their profession is “being good at what I do/finding answers and diagnoses” (27%), followed by relationships with and gratitude from patients (26%), making the world a better place (23%) and making good money at a job they like (12%). A few cited pride in their profession (6%) and teaching (2%). These figures are in line with last year’s responses.
The most challenging part of practicing cardiology is having so many rules and regulations (22%), followed by having to work long hours (16%), working with electronic health records (13%), trouble getting fair reimbursement (11%), danger/risk associated with treating COVID-19 patients (11%), dealing with difficult patients (8%) and worry about being sued (7%).
Bureaucratic tasks continue to be a burden for physicians in all specialties. On average, cardiologists spend 17.4 hours per week on paperwork and administration, similar to last year (16.9 hours per week) and to physicians overall (16.3 hours).
Despite the challenges, 86% of cardiologists said they would choose medicine again, and 92% would choose cardiology again, about the same as last year.
Most cardiologists (83%) plan to keep Medicare and/or Medicaid patients; only 1% say they won’t take new Medicare or Medicaid patients; and 16% are undecided.
Thirty-nine percent of cardiologists plan to participate in the Merit-based Incentive Payment System (MIPS) in 2021.
“The stakes of the Quality Payment Program – the program that incorporates MIPS – are high, with a 9% penalty applied to all Medicare reimbursement for failure to participate,” said Elizabeth Woodcock, MBA, CPC, president of physician practice consulting firm Woodcock & Associates, Atlanta.
“With margins already slim, most physicians can’t afford this massive penalty. It makes sense to protect your revenue by complying with at least the bare minimum,” she noted.
A version of this article first appeared on Medscape.com.
Despite the huge challenges of COVID-19, including a drop in patient visits, cardiologists reported an average increase in income in 2020 and remain among the top earners in medicine, according to the 2021 Medscape Cardiologist Compensation Report.
Although 46% of cardiologists reported some decline in compensation, average cardiologist income was $459,000 in 2020 – up from $438,000 in 2019.
Cardiologist pay is the third highest of all specialties in the overall 2021 Medscape Physician Compensation Report, which covers U.S. physicians as a whole and almost 18,000 physicians in 29 specialties.
Only plastic surgeons ($526,000) and orthopedists ($511,000) earned more than cardiologists in 2020.
On average among cardiologists, self-employment yields a somewhat higher paycheck than does being employed ($477,000 vs. $450,000).
Just like in last year’s report, nearly two-thirds (61%) of cardiologists overall say they feel fairly compensated.
The average incentive bonus payment for cardiologists in 2020 was 14% of total salary, about the same as last year. Two-thirds of cardiologists who earn an incentive bonus achieve more than three-quarters of their potential annual payment, up from 55% the prior year.
COVID challenges and the road back
The vast majority (92%) of cardiologists who saw a drop in income last year cited COVID-related issues such as job loss, working fewer hours, and seeing fewer patients.
Close to half (48%) of cardiologists who suffered financial or practice-related ill effects as a result of the pandemic expect their income to return to normal this year; 38% believe it will take 2 to 3 years. Notably, 45% of physicians overall said the pandemic did not cause them financial or practice-related harm.
Physician work hours generally declined for at least some time during the pandemic – and some physicians were furloughed – but most are now working about the same number of hours they did prior to COVID-19.
Cardiologists are back working an average of 57 hours per week. Perhaps not surprising, intensivists, infectious disease physicians, and public health/preventive medicine physicians are pulling longer hours now, about 6 or 7 more per week than before.
Although working about the same number of hours per week now as they did before the pandemic, physicians overall are typically seeing fewer patients because of time spent on medical office safety protocols, answering COVID-19–related questions and other factors.
Cardiologists are seeing an average decline in weekly patient visits of about 6% – from 77 to 72 patients. Pediatricians are experiencing the largest average declines – from 78 patients per week prior to 64 now, an 18% drop.
Among self-employed cardiologists, 43% believe that a drop in patient volume of up to one-quarter is permanent.
Most cardiologists remain happy at work
Despite COVID-19 and other professional challenges, most cardiologists (and physicians overall) continue to find their work rewarding.
Cardiologists say the most rewarding aspect of their profession is “being good at what I do/finding answers and diagnoses” (27%), followed by relationships with and gratitude from patients (26%), making the world a better place (23%) and making good money at a job they like (12%). A few cited pride in their profession (6%) and teaching (2%). These figures are in line with last year’s responses.
The most challenging part of practicing cardiology is having so many rules and regulations (22%), followed by having to work long hours (16%), working with electronic health records (13%), trouble getting fair reimbursement (11%), danger/risk associated with treating COVID-19 patients (11%), dealing with difficult patients (8%) and worry about being sued (7%).
Bureaucratic tasks continue to be a burden for physicians in all specialties. On average, cardiologists spend 17.4 hours per week on paperwork and administration, similar to last year (16.9 hours per week) and to physicians overall (16.3 hours).
Despite the challenges, 86% of cardiologists said they would choose medicine again, and 92% would choose cardiology again, about the same as last year.
Most cardiologists (83%) plan to keep Medicare and/or Medicaid patients; only 1% say they won’t take new Medicare or Medicaid patients; and 16% are undecided.
Thirty-nine percent of cardiologists plan to participate in the Merit-based Incentive Payment System (MIPS) in 2021.
“The stakes of the Quality Payment Program – the program that incorporates MIPS – are high, with a 9% penalty applied to all Medicare reimbursement for failure to participate,” said Elizabeth Woodcock, MBA, CPC, president of physician practice consulting firm Woodcock & Associates, Atlanta.
“With margins already slim, most physicians can’t afford this massive penalty. It makes sense to protect your revenue by complying with at least the bare minimum,” she noted.
A version of this article first appeared on Medscape.com.
Despite the huge challenges of COVID-19, including a drop in patient visits, cardiologists reported an average increase in income in 2020 and remain among the top earners in medicine, according to the 2021 Medscape Cardiologist Compensation Report.
Although 46% of cardiologists reported some decline in compensation, average cardiologist income was $459,000 in 2020 – up from $438,000 in 2019.
Cardiologist pay is the third highest of all specialties in the overall 2021 Medscape Physician Compensation Report, which covers U.S. physicians as a whole and almost 18,000 physicians in 29 specialties.
Only plastic surgeons ($526,000) and orthopedists ($511,000) earned more than cardiologists in 2020.
On average among cardiologists, self-employment yields a somewhat higher paycheck than does being employed ($477,000 vs. $450,000).
Just like in last year’s report, nearly two-thirds (61%) of cardiologists overall say they feel fairly compensated.
The average incentive bonus payment for cardiologists in 2020 was 14% of total salary, about the same as last year. Two-thirds of cardiologists who earn an incentive bonus achieve more than three-quarters of their potential annual payment, up from 55% the prior year.
COVID challenges and the road back
The vast majority (92%) of cardiologists who saw a drop in income last year cited COVID-related issues such as job loss, working fewer hours, and seeing fewer patients.
Close to half (48%) of cardiologists who suffered financial or practice-related ill effects as a result of the pandemic expect their income to return to normal this year; 38% believe it will take 2 to 3 years. Notably, 45% of physicians overall said the pandemic did not cause them financial or practice-related harm.
Physician work hours generally declined for at least some time during the pandemic – and some physicians were furloughed – but most are now working about the same number of hours they did prior to COVID-19.
Cardiologists are back working an average of 57 hours per week. Perhaps not surprising, intensivists, infectious disease physicians, and public health/preventive medicine physicians are pulling longer hours now, about 6 or 7 more per week than before.
Although working about the same number of hours per week now as they did before the pandemic, physicians overall are typically seeing fewer patients because of time spent on medical office safety protocols, answering COVID-19–related questions and other factors.
Cardiologists are seeing an average decline in weekly patient visits of about 6% – from 77 to 72 patients. Pediatricians are experiencing the largest average declines – from 78 patients per week prior to 64 now, an 18% drop.
Among self-employed cardiologists, 43% believe that a drop in patient volume of up to one-quarter is permanent.
Most cardiologists remain happy at work
Despite COVID-19 and other professional challenges, most cardiologists (and physicians overall) continue to find their work rewarding.
Cardiologists say the most rewarding aspect of their profession is “being good at what I do/finding answers and diagnoses” (27%), followed by relationships with and gratitude from patients (26%), making the world a better place (23%) and making good money at a job they like (12%). A few cited pride in their profession (6%) and teaching (2%). These figures are in line with last year’s responses.
The most challenging part of practicing cardiology is having so many rules and regulations (22%), followed by having to work long hours (16%), working with electronic health records (13%), trouble getting fair reimbursement (11%), danger/risk associated with treating COVID-19 patients (11%), dealing with difficult patients (8%) and worry about being sued (7%).
Bureaucratic tasks continue to be a burden for physicians in all specialties. On average, cardiologists spend 17.4 hours per week on paperwork and administration, similar to last year (16.9 hours per week) and to physicians overall (16.3 hours).
Despite the challenges, 86% of cardiologists said they would choose medicine again, and 92% would choose cardiology again, about the same as last year.
Most cardiologists (83%) plan to keep Medicare and/or Medicaid patients; only 1% say they won’t take new Medicare or Medicaid patients; and 16% are undecided.
Thirty-nine percent of cardiologists plan to participate in the Merit-based Incentive Payment System (MIPS) in 2021.
“The stakes of the Quality Payment Program – the program that incorporates MIPS – are high, with a 9% penalty applied to all Medicare reimbursement for failure to participate,” said Elizabeth Woodcock, MBA, CPC, president of physician practice consulting firm Woodcock & Associates, Atlanta.
“With margins already slim, most physicians can’t afford this massive penalty. It makes sense to protect your revenue by complying with at least the bare minimum,” she noted.
A version of this article first appeared on Medscape.com.
Physicians’ trust in health care leadership drops in pandemic
according to a survey conducted by NORC at the University of Chicago on behalf of the American Board of Internal Medicine Foundation.
Survey results, released May 21, indicate that 30% of physicians say their trust in the U.S. health care system and health care leadership has decreased during the pandemic. Only 18% reported an increase in trust.
Physicians, however, have great trust in their fellow clinicians.
In the survey of 600 physicians, 94% said they trust doctors within their practice; 85% trusted doctors outside of their practice; and 89% trusted nurses. That trust increased during the pandemic, with 41% saying their trust in fellow physicians rose and 37% saying their trust in nurses did.
In a separate survey, NORC asked patients about their trust in various aspects of health care. Among 2,069 respondents, a wide majority reported that they trust doctors (84%) and nurses (85%), but only 64% trusted the health care system as a whole. One in three consumers (32%) said their trust in the health care system decreased during the pandemic, compared with 11% who said their trust increased.
The ABIM Foundation released the research findings on May 21 as part of Building Trust, a national campaign that aims to boost trust among patients, clinicians, system leaders, researchers, and others.
