User login
Wellness vacations
It’s best practice to not set an alarm when on vacation. The point of vacation, after all, is to escape the rock-hard constraints of the daily grind. But the melody pulling me from slumber wasn’t coming from my phone. It was the ethereal chant of Fajr, morning prayer rising from surrounding mosques. I was in the medina of Marrakesh sleeping in a hotel that was once a home, called a riad. Some parts of the building date from the medieval period. Fajr occurs at dawn, before morning light. Getting from the bed to the toilet was treacherous – you must traverse cold, uneven steps to get there. Yet I had to get dressed: Morning yoga on our riad rooftop would start with sunrise. I guess even my vacations have agendas: I was in Morocco not only to holiday, but also to improve mind, body, and spirit.
For those who can afford them, your travel is fully arranged and activities such as yoga, cooking classes, hikes, and meditation are scheduled. This was my first wellness trip and it was transformative. Many times have I tried to disconnect from the distractions of life, but there is nothing so purifying as having no phone or Internet access. When I made peace with the reality that I couldn’t access EPIC or email, it was like a ringing in the ears had lifted: I could hear silence again.
This trip took us to three locations: Marrakesh, the Atlas Mountains, and the edge of the Sahara Desert. Yoga was prescribed twice a day. Morning practice was 90 minutes of shedding layers as the sun rose and our bodies warmed to increasingly difficult sequences. This was followed by Moroccan breakfast with fellow travelers from around the world. All were professionals and I wasn’t surprised to learn that burnout is common to many. I was surprised to realize that sharing stories with strangers about the vicissitudes of life was deeply bonding. (Or perhaps it was doing yoga inversions together.)
Also surprising was how easy it is to get lost in the maze that is Marrakesh. And yet, it was rewarding. Finding our way back through the mass of people, donkeys, and motorbikes along dark, unmarked alleys – without Waze – was intensely clarifying. Few things help you be present “in the moment” as being adrift and disoriented in a foreign city.
There was relaxation too. We made Khobz, traditional Moroccan bread by mixing just the right amounts of flour, yeast, sugar, oil, water, and salt. Knead, add, knead, add, and stop when done. We then walked a half mile to give our doughy creations to a baker who, with blackened calloused hands, worked an ancient communal oven. Then we waited patiently for the sardines ahead of us to finish baking first. I’ve no idea how long it all took – I had nowhere else to be.
The next day we hiked to a village in the Ourika Valley. There we had lunch at the home of a local Berber family. They served us their best tea, vegetable couscous, and lamb tagine while their chickens and donkeys watched us curiously. It was Thanksgiving (not on the Berber calendar of course) and sharing a meal prepared by a faraway stranger who doesn’t speak English makes you feel thankful in a refreshing way. Way more alike than different we are, I learned.
We finished our trip with a little desert “glamping.” The vast expanse of desert, interrupted by swirling winds and camel bellows quiets your mind, opens you to the immensity of life. That night we sat close to a bonfire and watched the Milky Way drift across the true black sky. I woke the next morning to the best night’s sleep I’ve had all year. My last wellness activity was unplanned, but meaningful nonetheless. As it happens, there’s no hot water in the desert and a bracingly cold shower marked the end of my treatment/vacation.
If the opposite of burned out is repleted, then I am. Also grateful to have such a transformative experience, for friends new and old who love me, and for hot water. Prescribe yourself one if you can.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
It’s best practice to not set an alarm when on vacation. The point of vacation, after all, is to escape the rock-hard constraints of the daily grind. But the melody pulling me from slumber wasn’t coming from my phone. It was the ethereal chant of Fajr, morning prayer rising from surrounding mosques. I was in the medina of Marrakesh sleeping in a hotel that was once a home, called a riad. Some parts of the building date from the medieval period. Fajr occurs at dawn, before morning light. Getting from the bed to the toilet was treacherous – you must traverse cold, uneven steps to get there. Yet I had to get dressed: Morning yoga on our riad rooftop would start with sunrise. I guess even my vacations have agendas: I was in Morocco not only to holiday, but also to improve mind, body, and spirit.
For those who can afford them, your travel is fully arranged and activities such as yoga, cooking classes, hikes, and meditation are scheduled. This was my first wellness trip and it was transformative. Many times have I tried to disconnect from the distractions of life, but there is nothing so purifying as having no phone or Internet access. When I made peace with the reality that I couldn’t access EPIC or email, it was like a ringing in the ears had lifted: I could hear silence again.
This trip took us to three locations: Marrakesh, the Atlas Mountains, and the edge of the Sahara Desert. Yoga was prescribed twice a day. Morning practice was 90 minutes of shedding layers as the sun rose and our bodies warmed to increasingly difficult sequences. This was followed by Moroccan breakfast with fellow travelers from around the world. All were professionals and I wasn’t surprised to learn that burnout is common to many. I was surprised to realize that sharing stories with strangers about the vicissitudes of life was deeply bonding. (Or perhaps it was doing yoga inversions together.)
Also surprising was how easy it is to get lost in the maze that is Marrakesh. And yet, it was rewarding. Finding our way back through the mass of people, donkeys, and motorbikes along dark, unmarked alleys – without Waze – was intensely clarifying. Few things help you be present “in the moment” as being adrift and disoriented in a foreign city.
There was relaxation too. We made Khobz, traditional Moroccan bread by mixing just the right amounts of flour, yeast, sugar, oil, water, and salt. Knead, add, knead, add, and stop when done. We then walked a half mile to give our doughy creations to a baker who, with blackened calloused hands, worked an ancient communal oven. Then we waited patiently for the sardines ahead of us to finish baking first. I’ve no idea how long it all took – I had nowhere else to be.
The next day we hiked to a village in the Ourika Valley. There we had lunch at the home of a local Berber family. They served us their best tea, vegetable couscous, and lamb tagine while their chickens and donkeys watched us curiously. It was Thanksgiving (not on the Berber calendar of course) and sharing a meal prepared by a faraway stranger who doesn’t speak English makes you feel thankful in a refreshing way. Way more alike than different we are, I learned.
We finished our trip with a little desert “glamping.” The vast expanse of desert, interrupted by swirling winds and camel bellows quiets your mind, opens you to the immensity of life. That night we sat close to a bonfire and watched the Milky Way drift across the true black sky. I woke the next morning to the best night’s sleep I’ve had all year. My last wellness activity was unplanned, but meaningful nonetheless. As it happens, there’s no hot water in the desert and a bracingly cold shower marked the end of my treatment/vacation.
If the opposite of burned out is repleted, then I am. Also grateful to have such a transformative experience, for friends new and old who love me, and for hot water. Prescribe yourself one if you can.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
It’s best practice to not set an alarm when on vacation. The point of vacation, after all, is to escape the rock-hard constraints of the daily grind. But the melody pulling me from slumber wasn’t coming from my phone. It was the ethereal chant of Fajr, morning prayer rising from surrounding mosques. I was in the medina of Marrakesh sleeping in a hotel that was once a home, called a riad. Some parts of the building date from the medieval period. Fajr occurs at dawn, before morning light. Getting from the bed to the toilet was treacherous – you must traverse cold, uneven steps to get there. Yet I had to get dressed: Morning yoga on our riad rooftop would start with sunrise. I guess even my vacations have agendas: I was in Morocco not only to holiday, but also to improve mind, body, and spirit.
For those who can afford them, your travel is fully arranged and activities such as yoga, cooking classes, hikes, and meditation are scheduled. This was my first wellness trip and it was transformative. Many times have I tried to disconnect from the distractions of life, but there is nothing so purifying as having no phone or Internet access. When I made peace with the reality that I couldn’t access EPIC or email, it was like a ringing in the ears had lifted: I could hear silence again.
This trip took us to three locations: Marrakesh, the Atlas Mountains, and the edge of the Sahara Desert. Yoga was prescribed twice a day. Morning practice was 90 minutes of shedding layers as the sun rose and our bodies warmed to increasingly difficult sequences. This was followed by Moroccan breakfast with fellow travelers from around the world. All were professionals and I wasn’t surprised to learn that burnout is common to many. I was surprised to realize that sharing stories with strangers about the vicissitudes of life was deeply bonding. (Or perhaps it was doing yoga inversions together.)
Also surprising was how easy it is to get lost in the maze that is Marrakesh. And yet, it was rewarding. Finding our way back through the mass of people, donkeys, and motorbikes along dark, unmarked alleys – without Waze – was intensely clarifying. Few things help you be present “in the moment” as being adrift and disoriented in a foreign city.
There was relaxation too. We made Khobz, traditional Moroccan bread by mixing just the right amounts of flour, yeast, sugar, oil, water, and salt. Knead, add, knead, add, and stop when done. We then walked a half mile to give our doughy creations to a baker who, with blackened calloused hands, worked an ancient communal oven. Then we waited patiently for the sardines ahead of us to finish baking first. I’ve no idea how long it all took – I had nowhere else to be.
The next day we hiked to a village in the Ourika Valley. There we had lunch at the home of a local Berber family. They served us their best tea, vegetable couscous, and lamb tagine while their chickens and donkeys watched us curiously. It was Thanksgiving (not on the Berber calendar of course) and sharing a meal prepared by a faraway stranger who doesn’t speak English makes you feel thankful in a refreshing way. Way more alike than different we are, I learned.
We finished our trip with a little desert “glamping.” The vast expanse of desert, interrupted by swirling winds and camel bellows quiets your mind, opens you to the immensity of life. That night we sat close to a bonfire and watched the Milky Way drift across the true black sky. I woke the next morning to the best night’s sleep I’ve had all year. My last wellness activity was unplanned, but meaningful nonetheless. As it happens, there’s no hot water in the desert and a bracingly cold shower marked the end of my treatment/vacation.
If the opposite of burned out is repleted, then I am. Also grateful to have such a transformative experience, for friends new and old who love me, and for hot water. Prescribe yourself one if you can.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Being whole
Medicine is a rewarding but demanding field. Part of being a professional is handling the stresses of the job. That ability is as important as tying strong horizontal mattress sutures, choosing correct antibiotics to treat staph, and gently breaking bad news.
The divorce and suicide rate among physicians are evidence that many physicians handle stress poorly. Our rates of depression, burnout, alcoholism, and substance abuse are further evidence of the suffering caused by unmitigated stress. It is endemic and destructive, harming physicians, their loved ones, and their patients. While this situation has long been true, in the past decade its importance has become better recognized. Some scholars have added physician wellness or fulfillment as a fourth aim of medical care to complement the triple aims of patient outcomes, consumer experience, and financial stewardship.
The sources of stress can be either external or internal. Internally, many physicians feel torn between competing professional roles. Recently one fellow in pediatric intensive care wrote an insightful reflective essay about two conflicting roles (“Virtue and Suffering: Where the Personal and Professional Collide,” Lauren Rissman, MD. reflectivemeded.org). One side is the potential benefits of technology and modern medical interventions. The other side is compassion and knowing when to say enough. Finding that balance – or boundary – or mixture is difficult. Even more difficult is helping patients/parents who are struggling with those choices.
Some old models of the doctor-patient relationship insisted on an emotional detachment to promote objectivity. This often is paired with using nondirective counseling. The admonishment for a physician to be nondirective comes up in end-of-life care choices in the ICU. It comes up in genetic counseling, particularly in the prenatal time frame, and when I do ethics consults requiring values clarification and mediation. But I also have found times during shared decision making when the model of a fully informed consumer choice is not valid. There are situations in which a paradigm of emotional detachment impairs the ability to convey empathy, compassion, and presence. Being detached also may prevent the moments of personal connection between doctor and patient that are the intangible rewards of the vocation. A good physician knows how to choose among these idealized models. It requires being genuine when employing a diverse bag of bedside tools.
