User login
Suicide increased 35% during 1999-2018 in the U.S.
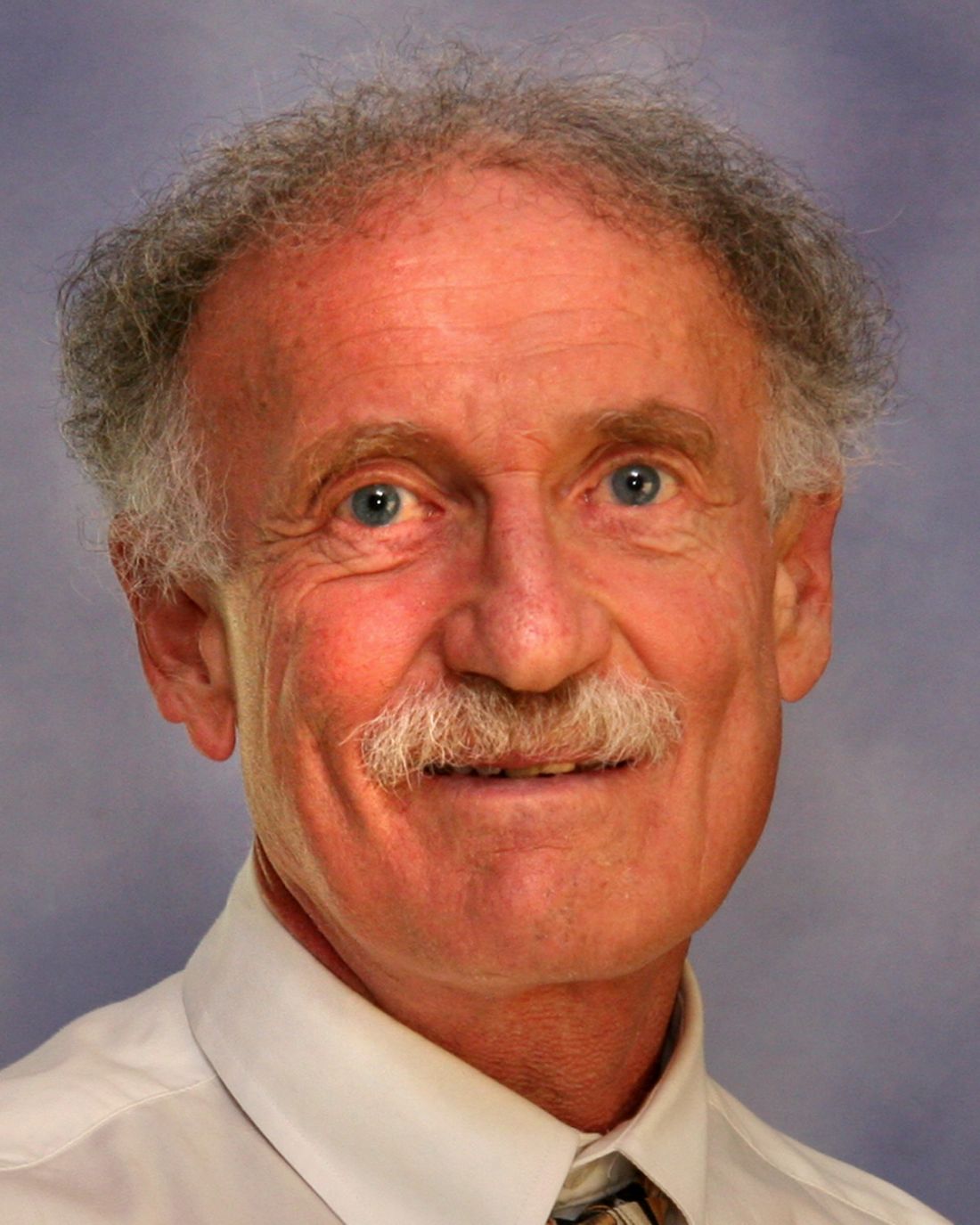
Age-adjusted suicide rate rose from 10.5 per 100,000 to 14.2 from 1999 to 2018, according to trends reported by the Centers for Disease Control and Prevention in a data brief.
Holly Hedegaard, MD, and colleagues from the National Center for Health Statistics within the CDC analyzed final mortality data from the National Vital Statistics System. As the second most common cause of death among Americans aged 10-34 years and the fourth most common among those aged 35-54 years, suicide is a major contributer to premature mortality.
at 22.8 and 6.2 per 100,000, respectively. Young people aged 10-14 years among both genders had the lowest rates of completing suicide, but it was men aged 75 years and older and women aged 45-64 years who had the highest rates. All of these trends were consistent throughout the study period.
Drawing from the 2013 National Center for Health Statistics Urban-Rural Classification Scheme for Counties, the researchers found that rural counties had significantly higher rates of suicide than did urban counties in 2018, and this was true for men and women. That said, suicide rates were still 3.5-3.9 times higher among men than among women regardless of urbanicity or rurality that year.
The full data brief can be found on the CDC website.
Age-adjusted suicide rate rose from 10.5 per 100,000 to 14.2 from 1999 to 2018, according to trends reported by the Centers for Disease Control and Prevention in a data brief.
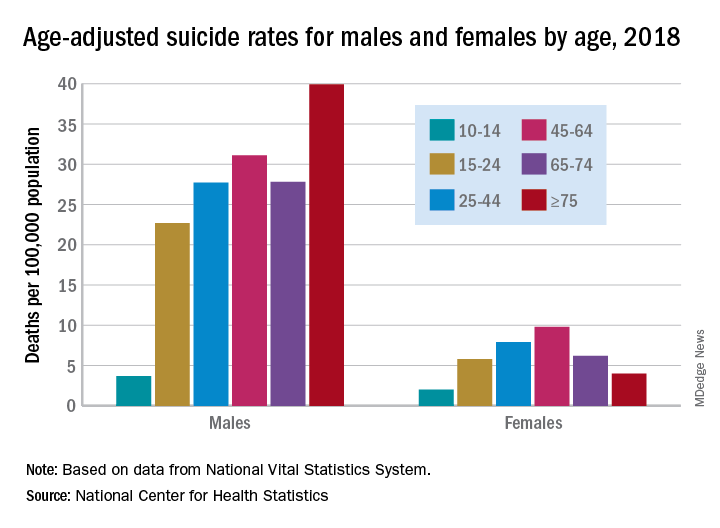
Holly Hedegaard, MD, and colleagues from the National Center for Health Statistics within the CDC analyzed final mortality data from the National Vital Statistics System. As the second most common cause of death among Americans aged 10-34 years and the fourth most common among those aged 35-54 years, suicide is a major contributer to premature mortality.
at 22.8 and 6.2 per 100,000, respectively. Young people aged 10-14 years among both genders had the lowest rates of completing suicide, but it was men aged 75 years and older and women aged 45-64 years who had the highest rates. All of these trends were consistent throughout the study period.
Drawing from the 2013 National Center for Health Statistics Urban-Rural Classification Scheme for Counties, the researchers found that rural counties had significantly higher rates of suicide than did urban counties in 2018, and this was true for men and women. That said, suicide rates were still 3.5-3.9 times higher among men than among women regardless of urbanicity or rurality that year.
The full data brief can be found on the CDC website.
Age-adjusted suicide rate rose from 10.5 per 100,000 to 14.2 from 1999 to 2018, according to trends reported by the Centers for Disease Control and Prevention in a data brief.
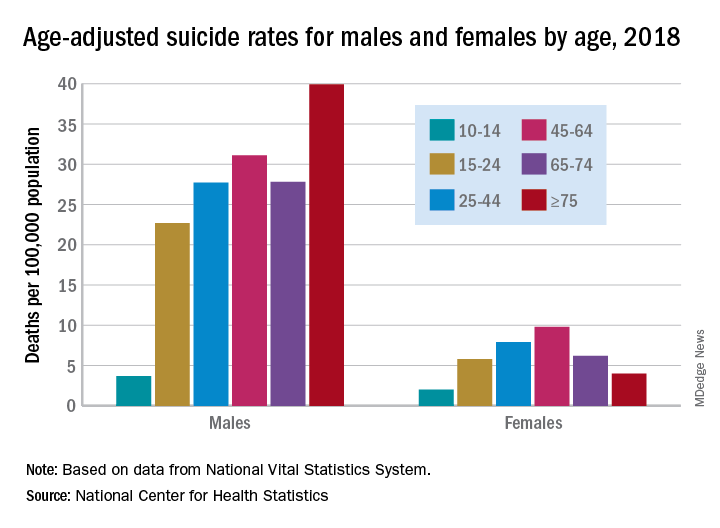
Holly Hedegaard, MD, and colleagues from the National Center for Health Statistics within the CDC analyzed final mortality data from the National Vital Statistics System. As the second most common cause of death among Americans aged 10-34 years and the fourth most common among those aged 35-54 years, suicide is a major contributer to premature mortality.
at 22.8 and 6.2 per 100,000, respectively. Young people aged 10-14 years among both genders had the lowest rates of completing suicide, but it was men aged 75 years and older and women aged 45-64 years who had the highest rates. All of these trends were consistent throughout the study period.
Drawing from the 2013 National Center for Health Statistics Urban-Rural Classification Scheme for Counties, the researchers found that rural counties had significantly higher rates of suicide than did urban counties in 2018, and this was true for men and women. That said, suicide rates were still 3.5-3.9 times higher among men than among women regardless of urbanicity or rurality that year.
The full data brief can be found on the CDC website.
Survey: COVID-19 is getting in our heads
As the COVID-19 pandemic sweeps across the United States, it is increasingly affecting those who are not infected. Social bonds are being broken, businesses are closing, jobs are being lost, and the stress is mounting.

In a poll conducted March 25-30, 45% of Americans said that stress resulting from the pandemic is having a negative impact on their mental health, compared with 32% expressing that view just 2 weeks earlier, the Kaiser Family Foundation reported April 2.
In the later survey, the effect looked like this: 19% of all respondents said that the pandemic has had a major negative impact and 26% said it has been minor so far. Women were more likely than men (24% vs. 15%) to report a major impact, as were blacks and Hispanic adults (both at 24%) compared with whites (17%), the KFF investigators said.
More Hispanic (44%) and black (42%) respondents also said that they had already lost their job, lost income, or had their hours reduced without pay as a result of the pandemic, compared with whites (36%). Among all respondents, 26% had lost income from a job or business and 28% had lost their job, been laid off, or had their hours reduced without pay, according to KFF.
A majority of respondents (57%) reported “being worried they will put themselves at risk of exposure to coronavirus because they can’t afford to stay home and miss work,” the researchers said. That figure is up from 35% in the earlier survey.
Anxiety about work-related exposure was even higher among hourly workers or those who get paid by the job (61%) and among employed adults who earn less than $40,000 annually (72%), they reported.
Overall, 72% of respondents said that their lives have been disrupted “a lot” or “some” by the coronavirus outbreak, and that is a jump of 32 percentage points over the previous poll, the investigators noted.
The disruption is expected to continue, it seems, as 74% believe that the worst is yet to come “in spite of the health, social and economic upheaval that Americans are already experiencing,” they wrote.
As the COVID-19 pandemic sweeps across the United States, it is increasingly affecting those who are not infected. Social bonds are being broken, businesses are closing, jobs are being lost, and the stress is mounting.

In a poll conducted March 25-30, 45% of Americans said that stress resulting from the pandemic is having a negative impact on their mental health, compared with 32% expressing that view just 2 weeks earlier, the Kaiser Family Foundation reported April 2.
In the later survey, the effect looked like this: 19% of all respondents said that the pandemic has had a major negative impact and 26% said it has been minor so far. Women were more likely than men (24% vs. 15%) to report a major impact, as were blacks and Hispanic adults (both at 24%) compared with whites (17%), the KFF investigators said.
More Hispanic (44%) and black (42%) respondents also said that they had already lost their job, lost income, or had their hours reduced without pay as a result of the pandemic, compared with whites (36%). Among all respondents, 26% had lost income from a job or business and 28% had lost their job, been laid off, or had their hours reduced without pay, according to KFF.
A majority of respondents (57%) reported “being worried they will put themselves at risk of exposure to coronavirus because they can’t afford to stay home and miss work,” the researchers said. That figure is up from 35% in the earlier survey.
Anxiety about work-related exposure was even higher among hourly workers or those who get paid by the job (61%) and among employed adults who earn less than $40,000 annually (72%), they reported.
Overall, 72% of respondents said that their lives have been disrupted “a lot” or “some” by the coronavirus outbreak, and that is a jump of 32 percentage points over the previous poll, the investigators noted.
The disruption is expected to continue, it seems, as 74% believe that the worst is yet to come “in spite of the health, social and economic upheaval that Americans are already experiencing,” they wrote.
As the COVID-19 pandemic sweeps across the United States, it is increasingly affecting those who are not infected. Social bonds are being broken, businesses are closing, jobs are being lost, and the stress is mounting.

In a poll conducted March 25-30, 45% of Americans said that stress resulting from the pandemic is having a negative impact on their mental health, compared with 32% expressing that view just 2 weeks earlier, the Kaiser Family Foundation reported April 2.
In the later survey, the effect looked like this: 19% of all respondents said that the pandemic has had a major negative impact and 26% said it has been minor so far. Women were more likely than men (24% vs. 15%) to report a major impact, as were blacks and Hispanic adults (both at 24%) compared with whites (17%), the KFF investigators said.
More Hispanic (44%) and black (42%) respondents also said that they had already lost their job, lost income, or had their hours reduced without pay as a result of the pandemic, compared with whites (36%). Among all respondents, 26% had lost income from a job or business and 28% had lost their job, been laid off, or had their hours reduced without pay, according to KFF.
A majority of respondents (57%) reported “being worried they will put themselves at risk of exposure to coronavirus because they can’t afford to stay home and miss work,” the researchers said. That figure is up from 35% in the earlier survey.
Anxiety about work-related exposure was even higher among hourly workers or those who get paid by the job (61%) and among employed adults who earn less than $40,000 annually (72%), they reported.
Overall, 72% of respondents said that their lives have been disrupted “a lot” or “some” by the coronavirus outbreak, and that is a jump of 32 percentage points over the previous poll, the investigators noted.
The disruption is expected to continue, it seems, as 74% believe that the worst is yet to come “in spite of the health, social and economic upheaval that Americans are already experiencing,” they wrote.
CBT by phone reduces depression in Parkinson’s disease
, according to trial results published in Neurology. The treatment’s effect on depression is “moderated by the reduction of negative thoughts,” the target of the intervention, the researchers said.
Telephone-based CBT may be a convenient option for patients, said lead study author Roseanne D. Dobkin, PhD, of the department of psychiatry at Rutgers Robert Wood Johnson Medical School in Piscataway, N.J., and the VA New Jersey Health Care System in Lyons. “A notable proportion of people with Parkinson’s [disease] do not receive the much needed mental health treatment to facilitate proactive coping with the daily challenges superimposed by their medical condition,” Dr. Dobkin said in a news release. “This study suggests that the effects of the [CBT] last long beyond when the treatment stopped and can be used alongside standard neurological care.”
An undertreated problem
Although depression affects about half of patients with Parkinson’s disease and is associated with physical and cognitive decline, it often goes overlooked and undertreated, the study authors said. Data about the efficacy and tolerability of antidepressants are mixed. CBT holds promise for reducing depression in Parkinson’s disease, prior research suggests, but patients may have limited access to in-person sessions because of physical and geographic barriers.
To assess the efficacy of telephone-based CBT for depression in Parkinson’s disease, compared with community-based treatment as usual, Dr. Dobkin and colleagues conducted a randomized controlled trial. Their study included 72 patients with Parkinson’s disease at an academic medical center. Participants had a depressive disorder, were between aged 35 and 85 years, had stable Parkinson’s disease and mental health treatment for at least 6 weeks, and had a family member or friend willing to participate in the study. The investigators excluded patients with possible dementia or marked cognitive impairment and active suicidal plans or intent.
Participants were randomly assigned to receive usual care plus telephone-based CBT or usual care only. Patients taking antidepressants were evenly divided between the groups.
Telephone-based CBT consisted of weekly 1-hour sessions for 10 weeks. During 6 months of follow-up, patients could receive one session per month if desired. The CBT “targeted negative thoughts (e.g., ‘I have no control’; ‘I am helpless’) and behaviors (e.g., avoidance, excessive worry, lack of exercise),” the investigators said. In addition, therapists trained patients’ care partners by telephone to help patients between sessions. Treatment as usual was defined by patients’ health care teams. For most participants in both groups, treatment as usual included taking antidepressant medication or receiving psychotherapy in the community.
Change in Hamilton Depression Rating Scale (HAM-D) score was the primary outcome. Secondary outcomes included whether patients considered their depression much improved and improvements in depression severity (as measured by the Beck Depression Inventory [BDI]), anxiety (as measured by the Hamilton Anxiety Rating Scale [HAM-A]), and quality of life. The researchers also assessed negative thinking using the Inference Questionnaire. Blinded raters assessed outcomes.
Sustained improvements
Thirty-seven patients were randomized to receive telephone-based CBT, and 35 were randomized to treatment as usual. Overall, 70% were taking antidepressants, and 14% continued receiving psychotherapy from community providers of their choice during the trial. Participants’ average age was 65 years, and 51% were female.
Post treatment, mean improvement in HAM-D score from baseline was 6.53 points in the telephone-based CBT group, compared with −0.27 points in the control group. “Effects at the end of treatment were maintained at 6-month follow-up,” the researchers reported.
About 40% of patients in the CBT group reported that their depression was much improved or very much improved, compared with none of the patients in the control group. Responders had mild to minimal symptomatology on the HAM-D, which indicates that the changes were clinically significant, the authors said.
Secondary outcomes also favored telephone-based CBT. “The intervention was feasible and highly acceptable, yielding an 88% retention rate over the 9-month trial,” Dr. Dobkin and colleagues said.
Compared with other control conditions, treatment-as-usual controls may enhance the effect size of an intervention, the authors noted. In addition, factors such as therapeutic relationship, time, and attention likely contribute to psychotherapy outcomes.
Success may hinge on cognitive ability
“The success of this trial highlights the need for further efficacy studies targeting neuropsychiatric manifestations of [Parkinson’s disease] and adds urgency to the discussion over policies regarding access to tele–mental health, especially for vulnerable populations with limited access to in-person mental health services,” Gregory M. Pontone, MD, and Kelly A. Mills, MD, wrote in an accompanying editorial. Dr. Pontone and Dr. Mills are affiliated with Johns Hopkins University in Baltimore.
“Only rudimentary evidence” exists to guide the treatment of depression in patients with Parkinson’s disease, the editorialists said. “Patient preference and tolerability suggest that nonpharmacologic therapies, such as CBT, are preferred as first-line treatment. Yet access to qualified CBT practitioners, especially those with a clinical knowledge of [Parkinson’s disease], is limited.”
Despite its advantages and the encouraging results, CBT may have important limitations as well, they said. Patients require a certain degree of cognitive ability to benefit from CBT, and the prevalence of dementia among patients with Parkinson’s disease is about 30%.
Nevertheless, the trial provided evidence of target engagement. “Though caveats include the single-blind design and potential confounding by time spent with patient and caregiver, the authors demonstrated that improvement was mediated by the mechanism of CBT – a reduction in negative thinking.”
The trial was funded by the Michael J. Fox Foundation for Parkinson’s Research and the Parkinson’s Alliance (Parkinson’s Unity Walk). Dr. Mills disclosed a patent pending for a system for phase-dependent cortical brain stimulation, National Institutes of Health funding, pending funding from the Michael J. Fox Foundation, and commercial research support from Global Kinetics Corporation. Dr. Pontone is a consultant for Acadia Pharmaceuticals.
SOURCE: Dobkin RD et al. Neurology. 2020 Apr 1. doi: 10.1212/WNL.0000000000009292.
, according to trial results published in Neurology. The treatment’s effect on depression is “moderated by the reduction of negative thoughts,” the target of the intervention, the researchers said.
Telephone-based CBT may be a convenient option for patients, said lead study author Roseanne D. Dobkin, PhD, of the department of psychiatry at Rutgers Robert Wood Johnson Medical School in Piscataway, N.J., and the VA New Jersey Health Care System in Lyons. “A notable proportion of people with Parkinson’s [disease] do not receive the much needed mental health treatment to facilitate proactive coping with the daily challenges superimposed by their medical condition,” Dr. Dobkin said in a news release. “This study suggests that the effects of the [CBT] last long beyond when the treatment stopped and can be used alongside standard neurological care.”
An undertreated problem
Although depression affects about half of patients with Parkinson’s disease and is associated with physical and cognitive decline, it often goes overlooked and undertreated, the study authors said. Data about the efficacy and tolerability of antidepressants are mixed. CBT holds promise for reducing depression in Parkinson’s disease, prior research suggests, but patients may have limited access to in-person sessions because of physical and geographic barriers.
To assess the efficacy of telephone-based CBT for depression in Parkinson’s disease, compared with community-based treatment as usual, Dr. Dobkin and colleagues conducted a randomized controlled trial. Their study included 72 patients with Parkinson’s disease at an academic medical center. Participants had a depressive disorder, were between aged 35 and 85 years, had stable Parkinson’s disease and mental health treatment for at least 6 weeks, and had a family member or friend willing to participate in the study. The investigators excluded patients with possible dementia or marked cognitive impairment and active suicidal plans or intent.
Participants were randomly assigned to receive usual care plus telephone-based CBT or usual care only. Patients taking antidepressants were evenly divided between the groups.
Telephone-based CBT consisted of weekly 1-hour sessions for 10 weeks. During 6 months of follow-up, patients could receive one session per month if desired. The CBT “targeted negative thoughts (e.g., ‘I have no control’; ‘I am helpless’) and behaviors (e.g., avoidance, excessive worry, lack of exercise),” the investigators said. In addition, therapists trained patients’ care partners by telephone to help patients between sessions. Treatment as usual was defined by patients’ health care teams. For most participants in both groups, treatment as usual included taking antidepressant medication or receiving psychotherapy in the community.
Change in Hamilton Depression Rating Scale (HAM-D) score was the primary outcome. Secondary outcomes included whether patients considered their depression much improved and improvements in depression severity (as measured by the Beck Depression Inventory [BDI]), anxiety (as measured by the Hamilton Anxiety Rating Scale [HAM-A]), and quality of life. The researchers also assessed negative thinking using the Inference Questionnaire. Blinded raters assessed outcomes.
Sustained improvements
Thirty-seven patients were randomized to receive telephone-based CBT, and 35 were randomized to treatment as usual. Overall, 70% were taking antidepressants, and 14% continued receiving psychotherapy from community providers of their choice during the trial. Participants’ average age was 65 years, and 51% were female.
Post treatment, mean improvement in HAM-D score from baseline was 6.53 points in the telephone-based CBT group, compared with −0.27 points in the control group. “Effects at the end of treatment were maintained at 6-month follow-up,” the researchers reported.
About 40% of patients in the CBT group reported that their depression was much improved or very much improved, compared with none of the patients in the control group. Responders had mild to minimal symptomatology on the HAM-D, which indicates that the changes were clinically significant, the authors said.
Secondary outcomes also favored telephone-based CBT. “The intervention was feasible and highly acceptable, yielding an 88% retention rate over the 9-month trial,” Dr. Dobkin and colleagues said.
Compared with other control conditions, treatment-as-usual controls may enhance the effect size of an intervention, the authors noted. In addition, factors such as therapeutic relationship, time, and attention likely contribute to psychotherapy outcomes.
Success may hinge on cognitive ability
“The success of this trial highlights the need for further efficacy studies targeting neuropsychiatric manifestations of [Parkinson’s disease] and adds urgency to the discussion over policies regarding access to tele–mental health, especially for vulnerable populations with limited access to in-person mental health services,” Gregory M. Pontone, MD, and Kelly A. Mills, MD, wrote in an accompanying editorial. Dr. Pontone and Dr. Mills are affiliated with Johns Hopkins University in Baltimore.
“Only rudimentary evidence” exists to guide the treatment of depression in patients with Parkinson’s disease, the editorialists said. “Patient preference and tolerability suggest that nonpharmacologic therapies, such as CBT, are preferred as first-line treatment. Yet access to qualified CBT practitioners, especially those with a clinical knowledge of [Parkinson’s disease], is limited.”
Despite its advantages and the encouraging results, CBT may have important limitations as well, they said. Patients require a certain degree of cognitive ability to benefit from CBT, and the prevalence of dementia among patients with Parkinson’s disease is about 30%.
Nevertheless, the trial provided evidence of target engagement. “Though caveats include the single-blind design and potential confounding by time spent with patient and caregiver, the authors demonstrated that improvement was mediated by the mechanism of CBT – a reduction in negative thinking.”
The trial was funded by the Michael J. Fox Foundation for Parkinson’s Research and the Parkinson’s Alliance (Parkinson’s Unity Walk). Dr. Mills disclosed a patent pending for a system for phase-dependent cortical brain stimulation, National Institutes of Health funding, pending funding from the Michael J. Fox Foundation, and commercial research support from Global Kinetics Corporation. Dr. Pontone is a consultant for Acadia Pharmaceuticals.
SOURCE: Dobkin RD et al. Neurology. 2020 Apr 1. doi: 10.1212/WNL.0000000000009292.
, according to trial results published in Neurology. The treatment’s effect on depression is “moderated by the reduction of negative thoughts,” the target of the intervention, the researchers said.
