User login
FDA adds diabetic kidney disease, heart failure indications to canagliflozin
The Food and Drug Administration has approved canagliflozin (Invokana) for the treatment of diabetic kidney disease and for reduction of the risk of hospitalization for heart failure in patients with type 2 diabetes and diabetic kidney disease, which makes it the first drug indicated for diabetic kidney disease treatment in 20 years.
FDA approval, which was announced in a press release by Janssen, the drug’s manufacturer, is based on results from the phase 3 CREDENCE trial. In that study patients with type 2 diabetes and chronic diabetic kidney disease received either 100 mg canagliflozin or placebo. Patients who received canagliflozin experienced a 30% reduction in the risk of the primary composite endpoint, which included end-stage kidney disease, doubling of serum creatinine, and renal or cardiovascular death. The risk of secondary outcomes were also reduced in patients receiving canagliflozin, including a 39% reduction in the risk of hospitalization for heart failure.
The most common adverse events associated with canagliflozin, according to the label, are female genital mycotic infections, urinary tract infection, and increased urination. Serious adverse events associated with canagliflozin include ketoacidosis, kidney problems, serious urinary tract infections, hypoglycemia, necrotizing fasciitis, serious allergic reaction, and bone fractures.
“The real battle to turn the tide on kidney disease is in early detection and slowing its progression so that patients stay healthier and fewer patients reach kidney failure,” LaVerne A. Burton, president and CEO of the American Kidney Fund, said in the press release. “We are so grateful that advances in kidney disease research are producing treatment options that help to slow the progression of diabetic kidney disease and reduce the risk of hospitalization for heart failure.”
Find the full press release on the Janssen website.
The Food and Drug Administration has approved canagliflozin (Invokana) for the treatment of diabetic kidney disease and for reduction of the risk of hospitalization for heart failure in patients with type 2 diabetes and diabetic kidney disease, which makes it the first drug indicated for diabetic kidney disease treatment in 20 years.
FDA approval, which was announced in a press release by Janssen, the drug’s manufacturer, is based on results from the phase 3 CREDENCE trial. In that study patients with type 2 diabetes and chronic diabetic kidney disease received either 100 mg canagliflozin or placebo. Patients who received canagliflozin experienced a 30% reduction in the risk of the primary composite endpoint, which included end-stage kidney disease, doubling of serum creatinine, and renal or cardiovascular death. The risk of secondary outcomes were also reduced in patients receiving canagliflozin, including a 39% reduction in the risk of hospitalization for heart failure.
The most common adverse events associated with canagliflozin, according to the label, are female genital mycotic infections, urinary tract infection, and increased urination. Serious adverse events associated with canagliflozin include ketoacidosis, kidney problems, serious urinary tract infections, hypoglycemia, necrotizing fasciitis, serious allergic reaction, and bone fractures.
“The real battle to turn the tide on kidney disease is in early detection and slowing its progression so that patients stay healthier and fewer patients reach kidney failure,” LaVerne A. Burton, president and CEO of the American Kidney Fund, said in the press release. “We are so grateful that advances in kidney disease research are producing treatment options that help to slow the progression of diabetic kidney disease and reduce the risk of hospitalization for heart failure.”
Find the full press release on the Janssen website.
The Food and Drug Administration has approved canagliflozin (Invokana) for the treatment of diabetic kidney disease and for reduction of the risk of hospitalization for heart failure in patients with type 2 diabetes and diabetic kidney disease, which makes it the first drug indicated for diabetic kidney disease treatment in 20 years.
FDA approval, which was announced in a press release by Janssen, the drug’s manufacturer, is based on results from the phase 3 CREDENCE trial. In that study patients with type 2 diabetes and chronic diabetic kidney disease received either 100 mg canagliflozin or placebo. Patients who received canagliflozin experienced a 30% reduction in the risk of the primary composite endpoint, which included end-stage kidney disease, doubling of serum creatinine, and renal or cardiovascular death. The risk of secondary outcomes were also reduced in patients receiving canagliflozin, including a 39% reduction in the risk of hospitalization for heart failure.
The most common adverse events associated with canagliflozin, according to the label, are female genital mycotic infections, urinary tract infection, and increased urination. Serious adverse events associated with canagliflozin include ketoacidosis, kidney problems, serious urinary tract infections, hypoglycemia, necrotizing fasciitis, serious allergic reaction, and bone fractures.
“The real battle to turn the tide on kidney disease is in early detection and slowing its progression so that patients stay healthier and fewer patients reach kidney failure,” LaVerne A. Burton, president and CEO of the American Kidney Fund, said in the press release. “We are so grateful that advances in kidney disease research are producing treatment options that help to slow the progression of diabetic kidney disease and reduce the risk of hospitalization for heart failure.”
Find the full press release on the Janssen website.
Heart disease raises risk of severe cutaneous adverse reactions to allopurinol
Researchers have found that patients with heart disease have an increased risk of hospitalization for severe cutaneous adverse reactions to allopurinol, with factors like chronic kidney disease and high initial dosage adding to that risk.
“Physicians who prescribe allopurinol should look for these risk factors so that they may consider initiating lower-dosage allopurinol and other precautions, which may prevent this rare but serious adverse reaction,” Chio Yokose, MD, of Massachusetts General Hospital in Boston and coauthors wrote in the Canadian Medical Association Journal.
To further investigate known associations between heart disease and severe cutaneous adverse reactions to allopurinol – including Stevens-Johnson syndrome and toxic epidermal necrolysis – the researchers used an administrative database known as Population Data BC to conduct a cohort study of allopurinol initiators in British Columbia between 1997 and 2015. Individuals with a history of severe cutaneous adverse reactions before starting allopurinol were excluded.
Of the 130,325 allopurinol users identified, 109 were hospitalized for allopurinol-associated severe cutaneous adverse reactions within 3 months of starting the drug. One in 655 allopurinol users with heart disease were admitted to the hospital for allopurinol-associated severe cutaneous adverse reaction (risk ratio = 1.53 per 1,000; 95% confidence interval, 1.10-2.06), compared with 1 in 1,548 allopurinol users without heart disease (risk ratio = 0.65 per 1,000; 95% CI, 0.50-0.82).
After multivariable analysis, other significant associations with hospital admission included chronic kidney disease (relative risk, 1.88; 95% CI, 1.17-3.02) and an initial allopurinol dosage greater than 100 mg/day (RR, 2.78; 95% CI, 1.75-4.43). In addition, patients with heart disease, chronic kidney disease, and an initial dosage greater than 100 mg/day had an 11-fold higher risk of hospital admission (RR, 11.13; 95% CI, 4.66-26.58).
The authors acknowledged their study’s limitations, including potential misclassification of reactions and comorbidities that can stem from a reliance on ICD codes. However, they also noted that “any misclassification is expected to be nondifferential” and bias results toward the null accordingly.
The study was funded by the Canadian Institutes of Health Research. One author reported receiving a grant from the National Institutes of Health and research support from AstraZeneca, along with consulting fees from Takeda, Selecta Biosciences, and Horizon. No other conflicts of interest were reported.
SOURCE: Yokose C et al. CMAJ. 2019 Sep 30. doi: 10.1503/cmaj.190339.
Researchers have found that patients with heart disease have an increased risk of hospitalization for severe cutaneous adverse reactions to allopurinol, with factors like chronic kidney disease and high initial dosage adding to that risk.
“Physicians who prescribe allopurinol should look for these risk factors so that they may consider initiating lower-dosage allopurinol and other precautions, which may prevent this rare but serious adverse reaction,” Chio Yokose, MD, of Massachusetts General Hospital in Boston and coauthors wrote in the Canadian Medical Association Journal.
To further investigate known associations between heart disease and severe cutaneous adverse reactions to allopurinol – including Stevens-Johnson syndrome and toxic epidermal necrolysis – the researchers used an administrative database known as Population Data BC to conduct a cohort study of allopurinol initiators in British Columbia between 1997 and 2015. Individuals with a history of severe cutaneous adverse reactions before starting allopurinol were excluded.
Of the 130,325 allopurinol users identified, 109 were hospitalized for allopurinol-associated severe cutaneous adverse reactions within 3 months of starting the drug. One in 655 allopurinol users with heart disease were admitted to the hospital for allopurinol-associated severe cutaneous adverse reaction (risk ratio = 1.53 per 1,000; 95% confidence interval, 1.10-2.06), compared with 1 in 1,548 allopurinol users without heart disease (risk ratio = 0.65 per 1,000; 95% CI, 0.50-0.82).
After multivariable analysis, other significant associations with hospital admission included chronic kidney disease (relative risk, 1.88; 95% CI, 1.17-3.02) and an initial allopurinol dosage greater than 100 mg/day (RR, 2.78; 95% CI, 1.75-4.43). In addition, patients with heart disease, chronic kidney disease, and an initial dosage greater than 100 mg/day had an 11-fold higher risk of hospital admission (RR, 11.13; 95% CI, 4.66-26.58).
The authors acknowledged their study’s limitations, including potential misclassification of reactions and comorbidities that can stem from a reliance on ICD codes. However, they also noted that “any misclassification is expected to be nondifferential” and bias results toward the null accordingly.
The study was funded by the Canadian Institutes of Health Research. One author reported receiving a grant from the National Institutes of Health and research support from AstraZeneca, along with consulting fees from Takeda, Selecta Biosciences, and Horizon. No other conflicts of interest were reported.
SOURCE: Yokose C et al. CMAJ. 2019 Sep 30. doi: 10.1503/cmaj.190339.
Researchers have found that patients with heart disease have an increased risk of hospitalization for severe cutaneous adverse reactions to allopurinol, with factors like chronic kidney disease and high initial dosage adding to that risk.
“Physicians who prescribe allopurinol should look for these risk factors so that they may consider initiating lower-dosage allopurinol and other precautions, which may prevent this rare but serious adverse reaction,” Chio Yokose, MD, of Massachusetts General Hospital in Boston and coauthors wrote in the Canadian Medical Association Journal.
To further investigate known associations between heart disease and severe cutaneous adverse reactions to allopurinol – including Stevens-Johnson syndrome and toxic epidermal necrolysis – the researchers used an administrative database known as Population Data BC to conduct a cohort study of allopurinol initiators in British Columbia between 1997 and 2015. Individuals with a history of severe cutaneous adverse reactions before starting allopurinol were excluded.
Of the 130,325 allopurinol users identified, 109 were hospitalized for allopurinol-associated severe cutaneous adverse reactions within 3 months of starting the drug. One in 655 allopurinol users with heart disease were admitted to the hospital for allopurinol-associated severe cutaneous adverse reaction (risk ratio = 1.53 per 1,000; 95% confidence interval, 1.10-2.06), compared with 1 in 1,548 allopurinol users without heart disease (risk ratio = 0.65 per 1,000; 95% CI, 0.50-0.82).
After multivariable analysis, other significant associations with hospital admission included chronic kidney disease (relative risk, 1.88; 95% CI, 1.17-3.02) and an initial allopurinol dosage greater than 100 mg/day (RR, 2.78; 95% CI, 1.75-4.43). In addition, patients with heart disease, chronic kidney disease, and an initial dosage greater than 100 mg/day had an 11-fold higher risk of hospital admission (RR, 11.13; 95% CI, 4.66-26.58).
The authors acknowledged their study’s limitations, including potential misclassification of reactions and comorbidities that can stem from a reliance on ICD codes. However, they also noted that “any misclassification is expected to be nondifferential” and bias results toward the null accordingly.
The study was funded by the Canadian Institutes of Health Research. One author reported receiving a grant from the National Institutes of Health and research support from AstraZeneca, along with consulting fees from Takeda, Selecta Biosciences, and Horizon. No other conflicts of interest were reported.
SOURCE: Yokose C et al. CMAJ. 2019 Sep 30. doi: 10.1503/cmaj.190339.
FROM THE CANADIAN MEDICAL ASSOCIATION JOURNAL
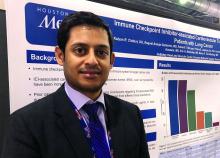
Cardiotoxicity after checkpoint inhibitor treatment seen early, linked to elevated biomarkers
PHILADELPHIA – , and occurred more frequently in patients with elevated biomarkers, in a retrospective cohort study reported at the annual scientific meeting of the Heart Failure Society of America.