High technology and highly invasive care pose dilemmas in assessing outcomes, minimizing suffering, and ensuring financial stewardship. When one addresses those different types of dilemmas happening simultaneously, the initial approach can be to separate the different influences into separate vectors. But when one does this on a regular basis, it fractures one’s self-image. To survive and flourish, the physician juggling these competing, conflicting goals must shun the split personality and seek to live as an integrated moral agent. This integration is not achieved by working harder or longer or even smarter. It requires time and effort directed to self-reflection. When pediatric ethicists get together at conferences, I notice that about one-half of them are neonatal ICU docs and one-quarter are pediatric ICU docs. Many view their work in ethics as a survival mechanism. We all are looking for answers to questions we may not be able to fully articulate.
In this short column I will not endeavor to offer a neat package of advice on how to achieve being whole. Dr. Rissman in her essay is just starting her career while I’m nearing the end of mine. It is a lifelong process to integrate oneself rather than exist in turmoil. It truly is a journey, not a destination. After a career dedicated to considering technology, compassion, and costs, I know there are no simple solutions. I also know that it is important to keep seeking better answers.
To encourage group discussion of ethical problems, I have heard facilitators say that there are no right and wrong answers. I strongly disagree. In ethics, there often is more than one correct answer. Ethicists can write books on why one right answer is slightly better than another right answer for a particular individual or population. We live for debates over such minutiae. In the real world of medical ethics, there also are definitely wrong answers.
Professional athletes know the importance of recovery after an intense workout. Muscles have accumulated microscopic tears that must heal. Professional physicians must develop a personal regimen of caring for overexertion of their own emotional and moral/spiritual muscles in order to remain whole.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
Medicine is a rewarding but demanding field. Part of being a professional is handling the stresses of the job. That ability is as important as tying strong horizontal mattress sutures, choosing correct antibiotics to treat staph, and gently breaking bad news.
The divorce and suicide rate among physicians are evidence that many physicians handle stress poorly. Our rates of depression, burnout, alcoholism, and substance abuse are further evidence of the suffering caused by unmitigated stress. It is endemic and destructive, harming physicians, their loved ones, and their patients. While this situation has long been true, in the past decade its importance has become better recognized. Some scholars have added physician wellness or fulfillment as a fourth aim of medical care to complement the triple aims of patient outcomes, consumer experience, and financial stewardship.
The sources of stress can be either external or internal. Internally, many physicians feel torn between competing professional roles. Recently one fellow in pediatric intensive care wrote an insightful reflective essay about two conflicting roles (“Virtue and Suffering: Where the Personal and Professional Collide,” Lauren Rissman, MD. reflectivemeded.org). One side is the potential benefits of technology and modern medical interventions. The other side is compassion and knowing when to say enough. Finding that balance – or boundary – or mixture is difficult. Even more difficult is helping patients/parents who are struggling with those choices.
Some old models of the doctor-patient relationship insisted on an emotional detachment to promote objectivity. This often is paired with using nondirective counseling. The admonishment for a physician to be nondirective comes up in end-of-life care choices in the ICU. It comes up in genetic counseling, particularly in the prenatal time frame, and when I do ethics consults requiring values clarification and mediation. But I also have found times during shared decision making when the model of a fully informed consumer choice is not valid. There are situations in which a paradigm of emotional detachment impairs the ability to convey empathy, compassion, and presence. Being detached also may prevent the moments of personal connection between doctor and patient that are the intangible rewards of the vocation. A good physician knows how to choose among these idealized models. It requires being genuine when employing a diverse bag of bedside tools.
High technology and highly invasive care pose dilemmas in assessing outcomes, minimizing suffering, and ensuring financial stewardship. When one addresses those different types of dilemmas happening simultaneously, the initial approach can be to separate the different influences into separate vectors. But when one does this on a regular basis, it fractures one’s self-image. To survive and flourish, the physician juggling these competing, conflicting goals must shun the split personality and seek to live as an integrated moral agent. This integration is not achieved by working harder or longer or even smarter. It requires time and effort directed to self-reflection. When pediatric ethicists get together at conferences, I notice that about one-half of them are neonatal ICU docs and one-quarter are pediatric ICU docs. Many view their work in ethics as a survival mechanism. We all are looking for answers to questions we may not be able to fully articulate.
In this short column I will not endeavor to offer a neat package of advice on how to achieve being whole. Dr. Rissman in her essay is just starting her career while I’m nearing the end of mine. It is a lifelong process to integrate oneself rather than exist in turmoil. It truly is a journey, not a destination. After a career dedicated to considering technology, compassion, and costs, I know there are no simple solutions. I also know that it is important to keep seeking better answers.
To encourage group discussion of ethical problems, I have heard facilitators say that there are no right and wrong answers. I strongly disagree. In ethics, there often is more than one correct answer. Ethicists can write books on why one right answer is slightly better than another right answer for a particular individual or population. We live for debates over such minutiae. In the real world of medical ethics, there also are definitely wrong answers.
Professional athletes know the importance of recovery after an intense workout. Muscles have accumulated microscopic tears that must heal. Professional physicians must develop a personal regimen of caring for overexertion of their own emotional and moral/spiritual muscles in order to remain whole.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
Medicine is a rewarding but demanding field. Part of being a professional is handling the stresses of the job. That ability is as important as tying strong horizontal mattress sutures, choosing correct antibiotics to treat staph, and gently breaking bad news.
The divorce and suicide rate among physicians are evidence that many physicians handle stress poorly. Our rates of depression, burnout, alcoholism, and substance abuse are further evidence of the suffering caused by unmitigated stress. It is endemic and destructive, harming physicians, their loved ones, and their patients. While this situation has long been true, in the past decade its importance has become better recognized. Some scholars have added physician wellness or fulfillment as a fourth aim of medical care to complement the triple aims of patient outcomes, consumer experience, and financial stewardship.
The sources of stress can be either external or internal. Internally, many physicians feel torn between competing professional roles. Recently one fellow in pediatric intensive care wrote an insightful reflective essay about two conflicting roles (“Virtue and Suffering: Where the Personal and Professional Collide,” Lauren Rissman, MD. reflectivemeded.org). One side is the potential benefits of technology and modern medical interventions. The other side is compassion and knowing when to say enough. Finding that balance – or boundary – or mixture is difficult. Even more difficult is helping patients/parents who are struggling with those choices.
Some old models of the doctor-patient relationship insisted on an emotional detachment to promote objectivity. This often is paired with using nondirective counseling. The admonishment for a physician to be nondirective comes up in end-of-life care choices in the ICU. It comes up in genetic counseling, particularly in the prenatal time frame, and when I do ethics consults requiring values clarification and mediation. But I also have found times during shared decision making when the model of a fully informed consumer choice is not valid. There are situations in which a paradigm of emotional detachment impairs the ability to convey empathy, compassion, and presence. Being detached also may prevent the moments of personal connection between doctor and patient that are the intangible rewards of the vocation. A good physician knows how to choose among these idealized models. It requires being genuine when employing a diverse bag of bedside tools.
High technology and highly invasive care pose dilemmas in assessing outcomes, minimizing suffering, and ensuring financial stewardship. When one addresses those different types of dilemmas happening simultaneously, the initial approach can be to separate the different influences into separate vectors. But when one does this on a regular basis, it fractures one’s self-image. To survive and flourish, the physician juggling these competing, conflicting goals must shun the split personality and seek to live as an integrated moral agent. This integration is not achieved by working harder or longer or even smarter. It requires time and effort directed to self-reflection. When pediatric ethicists get together at conferences, I notice that about one-half of them are neonatal ICU docs and one-quarter are pediatric ICU docs. Many view their work in ethics as a survival mechanism. We all are looking for answers to questions we may not be able to fully articulate.
In this short column I will not endeavor to offer a neat package of advice on how to achieve being whole. Dr. Rissman in her essay is just starting her career while I’m nearing the end of mine. It is a lifelong process to integrate oneself rather than exist in turmoil. It truly is a journey, not a destination. After a career dedicated to considering technology, compassion, and costs, I know there are no simple solutions. I also know that it is important to keep seeking better answers.
To encourage group discussion of ethical problems, I have heard facilitators say that there are no right and wrong answers. I strongly disagree. In ethics, there often is more than one correct answer. Ethicists can write books on why one right answer is slightly better than another right answer for a particular individual or population. We live for debates over such minutiae. In the real world of medical ethics, there also are definitely wrong answers.
Professional athletes know the importance of recovery after an intense workout. Muscles have accumulated microscopic tears that must heal. Professional physicians must develop a personal regimen of caring for overexertion of their own emotional and moral/spiritual muscles in order to remain whole.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
Cancer researchers win grants from DOD, GO2 Foundation
The GO2 Foundation for Lung Cancer has granted the 2019 Young Innovators Team Awards to two groups of investigators studying non-small cell lung cancer (NSCLC). Each group received $250,000 to support their work.
Yanxiang (Jessie) Guo, PhD, of Rutgers Cancer Institute of New Jersey, and Shawn Davidson, PhD, of Princeton University in New Jersey, won the award for their research on tumor metabolism and immunotherapy in KRAS-mutant NSCLC.
Dr. Guo and Dr. Davidson aim to prove that cancer cell metabolism affects the tumor microenvironment and leads to an impaired antitumor immune response. The pair’s ultimate goal is to overcome resistance to immunotherapy in KRAS-mutant NSCLC.
Matthew Bott, MD, of Memorial Sloan Kettering Cancer Center in New York, and Tuomas Tammela, MD, PhD, of Weill-Cornell Medical College in New York, won the award for their research on age-related differences in NSCLC.
Dr. Bott and Dr. Tammela aim to characterize differences in natural history and treatment response between younger and older patients with NSCLC. The main goal is to determine if different age groups require different approaches to treatment.
Two other researchers, both from Fox Chase Cancer Center in Philadelphia, received grants from the U.S. Department of Defense.
Jeffrey Peterson, PhD, was awarded a $1.4 million grant from the Department of Defense for his research on triple-negative breast cancer. Dr. Peterson will work with postdoctoral research fellows Alexander Beatty, PhD, and Tanu Singh, PhD, to determine if polyunsaturated fatty acids can be used to induce programmed cell death in triple-negative breast cancer.
Dr. Peterson theorizes that metastatic cells may be susceptible to preferential uptake of conjugated linoleic acid, which will trigger ferroptosis and destroy cancer cells without affecting normal cells. His ultimate goal is to set the stage for clinical trials of more effective, less toxic targeted therapies for triple-negative breast cancer.
Phillip Abbosh, MD, PhD, was awarded a $658,800 grant from the Department of Defense to investigate the role of the immune system and certain bacteria in mediating responses to therapy in bladder cancers.
Dr. Abbosh theorizes that a better understanding of the interaction between the immune system and bladder tumors could aid the development of new targeted therapies, and perhaps bacteria found in cancer patients’ bladders could be used to enhance treatment.
The GO2 Foundation for Lung Cancer has granted the 2019 Young Innovators Team Awards to two groups of investigators studying non-small cell lung cancer (NSCLC). Each group received $250,000 to support their work.
Yanxiang (Jessie) Guo, PhD, of Rutgers Cancer Institute of New Jersey, and Shawn Davidson, PhD, of Princeton University in New Jersey, won the award for their research on tumor metabolism and immunotherapy in KRAS-mutant NSCLC.
Dr. Guo and Dr. Davidson aim to prove that cancer cell metabolism affects the tumor microenvironment and leads to an impaired antitumor immune response. The pair’s ultimate goal is to overcome resistance to immunotherapy in KRAS-mutant NSCLC.
Matthew Bott, MD, of Memorial Sloan Kettering Cancer Center in New York, and Tuomas Tammela, MD, PhD, of Weill-Cornell Medical College in New York, won the award for their research on age-related differences in NSCLC.
Dr. Bott and Dr. Tammela aim to characterize differences in natural history and treatment response between younger and older patients with NSCLC. The main goal is to determine if different age groups require different approaches to treatment.
Two other researchers, both from Fox Chase Cancer Center in Philadelphia, received grants from the U.S. Department of Defense.
