User login
Use your court awareness to go faster in practice
Have you ever had a nightmare you’re running late? Recently I dreamt I was seeing patients on a ship, a little cruiser like the ones that give you tours of Boston Harbor, with low ceilings and narrow iron stairs. My nurse stood where what would have been the coffee and danish window. My first patient was a newborn (this was a nightmare, in case you forgot) who was enormous. She had a big belly and spindly legs that hung off the table. Uniform, umbilicated papules and pustules covered her body. At the sight of her, terror ripped through me – no clue. I rushed to the doctor lounge (nice the ship had one) and flipped channels on a little TV mounted on the ceiling. Suddenly, my nurse burst in, she was frantic because dozens of angry adults and crying children were crammed in the hallway. Apparently, I had been watching TV for hours and my whole clinic was now backed up.
Running-late dreams are common and usually relate to real life. For us, the clinic has been busy lately. Vaccinated patients are returning after a year with their skin cancers that have flourished and psoriasis covering them like kudzu. In particular, they “see the floor” better than other docs and therefore make continual adjustments to stay on pace. At its essence, they are using super-powers of observation to make decisions. It reminded me of a podcast about court awareness and great passers in basketball like the Charlotte Hornets’ LaMelo Ball and NBA great, Bill Bradley.
Bradley had an extraordinary ability to know where all the players were, and where they would be, at any given moment. He spent years honing this skill, noticing details in store windows as he stared straight ahead walking down a street. It’s reported his peripheral vision extended 5%-15% wider than average and he used it to gather more information and to process it more quickly. As a result he made outstanding decisions and fast, ultimately earning a spot in the Hall of Fame in Springfield.
Hall of Fame clinicians similarly take in a wider view than others and process that information quickly. They know how much time they have spent in the room, sense the emotional needs of the patient and anticipate the complexity of the problem. They quickly get to the critical questions and examinations that will make the diagnosis. They know the experience and skill of their medical assistant. They know the level of difficulty and even the temperament of patients who lie ahead on the schedule. All this is processed and used in moment-to-moment decision making. Do I sit down or stand up now? Can I excise this today, or reschedule? Do I ask another question? Do I step out of this room and see another in parallel while this biopsy is set up? And always, do I dare ask about grandkids or do I politely move on?
By broadening out their vision, they optimize their clinic, providing the best possible service, whether the day is busy or slow. I found their economy of motion also means they are less exhausted at the end of the day. I bet if when they dream of being on a ship, they’re sipping a Mai Tai, lounging on the deck.
For more on Bill Bradley and becoming more observant about your surroundings, you might appreciate the following:
www.newyorker.com/magazine/1965/01/23/a-sense-of-where-you-are and freakonomics.com/podcast/nsq-mindfulness/
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Have you ever had a nightmare you’re running late? Recently I dreamt I was seeing patients on a ship, a little cruiser like the ones that give you tours of Boston Harbor, with low ceilings and narrow iron stairs. My nurse stood where what would have been the coffee and danish window. My first patient was a newborn (this was a nightmare, in case you forgot) who was enormous. She had a big belly and spindly legs that hung off the table. Uniform, umbilicated papules and pustules covered her body. At the sight of her, terror ripped through me – no clue. I rushed to the doctor lounge (nice the ship had one) and flipped channels on a little TV mounted on the ceiling. Suddenly, my nurse burst in, she was frantic because dozens of angry adults and crying children were crammed in the hallway. Apparently, I had been watching TV for hours and my whole clinic was now backed up.
Running-late dreams are common and usually relate to real life. For us, the clinic has been busy lately. Vaccinated patients are returning after a year with their skin cancers that have flourished and psoriasis covering them like kudzu. In particular, they “see the floor” better than other docs and therefore make continual adjustments to stay on pace. At its essence, they are using super-powers of observation to make decisions. It reminded me of a podcast about court awareness and great passers in basketball like the Charlotte Hornets’ LaMelo Ball and NBA great, Bill Bradley.
Bradley had an extraordinary ability to know where all the players were, and where they would be, at any given moment. He spent years honing this skill, noticing details in store windows as he stared straight ahead walking down a street. It’s reported his peripheral vision extended 5%-15% wider than average and he used it to gather more information and to process it more quickly. As a result he made outstanding decisions and fast, ultimately earning a spot in the Hall of Fame in Springfield.
Hall of Fame clinicians similarly take in a wider view than others and process that information quickly. They know how much time they have spent in the room, sense the emotional needs of the patient and anticipate the complexity of the problem. They quickly get to the critical questions and examinations that will make the diagnosis. They know the experience and skill of their medical assistant. They know the level of difficulty and even the temperament of patients who lie ahead on the schedule. All this is processed and used in moment-to-moment decision making. Do I sit down or stand up now? Can I excise this today, or reschedule? Do I ask another question? Do I step out of this room and see another in parallel while this biopsy is set up? And always, do I dare ask about grandkids or do I politely move on?
By broadening out their vision, they optimize their clinic, providing the best possible service, whether the day is busy or slow. I found their economy of motion also means they are less exhausted at the end of the day. I bet if when they dream of being on a ship, they’re sipping a Mai Tai, lounging on the deck.
For more on Bill Bradley and becoming more observant about your surroundings, you might appreciate the following:
www.newyorker.com/magazine/1965/01/23/a-sense-of-where-you-are and freakonomics.com/podcast/nsq-mindfulness/
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Have you ever had a nightmare you’re running late? Recently I dreamt I was seeing patients on a ship, a little cruiser like the ones that give you tours of Boston Harbor, with low ceilings and narrow iron stairs. My nurse stood where what would have been the coffee and danish window. My first patient was a newborn (this was a nightmare, in case you forgot) who was enormous. She had a big belly and spindly legs that hung off the table. Uniform, umbilicated papules and pustules covered her body. At the sight of her, terror ripped through me – no clue. I rushed to the doctor lounge (nice the ship had one) and flipped channels on a little TV mounted on the ceiling. Suddenly, my nurse burst in, she was frantic because dozens of angry adults and crying children were crammed in the hallway. Apparently, I had been watching TV for hours and my whole clinic was now backed up.
Running-late dreams are common and usually relate to real life. For us, the clinic has been busy lately. Vaccinated patients are returning after a year with their skin cancers that have flourished and psoriasis covering them like kudzu. In particular, they “see the floor” better than other docs and therefore make continual adjustments to stay on pace. At its essence, they are using super-powers of observation to make decisions. It reminded me of a podcast about court awareness and great passers in basketball like the Charlotte Hornets’ LaMelo Ball and NBA great, Bill Bradley.
Bradley had an extraordinary ability to know where all the players were, and where they would be, at any given moment. He spent years honing this skill, noticing details in store windows as he stared straight ahead walking down a street. It’s reported his peripheral vision extended 5%-15% wider than average and he used it to gather more information and to process it more quickly. As a result he made outstanding decisions and fast, ultimately earning a spot in the Hall of Fame in Springfield.
Hall of Fame clinicians similarly take in a wider view than others and process that information quickly. They know how much time they have spent in the room, sense the emotional needs of the patient and anticipate the complexity of the problem. They quickly get to the critical questions and examinations that will make the diagnosis. They know the experience and skill of their medical assistant. They know the level of difficulty and even the temperament of patients who lie ahead on the schedule. All this is processed and used in moment-to-moment decision making. Do I sit down or stand up now? Can I excise this today, or reschedule? Do I ask another question? Do I step out of this room and see another in parallel while this biopsy is set up? And always, do I dare ask about grandkids or do I politely move on?
By broadening out their vision, they optimize their clinic, providing the best possible service, whether the day is busy or slow. I found their economy of motion also means they are less exhausted at the end of the day. I bet if when they dream of being on a ship, they’re sipping a Mai Tai, lounging on the deck.
For more on Bill Bradley and becoming more observant about your surroundings, you might appreciate the following:
www.newyorker.com/magazine/1965/01/23/a-sense-of-where-you-are and freakonomics.com/podcast/nsq-mindfulness/
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Internists’ patient visits rebound to near pre-COVID norms: Pay down slightly from previous year
Internists are seeing only 3% fewer patients than they did before the COVID-19 pandemic (72 per week on average now vs. 74 before the pandemic). Comparatively, for pediatricians, patient volume remains down 18%. Dermatologists, otolaryngologists, and orthopedists report that visits are down by about 15%.
The number of hours worked also rebounded for internists. In fact, some report working slightly more hours now than they did before the pandemic (52 hours a week, up from 50).
Pay for internists continues to hover near the bottom of the scale among specialties. In this year’s Medscape Internist Compensation Report 2021, internists averaged $248,000, down from $251,000 last year. Pediatricians were the lowest paid, at $221,000, followed by family physicians, at $236,000. Plastic surgeons made the most, at $526,000, followed by orthopedists, at $511,000.
It helped to be self-employed. These internists made $276,000 on average, compared with $238,000 for their employed counterparts.
Half say pay is fair
Internists are also near the bottom among specialists who feel they are fairly compensated. As in last year’s survey, just more than half of internists (52%) said they felt that they were fairly paid this year. By comparison, 79% of oncologists reported they were fairly compensated, which is on the high end regarding satisfaction, but only 44% of infectious diseases specialists felt that way.
Some indicators in the survey responses may help explain the dissatisfaction.
Internists are near the top in time spent on paperwork. On average, they spent 19.7 hours on paperwork and administration this year, up slightly from 18.5 last year. Infectious disease physicians spent the most time on those tasks (24.2 hours a week), and anesthesiologists spent the fewest, at 10.1 hours per week.
Administrative work was among many frustrations internists reported. The following are the top five most challenging aspects of the job, according to the respondents:
- Having so many rules and regulations (24%)
- Having to work long hours (16%)
- Dealing with difficult patients (16%)
- Working with electronic health records systems (11%)
- Danger/risk associated with treating COVID-19 patients (10%)
Conversely, the most rewarding aspects were “gratitude/relationships with patients” (31%); “knowing that I’m making the world a better place” (26%); and “being very good at what I do” (20%).
More than one-third lost income
More than one-third of internists (36%) reported that they lost some income during the past year.
Among those who lost income, 81% said they expect income to return to prepandemic levels within 3 years. Half of that group expected the rebound would come within the next year.
Slightly more than one-third of internists said they would participate in the merit-based incentive payment system (MIPS), and 12% said they would participate in advanced alternative payment models. The rest either said they would participate in neither, or they hadn’t decided.
“The stakes for the Quality Payment Program – the program that incorporates MIPS – are high, with a 9% penalty applied to all Medicare reimbursement for failure to participate,” says Elizabeth Woodcock, MBA, CPC, president of the physician practice consulting firm Woodcock and Associates, in Atlanta, Georgia.
“With margins already slim,” she told this news organization, “most physicians can’t afford this massive penalty.”
If they could choose again, most internists (76%) said they would choose medicine, which was almost the same number as physicians overall who would pick medicine again. Oncologists (88%) and ophthalmologists (87%) were the specialists most likely to choose medicine again. Those in physical medicine and rehabilitation were least likely to choose medicine again, at 67%.
But asked about their specialty, internists’ enthusiasm decreased. Only 68% said that they would make that same choice again.
That was up considerably, however, from the 2015 survey: For that year, only 25% said they would choose internal medicine again.
A version of this article first appeared on Medscape.com.
Internists are seeing only 3% fewer patients than they did before the COVID-19 pandemic (72 per week on average now vs. 74 before the pandemic). Comparatively, for pediatricians, patient volume remains down 18%. Dermatologists, otolaryngologists, and orthopedists report that visits are down by about 15%.
The number of hours worked also rebounded for internists. In fact, some report working slightly more hours now than they did before the pandemic (52 hours a week, up from 50).
Pay for internists continues to hover near the bottom of the scale among specialties. In this year’s Medscape Internist Compensation Report 2021, internists averaged $248,000, down from $251,000 last year. Pediatricians were the lowest paid, at $221,000, followed by family physicians, at $236,000. Plastic surgeons made the most, at $526,000, followed by orthopedists, at $511,000.
It helped to be self-employed. These internists made $276,000 on average, compared with $238,000 for their employed counterparts.
Half say pay is fair
Internists are also near the bottom among specialists who feel they are fairly compensated. As in last year’s survey, just more than half of internists (52%) said they felt that they were fairly paid this year. By comparison, 79% of oncologists reported they were fairly compensated, which is on the high end regarding satisfaction, but only 44% of infectious diseases specialists felt that way.
Some indicators in the survey responses may help explain the dissatisfaction.
Internists are near the top in time spent on paperwork. On average, they spent 19.7 hours on paperwork and administration this year, up slightly from 18.5 last year. Infectious disease physicians spent the most time on those tasks (24.2 hours a week), and anesthesiologists spent the fewest, at 10.1 hours per week.
Administrative work was among many frustrations internists reported. The following are the top five most challenging aspects of the job, according to the respondents:
- Having so many rules and regulations (24%)
- Having to work long hours (16%)
- Dealing with difficult patients (16%)
- Working with electronic health records systems (11%)
- Danger/risk associated with treating COVID-19 patients (10%)
Conversely, the most rewarding aspects were “gratitude/relationships with patients” (31%); “knowing that I’m making the world a better place” (26%); and “being very good at what I do” (20%).
More than one-third lost income
More than one-third of internists (36%) reported that they lost some income during the past year.
Among those who lost income, 81% said they expect income to return to prepandemic levels within 3 years. Half of that group expected the rebound would come within the next year.
Slightly more than one-third of internists said they would participate in the merit-based incentive payment system (MIPS), and 12% said they would participate in advanced alternative payment models. The rest either said they would participate in neither, or they hadn’t decided.
“The stakes for the Quality Payment Program – the program that incorporates MIPS – are high, with a 9% penalty applied to all Medicare reimbursement for failure to participate,” says Elizabeth Woodcock, MBA, CPC, president of the physician practice consulting firm Woodcock and Associates, in Atlanta, Georgia.
“With margins already slim,” she told this news organization, “most physicians can’t afford this massive penalty.”
If they could choose again, most internists (76%) said they would choose medicine, which was almost the same number as physicians overall who would pick medicine again. Oncologists (88%) and ophthalmologists (87%) were the specialists most likely to choose medicine again. Those in physical medicine and rehabilitation were least likely to choose medicine again, at 67%.
But asked about their specialty, internists’ enthusiasm decreased. Only 68% said that they would make that same choice again.
That was up considerably, however, from the 2015 survey: For that year, only 25% said they would choose internal medicine again.
A version of this article first appeared on Medscape.com.
Internists are seeing only 3% fewer patients than they did before the COVID-19 pandemic (72 per week on average now vs. 74 before the pandemic). Comparatively, for pediatricians, patient volume remains down 18%. Dermatologists, otolaryngologists, and orthopedists report that visits are down by about 15%.
The number of hours worked also rebounded for internists. In fact, some report working slightly more hours now than they did before the pandemic (52 hours a week, up from 50).
Pay for internists continues to hover near the bottom of the scale among specialties. In this year’s Medscape Internist Compensation Report 2021, internists averaged $248,000, down from $251,000 last year. Pediatricians were the lowest paid, at $221,000, followed by family physicians, at $236,000. Plastic surgeons made the most, at $526,000, followed by orthopedists, at $511,000.
It helped to be self-employed. These internists made $276,000 on average, compared with $238,000 for their employed counterparts.
Half say pay is fair
Internists are also near the bottom among specialists who feel they are fairly compensated. As in last year’s survey, just more than half of internists (52%) said they felt that they were fairly paid this year. By comparison, 79% of oncologists reported they were fairly compensated, which is on the high end regarding satisfaction, but only 44% of infectious diseases specialists felt that way.
Some indicators in the survey responses may help explain the dissatisfaction.
Internists are near the top in time spent on paperwork. On average, they spent 19.7 hours on paperwork and administration this year, up slightly from 18.5 last year. Infectious disease physicians spent the most time on those tasks (24.2 hours a week), and anesthesiologists spent the fewest, at 10.1 hours per week.
Administrative work was among many frustrations internists reported. The following are the top five most challenging aspects of the job, according to the respondents:
- Having so many rules and regulations (24%)
- Having to work long hours (16%)
- Dealing with difficult patients (16%)
- Working with electronic health records systems (11%)
- Danger/risk associated with treating COVID-19 patients (10%)
Conversely, the most rewarding aspects were “gratitude/relationships with patients” (31%); “knowing that I’m making the world a better place” (26%); and “being very good at what I do” (20%).
More than one-third lost income
More than one-third of internists (36%) reported that they lost some income during the past year.
Among those who lost income, 81% said they expect income to return to prepandemic levels within 3 years. Half of that group expected the rebound would come within the next year.
Slightly more than one-third of internists said they would participate in the merit-based incentive payment system (MIPS), and 12% said they would participate in advanced alternative payment models. The rest either said they would participate in neither, or they hadn’t decided.
“The stakes for the Quality Payment Program – the program that incorporates MIPS – are high, with a 9% penalty applied to all Medicare reimbursement for failure to participate,” says Elizabeth Woodcock, MBA, CPC, president of the physician practice consulting firm Woodcock and Associates, in Atlanta, Georgia.
“With margins already slim,” she told this news organization, “most physicians can’t afford this massive penalty.”
If they could choose again, most internists (76%) said they would choose medicine, which was almost the same number as physicians overall who would pick medicine again. Oncologists (88%) and ophthalmologists (87%) were the specialists most likely to choose medicine again. Those in physical medicine and rehabilitation were least likely to choose medicine again, at 67%.
But asked about their specialty, internists’ enthusiasm decreased. Only 68% said that they would make that same choice again.
