User login
Patients need physicians who see – and feel – beyond the EMR
CHICAGO – Speaking to a rapt audience of radiologists, an infectious disease physician who writes and teaches about the importance of human touch in medicine held sway at the opening session of the annual meeting of the Radiological Society of North America.
It wasn’t hard for Abraham Verghese, MD, to find points of commonality between those who sit in dark reading rooms and those who roam the wards.
The EMR, Dr. Verghese said, is a “system of epic disaster. It was not designed for ease of use; it was designed for billing. ... Frankly, we are the highest-paid clerical workers in the hospital, and that has to change. The Stone Age didn’t end because we ran out of stone; it ended because we had better ideas.”
The daily EMR click count for physicians has been estimated at 4,000, and it’s but part of the problem, said Dr. Verghese, professor of medicine at Stanford (Calif.) University. “For every hour of cumulative patient care, physicians spend 1½ hours on the computer, and another hour of our personal time at home dealing with our inbox,” he said. EMR systems may dominate clinical life for physicians, “but they were not built for our ease.”
Dr. Verghese is a practicing physician and medical educator, and is also the author of a body of fiction and nonfiction literature that delineates the physician-patient relationship. His TED-style talk followed opening remarks from Valerie Jackson, MD, the president of the Radiological Society of North America, who encouraged radiologists to reach out for a more direct connection with patients and with nonradiologist colleagues.
The patient connection – the human factor that leads many into the practice of medicine – can be eroded for myriad reasons, but health care systems that don’t elevate the physician-patient relationship do so at the peril of serious physician burnout, said Dr. Verghese. By some measures, and in some specialties, half of physicians score high on validated burnout indices – and a burned-out physician is at high risk for leaving the profession.
Dr. Verghese quoted the poet Anatole Broyard, who was treated for prostate cancer and wrote extensively about his experiences.
Wishing for a more personal connection with his physician, Mr. Broyard wrote: “I just wish he would brood on my situation for perhaps 5 minutes, that he would give me his whole mind just once, be bonded with me for a brief space, survey my soul as well as my flesh, to get at my illness, for each man is ill in his own way.”
It’s this opportunity for connection and contemplation that is sacrificed when, as Dr. Verghese said, “the patient in the bed has become a mere icon for the ‘real’ patient in the computer.”
Dr. Jackson, executive director of the American Board of Radiology, and Dr. Verghese both acknowledged that authentic patient connections can make practice more rewarding and reduce the risk of burnout.
Dr. Verghese also discussed other areas of risk when patients and their physicians are separated by an electronic divide.
“We are all getting distracted by our peripheral brains,” and patients may suffer when medical errors result from inattention and a reluctance to “trust what our eyes are showing us,” he said. He and his colleagues solicited and reported 208 vignettes of medical error. In 63% of the cases, the root cause of the error was failure to perform a physical examination (Am J Med. 2015 Dec;128[12]:1322-4.e3). “Patients have a front side – and a back side!” he said, to appreciative laughter. A careful physical exam, he said, involves inspecting – and palpating – both sides.
The act of putting hands on an unclothed patient for a physical exam would violate many societal norms, said Dr. Verghese, were it not for the special rules conferred on the physician-patient relationship.
“One individual in this dyad disrobes and allows touch. In any other context in this society, this is assault,” he said. “The very great privilege of our profession ... is that we are privileged to examine [patients’] bodies, and to touch.”
The gift of this ritual is not to be squandered, he said, adding that patients understand the special rhythm of the physical examination. “If you come in and do a half-assed probe of their belly and stick your stethoscope on top of their paper gown, they are on to you.”
Describing his own method for the physical exam, Dr. Verghese said that there’s something that feels commandeering and intrusive about beginning directly at the head, as one is taught. Instead, he offers an outstretched hand and begins with a handshake, noting grip strength, any tremor, hydration, and condition of skin and nails. Then, he caps the handshake with his other hand and slides two fingers over to the radial pulse, where he gathers more information, all the while strengthening his bond with his patient. His exam, he said, is his own, with its own rhythms and order which have not varied in decades.
Whatever the method, “this skill has to be passed on, and there is no easy way to do it. ... But when you examine well, you are preserving the ‘person-ality,’ the embodied identity of the patient.”
From the time of William Osler – and perhaps before – the physical examination has been a “symbolic centering on the body as a locus of personhood and disease,” said Dr. Verghese.
Dr. Jackson encouraged her radiologist peers to come out from the reading room to greet and connect with patients in the imaging suite. Similarly, Dr. Verghese said, technology can be used to “connect the image, or the biopsy report, or the lab test, to the personhood” of the patient. Bringing a tablet with imaging results or a laboratory readout to the bedside or the exam table and helping the patient place the findings on or within her own body marries the best of old and new.
He shared with the audience his practice for examining patients presenting with chronic fatigue – a condition that can be challenging to diagnose and manage.
These patients “come to you ready for you to join the long line of physicians who have disappointed them,” said Dr. Verghese, who at one time saw many such patients. He said that he developed a strategy of first listening, and then examining. “A very interesting thing happened – the voluble patient began to quiet down” under his examiner’s hands. If patients could, through his approach, relinquish their ceaseless quest for a definitive diagnosis “and instead begin a partnership toward wellness,” he felt he’d reached success. “It was because something magical had transpired in that encounter.”
Neither Dr. Verghese nor Dr. Jackson reported any conflicts of interest relevant to their presentations.
CHICAGO – Speaking to a rapt audience of radiologists, an infectious disease physician who writes and teaches about the importance of human touch in medicine held sway at the opening session of the annual meeting of the Radiological Society of North America.
It wasn’t hard for Abraham Verghese, MD, to find points of commonality between those who sit in dark reading rooms and those who roam the wards.
The EMR, Dr. Verghese said, is a “system of epic disaster. It was not designed for ease of use; it was designed for billing. ... Frankly, we are the highest-paid clerical workers in the hospital, and that has to change. The Stone Age didn’t end because we ran out of stone; it ended because we had better ideas.”
The daily EMR click count for physicians has been estimated at 4,000, and it’s but part of the problem, said Dr. Verghese, professor of medicine at Stanford (Calif.) University. “For every hour of cumulative patient care, physicians spend 1½ hours on the computer, and another hour of our personal time at home dealing with our inbox,” he said. EMR systems may dominate clinical life for physicians, “but they were not built for our ease.”
Dr. Verghese is a practicing physician and medical educator, and is also the author of a body of fiction and nonfiction literature that delineates the physician-patient relationship. His TED-style talk followed opening remarks from Valerie Jackson, MD, the president of the Radiological Society of North America, who encouraged radiologists to reach out for a more direct connection with patients and with nonradiologist colleagues.
The patient connection – the human factor that leads many into the practice of medicine – can be eroded for myriad reasons, but health care systems that don’t elevate the physician-patient relationship do so at the peril of serious physician burnout, said Dr. Verghese. By some measures, and in some specialties, half of physicians score high on validated burnout indices – and a burned-out physician is at high risk for leaving the profession.
Dr. Verghese quoted the poet Anatole Broyard, who was treated for prostate cancer and wrote extensively about his experiences.
Wishing for a more personal connection with his physician, Mr. Broyard wrote: “I just wish he would brood on my situation for perhaps 5 minutes, that he would give me his whole mind just once, be bonded with me for a brief space, survey my soul as well as my flesh, to get at my illness, for each man is ill in his own way.”
It’s this opportunity for connection and contemplation that is sacrificed when, as Dr. Verghese said, “the patient in the bed has become a mere icon for the ‘real’ patient in the computer.”
Dr. Jackson, executive director of the American Board of Radiology, and Dr. Verghese both acknowledged that authentic patient connections can make practice more rewarding and reduce the risk of burnout.
Dr. Verghese also discussed other areas of risk when patients and their physicians are separated by an electronic divide.
“We are all getting distracted by our peripheral brains,” and patients may suffer when medical errors result from inattention and a reluctance to “trust what our eyes are showing us,” he said. He and his colleagues solicited and reported 208 vignettes of medical error. In 63% of the cases, the root cause of the error was failure to perform a physical examination (Am J Med. 2015 Dec;128[12]:1322-4.e3). “Patients have a front side – and a back side!” he said, to appreciative laughter. A careful physical exam, he said, involves inspecting – and palpating – both sides.
The act of putting hands on an unclothed patient for a physical exam would violate many societal norms, said Dr. Verghese, were it not for the special rules conferred on the physician-patient relationship.
“One individual in this dyad disrobes and allows touch. In any other context in this society, this is assault,” he said. “The very great privilege of our profession ... is that we are privileged to examine [patients’] bodies, and to touch.”
The gift of this ritual is not to be squandered, he said, adding that patients understand the special rhythm of the physical examination. “If you come in and do a half-assed probe of their belly and stick your stethoscope on top of their paper gown, they are on to you.”
Describing his own method for the physical exam, Dr. Verghese said that there’s something that feels commandeering and intrusive about beginning directly at the head, as one is taught. Instead, he offers an outstretched hand and begins with a handshake, noting grip strength, any tremor, hydration, and condition of skin and nails. Then, he caps the handshake with his other hand and slides two fingers over to the radial pulse, where he gathers more information, all the while strengthening his bond with his patient. His exam, he said, is his own, with its own rhythms and order which have not varied in decades.
Whatever the method, “this skill has to be passed on, and there is no easy way to do it. ... But when you examine well, you are preserving the ‘person-ality,’ the embodied identity of the patient.”
From the time of William Osler – and perhaps before – the physical examination has been a “symbolic centering on the body as a locus of personhood and disease,” said Dr. Verghese.
Dr. Jackson encouraged her radiologist peers to come out from the reading room to greet and connect with patients in the imaging suite. Similarly, Dr. Verghese said, technology can be used to “connect the image, or the biopsy report, or the lab test, to the personhood” of the patient. Bringing a tablet with imaging results or a laboratory readout to the bedside or the exam table and helping the patient place the findings on or within her own body marries the best of old and new.
He shared with the audience his practice for examining patients presenting with chronic fatigue – a condition that can be challenging to diagnose and manage.
These patients “come to you ready for you to join the long line of physicians who have disappointed them,” said Dr. Verghese, who at one time saw many such patients. He said that he developed a strategy of first listening, and then examining. “A very interesting thing happened – the voluble patient began to quiet down” under his examiner’s hands. If patients could, through his approach, relinquish their ceaseless quest for a definitive diagnosis “and instead begin a partnership toward wellness,” he felt he’d reached success. “It was because something magical had transpired in that encounter.”
Neither Dr. Verghese nor Dr. Jackson reported any conflicts of interest relevant to their presentations.
CHICAGO – Speaking to a rapt audience of radiologists, an infectious disease physician who writes and teaches about the importance of human touch in medicine held sway at the opening session of the annual meeting of the Radiological Society of North America.
It wasn’t hard for Abraham Verghese, MD, to find points of commonality between those who sit in dark reading rooms and those who roam the wards.
The EMR, Dr. Verghese said, is a “system of epic disaster. It was not designed for ease of use; it was designed for billing. ... Frankly, we are the highest-paid clerical workers in the hospital, and that has to change. The Stone Age didn’t end because we ran out of stone; it ended because we had better ideas.”
The daily EMR click count for physicians has been estimated at 4,000, and it’s but part of the problem, said Dr. Verghese, professor of medicine at Stanford (Calif.) University. “For every hour of cumulative patient care, physicians spend 1½ hours on the computer, and another hour of our personal time at home dealing with our inbox,” he said. EMR systems may dominate clinical life for physicians, “but they were not built for our ease.”
Dr. Verghese is a practicing physician and medical educator, and is also the author of a body of fiction and nonfiction literature that delineates the physician-patient relationship. His TED-style talk followed opening remarks from Valerie Jackson, MD, the president of the Radiological Society of North America, who encouraged radiologists to reach out for a more direct connection with patients and with nonradiologist colleagues.
The patient connection – the human factor that leads many into the practice of medicine – can be eroded for myriad reasons, but health care systems that don’t elevate the physician-patient relationship do so at the peril of serious physician burnout, said Dr. Verghese. By some measures, and in some specialties, half of physicians score high on validated burnout indices – and a burned-out physician is at high risk for leaving the profession.
Dr. Verghese quoted the poet Anatole Broyard, who was treated for prostate cancer and wrote extensively about his experiences.
Wishing for a more personal connection with his physician, Mr. Broyard wrote: “I just wish he would brood on my situation for perhaps 5 minutes, that he would give me his whole mind just once, be bonded with me for a brief space, survey my soul as well as my flesh, to get at my illness, for each man is ill in his own way.”
It’s this opportunity for connection and contemplation that is sacrificed when, as Dr. Verghese said, “the patient in the bed has become a mere icon for the ‘real’ patient in the computer.”
Dr. Jackson, executive director of the American Board of Radiology, and Dr. Verghese both acknowledged that authentic patient connections can make practice more rewarding and reduce the risk of burnout.
Dr. Verghese also discussed other areas of risk when patients and their physicians are separated by an electronic divide.
“We are all getting distracted by our peripheral brains,” and patients may suffer when medical errors result from inattention and a reluctance to “trust what our eyes are showing us,” he said. He and his colleagues solicited and reported 208 vignettes of medical error. In 63% of the cases, the root cause of the error was failure to perform a physical examination (Am J Med. 2015 Dec;128[12]:1322-4.e3). “Patients have a front side – and a back side!” he said, to appreciative laughter. A careful physical exam, he said, involves inspecting – and palpating – both sides.
The act of putting hands on an unclothed patient for a physical exam would violate many societal norms, said Dr. Verghese, were it not for the special rules conferred on the physician-patient relationship.
“One individual in this dyad disrobes and allows touch. In any other context in this society, this is assault,” he said. “The very great privilege of our profession ... is that we are privileged to examine [patients’] bodies, and to touch.”
The gift of this ritual is not to be squandered, he said, adding that patients understand the special rhythm of the physical examination. “If you come in and do a half-assed probe of their belly and stick your stethoscope on top of their paper gown, they are on to you.”
Describing his own method for the physical exam, Dr. Verghese said that there’s something that feels commandeering and intrusive about beginning directly at the head, as one is taught. Instead, he offers an outstretched hand and begins with a handshake, noting grip strength, any tremor, hydration, and condition of skin and nails. Then, he caps the handshake with his other hand and slides two fingers over to the radial pulse, where he gathers more information, all the while strengthening his bond with his patient. His exam, he said, is his own, with its own rhythms and order which have not varied in decades.
Whatever the method, “this skill has to be passed on, and there is no easy way to do it. ... But when you examine well, you are preserving the ‘person-ality,’ the embodied identity of the patient.”
From the time of William Osler – and perhaps before – the physical examination has been a “symbolic centering on the body as a locus of personhood and disease,” said Dr. Verghese.
Dr. Jackson encouraged her radiologist peers to come out from the reading room to greet and connect with patients in the imaging suite. Similarly, Dr. Verghese said, technology can be used to “connect the image, or the biopsy report, or the lab test, to the personhood” of the patient. Bringing a tablet with imaging results or a laboratory readout to the bedside or the exam table and helping the patient place the findings on or within her own body marries the best of old and new.
He shared with the audience his practice for examining patients presenting with chronic fatigue – a condition that can be challenging to diagnose and manage.
These patients “come to you ready for you to join the long line of physicians who have disappointed them,” said Dr. Verghese, who at one time saw many such patients. He said that he developed a strategy of first listening, and then examining. “A very interesting thing happened – the voluble patient began to quiet down” under his examiner’s hands. If patients could, through his approach, relinquish their ceaseless quest for a definitive diagnosis “and instead begin a partnership toward wellness,” he felt he’d reached success. “It was because something magical had transpired in that encounter.”
Neither Dr. Verghese nor Dr. Jackson reported any conflicts of interest relevant to their presentations.
EXPERT ANALYSIS FROM RSNA 2019
Docs push back on surprise billing compromise
Compromise bipartisan legislation to address surprise medical bills is getting push back from physician groups.
Leadership from the House Energy and Commerce Committee and the Senate Health, Education, Labor, and Pensions Committee on Dec. 9 unveiled a compromise bill that includes rate-setting for small surprise billing and arbitration for larger ones at a lower threshold than what was originally proposed.
The new bill, part of a broader Lower Health Care Costs Act, would protect patients from surprise medical bills related to emergency care, holding them responsible for in-network cost-sharing rates for out-of-network care provided at an in-network facility without their informed consent. Out-of-network surprise bills would be applied to the patient’s in-network deductible.
Under the legislation, providers would be paid at minimum the local, market-based median in-network negotiated rate for services, with a median rate under a $750 threshold. When the median exceeds $750, the provider or insurer would be allowed to choose arbitration process to resolve payment disputes.
The bill also protects patients by banning out-of-network facilities and providers from sending balance bills for more than in-network cost-sharing amounts.
Physician groups, however, see the legislation as a giveback to insurers that puts health care professionals at a disadvantage when negotiating to be included in insurer networks.
At issue is the $750 threshold for optional arbitration.
“If you set the arbitration system in such a way that limits the ability of a physician to go to arbitration to settle a dispute between a health plan and the doctor, and if you say that can only be done when there [are] bills that are greater than $750 for a particular service, then the vast majority of services provided by doctors will not be able to go to arbitration,” Christian Shalgian, director of advocacy and health policy at the American College of Surgeons, said in an interview.
Cynthia Moran, executive vice president of government relations and health policy at the American College of Radiology, agreed.
“This particular product is going in a direction that we’re not comfortable with so we can’t support it on the basis of the benchmarks and the independent dispute resolution (IDR) process with the $750 threshold,” she said in an interview. The services radiologists provide tend to be in the $100-200 range, she said, so that would automatically exclude them from accessing arbitration. She also said that it is her understanding that many physician services will fall under that $750 threshold.
“That $750 is really going to mean that the vast majority of this policy is a benchmark-driven policy,” she said. “It is not going to be an IDR-driven policy and that is the crux of our objection to it.”