Jeffrey Peterson, PhD, was awarded a $1.4 million grant from the Department of Defense for his research on triple-negative breast cancer. Dr. Peterson will work with postdoctoral research fellows Alexander Beatty, PhD, and Tanu Singh, PhD, to determine if polyunsaturated fatty acids can be used to induce programmed cell death in triple-negative breast cancer.
Dr. Peterson theorizes that metastatic cells may be susceptible to preferential uptake of conjugated linoleic acid, which will trigger ferroptosis and destroy cancer cells without affecting normal cells. His ultimate goal is to set the stage for clinical trials of more effective, less toxic targeted therapies for triple-negative breast cancer.
Phillip Abbosh, MD, PhD, was awarded a $658,800 grant from the Department of Defense to investigate the role of the immune system and certain bacteria in mediating responses to therapy in bladder cancers.
Dr. Abbosh theorizes that a better understanding of the interaction between the immune system and bladder tumors could aid the development of new targeted therapies, and perhaps bacteria found in cancer patients’ bladders could be used to enhance treatment.
The GO2 Foundation for Lung Cancer has granted the 2019 Young Innovators Team Awards to two groups of investigators studying non-small cell lung cancer (NSCLC). Each group received $250,000 to support their work.
Yanxiang (Jessie) Guo, PhD, of Rutgers Cancer Institute of New Jersey, and Shawn Davidson, PhD, of Princeton University in New Jersey, won the award for their research on tumor metabolism and immunotherapy in KRAS-mutant NSCLC.
Dr. Guo and Dr. Davidson aim to prove that cancer cell metabolism affects the tumor microenvironment and leads to an impaired antitumor immune response. The pair’s ultimate goal is to overcome resistance to immunotherapy in KRAS-mutant NSCLC.
Matthew Bott, MD, of Memorial Sloan Kettering Cancer Center in New York, and Tuomas Tammela, MD, PhD, of Weill-Cornell Medical College in New York, won the award for their research on age-related differences in NSCLC.
Dr. Bott and Dr. Tammela aim to characterize differences in natural history and treatment response between younger and older patients with NSCLC. The main goal is to determine if different age groups require different approaches to treatment.
Two other researchers, both from Fox Chase Cancer Center in Philadelphia, received grants from the U.S. Department of Defense.
Jeffrey Peterson, PhD, was awarded a $1.4 million grant from the Department of Defense for his research on triple-negative breast cancer. Dr. Peterson will work with postdoctoral research fellows Alexander Beatty, PhD, and Tanu Singh, PhD, to determine if polyunsaturated fatty acids can be used to induce programmed cell death in triple-negative breast cancer.
Dr. Peterson theorizes that metastatic cells may be susceptible to preferential uptake of conjugated linoleic acid, which will trigger ferroptosis and destroy cancer cells without affecting normal cells. His ultimate goal is to set the stage for clinical trials of more effective, less toxic targeted therapies for triple-negative breast cancer.
Phillip Abbosh, MD, PhD, was awarded a $658,800 grant from the Department of Defense to investigate the role of the immune system and certain bacteria in mediating responses to therapy in bladder cancers.
Dr. Abbosh theorizes that a better understanding of the interaction between the immune system and bladder tumors could aid the development of new targeted therapies, and perhaps bacteria found in cancer patients’ bladders could be used to enhance treatment.
More than half of pediatric residents feel burned out
More than half of all pediatric residents report feeling burned out, in a trend that has now reached 3 years.
“The stable 54%-56% rate of burnout found during 2016-2018 in this study is similar to burnout rates previously reported in U.S. studies of pediatric residents,” Kathi Kemper, MD, Ohio State University, Columbus, and colleagues wrote (Pediatrics. 2019 Dec. 16. doi: 10.1542/peds.2019-1030).
The “alarming rate of physician burnout is a call to action on behalf of current trainees and future generations of doctors,” Jeanine Ronan, MD, of Children’s Hospital of Philadelphia, said in an accompanying editorial (Pediatrics. 2019 Dec. 16. doi: 10.1542/peds.2019-3210), adding that “although this concern was identified more than a decade ago, little progress has been made.”
The findings were based on the Pediatric Resident Burnout and Resilience Study Consortium surveys completed at 34 residency programs in 2016 (1,664 residents participated in the survey), 43 in 2017 (2,153 participated), and 49 in 2018 (2,241 participated). The 22-item Maslach Burnout Inventory Human Services Survey was used to assess burnout.
However, researchers noted that there were “no consistent significant differences between residents meeting criteria for burnout and those not meeting criteria for burnout in terms of any demographic characteristic,” the authors added.
For example, residency year and program size were associated with burnout in some years but not others.
There “were significant differences in burnout rates among postgraduate year 1 (PGY1), postgraduate year 2 (PGY2), and postgraduate year 3 (PGY3) in 2016 and 2017, but not in 2018,” the authors stated.
For 2016, burnout rates in PGY1, PGY2 and PGY3 were 36%, 34%, and 30%, respectively. In 2017, the rates changed to 33%, 36%, and 31%, respectively, while in 2018, the rates were reported to be 35% in the first postgraduate year and 33% each for the second and third postgraduate years.
Other findings from the survey revealed that residents who met the criteria for burnout reported worse mental health, more sleepiness, and greater stress, as well as lower mindfulness and self-compassion scores, less confidence in providing compassionate care, and lower levels of empathy and resilience.
“Residents who met the criteria for burnout were more likely to be on high-acuity rotations,” the Dr. Kemper and colleagues observed. “They were approximately twice as likely to report recently having made a medical error, more likely to report a work-life conflict, less likely to have had a vacation within the past month, and less likely to have had a recent weekend off than those who did not meet the criteria for burnout.
Additionally, residents reporting burnout “consistently reported significantly less satisfaction with support from family, spouse, friends, faculty, and colleagues,” the report states. “They also reported significantly lower quality of life, less satisfaction with their choice to go into pediatrics, and less satisfaction with their balance between personal and professional life.”
Dr. Ronan also noted that the survey “showed the negative impact of the environment on trainee performance and ability to cope with stress. Residency training programs should evaluate different scheduling and staffing models to determine if there are opportunities to enhance the learning environment.”
She also noted that given the link between electronic health record usage and administrative tasks and burnout, lessening administrative task burden on trainees may help decrease the rate of burnout.
Dr. Ronan added that mental health services also must be made readily available to trainees.
“The high burnout rate among pediatric residents must be addressed,” she said. “A comprehensive approach would include developing evidence-based training in mindfulness and coping techniques for the individual resident, an institutional approach to improve resident engagement and increase joy in the workplace, and the availability of mental health services when needed to address both urgent and chronic concerns.”
SOURCE: Kemper K et al. Pediatrics 2019 Dec 16. doi: 10.1542/peds.2019-1030.
More than half of all pediatric residents report feeling burned out, in a trend that has now reached 3 years.
“The stable 54%-56% rate of burnout found during 2016-2018 in this study is similar to burnout rates previously reported in U.S. studies of pediatric residents,” Kathi Kemper, MD, Ohio State University, Columbus, and colleagues wrote (Pediatrics. 2019 Dec. 16. doi: 10.1542/peds.2019-1030).
The “alarming rate of physician burnout is a call to action on behalf of current trainees and future generations of doctors,” Jeanine Ronan, MD, of Children’s Hospital of Philadelphia, said in an accompanying editorial (Pediatrics. 2019 Dec. 16. doi: 10.1542/peds.2019-3210), adding that “although this concern was identified more than a decade ago, little progress has been made.”
The findings were based on the Pediatric Resident Burnout and Resilience Study Consortium surveys completed at 34 residency programs in 2016 (1,664 residents participated in the survey), 43 in 2017 (2,153 participated), and 49 in 2018 (2,241 participated). The 22-item Maslach Burnout Inventory Human Services Survey was used to assess burnout.
However, researchers noted that there were “no consistent significant differences between residents meeting criteria for burnout and those not meeting criteria for burnout in terms of any demographic characteristic,” the authors added.
For example, residency year and program size were associated with burnout in some years but not others.
There “were significant differences in burnout rates among postgraduate year 1 (PGY1), postgraduate year 2 (PGY2), and postgraduate year 3 (PGY3) in 2016 and 2017, but not in 2018,” the authors stated.
For 2016, burnout rates in PGY1, PGY2 and PGY3 were 36%, 34%, and 30%, respectively. In 2017, the rates changed to 33%, 36%, and 31%, respectively, while in 2018, the rates were reported to be 35% in the first postgraduate year and 33% each for the second and third postgraduate years.
Other findings from the survey revealed that residents who met the criteria for burnout reported worse mental health, more sleepiness, and greater stress, as well as lower mindfulness and self-compassion scores, less confidence in providing compassionate care, and lower levels of empathy and resilience.
“Residents who met the criteria for burnout were more likely to be on high-acuity rotations,” the Dr. Kemper and colleagues observed. “They were approximately twice as likely to report recently having made a medical error, more likely to report a work-life conflict, less likely to have had a vacation within the past month, and less likely to have had a recent weekend off than those who did not meet the criteria for burnout.
Additionally, residents reporting burnout “consistently reported significantly less satisfaction with support from family, spouse, friends, faculty, and colleagues,” the report states. “They also reported significantly lower quality of life, less satisfaction with their choice to go into pediatrics, and less satisfaction with their balance between personal and professional life.”
Dr. Ronan also noted that the survey “showed the negative impact of the environment on trainee performance and ability to cope with stress. Residency training programs should evaluate different scheduling and staffing models to determine if there are opportunities to enhance the learning environment.”
She also noted that given the link between electronic health record usage and administrative tasks and burnout, lessening administrative task burden on trainees may help decrease the rate of burnout.
Dr. Ronan added that mental health services also must be made readily available to trainees.
“The high burnout rate among pediatric residents must be addressed,” she said. “A comprehensive approach would include developing evidence-based training in mindfulness and coping techniques for the individual resident, an institutional approach to improve resident engagement and increase joy in the workplace, and the availability of mental health services when needed to address both urgent and chronic concerns.”
SOURCE: Kemper K et al. Pediatrics 2019 Dec 16. doi: 10.1542/peds.2019-1030.
More than half of all pediatric residents report feeling burned out, in a trend that has now reached 3 years.
“The stable 54%-56% rate of burnout found during 2016-2018 in this study is similar to burnout rates previously reported in U.S. studies of pediatric residents,” Kathi Kemper, MD, Ohio State University, Columbus, and colleagues wrote (Pediatrics. 2019 Dec. 16. doi: 10.1542/peds.2019-1030).
The “alarming rate of physician burnout is a call to action on behalf of current trainees and future generations of doctors,” Jeanine Ronan, MD, of Children’s Hospital of Philadelphia, said in an accompanying editorial (Pediatrics. 2019 Dec. 16. doi: 10.1542/peds.2019-3210), adding that “although this concern was identified more than a decade ago, little progress has been made.”
The findings were based on the Pediatric Resident Burnout and Resilience Study Consortium surveys completed at 34 residency programs in 2016 (1,664 residents participated in the survey), 43 in 2017 (2,153 participated), and 49 in 2018 (2,241 participated). The 22-item Maslach Burnout Inventory Human Services Survey was used to assess burnout.
However, researchers noted that there were “no consistent significant differences between residents meeting criteria for burnout and those not meeting criteria for burnout in terms of any demographic characteristic,” the authors added.
For example, residency year and program size were associated with burnout in some years but not others.
There “were significant differences in burnout rates among postgraduate year 1 (PGY1), postgraduate year 2 (PGY2), and postgraduate year 3 (PGY3) in 2016 and 2017, but not in 2018,” the authors stated.
For 2016, burnout rates in PGY1, PGY2 and PGY3 were 36%, 34%, and 30%, respectively. In 2017, the rates changed to 33%, 36%, and 31%, respectively, while in 2018, the rates were reported to be 35% in the first postgraduate year and 33% each for the second and third postgraduate years.