Telephone-based CBT may be a convenient option for patients, said lead study author Roseanne D. Dobkin, PhD, of the department of psychiatry at Rutgers Robert Wood Johnson Medical School in Piscataway, N.J., and the VA New Jersey Health Care System in Lyons. “A notable proportion of people with Parkinson’s [disease] do not receive the much needed mental health treatment to facilitate proactive coping with the daily challenges superimposed by their medical condition,” Dr. Dobkin said in a news release. “This study suggests that the effects of the [CBT] last long beyond when the treatment stopped and can be used alongside standard neurological care.”
An undertreated problem
Although depression affects about half of patients with Parkinson’s disease and is associated with physical and cognitive decline, it often goes overlooked and undertreated, the study authors said. Data about the efficacy and tolerability of antidepressants are mixed. CBT holds promise for reducing depression in Parkinson’s disease, prior research suggests, but patients may have limited access to in-person sessions because of physical and geographic barriers.
To assess the efficacy of telephone-based CBT for depression in Parkinson’s disease, compared with community-based treatment as usual, Dr. Dobkin and colleagues conducted a randomized controlled trial. Their study included 72 patients with Parkinson’s disease at an academic medical center. Participants had a depressive disorder, were between aged 35 and 85 years, had stable Parkinson’s disease and mental health treatment for at least 6 weeks, and had a family member or friend willing to participate in the study. The investigators excluded patients with possible dementia or marked cognitive impairment and active suicidal plans or intent.
Participants were randomly assigned to receive usual care plus telephone-based CBT or usual care only. Patients taking antidepressants were evenly divided between the groups.
Telephone-based CBT consisted of weekly 1-hour sessions for 10 weeks. During 6 months of follow-up, patients could receive one session per month if desired. The CBT “targeted negative thoughts (e.g., ‘I have no control’; ‘I am helpless’) and behaviors (e.g., avoidance, excessive worry, lack of exercise),” the investigators said. In addition, therapists trained patients’ care partners by telephone to help patients between sessions. Treatment as usual was defined by patients’ health care teams. For most participants in both groups, treatment as usual included taking antidepressant medication or receiving psychotherapy in the community.
Change in Hamilton Depression Rating Scale (HAM-D) score was the primary outcome. Secondary outcomes included whether patients considered their depression much improved and improvements in depression severity (as measured by the Beck Depression Inventory [BDI]), anxiety (as measured by the Hamilton Anxiety Rating Scale [HAM-A]), and quality of life. The researchers also assessed negative thinking using the Inference Questionnaire. Blinded raters assessed outcomes.
Sustained improvements
Thirty-seven patients were randomized to receive telephone-based CBT, and 35 were randomized to treatment as usual. Overall, 70% were taking antidepressants, and 14% continued receiving psychotherapy from community providers of their choice during the trial. Participants’ average age was 65 years, and 51% were female.
Post treatment, mean improvement in HAM-D score from baseline was 6.53 points in the telephone-based CBT group, compared with −0.27 points in the control group. “Effects at the end of treatment were maintained at 6-month follow-up,” the researchers reported.
About 40% of patients in the CBT group reported that their depression was much improved or very much improved, compared with none of the patients in the control group. Responders had mild to minimal symptomatology on the HAM-D, which indicates that the changes were clinically significant, the authors said.
Secondary outcomes also favored telephone-based CBT. “The intervention was feasible and highly acceptable, yielding an 88% retention rate over the 9-month trial,” Dr. Dobkin and colleagues said.
Compared with other control conditions, treatment-as-usual controls may enhance the effect size of an intervention, the authors noted. In addition, factors such as therapeutic relationship, time, and attention likely contribute to psychotherapy outcomes.
Success may hinge on cognitive ability
“The success of this trial highlights the need for further efficacy studies targeting neuropsychiatric manifestations of [Parkinson’s disease] and adds urgency to the discussion over policies regarding access to tele–mental health, especially for vulnerable populations with limited access to in-person mental health services,” Gregory M. Pontone, MD, and Kelly A. Mills, MD, wrote in an accompanying editorial. Dr. Pontone and Dr. Mills are affiliated with Johns Hopkins University in Baltimore.
“Only rudimentary evidence” exists to guide the treatment of depression in patients with Parkinson’s disease, the editorialists said. “Patient preference and tolerability suggest that nonpharmacologic therapies, such as CBT, are preferred as first-line treatment. Yet access to qualified CBT practitioners, especially those with a clinical knowledge of [Parkinson’s disease], is limited.”
Despite its advantages and the encouraging results, CBT may have important limitations as well, they said. Patients require a certain degree of cognitive ability to benefit from CBT, and the prevalence of dementia among patients with Parkinson’s disease is about 30%.
Nevertheless, the trial provided evidence of target engagement. “Though caveats include the single-blind design and potential confounding by time spent with patient and caregiver, the authors demonstrated that improvement was mediated by the mechanism of CBT – a reduction in negative thinking.”
The trial was funded by the Michael J. Fox Foundation for Parkinson’s Research and the Parkinson’s Alliance (Parkinson’s Unity Walk). Dr. Mills disclosed a patent pending for a system for phase-dependent cortical brain stimulation, National Institutes of Health funding, pending funding from the Michael J. Fox Foundation, and commercial research support from Global Kinetics Corporation. Dr. Pontone is a consultant for Acadia Pharmaceuticals.
SOURCE: Dobkin RD et al. Neurology. 2020 Apr 1. doi: 10.1212/WNL.0000000000009292.
FROM NEUROLOGY
IV esketamine, ketamine equally effective for resistant depression
Intravenous (IV) esketamine is as safe and effective as IV ketamine for patients with treatment-resistant depression, new research suggests.
“Our study was the first randomized clinical trial directly comparing ketamine and esketamine in treatment-resistant depression,” senior investigator Lucas C. Quarantini, MD, PhD, division of psychiatry, Professor Edgard Santos University Hospital, Federal University of Bahia, Salvador, Brazil, said in an interview.
The findings showed that esketamine was not inferior to ketamine in remission of depressive symptoms 24 hours after a single IV dose, and the two treatments had similar side effect profiles, Dr. Quarantini said.
Furthermore, “our results showed that only the number of treatment failures was an important factor for the remission of symptoms,” he added.
The findings were scheduled to be presented at the Anxiety and Depression Association of America (ADAA) Conference 2020, along with publication in the Journal of Affective Disorders (2020 Mar 1;264:527-34). However, the ADAA conference was canceled in the wake of the coronavirus pandemic.
More treatment options
The randomized, double-blind noninferiority trial compared IV racemic ketamine and esketamine, two formulations of the glutamate NMDA receptor modulator drug. It included 63 participants (61.9% women; mean age, 47 years) with treatment-resistant major depressive disorder, as determined by DSM-5 criteria.
Participants were enrolled between March 2017 and June 2018 and randomized to receive a single subanesthetic dose of racemic ketamine (0.5 mg/kg; n = 29) or esketamine (0.25 mg/kg; n = 34) for 40 minutes.
Results showed esketamine to be noninferior to ketamine as determined by the Montgomery-Åsberg Depression Rating Scale (MADRS).
The difference of just 5.3% confirmed noninferiority.
Although ketamine showed a tendency to have a longer-lasting antidepressant effect compared with esketamine, the difference did not reach statistical significance and should be evaluated in future studies, the investigators noted.
Both treatments were safe and well tolerated. Consistent with previous studies, the most frequent side effects were dissociative symptoms, including derealization, depersonalization, and cardiovascular changes, and increased blood pressure and heart rate, which occurred equally in both groups. There were no serious adverse events in either study group.
The investigators noted that most of the previous research examining antidepressant effects of ketamine has used the IV racemic type. The current findings are particularly important for situations in which ketamine or intranasal esketamine, which was recently approved by the Food and Drug Administration, are unavailable, Dr. Quarantini said.
“What our study adds to what has been previously published is that the only way to really analyze if two drugs are equivalent is to compare them in a head-to-head trial; and that was what we did,” he said.
“Our findings bring a greater basis for practitioners from locations where intravenous esketamine is more easily obtainable than ketamine to use it as an affordable option for treating depressive patients,” Dr. Quarantini added.
“Since this [lack of availability] is the scenario here in Brazil, and probably in many other countries, all patients from these locations will benefit from this finding,” he said.
While further evaluating the study results to determine which clinical characteristics were predictive of remission of depressive symptoms, the researchers assessed several key factors. The median duration of disease progression was 12 months, median number of depressive episodes was five, and median number of therapeutic treatment failures was three.
The investigators also looked at the number of suicide attempts and degree of dissociative behavior.
Of these factors, the number of therapeutic failures was the only significant predictor of symptom remission, with an odds ratio of 1.46 for each prior therapeutic failure (95% CI, 1.08-1.99).
“To date, we have not found [other] studies with similar data,” Dr. Quarantini noted.
“Identifying remission predictors may contribute to selecting more suitable candidates for the intervention and result in more individualized and effective patient management,” the investigators wrote.
Consistent findings
Commenting on the findings, Gerard Sanacora, MD, PhD, professor of psychiatry at Yale University, New Haven, Conn., noted that key study limitations include the small sample size and lack of a placebo group.
Nevertheless, “I think it is fair to say that it is unlikely that the treatments are markedly different in their effects on depression over 24 hours,” he said in an interview.
Dr. Sanacora, director of the Yale Depression Research Program, was not involved with the current research.
The findings are “consistent with what we can extrapolate from other clinical trials examining racemic ketamine and esketamine separately,” he said.
Dr. Sanacora noted that because esketamine has been previously shown to be a more potent anesthetic than arketamine, the other component of racemic ketamine, it is “the primary form of ketamine used as an anesthetic agent in several regions of the world with the idea that it may be more selective for the desired anesthetic effect.”
Even with its limitations, the study does offer some notable yet preliminary insights, he added.
“It is interesting to see varying degrees of numerical differences between the two treatments at different time points,” Dr. Sanacora said. In addition, “there may be some differing effects between the two treatments over time, but we really do not have enough data to say much of anything [about that] with confidence at this point.”
The study was supported by the Programa de Pesquisa para o SUS through Fundação de Amparo à Pesquisa do Estado da Bahia. Dr. Quarantini has reported receiving consulting fees from Allergan, Abbott, Janssen Pharmaceuticals, and Lundbeck, and research fees from Janssen Pharmaceuticals. The other study authors’ disclosures are listed in the published article. Dr. Sanacora has reported consulting and/or conducting research from several pharmaceutical companies. He also holds shares in BioHaven Pharmaceuticals and is coinventor on a patent called “Glutamate Agents in the Treatment of Mental Disorders.”
A version of this article originally appeared on Medscape.com.
Intravenous (IV) esketamine is as safe and effective as IV ketamine for patients with treatment-resistant depression, new research suggests.
“Our study was the first randomized clinical trial directly comparing ketamine and esketamine in treatment-resistant depression,” senior investigator Lucas C. Quarantini, MD, PhD, division of psychiatry, Professor Edgard Santos University Hospital, Federal University of Bahia, Salvador, Brazil, said in an interview.
The findings showed that esketamine was not inferior to ketamine in remission of depressive symptoms 24 hours after a single IV dose, and the two treatments had similar side effect profiles, Dr. Quarantini said.
Furthermore, “our results showed that only the number of treatment failures was an important factor for the remission of symptoms,” he added.
The findings were scheduled to be presented at the Anxiety and Depression Association of America (ADAA) Conference 2020, along with publication in the Journal of Affective Disorders (2020 Mar 1;264:527-34). However, the ADAA conference was canceled in the wake of the coronavirus pandemic.
More treatment options
The randomized, double-blind noninferiority trial compared IV racemic ketamine and esketamine, two formulations of the glutamate NMDA receptor modulator drug. It included 63 participants (61.9% women; mean age, 47 years) with treatment-resistant major depressive disorder, as determined by DSM-5 criteria.
Participants were enrolled between March 2017 and June 2018 and randomized to receive a single subanesthetic dose of racemic ketamine (0.5 mg/kg; n = 29) or esketamine (0.25 mg/kg; n = 34) for 40 minutes.
Results showed esketamine to be noninferior to ketamine as determined by the Montgomery-Åsberg Depression Rating Scale (MADRS).
The difference of just 5.3% confirmed noninferiority.
Although ketamine showed a tendency to have a longer-lasting antidepressant effect compared with esketamine, the difference did not reach statistical significance and should be evaluated in future studies, the investigators noted.
Both treatments were safe and well tolerated. Consistent with previous studies, the most frequent side effects were dissociative symptoms, including derealization, depersonalization, and cardiovascular changes, and increased blood pressure and heart rate, which occurred equally in both groups. There were no serious adverse events in either study group.
The investigators noted that most of the previous research examining antidepressant effects of ketamine has used the IV racemic type. The current findings are particularly important for situations in which ketamine or intranasal esketamine, which was recently approved by the Food and Drug Administration, are unavailable, Dr. Quarantini said.
“What our study adds to what has been previously published is that the only way to really analyze if two drugs are equivalent is to compare them in a head-to-head trial; and that was what we did,” he said.
“Our findings bring a greater basis for practitioners from locations where intravenous esketamine is more easily obtainable than ketamine to use it as an affordable option for treating depressive patients,” Dr. Quarantini added.
“Since this [lack of availability] is the scenario here in Brazil, and probably in many other countries, all patients from these locations will benefit from this finding,” he said.
While further evaluating the study results to determine which clinical characteristics were predictive of remission of depressive symptoms, the researchers assessed several key factors. The median duration of disease progression was 12 months, median number of depressive episodes was five, and median number of therapeutic treatment failures was three.
The investigators also looked at the number of suicide attempts and degree of dissociative behavior.
Of these factors, the number of therapeutic failures was the only significant predictor of symptom remission, with an odds ratio of 1.46 for each prior therapeutic failure (95% CI, 1.08-1.99).
“To date, we have not found [other] studies with similar data,” Dr. Quarantini noted.
“Identifying remission predictors may contribute to selecting more suitable candidates for the intervention and result in more individualized and effective patient management,” the investigators wrote.
Consistent findings
Commenting on the findings, Gerard Sanacora, MD, PhD, professor of psychiatry at Yale University, New Haven, Conn., noted that key study limitations include the small sample size and lack of a placebo group.
Nevertheless, “I think it is fair to say that it is unlikely that the treatments are markedly different in their effects on depression over 24 hours,” he said in an interview.
Dr. Sanacora, director of the Yale Depression Research Program, was not involved with the current research.
The findings are “consistent with what we can extrapolate from other clinical trials examining racemic ketamine and esketamine separately,” he said.
Dr. Sanacora noted that because esketamine has been previously shown to be a more potent anesthetic than arketamine, the other component of racemic ketamine, it is “the primary form of ketamine used as an anesthetic agent in several regions of the world with the idea that it may be more selective for the desired anesthetic effect.”
Even with its limitations, the study does offer some notable yet preliminary insights, he added.
“It is interesting to see varying degrees of numerical differences between the two treatments at different time points,” Dr. Sanacora said. In addition, “there may be some differing effects between the two treatments over time, but we really do not have enough data to say much of anything [about that] with confidence at this point.”
The study was supported by the Programa de Pesquisa para o SUS through Fundação de Amparo à Pesquisa do Estado da Bahia. Dr. Quarantini has reported receiving consulting fees from Allergan, Abbott, Janssen Pharmaceuticals, and Lundbeck, and research fees from Janssen Pharmaceuticals. The other study authors’ disclosures are listed in the published article. Dr. Sanacora has reported consulting and/or conducting research from several pharmaceutical companies. He also holds shares in BioHaven Pharmaceuticals and is coinventor on a patent called “Glutamate Agents in the Treatment of Mental Disorders.”
A version of this article originally appeared on Medscape.com.
Intravenous (IV) esketamine is as safe and effective as IV ketamine for patients with treatment-resistant depression, new research suggests.
“Our study was the first randomized clinical trial directly comparing ketamine and esketamine in treatment-resistant depression,” senior investigator Lucas C. Quarantini, MD, PhD, division of psychiatry, Professor Edgard Santos University Hospital, Federal University of Bahia, Salvador, Brazil, said in an interview.
The findings showed that esketamine was not inferior to ketamine in remission of depressive symptoms 24 hours after a single IV dose, and the two treatments had similar side effect profiles, Dr. Quarantini said.
Furthermore, “our results showed that only the number of treatment failures was an important factor for the remission of symptoms,” he added.
The findings were scheduled to be presented at the Anxiety and Depression Association of America (ADAA) Conference 2020, along with publication in the Journal of Affective Disorders (2020 Mar 1;264:527-34). However, the ADAA conference was canceled in the wake of the coronavirus pandemic.
More treatment options
The randomized, double-blind noninferiority trial compared IV racemic ketamine and esketamine, two formulations of the glutamate NMDA receptor modulator drug. It included 63 participants (61.9% women; mean age, 47 years) with treatment-resistant major depressive disorder, as determined by DSM-5 criteria.
Participants were enrolled between March 2017 and June 2018 and randomized to receive a single subanesthetic dose of racemic ketamine (0.5 mg/kg; n = 29) or esketamine (0.25 mg/kg; n = 34) for 40 minutes.
Results showed esketamine to be noninferior to ketamine as determined by the Montgomery-Åsberg Depression Rating Scale (MADRS).
The difference of just 5.3% confirmed noninferiority.
Although ketamine showed a tendency to have a longer-lasting antidepressant effect compared with esketamine, the difference did not reach statistical significance and should be evaluated in future studies, the investigators noted.
Both treatments were safe and well tolerated. Consistent with previous studies, the most frequent side effects were dissociative symptoms, including derealization, depersonalization, and cardiovascular changes, and increased blood pressure and heart rate, which occurred equally in both groups. There were no serious adverse events in either study group.
The investigators noted that most of the previous research examining antidepressant effects of ketamine has used the IV racemic type. The current findings are particularly important for situations in which ketamine or intranasal esketamine, which was recently approved by the Food and Drug Administration, are unavailable, Dr. Quarantini said.
“What our study adds to what has been previously published is that the only way to really analyze if two drugs are equivalent is to compare them in a head-to-head trial; and that was what we did,” he said.
“Our findings bring a greater basis for practitioners from locations where intravenous esketamine is more easily obtainable than ketamine to use it as an affordable option for treating depressive patients,” Dr. Quarantini added.
“Since this [lack of availability] is the scenario here in Brazil, and probably in many other countries, all patients from these locations will benefit from this finding,” he said.
While further evaluating the study results to determine which clinical characteristics were predictive of remission of depressive symptoms, the researchers assessed several key factors. The median duration of disease progression was 12 months, median number of depressive episodes was five, and median number of therapeutic treatment failures was three.
The investigators also looked at the number of suicide attempts and degree of dissociative behavior.
Of these factors, the number of therapeutic failures was the only significant predictor of symptom remission, with an odds ratio of 1.46 for each prior therapeutic failure (95% CI, 1.08-1.99).
“To date, we have not found [other] studies with similar data,” Dr. Quarantini noted.
“Identifying remission predictors may contribute to selecting more suitable candidates for the intervention and result in more individualized and effective patient management,” the investigators wrote.
Consistent findings
Commenting on the findings, Gerard Sanacora, MD, PhD, professor of psychiatry at Yale University, New Haven, Conn., noted that key study limitations include the small sample size and lack of a placebo group.
Nevertheless, “I think it is fair to say that it is unlikely that the treatments are markedly different in their effects on depression over 24 hours,” he said in an interview.
Dr. Sanacora, director of the Yale Depression Research Program, was not involved with the current research.
The findings are “consistent with what we can extrapolate from other clinical trials examining racemic ketamine and esketamine separately,” he said.
Dr. Sanacora noted that because esketamine has been previously shown to be a more potent anesthetic than arketamine, the other component of racemic ketamine, it is “the primary form of ketamine used as an anesthetic agent in several regions of the world with the idea that it may be more selective for the desired anesthetic effect.”
Even with its limitations, the study does offer some notable yet preliminary insights, he added.
“It is interesting to see varying degrees of numerical differences between the two treatments at different time points,” Dr. Sanacora said. In addition, “there may be some differing effects between the two treatments over time, but we really do not have enough data to say much of anything [about that] with confidence at this point.”
The study was supported by the Programa de Pesquisa para o SUS through Fundação de Amparo à Pesquisa do Estado da Bahia. Dr. Quarantini has reported receiving consulting fees from Allergan, Abbott, Janssen Pharmaceuticals, and Lundbeck, and research fees from Janssen Pharmaceuticals. The other study authors’ disclosures are listed in the published article. Dr. Sanacora has reported consulting and/or conducting research from several pharmaceutical companies. He also holds shares in BioHaven Pharmaceuticals and is coinventor on a patent called “Glutamate Agents in the Treatment of Mental Disorders.”
A version of this article originally appeared on Medscape.com.
COVID-19: Mental health pros come to the aid of frontline comrades
Frontline COVID-19 healthcare workers across North America are dealing with unprecedented stress, but mental health therapists in both Canada and the US are doing their part to ensure the psychological well-being of their colleagues on the frontlines of the pandemic.
Over the past few weeks, thousands of licensed psychologists, psychotherapists, and social workers have signed up to offer free therapy sessions to healthcare professionals who find themselves psychologically overwhelmed by the pandemic’s economic, social, and financial fallout.
In Canada, the movement was started by Toronto psychotherapist Karen Dougherty, MA, who saw a social media post from someone in New York asking mental health workers to volunteer their time.
Inspired by this, Dougherty reached out to some of her close colleagues with a social media post of her own. A few days later, 450 people had signed up to volunteer and Ontario COVID-19 Therapists was born.
The sessions are provided by licensed Canadian psychotherapists and are free of charge to healthcare workers providing frontline COVID-19 care. After signing up online, users can choose from one of three therapists who will provide up to five free phone sessions.
In New York state, a similar initiative — which is not limited to healthcare workers — has gained incredible momentum. On March 21, Gov. Andrew Cuomo announced the creation of a statewide hotline [844-863-9314] to provide free mental health services to individuals sheltering at home who may be experiencing stress and anxiety as a result of COVID-19.
The governor called on mental-health professionals to volunteer their time and provide telephone and/or telehealth counseling. The New York State Psychiatric Association quickly got on board and encouraged its members to participate.
Just four days later, more than 6,000 mental health workers had volunteered their services, making New York the first state to address the mental health consequences of the pandemic in this way.
Self-care is vital for healthcare workers during the COVID-19 pandemic, particularly as stress mounts and workdays become longer and grimmer. Dougherty recommended that frontline workers manage overwhelming thoughts by limiting their intake of information about the virus.
Self-Care a “Selfless Act”
Clinicians need to balance the need to stay informed with the potential for information overload, which can contribute to anxiety, she said.
She also recommended that individuals continue to connect with loved ones while practicing social distancing. Equally important is talking to someone about the struggles people may be facing at work.
For Amin Azzam MD, MA, the benefits of these initiatives are obvious.
“There is always value in providing additional mental health services and tending to psychological well-being,” Azzam, adjunct professor of psychiatry, University of California, San Francisco and UC Berkeley, told Medscape Medical News.
“If there ever were a time when we can use all the emotional support possible, then it would be during a global pandemic,” added Azzam, who is also director of Open Learning Initiatives at Osmosis, a nonprofit health education company.
Azzam urged healthcare professionals to avail themselves of such resources as often as necessary.
“Taking care of ourselves is not a selfish act. When the oxygen masks come down on airplanes we are always instructed to put our own masks on first before helping those in need. It’s a sign of strength, not weakness, to seek emotional support,” he said.
However, it isn’t always easy. The longstanding stigma associated with seeking help for mental health issues has not stopped for COVID-19. Even workers who are in close daily contact with people infected with the virus are finding they’re not immune to the stigma associated with seeking mental health treatment, Azzam added.
“Nevertheless, the burden these frontline workers are facing is real…and often crushing. Some Ontario doctors have reported pretraumatic stress disorder, which they attribute to having watched the virus wreak havoc in other countries, and knowing that similar difficulties are headed their way,” he said.
A Growing Movement
Doris Grinspun, PhD, MSN, the CEO of Registered Nurses’ Association of Ontario (RNAO), said the province’s nurses are under intense pressure at work, then fear infecting family members once they come home. Some are even staying at hotels to ensure they don’t infect others, as reported by CBC News.
However, she added, most recognize the important role that psychotherapy can play, especially since many frontline healthcare workers find it difficult to speak with their families about the issues they face at work, for fear of adding stress to their family life as well.
“None of us are superhuman and immune to stress. When healthcare workers are facing workplace challenges never before seen in their lifetimes, they need opportunities to decompress to maintain their own health and well-being. This will help them pace themselves for the marathon — not sprint — to continue doing the important work of helping others,” said Azzam.
Given the attention it has garnered in such a short time, Azzam is hopeful that the free therapy movement will spread.
In Canada, mental health professionals in other provinces have already reached out to Dougherty, lending credence to the notion of a pan-Canadian network of therapists offering free services to healthcare workers during the outbreak.
In the US, other local initiatives are already underway.
“The one that I’m personally aware of is at my home institution at the University of California, San Francisco,” Azzam said. “We have a Care for the Caregiver program that is being greatly expanded at this time. As part of that initiative, the institution’s psychiatry department has solicited licensed mental health care providers to volunteer their time to provide those additional services.”
Azzam has also worked with colleagues developing a series of mental health tools that Osmosis has made available free of charge.