And by taking arbitration off the table, insurers have no incentive to negotiate in good faith with doctors to ensure that doctors are getting paid for the services they perform.
“For those situations where there is an out-of-network physician at an in-network facility, we believe that the patient should not have to pay any more for those emergency situations where they patient doesn’t get to choose their doctor,” Mr. Shalgian said. “The dispute really comes down to how much does the health plan have to pay the doctor.”
He noted that the legislation ties the rate to median in-network rates “and that’s a problem for us as well because of the fact that [this is] going to allow the health plans to set median in-network rates as the rate that they can pay the doctors.”
If the bill becomes law, “when you have a situation where you have an in-network physician trying to negotiate with a health plan to stay in network, that health plan now has more power in that negotiation because if [the physician] is making more than median in-network rates, then the health plan can say, ‘go out of network because we will just pay you median in-network’ at that point. That is a significant concern to us as well.”
Mr. Shalgian said that the ideal solution would be to eliminate the threshold entirely and just send disputes to arbitration. Recognizing that it might not be practical, the $750 threshold should be lowered.
ACS supported a $300 threshold, he added.
The bill is expected to be tacked on to one of the mandatory spending bills that Congress needs to pass by the end of the year.
The $750 threshold would be a savings generator for the government and an important bill such as this should be passed on its own merits, Mr. Shalgian said.
Ms. Moran called for Congress to take its time with the legislation.
“We do think that this whole issue needs more time for everyone to understand what the impact is on this first run of the solution and we think it should be slowed down a bit,” she said. “It should not go to the floor until you hear more from the providers [after] the providers figure out what the impact will be.”
The American Medical Association also called for Congress to slow down.
“The current proposal relies on benchmark rate setting that would serve only to benefit the bottom line of insurance companies at the expense of patients seeking a robust network of physicians for their care,” AMA President Patrice Harris, MD, said in a statement. “Rather than rushing to meet arbitrary deadlines, it is important to get this legislation right.”
Compromise bipartisan legislation to address surprise medical bills is getting push back from physician groups.
Leadership from the House Energy and Commerce Committee and the Senate Health, Education, Labor, and Pensions Committee on Dec. 9 unveiled a compromise bill that includes rate-setting for small surprise billing and arbitration for larger ones at a lower threshold than what was originally proposed.
The new bill, part of a broader Lower Health Care Costs Act, would protect patients from surprise medical bills related to emergency care, holding them responsible for in-network cost-sharing rates for out-of-network care provided at an in-network facility without their informed consent. Out-of-network surprise bills would be applied to the patient’s in-network deductible.
Under the legislation, providers would be paid at minimum the local, market-based median in-network negotiated rate for services, with a median rate under a $750 threshold. When the median exceeds $750, the provider or insurer would be allowed to choose arbitration process to resolve payment disputes.
The bill also protects patients by banning out-of-network facilities and providers from sending balance bills for more than in-network cost-sharing amounts.
Physician groups, however, see the legislation as a giveback to insurers that puts health care professionals at a disadvantage when negotiating to be included in insurer networks.
At issue is the $750 threshold for optional arbitration.
“If you set the arbitration system in such a way that limits the ability of a physician to go to arbitration to settle a dispute between a health plan and the doctor, and if you say that can only be done when there [are] bills that are greater than $750 for a particular service, then the vast majority of services provided by doctors will not be able to go to arbitration,” Christian Shalgian, director of advocacy and health policy at the American College of Surgeons, said in an interview.
Cynthia Moran, executive vice president of government relations and health policy at the American College of Radiology, agreed.
“This particular product is going in a direction that we’re not comfortable with so we can’t support it on the basis of the benchmarks and the independent dispute resolution (IDR) process with the $750 threshold,” she said in an interview. The services radiologists provide tend to be in the $100-200 range, she said, so that would automatically exclude them from accessing arbitration. She also said that it is her understanding that many physician services will fall under that $750 threshold.
“That $750 is really going to mean that the vast majority of this policy is a benchmark-driven policy,” she said. “It is not going to be an IDR-driven policy and that is the crux of our objection to it.”
And by taking arbitration off the table, insurers have no incentive to negotiate in good faith with doctors to ensure that doctors are getting paid for the services they perform.
“For those situations where there is an out-of-network physician at an in-network facility, we believe that the patient should not have to pay any more for those emergency situations where they patient doesn’t get to choose their doctor,” Mr. Shalgian said. “The dispute really comes down to how much does the health plan have to pay the doctor.”
He noted that the legislation ties the rate to median in-network rates “and that’s a problem for us as well because of the fact that [this is] going to allow the health plans to set median in-network rates as the rate that they can pay the doctors.”
If the bill becomes law, “when you have a situation where you have an in-network physician trying to negotiate with a health plan to stay in network, that health plan now has more power in that negotiation because if [the physician] is making more than median in-network rates, then the health plan can say, ‘go out of network because we will just pay you median in-network’ at that point. That is a significant concern to us as well.”
Mr. Shalgian said that the ideal solution would be to eliminate the threshold entirely and just send disputes to arbitration. Recognizing that it might not be practical, the $750 threshold should be lowered.
ACS supported a $300 threshold, he added.
The bill is expected to be tacked on to one of the mandatory spending bills that Congress needs to pass by the end of the year.
The $750 threshold would be a savings generator for the government and an important bill such as this should be passed on its own merits, Mr. Shalgian said.
Ms. Moran called for Congress to take its time with the legislation.
“We do think that this whole issue needs more time for everyone to understand what the impact is on this first run of the solution and we think it should be slowed down a bit,” she said. “It should not go to the floor until you hear more from the providers [after] the providers figure out what the impact will be.”
The American Medical Association also called for Congress to slow down.
“The current proposal relies on benchmark rate setting that would serve only to benefit the bottom line of insurance companies at the expense of patients seeking a robust network of physicians for their care,” AMA President Patrice Harris, MD, said in a statement. “Rather than rushing to meet arbitrary deadlines, it is important to get this legislation right.”
Compromise bipartisan legislation to address surprise medical bills is getting push back from physician groups.
Leadership from the House Energy and Commerce Committee and the Senate Health, Education, Labor, and Pensions Committee on Dec. 9 unveiled a compromise bill that includes rate-setting for small surprise billing and arbitration for larger ones at a lower threshold than what was originally proposed.
The new bill, part of a broader Lower Health Care Costs Act, would protect patients from surprise medical bills related to emergency care, holding them responsible for in-network cost-sharing rates for out-of-network care provided at an in-network facility without their informed consent. Out-of-network surprise bills would be applied to the patient’s in-network deductible.
Under the legislation, providers would be paid at minimum the local, market-based median in-network negotiated rate for services, with a median rate under a $750 threshold. When the median exceeds $750, the provider or insurer would be allowed to choose arbitration process to resolve payment disputes.
The bill also protects patients by banning out-of-network facilities and providers from sending balance bills for more than in-network cost-sharing amounts.
Physician groups, however, see the legislation as a giveback to insurers that puts health care professionals at a disadvantage when negotiating to be included in insurer networks.
At issue is the $750 threshold for optional arbitration.
“If you set the arbitration system in such a way that limits the ability of a physician to go to arbitration to settle a dispute between a health plan and the doctor, and if you say that can only be done when there [are] bills that are greater than $750 for a particular service, then the vast majority of services provided by doctors will not be able to go to arbitration,” Christian Shalgian, director of advocacy and health policy at the American College of Surgeons, said in an interview.
Cynthia Moran, executive vice president of government relations and health policy at the American College of Radiology, agreed.
“This particular product is going in a direction that we’re not comfortable with so we can’t support it on the basis of the benchmarks and the independent dispute resolution (IDR) process with the $750 threshold,” she said in an interview. The services radiologists provide tend to be in the $100-200 range, she said, so that would automatically exclude them from accessing arbitration. She also said that it is her understanding that many physician services will fall under that $750 threshold.
“That $750 is really going to mean that the vast majority of this policy is a benchmark-driven policy,” she said. “It is not going to be an IDR-driven policy and that is the crux of our objection to it.”
And by taking arbitration off the table, insurers have no incentive to negotiate in good faith with doctors to ensure that doctors are getting paid for the services they perform.
“For those situations where there is an out-of-network physician at an in-network facility, we believe that the patient should not have to pay any more for those emergency situations where they patient doesn’t get to choose their doctor,” Mr. Shalgian said. “The dispute really comes down to how much does the health plan have to pay the doctor.”
He noted that the legislation ties the rate to median in-network rates “and that’s a problem for us as well because of the fact that [this is] going to allow the health plans to set median in-network rates as the rate that they can pay the doctors.”
If the bill becomes law, “when you have a situation where you have an in-network physician trying to negotiate with a health plan to stay in network, that health plan now has more power in that negotiation because if [the physician] is making more than median in-network rates, then the health plan can say, ‘go out of network because we will just pay you median in-network’ at that point. That is a significant concern to us as well.”
Mr. Shalgian said that the ideal solution would be to eliminate the threshold entirely and just send disputes to arbitration. Recognizing that it might not be practical, the $750 threshold should be lowered.
ACS supported a $300 threshold, he added.
The bill is expected to be tacked on to one of the mandatory spending bills that Congress needs to pass by the end of the year.
The $750 threshold would be a savings generator for the government and an important bill such as this should be passed on its own merits, Mr. Shalgian said.
Ms. Moran called for Congress to take its time with the legislation.
“We do think that this whole issue needs more time for everyone to understand what the impact is on this first run of the solution and we think it should be slowed down a bit,” she said. “It should not go to the floor until you hear more from the providers [after] the providers figure out what the impact will be.”
The American Medical Association also called for Congress to slow down.
“The current proposal relies on benchmark rate setting that would serve only to benefit the bottom line of insurance companies at the expense of patients seeking a robust network of physicians for their care,” AMA President Patrice Harris, MD, said in a statement. “Rather than rushing to meet arbitrary deadlines, it is important to get this legislation right.”
Study: More pediatricians participating in global health opportunities
A look across nearly 3 decades finds that
Lead author Kevin Chan, MD, MPH, of the University of Toronto, and colleagues analyzed the responses of 668 pediatricians from the 2017 American Academy of Pediatrics Periodic Survey and compared the data with responses from 638 pediatricians collected in the 1989 periodic survey about pediatricians’ global health experiences and interests. Findings showed that participation in global health activities rose from 2% in 1989 to 5% in 2017, while interest in future global health experiences grew from 25% in 1989 to 32% in 2017. The study was published in Pediatrics.
Notable increases in global health participation were found in women (1% in 1989 to 5% in 2017) and men (3% in 1989 to 6% in 2017), subspecialists (3% in 1989 to 9% in 2017), and pediatricians who worked in medical school, hospital, or clinic settings (3% in 1989 to 8% in 2017).
In terms of age, pediatricians 50 years or older had a higher rate of a recent global health experience, with the largest increase in global health participation occurring in pediatricians 60 years and older (2% in 1989 to 9% in 2017), the study found.
Similarly, interest in future global health activities increased during the same time period for male and female pediatricians, for generalists and subspecialists, and for those working in medical school, hospital, or clinic settings. Clinical care and teaching settings were the most common preferences for future global health experiences in both 1989 and 2017. Administration and research were the least likely selected preferences in both surveys. Pediatricians affiliated with an academic institution, hospital, or clinic were more likely to have recently engaged in a global health activity and also were more likely express interest in such an opportunity, compared with solo pediatricians or those in small practices.
In an editorial accompanying the article, Suzinne Pak-Gorstein, MD, MPH, PhD, of the University of Washington, Seattle, said that the study highlights the importance of preparation for pediatricians who seek global health opportunities, particularly experiences that are short term.
“Ethical approaches to international work should be thoughtful and intentional, such as deciding to work with organizations that offer short-term experiences only in the context of long-term partnerships, considering the burden on local partners for hosting visitors, and insisting on a commitment to equitable collaborations that are mutually beneficial,” she wrote.
Dr. Pak-Gorstein added that future innovations in global health education can inspire learning experiences for pediatricians that utilize their passion and enthusiasm, while also enabling them to become more globally minded.
“In this way, pediatricians can be empowered to understand the world’s daunting challenges; respect cultural, religious, and socioeconomic differences; and facilitate dialogue and solutions for improving child health worldwide,” she concluded.
The survey was funded by the American Academy of Pediatrics. The study authors had no relevant financial disclosures. Dr. Pak-Gorstein said she received no funding for the editorial and had no relevant financial disclosures.
SOURCE: Chan K et al. Pediatrics. 2019 Dec 10. doi: 10.1542/peds.2019-1655.
A look across nearly 3 decades finds that
Lead author Kevin Chan, MD, MPH, of the University of Toronto, and colleagues analyzed the responses of 668 pediatricians from the 2017 American Academy of Pediatrics Periodic Survey and compared the data with responses from 638 pediatricians collected in the 1989 periodic survey about pediatricians’ global health experiences and interests. Findings showed that participation in global health activities rose from 2% in 1989 to 5% in 2017, while interest in future global health experiences grew from 25% in 1989 to 32% in 2017. The study was published in Pediatrics.
Notable increases in global health participation were found in women (1% in 1989 to 5% in 2017) and men (3% in 1989 to 6% in 2017), subspecialists (3% in 1989 to 9% in 2017), and pediatricians who worked in medical school, hospital, or clinic settings (3% in 1989 to 8% in 2017).
In terms of age, pediatricians 50 years or older had a higher rate of a recent global health experience, with the largest increase in global health participation occurring in pediatricians 60 years and older (2% in 1989 to 9% in 2017), the study found.
Similarly, interest in future global health activities increased during the same time period for male and female pediatricians, for generalists and subspecialists, and for those working in medical school, hospital, or clinic settings. Clinical care and teaching settings were the most common preferences for future global health experiences in both 1989 and 2017. Administration and research were the least likely selected preferences in both surveys. Pediatricians affiliated with an academic institution, hospital, or clinic were more likely to have recently engaged in a global health activity and also were more likely express interest in such an opportunity, compared with solo pediatricians or those in small practices.
In an editorial accompanying the article, Suzinne Pak-Gorstein, MD, MPH, PhD, of the University of Washington, Seattle, said that the study highlights the importance of preparation for pediatricians who seek global health opportunities, particularly experiences that are short term.
“Ethical approaches to international work should be thoughtful and intentional, such as deciding to work with organizations that offer short-term experiences only in the context of long-term partnerships, considering the burden on local partners for hosting visitors, and insisting on a commitment to equitable collaborations that are mutually beneficial,” she wrote.
Dr. Pak-Gorstein added that future innovations in global health education can inspire learning experiences for pediatricians that utilize their passion and enthusiasm, while also enabling them to become more globally minded.
“In this way, pediatricians can be empowered to understand the world’s daunting challenges; respect cultural, religious, and socioeconomic differences; and facilitate dialogue and solutions for improving child health worldwide,” she concluded.
The survey was funded by the American Academy of Pediatrics. The study authors had no relevant financial disclosures. Dr. Pak-Gorstein said she received no funding for the editorial and had no relevant financial disclosures.
SOURCE: Chan K et al. Pediatrics. 2019 Dec 10. doi: 10.1542/peds.2019-1655.
A look across nearly 3 decades finds that
Lead author Kevin Chan, MD, MPH, of the University of Toronto, and colleagues analyzed the responses of 668 pediatricians from the 2017 American Academy of Pediatrics Periodic Survey and compared the data with responses from 638 pediatricians collected in the 1989 periodic survey about pediatricians’ global health experiences and interests. Findings showed that participation in global health activities rose from 2% in 1989 to 5% in 2017, while interest in future global health experiences grew from 25% in 1989 to 32% in 2017. The study was published in Pediatrics.
Notable increases in global health participation were found in women (1% in 1989 to 5% in 2017) and men (3% in 1989 to 6% in 2017), subspecialists (3% in 1989 to 9% in 2017), and pediatricians who worked in medical school, hospital, or clinic settings (3% in 1989 to 8% in 2017).
In terms of age, pediatricians 50 years or older had a higher rate of a recent global health experience, with the largest increase in global health participation occurring in pediatricians 60 years and older (2% in 1989 to 9% in 2017), the study found.
Similarly, interest in future global health activities increased during the same time period for male and female pediatricians, for generalists and subspecialists, and for those working in medical school, hospital, or clinic settings. Clinical care and teaching settings were the most common preferences for future global health experiences in both 1989 and 2017. Administration and research were the least likely selected preferences in both surveys. Pediatricians affiliated with an academic institution, hospital, or clinic were more likely to have recently engaged in a global health activity and also were more likely express interest in such an opportunity, compared with solo pediatricians or those in small practices.
In an editorial accompanying the article, Suzinne Pak-Gorstein, MD, MPH, PhD, of the University of Washington, Seattle, said that the study highlights the importance of preparation for pediatricians who seek global health opportunities, particularly experiences that are short term.
“Ethical approaches to international work should be thoughtful and intentional, such as deciding to work with organizations that offer short-term experiences only in the context of long-term partnerships, considering the burden on local partners for hosting visitors, and insisting on a commitment to equitable collaborations that are mutually beneficial,” she wrote.
Dr. Pak-Gorstein added that future innovations in global health education can inspire learning experiences for pediatricians that utilize their passion and enthusiasm, while also enabling them to become more globally minded.
“In this way, pediatricians can be empowered to understand the world’s daunting challenges; respect cultural, religious, and socioeconomic differences; and facilitate dialogue and solutions for improving child health worldwide,” she concluded.
The survey was funded by the American Academy of Pediatrics. The study authors had no relevant financial disclosures. Dr. Pak-Gorstein said she received no funding for the editorial and had no relevant financial disclosures.
SOURCE: Chan K et al. Pediatrics. 2019 Dec 10. doi: 10.1542/peds.2019-1655.
