User login
Catheter ablation of AFib improves quality of life more than medications do
Background: Catheter ablation of AFib (primarily pulmonary vein isolation) has been shown to result in better maintenance of sinus rhythm than medications. Small studies of QOL have shown mixed results. Larger trials were needed.
Study design: Open-label randomized multisite clinical trial of catheter ablation (pulmonary vein isolation with additional ablation procedure at the treating physician discretion) versus standard rate and/or rhythm control medications (chosen by clinician discretion). Patients were included for paroxysmal or persistent AFib and either age 65 years or older or age younger than 65 years with one additional stroke risk factor. Quality of life surveys – the Atrial Fibrillation Effect on Quality of Life (AFEQT) questionnaire and the Mayo AF-Specific Symptom Inventory (MAFSI) – were completed at baseline, and at 3, 12, 24, 36, 48, and 60 months.
Setting: 126 centers in 10 countries.
Synopsis: The study included 2,204 patients with median age of 68 years, diagnosed with AFib a median of 1.1 years prior, who were followed for a median of 48 months. The median CHA2DS2-VASc score was 3.0.
Self-reported AFib dropped from 86.0% to 21.1% in the ablation group and from 83.7% to 39.8% in the medication group at 12 months. The AFEQT score (range 0-100, higher score indicating better QOL) increased from 62.9 to 86.4 in the ablation group and increased from 63.1 to 80.9 in the medication group (for a mean difference of 5.3 points [95% confidence interval, 3.7-6.9; P less than .001] favoring ablation). MAFSI symptom frequency score and symptom severity score also showed improvement in symptoms favoring ablation. Post hoc subgroup analysis showed that those with the most severe symptoms had the largest benefit from ablation.
The primary limitation is the lack of patient blinding (may bias self-reported symptoms).
While the CABANA trial efficacy study (published separately) showed that catheter ablation results in no significant difference in the combined outcome of death, disabling stroke, serious bleeding, or cardiac arrest, the CABANA QOL study, reviewed here, shows that ablation does result in improved QOL and reduced symptoms, compared with medical therapy.
Bottom line: Catheter ablation of AFib can be done safely and successfully at experienced centers. In patients with AFib-related symptoms, ablation reduces symptoms and improves QOL somewhat more than medications do. The most severely symptomatic patients appear to obtain the most benefit.
Citation: Packer DL et al. Effect of catheter ablation vs. antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation: The CABANA Randomized Clinical Trial. JAMA. 2019 Mar 15. doi: 10.1001/jama.2019.0693.
Dr. Stafford is a hospitalist at Duke University Health System.
Background: Catheter ablation of AFib (primarily pulmonary vein isolation) has been shown to result in better maintenance of sinus rhythm than medications. Small studies of QOL have shown mixed results. Larger trials were needed.
Study design: Open-label randomized multisite clinical trial of catheter ablation (pulmonary vein isolation with additional ablation procedure at the treating physician discretion) versus standard rate and/or rhythm control medications (chosen by clinician discretion). Patients were included for paroxysmal or persistent AFib and either age 65 years or older or age younger than 65 years with one additional stroke risk factor. Quality of life surveys – the Atrial Fibrillation Effect on Quality of Life (AFEQT) questionnaire and the Mayo AF-Specific Symptom Inventory (MAFSI) – were completed at baseline, and at 3, 12, 24, 36, 48, and 60 months.
Setting: 126 centers in 10 countries.
Synopsis: The study included 2,204 patients with median age of 68 years, diagnosed with AFib a median of 1.1 years prior, who were followed for a median of 48 months. The median CHA2DS2-VASc score was 3.0.
Self-reported AFib dropped from 86.0% to 21.1% in the ablation group and from 83.7% to 39.8% in the medication group at 12 months. The AFEQT score (range 0-100, higher score indicating better QOL) increased from 62.9 to 86.4 in the ablation group and increased from 63.1 to 80.9 in the medication group (for a mean difference of 5.3 points [95% confidence interval, 3.7-6.9; P less than .001] favoring ablation). MAFSI symptom frequency score and symptom severity score also showed improvement in symptoms favoring ablation. Post hoc subgroup analysis showed that those with the most severe symptoms had the largest benefit from ablation.
The primary limitation is the lack of patient blinding (may bias self-reported symptoms).
While the CABANA trial efficacy study (published separately) showed that catheter ablation results in no significant difference in the combined outcome of death, disabling stroke, serious bleeding, or cardiac arrest, the CABANA QOL study, reviewed here, shows that ablation does result in improved QOL and reduced symptoms, compared with medical therapy.
Bottom line: Catheter ablation of AFib can be done safely and successfully at experienced centers. In patients with AFib-related symptoms, ablation reduces symptoms and improves QOL somewhat more than medications do. The most severely symptomatic patients appear to obtain the most benefit.
Citation: Packer DL et al. Effect of catheter ablation vs. antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation: The CABANA Randomized Clinical Trial. JAMA. 2019 Mar 15. doi: 10.1001/jama.2019.0693.
Dr. Stafford is a hospitalist at Duke University Health System.
Background: Catheter ablation of AFib (primarily pulmonary vein isolation) has been shown to result in better maintenance of sinus rhythm than medications. Small studies of QOL have shown mixed results. Larger trials were needed.
Study design: Open-label randomized multisite clinical trial of catheter ablation (pulmonary vein isolation with additional ablation procedure at the treating physician discretion) versus standard rate and/or rhythm control medications (chosen by clinician discretion). Patients were included for paroxysmal or persistent AFib and either age 65 years or older or age younger than 65 years with one additional stroke risk factor. Quality of life surveys – the Atrial Fibrillation Effect on Quality of Life (AFEQT) questionnaire and the Mayo AF-Specific Symptom Inventory (MAFSI) – were completed at baseline, and at 3, 12, 24, 36, 48, and 60 months.
Setting: 126 centers in 10 countries.
Synopsis: The study included 2,204 patients with median age of 68 years, diagnosed with AFib a median of 1.1 years prior, who were followed for a median of 48 months. The median CHA2DS2-VASc score was 3.0.
Self-reported AFib dropped from 86.0% to 21.1% in the ablation group and from 83.7% to 39.8% in the medication group at 12 months. The AFEQT score (range 0-100, higher score indicating better QOL) increased from 62.9 to 86.4 in the ablation group and increased from 63.1 to 80.9 in the medication group (for a mean difference of 5.3 points [95% confidence interval, 3.7-6.9; P less than .001] favoring ablation). MAFSI symptom frequency score and symptom severity score also showed improvement in symptoms favoring ablation. Post hoc subgroup analysis showed that those with the most severe symptoms had the largest benefit from ablation.
The primary limitation is the lack of patient blinding (may bias self-reported symptoms).
While the CABANA trial efficacy study (published separately) showed that catheter ablation results in no significant difference in the combined outcome of death, disabling stroke, serious bleeding, or cardiac arrest, the CABANA QOL study, reviewed here, shows that ablation does result in improved QOL and reduced symptoms, compared with medical therapy.
Bottom line: Catheter ablation of AFib can be done safely and successfully at experienced centers. In patients with AFib-related symptoms, ablation reduces symptoms and improves QOL somewhat more than medications do. The most severely symptomatic patients appear to obtain the most benefit.
Citation: Packer DL et al. Effect of catheter ablation vs. antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation: The CABANA Randomized Clinical Trial. JAMA. 2019 Mar 15. doi: 10.1001/jama.2019.0693.
Dr. Stafford is a hospitalist at Duke University Health System.
High-dose tafamidis boosts survival in transthyretin amyloidosis cardiomyopathy
Treatment with oral tafamidis at 80 mg/day provided a significantly greater survival benefit than dosing at 20 mg/day in patients with transthyretin amyloid cardiomyopathy in the long-term extension of the landmark ATTR-ACT trial, Thibaud Damy, MD, PhD, reported at the European Society of Cardiology Heart Failure Discoveries virtual meeting.
Moreover, the superior survival benefit achieved by taking four 20-mg capsules of tafamidis (Vyndaqel) once daily – or its more convenient once-daily, single-capsule, 61-mg bioequivalent formulation marketed as Vyndamax – came at no cost in terms of side effects and toxicity, compared with low-dose therapy for this progressive multisystem disease, according to Dr. Damy, professor of cardiology at the University of Paris and head of the French National Referral Center for Cardiac Amyloidosis at Henri Mondor University Hospital, Créteil, France.
“There are no side effects with tafamidis,” he said. “It doesn’t act on any receptors, it just acts on the formation of amyloid fibrils, so there are no side effects at whatever dosage is used. And in ATTR-ACT there was actually a trend towards increased side effects in the placebo group because the amyloidosis is everywhere, so by decreasing the amyloidosis process you improve not only the heart but all the organs, and the patient has a better quality of life.”
ATTR-ACT (Transthyretin Amyloidosis Cardiomyopathy Clinical Trial) was a phase 3, double-blind study in which 441 patients with transthyretin amyloidosis cardiomyopathy (TAC) in 13 countries were randomized to tafamidis at either 80 mg or 20 mg per day or placebo and followed prospectively for 30 months. At 30 months, all-cause mortality was 29.5% in patients who received tafamidis, compared with 42.9% in controls, for a statistically significant and clinically important 30% relative risk reduction, establishing tafamidis as the first disease-modifying therapy for this disease (N Engl J Med. 2018 Sep 13;379[11]:1007-16).
Patients in the 80-mg group had a 20% reduction in the risk of death, compared with the 20-mg group, at 30 months in an analysis adjusted for baseline age, 6-minute walk distance, and N-terminal pro-B-type natriuretic peptide, all of which are known to impact survival in TAC. This between-group survival difference wasn’t statistically significant, providing one impetus for the subsequent long-term extension study, in which patients remained on their original dose of tafamidis, and the controls who’d been on placebo for 30 months were randomized 2:1 to tafamidis at 80 mg or 20 mg per day.
The primary endpoint in the long-term extension was a composite of all-cause mortality, heart transplantation, or implantation of a ventricular assist device. At a median follow-up of 39 months since ATTR-ACT began, the high-dose tafamidis group had an adjusted 33% reduction in the risk of this endpoint, compared with patients on 20 mg per day, a difference that barely missed statistical significance. At that point, everyone in the long-term extension was switched to the once-daily 61-mg formulation of tafamidis free acid, which is bioequivalent to four 20-mg capsules of tafamidis.
Dr. Damy’s key message: At a median of 51 months of follow-up, the group originally on 80 mg of tafamidis displayed a highly significant adjusted 43% reduction in risk of the composite endpoint, compared with those who had been on 20 mg per day.
Session chair Petar M. Seferovic, MD, PhD, pronounced the ATTR-ACT trial and its long-term extension “a breakthrough advancement.”
“This is the first time in human medical history that we have a drug which improves the long-term outcome, including survival, in patients with this form of hypertrophic cardiomyopathy. So this is extremely important. It’s one of the major steps forward in the treatment of patients with myocardial disease,” said Dr. Seferovic, president of the European Society of Cardiology Heart Failure Association and professor of internal medicine at the University of Belgrade, Serbia.
Discussant Loreena Hill, PhD, of Queen’s University in Belfast, Northern Ireland, observed that TAC is a devastating disease with a formidable symptom burden and an average survival of just 2-5 years after diagnosis.
“It is often underdiagnosed, and yet it is estimated to account for up to 13% of patients with heart failure and preserved ejection fraction,” she said, adding that she considers the long-term extension results “extremely positive.”
Nailing down the prevalence of hereditary TAC: the DISCOVERY study
TAC occurs when transthyretin, a transport protein, becomes destabilized and misfolds, promoting deposition of amyloid fibrils in the myocardium and elsewhere. In the heart, the result is progressive ventricular wall thickening and stiffness, manifest as restrictive cardiomyopathy and progressive nonischemic heart failure. The cause of transthyretin destabilization can be either autosomal dominant inheritance of any of more than 100 pathogenic mutations in the transthyretin gene identified to date or a spontaneous wild-type protein.
Dr. Damy was a coinvestigator in the recently published multicenter DISCOVERY study, in which 1,001 patients with clinically suspected cardiac amyloidosis, the great majority of them from the United States, were screened for pathogenic transthyretin genetic mutations. The overall prevalence of such mutations was 8% in the American patients, with the Val122Ile mutation being identified in 11% of African Americans (Amyloid. 2020 May 26;1-8).
The prevalence of wild-type amyloidosis causing TAC hasn’t yet been studied with anything approaching the rigor of DISCOVERY, but the available evidence suggests the wild-type version is roughly as common as the hereditary forms.
Although DISCOVERY and other studies indicate that TAC is far more common than generally realized, Pfizer has priced Vyndaqel and Vyndamax as though TAC is a rare disease, with a U.S. list price of around $225,000 per year.
“Obviously, the cost will go down over time,” Dr. Seferovic predicted.
Diagnosing TAC
Audience members mostly wanted to know how to identify individuals with TAC who are buried within the huge population of patients with heart failure with preserved ejection fraction. Dr. Damy said it’s actually a simple matter using a screening framework developed by an 11-member TAC expert panel on which he served. A definitive diagnosis can usually be achieved noninvasively at a low cost using bone scintigraphy, he added.
The panel recommended screening via bone scintigraphy in patients with an increased left ventricular wall thickness of 14 mm or more in men over age 65 and women older than 70 who either have heart failure or red flag symptoms.
These red flags for TAC include an echocardiographic finding of reduced longitudinal strain with relative apical sparing, a discrepancy between left ventricular wall thickness on imaging and normal or low-normal voltages on a standard 12-lead ECG, diffuse gadolinium enhancement or marked extracellular volume expansion on cardiac magnetic resonance imaging, a history of bilateral carpal tunnel syndrome, symptoms of polyneuropathy, and mildly increased serum troponin levels on multiple occasions (JACC Heart Fail. 2019 Aug;7[8]:709-16).
Dr. Damy reported receiving institutional research grant support from Pfizer, the study sponsor, and serving on a scientific advisory board for the company.
Treatment with oral tafamidis at 80 mg/day provided a significantly greater survival benefit than dosing at 20 mg/day in patients with transthyretin amyloid cardiomyopathy in the long-term extension of the landmark ATTR-ACT trial, Thibaud Damy, MD, PhD, reported at the European Society of Cardiology Heart Failure Discoveries virtual meeting.