These include a central site with educational material about COVID-19, a video about supporting educators’ mental health during high-stress periods; a video about managing students’ mental health during public health emergencies; a summary of recommended resources for psychological health in distressing times; and a YouTube Live event he held regarding tips for maximizing psychological health during stressful times.
This article first appeared on Medscape.com.
Frontline COVID-19 healthcare workers across North America are dealing with unprecedented stress, but mental health therapists in both Canada and the US are doing their part to ensure the psychological well-being of their colleagues on the frontlines of the pandemic.
Over the past few weeks, thousands of licensed psychologists, psychotherapists, and social workers have signed up to offer free therapy sessions to healthcare professionals who find themselves psychologically overwhelmed by the pandemic’s economic, social, and financial fallout.
In Canada, the movement was started by Toronto psychotherapist Karen Dougherty, MA, who saw a social media post from someone in New York asking mental health workers to volunteer their time.
Inspired by this, Dougherty reached out to some of her close colleagues with a social media post of her own. A few days later, 450 people had signed up to volunteer and Ontario COVID-19 Therapists was born.
The sessions are provided by licensed Canadian psychotherapists and are free of charge to healthcare workers providing frontline COVID-19 care. After signing up online, users can choose from one of three therapists who will provide up to five free phone sessions.
In New York state, a similar initiative — which is not limited to healthcare workers — has gained incredible momentum. On March 21, Gov. Andrew Cuomo announced the creation of a statewide hotline [844-863-9314] to provide free mental health services to individuals sheltering at home who may be experiencing stress and anxiety as a result of COVID-19.
The governor called on mental-health professionals to volunteer their time and provide telephone and/or telehealth counseling. The New York State Psychiatric Association quickly got on board and encouraged its members to participate.
Just four days later, more than 6,000 mental health workers had volunteered their services, making New York the first state to address the mental health consequences of the pandemic in this way.
Self-care is vital for healthcare workers during the COVID-19 pandemic, particularly as stress mounts and workdays become longer and grimmer. Dougherty recommended that frontline workers manage overwhelming thoughts by limiting their intake of information about the virus.
Self-Care a “Selfless Act”
Clinicians need to balance the need to stay informed with the potential for information overload, which can contribute to anxiety, she said.
She also recommended that individuals continue to connect with loved ones while practicing social distancing. Equally important is talking to someone about the struggles people may be facing at work.
For Amin Azzam MD, MA, the benefits of these initiatives are obvious.
“There is always value in providing additional mental health services and tending to psychological well-being,” Azzam, adjunct professor of psychiatry, University of California, San Francisco and UC Berkeley, told Medscape Medical News.
“If there ever were a time when we can use all the emotional support possible, then it would be during a global pandemic,” added Azzam, who is also director of Open Learning Initiatives at Osmosis, a nonprofit health education company.
Azzam urged healthcare professionals to avail themselves of such resources as often as necessary.
“Taking care of ourselves is not a selfish act. When the oxygen masks come down on airplanes we are always instructed to put our own masks on first before helping those in need. It’s a sign of strength, not weakness, to seek emotional support,” he said.
However, it isn’t always easy. The longstanding stigma associated with seeking help for mental health issues has not stopped for COVID-19. Even workers who are in close daily contact with people infected with the virus are finding they’re not immune to the stigma associated with seeking mental health treatment, Azzam added.
“Nevertheless, the burden these frontline workers are facing is real…and often crushing. Some Ontario doctors have reported pretraumatic stress disorder, which they attribute to having watched the virus wreak havoc in other countries, and knowing that similar difficulties are headed their way,” he said.
A Growing Movement
Doris Grinspun, PhD, MSN, the CEO of Registered Nurses’ Association of Ontario (RNAO), said the province’s nurses are under intense pressure at work, then fear infecting family members once they come home. Some are even staying at hotels to ensure they don’t infect others, as reported by CBC News.
However, she added, most recognize the important role that psychotherapy can play, especially since many frontline healthcare workers find it difficult to speak with their families about the issues they face at work, for fear of adding stress to their family life as well.
“None of us are superhuman and immune to stress. When healthcare workers are facing workplace challenges never before seen in their lifetimes, they need opportunities to decompress to maintain their own health and well-being. This will help them pace themselves for the marathon — not sprint — to continue doing the important work of helping others,” said Azzam.
Given the attention it has garnered in such a short time, Azzam is hopeful that the free therapy movement will spread.
In Canada, mental health professionals in other provinces have already reached out to Dougherty, lending credence to the notion of a pan-Canadian network of therapists offering free services to healthcare workers during the outbreak.
In the US, other local initiatives are already underway.
“The one that I’m personally aware of is at my home institution at the University of California, San Francisco,” Azzam said. “We have a Care for the Caregiver program that is being greatly expanded at this time. As part of that initiative, the institution’s psychiatry department has solicited licensed mental health care providers to volunteer their time to provide those additional services.”
Azzam has also worked with colleagues developing a series of mental health tools that Osmosis has made available free of charge.
These include a central site with educational material about COVID-19, a video about supporting educators’ mental health during high-stress periods; a video about managing students’ mental health during public health emergencies; a summary of recommended resources for psychological health in distressing times; and a YouTube Live event he held regarding tips for maximizing psychological health during stressful times.
This article first appeared on Medscape.com.
Frontline COVID-19 healthcare workers across North America are dealing with unprecedented stress, but mental health therapists in both Canada and the US are doing their part to ensure the psychological well-being of their colleagues on the frontlines of the pandemic.
Over the past few weeks, thousands of licensed psychologists, psychotherapists, and social workers have signed up to offer free therapy sessions to healthcare professionals who find themselves psychologically overwhelmed by the pandemic’s economic, social, and financial fallout.
In Canada, the movement was started by Toronto psychotherapist Karen Dougherty, MA, who saw a social media post from someone in New York asking mental health workers to volunteer their time.
Inspired by this, Dougherty reached out to some of her close colleagues with a social media post of her own. A few days later, 450 people had signed up to volunteer and Ontario COVID-19 Therapists was born.
The sessions are provided by licensed Canadian psychotherapists and are free of charge to healthcare workers providing frontline COVID-19 care. After signing up online, users can choose from one of three therapists who will provide up to five free phone sessions.
In New York state, a similar initiative — which is not limited to healthcare workers — has gained incredible momentum. On March 21, Gov. Andrew Cuomo announced the creation of a statewide hotline [844-863-9314] to provide free mental health services to individuals sheltering at home who may be experiencing stress and anxiety as a result of COVID-19.
The governor called on mental-health professionals to volunteer their time and provide telephone and/or telehealth counseling. The New York State Psychiatric Association quickly got on board and encouraged its members to participate.
Just four days later, more than 6,000 mental health workers had volunteered their services, making New York the first state to address the mental health consequences of the pandemic in this way.
Self-care is vital for healthcare workers during the COVID-19 pandemic, particularly as stress mounts and workdays become longer and grimmer. Dougherty recommended that frontline workers manage overwhelming thoughts by limiting their intake of information about the virus.
Self-Care a “Selfless Act”
Clinicians need to balance the need to stay informed with the potential for information overload, which can contribute to anxiety, she said.
She also recommended that individuals continue to connect with loved ones while practicing social distancing. Equally important is talking to someone about the struggles people may be facing at work.
For Amin Azzam MD, MA, the benefits of these initiatives are obvious.
“There is always value in providing additional mental health services and tending to psychological well-being,” Azzam, adjunct professor of psychiatry, University of California, San Francisco and UC Berkeley, told Medscape Medical News.
“If there ever were a time when we can use all the emotional support possible, then it would be during a global pandemic,” added Azzam, who is also director of Open Learning Initiatives at Osmosis, a nonprofit health education company.
Azzam urged healthcare professionals to avail themselves of such resources as often as necessary.
“Taking care of ourselves is not a selfish act. When the oxygen masks come down on airplanes we are always instructed to put our own masks on first before helping those in need. It’s a sign of strength, not weakness, to seek emotional support,” he said.
However, it isn’t always easy. The longstanding stigma associated with seeking help for mental health issues has not stopped for COVID-19. Even workers who are in close daily contact with people infected with the virus are finding they’re not immune to the stigma associated with seeking mental health treatment, Azzam added.
“Nevertheless, the burden these frontline workers are facing is real…and often crushing. Some Ontario doctors have reported pretraumatic stress disorder, which they attribute to having watched the virus wreak havoc in other countries, and knowing that similar difficulties are headed their way,” he said.
A Growing Movement
Doris Grinspun, PhD, MSN, the CEO of Registered Nurses’ Association of Ontario (RNAO), said the province’s nurses are under intense pressure at work, then fear infecting family members once they come home. Some are even staying at hotels to ensure they don’t infect others, as reported by CBC News.
However, she added, most recognize the important role that psychotherapy can play, especially since many frontline healthcare workers find it difficult to speak with their families about the issues they face at work, for fear of adding stress to their family life as well.
“None of us are superhuman and immune to stress. When healthcare workers are facing workplace challenges never before seen in their lifetimes, they need opportunities to decompress to maintain their own health and well-being. This will help them pace themselves for the marathon — not sprint — to continue doing the important work of helping others,” said Azzam.
Given the attention it has garnered in such a short time, Azzam is hopeful that the free therapy movement will spread.
In Canada, mental health professionals in other provinces have already reached out to Dougherty, lending credence to the notion of a pan-Canadian network of therapists offering free services to healthcare workers during the outbreak.
In the US, other local initiatives are already underway.
“The one that I’m personally aware of is at my home institution at the University of California, San Francisco,” Azzam said. “We have a Care for the Caregiver program that is being greatly expanded at this time. As part of that initiative, the institution’s psychiatry department has solicited licensed mental health care providers to volunteer their time to provide those additional services.”
Azzam has also worked with colleagues developing a series of mental health tools that Osmosis has made available free of charge.
These include a central site with educational material about COVID-19, a video about supporting educators’ mental health during high-stress periods; a video about managing students’ mental health during public health emergencies; a summary of recommended resources for psychological health in distressing times; and a YouTube Live event he held regarding tips for maximizing psychological health during stressful times.
This article first appeared on Medscape.com.
Routinely screen for depression in atopic dermatitis
Jonathan I. Silverberg, MD, PhD, declared in a video presentation during a virtual meeting held by the George Washington University department of dermatology.
The virtual meeting included presentations that had been slated for the annual meeting of the American Academy of Dermatology, which was canceled because of the COVID-19 pandemic.
Dr. Silverberg presented highlights of his recent study of depression screening rates in the National Ambulatory Medical Care Survey, an annual population-based survey by the National Center for Health Statistics. He and his coinvestigator analyzed 9,345 office visits for atopic dermatitis (AD) and 2,085 for psoriasis (Br J Dermatol. 2019 Oct 24. doi: 10.1111/bjd.18629.). The picture that emerged showed that there is much room for improvement.
“We found that depression screening rates were abysmally low in atopic dermatitis patients, with less than 2% patients being screened. There was very little difference in screening rates between patients on an advanced therapy, like systemic phototherapy or a biologic, compared to those who were just on topical therapy alone, meaning even the more severe patients aren’t being asked these questions. And no difference between dermatologists and primary care physicians,” said Dr. Silverberg, director of clinical research and contact dermatitis in the department of dermatology at George Washington University, Washington.
For Dr. Silverberg, known for his pioneering work documenting the marked yet often-underappreciated negative impact of AD on quality of life and mental health, these rock-bottom screening rates were particularly galling.
“There are very high rates of anxiety and depression amongst our patients with atopic dermatitis,” the dermatologist emphasized. “Mental health symptoms are an incredibly important domain in atopic dermatitis that we need to ask our patients about. We don’t ask enough.
“This to me is actually a very important symptom to measure. It’s not just a theoretical construct involved in understanding the burden of the disease, it’s something that’s actionable because most of these cases of mental health symptoms are reversible or modifiable with improved control of the atopic dermatitis,” he continued. “I use this as an indication to step up therapy. If a patient is clinically depressed and we believe that’s secondary to their chronic atopic dermatitis, this is a reason to step up therapy to something stronger.”
If the depressive symptoms don’t improve after stepping up the intensity of the dermatologic therapy, it’s probably time for the patient to see a mental health professional, Dr. Silverberg advised, adding, “I’m not telling every dermatology resident out there to become a psychiatrist.”
Depression and anxiety in AD: How common?
In an analysis of multiyear data from the Medical Expenditure Panel Surveys, an annual population-based project conducted by the Agency for Healthcare Research and Quality, Dr. Silverberg and a coinvestigator found that adults with AD were an adjusted 186% more likely than those without AD to screen positive for depressive symptoms on the two-item Patient Health Questionnaire (PHQ-2), with rates of 44.3% and 21.9%, respectively. The AD patients were also 500% more likely to screen positive for severe psychological distress, with a 25.9% rate of having a Kessler-6 index score of 13 or more, compared with 5.5% in adults without AD.
The rate of severe psychological distress was higher in adults with AD than in those with asthma, diabetes, hypertension, urticaria, or psoriasis, and was comparable with the rate in individuals with autoimmune disease (Ann Allergy Asthma Immunol. 2019 Aug;123[2]:179-85).
“It’s surprising when you think that the majority of the cases of atopic dermatitis in the population are mild and yet when you look at a population-based sample such as this you see a strong signal come up. It means that, with all the dilution of mild disease, the signal is still there. It emphasizes that even patients with mild disease get these depressive symptoms and psychosocial distress,” Dr. Silverberg observed.
In a separate analysis of the same national database, this time looking at Short Form-6D health utility scores – a measure of overall quality of life encompassing key domains including vitality, physical function, mental health, fatigue – adults with AD scored markedly worse than individuals with no chronic health disorders. Health utility scores were particularly low in adults with AD and comorbid symptoms of anxiety or depression, suggesting that those affective symptoms are major drivers of the demonstrably poor quality of life in adult AD (Ann Allergy Asthma Immunol. 2020 Jan;124[1]:88-9).
In the Atopic Dermatitis in America Study, Dr. Silverberg and coinvestigators cross-sectionally surveyed 2,893 adults using the seven-item Hospital Anxiety and Depression Scale anxiety (HADS-A) and depression (HADS-D) assessment instruments. Individuals with AD as determined using the modified U.K. Diagnostic Criteria had dramatically higher rates of both depression and anxiety. For example, the prevalence of a HADS-A score of 11 or more, which is considered to be case finding for clinically important anxiety, was 28.6% in adults with AD, nearly twice the 15.5% prevalence in those without the dermatologic disease. A HADS-D score of 11 or greater was present in 13.5% of subjects with AD and 9% of those without.
HADS-A and -D scores were higher in adults with moderate AD, compared with mild disease, and higher still in those with severe AD. Indeed, virtually all individuals with moderate to severe AD had symptoms of anxiety and depression, which in a large proportion had gone undiagnosed. A multivariate analysis strongly suggested that AD severity was the major driver of anxiety and depression in adults with AD (Br J Dermatol. 2019 Sep;181[3]:554-65).
An important finding was that 100% of adults with AD who had scores in the severe range on three validated measures of itch, frequency of symptoms, and lesion severity had borderline or abnormal scores on the HADS-A and -D.
“Of course, if you don’t ask, you’re not going to know about it,” Dr. Silverberg noted.
Dr. Silverberg reported receiving research grants from Galderma and GlaxoSmithKline and serving as a consultant to those pharmaceutical companies and more than a dozen others.
Jonathan I. Silverberg, MD, PhD, declared in a video presentation during a virtual meeting held by the George Washington University department of dermatology.
The virtual meeting included presentations that had been slated for the annual meeting of the American Academy of Dermatology, which was canceled because of the COVID-19 pandemic.
Dr. Silverberg presented highlights of his recent study of depression screening rates in the National Ambulatory Medical Care Survey, an annual population-based survey by the National Center for Health Statistics. He and his coinvestigator analyzed 9,345 office visits for atopic dermatitis (AD) and 2,085 for psoriasis (Br J Dermatol. 2019 Oct 24. doi: 10.1111/bjd.18629.). The picture that emerged showed that there is much room for improvement.
“We found that depression screening rates were abysmally low in atopic dermatitis patients, with less than 2% patients being screened. There was very little difference in screening rates between patients on an advanced therapy, like systemic phototherapy or a biologic, compared to those who were just on topical therapy alone, meaning even the more severe patients aren’t being asked these questions. And no difference between dermatologists and primary care physicians,” said Dr. Silverberg, director of clinical research and contact dermatitis in the department of dermatology at George Washington University, Washington.
For Dr. Silverberg, known for his pioneering work documenting the marked yet often-underappreciated negative impact of AD on quality of life and mental health, these rock-bottom screening rates were particularly galling.
“There are very high rates of anxiety and depression amongst our patients with atopic dermatitis,” the dermatologist emphasized. “Mental health symptoms are an incredibly important domain in atopic dermatitis that we need to ask our patients about. We don’t ask enough.
“This to me is actually a very important symptom to measure. It’s not just a theoretical construct involved in understanding the burden of the disease, it’s something that’s actionable because most of these cases of mental health symptoms are reversible or modifiable with improved control of the atopic dermatitis,” he continued. “I use this as an indication to step up therapy. If a patient is clinically depressed and we believe that’s secondary to their chronic atopic dermatitis, this is a reason to step up therapy to something stronger.”
If the depressive symptoms don’t improve after stepping up the intensity of the dermatologic therapy, it’s probably time for the patient to see a mental health professional, Dr. Silverberg advised, adding, “I’m not telling every dermatology resident out there to become a psychiatrist.”
Depression and anxiety in AD: How common?
In an analysis of multiyear data from the Medical Expenditure Panel Surveys, an annual population-based project conducted by the Agency for Healthcare Research and Quality, Dr. Silverberg and a coinvestigator found that adults with AD were an adjusted 186% more likely than those without AD to screen positive for depressive symptoms on the two-item Patient Health Questionnaire (PHQ-2), with rates of 44.3% and 21.9%, respectively. The AD patients were also 500% more likely to screen positive for severe psychological distress, with a 25.9% rate of having a Kessler-6 index score of 13 or more, compared with 5.5% in adults without AD.
The rate of severe psychological distress was higher in adults with AD than in those with asthma, diabetes, hypertension, urticaria, or psoriasis, and was comparable with the rate in individuals with autoimmune disease (Ann Allergy Asthma Immunol. 2019 Aug;123[2]:179-85).
“It’s surprising when you think that the majority of the cases of atopic dermatitis in the population are mild and yet when you look at a population-based sample such as this you see a strong signal come up. It means that, with all the dilution of mild disease, the signal is still there. It emphasizes that even patients with mild disease get these depressive symptoms and psychosocial distress,” Dr. Silverberg observed.
In a separate analysis of the same national database, this time looking at Short Form-6D health utility scores – a measure of overall quality of life encompassing key domains including vitality, physical function, mental health, fatigue – adults with AD scored markedly worse than individuals with no chronic health disorders. Health utility scores were particularly low in adults with AD and comorbid symptoms of anxiety or depression, suggesting that those affective symptoms are major drivers of the demonstrably poor quality of life in adult AD (Ann Allergy Asthma Immunol. 2020 Jan;124[1]:88-9).
In the Atopic Dermatitis in America Study, Dr. Silverberg and coinvestigators cross-sectionally surveyed 2,893 adults using the seven-item Hospital Anxiety and Depression Scale anxiety (HADS-A) and depression (HADS-D) assessment instruments. Individuals with AD as determined using the modified U.K. Diagnostic Criteria had dramatically higher rates of both depression and anxiety. For example, the prevalence of a HADS-A score of 11 or more, which is considered to be case finding for clinically important anxiety, was 28.6% in adults with AD, nearly twice the 15.5% prevalence in those without the dermatologic disease. A HADS-D score of 11 or greater was present in 13.5% of subjects with AD and 9% of those without.
HADS-A and -D scores were higher in adults with moderate AD, compared with mild disease, and higher still in those with severe AD. Indeed, virtually all individuals with moderate to severe AD had symptoms of anxiety and depression, which in a large proportion had gone undiagnosed. A multivariate analysis strongly suggested that AD severity was the major driver of anxiety and depression in adults with AD (Br J Dermatol. 2019 Sep;181[3]:554-65).
An important finding was that 100% of adults with AD who had scores in the severe range on three validated measures of itch, frequency of symptoms, and lesion severity had borderline or abnormal scores on the HADS-A and -D.
“Of course, if you don’t ask, you’re not going to know about it,” Dr. Silverberg noted.
Dr. Silverberg reported receiving research grants from Galderma and GlaxoSmithKline and serving as a consultant to those pharmaceutical companies and more than a dozen others.
Jonathan I. Silverberg, MD, PhD, declared in a video presentation during a virtual meeting held by the George Washington University department of dermatology.
The virtual meeting included presentations that had been slated for the annual meeting of the American Academy of Dermatology, which was canceled because of the COVID-19 pandemic.
Dr. Silverberg presented highlights of his recent study of depression screening rates in the National Ambulatory Medical Care Survey, an annual population-based survey by the National Center for Health Statistics. He and his coinvestigator analyzed 9,345 office visits for atopic dermatitis (AD) and 2,085 for psoriasis (Br J Dermatol. 2019 Oct 24. doi: 10.1111/bjd.18629.). The picture that emerged showed that there is much room for improvement.
“We found that depression screening rates were abysmally low in atopic dermatitis patients, with less than 2% patients being screened. There was very little difference in screening rates between patients on an advanced therapy, like systemic phototherapy or a biologic, compared to those who were just on topical therapy alone, meaning even the more severe patients aren’t being asked these questions. And no difference between dermatologists and primary care physicians,” said Dr. Silverberg, director of clinical research and contact dermatitis in the department of dermatology at George Washington University, Washington.
For Dr. Silverberg, known for his pioneering work documenting the marked yet often-underappreciated negative impact of AD on quality of life and mental health, these rock-bottom screening rates were particularly galling.
“There are very high rates of anxiety and depression amongst our patients with atopic dermatitis,” the dermatologist emphasized. “Mental health symptoms are an incredibly important domain in atopic dermatitis that we need to ask our patients about. We don’t ask enough.
“This to me is actually a very important symptom to measure. It’s not just a theoretical construct involved in understanding the burden of the disease, it’s something that’s actionable because most of these cases of mental health symptoms are reversible or modifiable with improved control of the atopic dermatitis,” he continued. “I use this as an indication to step up therapy. If a patient is clinically depressed and we believe that’s secondary to their chronic atopic dermatitis, this is a reason to step up therapy to something stronger.”
If the depressive symptoms don’t improve after stepping up the intensity of the dermatologic therapy, it’s probably time for the patient to see a mental health professional, Dr. Silverberg advised, adding, “I’m not telling every dermatology resident out there to become a psychiatrist.”
Depression and anxiety in AD: How common?
In an analysis of multiyear data from the Medical Expenditure Panel Surveys, an annual population-based project conducted by the Agency for Healthcare Research and Quality, Dr. Silverberg and a coinvestigator found that adults with AD were an adjusted 186% more likely than those without AD to screen positive for depressive symptoms on the two-item Patient Health Questionnaire (PHQ-2), with rates of 44.3% and 21.9%, respectively. The AD patients were also 500% more likely to screen positive for severe psychological distress, with a 25.9% rate of having a Kessler-6 index score of 13 or more, compared with 5.5% in adults without AD.
The rate of severe psychological distress was higher in adults with AD than in those with asthma, diabetes, hypertension, urticaria, or psoriasis, and was comparable with the rate in individuals with autoimmune disease (Ann Allergy Asthma Immunol. 2019 Aug;123[2]:179-85).
“It’s surprising when you think that the majority of the cases of atopic dermatitis in the population are mild and yet when you look at a population-based sample such as this you see a strong signal come up. It means that, with all the dilution of mild disease, the signal is still there. It emphasizes that even patients with mild disease get these depressive symptoms and psychosocial distress,” Dr. Silverberg observed.
In a separate analysis of the same national database, this time looking at Short Form-6D health utility scores – a measure of overall quality of life encompassing key domains including vitality, physical function, mental health, fatigue – adults with AD scored markedly worse than individuals with no chronic health disorders. Health utility scores were particularly low in adults with AD and comorbid symptoms of anxiety or depression, suggesting that those affective symptoms are major drivers of the demonstrably poor quality of life in adult AD (Ann Allergy Asthma Immunol. 2020 Jan;124[1]:88-9).
In the Atopic Dermatitis in America Study, Dr. Silverberg and coinvestigators cross-sectionally surveyed 2,893 adults using the seven-item Hospital Anxiety and Depression Scale anxiety (HADS-A) and depression (HADS-D) assessment instruments. Individuals with AD as determined using the modified U.K. Diagnostic Criteria had dramatically higher rates of both depression and anxiety. For example, the prevalence of a HADS-A score of 11 or more, which is considered to be case finding for clinically important anxiety, was 28.6% in adults with AD, nearly twice the 15.5% prevalence in those without the dermatologic disease. A HADS-D score of 11 or greater was present in 13.5% of subjects with AD and 9% of those without.
HADS-A and -D scores were higher in adults with moderate AD, compared with mild disease, and higher still in those with severe AD. Indeed, virtually all individuals with moderate to severe AD had symptoms of anxiety and depression, which in a large proportion had gone undiagnosed. A multivariate analysis strongly suggested that AD severity was the major driver of anxiety and depression in adults with AD (Br J Dermatol. 2019 Sep;181[3]:554-65).
An important finding was that 100% of adults with AD who had scores in the severe range on three validated measures of itch, frequency of symptoms, and lesion severity had borderline or abnormal scores on the HADS-A and -D.