Contacts with health care professionals increased among adults
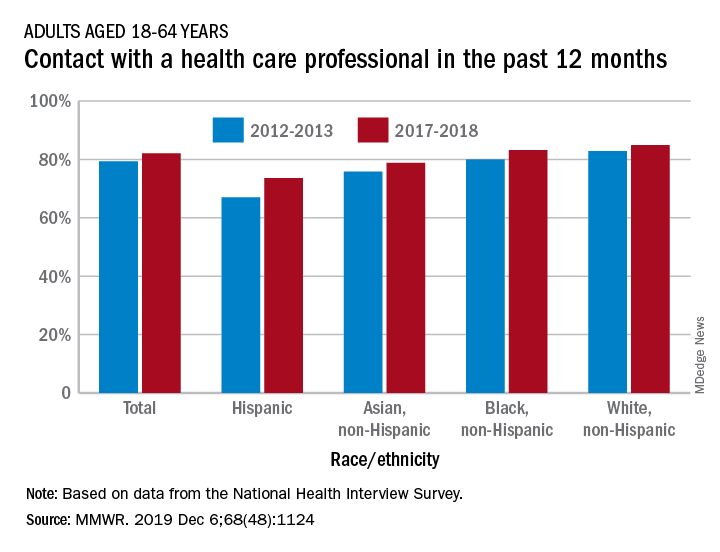
Adults aged 18-64 years were more likely to see or talk to a health care professional in 2017-2018 than they were in 2012-2013, according to the Centers for Disease Control and Prevention.
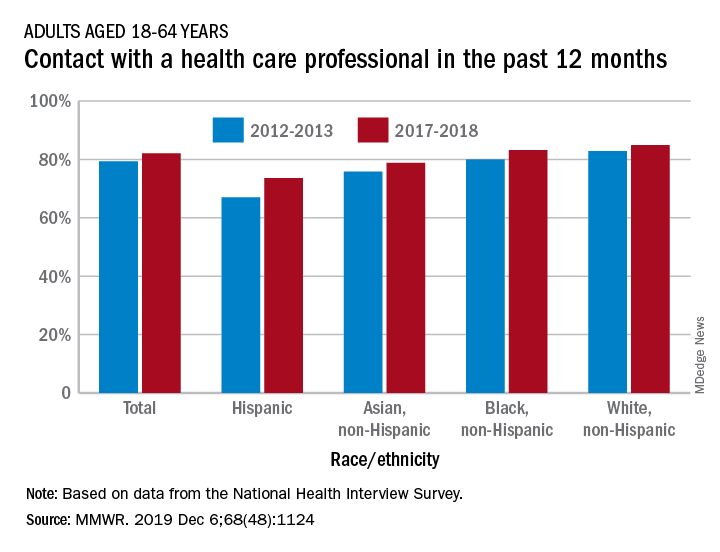
The percentage of American adults who had seen or talked to a health care professional in the past 12 months rose from 79.3% in 2012-2013 to 82.1% in 2017-2018, Michael E. Martinez, MPH, and Tainya C. Clarke, PhD, reported in the Morbidity and Mortality Weekly Report.
Analysis by race/ethnicity showed that Hispanic adults were still the least likely to have seen or talked to a health care professional in 2017-2018, even though they had the largest increase – more than six percentage points – between the two time periods, the CDC investigators reported.
White adults were the most likely to have seen or talked to a health care provider in both 2012-2013 and 2017-2018 but their 2.1-percentage-point increase over the course of the analysis was the smallest of the four groups included, based on data from the National Health Interview Survey.
SOURCE: Martinez ME, Clarke TC. MMWR. 2019 Dec 6;68(48):1124.
Adults aged 18-64 years were more likely to see or talk to a health care professional in 2017-2018 than they were in 2012-2013, according to the Centers for Disease Control and Prevention.
The percentage of American adults who had seen or talked to a health care professional in the past 12 months rose from 79.3% in 2012-2013 to 82.1% in 2017-2018, Michael E. Martinez, MPH, and Tainya C. Clarke, PhD, reported in the Morbidity and Mortality Weekly Report.
Analysis by race/ethnicity showed that Hispanic adults were still the least likely to have seen or talked to a health care professional in 2017-2018, even though they had the largest increase – more than six percentage points – between the two time periods, the CDC investigators reported.
White adults were the most likely to have seen or talked to a health care provider in both 2012-2013 and 2017-2018 but their 2.1-percentage-point increase over the course of the analysis was the smallest of the four groups included, based on data from the National Health Interview Survey.
SOURCE: Martinez ME, Clarke TC. MMWR. 2019 Dec 6;68(48):1124.
Adults aged 18-64 years were more likely to see or talk to a health care professional in 2017-2018 than they were in 2012-2013, according to the Centers for Disease Control and Prevention.
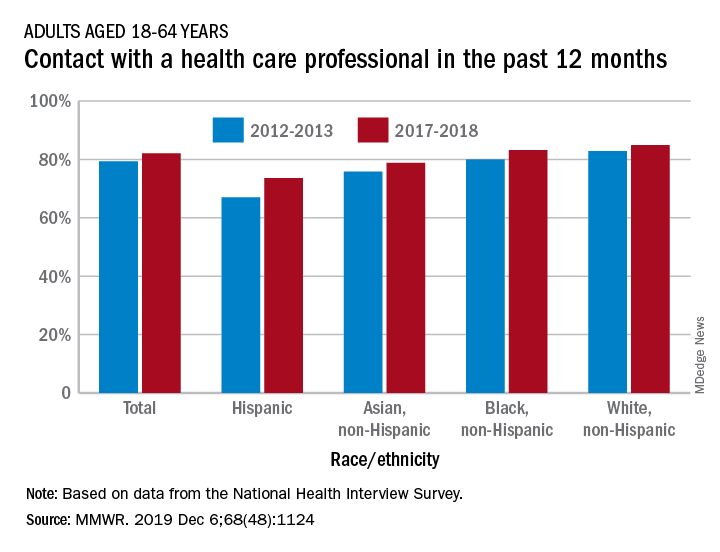
The percentage of American adults who had seen or talked to a health care professional in the past 12 months rose from 79.3% in 2012-2013 to 82.1% in 2017-2018, Michael E. Martinez, MPH, and Tainya C. Clarke, PhD, reported in the Morbidity and Mortality Weekly Report.
Analysis by race/ethnicity showed that Hispanic adults were still the least likely to have seen or talked to a health care professional in 2017-2018, even though they had the largest increase – more than six percentage points – between the two time periods, the CDC investigators reported.
White adults were the most likely to have seen or talked to a health care provider in both 2012-2013 and 2017-2018 but their 2.1-percentage-point increase over the course of the analysis was the smallest of the four groups included, based on data from the National Health Interview Survey.
SOURCE: Martinez ME, Clarke TC. MMWR. 2019 Dec 6;68(48):1124.
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
Negligent use of steroids
Question: Mr. M, a car mechanic, was treated with long-term ACTH and Kenalog after he developed severe contact dermatitis from daily exposure to petroleum-based solvents. His subsequent course was complicated by cataracts and osteoporosis. Which of the following is true in case he files a malpractice action?
A. Treatment with steroids was medically indicated for Mr. Mechanic’s dermatologic condition, so the doctor could not have breached the standard of care.
B. Under the “Learned Intermediary” doctrine, both the manufacturer and the prescribing doctor are jointly liable.
C. Corticosteroids are a known cause of osteoporosis and other complications, but not of cataracts, so that part of the malpractice action should be thrown out.
D. The plaintiff would prevail even if he could not find an expert witnesses to testify as to standard of care, since it is “common knowledge” that steroids cause osteoporosis.
E. Lack of informed consent may be his best legal theory of liability, as many jurisdictions now use the patient-centered standard, which does not require expert testimony.
Answer: E. The above hypothetical was modified from an old Montana case1 in which the patient failed in his negligence lawsuit because he did not have expert witnesses to testify as to standard of care and to adequacy of warning label. However, in some jurisdictions under today’s case law, informed consent relies on a subjective, i.e., patient-oriented standard, and expert testimony is unnecessary to prove breach of duty, although still needed to prove causation.
Steroid-related litigation
Steroid-related malpractice litigation is quite prevalent. In a retrospective study of a tertiary medical center from 1996 to 2008, Nash and coworkers identified 83 such cases.2 Steroids were prescribed for pain (23%), asthma or another pulmonary condition (20%), a dermatologic condition (18%), an autoimmune condition (17%), or allergies (6%).
Learned intermediary
“Drug reps” have a responsibility to inform doctors of both benefits and risks of their medications, a process termed “fair balance.” Generally speaking, if a doctor fails to warn the patient of a medication risk, and injury results, the patient may have a claim against the doctor but not the drug manufacturer. This is termed the “learned intermediary” doctrine, which is also applicable to medical devices such as dialysis equipment, breast implants, and blood products.
The justification is that manufacturers can reasonably rely on the treating doctor to warn of adverse effects, which are disclosed to the profession through their sales reps and in the package insert and PDR. The treating doctor, in turn, is expected to use his or her professional judgment to adequately warn the patient. It is simply not feasible for the manufacturer to directly warn every patient without usurping the doctor-patient relationship. However, where known complications were undisclosed to the FDA and the profession, then plaintiff attorneys can file class action lawsuits directed at the manufacturer.
Complications
Complications arising out of the use of steroids are typical examples of medical products liability. This may be on the basis of the doctor having prescribed the medication without a proper indication or where contraindicated, or may have prescribed “the wrong dose for the wrong patient by the wrong route.” In addition, there may have been a lack of informed consent, i.e., failure to explain the underlying condition and the material risks associated with using the drug. Other acts of negligence, e.g., vicarious liability, may also apply.
Corticosteroids such as Prednisone, Decadron, Kenalog, etc., are widely prescribed, and can cause serious complications, especially when used in high doses for extended periods. Examples include suppression of the immune system with supervening infections, steroid osteoporosis and fractures,3 aseptic necrosis, steroid diabetes, hypertension, emotional changes, weight gain, cataracts, neurological complications, and many others. As in all malpractice actions, the plaintiff bears the burden of proof covering the four requisite tort elements, i.e., duty, breach of duty, causation, and damages. Expert testimony is almost always needed in a professional negligence lawsuit.
Aseptic necrosis is a feared complication of steroid therapy.
A recent report4 featured a nurse in her 40s who developed aseptic necrosis of the right shoulder and both hips after taking high dose prednisone for 6 months. She was being treated for idiopathic thrombocytopenic purpura by a hematologist as well as sarcoidosis by a pulmonologist. The plaintiff claimed that both defendants negligently prescribed the medication for an extended period of time without proper monitoring, which caused her severe bone complications requiring a hip and shoulder replacement. The defendants maintained that the steroid medication was necessary to treat the life-threatening conditions from which the plaintiff suffered and that the dosage was carefully monitored and was not excessive. However, in a jury trial, the defendant hematologist and pulmonologist were each found 50% negligent, and the patient was awarded $4.1 million in damages.
In a case5 of steroid-related neurological sequelae, a Colorado jury awarded $14.9 million to a couple against an outpatient surgery center for negligently administering an epidural dose of Kenalog that rendered the patient paraplegic, and for failure to obtain informed consent. The jury awarded the woman, age 57, approximately $1.7 million in past and future medical expenses; $3.2 million in unspecified economic damages; and $6.5 million in past and future noneconomic damages such as pain and suffering. Her husband will receive $3.5 million in past and future noneconomic damages for loss of consortium, according to the verdict. Two years before the injection date of 2013, the drug maker had announced that Kenalog should not be used for epidural procedures because of cord complications including infarction and paraplegia.
Contributory role
The putative offending drug does not have to be the sole cause of injury; if it played a contributory role, the court may find the presence of liability. For example, a Kansas appeals court6 upheld a jury award of $2.88 million in the case of a 40-year-old man who took his life after neurologic complications followed an epidural injection. During one of patient’s visits for chronic low back pain, the defendant-anesthesiologist administered an epidural steroid injection into an area left swollen from a previous injection.
The patient developed neurologic symptoms, and lumbar puncture yielded green pus caused by methicillin-resistant Staphylococcus aureus. He went on to develop arachnoiditis, which left him with impotence, incontinence, and excruciating pain. His lawsuit contended the injection needle had passed through an infected edematous area, causing meningitis and arachnoiditis. Before the case went to trial, the patient took his life because of unremitting pain.
In March 2014, a Johnson County jury found the doctor 75% at fault and the clinic 25% at fault and awarded damages, which were reduced to $1.67 million because Kansas caps noneconomic damages at $250,000. The court rejected the defendants’ argument that the trial judge improperly instructed the jury it could find liability only if negligence “caused” rather than merely “contributed to” the patient’s death, holding that “... one who contributes to a wrongful death is a cause of that death as contemplated by the wrongful death statute.”
Dr. Tan is professor emeritus of medicine and former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at siang@hawaii.edu .
References
1. Hill v. Squibb Sons, E.R, 592 P.2d 1383 (Mont. 1979).
2. Nash JJ et al, Medical malpractice and corticosteroid use. Otolaryngol Head Neck Surg. 2011; 144:10-5.
3. Buckley L. et al, Glucocorticoid-Induced Osteoporosis. N Engl J Med 2018; 379:2547-56.
4. Zarin’s Jury Verdict: Review and Analysis. Article ID 40229, Philadelphia County.
5. Robbin Smith et al. v. The Surgery Center at Lone Tree, 2015-CV-30922, Douglas County District Court, Colo. Verdict for plaintiff, March 23, 2017.
6. Burnette v. Kimber L. Eubanks, M.D., & Paincare, P.A., 379 P.3d 372 (Kan. Ct. App. 2016).
Question: Mr. M, a car mechanic, was treated with long-term ACTH and Kenalog after he developed severe contact dermatitis from daily exposure to petroleum-based solvents. His subsequent course was complicated by cataracts and osteoporosis. Which of the following is true in case he files a malpractice action?
A. Treatment with steroids was medically indicated for Mr. Mechanic’s dermatologic condition, so the doctor could not have breached the standard of care.
B. Under the “Learned Intermediary” doctrine, both the manufacturer and the prescribing doctor are jointly liable.
C. Corticosteroids are a known cause of osteoporosis and other complications, but not of cataracts, so that part of the malpractice action should be thrown out.
D. The plaintiff would prevail even if he could not find an expert witnesses to testify as to standard of care, since it is “common knowledge” that steroids cause osteoporosis.
E. Lack of informed consent may be his best legal theory of liability, as many jurisdictions now use the patient-centered standard, which does not require expert testimony.
Answer: E. The above hypothetical was modified from an old Montana case1 in which the patient failed in his negligence lawsuit because he did not have expert witnesses to testify as to standard of care and to adequacy of warning label. However, in some jurisdictions under today’s case law, informed consent relies on a subjective, i.e., patient-oriented standard, and expert testimony is unnecessary to prove breach of duty, although still needed to prove causation.
Steroid-related litigation
Steroid-related malpractice litigation is quite prevalent. In a retrospective study of a tertiary medical center from 1996 to 2008, Nash and coworkers identified 83 such cases.2 Steroids were prescribed for pain (23%), asthma or another pulmonary condition (20%), a dermatologic condition (18%), an autoimmune condition (17%), or allergies (6%).
Learned intermediary
“Drug reps” have a responsibility to inform doctors of both benefits and risks of their medications, a process termed “fair balance.” Generally speaking, if a doctor fails to warn the patient of a medication risk, and injury results, the patient may have a claim against the doctor but not the drug manufacturer. This is termed the “learned intermediary” doctrine, which is also applicable to medical devices such as dialysis equipment, breast implants, and blood products.
The justification is that manufacturers can reasonably rely on the treating doctor to warn of adverse effects, which are disclosed to the profession through their sales reps and in the package insert and PDR. The treating doctor, in turn, is expected to use his or her professional judgment to adequately warn the patient. It is simply not feasible for the manufacturer to directly warn every patient without usurping the doctor-patient relationship. However, where known complications were undisclosed to the FDA and the profession, then plaintiff attorneys can file class action lawsuits directed at the manufacturer.
Complications
Complications arising out of the use of steroids are typical examples of medical products liability. This may be on the basis of the doctor having prescribed the medication without a proper indication or where contraindicated, or may have prescribed “the wrong dose for the wrong patient by the wrong route.” In addition, there may have been a lack of informed consent, i.e., failure to explain the underlying condition and the material risks associated with using the drug. Other acts of negligence, e.g., vicarious liability, may also apply.
Corticosteroids such as Prednisone, Decadron, Kenalog, etc., are widely prescribed, and can cause serious complications, especially when used in high doses for extended periods. Examples include suppression of the immune system with supervening infections, steroid osteoporosis and fractures,3 aseptic necrosis, steroid diabetes, hypertension, emotional changes, weight gain, cataracts, neurological complications, and many others. As in all malpractice actions, the plaintiff bears the burden of proof covering the four requisite tort elements, i.e., duty, breach of duty, causation, and damages. Expert testimony is almost always needed in a professional negligence lawsuit.
Aseptic necrosis is a feared complication of steroid therapy.
A recent report4 featured a nurse in her 40s who developed aseptic necrosis of the right shoulder and both hips after taking high dose prednisone for 6 months. She was being treated for idiopathic thrombocytopenic purpura by a hematologist as well as sarcoidosis by a pulmonologist. The plaintiff claimed that both defendants negligently prescribed the medication for an extended period of time without proper monitoring, which caused her severe bone complications requiring a hip and shoulder replacement. The defendants maintained that the steroid medication was necessary to treat the life-threatening conditions from which the plaintiff suffered and that the dosage was carefully monitored and was not excessive. However, in a jury trial, the defendant hematologist and pulmonologist were each found 50% negligent, and the patient was awarded $4.1 million in damages.