The findings support monitoring of cardiac biomarkers in the initial phase of checkpoint inhibitor treatment to identify patient at high cardiac risk, according to Kalyan R. Chitturi, DO, a resident physician with the DeBakey Heart and Vascular Center, Houston Methodist Hospital, who presented the results.
“It’s the early period that warrants the closest monitoring, as within the first 30-40 days, there’s higher risk,” Dr. Chitturi said in an interview. “When there was a biomarker elevation, it markedly increased the risk of MACE, warranting a closer vigilance during that time period.”
The retrospective study conducted by Dr. Chitturi and colleagues included a total of 252 patients with lung cancer who had been treated at one of seven different sites in Houston Methodist Cancer Center between Aug. 1, 2015, and Aug. 1, 2018.
Immune checkpoint inhibitors did not significantly increase the risk of MACE, compared with other lung cancer therapies, with incidences of 13.3% and 10.3%, respectively (P = .632), the investigators found.
However, MACE did occur earlier in the checkpoint inhibitor group, at a median time to event of 40 days, compared with 118 days in the patients not treated with checkpoint inhibitors, they found.
Risk of MACE with checkpoint inhibitor treatment was increased in patients with elevated troponin (hazard ratio, 2.48; 95% confidence interval, 1.18-5.21; P = .017) or elevated brain natriuretic peptide (HR, 5.77; 95% CI, 2.70-12.35; P less than .001), according to multivariate logistic regression analysis results.
These results suggest biomarkers such as cardiac troponin and brain natriuretic peptide are warranted to monitor patients in the early phase of checkpoint inhibitor treatment, according to Dr. Chitturi. “In the cost-benefit ratio of often-lethal MACE, it’s well worth it to collect these,” he said in the interview.
The results corroborate findings from some other recent studies, he noted. These include a recent study that linked elevated serum troponin to myocarditis in patients treated with immune checkpoint inhibitors (J Am Coll Cardiol. 2018 Apr 24;71[16]:1755-64).
Dr. Chitturi and coauthors reported no disclosures related to their presentation at the HFSA meeting.
SOURCE: Chitturi KR et al. HFSA 2019, Abstract 127.
PHILADELPHIA – , and occurred more frequently in patients with elevated biomarkers, in a retrospective cohort study reported at the annual scientific meeting of the Heart Failure Society of America.
The findings support monitoring of cardiac biomarkers in the initial phase of checkpoint inhibitor treatment to identify patient at high cardiac risk, according to Kalyan R. Chitturi, DO, a resident physician with the DeBakey Heart and Vascular Center, Houston Methodist Hospital, who presented the results.
“It’s the early period that warrants the closest monitoring, as within the first 30-40 days, there’s higher risk,” Dr. Chitturi said in an interview. “When there was a biomarker elevation, it markedly increased the risk of MACE, warranting a closer vigilance during that time period.”
The retrospective study conducted by Dr. Chitturi and colleagues included a total of 252 patients with lung cancer who had been treated at one of seven different sites in Houston Methodist Cancer Center between Aug. 1, 2015, and Aug. 1, 2018.
Immune checkpoint inhibitors did not significantly increase the risk of MACE, compared with other lung cancer therapies, with incidences of 13.3% and 10.3%, respectively (P = .632), the investigators found.
However, MACE did occur earlier in the checkpoint inhibitor group, at a median time to event of 40 days, compared with 118 days in the patients not treated with checkpoint inhibitors, they found.
Risk of MACE with checkpoint inhibitor treatment was increased in patients with elevated troponin (hazard ratio, 2.48; 95% confidence interval, 1.18-5.21; P = .017) or elevated brain natriuretic peptide (HR, 5.77; 95% CI, 2.70-12.35; P less than .001), according to multivariate logistic regression analysis results.
These results suggest biomarkers such as cardiac troponin and brain natriuretic peptide are warranted to monitor patients in the early phase of checkpoint inhibitor treatment, according to Dr. Chitturi. “In the cost-benefit ratio of often-lethal MACE, it’s well worth it to collect these,” he said in the interview.
The results corroborate findings from some other recent studies, he noted. These include a recent study that linked elevated serum troponin to myocarditis in patients treated with immune checkpoint inhibitors (J Am Coll Cardiol. 2018 Apr 24;71[16]:1755-64).
Dr. Chitturi and coauthors reported no disclosures related to their presentation at the HFSA meeting.
SOURCE: Chitturi KR et al. HFSA 2019, Abstract 127.
PHILADELPHIA – , and occurred more frequently in patients with elevated biomarkers, in a retrospective cohort study reported at the annual scientific meeting of the Heart Failure Society of America.
The findings support monitoring of cardiac biomarkers in the initial phase of checkpoint inhibitor treatment to identify patient at high cardiac risk, according to Kalyan R. Chitturi, DO, a resident physician with the DeBakey Heart and Vascular Center, Houston Methodist Hospital, who presented the results.
“It’s the early period that warrants the closest monitoring, as within the first 30-40 days, there’s higher risk,” Dr. Chitturi said in an interview. “When there was a biomarker elevation, it markedly increased the risk of MACE, warranting a closer vigilance during that time period.”
The retrospective study conducted by Dr. Chitturi and colleagues included a total of 252 patients with lung cancer who had been treated at one of seven different sites in Houston Methodist Cancer Center between Aug. 1, 2015, and Aug. 1, 2018.
Immune checkpoint inhibitors did not significantly increase the risk of MACE, compared with other lung cancer therapies, with incidences of 13.3% and 10.3%, respectively (P = .632), the investigators found.
However, MACE did occur earlier in the checkpoint inhibitor group, at a median time to event of 40 days, compared with 118 days in the patients not treated with checkpoint inhibitors, they found.
Risk of MACE with checkpoint inhibitor treatment was increased in patients with elevated troponin (hazard ratio, 2.48; 95% confidence interval, 1.18-5.21; P = .017) or elevated brain natriuretic peptide (HR, 5.77; 95% CI, 2.70-12.35; P less than .001), according to multivariate logistic regression analysis results.
These results suggest biomarkers such as cardiac troponin and brain natriuretic peptide are warranted to monitor patients in the early phase of checkpoint inhibitor treatment, according to Dr. Chitturi. “In the cost-benefit ratio of often-lethal MACE, it’s well worth it to collect these,” he said in the interview.
The results corroborate findings from some other recent studies, he noted. These include a recent study that linked elevated serum troponin to myocarditis in patients treated with immune checkpoint inhibitors (J Am Coll Cardiol. 2018 Apr 24;71[16]:1755-64).
Dr. Chitturi and coauthors reported no disclosures related to their presentation at the HFSA meeting.
SOURCE: Chitturi KR et al. HFSA 2019, Abstract 127.
REPORTING FROM HFSA 2019
MitraClip learning curve may top 200 cases
SAN FRANCISCO – It took in the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry from November 2013 to March 2018.
“These findings demonstrate the key role of operator experience in optimizing outcomes” of transcatheter mitral valve repair (TMVr) with MitraClip (Abbott Structural), said investigators, led by Adnan Chhatriwalla, MD, an interventional cardiologist at Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
“New operators may experience a ‘learning curve’ irrespective of the overall site experience or experience of other members of the Heart Team,” they wrote in the study (JACC Cardiovasc Interv. 2019 Sep 27. doi: 10.1016/j.jacc.2019.09.014).
“As TMVr becomes more prevalent in the U.S., it may be prudent for less experienced operators to be cognizant of where they sit on the ‘learning curve’ and to pay particular attention to case selection in their early experience, considering that more complex patients may be referred to more experienced centers for treatment when prudent,” they noted.
“The overall duration of the learning curve may exceed 200 cases,” Dr. Chhatriwalla said at the Transcatheter Cardiovascular Therapeutics annual meeting in a presentation that coincided with the study’s publication.
“This is a more complex procedure than [transcatheter aortic valve replacement], and the volume/outcome relationship is stronger. We are seeing issues that are related to early experience in low-volume programs. Public reporting so consumers can determine how many cases a center does is going to be critical,” said cardiothoracic surgeon Michael Mack, MD, director of the cardiovascular service line at a health system in Dallas, after the talk. He was one of the authors of the study.
The investigators compared outcomes among 549 operators who had done 1-25 MitraClip cases, 230 who had performed 26-50 cases, and 116 who had performed 50 or more.
Optimal procedural success – defined as less than or equal to 1+ residual mitral regurgitation (MR) without death or cardiac surgery – was 63.9%, 68.4%, and 75.1%, respectively, across the three groups (P less than .001). The “acceptable” procedural success rate – less than or equal to 2+ residual MR without death or cardiac surgery – was 91.4%, 92.4%, and 93.8% (P less than .001). No interaction was observed between the mechanism of mitral valve regurgitation and procedural outcomes.
Procedure time decreased as operators gained experience (145, 118, and 99 minutes), and atrial septal defect closure rates increased (0.9%, 1.4%, and 2.2%, respectively).
Composite complications rates also fell (9.7%, 8.1%, and 7.3%), driven mostly by less frequent cardiac perforation (1.0%, 1.1%, and 0.4%) and less frequent blood transfusion (9.6%, 8.6%, and 6.5%). The results were statistically significant.
“Adjusted learning curves for procedural success were visually evident after approximately 50 cases, and continued improvement in clinical outcomes was observed for the entire case sequence up to 200 cases,” the investigators wrote. The improvements could not be attributed to patient selection alone, they said.
More experienced operators were more likely to use more than one clip per case, and more frequently treated central and medial, as opposed to lateral, pathology. Operators with more than 50 cases were less likely to treat patients who had preexisting mitral stenosis or required home oxygen, and experienced operators were more likely to perform the procedure in unstable patients, when appropriate. The proportion of patients with functional MR – as opposed to degenerative disease – increased with increasing experience.
There were no statistically significant differences across the groups in stroke rates (P = .26), single-leaflet device attachments (P = .11), trans-septal complications (P = .25), urgent cardiac surgery (P = .42), or in-hospital mortality (P = .55).
Patients were a median of 81 years old, and most were white; 93% had 3+ or 4+ MR at baseline, and 86.3% had degenerative mitral disease. Two-thirds had atrial fibrillation/flutter.
The work was supported by the ACC/STS TVT Registry. Dr. Chhatriwalla is a proctor for Edwards Lifesciences and Medtronic, and is a speaker for Abbott, Edwards Lifesciences, and Medtronic. Dr. Mack has served as an investigator for Edwards Lifesciences and Abbott, and as a study chair for Medtronic. Other investigators reported similar industry disclosures.
The meeting is sponsored by the Cardiovascular Research Foundation.
SOURCE: Chhatriwalla A et. al. JACC Cardiovasc Interv. 2019 Sep 27. doi: 10.1016/j.jacc.2019.09.014.
SAN FRANCISCO – It took in the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry from November 2013 to March 2018.
“These findings demonstrate the key role of operator experience in optimizing outcomes” of transcatheter mitral valve repair (TMVr) with MitraClip (Abbott Structural), said investigators, led by Adnan Chhatriwalla, MD, an interventional cardiologist at Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
“New operators may experience a ‘learning curve’ irrespective of the overall site experience or experience of other members of the Heart Team,” they wrote in the study (JACC Cardiovasc Interv. 2019 Sep 27. doi: 10.1016/j.jacc.2019.09.014).
“As TMVr becomes more prevalent in the U.S., it may be prudent for less experienced operators to be cognizant of where they sit on the ‘learning curve’ and to pay particular attention to case selection in their early experience, considering that more complex patients may be referred to more experienced centers for treatment when prudent,” they noted.
“The overall duration of the learning curve may exceed 200 cases,” Dr. Chhatriwalla said at the Transcatheter Cardiovascular Therapeutics annual meeting in a presentation that coincided with the study’s publication.
“This is a more complex procedure than [transcatheter aortic valve replacement], and the volume/outcome relationship is stronger. We are seeing issues that are related to early experience in low-volume programs. Public reporting so consumers can determine how many cases a center does is going to be critical,” said cardiothoracic surgeon Michael Mack, MD, director of the cardiovascular service line at a health system in Dallas, after the talk. He was one of the authors of the study.