Richard J. Baron, MD, president and chief executive officer of the ABIM Foundation, said in an interview, “Clearly there’s lower trust in health care organization leaders and executives, and that’s troubling.
“Science by itself is not enough,” he said. “Becoming trustworthy has to be a core project of everybody in health care.”
Deterioration in physicians’ trust during the pandemic comes in part from failed promises of adequate personal protective equipment and some physicians’ loss of income as a result of the crisis, Dr. Baron said.
He added that the vaccine rollout was very uneven and that policies as to which elective procedures could be performed were handled differently in different parts of the country.
He also noted that, early on, transparency was lacking as to how many COVID patients hospitals were treating, which may have contributed to the decrease in trust in the system.
Fear of being known as ‘the COVID hospital’
Hospitals were afraid of being known as “the COVID hospital” and losing patients who were afraid to come there, Dr. Baron said.
He said the COVID-19 epidemic exacerbated problems regarding trust, but that trust has been declining for some time. The Building Trust campaign will focus on solutions in breaches of trust as physicians move increasingly toward being employees of huge systems, according to Dr. Baron.
However, trust works both ways, Dr. Baron notes. Physicians can be champions for their health care system or “throw the system under the bus,” he said.
For example, if a patient complains about the appointment system, clinicians who trust their institutions may say the system usually works and that they will try to make sure the patient has a better experience next time. Clinicians without trust may say they agree that the health care system doesn’t know what it is doing, and patients may further lose confidence when physicians validate their complaint, and patients may then go elsewhere.
78% of patients trust primary care doctor
When asked whether they trust their primary care physician, 78% of patients said yes. However, trust in doctors was higher among people who were older (90%), White (82%), or had high income (89%). Among people reporting lower trust, 25% said their physician spends too little time with them, and 14% said their doctor does not know or listen to them.
The survey shows that government agencies have work to do to earn trust. Responses indicate that 43% of physicians said they have “complete trust” in government health care agencies, such as the U.S. Food and Drug Administration and the Centers for Disease Control and Prevention, which is substantially higher than other parts of the health care system. However, trust in agencies declined for 43% of physician respondents and increased for 21%.
Dhruv Khullar, MD, MPP, of the department of health policy and economics at Weill Cornell Medical College in New York, told this news organization the survey results match what he sees anecdotally in medicine – that physicians have been losing trust in the system but not in their colleagues.
He said the sample size of 600 is enough to be influential, though he said he would like to know the response rate, which was not calculated for this survey.
He added that, in large part, physicians’ lack of trust in their systems may come from generally being asked to see more patients and to meet more metrics during the same or shorter periods.
Physicians’ lack of trust in the system can have significant consequences, he said. It can lead to burnout, which has been linked with poorer quality of care and physician turnover, he noted.
COVID-19 led some physicians to wonder whether their system had their best interests at heart, insofar as access to adequate medicines and supplies as well as emotional support were inconsistent, Dr. Khullar said.
He said that to regain trust health care systems need to ask themselves questions in three areas. The first is whether their goals are focused on the best interest of the organization or the best interest of the patient.
“Next is competency,” Dr. Khullar said. “Maybe your motives are right, but are you able to deliver? Are you delivering a good product, whether clinical services or something else?”
The third area is transparency, he said. “Are you going to be honest and forthright in what we’re doing and where we’re going?”
Caroline Pearson, senior vice president of health care strategy for NORC, said the emailed survey was conducted between Dec. 29, 2020, and Feb. 5, 2021, with a health care survey partner that maintains a nationwide panel of physicians across specialties.
She said this report is fairly novel insofar as surveys are more typically conducted regarding patients’ trust of their doctors or of the health care system.
Ms. Pearson said because health care is delivered in teams, understanding the level of trust among the entities helps ensure that care will be delivered effectively and seamlessly with high quality.
“We want our patients to trust our doctors, but we really want doctors to trust each other and trust the hospitals and systems in which they’re working,” she said.
Dr. Baron, Ms. Pearson, and Dr. Khullar report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a survey conducted by NORC at the University of Chicago on behalf of the American Board of Internal Medicine Foundation.
Survey results, released May 21, indicate that 30% of physicians say their trust in the U.S. health care system and health care leadership has decreased during the pandemic. Only 18% reported an increase in trust.
Physicians, however, have great trust in their fellow clinicians.
In the survey of 600 physicians, 94% said they trust doctors within their practice; 85% trusted doctors outside of their practice; and 89% trusted nurses. That trust increased during the pandemic, with 41% saying their trust in fellow physicians rose and 37% saying their trust in nurses did.
In a separate survey, NORC asked patients about their trust in various aspects of health care. Among 2,069 respondents, a wide majority reported that they trust doctors (84%) and nurses (85%), but only 64% trusted the health care system as a whole. One in three consumers (32%) said their trust in the health care system decreased during the pandemic, compared with 11% who said their trust increased.
The ABIM Foundation released the research findings on May 21 as part of Building Trust, a national campaign that aims to boost trust among patients, clinicians, system leaders, researchers, and others.
Richard J. Baron, MD, president and chief executive officer of the ABIM Foundation, said in an interview, “Clearly there’s lower trust in health care organization leaders and executives, and that’s troubling.
“Science by itself is not enough,” he said. “Becoming trustworthy has to be a core project of everybody in health care.”
Deterioration in physicians’ trust during the pandemic comes in part from failed promises of adequate personal protective equipment and some physicians’ loss of income as a result of the crisis, Dr. Baron said.
He added that the vaccine rollout was very uneven and that policies as to which elective procedures could be performed were handled differently in different parts of the country.
He also noted that, early on, transparency was lacking as to how many COVID patients hospitals were treating, which may have contributed to the decrease in trust in the system.
Fear of being known as ‘the COVID hospital’
Hospitals were afraid of being known as “the COVID hospital” and losing patients who were afraid to come there, Dr. Baron said.
He said the COVID-19 epidemic exacerbated problems regarding trust, but that trust has been declining for some time. The Building Trust campaign will focus on solutions in breaches of trust as physicians move increasingly toward being employees of huge systems, according to Dr. Baron.
However, trust works both ways, Dr. Baron notes. Physicians can be champions for their health care system or “throw the system under the bus,” he said.
For example, if a patient complains about the appointment system, clinicians who trust their institutions may say the system usually works and that they will try to make sure the patient has a better experience next time. Clinicians without trust may say they agree that the health care system doesn’t know what it is doing, and patients may further lose confidence when physicians validate their complaint, and patients may then go elsewhere.
78% of patients trust primary care doctor
When asked whether they trust their primary care physician, 78% of patients said yes. However, trust in doctors was higher among people who were older (90%), White (82%), or had high income (89%). Among people reporting lower trust, 25% said their physician spends too little time with them, and 14% said their doctor does not know or listen to them.
The survey shows that government agencies have work to do to earn trust. Responses indicate that 43% of physicians said they have “complete trust” in government health care agencies, such as the U.S. Food and Drug Administration and the Centers for Disease Control and Prevention, which is substantially higher than other parts of the health care system. However, trust in agencies declined for 43% of physician respondents and increased for 21%.
Dhruv Khullar, MD, MPP, of the department of health policy and economics at Weill Cornell Medical College in New York, told this news organization the survey results match what he sees anecdotally in medicine – that physicians have been losing trust in the system but not in their colleagues.
He said the sample size of 600 is enough to be influential, though he said he would like to know the response rate, which was not calculated for this survey.
He added that, in large part, physicians’ lack of trust in their systems may come from generally being asked to see more patients and to meet more metrics during the same or shorter periods.
Physicians’ lack of trust in the system can have significant consequences, he said. It can lead to burnout, which has been linked with poorer quality of care and physician turnover, he noted.
COVID-19 led some physicians to wonder whether their system had their best interests at heart, insofar as access to adequate medicines and supplies as well as emotional support were inconsistent, Dr. Khullar said.
He said that to regain trust health care systems need to ask themselves questions in three areas. The first is whether their goals are focused on the best interest of the organization or the best interest of the patient.
“Next is competency,” Dr. Khullar said. “Maybe your motives are right, but are you able to deliver? Are you delivering a good product, whether clinical services or something else?”
The third area is transparency, he said. “Are you going to be honest and forthright in what we’re doing and where we’re going?”
Caroline Pearson, senior vice president of health care strategy for NORC, said the emailed survey was conducted between Dec. 29, 2020, and Feb. 5, 2021, with a health care survey partner that maintains a nationwide panel of physicians across specialties.
She said this report is fairly novel insofar as surveys are more typically conducted regarding patients’ trust of their doctors or of the health care system.
Ms. Pearson said because health care is delivered in teams, understanding the level of trust among the entities helps ensure that care will be delivered effectively and seamlessly with high quality.
“We want our patients to trust our doctors, but we really want doctors to trust each other and trust the hospitals and systems in which they’re working,” she said.
Dr. Baron, Ms. Pearson, and Dr. Khullar report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a survey conducted by NORC at the University of Chicago on behalf of the American Board of Internal Medicine Foundation.
Survey results, released May 21, indicate that 30% of physicians say their trust in the U.S. health care system and health care leadership has decreased during the pandemic. Only 18% reported an increase in trust.
Physicians, however, have great trust in their fellow clinicians.
In the survey of 600 physicians, 94% said they trust doctors within their practice; 85% trusted doctors outside of their practice; and 89% trusted nurses. That trust increased during the pandemic, with 41% saying their trust in fellow physicians rose and 37% saying their trust in nurses did.
In a separate survey, NORC asked patients about their trust in various aspects of health care. Among 2,069 respondents, a wide majority reported that they trust doctors (84%) and nurses (85%), but only 64% trusted the health care system as a whole. One in three consumers (32%) said their trust in the health care system decreased during the pandemic, compared with 11% who said their trust increased.
The ABIM Foundation released the research findings on May 21 as part of Building Trust, a national campaign that aims to boost trust among patients, clinicians, system leaders, researchers, and others.
Richard J. Baron, MD, president and chief executive officer of the ABIM Foundation, said in an interview, “Clearly there’s lower trust in health care organization leaders and executives, and that’s troubling.
“Science by itself is not enough,” he said. “Becoming trustworthy has to be a core project of everybody in health care.”
Deterioration in physicians’ trust during the pandemic comes in part from failed promises of adequate personal protective equipment and some physicians’ loss of income as a result of the crisis, Dr. Baron said.
He added that the vaccine rollout was very uneven and that policies as to which elective procedures could be performed were handled differently in different parts of the country.
He also noted that, early on, transparency was lacking as to how many COVID patients hospitals were treating, which may have contributed to the decrease in trust in the system.
Fear of being known as ‘the COVID hospital’
Hospitals were afraid of being known as “the COVID hospital” and losing patients who were afraid to come there, Dr. Baron said.