In a case5 of steroid-related neurological sequelae, a Colorado jury awarded $14.9 million to a couple against an outpatient surgery center for negligently administering an epidural dose of Kenalog that rendered the patient paraplegic, and for failure to obtain informed consent. The jury awarded the woman, age 57, approximately $1.7 million in past and future medical expenses; $3.2 million in unspecified economic damages; and $6.5 million in past and future noneconomic damages such as pain and suffering. Her husband will receive $3.5 million in past and future noneconomic damages for loss of consortium, according to the verdict. Two years before the injection date of 2013, the drug maker had announced that Kenalog should not be used for epidural procedures because of cord complications including infarction and paraplegia.
Contributory role
The putative offending drug does not have to be the sole cause of injury; if it played a contributory role, the court may find the presence of liability. For example, a Kansas appeals court6 upheld a jury award of $2.88 million in the case of a 40-year-old man who took his life after neurologic complications followed an epidural injection. During one of patient’s visits for chronic low back pain, the defendant-anesthesiologist administered an epidural steroid injection into an area left swollen from a previous injection.
The patient developed neurologic symptoms, and lumbar puncture yielded green pus caused by methicillin-resistant Staphylococcus aureus. He went on to develop arachnoiditis, which left him with impotence, incontinence, and excruciating pain. His lawsuit contended the injection needle had passed through an infected edematous area, causing meningitis and arachnoiditis. Before the case went to trial, the patient took his life because of unremitting pain.
In March 2014, a Johnson County jury found the doctor 75% at fault and the clinic 25% at fault and awarded damages, which were reduced to $1.67 million because Kansas caps noneconomic damages at $250,000. The court rejected the defendants’ argument that the trial judge improperly instructed the jury it could find liability only if negligence “caused” rather than merely “contributed to” the patient’s death, holding that “... one who contributes to a wrongful death is a cause of that death as contemplated by the wrongful death statute.”
Dr. Tan is professor emeritus of medicine and former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at siang@hawaii.edu .
References
1. Hill v. Squibb Sons, E.R, 592 P.2d 1383 (Mont. 1979).
2. Nash JJ et al, Medical malpractice and corticosteroid use. Otolaryngol Head Neck Surg. 2011; 144:10-5.
3. Buckley L. et al, Glucocorticoid-Induced Osteoporosis. N Engl J Med 2018; 379:2547-56.
4. Zarin’s Jury Verdict: Review and Analysis. Article ID 40229, Philadelphia County.
5. Robbin Smith et al. v. The Surgery Center at Lone Tree, 2015-CV-30922, Douglas County District Court, Colo. Verdict for plaintiff, March 23, 2017.
6. Burnette v. Kimber L. Eubanks, M.D., & Paincare, P.A., 379 P.3d 372 (Kan. Ct. App. 2016).
Question: Mr. M, a car mechanic, was treated with long-term ACTH and Kenalog after he developed severe contact dermatitis from daily exposure to petroleum-based solvents. His subsequent course was complicated by cataracts and osteoporosis. Which of the following is true in case he files a malpractice action?
A. Treatment with steroids was medically indicated for Mr. Mechanic’s dermatologic condition, so the doctor could not have breached the standard of care.
B. Under the “Learned Intermediary” doctrine, both the manufacturer and the prescribing doctor are jointly liable.
C. Corticosteroids are a known cause of osteoporosis and other complications, but not of cataracts, so that part of the malpractice action should be thrown out.
D. The plaintiff would prevail even if he could not find an expert witnesses to testify as to standard of care, since it is “common knowledge” that steroids cause osteoporosis.
E. Lack of informed consent may be his best legal theory of liability, as many jurisdictions now use the patient-centered standard, which does not require expert testimony.
Answer: E. The above hypothetical was modified from an old Montana case1 in which the patient failed in his negligence lawsuit because he did not have expert witnesses to testify as to standard of care and to adequacy of warning label. However, in some jurisdictions under today’s case law, informed consent relies on a subjective, i.e., patient-oriented standard, and expert testimony is unnecessary to prove breach of duty, although still needed to prove causation.
Steroid-related litigation
Steroid-related malpractice litigation is quite prevalent. In a retrospective study of a tertiary medical center from 1996 to 2008, Nash and coworkers identified 83 such cases.2 Steroids were prescribed for pain (23%), asthma or another pulmonary condition (20%), a dermatologic condition (18%), an autoimmune condition (17%), or allergies (6%).
Learned intermediary
“Drug reps” have a responsibility to inform doctors of both benefits and risks of their medications, a process termed “fair balance.” Generally speaking, if a doctor fails to warn the patient of a medication risk, and injury results, the patient may have a claim against the doctor but not the drug manufacturer. This is termed the “learned intermediary” doctrine, which is also applicable to medical devices such as dialysis equipment, breast implants, and blood products.
The justification is that manufacturers can reasonably rely on the treating doctor to warn of adverse effects, which are disclosed to the profession through their sales reps and in the package insert and PDR. The treating doctor, in turn, is expected to use his or her professional judgment to adequately warn the patient. It is simply not feasible for the manufacturer to directly warn every patient without usurping the doctor-patient relationship. However, where known complications were undisclosed to the FDA and the profession, then plaintiff attorneys can file class action lawsuits directed at the manufacturer.
Complications
Complications arising out of the use of steroids are typical examples of medical products liability. This may be on the basis of the doctor having prescribed the medication without a proper indication or where contraindicated, or may have prescribed “the wrong dose for the wrong patient by the wrong route.” In addition, there may have been a lack of informed consent, i.e., failure to explain the underlying condition and the material risks associated with using the drug. Other acts of negligence, e.g., vicarious liability, may also apply.
Corticosteroids such as Prednisone, Decadron, Kenalog, etc., are widely prescribed, and can cause serious complications, especially when used in high doses for extended periods. Examples include suppression of the immune system with supervening infections, steroid osteoporosis and fractures,3 aseptic necrosis, steroid diabetes, hypertension, emotional changes, weight gain, cataracts, neurological complications, and many others. As in all malpractice actions, the plaintiff bears the burden of proof covering the four requisite tort elements, i.e., duty, breach of duty, causation, and damages. Expert testimony is almost always needed in a professional negligence lawsuit.
Aseptic necrosis is a feared complication of steroid therapy.
A recent report4 featured a nurse in her 40s who developed aseptic necrosis of the right shoulder and both hips after taking high dose prednisone for 6 months. She was being treated for idiopathic thrombocytopenic purpura by a hematologist as well as sarcoidosis by a pulmonologist. The plaintiff claimed that both defendants negligently prescribed the medication for an extended period of time without proper monitoring, which caused her severe bone complications requiring a hip and shoulder replacement. The defendants maintained that the steroid medication was necessary to treat the life-threatening conditions from which the plaintiff suffered and that the dosage was carefully monitored and was not excessive. However, in a jury trial, the defendant hematologist and pulmonologist were each found 50% negligent, and the patient was awarded $4.1 million in damages.
In a case5 of steroid-related neurological sequelae, a Colorado jury awarded $14.9 million to a couple against an outpatient surgery center for negligently administering an epidural dose of Kenalog that rendered the patient paraplegic, and for failure to obtain informed consent. The jury awarded the woman, age 57, approximately $1.7 million in past and future medical expenses; $3.2 million in unspecified economic damages; and $6.5 million in past and future noneconomic damages such as pain and suffering. Her husband will receive $3.5 million in past and future noneconomic damages for loss of consortium, according to the verdict. Two years before the injection date of 2013, the drug maker had announced that Kenalog should not be used for epidural procedures because of cord complications including infarction and paraplegia.
Contributory role
The putative offending drug does not have to be the sole cause of injury; if it played a contributory role, the court may find the presence of liability. For example, a Kansas appeals court6 upheld a jury award of $2.88 million in the case of a 40-year-old man who took his life after neurologic complications followed an epidural injection. During one of patient’s visits for chronic low back pain, the defendant-anesthesiologist administered an epidural steroid injection into an area left swollen from a previous injection.
The patient developed neurologic symptoms, and lumbar puncture yielded green pus caused by methicillin-resistant Staphylococcus aureus. He went on to develop arachnoiditis, which left him with impotence, incontinence, and excruciating pain. His lawsuit contended the injection needle had passed through an infected edematous area, causing meningitis and arachnoiditis. Before the case went to trial, the patient took his life because of unremitting pain.
In March 2014, a Johnson County jury found the doctor 75% at fault and the clinic 25% at fault and awarded damages, which were reduced to $1.67 million because Kansas caps noneconomic damages at $250,000. The court rejected the defendants’ argument that the trial judge improperly instructed the jury it could find liability only if negligence “caused” rather than merely “contributed to” the patient’s death, holding that “... one who contributes to a wrongful death is a cause of that death as contemplated by the wrongful death statute.”
Dr. Tan is professor emeritus of medicine and former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at siang@hawaii.edu .
References
1. Hill v. Squibb Sons, E.R, 592 P.2d 1383 (Mont. 1979).
2. Nash JJ et al, Medical malpractice and corticosteroid use. Otolaryngol Head Neck Surg. 2011; 144:10-5.
3. Buckley L. et al, Glucocorticoid-Induced Osteoporosis. N Engl J Med 2018; 379:2547-56.
4. Zarin’s Jury Verdict: Review and Analysis. Article ID 40229, Philadelphia County.
5. Robbin Smith et al. v. The Surgery Center at Lone Tree, 2015-CV-30922, Douglas County District Court, Colo. Verdict for plaintiff, March 23, 2017.
6. Burnette v. Kimber L. Eubanks, M.D., & Paincare, P.A., 379 P.3d 372 (Kan. Ct. App. 2016).
More states pushing plans to pay for telehealth care
More states are enacting laws that require private plans to cover telehealth services, but fair payment remains a challenge for providers, a new analysis finds.
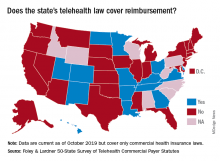
In 2019, 42 states and the District of Columbia had commercial payer telehealth laws, according to a December report by Foley & Lardner LLP, an international law firm. In contrast, about 30 states had such laws in 2015, according to a 2015 report by the National Conference of State Legislatures. Telehealth coverage laws generally require private plans to cover services provided via telehealth to the extent they cover in-person services of the same nature. The measures also frequently protect patients from cost-shifting, in which an insurer imposes higher deductibles or copays for telehealth services.
Private coverage for asynchronous telehealth and remote patient monitoring (RPM) is also growing. Twenty-four states mandate coverage for store and forward asynchronous telehealth, while 13 states require commercial health plans to cover RPM services, the analysis found. In addition, most telehealth coverage laws do not limit where a patient can receive telehealth services. However, some states, such as Arizona, Tennessee, and Washington, still require that patients be located in a particular clinical setting at the time of the telehealth consultation.
Overall, the landscape for reimbursement of telehealth services by commercial payers has improved, said Jacqueline Acosta, a health care attorney with Foley & Lardner and a coauthor of the report.
“[Foley& Lardner’s] 2017 report really noted that implementation [of telehealth] had really picked up both from providers and patients asking for telemedicine, but reimbursement still lagged behind,” Ms. Acosta said in an interview. “This one shows real progress on that front.”
However, the survey notes that payment parity for telehealth services remains lacking. Payment parity refers to insurers paying for telehealth services at the same or an equivalent rate as those delivered in-person. In 2019, 16 states had laws that specifically addressed reimbursement of telehealth services, but only 10 offer true payment parity, according to the Foley analysis. The 10 states with payment parity laws are Arkansas, Delaware, Georgia, Hawaii, Kentucky, Minnesota, Missouri, New Mexico, Utah, and Virginia. Other telehealth reimbursement measures often include ambiguity or allow room for payment negotiation, Ms. Acosta said.
She predicts that more payment parity laws and improved telehealth coverage laws are on the horizon for 2020 and beyond. California, for example, recently revised its telehealth law to require both coverage and payment parity for telehealth services. Mississippi meanwhile, recently expanded its law to include RPM coverage.
That states are revising existing laws and expanding their statutes shows an optimistic trend toward telehealth acceptance and coverage growth, Ms. Acosta said.
More states are enacting laws that require private plans to cover telehealth services, but fair payment remains a challenge for providers, a new analysis finds.
In 2019, 42 states and the District of Columbia had commercial payer telehealth laws, according to a December report by Foley & Lardner LLP, an international law firm. In contrast, about 30 states had such laws in 2015, according to a 2015 report by the National Conference of State Legislatures. Telehealth coverage laws generally require private plans to cover services provided via telehealth to the extent they cover in-person services of the same nature. The measures also frequently protect patients from cost-shifting, in which an insurer imposes higher deductibles or copays for telehealth services.
Private coverage for asynchronous telehealth and remote patient monitoring (RPM) is also growing. Twenty-four states mandate coverage for store and forward asynchronous telehealth, while 13 states require commercial health plans to cover RPM services, the analysis found. In addition, most telehealth coverage laws do not limit where a patient can receive telehealth services. However, some states, such as Arizona, Tennessee, and Washington, still require that patients be located in a particular clinical setting at the time of the telehealth consultation.
Overall, the landscape for reimbursement of telehealth services by commercial payers has improved, said Jacqueline Acosta, a health care attorney with Foley & Lardner and a coauthor of the report.
“[Foley& Lardner’s] 2017 report really noted that implementation [of telehealth] had really picked up both from providers and patients asking for telemedicine, but reimbursement still lagged behind,” Ms. Acosta said in an interview. “This one shows real progress on that front.”
However, the survey notes that payment parity for telehealth services remains lacking. Payment parity refers to insurers paying for telehealth services at the same or an equivalent rate as those delivered in-person. In 2019, 16 states had laws that specifically addressed reimbursement of telehealth services, but only 10 offer true payment parity, according to the Foley analysis. The 10 states with payment parity laws are Arkansas, Delaware, Georgia, Hawaii, Kentucky, Minnesota, Missouri, New Mexico, Utah, and Virginia. Other telehealth reimbursement measures often include ambiguity or allow room for payment negotiation, Ms. Acosta said.
She predicts that more payment parity laws and improved telehealth coverage laws are on the horizon for 2020 and beyond. California, for example, recently revised its telehealth law to require both coverage and payment parity for telehealth services. Mississippi meanwhile, recently expanded its law to include RPM coverage.
That states are revising existing laws and expanding their statutes shows an optimistic trend toward telehealth acceptance and coverage growth, Ms. Acosta said.
More states are enacting laws that require private plans to cover telehealth services, but fair payment remains a challenge for providers, a new analysis finds.
In 2019, 42 states and the District of Columbia had commercial payer telehealth laws, according to a December report by Foley & Lardner LLP, an international law firm. In contrast, about 30 states had such laws in 2015, according to a 2015 report by the National Conference of State Legislatures. Telehealth coverage laws generally require private plans to cover services provided via telehealth to the extent they cover in-person services of the same nature. The measures also frequently protect patients from cost-shifting, in which an insurer imposes higher deductibles or copays for telehealth services.
Private coverage for asynchronous telehealth and remote patient monitoring (RPM) is also growing. Twenty-four states mandate coverage for store and forward asynchronous telehealth, while 13 states require commercial health plans to cover RPM services, the analysis found. In addition, most telehealth coverage laws do not limit where a patient can receive telehealth services. However, some states, such as Arizona, Tennessee, and Washington, still require that patients be located in a particular clinical setting at the time of the telehealth consultation.
Overall, the landscape for reimbursement of telehealth services by commercial payers has improved, said Jacqueline Acosta, a health care attorney with Foley & Lardner and a coauthor of the report.
“[Foley& Lardner’s] 2017 report really noted that implementation [of telehealth] had really picked up both from providers and patients asking for telemedicine, but reimbursement still lagged behind,” Ms. Acosta said in an interview. “This one shows real progress on that front.”
However, the survey notes that payment parity for telehealth services remains lacking. Payment parity refers to insurers paying for telehealth services at the same or an equivalent rate as those delivered in-person. In 2019, 16 states had laws that specifically addressed reimbursement of telehealth services, but only 10 offer true payment parity, according to the Foley analysis. The 10 states with payment parity laws are Arkansas, Delaware, Georgia, Hawaii, Kentucky, Minnesota, Missouri, New Mexico, Utah, and Virginia. Other telehealth reimbursement measures often include ambiguity or allow room for payment negotiation, Ms. Acosta said.
She predicts that more payment parity laws and improved telehealth coverage laws are on the horizon for 2020 and beyond. California, for example, recently revised its telehealth law to require both coverage and payment parity for telehealth services. Mississippi meanwhile, recently expanded its law to include RPM coverage.
That states are revising existing laws and expanding their statutes shows an optimistic trend toward telehealth acceptance and coverage growth, Ms. Acosta said.
Health care: More uninsured as insurance costs grow faster
WASHINGTON – The number of uninsured grew in 2018 as the rate of health care spending grew, according to data from the Centers for Medicare & Medicaid Services.
A total of 30.7 million people in the United States were uninsured in 2018 – up 1 million from 2017. It was the second year in a row that the number of uninsured grew by that amount.
The newly uninsured came from the private insurance sector, which saw the number of insured decrease to 200.5 million in 2018 from 202.1 million in the previous year, partially offset by increases in Americans covered by Medicare and Medicaid.
The increase in uninsured people comes as the growth rate in health care spending rose to 4.6% in 2018 from 4.2% in 2017, though much of that growth in the rate of spending was attributed to the application of a health insurance tax in 2018 that Congress put a moratorium on in the previous year. The tax was part of the Affordable Care Act and was enacted in 2014.
“We see that health care spending reached $3.6 trillion, or $11,172 per person, and spending was faster,” Micah Hartman, statistician in the National Health Statistics Group in the CMS Office of the Actuary, said during a press conference to review the national health expenditure results. “The main reason for the acceleration was faster growth in the net cost of insurance, and that was particularly the case for private health insurance and also for Medicare.”
The net cost of insurance includes nonmedical expenses such as administration, taxes, and fees, as well as gains or losses for private health insurers. The ACA’s health insurance tax generated $14.3 billion in spending, according to Internal Revenue Service data.
Also contributing to the rise in the rate of growth was faster growth in medical prices, “and that was due to underlying economy-wide inflation, as well as the impacts of the tax,” Mr. Hartman said.