Moreover, the superior survival benefit achieved by taking four 20-mg capsules of tafamidis (Vyndaqel) once daily – or its more convenient once-daily, single-capsule, 61-mg bioequivalent formulation marketed as Vyndamax – came at no cost in terms of side effects and toxicity, compared with low-dose therapy for this progressive multisystem disease, according to Dr. Damy, professor of cardiology at the University of Paris and head of the French National Referral Center for Cardiac Amyloidosis at Henri Mondor University Hospital, Créteil, France.
“There are no side effects with tafamidis,” he said. “It doesn’t act on any receptors, it just acts on the formation of amyloid fibrils, so there are no side effects at whatever dosage is used. And in ATTR-ACT there was actually a trend towards increased side effects in the placebo group because the amyloidosis is everywhere, so by decreasing the amyloidosis process you improve not only the heart but all the organs, and the patient has a better quality of life.”
ATTR-ACT (Transthyretin Amyloidosis Cardiomyopathy Clinical Trial) was a phase 3, double-blind study in which 441 patients with transthyretin amyloidosis cardiomyopathy (TAC) in 13 countries were randomized to tafamidis at either 80 mg or 20 mg per day or placebo and followed prospectively for 30 months. At 30 months, all-cause mortality was 29.5% in patients who received tafamidis, compared with 42.9% in controls, for a statistically significant and clinically important 30% relative risk reduction, establishing tafamidis as the first disease-modifying therapy for this disease (N Engl J Med. 2018 Sep 13;379[11]:1007-16).
Patients in the 80-mg group had a 20% reduction in the risk of death, compared with the 20-mg group, at 30 months in an analysis adjusted for baseline age, 6-minute walk distance, and N-terminal pro-B-type natriuretic peptide, all of which are known to impact survival in TAC. This between-group survival difference wasn’t statistically significant, providing one impetus for the subsequent long-term extension study, in which patients remained on their original dose of tafamidis, and the controls who’d been on placebo for 30 months were randomized 2:1 to tafamidis at 80 mg or 20 mg per day.
The primary endpoint in the long-term extension was a composite of all-cause mortality, heart transplantation, or implantation of a ventricular assist device. At a median follow-up of 39 months since ATTR-ACT began, the high-dose tafamidis group had an adjusted 33% reduction in the risk of this endpoint, compared with patients on 20 mg per day, a difference that barely missed statistical significance. At that point, everyone in the long-term extension was switched to the once-daily 61-mg formulation of tafamidis free acid, which is bioequivalent to four 20-mg capsules of tafamidis.
Dr. Damy’s key message: At a median of 51 months of follow-up, the group originally on 80 mg of tafamidis displayed a highly significant adjusted 43% reduction in risk of the composite endpoint, compared with those who had been on 20 mg per day.
Session chair Petar M. Seferovic, MD, PhD, pronounced the ATTR-ACT trial and its long-term extension “a breakthrough advancement.”
“This is the first time in human medical history that we have a drug which improves the long-term outcome, including survival, in patients with this form of hypertrophic cardiomyopathy. So this is extremely important. It’s one of the major steps forward in the treatment of patients with myocardial disease,” said Dr. Seferovic, president of the European Society of Cardiology Heart Failure Association and professor of internal medicine at the University of Belgrade, Serbia.
Discussant Loreena Hill, PhD, of Queen’s University in Belfast, Northern Ireland, observed that TAC is a devastating disease with a formidable symptom burden and an average survival of just 2-5 years after diagnosis.
“It is often underdiagnosed, and yet it is estimated to account for up to 13% of patients with heart failure and preserved ejection fraction,” she said, adding that she considers the long-term extension results “extremely positive.”
Nailing down the prevalence of hereditary TAC: the DISCOVERY study
TAC occurs when transthyretin, a transport protein, becomes destabilized and misfolds, promoting deposition of amyloid fibrils in the myocardium and elsewhere. In the heart, the result is progressive ventricular wall thickening and stiffness, manifest as restrictive cardiomyopathy and progressive nonischemic heart failure. The cause of transthyretin destabilization can be either autosomal dominant inheritance of any of more than 100 pathogenic mutations in the transthyretin gene identified to date or a spontaneous wild-type protein.
Dr. Damy was a coinvestigator in the recently published multicenter DISCOVERY study, in which 1,001 patients with clinically suspected cardiac amyloidosis, the great majority of them from the United States, were screened for pathogenic transthyretin genetic mutations. The overall prevalence of such mutations was 8% in the American patients, with the Val122Ile mutation being identified in 11% of African Americans (Amyloid. 2020 May 26;1-8).
The prevalence of wild-type amyloidosis causing TAC hasn’t yet been studied with anything approaching the rigor of DISCOVERY, but the available evidence suggests the wild-type version is roughly as common as the hereditary forms.
Although DISCOVERY and other studies indicate that TAC is far more common than generally realized, Pfizer has priced Vyndaqel and Vyndamax as though TAC is a rare disease, with a U.S. list price of around $225,000 per year.
“Obviously, the cost will go down over time,” Dr. Seferovic predicted.
Diagnosing TAC
Audience members mostly wanted to know how to identify individuals with TAC who are buried within the huge population of patients with heart failure with preserved ejection fraction. Dr. Damy said it’s actually a simple matter using a screening framework developed by an 11-member TAC expert panel on which he served. A definitive diagnosis can usually be achieved noninvasively at a low cost using bone scintigraphy, he added.
The panel recommended screening via bone scintigraphy in patients with an increased left ventricular wall thickness of 14 mm or more in men over age 65 and women older than 70 who either have heart failure or red flag symptoms.
These red flags for TAC include an echocardiographic finding of reduced longitudinal strain with relative apical sparing, a discrepancy between left ventricular wall thickness on imaging and normal or low-normal voltages on a standard 12-lead ECG, diffuse gadolinium enhancement or marked extracellular volume expansion on cardiac magnetic resonance imaging, a history of bilateral carpal tunnel syndrome, symptoms of polyneuropathy, and mildly increased serum troponin levels on multiple occasions (JACC Heart Fail. 2019 Aug;7[8]:709-16).
Dr. Damy reported receiving institutional research grant support from Pfizer, the study sponsor, and serving on a scientific advisory board for the company.
Treatment with oral tafamidis at 80 mg/day provided a significantly greater survival benefit than dosing at 20 mg/day in patients with transthyretin amyloid cardiomyopathy in the long-term extension of the landmark ATTR-ACT trial, Thibaud Damy, MD, PhD, reported at the European Society of Cardiology Heart Failure Discoveries virtual meeting.
Moreover, the superior survival benefit achieved by taking four 20-mg capsules of tafamidis (Vyndaqel) once daily – or its more convenient once-daily, single-capsule, 61-mg bioequivalent formulation marketed as Vyndamax – came at no cost in terms of side effects and toxicity, compared with low-dose therapy for this progressive multisystem disease, according to Dr. Damy, professor of cardiology at the University of Paris and head of the French National Referral Center for Cardiac Amyloidosis at Henri Mondor University Hospital, Créteil, France.
“There are no side effects with tafamidis,” he said. “It doesn’t act on any receptors, it just acts on the formation of amyloid fibrils, so there are no side effects at whatever dosage is used. And in ATTR-ACT there was actually a trend towards increased side effects in the placebo group because the amyloidosis is everywhere, so by decreasing the amyloidosis process you improve not only the heart but all the organs, and the patient has a better quality of life.”
ATTR-ACT (Transthyretin Amyloidosis Cardiomyopathy Clinical Trial) was a phase 3, double-blind study in which 441 patients with transthyretin amyloidosis cardiomyopathy (TAC) in 13 countries were randomized to tafamidis at either 80 mg or 20 mg per day or placebo and followed prospectively for 30 months. At 30 months, all-cause mortality was 29.5% in patients who received tafamidis, compared with 42.9% in controls, for a statistically significant and clinically important 30% relative risk reduction, establishing tafamidis as the first disease-modifying therapy for this disease (N Engl J Med. 2018 Sep 13;379[11]:1007-16).
Patients in the 80-mg group had a 20% reduction in the risk of death, compared with the 20-mg group, at 30 months in an analysis adjusted for baseline age, 6-minute walk distance, and N-terminal pro-B-type natriuretic peptide, all of which are known to impact survival in TAC. This between-group survival difference wasn’t statistically significant, providing one impetus for the subsequent long-term extension study, in which patients remained on their original dose of tafamidis, and the controls who’d been on placebo for 30 months were randomized 2:1 to tafamidis at 80 mg or 20 mg per day.
The primary endpoint in the long-term extension was a composite of all-cause mortality, heart transplantation, or implantation of a ventricular assist device. At a median follow-up of 39 months since ATTR-ACT began, the high-dose tafamidis group had an adjusted 33% reduction in the risk of this endpoint, compared with patients on 20 mg per day, a difference that barely missed statistical significance. At that point, everyone in the long-term extension was switched to the once-daily 61-mg formulation of tafamidis free acid, which is bioequivalent to four 20-mg capsules of tafamidis.
Dr. Damy’s key message: At a median of 51 months of follow-up, the group originally on 80 mg of tafamidis displayed a highly significant adjusted 43% reduction in risk of the composite endpoint, compared with those who had been on 20 mg per day.
Session chair Petar M. Seferovic, MD, PhD, pronounced the ATTR-ACT trial and its long-term extension “a breakthrough advancement.”
“This is the first time in human medical history that we have a drug which improves the long-term outcome, including survival, in patients with this form of hypertrophic cardiomyopathy. So this is extremely important. It’s one of the major steps forward in the treatment of patients with myocardial disease,” said Dr. Seferovic, president of the European Society of Cardiology Heart Failure Association and professor of internal medicine at the University of Belgrade, Serbia.
Discussant Loreena Hill, PhD, of Queen’s University in Belfast, Northern Ireland, observed that TAC is a devastating disease with a formidable symptom burden and an average survival of just 2-5 years after diagnosis.
“It is often underdiagnosed, and yet it is estimated to account for up to 13% of patients with heart failure and preserved ejection fraction,” she said, adding that she considers the long-term extension results “extremely positive.”
Nailing down the prevalence of hereditary TAC: the DISCOVERY study
TAC occurs when transthyretin, a transport protein, becomes destabilized and misfolds, promoting deposition of amyloid fibrils in the myocardium and elsewhere. In the heart, the result is progressive ventricular wall thickening and stiffness, manifest as restrictive cardiomyopathy and progressive nonischemic heart failure. The cause of transthyretin destabilization can be either autosomal dominant inheritance of any of more than 100 pathogenic mutations in the transthyretin gene identified to date or a spontaneous wild-type protein.
Dr. Damy was a coinvestigator in the recently published multicenter DISCOVERY study, in which 1,001 patients with clinically suspected cardiac amyloidosis, the great majority of them from the United States, were screened for pathogenic transthyretin genetic mutations. The overall prevalence of such mutations was 8% in the American patients, with the Val122Ile mutation being identified in 11% of African Americans (Amyloid. 2020 May 26;1-8).
The prevalence of wild-type amyloidosis causing TAC hasn’t yet been studied with anything approaching the rigor of DISCOVERY, but the available evidence suggests the wild-type version is roughly as common as the hereditary forms.
Although DISCOVERY and other studies indicate that TAC is far more common than generally realized, Pfizer has priced Vyndaqel and Vyndamax as though TAC is a rare disease, with a U.S. list price of around $225,000 per year.
“Obviously, the cost will go down over time,” Dr. Seferovic predicted.
Diagnosing TAC
Audience members mostly wanted to know how to identify individuals with TAC who are buried within the huge population of patients with heart failure with preserved ejection fraction. Dr. Damy said it’s actually a simple matter using a screening framework developed by an 11-member TAC expert panel on which he served. A definitive diagnosis can usually be achieved noninvasively at a low cost using bone scintigraphy, he added.
The panel recommended screening via bone scintigraphy in patients with an increased left ventricular wall thickness of 14 mm or more in men over age 65 and women older than 70 who either have heart failure or red flag symptoms.
These red flags for TAC include an echocardiographic finding of reduced longitudinal strain with relative apical sparing, a discrepancy between left ventricular wall thickness on imaging and normal or low-normal voltages on a standard 12-lead ECG, diffuse gadolinium enhancement or marked extracellular volume expansion on cardiac magnetic resonance imaging, a history of bilateral carpal tunnel syndrome, symptoms of polyneuropathy, and mildly increased serum troponin levels on multiple occasions (JACC Heart Fail. 2019 Aug;7[8]:709-16).
Dr. Damy reported receiving institutional research grant support from Pfizer, the study sponsor, and serving on a scientific advisory board for the company.
FROM ESC HEART FAILURE 2020
QI initiative can decrease unnecessary IV treatment of asymptomatic hypertension
Background: Limited research suggests IV treatment of asymptomatic hypertension may be widespread and unhelpful. There is potential for unnecessary treatment to have adverse outcomes, such as hypotension.
Study design: Retrospective cohort study.
Setting: A single academic hospital.
Synopsis: Of 2,306 inpatients with asymptomatic hypertension, 11% were treated with IV medications to lower their blood pressure. Patients with indications for stricter blood pressure control (such as stroke, intracranial hemorrhage, aortic dissection) were excluded from the study. Following the baseline period, an education intervention was employed that included presentations, handouts, and posters. A second phase of quality improvement intervention included adjustment of the electronic medical record blood pressure alert parameters from more than 160/90 to more than 180/90. After these interventions, a lower percentage of patients received IV blood pressure medications for asymptomatic hypertension without a significant change in the number of rapid response calls, ICU transfers, or code blues. Limitations include that this is a single-center study and it is unclear if the performance improvement seen will be maintained over time.
Bottom line: IV antihypertensive use for asymptomatic hypertension is common despite lack of data to support its use, and reduced use is possible using quality improvement interventions.
Citation: Jacobs Z et al. Reducing unnecessary treatment of asymptomatic elevated blood pressure with intravenous medications on the general internal medicine wards: a quality improvement initiative. J Hosp Med. 2019 Mar;14(3):144-50.
Dr. Sharma is associate medical director for clinical education in hospital medicine at Duke Regional Hospital and an assistant professor of medicine at Duke University.
Background: Limited research suggests IV treatment of asymptomatic hypertension may be widespread and unhelpful. There is potential for unnecessary treatment to have adverse outcomes, such as hypotension.
Study design: Retrospective cohort study.
Setting: A single academic hospital.