Other findings from the survey revealed that residents who met the criteria for burnout reported worse mental health, more sleepiness, and greater stress, as well as lower mindfulness and self-compassion scores, less confidence in providing compassionate care, and lower levels of empathy and resilience.
“Residents who met the criteria for burnout were more likely to be on high-acuity rotations,” the Dr. Kemper and colleagues observed. “They were approximately twice as likely to report recently having made a medical error, more likely to report a work-life conflict, less likely to have had a vacation within the past month, and less likely to have had a recent weekend off than those who did not meet the criteria for burnout.
Additionally, residents reporting burnout “consistently reported significantly less satisfaction with support from family, spouse, friends, faculty, and colleagues,” the report states. “They also reported significantly lower quality of life, less satisfaction with their choice to go into pediatrics, and less satisfaction with their balance between personal and professional life.”
Dr. Ronan also noted that the survey “showed the negative impact of the environment on trainee performance and ability to cope with stress. Residency training programs should evaluate different scheduling and staffing models to determine if there are opportunities to enhance the learning environment.”
She also noted that given the link between electronic health record usage and administrative tasks and burnout, lessening administrative task burden on trainees may help decrease the rate of burnout.
Dr. Ronan added that mental health services also must be made readily available to trainees.
“The high burnout rate among pediatric residents must be addressed,” she said. “A comprehensive approach would include developing evidence-based training in mindfulness and coping techniques for the individual resident, an institutional approach to improve resident engagement and increase joy in the workplace, and the availability of mental health services when needed to address both urgent and chronic concerns.”
SOURCE: Kemper K et al. Pediatrics 2019 Dec 16. doi: 10.1542/peds.2019-1030.
FROM PEDIATRICS
Supreme Court weighs ACA back pay case
U.S. Supreme Court Justices heard oral arguments Dec. 10 in a case that centers on whether the federal government owes insurers billions based on an Affordable Care Act provision intended to help health plans mitigate risk under the law.
Maine Community Health Options v. United States, which consolidates several lawsuits against the government, involves the ACA’s risk corridor program, which required the U.S. Department of Health & Human Services to collect funds from profitable insurers that offered qualified health plans under the exchanges and distribute the funds to insurers with excessive losses.
Collections from profitable insurers under the program fell short in 2014, 2015, and 2016, while losses steadily grew, resulting in the HHS paying about 12 cents on the dollar in payments to insurers. More than 150 insurers now allege they were shortchanged and they want the Supreme Court to force the government to reimburse them $12 billion.
The U.S. Department of Justice counters that the government is not required to pay the plans because of appropriations measures passed by Congress in 2014 and later years that limited the funding available to compensate insurers for their losses. The federal government is not obligated to pay the insurers back for the losses and the suits should be dismissed, the DOJ attorneys argue.
The federal government and insurers have each experienced wins and losses at the lower court level. Most recently, the U.S. Court of Appeals for the Federal Circuit decided in favor of the government, ruling that while the ACA required the government to compensate the insurers for their losses, the appropriations measures repealed or suspended that requirement.
Insurers, economists, and state government led by both parties have weighed in on the case via court briefs.
The case could have important ramifications that have an impact on more than just insurers, said Timothy Jost, a health law expert and retired professor from Washington and Lee University in Lexington, Va.
“The insurers are left holding the bag, but a number of insurers went insolvent [due to the losses], so in those cases, the states are left holding the bag,” Mr. Jost said in an interview.
The outcome could influence future partnerships between the federal government and private entities, according to Katie Keith, an attorney and health law analyst who writes for the Health Affairs Blog. She noted that the U.S. Chamber of Commerce, which historically has not supported the ACA, sided with insurers in the case. In a court brief, attorneys for the chamber wrote that businesses make substantial financial investments to participate in federal programs, and their willingness to do so is based on having assurance that the government will honor its statutory commitments. If left uncorrected, the circuit’s decision “will have far-reaching consequences for myriad areas in which U.S. businesses partner with the federal government to provide vital goods and services,” chamber attorneys wrote.
“This is about more than the ACA. It’s about the fundamentals of public/private partnerships,” Ms. Keith said in an interview. “If you’re contracting with the government, can the government just break those promises or break those obligations after the fact? Folks at the chamber are making it about bigger, broader issues about what it means when the government partners with private organizations.”
Mr. Jost said it’s hard to say which way the Supreme Court will rule, but the fact that the court is reviewing the case speaks volumes.
“Its kind of hard to believe they’re going to order the federal government to pay $12 billion,” he said. “On the other hand, they didn’t have to take the case.”
A Supreme Court decision is expected in early 2020.
U.S. Supreme Court Justices heard oral arguments Dec. 10 in a case that centers on whether the federal government owes insurers billions based on an Affordable Care Act provision intended to help health plans mitigate risk under the law.
Maine Community Health Options v. United States, which consolidates several lawsuits against the government, involves the ACA’s risk corridor program, which required the U.S. Department of Health & Human Services to collect funds from profitable insurers that offered qualified health plans under the exchanges and distribute the funds to insurers with excessive losses.
Collections from profitable insurers under the program fell short in 2014, 2015, and 2016, while losses steadily grew, resulting in the HHS paying about 12 cents on the dollar in payments to insurers. More than 150 insurers now allege they were shortchanged and they want the Supreme Court to force the government to reimburse them $12 billion.
The U.S. Department of Justice counters that the government is not required to pay the plans because of appropriations measures passed by Congress in 2014 and later years that limited the funding available to compensate insurers for their losses. The federal government is not obligated to pay the insurers back for the losses and the suits should be dismissed, the DOJ attorneys argue.
The federal government and insurers have each experienced wins and losses at the lower court level. Most recently, the U.S. Court of Appeals for the Federal Circuit decided in favor of the government, ruling that while the ACA required the government to compensate the insurers for their losses, the appropriations measures repealed or suspended that requirement.
Insurers, economists, and state government led by both parties have weighed in on the case via court briefs.
The case could have important ramifications that have an impact on more than just insurers, said Timothy Jost, a health law expert and retired professor from Washington and Lee University in Lexington, Va.
“The insurers are left holding the bag, but a number of insurers went insolvent [due to the losses], so in those cases, the states are left holding the bag,” Mr. Jost said in an interview.
The outcome could influence future partnerships between the federal government and private entities, according to Katie Keith, an attorney and health law analyst who writes for the Health Affairs Blog. She noted that the U.S. Chamber of Commerce, which historically has not supported the ACA, sided with insurers in the case. In a court brief, attorneys for the chamber wrote that businesses make substantial financial investments to participate in federal programs, and their willingness to do so is based on having assurance that the government will honor its statutory commitments. If left uncorrected, the circuit’s decision “will have far-reaching consequences for myriad areas in which U.S. businesses partner with the federal government to provide vital goods and services,” chamber attorneys wrote.
“This is about more than the ACA. It’s about the fundamentals of public/private partnerships,” Ms. Keith said in an interview. “If you’re contracting with the government, can the government just break those promises or break those obligations after the fact? Folks at the chamber are making it about bigger, broader issues about what it means when the government partners with private organizations.”
Mr. Jost said it’s hard to say which way the Supreme Court will rule, but the fact that the court is reviewing the case speaks volumes.
“Its kind of hard to believe they’re going to order the federal government to pay $12 billion,” he said. “On the other hand, they didn’t have to take the case.”
A Supreme Court decision is expected in early 2020.
U.S. Supreme Court Justices heard oral arguments Dec. 10 in a case that centers on whether the federal government owes insurers billions based on an Affordable Care Act provision intended to help health plans mitigate risk under the law.
Maine Community Health Options v. United States, which consolidates several lawsuits against the government, involves the ACA’s risk corridor program, which required the U.S. Department of Health & Human Services to collect funds from profitable insurers that offered qualified health plans under the exchanges and distribute the funds to insurers with excessive losses.
Collections from profitable insurers under the program fell short in 2014, 2015, and 2016, while losses steadily grew, resulting in the HHS paying about 12 cents on the dollar in payments to insurers. More than 150 insurers now allege they were shortchanged and they want the Supreme Court to force the government to reimburse them $12 billion.
The U.S. Department of Justice counters that the government is not required to pay the plans because of appropriations measures passed by Congress in 2014 and later years that limited the funding available to compensate insurers for their losses. The federal government is not obligated to pay the insurers back for the losses and the suits should be dismissed, the DOJ attorneys argue.
The federal government and insurers have each experienced wins and losses at the lower court level. Most recently, the U.S. Court of Appeals for the Federal Circuit decided in favor of the government, ruling that while the ACA required the government to compensate the insurers for their losses, the appropriations measures repealed or suspended that requirement.
Insurers, economists, and state government led by both parties have weighed in on the case via court briefs.
The case could have important ramifications that have an impact on more than just insurers, said Timothy Jost, a health law expert and retired professor from Washington and Lee University in Lexington, Va.
“The insurers are left holding the bag, but a number of insurers went insolvent [due to the losses], so in those cases, the states are left holding the bag,” Mr. Jost said in an interview.
The outcome could influence future partnerships between the federal government and private entities, according to Katie Keith, an attorney and health law analyst who writes for the Health Affairs Blog. She noted that the U.S. Chamber of Commerce, which historically has not supported the ACA, sided with insurers in the case. In a court brief, attorneys for the chamber wrote that businesses make substantial financial investments to participate in federal programs, and their willingness to do so is based on having assurance that the government will honor its statutory commitments. If left uncorrected, the circuit’s decision “will have far-reaching consequences for myriad areas in which U.S. businesses partner with the federal government to provide vital goods and services,” chamber attorneys wrote.
“This is about more than the ACA. It’s about the fundamentals of public/private partnerships,” Ms. Keith said in an interview. “If you’re contracting with the government, can the government just break those promises or break those obligations after the fact? Folks at the chamber are making it about bigger, broader issues about what it means when the government partners with private organizations.”
Mr. Jost said it’s hard to say which way the Supreme Court will rule, but the fact that the court is reviewing the case speaks volumes.
“Its kind of hard to believe they’re going to order the federal government to pay $12 billion,” he said. “On the other hand, they didn’t have to take the case.”
A Supreme Court decision is expected in early 2020.
House passes drug pricing bill, likely ending its journey
The House of Representatives passed a partisan drug pricing bill, a move that likely ends its legislative journey as Senate Majority Leader Mitch McConnell (R-Ky.) has already signaled he will not bring it to the Senate floor.
The Elijah E. Cummings Lower Drug Costs Now Act (H.R. 3) passed Dec. 12 on a near party-line vote of 230-192, with two Republicans crossing the aisle to join the Democrats in support of the bill, and no Democrats voting against it. Four members from each party did not record votes.
“The American people are fed up with paying 3, 4, or 10 times more than people in other countries for the exact same drug,” House Energy and Commerce Committee Chairman Frank Pallone (D-N.J) said in a statement following the passage. “I’m proud that the House took decisive action today to finally level the playing field and provide real relief to the American people.”
H.R. 3 would give the secretary of Health and Human Services the ability to negotiate with drug manufacturers on the price of pharmaceuticals in Medicare Part D (and available in the commercial markets) using an international pricing benchmark and would penalize manufacturers who do not negotiate or fail to lower prices to be more in line with generally lower costs internationally.
Drug prices would need to be within 120% of the average price in a reference group of six nations: Australia, Canada, France, Germany, Japan, and the United Kingdom.
Savings from the lower costs that result from negotiations would be reinvested into medical research.
Passage of H.R. 3 would “lower ... medication by 65%” per year for women with breast cancer, Rep. Haley Stevens (D-Mich.) said during the floor debate.
The Congressional Budget Office estimated that the drug price negotiation provision would lower spending on pharmaceuticals by $465 billion over the next 10 years, offset partially by an increase in spending by $358 billion associated with provisions to provide dental, vision, and hearing coverage.