“Of course, if you don’t ask, you’re not going to know about it,” Dr. Silverberg noted.
Dr. Silverberg reported receiving research grants from Galderma and GlaxoSmithKline and serving as a consultant to those pharmaceutical companies and more than a dozen others.
The psychiatric clinic of the future
Despite the tremendous advances in psychiatry in recent years, the current clinical practice of psychiatry continues to rely on data from intermittent assessments along with subjective and unquantifiable accounts from patients and caregivers. Furthermore, there continues to be significant diagnostic variations among practitioners. Fortunately, technology to address these issues appears to be on the horizon.
How might the psychiatric clinic of the future look? What changes could we envision? These 4 critical factors may soon bring about dynamic changes in the way we practice psychiatry:
- precision psychiatry
- digital psychiatry
- technology-enhanced psychotherapy
- electronic health record (EHR) reforms.
In this article, we review how advances in each of these areas might lead to improved care for our patients.
Precision psychiatry
Precision psychiatry takes into account each patient’s variability in genes, environment, and lifestyle to determine individualized treatment and prevention strategies. It relies on pharmacogenomic testing as the primary tool. Pharmacogenomics is the study of variability in drug response due to heredity.
Emerging data on the clinical utility and cost-effectiveness of pharmacogenomic testing are encouraging, but its routine use is not well supported by current evidence.2 One limit to using pharmacogenomic testing is that many genes simultaneously exert an effect on the structure and function of neurons and associated pathophysiology. According to the International Society of Psychiatric Genetics, no single genetic variant is sufficient to cause psychiatric disorders such as depression, bipolar disorder, substance dependence, or schizophrenia. This limits the possibility of using genetic tests to establish a diagnosis.3
In the future, better algorithms could promote more accurate pharmacogenomics profiles for individual patients, which could influence treatment.
Precision psychiatry could lead to:
- identification of novel targets for new medications
- pharmacogenetic profiling of the patient to predict disease susceptibility and medication response
- personalized therapy: the right drug at the right dose for the right patient.
- improved efficacy and fewer adverse medication reactions.
Continue to: Digital psychiatry
Digital psychiatry
Integrating computer-based technology into psychiatric practice has given birth to a new frontier that could be called digital psychiatry. This might encompass the following:
- telepsychiatry
- social media with a mental health focus
- web-based applications/devices
- artificial intelligence (AI).
Telepsychiatry. Videoconferencing is the most widely used form of telepsychiatry. It provides patients with easier access to mental health treatment.4 Telepsychiatry has the potential to match patients and clinicians with similar cultural backgrounds, thus minimizing cultural gaps and misunderstandings. Most importantly, it is comparable to face-to-face interviews in terms of the reliability of assessment and treatment outcomes.5
Telepsychiatry might be particularly helpful for patients with restricted mobility, such as those who live in remote areas, nursing homes, or correctional facilities. In correctional settings, transferring prisoners is expensive and carries the risk of escape. In a small study (N = 86) conducted in Hong Kong, Chen et al6 found that using videoconferencing to conduct clinical interviews of inmates was cost-efficient and scored high in terms of patient acceptability.
Social media. Social media could be a powerful platform for early detection of mental illness. Staying connected with patients on social media could allow psychiatrists to be more aware of their patient’s mood fluctuations, which might lead to more timely assessments. Physicians could be automatically notified about changes in their patients’ social media activity that indicate changes in mental state, which could solicit immediate intervention and treatment. On the other hand, such use of social media could blur professional boundaries. Psychiatrists also could use social media to promote awareness of mental health and educate the public on ways to improve or maintain their mental well-being.7
Web-based applications/devices. Real-time monitoring through applications or internet-based smart devices creates a new avenue for patients to receive personalized assessments, treatment, and intervention.8 Smartwatches with internet connectivity may offer a glimpse of the wearer’s sleep architecture and duration, thus providing real-time data on patients who have insomnia. We can now passively collect objective data from devices, such as smartphones and laptops, to phenotype an individual’s mood and mental state, a process called digital phenotyping. The Table9 lists examples of the types of mental health–related metrics that can be captured by smartphones, smartwatches, and similar technology. Information from these devices can be accumulated to create a database that can be used to predict symptoms.10 For example, the way people use a smartphone’s keyboard, including latency time between space and character types, can be used to generate variables for data. This type of information is being studied for use in screening depression and passively assessing mood in real time.11
Continue to: Artificial intelligence
Artificial intelligence—the development of computer systems able to perform tasks that normally require human intelligence—is being increasingly used in psychiatry. Some studies have suggested AI can be used to identify patients’ risk of suicide12-15 or psychosis.16,17Kalanderian and Nasrallah18 reviewed several of these studies in
Other researchers have found clinical uses for machine learning, a subset of AI that uses methods to automatically detect patterns and make predictions based on those patterns. In one study, a machine learning analysis of functional MRI scans was able to identify 4 distinct subtypes of depression.19 In another study, a machine learning model was able to predict with 60% accuracy which patients with depression would respond to antidepressants.20
In the future, AI might be used to change mental health classification systems. Because many mental health disorders share similar symptom clusters, machine learning can help to identify associations between symptoms, behavior, brain function, and real-world function across different diagnoses, potentially affecting how we will classify mental disorders.21
Technology-enhanced psychotherapy
In the future, it might be common for psychotherapy to be provided by a computer, or “virtual therapist.” Several studies have evaluated the use of technology-enhanced psychotherapy.
Lucas et al22 investigated patients’ interactions with a virtual therapist. Participants were interviewed by an avatar named Ellie, who they saw on a TV screen. Half of the participants were told Ellie was not human, and half were told Ellie was being controlled remotely by a human. Three psychologists who were blinded to group allocations analyzed transcripts of the interviews and video recordings of participants’ facial expressions to quantify the participants’ fear, sadness, and other emotional responses during the interviews, as well as their openness to the questions. Participants who believed Ellie was fully automated reported significantly lower fear of self-disclosure and impression management (attempts to control how others perceive them) than participants who were told that Ellie was operated by a human. Additionally, participants who believed they were interacting with a computer were more open during the interview.22
Continue to: Researchers at the University of Southern California...
Researchers at the University of Southern California developed software that assessed 74 acoustic features, including pitch, volume, quality, shimmer, jitter, and prosody, to predict outcomes among patients receiving couples therapy. This software was able to predict marital discord at least as well as human therapists.23
Many mental health apps purport to implement specific components of psychotherapy. Many of these apps focus on cognitive-behavioral therapy worksheets, mindfulness exercises, and/or mood tracking. The features provided by such apps emulate the tasks and intended outcomes of traditional psychotherapy, but in an entirely decentralized venue.24
Some have expressed concern that an increased use of virtual therapists powered by AI might lead to a dehumanization of psychiatry (Box25,26).
Box
Whether there are aspects of the psychiatric patient encounter that cannot be managed by a “virtual clinician” created by artificial intelligence (AI) remains to be determined. Some of the benefits of using AI in this manner may be difficult to anticipate, or may be specific to an individual’s relationship with his/her clinician.25
On the other hand, AI systems blur previously assumed boundaries between reality and fiction, and this could have complex effects on patients. Similar to therapeutic relationships with a human clinician, there is the risk of transference of emotions, thoughts, and feelings to a virtual therapist powered by AI. Unlike with a psychiatrist or therapist, however, there is no person on the other side of this transference. Whether virtual clinicians will be able to manage such transference remains to be seen.
In Deep Medicine,26 cardiologist Eric Topol, MD, emphasizes a crucial component of a patient encounter that AI will be unlikely able to provide: empathy. Virtual therapists powered by AI will inherit the tasks best done by machines, leaving humans more time to do what they do best—providing empathy and being “present” for patients.
Electronic health record reforms
Although many clinicians find EHRs to be onerous and time-consuming, EHR technology is constantly improving, and EHRs have revolutionized documentation and order implementation. Several potential advances could improve clinical practice. For example, EHRs could incorporate a clinical decision support system that uses AI-based algorithms to assist psychiatrists with diagnosis, monitoring, and treatment.27 In the future, EHRs might have the ability to monitor and learn from errors and adverse events, and automatically design an algorithm to avoid them.28 They should be designed to better manage analysis of pharmacogenetic test results, which is challenging due to the amount and complexity of the data.29 Future EHRs should eliminate the non-intuitive and multi-click interfaces and cumbersome data searches of today’s EHRs.30
Technology brings new ethical considerations
Mental health interventions based on AI typically work with algorithms, and algorithms bring ethical issues. Mental health devices or systems that use AI could contain biases that have the potential to harm in unintended ways, such as a data-driven sexist or racist bias.31 This may require investing additional time to explain to patients (and their families) what an algorithm is and how it works in relation to the therapy provided.
Continue to: Another concern is patient...
Another concern is patient autonomy.32 For example, it would be ethically problematic if a patient were to assume that there was a human physician “at the other end” of a virtual therapist or other technology who is communicating or reviewing his/her messages. Similarly, an older adult or a patient with intellectual disabilities may not be able to understand advanced technology or what it does when it is installed in their home to monitor the patient’s activities. This would increase the risk of privacy violations, manipulation, or even coercion if the requirements for informed consent are not satisfied.
A flowchart for the future
Although current research and innovations typically target specific areas of psychiatry, these advances can be integrated by devising algorithms and protocols that will change the current practice of psychiatry. The Figure provides a glimpse of how the psychiatry clinic of the future might work. A maxim of management is that “the best way to predict the future is to create it.” However, the mere conception of a vision is not enough—working towards it is essential.
Bottom Line
With advances in technology, psychiatric practice will soon be radically different from what it is today. The expanded use of telepsychiatry, social media, artificial intelligence, and web-based applications/devices holds great promise for psychiatric assessment, diagnosis, and treatment, although certain ethical and privacy concerns need to be adequately addressed.
Related Resources
- National Institute of Mental Health. Technology and the future of mental health treatment. www.nimh.nih.gov/health/topics/technology-and-the-future-of-mental-health-treatment/index.shtml. Revised September 2019.
- Hays R, Farrell HM, Touros J. Mobile apps and mental health: using technology to quantify real-time clinical risk. Current Psychiatry. 2019;18(6):37-41.
- Torous J, Luo J, Chan SR. Mental health apps: what to tell patients. Current Psychiatry. 2018;17(3):21-25.
1. Pirmohamed M. Pharmacogenetics and pharmacogenomics. Br J Clin Pharmacol. 2001;52(4):345-347.
2. Benitez J, Cool CL, Scotti DJ. Use of combinatorial pharmacogenomic guidance in treating psychiatric disorders. Per Med. 2018;15(6):481-494.
3. Cannon TD. Candidate gene studies in the GWAS era: the MET proto-oncogene, neurocognition, and schizophrenia. Am J Psychiatry. 2010;167(4):4,369-372.
4. Greenwood J, Chamberlain C, Parker G. Evaluation of a rural telepsychiatry service. Australas Psychiatry. 2004;12(3):268-272.
5. Hubley S, Lynch SB, Schneck C, et al. Review of key telepsychiatry outcomes. World J Psychiatry. 2016;6(2):269-282.
6. Cheng KM, Siu BW, Yeung CC, et al. Telepsychiatry for stable Chinese psychiatric out-patients in custody in Hong Kong: a case-control pilot study. Hong Kong Med J. 2018;24(4):378-383.
7. Frankish K, Ryan C, Harris A. Psychiatry and online social media: potential, pitfalls and ethical guidelines for psychiatrists and trainees. Australasian Psychiatry. 2012;20(3):181-187.
8. de la Torre Díez I, Alonso SG, Hamrioui S, et al. IoT-based services and applications for mental health in the literature. J Med Syst. 2019;43(1):4-9.
9. Topol E. Deep Medicine. New York, NY: Basic Books; 2019:168.
10. Adams RA, Huys QJM, Roiser JP. Computational Psychiatry: towards a mathematically informed understanding of mental illness. J Neurol Neurosurg Psychiatry. 2016;87(1):53-63.
11. Insel TR. Bending the curve for mental health: technology for a public health approach. Am J Public Health. 2019;109(suppl 3):S168-S170.
12. Just MA, Pan L, Cherkassky VL, et al. Machine learning of neural representations of suicide and emotion concepts identifies suicidal youth. Nat Hum Behav. 2017;1:911-919.
13. Pestian J, Nasrallah H, Matykiewicz P, et al. Suicide note classification using natural language processing: a content analysis. Biomed Inform Insights. 2010;2010(3):19-28.
14. Walsh CG, Ribeiro JD, Franklin JC. Predicting risk of suicide attempts over time through machine learning. Clinical Psychological Science. 2017;5(3):457-469.
15. Pestian JP, Sorter M, Connolly B, et al; STM Research Group. A machine learning approach to identifying the thought markers of suicidal subjects: a prospective multicenter trial. Suicide Life Threat Behav. 2017;47(1):112-121.
16. Corcoran CM, Carrillo F, Fernández-Slezak D, et al. Prediction of psychosis across protocols and risk cohorts using automated language analysis. World Psychiatry. 2018;17(1):67-75.
17. Bedi G, Carrillo F, Cecchi GA, et al. Automated analysis of free speech predicts psychosis onset in high-risk youths. NPJ Schizophr. 2015;1:15030. doi: 10.1038/npjschz.2015.30.
18. Kalanderian H, Nasrallah HA. Artificial intelligence in psychiatry. Current Psychiatry. 2019;18(8):33-38.
19. Drysdale AT, Grosenick L, Downar J, et al. Resting-state connectivity biomarkers define neurophysiological subtypes of depression. Nat Med. 2017;23(1):28-38.
20. Chekroud AM, Zotti RJ, Shehzad Z, et al. Cross-trial prediction of treatment outcome in depression: a machine learning approach. Lancet Psychiatry. 2016;3(3):243-250.
21. Grisanzio KA, Goldstein-Piekarski AN, Wang MY, et al. Transdiagnostic symptom clusters and associations with brain, behavior, and daily function in mood, anxiety, and trauma disorders. JAMA Psychiatry. 2018;75(2):201-209.
22. Lucas G, Gratch J, King A, et al. It’s only a computer: virtual humans increase willingness to disclose. Computers in Human Behavior. 2014;37:94-100.
23. Nasir M, Baucom BR, Georgiou P, et al. Predicting couple therapy outcomes based on speech acoustic features. PLoS One. 2017;12(9):e0185123. doi: 10.1371/journal.pone.0185123.
24. Huguet A, Rao S, McGrath PJ, et al. A systematic review of cognitive behavioral therapy and behavioral activation apps for depression. PLoS One. 2016;11(5):e0154248. doi: 10.1371/journal.pone.0154248.
25. Scholten MR, Kelders SM, Van Gemert-Pijnen JE. Self-guided web-based interventions: scoping review on user needs and the potential of embodied conversational agents to address them. J Med Internet Res. 2017;19(11):e383.
26. Topol E. Deep Medicine. New York, NY: Basic Books; 2019:283-310.
27. Abramson EL, McGinnis S, Edwards A, et al. Electronic health record adoption and health information exchange among hospitals in New York State. J Eval Clin Pract. 2012;18(6):1156-1162.
28. Meeks DW, Smith MW, Taylor L, et al. An analysis of electronic health record-related patient safety concerns. J Am Med Inform Assoc. 2014;21(6):1053-1059.
29. Kho AN, Rasmussen LV, Connolly JJ, et al. Practical challenges in integrating genomic data into the electronic health record. Genet Med. 2013;15(10):772-778.
30. Ornstein SM, Oates RB, Fox GN. The computer-based medical record: current status. J Fam Pract. 1992;35(5):556-565.
31. Corea F. Machine ethics and artificial moral agents. In: Applied artificial intelligence: where AI can be used in business. Basel, Switzerland: Springer; 2019:33-41.
32. Beauchamp T, Childress J. Principles of biomedical ethics. 7th ed. New York, NY: Oxford University Press; 2012:44.
Despite the tremendous advances in psychiatry in recent years, the current clinical practice of psychiatry continues to rely on data from intermittent assessments along with subjective and unquantifiable accounts from patients and caregivers. Furthermore, there continues to be significant diagnostic variations among practitioners. Fortunately, technology to address these issues appears to be on the horizon.
How might the psychiatric clinic of the future look? What changes could we envision? These 4 critical factors may soon bring about dynamic changes in the way we practice psychiatry:
- precision psychiatry
- digital psychiatry
- technology-enhanced psychotherapy
- electronic health record (EHR) reforms.
In this article, we review how advances in each of these areas might lead to improved care for our patients.
Precision psychiatry
Precision psychiatry takes into account each patient’s variability in genes, environment, and lifestyle to determine individualized treatment and prevention strategies. It relies on pharmacogenomic testing as the primary tool. Pharmacogenomics is the study of variability in drug response due to heredity.
Emerging data on the clinical utility and cost-effectiveness of pharmacogenomic testing are encouraging, but its routine use is not well supported by current evidence.2 One limit to using pharmacogenomic testing is that many genes simultaneously exert an effect on the structure and function of neurons and associated pathophysiology. According to the International Society of Psychiatric Genetics, no single genetic variant is sufficient to cause psychiatric disorders such as depression, bipolar disorder, substance dependence, or schizophrenia. This limits the possibility of using genetic tests to establish a diagnosis.3
In the future, better algorithms could promote more accurate pharmacogenomics profiles for individual patients, which could influence treatment.
Precision psychiatry could lead to:
- identification of novel targets for new medications
- pharmacogenetic profiling of the patient to predict disease susceptibility and medication response
- personalized therapy: the right drug at the right dose for the right patient.
- improved efficacy and fewer adverse medication reactions.
Continue to: Digital psychiatry
Digital psychiatry
Integrating computer-based technology into psychiatric practice has given birth to a new frontier that could be called digital psychiatry. This might encompass the following:
- telepsychiatry
- social media with a mental health focus
- web-based applications/devices
- artificial intelligence (AI).
Telepsychiatry. Videoconferencing is the most widely used form of telepsychiatry. It provides patients with easier access to mental health treatment.4 Telepsychiatry has the potential to match patients and clinicians with similar cultural backgrounds, thus minimizing cultural gaps and misunderstandings. Most importantly, it is comparable to face-to-face interviews in terms of the reliability of assessment and treatment outcomes.5
Telepsychiatry might be particularly helpful for patients with restricted mobility, such as those who live in remote areas, nursing homes, or correctional facilities. In correctional settings, transferring prisoners is expensive and carries the risk of escape. In a small study (N = 86) conducted in Hong Kong, Chen et al6 found that using videoconferencing to conduct clinical interviews of inmates was cost-efficient and scored high in terms of patient acceptability.
Social media. Social media could be a powerful platform for early detection of mental illness. Staying connected with patients on social media could allow psychiatrists to be more aware of their patient’s mood fluctuations, which might lead to more timely assessments. Physicians could be automatically notified about changes in their patients’ social media activity that indicate changes in mental state, which could solicit immediate intervention and treatment. On the other hand, such use of social media could blur professional boundaries. Psychiatrists also could use social media to promote awareness of mental health and educate the public on ways to improve or maintain their mental well-being.7
Web-based applications/devices. Real-time monitoring through applications or internet-based smart devices creates a new avenue for patients to receive personalized assessments, treatment, and intervention.8 Smartwatches with internet connectivity may offer a glimpse of the wearer’s sleep architecture and duration, thus providing real-time data on patients who have insomnia. We can now passively collect objective data from devices, such as smartphones and laptops, to phenotype an individual’s mood and mental state, a process called digital phenotyping. The Table9 lists examples of the types of mental health–related metrics that can be captured by smartphones, smartwatches, and similar technology. Information from these devices can be accumulated to create a database that can be used to predict symptoms.10 For example, the way people use a smartphone’s keyboard, including latency time between space and character types, can be used to generate variables for data. This type of information is being studied for use in screening depression and passively assessing mood in real time.11
Continue to: Artificial intelligence
Artificial intelligence—the development of computer systems able to perform tasks that normally require human intelligence—is being increasingly used in psychiatry. Some studies have suggested AI can be used to identify patients’ risk of suicide12-15 or psychosis.16,17Kalanderian and Nasrallah18 reviewed several of these studies in
Other researchers have found clinical uses for machine learning, a subset of AI that uses methods to automatically detect patterns and make predictions based on those patterns. In one study, a machine learning analysis of functional MRI scans was able to identify 4 distinct subtypes of depression.19 In another study, a machine learning model was able to predict with 60% accuracy which patients with depression would respond to antidepressants.20
In the future, AI might be used to change mental health classification systems. Because many mental health disorders share similar symptom clusters, machine learning can help to identify associations between symptoms, behavior, brain function, and real-world function across different diagnoses, potentially affecting how we will classify mental disorders.21
Technology-enhanced psychotherapy
In the future, it might be common for psychotherapy to be provided by a computer, or “virtual therapist.” Several studies have evaluated the use of technology-enhanced psychotherapy.
Lucas et al22 investigated patients’ interactions with a virtual therapist. Participants were interviewed by an avatar named Ellie, who they saw on a TV screen. Half of the participants were told Ellie was not human, and half were told Ellie was being controlled remotely by a human. Three psychologists who were blinded to group allocations analyzed transcripts of the interviews and video recordings of participants’ facial expressions to quantify the participants’ fear, sadness, and other emotional responses during the interviews, as well as their openness to the questions. Participants who believed Ellie was fully automated reported significantly lower fear of self-disclosure and impression management (attempts to control how others perceive them) than participants who were told that Ellie was operated by a human. Additionally, participants who believed they were interacting with a computer were more open during the interview.22
Continue to: Researchers at the University of Southern California...
Researchers at the University of Southern California developed software that assessed 74 acoustic features, including pitch, volume, quality, shimmer, jitter, and prosody, to predict outcomes among patients receiving couples therapy. This software was able to predict marital discord at least as well as human therapists.23
Many mental health apps purport to implement specific components of psychotherapy. Many of these apps focus on cognitive-behavioral therapy worksheets, mindfulness exercises, and/or mood tracking. The features provided by such apps emulate the tasks and intended outcomes of traditional psychotherapy, but in an entirely decentralized venue.24
Some have expressed concern that an increased use of virtual therapists powered by AI might lead to a dehumanization of psychiatry (Box25,26).
Box
Whether there are aspects of the psychiatric patient encounter that cannot be managed by a “virtual clinician” created by artificial intelligence (AI) remains to be determined. Some of the benefits of using AI in this manner may be difficult to anticipate, or may be specific to an individual’s relationship with his/her clinician.25
On the other hand, AI systems blur previously assumed boundaries between reality and fiction, and this could have complex effects on patients. Similar to therapeutic relationships with a human clinician, there is the risk of transference of emotions, thoughts, and feelings to a virtual therapist powered by AI. Unlike with a psychiatrist or therapist, however, there is no person on the other side of this transference. Whether virtual clinicians will be able to manage such transference remains to be seen.
In Deep Medicine,26 cardiologist Eric Topol, MD, emphasizes a crucial component of a patient encounter that AI will be unlikely able to provide: empathy. Virtual therapists powered by AI will inherit the tasks best done by machines, leaving humans more time to do what they do best—providing empathy and being “present” for patients.
Electronic health record reforms
Although many clinicians find EHRs to be onerous and time-consuming, EHR technology is constantly improving, and EHRs have revolutionized documentation and order implementation. Several potential advances could improve clinical practice. For example, EHRs could incorporate a clinical decision support system that uses AI-based algorithms to assist psychiatrists with diagnosis, monitoring, and treatment.27 In the future, EHRs might have the ability to monitor and learn from errors and adverse events, and automatically design an algorithm to avoid them.28 They should be designed to better manage analysis of pharmacogenetic test results, which is challenging due to the amount and complexity of the data.29 Future EHRs should eliminate the non-intuitive and multi-click interfaces and cumbersome data searches of today’s EHRs.30
Technology brings new ethical considerations
Mental health interventions based on AI typically work with algorithms, and algorithms bring ethical issues. Mental health devices or systems that use AI could contain biases that have the potential to harm in unintended ways, such as a data-driven sexist or racist bias.31 This may require investing additional time to explain to patients (and their families) what an algorithm is and how it works in relation to the therapy provided.
Continue to: Another concern is patient...
Another concern is patient autonomy.32 For example, it would be ethically problematic if a patient were to assume that there was a human physician “at the other end” of a virtual therapist or other technology who is communicating or reviewing his/her messages. Similarly, an older adult or a patient with intellectual disabilities may not be able to understand advanced technology or what it does when it is installed in their home to monitor the patient’s activities. This would increase the risk of privacy violations, manipulation, or even coercion if the requirements for informed consent are not satisfied.
A flowchart for the future
Although current research and innovations typically target specific areas of psychiatry, these advances can be integrated by devising algorithms and protocols that will change the current practice of psychiatry. The Figure provides a glimpse of how the psychiatry clinic of the future might work. A maxim of management is that “the best way to predict the future is to create it.” However, the mere conception of a vision is not enough—working towards it is essential.
Bottom Line
With advances in technology, psychiatric practice will soon be radically different from what it is today. The expanded use of telepsychiatry, social media, artificial intelligence, and web-based applications/devices holds great promise for psychiatric assessment, diagnosis, and treatment, although certain ethical and privacy concerns need to be adequately addressed.
Related Resources
- National Institute of Mental Health. Technology and the future of mental health treatment. www.nimh.nih.gov/health/topics/technology-and-the-future-of-mental-health-treatment/index.shtml. Revised September 2019.