Synopsis: Of 2,306 inpatients with asymptomatic hypertension, 11% were treated with IV medications to lower their blood pressure. Patients with indications for stricter blood pressure control (such as stroke, intracranial hemorrhage, aortic dissection) were excluded from the study. Following the baseline period, an education intervention was employed that included presentations, handouts, and posters. A second phase of quality improvement intervention included adjustment of the electronic medical record blood pressure alert parameters from more than 160/90 to more than 180/90. After these interventions, a lower percentage of patients received IV blood pressure medications for asymptomatic hypertension without a significant change in the number of rapid response calls, ICU transfers, or code blues. Limitations include that this is a single-center study and it is unclear if the performance improvement seen will be maintained over time.
Bottom line: IV antihypertensive use for asymptomatic hypertension is common despite lack of data to support its use, and reduced use is possible using quality improvement interventions.
Citation: Jacobs Z et al. Reducing unnecessary treatment of asymptomatic elevated blood pressure with intravenous medications on the general internal medicine wards: a quality improvement initiative. J Hosp Med. 2019 Mar;14(3):144-50.
Dr. Sharma is associate medical director for clinical education in hospital medicine at Duke Regional Hospital and an assistant professor of medicine at Duke University.
Background: Limited research suggests IV treatment of asymptomatic hypertension may be widespread and unhelpful. There is potential for unnecessary treatment to have adverse outcomes, such as hypotension.
Study design: Retrospective cohort study.
Setting: A single academic hospital.
Synopsis: Of 2,306 inpatients with asymptomatic hypertension, 11% were treated with IV medications to lower their blood pressure. Patients with indications for stricter blood pressure control (such as stroke, intracranial hemorrhage, aortic dissection) were excluded from the study. Following the baseline period, an education intervention was employed that included presentations, handouts, and posters. A second phase of quality improvement intervention included adjustment of the electronic medical record blood pressure alert parameters from more than 160/90 to more than 180/90. After these interventions, a lower percentage of patients received IV blood pressure medications for asymptomatic hypertension without a significant change in the number of rapid response calls, ICU transfers, or code blues. Limitations include that this is a single-center study and it is unclear if the performance improvement seen will be maintained over time.
Bottom line: IV antihypertensive use for asymptomatic hypertension is common despite lack of data to support its use, and reduced use is possible using quality improvement interventions.
Citation: Jacobs Z et al. Reducing unnecessary treatment of asymptomatic elevated blood pressure with intravenous medications on the general internal medicine wards: a quality improvement initiative. J Hosp Med. 2019 Mar;14(3):144-50.
Dr. Sharma is associate medical director for clinical education in hospital medicine at Duke Regional Hospital and an assistant professor of medicine at Duke University.
Spinning of results common in industry-sponsored interventional cardiovascular trials
As the rigor of COVID-19 research comes under increasing scrutiny, a deep dive into contemporary trials of invasive cardiovascular interventions finds intricate ties with industry and the art of spin on full display.
After examining 216 randomized, controlled trials published in the past decade, researchers found that more than half (53.2%) were commercially funded. In 18.3% of these trials, the sponsor was involved with the trial conduct and reporting.
Commercially sponsored trials were significantly more likely to report results that favored the experimental therapy than trials without commercial sponsorship (64.3% vs. 48.5%; P = .02).
The association remained statistically significant after adjustment for differences in trial characteristics (exponent of regression coefficient beta, 2.80; 95% confidence interval, 1.09-7.18; P = .03), the authors reported in JAMA Internal Medicine.
“To make this clear, this is not an attack on industry-sponsored trials,” study author and cardiac surgeon Mario Gaudino, MD, of New York–Presbyterian and Weill Cornell Medical Center, New York, said in an interview. “Because industry has more money, they have the best trialists, the best research organization. So they generally do a pretty good trial; they’re larger, they have a higher Fragility Index, which means they’re more solid.
“And, most importantly, more than half of the trials were sponsored by industry,” he said. “So without industry, there wouldn’t be half the research in that 10-year period we explored.”
Previous research in cardiology and in other fields has shown that trials supported by for-profit organizations are more likely to report positive findings. The explanations often focus on bias and differential quality in how the trials were designed and reported.
In the present analysis, however, the authors found no difference between trials with and without industry funding in terms of estimated treatment effect, length of follow-up, use of composite or clinically significant outcomes, or outcome modification, compared with the published protocol.
Part of the explanation may be that industry-sponsored trials more often used a noninferiority design (26.1% vs. 14.9%) and had a higher loss of patients to follow-up (median of sample, 1.0% vs. 0.1%), Dr. Gaudino said. “But I think more, in general, it’s not so much a difference in the measurable characteristics of the trial. It’s the selection of the sites that participate, the patient population that is targeted that makes the trial very likely to get the result that industry would like to see.”
“Just think of the differences in the transcatheter MitraClip results between MITRA-FR and COAPT – basically they were related to the fact they enrolled different patients,” he said.
Significant spin
The analysis included 216 coronary, vascular, and structural interventional cardiology and vascular and cardiac surgical randomized, controlled trials published from January 2008 to May 31, 2019. Most were multicenter trials (78.7%); 58% originated from Europe, 12% from North America, and 10.6% from Asia.
One in six trials (16.2%) were not prospectively registered before the start of enrollment, and at least one major discrepancy existed between the registered and published primary outcome in 38% of registered trials.
“If you don’t register the trial then you can make all the changes you want to the protocol up until the moment you publish,” Dr. Gaudino observed. “There really is no rational justification for not registering a trial.”
Overall, the trials were not particularly robust, he noted. In 62 trials in which the Fragility Index was measured, only a median of five patients experiencing a different outcome in a commercially sponsored trial would change statistically significant results to nonsignificant. For noncommercially sponsored trials, that number was 4.5 and in four trials; the change in condition of only one patient was needed to switch the statistical significance.
“This finding is concerning given the substantial role that [randomized, controlled trials] results play in federal device approvals, payer criteria, and clinical consensus guidelines,” the authors wrote.
The authors also looked for interpretation bias in the trials. In the 84 trials with nonsignificant differences in the primary outcomes, 65.5% contained spin, such as focusing on statistically significant secondary outcomes or interpreting nonsignificant primary outcomes as showing treatment equivalence or comparable effectiveness. Spin was present in 80.6% of the trials with commercial sponsorship and in 54.2% without (P = .02) – a finding that remained significant after trial differences were controlled for (beta, 4.64; 95% CI, 1.05-20.54; P = .04).
A pivot point
“It’s just another paper showing there are issues with conflicts of interest in industry trials. I’m not particularly surprised,” said David Moher, PhD, MSc, director of the Centre for Journalology, based at the Ottawa Hospital Research Institute.
“It’s sort of high time people from all sides sat down together and tried to resolve how to actually move forward with industry wanting to do trials,” he said. “They are hugely important in drug development. How can these trials be done where the impact of industry and, for that matter, academia is minimized?”
Dr. Gaudino suggested the “ideal situation” would be to have industry put its funding into an existing funding organization, such as the National Institutes of Health or a newly created independent organization – a concept that has been floated before without much forward movement.
“We may be at a pivot point,” Dr. Moher said. “It’s quite clear that COVID has indicated some serious problems with how trials are done, how they’re disseminated, the notion of open science. I think this could be an opportunity. Whether there is so much noise, whether anybody will be able to take any of these initiative forward, I don’t know.”
No matter how trial funding is revised, patients must be brought to the table, he said.
“What frustrates me quite a bit is this almost parental view of all of this – the scientists know best, industry knows best,” Dr. Moher said. “We actually need the most important groups: patients and the public. They need to have an enormous amount of say in how this actually is formed.”
Commenting further, Dr. Moher said that “industry and academia can only do trials when they have patients willing to participate, and yet in the discussions you and I are having, what do patients think about spin in trials? I would imagine they would be horrified that they are going into studies – in a sense in many cases risking their lives – and yet people are spinning the results.”
Dr. Gaudino and Dr. Moher reported having no relevant conflicts of interest.
A version of this story originally appeared on Medscape.com.
As the rigor of COVID-19 research comes under increasing scrutiny, a deep dive into contemporary trials of invasive cardiovascular interventions finds intricate ties with industry and the art of spin on full display.
After examining 216 randomized, controlled trials published in the past decade, researchers found that more than half (53.2%) were commercially funded. In 18.3% of these trials, the sponsor was involved with the trial conduct and reporting.
Commercially sponsored trials were significantly more likely to report results that favored the experimental therapy than trials without commercial sponsorship (64.3% vs. 48.5%; P = .02).
The association remained statistically significant after adjustment for differences in trial characteristics (exponent of regression coefficient beta, 2.80; 95% confidence interval, 1.09-7.18; P = .03), the authors reported in JAMA Internal Medicine.
“To make this clear, this is not an attack on industry-sponsored trials,” study author and cardiac surgeon Mario Gaudino, MD, of New York–Presbyterian and Weill Cornell Medical Center, New York, said in an interview. “Because industry has more money, they have the best trialists, the best research organization. So they generally do a pretty good trial; they’re larger, they have a higher Fragility Index, which means they’re more solid.
“And, most importantly, more than half of the trials were sponsored by industry,” he said. “So without industry, there wouldn’t be half the research in that 10-year period we explored.”
Previous research in cardiology and in other fields has shown that trials supported by for-profit organizations are more likely to report positive findings. The explanations often focus on bias and differential quality in how the trials were designed and reported.
In the present analysis, however, the authors found no difference between trials with and without industry funding in terms of estimated treatment effect, length of follow-up, use of composite or clinically significant outcomes, or outcome modification, compared with the published protocol.
Part of the explanation may be that industry-sponsored trials more often used a noninferiority design (26.1% vs. 14.9%) and had a higher loss of patients to follow-up (median of sample, 1.0% vs. 0.1%), Dr. Gaudino said. “But I think more, in general, it’s not so much a difference in the measurable characteristics of the trial. It’s the selection of the sites that participate, the patient population that is targeted that makes the trial very likely to get the result that industry would like to see.”
“Just think of the differences in the transcatheter MitraClip results between MITRA-FR and COAPT – basically they were related to the fact they enrolled different patients,” he said.
Significant spin
The analysis included 216 coronary, vascular, and structural interventional cardiology and vascular and cardiac surgical randomized, controlled trials published from January 2008 to May 31, 2019. Most were multicenter trials (78.7%); 58% originated from Europe, 12% from North America, and 10.6% from Asia.
One in six trials (16.2%) were not prospectively registered before the start of enrollment, and at least one major discrepancy existed between the registered and published primary outcome in 38% of registered trials.
“If you don’t register the trial then you can make all the changes you want to the protocol up until the moment you publish,” Dr. Gaudino observed. “There really is no rational justification for not registering a trial.”
Overall, the trials were not particularly robust, he noted. In 62 trials in which the Fragility Index was measured, only a median of five patients experiencing a different outcome in a commercially sponsored trial would change statistically significant results to nonsignificant. For noncommercially sponsored trials, that number was 4.5 and in four trials; the change in condition of only one patient was needed to switch the statistical significance.
“This finding is concerning given the substantial role that [randomized, controlled trials] results play in federal device approvals, payer criteria, and clinical consensus guidelines,” the authors wrote.
The authors also looked for interpretation bias in the trials. In the 84 trials with nonsignificant differences in the primary outcomes, 65.5% contained spin, such as focusing on statistically significant secondary outcomes or interpreting nonsignificant primary outcomes as showing treatment equivalence or comparable effectiveness. Spin was present in 80.6% of the trials with commercial sponsorship and in 54.2% without (P = .02) – a finding that remained significant after trial differences were controlled for (beta, 4.64; 95% CI, 1.05-20.54; P = .04).
A pivot point
“It’s just another paper showing there are issues with conflicts of interest in industry trials. I’m not particularly surprised,” said David Moher, PhD, MSc, director of the Centre for Journalology, based at the Ottawa Hospital Research Institute.
“It’s sort of high time people from all sides sat down together and tried to resolve how to actually move forward with industry wanting to do trials,” he said. “They are hugely important in drug development. How can these trials be done where the impact of industry and, for that matter, academia is minimized?”
Dr. Gaudino suggested the “ideal situation” would be to have industry put its funding into an existing funding organization, such as the National Institutes of Health or a newly created independent organization – a concept that has been floated before without much forward movement.
“We may be at a pivot point,” Dr. Moher said. “It’s quite clear that COVID has indicated some serious problems with how trials are done, how they’re disseminated, the notion of open science. I think this could be an opportunity. Whether there is so much noise, whether anybody will be able to take any of these initiative forward, I don’t know.”
No matter how trial funding is revised, patients must be brought to the table, he said.
“What frustrates me quite a bit is this almost parental view of all of this – the scientists know best, industry knows best,” Dr. Moher said. “We actually need the most important groups: patients and the public. They need to have an enormous amount of say in how this actually is formed.”
Commenting further, Dr. Moher said that “industry and academia can only do trials when they have patients willing to participate, and yet in the discussions you and I are having, what do patients think about spin in trials? I would imagine they would be horrified that they are going into studies – in a sense in many cases risking their lives – and yet people are spinning the results.”
Dr. Gaudino and Dr. Moher reported having no relevant conflicts of interest.
A version of this story originally appeared on Medscape.com.
As the rigor of COVID-19 research comes under increasing scrutiny, a deep dive into contemporary trials of invasive cardiovascular interventions finds intricate ties with industry and the art of spin on full display.
After examining 216 randomized, controlled trials published in the past decade, researchers found that more than half (53.2%) were commercially funded. In 18.3% of these trials, the sponsor was involved with the trial conduct and reporting.
Commercially sponsored trials were significantly more likely to report results that favored the experimental therapy than trials without commercial sponsorship (64.3% vs. 48.5%; P = .02).
The association remained statistically significant after adjustment for differences in trial characteristics (exponent of regression coefficient beta, 2.80; 95% confidence interval, 1.09-7.18; P = .03), the authors reported in JAMA Internal Medicine.
“To make this clear, this is not an attack on industry-sponsored trials,” study author and cardiac surgeon Mario Gaudino, MD, of New York–Presbyterian and Weill Cornell Medical Center, New York, said in an interview. “Because industry has more money, they have the best trialists, the best research organization. So they generally do a pretty good trial; they’re larger, they have a higher Fragility Index, which means they’re more solid.
“And, most importantly, more than half of the trials were sponsored by industry,” he said. “So without industry, there wouldn’t be half the research in that 10-year period we explored.”
Previous research in cardiology and in other fields has shown that trials supported by for-profit organizations are more likely to report positive findings. The explanations often focus on bias and differential quality in how the trials were designed and reported.