That was up considerably, however, from the 2015 survey: For that year, only 25% said they would choose internal medicine again.
A version of this article first appeared on Medscape.com.
Less ambulatory care occurred than expected in pandemic, according to study
according to an analysis of national claims data from Jan. 1, 2019, to Oct. 31, 2020.
“The COVID-19 pandemic has seriously disrupted access to U.S. ambulatory care, endangering population health,” said John N. Mafi, MD, of the University of California, Los Angeles, in a presentation at the annual meeting of the Society of General Internal Medicine.
Dr. Mafi and colleagues conducted the analysis, which included 20 monthly cohorts, and measured outpatient visit rates per 100 members across all 20 study months. The researchers used a “difference-in-differences study design” and compared changes in rates of ambulatory care visits in January-February 2019 through September-October 2019 with the same periods in 2020.
They found that overall utilization fell to 68.9% of expected rates. This number increased to 82.6% of expected rates by May-June 2020 and to 87.7% of expected rates by July-August 2020.
To examine the impact of COVID-19 on U.S. ambulatory care patterns, the researchers identified 10.4 million individuals aged 18 years and older using the MedInsight research claims database. This database included Medicaid, commercial, dual eligible (receiving both Medicare and Medicaid benefits), Medicare Advantage (MA), and Medicare fee-for-service (FFS) patients. The average age of the individuals studied was 52 years, and 55% of the population were women. The researchers measured outpatient visit rates per 100 beneficiaries for several types of ambulatory care visits: emergency, urgent care, office, physical exams, preventive, alcohol/drug, and psychiatric care.
The researchers verified parallel trends in visits between 2018 and 2019 to establish a historical benchmark and divided the patient population into three groups based on insurance enrollment (continuously enrolled, not continuously enrolled, and fully enrolled) to account for new members adding insurance and disrupted coverage caused by job losses or other factors. The trends in ambulatory care utilization were similar between cohorts across the groups.
The rebound seen by the summer of 2020 showed variation when broken out by insurance type: 94.0% for Medicare FFS; 88.9% for commercial insurance; 86.3% for Medicare Advantage; 83.6% for dual eligible; and 78.0% for Medicaid.
“The big picture is that utilization looks similar across the three groups and has not attained prepandemic levels,” Dr. Mafi said.
When the results were divided by service type, utilization rates remained below expected rates while needs remain similar for U.S. Preventive Services Task Force–recommended preventive screening services, Dr. Mafi noted. The demand for psychiatric and substance use services has increased, but use rates are below expected rates. In addition, both avoidable and nonavoidable ED utilization both remained below expected rates.
In-person visits are down across insurance groups, but virtual visits are skyrocketing, across all insurance groups, Dr. Mafi added. However, virtual care visits have not completely compensated for declines in in-person visits, notably among dual-eligible and Medicaid insurance members.
Takeaways for policy makers include the fact that, while some reductions in unnecessary care, such as avoidable ED visits, may be beneficial, the “reduced USPSTF-recommended cancer and other evidence-based disease prevention may worsen health outcomes, particularly for Medicaid beneficiaries,” he said.
Outreach and outcomes
The study is important because “understanding ambulatory care patterns during the pandemic can highlight vulnerabilities and opportunities in our health care system,” Dr. Mafi said in an interview.
“While the COVID-19 pandemic has seriously disrupted access to U.S. ambulatory care, most studies have focused on the early months of the pandemic,” he noted.
Dr. Mafi said he was not surprised that ambulatory care utilization has not rebounded among Medicaid beneficiaries relative to other insurance groups.
“Medicaid beneficiaries are underresourced individuals who are disproportionately racial/ethnic minorities, and they historically have had difficulties accessing care. Our data suggest that the COVID-19 pandemic may be widening these preexisting inequities in access to ambulatory care,” he observed.
The study findings were limited by the use of the MedInsight research dataset, which is a convenience sample; and, therefore, the results might not be generalizable nationally, Dr. Mafi said. “However, it does include beneficiaries from all major insurance types across all 50 U.S. states. Additionally, our analysis was completed at the population level rather than the patient level, and so we were unable to account for patient-level characteristics such as clinical complexity,” he explained.
“The take-home message for clinicians is that our patients with Medicaid insurance may need additional efforts to overcome barriers to accessing ambulatory care, such as creating robust telemedicine outreach programs,” said Dr. Mafi. “Policy makers should also consider providing additional support and resources to safety net health systems who disproportionately care for Medicaid beneficiaries, such as higher reimbursements for both in-person and telemedicine visits.”
More research is needed, he emphasized. “We urgently need further inquiry into the impact of this persistently deferred ambulatory care utilization on important health outcomes such as preventable death/disability and quality of care.”
COVID consequences challenge ambulatory care
“These study findings mirror what we are seeing in primary care settings,” Maureen Lyons, MD, of Washington University. St. Louis, said in an interview. “With the pandemic, there are many additional barriers for patients accessing care, and these barriers have disproportionately impacted those who are already disadvantaged.
“From clinical experience, there are barriers directly related to COVID-19, such as the risk of infection or discomfort being in a clinic setting with other people. However, there also are barriers related to change in financial situation or insurance related to changes or loss of employment,” she said.
“Additionally, many patients have needed to take on increased responsibilities in other areas of their lives, such as caring for an ill family member or being responsible for children’s virtual school,” she said. These new responsibilities can lead people to skip or postpone ambulatory care visits.
“Loss of ambulatory care is likely to lead to increases in preventable illnesses with long-lasting effects,” Dr. Lyons noted. “Studying this in a robust fashion, as Dr. Mafi and colleagues have done, is a critical step in understanding and addressing this urgent need.”
Dr. Mafi noted that the data he presented is preliminary, and that he and his team hope to publish finalized estimates of ambulatory utilization rates in a forthcoming scientific paper.
The study was a collaboration between UCLA and Millman MedInsight, an actuarial health analytics company. Several coauthors are Millman employees. Dr. Mafi and the other researchers had no other relevant financial conflicts to disclose. Dr. Lyons had no financial conflicts to disclose.
according to an analysis of national claims data from Jan. 1, 2019, to Oct. 31, 2020.
“The COVID-19 pandemic has seriously disrupted access to U.S. ambulatory care, endangering population health,” said John N. Mafi, MD, of the University of California, Los Angeles, in a presentation at the annual meeting of the Society of General Internal Medicine.
Dr. Mafi and colleagues conducted the analysis, which included 20 monthly cohorts, and measured outpatient visit rates per 100 members across all 20 study months. The researchers used a “difference-in-differences study design” and compared changes in rates of ambulatory care visits in January-February 2019 through September-October 2019 with the same periods in 2020.
They found that overall utilization fell to 68.9% of expected rates. This number increased to 82.6% of expected rates by May-June 2020 and to 87.7% of expected rates by July-August 2020.
To examine the impact of COVID-19 on U.S. ambulatory care patterns, the researchers identified 10.4 million individuals aged 18 years and older using the MedInsight research claims database. This database included Medicaid, commercial, dual eligible (receiving both Medicare and Medicaid benefits), Medicare Advantage (MA), and Medicare fee-for-service (FFS) patients. The average age of the individuals studied was 52 years, and 55% of the population were women. The researchers measured outpatient visit rates per 100 beneficiaries for several types of ambulatory care visits: emergency, urgent care, office, physical exams, preventive, alcohol/drug, and psychiatric care.
The researchers verified parallel trends in visits between 2018 and 2019 to establish a historical benchmark and divided the patient population into three groups based on insurance enrollment (continuously enrolled, not continuously enrolled, and fully enrolled) to account for new members adding insurance and disrupted coverage caused by job losses or other factors. The trends in ambulatory care utilization were similar between cohorts across the groups.
The rebound seen by the summer of 2020 showed variation when broken out by insurance type: 94.0% for Medicare FFS; 88.9% for commercial insurance; 86.3% for Medicare Advantage; 83.6% for dual eligible; and 78.0% for Medicaid.
“The big picture is that utilization looks similar across the three groups and has not attained prepandemic levels,” Dr. Mafi said.
When the results were divided by service type, utilization rates remained below expected rates while needs remain similar for U.S. Preventive Services Task Force–recommended preventive screening services, Dr. Mafi noted. The demand for psychiatric and substance use services has increased, but use rates are below expected rates. In addition, both avoidable and nonavoidable ED utilization both remained below expected rates.
In-person visits are down across insurance groups, but virtual visits are skyrocketing, across all insurance groups, Dr. Mafi added. However, virtual care visits have not completely compensated for declines in in-person visits, notably among dual-eligible and Medicaid insurance members.
Takeaways for policy makers include the fact that, while some reductions in unnecessary care, such as avoidable ED visits, may be beneficial, the “reduced USPSTF-recommended cancer and other evidence-based disease prevention may worsen health outcomes, particularly for Medicaid beneficiaries,” he said.
Outreach and outcomes
The study is important because “understanding ambulatory care patterns during the pandemic can highlight vulnerabilities and opportunities in our health care system,” Dr. Mafi said in an interview.
“While the COVID-19 pandemic has seriously disrupted access to U.S. ambulatory care, most studies have focused on the early months of the pandemic,” he noted.
Dr. Mafi said he was not surprised that ambulatory care utilization has not rebounded among Medicaid beneficiaries relative to other insurance groups.
“Medicaid beneficiaries are underresourced individuals who are disproportionately racial/ethnic minorities, and they historically have had difficulties accessing care. Our data suggest that the COVID-19 pandemic may be widening these preexisting inequities in access to ambulatory care,” he observed.
The study findings were limited by the use of the MedInsight research dataset, which is a convenience sample; and, therefore, the results might not be generalizable nationally, Dr. Mafi said. “However, it does include beneficiaries from all major insurance types across all 50 U.S. states. Additionally, our analysis was completed at the population level rather than the patient level, and so we were unable to account for patient-level characteristics such as clinical complexity,” he explained.
“The take-home message for clinicians is that our patients with Medicaid insurance may need additional efforts to overcome barriers to accessing ambulatory care, such as creating robust telemedicine outreach programs,” said Dr. Mafi. “Policy makers should also consider providing additional support and resources to safety net health systems who disproportionately care for Medicaid beneficiaries, such as higher reimbursements for both in-person and telemedicine visits.”
More research is needed, he emphasized. “We urgently need further inquiry into the impact of this persistently deferred ambulatory care utilization on important health outcomes such as preventable death/disability and quality of care.”
COVID consequences challenge ambulatory care
“These study findings mirror what we are seeing in primary care settings,” Maureen Lyons, MD, of Washington University. St. Louis, said in an interview. “With the pandemic, there are many additional barriers for patients accessing care, and these barriers have disproportionately impacted those who are already disadvantaged.
“From clinical experience, there are barriers directly related to COVID-19, such as the risk of infection or discomfort being in a clinic setting with other people. However, there also are barriers related to change in financial situation or insurance related to changes or loss of employment,” she said.
“Additionally, many patients have needed to take on increased responsibilities in other areas of their lives, such as caring for an ill family member or being responsible for children’s virtual school,” she said. These new responsibilities can lead people to skip or postpone ambulatory care visits.
“Loss of ambulatory care is likely to lead to increases in preventable illnesses with long-lasting effects,” Dr. Lyons noted. “Studying this in a robust fashion, as Dr. Mafi and colleagues have done, is a critical step in understanding and addressing this urgent need.”
Dr. Mafi noted that the data he presented is preliminary, and that he and his team hope to publish finalized estimates of ambulatory utilization rates in a forthcoming scientific paper.
The study was a collaboration between UCLA and Millman MedInsight, an actuarial health analytics company. Several coauthors are Millman employees. Dr. Mafi and the other researchers had no other relevant financial conflicts to disclose. Dr. Lyons had no financial conflicts to disclose.
according to an analysis of national claims data from Jan. 1, 2019, to Oct. 31, 2020.
“The COVID-19 pandemic has seriously disrupted access to U.S. ambulatory care, endangering population health,” said John N. Mafi, MD, of the University of California, Los Angeles, in a presentation at the annual meeting of the Society of General Internal Medicine.
Dr. Mafi and colleagues conducted the analysis, which included 20 monthly cohorts, and measured outpatient visit rates per 100 members across all 20 study months. The researchers used a “difference-in-differences study design” and compared changes in rates of ambulatory care visits in January-February 2019 through September-October 2019 with the same periods in 2020.
They found that overall utilization fell to 68.9% of expected rates. This number increased to 82.6% of expected rates by May-June 2020 and to 87.7% of expected rates by July-August 2020.
To examine the impact of COVID-19 on U.S. ambulatory care patterns, the researchers identified 10.4 million individuals aged 18 years and older using the MedInsight research claims database. This database included Medicaid, commercial, dual eligible (receiving both Medicare and Medicaid benefits), Medicare Advantage (MA), and Medicare fee-for-service (FFS) patients. The average age of the individuals studied was 52 years, and 55% of the population were women. The researchers measured outpatient visit rates per 100 beneficiaries for several types of ambulatory care visits: emergency, urgent care, office, physical exams, preventive, alcohol/drug, and psychiatric care.
The researchers verified parallel trends in visits between 2018 and 2019 to establish a historical benchmark and divided the patient population into three groups based on insurance enrollment (continuously enrolled, not continuously enrolled, and fully enrolled) to account for new members adding insurance and disrupted coverage caused by job losses or other factors. The trends in ambulatory care utilization were similar between cohorts across the groups.
The rebound seen by the summer of 2020 showed variation when broken out by insurance type: 94.0% for Medicare FFS; 88.9% for commercial insurance; 86.3% for Medicare Advantage; 83.6% for dual eligible; and 78.0% for Medicaid.
“The big picture is that utilization looks similar across the three groups and has not attained prepandemic levels,” Dr. Mafi said.
When the results were divided by service type, utilization rates remained below expected rates while needs remain similar for U.S. Preventive Services Task Force–recommended preventive screening services, Dr. Mafi noted. The demand for psychiatric and substance use services has increased, but use rates are below expected rates. In addition, both avoidable and nonavoidable ED utilization both remained below expected rates.
In-person visits are down across insurance groups, but virtual visits are skyrocketing, across all insurance groups, Dr. Mafi added. However, virtual care visits have not completely compensated for declines in in-person visits, notably among dual-eligible and Medicaid insurance members.
Takeaways for policy makers include the fact that, while some reductions in unnecessary care, such as avoidable ED visits, may be beneficial, the “reduced USPSTF-recommended cancer and other evidence-based disease prevention may worsen health outcomes, particularly for Medicaid beneficiaries,” he said.
Outreach and outcomes
The study is important because “understanding ambulatory care patterns during the pandemic can highlight vulnerabilities and opportunities in our health care system,” Dr. Mafi said in an interview.
“While the COVID-19 pandemic has seriously disrupted access to U.S. ambulatory care, most studies have focused on the early months of the pandemic,” he noted.
Dr. Mafi said he was not surprised that ambulatory care utilization has not rebounded among Medicaid beneficiaries relative to other insurance groups.
“Medicaid beneficiaries are underresourced individuals who are disproportionately racial/ethnic minorities, and they historically have had difficulties accessing care. Our data suggest that the COVID-19 pandemic may be widening these preexisting inequities in access to ambulatory care,” he observed.
The study findings were limited by the use of the MedInsight research dataset, which is a convenience sample; and, therefore, the results might not be generalizable nationally, Dr. Mafi said. “However, it does include beneficiaries from all major insurance types across all 50 U.S. states. Additionally, our analysis was completed at the population level rather than the patient level, and so we were unable to account for patient-level characteristics such as clinical complexity,” he explained.
“The take-home message for clinicians is that our patients with Medicaid insurance may need additional efforts to overcome barriers to accessing ambulatory care, such as creating robust telemedicine outreach programs,” said Dr. Mafi. “Policy makers should also consider providing additional support and resources to safety net health systems who disproportionately care for Medicaid beneficiaries, such as higher reimbursements for both in-person and telemedicine visits.”
More research is needed, he emphasized. “We urgently need further inquiry into the impact of this persistently deferred ambulatory care utilization on important health outcomes such as preventable death/disability and quality of care.”
COVID consequences challenge ambulatory care
“These study findings mirror what we are seeing in primary care settings,” Maureen Lyons, MD, of Washington University. St. Louis, said in an interview. “With the pandemic, there are many additional barriers for patients accessing care, and these barriers have disproportionately impacted those who are already disadvantaged.
“From clinical experience, there are barriers directly related to COVID-19, such as the risk of infection or discomfort being in a clinic setting with other people. However, there also are barriers related to change in financial situation or insurance related to changes or loss of employment,” she said.
“Additionally, many patients have needed to take on increased responsibilities in other areas of their lives, such as caring for an ill family member or being responsible for children’s virtual school,” she said. These new responsibilities can lead people to skip or postpone ambulatory care visits.
“Loss of ambulatory care is likely to lead to increases in preventable illnesses with long-lasting effects,” Dr. Lyons noted. “Studying this in a robust fashion, as Dr. Mafi and colleagues have done, is a critical step in understanding and addressing this urgent need.”
Dr. Mafi noted that the data he presented is preliminary, and that he and his team hope to publish finalized estimates of ambulatory utilization rates in a forthcoming scientific paper.
The study was a collaboration between UCLA and Millman MedInsight, an actuarial health analytics company. Several coauthors are Millman employees. Dr. Mafi and the other researchers had no other relevant financial conflicts to disclose. Dr. Lyons had no financial conflicts to disclose.