He said the COVID-19 epidemic exacerbated problems regarding trust, but that trust has been declining for some time. The Building Trust campaign will focus on solutions in breaches of trust as physicians move increasingly toward being employees of huge systems, according to Dr. Baron.
However, trust works both ways, Dr. Baron notes. Physicians can be champions for their health care system or “throw the system under the bus,” he said.
For example, if a patient complains about the appointment system, clinicians who trust their institutions may say the system usually works and that they will try to make sure the patient has a better experience next time. Clinicians without trust may say they agree that the health care system doesn’t know what it is doing, and patients may further lose confidence when physicians validate their complaint, and patients may then go elsewhere.
78% of patients trust primary care doctor
When asked whether they trust their primary care physician, 78% of patients said yes. However, trust in doctors was higher among people who were older (90%), White (82%), or had high income (89%). Among people reporting lower trust, 25% said their physician spends too little time with them, and 14% said their doctor does not know or listen to them.
The survey shows that government agencies have work to do to earn trust. Responses indicate that 43% of physicians said they have “complete trust” in government health care agencies, such as the U.S. Food and Drug Administration and the Centers for Disease Control and Prevention, which is substantially higher than other parts of the health care system. However, trust in agencies declined for 43% of physician respondents and increased for 21%.
Dhruv Khullar, MD, MPP, of the department of health policy and economics at Weill Cornell Medical College in New York, told this news organization the survey results match what he sees anecdotally in medicine – that physicians have been losing trust in the system but not in their colleagues.
He said the sample size of 600 is enough to be influential, though he said he would like to know the response rate, which was not calculated for this survey.
He added that, in large part, physicians’ lack of trust in their systems may come from generally being asked to see more patients and to meet more metrics during the same or shorter periods.
Physicians’ lack of trust in the system can have significant consequences, he said. It can lead to burnout, which has been linked with poorer quality of care and physician turnover, he noted.
COVID-19 led some physicians to wonder whether their system had their best interests at heart, insofar as access to adequate medicines and supplies as well as emotional support were inconsistent, Dr. Khullar said.
He said that to regain trust health care systems need to ask themselves questions in three areas. The first is whether their goals are focused on the best interest of the organization or the best interest of the patient.
“Next is competency,” Dr. Khullar said. “Maybe your motives are right, but are you able to deliver? Are you delivering a good product, whether clinical services or something else?”
The third area is transparency, he said. “Are you going to be honest and forthright in what we’re doing and where we’re going?”
Caroline Pearson, senior vice president of health care strategy for NORC, said the emailed survey was conducted between Dec. 29, 2020, and Feb. 5, 2021, with a health care survey partner that maintains a nationwide panel of physicians across specialties.
She said this report is fairly novel insofar as surveys are more typically conducted regarding patients’ trust of their doctors or of the health care system.
Ms. Pearson said because health care is delivered in teams, understanding the level of trust among the entities helps ensure that care will be delivered effectively and seamlessly with high quality.
“We want our patients to trust our doctors, but we really want doctors to trust each other and trust the hospitals and systems in which they’re working,” she said.
Dr. Baron, Ms. Pearson, and Dr. Khullar report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
First issue vs. April 2021 issue: Much has changed since 1971
For the first readers of Family Practice News, it started with this: “How safe is the pill? An extensive epidemiologic study being carried out in the United Kingdom by the Royal College of General Practitioners is expected to provide definitive answers to this question within the next few years.”
That was the first paragraph of the lead article on the front page of our very first issue, published in October 1971. The report on oral contraceptives, coming from the annual meeting of the British Medical Association in Leicester, largely focused on recruiting – noting that “all women in the study are married” – and data-gathering methods.
That first issue also covered such topics as the effect of “early and frequent coitus” on cervical dysplasia incidence (p. 4), breast cancer in men (p. 13), and treatment of prostate inflammation in patients with impotence (p. 34).
Our April 2021 issue included five articles related to the COVID-19 pandemic, starting on the front page and featuring a photo – a physician sitting at a computer, wearing a mask – and a topic – vaccine-hesitant patients.
Business of medicine today vs. in 1971
At the time of publication of our first issue the United States was in the midst of a 90-day freeze on wages and prices ordered by President Richard Nixon. Two articles in that first issue discussed the subject: “Freeze clouds future of health insurance plans” and “Freeze lets physicians ‘stabilize’ office fees.”
Besides COVID-19, here are some other topics covered in April 2021 but not in 1971: lessons learned from an electronic health records conversion, competition for physicians in the form of a “virtual primary care service” offered by United Healthcare, and the sleep effects of smartphone “addiction.”
Technology, clearly, plays a much larger role in physicians’ lives these days.
Similarities between issues
Not everything has changed, of course. We were informing physicians about heart disease in 1971 with “Primary MD can treat most vascular cases” and “Job satisfaction can help prevent heart disease.”
A look at the latest issue uncovered “Link clinched between high-glycemic index diets and cardiovascular disease events” and “Ultraprocessed ‘healthy’ foods raise cardiovascular disease events risk.” Diabetes is another topic that we have began covering since day one and continue to consider to be relevant to practicing family medicine. “Family attitude key to diabetic’s state” was published in our first issue and “Type 1 diabetes prevention moves toward reality as studies published” ran in our April 2021 issue.
The photos in that first issue, however, present a somewhat jarring counterpoint to our latest issue. The faces that look back from 50 years ago are men’s faces: 29 men, to be exact. There were no photos of women physicians in that issue.
That was not the case in April of 2021. Of the 26 physicians or research scientists who appeared in photos in that issue, 8 were women. Plus, three of those women appeared on the cover.
Among the photos from 1971 were 6 of the 14 founding members of our editorial advisory board, who were, again, all men. Our current board consists of 13 men and 8 women.
Times have changed.
This article was updated 5/27/21.
For the first readers of Family Practice News, it started with this: “How safe is the pill? An extensive epidemiologic study being carried out in the United Kingdom by the Royal College of General Practitioners is expected to provide definitive answers to this question within the next few years.”
That was the first paragraph of the lead article on the front page of our very first issue, published in October 1971. The report on oral contraceptives, coming from the annual meeting of the British Medical Association in Leicester, largely focused on recruiting – noting that “all women in the study are married” – and data-gathering methods.
That first issue also covered such topics as the effect of “early and frequent coitus” on cervical dysplasia incidence (p. 4), breast cancer in men (p. 13), and treatment of prostate inflammation in patients with impotence (p. 34).
Our April 2021 issue included five articles related to the COVID-19 pandemic, starting on the front page and featuring a photo – a physician sitting at a computer, wearing a mask – and a topic – vaccine-hesitant patients.
Business of medicine today vs. in 1971
At the time of publication of our first issue the United States was in the midst of a 90-day freeze on wages and prices ordered by President Richard Nixon. Two articles in that first issue discussed the subject: “Freeze clouds future of health insurance plans” and “Freeze lets physicians ‘stabilize’ office fees.”
Besides COVID-19, here are some other topics covered in April 2021 but not in 1971: lessons learned from an electronic health records conversion, competition for physicians in the form of a “virtual primary care service” offered by United Healthcare, and the sleep effects of smartphone “addiction.”
Technology, clearly, plays a much larger role in physicians’ lives these days.
Similarities between issues
Not everything has changed, of course. We were informing physicians about heart disease in 1971 with “Primary MD can treat most vascular cases” and “Job satisfaction can help prevent heart disease.”
A look at the latest issue uncovered “Link clinched between high-glycemic index diets and cardiovascular disease events” and “Ultraprocessed ‘healthy’ foods raise cardiovascular disease events risk.” Diabetes is another topic that we have began covering since day one and continue to consider to be relevant to practicing family medicine. “Family attitude key to diabetic’s state” was published in our first issue and “Type 1 diabetes prevention moves toward reality as studies published” ran in our April 2021 issue.
The photos in that first issue, however, present a somewhat jarring counterpoint to our latest issue. The faces that look back from 50 years ago are men’s faces: 29 men, to be exact. There were no photos of women physicians in that issue.
That was not the case in April of 2021. Of the 26 physicians or research scientists who appeared in photos in that issue, 8 were women. Plus, three of those women appeared on the cover.
Among the photos from 1971 were 6 of the 14 founding members of our editorial advisory board, who were, again, all men. Our current board consists of 13 men and 8 women.
Times have changed.
This article was updated 5/27/21.
For the first readers of Family Practice News, it started with this: “How safe is the pill? An extensive epidemiologic study being carried out in the United Kingdom by the Royal College of General Practitioners is expected to provide definitive answers to this question within the next few years.”
That was the first paragraph of the lead article on the front page of our very first issue, published in October 1971. The report on oral contraceptives, coming from the annual meeting of the British Medical Association in Leicester, largely focused on recruiting – noting that “all women in the study are married” – and data-gathering methods.
That first issue also covered such topics as the effect of “early and frequent coitus” on cervical dysplasia incidence (p. 4), breast cancer in men (p. 13), and treatment of prostate inflammation in patients with impotence (p. 34).
Our April 2021 issue included five articles related to the COVID-19 pandemic, starting on the front page and featuring a photo – a physician sitting at a computer, wearing a mask – and a topic – vaccine-hesitant patients.
Business of medicine today vs. in 1971
At the time of publication of our first issue the United States was in the midst of a 90-day freeze on wages and prices ordered by President Richard Nixon. Two articles in that first issue discussed the subject: “Freeze clouds future of health insurance plans” and “Freeze lets physicians ‘stabilize’ office fees.”
Besides COVID-19, here are some other topics covered in April 2021 but not in 1971: lessons learned from an electronic health records conversion, competition for physicians in the form of a “virtual primary care service” offered by United Healthcare, and the sleep effects of smartphone “addiction.”
Technology, clearly, plays a much larger role in physicians’ lives these days.
Similarities between issues
Not everything has changed, of course. We were informing physicians about heart disease in 1971 with “Primary MD can treat most vascular cases” and “Job satisfaction can help prevent heart disease.”
A look at the latest issue uncovered “Link clinched between high-glycemic index diets and cardiovascular disease events” and “Ultraprocessed ‘healthy’ foods raise cardiovascular disease events risk.” Diabetes is another topic that we have began covering since day one and continue to consider to be relevant to practicing family medicine. “Family attitude key to diabetic’s state” was published in our first issue and “Type 1 diabetes prevention moves toward reality as studies published” ran in our April 2021 issue.
The photos in that first issue, however, present a somewhat jarring counterpoint to our latest issue. The faces that look back from 50 years ago are men’s faces: 29 men, to be exact. There were no photos of women physicians in that issue.
That was not the case in April of 2021. Of the 26 physicians or research scientists who appeared in photos in that issue, 8 were women. Plus, three of those women appeared on the cover.
Among the photos from 1971 were 6 of the 14 founding members of our editorial advisory board, who were, again, all men. Our current board consists of 13 men and 8 women.