- Hays R, Farrell HM, Touros J. Mobile apps and mental health: using technology to quantify real-time clinical risk. Current Psychiatry. 2019;18(6):37-41.
- Torous J, Luo J, Chan SR. Mental health apps: what to tell patients. Current Psychiatry. 2018;17(3):21-25.
Despite the tremendous advances in psychiatry in recent years, the current clinical practice of psychiatry continues to rely on data from intermittent assessments along with subjective and unquantifiable accounts from patients and caregivers. Furthermore, there continues to be significant diagnostic variations among practitioners. Fortunately, technology to address these issues appears to be on the horizon.
How might the psychiatric clinic of the future look? What changes could we envision? These 4 critical factors may soon bring about dynamic changes in the way we practice psychiatry:
- precision psychiatry
- digital psychiatry
- technology-enhanced psychotherapy
- electronic health record (EHR) reforms.
In this article, we review how advances in each of these areas might lead to improved care for our patients.
Precision psychiatry
Precision psychiatry takes into account each patient’s variability in genes, environment, and lifestyle to determine individualized treatment and prevention strategies. It relies on pharmacogenomic testing as the primary tool. Pharmacogenomics is the study of variability in drug response due to heredity.
Emerging data on the clinical utility and cost-effectiveness of pharmacogenomic testing are encouraging, but its routine use is not well supported by current evidence.2 One limit to using pharmacogenomic testing is that many genes simultaneously exert an effect on the structure and function of neurons and associated pathophysiology. According to the International Society of Psychiatric Genetics, no single genetic variant is sufficient to cause psychiatric disorders such as depression, bipolar disorder, substance dependence, or schizophrenia. This limits the possibility of using genetic tests to establish a diagnosis.3
In the future, better algorithms could promote more accurate pharmacogenomics profiles for individual patients, which could influence treatment.
Precision psychiatry could lead to:
- identification of novel targets for new medications
- pharmacogenetic profiling of the patient to predict disease susceptibility and medication response
- personalized therapy: the right drug at the right dose for the right patient.
- improved efficacy and fewer adverse medication reactions.
Continue to: Digital psychiatry
Digital psychiatry
Integrating computer-based technology into psychiatric practice has given birth to a new frontier that could be called digital psychiatry. This might encompass the following:
- telepsychiatry
- social media with a mental health focus
- web-based applications/devices
- artificial intelligence (AI).
Telepsychiatry. Videoconferencing is the most widely used form of telepsychiatry. It provides patients with easier access to mental health treatment.4 Telepsychiatry has the potential to match patients and clinicians with similar cultural backgrounds, thus minimizing cultural gaps and misunderstandings. Most importantly, it is comparable to face-to-face interviews in terms of the reliability of assessment and treatment outcomes.5
Telepsychiatry might be particularly helpful for patients with restricted mobility, such as those who live in remote areas, nursing homes, or correctional facilities. In correctional settings, transferring prisoners is expensive and carries the risk of escape. In a small study (N = 86) conducted in Hong Kong, Chen et al6 found that using videoconferencing to conduct clinical interviews of inmates was cost-efficient and scored high in terms of patient acceptability.
Social media. Social media could be a powerful platform for early detection of mental illness. Staying connected with patients on social media could allow psychiatrists to be more aware of their patient’s mood fluctuations, which might lead to more timely assessments. Physicians could be automatically notified about changes in their patients’ social media activity that indicate changes in mental state, which could solicit immediate intervention and treatment. On the other hand, such use of social media could blur professional boundaries. Psychiatrists also could use social media to promote awareness of mental health and educate the public on ways to improve or maintain their mental well-being.7
Web-based applications/devices. Real-time monitoring through applications or internet-based smart devices creates a new avenue for patients to receive personalized assessments, treatment, and intervention.8 Smartwatches with internet connectivity may offer a glimpse of the wearer’s sleep architecture and duration, thus providing real-time data on patients who have insomnia. We can now passively collect objective data from devices, such as smartphones and laptops, to phenotype an individual’s mood and mental state, a process called digital phenotyping. The Table9 lists examples of the types of mental health–related metrics that can be captured by smartphones, smartwatches, and similar technology. Information from these devices can be accumulated to create a database that can be used to predict symptoms.10 For example, the way people use a smartphone’s keyboard, including latency time between space and character types, can be used to generate variables for data. This type of information is being studied for use in screening depression and passively assessing mood in real time.11
Continue to: Artificial intelligence
Artificial intelligence—the development of computer systems able to perform tasks that normally require human intelligence—is being increasingly used in psychiatry. Some studies have suggested AI can be used to identify patients’ risk of suicide12-15 or psychosis.16,17Kalanderian and Nasrallah18 reviewed several of these studies in
Other researchers have found clinical uses for machine learning, a subset of AI that uses methods to automatically detect patterns and make predictions based on those patterns. In one study, a machine learning analysis of functional MRI scans was able to identify 4 distinct subtypes of depression.19 In another study, a machine learning model was able to predict with 60% accuracy which patients with depression would respond to antidepressants.20
In the future, AI might be used to change mental health classification systems. Because many mental health disorders share similar symptom clusters, machine learning can help to identify associations between symptoms, behavior, brain function, and real-world function across different diagnoses, potentially affecting how we will classify mental disorders.21
Technology-enhanced psychotherapy
In the future, it might be common for psychotherapy to be provided by a computer, or “virtual therapist.” Several studies have evaluated the use of technology-enhanced psychotherapy.
Lucas et al22 investigated patients’ interactions with a virtual therapist. Participants were interviewed by an avatar named Ellie, who they saw on a TV screen. Half of the participants were told Ellie was not human, and half were told Ellie was being controlled remotely by a human. Three psychologists who were blinded to group allocations analyzed transcripts of the interviews and video recordings of participants’ facial expressions to quantify the participants’ fear, sadness, and other emotional responses during the interviews, as well as their openness to the questions. Participants who believed Ellie was fully automated reported significantly lower fear of self-disclosure and impression management (attempts to control how others perceive them) than participants who were told that Ellie was operated by a human. Additionally, participants who believed they were interacting with a computer were more open during the interview.22
Continue to: Researchers at the University of Southern California...
Researchers at the University of Southern California developed software that assessed 74 acoustic features, including pitch, volume, quality, shimmer, jitter, and prosody, to predict outcomes among patients receiving couples therapy. This software was able to predict marital discord at least as well as human therapists.23
Many mental health apps purport to implement specific components of psychotherapy. Many of these apps focus on cognitive-behavioral therapy worksheets, mindfulness exercises, and/or mood tracking. The features provided by such apps emulate the tasks and intended outcomes of traditional psychotherapy, but in an entirely decentralized venue.24
Some have expressed concern that an increased use of virtual therapists powered by AI might lead to a dehumanization of psychiatry (Box25,26).
Box
Whether there are aspects of the psychiatric patient encounter that cannot be managed by a “virtual clinician” created by artificial intelligence (AI) remains to be determined. Some of the benefits of using AI in this manner may be difficult to anticipate, or may be specific to an individual’s relationship with his/her clinician.25
On the other hand, AI systems blur previously assumed boundaries between reality and fiction, and this could have complex effects on patients. Similar to therapeutic relationships with a human clinician, there is the risk of transference of emotions, thoughts, and feelings to a virtual therapist powered by AI. Unlike with a psychiatrist or therapist, however, there is no person on the other side of this transference. Whether virtual clinicians will be able to manage such transference remains to be seen.
In Deep Medicine,26 cardiologist Eric Topol, MD, emphasizes a crucial component of a patient encounter that AI will be unlikely able to provide: empathy. Virtual therapists powered by AI will inherit the tasks best done by machines, leaving humans more time to do what they do best—providing empathy and being “present” for patients.
Electronic health record reforms
Although many clinicians find EHRs to be onerous and time-consuming, EHR technology is constantly improving, and EHRs have revolutionized documentation and order implementation. Several potential advances could improve clinical practice. For example, EHRs could incorporate a clinical decision support system that uses AI-based algorithms to assist psychiatrists with diagnosis, monitoring, and treatment.27 In the future, EHRs might have the ability to monitor and learn from errors and adverse events, and automatically design an algorithm to avoid them.28 They should be designed to better manage analysis of pharmacogenetic test results, which is challenging due to the amount and complexity of the data.29 Future EHRs should eliminate the non-intuitive and multi-click interfaces and cumbersome data searches of today’s EHRs.30
Technology brings new ethical considerations
Mental health interventions based on AI typically work with algorithms, and algorithms bring ethical issues. Mental health devices or systems that use AI could contain biases that have the potential to harm in unintended ways, such as a data-driven sexist or racist bias.31 This may require investing additional time to explain to patients (and their families) what an algorithm is and how it works in relation to the therapy provided.
Continue to: Another concern is patient...
Another concern is patient autonomy.32 For example, it would be ethically problematic if a patient were to assume that there was a human physician “at the other end” of a virtual therapist or other technology who is communicating or reviewing his/her messages. Similarly, an older adult or a patient with intellectual disabilities may not be able to understand advanced technology or what it does when it is installed in their home to monitor the patient’s activities. This would increase the risk of privacy violations, manipulation, or even coercion if the requirements for informed consent are not satisfied.
A flowchart for the future
Although current research and innovations typically target specific areas of psychiatry, these advances can be integrated by devising algorithms and protocols that will change the current practice of psychiatry. The Figure provides a glimpse of how the psychiatry clinic of the future might work. A maxim of management is that “the best way to predict the future is to create it.” However, the mere conception of a vision is not enough—working towards it is essential.
Bottom Line
With advances in technology, psychiatric practice will soon be radically different from what it is today. The expanded use of telepsychiatry, social media, artificial intelligence, and web-based applications/devices holds great promise for psychiatric assessment, diagnosis, and treatment, although certain ethical and privacy concerns need to be adequately addressed.
Related Resources
- National Institute of Mental Health. Technology and the future of mental health treatment. www.nimh.nih.gov/health/topics/technology-and-the-future-of-mental-health-treatment/index.shtml. Revised September 2019.
- Hays R, Farrell HM, Touros J. Mobile apps and mental health: using technology to quantify real-time clinical risk. Current Psychiatry. 2019;18(6):37-41.
- Torous J, Luo J, Chan SR. Mental health apps: what to tell patients. Current Psychiatry. 2018;17(3):21-25.
1. Pirmohamed M. Pharmacogenetics and pharmacogenomics. Br J Clin Pharmacol. 2001;52(4):345-347.
2. Benitez J, Cool CL, Scotti DJ. Use of combinatorial pharmacogenomic guidance in treating psychiatric disorders. Per Med. 2018;15(6):481-494.
3. Cannon TD. Candidate gene studies in the GWAS era: the MET proto-oncogene, neurocognition, and schizophrenia. Am J Psychiatry. 2010;167(4):4,369-372.
4. Greenwood J, Chamberlain C, Parker G. Evaluation of a rural telepsychiatry service. Australas Psychiatry. 2004;12(3):268-272.
5. Hubley S, Lynch SB, Schneck C, et al. Review of key telepsychiatry outcomes. World J Psychiatry. 2016;6(2):269-282.
6. Cheng KM, Siu BW, Yeung CC, et al. Telepsychiatry for stable Chinese psychiatric out-patients in custody in Hong Kong: a case-control pilot study. Hong Kong Med J. 2018;24(4):378-383.
7. Frankish K, Ryan C, Harris A. Psychiatry and online social media: potential, pitfalls and ethical guidelines for psychiatrists and trainees. Australasian Psychiatry. 2012;20(3):181-187.
8. de la Torre Díez I, Alonso SG, Hamrioui S, et al. IoT-based services and applications for mental health in the literature. J Med Syst. 2019;43(1):4-9.
9. Topol E. Deep Medicine. New York, NY: Basic Books; 2019:168.
10. Adams RA, Huys QJM, Roiser JP. Computational Psychiatry: towards a mathematically informed understanding of mental illness. J Neurol Neurosurg Psychiatry. 2016;87(1):53-63.
11. Insel TR. Bending the curve for mental health: technology for a public health approach. Am J Public Health. 2019;109(suppl 3):S168-S170.
12. Just MA, Pan L, Cherkassky VL, et al. Machine learning of neural representations of suicide and emotion concepts identifies suicidal youth. Nat Hum Behav. 2017;1:911-919.
13. Pestian J, Nasrallah H, Matykiewicz P, et al. Suicide note classification using natural language processing: a content analysis. Biomed Inform Insights. 2010;2010(3):19-28.
14. Walsh CG, Ribeiro JD, Franklin JC. Predicting risk of suicide attempts over time through machine learning. Clinical Psychological Science. 2017;5(3):457-469.
15. Pestian JP, Sorter M, Connolly B, et al; STM Research Group. A machine learning approach to identifying the thought markers of suicidal subjects: a prospective multicenter trial. Suicide Life Threat Behav. 2017;47(1):112-121.
16. Corcoran CM, Carrillo F, Fernández-Slezak D, et al. Prediction of psychosis across protocols and risk cohorts using automated language analysis. World Psychiatry. 2018;17(1):67-75.
17. Bedi G, Carrillo F, Cecchi GA, et al. Automated analysis of free speech predicts psychosis onset in high-risk youths. NPJ Schizophr. 2015;1:15030. doi: 10.1038/npjschz.2015.30.
18. Kalanderian H, Nasrallah HA. Artificial intelligence in psychiatry. Current Psychiatry. 2019;18(8):33-38.
19. Drysdale AT, Grosenick L, Downar J, et al. Resting-state connectivity biomarkers define neurophysiological subtypes of depression. Nat Med. 2017;23(1):28-38.
20. Chekroud AM, Zotti RJ, Shehzad Z, et al. Cross-trial prediction of treatment outcome in depression: a machine learning approach. Lancet Psychiatry. 2016;3(3):243-250.
21. Grisanzio KA, Goldstein-Piekarski AN, Wang MY, et al. Transdiagnostic symptom clusters and associations with brain, behavior, and daily function in mood, anxiety, and trauma disorders. JAMA Psychiatry. 2018;75(2):201-209.
22. Lucas G, Gratch J, King A, et al. It’s only a computer: virtual humans increase willingness to disclose. Computers in Human Behavior. 2014;37:94-100.
23. Nasir M, Baucom BR, Georgiou P, et al. Predicting couple therapy outcomes based on speech acoustic features. PLoS One. 2017;12(9):e0185123. doi: 10.1371/journal.pone.0185123.
24. Huguet A, Rao S, McGrath PJ, et al. A systematic review of cognitive behavioral therapy and behavioral activation apps for depression. PLoS One. 2016;11(5):e0154248. doi: 10.1371/journal.pone.0154248.
25. Scholten MR, Kelders SM, Van Gemert-Pijnen JE. Self-guided web-based interventions: scoping review on user needs and the potential of embodied conversational agents to address them. J Med Internet Res. 2017;19(11):e383.
26. Topol E. Deep Medicine. New York, NY: Basic Books; 2019:283-310.
27. Abramson EL, McGinnis S, Edwards A, et al. Electronic health record adoption and health information exchange among hospitals in New York State. J Eval Clin Pract. 2012;18(6):1156-1162.
28. Meeks DW, Smith MW, Taylor L, et al. An analysis of electronic health record-related patient safety concerns. J Am Med Inform Assoc. 2014;21(6):1053-1059.
29. Kho AN, Rasmussen LV, Connolly JJ, et al. Practical challenges in integrating genomic data into the electronic health record. Genet Med. 2013;15(10):772-778.
30. Ornstein SM, Oates RB, Fox GN. The computer-based medical record: current status. J Fam Pract. 1992;35(5):556-565.
31. Corea F. Machine ethics and artificial moral agents. In: Applied artificial intelligence: where AI can be used in business. Basel, Switzerland: Springer; 2019:33-41.
32. Beauchamp T, Childress J. Principles of biomedical ethics. 7th ed. New York, NY: Oxford University Press; 2012:44.
1. Pirmohamed M. Pharmacogenetics and pharmacogenomics. Br J Clin Pharmacol. 2001;52(4):345-347.
2. Benitez J, Cool CL, Scotti DJ. Use of combinatorial pharmacogenomic guidance in treating psychiatric disorders. Per Med. 2018;15(6):481-494.
3. Cannon TD. Candidate gene studies in the GWAS era: the MET proto-oncogene, neurocognition, and schizophrenia. Am J Psychiatry. 2010;167(4):4,369-372.
4. Greenwood J, Chamberlain C, Parker G. Evaluation of a rural telepsychiatry service. Australas Psychiatry. 2004;12(3):268-272.
5. Hubley S, Lynch SB, Schneck C, et al. Review of key telepsychiatry outcomes. World J Psychiatry. 2016;6(2):269-282.
6. Cheng KM, Siu BW, Yeung CC, et al. Telepsychiatry for stable Chinese psychiatric out-patients in custody in Hong Kong: a case-control pilot study. Hong Kong Med J. 2018;24(4):378-383.
7. Frankish K, Ryan C, Harris A. Psychiatry and online social media: potential, pitfalls and ethical guidelines for psychiatrists and trainees. Australasian Psychiatry. 2012;20(3):181-187.
8. de la Torre Díez I, Alonso SG, Hamrioui S, et al. IoT-based services and applications for mental health in the literature. J Med Syst. 2019;43(1):4-9.
9. Topol E. Deep Medicine. New York, NY: Basic Books; 2019:168.
10. Adams RA, Huys QJM, Roiser JP. Computational Psychiatry: towards a mathematically informed understanding of mental illness. J Neurol Neurosurg Psychiatry. 2016;87(1):53-63.
11. Insel TR. Bending the curve for mental health: technology for a public health approach. Am J Public Health. 2019;109(suppl 3):S168-S170.
12. Just MA, Pan L, Cherkassky VL, et al. Machine learning of neural representations of suicide and emotion concepts identifies suicidal youth. Nat Hum Behav. 2017;1:911-919.
13. Pestian J, Nasrallah H, Matykiewicz P, et al. Suicide note classification using natural language processing: a content analysis. Biomed Inform Insights. 2010;2010(3):19-28.
14. Walsh CG, Ribeiro JD, Franklin JC. Predicting risk of suicide attempts over time through machine learning. Clinical Psychological Science. 2017;5(3):457-469.
15. Pestian JP, Sorter M, Connolly B, et al; STM Research Group. A machine learning approach to identifying the thought markers of suicidal subjects: a prospective multicenter trial. Suicide Life Threat Behav. 2017;47(1):112-121.
16. Corcoran CM, Carrillo F, Fernández-Slezak D, et al. Prediction of psychosis across protocols and risk cohorts using automated language analysis. World Psychiatry. 2018;17(1):67-75.
17. Bedi G, Carrillo F, Cecchi GA, et al. Automated analysis of free speech predicts psychosis onset in high-risk youths. NPJ Schizophr. 2015;1:15030. doi: 10.1038/npjschz.2015.30.
18. Kalanderian H, Nasrallah HA. Artificial intelligence in psychiatry. Current Psychiatry. 2019;18(8):33-38.
19. Drysdale AT, Grosenick L, Downar J, et al. Resting-state connectivity biomarkers define neurophysiological subtypes of depression. Nat Med. 2017;23(1):28-38.
20. Chekroud AM, Zotti RJ, Shehzad Z, et al. Cross-trial prediction of treatment outcome in depression: a machine learning approach. Lancet Psychiatry. 2016;3(3):243-250.
21. Grisanzio KA, Goldstein-Piekarski AN, Wang MY, et al. Transdiagnostic symptom clusters and associations with brain, behavior, and daily function in mood, anxiety, and trauma disorders. JAMA Psychiatry. 2018;75(2):201-209.
22. Lucas G, Gratch J, King A, et al. It’s only a computer: virtual humans increase willingness to disclose. Computers in Human Behavior. 2014;37:94-100.
23. Nasir M, Baucom BR, Georgiou P, et al. Predicting couple therapy outcomes based on speech acoustic features. PLoS One. 2017;12(9):e0185123. doi: 10.1371/journal.pone.0185123.
24. Huguet A, Rao S, McGrath PJ, et al. A systematic review of cognitive behavioral therapy and behavioral activation apps for depression. PLoS One. 2016;11(5):e0154248. doi: 10.1371/journal.pone.0154248.
25. Scholten MR, Kelders SM, Van Gemert-Pijnen JE. Self-guided web-based interventions: scoping review on user needs and the potential of embodied conversational agents to address them. J Med Internet Res. 2017;19(11):e383.
26. Topol E. Deep Medicine. New York, NY: Basic Books; 2019:283-310.
27. Abramson EL, McGinnis S, Edwards A, et al. Electronic health record adoption and health information exchange among hospitals in New York State. J Eval Clin Pract. 2012;18(6):1156-1162.
28. Meeks DW, Smith MW, Taylor L, et al. An analysis of electronic health record-related patient safety concerns. J Am Med Inform Assoc. 2014;21(6):1053-1059.
29. Kho AN, Rasmussen LV, Connolly JJ, et al. Practical challenges in integrating genomic data into the electronic health record. Genet Med. 2013;15(10):772-778.
30. Ornstein SM, Oates RB, Fox GN. The computer-based medical record: current status. J Fam Pract. 1992;35(5):556-565.
31. Corea F. Machine ethics and artificial moral agents. In: Applied artificial intelligence: where AI can be used in business. Basel, Switzerland: Springer; 2019:33-41.
32. Beauchamp T, Childress J. Principles of biomedical ethics. 7th ed. New York, NY: Oxford University Press; 2012:44.
As physicians, accountability is part of our innate identity
Recently, Nicolas Badre, MD, challenged psychiatrists who care for patients involved in the legal system. He encouraged “a resurgence of personal accountability and responsibility.”
Using the chronically disenfranchised patients who are repetitiously shuttled between jails and mental hospitals as examples, he pointed out that we psychiatrists must “step up to the plate” and approach clinical problems with the attitude that “the buck stops with me.” As Dr. Badre pointed out, this is especially true when dealing with large, complex systems in which fragmented care exists without clear leadership. This, in turn, allows for a dissolution of accountability.
Accountability is a natural continuation of our training as physicians. We all remember the transition from medical student to intern, the steep learning curve as well as growth and maturation during this changeover. A dramatic transformation occurs over the course of 1 year, from medical students who tag along learning from patients to interns expected to be on their own for endless hours.
Over the course of those hours, we came to the understanding that people’s lives were in our hands. This causes a shift in our identity. This process continues throughout residency and onward in our careers. At some point, it becomes part of our innate identity as physicians or our professional sense of self – which is hard to describe to nonphysicians.
A profound example of a sense of accountability within the medical profession can be found in “How We Live,” a book by National Book Award winner Sherwin B. Nuland, MD. In the book, the late Dr. Nuland recounted how, as a 49-year-old seasoned surgeon working at Yale University, New Haven, Conn., and casually rounding on patients, he heard a frantic message: “Any general surgeon! Any general surgeon! Go immediately to the operating room – immediately – any general surgeon!”
The case involved a 42-year-old wife and mother who had been rushed to the ED after having been found in the community in a profound state of shock. In the ED, it was suspected that the patient was bleeding heavily from a ruptured tubal pregnancy. She was sped rapidly to the operating room with an undetectable blood pressure and a barely palpable pulse. The on-call ob.gyn. had been summoned from home, and he rushed to the operating room along with his department chairman.
Because the woman had lost much of her blood supply, there was no time for crossmatching. The anesthesiologist had placed large-bore intravenous lines and transfused her with O-negative blood (the universal donor blood type) to try maintain some level of blood pressure. Before she could be even fully anesthetized, the ob.gyn had made an incision in her lower abdomen. The bleeding he encountered was profound.
After a quick evaluation, the ob.gyn. realized that the blood was coming from above, not below, leading to the emergency page that Dr. Nuland heard. Dr. Nuland described bounding up the stairs three at a time. He recalled: “[A] very real apprehension had entered my mind. I might encounter a situation that was beyond me, something that I might make even worse, something that would cause me to regret for the rest of my life that I had answered the page’s insistent call instead of simply turning my back on its urgency and slinking off to my car before anyone noticed I was there.”
However, he could not see himself doing such a thing and he rushed up to the operating room because, “walking away from that kind of cry for help would have violated every precept taught me by my life and my training, and every bit of moral sense I had. … . I bear an obsessive preoccupation with accepting responsibility, amounting really to a compulsively neurotic sense of duty.”
And yet in the next few seconds, as he was running to the operating room, he wondered: “Am I about to botch something up? Will I, in one quick stroke of ineptness and fate, bring my career crashing down around my feet and with it my sense of what I am? Am I on my way to destroy an unknown patient and myself at the same time?”
In Dr. Nuland’s thoughts lie the conundrum of responsibility for physicians. Thankfully for Dr. Nuland, he was able to save the day and diagnose a rare case of rupture of an aneurysm of the splenic artery and keep the patient alive. This dramatic story involved a surgical colleague who had to make split-second decisions while a patient’s life hanged in the balance, but the same principles apply to us as psychiatrists.
I would note that, in the above example of the surgical patient, the “system” for saving the woman’s life was well organized and resourced to allow for a comprehensive and time-limited intervention into a life-threatening situation. There was an operating room staffed by various professionals who all had a defined role. It required the leader, Dr. Nuland, to step in, make the right diagnosis, and then issue commands to the identified professionals who all recognized his leadership and were skilled in carrying out their assigned duties. Dr. Nuland clearly was the leader once he took charge.