The investigators compared outcomes among 549 operators who had done 1-25 MitraClip cases, 230 who had performed 26-50 cases, and 116 who had performed 50 or more.
Optimal procedural success – defined as less than or equal to 1+ residual mitral regurgitation (MR) without death or cardiac surgery – was 63.9%, 68.4%, and 75.1%, respectively, across the three groups (P less than .001). The “acceptable” procedural success rate – less than or equal to 2+ residual MR without death or cardiac surgery – was 91.4%, 92.4%, and 93.8% (P less than .001). No interaction was observed between the mechanism of mitral valve regurgitation and procedural outcomes.
Procedure time decreased as operators gained experience (145, 118, and 99 minutes), and atrial septal defect closure rates increased (0.9%, 1.4%, and 2.2%, respectively).
Composite complications rates also fell (9.7%, 8.1%, and 7.3%), driven mostly by less frequent cardiac perforation (1.0%, 1.1%, and 0.4%) and less frequent blood transfusion (9.6%, 8.6%, and 6.5%). The results were statistically significant.
“Adjusted learning curves for procedural success were visually evident after approximately 50 cases, and continued improvement in clinical outcomes was observed for the entire case sequence up to 200 cases,” the investigators wrote. The improvements could not be attributed to patient selection alone, they said.
More experienced operators were more likely to use more than one clip per case, and more frequently treated central and medial, as opposed to lateral, pathology. Operators with more than 50 cases were less likely to treat patients who had preexisting mitral stenosis or required home oxygen, and experienced operators were more likely to perform the procedure in unstable patients, when appropriate. The proportion of patients with functional MR – as opposed to degenerative disease – increased with increasing experience.
There were no statistically significant differences across the groups in stroke rates (P = .26), single-leaflet device attachments (P = .11), trans-septal complications (P = .25), urgent cardiac surgery (P = .42), or in-hospital mortality (P = .55).
Patients were a median of 81 years old, and most were white; 93% had 3+ or 4+ MR at baseline, and 86.3% had degenerative mitral disease. Two-thirds had atrial fibrillation/flutter.
The work was supported by the ACC/STS TVT Registry. Dr. Chhatriwalla is a proctor for Edwards Lifesciences and Medtronic, and is a speaker for Abbott, Edwards Lifesciences, and Medtronic. Dr. Mack has served as an investigator for Edwards Lifesciences and Abbott, and as a study chair for Medtronic. Other investigators reported similar industry disclosures.
The meeting is sponsored by the Cardiovascular Research Foundation.
SOURCE: Chhatriwalla A et. al. JACC Cardiovasc Interv. 2019 Sep 27. doi: 10.1016/j.jacc.2019.09.014.
SAN FRANCISCO – It took in the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry from November 2013 to March 2018.
“These findings demonstrate the key role of operator experience in optimizing outcomes” of transcatheter mitral valve repair (TMVr) with MitraClip (Abbott Structural), said investigators, led by Adnan Chhatriwalla, MD, an interventional cardiologist at Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
“New operators may experience a ‘learning curve’ irrespective of the overall site experience or experience of other members of the Heart Team,” they wrote in the study (JACC Cardiovasc Interv. 2019 Sep 27. doi: 10.1016/j.jacc.2019.09.014).
“As TMVr becomes more prevalent in the U.S., it may be prudent for less experienced operators to be cognizant of where they sit on the ‘learning curve’ and to pay particular attention to case selection in their early experience, considering that more complex patients may be referred to more experienced centers for treatment when prudent,” they noted.
“The overall duration of the learning curve may exceed 200 cases,” Dr. Chhatriwalla said at the Transcatheter Cardiovascular Therapeutics annual meeting in a presentation that coincided with the study’s publication.
“This is a more complex procedure than [transcatheter aortic valve replacement], and the volume/outcome relationship is stronger. We are seeing issues that are related to early experience in low-volume programs. Public reporting so consumers can determine how many cases a center does is going to be critical,” said cardiothoracic surgeon Michael Mack, MD, director of the cardiovascular service line at a health system in Dallas, after the talk. He was one of the authors of the study.
The investigators compared outcomes among 549 operators who had done 1-25 MitraClip cases, 230 who had performed 26-50 cases, and 116 who had performed 50 or more.
Optimal procedural success – defined as less than or equal to 1+ residual mitral regurgitation (MR) without death or cardiac surgery – was 63.9%, 68.4%, and 75.1%, respectively, across the three groups (P less than .001). The “acceptable” procedural success rate – less than or equal to 2+ residual MR without death or cardiac surgery – was 91.4%, 92.4%, and 93.8% (P less than .001). No interaction was observed between the mechanism of mitral valve regurgitation and procedural outcomes.
Procedure time decreased as operators gained experience (145, 118, and 99 minutes), and atrial septal defect closure rates increased (0.9%, 1.4%, and 2.2%, respectively).
Composite complications rates also fell (9.7%, 8.1%, and 7.3%), driven mostly by less frequent cardiac perforation (1.0%, 1.1%, and 0.4%) and less frequent blood transfusion (9.6%, 8.6%, and 6.5%). The results were statistically significant.
“Adjusted learning curves for procedural success were visually evident after approximately 50 cases, and continued improvement in clinical outcomes was observed for the entire case sequence up to 200 cases,” the investigators wrote. The improvements could not be attributed to patient selection alone, they said.
More experienced operators were more likely to use more than one clip per case, and more frequently treated central and medial, as opposed to lateral, pathology. Operators with more than 50 cases were less likely to treat patients who had preexisting mitral stenosis or required home oxygen, and experienced operators were more likely to perform the procedure in unstable patients, when appropriate. The proportion of patients with functional MR – as opposed to degenerative disease – increased with increasing experience.
There were no statistically significant differences across the groups in stroke rates (P = .26), single-leaflet device attachments (P = .11), trans-septal complications (P = .25), urgent cardiac surgery (P = .42), or in-hospital mortality (P = .55).
Patients were a median of 81 years old, and most were white; 93% had 3+ or 4+ MR at baseline, and 86.3% had degenerative mitral disease. Two-thirds had atrial fibrillation/flutter.
The work was supported by the ACC/STS TVT Registry. Dr. Chhatriwalla is a proctor for Edwards Lifesciences and Medtronic, and is a speaker for Abbott, Edwards Lifesciences, and Medtronic. Dr. Mack has served as an investigator for Edwards Lifesciences and Abbott, and as a study chair for Medtronic. Other investigators reported similar industry disclosures.
The meeting is sponsored by the Cardiovascular Research Foundation.
SOURCE: Chhatriwalla A et. al. JACC Cardiovasc Interv. 2019 Sep 27. doi: 10.1016/j.jacc.2019.09.014.
REPORTING FROM TCT 2019
Ticagrelor monotherapy tops DAPT for high-risk PCI patients
SAN FRANCISCO – After 3 months of ticagrelor (Brilinta) plus aspirin following cardiac stenting, stopping the aspirin but continuing the ticagrelor resulted in less bleeding with no increase in ischemic events in a randomized trial with more than 7,000 drug-eluting stent patients at high risk for both.
“This was a superior therapy” to staying on both drugs, the more usual approach, said lead investigator Roxana Mehran, MD, director of interventional cardiovascular research and clinical trials at the Icahn School of Medicine at Mount Sinai, New York.
“We can’t say this is for all comers, but for patients whose physician felt comfortable putting them on aspirin and ticagrelor,” who tolerated it well for the first 3 months, and who had clinical and angiographic indications of risk, “I think these patients can be peeled away” from aspirin, she said in a presentation at the Transcatheter Cardiovascular Therapeutics annual meeting that coincided with publication of the trial, dubbed TWILIGHT (Ticagrelor with Aspirin or Alone in High-Risk Patients after Coronary Intervention).
Interventional cardiologists have long sought the sweet spot for dual-antiplatelet therapy (DAPT) after stenting; the idea is to maximize thrombosis prevention while minimizing bleeding risk. The trial supports the trend in recent years towards shorter DAPT. Often, however, it’s the P2Y12 inhibitor – ticagrelor, clopidogrel (Plavix), or prasugrel (Effient) – that goes first, not the aspirin.
Responding to an audience question about why the trial didn’t include an aspirin monotherapy arm, Dr. Mehran said that aspirin alone wouldn’t have been sufficient in high-risk patients “in whom you have almost 70% acute coronary syndrome.” She added that her team has data showing that aspirin itself doesn’t have much effect on blood thrombogenicity.
The 7,119 patients in TWILIGHT were on ticagrelor 90 mg twice daily and aspirin 81-100 mg daily for 3 months, then evenly randomized to continued treatment or ticagrelor plus an aspirin placebo for a year.
Subjects had to have at least one clinical and angiographic finding that put them at high risk for bleeding or an ischemic event, such as chronic kidney disease, acute coronary syndrome, diabetes, or a bifurcated target lesion treated with two stents.
One year after randomization, 4% in the ticagrelor monotherapy group versus 7.1% in the ticagrelor plus aspirin arm reached the primary end point, actionable (type 2), severe (type 3), or fatal (type 5) bleeding on the Bleeding Academic Research Consortium scale (hazard ratio, 0.56; 95% confidence interval, 0.45 - 0.68, P less than .001).
The incidence of death from any cause, nonfatal myocardial infarction, or nonfatal stroke was 3.9% in both groups (HR, 0.99; 95% CI, 0.78-1.25; P less than .001 for noninferiority).
There were more ischemic strokes in the ticagrelor monotherapy arm (0.5% versus 0.2%). All-cause mortality (1.3% versus 1%) and stent thrombosis (0.6% versus 0.4%) were more frequent in the ticagrelor/aspirin group, but the differences were not statistically significant.
The two groups were well balanced. The mean age was 65 years, 23.8% of the patients were female, 37% had diabetes, and 65% had percutaneous coronary intervention for an acute coronary syndrome. Almost two-thirds had multivessel disease. Mean stent length was about 40 mm. The trial excluded patients with prior strokes.
Almost 2,000 patients originally enrolled in the trial never made it to randomization because they had a major bleeding or ischemic event in the 3-month run up, or dyspnea or some other reaction to ticagrelor.
The recent STOPDAPT-2 trial had a similar outcome – less bleeding with no increase in ischemic events – with clopidogrel monotherapy after a month-long run in of dual therapy with aspirin, versus continued treatment with both, in patients at low risk for ischemic events after stenting (JAMA. 2019 Jun 25;321[24]:2414-27).
Another recent study, GLOBAL LEADERS, concluded that 1 month of DAPT followed by ticagrelor monotherapy for 23 months was not superior to 12 months of DAPT followed by a year of aspirin. There was a numerical advantage for solo ticagrelor on death, myocardial infarction, and bleeding, but it did not reach statistical significance (Lancet. 2018 Sep 15;392[10151]:940-9).
The work was funded by ticagrelor’s maker, AstraZeneca. Dr. Mehran reported consulting and other relationships with Abbott, Janssen, and other companies.
SOURCE: Mehran A et al. N Engl J Med. 2019 Sep 26. doi: 10.1056/NEJMoa1908419.
SAN FRANCISCO – After 3 months of ticagrelor (Brilinta) plus aspirin following cardiac stenting, stopping the aspirin but continuing the ticagrelor resulted in less bleeding with no increase in ischemic events in a randomized trial with more than 7,000 drug-eluting stent patients at high risk for both.
“This was a superior therapy” to staying on both drugs, the more usual approach, said lead investigator Roxana Mehran, MD, director of interventional cardiovascular research and clinical trials at the Icahn School of Medicine at Mount Sinai, New York.
“We can’t say this is for all comers, but for patients whose physician felt comfortable putting them on aspirin and ticagrelor,” who tolerated it well for the first 3 months, and who had clinical and angiographic indications of risk, “I think these patients can be peeled away” from aspirin, she said in a presentation at the Transcatheter Cardiovascular Therapeutics annual meeting that coincided with publication of the trial, dubbed TWILIGHT (Ticagrelor with Aspirin or Alone in High-Risk Patients after Coronary Intervention).