Despite this growth in the rate of spending, health care spending as a percentage of GDP fell slightly from 17.9% in 2017 in 17.7%, as the GDP grew faster than health care spending in 2018.
The faster growth in prices more than offset the slightly slower growth in the use and intensity of medical services, CMS reported.
The growth rate on spending on physician and clinical services slowed to 4.1% in 2018 from 4.7% in 2017. Overall spending on physician and clinical services in 2018 reached $725.6 billion and accounted for 20% of overall health care spending.
Spending on hospital services also slowed, but only slightly, dropping to a growth rate of 4.5% from 4.7% during this period. Hospital spending in 2018, at $1.2 trillion, accounted for 33% of overall health care spending.
On a personal level, overall growth in personal health care spending held steady with growth rate of 4.1% in 2018, the same as 2017, though individual components that feed into the figure varied. For example, growth rate in the spending on retail pharmaceuticals rose to 2.5% from 1.4% during this period. Spending on retail pharmaceuticals reached $335 billion and accounted for 9% of overall health care spending.
Another factor in the rising growth rate in spending came from employer-sponsored insurance.
“Growth in health spending by private business was due to faster growth in employer contributions to private health insurance premiums,” Anne B. Martin, economist in the National Health Statistics Group, said during the press conference. There also was faster growth in spending by the federal government, “driven mainly by faster growth in the federally funded portions of Medicare and Medicaid.”
Spending by private health insurance grew at a rate of 5.8% and reached $1.2 trillion in 2018. Medicare spending grew by 6.4% and reached $750.2 billion, while Medicaid spending grew 3.0%, reaching $597.4 billion.
SOURCE: Hartman M et al. Health Affairs. 2019. doi: 10.1377/hlthaff.2019.00451
WASHINGTON – The number of uninsured grew in 2018 as the rate of health care spending grew, according to data from the Centers for Medicare & Medicaid Services.
A total of 30.7 million people in the United States were uninsured in 2018 – up 1 million from 2017. It was the second year in a row that the number of uninsured grew by that amount.
The newly uninsured came from the private insurance sector, which saw the number of insured decrease to 200.5 million in 2018 from 202.1 million in the previous year, partially offset by increases in Americans covered by Medicare and Medicaid.
The increase in uninsured people comes as the growth rate in health care spending rose to 4.6% in 2018 from 4.2% in 2017, though much of that growth in the rate of spending was attributed to the application of a health insurance tax in 2018 that Congress put a moratorium on in the previous year. The tax was part of the Affordable Care Act and was enacted in 2014.
“We see that health care spending reached $3.6 trillion, or $11,172 per person, and spending was faster,” Micah Hartman, statistician in the National Health Statistics Group in the CMS Office of the Actuary, said during a press conference to review the national health expenditure results. “The main reason for the acceleration was faster growth in the net cost of insurance, and that was particularly the case for private health insurance and also for Medicare.”
The net cost of insurance includes nonmedical expenses such as administration, taxes, and fees, as well as gains or losses for private health insurers. The ACA’s health insurance tax generated $14.3 billion in spending, according to Internal Revenue Service data.
Also contributing to the rise in the rate of growth was faster growth in medical prices, “and that was due to underlying economy-wide inflation, as well as the impacts of the tax,” Mr. Hartman said.
Despite this growth in the rate of spending, health care spending as a percentage of GDP fell slightly from 17.9% in 2017 in 17.7%, as the GDP grew faster than health care spending in 2018.
The faster growth in prices more than offset the slightly slower growth in the use and intensity of medical services, CMS reported.
The growth rate on spending on physician and clinical services slowed to 4.1% in 2018 from 4.7% in 2017. Overall spending on physician and clinical services in 2018 reached $725.6 billion and accounted for 20% of overall health care spending.
Spending on hospital services also slowed, but only slightly, dropping to a growth rate of 4.5% from 4.7% during this period. Hospital spending in 2018, at $1.2 trillion, accounted for 33% of overall health care spending.
On a personal level, overall growth in personal health care spending held steady with growth rate of 4.1% in 2018, the same as 2017, though individual components that feed into the figure varied. For example, growth rate in the spending on retail pharmaceuticals rose to 2.5% from 1.4% during this period. Spending on retail pharmaceuticals reached $335 billion and accounted for 9% of overall health care spending.
Another factor in the rising growth rate in spending came from employer-sponsored insurance.
“Growth in health spending by private business was due to faster growth in employer contributions to private health insurance premiums,” Anne B. Martin, economist in the National Health Statistics Group, said during the press conference. There also was faster growth in spending by the federal government, “driven mainly by faster growth in the federally funded portions of Medicare and Medicaid.”
Spending by private health insurance grew at a rate of 5.8% and reached $1.2 trillion in 2018. Medicare spending grew by 6.4% and reached $750.2 billion, while Medicaid spending grew 3.0%, reaching $597.4 billion.
SOURCE: Hartman M et al. Health Affairs. 2019. doi: 10.1377/hlthaff.2019.00451
WASHINGTON – The number of uninsured grew in 2018 as the rate of health care spending grew, according to data from the Centers for Medicare & Medicaid Services.
A total of 30.7 million people in the United States were uninsured in 2018 – up 1 million from 2017. It was the second year in a row that the number of uninsured grew by that amount.
The newly uninsured came from the private insurance sector, which saw the number of insured decrease to 200.5 million in 2018 from 202.1 million in the previous year, partially offset by increases in Americans covered by Medicare and Medicaid.
The increase in uninsured people comes as the growth rate in health care spending rose to 4.6% in 2018 from 4.2% in 2017, though much of that growth in the rate of spending was attributed to the application of a health insurance tax in 2018 that Congress put a moratorium on in the previous year. The tax was part of the Affordable Care Act and was enacted in 2014.
“We see that health care spending reached $3.6 trillion, or $11,172 per person, and spending was faster,” Micah Hartman, statistician in the National Health Statistics Group in the CMS Office of the Actuary, said during a press conference to review the national health expenditure results. “The main reason for the acceleration was faster growth in the net cost of insurance, and that was particularly the case for private health insurance and also for Medicare.”
The net cost of insurance includes nonmedical expenses such as administration, taxes, and fees, as well as gains or losses for private health insurers. The ACA’s health insurance tax generated $14.3 billion in spending, according to Internal Revenue Service data.
Also contributing to the rise in the rate of growth was faster growth in medical prices, “and that was due to underlying economy-wide inflation, as well as the impacts of the tax,” Mr. Hartman said.
Despite this growth in the rate of spending, health care spending as a percentage of GDP fell slightly from 17.9% in 2017 in 17.7%, as the GDP grew faster than health care spending in 2018.
The faster growth in prices more than offset the slightly slower growth in the use and intensity of medical services, CMS reported.
The growth rate on spending on physician and clinical services slowed to 4.1% in 2018 from 4.7% in 2017. Overall spending on physician and clinical services in 2018 reached $725.6 billion and accounted for 20% of overall health care spending.
Spending on hospital services also slowed, but only slightly, dropping to a growth rate of 4.5% from 4.7% during this period. Hospital spending in 2018, at $1.2 trillion, accounted for 33% of overall health care spending.
On a personal level, overall growth in personal health care spending held steady with growth rate of 4.1% in 2018, the same as 2017, though individual components that feed into the figure varied. For example, growth rate in the spending on retail pharmaceuticals rose to 2.5% from 1.4% during this period. Spending on retail pharmaceuticals reached $335 billion and accounted for 9% of overall health care spending.
Another factor in the rising growth rate in spending came from employer-sponsored insurance.
“Growth in health spending by private business was due to faster growth in employer contributions to private health insurance premiums,” Anne B. Martin, economist in the National Health Statistics Group, said during the press conference. There also was faster growth in spending by the federal government, “driven mainly by faster growth in the federally funded portions of Medicare and Medicaid.”
Spending by private health insurance grew at a rate of 5.8% and reached $1.2 trillion in 2018. Medicare spending grew by 6.4% and reached $750.2 billion, while Medicaid spending grew 3.0%, reaching $597.4 billion.
SOURCE: Hartman M et al. Health Affairs. 2019. doi: 10.1377/hlthaff.2019.00451
Thanksgiving took a bite out of HealthCare.gov
Health care insurance may have taken a bit of a back seat to turkey and shopping last week as according to the Centers for Medicare & Medicaid Services.
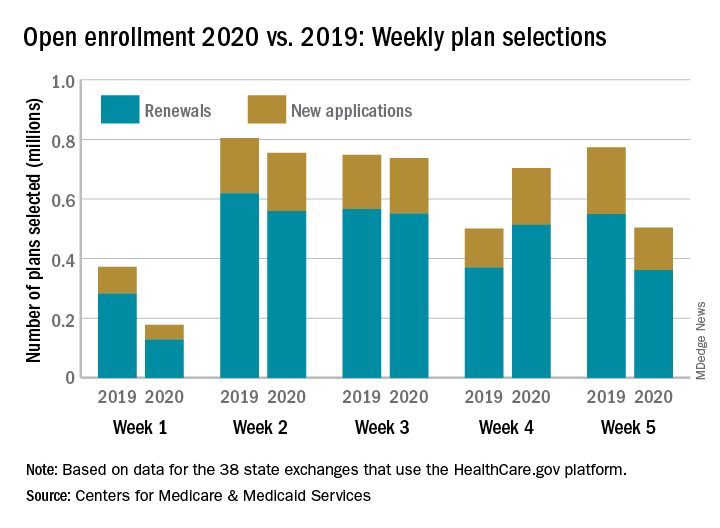
Consumers selected 28% fewer plans during week 5 (Nov. 24-30) of Open Enrollment 2020 than in week 4. A similar drop of 33% occurred last year between week 3 of open enrollment and week 4, which included Thanksgiving and Black Friday, CMS data show.
Through week 5, total plans selections for 2020 health insurance coverage came in at almost 2.9 million, which is down about 10% from last year’s 5-week total of 3.2 million for 2019 coverage.
The HealthCare.gov platform is being used by 38 states for the 2020 benefit year, and so far Florida residents have selected the most plans, almost 797,000. Texas is next with just over 400,000 selections, followed by Georgia with 173,000 and North Carolina with 162,000, CMS reported Dec. 4.
Health care insurance may have taken a bit of a back seat to turkey and shopping last week as according to the Centers for Medicare & Medicaid Services.
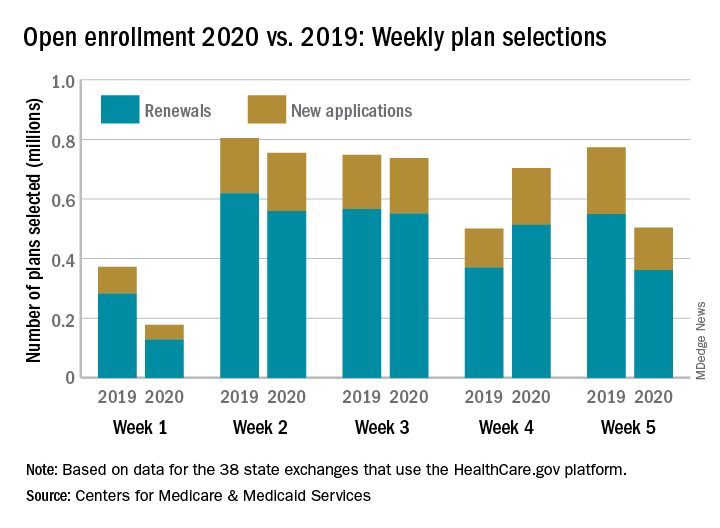
Consumers selected 28% fewer plans during week 5 (Nov. 24-30) of Open Enrollment 2020 than in week 4. A similar drop of 33% occurred last year between week 3 of open enrollment and week 4, which included Thanksgiving and Black Friday, CMS data show.
Through week 5, total plans selections for 2020 health insurance coverage came in at almost 2.9 million, which is down about 10% from last year’s 5-week total of 3.2 million for 2019 coverage.
The HealthCare.gov platform is being used by 38 states for the 2020 benefit year, and so far Florida residents have selected the most plans, almost 797,000. Texas is next with just over 400,000 selections, followed by Georgia with 173,000 and North Carolina with 162,000, CMS reported Dec. 4.
Health care insurance may have taken a bit of a back seat to turkey and shopping last week as according to the Centers for Medicare & Medicaid Services.
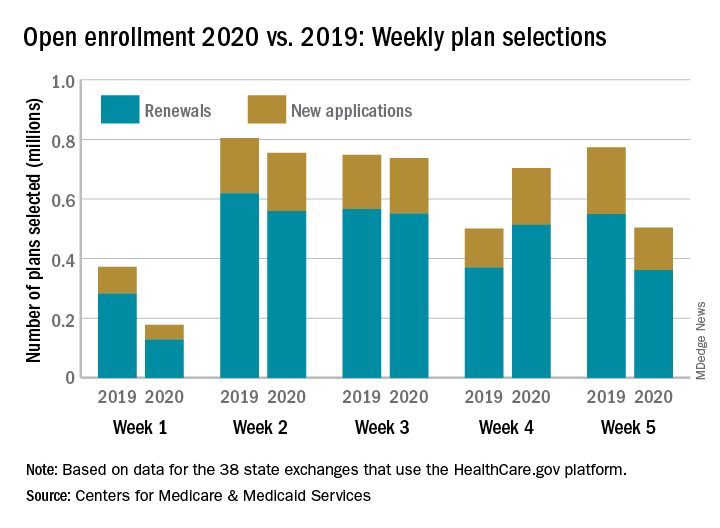
Consumers selected 28% fewer plans during week 5 (Nov. 24-30) of Open Enrollment 2020 than in week 4. A similar drop of 33% occurred last year between week 3 of open enrollment and week 4, which included Thanksgiving and Black Friday, CMS data show.
Through week 5, total plans selections for 2020 health insurance coverage came in at almost 2.9 million, which is down about 10% from last year’s 5-week total of 3.2 million for 2019 coverage.
The HealthCare.gov platform is being used by 38 states for the 2020 benefit year, and so far Florida residents have selected the most plans, almost 797,000. Texas is next with just over 400,000 selections, followed by Georgia with 173,000 and North Carolina with 162,000, CMS reported Dec. 4.
Millennials in Medicine: Cross-Trained Physicians Not Valued in Medical Marketplace
Millennials, defined as those born between 1981 and 1996, currently comprise 15% of all active physicians in the US.1,2 A recent survey found that nearly 4 of 5 US millennial physicians have a desire for cross-sectional work in areas beyond patient care, such as academic research, health care consulting, entrepreneurship, and health care administration.3
For employers and educators, a better understanding of these preferences, through consideration of the unique education and skill set of the millennial physician workforce, may lead to more effective recruitment of young physicians and improved health systems, avoiding a mismatch between health care provider skills and available jobs that can be costly for both employers and employees.4
This article describes how US millennial physicians are choosing to cross-train (obtaining multiple degrees and/or completing combined medical residency training) throughout undergraduate, medical, and graduate medical education. We also outline ways in which the current physician marketplace may not match the skills of this population and suggest some ways that health care organizations could capitalize on this trend toward more cross-trained personnel in order to effectively recruit and retain the next generation of physicians.
Millennial Education
Undergraduates
The number of interdisciplinary undergraduate majors increased by almost 250% from 1975 to 2000.5 In 2010, nearly 20% of US college students graduated with 2 majors, representing a 70% increase in double majors between 2001 and 2011.6,7 One emerging category of interdisciplinary majors in US colleges is health humanities programs, which have quadrupled since 2000.8
Medical school applicants and matriculants reflect this trend. Whereas in 1994, only 19% of applicants to medical school held nonscience degrees, about one-third of applicants now hold such degrees.9,10 We have found no aggregated data on double majors entering US medical schools, but public class profiles suggest that medical school matriculants mirror their undergraduate counterparts in their tendency to hold double majors. In 2016, for example, 15% of the incoming class at the University of Michigan Medical School was composed of double majors, increasing to over 25% in 2017.11
Medical Students
Early dual-degree programs in undergraduate medical training were reserved for MD/PhD programs.12 Most US MD/PhD programs (90 out of 151) now offer doctorates in social sciences, humanities, or other nontraditional fields of graduate medical study, reflecting a shift in interests of those seeking dual-degree training in undergraduate medical education.13 While only 3 MD/PhD programs in the 1970s included trainees in the social sciences, 17 such programs exist today.14
Interest in dual-degree programs offering master’s level study has also increased over the past decade. In 2017, 87 medical schools offered programs for students to pursue a master of public health (MPH) and 41 offered master of science degrees in various fields, up from 52 and 37 institutions, respectively in 2006.15 The number of schools offering combined training in nonscience fields has also grown, with 63 institutions now offering a master of business administration (MBA), nearly double the number offered in 2006.15 At some institutions more than 20% of students are earning a master’s degree or doctorate in addition to their MD degree.16
Residents
The authors found no documentation of US residency training programs, outside of those in the specialty of preventive medicine, providing trainees with formal opportunities to obtain an MBA or MPH prior to 2001.17 However, of the 510 internal medicine residency programs listed on the American Medical Association residency and fellowship database (freida.ama-assn.org), 45 identified as having established a pathway for residents to pursue an MBA, MPH, or PhD during residency.18
Over the past 20 years, combined residency programs have increased 49% (from 128 to 191), which is triple the 16% rate (1,350 to 1,562) of increase in programs in internal medicine, pediatrics, family medicine, psychiatry, and emergency medicine.19,20 A 2009 moratorium on the creation of new combined residency programs in psychiatry and neurology was lifted in 2016and is likely to increase the rate of total combined programs.21
The Table shows the number of categorical and combined residency programs available in 1996 and in 2016. Over 2 decades, 17 new specialty combinations became available for residency training. While there were no combined training programs within these 17 new combinations in 1996,there were 66 programs with these combinations in 2016.19,20
Although surgical specialties are notably absent from the list of combined residency options, likely due to the duration of surgical training, some surgical training programs do offer pathways that culminate in combined degrees,22 and a high number of surgery program directors agree that residents should receive formal training in business and practice management.23
The Medical Job Market
Although today’s young physicians are cross-trained in multiple disciplines, the current job market may not directly match these skill sets. Of the 7,235 jobs listed by the New England Journal of Medicine (NEJM) career center (www.nejmcareercenter.org/jobs), only 54 were targeted at those with combined training, the majority of which were aimed at those trained in internal medicine/pediatrics. Of the combined specialties in the Table, formal positions were listed for only 6.24 A search of nearly 1,500 federal medical positions on USAJOBS (www.usajobs.gov) found only 4 jobs that combined specialties, all restricted to internal medicine/pediatrics.25 When searching for jobs containing the terms MBA, MPH, and public health there were only 8 such positions on NEJM and 7 on USAJOBS.24,25 Although the totality of the medical marketplace may not be best encompassed by these sources, the authors believe NEJM and USAJOBS are somewhat representative of the opportunities for physicians in the US.