In the present analysis, however, the authors found no difference between trials with and without industry funding in terms of estimated treatment effect, length of follow-up, use of composite or clinically significant outcomes, or outcome modification, compared with the published protocol.
Part of the explanation may be that industry-sponsored trials more often used a noninferiority design (26.1% vs. 14.9%) and had a higher loss of patients to follow-up (median of sample, 1.0% vs. 0.1%), Dr. Gaudino said. “But I think more, in general, it’s not so much a difference in the measurable characteristics of the trial. It’s the selection of the sites that participate, the patient population that is targeted that makes the trial very likely to get the result that industry would like to see.”
“Just think of the differences in the transcatheter MitraClip results between MITRA-FR and COAPT – basically they were related to the fact they enrolled different patients,” he said.
Significant spin
The analysis included 216 coronary, vascular, and structural interventional cardiology and vascular and cardiac surgical randomized, controlled trials published from January 2008 to May 31, 2019. Most were multicenter trials (78.7%); 58% originated from Europe, 12% from North America, and 10.6% from Asia.
One in six trials (16.2%) were not prospectively registered before the start of enrollment, and at least one major discrepancy existed between the registered and published primary outcome in 38% of registered trials.
“If you don’t register the trial then you can make all the changes you want to the protocol up until the moment you publish,” Dr. Gaudino observed. “There really is no rational justification for not registering a trial.”
Overall, the trials were not particularly robust, he noted. In 62 trials in which the Fragility Index was measured, only a median of five patients experiencing a different outcome in a commercially sponsored trial would change statistically significant results to nonsignificant. For noncommercially sponsored trials, that number was 4.5 and in four trials; the change in condition of only one patient was needed to switch the statistical significance.
“This finding is concerning given the substantial role that [randomized, controlled trials] results play in federal device approvals, payer criteria, and clinical consensus guidelines,” the authors wrote.
The authors also looked for interpretation bias in the trials. In the 84 trials with nonsignificant differences in the primary outcomes, 65.5% contained spin, such as focusing on statistically significant secondary outcomes or interpreting nonsignificant primary outcomes as showing treatment equivalence or comparable effectiveness. Spin was present in 80.6% of the trials with commercial sponsorship and in 54.2% without (P = .02) – a finding that remained significant after trial differences were controlled for (beta, 4.64; 95% CI, 1.05-20.54; P = .04).
A pivot point
“It’s just another paper showing there are issues with conflicts of interest in industry trials. I’m not particularly surprised,” said David Moher, PhD, MSc, director of the Centre for Journalology, based at the Ottawa Hospital Research Institute.
“It’s sort of high time people from all sides sat down together and tried to resolve how to actually move forward with industry wanting to do trials,” he said. “They are hugely important in drug development. How can these trials be done where the impact of industry and, for that matter, academia is minimized?”
Dr. Gaudino suggested the “ideal situation” would be to have industry put its funding into an existing funding organization, such as the National Institutes of Health or a newly created independent organization – a concept that has been floated before without much forward movement.
“We may be at a pivot point,” Dr. Moher said. “It’s quite clear that COVID has indicated some serious problems with how trials are done, how they’re disseminated, the notion of open science. I think this could be an opportunity. Whether there is so much noise, whether anybody will be able to take any of these initiative forward, I don’t know.”
No matter how trial funding is revised, patients must be brought to the table, he said.
“What frustrates me quite a bit is this almost parental view of all of this – the scientists know best, industry knows best,” Dr. Moher said. “We actually need the most important groups: patients and the public. They need to have an enormous amount of say in how this actually is formed.”
Commenting further, Dr. Moher said that “industry and academia can only do trials when they have patients willing to participate, and yet in the discussions you and I are having, what do patients think about spin in trials? I would imagine they would be horrified that they are going into studies – in a sense in many cases risking their lives – and yet people are spinning the results.”
Dr. Gaudino and Dr. Moher reported having no relevant conflicts of interest.
A version of this story originally appeared on Medscape.com.
Lancet, NEJM retract studies on hydroxychloroquine for COVID-19
The Lancet announced today that it has retracted a highly cited study that suggested hydroxychloroquine may cause more harm than benefit in patients with COVID-19. Hours later, the New England Journal of Medicine announced that it had retracted a second article by some of the same authors, also on heart disease and COVID-19.
The Lancet article, titled “Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: A multinational registry analysis” was originally published online May 22. The NEJM article, “Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19” was initially published May 1.
Three authors of the Lancet article, Mandeep R. Mehra, MD, Frank Ruschitzka, MD, and Amit N. Patel, MD, wrote in a letter that the action came after concerns were raised about the integrity of the data, and about how the analysis was conducted by Chicago-based Surgisphere Corp and study coauthor Sapan Desai, MD, Surgisphere’s founder and CEO.
The authors asked for an independent third-party review of Surgisphere to evaluate the integrity of the trial elements and to replicate the analyses in the article.
“Our independent peer reviewers informed us that Surgisphere would not transfer the full dataset, client contracts, and the full ISO audit report to their servers for analysis, as such transfer would violate client agreements and confidentiality requirements,” the authors wrote.
Therefore, reviewers were not able to conduct the review and notified the authors they would withdraw from the peer-review process.
The Lancet said in a statement: “The Lancet takes issues of scientific integrity extremely seriously, and there are many outstanding questions about Surgisphere and the data that were allegedly included in this study. Following guidelines from the Committee on Publication Ethics and International Committee of Medical Journal Editors, institutional reviews of Surgisphere’s research collaborations are urgently needed.”
The authors wrote, “We can never forget the responsibility we have as researchers to scrupulously ensure that we rely on data sources that adhere to our high standards. Based on this development, we can no longer vouch for the veracity of the primary data sources. Due to this unfortunate development, the authors request that the paper be retracted.
“We all entered this collaboration to contribute in good faith and at a time of great need during the COVID-19 pandemic. We deeply apologize to you, the editors, and the journal readership for any embarrassment or inconvenience that this may have caused.”
In a similar, if briefer, note, the authors requested that the New England Journal of Medicine retract the earlier article as well. The retraction notice on the website reads: “Because all the authors were not granted access to the raw data and the raw data could not be made available to a third-party auditor, we are unable to validate the primary data sources underlying our article, ‘Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19.’ We therefore request that the article be retracted. We apologize to the editors and to readers of the Journal for the difficulties that this has caused.”
Both journals had already published “Expression of Concern” notices about the articles. The expression of concern followed an open letter, endorsed by more than 200 scientists, ethicists, and clinicians and posted on May 28, questioning the data and ethics of the study.
A version of this article originally appeared on Medscape.com.
The Lancet announced today that it has retracted a highly cited study that suggested hydroxychloroquine may cause more harm than benefit in patients with COVID-19. Hours later, the New England Journal of Medicine announced that it had retracted a second article by some of the same authors, also on heart disease and COVID-19.
The Lancet article, titled “Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: A multinational registry analysis” was originally published online May 22. The NEJM article, “Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19” was initially published May 1.
Three authors of the Lancet article, Mandeep R. Mehra, MD, Frank Ruschitzka, MD, and Amit N. Patel, MD, wrote in a letter that the action came after concerns were raised about the integrity of the data, and about how the analysis was conducted by Chicago-based Surgisphere Corp and study coauthor Sapan Desai, MD, Surgisphere’s founder and CEO.
The authors asked for an independent third-party review of Surgisphere to evaluate the integrity of the trial elements and to replicate the analyses in the article.
“Our independent peer reviewers informed us that Surgisphere would not transfer the full dataset, client contracts, and the full ISO audit report to their servers for analysis, as such transfer would violate client agreements and confidentiality requirements,” the authors wrote.
Therefore, reviewers were not able to conduct the review and notified the authors they would withdraw from the peer-review process.
The Lancet said in a statement: “The Lancet takes issues of scientific integrity extremely seriously, and there are many outstanding questions about Surgisphere and the data that were allegedly included in this study. Following guidelines from the Committee on Publication Ethics and International Committee of Medical Journal Editors, institutional reviews of Surgisphere’s research collaborations are urgently needed.”
The authors wrote, “We can never forget the responsibility we have as researchers to scrupulously ensure that we rely on data sources that adhere to our high standards. Based on this development, we can no longer vouch for the veracity of the primary data sources. Due to this unfortunate development, the authors request that the paper be retracted.
“We all entered this collaboration to contribute in good faith and at a time of great need during the COVID-19 pandemic. We deeply apologize to you, the editors, and the journal readership for any embarrassment or inconvenience that this may have caused.”
In a similar, if briefer, note, the authors requested that the New England Journal of Medicine retract the earlier article as well. The retraction notice on the website reads: “Because all the authors were not granted access to the raw data and the raw data could not be made available to a third-party auditor, we are unable to validate the primary data sources underlying our article, ‘Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19.’ We therefore request that the article be retracted. We apologize to the editors and to readers of the Journal for the difficulties that this has caused.”
Both journals had already published “Expression of Concern” notices about the articles. The expression of concern followed an open letter, endorsed by more than 200 scientists, ethicists, and clinicians and posted on May 28, questioning the data and ethics of the study.
A version of this article originally appeared on Medscape.com.
The Lancet announced today that it has retracted a highly cited study that suggested hydroxychloroquine may cause more harm than benefit in patients with COVID-19. Hours later, the New England Journal of Medicine announced that it had retracted a second article by some of the same authors, also on heart disease and COVID-19.
The Lancet article, titled “Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: A multinational registry analysis” was originally published online May 22. The NEJM article, “Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19” was initially published May 1.
Three authors of the Lancet article, Mandeep R. Mehra, MD, Frank Ruschitzka, MD, and Amit N. Patel, MD, wrote in a letter that the action came after concerns were raised about the integrity of the data, and about how the analysis was conducted by Chicago-based Surgisphere Corp and study coauthor Sapan Desai, MD, Surgisphere’s founder and CEO.
The authors asked for an independent third-party review of Surgisphere to evaluate the integrity of the trial elements and to replicate the analyses in the article.
“Our independent peer reviewers informed us that Surgisphere would not transfer the full dataset, client contracts, and the full ISO audit report to their servers for analysis, as such transfer would violate client agreements and confidentiality requirements,” the authors wrote.
Therefore, reviewers were not able to conduct the review and notified the authors they would withdraw from the peer-review process.
The Lancet said in a statement: “The Lancet takes issues of scientific integrity extremely seriously, and there are many outstanding questions about Surgisphere and the data that were allegedly included in this study. Following guidelines from the Committee on Publication Ethics and International Committee of Medical Journal Editors, institutional reviews of Surgisphere’s research collaborations are urgently needed.”
The authors wrote, “We can never forget the responsibility we have as researchers to scrupulously ensure that we rely on data sources that adhere to our high standards. Based on this development, we can no longer vouch for the veracity of the primary data sources. Due to this unfortunate development, the authors request that the paper be retracted.
“We all entered this collaboration to contribute in good faith and at a time of great need during the COVID-19 pandemic. We deeply apologize to you, the editors, and the journal readership for any embarrassment or inconvenience that this may have caused.”
In a similar, if briefer, note, the authors requested that the New England Journal of Medicine retract the earlier article as well. The retraction notice on the website reads: “Because all the authors were not granted access to the raw data and the raw data could not be made available to a third-party auditor, we are unable to validate the primary data sources underlying our article, ‘Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19.’ We therefore request that the article be retracted. We apologize to the editors and to readers of the Journal for the difficulties that this has caused.”
Both journals had already published “Expression of Concern” notices about the articles. The expression of concern followed an open letter, endorsed by more than 200 scientists, ethicists, and clinicians and posted on May 28, questioning the data and ethics of the study.
A version of this article originally appeared on Medscape.com.
RA raises cardiac risk even without CAD
In patients with rheumatoid arthritis (RA), strategies to prevent cardiovascular events, such as treating hypertension, encouraging patients to stop smoking, and reinforcing statin therapy, may be especially important, regardless of whether they have a history of coronary artery disease because their risk for adverse cardiovascular outcomes is significantly greater than for patients who have neither RA nor coronary artery disease (CAD), a large population-based study from Denmark suggests.
“Among patients with RA, risk stratification by presence or absence of documented CAD may allow for screening and personalized treatment strategies,” wrote Brian B. Løgstrup, MD, PhD, DMSc, of Aarhus (Denmark) University Hospital, and his colleagues.
The study, published in Annals of the Rheumatic Diseases, analyzed 125,331 patients with and without CAD in the Western Denmark Heart Registry who had coronary angiography from 2003 through 2016. The cohort included 671 RA patients with no confirmed CAD and 1,061 RA patients who had CAD.
The study makes a significant contribution to the literature in reporting on the additive risk of RA and CAD, said Christie M. Bartels, MD, associate professor in the division of rheumatology at the University of Wisconsin, Madison. “Even among patients with both conditions [RA and CVD], they were less likely to get statin therapy,” she said, noting that the 82.6% of study patients with both CAD and RA were on statins vs. 86.5% of those with CAD alone, while the former had significantly higher rates of hypertension – 64.3% vs. 58.8%. “We’re doing a less effective job on secondary prevention,” she said. The anti-inflammatory properties of statins can also have an additive benefit in RA, she noted.
“This study shows that the rheumatologist can play a role in reinforcing the importance of primary and secondary cardiovascular disease prevention – meaning hypertension control, counseling patients to stop smoking and following up on statin therapy in RA,” Dr. Bartels added.
The study presents two novel findings, Dr. Løgstrup and colleagues noted:
- That RA confers a statistically significant, “but numerically marginally,” heightened risk of cardiovascular events other than stroke.
- Among patients with CAD, RA confers an increased risk of cardiac and all-cause death as well as MI and major adverse cardiovascular events (MACE).
“These finding indicate that RA may have a potential impact for precipitating cardiovascular events beyond CAD and, even more importantly, that RA seems to exacerbate the clinical risk of cardiovascular events in the presence of CAD,” Dr. Løgstrup and colleagues wrote.
The study found that patients with neither RA nor CAD had the lowest 10-year rates of MI (2.7%), ischemic stroke (2.9%), all-cause death (21.6%), cardiac death (2.3%), and MACE (7.3%).
By comparison, those with RA but no CAD had 10-year rates of 3.8% for MI, 5.5% for stroke, 35.6% for all-cause death, 3% for cardiac death, and 11.5% for MACE. Rates for those outcomes for people with CAD but no RA were 9.9% for MI, 4.6% for stroke, 33.3% for all-cause death, 7% for cardiac death, and 19.1% for MACE.