FROM SGIM 2021
Telemedicine is popular among Mohs surgeons – for now
A majority of
A variety of factors combine to make it “very difficult for surgeons to make long-term plans for implementing telemedicine in their practices,” said Mario Maruthur, MD, who presented the findings at the annual meeting of the American College of Mohs Surgery. “Telemedicine likely has a role in Mohs practices, particularly with postop follow-up visits. However, postpandemic reimbursement and regulatory issues need to be formally laid out before Mohs surgeons are able to incorporate it into their permanent work flow.”
Dr. Maruthur, a Mohs surgery and dermatologic oncology fellow at Memorial Sloan Kettering Cancer Center, New York, and colleagues sent a survey to ACMS members in September and October 2020. “We saw first-hand in our surgical practice that telemedicine quickly became an important tool when the pandemic surged in the spring of 2020,” he said. Considering that surgical practices are highly dependent on in-person visits, the impetus for this study was to assess to what degree Mohs practices from across the spectrum, including academic and private practices, embraced telemedicine during the pandemic, and “what these surgical practices used telemedicine for, how it was received by their patients, which telemedicine platforms were most often utilized, and lastly, what are their plans if any for incorporating telemedicine into their surgical practices after the pandemic subsides.”
The researchers received responses from 115 surgeons representing all regions of the country (40% Northeast, 21% South, 21% Midwest, and 18% West). Half practiced in urban areas (37%) and large cities (13%), and 40% were in an academic setting versus 36% in a single-specialty private practice.
More than 70% of the respondents said their case load fell by at least 75% during the initial surge of the pandemic; 80% turned to telemedicine, compared with just 23% who relied on the technology prior to the pandemic. The most commonly used telemedicine technologies were FaceTime, Zoom, Doximity, and Epic.
Mohs surgeons reported most commonly using telemedicine for postsurgery management (77% of the total 115 responses). “Telemedicine is a great fit for this category of visits as they allow the surgeon to view the surgical site and answer any questions they patient may have,” Dr. Maruthur said. “If the surgeon does suspect a postop infection or other concern based on a patient’s signs or symptoms, they can easily schedule the patient for an in-person assessment. We suspect that postop follow-up visits may be the best candidate for long-term use of telemedicine in Mohs surgery practices.”
Surgeons also reported using telemedicine for “spot checks” (61%) and surgical consultations (59%).
However, Dr. Maruther noted that preoperative assessments and spot checks can be difficult to perform using telemedicine. “The quality of the video image is not always great, patients can have a difficult time pointing the camera at the right spot and at the right distance. Even appreciating the actual size of the lesion are all difficult over a video encounter. And there is a lot of information gleaned from in-person physical examination, such as whether the lesion is fixed to a deeper structure and whether there are any nearby scars or other suspicious lesions.”
Nearly three-quarters of the surgeons using the technology said most or all patients were receptive to telemedicine.
However, the surgeons reported multiple barriers to the use of telemedicine: Limitations when compared with physical exams (88%), fitting it into the work flow (58%), patient response and training (57%), reimbursement concerns (50%), implementation of the technology (37%), regulations such as HIPAA (24%), training of staff (17%), and licensing (8%).
In an interview, Sumaira Z. Aasi, MD, director of Mohs and dermatologic surgery, Stanford University, agreed that there are many obstacles to routine use of telemedicine by Mohs surgeons. “As surgeons, we rely on the physical and tactile exam to get a sense of the size and extent of the cancer and characteristics such as the laxity of the surrounding tissue whether the tumor is fixed,” she said. “It is very difficult to access this on a telemedicine visit.”
In addition, she said, “many of our patients are in the elderly population, and some may not be comfortable using this technology. Also, it’s not a work flow that we are comfortable or familiar with. And I think that the technology has to improve to allow for better resolution of images as we ‘examine’ patients through a telemedicine visit.”
She added that “another con is there is a reliance on having the patient point out lesions of concern. Many cancers are picked by a careful in-person examination by a qualified physician/dermatologist/Mohs surgeon when the lesion is quite small or subtle and not even noticed by the patient themselves. This approach invariably leads to earlier biopsies and earlier treatments that can prevent morbidity and save health care money.”
On the other hand, she said, telemedicine “may save patients some time and money in terms of the effort and cost of transportation to come in for simpler postoperative medical visits that are often short in their very nature, such as postop check-ups.”
Most of the surgeons surveyed (69%) said telemedicine probably or definitely deserves a place in the practice Mohs surgery, but only 50% said they’d like to or would definitely pursue giving telemedicine a role in their practices once the pandemic is over.
“At the start of the pandemic, many regulations in areas such as HIPAA were eased, and reimbursements were increased, which allowed telemedicine to be quickly adopted,” Dr. Maruther said. “The government and payers have yet to decide which regulations and reimbursements will be in place after the pandemic. That makes it very difficult for surgeons to make long-term plans for implementing telemedicine in their practices.”
Dr. Aasi predicted that telemedicine will become more appealing to patients and physicians as it its technology and usability improves. More familiarity with its use will also be helpful, she said, and surgeons will be more receptive as it’s incorporated into efficient daily work flow.
The study was funded in part by the National Institutes of Health.
A majority of
A variety of factors combine to make it “very difficult for surgeons to make long-term plans for implementing telemedicine in their practices,” said Mario Maruthur, MD, who presented the findings at the annual meeting of the American College of Mohs Surgery. “Telemedicine likely has a role in Mohs practices, particularly with postop follow-up visits. However, postpandemic reimbursement and regulatory issues need to be formally laid out before Mohs surgeons are able to incorporate it into their permanent work flow.”
Dr. Maruthur, a Mohs surgery and dermatologic oncology fellow at Memorial Sloan Kettering Cancer Center, New York, and colleagues sent a survey to ACMS members in September and October 2020. “We saw first-hand in our surgical practice that telemedicine quickly became an important tool when the pandemic surged in the spring of 2020,” he said. Considering that surgical practices are highly dependent on in-person visits, the impetus for this study was to assess to what degree Mohs practices from across the spectrum, including academic and private practices, embraced telemedicine during the pandemic, and “what these surgical practices used telemedicine for, how it was received by their patients, which telemedicine platforms were most often utilized, and lastly, what are their plans if any for incorporating telemedicine into their surgical practices after the pandemic subsides.”
The researchers received responses from 115 surgeons representing all regions of the country (40% Northeast, 21% South, 21% Midwest, and 18% West). Half practiced in urban areas (37%) and large cities (13%), and 40% were in an academic setting versus 36% in a single-specialty private practice.
More than 70% of the respondents said their case load fell by at least 75% during the initial surge of the pandemic; 80% turned to telemedicine, compared with just 23% who relied on the technology prior to the pandemic. The most commonly used telemedicine technologies were FaceTime, Zoom, Doximity, and Epic.
Mohs surgeons reported most commonly using telemedicine for postsurgery management (77% of the total 115 responses). “Telemedicine is a great fit for this category of visits as they allow the surgeon to view the surgical site and answer any questions they patient may have,” Dr. Maruthur said. “If the surgeon does suspect a postop infection or other concern based on a patient’s signs or symptoms, they can easily schedule the patient for an in-person assessment. We suspect that postop follow-up visits may be the best candidate for long-term use of telemedicine in Mohs surgery practices.”
Surgeons also reported using telemedicine for “spot checks” (61%) and surgical consultations (59%).
However, Dr. Maruther noted that preoperative assessments and spot checks can be difficult to perform using telemedicine. “The quality of the video image is not always great, patients can have a difficult time pointing the camera at the right spot and at the right distance. Even appreciating the actual size of the lesion are all difficult over a video encounter. And there is a lot of information gleaned from in-person physical examination, such as whether the lesion is fixed to a deeper structure and whether there are any nearby scars or other suspicious lesions.”
Nearly three-quarters of the surgeons using the technology said most or all patients were receptive to telemedicine.
However, the surgeons reported multiple barriers to the use of telemedicine: Limitations when compared with physical exams (88%), fitting it into the work flow (58%), patient response and training (57%), reimbursement concerns (50%), implementation of the technology (37%), regulations such as HIPAA (24%), training of staff (17%), and licensing (8%).
In an interview, Sumaira Z. Aasi, MD, director of Mohs and dermatologic surgery, Stanford University, agreed that there are many obstacles to routine use of telemedicine by Mohs surgeons. “As surgeons, we rely on the physical and tactile exam to get a sense of the size and extent of the cancer and characteristics such as the laxity of the surrounding tissue whether the tumor is fixed,” she said. “It is very difficult to access this on a telemedicine visit.”
In addition, she said, “many of our patients are in the elderly population, and some may not be comfortable using this technology. Also, it’s not a work flow that we are comfortable or familiar with. And I think that the technology has to improve to allow for better resolution of images as we ‘examine’ patients through a telemedicine visit.”
She added that “another con is there is a reliance on having the patient point out lesions of concern. Many cancers are picked by a careful in-person examination by a qualified physician/dermatologist/Mohs surgeon when the lesion is quite small or subtle and not even noticed by the patient themselves. This approach invariably leads to earlier biopsies and earlier treatments that can prevent morbidity and save health care money.”
On the other hand, she said, telemedicine “may save patients some time and money in terms of the effort and cost of transportation to come in for simpler postoperative medical visits that are often short in their very nature, such as postop check-ups.”
Most of the surgeons surveyed (69%) said telemedicine probably or definitely deserves a place in the practice Mohs surgery, but only 50% said they’d like to or would definitely pursue giving telemedicine a role in their practices once the pandemic is over.
“At the start of the pandemic, many regulations in areas such as HIPAA were eased, and reimbursements were increased, which allowed telemedicine to be quickly adopted,” Dr. Maruther said. “The government and payers have yet to decide which regulations and reimbursements will be in place after the pandemic. That makes it very difficult for surgeons to make long-term plans for implementing telemedicine in their practices.”
Dr. Aasi predicted that telemedicine will become more appealing to patients and physicians as it its technology and usability improves. More familiarity with its use will also be helpful, she said, and surgeons will be more receptive as it’s incorporated into efficient daily work flow.
The study was funded in part by the National Institutes of Health.
A majority of
A variety of factors combine to make it “very difficult for surgeons to make long-term plans for implementing telemedicine in their practices,” said Mario Maruthur, MD, who presented the findings at the annual meeting of the American College of Mohs Surgery. “Telemedicine likely has a role in Mohs practices, particularly with postop follow-up visits. However, postpandemic reimbursement and regulatory issues need to be formally laid out before Mohs surgeons are able to incorporate it into their permanent work flow.”
Dr. Maruthur, a Mohs surgery and dermatologic oncology fellow at Memorial Sloan Kettering Cancer Center, New York, and colleagues sent a survey to ACMS members in September and October 2020. “We saw first-hand in our surgical practice that telemedicine quickly became an important tool when the pandemic surged in the spring of 2020,” he said. Considering that surgical practices are highly dependent on in-person visits, the impetus for this study was to assess to what degree Mohs practices from across the spectrum, including academic and private practices, embraced telemedicine during the pandemic, and “what these surgical practices used telemedicine for, how it was received by their patients, which telemedicine platforms were most often utilized, and lastly, what are their plans if any for incorporating telemedicine into their surgical practices after the pandemic subsides.”
The researchers received responses from 115 surgeons representing all regions of the country (40% Northeast, 21% South, 21% Midwest, and 18% West). Half practiced in urban areas (37%) and large cities (13%), and 40% were in an academic setting versus 36% in a single-specialty private practice.
More than 70% of the respondents said their case load fell by at least 75% during the initial surge of the pandemic; 80% turned to telemedicine, compared with just 23% who relied on the technology prior to the pandemic. The most commonly used telemedicine technologies were FaceTime, Zoom, Doximity, and Epic.
Mohs surgeons reported most commonly using telemedicine for postsurgery management (77% of the total 115 responses). “Telemedicine is a great fit for this category of visits as they allow the surgeon to view the surgical site and answer any questions they patient may have,” Dr. Maruthur said. “If the surgeon does suspect a postop infection or other concern based on a patient’s signs or symptoms, they can easily schedule the patient for an in-person assessment. We suspect that postop follow-up visits may be the best candidate for long-term use of telemedicine in Mohs surgery practices.”
Surgeons also reported using telemedicine for “spot checks” (61%) and surgical consultations (59%).
However, Dr. Maruther noted that preoperative assessments and spot checks can be difficult to perform using telemedicine. “The quality of the video image is not always great, patients can have a difficult time pointing the camera at the right spot and at the right distance. Even appreciating the actual size of the lesion are all difficult over a video encounter. And there is a lot of information gleaned from in-person physical examination, such as whether the lesion is fixed to a deeper structure and whether there are any nearby scars or other suspicious lesions.”
Nearly three-quarters of the surgeons using the technology said most or all patients were receptive to telemedicine.
However, the surgeons reported multiple barriers to the use of telemedicine: Limitations when compared with physical exams (88%), fitting it into the work flow (58%), patient response and training (57%), reimbursement concerns (50%), implementation of the technology (37%), regulations such as HIPAA (24%), training of staff (17%), and licensing (8%).
In an interview, Sumaira Z. Aasi, MD, director of Mohs and dermatologic surgery, Stanford University, agreed that there are many obstacles to routine use of telemedicine by Mohs surgeons. “As surgeons, we rely on the physical and tactile exam to get a sense of the size and extent of the cancer and characteristics such as the laxity of the surrounding tissue whether the tumor is fixed,” she said. “It is very difficult to access this on a telemedicine visit.”
In addition, she said, “many of our patients are in the elderly population, and some may not be comfortable using this technology. Also, it’s not a work flow that we are comfortable or familiar with. And I think that the technology has to improve to allow for better resolution of images as we ‘examine’ patients through a telemedicine visit.”
She added that “another con is there is a reliance on having the patient point out lesions of concern. Many cancers are picked by a careful in-person examination by a qualified physician/dermatologist/Mohs surgeon when the lesion is quite small or subtle and not even noticed by the patient themselves. This approach invariably leads to earlier biopsies and earlier treatments that can prevent morbidity and save health care money.”
On the other hand, she said, telemedicine “may save patients some time and money in terms of the effort and cost of transportation to come in for simpler postoperative medical visits that are often short in their very nature, such as postop check-ups.”
Most of the surgeons surveyed (69%) said telemedicine probably or definitely deserves a place in the practice Mohs surgery, but only 50% said they’d like to or would definitely pursue giving telemedicine a role in their practices once the pandemic is over.
“At the start of the pandemic, many regulations in areas such as HIPAA were eased, and reimbursements were increased, which allowed telemedicine to be quickly adopted,” Dr. Maruther said. “The government and payers have yet to decide which regulations and reimbursements will be in place after the pandemic. That makes it very difficult for surgeons to make long-term plans for implementing telemedicine in their practices.”
Dr. Aasi predicted that telemedicine will become more appealing to patients and physicians as it its technology and usability improves. More familiarity with its use will also be helpful, she said, and surgeons will be more receptive as it’s incorporated into efficient daily work flow.
The study was funded in part by the National Institutes of Health.
FROM THE ACMS ANNUAL MEETING
Pediatricians see drop in income during the pandemic
The average income for pediatricians declined slightly from 2019 to 2020, according to the Medscape Pediatrician Compensation Report 2021.

The report, which was conducted between October 2020 and February 2021, found that the average pediatrician income was down $11,000 – from $232,000 in 2019 to $221,000 in 2020, with 48% of pediatricians reporting at least some decline in compensation.
The specialty also earned the least amount of money in 2020, compared with all of the other specialties, which isn’t surprising since pediatricians have been among the lowest-paid physician specialties since 2013. The highest-earning specialty was plastic surgery with an average income of $526,000 annually.
Most pediatricians who saw a drop in income cited pandemic-related issues such as job loss, fewer hours, and fewer patients.
Jesse Hackell, MD, vice president and chief operating officer of Ponoma Pediatrics in New York, said in an interview the reduced wages pediatricians saw in 2020 didn’t surprise him because many pediatric offices saw a huge drop in visits that were not urgent.
“[The report] shows that procedural specialties tended to do a lot better than the nonprocedural specialties,” Dr. Hackell said. “That’s because, during the shutdown, if you broke your leg, you still needed the orthopedist. And even though the hospitals weren’t doing elective surgeries, they were certainly doing the emergency stuff.”
Meanwhile, in pediatrician offices, where Dr. Hackell said office visits dropped 70%-80% at the beginning of the pandemic, “parents weren’t going to bring a healthy kid out for routine visits and they weren’t going to bring a kid out for minor illnesses and expose them to possibly communicable diseases in the office.”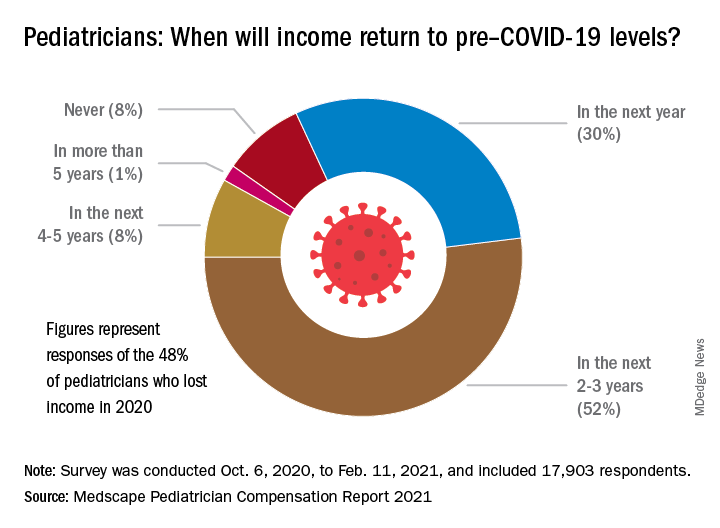
About 52% of pediatricians who lost income because of the pandemic believe their income levels will return to normal in 2-3 years. Meanwhile 30% of pediatricians expect their income to return to normal within a year, and 8% believe it will take 4 years for them to bounce back.