Times have changed.
This article was updated 5/27/21.
Family physicians’ compensation levels stable in pandemic
to $236,000, up from $234,000 last year, even as many practices saw a decrease in hours and patient visits during the pandemic.
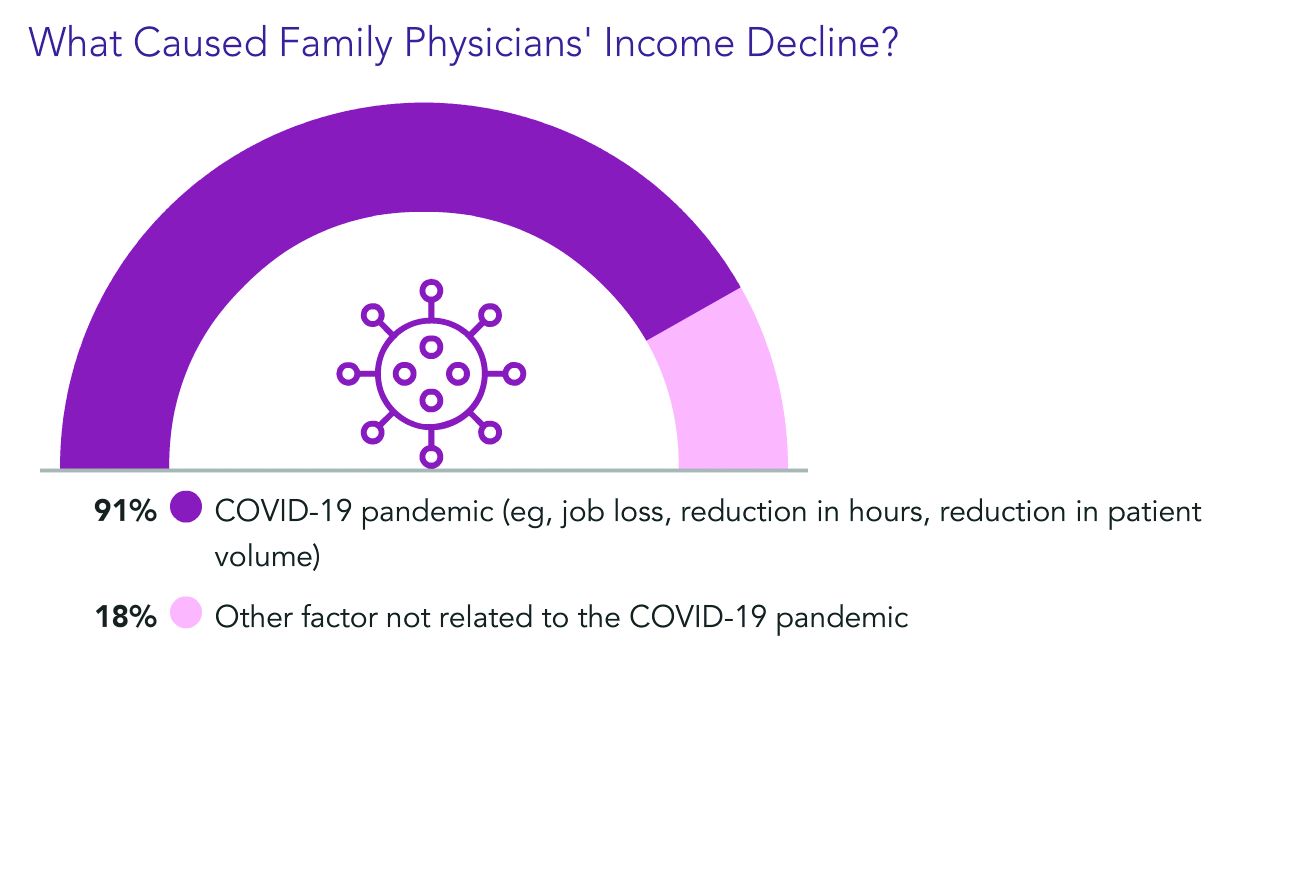
Only pediatricians earned less ($221,000) according to the Medscape Family Physician Compensation Report 2021. Plastic surgeons topped this year’s list, at $526,000, followed by orthopedists, at $511,000, and cardiologists, at $459,000.
Family physicians ranked in the middle of specialties in terms of the percentages of physicians who thought they were fairly compensated: 57% of family physicians said they were fairly paid, and 79% of oncologists said they were. Only 44% of infectious disease physicians said they were fairly compensated.
Survey answers indicate, though, that pay isn’t driving family physicians’ satisfaction.
Only 10% of family physicians in the survey said that “making good money at a job I like” was the most rewarding aspect of the job. The top two answers by far were “gratitude/relationships with patients” (chosen by 34%) and “knowing I’m making the world a better place” (27%). Respondents could choose more than one answer.
Despite the small uptick in earnings overall in the specialty, more than one-third of family physicians (36%) reported a decline in compensation in this year’s survey, which included 18,000 responses from physicians in 29 specialties.
Male family physicians continue to be paid much more than their female colleagues, this year 29% more, widening the gap from 26% last year. Overall, men in primary care earned 27% more than their female colleagues, and male specialists earned 33% more.
As for decline in patients seen in some specialties, family physicians are holding their own.
Whereas pediatricians have seen a drop of 18% in patient visits, family physicians saw a decline of just 5%, from an average of 81 to 77 patients per week.
Most expect return to normal pay within 3 years
Most family physicians (83%) who incurred financial losses this year said they expect that income will return to normal within 3 years. More than one-third of that group (38%) said they expect compensation to get back to normal in the next year.
Almost all of the family physicians who lost income (91%) pointed the finger at COVID-19. Respondents could choose more than one answer, and 18% said other factors were also to blame.
Family physicians averaged $27,000 in incentive bonuses, higher than those in internal medicine, pediatrics, and psychiatry. Orthopedists had by far the highest bonuses, at $116,000.
For family physicians who received a bonus this year, the amount equaled about 12% of their salary, up from 10% last year. Bonuses are usually based on productivity but can also be tied to patient satisfaction, clinical processes, and other factors.
The number of family physicians who achieved more than three-quarters of their potential annual bonus rose to 61% this year, up from 55%.
17 hours a week on administrative tasks
The survey also ranked specialties by the amount of time physicians spent on paperwork and administrative tasks, including participation in professional organizations and clinical reading.
Family physicians fell squarely in the middle, with 17 hours per week spent on such tasks. Infectious disease physicians spent the most time, at 24.2 hours a week, and anesthesiologists spent the least, at 10.1.
Work hours declined for many physicians during the pandemic, and some were furloughed.
But, like most physicians, family physicians are once more working normal hours. They average 49 hours per week, which is slightly more than before the pandemic.
Specialists whose weekly hours are above normal are infectious disease physicians, intensivists, and public health and preventive medicine physicians; all are working 6 to 7 hours a week more than usual, according to the survey responses.
Responses also turned up some uncertainty on the future makeup of patient panels.
Most family physicians (69%) said they would continue to take new and current Medicare/Medicaid patients.
However, close to one-third of family physicians said they would stop treating at least some patients they already have and will not take new ones or haven’t decided yet.
A version of this article first appeared on Medscape.com.
to $236,000, up from $234,000 last year, even as many practices saw a decrease in hours and patient visits during the pandemic.
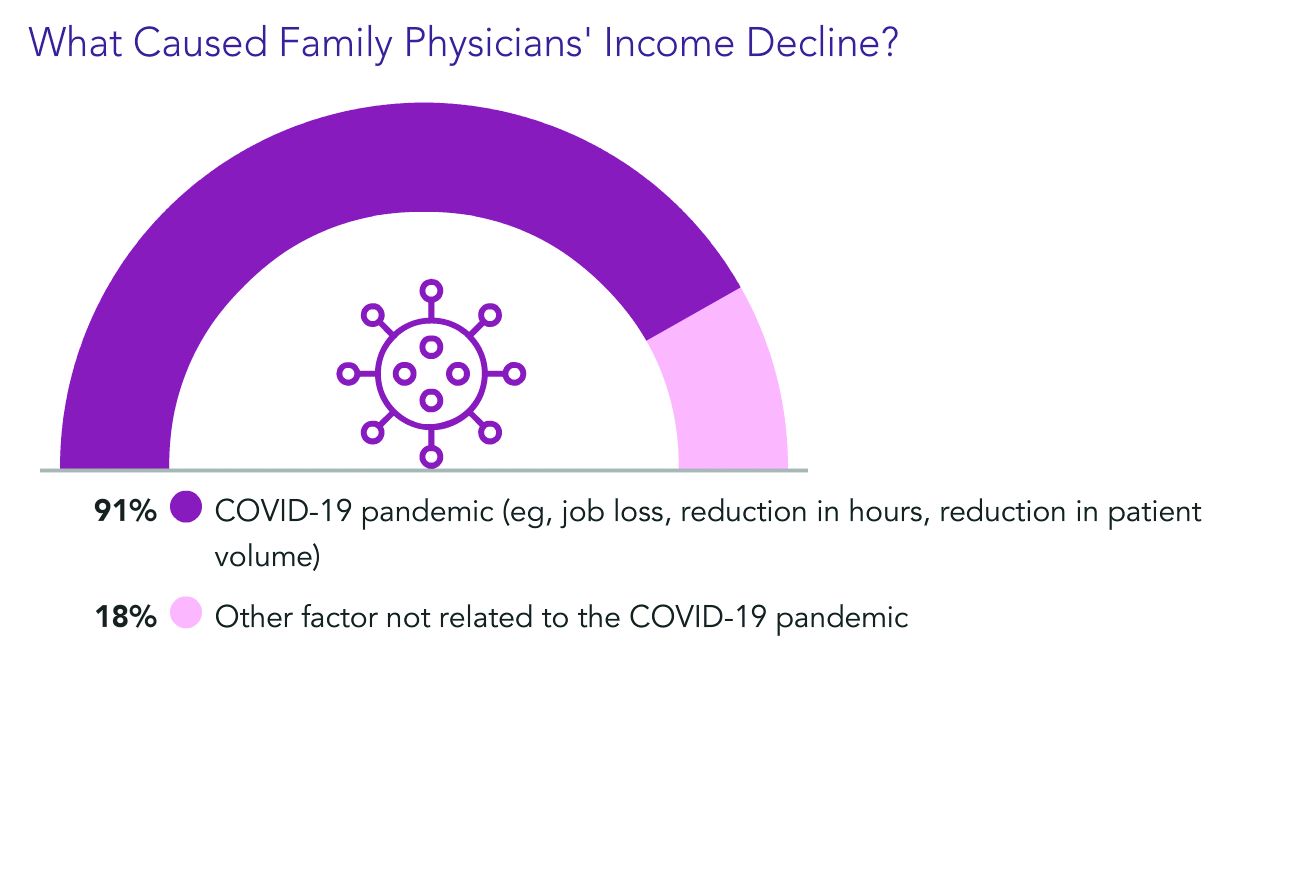
Only pediatricians earned less ($221,000) according to the Medscape Family Physician Compensation Report 2021. Plastic surgeons topped this year’s list, at $526,000, followed by orthopedists, at $511,000, and cardiologists, at $459,000.