Interventional cardiologists have long sought the sweet spot for dual-antiplatelet therapy (DAPT) after stenting; the idea is to maximize thrombosis prevention while minimizing bleeding risk. The trial supports the trend in recent years towards shorter DAPT. Often, however, it’s the P2Y12 inhibitor – ticagrelor, clopidogrel (Plavix), or prasugrel (Effient) – that goes first, not the aspirin.
Responding to an audience question about why the trial didn’t include an aspirin monotherapy arm, Dr. Mehran said that aspirin alone wouldn’t have been sufficient in high-risk patients “in whom you have almost 70% acute coronary syndrome.” She added that her team has data showing that aspirin itself doesn’t have much effect on blood thrombogenicity.
The 7,119 patients in TWILIGHT were on ticagrelor 90 mg twice daily and aspirin 81-100 mg daily for 3 months, then evenly randomized to continued treatment or ticagrelor plus an aspirin placebo for a year.
Subjects had to have at least one clinical and angiographic finding that put them at high risk for bleeding or an ischemic event, such as chronic kidney disease, acute coronary syndrome, diabetes, or a bifurcated target lesion treated with two stents.
One year after randomization, 4% in the ticagrelor monotherapy group versus 7.1% in the ticagrelor plus aspirin arm reached the primary end point, actionable (type 2), severe (type 3), or fatal (type 5) bleeding on the Bleeding Academic Research Consortium scale (hazard ratio, 0.56; 95% confidence interval, 0.45 - 0.68, P less than .001).
The incidence of death from any cause, nonfatal myocardial infarction, or nonfatal stroke was 3.9% in both groups (HR, 0.99; 95% CI, 0.78-1.25; P less than .001 for noninferiority).
There were more ischemic strokes in the ticagrelor monotherapy arm (0.5% versus 0.2%). All-cause mortality (1.3% versus 1%) and stent thrombosis (0.6% versus 0.4%) were more frequent in the ticagrelor/aspirin group, but the differences were not statistically significant.
The two groups were well balanced. The mean age was 65 years, 23.8% of the patients were female, 37% had diabetes, and 65% had percutaneous coronary intervention for an acute coronary syndrome. Almost two-thirds had multivessel disease. Mean stent length was about 40 mm. The trial excluded patients with prior strokes.
Almost 2,000 patients originally enrolled in the trial never made it to randomization because they had a major bleeding or ischemic event in the 3-month run up, or dyspnea or some other reaction to ticagrelor.
The recent STOPDAPT-2 trial had a similar outcome – less bleeding with no increase in ischemic events – with clopidogrel monotherapy after a month-long run in of dual therapy with aspirin, versus continued treatment with both, in patients at low risk for ischemic events after stenting (JAMA. 2019 Jun 25;321[24]:2414-27).
Another recent study, GLOBAL LEADERS, concluded that 1 month of DAPT followed by ticagrelor monotherapy for 23 months was not superior to 12 months of DAPT followed by a year of aspirin. There was a numerical advantage for solo ticagrelor on death, myocardial infarction, and bleeding, but it did not reach statistical significance (Lancet. 2018 Sep 15;392[10151]:940-9).
The work was funded by ticagrelor’s maker, AstraZeneca. Dr. Mehran reported consulting and other relationships with Abbott, Janssen, and other companies.
SOURCE: Mehran A et al. N Engl J Med. 2019 Sep 26. doi: 10.1056/NEJMoa1908419.
SAN FRANCISCO – After 3 months of ticagrelor (Brilinta) plus aspirin following cardiac stenting, stopping the aspirin but continuing the ticagrelor resulted in less bleeding with no increase in ischemic events in a randomized trial with more than 7,000 drug-eluting stent patients at high risk for both.
“This was a superior therapy” to staying on both drugs, the more usual approach, said lead investigator Roxana Mehran, MD, director of interventional cardiovascular research and clinical trials at the Icahn School of Medicine at Mount Sinai, New York.
“We can’t say this is for all comers, but for patients whose physician felt comfortable putting them on aspirin and ticagrelor,” who tolerated it well for the first 3 months, and who had clinical and angiographic indications of risk, “I think these patients can be peeled away” from aspirin, she said in a presentation at the Transcatheter Cardiovascular Therapeutics annual meeting that coincided with publication of the trial, dubbed TWILIGHT (Ticagrelor with Aspirin or Alone in High-Risk Patients after Coronary Intervention).
Interventional cardiologists have long sought the sweet spot for dual-antiplatelet therapy (DAPT) after stenting; the idea is to maximize thrombosis prevention while minimizing bleeding risk. The trial supports the trend in recent years towards shorter DAPT. Often, however, it’s the P2Y12 inhibitor – ticagrelor, clopidogrel (Plavix), or prasugrel (Effient) – that goes first, not the aspirin.
Responding to an audience question about why the trial didn’t include an aspirin monotherapy arm, Dr. Mehran said that aspirin alone wouldn’t have been sufficient in high-risk patients “in whom you have almost 70% acute coronary syndrome.” She added that her team has data showing that aspirin itself doesn’t have much effect on blood thrombogenicity.
The 7,119 patients in TWILIGHT were on ticagrelor 90 mg twice daily and aspirin 81-100 mg daily for 3 months, then evenly randomized to continued treatment or ticagrelor plus an aspirin placebo for a year.
Subjects had to have at least one clinical and angiographic finding that put them at high risk for bleeding or an ischemic event, such as chronic kidney disease, acute coronary syndrome, diabetes, or a bifurcated target lesion treated with two stents.
One year after randomization, 4% in the ticagrelor monotherapy group versus 7.1% in the ticagrelor plus aspirin arm reached the primary end point, actionable (type 2), severe (type 3), or fatal (type 5) bleeding on the Bleeding Academic Research Consortium scale (hazard ratio, 0.56; 95% confidence interval, 0.45 - 0.68, P less than .001).
The incidence of death from any cause, nonfatal myocardial infarction, or nonfatal stroke was 3.9% in both groups (HR, 0.99; 95% CI, 0.78-1.25; P less than .001 for noninferiority).
There were more ischemic strokes in the ticagrelor monotherapy arm (0.5% versus 0.2%). All-cause mortality (1.3% versus 1%) and stent thrombosis (0.6% versus 0.4%) were more frequent in the ticagrelor/aspirin group, but the differences were not statistically significant.
The two groups were well balanced. The mean age was 65 years, 23.8% of the patients were female, 37% had diabetes, and 65% had percutaneous coronary intervention for an acute coronary syndrome. Almost two-thirds had multivessel disease. Mean stent length was about 40 mm. The trial excluded patients with prior strokes.
Almost 2,000 patients originally enrolled in the trial never made it to randomization because they had a major bleeding or ischemic event in the 3-month run up, or dyspnea or some other reaction to ticagrelor.
The recent STOPDAPT-2 trial had a similar outcome – less bleeding with no increase in ischemic events – with clopidogrel monotherapy after a month-long run in of dual therapy with aspirin, versus continued treatment with both, in patients at low risk for ischemic events after stenting (JAMA. 2019 Jun 25;321[24]:2414-27).
Another recent study, GLOBAL LEADERS, concluded that 1 month of DAPT followed by ticagrelor monotherapy for 23 months was not superior to 12 months of DAPT followed by a year of aspirin. There was a numerical advantage for solo ticagrelor on death, myocardial infarction, and bleeding, but it did not reach statistical significance (Lancet. 2018 Sep 15;392[10151]:940-9).
The work was funded by ticagrelor’s maker, AstraZeneca. Dr. Mehran reported consulting and other relationships with Abbott, Janssen, and other companies.
SOURCE: Mehran A et al. N Engl J Med. 2019 Sep 26. doi: 10.1056/NEJMoa1908419.
REPORTING FROM TCT 2019
AF risk is elevated after early-stage breast cancer diagnosis
Women with early-stage breast cancer are at elevated risk for atrial fibrillation (AF) short term and, to a lesser extent, long term, finds a large Canadian cohort study. Risk was higher for those who had received chemotherapy but not tied to specific cardiotoxic drugs or drug classes.
“Cardiovascular disease is a particularly pertinent clinical concern for women diagnosed with early-stage breast cancer,” note the investigators, led by Husam Abdel-Qadir, MD, PhD, FRCPC, Cardiology Clinic, Women’s College Hospital, Toronto. “Many early-stage breast cancer survivors are older than 65 years and have hypertension, diabetes, or left ventricular dysfunction. Accordingly, a diagnosis of AF would translate to a clinically relevant stroke risk for many early-stage breast cancer survivors.”
The investigators undertook a population-based retrospective cohort study of women in the province of Ontario with stage I-III breast cancer diagnosed between April 2007 and December 2016, matching them 1:3 to cancer-free control women on birth year and receipt of breast imaging.
An initial analysis, based on 95,539 breast cancer patients and 217,456 cancer-free controls, showed that the former and latter groups did not differ significantly on the prevalence of preexisting AF (5.3% vs. 5.2%; P = .21), according to results reported in JAMA Network Open.
Main analyses excluded women with preexisting AF, leaving 68,113 breast cancer patients and 204,330 cancer-free controls having a mean follow-up of 5.7 years. Both groups had a mean age of 60 years at baseline, and prevalences of cardiovascular comorbidities were similar. Within the breast cancer group, 50.4% had left-sided disease; overall, 53.2% received chemotherapy and 71.7% received radiation therapy.
At 10 years after diagnosis, breast cancer patients had a small but significant increase in AF incidence relative to control peers (7.4% vs. 6.8%; P less than .001). When the investigators looked at specific time periods, survivors had a significantly elevated AF risk in year 1 postdiagnosis (hazard ratio, 2.16) and after year 5 postdiagnosis (hazard ratio, 1.20), but not during years 2 through 5.
Analyses beginning 1 year after diagnosis showed a slightly smaller but still significant elevation of AF incidence for the breast cancer group at 9 years of follow-up (10 years after diagnosis) (7.0% vs. 6.5%; P less than .001).
Among breast cancer patients, those who received chemotherapy had a higher risk of AF than those who did not (adjusted hazard ratio, 1.23); however, this elevation of risk was not specifically tied to receipt of anthracyclines or trastuzumab (Herceptin) versus other chemotherapy. Risk was not elevated for those who received radiation therapy.
“Our study findings suggest that a diagnosis of early-stage breast cancer may be associated with a small increase in the risk of AF compared with that for cancer-free women,” Dr. Abdel-Qadir and coinvestigators noted. “Since the absolute risk is small, this finding does not warrant routine surveillance but rather should prompt consideration of AF in the differential diagnosis for women with compatible symptoms.
“The early and late periods of increased AF risk in early-stage breast cancer survivors warrant focused research to better understand the underlying causes and subsequent implications,” they concluded.
Dr. Abdel-Qadir reported receiving grants from the Canadian Cardiovascular Society during the conduct of the study, speaker fees from Amgen, and an honorarium for clinical events adjudication committee membership from the Canadian Vigour Centre for a study funded by AstraZeneca. The study was funded by the Canadian Cardiovascular Society Atrial Fibrillation Research Award.
SOURCE: Abdel-Qadir H et al. JAMA Netw Open. 2019 Sep 4;2(9):e1911838.
Women with early-stage breast cancer are at elevated risk for atrial fibrillation (AF) short term and, to a lesser extent, long term, finds a large Canadian cohort study. Risk was higher for those who had received chemotherapy but not tied to specific cardiotoxic drugs or drug classes.
“Cardiovascular disease is a particularly pertinent clinical concern for women diagnosed with early-stage breast cancer,” note the investigators, led by Husam Abdel-Qadir, MD, PhD, FRCPC, Cardiology Clinic, Women’s College Hospital, Toronto. “Many early-stage breast cancer survivors are older than 65 years and have hypertension, diabetes, or left ventricular dysfunction. Accordingly, a diagnosis of AF would translate to a clinically relevant stroke risk for many early-stage breast cancer survivors.”
The investigators undertook a population-based retrospective cohort study of women in the province of Ontario with stage I-III breast cancer diagnosed between April 2007 and December 2016, matching them 1:3 to cancer-free control women on birth year and receipt of breast imaging.