Physician work hours generally declined for some time during the pandemic, according to the report. However, most pediatricians are working about the same number of hours as they did before the pandemic, which is 47 hours per week.
Despite working the same number of hours per week that they did prepandemic, they are seeing fewer patients. They are currently seeing on average 64 patients per week, compared with the 78 patients they used to see weekly before the pandemic.
Dr. Hackell said that might be because pediatric offices are trying to make up the loss of revenue during the beginning of the pandemic, from the reduced number of well visits and immunizations, in the second half of the year with outreach.
“Since about June 2020, we’ve been making concerted efforts to remind parents that preventing other infectious diseases is critically important,” Dr. Hackell explained. “And so actually, for the second half of the year, many of us saw more well visits and immunization volume than in 2019 as we sought to make up the gap. It wasn’t that we were seeing more overall, but we’re trying to make up the gap that happened from March, April, May, [and] June.”
Most pediatricians find their work rewarding. One-third say the most rewarding part of their job is gratitude from and relationships with their patients. Meanwhile, 31% of pediatricians said knowing they are making the world a better place was a rewarding part of their job. Only 8% of them said making money was a rewarding part of their job.
Dr. Hackell said he did not go into pediatrics to make money, it was because he found it stimulating and has “no complaints.”
“I’ve been a pediatrician for 40 years and I wouldn’t do anything else,” Dr. Hackell said. “I don’t know that there’s anything that I would find as rewarding as the relationships that I’ve had over 40 years with my patients. You know, getting invited to weddings of kids who I saw when they were newborns is pretty impressive. It’s the gratification of having ongoing relationships with families.”
Furthermore, the report revealed that 77% of pediatricians said they would pick medicine again if they had a choice, and 82% said they would choose the same specialty.
The experts disclosed no relevant financial interests.
*This story was updated on 5/18/2021.
The average income for pediatricians declined slightly from 2019 to 2020, according to the Medscape Pediatrician Compensation Report 2021.

The report, which was conducted between October 2020 and February 2021, found that the average pediatrician income was down $11,000 – from $232,000 in 2019 to $221,000 in 2020, with 48% of pediatricians reporting at least some decline in compensation.
The specialty also earned the least amount of money in 2020, compared with all of the other specialties, which isn’t surprising since pediatricians have been among the lowest-paid physician specialties since 2013. The highest-earning specialty was plastic surgery with an average income of $526,000 annually.
Most pediatricians who saw a drop in income cited pandemic-related issues such as job loss, fewer hours, and fewer patients.
Jesse Hackell, MD, vice president and chief operating officer of Ponoma Pediatrics in New York, said in an interview the reduced wages pediatricians saw in 2020 didn’t surprise him because many pediatric offices saw a huge drop in visits that were not urgent.
“[The report] shows that procedural specialties tended to do a lot better than the nonprocedural specialties,” Dr. Hackell said. “That’s because, during the shutdown, if you broke your leg, you still needed the orthopedist. And even though the hospitals weren’t doing elective surgeries, they were certainly doing the emergency stuff.”
Meanwhile, in pediatrician offices, where Dr. Hackell said office visits dropped 70%-80% at the beginning of the pandemic, “parents weren’t going to bring a healthy kid out for routine visits and they weren’t going to bring a kid out for minor illnesses and expose them to possibly communicable diseases in the office.”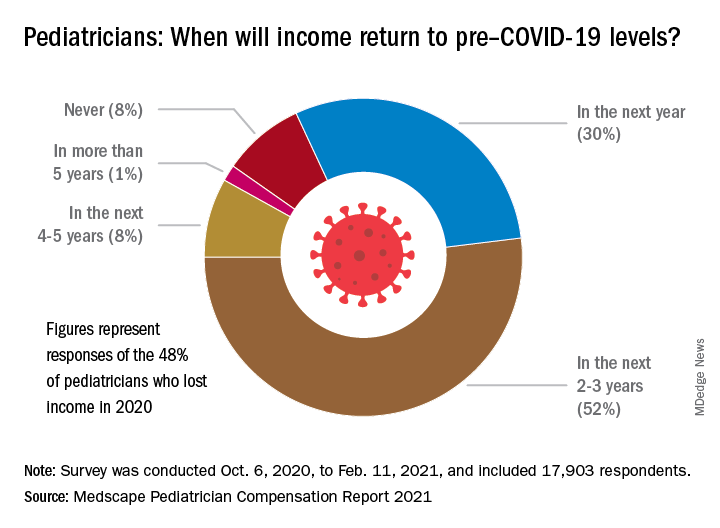
About 52% of pediatricians who lost income because of the pandemic believe their income levels will return to normal in 2-3 years. Meanwhile 30% of pediatricians expect their income to return to normal within a year, and 8% believe it will take 4 years for them to bounce back.
Physician work hours generally declined for some time during the pandemic, according to the report. However, most pediatricians are working about the same number of hours as they did before the pandemic, which is 47 hours per week.
Despite working the same number of hours per week that they did prepandemic, they are seeing fewer patients. They are currently seeing on average 64 patients per week, compared with the 78 patients they used to see weekly before the pandemic.
Dr. Hackell said that might be because pediatric offices are trying to make up the loss of revenue during the beginning of the pandemic, from the reduced number of well visits and immunizations, in the second half of the year with outreach.
“Since about June 2020, we’ve been making concerted efforts to remind parents that preventing other infectious diseases is critically important,” Dr. Hackell explained. “And so actually, for the second half of the year, many of us saw more well visits and immunization volume than in 2019 as we sought to make up the gap. It wasn’t that we were seeing more overall, but we’re trying to make up the gap that happened from March, April, May, [and] June.”
Most pediatricians find their work rewarding. One-third say the most rewarding part of their job is gratitude from and relationships with their patients. Meanwhile, 31% of pediatricians said knowing they are making the world a better place was a rewarding part of their job. Only 8% of them said making money was a rewarding part of their job.
Dr. Hackell said he did not go into pediatrics to make money, it was because he found it stimulating and has “no complaints.”
“I’ve been a pediatrician for 40 years and I wouldn’t do anything else,” Dr. Hackell said. “I don’t know that there’s anything that I would find as rewarding as the relationships that I’ve had over 40 years with my patients. You know, getting invited to weddings of kids who I saw when they were newborns is pretty impressive. It’s the gratification of having ongoing relationships with families.”
Furthermore, the report revealed that 77% of pediatricians said they would pick medicine again if they had a choice, and 82% said they would choose the same specialty.
The experts disclosed no relevant financial interests.
*This story was updated on 5/18/2021.
The average income for pediatricians declined slightly from 2019 to 2020, according to the Medscape Pediatrician Compensation Report 2021.

The report, which was conducted between October 2020 and February 2021, found that the average pediatrician income was down $11,000 – from $232,000 in 2019 to $221,000 in 2020, with 48% of pediatricians reporting at least some decline in compensation.
The specialty also earned the least amount of money in 2020, compared with all of the other specialties, which isn’t surprising since pediatricians have been among the lowest-paid physician specialties since 2013. The highest-earning specialty was plastic surgery with an average income of $526,000 annually.
Most pediatricians who saw a drop in income cited pandemic-related issues such as job loss, fewer hours, and fewer patients.
Jesse Hackell, MD, vice president and chief operating officer of Ponoma Pediatrics in New York, said in an interview the reduced wages pediatricians saw in 2020 didn’t surprise him because many pediatric offices saw a huge drop in visits that were not urgent.
“[The report] shows that procedural specialties tended to do a lot better than the nonprocedural specialties,” Dr. Hackell said. “That’s because, during the shutdown, if you broke your leg, you still needed the orthopedist. And even though the hospitals weren’t doing elective surgeries, they were certainly doing the emergency stuff.”
Meanwhile, in pediatrician offices, where Dr. Hackell said office visits dropped 70%-80% at the beginning of the pandemic, “parents weren’t going to bring a healthy kid out for routine visits and they weren’t going to bring a kid out for minor illnesses and expose them to possibly communicable diseases in the office.”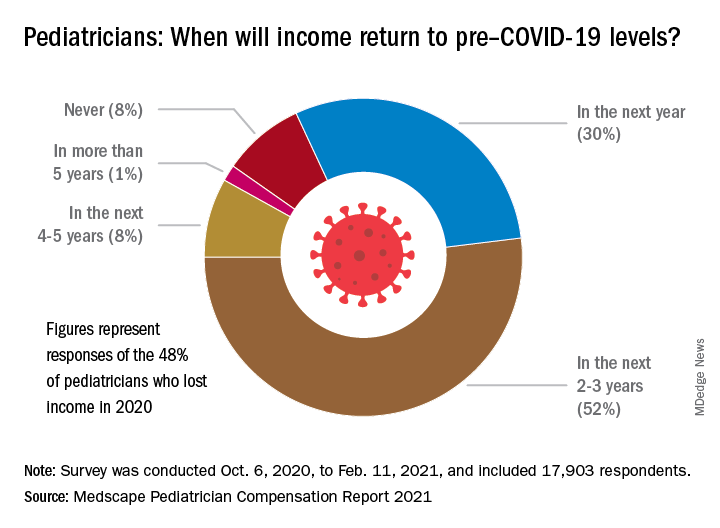
About 52% of pediatricians who lost income because of the pandemic believe their income levels will return to normal in 2-3 years. Meanwhile 30% of pediatricians expect their income to return to normal within a year, and 8% believe it will take 4 years for them to bounce back.
Physician work hours generally declined for some time during the pandemic, according to the report. However, most pediatricians are working about the same number of hours as they did before the pandemic, which is 47 hours per week.
Despite working the same number of hours per week that they did prepandemic, they are seeing fewer patients. They are currently seeing on average 64 patients per week, compared with the 78 patients they used to see weekly before the pandemic.
Dr. Hackell said that might be because pediatric offices are trying to make up the loss of revenue during the beginning of the pandemic, from the reduced number of well visits and immunizations, in the second half of the year with outreach.
“Since about June 2020, we’ve been making concerted efforts to remind parents that preventing other infectious diseases is critically important,” Dr. Hackell explained. “And so actually, for the second half of the year, many of us saw more well visits and immunization volume than in 2019 as we sought to make up the gap. It wasn’t that we were seeing more overall, but we’re trying to make up the gap that happened from March, April, May, [and] June.”
Most pediatricians find their work rewarding. One-third say the most rewarding part of their job is gratitude from and relationships with their patients. Meanwhile, 31% of pediatricians said knowing they are making the world a better place was a rewarding part of their job. Only 8% of them said making money was a rewarding part of their job.
Dr. Hackell said he did not go into pediatrics to make money, it was because he found it stimulating and has “no complaints.”
“I’ve been a pediatrician for 40 years and I wouldn’t do anything else,” Dr. Hackell said. “I don’t know that there’s anything that I would find as rewarding as the relationships that I’ve had over 40 years with my patients. You know, getting invited to weddings of kids who I saw when they were newborns is pretty impressive. It’s the gratification of having ongoing relationships with families.”
Furthermore, the report revealed that 77% of pediatricians said they would pick medicine again if they had a choice, and 82% said they would choose the same specialty.
The experts disclosed no relevant financial interests.
*This story was updated on 5/18/2021.
Are more naturopaths trying to compete with docs?
Jon Hislop, MD, PhD, hadn’t been in practice very long before patients began coming to him with requests to order tests that their naturopaths had recommended.
The family physician in North Vancouver, British Columbia, knew little about naturopathy but began researching it.
“I was finding that some of what the naturopaths were telling them was a little odd. Some of the tests they were asking for were unnecessary,” Dr. Hislop said.
The more he learned about naturopathy, the more appalled he became. He eventually took to Twitter, where he wages a campaign against naturopathy and alternative medicine.
“There is no alternative medicine,” he said. “There’s medicine and there’s other stuff. We need to stick to medicine and stay away from the other stuff.”
Dr. Hislop is not alone in his criticism of naturopathic medicine. Professional medical societies almost universally oppose naturopathy, but that has not stopped its spread or prevented it from becoming part of some health care systems.
Americans spent $30.2 billion on out-of-pocket complementary health care, according to a 2016 report from the National Institutes of Health. That includes everything from herbal supplements and massage therapy to chiropractic care.
What is naturopathic medicine?
Naturopathy came to the United States from Germany in the 1800s, but some of its practices are thousands of years old. Naturopathic treatments include homeopathy, IV vitamin infusions, acupuncture, Reiki, and herbal supplements.
Naturopathy is based on the belief that the body has an innate ability to heal itself. It discourages drugs and surgery in favor of supplements, herbs, and other so-called natural treatments. Much of it centers around addressing lifestyle issues and counseling patients to improve their diets, quit smoking, exercise more, lose weight, etc., in order to address the root causes of some health problems.
Practitioners are critical of Western medicine for what they regard as an over-reliance on drugs and technology and for treating symptoms rather than the causes of disease.
“We get a lot of people who are at the end of their ropes, people with hard-to-diagnose diseases who know they are sick but whose labs are normal,” said Jaquel Patterson, ND, former president of the American Association of Naturopathic Physicians (AANP) and medical director of a naturopathic practice in Connecticut.
Separate training and licensing
There are major differences among naturopaths.
At one extreme are unlicensed, self-taught “healers,” who can embrace everything from homeopathy to aromatherapy.
At the other end are naturopathic doctors (NDs), who are more likely to become part of health care systems. These caregivers are trained and licensed, though not by the same institutions as traditional physicians.
To be licensed, NDs must graduate from one of seven accredited naturopathic medical schools in the United States and Canada. In addition to a standard medical curriculum, schools require graduates to complete 4 years of training in clinical nutrition, acupuncture, homeopathic medicine, botanical medicine, physical medicine, and counseling. Medical students intern in clinical settings for 2 years.
NDs are eager to distinguish themselves from their uncredentialed counterparts.
“Some people go to a weekend class and call themselves naturopaths. That’s very concerning. I don’t want those people to be licensed either,” said Hallie Armstrong, ND, who practices in Michigan.
In the United States, there are 6,000 practicing NDs and an unknown number of unlicensed naturopathic healers.
Can naturopaths call themselves ‘physicians’?
Twenty-two states, the District of Columbia, Puerto Rico, and the U.S. Virgin Islands have licensing or registration laws for naturopathic doctors. Three states – South Carolina, Tennessee, and Florida – prohibit practicing naturopathic medicine without a license, according to the AANP.
States that license NDs differ in what they permit them to do.
Nine states allow licensed NDs to use the term “physician,” although this is prohibited in seven states. Most licensed states allow naturopathic practitioners some prescribing authority, including the prescribing of many controlled substances, although only a few states permit full prescribing rights. Most states that license NDs allow them to prescribe and administer nonprescription therapeutic substances, drugs, and therapies.
Twelve states and the District of Columbia allow licensed naturopathic doctors to perform some minor procedures, such as stitching up wounds. Additionally, 13 states allow NDs to order diagnostic tests.
Although the AANP lobbies to get licensure in more states and to expand the activities that NDs can perform, the medical establishment in those states nearly always opposes the legislation, as do national organizations, such as the American Academy of Family Physicians and the American College of Physicians.
“They absolutely will not stop until they get licenses. They’ve done a really good job of selling themselves as legitimate health care professionals to state legislatures,” said David Gorski, MD, PhD, FACS, a surgical oncologist and managing editor of Science-Based Medicine, a blog that attacks unproven medical claims and defends traditional medicine. Naturopathy is a favorite target.
Are naturopaths gaining ground anyway?
Despite the opposition of the medical establishment and many individual health care professionals, a growing number of health care systems are adopting alternative medicine.
In 2018, the AANP stated that 28 prominent health systems, hospitals, and cancer treatment centers had one or more licensed NDs on staff. Among them were Cancer Treatment Centers of America, Cedars-Sinai, Columbia University’s Herbert Irving Comprehensive Cancer Center, and the Fred Hutchinson Cancer Research Center.
Other health care systems may not have NDs on staff but provide naturopathic treatments, usually under the heading of “complementary medicine” or “integrative medicine.” For example, the Cleveland Clinic’s Center for Integrative and Lifestyle Medicine offers acupuncture, Chinese herbal medicine, Reiki, yoga, and culinary medicine.
Critics find this appalling.
“I think it’s a mistake to integrate that kind of practice into a science-based health care setting. If we learned anything over the past year, it’s that medicine based on magical thinking is dangerous,” said Timothy Caulfield, LLM, FCAHS, research director at the Health Law Institute of the University of Alberta, Edmonton.
Dr. Gorski added: “I’m not exactly sure why doctors who should know better have become more accepting of practices that aren’t science-based or are outright quackery.”
Becoming part of the system
Beaumont Health, Michigan’s largest health care system, added integrative medicine in 2006 and hired its first naturopathic practitioners a year later.
The integrative practitioners began in oncology, offering such things as massage therapy, acupuncture, guided imagery, and Reiki. “Very quickly, people outside oncology began saying, ‘I’ve got a cardiology patient who would really benefit from this ... I’ve got a GI patient who could benefit from this...,’” said Maureen Anderson, MD, medical director of Beaumont Integrative Medicine.
Beaumont now offers integrative medicine at three locations. They average 20,000 visits a year and work with 50 to 60 practitioners, many of whom work part-time.