An outpatient psychiatrist facing a suicidal patient must deal with a different set of challenges, often involving various complex systems as well as multiple barriers. Clinical barriers include available interdisciplinary resources/personnel to assist not only with the critical encounter, but also with extended evaluation and treatment in a secure, well-resourced environment. Administrative barriers can include justifying the optimal treatment plan to payors. Our lethal patients often require both outpatient and inpatient services with sometimes-conflicting agendas. In a recent article, I pointed out some of the vexing problems that arise when communication and collaboration are poor between inpatient and outpatient psychiatrists. In such complex environments, it is less clear what is involved in the outpatient psychiatrist stepping up to the plate and asserting leadership.
An emotionally wrenching article about an emergency physician, Matthew E. Seaman, MD, who died by suicide, reminds us of the potential for suicide in a complicated patient (in this case, a medical colleague) involving complex systems. Plagued by a review of his care by the medical board (they had forced him to surrender his medical license and allowed the allegations to go public in lieu of further disciplinary proceedings), a subsequent lawsuit and an ultimate attempt by the plaintiff to obtain Dr. Seaman’s personal assets led to his worsening mental health. According to his wife, also a physician, he was getting “more depressed by the insults and assaults on his integrity and professionalism.”
Just before the investigation, he had received a 30-year pin from the American Board of Emergency Medicine for his “dedication to the specialty.” He fell into a deep depression from which he could not recover despite several psychiatric admissions and several medication trials. Along with his depression, he suffered from severe anxiety, a known risk factor for suicide. Dr. Seaman was feeling overwhelmed by the lengthy legal process targeting him as being negligent. He begged his attorney to settle the case, but his insurance carrier would not allow it. According to his wife: “All sense of human worth had been beaten out of him.”
Dr. Seaman had been known as resilient. He could handle complex ED situations, including simultaneously dealing with multiple traumas. He previously had been named in three malpractice lawsuits and had prevailed in each one. But his resilience had greatly diminished, and he became overwhelmed. He previously had, as a physician, been able to step up to the plate of accountability. But now, because of a confluence of depression and anxiety as well as the “insults and assaults on his integrity and professionalism,” he found life to be unbearable with the resulting tragic end.
So how would we as psychiatrists step up to the plate and be accountable when faced with a struggling fellow physician at risk for suicide such as Dr. Seaman?
Be aware of relevant risk factors
In addition to being aware of the usual risk factors for suicide, it would behoove us to also understand how physician suicides differ from suicides among nonphysicians.1 For example, physicians who have died by suicide were far more likely to have experienced job-related problems than nonphysicians, but less likely to have experienced the recent death of a loved one. Also noteworthy is that physicians who end their lives were more often married. In addition, Michael F. Myers, MD, a psychiatrist who has studied physician suicides, noted in the article about Dr. Seaman that struggling physicians are likely to suffer from shame and embarrassment.
Consider shame, burdensomeness, and secrecy
When suicide risk factors are taught to students and professionals, rarely is shame mentioned. Perhaps it is not a common risk factor in the general population, but shame and its cousin, disgrace, are known risk factors that likely apply more to people – such as physicians – who have built a reputation over their careers. One whole chapter is given to disgrace suicides in a book about suicide notes.2 A reputation often is one of the most important factors for professionals, which creates their sense of identity and, by extension, a sense of purpose in life.
When a doctor perceives that his or her reputation is being destroyed, it can produce a profound sense of shame, one of the most powerful of negative emotions.3 Another feature among completed suicides that applies more generally is perceived burdensomeness, according to Thomas E. Joiner Jr., PhD, one of the deep and innovative researchers in the field of suicidology.4 Once a doctor starts feeling that he has been a failure in his professional life and starts ruminating about it, the feelings of failure may generalize to other areas of his life, so that he starts feeling that he is a burden to his spouse. This, then, only increases his shame.
The issue of secrecy also is noteworthy. I was struck reading a book by Dr. Myers on physician suicide by the many spouses and family members who were caught completely unaware of problems when their spouse, a doctor, ended their lives by suicide.5 The doctors hid their problems well, perhaps not wanting to burden their family members. Also, if feelings of shame are an issue, then concealment tends to occur. This concealment of suicidality runs counter to the current narrative among some in the professional community that suicides are preventable (this despite the continuing increase in rates of suicide at the same time that there are increases in mental health services and suicide prevention programs).6
As pointed out in some of the letters quoted in Dr. Myers’s book, those who completed suicide are smart and know how to hide their symptoms well. Although Dr. Seaman’s wife, Linda Seaman, MD, was aware of her husband’s suicidality, when he eventually determined that he was going to end his life, he apparently did not reveal his more serious intention to her. Aside from spouses and family, determined suicide completers often hide their intentions from their clinicians.7
Attempt to obtain collateral information
By being aware of the usual and less-usual risk factors for suicide that our physician colleagues may present with as explained above, we can use strategies for mitigating risk. If secrecy because of shame and embarrassment prevents our physician patient from being fully candid, include the spouse or another significant family member in sessions. While the physician might hide his suicidal intent from both the clinician and spouse, it remains prudent to include the spouse in the treatment plan. Give the spouse a telephone number with which they can contact you if they notice any worrisome change in functioning or behavior. Collateral information often is helpful. (Example: Is the patient not eating, not sleeping, or giving away valued possessions?)
Assess for competency
In Dr. Seaman’s case, it was noted that, with a trial approaching, Dr. Seaman had written in a journal entry that he could not mentally endure a trial. “For me, the stress is overwhelming.” Such a patient, suffering from severe depression, often is unable to properly assist his attorney in his defense. The outpatient psychiatrist can notify the court or one of the attorneys that the competency of the physician patient is questionable (or express a definite opinion of incompetency), and offer the opinion that it would be best to postpone further legal action until the patient is in a more healthy state of mind.
Know when hospitalization is needed
Obviously, the process will go smoother if the admission is voluntary. If the patient physician resists and the psychiatrist believes that the risk for self-harm is too high for the physician patient to remain as an outpatient, try to get a spouse or family member to persuade him to be admitted. An involuntary admission opens up a whole new can of worms and may fracture the therapeutic alliance.
In the end, it might be better to take that risk rather than having a dead patient on your hands. If a hospitalization is necessary, contact the admitting psychiatrist and verbally express your concerns and the reasons why a hospitalization is needed. Ask the inpatient psychiatrist to contact you when a discharge is approaching so that you have an opportunity to ask relevant questions.
For example, during his second psychiatric admission, as the time for discharge was approaching, Dr. Seaman wrote: “I am not well enough for discharge. I am still mentally ill.” Ask the inpatient doctor whether the patient has gotten sufficiently better and he feels confident he can function as an outpatient. If there is a conflicting opinion about the readiness of the patient for discharge, notify the medical director of the service or an administrator about your concerns.
Ask for consultation
At any stage of the process consider getting consultation for a trusted colleague or senior clinician if you are failing to make progress. Sometimes it helps to get the perspective from a fresh pair of eyes or ears.
Get a reality check
Having recounted the inspiring story of Dr. Nuland’s magnificent efforts and joyous success in preserving a life that was on the verge of being lost in the battle against death at the last possible second, I would note the following: Surgeons will tell you that, despite their most heroic efforts and teamwork, there are times when luck runs out and the patient dies on the operating table. Also, small lapses, which all mortals are prone to despite their best efforts at conscientiousness, sometimes can lead to a bad outcome.
Similarly, in psychiatry, no matter how much effort we put into saving a life, sometimes it is all to no avail. Despite all we have learned about suicide and its risk factors, and no matter how much care we take to contain risk, our patients who are determined will find a way of ending their own lives. The vexing problem of suicide seems intractable. A suicide among our patients humbles us, but also hopefully inspires us to keep trying harder to step up to the plate of accountability.
In conclusion, for us physicians, accountability is not a facet, a trait, or even a pursuit, accountability is at the core of who are and how we define ourselves. Accountability is the reason we leap stairs three at time when we are urgently paged. Accountability is the reason malpractice lawsuits cut at the core of our self-image. Accountability allows us to always have hope for a positive outcome, despite overwhelming barriers, and gives our lives a sense of purpose.
For me, in preparing this article, accountability was reviewing and studying physician suicide and then applying best practices in risk assessment after reading the tragic story of Dr. Seaman. I hope I inspire you to do the same in the pursuit of helping our vulnerable patients.
Learning how to care for our complex patients is a never-ending journey.
References
1. Gold KJ. Gen Hosp Psychiatry. 2013 Jan;35(1):45-9.
2. Etkind M. ...Or Not to Be: A Collection of Suicide Notes. New York: Riverhead Books, 1997.
3. Lamia LC. Shame: A concealed, contagious, and dangerous emotion. Psychology Today. 2011 Apr 4.
4. Joiner TE. Why People Die by Suicide. Cambridge: Harvard University Press, 2005.
5. Myers MF. Why Physicians Die by Suicide. 2017.
6. National Institutes of Health. Suicide Prevention. https://www.nimh.nih.gov/health/topics/suicide-prevention/index.shtml.
7. Levy AG et al. JAMA Netw Open. 2019 Aug 14. doi: 10.1001/jamanetworkopen.2019.9277.
Dr. Kausch is a clinical and forensic psychiatrist who is on the faculty at Case Western Reserve University, Cleveland, as an assistant clinical professor. He spends most of his time seeing patients through the Akron General/Cleveland Clinic health system. He has published in the area of forensic psychiatry, addictions, pathological gambling, and suicide. He has recently taken an interest in conducting marital therapy and is now publishing in that area as well.
Recently, Nicolas Badre, MD, challenged psychiatrists who care for patients involved in the legal system. He encouraged “a resurgence of personal accountability and responsibility.”
Using the chronically disenfranchised patients who are repetitiously shuttled between jails and mental hospitals as examples, he pointed out that we psychiatrists must “step up to the plate” and approach clinical problems with the attitude that “the buck stops with me.” As Dr. Badre pointed out, this is especially true when dealing with large, complex systems in which fragmented care exists without clear leadership. This, in turn, allows for a dissolution of accountability.
Accountability is a natural continuation of our training as physicians. We all remember the transition from medical student to intern, the steep learning curve as well as growth and maturation during this changeover. A dramatic transformation occurs over the course of 1 year, from medical students who tag along learning from patients to interns expected to be on their own for endless hours.
Over the course of those hours, we came to the understanding that people’s lives were in our hands. This causes a shift in our identity. This process continues throughout residency and onward in our careers. At some point, it becomes part of our innate identity as physicians or our professional sense of self – which is hard to describe to nonphysicians.
A profound example of a sense of accountability within the medical profession can be found in “How We Live,” a book by National Book Award winner Sherwin B. Nuland, MD. In the book, the late Dr. Nuland recounted how, as a 49-year-old seasoned surgeon working at Yale University, New Haven, Conn., and casually rounding on patients, he heard a frantic message: “Any general surgeon! Any general surgeon! Go immediately to the operating room – immediately – any general surgeon!”
The case involved a 42-year-old wife and mother who had been rushed to the ED after having been found in the community in a profound state of shock. In the ED, it was suspected that the patient was bleeding heavily from a ruptured tubal pregnancy. She was sped rapidly to the operating room with an undetectable blood pressure and a barely palpable pulse. The on-call ob.gyn. had been summoned from home, and he rushed to the operating room along with his department chairman.
Because the woman had lost much of her blood supply, there was no time for crossmatching. The anesthesiologist had placed large-bore intravenous lines and transfused her with O-negative blood (the universal donor blood type) to try maintain some level of blood pressure. Before she could be even fully anesthetized, the ob.gyn had made an incision in her lower abdomen. The bleeding he encountered was profound.
After a quick evaluation, the ob.gyn. realized that the blood was coming from above, not below, leading to the emergency page that Dr. Nuland heard. Dr. Nuland described bounding up the stairs three at a time. He recalled: “[A] very real apprehension had entered my mind. I might encounter a situation that was beyond me, something that I might make even worse, something that would cause me to regret for the rest of my life that I had answered the page’s insistent call instead of simply turning my back on its urgency and slinking off to my car before anyone noticed I was there.”
However, he could not see himself doing such a thing and he rushed up to the operating room because, “walking away from that kind of cry for help would have violated every precept taught me by my life and my training, and every bit of moral sense I had. … . I bear an obsessive preoccupation with accepting responsibility, amounting really to a compulsively neurotic sense of duty.”
And yet in the next few seconds, as he was running to the operating room, he wondered: “Am I about to botch something up? Will I, in one quick stroke of ineptness and fate, bring my career crashing down around my feet and with it my sense of what I am? Am I on my way to destroy an unknown patient and myself at the same time?”
In Dr. Nuland’s thoughts lie the conundrum of responsibility for physicians. Thankfully for Dr. Nuland, he was able to save the day and diagnose a rare case of rupture of an aneurysm of the splenic artery and keep the patient alive. This dramatic story involved a surgical colleague who had to make split-second decisions while a patient’s life hanged in the balance, but the same principles apply to us as psychiatrists.
I would note that, in the above example of the surgical patient, the “system” for saving the woman’s life was well organized and resourced to allow for a comprehensive and time-limited intervention into a life-threatening situation. There was an operating room staffed by various professionals who all had a defined role. It required the leader, Dr. Nuland, to step in, make the right diagnosis, and then issue commands to the identified professionals who all recognized his leadership and were skilled in carrying out their assigned duties. Dr. Nuland clearly was the leader once he took charge.
An outpatient psychiatrist facing a suicidal patient must deal with a different set of challenges, often involving various complex systems as well as multiple barriers. Clinical barriers include available interdisciplinary resources/personnel to assist not only with the critical encounter, but also with extended evaluation and treatment in a secure, well-resourced environment. Administrative barriers can include justifying the optimal treatment plan to payors. Our lethal patients often require both outpatient and inpatient services with sometimes-conflicting agendas. In a recent article, I pointed out some of the vexing problems that arise when communication and collaboration are poor between inpatient and outpatient psychiatrists. In such complex environments, it is less clear what is involved in the outpatient psychiatrist stepping up to the plate and asserting leadership.
An emotionally wrenching article about an emergency physician, Matthew E. Seaman, MD, who died by suicide, reminds us of the potential for suicide in a complicated patient (in this case, a medical colleague) involving complex systems. Plagued by a review of his care by the medical board (they had forced him to surrender his medical license and allowed the allegations to go public in lieu of further disciplinary proceedings), a subsequent lawsuit and an ultimate attempt by the plaintiff to obtain Dr. Seaman’s personal assets led to his worsening mental health. According to his wife, also a physician, he was getting “more depressed by the insults and assaults on his integrity and professionalism.”
Just before the investigation, he had received a 30-year pin from the American Board of Emergency Medicine for his “dedication to the specialty.” He fell into a deep depression from which he could not recover despite several psychiatric admissions and several medication trials. Along with his depression, he suffered from severe anxiety, a known risk factor for suicide. Dr. Seaman was feeling overwhelmed by the lengthy legal process targeting him as being negligent. He begged his attorney to settle the case, but his insurance carrier would not allow it. According to his wife: “All sense of human worth had been beaten out of him.”
Dr. Seaman had been known as resilient. He could handle complex ED situations, including simultaneously dealing with multiple traumas. He previously had been named in three malpractice lawsuits and had prevailed in each one. But his resilience had greatly diminished, and he became overwhelmed. He previously had, as a physician, been able to step up to the plate of accountability. But now, because of a confluence of depression and anxiety as well as the “insults and assaults on his integrity and professionalism,” he found life to be unbearable with the resulting tragic end.
So how would we as psychiatrists step up to the plate and be accountable when faced with a struggling fellow physician at risk for suicide such as Dr. Seaman?
Be aware of relevant risk factors
In addition to being aware of the usual risk factors for suicide, it would behoove us to also understand how physician suicides differ from suicides among nonphysicians.1 For example, physicians who have died by suicide were far more likely to have experienced job-related problems than nonphysicians, but less likely to have experienced the recent death of a loved one. Also noteworthy is that physicians who end their lives were more often married. In addition, Michael F. Myers, MD, a psychiatrist who has studied physician suicides, noted in the article about Dr. Seaman that struggling physicians are likely to suffer from shame and embarrassment.
Consider shame, burdensomeness, and secrecy
When suicide risk factors are taught to students and professionals, rarely is shame mentioned. Perhaps it is not a common risk factor in the general population, but shame and its cousin, disgrace, are known risk factors that likely apply more to people – such as physicians – who have built a reputation over their careers. One whole chapter is given to disgrace suicides in a book about suicide notes.2 A reputation often is one of the most important factors for professionals, which creates their sense of identity and, by extension, a sense of purpose in life.
When a doctor perceives that his or her reputation is being destroyed, it can produce a profound sense of shame, one of the most powerful of negative emotions.3 Another feature among completed suicides that applies more generally is perceived burdensomeness, according to Thomas E. Joiner Jr., PhD, one of the deep and innovative researchers in the field of suicidology.4 Once a doctor starts feeling that he has been a failure in his professional life and starts ruminating about it, the feelings of failure may generalize to other areas of his life, so that he starts feeling that he is a burden to his spouse. This, then, only increases his shame.
The issue of secrecy also is noteworthy. I was struck reading a book by Dr. Myers on physician suicide by the many spouses and family members who were caught completely unaware of problems when their spouse, a doctor, ended their lives by suicide.5 The doctors hid their problems well, perhaps not wanting to burden their family members. Also, if feelings of shame are an issue, then concealment tends to occur. This concealment of suicidality runs counter to the current narrative among some in the professional community that suicides are preventable (this despite the continuing increase in rates of suicide at the same time that there are increases in mental health services and suicide prevention programs).6
As pointed out in some of the letters quoted in Dr. Myers’s book, those who completed suicide are smart and know how to hide their symptoms well. Although Dr. Seaman’s wife, Linda Seaman, MD, was aware of her husband’s suicidality, when he eventually determined that he was going to end his life, he apparently did not reveal his more serious intention to her. Aside from spouses and family, determined suicide completers often hide their intentions from their clinicians.7
Attempt to obtain collateral information
By being aware of the usual and less-usual risk factors for suicide that our physician colleagues may present with as explained above, we can use strategies for mitigating risk. If secrecy because of shame and embarrassment prevents our physician patient from being fully candid, include the spouse or another significant family member in sessions. While the physician might hide his suicidal intent from both the clinician and spouse, it remains prudent to include the spouse in the treatment plan. Give the spouse a telephone number with which they can contact you if they notice any worrisome change in functioning or behavior. Collateral information often is helpful. (Example: Is the patient not eating, not sleeping, or giving away valued possessions?)
Assess for competency
In Dr. Seaman’s case, it was noted that, with a trial approaching, Dr. Seaman had written in a journal entry that he could not mentally endure a trial. “For me, the stress is overwhelming.” Such a patient, suffering from severe depression, often is unable to properly assist his attorney in his defense. The outpatient psychiatrist can notify the court or one of the attorneys that the competency of the physician patient is questionable (or express a definite opinion of incompetency), and offer the opinion that it would be best to postpone further legal action until the patient is in a more healthy state of mind.
Know when hospitalization is needed
Obviously, the process will go smoother if the admission is voluntary. If the patient physician resists and the psychiatrist believes that the risk for self-harm is too high for the physician patient to remain as an outpatient, try to get a spouse or family member to persuade him to be admitted. An involuntary admission opens up a whole new can of worms and may fracture the therapeutic alliance.
In the end, it might be better to take that risk rather than having a dead patient on your hands. If a hospitalization is necessary, contact the admitting psychiatrist and verbally express your concerns and the reasons why a hospitalization is needed. Ask the inpatient psychiatrist to contact you when a discharge is approaching so that you have an opportunity to ask relevant questions.
For example, during his second psychiatric admission, as the time for discharge was approaching, Dr. Seaman wrote: “I am not well enough for discharge. I am still mentally ill.” Ask the inpatient doctor whether the patient has gotten sufficiently better and he feels confident he can function as an outpatient. If there is a conflicting opinion about the readiness of the patient for discharge, notify the medical director of the service or an administrator about your concerns.
Ask for consultation
At any stage of the process consider getting consultation for a trusted colleague or senior clinician if you are failing to make progress. Sometimes it helps to get the perspective from a fresh pair of eyes or ears.
Get a reality check
Having recounted the inspiring story of Dr. Nuland’s magnificent efforts and joyous success in preserving a life that was on the verge of being lost in the battle against death at the last possible second, I would note the following: Surgeons will tell you that, despite their most heroic efforts and teamwork, there are times when luck runs out and the patient dies on the operating table. Also, small lapses, which all mortals are prone to despite their best efforts at conscientiousness, sometimes can lead to a bad outcome.
Similarly, in psychiatry, no matter how much effort we put into saving a life, sometimes it is all to no avail. Despite all we have learned about suicide and its risk factors, and no matter how much care we take to contain risk, our patients who are determined will find a way of ending their own lives. The vexing problem of suicide seems intractable. A suicide among our patients humbles us, but also hopefully inspires us to keep trying harder to step up to the plate of accountability.
In conclusion, for us physicians, accountability is not a facet, a trait, or even a pursuit, accountability is at the core of who are and how we define ourselves. Accountability is the reason we leap stairs three at time when we are urgently paged. Accountability is the reason malpractice lawsuits cut at the core of our self-image. Accountability allows us to always have hope for a positive outcome, despite overwhelming barriers, and gives our lives a sense of purpose.
For me, in preparing this article, accountability was reviewing and studying physician suicide and then applying best practices in risk assessment after reading the tragic story of Dr. Seaman. I hope I inspire you to do the same in the pursuit of helping our vulnerable patients.
Learning how to care for our complex patients is a never-ending journey.
References
1. Gold KJ. Gen Hosp Psychiatry. 2013 Jan;35(1):45-9.
2. Etkind M. ...Or Not to Be: A Collection of Suicide Notes. New York: Riverhead Books, 1997.
3. Lamia LC. Shame: A concealed, contagious, and dangerous emotion. Psychology Today. 2011 Apr 4.
4. Joiner TE. Why People Die by Suicide. Cambridge: Harvard University Press, 2005.
5. Myers MF. Why Physicians Die by Suicide. 2017.
6. National Institutes of Health. Suicide Prevention. https://www.nimh.nih.gov/health/topics/suicide-prevention/index.shtml.
7. Levy AG et al. JAMA Netw Open. 2019 Aug 14. doi: 10.1001/jamanetworkopen.2019.9277.
Dr. Kausch is a clinical and forensic psychiatrist who is on the faculty at Case Western Reserve University, Cleveland, as an assistant clinical professor. He spends most of his time seeing patients through the Akron General/Cleveland Clinic health system. He has published in the area of forensic psychiatry, addictions, pathological gambling, and suicide. He has recently taken an interest in conducting marital therapy and is now publishing in that area as well.
Recently, Nicolas Badre, MD, challenged psychiatrists who care for patients involved in the legal system. He encouraged “a resurgence of personal accountability and responsibility.”
Using the chronically disenfranchised patients who are repetitiously shuttled between jails and mental hospitals as examples, he pointed out that we psychiatrists must “step up to the plate” and approach clinical problems with the attitude that “the buck stops with me.” As Dr. Badre pointed out, this is especially true when dealing with large, complex systems in which fragmented care exists without clear leadership. This, in turn, allows for a dissolution of accountability.
Accountability is a natural continuation of our training as physicians. We all remember the transition from medical student to intern, the steep learning curve as well as growth and maturation during this changeover. A dramatic transformation occurs over the course of 1 year, from medical students who tag along learning from patients to interns expected to be on their own for endless hours.
Over the course of those hours, we came to the understanding that people’s lives were in our hands. This causes a shift in our identity. This process continues throughout residency and onward in our careers. At some point, it becomes part of our innate identity as physicians or our professional sense of self – which is hard to describe to nonphysicians.
A profound example of a sense of accountability within the medical profession can be found in “How We Live,” a book by National Book Award winner Sherwin B. Nuland, MD. In the book, the late Dr. Nuland recounted how, as a 49-year-old seasoned surgeon working at Yale University, New Haven, Conn., and casually rounding on patients, he heard a frantic message: “Any general surgeon! Any general surgeon! Go immediately to the operating room – immediately – any general surgeon!”
The case involved a 42-year-old wife and mother who had been rushed to the ED after having been found in the community in a profound state of shock. In the ED, it was suspected that the patient was bleeding heavily from a ruptured tubal pregnancy. She was sped rapidly to the operating room with an undetectable blood pressure and a barely palpable pulse. The on-call ob.gyn. had been summoned from home, and he rushed to the operating room along with his department chairman.
Because the woman had lost much of her blood supply, there was no time for crossmatching. The anesthesiologist had placed large-bore intravenous lines and transfused her with O-negative blood (the universal donor blood type) to try maintain some level of blood pressure. Before she could be even fully anesthetized, the ob.gyn had made an incision in her lower abdomen. The bleeding he encountered was profound.
After a quick evaluation, the ob.gyn. realized that the blood was coming from above, not below, leading to the emergency page that Dr. Nuland heard. Dr. Nuland described bounding up the stairs three at a time. He recalled: “[A] very real apprehension had entered my mind. I might encounter a situation that was beyond me, something that I might make even worse, something that would cause me to regret for the rest of my life that I had answered the page’s insistent call instead of simply turning my back on its urgency and slinking off to my car before anyone noticed I was there.”
However, he could not see himself doing such a thing and he rushed up to the operating room because, “walking away from that kind of cry for help would have violated every precept taught me by my life and my training, and every bit of moral sense I had. … . I bear an obsessive preoccupation with accepting responsibility, amounting really to a compulsively neurotic sense of duty.”