For patients with both RA and CAD, 10-year rates were 12.2% for MI, 4.4% for stroke, 49% for all-cause death, 10.9% for cardiac death, and 24.3% for MACE.
The researchers also performed a risk adjustment analysis based on potential confounding variables across the different groups, such as age, gender, comorbidities including diabetes and hypertension, active smoking status, and anticoagulant, antiplatelet, and statin therapy. The adjusted analysis revealed that patients with RA alone had a 63% greater risk of MI, 68% greater risk for stroke, 42% greater risk for all-cause death, 25% greater risk for cardiac death, and 60% greater risk for MACE than did people who had neither RA nor CAD.
For people with both RA and CAD, the adjusted risks were significantly higher when compared to people with neither: more than four times greater for MI and MACE, 55% greater for stroke, almost double for all-cause death, and 3.7 times greater for cardiac death. People with CAD but no RA also had higher adjusted risk rates compared to people with neither, but had variable rates when compared to people with RA but no CAD, and significantly lower adjusted rates compared to people with both.
The nature of CAD was also a factor, Dr. Løgstrup and colleagues noted. “We found more non-obstructive CAD but no increased incidence of one-vessel, two-vessel, and three-vessel disease in patients with RA than in patients without RA,” they wrote. That’s in line with other published studies (Semin Arthritis Rheum. 2010;40[3]:215–21 and J Rheumatol. 2007;34[5]:937–42), but counter to a study that found increased plaque burden and higher rates of multivessel disease among people with RA (Ann Rheum Dis. 2014;73:1797–804). Differences in methodology, vessel disease definitions, and study population may explain these deviations.
The study authors did not declare any outside source of funding or any competing interests.
Dr. Bartels disclosed receiving institutional grant funding through Pfizer.
SOURCE: Løgstrup BB et al. Ann Rheum Dis. 2020 May 29. doi: 10.1136/annrheumdis-2020-217154.
In patients with rheumatoid arthritis (RA), strategies to prevent cardiovascular events, such as treating hypertension, encouraging patients to stop smoking, and reinforcing statin therapy, may be especially important, regardless of whether they have a history of coronary artery disease because their risk for adverse cardiovascular outcomes is significantly greater than for patients who have neither RA nor coronary artery disease (CAD), a large population-based study from Denmark suggests.
“Among patients with RA, risk stratification by presence or absence of documented CAD may allow for screening and personalized treatment strategies,” wrote Brian B. Løgstrup, MD, PhD, DMSc, of Aarhus (Denmark) University Hospital, and his colleagues.
The study, published in Annals of the Rheumatic Diseases, analyzed 125,331 patients with and without CAD in the Western Denmark Heart Registry who had coronary angiography from 2003 through 2016. The cohort included 671 RA patients with no confirmed CAD and 1,061 RA patients who had CAD.
The study makes a significant contribution to the literature in reporting on the additive risk of RA and CAD, said Christie M. Bartels, MD, associate professor in the division of rheumatology at the University of Wisconsin, Madison. “Even among patients with both conditions [RA and CVD], they were less likely to get statin therapy,” she said, noting that the 82.6% of study patients with both CAD and RA were on statins vs. 86.5% of those with CAD alone, while the former had significantly higher rates of hypertension – 64.3% vs. 58.8%. “We’re doing a less effective job on secondary prevention,” she said. The anti-inflammatory properties of statins can also have an additive benefit in RA, she noted.
“This study shows that the rheumatologist can play a role in reinforcing the importance of primary and secondary cardiovascular disease prevention – meaning hypertension control, counseling patients to stop smoking and following up on statin therapy in RA,” Dr. Bartels added.
The study presents two novel findings, Dr. Løgstrup and colleagues noted:
- That RA confers a statistically significant, “but numerically marginally,” heightened risk of cardiovascular events other than stroke.
- Among patients with CAD, RA confers an increased risk of cardiac and all-cause death as well as MI and major adverse cardiovascular events (MACE).
“These finding indicate that RA may have a potential impact for precipitating cardiovascular events beyond CAD and, even more importantly, that RA seems to exacerbate the clinical risk of cardiovascular events in the presence of CAD,” Dr. Løgstrup and colleagues wrote.
The study found that patients with neither RA nor CAD had the lowest 10-year rates of MI (2.7%), ischemic stroke (2.9%), all-cause death (21.6%), cardiac death (2.3%), and MACE (7.3%).
By comparison, those with RA but no CAD had 10-year rates of 3.8% for MI, 5.5% for stroke, 35.6% for all-cause death, 3% for cardiac death, and 11.5% for MACE. Rates for those outcomes for people with CAD but no RA were 9.9% for MI, 4.6% for stroke, 33.3% for all-cause death, 7% for cardiac death, and 19.1% for MACE.
For patients with both RA and CAD, 10-year rates were 12.2% for MI, 4.4% for stroke, 49% for all-cause death, 10.9% for cardiac death, and 24.3% for MACE.
The researchers also performed a risk adjustment analysis based on potential confounding variables across the different groups, such as age, gender, comorbidities including diabetes and hypertension, active smoking status, and anticoagulant, antiplatelet, and statin therapy. The adjusted analysis revealed that patients with RA alone had a 63% greater risk of MI, 68% greater risk for stroke, 42% greater risk for all-cause death, 25% greater risk for cardiac death, and 60% greater risk for MACE than did people who had neither RA nor CAD.
For people with both RA and CAD, the adjusted risks were significantly higher when compared to people with neither: more than four times greater for MI and MACE, 55% greater for stroke, almost double for all-cause death, and 3.7 times greater for cardiac death. People with CAD but no RA also had higher adjusted risk rates compared to people with neither, but had variable rates when compared to people with RA but no CAD, and significantly lower adjusted rates compared to people with both.
The nature of CAD was also a factor, Dr. Løgstrup and colleagues noted. “We found more non-obstructive CAD but no increased incidence of one-vessel, two-vessel, and three-vessel disease in patients with RA than in patients without RA,” they wrote. That’s in line with other published studies (Semin Arthritis Rheum. 2010;40[3]:215–21 and J Rheumatol. 2007;34[5]:937–42), but counter to a study that found increased plaque burden and higher rates of multivessel disease among people with RA (Ann Rheum Dis. 2014;73:1797–804). Differences in methodology, vessel disease definitions, and study population may explain these deviations.
The study authors did not declare any outside source of funding or any competing interests.
Dr. Bartels disclosed receiving institutional grant funding through Pfizer.
SOURCE: Løgstrup BB et al. Ann Rheum Dis. 2020 May 29. doi: 10.1136/annrheumdis-2020-217154.
In patients with rheumatoid arthritis (RA), strategies to prevent cardiovascular events, such as treating hypertension, encouraging patients to stop smoking, and reinforcing statin therapy, may be especially important, regardless of whether they have a history of coronary artery disease because their risk for adverse cardiovascular outcomes is significantly greater than for patients who have neither RA nor coronary artery disease (CAD), a large population-based study from Denmark suggests.
“Among patients with RA, risk stratification by presence or absence of documented CAD may allow for screening and personalized treatment strategies,” wrote Brian B. Løgstrup, MD, PhD, DMSc, of Aarhus (Denmark) University Hospital, and his colleagues.
The study, published in Annals of the Rheumatic Diseases, analyzed 125,331 patients with and without CAD in the Western Denmark Heart Registry who had coronary angiography from 2003 through 2016. The cohort included 671 RA patients with no confirmed CAD and 1,061 RA patients who had CAD.
The study makes a significant contribution to the literature in reporting on the additive risk of RA and CAD, said Christie M. Bartels, MD, associate professor in the division of rheumatology at the University of Wisconsin, Madison. “Even among patients with both conditions [RA and CVD], they were less likely to get statin therapy,” she said, noting that the 82.6% of study patients with both CAD and RA were on statins vs. 86.5% of those with CAD alone, while the former had significantly higher rates of hypertension – 64.3% vs. 58.8%. “We’re doing a less effective job on secondary prevention,” she said. The anti-inflammatory properties of statins can also have an additive benefit in RA, she noted.
“This study shows that the rheumatologist can play a role in reinforcing the importance of primary and secondary cardiovascular disease prevention – meaning hypertension control, counseling patients to stop smoking and following up on statin therapy in RA,” Dr. Bartels added.
The study presents two novel findings, Dr. Løgstrup and colleagues noted:
- That RA confers a statistically significant, “but numerically marginally,” heightened risk of cardiovascular events other than stroke.
- Among patients with CAD, RA confers an increased risk of cardiac and all-cause death as well as MI and major adverse cardiovascular events (MACE).
“These finding indicate that RA may have a potential impact for precipitating cardiovascular events beyond CAD and, even more importantly, that RA seems to exacerbate the clinical risk of cardiovascular events in the presence of CAD,” Dr. Løgstrup and colleagues wrote.
The study found that patients with neither RA nor CAD had the lowest 10-year rates of MI (2.7%), ischemic stroke (2.9%), all-cause death (21.6%), cardiac death (2.3%), and MACE (7.3%).
By comparison, those with RA but no CAD had 10-year rates of 3.8% for MI, 5.5% for stroke, 35.6% for all-cause death, 3% for cardiac death, and 11.5% for MACE. Rates for those outcomes for people with CAD but no RA were 9.9% for MI, 4.6% for stroke, 33.3% for all-cause death, 7% for cardiac death, and 19.1% for MACE.
For patients with both RA and CAD, 10-year rates were 12.2% for MI, 4.4% for stroke, 49% for all-cause death, 10.9% for cardiac death, and 24.3% for MACE.
The researchers also performed a risk adjustment analysis based on potential confounding variables across the different groups, such as age, gender, comorbidities including diabetes and hypertension, active smoking status, and anticoagulant, antiplatelet, and statin therapy. The adjusted analysis revealed that patients with RA alone had a 63% greater risk of MI, 68% greater risk for stroke, 42% greater risk for all-cause death, 25% greater risk for cardiac death, and 60% greater risk for MACE than did people who had neither RA nor CAD.
For people with both RA and CAD, the adjusted risks were significantly higher when compared to people with neither: more than four times greater for MI and MACE, 55% greater for stroke, almost double for all-cause death, and 3.7 times greater for cardiac death. People with CAD but no RA also had higher adjusted risk rates compared to people with neither, but had variable rates when compared to people with RA but no CAD, and significantly lower adjusted rates compared to people with both.
The nature of CAD was also a factor, Dr. Løgstrup and colleagues noted. “We found more non-obstructive CAD but no increased incidence of one-vessel, two-vessel, and three-vessel disease in patients with RA than in patients without RA,” they wrote. That’s in line with other published studies (Semin Arthritis Rheum. 2010;40[3]:215–21 and J Rheumatol. 2007;34[5]:937–42), but counter to a study that found increased plaque burden and higher rates of multivessel disease among people with RA (Ann Rheum Dis. 2014;73:1797–804). Differences in methodology, vessel disease definitions, and study population may explain these deviations.
The study authors did not declare any outside source of funding or any competing interests.
Dr. Bartels disclosed receiving institutional grant funding through Pfizer.
SOURCE: Løgstrup BB et al. Ann Rheum Dis. 2020 May 29. doi: 10.1136/annrheumdis-2020-217154.
FROM ANNALS OF THE RHEUMATIC DISEASES
More fatalities in heart transplant patients with COVID-19
COVID-19 infection is associated with a high risk for mortality in heart transplant (HT) recipients, a new case series suggests.
Investigators looked at data on 28 patients with a confirmed diagnosis of COVID-19 who received a HT between March 1, 2020, and April 24, 2020 and found a case-fatality rate of 25%.
“The high case fatality in our case series should alert physicians to the vulnerability of heart transplant recipients during the COVID-19 pandemic,” senior author Nir Uriel, MD, MSc, professor of medicine at Columbia University, New York, said in an interview.
“These patients require extra precautions to prevent the development of infection,” said Dr. Uriel, who is also a cardiologist at New York Presbyterian/Columbia University Irving Medical Center.
The study was published online May 13 in JAMA Cardiology.
Similar presentation
HT recipients can have several comorbidities after the procedure, including hypertension, diabetes, cardiac allograft vasculopathy, and ongoing immunosuppression, all of which can place them at risk for infection and adverse outcomes with COVID-19 infection, the authors wrote.
The researchers therefore embarked on a case series looking at 28 HT recipients with COVID-19 infection (median age, 64.0 years; interquartile range, 53.5-70.5; 79% male) to “describe the outcomes of recipients of HT who are chronically immunosuppressed and develop COVID-19 and raise important questions about the role of the immune system in the process.”
The median time from HT to study period was 8.6 (IQR, 4.2-14.5) years. Most patients had numerous comorbidities.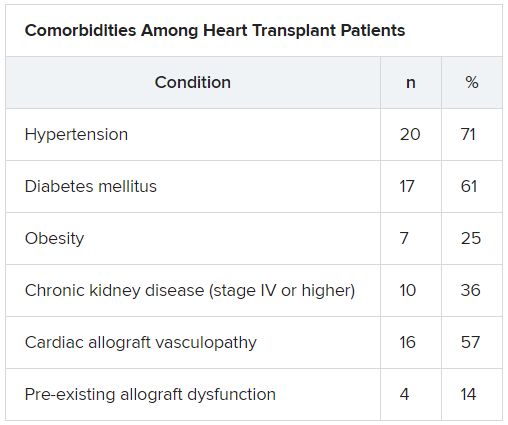
“The presentation of COVID-19 was similar to nontransplant patients with fever, dyspnea, cough, and GI symptoms,” Dr. Uriel reported.
No protective effect
Twenty-two patients (79%) required admission to the hospital, seven of whom (25%) required admission to the ICU and mechanical ventilation.
Despite the presence of immunosuppressive therapy, all patients had significant elevation of inflammatory biomarkers (median peak high-sensitivity C-reactive protein [hs-CRP], 11.83 mg/dL; IQR, 7.44-19.26; median peak interleukin [IL]-6, 105 pg/mL; IQR, 38-296).
Three-quarters had myocardial injury, with a median high-sensitivity troponin T of 0.055 (0.0205 - 0.1345) ng/mL.
Treatments of COVID-19 included hydroxychloroquine (18 patients; 78%), high-dose corticosteroids (eight patients; 47%), and IL-6 receptor antagonists (six patients; 26%).
Moreover, during hospitalization, mycophenolate mofetil was discontinued in most (70%) patients, and one-quarter had a reduction in their calcineurin inhibitor dose.