The bill also includes mandatory rebates to the federal government when a drug’s price rises faster than the rate of inflation. It includes an annual cap on out-of-pocket spending on pharmaceuticals of $2,000 for Medicare Part D participants.
The bill was contentious from its introduction, which erased bipartisan work across the committees of jurisdiction, including a number of individual bills that passed at the committee level with bipartisan support.
The price negotiation scheme, using the international benchmark, was a key point of objection, which some argued was more akin to price-setting.
“Government price setting will kill innovation in clinical areas where it is most needed,” Rep. George Holding (R-N.C.) said during the floor debate. “The pricing scheme outlined in H.R. 3 would disincentivize research and development for drugs that are first in their class, such as the future cure for Alzheimer’s.”
The CBO estimates that if the bill were enacted, “8 fewer drugs would be introduced to the U.S. market over the 2020-2029 period, and about 30 fewer drugs over the subsequent decade.”
An amendment offered by House Energy and Commerce Committee Ranking Member Greg Walden (R-Ore.) attempted to replace the language of H.R. 3 with substitute language that collected all the individual drug pricing–related bills that had previously passed with bipartisan support at the committee level, but that was voted down by 223-201 vote with 12 members not voting.
Rep. Walden noted that policies within his substitute “unanimously passed the Energy and Commerce Committee earlier this year. They would have unanimously passed on this House floor had a poison pill not been put in up in the Rules Committee.”
Rep. Katie Porter (D-Calif.) countered that Rep. Walden’s amendment “doesn’t tackle the fundamental problem, which is reducing drug prices. This amendment fails to solve the main problem of actually lowering drug prices.”
The House of Representatives passed a partisan drug pricing bill, a move that likely ends its legislative journey as Senate Majority Leader Mitch McConnell (R-Ky.) has already signaled he will not bring it to the Senate floor.
The Elijah E. Cummings Lower Drug Costs Now Act (H.R. 3) passed Dec. 12 on a near party-line vote of 230-192, with two Republicans crossing the aisle to join the Democrats in support of the bill, and no Democrats voting against it. Four members from each party did not record votes.
“The American people are fed up with paying 3, 4, or 10 times more than people in other countries for the exact same drug,” House Energy and Commerce Committee Chairman Frank Pallone (D-N.J) said in a statement following the passage. “I’m proud that the House took decisive action today to finally level the playing field and provide real relief to the American people.”
H.R. 3 would give the secretary of Health and Human Services the ability to negotiate with drug manufacturers on the price of pharmaceuticals in Medicare Part D (and available in the commercial markets) using an international pricing benchmark and would penalize manufacturers who do not negotiate or fail to lower prices to be more in line with generally lower costs internationally.
Drug prices would need to be within 120% of the average price in a reference group of six nations: Australia, Canada, France, Germany, Japan, and the United Kingdom.
Savings from the lower costs that result from negotiations would be reinvested into medical research.
Passage of H.R. 3 would “lower ... medication by 65%” per year for women with breast cancer, Rep. Haley Stevens (D-Mich.) said during the floor debate.
The Congressional Budget Office estimated that the drug price negotiation provision would lower spending on pharmaceuticals by $465 billion over the next 10 years, offset partially by an increase in spending by $358 billion associated with provisions to provide dental, vision, and hearing coverage.
The bill also includes mandatory rebates to the federal government when a drug’s price rises faster than the rate of inflation. It includes an annual cap on out-of-pocket spending on pharmaceuticals of $2,000 for Medicare Part D participants.
The bill was contentious from its introduction, which erased bipartisan work across the committees of jurisdiction, including a number of individual bills that passed at the committee level with bipartisan support.
The price negotiation scheme, using the international benchmark, was a key point of objection, which some argued was more akin to price-setting.
“Government price setting will kill innovation in clinical areas where it is most needed,” Rep. George Holding (R-N.C.) said during the floor debate. “The pricing scheme outlined in H.R. 3 would disincentivize research and development for drugs that are first in their class, such as the future cure for Alzheimer’s.”
The CBO estimates that if the bill were enacted, “8 fewer drugs would be introduced to the U.S. market over the 2020-2029 period, and about 30 fewer drugs over the subsequent decade.”
An amendment offered by House Energy and Commerce Committee Ranking Member Greg Walden (R-Ore.) attempted to replace the language of H.R. 3 with substitute language that collected all the individual drug pricing–related bills that had previously passed with bipartisan support at the committee level, but that was voted down by 223-201 vote with 12 members not voting.
Rep. Walden noted that policies within his substitute “unanimously passed the Energy and Commerce Committee earlier this year. They would have unanimously passed on this House floor had a poison pill not been put in up in the Rules Committee.”
Rep. Katie Porter (D-Calif.) countered that Rep. Walden’s amendment “doesn’t tackle the fundamental problem, which is reducing drug prices. This amendment fails to solve the main problem of actually lowering drug prices.”
The House of Representatives passed a partisan drug pricing bill, a move that likely ends its legislative journey as Senate Majority Leader Mitch McConnell (R-Ky.) has already signaled he will not bring it to the Senate floor.
The Elijah E. Cummings Lower Drug Costs Now Act (H.R. 3) passed Dec. 12 on a near party-line vote of 230-192, with two Republicans crossing the aisle to join the Democrats in support of the bill, and no Democrats voting against it. Four members from each party did not record votes.
“The American people are fed up with paying 3, 4, or 10 times more than people in other countries for the exact same drug,” House Energy and Commerce Committee Chairman Frank Pallone (D-N.J) said in a statement following the passage. “I’m proud that the House took decisive action today to finally level the playing field and provide real relief to the American people.”
H.R. 3 would give the secretary of Health and Human Services the ability to negotiate with drug manufacturers on the price of pharmaceuticals in Medicare Part D (and available in the commercial markets) using an international pricing benchmark and would penalize manufacturers who do not negotiate or fail to lower prices to be more in line with generally lower costs internationally.
Drug prices would need to be within 120% of the average price in a reference group of six nations: Australia, Canada, France, Germany, Japan, and the United Kingdom.
Savings from the lower costs that result from negotiations would be reinvested into medical research.
Passage of H.R. 3 would “lower ... medication by 65%” per year for women with breast cancer, Rep. Haley Stevens (D-Mich.) said during the floor debate.
The Congressional Budget Office estimated that the drug price negotiation provision would lower spending on pharmaceuticals by $465 billion over the next 10 years, offset partially by an increase in spending by $358 billion associated with provisions to provide dental, vision, and hearing coverage.
The bill also includes mandatory rebates to the federal government when a drug’s price rises faster than the rate of inflation. It includes an annual cap on out-of-pocket spending on pharmaceuticals of $2,000 for Medicare Part D participants.
The bill was contentious from its introduction, which erased bipartisan work across the committees of jurisdiction, including a number of individual bills that passed at the committee level with bipartisan support.
The price negotiation scheme, using the international benchmark, was a key point of objection, which some argued was more akin to price-setting.
“Government price setting will kill innovation in clinical areas where it is most needed,” Rep. George Holding (R-N.C.) said during the floor debate. “The pricing scheme outlined in H.R. 3 would disincentivize research and development for drugs that are first in their class, such as the future cure for Alzheimer’s.”
The CBO estimates that if the bill were enacted, “8 fewer drugs would be introduced to the U.S. market over the 2020-2029 period, and about 30 fewer drugs over the subsequent decade.”
An amendment offered by House Energy and Commerce Committee Ranking Member Greg Walden (R-Ore.) attempted to replace the language of H.R. 3 with substitute language that collected all the individual drug pricing–related bills that had previously passed with bipartisan support at the committee level, but that was voted down by 223-201 vote with 12 members not voting.
Rep. Walden noted that policies within his substitute “unanimously passed the Energy and Commerce Committee earlier this year. They would have unanimously passed on this House floor had a poison pill not been put in up in the Rules Committee.”
Rep. Katie Porter (D-Calif.) countered that Rep. Walden’s amendment “doesn’t tackle the fundamental problem, which is reducing drug prices. This amendment fails to solve the main problem of actually lowering drug prices.”
Medtwitter embraces incoming student’s excitement
When Melissa Gonzalez excitedly tweeted that she had been accepted to medical school earlier this year, she had no idea the tweet would draw attention and responses from people across the country.
The tweet, which shared that Ms. Gonzalez was the daughter of Mexican immigrants, received more than 300,000 likes and another 23,000 retweets from physicians, medical associations, students, and graduates alike. In this video, Ms. Gonzalez, who was accepted to Keck School of Medicine of the University of Southern California, Los Angeles, speaks of her journey to medical school.
When Melissa Gonzalez excitedly tweeted that she had been accepted to medical school earlier this year, she had no idea the tweet would draw attention and responses from people across the country.
The tweet, which shared that Ms. Gonzalez was the daughter of Mexican immigrants, received more than 300,000 likes and another 23,000 retweets from physicians, medical associations, students, and graduates alike. In this video, Ms. Gonzalez, who was accepted to Keck School of Medicine of the University of Southern California, Los Angeles, speaks of her journey to medical school.
When Melissa Gonzalez excitedly tweeted that she had been accepted to medical school earlier this year, she had no idea the tweet would draw attention and responses from people across the country.
The tweet, which shared that Ms. Gonzalez was the daughter of Mexican immigrants, received more than 300,000 likes and another 23,000 retweets from physicians, medical associations, students, and graduates alike. In this video, Ms. Gonzalez, who was accepted to Keck School of Medicine of the University of Southern California, Los Angeles, speaks of her journey to medical school.
Paid (and unpaid) time off
Many medical offices are following a popular trend in the business world: They are replacing employee sick leave, vacation, and any other miscellaneous time benefits with a combination of all of them, collectively referred to as “, and you should carefully consider all the pros and cons before adopting it.
Employees generally like the concept because most never use all their sick leave. Allowing them to take the difference as extra vacation time makes them happy, and makes your office more attractive to excellent prospects. They also appreciate being treated more like adults who can make time off decisions for themselves.
Employers like it because there is less paperwork and less abuse of sick leave. They don’t have to make any decisions about whether an employee is really sick or not; reasons for absence are now irrelevant, so feigned illnesses are a thing of the past. If an employee requests a day off with adequate notice, and there is adequate coverage of that employee’s duties, you don’t need to know (or care) about the reason for the request.
Critics say employees are absent more frequently under a PTO system, since employees who never used their full allotment of sick leave will typically use all of their PTO; but that, in a sense, is the idea. Time off is necessary and important for good office morale, and should be taken by all employees, as well as by all employers. (Remember Eastern’s First Law: Your last words will NOT be, “I wish I had spent more time in the office.”)
Besides, you should be suspicious of any employee who won’t take vacations. They are often embezzlers who fear that their illicit modus operandi will be discovered during their absence. (More on that next month.)
Most extra absences can be controlled by requiring prior approval for any time off, except emergencies. Critics point out that you are then replacing decisions about what constitutes an illness with decisions about what constitutes an emergency; but many criteria for emergencies can be settled upon in advance.
Some experts suggest dealing with increased absenteeism by allowing employees to take salary in exchange for unused PTO. I disagree because again, time off should be taken. If you want to allow PTO to be paid as salary, set a limit – say, 10%. Use the rest, or lose it.
A major issue with PTO is the possibility that employees will resist staying home when they are actually sick. Some businesses have found that employees tend to view all PTO as vacation time, and don’t want to “waste” any of it on illness. You should make it very clear that sick employees must stay home, and if they come to work sick, they will be sent home. You have an obligation to protect the rest of your employees, not to mention your patients (especially those who are elderly or immunocompromised) from a staff member with a potentially communicable illness.
Other clear guidelines should be established as well. Make sure everyone knows they will have to request PTO in advance, except for emergencies. First define “in advance” (72 hours? A week?), and then “emergency,” and put these definitions in writing. Illnesses are emergencies, of course, but what about waking up with a bad hangover? A sick child qualifies if your employee is the only available caregiver, but what about a malfunctioning car? Some circumstances will necessarily be decided on a case-by-case basis; but the more situations you can anticipate and settle in advance, the fewer hassles you will have.