And yet in the next few seconds, as he was running to the operating room, he wondered: “Am I about to botch something up? Will I, in one quick stroke of ineptness and fate, bring my career crashing down around my feet and with it my sense of what I am? Am I on my way to destroy an unknown patient and myself at the same time?”
In Dr. Nuland’s thoughts lie the conundrum of responsibility for physicians. Thankfully for Dr. Nuland, he was able to save the day and diagnose a rare case of rupture of an aneurysm of the splenic artery and keep the patient alive. This dramatic story involved a surgical colleague who had to make split-second decisions while a patient’s life hanged in the balance, but the same principles apply to us as psychiatrists.
I would note that, in the above example of the surgical patient, the “system” for saving the woman’s life was well organized and resourced to allow for a comprehensive and time-limited intervention into a life-threatening situation. There was an operating room staffed by various professionals who all had a defined role. It required the leader, Dr. Nuland, to step in, make the right diagnosis, and then issue commands to the identified professionals who all recognized his leadership and were skilled in carrying out their assigned duties. Dr. Nuland clearly was the leader once he took charge.
An outpatient psychiatrist facing a suicidal patient must deal with a different set of challenges, often involving various complex systems as well as multiple barriers. Clinical barriers include available interdisciplinary resources/personnel to assist not only with the critical encounter, but also with extended evaluation and treatment in a secure, well-resourced environment. Administrative barriers can include justifying the optimal treatment plan to payors. Our lethal patients often require both outpatient and inpatient services with sometimes-conflicting agendas. In a recent article, I pointed out some of the vexing problems that arise when communication and collaboration are poor between inpatient and outpatient psychiatrists. In such complex environments, it is less clear what is involved in the outpatient psychiatrist stepping up to the plate and asserting leadership.
An emotionally wrenching article about an emergency physician, Matthew E. Seaman, MD, who died by suicide, reminds us of the potential for suicide in a complicated patient (in this case, a medical colleague) involving complex systems. Plagued by a review of his care by the medical board (they had forced him to surrender his medical license and allowed the allegations to go public in lieu of further disciplinary proceedings), a subsequent lawsuit and an ultimate attempt by the plaintiff to obtain Dr. Seaman’s personal assets led to his worsening mental health. According to his wife, also a physician, he was getting “more depressed by the insults and assaults on his integrity and professionalism.”
Just before the investigation, he had received a 30-year pin from the American Board of Emergency Medicine for his “dedication to the specialty.” He fell into a deep depression from which he could not recover despite several psychiatric admissions and several medication trials. Along with his depression, he suffered from severe anxiety, a known risk factor for suicide. Dr. Seaman was feeling overwhelmed by the lengthy legal process targeting him as being negligent. He begged his attorney to settle the case, but his insurance carrier would not allow it. According to his wife: “All sense of human worth had been beaten out of him.”
Dr. Seaman had been known as resilient. He could handle complex ED situations, including simultaneously dealing with multiple traumas. He previously had been named in three malpractice lawsuits and had prevailed in each one. But his resilience had greatly diminished, and he became overwhelmed. He previously had, as a physician, been able to step up to the plate of accountability. But now, because of a confluence of depression and anxiety as well as the “insults and assaults on his integrity and professionalism,” he found life to be unbearable with the resulting tragic end.
So how would we as psychiatrists step up to the plate and be accountable when faced with a struggling fellow physician at risk for suicide such as Dr. Seaman?
Be aware of relevant risk factors
In addition to being aware of the usual risk factors for suicide, it would behoove us to also understand how physician suicides differ from suicides among nonphysicians.1 For example, physicians who have died by suicide were far more likely to have experienced job-related problems than nonphysicians, but less likely to have experienced the recent death of a loved one. Also noteworthy is that physicians who end their lives were more often married. In addition, Michael F. Myers, MD, a psychiatrist who has studied physician suicides, noted in the article about Dr. Seaman that struggling physicians are likely to suffer from shame and embarrassment.
Consider shame, burdensomeness, and secrecy
When suicide risk factors are taught to students and professionals, rarely is shame mentioned. Perhaps it is not a common risk factor in the general population, but shame and its cousin, disgrace, are known risk factors that likely apply more to people – such as physicians – who have built a reputation over their careers. One whole chapter is given to disgrace suicides in a book about suicide notes.2 A reputation often is one of the most important factors for professionals, which creates their sense of identity and, by extension, a sense of purpose in life.
When a doctor perceives that his or her reputation is being destroyed, it can produce a profound sense of shame, one of the most powerful of negative emotions.3 Another feature among completed suicides that applies more generally is perceived burdensomeness, according to Thomas E. Joiner Jr., PhD, one of the deep and innovative researchers in the field of suicidology.4 Once a doctor starts feeling that he has been a failure in his professional life and starts ruminating about it, the feelings of failure may generalize to other areas of his life, so that he starts feeling that he is a burden to his spouse. This, then, only increases his shame.
The issue of secrecy also is noteworthy. I was struck reading a book by Dr. Myers on physician suicide by the many spouses and family members who were caught completely unaware of problems when their spouse, a doctor, ended their lives by suicide.5 The doctors hid their problems well, perhaps not wanting to burden their family members. Also, if feelings of shame are an issue, then concealment tends to occur. This concealment of suicidality runs counter to the current narrative among some in the professional community that suicides are preventable (this despite the continuing increase in rates of suicide at the same time that there are increases in mental health services and suicide prevention programs).6
As pointed out in some of the letters quoted in Dr. Myers’s book, those who completed suicide are smart and know how to hide their symptoms well. Although Dr. Seaman’s wife, Linda Seaman, MD, was aware of her husband’s suicidality, when he eventually determined that he was going to end his life, he apparently did not reveal his more serious intention to her. Aside from spouses and family, determined suicide completers often hide their intentions from their clinicians.7
Attempt to obtain collateral information
By being aware of the usual and less-usual risk factors for suicide that our physician colleagues may present with as explained above, we can use strategies for mitigating risk. If secrecy because of shame and embarrassment prevents our physician patient from being fully candid, include the spouse or another significant family member in sessions. While the physician might hide his suicidal intent from both the clinician and spouse, it remains prudent to include the spouse in the treatment plan. Give the spouse a telephone number with which they can contact you if they notice any worrisome change in functioning or behavior. Collateral information often is helpful. (Example: Is the patient not eating, not sleeping, or giving away valued possessions?)
Assess for competency
In Dr. Seaman’s case, it was noted that, with a trial approaching, Dr. Seaman had written in a journal entry that he could not mentally endure a trial. “For me, the stress is overwhelming.” Such a patient, suffering from severe depression, often is unable to properly assist his attorney in his defense. The outpatient psychiatrist can notify the court or one of the attorneys that the competency of the physician patient is questionable (or express a definite opinion of incompetency), and offer the opinion that it would be best to postpone further legal action until the patient is in a more healthy state of mind.
Know when hospitalization is needed
Obviously, the process will go smoother if the admission is voluntary. If the patient physician resists and the psychiatrist believes that the risk for self-harm is too high for the physician patient to remain as an outpatient, try to get a spouse or family member to persuade him to be admitted. An involuntary admission opens up a whole new can of worms and may fracture the therapeutic alliance.
In the end, it might be better to take that risk rather than having a dead patient on your hands. If a hospitalization is necessary, contact the admitting psychiatrist and verbally express your concerns and the reasons why a hospitalization is needed. Ask the inpatient psychiatrist to contact you when a discharge is approaching so that you have an opportunity to ask relevant questions.
For example, during his second psychiatric admission, as the time for discharge was approaching, Dr. Seaman wrote: “I am not well enough for discharge. I am still mentally ill.” Ask the inpatient doctor whether the patient has gotten sufficiently better and he feels confident he can function as an outpatient. If there is a conflicting opinion about the readiness of the patient for discharge, notify the medical director of the service or an administrator about your concerns.
Ask for consultation
At any stage of the process consider getting consultation for a trusted colleague or senior clinician if you are failing to make progress. Sometimes it helps to get the perspective from a fresh pair of eyes or ears.
Get a reality check
Having recounted the inspiring story of Dr. Nuland’s magnificent efforts and joyous success in preserving a life that was on the verge of being lost in the battle against death at the last possible second, I would note the following: Surgeons will tell you that, despite their most heroic efforts and teamwork, there are times when luck runs out and the patient dies on the operating table. Also, small lapses, which all mortals are prone to despite their best efforts at conscientiousness, sometimes can lead to a bad outcome.
Similarly, in psychiatry, no matter how much effort we put into saving a life, sometimes it is all to no avail. Despite all we have learned about suicide and its risk factors, and no matter how much care we take to contain risk, our patients who are determined will find a way of ending their own lives. The vexing problem of suicide seems intractable. A suicide among our patients humbles us, but also hopefully inspires us to keep trying harder to step up to the plate of accountability.
In conclusion, for us physicians, accountability is not a facet, a trait, or even a pursuit, accountability is at the core of who are and how we define ourselves. Accountability is the reason we leap stairs three at time when we are urgently paged. Accountability is the reason malpractice lawsuits cut at the core of our self-image. Accountability allows us to always have hope for a positive outcome, despite overwhelming barriers, and gives our lives a sense of purpose.
For me, in preparing this article, accountability was reviewing and studying physician suicide and then applying best practices in risk assessment after reading the tragic story of Dr. Seaman. I hope I inspire you to do the same in the pursuit of helping our vulnerable patients.
Learning how to care for our complex patients is a never-ending journey.
References
1. Gold KJ. Gen Hosp Psychiatry. 2013 Jan;35(1):45-9.
2. Etkind M. ...Or Not to Be: A Collection of Suicide Notes. New York: Riverhead Books, 1997.
3. Lamia LC. Shame: A concealed, contagious, and dangerous emotion. Psychology Today. 2011 Apr 4.
4. Joiner TE. Why People Die by Suicide. Cambridge: Harvard University Press, 2005.
5. Myers MF. Why Physicians Die by Suicide. 2017.
6. National Institutes of Health. Suicide Prevention. https://www.nimh.nih.gov/health/topics/suicide-prevention/index.shtml.
7. Levy AG et al. JAMA Netw Open. 2019 Aug 14. doi: 10.1001/jamanetworkopen.2019.9277.
Dr. Kausch is a clinical and forensic psychiatrist who is on the faculty at Case Western Reserve University, Cleveland, as an assistant clinical professor. He spends most of his time seeing patients through the Akron General/Cleveland Clinic health system. He has published in the area of forensic psychiatry, addictions, pathological gambling, and suicide. He has recently taken an interest in conducting marital therapy and is now publishing in that area as well.
Burnout: A concept that rebrands mental illness for professionals
Over the past years, I have had the opportunity to attend countless lectures on burnout provided by colleagues spanning across many fields in mental health and health care in general. The talks generally follow a common narration: 1. Your work is important and meaningful to many. 2. Your work requires significant training, dedication, and passion. 3. While you get personal gratification from your work, it does come with a cost. 4. This cost can be great and can affect you physically and mentally. 5. This cost is called burnout.
Burnout is described as irritability (poor mood), low energy, poor concentration, difficulty appreciating enjoyable things (anhedonia), and poor sleep, among other symptoms, as a result of work stress. At this point in the lectures, I usually ask whomever is sitting next to me: “I came in late, is this a lecture on depression?” to which the answer is typically “No! Of course not, this is about ‘burnout’ not mental illness.” And here lies a concern about burnout: Is burnout a concept describing depression that we have repackaged to protect professionals from the stigmatization of mental illness? Does our tendency not to characterize patients’ struggles as burnout stigmatize them – and imply that their employment is not challenging to cause burnout?
According to the literature, a range of factors affects burnout in professionals: lack of control, unclear job expectations, dysfunctional workplace dynamics, extremes of activity, lack of social support, work-life imbalance. Contrary to depression, burnout is not caused by neurobiological problems. Patients with burnout don’t have chemical imbalances, hyperactive default mode networks, or overactive amygdalas. Burnout is caused by social factors and affects dedicated, caring, and exceptional individuals who have been pushed outside their window of tolerance.
Literature suggests a variety of remedies to treat burnout: Reevaluate your employment, discuss occupational concerns with your supervisor, discuss with colleagues, receive help from your social support system, and seek human resources services. In addition, experts recommend engaging in relaxing activities, improving your sleep hygiene, exercising regularly, and participating in mindfulness to reduce symptoms. Contrary to depression, burnout does not require individuals to fix their maladaptive thoughts or discover inadequate unconscious beliefs that may be affecting their work. Contrary to depression, burnout does not require the rebalancing of neurochemistry using psychotropic medication.
The concept of burnout engenders concerns. I fear that it divides physicians and patients into two different classes and thus further stigmatizes those with mental illness. It implies that we physicians are somehow immune from mental illness and its consequences. We do not suffer from brain abnormalities, we do not require mind-altering medications, we are not “mentally ill.” Contrarily, at times it might be implied that patients’ jobs are not important enough to cause burnout; if they feel sad, anhedonic, have poor energy and poor sleep, it is because they have mental illness. Their brains are inadequate and flawed. But for physicians, our brains are intact, just pushed beyond human capabilities.
I should point out that I do not think that burnout experts believe or desire to promote such concepts. I am not aware of burnout experts championing physician exceptionalism or promoting the stigmatization of patients. I believe that this problem is an unintended consequence, a side effect, of the idea of burnout itself.
Another concern I have is that the concept of burnout may actually hinder physicians from seeking necessary and appropriate professional services to address symptoms. Interestingly, most lectures I have attended on burnout have not discussed the concerning number of physicians who end their lives by suicide. There was a time when I argued against the removal of the grief exclusion in the DSM; I worried that we were pathologizing natural emotional reactions to trauma. However, I have come to realize that, if someone is debilitated by depression, seeking professional help should not be predicated on the trigger. As such, I would recommend the vast number of physicians who state burnout in surveys to seriously consider the possibility that they may, in fact, be suffering from mental illness. We encourage our patients to seek help and speak out against stigmatization; isn’t it time that we as professionals should not be afraid to do the same?
I have concerns about the concept of burnout, but I certainly do not think that we should get rid of the idea. On the contrary, I applaud this attempt at de-pathologizing, and de-medicalizing human suffering. As many have argued with more or less success and controversy of the years, many emotional problems are not best suited to be treated by psychotropic medication or even psychiatry. I think that psychiatry should embrace paradigms that include social and occupational constructs of emotional pain, not rooted in diseases and/or chemical imbalances. Such paradigms should, furthermore, not be limited to certain professions or life circumstances. We are all affected by human suffering. Access and willingness to appropriate care or support should not be granted only to those with a mental illness diagnosis.
Burnout is a promising idea that challenges our conceptualization of mental disorders. Burnout brings a humanity to emotional pain frequently lost in the medicalized diagnoses of the DSM. Psychiatry should seriously consider opening its door to nonmedicalized understanding of psychological suffering. By opening those doors, we begin to create a less medicalized construct for human suffering. We begin to create one based on shared human experience.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings is chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Springer, 2019).
Over the past years, I have had the opportunity to attend countless lectures on burnout provided by colleagues spanning across many fields in mental health and health care in general. The talks generally follow a common narration: 1. Your work is important and meaningful to many. 2. Your work requires significant training, dedication, and passion. 3. While you get personal gratification from your work, it does come with a cost. 4. This cost can be great and can affect you physically and mentally. 5. This cost is called burnout.
Burnout is described as irritability (poor mood), low energy, poor concentration, difficulty appreciating enjoyable things (anhedonia), and poor sleep, among other symptoms, as a result of work stress. At this point in the lectures, I usually ask whomever is sitting next to me: “I came in late, is this a lecture on depression?” to which the answer is typically “No! Of course not, this is about ‘burnout’ not mental illness.” And here lies a concern about burnout: Is burnout a concept describing depression that we have repackaged to protect professionals from the stigmatization of mental illness? Does our tendency not to characterize patients’ struggles as burnout stigmatize them – and imply that their employment is not challenging to cause burnout?
According to the literature, a range of factors affects burnout in professionals: lack of control, unclear job expectations, dysfunctional workplace dynamics, extremes of activity, lack of social support, work-life imbalance. Contrary to depression, burnout is not caused by neurobiological problems. Patients with burnout don’t have chemical imbalances, hyperactive default mode networks, or overactive amygdalas. Burnout is caused by social factors and affects dedicated, caring, and exceptional individuals who have been pushed outside their window of tolerance.
Literature suggests a variety of remedies to treat burnout: Reevaluate your employment, discuss occupational concerns with your supervisor, discuss with colleagues, receive help from your social support system, and seek human resources services. In addition, experts recommend engaging in relaxing activities, improving your sleep hygiene, exercising regularly, and participating in mindfulness to reduce symptoms. Contrary to depression, burnout does not require individuals to fix their maladaptive thoughts or discover inadequate unconscious beliefs that may be affecting their work. Contrary to depression, burnout does not require the rebalancing of neurochemistry using psychotropic medication.
The concept of burnout engenders concerns. I fear that it divides physicians and patients into two different classes and thus further stigmatizes those with mental illness. It implies that we physicians are somehow immune from mental illness and its consequences. We do not suffer from brain abnormalities, we do not require mind-altering medications, we are not “mentally ill.” Contrarily, at times it might be implied that patients’ jobs are not important enough to cause burnout; if they feel sad, anhedonic, have poor energy and poor sleep, it is because they have mental illness. Their brains are inadequate and flawed. But for physicians, our brains are intact, just pushed beyond human capabilities.
I should point out that I do not think that burnout experts believe or desire to promote such concepts. I am not aware of burnout experts championing physician exceptionalism or promoting the stigmatization of patients. I believe that this problem is an unintended consequence, a side effect, of the idea of burnout itself.
Another concern I have is that the concept of burnout may actually hinder physicians from seeking necessary and appropriate professional services to address symptoms. Interestingly, most lectures I have attended on burnout have not discussed the concerning number of physicians who end their lives by suicide. There was a time when I argued against the removal of the grief exclusion in the DSM; I worried that we were pathologizing natural emotional reactions to trauma. However, I have come to realize that, if someone is debilitated by depression, seeking professional help should not be predicated on the trigger. As such, I would recommend the vast number of physicians who state burnout in surveys to seriously consider the possibility that they may, in fact, be suffering from mental illness. We encourage our patients to seek help and speak out against stigmatization; isn’t it time that we as professionals should not be afraid to do the same?
I have concerns about the concept of burnout, but I certainly do not think that we should get rid of the idea. On the contrary, I applaud this attempt at de-pathologizing, and de-medicalizing human suffering. As many have argued with more or less success and controversy of the years, many emotional problems are not best suited to be treated by psychotropic medication or even psychiatry. I think that psychiatry should embrace paradigms that include social and occupational constructs of emotional pain, not rooted in diseases and/or chemical imbalances. Such paradigms should, furthermore, not be limited to certain professions or life circumstances. We are all affected by human suffering. Access and willingness to appropriate care or support should not be granted only to those with a mental illness diagnosis.
Burnout is a promising idea that challenges our conceptualization of mental disorders. Burnout brings a humanity to emotional pain frequently lost in the medicalized diagnoses of the DSM. Psychiatry should seriously consider opening its door to nonmedicalized understanding of psychological suffering. By opening those doors, we begin to create a less medicalized construct for human suffering. We begin to create one based on shared human experience.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings is chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Springer, 2019).
Over the past years, I have had the opportunity to attend countless lectures on burnout provided by colleagues spanning across many fields in mental health and health care in general. The talks generally follow a common narration: 1. Your work is important and meaningful to many. 2. Your work requires significant training, dedication, and passion. 3. While you get personal gratification from your work, it does come with a cost. 4. This cost can be great and can affect you physically and mentally. 5. This cost is called burnout.
Burnout is described as irritability (poor mood), low energy, poor concentration, difficulty appreciating enjoyable things (anhedonia), and poor sleep, among other symptoms, as a result of work stress. At this point in the lectures, I usually ask whomever is sitting next to me: “I came in late, is this a lecture on depression?” to which the answer is typically “No! Of course not, this is about ‘burnout’ not mental illness.” And here lies a concern about burnout: Is burnout a concept describing depression that we have repackaged to protect professionals from the stigmatization of mental illness? Does our tendency not to characterize patients’ struggles as burnout stigmatize them – and imply that their employment is not challenging to cause burnout?
According to the literature, a range of factors affects burnout in professionals: lack of control, unclear job expectations, dysfunctional workplace dynamics, extremes of activity, lack of social support, work-life imbalance. Contrary to depression, burnout is not caused by neurobiological problems. Patients with burnout don’t have chemical imbalances, hyperactive default mode networks, or overactive amygdalas. Burnout is caused by social factors and affects dedicated, caring, and exceptional individuals who have been pushed outside their window of tolerance.
Literature suggests a variety of remedies to treat burnout: Reevaluate your employment, discuss occupational concerns with your supervisor, discuss with colleagues, receive help from your social support system, and seek human resources services. In addition, experts recommend engaging in relaxing activities, improving your sleep hygiene, exercising regularly, and participating in mindfulness to reduce symptoms. Contrary to depression, burnout does not require individuals to fix their maladaptive thoughts or discover inadequate unconscious beliefs that may be affecting their work. Contrary to depression, burnout does not require the rebalancing of neurochemistry using psychotropic medication.
The concept of burnout engenders concerns. I fear that it divides physicians and patients into two different classes and thus further stigmatizes those with mental illness. It implies that we physicians are somehow immune from mental illness and its consequences. We do not suffer from brain abnormalities, we do not require mind-altering medications, we are not “mentally ill.” Contrarily, at times it might be implied that patients’ jobs are not important enough to cause burnout; if they feel sad, anhedonic, have poor energy and poor sleep, it is because they have mental illness. Their brains are inadequate and flawed. But for physicians, our brains are intact, just pushed beyond human capabilities.
I should point out that I do not think that burnout experts believe or desire to promote such concepts. I am not aware of burnout experts championing physician exceptionalism or promoting the stigmatization of patients. I believe that this problem is an unintended consequence, a side effect, of the idea of burnout itself.
Another concern I have is that the concept of burnout may actually hinder physicians from seeking necessary and appropriate professional services to address symptoms. Interestingly, most lectures I have attended on burnout have not discussed the concerning number of physicians who end their lives by suicide. There was a time when I argued against the removal of the grief exclusion in the DSM; I worried that we were pathologizing natural emotional reactions to trauma. However, I have come to realize that, if someone is debilitated by depression, seeking professional help should not be predicated on the trigger. As such, I would recommend the vast number of physicians who state burnout in surveys to seriously consider the possibility that they may, in fact, be suffering from mental illness. We encourage our patients to seek help and speak out against stigmatization; isn’t it time that we as professionals should not be afraid to do the same?
I have concerns about the concept of burnout, but I certainly do not think that we should get rid of the idea. On the contrary, I applaud this attempt at de-pathologizing, and de-medicalizing human suffering. As many have argued with more or less success and controversy of the years, many emotional problems are not best suited to be treated by psychotropic medication or even psychiatry. I think that psychiatry should embrace paradigms that include social and occupational constructs of emotional pain, not rooted in diseases and/or chemical imbalances. Such paradigms should, furthermore, not be limited to certain professions or life circumstances. We are all affected by human suffering. Access and willingness to appropriate care or support should not be granted only to those with a mental illness diagnosis.
Burnout is a promising idea that challenges our conceptualization of mental disorders. Burnout brings a humanity to emotional pain frequently lost in the medicalized diagnoses of the DSM. Psychiatry should seriously consider opening its door to nonmedicalized understanding of psychological suffering. By opening those doors, we begin to create a less medicalized construct for human suffering. We begin to create one based on shared human experience.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings is chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Springer, 2019).
Complexity of suicidal ideation, behavior points to need for new treatments
LAS VEGAS – More than 10 years ago, Gerard Sanacora, PhD, MD, came across a study in the medical literature that stopped him in his tracks.
For the study, Austrian neurologist Eberhard A. Deisenhammer, MD, and colleagues sought to determine the length of the period between consideration and accomplishment of a suicide attempt (J Clin Psychiatry. 2009;70[1]:19-24). To do so, they interviewed 82 patients who were referred to a psychiatric university hospital after a suicide attempt. Nearly half of the patients (48%) reported that the period between the first current thought of suicide and the actual attempt had lasted 10 minutes or less.
“When you’re talking about treating suicide behavior, there are so many components: the impulsivity component, the resilience component – all these things that can’t be measured with a simple outcome measure,” Dr. Sanacora said at an annual psychopharmacology update held by the Nevada Psychiatric Association. “That’s one of the real challenges. It requires us to take a good look at how we’re treating these patients in general.”
It also underscores the need for new treatments that target suicidal ideation and behavior.
“There is increasing evidence that ketamine and esketamine can produce effects that could be used in the treatment of mood disorder patients with suicidal ideation or behavior,” said Dr. Sanacora, professor of psychiatry at Yale University, New Haven, Conn. “However, there are many challenges to performing the studies that are required to more definitively demonstrate rapid and sustained improvement in suicide risks.”
The global 12-month prevalence of nonfatal suicide attempts is about 0.3% to 0.4%, and the lifetime prevalence is 3%, “which is pretty shocking,” he said. In the United States, there are more than 30 suicide attempts for each suicide death. At the same time, a World Health Organization community survey conducted in 21 countries found that the 12-month prevalence of suicidal ideation was about 2%, and that the lifetime prevalence was 9%. “These are large numbers that we’re talking about internationally,” said Dr. Sanacora, who also directs the Yale Depression Research Program. In 2013, suicidal ideation constituted nearly 1% of all adult ED visits in the United States, with conservative costs of $2.2 billion. “Every step along the process takes a large toll on the health care system and society, from the top level of completed suicide to suicidal ideation,” he said.