“Heart transplant recipients generally require more intense immunosuppressive therapy than most other solid organ transplant recipients, and this high baseline immunosuppression increases their propensity to develop infections and their likelihood of experiencing severe manifestations of infections,” Dr. Uriel commented.
“With COVID-19, in which the body’s inflammatory reaction appears to play a role in disease severity, there has been a question of whether immunosuppression may offer a protective effect,” he continued.
“This case series suggests that this is not the case, although this would need to be confirmed in larger studies,” he said.
Low threshold
Among the 22 patients who were admitted to the hospital, half were discharged home and four (18%) were still hospitalized at the end of the study.
Of the seven patients who died, two died at the study center, and five died in an outside institution.
“In the HT population, social distancing (or isolation), strict use of masks when in public, proper handwashing, and sanitization of surfaces are of paramount importance in the prevention of COVID-19 infection,” Dr. Uriel stated.
“In addition, we have restricted these patients’ contact with the hospital as much as possible during the pandemic,” he said.
However, “there should be a low threshold to hospitalize heart transplant patients who develop infection with COVID-19. Furthermore, in our series, outcomes were better for patients hospitalized at the transplant center; therefore, strong consideration should be given to transferring HT patients when hospitalized at another hospital,” he added.
The authors emphasized that COVID-19 patients “will require ongoing monitoring in the recovery phase, as an immunosuppression regimen is reintroduced and the consequences to the allograft itself become apparent.”
Vulnerable population
Commenting on the study, Mandeep R. Mehra, MD, MSc, William Harvey Distinguished Chair in Advanced Cardiovascular Medicine at Brigham and Women’s Hospital, Boston, suggested that “in epidemiological terms, [the findings] might not look as bad as the way they are reflected in the paper.”
Given that Columbia is “one of the larger heart transplant centers in the U.S., following probably 1,000 patients, having only 22 out of perhaps thousands whom they transplanted or are actively following would actually represent a low serious infection rate,” said Dr. Mehra, who is also the executive director of the Center for Advanced Heart Disease at Brigham and Women’s Hospital and a professor of medicine at Harvard Medical School, also in Boston.
“We must not forget to emphasize that, when assessing these case fatality rates, we must look at the entire population at risk, not only the handful that we were able to observe,” explained Dr. Mehra, who was not involved with the study.
Moreover, the patients were “older and had comorbidities, with poor underlying kidney function and other complications, and underlying coronary artery disease in the transplanted heart,” so “it would not surprise me that they had such a high fatality rate, since they had a high degree of vulnerability,” he said.
Dr. Mehra, who is also the editor-in-chief of the Journal of Heart and Lung Transplantation, said that the journal has received manuscripts still in the review process that suggest different fatality rates than those found in the current case series.
However, he acknowledged that, because these are patients with serious vulnerability due to underlying heart disease, “you can’t be lackadaisical and need to do everything to decrease this vulnerability.”
The authors noted that, although their study did not show a protective effect from immunosuppression against COVID-19, further studies are needed to assess each individual immunosuppressive agent and provide a definitive answer.
The study was supported by a grant to one of the investigators from the National Heart, Lung, and Blood Institute. Dr. Uriel reports no relevant financial relationships. The other authors’ disclosures are listed in the publication. Dr. Mehra reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
COVID-19 infection is associated with a high risk for mortality in heart transplant (HT) recipients, a new case series suggests.
Investigators looked at data on 28 patients with a confirmed diagnosis of COVID-19 who received a HT between March 1, 2020, and April 24, 2020 and found a case-fatality rate of 25%.
“The high case fatality in our case series should alert physicians to the vulnerability of heart transplant recipients during the COVID-19 pandemic,” senior author Nir Uriel, MD, MSc, professor of medicine at Columbia University, New York, said in an interview.
“These patients require extra precautions to prevent the development of infection,” said Dr. Uriel, who is also a cardiologist at New York Presbyterian/Columbia University Irving Medical Center.
The study was published online May 13 in JAMA Cardiology.
Similar presentation
HT recipients can have several comorbidities after the procedure, including hypertension, diabetes, cardiac allograft vasculopathy, and ongoing immunosuppression, all of which can place them at risk for infection and adverse outcomes with COVID-19 infection, the authors wrote.
The researchers therefore embarked on a case series looking at 28 HT recipients with COVID-19 infection (median age, 64.0 years; interquartile range, 53.5-70.5; 79% male) to “describe the outcomes of recipients of HT who are chronically immunosuppressed and develop COVID-19 and raise important questions about the role of the immune system in the process.”
The median time from HT to study period was 8.6 (IQR, 4.2-14.5) years. Most patients had numerous comorbidities.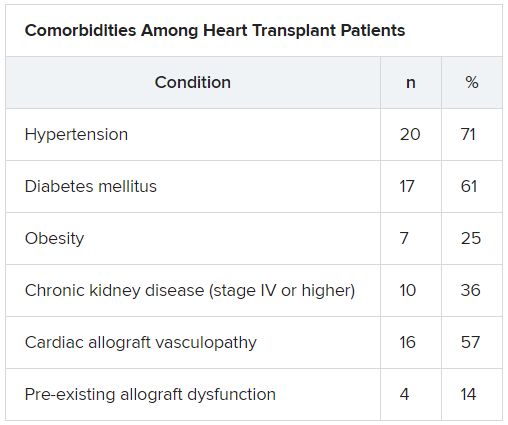
“The presentation of COVID-19 was similar to nontransplant patients with fever, dyspnea, cough, and GI symptoms,” Dr. Uriel reported.
No protective effect
Twenty-two patients (79%) required admission to the hospital, seven of whom (25%) required admission to the ICU and mechanical ventilation.
Despite the presence of immunosuppressive therapy, all patients had significant elevation of inflammatory biomarkers (median peak high-sensitivity C-reactive protein [hs-CRP], 11.83 mg/dL; IQR, 7.44-19.26; median peak interleukin [IL]-6, 105 pg/mL; IQR, 38-296).
Three-quarters had myocardial injury, with a median high-sensitivity troponin T of 0.055 (0.0205 - 0.1345) ng/mL.
Treatments of COVID-19 included hydroxychloroquine (18 patients; 78%), high-dose corticosteroids (eight patients; 47%), and IL-6 receptor antagonists (six patients; 26%).
Moreover, during hospitalization, mycophenolate mofetil was discontinued in most (70%) patients, and one-quarter had a reduction in their calcineurin inhibitor dose.
“Heart transplant recipients generally require more intense immunosuppressive therapy than most other solid organ transplant recipients, and this high baseline immunosuppression increases their propensity to develop infections and their likelihood of experiencing severe manifestations of infections,” Dr. Uriel commented.
“With COVID-19, in which the body’s inflammatory reaction appears to play a role in disease severity, there has been a question of whether immunosuppression may offer a protective effect,” he continued.
“This case series suggests that this is not the case, although this would need to be confirmed in larger studies,” he said.
Low threshold
Among the 22 patients who were admitted to the hospital, half were discharged home and four (18%) were still hospitalized at the end of the study.
Of the seven patients who died, two died at the study center, and five died in an outside institution.
“In the HT population, social distancing (or isolation), strict use of masks when in public, proper handwashing, and sanitization of surfaces are of paramount importance in the prevention of COVID-19 infection,” Dr. Uriel stated.
“In addition, we have restricted these patients’ contact with the hospital as much as possible during the pandemic,” he said.
However, “there should be a low threshold to hospitalize heart transplant patients who develop infection with COVID-19. Furthermore, in our series, outcomes were better for patients hospitalized at the transplant center; therefore, strong consideration should be given to transferring HT patients when hospitalized at another hospital,” he added.
The authors emphasized that COVID-19 patients “will require ongoing monitoring in the recovery phase, as an immunosuppression regimen is reintroduced and the consequences to the allograft itself become apparent.”
Vulnerable population
Commenting on the study, Mandeep R. Mehra, MD, MSc, William Harvey Distinguished Chair in Advanced Cardiovascular Medicine at Brigham and Women’s Hospital, Boston, suggested that “in epidemiological terms, [the findings] might not look as bad as the way they are reflected in the paper.”
Given that Columbia is “one of the larger heart transplant centers in the U.S., following probably 1,000 patients, having only 22 out of perhaps thousands whom they transplanted or are actively following would actually represent a low serious infection rate,” said Dr. Mehra, who is also the executive director of the Center for Advanced Heart Disease at Brigham and Women’s Hospital and a professor of medicine at Harvard Medical School, also in Boston.
“We must not forget to emphasize that, when assessing these case fatality rates, we must look at the entire population at risk, not only the handful that we were able to observe,” explained Dr. Mehra, who was not involved with the study.
Moreover, the patients were “older and had comorbidities, with poor underlying kidney function and other complications, and underlying coronary artery disease in the transplanted heart,” so “it would not surprise me that they had such a high fatality rate, since they had a high degree of vulnerability,” he said.
Dr. Mehra, who is also the editor-in-chief of the Journal of Heart and Lung Transplantation, said that the journal has received manuscripts still in the review process that suggest different fatality rates than those found in the current case series.
However, he acknowledged that, because these are patients with serious vulnerability due to underlying heart disease, “you can’t be lackadaisical and need to do everything to decrease this vulnerability.”
The authors noted that, although their study did not show a protective effect from immunosuppression against COVID-19, further studies are needed to assess each individual immunosuppressive agent and provide a definitive answer.
The study was supported by a grant to one of the investigators from the National Heart, Lung, and Blood Institute. Dr. Uriel reports no relevant financial relationships. The other authors’ disclosures are listed in the publication. Dr. Mehra reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
COVID-19 infection is associated with a high risk for mortality in heart transplant (HT) recipients, a new case series suggests.
Investigators looked at data on 28 patients with a confirmed diagnosis of COVID-19 who received a HT between March 1, 2020, and April 24, 2020 and found a case-fatality rate of 25%.
“The high case fatality in our case series should alert physicians to the vulnerability of heart transplant recipients during the COVID-19 pandemic,” senior author Nir Uriel, MD, MSc, professor of medicine at Columbia University, New York, said in an interview.
“These patients require extra precautions to prevent the development of infection,” said Dr. Uriel, who is also a cardiologist at New York Presbyterian/Columbia University Irving Medical Center.
The study was published online May 13 in JAMA Cardiology.
Similar presentation
HT recipients can have several comorbidities after the procedure, including hypertension, diabetes, cardiac allograft vasculopathy, and ongoing immunosuppression, all of which can place them at risk for infection and adverse outcomes with COVID-19 infection, the authors wrote.
The researchers therefore embarked on a case series looking at 28 HT recipients with COVID-19 infection (median age, 64.0 years; interquartile range, 53.5-70.5; 79% male) to “describe the outcomes of recipients of HT who are chronically immunosuppressed and develop COVID-19 and raise important questions about the role of the immune system in the process.”
The median time from HT to study period was 8.6 (IQR, 4.2-14.5) years. Most patients had numerous comorbidities.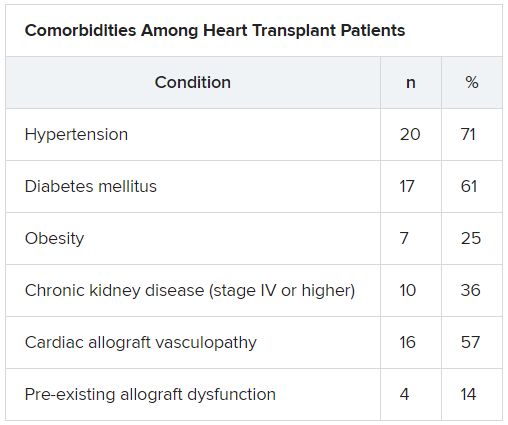
“The presentation of COVID-19 was similar to nontransplant patients with fever, dyspnea, cough, and GI symptoms,” Dr. Uriel reported.
No protective effect
Twenty-two patients (79%) required admission to the hospital, seven of whom (25%) required admission to the ICU and mechanical ventilation.
Despite the presence of immunosuppressive therapy, all patients had significant elevation of inflammatory biomarkers (median peak high-sensitivity C-reactive protein [hs-CRP], 11.83 mg/dL; IQR, 7.44-19.26; median peak interleukin [IL]-6, 105 pg/mL; IQR, 38-296).
Three-quarters had myocardial injury, with a median high-sensitivity troponin T of 0.055 (0.0205 - 0.1345) ng/mL.
Treatments of COVID-19 included hydroxychloroquine (18 patients; 78%), high-dose corticosteroids (eight patients; 47%), and IL-6 receptor antagonists (six patients; 26%).
Moreover, during hospitalization, mycophenolate mofetil was discontinued in most (70%) patients, and one-quarter had a reduction in their calcineurin inhibitor dose.
“Heart transplant recipients generally require more intense immunosuppressive therapy than most other solid organ transplant recipients, and this high baseline immunosuppression increases their propensity to develop infections and their likelihood of experiencing severe manifestations of infections,” Dr. Uriel commented.
“With COVID-19, in which the body’s inflammatory reaction appears to play a role in disease severity, there has been a question of whether immunosuppression may offer a protective effect,” he continued.
“This case series suggests that this is not the case, although this would need to be confirmed in larger studies,” he said.
Low threshold
Among the 22 patients who were admitted to the hospital, half were discharged home and four (18%) were still hospitalized at the end of the study.
Of the seven patients who died, two died at the study center, and five died in an outside institution.
“In the HT population, social distancing (or isolation), strict use of masks when in public, proper handwashing, and sanitization of surfaces are of paramount importance in the prevention of COVID-19 infection,” Dr. Uriel stated.
“In addition, we have restricted these patients’ contact with the hospital as much as possible during the pandemic,” he said.
However, “there should be a low threshold to hospitalize heart transplant patients who develop infection with COVID-19. Furthermore, in our series, outcomes were better for patients hospitalized at the transplant center; therefore, strong consideration should be given to transferring HT patients when hospitalized at another hospital,” he added.
The authors emphasized that COVID-19 patients “will require ongoing monitoring in the recovery phase, as an immunosuppression regimen is reintroduced and the consequences to the allograft itself become apparent.”
Vulnerable population
Commenting on the study, Mandeep R. Mehra, MD, MSc, William Harvey Distinguished Chair in Advanced Cardiovascular Medicine at Brigham and Women’s Hospital, Boston, suggested that “in epidemiological terms, [the findings] might not look as bad as the way they are reflected in the paper.”
Given that Columbia is “one of the larger heart transplant centers in the U.S., following probably 1,000 patients, having only 22 out of perhaps thousands whom they transplanted or are actively following would actually represent a low serious infection rate,” said Dr. Mehra, who is also the executive director of the Center for Advanced Heart Disease at Brigham and Women’s Hospital and a professor of medicine at Harvard Medical School, also in Boston.
