User login
Write an exercise Rx to improve patients' cardiorespiratory fitness
It is well-known that per capita health care spending in the United States is more than twice the average in other developed countries1; nevertheless, the overall health care ranking of the US is near the bottom compared to other countries in this group.2 Much of the reason for this poor relative showing lies in the fact that the US has employed a somewhat traditional fee-for-service health care model that does not incentivize efforts to promote health and wellness or prevent chronic disease. The paradigm of promoting physical activity for its disease-preventing and treatment benefits has not been well-integrated in the US health care system.
In this article, we endeavor to provide better understanding of the barriers that keep family physicians from routinely promoting physical activity in clinical practice; define tools and resources that can be used in the clinical setting to promote physical activity; and delineate areas for future work.
Glaring hole in US physical activity education
Many primary care physicians feel underprepared to prescribe or motivate patients to exercise. The reason for that lack of preparedness likely relates to a medical education system that does not spend time preparing physicians to perform this critical task. A study showed that, on average, medical schools require only 8 hours of physical activity education in their curriculum during the 4 years of schooling.3 Likewise, the average primary care residency program offers only 3 hours of didactic training on physical activity, nutrition, and obesity.4 The problem extends to sports medicine fellowship training, in which a 2019 survey showed that 63% of fellows were never taught how to write an exercise prescription in their training program.5
Without education on physical activity, medical students, residents, and fellows are woefully underprepared to realize the therapeutic value of physical activity in patient care, comprehend current physical activity guidelines, appropriately motivate patients to engage in exercise, and competently discuss exercise prescriptions in different disease states. Throughout their training, it is imperative for medical professionals to be educated on the social determinants of health, which include the conditions in which people live, work, and play. These environmental variables can contribute to health inequities that create additional barriers to improvement in physical fitness.6
National guidelines on physical activity
The 2018 National Physical Activity Guidelines detail recommendations for children, adolescents, adults, and special populations.7 The guidelines define physical activity as bodily movement produced by skeletal muscles that result in energy expenditure above resting baseline levels, and includes all types, intensities, and domains of activity. Exercise is a subset of physical activity characterized as planned, structured, repetitive, and designed to improve or maintain physical fitness, physical performance, or health.
Highlights from the 2018 guidelines include7:
- Preschool-aged children (3 to 5 years of age) should be physically active throughout the day, with as much as 3 hours per day of physical activity of all intensities—light, moderate, and vigorous.
- Older children and adolescents (6 to 17 years) should accumulate 60 minutes per day of moderate-to-vigorous physical activity, including aerobic, muscle-strengthening, and bone-strengthening activities.
- Adults of all ages should achieve approximately 150 to 300 minutes of moderate or 75 to 150 minutes of vigorous physical activity (or an equivalent combination) per week, along with at least 2 days per week of muscle-strengthening activities. Other types of physical activity include flexibility, balance, bone-strengthening, and mind–body exercises.
3-step framework for enhancing physical activity counseling
Merely knowing that physical activity is healthy is not enough, during a patient encounter, to increase the level of physical activity. Therefore, it is imperative to learn and adopt a framework that has proved to yield successful outcomes. The Screening, Brief Intervention, and Referral to Treatment (SBIRT) framework, which has predominantly been used to change patient behavior related to alcohol and substance use, is now being utilized by some providers to promote physical activity.8 We apply the SBIRT approach in this article, although research is lacking on its clinical utility and outcome measures.
Continue to: SBIRT
SBIRT: Screening
An office visit provides an opportunity to understand a patient’s level of physical activity. Often, understanding a patient’s baseline level of activity is only asked during a thorough social history, which might not be performed during patient encounters. As physical activity is the primary determinant of cardiorespiratory fitness (CRF), some health care systems have begun delineating physical activity levels as a vital sign to ensure that the assessment of physical activity is a standard part of every clinical encounter. At a minimum, this serves as a prompt and provides an opportunity to start a conversation around improving physical activity levels when guidelines are not being met.
The exercise vital sign. Assessment and documentation of physical activity in the electronic health record are not yet standardized; however, Kaiser Permanente health plans have implemented the exercise vital sign, or EVS, in its HealthConnect (Epic Systems) electronic health record. The EVS incorporates information about a patient’s:
- days per week of moderate-to-strenuous exercise (eg, a brisk walk)
- minutes per day, on average, of exercise at this level.
The physical activity vital sign. Intermountain Healthcare implemented the physical activity vital sign, or PAVS, in its iCentra (Cerner Corp.) electronic health record. The 3-question PAVS assessment asks:
- On average, how many days of the week do you perform physical activity or exercise?
- On average, how many total minutes of physical activity or exercise do you perform on those days?
- How would you describe the intensity of your physical activity or exercise: Light (ie, a casual walk)? Moderate (a brisk walk)? Or vigorous (jogging)?
PAVS includes a fourth data point: The physician–user documents whether the patient was counseled to start, increase, maintain, or modify physical activity or exercise.
EVS and the PAVS have demonstrated validity.9-11
Continue to: Cardiorespiratory fitness as a vital sign
Cardiorespiratory fitness as a vital sign. In 2016, the American Heart Association (AHA) asserted the importance of assessing CRF as a clinical vital sign.12 CRF is commonly expressed as maximal oxygen consumption (VO2max = O2 mL/kg/min) and measured through cardiopulmonary exercise testing (CPET), considered the gold standard by combining conventional graded exercise testing with ventilatory expired gas analysis. CPET is more objective and precise than equations estimating CRF that are derived from peak work rate. AHA recommended that efforts to improve CRF should become standard in clinical encounters, explaining that even a small increase in CRF (eg, 1 or 2 metabolic equivalentsa [METs]) is associated with a considerably (10% to 30%) lower rate of adverse cardiovascular events.12
De Souza de Silva and colleagues revealed an association between each 1-MET increase in CRF and per-person annual health care cost savings (adjusted for age and presence of cardiovascular disease) of $3272 (normal-weight patients), $4252 (overweight), and $6103 (obese).13 In its 2016 scientific statement on CRF as a vital sign, AHA listed several methods of estimating CRF and concluded that, although CPET involves a higher level of training, proficiency, equipment, and, therefore, cost, the independent and additive information obtained justifies its use in many patients.12
CASE
Mary Q, 68 years of age, presents for an annual well-woman examination. Body mass index is 32; resting heart rate (HR), 73 bpm; and blood pressure, 126/74 mm Hg. She reports being inactive, except for light walking every day with her dog around the neighborhood, which takes them approximately 15 minutes. She denies any history or signs and symptoms of cardiovascular, metabolic, or renal disease.
You consider 3 questions before taking next steps regarding increasing Ms. Q’s activity level:
- What is her PAVS?
- Does she need medical clearance before starting an exercise program?
- What would an evidence-based cardiovascular exercise prescription for Ms. Q look like?
SBIRT: Brief intervention
When a patient does not meet the recommended level of physical activity, you have an opportunity to deliver a brief intervention. To do this effectively, you must have adequate understanding of the patient’s receptivity for change. The transtheoretical, or Stages of Change, model proposes that a person typically goes through 5 stages of growth—pre-contemplation, contemplation, preparation, action, and maintenance—in the process of lifestyle modification. This model highlights the different approaches to exercise adoption and maintenance that need to be taken, based on a given patient’s stage at the moment.
Continue to: Using this framework...
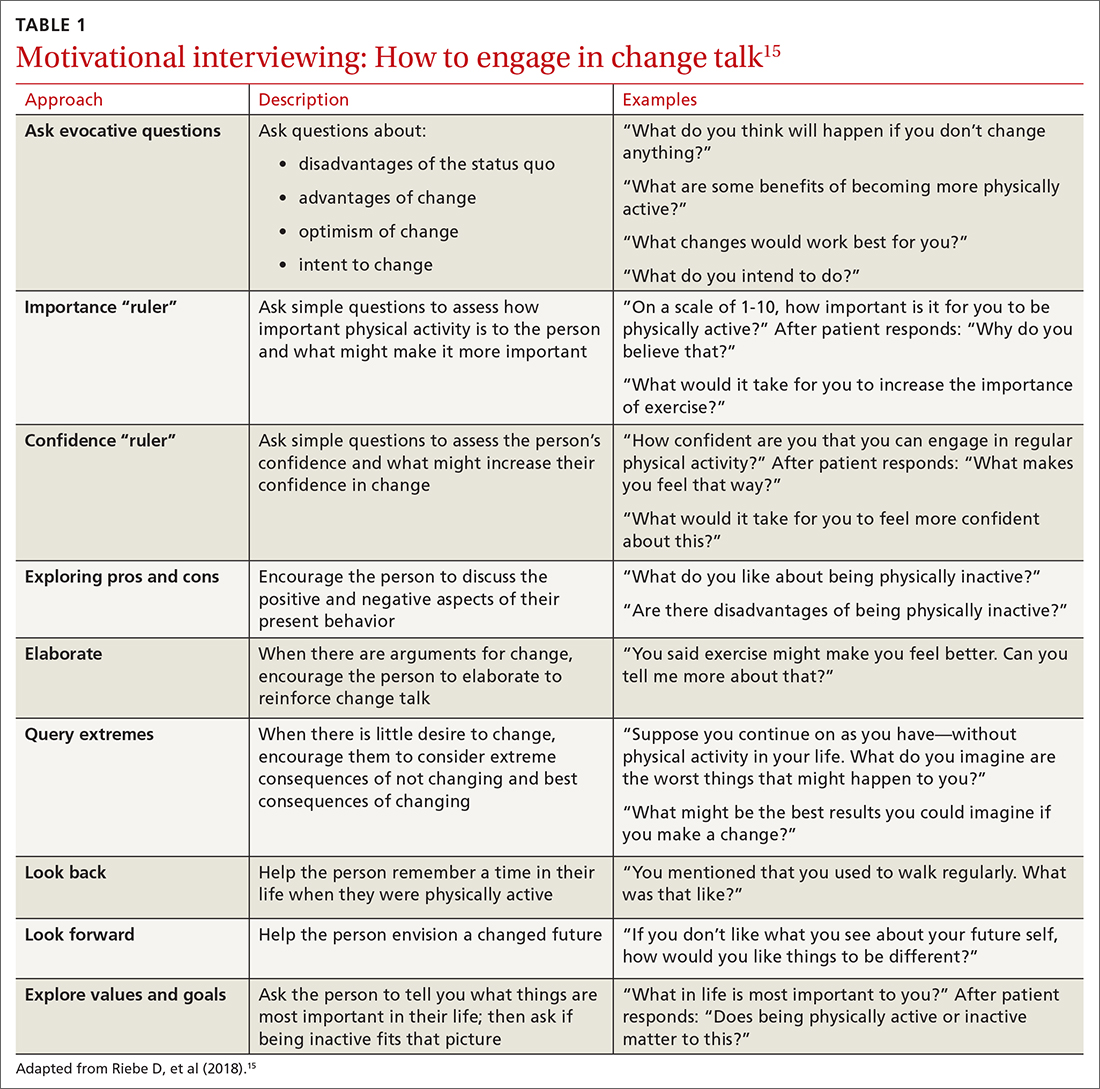
Using this framework, you can help patients realize intrinsic motivation that can facilitate progression through each stage, utilizing techniques such as motivational interviewing—so-called change talk—to increase self-efficacy.14TABLE 115 provides examples of motivational interviewing techniques that can be used during a patient encounter to improve health behaviors, such as physical activity.
Writing the exercise prescription
A patient who wants to increase their level of physical activity should be offered a formal exercise prescription, which has been shown to increase the level of physical activity, particularly in older patients. In fact, a study conducted in Spain in the practices of family physicians found that older patients who received a physical activity prescription increased their activity by 131 minutes per week; and compared to control patients, they doubled the minutes per week devoted to moderate or vigorous physical activity.16
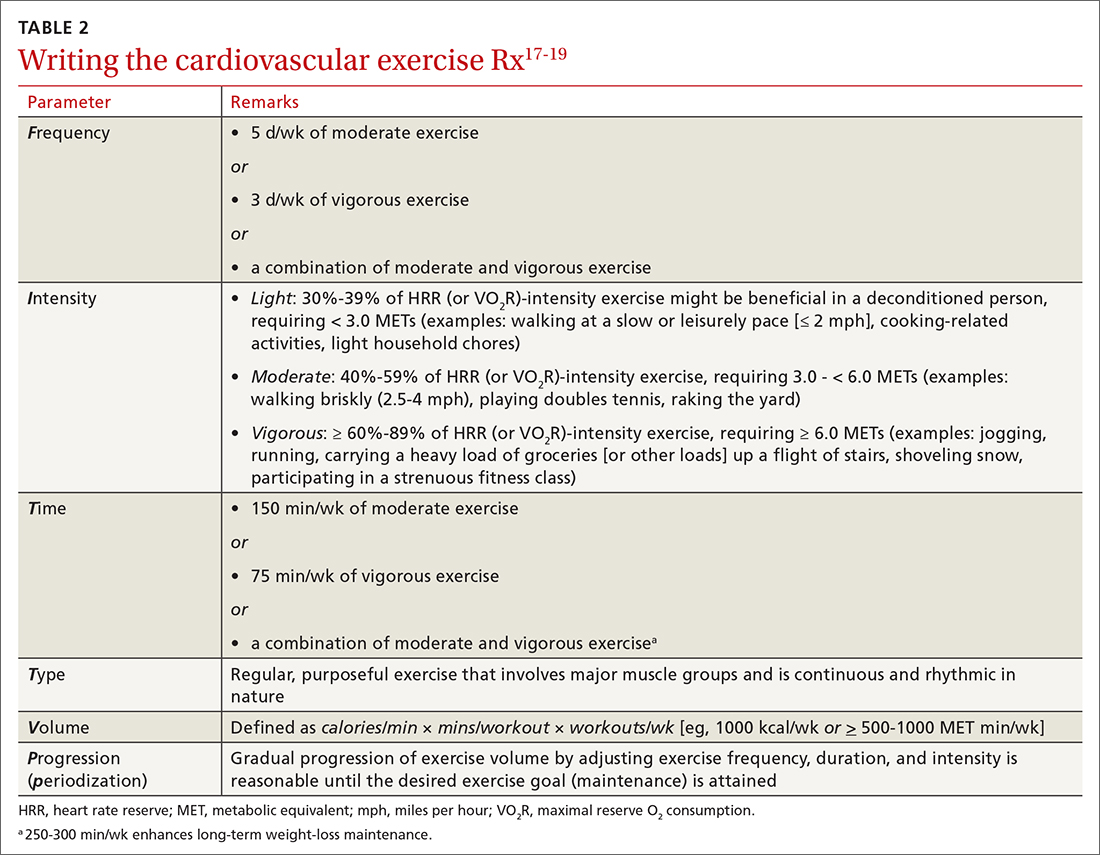
FITT-VP. The basics of a cardiovascular exercise prescription can be found in the FITT-VP (Frequency, Intensity, Time, Type, Volume, and [monitoring of] Progression) framework (TABLE 217-19). For most patients, this model includes 3 to 5 days per week of moderate-to-vigorous physical activity for 30 to 60 minutes per session. For patients with established chronic disease, physical activity provides health benefits but might require modification. Disease-specific patient handouts for exercise can be downloaded, at no cost, through the American College of Sports Medicine (ACSM) “Exercise Is Medicine” program, which can be found at: www.exerciseismedicine.org/support_page.php/rx-for-health-series.
Determining intensity level. Although CPET is the gold standard for determining a patient’s target intensity level, such a test might be impracticable for a given patient. Surrogate markers of target intensity level can be obtained by measuring maximum HR (HRmax), using a well-known equation20:
HRmax = 220 – age
which is then multiplied by intensity range:
- light: 30%-39%
- moderate: 40%-59%
- vigorous: 60%-89%
or, more preferably, by calculating the HR training zone while accounting for HR at rest (HRrest). This is accomplished by calculating the HR reserve (HRR) (ie, HRR = HRmax – HRrest) and then calculating the target heart rate (THR)21:
THR = [HRR × %intensity] + HRrest
Continue to: The THR calculation...
The THR calculation is performed twice, once with a lower %intensity and again with a higher %intensity to develop a training zone based on HRR.
The HRR equation is more accurate than calculating HRmax from 220 – age, because HRR accounts for resting HR, which is often lower in people who are better conditioned.
Another method of calculating intensity for patients who are beginning a physical activity program is the rating of perceived exertion (RPE), which is graded on a scale of 6 to 20: Moderate exercise correlates with an RPE of 12 to 13 (“somewhat hard”); vigorous exercise correlates with an RPE of 14 to 16 (“hard”). By adding a zero to the rating on the RPE scale, the corresponding HR in a healthy adult can be estimated when they are performing an activity at that perceived intensity.22 Moderate exercise therefore correlates with a HR of 120 and 130 bpm.
The so-called talk test can also guide exercise intensity: Light-intensity activity correlates with an ability to sing; moderate-intensity physical activity likely allows the patient to still hold a conversation; and vigorous-intensity activity correlates with an inability to carry on a conversation while exercising.
An exercise prescription should be accompanied by a patient-derived goal, which can be reassessed during a follow-up visit. So-called SMART goals (Specific, Measurable, Achievable, Relevant, and Time-bound) are tools to help patients set personalized and realistic expectations for physical activity. Meeting the goal of approximately 150 to 300 minutes of moderate or 75 to 150 minutes of vigorous physical activity (or an equivalent combination) per week is ideal, but a patient needs to start where they are, at the moment, and gradually increase activity by setting what for them are realistic and sustainable goals.
Continue to: CASE
CASE
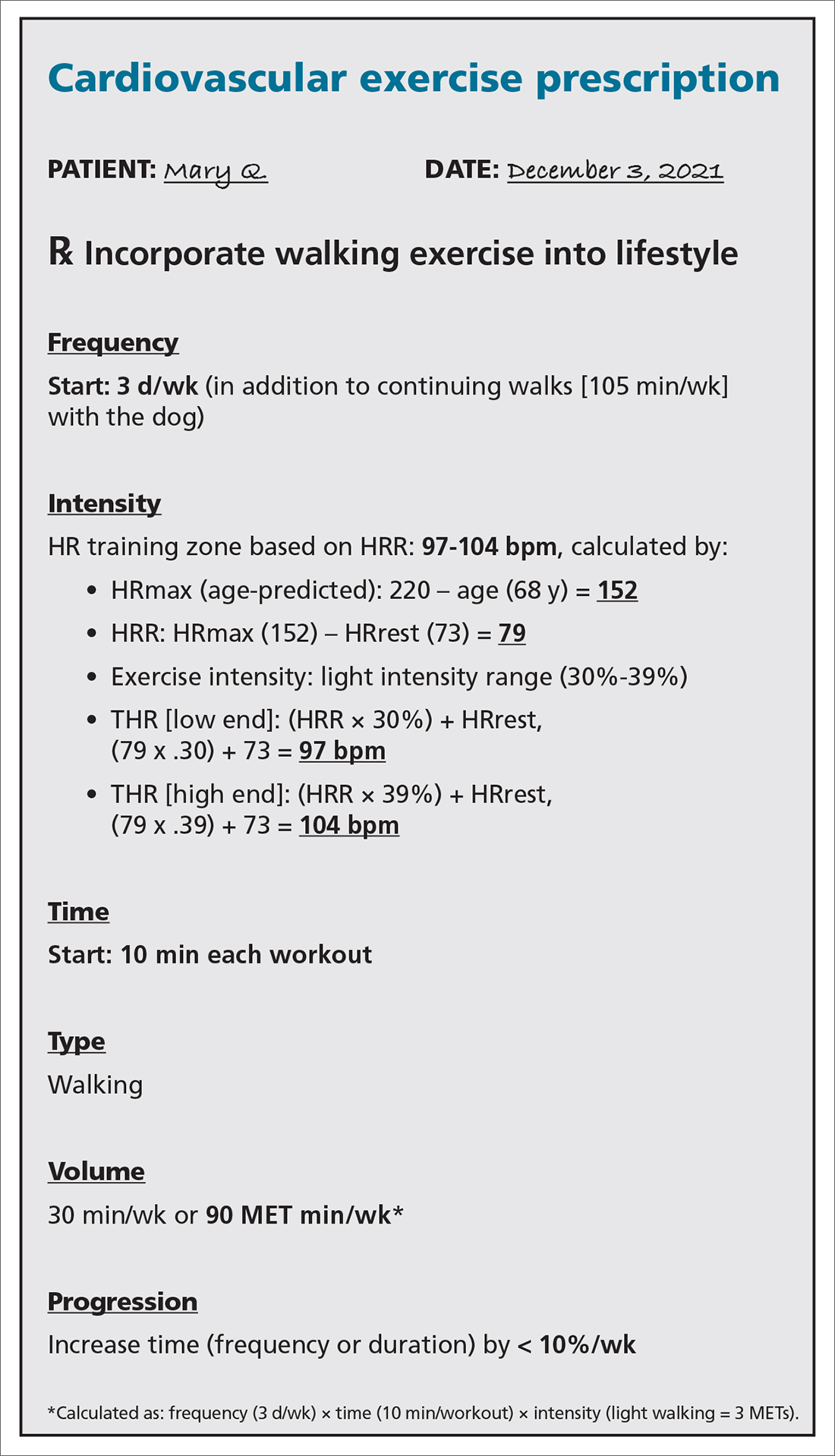
With a PAVS of 105 minutes (ie, 15 minutes per day × 7 days) of weekly light-to-moderate exercise walking her dog, Ms. Q does not satisfy current physical activity guidelines. She needs an exercise prescription to incorporate into her lifestyle (see “Cardiovascular exercise prescription,” at left).
First, based on ACSM pre-participation guidelines, Ms. Q does not need medical clearance before initiating light-to-moderate exercise and gradually progressing to vigorous-intensity exercise.
Second, in addition to walking the dog for 105 minutes a week, you:
- advise her to start walking for 10 minutes, 3 times per week, at a pace that keeps her HR at 97-104 bpm.
- encourage her to gradually increase the frequency or duration of her walks by no more than 10% per week.
SBIRT: Referral for treatment
When referring a patient to a fitness program or professional, it is essential to consider their preferences, resources, and environment.23 Community fitness partners are often an excellent referral option for a patient seeking guidance or structure for their exercise program. Using the ACSM ProFinder service, (www.acsm.org/get-stay-certified/find-a-pro) you can search for exercise professionals who have achieved the College’s Gold Standard credential.