Medical jobs tailored to cross-trained physicians do not appear to have kept pace with the numbers of such specialists currently in medical school and residency training. Though millennials are cross-training in increasing numbers, we surmise that they are not doing so as a direct result of the job market.
Future Medicine
Regardless of the mismatch between cross-trained physicians and the current job market, millennials may be well suited for future health systems. In 2001, the National Academies of Sciences, Engineering and Medicine (NASEM) called for increasing interdisciplinary training and improving cross-functional team performance as a major goal for health care providers in twenty-first century health systems.26 NASEM also recommended that academic medical centers develop medical leaders who can manage systems changes required to enhance health, a proposal supported by the fact that hospitals with medically trained CEOs outperform others.27,28
Public Health 3.0, a federal initiative to improve and integrate public health efforts, also emphasizes cross-disciplinary teams and cross-sector partnerships,29 while the Centers for Medicare and Medicaid Services (CMS) has incentivized the development of interprofessional health care teams.30 While cross-training does not automatically connote interdisciplinary training, we believe that cross-training may reveal or develop an interdisciplinary mind-set that may support and embrace interdisciplinary performance. Finally, the US Department of Health and Human Services’ (HHS) Strategic Goals emphasize integrated care for vulnerable populations, something that cross-trained physicians may be especially poised to accomplish.31
A Path Forward
The education, training, and priorities of young physicians demonstrates career interests that diverge from mainstream, traditional options. Data provided herein describe the increasing rates at which millennial physicians are cross-training and have suggested that the current marketplace may not match the interests of this population. The ultimate question is where such cross-trained physicians fit into today’s (or tomorrow’s) health system?
It may be easiest to deploy cross-trained physicians in their respective clinical departments (eg, having a physician trained in internal medicine and pediatrics perform clinical duties in both a medicine department and a pediatrics department). But < 40% of dual-boarded physicians practice both specialties in which they’re trained, so other opportunities should be pursued.32,33 One strategy may be to embrace the promise of interdisciplinary care, as supported by Public Health 3.0 and NASEM.26,29 Our evidence may demonstrate that the interdisciplinary mind-set may be more readily evident in the millennial generation, and that this mind-set may improve interdisciplinary care.
As health is impacted both by direct clinical care as well as programs designed to address population health, cross-trained physicians may be better equipped to integrate aspects of clinical care spanning a variety of clinical fields as well as orchestrating programs designed to improve health at the population level. This mind-set may be best captured by organizations willing to adapt their medical positions to emphasize multidisciplinary training, skills, and capabilities. For example, a physician trained in internal medicine and psychiatry may have the unique training and skill-set to establish an integrated behavioral health clinic that crosses boundaries between traditional departments, emphasizing the whole health of the clinic’s population and not simply focusing on providing services of a particular specialty. Hiring cross-trained physicians throughout such a clinic may benefit the operations of the clinic and improve not only the services provided, but ultimately, the health of that clinic’s patients. By embracing cross-trained physicians, health care organizations and educators may better meet the needs of their employees, likely resulting in a more cost-effective investment for employers, employees, and the health system as a whole.4 Additionally, patient health may also improve.
There is evidence that cross-trained physicians are already likely to hold leadership positions compared with their categorically-trained counterparts, and this may reflect the benefits of an interdisciplinary mind-set.33 Perhaps a cross-trained physician is more likely to see beyond standard, specialty-based institutional barriers and develop processes and programs designed for overall patient benefit. Leadership is a skill that many millennials clearly wish to enhance throughout their career.34 Recruiting cross-trained physicians for leadership positions may reveal synergies between such training and an ability to lead health care organizations into the future.
Many millennial physicians are bringing a new set of skills into the medical marketplace. Health organizations should identify ways to recruit for these skills and deploy them within their systems in order to have more dedicated, engaged employees, more effective health systems, and ultimately, healthier patients.
Acknowledgments
Data from this analysis were presented at the 10th Consortium of Universities for Global Health conference in 2019.35
1. Dimock M. Defining generations: where millennials end and generation Z begins. http://www.pewresearch.org/fact-tank/2018/03/01/defining-generations-where-millennials-end-and-post-millennials-begin/. Published January 17, 2019. Accessed November 7, 2019.
2. IHS Inc. The complexities of physician supply and demand: projections from 2014 to 2025. Final report. https://www.modernhealthcare.com/assets/pdf/CH10888123.pdf. Published April 5, 2016. Accessed November 7, 2019.
3. Miller RN. Millennial physicians sound off on state of medicine today. https://wire.ama-assn.org/life-career/millennial-physicians-sound-state-medicine-today. Published March 27, 2017. Accessed November 7, 2019.
4. World Economic Forum. Matching skills and labour market needs: building social partnerships for better skills and better jobs. http://www3.weforum.org/docs/GAC/2014/WEF_GAC_Employment_MatchingSkillsLabourMarket_Report_2014.pdf. Published January 2014. Accessed November 7, 2019.
5. Brint SG, Turk-Bicakci L, Proctor K, Murphy SP. Expanding the social frame of knowledge: interdisciplinary, degree-granting fields in American Colleges and Universities, 1975–2000. Rev High Ed. 2009;32(2):155-183.
6. National Science Foundation. National survey of college graduates. https://www.nsf.gov/statistics/srvygrads. Updated February 2019. Accessed November 7, 2019.
7. Simon CC. Major decisions. New York Times. November 2, 2012. http://www.nytimes.com/2012/11/04/education/edlife/choosing-one-college-major-out-of-hundreds.html. Accessed November 7, 2019.
8. Berry SL, Erin GL, Therese J. Health humanities baccalaureate programs in the United States. http://www.hiram.edu/wp-content/uploads/2017/09/HHBP2017.pdf. Published September 2017. Accessed November 7, 2019.
9. Sorensen NE, Jackson JR. Science majors and nonscience majors entering medical school: acceptance rates and academic performance. NACADA J. 1997;17(1):32-41.
10. Association of American Medical Colleges. Table A-17: MCAT and GPAs for applicants and matriculants to U.S. medical schools by primary undergraduate major, 2019-2020. https://www.aamc.org/download/321496/data/factstablea17.pdf. Published October 16, 2019. Accessed November 7, 2019.
11. University of Michigan Medical School. Many paths, one destination: medical school welcomes its 170th class of medical students. https://medicine.umich.edu/medschool/news/many-paths-one-destination-medical-school-welcomes-its-170th-class-medical-students. Updated July 29, 2016. Accessed November 7, 2019.
12. Harding CV, Akabas MH, Andersen OS. History and outcomes of 50 years of physician-scientist training in medical scientist training programs. Acad Med. 2017; 92(10):1390-1398.
13. Association of American Medical Colleges. MD-PhD in “social sciences or humanities” and “other non-traditional fields of graduate study” - by school. https://students-residents.aamc.org/choosing-medical-career/careers-medical-research/md-phd-dual-degree-training/non-basic-science-phd-training-school/. Accessed November 8, 2019.
14. Holmes SM, Karlin J, Stonington SD, Gottheil DL. The first nationwide survey of MD-PhDs in the social sciences and humanities: training patterns and career choices. BMC Med Educ. 2017;17(1):60.
15. Association of American Medical Colleges Combined degrees and early acceptance programs. https://www.aamc.org/data-reports/curriculum-reports/interactive-data/combined-degrees-and-early-acceptance-programs. Accessed November 8, 2019.
16. Tufts University School of Medicine. 2023 class profile. http://medicine.tufts.edu/Education/MD-Programs/Doctor-of-Medicine/Class-Profile. Published 2015. Accessed November 8, 2019.
17. Zweifler J, Evan R. Development of a residency/MPH program. Family Med. 2001;33(6):453-458.
18. American Medical Association. The AMA residency and fellowship database. http://freida.ama-assn.org/Freida. Accessed November 7, 2019.
19. National Resident Matching Program. NRMP data. http://www.nrmp.org/wp-content/uploads/2013/08/resultsanddata1996.pdf. Published March 1996. Accessed November 7, 2019.
20. Brotherton SE, Etzel SI. Graduate medical education, 2016-2017. JAMA. 2017;318(23):2368-2387.
21. American Board of Psychiatry and Neurology. Update for psychiatry GME programs on combined training program accreditation/approval February 2012. https://www.umassmed.edu/globalassets/neuropsychiatry/files/combined-program-letter.pdf. Accessed November 7, 2019.
22. Massachusetts General Hospital. Surgical residency program. https://www.massgeneral.org/surgery/education/residency.aspx?id=77. Accessed November 7, 2019.
23. Lusco VC, Martinez SA, Polk HC Jr. Program directors in surgery agree that residents should be formally trained in business and practice management. Am J Surg. 2005;189(1):11-13.
24. New England Journal of Medicine. NEJM CareerCenter. http://www.nejmcareercenter.org. Accessed November 7, 2019.
25. US Office of Personnel Management. USAJOBS. https://www.usajobs.gov. Accessed November 7, 2019.
26. Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. http://www.nationalacademies.org/hmd/~/media/Files/Report%20Files/2001/Crossing-the-Quality-Chasm/Quality%20Chasm%202001%20%20report%20brief.pdf. Published March 2001. Accessed November 7, 2019.
27. Kohn LT, ed; Committee on the Roles of Academic Health Centers in the 21st Century; Institute of Medicine of the National Academies. Academic Health Centers: Leading Change in the 21st Century. National Academy Press: Washington, DC; 2004.
28. Goodall AH. Physician-leaders and hospital performance: is there an association? http://ftp.iza.org/dp5830.pdf. Published July 2011. Accessed November 7, 2019.
29. US Department of Health and Human Services, Office of the Assistant Secretary for Health. Public health 3.0: a call to action to create a 21st century public health infrastructure. https://www.healthypeople.gov/sites/default/files/Public-Health-3.0-White-Paper.pdf. Accessed November 7, 2019.
30. Centers for Medicare and Medicaid Services. Health care innovation awards round one project profiles. http://innovation.cms.gov/files/x/hcia-project-profiles.pdf. Updated December 2013. Accessed November 7, 2019.
31. US Department of Health and Human Services. Strategic Objective 1.3: Improve Americans’ access to healthcare and expand choices of care and service options. https://www.hhs.gov/about/strategic-plan/strategic-goal-1/index.html#obj_1_3. Updated March 18, 2019. Accessed November 7, 2019.
32. Kessler CS, Stallings LA, Gonzalez AA, Templeman TA. Combined residency training in emergency medicine and internal medicine: an update on career outcomes and job satisfaction. Acad Emerg Med. 2009;16(9):894-899.
33. Summergrad P, Silberman E, Price LL. Practice and career outcomes of double-boarded psychiatrists. Psychosomatics. 2011;52(6):537-543.
34. Rigoni B, Adkins A. What millennials want from a new job. Harvard Business Rev. May 11, 2016. https://hbr.org/2016/05/what-millennials-want-from-a-new-job. Accessed November 7, 2019.
35. Jung P, Smith C. Medical millennials: a mismatch between training preferences and employment opportunities. Lancet Glob Health. 2019;7(suppl 1):S38.
Millennials, defined as those born between 1981 and 1996, currently comprise 15% of all active physicians in the US.1,2 A recent survey found that nearly 4 of 5 US millennial physicians have a desire for cross-sectional work in areas beyond patient care, such as academic research, health care consulting, entrepreneurship, and health care administration.3
For employers and educators, a better understanding of these preferences, through consideration of the unique education and skill set of the millennial physician workforce, may lead to more effective recruitment of young physicians and improved health systems, avoiding a mismatch between health care provider skills and available jobs that can be costly for both employers and employees.4
This article describes how US millennial physicians are choosing to cross-train (obtaining multiple degrees and/or completing combined medical residency training) throughout undergraduate, medical, and graduate medical education. We also outline ways in which the current physician marketplace may not match the skills of this population and suggest some ways that health care organizations could capitalize on this trend toward more cross-trained personnel in order to effectively recruit and retain the next generation of physicians.
Millennial Education
Undergraduates
The number of interdisciplinary undergraduate majors increased by almost 250% from 1975 to 2000.5 In 2010, nearly 20% of US college students graduated with 2 majors, representing a 70% increase in double majors between 2001 and 2011.6,7 One emerging category of interdisciplinary majors in US colleges is health humanities programs, which have quadrupled since 2000.8
Medical school applicants and matriculants reflect this trend. Whereas in 1994, only 19% of applicants to medical school held nonscience degrees, about one-third of applicants now hold such degrees.9,10 We have found no aggregated data on double majors entering US medical schools, but public class profiles suggest that medical school matriculants mirror their undergraduate counterparts in their tendency to hold double majors. In 2016, for example, 15% of the incoming class at the University of Michigan Medical School was composed of double majors, increasing to over 25% in 2017.11
Medical Students
Early dual-degree programs in undergraduate medical training were reserved for MD/PhD programs.12 Most US MD/PhD programs (90 out of 151) now offer doctorates in social sciences, humanities, or other nontraditional fields of graduate medical study, reflecting a shift in interests of those seeking dual-degree training in undergraduate medical education.13 While only 3 MD/PhD programs in the 1970s included trainees in the social sciences, 17 such programs exist today.14
Interest in dual-degree programs offering master’s level study has also increased over the past decade. In 2017, 87 medical schools offered programs for students to pursue a master of public health (MPH) and 41 offered master of science degrees in various fields, up from 52 and 37 institutions, respectively in 2006.15 The number of schools offering combined training in nonscience fields has also grown, with 63 institutions now offering a master of business administration (MBA), nearly double the number offered in 2006.15 At some institutions more than 20% of students are earning a master’s degree or doctorate in addition to their MD degree.16
Residents
The authors found no documentation of US residency training programs, outside of those in the specialty of preventive medicine, providing trainees with formal opportunities to obtain an MBA or MPH prior to 2001.17 However, of the 510 internal medicine residency programs listed on the American Medical Association residency and fellowship database (freida.ama-assn.org), 45 identified as having established a pathway for residents to pursue an MBA, MPH, or PhD during residency.18
Over the past 20 years, combined residency programs have increased 49% (from 128 to 191), which is triple the 16% rate (1,350 to 1,562) of increase in programs in internal medicine, pediatrics, family medicine, psychiatry, and emergency medicine.19,20 A 2009 moratorium on the creation of new combined residency programs in psychiatry and neurology was lifted in 2016and is likely to increase the rate of total combined programs.21
The Table shows the number of categorical and combined residency programs available in 1996 and in 2016. Over 2 decades, 17 new specialty combinations became available for residency training. While there were no combined training programs within these 17 new combinations in 1996,there were 66 programs with these combinations in 2016.19,20
Although surgical specialties are notably absent from the list of combined residency options, likely due to the duration of surgical training, some surgical training programs do offer pathways that culminate in combined degrees,22 and a high number of surgery program directors agree that residents should receive formal training in business and practice management.23
The Medical Job Market
Although today’s young physicians are cross-trained in multiple disciplines, the current job market may not directly match these skill sets. Of the 7,235 jobs listed by the New England Journal of Medicine (NEJM) career center (www.nejmcareercenter.org/jobs), only 54 were targeted at those with combined training, the majority of which were aimed at those trained in internal medicine/pediatrics. Of the combined specialties in the Table, formal positions were listed for only 6.24 A search of nearly 1,500 federal medical positions on USAJOBS (www.usajobs.gov) found only 4 jobs that combined specialties, all restricted to internal medicine/pediatrics.25 When searching for jobs containing the terms MBA, MPH, and public health there were only 8 such positions on NEJM and 7 on USAJOBS.24,25 Although the totality of the medical marketplace may not be best encompassed by these sources, the authors believe NEJM and USAJOBS are somewhat representative of the opportunities for physicians in the US.
Medical jobs tailored to cross-trained physicians do not appear to have kept pace with the numbers of such specialists currently in medical school and residency training. Though millennials are cross-training in increasing numbers, we surmise that they are not doing so as a direct result of the job market.
Future Medicine
Regardless of the mismatch between cross-trained physicians and the current job market, millennials may be well suited for future health systems. In 2001, the National Academies of Sciences, Engineering and Medicine (NASEM) called for increasing interdisciplinary training and improving cross-functional team performance as a major goal for health care providers in twenty-first century health systems.26 NASEM also recommended that academic medical centers develop medical leaders who can manage systems changes required to enhance health, a proposal supported by the fact that hospitals with medically trained CEOs outperform others.27,28
Public Health 3.0, a federal initiative to improve and integrate public health efforts, also emphasizes cross-disciplinary teams and cross-sector partnerships,29 while the Centers for Medicare and Medicaid Services (CMS) has incentivized the development of interprofessional health care teams.30 While cross-training does not automatically connote interdisciplinary training, we believe that cross-training may reveal or develop an interdisciplinary mind-set that may support and embrace interdisciplinary performance. Finally, the US Department of Health and Human Services’ (HHS) Strategic Goals emphasize integrated care for vulnerable populations, something that cross-trained physicians may be especially poised to accomplish.31
A Path Forward
The education, training, and priorities of young physicians demonstrates career interests that diverge from mainstream, traditional options. Data provided herein describe the increasing rates at which millennial physicians are cross-training and have suggested that the current marketplace may not match the interests of this population. The ultimate question is where such cross-trained physicians fit into today’s (or tomorrow’s) health system?