What about unpaid time off? There are two basic options: Don’t allow it at all, or require employees to submit a written request, explaining why they need it, and why it’s a special situation and won’t be a regular occurrence. Even if you (almost) always approve such requests, forcing your employees to jump through a hoop or two makes it far less likely that anyone will abuse the privilege. And it allows you to make judgments on a case-by-case basis, while still being able to honestly say you offer it as a blanket policy to all employees.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Many medical offices are following a popular trend in the business world: They are replacing employee sick leave, vacation, and any other miscellaneous time benefits with a combination of all of them, collectively referred to as “, and you should carefully consider all the pros and cons before adopting it.
Employees generally like the concept because most never use all their sick leave. Allowing them to take the difference as extra vacation time makes them happy, and makes your office more attractive to excellent prospects. They also appreciate being treated more like adults who can make time off decisions for themselves.
Employers like it because there is less paperwork and less abuse of sick leave. They don’t have to make any decisions about whether an employee is really sick or not; reasons for absence are now irrelevant, so feigned illnesses are a thing of the past. If an employee requests a day off with adequate notice, and there is adequate coverage of that employee’s duties, you don’t need to know (or care) about the reason for the request.
Critics say employees are absent more frequently under a PTO system, since employees who never used their full allotment of sick leave will typically use all of their PTO; but that, in a sense, is the idea. Time off is necessary and important for good office morale, and should be taken by all employees, as well as by all employers. (Remember Eastern’s First Law: Your last words will NOT be, “I wish I had spent more time in the office.”)
Besides, you should be suspicious of any employee who won’t take vacations. They are often embezzlers who fear that their illicit modus operandi will be discovered during their absence. (More on that next month.)
Most extra absences can be controlled by requiring prior approval for any time off, except emergencies. Critics point out that you are then replacing decisions about what constitutes an illness with decisions about what constitutes an emergency; but many criteria for emergencies can be settled upon in advance.
Some experts suggest dealing with increased absenteeism by allowing employees to take salary in exchange for unused PTO. I disagree because again, time off should be taken. If you want to allow PTO to be paid as salary, set a limit – say, 10%. Use the rest, or lose it.
A major issue with PTO is the possibility that employees will resist staying home when they are actually sick. Some businesses have found that employees tend to view all PTO as vacation time, and don’t want to “waste” any of it on illness. You should make it very clear that sick employees must stay home, and if they come to work sick, they will be sent home. You have an obligation to protect the rest of your employees, not to mention your patients (especially those who are elderly or immunocompromised) from a staff member with a potentially communicable illness.
Other clear guidelines should be established as well. Make sure everyone knows they will have to request PTO in advance, except for emergencies. First define “in advance” (72 hours? A week?), and then “emergency,” and put these definitions in writing. Illnesses are emergencies, of course, but what about waking up with a bad hangover? A sick child qualifies if your employee is the only available caregiver, but what about a malfunctioning car? Some circumstances will necessarily be decided on a case-by-case basis; but the more situations you can anticipate and settle in advance, the fewer hassles you will have.
What about unpaid time off? There are two basic options: Don’t allow it at all, or require employees to submit a written request, explaining why they need it, and why it’s a special situation and won’t be a regular occurrence. Even if you (almost) always approve such requests, forcing your employees to jump through a hoop or two makes it far less likely that anyone will abuse the privilege. And it allows you to make judgments on a case-by-case basis, while still being able to honestly say you offer it as a blanket policy to all employees.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Many medical offices are following a popular trend in the business world: They are replacing employee sick leave, vacation, and any other miscellaneous time benefits with a combination of all of them, collectively referred to as “, and you should carefully consider all the pros and cons before adopting it.
Employees generally like the concept because most never use all their sick leave. Allowing them to take the difference as extra vacation time makes them happy, and makes your office more attractive to excellent prospects. They also appreciate being treated more like adults who can make time off decisions for themselves.
Employers like it because there is less paperwork and less abuse of sick leave. They don’t have to make any decisions about whether an employee is really sick or not; reasons for absence are now irrelevant, so feigned illnesses are a thing of the past. If an employee requests a day off with adequate notice, and there is adequate coverage of that employee’s duties, you don’t need to know (or care) about the reason for the request.
Critics say employees are absent more frequently under a PTO system, since employees who never used their full allotment of sick leave will typically use all of their PTO; but that, in a sense, is the idea. Time off is necessary and important for good office morale, and should be taken by all employees, as well as by all employers. (Remember Eastern’s First Law: Your last words will NOT be, “I wish I had spent more time in the office.”)
Besides, you should be suspicious of any employee who won’t take vacations. They are often embezzlers who fear that their illicit modus operandi will be discovered during their absence. (More on that next month.)
Most extra absences can be controlled by requiring prior approval for any time off, except emergencies. Critics point out that you are then replacing decisions about what constitutes an illness with decisions about what constitutes an emergency; but many criteria for emergencies can be settled upon in advance.
Some experts suggest dealing with increased absenteeism by allowing employees to take salary in exchange for unused PTO. I disagree because again, time off should be taken. If you want to allow PTO to be paid as salary, set a limit – say, 10%. Use the rest, or lose it.
A major issue with PTO is the possibility that employees will resist staying home when they are actually sick. Some businesses have found that employees tend to view all PTO as vacation time, and don’t want to “waste” any of it on illness. You should make it very clear that sick employees must stay home, and if they come to work sick, they will be sent home. You have an obligation to protect the rest of your employees, not to mention your patients (especially those who are elderly or immunocompromised) from a staff member with a potentially communicable illness.
Other clear guidelines should be established as well. Make sure everyone knows they will have to request PTO in advance, except for emergencies. First define “in advance” (72 hours? A week?), and then “emergency,” and put these definitions in writing. Illnesses are emergencies, of course, but what about waking up with a bad hangover? A sick child qualifies if your employee is the only available caregiver, but what about a malfunctioning car? Some circumstances will necessarily be decided on a case-by-case basis; but the more situations you can anticipate and settle in advance, the fewer hassles you will have.
What about unpaid time off? There are two basic options: Don’t allow it at all, or require employees to submit a written request, explaining why they need it, and why it’s a special situation and won’t be a regular occurrence. Even if you (almost) always approve such requests, forcing your employees to jump through a hoop or two makes it far less likely that anyone will abuse the privilege. And it allows you to make judgments on a case-by-case basis, while still being able to honestly say you offer it as a blanket policy to all employees.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
‘Real-world’ data show CAR T therapies are cost effective
ORLANDO – Chimeric antigen receptor (CAR) T-cell therapy has been hailed as a major advance and a game changer, but their cost has redefined the meaning of “expensive.”
However, new “real-world” data now suggests that CAR T-cell therapy may actually be cost effective, as it may lower other expenses related to the illness.
When used in a population of older adults with non-Hodgkin lymphoma, these new data show that CAR T-cell therapy cut related expenditures, compared with health care costs prior to receiving this treatment.
“CAR T therapy was associated with fewer hospitalizations, shorter time in the hospital, fewer ED visits, and lower total health care costs,” said lead study author Karl M. Kilgore, PhD, of Avalere Health in Washington, D.C.
He presented the findings at the 2019 annual meeting of the American Society of Hematology (abstract 793).
CAR T-cell therapies were approved in the United States in 2017. First came tisagenlecleucel (Kymriah, Novartis), for the treatment of pediatric and young adult patients with acute lymphoblastic leukemia, with a price tag of $475,000. Closely following it was axicabtagene ciloleucel (Yescarta, Kite/Gliead), indicated for adult patients with relapsed/refractory aggressive B-cell non-Hodgkin lymphoma who are ineligible for autologous stem cell transplant, with a price tag of $373,000.
The formidable price tags sent shock waves through the blood cancers community, which is struggling to incorporate this novel approach because of the remarkable responses that have been seen.
Real-world experience
In the current study, Dr. Kilgore and colleagues evaluated the demographic and clinical characteristics of Medicare patients who received CAR T therapy (axicabtagene ciloleucel or tisagenlecleucel) and then compared health care utilization, costs, and outcomes pre– and post–CAR T therapy.
“The goal of this study was to look at the real use of CAR T-cell therapy and real-world data on the use of these therapies,” said Dr. Kilgore. “And to look at health care utilization.”
Data was obtained from the Centers for Medicare & Medicaid Services 100% Medicare Fee-for-Service Part A and B claims data, and patients were included in the study if they had been diagnosed with lymphoma and received CAR T therapy between Oct. 1, 2017, and Sept. 30, 2018.
A total of 177 patients met all of the inclusion criteria and were included in the analysis.
The average age was 70 years, more than half (58.8%) were male, and they were primarily white (87.6%). Nearly all patients (91.5%) had a primary diagnosis of diffuse large B-cell lymphoma (DLBCL), as well as multiple comorbidities with 74.6% having a Charlson Comorbidity Index score of 3 or less. Fewer than 5% of patients had undergone a previous autologous stem cell transplant, and 51% had one or more comorbidities that would have disqualified them from participating in CAR T clinical trials (for example, renal failure, heart failure, recent history of deep vein thrombosis/pulmonary embolism).
Just over half of participants (52%) had been treated with intravenous chemotherapy in the 6 months prior to receiving CAR T-cell therapy, and 60% received outpatient lymphodepletion.
During their index episode of care for CAR T infusion, the patients spent a median of 16 days (interquartile range, 10) in the hospital during and 45.5% required ICU care after infusion. In the 6-month period prior to CAR T-cell therapy (preindex), 51.2% had been hospitalized at least once, and almost 20% had three or more periods of hospitalization. Of that group, 27.1% were readmitted during the postindex period.
Among patients who required hospitalization, the median length of stay preindex was 7 days and 5 days post index. The number of ED visits was also lower in the post versus preindex (15.8% vs. 29.9%).
“Patients spent 17% less time in the hospital 6 months after CAR T-cell therapy than before,” he said.
While there were no deaths during the postindex period, a small percentage (less than 5%) were admitted to hospice care. It is unclear if any patients received chemotherapy during the 100-day postindex period, which would suggest disease progression. However, the authors note that claims for the period might be lagging behind for some patients.
Dr. Kilgore pointed out that half of the patients had one or more chronic conditions that, in some cases, would have excluded them from clinical trials. “But 73% remain alive at 6 months,” he said. “We have data that goes out to 21 months, and over 50% are still alive at almost 2 years.”
As for cost, the median total health care costs during the preindex period were $51,999 (mean, 58,820; standard deviation, 45,701) and $14,014 post index (mean, 23,738; SD, 29,698). This extrapolates into $9,749 pre- versus $7,121 post index for each patient per month, which is a 27% decrease in expenditures.
Dr. Kilgore explained that the total paid amounts for CAR T from all sources (Medicare and patient) varied significantly, depending on whether patients were treated in a clinical trial and whether the hospital was reimbursed under standard Medicare prospective payment system for inpatient facilities or through the PPS-exempt payment system.
Impressive survival
Commenting on the study, Sarah Rutherford, MD, a hematologist at Weill Cornell Medical College, New York, and New York–Presbyterian, believes that the key takeaway from this study is that the majority of participants – who were older and sicker than many enrolled on CAR T-cell clinical trials – did quite well.
“Diffuse large B-cell lymphoma is a disease that usually causes people to die quickly if they are refractory to multiple lines of therapy, so the 6-month survival of 75% in this patient population is impressive,” she said. “A large proportion of these patients are likely to have died had they not received CAR T-cell therapy.”
Dr. Rutherford noted that the study authors analyzed the costs associated with patients in the pre– and post–CAR T-cell setting, finding that health care costs were lower following CAR T-cell therapy in this Medicare patient subset, compared with costs prior to the therapy.