Because Michigan does not license NDs, their scope of practice at Beaumont is limited. They take patient histories, provide advice on nutrition, diet, and exercise, and prescribe herbs and supplements. Beaumont operates its own herbal and supplement pharmacy.
NDs work under the medical supervision of Dr. Anderson, an emergency medicine physician who became interested in naturopathy because she thought traditional medicine doesn’t do a good job of providing care for chronic conditions. Any initial skepticism on the part of the medical staff has been overcome by seeing the benefits naturopathy provides, Dr. Anderson said. The claim is echoed by Mr. Armstrong, an ND who works in the system part-time: “As soon as [doctors] understand our schooling and where we’re coming from and understand that we want to do the same things, then they’re very accepting.”
The University of California, Irvine, health care system has one of the largest naturopathic medicine programs in the country, the result of a $200 million donation in 2017 from a couple who champion alternative medicine. The Susan Samueli Integrative Health Institute includes 28 health care professionals, including MDs, NDs, RNs, acupuncturists, dietitians, yoga instructors, and others. It includes a research arm, which is focused primarily on acupuncture.
The alternative medicine offerings benefit the system, said Kim Hecht, DO, medical director of inpatient and ambulatory services at the Samueli Institute.
“I’m not against traditional medicine, because I think everything has a time and a place,” Dr. Hecht said. However, she rejects the idea that MDs can offer the same holistic approach as NDs.
“Medical science likes to say we’re interested in treating the whole person, but if you look at medical school courses, that’s not what’s being taught,” she said.
The chance to work within a traditional health care system was attractive to Arvin Jenab, ND, medical director of naturopathic medicine at the institute.
“It offers the opportunity to refine our medicine and trim the things that aren’t necessary or are controversial and concentrate on the things at the core of what we do,” he said.
UCI Health practices a conservative model of naturopathy that supports traditional practitioners, Mr. Jenab said.
Is there any harm?
Some patients clearly want what naturopathy offers. So what’s the harm?
Health care systems that integrate alternative medicine legitimize it and lower the overall standard of care, Mr. Caulfield said. Most naturopathy claims are not backed by evidence, and making it available to patients amounts to deceiving them, he said.
“If there’s good science behind it, it’s not going to be alternative medicine; it’s going to be medicine,” Mr. Caulfield said.
Family physician Dr. Hislop said that refusing to order naturopath-recommended tests interferes with his relationships with patients and often requires lengthy conversations to explain the problems with naturopathy.
Naturopathic medicine can deter patients from seeking proven conventional treatments, which can put their health at risk, Dr. Gorski said.
Some naturopaths could potentially be harmful.
In 2017, a California woman died after receiving an IV preparation of curcumin, a chemical constituent in the Indian spice turmeric featured in alternative medicine. The U.S. Food and Drug Administration found that the treating ND mixed the curcumin emulsion product with ungraded castor oil that had a warning label stating: “CAUTION: For manufacturing or laboratory use only.”
Because naturopathic care is generally not covered by insurance, it can also be expensive for patients who pay out of pocket.
Ironically, the mainstream health care system helps create the environment in which naturopathic medicine thrives.
It offers patients a more relaxed and personal alternative to rushed visits with harried doctors scrambling to see the required number of patients in a day. By contrast, an initial visit with an ND might last a leisurely 60 minutes, with 30-minute follow-up appointments.
Mr. Caulfield acknowledged that the relaxed naturopathic approach can be more attractive to patients but said the answer is to reform the current system: “You don’t fix a broken arm by acupuncture.”
A version of this article first appeared on Medscape.com.
Jon Hislop, MD, PhD, hadn’t been in practice very long before patients began coming to him with requests to order tests that their naturopaths had recommended.
The family physician in North Vancouver, British Columbia, knew little about naturopathy but began researching it.
“I was finding that some of what the naturopaths were telling them was a little odd. Some of the tests they were asking for were unnecessary,” Dr. Hislop said.
The more he learned about naturopathy, the more appalled he became. He eventually took to Twitter, where he wages a campaign against naturopathy and alternative medicine.
“There is no alternative medicine,” he said. “There’s medicine and there’s other stuff. We need to stick to medicine and stay away from the other stuff.”
Dr. Hislop is not alone in his criticism of naturopathic medicine. Professional medical societies almost universally oppose naturopathy, but that has not stopped its spread or prevented it from becoming part of some health care systems.
Americans spent $30.2 billion on out-of-pocket complementary health care, according to a 2016 report from the National Institutes of Health. That includes everything from herbal supplements and massage therapy to chiropractic care.
What is naturopathic medicine?
Naturopathy came to the United States from Germany in the 1800s, but some of its practices are thousands of years old. Naturopathic treatments include homeopathy, IV vitamin infusions, acupuncture, Reiki, and herbal supplements.
Naturopathy is based on the belief that the body has an innate ability to heal itself. It discourages drugs and surgery in favor of supplements, herbs, and other so-called natural treatments. Much of it centers around addressing lifestyle issues and counseling patients to improve their diets, quit smoking, exercise more, lose weight, etc., in order to address the root causes of some health problems.
Practitioners are critical of Western medicine for what they regard as an over-reliance on drugs and technology and for treating symptoms rather than the causes of disease.
“We get a lot of people who are at the end of their ropes, people with hard-to-diagnose diseases who know they are sick but whose labs are normal,” said Jaquel Patterson, ND, former president of the American Association of Naturopathic Physicians (AANP) and medical director of a naturopathic practice in Connecticut.
Separate training and licensing
There are major differences among naturopaths.
At one extreme are unlicensed, self-taught “healers,” who can embrace everything from homeopathy to aromatherapy.
At the other end are naturopathic doctors (NDs), who are more likely to become part of health care systems. These caregivers are trained and licensed, though not by the same institutions as traditional physicians.
To be licensed, NDs must graduate from one of seven accredited naturopathic medical schools in the United States and Canada. In addition to a standard medical curriculum, schools require graduates to complete 4 years of training in clinical nutrition, acupuncture, homeopathic medicine, botanical medicine, physical medicine, and counseling. Medical students intern in clinical settings for 2 years.
NDs are eager to distinguish themselves from their uncredentialed counterparts.
“Some people go to a weekend class and call themselves naturopaths. That’s very concerning. I don’t want those people to be licensed either,” said Hallie Armstrong, ND, who practices in Michigan.
In the United States, there are 6,000 practicing NDs and an unknown number of unlicensed naturopathic healers.
Can naturopaths call themselves ‘physicians’?
Twenty-two states, the District of Columbia, Puerto Rico, and the U.S. Virgin Islands have licensing or registration laws for naturopathic doctors. Three states – South Carolina, Tennessee, and Florida – prohibit practicing naturopathic medicine without a license, according to the AANP.
States that license NDs differ in what they permit them to do.
Nine states allow licensed NDs to use the term “physician,” although this is prohibited in seven states. Most licensed states allow naturopathic practitioners some prescribing authority, including the prescribing of many controlled substances, although only a few states permit full prescribing rights. Most states that license NDs allow them to prescribe and administer nonprescription therapeutic substances, drugs, and therapies.
Twelve states and the District of Columbia allow licensed naturopathic doctors to perform some minor procedures, such as stitching up wounds. Additionally, 13 states allow NDs to order diagnostic tests.
Although the AANP lobbies to get licensure in more states and to expand the activities that NDs can perform, the medical establishment in those states nearly always opposes the legislation, as do national organizations, such as the American Academy of Family Physicians and the American College of Physicians.
“They absolutely will not stop until they get licenses. They’ve done a really good job of selling themselves as legitimate health care professionals to state legislatures,” said David Gorski, MD, PhD, FACS, a surgical oncologist and managing editor of Science-Based Medicine, a blog that attacks unproven medical claims and defends traditional medicine. Naturopathy is a favorite target.
Are naturopaths gaining ground anyway?
Despite the opposition of the medical establishment and many individual health care professionals, a growing number of health care systems are adopting alternative medicine.
In 2018, the AANP stated that 28 prominent health systems, hospitals, and cancer treatment centers had one or more licensed NDs on staff. Among them were Cancer Treatment Centers of America, Cedars-Sinai, Columbia University’s Herbert Irving Comprehensive Cancer Center, and the Fred Hutchinson Cancer Research Center.
Other health care systems may not have NDs on staff but provide naturopathic treatments, usually under the heading of “complementary medicine” or “integrative medicine.” For example, the Cleveland Clinic’s Center for Integrative and Lifestyle Medicine offers acupuncture, Chinese herbal medicine, Reiki, yoga, and culinary medicine.
Critics find this appalling.
“I think it’s a mistake to integrate that kind of practice into a science-based health care setting. If we learned anything over the past year, it’s that medicine based on magical thinking is dangerous,” said Timothy Caulfield, LLM, FCAHS, research director at the Health Law Institute of the University of Alberta, Edmonton.
Dr. Gorski added: “I’m not exactly sure why doctors who should know better have become more accepting of practices that aren’t science-based or are outright quackery.”
Becoming part of the system
Beaumont Health, Michigan’s largest health care system, added integrative medicine in 2006 and hired its first naturopathic practitioners a year later.
The integrative practitioners began in oncology, offering such things as massage therapy, acupuncture, guided imagery, and Reiki. “Very quickly, people outside oncology began saying, ‘I’ve got a cardiology patient who would really benefit from this ... I’ve got a GI patient who could benefit from this...,’” said Maureen Anderson, MD, medical director of Beaumont Integrative Medicine.
Beaumont now offers integrative medicine at three locations. They average 20,000 visits a year and work with 50 to 60 practitioners, many of whom work part-time.
Because Michigan does not license NDs, their scope of practice at Beaumont is limited. They take patient histories, provide advice on nutrition, diet, and exercise, and prescribe herbs and supplements. Beaumont operates its own herbal and supplement pharmacy.
NDs work under the medical supervision of Dr. Anderson, an emergency medicine physician who became interested in naturopathy because she thought traditional medicine doesn’t do a good job of providing care for chronic conditions. Any initial skepticism on the part of the medical staff has been overcome by seeing the benefits naturopathy provides, Dr. Anderson said. The claim is echoed by Mr. Armstrong, an ND who works in the system part-time: “As soon as [doctors] understand our schooling and where we’re coming from and understand that we want to do the same things, then they’re very accepting.”
The University of California, Irvine, health care system has one of the largest naturopathic medicine programs in the country, the result of a $200 million donation in 2017 from a couple who champion alternative medicine. The Susan Samueli Integrative Health Institute includes 28 health care professionals, including MDs, NDs, RNs, acupuncturists, dietitians, yoga instructors, and others. It includes a research arm, which is focused primarily on acupuncture.
The alternative medicine offerings benefit the system, said Kim Hecht, DO, medical director of inpatient and ambulatory services at the Samueli Institute.
“I’m not against traditional medicine, because I think everything has a time and a place,” Dr. Hecht said. However, she rejects the idea that MDs can offer the same holistic approach as NDs.
“Medical science likes to say we’re interested in treating the whole person, but if you look at medical school courses, that’s not what’s being taught,” she said.
The chance to work within a traditional health care system was attractive to Arvin Jenab, ND, medical director of naturopathic medicine at the institute.
“It offers the opportunity to refine our medicine and trim the things that aren’t necessary or are controversial and concentrate on the things at the core of what we do,” he said.
UCI Health practices a conservative model of naturopathy that supports traditional practitioners, Mr. Jenab said.
Is there any harm?
Some patients clearly want what naturopathy offers. So what’s the harm?
Health care systems that integrate alternative medicine legitimize it and lower the overall standard of care, Mr. Caulfield said. Most naturopathy claims are not backed by evidence, and making it available to patients amounts to deceiving them, he said.
“If there’s good science behind it, it’s not going to be alternative medicine; it’s going to be medicine,” Mr. Caulfield said.
Family physician Dr. Hislop said that refusing to order naturopath-recommended tests interferes with his relationships with patients and often requires lengthy conversations to explain the problems with naturopathy.
Naturopathic medicine can deter patients from seeking proven conventional treatments, which can put their health at risk, Dr. Gorski said.
Some naturopaths could potentially be harmful.
In 2017, a California woman died after receiving an IV preparation of curcumin, a chemical constituent in the Indian spice turmeric featured in alternative medicine. The U.S. Food and Drug Administration found that the treating ND mixed the curcumin emulsion product with ungraded castor oil that had a warning label stating: “CAUTION: For manufacturing or laboratory use only.”
Because naturopathic care is generally not covered by insurance, it can also be expensive for patients who pay out of pocket.
Ironically, the mainstream health care system helps create the environment in which naturopathic medicine thrives.
It offers patients a more relaxed and personal alternative to rushed visits with harried doctors scrambling to see the required number of patients in a day. By contrast, an initial visit with an ND might last a leisurely 60 minutes, with 30-minute follow-up appointments.
Mr. Caulfield acknowledged that the relaxed naturopathic approach can be more attractive to patients but said the answer is to reform the current system: “You don’t fix a broken arm by acupuncture.”
A version of this article first appeared on Medscape.com.
Jon Hislop, MD, PhD, hadn’t been in practice very long before patients began coming to him with requests to order tests that their naturopaths had recommended.
The family physician in North Vancouver, British Columbia, knew little about naturopathy but began researching it.
“I was finding that some of what the naturopaths were telling them was a little odd. Some of the tests they were asking for were unnecessary,” Dr. Hislop said.
The more he learned about naturopathy, the more appalled he became. He eventually took to Twitter, where he wages a campaign against naturopathy and alternative medicine.
“There is no alternative medicine,” he said. “There’s medicine and there’s other stuff. We need to stick to medicine and stay away from the other stuff.”
Dr. Hislop is not alone in his criticism of naturopathic medicine. Professional medical societies almost universally oppose naturopathy, but that has not stopped its spread or prevented it from becoming part of some health care systems.
Americans spent $30.2 billion on out-of-pocket complementary health care, according to a 2016 report from the National Institutes of Health. That includes everything from herbal supplements and massage therapy to chiropractic care.
What is naturopathic medicine?
Naturopathy came to the United States from Germany in the 1800s, but some of its practices are thousands of years old. Naturopathic treatments include homeopathy, IV vitamin infusions, acupuncture, Reiki, and herbal supplements.
Naturopathy is based on the belief that the body has an innate ability to heal itself. It discourages drugs and surgery in favor of supplements, herbs, and other so-called natural treatments. Much of it centers around addressing lifestyle issues and counseling patients to improve their diets, quit smoking, exercise more, lose weight, etc., in order to address the root causes of some health problems.
Practitioners are critical of Western medicine for what they regard as an over-reliance on drugs and technology and for treating symptoms rather than the causes of disease.
“We get a lot of people who are at the end of their ropes, people with hard-to-diagnose diseases who know they are sick but whose labs are normal,” said Jaquel Patterson, ND, former president of the American Association of Naturopathic Physicians (AANP) and medical director of a naturopathic practice in Connecticut.
Separate training and licensing
There are major differences among naturopaths.
At one extreme are unlicensed, self-taught “healers,” who can embrace everything from homeopathy to aromatherapy.
At the other end are naturopathic doctors (NDs), who are more likely to become part of health care systems. These caregivers are trained and licensed, though not by the same institutions as traditional physicians.
To be licensed, NDs must graduate from one of seven accredited naturopathic medical schools in the United States and Canada. In addition to a standard medical curriculum, schools require graduates to complete 4 years of training in clinical nutrition, acupuncture, homeopathic medicine, botanical medicine, physical medicine, and counseling. Medical students intern in clinical settings for 2 years.
NDs are eager to distinguish themselves from their uncredentialed counterparts.
“Some people go to a weekend class and call themselves naturopaths. That’s very concerning. I don’t want those people to be licensed either,” said Hallie Armstrong, ND, who practices in Michigan.
In the United States, there are 6,000 practicing NDs and an unknown number of unlicensed naturopathic healers.
Can naturopaths call themselves ‘physicians’?
Twenty-two states, the District of Columbia, Puerto Rico, and the U.S. Virgin Islands have licensing or registration laws for naturopathic doctors. Three states – South Carolina, Tennessee, and Florida – prohibit practicing naturopathic medicine without a license, according to the AANP.
States that license NDs differ in what they permit them to do.
Nine states allow licensed NDs to use the term “physician,” although this is prohibited in seven states. Most licensed states allow naturopathic practitioners some prescribing authority, including the prescribing of many controlled substances, although only a few states permit full prescribing rights. Most states that license NDs allow them to prescribe and administer nonprescription therapeutic substances, drugs, and therapies.
Twelve states and the District of Columbia allow licensed naturopathic doctors to perform some minor procedures, such as stitching up wounds. Additionally, 13 states allow NDs to order diagnostic tests.
Although the AANP lobbies to get licensure in more states and to expand the activities that NDs can perform, the medical establishment in those states nearly always opposes the legislation, as do national organizations, such as the American Academy of Family Physicians and the American College of Physicians.
“They absolutely will not stop until they get licenses. They’ve done a really good job of selling themselves as legitimate health care professionals to state legislatures,” said David Gorski, MD, PhD, FACS, a surgical oncologist and managing editor of Science-Based Medicine, a blog that attacks unproven medical claims and defends traditional medicine. Naturopathy is a favorite target.
Are naturopaths gaining ground anyway?
Despite the opposition of the medical establishment and many individual health care professionals, a growing number of health care systems are adopting alternative medicine.
In 2018, the AANP stated that 28 prominent health systems, hospitals, and cancer treatment centers had one or more licensed NDs on staff. Among them were Cancer Treatment Centers of America, Cedars-Sinai, Columbia University’s Herbert Irving Comprehensive Cancer Center, and the Fred Hutchinson Cancer Research Center.