An initial analysis, based on 95,539 breast cancer patients and 217,456 cancer-free controls, showed that the former and latter groups did not differ significantly on the prevalence of preexisting AF (5.3% vs. 5.2%; P = .21), according to results reported in JAMA Network Open.
Main analyses excluded women with preexisting AF, leaving 68,113 breast cancer patients and 204,330 cancer-free controls having a mean follow-up of 5.7 years. Both groups had a mean age of 60 years at baseline, and prevalences of cardiovascular comorbidities were similar. Within the breast cancer group, 50.4% had left-sided disease; overall, 53.2% received chemotherapy and 71.7% received radiation therapy.
At 10 years after diagnosis, breast cancer patients had a small but significant increase in AF incidence relative to control peers (7.4% vs. 6.8%; P less than .001). When the investigators looked at specific time periods, survivors had a significantly elevated AF risk in year 1 postdiagnosis (hazard ratio, 2.16) and after year 5 postdiagnosis (hazard ratio, 1.20), but not during years 2 through 5.
Analyses beginning 1 year after diagnosis showed a slightly smaller but still significant elevation of AF incidence for the breast cancer group at 9 years of follow-up (10 years after diagnosis) (7.0% vs. 6.5%; P less than .001).
Among breast cancer patients, those who received chemotherapy had a higher risk of AF than those who did not (adjusted hazard ratio, 1.23); however, this elevation of risk was not specifically tied to receipt of anthracyclines or trastuzumab (Herceptin) versus other chemotherapy. Risk was not elevated for those who received radiation therapy.
“Our study findings suggest that a diagnosis of early-stage breast cancer may be associated with a small increase in the risk of AF compared with that for cancer-free women,” Dr. Abdel-Qadir and coinvestigators noted. “Since the absolute risk is small, this finding does not warrant routine surveillance but rather should prompt consideration of AF in the differential diagnosis for women with compatible symptoms.
“The early and late periods of increased AF risk in early-stage breast cancer survivors warrant focused research to better understand the underlying causes and subsequent implications,” they concluded.
Dr. Abdel-Qadir reported receiving grants from the Canadian Cardiovascular Society during the conduct of the study, speaker fees from Amgen, and an honorarium for clinical events adjudication committee membership from the Canadian Vigour Centre for a study funded by AstraZeneca. The study was funded by the Canadian Cardiovascular Society Atrial Fibrillation Research Award.
SOURCE: Abdel-Qadir H et al. JAMA Netw Open. 2019 Sep 4;2(9):e1911838.
Women with early-stage breast cancer are at elevated risk for atrial fibrillation (AF) short term and, to a lesser extent, long term, finds a large Canadian cohort study. Risk was higher for those who had received chemotherapy but not tied to specific cardiotoxic drugs or drug classes.
“Cardiovascular disease is a particularly pertinent clinical concern for women diagnosed with early-stage breast cancer,” note the investigators, led by Husam Abdel-Qadir, MD, PhD, FRCPC, Cardiology Clinic, Women’s College Hospital, Toronto. “Many early-stage breast cancer survivors are older than 65 years and have hypertension, diabetes, or left ventricular dysfunction. Accordingly, a diagnosis of AF would translate to a clinically relevant stroke risk for many early-stage breast cancer survivors.”
The investigators undertook a population-based retrospective cohort study of women in the province of Ontario with stage I-III breast cancer diagnosed between April 2007 and December 2016, matching them 1:3 to cancer-free control women on birth year and receipt of breast imaging.
An initial analysis, based on 95,539 breast cancer patients and 217,456 cancer-free controls, showed that the former and latter groups did not differ significantly on the prevalence of preexisting AF (5.3% vs. 5.2%; P = .21), according to results reported in JAMA Network Open.
Main analyses excluded women with preexisting AF, leaving 68,113 breast cancer patients and 204,330 cancer-free controls having a mean follow-up of 5.7 years. Both groups had a mean age of 60 years at baseline, and prevalences of cardiovascular comorbidities were similar. Within the breast cancer group, 50.4% had left-sided disease; overall, 53.2% received chemotherapy and 71.7% received radiation therapy.
At 10 years after diagnosis, breast cancer patients had a small but significant increase in AF incidence relative to control peers (7.4% vs. 6.8%; P less than .001). When the investigators looked at specific time periods, survivors had a significantly elevated AF risk in year 1 postdiagnosis (hazard ratio, 2.16) and after year 5 postdiagnosis (hazard ratio, 1.20), but not during years 2 through 5.
Analyses beginning 1 year after diagnosis showed a slightly smaller but still significant elevation of AF incidence for the breast cancer group at 9 years of follow-up (10 years after diagnosis) (7.0% vs. 6.5%; P less than .001).
Among breast cancer patients, those who received chemotherapy had a higher risk of AF than those who did not (adjusted hazard ratio, 1.23); however, this elevation of risk was not specifically tied to receipt of anthracyclines or trastuzumab (Herceptin) versus other chemotherapy. Risk was not elevated for those who received radiation therapy.
“Our study findings suggest that a diagnosis of early-stage breast cancer may be associated with a small increase in the risk of AF compared with that for cancer-free women,” Dr. Abdel-Qadir and coinvestigators noted. “Since the absolute risk is small, this finding does not warrant routine surveillance but rather should prompt consideration of AF in the differential diagnosis for women with compatible symptoms.
“The early and late periods of increased AF risk in early-stage breast cancer survivors warrant focused research to better understand the underlying causes and subsequent implications,” they concluded.
Dr. Abdel-Qadir reported receiving grants from the Canadian Cardiovascular Society during the conduct of the study, speaker fees from Amgen, and an honorarium for clinical events adjudication committee membership from the Canadian Vigour Centre for a study funded by AstraZeneca. The study was funded by the Canadian Cardiovascular Society Atrial Fibrillation Research Award.
SOURCE: Abdel-Qadir H et al. JAMA Netw Open. 2019 Sep 4;2(9):e1911838.
FROM JAMA NETWORK OPEN
Dual therapy best for AFib with ACS no matter the treatment strategy
SAN FRANCISCO – Anticoagulation with apixaban and a P2Y12 inhibitor without aspirin provides superior safety and similar efficacy in patients with atrial fibrillation who have an acute coronary syndrome, compared with regimens that include vitamin K antagonists, aspirin, or both.
The findings come from a prespecified analysis of data from the AUGUSTUS trial presented by Stephan Windecker, MD, at the Transcatheter Cardiovascular Therapeutics annual meeting.
“This study adds very important information [to the notion] that triple therapy in the setting of atrial fibrillation and PCI [percutaneous coronary intervention] is really not the way to go,” Ori Ben-Yehuda, MD, FACC, executive director of the Cardiovascular Research Foundation’s Clinical Trials Center, said during a media briefing.
In the recent multicenter AUGUSTUS trial, Dr. Windecker, of the department of cardiology at Bern University Hospital, Switzerland, and colleagues found that among 4,614 patients with atrial fibrillation and a recent acute coronary syndrome or PCI treated with a P2Y12 inhibitor, apixaban without aspirin resulted in less bleeding, fewer hospitalizations, and no significant differences in ischemic events compared with regimens that included a vitamin K antagonist (VKA), aspirin, or both (N Engl J Med. 2019;380:1509-24). For this prespecified analysis, the researchers used a 2×2 factorial design to compare apixaban with VKA and aspirin with placebo in the AUGUSTUS trial participants with ACS treated medically (group 1; 1,097 patients, or 24%), those with ACS treated with PCI (group 2; 1,714 patients, or 37%), and those undergoing elective PCI (group 3; 1,784 patients, or 39%). The outcomes of interest were bleeding, death, and hospitalization as well as death and ischemic events by antithrombotic strategy in the study participants. This marks the only trial in the field that included patients with ACS managed medically, Dr. Windecker said.
At baseline, the median age of patients was 71 years, 30% were female, 36% had diabetes, and 45% had heart failure. Patients managed medically were younger (a median age of 70) and more frequently female; 57% presented with heart failure. The groups had identical CHA2DS2VASc scores (4), and very similar HAS-BLED scores (2 in groups 1 and 2, and 3 in group 3).
Apixaban compared with VKA showed lower International Society on Thrombosis and Haemostasis–defined major or clinically relevant nonmajor bleeding among patients in group 1 (HR, 0.44), group 2 (HR, 0.68), and group 3 (HR, 0.82) (P for interaction = .052). Apixaban compared with VKA reduced death or hospitalization among patients in group 1 (HR, 0.71), group 2 (HR 0.88), and group 3 (HR, 0.87) (P for interaction = .345). Compared with VKA, apixaban resulted in a similar effect on death and ischemic events among patients in all three treatment groups (P for interaction = .356).
Compared with placebo, aspirin had a higher rate of bleeding among patients in group 1 (HR, 1.49), group 2 (HR, 2.02) and group 3 (HR, 1.91) (P for interaction = .479). For the same comparison, there was no difference in outcomes among the three groups for the composite of death or hospitalization and death and ischemic events.
“The overall results of the AUGUSTUS trial are consistent across the three clinically important subgroups,” Dr. Windecker said. The reasons why patients received medical therapy remain unclear, “because it was at the physician’s discretion as to whether they were treated medically or underwent PCI,” he said. “The proportion very much reflects our clinical practice, where 20%-25% of patients are treated medically. What was surprising for me is that I would have anticipated there would be more elderly patients with comorbidities, but I did anticipate that there would be more female patients (in this subgroup).”
Robert A. Harrington, MD, an interventional cardiologist at Stanford (Calif.) University who served on the Data Safety and Monitoring Board for the trial, noted that the patients with atrial fibrillation represent 7%-10% of all ACS patients, “so it’s a big population,” he said. “What’s been disappointing is that none of the trials have been big enough to uncouple the bleeding vs. ischemic issue. We don’t know the answer for how long do you need the triple therapy versus when you can switch to the double therapy.”
Dr. Windecker said that the optimal duration of short-term aspirin remains unclear in this patient population. “Whether there is a benefit of giving aspirin for 2 weeks or 4 weeks remains unanswered,” he said. “Triple therapy is not the way to go, but we need to fine-tune, and probably individualize, which patients may benefit from a certain duration of aspirin.”
The study results were published online at the time of presentation (Circulation 2019 Sep 26. doi: 10.1161/CIRCULATIONAHA.119.043308.
AUGUSTUS was funded by Bristol-Myers Squibb and Pfizer Inc. Dr. Windecker reported having received institutional research and educational grants to Bern University Hospital from Abbott, Amgen, Bayer, BMS, CSL Behring, Boston Scientific, Biotronik, Edwards Lifesciences, Medtronic, Polares, and Sinomed. His coauthors reported having numerous financial ties to the pharmaceutical and device industries.
SOURCE: Windecker S. TCT 2019, Late-Breaking Trials 1 session.
SAN FRANCISCO – Anticoagulation with apixaban and a P2Y12 inhibitor without aspirin provides superior safety and similar efficacy in patients with atrial fibrillation who have an acute coronary syndrome, compared with regimens that include vitamin K antagonists, aspirin, or both.
The findings come from a prespecified analysis of data from the AUGUSTUS trial presented by Stephan Windecker, MD, at the Transcatheter Cardiovascular Therapeutics annual meeting.
“This study adds very important information [to the notion] that triple therapy in the setting of atrial fibrillation and PCI [percutaneous coronary intervention] is really not the way to go,” Ori Ben-Yehuda, MD, FACC, executive director of the Cardiovascular Research Foundation’s Clinical Trials Center, said during a media briefing.
In the recent multicenter AUGUSTUS trial, Dr. Windecker, of the department of cardiology at Bern University Hospital, Switzerland, and colleagues found that among 4,614 patients with atrial fibrillation and a recent acute coronary syndrome or PCI treated with a P2Y12 inhibitor, apixaban without aspirin resulted in less bleeding, fewer hospitalizations, and no significant differences in ischemic events compared with regimens that included a vitamin K antagonist (VKA), aspirin, or both (N Engl J Med. 2019;380:1509-24). For this prespecified analysis, the researchers used a 2×2 factorial design to compare apixaban with VKA and aspirin with placebo in the AUGUSTUS trial participants with ACS treated medically (group 1; 1,097 patients, or 24%), those with ACS treated with PCI (group 2; 1,714 patients, or 37%), and those undergoing elective PCI (group 3; 1,784 patients, or 39%). The outcomes of interest were bleeding, death, and hospitalization as well as death and ischemic events by antithrombotic strategy in the study participants. This marks the only trial in the field that included patients with ACS managed medically, Dr. Windecker said.