Gym memberships or fitness programs might be part of the extra coverage offered by Medicare Advantage Plans, other Medicare health plans, or Medicare Supplement Insurance (Medigap) plans.24
Continue to: CASE
CASE
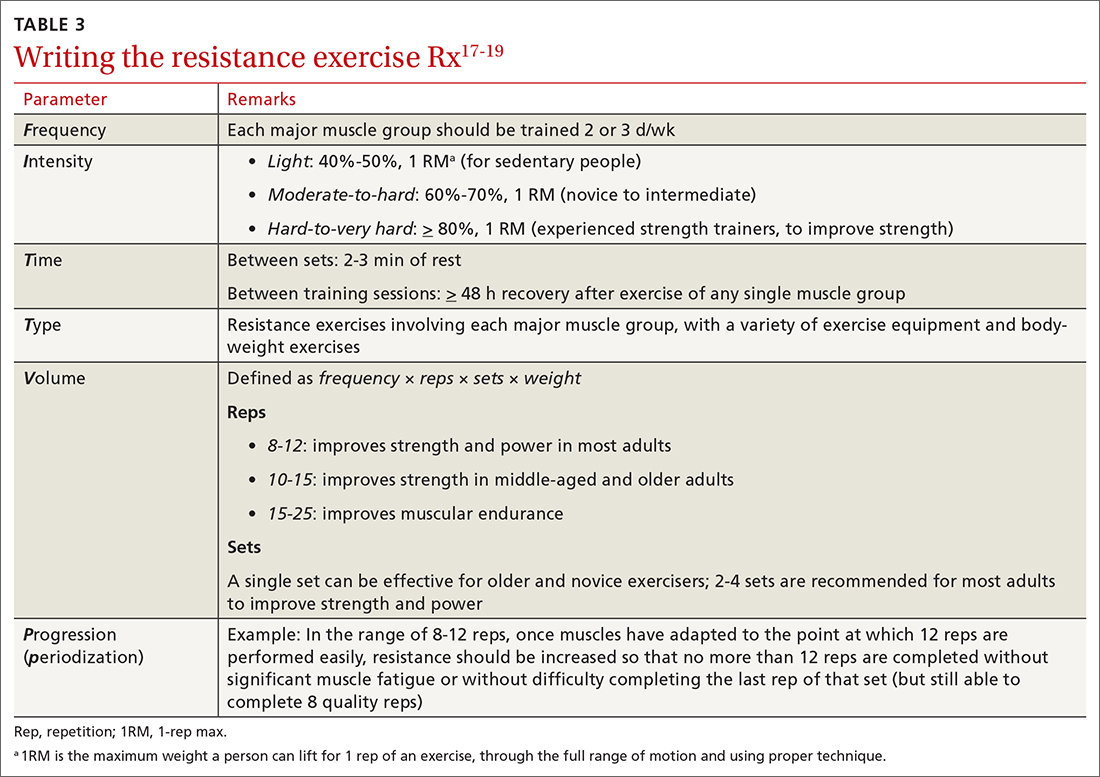
After providing Ms. Q with her exercise prescription, you refer her to a local gym that participates in the Silver Sneakers fitness and wellness program (for adults ≥ 65 years of age in eligible Medicare plans) to determine whether she qualifies to begin resistance and flexibility training, for which you will write a second exercise prescription (TABLE 317-19).
Pre-participation screening
Updated 2015 ACSM exercise pre-participation health screening recommendations attempt to decrease possible barriers to people who are becoming more physically active, by minimizing unnecessary referral to health care providers before they change their level of physical activity. ACSM recommendations on exercise clearance include this guidance25:
- For a patient who is asymptomatic and already physically active—regardless of whether they have known cardiovascular, metabolic, or renal disease—medical clearance is unnecessary for moderate-intensity exercise.
- Any patient who has been physically active and asymptomatic but who becomes symptomatic during exercise should immediately discontinue such activity and undergo medical evaluation.
- For a patient who is inactive, asymptomatic, and who does not have known cardiovascular, metabolic, or renal disease, medical clearance for light- or moderate-intensity exercise is unnecessary.
- For inactive, asymptomatic patients who have known cardiovascular, metabolic, or renal disease, medical clearance is recommended.
Digital health
Smartwatches and health apps (eg, CardioCoach, Fitbit, Garmin Connect, Nike Training Club, Strava, and Training Peaks) can provide workouts and offer patients the ability to collect information and even connect with other users through social media platforms. This information can be synced to Apple Health platforms for iPhones (www.apple.com/ios/health/) or through Google Fit (www.google.com/fit/) on Android devices. Primary care physicians who become familiar with health apps might find them useful for select patients who want to use technology to improve their physical activity level.
However, data on the value of using digital apps for increasing physical activity, in relation to their cost, are limited. Additional research is needed to assess their validity.
Billing and coding
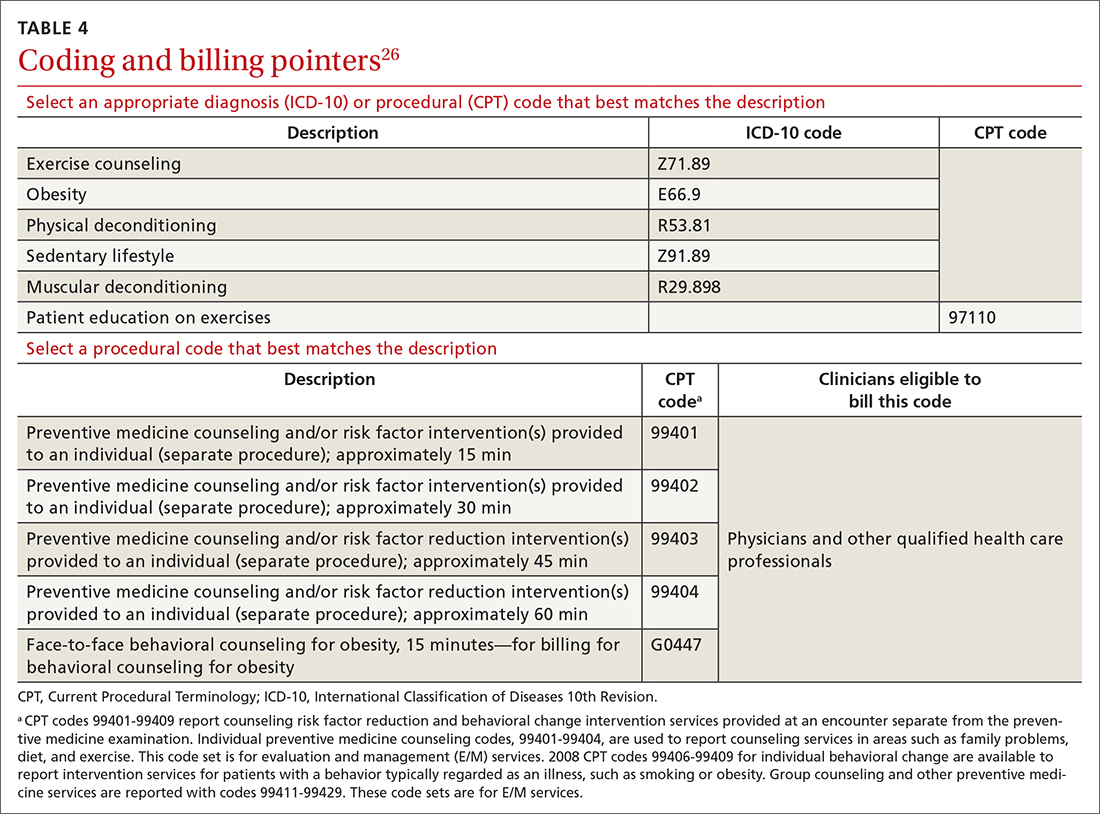
For most patients, the physical activity assessment, prescription, and referral are performed in the context of treating another condition (eg, hypertension, type 2 diabetes, obesity, depression) or during a preventive health examination, and are typically covered without additional charge to the patient. An evaluation and management visit for an established patient could be used to bill if > 50% of the office visit was spent face-to-face with a physician, with patient counseling and coordination of care.
Continue to: Physicians and physical therapists...
Physicians and physical therapists can use the therapeutic exercise code (Current Procedural Terminology code 97110) when teaching patients exercises to develop muscle strength and endurance, joint range of motion, and flexibility26 (TABLE 426).
Conclusion
Physical activity and CRF are strong predictors of premature mortality, even compared to other risk factors, such as cigarette smoking, hypertension, hypercholesterolemia, and type 2 diabetes.27 Brief physical activity assessment and counseling is an efficient, effective, and cost-effective means to increase physical activity, and presents a unique opportunity for you to encourage lifestyle-based strategies for reducing cardiovascular risk.28
However, it is essential to meet patients where they are before trying to have them progress; it is therefore imperative to assess the individual patient’s level of activity using PAVS. With that information in hand, you can personalize physical activity advice; determine readiness for change and potential barriers for change; assist the patient in setting SMART goals; and arrange follow-up to assess adherence to the exercise prescription. Encourage the patient to call their health insurance plan to determine whether a gym membership or fitness program is covered.
Research is needed to evaluate the value of using digital apps, in light of their cost, to increase physical activity and improve CRF in a clinical setting. Prospective trials should be initiated to determine how routine implementation of CRF assessment in primary care alters the trajectory of clinical care. It is hoped that future research will answer the question: Would such an approach improve clinical outcomes and reduce health care expenditures?12
a Defined as O2 consumed while sitting at rest; equivalent to 3.5 mL of O2 × kg of body weight × min.
CORRESPONDENCE
Matthew Kampert, DO, MS, Sports Medicine, 5555 Transportation Boulevard, Cleveland, OH 44125; kamperm@ccf.org
1. Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries. JAMA. 2018;319:1024-1039. doi: 10.1001/jama.2018.1150
2. Tikkanen R, Abrams MK. U.S. health care from a global perspective, 2019: higher spending, worse outcomes? The Commonwealth Fund Website. January 30, 2020. Accessed November 16, 2021. www.commonwealthfund.org/publications/issue-briefs/2020/jan/us-health-care-global-perspective-2019
3. Stoutenberg M, Stasi S, Stamatakis E, et al. Physical activity training in US medical schools: preparing future physicians to engage in primary prevention. Phys Sportsmed. 2015;43:388-394. doi: 10.1080/00913847.2015.1084868
4. Antognoli EL, Seeholzer EL, Gullett H, et al. Primary care resident training for obesity, nutrition, and physical activity counseling: a mixed-methods study. Health Promot Pract. 2017;18:672-680. doi: 10.1177/1524839916658025
5. Asif IM, Drezner JA. Sports and exercise medicine education in the USA: call to action. Br J Sports Med. 2020;54:195-196. doi: 10.1136/bjsports-2019-101104
6. Douglas JA, Briones MD, Bauer EZ, et al. Social and environmental determinants of physical activity in urban parks: testing a neighborhood disorder model. Prev Med. 2018;109:119-124. doi: 10.1016/j.ypmed.2018.01.013
7. 2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC: US Department of Health & Human Services; 2018. Accessed November 15, 2021. https://health.gov/sites/default/files/2019-09/PAG_Advisory_Committee_Report.pdf
8. Avis JL, Cave AL, Donaldson S, et al. Working with parents to prevent childhood obesity: protocol for a primary care-based ehealth study. JMIR Res Protoc. 2015;4:e35. doi:10.2196/resprot.4147
9. Ball TJ, Joy EA, Gren LH, et al. Concurrent validity of a self-reported physical activity ‘vital sign’ questionnaire with adult primary care patients. Prev Chronic Dis. 2016;13:e16. doi: 10.5888/pcd13.150228
10. Ball TJ, Joy EA, Gren LH, et al. Predictive validity of an adult physical activity “vital sign” recorded in electronic health records. J Phys Act Health. 2016;13:403-408. doi: 10.1123/jpah.2015-0210
11. Coleman KJ, Ngor E, Reynolds K, et al. Initial validation of an exercise “vital sign” in electronic medical records. Med Sci Sports Exerc. 2012;44:2071-2076. doi: 10.1249/MSS.0b013e3182630ec1
12. Ross R, Blair SN, Arena R, et al; ; ; ; ; ; . Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation. 2016;134:e653-e699. doi: 10.1161/CIR.0000000000000461
13. de Souza de Silva CG, Kokkinos PP, Doom R, et al. Association between cardiorespiratory fitness, obesity, and health care costs: The Veterans Exercise Testing Study. Int J Obes (Lond). 2019;43:2225-2232. doi: 10.1038/s41366-018-0257-0
14. Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38-48. doi: 10.4278/0890-1171-12.1.38
15. Riebe D, Ehrman JK, Liguori G, et al. Methods for evoking change talk. In: ACSM’s Guidelines for Exercise Testing and Prescription. 10th ed. Wolters Kluwer; 2018.
16. Grandes G, Sanchez A, Sanchez-Pinilla RO, et al. Effectiveness of physical activity advice and prescription by physicians in routine primary care: a cluster randomized trial. Arch Intern Med. 2009;169:694-701. doi: 10.1001/archinternmed.2009.23
17. McNeill LH, Kreuter MW, Subramanian SV. Social environment and physical activity: a review of concepts and evidence. Soc Sci Med. 2006;63:1011-1022. doi: 10.1016/j.socscimed.2006.03.012
18. Garber CE, Blissmer BE, Deschenes MR, et al; American College of Sports Medicine. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Position stand. Med Sci Sport Exerc. 2011;43:1334-1359. doi: 10.1249/MSS.0b013e318213fefb
19. Donnelly JE, Blair SN, Jakicic JM, et al; American College of Sports Medicine. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Position stand. Med Sci Sport Exerc. 2009;41:459-471. doi: 10.1249/MSS.0b013e3181949333
20. Fox SM 3rd, Naughton JP, Haskell WL. Physical activity and the prevention of coronary heart disease. Ann Clin Res. 1971;3:404-432.
21. Karvonen MJ, Kentala E, Mustala O. The effects of training on heart rate; a longitudinal study. Ann Med Exp Biol Fenn. 1957;35:307-315.
22. The Borg RPE scale. In: Borg G. Borg’s Perceived Exertion and Pain Scales. Human Kinetics; 1998:29-38.
23. Ratamess NA, Alvar BA, Evetoch TK, et al; American College of Sports Medicine. Progression models in resistance training for healthy adults. Position stand. Med Sci Sport Exerc. 2009;41:687-708. doi: 10.1249/MSS.0b013e3181915670
24. Gym memberships & fitness programs. Medicare.gov. Baltimore, MD: US Centers for Medicare and Medicaid Services. Accessed November 16, 2021. www.medicare.gov/coverage/gym-memberships-fitness-programs
25. Riebe D, Franklin BA, Thompson PD, et al. Updating ACSM’s recommendations for exercise preparticipation health screening. Med Sci Sports Exerc. 2015;47:2473-2479. doi: 10.1249/MSS.0000000000000664
26. Physical Activity Related Current Procedural Terminology (CPT®) Codes. Physical Activity Alliance website. Accessed November 16, 2021. https://paamovewithus.org/wp-content/uploads/2020/11/PAA-Physical-Activity-CPT-Codes-Nov-2020-AMA-Approved-Final-1.pdf
27. Blair SN. Physical inactivity: the biggest public health problem of the 21st century Br J Sports Med. 2009;43:1-2.
28. Vuori IM, Lavie CJ, Blair SN. Physical activity promotion in the health care system. Mayo Clin Proc. 2013;88:1446-1461. doi: 10.1016/j.mayocp.2013.08.020
It is well-known that per capita health care spending in the United States is more than twice the average in other developed countries1; nevertheless, the overall health care ranking of the US is near the bottom compared to other countries in this group.2 Much of the reason for this poor relative showing lies in the fact that the US has employed a somewhat traditional fee-for-service health care model that does not incentivize efforts to promote health and wellness or prevent chronic disease. The paradigm of promoting physical activity for its disease-preventing and treatment benefits has not been well-integrated in the US health care system.
In this article, we endeavor to provide better understanding of the barriers that keep family physicians from routinely promoting physical activity in clinical practice; define tools and resources that can be used in the clinical setting to promote physical activity; and delineate areas for future work.
Glaring hole in US physical activity education
Many primary care physicians feel underprepared to prescribe or motivate patients to exercise. The reason for that lack of preparedness likely relates to a medical education system that does not spend time preparing physicians to perform this critical task. A study showed that, on average, medical schools require only 8 hours of physical activity education in their curriculum during the 4 years of schooling.3 Likewise, the average primary care residency program offers only 3 hours of didactic training on physical activity, nutrition, and obesity.4 The problem extends to sports medicine fellowship training, in which a 2019 survey showed that 63% of fellows were never taught how to write an exercise prescription in their training program.5
Without education on physical activity, medical students, residents, and fellows are woefully underprepared to realize the therapeutic value of physical activity in patient care, comprehend current physical activity guidelines, appropriately motivate patients to engage in exercise, and competently discuss exercise prescriptions in different disease states. Throughout their training, it is imperative for medical professionals to be educated on the social determinants of health, which include the conditions in which people live, work, and play. These environmental variables can contribute to health inequities that create additional barriers to improvement in physical fitness.6
National guidelines on physical activity
The 2018 National Physical Activity Guidelines detail recommendations for children, adolescents, adults, and special populations.7 The guidelines define physical activity as bodily movement produced by skeletal muscles that result in energy expenditure above resting baseline levels, and includes all types, intensities, and domains of activity. Exercise is a subset of physical activity characterized as planned, structured, repetitive, and designed to improve or maintain physical fitness, physical performance, or health.
Highlights from the 2018 guidelines include7:
- Preschool-aged children (3 to 5 years of age) should be physically active throughout the day, with as much as 3 hours per day of physical activity of all intensities—light, moderate, and vigorous.
- Older children and adolescents (6 to 17 years) should accumulate 60 minutes per day of moderate-to-vigorous physical activity, including aerobic, muscle-strengthening, and bone-strengthening activities.
- Adults of all ages should achieve approximately 150 to 300 minutes of moderate or 75 to 150 minutes of vigorous physical activity (or an equivalent combination) per week, along with at least 2 days per week of muscle-strengthening activities. Other types of physical activity include flexibility, balance, bone-strengthening, and mind–body exercises.
3-step framework for enhancing physical activity counseling
Merely knowing that physical activity is healthy is not enough, during a patient encounter, to increase the level of physical activity. Therefore, it is imperative to learn and adopt a framework that has proved to yield successful outcomes. The Screening, Brief Intervention, and Referral to Treatment (SBIRT) framework, which has predominantly been used to change patient behavior related to alcohol and substance use, is now being utilized by some providers to promote physical activity.8 We apply the SBIRT approach in this article, although research is lacking on its clinical utility and outcome measures.
Continue to: SBIRT
SBIRT: Screening
An office visit provides an opportunity to understand a patient’s level of physical activity. Often, understanding a patient’s baseline level of activity is only asked during a thorough social history, which might not be performed during patient encounters. As physical activity is the primary determinant of cardiorespiratory fitness (CRF), some health care systems have begun delineating physical activity levels as a vital sign to ensure that the assessment of physical activity is a standard part of every clinical encounter. At a minimum, this serves as a prompt and provides an opportunity to start a conversation around improving physical activity levels when guidelines are not being met.
The exercise vital sign. Assessment and documentation of physical activity in the electronic health record are not yet standardized; however, Kaiser Permanente health plans have implemented the exercise vital sign, or EVS, in its HealthConnect (Epic Systems) electronic health record. The EVS incorporates information about a patient’s:
- days per week of moderate-to-strenuous exercise (eg, a brisk walk)
- minutes per day, on average, of exercise at this level.
The physical activity vital sign. Intermountain Healthcare implemented the physical activity vital sign, or PAVS, in its iCentra (Cerner Corp.) electronic health record. The 3-question PAVS assessment asks:
- On average, how many days of the week do you perform physical activity or exercise?
- On average, how many total minutes of physical activity or exercise do you perform on those days?
- How would you describe the intensity of your physical activity or exercise: Light (ie, a casual walk)? Moderate (a brisk walk)? Or vigorous (jogging)?
PAVS includes a fourth data point: The physician–user documents whether the patient was counseled to start, increase, maintain, or modify physical activity or exercise.
EVS and the PAVS have demonstrated validity.9-11
Continue to: Cardiorespiratory fitness as a vital sign
Cardiorespiratory fitness as a vital sign. In 2016, the American Heart Association (AHA) asserted the importance of assessing CRF as a clinical vital sign.12 CRF is commonly expressed as maximal oxygen consumption (VO2max = O2 mL/kg/min) and measured through cardiopulmonary exercise testing (CPET), considered the gold standard by combining conventional graded exercise testing with ventilatory expired gas analysis. CPET is more objective and precise than equations estimating CRF that are derived from peak work rate. AHA recommended that efforts to improve CRF should become standard in clinical encounters, explaining that even a small increase in CRF (eg, 1 or 2 metabolic equivalentsa [METs]) is associated with a considerably (10% to 30%) lower rate of adverse cardiovascular events.12
De Souza de Silva and colleagues revealed an association between each 1-MET increase in CRF and per-person annual health care cost savings (adjusted for age and presence of cardiovascular disease) of $3272 (normal-weight patients), $4252 (overweight), and $6103 (obese).13 In its 2016 scientific statement on CRF as a vital sign, AHA listed several methods of estimating CRF and concluded that, although CPET involves a higher level of training, proficiency, equipment, and, therefore, cost, the independent and additive information obtained justifies its use in many patients.12
CASE
Mary Q, 68 years of age, presents for an annual well-woman examination. Body mass index is 32; resting heart rate (HR), 73 bpm; and blood pressure, 126/74 mm Hg. She reports being inactive, except for light walking every day with her dog around the neighborhood, which takes them approximately 15 minutes. She denies any history or signs and symptoms of cardiovascular, metabolic, or renal disease.
You consider 3 questions before taking next steps regarding increasing Ms. Q’s activity level:
- What is her PAVS?
- Does she need medical clearance before starting an exercise program?
- What would an evidence-based cardiovascular exercise prescription for Ms. Q look like?
SBIRT: Brief intervention
When a patient does not meet the recommended level of physical activity, you have an opportunity to deliver a brief intervention. To do this effectively, you must have adequate understanding of the patient’s receptivity for change. The transtheoretical, or Stages of Change, model proposes that a person typically goes through 5 stages of growth—pre-contemplation, contemplation, preparation, action, and maintenance—in the process of lifestyle modification. This model highlights the different approaches to exercise adoption and maintenance that need to be taken, based on a given patient’s stage at the moment.