It may be easiest to deploy cross-trained physicians in their respective clinical departments (eg, having a physician trained in internal medicine and pediatrics perform clinical duties in both a medicine department and a pediatrics department). But < 40% of dual-boarded physicians practice both specialties in which they’re trained, so other opportunities should be pursued.32,33 One strategy may be to embrace the promise of interdisciplinary care, as supported by Public Health 3.0 and NASEM.26,29 Our evidence may demonstrate that the interdisciplinary mind-set may be more readily evident in the millennial generation, and that this mind-set may improve interdisciplinary care.
As health is impacted both by direct clinical care as well as programs designed to address population health, cross-trained physicians may be better equipped to integrate aspects of clinical care spanning a variety of clinical fields as well as orchestrating programs designed to improve health at the population level. This mind-set may be best captured by organizations willing to adapt their medical positions to emphasize multidisciplinary training, skills, and capabilities. For example, a physician trained in internal medicine and psychiatry may have the unique training and skill-set to establish an integrated behavioral health clinic that crosses boundaries between traditional departments, emphasizing the whole health of the clinic’s population and not simply focusing on providing services of a particular specialty. Hiring cross-trained physicians throughout such a clinic may benefit the operations of the clinic and improve not only the services provided, but ultimately, the health of that clinic’s patients. By embracing cross-trained physicians, health care organizations and educators may better meet the needs of their employees, likely resulting in a more cost-effective investment for employers, employees, and the health system as a whole.4 Additionally, patient health may also improve.
There is evidence that cross-trained physicians are already likely to hold leadership positions compared with their categorically-trained counterparts, and this may reflect the benefits of an interdisciplinary mind-set.33 Perhaps a cross-trained physician is more likely to see beyond standard, specialty-based institutional barriers and develop processes and programs designed for overall patient benefit. Leadership is a skill that many millennials clearly wish to enhance throughout their career.34 Recruiting cross-trained physicians for leadership positions may reveal synergies between such training and an ability to lead health care organizations into the future.
Many millennial physicians are bringing a new set of skills into the medical marketplace. Health organizations should identify ways to recruit for these skills and deploy them within their systems in order to have more dedicated, engaged employees, more effective health systems, and ultimately, healthier patients.
Acknowledgments
Data from this analysis were presented at the 10th Consortium of Universities for Global Health conference in 2019.35
Millennials, defined as those born between 1981 and 1996, currently comprise 15% of all active physicians in the US.1,2 A recent survey found that nearly 4 of 5 US millennial physicians have a desire for cross-sectional work in areas beyond patient care, such as academic research, health care consulting, entrepreneurship, and health care administration.3
For employers and educators, a better understanding of these preferences, through consideration of the unique education and skill set of the millennial physician workforce, may lead to more effective recruitment of young physicians and improved health systems, avoiding a mismatch between health care provider skills and available jobs that can be costly for both employers and employees.4
This article describes how US millennial physicians are choosing to cross-train (obtaining multiple degrees and/or completing combined medical residency training) throughout undergraduate, medical, and graduate medical education. We also outline ways in which the current physician marketplace may not match the skills of this population and suggest some ways that health care organizations could capitalize on this trend toward more cross-trained personnel in order to effectively recruit and retain the next generation of physicians.
Millennial Education
Undergraduates
The number of interdisciplinary undergraduate majors increased by almost 250% from 1975 to 2000.5 In 2010, nearly 20% of US college students graduated with 2 majors, representing a 70% increase in double majors between 2001 and 2011.6,7 One emerging category of interdisciplinary majors in US colleges is health humanities programs, which have quadrupled since 2000.8
Medical school applicants and matriculants reflect this trend. Whereas in 1994, only 19% of applicants to medical school held nonscience degrees, about one-third of applicants now hold such degrees.9,10 We have found no aggregated data on double majors entering US medical schools, but public class profiles suggest that medical school matriculants mirror their undergraduate counterparts in their tendency to hold double majors. In 2016, for example, 15% of the incoming class at the University of Michigan Medical School was composed of double majors, increasing to over 25% in 2017.11
Medical Students
Early dual-degree programs in undergraduate medical training were reserved for MD/PhD programs.12 Most US MD/PhD programs (90 out of 151) now offer doctorates in social sciences, humanities, or other nontraditional fields of graduate medical study, reflecting a shift in interests of those seeking dual-degree training in undergraduate medical education.13 While only 3 MD/PhD programs in the 1970s included trainees in the social sciences, 17 such programs exist today.14
Interest in dual-degree programs offering master’s level study has also increased over the past decade. In 2017, 87 medical schools offered programs for students to pursue a master of public health (MPH) and 41 offered master of science degrees in various fields, up from 52 and 37 institutions, respectively in 2006.15 The number of schools offering combined training in nonscience fields has also grown, with 63 institutions now offering a master of business administration (MBA), nearly double the number offered in 2006.15 At some institutions more than 20% of students are earning a master’s degree or doctorate in addition to their MD degree.16
Residents
The authors found no documentation of US residency training programs, outside of those in the specialty of preventive medicine, providing trainees with formal opportunities to obtain an MBA or MPH prior to 2001.17 However, of the 510 internal medicine residency programs listed on the American Medical Association residency and fellowship database (freida.ama-assn.org), 45 identified as having established a pathway for residents to pursue an MBA, MPH, or PhD during residency.18
Over the past 20 years, combined residency programs have increased 49% (from 128 to 191), which is triple the 16% rate (1,350 to 1,562) of increase in programs in internal medicine, pediatrics, family medicine, psychiatry, and emergency medicine.19,20 A 2009 moratorium on the creation of new combined residency programs in psychiatry and neurology was lifted in 2016and is likely to increase the rate of total combined programs.21
The Table shows the number of categorical and combined residency programs available in 1996 and in 2016. Over 2 decades, 17 new specialty combinations became available for residency training. While there were no combined training programs within these 17 new combinations in 1996,there were 66 programs with these combinations in 2016.19,20
Although surgical specialties are notably absent from the list of combined residency options, likely due to the duration of surgical training, some surgical training programs do offer pathways that culminate in combined degrees,22 and a high number of surgery program directors agree that residents should receive formal training in business and practice management.23
The Medical Job Market
Although today’s young physicians are cross-trained in multiple disciplines, the current job market may not directly match these skill sets. Of the 7,235 jobs listed by the New England Journal of Medicine (NEJM) career center (www.nejmcareercenter.org/jobs), only 54 were targeted at those with combined training, the majority of which were aimed at those trained in internal medicine/pediatrics. Of the combined specialties in the Table, formal positions were listed for only 6.24 A search of nearly 1,500 federal medical positions on USAJOBS (www.usajobs.gov) found only 4 jobs that combined specialties, all restricted to internal medicine/pediatrics.25 When searching for jobs containing the terms MBA, MPH, and public health there were only 8 such positions on NEJM and 7 on USAJOBS.24,25 Although the totality of the medical marketplace may not be best encompassed by these sources, the authors believe NEJM and USAJOBS are somewhat representative of the opportunities for physicians in the US.
Medical jobs tailored to cross-trained physicians do not appear to have kept pace with the numbers of such specialists currently in medical school and residency training. Though millennials are cross-training in increasing numbers, we surmise that they are not doing so as a direct result of the job market.
Future Medicine
Regardless of the mismatch between cross-trained physicians and the current job market, millennials may be well suited for future health systems. In 2001, the National Academies of Sciences, Engineering and Medicine (NASEM) called for increasing interdisciplinary training and improving cross-functional team performance as a major goal for health care providers in twenty-first century health systems.26 NASEM also recommended that academic medical centers develop medical leaders who can manage systems changes required to enhance health, a proposal supported by the fact that hospitals with medically trained CEOs outperform others.27,28
Public Health 3.0, a federal initiative to improve and integrate public health efforts, also emphasizes cross-disciplinary teams and cross-sector partnerships,29 while the Centers for Medicare and Medicaid Services (CMS) has incentivized the development of interprofessional health care teams.30 While cross-training does not automatically connote interdisciplinary training, we believe that cross-training may reveal or develop an interdisciplinary mind-set that may support and embrace interdisciplinary performance. Finally, the US Department of Health and Human Services’ (HHS) Strategic Goals emphasize integrated care for vulnerable populations, something that cross-trained physicians may be especially poised to accomplish.31
A Path Forward
The education, training, and priorities of young physicians demonstrates career interests that diverge from mainstream, traditional options. Data provided herein describe the increasing rates at which millennial physicians are cross-training and have suggested that the current marketplace may not match the interests of this population. The ultimate question is where such cross-trained physicians fit into today’s (or tomorrow’s) health system?
It may be easiest to deploy cross-trained physicians in their respective clinical departments (eg, having a physician trained in internal medicine and pediatrics perform clinical duties in both a medicine department and a pediatrics department). But < 40% of dual-boarded physicians practice both specialties in which they’re trained, so other opportunities should be pursued.32,33 One strategy may be to embrace the promise of interdisciplinary care, as supported by Public Health 3.0 and NASEM.26,29 Our evidence may demonstrate that the interdisciplinary mind-set may be more readily evident in the millennial generation, and that this mind-set may improve interdisciplinary care.
As health is impacted both by direct clinical care as well as programs designed to address population health, cross-trained physicians may be better equipped to integrate aspects of clinical care spanning a variety of clinical fields as well as orchestrating programs designed to improve health at the population level. This mind-set may be best captured by organizations willing to adapt their medical positions to emphasize multidisciplinary training, skills, and capabilities. For example, a physician trained in internal medicine and psychiatry may have the unique training and skill-set to establish an integrated behavioral health clinic that crosses boundaries between traditional departments, emphasizing the whole health of the clinic’s population and not simply focusing on providing services of a particular specialty. Hiring cross-trained physicians throughout such a clinic may benefit the operations of the clinic and improve not only the services provided, but ultimately, the health of that clinic’s patients. By embracing cross-trained physicians, health care organizations and educators may better meet the needs of their employees, likely resulting in a more cost-effective investment for employers, employees, and the health system as a whole.4 Additionally, patient health may also improve.
There is evidence that cross-trained physicians are already likely to hold leadership positions compared with their categorically-trained counterparts, and this may reflect the benefits of an interdisciplinary mind-set.33 Perhaps a cross-trained physician is more likely to see beyond standard, specialty-based institutional barriers and develop processes and programs designed for overall patient benefit. Leadership is a skill that many millennials clearly wish to enhance throughout their career.34 Recruiting cross-trained physicians for leadership positions may reveal synergies between such training and an ability to lead health care organizations into the future.
Many millennial physicians are bringing a new set of skills into the medical marketplace. Health organizations should identify ways to recruit for these skills and deploy them within their systems in order to have more dedicated, engaged employees, more effective health systems, and ultimately, healthier patients.
Acknowledgments
Data from this analysis were presented at the 10th Consortium of Universities for Global Health conference in 2019.35
1. Dimock M. Defining generations: where millennials end and generation Z begins. http://www.pewresearch.org/fact-tank/2018/03/01/defining-generations-where-millennials-end-and-post-millennials-begin/. Published January 17, 2019. Accessed November 7, 2019.
2. IHS Inc. The complexities of physician supply and demand: projections from 2014 to 2025. Final report. https://www.modernhealthcare.com/assets/pdf/CH10888123.pdf. Published April 5, 2016. Accessed November 7, 2019.
3. Miller RN. Millennial physicians sound off on state of medicine today. https://wire.ama-assn.org/life-career/millennial-physicians-sound-state-medicine-today. Published March 27, 2017. Accessed November 7, 2019.
4. World Economic Forum. Matching skills and labour market needs: building social partnerships for better skills and better jobs. http://www3.weforum.org/docs/GAC/2014/WEF_GAC_Employment_MatchingSkillsLabourMarket_Report_2014.pdf. Published January 2014. Accessed November 7, 2019.
5. Brint SG, Turk-Bicakci L, Proctor K, Murphy SP. Expanding the social frame of knowledge: interdisciplinary, degree-granting fields in American Colleges and Universities, 1975–2000. Rev High Ed. 2009;32(2):155-183.
6. National Science Foundation. National survey of college graduates. https://www.nsf.gov/statistics/srvygrads. Updated February 2019. Accessed November 7, 2019.
7. Simon CC. Major decisions. New York Times. November 2, 2012. http://www.nytimes.com/2012/11/04/education/edlife/choosing-one-college-major-out-of-hundreds.html. Accessed November 7, 2019.
8. Berry SL, Erin GL, Therese J. Health humanities baccalaureate programs in the United States. http://www.hiram.edu/wp-content/uploads/2017/09/HHBP2017.pdf. Published September 2017. Accessed November 7, 2019.
9. Sorensen NE, Jackson JR. Science majors and nonscience majors entering medical school: acceptance rates and academic performance. NACADA J. 1997;17(1):32-41.
10. Association of American Medical Colleges. Table A-17: MCAT and GPAs for applicants and matriculants to U.S. medical schools by primary undergraduate major, 2019-2020. https://www.aamc.org/download/321496/data/factstablea17.pdf. Published October 16, 2019. Accessed November 7, 2019.
11. University of Michigan Medical School. Many paths, one destination: medical school welcomes its 170th class of medical students. https://medicine.umich.edu/medschool/news/many-paths-one-destination-medical-school-welcomes-its-170th-class-medical-students. Updated July 29, 2016. Accessed November 7, 2019.
12. Harding CV, Akabas MH, Andersen OS. History and outcomes of 50 years of physician-scientist training in medical scientist training programs. Acad Med. 2017; 92(10):1390-1398.
13. Association of American Medical Colleges. MD-PhD in “social sciences or humanities” and “other non-traditional fields of graduate study” - by school. https://students-residents.aamc.org/choosing-medical-career/careers-medical-research/md-phd-dual-degree-training/non-basic-science-phd-training-school/. Accessed November 8, 2019.
14. Holmes SM, Karlin J, Stonington SD, Gottheil DL. The first nationwide survey of MD-PhDs in the social sciences and humanities: training patterns and career choices. BMC Med Educ. 2017;17(1):60.
15. Association of American Medical Colleges Combined degrees and early acceptance programs. https://www.aamc.org/data-reports/curriculum-reports/interactive-data/combined-degrees-and-early-acceptance-programs. Accessed November 8, 2019.
16. Tufts University School of Medicine. 2023 class profile. http://medicine.tufts.edu/Education/MD-Programs/Doctor-of-Medicine/Class-Profile. Published 2015. Accessed November 8, 2019.
17. Zweifler J, Evan R. Development of a residency/MPH program. Family Med. 2001;33(6):453-458.
18. American Medical Association. The AMA residency and fellowship database. http://freida.ama-assn.org/Freida. Accessed November 7, 2019.
19. National Resident Matching Program. NRMP data. http://www.nrmp.org/wp-content/uploads/2013/08/resultsanddata1996.pdf. Published March 1996. Accessed November 7, 2019.
20. Brotherton SE, Etzel SI. Graduate medical education, 2016-2017. JAMA. 2017;318(23):2368-2387.
21. American Board of Psychiatry and Neurology. Update for psychiatry GME programs on combined training program accreditation/approval February 2012. https://www.umassmed.edu/globalassets/neuropsychiatry/files/combined-program-letter.pdf. Accessed November 7, 2019.
22. Massachusetts General Hospital. Surgical residency program. https://www.massgeneral.org/surgery/education/residency.aspx?id=77. Accessed November 7, 2019.
23. Lusco VC, Martinez SA, Polk HC Jr. Program directors in surgery agree that residents should be formally trained in business and practice management. Am J Surg. 2005;189(1):11-13.
24. New England Journal of Medicine. NEJM CareerCenter. http://www.nejmcareercenter.org. Accessed November 7, 2019.
25. US Office of Personnel Management. USAJOBS. https://www.usajobs.gov. Accessed November 7, 2019.
26. Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. http://www.nationalacademies.org/hmd/~/media/Files/Report%20Files/2001/Crossing-the-Quality-Chasm/Quality%20Chasm%202001%20%20report%20brief.pdf. Published March 2001. Accessed November 7, 2019.
27. Kohn LT, ed; Committee on the Roles of Academic Health Centers in the 21st Century; Institute of Medicine of the National Academies. Academic Health Centers: Leading Change in the 21st Century. National Academy Press: Washington, DC; 2004.
28. Goodall AH. Physician-leaders and hospital performance: is there an association? http://ftp.iza.org/dp5830.pdf. Published July 2011. Accessed November 7, 2019.
29. US Department of Health and Human Services, Office of the Assistant Secretary for Health. Public health 3.0: a call to action to create a 21st century public health infrastructure. https://www.healthypeople.gov/sites/default/files/Public-Health-3.0-White-Paper.pdf. Accessed November 7, 2019.
30. Centers for Medicare and Medicaid Services. Health care innovation awards round one project profiles. http://innovation.cms.gov/files/x/hcia-project-profiles.pdf. Updated December 2013. Accessed November 7, 2019.
31. US Department of Health and Human Services. Strategic Objective 1.3: Improve Americans’ access to healthcare and expand choices of care and service options. https://www.hhs.gov/about/strategic-plan/strategic-goal-1/index.html#obj_1_3. Updated March 18, 2019. Accessed November 7, 2019.
32. Kessler CS, Stallings LA, Gonzalez AA, Templeman TA. Combined residency training in emergency medicine and internal medicine: an update on career outcomes and job satisfaction. Acad Emerg Med. 2009;16(9):894-899.
33. Summergrad P, Silberman E, Price LL. Practice and career outcomes of double-boarded psychiatrists. Psychosomatics. 2011;52(6):537-543.