Other health care systems may not have NDs on staff but provide naturopathic treatments, usually under the heading of “complementary medicine” or “integrative medicine.” For example, the Cleveland Clinic’s Center for Integrative and Lifestyle Medicine offers acupuncture, Chinese herbal medicine, Reiki, yoga, and culinary medicine.
Critics find this appalling.
“I think it’s a mistake to integrate that kind of practice into a science-based health care setting. If we learned anything over the past year, it’s that medicine based on magical thinking is dangerous,” said Timothy Caulfield, LLM, FCAHS, research director at the Health Law Institute of the University of Alberta, Edmonton.
Dr. Gorski added: “I’m not exactly sure why doctors who should know better have become more accepting of practices that aren’t science-based or are outright quackery.”
Becoming part of the system
Beaumont Health, Michigan’s largest health care system, added integrative medicine in 2006 and hired its first naturopathic practitioners a year later.
The integrative practitioners began in oncology, offering such things as massage therapy, acupuncture, guided imagery, and Reiki. “Very quickly, people outside oncology began saying, ‘I’ve got a cardiology patient who would really benefit from this ... I’ve got a GI patient who could benefit from this...,’” said Maureen Anderson, MD, medical director of Beaumont Integrative Medicine.
Beaumont now offers integrative medicine at three locations. They average 20,000 visits a year and work with 50 to 60 practitioners, many of whom work part-time.
Because Michigan does not license NDs, their scope of practice at Beaumont is limited. They take patient histories, provide advice on nutrition, diet, and exercise, and prescribe herbs and supplements. Beaumont operates its own herbal and supplement pharmacy.
NDs work under the medical supervision of Dr. Anderson, an emergency medicine physician who became interested in naturopathy because she thought traditional medicine doesn’t do a good job of providing care for chronic conditions. Any initial skepticism on the part of the medical staff has been overcome by seeing the benefits naturopathy provides, Dr. Anderson said. The claim is echoed by Mr. Armstrong, an ND who works in the system part-time: “As soon as [doctors] understand our schooling and where we’re coming from and understand that we want to do the same things, then they’re very accepting.”
The University of California, Irvine, health care system has one of the largest naturopathic medicine programs in the country, the result of a $200 million donation in 2017 from a couple who champion alternative medicine. The Susan Samueli Integrative Health Institute includes 28 health care professionals, including MDs, NDs, RNs, acupuncturists, dietitians, yoga instructors, and others. It includes a research arm, which is focused primarily on acupuncture.
The alternative medicine offerings benefit the system, said Kim Hecht, DO, medical director of inpatient and ambulatory services at the Samueli Institute.
“I’m not against traditional medicine, because I think everything has a time and a place,” Dr. Hecht said. However, she rejects the idea that MDs can offer the same holistic approach as NDs.
“Medical science likes to say we’re interested in treating the whole person, but if you look at medical school courses, that’s not what’s being taught,” she said.
The chance to work within a traditional health care system was attractive to Arvin Jenab, ND, medical director of naturopathic medicine at the institute.
“It offers the opportunity to refine our medicine and trim the things that aren’t necessary or are controversial and concentrate on the things at the core of what we do,” he said.
UCI Health practices a conservative model of naturopathy that supports traditional practitioners, Mr. Jenab said.
Is there any harm?
Some patients clearly want what naturopathy offers. So what’s the harm?
Health care systems that integrate alternative medicine legitimize it and lower the overall standard of care, Mr. Caulfield said. Most naturopathy claims are not backed by evidence, and making it available to patients amounts to deceiving them, he said.
“If there’s good science behind it, it’s not going to be alternative medicine; it’s going to be medicine,” Mr. Caulfield said.
Family physician Dr. Hislop said that refusing to order naturopath-recommended tests interferes with his relationships with patients and often requires lengthy conversations to explain the problems with naturopathy.
Naturopathic medicine can deter patients from seeking proven conventional treatments, which can put their health at risk, Dr. Gorski said.
Some naturopaths could potentially be harmful.
In 2017, a California woman died after receiving an IV preparation of curcumin, a chemical constituent in the Indian spice turmeric featured in alternative medicine. The U.S. Food and Drug Administration found that the treating ND mixed the curcumin emulsion product with ungraded castor oil that had a warning label stating: “CAUTION: For manufacturing or laboratory use only.”
Because naturopathic care is generally not covered by insurance, it can also be expensive for patients who pay out of pocket.
Ironically, the mainstream health care system helps create the environment in which naturopathic medicine thrives.
It offers patients a more relaxed and personal alternative to rushed visits with harried doctors scrambling to see the required number of patients in a day. By contrast, an initial visit with an ND might last a leisurely 60 minutes, with 30-minute follow-up appointments.
Mr. Caulfield acknowledged that the relaxed naturopathic approach can be more attractive to patients but said the answer is to reform the current system: “You don’t fix a broken arm by acupuncture.”
A version of this article first appeared on Medscape.com.
Doctors prescribe fewer statins in the afternoon
Primary care physicians are more likely to write a prescription for statins for their patients at risk for cardiovascular adverse events in the morning than in the afternoon, new research suggests.
In an observational cohort study, researchers from the nudge unit, University of Pennsylvania, Philadelphia, found that patients who had the first appointments of the day were most likely to have statins prescribed for them, and that this likelihood decreased as the day went on.
The study was published online May 11, 2021, in JAMA Network Open.
“Physicians are faced with decision fatigue, where they are seeing 20 patients in a day and may not have the mental bandwidth or cognitive bandwidth to fully think through every decision for every patient and to make all the appropriate decisions all of the time,” lead author Allison J. Hare, medical student and clinical informatics fellow in the nudge unit, said in an interview.
The Penn Medicine nudge unit attempts to better align clinician decision-making with current standards in best practices for the provision of various therapies, Ms. Hare explained.
“As we see more and more best-practice guidelines come out, we also see that there is a gap in the intention to treat and actual provision of these therapies,” she said. “There are also increasing expectations for clinicians to provide all of these different evidence-backed therapies. It can be hard to keep up with all these guidelines, especially when you are expected to take care of more and more patients, more and more efficiently.”
Guideline-directed statin therapy has been demonstrated to reduce the risk for major adverse cardiovascular events, yet 50% of statin-eligible patients have not been prescribed one.
“In our prior work at the nudge unit, we observed that rates of preventive care, including flu vaccination and cancer screening, declined as the clinic day progressed. We wanted to see if this occurred with statin scripts,” Ms. Hare said.
The researchers obtained data from 28 Penn Medicine primary care practices that included 10,757 patients at risk for heart disease for the period from March 2019 to February 2020.
Their mean age was 66.0 years (standard deviation, 10.5 years), 5,072 (47.2%) were female, and 7,071 (65.7%) were White. Patient characteristics were similar between morning and afternoon appointments.
All patients had clinical atherosclerotic cardiovascular disease, familial hypercholesterolemia, or LDL cholesterol of at least 190 mg/dL, conditions which qualified them for statins based on the U.S. Preventive Services Task Force guidelines.
The appointment times for each patient were broken down into hour blocks, ranging from the 8:00 a.m. hour to the 4:00 p.m. hour, which bookend open times in most practices.
Overall, statins were prescribed in 36% (n = 3,864) of visits.
The data showed a clear decline in statin prescribing as the day went on. For example, compared with patients who came in at 8:00 a.m. (the reference group), patients who came in at 9:00 a.m. were 12% less likely to get a prescription.
Patients coming in for noon appointments were 37% less likely to get a statin prescription, which made them the least likely to get a script. After the noon visits, there was a slight increase, but the likelihood of a statin prescription remained 27% less likely or worse for the rest of the day.
“In the context of the myriad tasks that clinicians are faced with doing for a single patient, and then also within the context of seeing 20 patients in 15-minute increments, it is easy to see how certain things fall through the cracks,” Ms. Hare said. “It’s impossible for any clinician to remember every single little thing for their patient every single time, so if we can augment the clinician’s ability to make those appropriate decisions with electronic tools, we can narrow that gap a little bit.”
Why the variability?
“The nudge unit uses prompts to ask the physician about prescribing statins. The question is, what is causing the variability in statin prescriptions?” Nieca Goldberg, MD, medical director of the New York University women’s heart program, said in an interview.
“Is it fatigue, lack of familiarity of guidelines, or is this due to the volume of patients and lack of time to discuss the therapy and make a shared decision with their patient? The answer to these questions was not part of the study,” said Dr. Goldberg, who is also an American Heart Association volunteer expert. “It would be interesting to know the thoughts of the physicians who were studied after they were informed of the results. Also, having a nudge to write the prescription will increase the prescriptions of statins, but will patients take the medication?”
The study was funded in part by a grant from the National Institute on Aging. Ms. Hare and Dr. Goldberg reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Primary care physicians are more likely to write a prescription for statins for their patients at risk for cardiovascular adverse events in the morning than in the afternoon, new research suggests.
In an observational cohort study, researchers from the nudge unit, University of Pennsylvania, Philadelphia, found that patients who had the first appointments of the day were most likely to have statins prescribed for them, and that this likelihood decreased as the day went on.
The study was published online May 11, 2021, in JAMA Network Open.
“Physicians are faced with decision fatigue, where they are seeing 20 patients in a day and may not have the mental bandwidth or cognitive bandwidth to fully think through every decision for every patient and to make all the appropriate decisions all of the time,” lead author Allison J. Hare, medical student and clinical informatics fellow in the nudge unit, said in an interview.
The Penn Medicine nudge unit attempts to better align clinician decision-making with current standards in best practices for the provision of various therapies, Ms. Hare explained.
“As we see more and more best-practice guidelines come out, we also see that there is a gap in the intention to treat and actual provision of these therapies,” she said. “There are also increasing expectations for clinicians to provide all of these different evidence-backed therapies. It can be hard to keep up with all these guidelines, especially when you are expected to take care of more and more patients, more and more efficiently.”
Guideline-directed statin therapy has been demonstrated to reduce the risk for major adverse cardiovascular events, yet 50% of statin-eligible patients have not been prescribed one.
“In our prior work at the nudge unit, we observed that rates of preventive care, including flu vaccination and cancer screening, declined as the clinic day progressed. We wanted to see if this occurred with statin scripts,” Ms. Hare said.
The researchers obtained data from 28 Penn Medicine primary care practices that included 10,757 patients at risk for heart disease for the period from March 2019 to February 2020.
Their mean age was 66.0 years (standard deviation, 10.5 years), 5,072 (47.2%) were female, and 7,071 (65.7%) were White. Patient characteristics were similar between morning and afternoon appointments.
All patients had clinical atherosclerotic cardiovascular disease, familial hypercholesterolemia, or LDL cholesterol of at least 190 mg/dL, conditions which qualified them for statins based on the U.S. Preventive Services Task Force guidelines.
The appointment times for each patient were broken down into hour blocks, ranging from the 8:00 a.m. hour to the 4:00 p.m. hour, which bookend open times in most practices.
Overall, statins were prescribed in 36% (n = 3,864) of visits.
The data showed a clear decline in statin prescribing as the day went on. For example, compared with patients who came in at 8:00 a.m. (the reference group), patients who came in at 9:00 a.m. were 12% less likely to get a prescription.
Patients coming in for noon appointments were 37% less likely to get a statin prescription, which made them the least likely to get a script. After the noon visits, there was a slight increase, but the likelihood of a statin prescription remained 27% less likely or worse for the rest of the day.
“In the context of the myriad tasks that clinicians are faced with doing for a single patient, and then also within the context of seeing 20 patients in 15-minute increments, it is easy to see how certain things fall through the cracks,” Ms. Hare said. “It’s impossible for any clinician to remember every single little thing for their patient every single time, so if we can augment the clinician’s ability to make those appropriate decisions with electronic tools, we can narrow that gap a little bit.”
Why the variability?
“The nudge unit uses prompts to ask the physician about prescribing statins. The question is, what is causing the variability in statin prescriptions?” Nieca Goldberg, MD, medical director of the New York University women’s heart program, said in an interview.
“Is it fatigue, lack of familiarity of guidelines, or is this due to the volume of patients and lack of time to discuss the therapy and make a shared decision with their patient? The answer to these questions was not part of the study,” said Dr. Goldberg, who is also an American Heart Association volunteer expert. “It would be interesting to know the thoughts of the physicians who were studied after they were informed of the results. Also, having a nudge to write the prescription will increase the prescriptions of statins, but will patients take the medication?”
The study was funded in part by a grant from the National Institute on Aging. Ms. Hare and Dr. Goldberg reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Primary care physicians are more likely to write a prescription for statins for their patients at risk for cardiovascular adverse events in the morning than in the afternoon, new research suggests.
In an observational cohort study, researchers from the nudge unit, University of Pennsylvania, Philadelphia, found that patients who had the first appointments of the day were most likely to have statins prescribed for them, and that this likelihood decreased as the day went on.
The study was published online May 11, 2021, in JAMA Network Open.
“Physicians are faced with decision fatigue, where they are seeing 20 patients in a day and may not have the mental bandwidth or cognitive bandwidth to fully think through every decision for every patient and to make all the appropriate decisions all of the time,” lead author Allison J. Hare, medical student and clinical informatics fellow in the nudge unit, said in an interview.
The Penn Medicine nudge unit attempts to better align clinician decision-making with current standards in best practices for the provision of various therapies, Ms. Hare explained.
“As we see more and more best-practice guidelines come out, we also see that there is a gap in the intention to treat and actual provision of these therapies,” she said. “There are also increasing expectations for clinicians to provide all of these different evidence-backed therapies. It can be hard to keep up with all these guidelines, especially when you are expected to take care of more and more patients, more and more efficiently.”
Guideline-directed statin therapy has been demonstrated to reduce the risk for major adverse cardiovascular events, yet 50% of statin-eligible patients have not been prescribed one.
“In our prior work at the nudge unit, we observed that rates of preventive care, including flu vaccination and cancer screening, declined as the clinic day progressed. We wanted to see if this occurred with statin scripts,” Ms. Hare said.
The researchers obtained data from 28 Penn Medicine primary care practices that included 10,757 patients at risk for heart disease for the period from March 2019 to February 2020.
Their mean age was 66.0 years (standard deviation, 10.5 years), 5,072 (47.2%) were female, and 7,071 (65.7%) were White. Patient characteristics were similar between morning and afternoon appointments.
All patients had clinical atherosclerotic cardiovascular disease, familial hypercholesterolemia, or LDL cholesterol of at least 190 mg/dL, conditions which qualified them for statins based on the U.S. Preventive Services Task Force guidelines.
The appointment times for each patient were broken down into hour blocks, ranging from the 8:00 a.m. hour to the 4:00 p.m. hour, which bookend open times in most practices.
Overall, statins were prescribed in 36% (n = 3,864) of visits.
The data showed a clear decline in statin prescribing as the day went on. For example, compared with patients who came in at 8:00 a.m. (the reference group), patients who came in at 9:00 a.m. were 12% less likely to get a prescription.
Patients coming in for noon appointments were 37% less likely to get a statin prescription, which made them the least likely to get a script. After the noon visits, there was a slight increase, but the likelihood of a statin prescription remained 27% less likely or worse for the rest of the day.
“In the context of the myriad tasks that clinicians are faced with doing for a single patient, and then also within the context of seeing 20 patients in 15-minute increments, it is easy to see how certain things fall through the cracks,” Ms. Hare said. “It’s impossible for any clinician to remember every single little thing for their patient every single time, so if we can augment the clinician’s ability to make those appropriate decisions with electronic tools, we can narrow that gap a little bit.”
Why the variability?
“The nudge unit uses prompts to ask the physician about prescribing statins. The question is, what is causing the variability in statin prescriptions?” Nieca Goldberg, MD, medical director of the New York University women’s heart program, said in an interview.
“Is it fatigue, lack of familiarity of guidelines, or is this due to the volume of patients and lack of time to discuss the therapy and make a shared decision with their patient? The answer to these questions was not part of the study,” said Dr. Goldberg, who is also an American Heart Association volunteer expert. “It would be interesting to know the thoughts of the physicians who were studied after they were informed of the results. Also, having a nudge to write the prescription will increase the prescriptions of statins, but will patients take the medication?”
The study was funded in part by a grant from the National Institute on Aging. Ms. Hare and Dr. Goldberg reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Online patient reviews and HIPAA
In 2013, a California hospital paid $275,000 to settle claims that it violated the HIPAA privacy rule when it disclosed a patient’s health information in response to a negative online review. More recently, a Texas dental practice paid a substantial fine to the Department of Health & Human Services, which enforces HIPAA, after it responded to unfavorable Yelp reviews with patient names and details of their health conditions, treatment plans, and cost information. In addition to the fine, the practice agreed to 2 years of monitoring by HHS for compliance with HIPAA rules.
Most physicians have had the unpleasant experience of finding a negative online review from a disgruntled patient or family member. Some are justified, many are not; either way, your first impulse will often be to post a response – but that is almost always a bad idea. “Social media is not the place for providers to discuss a patient’s care,” an HHS official said in a statement issued about the dental practice case in 2016. “Doctors and dentists must think carefully about patient privacy before responding to online reviews.”
Any information that could be used to identify a patient is a HIPAA breach. This is true even if the patient has already disclosed information, because doing so does not nullify their HIPAA rights, and HIPAA provides no exceptions for responses. Even acknowledging that the reviewer was in fact your patient could, in some cases, be considered a violation.