Continue to: Using this framework...
Using this framework, you can help patients realize intrinsic motivation that can facilitate progression through each stage, utilizing techniques such as motivational interviewing—so-called change talk—to increase self-efficacy.14TABLE 115 provides examples of motivational interviewing techniques that can be used during a patient encounter to improve health behaviors, such as physical activity.
Writing the exercise prescription
A patient who wants to increase their level of physical activity should be offered a formal exercise prescription, which has been shown to increase the level of physical activity, particularly in older patients. In fact, a study conducted in Spain in the practices of family physicians found that older patients who received a physical activity prescription increased their activity by 131 minutes per week; and compared to control patients, they doubled the minutes per week devoted to moderate or vigorous physical activity.16
FITT-VP. The basics of a cardiovascular exercise prescription can be found in the FITT-VP (Frequency, Intensity, Time, Type, Volume, and [monitoring of] Progression) framework (TABLE 217-19). For most patients, this model includes 3 to 5 days per week of moderate-to-vigorous physical activity for 30 to 60 minutes per session. For patients with established chronic disease, physical activity provides health benefits but might require modification. Disease-specific patient handouts for exercise can be downloaded, at no cost, through the American College of Sports Medicine (ACSM) “Exercise Is Medicine” program, which can be found at: www.exerciseismedicine.org/support_page.php/rx-for-health-series.
Determining intensity level. Although CPET is the gold standard for determining a patient’s target intensity level, such a test might be impracticable for a given patient. Surrogate markers of target intensity level can be obtained by measuring maximum HR (HRmax), using a well-known equation20:
HRmax = 220 – age
which is then multiplied by intensity range:
- light: 30%-39%
- moderate: 40%-59%
- vigorous: 60%-89%
or, more preferably, by calculating the HR training zone while accounting for HR at rest (HRrest). This is accomplished by calculating the HR reserve (HRR) (ie, HRR = HRmax – HRrest) and then calculating the target heart rate (THR)21:
THR = [HRR × %intensity] + HRrest
Continue to: The THR calculation...
The THR calculation is performed twice, once with a lower %intensity and again with a higher %intensity to develop a training zone based on HRR.
The HRR equation is more accurate than calculating HRmax from 220 – age, because HRR accounts for resting HR, which is often lower in people who are better conditioned.
Another method of calculating intensity for patients who are beginning a physical activity program is the rating of perceived exertion (RPE), which is graded on a scale of 6 to 20: Moderate exercise correlates with an RPE of 12 to 13 (“somewhat hard”); vigorous exercise correlates with an RPE of 14 to 16 (“hard”). By adding a zero to the rating on the RPE scale, the corresponding HR in a healthy adult can be estimated when they are performing an activity at that perceived intensity.22 Moderate exercise therefore correlates with a HR of 120 and 130 bpm.
The so-called talk test can also guide exercise intensity: Light-intensity activity correlates with an ability to sing; moderate-intensity physical activity likely allows the patient to still hold a conversation; and vigorous-intensity activity correlates with an inability to carry on a conversation while exercising.
An exercise prescription should be accompanied by a patient-derived goal, which can be reassessed during a follow-up visit. So-called SMART goals (Specific, Measurable, Achievable, Relevant, and Time-bound) are tools to help patients set personalized and realistic expectations for physical activity. Meeting the goal of approximately 150 to 300 minutes of moderate or 75 to 150 minutes of vigorous physical activity (or an equivalent combination) per week is ideal, but a patient needs to start where they are, at the moment, and gradually increase activity by setting what for them are realistic and sustainable goals.
Continue to: CASE
CASE
With a PAVS of 105 minutes (ie, 15 minutes per day × 7 days) of weekly light-to-moderate exercise walking her dog, Ms. Q does not satisfy current physical activity guidelines. She needs an exercise prescription to incorporate into her lifestyle (see “Cardiovascular exercise prescription,” at left).
First, based on ACSM pre-participation guidelines, Ms. Q does not need medical clearance before initiating light-to-moderate exercise and gradually progressing to vigorous-intensity exercise.
Second, in addition to walking the dog for 105 minutes a week, you:
- advise her to start walking for 10 minutes, 3 times per week, at a pace that keeps her HR at 97-104 bpm.
- encourage her to gradually increase the frequency or duration of her walks by no more than 10% per week.
SBIRT: Referral for treatment
When referring a patient to a fitness program or professional, it is essential to consider their preferences, resources, and environment.23 Community fitness partners are often an excellent referral option for a patient seeking guidance or structure for their exercise program. Using the ACSM ProFinder service, (www.acsm.org/get-stay-certified/find-a-pro) you can search for exercise professionals who have achieved the College’s Gold Standard credential.
Gym memberships or fitness programs might be part of the extra coverage offered by Medicare Advantage Plans, other Medicare health plans, or Medicare Supplement Insurance (Medigap) plans.24
Continue to: CASE
CASE
After providing Ms. Q with her exercise prescription, you refer her to a local gym that participates in the Silver Sneakers fitness and wellness program (for adults ≥ 65 years of age in eligible Medicare plans) to determine whether she qualifies to begin resistance and flexibility training, for which you will write a second exercise prescription (TABLE 317-19).
Pre-participation screening
Updated 2015 ACSM exercise pre-participation health screening recommendations attempt to decrease possible barriers to people who are becoming more physically active, by minimizing unnecessary referral to health care providers before they change their level of physical activity. ACSM recommendations on exercise clearance include this guidance25:
- For a patient who is asymptomatic and already physically active—regardless of whether they have known cardiovascular, metabolic, or renal disease—medical clearance is unnecessary for moderate-intensity exercise.
- Any patient who has been physically active and asymptomatic but who becomes symptomatic during exercise should immediately discontinue such activity and undergo medical evaluation.
- For a patient who is inactive, asymptomatic, and who does not have known cardiovascular, metabolic, or renal disease, medical clearance for light- or moderate-intensity exercise is unnecessary.
- For inactive, asymptomatic patients who have known cardiovascular, metabolic, or renal disease, medical clearance is recommended.
Digital health
Smartwatches and health apps (eg, CardioCoach, Fitbit, Garmin Connect, Nike Training Club, Strava, and Training Peaks) can provide workouts and offer patients the ability to collect information and even connect with other users through social media platforms. This information can be synced to Apple Health platforms for iPhones (www.apple.com/ios/health/) or through Google Fit (www.google.com/fit/) on Android devices. Primary care physicians who become familiar with health apps might find them useful for select patients who want to use technology to improve their physical activity level.
However, data on the value of using digital apps for increasing physical activity, in relation to their cost, are limited. Additional research is needed to assess their validity.
Billing and coding
For most patients, the physical activity assessment, prescription, and referral are performed in the context of treating another condition (eg, hypertension, type 2 diabetes, obesity, depression) or during a preventive health examination, and are typically covered without additional charge to the patient. An evaluation and management visit for an established patient could be used to bill if > 50% of the office visit was spent face-to-face with a physician, with patient counseling and coordination of care.
Continue to: Physicians and physical therapists...
Physicians and physical therapists can use the therapeutic exercise code (Current Procedural Terminology code 97110) when teaching patients exercises to develop muscle strength and endurance, joint range of motion, and flexibility26 (TABLE 426).
Conclusion
Physical activity and CRF are strong predictors of premature mortality, even compared to other risk factors, such as cigarette smoking, hypertension, hypercholesterolemia, and type 2 diabetes.27 Brief physical activity assessment and counseling is an efficient, effective, and cost-effective means to increase physical activity, and presents a unique opportunity for you to encourage lifestyle-based strategies for reducing cardiovascular risk.28
However, it is essential to meet patients where they are before trying to have them progress; it is therefore imperative to assess the individual patient’s level of activity using PAVS. With that information in hand, you can personalize physical activity advice; determine readiness for change and potential barriers for change; assist the patient in setting SMART goals; and arrange follow-up to assess adherence to the exercise prescription. Encourage the patient to call their health insurance plan to determine whether a gym membership or fitness program is covered.
Research is needed to evaluate the value of using digital apps, in light of their cost, to increase physical activity and improve CRF in a clinical setting. Prospective trials should be initiated to determine how routine implementation of CRF assessment in primary care alters the trajectory of clinical care. It is hoped that future research will answer the question: Would such an approach improve clinical outcomes and reduce health care expenditures?12
a Defined as O2 consumed while sitting at rest; equivalent to 3.5 mL of O2 × kg of body weight × min.
CORRESPONDENCE
Matthew Kampert, DO, MS, Sports Medicine, 5555 Transportation Boulevard, Cleveland, OH 44125; kamperm@ccf.org
It is well-known that per capita health care spending in the United States is more than twice the average in other developed countries1; nevertheless, the overall health care ranking of the US is near the bottom compared to other countries in this group.2 Much of the reason for this poor relative showing lies in the fact that the US has employed a somewhat traditional fee-for-service health care model that does not incentivize efforts to promote health and wellness or prevent chronic disease. The paradigm of promoting physical activity for its disease-preventing and treatment benefits has not been well-integrated in the US health care system.
In this article, we endeavor to provide better understanding of the barriers that keep family physicians from routinely promoting physical activity in clinical practice; define tools and resources that can be used in the clinical setting to promote physical activity; and delineate areas for future work.
Glaring hole in US physical activity education
Many primary care physicians feel underprepared to prescribe or motivate patients to exercise. The reason for that lack of preparedness likely relates to a medical education system that does not spend time preparing physicians to perform this critical task. A study showed that, on average, medical schools require only 8 hours of physical activity education in their curriculum during the 4 years of schooling.3 Likewise, the average primary care residency program offers only 3 hours of didactic training on physical activity, nutrition, and obesity.4 The problem extends to sports medicine fellowship training, in which a 2019 survey showed that 63% of fellows were never taught how to write an exercise prescription in their training program.5
Without education on physical activity, medical students, residents, and fellows are woefully underprepared to realize the therapeutic value of physical activity in patient care, comprehend current physical activity guidelines, appropriately motivate patients to engage in exercise, and competently discuss exercise prescriptions in different disease states. Throughout their training, it is imperative for medical professionals to be educated on the social determinants of health, which include the conditions in which people live, work, and play. These environmental variables can contribute to health inequities that create additional barriers to improvement in physical fitness.6
National guidelines on physical activity
The 2018 National Physical Activity Guidelines detail recommendations for children, adolescents, adults, and special populations.7 The guidelines define physical activity as bodily movement produced by skeletal muscles that result in energy expenditure above resting baseline levels, and includes all types, intensities, and domains of activity. Exercise is a subset of physical activity characterized as planned, structured, repetitive, and designed to improve or maintain physical fitness, physical performance, or health.
Highlights from the 2018 guidelines include7:
- Preschool-aged children (3 to 5 years of age) should be physically active throughout the day, with as much as 3 hours per day of physical activity of all intensities—light, moderate, and vigorous.
- Older children and adolescents (6 to 17 years) should accumulate 60 minutes per day of moderate-to-vigorous physical activity, including aerobic, muscle-strengthening, and bone-strengthening activities.
- Adults of all ages should achieve approximately 150 to 300 minutes of moderate or 75 to 150 minutes of vigorous physical activity (or an equivalent combination) per week, along with at least 2 days per week of muscle-strengthening activities. Other types of physical activity include flexibility, balance, bone-strengthening, and mind–body exercises.
3-step framework for enhancing physical activity counseling
Merely knowing that physical activity is healthy is not enough, during a patient encounter, to increase the level of physical activity. Therefore, it is imperative to learn and adopt a framework that has proved to yield successful outcomes. The Screening, Brief Intervention, and Referral to Treatment (SBIRT) framework, which has predominantly been used to change patient behavior related to alcohol and substance use, is now being utilized by some providers to promote physical activity.8 We apply the SBIRT approach in this article, although research is lacking on its clinical utility and outcome measures.
Continue to: SBIRT
SBIRT: Screening
An office visit provides an opportunity to understand a patient’s level of physical activity. Often, understanding a patient’s baseline level of activity is only asked during a thorough social history, which might not be performed during patient encounters. As physical activity is the primary determinant of cardiorespiratory fitness (CRF), some health care systems have begun delineating physical activity levels as a vital sign to ensure that the assessment of physical activity is a standard part of every clinical encounter. At a minimum, this serves as a prompt and provides an opportunity to start a conversation around improving physical activity levels when guidelines are not being met.
The exercise vital sign. Assessment and documentation of physical activity in the electronic health record are not yet standardized; however, Kaiser Permanente health plans have implemented the exercise vital sign, or EVS, in its HealthConnect (Epic Systems) electronic health record. The EVS incorporates information about a patient’s:
- days per week of moderate-to-strenuous exercise (eg, a brisk walk)
- minutes per day, on average, of exercise at this level.
The physical activity vital sign. Intermountain Healthcare implemented the physical activity vital sign, or PAVS, in its iCentra (Cerner Corp.) electronic health record. The 3-question PAVS assessment asks:
- On average, how many days of the week do you perform physical activity or exercise?
- On average, how many total minutes of physical activity or exercise do you perform on those days?
- How would you describe the intensity of your physical activity or exercise: Light (ie, a casual walk)? Moderate (a brisk walk)? Or vigorous (jogging)?
PAVS includes a fourth data point: The physician–user documents whether the patient was counseled to start, increase, maintain, or modify physical activity or exercise.
EVS and the PAVS have demonstrated validity.9-11
Continue to: Cardiorespiratory fitness as a vital sign
Cardiorespiratory fitness as a vital sign. In 2016, the American Heart Association (AHA) asserted the importance of assessing CRF as a clinical vital sign.12 CRF is commonly expressed as maximal oxygen consumption (VO2max = O2 mL/kg/min) and measured through cardiopulmonary exercise testing (CPET), considered the gold standard by combining conventional graded exercise testing with ventilatory expired gas analysis. CPET is more objective and precise than equations estimating CRF that are derived from peak work rate. AHA recommended that efforts to improve CRF should become standard in clinical encounters, explaining that even a small increase in CRF (eg, 1 or 2 metabolic equivalentsa [METs]) is associated with a considerably (10% to 30%) lower rate of adverse cardiovascular events.12
De Souza de Silva and colleagues revealed an association between each 1-MET increase in CRF and per-person annual health care cost savings (adjusted for age and presence of cardiovascular disease) of $3272 (normal-weight patients), $4252 (overweight), and $6103 (obese).13 In its 2016 scientific statement on CRF as a vital sign, AHA listed several methods of estimating CRF and concluded that, although CPET involves a higher level of training, proficiency, equipment, and, therefore, cost, the independent and additive information obtained justifies its use in many patients.12
CASE
Mary Q, 68 years of age, presents for an annual well-woman examination. Body mass index is 32; resting heart rate (HR), 73 bpm; and blood pressure, 126/74 mm Hg. She reports being inactive, except for light walking every day with her dog around the neighborhood, which takes them approximately 15 minutes. She denies any history or signs and symptoms of cardiovascular, metabolic, or renal disease.
You consider 3 questions before taking next steps regarding increasing Ms. Q’s activity level:
- What is her PAVS?
- Does she need medical clearance before starting an exercise program?
- What would an evidence-based cardiovascular exercise prescription for Ms. Q look like?
SBIRT: Brief intervention
When a patient does not meet the recommended level of physical activity, you have an opportunity to deliver a brief intervention. To do this effectively, you must have adequate understanding of the patient’s receptivity for change. The transtheoretical, or Stages of Change, model proposes that a person typically goes through 5 stages of growth—pre-contemplation, contemplation, preparation, action, and maintenance—in the process of lifestyle modification. This model highlights the different approaches to exercise adoption and maintenance that need to be taken, based on a given patient’s stage at the moment.
Continue to: Using this framework...
Using this framework, you can help patients realize intrinsic motivation that can facilitate progression through each stage, utilizing techniques such as motivational interviewing—so-called change talk—to increase self-efficacy.14TABLE 115 provides examples of motivational interviewing techniques that can be used during a patient encounter to improve health behaviors, such as physical activity.
Writing the exercise prescription
A patient who wants to increase their level of physical activity should be offered a formal exercise prescription, which has been shown to increase the level of physical activity, particularly in older patients. In fact, a study conducted in Spain in the practices of family physicians found that older patients who received a physical activity prescription increased their activity by 131 minutes per week; and compared to control patients, they doubled the minutes per week devoted to moderate or vigorous physical activity.16
FITT-VP. The basics of a cardiovascular exercise prescription can be found in the FITT-VP (Frequency, Intensity, Time, Type, Volume, and [monitoring of] Progression) framework (TABLE 217-19). For most patients, this model includes 3 to 5 days per week of moderate-to-vigorous physical activity for 30 to 60 minutes per session. For patients with established chronic disease, physical activity provides health benefits but might require modification. Disease-specific patient handouts for exercise can be downloaded, at no cost, through the American College of Sports Medicine (ACSM) “Exercise Is Medicine” program, which can be found at: www.exerciseismedicine.org/support_page.php/rx-for-health-series.
Determining intensity level. Although CPET is the gold standard for determining a patient’s target intensity level, such a test might be impracticable for a given patient. Surrogate markers of target intensity level can be obtained by measuring maximum HR (HRmax), using a well-known equation20:
HRmax = 220 – age
which is then multiplied by intensity range:
- light: 30%-39%
- moderate: 40%-59%
- vigorous: 60%-89%
or, more preferably, by calculating the HR training zone while accounting for HR at rest (HRrest). This is accomplished by calculating the HR reserve (HRR) (ie, HRR = HRmax – HRrest) and then calculating the target heart rate (THR)21:
THR = [HRR × %intensity] + HRrest
Continue to: The THR calculation...
The THR calculation is performed twice, once with a lower %intensity and again with a higher %intensity to develop a training zone based on HRR.
The HRR equation is more accurate than calculating HRmax from 220 – age, because HRR accounts for resting HR, which is often lower in people who are better conditioned.
Another method of calculating intensity for patients who are beginning a physical activity program is the rating of perceived exertion (RPE), which is graded on a scale of 6 to 20: Moderate exercise correlates with an RPE of 12 to 13 (“somewhat hard”); vigorous exercise correlates with an RPE of 14 to 16 (“hard”). By adding a zero to the rating on the RPE scale, the corresponding HR in a healthy adult can be estimated when they are performing an activity at that perceived intensity.22 Moderate exercise therefore correlates with a HR of 120 and 130 bpm.
The so-called talk test can also guide exercise intensity: Light-intensity activity correlates with an ability to sing; moderate-intensity physical activity likely allows the patient to still hold a conversation; and vigorous-intensity activity correlates with an inability to carry on a conversation while exercising.
An exercise prescription should be accompanied by a patient-derived goal, which can be reassessed during a follow-up visit. So-called SMART goals (Specific, Measurable, Achievable, Relevant, and Time-bound) are tools to help patients set personalized and realistic expectations for physical activity. Meeting the goal of approximately 150 to 300 minutes of moderate or 75 to 150 minutes of vigorous physical activity (or an equivalent combination) per week is ideal, but a patient needs to start where they are, at the moment, and gradually increase activity by setting what for them are realistic and sustainable goals.
Continue to: CASE
CASE
With a PAVS of 105 minutes (ie, 15 minutes per day × 7 days) of weekly light-to-moderate exercise walking her dog, Ms. Q does not satisfy current physical activity guidelines. She needs an exercise prescription to incorporate into her lifestyle (see “Cardiovascular exercise prescription,” at left).
First, based on ACSM pre-participation guidelines, Ms. Q does not need medical clearance before initiating light-to-moderate exercise and gradually progressing to vigorous-intensity exercise.
Second, in addition to walking the dog for 105 minutes a week, you:
- advise her to start walking for 10 minutes, 3 times per week, at a pace that keeps her HR at 97-104 bpm.
- encourage her to gradually increase the frequency or duration of her walks by no more than 10% per week.
SBIRT: Referral for treatment
When referring a patient to a fitness program or professional, it is essential to consider their preferences, resources, and environment.23 Community fitness partners are often an excellent referral option for a patient seeking guidance or structure for their exercise program. Using the ACSM ProFinder service, (www.acsm.org/get-stay-certified/find-a-pro) you can search for exercise professionals who have achieved the College’s Gold Standard credential.
Gym memberships or fitness programs might be part of the extra coverage offered by Medicare Advantage Plans, other Medicare health plans, or Medicare Supplement Insurance (Medigap) plans.24
Continue to: CASE
CASE
After providing Ms. Q with her exercise prescription, you refer her to a local gym that participates in the Silver Sneakers fitness and wellness program (for adults ≥ 65 years of age in eligible Medicare plans) to determine whether she qualifies to begin resistance and flexibility training, for which you will write a second exercise prescription (TABLE 317-19).
Pre-participation screening
Updated 2015 ACSM exercise pre-participation health screening recommendations attempt to decrease possible barriers to people who are becoming more physically active, by minimizing unnecessary referral to health care providers before they change their level of physical activity. ACSM recommendations on exercise clearance include this guidance25:
- For a patient who is asymptomatic and already physically active—regardless of whether they have known cardiovascular, metabolic, or renal disease—medical clearance is unnecessary for moderate-intensity exercise.
- Any patient who has been physically active and asymptomatic but who becomes symptomatic during exercise should immediately discontinue such activity and undergo medical evaluation.
- For a patient who is inactive, asymptomatic, and who does not have known cardiovascular, metabolic, or renal disease, medical clearance for light- or moderate-intensity exercise is unnecessary.
- For inactive, asymptomatic patients who have known cardiovascular, metabolic, or renal disease, medical clearance is recommended.
Digital health
Smartwatches and health apps (eg, CardioCoach, Fitbit, Garmin Connect, Nike Training Club, Strava, and Training Peaks) can provide workouts and offer patients the ability to collect information and even connect with other users through social media platforms. This information can be synced to Apple Health platforms for iPhones (www.apple.com/ios/health/) or through Google Fit (www.google.com/fit/) on Android devices. Primary care physicians who become familiar with health apps might find them useful for select patients who want to use technology to improve their physical activity level.
However, data on the value of using digital apps for increasing physical activity, in relation to their cost, are limited. Additional research is needed to assess their validity.
Billing and coding
For most patients, the physical activity assessment, prescription, and referral are performed in the context of treating another condition (eg, hypertension, type 2 diabetes, obesity, depression) or during a preventive health examination, and are typically covered without additional charge to the patient. An evaluation and management visit for an established patient could be used to bill if > 50% of the office visit was spent face-to-face with a physician, with patient counseling and coordination of care.