“I think CAR T-cell use is certainly justified given the lack of efficacious therapies in relapsed and refractory DLBCL patients, and this study indicates that there may be a financial benefit as well, though the actual costs associated with CAR T-cell therapy were not included in the analysis,” she told Medscape Medical News.
Also weighing in on the study, James Essell, MD, from the U.S. Oncology Network, pointed out that CAR T-cell therapy is changing the paradigm of treatment. For example, refractory lymphoma has a life expectancy of about 6 months. “But with newer data we’re seeing about 50% of patients alive at 3 years after CAR T-cell therapy and we’re thinking that will equate into a cure,” he said.
Dr. Essell explained that, in the past, the scenario would be 6 months of chemotherapy, relapse, other chemotherapy, relapse, and then CAR T, but several clinical trials are now looking at giving CAR T at first relapse. “Instead of waiting until they’ve had a transplant, which is going to be about $100,000 at least, they are going to be randomized between autologous transplant and CAR T up front,” he said.
“We are also doing clinical trials through the network for patients who are not candidates for an autologous transplant,” Dr. Essell continued. “They will go straight to CAR-T therapy and that will really increase the cure rate because these are people who weren’t eligible for any curative therapy – and now they are being given a chance.”
Whether CAR T-cell use will expand to broader populations will depend on the results of the randomized trials that are ongoing now, he added.
“That’s our hypotheses right now, but they are being studied in a wide range of hematologic cancers, and in addition, there is a lot of research in solid tumors,” Dr. Essell said. “I don’t think you’d see this mass amount of research and dollars being poured into it if people didn’t think it was going to be a game changer.”
Dr. Kilgore has disclosed research funding from Kite Pharma. Several of the other coauthors have disclosed relationships with industry, which are noted in the abstract. Dr. Essell has disclosed no relevant financial relationships.
A version of this story originally appeared on Medscape.com.
ORLANDO – Chimeric antigen receptor (CAR) T-cell therapy has been hailed as a major advance and a game changer, but their cost has redefined the meaning of “expensive.”
However, new “real-world” data now suggests that CAR T-cell therapy may actually be cost effective, as it may lower other expenses related to the illness.
When used in a population of older adults with non-Hodgkin lymphoma, these new data show that CAR T-cell therapy cut related expenditures, compared with health care costs prior to receiving this treatment.
“CAR T therapy was associated with fewer hospitalizations, shorter time in the hospital, fewer ED visits, and lower total health care costs,” said lead study author Karl M. Kilgore, PhD, of Avalere Health in Washington, D.C.
He presented the findings at the 2019 annual meeting of the American Society of Hematology (abstract 793).
CAR T-cell therapies were approved in the United States in 2017. First came tisagenlecleucel (Kymriah, Novartis), for the treatment of pediatric and young adult patients with acute lymphoblastic leukemia, with a price tag of $475,000. Closely following it was axicabtagene ciloleucel (Yescarta, Kite/Gliead), indicated for adult patients with relapsed/refractory aggressive B-cell non-Hodgkin lymphoma who are ineligible for autologous stem cell transplant, with a price tag of $373,000.
The formidable price tags sent shock waves through the blood cancers community, which is struggling to incorporate this novel approach because of the remarkable responses that have been seen.
Real-world experience
In the current study, Dr. Kilgore and colleagues evaluated the demographic and clinical characteristics of Medicare patients who received CAR T therapy (axicabtagene ciloleucel or tisagenlecleucel) and then compared health care utilization, costs, and outcomes pre– and post–CAR T therapy.
“The goal of this study was to look at the real use of CAR T-cell therapy and real-world data on the use of these therapies,” said Dr. Kilgore. “And to look at health care utilization.”
Data was obtained from the Centers for Medicare & Medicaid Services 100% Medicare Fee-for-Service Part A and B claims data, and patients were included in the study if they had been diagnosed with lymphoma and received CAR T therapy between Oct. 1, 2017, and Sept. 30, 2018.
A total of 177 patients met all of the inclusion criteria and were included in the analysis.
The average age was 70 years, more than half (58.8%) were male, and they were primarily white (87.6%). Nearly all patients (91.5%) had a primary diagnosis of diffuse large B-cell lymphoma (DLBCL), as well as multiple comorbidities with 74.6% having a Charlson Comorbidity Index score of 3 or less. Fewer than 5% of patients had undergone a previous autologous stem cell transplant, and 51% had one or more comorbidities that would have disqualified them from participating in CAR T clinical trials (for example, renal failure, heart failure, recent history of deep vein thrombosis/pulmonary embolism).
Just over half of participants (52%) had been treated with intravenous chemotherapy in the 6 months prior to receiving CAR T-cell therapy, and 60% received outpatient lymphodepletion.
During their index episode of care for CAR T infusion, the patients spent a median of 16 days (interquartile range, 10) in the hospital during and 45.5% required ICU care after infusion. In the 6-month period prior to CAR T-cell therapy (preindex), 51.2% had been hospitalized at least once, and almost 20% had three or more periods of hospitalization. Of that group, 27.1% were readmitted during the postindex period.
Among patients who required hospitalization, the median length of stay preindex was 7 days and 5 days post index. The number of ED visits was also lower in the post versus preindex (15.8% vs. 29.9%).
“Patients spent 17% less time in the hospital 6 months after CAR T-cell therapy than before,” he said.
While there were no deaths during the postindex period, a small percentage (less than 5%) were admitted to hospice care. It is unclear if any patients received chemotherapy during the 100-day postindex period, which would suggest disease progression. However, the authors note that claims for the period might be lagging behind for some patients.
Dr. Kilgore pointed out that half of the patients had one or more chronic conditions that, in some cases, would have excluded them from clinical trials. “But 73% remain alive at 6 months,” he said. “We have data that goes out to 21 months, and over 50% are still alive at almost 2 years.”
As for cost, the median total health care costs during the preindex period were $51,999 (mean, 58,820; standard deviation, 45,701) and $14,014 post index (mean, 23,738; SD, 29,698). This extrapolates into $9,749 pre- versus $7,121 post index for each patient per month, which is a 27% decrease in expenditures.
Dr. Kilgore explained that the total paid amounts for CAR T from all sources (Medicare and patient) varied significantly, depending on whether patients were treated in a clinical trial and whether the hospital was reimbursed under standard Medicare prospective payment system for inpatient facilities or through the PPS-exempt payment system.
Impressive survival
Commenting on the study, Sarah Rutherford, MD, a hematologist at Weill Cornell Medical College, New York, and New York–Presbyterian, believes that the key takeaway from this study is that the majority of participants – who were older and sicker than many enrolled on CAR T-cell clinical trials – did quite well.
“Diffuse large B-cell lymphoma is a disease that usually causes people to die quickly if they are refractory to multiple lines of therapy, so the 6-month survival of 75% in this patient population is impressive,” she said. “A large proportion of these patients are likely to have died had they not received CAR T-cell therapy.”
Dr. Rutherford noted that the study authors analyzed the costs associated with patients in the pre– and post–CAR T-cell setting, finding that health care costs were lower following CAR T-cell therapy in this Medicare patient subset, compared with costs prior to the therapy.
“I think CAR T-cell use is certainly justified given the lack of efficacious therapies in relapsed and refractory DLBCL patients, and this study indicates that there may be a financial benefit as well, though the actual costs associated with CAR T-cell therapy were not included in the analysis,” she told Medscape Medical News.
Also weighing in on the study, James Essell, MD, from the U.S. Oncology Network, pointed out that CAR T-cell therapy is changing the paradigm of treatment. For example, refractory lymphoma has a life expectancy of about 6 months. “But with newer data we’re seeing about 50% of patients alive at 3 years after CAR T-cell therapy and we’re thinking that will equate into a cure,” he said.
Dr. Essell explained that, in the past, the scenario would be 6 months of chemotherapy, relapse, other chemotherapy, relapse, and then CAR T, but several clinical trials are now looking at giving CAR T at first relapse. “Instead of waiting until they’ve had a transplant, which is going to be about $100,000 at least, they are going to be randomized between autologous transplant and CAR T up front,” he said.
“We are also doing clinical trials through the network for patients who are not candidates for an autologous transplant,” Dr. Essell continued. “They will go straight to CAR-T therapy and that will really increase the cure rate because these are people who weren’t eligible for any curative therapy – and now they are being given a chance.”
Whether CAR T-cell use will expand to broader populations will depend on the results of the randomized trials that are ongoing now, he added.
“That’s our hypotheses right now, but they are being studied in a wide range of hematologic cancers, and in addition, there is a lot of research in solid tumors,” Dr. Essell said. “I don’t think you’d see this mass amount of research and dollars being poured into it if people didn’t think it was going to be a game changer.”
Dr. Kilgore has disclosed research funding from Kite Pharma. Several of the other coauthors have disclosed relationships with industry, which are noted in the abstract. Dr. Essell has disclosed no relevant financial relationships.
A version of this story originally appeared on Medscape.com.
ORLANDO – Chimeric antigen receptor (CAR) T-cell therapy has been hailed as a major advance and a game changer, but their cost has redefined the meaning of “expensive.”
However, new “real-world” data now suggests that CAR T-cell therapy may actually be cost effective, as it may lower other expenses related to the illness.
When used in a population of older adults with non-Hodgkin lymphoma, these new data show that CAR T-cell therapy cut related expenditures, compared with health care costs prior to receiving this treatment.
“CAR T therapy was associated with fewer hospitalizations, shorter time in the hospital, fewer ED visits, and lower total health care costs,” said lead study author Karl M. Kilgore, PhD, of Avalere Health in Washington, D.C.
He presented the findings at the 2019 annual meeting of the American Society of Hematology (abstract 793).
CAR T-cell therapies were approved in the United States in 2017. First came tisagenlecleucel (Kymriah, Novartis), for the treatment of pediatric and young adult patients with acute lymphoblastic leukemia, with a price tag of $475,000. Closely following it was axicabtagene ciloleucel (Yescarta, Kite/Gliead), indicated for adult patients with relapsed/refractory aggressive B-cell non-Hodgkin lymphoma who are ineligible for autologous stem cell transplant, with a price tag of $373,000.
The formidable price tags sent shock waves through the blood cancers community, which is struggling to incorporate this novel approach because of the remarkable responses that have been seen.
Real-world experience
In the current study, Dr. Kilgore and colleagues evaluated the demographic and clinical characteristics of Medicare patients who received CAR T therapy (axicabtagene ciloleucel or tisagenlecleucel) and then compared health care utilization, costs, and outcomes pre– and post–CAR T therapy.
“The goal of this study was to look at the real use of CAR T-cell therapy and real-world data on the use of these therapies,” said Dr. Kilgore. “And to look at health care utilization.”
Data was obtained from the Centers for Medicare & Medicaid Services 100% Medicare Fee-for-Service Part A and B claims data, and patients were included in the study if they had been diagnosed with lymphoma and received CAR T therapy between Oct. 1, 2017, and Sept. 30, 2018.
A total of 177 patients met all of the inclusion criteria and were included in the analysis.
The average age was 70 years, more than half (58.8%) were male, and they were primarily white (87.6%). Nearly all patients (91.5%) had a primary diagnosis of diffuse large B-cell lymphoma (DLBCL), as well as multiple comorbidities with 74.6% having a Charlson Comorbidity Index score of 3 or less. Fewer than 5% of patients had undergone a previous autologous stem cell transplant, and 51% had one or more comorbidities that would have disqualified them from participating in CAR T clinical trials (for example, renal failure, heart failure, recent history of deep vein thrombosis/pulmonary embolism).
Just over half of participants (52%) had been treated with intravenous chemotherapy in the 6 months prior to receiving CAR T-cell therapy, and 60% received outpatient lymphodepletion.
During their index episode of care for CAR T infusion, the patients spent a median of 16 days (interquartile range, 10) in the hospital during and 45.5% required ICU care after infusion. In the 6-month period prior to CAR T-cell therapy (preindex), 51.2% had been hospitalized at least once, and almost 20% had three or more periods of hospitalization. Of that group, 27.1% were readmitted during the postindex period.