According to 2016 data from the Centers for Disease Control and Prevention, nearly 10 million people in the United States have seriously considered suicide, about 2.5 million made a plan, about 1 million attempted suicide, and about 40,000 completed suicide. “We have to think about what we’re treating,” Dr. Sanacora said. “Are we treating the suicidal ideation, or are we trying to prevent completed suicides?”
A prior history of attempted suicide is the strongest single predictive factor of a completed suicide. “In fact, the risk of dying by suicide is approximately 100 times than that of the general population within 1 year of an index attempt,” he said. Another major risk factor is having a previous psychiatric hospitalization. In fact, up to 41% of those who completed suicide had been psychiatric inpatients within the previous year, and as many as 9% of suicides occurred within 1 day of discharge from psychiatric inpatient care. Other identified risk factors include marital status, belonging to a sexual minority, occupation, military service, general medical comorbidities, diagnosis of personality disorder, chronic pain, traumatic brain injury, childhood abuse, location of residence, access to firearms, and family history of suicide. Protective factors include having a strong social support network, being a parent, and religiosity. “These are things that typically aren’t part of a treatment, but they can be woven into a treatment plan in some way,” he said.
Other identified risk symptoms include feelings of worthlessness and hopelessness, the combination of depression and anxiety, and psychosis, regardless of the specific diagnosis.
Medical stabilization constitutes the first step in the standard treatment approach to suicidal ideation and behavior. “You want to make sure the person is hospitalized and take care of any injuries that may have been sustained in the suicide attempt,” Dr. Sanacora said. The next step is reducing the immediate risks. “For the most part, that’s making sure the individual is in a safe setting commensurate with the level of risk,” he said. “You want to remove any other risks that could be around them. Then, you want to assure that an appropriate level of follow-up is provided on stepdown to lower levels of care. That year after hospitalization puts you at incredible risk, so we want to make sure we’re not just treating something in the acute phase and then not having longer-term follow-up for it.”
Existing treatments that have some evidence to help with the treatment of suicidal ideation and behavior include the use of antidepressants, lithium, and clozapine, but these agents are far from fast-acting for a patient in crisis. “In addition, a lot of docs are hesitant to give lithium because it has the potential of overdose itself,” Dr. Sanacora said. With clozapine, he continued, “there is some level of confounding by indication because, when you’re giving clozapine, it’s usually a more reliable patient, one who is not at risk of self-harm.”
The STAR*D (Sequenced Treatment Alternatives to Relieve Depression) trial demonstrated that, for the patients who do not respond to the first two levels of treatment with citalopram, their chances of having a remission by getting a third or fourth level of treatment is reduced to below 15% (Am J Psychiatry. 2006;163[1]:28-40).
“This suggests that, with our current armamentarium, we are limited,” said Dr. Sanacora, who is also codirector of the Yale New Haven Hospital Interventional Psychiatry Service. In the STAR*D trial, the time to response to citalopram was 6 weeks in 50% of patients. “So, when somebody is going through a crisis and is at imminent risk for suicide, and you tell them, ‘You’ll be 50% better in 6 weeks,’ that’s hard to swallow,” he said.
Recent studies of ketamine and esketamine have demonstrated a rapid onset of effect in patients with major depressive disorder, but whether they alter suicidal ideation and behavior remains unclear. “If you are wanting to improve suicidal ideation and behavior, what outcome measure are you using to do this?” Dr. Sanacora asked. “It may seem simple, but it’s not. To do a clinical trial, you would need large sample sizes to look at behavior as an outcome. In fact, even retrospective studies on this topic don’t have enough events to give you statistical meaning.” This leaves clinicians to consider scales that have been used for examining suicidal ideation and behavior over the years, including the MINI suicidality module, the SAD PERSONS scale, and the Suicide Intent Scale. “However, while they could have some value to be used clinically, these scales really don’t have great value as outcome measures,” Dr. Sanacora said.
There also have been attempts to develop scales that capture changes in suicidal ideation and behavior over time, including the C-SSRS (Columbia-Suicide Severity Rating Scale) and the Sheehan Suicidality Tracking Scale. “The sad thing is, none of these measures have been proven to be very useful clinically,” he said. “They may have some level of sensitivity and specificity, but their actual predictive value is not great. So using these clinically is somewhat difficult.”
In 2018, Dr. Sanacora and his colleagues published results from a systematic review and individual participant data meta-analysis examining the effects of a single dose of ketamine on suicidal ideation (Am J Psychiatry. 2018;175[2]:150-8). The analysis included 167 participants with suicidal ideation at baseline. “Within 24 hours there was a very clear decrease in suicidal ideation in terms of clinician-reported scale,” he said. “Over 50% of patients reported having minimal or no ideation after treatment. That was maintained for 7 days.” Effect sizes were moderate to large at all time points post dose.
In the largest meta-analysis of its kind to date, researchers reviewed 15 independent trials of ketamine for suicide ideation in 572 adults with psychiatric disorders, all with a single dose of drug with varying routes and dosages (Aust N Z J Psychiatry. 2020;54[1]:29-45). The researchers in that study concluded that ketamine “may have a role in acute treatment for suicidality. However, there is clearly a need for clinical measures to ensure persistence of any benefits.”
Esketamine, which was approved in March 2019 for major depressive disorder, also shows promise in patients with suicidal ideation and behavior. In a double-blind, multicenter, proof-of-concept study, researchers randomized 68 participants to receive esketamine (84 mg) or placebo twice weekly for 4 weeks, in addition to comprehensive standard-of-care treatment (Am J Psychiatry. 2018;175[7]:620-30). The primary efficacy endpoint was change in score from baseline to 4 hours after initial dose on the MADRS (Montgomery-Asberg Depression Rating Scale). “There was a nice effect in the antidepressant response, compared with placebo. It hit the primary endpoint at 4 hours. The patients got treated twice a week for 4 weeks. People got better quickly and stayed well moving on.” The researchers also found that the rate of remission at day 25 was 60% in the esketamine group, compared with 42% in the placebo group. “The take-home message is that, even without the esketamine, the remission rate was 42% at day 25. That means if you’re giving people really good care, meaning that you’re seeing them twice a week and they’re inpatient until they’re able to go outpatient, people can do pretty well with that level of care.”
Meanwhile, In a proof-of-concept trial, 18 depressed subjects with acute suicidal ideation who presented to the emergency department and required hospitalization were randomized to either IV ketamine 0.2 mg/kg or to saline placebo (Depress Anxiety. 2019 Nov 16. doi: 10.1002/da.22975). Ninety minutes after infusion, 88% of patients in the ketamine group had achieved remission of suicidal ideation, compared with 33% in the placebo group (P less than .05). No serious adverse events were noted.
“There is a clear need for new treatments targeting suicidal ideation and behavior,” Dr. Sanacora concluded. “Any plan to institute a rapid-acting treatment for individuals with imminent risk of suicidal behavior must be placed in the context of a larger comprehensive treatment plan. Getting somebody to feel better in the short run is great, but you really have to think about the whole treatment plan.”
Dr. Sanacora reported having received grants and research support from numerous pharmaceutical companies. He also holds an ownership interest in Biohaven Pharmaceuticals.
LAS VEGAS – More than 10 years ago, Gerard Sanacora, PhD, MD, came across a study in the medical literature that stopped him in his tracks.
For the study, Austrian neurologist Eberhard A. Deisenhammer, MD, and colleagues sought to determine the length of the period between consideration and accomplishment of a suicide attempt (J Clin Psychiatry. 2009;70[1]:19-24). To do so, they interviewed 82 patients who were referred to a psychiatric university hospital after a suicide attempt. Nearly half of the patients (48%) reported that the period between the first current thought of suicide and the actual attempt had lasted 10 minutes or less.
“When you’re talking about treating suicide behavior, there are so many components: the impulsivity component, the resilience component – all these things that can’t be measured with a simple outcome measure,” Dr. Sanacora said at an annual psychopharmacology update held by the Nevada Psychiatric Association. “That’s one of the real challenges. It requires us to take a good look at how we’re treating these patients in general.”
It also underscores the need for new treatments that target suicidal ideation and behavior.
“There is increasing evidence that ketamine and esketamine can produce effects that could be used in the treatment of mood disorder patients with suicidal ideation or behavior,” said Dr. Sanacora, professor of psychiatry at Yale University, New Haven, Conn. “However, there are many challenges to performing the studies that are required to more definitively demonstrate rapid and sustained improvement in suicide risks.”
The global 12-month prevalence of nonfatal suicide attempts is about 0.3% to 0.4%, and the lifetime prevalence is 3%, “which is pretty shocking,” he said. In the United States, there are more than 30 suicide attempts for each suicide death. At the same time, a World Health Organization community survey conducted in 21 countries found that the 12-month prevalence of suicidal ideation was about 2%, and that the lifetime prevalence was 9%. “These are large numbers that we’re talking about internationally,” said Dr. Sanacora, who also directs the Yale Depression Research Program. In 2013, suicidal ideation constituted nearly 1% of all adult ED visits in the United States, with conservative costs of $2.2 billion. “Every step along the process takes a large toll on the health care system and society, from the top level of completed suicide to suicidal ideation,” he said.
According to 2016 data from the Centers for Disease Control and Prevention, nearly 10 million people in the United States have seriously considered suicide, about 2.5 million made a plan, about 1 million attempted suicide, and about 40,000 completed suicide. “We have to think about what we’re treating,” Dr. Sanacora said. “Are we treating the suicidal ideation, or are we trying to prevent completed suicides?”
A prior history of attempted suicide is the strongest single predictive factor of a completed suicide. “In fact, the risk of dying by suicide is approximately 100 times than that of the general population within 1 year of an index attempt,” he said. Another major risk factor is having a previous psychiatric hospitalization. In fact, up to 41% of those who completed suicide had been psychiatric inpatients within the previous year, and as many as 9% of suicides occurred within 1 day of discharge from psychiatric inpatient care. Other identified risk factors include marital status, belonging to a sexual minority, occupation, military service, general medical comorbidities, diagnosis of personality disorder, chronic pain, traumatic brain injury, childhood abuse, location of residence, access to firearms, and family history of suicide. Protective factors include having a strong social support network, being a parent, and religiosity. “These are things that typically aren’t part of a treatment, but they can be woven into a treatment plan in some way,” he said.
Other identified risk symptoms include feelings of worthlessness and hopelessness, the combination of depression and anxiety, and psychosis, regardless of the specific diagnosis.
Medical stabilization constitutes the first step in the standard treatment approach to suicidal ideation and behavior. “You want to make sure the person is hospitalized and take care of any injuries that may have been sustained in the suicide attempt,” Dr. Sanacora said. The next step is reducing the immediate risks. “For the most part, that’s making sure the individual is in a safe setting commensurate with the level of risk,” he said. “You want to remove any other risks that could be around them. Then, you want to assure that an appropriate level of follow-up is provided on stepdown to lower levels of care. That year after hospitalization puts you at incredible risk, so we want to make sure we’re not just treating something in the acute phase and then not having longer-term follow-up for it.”
Existing treatments that have some evidence to help with the treatment of suicidal ideation and behavior include the use of antidepressants, lithium, and clozapine, but these agents are far from fast-acting for a patient in crisis. “In addition, a lot of docs are hesitant to give lithium because it has the potential of overdose itself,” Dr. Sanacora said. With clozapine, he continued, “there is some level of confounding by indication because, when you’re giving clozapine, it’s usually a more reliable patient, one who is not at risk of self-harm.”
The STAR*D (Sequenced Treatment Alternatives to Relieve Depression) trial demonstrated that, for the patients who do not respond to the first two levels of treatment with citalopram, their chances of having a remission by getting a third or fourth level of treatment is reduced to below 15% (Am J Psychiatry. 2006;163[1]:28-40).
“This suggests that, with our current armamentarium, we are limited,” said Dr. Sanacora, who is also codirector of the Yale New Haven Hospital Interventional Psychiatry Service. In the STAR*D trial, the time to response to citalopram was 6 weeks in 50% of patients. “So, when somebody is going through a crisis and is at imminent risk for suicide, and you tell them, ‘You’ll be 50% better in 6 weeks,’ that’s hard to swallow,” he said.
Recent studies of ketamine and esketamine have demonstrated a rapid onset of effect in patients with major depressive disorder, but whether they alter suicidal ideation and behavior remains unclear. “If you are wanting to improve suicidal ideation and behavior, what outcome measure are you using to do this?” Dr. Sanacora asked. “It may seem simple, but it’s not. To do a clinical trial, you would need large sample sizes to look at behavior as an outcome. In fact, even retrospective studies on this topic don’t have enough events to give you statistical meaning.” This leaves clinicians to consider scales that have been used for examining suicidal ideation and behavior over the years, including the MINI suicidality module, the SAD PERSONS scale, and the Suicide Intent Scale. “However, while they could have some value to be used clinically, these scales really don’t have great value as outcome measures,” Dr. Sanacora said.
There also have been attempts to develop scales that capture changes in suicidal ideation and behavior over time, including the C-SSRS (Columbia-Suicide Severity Rating Scale) and the Sheehan Suicidality Tracking Scale. “The sad thing is, none of these measures have been proven to be very useful clinically,” he said. “They may have some level of sensitivity and specificity, but their actual predictive value is not great. So using these clinically is somewhat difficult.”
In 2018, Dr. Sanacora and his colleagues published results from a systematic review and individual participant data meta-analysis examining the effects of a single dose of ketamine on suicidal ideation (Am J Psychiatry. 2018;175[2]:150-8). The analysis included 167 participants with suicidal ideation at baseline. “Within 24 hours there was a very clear decrease in suicidal ideation in terms of clinician-reported scale,” he said. “Over 50% of patients reported having minimal or no ideation after treatment. That was maintained for 7 days.” Effect sizes were moderate to large at all time points post dose.
In the largest meta-analysis of its kind to date, researchers reviewed 15 independent trials of ketamine for suicide ideation in 572 adults with psychiatric disorders, all with a single dose of drug with varying routes and dosages (Aust N Z J Psychiatry. 2020;54[1]:29-45). The researchers in that study concluded that ketamine “may have a role in acute treatment for suicidality. However, there is clearly a need for clinical measures to ensure persistence of any benefits.”
Esketamine, which was approved in March 2019 for major depressive disorder, also shows promise in patients with suicidal ideation and behavior. In a double-blind, multicenter, proof-of-concept study, researchers randomized 68 participants to receive esketamine (84 mg) or placebo twice weekly for 4 weeks, in addition to comprehensive standard-of-care treatment (Am J Psychiatry. 2018;175[7]:620-30). The primary efficacy endpoint was change in score from baseline to 4 hours after initial dose on the MADRS (Montgomery-Asberg Depression Rating Scale). “There was a nice effect in the antidepressant response, compared with placebo. It hit the primary endpoint at 4 hours. The patients got treated twice a week for 4 weeks. People got better quickly and stayed well moving on.” The researchers also found that the rate of remission at day 25 was 60% in the esketamine group, compared with 42% in the placebo group. “The take-home message is that, even without the esketamine, the remission rate was 42% at day 25. That means if you’re giving people really good care, meaning that you’re seeing them twice a week and they’re inpatient until they’re able to go outpatient, people can do pretty well with that level of care.”
Meanwhile, In a proof-of-concept trial, 18 depressed subjects with acute suicidal ideation who presented to the emergency department and required hospitalization were randomized to either IV ketamine 0.2 mg/kg or to saline placebo (Depress Anxiety. 2019 Nov 16. doi: 10.1002/da.22975). Ninety minutes after infusion, 88% of patients in the ketamine group had achieved remission of suicidal ideation, compared with 33% in the placebo group (P less than .05). No serious adverse events were noted.
“There is a clear need for new treatments targeting suicidal ideation and behavior,” Dr. Sanacora concluded. “Any plan to institute a rapid-acting treatment for individuals with imminent risk of suicidal behavior must be placed in the context of a larger comprehensive treatment plan. Getting somebody to feel better in the short run is great, but you really have to think about the whole treatment plan.”
Dr. Sanacora reported having received grants and research support from numerous pharmaceutical companies. He also holds an ownership interest in Biohaven Pharmaceuticals.
LAS VEGAS – More than 10 years ago, Gerard Sanacora, PhD, MD, came across a study in the medical literature that stopped him in his tracks.
For the study, Austrian neurologist Eberhard A. Deisenhammer, MD, and colleagues sought to determine the length of the period between consideration and accomplishment of a suicide attempt (J Clin Psychiatry. 2009;70[1]:19-24). To do so, they interviewed 82 patients who were referred to a psychiatric university hospital after a suicide attempt. Nearly half of the patients (48%) reported that the period between the first current thought of suicide and the actual attempt had lasted 10 minutes or less.
“When you’re talking about treating suicide behavior, there are so many components: the impulsivity component, the resilience component – all these things that can’t be measured with a simple outcome measure,” Dr. Sanacora said at an annual psychopharmacology update held by the Nevada Psychiatric Association. “That’s one of the real challenges. It requires us to take a good look at how we’re treating these patients in general.”
It also underscores the need for new treatments that target suicidal ideation and behavior.
“There is increasing evidence that ketamine and esketamine can produce effects that could be used in the treatment of mood disorder patients with suicidal ideation or behavior,” said Dr. Sanacora, professor of psychiatry at Yale University, New Haven, Conn. “However, there are many challenges to performing the studies that are required to more definitively demonstrate rapid and sustained improvement in suicide risks.”
The global 12-month prevalence of nonfatal suicide attempts is about 0.3% to 0.4%, and the lifetime prevalence is 3%, “which is pretty shocking,” he said. In the United States, there are more than 30 suicide attempts for each suicide death. At the same time, a World Health Organization community survey conducted in 21 countries found that the 12-month prevalence of suicidal ideation was about 2%, and that the lifetime prevalence was 9%. “These are large numbers that we’re talking about internationally,” said Dr. Sanacora, who also directs the Yale Depression Research Program. In 2013, suicidal ideation constituted nearly 1% of all adult ED visits in the United States, with conservative costs of $2.2 billion. “Every step along the process takes a large toll on the health care system and society, from the top level of completed suicide to suicidal ideation,” he said.
According to 2016 data from the Centers for Disease Control and Prevention, nearly 10 million people in the United States have seriously considered suicide, about 2.5 million made a plan, about 1 million attempted suicide, and about 40,000 completed suicide. “We have to think about what we’re treating,” Dr. Sanacora said. “Are we treating the suicidal ideation, or are we trying to prevent completed suicides?”
A prior history of attempted suicide is the strongest single predictive factor of a completed suicide. “In fact, the risk of dying by suicide is approximately 100 times than that of the general population within 1 year of an index attempt,” he said. Another major risk factor is having a previous psychiatric hospitalization. In fact, up to 41% of those who completed suicide had been psychiatric inpatients within the previous year, and as many as 9% of suicides occurred within 1 day of discharge from psychiatric inpatient care. Other identified risk factors include marital status, belonging to a sexual minority, occupation, military service, general medical comorbidities, diagnosis of personality disorder, chronic pain, traumatic brain injury, childhood abuse, location of residence, access to firearms, and family history of suicide. Protective factors include having a strong social support network, being a parent, and religiosity. “These are things that typically aren’t part of a treatment, but they can be woven into a treatment plan in some way,” he said.
Other identified risk symptoms include feelings of worthlessness and hopelessness, the combination of depression and anxiety, and psychosis, regardless of the specific diagnosis.
Medical stabilization constitutes the first step in the standard treatment approach to suicidal ideation and behavior. “You want to make sure the person is hospitalized and take care of any injuries that may have been sustained in the suicide attempt,” Dr. Sanacora said. The next step is reducing the immediate risks. “For the most part, that’s making sure the individual is in a safe setting commensurate with the level of risk,” he said. “You want to remove any other risks that could be around them. Then, you want to assure that an appropriate level of follow-up is provided on stepdown to lower levels of care. That year after hospitalization puts you at incredible risk, so we want to make sure we’re not just treating something in the acute phase and then not having longer-term follow-up for it.”
Existing treatments that have some evidence to help with the treatment of suicidal ideation and behavior include the use of antidepressants, lithium, and clozapine, but these agents are far from fast-acting for a patient in crisis. “In addition, a lot of docs are hesitant to give lithium because it has the potential of overdose itself,” Dr. Sanacora said. With clozapine, he continued, “there is some level of confounding by indication because, when you’re giving clozapine, it’s usually a more reliable patient, one who is not at risk of self-harm.”
The STAR*D (Sequenced Treatment Alternatives to Relieve Depression) trial demonstrated that, for the patients who do not respond to the first two levels of treatment with citalopram, their chances of having a remission by getting a third or fourth level of treatment is reduced to below 15% (Am J Psychiatry. 2006;163[1]:28-40).
“This suggests that, with our current armamentarium, we are limited,” said Dr. Sanacora, who is also codirector of the Yale New Haven Hospital Interventional Psychiatry Service. In the STAR*D trial, the time to response to citalopram was 6 weeks in 50% of patients. “So, when somebody is going through a crisis and is at imminent risk for suicide, and you tell them, ‘You’ll be 50% better in 6 weeks,’ that’s hard to swallow,” he said.
Recent studies of ketamine and esketamine have demonstrated a rapid onset of effect in patients with major depressive disorder, but whether they alter suicidal ideation and behavior remains unclear. “If you are wanting to improve suicidal ideation and behavior, what outcome measure are you using to do this?” Dr. Sanacora asked. “It may seem simple, but it’s not. To do a clinical trial, you would need large sample sizes to look at behavior as an outcome. In fact, even retrospective studies on this topic don’t have enough events to give you statistical meaning.” This leaves clinicians to consider scales that have been used for examining suicidal ideation and behavior over the years, including the MINI suicidality module, the SAD PERSONS scale, and the Suicide Intent Scale. “However, while they could have some value to be used clinically, these scales really don’t have great value as outcome measures,” Dr. Sanacora said.
There also have been attempts to develop scales that capture changes in suicidal ideation and behavior over time, including the C-SSRS (Columbia-Suicide Severity Rating Scale) and the Sheehan Suicidality Tracking Scale. “The sad thing is, none of these measures have been proven to be very useful clinically,” he said. “They may have some level of sensitivity and specificity, but their actual predictive value is not great. So using these clinically is somewhat difficult.”
In 2018, Dr. Sanacora and his colleagues published results from a systematic review and individual participant data meta-analysis examining the effects of a single dose of ketamine on suicidal ideation (Am J Psychiatry. 2018;175[2]:150-8). The analysis included 167 participants with suicidal ideation at baseline. “Within 24 hours there was a very clear decrease in suicidal ideation in terms of clinician-reported scale,” he said. “Over 50% of patients reported having minimal or no ideation after treatment. That was maintained for 7 days.” Effect sizes were moderate to large at all time points post dose.
In the largest meta-analysis of its kind to date, researchers reviewed 15 independent trials of ketamine for suicide ideation in 572 adults with psychiatric disorders, all with a single dose of drug with varying routes and dosages (Aust N Z J Psychiatry. 2020;54[1]:29-45). The researchers in that study concluded that ketamine “may have a role in acute treatment for suicidality. However, there is clearly a need for clinical measures to ensure persistence of any benefits.”
Esketamine, which was approved in March 2019 for major depressive disorder, also shows promise in patients with suicidal ideation and behavior. In a double-blind, multicenter, proof-of-concept study, researchers randomized 68 participants to receive esketamine (84 mg) or placebo twice weekly for 4 weeks, in addition to comprehensive standard-of-care treatment (Am J Psychiatry. 2018;175[7]:620-30). The primary efficacy endpoint was change in score from baseline to 4 hours after initial dose on the MADRS (Montgomery-Asberg Depression Rating Scale). “There was a nice effect in the antidepressant response, compared with placebo. It hit the primary endpoint at 4 hours. The patients got treated twice a week for 4 weeks. People got better quickly and stayed well moving on.” The researchers also found that the rate of remission at day 25 was 60% in the esketamine group, compared with 42% in the placebo group. “The take-home message is that, even without the esketamine, the remission rate was 42% at day 25. That means if you’re giving people really good care, meaning that you’re seeing them twice a week and they’re inpatient until they’re able to go outpatient, people can do pretty well with that level of care.”
Meanwhile, In a proof-of-concept trial, 18 depressed subjects with acute suicidal ideation who presented to the emergency department and required hospitalization were randomized to either IV ketamine 0.2 mg/kg or to saline placebo (Depress Anxiety. 2019 Nov 16. doi: 10.1002/da.22975). Ninety minutes after infusion, 88% of patients in the ketamine group had achieved remission of suicidal ideation, compared with 33% in the placebo group (P less than .05). No serious adverse events were noted.
“There is a clear need for new treatments targeting suicidal ideation and behavior,” Dr. Sanacora concluded. “Any plan to institute a rapid-acting treatment for individuals with imminent risk of suicidal behavior must be placed in the context of a larger comprehensive treatment plan. Getting somebody to feel better in the short run is great, but you really have to think about the whole treatment plan.”
Dr. Sanacora reported having received grants and research support from numerous pharmaceutical companies. He also holds an ownership interest in Biohaven Pharmaceuticals.
EXPERT ANALYSIS FROM NPA 2020