Continue to: Physicians and physical therapists...
Physicians and physical therapists can use the therapeutic exercise code (Current Procedural Terminology code 97110) when teaching patients exercises to develop muscle strength and endurance, joint range of motion, and flexibility26 (TABLE 426).
Conclusion
Physical activity and CRF are strong predictors of premature mortality, even compared to other risk factors, such as cigarette smoking, hypertension, hypercholesterolemia, and type 2 diabetes.27 Brief physical activity assessment and counseling is an efficient, effective, and cost-effective means to increase physical activity, and presents a unique opportunity for you to encourage lifestyle-based strategies for reducing cardiovascular risk.28
However, it is essential to meet patients where they are before trying to have them progress; it is therefore imperative to assess the individual patient’s level of activity using PAVS. With that information in hand, you can personalize physical activity advice; determine readiness for change and potential barriers for change; assist the patient in setting SMART goals; and arrange follow-up to assess adherence to the exercise prescription. Encourage the patient to call their health insurance plan to determine whether a gym membership or fitness program is covered.
Research is needed to evaluate the value of using digital apps, in light of their cost, to increase physical activity and improve CRF in a clinical setting. Prospective trials should be initiated to determine how routine implementation of CRF assessment in primary care alters the trajectory of clinical care. It is hoped that future research will answer the question: Would such an approach improve clinical outcomes and reduce health care expenditures?12
a Defined as O2 consumed while sitting at rest; equivalent to 3.5 mL of O2 × kg of body weight × min.
CORRESPONDENCE
Matthew Kampert, DO, MS, Sports Medicine, 5555 Transportation Boulevard, Cleveland, OH 44125; kamperm@ccf.org
1. Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries. JAMA. 2018;319:1024-1039. doi: 10.1001/jama.2018.1150
2. Tikkanen R, Abrams MK. U.S. health care from a global perspective, 2019: higher spending, worse outcomes? The Commonwealth Fund Website. January 30, 2020. Accessed November 16, 2021. www.commonwealthfund.org/publications/issue-briefs/2020/jan/us-health-care-global-perspective-2019
3. Stoutenberg M, Stasi S, Stamatakis E, et al. Physical activity training in US medical schools: preparing future physicians to engage in primary prevention. Phys Sportsmed. 2015;43:388-394. doi: 10.1080/00913847.2015.1084868
4. Antognoli EL, Seeholzer EL, Gullett H, et al. Primary care resident training for obesity, nutrition, and physical activity counseling: a mixed-methods study. Health Promot Pract. 2017;18:672-680. doi: 10.1177/1524839916658025
5. Asif IM, Drezner JA. Sports and exercise medicine education in the USA: call to action. Br J Sports Med. 2020;54:195-196. doi: 10.1136/bjsports-2019-101104
6. Douglas JA, Briones MD, Bauer EZ, et al. Social and environmental determinants of physical activity in urban parks: testing a neighborhood disorder model. Prev Med. 2018;109:119-124. doi: 10.1016/j.ypmed.2018.01.013
7. 2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC: US Department of Health & Human Services; 2018. Accessed November 15, 2021. https://health.gov/sites/default/files/2019-09/PAG_Advisory_Committee_Report.pdf
8. Avis JL, Cave AL, Donaldson S, et al. Working with parents to prevent childhood obesity: protocol for a primary care-based ehealth study. JMIR Res Protoc. 2015;4:e35. doi:10.2196/resprot.4147
9. Ball TJ, Joy EA, Gren LH, et al. Concurrent validity of a self-reported physical activity ‘vital sign’ questionnaire with adult primary care patients. Prev Chronic Dis. 2016;13:e16. doi: 10.5888/pcd13.150228
10. Ball TJ, Joy EA, Gren LH, et al. Predictive validity of an adult physical activity “vital sign” recorded in electronic health records. J Phys Act Health. 2016;13:403-408. doi: 10.1123/jpah.2015-0210
11. Coleman KJ, Ngor E, Reynolds K, et al. Initial validation of an exercise “vital sign” in electronic medical records. Med Sci Sports Exerc. 2012;44:2071-2076. doi: 10.1249/MSS.0b013e3182630ec1
12. Ross R, Blair SN, Arena R, et al; ; ; ; ; ; . Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation. 2016;134:e653-e699. doi: 10.1161/CIR.0000000000000461
13. de Souza de Silva CG, Kokkinos PP, Doom R, et al. Association between cardiorespiratory fitness, obesity, and health care costs: The Veterans Exercise Testing Study. Int J Obes (Lond). 2019;43:2225-2232. doi: 10.1038/s41366-018-0257-0
14. Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38-48. doi: 10.4278/0890-1171-12.1.38
15. Riebe D, Ehrman JK, Liguori G, et al. Methods for evoking change talk. In: ACSM’s Guidelines for Exercise Testing and Prescription. 10th ed. Wolters Kluwer; 2018.
16. Grandes G, Sanchez A, Sanchez-Pinilla RO, et al. Effectiveness of physical activity advice and prescription by physicians in routine primary care: a cluster randomized trial. Arch Intern Med. 2009;169:694-701. doi: 10.1001/archinternmed.2009.23
17. McNeill LH, Kreuter MW, Subramanian SV. Social environment and physical activity: a review of concepts and evidence. Soc Sci Med. 2006;63:1011-1022. doi: 10.1016/j.socscimed.2006.03.012
18. Garber CE, Blissmer BE, Deschenes MR, et al; American College of Sports Medicine. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Position stand. Med Sci Sport Exerc. 2011;43:1334-1359. doi: 10.1249/MSS.0b013e318213fefb
19. Donnelly JE, Blair SN, Jakicic JM, et al; American College of Sports Medicine. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Position stand. Med Sci Sport Exerc. 2009;41:459-471. doi: 10.1249/MSS.0b013e3181949333
20. Fox SM 3rd, Naughton JP, Haskell WL. Physical activity and the prevention of coronary heart disease. Ann Clin Res. 1971;3:404-432.
21. Karvonen MJ, Kentala E, Mustala O. The effects of training on heart rate; a longitudinal study. Ann Med Exp Biol Fenn. 1957;35:307-315.
22. The Borg RPE scale. In: Borg G. Borg’s Perceived Exertion and Pain Scales. Human Kinetics; 1998:29-38.
23. Ratamess NA, Alvar BA, Evetoch TK, et al; American College of Sports Medicine. Progression models in resistance training for healthy adults. Position stand. Med Sci Sport Exerc. 2009;41:687-708. doi: 10.1249/MSS.0b013e3181915670
24. Gym memberships & fitness programs. Medicare.gov. Baltimore, MD: US Centers for Medicare and Medicaid Services. Accessed November 16, 2021. www.medicare.gov/coverage/gym-memberships-fitness-programs
25. Riebe D, Franklin BA, Thompson PD, et al. Updating ACSM’s recommendations for exercise preparticipation health screening. Med Sci Sports Exerc. 2015;47:2473-2479. doi: 10.1249/MSS.0000000000000664
26. Physical Activity Related Current Procedural Terminology (CPT®) Codes. Physical Activity Alliance website. Accessed November 16, 2021. https://paamovewithus.org/wp-content/uploads/2020/11/PAA-Physical-Activity-CPT-Codes-Nov-2020-AMA-Approved-Final-1.pdf
27. Blair SN. Physical inactivity: the biggest public health problem of the 21st century Br J Sports Med. 2009;43:1-2.
28. Vuori IM, Lavie CJ, Blair SN. Physical activity promotion in the health care system. Mayo Clin Proc. 2013;88:1446-1461. doi: 10.1016/j.mayocp.2013.08.020
1. Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries. JAMA. 2018;319:1024-1039. doi: 10.1001/jama.2018.1150
2. Tikkanen R, Abrams MK. U.S. health care from a global perspective, 2019: higher spending, worse outcomes? The Commonwealth Fund Website. January 30, 2020. Accessed November 16, 2021. www.commonwealthfund.org/publications/issue-briefs/2020/jan/us-health-care-global-perspective-2019
3. Stoutenberg M, Stasi S, Stamatakis E, et al. Physical activity training in US medical schools: preparing future physicians to engage in primary prevention. Phys Sportsmed. 2015;43:388-394. doi: 10.1080/00913847.2015.1084868
4. Antognoli EL, Seeholzer EL, Gullett H, et al. Primary care resident training for obesity, nutrition, and physical activity counseling: a mixed-methods study. Health Promot Pract. 2017;18:672-680. doi: 10.1177/1524839916658025
5. Asif IM, Drezner JA. Sports and exercise medicine education in the USA: call to action. Br J Sports Med. 2020;54:195-196. doi: 10.1136/bjsports-2019-101104
6. Douglas JA, Briones MD, Bauer EZ, et al. Social and environmental determinants of physical activity in urban parks: testing a neighborhood disorder model. Prev Med. 2018;109:119-124. doi: 10.1016/j.ypmed.2018.01.013
7. 2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC: US Department of Health & Human Services; 2018. Accessed November 15, 2021. https://health.gov/sites/default/files/2019-09/PAG_Advisory_Committee_Report.pdf
8. Avis JL, Cave AL, Donaldson S, et al. Working with parents to prevent childhood obesity: protocol for a primary care-based ehealth study. JMIR Res Protoc. 2015;4:e35. doi:10.2196/resprot.4147
9. Ball TJ, Joy EA, Gren LH, et al. Concurrent validity of a self-reported physical activity ‘vital sign’ questionnaire with adult primary care patients. Prev Chronic Dis. 2016;13:e16. doi: 10.5888/pcd13.150228
10. Ball TJ, Joy EA, Gren LH, et al. Predictive validity of an adult physical activity “vital sign” recorded in electronic health records. J Phys Act Health. 2016;13:403-408. doi: 10.1123/jpah.2015-0210
11. Coleman KJ, Ngor E, Reynolds K, et al. Initial validation of an exercise “vital sign” in electronic medical records. Med Sci Sports Exerc. 2012;44:2071-2076. doi: 10.1249/MSS.0b013e3182630ec1
12. Ross R, Blair SN, Arena R, et al; ; ; ; ; ; . Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation. 2016;134:e653-e699. doi: 10.1161/CIR.0000000000000461
13. de Souza de Silva CG, Kokkinos PP, Doom R, et al. Association between cardiorespiratory fitness, obesity, and health care costs: The Veterans Exercise Testing Study. Int J Obes (Lond). 2019;43:2225-2232. doi: 10.1038/s41366-018-0257-0
14. Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38-48. doi: 10.4278/0890-1171-12.1.38
15. Riebe D, Ehrman JK, Liguori G, et al. Methods for evoking change talk. In: ACSM’s Guidelines for Exercise Testing and Prescription. 10th ed. Wolters Kluwer; 2018.
16. Grandes G, Sanchez A, Sanchez-Pinilla RO, et al. Effectiveness of physical activity advice and prescription by physicians in routine primary care: a cluster randomized trial. Arch Intern Med. 2009;169:694-701. doi: 10.1001/archinternmed.2009.23
17. McNeill LH, Kreuter MW, Subramanian SV. Social environment and physical activity: a review of concepts and evidence. Soc Sci Med. 2006;63:1011-1022. doi: 10.1016/j.socscimed.2006.03.012
18. Garber CE, Blissmer BE, Deschenes MR, et al; American College of Sports Medicine. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Position stand. Med Sci Sport Exerc. 2011;43:1334-1359. doi: 10.1249/MSS.0b013e318213fefb
19. Donnelly JE, Blair SN, Jakicic JM, et al; American College of Sports Medicine. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Position stand. Med Sci Sport Exerc. 2009;41:459-471. doi: 10.1249/MSS.0b013e3181949333
20. Fox SM 3rd, Naughton JP, Haskell WL. Physical activity and the prevention of coronary heart disease. Ann Clin Res. 1971;3:404-432.
21. Karvonen MJ, Kentala E, Mustala O. The effects of training on heart rate; a longitudinal study. Ann Med Exp Biol Fenn. 1957;35:307-315.
22. The Borg RPE scale. In: Borg G. Borg’s Perceived Exertion and Pain Scales. Human Kinetics; 1998:29-38.
23. Ratamess NA, Alvar BA, Evetoch TK, et al; American College of Sports Medicine. Progression models in resistance training for healthy adults. Position stand. Med Sci Sport Exerc. 2009;41:687-708. doi: 10.1249/MSS.0b013e3181915670
24. Gym memberships & fitness programs. Medicare.gov. Baltimore, MD: US Centers for Medicare and Medicaid Services. Accessed November 16, 2021. www.medicare.gov/coverage/gym-memberships-fitness-programs
25. Riebe D, Franklin BA, Thompson PD, et al. Updating ACSM’s recommendations for exercise preparticipation health screening. Med Sci Sports Exerc. 2015;47:2473-2479. doi: 10.1249/MSS.0000000000000664
26. Physical Activity Related Current Procedural Terminology (CPT®) Codes. Physical Activity Alliance website. Accessed November 16, 2021. https://paamovewithus.org/wp-content/uploads/2020/11/PAA-Physical-Activity-CPT-Codes-Nov-2020-AMA-Approved-Final-1.pdf
27. Blair SN. Physical inactivity: the biggest public health problem of the 21st century Br J Sports Med. 2009;43:1-2.
28. Vuori IM, Lavie CJ, Blair SN. Physical activity promotion in the health care system. Mayo Clin Proc. 2013;88:1446-1461. doi: 10.1016/j.mayocp.2013.08.020
PRACTICE RECOMMENDATIONS
› Encourage children and adolescents (6 to 17 years of age) to engage in 60 min of moderate-to-vigorous physical activity, including aerobic, muscle-strengthening, and bone-strengthening endeavors on most, if not all, days of the week. A
› Encourage adults to perform approximately 150 to 300 min of moderate or 75 to 150 min of vigorous physical activity (or an equivalent combination) per week, along with moderate-intensity muscle-strengthening activities on ≥ 2 days per week. A
› Counsel patients that even a small (eg, 1-2 metabolic equivalents) increase in cardiorespiratory fitness is associated with a 10% to 30% lower rate of adverse events. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
New data on rare myocarditis after COVID-19 vaccination
Adolescents and adults younger than age 21 who develop myocarditis after mRNA COVID-19 vaccination frequently have abnormal findings on cardiac MRI (cMRI) but most have a mild clinical course with rapid resolution of symptoms, a new study concludes.
“This study supports what we’ve been seeing. People identified and treated early and appropriately for the rare complication of COVID-19 vaccine-related myocarditis typically experienced only mild cases and short recovery times,” American Heart Association President Donald M. Lloyd-Jones, MD, said in a podcast.
“Overwhelmingly, the data continue to indicate [that] the benefits of COVID-19 vaccine far outweigh any very rare risks of adverse events from the vaccine, including myocarditis,” Dr. Lloyd-Jones added.
The study was published online Dec. 6 in Circulation.
Using data from 26 pediatric medical centers across the United States and Canada, the researchers reviewed the medical records of 139 patients younger than 21 with suspected myocarditis within 1 month of receiving a COVID-19 vaccination.
They made the following key observations:
- Most patients were male (90.6%), White (66.2%) and with a median age of 15.8 years.
- Suspected myocarditis occurred in 136 patients (97.8%) following mRNA vaccine, with 131 (94.2%) following the Pfizer-BioNTech vaccine; 128 cases (91.4%) occurred after the second dose.
- Symptoms started a median of 2 days (range 0 to 22 days) following vaccination administration.
- Chest pain was the most common symptom (99.3%), with fever present in 30.9% of patients and shortness of breath in 27.3%.
- Patients were treated with nonsteroidal anti-inflammatory drugs (81.3%), intravenous immunoglobulin (21.6%), glucocorticoids (21.6%), colchicine (7.9%) or no anti-inflammatory therapies (8.6%).
- Twenty-six patients (18.7%) were admitted to the intensive care unit; 2 received inotropic/vasoactive support; none required extracorporeal membrane oxygenation or died.
- Median time spent in the hospital was 2 days.
- A total of 111 patients had elevated troponin I (8.12 ng/mL) and 28 had elevated troponin T (0.61 ng/mL).
- More than two-thirds (69.8%) had abnormal electrocardiograms and/or arrhythmias (7 with nonsustained ventricular tachycardia).
- Twenty-six patients (18.7%) had left ventricular ejection fraction (LVEF) less than 55% on echocardiogram; LVEF had returned to normal in the 25 who returned for follow-up.
- 75 of 97 patients (77.3%) who underwent cMRI at a median of 5 days from symptom onset had abnormal findings; 74 (76.3%) had late gadolinium enhancement, 54 (55.7%) had myocardial edema, and 49 (50.5%) met Lake Louise criteria for myocarditis.
“These data suggest that most cases of suspected COVID-19 vaccine–related myocarditis in people younger than 21 are mild and resolve quickly,” corresponding author Dongngan Truong, MD, Division of Pediatric Cardiology, University of Utah and Primary Children’s Hospital, Salt Lake City, said in a statement.
“We were very happy to see that type of recovery. However, we are awaiting further studies to better understand the long-term outcomes of patients who have had COVID-19 vaccination-related myocarditis. We also need to study the risk factors and mechanisms for this rare complication,” Dr. Truong added.
Dr. Lloyd-Jones said these findings support the AHA’s position that COVID-19 vaccines are “safe, highly effective, and fundamental to saving lives, protecting our families and communities against COVID-19, and ending the pandemic.”
The study received no funding. Dr. Truong consults for Pfizer on vaccine-associated myocarditis. A complete list of author disclosures is available with the original article.
A version of this article first appeared on Medscape.com.
Adolescents and adults younger than age 21 who develop myocarditis after mRNA COVID-19 vaccination frequently have abnormal findings on cardiac MRI (cMRI) but most have a mild clinical course with rapid resolution of symptoms, a new study concludes.
“This study supports what we’ve been seeing. People identified and treated early and appropriately for the rare complication of COVID-19 vaccine-related myocarditis typically experienced only mild cases and short recovery times,” American Heart Association President Donald M. Lloyd-Jones, MD, said in a podcast.
“Overwhelmingly, the data continue to indicate [that] the benefits of COVID-19 vaccine far outweigh any very rare risks of adverse events from the vaccine, including myocarditis,” Dr. Lloyd-Jones added.
The study was published online Dec. 6 in Circulation.
Using data from 26 pediatric medical centers across the United States and Canada, the researchers reviewed the medical records of 139 patients younger than 21 with suspected myocarditis within 1 month of receiving a COVID-19 vaccination.
They made the following key observations:
- Most patients were male (90.6%), White (66.2%) and with a median age of 15.8 years.
- Suspected myocarditis occurred in 136 patients (97.8%) following mRNA vaccine, with 131 (94.2%) following the Pfizer-BioNTech vaccine; 128 cases (91.4%) occurred after the second dose.
- Symptoms started a median of 2 days (range 0 to 22 days) following vaccination administration.
- Chest pain was the most common symptom (99.3%), with fever present in 30.9% of patients and shortness of breath in 27.3%.
- Patients were treated with nonsteroidal anti-inflammatory drugs (81.3%), intravenous immunoglobulin (21.6%), glucocorticoids (21.6%), colchicine (7.9%) or no anti-inflammatory therapies (8.6%).
- Twenty-six patients (18.7%) were admitted to the intensive care unit; 2 received inotropic/vasoactive support; none required extracorporeal membrane oxygenation or died.
- Median time spent in the hospital was 2 days.
- A total of 111 patients had elevated troponin I (8.12 ng/mL) and 28 had elevated troponin T (0.61 ng/mL).
- More than two-thirds (69.8%) had abnormal electrocardiograms and/or arrhythmias (7 with nonsustained ventricular tachycardia).
- Twenty-six patients (18.7%) had left ventricular ejection fraction (LVEF) less than 55% on echocardiogram; LVEF had returned to normal in the 25 who returned for follow-up.
- 75 of 97 patients (77.3%) who underwent cMRI at a median of 5 days from symptom onset had abnormal findings; 74 (76.3%) had late gadolinium enhancement, 54 (55.7%) had myocardial edema, and 49 (50.5%) met Lake Louise criteria for myocarditis.
“These data suggest that most cases of suspected COVID-19 vaccine–related myocarditis in people younger than 21 are mild and resolve quickly,” corresponding author Dongngan Truong, MD, Division of Pediatric Cardiology, University of Utah and Primary Children’s Hospital, Salt Lake City, said in a statement.
“We were very happy to see that type of recovery. However, we are awaiting further studies to better understand the long-term outcomes of patients who have had COVID-19 vaccination-related myocarditis. We also need to study the risk factors and mechanisms for this rare complication,” Dr. Truong added.
Dr. Lloyd-Jones said these findings support the AHA’s position that COVID-19 vaccines are “safe, highly effective, and fundamental to saving lives, protecting our families and communities against COVID-19, and ending the pandemic.”
The study received no funding. Dr. Truong consults for Pfizer on vaccine-associated myocarditis. A complete list of author disclosures is available with the original article.
A version of this article first appeared on Medscape.com.
Adolescents and adults younger than age 21 who develop myocarditis after mRNA COVID-19 vaccination frequently have abnormal findings on cardiac MRI (cMRI) but most have a mild clinical course with rapid resolution of symptoms, a new study concludes.
“This study supports what we’ve been seeing. People identified and treated early and appropriately for the rare complication of COVID-19 vaccine-related myocarditis typically experienced only mild cases and short recovery times,” American Heart Association President Donald M. Lloyd-Jones, MD, said in a podcast.
“Overwhelmingly, the data continue to indicate [that] the benefits of COVID-19 vaccine far outweigh any very rare risks of adverse events from the vaccine, including myocarditis,” Dr. Lloyd-Jones added.
The study was published online Dec. 6 in Circulation.
Using data from 26 pediatric medical centers across the United States and Canada, the researchers reviewed the medical records of 139 patients younger than 21 with suspected myocarditis within 1 month of receiving a COVID-19 vaccination.
They made the following key observations:
- Most patients were male (90.6%), White (66.2%) and with a median age of 15.8 years.
- Suspected myocarditis occurred in 136 patients (97.8%) following mRNA vaccine, with 131 (94.2%) following the Pfizer-BioNTech vaccine; 128 cases (91.4%) occurred after the second dose.
- Symptoms started a median of 2 days (range 0 to 22 days) following vaccination administration.
- Chest pain was the most common symptom (99.3%), with fever present in 30.9% of patients and shortness of breath in 27.3%.