“We must not forget to emphasize that, when assessing these case fatality rates, we must look at the entire population at risk, not only the handful that we were able to observe,” explained Dr. Mehra, who was not involved with the study.
Moreover, the patients were “older and had comorbidities, with poor underlying kidney function and other complications, and underlying coronary artery disease in the transplanted heart,” so “it would not surprise me that they had such a high fatality rate, since they had a high degree of vulnerability,” he said.
Dr. Mehra, who is also the editor-in-chief of the Journal of Heart and Lung Transplantation, said that the journal has received manuscripts still in the review process that suggest different fatality rates than those found in the current case series.
However, he acknowledged that, because these are patients with serious vulnerability due to underlying heart disease, “you can’t be lackadaisical and need to do everything to decrease this vulnerability.”
The authors noted that, although their study did not show a protective effect from immunosuppression against COVID-19, further studies are needed to assess each individual immunosuppressive agent and provide a definitive answer.
The study was supported by a grant to one of the investigators from the National Heart, Lung, and Blood Institute. Dr. Uriel reports no relevant financial relationships. The other authors’ disclosures are listed in the publication. Dr. Mehra reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Ticagrelor gets FDA nod for DAPT in high-risk patients with CAD
The Food and Drug Administration has approved ticagrelor (Brilinta/Brilique, AstraZeneca) for use with aspirin to cut the risk for a first myocardial infarction or stroke in high-risk patients with coronary artery disease (CAD) but no history of MI or stroke, AstraZeneca announced today.
The new indication is based on the results of THEMIS (Effect of Ticagrelor on Health Outcomes in Diabetes Mellitus Patients Intervention Study), in which such patients with both CAD and type 2 diabetes on dual-antiplatelet therapy that included ticagrelor 60 mg twice-daily showed a 10% drop in risk for major adverse cardiac events, compared with aspirin alone over about 3 years. The absolute difference was 0.8% in the 42-country trial with more than 19,000 patients.
Patients falling under the new indication do not need to have diabetes, although THEMIS had entered patients with diabetes and CAD, the latter defined as a 50% or greater narrowing of a coronary artery or a history of coronary revascularization but without a history of MI or stroke.
The trial showed a significant reduction in the rate of the primary efficacy end point (P = .04), a composite of cardiovascular death, MI, and stroke. But the risk of TIMI (Thrombolysis in Myocardial Infarction) bleeding classification major bleeding was more than doubled in the ticagrelor group (P < .001) and the risk for intracranial hemorrhage went up 71% (P = .005). Net clinical benefit didn't differ significantly between the groups in an exploratory analysis.
The benefit of dual-antiplatelet therapy with ticagrelor for the primary efficacy end point was even more pronounced in a prespecified THEMIS subanalysis of more than 11,000 patients with a history of percutaneous coronary intervention. In this group, the risk for intracerebral hemorrhage didn't differ significantly between the groups, and the net clinical benefit favored ticagrelor by a significant 15%.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration has approved ticagrelor (Brilinta/Brilique, AstraZeneca) for use with aspirin to cut the risk for a first myocardial infarction or stroke in high-risk patients with coronary artery disease (CAD) but no history of MI or stroke, AstraZeneca announced today.
The new indication is based on the results of THEMIS (Effect of Ticagrelor on Health Outcomes in Diabetes Mellitus Patients Intervention Study), in which such patients with both CAD and type 2 diabetes on dual-antiplatelet therapy that included ticagrelor 60 mg twice-daily showed a 10% drop in risk for major adverse cardiac events, compared with aspirin alone over about 3 years. The absolute difference was 0.8% in the 42-country trial with more than 19,000 patients.
Patients falling under the new indication do not need to have diabetes, although THEMIS had entered patients with diabetes and CAD, the latter defined as a 50% or greater narrowing of a coronary artery or a history of coronary revascularization but without a history of MI or stroke.
The trial showed a significant reduction in the rate of the primary efficacy end point (P = .04), a composite of cardiovascular death, MI, and stroke. But the risk of TIMI (Thrombolysis in Myocardial Infarction) bleeding classification major bleeding was more than doubled in the ticagrelor group (P < .001) and the risk for intracranial hemorrhage went up 71% (P = .005). Net clinical benefit didn't differ significantly between the groups in an exploratory analysis.
The benefit of dual-antiplatelet therapy with ticagrelor for the primary efficacy end point was even more pronounced in a prespecified THEMIS subanalysis of more than 11,000 patients with a history of percutaneous coronary intervention. In this group, the risk for intracerebral hemorrhage didn't differ significantly between the groups, and the net clinical benefit favored ticagrelor by a significant 15%.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration has approved ticagrelor (Brilinta/Brilique, AstraZeneca) for use with aspirin to cut the risk for a first myocardial infarction or stroke in high-risk patients with coronary artery disease (CAD) but no history of MI or stroke, AstraZeneca announced today.
The new indication is based on the results of THEMIS (Effect of Ticagrelor on Health Outcomes in Diabetes Mellitus Patients Intervention Study), in which such patients with both CAD and type 2 diabetes on dual-antiplatelet therapy that included ticagrelor 60 mg twice-daily showed a 10% drop in risk for major adverse cardiac events, compared with aspirin alone over about 3 years. The absolute difference was 0.8% in the 42-country trial with more than 19,000 patients.
Patients falling under the new indication do not need to have diabetes, although THEMIS had entered patients with diabetes and CAD, the latter defined as a 50% or greater narrowing of a coronary artery or a history of coronary revascularization but without a history of MI or stroke.
The trial showed a significant reduction in the rate of the primary efficacy end point (P = .04), a composite of cardiovascular death, MI, and stroke. But the risk of TIMI (Thrombolysis in Myocardial Infarction) bleeding classification major bleeding was more than doubled in the ticagrelor group (P < .001) and the risk for intracranial hemorrhage went up 71% (P = .005). Net clinical benefit didn't differ significantly between the groups in an exploratory analysis.
The benefit of dual-antiplatelet therapy with ticagrelor for the primary efficacy end point was even more pronounced in a prespecified THEMIS subanalysis of more than 11,000 patients with a history of percutaneous coronary intervention. In this group, the risk for intracerebral hemorrhage didn't differ significantly between the groups, and the net clinical benefit favored ticagrelor by a significant 15%.
A version of this article originally appeared on Medscape.com.
Deprescribing hypertension meds can be safe in older patients
Some patients aged 80 years or older can potentially cut back on their number of antihypertensive meds, under physician guidance, without an important loss of blood pressure (BP) control, researchers concluded based on their randomized multicenter trial.
Deprescription of one of at least two antihypertensive meds in such patients was found noninferior to usual care in keeping systolic BP below 150 mm Hg at 12 weeks, in the study that randomly assigned only patients who were considered appropriate for BP-med reduction by their primary care physicians.
Major trials that have shaped some contemporary hypertension guidelines, notably SPRINT, in general have not included such older patients with hypertension along with other chronic conditions, such as diabetes or a history of stroke. So “it’s difficult to know whether their data are relevant for frail, multimorbid patients. In fact, the guidelines say you should use some clinical judgment when applying the results of SPRINT to the kind of patients seen in clinical practice,” James P. Sheppard, PhD, of University of Oxford (England) said in an interview.
The current study, called Optimising Treatment for Mild Systolic Hypertension in the Elderly (OPTIMISE), entered “patients in whom the benefits of taking blood pressure-lowering treatments might start to be outweighed by the potential harms,” Dr. Sheppard said.
The trial is meant to provide something of an otherwise-scant evidence base for how to deprescribe antihypertensive medications, said Dr. Sheppard, who is lead author on the report published May 25 in JAMA.
Of the trial’s 282 patients randomly assigned to the drug-reduction group, 86.4% reached the primary endpoint goal of systolic BP less than 150 mm Hg, compared with 87.7% of the 287 patients on usual care, a difference which in adjusted analysis met the predetermined standard for noninferiority.
The intervention group reduced its number of antihypertensive agents by a mean of 0.6 per patient, which the authors described as “a modest reduction.” However, they noted, drugs that were taken away could be reintroduced as judged necessary by the physicians, yet most of the group sustained their reductions until the end of the 12 weeks.
Had the primary endpoint instead specified a threshold of 130 mm Hg for BP control, which is more consistent with SPRINT and some guidelines in the United States, “the deprescribing strategy would have failed to be considered noninferior to usual care” as calculated by the OPTIMISE authors themselves, observed an accompanying editorial.
The 150 mm Hg threshold chosen by the trialists for the primary endpoint, therefore, “was somewhat of a low bar,” wrote Eric D. Peterson, MD, MPH, of Duke University, Durham, N.C., and Michael W. Rich, MD, of Washington University School of Medicine, St. Louis, Mo.
“Here in the UK it wouldn’t be considered a low bar,” Dr. Sheppard said in an interview. The National Institute for Health and Care Excellence guidelines in Britain “recommends that you treat people over the age of 18 regardless of whether they have any other conditions and to 150 mm Hg systolic.”
The study’s general practitioners, he said, “did what we told them to do, and as a result, two-thirds of the patients were able to reduce their medications. If we had a lower threshold for treatment, it’s possible that more patients might have had medications reintroduced. I think you still could have potentially ended up with a noninferior result.”
Participating physicians were instructed to enroll only “patients who, in their opinion, might potentially benefit from medication reduction due to one or more of the following existing characteristics: polypharmacy, comorbidity, nonadherence or dislike of medicines, or frailty,” the report notes.
They chose which antihypertensives would be dropped for each patient and “were given a medication reduction algorithm to assist with this decision.” Physicians also followed a guide for monitoring for safety issues and were told to reintroduce medications if systolic BP exceeded 150 mm Hg or diastolic BP rose above 90 mm Hg for more than 1 week or in the event of adverse events or signs of accelerated hypertension, the group wrote.
In the deprescription group, the mean systolic BP rose 4.3 points from baseline to 12 weeks, from 129.4 to 133.7 mm Hg. For those given usual care, mean systolic BP went from 130.5 to 130.8 mm Hg. Adjusted, the mean change in systolic BP was 3.4 mm Hg greater (P = .005) in the intervention group. The corresponding adjusted mean change in diastolic BP was a 2.2 mm Hg increase in the intervention group (P = .001).
Although the difference seems minimal, wrote Dr. Peterson and Dr. Rich, “such differences in BP can potentially lead to long-term differences in outcomes at the population level.”
Also, they pointed out, only about 10% of patients screened for enrollment actually entered the study, which brings into question the study’s generalizability, and “patients in the trial had relatively well-controlled BP at baseline.”
Dr. Sheppard said patients in the original screened population, taken from a national database, were directly invited to participate en masse by conventional mail, based on broad inclusion criteria. Far more than the number needed were invited, and nearly all of those excluded from the study had simply not responded to the invitation.
As for greater increases in systolic and diastolic pressures in the deprescribing group, the OPTIMISE authors acknowledged that “caution should be exercised when adopting this approach in routine clinical practice.”
His own view, Dr. Sheppard said, “is that there are some patients who will definitely benefit from intensive blood pressure lowering like you saw in the SPRINT trial. And there’s other patients who will benefit from deprescribing and having a slightly higher target. Those sorts of things very much need to be individualized at the patient level.”
And ideally, he added, clinicians in practice should probably be even more selective in choosing patients for a deprescribing strategy, “and focus on people who are at the highest risk of adverse events.”
Dr. Sheppard has disclosed no relevant financial relationships; disclosures for the other authors are in the report. Dr. Peterson disclosed receiving personal fees from Cerner and Livongo and grants and personal fees from AstraZeneca, Janssen, and Amgen; Dr. Rick has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Some patients aged 80 years or older can potentially cut back on their number of antihypertensive meds, under physician guidance, without an important loss of blood pressure (BP) control, researchers concluded based on their randomized multicenter trial.
Deprescription of one of at least two antihypertensive meds in such patients was found noninferior to usual care in keeping systolic BP below 150 mm Hg at 12 weeks, in the study that randomly assigned only patients who were considered appropriate for BP-med reduction by their primary care physicians.
Major trials that have shaped some contemporary hypertension guidelines, notably SPRINT, in general have not included such older patients with hypertension along with other chronic conditions, such as diabetes or a history of stroke. So “it’s difficult to know whether their data are relevant for frail, multimorbid patients. In fact, the guidelines say you should use some clinical judgment when applying the results of SPRINT to the kind of patients seen in clinical practice,” James P. Sheppard, PhD, of University of Oxford (England) said in an interview.
The current study, called Optimising Treatment for Mild Systolic Hypertension in the Elderly (OPTIMISE), entered “patients in whom the benefits of taking blood pressure-lowering treatments might start to be outweighed by the potential harms,” Dr. Sheppard said.
The trial is meant to provide something of an otherwise-scant evidence base for how to deprescribe antihypertensive medications, said Dr. Sheppard, who is lead author on the report published May 25 in JAMA.
Of the trial’s 282 patients randomly assigned to the drug-reduction group, 86.4% reached the primary endpoint goal of systolic BP less than 150 mm Hg, compared with 87.7% of the 287 patients on usual care, a difference which in adjusted analysis met the predetermined standard for noninferiority.
The intervention group reduced its number of antihypertensive agents by a mean of 0.6 per patient, which the authors described as “a modest reduction.” However, they noted, drugs that were taken away could be reintroduced as judged necessary by the physicians, yet most of the group sustained their reductions until the end of the 12 weeks.
Had the primary endpoint instead specified a threshold of 130 mm Hg for BP control, which is more consistent with SPRINT and some guidelines in the United States, “the deprescribing strategy would have failed to be considered noninferior to usual care” as calculated by the OPTIMISE authors themselves, observed an accompanying editorial.
The 150 mm Hg threshold chosen by the trialists for the primary endpoint, therefore, “was somewhat of a low bar,” wrote Eric D. Peterson, MD, MPH, of Duke University, Durham, N.C., and Michael W. Rich, MD, of Washington University School of Medicine, St. Louis, Mo.
“Here in the UK it wouldn’t be considered a low bar,” Dr. Sheppard said in an interview. The National Institute for Health and Care Excellence guidelines in Britain “recommends that you treat people over the age of 18 regardless of whether they have any other conditions and to 150 mm Hg systolic.”