At baseline, the median age of patients was 71 years, 30% were female, 36% had diabetes, and 45% had heart failure. Patients managed medically were younger (a median age of 70) and more frequently female; 57% presented with heart failure. The groups had identical CHA2DS2VASc scores (4), and very similar HAS-BLED scores (2 in groups 1 and 2, and 3 in group 3).
Apixaban compared with VKA showed lower International Society on Thrombosis and Haemostasis–defined major or clinically relevant nonmajor bleeding among patients in group 1 (HR, 0.44), group 2 (HR, 0.68), and group 3 (HR, 0.82) (P for interaction = .052). Apixaban compared with VKA reduced death or hospitalization among patients in group 1 (HR, 0.71), group 2 (HR 0.88), and group 3 (HR, 0.87) (P for interaction = .345). Compared with VKA, apixaban resulted in a similar effect on death and ischemic events among patients in all three treatment groups (P for interaction = .356).
Compared with placebo, aspirin had a higher rate of bleeding among patients in group 1 (HR, 1.49), group 2 (HR, 2.02) and group 3 (HR, 1.91) (P for interaction = .479). For the same comparison, there was no difference in outcomes among the three groups for the composite of death or hospitalization and death and ischemic events.
“The overall results of the AUGUSTUS trial are consistent across the three clinically important subgroups,” Dr. Windecker said. The reasons why patients received medical therapy remain unclear, “because it was at the physician’s discretion as to whether they were treated medically or underwent PCI,” he said. “The proportion very much reflects our clinical practice, where 20%-25% of patients are treated medically. What was surprising for me is that I would have anticipated there would be more elderly patients with comorbidities, but I did anticipate that there would be more female patients (in this subgroup).”
Robert A. Harrington, MD, an interventional cardiologist at Stanford (Calif.) University who served on the Data Safety and Monitoring Board for the trial, noted that the patients with atrial fibrillation represent 7%-10% of all ACS patients, “so it’s a big population,” he said. “What’s been disappointing is that none of the trials have been big enough to uncouple the bleeding vs. ischemic issue. We don’t know the answer for how long do you need the triple therapy versus when you can switch to the double therapy.”
Dr. Windecker said that the optimal duration of short-term aspirin remains unclear in this patient population. “Whether there is a benefit of giving aspirin for 2 weeks or 4 weeks remains unanswered,” he said. “Triple therapy is not the way to go, but we need to fine-tune, and probably individualize, which patients may benefit from a certain duration of aspirin.”
The study results were published online at the time of presentation (Circulation 2019 Sep 26. doi: 10.1161/CIRCULATIONAHA.119.043308.
AUGUSTUS was funded by Bristol-Myers Squibb and Pfizer Inc. Dr. Windecker reported having received institutional research and educational grants to Bern University Hospital from Abbott, Amgen, Bayer, BMS, CSL Behring, Boston Scientific, Biotronik, Edwards Lifesciences, Medtronic, Polares, and Sinomed. His coauthors reported having numerous financial ties to the pharmaceutical and device industries.
SOURCE: Windecker S. TCT 2019, Late-Breaking Trials 1 session.
SAN FRANCISCO – Anticoagulation with apixaban and a P2Y12 inhibitor without aspirin provides superior safety and similar efficacy in patients with atrial fibrillation who have an acute coronary syndrome, compared with regimens that include vitamin K antagonists, aspirin, or both.
The findings come from a prespecified analysis of data from the AUGUSTUS trial presented by Stephan Windecker, MD, at the Transcatheter Cardiovascular Therapeutics annual meeting.
“This study adds very important information [to the notion] that triple therapy in the setting of atrial fibrillation and PCI [percutaneous coronary intervention] is really not the way to go,” Ori Ben-Yehuda, MD, FACC, executive director of the Cardiovascular Research Foundation’s Clinical Trials Center, said during a media briefing.
In the recent multicenter AUGUSTUS trial, Dr. Windecker, of the department of cardiology at Bern University Hospital, Switzerland, and colleagues found that among 4,614 patients with atrial fibrillation and a recent acute coronary syndrome or PCI treated with a P2Y12 inhibitor, apixaban without aspirin resulted in less bleeding, fewer hospitalizations, and no significant differences in ischemic events compared with regimens that included a vitamin K antagonist (VKA), aspirin, or both (N Engl J Med. 2019;380:1509-24). For this prespecified analysis, the researchers used a 2×2 factorial design to compare apixaban with VKA and aspirin with placebo in the AUGUSTUS trial participants with ACS treated medically (group 1; 1,097 patients, or 24%), those with ACS treated with PCI (group 2; 1,714 patients, or 37%), and those undergoing elective PCI (group 3; 1,784 patients, or 39%). The outcomes of interest were bleeding, death, and hospitalization as well as death and ischemic events by antithrombotic strategy in the study participants. This marks the only trial in the field that included patients with ACS managed medically, Dr. Windecker said.
At baseline, the median age of patients was 71 years, 30% were female, 36% had diabetes, and 45% had heart failure. Patients managed medically were younger (a median age of 70) and more frequently female; 57% presented with heart failure. The groups had identical CHA2DS2VASc scores (4), and very similar HAS-BLED scores (2 in groups 1 and 2, and 3 in group 3).
Apixaban compared with VKA showed lower International Society on Thrombosis and Haemostasis–defined major or clinically relevant nonmajor bleeding among patients in group 1 (HR, 0.44), group 2 (HR, 0.68), and group 3 (HR, 0.82) (P for interaction = .052). Apixaban compared with VKA reduced death or hospitalization among patients in group 1 (HR, 0.71), group 2 (HR 0.88), and group 3 (HR, 0.87) (P for interaction = .345). Compared with VKA, apixaban resulted in a similar effect on death and ischemic events among patients in all three treatment groups (P for interaction = .356).
Compared with placebo, aspirin had a higher rate of bleeding among patients in group 1 (HR, 1.49), group 2 (HR, 2.02) and group 3 (HR, 1.91) (P for interaction = .479). For the same comparison, there was no difference in outcomes among the three groups for the composite of death or hospitalization and death and ischemic events.
“The overall results of the AUGUSTUS trial are consistent across the three clinically important subgroups,” Dr. Windecker said. The reasons why patients received medical therapy remain unclear, “because it was at the physician’s discretion as to whether they were treated medically or underwent PCI,” he said. “The proportion very much reflects our clinical practice, where 20%-25% of patients are treated medically. What was surprising for me is that I would have anticipated there would be more elderly patients with comorbidities, but I did anticipate that there would be more female patients (in this subgroup).”
Robert A. Harrington, MD, an interventional cardiologist at Stanford (Calif.) University who served on the Data Safety and Monitoring Board for the trial, noted that the patients with atrial fibrillation represent 7%-10% of all ACS patients, “so it’s a big population,” he said. “What’s been disappointing is that none of the trials have been big enough to uncouple the bleeding vs. ischemic issue. We don’t know the answer for how long do you need the triple therapy versus when you can switch to the double therapy.”
Dr. Windecker said that the optimal duration of short-term aspirin remains unclear in this patient population. “Whether there is a benefit of giving aspirin for 2 weeks or 4 weeks remains unanswered,” he said. “Triple therapy is not the way to go, but we need to fine-tune, and probably individualize, which patients may benefit from a certain duration of aspirin.”
The study results were published online at the time of presentation (Circulation 2019 Sep 26. doi: 10.1161/CIRCULATIONAHA.119.043308.
AUGUSTUS was funded by Bristol-Myers Squibb and Pfizer Inc. Dr. Windecker reported having received institutional research and educational grants to Bern University Hospital from Abbott, Amgen, Bayer, BMS, CSL Behring, Boston Scientific, Biotronik, Edwards Lifesciences, Medtronic, Polares, and Sinomed. His coauthors reported having numerous financial ties to the pharmaceutical and device industries.
SOURCE: Windecker S. TCT 2019, Late-Breaking Trials 1 session.
AT TCT 2019
Click for Credit: Psoriasis relief; Stress & CV problems; more
Here are 5 articles from the October issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Bronchiolitis is a feared complication of connective tissue disease
To take the posttest, go to: https://bit.ly/2klWpRb
Expires April 8, 2020
2. Stress incontinence surgery improves sexual dysfunction
To take the posttest, go to: https://bit.ly/2m0wb71
Expires April 10, 2020
3. Survey finds psoriasis patients seek relief with alternative therapies
To take the posttest, go to: https://bit.ly/2lZZDtO
Expires April 10, 2020
4. New data further suggest that stress does a number on the CV system
To take the posttest, go to: https://bit.ly/2lR31ax
Expires April 11, 2020
5. Rate of objects ingested by young children increased over last two decades
To take the posttest, go to: https://bit.ly/2mmYptb
Expires April 12, 2020
Here are 5 articles from the October issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Bronchiolitis is a feared complication of connective tissue disease
To take the posttest, go to: https://bit.ly/2klWpRb
Expires April 8, 2020
2. Stress incontinence surgery improves sexual dysfunction
To take the posttest, go to: https://bit.ly/2m0wb71
Expires April 10, 2020
3. Survey finds psoriasis patients seek relief with alternative therapies
To take the posttest, go to: https://bit.ly/2lZZDtO
Expires April 10, 2020
4. New data further suggest that stress does a number on the CV system
To take the posttest, go to: https://bit.ly/2lR31ax
Expires April 11, 2020
5. Rate of objects ingested by young children increased over last two decades
To take the posttest, go to: https://bit.ly/2mmYptb
Expires April 12, 2020
Here are 5 articles from the October issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Bronchiolitis is a feared complication of connective tissue disease
To take the posttest, go to: https://bit.ly/2klWpRb
Expires April 8, 2020
2. Stress incontinence surgery improves sexual dysfunction
To take the posttest, go to: https://bit.ly/2m0wb71
Expires April 10, 2020
3. Survey finds psoriasis patients seek relief with alternative therapies
To take the posttest, go to: https://bit.ly/2lZZDtO
Expires April 10, 2020
4. New data further suggest that stress does a number on the CV system
To take the posttest, go to: https://bit.ly/2lR31ax
Expires April 11, 2020
5. Rate of objects ingested by young children increased over last two decades
To take the posttest, go to: https://bit.ly/2mmYptb
Expires April 12, 2020
Skip supplemental O2 in nonhypoxic ACS
PARIS – A massive randomized trial that included all New Zealanders with a suspected acute coronary syndrome during a 2-year period has provided definitive evidence that giving high-flow supplemental oxygen to those who are nonhypoxemic is of no clinical benefit, although it wasn’t harmful, either.

“Patients who have a normal blood oxygen saturation level are very unlikely to benefit from supplemental oxygen,” Ralph Stewart, MbChB, said in presenting the results of the NZOTACS (New Zealand Oxygen Therapy in Acute Coronary Syndromes) trial at the annual congress of the European Society of Cardiology.
“It’s amazing that oxygen has been used in patients with suspected heart attack for over 50 years, and during that time there’s never been definite evidence that it improves outcomes. And more recently some have even suggested giving high-level oxygen might actually cause harm,” observed Dr. Stewart, a cardiologist at Auckland City Hospital and the University of Auckland (New Zealand).
The primary outcome in NZOTACS was 30-day all-cause mortality. In the overall study population, the rate was 3.0% in the group assigned to the routine high-flow oxygen protocol and closely similar at 3.1% in those randomized to the conservative oxygen strategy. And there was reassuringly no signal that the liberal oxygen protocol caused any harm.
To conduct this cluster randomized crossover trial, Dr. Stewart and his coinvestigators divided New Zealand into quadrants and, taking advantage of the coordinated health care systems operative in the nation of 4.8 million, they arranged for all ambulances, emergency departments, and hospitals in each geographic region to utilize each supplemental oxygen strategy for a total of 12 months.