- Patients were treated with nonsteroidal anti-inflammatory drugs (81.3%), intravenous immunoglobulin (21.6%), glucocorticoids (21.6%), colchicine (7.9%) or no anti-inflammatory therapies (8.6%).
- Twenty-six patients (18.7%) were admitted to the intensive care unit; 2 received inotropic/vasoactive support; none required extracorporeal membrane oxygenation or died.
- Median time spent in the hospital was 2 days.
- A total of 111 patients had elevated troponin I (8.12 ng/mL) and 28 had elevated troponin T (0.61 ng/mL).
- More than two-thirds (69.8%) had abnormal electrocardiograms and/or arrhythmias (7 with nonsustained ventricular tachycardia).
- Twenty-six patients (18.7%) had left ventricular ejection fraction (LVEF) less than 55% on echocardiogram; LVEF had returned to normal in the 25 who returned for follow-up.
- 75 of 97 patients (77.3%) who underwent cMRI at a median of 5 days from symptom onset had abnormal findings; 74 (76.3%) had late gadolinium enhancement, 54 (55.7%) had myocardial edema, and 49 (50.5%) met Lake Louise criteria for myocarditis.
“These data suggest that most cases of suspected COVID-19 vaccine–related myocarditis in people younger than 21 are mild and resolve quickly,” corresponding author Dongngan Truong, MD, Division of Pediatric Cardiology, University of Utah and Primary Children’s Hospital, Salt Lake City, said in a statement.
“We were very happy to see that type of recovery. However, we are awaiting further studies to better understand the long-term outcomes of patients who have had COVID-19 vaccination-related myocarditis. We also need to study the risk factors and mechanisms for this rare complication,” Dr. Truong added.
Dr. Lloyd-Jones said these findings support the AHA’s position that COVID-19 vaccines are “safe, highly effective, and fundamental to saving lives, protecting our families and communities against COVID-19, and ending the pandemic.”
The study received no funding. Dr. Truong consults for Pfizer on vaccine-associated myocarditis. A complete list of author disclosures is available with the original article.
A version of this article first appeared on Medscape.com.
AHA challenges diet doctor’s study alleging COVID vax risks
An abstract and poster presentation questioning the safety of mRNA-based COVID-19 vaccines, embraced by some and lambasted by others, has drawn an “expression of concern” from the American Heart Association, along with a bid for correction.
The abstract in question concludes that COVID vaccines “dramatically increase” levels of certain inflammatory biomarkers, and therefore, the 5-year risk of acute coronary syndromes (ACS), based on pre- and post-vaccination results of an obscure blood panel called the PULS Cardiac Test (GD Biosciences). The findings were presented at the AHA’s 2021 Scientific Sessionsas, an uncontrolled observational study of 566 patients in a preventive cardiology practice.
Some on social media have seized on the abstract as evidence of serious potential harm from the two available mRNA-based SARS-CoV-2 vaccines, BNT162b2 (Pfizer-BioNTech) and mRNA-1273 (Moderna). But others contend that the study’s described design and findings are specious and its conclusions overstated.
They also point to the notoriety of its one listed author, Steven R. Gundry, MD, who promotes his diet books and supplements as well as fringe, highly criticized theories about diet and disease on several websites, including drgundry.com. Dr. Gundry has not responded to requests for an interview.
Dr. Gundry’s abstract from the AHA Scientific Sessions 2021, available on the meeting’s program planner, was marked with an “expression of concern” by the AHA that is to stand “until a suitable correction is published, to indicate that the abstract in its current version may not be reliable.”
The expression of concern statement, also published online Nov. 24 in Circulation, says “potential errors in the abstract” were brought to the attention of the meeting planners. “Specifically, there are several typographical errors, there is no data in the abstract regarding myocardial T-cell infiltration, there are no statistical analyses for significance provided, and the author is not clear that only anecdotal data was used.”
The biomarker elevations on which the abstract’s conclusions are based included hepatocyte growth factor, “which serves as a marker for chemotaxis of T-cells into epithelium and cardiac tissue,” it states.
“The expression of concern about the abstract will remain in place until a correction is accepted and published” in Circulation, AHA spokesperson Suzanne Grant told this news organization by email.
“The specific data needed will be up to the abstract author to determine and supply,” she said, noting that Dr. Gundry “has been in communication with the journal throughout this process.”
Submitting researchers “must always attest to the validity of the abstract,” Ms. Grant said. “Abstracts are then curated by independent review panels, blinded to the identities of the abstract authors, and are considered based on the potential to add to the diversity of scientific issues and views discussed at the meeting.”
Regarding the AHA’s system for vetting abstracts vying for acceptance to the scientific sessions, she said it is not primarily intended to “evaluate scientific validity” and that the organization is “currently reviewing its existing abstract submission processes.”
A recent Reuters report reviews the controversy and provides links to criticisms of the study on social media.
A version of this article first appeared on Medscape.com.
An abstract and poster presentation questioning the safety of mRNA-based COVID-19 vaccines, embraced by some and lambasted by others, has drawn an “expression of concern” from the American Heart Association, along with a bid for correction.
The abstract in question concludes that COVID vaccines “dramatically increase” levels of certain inflammatory biomarkers, and therefore, the 5-year risk of acute coronary syndromes (ACS), based on pre- and post-vaccination results of an obscure blood panel called the PULS Cardiac Test (GD Biosciences). The findings were presented at the AHA’s 2021 Scientific Sessionsas, an uncontrolled observational study of 566 patients in a preventive cardiology practice.
Some on social media have seized on the abstract as evidence of serious potential harm from the two available mRNA-based SARS-CoV-2 vaccines, BNT162b2 (Pfizer-BioNTech) and mRNA-1273 (Moderna). But others contend that the study’s described design and findings are specious and its conclusions overstated.
They also point to the notoriety of its one listed author, Steven R. Gundry, MD, who promotes his diet books and supplements as well as fringe, highly criticized theories about diet and disease on several websites, including drgundry.com. Dr. Gundry has not responded to requests for an interview.
Dr. Gundry’s abstract from the AHA Scientific Sessions 2021, available on the meeting’s program planner, was marked with an “expression of concern” by the AHA that is to stand “until a suitable correction is published, to indicate that the abstract in its current version may not be reliable.”
The expression of concern statement, also published online Nov. 24 in Circulation, says “potential errors in the abstract” were brought to the attention of the meeting planners. “Specifically, there are several typographical errors, there is no data in the abstract regarding myocardial T-cell infiltration, there are no statistical analyses for significance provided, and the author is not clear that only anecdotal data was used.”
The biomarker elevations on which the abstract’s conclusions are based included hepatocyte growth factor, “which serves as a marker for chemotaxis of T-cells into epithelium and cardiac tissue,” it states.
“The expression of concern about the abstract will remain in place until a correction is accepted and published” in Circulation, AHA spokesperson Suzanne Grant told this news organization by email.
“The specific data needed will be up to the abstract author to determine and supply,” she said, noting that Dr. Gundry “has been in communication with the journal throughout this process.”
Submitting researchers “must always attest to the validity of the abstract,” Ms. Grant said. “Abstracts are then curated by independent review panels, blinded to the identities of the abstract authors, and are considered based on the potential to add to the diversity of scientific issues and views discussed at the meeting.”
Regarding the AHA’s system for vetting abstracts vying for acceptance to the scientific sessions, she said it is not primarily intended to “evaluate scientific validity” and that the organization is “currently reviewing its existing abstract submission processes.”
A recent Reuters report reviews the controversy and provides links to criticisms of the study on social media.
A version of this article first appeared on Medscape.com.
An abstract and poster presentation questioning the safety of mRNA-based COVID-19 vaccines, embraced by some and lambasted by others, has drawn an “expression of concern” from the American Heart Association, along with a bid for correction.
The abstract in question concludes that COVID vaccines “dramatically increase” levels of certain inflammatory biomarkers, and therefore, the 5-year risk of acute coronary syndromes (ACS), based on pre- and post-vaccination results of an obscure blood panel called the PULS Cardiac Test (GD Biosciences). The findings were presented at the AHA’s 2021 Scientific Sessionsas, an uncontrolled observational study of 566 patients in a preventive cardiology practice.
Some on social media have seized on the abstract as evidence of serious potential harm from the two available mRNA-based SARS-CoV-2 vaccines, BNT162b2 (Pfizer-BioNTech) and mRNA-1273 (Moderna). But others contend that the study’s described design and findings are specious and its conclusions overstated.
They also point to the notoriety of its one listed author, Steven R. Gundry, MD, who promotes his diet books and supplements as well as fringe, highly criticized theories about diet and disease on several websites, including drgundry.com. Dr. Gundry has not responded to requests for an interview.
Dr. Gundry’s abstract from the AHA Scientific Sessions 2021, available on the meeting’s program planner, was marked with an “expression of concern” by the AHA that is to stand “until a suitable correction is published, to indicate that the abstract in its current version may not be reliable.”
The expression of concern statement, also published online Nov. 24 in Circulation, says “potential errors in the abstract” were brought to the attention of the meeting planners. “Specifically, there are several typographical errors, there is no data in the abstract regarding myocardial T-cell infiltration, there are no statistical analyses for significance provided, and the author is not clear that only anecdotal data was used.”
The biomarker elevations on which the abstract’s conclusions are based included hepatocyte growth factor, “which serves as a marker for chemotaxis of T-cells into epithelium and cardiac tissue,” it states.
“The expression of concern about the abstract will remain in place until a correction is accepted and published” in Circulation, AHA spokesperson Suzanne Grant told this news organization by email.
“The specific data needed will be up to the abstract author to determine and supply,” she said, noting that Dr. Gundry “has been in communication with the journal throughout this process.”
Submitting researchers “must always attest to the validity of the abstract,” Ms. Grant said. “Abstracts are then curated by independent review panels, blinded to the identities of the abstract authors, and are considered based on the potential to add to the diversity of scientific issues and views discussed at the meeting.”
Regarding the AHA’s system for vetting abstracts vying for acceptance to the scientific sessions, she said it is not primarily intended to “evaluate scientific validity” and that the organization is “currently reviewing its existing abstract submission processes.”
A recent Reuters report reviews the controversy and provides links to criticisms of the study on social media.
A version of this article first appeared on Medscape.com.
Higher resting heart rate tied to increased dementia risk
independent of the presence of cardiovascular disease (CVD) risk factors, new research shows.
“RHR is easy to measure and might be used to identify older people potentially at high risk of dementia and cognitive decline for early interventions,” Yume Imahori, MD, PhD, with the Aging Research Center, Karolinska Institutet, Stockholm, said in an interview.
“Health care professionals should be aware of potential cognitive consequences associated with elevated RHR in older people and may advise older people with high RHR to have a follow-up assessment of cognitive function,” Dr. Imahori said.
The study was published online Dec. 3, 2021, in Alzheimer’s & Dementia.
Heart-brain connection
The findings are based on 2,147 adults (62% women) aged 60 years and older (mean age, 70.6 years) from the population-based Swedish National Aging and Care in Kungsholmen (SNAC-K) study. All were free of dementia at baseline and were followed regularly from 2001-2004 to 2013-2016.
The average RHR at baseline was 65.7 bpm. Individuals in higher RHR groups were older, less educated, and were more likely to be smokers and sedentary and to have hypertension. There were no differences among RHR groups in the prevalence of CVD at baseline.
During a median follow-up of 11.4 years, 289 participants were diagnosed with dementia.
In the fully adjusted model, participants with RHR of 80 bpm or higher had a 55% increased risk of developing dementia, compared with peers with lower RHR of 60 to 69 bpm (hazard ratio, 1.55; 95% CI, 1.06-2.27).
“This association was not due to underlying cardiovascular diseases such as atrial fibrillation and heart failure, which is important because elevated RHR is often related to heart disease,” Dr. Imahori said in an interview.
Regarding cognitive function, Mini-Mental State Examination scores declined over time during the follow-up period in all RHR groups, but participants with RHR 70-79 and 80+ bpm had a greater decline, compared with those with lower RHR of 60-69 bpm.
Dr. Imahori said these findings are in line with data from the U.S. Atherosclerosis Risk in Communities study linking elevated RHR of 80+ bpm in midlife to dementia and cognitive decline in late life.
Public health implications
Reached for comment, Claire Sexton, DPhil, Alzheimer’s Association director of scientific programs and outreach, said this study adds to the “growing body of research showing the health of the heart and brain are closely connected. However, this study only shows a correlation between resting heart rate and cognition, not causation. More research is needed.
“Evidence shows that other risk factors for cardiovascular disease and stroke – obesity, high blood pressure, and diabetes – negatively impact your cognitive health,” Dr. Sexton said in an interview.
“The Alzheimer’s Association believes the conversation about heart health management is something everyone should be having with their doctor,” she said.
“There are things you can do today to lower your risk for cardiovascular disease, including regular exercise and maintaining a healthy diet. Improving your heart health is an important step to maintaining your brain health as you age,” Dr. Sexton added.
SNAC-K is supported by the Swedish Ministry of Health and Social Affairs and the participating county councils and municipalities and in part by additional grants from the Swedish Research Council and the Swedish Research Council for Health, Working Life and Welfare. Dr. Imahori and Dr. Sexton disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
independent of the presence of cardiovascular disease (CVD) risk factors, new research shows.
“RHR is easy to measure and might be used to identify older people potentially at high risk of dementia and cognitive decline for early interventions,” Yume Imahori, MD, PhD, with the Aging Research Center, Karolinska Institutet, Stockholm, said in an interview.
“Health care professionals should be aware of potential cognitive consequences associated with elevated RHR in older people and may advise older people with high RHR to have a follow-up assessment of cognitive function,” Dr. Imahori said.
The study was published online Dec. 3, 2021, in Alzheimer’s & Dementia.
Heart-brain connection
The findings are based on 2,147 adults (62% women) aged 60 years and older (mean age, 70.6 years) from the population-based Swedish National Aging and Care in Kungsholmen (SNAC-K) study. All were free of dementia at baseline and were followed regularly from 2001-2004 to 2013-2016.
The average RHR at baseline was 65.7 bpm. Individuals in higher RHR groups were older, less educated, and were more likely to be smokers and sedentary and to have hypertension. There were no differences among RHR groups in the prevalence of CVD at baseline.
During a median follow-up of 11.4 years, 289 participants were diagnosed with dementia.
In the fully adjusted model, participants with RHR of 80 bpm or higher had a 55% increased risk of developing dementia, compared with peers with lower RHR of 60 to 69 bpm (hazard ratio, 1.55; 95% CI, 1.06-2.27).
“This association was not due to underlying cardiovascular diseases such as atrial fibrillation and heart failure, which is important because elevated RHR is often related to heart disease,” Dr. Imahori said in an interview.
Regarding cognitive function, Mini-Mental State Examination scores declined over time during the follow-up period in all RHR groups, but participants with RHR 70-79 and 80+ bpm had a greater decline, compared with those with lower RHR of 60-69 bpm.
Dr. Imahori said these findings are in line with data from the U.S. Atherosclerosis Risk in Communities study linking elevated RHR of 80+ bpm in midlife to dementia and cognitive decline in late life.
Public health implications
Reached for comment, Claire Sexton, DPhil, Alzheimer’s Association director of scientific programs and outreach, said this study adds to the “growing body of research showing the health of the heart and brain are closely connected. However, this study only shows a correlation between resting heart rate and cognition, not causation. More research is needed.
“Evidence shows that other risk factors for cardiovascular disease and stroke – obesity, high blood pressure, and diabetes – negatively impact your cognitive health,” Dr. Sexton said in an interview.
“The Alzheimer’s Association believes the conversation about heart health management is something everyone should be having with their doctor,” she said.
“There are things you can do today to lower your risk for cardiovascular disease, including regular exercise and maintaining a healthy diet. Improving your heart health is an important step to maintaining your brain health as you age,” Dr. Sexton added.
SNAC-K is supported by the Swedish Ministry of Health and Social Affairs and the participating county councils and municipalities and in part by additional grants from the Swedish Research Council and the Swedish Research Council for Health, Working Life and Welfare. Dr. Imahori and Dr. Sexton disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
independent of the presence of cardiovascular disease (CVD) risk factors, new research shows.
“RHR is easy to measure and might be used to identify older people potentially at high risk of dementia and cognitive decline for early interventions,” Yume Imahori, MD, PhD, with the Aging Research Center, Karolinska Institutet, Stockholm, said in an interview.
“Health care professionals should be aware of potential cognitive consequences associated with elevated RHR in older people and may advise older people with high RHR to have a follow-up assessment of cognitive function,” Dr. Imahori said.
The study was published online Dec. 3, 2021, in Alzheimer’s & Dementia.
Heart-brain connection
The findings are based on 2,147 adults (62% women) aged 60 years and older (mean age, 70.6 years) from the population-based Swedish National Aging and Care in Kungsholmen (SNAC-K) study. All were free of dementia at baseline and were followed regularly from 2001-2004 to 2013-2016.
The average RHR at baseline was 65.7 bpm. Individuals in higher RHR groups were older, less educated, and were more likely to be smokers and sedentary and to have hypertension. There were no differences among RHR groups in the prevalence of CVD at baseline.
During a median follow-up of 11.4 years, 289 participants were diagnosed with dementia.
In the fully adjusted model, participants with RHR of 80 bpm or higher had a 55% increased risk of developing dementia, compared with peers with lower RHR of 60 to 69 bpm (hazard ratio, 1.55; 95% CI, 1.06-2.27).
“This association was not due to underlying cardiovascular diseases such as atrial fibrillation and heart failure, which is important because elevated RHR is often related to heart disease,” Dr. Imahori said in an interview.
Regarding cognitive function, Mini-Mental State Examination scores declined over time during the follow-up period in all RHR groups, but participants with RHR 70-79 and 80+ bpm had a greater decline, compared with those with lower RHR of 60-69 bpm.
Dr. Imahori said these findings are in line with data from the U.S. Atherosclerosis Risk in Communities study linking elevated RHR of 80+ bpm in midlife to dementia and cognitive decline in late life.
Public health implications
Reached for comment, Claire Sexton, DPhil, Alzheimer’s Association director of scientific programs and outreach, said this study adds to the “growing body of research showing the health of the heart and brain are closely connected. However, this study only shows a correlation between resting heart rate and cognition, not causation. More research is needed.
“Evidence shows that other risk factors for cardiovascular disease and stroke – obesity, high blood pressure, and diabetes – negatively impact your cognitive health,” Dr. Sexton said in an interview.
“The Alzheimer’s Association believes the conversation about heart health management is something everyone should be having with their doctor,” she said.
“There are things you can do today to lower your risk for cardiovascular disease, including regular exercise and maintaining a healthy diet. Improving your heart health is an important step to maintaining your brain health as you age,” Dr. Sexton added.
SNAC-K is supported by the Swedish Ministry of Health and Social Affairs and the participating county councils and municipalities and in part by additional grants from the Swedish Research Council and the Swedish Research Council for Health, Working Life and Welfare. Dr. Imahori and Dr. Sexton disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ALZHEIMER’S & DEMENTIA
Blood pressure control worsened during COVID pandemic
Blood pressure control declined in both men and women with the onset of the COVID-19 pandemic in the United States in 2020, especially among women and older adults, according to a new analysis.
“We know that even small rises in blood pressure increase one’s risk of stroke and other adverse cardiovascular disease events,” lead author Luke J. Laffin, MD, codirector, Center for Blood Pressure Disorders, Cleveland Clinic, Ohio, said in a news release.
The researchers say increases in systolic BP among U.S. adults during the COVID-19 pandemic “could signal a forthcoming increase in incident cardiovascular disease mortality.”
Their study was published online Dec. 6 in Circulation.
Dr. Laffin and colleagues analyzed BP data from 464,585 U.S. adults (mean age, 46, 54% women) who had their BP measured as part of employee health screening annually from 2018 through 2020.
They found that BP levels went up between April and Dec. of 2020 – around the same time stay-at-home orders and other restrictions were put in place.
During this pandemic period, average monthly increases in BP ranged from 1.10 to 2.50 mm Hg higher for systolic BP and 0.14 to 0.53 mm Hg higher for diastolic BP, compared with the prepandemic period of April to Dec. 2019.
Increases in systolic and diastolic BP were seen among men and women and across age groups. Larger increases were evident in women for both systolic and diastolic BP: in older individuals for systolic BP and in younger individuals for diastolic BP (all P < .0001).
Dr. Laffin and colleagues also assessed changes in BP category based on current American Heart Association blood pressure guidelines (normal, elevated, stage 1, or stage 2 hypertension).
During the pandemic, more adults (26.8%) were recategorized to a higher BP category, whereas only 22% moved to a lower BP category, compared with before the pandemic.
“At the start of the pandemic, most people were not taking good care of themselves. Increases in blood pressure were likely related to changes in eating habits, increased alcohol consumption, less physical activity, decreased medication adherence, more emotional stress, and poor sleep,” Dr. Laffin said.
However, the increases in BP during the pandemic could not be explained by weight gain, the researchers note, because the observed changes in weight during the pandemic were similar to the prepandemic period among 86% of adults completing weight data.
The study authors are following up on these results to determine if this trend continued in 2021.
“Unfortunately, this research confirms what is being seen across the country – the COVID-19 pandemic has had and will continue to have long-reaching health impacts across the country and particularly related to uncontrolled hypertension,” Eduardo Sanchez, MD, MPH, the AHA’s chief medical officer for prevention, said in the news release.
“These results validate why the American Heart Association’s National Hypertension Control Initiative (NHCI) is critically important,” he said.
“With a particular emphasis on historically under-resourced communities in the United States, the comprehensive program supports health care teams at community health centers through regular blood pressure management training; technical assistance and resources that include the proper blood pressure measurement technique; self-measured blood pressure monitoring and management; medication adherence; and healthy lifestyle services,” Dr. Sanchez noted.
The study had no specific funding. Dr. Laffin is a paid consultant for Medtronic and medical advisor for LucidAct Health.
A version of this article first appeared on Medscape.com.
Blood pressure control declined in both men and women with the onset of the COVID-19 pandemic in the United States in 2020, especially among women and older adults, according to a new analysis.
“We know that even small rises in blood pressure increase one’s risk of stroke and other adverse cardiovascular disease events,” lead author Luke J. Laffin, MD, codirector, Center for Blood Pressure Disorders, Cleveland Clinic, Ohio, said in a news release.
The researchers say increases in systolic BP among U.S. adults during the COVID-19 pandemic “could signal a forthcoming increase in incident cardiovascular disease mortality.”