Among patients who required hospitalization, the median length of stay preindex was 7 days and 5 days post index. The number of ED visits was also lower in the post versus preindex (15.8% vs. 29.9%).
“Patients spent 17% less time in the hospital 6 months after CAR T-cell therapy than before,” he said.
While there were no deaths during the postindex period, a small percentage (less than 5%) were admitted to hospice care. It is unclear if any patients received chemotherapy during the 100-day postindex period, which would suggest disease progression. However, the authors note that claims for the period might be lagging behind for some patients.
Dr. Kilgore pointed out that half of the patients had one or more chronic conditions that, in some cases, would have excluded them from clinical trials. “But 73% remain alive at 6 months,” he said. “We have data that goes out to 21 months, and over 50% are still alive at almost 2 years.”
As for cost, the median total health care costs during the preindex period were $51,999 (mean, 58,820; standard deviation, 45,701) and $14,014 post index (mean, 23,738; SD, 29,698). This extrapolates into $9,749 pre- versus $7,121 post index for each patient per month, which is a 27% decrease in expenditures.
Dr. Kilgore explained that the total paid amounts for CAR T from all sources (Medicare and patient) varied significantly, depending on whether patients were treated in a clinical trial and whether the hospital was reimbursed under standard Medicare prospective payment system for inpatient facilities or through the PPS-exempt payment system.
Impressive survival
Commenting on the study, Sarah Rutherford, MD, a hematologist at Weill Cornell Medical College, New York, and New York–Presbyterian, believes that the key takeaway from this study is that the majority of participants – who were older and sicker than many enrolled on CAR T-cell clinical trials – did quite well.
“Diffuse large B-cell lymphoma is a disease that usually causes people to die quickly if they are refractory to multiple lines of therapy, so the 6-month survival of 75% in this patient population is impressive,” she said. “A large proportion of these patients are likely to have died had they not received CAR T-cell therapy.”
Dr. Rutherford noted that the study authors analyzed the costs associated with patients in the pre– and post–CAR T-cell setting, finding that health care costs were lower following CAR T-cell therapy in this Medicare patient subset, compared with costs prior to the therapy.
“I think CAR T-cell use is certainly justified given the lack of efficacious therapies in relapsed and refractory DLBCL patients, and this study indicates that there may be a financial benefit as well, though the actual costs associated with CAR T-cell therapy were not included in the analysis,” she told Medscape Medical News.
Also weighing in on the study, James Essell, MD, from the U.S. Oncology Network, pointed out that CAR T-cell therapy is changing the paradigm of treatment. For example, refractory lymphoma has a life expectancy of about 6 months. “But with newer data we’re seeing about 50% of patients alive at 3 years after CAR T-cell therapy and we’re thinking that will equate into a cure,” he said.
Dr. Essell explained that, in the past, the scenario would be 6 months of chemotherapy, relapse, other chemotherapy, relapse, and then CAR T, but several clinical trials are now looking at giving CAR T at first relapse. “Instead of waiting until they’ve had a transplant, which is going to be about $100,000 at least, they are going to be randomized between autologous transplant and CAR T up front,” he said.
“We are also doing clinical trials through the network for patients who are not candidates for an autologous transplant,” Dr. Essell continued. “They will go straight to CAR-T therapy and that will really increase the cure rate because these are people who weren’t eligible for any curative therapy – and now they are being given a chance.”
Whether CAR T-cell use will expand to broader populations will depend on the results of the randomized trials that are ongoing now, he added.
“That’s our hypotheses right now, but they are being studied in a wide range of hematologic cancers, and in addition, there is a lot of research in solid tumors,” Dr. Essell said. “I don’t think you’d see this mass amount of research and dollars being poured into it if people didn’t think it was going to be a game changer.”
Dr. Kilgore has disclosed research funding from Kite Pharma. Several of the other coauthors have disclosed relationships with industry, which are noted in the abstract. Dr. Essell has disclosed no relevant financial relationships.
A version of this story originally appeared on Medscape.com.
2020 open enrollment: HealthCare.gov heats up in week 6
HealthCare.gov just had its busiest week of the 2020 open enrollment season, but the plan count for all consumers continues to run below last year’s total through 6 weeks, according to the Centers for Medicare & Medicaid Services.
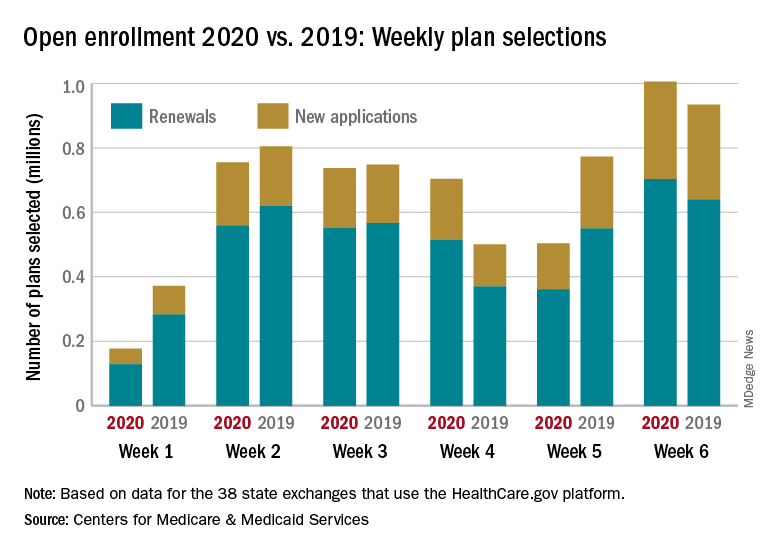
Just over 1 million plans – 302,000 new consumers and 703,000 renewals – were selected during the week of Dec. 1-7, eclipsing the season high of 755,000 from week 2 of open enrollment for the 38 states using the HealthCare.gov platform for the 2020 coverage year, CMS reported Dec. 12.
That brings the cumulative count for the 2020 open enrollment to almost 3.9 million plans through 6 weeks, compared with over 4.1 million selections last year for 2019 coverage, CMS said. If recent history is any indication, though, the cumulative total for 2020 can be expected to approximately double in the final week, as has occurred in the previous 2 years.
Last year, the cumulative total went from 4.1 million after 6 weeks to a final tally of 8.4 million after 7 weeks, and in 2017 it rose from 4.7 million through 6 weeks to a season-ending 8.8 million. Comparisons with seasons before that are not as relevant, because the open-enrollment period was about twice as long, extending through the end of January.
The 2020 open enrollment started Nov. 1 and will end Dec. 15, and week 7 actually ends Dec. 14, so there will be a 1-day week 8 after that.
HealthCare.gov just had its busiest week of the 2020 open enrollment season, but the plan count for all consumers continues to run below last year’s total through 6 weeks, according to the Centers for Medicare & Medicaid Services.
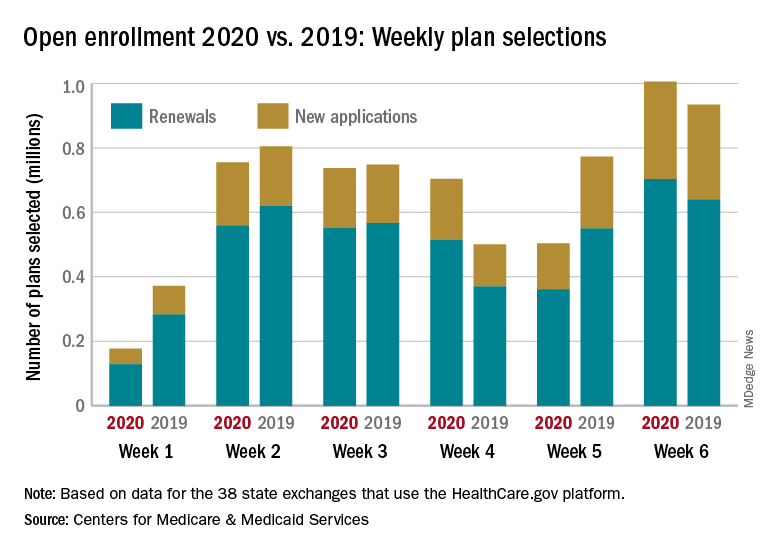
Just over 1 million plans – 302,000 new consumers and 703,000 renewals – were selected during the week of Dec. 1-7, eclipsing the season high of 755,000 from week 2 of open enrollment for the 38 states using the HealthCare.gov platform for the 2020 coverage year, CMS reported Dec. 12.
That brings the cumulative count for the 2020 open enrollment to almost 3.9 million plans through 6 weeks, compared with over 4.1 million selections last year for 2019 coverage, CMS said. If recent history is any indication, though, the cumulative total for 2020 can be expected to approximately double in the final week, as has occurred in the previous 2 years.
Last year, the cumulative total went from 4.1 million after 6 weeks to a final tally of 8.4 million after 7 weeks, and in 2017 it rose from 4.7 million through 6 weeks to a season-ending 8.8 million. Comparisons with seasons before that are not as relevant, because the open-enrollment period was about twice as long, extending through the end of January.
The 2020 open enrollment started Nov. 1 and will end Dec. 15, and week 7 actually ends Dec. 14, so there will be a 1-day week 8 after that.
HealthCare.gov just had its busiest week of the 2020 open enrollment season, but the plan count for all consumers continues to run below last year’s total through 6 weeks, according to the Centers for Medicare & Medicaid Services.
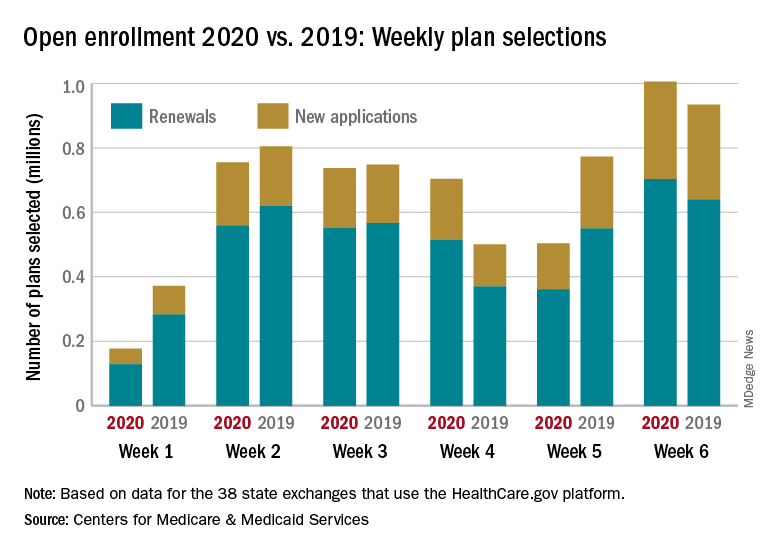
Just over 1 million plans – 302,000 new consumers and 703,000 renewals – were selected during the week of Dec. 1-7, eclipsing the season high of 755,000 from week 2 of open enrollment for the 38 states using the HealthCare.gov platform for the 2020 coverage year, CMS reported Dec. 12.
That brings the cumulative count for the 2020 open enrollment to almost 3.9 million plans through 6 weeks, compared with over 4.1 million selections last year for 2019 coverage, CMS said. If recent history is any indication, though, the cumulative total for 2020 can be expected to approximately double in the final week, as has occurred in the previous 2 years.
Last year, the cumulative total went from 4.1 million after 6 weeks to a final tally of 8.4 million after 7 weeks, and in 2017 it rose from 4.7 million through 6 weeks to a season-ending 8.8 million. Comparisons with seasons before that are not as relevant, because the open-enrollment period was about twice as long, extending through the end of January.
The 2020 open enrollment started Nov. 1 and will end Dec. 15, and week 7 actually ends Dec. 14, so there will be a 1-day week 8 after that.