In the liberal oxygen strategy, patients with suspected ACS on the basis of ischemic chest pain or ECG changes received high-flow oxygen by face mask at 6-8 L/min regardless of their blood oxygen saturation (SaO2) level. The oxygen was stopped only upon clinical resolution of myocardial ischemia. In contrast, in the low-oxygen protocol, supplemental oxygen was reserved for patients with an initial SaO2 below 90%, with a target SaO2 of 90%-94%.
Roughly 90% of the nearly 41,000 study participants had a normal SaO2 of 90% or more. Their 30-day mortality was 2.1% with the high-oxygen protocol and similar at 1.9% with the conservative oxygen protocol.
In contrast, there was a suggestion of benefit for the routine liberal oxygen strategy in the subgroup of patients with ST-elevation MI. Their 30-day mortality was 8.8% with high-flow oxygen and 10.6% with the conservative oxygen protocol. The resultant 19% relative risk reduction barely missed statistical significance. There was also a trend for possible benefit of routine high-flow oxygen in the roughly 12% of NZOTACS participants with an SaO2 below 95%, a lower bar than the 90% SaO2 that defines hypoxemia. Their death rate at 30 days was 10.1% if they got supplemental oxygen and 11.1% if they only received oxygen in the event their SaO2 was below 90%. But these exploratory findings must be viewed as hypothesis-generating, and a large confirmatory study would be required, Dr. Stewart noted.
Discussant Robin Hofmann, MD, PhD, commented that, based on the NZOTACS results, he believes a couple of changes to the current ESC guidelines on management of ACS are in order. The guidelines now state that oxygen is indicated in patients with suspected ACS and hypoxemia as defined by an SaO2 below 90%, giving that recommendation a Class I Level of Evidence C. That should now be upgraded to the strongest-possible Class I A recommendation, according to Dr. Hofmann, a cardiologist at the Karolinska Institute in Stockholm.
The ESC guidelines also state that oxygen isn’t routinely recommended in patients with an SaO2 of 90% or more, rating that guidance Class III B. On the basis of NZOTACS coupled with earlier far smaller studies, that should be changed to a Class III A recommendation, meaning simply don’t do it. The hint provided by NZOTACS of a possible small benefit for oxygen in patients with an SaO2 below 95% isn’t strong enough evidence to carry the day, in Dr. Hofmann’s view.
Dr. Stewart and Dr. Hofmann reported having no financial conflicts of interest. The NZOTACS trial was funded by the National Heart Foundation of New Zealand.
SOURCE: Stewart R. ESC 2019, Hotline Session 2.
PARIS – A massive randomized trial that included all New Zealanders with a suspected acute coronary syndrome during a 2-year period has provided definitive evidence that giving high-flow supplemental oxygen to those who are nonhypoxemic is of no clinical benefit, although it wasn’t harmful, either.

“Patients who have a normal blood oxygen saturation level are very unlikely to benefit from supplemental oxygen,” Ralph Stewart, MbChB, said in presenting the results of the NZOTACS (New Zealand Oxygen Therapy in Acute Coronary Syndromes) trial at the annual congress of the European Society of Cardiology.
“It’s amazing that oxygen has been used in patients with suspected heart attack for over 50 years, and during that time there’s never been definite evidence that it improves outcomes. And more recently some have even suggested giving high-level oxygen might actually cause harm,” observed Dr. Stewart, a cardiologist at Auckland City Hospital and the University of Auckland (New Zealand).
The primary outcome in NZOTACS was 30-day all-cause mortality. In the overall study population, the rate was 3.0% in the group assigned to the routine high-flow oxygen protocol and closely similar at 3.1% in those randomized to the conservative oxygen strategy. And there was reassuringly no signal that the liberal oxygen protocol caused any harm.
To conduct this cluster randomized crossover trial, Dr. Stewart and his coinvestigators divided New Zealand into quadrants and, taking advantage of the coordinated health care systems operative in the nation of 4.8 million, they arranged for all ambulances, emergency departments, and hospitals in each geographic region to utilize each supplemental oxygen strategy for a total of 12 months.
In the liberal oxygen strategy, patients with suspected ACS on the basis of ischemic chest pain or ECG changes received high-flow oxygen by face mask at 6-8 L/min regardless of their blood oxygen saturation (SaO2) level. The oxygen was stopped only upon clinical resolution of myocardial ischemia. In contrast, in the low-oxygen protocol, supplemental oxygen was reserved for patients with an initial SaO2 below 90%, with a target SaO2 of 90%-94%.
Roughly 90% of the nearly 41,000 study participants had a normal SaO2 of 90% or more. Their 30-day mortality was 2.1% with the high-oxygen protocol and similar at 1.9% with the conservative oxygen protocol.
In contrast, there was a suggestion of benefit for the routine liberal oxygen strategy in the subgroup of patients with ST-elevation MI. Their 30-day mortality was 8.8% with high-flow oxygen and 10.6% with the conservative oxygen protocol. The resultant 19% relative risk reduction barely missed statistical significance. There was also a trend for possible benefit of routine high-flow oxygen in the roughly 12% of NZOTACS participants with an SaO2 below 95%, a lower bar than the 90% SaO2 that defines hypoxemia. Their death rate at 30 days was 10.1% if they got supplemental oxygen and 11.1% if they only received oxygen in the event their SaO2 was below 90%. But these exploratory findings must be viewed as hypothesis-generating, and a large confirmatory study would be required, Dr. Stewart noted.
Discussant Robin Hofmann, MD, PhD, commented that, based on the NZOTACS results, he believes a couple of changes to the current ESC guidelines on management of ACS are in order. The guidelines now state that oxygen is indicated in patients with suspected ACS and hypoxemia as defined by an SaO2 below 90%, giving that recommendation a Class I Level of Evidence C. That should now be upgraded to the strongest-possible Class I A recommendation, according to Dr. Hofmann, a cardiologist at the Karolinska Institute in Stockholm.
The ESC guidelines also state that oxygen isn’t routinely recommended in patients with an SaO2 of 90% or more, rating that guidance Class III B. On the basis of NZOTACS coupled with earlier far smaller studies, that should be changed to a Class III A recommendation, meaning simply don’t do it. The hint provided by NZOTACS of a possible small benefit for oxygen in patients with an SaO2 below 95% isn’t strong enough evidence to carry the day, in Dr. Hofmann’s view.
Dr. Stewart and Dr. Hofmann reported having no financial conflicts of interest. The NZOTACS trial was funded by the National Heart Foundation of New Zealand.
SOURCE: Stewart R. ESC 2019, Hotline Session 2.
PARIS – A massive randomized trial that included all New Zealanders with a suspected acute coronary syndrome during a 2-year period has provided definitive evidence that giving high-flow supplemental oxygen to those who are nonhypoxemic is of no clinical benefit, although it wasn’t harmful, either.

“Patients who have a normal blood oxygen saturation level are very unlikely to benefit from supplemental oxygen,” Ralph Stewart, MbChB, said in presenting the results of the NZOTACS (New Zealand Oxygen Therapy in Acute Coronary Syndromes) trial at the annual congress of the European Society of Cardiology.
“It’s amazing that oxygen has been used in patients with suspected heart attack for over 50 years, and during that time there’s never been definite evidence that it improves outcomes. And more recently some have even suggested giving high-level oxygen might actually cause harm,” observed Dr. Stewart, a cardiologist at Auckland City Hospital and the University of Auckland (New Zealand).
The primary outcome in NZOTACS was 30-day all-cause mortality. In the overall study population, the rate was 3.0% in the group assigned to the routine high-flow oxygen protocol and closely similar at 3.1% in those randomized to the conservative oxygen strategy. And there was reassuringly no signal that the liberal oxygen protocol caused any harm.
To conduct this cluster randomized crossover trial, Dr. Stewart and his coinvestigators divided New Zealand into quadrants and, taking advantage of the coordinated health care systems operative in the nation of 4.8 million, they arranged for all ambulances, emergency departments, and hospitals in each geographic region to utilize each supplemental oxygen strategy for a total of 12 months.
In the liberal oxygen strategy, patients with suspected ACS on the basis of ischemic chest pain or ECG changes received high-flow oxygen by face mask at 6-8 L/min regardless of their blood oxygen saturation (SaO2) level. The oxygen was stopped only upon clinical resolution of myocardial ischemia. In contrast, in the low-oxygen protocol, supplemental oxygen was reserved for patients with an initial SaO2 below 90%, with a target SaO2 of 90%-94%.
Roughly 90% of the nearly 41,000 study participants had a normal SaO2 of 90% or more. Their 30-day mortality was 2.1% with the high-oxygen protocol and similar at 1.9% with the conservative oxygen protocol.
In contrast, there was a suggestion of benefit for the routine liberal oxygen strategy in the subgroup of patients with ST-elevation MI. Their 30-day mortality was 8.8% with high-flow oxygen and 10.6% with the conservative oxygen protocol. The resultant 19% relative risk reduction barely missed statistical significance. There was also a trend for possible benefit of routine high-flow oxygen in the roughly 12% of NZOTACS participants with an SaO2 below 95%, a lower bar than the 90% SaO2 that defines hypoxemia. Their death rate at 30 days was 10.1% if they got supplemental oxygen and 11.1% if they only received oxygen in the event their SaO2 was below 90%. But these exploratory findings must be viewed as hypothesis-generating, and a large confirmatory study would be required, Dr. Stewart noted.
Discussant Robin Hofmann, MD, PhD, commented that, based on the NZOTACS results, he believes a couple of changes to the current ESC guidelines on management of ACS are in order. The guidelines now state that oxygen is indicated in patients with suspected ACS and hypoxemia as defined by an SaO2 below 90%, giving that recommendation a Class I Level of Evidence C. That should now be upgraded to the strongest-possible Class I A recommendation, according to Dr. Hofmann, a cardiologist at the Karolinska Institute in Stockholm.
The ESC guidelines also state that oxygen isn’t routinely recommended in patients with an SaO2 of 90% or more, rating that guidance Class III B. On the basis of NZOTACS coupled with earlier far smaller studies, that should be changed to a Class III A recommendation, meaning simply don’t do it. The hint provided by NZOTACS of a possible small benefit for oxygen in patients with an SaO2 below 95% isn’t strong enough evidence to carry the day, in Dr. Hofmann’s view.
Dr. Stewart and Dr. Hofmann reported having no financial conflicts of interest. The NZOTACS trial was funded by the National Heart Foundation of New Zealand.
SOURCE: Stewart R. ESC 2019, Hotline Session 2.
REPORTING FROM THE ESC CONGRESS 2019
Beta-blockers effective, safe for HFrEF with renal dysfunction
PARIS – Beta-blocking drugs were as effective for improving survival in patients with moderately severe renal dysfunction as they were in patients with normal renal function in a meta-analysis of more than 13,000 patients, a finding that seemed to solidify the role for this drug class for essentially all similar heart failure patients, regardless of their renal function.
This evidence could reshape usual care because “renal impairment is often considered a barrier in clinical practice” for starting a beta-blocker drug in patients with heart failure with reduced ejection fraction (HFrEF), Dipak Kotecha, MBChB, said at the annual congress of the European Society of Cardiology.
“We have shown with sufficient sample size that beta-blockers are effective in reducing mortality in patient with HFrEF and in sinus rhythm, even in those with an eGFR [estimated glomerular filtration rate] of 30-44 mL/min per 1.73 m2,” said Dr. Kotecha, a cardiologist at the University of Birmingham (England). “The results suggest that renal impairment should not obstruct the prescription and maintenance of beta-blockers in patients with HFrEF.”
“This important study was a novel attempt to look at [HFrEF] patients with renal insufficiency to see whether they received the same benefit from beta-blockers as other patients, and they did. So renal insufficiency is not a reason to withhold beta-blockers” from these patients, commented Mariell Jessup, MD, a heart failure physician and chief science and medical officer for the American Heart Association in Dallas. “The onus is on clinicians to find a reason not to give a beta-blocker to a patient with HFrEF because they are generally well tolerated and they can have enormous benefit, as we saw in this study,” she said in a video interview.