Family physicians ranked in the middle of specialties in terms of the percentages of physicians who thought they were fairly compensated: 57% of family physicians said they were fairly paid, and 79% of oncologists said they were. Only 44% of infectious disease physicians said they were fairly compensated.
Survey answers indicate, though, that pay isn’t driving family physicians’ satisfaction.
Only 10% of family physicians in the survey said that “making good money at a job I like” was the most rewarding aspect of the job. The top two answers by far were “gratitude/relationships with patients” (chosen by 34%) and “knowing I’m making the world a better place” (27%). Respondents could choose more than one answer.
Despite the small uptick in earnings overall in the specialty, more than one-third of family physicians (36%) reported a decline in compensation in this year’s survey, which included 18,000 responses from physicians in 29 specialties.
Male family physicians continue to be paid much more than their female colleagues, this year 29% more, widening the gap from 26% last year. Overall, men in primary care earned 27% more than their female colleagues, and male specialists earned 33% more.
As for decline in patients seen in some specialties, family physicians are holding their own.
Whereas pediatricians have seen a drop of 18% in patient visits, family physicians saw a decline of just 5%, from an average of 81 to 77 patients per week.
Most expect return to normal pay within 3 years
Most family physicians (83%) who incurred financial losses this year said they expect that income will return to normal within 3 years. More than one-third of that group (38%) said they expect compensation to get back to normal in the next year.
Almost all of the family physicians who lost income (91%) pointed the finger at COVID-19. Respondents could choose more than one answer, and 18% said other factors were also to blame.
Family physicians averaged $27,000 in incentive bonuses, higher than those in internal medicine, pediatrics, and psychiatry. Orthopedists had by far the highest bonuses, at $116,000.
For family physicians who received a bonus this year, the amount equaled about 12% of their salary, up from 10% last year. Bonuses are usually based on productivity but can also be tied to patient satisfaction, clinical processes, and other factors.
The number of family physicians who achieved more than three-quarters of their potential annual bonus rose to 61% this year, up from 55%.
17 hours a week on administrative tasks
The survey also ranked specialties by the amount of time physicians spent on paperwork and administrative tasks, including participation in professional organizations and clinical reading.
Family physicians fell squarely in the middle, with 17 hours per week spent on such tasks. Infectious disease physicians spent the most time, at 24.2 hours a week, and anesthesiologists spent the least, at 10.1.
Work hours declined for many physicians during the pandemic, and some were furloughed.
But, like most physicians, family physicians are once more working normal hours. They average 49 hours per week, which is slightly more than before the pandemic.
Specialists whose weekly hours are above normal are infectious disease physicians, intensivists, and public health and preventive medicine physicians; all are working 6 to 7 hours a week more than usual, according to the survey responses.
Responses also turned up some uncertainty on the future makeup of patient panels.
Most family physicians (69%) said they would continue to take new and current Medicare/Medicaid patients.
However, close to one-third of family physicians said they would stop treating at least some patients they already have and will not take new ones or haven’t decided yet.
A version of this article first appeared on Medscape.com.
to $236,000, up from $234,000 last year, even as many practices saw a decrease in hours and patient visits during the pandemic.
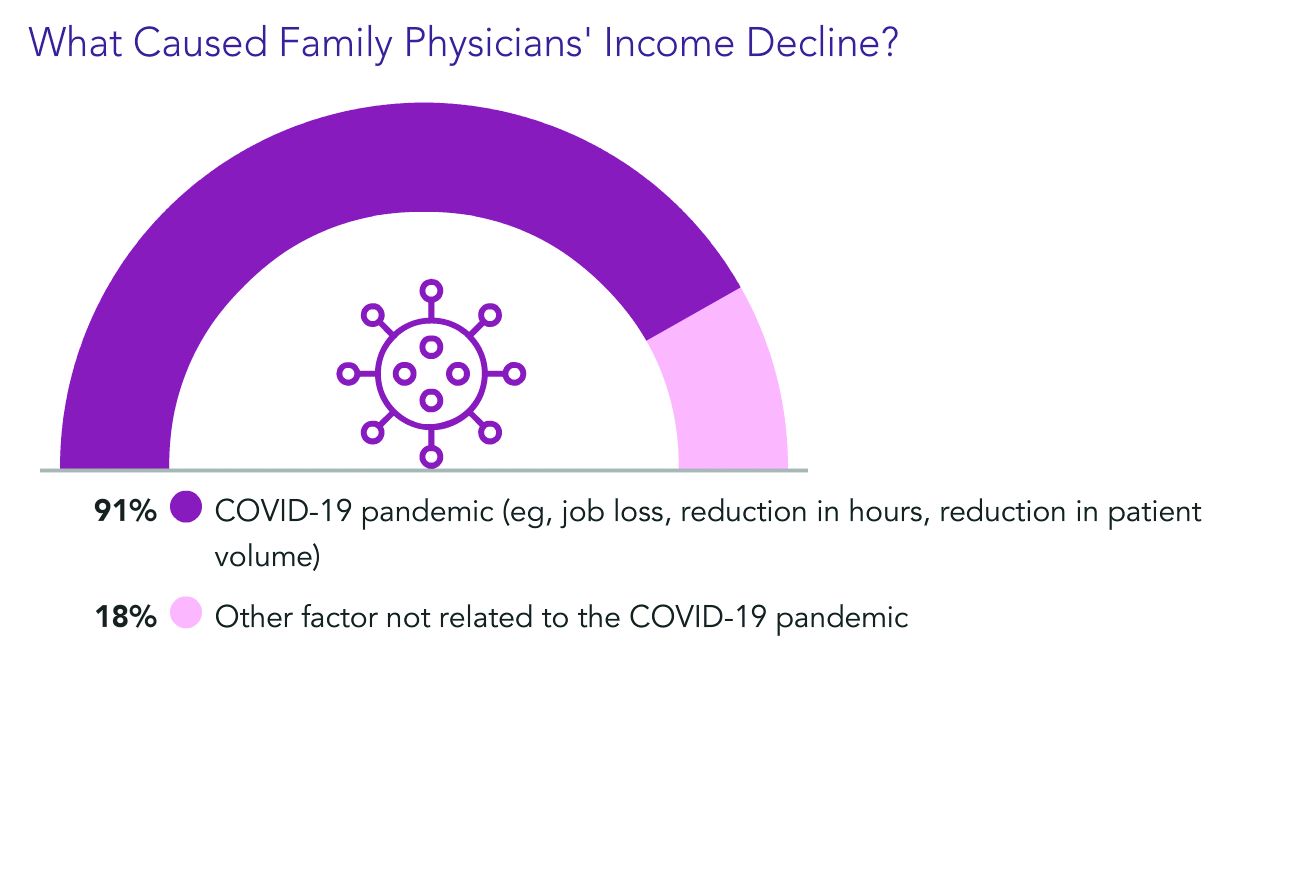
Only pediatricians earned less ($221,000) according to the Medscape Family Physician Compensation Report 2021. Plastic surgeons topped this year’s list, at $526,000, followed by orthopedists, at $511,000, and cardiologists, at $459,000.
Family physicians ranked in the middle of specialties in terms of the percentages of physicians who thought they were fairly compensated: 57% of family physicians said they were fairly paid, and 79% of oncologists said they were. Only 44% of infectious disease physicians said they were fairly compensated.
Survey answers indicate, though, that pay isn’t driving family physicians’ satisfaction.
Only 10% of family physicians in the survey said that “making good money at a job I like” was the most rewarding aspect of the job. The top two answers by far were “gratitude/relationships with patients” (chosen by 34%) and “knowing I’m making the world a better place” (27%). Respondents could choose more than one answer.
Despite the small uptick in earnings overall in the specialty, more than one-third of family physicians (36%) reported a decline in compensation in this year’s survey, which included 18,000 responses from physicians in 29 specialties.
Male family physicians continue to be paid much more than their female colleagues, this year 29% more, widening the gap from 26% last year. Overall, men in primary care earned 27% more than their female colleagues, and male specialists earned 33% more.
As for decline in patients seen in some specialties, family physicians are holding their own.
Whereas pediatricians have seen a drop of 18% in patient visits, family physicians saw a decline of just 5%, from an average of 81 to 77 patients per week.
Most expect return to normal pay within 3 years
Most family physicians (83%) who incurred financial losses this year said they expect that income will return to normal within 3 years. More than one-third of that group (38%) said they expect compensation to get back to normal in the next year.
Almost all of the family physicians who lost income (91%) pointed the finger at COVID-19. Respondents could choose more than one answer, and 18% said other factors were also to blame.
Family physicians averaged $27,000 in incentive bonuses, higher than those in internal medicine, pediatrics, and psychiatry. Orthopedists had by far the highest bonuses, at $116,000.
For family physicians who received a bonus this year, the amount equaled about 12% of their salary, up from 10% last year. Bonuses are usually based on productivity but can also be tied to patient satisfaction, clinical processes, and other factors.
The number of family physicians who achieved more than three-quarters of their potential annual bonus rose to 61% this year, up from 55%.
17 hours a week on administrative tasks
The survey also ranked specialties by the amount of time physicians spent on paperwork and administrative tasks, including participation in professional organizations and clinical reading.
Family physicians fell squarely in the middle, with 17 hours per week spent on such tasks. Infectious disease physicians spent the most time, at 24.2 hours a week, and anesthesiologists spent the least, at 10.1.
Work hours declined for many physicians during the pandemic, and some were furloughed.
But, like most physicians, family physicians are once more working normal hours. They average 49 hours per week, which is slightly more than before the pandemic.
Specialists whose weekly hours are above normal are infectious disease physicians, intensivists, and public health and preventive medicine physicians; all are working 6 to 7 hours a week more than usual, according to the survey responses.
Responses also turned up some uncertainty on the future makeup of patient panels.
Most family physicians (69%) said they would continue to take new and current Medicare/Medicaid patients.
However, close to one-third of family physicians said they would stop treating at least some patients they already have and will not take new ones or haven’t decided yet.
A version of this article first appeared on Medscape.com.
Ob.gyn. pay up slightly during pandemic, survey finds
Although 45% of ob.gyns. reported some decline in compensation during the pandemic, they earned more income in 2020 than they did in 2019, according to the 2021 Medscape Ob/Gyn Compensation Report.