Responding to good reviews can get you in trouble too, for the same reasons. In 2016, a physical therapy practice paid a $25,000 fine after it posted patient testimonials, “including full names and full-face photographic images to its website without obtaining valid, HIPAA-compliant authorizations.”
And by the way, most malpractice policies specifically exclude disciplinary fines and settlements from coverage.
All of that said,
- Ignore them. This is your best choice most of the time. Most negative reviews have minimal impact and simply do not deserve a response; responding may pour fuel on the fire. Besides, an occasional negative review actually lends credibility to a reviewing site and to the positive reviews posted on that site. Polls show that readers are suspicious of sites that contain only rave reviews. They assume such reviews have been “whitewashed” – or just fabricated.
- Solicit more reviews to that site. The more you can obtain, the less impact any complaints will have, since you know the overwhelming majority of your patients are happy with your care and will post a positive review if asked. Solicit them on your website, on social media, or in your email reminders. To be clear, you must encourage reviews from all patients, whether they have had a positive experience or not. If you invite only the satisfied ones, you are “filtering,” which can be perceived as false or deceptive advertising. (Google calls it “review-gating,” and according to their guidelines, if they catch you doing it they will remove all of your reviews.)
- Respond politely. In those rare cases where you feel you must respond, do so without acknowledging that the individual was a patient, or disclosing any information that may be linked to the patient. For example, you can say that you provide excellent and appropriate care, or describe your general policies. Be polite, professional, and sensitive to the patient’s position. Readers tend to respect and sympathize with a doctor who responds in a professional, respectful manner and does not trash the complainant in retaliation.
- Take the discussion offline. Sometimes the person posting the review is just frustrated and wants to be heard. In those cases, consider contacting the patient and offering to discuss their concerns privately. If you cannot resolve your differences, try to get the patient’s written permission to post a response to their review. If they refuse, you can explain that, thereby capturing the moral high ground.
If the review contains false or defamatory content, that’s a different situation entirely; you will probably need to consult your attorney.
Regardless of how you handle negative reviews, be sure to learn from them. Your critics, as the song goes, are not always evil – and not always wrong. Complaints give you a chance to review your office policies and procedures and your own conduct, identify weaknesses, and make changes as necessary. At the very least, the exercise will help you to avoid similar complaints in the future. Don’t let valuable opportunities like that pass you by.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@frontlinemedcom.com.
In 2013, a California hospital paid $275,000 to settle claims that it violated the HIPAA privacy rule when it disclosed a patient’s health information in response to a negative online review. More recently, a Texas dental practice paid a substantial fine to the Department of Health & Human Services, which enforces HIPAA, after it responded to unfavorable Yelp reviews with patient names and details of their health conditions, treatment plans, and cost information. In addition to the fine, the practice agreed to 2 years of monitoring by HHS for compliance with HIPAA rules.
Most physicians have had the unpleasant experience of finding a negative online review from a disgruntled patient or family member. Some are justified, many are not; either way, your first impulse will often be to post a response – but that is almost always a bad idea. “Social media is not the place for providers to discuss a patient’s care,” an HHS official said in a statement issued about the dental practice case in 2016. “Doctors and dentists must think carefully about patient privacy before responding to online reviews.”
Any information that could be used to identify a patient is a HIPAA breach. This is true even if the patient has already disclosed information, because doing so does not nullify their HIPAA rights, and HIPAA provides no exceptions for responses. Even acknowledging that the reviewer was in fact your patient could, in some cases, be considered a violation.
Responding to good reviews can get you in trouble too, for the same reasons. In 2016, a physical therapy practice paid a $25,000 fine after it posted patient testimonials, “including full names and full-face photographic images to its website without obtaining valid, HIPAA-compliant authorizations.”
And by the way, most malpractice policies specifically exclude disciplinary fines and settlements from coverage.
All of that said,
- Ignore them. This is your best choice most of the time. Most negative reviews have minimal impact and simply do not deserve a response; responding may pour fuel on the fire. Besides, an occasional negative review actually lends credibility to a reviewing site and to the positive reviews posted on that site. Polls show that readers are suspicious of sites that contain only rave reviews. They assume such reviews have been “whitewashed” – or just fabricated.
- Solicit more reviews to that site. The more you can obtain, the less impact any complaints will have, since you know the overwhelming majority of your patients are happy with your care and will post a positive review if asked. Solicit them on your website, on social media, or in your email reminders. To be clear, you must encourage reviews from all patients, whether they have had a positive experience or not. If you invite only the satisfied ones, you are “filtering,” which can be perceived as false or deceptive advertising. (Google calls it “review-gating,” and according to their guidelines, if they catch you doing it they will remove all of your reviews.)
- Respond politely. In those rare cases where you feel you must respond, do so without acknowledging that the individual was a patient, or disclosing any information that may be linked to the patient. For example, you can say that you provide excellent and appropriate care, or describe your general policies. Be polite, professional, and sensitive to the patient’s position. Readers tend to respect and sympathize with a doctor who responds in a professional, respectful manner and does not trash the complainant in retaliation.
- Take the discussion offline. Sometimes the person posting the review is just frustrated and wants to be heard. In those cases, consider contacting the patient and offering to discuss their concerns privately. If you cannot resolve your differences, try to get the patient’s written permission to post a response to their review. If they refuse, you can explain that, thereby capturing the moral high ground.
If the review contains false or defamatory content, that’s a different situation entirely; you will probably need to consult your attorney.
Regardless of how you handle negative reviews, be sure to learn from them. Your critics, as the song goes, are not always evil – and not always wrong. Complaints give you a chance to review your office policies and procedures and your own conduct, identify weaknesses, and make changes as necessary. At the very least, the exercise will help you to avoid similar complaints in the future. Don’t let valuable opportunities like that pass you by.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@frontlinemedcom.com.
In 2013, a California hospital paid $275,000 to settle claims that it violated the HIPAA privacy rule when it disclosed a patient’s health information in response to a negative online review. More recently, a Texas dental practice paid a substantial fine to the Department of Health & Human Services, which enforces HIPAA, after it responded to unfavorable Yelp reviews with patient names and details of their health conditions, treatment plans, and cost information. In addition to the fine, the practice agreed to 2 years of monitoring by HHS for compliance with HIPAA rules.
Most physicians have had the unpleasant experience of finding a negative online review from a disgruntled patient or family member. Some are justified, many are not; either way, your first impulse will often be to post a response – but that is almost always a bad idea. “Social media is not the place for providers to discuss a patient’s care,” an HHS official said in a statement issued about the dental practice case in 2016. “Doctors and dentists must think carefully about patient privacy before responding to online reviews.”
Any information that could be used to identify a patient is a HIPAA breach. This is true even if the patient has already disclosed information, because doing so does not nullify their HIPAA rights, and HIPAA provides no exceptions for responses. Even acknowledging that the reviewer was in fact your patient could, in some cases, be considered a violation.
Responding to good reviews can get you in trouble too, for the same reasons. In 2016, a physical therapy practice paid a $25,000 fine after it posted patient testimonials, “including full names and full-face photographic images to its website without obtaining valid, HIPAA-compliant authorizations.”
And by the way, most malpractice policies specifically exclude disciplinary fines and settlements from coverage.
All of that said,
- Ignore them. This is your best choice most of the time. Most negative reviews have minimal impact and simply do not deserve a response; responding may pour fuel on the fire. Besides, an occasional negative review actually lends credibility to a reviewing site and to the positive reviews posted on that site. Polls show that readers are suspicious of sites that contain only rave reviews. They assume such reviews have been “whitewashed” – or just fabricated.
- Solicit more reviews to that site. The more you can obtain, the less impact any complaints will have, since you know the overwhelming majority of your patients are happy with your care and will post a positive review if asked. Solicit them on your website, on social media, or in your email reminders. To be clear, you must encourage reviews from all patients, whether they have had a positive experience or not. If you invite only the satisfied ones, you are “filtering,” which can be perceived as false or deceptive advertising. (Google calls it “review-gating,” and according to their guidelines, if they catch you doing it they will remove all of your reviews.)
- Respond politely. In those rare cases where you feel you must respond, do so without acknowledging that the individual was a patient, or disclosing any information that may be linked to the patient. For example, you can say that you provide excellent and appropriate care, or describe your general policies. Be polite, professional, and sensitive to the patient’s position. Readers tend to respect and sympathize with a doctor who responds in a professional, respectful manner and does not trash the complainant in retaliation.
- Take the discussion offline. Sometimes the person posting the review is just frustrated and wants to be heard. In those cases, consider contacting the patient and offering to discuss their concerns privately. If you cannot resolve your differences, try to get the patient’s written permission to post a response to their review. If they refuse, you can explain that, thereby capturing the moral high ground.
If the review contains false or defamatory content, that’s a different situation entirely; you will probably need to consult your attorney.
Regardless of how you handle negative reviews, be sure to learn from them. Your critics, as the song goes, are not always evil – and not always wrong. Complaints give you a chance to review your office policies and procedures and your own conduct, identify weaknesses, and make changes as necessary. At the very least, the exercise will help you to avoid similar complaints in the future. Don’t let valuable opportunities like that pass you by.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@frontlinemedcom.com.
HHS prohibits discrimination against LGBTQ patients: Action reverses Trump-era policy
The Biden administration is reversing a Trump-era policy that allowed health care providers to bar services to lesbian, gay, bisexual, transgender, or queer (LGBTQ) patients.
The U.S. Department of Health and Human Services gave notice on Monday that it would interpret the Affordable Care Act’s Section 1557 – which bars discrimination on the basis of sex – to include discrimination on the basis of sexual orientation or gender identity. The department said its position is consistent with a June 2020 U.S. Supreme Court ruling in Bostock v. Clayton County, GA. The ruling determined that the Civil Rights Act’s prohibition of employment discrimination on the basis of sex includes sexual orientation and gender identity.
“The mission of our Department is to enhance the health and well-being of all Americans, no matter their gender identity or sexual orientation,” said HHS Assistant Secretary for Health Rachel Levine, MD, in a statement released Monday.
“All people need access to health care services to fix a broken bone, protect their heart health, and screen for cancer risk,” she said. “No one should be discriminated against when seeking medical services because of who they are.”
Many physician organizations applauded the decision.
“The Biden administration did the right thing by terminating a short-lived effort to allow discrimination based on gender or sexual orientation when seeking health care,” said Susan R. Bailey, MD, president of the American Medical Association, in a statement.
When, in 2019, the Trump administration proposed to allow providers to deny care to LGBTQ people, the AMA said in a letter to the HHS that its interpretation “was contrary to the intent and the plain language of the law.”
Now, said Bailey, the AMA welcomes the Biden administration’s interpretation. It “is a victory for health equity and ends a dismal chapter in which a federal agency sought to remove civil rights protections,” she said.
An alliance of patient groups – including the American Cancer Society, the American Cancer Society Cancer Action Network, the American Heart Association, the American Lung Association, the Epilepsy Foundation, the National Multiple Sclerosis Society, and the National Organization for Rare Disorders – also applauded the new policy. “This community already faces significant health disparities,” the groups noted in a statement. People with chronic illness such as HIV and cancer “need to be able to access care quickly and without fear of discrimination,” they said.
The groups had filed a friend of the court brief in a case against the Trump administration rule.
“We welcome this positive step to ensure access is preserved without hindrance, as intended by the health care law,” they said.
Twenty-two states and Washington, D.C. – led by former California Attorney General Xavier Becerra, who is now HHS secretary – sued the Trump administration in July 2020, aiming to overturn the rule.
Chase Strangio, deputy director for Trans Justice with the American Civil Liberties Union LGBTQ & HIV Project, noted that the HHS announcement was crucial in the face of efforts in multiple states to bar health care for transgender youth. “The Biden administration has affirmed what courts have said for decades: Discrimination against LGBTQ people is against the law. It also affirms what transgender people have long said: Gender-affirming care is life-saving care,” he said in a statement.
Lambda Legal, which led another lawsuit against the Trump administration rule, said it welcomed the HHS action but noted in a statement by the organization’s senior attorney, Omar Gonzalez-Pagan, that it “does not address significant aspects of the Trump-era rule that we and others have challenged in court.”
The Trump rule also “limited the remedies available to people who face health disparities, limited access to health care for people with Limited English Proficiency, unlawfully incorporated religious exemptions, and dramatically reduced the number of health care entities and insurance subject to the rule, all of which today’s action does not address,” said Gonzalez-Pagan.
“We encourage Secretary Xavier Becerra and the Biden administration to take additional steps to ensure that all LGBTQ people are completely covered wherever and whenever they may encounter discrimination during some of the most delicate and precarious moments of their lives: When seeking health care,” he said.
A version of this article first appeared on Medscape.com.
The Biden administration is reversing a Trump-era policy that allowed health care providers to bar services to lesbian, gay, bisexual, transgender, or queer (LGBTQ) patients.
The U.S. Department of Health and Human Services gave notice on Monday that it would interpret the Affordable Care Act’s Section 1557 – which bars discrimination on the basis of sex – to include discrimination on the basis of sexual orientation or gender identity. The department said its position is consistent with a June 2020 U.S. Supreme Court ruling in Bostock v. Clayton County, GA. The ruling determined that the Civil Rights Act’s prohibition of employment discrimination on the basis of sex includes sexual orientation and gender identity.
“The mission of our Department is to enhance the health and well-being of all Americans, no matter their gender identity or sexual orientation,” said HHS Assistant Secretary for Health Rachel Levine, MD, in a statement released Monday.
“All people need access to health care services to fix a broken bone, protect their heart health, and screen for cancer risk,” she said. “No one should be discriminated against when seeking medical services because of who they are.”
Many physician organizations applauded the decision.
“The Biden administration did the right thing by terminating a short-lived effort to allow discrimination based on gender or sexual orientation when seeking health care,” said Susan R. Bailey, MD, president of the American Medical Association, in a statement.
When, in 2019, the Trump administration proposed to allow providers to deny care to LGBTQ people, the AMA said in a letter to the HHS that its interpretation “was contrary to the intent and the plain language of the law.”
Now, said Bailey, the AMA welcomes the Biden administration’s interpretation. It “is a victory for health equity and ends a dismal chapter in which a federal agency sought to remove civil rights protections,” she said.
An alliance of patient groups – including the American Cancer Society, the American Cancer Society Cancer Action Network, the American Heart Association, the American Lung Association, the Epilepsy Foundation, the National Multiple Sclerosis Society, and the National Organization for Rare Disorders – also applauded the new policy. “This community already faces significant health disparities,” the groups noted in a statement. People with chronic illness such as HIV and cancer “need to be able to access care quickly and without fear of discrimination,” they said.
The groups had filed a friend of the court brief in a case against the Trump administration rule.
“We welcome this positive step to ensure access is preserved without hindrance, as intended by the health care law,” they said.
Twenty-two states and Washington, D.C. – led by former California Attorney General Xavier Becerra, who is now HHS secretary – sued the Trump administration in July 2020, aiming to overturn the rule.
Chase Strangio, deputy director for Trans Justice with the American Civil Liberties Union LGBTQ & HIV Project, noted that the HHS announcement was crucial in the face of efforts in multiple states to bar health care for transgender youth. “The Biden administration has affirmed what courts have said for decades: Discrimination against LGBTQ people is against the law. It also affirms what transgender people have long said: Gender-affirming care is life-saving care,” he said in a statement.
Lambda Legal, which led another lawsuit against the Trump administration rule, said it welcomed the HHS action but noted in a statement by the organization’s senior attorney, Omar Gonzalez-Pagan, that it “does not address significant aspects of the Trump-era rule that we and others have challenged in court.”
The Trump rule also “limited the remedies available to people who face health disparities, limited access to health care for people with Limited English Proficiency, unlawfully incorporated religious exemptions, and dramatically reduced the number of health care entities and insurance subject to the rule, all of which today’s action does not address,” said Gonzalez-Pagan.
“We encourage Secretary Xavier Becerra and the Biden administration to take additional steps to ensure that all LGBTQ people are completely covered wherever and whenever they may encounter discrimination during some of the most delicate and precarious moments of their lives: When seeking health care,” he said.
A version of this article first appeared on Medscape.com.
The Biden administration is reversing a Trump-era policy that allowed health care providers to bar services to lesbian, gay, bisexual, transgender, or queer (LGBTQ) patients.
The U.S. Department of Health and Human Services gave notice on Monday that it would interpret the Affordable Care Act’s Section 1557 – which bars discrimination on the basis of sex – to include discrimination on the basis of sexual orientation or gender identity. The department said its position is consistent with a June 2020 U.S. Supreme Court ruling in Bostock v. Clayton County, GA. The ruling determined that the Civil Rights Act’s prohibition of employment discrimination on the basis of sex includes sexual orientation and gender identity.
“The mission of our Department is to enhance the health and well-being of all Americans, no matter their gender identity or sexual orientation,” said HHS Assistant Secretary for Health Rachel Levine, MD, in a statement released Monday.
“All people need access to health care services to fix a broken bone, protect their heart health, and screen for cancer risk,” she said. “No one should be discriminated against when seeking medical services because of who they are.”
Many physician organizations applauded the decision.
“The Biden administration did the right thing by terminating a short-lived effort to allow discrimination based on gender or sexual orientation when seeking health care,” said Susan R. Bailey, MD, president of the American Medical Association, in a statement.
When, in 2019, the Trump administration proposed to allow providers to deny care to LGBTQ people, the AMA said in a letter to the HHS that its interpretation “was contrary to the intent and the plain language of the law.”
Now, said Bailey, the AMA welcomes the Biden administration’s interpretation. It “is a victory for health equity and ends a dismal chapter in which a federal agency sought to remove civil rights protections,” she said.