The analysis run by Dr. Kotecha and associates used data collected in 11 of the pivotal randomized, controlled trial run for beta-blockers during the 1990s and early 2000s, with each study comparing bucindolol, bisoprolol, carvedilol, metoprolol XL, or nebivolol against placebo. The studies collectively enrolled 18,637 patients, which the investigators whittled down in their analysis to 17,433 after excluding patients with a left ventricular ejection fraction below 50% or who were undocumented. The subgroup with HFrEF included 13,861 patient in sinus rhythm at entry, 2,879 with atrial fibrillation, and 693 with an unknown atrial status. The main analysis ran in the 13,861 patients with HFrEF and in sinus rhythm; 14% of this cohort had an eGFR of 30-44 mL/min per 1.73 m2 and 27% had an eGFR of 45-59 mL/min per 1.73 m2. The median age of all patients in the main analysis was 65 years, 23% were women, and their median left ventricular ejection fraction was 27%.
During follow-up of about 3 years, the impact of beta-blocker treatment on survival, compared with placebo, was “substantial” for all strata of patients by renal function, except for those with eGFRs below 30 mL/min per 1.73 m2. (Survival was similar regardless of beta-blocker treatment in the small number of patients with severe renal dysfunction.) The number needed to treat to prevent 1 death in patients with an eGFR of 30-44 mL/min per 1.73 m2 was 21, the same as among patients with an eGFR of 90 mL/min per 1.73 m2 or more, Dr. Kotecha said.
Among the subgroup of patients with atrial fibrillation, beta-blockers appeared to exert no survival benefit, compared with placebo. The investigators did not assess the survival benefits exerted by any individual beta-blocker, compared with the others, and Dr. Kotecha stressed that “my belief is that this is a class effect” and is roughly similar across all the beta-blockers used in the studies.
The analysis also showed good safety and tolerability of the beta-blockers in patients with renal dysfunction. The incidence of adverse events leading to treatment termination was very similar in the beta-blocker and placebo arms, and more than three-quarters of patients in each of the two subgroups with renal dysfunction were maintained on more than 50% of their target beta-blocker dosage.
Dr. Kotecha has been an advisor to Bayer, a speaker on behalf of Atricure, and has received research funding from GlaxoSmithKline and Menarini. Dr. Jessup had no disclosures.
This analysis of individual patient data is very important and extends our knowledge. The results confirm that beta-blocker treatment reduces mortality in patients with heart failure with reduced ejection fraction (HFrEF) and in sinus rhythm who also have moderately severe renal dysfunction with an estimated glomerular filtration rate as low as 30-44 mL/min per 1.73 m2. This is good news for patients with HFrEF and kidney disease. Clinicians often use comorbidities as a reason not to prescribe or up-titrate beta-blockers. These results show that beta-blockers can be used at guideline-directed dosages, even in patients with renal dysfunction. The findings highlight the importance of not looking for excuses to not treat patients with a beta-blocker. Do not worry about renal function.
Theresa A. McDonagh, MD, professor of cardiology at King’s College, London, made these comments as designated discussant for Dr. Kotecha’s report. She had no disclosures.
This analysis of individual patient data is very important and extends our knowledge. The results confirm that beta-blocker treatment reduces mortality in patients with heart failure with reduced ejection fraction (HFrEF) and in sinus rhythm who also have moderately severe renal dysfunction with an estimated glomerular filtration rate as low as 30-44 mL/min per 1.73 m2. This is good news for patients with HFrEF and kidney disease. Clinicians often use comorbidities as a reason not to prescribe or up-titrate beta-blockers. These results show that beta-blockers can be used at guideline-directed dosages, even in patients with renal dysfunction. The findings highlight the importance of not looking for excuses to not treat patients with a beta-blocker. Do not worry about renal function.
Theresa A. McDonagh, MD, professor of cardiology at King’s College, London, made these comments as designated discussant for Dr. Kotecha’s report. She had no disclosures.
This analysis of individual patient data is very important and extends our knowledge. The results confirm that beta-blocker treatment reduces mortality in patients with heart failure with reduced ejection fraction (HFrEF) and in sinus rhythm who also have moderately severe renal dysfunction with an estimated glomerular filtration rate as low as 30-44 mL/min per 1.73 m2. This is good news for patients with HFrEF and kidney disease. Clinicians often use comorbidities as a reason not to prescribe or up-titrate beta-blockers. These results show that beta-blockers can be used at guideline-directed dosages, even in patients with renal dysfunction. The findings highlight the importance of not looking for excuses to not treat patients with a beta-blocker. Do not worry about renal function.
Theresa A. McDonagh, MD, professor of cardiology at King’s College, London, made these comments as designated discussant for Dr. Kotecha’s report. She had no disclosures.
PARIS – Beta-blocking drugs were as effective for improving survival in patients with moderately severe renal dysfunction as they were in patients with normal renal function in a meta-analysis of more than 13,000 patients, a finding that seemed to solidify the role for this drug class for essentially all similar heart failure patients, regardless of their renal function.
This evidence could reshape usual care because “renal impairment is often considered a barrier in clinical practice” for starting a beta-blocker drug in patients with heart failure with reduced ejection fraction (HFrEF), Dipak Kotecha, MBChB, said at the annual congress of the European Society of Cardiology.
“We have shown with sufficient sample size that beta-blockers are effective in reducing mortality in patient with HFrEF and in sinus rhythm, even in those with an eGFR [estimated glomerular filtration rate] of 30-44 mL/min per 1.73 m2,” said Dr. Kotecha, a cardiologist at the University of Birmingham (England). “The results suggest that renal impairment should not obstruct the prescription and maintenance of beta-blockers in patients with HFrEF.”
“This important study was a novel attempt to look at [HFrEF] patients with renal insufficiency to see whether they received the same benefit from beta-blockers as other patients, and they did. So renal insufficiency is not a reason to withhold beta-blockers” from these patients, commented Mariell Jessup, MD, a heart failure physician and chief science and medical officer for the American Heart Association in Dallas. “The onus is on clinicians to find a reason not to give a beta-blocker to a patient with HFrEF because they are generally well tolerated and they can have enormous benefit, as we saw in this study,” she said in a video interview.
The analysis run by Dr. Kotecha and associates used data collected in 11 of the pivotal randomized, controlled trial run for beta-blockers during the 1990s and early 2000s, with each study comparing bucindolol, bisoprolol, carvedilol, metoprolol XL, or nebivolol against placebo. The studies collectively enrolled 18,637 patients, which the investigators whittled down in their analysis to 17,433 after excluding patients with a left ventricular ejection fraction below 50% or who were undocumented. The subgroup with HFrEF included 13,861 patient in sinus rhythm at entry, 2,879 with atrial fibrillation, and 693 with an unknown atrial status. The main analysis ran in the 13,861 patients with HFrEF and in sinus rhythm; 14% of this cohort had an eGFR of 30-44 mL/min per 1.73 m2 and 27% had an eGFR of 45-59 mL/min per 1.73 m2. The median age of all patients in the main analysis was 65 years, 23% were women, and their median left ventricular ejection fraction was 27%.
During follow-up of about 3 years, the impact of beta-blocker treatment on survival, compared with placebo, was “substantial” for all strata of patients by renal function, except for those with eGFRs below 30 mL/min per 1.73 m2. (Survival was similar regardless of beta-blocker treatment in the small number of patients with severe renal dysfunction.) The number needed to treat to prevent 1 death in patients with an eGFR of 30-44 mL/min per 1.73 m2 was 21, the same as among patients with an eGFR of 90 mL/min per 1.73 m2 or more, Dr. Kotecha said.
Among the subgroup of patients with atrial fibrillation, beta-blockers appeared to exert no survival benefit, compared with placebo. The investigators did not assess the survival benefits exerted by any individual beta-blocker, compared with the others, and Dr. Kotecha stressed that “my belief is that this is a class effect” and is roughly similar across all the beta-blockers used in the studies.
The analysis also showed good safety and tolerability of the beta-blockers in patients with renal dysfunction. The incidence of adverse events leading to treatment termination was very similar in the beta-blocker and placebo arms, and more than three-quarters of patients in each of the two subgroups with renal dysfunction were maintained on more than 50% of their target beta-blocker dosage.
Dr. Kotecha has been an advisor to Bayer, a speaker on behalf of Atricure, and has received research funding from GlaxoSmithKline and Menarini. Dr. Jessup had no disclosures.
PARIS – Beta-blocking drugs were as effective for improving survival in patients with moderately severe renal dysfunction as they were in patients with normal renal function in a meta-analysis of more than 13,000 patients, a finding that seemed to solidify the role for this drug class for essentially all similar heart failure patients, regardless of their renal function.
This evidence could reshape usual care because “renal impairment is often considered a barrier in clinical practice” for starting a beta-blocker drug in patients with heart failure with reduced ejection fraction (HFrEF), Dipak Kotecha, MBChB, said at the annual congress of the European Society of Cardiology.
“We have shown with sufficient sample size that beta-blockers are effective in reducing mortality in patient with HFrEF and in sinus rhythm, even in those with an eGFR [estimated glomerular filtration rate] of 30-44 mL/min per 1.73 m2,” said Dr. Kotecha, a cardiologist at the University of Birmingham (England). “The results suggest that renal impairment should not obstruct the prescription and maintenance of beta-blockers in patients with HFrEF.”
“This important study was a novel attempt to look at [HFrEF] patients with renal insufficiency to see whether they received the same benefit from beta-blockers as other patients, and they did. So renal insufficiency is not a reason to withhold beta-blockers” from these patients, commented Mariell Jessup, MD, a heart failure physician and chief science and medical officer for the American Heart Association in Dallas. “The onus is on clinicians to find a reason not to give a beta-blocker to a patient with HFrEF because they are generally well tolerated and they can have enormous benefit, as we saw in this study,” she said in a video interview.
The analysis run by Dr. Kotecha and associates used data collected in 11 of the pivotal randomized, controlled trial run for beta-blockers during the 1990s and early 2000s, with each study comparing bucindolol, bisoprolol, carvedilol, metoprolol XL, or nebivolol against placebo. The studies collectively enrolled 18,637 patients, which the investigators whittled down in their analysis to 17,433 after excluding patients with a left ventricular ejection fraction below 50% or who were undocumented. The subgroup with HFrEF included 13,861 patient in sinus rhythm at entry, 2,879 with atrial fibrillation, and 693 with an unknown atrial status. The main analysis ran in the 13,861 patients with HFrEF and in sinus rhythm; 14% of this cohort had an eGFR of 30-44 mL/min per 1.73 m2 and 27% had an eGFR of 45-59 mL/min per 1.73 m2. The median age of all patients in the main analysis was 65 years, 23% were women, and their median left ventricular ejection fraction was 27%.
During follow-up of about 3 years, the impact of beta-blocker treatment on survival, compared with placebo, was “substantial” for all strata of patients by renal function, except for those with eGFRs below 30 mL/min per 1.73 m2. (Survival was similar regardless of beta-blocker treatment in the small number of patients with severe renal dysfunction.) The number needed to treat to prevent 1 death in patients with an eGFR of 30-44 mL/min per 1.73 m2 was 21, the same as among patients with an eGFR of 90 mL/min per 1.73 m2 or more, Dr. Kotecha said.
Among the subgroup of patients with atrial fibrillation, beta-blockers appeared to exert no survival benefit, compared with placebo. The investigators did not assess the survival benefits exerted by any individual beta-blocker, compared with the others, and Dr. Kotecha stressed that “my belief is that this is a class effect” and is roughly similar across all the beta-blockers used in the studies.
The analysis also showed good safety and tolerability of the beta-blockers in patients with renal dysfunction. The incidence of adverse events leading to treatment termination was very similar in the beta-blocker and placebo arms, and more than three-quarters of patients in each of the two subgroups with renal dysfunction were maintained on more than 50% of their target beta-blocker dosage.
Dr. Kotecha has been an advisor to Bayer, a speaker on behalf of Atricure, and has received research funding from GlaxoSmithKline and Menarini. Dr. Jessup had no disclosures.
REPORTING FROM THE ESC CONGRESS 2019