Their study was published online Dec. 6 in Circulation.
Dr. Laffin and colleagues analyzed BP data from 464,585 U.S. adults (mean age, 46, 54% women) who had their BP measured as part of employee health screening annually from 2018 through 2020.
They found that BP levels went up between April and Dec. of 2020 – around the same time stay-at-home orders and other restrictions were put in place.
During this pandemic period, average monthly increases in BP ranged from 1.10 to 2.50 mm Hg higher for systolic BP and 0.14 to 0.53 mm Hg higher for diastolic BP, compared with the prepandemic period of April to Dec. 2019.
Increases in systolic and diastolic BP were seen among men and women and across age groups. Larger increases were evident in women for both systolic and diastolic BP: in older individuals for systolic BP and in younger individuals for diastolic BP (all P < .0001).
Dr. Laffin and colleagues also assessed changes in BP category based on current American Heart Association blood pressure guidelines (normal, elevated, stage 1, or stage 2 hypertension).
During the pandemic, more adults (26.8%) were recategorized to a higher BP category, whereas only 22% moved to a lower BP category, compared with before the pandemic.
“At the start of the pandemic, most people were not taking good care of themselves. Increases in blood pressure were likely related to changes in eating habits, increased alcohol consumption, less physical activity, decreased medication adherence, more emotional stress, and poor sleep,” Dr. Laffin said.
However, the increases in BP during the pandemic could not be explained by weight gain, the researchers note, because the observed changes in weight during the pandemic were similar to the prepandemic period among 86% of adults completing weight data.
The study authors are following up on these results to determine if this trend continued in 2021.
“Unfortunately, this research confirms what is being seen across the country – the COVID-19 pandemic has had and will continue to have long-reaching health impacts across the country and particularly related to uncontrolled hypertension,” Eduardo Sanchez, MD, MPH, the AHA’s chief medical officer for prevention, said in the news release.
“These results validate why the American Heart Association’s National Hypertension Control Initiative (NHCI) is critically important,” he said.
“With a particular emphasis on historically under-resourced communities in the United States, the comprehensive program supports health care teams at community health centers through regular blood pressure management training; technical assistance and resources that include the proper blood pressure measurement technique; self-measured blood pressure monitoring and management; medication adherence; and healthy lifestyle services,” Dr. Sanchez noted.
The study had no specific funding. Dr. Laffin is a paid consultant for Medtronic and medical advisor for LucidAct Health.
A version of this article first appeared on Medscape.com.
Blood pressure control declined in both men and women with the onset of the COVID-19 pandemic in the United States in 2020, especially among women and older adults, according to a new analysis.
“We know that even small rises in blood pressure increase one’s risk of stroke and other adverse cardiovascular disease events,” lead author Luke J. Laffin, MD, codirector, Center for Blood Pressure Disorders, Cleveland Clinic, Ohio, said in a news release.
The researchers say increases in systolic BP among U.S. adults during the COVID-19 pandemic “could signal a forthcoming increase in incident cardiovascular disease mortality.”
Their study was published online Dec. 6 in Circulation.
Dr. Laffin and colleagues analyzed BP data from 464,585 U.S. adults (mean age, 46, 54% women) who had their BP measured as part of employee health screening annually from 2018 through 2020.
They found that BP levels went up between April and Dec. of 2020 – around the same time stay-at-home orders and other restrictions were put in place.
During this pandemic period, average monthly increases in BP ranged from 1.10 to 2.50 mm Hg higher for systolic BP and 0.14 to 0.53 mm Hg higher for diastolic BP, compared with the prepandemic period of April to Dec. 2019.
Increases in systolic and diastolic BP were seen among men and women and across age groups. Larger increases were evident in women for both systolic and diastolic BP: in older individuals for systolic BP and in younger individuals for diastolic BP (all P < .0001).
Dr. Laffin and colleagues also assessed changes in BP category based on current American Heart Association blood pressure guidelines (normal, elevated, stage 1, or stage 2 hypertension).
During the pandemic, more adults (26.8%) were recategorized to a higher BP category, whereas only 22% moved to a lower BP category, compared with before the pandemic.
“At the start of the pandemic, most people were not taking good care of themselves. Increases in blood pressure were likely related to changes in eating habits, increased alcohol consumption, less physical activity, decreased medication adherence, more emotional stress, and poor sleep,” Dr. Laffin said.
However, the increases in BP during the pandemic could not be explained by weight gain, the researchers note, because the observed changes in weight during the pandemic were similar to the prepandemic period among 86% of adults completing weight data.
The study authors are following up on these results to determine if this trend continued in 2021.
“Unfortunately, this research confirms what is being seen across the country – the COVID-19 pandemic has had and will continue to have long-reaching health impacts across the country and particularly related to uncontrolled hypertension,” Eduardo Sanchez, MD, MPH, the AHA’s chief medical officer for prevention, said in the news release.
“These results validate why the American Heart Association’s National Hypertension Control Initiative (NHCI) is critically important,” he said.
“With a particular emphasis on historically under-resourced communities in the United States, the comprehensive program supports health care teams at community health centers through regular blood pressure management training; technical assistance and resources that include the proper blood pressure measurement technique; self-measured blood pressure monitoring and management; medication adherence; and healthy lifestyle services,” Dr. Sanchez noted.
The study had no specific funding. Dr. Laffin is a paid consultant for Medtronic and medical advisor for LucidAct Health.
A version of this article first appeared on Medscape.com.
Metabolites implicated in CHD development in African Americans
Selected metabolic biomarkers may influence disease risk and progression in African American and White persons in different ways, a cohort study of the landmark Jackson Heart Study has found.
The investigators identified 22 specific metabolites that seem to influence incident CHD risk in African American patients – 13 metabolites that were also replicated in a multiethnic population and 9 novel metabolites that include N-acylamides and leucine, a branched-chain amino acid.
“To our knowledge, this is the first time that an N-acylamide as a class of molecule has been shown to be associated with incident coronary heart disease,” lead study author Daniel E. Cruz, MD, an instructor at Harvard Medical School in the division of cardiovascular medicine at Beth Israel Deaconess Medical Center in Boston, said in an interview.
The researchers analyzed targeted plasma metabolomic profiles of 2,346 participants in the Jackson Heart Study, a prospective population-based cohort study in the Mississippi city that included 5,306 African American patients evaluated over 15 years. They then performed a replication analysis of CHD-associated metabolites among 1,588 multiethnic participants in the Women’s Health Initiative, another population-based cohort study that included 161,808 postmenopausal women, also over 15 years. In all, the study, published in JAMA Cardiology, identified 46 metabolites that were associated with incident CHD up to 16 years before the incident event
Dr. Cruz said the “most interesting” findings were the roles of the N-acylamide linoleoyl ethanolamide and leucine. The former is of interest “because it is a lipid-signaling molecule that has been shown to have anti-inflammatory effects on macrophages; the influence and effects on macrophages are of particular interest because of macrophages’ central role in atherosclerosis and coronary heart disease,” he said.
Leucine draws interest because, in this study population, it was linked to a reduced risk of incident CHD. The researchers cited four previous studies in predominantly non-Hispanic White populations that found no association between branched-chain amino acids and incident CHD in Circulation, Stroke Circulation: Genomic and Precision Medicine, and Atherosclerosis. Other branched-amino acids included in the analysis trended toward a decreased risk of CHD, but those didn’t achieve the same statistical significance as that of leucine, Dr. Cruz said.
“In some of the analyses we did, there was a subset of metabolites that the associations with CHD appeared to be different between self-identified African Americans in the Jackson cohort vs. self-identified non-Hispanic Whites, and leucine was one of them,” Dr. Cruz said.
He emphasized that this study “is not a genetic analysis” because the participants self-identified their race. “So our next step is to figure out why this difference appears between these self-identified groups,” Dr. Cruz said. “We suspect environmental factors play a role – psychological stress, diet, income level, to name a few – but we are also interested to see if there are genetic causes.”
The results “are not clinically applicable,” Dr. Cruz said, but they do point to a need for more ethnically and racially diverse study populations. “The big picture is that, before we go implementing novel biomarkers into clinical practice, we need to make sure that they are accurate across different populations of people,” he said. “The only way to do this is to study different groups with the same rigor and vigor and thoughtfulness as any other group.”
These findings fall in line with other studies that found other nonmetabolomic biomarkers have countervailing effects on CHD risk in African Americans and non-Hispanic Whites, said Christie M. Ballantyne, MD, chief of cardiology at Baylor College of Medicine in Houston. For example, African Americans have been found to have lower triglyceride and HDL cholesterol levels than those of Whites.
The study “points out that there may be important biological differences in the metabolic pathways and abnormalities in the development of CHD between races,” Dr. Ballantyne said. “This further emphasizes both the importance and challenge of testing therapies in multiple racial/ethnic groups and with more even representation between men and women.”
Combining metabolomic profiling along with other biomarkers and possibly genetics may be helpful to “personalize” therapies in the future, he added.
Dr. Cruz and Dr. Ballantyne have no relevant relationships to disclose.
Selected metabolic biomarkers may influence disease risk and progression in African American and White persons in different ways, a cohort study of the landmark Jackson Heart Study has found.
The investigators identified 22 specific metabolites that seem to influence incident CHD risk in African American patients – 13 metabolites that were also replicated in a multiethnic population and 9 novel metabolites that include N-acylamides and leucine, a branched-chain amino acid.
“To our knowledge, this is the first time that an N-acylamide as a class of molecule has been shown to be associated with incident coronary heart disease,” lead study author Daniel E. Cruz, MD, an instructor at Harvard Medical School in the division of cardiovascular medicine at Beth Israel Deaconess Medical Center in Boston, said in an interview.
The researchers analyzed targeted plasma metabolomic profiles of 2,346 participants in the Jackson Heart Study, a prospective population-based cohort study in the Mississippi city that included 5,306 African American patients evaluated over 15 years. They then performed a replication analysis of CHD-associated metabolites among 1,588 multiethnic participants in the Women’s Health Initiative, another population-based cohort study that included 161,808 postmenopausal women, also over 15 years. In all, the study, published in JAMA Cardiology, identified 46 metabolites that were associated with incident CHD up to 16 years before the incident event
Dr. Cruz said the “most interesting” findings were the roles of the N-acylamide linoleoyl ethanolamide and leucine. The former is of interest “because it is a lipid-signaling molecule that has been shown to have anti-inflammatory effects on macrophages; the influence and effects on macrophages are of particular interest because of macrophages’ central role in atherosclerosis and coronary heart disease,” he said.
Leucine draws interest because, in this study population, it was linked to a reduced risk of incident CHD. The researchers cited four previous studies in predominantly non-Hispanic White populations that found no association between branched-chain amino acids and incident CHD in Circulation, Stroke Circulation: Genomic and Precision Medicine, and Atherosclerosis. Other branched-amino acids included in the analysis trended toward a decreased risk of CHD, but those didn’t achieve the same statistical significance as that of leucine, Dr. Cruz said.
“In some of the analyses we did, there was a subset of metabolites that the associations with CHD appeared to be different between self-identified African Americans in the Jackson cohort vs. self-identified non-Hispanic Whites, and leucine was one of them,” Dr. Cruz said.
He emphasized that this study “is not a genetic analysis” because the participants self-identified their race. “So our next step is to figure out why this difference appears between these self-identified groups,” Dr. Cruz said. “We suspect environmental factors play a role – psychological stress, diet, income level, to name a few – but we are also interested to see if there are genetic causes.”
The results “are not clinically applicable,” Dr. Cruz said, but they do point to a need for more ethnically and racially diverse study populations. “The big picture is that, before we go implementing novel biomarkers into clinical practice, we need to make sure that they are accurate across different populations of people,” he said. “The only way to do this is to study different groups with the same rigor and vigor and thoughtfulness as any other group.”
These findings fall in line with other studies that found other nonmetabolomic biomarkers have countervailing effects on CHD risk in African Americans and non-Hispanic Whites, said Christie M. Ballantyne, MD, chief of cardiology at Baylor College of Medicine in Houston. For example, African Americans have been found to have lower triglyceride and HDL cholesterol levels than those of Whites.
The study “points out that there may be important biological differences in the metabolic pathways and abnormalities in the development of CHD between races,” Dr. Ballantyne said. “This further emphasizes both the importance and challenge of testing therapies in multiple racial/ethnic groups and with more even representation between men and women.”
Combining metabolomic profiling along with other biomarkers and possibly genetics may be helpful to “personalize” therapies in the future, he added.
Dr. Cruz and Dr. Ballantyne have no relevant relationships to disclose.
Selected metabolic biomarkers may influence disease risk and progression in African American and White persons in different ways, a cohort study of the landmark Jackson Heart Study has found.
The investigators identified 22 specific metabolites that seem to influence incident CHD risk in African American patients – 13 metabolites that were also replicated in a multiethnic population and 9 novel metabolites that include N-acylamides and leucine, a branched-chain amino acid.
“To our knowledge, this is the first time that an N-acylamide as a class of molecule has been shown to be associated with incident coronary heart disease,” lead study author Daniel E. Cruz, MD, an instructor at Harvard Medical School in the division of cardiovascular medicine at Beth Israel Deaconess Medical Center in Boston, said in an interview.
The researchers analyzed targeted plasma metabolomic profiles of 2,346 participants in the Jackson Heart Study, a prospective population-based cohort study in the Mississippi city that included 5,306 African American patients evaluated over 15 years. They then performed a replication analysis of CHD-associated metabolites among 1,588 multiethnic participants in the Women’s Health Initiative, another population-based cohort study that included 161,808 postmenopausal women, also over 15 years. In all, the study, published in JAMA Cardiology, identified 46 metabolites that were associated with incident CHD up to 16 years before the incident event
Dr. Cruz said the “most interesting” findings were the roles of the N-acylamide linoleoyl ethanolamide and leucine. The former is of interest “because it is a lipid-signaling molecule that has been shown to have anti-inflammatory effects on macrophages; the influence and effects on macrophages are of particular interest because of macrophages’ central role in atherosclerosis and coronary heart disease,” he said.
Leucine draws interest because, in this study population, it was linked to a reduced risk of incident CHD. The researchers cited four previous studies in predominantly non-Hispanic White populations that found no association between branched-chain amino acids and incident CHD in Circulation, Stroke Circulation: Genomic and Precision Medicine, and Atherosclerosis. Other branched-amino acids included in the analysis trended toward a decreased risk of CHD, but those didn’t achieve the same statistical significance as that of leucine, Dr. Cruz said.
“In some of the analyses we did, there was a subset of metabolites that the associations with CHD appeared to be different between self-identified African Americans in the Jackson cohort vs. self-identified non-Hispanic Whites, and leucine was one of them,” Dr. Cruz said.
He emphasized that this study “is not a genetic analysis” because the participants self-identified their race. “So our next step is to figure out why this difference appears between these self-identified groups,” Dr. Cruz said. “We suspect environmental factors play a role – psychological stress, diet, income level, to name a few – but we are also interested to see if there are genetic causes.”
The results “are not clinically applicable,” Dr. Cruz said, but they do point to a need for more ethnically and racially diverse study populations. “The big picture is that, before we go implementing novel biomarkers into clinical practice, we need to make sure that they are accurate across different populations of people,” he said. “The only way to do this is to study different groups with the same rigor and vigor and thoughtfulness as any other group.”
These findings fall in line with other studies that found other nonmetabolomic biomarkers have countervailing effects on CHD risk in African Americans and non-Hispanic Whites, said Christie M. Ballantyne, MD, chief of cardiology at Baylor College of Medicine in Houston. For example, African Americans have been found to have lower triglyceride and HDL cholesterol levels than those of Whites.
The study “points out that there may be important biological differences in the metabolic pathways and abnormalities in the development of CHD between races,” Dr. Ballantyne said. “This further emphasizes both the importance and challenge of testing therapies in multiple racial/ethnic groups and with more even representation between men and women.”
Combining metabolomic profiling along with other biomarkers and possibly genetics may be helpful to “personalize” therapies in the future, he added.
Dr. Cruz and Dr. Ballantyne have no relevant relationships to disclose.
FROM JAMA CARDIOLOGY
Apixaban outmatches rivaroxaban for VTE in study
Recurrent venous thromboembolism (VTE) – a composite of pulmonary embolism and deep vein thrombosis – was the primary effectiveness outcome in the retrospective analysis of new-user data from almost 40,000 patients, which was published in Annals of Internal Medicine. Safety was evaluated through a composite of intracranial and gastrointestinal bleeding.
After a median follow-up of 102 days in the apixaban group and 105 days in the rivaroxaban group, apixaban demonstrated superiority for both primary outcomes.
These real-world findings may guide selection of initial anticoagulant therapy, reported lead author Ghadeer K. Dawwas, PhD, MSc, MBA, of the University of Pennsylvania, Philadelphia, and colleagues.
“Randomized clinical trials comparing apixaban with rivaroxaban in patients with VTE are under way (for example, COBRRA (NCT03266783),” the investigators wrote. “Until the results from these trials become available (The estimated completion date for COBRRA is December 2023.), observational studies that use existing data can provide evidence on the effectiveness and safety of these alternatives to inform clinical practice.”
In the new research, apixaban was associated with a 23% lower rate of recurrent VTE (hazard ratio, 0.77; 95% confidence interval, 0.69-0.87), including a 15% lower rate of deep vein thrombosis and a 41% lower rate of pulmonary embolism. Apixaban was associated with 40% fewer bleeding events (HR, 0.60; 95% CI, 0.53-0.69]), including a 40% lower rate of GI bleeding and a 46% lower rate of intracranial bleeding.
The study involved 37,236 patients with VTE, all of whom were diagnosed in at least one inpatient encounter and initiated direct oral anticoagulant (DOAC) therapy within 30 days, according to Optum’s deidentified Clinformatics Data Mart Database. Patients were evenly split into apixaban and rivaroxaban groups, with 18,618 individuals in each. Propensity score matching was used to minimize differences in baseline characteristics.
Apixaban was associated with an absolute reduction in recurrent VTE of 0.6% and 1.1% over 2 and 6 months, respectively, as well as reductions in bleeding of 1.1% and 1.5% over the same respective time periods.
The investigators noted that these findings were maintained in various sensitivity and subgroup analyses, including a model in which patients with VTE who had transient risk factors were compared with VTE patients exhibiting chronic risk factors.
“These findings suggest that apixaban has superior effectiveness and safety, compared with rivaroxaban and may provide guidance to clinicians and patients regarding selection of an anticoagulant for treatment of VTE,” Dr. Dawwas and colleagues concluded.
Study may have missed some nuance in possible outcomes, according to vascular surgeon
Thomas Wakefield, MD, a vascular surgeon and a professor of surgery at the University of Michigan Health Frankel Cardiovascular Center, Ann Arbor, generally agreed with the investigators’ conclusion, although he noted that DOAC selection may also be influenced by other considerations.
“The results of this study suggest that, when choosing an agent for an individual patient, apixaban does appear to have an advantage over rivaroxaban related to recurrent VTE and bleeding,” Dr. Wakefield said in an interview. “One must keep in mind that these are not the only factors that are considered when choosing an agent and these are not the only two DOACs available. For example, rivaroxaban is given once per day while apixaban is given twice per day, and rivaroxaban has been shown to be successful in the treatment of other thrombotic disorders.”
Dr. Wakefield also pointed out that the study may have missed some nuance in possible outcomes.
“The current study looked at severe outcomes that resulted in inpatient hospitalization, so the generalization to strictly outpatient treatment and less severe outcomes cannot be inferred,” he said.
Damon E. Houghton, MD, of the department of medicine and a consultant in the department of vascular medicine and hematology at Mayo Clinic, Rochester, Minn., called the study a “very nice analysis,” highlighting the large sample size.
“The results are not a reason to abandon rivaroxaban altogether, but do suggest that, when otherwise appropriate for a patient, apixaban should be the first choice,” Dr. Houghton said in a written comment. “Hopefully this analysis will encourage more payers to create financial incentives that facilitate the use of apixaban in more patients.”
Randomized trial needed, says hematologist
Colleen Edwards, MD, of the departments of medicine, hematology, and medical oncology, at the Icahn School of Medicine at Mount Sinai, New York, had a more guarded view of the findings than Dr. Wakefield and Dr. Houghton.
“[The investigators] certainly seem to be doing a lot of statistical gymnastics in this paper,” Dr. Edwards said in an interview. “They used all kinds of surrogates in place of real data that you would get from a randomized trial.”
For example, Dr. Edwards noted the use of prescription refills as a surrogate for medication adherence, and emphasized that inpatient observational data may not reflect outpatient therapy.
“Inpatients are constantly missing their medicines all the time,” she said. “They’re holding it for procedures, they’re NPO, they’re off the floor, so they missed their medicine. So it’s just a very different patient population than the outpatient population, which is where venous thromboembolism is treated now, by and large.”
Although Dr. Edwards suggested that the findings might guide treatment selection “a little bit,” she noted that insurance constraints and costs play a greater role, and ultimately concluded that a randomized trial is needed to materially alter clinical decision-making.
“I think we really have to wait for randomized trial before we abandon our other choices,” she said.
The investigators disclosed relationships with Merck, Celgene, UCB, and others. Dr. Wakefield reported awaiting disclosures. Dr. Houghton and Dr. Edwards reported no relevant conflicts of interest.
Recurrent venous thromboembolism (VTE) – a composite of pulmonary embolism and deep vein thrombosis – was the primary effectiveness outcome in the retrospective analysis of new-user data from almost 40,000 patients, which was published in Annals of Internal Medicine. Safety was evaluated through a composite of intracranial and gastrointestinal bleeding.
After a median follow-up of 102 days in the apixaban group and 105 days in the rivaroxaban group, apixaban demonstrated superiority for both primary outcomes.
These real-world findings may guide selection of initial anticoagulant therapy, reported lead author Ghadeer K. Dawwas, PhD, MSc, MBA, of the University of Pennsylvania, Philadelphia, and colleagues.
“Randomized clinical trials comparing apixaban with rivaroxaban in patients with VTE are under way (for example, COBRRA (NCT03266783),” the investigators wrote. “Until the results from these trials become available (The estimated completion date for COBRRA is December 2023.), observational studies that use existing data can provide evidence on the effectiveness and safety of these alternatives to inform clinical practice.”