An alliance of patient groups – including the American Cancer Society, the American Cancer Society Cancer Action Network, the American Heart Association, the American Lung Association, the Epilepsy Foundation, the National Multiple Sclerosis Society, and the National Organization for Rare Disorders – also applauded the new policy. “This community already faces significant health disparities,” the groups noted in a statement. People with chronic illness such as HIV and cancer “need to be able to access care quickly and without fear of discrimination,” they said.
The groups had filed a friend of the court brief in a case against the Trump administration rule.
“We welcome this positive step to ensure access is preserved without hindrance, as intended by the health care law,” they said.
Twenty-two states and Washington, D.C. – led by former California Attorney General Xavier Becerra, who is now HHS secretary – sued the Trump administration in July 2020, aiming to overturn the rule.
Chase Strangio, deputy director for Trans Justice with the American Civil Liberties Union LGBTQ & HIV Project, noted that the HHS announcement was crucial in the face of efforts in multiple states to bar health care for transgender youth. “The Biden administration has affirmed what courts have said for decades: Discrimination against LGBTQ people is against the law. It also affirms what transgender people have long said: Gender-affirming care is life-saving care,” he said in a statement.
Lambda Legal, which led another lawsuit against the Trump administration rule, said it welcomed the HHS action but noted in a statement by the organization’s senior attorney, Omar Gonzalez-Pagan, that it “does not address significant aspects of the Trump-era rule that we and others have challenged in court.”
The Trump rule also “limited the remedies available to people who face health disparities, limited access to health care for people with Limited English Proficiency, unlawfully incorporated religious exemptions, and dramatically reduced the number of health care entities and insurance subject to the rule, all of which today’s action does not address,” said Gonzalez-Pagan.
“We encourage Secretary Xavier Becerra and the Biden administration to take additional steps to ensure that all LGBTQ people are completely covered wherever and whenever they may encounter discrimination during some of the most delicate and precarious moments of their lives: When seeking health care,” he said.
A version of this article first appeared on Medscape.com.
How I got started in advocacy
Rheumatology News and the Coalition of State Rheumatology Organizations have partnered together to keep rheumatologists regularly informed on the advocacy issues of the day and perhaps inspire those who may be on the fence about finding “room” in their lives for action. This inaugural piece tells how CSRO President Dr. Madelaine (Mattie) A. Feldman views advocacy and how she found her way to action.
As a rheumatologist in private practice for 30 years, with husband and kids (and now grandkids), an active social life, and an exercise regimen, I realized if I were to become active in advocacy I would have to make room for it in my busy schedule. We all come up against the question of where will we find the time for a new hobby, exercise, joining a new organization, or even just eating right? Next comes the priority list discussion. How important is advocacy for my patients, my specialty, and my profession? Ultimately, how important is it for me? Where did that desire to get involved even come from? Why have I become so passionate about the issues?
For me, the answer to these questions goes back to the 1960s when I was growing up in New Orleans. My mom participated in civil rights protests, which did not make our family popular in the neighborhood, back when the KKK put flyers on everyone’s screen door. My mother didn’t care and told me that, no matter what people said, it was our duty to stand up for what was right. That was a long time ago and sadly my mom passed away just a year after I was old enough to vote. Her words have stayed with me and are more important now than ever.
Striving for justice despite how formidable the foe is requires an inner knowing that what you are doing is meaningful and will make a difference maybe not now, maybe not next year. At some point you must believe that your efforts will create a change for the better, small as it may be. My “saying” on Twitter (@MattieRheumMD) is “I’ll keep doing what I’m doing until my cynicism catches up to my passion.”
The story about my mom is just one of the many stories in my life taking me to where I am today. We all have them. I think the reason many of us go into rheumatology may be similar to the reasoning that leads one to advocacy efforts. At this point in time we can’t yet offer a cure, but we can point to a path that leads to improvements in the lives of our patients. I have to remind myself of that, every time there is an advocacy battle ahead, whether with insurance companies or the government ... increments are important.
The four Ps of advocacy
Living with compromise is hard, particularly when working within a system that needs a complete overhaul. Still, compromise is the key to getting anything done. Compromise is one of the four Ps of advocacy. I realize that compromise doesn’t start with a P, but it is such an integral part of advocacy, I am making allowances for it. The other Ps include patience, persistence/perseverance, and passion. I’m sure there are many others that could be part of the P family, like planning and performance, but let’s stick with these.
You don’t need to have all of these qualities when you start on the road to action in advocacy. For example, my passion came first. It developed when my patients could not get access to the treatments they needed. For many reasons, the medications were either unavailable (i.e., not on formulary, tiered very high) or unaffordable (i.e., copay too high, deductible too high). My passion deepened when I saw the hypocrisy within the drug-supply channel and the mistruths being told by those who profit from this channel. It wasn’t the “profit” part that bothered me, as I’m a believer in the free market. But this was not free market, and the companies were actually profiteering on the backs of my patients and justifying it by claiming they were saving the health care system billions of dollars. The fallacy of that claim and the players in this broken system are stories for another day.
Persistence came next for me. If you let up on the message, things might not only stay the same but could get worse. Perseverance is part of persistence because you need it to keep knocking on the same door even after that door is metaphorically (hopefully not literally) slammed in your face. Often, I will feel like a broken record and think that everyone has already heard the issues, not only from me but also from my fellow advocates. But never underestimate how many times a message, particularly on a difficult issue to understand, needs to be heard before it is fully comprehended.
Patience is one of the more difficult attributes to practice when you want action. I want things to happen yesterday – not tomorrow and definitely not next year. I have learned that the wheels of change turn quite slowly in this arena, sometimes pausing for inordinately long periods of time. I realize now that during the long wait, new facts can arise, allowing me to shape a different advocacy approach, one that ultimately bolsters my case. It still is very difficult to hear that a piece of legislation that seemed to be moving forward suddenly died and won’t be heard again until the next session. With patience you move forward with a smile, maybe a half-hearted one, but a smile nonetheless. This just makes life better.
Then there is compromise. This took me the longest to understand, particularly on the issues where my passion ran the deepest. Here is where passion could potentially get in the way of action. Feeling very strongly about an issue makes it difficult to let any piece of your ideal end result fall by the wayside. Here is where the saying “the perfect is the enemy of the good” comes into play. Just because you can’t have it all, doesn’t mean you can’t do good by achieving just part of what you have been striving for. Remember if you seek perfection, without compromise, you may lose the entire battle. Is there such a thing as compromising too much? I think so, but that may just be my passion speaking.
Rheumatology News and the Coalition of State Rheumatology Organizations started this column to keep you informed about current advocacy issues in rheumatology and perhaps inspire those who may be on the fence about finding “room” in their lives for action.
Advocacy doesn’t have to take up much room in your life. It can be as simple as clicking on CSRO.info/map, finding your state, and taking action by writing a letter to your representative on an important piece of legislation, like an accumulator adjustment ban (lots more on that in future columns). Or maybe just finding the time to read this column is all the action you have room for. We all have different amounts of space for any particular activity in our busy lives. It seems one of my stories from childhood created that space for advocacy in my life. I guess you could say it created a “Rheum” for Action.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is President of the CSRO, chair of the Alliance for Safe Biologic Medicines, and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at rhnews@mdedge.com.
Rheumatology News and the Coalition of State Rheumatology Organizations have partnered together to keep rheumatologists regularly informed on the advocacy issues of the day and perhaps inspire those who may be on the fence about finding “room” in their lives for action. This inaugural piece tells how CSRO President Dr. Madelaine (Mattie) A. Feldman views advocacy and how she found her way to action.
As a rheumatologist in private practice for 30 years, with husband and kids (and now grandkids), an active social life, and an exercise regimen, I realized if I were to become active in advocacy I would have to make room for it in my busy schedule. We all come up against the question of where will we find the time for a new hobby, exercise, joining a new organization, or even just eating right? Next comes the priority list discussion. How important is advocacy for my patients, my specialty, and my profession? Ultimately, how important is it for me? Where did that desire to get involved even come from? Why have I become so passionate about the issues?
For me, the answer to these questions goes back to the 1960s when I was growing up in New Orleans. My mom participated in civil rights protests, which did not make our family popular in the neighborhood, back when the KKK put flyers on everyone’s screen door. My mother didn’t care and told me that, no matter what people said, it was our duty to stand up for what was right. That was a long time ago and sadly my mom passed away just a year after I was old enough to vote. Her words have stayed with me and are more important now than ever.
Striving for justice despite how formidable the foe is requires an inner knowing that what you are doing is meaningful and will make a difference maybe not now, maybe not next year. At some point you must believe that your efforts will create a change for the better, small as it may be. My “saying” on Twitter (@MattieRheumMD) is “I’ll keep doing what I’m doing until my cynicism catches up to my passion.”
The story about my mom is just one of the many stories in my life taking me to where I am today. We all have them. I think the reason many of us go into rheumatology may be similar to the reasoning that leads one to advocacy efforts. At this point in time we can’t yet offer a cure, but we can point to a path that leads to improvements in the lives of our patients. I have to remind myself of that, every time there is an advocacy battle ahead, whether with insurance companies or the government ... increments are important.
The four Ps of advocacy
Living with compromise is hard, particularly when working within a system that needs a complete overhaul. Still, compromise is the key to getting anything done. Compromise is one of the four Ps of advocacy. I realize that compromise doesn’t start with a P, but it is such an integral part of advocacy, I am making allowances for it. The other Ps include patience, persistence/perseverance, and passion. I’m sure there are many others that could be part of the P family, like planning and performance, but let’s stick with these.
You don’t need to have all of these qualities when you start on the road to action in advocacy. For example, my passion came first. It developed when my patients could not get access to the treatments they needed. For many reasons, the medications were either unavailable (i.e., not on formulary, tiered very high) or unaffordable (i.e., copay too high, deductible too high). My passion deepened when I saw the hypocrisy within the drug-supply channel and the mistruths being told by those who profit from this channel. It wasn’t the “profit” part that bothered me, as I’m a believer in the free market. But this was not free market, and the companies were actually profiteering on the backs of my patients and justifying it by claiming they were saving the health care system billions of dollars. The fallacy of that claim and the players in this broken system are stories for another day.
Persistence came next for me. If you let up on the message, things might not only stay the same but could get worse. Perseverance is part of persistence because you need it to keep knocking on the same door even after that door is metaphorically (hopefully not literally) slammed in your face. Often, I will feel like a broken record and think that everyone has already heard the issues, not only from me but also from my fellow advocates. But never underestimate how many times a message, particularly on a difficult issue to understand, needs to be heard before it is fully comprehended.
Patience is one of the more difficult attributes to practice when you want action. I want things to happen yesterday – not tomorrow and definitely not next year. I have learned that the wheels of change turn quite slowly in this arena, sometimes pausing for inordinately long periods of time. I realize now that during the long wait, new facts can arise, allowing me to shape a different advocacy approach, one that ultimately bolsters my case. It still is very difficult to hear that a piece of legislation that seemed to be moving forward suddenly died and won’t be heard again until the next session. With patience you move forward with a smile, maybe a half-hearted one, but a smile nonetheless. This just makes life better.
Then there is compromise. This took me the longest to understand, particularly on the issues where my passion ran the deepest. Here is where passion could potentially get in the way of action. Feeling very strongly about an issue makes it difficult to let any piece of your ideal end result fall by the wayside. Here is where the saying “the perfect is the enemy of the good” comes into play. Just because you can’t have it all, doesn’t mean you can’t do good by achieving just part of what you have been striving for. Remember if you seek perfection, without compromise, you may lose the entire battle. Is there such a thing as compromising too much? I think so, but that may just be my passion speaking.
Rheumatology News and the Coalition of State Rheumatology Organizations started this column to keep you informed about current advocacy issues in rheumatology and perhaps inspire those who may be on the fence about finding “room” in their lives for action.
Advocacy doesn’t have to take up much room in your life. It can be as simple as clicking on CSRO.info/map, finding your state, and taking action by writing a letter to your representative on an important piece of legislation, like an accumulator adjustment ban (lots more on that in future columns). Or maybe just finding the time to read this column is all the action you have room for. We all have different amounts of space for any particular activity in our busy lives. It seems one of my stories from childhood created that space for advocacy in my life. I guess you could say it created a “Rheum” for Action.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is President of the CSRO, chair of the Alliance for Safe Biologic Medicines, and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at rhnews@mdedge.com.
Rheumatology News and the Coalition of State Rheumatology Organizations have partnered together to keep rheumatologists regularly informed on the advocacy issues of the day and perhaps inspire those who may be on the fence about finding “room” in their lives for action. This inaugural piece tells how CSRO President Dr. Madelaine (Mattie) A. Feldman views advocacy and how she found her way to action.
As a rheumatologist in private practice for 30 years, with husband and kids (and now grandkids), an active social life, and an exercise regimen, I realized if I were to become active in advocacy I would have to make room for it in my busy schedule. We all come up against the question of where will we find the time for a new hobby, exercise, joining a new organization, or even just eating right? Next comes the priority list discussion. How important is advocacy for my patients, my specialty, and my profession? Ultimately, how important is it for me? Where did that desire to get involved even come from? Why have I become so passionate about the issues?
For me, the answer to these questions goes back to the 1960s when I was growing up in New Orleans. My mom participated in civil rights protests, which did not make our family popular in the neighborhood, back when the KKK put flyers on everyone’s screen door. My mother didn’t care and told me that, no matter what people said, it was our duty to stand up for what was right. That was a long time ago and sadly my mom passed away just a year after I was old enough to vote. Her words have stayed with me and are more important now than ever.
Striving for justice despite how formidable the foe is requires an inner knowing that what you are doing is meaningful and will make a difference maybe not now, maybe not next year. At some point you must believe that your efforts will create a change for the better, small as it may be. My “saying” on Twitter (@MattieRheumMD) is “I’ll keep doing what I’m doing until my cynicism catches up to my passion.”
The story about my mom is just one of the many stories in my life taking me to where I am today. We all have them. I think the reason many of us go into rheumatology may be similar to the reasoning that leads one to advocacy efforts. At this point in time we can’t yet offer a cure, but we can point to a path that leads to improvements in the lives of our patients. I have to remind myself of that, every time there is an advocacy battle ahead, whether with insurance companies or the government ... increments are important.
The four Ps of advocacy
Living with compromise is hard, particularly when working within a system that needs a complete overhaul. Still, compromise is the key to getting anything done. Compromise is one of the four Ps of advocacy. I realize that compromise doesn’t start with a P, but it is such an integral part of advocacy, I am making allowances for it. The other Ps include patience, persistence/perseverance, and passion. I’m sure there are many others that could be part of the P family, like planning and performance, but let’s stick with these.
You don’t need to have all of these qualities when you start on the road to action in advocacy. For example, my passion came first. It developed when my patients could not get access to the treatments they needed. For many reasons, the medications were either unavailable (i.e., not on formulary, tiered very high) or unaffordable (i.e., copay too high, deductible too high). My passion deepened when I saw the hypocrisy within the drug-supply channel and the mistruths being told by those who profit from this channel. It wasn’t the “profit” part that bothered me, as I’m a believer in the free market. But this was not free market, and the companies were actually profiteering on the backs of my patients and justifying it by claiming they were saving the health care system billions of dollars. The fallacy of that claim and the players in this broken system are stories for another day.
Persistence came next for me. If you let up on the message, things might not only stay the same but could get worse. Perseverance is part of persistence because you need it to keep knocking on the same door even after that door is metaphorically (hopefully not literally) slammed in your face. Often, I will feel like a broken record and think that everyone has already heard the issues, not only from me but also from my fellow advocates. But never underestimate how many times a message, particularly on a difficult issue to understand, needs to be heard before it is fully comprehended.
Patience is one of the more difficult attributes to practice when you want action. I want things to happen yesterday – not tomorrow and definitely not next year. I have learned that the wheels of change turn quite slowly in this arena, sometimes pausing for inordinately long periods of time. I realize now that during the long wait, new facts can arise, allowing me to shape a different advocacy approach, one that ultimately bolsters my case. It still is very difficult to hear that a piece of legislation that seemed to be moving forward suddenly died and won’t be heard again until the next session. With patience you move forward with a smile, maybe a half-hearted one, but a smile nonetheless. This just makes life better.
Then there is compromise. This took me the longest to understand, particularly on the issues where my passion ran the deepest. Here is where passion could potentially get in the way of action. Feeling very strongly about an issue makes it difficult to let any piece of your ideal end result fall by the wayside. Here is where the saying “the perfect is the enemy of the good” comes into play. Just because you can’t have it all, doesn’t mean you can’t do good by achieving just part of what you have been striving for. Remember if you seek perfection, without compromise, you may lose the entire battle. Is there such a thing as compromising too much? I think so, but that may just be my passion speaking.
Rheumatology News and the Coalition of State Rheumatology Organizations started this column to keep you informed about current advocacy issues in rheumatology and perhaps inspire those who may be on the fence about finding “room” in their lives for action.
Advocacy doesn’t have to take up much room in your life. It can be as simple as clicking on CSRO.info/map, finding your state, and taking action by writing a letter to your representative on an important piece of legislation, like an accumulator adjustment ban (lots more on that in future columns). Or maybe just finding the time to read this column is all the action you have room for. We all have different amounts of space for any particular activity in our busy lives. It seems one of my stories from childhood created that space for advocacy in my life. I guess you could say it created a “Rheum” for Action.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is President of the CSRO, chair of the Alliance for Safe Biologic Medicines, and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at rhnews@mdedge.com.