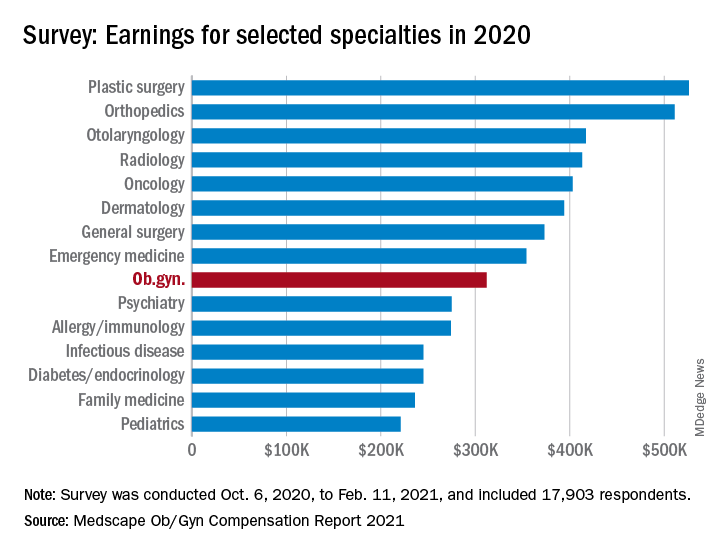
The report, which surveyed nearly 18,000 physicians in more than 29 specialties, found that ob.gyns.’ income level was $312,000 in 2020, compared with $308,000 in 2019.
Despite the $4,000 increase, they still ranked near the bottom half in comparison with all other specialties. The lowest-paid specialties were public health & preventive medicine ($237,000), family medicine ($236,000), and pediatrics ($221,000), and the top earning specialties were plastic surgery ($526,000), orthopedics ($511,000), and cardiology ($459,000).
Optimistic about financial bounce back
Most ob.gyns. who experienced income loss cited job loss, reduction in hours, and lower patient volume because of the COVID-19 pandemic as reasons for their wage decline.
The specialty’s average incentive bonus, which is usually based on productivity and can be tied to patient satisfaction and clinical processes, was $48,000, and accounted for about 14% of total salary.
Of the ob.gyns. who reported financial losses during the pandemic, 41% expect their income to return to normal this year. However, 45% believe it will take 2-3 years to bounce back from the pandemic’s financial effect. About 11% believe they will never return to their pre–COVID-19 income.
Working similar hours, seeing fewer patients
The survey also found that ob.gyns. are back to working about the same number of hours they did prepandemic. Ob.gyns. currently work on average 54 hours per week, compared with the 56 hours per week they worked before the pandemic. However, they are only seeing 76 patients per week, compared with 81 patients per week before the pandemic.
Ob.gyns. reported spending 15.1 hours per week on medical-related work outside of patient visits, including paperwork, EHR documentation, administrative and managerial work, and clinical reading. The time required was slightly longer than last year (14.3 hours per week).
Similar to last year’s report, 55% of ob.gyns. said they are fairly compensated. Around 34% of them said the most rewarding part of their job is the relationships they have with their patients, followed by helping others (23%), and being good at what they do (22%). Only 11% said money was the most rewarding part of their job.
Challenges
The pandemic has brought many challenges for physicians, including financial difficulties and the potential to be exposed to SARS-CoV-2. However, when asked about the most challenging part of their job, only 4% of ob.gyns. said the danger or risk associated with treating patients with COVID-19 was the most challenging aspect of their job. By contrast, 21% of ob.gyns. said working long hours and having so many rules and regulations bog down their daily work.
Despite the pandemic-related challenges, 74% of ob.gyns. said they would choose medicine again and work in the same specialty.
A version of this article first appeared on Medscape.com.
Although 45% of ob.gyns. reported some decline in compensation during the pandemic, they earned more income in 2020 than they did in 2019, according to the 2021 Medscape Ob/Gyn Compensation Report.
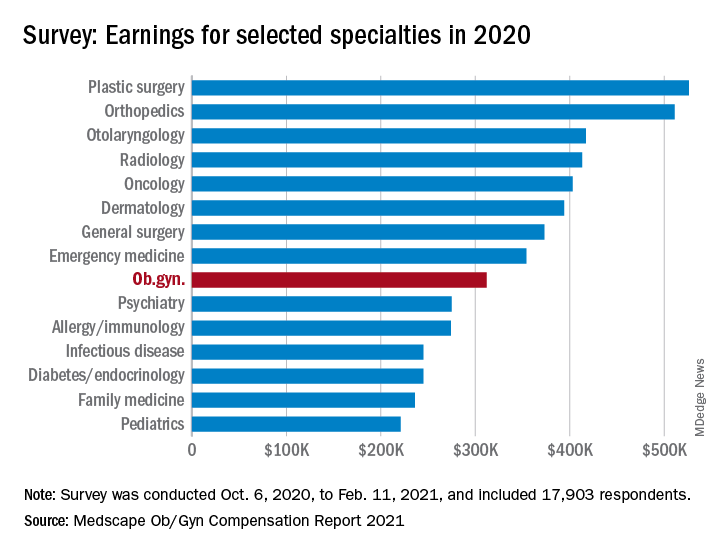
The report, which surveyed nearly 18,000 physicians in more than 29 specialties, found that ob.gyns.’ income level was $312,000 in 2020, compared with $308,000 in 2019.
Despite the $4,000 increase, they still ranked near the bottom half in comparison with all other specialties. The lowest-paid specialties were public health & preventive medicine ($237,000), family medicine ($236,000), and pediatrics ($221,000), and the top earning specialties were plastic surgery ($526,000), orthopedics ($511,000), and cardiology ($459,000).
Optimistic about financial bounce back
Most ob.gyns. who experienced income loss cited job loss, reduction in hours, and lower patient volume because of the COVID-19 pandemic as reasons for their wage decline.
The specialty’s average incentive bonus, which is usually based on productivity and can be tied to patient satisfaction and clinical processes, was $48,000, and accounted for about 14% of total salary.
Of the ob.gyns. who reported financial losses during the pandemic, 41% expect their income to return to normal this year. However, 45% believe it will take 2-3 years to bounce back from the pandemic’s financial effect. About 11% believe they will never return to their pre–COVID-19 income.
Working similar hours, seeing fewer patients
The survey also found that ob.gyns. are back to working about the same number of hours they did prepandemic. Ob.gyns. currently work on average 54 hours per week, compared with the 56 hours per week they worked before the pandemic. However, they are only seeing 76 patients per week, compared with 81 patients per week before the pandemic.
Ob.gyns. reported spending 15.1 hours per week on medical-related work outside of patient visits, including paperwork, EHR documentation, administrative and managerial work, and clinical reading. The time required was slightly longer than last year (14.3 hours per week).
Similar to last year’s report, 55% of ob.gyns. said they are fairly compensated. Around 34% of them said the most rewarding part of their job is the relationships they have with their patients, followed by helping others (23%), and being good at what they do (22%). Only 11% said money was the most rewarding part of their job.
Challenges
The pandemic has brought many challenges for physicians, including financial difficulties and the potential to be exposed to SARS-CoV-2. However, when asked about the most challenging part of their job, only 4% of ob.gyns. said the danger or risk associated with treating patients with COVID-19 was the most challenging aspect of their job. By contrast, 21% of ob.gyns. said working long hours and having so many rules and regulations bog down their daily work.
Despite the pandemic-related challenges, 74% of ob.gyns. said they would choose medicine again and work in the same specialty.
A version of this article first appeared on Medscape.com.
Although 45% of ob.gyns. reported some decline in compensation during the pandemic, they earned more income in 2020 than they did in 2019, according to the 2021 Medscape Ob/Gyn Compensation Report.
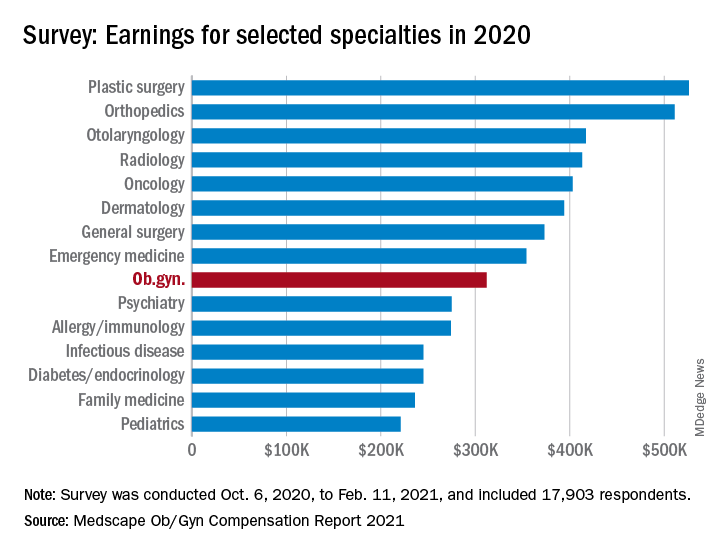
The report, which surveyed nearly 18,000 physicians in more than 29 specialties, found that ob.gyns.’ income level was $312,000 in 2020, compared with $308,000 in 2019.
Despite the $4,000 increase, they still ranked near the bottom half in comparison with all other specialties. The lowest-paid specialties were public health & preventive medicine ($237,000), family medicine ($236,000), and pediatrics ($221,000), and the top earning specialties were plastic surgery ($526,000), orthopedics ($511,000), and cardiology ($459,000).
Optimistic about financial bounce back
Most ob.gyns. who experienced income loss cited job loss, reduction in hours, and lower patient volume because of the COVID-19 pandemic as reasons for their wage decline.
The specialty’s average incentive bonus, which is usually based on productivity and can be tied to patient satisfaction and clinical processes, was $48,000, and accounted for about 14% of total salary.
Of the ob.gyns. who reported financial losses during the pandemic, 41% expect their income to return to normal this year. However, 45% believe it will take 2-3 years to bounce back from the pandemic’s financial effect. About 11% believe they will never return to their pre–COVID-19 income.
Working similar hours, seeing fewer patients
The survey also found that ob.gyns. are back to working about the same number of hours they did prepandemic. Ob.gyns. currently work on average 54 hours per week, compared with the 56 hours per week they worked before the pandemic. However, they are only seeing 76 patients per week, compared with 81 patients per week before the pandemic.
Ob.gyns. reported spending 15.1 hours per week on medical-related work outside of patient visits, including paperwork, EHR documentation, administrative and managerial work, and clinical reading. The time required was slightly longer than last year (14.3 hours per week).
Similar to last year’s report, 55% of ob.gyns. said they are fairly compensated. Around 34% of them said the most rewarding part of their job is the relationships they have with their patients, followed by helping others (23%), and being good at what they do (22%). Only 11% said money was the most rewarding part of their job.
Challenges
The pandemic has brought many challenges for physicians, including financial difficulties and the potential to be exposed to SARS-CoV-2. However, when asked about the most challenging part of their job, only 4% of ob.gyns. said the danger or risk associated with treating patients with COVID-19 was the most challenging aspect of their job. By contrast, 21% of ob.gyns. said working long hours and having so many rules and regulations bog down their daily work.