In the new research, apixaban was associated with a 23% lower rate of recurrent VTE (hazard ratio, 0.77; 95% confidence interval, 0.69-0.87), including a 15% lower rate of deep vein thrombosis and a 41% lower rate of pulmonary embolism. Apixaban was associated with 40% fewer bleeding events (HR, 0.60; 95% CI, 0.53-0.69]), including a 40% lower rate of GI bleeding and a 46% lower rate of intracranial bleeding.
The study involved 37,236 patients with VTE, all of whom were diagnosed in at least one inpatient encounter and initiated direct oral anticoagulant (DOAC) therapy within 30 days, according to Optum’s deidentified Clinformatics Data Mart Database. Patients were evenly split into apixaban and rivaroxaban groups, with 18,618 individuals in each. Propensity score matching was used to minimize differences in baseline characteristics.
Apixaban was associated with an absolute reduction in recurrent VTE of 0.6% and 1.1% over 2 and 6 months, respectively, as well as reductions in bleeding of 1.1% and 1.5% over the same respective time periods.
The investigators noted that these findings were maintained in various sensitivity and subgroup analyses, including a model in which patients with VTE who had transient risk factors were compared with VTE patients exhibiting chronic risk factors.
“These findings suggest that apixaban has superior effectiveness and safety, compared with rivaroxaban and may provide guidance to clinicians and patients regarding selection of an anticoagulant for treatment of VTE,” Dr. Dawwas and colleagues concluded.
Study may have missed some nuance in possible outcomes, according to vascular surgeon
Thomas Wakefield, MD, a vascular surgeon and a professor of surgery at the University of Michigan Health Frankel Cardiovascular Center, Ann Arbor, generally agreed with the investigators’ conclusion, although he noted that DOAC selection may also be influenced by other considerations.
“The results of this study suggest that, when choosing an agent for an individual patient, apixaban does appear to have an advantage over rivaroxaban related to recurrent VTE and bleeding,” Dr. Wakefield said in an interview. “One must keep in mind that these are not the only factors that are considered when choosing an agent and these are not the only two DOACs available. For example, rivaroxaban is given once per day while apixaban is given twice per day, and rivaroxaban has been shown to be successful in the treatment of other thrombotic disorders.”
Dr. Wakefield also pointed out that the study may have missed some nuance in possible outcomes.
“The current study looked at severe outcomes that resulted in inpatient hospitalization, so the generalization to strictly outpatient treatment and less severe outcomes cannot be inferred,” he said.
Damon E. Houghton, MD, of the department of medicine and a consultant in the department of vascular medicine and hematology at Mayo Clinic, Rochester, Minn., called the study a “very nice analysis,” highlighting the large sample size.
“The results are not a reason to abandon rivaroxaban altogether, but do suggest that, when otherwise appropriate for a patient, apixaban should be the first choice,” Dr. Houghton said in a written comment. “Hopefully this analysis will encourage more payers to create financial incentives that facilitate the use of apixaban in more patients.”
Randomized trial needed, says hematologist
Colleen Edwards, MD, of the departments of medicine, hematology, and medical oncology, at the Icahn School of Medicine at Mount Sinai, New York, had a more guarded view of the findings than Dr. Wakefield and Dr. Houghton.
“[The investigators] certainly seem to be doing a lot of statistical gymnastics in this paper,” Dr. Edwards said in an interview. “They used all kinds of surrogates in place of real data that you would get from a randomized trial.”
For example, Dr. Edwards noted the use of prescription refills as a surrogate for medication adherence, and emphasized that inpatient observational data may not reflect outpatient therapy.
“Inpatients are constantly missing their medicines all the time,” she said. “They’re holding it for procedures, they’re NPO, they’re off the floor, so they missed their medicine. So it’s just a very different patient population than the outpatient population, which is where venous thromboembolism is treated now, by and large.”
Although Dr. Edwards suggested that the findings might guide treatment selection “a little bit,” she noted that insurance constraints and costs play a greater role, and ultimately concluded that a randomized trial is needed to materially alter clinical decision-making.
“I think we really have to wait for randomized trial before we abandon our other choices,” she said.
The investigators disclosed relationships with Merck, Celgene, UCB, and others. Dr. Wakefield reported awaiting disclosures. Dr. Houghton and Dr. Edwards reported no relevant conflicts of interest.
Recurrent venous thromboembolism (VTE) – a composite of pulmonary embolism and deep vein thrombosis – was the primary effectiveness outcome in the retrospective analysis of new-user data from almost 40,000 patients, which was published in Annals of Internal Medicine. Safety was evaluated through a composite of intracranial and gastrointestinal bleeding.
After a median follow-up of 102 days in the apixaban group and 105 days in the rivaroxaban group, apixaban demonstrated superiority for both primary outcomes.
These real-world findings may guide selection of initial anticoagulant therapy, reported lead author Ghadeer K. Dawwas, PhD, MSc, MBA, of the University of Pennsylvania, Philadelphia, and colleagues.
“Randomized clinical trials comparing apixaban with rivaroxaban in patients with VTE are under way (for example, COBRRA (NCT03266783),” the investigators wrote. “Until the results from these trials become available (The estimated completion date for COBRRA is December 2023.), observational studies that use existing data can provide evidence on the effectiveness and safety of these alternatives to inform clinical practice.”
In the new research, apixaban was associated with a 23% lower rate of recurrent VTE (hazard ratio, 0.77; 95% confidence interval, 0.69-0.87), including a 15% lower rate of deep vein thrombosis and a 41% lower rate of pulmonary embolism. Apixaban was associated with 40% fewer bleeding events (HR, 0.60; 95% CI, 0.53-0.69]), including a 40% lower rate of GI bleeding and a 46% lower rate of intracranial bleeding.
The study involved 37,236 patients with VTE, all of whom were diagnosed in at least one inpatient encounter and initiated direct oral anticoagulant (DOAC) therapy within 30 days, according to Optum’s deidentified Clinformatics Data Mart Database. Patients were evenly split into apixaban and rivaroxaban groups, with 18,618 individuals in each. Propensity score matching was used to minimize differences in baseline characteristics.
Apixaban was associated with an absolute reduction in recurrent VTE of 0.6% and 1.1% over 2 and 6 months, respectively, as well as reductions in bleeding of 1.1% and 1.5% over the same respective time periods.
The investigators noted that these findings were maintained in various sensitivity and subgroup analyses, including a model in which patients with VTE who had transient risk factors were compared with VTE patients exhibiting chronic risk factors.
“These findings suggest that apixaban has superior effectiveness and safety, compared with rivaroxaban and may provide guidance to clinicians and patients regarding selection of an anticoagulant for treatment of VTE,” Dr. Dawwas and colleagues concluded.
Study may have missed some nuance in possible outcomes, according to vascular surgeon
Thomas Wakefield, MD, a vascular surgeon and a professor of surgery at the University of Michigan Health Frankel Cardiovascular Center, Ann Arbor, generally agreed with the investigators’ conclusion, although he noted that DOAC selection may also be influenced by other considerations.
“The results of this study suggest that, when choosing an agent for an individual patient, apixaban does appear to have an advantage over rivaroxaban related to recurrent VTE and bleeding,” Dr. Wakefield said in an interview. “One must keep in mind that these are not the only factors that are considered when choosing an agent and these are not the only two DOACs available. For example, rivaroxaban is given once per day while apixaban is given twice per day, and rivaroxaban has been shown to be successful in the treatment of other thrombotic disorders.”
Dr. Wakefield also pointed out that the study may have missed some nuance in possible outcomes.
“The current study looked at severe outcomes that resulted in inpatient hospitalization, so the generalization to strictly outpatient treatment and less severe outcomes cannot be inferred,” he said.
Damon E. Houghton, MD, of the department of medicine and a consultant in the department of vascular medicine and hematology at Mayo Clinic, Rochester, Minn., called the study a “very nice analysis,” highlighting the large sample size.
“The results are not a reason to abandon rivaroxaban altogether, but do suggest that, when otherwise appropriate for a patient, apixaban should be the first choice,” Dr. Houghton said in a written comment. “Hopefully this analysis will encourage more payers to create financial incentives that facilitate the use of apixaban in more patients.”
Randomized trial needed, says hematologist
Colleen Edwards, MD, of the departments of medicine, hematology, and medical oncology, at the Icahn School of Medicine at Mount Sinai, New York, had a more guarded view of the findings than Dr. Wakefield and Dr. Houghton.
“[The investigators] certainly seem to be doing a lot of statistical gymnastics in this paper,” Dr. Edwards said in an interview. “They used all kinds of surrogates in place of real data that you would get from a randomized trial.”
For example, Dr. Edwards noted the use of prescription refills as a surrogate for medication adherence, and emphasized that inpatient observational data may not reflect outpatient therapy.
“Inpatients are constantly missing their medicines all the time,” she said. “They’re holding it for procedures, they’re NPO, they’re off the floor, so they missed their medicine. So it’s just a very different patient population than the outpatient population, which is where venous thromboembolism is treated now, by and large.”
Although Dr. Edwards suggested that the findings might guide treatment selection “a little bit,” she noted that insurance constraints and costs play a greater role, and ultimately concluded that a randomized trial is needed to materially alter clinical decision-making.
“I think we really have to wait for randomized trial before we abandon our other choices,” she said.
The investigators disclosed relationships with Merck, Celgene, UCB, and others. Dr. Wakefield reported awaiting disclosures. Dr. Houghton and Dr. Edwards reported no relevant conflicts of interest.
FROM ANNALS OF INTERNAL MEDICINE
Care via video teleconferencing can be as effective as in-person for some conditions
This was a finding of a new study published in Annals of Internal Medicine involving a review of literature on video teleconferencing (VTC) visits, which was authored by Jordan Albritton, PhD, MPH and his colleagues.
The authors found generally comparable patient outcomes as well as no differences in health care use, patient satisfaction, and quality of life when visits conducted using VTC were compared with usual care.
While VTC may work best for monitoring patients with chronic conditions, it can also be effective for acute care, said Dr. Albritton, who is a research public health analyst at RTI International in Research Triangle Park, N.C., in an interview.
The investigators analyzed 20 randomized controlled trials of at least 50 patients and acceptable risk of bias in which VTC was used either for main or adjunct care delivery. Published from 2013 to 2019, these studies looked at care for diabetes and pain management, as well as some respiratory, neurologic, and cardiovascular conditions. Studies comparing VTC with usual care that did not involve any added in-person care were more likely to favor the VTC group, the investigators found.
“We excluded conditions such as substance use disorders, maternal care, and weight management for which there was sufficient prior evidence of the benefit of VTC,” Dr. Albritton said in an interview. “But I don’t think our results would have been substantially different if we had included these other diseases. We found general evidence in the literature that VTC is effective for a broader range of conditions.”
In some cases, such as if changes in a patient’s condition triggered an automatic virtual visit, the author said he thinks VTC may lead to even greater effectiveness.
“The doctor and patient could figure out on the spot what’s going on and perhaps change the medication,” Dr. Albritton explained.
In general agreement is Julia L. Frydman, MD, assistant professor in the Brookdale Department of Geriatric and Palliative Medicine at Icahn School of Medicine at Mount Sinai in New York, who was not involved in the RTI research.
“Telemedicine has promise across many medical subspecialties, and what we need now are more studies to understand the perspectives of patients, caregivers, and clinicians as well as the impact of telemedicine on health outcomes and healthcare utilization.”
In acknowledgment of their utility, video visits are on the rise in the United States. A 2020 survey found that 22% of patients and 80% of physicians reported having participated in a video visit, three times the rate of the previous year. The authors noted that policy changes enacted to support telehealth strategies during the pandemic are expected to remain in place, and although patients are returning to in-person care, the virtual visit market will likely continue growing.
Increased telemedicine use by older adults
“We’ve seen an exciting expansion of telemedicine use among older adults, and we need to focus on continuing to meet their needs,” Dr. Frydman said.
In a recent study of televisits during the pandemic, Dr. Frydman’s group found a fivefold greater uptake of remote consultations by seniors – from 5% to 25%. Although in-person visits were far more common among older adults.
A specific advantage of video-based over audio-only telehealth, noted Dr. Albritton, is that physicians can directly observe patients in their home environment. Sharing that view is Deepa Iyengar, MBBS/MD,MPH, professor of family medicine at McGovern Medical School at The University of Texas Health Science Center at Houston, where, she said, “the pandemic has put VTC use into overdrive.”
According to Dr. Iyengar, who was not involved in the RTI research, the video component definitely represents value-added over phone calls. “You can pick up visual cues on video that you might not see if the patient came in and you can see what the home environment is like – whether there are a lot of loose rugs on the floor or broken or missing light bulbs,” she said in an interview.
‘VTC is here to stay’
In other parts of the country, doctors are finding virtual care useful – and more common. “VTC is here to stay, for sure – the horse is out of the barn,” said Cheryl L. Wilkes, MD, an internist at Northwestern Medicine and assistant professor of medicine at Northwestern University in Chicago. “The RTI study shows no harm from VTC and also shows it may even improve clinical outcomes.”
Video visits can also save patients high parking fees at clinics and spare the sick or elderly from having to hire caregivers to bring them into the office or from having to walk blocks in dangerous weather conditions, she added. “And I can do a virtual visit on the fly or at night when a relative or caregiver is home from work to be there with the patient.”
In addition to being beneficial for following up with patients with chronic diseases such as hypertension or diabetes, VTC may be able to replace some visits that have traditionally required hands-on care, said Dr. Wilkes.
She said she knows a cardiologist who has refined a process whereby a patient – say, one who may have edema – is asked to perform a maneuver via VTC and then display the result to the doctor: The doctor says, “put your leg up and press on it hard for 10 seconds and then show me what it looks like,” according to Dr. Wilkes.
The key now is to identify the best persons across specialties from neurology to rheumatology to videotape ways they’ve created to help their patients participate virtually in consults traditionally done at the office, Dr. Wilkes noted.
But some conditions will always require palpation and the use of a stethoscope, according Dr. Iyengar.
“If someone has an ulcer, I have to be able to feel it,” she said.
And while some maternity care can be given virtually – for instance, if a mother-to be develops a bad cold – hands-on obstetrical care to check the position and health of the baby obviously has to be done in person. “So VTC is definitely going to be a welcome addition but not a replacement,” Dr. Iyengar said.
Gaps in research on VTC visits
Many questions remain regarding the overall usefulness of VTC visits for certain patient groups, according to the authors.
They highlighted, for example, the dearth of data on subgroups or on underserved and vulnerable populations, with no head-to-head studies identified in their review. In addition, they found no studies examining VTC versus usual care for patients with concurrent conditions or on its effect on health equity and disparities.
“It’s now our job to understand the ongoing barriers to telemedicine access, including the digital divide and the usability of telemedicine platforms, and design interventions that overcome them,” Dr. Frydman said. “At the same time, we need to make sure we’re understanding and respecting the preferences of older adults in terms of how they access health care.”
This study was supported by the Patient-Centered Outcomes Research Institute (PCORI). Dr. Albritton is employed by RTI International, the contractor responsible for conducting the research and developing the manuscript. Several coauthors disclosed support from or contracts with PCORI. One coauthor’s spouse holds stock in private health companies. Dr. Frydman, Dr. Iyengar, and Dr. Wilkes disclosed no competing interests relevant to their comments.
This was a finding of a new study published in Annals of Internal Medicine involving a review of literature on video teleconferencing (VTC) visits, which was authored by Jordan Albritton, PhD, MPH and his colleagues.
The authors found generally comparable patient outcomes as well as no differences in health care use, patient satisfaction, and quality of life when visits conducted using VTC were compared with usual care.
While VTC may work best for monitoring patients with chronic conditions, it can also be effective for acute care, said Dr. Albritton, who is a research public health analyst at RTI International in Research Triangle Park, N.C., in an interview.
The investigators analyzed 20 randomized controlled trials of at least 50 patients and acceptable risk of bias in which VTC was used either for main or adjunct care delivery. Published from 2013 to 2019, these studies looked at care for diabetes and pain management, as well as some respiratory, neurologic, and cardiovascular conditions. Studies comparing VTC with usual care that did not involve any added in-person care were more likely to favor the VTC group, the investigators found.
“We excluded conditions such as substance use disorders, maternal care, and weight management for which there was sufficient prior evidence of the benefit of VTC,” Dr. Albritton said in an interview. “But I don’t think our results would have been substantially different if we had included these other diseases. We found general evidence in the literature that VTC is effective for a broader range of conditions.”
In some cases, such as if changes in a patient’s condition triggered an automatic virtual visit, the author said he thinks VTC may lead to even greater effectiveness.
“The doctor and patient could figure out on the spot what’s going on and perhaps change the medication,” Dr. Albritton explained.
In general agreement is Julia L. Frydman, MD, assistant professor in the Brookdale Department of Geriatric and Palliative Medicine at Icahn School of Medicine at Mount Sinai in New York, who was not involved in the RTI research.
“Telemedicine has promise across many medical subspecialties, and what we need now are more studies to understand the perspectives of patients, caregivers, and clinicians as well as the impact of telemedicine on health outcomes and healthcare utilization.”
In acknowledgment of their utility, video visits are on the rise in the United States. A 2020 survey found that 22% of patients and 80% of physicians reported having participated in a video visit, three times the rate of the previous year. The authors noted that policy changes enacted to support telehealth strategies during the pandemic are expected to remain in place, and although patients are returning to in-person care, the virtual visit market will likely continue growing.
Increased telemedicine use by older adults
“We’ve seen an exciting expansion of telemedicine use among older adults, and we need to focus on continuing to meet their needs,” Dr. Frydman said.
In a recent study of televisits during the pandemic, Dr. Frydman’s group found a fivefold greater uptake of remote consultations by seniors – from 5% to 25%. Although in-person visits were far more common among older adults.
A specific advantage of video-based over audio-only telehealth, noted Dr. Albritton, is that physicians can directly observe patients in their home environment. Sharing that view is Deepa Iyengar, MBBS/MD,MPH, professor of family medicine at McGovern Medical School at The University of Texas Health Science Center at Houston, where, she said, “the pandemic has put VTC use into overdrive.”
According to Dr. Iyengar, who was not involved in the RTI research, the video component definitely represents value-added over phone calls. “You can pick up visual cues on video that you might not see if the patient came in and you can see what the home environment is like – whether there are a lot of loose rugs on the floor or broken or missing light bulbs,” she said in an interview.
‘VTC is here to stay’
In other parts of the country, doctors are finding virtual care useful – and more common. “VTC is here to stay, for sure – the horse is out of the barn,” said Cheryl L. Wilkes, MD, an internist at Northwestern Medicine and assistant professor of medicine at Northwestern University in Chicago. “The RTI study shows no harm from VTC and also shows it may even improve clinical outcomes.”
Video visits can also save patients high parking fees at clinics and spare the sick or elderly from having to hire caregivers to bring them into the office or from having to walk blocks in dangerous weather conditions, she added. “And I can do a virtual visit on the fly or at night when a relative or caregiver is home from work to be there with the patient.”
In addition to being beneficial for following up with patients with chronic diseases such as hypertension or diabetes, VTC may be able to replace some visits that have traditionally required hands-on care, said Dr. Wilkes.
She said she knows a cardiologist who has refined a process whereby a patient – say, one who may have edema – is asked to perform a maneuver via VTC and then display the result to the doctor: The doctor says, “put your leg up and press on it hard for 10 seconds and then show me what it looks like,” according to Dr. Wilkes.
The key now is to identify the best persons across specialties from neurology to rheumatology to videotape ways they’ve created to help their patients participate virtually in consults traditionally done at the office, Dr. Wilkes noted.
But some conditions will always require palpation and the use of a stethoscope, according Dr. Iyengar.
“If someone has an ulcer, I have to be able to feel it,” she said.
And while some maternity care can be given virtually – for instance, if a mother-to be develops a bad cold – hands-on obstetrical care to check the position and health of the baby obviously has to be done in person. “So VTC is definitely going to be a welcome addition but not a replacement,” Dr. Iyengar said.
Gaps in research on VTC visits
Many questions remain regarding the overall usefulness of VTC visits for certain patient groups, according to the authors.
They highlighted, for example, the dearth of data on subgroups or on underserved and vulnerable populations, with no head-to-head studies identified in their review. In addition, they found no studies examining VTC versus usual care for patients with concurrent conditions or on its effect on health equity and disparities.
“It’s now our job to understand the ongoing barriers to telemedicine access, including the digital divide and the usability of telemedicine platforms, and design interventions that overcome them,” Dr. Frydman said. “At the same time, we need to make sure we’re understanding and respecting the preferences of older adults in terms of how they access health care.”
This study was supported by the Patient-Centered Outcomes Research Institute (PCORI). Dr. Albritton is employed by RTI International, the contractor responsible for conducting the research and developing the manuscript. Several coauthors disclosed support from or contracts with PCORI. One coauthor’s spouse holds stock in private health companies. Dr. Frydman, Dr. Iyengar, and Dr. Wilkes disclosed no competing interests relevant to their comments.
This was a finding of a new study published in Annals of Internal Medicine involving a review of literature on video teleconferencing (VTC) visits, which was authored by Jordan Albritton, PhD, MPH and his colleagues.
The authors found generally comparable patient outcomes as well as no differences in health care use, patient satisfaction, and quality of life when visits conducted using VTC were compared with usual care.
While VTC may work best for monitoring patients with chronic conditions, it can also be effective for acute care, said Dr. Albritton, who is a research public health analyst at RTI International in Research Triangle Park, N.C., in an interview.
The investigators analyzed 20 randomized controlled trials of at least 50 patients and acceptable risk of bias in which VTC was used either for main or adjunct care delivery. Published from 2013 to 2019, these studies looked at care for diabetes and pain management, as well as some respiratory, neurologic, and cardiovascular conditions. Studies comparing VTC with usual care that did not involve any added in-person care were more likely to favor the VTC group, the investigators found.
“We excluded conditions such as substance use disorders, maternal care, and weight management for which there was sufficient prior evidence of the benefit of VTC,” Dr. Albritton said in an interview. “But I don’t think our results would have been substantially different if we had included these other diseases. We found general evidence in the literature that VTC is effective for a broader range of conditions.”
In some cases, such as if changes in a patient’s condition triggered an automatic virtual visit, the author said he thinks VTC may lead to even greater effectiveness.
“The doctor and patient could figure out on the spot what’s going on and perhaps change the medication,” Dr. Albritton explained.
In general agreement is Julia L. Frydman, MD, assistant professor in the Brookdale Department of Geriatric and Palliative Medicine at Icahn School of Medicine at Mount Sinai in New York, who was not involved in the RTI research.