The study’s general practitioners, he said, “did what we told them to do, and as a result, two-thirds of the patients were able to reduce their medications. If we had a lower threshold for treatment, it’s possible that more patients might have had medications reintroduced. I think you still could have potentially ended up with a noninferior result.”
Participating physicians were instructed to enroll only “patients who, in their opinion, might potentially benefit from medication reduction due to one or more of the following existing characteristics: polypharmacy, comorbidity, nonadherence or dislike of medicines, or frailty,” the report notes.
They chose which antihypertensives would be dropped for each patient and “were given a medication reduction algorithm to assist with this decision.” Physicians also followed a guide for monitoring for safety issues and were told to reintroduce medications if systolic BP exceeded 150 mm Hg or diastolic BP rose above 90 mm Hg for more than 1 week or in the event of adverse events or signs of accelerated hypertension, the group wrote.
In the deprescription group, the mean systolic BP rose 4.3 points from baseline to 12 weeks, from 129.4 to 133.7 mm Hg. For those given usual care, mean systolic BP went from 130.5 to 130.8 mm Hg. Adjusted, the mean change in systolic BP was 3.4 mm Hg greater (P = .005) in the intervention group. The corresponding adjusted mean change in diastolic BP was a 2.2 mm Hg increase in the intervention group (P = .001).
Although the difference seems minimal, wrote Dr. Peterson and Dr. Rich, “such differences in BP can potentially lead to long-term differences in outcomes at the population level.”
Also, they pointed out, only about 10% of patients screened for enrollment actually entered the study, which brings into question the study’s generalizability, and “patients in the trial had relatively well-controlled BP at baseline.”
Dr. Sheppard said patients in the original screened population, taken from a national database, were directly invited to participate en masse by conventional mail, based on broad inclusion criteria. Far more than the number needed were invited, and nearly all of those excluded from the study had simply not responded to the invitation.
As for greater increases in systolic and diastolic pressures in the deprescribing group, the OPTIMISE authors acknowledged that “caution should be exercised when adopting this approach in routine clinical practice.”
His own view, Dr. Sheppard said, “is that there are some patients who will definitely benefit from intensive blood pressure lowering like you saw in the SPRINT trial. And there’s other patients who will benefit from deprescribing and having a slightly higher target. Those sorts of things very much need to be individualized at the patient level.”
And ideally, he added, clinicians in practice should probably be even more selective in choosing patients for a deprescribing strategy, “and focus on people who are at the highest risk of adverse events.”
Dr. Sheppard has disclosed no relevant financial relationships; disclosures for the other authors are in the report. Dr. Peterson disclosed receiving personal fees from Cerner and Livongo and grants and personal fees from AstraZeneca, Janssen, and Amgen; Dr. Rick has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Some patients aged 80 years or older can potentially cut back on their number of antihypertensive meds, under physician guidance, without an important loss of blood pressure (BP) control, researchers concluded based on their randomized multicenter trial.
Deprescription of one of at least two antihypertensive meds in such patients was found noninferior to usual care in keeping systolic BP below 150 mm Hg at 12 weeks, in the study that randomly assigned only patients who were considered appropriate for BP-med reduction by their primary care physicians.
Major trials that have shaped some contemporary hypertension guidelines, notably SPRINT, in general have not included such older patients with hypertension along with other chronic conditions, such as diabetes or a history of stroke. So “it’s difficult to know whether their data are relevant for frail, multimorbid patients. In fact, the guidelines say you should use some clinical judgment when applying the results of SPRINT to the kind of patients seen in clinical practice,” James P. Sheppard, PhD, of University of Oxford (England) said in an interview.
The current study, called Optimising Treatment for Mild Systolic Hypertension in the Elderly (OPTIMISE), entered “patients in whom the benefits of taking blood pressure-lowering treatments might start to be outweighed by the potential harms,” Dr. Sheppard said.
The trial is meant to provide something of an otherwise-scant evidence base for how to deprescribe antihypertensive medications, said Dr. Sheppard, who is lead author on the report published May 25 in JAMA.
Of the trial’s 282 patients randomly assigned to the drug-reduction group, 86.4% reached the primary endpoint goal of systolic BP less than 150 mm Hg, compared with 87.7% of the 287 patients on usual care, a difference which in adjusted analysis met the predetermined standard for noninferiority.
The intervention group reduced its number of antihypertensive agents by a mean of 0.6 per patient, which the authors described as “a modest reduction.” However, they noted, drugs that were taken away could be reintroduced as judged necessary by the physicians, yet most of the group sustained their reductions until the end of the 12 weeks.
Had the primary endpoint instead specified a threshold of 130 mm Hg for BP control, which is more consistent with SPRINT and some guidelines in the United States, “the deprescribing strategy would have failed to be considered noninferior to usual care” as calculated by the OPTIMISE authors themselves, observed an accompanying editorial.
The 150 mm Hg threshold chosen by the trialists for the primary endpoint, therefore, “was somewhat of a low bar,” wrote Eric D. Peterson, MD, MPH, of Duke University, Durham, N.C., and Michael W. Rich, MD, of Washington University School of Medicine, St. Louis, Mo.
“Here in the UK it wouldn’t be considered a low bar,” Dr. Sheppard said in an interview. The National Institute for Health and Care Excellence guidelines in Britain “recommends that you treat people over the age of 18 regardless of whether they have any other conditions and to 150 mm Hg systolic.”
The study’s general practitioners, he said, “did what we told them to do, and as a result, two-thirds of the patients were able to reduce their medications. If we had a lower threshold for treatment, it’s possible that more patients might have had medications reintroduced. I think you still could have potentially ended up with a noninferior result.”
Participating physicians were instructed to enroll only “patients who, in their opinion, might potentially benefit from medication reduction due to one or more of the following existing characteristics: polypharmacy, comorbidity, nonadherence or dislike of medicines, or frailty,” the report notes.
They chose which antihypertensives would be dropped for each patient and “were given a medication reduction algorithm to assist with this decision.” Physicians also followed a guide for monitoring for safety issues and were told to reintroduce medications if systolic BP exceeded 150 mm Hg or diastolic BP rose above 90 mm Hg for more than 1 week or in the event of adverse events or signs of accelerated hypertension, the group wrote.
In the deprescription group, the mean systolic BP rose 4.3 points from baseline to 12 weeks, from 129.4 to 133.7 mm Hg. For those given usual care, mean systolic BP went from 130.5 to 130.8 mm Hg. Adjusted, the mean change in systolic BP was 3.4 mm Hg greater (P = .005) in the intervention group. The corresponding adjusted mean change in diastolic BP was a 2.2 mm Hg increase in the intervention group (P = .001).
Although the difference seems minimal, wrote Dr. Peterson and Dr. Rich, “such differences in BP can potentially lead to long-term differences in outcomes at the population level.”
Also, they pointed out, only about 10% of patients screened for enrollment actually entered the study, which brings into question the study’s generalizability, and “patients in the trial had relatively well-controlled BP at baseline.”
Dr. Sheppard said patients in the original screened population, taken from a national database, were directly invited to participate en masse by conventional mail, based on broad inclusion criteria. Far more than the number needed were invited, and nearly all of those excluded from the study had simply not responded to the invitation.
As for greater increases in systolic and diastolic pressures in the deprescribing group, the OPTIMISE authors acknowledged that “caution should be exercised when adopting this approach in routine clinical practice.”
His own view, Dr. Sheppard said, “is that there are some patients who will definitely benefit from intensive blood pressure lowering like you saw in the SPRINT trial. And there’s other patients who will benefit from deprescribing and having a slightly higher target. Those sorts of things very much need to be individualized at the patient level.”
And ideally, he added, clinicians in practice should probably be even more selective in choosing patients for a deprescribing strategy, “and focus on people who are at the highest risk of adverse events.”
Dr. Sheppard has disclosed no relevant financial relationships; disclosures for the other authors are in the report. Dr. Peterson disclosed receiving personal fees from Cerner and Livongo and grants and personal fees from AstraZeneca, Janssen, and Amgen; Dr. Rick has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FDA okays emergency use for Impella RP in COVID-19 right heart failure
The Food and Drug Administration issued an emergency use authorization for use of the Impella RP heart pump system in COVID-19 patients with right heart failure or decompensation, Abiomed announced June 1.
“Based on extrapolation of data from the approved indication and reported clinical experience, FDA has concluded that the Impella RP may be effective at providing temporary right ventricular support for the treatment of acute right heart failure or decompensation caused by COVID-19 complications, including PE [pulmonary embolism],” the letter noted.
It cited, for example, use of the temporary heart pump in a 59-year-old woman suffering from COVID-19 who went into right ventricular failure and became hypotensive after an acute PE was removed. After placement of the device, the patient experienced a “dramatic and immediate” improvement in arterial pressure and the device was removed on the fifth day, according to Amir Kaki, MD, and Ted Schreiber, MD, of Ascension St. John Hospital, Detroit, whose review of the case has been posted online.
“Acute pulmonary embolism is clearly being recognized as a life-threatening manifestation of COVID-19. Impella RP is an important tool to help cardiologists save lives during this pandemic,” Dr. Kaki said in the letter. “As we have demonstrated in our series of patients, early recognition of right ventricular dysfunction and early placement of the Impella RP for patients who are hypotensive can be lifesaving.”
Other data cited in support of the Impella RP emergency use authorization (EUA) include a 2019 series of hemodynamically unstable patients with PE in Japan and a 2017 case report of a 47-year-old man with right ventricular failure, profound shock, and a massive PE.
The FDA granted premarket approval of the Impella RP system in 2017 to provide temporary right ventricular support for up to 14 days in patients with a body surface area of at least 1.5 m2 who develop acute right heart failure or decompensation following left ventricular assist device implantation, MI, heart transplant, or open-heart surgery.
The EUA indication for the Impella RP system is to provide temporary right ventricular support for up to 14 days in critical care patients with a body surface area of at least 1.5 m2 for the treatment of acute right heart failure or decompensation caused by complications related to COVID-19, including PE.
The Impella RP is authorized only for emergency use under the EUA and only for the duration of the circumstances justifying use of EUAs, the letter noted.
Last year, concerns were raised about off-indication use after interim results from a postapproval study suggested a higher risk for death than seen in premarket studies treated with the temporary heart pump.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration issued an emergency use authorization for use of the Impella RP heart pump system in COVID-19 patients with right heart failure or decompensation, Abiomed announced June 1.
“Based on extrapolation of data from the approved indication and reported clinical experience, FDA has concluded that the Impella RP may be effective at providing temporary right ventricular support for the treatment of acute right heart failure or decompensation caused by COVID-19 complications, including PE [pulmonary embolism],” the letter noted.
It cited, for example, use of the temporary heart pump in a 59-year-old woman suffering from COVID-19 who went into right ventricular failure and became hypotensive after an acute PE was removed. After placement of the device, the patient experienced a “dramatic and immediate” improvement in arterial pressure and the device was removed on the fifth day, according to Amir Kaki, MD, and Ted Schreiber, MD, of Ascension St. John Hospital, Detroit, whose review of the case has been posted online.
“Acute pulmonary embolism is clearly being recognized as a life-threatening manifestation of COVID-19. Impella RP is an important tool to help cardiologists save lives during this pandemic,” Dr. Kaki said in the letter. “As we have demonstrated in our series of patients, early recognition of right ventricular dysfunction and early placement of the Impella RP for patients who are hypotensive can be lifesaving.”
Other data cited in support of the Impella RP emergency use authorization (EUA) include a 2019 series of hemodynamically unstable patients with PE in Japan and a 2017 case report of a 47-year-old man with right ventricular failure, profound shock, and a massive PE.
The FDA granted premarket approval of the Impella RP system in 2017 to provide temporary right ventricular support for up to 14 days in patients with a body surface area of at least 1.5 m2 who develop acute right heart failure or decompensation following left ventricular assist device implantation, MI, heart transplant, or open-heart surgery.
The EUA indication for the Impella RP system is to provide temporary right ventricular support for up to 14 days in critical care patients with a body surface area of at least 1.5 m2 for the treatment of acute right heart failure or decompensation caused by complications related to COVID-19, including PE.
The Impella RP is authorized only for emergency use under the EUA and only for the duration of the circumstances justifying use of EUAs, the letter noted.
Last year, concerns were raised about off-indication use after interim results from a postapproval study suggested a higher risk for death than seen in premarket studies treated with the temporary heart pump.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration issued an emergency use authorization for use of the Impella RP heart pump system in COVID-19 patients with right heart failure or decompensation, Abiomed announced June 1.
“Based on extrapolation of data from the approved indication and reported clinical experience, FDA has concluded that the Impella RP may be effective at providing temporary right ventricular support for the treatment of acute right heart failure or decompensation caused by COVID-19 complications, including PE [pulmonary embolism],” the letter noted.
It cited, for example, use of the temporary heart pump in a 59-year-old woman suffering from COVID-19 who went into right ventricular failure and became hypotensive after an acute PE was removed. After placement of the device, the patient experienced a “dramatic and immediate” improvement in arterial pressure and the device was removed on the fifth day, according to Amir Kaki, MD, and Ted Schreiber, MD, of Ascension St. John Hospital, Detroit, whose review of the case has been posted online.
“Acute pulmonary embolism is clearly being recognized as a life-threatening manifestation of COVID-19. Impella RP is an important tool to help cardiologists save lives during this pandemic,” Dr. Kaki said in the letter. “As we have demonstrated in our series of patients, early recognition of right ventricular dysfunction and early placement of the Impella RP for patients who are hypotensive can be lifesaving.”
Other data cited in support of the Impella RP emergency use authorization (EUA) include a 2019 series of hemodynamically unstable patients with PE in Japan and a 2017 case report of a 47-year-old man with right ventricular failure, profound shock, and a massive PE.
The FDA granted premarket approval of the Impella RP system in 2017 to provide temporary right ventricular support for up to 14 days in patients with a body surface area of at least 1.5 m2 who develop acute right heart failure or decompensation following left ventricular assist device implantation, MI, heart transplant, or open-heart surgery.
The EUA indication for the Impella RP system is to provide temporary right ventricular support for up to 14 days in critical care patients with a body surface area of at least 1.5 m2 for the treatment of acute right heart failure or decompensation caused by complications related to COVID-19, including PE.
The Impella RP is authorized only for emergency use under the EUA and only for the duration of the circumstances justifying use of EUAs, the letter noted.
Last year, concerns were raised about off-indication use after interim results from a postapproval study suggested a higher risk for death than seen in premarket studies treated with the temporary heart pump.
A version of this article originally appeared on Medscape.com.