Despite the pandemic-related challenges, 74% of ob.gyns. said they would choose medicine again and work in the same specialty.
A version of this article first appeared on Medscape.com.
ID doctors have the most paperwork, administrative demands
Infectious disease physicians are among the doctors carrying the largest burdens in the COVID-19 pandemic.
Perhaps not surprisingly, they were the specialists least likely to feel they were fairly compensated in the Medscape Infectious Diseases Physician Compensation Report 2021.
Only 44% said the pay was fair (down from 51% the prior year) compared with those at the high end – 79% in oncology, 69% in psychiatry, and 68% in plastic surgery who answered that way.
Income, which averaged $245,000, varied little from the previous year overall, according to the survey, but nearly one-third of ID physicians saw a decline in pay.
Again this year, ID physicians ranked near the bottom on the compensation spectrum. Pediatricians were lowest paid at $221,000. Plastic surgeons topped the chart at $526,000, followed by orthopedists at $511,000.
At the same time, the ID specialty is facing increasing shortages, a gap made even more visible in the pandemic. Medscape reported last year that nearly 80% of U.S. counties have no infectious disease specialists.
Thomas File Jr., MD, last year’s president of the Infectious Diseases Society of America, emphasized that COVID-19 is not the only threat that ID specialists have had to deal with or will have. He cited the threats that Zika and SARS posed in past years.
“COVID-19 illustrates the need for more trained ID specialists, because we know we’re going to be seeing more outbreaks in the future,” he said in an interview at the onset of the pandemic in March 2020.
Longer hours in pandemic
ID physicians’ hours generally increased during the pandemic, and they remain inflated by 8 hours per week (60 compared with 52 prepandemic) as the nation struggles to manage continuing COVID-19 infections. Physicians in critical care and public health and preventive medicine are seeing heavier workloads as well, by an average of 6-7 hours per week.
At the same time, ID physicians spent the most time of physicians in all specialties on paperwork and administrative tasks. Those tasks, which include electronic health record entry and clinical reading, took ID doctors 24.2 hours a week, more the twice the hours spent by those in anesthesiology (10.1), ophthalmology (10.3), and radiology (11.6).
The 24.2 hours was a substantial increase from the last report, when ID physicians said they spent 18.5 hours on the tasks.
The survey asked about the most challenging part of the job. ID physicians reported “long hours” as number one followed by “having so many rules and regulations.”
Only 4% said the danger or risk associated with treating COVID-19 patients was the most challenging part.
The top two aspects of their work they deemed most rewarding were “being very good at what I do” (chosen by 33%) and “knowing that I’m making the world a better place” (31%).
Patient volume up 17%
ID physicians reported seeing 78 patients per week in this report compared with 66 prepandemic, a 17% increase. Conversely, pediatricians saw an 18% drop in patient visits, followed by dermatologists, orthopedists and otolaryngologists (all down about 15%).
Despite the challenges and dissatisfaction with pay, the great majority of ID physicians said they would choose both medicine (83%) and their specialty (89%, up from 85% last year) again.
A version of this article first appeared on Medscape.com.
Infectious disease physicians are among the doctors carrying the largest burdens in the COVID-19 pandemic.
Perhaps not surprisingly, they were the specialists least likely to feel they were fairly compensated in the Medscape Infectious Diseases Physician Compensation Report 2021.
Only 44% said the pay was fair (down from 51% the prior year) compared with those at the high end – 79% in oncology, 69% in psychiatry, and 68% in plastic surgery who answered that way.
Income, which averaged $245,000, varied little from the previous year overall, according to the survey, but nearly one-third of ID physicians saw a decline in pay.
Again this year, ID physicians ranked near the bottom on the compensation spectrum. Pediatricians were lowest paid at $221,000. Plastic surgeons topped the chart at $526,000, followed by orthopedists at $511,000.
At the same time, the ID specialty is facing increasing shortages, a gap made even more visible in the pandemic. Medscape reported last year that nearly 80% of U.S. counties have no infectious disease specialists.
Thomas File Jr., MD, last year’s president of the Infectious Diseases Society of America, emphasized that COVID-19 is not the only threat that ID specialists have had to deal with or will have. He cited the threats that Zika and SARS posed in past years.
“COVID-19 illustrates the need for more trained ID specialists, because we know we’re going to be seeing more outbreaks in the future,” he said in an interview at the onset of the pandemic in March 2020.
Longer hours in pandemic
ID physicians’ hours generally increased during the pandemic, and they remain inflated by 8 hours per week (60 compared with 52 prepandemic) as the nation struggles to manage continuing COVID-19 infections. Physicians in critical care and public health and preventive medicine are seeing heavier workloads as well, by an average of 6-7 hours per week.
At the same time, ID physicians spent the most time of physicians in all specialties on paperwork and administrative tasks. Those tasks, which include electronic health record entry and clinical reading, took ID doctors 24.2 hours a week, more the twice the hours spent by those in anesthesiology (10.1), ophthalmology (10.3), and radiology (11.6).
The 24.2 hours was a substantial increase from the last report, when ID physicians said they spent 18.5 hours on the tasks.
The survey asked about the most challenging part of the job. ID physicians reported “long hours” as number one followed by “having so many rules and regulations.”
Only 4% said the danger or risk associated with treating COVID-19 patients was the most challenging part.
The top two aspects of their work they deemed most rewarding were “being very good at what I do” (chosen by 33%) and “knowing that I’m making the world a better place” (31%).
Patient volume up 17%
ID physicians reported seeing 78 patients per week in this report compared with 66 prepandemic, a 17% increase. Conversely, pediatricians saw an 18% drop in patient visits, followed by dermatologists, orthopedists and otolaryngologists (all down about 15%).
Despite the challenges and dissatisfaction with pay, the great majority of ID physicians said they would choose both medicine (83%) and their specialty (89%, up from 85% last year) again.
A version of this article first appeared on Medscape.com.
Infectious disease physicians are among the doctors carrying the largest burdens in the COVID-19 pandemic.
Perhaps not surprisingly, they were the specialists least likely to feel they were fairly compensated in the Medscape Infectious Diseases Physician Compensation Report 2021.
Only 44% said the pay was fair (down from 51% the prior year) compared with those at the high end – 79% in oncology, 69% in psychiatry, and 68% in plastic surgery who answered that way.
Income, which averaged $245,000, varied little from the previous year overall, according to the survey, but nearly one-third of ID physicians saw a decline in pay.
Again this year, ID physicians ranked near the bottom on the compensation spectrum. Pediatricians were lowest paid at $221,000. Plastic surgeons topped the chart at $526,000, followed by orthopedists at $511,000.
At the same time, the ID specialty is facing increasing shortages, a gap made even more visible in the pandemic. Medscape reported last year that nearly 80% of U.S. counties have no infectious disease specialists.
Thomas File Jr., MD, last year’s president of the Infectious Diseases Society of America, emphasized that COVID-19 is not the only threat that ID specialists have had to deal with or will have. He cited the threats that Zika and SARS posed in past years.
“COVID-19 illustrates the need for more trained ID specialists, because we know we’re going to be seeing more outbreaks in the future,” he said in an interview at the onset of the pandemic in March 2020.
Longer hours in pandemic
ID physicians’ hours generally increased during the pandemic, and they remain inflated by 8 hours per week (60 compared with 52 prepandemic) as the nation struggles to manage continuing COVID-19 infections. Physicians in critical care and public health and preventive medicine are seeing heavier workloads as well, by an average of 6-7 hours per week.
At the same time, ID physicians spent the most time of physicians in all specialties on paperwork and administrative tasks. Those tasks, which include electronic health record entry and clinical reading, took ID doctors 24.2 hours a week, more the twice the hours spent by those in anesthesiology (10.1), ophthalmology (10.3), and radiology (11.6).
The 24.2 hours was a substantial increase from the last report, when ID physicians said they spent 18.5 hours on the tasks.
The survey asked about the most challenging part of the job. ID physicians reported “long hours” as number one followed by “having so many rules and regulations.”
Only 4% said the danger or risk associated with treating COVID-19 patients was the most challenging part.
The top two aspects of their work they deemed most rewarding were “being very good at what I do” (chosen by 33%) and “knowing that I’m making the world a better place” (31%).
Patient volume up 17%
ID physicians reported seeing 78 patients per week in this report compared with 66 prepandemic, a 17% increase. Conversely, pediatricians saw an 18% drop in patient visits, followed by dermatologists, orthopedists and otolaryngologists (all down about 15%).
Despite the challenges and dissatisfaction with pay, the great majority of ID physicians said they would choose both medicine (83%) and their specialty (89%, up from 85% last year) again.
A version of this article first appeared on Medscape.com.
AHA/ACC guidance on ethics, professionalism in cardiovascular care
The American Heart Association and the American College of Cardiology have issued a new report on medical ethics and professionalism in cardiovascular medicine.
The report addresses a variety of topics including diversity, equity, inclusion, and belonging; racial, ethnic and gender inequities; conflicts of interest; clinician well-being; data privacy; social justice; and modern health care delivery systems.
The 54-page report is based on the proceedings of the joint 2020 Consensus Conference on Professionalism and Ethics, held Oct. 19 and 20, 2020. It was published online May 11 in Circulation and the Journal of the American College of Cardiology .
The 2020 consensus conference on professionalism and ethics came at a time even more fraught than the eras of the three previous meetings on the same topics, held in 1989, 1997, and 2004, the writing group notes.
“We have seen the COVID-19 pandemic challenge the physical and economic health of the entire country, coupled with a series of national tragedies that have awakened the call for social justice,” conference cochair C. Michael Valentine, MD, said in a news release.
“There is no better time than now to review, evaluate, and take a fresh perspective on medical ethics and professionalism,” said Dr. Valentine, professor of medicine at the Heart and Vascular Center, University of Virginia, Charlottesville.
“We hope this report will provide cardiovascular professionals and health systems with the recommendations and tools they need to address conflicts of interest; racial, ethnic, and gender inequities; and improve diversity, inclusion, and wellness among our workforce,” Dr. Valentine added. “The majority of our members are now employed and must be engaged as the leaders for change in cardiovascular care.”
Road map to improve diversity, achieve allyship
The writing committee was made up of a diverse group of cardiologists, internists, and associated health care professionals and laypeople and was organized into five task forces, each addressing a specific topic: conflicts of interest; diversity, equity, inclusion, and belonging; clinician well-being; patient autonomy, privacy, and social justice in health care; and modern health care delivery.
The report serves as a road map to achieve equity, inclusion, and belonging among cardiovascular professionals and calls for ongoing assessment of the professional culture and climate, focused on improving diversity and achieving effective allyship, the writing group says.
The report proposes continuous training to address individual, structural, and systemic racism, sexism, homophobia, classism, and ableism.