“Telemedicine has promise across many medical subspecialties, and what we need now are more studies to understand the perspectives of patients, caregivers, and clinicians as well as the impact of telemedicine on health outcomes and healthcare utilization.”
In acknowledgment of their utility, video visits are on the rise in the United States. A 2020 survey found that 22% of patients and 80% of physicians reported having participated in a video visit, three times the rate of the previous year. The authors noted that policy changes enacted to support telehealth strategies during the pandemic are expected to remain in place, and although patients are returning to in-person care, the virtual visit market will likely continue growing.
Increased telemedicine use by older adults
“We’ve seen an exciting expansion of telemedicine use among older adults, and we need to focus on continuing to meet their needs,” Dr. Frydman said.
In a recent study of televisits during the pandemic, Dr. Frydman’s group found a fivefold greater uptake of remote consultations by seniors – from 5% to 25%. Although in-person visits were far more common among older adults.
A specific advantage of video-based over audio-only telehealth, noted Dr. Albritton, is that physicians can directly observe patients in their home environment. Sharing that view is Deepa Iyengar, MBBS/MD,MPH, professor of family medicine at McGovern Medical School at The University of Texas Health Science Center at Houston, where, she said, “the pandemic has put VTC use into overdrive.”
According to Dr. Iyengar, who was not involved in the RTI research, the video component definitely represents value-added over phone calls. “You can pick up visual cues on video that you might not see if the patient came in and you can see what the home environment is like – whether there are a lot of loose rugs on the floor or broken or missing light bulbs,” she said in an interview.
‘VTC is here to stay’
In other parts of the country, doctors are finding virtual care useful – and more common. “VTC is here to stay, for sure – the horse is out of the barn,” said Cheryl L. Wilkes, MD, an internist at Northwestern Medicine and assistant professor of medicine at Northwestern University in Chicago. “The RTI study shows no harm from VTC and also shows it may even improve clinical outcomes.”
Video visits can also save patients high parking fees at clinics and spare the sick or elderly from having to hire caregivers to bring them into the office or from having to walk blocks in dangerous weather conditions, she added. “And I can do a virtual visit on the fly or at night when a relative or caregiver is home from work to be there with the patient.”
In addition to being beneficial for following up with patients with chronic diseases such as hypertension or diabetes, VTC may be able to replace some visits that have traditionally required hands-on care, said Dr. Wilkes.
She said she knows a cardiologist who has refined a process whereby a patient – say, one who may have edema – is asked to perform a maneuver via VTC and then display the result to the doctor: The doctor says, “put your leg up and press on it hard for 10 seconds and then show me what it looks like,” according to Dr. Wilkes.
The key now is to identify the best persons across specialties from neurology to rheumatology to videotape ways they’ve created to help their patients participate virtually in consults traditionally done at the office, Dr. Wilkes noted.
But some conditions will always require palpation and the use of a stethoscope, according Dr. Iyengar.
“If someone has an ulcer, I have to be able to feel it,” she said.
And while some maternity care can be given virtually – for instance, if a mother-to be develops a bad cold – hands-on obstetrical care to check the position and health of the baby obviously has to be done in person. “So VTC is definitely going to be a welcome addition but not a replacement,” Dr. Iyengar said.
Gaps in research on VTC visits
Many questions remain regarding the overall usefulness of VTC visits for certain patient groups, according to the authors.
They highlighted, for example, the dearth of data on subgroups or on underserved and vulnerable populations, with no head-to-head studies identified in their review. In addition, they found no studies examining VTC versus usual care for patients with concurrent conditions or on its effect on health equity and disparities.
“It’s now our job to understand the ongoing barriers to telemedicine access, including the digital divide and the usability of telemedicine platforms, and design interventions that overcome them,” Dr. Frydman said. “At the same time, we need to make sure we’re understanding and respecting the preferences of older adults in terms of how they access health care.”
This study was supported by the Patient-Centered Outcomes Research Institute (PCORI). Dr. Albritton is employed by RTI International, the contractor responsible for conducting the research and developing the manuscript. Several coauthors disclosed support from or contracts with PCORI. One coauthor’s spouse holds stock in private health companies. Dr. Frydman, Dr. Iyengar, and Dr. Wilkes disclosed no competing interests relevant to their comments.
FROM ANNALS OF INTERNAL MEDICINE
No serious CV risks for elderly after Pfizer COVID-19 vaccine
A French population-based study provides further evidence that the BNT162b2 Pfizer-BioNTech mRNA COVID-19 vaccine does not increase the short-term risk for serious cardiovascular adverse events in older people.
The study showed no increased risk of myocardial infarction (MI), stroke, or pulmonary embolism (PE) following vaccination in adults aged 75 years or older in the 14 days following vaccination.
“These findings regarding the BNT162b2 vaccine’s short-term cardiovascular safety profile in older people are reassuring. They should be taken into account by doctors when considering implementing a third dose of the vaccine in older people,” Marie Joelle Jabagi, PharmD, PhD, with the French National Agency for Medicines and Health Products Safety, Saint-Denis, France, said in an interview.
The study was published as a research letter online Nov. 22 in JAMA.
The Pfizer-BioNTech mRNA vaccine was the first SARS-CoV-2 vaccine authorized in France and has been widely used in older people. The phase 3 trials of the vaccine showed no increase in cardiovascular events, but older people were underrepresented in the trials.
As of April 30, 2021, nearly 3.9 million French adults aged 75 or older had received at least one dose of the Pfizer COVID-19 vaccine and 3.2 million had received two doses.
Using the French National Health Data System linked to the national COVID-19 vaccination database, Dr. Jabagi and her colleagues identified all unvaccinated or vaccinated adults aged 75 and older who were hospitalized between Dec. 15, 2020, and April 30, 2021, for acute MI, hemorrhagic or ischemic stroke, or PE.
During the 4.5-month study period, 11,113 elderly were hospitalized for acute MI, 17,014 for ischemic stroke, 4,804 for hemorrhagic stroke, and 7,221 for PE. Of these, 58.6%, 54.0%, 42.7%, and 55.3%, respectively, had received at least one dose of vaccine.
In the 14 days following receipt of either dose, no significant increased risk was found for any outcome, the investigators report.
The relative incidence (RI) for MI after the first and second dose was 0.97 (95% CI, 0.88-1.06) and 1.04 (95% CI, 0.93-1.16), respectively.
For ischemic stroke, the RI was 0.90 after the first dose (95% CI, 0.84-0.98) and 0.92 (95% CI, 0.84-1.02) after the second; for hemorrhagic stroke, the RI was 0.90 (95% CI, 0.78-1.04) and 0.97 (95% CI, 0.81-1.15), respectively.
For PE, the RI was 0.85 (95% CI, 0.75-0.96) after the first dose and 1.10 (95% CI, 0.95-1.26) after the second dose.
There was also no significant increase for any of the cardiovascular events when the exposure risk window was subdivided into 1 to 7 days and 8 to 14 days.
“Evaluating the short-term risk of hospitalization for severe cardiovascular events after the BNT162b2 mRNA vaccine in older people was a priority, especially after signals for hypertension and cardiovascular, thromboembolic, and hemorrhagic events have been issued from spontaneous notification data,” Dr. Jabagi said in an interview.
“The results of this nationwide study provide further solid evidence regarding the lack of increase of serious cardiovascular adverse events in older people in the 14 days following both doses of the vaccine,” Dr. Jabagi said.
The French study supports a recent U.S. study of more than 6 million people demonstrating that serious health risks were no more common in the first 3 weeks after Pfizer/BioNTech or Moderna COVID-19 vaccination compared with 22 to 42 days later.
As previously reported by this news organization, mRNA vaccination was not associated with greater risks for Guillain-Barré syndrome, myocarditis/pericarditis, stroke, or 20 other serious outcomes.
The current study had no specific funding. Dr. Jabagi and colleagues have declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
A French population-based study provides further evidence that the BNT162b2 Pfizer-BioNTech mRNA COVID-19 vaccine does not increase the short-term risk for serious cardiovascular adverse events in older people.
The study showed no increased risk of myocardial infarction (MI), stroke, or pulmonary embolism (PE) following vaccination in adults aged 75 years or older in the 14 days following vaccination.
“These findings regarding the BNT162b2 vaccine’s short-term cardiovascular safety profile in older people are reassuring. They should be taken into account by doctors when considering implementing a third dose of the vaccine in older people,” Marie Joelle Jabagi, PharmD, PhD, with the French National Agency for Medicines and Health Products Safety, Saint-Denis, France, said in an interview.
The study was published as a research letter online Nov. 22 in JAMA.
The Pfizer-BioNTech mRNA vaccine was the first SARS-CoV-2 vaccine authorized in France and has been widely used in older people. The phase 3 trials of the vaccine showed no increase in cardiovascular events, but older people were underrepresented in the trials.
As of April 30, 2021, nearly 3.9 million French adults aged 75 or older had received at least one dose of the Pfizer COVID-19 vaccine and 3.2 million had received two doses.
Using the French National Health Data System linked to the national COVID-19 vaccination database, Dr. Jabagi and her colleagues identified all unvaccinated or vaccinated adults aged 75 and older who were hospitalized between Dec. 15, 2020, and April 30, 2021, for acute MI, hemorrhagic or ischemic stroke, or PE.
During the 4.5-month study period, 11,113 elderly were hospitalized for acute MI, 17,014 for ischemic stroke, 4,804 for hemorrhagic stroke, and 7,221 for PE. Of these, 58.6%, 54.0%, 42.7%, and 55.3%, respectively, had received at least one dose of vaccine.
In the 14 days following receipt of either dose, no significant increased risk was found for any outcome, the investigators report.
The relative incidence (RI) for MI after the first and second dose was 0.97 (95% CI, 0.88-1.06) and 1.04 (95% CI, 0.93-1.16), respectively.
For ischemic stroke, the RI was 0.90 after the first dose (95% CI, 0.84-0.98) and 0.92 (95% CI, 0.84-1.02) after the second; for hemorrhagic stroke, the RI was 0.90 (95% CI, 0.78-1.04) and 0.97 (95% CI, 0.81-1.15), respectively.
For PE, the RI was 0.85 (95% CI, 0.75-0.96) after the first dose and 1.10 (95% CI, 0.95-1.26) after the second dose.
There was also no significant increase for any of the cardiovascular events when the exposure risk window was subdivided into 1 to 7 days and 8 to 14 days.
“Evaluating the short-term risk of hospitalization for severe cardiovascular events after the BNT162b2 mRNA vaccine in older people was a priority, especially after signals for hypertension and cardiovascular, thromboembolic, and hemorrhagic events have been issued from spontaneous notification data,” Dr. Jabagi said in an interview.
“The results of this nationwide study provide further solid evidence regarding the lack of increase of serious cardiovascular adverse events in older people in the 14 days following both doses of the vaccine,” Dr. Jabagi said.
The French study supports a recent U.S. study of more than 6 million people demonstrating that serious health risks were no more common in the first 3 weeks after Pfizer/BioNTech or Moderna COVID-19 vaccination compared with 22 to 42 days later.
As previously reported by this news organization, mRNA vaccination was not associated with greater risks for Guillain-Barré syndrome, myocarditis/pericarditis, stroke, or 20 other serious outcomes.
The current study had no specific funding. Dr. Jabagi and colleagues have declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
A French population-based study provides further evidence that the BNT162b2 Pfizer-BioNTech mRNA COVID-19 vaccine does not increase the short-term risk for serious cardiovascular adverse events in older people.
The study showed no increased risk of myocardial infarction (MI), stroke, or pulmonary embolism (PE) following vaccination in adults aged 75 years or older in the 14 days following vaccination.
“These findings regarding the BNT162b2 vaccine’s short-term cardiovascular safety profile in older people are reassuring. They should be taken into account by doctors when considering implementing a third dose of the vaccine in older people,” Marie Joelle Jabagi, PharmD, PhD, with the French National Agency for Medicines and Health Products Safety, Saint-Denis, France, said in an interview.
The study was published as a research letter online Nov. 22 in JAMA.
The Pfizer-BioNTech mRNA vaccine was the first SARS-CoV-2 vaccine authorized in France and has been widely used in older people. The phase 3 trials of the vaccine showed no increase in cardiovascular events, but older people were underrepresented in the trials.
As of April 30, 2021, nearly 3.9 million French adults aged 75 or older had received at least one dose of the Pfizer COVID-19 vaccine and 3.2 million had received two doses.
Using the French National Health Data System linked to the national COVID-19 vaccination database, Dr. Jabagi and her colleagues identified all unvaccinated or vaccinated adults aged 75 and older who were hospitalized between Dec. 15, 2020, and April 30, 2021, for acute MI, hemorrhagic or ischemic stroke, or PE.
During the 4.5-month study period, 11,113 elderly were hospitalized for acute MI, 17,014 for ischemic stroke, 4,804 for hemorrhagic stroke, and 7,221 for PE. Of these, 58.6%, 54.0%, 42.7%, and 55.3%, respectively, had received at least one dose of vaccine.
In the 14 days following receipt of either dose, no significant increased risk was found for any outcome, the investigators report.
The relative incidence (RI) for MI after the first and second dose was 0.97 (95% CI, 0.88-1.06) and 1.04 (95% CI, 0.93-1.16), respectively.
For ischemic stroke, the RI was 0.90 after the first dose (95% CI, 0.84-0.98) and 0.92 (95% CI, 0.84-1.02) after the second; for hemorrhagic stroke, the RI was 0.90 (95% CI, 0.78-1.04) and 0.97 (95% CI, 0.81-1.15), respectively.
For PE, the RI was 0.85 (95% CI, 0.75-0.96) after the first dose and 1.10 (95% CI, 0.95-1.26) after the second dose.
There was also no significant increase for any of the cardiovascular events when the exposure risk window was subdivided into 1 to 7 days and 8 to 14 days.
“Evaluating the short-term risk of hospitalization for severe cardiovascular events after the BNT162b2 mRNA vaccine in older people was a priority, especially after signals for hypertension and cardiovascular, thromboembolic, and hemorrhagic events have been issued from spontaneous notification data,” Dr. Jabagi said in an interview.
“The results of this nationwide study provide further solid evidence regarding the lack of increase of serious cardiovascular adverse events in older people in the 14 days following both doses of the vaccine,” Dr. Jabagi said.
The French study supports a recent U.S. study of more than 6 million people demonstrating that serious health risks were no more common in the first 3 weeks after Pfizer/BioNTech or Moderna COVID-19 vaccination compared with 22 to 42 days later.
As previously reported by this news organization, mRNA vaccination was not associated with greater risks for Guillain-Barré syndrome, myocarditis/pericarditis, stroke, or 20 other serious outcomes.
The current study had no specific funding. Dr. Jabagi and colleagues have declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
AHA statement on impact of major life events on physical activity
Physical activity levels may decline during major life events, and it’s important for health care professionals to encourage patients to maintain regular physical activity during times of significant changes in their lives, the American Heart Association says in a new scientific statement.
With this statement, “We hope health care providers, public health workers, and individuals understand that a major life change can lead to decreases in physical activity or increases in sedentary behavior,” writing group chair Abbi D. Lane-Cordova, PhD, said in an interview.
The statement includes “tips for screening for physical activity and talking to people about their activity during these big life events and resources that can be used by health care providers to help people achieve healthy levels of physical activity,” said Dr. Lane-Cordova, assistant professor in exercise science, Arnold School of Public Health, University of South Carolina, Columbia.
The statement was published online Dec. 1 in the journal Circulation.
The AHA Committee on Physical Activity, part of the organization’s Council on Lifestyle and Cardiometabolic Health, began discussing this topic back in 2019, Dr. Lane-Cordova explained.
“We spoke as a group about how much activity levels can change when something big happens in life, like becoming a parent or retiring. The change in activity behavior (physical activity or sedentary behavior) is important because these activity behaviors can influence heart health,” she said.
The group started work on the scientific statement in early 2020 – “and then the pandemic hit, and it seemed more important than ever to create awareness and a resource for people to help improve, or at least maintain, favorable activity behaviors when there’s a profound change or event in life,” Dr. Lane-Cordova said.
Some more vulnerable than others
The writing group examined data on 17 different life events or transitions and found evidence that physical activity levels may decline during nine events: beginning a new school (elementary, middle, high school, or college); a first job or career change; a marriage or civil union; pregnancy; parenting; retirement; or moving into a long-term care facility.
The authors also identified individuals who may be particularly susceptible to lower levels of physical activity in general and during important life events. They include those with lower levels of education; those who live alone; those who lack access to a safe outdoor space; Black Americans; some members of the LGBTQ+ community; and women who are pregnant and new parents.
They offer practical strategies for health care professionals to support routine physical activity levels during major life events and transitions. These include asking simple questions about how life transitions may be changing physical activity patterns and encouraging the use of wearable step trackers to monitor levels and changes.
“It’s important to maintain or improve physical activity when major life events happen, which is often a time when exercise is most needed,” Dr. Lane-Cordova said in a news release.
“Clinicians should express compassion as they ask about life transitions and initiate conversations about physical activity during life events and transitions,” the writing group advises.
The group also says its important “to look beyond the health care setting and engage organizations, communities, workplaces, faith-based communities, and assisted living facilities to promote physical activity.”
The statement provides a list of resources for individuals and health care professionals, many of which are free and online.
This research had no commercial funding. Members of the writing group have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Physical activity levels may decline during major life events, and it’s important for health care professionals to encourage patients to maintain regular physical activity during times of significant changes in their lives, the American Heart Association says in a new scientific statement.
With this statement, “We hope health care providers, public health workers, and individuals understand that a major life change can lead to decreases in physical activity or increases in sedentary behavior,” writing group chair Abbi D. Lane-Cordova, PhD, said in an interview.
The statement includes “tips for screening for physical activity and talking to people about their activity during these big life events and resources that can be used by health care providers to help people achieve healthy levels of physical activity,” said Dr. Lane-Cordova, assistant professor in exercise science, Arnold School of Public Health, University of South Carolina, Columbia.
The statement was published online Dec. 1 in the journal Circulation.
The AHA Committee on Physical Activity, part of the organization’s Council on Lifestyle and Cardiometabolic Health, began discussing this topic back in 2019, Dr. Lane-Cordova explained.
“We spoke as a group about how much activity levels can change when something big happens in life, like becoming a parent or retiring. The change in activity behavior (physical activity or sedentary behavior) is important because these activity behaviors can influence heart health,” she said.
The group started work on the scientific statement in early 2020 – “and then the pandemic hit, and it seemed more important than ever to create awareness and a resource for people to help improve, or at least maintain, favorable activity behaviors when there’s a profound change or event in life,” Dr. Lane-Cordova said.
Some more vulnerable than others
The writing group examined data on 17 different life events or transitions and found evidence that physical activity levels may decline during nine events: beginning a new school (elementary, middle, high school, or college); a first job or career change; a marriage or civil union; pregnancy; parenting; retirement; or moving into a long-term care facility.
The authors also identified individuals who may be particularly susceptible to lower levels of physical activity in general and during important life events. They include those with lower levels of education; those who live alone; those who lack access to a safe outdoor space; Black Americans; some members of the LGBTQ+ community; and women who are pregnant and new parents.
They offer practical strategies for health care professionals to support routine physical activity levels during major life events and transitions. These include asking simple questions about how life transitions may be changing physical activity patterns and encouraging the use of wearable step trackers to monitor levels and changes.
“It’s important to maintain or improve physical activity when major life events happen, which is often a time when exercise is most needed,” Dr. Lane-Cordova said in a news release.
“Clinicians should express compassion as they ask about life transitions and initiate conversations about physical activity during life events and transitions,” the writing group advises.
The group also says its important “to look beyond the health care setting and engage organizations, communities, workplaces, faith-based communities, and assisted living facilities to promote physical activity.”
The statement provides a list of resources for individuals and health care professionals, many of which are free and online.
This research had no commercial funding. Members of the writing group have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Physical activity levels may decline during major life events, and it’s important for health care professionals to encourage patients to maintain regular physical activity during times of significant changes in their lives, the American Heart Association says in a new scientific statement.
With this statement, “We hope health care providers, public health workers, and individuals understand that a major life change can lead to decreases in physical activity or increases in sedentary behavior,” writing group chair Abbi D. Lane-Cordova, PhD, said in an interview.
The statement includes “tips for screening for physical activity and talking to people about their activity during these big life events and resources that can be used by health care providers to help people achieve healthy levels of physical activity,” said Dr. Lane-Cordova, assistant professor in exercise science, Arnold School of Public Health, University of South Carolina, Columbia.
The statement was published online Dec. 1 in the journal Circulation.
The AHA Committee on Physical Activity, part of the organization’s Council on Lifestyle and Cardiometabolic Health, began discussing this topic back in 2019, Dr. Lane-Cordova explained.
“We spoke as a group about how much activity levels can change when something big happens in life, like becoming a parent or retiring. The change in activity behavior (physical activity or sedentary behavior) is important because these activity behaviors can influence heart health,” she said.
The group started work on the scientific statement in early 2020 – “and then the pandemic hit, and it seemed more important than ever to create awareness and a resource for people to help improve, or at least maintain, favorable activity behaviors when there’s a profound change or event in life,” Dr. Lane-Cordova said.
Some more vulnerable than others
The writing group examined data on 17 different life events or transitions and found evidence that physical activity levels may decline during nine events: beginning a new school (elementary, middle, high school, or college); a first job or career change; a marriage or civil union; pregnancy; parenting; retirement; or moving into a long-term care facility.
The authors also identified individuals who may be particularly susceptible to lower levels of physical activity in general and during important life events. They include those with lower levels of education; those who live alone; those who lack access to a safe outdoor space; Black Americans; some members of the LGBTQ+ community; and women who are pregnant and new parents.
They offer practical strategies for health care professionals to support routine physical activity levels during major life events and transitions. These include asking simple questions about how life transitions may be changing physical activity patterns and encouraging the use of wearable step trackers to monitor levels and changes.
“It’s important to maintain or improve physical activity when major life events happen, which is often a time when exercise is most needed,” Dr. Lane-Cordova said in a news release.
“Clinicians should express compassion as they ask about life transitions and initiate conversations about physical activity during life events and transitions,” the writing group advises.
The group also says its important “to look beyond the health care setting and engage organizations, communities, workplaces, faith-based communities, and assisted living facilities to promote physical activity.”
The statement provides a list of resources for individuals and health care professionals, many of which are free and online.
This research had no commercial funding. Members of the writing group have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.