34. Rigoni B, Adkins A. What millennials want from a new job. Harvard Business Rev. May 11, 2016. https://hbr.org/2016/05/what-millennials-want-from-a-new-job. Accessed November 7, 2019.
35. Jung P, Smith C. Medical millennials: a mismatch between training preferences and employment opportunities. Lancet Glob Health. 2019;7(suppl 1):S38.
1. Dimock M. Defining generations: where millennials end and generation Z begins. http://www.pewresearch.org/fact-tank/2018/03/01/defining-generations-where-millennials-end-and-post-millennials-begin/. Published January 17, 2019. Accessed November 7, 2019.
2. IHS Inc. The complexities of physician supply and demand: projections from 2014 to 2025. Final report. https://www.modernhealthcare.com/assets/pdf/CH10888123.pdf. Published April 5, 2016. Accessed November 7, 2019.
3. Miller RN. Millennial physicians sound off on state of medicine today. https://wire.ama-assn.org/life-career/millennial-physicians-sound-state-medicine-today. Published March 27, 2017. Accessed November 7, 2019.
4. World Economic Forum. Matching skills and labour market needs: building social partnerships for better skills and better jobs. http://www3.weforum.org/docs/GAC/2014/WEF_GAC_Employment_MatchingSkillsLabourMarket_Report_2014.pdf. Published January 2014. Accessed November 7, 2019.
5. Brint SG, Turk-Bicakci L, Proctor K, Murphy SP. Expanding the social frame of knowledge: interdisciplinary, degree-granting fields in American Colleges and Universities, 1975–2000. Rev High Ed. 2009;32(2):155-183.
6. National Science Foundation. National survey of college graduates. https://www.nsf.gov/statistics/srvygrads. Updated February 2019. Accessed November 7, 2019.
7. Simon CC. Major decisions. New York Times. November 2, 2012. http://www.nytimes.com/2012/11/04/education/edlife/choosing-one-college-major-out-of-hundreds.html. Accessed November 7, 2019.
8. Berry SL, Erin GL, Therese J. Health humanities baccalaureate programs in the United States. http://www.hiram.edu/wp-content/uploads/2017/09/HHBP2017.pdf. Published September 2017. Accessed November 7, 2019.
9. Sorensen NE, Jackson JR. Science majors and nonscience majors entering medical school: acceptance rates and academic performance. NACADA J. 1997;17(1):32-41.
10. Association of American Medical Colleges. Table A-17: MCAT and GPAs for applicants and matriculants to U.S. medical schools by primary undergraduate major, 2019-2020. https://www.aamc.org/download/321496/data/factstablea17.pdf. Published October 16, 2019. Accessed November 7, 2019.
11. University of Michigan Medical School. Many paths, one destination: medical school welcomes its 170th class of medical students. https://medicine.umich.edu/medschool/news/many-paths-one-destination-medical-school-welcomes-its-170th-class-medical-students. Updated July 29, 2016. Accessed November 7, 2019.
12. Harding CV, Akabas MH, Andersen OS. History and outcomes of 50 years of physician-scientist training in medical scientist training programs. Acad Med. 2017; 92(10):1390-1398.
13. Association of American Medical Colleges. MD-PhD in “social sciences or humanities” and “other non-traditional fields of graduate study” - by school. https://students-residents.aamc.org/choosing-medical-career/careers-medical-research/md-phd-dual-degree-training/non-basic-science-phd-training-school/. Accessed November 8, 2019.
14. Holmes SM, Karlin J, Stonington SD, Gottheil DL. The first nationwide survey of MD-PhDs in the social sciences and humanities: training patterns and career choices. BMC Med Educ. 2017;17(1):60.
15. Association of American Medical Colleges Combined degrees and early acceptance programs. https://www.aamc.org/data-reports/curriculum-reports/interactive-data/combined-degrees-and-early-acceptance-programs. Accessed November 8, 2019.
16. Tufts University School of Medicine. 2023 class profile. http://medicine.tufts.edu/Education/MD-Programs/Doctor-of-Medicine/Class-Profile. Published 2015. Accessed November 8, 2019.
17. Zweifler J, Evan R. Development of a residency/MPH program. Family Med. 2001;33(6):453-458.
18. American Medical Association. The AMA residency and fellowship database. http://freida.ama-assn.org/Freida. Accessed November 7, 2019.
19. National Resident Matching Program. NRMP data. http://www.nrmp.org/wp-content/uploads/2013/08/resultsanddata1996.pdf. Published March 1996. Accessed November 7, 2019.
20. Brotherton SE, Etzel SI. Graduate medical education, 2016-2017. JAMA. 2017;318(23):2368-2387.
21. American Board of Psychiatry and Neurology. Update for psychiatry GME programs on combined training program accreditation/approval February 2012. https://www.umassmed.edu/globalassets/neuropsychiatry/files/combined-program-letter.pdf. Accessed November 7, 2019.
22. Massachusetts General Hospital. Surgical residency program. https://www.massgeneral.org/surgery/education/residency.aspx?id=77. Accessed November 7, 2019.
23. Lusco VC, Martinez SA, Polk HC Jr. Program directors in surgery agree that residents should be formally trained in business and practice management. Am J Surg. 2005;189(1):11-13.
24. New England Journal of Medicine. NEJM CareerCenter. http://www.nejmcareercenter.org. Accessed November 7, 2019.
25. US Office of Personnel Management. USAJOBS. https://www.usajobs.gov. Accessed November 7, 2019.
26. Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. http://www.nationalacademies.org/hmd/~/media/Files/Report%20Files/2001/Crossing-the-Quality-Chasm/Quality%20Chasm%202001%20%20report%20brief.pdf. Published March 2001. Accessed November 7, 2019.
27. Kohn LT, ed; Committee on the Roles of Academic Health Centers in the 21st Century; Institute of Medicine of the National Academies. Academic Health Centers: Leading Change in the 21st Century. National Academy Press: Washington, DC; 2004.
28. Goodall AH. Physician-leaders and hospital performance: is there an association? http://ftp.iza.org/dp5830.pdf. Published July 2011. Accessed November 7, 2019.
29. US Department of Health and Human Services, Office of the Assistant Secretary for Health. Public health 3.0: a call to action to create a 21st century public health infrastructure. https://www.healthypeople.gov/sites/default/files/Public-Health-3.0-White-Paper.pdf. Accessed November 7, 2019.
30. Centers for Medicare and Medicaid Services. Health care innovation awards round one project profiles. http://innovation.cms.gov/files/x/hcia-project-profiles.pdf. Updated December 2013. Accessed November 7, 2019.
31. US Department of Health and Human Services. Strategic Objective 1.3: Improve Americans’ access to healthcare and expand choices of care and service options. https://www.hhs.gov/about/strategic-plan/strategic-goal-1/index.html#obj_1_3. Updated March 18, 2019. Accessed November 7, 2019.
32. Kessler CS, Stallings LA, Gonzalez AA, Templeman TA. Combined residency training in emergency medicine and internal medicine: an update on career outcomes and job satisfaction. Acad Emerg Med. 2009;16(9):894-899.
33. Summergrad P, Silberman E, Price LL. Practice and career outcomes of double-boarded psychiatrists. Psychosomatics. 2011;52(6):537-543.
34. Rigoni B, Adkins A. What millennials want from a new job. Harvard Business Rev. May 11, 2016. https://hbr.org/2016/05/what-millennials-want-from-a-new-job. Accessed November 7, 2019.
35. Jung P, Smith C. Medical millennials: a mismatch between training preferences and employment opportunities. Lancet Glob Health. 2019;7(suppl 1):S38.
Improving Veteran Care With the Mission Act
NATIONAL HARBOR, MD–The US Department of Veterans Affairs (VA) is in the midst of a significant change in the way it will deliver care to veterans. Agency officials remain optimistic that the change will be for the better, and early indications are positive.
The change is being driven by the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks (Mission) Act of 2018, a bill that opens health services options for veterans and integrates VA-administered care and care from community-based providers.
“This is change that is enhancing their experience in the system, and this is enhancing their options and the quality of the options in the system,” Jennifer MacDonald, MD, chief consultant to the principal deputy undersecretary for health at the VA, said during a December 3 session at the AMSUS 2019 annual meeting. “We need also for our workforce to understand how important they are to us across this degree of change.”
Dr. MacDonald highlighted integration with community-based care, including a community urgent care provision that allows veterans to access urgent care facilities and receive care without the need for prior authorization.
“The important piece about that is that we are also looking at the way this care has been accessed,” she said. “By and large, what we have seen from the data is that veterans are indeed seeking community urgent care at a site close to home. This may be CVS or Walgreens. It may be a stand-alone urgent care with a bit more functionality than those Minute Clinics tend to have. We are seeing veterans typically access care through those sites for those minor concerns and illnesses.”
However, she noted that this type of access does not alter the role the VA plays in administration of health care services.
“We are seeing them come back to VA for the majority of their care and for their core care–when there are serious issues, when insulin needs to be adjusted for diabetes, when there are heart disease medications that need to be refilled–we are seeing veterans not seek out urgent care, but come to us, and that is exactly what we want,” she said. “We want the continuity of care to continue and we want to help guide people to the right care, right place, right time.”
Dr. MacDonald also highlighted the expansion of a program that provides a stipend to caregivers that allows veterans to avoid institutionalization and remain within the community under that caregiver’s (a family or friend) supervision. This will expand by year’s end to Vietnam War-era veterans and within 2 years, to veterans that fall between the Vietnam War-era and the September 11, 2001, terrorist attacks.
“We wanted to do this equitably across all eras of veterans,” she said. “This now gives us that opportunity.”
Telehealth also plays a key role.
“For the first time ever, VA now has what we term ‘anywhere-to-anywhere’ telehealth under the Mission Act, an enormous opportunity for us,” she said. “Since we stretch … from New York City to Guam, we need the opportunity to provide care where it may be difficult to recruit and retain providers wherever veterans choose to live,” she said. “We believe that we should be able to meet people where they are regardless of where they choose to live. That’s an aspirational vision, but it is one we believe is exceptionally important and indeed we are moving toward that.”
These are just the beginning; the full implementation of the act goes out to 2034.
According to Dr. MacDonald, the agency is working hard to engage both veterans and the workforce to keep tabs on how the implementation is going.
“It’s a fundamental change in the day-to-day business that they’ve been doing, sometimes for years, and so extremely important across this change is that we have set up processes and now a joint operations center and a number of forums to hear directly from our front line and make sure that their issues are our issues in central office, in DC here, and that they feel heard and that they know that when they have needs, those needs are actioned,” she said.
The VA, under the Mission Act, is also working hard to engage health care providers in the community, including making VA training to community partners, including training on opioid use, suicide prevent and military culture.
However, all these change are for naught if the veterans are not on board. But so far, Dr. MacDonald said the early feedback is very positive.
She cited a VFW survey that asked a question about the Mission Act changes so far and whether they would recommend the VA to other veterans. Ninety percent of the respondents answered they would.
“That’s our marker that we are getting somewhere with these changes and the way we do business,” she said. “That is what we want to see continue to increase.”
NATIONAL HARBOR, MD–The US Department of Veterans Affairs (VA) is in the midst of a significant change in the way it will deliver care to veterans. Agency officials remain optimistic that the change will be for the better, and early indications are positive.
The change is being driven by the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks (Mission) Act of 2018, a bill that opens health services options for veterans and integrates VA-administered care and care from community-based providers.
“This is change that is enhancing their experience in the system, and this is enhancing their options and the quality of the options in the system,” Jennifer MacDonald, MD, chief consultant to the principal deputy undersecretary for health at the VA, said during a December 3 session at the AMSUS 2019 annual meeting. “We need also for our workforce to understand how important they are to us across this degree of change.”
Dr. MacDonald highlighted integration with community-based care, including a community urgent care provision that allows veterans to access urgent care facilities and receive care without the need for prior authorization.
“The important piece about that is that we are also looking at the way this care has been accessed,” she said. “By and large, what we have seen from the data is that veterans are indeed seeking community urgent care at a site close to home. This may be CVS or Walgreens. It may be a stand-alone urgent care with a bit more functionality than those Minute Clinics tend to have. We are seeing veterans typically access care through those sites for those minor concerns and illnesses.”
However, she noted that this type of access does not alter the role the VA plays in administration of health care services.
“We are seeing them come back to VA for the majority of their care and for their core care–when there are serious issues, when insulin needs to be adjusted for diabetes, when there are heart disease medications that need to be refilled–we are seeing veterans not seek out urgent care, but come to us, and that is exactly what we want,” she said. “We want the continuity of care to continue and we want to help guide people to the right care, right place, right time.”
Dr. MacDonald also highlighted the expansion of a program that provides a stipend to caregivers that allows veterans to avoid institutionalization and remain within the community under that caregiver’s (a family or friend) supervision. This will expand by year’s end to Vietnam War-era veterans and within 2 years, to veterans that fall between the Vietnam War-era and the September 11, 2001, terrorist attacks.
“We wanted to do this equitably across all eras of veterans,” she said. “This now gives us that opportunity.”
Telehealth also plays a key role.
“For the first time ever, VA now has what we term ‘anywhere-to-anywhere’ telehealth under the Mission Act, an enormous opportunity for us,” she said. “Since we stretch … from New York City to Guam, we need the opportunity to provide care where it may be difficult to recruit and retain providers wherever veterans choose to live,” she said. “We believe that we should be able to meet people where they are regardless of where they choose to live. That’s an aspirational vision, but it is one we believe is exceptionally important and indeed we are moving toward that.”
These are just the beginning; the full implementation of the act goes out to 2034.
According to Dr. MacDonald, the agency is working hard to engage both veterans and the workforce to keep tabs on how the implementation is going.
“It’s a fundamental change in the day-to-day business that they’ve been doing, sometimes for years, and so extremely important across this change is that we have set up processes and now a joint operations center and a number of forums to hear directly from our front line and make sure that their issues are our issues in central office, in DC here, and that they feel heard and that they know that when they have needs, those needs are actioned,” she said.
The VA, under the Mission Act, is also working hard to engage health care providers in the community, including making VA training to community partners, including training on opioid use, suicide prevent and military culture.
However, all these change are for naught if the veterans are not on board. But so far, Dr. MacDonald said the early feedback is very positive.
She cited a VFW survey that asked a question about the Mission Act changes so far and whether they would recommend the VA to other veterans. Ninety percent of the respondents answered they would.
“That’s our marker that we are getting somewhere with these changes and the way we do business,” she said. “That is what we want to see continue to increase.”
NATIONAL HARBOR, MD–The US Department of Veterans Affairs (VA) is in the midst of a significant change in the way it will deliver care to veterans. Agency officials remain optimistic that the change will be for the better, and early indications are positive.
The change is being driven by the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks (Mission) Act of 2018, a bill that opens health services options for veterans and integrates VA-administered care and care from community-based providers.
“This is change that is enhancing their experience in the system, and this is enhancing their options and the quality of the options in the system,” Jennifer MacDonald, MD, chief consultant to the principal deputy undersecretary for health at the VA, said during a December 3 session at the AMSUS 2019 annual meeting. “We need also for our workforce to understand how important they are to us across this degree of change.”
Dr. MacDonald highlighted integration with community-based care, including a community urgent care provision that allows veterans to access urgent care facilities and receive care without the need for prior authorization.
“The important piece about that is that we are also looking at the way this care has been accessed,” she said. “By and large, what we have seen from the data is that veterans are indeed seeking community urgent care at a site close to home. This may be CVS or Walgreens. It may be a stand-alone urgent care with a bit more functionality than those Minute Clinics tend to have. We are seeing veterans typically access care through those sites for those minor concerns and illnesses.”
However, she noted that this type of access does not alter the role the VA plays in administration of health care services.
“We are seeing them come back to VA for the majority of their care and for their core care–when there are serious issues, when insulin needs to be adjusted for diabetes, when there are heart disease medications that need to be refilled–we are seeing veterans not seek out urgent care, but come to us, and that is exactly what we want,” she said. “We want the continuity of care to continue and we want to help guide people to the right care, right place, right time.”
Dr. MacDonald also highlighted the expansion of a program that provides a stipend to caregivers that allows veterans to avoid institutionalization and remain within the community under that caregiver’s (a family or friend) supervision. This will expand by year’s end to Vietnam War-era veterans and within 2 years, to veterans that fall between the Vietnam War-era and the September 11, 2001, terrorist attacks.
“We wanted to do this equitably across all eras of veterans,” she said. “This now gives us that opportunity.”
Telehealth also plays a key role.
“For the first time ever, VA now has what we term ‘anywhere-to-anywhere’ telehealth under the Mission Act, an enormous opportunity for us,” she said. “Since we stretch … from New York City to Guam, we need the opportunity to provide care where it may be difficult to recruit and retain providers wherever veterans choose to live,” she said. “We believe that we should be able to meet people where they are regardless of where they choose to live. That’s an aspirational vision, but it is one we believe is exceptionally important and indeed we are moving toward that.”
These are just the beginning; the full implementation of the act goes out to 2034.
According to Dr. MacDonald, the agency is working hard to engage both veterans and the workforce to keep tabs on how the implementation is going.
“It’s a fundamental change in the day-to-day business that they’ve been doing, sometimes for years, and so extremely important across this change is that we have set up processes and now a joint operations center and a number of forums to hear directly from our front line and make sure that their issues are our issues in central office, in DC here, and that they feel heard and that they know that when they have needs, those needs are actioned,” she said.
The VA, under the Mission Act, is also working hard to engage health care providers in the community, including making VA training to community partners, including training on opioid use, suicide prevent and military culture.
However, all these change are for naught if the veterans are not on board. But so far, Dr. MacDonald said the early feedback is very positive.
She cited a VFW survey that asked a question about the Mission Act changes so far and whether they would recommend the VA to other veterans. Ninety percent of the respondents answered they would.
“That’s our marker that we are getting somewhere with these changes and the way we do business,” she said. “That is what we want to see continue to increase.”