It offers recommendations for championing equity in patient care that include an annual review of practice records to look for differences in patient treatment by race, ethnicity, zip code, and primary language.
The report calls for a foundation of training in allyship and antiracism as part of medical school course requirements and experiences: A required course on social justice, race, and racism as part of the first-year curriculum; school programs and professional organizations supporting students, trainees, and members in allyship and antiracism action; and facilitating immersion and partnership with surrounding communities.
“As much as 80% of a person’s health is determined by the social and economic conditions of their environment,” consensus cochair Ivor Benjamin, MD, said in the release.
“To achieve social justice and mitigate health disparities, we must go to the margins and shift our discussions to be inclusive of populations such as rural and marginalized groups from the perspective of health equity lens for all,” said Dr. Benjamin, professor of medicine, Medical College of Wisconsin, Milwaukee.
The report also highlights the need for psychosocial support of the cardiovascular community and recommends that health care organizations prioritize regular assessment of clinicians’ well-being and engagement.
It also recommends addressing the well-being of trainees in postgraduate training programs and calls for an ombudsman program that allows for confidential reporting of mistreatment and access to support.
The report also highlights additional opportunities to:
- improve the efficiency of health information technology, such as electronic health records, and reduce the administrative burden
- identify and assist clinicians who experience mental health conditions, , or
- emphasize patient autonomy using shared decision-making and patient-centered care that is supportive of the individual patient’s values
- increase privacy protections for patient data used in research
- maintain integrity as new ways of delivering care, such as telemedicine, team-based care approaches, and physician-owned specialty centers emerge
- perform routine audits of electronic health records to promote optimal patient care, as well as ethical medical practice
- expand and make mandatory the reporting of intellectual or associational interests in addition to relationships with industry
The report’s details and recommendations will be presented and discussed Saturday, May 15, at 8:00 AM ET, during ACC.21. The session is titled Diversity and Equity: The Means to Expand Inclusion and Belonging.
The AHA will present a live webinar and six-episode podcast series (available on demand) to highlight the report’s details, dialogue, and actionable steps for cardiovascular and health care professionals, researchers, and educators.
This research had no commercial funding. The list of 40 volunteer committee members and coauthors, including their disclosures, are listed in the original report.
A version of this article first appeared on Medscape.com.
The American Heart Association and the American College of Cardiology have issued a new report on medical ethics and professionalism in cardiovascular medicine.
The report addresses a variety of topics including diversity, equity, inclusion, and belonging; racial, ethnic and gender inequities; conflicts of interest; clinician well-being; data privacy; social justice; and modern health care delivery systems.
The 54-page report is based on the proceedings of the joint 2020 Consensus Conference on Professionalism and Ethics, held Oct. 19 and 20, 2020. It was published online May 11 in Circulation and the Journal of the American College of Cardiology .
The 2020 consensus conference on professionalism and ethics came at a time even more fraught than the eras of the three previous meetings on the same topics, held in 1989, 1997, and 2004, the writing group notes.
“We have seen the COVID-19 pandemic challenge the physical and economic health of the entire country, coupled with a series of national tragedies that have awakened the call for social justice,” conference cochair C. Michael Valentine, MD, said in a news release.
“There is no better time than now to review, evaluate, and take a fresh perspective on medical ethics and professionalism,” said Dr. Valentine, professor of medicine at the Heart and Vascular Center, University of Virginia, Charlottesville.
“We hope this report will provide cardiovascular professionals and health systems with the recommendations and tools they need to address conflicts of interest; racial, ethnic, and gender inequities; and improve diversity, inclusion, and wellness among our workforce,” Dr. Valentine added. “The majority of our members are now employed and must be engaged as the leaders for change in cardiovascular care.”
Road map to improve diversity, achieve allyship
The writing committee was made up of a diverse group of cardiologists, internists, and associated health care professionals and laypeople and was organized into five task forces, each addressing a specific topic: conflicts of interest; diversity, equity, inclusion, and belonging; clinician well-being; patient autonomy, privacy, and social justice in health care; and modern health care delivery.
The report serves as a road map to achieve equity, inclusion, and belonging among cardiovascular professionals and calls for ongoing assessment of the professional culture and climate, focused on improving diversity and achieving effective allyship, the writing group says.
The report proposes continuous training to address individual, structural, and systemic racism, sexism, homophobia, classism, and ableism.
It offers recommendations for championing equity in patient care that include an annual review of practice records to look for differences in patient treatment by race, ethnicity, zip code, and primary language.
The report calls for a foundation of training in allyship and antiracism as part of medical school course requirements and experiences: A required course on social justice, race, and racism as part of the first-year curriculum; school programs and professional organizations supporting students, trainees, and members in allyship and antiracism action; and facilitating immersion and partnership with surrounding communities.
“As much as 80% of a person’s health is determined by the social and economic conditions of their environment,” consensus cochair Ivor Benjamin, MD, said in the release.
“To achieve social justice and mitigate health disparities, we must go to the margins and shift our discussions to be inclusive of populations such as rural and marginalized groups from the perspective of health equity lens for all,” said Dr. Benjamin, professor of medicine, Medical College of Wisconsin, Milwaukee.
The report also highlights the need for psychosocial support of the cardiovascular community and recommends that health care organizations prioritize regular assessment of clinicians’ well-being and engagement.
It also recommends addressing the well-being of trainees in postgraduate training programs and calls for an ombudsman program that allows for confidential reporting of mistreatment and access to support.
The report also highlights additional opportunities to:
- improve the efficiency of health information technology, such as electronic health records, and reduce the administrative burden
- identify and assist clinicians who experience mental health conditions, , or
- emphasize patient autonomy using shared decision-making and patient-centered care that is supportive of the individual patient’s values
- increase privacy protections for patient data used in research
- maintain integrity as new ways of delivering care, such as telemedicine, team-based care approaches, and physician-owned specialty centers emerge
- perform routine audits of electronic health records to promote optimal patient care, as well as ethical medical practice
- expand and make mandatory the reporting of intellectual or associational interests in addition to relationships with industry
The report’s details and recommendations will be presented and discussed Saturday, May 15, at 8:00 AM ET, during ACC.21. The session is titled Diversity and Equity: The Means to Expand Inclusion and Belonging.
The AHA will present a live webinar and six-episode podcast series (available on demand) to highlight the report’s details, dialogue, and actionable steps for cardiovascular and health care professionals, researchers, and educators.
This research had no commercial funding. The list of 40 volunteer committee members and coauthors, including their disclosures, are listed in the original report.
A version of this article first appeared on Medscape.com.
The American Heart Association and the American College of Cardiology have issued a new report on medical ethics and professionalism in cardiovascular medicine.
The report addresses a variety of topics including diversity, equity, inclusion, and belonging; racial, ethnic and gender inequities; conflicts of interest; clinician well-being; data privacy; social justice; and modern health care delivery systems.
The 54-page report is based on the proceedings of the joint 2020 Consensus Conference on Professionalism and Ethics, held Oct. 19 and 20, 2020. It was published online May 11 in Circulation and the Journal of the American College of Cardiology .
The 2020 consensus conference on professionalism and ethics came at a time even more fraught than the eras of the three previous meetings on the same topics, held in 1989, 1997, and 2004, the writing group notes.
“We have seen the COVID-19 pandemic challenge the physical and economic health of the entire country, coupled with a series of national tragedies that have awakened the call for social justice,” conference cochair C. Michael Valentine, MD, said in a news release.
“There is no better time than now to review, evaluate, and take a fresh perspective on medical ethics and professionalism,” said Dr. Valentine, professor of medicine at the Heart and Vascular Center, University of Virginia, Charlottesville.
“We hope this report will provide cardiovascular professionals and health systems with the recommendations and tools they need to address conflicts of interest; racial, ethnic, and gender inequities; and improve diversity, inclusion, and wellness among our workforce,” Dr. Valentine added. “The majority of our members are now employed and must be engaged as the leaders for change in cardiovascular care.”
Road map to improve diversity, achieve allyship
The writing committee was made up of a diverse group of cardiologists, internists, and associated health care professionals and laypeople and was organized into five task forces, each addressing a specific topic: conflicts of interest; diversity, equity, inclusion, and belonging; clinician well-being; patient autonomy, privacy, and social justice in health care; and modern health care delivery.
The report serves as a road map to achieve equity, inclusion, and belonging among cardiovascular professionals and calls for ongoing assessment of the professional culture and climate, focused on improving diversity and achieving effective allyship, the writing group says.
The report proposes continuous training to address individual, structural, and systemic racism, sexism, homophobia, classism, and ableism.
It offers recommendations for championing equity in patient care that include an annual review of practice records to look for differences in patient treatment by race, ethnicity, zip code, and primary language.
The report calls for a foundation of training in allyship and antiracism as part of medical school course requirements and experiences: A required course on social justice, race, and racism as part of the first-year curriculum; school programs and professional organizations supporting students, trainees, and members in allyship and antiracism action; and facilitating immersion and partnership with surrounding communities.
“As much as 80% of a person’s health is determined by the social and economic conditions of their environment,” consensus cochair Ivor Benjamin, MD, said in the release.
“To achieve social justice and mitigate health disparities, we must go to the margins and shift our discussions to be inclusive of populations such as rural and marginalized groups from the perspective of health equity lens for all,” said Dr. Benjamin, professor of medicine, Medical College of Wisconsin, Milwaukee.
The report also highlights the need for psychosocial support of the cardiovascular community and recommends that health care organizations prioritize regular assessment of clinicians’ well-being and engagement.
It also recommends addressing the well-being of trainees in postgraduate training programs and calls for an ombudsman program that allows for confidential reporting of mistreatment and access to support.
The report also highlights additional opportunities to:
- improve the efficiency of health information technology, such as electronic health records, and reduce the administrative burden
- identify and assist clinicians who experience mental health conditions, , or
- emphasize patient autonomy using shared decision-making and patient-centered care that is supportive of the individual patient’s values
- increase privacy protections for patient data used in research
- maintain integrity as new ways of delivering care, such as telemedicine, team-based care approaches, and physician-owned specialty centers emerge
- perform routine audits of electronic health records to promote optimal patient care, as well as ethical medical practice
- expand and make mandatory the reporting of intellectual or associational interests in addition to relationships with industry
The report’s details and recommendations will be presented and discussed Saturday, May 15, at 8:00 AM ET, during ACC.21. The session is titled Diversity and Equity: The Means to Expand Inclusion and Belonging.
The AHA will present a live webinar and six-episode podcast series (available on demand) to highlight the report’s details, dialogue, and actionable steps for cardiovascular and health care professionals, researchers, and educators.
This research had no commercial funding. The list of 40 volunteer committee members and coauthors, including their disclosures, are listed in the original report.
A version of this article first appeared on Medscape.com.








